

WELCOME OUR VALUES
Respect
Value the rights, beliefs and choices of every individual
Take responsibility for our decisions and actions
Work together to create value in health
Welcome to NCN Health, a small rural health service providing a range of health programs for our local community.
This booklet will provide you with important information for before, during your stay and discharge from our health service.
It is designed to help consumers, their families, carers and other support people get the most out of their health care. Being actively involved, and working in partnership with healthcare providers can help ensure you get the care that is right for you
You can use the information in this booklet when you talk to your doctors and healthcare providers, including nurses, pharmacists, specialists, allied health and mental health workers.
We hope you find this booklet useful, if you need any more information the staff will be happy to help
Interpreters
Please let us know if you need an interpreter. Printed information is available in many languages from the Department of Health website wwwhealthvicgovau If you require copies please let us know and we will arrange this for you.

HOSPITAL IN THE HOME (HITH) GENERAL INFORMATION
Admission to NCN@HOME HITH Program
Patients can be admitted to the NCN@Home HITH program by a number of sources:
Admissions from GP clinic
NCN Health Acute Ward or Urgent Care Centres
NCN Health Community Health and Wellbeing services
Residential Aged Care Facilities
Other Health Services
The treating doctor will complete a patient history and examination prior to the patient being admitted.
NCN Health HITH program
NCN@Home provides home-based care for patients who would otherwise require a stay in hospital.
Treatment is provided in your own home by the District Nursing staff in consultation with your own doctor.
Who can be treated in the NCN@Home program?
You can be treated in the program if:
Your condition is stable and you do not require 24-hour monitoring in a hospital ward,
You agree to share responsibility for your own medical care in your home environment,
You have support people available, a telephone and access to transport.
Who will care for me at home?
A nurse will visit daily as required to provide care, treatment and to monitor your progress. Access to advice is available 24-hours a day via telephone. A family member and/or support person should be available to assist with your daily needs. However, services such as home help or meals on wheels can be arranged if required.
When do I see my doctor?
You will need to be regularly reviewed by your treating doctor. The medical reviews may occur at home via telehealth, or at the GP Clinic.
What if I need help or advice?
Advice is available 24 hours a day by telephone. If problems cannot be solved over the telephone, you may need to return to hospital for review and/or additional treatment. Family or friends may need to provide transport in these circumstances
Health and safety
NCN Health is committed to ensuring a healthy and safe environment for its staff, patients and visitors.
Reporting a Hazard: If you observe a condition or activity that you believe has the potential to cause harm please report it as soon as possible to a staff member, who will take the appropriate action.
General Information
Smoke Free: NCN Health is proud to be a totally smoke free facility. It is illegal to smoke within 4 metres of any doorway.
Smoking is not allowed in the buildings or the hospital grounds.
We ask that you also refrain from smoking whilst our staff are visiting you in your home.
Patients who smoke may speak with staff to discuss their needs and access support. We can provide you with resources to help stop smoking.
Advocacy
An advocate is someone you choose to have support you when accessing services. The aim is to protect you if you are not able to speak up for yourself or to help you receive equal rights.
Not everyone needs or wants an Advocate but it is important to know it is an option for you.
Advocates can:
Support you to speak out on your own behalf
Speak for you to service providers and other groups
Refer you to other services
Ensure you are being listened to Provide information on rights
Who can be an Advocate?
Anyone can be an Advocate. An Advocate does not need to be an expert. They need to be able to listen and follow steps to resolve a complaint.
They are not a legal representative and do not receive payment. An example is a good friend whom you trust and will have your best interests at heart.
The Older Persons Advocacy Network (OPAN) is funded to provide free, confidential and independent advocacy support to older people, their families and representatives across Australia.
For more information, speak to the nursing staff or contact one of the services listed on the righthand side of the page.
72 Wyndham Street Shepparton Victoria 3630 (03) 5822 1944 www.riac.org.au
Senior Rights Victoria Level 4, 98 Elizabeth Street Melbourne Victoria 3000 1300 368 821 www.seniorsrights.org.au
Elders Rights Advocacy
Level 2,85 Queen Street Melbourne Victoria 3000 1800 700 600 www.era.asn.au
Office of the Public Advocate Level 5,436 Lonsdale Street Melbourne Victoria 3000 1300 309 337 www.publicadvocate.vic.gov.au

Feedback (Concerns, Compliments & Suggestions)
NCN Health is dedicated to providing quality care and service to our community.
Feedback can be given in the following ways;
We appreciate all feedback about the services and care provided, including; compliments, complaints and suggestions. All feedback helps improve our service to you.
All feedback including complaints are managed to ensure your confidentiality is maintained
You may choose to remain anonymous when providing feedback, however providing contact details allows us to discuss your feedback with you and advise you of the actions taken in response to your feedback.
By speaking directly to the Nurse
Unit Manager or health professional in the relevant area
Paper copies of the NCN Health
Consumer Feedback Form are available in each reception area
You can also download a printable version of the feedback form on the NCN Health website:
https://ncnhealth.org.au/contact/ Share your experience online at CareOpinion, your information can reamain private and will be followed up by the health service
https://www.careopinion.org.au/
Feedback can also be provided to the Feedback Officer via the following options:
T: (03) 5866 9444
E: ncnhealth@ncnhealthorgau
E:
E: ncnhealth@ncnhealthorgau
If you believe your concerns have not been addressed, you may contact:
Health Complaints Commissioner Level 26, 570 Burke Street Melbourne Vic 3000
Phone: 1300 582 113 Email: hcc@hcc.vic.gov.au
Advance Care Directive
What is an Advance Care Directive
Advance Care Directive is for everyone. It is a way to let your family and doctors know how you want to be cared for if you become unable to make decisions.
If you are sick or injured and cannot make your own decisions about treatment, your family may be asked to make decisions about your care such as;
Resuscitation and life support
High risk surgery
Permanent tube feeding
Hospital or nursing home admissions

How can an Advance Care Directive help me?
You can make these decisions ahead of time, or you can discuss and write down your preferences so these can be followed.
When should I start an Advance Care Directive?
Most people do not make good decisions during a time of stress It is a good idea to plan when you are well and your health is stable.
This gives you enough time to think clearly and talk about your preferences with your family and doctor.
What are the benefits of an Advance Care Directive?
Peace of mind
Makes things easier for your family
Helps doctors and others who care for you to know what you want and what you do not want.
Advance Care Directive
How do I do an Advance Care Directive?
There are four (4) key steps you can take now:
Talk about your views and preferences with your family, doctor, carers and close friends Appoint an Enduring Power of Attorney (medical) who can make health care decisions on your behalf if needed. Write down your views and preferences for your family and doctors in a document called an ‘Advance Care Directive’
Give copies of your Advance Care Directive to your family, doctor and hospital staff on admission
If you still need further information, staff will be available to discuss and Advance Care Directive with you during your admission, if you wish to take the Advance Care Directive
Form home please discuss this with the staff.
What is a Substitute Decision Maker / Power of Attorney?
A Substitute Decision Maker/Power of Attorney is a legal document where you can nominate a person to manage your medical or financial decisions.
It is advised that this is completed before any acute medical illness or condition occurs It may not be possible for this document to be attended to once you become unwell.
You can get the forms to fill out an Enduring Power of Attorney from the Office of the Public Advocate website.
You can also speak with nursing staff or your medical officer for more information.
Website:
www.publicadvocate.vic.gov.au
Telephone: 1300 309 337
Goals of Care
Goals of care describe what a patient wants to achieve during an episode of care, within the context of their clinical situation Goals of care are the clinical and personal goals for that patient’s episode of care that are determined through a shared decision-making process
Identify goals of care when the patient is admitted
The treating team works with the patient and family to identify goals of care
Goals of care inform medical decision-making and limitations of medical treatment (resuscitation plan)
Medical management aligns with the patient’s values and preferences from the point of admission.
Revisit goals of care when:
The patient is re-admitted to hospital
There are significant changes in the patient’s condition or circumstances
The patient, substitute decision maker or family request it
The patient, substitute decision maker or family expresses concerns
About goals of care
Active medical treatments and end of life care are not mutually exclusive Goals of care are reflected in the clinical treatment plan, limitations of medical treatment (resuscitation plan) and advance care planning.

Goals of care guide treatment at times of crisis
Crisis’ often occur after hours. Without documented goals of care, clinicians who don’t know the patient are forced to make decisions in the heat of the moment and without the input of the patient or substitute decision maker.


Who may be involved in your care
During your admission there may be several staff who will care for you, this may include:
Nursing staff
Your doctor or the doctor providing after hours coverage
Allied health professionals
Nursing visits
Each visit the nursing staff will check your vital signs (blood pressure, pulse, temperature, breaths, oxygen saturation and pain levels)
They will also complete a care plan. This will include them questioning you about if you are managing with activities of daily life, for example toileting, preparing and eating meals and hygiene.
Nurses will also complete the required care for the visit and complete paperwork to ensure an accurate record of your health journey.
Doctors’ visits
While you are on the NCN@HomeHITH program a doctor will be managing your care.
You will need to have a doctor’s visit to determine your initial and ongoing needs, to order investigations and medications.
Further doctors’ visits may be required to assess if the current care is appropriate and to make changes as required.
Telehealth visits can be arranged if these suit both the doctor and patient.
Allied Health Professionals
If, during a nursing or medical visit a need for an allied health professional (physiotherapist, occupational therapist, exercise physiologist, dietitian, social worker, diabetes educator, chronic disease worker) is recognised a referral can be completed.
It is our aim to have an appointment set up prior to the program ending.
In some situations, a telehealth appointment may be arranged for you ensuring you have access to appropriate and timely care.

COMMUNICATING FOR SAFETY
When our clinicians talk with each other they are encouraged to use a structured communication tool. The structure we encourage is ISBAR.
I: Identify
S: Situation
B: Background
A: Assessment
R: Request/recommendations
When talking with our clients we are encouraged to use common language and to avoid using jargon and medical terms
If your care provider forgets this please remind them as our aim is that you have a good understanding of the information we provide

Also feel free to check back to confirm what you understand is correct, do this as often as you feel you need
It’s a good idea to write down any questions that you may want to ask our staff between visits, have a pen and paper available for this Bring out your questions and get the carer to go through them with you at the visit.

COMPREHENSIVE CARE
Preventing Falls
Staff will help you to stop falling by:
Assessing your risk of falling and discuss the results with you
Developing a falls prevention care plan suited to your needs
Refer you to other staff who specialise in different areas

Organise visits by Occupational Therapists or Physiotherapists to help make your home safer, or to suggest changes to it or equipment to help you move safely
What can you do to reduce your risk of falling?
Wear laced up or snug fitting shoes or slippers with rubber soles
Use your usual walking aids and if you need any assistance, tell us
Don’t rush – take your time
Get your balance before moving away from the bed or chair
Be careful walking around in the dark, especially going to the toilet at night
If you do fall while on the HITH program it is important to report the fall to our staff.
Once you are safe (call an ambulance if you require this ‘000’) contact the nurse on the numbers provided on admission.
COMPREHENSIVE CARE

Preventing Pressure Ulcers

What can you do?
Keep your skin clean and dry
Avoid any products that dry out your skin Apply moisturiser to dry skin
Protect bony areas like your ankles, shoulder blades or elbows
Avoid anything that causes friction or shearing (pulling).
Staff will:
Encourage and assist you to change positions frequently
Provide you with a special mattress or cushion for support
Encourage you to look at your skin daily and let the nurse know about any change you see.
What can you do to reduce your risk of pressure ulcers?
Sit out of bed rather than sitting up in bed
Move as frequently as possible Even small changes in how you sit or lie makes a difference
Walk around every few hours if you can.
PREVENTING AND CONTROLLING INFECTIONS
Hand hygiene is an important factor in reducing infections Our hands may look clean but germs are invisible to our eyes.
What can you do?
Use soap and water when hands are visibly dirty
Use alcohol-based hand rub when hands are visibly clean
Tell us if you have diarrhoea or vomiting.

Staff will perform the ‘Five Moments’of hand hygiene:
Before touching a patient
Before clean / aseptic procedures
After body fluid exposure / risk
After touching a patient
After touching patient surroundings.
How can you prevent infections?
Wash hands regularly, or use an alcohol-based product to help stop the spread of infections

Wash your hands before and after visiting the toilet, and before all meals
Do not hesitate to ask our staff if they have washed their hands.
BLOOD MANAGEMENT
Preventing Blood Clots
Staff will help you to prevent blood clots by:
What can you do to reduce your risk of blood clots


Advising you to sit out of bed and mobilise frequently Refer you to other staff who specialise in different areas. Move as often as you can. This helps to keep the blood flowing in your leg veins
Try to do simple leg and ankle exercises Drink fluids as recommended.
MEDICATION SAFETY
Medications
Doctors and nurses need to know about all the medicines you use so they can make the right decisions about your health Medicines include prescription, over the counter, herbal and natural medicines, and come in different forms such as tablets, lotions and patches.

Staff will:

Check what medication you are currently taking Explain what medications you are taking and why.
What can you do?
Tell us if you don’t understand what your medicines are for Tell us if you have any allergies
Tell us if you do not feel well
Tell us if you think your condition has changed
Tell us if you think your medications have been missed.
Leaving the Hospital in the Home (HITH) Program


Questions you can ask:
Can you explain to me which treatment I need nowand in the future?
When are my follow-up appointments?
Will I be given a discharge plan?
Will you send my discharge plan to my GP?
What Happens During HITH Discharge?
We will discharge you when you no longer need to receive HITH care, this is usually when you no longer need daily care.
During the discharge process, members of our team will provide you with the information you need to make this transition successfully.
Our team should discuss the following with you:
Your medical condition at the time of discharge
What kinds of follow-up care you will need, such as physiotherapy
What medications you need to take, including why, when, and how to take them, and possible side effects to watch for
What medical equipment you will need, and how to get it
When and how you will receive test results
Instructions on food and drink, exercise, and activities to avoid
Phone numbers to call if you have a question or problem
Days and times of your follow-up appointments, or information about how to make appointments
24 - 48 hrs after you are discharged one of our nursing team will call you to check how you are going and if you have any concerns. During this phone call, you will also be asked to answer a short patient survey that will provide us with feedback to change and improve our service
Leaving Hospital in the Home (HITH) - Payments
Public patients have their medical costs, except for discharge medicines, covered by Medicare
As a patient under the HITH program you are only responsible for paying for your medications
Protecting patient privacy is something we value at NCN Health.
Throughout the service patients, clients, residents and visitors are made aware of why their information is collected, used, and disclosed. Wherever possible, we will provide patients, residents and clients with choices about how their information is used and to whom it is disclosed.
Confidentiality of health information is assured Information is stored in a secure manner, both paper-based and electronically. We support, promote and comply with the 11 Health Privacy Principles.
Client information will only be used and disclosed for the purposes for which it was collected and be protected from misuse.
The collection or sharing of information is limited to that which is necessary, rather than what may be useful in the future.
We make every effort to be clear about the purposes for which information is being shared.
We will also be open with patients, clients, residents, visitors, family members and other stakeholders about why information is being shared and with whom, what will happen to it, and how it maybe accessed and corrected it if necessary.
Use of Your Medical Records
During your treatment doctors, nurses and other health care professionals will need to collect information about you This information is important because it will assist in planning your treatment.
Information relating to your health care may be shared with other health care professionals or other health care facilities where they are continuing with your care
The information may also be used in reviews and audits, in which case all information remains confidential and is not identified
Your information cannot be released to any person(s) not involved in your continuing care unless your consent is obtained, or if it is required by law All medical records remain the property of NCN Health.
Access to your Medical Records and Disclosure of your Information.
Your information can only be accessed and/or disclosed by your treatment team for the purpose of your ongoing care It cannot be accessed by your relatives or friends without your consent.
Your information may also be shared with external organisations as a requirement by law. If you have any concerns about your information being shared with other health care providers or services, please speak to a member of the health care team
Freedom of Information Act 1982
People may have access to information held in their medical record through the Freedom of Information Act.
All applications for information must be processed by the Freedom of Information Officer These incur a request / application fee and may take up to 45 days to process.
Inquiries can be made in person or in writing addressed to:
Nathalia:
The Freedom of Information Officer
NCN Health Nathalia
36-44 McDonnell Street
Nathalia Victoria 3638
Cobram:
The Freedom of Information Officer
NCN Health Cobram
PO Box 252
Cobram Victoria 3644
Numurkah:
The Freedom of Information Officer
NCN Health Numurkah
PO Box 128
Numurkah Victoria 3636
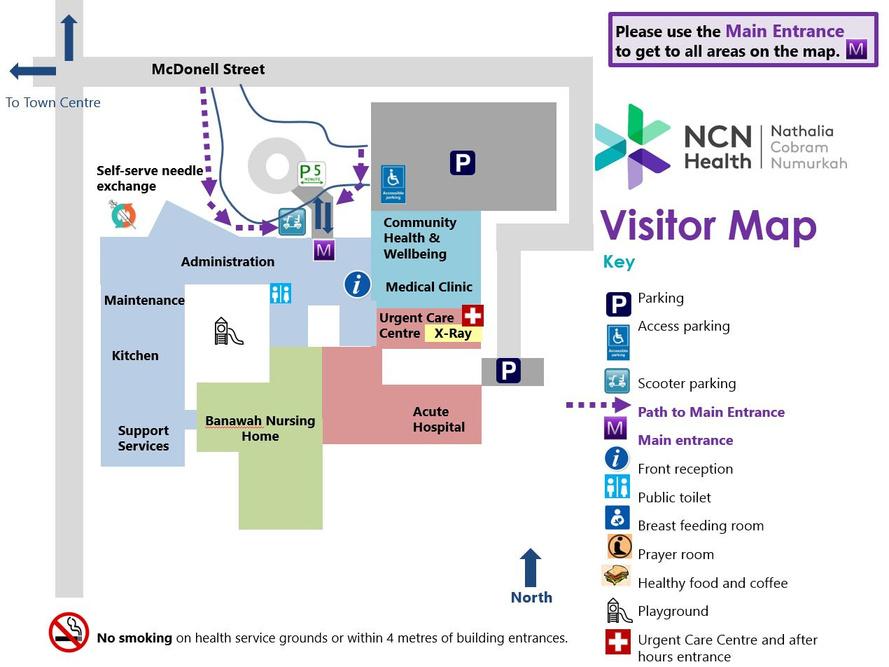
Visitor Maps - Nathalia Campus

Visitor Maps - Cobram Campus


Visitor Maps - Numurkah Campus


Contacts Details:
Ambulance 000
Nathalia District Nursing Service (DNS):
M 0417 362 789
Cobram District Nursing Service (DNS):

T (03) 5871 0917
M 0418 819 842
Numurkah District Nursing Service (DNS):
T (03) 5862 0564
M 0407 620 038
After Hours
Nathalia
M 0419 554 083
Cobram
M 0459 895 214
Numurkah
T (03) 5862 0519
Nathalia Campus
36-44 McDonell St, Nathalia VIC 3638
T: (03) 5866 9444
E: ncnnathalia@ncnhealth.org.au


Cobram Campus
24-32 Broadway St, Cobram VIC 3644
PO Box 252, Cobram VIC 3644
T: (03) 5871 0777
E: ncncobram@ncnhealth.org.au
Numurkah Campus
2 Katamatite Rd, Numurkah VIC 3636
PO Box 128, Numurkah VIC 3636
T: (03) 5862 0555
E: ncnnumurkah@ncnhealth.org.au
