MORE TARIFF PAIN FOR FRAME DISTRIBUTORS
Australian Border Force plans to expand its border tax to now incorporate metal frames
PREMIUM HYDROPHOBIC IOL with PUre Refractive Optics (PRO) TEchnology

For your daily range of vision
30
THE ISSUES FACING MODERN-DAY CATARACT


Three surgeons provide a bird’s eye view on the current state of cataract surgery
52
OCULAR ASSOCIATIONS IN PREGNANCY
The practitioner’s duty is heightened because they have two patients to consider
03
JULY 2023
AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975
You’d look good in Specsavers

If you love the idea of a fulfilling career in optometry, where you’ll have access to the latest technology and be part of a business that’s focused on advancing your career, you’ll shine at Specsavers.

FURTHER TARIFF PAIN FOR EYEWEAR FRAME DISTRIBUTORS COMES AT A 'DIFFICULT' TIME
An Australia Border Force (ABF) decision to reinstate a 5% border tax beyond acetate eyewear to now cover metal frames will likely hurt the independent optical market further, industry figures have warned, as the Optical Distributors and Manufacturers Association (ODMA) vows to keep advocating against the move.
It comes after the border authority issued a fresh alert on 24 May 2023 outlining its intention to revoke tariff concession order (TCO) TC 0315708, which covers metal spectacle frames.
Twelve months earlier, the same order was made against plastic frames, in a decision that blindsided the industry. With almost immediate effect, eyewear wholesalers who imported product from Europe

– for which there is no free trade agreement – needed to pay a 5% duty rate at the border, which they were previously exempt from.
Responding to the latest ABF decision on metal frames, Safilo Asia Pacific senior director Mr David Pearson said it was “a very poor decision and will only result in putting additional costs on consumers and pressure on the industry”.
“There will be no gain for optical industry or consumers, and it is likely that independent practices will bear the majority of the impact,” he said, noting that Safilo is a major supplier to independent optical practices in Australia.
Mr Mark Wymond, managing director of independent wholesalers Eyes Right Optical,
Modstyle and Sunglass Collective, was also disappointed by the move.
“This tariff only hurts the independent frame suppliers, it doesn’t touch some of the multi-nationals, and it is a ridiculous cash grab by a mislead government,” he said.
“Putting my economist hat on, let’s hope that the government has revoked this tariff concession to then use it to bargain an improved free trade deal with the EU.”
Eyecare Plus general manager Mr Philip Rose said the independent optometry network was disappointed by the TCO decisions that came at a difficult time for Australian consumers.
“The 5% will be added to the wholesale cost and ultimately patients will be paying more for their glasses. This has come at a time when inflation and the cost of living is at an all time high, with families struggling to pay for mortgages/rent, food and other
continued page 8
AUSSIE DEVICE USES ULTRASOUND TO NON-INVASIVELY DELIVER EYE THERAPIES
A Melbourne biotech company founded by ophthalmologist Dr Harry Unger and Mr Mark Unger has developed an investigational device that uses ultrasound to deliver therapies non-invasively through ocular tissues, offering advantages over the standard of care for some retinal and corneal diseases.
The handheld system is being developed by muPharma and comprises a reusable ultrasound actuator and a disposable, sterile tip. The tip features a solid, non-reactive substrate with fabricated features to hold the relevant drug. The mechanism of action, called sonophoresis, involves gentle ultrasonic vibration causing cavitation in tissue – this
“opens” the inter-cellular spaces and makes cell surface membranes more permeable.
This technology has also been shown to have applications in immunology, delivering vaccines to the inside of the lip.
In ophthalmology, the muPharma device could replace intravitreal injections for age-related macular degeneration (AMD) and avoid removal of the corneal-epithelium for corneal cross-linking treatment.
muPharma managing director Mark Unger who is an Adjunct Senior Research Fellow at the Monash Institute of Pharmaceutical Sciences and an Honorary Fellow at The University of Melbourne Department of Ophthalmology,
said overcoming the need for eye injections could alleviate patient fear, a predominant cause of non-compliance.
“Our device also removes the significant risks associated with injections into the eye, including raising intraocular pressure as only the drug – and not the solution – in which it is dissolved, is delivered which is not only advantageous for wet-form AMD, but also opens new dry-form AMD treatment options,” he said.
“muPharma’s device provides convenience for patients who could potentially drive and work shortly after treatment and not need carers unless otherwise required
continued page 8
Specsavers’ global sustainability team is setting ambitious targets, including carbon net zero by 2050, explains CATHY RENNIE MATOS, who is responsible for driving it at a regional level. page 60

AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975 JULY 2023
Metal eyewear from certain countries are set to cost 5% more to import into Australia.
Treating a wide range of patients with a unique ZEISS optic. ZEISS CT LUCIA 621P/PY
The CT LUCIA from ZEISS is the new aspheric monofocal IOL in the hydrophobic ZEISS cataract portfolio.

With excellent stability, an improved injector system and a design that is uniquely forgiving to decentration, it delivers consistent visual outcomes for a broad range of patients and surgical situations.

Benefit from:
• Consistent visual outcomes* thanks to the patented ZEISS Optic (ZO) Asphericity Concept

• Excellent stability through the use of an optic-haptic junction and step-valued C-loop haptic
• Intuitive injector handling due to latest improvements to the fully preloaded injector system
*The data is taken from a simulation. The transferability of the results of such a simulation to patients with an actual implanted intraocular lens has not yet been scientifically proven. Whether the simulated impressions correspond to the actual visual impressions must be clarified in future invasive studies. www.zeiss.com/LUCIA ZEISS AU: 1300 365 470 med.au@zeiss.com Carl Zeiss Pty Ltd, NSW 2113 AUSTRALIA.
IN THIS ISSUE
Cataract surgery is the most-performed operation in Australia, so it’s unsurprising to discover that it’s at the epicentre of ophthalmic innovation. The almost-immediate impact on people’s lives means it’s also one of the most effective surgeries available – and let’s face it, it’s a reliable income source for most ophthalmologists.
But there’s a common industry saying that there’s “no free lunch” in optics. There’s always room for improvement, and ophthalmologists have seen their share of over-hyped IOLs. Innovation isn’t always linear, nor does it regularly advance in leaps – and this is perhaps the case in cataract surgery amid an era of optimisation.
DRY EYE DIET
CORRECT CALCULATION
Many of these innovations can be found in this issue with a special focus on cataract surgery. Take premium IOLs for example. For years, multifocals were the go-to for spectacle independence, but this came at a cost of visual disturbances. Extended depth of focus (EDOF) IOLs previously offered the double whammy – some spectacle dependence and some visual disturbances – but in recent years manufacturers have cracked the code and the tide is now turning in EDOF’s favour.
IOL materials are another example of innovation. Hydrophobic and hydrophilic acrylic are the two main choices today. Both are imperfect, and Adelaide’s Dr Ben LaHood covers this on page 44. Alcon’s R&D team have also emerged with the Clareon IOL family with an improved hydrophobic material, which has now been applied to its PanOptix trifocal (page 42).
IOL MATERIALS
IN TOUCH
Incremental advances in phaco, around since the 1960s, have also led to big advantages. The Swiss-made Sophi system is one of the newest to Australia (page 40), with the most notable of these being its completely cable-free design.



In terms of policy, Australia enjoys access to advanced IOLs and is often a testing ground due to its favourable regulatory system. But wait times in the public system remain an issue. Thankfully, NSW – one of the worst-performers – has responded with changes to the urgency of cataract surgery for the second eye.


Australian cataract surgery is by no means the finished product, but it’s clear from the level of activity that it punches well above its weight as surgeons seek the best for their patients.

INSIGHT July 2023 5 27 44 36
62
IPL inventor Dr Rolando Toyos was in Australia discussing the link between nutrition and the ocular surface.
Dr Ben LaHood on why the negativity surrounding hydrophilic IOLs is blown out of proportion.
A WA couple have combined their knowledge to develop a new automated software to process toric IOL calculations.
Ophthalmology Updates! is returning, ensuring eye doctors remain abreast of the latest in each subspecialty.
MYLES HUME Editor FEATURES JULY 2023 07 UPFRONT 09 NEWS THIS MONTH 69 OPTICAL DISPENSING 70 ORTHOPTICS AUSTRALIA 71 MANAGEMENT 72 SOAPBOX 73 CLASSIFIEDS/CALENDAR 74 PEOPLE ON THE MOVE EVERY ISSUE
NO ROOM FOR CATARACT COMPLACENCY EDITORIAL
Modernising phaco
Sophi is a complete revolution, intended to make the work of ophthalmologists and the surgical team simpler, safer, and more efficient.
Using a “Lean” philosophy, Sophi was designed to enhance cataract workflow by minimising unnecessary waste of time, materials, and energy.
Mobility
A truly wireless system offering flexibility and easy handling.
Simplicity
Simplicity
Compact footprint and modern, intuitive design.

Safety
Smart at every procedure step – ensuring fluidics and integrity.



Contact Designs For Vision today to arrange a trial.
Call 1800 225 307
dfv.com.au
DV1381-0523
UPFRONT
Just as Insight went to print, OPTOMETRIST WAREHOUSE, part of the Chemist Warehouse Group in Australia, and EyRIS, a Singapore-based healthcare technology company specialising in artificial intelligence (AI) healthcare solutions, announced they have signed a Memorandum of Understanding (MOU) to collaborate on a ground-breaking study focused on the effectiveness of AI in screening diabetic retinopathy. The study will span a period of 36
WEIRD
A new case study published in the journal Drug Science has suggested the psychedelic compound psilocybin may temporarily reverse colour blindness. The study outlined the experience of a 35-year-old man with mild red-green colour blindness. After taking 5 grams of psilocybin-containing magic mushrooms, he reported temporary improvement in his condition, posing new questions about psilocybin’s potential for lasting changes to the visual system for some people.
WONDERFUL
An “accidental miracle” has seen a Kiwi woman with glaucoma experience vision improvements. Radio NZ reported that well-known author Lynley Hood was diagnosed with glaucoma 12 years ago. Recently, she took part in a clinical trial for chronic pain treatment due to a pelvis fracture. She was in the placebo group who had an electrical current pass across their scalp, which ultimately improved her vision allowing her to return to activities such as reading and writing.
WACKY
Scientists have explored how the brain manages auditory and visual information when one eye is temporarily covered. Writing in NeuroImage, the Italian-German research team highlighted that a short period of monocular deprivation affects auditory processing, resulting in a selective increase in neural responses to sounds. The findings could provide insight for rehabilitation from different diseases and conditions, including amblyopia.
months and involve a large sample size of diabetic patients across various regions in Australia. IN OTHER NEWS, findings from the Australian Healthcare Index June 2023 report, supported by Healthengine and Australian Patients Association, reflect the healthcare system is under continued strain. Patient satisfaction with the healthcare system in Australia has dropped from 7.8 out of 10 in March 2021 to 7.0 out of 10 in June 2023. According to the report, 42% of Australians go less often to the GP due to out-of-pocket costs;
that jumps to one in two (51%) in the 18-34-year-old age bracket. FINALLY, Dr Shuan Dai, director of ophthalmology at Queensland Children’s Hospital, and Dr Ann Webber, senior paediatric optometrist, and their partners Ms Hong Duan and Mr Brad Gregory, are trekking sections of the Larapinta Trail in Alice Springs during NAIDOC week (2–9 July) to support the Children's Hospital Foundation. The Trek for Sick Kids aims to raise $20,000 for the foundation, which plays a vital role in enhancing the lives of sick and injured children.
Published by: 379 Docklands Drive, Docklands VIC 3008 T: 03 9690 8766 www.primecreative.com.au
Chief Operating Officer Christine Clancy christine.clancy@primecreative.com.au
Group Managing Editor Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Journalist Rhiannon Bowman rhiannon.bowman@primecreative.com.au
Commissioning Editor, Healthcare Education Jeff Megahan Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Salma Kennedy salma.kennedy@primecreative.com.au
Design Production Manager Michelle Weston michelle.weston@primecreative.com.au
The visual system is affected in approximately 25% of patients with preeclampsia during pregnancy. Page 53

WHAT'S
26-29 JULY
AUSCRS 2023 will be the first event for Dr Jacqueline Beltz and Prof Gerard Sutton as co-presidents, taking place at the Sheraton Mirage, Port Douglas. www.auscrs.org.au
Head of Design Blake Storey
Art Director Bea Barthelson Subscriptions
T: 03 9690 8766 subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright – No part of this publication be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.

INSIGHT July 2023 7
NEXT MONTH OPHTHALMOLOGY UPDATES!
AUGUST
place at Fullerton Hotel, Sydney, the conference is an ideal chance for eye doctors to brush up on common subspecialty topics.
THIS MONTH OPHTHALMOLOGY AUSCRS 2023
26-27
Taking
ophthalmologyupdates.com
Complete calendar page 73. insightnews.com.au
STAT
WORK
PHILANTHROPIC
ON
'FRAMES SUPPLIERS ARE FACING RISING COSTS'
continued from page 3
everyday goods,” he said.
TCOs are an Australian Government revenue concession that exists where there are no known Australian manufacturers of certain products that are substitutable for imported goods.
The TCO on eyewear meant importers did not need to pay the 5% duty rate in Australia. But that came to an end in May 2022 after Port Macquarie-based Optex Australia notified the ABF that it produces acetate eyewear in Australia.
The move has hit importers of European eyewear the hardest because Australia doesn’t have a free trade agreement with the continent yet. The vast majority of optical frames sold in Australia are imported, with most of these from the European Union.
The industry was bracing for the revocation of the metal frames TCO, after ABF signalled it would do so last year.
“Whilst this news is not entirely unexpected, it is very frustrating and I feel for frames suppliers that are already facing many rising costs,” ODMA CEO Ms Amanda Trotman said.
According to ODMA, the production capacity of the manufacturer who complained to the ABF is thought to be in the low thousands. The association said revoking the eyewear TCO means the $4 billion optical dispensing and eyewear industry – selling more than five million
frames each year – is now faced with a 5% tariff on millions of frames imported annually.
This decision, after decades of nil tariffs for the industry, has increased costs for retailers and consumers, exacerbating cost of living pressures on the millions of Australians who use optical products, as well as putting upward pressure on inflation, ODMA stated.
ODMA SEEKS ANSWERS
Now with the TCO revoked for metal frames, Trotman said this was not unexpected given The Customs Delegate took a broad view on what constituted producing substitutable goods when the decision was made to revoke the concession on plastic frames in 2022.
ODMA is still waiting on an update from the Minister of Home Affairs Office despite multiple requests. It was advised that the department requested the ABF explain further the decision it made in 2022 beyond its ODMA appeal response – and that an update would be provided.
“We have been keeping ODMA members updated on the matter and encouraged members to themselves write to the minister’s office. As recent as last week, another letter was sent to the Minister of Home Affairs instigated by an ODMA member via a Federal Member of Parliament,” Trotman said.
ODMA said it would now seek to
appeal the latest intention to revoke the metal frames TCO. At the time of writing, interested parties have until close of business 21 June 2023 to provide written reasons why the ABF should not go through with its plan. ODMA will do this, as well as seek further regulatory advice on other avenues to pursue.
“One further avenue to pursue of course is a broader consumer focused media campaign on the situation given costs often have to be passed on to those selling the eyewear and they often need to pass that increase on to the consumer as there are just so many pressures on costs for every business currently,” Trotman said.
Meanwhile, ODMA is continuing to keep tabs on the EU Free Trade Agreement, which would nullify tariffs imposed by ABF on the large volumes of eyewear coming from Europe.
Trotman said there had been progress on this front following recent comments from Prime Minister Anthony Albanese in the UK.
“ODMA is concerned that these revocation decisions create significant additional red tape and uncertainly for our members who are now faced with further administrative burdens when determining which products and countries the tariff applies to. It is ODMA’s view that the reimposition of these tariffs does little to nothing to assist Australian industry and is to the detriment of Australian consumers,” Trotman added.
DEVICE AIDS 'EPI-ON' METHOD FOR CORNEAL CROSS-LINKING
continued from page 3
because of general debility. There is also potential for increased ophthalmologist productivity to perform more complex and profitable procedures through having supervised para-medical staff provide treatment.”
Given its route of delivery, Mark Unger said there is also the possibility of needing lower anti-VEGF doses.
For corneal cross-linking, the muPharma device offers an “epi-on” method of rapidly, safely and effectively delivering riboflavin into the cornea without the need to remove the corneal epithelium.
“Riboflavin formulations delivered by the muPharma device do not require any

epithelial enhancers and the cross-linking procedure can be done in keeping with well-established and approved FDA clinical protocols that have demonstrated clinical efficacy,” he said.
The muPharma concept was developed by Dr Harry Unger, building on a previous, but ultimately limited, ultrasound-based system he conceived using a polymer gel to hold and release drugs.
During the past decade, the muPharma device has been developed at the Melbourne Centre for Nanofabrication under Professor Nicolas Voelcker (scientific director at MCN). Dr Harry Unger is chairman, guiding the company’s research direction in ophthalmology, and Dr Glenn Begley, previously the
muPharma’s ultrasound-based ocular drug delivery device.
CEO of BioCurate and vice-president of Oncology Global Research at Amgen, is the medical director.

Although using ultrasound to deliver drugs into skin is well established, Mark Unger said muPharma’s technology for ocular and mucosal membrane delivery “is highly novel” with various granted patents globally. Extensive histology and functional analysis has shown the technology does not damage any ocular tissue.
“The device has also been used in a small number of human subjects (with ethics approval) and was well tolerated and without adverse sequelae. Follow-on human trials for ocular biologics and riboflavin are being planned.”
8 INSIGHT July 2023
NEWS
“ONE FURTHER AVENUE TO PURSUE OF COURSE IS A BROADER CONSUMER FOCUSED MEDIA CAMPAIGN ON THE SITUATION GIVEN COSTS OFTEN HAVE TO BE PASSED ON TO THOSE SELLING THE EYEWEAR AND THEY OFTEN NEED TO PASS THAT INCREASE ON TO THE CONSUMER.”
AMANDA TROTMAN, ODMA
US INVESTOR BACKS AUSSIE AI INNOVATION



New York-based health technology company Ascertain is investing US$12 million (AU$18 m) in Eyetelligence, a Melbourne-based company which uses advanced artificial intelligence (AI) technology and retinal imaging to screen for eye and systemic diseases.
The technology is based on the inventions of Dr Mingguang He, a leading clinician-scientist at the University of Melbourne and the Centre for Eye Research Australia, who was joined by commercial healthcare leader Mr Jason Sun to found Eyetelligence.

Eyetelligence has developed a suite of clinically validated and regulatory approved AI-enabled products already being commercialised in the Australian, New Zealand, European, and Japanese markets. Eyetelligence’s products are used within the Bupa Optical and George & Matilda optometry networks in Australia.
“The three most common eye diseases – diabetic retinopathy, age-related macular degeneration and glaucoma – can be detected far earlier with algorithmic retinal image analysis. These three diseases, however, are just the tip of the iceberg,” He said.
“The eye is a window through which we can discern any disease that affects the microvascular system. This technology allows clinicians to act faster and prevent significant impacts on quality of life.”
He said he welcomed the support of creation platform Ascertain, which sees the potential of Eyetelligence’s technology for the US.
“[Ascertain] is committed to identifying and accelerating the use of emerging AI technologies to drive significant health benefits globally,” He said.
Eyetelligence is the first international investment by Ascertain, a first of its kind partnership between Aegis Ventures, a next-generation healthcare-focused venture studio, and Northwell Health, one of the largest health systems in the US.




Mr Daniel Boyer, deputy CEO of the Australian Trade and Investment Commission (Austrade) said Australia has a successful track record of health
and biomedical innovations that have been scaled up internationally.

“Our world-class universities, highly skilled talent and complementary regulatory environment make our healthtech ecosystem a global leader,” Boyer said.
“Ascertain’s investment in Eyetelligence is a nod to Australia’s cutting-edge biotech sector and shows we are increasingly a partner of choice for US investors.”

Eyetelligence will be rebranded and launched in the US as Optain and aims to enable non-invasive point-of-care technology to diagnose a range of diseases more rapidly, cost-effectively, and accessibly.
Mr Jeff Dunkel, CEO of Optain, said by enabling earlier diagnosis and treatment, the technology can drive better patient outcomes and cost savings across health systems.
“The healthcare industry has made a concerted effort in recent years to shift treatment from reactive care to proactive, preventive care, but many of the legacy screening and diagnostic technologies used by clinicians today are expensive and inaccessible,” Dunkel said.
“Optain will accelerate that shift and make preventive care ubiquitous by placing smarter, faster, and more efficient diagnostic tools in the hands of clinicians everywhere.
“Optain’s first goal is to expand access to screenings and diagnosis for preventable eye disease, closing critical health equity gaps, particularly in underserved communities where diagnostic and screening tools aren’t available,” he said.
Eyetelligence will continue to expand under its current brand in Australia and other international markets.






















 Melbourne-based Eyetelligence co-founder Dr Mingguang He.
Melbourne-based Eyetelligence co-founder Dr Mingguang He.
IN BRIEF
O=MEGA23 UPDATE
Myopia management will be a major focus of O=MEGA23 in partnership with the 4th World Congress of Optometry (WCO), featuring updates across several presentations. The event, taking place in Melbourne in September, will include a session by Drs Paul and Kate Gifford, founders of Myopia Profile. “Our presentation will outline the latest research on the knowns and the unknowns for several unanswered questions in myopia management. The knowns will be translated into actionable clinical advice and management pathways, and the unknowns detailed to support practitioner communication,” Kate said. Plenary speaker Professor Mark Bullimore will also be discussing myopia, supported by CooperVision, a major platinum sponsor of O=MEGA23.
LOST APPEAL
An optometrist who tampered with over 400 glasses prescriptions has lost a bid to have their five-year disqualification set aside. The practitioner went to the South Australia Court of Appeal challenging an order made in the Supreme Court that extended their original disqualification period from one to five years, and ordered the optometrist to pay the Optometry Board of Australia’s costs. The misconduct related to the tampering of glasses prescriptions between February 2015 and January 2016 when the optometrist used their log-in credentials to change patient records entered by another optometrist 410 times. Due to this, 313 sets of glasses manufactured for patients from a total of 359 scripts were defective. In the remaining cases, alterations were corrected before the glasses were made.
EYEGLASSES RULE
The US Federal Trade Commission (FTC) is proposing changes to its Eyeglasses Rule, in its latest clampdown on optometrists. The pre-existing regulation meant patients had the right to obtain their spectacle prescription at no extra charge once their eye exam has been completed, allowing them to shop around for the best deal. But based on public comments and consumer reports, the FTC said it was apparent some practitioners were not following this. In response, the regulator is proposing eyecare professionals not only get a signed confirmation when they release prescriptions to patients, but also to keep a record of that confirmation for at least three years. A similar measure has been implemented for contact lenses.
BID TO FAST-TRACK OVERSEASTRAINED PRACTITIONERS INTO STRETCHED SYSTEM
Ahpra and the National Boards has welcomed an independent review to cut the red tape and costs for qualified internationally trained practitioners wanting to work in Australia’s health system. If introduced, the measure could alleviate workforce shortages in regional areas that have struggled especially when it comes to specialist eyecare services.

Released on 28 April 2023, the ‘Independent Review of Overseas Health Practitioner Regulatory Settings Interim Report’, led by Ms Robyn Kruk AO, recommends measures to immediately boost the health workforce and ensure Australia is a competitive destination for the global health workforce, while maintaining quality and safety.
According to the report, employers and health practitioners say Australia’s registration and immigration processes are often slower, more complex and expensive than other countries. For example, recruiting an overseas GP can take up to 21 months and cost more than $25,000 even for cohorts from fast-tracked countries, while an overseas trained nurse can pay over $20,000 and take 35 months to get their qualifications recognised.
Interim findings of the Kruk review include:
• Improving regulation timeframes and consistency by making registration assessment a core process under the bolstered stewardship of Ahpra
• Fast tracking approvals for practitioners from trusted countries by expanding the use of competent authority pathways
• Cutting red tape by removing duplications such as having to submit multiple criminal history checks while speeding up the allocation of Medicare provider numbers
• Improving monitoring and publishing data outlining health workforce shortages, distribution and skills to better inform planning and policy
• Reviewing current standards, including English language and recency of practice requirements.
“The severe shortage of healthcare professionals across Australia’s health systems is a real and significant risk to patient safety,” Ahpra CEO Mr Martin Fletcher said.
“While a system-wide overhaul is needed to better align the qualifications recognised by Australian medical colleges and cut duplication of processes across authorities, Ahpra and the National Boards welcome the
opportunity to be stewards for changes that will strengthen the nation’s health system immediately and in the long-term.
“Patient safety will always be the paramount priority in registering any practitioner. But by eliminating needless duplication, easing bureaucratic delays and better recognising the experience of overseas health professionals, we can attract the best and most suited to Australia, sooner.”
A move to a single portal for international applicants to lodge all their paperwork to Ahpra (covering migration, registration and employment) would also remove duplicity in the system. A “tell us once” approach would significantly cut the time and expense of navigating the current system, Ahpra stated.
“Australia’s health regulation system is the safest in the world. This isn’t an accident. We have a rigorous process to ensure those registered to care for the community are adequately trained and qualified,” Fletcher said.
“We know that registration and migration processes are not the easiest to navigate. We have been working closely with relevant agencies to streamline this and are pleased that we are already seeing a positive impact with overseas-based practitioner registration back to pre-pandemic levels.”
In ophthalmology, a 2018 report into workforce shortage recommended an increased intake of trainees to counter the predicted undersupply of ophthalmologists in 2030 of three per year from 2019 –compounding. Along with a maldistribution of ophthalmologists who disproportionately mostly work in urban locations, it highlighted “a higher-than-average reliance” on international medical graduates.
And in optometry, a Deloitte Access Economics report commissioned by Specsavers calculated that the number of optometrists required to support the level of clinical demand is projected to grow from 4,234 in 2018 to 7,841 by 2037.
The National Registration and Accreditation Scheme has allowed Australia’s registered health workforce to increase every year through both domestic graduates and international recruits.
According to Ahpra, it has already begun streamlining the registration process to make it simpler for registrants, including changes to English language requirements that allow applicants to resit specific parts of the test rather than restarting the entire process.

10 INSIGHT July 2023 NEWS
A system-wide overhaul is needed to cut duplication of processes.



PREMIUM HYDROPHOBIC IOL with PUre Refractive Optics (PRO) TEchnology For your daily range of vision © 2023 Bausch & Lomb Incorporated. ®/TM denote trademarks of Bausch & Lomb Incorporated and its affiliates. Bausch & Lomb (Australia) Pty Ltd. ABN 88 000 222 408. Level 2, 12 Help Street, Chatswood NSW 2067 Australia. (Ph 1800 251 150) New Zealand Distributor: Toomac Ophthalmic. 32D Poland Road, Glenfield 0627 Auckland New Zealand (Ph 0508 443 5347) LUX.0005.AU.23 For more information please contact your Bausch + Lomb Territory Manager, Customer Service at Customer.Service@bausch.com or scan the code to receive a call back.
WAND OPTOMETRISTS JOIN GEORGE & MATILDA EYECARE AS PART OF EXIT STRATEGY

G eorge & Matilda Eyecare (G&M) has expanded its network with the addition of Mr Sean and Ms Robyn Wand from Wand Optometrists in Toukley on the NSW Central Coast, which has been in operation for more than 45 years.

G&M said the acquisition complements the network’s growth plan for the mid-north coast of NSW, following its partnership with Rolfe Optometry Group late in 2022.
Sean and Robyn both graduated from UNSW, and after a stint working in the UK, they returned to Australia in 1993 to start a family and a business, purchasing a practice established in Toukley in 1978 from a Sydney optometrist who was travelling to and from the city.
“Sean and Robyn each have over 36 years of industry experience and demonstrate our key values by putting patients first every single day,” G&M’s general manager of partnerships Ms Cassie Gersbach , said.
“They pride themselves on integrity having formed trusted long term, multi-generational relationships. Those relationships continue through the community by working with local GPs and ophthalmologists to manage a high level of patient care for the Toukley community.”
Sean shared why they chose George & Matilda Eyecare as part of their exit strategy.
“Growing the practice has been exactly like raising a child. So, we are keen for our patients to continue to be looked after long into the future. We are excited that G&M will make this happen. We would have hated to simply close our doors and walk away when we decided to retire,” he said.
Sean said G&M’s growth in their area was also appealing, giving them confidence in the knowledge they can be supported and helped by other members in the group, and vice versa.
“We like that G&M have taken seven years to refine their model. Then, with confidence, move into expansion. We

can see already that they know a lot more about running a business than we do. We are looking forward to seeing our practice being invigorated by the change,” he said.
He described the process of selling the practice to G&M as transparent and supportive.
“Any questions or concerns have always been addressed with transparency and ease. We’ve had help and support getting the financials and information needed regarding the sale of the business. There’s been no pressure and we’ve worked at a pace which suited us to get where we needed to be to make our final decision.
“Anyone in our position will know that it is increasingly more complex to market and run a business. The best way to grow is to bring people who have tried and tested systems and who have access to the latest data and technology. After 30 years, Robyn was ready to retire. So, it was better to handover the management side so I could concentrate best on being the clinician without any worry,” he said.
G&M said it is clear on its strategy for bridging the gap geographically across key areas and will have more announcements to share shortly.
WYNDHAM CLINIC PRIVATE HOSPITAL INCREASES OPHTHALMIC LIST CAPACITY
Wyndham Clinic Private Hospital, located in Victoria, is expanding its ophthalmic presence and increasing theatre time for private lists.
The move has coincided with leadership changes within the hospital, now being led by CEO Ms Frances Jordan who has worked across Australia and most recently in Geelong, and the eastern and northern suburbs of Melbourne.

After joining Wyndham Clinic Private Hospital in March 2023, she is focused on growing the day surgery’s ophthalmic surgery footprint, committing to an investment in new equipment and another ophthalmic operating theatre to bring the total number to three.
“When I arrived here it was evident the deep experience of the theatre staff in ophthalmic work, especially from The Royal Victorian Eye and Ear Hospital (Eye and Ear). We are investing in making Wyndham a leading hospital for ophthalmic procedures in Melbourne’s West,” she said.
Wyndham Clinic is now offering to current and prospective ophthalmologists: new ophthalmic lists now available Monday to Friday, experienced theatre staff from the Eye and Ear with high volume capacity, the Centurion phaco system and Active Sentry technology with six new Active Sentry handpieces about to be acquired.
The facility also offers increased surgical trays to cater for MIGS, trabeculectomy, strabismus, pterygium, and oculoplastics, as well as capability for plastics, and competitive uninsured rates. There is access to a private consulting room if necessary.
Wyndham is located 20 minutes from the West Gate Bridge and in Australia’s fastest growing Local Government
Wyndham Clinic has plenty of parking for patients and complimentary parking for specialists, and offers easy access to the Princes Freeway.
Contact Sally Bebawy on 0421 713 747 to discuss opportunities.
12 INSIGHT July 2023 NEWS
From left: Robyn Wand, Sean Wand, practice manager Chris Drzewiecki, and optometrist Stephanie Ngo.
Frances Jordan, Wyndham Clinic Private Hospital.




1800 637 654 @eyesrightoptical
SPECSAVERS ANNOUNCE SPEAKERS AHEAD OF CLINICAL CONFERENCE IN SYDNEY
Organisers of the 2023 Specsavers Clinical Conference (SCC 2023) have unveiled a high-powered line-up of ophthalmologists who will present at the two-day CPD event, providing insights into some of the most pertinent issues optometrists face in the consulting room.
Dr Brendan Cronin (keratoconus and allergies), Dr Shenton Chew (glaucoma), Dr Lindsay McGrath (suspicious intraocular lesions and masquerades), Dr Robyn Troutbeck (inflammatory eye disease), Associate Professor Chameen Samarawickrama (keratitis presentations) and Dr Kate Reid (optic nerve stroke and dangerous headaches) are among key speakers confirmed for the event taking place 28-29 October.
SCC, now in its 12th year, will feature an in-person conference at the Hotel Sofitel Sydney Darling Harbour. This will be in addition to a live broadcast across Australia and New Zealand, using the latest technology, and a custom-built platform including a website and app. Specsavers says SCC 2023 will aim to deliver a seamless experience for delegates, whether they are attending in person or watching at home.
The event is considered one of the most popular events on the annual optometry calendar and provides optometrists with two days of CPD content.
The full program for SCC 2023 has been announced on the Specsavers website, and also includes:
• M yopia management – Dr Rushmia Karim
• T he paediatric eye exam – Dr Shanel Sharma
• R etinal detachment – Professor Adrian Fung
• S ystemic medications that optometrists should know – Ljubica Bukorovic
• B eyond the Eyes and to the Brain – TBC
• D iabetic Retinopathy – TBC
In addition to the clinical program, SCC 2023 will features winners of the annual Dame Mary Perkins Award for outstanding patient care and the Doug Perkins Medal, which is awarded to
one Australian and one New Zealand store each year that consistently demonstrates high standards of clinical excellence.
Specsavers ANZ director of optometry Dr Ben Ashby will also provide an update on the company’s operations across the region.
Limited places will be available to attend the conference live in-person at Sofitel Sydney Darling Harbour.

“One of Specsavers key focuses is ensuring the ongoing professional development of our optometrists,” Specsavers head of professional development Ms Cindy Nguyen said.
“We pride ourselves on delivering a range of experiences across the year to ensure that our optometrists stay ahead of new trends and technology and are at the forefront of clinical practice,” she said.
“Offering SCC as an online or ‘virtual’ event over the past few years has enabled us to ensure our optometrists have access to this valuable education, no matter where they are located. So, we wanted to make sure we continued to deliver that, as well as delivering an exciting in-person conference for those who prefer to travel and attend in person.”
HOW THOROUGH ARE YOUR PATIENT RECORDS?
To help practitioners, including optometrists, better understand and meet their health record management obligations, seven of Ahpra’s national boards have developed two new health record management resources.
The resources are available on Ahpra’s Resources page. The tools include a summary of the guidance about record management given in the shared Code of conduct, and a self-reflective tool to help assess the adequacy of record keeping and management practices.
The one-page summary, Managing health records – Summary of obligations, aims to help practitioners meet their health record management requirements.
“It summarises the information in the Code of conduct about health record
management requirements and brings all the guidance on record keeping and management from the code into a single document,” Ahpra said.
The agency said the Managing health records – Self-reflective tool is designed to help practitioners reflect on their record keeping and management processes.

“The interactive tool aims to help practitioners assess how they manage their health records and to identify opportunities for improvement,” it said.
The tools have been developed by the following National Boards for the relevant professions:

• C hiropractic
• M edical Radiation Practice
• O ccupational Therapy
• O ptometry
• O steopathy
• P hysiotherapy
• Podiatry
“All registered health practitioners must keep good health records. Good records contribute to the continuity of healthcare and help keep the public safe,” Ahpra said.
National Board’s expectations about health records are outlined in their respective codes of conduct or ethics. In addition to these requirements, practitioners must also consider state, territory or Commonwealth legislation about health records and privacy that may apply.
The new resources, along with several others covering a range of topics to support practitioner’s practice, are available on Ahpra’s Resources page.
14 INSIGHT July 2023 NEWS
The in-person aspect of the conference will be held at the Hotel Sofitel Sydney, in Darling Harbour.
A self-reflective tool helps assess the adequacy of record keeping.

CHATGPT SCORES NEARLY 50% ON OPHTHALMOLOGY PRACTICE EXAM
A study of ChatGPT found the artificial intelligence (AI) tool answered less than half of the test questions correctly in a study resource commonly used by trainee ophthalmologists when preparing for certification.
The study, published in JAMA Ophthalmology and led by St Michael’s Hospital in Toronto, Canada, found ChatGPT correctly answered 46% of questions when initially conducted in January 2023. When researchers conducted the same test one month later, the bot scored more than 10% higher.
The researchers noted the potential of AI in medicine and exam preparation has garnered excitement since ChatGPT became publicly available in November 2022. It’s also raising concern for the potential of incorrect information and cheating in academia. ChatGPT is free, available to anyone with an internet connection, and works in a conversational manner.
“ChatGPT may have an increasing role in medical education and clinical practice over time, however it is important to stress the responsible use of such AI systems,” said

Dr Rajeev Muni, principal investigator of the study and a researcher at the Li Ka Shing Knowledge Institute at St Michael’s.
“ChatGPT as used in this investigation did not answer sufficient multiple choice questions correctly for it to provide substantial assistance in preparing for board certification at this time.”
Researchers used a dataset of practice multiple choice questions from the free trial of OphthoQuestions, a common resource for board certification exam preparation. Of 125 text-based multiple-choice questions, ChatGPT answered 58 (46%) questions correctly when the study was first conducted in January 2023. Researchers repeated
the analysis in February 2023, and the performance improved to 58%.
“ChatGPT is an artificial intelligence system that has tremendous promise in medical education. Though it provided incorrect answers to board certification questions in ophthalmology about half the time, we anticipate that ChatGPT’s body of knowledge will rapidly evolve,” said Dr Marko Popovic, a co-author of the study.
ChatGPT closely matched how trainees answer questions, and selected the same multiple-choice response as the most common answer provided by ophthalmology trainees 44% of the time.
ChatGPT selected the multiple-choice response that was least popular among ophthalmology trainees 11% of the time, second least popular 18% of the time, and second most popular 22% of the time.
“ChatGPT performed most accurately on general medicine questions, answering 79% of them correctly. On the other hand, its accuracy was considerably lower on questions for ophthalmology subspecialties,” said Mr Andrew Mihalache, lead author.
ACO MAKES HISTORY WITH WOMEN-LED COUNCIL

The Australian College of Optometry (ACO) has announced Associate Professor Lauren Ayton and Ms Theodora Elia-Adams have been appointed vice president and treasurer respectively.
They join ACO’s first female president, Ms Sophie Koh, marking the first time in the college’s history that women concurrently hold the roles president, vice president and treasurer.
“I am honoured to serve alongside a diverse group of individuals who are dedicated to best governance and the continued good work of the ACO. It’s a strong recipe to steer an organisation,” Koh said.
The announcement follows the ACO and National Vision Research Institute’s (NVRI) first in-person Annual General Meeting in four years on 31 May.
Ayton and Dr Michelle Waugh, both returning council members, were reappointed for a further two-year term.
Mr Roman Serebrianik, a former ACO optometrist of 14 years with experience in senior policy and advocacy roles at Vision
2020 Australia and the Stroke Foundation (current) was also elected to the council.
Ms Denise Gronow, immediate past treasurer of seven years, will remain on council.
Outgoing council member and vice president, Mr Tim Powell, was acknowledged for his valuable contributions to the ACO during his five-year tenure and his exemplary stewardship.
Koh and ACO CEO Mr Pete Haydon also welcomed questions from attendees at the AGM on the transition currently underway at the ACO to improve organisational stability and secure continued delivery of ACO’s public health, education and research work into the future.
“The ACO’s new strategic plan offers us a once in a generation opportunity to bring about change and the council is enthusiastic to continue working with Pete and staff to take ACO to its new heights,” Koh said.
The ACO 2022’s Annual Report was also launched during the AGM and can be viewed online at www.aco.org.au/aco-publications/.
AWARD WINNERS
Members and stakeholders who attended the AGM also celebrated recent ACO achievements with the following awards: ACO Outstanding University Graduate Award
Australian Universities are invited to nominate their most outstanding optometry graduate through combined evaluation of academic excellence and professional commitment.
Awarded to: Kayla Adams (Deakin University), Amy Ricks (Flinders University), Mahmoud Haddara (University of Melbourne), Johnson Tran (UNSW Sydney) and Vyasa Bliss (Queensland University of Technology).
Outstanding Graduate Award for ACO Certificate in Ocular Therapeutics
This award is granted in recognition of the candidate who has achieved the highest score across all assessments for their graduating year of the ACO Certificate in Ocular Therapeutics.
Awarded to: Hetal Dagar.
16 INSIGHT July 2023 NEWS
When researchers conducted the same test one month later, the bot scored more than 10% higher.
From left: Associate Professor Lauren Ayton, Sophie Koh, and Theodora Elia-Adams.
For more information, contact your Bausch + Lomb Territory Manager or Bausch + Lomb Customer Service 1800 251 150 MIOCHOL® -E Acetylcholine Chloride 20mg/2 mL Rapid Miosis Latex free* MIOSIS IN THE BLINK OF AN EYE *Free from natural rubber latex. Material was prepared in December 2022 © 2022 Bausch & Lomb Incorporated. ®/TM are trademarks of Bausch & Lomb Incorporated or its affiliates. Bausch & Lomb (Australia) Pty Ltd. ABN 88 000 222 408. Level 2, 12 Help Street, Chatswood NSW 2067 Australia. (Ph 1800 251 150) MIO.0002.AU.22 Always review product information before prescribing these medications. Product information is available on request from Bausch + Lomb on 1800 251 150.
GLOBAL EYEWEAR BRAND EXPANDS IN GULF REGION

EssilorLuxottica has penned a joint venture agreement with Chalhoub Group to expand its eyewear retail presence in the Middle East’s Gulf region.
The deal, announced 10 May, aims to shape the eyewear category in the Gulf Cooperation Council (GCC) region, combining EssilorLuxottica’s eyewear expertise, technology, and brands, with Chalhoub Group’s understanding of the region’s consumers.
The new partnership is said to represent an important step for EssilorLuxottica in raising the segment’s visibility and standards by increasing consumer engagement with high quality premium brands. It will also support Chalhoub Group’s expansion into the rapidly growing eyewear category using the group’s expertise in luxury retail.
Mr Francesco Milleri, chairman and CEO at EssilorLuxottica, was pleased to partner with Chalhoub Group to grow the eyewear category in “the highly dynamic” GCC region.
“This move will allow us to complement our existing and deeply rooted network of customers in the region, whom EssilorLuxottica is committed to continue serving with high quality products and solutions,” he said.
“Leveraging on Chalhoub Group’s extensive knowledge and retail presence in the region, we will raise the visibility and quality of the entire industry and reinvent the omnichannel consumer journey together, resulting in a more engaging retail experience for consumers.”
Mr Patrick Chalhoub, group president at Chalhoub Group, said eyewear represented a new vertical that had significant potential for growth and innovation, with high demand from the firm’s regional luxury consumers.
“EssilorLuxottica is a partner of choice with their fashionable, elegant products, and brand portfolio; their core values of helping people to ‘see more and be more’, alongside their growth ambition in the GCC region, complements our group’s purpose to inspire and delight customers.”
A series of mono-brand and multi-brand stores will be launched in the GCC for EssilorLuxottica’s core and iconic global eyewear brands, including Ray-Ban, Persol, and Oliver Peoples, allowing the brand to expand its global footprint in the GCC region.
EARLY ADOPTERS SHARE THEIR EXPERIENCE USING ZEISS CATARACT WORKFLOW
Early adopters who have been trialling the latest innovations in cataract workflow from ZEISS over the past 12 months are now sharing their experience as part of a nation-wide roadshow.

Having commenced in Perth, then Melbourne, the next stop for the roadshow will be at the Sydney QT Hotel on 3 August.
Dr Smita Agarwal, Dr Amir Hamid, Dr Brad Townsend and Dr Weng Sehu will be participating in the conversation on how to take cataract workflow to the next step with ZEISS devices and applications.
At the first roadshow in Perth, international surgeons Dr Amir Hamid and Dr Tun Kuan Yeo, as well as Perth based Dr Andrea Ang and Associate Professor Angus Turner, stepped the audience through ZEISS’s Cataract Workflow.
“The workflow’s first stop was in the clinic with surgery planner EQ Workplace, which assists in streamlining processes and saving time in the clinic,” ZEISS said.
“Next, we continued to the operating room with the innovative QUATERA 700 phaco pump system fluidics and concluded the workflow with the first monofocal C-loop hydrophobic IOL in

the ZEISS portfolio, the CT LUCIA 621, with the unique ZEISS optic.”
Best practices were shared with the audience as well as tips to allow for a smooth and easy transition to the latest technology available.
The ZEISS Cataract Workflow roadshow continued to Melbourne in early May.
Early adopters Dr Anton van Heerden and Dr Georgia Cleary discussed their experience with the Cataract Workflow and how it enabled greater efficiency without compromise.
ZEISS has also completed two registrar events in Brisbane and Sydney and is holding a third in Melbourne in July.
NORLASE SECURES MAJOR FUNDING

Danish ophthalmic laser manufacturer Norlase – whose lasers are available in Australia via OptiMed – has announced its biggest investment round thus far. The US$11 million (AU$17 m) in funding was led by London-based firm West Hill Capital.
It comes on the heels of the FDA clearance and CE mark approval of the company’s most advanced product to date, the ECHO pattern laser. It will enable Norlase to accelerate the production ramp-up of the system, as well as its other cutting edge laser treatment solutions.
“In four short years, Norlase has brought three revolutionary laser solutions to market,” said Norlase CEO and co-founder Oliver Hvidt.
“With the introduction of ECHO, we are ushering in a new chapter for pattern laser products. This incredible technology reduces what is today a large, 100-pound piece of equipment, into a device you can hold in the palm of your hand and easily attach to existing slit-lamps.
“It’s the convenient and affordable pattern laser that the market has been waiting for. The launch of ECHO in the USA and EU, combined with the growing demand for our LION laser indirect ophthalmoscope and LEAF single-spot laser, means we need to drastically expand our production and global market presence. We are excited about this challenge and thankful for the support of our investors.”
18 INSIGHT July 2023
A series of branded stores will be launched in the region.
ECHO attaches directly to compatible slit lamps.
NEWS
At the roadshow events, the audience is taken through ZEISS’s Cataract Workflow.

GROW YOUR CAREER WITH US www.georgeandmatilda.com.au Email Sam at opportunities@georgeandmatilda.com.au or scan the QR code further study leadership partnership specialty interests
Lions Eye Institute:
ONE MILLION REASONS TO CELEBRATE 40 YEARS
The Lions Eye Institute is celebrating two major milestones in 2023: its 40th anniversary of saving and restoring the sight of Western Australians, as well as one million patient visits since the institute first started treating patients.

Lions Eye Institute (LEI) was the brainchild of Professor Ian Constable AO, which all began in 1983. He was recruited to Australia from Boston, US, and was attracted to the role as he could see the significant need for improved eye healthcare in Western Australia.
“When I arrived in 1975, eye surgery was not universally available. Patients had to travel interstate for some conditions. Rural and remote services were very limited,” Constable says.
At the time, Perth-based Lions clubs had established and were running a very successful Glaucoma Detection Clinic, operated from a now-iconic caravan. The clubs went on to form the Lions Save-Sight Foundation WA to expand on this work, resulting in LEI as its known today.

Over the years, the leadership baton has passed from Constable to Professor David Mackey AO and then to current managing director Professor Bill Morgan.
As a not-for-profit organisation, ongoing philanthropic support has been the cornerstone of LEI, leading to major discoveries, breakthroughs and inventions.
Some of these include:
• Inventing the first soft artificial cornea
• Discovering gene therapy to treat wet age-related macular degeneration

• Inventing the XEN Gel Stent, the most used surgical glaucoma implant in the world, and the Virna Glaucoma Drainage Device, an affordable treatment for glaucoma used in Indonesia
• Creating the Barrett Universal II Formula used in cataract surgery
• Pioneering the central retinal vein occlusion (CRVO) bypass laser surgery procedure, a world-first cure for CRVO
• Making a significant scientific discovery into cytomegalovirus infections,
“Over the last 40 years, the Lions Eye Institute has discovered many new sight-saving treatments and therapies,” Morgan says. “This is largely due to the ability of our medical researchers to work closely with our ophthalmologists, some of whom are researchers themselves, to ensure that patients receive the best possible and most advanced treatment available.
“However, none of this would be possible without the early and ongoing support of Lions clubs, the Lions Save-Sight Foundation WA, federal and state governments and the generosity of philanthropic supporters.”
For people living with glaucoma, the invention of the XEN Gel Stent has saved sight and changed lives. Co-invented by Morgan and Professor Dao-Yi Yu AM, the device was one of the first commercially available minimally invasive surgical devices (MIGS) to treat glaucoma.
Morgan says uncovering advances in treatments such as XEN were the driving force behind the LEI’s significant and ongoing commitment to world-class medical research and its translation into clinical practice.
“The need has never been greater for LEI to discover new treatments and cures for eye diseases, in order to provide better vision for all. We have a strong focus on the future eyecare needs of Western Australians and beyond,” he adds.
LEI IN 2023
Since its beginnings on the Queen Elizabeth II Medical Centre in Nedlands, LEI has opened clinics in Murdoch, Midland and Broome.
In 2013, it introduced Lions Outback Vision to provide eye health care to the state’s remote, rural and Indigenous communities. Over the decades, LEI has undertaken clinical and research work in neighbouring countries such as Indonesia.
The institute also comprises a day surgery, Lions Eye Bank, Lions Laser Vision, a Clinical Trials Centre, optometry clinic and research laboratories. Over four decades, LEI has grown to now:
• See up to 80,000 patients across Western Australia each year
• U ndertake more than 70 clinical trials per annum
• Employ approximately 300 people
• Facilitate approximately 400 corneal and scleral transplants per annum
• Receive up to $5 million in donated gifts each year.
In recent years LEI has partnered with The University of Western Australia to establish the state’s first optometry school. The institute is also expanding research capacity with the appointment of two new professorial chair positions. These collaborations support LEI’s commitment to teaching the next generation of eye healthcare professionals.
The Lions Eye Institute’s 40th anniversary is being celebrated throughout 2023.
20 INSIGHT July 2023
EYECARE
A staff celebration to mark 40 years of saving sight at the Lions Eye Institute, and to recognise a milestone birthday for founder and Patron Professor Ian Constable AO.
The original Glaucoma Detection Service caravan, circa 1964. Credit Arthur Nutt, City of Perth Lions Club.


Make trial lenses easy with MyAlcon FitSCAN ordering Happier and more satisfied customers More efficiency for your practice More fits, more sales* ©2023 Alcon Laboratories Pty Ltd. AUS: 1800 224 153; Auckland NZ: 0800 101 106. ANZ-VC-2200026 * Subject to availability of stock from Alcon. Subject to the individual eye care professional’s experience.
Optometrist
EyeQ
“It saves us it actually makes our better.” t i me product ivity Watch this video to find out more ,
Mark Koszek Clinical
& Professional Education Officer,
Optometrists
OPTOMETRIST STARTS CAREER IN Australia’s Red Centre
After graduating from the Master of Optometry program at QUT in 2022, BIANCA ROMEO started her career in Alice Springs. It’s a unique challenge already providing a host of rich experiences, just months into the role.


Moving to one of the most isolated parts of Australia where health resources are scarce and one’s clinical skills are tested daily might seem like a tough way to begin an optometry career, but for Ms Bianca Romeo it made perfect sense.

“I have always wanted to work in a regional/remote community upon graduating, and through my EssilorLuxottica Cadetship, the opportunity to work in Alice Springs popped up and it sounded like a good challenge. It would also allow me to provide a much-needed service in an area that is incredibly isolated from the rest of Australia,” she explains.
“These areas really struggle to find healthcare workers who will stay on a permanent basis, and establishing a connection within the community is important for building rapport and ensuring that patients feel comfortable returning for follow up care, knowing they are going to be seeing the same optometrist.”
Today, Romeo is the only full time optometrist within Alice Springs OPSM store. She’s mentored by the practice’s part-time optometrist, Ms Emily Procopis, who has been in there since 2006.
While many graduates seek the security of a metropolitan job, or one close to their family, Romeo’s attraction to a regional and remote career perhaps has origins to her childhood. Born in rural South Australia (Berri), she grew up in regional Queensland (Withcott and Toowoomba) before relocating to Brisbane to study optometry.
Her first introduction to the EssilorLuxottica network came during her second year of study at OPSM Fairfield Gardens. She was awarded a cadetship in 2021, which provided opportunities to work in regional and
remote areas of Australia and New Zealand with EssilorLuxottica upon graduating.
This took her to Alice Springs in 2023. Here, she has found some similarities to her experience in Brisbane: testing vision, prescribing spectacles and diagnosing and treating eye disease. However, a notable difference is fewer resources available to patients.
“As such, I am exposed to a lot more diabetic patients with more severe diabetic changes, as well as more opaque corneas from injury or trichiasis. Challenges include testing patients who do not speak English, as well as knowing what should be referred to ophthalmology and what should be monitored in an optometry setting,” Romeo explains.

“As our only local ophthalmology services are public services, I have to consider the urgency of referral and likelihood of treatment and intervention more carefully than I would in a metro setting. I have enjoyed this challenge, and really appreciate the opportunity it provides for me to enhance my clinical decision making and diagnostic capabilities, as well as adapting my testing style for non-verbal patients or patients who do not speak English.”
Procopis, her mentor, has played a major role in educating Romeo about what services are available in Alice Springs, including what ophthalmology services can be provided locally at the Alice Springs Hospital, and those that need to be referred elsewhere, such as Adelaide.
“ She has also encouraged and supported me reaching out to other local optometrists for advice,” Romeo adds.
Beyond the consulting room, she is having an impact through outreach
22 INSIGHT July 2023
PROFILE
Bianca Romeo on a 2022 OneSight trip.
Bianca Romeo enjoys what the Northern Territory has to offer with her partner.
clinics. Before becoming a qualified optometrist, as part of an optometry student placement in 2022, she travelled to Cooktown, Hopevale and Coen in Queensland with the OneSight EssilorLuxottica Foundation to provide screenings and glasses where needed for Aboriginal and Torres Strait Islander school children. Through this work she was introduced to Mr Wayne Tennent, who heads OneSight across Australia, New Zealand and the Pacific. This connection served her well upon moving to Alice Springs.
BETTER VISION. X-TRA CLEAN.
Tennent facilitated a key meeting with Dr Tim Henderson, the ophthalmologist at the Alice Springs Hospital. Recently, Romeo accompanied Henderson – as well as his support staff, a registrar, orthoptist and Aboriginal liaison officer – on an ophthalmology trip to Docker River.

“Dr Tim Henderson and the Alice Springs Hospital provide ophthalmology clinics for patients in remote communities, which is incredibly beneficial as it allows patients to receive necessary eyecare without having to travel to the hospital, which for Docker River is a seven-hour drive away,” she says.
“He can provide thorough eye examinations, deliver treatments to patients, and identify any patients who will require further assessment at the Alice Springs Hospital in the future.”
Something that stood out to Romeo was the relationships and trust staff at the community health centre had built with patients in Docker River. In fact, they pick up patients who are due to see Henderson, because the majority wouldn’t attend their appointment otherwise.
“This really highlighted how important it is that the hospital and Dr Henderson provide services locally to these patients, as it improves attendance at appointments and subsequently improves their eye health outcomes. These patients are less likely to be able to attend appointments that are held at the hospital seven hours away,” she says.
“I find outreach clinics incredibly rewarding, as I know I am truly making a difference when providing these services. It really does open your eyes to the gaps in healthcare in remote areas and having that exposure encourages you to continue to participate in further clinics. I am very grateful to OneSight for providing me with these eye-opening opportunities, and look forward to attending clinics with them in the future.”
Available with Biometric Intelligent Glasses.
For more information, speak to your local Rodenstock Account Manager.

Go to: rodenstock.com/bigvisionforall X-tra Clean Finish by Rodenstock – so smooth, nothing sticks.
From left: OneSight EssilorLuxottica Foundation’s Wayne Tennent, Bianca Romeo, Alice Springs ophthalmologist Dr Tim Henderson, registrar Dr Ella Berry, principal orthoptist Lina Li and eye Aboriginal liaison officer Veronica Stafford.
Ohlrich Eye Centre:
A 50-YEAR OPHTHALMIC LEGACY
The Ohlrich Eye Centre has been providing ophthalmic care to the Brisbane community out of the same building for more than 50 years. Insight reflects on the Ohlrich legacy, and what the future holds for this iconic practice.


Ophthalmology has grown and changed since Dr John Ohlrich established the Ohlrich Eye Centre in 1975. With his son, Dr Stephen Ohlrich, at the helm, the practice has remained firmly at the forefront of ophthalmic expertise. Now, as Stephen nears retirement, he is preparing to pass the baton to the next generation. Located in Coorparoo, the family practice is going on the market for the first time in five decades. Today, Stephen reflects on his family’s legacy and the progress of ophthalmology.
“It was a different world when my father, John, opened the practice. At that time, there were only about 100 ophthalmologists across Australia. Now, there are 10 times as many,” Stephen explains.
Dr John Ohlrich was part of the inaugural venture of the National Trachoma and Eye health program with Professor Fred Hollows at “a time when an ophthalmic consultation could be and, in this case, was, conducted on the tail gate of a flat-bed truck,” Stephen reflects.
John believed in research, teaching and improving the delivery of eyecare. “Blindness is both treatable and preventable,” was his mantra, Stephen recalls.
“He wanted a professorial eye unit, and he single-handedly raised the funds to support this venture,” Stephen says. “In order to achieve this, he raised the sleeping giant of fund raising – the Lions. At one memorable Lions branch meeting he announced ‘I will sell 100 dozen Lion’s Christmas cakes. What are the rest of you going to do?’. As a medical student, I delivered these cakes to all the ophthalmology practices in Brisbane in my rusty Holden ute.”
Ultimately, John raised the money to establish a Chair of Ophthalmology in Queensland. He was also instrumental in establishing the Prevent Blindness Foundation, the Lions research building at Princess Alexandra Hospital, and the Queensland Eye Bank.
Stephen, following in his father’s footsteps, completed his training as an ophthalmologist in 1995. He did three years basic training in Queensland and two year-long fellowships in the United Kingdom. Upon graduation, he joined his father at Ohlrich Eye Centre, and together they built the practice into a community-oriented centre renowned for excellent patient care.
Both John and Stephen also played a vital role in the public hospital system. They worked at the Princess Alexandra Hospital for a combined 49 years (John from 1969-2000, Stephen from 1986-2018), caring for the eye health of thousands of patients and participating in the training of all the ophthalmology registrars of the day.
Stephen was also part of the Queensland Qualification and Education Committee for 10 years.
“During that time, I was the chairman for six years serving on the Federal Qualification and Education Committee. That’s when I started the Friday afternoon teaching sessions, which were done at the Princess Alexandra Hospital –attended by all the registrars from the Queensland training program,” he says.
“Subsequent to that, I was a RANZCO examiner for the clinical examination (RACE) for 10 years. Every registrar who has completed their training since 1969 in Brisbane has, at some stage, been supervised by Dad or me.”
In 2004, John passed away, leaving the practice and all its patients in Stephen’s care. Some of these patients had been treated at Ohlrich Eye Centre for more than 30 years, with a variety of chronic eye conditions, requiring careful management. Stephen continued to care for these people, and further grew the client base with cataract and macular degeneration patients. To this day, Stephen continues to run the clinic as a comprehensive ophthalmology practice with a subspecialty in oculoplastic surgery. He commonly performs tumour reconstructive surgery of the periorbital region.
As advances in technology have allowed optometrists to diagnose and treat more than they used to, the tendency is for patients to be referred on to subspecialty ophthalmologists. Stephen, however, continued practising as a

24 INSIGHT July 2023
Dr Stephen Ohlrich in his rooms at the Ohlrich Eye Centre, with a portrait of his late father Dr John Ohlrich on the wall behind.
PROFILE
Dr Stephen Ohlrich assessing a patient in his main consultation room at the Ohlrich Eye Centre.
comprehensive ophthalmologist because, being a RANZCO examiner, he was required to have proficiency across all areas of ophthalmology.

He further reflected that “cataract surgery has become a very common operation that we do much earlier” with patients expecting “excellent surgical results and spectacle independence.”
However, he says the biggest change during his career has been the improved treatment for macular degeneration. When he first started, after a patient got neovascular age-related macular degeneration and lost central vision, no more could be done.

“Now, with regular intravitreal injections to slow the progress of the disease, patients keep coming back through the door, so you get to know them quite well,” he says.
Over the years, Stephen has kept the practice’s equipment up-to-date with every new technological advancement in the field. The state-of-the-art machines at the practice are a far cry from the original field machine with all its patient data saved on floppy disks.
“The first thing I did was install a visual field machine, which was hardly avant-garde,” Stephen remembers fondly.
Now, Stephen is looking to retire, and hopes to see the Ohlrich Eye Centre passed on to another ophthalmologist with a focus on comprehensive eyecare.
“It’s a solo practice, but could possibly have two ophthalmologists here. I think young fellows by-and-large want to be subspecialists, but if there is an ophthalmologist out there who wants to use their comprehensive ophthalmology skills in an inner city setting, they would need a head start, and I think this would be the ideal base for them.”
It’s more than a practice up for sale; it’s a piece of ophthalmic history and the opportunity to continue a well-established legacy.
“FOR AN OPHTHALMOLOGIST WHO WANTS TO USE THEIR COMPREHENSIVE OPHTHALMOLOGY SKILLS IN AN INNER CITY SETTING, THE OHLRICH EYE CENTRE WOULD BE AN IDEAL BASE.”
Dr Stephen Ohlrich has invested in state-of-the-art equipment for the Ohlrich Eye Centre since 1996.

Grow your business with Afterpay. Discover what top healthcare brands already know: Afterpay helps care for your customers and your business. Sign up to reach over 4 million Aussies & Kiwis who use Afterpay.* *Afterpay user data Good for your patients. Good for your business. Eligibility criteria and T&Cs apply. Please see afterpay.com for full terms. See how Bailey Nelson grew with Afterpay.
Challenging
DRY EYE DOGMA
World renowned dry eye expert Dr Rolando Toyos was recently in Australia to promote his new book. He tells Insight about his mission to dismantle many of the belief systems around dry eye disease, and why the answer often lies much deeper within patients.
When Dr Rolando Toyos tried to convince the world intense pulsed light (IPL) therapy had applications in eyecare, it took many years until a company finally agreed to commercialise the technology. The approach remains a gold standard treatment in dry eye disease (DED) today, and now he is on a new crusade to compel the industry to change its ways.

Through several decades researching DED – long before it became a part of mainstream eyecare – Toyos says diet is one of, if not the biggest, influencer on outcomes. It fits with his approach that DED goes much deeper than the surface of the eye; instead it’s a skin gland condition linked to systemic issues within the patient.
Toyos’ efforts have manifested in his latest book: Toyos Dry Eye Diet – What to eat to heal your dry eyes. He was in Australia at the beginning of May, linking up with Lumenis and Ms Liz Barrett’s Dry Eye Solution, to promote his work aimed at dry eye sufferers and eyecare professionals who see these patients. For several years, Toyos discussed diet with DED patients, but around 18 months ago he became more radical in his approach telling patients exactly what to eat, and what to eliminate. With demonstrable improvements in their DED signs and symptoms, Toyos wanted to share his work with the broader community in a book that fuses his clinical experience with scientific and lifespan studies, as well as research into Blue Zone populations where centenarians exist in disproportionately high numbers.
“To achieve a paradigm shift in our field, it’s not like the tech world where a new app comes along and supersedes older technology immediately. It takes about 20 years in medicine – this has been researched and can also be seen in the time it took from when I started promoting IPL to the time it gained acceptance,” he says.
Toyos has been researching DED for more than 25 years. When he started there wasn’t many doctors concentrating on it.
“That was bad, and now we have many doctors concentrating on it, but they’re treating wrong; I’m talking about the traditional way we’ve been taught with warm compresses, lid scrubs, artificial tears, and doxycycline. In terms of ‘dry eye specialists’, I would say about 5% of them are really honing in on diet, and that’s the reason why I wrote this book,” he says.
“For the paradigm shift to happen, we need a new crop of doctors trained in a new way and the older doctors to dump what they have learned previously. There needs to be an unlearning phase, followed by a new learning phase and then implementation. We’re still in the unlearning phase; I can see it in people’s eyes when I’m lecturing. I say don’t do A, B, C and D, and many will say they have been giving artificial tears or doxycycline forever, isn’t that good? We need to completely change our approach.”
IT BEGINS IN THE GUT
In the ophthalmic world, Toyos is most famous for discovering IPL’s applications in DED.
In 2001, after incorporating aesthetics into his general ophthalmology practice, he used IPL to coagulate the abnormal telangiectasias of the skin in rosacea and to perform facial rejuvenation. Some with meibomian gland dysfunction (MGD) reported IPL had not only improved their skin but also their DED symptoms. After studying further, his team began investigating how to optimise IPL for DED, which led to Toyos working with DermaMed to bring the first DED IPL system to market, before later working with Lumenis.
Toyos has also developed the Toyos Protocol used to treat dry eye by doctors and other researchers around the world, and authored his first book in 2015: Dry Eye Disease Treatment in the Year 2020, detailing proven treatments, discarding ideas that have failed but continue to exist and offering a glimpse into the future.
Since publishing this work, he says the science has exploded about what changes can be made at the cellular level through diet and supplementation. Researching how this relates to DED has led him down rabbit holes and even required some “unlearning” on his part, but the science points to lifestyle, diet and nutrition as a key factor in DED, with benefits beyond the discomfort patients feel in their eyes.
“DED patients are a difficult group because there are so many problems that can affect the tear film. My definition is different than others, I see it as a skin gland condition that can be affected by systemic problems. All these factors come into play and that creates a poor tear and inflamed tear that starts to affect the ocular structures. Then, over time, it becomes a problem of chronic pain, which starts to affect the psychology of patients,” he explains.
“In my view, dry eye disease is a dermatological disease, it’s an eye disease, an immunological disease, and when you start talking about issues affecting the skin and glands, you’re really talking about issues like diet, lifestyle, and other aspects to help the overall systemic problem that enable you to ultimately improve the tear.”
For Toyos, this often begins in the gut. Even five years ago, he says gut bacteria wasn’t part of the DED conversation, but research in this area has accelerated in more recent years. The gut is where the body’s immunology stems from, but an acidic gut with bad bacteria causes the inflammatory mediators in the body to heighten, while a healthy gut will decrease inflammatory cytokines, having a positive downstream effect on DED.
“I’ve always talked to patients about diet, but I was never very specific. The conversation was more like: ‘don’t eat these inflammatory foods, let me put you on an anti-inflammatory diet’,” he says.

“But a year and a half ago, I started giving patients a specific list of what foods I wanted them to eat, while eliminating everything else. This is to build up their good gut bacteria and it’s something I looked at with stool samples, working with dieticians. It was working. Then patients move on to a different, overall diet after two months and it’s performing great. I’ve also found the uptake is so much better now that I explain each food and why.”
Toyos says many of the foods within his DED diet have been linked with increase life expectancy.
INSIGHT July 2023 27
DRY EYE
Dr Rolando Toyos is Honorary President of the International Dry Eye Academy.
“IN TERMS OF ‘DRY EYE SPECIALISTS’, I WOULD SAY ABOUT 5% OF THEM ARE REALLY HONING IN ON DIET, AND THAT’S THE REASON WHY I WROTE THIS BOOK.”
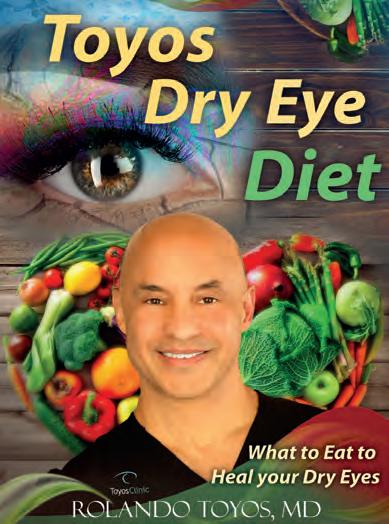
“Some patients have a wake-up call of a heart attack to really change their health and lifestyle. When I’m talking to patients, I’m telling them this is your wake up call, your dry eye is sending a signal to make yourself better.”
BERRIES, MUSHROOMS, SOY AND MORE
When a DED patient enters Toyos’ clinic, the first thing he’s looking at is their skin; around 90% of patients with a skin condition such as acne or rosacea will have a DED problem affecting either the meibomian or lacrimal glands. Next, he’s looking at the medication they take and other medical problems.
“For example, patients with rheumatoid arthritis or diabetes are at more risk of developing DED. Many of the medications they’re taking can have an impact too: oral anti-histamines, psychology medications, and statins for cholesterol, but it goes beyond that now,” he says.
“We’ve got patients that have been taking something like doxycycline for years to control inflammation, but that’s actually killing all of the good gut bacteria. Now we realise that the immunological heart of our health is controlled by our gut, so if you’re killing your good gut bacteria and bad gut bacteria is taking over your gastrointestinal system, that’s going to affect your eye health.
“The way I see it: if you want to be a dry eye specialist, you have to start reading not only eye journals, but what’s going on in dermatology, anti-ageing, immunology, and nutrition.”

Once Toyos has a clear picture of the patient’s dermatology and medication list, before getting to the slit lamp, he’s then discussing diet. In the past 40 years, he says the Western world has moved away from a more planted-based diet to one that consumes more meat, and ultra-processed foods, leading to heightened and/or chronic inflammation.

The patient’s individual profile will impact what sort of diet is ultimately prescribed. For example, one of the toughest cases is a DED patient with allergen (around 60% of all DED cases). He says there is a study showing in these patients mushroom intake can decrease signs and symptoms of allergy. Elsewhere, there’s specific studies showing supplementation of resveratrol (found in grapes, wine, berries, and more) can decrease DED signs and symptoms. Lutein and zeaxanthin (found in many vegetable) can also do the same.
“Alcohol intake has also been looked at and shows it will affect women more than men in DED signs and symptoms,” Toyos adds.
“Another study looked at the intake of soy – an oestrogen mimicker – to see if that would decrease the hot flushes women experience in menopause, and it actually didn’t decrease hot flushes but instead decreased the signs and symptoms of DED.”
When looking at the positive affect of probiotics in DED, Toyos says there’s evidence to support this, but warns it’s limited. This is because the study in question did not take stool samples, therefore they could ascertain whether the patient’s gut health had actually improved along with their DED.
“But we know if we can improve gut bacteria, this will improve the signs and symptoms of DED, and the only thing that’s really been shown to do that is a switch in diet. It’s about turning the acidic GI tract into a more basic GI,
28 INSIGHT July 2023 DRY EYE
– DR ROLANDO TOYOS, OPHTHALMOLOGIST
Proceeds from Toyos Dry Eye Diet – What to eat to heal your dry eyes, will go towards helping the disadvantaged.
Dr Rolando Toyos perfomring a Lumenis OptiLight demonstration in Sydney on his recent tour of Australia.
bacteria in our body – and probiotic, which will populate the gut with bacteria. That’s what is contained in my starter diet.”
Toyos says a lot of research is focused on sirtuins – a family of signalling proteins involved in metabolic regulation – that are thought to prolong life and improve mitochondria function. Some foods such as strawberries and blueberries contain sirtuin-activating compounds (STACs), so these are abundant in Toyos’ DED diet.
“For example, apples have a lot of quercetin, which is a STAC. Not only that, apples also have a role with the tumour suppressor gene maspin, so I have my
Introducing Second generation Reflex™ technology for on or off-axis treatment in YAG & SLT modes

patients eating a lot of apples because it’s also a prebiotic, probiotic,” he says, adding that walking and exercise are sirtuin-activating activity.
Once patients finish the starter diet, Toyos advises them to adopt the 90:10 rule when it comes to eating health and unhealthy foods, as adopted by Blue Zone populations. If alcohol is to be consumed, it’s red wine.
DRY EYE AND FAD DIETS
In his clinic, Toyos persuades many patients off fad diets. In fact, so much so, he has devoted a section in his new book arguing why most modern-day diets are counterproductive in DED.
He’s also included a DED glossary where he gives his take on several common treatments. Here, readers can find out why he’s against the use of artificial tears, lid scrubs, warm compresses.
“This isn’t anecdotal or what I think, it’s backed by research. I discuss the research and if there’s positive or negative, I’ve mentioned them both, so a clinician can go through and make their own informed decision,” he says.
“This book took me two years to write, and the reason is that each rabbit hole I went down would lead to three more. It’s a very complex field, and I think it does take a clinician to decipher it all. You could probably find a research paper that will justify any point of view.”
With all proceeds from the book going towards the Toyos Foundation providing free eyecare to the underprivileged, Toyos says eyecare professionals shouldn’t be afraid to shake up their approach, and begin getting to the root of their patients’ DED.


“When looking at ways to make somebody to change their diet, out of friends, family, TV and other influences, the number one approach is a recommendation by a doctor,” he says.
“We hold a lot of power, and it’s time we used it.”
•PROcap™ Premium Refractive Outcome Capsulotomy
Restoring the baseline best quality of vision
• SLT A proven first line therapy for treatment of primary open-angle glaucoma1
•Advanced Active cooling cavity technology with optimal optical breakdown < 1.4 mJ2
• Imprint™ Heads-up-display and energy control at the joystick enabling you to focus entirely on the patient
 Dr Rolando Toyos, now a director of Dry Eye Solution, along with the company’s CEO and founder Liz Barrett, and director Mr Andy McKie.
Dr Rolando Toyos, now a director of Dry Eye Solution, along with the company’s CEO and founder Liz Barrett, and director Mr Andy McKie.



©2023 Rayner Group, all rights reserved. Rayner and RayOne are proprietary marks of Rayner. All other trademarks are property of their respective owners. Rayner, 10 Dominion Way, Worthing, West Sussex, BN14 8AQ. Registered in England: 615539. EC 2023-30 AU 03/23 MADE IN UK Extending range without compromise 1. Ferreira TB. Comparison of visual outcomes of a monofocal, two enhanced monofocals and two extended depth of focus intraocular lenses. Presented at ESCRS 2022. 2. RayOne EMV: First Clinical Results, Rayner. Oct 2020. 3. Rayner RayPRO, data on file. 4. Rayner, data on file. 5. Rayner Peer2Peer webinar. May 2022. 6. Royo, M. RayOne EMV and TECNIS Eyhance: A Comparative Clinical Defocus Curve. Data on file. 2021. 7. Bhogal-Bhamra GK, Sheppard AL, Kolli S, Wolffsohn JS. J Refract Surg. 2019;35(1):48-53. • Increased range of focus: Up to 1.5 D1,4,6 with an emmetropic target. • High quality vision: Truly non-diffractive IOL with monofocals levels of contrast sensitivity1, dysphotopsia2,5 and high levels of patient satisfaction.3 Now available on the rotationally stable RayOne toric platform.7 RayOne EMV & EMV Toric offers: TORIC NOW AVAILABLE Leading surgeons from around the world share their real-world experience with RayOne EMV - watch engaging webinars, listen to insightful interviews and podcasts, and read interesting case study articles. Visit www.rayner.com/peer2peer to access videos and articles, download resources and join future events and discussions. Join the conversation Search for #Peer2Peer P eerP eer For more information call your Rayner representative or 1300RAYNER
Choice, training and equity –
THE ISSUES FACING MODERN-DAY CATARACT
Three surgeons provide a bird’s eye view on the current state of cataract surgery in Australia, including equity and accessibility to the latest advanced intraocular lenses, and how training is adapting to produce more skilled surgeons for tomorrow.
“
In the public system, intraocular lens (IOL) selection for cataract patients shouldn’t be seen as a conveyor belt where you can have any colour you want, as long as it’s black.”
This is the view of Dr Ben LaHood, a New Zealand-born cataract and refractive specialist who is outspoken on the inequity between the cataract patient experience in the public versus private system in Australia, where he practises today.

Working across both settings, LaHood is well-placed to highlight what Australia is doing well, and what areas require improvement. But he is not a lone voice in how Australia can provide better cataract surgery outcomes and experiences for patients.
Dr Jacqueline Beltz and Dr Ben Connell, both Melbourne-based, also have opinions on how surgeons’ decision-making can generate better results in 2023, which they share with Insight in this article. LaHood, Beltz and Connell – all leading cataract surgeons in their own right – also share how advanced technology is giving patients greater choice and therefore greater expectations about glasses independence, but more on this later.
First up, does Australia need to address the gap in access to advanced IOLs in public and private systems?
Speaking from his experience in private practice at Adelaide Eye and Laser Centre, LaHood says surgeons, himself included, are unquestionably performing cataract surgery on patients in private practice at an earlier age, and their expectations are higher.


But it’s a different dynamic in public hospitals, something he is familiar with through his role at the Queen Elizabeth Hospital in Adelaide.
“The idea of treating the potentially older, more difficult, denser cataract patient in public differently to the earlier, younger, easier cataract in private, has been quite ageist,” LaHood says.
“We imagine that these older patients come into the public system, have low expectations, and accept average outcomes. But we’re all living longer. The vision we’re giving people is going to dictate how they see for the rest of their life, so it’s vitally important.”
“I BELIEVE VERY STRONGLY THAT WHETHER A PATIENT HAS CATARACT SURGERY IN PUBLIC OR PRIVATE, THEY SHOULD RECEIVE THE SAME LEVEL OF CARE ... MOST IMPORTANTLY, WE SHOULD BE ABLE TO IMPLANT THE SAME IOL.”
DR BEN LAHOOD OPHTHALMOLOGIST
To that end, in his role at the Queen Elizabeth Hospital preparing trainees to work in private practice, LaHood urges cataract surgeons to consider the patient’s refractive outcome in more detail.
“In my public health capacity, part of my job is instilling a refractive-surgeon mentality into cataract surgery – we’re not only removing opacity; we’re giving the patient a once-in-their lifetime opportunity to have the best vision they possibly can, sometimes better than when they were young. Subspecialising in cataract surgery makes you think more and more about the potential outcomes, rather than only the procedure,” LaHood says.
Despite perceived ageism in how cataract patients in the public versus private system are treated, overall LaHood believes Australia is performing well compared to other countries.
He says a patient with private health insurance in Australia can have any IOL they want, regardless of cost.
“In other countries, that would require partial payment – or complete payment for certain IOLs – even as basic as needing to charge for a toric IOL. Whereas, in Australia, I can see a patient, we can discuss all the options, and for an insured patient it doesn’t matter which lens they select, my fee is the same, regardless of which lens I’m implanting,” he says.
INSIGHT July 2023 31
CATARACT
Conversely, LaHood adds, it’s difficult to be seen in the public system in a reasonable period of time for cataract assessment – and that’s still
The delay can result in loss of independence, functional decline, and increase risk of falls. The problem, LaHood says, relates back to training more surgeons, funding more training positions in the public system – and making those public positions more appealing.
“In the New Zealand system, for instance, it is very common to work the majority of your time in public and a minority in private, whereas, in Australia, I work one tenth of my week in public, and even that is seen as basically doing some charity work. This is the system that trained me – I should be giving back more than that, but it’s seen as acceptable. The culture in Australia around how much we give back to the public system is not healthy and I am part of this problem,” he says.
“When you have a choice between a massively overbooked, stressful public clinic where staff feel burnt out and underappreciated, or a calm, controlled private environment where you also earn a lot more, it’s no surprise what the majority of us prefer. I don’t know the exact solution, but if you consider we have an aging population and a growing number of treatments to keep people seeing well for longer, the obvious solution to me would seem to be to increase the workforce. In my opinion this needs to be a combination of more trainees and also delegating tasks such as intravitreal injections to trained nurses. This worked well in New Zealand so I don’t know why we aren’t doing it in Australia.”
L aHood’s views may seem contentious to some, but he is considered a leader in his field. At 39 years of age, he was Australia’s youngest nominee listed among the top 100 in their field globally in the 2023 Power List, compiled by The Ophthalmologist magazine.
“My views have been seen as controversial, but they shouldn’t be.
I believe very strongly that whether a patient has cataract surgery in public or private, they should receive the same level of care. That means they should have a safe surgeon operating in a safe environment, and most importantly, we should be able to implant the same IOL. It shouldn’t be elitist,” LaHood says.

“I don’t know how much of that mentality stems from being brought up to treat the CEO the same as the cleaner, but I think it’s as simple as that. If we stop and look at the benefits of the latest advanced technology lenses – multifocal, extended depth of focus lenses – the arguments against implanting them in public patients are not valid.”
One of the main arguments against it is cost, but as LaHood points out, the cost of advanced IOL implants compared to other prostheses like a hip or a knee joint replacement, is minimal.
“If we performed a proper cost analysis and factor in ongoing need for glasses, ongoing trips to an optometrist, potential loss of independence, time out of work for family members to take patients to appointments, it would be overwhelmingly in favour of properly correcting a patient’s vision fairly. Admittedly, advanced technology lenses aren’t for everyone, but we should be able to offer it to them,” LaHood says.
“Another [invalid] argument is we must have a point of difference to incentivise patients to use the private system to take some burden off the public system, but there’s still enough incentive in the private system with patients getting to choose their surgeon and surgery date more precisely. I don’t think that would stop a patient having surgery in private because they felt that they were getting the same IOL as in public.”
Multifocal and toric IOLs offer a greater range and quality of vision. However, that may come with a trade off in terms of visual side effects or risks. Patient selection and counselling are crucial to match the right patient and IOL option. Concerns that clinics will be overrun with unhappy patients who inappropriately received a more premium IOL option in the public system are also unwarranted, LaHood says.
“At the moment, toric lenses are considered advanced, but they should be considered the most basic device we have. I’m often asked about toric lenses and the low threshold in the public system because surgeons are worried their clinic will be inundated with unhappy patients who need a lens rotation,” he says.


“We’ve been implanting toric lenses and multifocal IOLs for years at Queen Elizabeth Hospital in Adelaide and we’re not seeing a tidal wave of unhappy patients. I’m standing on the shoulders of giants like Dr Michael Goggin who drove this with ZEISS and Bausch + Lomb and really pushed this program along. Unhappy patients are super rare, as long as the preoperative counselling is appropriate, and the surgery is executed well – as it should be with every patient.”
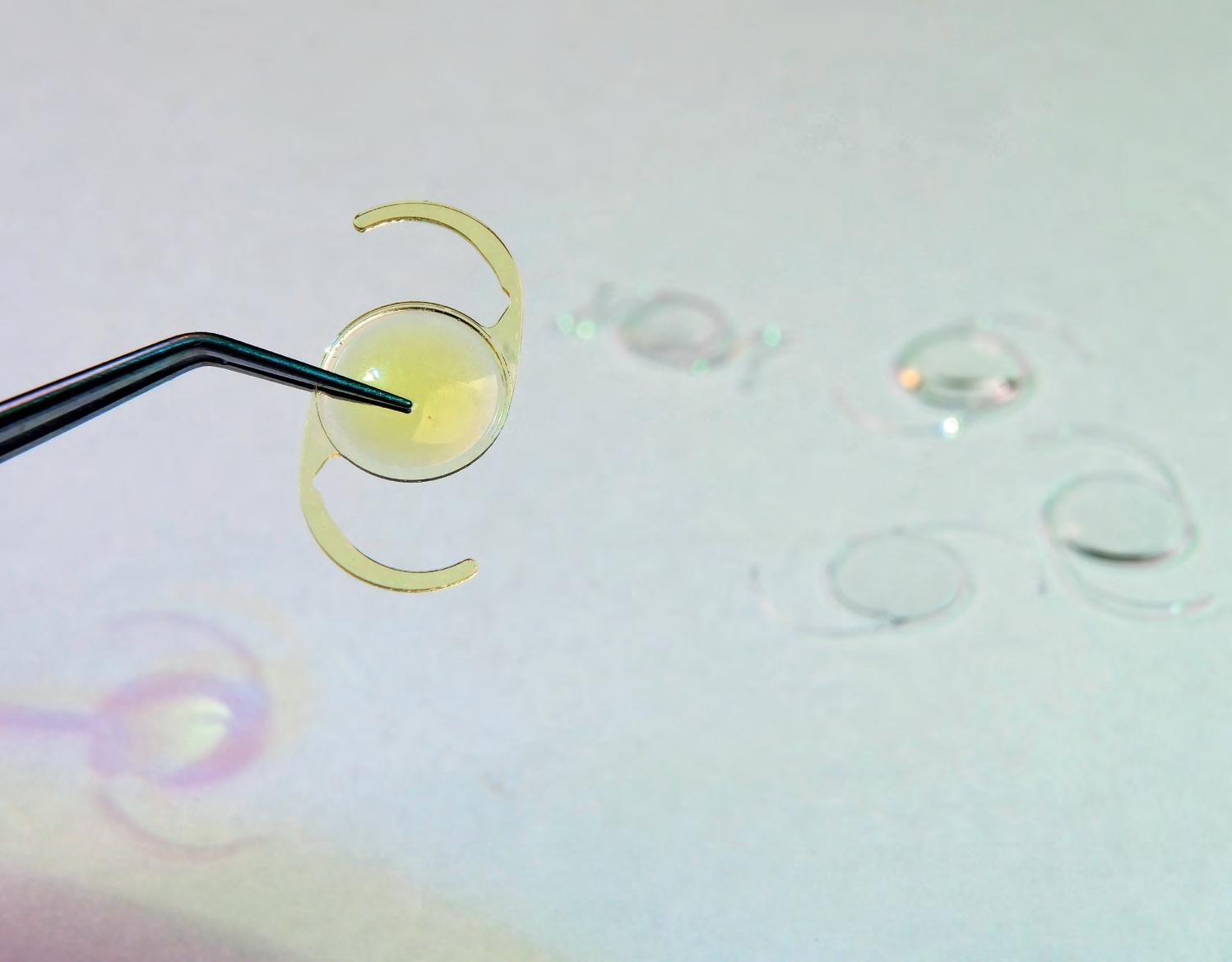
32 INSIGHT July 2023 CATARACT
Australian surgeons and patients are gaining access to an expanding suite of IOL types and designs.
“ADVANCED IOLS ARE A RELATIVELY NEW CATEGORY WITHIN CATARACT SURGERY AND SO FAR, IT HAS MAINLY BEEN UP TO CONSULTANT OPHTHALMOLOGISTS TO SEEK OUT TRAINING AND EXPERIENCE OF THEIR OWN ACCORD.”
DR JACQUELINE BELTZ OPHTHALMOLOGIST
TRAIN TRAINEES TO BECOME CAPABLE, ADAPTIVE, INNOVATIVE
Like LaHood, ophthalmologist Dr Jacqueline Beltz splits her time between public (75%) and private (25%) practice, which equates to about four days a week at the Royal Victorian Eye and Ear Hospital and one to one-and-a-half days private at Eye Surgery Associates in Melbourne.
Among several leadership roles, she directs the Advanced Cataract Fellowship at the Eye and Ear, a role she says allows her to directly supervise and execute complex cataract surgeries for public patients.
She was also recently appointed co-president of Australasian Society for Cataract and Refractive Surgeons (AUSCRS) with Professor Gerrard Sutton, a position that recognises her preeminent standing in cataract surgery in Australia.
“We are very fortunate in Australia to have access to such a high level of surgical training and excellence as well as the technologies, particularly resources for pre-operative measurements and conversations as well as IOL technology and instrumentation that it takes to achieve excellent results,” she says.
“We are one of few countries that can provide toric IOLs to many of our patients without additional cost. The fact that we can provide astigmatism correction without having to justify or consent patients to additional cost really leads us to the very best results.”
Furthermore, she adds, surgeons in Australia can also provide presbyopia correcting IOLs for many of their patients without additional cost.


“Working patients up for these technologies takes additional time and resources and sometimes extra visits that we are often able to provide.”
Beltz points out that recently, in Victoria, a team of ophthalmologists,

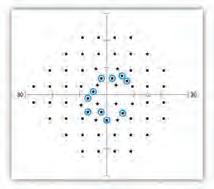




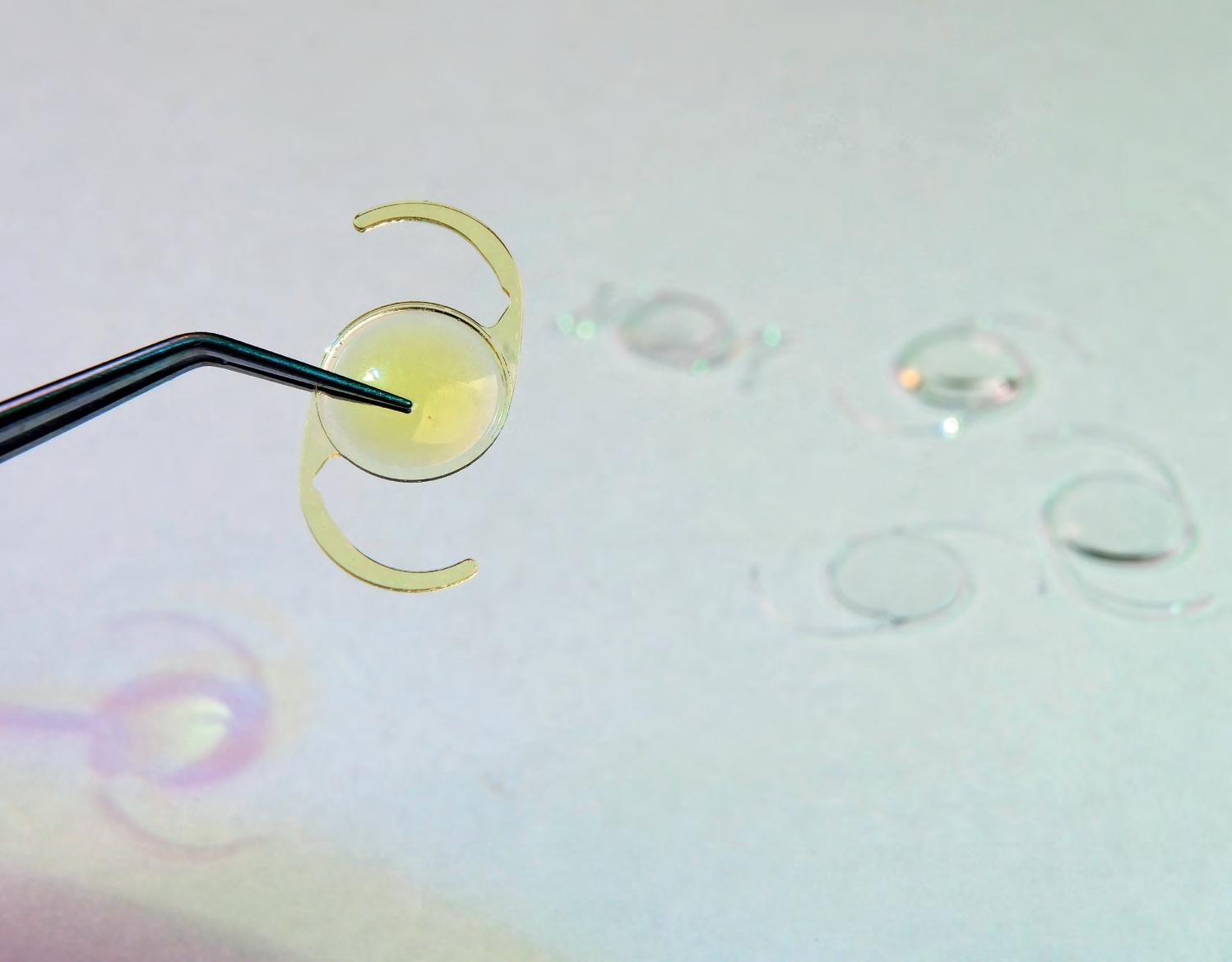
Dr Jacqueline Beltz says there is more to achieving excellent refractive outcomes than just access to lenses.
orthoptists, executives and industry representatives collaborated to reduce the cut off for astigmatism correcting IOLs.
“This means more patients can be free of spectacles, at least for distance vision, after cataract surgery. The same team have also been successful in gaining access to some IOLs with a small degree of extended depth of focus,” she says.
“We have also been able to introduce presbyopia correction at the time of cataract surgery as a structured surgical training program for thirdand fourth-year ophthalmology trainees. The hope is that this program will help to close the gap between private and public cataract surgery in Victoria.”
B eltz agrees with LaHood that there still exists a gap between what surgeons can offer their patients in public versus private.
“There is no lower limit to astigmatism correction in private and so I can strive to correct as much as possible of the pre-existing astigmatism for my patients in private practice,” she says
“In public, at least in Victoria, many patients unfortunately still fall below the threshold for astigmatism correction, and this might lead them to needing glasses for all distances after cataract surgery.”
She continues: “Similarly, despite our new program [for third- and fourth-year ophthalmology trainees], there still remains better access to presbyopia correction at the time of cataract surgery, meaning the reduction of glasses also for near work after cataract surgery, between
private and public patients.”
Beltz recently completed six years as director of training for ophthalmology in Victoria, and through that role, plus her involvement with trainees at the Eye and Ear Hospital and utilising her Masters of Surgical Education, has been heavily involved in restructuring the microsurgical training program, particularly for cataract surgery in Victoria.
“In 2017 I introduced structured virtual reality and lab-based microsurgical training as an essential pre-requisite to starting live surgery in Victoria. Mind-training with high performance psychologists also became a part of that training program in 2019,” Beltz explains.
Having seen the program’s success, RANZCO introduced mandatory virtual reality training for all ophthalmology trainees in Australia and New Zealand in 2023.
Her wealth of experience in training makes her well-placed to provide insight into how advanced lenses fit into the IOL landscape.
“Advanced IOLs are a relatively new category within cataract surgery and so far, it has mainly been up to consultant ophthalmologists to seek out training and experience of their own accord,” she says.
“This has led to quite a variation in comfort with these technologies as well as results. I believe the time is right now for all trainee ophthalmologists to be training with these technologies.”
While training programs use current technologies, Beltz says they’re focusing on the skills and mindset that it takes to safely and expertly pick up new techniques and technologies.
“Hopefully, in this way, we can help our current trainees to become capable, adaptive, and innovative experts who are ready to develop the next generation of technologies and become much better ophthalmologists than we are today.”
Beltz says the profession is working to improve training in advanced IOL use – meaning patient selection, optimisation, conversations, IOL calculations, surgical techniques, post operative assessments and audit, and dealing with problems or complications or the need for refractive enhancements.

“Third- and fourth-year trainees in Victoria now all have access to this program that includes structured training across all of those areas as well as access to a certain number of IOLs to use throughout their training,” she says.
It was important to Beltz, when developing this program, that it did more than merely provide trainees with premium IOLs to use.
“There is a lot more to achieving excellent refractive outcomes than just access to lenses. Our program, run through the GENEYE platform, which is a part of Eye and Ear education, will help us to close the gap between private and public refractive outcomes over the next few years,” she says.
“While training in presbyopia correction has become essential and is likely to continue to be an important part of our training program, removing a threshold for astigmatism correction would make the greatest difference to our patient outcomes, in my opinion.”
GREAT EXPECTATIONS
Cataract, refractive and corneal surgeon Dr Ben Connell believes strongly in the value of data, specifically in the outcomes of cataract surgery. He says reflecting on his own results guides him to give subsequent patients better information on how they’re going to go with surgery.
“ I think it’s important as doctors that we look at our results, we reflect on them, and we make adjustments for future practice. As a cyclist who uses Strava, I find it amazing that we can have detailed data about our leisure activities, but with professional activities, we don’t get that same thorough feedback.”
Connell, who, similarly to Beltz, splits his time 20% in public practice at the Eye and Ear Hospital, 80% in private at Eye Surgery Associates, says lens technology has improved to such a degree over the past 15 to

34 INSIGHT July 2023 CATARACT
Dr Jacqueline Beltz meditating at GENEYE in 2019, a training program designed for ophthalmologists to perform high performance eyecare and surgery.
20 years, there are now increased options where patients can have their glasses dependence significantly reduced.
“When patients come to see me, they are a lot more aware of their options, and I think as an ophthalmologist, we have to consider them. There are limitations, but the newer types of advanced lenses do have great outcomes in the appropriate patient. Patients are a lot more aware of those outcomes, and we need to think a lot more about them,” Connell says.
“Ten years ago, the only option for patients wanting to reduce their glasses dependence was multifocal lenses but patients would often experience issues with night vision where they would see rings around lights and halos. Now, the extended depth of focus and monofocal-plus lenses offers patients a lot more glasses independence at the intermediate vision range – used in 80% of their day – with fewer night vision symptoms; that’s a great outcome.”
But improved lens technology and more options has given rise to a new challenge for Connell.
“The biggest challenge for me – and this is where my practice has changed a lot – is managing patients’ expectations. When discussing newer lens options, I prefer to use the term ‘reduced glasses dependence’ instead of ‘spectacle free’ because there may be some circumstances where the patient might still need glasses. It’s important to manage their expectations in that respect,” he says.
As well as regularly reviewing his cataract surgery results, Connell sees immense value in patient reported outcomes.

“There’s often an overlap between what surgeons consider important and what the patient does; accurate refractive outcomes and reduced glasses dependence to name two. But there are other factors where there’s room for improvement,” he explains.


“I don’t think our profession systematically looks at patient reported outcomes pre and post-surgery. We tend to look at short term refractive outcomes but there’s a range of other outcomes that are equally important, such as reducing the patient’s risk of having a fall and improving their quality-of-life – those are outcomes we don’t really look at.”

Connell sums up: “I think there’s a lot of technology that’s underutilised. There should be more surgeons using toric lenses because it gives patient’s better vision without glasses, and it reduces their astigmatism. Surgeons need to increase their use of newer lenses and familiarise themselves and become more confident with them. I think that’s where there’s room for improvement.
“Overall, surgical techniques are improving, our complication rates are getting lower, we’re accurate with predicting to what degree a patient will require glasses after surgery, and generally speaking, patient satisfaction levels are incredibly high.”

Wyndham Clinic Day Surgery offers you • 2 theatres and large recovery areas • We are located just 20mins from the Westgate Bridge • Ex RVEEH clinical staff with high volume capacity • Very competitive uninsured rates • Easy access and great value parking for patients • Centurion Phaco system with active sentry technology • MIGS, Trabeculectomy, Strabismus, Pterygium and Ocuplastic Wyndham Clinic Private Hospital 242A Hoppers Lane Werribee VIC 3030 Phone: (03) 9731 6646 Fax: (03) 9748 7057 Sally Bebawy Business Development Manager Phone: 0421 713 747 Email: sbebawy@wyndham.clinic Web: www.wyndhamclinic.com.au/ophthalmology Contact us today to discuss opportunities. Secure your private theatre list now - Monday to Friday.
“THERE’S OFTEN AN OVERLAP BETWEEN WHAT SURGEONS CONSIDER IMPORTANT AND WHAT THE PATIENT DOES ... BUT THERE ARE OTHER FACTORS WHERE THERE’S ROOM FOR IMPROVEMENT.”
DR BEN CONNELL OPHTHALMOLOGIST
The solution FOR TIME-POOR CATARACT CLINICS
With manual processes and multiple data points, it’s little surprise cataract surgery is one of the largest sources of ‘never events’. Toric IOL calculations, in particular, are a major drain on staff time too. A WA couple have combined their automation and medical knowledge to create a program that eliminates these issues for busy eye clinics.
Some weeks at home, early in the morning before his children wake, Dr Lasitha Jayasinghe opens the DropBox and can review, in detail, up to 60 toric intraocular lens (IOL) calculations. It’s a manual and tedious task. He knows there are better ways to spend his time, but it’s a price worth paying to avoid the nightmare scenario of implanting the incorrect lens.
Jayasinghe, who trained in his native country Sri Lanka before moving to Australia in 2016, is one of three ophthalmologists at Southwest Eye Surgeons. Each year, the high-volume clinic can see up to 3,000 cataract patients across its two practices in Bunbury and Busselton, serving a vast community across Western Australia’s southwest.
Like other parts of Australia, the state boasts a high rate of toric IOL implantations – available to patients in the public system through Medicare, even those with very low astigmatism. It is a stark contrast to what Jayasinghe had experienced in other health systems where torics were only accessible to a select few.
Considering 95-97% of his cataract cases today receive a toric IOL –requiring a more involved work-up phase – traditionally Jayasinghe was one
of three people who would manually review results provided by online toric calculators. A key part of this was ensuring each patient’s biometry data was entered correctly in the first place, often by an ophthalmic nurse.
One of those nurses was Ms Gabrielle Holt. With more than a decade of nursing experience, she was well-versed in this cumbersome aspect of cataract surgery work.
Thinking there must be a better way, she enlisted her partner Mr Ryan Schulte – a software engineer – and with their combined expertise they set out to develop a system that would create greater efficiencies and confidence in the final toric calculation.
They established Schulte Holt Technology and in February 2022 launched the Schulte Holt Toric IOL Calculator Processor. The system automatically runs the surgeon’s calculations with the Barrett, Kane and EVO toric calculators, providing a full PDF printout instantly. Soon, it will also incorporate the Holliday and Haigis formulas.
The key to the technology is the use of automation to pre-populate biometry data into the calculator – straight from the measurement device. Each surgeon within the clinic can then have the processor customised for their preferences, including surgically induced astigmatism, incision location and preferred IOLs.
Before bringing the concept to life, Schulte, with a non-ophthalmic background in robotics and software development, was surprised to learn many practices in 2023 were performing this task manually.
“I showed him how extremely tedious and time consuming toric IOL calculations are, and the potential for it to be riddled with errors,” Holt says. “He was also surprised at the volume of calculations that we do at any given time.
“In many practices, toric calculations aren’t usually done during patient time, it’ll be at the end of the day when you’re fatigued after seeing patients all day. We’ve developed a system that’s machine agnostic, meaning any machine that can abstract biometric measurements can be incorporated into the program. It was also designed with the purpose of completing high numbers of IOL toric calculations to keep up with increasing demand for cataract surgery, and to reduce errors during calculations and therefore increase patient safety.”
CREATING MORE MENTAL BANDWIDTH
As an ophthalmologist with a high volume of toric IOL patients, every minute is valuable to Jayasinghe, but what’s also important is a clear mind and ability to focus.

Knowing that the pre-populated data is accurate, when he receives the results from the Schulte Holt processor, his priority becomes IOL selection, and understanding what will be required on the operating table.
“Since implementing the Schulte Holt processor, it has freed up a few hours per month, but it has afforded me more mental capacity and less mental strain when planning for my surgeries,” he says.
“There’s also a financial benefit for our clinics too. It means our staff are spending a lot less time on manual data entry. When you extrapolate that across 3,000 cases a year, that is a significant time saving that frees them up for other tasks.”
To demonstrate the effectiveness and accuracy of the Schulte Holt IOL processor in comparison to manually input data, a study was performed at Southwest Eye Surgeons.
This involved 352 manual IOL calculations versus 696 calculations with Schulte Holt’s software. The Barrett Toric IOL Calculator was the formula of choice.
The manually-calculated torics took 371 minutes, or 1.05 minutes per calculation. Of these, 40 mistakes were identified and needed to be redone. During the manual data input, 25 distractions occurred for the user inputting data, such as patients requiring assistance (7), phone calls (3), other staff members requiring assistance (15). Importantly, distraction tracking is not relevant for the Schulte Holt processor as it runs in the background constantly.
By comparison, the automated process involving the Schulte Holt took much less time.
After biometric measurements were captured on a ZEISS IOL Master 700,
36 INSIGHT July 2023
CATARACT
Dr Lasitha Jayasinghe assesses a patient post-cataract surgery.
the system was automatically set up to upload a PDF into the Schulte Holt processor, without adding extra steps or time to the procedure. The user then needs to open the program on the desktop computer and hit ‘run’.
The Schulte Holt processor took 138 minutes for 696 toric IOL calculations, or 0.19 minutes per calculation (the most current version has recorded speeds of 0.05 minutes per calculation).
The Schulte Holt processor recorded seven errors during this study: six were due to only the left eye being uploaded which caused an error in the code, while another was because no white-to-white value had been recorded. In all cases, mistakes were easy to identify because there was no toric IOL calculation completed. The errors have now been rectified within the program coding.
Since implementing the technology, Jayasinghe has been impressed by many other features, including the way in which the information is presented.
“The way it is formatted gives a very clear picture for me to refer to during surgery. Between cases you may only have a few minutes, so it helps me to quickly understand important information, such as the axis of the lens,” he says.
“There’s also a huge advantage for surgeons who use an optimised A Constant. Traditionally, you have to enter this manually into a toric calculator each time, but if you use the Schulte Holt processor you can key it in once and that’s it.
“Every surgeon has their preferences, so being able to create a profile for each surgeon and incorporate an optimised A Constant is a major advance. There aren’t many, if any, other programs that can do this with one click. It’s useful for us as surgeons in WA who often need to work with multiple types of IOLs depending on what is available locally at any given time. We don’t always have the same access to all IOL types like in metro areas when last-minute scheduling is needed due to logistic reasons.”
RESPONSIVE TO AN EVOLVING MARKET

It’s been a labour of love for Holt and Schulte to develop the software, but they are excited to see it working in real world clinics. The development phase involved robust feedback from four ophthalmologists affiliated with Southwest Eye Surgeons.
“Ryan is extremely efficient at learning new information. When working with the surgeons he was picking their brains non-stop,” Holt says.
“Considering how differently each surgeon works, it’s been quite an accomplishment to customise it to a level that suited every single one of those involved in the test phase.”
Now the program is fully operational, it’s all about optimisation with plans to continuously add and update calculators on the platform. As new IOLs come
to market, the company can enter these into the software’s backend and make them immediately available to ophthalmologists using the processor.
Holt says this is a distinct advantage, especially for practices who might be relying on calculators built into their biometer.
“While these use great calculators, they have significant limitations. They work well in isolated environments, but the way that clinics have changed and the volume they’re dealing with, it’s not suitable anymore. Often, to add new IOLs someone has to visit the practice and enter this manually – which then leaves them vulnerable to more errors.”
For practices considering bringing the Schulte Holt processor into their workflow, Holt says they can trial the technology before committing to it. If they decide to become a customer, it involves an upfront payment, and then a smaller, ongoing subscription fee which covers all updates and maintenance costs.
“When installing the system, we can either do it remotely or visit the practice – we personally integrate it into the clinic. We watch how they normally run their practice and give advice on how they can do so more efficiently with customisations to our processor,” Holt says.
“We include training for staff to perform customisations. This includes setting it up so that immediately after biometry, the system immediately runs the toric calculations. Or if a clinic prefers to run them all at once, we can cater for this as well. For certain doctors, they receive a print out PDF straightaway, which means we can pair it with the measurement data, while others doctors prefer theirs to be online.
“The second the measurements are captured, the toric calculations are completed, it’s such a significant time-saver for practices, and eliminates worries about human error.”
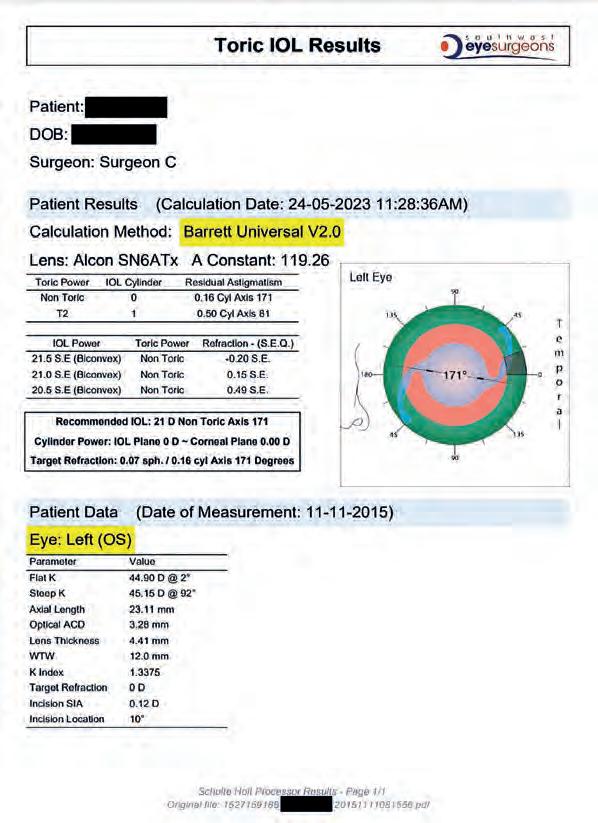
INSIGHT July 2023 37
Gabrielle Holt, with an ophthalmic nursing background, and her software engineer partner Ryan Schulte have combined their experience to develop the Schulte Holt Toric IOL Calculator Processor.
Schulte Holt Technology’s toric IOL processor is designed to deliver results instantly in an easy-to-read print-out for the patient.
NO ONE DREAMS OF SILVER
PanOptix® is the most implanted trifocal IOL worldwide and delivers an exceptional high-quality visual experience from far to near, with 99% patient satisfaction.*1-4


Please refer to relevant product direction for use for complete list of indications, contraindications and warnings.
* Based on global Clareon® PanOptix® and AcrySof® PanOptix® unit sales 2021–2022.
† Pooled binocular defocus curve data from six individual studies. Snellen VA was converted from logMAR VA. A Snellen notation of 20/20^-2 or better indicates a logMAR VA of 0.04 or better, which means ≥3 of the 5 ETDRS chart letters in the line were identified correctly.
§ Defined as Miyata grade 0, <25mv/mm2 over 3 years (n=138), and over 9 years (n=20), respectively.
References: 1. Market Scope 2022 IOL Market Report. 2. Alcon data on file, 2022 [REF-18881]. 3. Clareon® PanOptix® Directions for Use_09/2021. 4. Modi S et al. Visual and Patient-Reported Outcomes of a Diffractive Trifocal Intraocular Lens Compared with Those of a Monofocal Intraocular Lens. Ophthalmol 2021;128(2):197–207. 5. Alcon data on file, 2022 [REF-17351]. 6. Lwowski C et al. Visual and patient-reported factors leading to satisfaction after implantation of diffractive EDOF and trifocal intraocular lenses. J Cataract Refract Surg 2022;48(4):421–428. 7. Lane S et al. Evaluation of intraocular lens mechanical stability. J Cataract Refract Surg 2019;45(4):501–6. 8. Alcon data on file, 2019 [REF-05749]. 9. Clareon® PanOptix® Toric Directions for Use. 10. Alcon data on file, 2017 [REF-00516]. 11. Alcon data on file, 2020 [REF-10587]. 12. Stanojcic N et al. Visual and refractive outcomes and glistenings occurrence after implantation of 2 hydrophobic acrylic aspheric monofocal IOLs. J Cataract Refract Surg 2020;46(7):986–94. 13. Oshika T et al. Mid-term and long-term clinical assessments of a new 1-piece hydrophobic acrylic IOL with hydroxyethyl methacrylate. J Cataract Refract Surg 2020;46(5):682–87. 14. Maxwell A et al. Long-term effectiveness and safety of a three-piece acrylic hydrophobic intraocular lens modified with hydroxyethyl methacrylate: an open-label, 3-year follow-up study. Clin Ophthalmol 2018;12:2031–37. 15. Alcon data on file, 2019 [REF-13093].
© 2023
Auckland,
Zealand.
Alcon Inc. Alcon Laboratories (Australia) Pty Ltd. ABN: 88 000 740 830. Phone: 1300 224 153.
New
Phone: 0800 809 189. ALC1892 04/23 ANZ-CPO-2300005
COMINGSOON
CHOOSE THE GLOBAL LEADER IN TRIFOCAL IOLs*1,2
• Full range of excellent vision with 20/20 vision at all distances.†4
• True comfort at intermediate distance with a natural focal point of 60cm. 5,6
• >9/10 patients are spectacle independent. 5
• Excellent clarity and stability with the glistening-free Clareon® IOL material.§7-14

• Over 2.2 million implants worldwide. 2
• Consistent and controlled IOL delivery with the Clareon® Monarch IV delivery system.15
Taking the
FUSS OUT OF PHACO
The phaco machine needs to act as a trusty friend to the cataract surgeon, offering an energy supply that efficiently emulsifies the lens while maintaining excellent fluidics for anterior chamber stability. A new system in Australia achieves this – and goes much further in terms of safety and simplicity.
For Melbourne-based glaucoma specialist and cataract surgeon Dr Brian Ang, surgery can be stressful enough – especially when things don’t go to plan. In such instances, the surgeon needs to fall back on their training, and trust the equipment won’t complicate matters further.

In cataract surgery, the phacoemulsification (phaco) system is one of the key items in the ophthalmologist’s toolkit. The technology was first developed by Mr Charles Kelman in 1967 in what was considered a major leap forward, allowing the removal of an emulsified cataractous lens through a much smaller incision. With its evolution over the ensuing decades, surgeons have come to expect safety, performance, efficiency, familiarity, and simplicity from their phaco machine. And in more recent times, they want a system that’s eco-friendly.
Ang’s pre-existing phaco system had not been updated for some years. It wasn’t able to maintain anterior chamber stability as well as the newer systems could and didn’t have a dual linear function (separating vacuum/ aspiration from phaco) on its foot pedal.
Some of his overseas peers had been using the Sophi phaco system, developed in Switzerland and introduced into Australia by Designs For Vision (DFV), a Paragon brand. The device has been designed with mobility, simplicity, and safety in mind – and in the world of cataract surgery, it’s all about optimisation to improve the experience for surgeons and patients.
“When doing cataract surgery, I want to have the reassurance that the system will work as intended – there is no point adding extra stress by using inefficient and difficult-to-use phaco systems,” Ang explains.
“Some of my colleagues in Europe are already using the Sophi phaco system and have spoken highly about it. I like the excellent anterior chamber stability, minimal post-occlusion surge, and the dual linear setting which I use when chopping. I also love how the foot pedal can be moved over the floor like a hovercraft.”
“The system has done very well so far, even in difficult cases. I think it is a great phaco system that ticks the two essential criteria for me: safety and performance.”
OUTWARD SIMPLICITY DUE TO COMPLEXITY WITHIN
Sophi has been designed to satisfy several requirements in modern-day cataract surgery, but its fast and responsive Triple Pump Fluidics is the key. It offers higher anterior chamber stability due to its IOP Control Pump infusion, which does not rely on gravity or infusion pressure. The dedicated Infusion Pump controls the anterior chamber by measuring flow and pressure of irrigation, and responding to pressure changes. Meanwhile, the surgeon can choose their preferred aspiration (Peristaltic Pump aspiration or Clean Venturi aspiration).
According to Mr George Krokidis, national surgical product manager for DFV, the system is highly mobile. Being the first battery-operated phaco system (lasting for up to 20 surgeries), it operates free from any

connection cables, including power, data, and air lines. It is also equipped with an integrated air compressor. Importantly, its pedal is also cable free.
“Sophi’s mobility is the result of its smart design: it’s completely wireless, has a small footprint – a great space saver in theatre – with a mono-brake handle, a ‘hover’ pedal, rotatable display, and tray,” he says.
“With so much already going on in theatre, and increased use of new technologies with additional monitors and cables, it’s refreshing to have a new system that bucks this trend and keeps to a minimal space. Bluetooth connectivity to other devices also makes Sophi future-ready.”
Sophi’s manufacturer has also prioritised simplicity in its design. This is achieved by using modern assistance systems, and clever use of the latest technology. This includes an intuitive and fast graphical user interface and set-up, voice audio and visual sensory info/feedback to assist the surgeon and surgical team.
Safety and hygiene is the third most important element. The system contains what is described as a world-first Clean Venturi system and automated Cassette Slot-In-System which helps to reduce the risk of contamination.
“The automated Cassette Slot-In-System reduces the risk of contamination, and with the Clean Venturi system foil prevents contamination of the device and air with patient’s eye fluids. The Cassette Control Guard also helps to monitor the cassette’s expiry date.”
Sophi’s smart design of consumables also leads to high functionality and economic benefits, while offering waste reduction from a lean and (optional) reusable cassette.
“The system uses a lean cassette for less waste, and allows the use of glass or plastic bottles, or bags of balanced salt solution (BSS). Moreover, the use of the ‘day cassette’ and disposable tubing significantly reduces the waste per case,” Krokidis says.
40 INSIGHT July 2023
CATARACT
Sophi, with a cable-free design, satisfies many requirements of modern day ophthalmic surgeons.
FEATURES IMPRESS EXPERIENCED OPHTHALMOLOGIST
Sophi’s attention to waste reduction was one of the attributes that stood out for Dr Robert Harvey, an ophthalmologist based in rural Victoria.
“In terms of features that have impressed me the most since installation, the lack of wires and tubes gives a clean streamlined appearance. Each patient has a cassette with tubes leading to the lightweight handpiece, but the bottle of BSS lasts for several patients leading to significant cost savings,” he says.
Harvey has more than 20 years of ophthalmic experience in the UK and Australia and today is a general ophthalmologist who subspecialises in glaucoma. Inevitably this means he treats many eyes with shallow anterior chambers and loose zonules through pseudoexfoliation.

“The phaco machine needs to be reliable with excellent power to get through tough cataracts and maintain excellent fluidics to keep the anterior chamber stable,” he says.
“The machine is easy to set up. The foot pedal is wireless and usually locked in position or glides like an ice puck when getting positioned. All functions are configurable, and the machine gives verbal feedback.”
Overall, Harvey has been pleased with his patient outcomes after using the system. Although dense cataracts are not the norm in Australia, Sophi handles these effectively thanks to a ‘High Vac’ designed phaco tip and the use of sinusoidal signal to control the handpiece. This means the energy used is more efficient and considerably reduced.
“Corneas are clear post-operatively. Dense cataracts can be demolished by increasing the frequency of pulses,” Harvey says. “DFV supplied the demo machine which we have now purchased and they provide valuable in theatre training for the surgeon and theatre nurses.”

Revolutionising
Fast, error free Toric calculations. Get in touch with us today for a free trial. Web: www.schulteholt.com Email: team@schulteholt.com Schulte Holt Technology
CATARACT TECHNOLOGY
Since using the Sophi phaco system, Dr Brian Ang (left) likes the excellent anterior chamber stability it offers, in addition to minimal post-occlusion surge, and its dual linear setting.
A NEW LEVEL
of clarity
Alcon’s Clareon hydrophobic acrylic IOL material has been applied to its leading trifocal intraocular lens design. Melbourne’s DR UDAY BHATT has had early access with the lens and discusses his initial impressions.
When the R&D experts at Alcon developed the company’s most advanced* intraocular lens (IOL) material to date, Clareon, Melbourne ophthalmologist Dr Uday Bhatt found himself in the first cache of surgeons globally to implant these IOLs. The intention was to assess how the material, in a monofocal design at the time, would perform over a three-year period.
“I was among approximately 12 surgeons in the world approached for the trial, and I contributed about 40 patients out of the 215 enrolled patients (424 eyes) across 19 multinational sites,” he says. “In fact, with a significant number of patients ready to go, I was the first in the world to implant a Clareon IOL at Vision Eye Institute (VEI), Footscray.”
This wasn’t the first time Bhatt was an early adopter of IOL technology. He was also the first to use Alcon’s AcrySof PanOptix trifocal in Australia and has implanted many AcrySof IQ Vivity extended depth of focus IOLs, among the highest in the world to date. In addition, he has been an investigator in several ground-breaking research projects investigating the latest IOLs and glaucoma therapies.
When using the first Clareon IOL – made from a hydrophobic acrylic with increased water content compared to AcrySof – Bhatt was immediately impressed with the clarity of the new material. The study he’s referring to also involved Dr Tim Roberts, affiliated with the University of Sydney and VEI, and results were published in February 2023. At three years, 100% of eyes implanted with the Clareon IOL presented with Grade 0 glistenings; and 92.9% of eyes (394/424) had either no posterior capsular opacification (PCO) or clinically non-significant PCO. Visual outcomes were excellent and stable over the three-year study period.1
Today, the clarity of Clareon persists several years later in his trial patients, with the optical performance he has come to expect from around two decades of implanting Alcon IOLs.
Clareon first became available to Australian ophthalmologists as a monofocal in 2018, followed by the toric version in 2020. Alcon’s PanOptix is the next IOL to be rolled out widely as part of the Clareon IOL family. It became available in Australia in June 2023, with Bhatt gaining early access to implant the IOL in a number of patients in Melbourne. Clareon PanOptix Toric will also be part of the launch.

As Bhatt explains, one of Alcon’s key motivations behind Clareon, on the basis of listening to surgeons, was to build on Alcon’s AcrySof platform which has been implanted in well over 125 million eyes globally. 2
Specifically, Clareon has sought to further improve optical clarity, an important parameter in the quality assessment of IOLs. The material clarity is born out of a glistening-free material (defined as Miyata grade 0 or <25mv/mm2) that Alcon says has among the lowest levels of haze and subsurface nanoglistenings (SSNGs) compared to leading competitor IOLs. 3-7†
With the Clareon material now applied to the PanOptix design, Bhatt says he is now able to deliver even greater outcomes for his patients seeking spectacle independence with a trifocal IOL.
“Seeing how Clareon has performed in monofocal and toric versions of IOLs, we can see the material has withstood the test of time. It’s an excellent material, particularly in terms of maintaining optical clarity,” he says.
Bhatt says having a glistening-free material is arguably more important on a multifocal lens like PanOptix. These fluid-filled microvacuoles might add to scattering of light resulting in dysphotopsia, decreased contrast sensitivity, and other photic phenomena that interfere with vision and are associated with diffractive multifocal IOLs. Coupled with known visual disturbances that can occur in low light with a diffractive lens design, this could become more problematic on a trifocal IOL.
“So, for that reason, it’s very important this platform is extremely robust. There’s no doubt the Clareon platform has been tested properly and I’m looking forward to Alcon rolling out this new lens material across its portfolio. They had a good lens (with AcrySof), and now we have an even better one with Clareon.”
EARLY RESULTS
A key part of the design is a proprietary edge to help reduce glare and posterior capsular opacification. 8 The lens’ STABLEFORCE Haptics also provide superior axial and rotational stability. 8-14 In addition, Clareon has been extensively researched, with inclusion in 30 published studies worldwide, while Clareon Monofocal and Clareon Toric IOLs have already been implanted in more than one million eyes across more than 70 countries.15
The latest Clareon PanOptix lens is designed to mitigate the effects of presbyopia by providing improved intermediate and near visual acuity

42 INSIGHT July 2023
CATARACT
Clareon PanOptix IOLS are inserted using the reusable Clareon Monarch IV Delivery System.
The Clareon PanOptix IOL is now available to Australian surgeons.
while maintaining comparable distance visual acuity with a reduced need for glasses, compared to a monofocal IOL.
According to Alcon, Clareon PanOptix has been demonstrated to achieve:
• 6/6 visual acuity at distance, intermediate and near 16
• A m ore natural intermediate focal point at 60 cm vs 80 cm17-21
• 9 6% of patients achieve spectacle independence 22,24
• 9 9% of PanOptix patients would have the same lens implanted again16
Bhatt’s own one-week post-operative data for 12 patients that had Clareon PanOptix shows all patients except one have achieved 6/6 or better uncorrected distant visual acuity (UCDVA) and N6 or better uncorrected near visual acuity (UCNVA). The one patient that has not achieved this has some post-op inflammation and corneal oedema due to high intraocular pressure post-op and is improving slowly.
Clareon PanOptix Toric is also available for astigmatic patients, continuing the Alcon legacy of optimised rotational stability. 8-14
In trials, 95% of Clareon IOLs had an absolute rotation of ≤5° 24,25 on day one of surgery, and after six months there was a 2° mean absolute rotation of the lens. 24
“It’s still quite early, but my early post-operative results are looking fantastic in terms of visual outcomes with Clareon PanOptix,” Bhatt says. “We will need to follow them up for a bit longer, and soon I would have implanted the Clareon PanOptix in another 15 to 17 patients, so that will be a reasonable number to begin understanding its performance.”
For Bhatt, the real advance with the Clareon portfolio is that it leverages many of the same design characteristics and optics that he appreciates from Alcon to help deliver the consistent outcomes surgeons expect.

“The design of Alcon lenses are very well tested, so I think it’s important that the shape, the design and other elements like the haptics to facilitate accurate centration within the capsular bag are maintained. The legacy is there, and Alcon has built on this with an improved material,” he says.

“Clareon will remain my go-to family of IOLs. Generally, when you have used these lenses in trial settings you tend to know a lot more about them. And if you’re happy with the outcomes in various testing conditions, then you can be confident about their performance in day-to-day lives.”
NEW DELIVERY SYSTEM
Clareon Monofocal and Toric have been available on the AutonoMe delivery system, described as the first and only automated, disposable, pre-loaded IOL injector. This is Alcon’s latest generation delivery system.
Clareon PanOptix are inserted using the reusable Clareon Monarch IV Delivery System. This manual IOL injector has been designed specifically for the Clareon material.

Some key features of the delivery system include 26 :
• Enlarged thread weight and twist knob for precise speed and control
• A n improved thread design to reduce the number of rotations compared to Monarch III
• A precisely engineered plunger tip that uniquely grips the Clareon IOL for consistent planar deliveries
• B alanced weight to accommodate any surgeon technique
“This new lens loading system is much improved and works seamlessly with this lens, in my experience,” says Bhatt. “It holds the IOL much better and inserts it nicely into the eye, and maintains its position while delivering. It also features an enlarged thread, which means you can inject the IOL faster into the eye, if you wish to.”
* Based on Alcon’s range of IOLs
† Over 3 years (n=138), and over 9 years (n=20), respectively
REFERENCES:
1. N uijts R, Bhatt U, Nanavaty MA, Roberts TV, Peterson R, Teus MA. Three-Year Multinational Clinical Study on an Aspheric Hydrophobic Acrylic Intraocular Lens. J Cataract Refract Surg. 2023 Feb 22. doi: 10.1097/j.jcrs.0000000000001173. Epub ahead of print. PMID: 36848238.
2. A lcon Announces Launch of AcrySof IQ Vivity, the First and Only Non-Diffractive Extended Depth of Focus Intraocular Lens in the U.S. https://www.alcon.com/media-release/al con-announces-launch-acrysof-iq-vivity-first-and-only-non-diffractive-extended.
3. S tanojcic N et al. Visual and refractive outcomes and glistenings after implantation of 2 hydrophobic acrylic aspheric monofocal IOLs. J Cataract Refract Surg 2020;46:986-994.
4. O shika T et al. Mid-term and long-term clinical assessments of a new 1-piece hydrophobic acrylic IOL with hydroxyethyl methacrylate. J Cataract Refract Surg 2020;46:682-687.
5. M axwell A et al. Long-term effectiveness and safety of a three-piece acrylic hydrophobic intraocular lens modified with hydroxyethyl-methacrylate: an open-label, 3-year follow-up study. Clinical Ophthalmology 2018:12;2031-2037.
6. Werner L, Thatthamla I, Ong M, Schatz H, Garcia-Gonzalez M, Gros-Otero J, Cañones-Zafra R, Teus MA. Evaluation of clarity characteristics in a new hydrophobic acrylic IOL in comparison to commercially available IOLs. J Cataract Refract Surg. 2019 Oct;45(10):14901497. Doi: 10.1016/j.jcrs.2019.05.017. Epub 2019 Aug 6. PMID: 31399323.
7. C lareon® IOL Directions for Use.
8. D as KK, Werner L, Collins S, Hong X. In vitro and schematic model eye assessment of glare or positive dysphotopsia-type photic phenomena: Comparison of a new material IOL to other monofocal IOLs. J Cataract Refract Surg. 2019 Feb;45(2):219-227. Doi: 10.1016/j. jcrs.2018.09.017. Epub 2018 Nov 22. PMID: 30471850.
9. L ane, S., Collins, S., Das, K. K., Maass, S., Thatthamla, I., Schatz, H., … & Jain, R. (2019). Evaluation of intraocular lens mechanical stability. Journal of Cataract & Refractive Surgery, 45(4), 501-506.
10. T DOC-0054028 (2017) - Clareon SY60WF Axial Displacement Study at Varied Compressions.
11. K ramer BA, Hardten DR, Berdahl JP. Rotation Characteristics of Three Toric Monofocal Intraocular Lenses. Clin Ophthalmol. 2020 Dec 16;14:4379-4384. doi: 10.2147/OPTH. S285818. PMID: 33364742; PMCID: PMC7751684.
12. L ee BS, Chang DF. Comparison of the Rotational Stability of Two Toric Intraocular Lenses in 1273 Consecutive Eyes. Ophthalmology. 2018 Sep;125(9):1325-1331. doi: 10.1016/j. ophtha.2018.02.012. Epub 2018 Mar 12. PMID: 29544960.
13. O shika T, Fujita Y, Hirota A, Inamura M, Inoue Y, Miyata K, Miyoshi T, Nakano S, Nishimura T, Sugita T. Comparison of incidence of repositioning surgery to correct misalignment with three toric intraocular lenses. Eur J Ophthalmol. 2020 Jul;30(4):680-684. doi: 10.1177/1120672119834469. Epub 2019 Mar 6. PMID: 30841757.
14 C lareon® Vivity Directions for Use.
15. A lcon Strengthens Leadership in IOL Innovation with Launch of Clareon Portfolio in the U.S. https://www.alcon.com/media-release/alcon-strengthens-leadership-iol-innovation-launch-clareon-portfolio-us.
16 C lareon® PanOptix® IOL Directions for Use.
17. Kohnen T. First implantation of a diffractive quadrafocal (trifocal) intraocular lens. J Cataract Refract Surg. 2015;41(10):2330–2332.
18. C harness N et al. Monitor viewing distance for younger and older workers. Proceedings of theHumanFactorsandErgonomicsSocietyAnnualMeeting.2008;52(19):1614–1617.
19. AverageofAmericanOSHA,CanadianOSHAandAmericanOptometricAssocationRecommendationsforComputerMonitorDistances.www.aoa.org.(July,2015).
20. P lagenhoefSetal.Anatomical data for analyzing human motion. Research Quarterly for Exercise and Sport. 1983;54:169–178.
21. W hat is the average male height? Average Height. https://www.averageheight.co/average-male-height. Accessed November 11, 2022.
22 B öhm M et al. Defocus curves of 4 presbyopia- correcting IOL designs: Diffractive panfocal, diffractive trifocal, segmental refractive, and extended-depth-of-focus. J Cataract Refract Surg. 2019;45(11):1625–1636.
23. Kohnen T et al. Visual Performance of a Quadrifocal (Trifocal) Intraocular Lens Following Removal of the Crystalline Lens. Am J Ophthalmol. 2017;184:52–62.
24. C lareon Toric IOL Directions for Use.
25. A lcon Data on File, 2019. [TDOC-0055470].
26. C lareon® Monarch® IV Directions for Use.
INSIGHT July 2023 43
"SEEING HOW CLAREON HAS PERFORMED IN MONOFOCAL AND TORIC VERSIONS OF IOLS, WE CAN SEE THE MATERIAL HAS WITHSTOOD THE TEST OF TIME. IT’S AN EXCELLENT MATERIAL.”
DR UDAY BHATT OPHTHALMOLOGIST
FOR HYDROPHILIC IOLS The case
In the ongoing quest to produce an intraocular lens (IOL) that closely imitates a healthy crystalline lens, manufacturers have walked a narrow tightrope when it comes to IOL materials. Biocompatibility, clarity, foldability, and an ability to apply advanced optical designs are all vital factors when bringing a lens to market, with diminishingly less room for compromise.
Today, two categories of acrylic materials have come to dominate the IOL market: hydrophobic and hydrophilic.
At a chemical level, their differences boil down to their water content, with hydrophilic usually comprising 18–38% water compared to ≤5% for hydrophobic.1
But do their differences go much deeper than this? Some would say yes, when considering the surgical experience, stability, visual outcomes and complication rates of these two materials. In fact, the debate around the use of hydrophilic IOLs, in particular, has intensified to the point of some calling for a ban on the material.
How it has reached this point is perplexing to renowned cataract and refractive surgeon Dr Ben LaHood, a consultant ophthalmologist at Adelaide Eye and Laser Centre, The Queen Elizabeth Hospital in Adelaide, and senior lecturer at the University of Adelaide.
He believes the war being waged on hydrophilic acrylic IOLs is unjustified, saying the industry should be engaged in a more nuanced conversation about judicious use and the potential for optimal outcomes.
“The biggest issue that’s reared its head in the last decade has been the potential for hydrophilic acrylic IOLs to absorb different molecules and become opaque. The potential for opacifications is the most publicly known downside of hydrophilic materials – and it’s been so big that there’s even been calls for manufacturers to stop producing them. I think that would be an unwise move because what we’re talking about is the absolutely tiny risk of an absolutely tiny risk,” he says.
“Hydrophilic IOLs have so many positive attributes, such as excellent optical clarity and unique optical designs. In terms of optimal outcomes, we’re aiming for minimal residual refractive error; the smaller the incision, the less surgically induced astigmatism we may create. This means we can potentially leave the eye very similar to its preoperative measurement.
Therefore, outcomes with hydrophilic IOLs could potentially be more predictable than a larger incision for hydrophobic implantation. 2
“When you consider these factors, it’s my view that the worry about opacities has been blown out of proportion.”
THE PROS AND CONS
Looking at hydrophobic IOLs, LaHood says they too can have great optical clarity and are stiffer which can help provide long term stability within the capsular bag. However, in his experience they can be more challenging to insert safely through smaller incisions, and some designs have been more susceptible to glistenings. 3 These fluid-filled microvacuoles can scatter light resulting in dysphotopsia, decreased contrast sensitivity, and other photic phenomena that interfere with vision1, 4-6 and, in severe cases, may require explantation.
“Today we have some great hydrophobic materials that don’t appear to have glistenings long-term, which is fantastic, but these lenses are still limited in the ease that manufacturers can apply more complex optical designs on to the surfaces and how easily we can fold them to insert through a tiny incision.”

When it comes to hydrophilic IOLs, he says greater flexibility in the material means surgeons can insert them through smaller incisions.
"The IOL then unfolds within the eye effortlessly to assume its final position quickly,7 which is especially useful when implanting toric IOLs where the slower unfolding or self-adherence seen with some hydrophobic acrylic IOLs can be time-consuming and may lead to rotation if the surgeon is impatient, 8-9 he says.
“Hydrophilic IOLs tend to have more complex haptic designs to maintain their position – being a softer material they can be more easily distorted by the changes of the capsular bag over time. 9 ”
Hydrophilic IOLs – which have existed for some four decades – account for around a third of IOLs implanted worldwide today. From an optical design and manufacturing point of view, it is considered easier to develop advanced optics on a hydrophilic. IOL manufacturer Rayner is one company that has adopted the hydrophilic material for its new RayOne EMV platform featuring a non-diffractive design that provides patients with an enhanced range of vision.
44 INSIGHT July 2023
CATARACT
When a surgeon selects an IOL for cataract surgery in 2023, there are usually two acrylic materials to choose from. DR BEN LAHOOD discusses their differences and why he believes calls to limit the use of one material type are unfounded.
Rayner is one company that has adopted the hydrophilic material for its new RayOne EMV platform.
When it comes to hydrophilic IOLs, LaHood believes the discussion should steer way from blanket bans, to thinking about patient candidates.
Studies have highlighted reports of calcification of hydrophilic IOLs in patients with a break down of their blood/eye barrier such as diabetics, who underwent procedures using intraocular instillation of air or gas, such as Descemet membrane endothelial keratoplasty (DMEK), pars plana vitrectomy or Descemet stripping endothelial keratoplasty (DSEK).11 Since surgeons cannot predict perfectly which patients may one day require keratoplasty or pars plana vitrectomy surgeries, the suggestion emerged that surgeons should avoid hydrophilic IOL use.
In his 10 years of implanting and observing hydrophilic IOLs, LaHood has not encountered a hydrophilic IOL opacity, and struggles to think of a colleague who has as well. That’s not to say these cases don’t exist, but improved manufacturing processes coupled with judicious use would ensure opacities become “vanishingly rare”.
If there is the potential for gas inside the eye and/or diabetes, when the intersection of those two conditions occurs, he would avoid a hydrophilic IOL.
“Specifically, in the case of a patient requiring an endothelial keratoplasty for severe Fuchs dystrophy, I would probably avoid any type of multifocal lens design because I don’t want to put something diffractive behind an already irregular surface. That would leave me with my monofocal choice, a hydrophobic IOL, so it doesn’t alter my thinking much there.”
LaHood considers that patients who may require retinal surgery longer term are also known to be at higher risk for a breakdown of their blood vessel barrier, changing the chemistry within their eye, and gas injection, which could lead to IOL opacity.
“This is a very small group of patients where I’d be unlikely to implant a multifocal lens in anyway because of their already-compromised macula, leading to using my hydrophobic monofocal IOL of choice. It doesn’t greatly alter my practice, particularly, but for surgeons who are using hydrophilic IOLs consistently, that’s where they may want to consider their use," he says.
Alternatively, there has been significant advancement in adaptive techniques that serves as valuable tools in the surgeon’s arsenal to safeguard IOLs against opacification, irrespective of the material employed. One approach is the reduction of air/gas exposure both in terms of volume and duration.12-14 Additionally, irrigation with saline solution for a brief period has been proposed as a strategy to facilitate passive diffusion and remove excess of calcium ions. Furthermore, researchers are also developing IOL tests that can help identify a material’s susceptibility to calcification in the eye.
In the case of posterior capsular opacification (PCO) – the most common of late postoperative cataract surgery complications – LaHood says it is accepted these rates are higher in hydrophilic IOL cases.11 In his own clinic, YAG capsulotomies for PCO are performed on 5% of his hydrophilic patients, and 2% of his hydrophobic cases.

However, it should be noted that material alone is not the sole influencing factor when it comes to preventing PCO development, and
that not all hydrophobic acrylic lenses are automatically superior in this regard. In fact, there is significant overlap, and certain hydrophilic IOLs with specially designed and optimised anti-PCO features can outperform certain hydrophobic lenses.15

Given the frequency and low risk of capsulotomies, LaHood doesn’t believe the differences in PCO rates should be a major factor when selecting IOL materials. For some surgeons implanting advanced trifocal IOLs, this procedure is a routine step in the months following surgery anyway.
A CASE STUDY
One of the newest hydrophilic IOLs to join LaHood’s armamentarium is the RayOne EMV.
Manufacturer Rayner says the platform offers up to 1.5 D increased range of focus (emmetropic targeting)16-18 , monofocal levels of contrast sensitivity 17 and dysphotopsia.19,20 The company recently released a toric variant, developed with renowned Australian ophthalmologist Professor Graham Barrett.
RayOne EMV IOLs are made from Rayacryl (Rayner’s own hydrophilic acrylic material), with the company reporting zero primary opacifications in more than 10 million implantations.
To ensure its stability, a 360° square edge design helps reduce epithelial cell migration, including at the haptic-optic junction. 21 According to the company, this has resulted in extremely low YAG capsulotomy rates, comparable with hydrophobic acrylic lenses with square-edge optics. 21 LaHood breaks his IOL options into three main groups: a solid monofocal he’s familiar with, a trusted trifocal, plus an extended range of vision/monofocal-plus IOL. RayOne EMV fits within the latter category.
The first patients he trialled the lens in were young adult patients with traumatic cataracts. He chose the RayOne IOL for its ability to provide a natural range of vision, without compromising distance visual acuity, a problem in some EDOF designs.

“It will go through a small incision, looks beautifully clear within the eye and seems to have good rotational stability so far. It does have large and unusual haptics, which is a requirement of hydrophilic IOLs to maintain the stability in the capsular bag, so there has been a learning curve when it comes to injecting it into the eye and ensuring consistent orientation,” he says.
“Interestingly, none of my RayOne EMV patients have required a capsulotomy – and many of these people are at high risk of PCO. This is very important and something we want to avoid because we know one of the risk factors for retinal detachment in young people is disrupting the posterior capsule. I chose this lens for the optical outcome it provides, but this has been a nice side-effect.”
NOTE: References will appear in the online version of this article, and are available upon request.
INSIGHT July 2023 45
“THIS GREATER FLEXIBILITY IN THE MATERIAL MEANS WE CAN INSERT HYDROPHILIC IOLS THROUGH SMALLER INCISIONS. THE IOL THEN UNFOLDS WITHIN THE EYE EFFORTLESSLY TO ASSUME ITS FINAL POSITION QUICKLY.”
DR BEN LAHOOD OPHTHALMOLOGIST
An implanted hydrophilic acrylic IOL.
THE LATEST AND GREATEST FROM
ASCRS 2023
Each year Sydney cataract and refractive surgeon DR PETER SUMICH blocks out his calendar to attend the American Society of Cataract and Refractive Surgery’s annual conference. He provides an update on the latest innovations in global ophthalmology and their relevance to Australia.

ASCRS 2023 saw the world’s leading cataract and refractive surgeons descend on the vibrant melting pot of San Diego, California. Several concurrences contributed to a festival city atmosphere, with 5th Street closed to traffic and outdoor diners lining the streets. The Padres baseball team were playing the Dodgers at Petco Stadium; the streets were closed for Cinco de Mayo (5 May, to celebrate the Mexican victory in battle against the US) and the ASCRS circus was in town.
I have been going to the American Society of Cataract and Refractive Surgery’s annual conference for 25 years and something felt oddly different this year. It wasn’t just that corporate sponsorship and promotional excess had lessened. I realised that the wrinkle in time caused by three years of COVID has seen a changing of the guard at ASCRS and some cultural changes.
There were far more female representatives on senior panels than in previous years. They were impressive, eloquent and advanced. There were younger main speakers, formerly the sidekicks of the headliners; young presenters who had served their time in the minor sessions. The former headliners seemed to have receded into roles as father-figure convenors, rather than unabashed industry spruikers and opinion makers. What hasn’t changed is the excellent standard of presentations and the performative nature of the speakers. Nobody does a conference like the Americans.
IOL UPDATE AND AI
A key theme was the trend away from multifocal IOLs and the increasing adoption of EDOF lenses. These lenses provide a reasonable degree of spectacle independence without the well documented downsides of diffractive multifocal optics. Multifocal IOLs are exquisitely sensitive to any residual refractive error and tear film imperfections.
Dr Warren Hill noted that the wavefront displacement of an EDOF creates an altered path length without spherical aberration and excessive loss of contrast.
He noted that whilst the most demanding of presbyopes will continue to want full multifocal IOL spectacle freedom, the safety margins of EDOF technology can be pushed to a point where most would be satisfied.

Occasionally it needs to be emphasised that the most crucial refractive interface remains a stable tear film. Around 50% of the population are affected by dry eye. Many new devices were demonstrated in Trades Hall which heat, massage, squeeze or otherwise modify meibomian gland disease. Special guest comedian Ken Jeong, famous for his role in The Hangover movies, humorously presented his personal story of dry eye and how it affected his life. A massive immediate unmet need for dry eye management exists. An obvious commercial opportunity awaits optometrists to provide dry eye clinical services outside of Medicare.
Artificial intelligence (AI) was trending. In biometry it has become a genuine option. Several large, big data groups are beginning the collection of post-surgical refractive data to derive new biometry relationships beyond
46 INSIGHT July 2023
CATARACT
Many new devices were on display that heat, massage, squeeze or otherwise modify meibomian gland disease, a key factor when optimising cataract outcomes.
ASCRS 2023 was hosted in San Diego.
gender in 97% of people by looking at a retina. It can see a relationship which is beyond the unassisted human mind to correlate. Disturbingly, we cannot interrogate the AI to ask how it knows because it has not been programmed to explain it to us.
Those things being said, we are near the biologic floor of biometry prediction now. The cornea, zonules, IOL tilt and capsule are the largest unknowns in any given patient. Interestingly, the post operative refraction, which can vary in a patient from day-to-day and between refractionists, is a significant error source in refractive results analysis.
What biometry fails, post operative manipulations can refine. The LAL, or light adjustable lens, had another outing at ASCRS this year. The lens is a photopolymer which can shape change upon UV exposure. It is a rather clumsy procedure in which a patient with post cataract refractive error is given a treating dose of UV which photopolymerises the IOL and creates a shape change. Then the patient must wear sunglasses for a few months to avoid any environmental UV exposure and then requires a fixing dose of UV to ‘lock in’ the changes.
The LAL is unlikely to be widely adopted in Australia. Here we can make post operative refinements with sulcus based piggyback lenses (US does not have them) and excimer corneal laser enhancements (PRK or LASIK). Enhancements are not easily available in the US under managed care, because it constitutes extra billing which is disallowed under most contracts. Therefore, to assure a refractive outcome a patient must self-insure, receive a premium lens or pathway, and lose insurance coverage. Yet again we are witnessing the perverse incentives that US managed care creates.
ASCRS wouldn’t be complete without the latest iteration of an accommodating lens implant.


The Jellisee accommodating IOL was presented and looks as good as any of the accommodating lens technologies to date. It is modelled on a fluid filled paediatric crystalline lens which has a stronger elastic anterior capsule, such that it is permanently accommodated. Dis-accommodation is necessary for distance viewing and is achieved by residual ciliary muscle activity. The curvature changes take place on the anterior capsule, thus making the posterior capsule irrelevant. Early human implants have demonstrated some success in pilot stages with accommodation up to 7D.
Sometimes everyday items can be reimagined. A new phaco handpiece was demonstrated by Dr Elizabeth Yeu. The ZEISS Micor 700 contains all the flow pumps in a small handpiece with no phaco machine needed. It requires only irrigating fluid plugged into the handpiece and takes a fraction of the time to set up. It is not traditional phacoemulsification. It seems to rely on mechanical energy with no ultrasound. Whether it is applicable to cataracts of all densities was uncertain to me.
THE LATEST IN GLAUCOMA
The Innovators session is always stimulating. A new femtosecond laser procedure forming a trabeculotomy was demonstrated. Using a patient interface which includes a gonioscope, the laser is aimed at the trabecular meshwork creating a slit trabeculotomy which was patent up to several months. With the current Glaukos iStent, the trabecular Glaukos iDose slow-release implant and then this new femto laser, we may see glaucoma evolve into a purely surgical disease. It might be time to consider selling your shares in topical glaucoma medication companies!
It is truly remarkable to see the continued innovations that are occurring in ophthalmology. Most originate with small companies and enthusiastic researchers based on a clever clinical idea, a cross fertilisation with science industry, and commercialisation by a major player. So, if you have an innovative idea, it might be worth making a start on it today.
THE WELLNESS SESSION
What is happiness? During the wellness session, Dr Daniel Lerner excerpted parts of his book Goodness, Greatness and Grit. The brief takeaway is that happiness is not just raw success or money. Positive emotions in life can be self-reinforcing. Keep a gratitude journal about the things you are grateful for. Take a three-minute breathing break from work twice a day to sit, breathe quietly and relax. Engage with others using your character strengths at work
and enjoy what they have to offer to you. Keep your key home relationships healthy by reaching out to your loved ones every day, ask for help when you need it and offer help when it’s requested. Find activities that give you true meaning to your life by helping other people or making the world a better place.
AUSSIES MATCHING IT ON WORLD STAGE
When I attend conferences, I am looking to learn new ideas but also to self-check that I am thinking in the right ways. I think we all do this. What is profoundly obvious is that Australian ophthalmology is at or above the standards overseas. This is due to our mostly reasonable regulatory system allowing devices to be used here, our clinical independence from insurers and our excellent AUSCRS conference which parses and debates new technology and techniques.
Professor Graham Barrett deserves great credit for setting up AUSCRS and has created the local milieu for cataract and refractive surgeons to adopt early and develop expertise rapidly. AUSCRS will be held in Port Douglas on 26-29 July and the new co-presidents Professor Gerard Sutton and Dr Jacqui Beltz will no doubt continue the tradition of academic debate, lighthearted repartee and social generosity. If you missed ASCRS, then get to Port Douglas in July.
INSIGHT July 2023 47
Special guest comedian Ken Jeong presented his personal story of dry eye.
An ASCRS Australian contingent visiting Yosemite post-conference. From left: Dr Andrew Atkins, Dr Shish Lal, Dr Gagan Khannah and Dr Peter Sumich.
The first age-related myopia management solution from ZEISS.
Full UV Protection
ZEISS MyoCare lenses with two designs for specific age groups

• C.A.R.E® Technology creating alternating defocus and correction zones in a ring-like pattern.
• ClearFocus design ensuring clarity of vision in all directions of gaze whilst effectively managing myopia progression.
• Available in a wide range of materials and indices.
zeiss.com.au/vision
Scan to watch

At the completion of this article, the reader should be able to improve their co-management of cataract patients.
Including:
• Understand the rationale for pre-operative patient education, and review an example
• Review the benefits and limitation of the different types of intraocular lenses
• Develop conditions for improved pre- and post-operative care of cataract patients
PRACTICAL CATARACT CO-MANAGEMENT
As demand for cataract surgery increases, optometrists are playing a greater role in the patient journey. In this collaborative article, optometrist KRISTIE BUTLER and ophthalmologist Dr LEWIS LEVITZ explain the definition of ‘skillful co-management’ and why it’s never been more important for optometrists to remain abreast of the newest cataract technologies, procedures and protocols.
PRACTICAL CATARACT CO-MANAGEMENT
When it comes to cataract surgery and intraocular lens (IOL) selection, optometrists are in the privileged position of not just assessing eye health, but also of knowing their patients’ personalities, likes and dislikes as optometrists have often known them, and sometimes their families, for some time.



While most patients have heard the term ‘cataract’ and know someone who has had surgery, many are unaware of what is involved. Optometrists are tasked with the important job of patient education. That is: explaining what a cataract actually is, outlining the surgery and helping them understand the differences between the available IOLs. This is all done prior to referral for potential surgery.
Lifestyle, hobbies and profession as well as any unique visual requirements and personality traits must be acknowledged when selecting an IOL. This is in addition to ocular health, general health, previous ocular surgery and refractive error considerations. An increased significance is now placed on the visual outcomes of cataract surgery. Some patients, for example, will be hoping to achieve spectacle independence following cataract surgery. Getting a feel for your patient’s expectations is crucial for achieving successful results.
This case report describes how we explored a typical cataract patient’s option and came to a tentative decision regarding IOLs before referring her to the ophthalmologist.
CASE REPORT
At the optometry practice with Kristie Butler: Mrs X, a 67-year-old female attended the practice with complaints of deteriorating vision. Her prescription, unchanged from her previous test over 12 months ago, was R +1.50 VA 6/7.5-2, L +1.75/-0.50x10 VA 6/9-2, Add +2.25. Her acuities had dropped a line in both eyes since her last test.

Slit lamp exam revealed anterior cortical and nuclear sclerotic cataracts and a healthy ocular surface (Figure 1). Fundus exam and OCT showed healthy optic nerves and maculae and her intraocular pressures were normal. It was
evident her cataracts were the cause of her symptoms and acuity reduction. As she was unhappy with her current vision, we began the discussion about cataracts and their treatment.
I explained how her cataract would be replaced with an IOL. New technology means that there would be a variety of IOLs that could be offered depending on her particular needs.
Monofocal IOLs
Monofocal IOLs would be her first option, providing good vision at one distance only. Taking into account her prior refractive history of emmetropia until her late 40s, monofocal IOLs would be set for distance and she would require reading glasses for all of her close tasks, such as reading, using a tablet and her crosswords, all of which she enjoys.
Monovision IOLs
We then discussed monovision, having her non-dominant eye set for near, thus decreasing spectacle dependence. She was very interested in having some near vision without having to wear glasses but felt she would have trouble tolerating the distance blur in one eye.
This is a better option for myopes, especially those used to monovision in contact lenses.
Multifocal IOLs
Her interest in potentially not having to wear reading glasses led us to talk about multifocal/ trifocal IOLs and the extended depth of focus (EDOF) IOL. I explained how multifocal IOLs will give her good distance and near vision, however she may see haloes around lights at night. Even though she seems fairly easy going, does not have precise visual requirements and has no other pathology, this did not appeal to her as she often has to drive at night.
Extended
depth of focus (EDOF) IOLs
EDOF IOLs are the latest innovation in addressing presbyopia at the time of cataract surgery. They give a good functional range of vision, with good distance and intermediate vision and reasonable near vision, with less side effects than the multifocal IOL. This will enable her to accomplish most daily tasks, such as driving, cooking, cleaning etc. without glasses, although she may have to wear reading glasses for books or fine print. These days there are a variety of lenses which can offer a patient an extended depth of focus but which are not truly ‘multifocal’. These use different qualities of light to offer a range of vision while trying to decrease the unwanted visual phenomena which can accompany a
INSIGHT July 2023 49
CLINICAL CPD HOURS This activity meets the OBA registration standards for CPD
CPD
LEARNING OBJECTIVES:
Kristie Butler BOptom, GCOT
Dr Lewis Levitz MBBCh MMed, FCS(SA)Ophth, FRCSEd, FRANZCO Vision Eye Institute
“GETTING A FEEL FOR YOUR PATIENT’S EXPECTATIONS IS CRUCIAL FOR ACHIEVING SUCCESSFUL RESULTS.”
FIGURE 1. Cortical and nuclear sclerotic cataract
diffractive multifocal lens. 2 These include, among others, the Vivity (Alcon), Eyhance and Symfony (Johnson & Johnson), Lentis (Teleon Surgical), RayOne EMV (Raynere), IC8 (AcuFocus), and the At Lara (Carl Zeis Meditec).
The type of implant is less important that the communication between the optometrist and the ophthalmologist so that the optometrist is aware which type of lens was used.
We both believed the EDOF IOL would be a good fit for her lifestyle, so this was noted in my referral to the ophthalmologist. I explained that the ophthalmologist would take different measurements and assess her eyes further before helping her come to a final decision.
With the ophthalmologist, Dr Lewis Levtiz: Ophthalmology today is as much about managing expectations as it is about providing eyecare.
When a patient is referred for a cataract assessment, they know that they will probably be offered an operation. They have certain questions on their mind: ‘Do I really have a cataract?’, ‘Do I trust the doctor?’, ‘How long will I be away from work, golf, swimming, driving?’, ‘Where will it be done?’ ‘How long will the recovery take?’. I assume that each patient has all of these questions when they walk in the door. The answers that the attending ophthalmologist gives must take into account the patient’s pathology, comorbidity, expectations, personality and possible changing visual needs.

The ‘discussion’ vs the ‘excuse’
The more time spent discussing the various options and the compromises inherent in each, the better it is for all. The patient regards an educational talk held before an operation

as a ‘discussion’, while the same talk held afterwards is regarded as an ‘excuse’.
Once the diagnosis of cataract as the cause of the patient’s visual loss is confirmed, it’s vital to discuss the condition of the patient’s macular and cornea. If the patient has macular disease, then now is the time to mention it. If the cornea is dry or has irregular astigmatism, then mentioning it before discussing lens options enables the ophthalmologist to guide the patient away from choices they might want to
make, but may not be in their interests.
As part of my standard approach, after these vital topics have been communicated, I then give a few minutes over to discussing options, briefly stating what the benefit of each lens may be for that particular patient. Because I know that the referring optometrist has already mentioned these concepts, and the person may have had time to mull them over, the discussion on options is made much easier.
Monofocal intraocular lenses
Monofocal lenses placed in both eyes with a similar refractive target is still a good choice for many. I explained to Mrs X that monovision probably will give the best and sharpest single image. She will still maintain good binocular vision. It is a good option for anyone happy to continue using their reading or multifocal glasses.
The downside is that if she chooses this option is that she may still need to wear glasses for reading. In order for her not to regard the cataract operation as a ‘failure,’ it’s important to clearly explain this possibility beforehand.
Monovision
Giving Mrs X the tried and tested option of correcting her dominant eye for plano and then leaving her non-dominant eye slightly myopic is also a choice. True monovision would mean she was left with a script of -1.00 whereas mini monovision is when the non-dominant eye is left with a script of between -0.5 to-0.75. This is both achievable and yet also not always achievable. There are so many individual
50 INSIGHT July 2023
“THE TYPE OF IMPLANT IS LESS IMPORTANT THAT THE COMMUNICATION BETWEEN THE OPTOMETRIST AND THE OPHTHALMOLOGIST SO THAT THE OPTOMETRIST IS AWARE WHICH TYPE OF LENS WAS USED.”
CPD
Ophthalmology can be as much about managing expectations as it is about providing eyecare.
Cataracts are the most common elective surgery diagnosis in Australia. More than 250,000 people undergo the procedure each year.
variables, notwithstanding the fact that most lenses only come in 0.5 increments, that this option cannot be guaranteed.
The monovision lens option is great for people who have used contact lenses and are used to monovision. 3 Mrs X has not used contact lenses previously. (Mrs X also has cataracts so a contact lens trial would not be a true reflection of what her outcome would be). The best thing about offering her monovision is that if she is unhappy, she can be referred for corneal refractive surgery after three months and be left emmetropic again. Mrs X turned down this offer.
Multifocal lenses
Mrs X was then offered multifocal lenses as she expressed a wish to be independent of glasses. As she was hyperopic before, I had no hesitation in offering her multifocal lenses. 4,5,6,7 I explained that she will still need glasses for near work in poor light.
Mrs X was told that she will have halos around light at night and that it may take time to adjust to this ‘new way of seeing’. 8 Pupil size, although important with the older diffractive multifocal lenses, is not as much of a contra-indication with the newer diffractive lenses. 9 It is important to stress that corneal pathology or macular pathology will degrade the vision. The OCT scan which accompanied her from her optometrist visit gave me reassurance that she would do well. However, Mrs X was not keen on the idea of night time halos.
Extended depth of focus (EDOF) lenses
I explained to Mrs X that EDOF lenses are a compromise between monofocal lenses and multifocal lenses.10 There are various types on the market, which may give vision equal to that of a monofocal lens with the advantage of reading at arm’s length.11 There are also much fewer nocturnal dysphotopsia than with multifocal lenses.
A very recent study showed that an EDOF lens gave comparable distance vision as a monofocal lens but with the advantage of being able to read two extra lines at intermediate distance. There was no statistical difference in the patients reporting unwanted visual phenomenon, however these were reported less frequently in the monofocal group.12
I p romised that I would let the referring optometrist know exactly what lens was used, as performing a post-operative refraction on someone with an EDOF lens is different to that performed with a monofocal lens. The patient with the EDOF lens should be left ‘more plus’ than with a monofocal lens.
As Mrs X had realistic expectations, and was willing to accept that she will still need to use reading glasses, I offered her an EDOF lens. She had uncomplicated surgery on each eye two weeks apart. She was given a combination of antibiotic drops for 10 days and steroid drops
for one month. She was then referred back to her referring optometrist for review.
First post-operative visit
Mrs X could be seen either by her optometrist of her ophthalmologist for a day one post-operative visit.
Her vison would be assessed, but this is often variable and will depend on the amount of ultrasound power needed to remove the cataract and the health of the endothelium. Although the post-operative vision is usually much better than the pre-operative vision, a pinhole vision may need to be used in the occasional case.
The cornea would be assessed next. There may be a small collection of viscoelastic on the endothelium. This usually disappears in a day. The site of the corneal incision is checked to see that there is no iris prolapse.
The pupil may be normal or still slightly dilated on day one. Sometimes, the pupil looks irregular from the dilation. This should not be confused with a peaked pupil due to vitreous in the anterior chamber which can be more serious.
The lens should be seen sitting behind the anterior capsule in uncomplicated cases. Certain surgeons prefer that intraocular pressure not be taken on day one to avoid pressure on the wound, but an I-Care tonometry reading is reasonable. A slightly elevated pressure need not be treated as it may be due to retained viscoelastic.
Return visit at the optometrist’s rooms
Our patient attended my optometric practice for her final check a week after her four-week post-op visit. I was aware she had received the EDOF IOL and knew what to expect at the follow-up as I had received several correspondence letters from the ophthalmologist.
Her unaided acuities were R 6/6, L 6/6-2, near N6 at 40 cm. She was very happy with her vision. She could use her phone and tablet unaided and felt she only needed reading glasses for her crosswords and books. Final refraction was R plano VA 6/6, L -0.25/-0.25x180 VA 6/6, Add +2.25.
CONCLUSION
A thorough eye test and informed discussion regarding choice of IOL with an optometrist made our patient’s experience with the ophthalmologist and subsequent cataract surgery that much smoother.
Patient confidence in their IOL selection grows when they have consulted with two separate eye professionals prior to surgery. Ultimately, this leads to better visual outcomes and greater patient satisfaction.
REFERENCES:
1. A ustralian Institute of Health and Welfare. Admitted patient care 2016–17: Australian hospital statistics. Health services series no. 84. Cat. no. HSE 201. Canberra: AIHW; 2018.
2. K anclerz P, Toto F, Grzybowski A, Alio JL. Extended Depth-of-Field Intraocular Lenses: An Update. Asia Pac J Ophthalmol (Phila). 2020; 9 (3): 194-202.
3. L abiris G, Giarmoukakis A, Patsiamanidi M, Papadopoulos Z, Kozobolis VP. Mini-monovision versus multifocal intraocular lens implantation. J Cataract Refract Surg. 2015;
4. R uiz-Mesa R, Abengózar-Vela A, Ruiz-Santos M. A comparative study of the visual outcomes between a new trifocal and an extended depth of focus intraocular lens. Eur J Ophthalmol. 2018;
5. D e Vries NE, Nuijts RMMA. Multifocal intraocular lenses in cataract surgery: Literature review of benefits and side effects. Vol. 39, Journal of Cataract and Refractive Surgery. 2013. p. 268–78.
6. Kohnen T, Herzog M, Hemkeppler E, Schönbrunn S, De Lorenzo N, Petermann K, et al. Visual Performance of a Quadrifocal (Trifocal) Intraocular Lens Following Removal of the Crystalline Lens. Am J Ophthalmol. 2017;
7. S udhir RR, Dey A, Bhattacharrya S, Bahulayan A. Acrysof IQ panoptix intraocular lens versus extended depth of focus intraocular lens and trifocal intraocular lens: A clinical overview. Asia-Pacific Journal of Ophthalmology. 2019.
8. L awless M, Hodge C, Reich J, Levitz L, Bhatt UK, McAlinden C, et al. Visual and refractive outcomes following implantation of a new trifocal intraocular lens. Eye Vis. 2017;
9. B raga-Mele R, Chang D, Dewey S, Foster G, Henderson BA, Hill W, et al. Multifocal intraocular lenses: Relative indications and contraindications for implantation. Vol. 40, Journal of Cataract and Refractive Surgery. 2014. p. 313–22.

10. P alomino-Bautista C, Sánchez-Jean R, Carmona-Gonzalez D, Piñero DP, Molina-Martín A. Depth of field measures in pseudophakic eyes implanted with different type of presbyopia-correcting IOLS. Sci Rep. 2021;
11 K anclerz P, Toto F, Grzybowski A, Alio JL. Extended depth-of-field intraocular lenses: An update. Asia-Pacific Journal of Ophthalmology. 2020.
12. P antanelli SM, O'Rourke T, Bolognia O, Scruggs K, Longenecker A, Lehman E. Vision and patient-reported outcomes with nondiffractive EDOF or neutral aspheric monofocal intraocular lenses. J Cataract Refract Surg. 2023; 49 (4): 360-366.
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
INSIGHT July 2023 51
A multifocal IOL was discussed with the patient, but she chose to avoid this option due to a requirement for night time driving without visual disturbances, such as haloes.
If, like Chanuka, you love the idea of a fulfilling career in optometry with lots of opportunities to progress, you’ll shine at Specsavers. join.specsavers.com/au/find-a-job


an ambitious
look good in Specsavers
Chanuka Optometrist Are you
person? You’d
At the completion of this article, the reader should be able to improve their understanding of ocular associations in pregnancy.
Including:
• Recognise pregnancy-related physiological ocular changes.
• U nd erstand the rationale for revising standard clinical protocols when treating a pregnant patient.
• U nderstand how pregnancy can modify pre-existing ocular pathologies
• Id entify ophthalmic conditions due to pregnancy complications which necessitate referral
OCULAR ASSOCIATIONS IN PREGNANCY
Profound systemic and ocular changes can take place during pregnancy, making it vital for clinicians to understand how these changes can affect the health and vision of expectant patients. As Associate Professor SUDHA CUGATI and Professor CELIA CHEN point out, the practitioner’s duty is heightened because they have two patients to think of.
The eyes can undergo physiological and pathological changes in pregnancy. Some changes exacerbate pre-existing eye conditions while other conditions manifest for the first time during pregnancy. Early recognition and management are essential to prevent sight-threatening complications.
While treating a pregnant patient, it’s essential to remember that you are dealing with two people – the pregnant woman and the foetus. In addition, some obstetric complications can be associated with ophthalmic signs, so prompt recognition of these eye findings may be lifesaving for both the mother and the foetus.
The aim of this article is to improve awareness of the potential ocular complications in pregnancy, to help recognise the indications for prompt referral to a specialist to preserve sight, and maintain maternal and foetal safety. The safety of the use of common ophthalmological medications will also be discussed.
PHYSIOLOGICAL OCULAR CHANGES IN PREGNANCY
• Eyelids
Hormonal changes in pregnancy can result in melasma, an increased pigmentation around the eyes and cheeks. It normally does not require any active intervention and tends to fade slowly after pregnancy.
• Co rnea
During the second and third trimesters of pregnancy, corneal thickness can increase up to 16 microns and curvature can increase by an average of 1 diopter sphere resulting in refractive changes which returns to normal soon after delivery.
Corneal sensitivity can also decrease during pregnancy and can return to normal by two months postpartum. Reduction in corneal sensitivity can increase the risk of infections. There is also an increased prevalence of dry eyes in pregnancy which increases with gestational age. 2
REFRACTIVE CHANGES AND ISSUES DURING PREGNANCY3
• M yopia in Pregnancy
Myopic shift in the lens results from increased
lens curvature in pregnancy, resulting in a change in refraction. In addition, a temporary loss of accommodation can be seen in the immediate post-partum period. These lenticular changes also indicate that new glasses or refractive surgeries should be withheld during pregnancy. Patients who are high myopes are not at an increased risk of retinal detachment during delivery and spontaneous vaginal delivery is not contraindicated in these patients.
• C ontact lens intolerance
Many pregnant women develop contact lens intolerance which could be explained to be due to the changes in corneal curvature and thickness, as well as dry eyes. It is advisable not to prescribe new contact lenses during pregnancy.
• R efractive eye surgery and pregnancy
Due to the changes in the corneal curvature and myopic shift, it is recommended that refractive surgery be avoided during pregnancy and until after the refraction is stable postpartum.
A. PRE-EXISTING EYE CONDITION MODIFIED DURING PREGNANCY
• D iabetic Retinopathy (DR)
Progression of DR can be seen in the second and third trimester of pregnancy in patients with
A/Prof Sudha Cugati

MBBS, MS, PhD, FRANZCO
Consultant Ophthalmologist, Modbury Hospital, South Australia

Prof Celia Chen

MBBS, MPH, PhD, FRANZCO
Academic Professor, Flinders University
Clinical Professor, University of South Australia
Type 1 and Type 2 Diabetes (Figure 1 A and 1 B).
The degree of DR at the start of pregnancy, glycosylated haemoglobin (HbA1C) control, duration of diabetes and presence of hypertension are known risk factors for worsening of DR in pregnancy.
Diabetic macular oedema (DME), resulting in severe vision loss, may develop during pregnancy. Improvement and regression of DR tend to occur postpartum.
Physiological ocular changes in pregnancy
Pathological pre-existing eye condition worsening during pregnancy
Pathological eye condition that occurs for the first-time in pregnancy
Pathological systemic pregnancy complications leading to eye conditions Melasma
• HELLP s yndrome
• Pituitary adenoma
• Thrombocytopenic Purpura
• Grave’s disease
INSIGHT July 2023 53
CLINICAL CPD HOURS This activity meets the OBA registration standards for CPD
CPD
LEARNING OBJECTIVES:
Diabe tic Retinopathy
Cen tral serous chorioretinopathy
Preeclampsia and Eclampsia
thickness and curvature • Glaucoma* • Uv eal Melanoma• Diss eminated intravascular coagulopathy
changes • Idiopathic intracranial hypertension
Meningiomas
•
•
•
Cornea
Refractive
•
• An tiphospholipid antibody syndrome
* Pregnancy-related physiological changes may be protective against glaucoma with reduced intraocular pressure during pregnancy.
TABLE 1. TABLE SHOWING THE OPHTHALMIC ASSOCIATIONS IN PREGNANCY
Ocular examination is recommended before conception and during the first trimester of pregnancy. 4
Appropriate and prompt referral should be made to an ophthalmologist if there is a progression of DR or if severe DR is noted at the onset. Laser photocoagulation is recommended prior to pregnancy in patients with severe non proliferative diabetic retinopathy. 5

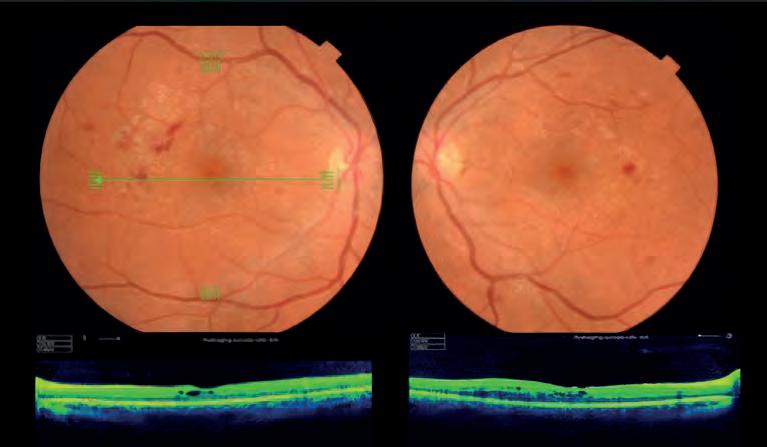
In patients with DME, intravitreal steroids may be a safer alternative to intravitreal anti-vascular endothelial growth factor (VEGF), the safety of these agents is not established in pregnancy.
Patients with gestational diabetes are usually checked at 28 weeks of gestation. The risk of developing DR in patients with gestational diabetes is less than 1%. Ophthalmological assessment is usually not essential in these patients.
• G laucoma
Pregnancy is protective against glaucoma. Increased progesterone level during pregnancy
causes increased the uveoscleral outflow, thus reducing the intraocular pressure (IOP). The level of female sex hormones during pregnancy are also neuroprotective to the optic nerve. These physiological effects and IOP return to baseline three months postpartum. In pregnant patients with glaucoma, the IOP may decrease, thus requiring fewer glaucoma drops. 6 Certain IOP-lowering medications are contraindicated in pregnancy which will be discussed later in the article.
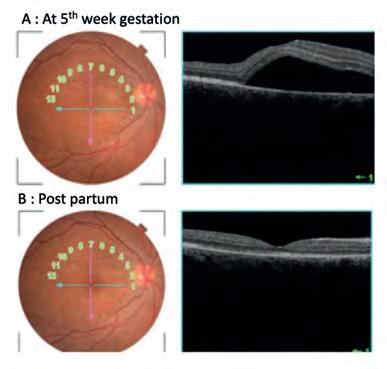
• I diopathic Intracranial hypertension (IIH)
In a patient with pre-existing IIH, weight gain during pregnancy may worsen the intracranial hypertension. Therefore, regular monitoring, usually at the first trimester, at the end of the second trimester and the six weeks postpartum is recommended. If a significant increase in optic nerve swelling is noted with increase in OCT retinal nerve fiber layer thickness, then there are measures that may help to temporise and lower
B:
the intracranial pressure with lumbar puncture or lumbar drain.
The presence of IIH is not a contraindication to normal delivery.
The usual medication used to treat IIH is acetazolamide, a carbonic anhydrase inhibitor. It is a class B2 medication – drugs which have been taken by only a limited number of pregnant women. There are reports of teratogenic effect with midline cleft syndrome in animal models but not human. In general, most patients prefer to be off the medication when trying to conceive. However, if required, acetazolamide has been demonstrated to be relatively safe in pregnancy and can be used in patients with IIH. These should be in consultation with the treating neuro-ophthalmologist and obstetrician.
• M eningiomas
Meningiomas, a typically slow growing tumor, can have an accelerated growth in pregnancy due to increasing estrogen and progesterone levels and vascular endothelial growth factors. Pregnant patients with known meningioma in the sellar and suprasellar region that may result in compressive optic neuropathy, should therefore be referred and monitored to a neuro-ophthalmologists with ongoing follow-up.
B. PATHOLOGICAL CONDITIONS OCCURRING FOR THE FIRST TIME IN PREGNANCY
• C entral serous chorioretinopathy (CSCR) Pregnancy increases the risk of CSCR due to the increased cortisol levels and other hormonal changes. Patients often note mild vision blurring and colour changes. Examination usually shows a hyperopic shift due to elevation of the macula and OCT can confirm the CSCR changes (Figure 2). It can occur in all trimesters of pregnancy and can resolve spontaneously,
54 INSIGHT July 2023
FIGURE 1A. Fundus photographs (top panel) and OCT imaging (bottom panel) of a 22-year-old female at 15 weeks gestation with type II diabetes. (Visual acuity 6/18 OU. HbA1c: 7.5%)
CPD
FIGURE 1B. Fundus examination and OCT of the same patient at 20 weeks gestation review showing worsening of diabetic retinopathy and macular oedema in both eyes (Visual acuity 6/36 OU. HbA1c: 7.3%)
FIGURES 2A AND 2B.
A: Pregnant patient noted blurry vision in the right eye at five weeks gestation and examination showed 6/15 vision, that improved to 6/9 with +1.0 DS correction. OCT of the right eye (right panel) showed a CSCR.
The condition resolved spontaneously post-partum, but the patient had unaided vision of 6/7.5 with subjective metamorphopsia and colour vision changes.
usually over 6-8 weeks or by the time of postpartum.7 CSCR can recur in subsequent pregnancy. It is important to educate the patients about the natural course of the disease.
• U veal melanoma
Ocular melanoma is more prevalent and tends to progress rapidly in pregnant women compared with non-pregnant women. 8 The mechanism of tumour growth during pregnancy is unclear as hormonal correlation in pathophysiology of melanoma has not yet been established. Patients with known melanoma or newly detected uveal melanoma should prompt a referral to an ophthalmologist with interest and expertise in ocular oncology.
C. OPHTHALMIC ASSOCIATIONS DUE TO COMPLICATIONS IN PREGNANCY
The following conditions in pregnancy can be associated with visual symptoms. It is important to recognise these conditions and an appropriate referral should be made to the ophthalmologists.
• Preeclampsia and Eclampsia
Preeclampsia causes severe arteriolar spasm due to vasospasm and increased resistance to blood flow and generalised constriction of retinal arterioles. The visual system is affected in approximately 25% of patients with preeclampsia and 50% of patients with eclampsia. Patients can present with symptoms of blurred vision, visual field defects and diplopia. Fundus findings in preeclampsia may include retinal arteriole narrowing, tortuosity, retinal haemorrhage, and optic nerve swelling (Figure 3). Occasionally patients can present
with acute vision loss due to serous retinal detachment (RD) or cortical blindness. Presence of these changes in pregnancy warrants urgent referral to her obstetrician for blood pressure monitoring and management.
• Disseminated intravascular coagulopathy (DIC) DIC, a major emergency in pregnancy, is caused by the disruption of coagulation pathways (intrinsic and extrinsic), resulting in formation of small thrombi in small vessels generalised or localised in the body.
RED FLAG SYMPTOMS ASSOCIATED EYE CONDITION
Transient vision loss (Vision returns to normal <24hrs)
Sudden painless vision loss (>24hrs)
Sudden painful vision loss
Papilledema, amarosis fugax
Retinal artery or vein occlusion, serous retinal detachment, vitreous hemorrhage, and optic disc ischemia

Glaucoma, acute angle closure glaucoma, optic disc neuritis (pain with eye movement >50% of cases), intraocular infection
Patients with DIC can present with complaints of blurred vision, visual field defects or metamorphopsia, either due to central choroidopathy or serous RD. A characteristic of these presentations is a bilateral involvement. These women require prompt management by the obstetrician to prevent systemic complications.
• Haemolysis, elevated liver enzymes, low platelets (HELLP syndrome)
HELLP syndrome is a severe variant to pre-eclampsia and eclampsia. Patients can present with symptoms of acute vision loss. Fundoscopy may reveal retinal artery and vein occlusions, serous RDs (Figure 4) and Purtscher-like retinopathy with multiple white retinal patches and retinal haemorrhages.
Sudden loss of visual field
Optic neuritis, meningioma, branch retinal artery or vein occlusion, occipital lobe pathology, optic tract lesion, glaucoma, Diplopia Monocular (Symptom can be elicited from one eye only)
Diplopia Binocular (symptoms present when two eyes are open)
Refractive error, corneal disease, iris pathology
Cranial nerve palsies – 3rd/4th/5th/6th
SYMPTOMS OF INTERMEDIATE URGENCY
Gradual painless loss of vision (over months or years)
Refractive error, glaucoma, diabetic retinopathy or associated DME, OTHER NON-URGENT SYMPTOMS
Burning/itching/tearing without pain
Blepharitis, dry-eye syndrome, conjunctivitis, contact lens related problems,
vision or visual field change should always be discussed with an ophthalmologist.
• A ntiphospholipid Antibody Syndrome (APS) APS is an autoimmune condition and 14-18% of patients present with ocular symptoms. Clinical signs include conjunctival microaneurysms or telangiectasia, episcleritis, keratitis and iritis. Posterior segment manifestations include RD, posterior scleritis, vitritis, retinal arterial and vein thrombosis. Patients are treated with long-term anticoagulants and visual prognosis is good. Patients should be promptly referred to their physician and ophthalmologist for further management.
• Thrombocytopenic Purpura (TTP) TTP, a haematological disorder, is characterised by microangiopathic haemolytic anaemia and thrombocytopenia, renal failure and neurological disturbances which can occur during pregnancy.
About 10% of patients with TTP can develop ocular complications; these can include retinal findings of arteriolar constriction, exudates, retinal haemorrhage and serous RD and optic atrophy. Visual field test may
INSIGHT July 2023 55
* This table is a guide only. Each patient with acute
TABLE 2. * VISION CHANGE IN PREGNANT FEMALE, A GUIDE FOR PATIENT SYMPTOMATOLOGY
FIGURE 3. A 34-week pregnant patient with no previous medical history presented with bilateral blurry vision. A: Fundoscopy at the time revealed bilateral disc oedema (D) with peripapillary haemorrhage (H), hard exudate (E) and cotton wool spots (C). Blood pressure was 220/160 suggesting pre-eclampsia. The woman had induced labour. At four weeks postpartum (B), the retinal findings improved, especially the bilateral disc oedema. There are residual lipid exudates in circinate pattern (arrow).
show a homonymous hemianopia if there are cerebrovascular accidents affecting the retrochiasmal pathway.
• G rave’s disease
In a pregnant patient with pre-existing Grave’s disease, thyroid eye disease may have an accelerated progression in 1-2 % of these women, especially in the first trimester and postpartum. Ophthalmic examination includes orbitopathy includes proptosis, lid lag, periorbital edema extraocular muscle enlargement and fibrosis, optic neuropathy and dry eyes.

• Pituitary adenoma
A previously undetected pituitary adenoma may manifest itself during pregnancy because of the physiological pituitary gland enlargement during pregnancy.
If any pregnant patient presents with headache, decreased visual acuity and diplopia, visual field changes especially of bitemporal hemianopia, she should be referred to an ophthalmologist and/or general practitioner promptly so that appropriate investigations with neuroimaging are performed. 9
These patients will need a baseline ophthalmic evaluation including field evaluation and OCT retinal nerve fiber layer thickness and ganglion cell plot, that will help to guide the chronicity of any chiasmal compression. Most adenomas will regress following pregnancy leaving no vision compromise postpartum.
• O cclusive vascular disorders
Arterial occlusion in the form of central retinal artery occlusion (CRAO) and branch retinal artery occlusion (BRAO) can occur in pregnant patients with hypercoagulability state. Patients can present with sudden onset of painless vision loss or visual field disturbances.
OPHTHALMIC MEDICATIONS DURING PREGNANCY
Risk of ophthalmic drugs to the foetus needs to be considered while treating a pregnant mother. Any medication should be used in a pregnant woman only if the benefit to the mother outweighs risk to the foetus.
Systemic absorption of topical medications (more commonly with drops than ointment) can occur via the conjunctival vessels or the nasal mucosa. Systemic absorption can be reduced by nasolacrimal occlusion for a few minutes after instillation of drops.
In addition, drugs should be used at the minimal effective dose and for the minimal duration. If possible, they should be avoided in the first trimester.10,11
CONCLUSION
Physiological ophthalmic manifestations are common in pregnancy and may account for majority of patient’s symptoms. However, it is important to recognise pathological ocular diseases that can be encountered
TOPICAL MEDICATION
Lubricant eyedrops
CATEGORY A CATEGORY BCATEGORY C
• Hypromellose
• Carbomer
• Polyvinyl alcohol
• Carmellose
• Hy droxyethyl cellulose
Anti-allergic drops
Diagnostics
• Mas t cell stabilisers• An tihistamines
• Tropicamide (except multidose)
• Cy clopentolate (except multidose)
• Fluorescein
• Phen ylephrine
Glaucoma drops
• Alpha 2 adrenergics (safest & 1st choice)
• Prostaglandin Analogue
• Carbonic anh ydrase inhibitors
• Cholinergic
• B eta Blockers
Antibiotics & Antivirals
Miscellaneous

• Cephalosporin
• Aciclovir
• Lignoc aine
• Chloramphenicol
• Tetracaine
• Atropine/ Homatropine
CATEGORY A – Drugs taken by a large number of pregnant women with no proven evidence of harmful effect to foetus CATEGORY B – Drugs taken by limited number of pregnant women without harmful effect on foetus with or without supporting animal studies CATEGORY C – Drugs that have caused or suspected to have caused harmful effect to the foetus without causing malformations
REFERENCES:
1. Q in Q, Chen C, Cugati S. Ophthalmic associations in pregnancy. Australian journal of general practice. 2020; 49 (10): 673-80.
2. D uran M, Güngör İ. The effect of pregnancy on tear osmolarity. Contact lens & anterior eye. 2019; 42 (2): 196-9.
3. S harma S, Rekha W, Sharma T, Downey G. Refractive issues in pregnancy. Australian & New Zealand journal of obstetrics & gynaecology. 2006;46(3):186-8.
4. F laxel CJ, Adelman RA, Bailey ST, Fawzi A, Lim JI, Vemulakonda GA, et al. Diabetic Retinopathy Preferred Practice Pattern. Ophthalmology (Rochester, Minn). 2020; 127 (1): P66-P145.
5. E rrera M-HMD, Kohly RPMDP, da Cruz LMDP. Pregnancy-associated Retinal Diseases and Their Management. Survey of op hthalmology. 2013; 58 (2): 127-42.
6. R azeghinejad MRMD, Tania Tai TYMD, Fudemberg SJMD, Katz LJMD. Pregnancy and Glaucoma. Survey of ophthalmology. 2011; 56 (4):324-35.
7. D aruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N, et al. Central serous chorioretinopathy: Recent findings and new physiopathology hypothesis. Progress in retinal and eye research. 2015; 48: 82-118.
8. S eddon JM, MacLaughlin DT, Albert DM, Gragoudas ES, Ference M. Uveal melanomas presenting during pregnancy and the investigation of oestrogen receptors in melanomas. British journal of ophthalmology. 1982; 66 (11): 695-704.
9. B rewington TE, Clark CC, Amin N, Venable HP. The effect of pregnancy on the peripheral visual field. Journal of the National Medical Association. 1974; 66 (4): 330-1.
10. A ppendix 7 - Ophthalmic Drug Use in Pregnancy. In: Jackson TL, editor. Moorfields Manual of Ophthalmology: Mosby Ltd. p. 702-6.
in pregnancy either de novo or as a result of complications during pregnancy.
Patients presenting with red flag symptoms and signs should be referred to an ophthalmologist. In addition, pre-existing eye conditions need to be cautiously monitored during pregnancy to avoid blinding eye diseases. While systemic absorption of ophthalmic medications is small, medications should be avoided unless necessary during pregnancy to prevent foetal harm.
11. C hung CY, Kwok AKH, Chung KL. Use of ophthalmic medications during pregnancy. = Xianggang yi xue za zhi. 2004; 10 (3): 191.
scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
56 INSIGHT July 2023
Insight readers can
NOTE:
TABLE 3. LIST OF TOPICAL MEDICATIONS COMMONLY USED IN OPTOMETRY AND THEIR SAFETY DURING PREGNANCY
CPD
FIGURE 4. A 26-year-old patient at 30-week gestation had acute loss of vision in the left eye. Examination revealed a macular off inferior serous retinal detachment (white arrows) and retinal haemorrhage (H). Urgent obstetrics referral revealed elevated liver enzyme and low platelet count confirming HELLP syndrome.





An age-related
APPROACH TO MYOPIA CONTROL
ZEISS Vision Care has more than a decade of experience developing lenses to manage myopia. Now the company is bringing its latest innovation to Australia and New Zealand – an age-related solution comprising two lens design options.
One of the key challenges for manufacturers developing spectacles lenses for myopia management is finding the optimal compromise. It’s the sweet-spot, accounting for the interplay between a maximised treatment zone, together with a minimised central zone that provides clear vision, while ensuring the control effect is maintained at all gaze angles.
Once satisfied, these elements address a fourth factor: wear time – a major contributor for putting the brakes on myopia, with increasing efficacy for longer hours of daily wear.
Two new myopia spectacle lens designs from ZEISS Vison Care have been designed with these requirements in mind, seeing the company become the latest to bring a lens to market for progressing myopes in Australia and New Zealand.
The company’s ZEISS MyoCare lenses will be released to Australian and New Zealand optometry practices in July 2023. The company has developed a unique, patented design (which will be detailed later in this article), but of more interest to ophthalmic professionals is the way in which ZEISS is structuring the portfolio.
It’s taking a different approach by offering an “age-related myopia management lens solution”. This involves two distinct designs: one for children under the age of 10 (ZEISS MyoCare with a 7 mm diameter clear zone), and another for children 10 and older (ZEISS MyoCare S with a 9 mm diameter clear zone).
“These represent a softer and a harder version of the ZEISS MyoCare lens design, respectively,” Ms Elmarie Pretorius, professional services manager for ZEISS Vision Care Australia & New Zealand, says.
“Two prototypes went into trials in China, and after six months the intention was to release one to the wider market, and that was the harder design with a smaller central zone and a higher plus in the periphery (ZEISS MyoCare).
“But when we received our 12-month results, there was a clearly stated graph that showed a strong emmetropic growth ratio in the 6-9 years age group with our harder ZEISS MyoCare design. But this further improved significantly in the 10 and older age group with the softer design (ZEISS MyoCare S). That’s why we are launching an age-specific solution.”
While ZEISS MyoCare lenses represent one of the latest innovations in Australian myopia care, the company has had a presence in this space for some years. Eyecare professionals may be familiar with ZEISS MyoVision Pro lenses – a single vision option for children between the ages of six and 12.

The older ZEISS MyoVision lenses were based on peripheral defocus, but Pretorius says the research now points to the concept of “simultaneous competing defocus” as inhering a stronger growth stop signal in myopia.
Based on these developments, ZEISS’ R&D department has incorporated significant improvements in the new ZEISS MyoCare portfolio, which has been inspired by the ring-like imprints on the cornea following orthokeratology treatment.
In terms of efficacy, both ZEISS MyoCare lens design variants are now the subject of a multi-centre randomised controlled two-year clinical trial to assess their safety and effectiveness. Pretorius says the latest data after 12 months shows participants wearing the ZEISS MyoCare design are 63% closer to the emmetropic growth curve. Meanwhile, those wearing ZEISS MyoCare S were 86% closer to normal emmetropic growth. (NOTE: be mindful when comparing data. Other lens designs may compare to control groups, for example).
To achieve this, ZEISS MyoCare’s design adopts annular cylindrical microstructures to induce simultaneous competing myopic blur on the peripheral retina to slow myopia progression. The company’s patented Cylindrical Annular Refractive Elements (C.A.R.E.) Technology incorporates
58 INSIGHT July 2023
MYOPIA
alternating defocus and correction zones expanding towards the periphery of the lens. These elements are so small in dimension that special optical methods are required to make them visible.
“What also makes the ZEISS MyoCare lens unique is the use of a cylindrical shape in the functional zone, where the height, width and size of the microstructures creates the blur effect as part of simultaneous competing defocus,” Pretorius says.
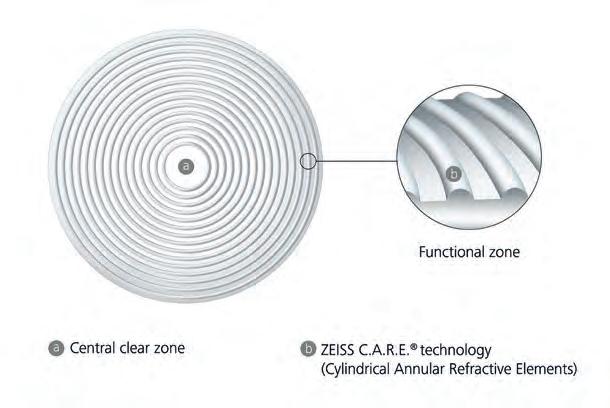
“As opposed to a normal spherical or aspherical lenslet in the treatment zone, our approach means that light coming in and falling on that cylindrical shape causes a blended distribution of blur, which is less perceived by the child, helping to improve adaptability and wearability of the lens, while creating the strongest stop signal to prevent the eye elongating.”
TREATMENT EFFECT AT ALL GAZE ANGLES
Compared to contact lenses and ortho-k, spectacle lenses are thought to offer distinct advantages as a myopia management intervention in children. They are easy-to-fit, affordable, mostly well accepted and tolerated, and minimally invasive.
But to make spectacle lenses work for myopia control, it requires some clever optical science that equally accounts for a treatment zone that slows myopia progression, as well as a clear zone that provides sharp vision to correct the patient’s refractive error.
With a 9 mm diameter of the clear zone for MyoCare S and a 7 mm diameter for ZEISS MyoCare, the clear zone needs to provide enough space for children to pursue their typical daily activities without any accommodation issues during near tasks like reading or writing. At the same time, ZEISS realised the need to keep the clear zone as small as possible to establish an effective functional zone projecting myopic defocus on the near peripheral retina close to the fovea.
The lens also needs to account for constant movement of the eye, ensuring the intended correction and myopic defocus is maintained for all gaze angles.
Pretorius says ZEISS addresses this by using ClearFocus design, a freeform back surface that not only provides the correct lens power for all viewing angles, but minimises unwanted hyperopic defocus independent of gaze direction.
“With a standard back surface, when a patient looks on an angle or to the side, they’re potentially not getting the same level of effectiveness compared to a flatter back surface,” Pretorius says.
“Because we’ve got a freeform back design, we’re able to minimise unintended hyperopic defocus for oblique views through the lens periphery.”
AUSTRALIA & NEW ZEALAND LAUNCH
ZEISS MyoCare has been in use in China for more than a year, and became available in Europe in April 2023. The longer wait for Australian optometry practices means local eyecare professionals can access the lenses in 1.5, 1.6 and 1.67 indexes, as opposed to only 1.59 index (polycarbonate).
Australian and New Zealand optical practices can expect several ZEISS MyoCare launch events across the country, in addition to promotional events in collaboration with eyewear companies that have designed frames for myopia control lenses.
“These frames will feature markings to ensure the lenses are dispensed in the correct fashion,” Pretorius says.
“We also know a lot of optometrists are confident in managing myopia, but many others wanting to get started might be lacking confidence or are unsure where to start. We will be creating material to help them understand the lens technology, as well as how to communicate its benefits to patients.”
In addition to this, Pretorius says ZEISS will be releasing a seven-part webinar series to help optical dispensers and assistants improve their myopia knowledge. The launch events will be CPD-accredited for optometrists, and the company will be speaking to ophthalmologists to ensure they have an understanding of the ZEISS MyoCare design.
ZEISS is also putting the final touches on an attractive warranty structure, as an indication of its confidence in the product, Pretorius says.
MYOPIA – A GLOBAL ISSUE
ZEISS recognises the magnitude of the myopia problem. However, years of research show that prevalence differs and the risks associated with progressive myopia require specific solutions for different target groups.
It’s predicted myopia prevalence will climb to 50% by 2050. Despite being a global challenge, there are regional differences. For example, up to 90% of the urban youth of 20 years and younger are affected in Southeast Asia, while rates in Europe are much lower. Currently, 36% of Australians and New Zealanders are estimated to have myopia, but this could rise to a staggering 55% by 2050, with Australia expected to have 4.1 million high myopes by then.
With much of the research emerging from East Asian countries, the company set out to understand the refractive development in Caucasian children.
In 2014, ZEISS partnered with the Leipzig Research Center for Civilization Diseases of the University of Leipzig which started the LIFE Child study in 2011 – one of the biggest population-based longitudinal cohort studies in Europe. The study monitors child development from birth to adulthood and to understand factors associated with health and disease. The so-called ‘eye health cohort’ now consists of approximately 2,000 children aged between three and 16 years. These participants are invited to attend annual follow-ups where refraction, visual acuity and axial length of the eye are recorded and monitored longitudinally.
Separately, ZEISS partnered with Euronet Market Research to analyse ocular history data collected in over 400 optician shops across Germany from more than 500,000 subjects aged between 0 and 20 years to validate that the study results reflect what is observed in real-world eyecare practices.
The combined insights from these studies point to a trend of increasing myopia prevalence in Europe – similar to what is seen in North America, India and Australia, but to a much smaller extent than what is observed in East Asia.
“We looked at the refractive development of the eye from kids across multiple multicultural ethnicities, and concluded they’re very similar in how they develop, so it appears to be the influence of genetics and external factors driving higher prevalence in East Asia,” Ms Elmarie Pretorius, professional services manager for ZEISS Vision Care Australia & New Zealand, says.
“Because we’ve seen that myopia is rising across the world, as a company we decided to do more about it, and that’s provided the research and basis of our new lens design.”
INSIGHT July 2023 59
The company’s lens comprises a central clear zone (a), and a functional zone with patented Cylindrical Annular Refractive Elements (C.A.R.E.) Technology (b) that incorporates alternating defocus and correction zones expanding towards the periphery of the lens.
Think globally,
Specsavers’ global sustainability team is setting ambitious targets, including carbon net zero by 2050.
CATHY RENNIE MATOS will be responsible for driving this at a regional level and discusses what steps are taking place now, and what lies ahead.
When Ms Cathy Rennie Matos sat down to discuss her new role within Specsavers Australia & New Zealand, she was packing her bag for a business trip to Europe to meet her counterparts in the company’s global sustainability team for the first time.
“I’m going to spend time with my colleagues from the UK and Northern Europe, as well as our subject matter experts, and look at how they’re managing matters such as recycling and waste,” Matos says.
“There’s a lot that Northern Europe, as a region, is doing in the sustainability space, in terms of its infrastructure and the way it approaches waste, and I’m interested in better understanding that for our operations in Australia and New Zealand.”
With a communications and marketing background, Matos has been head of public relations at Specsavers ANZ for the past five years but performing a dual PR-sustainability role for the last two. She then transitioned into the newly created head of sustainability position at Specsavers ANZ in March 2023.
It’s an issue the company has taken seriously for some time. But the appointment of Specsavers global CEO Mr John Perkins as chief sustainability officer is perhaps indicative of an even greater emphasis on issues such as energy consumption, packaging, and the suppliers it does business with.
Increasingly, consumers are also seeking out the products and services of environmentally conscious optical products and businesses.
Perkins’ appointment set in motion a process of creating a sustainability agenda that would form part of the company’s long-term framework,
ACT LOCALLY
including what structures were needed within the organisation to deliver on its sustainability ambitions.
“We want to continue to change lives through better sight and hearing, but we want to do it in a way that is better for our people, our communities and our planet,” Matos says.
Specsavers’ global sustainability team further identified its ambitions within the three pillars of: people, communities, and planet. It wants to be carbon net zero by 2050 and reduce the environmental impact of its operations and material consumption, including product, packaging, water, resource management and waste.

“We also want to empower our people to be able to make a difference themselves in their local communities and live and work more sustainably. That includes volunteerism and supporting fundraising efforts, diversity and inclusion, and health and wellbeing programs,” Matos says.
“In the community, our ambition is to enhance access to sight and hearing care services and support for people in our communities who are facing barriers to care, whether it be geography, language, or cost.”
The company is working with a group of subject matter experts as part of its global sustainability team to develop strategies and support each region in delivering on its goals.
“We’ve got a carbon expert, a packaging and waste expert, and we’ve recently brought on board a materials expert who will work closely with our supply chain and product teams on the materials that go into our products,” Matos says.
CARBON CRUSADE
The biggest contributor to carbon emissions in the optics industry derives from the purchase of goods and services, predominantly contact lenses, frames and spectacle lenses, and the manufacture of optical equipment. Transport and distribution, capital expenditure, and business travel contribute to a lesser degree.
As Matos explains, carbon emissions are divided by scope; Scope 1 are direct emissions from sources owned or controlled by a company; Scope 2 are
60 INSIGHT July 2023
SUSTAINABILITY
Specsavers Cannonvale store operates using 100% renewable electricity.
indirect emissions from purchased electricity, steam, heat, and cooling, and Scope 3 are all other emissions associated with a company’s activities.
“We’ve been working globally with an agency called Carbon Intelligence on establishing our carbon baseline and are in the process of taking a recommendation on an interim target for Scope 1 and 2, as well as an interim target for Scope 3, to our executive board,” Matos says.
“From Specsavers’ perspective, our electricity usage and the F gas that comes from air conditioning units within stores fall under Scope 1 and 2. We need to be transitioning to renewable energy.”
The company’s carbon reduction plan is aligned with the globally recognised Science Based Targets initiative (SBTi), a gold-class standard which provides companies with a clearly defined path to reducing emissions in line with the Paris Agreement to limit global temperature increase to below 1.5 degrees.
It is starting to make inroads; the company moved all its centrally-procured electricity over to a renewable tariff as of January.
“I’ve also been working with the Australian Retailers Association, who have been holding workshops on getting to net zero,” Matos says. “Speaking to other retailers, a lot of organisations are currently navigating how to do this. We are fortunate because, being a global organisation, we were able to bring in external consultants to help us. Optometry Australia has also brought a consultant on board for the same purpose.”
SUPPLIER ENGAGEMENT
Having set its interim and long-term carbon emission targets, Matos says Specsavers is now starting to focus on what its carbon reduction strategy looks like.

A big part of that is in supplier engagement. “We need to be working as an industry with our suppliers to get where we need to. We can only do it by collaborating,” she says.
“Our supply chain team is starting to have those conversations, especially with our biggest suppliers. That’s going to happen over a long period of time. We need to understand where they are on the sustainability journey, and where we can lean in and offer support. Some may not be as far along as others, but we can learn from, and support, each other through it.”
As Matos points out, there are several companies within the optical industry that have started devoting more resources to developing a sustainability charter. It is, in part, driven by consumer demand.
“We conduct consumer research a couple of times a year to get a feel from consumers about what they think is important. They are becoming savvier, and their expectations of organisations are rising in terms of materials, waste, and working on becoming carbon net zero. We have had feedback from customers asking whether a particular type of daily contact lens is available as a monthly so there’s less waste. I think we’ll see more of that,” Matos says.
As someone familiar with the machinations of PR, Matos says she is noticing a discernible increase in the amount of advertising from organisations in Australia promoting what they’re doing in the sustainability space.
“It’s right at the top of the ACCC’s agenda. As more government regulation comes in, I think we’ll continue to see growing consumer expectations. But it’s not about doing it because that’s what consumers want; it’s because it’s the right thing to do, in terms of the environment and business resilience,” she says.
“SPECSAVERS ANZ BECAME A SIGNATORY TO THE AUSTRALIAN PACKAGING COVENANT LAST YEAR AND WE’VE GOT TARGETS OVER THE NEXT SEVEN YEARS ALIGNED WITH AUSTRALIA’S 2025 NATIONAL PACKAGING TARGETS.”
CATHY RENNIE MATOS SPECSAVERS

we’re saying. Ours is a complex industry and I think we have a responsibility to make sure we’re educating consumers.”
PACKAGING PROTOCOL
A carbon reduction plan that is aligned with SBTi is one of the more immediate actions Specsavers is taking towards implementing its sustainability initiatives, but Matos says the company is also undertaking several packaging-related projects.
“Working with an expert in materials and looking at how we can reduce the environmental impact of packaging. That includes how we can reduce the amount of plastic we use, how we can make packaging more recyclable, and made from recycled materials,” she says.
“Specsavers ANZ became a signatory to the Australian Packaging Covenant last year and we’ve got targets over the next seven years aligned with Australia’s 2025 National Packaging Targets.”
Matos and her team are investigating whether the company has the infrastructure in place to capitalise on recycling opportunities. It started recycling demo lenses last year and is working this year on glasses recycling to complement glasses reuse.
“We have worked with Lions Recycle For Sight for many years but not all glasses can be reused. We’re working hard to find a solution to recycle frames and lenses that can’t be reused, such as display models, for instance,” Matos says.
“Most of our packaging sits within the supply chain. From a customer’s perspective, if they purchase and pick up through a store, they receive their glasses in a case with a lens cloth in a carry bag. For us, it’s about figuring out how we can reduce the amount of plastic that we have within the supply chain that ends up in store, and looking at how we can ensure that stores can recycle any plastic that does get to store level.”
Before Matos can meet with her sustainably-minded counterparts in northern Europe, she is first boarding a flight to the Northern Territory.
“I’m taking our executive board up to Alice Springs on a cultural learning trip [in May] – it falls within our ‘People’ pillar in our sustainability agenda,” she explains.

“Last year the board signed off on a plan to better integrate Aboriginal and Torres Strait Islander culture into the business. As part of that, we’ve recently introduced cultural protocols across the business, and are going to be rolling out cultural learning and awareness training this year.
“As part of the board’s cultural learning, they are meeting with some of The Fred Hollows Foundation program partners in the Alice Springs Hospital and the Central Australian Aboriginal Congress to better understand some of the challenges they face in delivering eye care to Aboriginal and Torres Strait Islander communities. We support both of those programs through our support of The Fred Hollows Foundation.”
INSIGHT July 2023 61
A FRONT ROW SEAT TO OPHTHALMIC SUBSPECIALTIES
Ophthalmology Updates! is a two-day conference bringing together the brightest minds from each ophthalmic subspecialty to update attendees on their field. It is returning in August 2023 with ABC’s Dr Norman Swan as the special guest speaker.
Brainchild of Sydney retinal ophthalmologist Professor Adrian Fung, the Ophthalmology Updates! Conference was born out of the need that all ophthalmologists require constant upskilling in ophthalmic subspecialty topics.
Started in 2016, it is returning as a stand-alone event in August 2023, following a hiatus in 2020 and 2021 due to COVID, and was combined with RANZCO’s NSW conference in 2022.
“I founded the concept of Ophthalmology Updates! because I realised, when I came out of fellowship, I knew a lot about my subspecialty, but I was losing touch with other subspecialties, so it was a good way to keep up-to-date with what’s going on in all subspecialties,” Fung says.

Taking place on 26-27 August at Fullerton Hotel in Sydney, the event is designed for general ophthalmologists who want to consolidate their knowledge and learn about new advances in a range of subspecialties; for subspecialty ophthalmologists who want a refresher on other subspecialties; and for registrars preparing for RANZCO examinations.

Invited speakers prepare a three-part presentation, each lasting 15 minutes, on a common subspecialty condition, a ‘frontier’ topic on a topical subject (but not in trials or experimental), and a case-based discussion.
“Common conditions are not necessarily covered a lot in conferences because they’re assumed knowledge but as we progress in our careers, the field can move on, frontier topics change from year-to-year depending on what is topical in that year,” Fung says.
“We try to keep it clinically applicable for current ophthalmologists, so even though there might be treatments in the pipeline, we tend to focus on therapeutics – or imaging or diagnostics – which are TGA-approved and PBS-listed because we want it to be something that is practical and useful to the clinician.”
Fung says it was timely to invite Dr Norman Swan, a multi-award winning producer, broadcaster and investigative journalist, as guest speaker this year to discuss medicine and the media.
“There has been a lot in the media about Medicare fraud, ongoing issues regarding the Medicare rebate, and issues about unprofessional practice of doctors. I was interested in exploring that idea, and Dr Swan is both a doctor and well known in
BUT THAT’S FINE.”
the media, getting his understanding of how these stories make it into the media, who controls that narrative, and what are the politics behind it.”
Fung expects about 200 to 250 delegates to attend, which he says is in keeping with the conference’s informal atmosphere.
“One of the main focuses of the conference is we dedicate a lot of time to discussion and Q&A,” he says.
“We want all attendees to be able to ask questions. Sometimes the discussion might go on a tangent, but that’s fine. We want to ensure there is enough time to have a discussion, either with the speaker or the chair, or as a group. Keeping attendance between 200-250 in the Heritage Ballroom at the Fullerton is very conducive to discussion and doesn’t feel intimidating to anybody to ask a question.”
The event also includes a dinner, which will this year be held at Bennelong Restaurant at Sydney Opera House, on Saturday 26 August. The conference is approved for 12 Level 1 RANZCO and 10 Orthoptic Australia CPD Points.
For more information, visit www. ophthalmologyupdates.com.
62 INSIGHT July 2023
EVENT: PREVIEW
PROF ADRIAN FUNG, CONVENOR
OCULOPLASTICS, SAT 26 AUG PROFESSOR DINESH SELVA

Professor Selva was appointed to the foundation chair of Ophthalmology & Visual Sciences at the University of Adelaide in 2004. He is Chairman of the South Australian Institute of Ophthalmology, University of Adelaide and has published over 600 peer-reviewed papers and book chapters. In his lecture on oculoplastics, he will discuss surgical video vignettes and endoscopic orbital surgery.
TOXOPLASMOSIS & LEADERSHIP, SAT 26 AUG

PROFESSOR JUSTINE SMITH

Professor Smith is an ophthalmologist-scientist, co-appointed as Matthew Flinders Distinguished Professor at Flinders University and Senior Consultant at Flinders Medical Centre. She will provide a toxoplasmosis update, as well as discuss medical journal publishing in 2023 and share what she learnt during her time as president and executive vice president of the Association for Research in Vision and Ophthalmology.
MEDICAL RETINA, SAT 26 AUG PROFESSOR ROBYN GUYMER

Deputy director of the Centre for Eye Research Australia and a senior retinal specialist at the Royal Victorian Eye and Ear Hospital, Professor Guymer will be discussing emerging treatments for neovascular AMD and geographic atrophy. She is currently investigating new strategies for treating early stages of AMD and is working to identify novel imaging and functional biomarkers and surrogate endpoints to improve the feasibility of conducting early intervention trials.
GLAUCOMA, SAT 26 AUG DR NATHAN KERR
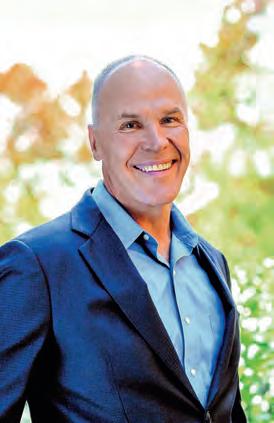


Integrating Alcon’s Hydrus microstent into clinical practice for primary open-angle glaucoma, plus new approaches to the subconjunctival space will be addressed in Dr Kerr’s presentation. Having completed a prestigious glaucoma fellowship at Moorfields Eye Hospital, he serves as a glaucoma section editor for Clinical and Experimental Ophthalmology and is a principal investigator in glaucoma at the Centre for Eye Research Australia.
CATARACT, SAT 26 AUG ASSOCIATE PROFESSOR MICHAEL LAWLESS
A/Prof Lawless was the first ophthalmologist in Australia and New Zealand to perform SMILE Pro and one of the first in the world to perform LASIK using the ZEISS Visumax 800 laser system. His lecture will provide 10 pointers that surgeons can implement to make them better cataract and refractive surgeons, as well as discuss the latest IOL technologies and their role in practice.
MEDICINE & THE MEDIA, SAT 26 AUG DR NORMAN SWAN

An expert on medicine and the media, special guest speaker Dr Norman Swan co-hosts ABC Radio National’s Health Report and co-hosted Coronacast, a podcast on coronavirus during the COVID-19 pandemic. Swan is also a reporter and commentator on ABC’s 7.30, Midday, News Breakfast and Four Corners. He is a past winner of the Gold Walkley and has won other Walkleys including one with his Coronacast colleagues in 2020.
NEURO-OPHTHALMOLOGY, SUN 27 AUG PROFESSOR CELIA CHEN
Professor Chen is a clinical professor with University of South Australia and consultant neuro-ophthalmologist/clinician-scientist at Flinders University. She is the current president of the Neuro-Ophthalmic Society of Australia. Chen’s lecture will focus on arterial occlusions to the eye, from retinal emboli to ocular ischaemic syndrome. She will also address what’s new in idiopathic intracranial hypertension.

INSIGHT July 2023 63
INVITED SPEAKERS
Targeted
APPROACH INCREASES UPTAKE OF DIABETES EYE CHECKS
There are up to 1.9 million people living with diabetes in Australia. Of those, research suggests 800,000 don’t access routine eyecare services. This was the impetus to establish diabetes eye check reminder system KeepSight in 2018. How is the initiative faring five years on?


KeepSight’s mission is to eliminate vision loss to diabetes in Australia by increasing the number of people accessing routine diabetes eyecare – connecting people with diabetes to the eye checks that they need.

Most of the people who are already part of the KeepSight program are referred by their optometrist. Specsavers is the program’s founding optometry partner, and registers around 2,000 new patients with diabetes plus 3,500 follow up appointments to the program each week. Other major providers, including Luxottica, are also integrated with the program and with recent integrations with Optomate and support from Optometry Australia, other providers are also beginning to increase their referral rates to KeepSight.
According to Diabetes Australia (DA), this support from the sector is invaluable to the success of the program. Integration means a streamlined, efficient sign-up process for both people with diabetes and providers. It also reinforces the importance of the KeepSight message through endorsement from a health professional. But despite that, some people with diabetes are hard to engage.
DA’s KeepSight program director Ms Taryn Black says there are a multitude of reasons why people might not be engaging in regular eye checks.
“Diabetes is a complex condition and people living with it have a lot to manage. It is relentless. There is never a day off. Often people are also dealing with other, potentially more urgent complications. So, the need to have an eye check may be down the pecking order of priority,” she says.
“And as we know, diabetic retinopathy can be asymptomatic. People might think their vision is fine so there is no need to prioritise a check right now.
“On top of this, there may be other concerns that people have – the cost, accessibility to an eyecare provider, worry that having an eye check may hurt or that the check might actually find a problem – there are many potential barriers.”
DA says this is where KeepSight plays an important role. The KeepSight team routinely engages with people with diabetes encouraging them to sign up for checks but also working to allay any other barrier or concerns they may have.
This work to drive more people with diabetes into the clinic for a check is a critical piece of the KeepSight effort, Black says.
“We have a unique opportunity to be able to directly connect with people with diabetes via the National Diabetes Services Scheme (NDSS).”
KeepSight is employing a multi-pronged approach to communicating with people with diabetes about eye health.
Increasingly DA is much more targeted in the way it communicates. It achieves this by developing messaging targeted to particular groups or cohorts.
“This might be people who are newly diagnosed, or those who have lived with diabetes for many years. It might also be people in regional and remote areas, versus those in metro areas. It might be people who have started the sign-up process previously who, for whatever reason, didn’t complete it,” Black says.
“All of these groups require a subtle nuancing in the message which speaks to their unique challenges – but it is essentially the same message –register for reminders and get your eyes checked – it’s really important.”
In the most recent activation, the team observed a six-times improvement in response, simply by adapting the message to speak more directly to the person’s individual experience and reinforcing the message with a follow up communication.
In addition to direct communications, the KeepSight team adopts what it calls an ‘always on’ approach to marketing and communication. There is always something in market encouraging people to sign up and reinforcing the diabetes eye health message. This might include social media or digital advertising, media articles, or advertising in key publications.
The goal is to build exposure so that people see the diabetes eye health message everywhere.
It is this layered approach that the KeepSight team hopes will continue to bring people into eyecare providers for a check.
“KeepSight’s mission is to direct people with diabetes into routine eye care and remind them to keep going back. That is then where the eyecare sector’s role really comes into play – to provide quality and reassuring, specialist diabetes eyecare,” Black says.
“It really is a wrap-around effort to support people with diabetes to prioritise their eyes and we are grateful for the support of providers like Specsavers who are so committed to this important cause, providing not just financial support but also industry expertise and insight.”
64 INSIGHT July 2023
EYECARE
“DIABETES IS A COMPLEX CONDITION AND PEOPLE LIVING WITH IT HAVE A LOT TO MANAGE. IT IS RELENTLESS. THERE IS NEVER A DAY OFF.”
TARYN BLACK DIABETES AUSTRALIA
Insight Dry Eye Directory returning in 2023

The October 2023 issue will feature the Insight Dry Eye Directory, Australia’s most comprehensive source for dry eye care.
Back by popular demand, this all-in-one resource is a valuable purchasing guide for practices, showcasing available Therapies and Diagnostics in Australia. It will also feature a comprehensive list of dedicated Dry Eye Clinics.
It’s FREE and EASY for you to list your products or services.
If you operate a dry eye clinic, or are a supplier of dry eye products, scan the QR code to organise you listing, or visit insightnews.com.au/dry-eye-directory-2023
Scan HERE to arrange your listing.

To amplify your product via advertising, contact Insight BDM Luke Ronca: 0402 718 081 or luke.ronca@primecreative.com.au
www.insightnews.com.au

AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975
Inside the
GLAUCOMA COLLABORATIVE CARE CLINIC
The Royal Victorian Eye and Ear Hospital and the Australian College of Optometry established the Glaucoma Collaborative Care clinic almost seven years ago and celebrated the 200th clinic during World Glaucoma Week in March. What has contributed to the clinic’s success?
The Glaucoma Collaborative Care clinic (GCC) was initiated by The Royal Victorian Eye and Ear Hospital (the Eye and Ear) in response to rising glaucoma levels and aims to alleviate pressure on in-demand public health ophthalmologists and ensure appropriate care for patients. Originally serving as a pilot project in partnership with the Australian College of Optometry (ACO) between 2016-2017, the clinic was based on RANZCO’s new model of collaborative glaucoma care guidelines.
The clinic provides diagnostic and ophthalmic review for low risk and glaucoma suspect patients from the Eye and Ear. The program has been developed for patient-centred, cost-effective care. Its primary focus is on facilitating community-based follow-up when appropriate, while improving access to specialist hospital-based care for patients with diagnosed glaucoma who are at higher risk of disease progression. In other words, scarce glaucoma specialist resources are being directed to the most at-risk cases.
Running fortnightly from the ACO’s Carlton clinic, the GCC clinic is said to be an example of how a team-based approach involving ophthalmologists, optometrists and orthoptists is integral to supporting positive, more sustainable eyecare outcomes.
FOSTERING A CLINICAL DIALOGUE
Lead optometrist of ocular disease services at the ACO, Ms Janelle Scully, was involved in a previous collaboration evaluating which general referrals from the Eye and Ear could be triaged to primary care and leapt at the opportunity to be involved when it pivoted into a glaucoma-specific collaboration.
A team of four optometrists and an ophthalmologist from the Eye and Ear – usually Associate Professor George Kong, who is sometimes joined by a glaucoma fellow – aim to see about 20 patients at the GCC clinic every fortnight.
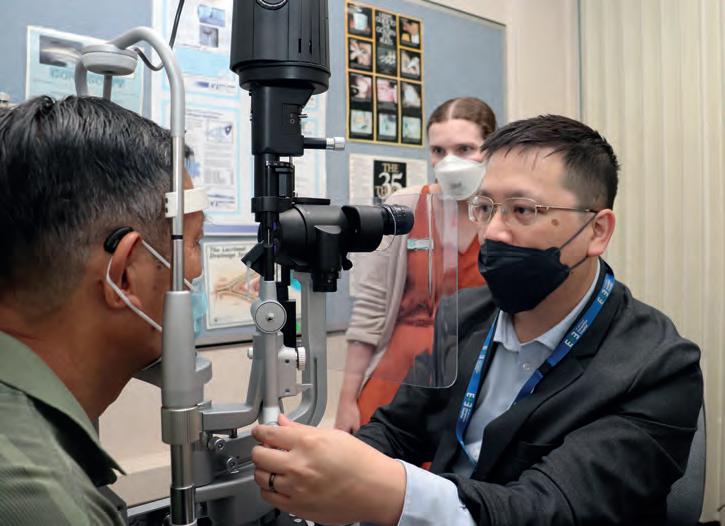
“Based on their referral, the patients that we see at GCC are thought to be low risk, or potentially suitable for community care. Sometimes they’ll be existing patients from another clinic at the Eye and Ear, such as the medical retina clinic. Depending on the triage process by the glaucoma team at the Eye and Ear, they might be referred to GCC,” Scully says.
“With the cost-of-living pressures, and demand on public hospitals, the Eye and Ear determine which patients can be safely managed in a community setting. We also assess the patients we see at GCC to identify which patients can receive ongoing care at the ACO, or their local optometrist. All the patients that are seen at the clinic get a full outcome letter that goes to their referrer and their GP, so everyone knows the care pathway going forward.”
Some of the patients have never been treated for glaucoma, or don’t have an existing diagnosis, but might be a glaucoma suspect. Others might be new immigrants to Australia or might have received glaucoma care at a previous hospital interstate and are now transferring their care to the public system in Victoria.
From a pilot to a program running for nearly seven years, the clinic has proven clinically effective and beneficial, although it has faced challenges, including remaining open during COVID. For Scully, it has also facilitated professional relationships between optometry and ophthalmology.
“We’re improving clinical relationships. Working with the ophthalmologists and glaucoma fellows that have rotated through the clinic throughout the last seven years has been fantastic in fostering clinical discussions about what their thoughts are on various cases. It really informs our thoughts about the other patients that we see. It also gives the ophthalmologists some insight into how optometrists think and what we’re concerned about,” she says.
“Interestingly, a number of the recent glaucoma fellows are former optometrists. A small but significant number of former optometrists have been going through the medical school pathway and ophthalmology training.”
Scully believes people are generally unaware of the limitations of the public system when it comes to treating glaucoma. Furthermore, in conjunction with an ageing population, she thinks the increasing use of technology allowing eyecare practitioners to detect glaucoma earlier means they’re finding more glaucoma and therefore needing to manage a growing number of patients.
“It’s going to be critical going forward that, with the number of patients that will have glaucoma, that optometry and ophthalmology working together is the only way we’re going to be able to manage the massive load of patients that need care. And that’s not just in the public system, that’s in regional areas. A solid link between primary care optometry and secondary and tertiary care ophthalmology is what is going to help get the best outcome for all patients,” she says.
NOT WITHOUT CHALLENGES
Dr Catherine Green, head of the glaucoma unit at the Eye and Ear for more than 10 years, has advocated for the collaborative clinic since the start and believes its progressive approach to care has made a difference to glaucoma patients.
“The Eye and Ear is without doubt the largest glaucoma service in Victoria, but I think it’s the largest in Australia in the public system. Our unit has about 15 to 17 consultants, and we see over 10,000 outpatients per year and perform the majority of glaucoma surgery for the state of Victoria in the public system, including very complex disease,” Green says.
66 INSIGHT July 2023
GLAUCOMA
Ophthalmologist Dr George Kong and optometrist Janelle Scully assess a patient attending the Glaucoma Collaborative Care clinic.
“We have allied eyecare practitioners working alongside ophthalmologists in real time that not only optimises the efficiency of testing and diagnosis, plus the opportunity for a management plan. If a patient requires treatment, treatment can be initiated, or if they require laser treatment, they can be directly referred to the Eye and Ear without the need for another appointment,” she says.

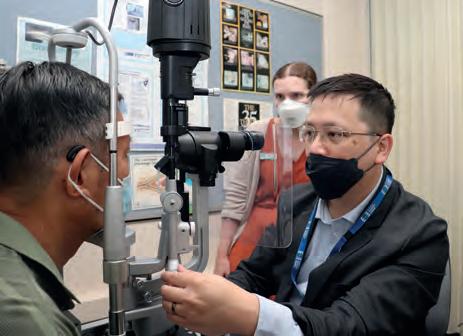
“There’s also an opportunity for a patient to be discharged, either to the referring optometrist or to another community optometrist, and, as the ACO also has a glaucoma monitoring clinic that that they run separately, there is an easy pathway back to the hospital if a patient requires that.”
Green says the collaborative project has reduced the Eye and Ear’s waitlist for new patients, and demonstrated it is a safe program with high patient satisfaction – in terms of cost, waiting times, the care they received, and outcomes – and practitioner satisfaction.

Yet there have been challenges, nominally staff retention and identifying ophthalmologists who are available to be on site at the ACO on the given day, and COVID-related interruptions.
“As a result, we’re probably not getting the volume of patients in terms of the numbers of patients that the clinic was designed to provide care for. We’re probably under servicing in terms of meeting that goal. I see that very
service, including the GCC.”
Green also highlights a separate project she is leading, built on the back of the successful GCC project.
“We [the Eye and Ear] have been running for the last few years the Glaucoma Community Collaborative Care project where we have partnered with a select group of 20 optometrists who have been identified in specific geographical areas – some in outer suburbs and some in the country – that are relevant to our patient population,” she says.
“The GCC at the ACO was designed for patients who are suitable for ongoing optometric care but there is a group of patients who are low risk but cannot be discharged from care. They still need to see an ophthalmologist every year or two but could potentially see another eyecare practitioner for other visits if they’re stable. So for this population of patients, we’ve established the community project. Those patients are not discharged from the Eye and Ear hospital; they remain under our care but for probably three out of four of their appointments, they don’t come to the hospital, they get seen by a community optometrist, specially selected and trained by the Eye and Ear.”
The optometrist then generates a report that is virtually reviewed by an ophthalmologist at the Eye and Ear.
“We are then able to identify if there are patients out there that we thought were low risk who are progressing. So that’s another program, also highly successful, which has gone from a pilot to ‘business as usual’.”
Green says this program too has had its challenges, primarily with workforce movement, but again, clinician and patient satisfaction is high.
“We identify a site and we identify an optometrist, and then that optometrist moves somewhere else. That’s been one of the challenges of that particular project, but it’s manageable, we’ve got systems in place for it,” she says.
“The bottom line is we’re providing patients with an alternative place to have care, we’re providing access for them when they might not have been able to receive an appointment in a timely fashion.”
INSIGHT July 2023 67
“AS THE HUB OF GLAUCOMA IN THE PUBLIC SYSTEM, WE HAVE A SITUATION OF DEMAND OUTSTRIPPING OUR ABILITY TO PROVIDE SERVICES.”
DR CATHERINE GREEN EYE AND EAR HOSPITAL
The Glaucoma Collaborative Care clinic team (L-R) clinical assistant Dr Ashim Dey; optometrists Dr Josephine Li, Joe Waterman, Tracy Tran, Janelle Scully; ophthalmologist Dr George Kong and optometrist Iris Huang celebrate its 200th clinic.
3





NEW BRANDS COMING SOON... SEE YOU AT OMEGA23! Proj ect Gree n ey ew ea r LAUNCHING AT OMEGA23
A PERSONALISED FRAME – JUST FOR YOU
Eyewear is not only a functional tool for correcting vision, but also an expression of personal identity. The right pair of spectacles can enhance one’s features and make a statement to complement one’s style. However, finding the perfect pair of spectacles can be challenging. That’s where tailor-made eyewear comes in.
To learn more about the concept and process of tailor-made eyewear, we interviewed the founder and designer of Madebyavision, who has a wealth of experience in the industry and a passion for creating beautiful, functional, and meaningful glasses. The designer offers a personalised approach to frames that is as unique as each customer.
Most glasses are mass-produced and are designed to fit a standard model, which may not suit everyone’s needs or preferences. To create a one-of-a-kind design that reflects the customer’s personality and style, the designer offers a comprehensive consultation process incorporating various factors such as the customer’s face shape, skin tone, and wardrobe.

The process of creating tailor-made eyewear starts with a consultation with the customer, and taking precise measurements of their face, nose, and temples. Based on that, the frame is designed to fit the customer’s features

and accentuate their best qualities. There are more than 200 different colours of premium acetate for customers to choose, which is harder, higher quality, and shinier than regular plastic. The customer can choose the colour, texture, and finishing of the acetate, including raw finishing for a textured and patterned look, or high polish for a shiny and smooth finish. There is an option to customise the detailing, such as diamond cutting, to add a touch of sophistication and individuality. The result of a tailor-made design is unique and only one in the whole world.
However, the process of creating tailor-made eyewear is not just about selecting options and materials. The biggest challenge in creating tailor-made eyewear is fully understanding the customer’s needs and expectations. As eyewear is a personal and emotional product, the consultation process requires a lot of communication and trust between the designer and the customer.

Therefore, the consultation process has to be customer-focused. Based on the customer’s input, adjustment of design applied on the front size and temple length ensures the perfect fit. The initial cutting of the front and temple is important to reconfirm the design with the customer. Despite the challenges, there’s great reward in creating glasses that reflect the customer’s individuality and style.
In conclusion, tailor-made eyewear is a personalised and innovative approach to frames that offers endless options and design possibilities. While the process of tailor-made eyewear may require more time and effort than buying off-the-shelf glasses, the rewards in terms of comfort, durability, and exclusivity are worth it. Tailor-made eyewear can be a transformational investment for customer engagement, optical dispensers, and optical practices.
Following the interview, I felt motivated to enhance my skills beyond my usual dispensing techniques by creating my own eyewear. In April, I participated in the “Make your own eyewear workshop” at Chris Savage’s Marrickville studio in Sydney, following the Optical Dispensers Australia (ODA) Conference. It was an enlightening experience to be guided through a step-by-step process to craft my own glasses. Possessing this specialised skill would be advantageous for an optical dispenser to expand their skill set and differentiate their service from other optical practices. I would recommend it to any optical dispenser who is interested in learning how to design their own frames.
ABOUT THE AUTHOR: Gladys Mak is an experienced optical dispenser with diverse industry background both in Australia and internationally. She has extensive experience in frame manufacturing and product development, and is an Advisory Board Member of Optical Dispensers Australia.

DISPENSING INSIGHT July 2023 69
Gladys Mak’s own handmade glasses from Chris Savage’s workshop at Marrickville studio in Sydney in April.
TAILOR-MADE EYEWEAR ISN’T THE NORM NOWADAYS, BUT OFFERS A PERSONALISED AND INNOVATIVE APPROACH WITH ENDLESS OPTIONS AND DESIGN POSSIBILITIES, WRITES GLADYS MAK.
GLADYS MAK
“AS EYEWEAR IS A PERSONAL AND EMOTIONAL PRODUCT, THE CONSULTATION PROCESS REQUIRES A LOT OF COMMUNICATION AND TRUST.”
When creating customised eyewear, the customer can choose the colour, texture, and finishing of the acetate, including raw finishing for a textured and patterned look, or high polish for a shiny and smooth finish. Image: madebyavision
NEW RESOURCES TO HELP EYECARE PROFESSIONALS SUPPORT PATIENTS WITH MACULAR DISEASE

ORTHOPTISTS, OPTOMETRISTS, AND OPHTHALMOLOGISTS WILL HAVE A LEADING ROLE TO PLAY IN THE SUCCESS OF THE MY EYES PROGRAM THE MDFA IS LAUNCHING IN THE LATTER HALF OF 2023, CEO DR KATHY CHAPMAN EXPLAINS.
Supporting people living with macular disease is integral to the work of Macular Disease Foundation Australia (MDFA). This support extends to the eye healthcare professionals, particularly orthoptists and optometrists, who work at the frontline to deliver patients with primary eyecare.
To assist, MDFA has new online education courses to help orthoptists and optometrists better detect and manage inherited retinal diseases (IRDs) – Australia’s leading cause of irreversible legal blindness in working-age adults.
In Australia, one in every 1,500 children is born with an IRD.
MDFA’s courses for health professionals are funded by the Commonwealth Government under the National Strategic Action Plan for Macular Disease – a coordinated national response to macular disease in Australia.
One of the action plan’s key recommendations was improving health professionals’ knowledge of macular disease through education.
Healthcare professionals, particularly orthoptists and optometrists, play a valuable role in detecting and managing vision loss and blindness. The better equipped a healthcare professional is, the better the outcome for patients.
Working with some of Australia’s leading retinal specialists, MDFA has developed a self-paced course which includes education on how to best detect and image IRDs, key signs and symptoms, managing and reducing modifiable risk, and ensuring high-risk individuals are having regular eye examinations. The course also gives health professionals the necessary information to link patients diagnosed with inherited retinal diseases with appropriate supports and services.
This free, accredited course on IRDs will be launching soon and will be available to access via the MDFA website at www.mdfoundation.com.au or by using the QR code below.

A NEW WAY TO SUPPORT PEOPLE WITH MACULAR DISEASE
Orthoptists are a critical part of the healthcare team for people with macular disease. Over the coming year, MDFA sees orthoptists playing
an even greater role for their patients by connecting them to the upcoming My Eyes program.
Over the past two years, MDFA has invested in research to hear directly from people with macular disease, the people who care for them, and the people who treat them.
We are using this information to develop the very first patient support program for all people living with macular disease – based on their own needs and experiences. This new program is called My Eyes.
My Eyes focuses on three pillars of support – health information, emotional and practical – tailored to a patient’s own situation. Participants receive resources to live well with their macular disease and improve their health literacy. Connecting your patients to the program will ensure they get the very best of care in between their visits to their eye health professional.
MDFA will launch the My Eyes program in the latter half of 2023. Orthoptists, optometrists, and ophthalmologists – the triad of optimum eyecare – will have a leading role to play in the success of the My Eyes program. If your clinic is interested in connecting your patients into the My Eyes program when it becomes available, please contact the support team at myeyes@ mdfoundation.com.au.
ABOUT THE AUTHOR: KATHY CHAPMAN is the CEO of the Macular Disease Foundation Australia, the national peak body representing the 1.8 million Australians living with macular disease.

ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community. Visit: orthoptics.org.au

70 INSIGHT July 2023
DR KATHY CHAPMAN, MDFA
“THE BETTER EQUIPPED A HEALTHCARE PROFESSIONAL IS, THE BETTER THE OUTCOME FOR PATIENTS.”
Macular Disease Foundation Australia has invested in research to hear directly from people with macular disease, the people who care for them, and the people who treat them.
RETHINKING APPROACHES TO WORKPLACE PSYCHOSOCIAL RISKS
ONE OF YOUR JUNIOR EMPLOYEES SEEMS INCREASINGLY WITHDRAWN AND ANXIOUS. YESTERDAY AFTERNOON SHE LOOKED
AS IF SHE HAD BEEN CRYING. WHEN YOU ASK HER, SHE SAYS EVERYTHING IS FINE. WHAT MORE DO YOU NEED TO DO?
Changes to work health and safety regulations will require employers to take a proactive approach to managing risks to employees’ mental health and wellbeing.
Responses such as resilience initiatives imply the problem is with an individual’s ability to cope, rather than the work environment.
“CRITICS SUGGEST ONE PROBLEM WITH APPROACHES
The changing approach is reflected in the Model Work Health and Safety (WHS) regulations, which now require employers to use a risk-based approach to managing workplace psychosocial hazards, as they would manage other risks to the health and safety of workers. This requirement is progressively being incorporated into state and territory legislation.
To support the changes, Safe Work Australia’s 2022 Model Code of Practice on Managing psychosocial hazards at work (model code) provides practical guidance to help organisations meet their WHS responsibilities.

WHAT ARE PSYCHOSOCIAL HAZARDS?
The term covers aspects of the work environment, design or interactions that may cause psychological or physical harm.
Psychosocial hazards will be different in each workplace but can include issues such as escalating workload leading to long hours or missing breaks; repetitive work; pressure of financial targets; patient distress; inappropriate patient behaviours; isolation; interpersonal conflict; or bullying, harassment or discrimination.
Risks can occur in combination, and ongoing low-level stresses may make a worker more vulnerable to harm from a single severe incident.
A NEED TO RETHINK CURRENT APPROACHES
Employers’ duty to protect workers’ psychological health and safety is not new and your workplace may already have policies and programs to support the mental wellbeing of workers in the workplace.

However, the increasing cost and frequency of workplace psychological injuries suggests current approaches have failed to prevent psychological harm to workers.
For example, between 2019 and 2022, the Medical Training Surveys consistently report around one third of respondents had experienced or witnessed bullying, harassment, discrimination or racism in the past 12 months. The person responsible in a number of these cases was another healthcare colleague.
Even though most respondents said their organisation had relevant policies, most of the respondents to the survey were unwilling to report the incident.
TOWARDS A RISK MANAGEMENT MODEL
Critics suggest one problem with approaches to date is they assume workplace stress is ‘normal’ or unavoidable. Responses such as resilience initiatives imply the problem is with an individual’s ability to cope, rather than the work environment. Health and safety authorities and regulators now consider many psychosocial hazards arise from work design. They have the potential to harm all workers and should be managed using the same risk assessment approach as physical risks.
FOCUS ON CHANGES TO WORKPLACE DESIGN
The new model code is clear that it will not be enough to simply rely on policies or employee assistance programs in response to the risks.
These have a place as part of the response. However, they are the least reliable means of controlling risks and provide the lowest level of protection. They rely on people understanding and following them, and do not address the underlying causes.
In the case of physical risks, employers need to implement effective controls such as safety shut-off systems for medical equipment, as well as policies on disposing of hazardous material. Now employers will also need to show the steps they took to
change work design or alter the environment to remove or reduce psychosocial risks.
CREATIVE PROBLEM-SOLVING IN YOUR WORKPLACE
The message to employers and business owners is not to wait for workers to complain or become unwell. Instead, consult with workers to:
• Identify aspects of work and situations that could cause harm;
• Assess the risk, likelihood and severity of potential harm;
• Implement control measures to eliminate or minimise the risk of harm; and
• Review the control measures and modify if necessary.
It is important to encourage all workers to be involved. However, everyone does not need to agree on the list of risks. Some may thrive under pressure or enjoy routine, while others may become burned out. Even if only some workers identify a risk, it should still be managed through the risk assessment process.
As well as coming up with suggestions for your practice, the process may itself help mitigate stress by reassuring workers that managers are aware of their concerns –provided some action is taken to address the issues after they are identified.
MANAGEMENT INSIGHT July 2023 71
TO DATE IS THEY ASSUME WORKPLACE STRESS IS ‘NORMAL’ OR UNAVOIDABLE.”
ABOUT THE AUTHOR: TRACEY PICKETT BA, LLB, is a Legal and Policy Advisor for Avant.
THE DIFFICULTY IN FINDING SUITABLE FRONT-OF-HOUSE STAFF
At the time, 58% of respondents were having difficulty recruiting non-optometry practice staff.
The issue was affecting metropolitan practices more than those in regional areas in Victoria and South Australia, and since conducting the survey, we have been visiting practices in both states to ensure we continue to be well-informed about the reality of life for our members.
being the first point-of-contact for the majority of the community, which goes above and beyond traditional retail roles. This ties into the orientation of optometry practices as places focussed on the wellbeing of our communities, giving optometric employees a chance to contribute to quality-of-life for hundreds if not thousands of individuals over time.
 BY ILSA HAMPTON
BY ILSA HAMPTON
Practice managers, receptionists, optical assistants and qualified optical dispensers all play critical roles in viable optometry practices in 2023. But for many practice owners, finding suitable people to fill these front-of-house positions has become increasingly difficult.
Not only does a shortage of front-of-house staff mean a reduction in the ability to manage practices and dispense glasses to patients, but it can also mean busy optometrists have to add dispensing duties to their often-overloaded days. This means less time for optometry appointments at a time when patients in some places are still catching up on caring for their eyes post-COVID lockdowns. Shortages of these staff make some practices even question their viability.
Last year, Optometry Victoria South Australia (OV/SA) was alerted to this issue by our members. This prompted a member survey to assess the extent of the issue and help determine our role in finding solutions, noting that workforce shortages were and are being experienced across multiple industries simultaneously in Australia.
Two of the primary reasons cited in the OV/SA survey regarding the workforce shortage was an insufficient pool of suitable workers, and the fact that the pandemic had changed how people feel about public-facing work. Part of the social context for these challenges is the great values re-alignment that many of us have embraced in the last couple of years; sometimes called the ‘great resignation’, large numbers of people have reconsidered their priorities in light of their values, which in turn has impacted workplaces.
When considering our role in the face of these challenges, we started to explore what we could offer our members that might give them a greater chance to find people for their front-of-house roles. Rather than using their usual channels to find people, such as Seek, we considered how we might be able to help practices reach people in their local communities in different ways.
Of course, we didn’t want them to find just anyone. One of the best-kept secrets across the cities and towns of Victoria and South Australia is the amazing opportunity to contribute directly to the quality-of-life of others by working in an optometry practice. This is why we are suggesting our members don’t use the frameworks or discourse of ‘retail’ when recruiting for these roles, which implies a focus on profits and sales.
Front-of-house staff aren’t just salespeople – they often need to have a general understanding of eye conditions and be able to identify patient requirements. Often, they also take on a role similar to a medical receptionist, managing and optimising practitioner patient books and
This is why OV/SA has launched our new, content-rich resource to support our members with this challenge of finding strong front-of-house staff. The resource was developed after speaking with people from a range of networks, and was then shared in draft form with some members and updated before receiving feedback from our State Advisory Committee, which is itself made up of a diverse range of members. We then field-tested with both practice owners as well as prospective front-of-house employees, and used this feedback to make final changes and ensure it would have the best chance of being useful for members.
The challenge of recruitment within the optometry sector is further corroborated by the recent creation of ProVision’s Optometry Recruitment Kit, and we’re pleased to find that OV/SA’s resource complements this kit. By utilising OV/SA’s resource in conjunction with ProVision’s Kit, we believe optometrists will be well-equipped to try some new approaches for recruitment of front-of-house staff, finding people who are motivated by a desire to serve, recognise the potential career paths with optical dispensing training, and are keen to learn all it takes to give patients the best possible experience.
Name: Ilsa Hampton
Qualifications: GAICD, MPH, Grad Cert Mgt, Grad Dip Ed, BA
Affiliations: Optometry Victoria South Australia
Position: CEO
Location: Melbourne
Time in industry: 15 months
TWO OF THE PRIMARY REASONS CITED IN THE OV/SA SURVEY REGARDING THE WORKFORCE SHORTAGE WAS AN INSUFFICIENT POOL OF SUITABLE WORKERS, AND THE FACT THAT THE PANDEMIC HAD CHANGED HOW PEOPLE FEEL ABOUT PUBLIC-FACING WORK.
72 INSIGHT July 2023 SOAPBOX
2023 CALENDAR
JULY
AUSCRS 2023
Port Douglas, Australia 26 – 29 July auscrs.org.au/2023-conference
AUGUST
TASMANIA LIFESTYLE CONGRESS (TLC)
Hobart, Tasmania
5 – 6 August taslifestylecongress.com.au
WORLD CONFERENCE ON OPHTHALMOLOGY & EYECARE
Rome, Italy
21 – 23 August eyecare.thepeopleevents.com
OPHTHALMOLOGY UPDATES!
Sydney, Australia
26– 27 August ophthalmologyupdates.com
SEPTEMBER
ORTHOKERATOLOGY
SOCIETY OF OCEANIA CONFERENCE
Gold Coast, Australia
1 – 3 September www.facebook.com/OrthoKSO/
O=MEGA23 & WORLD CONGRESS OF OPTOMETRY
Melbourne, Australia
8 – 10 September omega-event.org
EUROPEAN SOCIETY OF CATARACT & REFRACTIVE SURGEONS CONGRESS
Vienna, Austria
8 – 12 September congress.escrs.org/
INTERNATIONAL VISION EXPO WEST
Las Vegas, US 14 – 17 September west.visionexpo.com
SILMO PARIS
Paris, France
29 September – 2 October event.silmoparis.com/2023/en/
OCTOBER
RANZCO SCIENTIFIC CONGRESS
Perth, Australia 20 – 24 October ranzco.edu/events
ORTHOPTICS AUSTRALIA ANNUAL CONFERENCE
Perth, Australia
21 – 24 October orthoptics.org.au
EYECARE PLUS BOOTCAMP AND AGM
Sydney, Australia
27 – 28 October y.safier@eyecareplus.com.au
NOVEMBER
HONG KONG INTERNATIONAL OPTIC FAIR
Hong Kong
8 – 10 November hktdc.com/event/hkopticalfair/en
SILMO ISTANBUL
Istanbul, Turkey
23 – 26 November silmoistanbul.com/en
To list an event in our calendar email: myles.hume@primecreative.com.au
DECEMBER
ASIA PACIFIC TELEOPHTHALMOLOGY SOCIETY CONGRESS
Pattaya, Thailand
2 – 3 December 2023.asiateleophth.org
THE 16TH CONGRESS OF THE ASIA-PACIFIC VITREO-RETINA SOCIETY (APVRS) 2023
Hong Kong
8 – 10 December 2023.apvrs.org
FEBRUARY 2024
MIDO EYEWEAR SHOW
Milan, Italy 3 – 5 February mido.com
31ST ANNUAL AUSTRALIAN AND NEW ZEALAND GLAUCOMA SOCIETY (ANZGS) CONGRESS 23
Hobart, Tasmania
16 – 19 February anzgsconference.com
$30k Sign-on bonus Optometrist opportunities across Australia
2023 is shaping up to be another year of next-level growth for Specsavers, with 4 new stores already opened and many more scheduled to come. This growth is creating more opportunities for optometrists like you to join us. We offer flexible rosters to support work/life balance, access to the latest technology (including OCT in every store free for every patient) and extremely attractive salaries – with $30k sign-on bonuses in selected locations. We will also provide you with excellent opportunities for career development – including pathway to Partnership, outreach opportunities and the chance to mentor new graduates. There is no better time to join!
Specsavers Stawell and Horsham –Optometry opportunity Specsavers Stawell and Horsham are looking for a full time Optometrist to join their team. You will be based at our Stawell store, however travel to Horsham once a week would also be required. Stawell is a one test room store, offering fully automated equipment including OCT - which is free for every patient. You will work with a friendly, long standing team,
including experienced retail staffmaking handovers a breeze. If you’re a nature lover, this is the town for you - with Stawell being only a 20 minute drive from the Grampians National Park! The town itself also has all the amenities you need. We’re offering a generous $165,000 package for this role, so what are you waiting for?
Locum opportunity at Bundaberg
Specsavers in Bundaberg have a fantastic opportunity for experienced and professional locum optometrists to provide excellent eyecare on an ongoing basis starting in June. Both Specsavers Bundaberg practices have highly motivated and passionate teams who work with you allowing you to deliver optimum patient care and the best customer experience that Specsavers is known for. All travel and accommodation will be provided and booked for you with attractive rates available and block bookings on offer to fill up your diary.
Optometrist opportunity –
Specsavers Whakatane, NZ
Specsavers Whakatane is seeking a motivated and skilled optometrist to join their dynamic team. As a Specsavers optometrist, you will have access to state-of-the-art
equipment, ongoing training and development opportunities, and the support of a dedicated team of optical professionals. Whakatane is a brilliant location, only a stone’s throw away from the Tauranga, but with the opportunity to work with plenty of exciting pathology and away from the busy city traffic. With a strong focus on work-life balance, Specsavers is the perfect place to take your career to the next level. Apply now to join our team in Porirua and make a difference in the lives of the local community.
Early Bird Package for Graduate Optometrist
The Specsavers Graduate Recruitment Team have selected a number of regional opportunities for the Specsavers ‘Early Bird Package’ which offers our highest sign on bonus yet! The opportunities are throughout NSW, QLD, NT, TAS, SA & WA. With continued growth in providing excellent eyecare to patients, now is an exciting time to join a company that is leading and defining the future of the optical industry. At Specsavers you will have access to cutting edge technology, and access to our comprehensive two-year Graduate Program providing newly qualified optometrist with support to assist your development.
LET’S TALK!
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Australia Optometrist employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Matthew Cooney matthew.cooney@specsavers.com or 0447 276 483
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795 499
Graduate employment enquiries: apac.graduateteam@specsavers.com
Specsavers YOUR CAREER, NO LIMITS Visit spectrum-anz.com
All Specsavers stores now with OCT







MOVE monthly bulletin to keep the Australian ophthalmic sector updated on new appointments and personnel changes, nationally and globally. CAREER People 74 INSIGHT July 2023
ON THE







YOUR
Join OPSM, Australia’s largest optometry network. We’ll always have the capacity to give you more opportunities, more choice, and more time interacting with your patients. Accelerate your career aspirations with OPSM. Visit opsm.com.au/careers today.
DEDICATED TIME WITH
PATIENTS
























































 Melbourne-based Eyetelligence co-founder Dr Mingguang He.
Melbourne-based Eyetelligence co-founder Dr Mingguang He.












































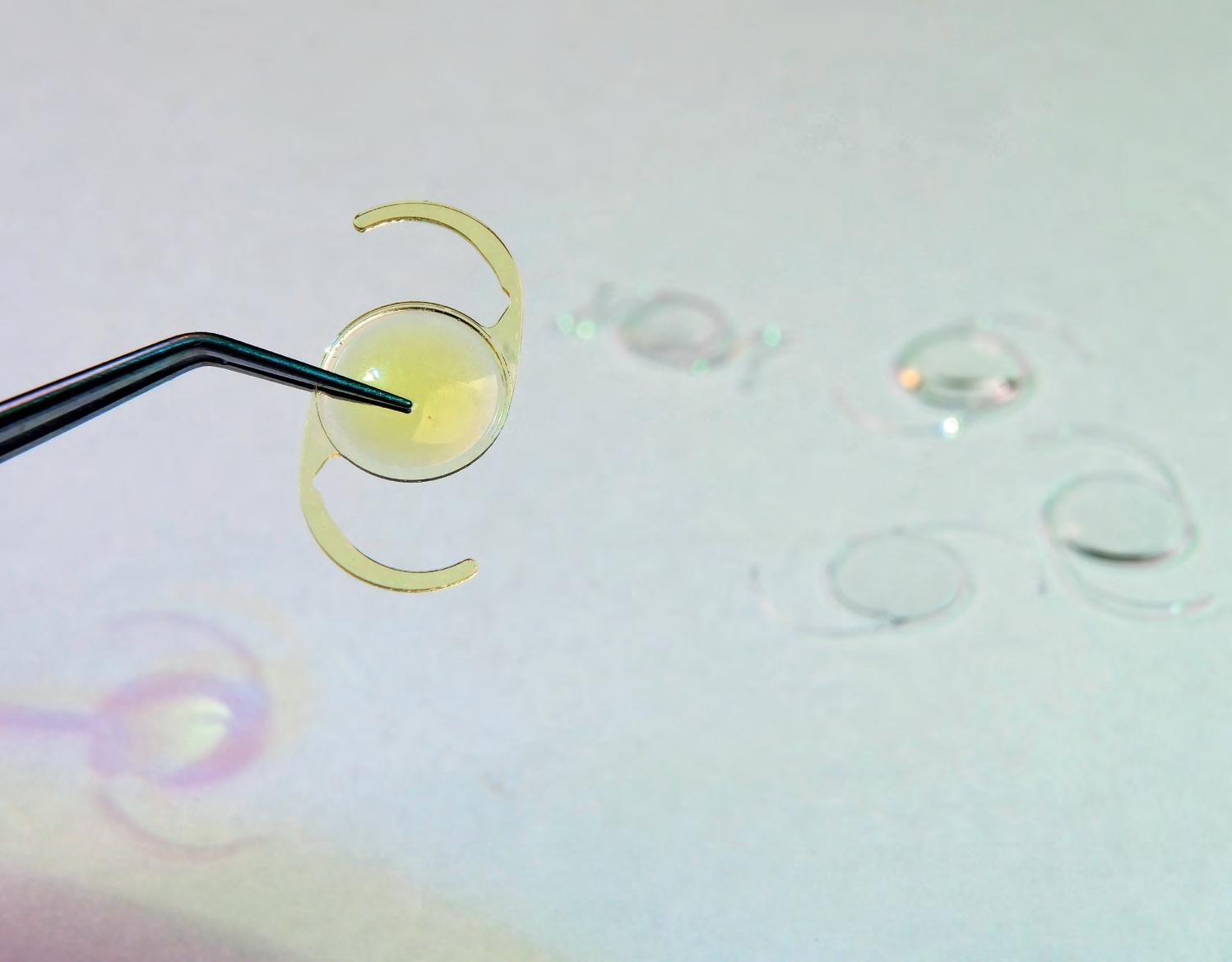



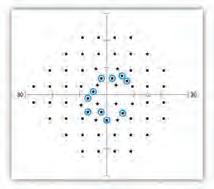









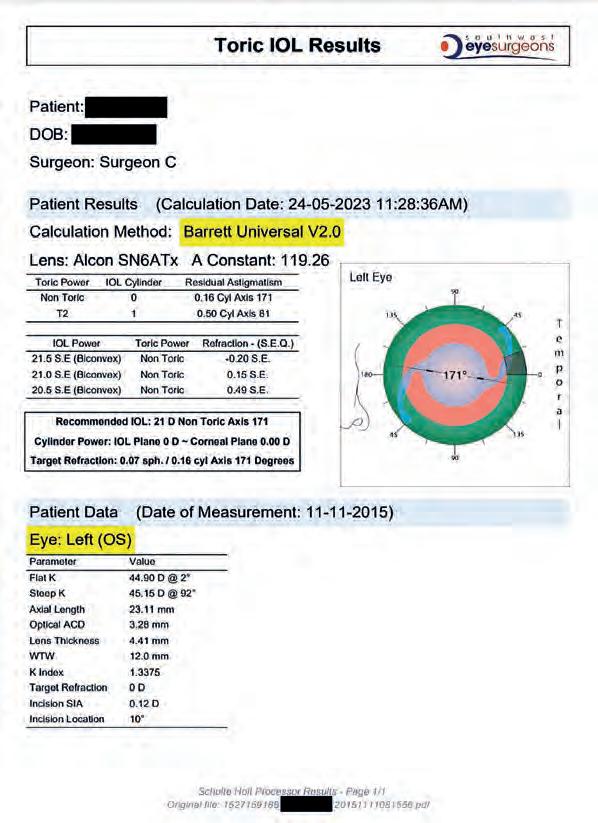





























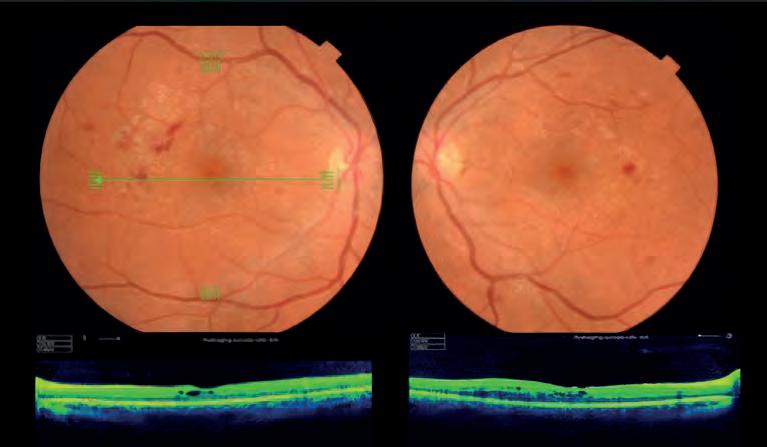
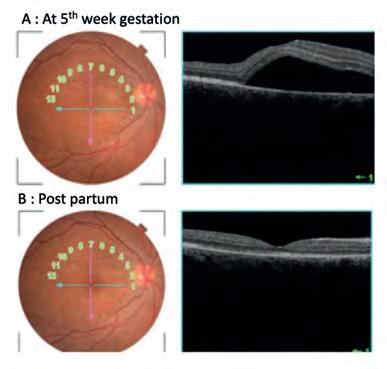








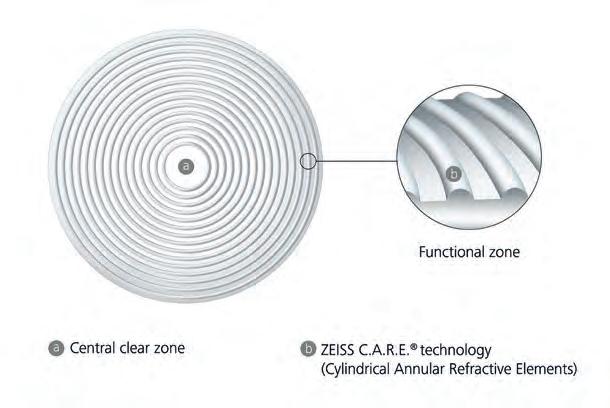



















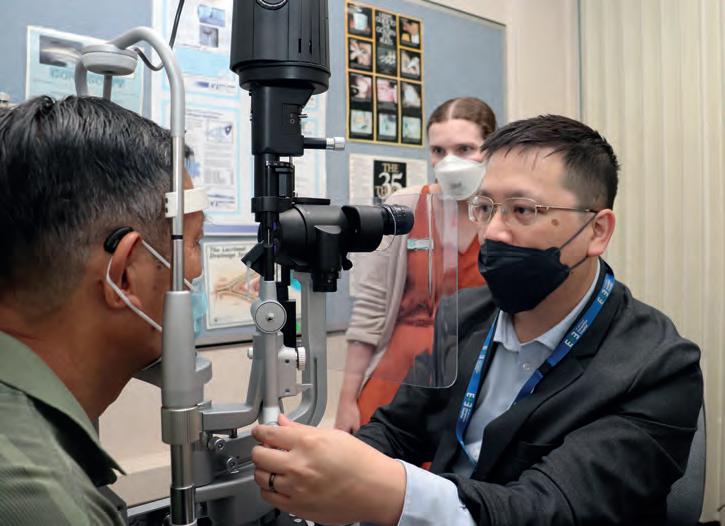

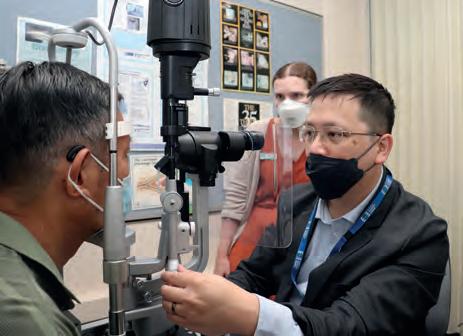















 BY ILSA HAMPTON
BY ILSA HAMPTON













