Core Competencies of Healthcare Professionals involved in Older People’s care
Entrustable Professional Activities (EPAs)
Professor Tahir Masud
Professor of Geriatric Medicine, Nottingham, UK

Past President of the British Geriatrics Society (BGS)
Director of Education and Training,
European Geriatric Medicine Society (EuGMS) Executive Board
Joint Report 2011: WHO
National Institute of Health
National Institute of Ageing
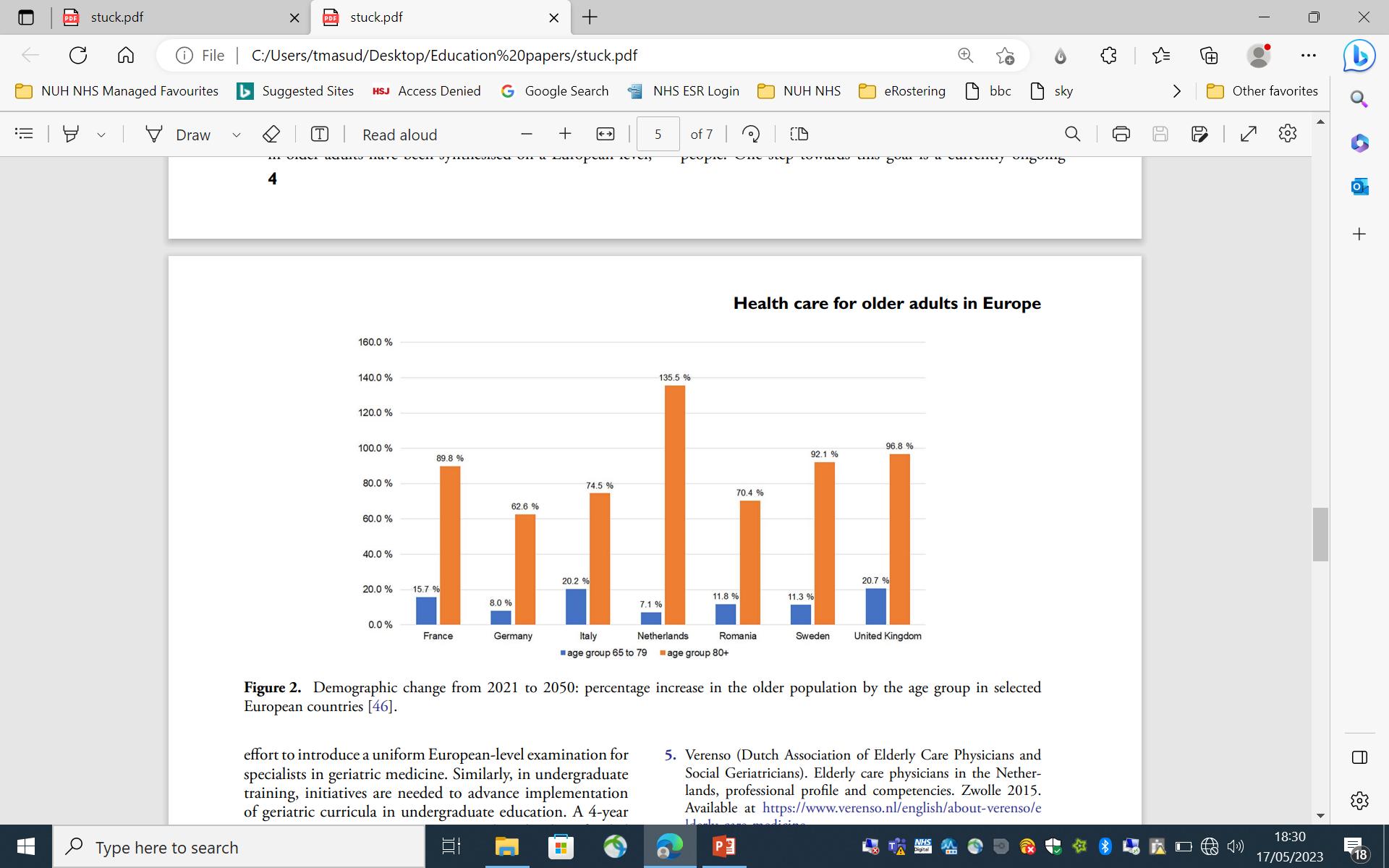
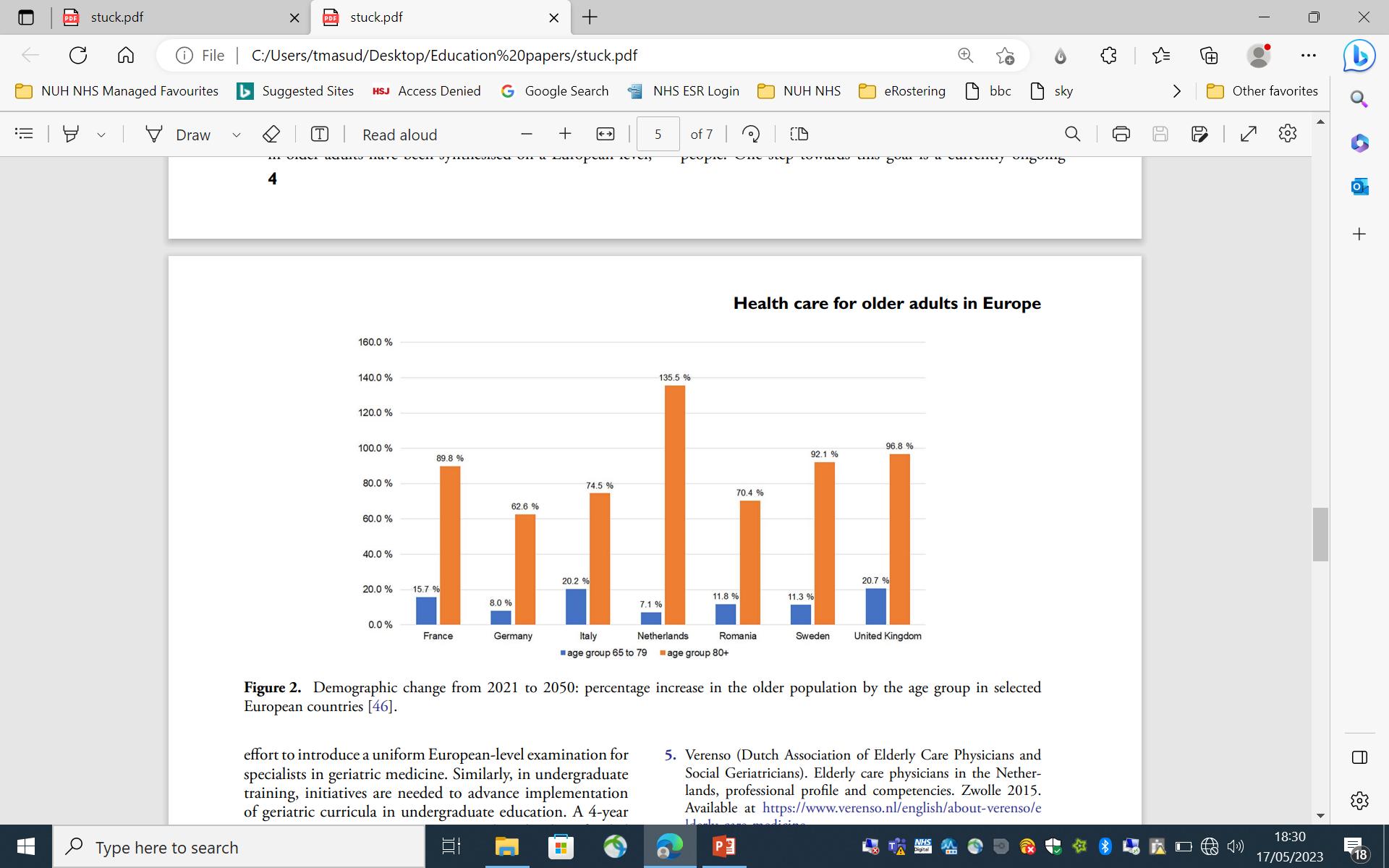
“Oldest Old” (>85 years) are projected to increase globally by 351% between 2010 and 2050
Report: Ageing in the European Union Rechel et al 2013 Lancet
“Workforce providing healthcare for older people should be expanded and that health workers should be trained appropriately”
Silver Paper: Report of a European summit on Age Related Disease
Ageing Clin Exp Res 2009
Cruz-Jentoft AJ, Franco A, Sommer P, Baeyens JP, Jankowska E, Maggi A, Ponikowski P, Rys A, Szczerbinska K, Michel JP, Milewicz A
“The research literature suggests that support for geriatrics in national undergraduate curricula is key to delivery of teaching in the speciality”
European Union of Medical Specialists
(UEMS)- Geriatric Medicine Section
Updated Lit Review
2009-2012 (TM)
First draft Pre-Delphi
European Undergraduate Geriatric Medicine Curriculum
Dec 2012 (TM,AS)
•A.Stuck
•T.Masud
•K.Mulpeter
•A.Blundell
•A.Gordon
•K.Singler
•R.Roller-Wirnsberger
UEMS Subgroup + Experts
Final draft Pre-Delphi
European Undergraduate Geriatric Medicine
Curriculum Jan 2013
12 paragraphs/domains
DELPHI PROCESS
3 rounds
Feb-April 2013 (AS)
Delphi Process
Austria Thomas Frühwald
Austria Georg Pinter
Belgium Margareta Lambert
Belgium Jean Petermans
Bulgaria Toni Staykova
Czech Republic Eva Topinková
Denmark Ellen Holm
Denmark Susanne van der Mark
Estonia Helgi Kolk
Finland Maria Nuotio
Finland Jaakko Valvanne
France Alain Franco
Germany Dieter Lüttje
Greece George C. Spatharakis
Hungary Gyula Bakó
Iceland Pálmi V. Jónsson
Ireland Ken Mulpeter
Israel A. Mark Clarfield
Italy Mario Barbagallo
Italy Renzo Rozzini
Lithuania Jūratė Macijauskienė
Malta Anthony Fiorini
Malta Mark A. Vassallo
Netherlands Jaap Krulder
Norway Thomas Svendsen
Poland Katarzyna Wieczorowska-Tobis
Portugal Gorjão Clara
Romania Gabriel-Ioan Prada
Serbia Mladen Davidovic
Serbia Predrag Erceg
Slovakia Stefan Krajcik
Slovenia Gregor Veninsék
Spain Sergio Ariño-Blasco
Sweden Anne Ekdahl
Sweden Maria Eriksdotter
Switzerland Christophe J. Büla
Switzerland Andreas E. Stuck
Turkey Mustafa Cankurtaran
Turkey Asli Curgunlu
United Kingdom Tahir Masud
Expert Adrian Blundell
Expert Adrian Goeldlin
Expert Adam Gordon
Expert Regina Roller-Wirnsberger
Expert Katrin Singler
Expert Arturo Vilches-Moraga
29 countries
n = 46


Ten Broad Domains
1. Respect for Older Patients
2. Principles of Ageing
3. Common Medical Conditions in Older People
4. Geriatric Assessment
5. Medication Use in Older People
6. Older peoples Response to Illness: Impairments/Disabilities/Handicaps
7. Ethical and Legal Issues
8. Role of other Healthcare and Social Care Professions
9. Healthcare in Different Settings
10. Specific Regional Health and Social Care Aspects
Masud T et al Age Ageing 2014
Curricular Mapping/Surveys and Audits

Local or National exam
Examinations
Qs Qs European Curriculum Curriculum mapping Identify Gaps Formulate new Qs
Final
Questions Bank Medical Schools
Improving Assessment of Knowledge in Geriatric Medicine- Undergraduates Curricular Mapping
Relaunch of Plan: Update of European Undergraduate Curriculum in
Updated Literature Search
1. Scoping review on literature
2. Scoping review on EPAs and how they applied in other specialities
Curriculum Development Panel reviews literature search and produces first version of Revised Curriculum
Delphi rounds (2 or 3) with a separate Delphi Panel
Prepare Publication of Revised Curriculum for submission to Age and Ageing
Future Plans
• Translation into languages


• Implementation into Medical schools / Curriculum Mapping / Audits

2021:
GM
11
1st Scoping Review
Results
Records identified through database searching
(18th May, 2021), n = 2,503
Records after removal of duplicates, conference abstracts, nursing or pediatric titles, n = 1,136
Records screened, n = 1,136
Excluded, n = 743
Studies included in the review, n = 367
Full-text articles assessed for eligibility, n = 393 Excluded, n = 26 13
Major themes
Six major themes were identified:
• Curricula
• Curricular topics
• Teaching methods
• Teaching settings
• Medical students’ skills
• Medical students’ attitudes
14
Curricular topics
Curricular topics:
• Delirium
• Pharmacotherapeutics (e.g. deprescribing)
• Healthy ageing and health promotion (e.g. vaccinations)
• Frailty
• Malnutrition
• Elder abuse
• Social gerontology
• Telemedicine
15
Curricular topics: healthy ageing
Intervention to promote healthy ageing:
• Deprescribing
• Exercise prescription
• Management of cardiovascular risk factors
• Vaccinations
• Nutrition
16
Teaching methods
Teaching methods:
• Clinical placements
• Interprofessional education
• Senior mentor programmes, intergenerational contact
• Simulation games, Serious games
• E-learning
• Service learning
• Short-term research training programs
• Student journaling
Vertical Integration
17
Teaching settings
Teaching settings:
• Acute-care hospitals (geriatric wards versus non-geriatric wards)
• Rehabilitation settings
• Home visits
• Nursing homes (empathy, more holistic approach)
18
2nd Scoping Review

19
• Entrustable Professional Activities” (EPAs) have become a popular component of competency-based medical education as a new approach for operationalising learning outcomes
• Originally, EPAs were mainly used for postgraduate medical education [9], including geriatric postgraduate specialty training (AGS, UEMS)
• There is a growing interest in the use of EPAs in undergraduate medical education
• In this context, EPAs are defined as units of professional activities, which medical students can be entrusted to perform with distant supervision alone
AIM
• to evaluate whether, and if so how, current undergraduate curricula including EPAs address geriatric learning objectives
(by mapping to the 2014 European Undergraduate Geriatric Medicine Curriculum)
Search
• Of 1311 hits, we found 9 undergraduate curricula that met the inclusion criteria
20
INTRODUCTION
Section 4—Multidisciplinary team-working and services
4a: Graduates should understand and respect the roles and expertise of other health and social care professionals by:
4b: Graduates should know about care of older patients in different settings and about specific aspects of health and social care in their region/country by:
Section 5—Prescribing in geriatric medicine
5: Graduates should understand the principles of treatment, including the appropriate and safe use of medicines as a basis for prescribing , by:
Section 6—Ethicolegal aspects of geriatric medicine
6: Graduates should understand the main ethical and legal issues arising in the care of older patients by:
Section 7—Research in ageing and geriatric medicine
7: Graduates should understand the intricacies of undertaking and interpreting research in older people by:
25
Pearson G et al
Section 5—Prescribing in geriatric medicine
5: Graduates should understand the principles of treatment, including the appropriate and safe use of medicines as a basis for prescribing , by:
i. Describing the effect of ageing upon pharmacodynamics and pharmacokinetics.
ii. Defining the concept of polypharmacy in older people.
iii. Engaging in medicines optimisation with older patients, accounting for physiological differences, drug–drug interactions, multi-morbidity, frailty, adverse drug reactions and patient preference, and considering objective assessment tools available for medication reviews where appropriate (e.g. STOPP/START, STOPPFall, anti-cholinergic calculators and levodopa equivalence calculators).
iv. Discussing the factors affecting medication concordance with older patients and the detection and management of drug underuse/overuse.
v. Prescribing safely for the conditions defined in section 3, and to manage symptoms occurring at the end of life.
26
Pearson g et al
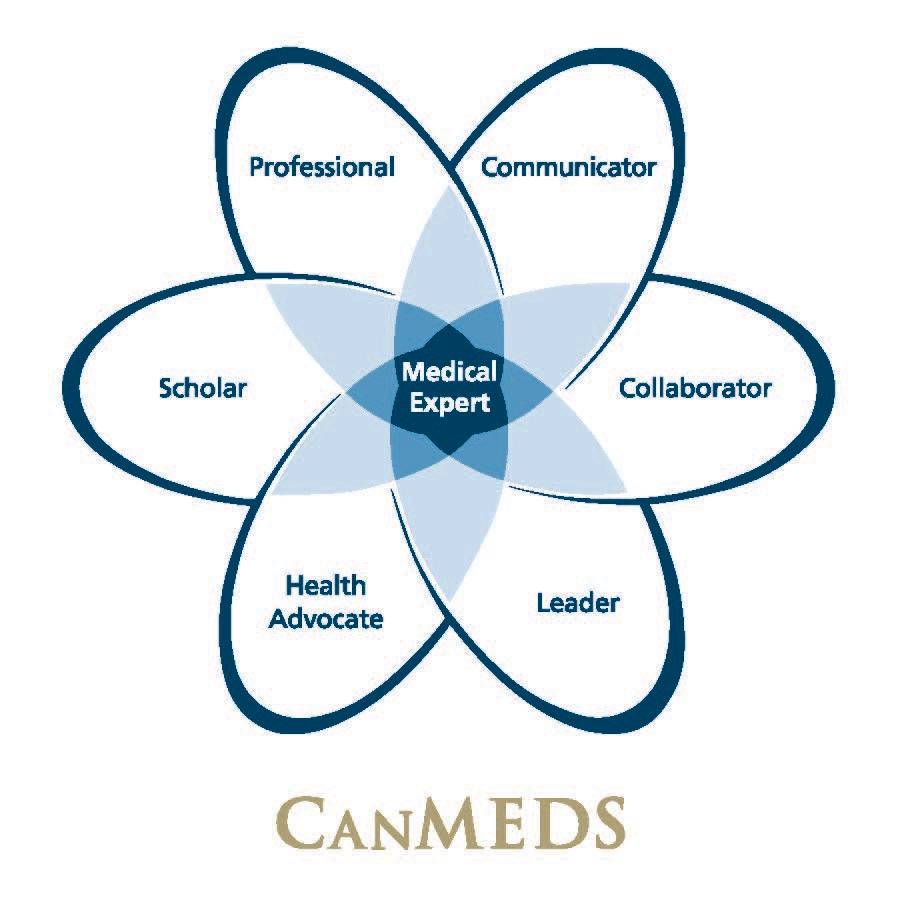
Competency-Based Medical Education

“Copyright © 2015 The Royal College of Physicians and Surgeons of Canada. https://www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e Reproduced with permission.”
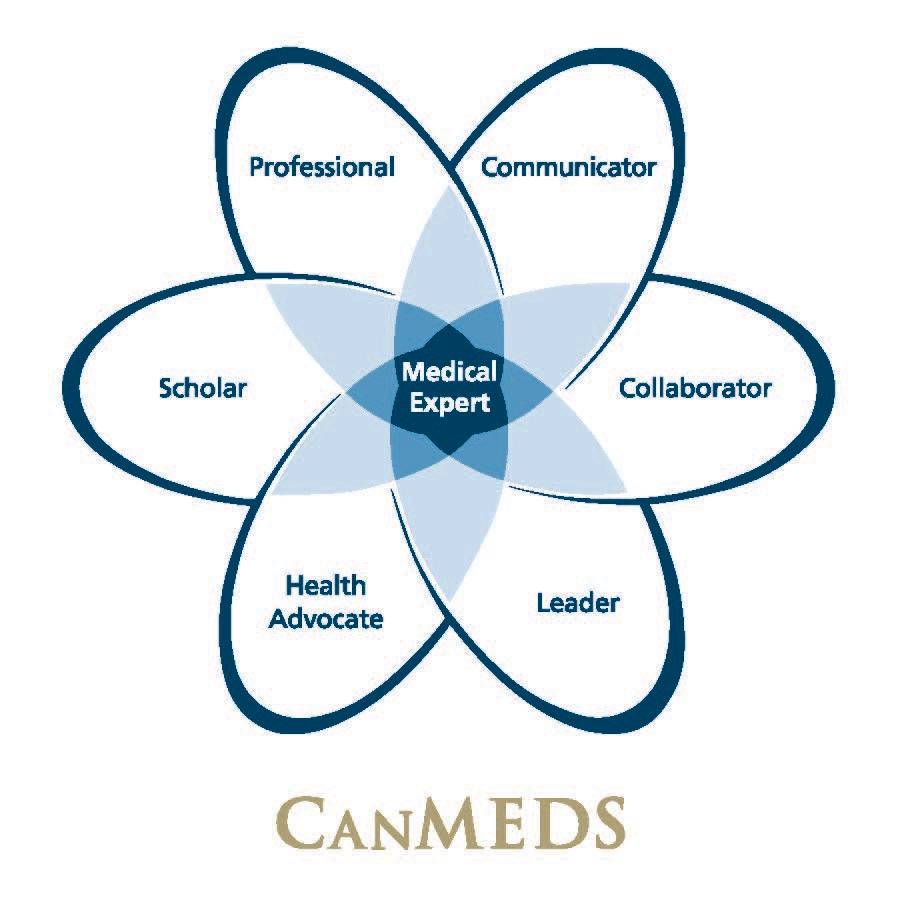
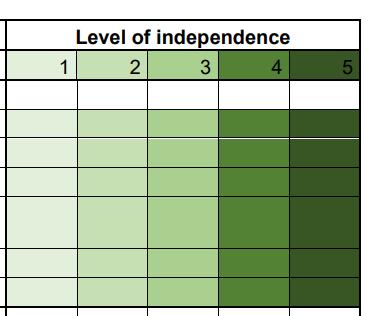
Entrustable Professional Activity EPA

… Is a unit of professional practice that can be fully entrusted to a resident, as soon as he or she has demonstrated the necessary competence to execute this activity unsupervised


ten
SIME | UEMS| PCBME | Monika Brodmann Maeder | 27.April 2023 Brussels
Cate 2005
1. Managing community liaison and practice
• Performs a comprehensive assessment (which includes physical, functional, social, environmental, psychological and spiritual concerns) of older people in community settings
• Manages acute illness, comorbidities (including dementia) and other problems safely in community settings, including in patient’s homes and care homes (with or without a hospital at home service)
• Able to discuss uncertainty and balance benefits/burdens of hospital versus home treatment
• Manages rehabilitation in community settings, including patient’s homes, care homes and community inpatient rehabilitation.
• Performs an assessment of mental capacity
• Performs a medication review
• Formulates an appropriate differential diagnosis, problem list, and individualised management plan taking into account patient preferences
• Understands the various agencies involved in community care, (including voluntary, social prescribing and third sector)
• Promotes multidisciplinary team working
• Demonstrates a flexible approach to care which crosses the traditional division between primary and secondary car
• Identifies patients with limited reversibility of their medical condition, is able to discuss end of life, undertake advance care planning conversations (including community DNACPR) and determine palliative care needs
To be added to the info icon text against the specialty CiP 5
To auto-populate and display the latest comment made by the Specialty Educational Supervisor here.
Level 1
Level 2
Level 3
Level 4
Please provide comments to justify your rating and identify any areas of concern or excellence
37
E.g No. 5
Subspecialty Training: Themed for Service Geriatric Medicine CiPs (EPAs)
1. Able to manage older patients presenting with fracture and is able to provide a comprehensive ortho-geriatric and bone health service
2. Able to assess patients with urinary and faecal incontinence and is able to provide a continence service for a specific patient group in conjunction with specialist nursing, therapy and surgical colleagues
3. Able to manage ill or disabled older people in a hospital at home, intermediate care and community setting and is able to provide a comprehensive community geriatric medicine service
4. Able to manage patients with a wide range of movement disorders at any stage and is able to develop a movement disorders service for older people
38

Overall Project lead: Marina Kotsani



Rational
• Geriatric Medicine (GM) skills and competencies are increasingly required
• Heterogeneous historical GM development among countries
• Pragmatic and feasible solutions should be investigated for countries with emerging GM (training of existing workforce)
• Need for core GM competencies across all settings (and a standardized approach in all countries?)