Doctors urged to speak up for health justice

HE UNIVERSITY OF WESTERN CAPE (UWC), School of Public Health (SoPH), and Peoples Health Movement South Africa (PHM-SA) recently hosted their annual David Sanders Lecture in Public Health and Social Justice. This year's theme, 'Health Justice is Social Justice: The duty to speak up and out’, was delivered by Fatima Hassan, a renowned human rights lawyer and director of the Health Justice Initiative (HJI). Her speech was a powerful call to action, urging the public health community to confront systemic inequalities and advocate for health justice both locally and globally. Honouring the legacy of David Sanders, a tireless advocate for social justice and health equity, Hassan emphasised the importance of continuing his work, particularly in addressing critical global health issues. One of the most pressing issues she highlighted was the ongoing genocide in Gaza and its devastating impact on health services.

“David was certainly
not afraid to call out public health inequality, social injustice, apartheid, or genocide. He would have been at the forefront of local solidarity efforts including, I know, fully supporting the current efforts of training a recently arrived cohort of Gazan medical students at UCT, Pretoria, and Wits to complete their medical degrees because their universities and medical schools have been destroyed by Israeli occupation forces.”
THE CRISIS IN GAZA
Hassan painted a grim picture of the situation in Gaza, where health services and workers are being intentionally targeted.
“There is a deliberate obliteration of health services and the intentional targeting of health workers through assassinations, killings, and abductions.” She cited warnings from UN officials about the potential extermination of the population if the violence continues. “We must stand in solidarity with the people of Gaza,” she urged, “and support efforts to rebuild their health system.”
She proposed practical measures such as training Gazan medical students in SA to
The benefits of

help address the dire shortage of healthcare professionals in the region.
SA’S
HEALTHCARE INEQUALITY
Turning her attention to SA, Hassan critiqued the healthcare system, which she described as suffering from extreme inequality rooted in apartheid and colonialism.
“But inequality is by design, human-made, thriving on a global backdrop of staggering economic inequality and global trade, regulatory, and economic policies or rules that ignore the economic upliftment of poor people in the Global South especially.
These systems force us to rely on charity, donations, and what I call ‘voluntary benevolence’ from philanthrocapitalists and richer governments, usually in exchange for something else.” She called for urgent reforms in both the public and private healthcare sectors, highlighting the inefficiencies and high costs that lead to poor health outcomes. “Our healthcare system is failing the most vulnerable among us,” she said. “We must engage with the NHI plans to ensure that they address
these systemic issues.”
GLOBAL ECONOMIC INEQUALITY & HEALTH
Hassan placed SA's health crisis within a broader global context of economic inequality. She criticised austerity measures and the reliance on charity instead of systemic change. “Charity is not a substitute for justice,” she said. She also highlighted the monopolistic practices of the pharmaceutical industry during the Covid-19 pandemic, which exacerbated health disparities and resulted in preventable deaths. “In Covid, the creed of intellectual property fundamentalism preached to us by the ultra-wealthy and by pharmaceutical corporations was to tell us to monopolise and privatise the manufacture and supply of publicly created vaccines, medicines, etc, while relying on voluntary market measures – not effective regulation or compulsory measures – to ensure access. That creed has failed us.”
THE FIGHT FOR VACCINE EQUITY
Recounting the legal struggles of the
probiotics in acute and chronic conditions


Health Justice Initiative (HJI) to access vaccine procurement contracts during the Covid-19 pandemic, Hassan revealed a lack of transparency and exploitative terms imposed by pharmaceutical companies, which undermined public health and democracy. “We were treated as beggars for vaccines,” she said, quoting president Cyril Ramaphosa. She emphasised the need for transparency in procurement processes and advocated for a legally binding international agreement to ensure fair terms in future health crises.
CritiquingtheNHI system, Hassan pointedoutsystemic issues such as marketpower, secrecy,andlackof accountability that could hinder equitable healthcare access
“SA participated in several vaccine research trials, contributing to the research and development of front-runner vaccines. But the gap between the speed of science and the ability to vaccinate or treat people in the Global South remained wide,” Hassan said. “The same thing is playing out again: With Mpox, Africa does not have enough vaccines and is now desperate for supplies, while Northern countries stockpile, and while we wait for real technology transfer licenses. Ironically, with the current Mpox cases in the Global North, research has accelerated, more than it has in previous decades when Mpox was confined to Central and East Africa. It should be clear
to everyone that diseases and outbreaks know no borders. Hoarding supplies or manufacturing know-how is a selfdefeating public health strategy.”
THE TRIPS WAIVER PROPOSAL
Hassan discussed the TRIPS Waiver Proposal, which SA and India proposed to the World Trade Organization (WTO) to allow affordable access to vaccines and technology during the pandemic. She highlighted the opposition from wealthier nations, which she argued was driven by profit motives rather than public health concerns. "We must continue to fight for equitable access to life-saving medicines," she urged.
CRITIQUE OF THE NHI SYSTEM
Critiquing the NHI system, Hassan pointed out systemic issues such as market power, secrecy, and lack of accountability that could hinder equitable healthcare access. Raising concerns about governance, the need for a robust local manufacturing industry, and the impact of corruption and xenophobia on healthcare delivery, she said: “We cannot achieve health justice without addressing these systemic barriers. Sadly, the political gamesmanship over NHI is coming across as unaccountable, arrogant, and nonengaging. This will not build our health system. Frankly, we are in a health crisis, and I hope that people can see the signs.”
SOLIDARITY WITH GAZA
Drawing parallels between SA’s struggles and the situation in Gaza, Hassan emphasised the need for international solidarity and action.
She recommended practical measures such as supporting calls for a ceasefire, rebuilding Gaza's health system, and providing scholarships for Palestinian medical students. She also encouraged
academic institutions to adopt Boycott, Divestment, and Sanctions (BDS) resolutions against Israeli institutions. “We have a moral obligation to speak out against injustices,” she said. “Health justice is inextricably linked to social justice.”
CALL TO ACTION
Hassan concluded her lecture with a powerful call to action, urging the public health community to confront systemic inequalities and advocate for health justice both locally and globally. “We must honour David Sanders’ legacy by continuing his work,” she said.
“We all have a duty to speak out and speak up. If we remain silent, the inequities which we are supposed to challenge in our work will be exacerbated, and the impunity of tyrannical regimes will continue. And that will only make our field complicit – both today and every day.
Sadly,thepolitical gamesmanship over NHI is comingacrossas unaccountable, arrogantand nonengaging
This is why health justice is intrinsically linked to social justice.” Hassan’s address was a powerful reminder of the importance of health justice. Her call to action resonated with the audience, urging them to confront systemic inequalities and advocate for health justice both locally and globally.
As she so eloquently stated, “Health justice is social justice. We have a duty to speak up and out.”
The human rights of health

EAR DEVOTED READERS,
In this issue, we begin with a highlight from the annual David Sanders Lecture, hosted by the University of Western Cape and Peoples Health Movement South Africa. Human rights lawyer Fatima Hassan passionately discusses the intersection of health justice and social justice, urging the public health community to tackle systemic inequalities and advocate for global health justice. Our coverage continues with a focus on the alarming HIV prevalence in Mpumalanga, where a recent survey reveals significant disparities in awareness and treatment among youth. This calls for urgent public health interventions to address these gaps. The 2024 Lancet Commission report on dementia is another key feature, identifying 14 modifiable risk factors
that could prevent or delay a significant percentage of cases, advocating for early intervention. We highlight the emergence of monoclonal antibodies as a promising malaria prevention strategy, with a phase 2 trial showing encouraging results for children.
Additionally, we review treatment options for seasonal allergic rhinitis and chronic kidney disease, stressing the need for patient education and individualised care.
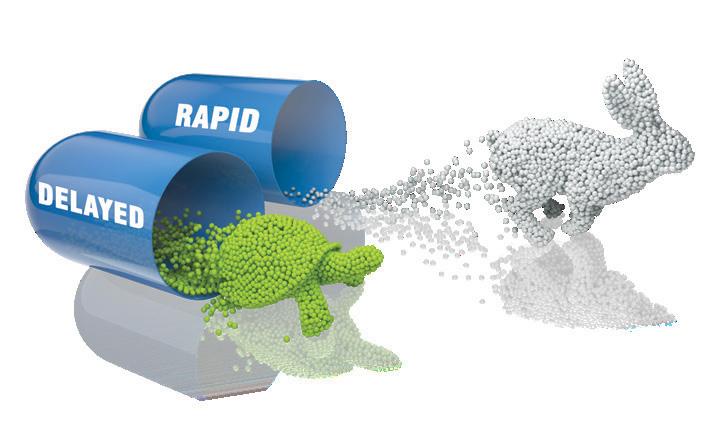
Look out for our three CPD articles, available online at www.medicalchronicle.co.za. In The benefits of multistrain probiotics in acute and chronic conditions, Dr lhaam Mohamed discusses the benefits of multi-strain probiotics in both acute and chronic health conditions, emphasising the importance of the gut microbiome and the concept of dysbiosis.
We also examine a comprehensive approach to managing osteoarthritis, a prevalent degenerative joint disease that affects around 528 million people worldwide.
If you missed any of our recent webinars, the good news is that you can watch the recording and still earn your CPD point. Find the summaries of the webinars in our webinar reports.


Mpumalanga's HIV crisis urgent interventions needed
Mpumalanga province faces a critical public health challenge as 6th National HIV prevalence, incidence, and behaviour survey reveals the highest HIV prevalence rate in SA, necessitating urgent interventions and targeted strategies. Mpumalanga's HIV crisis: urgent interventions needed.
By Nicky Belseck, medical journalist
PUMALANGA PROVINCE
MADE headlines for all the wrong reasons when the Human Sciences Research Council (HSRC) unveiled the key findings of the Sixth South African HIV Prevalence, Incidence, and Behaviour Survey (SABSSM VI) last month. The results highlight a critical public health issue, with Mpumalanga recording the highest HIV prevalence rate in SA.
HIV PREVALENCE AND DEMOGRAPHICS
Mpumalanga's HIV prevalence rate stands at a staggering 17.4% as of 2022, translating to approximately 890 000 people living with HIV (PLHIV). This marks an increase of 30 000 individuals since 2017. The prevalence among youth aged 1524 years is 7.8%, with males at 9.8% and females at 6.3%. For adults aged 25-49 years, the prevalence rises significantly to 26.4%, with females at 31.9% and males at 19.9%. The highest prevalence is observed in the 45-49 age group at 40.8%.
GEOGRAPHICAL DISPARITIES
The survey revealed notable geographical disparities in HIV prevalence across Mpumalanga's districts. Gert Sibande district has the highest rate at 20.5%, followed by Ehlanzeni at 16%, and Nkangala at 13.1%. Rural areas exhibit higher prevalence rates compared to urban settings, indicating a need for targeted interventions in these regions.
ANTIRETROVIRAL TREATMENT (ART) AND VIRAL LOAD SUPPRESSION
ART coverage has improved significantly, rising from 65.4% in 2017 to 81.8% in 2022. Approximately 630 000 PLHIV are now receiving treatment. However, ART coverage among adolescents and youth aged 15-24 years is lower at 56.4%, compared to 83.9% for those aged 25-49 years. The viral load suppression (VLS) rate in Mpumalanga is 82.5%, an increase from 60.0% in 2017, with males showing a higher suppression rate (84.6%) compared to
females (81.9%).
AWARENESS AND TREATMENT GAPS
The survey found that 87.3% of PLHIV aged 15 years and older were aware of their HIV status, and 94.5% of those diagnosed were on ART. Among those on ART, 94% achieved viral suppression. However, only 70.6% of adolescents and youth were aware of their status, highlighting a significant gap in awareness and treatment among younger populations. Over 160 000 individuals are not receiving treatment, posing a risk for further transmission of the virus.
BEHAVIOURAL INSIGHTS AND PREVENTION
The survey noted a decrease in early sexual debut among adolescents, from 13.3% in 2017 to 5.4% in 2022. However, 5.1% reported having multiple sexual partners, with higher rates among males (7.4%) than females (2.7%). Condom use with the most recent partner was reported at 46.1%, indicating inconsistencies in preventive behaviours. Self-reported circumcision rates increased from 63.7% in 2017 to 71.8% in 2022, with higher rates in rural informal areas.
PRE-EXPOSURE PROPHYLAXIS (PREP) AWARENESS AND UPTAKE
Awareness of PrEP among sexually active adults was 43.0%, but only 8.4% had used it. Willingness to use PrEP was higher among females (61.4%) compared to males (45.7%). This indicates a need for increased education and access to PrEP as a preventive measure.
RECOMMENDATIONS AND URGENT INTERVENTIONS
The findings underscore both progress and ongoing challenges in addressing the HIV epidemic in Mpumalanga. Overall principal investigator of the study, the HSRC’s Professor Khangelani Zuma, emphasised the urgent need for significant interventions to address the rising infection rates.
“We recommend a continued focus on increasing coverage and demand for medical male circumcision among males aged 15 years and older. We must also enhance public awareness and uptake of effective HIV prevention measures, such as regular HIV testing, condoms, and PrEP,” he said. While there have been improvements in
ART coverage and viral load suppression, significant challenges remain in awareness, treatment gaps, and consistent preventive behaviours, particularly among youth and in rural areas. The findings highlight the need for continued efforts to address these issues and reduce the impact of HIV in Mpumalanga Province.


H HealthONE Enterprise simpler,
smarter, and
safer patient centred healthcare
Healthcare solutions provider Altron HealthTech will soon be launching the modernised HealthONE Enterprise.
ealthONE ENTERPRISE OFFERS
many exciting features such as the ability to book an appointment; maintain electronic health records with surgical and medical histories; allow clinicians to manage scripts and medications; electronic scripting and referrals; manage chronic and acute conditions; and better management of
overall patient health. It also provides process efficiencies for medical professionals with a simple click. A multidiscipline, platform, and cloud-based solution, it has been designed for use in, amongst others, primary healthcare management in hospitals and clinics.
Electronic health records allow healthcare practitioners instant access




to a patient’s healthcare journey including the ability to upload a patient’s Xray images and pathology results, allowing them to make more informed decisions based on all the available information and alleviating the need to run duplicate tests. As healthcare providers increasingly look to provide personalised healthcare solutions tailored to an individual’s unique needs,

















HealthONE Enterprise provides a patientcentred approach to managing the entire patient healthcare journey. Its platform architecture offers the capability to collect vast amounts of data, providing valuable insights, preferences and trends which can be leveraged by clinicians. The system facilitates informed decision-making and automates processes to save costs, boost productivity and free up medical staff to provide quality healthcare rather than spending time on administrative tasks. Built on the latest technology and security protocols, HealthONE Enterprise is POPIA compliant and secures healthcare records to ensure patient privacy and to protect personal information.
The solution has the benefit of being scalable and interoperable with several third-party systems and devices including HR systems, pathology systems and medical devices such as e-vitals, audiometry, spirometry, and vision devices. It is also customisable according to a healthcare provider’s unique requirements. Rich reporting and trend analysis functionality provide actionable insights into the healthcare histories of patients.
We take care of our clients’ administrative, financial and clinical supportneeds, allowingthemtofocus ontheirpatients,in theprocessimproving patientoutcomes
Altron HealthTech’s practice management applications, electronic health records solutions, claims management systems and data insight capabilities, run seamlessly in the background of HealthONE Enterprise. “We take care of our clients’ administrative, financial and clinical support needs, allowing them to focus on their patients, in the process improving patient outcomes,” says Altron HealthTech MD, Leslie Moodley.



Altron HealthTech has a 30-year tradition of providing innovative technology solutions. The company’s strategy is focused on solving real problems through best-in-class technology while its core strategy is innovation. This position was bolstered by the launch of HealthONE Cloud in 2021, a clinical offering which was well received by the market.
Technology industry leader Altron is a proudly South African platform and IT services company founded in 1965. The company specialises in harnessing the power of data, technology, and human ingenuity to solve real-world problems.

Your career supports so much of what’s important in your life. As the world’s leading medical defence organisation, we can help you keep it all safe, with the best medical protection money can buy. As well as indemnity, we’re here to support you with complaints, complex legal challenges, 24/7 emergency medicolegal advice, and much more.
of dementia cases preventable
Unlocking dementia prevention, the 2024 Lancet Commission Report identified 14 key risk factors to prevent or delay onset in up to 45% of dementia cases.
By Nicky Belseck, medical journalist
ITH A COMPREHENSIVE overview
of the latest findings, the 2024 update of the Lancet Commission on dementia provides new hopeful evidence about the prevention, intervention, and care of dementia. This report is particularly significant given the global aging population and the increasing prevalence of dementia.
Notably, the report highlighted 14 modifiable risk factors that, if addressed, could prevent, or delay up to 45% of dementia cases. These included: untreated vision loss, high LDL cholesterol, education level, hearing loss, hypertension, smoking, obesity, diabetes, depression, physical inactivity, excessive alcohol consumption, traumatic brain injury, air pollution, and social isolation. Addressing these factors through early and continuous intervention throughout life can significantly reduce the incidence of dementia.
Emphasising a life-course approach, the report suggested that risk factors can be modified at any age. Tailored
interventions for high-risk individuals are recommended to maximise the potential for dementia prevention. According to the authors, Prof Livingston et al, access to quality education and promoting cognitive, physical, and social activities in midlife and later life are essential for reducing dementia risk. Engaging in these activities enhances cognitive reserve, helping individuals withstand neuropathological changes without developing dementia symptoms.
Strong evidence indicates that treating hearing loss and depression can effectively lower dementia risk, with the use of hearing aids showing significant benefits.
Improved cognitive health is linked to reduced air pollution, with protective measures against traumatic brain injury, especially in contact sports, is also recommended. The report calls for national and international policy changes to prioritise dementia risk reduction. These policies should focus on equity and accessibility for high-risk populations, ensuring that














interventions are available to those who need them most. For individuals diagnosed with dementia, person-centred care is advocated. This includes the use of cholinesterase inhibitors and memantine for Alzheimer’s and Lewy body dementia, along with managing neuropsychiatric symptoms.
There is optimism regarding new disease-modifying treatments for Alzheimer’s disease. However, concerns about side effects and accessibility remain, highlighting the need for further research and development. Prof Livingston et al. stressed the importance of equitable access to care and interventions, particularly for marginalised and lower socioeconomic groups. These groups often face a higher burden of modifiable risk factors and require targeted support. Acknowledging the complexities of studying dementia prevention, the report emphasised the need for a life-course approach to understand how various factors influence dementia risk over time. The importance of diversity
and inclusivity in dementia research was highlighted with Prof Livingston et al. explaining that many studies predominantly involve participants from high-income countries, potentially leading to biased findings. Ensuring diverse representation in research is crucial for developing effective interventions. Emphasising the increased risk of dementia associated with traumatic brain injury and depression, the authors said better management of these conditions is advocated to reduce dementia risk. Overall, the report provided a hopeful outlook on dementia prevention and care. By addressing modifiable risk factors through individual actions and systemic policy changes, we can improve the lives of individuals living with dementia and their families. A comprehensive approach that includes lifestyle modifications, social engagement, mental health support, and innovative technological solutions is essential to effectively tackle the growing challenge of dementia.
South African and Australian health product regulators to share regulatory expertise
The South African Health Products Regulatory Authority (SAHPRA) and the Australian Therapeutic Goods Administration (TGA) have formalised their collaboration by signing a Memorandum of Understanding (MoU). This agreement aims to enhance cooperation between the two regulatory bodies.
THE MOU AIMS to build on the existing relationship between SAHPRA and TGA, enhancing their ability to assess medical products and therapeutic goods, and to monitor these products for ongoing efficacy, safety, and quality after registration.
AREAS OF COOPERATION
SAHPRA and TGA will engage in data sharing to improve their regulatory functions. This collaboration will focus on the evaluation and approval of medical products and therapeutic goods, as well as their ongoing monitoring for efficacy and safety, and the surveillance of adverse reactions. Dr Boitumelo SemeteMakokotlela, chief executive officer of SAHPRA, stated that the agreement with TGA extends the reach of both regulators' pharmacovigilance programmes and enhances their internal expertise." This
partnership allows us to leverage each other's strengths and regulatory outcomes in the evaluation of health products, both pre- and post-registration. This will improve therapeutic outcomes for the populations we serve and strengthen our postregistration surveillance for efficacy, safety, and quality," said Dr Semete-Makokotlela. Prof Anthony Lawler, deputy secretary at the Australian Government Department of Health and Aged Care and head of the TGA, commented: “TGA is delighted to have formalised our collaborative relationship with SAHPRA through this international agreement. We look forward to working closely with our South African counterparts to share critical regulatory information, ensuring the continued safety, quality, and efficacy of therapeutic products available in the market.”
Source: SAHPRA

Fighting Acute Malnutrition with Cooking Classes in Nigeria
Since April 2024, Doctors Without Borders (MSF)-supported healthcare facilities in the northwest and northeast of Nigeria have witnessed a drastic increase in acute malnutrition cases, mostly in children. There was also a shocking 80% increase in acute malnutrition cases compared to the same period last year. With already limited resources, MSF struggled to meet the needs of so many patients. To make up for this gap, an outreach team was formed to get to the root cause of the problem.
MSF health promotion supervisor in Kebbi, Maryam Muhammad and her outreach team now travel from village to village in a car packed with cooking utensils and essential ingredients, such as soya beans, sorghum, moringa leaves, palm oil, and groundnuts.
The MSF team teaches communities a recipe based on a classic Nigerian porridge called ‘kwash pap’, but instead of the traditional flour, we use Tom Brown flour. Tom Brown is a flour that nutritionists have improved over the years to become a valuable and efficient tool for preventing and treating moderate acute malnutrition. Between January and May 2024, Maryam and the health promotion team organised 554 demonstrations around Kebbi, and more than 13,300 people attended these events, including 1,461 men.
FIND OUT HOW YOU CAN WORK WITH US: VISIT: MSF.ORG.ZA/WORK-WITH-US
©Georg Gassauer

This kind of cooking demonstration is crucial because people understand that they can prevent their children from becoming acutely malnourished rather than bringing them to a facility to treat them. Prevention will always be better than cure. MSF will not remain here forever, so sustainable approaches are needed to reduce severe acute malnutrition. And we know that the people we train today will pass the recipe to others.
- Maryam Muhammad, MSF health promotion supervisor in Kebbi.

Lost to follow-up
Addressing TB challenges in SA
Insights from the Annual Steve Biko Bioethics Lecture where prominent health activist Russell Rensburg tackled legal and ethical measures to combat TB in SA.
By Nicky Belseck, medical journalist
THE CRITICAL ISSUE of TB in SA was the focus of the Annual Steve Biko Bioethics Lecture, held last month. The lecture, ‘Lost to Follow Up: TB in SA – Translating the Obligation to Take Legal and Other Measures to Realise the Right to Health,’ was delivered by Dr Russell Rensburg, the director of the Rural Health Advocacy Project SA, and a prominent health activist with over 20 years of experience in health system strengthening, particularly in rural areas.
Dr Rensburg highlighted several critical issues related to TB in SA, emphasising the severity of the TB epidemic in the country, noting the high rates of infection and the challenges in managing and treating the disease effectively, with the focus on the issue of patients being ‘lost to follow-up'. This term refers to patients who start TB treatment but do not complete it, leading to higher rates of drug resistance and continued transmission of the disease.
Discussing the legal and policy obligations of the SA government to ensure the right to health, Dr Rensburg emphasised the need for robust legal measures and policies to support TB patients and ensure they complete their treatment. He underscored the importance of strengthening health systems to be more responsive and effective in managing TB, this includes improving public finance allocation processes to ensure adequate resources are directed towards TB control
and treatment. Equitable access to quality healthcare, particularly for rural communities, was another key point. Dr Rensburg pointed out the disparities in healthcare access and the impact this has on TB treatment outcomes. Touching on the broader issue of socio-economic rights and how they are intertwined with health outcomes, Dr Rensburg argued for a more integrated approach to healthcare that considers the social determinants of health.
Community engagement and advocacy were highlighted as crucial elements in addressing TB, with Dr Rensburg calling for greater involvement of communities in TB control efforts and for policies that are informed by the lived experiences of those affected by the disease.
Strengthening health systems to ensure they are more responsive and capable of managing TB effectively was a primary recommendation. This includes improving infrastructure, increasing the availability of diagnostic tools, and ensuring a steady supply of medications. Aligning public finance allocation processes with the goal of advancing socio-economic rights, including the right to health, was also emphasised. This means prioritising funding for TB programmes and ensuring that resources are distributed equitably, particularly to rural and underserved communities.
Implementing and enforcing robust legal and policy frameworks that support TB control efforts was another key measure
raised by Dr Rensburg. This includes enacting laws that protect the rights of TB patients and ensure they have access to necessary treatments and support services. Awareness campaigns that inform the public about TB prevention, symptoms, and the importance of completing treatment regimens to prevent the spread of the disease are essential.
Addressing the shortage of healthcare workers is also vital. Dr Rensburg said that the development of the National Human Resources for Health Strategy 2030 aims to train and retain more healthcare professionals, particularly in rural areas where the burden of TB is often highest. He explained that implementing robust monitoring and evaluation systems to track the progress of TB control programmes is vital as this helps in identifying gaps and making necessary adjustments to improve outcomes. And described collaboration between various stakeholders, including government agencies, non-governmental organisations, and international partners, as crucial to create a unified and effective response to TB.
Addressing the socio-economic factors contributing to TB in SA, Dr Rensburg said high levels of poverty limit access to healthcare, nutritious food, and adequate living conditions, all of which are crucial for preventing and managing TB. Poor individuals are more likely to live in overcrowded and poorly
ventilated environments, which facilitate the transmission of TB. Limited access to quality healthcare services, particularly in rural and underserved areas, hampers early diagnosis and effective treatment of TB. This includes a shortage of healthcare facilities, medical professionals, and diagnostic tools, Dr Rensburg explained.
Low levels of education and health literacy can lead to a lack of awareness about TB symptoms, transmission, and the importance of completing treatment. This can result in delayed diagnosis and poor adherence to treatment regimens, he warned. Unfortunately, stigma associated with TB and HIV can discourage individuals from seeking diagnosis and treatment.
Discrimination in healthcare settings can further deter people from accessing necessary services, Dr Rensburg said, and inadequate public health infrastructure, including insufficient funding and resources for TB control programmes, can impede efforts to manage and reduce TB incidence. This includes challenges in implementing effective contact tracing, treatment adherence support, and public health education campaigns.
Dr Rensburg’s lecture was a call to action for healthcare professionals, policymakers, and advocates to work together to address the socio-economic factors contributing to health disparities and to ensure that all South Africans have access to the healthcare they need.


Date: 5 November 2024
Time: 7pm
Topic: Lacosamide – A practical update on the new anti-seizure medication
Speaker: Dr James Butler and Dr Sally Ackermann

CLICK TO REGISTER https://bit.ly/MacleodsWebinar5Nov24
Dr Butler is a neurologist who specialises in epilepsy, including epilepsy surgery. He qualified from the University of Cape Town in 1988, completed his neurology training at the same institution in 1995, and finished a two-year fellowship in epilepsy at the Epilepsy Unit in the Department of Neurological Sciences, University of Western Ontario, Canada from 1996 to 1998. He completed six university courses in clinical epidemiology and biostatistics from the same institution. He was subsequently appointed as a consultant neurologist at the University of Stellenbosch, before starting the Epilepsy Unit at Constantiaberg Hospital, Cape Town in 2000. He subsequently established a research unit in the same hospital, is affiliated as a part-time consultant to the Neurology Department at the University of Cape Town and the University of Stellenbosch, and has published 18 articles in international peer-reviewed journals, including one of the few completed randomised controlled trials of epilepsy surgery in adults. He serves as a member of the Neurological Association of South Africa executive committee. He holds a weekly Friday morning neurosciences meeting and a weekly EEG meeting, attended by members of the two local universities and neurologists, neurosurgeons, neuroradiologists, neuropathologist and neuropsychologists from across the country.




CPD course: Stock management strategies for healthcare practices
Proper stock management is essential for the efficient operation of any healthcare practice, regardless of its size. In a field where patient care and safety are top priorities, maintaining an organised, well-monitored inventory ensures that vital supplies are always available, wastage is minimised, and regulatory requirements are met.
THERE ARE FIVE reasons why proper stock management is crucial, followed by an overview of the new Stock Management Course provided by GoodX Online Short Courses, which offers a stepby-step guide on mastering this skill:
1. Ensures availability of essential supplies
Healthcare providers rely on immediate access to critical supplies. Effective stock management ensures that these items are always on hand when needed, preventing treatment delays that could affect patient outcomes. Ensuring that supplies are always well-stocked keeps patient care seamless and uninterrupted.
2. Prevents expired or outdated stock
A significant part of stock management is ensuring that medical supplies with expiration dates are monitored and rotated appropriately. Using expired items can lead to safety risks and regulatory violations. Proper stock control ensures that all supplies are used before their expiration date, helping the practice maintain patient safety and regulatory compliance.
3. Reduces wastage and cost
Over-ordering and unused stock can lead to significant wastage and unnecessary costs. Proper stock management practices prevent over-purchasing and reduce the risk of having unused, expired items. This helps healthcare practices save money, optimise budgets, and use resources more effectively.
4. Improves workflow efficiency
An organised inventory system allows healthcare workers to access necessary supplies quickly and easily. When stock is appropriately managed, time is saved, and workflow efficiency improves, allowing staff to focus on what matters most: patient care.
5. Compliance with regulatory requirements
Healthcare facilities are required to follow strict regulations regarding stock management and traceability. These regulations are in place to protect patients and ensure safe handling of medical supplies. Proper inventory management helps practices meet these requirements and avoid costly fines or legal issues.
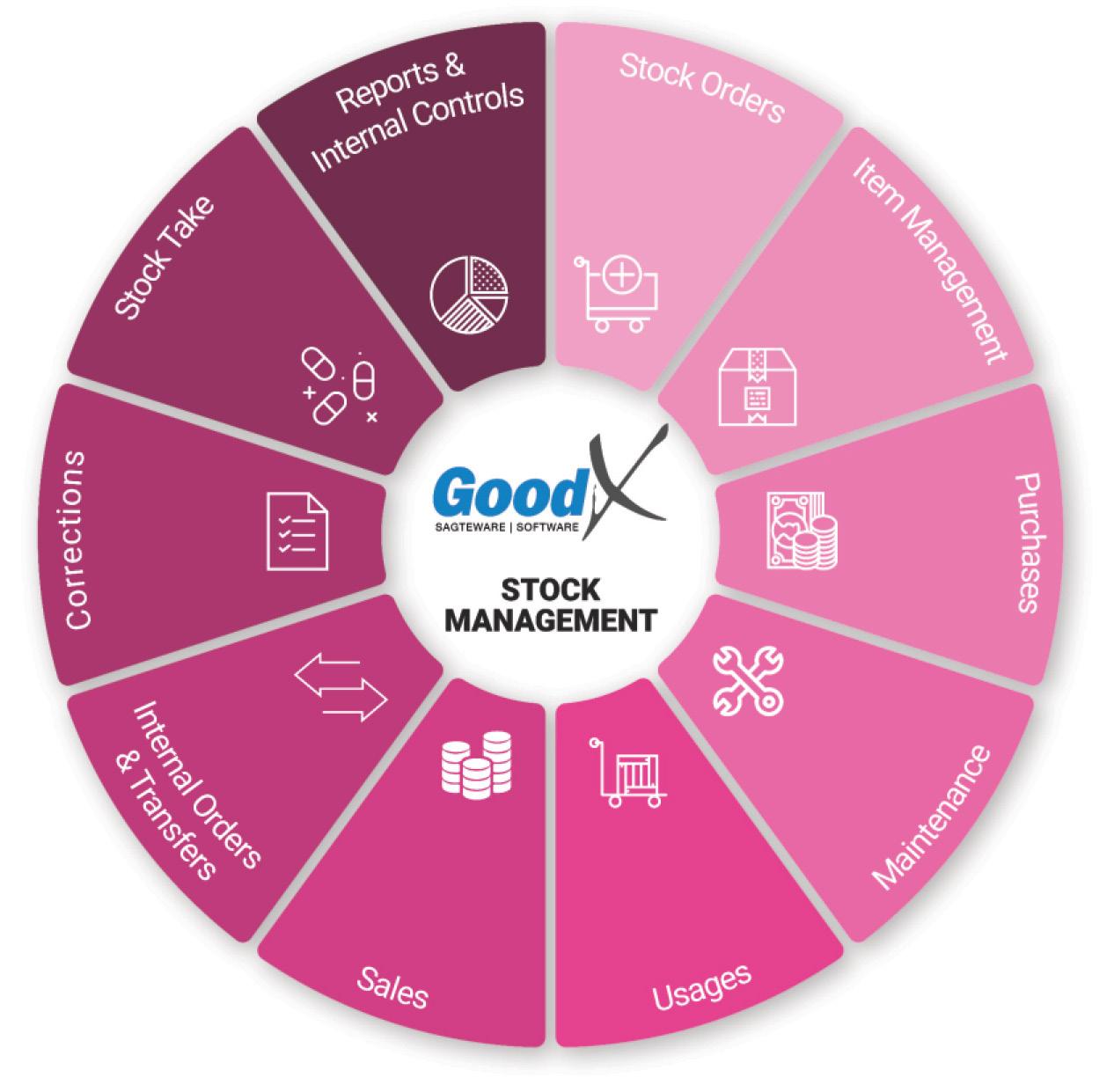
A STEP-BY-STEP GUIDE TO MANAGING STOCK IN A HEALTHCARE PRACTICE
To help healthcare professionals develop an efficient stock management system, our New Stock Management CPD Course offers comprehensive, step-by-step instructions supported by many diagrams to make the theoretical knowledge more understandable. The following key topics are covered in the course:
1. Understanding stock management
This introductory module explains the fundamentals of stock management in healthcare settings. You’ll learn why stock management is crucial to patient care, efficiency, and financial sustainability, setting the foundation for mastering inventory control.
2. Stock orders
Accurate stock orders are key to maintaining balanced inventory levels. This module teaches best practices for assessing stock needs, forecasting demand, and setting up automated ordering systems with reliable suppliers. You’ll also learn how to streamline the ordering process to avoid delays.
3. Stock item management
This section covers how to organise and classify different types of stock for easy access and monitoring. You'll learn about labelling systems, digital tracking, and storage solutions that prevent errors, such as stocking expired items or losing supplies.
4. Stock purchases
Understanding how to make smart
can save time and money. This module will teach you how to negotiate better deals with suppliers, how to determine when to make bulk purchases, and how to evaluate vendors for reliability and quality.
5. Stock maintenance
Maintaining stock goes beyond just placing orders. In this module, you’ll learn about regular inspections, stock rotation methods, and procedures for ensuring the quality and integrity of stored supplies. Effective maintenance keeps stock in good condition and prevents wastage due to damages or expirations.
6. Stock usages
Tracking stock usage is key to maintaining appropriate stock levels. This section covers how to monitor daily consumption patterns, identify trends in stock usage, and adjust future stock orders accordingly to prevent overstocking or shortages.
7. Stock sales
Some healthcare practices sell medical supplies, such as equipment or supplements, to patients. In this module, you’ll learn how to handle inventory that is also sold, ensuring that sales and in-house use of supplies are efficiently managed without disrupting patient care.
8. Internal stock orders and transfers
Large healthcare practices often need to transfer stock between departments or locations. This module covers best practices for managing internal stock transfers, ensuring that all areas of the practice are adequately supplied without causing or wastage.
9. Stock corrections
Mistakes in inventory management can occur, such as incorrect orders, damaged goods, or lost stock. This section teaches how to identify, record, and correct stock discrepancies efficiently, helping you minimise the impact on patient care and finances.
10. Stock take
A regular stock take involves physically counting all inventory to ensure that records match actual stock levels. This module provides guidelines for conducting thorough stock takes and adjusting inventory systems based on the results.
11. Stock reports
Tracking and analysing stock performance is essential for continuous improvement.
In this module, you’ll learn how to generate accurate reports on stock usage, find inefficiencies, and make data-driven decisions to enhance inventory management.
12. Implementing stock management
This final module provides an approach to implementing stock management systems in a healthcare setting.
Visit www.goodx.healthcare/onlinecourses and download the new Stock Management Course prospectus, which provides a detailed, step-by-step guide to help healthcare professionals master the principles and practices of inventory control, leading to better patient care and improved operational efficiency.



Date: 28 November 2024
Time: 7pm
Topic: Acne: Combination vs Mono Therapy Treatment
Speaker: Dr Lev Naidoo
CLICK TO REGISTER https://bit.ly/GlenmarkWebinar28Nov24
Dr Lev Naidoo completed her studies at the University of KZN, graduating MBChB - cum laude and obtaining the Fellowship of the College of Dermatology with distinction. She completed a short-term fellowship in Epidemiology at The University of Columbia, New York, and obtained her Masters in Medicine thereafter. Post- fellowship she remained at The University of KZN as a consultant and lecturer. She relocated to Johannesburg in 2018 where she founded The Dermatology Room in Hyde Park. She serves as an executive committee member of the

Aesthetic and Anti-aging Medicine Society of South Africa and the South African Society for Dermatological Surgery. She is co-founder of iClass Anatomy Africa, the African Affiliate of iClass anatomy. Dr Lev has enjoyed working with and assists as a KOL for several leading skincare and aesthetic companies. She continues to enjoy teaching, practicing medical and aesthetic dermatology and optimising safe and effective treatment protocols that integrate clinical procedures together with optimal skincare regimes.

Acne vulgaris is a common condition that requires a multifaceted management strategy.
A Acne and its management
CNE VULGARIS IS a widespread dermatological condition that primarily affects adolescents and young adults, characterised by various lesions such as comedones, papules, pustules, nodules, and cysts. This condition can lead to significant physical and psychological distress. The pathogenesis of acne is multifactorial, involving increased sebum production, follicular hyperkeratinisation, colonisation by Cutibacterium acnes, and inflammation.
Management of acne involves a combination of topical and systemic therapies tailored to the severity of the condition. Topical treatments include retinoids like adapalene, tretinoin, and tazarotene, which normalise keratinisation and reduce inflammation. Benzoyl peroxide (BPO) is another key topical agent with antimicrobial properties against C. acnes, often used in conjunction with other treatments to enhance efficacy and minimise antibiotic resistance. Topical antibiotics, such as clindamycin and erythromycin, are also utilised but are typically combined with BPO to mitigate resistance concerns.
Combination therapies, particularly the fixed-dose combination of adapalene and BPO, have shown superior efficacy compared to monotherapies. Clinical studies indicate that this combination significantly reduces both inflammatory and noninflammatory lesions, with improvements often visible within the first week of treatment. The combination addresses four critical factors of acne: excessive sebum production, abnormal keratinisation, bacterial colonisation, and inflammation. Patient compliance is vital for successful acne treatment, particularly during the recommended 12-week treatment period. Simplifying the treatment regimen, managing side effects, and providing psychological support can enhance adherence. Common side effects of the combination gel include skin irritation and dryness, which can be managed with non-comedogenic moisturisers and adjustments in application frequency. Educating patients about the chronic nature of acne and setting realistic expectations for treatment outcomes are essential for improving compliance.
Systemic therapies for acne include oral antibiotics, such as tetracyclines, which are effective for moderate to severe inflammatory acne, and hormonal therapies like combined oral contraceptives and antiandrogens for female patients. Isotretinoin is a potent oral retinoid reserved for severe cases, requiring careful monitoring due to potential side effects.
In addition to pharmacological treatments, physical modalities like lasers and light therapies, as well as chemical peels, can aid in acne management. Emerging evidence suggests that dietary
factors, particularly high glycemic index diets and certain dairy products, may exacerbate acne, indicating that dietary counseling could be beneficial.
Effective acne management necessitates a collaborative approach between healthcare providers and patients, emphasising education about the condition, treatment adherence,
and potential side effects. Regular follow-up visits are crucial for monitoring treatment response and making necessary adjustments.
CONCLUSION
In conclusion, evidence-based guidelines advocate for a combination of topical and systemic therapies tailored to individual

patient needs. The adapalene and BPO combination remains a first-line treatment, effectively addressing the key factors contributing to acne while highlighting the importance of patient compliance and education in achieving optimal treatment outcomes. Ongoing research continues to enhance understanding and management of this prevalent condition.
The benefits of multistrain probiotics in acute and
chronic conditions
Dr Ilhaam Mohamed discusses the benefits of multi-strain probiotics in both acute and chronic health conditions, emphasising the importance of the gut microbiome and the concept of dysbiosis, which refers to an imbalance in gut microbial communities.
DYSBIOSIS DISRUPTS NORMAL digestive and immune functions and is not solely linked to antibiotic use, with its effects extending beyond gut health. Probiotics, defined as live microorganisms
that confer health benefits when administered in adequate amounts, play a crucial role in maintaining gut health by modulating immune responses, producing bioactive compounds, and enhancing
intestinal barrier function.
Probiotics improve health through various mechanisms, including suppressing inflammation, modulating immune responses, and restoring gut microbial

balance. They can be combined with prebiotics to create synbiotics, which work synergistically to enhance gut health. The text highlights the advantages of multi-strain probiotics over single-strain preparations, noting that the combination of different strains can lead to synergistic effects that enhance health outcomes.

Health


Clinical applications of probiotics are explored across various conditions, including paediatric diseases, adult health issues, and systemic applications beyond gastrointestinal health. In paediatric medicine, probiotics are used for conditions like necrotizing enterocolitis, acute gastroenteritis, and antibiotic-associated diarrhea. In adults, they have shown good evidence for preventing Clostridium difficile diarrhoea and antibiotic-associated diarrhoea, as well as aiding in immune response and Helicobacter pylori eradication. Specific benefits are noted in areas such as colorectal cancer, oral health, type 2 diabetes mellitus, cholesterol metabolism, allergic diseases, and women's health.
Certain probiotic strains, such as Lactobacillus reuteri, are effective in reducing colic in infants, while others can help manage colorectal cancer by reducing carcinogen levels and improving intestinal barrier function. The document concludes by acknowledging the ongoing research into probiotics and their mechanisms of action, suggesting that future studies will further elucidate their therapeutic potential. It emphasises the promise of using multi-strain probiotics for treating various diseases, while also calling for rigorous testing of probiotic strains in clinical settings to validate their efficacy.
The document discusses the benefits of multi-strain probiotics in both acute and chronic health conditions, emphasising the importance of the gut microbiome and the concept of dysbiosis, which refers to an imbalance in gut microbial communities.
Dysbiosis disrupts normal digestive and immune functions and is not solely linked to antibiotic use, with its effects extending beyond gut health. Probiotics, defined as live microorganisms that confer health benefits when administered in adequate amounts, play a crucial role in maintaining gut health by modulating immune responses, producing bioactive compounds, and enhancing intestinal barrier function.
Probiotics improve health through various mechanisms, including suppressing inflammation, modulating immune responses, and restoring gut microbial balance. They can be combined with prebiotics to create
which work synergistically to enhance gut health.
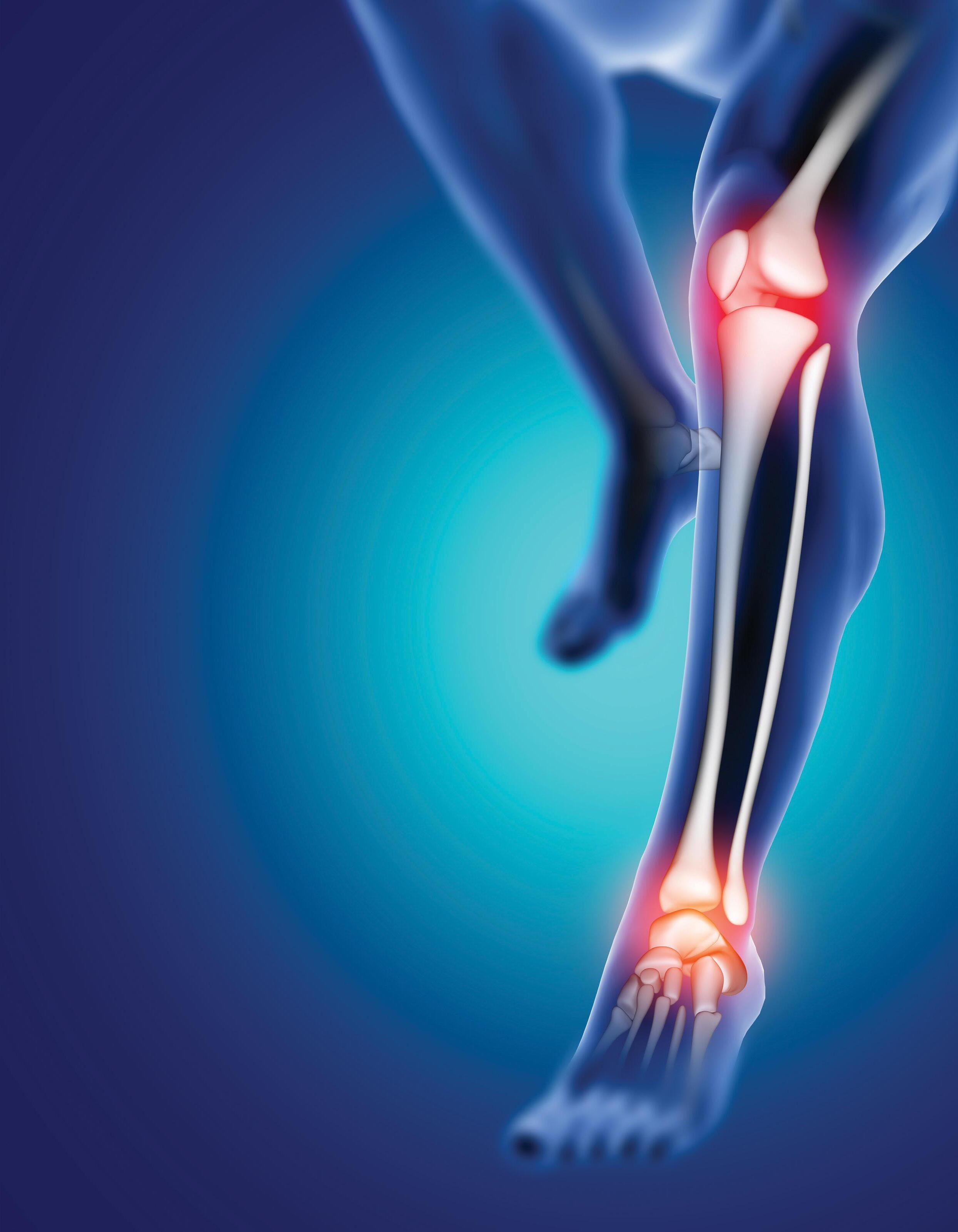
A comprehensive approach to managing osteoarthritis
Osteoarthritis (OA) is a prevalent degenerative joint disease that affects around 528 million people worldwide, with a significant rise in cases since 1990.
OA PREDOMINANTLY IMPACTS individuals over the age of 55, especially women, and commonly involves the knee, hip, and hand joints.
The pathophysiology of OA is intricate, involving the degradation of cartilage and alterations in the underlying bone structure. The lack of effective treatments to prevent cartilage and bone deterioration underscores the need for personalised therapeutic approaches that consider the specific phenotypes and endotypes of OA.
These phenotypes can be influenced by various factors, including inflammation, pain, metabolic syndrome, and cellular aging. OA often initiates due to mechanical overload, necessitating targeted treatment strategies.
Differential diagnoses for OA include several other conditions that exhibit similar symptoms, such as rheumatoid arthritis, psoriatic arthritis, gout, and others. Accurate diagnosis typically requires a combination of clinical assessments, imaging techniques, and laboratory tests.
Current treatment modalities for OA are advancing, with clinical trials exploring methods to regenerate cartilage and target inflammatory mediators through intraarticular injections. Pain management strategies often involve inhibiting nerve growth factor activity, although existing therapies have not significantly altered disease progression or reduced the necessity for joint replacements in severe cases. Promising therapeutic options include anabolic drugs like sprifermin and BMP-7, stem cell therapy, extracellular vesicles, and anti-cytokine therapies.
Intra-articular injections, such as corticosteroids and hyaluronic acid, are common pharmacological treatments. While corticosteroid injections can provide substantial pain relief, they may lead to cartilage volume loss over time. Hyaluronic acid injections have been linked to a slower progression of knee OA. Platelet-rich plasma injections, which contain elevated levels of growth factors, have shown potential for pain relief and functional improvement compared to hyaluronic acid or saline, although the clinical efficacy of PRP remains debated due to variability in preparation methods and inconsistent results.
Lifestyle modifications, particularly exercise and weight management, are crucial in OA management. Evidence supports the short-term benefits of exercise on pain and function, with longterm effectiveness linked to adherence to home-based exercise programmes. Weight reduction can alleviate stress on affected
joints and may slow cartilage loss.
Physical activity is essential for improving pain, physical function, and overall quality of life in OA patients. The World Health
Organization is also working to enhance access to care for individuals with OA through rehabilitation initiatives and promoting healthy ageing.

Continued research into phenotypespecific therapies and a multifaceted treatment approach is recommended to improve patient outcomes.
Osteoarthritis









The effective and safe choice for osteoarthritis patients
Improves joint function
Effective in the management of pain
Optimum molecular weight allows endogenous hyaluronic acid synthesis for better mobility of the knee total knee replacement

Worldwide,every30minutesapersonwhosuffers astrokeandcould havebeensavedeitherpasses awayorsuffersalife-changingbraininjury becausetheyweren’t treatedinahospitalthat followstheinternationallyrecognisedcriteriain strokemanagement.
Time is brain

ITHIN MINUTES OF a stroke occurring, brain cells begin to die.
This critical neurological damage means that time is of the utmost essence for the patient. Specialist neurologist at Netcare The Bay Hospital, Dr Naazim Siddi Ganie, elaborates on the gravity of the situation: “When the blood supply to the affected part of the brain is interrupted or reduced, brain tissue can no longer get the oxygen and nutrients it needs.
This makes a stroke a medical emergency that requires prompt treatment. The mantra ‘Time is brain’ underscores a crucial reality: within minutes of a stroke occurring, brain cells begin to die, making rapid medical intervention paramount.”
This urgency is a defining factor in the treatment protocols at Netcare The Bay Hospital in Richards Bay, which recently received the prestigious Gold Award from the World Stroke Organization (WSO) and the Angels Initiative for its excellence in stroke care. Dr Ganie explains that having a stroke remains one of the leading causes of disability and death worldwide: “In South Africa, the challenge is even more pressing, especially in underserved areas like Richards Bay and other areas of Northern KwaZulu-Natal.”
According to the World Stroke Organization (WSO) Angels Initiative, worldwide, every 30 minutes, a person who suffers a stroke and could have been saved
either passes away or suffers a life-changing brain injury because they weren’t treated in a hospital that follows the internationally recognised criteria in stroke management.
CAN STROKES BE PREVENTED?
Dr Ganie explains that following a healthy lifestyle may prevent most strokes. He recommends maintaining a healthy weight, exercising regularly, reducing stress levels, limiting alcohol intake and quitting cigarettes if you’re a smoker. “It is also imperative to manage conditions like high blood pressure, atrial fibrillation (a type of abnormal heart rhythm), diabetes, and high cholesterol”, he adds.
However, some strokes are caused by unavoidable factors. “Ageing contributes to an increased risk of stroke. Women, unfortunately, have an increased risk of stroke after menopause. In addition, family history also plays a role. Genetic conditions like familial high blood pressure and cholesterol or clotting disorders, for example, also increase the risk of a stroke.”
DIFFERENT TYPES OF STROKES
Dr Ganie explains that around 85% of all strokes are ischaemic strokes caused by a blood clot. They occur when a major blood vessel in the brain is blocked, either by a blood clot or by a build-up of fatty deposits and cholesterol known as plaque.
“A haemorrhagic stroke occurs when a
blood vessel in the brain bursts, flooding nearby tissue with blood. This causes pressure and irritation to the delicate brain tissue.” Dr Ganie stresses that a transient ischemic attack (TIA) – which is when blood flow to part of the brain is reduced by a clot or fatty deposit – can result in symptoms similar to a stroke but that the damage is not permanent.
THERE IS CAUSE FOR OPTIMISM FOR STROKE PATIENTS
According to Dr Ganie, Netcare The Bay Hospital offers cutting edge treatments for stroke patients, including thrombolytic therapy, which dissolves blood clots and restores blood flow to the brain. They also facilitate mechanical thrombectomies, a minimally invasive procedure to remove clots from large arteries. “Both treatments have been shown to significantly reduce disability and improve survival rates when administered promptly.”
Dr Ganie and his team ensure patients receive a comprehensive rehabilitation programme designed to help them regain as much function as possible to reintegrate into their communities.
“This holistic approach acknowledges that while acute intervention is critical, longterm recovery is just as important. After discharge, stroke survivors are connected with physiotherapists, speech therapists, and occupational therapists to help them
recover lost abilities and improve their quality of life. The hospital also provides ongoing support through regular follow-up appointments, ensuring patients receive continuous care throughout their recovery journey.” The hospital's stroke team works closely with local paramedics, equipping them with the knowledge and tools needed to quickly recognise and act on suspected stroke cases. Dr Ganie says this pre-hospital coordination means the team is prepared even before the patient arrives, ensuring that precious minutes are saved. “Once the patient is in the emergency department, the team jumps into action with a clearly defined protocol that minimises delays in diagnostic imaging and treatment decisions.”
EDUCATION
IS KEY
“An easy way to remember the signs of a stroke is to use the acronym FAST:
• Face drooping
• Arm weakness
• Speech difficulty
• Time to call emergency services.
Dr Ganie says this is important because many patients get to healthcare facilities too late. “If they’d arrived earlier, they could benefit from treatments such as thrombolysis or mechanical thrombectomy, both of which can dramatically improve outcomes if administered within the golden window.”
For adult patients with type 2 diabetes1,2


PROVEN GLYCAEMIC CONTROL*2-4



PROVEN CV RISK REDUCTION † 3-5
PROVEN



References: 1. OzempicR Approved Professional Information, 17 February 2023. 2. Rodbard HW, Lingvay I, Reed J, et al Semaglutide Added to Basal Insulin in Type 2 Diabetes (SUSTAIN 5): A Randomized, Controlled Trial. J Clin Endocrinol Metab 2018;103(6):2291-2301. 3. Lingvay I, Catarig AM, Frías JP, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes (SUSTAIN 8): a double-blind, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol 2019;7(11):834-844. 4. Capehorn MS, Catarig AM, Furberg JK, et al. Efficacy and safety of once-weekly semaglutide 1.0 mg vs once-daily liraglutide 1.2 mg as add-on to 1-3 oral antidiabetic drugs in subjects with type 2 diabetes (SUSTAIN 10). Diabetes Metab 2020;46(2):100-109. 5. Marso SP, Bain SC, Consoli A, et al. SUSTAIN-6 Investigators. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016;375(19):1834-1844. 6. Davies MJ, Aroda VR, Collins BS, et al. Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2022;45(11):2753-2786.
Abbreviated Professional Information
Scheduling status: S4 Name of the medicine: Ozempic® Qualitative and quantitative composition: Semaglutide 1,34 mg/ml. Therapeutic indication: Ozempic® is indicated: a) for the treatment of adults with insufficiently controlled type 2 diabetes mellitus as an adjunct to diet and exercise • as monotherapy when metformin is considered inappropriate due to intolerance or contraindications. • as combination therapy with oral anti-diabetic medicines (metformin, thiazolidinediones, sulphonylurea), basal insulin with or without metformin and pre-mix insulin. b) to reduce the risk of major adverse cardiovascular events (cardiovascular death, non-fatal myocardial infarction or non-fatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease. Posology and method of administration: Ozempic® starting dose is 0,25 mg once weekly. After 4 weeks, the dose should be increased to 0,5 mg once weekly. After at least 4 weeks with a dose of 0,5 mg once weekly, the dose can be increased to 1 mg once weekly to further improve glycaemic control. Ozempic® is to be administered once weekly at any time of the day, with or without meals. Ozempic® is to be injected subcutaneously in the abdomen, in the thigh or in the upper arm. The injection site can be changed without dose adjustment. Ozempic® should not be administered intravenously or intramuscularly. The day of weekly administration can be changed if necessary as long as the time between two doses is at least 2 days (>48 hours). When Ozempic® is added to existing sodium-glucose cotransporter 2 (SGLT2) inhibitor therapy, the current dose of SGLT2 inhibitor can be continued unchanged. Contraindications: Hypersensitivity to semaglutide or to any of the excipients, a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2), pregnancy and lactation. Special warnings and precautions for use: Ozempic® should not be used in patients with type 1 diabetes mellitus or for the treatment of diabetic ketoacidosis. Ozempic® is not a substitute for insulin. Acute pancreatitis has been observed with the use of Ozempic®. Patients should be informed of the characteristic symptoms of acute pancreatitis. If pancreatitis is suspected, Ozempic® should be discontinued; if confirmed, Ozempic® should not be restarted. Patients treated with Ozempic® in combination with a sulfonylurea or insulin may have an increased risk of hypoglycaemia. The risk of hypoglycaemia can be lowered by reducing the dose of sulfonylurea or insulin when initiating treatment with Ozempic®. Risk of Thyroid C-cell Tumours: Cases of MTC in patients treated with liraglutide, another GLP-1 receptor agonist have been reported in the post marketing period; the data in these reports are insufficient to establish or exclude a causal relationship between MTC and GLP-1 receptor agonist use in humans. Interaction with other medicines and other forms of interaction: In vitro studies have shown very low potential for Ozempic® to inhibit or induce CYP enzymes and to inhibit drug transporters. The delay of gastric emptying with Ozempic® may influence the absorption of concomitantly administered oral medicines. The potential effect of Ozempic® on the absorption of co-administered oral medicines was studied in trials at Ozempic® 1 mg steady state exposure. Fertility, pregnancy and lactation: Ozempic® is contraindicated during pregnancy and lactation. Undesirable effects: The most frequently reported adverse reactions with Ozempic® in clinical trials were gastrointestinal disorders, including nausea, diarrhoea and vomiting. Adverse reactions by system organ class and absolute frequencies identified in all phase 3a trials listed here as Very common (≥1/10): Hypoglycaemia when used with insulin or sulfonylurea, nausea, diarrhoea; Common (≥1/100 to <1/10): Hypoglycaemia when used with other OADs, decreased appetite, dizziness, diabetic retinopathy complications, vomiting, abdominal pain, abdominal distension, constipation, dyspepsia, gastritis, gastrooesophageal reflux disease, eructation, flatulence, cholelithiasis, fatigue, increased lipase, increased amylase, weight decreased; Uncommon (≥1/1,000 to <1/100): hypersensitivity, dysgeusia, increased heart rate, injection site reactions, hypersensitivity, acute pancreatitis; Rare (≥1/10,000 to <1/1,000): anaphylactic reaction.Frequency unknown: angioedema. Overdose: There is no specific antidote for overdose with Ozempic®. In the event of overdose, appropriate supportive treatment should be initiated according to the patient’s clinical signs and symptoms. A prolonged period of observation and treatment for these symptoms may be necessary, taking into account the long half-life of Ozempic® of approximately 1 week. Reg. No.: 53/21.13/0497. For full prescribing information, refer to the Professional Information approved by the Medicines Regulatory Authority.
Nordisk (Pty) Ltd. Reg. No.: 1959/000833/07. 150 Rivonia Road, 10 Marion Street Office Park, Building C1, Sandton, Johannesburg, 2196, South Africa. Tel: (011) 202 0500. Fax: (011) 807
The first 1000 days
“The first 1000 days is a time of potential and enormous vulnerability” – UP maternal and child health expert during inaugural address.
PROF UTE FEUCHT, a leading expert in maternal and child health based at the University of Pretoria (UP), shed light on the importance of the first 1000 days of life – from conception to age two. Her lecture also highlighted how placental function, maternal health and early childhood factors influence lifelong health outcomes.
Drawing from her research, Prof Feucht laid out the interconnected risk factors for suboptimal foetal growth and postnatal well-being, particularly the impact of maternal HIV infection on children, even when the children remain uninfected with the virus.
Most stillbirths occurmainlyin apparentlylow-risk pregnancies, and are coded as“unexplained stillbirths”
The inaugural address was held at UP’s Senate Hall, with Vice-Principal: Academic Prof Loretta Feris; Dean of the Faculty of Health Sciences Prof Tiaan de Jager; and other deans in attendance, along with Prof Feucht’s family members. Prof Feucht is the director of UP’s Centre for Maternal, Fetal, Newborn and Child Health Care Strategies at the university.
Prof Feucht began her lecture by exploring foetal growth restriction, a condition where a foetus doesn’t reach its genetic growth potential due to placental insufficiency.
“This condition has far-reaching consequences, including stillbirths, neonatal deaths and childhood growth disturbances, as well as conditions that can manifest later in life as non-communicable diseases like diabetes and hypertension,” she explained.
Prof Feucht added that data from the South African mortality auditing programmes in the public sector health facilities shows that most stillbirths occur mainly in apparently low-risk pregnancies, and are coded as 'unexplained stillbirths'. In addition, these stillbirths are mostly antenatal, meaning they are not
intrapartum, therefore not linked to the quality of care that the mother receives during the delivery.
She also drew data from the Siyakhula study, which examined HIV-exposed uninfected infants in South Africa. The study found that these children, even without vertical HIV transmission, were more likely to suffer from stunted growth due to changes in their intrauterine environment.

“The Umbiflow studies, which used Doppler ultrasound technology to assess placental blood flow, showed the potential for this technology to prevent stillbirths and identify at-risk pregnancies,” Prof Feucht said. “The studies, conducted across South Africa and other low- and middleincome countries, revealed alarming rates of placental insufficiency in seemingly healthy women. The prevalence of abnormal Dopplers – indicating insufficient blood flow to the foetus – was found to be 10 times higher in these low- and middle-income countries compared to high-income settings.”
THE FIRST 1000 DAYS
Prof Feucht said that 80% of a baby’s brain growth occurs within the first 1000 days, the crucial period from conception to a child’s second birthday.
“This is a time of tremendous potential and enormous vulnerability, where the foundation for future health, growth and neurodevelopment is laid,” she said. “Poor foetal growth and development during these early stages, particularly due to conditions like foetal growth restriction, can lead to life-long disadvantages.”
Prof Feucht went on to draw attention to the developmental origins of health and disease hypothesis, which suggests that a foetus makes genetic adaptations in response to its environment. These adaptations, while initially protective, may predispose an individual to chronic diseases in adulthood if the predicted environment doesn’t match reality.
Theprevalenceof abnormalDopplers–indicatinginsufficient blood low to the foetus – was found to be 10 timeshigherin these low- and middleincome countriescompared tohigh-income settings
When it comes to postnatal care, particularly for vulnerable infants born to mothers living with HIV, or those experiencing placental insufficiency, Prof

track the growth and development of infants up
24 months. These studies found that children exposed to both HIV and placental insufficiency were at significantly higher risk for stunted growth and cognitive delays.
THE FUTURE
To identify and address these risks, Prof Feucht called for better integration of care for mothers and infants in South Africa’s healthcare system. “Streamlined, holistic care for both mother and child at primary healthcare centres would reduce the number of visits needed for family planning, HIV-related care and routine infant checkups and immunisations, ultimately leading to better health outcomes for both,” she said. Additionally, her research group is now conducting research to elucidate the reasons for placental insufficiency in the South African setting. Prof Feucht quoted a recent Lancet report which stated: “The fact that every fourth baby in the world is born too soon or born too small is a concern for human rights, public health, the national economy and development.” Addressing this issue is vital for ensuring a healthier future for all, she emphasised.
Experience the freedom* with a 2-in-1 insulin co-formulation providing basal and mealtime control1-5

Targets both FPG and PPG for HbA1c control1,3,6,7 Ryzodeg®
Once-

ability to concentrate and react may be impaired as a result of hypoglycaemia. Patients must be advised to take precautions to avoid hypoglycaemia while driving or operating machinery. Hyperglycaemia: Ryzodeg® should not be used to treat severe hyperglycaemia. Inadequate dosing and/or discontinuation of treatment in patients requiring insulin may lead to hyperglycaemia and potentially to diabetic ketoacidosis, which is potentially lethal. Concomitant illness, especially infections, may lead to hyperglycaemia and thereby cause an increased insulin requirement. Transferring to a new type, brand, or manufacturer of insulin must be done under strict medical supervision. Interactions: When using Ryzodeg® in combination with thiazolidinediones, patients should be observed for signs and symptoms of congestive heart failure, weight gain and oedema. Thiazolidinediones should be discontinued if any deterioration in cardiac function occurs. The following substances may reduce the insulin requirement: Oral antidiabetic medicines, glucagon-like peptide-1 (GLP-1) receptor agonists, monoamine oxidase inhibitors (MAOI), beta-blockers, angiotensin converting enzyme (ACE) inhibitors, salicylates, anabolic steroids and sulphonamides. The following substances may increase the insulin requirement: oral contraceptive, thiazides, glucocorticoids, thyroid hormones, sympathomimetics, growth hormones and danazol. Beta-blocking medicines may mask the symptoms of hypoglycaemia and may reduce the body’s response to hypoglycaemia. Octreotide and lanreotide may either increase or decrease the insulin requirement. Alcohol may intensify or reduce the hypoglycaemic effect of insulin. Insulin antibodies: Ryzodeg® administration may cause insulin antibodies to form. In rare cases, the presence of such insulin antibodies may necessitate adjustment of the insulin dose to correct a tendency to hyper- or hypoglycaemia. Immediate-type allergic reactions to either insulin itself or the excipients may potentially be life threatening. Skin and subcutaneous tissue disorders: Injection site reactions may occur. Patients must be instructed to perform continuous rotation of the injection site to reduce the risk of developing lipodystrophy (including lipohypertrophy, lipoatrophy) and cutaneous amyloidosis. There is a potential risk of delayed insulin absorption and worsened glycaemic control following insulin injections at sites with these reactions. A sudden change in the injection site to an unaffected area has been reported to result in hypoglycaemia. Blood glucose monitoring is recommended after the change in the injection site from an affected to an unaffected area, and dose adjustment of antidiabetic medications may be considered. In children, extra care should be taken to match insulin doses with food intake and physical activities to minimise the risk of hypoglycaemia. Paediatric population: Ryzodeg® may be associated with higher occurrence of severe hypoglycaemia compared to a basal-bolus regimen in the paediatric population, particularly in children 2 to 5 years old. For this age group, Ryzodeg® should be considered on an individual basis. Insulin initiation and glucose control intensification: Intensification or rapid improvement in glucose control has been associated with transitory, reversible ophthalmologic refraction disorder, worsening of diabetic retinopathy, and acute painful peripheral neuropathy. However, long-term glycaemic control decreases the risk of diabetic retinopathy and neuropathy. Fertility, pregnancy and lactation: Safety has not been established in pregnancy and lactation and Ryzodeg® should not be recommended for use during pregnancy. Posology and administration: Ryzodeg® can be administered once- or twice-daily with the main meal(s). When needed, the patient can change the time of administration, if Ryzodeg® is dosed with a main meal. The potency of insulin analogues, including Ryzodeg®, is expressed in units (U). 1 unit (U) Ryzodeg® corresponds to 1 international unit (IU) of human insulin and one unit of all other insulin analogues. In patients with type 2 diabetes mellitus, Ryzodeg® can be combined with oral anti-diabetic products approved for use with insulin, with or without bolus insulin. When using Ryzodeg® once-daily, it is recommended to consider changing to twice-daily when reaching 60 units. Split the dose based on individual patient’s needs and administer with main meals. In type 1 diabetes mellitus, Ryzodeg® is combined with short-/rapid-acting insulin at the remaining meals. Ryzodeg® is to be dosed in accordance with individual patients’ needs. Dose-adjustments are recommended to be primarily based on pre-breakfast glucose measurements. An adjustment of dose may be necessary if patients undertake increased physical activity, change their usual diet or during concomitant illness. Initiation: For patients with type 2 diabetes mellitus, the recommended total daily starting dose of Ryzodeg® is 10 units once daily with meal(s) followed by individual dosage adjustments. For patients with type 1 diabetes mellitus, Ryzodeg® is to be used once-daily at a mealtime and a short-/rapid-acting insulin should be used at the remaining meals with individual dosage adjustments. The recommended starting dose of Ryzodeg® is 60 - 70 % of the total daily insulin requirements. Transfer from other insulin medicines: Close glucose monitoring is recommended during transfer and in the following weeks. Patients with type 2 diabetes: Patients switching from once-daily basal or premix insulin therapy can be converted unit-to-unit to once- or twice-daily Ryzodeg® at the same total insulin dose as the patient’s previous total daily insulin dose. Patients switching from more than once-daily basal or premix insulin therapy can be converted
In general, patients are initiated on the same number of basal units. Doses and timing of concomitant antidiabetic treatment may need to be adjusted. Patients with type 1 diabetes: For patients with type 1 diabetes mellitus, the recommended starting dose of Ryzodeg® is 60 - 70 % of the total daily insulin requirements in combination with short-/rapid-acting insulin at the remaining meals followed by individual dosage adjustments. Doses and timing of concurrent short-/rapid-acting insulin products may need to be adjusted. Flexibility: Ryzodeg® allows for flexibility in the timing of insulin administration if it is dosed with the main meal(s). If a dose of Ryzodeg® is missed, the patient can take the next dose with the next main meal of that day, and thereafter resume the usual dosing schedule. Patients should not take an extra dose to make up for

Adcock Ingram Critical Care partners with Global MedTech Giant Medline
Adcock Ingram Critical Care, a leading manufacturer and supplier of hospital and critical care products in Southern Africa, is taking another step towards improving patient care in the region through a strategic alliance with Medline.
EDLINE IS ONE of the world’s largest manufacturers and distributors of medical supplies and services, with annual global sales in excess of US$23 billion. The partnership solidifies Adcock Ingram Critical Care as the exclusive distributor of Medline’s products in Southern Africa and is a testament to its commitment to provide quality products that improve the health and lives of people in the markets they serve.
Ranked as one of Forbes largest private companies, Medline delivers world-class products, robust supply chain resources and clinical practice expertise to clients in more than 125 countries. Medline’s innovative and cutting-edge MedTech portfolio includes more than 550,000 products, serving the entire continuum of care. Its extensive reach and product range have transformed healthcare delivery worldwide, making it a key player in driving efficiency and improving patient outcomes.
By partnering with Adcock Ingram Critical Care, Medline is bringing its global
expertise to South Africa, strengthening the country’s healthcare infrastructure at a time when it is most needed.
“This is another milestone in our commitment to ensure that every South African can access the care they deserve. Together with Medline, we can help to build a stronger, healthier South Africa,” says Colin Sheen, managing director, Adcock Ingram Critical Care.
A STRATEGIC ALLIANCE WITH NATIONAL IMPACT
For decades, Adcock Ingram Critical Care has been delivering essential medical solutions to the nation, from Medicine Delivery in Hospital Care to Renal Care, Transfusion Therapies, Infusion Systems and most recently Wound & Stoma Care. The strategic alliance with Medline will ensure expanded and continued medical access and support healthcare providers and patients across South Africa and Southern Africa.
“The Strategic Alliance with Medline is




a significant milestone for us,” says Sheen. “This partnership will provide medical professionals across the country with access to world-class medical supplies and technology, empowering them to deliver better care and improved patient outcomes.”
Beyond its business scope and as part of its larger mission, Adcock Ingram Critical Care is connecting global medical innovations with local requirements, ensuring that hospitals, clinics, and healthcare providers – even in the most remote areas – have access to the essential tools needed to save lives.






outcomes and contributing to a stronger medical care system.”
IMPROVING HEALTHCARE FOR A STRONGER NATION

























































South Africa is one of the largest medical technology markets in Africa and the Middle East, valued at over R21 billion in 2021 and projected to grow to R29.6 billion by 2025. As the demand for access to quality healthcare services increases, strategic alliances like Adcock Ingram Critical Care and Medline are vital in ensuring that healthcare providers are equipped at providing medical services and improving access in both urban and rural clinical settings.

“Adcock Ingram Critical Care’s knowledge of the South African medical sector, combined with Medline’s worldclass products, creates a powerful synergy,” says Salam Hadla, Medline’s Vice president for the Middle East & Africa Region. “We are excited to partner with Adcock Ingram Critical Care to help advance care standards across Southern Africa. Our shared mission is to offer healthcare providers the highest quality products, ensuring better clinical








































































Chronic pelvic pain Are current diagnostic & treatment methods effective?
Chronic pelvic pain (CPP) is a significant health issue affecting approximately one in six women in the UK, characterised by persistent pain in the lower abdomen or pelvis lasting over six months.
CPP IS MULTIFACETED, with biological, psychological, and social factors contributing to its complexity.
Common biological causes include pelvic inflammatory disease, endometriosis, and chronic inflammation. Psychological factors such as depression, anxiety, and trauma also play a crucial role, leading to debilitating symptoms that can disrupt daily life, work, and sexual function. Consequently, managing CPP requires a comprehensive, multidisciplinary approach.
Diagnostic methods for CPP involve clinical assessments, imaging techniques, and, when necessary, surgical interventions. Non-invasive methods like transvaginal ultrasound and MRI are recommended before considering laparoscopy, which, although traditionally regarded as the gold standard for diagnosis, should be used judiciously due to associated risks and costs. Studies indicate that a significant percentage of women undergoing laparoscopy do not have identifiable pathologies, underscoring the need for a more nuanced diagnostic approach.
Effective management of CPP necessitates a multidimensional treatment strategy that addresses the bio-psychosocial needs of patients. Pharmacological treatments often focus on symptom control, with options including hormonal therapies, analgesics, and dietary modifications. Hormonal treatments, such as oral contraceptives and GnRH analogues, have shown efficacy in reducing pain, particularly for cyclical pelvic pain. However, potential side effects and the patient's overall health must be considered when prescribing these medications.
Surgical interventions, including laparoscopy, can serve both diagnostic and therapeutic purposes. While laparoscopy can identify certain pathologies, its effectiveness varies, and it is not universally applicable. The RCOG advises against using surgery for minor adhesions, as the long-term benefits remain inconclusive. Other surgical options, such as laparoscopic uterine nerve ablation, have been explored but may not address the full spectrum of CPP symptoms.
Psychosocial factors significantly influence CPP, with high rates of anxiety and depression reported among affected women. Cognitive Behavioral Therapy (CBT) has been recognised as a potential treatment for chronic pain syndromes, including CPP, although research on its long-term effectiveness is limited. Emerging complementary therapies, such as yoga and gentle exercise, have shown promise in improving quality of life and pain management for women with CPP.
Current guidelines from the National Institute for Health and Care Excellence
(NICE) do not specifically address treatments for CPP, while the RCOG and EAU outline various treatment options, many of which lack robust evidence for long-term effectiveness. There is a pressing need for a multi-modal approach that combines medical, psychological,
and complementary therapies to optimise symptom management. In conclusion, CPP is a prevalent and distressing condition that requires a nuanced management approach. The treatment landscape suggests that relying on a single method is often insufficient. Instead, a combination of
medical, psychological, and complementary therapies should be considered to enhance patient outcomes.
Source: Dale, R. Chronic pelvic pain: how effective are current diagnostic and treatment guidelines in the field of chronic pelvic pain? Pain News 2024;22(2):64–69. The British Pain Society 2024.

• Effective multimodal combination2

• Breaks the pain/anxiety cycle1,3,4
• Delivers effective opioid-sparing analgesia1
CLINICAL | CARDIAC
Combination therapy in hypertension
Exploring compliance, efficacy and side effects of telmisartan and amlodipine as a fixed-dose combination.
C
ARDIOVASCULAR DISEASES
(CVD) are the leading cause of death worldwide. High blood pressure (BP) is the primary global risk factor for all-cause preventable morbidity and mortality. Globally, only about 14% of patients achieve BP control to systolic BP <140 mm Hg and diastolic BP <90 mm Hg. Most patients (>60%) require two or more drugs to achieve BP control, yet poor adherence to therapy is a major barrier to achieving this control.
Fixed-dose combinations (FDCs) of BPlowering drugs are one means to improve BP control through greater adherence and efficacy, with favourable safety and cost profiles. The authors present a review of the supporting data from a successful application to the World Health Organization (WHO) for the inclusion of FDCs of two BP-lowering drugs on the 21st WHO Essential Medicines List. The authors discuss the efficacy and safety of FDCs of two BP-lowering drugs for the management of hypertension in adults, relevant hypertension guideline recommendations, and the estimated cost of such therapies.1
High blood pressure (BP) is a leading cause of CVD and a key global risk factor for preventable morbidity and mortality. In 2010, the worldwide prevalence of hypertension (systolic BP [SBP] ≥140mmHg or diastolic BP [DBP] ≥90mmHg or both, or use of BP-lowering drug) among adults (age ≥20 years) was estimated to be 1.4 billion. Of these, 36.9% (33.8%-40.0%) received BP-lowering drug(s) but only 13.8% (11.4%-16.3%) had BP controlled to SBP <140mm Hg and DBP <90mmHg.1
Most patients (>60%) with hypertension require two or more drugs to achieve optimal BP control. However, less than one-third of those treated receive such therapy. Other major causes of poor BP control among treated individuals include lack of adherence to prescribed drugs and therapeutic inertia (lack of treatment intensification despite uncontrolled BP).
Doubling the present global hypertension control rate to 25%, which is feasible if two-drug BP-lowering fixed-dose combinations (FDCs) were widely prescribed, could increase the number of patients with controlled hypertension by 80 million and could prevent two million stroke and heart attack events and more than 600 000 cardiovascular-related deaths
over five years. Major international clinical practice guidelines for the management of hypertension have begun recommending FDCs, yet FDCs are not widely available, which is due, at least in part, because they had not been designated as an essential medicine until recently.1
TWO-DRUG BP-LOWERING FDCS FOR INCLUSION IN THE WHO EML
Inclusion of a medicine on the World Health Organization (WHO) Essential Medicines List (EML) offers one mechanism for increasing its availability, affordability, and accessibility. WHO defines essential medicines as “those that satisfy the priority health care needs of the population.”
Selection of these medicines is based on the relevance to public health, evidence of benefits and harms, and cost-effectiveness. The underpinning rationale for nominating essential medicines is to ensure their continuous availability in health systems, in specific appropriate dosage form, of assured quality, and at an affordable price.2
The selection of classes of BP-lowering drugs was based on several international hypertension guidelines. Among the available classes of BP-lowering drugs, guidelines recommend preferential use of thiazide/thiazide-like diuretics, angiotensinconverting enzyme (ACE) inhibitors (ACEIs), angiotensin receptor blockers (ARBs), and calcium channel blockers (CCBs) for the pharmacological management of hypertension because of the evidence of a reduction in CVD events with these classes. Among these, guidelines recommend twodrug BP-lowering FDCs of the following classes: an ACEI or ARB in combination with either a thiazide/thiazide-like diuretic or a CCB. We selected drugs from these classes in the WHO EML application based on the extent of current use, availability, and price.2
The rationale supporting the proposed FDCs is summarised below.
TELMISARTAN/AMLODIPINE
Among the ARBs available for commercial use, telmisartan stands out with its extended half-life of ~24-hours. This extended half-life strongly implies that telmisartan is equipped with a prolonged efficacy, thereby ensuring effective control of BP over the course of a single daily dose.3
Furthermore, telmisartan boasts a unique attribute that sets it apart from


its ARB counterparts: Its notably high lipophilicity. This quality enhances its ability to permeate tissues, facilitate intracellular absorption, and optimise bioavailability. This heightened lipophilicity is mirrored in its substantial volume of distribution, measuring around 500 liters. Notably, this elevated lipophilicity, particularly when compared to compounds like losartan, may confer advantageous vascular protection.3
A distinguishing characteristic that sets telmisartan apart from other ARBs is its status as a non-prodrug. This distinction implies that the compound's anti-hypertensive potency is directly associated with the activity of the parent compound, without requiring any conversion or activation steps.3
The efficacy of telmisartan as monotherapy has been extensively studied. Various studies used ambulatory BP monitoring (ABPM) to examine if telmisartan’s prolonged half-life results in sustained BP control throughout the day.3
In a study comparing telmisartan with a long-acting CCB, both treatments yielded similar reductions in clinical BP in patients living with mild-to-moderate hypertension. However, telmisartan demonstrated a greater reduction in mean DBP during the nighttime and the last four hours of the dosing interval compared to the CCB. In studies involving ramipril (an ACEi) and losartan, telmisartan exhibited superior reductions in mean SBP and DBP during the last six hours of the dosing interval.3
Studies investigating fixed-dose combination therapy with telmisartan, and hydrochlorothiazide (HCTZ) resulted in significant reductions in SBP and DBP compared to losartan/HCTZ.3
Telmisartan's effectiveness was also highlighted in specific patient populations. In overweight patients with hypertension, telmisartan-based treatment demonstrated significant reductions in daytime and nighttime mean BP, helping to mitigate the
risks associated with metabolic syndrome.3
In elderly patients with systolic hypertension, telmisartan/HCTZ was at least as effective as amlodipine/HCTZ in reducing SBP, with fewer drug-related adverse events reported in the telmisartan group.3 Amlodipine is a widely used and low-priced drug. Amlodipine has been demonstrated to be effective across a broad range of race/ethnic groups and reduces the need for laboratory testing for electrolytes and renal function. Peripheral oedema is a common adverse effect of amlodipine. Concomitant use of an ACEI or ARB with amlodipine reduces the incidence of pedal oedema by 38% (relative risk [RR] 0.62; 95% UI 0.53-0.74; P < .00001) and risk of withdrawal due to peripheral oedema by 62% (RR 0.38; 95% CI, 0.22-0.66, P=0.002).2 The treatment of chronic diseases such as hypertension and dyslipidaemia can be negatively impacted by poor levels of patient compliance with medication. For such patients, reducing the number of pills and improving convenience could improve outcomes.2
CONCLUSIONS
Fixed-dose combinations of BP-lowering drugs for treating high BP improve clinical outcomes, are well-tolerated, and can lead to greater availability and affordability globally.1
REFERENCES
1. Salam A, Huffman MD, Kanukula R, et al. Two-drug fixed-dose combinations of blood pressure-lowering drugs as WHO essential medicines: An overview of efficacy, safety, and cost. J Clin Hypertens. 2020; 22: 1769–1779. https://doi.org/10.1111/jch.14009
2. Jin X, Kim MH, Han KH, et al. Efficacy and safety of co-administered telmisartan/amlodipine and rosuvastatin in subjects with hypertension and dyslipidemia. J Clin Hypertens (Greenwich). 2020 Oct;22(10):1835-1845. doi: 10.1111/jch.13893. Epub 2020 Sep 16. PMID: 32937023; PMCID: PMC7692919.
3. Gosse P. A review of telmisartan in the treatment of hypertension: blood pressure control in the early morning hours. Vasc Health Risk Manag, 2006.









Efficacy and safety in treating seasonal allergic rhinitis
Seasonal allergic rhinitis (SAR) is a common condition that significantly impacts the quality of life of millions of individuals
CHARACTERISED BY SYMPTOMS such as nasal congestion, sneezing, itching, and rhinorrhoea, SAR can also affect ocular health, leading to itchy and watery eyes. The management of SAR often involves the use of antihistamines and corticosteroids, either as monotherapy or in combination. This article delves into a recent phase 2 clinical trial that evaluates the efficacy and safety of GSP301, a fixeddose combination nasal spray containing olopatadine (an antihistamine) and mometasone (a corticosteroid), in treating SAR.
STUDY DESIGN AND METHODOLOGY
The study was a double-blind, parallelgroup trial involving 1111 patients aged 12 and older who were diagnosed with SAR. The participants were randomised to receive either twice-daily or once-daily GSP301, monotherapy with olopatadine or mometasone, or a placebo for a duration of 14 days. The primary endpoint of the study was the change in the reflective Total Nasal Symptom Score (rTNSS) from baseline. Secondary endpoints included changes in instantaneous TNSS (iTNSS), ocular symptoms, and quality of life measures.
PRIMARY ENDPOINT RESULTS
The results of the study indicated that twice-daily GSP301 significantly improved rTNSS compared to placebo, as well as twice-daily olopatadine and mometasone. Specifically, the twice-daily GSP301 regimen demonstrated a marked reduction in nasal symptoms, highlighting its superior efficacy over the individual components and
placebo. The once-daily GSP301 regimen also showed significant improvements over placebo and once-daily olopatadine, although it did not outperform mometasone in this dosing schedule.
SECONDARY ENDPOINT RESULTS
In addition to the primary endpoint, the study also assessed secondary endpoints, which provided further insights into the efficacy of GSP301. Both dosing regimens of GSP301 led to statistically significant improvements in nasal symptoms compared to placebo.
Notably, the twice-daily GSP301 regimen showed superior results over twice-daily mometasone, underscoring its potential as a robust treatment option for SAR. The onset of action for once-daily GSP301 was significant at 150 minutes post-dose, indicating a relatively rapid relief of symptoms. This is particularly important for patients seeking quick alleviation of SAR symptoms.
OCULAR SYMPTOMS AND QUALITY OF LIFE
Ocular symptoms, which are often associated with SAR, were also evaluated in the study. The results revealed that GSP301 was effective in reducing ocular symptoms, thereby providing comprehensive relief for patients. Quality of life assessments further demonstrated that both GSP301 regimens resulted in meaningful enhancements across various domains compared to placebo. These improvements in quality of life are crucial, as SAR can significantly impact daily activities and overall well-being.
SAFETY AND TOLERABILITY
The safety and tolerability of GSP301 were also key aspects of the study. Adverse events were reported in 10.8% of patients receiving twice-daily GSP301, 9.5% for once-daily GSP301, and 8.2% for placebo. The most common adverse events were mild to moderate in nature, primarily headaches and dysgeusia (altered taste). Importantly, no serious adverse events were linked to the treatment, suggesting that GSP301 is generally well tolerated.
CONCLUSION
The findings of this phase 2 clinical trial indicate that GSP301 is an effective and safe option for managing symptoms of SAR. The fixed-dose combination of olopatadine and mometasone in GSP301 provides significant improvements in nasal and ocular symptoms, enhancing patients' quality of life. The twice-daily regimen, in particular, demonstrated superior efficacy over the individual components and placebo, making it a promising treatment option for SAR.
The study supports further evaluation of GSP301 in later phase trials to confirm its efficacy and safety in a larger patient population. As SAR continues to affect millions of individuals, the development of effective and well-tolerated treatments like GSP301 is essential in improving patient outcomes and quality of life.
IMPLICATIONS FOR CLINICAL PRACTICE
For healthcare professionals, the results of this study offer valuable insights into the management of SAR. The combination of
an antihistamine and a corticosteroid in a single nasal spray provides a convenient and effective treatment option for patients. The rapid onset of action and significant improvements in both nasal and ocular symptoms make GSP301 a compelling choice for managing SAR.In clinical practice, the use of GSP301 could potentially reduce the need for multiple medications, simplifying treatment regimens and improving patient adherence. The favourable safety profile further supports its use in a broad patient population, including adolescents and adults.
FUTURE DIRECTIONS
The promising results of this phase 2 trial pave the way for further research into GSP301. Future studies should focus on larger, more diverse patient populations to confirm the findings and explore longterm safety and efficacy. Additionally, investigating the use of GSP301 in other allergic conditions, such as perennial allergic rhinitis, could expand its therapeutic potential. In conclusion, GSP301 represents a significant advancement in the treatment of SAR, offering a combination of efficacy, safety, and convenience. As research continues, it holds the potential to become a cornerstone in the management of allergic rhinitis, improving the lives of patients worldwide.
REFERENCE
Andrews, Charles P. et al. Efficacy and safety of twice-daily and once-daily olopatadine-mometasone combination nasal spray for seasonal allergic rhinitis. Annals of Allergy, Asthma & Immunology. 2020;124:171178.e2. https://doi.org/10.1016/j.anai.2019.11.007.





The SA guideline choice for AOMT
Acute otitis media with tympanostomy tubes (AOMT) is a common condition in paediatric patients, often requiring effective and timely treatment to prevent complications.
A
CCORDING TO THE RSA guidelines, topical ciprofloxacin/dexamethasone otic suspension (ciprofloxacin/ dexamethasone) is the recommended choice for managing AOMT. This recommendation is supported by several studies highlighting its superior efficacy and safety profile compared to other treatments.
HIGHER CURE RATES WITH CIPROFLOXACIN/DEXAMETHASONE VS ORAL AMOXICILLIN/ CLAVULANIC ACID
A study by Dohar et al. compared the effectiveness of ciprofloxacin/ dexamethasone with oral amoxicillin/ clavulanic acid (AMOX/CLAV) in treating
AOMT. The study involved 80 children aged six months to 12 years, who were randomly assigned to receive either ciprofloxacin/dexamethasone (four drops twice daily for seven days) or AMOX/CLAV (600 mg every 12 hours for 10 days).
The results were compelling:
• The median time to cessation of

twice daily dosage1 for use in babies from 6 months (in AOMT**) through adults, including the elderly1,2


* AOE: Acute Otitis Externa ** AOMT: Acute Otitis Media with Tympanotomy Tubes. References: 1. Cilodex® Approved Professional Information, 13 April 2022. 2. Daniel SJ, et al. Guidelines for the treatment of tympanostomy tube otorrhoea. J Otolaryngol 2005;34(S2):S60-S63. For full prescribing
by the South African Health Products Regulatory Authority. S4 CILODEX® Ear Drops, suspension. 1 ml of suspension contains 3 mg ciprofloxacin (as hydrochloride) and 1 mg dexamethasone preserved with benzalkonium chloride 0,01% (m/v). A39/16.2/0544. Novartis SA (Pty) Ltd. Magwa Crescent West, Waterfall City, Jukskei View, 2090. Tel. (011) 347 6600. Co. Reg. No. 1946/020671/07. Novartis Adverse Drug Reaction Reporting: Email: patientsafety.sacg@novartis.com. Web: www.novartis.com/report. Tel: 0861 929-929. Marketed and Distributed by Adcock Ingram Limited. Co. Reg. No. 1949/034385/06. Private Bag X69, Bryanston, 2021, South Africa. Customer Care: 0860 ADCOCK/232625. www.adcock.com FA-11263392. Exp.: 09/2026.

hr Cilodex 2024 ad new look 2.indd 1 2024/09/20 12:35
otorrhoea was significantly shorter for the ciprofloxacin/dexamethasone group (four days) compared to the AMOX/CLAV group (seven days)
• The clinical cure rate was higher in the ciprofloxacin/dexamethasone group, with 85% achieving clinical cure versus 59% in the AMOX/CLAV group
• Adverse events were less frequent with ciprofloxacin/dexamethasone, with ear pain reported in 5.1% of cases, while AMOX/CLAV was associated with higher rates of diarrhoea (19.5%), dermatitis (7.3%), and gastroenteritis (4.9%).
These findings support the use of ciprofloxacin/dexamethasone as a more effective and safer treatment option for AOMT compared to oral antibiotics.
CIPROFLOXACIN/DEXAMETHASONE VS OFLOXACIN: SUPERIOR CLINICAL AND MICROBIOLOGICAL OUTCOMES
Another study by Roland et al. evaluated the efficacy of ciprofloxacin/dexamethasone compared to ofloxacin in children with AOMT. This randomised trial included 599 participants aged six months to 12 years, who received either Ciprofloxacin/ dexamethasone (four drops twice daily for seven days) or ofloxacin (five drops twice daily for 10 days). The key findings were: • Ciprofloxacin/dexamethasone achieved a clinical cure rate of 90% compared to 78% for ofloxacin
• The microbiologic success rate was 92% for ciprofloxacin/dexamethasone versus 81.8% for ofloxacin
• Treatment failures were lower in the ciprofloxacin/dexamethasone group (4.4% vs 14.1%).
The median time to cessation of otorrhoea was shorter for ciprofloxacin/ dexamethasone (four days) compared to ofloxacin (six days). These results demonstrate that ciprofloxacin/ dexamethasone is not only more effective in achieving clinical and microbiological cure but also provides quicker symptom resolution compared to ofloxacin.
CONCLUSION
The evidence from these studies underscores the efficacy and safety of ciprofloxacin/dexamethasone in treating AOMT. With higher cure rates, quicker resolution of symptoms, and fewer adverse effects, Ciprofloxacin/dexamethasone stands out as the preferred treatment option.
The RSA guidelines rightly recommend ciprofloxacin/dexamethasone for managing AOMT, ensuring better outcomes for paediatric patients.
Ocular comorbidities in rosacea
Rosacea, a chronic inflammatory skin condition, has long been known to affect the skin, but its impact on ocular health is less frequently discussed.
RECENT STUDY PROVIDES valuable insights into the ocular complications associated with rosacea.
The study analysed data from 12 936 rosacea patients and an equal number of matched controls over a 12-year period. The findings reveal significant associations between rosacea and several eye conditions, including blepharitis, conjunctivitis, glaucoma, dry eye syndrome, and chalazion. Notably, the risk for chalazion is particularly pronounced in female patients and those under 50 years of age.
KEY FINDINGS
Blepharitis: The most common ocular condition associated with rosacea, with an adjusted odds ratio (aOR) of 3.44.
Conjunctivitis: Found to have an a OR of 1.65.
Glaucoma: Patients with rosacea have an aOR of 1.93 for developing glaucoma. Dry eye syndrome: An aOR of 1.89 was observed.
Chalazion: Particularly prevalent in women and younger patients, with an a OR of 3.26.
The associations between rosacea and these ocular conditions may be multifactorial, involving inflammation, skin barrier disruption, and an increased presence of Demodex mites, which can exacerbate eyelid inflammation and contribute to conditions like dry eye syndrome.
CLINICAL IMPLICATIONS
The research underscores the necessity for clinicians to be vigilant in monitoring ocular symptoms in rosacea patients. Collaborative care with ophthalmologists is advocated to ensure early detection and management of these associated eye conditions. Untreated dry eye, for instance, can lead to severe consequences, including corneal damage and potential vision loss.
Subgroup analyses reveal that both women and men with rosacea show significant associations with ocular conditions, with women particularly affected by blepharitis and chalazion. Individuals aged 50 and older have significant associations with various ocular disorders, while those under 50 exhibit even stronger correlations, especially with blepharitis and glaucoma.
TREATMENT CONSIDERATIONS
While oral doxycycline can improve meibomian gland function, isotretinoin may worsen eye symptoms and should be used cautiously. An unexpected finding was the increased risk of glaucoma among rosacea patients, potentially linked to corticosteroid use, which can elevate intraocular pressure. Regular ophthalmic screenings are
recommended for those with a history of steroid use or family history of glaucoma.
STUDY LIMITATIONS AND FUTURE RESEARCH:
Further research in diverse populations
is encouraged to enhance understanding and management of rosacea and its ocular implications. This study provides a crucial foundation for future investigations and highlights the need for comprehensive care in patients with rosacea to address both
dermatological and ocular health.
REFERENCE
Rosacea: A Case-Control Study Based on Seven Institutions. J Clin Med. 2021:29;10(13):2897. doi: 10.3390/jcm10132897. PMID: 34209731; PMCID:

and











































































An anti-infective and corticosteroid combination to treat a wide range of ocular infl ammation with infection or a risk of infection 1













0,5 % Loteprednol Etabonate with site-specific, high anti-inflammatory e cacy 2-4 0,3 % Tobramycin with broad spectrum activity 5 Reduced propensity for elevation in intraocular pressure 6









































Ther. 2012;34:1259–1272. 5. Comstock TL, Holland EJ. Loteprednol and tobramycin in combination: a review of their impact on current treatment regimens. Expert Opin Pharmacother. 2010 ;11(5):843-52. 6. Lane SS, Holland EJ. Loteprednol etabonate 0.5% versus prednisolone acetate 1.0% for the treatment of inflammation after cataract surgery. J Cataract Refract Surg. 2013:39(2):168-73.

Revelation trial: Drug-coated balloon shows promise in treating STEMI
The Revelation trial has provided significant insights into the treatment of acute myocardial infarction (AMI), particularly in patients with ST-segment elevation myocardial infarction (STEMI).










on the primary endpoint of fractional flow reserve (FFR) assessed at nine months.



designed to evaluate the non-inferiority of DES, thus meeting the primary endpoint.














SUSTAINED SAFETY AND FEASIBILITY AT 24 MONTHS


At the 24-month follow-up, the DCB continued to demonstrate sustained safety and feasibility. The clinical outcomes were excellent and comparable to those achieved with contemporary DES. This long-term data supports the 'leave nothing behind' strategy, which is an appealing alternative to traditional stenting methods.
KEY FINDINGS
Several key findings emerged from the Revelation trial:
1. Primary endpoint (FFR): There was no significant difference between the DCB and DES groups at the nine-month follow-up, confirming the non-inferiority of the DCB.

2. Secondary endpoints: The trial reported low rates of major adverse cardiac events (MACE), stent thrombosis, and major bleeding in both treatment groups. Importantly, no cardiac deaths were reported in either group, underscoring the safety of the DCB.
3. Target lesion revascularisation (TLR): The rate of TLR events was low, with only one additional TLR occurring in the DCB group between the nine-month and twoyear follow-ups. This finding highlights the durability of the DCB's effectiveness over time.
CLINICAL IMPLICATIONS


The Revelation trial's findings suggest that the paclitaxel DCB is a safe and effective option for treating patients with STEMI. The comparable outcomes to secondgeneration DES provide clinicians with a viable alternative that aligns with the 'leave nothing behind' strategy. This approach could potentially reduce the long-term complications associated with permanent implants.
CONCLUSION



In conclusion, the Revelation trial has demonstrated that the paclitaxel DCB is a promising treatment for STEMI, offering outcomes on par with second-generation DES. The sustained safety and feasibility observed at the 24-month follow-up further support its use in clinical practice. As the medical community continues to seek innovative solutions for AMI treatment, the paclitaxel DCB represents a significant advancement in interventional cardiology.
REFERENCE
Niehe S.R. et al. Two-Year Clinical Outcomes of the REVELATION Study: Sustained Safety and Feasibility of Paclitaxel-Coated Balloon Angioplasty Versus DrugEluting Stent in Acute Myocardial Infarction. J Invasive Cardiol. 2022;34(1):E39-E42; 2.
From mother to baby Iron deficiency and its effects on neurocognitive growth
Iron is a vital nutrient for cellular functions, especially during pregnancy, where its demand increases significantly due to the expansion of maternal blood volume and the development of the fetus.
IRON DEFICIENCY IN pregnant women can lead to severe consequences, including maternal illness, low birth weight, prematurity, and intrauterine growth restriction. The fetal brain is particularly vulnerable to iron deficiency, which can be exacerbated by maternal conditions such as hypertension, smoking, or glucose intolerance. Research has linked low maternal iron intake to neurodevelopmental disorders in children, including autism and schizophrenia.
Iron is crucial for the fetus to meet its metabolic needs and to build iron stores for the first six months of life. Iron deficiency is prevalent, affecting up to 80% of pregnant women in low- and middle-income countries and around 45% in wealthier nations. The placenta also requires significant iron and can store it to mitigate maternal deficiencies. Adequate fetal iron loading is vital to prevent postnatal iron deficiency, which is associated with long-term neurodevelopmental issues.
Routinescreening for iron status in newborns is often neglected,despite thehighprevalenceof irondeficiency
Anaemia is a late-stage indicator of iron deficiency, as iron is prioritised for red blood cell production over other tissues, including the brain. Biomarkers like serum ferritin are more sensitive for assessing iron status than haemoglobin levels alone, which may overlook early deficiency stages.
Routine screening for iron status in newborns is often neglected, despite the high prevalence of iron deficiency. Delayed cord clamping can enhance iron levels in neonates, providing sufficient iron for growth in the first few months. While haemoglobin concentration is commonly used to assess iron status, it is not sensitive enough to detect early deficiency, which can lead to anemia. Other biomarkers, such as serum ferritin, total iron binding capacity saturation (%TSAT), and hepcidin, are more effective in diagnosing iron deficiency anemia (IDA) and distinguishing it from other causes of anemia.
Iron deficiency and IDA are not synonymous. IDA occurs when iron deficiency leads to anaemia. Non-anaemic stages of deficiency can still impair tissue function, including brain development. Children with pre-anaemic iron deficiency may face cognitive and behavioural issues,
highlighting the importance of iron for brain health even before anaemia develops.
CONCLUSION
The consequences of maternal iron deficiency can have immediate and long-
term effects on fetal brain development, potentially leading to altered brain structure and cognitive dysfunction in children, even if iron levels normalise later. Low iron status in infancy is associated with developmental delays and increased risks of mental health issues later in life.
REFERENCE
Georgieff, Michael K. Iron Deficiency in Pregnancy. Am J Obstet Gynecol. 2020;223(4): 516–524. doi:10.1016/j.ajog.2020.03.006.


Evaluation and management of chronic kidney disease
A summary of clinical practice guidelines.
Cwww.kidney-international.org chapter2
HRONIC KIDNEY DISEASE (CKD) management is a multifaceted approach aimed at slowing disease progression, managing complications, and enhancing the quality of life for patients. The main points of CKD management are illustrated in the following article.
1. Early detection and screening
Regular screening is crucial, especially for high-risk populations such as those with diabetes or hypertension. This involves measuring the albumin-to-creatinine ratio (ACR) and estimating glomerular filtration rate (eGFR) to identify kidney damage early, allowing for timely interventions.
2. Risk assessment and monitoring
Continuous monitoring of kidney function and associated risk factors is essential. Significant changes in eGFR (greater than 20%) or a doubling of ACR should prompt further evaluation. Albuminuria and proteinuria are key indicators of CKD progression, and regular assessments help in tailoring management strategies.
3. Medication management
Specific medications, such as sodiumglucose cotransporter-2 inhibitors (SGLT2i) and mineralocorticoid receptor antagonists (MRAs), are recommended for managing CKD and related conditions like diabetes and hypertension. Careful management is necessary to prevent nephrotoxicity and complications such as hyperkalemia, with regular medication reviews to optimise treatment.
CKD is classified based on:
• Cause (C)
• GFR (G)
• Albuminuria (A)
Kidney failure Severely
Low risk (if no other markers of kidney disease, no CKD)
Moderately increased risk
their specific health profiles.
High risk
Very high risk
Figure13|Frequencyofmonitoringglomerular filtrationrate(GFR)andalbuminuriainpeoplewithchronickidneydisease(CKD). AlbuminuriaandGFRgridreflectstheriskofprogressionbyintensityofcoloring(green,yellow,orange,red,anddeepred).Thenumbersinthe boxesareaguidetothefrequencyofmonitoring(numberoftimesperyear).ReproducedfromdeBoerIH,KhuntiK,SaduskyT,etal.Diabetes managementinchronickidneydisease:aconsensusreportbytheAmericanDiabetesAssociation(ADA)andKidneyDisease:ImprovingGlobal Outcomes(KDIGO). KidneyInt.2022;102:974 –989.29 Copyright ª 2022,InternationalSocietyofNephrology,AmericanDiabetesAssociation,and KDIGO.PublishedbyElsevierInc.andAmericanDiabetesAssociation.Allrightsreserved.
4. Comprehensive treatment strategies
Effective management of comorbid conditions, particularly hypertension and diabetes, is critical. Lifestyle modifications, including dietary changes (eg, low sodium and protein intake) and maintaining a target systolic blood pressure below 130/80 mmHg, are recommended to reduce CKD progression.
PATIENTS AT HIGHER RISK OF CKD PROGRESSION
Table 1 visually categorises patients based on their CKD stage and associated risks for kidney failure. The heat map illustrates the relationship between eGFR and albuminuria levels, highlighting varying risks of progression to kidney failure. It emphasises the need for individualised risk assessment, as patients within the same CKD stage can have significantly different risks based on
Assess albuminuria and GFR more frequently for individuals at higher risk of CKD progression when it will influence therapeutic decisions. Previous guidelines have recommended routine monitoring of albuminuria and GFR, suggesting annual monitoring for those with CKD stages G1–G2, every six months for CKD stage G3, every three months for CKD stage G4, and every six weeks for CKD stage G5. Given the increased risk of disease progression, individuals at higher risk should undergo more frequent monitoring. This may be particularly necessary for those with changing clinical status, intercurrent events, and following therapeutic interventions to assess response, adherence, and ensure safety. Additionally, the risk of progression may vary by the etiology of CKD within a specific stage based on GFR and albuminuria or proteinuria.
5. Kidney replacement therapy (KRT) planning
Planning for KRT should begin when eGFR falls below 15 ml/min or when complications arise. Early discussions about dialysis initiation, especially for paediatric patients, should involve caregivers to ensure informed decision-making.
PracticePoint2.1.4:AmongpeoplewithCKDwhoinitiate hemodynamicallyactivetherapies,GFRreductionsof >30%onsubsequenttestingexceedtheexpectedvariability andwarrantevaluation.
6. Symptom management and quality of life
AcuteeGFRdeclineafterintensiveBPcontrolhasbeen observedinpeoplewithCKD,withreductionsof10%–20% beingtypicalwithinthe first3monthsoftreatment.These declinesineGFRarehemodynamicallymediated,representingaresponsetoBPfallingbelowthelowerthresholdofa person ’sautoregulatoryresponse.Formany,thisinitial declineineGFRistransientandwillstabilizeorresolveover time,asresettingoftheautoregulatoryfunctionoccurs.Thus, acuterisesinSCr(ordeclinesineGFR)of <20%–30%are expectedanddonotwarrantchangesintherapeuticagents, whichmaybeimportantforcardio-andkidney-protective effectsinthelongterm.Thisphenomenonisespecially commonwhenusingACEi/angiotensinIIreceptorblockers (ARBs),astheybothlowerBPandalterarteriolar flow throughtheglomeruli,andSGLT2ithroughsimilarhemo-
This tool aids in prioritising management strategies and tailoring interventions based on individual patient risk profiles, ensuring that high-risk patients receive more intensive monitoring and care.
Addressing symptoms such as fatigue, pruritus, and psychological distress is vital for improving the quality of life in CKD patients. A multidisciplinary approach is recommended for effective symptom management and nutritional support.
7. Patient education and engagement
Tailored education programmes that include care partners are essential for promoting self-management and adherence to treatment plans. Engaging patients in their care enhances their understanding and involvement in decision-making.
8. Transitioning care
Special considerations are needed for transitioning young patients from paediatric to adult care, requiring careful planning and follow-up to ensure continuity of care.
9. Research and future directions
Ongoing research is necessary to refine CKD management strategies, develop better biomarkers, and improve risk prediction models. The guidelines advocate for inclusive studies to enhance understanding and treatment of CKD across diverse populations.
CONCLUSION
“nondipper” whoreceivedSGLT2i,exceptinunusualcases whentheacute “dip” ineGFRwas >30%frombaseline. These fi ndingswereconsistentacrossallsubgroups. AsignificantdropineGFR(>30%)whileinitiatingantihypertensiveagents,renin-angiotensinsysteminhibitors (RASi),mineralocorticoidreceptorantagonists(MRA),or SGLT2ishouldpromptareviewintoothercausesandwarrantsclosemonitoring.However,healthcareprovidersshould avoidtheurgetostopthesekidney-protectiveagents, particularlybecausetheseearlier “dips” aretypicallyreversible andnotanindicationofdrugtoxicity.
Effective CKD management requires a collaborative, patient-centred approach that integrates risk assessment, lifestyle changes, medication management, and continuous monitoring to optimise patient care and outcomes.
PracticePoint2.1.5:Foralbuminuriamonitoringofpeople withCKD,adoublingoftheACRonasubsequenttest exceedslaboratoryvariabilityandwarrantsevaluation.
REFERENCE
Small fluctuationsinalbuminuriaorproteinurialevels maynotindicatediseaseprogression.Appreciationoffactors thatimpactalbuminuriaandchangesinthemeasureis importantforhealthcareproviders.Routinesurveillanceus-
TARGETED CARDIO-RENALMETABOLIC PROTECTION¹
AN APPLE A DAY
(or more precisely, an analogue of a chemical in the bark of an apple tree) keeps type 2 diabetes, cardiovascular disease and kidney disease away2,3

Introducing Cipla’s new SGLT2 inhibitors




Dapagliflozin 5 mg; 10 mg
Dapagliflozin 5 mg; 10 mg Metformin hydrochloride 1 000 mg (extended release)
SAGALATIN & SYNGLUTRA, going beyond glucose lowering⁴at up to a 30 % costing saving to the originator5
S4 Reg. No. 53/21.2/0720. Sagalatin 5. Each film-coated tablet contains dapagliflozin propanediol equivalent to 5 mg dapagliflozin.
S4 Reg. No. 53/21.2/0721. Sagalatin 10. Each film-coated tablet contains dapagliflozin propanediol equivalent to 10 mg dapagliflozin. S4 Reg. No. 53/21.1/0651. Synglutra 5/1000. Each film-coated tablet contains the equivalent of 5 mg dapagliflozin (as dapagliflozin propanediol) and 1 000 mg of metformin hydrochloride. S4 Reg. No. 53/21.1/0652. Synglutra 10/1000. Each film-coated tablet contains the equivalent of 10 mg dapagliflozin (as dapagliflozin propanediol) and 1 000 mg of metformin hydrochloride. For full prescribing information, refer to the Professional Information approved by the medicine’s regulatory authority. References: 1. Salvatore, T., Galiero, R., Caturano, A., Rinaldi, L., Di Martino, A., Albanese, G., Di Salvo, J., Epifani, R., Marfella, R., Docimo, G., Lettieri, M., Sardu, C. and Sasso, F.C. (2022). An Overview of the Cardiorenal Protective Mechanisms of SGLT2 Inhibitors. Int J Mol Sci. Mar 26;23(7):3651. doi: 10.3390/ijms23073651. PMID: 35409011; PMCID: PMC8998569. 2. Ehrenkranz, J.R., Lewis, N.G., Kahn, C.R. and Roth, J. Phlorizin. (2005): a review. Diabetes Metab Res Rev. Jan-Feb;21(1):31-8. doi: 10.1002/dmrr.532. PMID: 15624123. 3. Zelniker, T.A. and Braunwald, E. (2018). Cardiac and Renal Effects of Sodium-Glucose Co-Transporter 2 Inhibitors in Diabetes: JACC State-of-the-Art Review. J Am Coll Cardiol. Oct 9;72(15):1845-1855. doi: 10.1016/j.jacc.2018.06.040. Epub 2018 Jul 31. PMID: 30075873. 4. Ni, L., Yuan, C., Chen, G., Zhang, C. and Wu, X. (2020).SGLT2i: beyond the glucose-lowering effect. Cardiovasc Diabetol. Jun 26;19(1):98. 5. Department of Health Pricing schedule, effective 15 May 2023. CIPLA MEDPRO (PTY) LTD. Co. Reg. No. 1995/004182/07. Building 9, Parc du Cap, Mispel Street, Bellville, 7530, RSA. Website: www.cipla.co.za Customer Care: 080 222 6662. [1110635708a]
ESC’s 2024 key recommendations for atrial fibrillation management
The 2024 European Society of Cardiology (ESC) guidelines for the management of atrial fibrillation (AF) present a comprehensive approach to diagnosing and treating this common heart rhythm disorder.
DEVELOPED IN COLLABORATION with the European Association for Cardio-Thoracic Surgery (EACTS), these recommendations aim to enhance patient care through tailored strategies.
The ESC guidelines aim to assist health professionals in making the best diagnostic and therapeutic decisions for patients. These guidelines are freely available and do not override the responsibility of health professionals to make decisions based on individual patient conditions and consultations.
The guidelines represent the ESC's official position and are regularly updated based on new evidence. The task force responsible for these guidelines includes diverse professionals and patient representatives. They critically review literature, assess risk-benefit ratios, and evaluate patient-reported outcomes. Recommendations are voted on, requiring at least 75% agreement, and conflicts of interest are managed according to ESC rules. The ESC Clinical Practice Guidelines (CPG) Committee oversees the preparation and approval of new guidelines, which undergo multiple rounds of peer review. The guidelines are based on published evidence, primarily clinical trials and meta-analyses. Off-label medication use is included if supported by sufficient evidence, but final decisions rest with the responsible health professional.
A patient-centred and integrated approach to AF management means working with a model of care that respects the patient’s experience, values, needs, and preferences for planning, co-ordination, and delivery of care. A central component of this model is the therapeutic relationship between the patient and the multidisciplinary team of healthcare professionals.
The 2024 guidelines focus on atrial fibrillation (AF), a common heart condition with significant health impacts. The AFCARE framework emphasises managing comorbidities and risk factors, avoiding stroke and thromboembolism, reducing symptoms through rate and rhythm control, and dynamic reassessment. Patient empowerment and shared decision-making are crucial for better outcomes.
The guidelines also address the need for healthcare professionals to work within local multidisciplinary teams and highlight the importance of guideline adherence, as demonstrated by the ESC's STEEER-AF trial. The 2024 guidelines aim to improve readability, implementation, and patient outcomes, with a patient version available online.
DIAGNOSTIC EVALUATION
A transthoracic echocardiogram is recommended for evaluating new cases of atrial fibrillation. This non-invasive imaging technique provides crucial insights into cardiac structure and function, assisting in determining the appropriate management pathway.
PATIENT-CENTRED MANAGEMENT
The guidelines emphasise the importance of patient education and a multidisciplinary approach. This strategy involves collaboration among various healthcare professionals to ensure that patients receive comprehensive care tailored to their individual needs. Engaging patients in their treatment plans enhances adherence and overall outcomes.
COMORBIDITY MANAGEMENT
Managing comorbidities is essential for patients with AF. Recommendations include:
• Diuretics for patients with heart failure,
which can help alleviate symptoms and improve quality of life.
• Sodium-glucose cotransporter-2 inhibitors are encouraged for heart failure patients with AF, offering dual benefits in managing heart function and glycemic control.
• Effective glycemic control is critical for diabetic patients with AF to minimise complications and improve cardiovascular health.
• For patients with a body mass index (BMI) of 40kg/m² or higher, bariatric surgery may be considered as a treatment option to help reduce weight and potentially improve AF outcomes.
• Management of obstructive sleep apnea is also recommended, as addressing this condition can improve heart rhythm stability and overall health.
ANTICOAGULATION STRATEGIES
Initiating oral anticoagulation is advised for AF patients at elevated risk of thromboembolic events. A CHA₂DS ₂-VA score of two or more indicates a strong need for anticoagulation, while a score of one warrants consideration for treatment. The guidelines support the use of direct oral anticoagulants (DOACs) over vitamin K antagonists (VKAs) for patients undergoing cardioversion, owing to their safety profile and ease of use.
ANTITHROMBOTIC THERAPY
POST-ACS
For patients with atrial fibrillation undergoing percutaneous coronary intervention (PCI) or those with acute coronary syndrome (ACS), a prolonged triple therapy approach may be beneficial. This involves using anticoagulants alongside antiplatelet therapy, carefully balancing the risks of thrombosis and bleeding based on
C A R E
individual patient profiles.
MANAGEMENT OF STROKE RISK
The guidelines clarify that antiplatelet drugs should not be combined with oral anticoagulants for the purpose of stroke prevention. For patients on anticoagulation who experience an ischemic stroke, a thorough diagnostic work-up is recommended to explore the underlying causes and adjust treatment as necessary.
RATE AND RHYTHM CONTROL
Effective management of heart rate is crucial for patients with AF. The guidelines recommend specific drugs and strategies for rate control therapy, ensuring patients maintain an appropriate heart rate and rhythm. Catheter ablation is advised for patients experiencing recurrent AF or those who develop bradycardia following initial ablation procedures. This invasive technique can help restore normal heart rhythm and alleviate symptoms.
BLEEDING RISK MANAGEMENT
Assessing and managing modifiable bleeding risk factors is essential for patients on anticoagulants. The guidelines recommend using the HAS-BLED score to evaluate bleeding risk, allowing clinicians to tailor anticoagulation strategies accordingly.
SURGICAL INTERVENTIONS
In cases where AF patients are undergoing endoscopic or hybrid AF ablation, surgical left atrial appendage occlusion may be considered as an adjunct to oral anticoagulation. This procedure can help reduce the risk of thromboembolic events in high-risk patients.
CONCLUSION
The 2024 ESC guidelines for the management of atrial fibrillation provide a detailed roadmap for healthcare professionals. By focusing on comprehensive diagnostic evaluations, patient-centered management, and tailored treatment strategies, these recommendations aim to improve patient outcomes and enhance the quality of care for those living with atrial fibrillation.
REFERENCE
Van Gelder IC, Rienstra M, Bunting KV, et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2024 Sep 29;45(36):3314-3414. doi: 10.1093/eurheartj/ehae176. PMID: 39210723.
Apixaban is better than warfarin at preventing stroke and systemic embolism with less major bleeding.**

Fibranix 2,5 / 5
Apixaban 2,5 mg; 5 mg
INDICATIONS:2

• Prevention of stroke and systemic embolism (SE) in patients with nonvalvular atrial fibrillation (NVAF) with one or more risk factors.
• Treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE), and prevention of recurrent DVT and PE.
• Prevention of venous thromboembolic events (VTE) in adult patients who have undergone elective hip or knee replacement surgery.
* Efficacy defined as stroke and SE prevention vs warfarin; safety defined as less bleeding and mortality vs warfarin. Both seen in a study on patients with non valvular atrial fibrillation.1
** The rate of stroke or systemic embolism was significantly lower on apixaban (1,27 % / year) compared with warfarin (1,6 % / year, hazard ratio (HR) 0,79, p < 0,001). The major bleeding rate was 2,13 % per year with apixaban and 3,09 % per year with warfarin (hazard ratio, 0,69; 95 % CI, 0,60 to 0,80; p < 0,001).1

Know your body: A woman’s guide to prevention and control
When it comes to cervical cancer, forewarned is forearmed. Cervical cancer is the second most common cancer affecting women in South Africa, with one in every 42 women facing a lifetime risk, according to the Cancer Association of South Africa (CANSA).
WHILE THESE STATISTICS may seem alarming, it’s never too late to arm yourself with knowledge and take proactive steps to reduce your risk.
Globally, cervical cancer ranks as the fourth most diagnosed cancer among women, but in South Africa, it's the second most prevalent, trailing only breast cancer. This type of cancer occurs when abnormal cells develop in the cervix, the bridge between the uterus and vagina. The main culprit behind cervical cancer is the human papillomavirus (HPV), but there’s a silver lining: it’s largely preventable with the HPV vaccine and regular screenings. Early detection is crucial, especially since this cancer disproportionately impacts women with limited access to healthcare.
THE POWER OF REGULAR SCREENING AND PAP SMEARS
An annual pap smear is more than just a routine check-up, it’s a lifesaver. This simple test can detect cancerous and precancerous cells, giving you the opportunity to address issues before they escalate. Women with private healthcare often adhere more strictly to regular screenings, benefiting from early intervention. However, in public healthcare,
barriers like limited resources and fear of a positive diagnosis can delay these essential checks, leading to late-stage diagnosis when treatment becomes more challenging.
While funding for regular screening can be a hurdle, options do exist. Government healthcare facilities provide screenings, though wait times can be long due to high demand. The good news is that affordable pap smears are available at pharmacies like Dis-Chem and Clicks, making it easier to prioritise your health.
Tackling the fear factor is tougher, but it’s vital to remove the stigma around testing. Awareness campaigns need to emphasise that knowledge is power— catching potential problems early leads to better outcomes. Ignoring symptoms doesn’t make them disappear; it only allows them to grow into bigger, more complex issues.
UNDERSTANDING YOUR RISK AND REDUCING IT
Several factors can increase your risk of developing cervical cancer, but there are ways to mitigate them.
Human Papillomavirus (HPV): HPV is a widespread infection, with 70% of
people contracting it at some point in their lives. Two strains, HPV-16 and HPV-18 are responsible for over 70% of cervical cancer cases. South Africa has made strides in rolling out the HPV vaccine, especially for girls aged nine to 15 years, through the Department of Health’s HPV School Vaccination Programme. Vaccination is the most effective method to lower your risk, preventing 90% of cervical and anal cancers caused by HPV.
OTHER FACTORS CAN INCREASE HPV
RISK INCLUDING:
Early sexual activity at a younger age increases your risk of contracting HPV and, subsequently, cervical cancer. The best prevention is comprehensive sex education, with open conversations between parents, caregivers, and children.
Smoking tobacco not only harms your lungs but also thins your blood vessels, increasing your risk of cervical cancer. Smokers who contract HPV are more likely to experience prolonged infections that don’t clear up. The best option is to quit smoking cigarettes but if not, tobacco harm reduction should be considered – using products such as nicotine replacement

By Dr Motlatsi Mokoape, Specialist Obstetrician & Gynaecologist
therapies, heat not burn products, and oral nicotine which are better alternatives as they don’t combust tobacco which causes harmful toxins.
Polygamous marriages can expose women to higher risks of infections, which can lead to cervical cancer. Awareness of these risks and adherence to regular health screenings are essential for prevention.
Multiple sexual partners, the more sexual partners you have, the greater your risk of contracting HPV and other sexually transmitted infections (STIs), including herpes, chlamydia, gonorrhea, syphilis, and HIV/AIDS, all of which can increase your chances of developing cervical cancer. Practicing safe sex and reducing the number of partners are key preventative measures.
EMPOWER YOURSELF
I urge all women to take charge of their health by adopting preventative measures to lower their risk of cervical cancer. Regular health screenings, vaccinations, proper nutrition, exercise, and self-care are essential tools in your arsenal against this disease. Remember, knowledge and action are your best defences.
Recent advances in malaria
Malaria remains the world’s leading parasitic disease, predominantly affecting the African region, with Plasmodium falciparum being the deadliest species.
BETWEEN 2000 AND 2015, malaria incidence and mortality rates decreased significantly due to international efforts and interventions like insecticide-treated bed nets and artemisinin-based therapies.
However, from 2015 to 2020, there was a troubling increase in cases and deaths, with about 627 000 fatalities reported in 2021. Contributing factors include resource diversion due to Covid-19, emerging drug-resistant strains, and insecticide resistance.
Research for improved malaria control is ongoing. In 2021, the World Health Organization (WHO) recommended the RTS,S/AS01 vaccine for children and recently approved the R21/Matrix-M vaccine, though neither met the WHO's efficacy target of 75%. WHO also advocates for malaria chemoprevention in high-risk groups, such as young children and pregnant women, although complex dosing schedules hinder implementation.
MONOCLONAL ANTIBODIES IN MALARIA PREVENTION
Monoclonal antibodies present a promising approach to malaria prevention, especially for vulnerable populations like children. A phase 2 trial in Mali evaluated a longacting monoclonal antibody targeting the circumsporozoite protein of P. falciparum, revealing protective efficacy of 75% to 88% in adults. This led to the development of L9LS, a human IgG1 monoclonal antibody, which has shown greater potency in preclinical models.
CLINICAL TRIAL FINDINGS
A study published in The New England Journal of Medicine assessed the safety and efficacy of L9LS in children aged 6-10 years in a malaria-endemic area in Mali. The trial included healthy participants and monitored them for six months post-administration during the malaria transmission season. The primary endpoint was the first asymptomatic P. falciparum infection, while the secondary endpoint involved clinical malaria cases.
No safety issues were noted, and asymptomatic infections occurred in 48% of the 150mg group and 40% in the 300 mg group, compared to 81% in the placebo group. L9LS demonstrated 66% efficacy at the 150mg dose and 70% at 300mg against P. falciparum infections. Efficacy against clinical malaria was 67% and 77%, respectively.
This study indicated that a single subcutaneous dose of L9LS could provide substantial protection against malaria in
children. While existing vaccination and chemoprevention strategies face limitations, L9LS could complement or enhance current efforts, especially in high-risk populations.
The trial supports administering L9LS to school-aged children before the malaria season to reduce morbidity, highlighting its potential role in improving coverage among
vulnerable groups.
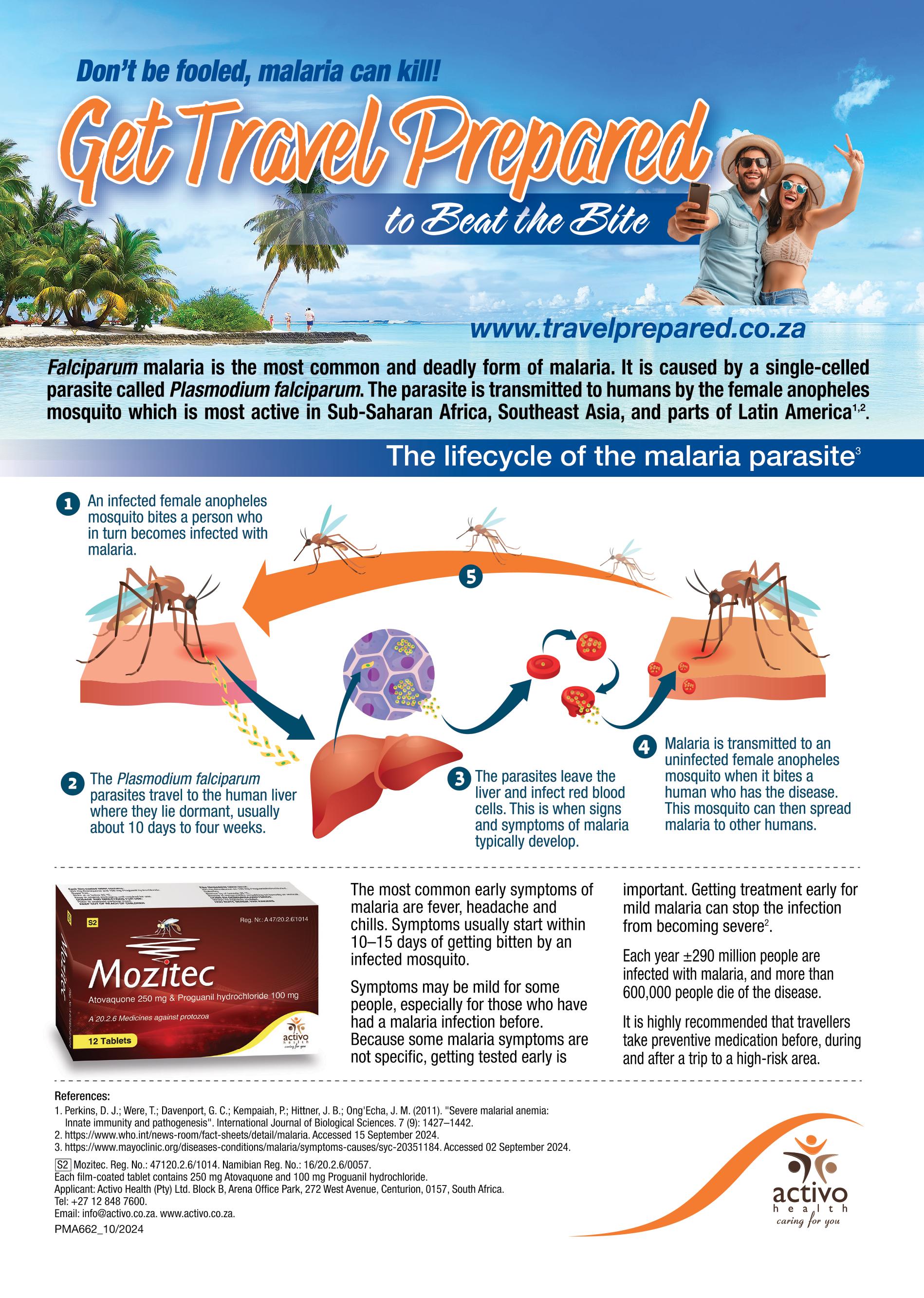
Contraception: Multifactor considerations
Dr Tobie De Villiers recently presented a CPD-accredited webinar about contraception. This was sponsored by Cipla. The following article is a summary of his presentation.
To watch a replay of this webinar and still earn a CPD point, go to: https://event.webinarjam.com/go/ replay/843/r46v4iv3ptw6nh036fl. Email john.woodford@newmedia.co.za to let him know to allocate your point/ request an attendance certificate for those who don’t fall under the HPCSA.
THE LANDSCAPE OF contraception has evolved significantly since the introduction of combined oral contraceptives (COCs) in 1960. Initially, these contraceptives contained high doses of oestrogen and progesterone, which led to notable adverse effects, including an increased risk of venous thromboembolism. Modern formulations have since reduced these doses, addressing many of the early concerns about side effects.
MECHANISM OF ACTION
COCs work through multiple mechanisms:
• Suppression of ovulation: Preventing the release of eggs from the ovaries
• Modification of the endometrium: Making it less suitable for implantation
• Changes to cervical mucus: Making it more difficult for sperm to enter the uterus.
ROLE OF OESTROGEN
Oestrogen is crucial in COCs for several reasons:
• Enhances the effectiveness of progestins
• Improves menstrual patterns
• Prevents estrogen deficiency.
Different types of oestrogen used in COCs include natural oestrogen (E2), synthetic ethinyl oestradiol (EE), and foetal oestrogen (E4). These are classified based on their dosage and type.
PROGESTINS IN COCs
Progestins, synthetic derivatives of progesterone, are added to COCs to protect
the endometrium and suppress ovulation. They vary in their effects on other hormone receptors, influencing their clinical utility and side effect profiles. Progestins are categorised based on their origin, potency, and receptor activity, highlighting that not all progestins are the same.
CLASSIFICATIONS OF COCs
COCs are classified based on:
• Types of oestrogen and progestin
• Dosages
• Special effects, such as anti-androgenic properties.
Benefits of oral contraceptives
Oral contraceptives offer several benefits, including:
• Improvement of menstrual symptoms

• Reduction of iron deficiency anaemia
• Decreased risk of certain cancers.
RISKS AND GUIDELINES
Despite their benefits, COCs are associated with risks, particularly the risk of pulmonary embolism. It is recommended that women can continue using COCs until menopause or the age of 50-55, with a transition to non-hormonal contraception thereafter.
CONCLUSION
Understanding the various components and classifications of oral contraceptives, their mechanisms of action, benefits, and associated risks is crucial.
This knowledge helps in making informed decisions about their use in different age groups.
A practical approach to managing GERD
Dr Nazeer Chopdat, a consultant gastroenterologist, recently presented a gastroenterology webinar for Medical Chronicle. This CPD-accredited event was sponsored by Adcock.
To watch a replay of this webinar and still earn a CPD point, go to: https://event.webinarjam.com/go/ replay/845/7worwh71yu402azqgbw. Email john.woodford@newmedia.co.za to let him know to allocate your point/ request an attendance certificate for those who don’t fall under the HPCSA.
GASTROESOPHAGEAL REFLUX DISEASE (GERD) is a prevalent condition affecting approximately 25% of the Western population, with a lower incidence in Asia. It is most commonly seen in individuals aged 60-70 years and is increasingly recognised in older adults. Dr Chopdat's presentation provides a comprehensive overview of GERD, covering its epidemiology, pathophysiology, clinical presentation, diagnosis, treatment options, and unmet needs in management.
CLINICAL PRESENTATION AND DIAGNOSIS
GERD presents with a variety of symptoms, including heartburn, dysphagia, and nocturnal choking. Atypical symptoms such as chronic cough and laryngitis are also associated with the condition. Alarm symptoms, which necessitate urgent referral, include dysphagia, odynophagia, weight loss, and gastrointestinal bleeding. Diagnosis of GERD is multifaceted, involving empiric trials, endoscopy, and pH monitoring to evaluate acid exposure and symptom correlation. Manometry is also utilised to assess motility disorders related to GERD. The Montreal definition
of GERD differentiates between non-erosive reflux disease (NERD) and erosive esophagitis (EE).
TREATMENT APPROACH
The treatment of GERD aims to enhance lower oesophageal sphincter (LES) pressure, improve oesophageal acid clearance, facilitate gastric emptying, and protect the oesophageal lining. Dr Chopdat outlines a structured treatment approach in three phases:
1. Lifestyle modifications: Recommendations include elevating the head of the bed, reducing fat intake, quitting smoking, avoiding lying down after meals, losing weight, limiting alcohol, and wearing loose clothing. While these changes may not completely alleviate symptoms, they can significantly improve them.
2. Pharmacologic intervention: Standard or high-dose antisecretory therapy is employed, with proton pump inhibitors (PPIs) proving more effective than H2 receptor antagonists in healing erosive oesophagitis and providing symptom relief. Timing of medication administration is crucial, particularly for PPIs, which should be taken before meals for optimal
effectiveness. Potential reasons for PPI therapy failure, such as compliance issues and weakly acidic reflux, are also addressed.
3. Surgical intervention: This is considered for patients unresponsive to pharmacologic treatment or those with severe complications. Laparoscopic fundoplication is presented as an effective option for refractory GERD, offering high patient satisfaction and long-term symptom relief, although it may lead to side effects like bloating and dysphagia. Alternative treatments, such as magnetic sphincter augmentation (LINX), show promise in improving quality of life and reducing PPI dependence.
SPECIAL CONSIDERATIONS AND UNMET NEEDS
In pregnancy, two-thirds of women experience heartburn, typically resolving post-delivery. Treatment during pregnancy should prioritise lifestyle changes, followed by antacids and H2RAs, which are generally safe. Unmet needs in GERD management include breakthrough symptoms and the necessity for improved medication adherence. The introduction of dexlansoprazole, a newer PPI, is highlighted

for its superior acid control and longer duration of action, making it a promising option for GERD patients. Other treatment options include potassium-competitive acid blockers (P-CABs), pain modulators, and baclofen for reducing transient LES relaxations.
Endoscopic treatments are described as relatively new and may benefit select patients with well-documented GERD responsive to PPIs. The presentation includes case studies that illustrate the complexities of GERD management, emphasising the need for lifestyle changes, appropriate medication use, and potential surgical or endoscopic interventions for refractory cases.
CONCLUSION
Dr Chopdat's presentation underscores the multifaceted approach required for effective GERD management, integrating both medical and surgical options while addressing the challenges of long-term PPI therapy and the necessity for individualised patient care. By adopting a comprehensive treatment strategy, healthcare professionals can significantly improve the quality of life for patients suffering from GERD.
Why shouldn’t you treat all your seasonal allergic rhinitis patients the same?
Seasonal allergic rhinitis (SAR) is a prevalent condition affecting a significant portion of the population, particularly in South Africa.
PROF JONATHAN PETER from the Division of Allergology and Clinical Immunology at the University of Cape Town presented a comprehensive overview of the complexities and nuances in treating SAR during a Medical Chronicle webinar on 17 September. This webinar was sponsored by Glenmark. This article is a summary of the presentation.
PREVALENCE AND CO-MORBIDITIES
Allergic rhinitis and asthma are common in South Africa, with 20%-30% of adolescents in certain areas affected. Asthma affects 1 in 10 individuals, with 70% of these cases co-morbid with allergic rhinitis. The prevalence is increasing in lowand middle-income countries (LMICs).
DIAGNOSIS AND MISCONCEPTIONS
A critical starting point is distinguishing allergic rhinitis from other types of rhinitis. Allergies typically cause itching, which antihistamines can relieve, whereas most
rhinitis cases are irritant-based, and nasal steroids may not be effective. Normal adults can experience three-five viral upper respiratory tract infections per year, and many cases of clinically diagnosed rhinosinusitis resolve without antibiotics. Intranasal steroids require at least two weeks to be effective in allergic rhinitis, and food allergy tests are not recommended for diagnosing allergic rhinitis.
SYMPTOM MONITORING AND SEASONAL VARIABILITY
Patients often present with multiple common syndromes, and it is essential to detail symptoms for monitoring. Major symptoms include nasal obstruction, rhinorrhea, itching, and sneezing. Seasonal allergic rhinitis can vary significantly from season to season, influenced by local weather conditions and extreme weather events. For instance, the 2017 Cape Town drought led to the highest peak of grass pollen in the 2010-2020 decade.
CITY PROFILES AND POLLEN TYPES
Different cities in South Africa have distinct pollen profiles. For example:
• Cape Town: Cypress, grass, pine, gum
• Bloemfontein: Grass, false olive, ash, elm
• Johannesburg: Plane, grass, mulberry, cypress
• Pretoria: Grass, mulberry, birch, plane
• Kimberley: Grass, olive, mulberry
• Durban: Grass, mulberry, ferns, birch
• Gqeberha: Grass, cypress, gum.
EMPOWERING PATIENTS AND MANAGEMENT STRATEGIES
Empowering patients with knowledge about their condition and local pollen counts is crucial. Simplified management strategies should target specific symptoms and timing. Combination therapy in a single device offers broader disease coverage, faster symptom control, and improved patient compliance. Intranasal corticosteroids and antihistamines are effective, with

combination therapy providing uniform distribution and no runoff.
ALLERGEN IMMUNOTHERAPY
Allergen immunotherapy (AIT) is an effective add-on treatment for uncontrolled allergic rhinitis. Both subcutaneous (SCIT) and sublingual (SLIT) immunotherapy have shown benefits, including reduced symptoms, decreased medication use, and prevention of new-onset asthma.
CONCLUSION
Rhinitis is often multifactorial and not always allergic. Understanding the complexities of pollinosis and local pollen patterns is essential for effective management. Empowering patients and considering all available treatment options, including allergen immunotherapy, can significantly improve outcomes.
For more information and to empower your patients, visit www.pollencount.co.za.
Emerging trends in the diagnosis and management of spring allergies: What healthcare professionals need to know
THIS ARTICLE HIGHLIGHTS the key points from a recent presentation by Dr Thulja Trikamjee on the diagnosis and management of spring allergies, focusing on the latest trends and best practices for healthcare professionals. This webinar was sponsored by Thermo Fisher Scientific. Dr Tricomi, a pediatrician and allergist from the University of Cape Town Lung Institute, highlights the rising prevalence of allergies during spring and the critical need for effective management strategies.
UNDERSTANDING RHINITIS
Allergic rhinitis
Allergic rhinitis is defined as an immunologic nasal response primarily mediated by immunoglobulin E (IgE). The global prevalence is 10%-40%, making it a major public health issue. It affects quality of life, school performance, and imposes an economic burden.
Non-allergic rhinitis
Non-allergic rhinitis is defined as rhinitis symptoms in the absence of
identifiable allergy, structural abnormality, or sinus disease.
DIAGNOSIS OF ALLERGIC RHINITIS
Take a detailed patient history, including family history of allergic diseases. Examination of the whole patient, focusing on growth, facial features, and nasal examination. Consideration of other symptoms like asthma, eczema, ENT problems, and food allergies.
TESTING FOR ALLERGENSPECIFIC IgE
Skin prick or blood tests identify allergens. Interpret IgE testing in the context of clinical history to avoid false positives and negatives. Dr Tricomi critiques the use of broad allergen panels and advocates for targeted testing based on individual histories.
Management principles:
1. Allergen avoidance is a key strategy in managing allergic rhinitis. 2. Pharmacotherapy is used to control symptoms.
3. Immunotherapy should be considered for patients who respond poorly to optimal treatment.
Steps include correct allergy diagnosis, assessment of adherence, and demonstration of uncontrolled disease during allergen exposure.
OVERVIEW
Key points discussed include the significant impact of allergic rhinitis on quality of life, including sleep disturbances, productivity issues, and academic performance in children. The economic burden of allergies is substantial, with over $30 billion spent annually in the US on over-the-counter medications. Dr Tricomi connects allergic rhinitis to other health issues, such as ADHD and autism spectrum disorders, emphasising that untreated allergies can worsen these conditions. Dr Tricomi stresses that allergic rhinitis is often underestimated, with prevalence rates between 10% and 40%, and many individuals remain undiagnosed, posing a public health concern. The concept of the 'allergic march' is introduced,

illustrating how allergies can evolve from skin conditions in infancy to respiratory issues like asthma in later childhood. The discussion also highlights the need for personalised treatment plans, including the use of antihistamines and intranasal corticosteroids, tailored to the frequency and severity of symptoms. The importance of collaboration between allergists and ENT specialists is noted, particularly in managing complications like chronic sinusitis.
CONCLUSION
Spring allergies, particularly allergic rhinitis, pose a significant challenge for healthcare professionals. By understanding the latest trends in diagnosis and management, including the importance of allergen avoidance, pharmacotherapy, and immunotherapy, healthcare professionals can improve patient outcomes and quality of life. The webinar emphasises the necessity for comprehensive management of allergic diseases, advocating for evidence-based approaches that improve patient quality of life.

Global Health and Disease Burden in Africa
The Global Burden of Disease is a systematic, scientific report designed to quantify loss due to disease, injuries and risk factors by age, sex, and geography for specific points in time.
THE GLOBAL BURDEN of Disease report highlights the significant health challenges faced by Africa, emphasising the need for effective public health policies and interventions. The report quantifies the loss of healthy life due to diseases, injuries, and risk factors, using measures such as Disability Adjusted Life Years (DALYs) and Quality Adjusted Life Years (QALYs). In Africa, nearly 630 million years of healthy life are lost annually, resulting in an economic burden exceeding 2.4 trillion International Dollars. The World Health Organization (WHO) suggests that implementing essential health services could nearly halve this cost.
Despite progress in disease eradication and control, many Sustainable Development Goals (SDGs) remain unmet, partly due to the Covid-19 pandemic. Global health aims to improve health outcomes for vulnerable populations and reduce disparities in low-resource settings through research, education, and collaborative efforts. The focus is on achieving health equity for all.
GLOBAL HEALTH
Over the past two decades, the global health landscape has transformed, with people living longer and the population aging. While child mortality has decreased, the burden of disease is increasingly characterised by disabilities rather than premature deaths. In sub-Saharan Africa, communicable diseases, maternal, nutritional, and newborn diseases still dominate health challenges. However, there has been notable progress in reducing mortality from communicable diseases, particularly in early childhood.
THE GLOBAL BURDEN OF DISEASE
The health status of the African population is poor, hindering economic and social development. In 2015, diseases in Africa accounted for an estimated 704 million DALYs, with communicable diseases contributing significantly to this burden. Five countries: Democratic Republic of Congo, Ethiopia, Nigeria, South Africa, and Tanzania, accounted for nearly half of the total DALYs in the region. The economic impact of ill health varies by age, disease category, and economic group.
HIV/AIDS and malaria were major health concerns in the early 2000s, but their relative burdens have decreased over the past two decades. Sub-Saharan Africa has made progress in reducing mortality rates since 1970, although some countries, like Mozambique, have seen rising mortality rates among specific age groups. Noncommunicable diseases (NCDs) such as stroke, diabetes, and mental health issues have increased, particularly in upper-middleincome countries.
Road accidents and interpersonal violence have also emerged as significant health threats in developing nations. In sub-Saharan Africa, a higher percentage of health years lost are due to disabilities, including depression and chronic pain. Nutritional deficiencies, particularly iron deficiency anaemia, have a more substantial impact in sub-Saharan Africa compared to global averages. Key risk factors for premature death and disability include undernutrition and household air pollution, with substantial progress made in reducing childhood underweight and vitamin deficiencies. Alcohol use, high blood pressure, and smoking are significant contributors to health loss in many African countries. In upper-middle-income nations, high fasting plasma glucose and body mass index are major health concerns, while childhood underweight remains a primary risk factor in lower-income countries.
The burden of disease encompasses the cumulative consequences of diseases, including health, social, and economic costs. Globally, non-communicable diseases account for the majority of the burden, followed by communicable diseases and injuries. South Africa faces a quadruple burden of disease, including HIV/AIDS, TB, maternal and childhood mortality, and NCDs.
TB remains a leading cause of death in South Africa, with significant cases reported in recent years. Other infectious diseases, such as malaria and cholera, continue to pose risks. The African CDC reports various infectious diseases affecting the continent, including anthrax, avian influenza, and Ebola.
Infectious diseases can perpetuate poverty and undermine community resilience, leading to severe economic consequences. Although the global
incidence of infectious diseases has declined since 2000, they still impose significant health and economic burdens.
PROGRESS WITH DISEASE BURDEN IN AFRICA
Progress has been made in addressing disease burdens in Africa. Algeria became the third African country to be certified malaria-free in 2019, following Mauritius and Morocco. Several countries, including Botswana and South Africa, are committed to malaria elimination. The decline in new HIV infections is notable, with significant reductions reported in Eastern and Southern Africa. By 2022, two-thirds of people living with HIV globally were receiving treatment, with substantial access to antiretroviral therapy in sub-Saharan Africa.
In terms of TB, 18 African countries are among the 30 high-burden countries globally, accounting for a significant percentage of cases. Progress towards the End TB Strategy has been mixed, with some countries achieving milestones while others have seen reversals in progress.
By 2022, 42 African countries had eradicated Guinea worm disease, and several others had eliminated various public health problems. The ongoing efforts to combat diseases in Africa reflect a commitment to improving health outcomes and addressing the complex challenges posed by both communicable and non-communicable diseases. The report underscores the importance of continued investment in health systems, research, and collaborative interventions to achieve better health for all in the region. The report also highlights the importance of addressing social determinants of health, such as education, income, and living conditions, which significantly impact health outcomes. Improving access to clean water, sanitation, and hygiene (WASH) services is crucial in preventing infectious diseases and improving overall health. Additionally, strengthening health systems, including workforce training, infrastructure development, and supply chain management, is essential for delivering quality health services. The role of international partnerships and collaborations in addressing global health challenges

cannot be overstated. Organisations such as the WHO, the Global Fund, and Gavi, the Vaccine Alliance, play a critical role in supporting health initiatives in Africa. These partnerships facilitate the sharing of knowledge, resources, and best practices, enabling countries to implement effective health interventions.
Furthermore, the report emphasises the need for innovative approaches to healthcare delivery, including the use of digital health technologies.
Telemedicine, mobile health applications, and electronic health records can enhance access to health services, particularly in remote and underserved areas. These technologies also enable better data collection and analysis, supporting evidence-based decision-making and improving health outcomes. The report calls for increased investment in health research and development to address the unique health challenges faced by African countries. Research on diseases prevalent in the region, such as malaria, HIV/AIDS, and TB, is crucial for developing effective treatments and interventions. Additionally, research on non-communicable diseases, mental health, and health systems strengthening is essential for addressing the evolving health needs of the population.
CONCLUSION
In conclusion, the Global Burden of Disease report provides a comprehensive overview of the health challenges faced by Africa and underscores the need for concerted efforts to improve health outcomes. By addressing the social determinants of health, strengthening health systems, fostering international partnerships, and leveraging innovative technologies, significant progress can be made in reducing the burden of disease and achieving health equity for all. Continued investment in health research and development is essential for developing effective interventions and ensuring sustainable health improvements in the region. The report serves as a call to action for governments, health organisations, and stakeholders to work together in addressing the complex health challenges faced by Africa and improving the health and wellbeing of its population.
PLACEBO
"C Heart smart Netcare's CVD crusade

Marking a pivotal step forward in the fight against cardiovascular disease (CVD) in the Western Cape, Netcare hospitals in the province are launching an initiative to champion heart health awareness and CVD prevention.
ARDIOVASCULAR DISEASE
is the leading cause of death worldwide, claiming an estimated 17.9 million lives each year, according to the World Health Organization. This staggering statistic highlights the urgent need for proactive heart health measures,” asserts Dr Louis Van Der Hoven, regional general manager of Netcare Western Cape.
“For us at Netcare, this is a tangible commitment to community wellbeing,” says Dr Van Der Hoven. “By offering free health checks and expert advice, we aim to empower individuals to take control of their heart health.”
The Healthy Heart Drive will take place in the reception areas at four key facilities: Netcare Christiaan Barnard Memorial, Netcare Blaauwberg, Netcare N1 City and Netcare Kuilsriver hospitals. These hospitals will provide free blood pressure and cholesterol checks and consultations with dietitians and physiotherapists for expert preventative care advice. This comprehensive approach tackles heart health from all angles, including diet, exercise, stress management and medical intervention.
Dr Shaheen Pandie, a cardiologist at Netcare Christiaan Barnard Memorial Hospital, is one of the healthcare professionals behind the initiative and is committed to highlighting the dangers and prevalence of undiagnosed coronary artery disease. "Early screening isn't just important – it's lifesaving. And in a cardiac emergency, swift access to the best care is crucial," he emphasises.
"The belief that heart disease only affects older adults is dangerously outdated," warns Dr Pandie. "Today, we see heart disease and its risk factors rising alarmingly among younger people, driven significantly by the global obesity crisis."
REVAMP
YOUR
DIET AND LIFESTYLE FOR BETTER HEART HEALTH
“The typical South African diet, rich in refined carbohydrates and saturated fats, severely jeopardises heart health. Simple changes, like reducing red meat, opting for lean meats, and incorporating more plantbased foods, can make a huge difference. Cutting back on refined carbs, embracing whole grains, and choosing fat-free or lowfat dairy are equally important steps worth taking,” advises Dr Pandie.
“Regular blood pressure and cholesterol checks are essential. A study in The Lancet shows that 50% of people in sub-Saharan Africa are undiagnosed. Elevated cholesterol is especially underdiagnosed in Afrikaners and Indians of Gujarati descent. The obesity pandemic worsens both hypertension and dyslipidaemia – unhealthy levels of fats in the blood – which raise the risk of heart disease.
“Lifestyle changes like regular exercise, healthy eating, weight loss, and quitting smoking can drastically reduce heart disease risk. Therefore, engaging in cardiovascular exercise for at least 30 minutes daily or five times a week is important. Quitting smoking is one of the most effective ways to prevent heart attacks and strokes,” he recommends.
A SPECIAL MESSAGE TO THE PILLARS OF THE COMMUNITY
Dr Pandie highlights the incredible strength and resilience of South African women, who are often society's caregivers. However, he emphasises the importance of women prioritising their own health.
EDITORIAL
EDITOR: Claire Rush McMillan
Claire.Rush@newmedia.co.za
NEWS WRITER: Nicky Belseck
Nicky.Belseck@newmedia.co.za
SUB-EDITOR: Gill Abrahams
EDITORIAL CONTRIBUTORS
Dr Ilhaam Mohamed, Prof Morgan Chetty.
LAYOUT & DESIGN: Naresh Budraj
ADVERTISING
ADVERTISING EXECUTIVES
Anel du Plooy - Tel: 082 786 9517
Anel.duPlooy@newmedia.co.za
Cindy Riederer - Tel: 082 492 0229
Cindy.Riederer@newmedia.co.za
DISTRIBUTION & SUBSCRIPTIONS
Felicity Garbers
Email: felicity.garbers@newmedia.co.za
Update your details here: www.medicalacademic.co.za
PUBLISHING TEAM
GENERAL MANAGER: Dev Naidoo
HEAD OF COMMERCIAL: B2B: Johann Gerber
Email: Johann.Gerber@newmedia.co.za
TIME TO TAKE CHARGE OF YOUR HEART HEALTH
For those with genetically high cholesterol, a combination of lifestyle changes and medical interventions is essential. To maintain good heart health, embrace a Mediterranean-based diet and reduce trans fats, which are the unhealthy fats found in processed foods.
Stress is another significant risk factor for heart attacks. "Stress can elevate blood pressure and other heart disease risk factors,” warns Dr Pandie. He recommends early mental health interventions and stress management techniques such as mindfulness and regular exercise.
“The Healthy Heart Drive is a powerful initiative that empowers individuals to take control of their wellbeing. However, true change begins with you – take ownership of your health through early screening and healthier lifestyle choices.“
Heart disease is a silent killer, but early diagnosis can be a lifesaver. Take charge – get screened. Understand your family's cardiovascular history and that of your partner. Break free from a sedentary lifestyle by engaging in daily physical activities like swimming or hiking. Plan your meals to include heart-healthy options and commit to regular exercise. It's time to break a sweat! Your heart will thank you, and so will your loved ones. Together, we can beat heart disease and build a healthier, happier future," concludes Dr Pandie. .
“Despite facing significant challenges like obesity, hypertension and high cholesterol, South African women have the power to transform their wellbeing. By seeking timely medical care and staying informed about their unique heart health needs, they can continue to nurture their families while also nurturing themselves. Recognising and addressing these health issues can lead to longer, healthier, and happier lives for these indispensable pillars of our community,” he notes.
DIGITAL MANAGER: Varushka Padayachi
PRODUCTION MANAGER: Angela Silver
ART DIRECTOR: David Kyslinger
CONTACT
Johannesburg Office
Building 13, The Woodlands Office Park, 20 Woodlands Drive, Woodmead, Sandton PO Box 784698, Sandton 2146 +27 11 867 6111
COVER PRICE
Medical Chronicle per issue R60.00 VAT Incl.
Published by New Media, a division of Media24 (Pty) Ltd Printed and bound by Novus Print - Montague Gardens, Cape Town
MANAGEMENT TEAM
CEO : Aileen Lamb
COMMERCIAL DIRECTOR: Maria Tiganis
STRATEGY DIRECTOR: Andrew Nunneley
CHIEF FINANCIAL OFFICER: Venette Malone
Interim CEO: MEDIA24: Raj Lalbahadur
HEAD OFFICE
Cape Town
11 Shelley Road, Salt River, Cape Town PO Box 440, Green Point 8051 +27 021 406 2002 Unless