









Dr Ushma Narsai Avant member

anddeductions for








Of course, more money is always welcomed, but is that the solution when it hasn’t necessarily worked in the past? More money may not mean better understanding
Andrea Downey | Managing Editor
Women’s health has been in the spotlight after the Federal Government committed billions in the budget to improve access to medications for menopause, IVF and endometriosis, among others.
Yet in putting together this magazine one thing stood out - women’s health still has a way to go. Whether it’s more research, funding, clinician training or access to services.
Women tend to miss out at all stages in their lives. It can still take years to get a diagnosis for conditions like endometriosis and there’s still confusion about how best to medically support women at different stages of their lives.
You can’t say hormone replacement therapy without it being surrounded by some controversy – largely based on a study that linked oral oestrogen plus progestogen to breast cancer, which was later discounted.
But it still causes confusion and debate among clinicians today. While that debate continues, women going through menopause – sometimes dealing with unbearable symptoms – are missing out.
Elsewhere, period poverty still exists in WA with some women struggling to access period products.
Of course, more money is always welcomed, but is that the solution when it hasn’t necessarily worked in the past? More money may not mean better understanding.
On a separate note, Medical Forum is now delivering CPD verified content.

Complete the self-reflection and claim your CPD time, please scan here
This month you can tick off 6.5 hours of CPD if you complete each verified piece of content, or you can pick and choose what works for you and complete 30 minutes per piece.
Look for the QR code throughout the magazine to complete your self-reflection and claim your CPD time.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.







PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Classifieds Manager
Paul Riessen 08 9203 5222 paul@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au



















A new immunisation program to protect babies against respiratory syncytial virus (RSV) reduced hospitalisation rates across three hospitals by almost 90%.
An Australian-first study into the effectiveness of the long-acting monoclonal antibody Beyfortus (nirsevimab) also found the program helped more than 500 WA families avoid a hospital stay.
Led by researchers at the Wesfarmers Centre of Vaccines and Infectious Diseases at the Kids Research Institute Australia, the REVIVE study investigated RSVrelated hospital admissions following the introduction of WA’s immunisation program.
RSV is a life-threatening virus that affects the airways and lungs and is responsible for sending 3.6 million children to hospitals worldwide each year.
In 2024, WA became the first state to offer a free RSV immunisation program for all babies born throughout the winter season.
Lead author Dr Ushma Wadia said the study made WA the first place in the southern hemisphere to successfully demonstrate the impact of RSV immunisation in young babies.
“More than 24,000 doses of nirsevimab were distributed throughout April to September last year,
The cost-of-living crisis is disproportionately affecting women who are twice as likely as men to say they cannot afford a prescription for themselves or their family due to high prices.
The number of women who said they could not afford medicine has also increased by one third since 2022, rising to one in four.
That figure is even higher for women aged 35-54 with one in three unable to afford their medication.
The results come from independent research by Insightfully, a market research company, who spoke to more than 2800 women nationally.
It prompted a call from community pharmacists for the Federal Government to cut out-of-pocket medicine costs.
Pharmacy Guild of Australia National President Professor Trent Twomey said: “In Australian families, women are often the primary caregivers and

providing coverage to 85% of newborns and 66% of a ‘catch-up’ cohort of babies in the lead-up to their first winter season,” she said.
The project also investigated the effect immunisation had on the severity of RSV cases, with recipients found to be 60% less likely to require oxygen or assistance with their breathing if admitted with RSV.
Immunisation Foundation of Australia director Catherine Hughes said the results were reassuring for new parents.
“This is probably the biggest public health initiative in the last 20 years and is a real game-changer in the protection of our most vulnerable children.”
A $174.5 million national RSV immunisation program began in April with jabs available for all pregnant women and eligible infants.
the family’s health manager – taking responsibility for making health appointments and filling and paying for prescription medicines.
“Australians should be able to access the medicine they need to keep themselves and their family healthy.”
The Federal Government announced a reduction of the cost of medicines on the Pharmaceutical Benefits Scheme (PBS) in its most recent budget, capping the price of scripts at $25.
Free flu vaccinations will be available across WA for a fourth winter ahead of what is expected to be a higherthan-average flu season.
Running from 1 May to 30 June all people aged five to 65 who are not eligible for a jab under the National Immunisation Program will be able to access the vaccine free of charge.
General practices, community pharmacies, Aboriginal Medical Services, nurse practitioner clinics,
corporate vaccination service providers and community health clinics may all participate in the program, WA Health said.
The program is available to anyone in WA, including interstate and international visitors and those without a Medicare card.
RACGP Vice President and WA Chair Ramya Raman said: “This year, we’re witnessing record case numbers, and it’s vital that we get as many people vaccinated as possible.
“Unfortunately, vaccination rates are falling. For children aged five and under, vaccination coverage was only 30.3% in 2023 and just 25.8% last year.”
Australia has already recorded more than 48,000 cases of lab-confirmed influenza this year, which is 50% higher than this time last year. WA has recorded more than 3000 flu cases this year.

Exercise could potentially reduce the recurrence rate of breast cancer, new ECU research has found.
The study found that despite the advances made in breast cancer treatment, recurrence remains common and continued to contribute to higher mortality risks. In more aggressive cancers, the risk of recurrence can be as high as between 20% to 30%.
PhD student Francesco Bettariga investigated the effects of exercise in women with non-metastatic breast cancer and found a combination of resistance and aerobic exercise could reduce proinflammatory biomarkers.
While the exact reason for the reduction in inflammation is still being investigated, Mr Bettariga suggested a chemical reaction in the muscles, or an increase in muscle mass, could be behind it.
“What our research was able to confirm was that a combination of both resistance and aerobic exercises had the greatest potential to reduce inflammation.
“While there are currently no guidelines on how much exercise
to do, we would suggest moderate to high intensity aerobic exercises two to three times weekly, with resistance training added in a few times per week.”
Sexual misconduct to be permanently listed
Doctors found to have committed sexual misconduct will have it permanently published on their public registrar record in a move the regulator says will protect patients.
Ahpra’s amendments will also provide increased protections for people who make complaints about health practitioners, including making it an offence for practitioners to enter into non-disclosure agreements that prevent complaints being made to health regulators.
Acting chief executive Kym Ayscough said: “Everybody has the right to expect their practitioner to be safe and fit to practise, and these reforms strengthen that right.
“We support these changes, which align with the range of reforms that Ahpra and the National Boards are progressing as part of our actions to improve public safety involving sexual misconduct in healthcare.”
A nationally consistent process for practitioners to regain registration, where their registration has
previously been cancelled or they have been disqualified from registration, will also be established. At the same time, the RACGP has taken aim at the length of time the regulator takes to resolve matters.
In a submission to The National Health Practitioner Ombudsman on Ahpra’s immediate action powers, it said doctors had raised a range of concerns, including frustration with the time taken to receive an outcome for a matter that led to immediate action.
“Practitioners frequently report inadequate communication about investigation progress, leaving them in prolonged uncertainty,” the College said.
“Practitioners subject to immediate action restrictions do not appear to receive regular updates or have any stages of the regulatory process clearly communicated to them.
“The impact of the regulatory system on practitioner wellbeing has been well documented, with several cases of notifications leading to suicide by those under investigation.”
A project to empower WA women to prioritise self-care and engage in their own wellbeing has been awarded funding to expand across the State.
She Speaks, an initiative by ECU, will receive $50,000 funding from the WA Department of Communities Women’s Grants for a Stronger Future program to support the delivery of workshops from Broome to Esperance.
Western Australian statistics show concerning trends, with one in five women diagnosed with mental health conditions, eight out of 10 women not doing enough physical activity, and one in four taking on unpaid caring responsibilities that often take precedence over personal wellbeing.
She Speaks, which already operates in Perth, aims to change how women perceive, articulate, and implement self-care practices in their everyday lives.
ECU Research Fellow and SheSpeaks founder Professor Narelle Lemon said: “This funding validates the importance of our work and allows the project to support women in regions where wellbeing resources are more limited.

“We're not offering a one-size-fits-all approach, we’re providing women with a diverse set of tools and the knowledge to select the right tools for different situations.”
Western Australia’s best and brightest rural clinicians were celebrated at the 2025 WA Rural Health Excellence Awards.
This year’s winners represent nearly every region of WA, with the winners recognised for their exceptional work towards improving health outcomes in the State.
Rural Health West chief executive Professor Catherine Elliot said the winners displayed common themes of innovation, cultural connection, and a commitment to addressing the unique health challenges faced by rural communities.
“From nominees to finalists to winners, the calibre of those recognised is outstanding,” she said.
“Their professionalism, innovation, and dedication inspire us all, and their work underscores the vital role of rural healthcare in building healthier, more connected communities.”
Winners include:
• Aboriginal Health Professional of the Year: Soleil White, Broome Regional Aboriginal Medical Service, and Sharon Lockyer, WA Country Health Service – Pilbara
• Allied Health Professional of the Year: Bryan Fleming, Lake Grace Dental and Dalyellup Dental
• Clinical Leader of the Year (joint winners): David and Hayley Rigby, Pilbara Therapy Services
• Community Health Professional of the Year: Debra Collins,


Morawa, and Alexandra Naylor, Goldfields Family Dental
• General Practitioner of the Year: Susannah Warwick, Derby Aboriginal Health Service
• Health Team of the Year: Lions Outback Vision, Kimberley and Perth
Associate Professor Emmeline Lee has been appointed the new Director of BreastScreen WA. Dr Lee is a locally trained radiologist with 20 years of experience in women’s imaging. She replaces Associate Professor Liz Wylie who has retired.

Works are now underway on the expansion of the Sir Charles Gairdner Hospital emergency department.
A tender has also been awarded to Cooper & Oxley to build a 10-bed pod for SCGH intensive care unit.

• Nurse or Midwife of the Year: Nicholas Corsair, Kimberley Renal Services
• Specialist of the Year: Apaks Dede, WA Country Health Service, Midwest
• Young Professional of the Year: Tylah Bedford, Yura Yungi Medical Service Aboriginal Corporation
• WACHS Intern of the Year: Holly Reid, Great Southern
• WACHS Resident Medical Officer of the Year: Xavier Cornwall, South West
• Chairmans’ Award: Bryan Fleming, Lake Grace Dental and Dalyellup Dental
The awards were celebrated at a gala event and are organised annually by Rural Health West and WA Country Health Service.
Professor Michael Kidd has been appointed as Australia’s new Chief Medical Officer, taking up the post in June. Professor Kidd was formerly President of the Royal Australian College of Practitioners and served as Deputy Chief Medical Officer and Principal Medical Advisor with the Department of Health and Aged Care during the COVID-19 pandemic.


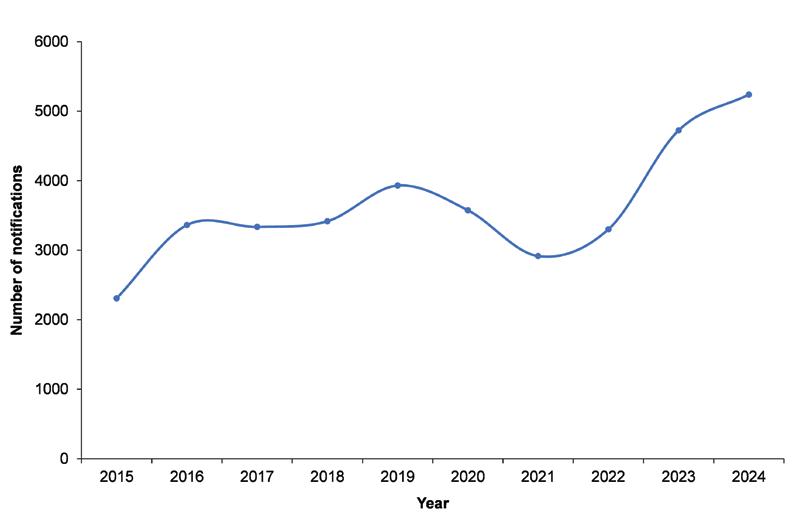
Last year saw the highest ever number of gonorrhoea notifications in WA, following a decline in notifications in 2020 and 2021 due to COVID-19-related travel restrictions limiting importation of overseas strains.
Opportunistic testing is important for prompt diagnosis and treatment because 80% of people with uncomplicated gonococcal cervicitis, most people with gonococcal pharyngitis or proctitis, and 10-15% of people with gonococcal urethritis have no symptoms.
Routine sexually transmissible infection (STI) testing every three months is recommended for people who may be at higher risk, such as men who have sex with men. Ask the patient about sexual practices to ensure correct specimen collection sites.
How to test for gonorrhoea
Consider routinely offering throat and rectal swabs in addition to a first void urine (FVU) for people with a penis and self-obtained lower vaginal swab (SOLVS) for people with a cervix, as well as blood-borne virus (HCV, HBV, HIV) and syphilis serology.
Consider gonococcal urethritis in sexually active patients presenting
with dysuria or symptoms of a urinary tract infection. Make sure to collect a FVU for gonorrhoea and chlamydia PCR, in addition to a mid-stream sample for culture. This enables diagnosis of both conditions.
People with urethral or cervical discharge should have a swab of
the discharge collected for culture and antimicrobial resistance (AMR) testing, in addition to a PCR test. Culture enables identification of AMR strains – especially ceftriaxone resistance – which is important because they are highly prevalent in many south-east Asian countries frequented by Australians.
Number of gonorrhoea notifications in WA from 2015 to 2024


Opportunistic and routine STI testing every three to 12 months depending on risk is important because most STIs do not show any symptoms
Consider gonococcal urethritis in sexually active patients presenting with dysuria or symptoms of a urinary tract infection. Collect first void urine for gonorrhoea and chlamydia PCR, and a mid-stream sample for culture
Ceftriaxone 500mg in 2mL 1% lignocaine as an intramuscular injection, given with oral azithromycin – 2g for pharyngeal, and 1g for rectal infections – or 100mg doxycycline daily for 1 week remains the mainstay of gonorrhoea treatment.
Empirical treatment of sexually active people who present with a urethral or vaginal discharge is important to prevent complications in the patient. It can also limit community transmission by reducing the duration of infectivity.
Ceftriaxone 500mg in 2mL 1% lignocaine as an intramuscular injection, given with oral azithromycin – 2g for pharyngeal, and 1g for rectal infections – or 100mg doxycycline daily for 1 week remains the mainstay of gonorrhoea treatment.
As with all STIs, partners should be informed promptly so they can be tested and offered empirical treatment while awaiting pathology testing. This will interrupt ongoing transmission back to the index case and others in the community.
Routinely and opportunistically offering STI testing helps patients feel comfortable and willing to discuss their sexual health.
Examples of conversation starters could include:
Young people: “STIs are very common among people of your age, and most STIs do not show any symptoms. We encourage all sexually active young people to get tested regularly.”
Aboriginal people (MBS item 715): “As part of your health check we also ask about your sexual health. Are you happy if I ask some questions today? You might feel a bit embarrassed, but I ask everyone the same questions
Preparing swabs for patient self-collection
1. Show the swab to the patient.
2. Label all tubes and urine jar with the patient’s details to avoid handling the tube after the patient returns the specimen.
3. Moisten the tip of the swab with saline or sterile water.
4. Put all equipment in the specimen bag and hand to the patient.
5. Review the collection process with the patient and remind them to put the swab inside the tube, seal the tube and put the sealed tube inside the specimen bag.
Clinician collected specimens
• If patients have any symptoms, a physical examination and clinician collected swab samples are recommended.
• Throat swabs are difficult for patients to collect, therefore clinician collected throat swabs are recommended for symptomatic and asymptomatic patients.

and it helps me to know what to test you for depending on your risks. Do you have any questions before we start?”
Reproductive health consultations: “While you’re here for advice about contraception/cervical screening it’s a good time to talk about other areas of sexual health, like having a sexual health check-up…”
Antenatal and pre-pregnancy consultations: “STIs are common among people of reproductive age and most STIs do not show any symptoms, but they can cause serious illness in mothers and babies, including stillbirth.
“We encourage everyone who is pregnant or contemplating pregnancy to have a sexual health check-up. We also encourage pregnant people to have syphilis testing at their first pregnancy checkup and at 28 and 36 weeks, so that if they have an STI it can be treated early before it affects mum’s or baby’s health.”
Most patients can collect their own FVU, SOLVS and rectal swab for opportunistic STI testing. Throat swabs are best collected by a clinician.

The use of menopause replacement therapy has once again hit the headlines, with female doctors in public debate and many GPs left scratching their heads, as Cathy O’Leary reports.
HRT and controversy have long been bedfellows, but debate over the use of treatment – now referred to as menopause hormone therapy – has intensified in Australia in recent months.
A public forum called ‘So Hot Right Now’, held at the Sydney Opera House in March, developed into something of a flashpoint over the science of MHT, which spilt over to Perth shortly after.
Organised by two Australian GPs, consultants and patient advocates, the Sydney event featured GP Dr Louise Newson who runs a highprofile menopause clinic in the UK.
She has faced criticism for her hormone prescribing practices which use high doses, but she insists they are safe and provide women with what they need and want.
A few days after her Sydney appearance, Dr Newson gave a series of talks to doctors and
women in Perth, organised by Hera, a menopause and women’s health clinic.
She told her audiences that without MHT, many menopausal women were suffering debilitating symptoms like brain fog and faced increased risks from diseases linked to inflammation like cardiovascular disease, which she said “shouldn’t be happening in 2025”.
Both events have shone a spotlight on how debate about MHT has rapidly expanded and become emotionally charged, particularly around the dosage of hormones being prescribed by a new breed of female doctors.
Challenging the old guard
claim menopause is being overmedicalised, arguing that this trivialises the valid experiences of women who are often at their wit’s end.
The conversation has become more nuanced, with focus not just on symptom control but also the diseases influenced by low hormone levels, such as heart disease, diabetes, dementia, autoimmune disease and cancer.

These doctors are openly challenging the status quo and
Perth menopause specialist and women’s health GP Dr Sunita Chelvanayagam co-founded the Hera clinic – the first GP-led menopause clinic in WA – in 2023 with Dr Michelle Cotellessa.
She told Medical Forum they wanted Dr Newson to speak in Perth because perimenopause and menopause needed to be part of
the conversation for women and no longer swept under the carpet as a taboo subject.
Dr Chelvanayagam says that while 20% of women sail through menopause relatively unscathed, 80% struggle, not just with hot flushes, but with palpitations, fatigue, wild mood swings and heavy periods. For some the symptoms were severe.
Oestrogen depletion at menopause could also contribute to rapid muscle and bone loss, cognitive decline, elevated cholesterol and poor glucose metabolism.
“A lot of women want to take control of their health and we’re living so much longer but many women are in that sandwich era of looking after children, looking after older parents and working full time, so life is very busy,” she said.
“We see a lot of women who feel a bit indulgent sitting down and telling their story, but they've never been able to do that with a GP because no one's got the time.
“I think GPs want to first do no harm, and sometimes that means taking the path of least resistance based on what we know.”
She said menopausal women were clutching at anything that could help them, but often came in saying they did not know what they should do.
“I think HRT's been under so much scrutiny in a way no other medicine has,” she added.
“We use many medications off label – we use them for things like epilepsy and nerve pain – there’s so much that we use off label because that's medicine, and no one bats an eyelid.
“Hormones now are very body identical, and there’s a lot of nuances in the dose, yet that raises questions.”
Dr Chelvanayagam said women now spent many years in a menopausal state, far more than their ancestors.
“Some women don’t think it's very natural to have HRT, but it's not natural to be menopausal as long as we are,” she said.
“We are meant to be pregnant, breastfeeding, then menopausal, but we spend decades and decades doing a lot more than
we should. That’s where replacing hormones comes in, particularly in terms of brain function.
“It’s not about reversing ageing or a cosmetic improvement, it’s about helping with the risk of heart disease, osteoporosis and potentially dementia.
“We’re the sum of all our genetic predispositions to other chronic illnesses, so it’s not just one thing.”
But some women’s health experts remain worried about what they regard as excessive and potentially unsafe dosages of hormones prescribed by some of their peers.
Organisations like the Australasian Menopause Society say advice and treatments for menopause should be evidence-based and consensusbased.
Where there is some consensus in the medical profession is that the attention being given to this important area of women’s health is long overdue, so some debate is to be expected.
In the spotlight
Menopause has gone from forgotten cousin to political asset – the subject of a recent Senate inquiry and ensuing promises of funding by the major parties, including a new rebate for menopause health assessments from July this year.
That was upended in 2002 after a big US study, the Women’s Health Initiative, reported a link between the risk of breast cancer, venous thromboembolism and coronary heart disease in women taking oral oestrogen plus progestogen.
It scared off millions of women and their doctors around the world from using the therapy, leading to a dramatic reduction in prescribing.
While the risks were later reassessed and largely discounted, the HRT hangover remained, only to be reignited last year by a series of articles in The Lancet suggesting that menopause was being overmedicalised and wrongly treated like a disease, resulting in some women getting unnecessary treatment.
There was strong backlash to The Lancet articles, including from Professor Bronwyn Stuckey, medical director at Keogh Institute for Medical Research, consultant physician at Sir Charles Gairdner Hospital’s Department of Endocrinology and Diabetes, and Clinical Professor at UWA’s School of Medicine.

She worries that women are missing out on treatment that could not only reduce severe symptoms but also help stave off chronic diseases.
Three new body identical hormone medications were also added to the Pharmaceutical Benefits Scheme earlier this year, the first additions in more than 20 years and saving some women almost $550 a year.
It is a far cry from decades past, when some women resorted to carrying around paper fans and hanging a wet cloth around their necks as they struggled with what was termed ‘the change of life’.
For those faced with severe menopausal symptoms, it was not so much a change of life as lifechanging, as they were forced to endure debilitating hot flushes, night sweats and mood swings.
But just as the contraceptive pill revolutionised women’s control over their fertility, hormone replacement therapy came into its own, offering women the chance to get their life back on track.
Prof Stuckey told Medical Forum that despite advances in understanding of the risks and benefits of menopausal hormone therapy, outdated research continued to raise concerns for both patients and their clinicians.
“I don't think my own position has changed much at all over the years. There’s no doubt that menopause is an oestrogen deficient state,” she said.
“You can't argue that it's not that, so what are critics talking about? There is good evidence that oestrogen has a lot of protective effects bone-wise and cardiovascular-wise.
“Let's not forget quality of life. You prescribe hormone replacement therapy to a patient and they say, ‘oh my God I feel much better’ or ‘you saved my life’.
Obstetrician and gynaecologist Jared Watts has completed three assignments with Médecins Sans Frontières/Doctors Without Borders (MSF) in Nigeria, Syria, and Sierra Leone.

Not only was the work rewarding, but it helped him develop skills to manage challenging cases in remote Western Australia. Why did you want to work with MFS?
When I started working in the Kimberley, I had a contract that allowed me to work overseas with MSF. I was instantly attracted to their principles of impartiality, neutrality and independence.
For me, it is an organisation that always aims to provide the best care possible, irrespective of where or who the patient is. I saw these principles in action and have never looked back.
What experience did you have that prepared you for working with MSF?
Before MSF, I worked for two years in rural parts of WA, which is the best pre-departure experience someone can have. I also undertook a post-grad qualification in tropical medicine and global health, which helped me understand the health issues in the areas MSF works.
MSF also has a support network of international staff. Before my
first assignment I spoke to an experienced doctor about my concerns, which was a huge help.
What is a memorable moment for you on assignment?
In Syria, I worked to rebuild a service in a hospital that had previously been occupied by Islamic State. The team was made up of professionals from engineers to nurse managers, orthopaedic surgeons, obstetricians, midwives and translators.
It grew so quickly because of the high demand for medical care. I remember walking into the birth suite one day at 8am and walking out at 8:04am having seen five babies born.
The passion, hard work and dedication of all the staff was incredible. To see a service start and grow so quickly was something I will never forget.
What did you learn from working overseas?
Right from my first assignment, I learnt so much about providing care in remote emergency settings. When I was in Nigeria, I worked with local doctors who taught me

a lot about operating on difficult and complicated cases with limited resources. In Australia, we aim for complicated cases or births to occur in tertiary hospitals, with all their available equipment and expertise, but we know unexpected births and emergencies can still occur anywhere.
Since being back in Australia, I have taught the skills I learnt on assignment to many rural doctors, helping improve the emergency obstetric care we provide across rural and remote areas.
What advice would you give to someone considering working with MSF?
Do it. It can seem a little scary to start with, but the support MSF gives you is incredible. You learn a lot and often don’t want to leave.
MSF is recruiting obstetriciangynaecologists, surgeons, anaesthetists and paediatricians to work on humanitarian projects.

continued from Page 11
“I think that people who haven't been through it, or people who've had an easy menopause, and men of course, don't realise what a change in the oestrogen levels does to women – palpitations, hot flushes, not sleeping, vaginal dryness and sex hurting.
“And they've got to put up with that for the rest of their lives if you don't do something.”
Prof Stuckey said what had changed since the WHI study was a real push to optimise which progestogen doctors used and the way they gave it.
“From the cardiovascular point of view, that was known for quite a while, but the effect of the progesterone on breast cancer risk was a good take home message from the study.”
Prof Stuckey says persistent claims of over-medicalising menopause are nonsensical.
“When you think of the medicalisation of obstetric practices, the medicalisation of treatment of infectious disease, using antiseptics when you deliver a baby – these things have meant that women's lifespan has increased past child-bearing age,” she said.
“Doctors have caused this, so with menopause they should also be responsible for things like osteoporosis and female cardiovascular disease – all of those things that come after menopause.”
She also targeted men “with intact testes” who did not understand how horrendously some women suffered in menopause.
“If their testosterone dropped off, then they'd understand,” she said.
Prof Stuckey said she was deeply concerned about some of the longterm effects of low hormone levels.
“It's not just symptomatic menopause, it’s things that happen like the bone loss,” she said.
“After the WHI study women started to avoid hormone replacement therapy for maintenance of bone density and so now we’re stuck with people in their early 50s who are on weapons

grade anti-resorptive therapy like bisphosphonates, which are not so much of a problem, but Prolia (denosumab) is a big problem.
“If you put somebody who's in their 50s on it, you know there's no approved protocol for exit strategies with that.
“And then you get these rebound multiple vertebral fractures in people if they stop it.”
But Prof Stuckey is wary of some aspects of the new wave of enthusiasm for menopause treatment and some of the hormone doses being used.
“We have this push by people who seem to have discovered menopause after not having wanted to touch it with a barge pole,” she said.
“I agree some people need higher doses than others, but I think with the sort of doses Louise Newson uses you are going to run into the trouble of tachyphylaxis, where the higher the dose you give the more people are dependent on a high dose.
“For instance, the worst time for hot flushes is perimenopause when the oestrogen is swinging up to very high levels and then plummeting down to low levels, so that sort of fall in oestrogen triggers symptoms and if you keep chasing that you get into a bit of trouble with tachyphylaxis.
“Younger people definitely need higher doses than older people, but everybody's different. With some people you can maintain their bone density and their quality of life on a smidgeon of oestrogen and some people you need to use high doses.
“Some people are happy with oral and some people you need to use transdermal.”
While the lack of consensus on MHT makes it difficult for GPs to decide how best to help their patients, a view now being embraced by many clinicians is that while MHT has a firm place in the treatment bag, the dose and delivery need be individualised rather than a onesize-fits-all.
It is an approach that Prof Stuckey supports.
“You definitely can't have one therapeutic formula in your kit bag, you have to know what all the others do and what they don't do,” she said.
Dr Chelvanayagam also welcomes a personalised approach.
“I think it's good for women to hear what is actually a good news story, that there is something they can do, no matter if it involves taking hormones or not,” she said.
“It's not indulgent, it is a good thing to do something about your health.
“There are many different ways of going about it, but it's really about optimising through a range of things including exercise, diet, social connection.
“It’s giving women quality of life when we're so conditioned by society to just muddle on and keep going.
“I think it is the most transformational medicine we've ever come across as doctors and it's not always easy, but when you talk to women and then see how well they do, that's really amazing.”
ED: Additional resources can be found in the Practitioner Toolkit for Managing Menopause.
Primary care plays a vital role in preventative health and reducing strain on secondary care services. But ‘GP deserts’ are hindering people’s access to care and putting pressure on our GP workforce.
By Andrea Downey

It’s an age-old problem in health – there are not enough resources to support the growing number of patients needing care and the ensuing pressure that is putting on the healthcare system.
The importance of primary care is known. People who see their GP regularly can manage their health better and are less likely to end up in hospital.
But so-called ‘GP deserts’ are resulting in thousands of West Australians missing out on essential check-ups, screening, medication management and other services GPs provide.
The re-elected State Government has a new focus on preventative health, designating a whole portfolio under Minister for Preventative Health Sabine Winton.
Premier Roger Cook wants to make WA the “healthiest state in Australia”, but can that be achieved, and the goal of preventative health be realised, while some still struggle to access a GP?
Geographical barriers
Research from the Grattan Institute shows around half a million Australians live in GP deserts, where they receive 40% fewer GP services than the national average.
Most GP deserts are in WA, remote Queensland and the Northern Territory.
While the term desert conjures up images of remote towns, some metropolitan areas in WA are also at the mercy of a shortage of GP services.
Peter Breadon, Program Director of Health and Aged Care at the Grattan Institute, said a number of factors were at play in WA, including our unique geography.
“There are lots of parts of rural WA that are GP deserts and WA does worse than most other states in Australia. It really is a state where urgent investment is needed,” he told Medical Forum
“It’s partly the geography, but there’s also been rapid population growth which is hard for services to keep up with. Those things probably play a part.”
The areas worst hit are remote regions such as the Pilbara and Kimberley, but metropolitan regions including Cottesloe and South Perth are also falling behind.
The Federal Government has confirmed nine new Distribution Priority Areas in WA, the majority of those in metropolitan regions, as the State grapples with GP shortages.
However, the new DPAs are not in areas considered a GP desert by the Grattan Institute, raising questions on whether a new approach is needed.
Mr Breadon said there needs to be a more targeted approach to addressing primary care shortages.
“One thing we've seen in Australian policy over the years is this focus on investing and measuring access by remoteness levels. And certainly, areas that are more remote across Australia tend to have lower levels of services, and there are more of those areas in Western Australia, however it's not a perfect correlation.
“We're arguing to move away from the characteristics that, on average, are associated with lower levels of care to just target those areas with lower levels of care, whether they're in a city, a town, or a remote area.
“Targeting investment at low levels of care is the way to do it.”
The Grattan Institute defines a GP desert as an area that has below 4.5 GP services per person.
Those considered to be on the cusp of becoming a GP desert have below 4.9 GP services per person.
Using the latest Medicare-subsidised data, it has determined there are six GP deserts in WA and four areas on the brink of becoming one.
The Kimberley, East Pilbara, West Pilbara, Esperance, South Perth and Cottesloe were all found to have less than 4.5 GP services per person. The worst hit was West Pilbara with 2.9 services per person.
The Gascoyne, South Wheatbelt, Perth City and Manjimup were noted as almost a GP desert.
Adding to the problem are high vacancy rates and retention issues alongside dissatisfaction with incentives in rural areas.
In a recent survey of GPs, Rural Health West found 44% of respondents had experienced excessive workloads in the past 12 months, 43% said recruiting more staff was a challenge and 44% said they faced problems with staff turnover.
Catherine Elliott said a range of programs were being delivered to support health professionals on the ground, but funding was constrained.

As of 21 March, there were 78 GP vacancies in the State’s rural and remote areas, according to data provided by Rural Health West. Some of these are GPs wanting to grow their practice, but others are where a GP is absent.
Across the full health workforce there were 159 vacancies, predominantly nurses, physiotherapists and speech pathologists. The Kimberley was the worst hit region with 39 vacancies, followed by the South West with 32 and the Wheatbelt with 20.
Retention rates are further adding pressure to the system. Five-year turnover rates in some areas of WA were as high as 62%, Rural Health West data shows.
In the Kimberley the rate was 52%, the Inner Regional area was 62% and the Pilbara and Goldfields sat at 47% and 46% (see graphic for the full regional breakdown).
WA saw a 31% increase in the number of GPs training in 2025, bolstered by 67% growth in the number of registrars training as specialist GPs on a rural pathway, RACGP figures show.
But the College’s latest Health of the Nation survey found WA has just 99 GPs per 100,000 people, lagging far behind States such as Victoria and NSW which has 116.
Nationally, Department of Health data show a shortage of 2400 fulltime equivalent GPs, forecast to grow to 8900 by 2048.
The result is an overloaded workforce at risk of burnout.
“If we’re serious about equity for rural communities, we must keep listening to the workforce and backing them with the resources they need.”

“The message from rural health professionals is consistent and clear: many locations are facing critical workforce shortages that create inequity of healthcare for rural communities,” she said.
“It's not just about workforce numbers – it's about burnout, barriers to training, and the pressure of delivering quality care with limited support.
Source: Rural Health West
Albany-based GP and AMA(WA) Chair Rural Doctors Practice Group Dr Paddy Glackin said general practitioners in regional areas often take on more responsibility than their urban counterparts, such as running local emergency departments.
“There is a relatively small number of doctors forced to carry out an awful lot of responsibility, and that’s very pressurising,” he told Medical Forum
Then there is difficulty finding the balance between the need for GP services and patient demand.
continued on Page 17


By completing this survey, you have the chance to win a $1000 Luxury Escapes voucher. Additional entries available if you update your postal address or email address at the end of the survey.




continued from Page 15
“You need a certain population to be able to support a GP, but you also need a certain number of GPs to be able to run a truly sustainable service,” Dr Glackin said.
“As a result, there are country GP practices struggling to get enough work to maintain a sustainable practice compared to their metro counterparts.
“Then word gets around of ‘don't go and work there because they're burnt out’. So, consequently, people go somewhere they won’t get burnt out or where they are in a more collegiate, supportive and wellstructured environment.
“Look at the impact on small towns like Norseman, which had a GP for close to 20 years who provided general practice services and also worked in the hospital and did a huge amount of work in that community.
“Then when it was time for him to move on, they found it next to impossible to find anybody who can replace the huge amount of work that doctor did.
“There’s quite high turnover in country practice. It’s really tough.”
Mr Breadon added that GPs and other healthcare workers could experience “moral injury” when they felt they were not meeting the needs of their patients because they were too stressed.
“That can be a downward spiral where people leave those areas, or stop working, or work less, further diminishing the amount of care that's available,” he said.
“There are big economic and health system consequences from these gaps in access to care.”
As regional and rural towns struggle to fill GP vacancies, local governments have stepped in to offer huge incentives and salary packages.
The Wheatbelt Shire of Quairading made headlines in 2023 after offering a $1 million salary package for a new GP, including housing.
It is not the only regional area to
offer such large sums. Last year Livingston Medical advertised a GP role in Bremer Bay for up to $450,000 plus a house and car.
Similar situations are being seen elsewhere in Australia where GP shortages persist, including Queensland.
But Dr Glackin said these bidding wars can be “very problematic”, adding that he is aware of some local governments spending large portions of their budget on GP incentives, which then limits their capacity to provide other essential services.
Dr Michael Livingston, founder of Livingston Medical which has provided medical services in country WA since 2013, said the secret to attracting and retaining GPs is to treat them like human beings.
As part of his work setting up clinics in rural areas, Dr Livingston often negotiates housing and car packages with local governments to make the transition to country work easier.
“Whatever site we get, I don’t ask people to do something I wouldn’t do myself,” he said. “So, for every single one of these locations I always go in first so that when the next person comes in it’s streamlined.”
Mr Breadon argues that the situation needs cross-government intervention, calling for a minimum care threshold to be put into the National Health Reform Agreement to “draw a line in the sand on what we consider to be insufficient”.
“In areas that persistently fall below that threshold of acceptable levels of care, we argue that Commonwealth and State Governments should work together to fill those gaps with what's sometimes called cocommissioning,” he said.
“Funding should be unlocked on a population health needs basis to identify the gap in care and give an investment to fill those gaps.”
That funding, he said, should be based on a salaried model as many of the traditional subsidies do not work to attract and retain clinicians.
Of course, at the heart of this issue is patients – often the most vulnerable – who are missing out on care.
Most GP deserts are located in areas where patients are typically sicker and poorer. Some are missing out on care altogether.
Data from the Grattan Institute shows last year 8% of people aged 65 and over in these areas didn’t see a GP at all, compared to less than 1% of the rest of the country.
People living in these areas are almost twice as likely to go to hospital for a condition that might have been avoided with good primary care, or to die from an avoidable cause.
“If you’re adding GP services anywhere in Australia, these are the most important places to start,” Mr Breadon said.
“On average they need care more than other parts of Australia because people there tend to be sicker, more disadvantaged, and in many cases they have lower bulk billing rates. We really wanted to shine a light on those places with the very lowest level of care to start investing there.”
Dr Glackin said a lack of access to GPs creates a vicious cycle where patients get sicker, eventually needing further care.
“When you become unwell, you've got less access to diagnostic modalities, you've got less access to specialist care than what would be delivered in the city to support your GP and to help advise on your treatment. You lose out at every level.”
But despite its challenges, Dr Glackin wouldn’t work anywhere else.
“I really enjoy my work, it's endlessly fascinating, I love the variety. Tomorrow I'll be working in a local emergency department.
“It's challenging, it's exciting, you work much closer to the top of your scope of practice.
“I think that's very rewarding, and the level of care and support you can provide to patients, families and communities is great.”
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
While Dr Brigid Corrigan’s specialty might be breast surgery, her plastic surgery skills are also in demand for skin cancer removal and hand reconstruction.
By Ara Jansen

Despite having a dad and grandparents who were doctors, plastic surgeon Dr Brigid Corrigan says there was never any pressure on her to become one.
Her family moved from the UK when she was nine and her dad became a country GP in Narrogin.
“I don’t really know why, but I know in high school it was what I thought about and kept coming back to,” says Brigid, who from a very young age had a strong feeling this was the direction she was headed.
“I did a year of science and then went into medicine as I didn’t get into medicine first. It wasn’t until my fourth year that I became attracted to the practical stuff and knew I wanted to be hands-on in medicine.”
Throughout medical school at UWA Brigid thought she would become a general surgeon and didn’t get much exposure to plastics.
As a second-year resident at Royal Perth Hospital she did a rotation through plastic surgery which piqued her interest and, like many other doctors, was encouraged by an enthusiastic and knowledgeable group of people already working in the specialty.
“That made a big difference,” she says. “They seemed to love it and really encouraged my exploring it. As residents we rotated through a number of specialties and sometimes it really is the people you work with who help you enjoy it rather than the subject.
“Following three years as an intern and resident at RPH, I became a service surgical registrar and subsequently applied for plastic surgery training.”
Awarded a fellowship of the Royal Australian College of Surgeons in plastic and reconstructive surgery in 2008, Brigid did post-fellowship training in Ireland, England and Melbourne.
At Oxford her fellowship focussed on breast reconstruction, sarcoma, hand and microvascular surgery. She did further study during a six-month advanced aesthetic surgery fellowship at the Melbourne Institute of Plastic Surgery before returning to Perth in 2010.
As a specialist plastic surgeon, Brigid does a lot of emergency hand surgery and reconstructive hand surgery. This injury makes up a significant part of her work at Royal Perth, where she works a day and a half a week.
She enjoys the benefits of being able to teach and train registrars and the variety of cases tends to be wider. She likes having the freedom to be able to work in both the public and private space.
“At my RPH clinic I see a lot of complex patients, many of whom would not be able to access treatment privately. I get great satisfaction looking after these patients.”
You’ll also find her amidst a busy list at St John of God in Subiaco and the Wexford Medical Clinic in Murdoch. Along with six colleagues she owns Handoc, which treats hand injuries. Their Handoc app is a practical hand injury management guide.
“Hands are one of the most commonly injured parts of the


body because they are in harm’s way. There are lots of work injuries on places like mining sites – crush injuries or loss of fingertips and sewing on fingers. Half of workplace accidents I see are hand injuries.”
Breast surgery remains a major subspecialty interest – reconstruction, particularly for cancer patients, alongside augmentation, reduction and revision surgery.
Working almost always with adults, sometimes she might consult with a young girl with developmental breast issues. Her most common
procedures on the cosmetic side are breast procedures, especially breast reductions. She also does a range of reconstructive procedures including skin cancer management.
When asked whether she finds any conflict between cosmetic surgery versus emergency or necessary surgeries, she says it’s often not as black and white as people think. For example, for someone with very big breasts, a reduction surgery might be considered cosmetic yet there are many functional benefits, as well as psychological benefits.
Over

Perth Radiological Clinic offers a comprehensive range of women’s imaging services including:
• Obstetric ultrasound including first trimester screening and cervical length assessment
• Gynaecological ultrasound imaging
• Pelvic MRI and pelvic floor ultrasound
• Endometriosis MRI
• Five breast imaging clinics across the metropolitan area (North, South, East and Central) for ultimate patient convenience
• All breast imaging modalities and breast biopsies performed including—
- Breast implant volumetric assessment, using low dose CT
- Digital mammography
- 3D mammography (tomosynthesis)
- Breast MRI.
Doctor Priority Line for urgent bookings and enquiries

continued from Page 21
“With a breast reduction, it can make a huge difference to quality of life, including relief from neck, back and shoulder pain. In some patient reported outcome studies, breast reduction has been shown to improve quality of life to the same extent as a hip or knee replacement can.
“When procedures are purely cosmetic, expectation management and educating patients on realistic outcomes is paramount. You tend to go a bit more slowly in terms of assessing the patient generally, just to be sure they are going to be happy with the outcome and satisfied with their surgery.
“Everyone has their own definition of what is beautiful. With aesthetic practices we are always trying to ascertain what our patients want to achieve and being honest about what is feasible.
“We have become a lot more aware of patients who have other mental health issues and work to address those first, referring on to psychologists where appropriate.”
One of the aspects of her work she enjoys is the problem-solving, particularly in reconstructive work, like during microvascular surgery to join and repair damaged blood vessels.
“My favourite type of surgery changes but I do love the variety. Some operations are lengthy, like using the patient’s own tissue in autologous breast reconstruction. That takes about 10 hours for bilateral DIEP flaps.
“I would not like to be doing that one every day but it’s very rewarding surgery and most of these patients get good outcomes and are very grateful patients. On other days you could do six skin cancer operations in a morning which is a less taxing, but still important surgery.
“Outside of work I try and stay reasonably fit and like being active outdoors. I’m mostly a walker and often walk with a group of girlfriends. Two female doctor friends and I walk every Saturday morning, have breakfast and often it becomes a debrief of our week.”
For relaxation she sings in a community choir which puts on public concerts a few times a year. She finds it a fun and good way to meet different people. Plus, it doesn’t require her hands.
Brigid is a volunteer and a board director with Rafiki, a Perth-based not-for-profit which supports health and education services in Tanzania. Among other initiatives, the group teaches and trains local surgeons at the Plastic and Reconstructive unit at the Muhimbili National Hospital, which is now part of a pathway training the country’s first incountry plastic and reconstructive surgeons.
Most of Brigid’s surgery for Rafiki has been for cleft lip and palate operations and burns releases. She’s also an active member of the Australian Access to Breast Reconstruction Collaborative Group. Formed in 2020, it’s an Australian group comprising
clinicians and consumer advocates which believes that “all women in Australia requiring mastectomy for the management of their breast cancer have timely access to breast reconstruction regardless of geographical location or financial circumstance”.
Brigid says this is important because women in both cities and regional areas need to be aware of what their reconstruction options are and to be able to access them if they choose to.
Brigid is currently vice president of the Australian Society of Plastic Surgeons and is on the AMA(WA) Council and chair of its private specialist practice group. She enjoys the advocacy work involved in both of roles and the chance to have some involvement in influencing health policy.
By David Andrew

Doctors dedicate their lives to evidence-based patient health, yet when it comes to finances many abandon this rigour, choosing an ad hoc approach.
Yet failing to plan adequately can leave you in the ‘retirement red zone’ – a point where your financial resources fall short of sustaining the lifestyle you’ve worked so hard to achieve.
For high-income professionals like doctors, this is avoidable with the right strategies.
What Is the retirement red zone?
The retirement red zone refers to a scenario where your retirement assets are depleted prematurely. This can happen due to poor
planning, insufficient savings, or underestimating future expenses like helping family and inflation.
For affluent families, the stakes are higher because tax inefficiencies and unstructured plans can erode wealth faster than expected.
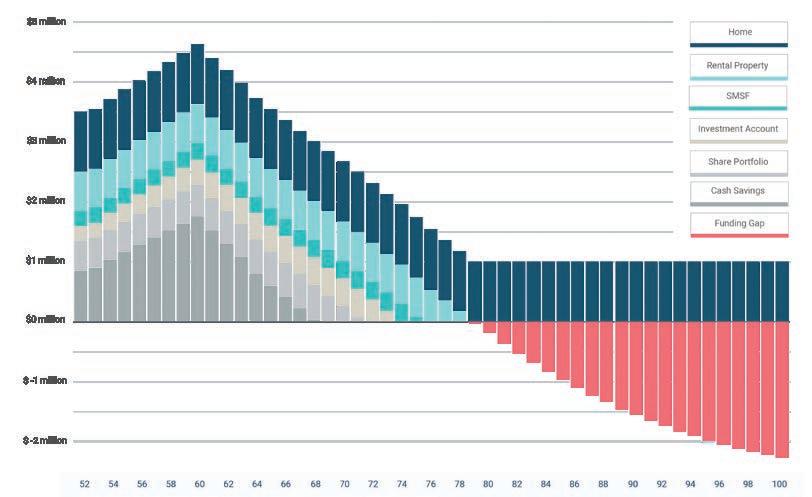
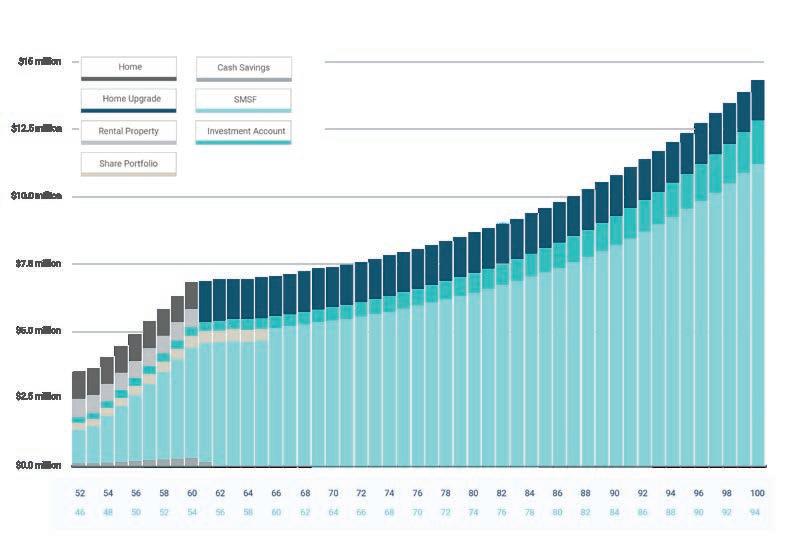
The retirement scenario below is typical. It shows the retirement red zone, where retirement assets are exhausted well before your life expectancy. In the red zone, the only funding remedies are to downsize your home or apply for the Age Pension.
Doctors face unique challenges when it comes to retirement planning.
Late career start: Many begin earning substantial incomes later
than other professionals due to lengthy training, meaning they have fewer years to benefit from the power of compound interest
High tax burden: Without proper structuring, a significant portion of income and investment can be lost to taxes.
Limited time: Busy schedules often leave little time for dealing with dayto-day finances, let alone planning for the long-term.
These factors make it essential to develop a robust retirement strategy tailored to your needs. The time to start is in your forties – or even earlier – but many wait too late into their fifties.
There are a number of things you can do to avoid slipping into the retirement red zone.
Retirement isn’t just about money; it’s about purpose and fulfilment. Ask yourself:
• How will you spend your time?
• What goals do you want to achieve?
• Who do you want to spend more time with?
• Who do you want to help?
• What adventures and travel are you planning?
Having clarity on these questions helps shape not only your lifestyle but also your financial plan. Tools like a Retirement Goal Planner can help prioritise what matters most.

A common concern is whether you’ll have enough money. Many academic researchers have considered this problem and concluded that the 4% rule is a great start.
This rule suggests that you will need a capital sum of 25 times your annual spending, plus any lump sums to ensure your retirement savings will last your lifetime.
In our experience, the 4% rule is a good start, but the rule can overstate the capital you need for a comfortable retirement.
The best way to establish the capital you need is to undertake detailed financial modelling based on your actual requirements. This takes the problem out of the realms of theory and into evidence-based strategy.
This kind of modelling provides pathway certainty, where you base your spending expectations on clear goals and a strategy optimised for tax, saving and then spending.
Back when your grandparents retired, they probably expected to live another 10 years at most. Now, you could live well into your nineties.
The inflation experience over the past few years tells us that the purchasing power of your money is not guaranteed. Inflation is an invisible force that gradually eats away at your wealth and, if left unchecked, it can severely impact your lifestyle in retirement.
For instance, keeping $2 million in cash might feel safe, but over time its value diminishes. What your $2 million can buy today will cost about $3.6 million in 20 years’ time assuming inflation of 3%.
Build a resilient investment plan
If taking an evidence-based approach to medicine make sense, then it translates to investing.
History shows that markets reward investors for the capital they supply. Since 1926 the S&P 500 index has returned an average of about 10% each year. There is no reason to believe this won’t continue in the future, so your challenge is securing your fair share of this return.
Academic research confirms that strategies like stock-picking or market timing rarely work. Instead,
evidence points to steady growth through disciplined low-cost investment strategies.
Retirement should be a time of freedom and fulfilment, not financial stress.
By taking steps now, you can avoid the retirement red zone and secure the future you deserve. Define your goals, plan for inflation and taxes, and seek professional advice where needed.
Your financial health is as important as the care you provide others.
If you would like to have a conversation with someone to secure your retirement, please reach out.
Medicine shortages in Australia have reached an unprecedented level in recent months, particularly in remote and regional WA. How are people coping and what can we expect going forward?

Pharmacist Ben Teo and his family have run the community pharmacy in Karratha for several years. Prior to that they ran a pharmacy in Carnarvon for seven years.
They love living in the far north of Western Australia, but lately doing his job has proved challenging. Unprecedented medication shortages across the country have proved difficult to manage for doctors, pharmacists and patients.
“I guess it started around COVID. I’d like to say it has got a bit better, but it’s still a daily draining task,” Mr Teo said of the shortages.
“We have one staff member sitting on the computer just to keep updated.”
Mr Teo says these shortages are the worst he has ever seen in his time as a pharmacist. Some, he explains, are quite simple in that it’s just a phone call to get a substitute and that is doubled up for the short term.
But with ADHD or diabetes medicines, it’s not that simple.
“They will potentially have to go back to the GP for monitoring and ongoing intervention, which then puts more pressure on the whole health system.”
Therein lies the nub – the entire health system, patients and the economics of the structure have been affected, resulting in an Australia-wide cry for better management and communication of potential shortages.
There are currently more than 400 medicine shortages across the country, according to the Therapeutic Goods Association (TGA) as well as a worldwide shortage reported by the World Health Organization.
In Australia the list of shortages includes pain management medications, some antibiotics and diabetes medications.
Supply of hormone replacement therapy estradiol-containing transdermal patches is also impacted, with pharmacists able to dispense an alternative brand or
strength as of November 2024 as the TGA looks to mitigate shortages. As a result, there have been calls for a more streamlined approach to dealing with these shortages in Australia in the hope it prevents similar long-term shortages in the future.
The TGA said late last year it was “pursuing a program of regulatory, digital and process improvements to address high priority issues and further reduce the impact of medicine supply disruptions”.
In June 2024 the TGA held discussions to identify priority areas for potential reform, which were provided to the Federal Government.
In November it announced proposed improvements to its monitoring and management of medicine shortages and discontinuations.
But in January this year the Australian Medical Association
(AMA) called for a dedicated forum to provide ongoing advice and solutions.
AMA President Dr Danielle McMullen said such a forum could significantly improve communication to doctors, patients and all other relevant stakeholders.
• change in demand due to changes in health practitioner
clinical practice guidelines
• shortage of raw ingredients
• discontinuation

“One issue that persists is the challenge of timely, accurate and consistent communication regarding medicine shortages. These shortages affect so many people in our community, including doctors, pharmacists and, crucially, patients.
“Medicine shortages and other disruptions have a profound effect on the community and inadequate communication can result in additional costs for patients, for whom there is often little transparency or forewarning.
“We appreciate the nature of medicine shortages are unpredictable, but this is about giving us the best possible chance to respond to supply disruptions, which remain prevalent in the postCOVID era.”
Speaking to Medical Forum, Dr McMullen said the proposed forum is a way to improve transparency and awareness of mechanisms that help manage shortages.
“A forum of stakeholders would help make sure that the whole sector is on the same page, both about existing shortages and looking forward, because sometimes they can predict those,” Dr McMullen said.
To some extent, medicine shortages or delays are expected, partly due to raw material shortages and fluctuations in demand. But the ‘why’ of recent shortages, their length and breadth is a complicated answer.
According to Diabetes WA the global shortage of Ozempic started in 2022. There are several factors that contribute to a disruption in the supply of medications, these include:
• disruptions in the manufacturing plants
natural disasters
• local or international challenges in manufacture and or transportation
• product recalls due to unexpected quality and safety issues.
In light of the pressure this is placing on healthcare providers, and of course patients, the TGA and other groups have scrambled to find a way to improve and avoid.
In April 2024, the TGA released a research report entitled Understanding the Medicine Shortages in Australia.
Insights found that in some cases it was “too little too late” and that “consumers have been left to find solutions themselves”.
Solutions ranged from considering ways to increase production and supply of medicines to Australia through on-shore manufacturing; partnering with overseas allies for stock exchanges; ensuring equitable distribution and allocation of stock across the country; and implementing purchase limits to ensure fair distribution.
Progress is slow moving. To mitigate a national shortage of IV fluids the Federal Government in March struck a $40m deal with Baxter Healthcare to expand their production facility in Sydney$20m in federal funding will be matched by the company.
While there have been positive steps, one particularly worrying impact is on palliative care which has faced dire shortages in the past 12 months.
For 60-year-old Linda Summerton, the experience of trying to find suitable end-of-life medicine for her 86-year-old mother was devastating.
In 2024 her mother started using Ordine – liquid morphine – for the pain every day.
“It got to July, August, and we went to the chemist to fill it and they said ‘We don’t have any’,” says Linda, a palliative care nurse for 22 years.
They were told there were no alternatives, so they went back to their GP and were given a script for Oxycodone.
“Most people know that morphine is the gold standard for pain and shortness of breath, but mum started on the Oxy. She said it wasn’t as effective.”
This lasted three months.
“One day I rang eight different pharmacies trying to find Ordine,” Linda adds.
Finally, around September, they were able to access the drug.
“I felt like I had won the lottery,” Linda says. “My mum is in a wheelchair so going back and forward to the GP made the entire experience even more difficult.”
Being a nurse, Linda had heard about the coming shortages, but she says they were told alternative brands would be available.
“This is a drug that’s mainly for palliative care patients and end-oflife patients. It’s not a time when you want more uncertainty, there’s enough uncertainty. I’ve never known a shortage like that before.”
Dr Peter Allcroft, Chair of Palliative Care Australia, has suggested people are ending up in hospital as a result of being unable to access pain medicines.
Despite sector representations to the Minister for Health, the TGA and the Department of Health and Aged Care, there has been little progress toward ensuring a stable supply of these life-changing drugs, PCA said in a statement.

Diagnosed in 2019 with pulmonary fibrosis, her mother –who is still alive – was relatively stable until she started suffering from shortness of breath in 2023.
“People, including children, are dying without adequate pain relief,” Dr Allcroft says.
The current situation has been building over several years and has become especially challenging
Ovulation Induction & Ovulation Tracking (OI/OT)
Intrauterine Insemination (IUI)
Our Fertility Specialists in WA

Dr Gayatri Borude
MBBS, MD, DNB, FRANZCOG, FACOG, FMAS
Clinical Director (WA), Fertility Specialist, Obstetrician & Gynaecologist
In Vitro Fertilisation (IVF)
Intracytoplasmic Sperm Injection (ICSI)

Frozen Embryo Transfer (FET)
Donor Program Egg Freezing

Dr Mahalakshmi Ragunath
MBBS, DGO, MRCOG, MSc, FRCOG, FRANZCOG
Fertility Specialist, Obstetrician & Gynaecologist
Perth 9 Perilya Road, Craigie WA

Dr Shanthi Srinivasan
MBBS, MD, DNB, FNB(Rep Medicine), FRANZCOG
Fertility Specialist, Obstetrician & Gynaecologist

continued from Page 27
in the last 12 months as global supply chains and pharmaceutical companies falter and reprioritise.
Adding to the distress is cost, with many of the alternative medications not subsidised through the Pharmaceutical Benefits Scheme (PBS).
One of the most startling examples is hydromorphone SR, a medication used to treat acute and chronic pain, which costs the public $182 for 32mg. The overseas alternative, which is not PBS-listed, is $4209 for 100 tablets – 23 times more expensive.
Dr Meera Agar, PCA Board Chair, tells Medical Forum they first heard certain medications would be discontinued 18 months ago, with only a couple of months’ notice.
“We’ve been working closely with the medical shortages section of the TGA… but that’s not the end of the story,” she says.
Mr Ngeow says 90% of Australian medicine is imported and, on top of that, there’s the tyranny of distance, particularly in WA.
“We are the largest health jurisdiction in the world,” Mr Ngeow told Medical Forum. “We have a low population density, and we are at the end of a complex worldwide supply train.
“So shortages will be felt disproportionately in WA compared to anywhere else in the world.”
He explains there were issues during COVID and “I don’t think we’ve ever really seen a catch-up from that point”.

Due to the pressure of shortages, pharmacists are working harder than ever, he says.
“It’s that extra thing they need to handle. They are just doing more in general.”
Going forward, Mr Ngeow says there’s a lot more that can be done if “we can get some small regulatory changes in the State”.
“Having that clear signalling helps if you know it’s only going to be a shortage for a month –there’s probably some people who can hold out. We can use existing supplies if it’s going to be 12 months, then you can probably change people to a different medicine. So, it’s really understanding the recommended action as well as what’s happening in more detail.”
Dr McMullen knows this first-hand; she’s a GP and describes the shortages as “endlessly frustrating”.
“We get feedback from AMA members about having to double check another system all the time. You get phone calls back from frustrated patients.”
It seems that the ‘why’ of how it came to this is multi-layered and complex, with much out of Australia’s control.
However, information sharing and greater awareness of existing and forecasted supply disruptions can be improved.
The next questions are around what medication replaces that?
And what about clinicians who need to explain how to use the new formulation?
“The flow-on parts have not really been tackled,” Dr Agar says. “So that’s a more immediate issue.
“There’s a resource issue but also access to a clinician who can prescribe it, to actually finding stock.
“It’s that whole pathway. Then the next script you’ve got to do it again because you can’t guarantee that once you’ve been on the replacement it’s going to be available for your next month’s script.”
Fixing the issue
Also at the frontline of the shortages are pharmacists. Andrew Ngeow, President of the WA Branch of the Pharmacy Guild of Australia, has some inciteful views on how to ease the pressure.
With pressures on GPs and organisations saying there is no end in sight to the medication shortages in the short to mediumterm, he believes pharmacists should be given the power to make decisions on prescriptions to help ease the pressure where it is safe to do so.
“For example, if you can’t get a 20mg tablet, a pharmacist should be able to give you two 10mg tablets,” Mr Ngeow said, adding that the Guild has spoken to departments and government on this subject.

“We will see where that lands. Hopefully sooner rather than later.”
What about the GPs themselves? Dr McMullen says going forward the right mechanisms need to be in place to communicate these shortages and secure alternative suppliers.
The Pharmacy Guild of Australia has called on the Federal Government to reinstate the Medicine Shortage Working Party, which was disbanded in 2021.
The current approach to managing medicine shortages is too shortterm and reactive, says National President of the Pharmacy Guild, Trent Twomey.
“It doesn’t address the root cause of shortages, and patients continue to suffer. Information sharing and greater awareness of existing and forecasted supply disruptions is crucial to making sure Australian patients have the medicine they need.”
As Ms Summerton says of her mother’s experience: “I knew morphine shortages were coming, but there was not enough planning or foresight. It should never have happened, we’re talking about elderly people at the end of their life.”
The Breast Clinic at Hollywood is a part of the Perth Breast Cancer Institute in the Breast Cancer Research Centre WA and is the domain of two breast physicians – Dr Susie Kitchin
MBBS FRACGP and Dr Pamela Thompson
MBBS(Hons) FRACGP DCH.

Both are UWA graduates, and each has over 12 years’ experience working in public and private breast disciplines, with a background of rural and city GP work, which brings a holistic attitude to the care they provide all their patients.
The institute’s Breast Clinic is a valuable resource for patients and GP colleagues – offering a specialised level of care, support, advice and information.
The Breast Clinic is available to any patient with breast tissue wanting personalised, expert breast care in a safe, inclusive environment.
Patients can self-refer, GPs can refer their patients as well as other specialists, and all will receive prompt and appropriate management.
Referrals can be phoned, emailed or faxed and will be triaged within 24 hours. The Breast Clinic has standard longer appointments, which allow us to understand patients’ concerns, complete thorough examinations and provide advice and followup plans that inform and reassure patients as they go through this challenging phase of their lives.
It is important to know that the Breast Clinic is a service available to everyone.
Key groups we manage include patients with benign disease needing regular follow up, patients with new symptoms of a lump, pain or others that needs investigation, people with a family history who want evaluation of their own personal risk, people starting or continuing their routine screening program, breast cancer diagnosis, management and survivorship.
Screening is available to all women though BSWA. However, the Breast Clinic also provides a screening service for patients who may want a more personalised approach. Some may have a higher risk of breast cancer that warrants further investigation than mammogram alone or want a timely approach to their screening needs.
Our clinic provides a same-day service with clinical examination, imaging completed, and results discussed on the day, so there is no waiting anxiously for outcomes. The reassurance of one day care helps minimise the natural worry that
people can experience during their screening process.
When a biopsy is required, this is also completed in the quickest time frame. When an onward referral is necessary, the availability of the team at the Perth Breast Cancer Institute allows soonest appointments and ideal continuity of care.
Our goal is to provide timely, empathic, evidence-based care to all our patients in a safe and welcoming environment and also help women to take responsibility for their own health and wellbeing through education and support.
That includes educating people to know what their own normal breast feels like, coaching them to do a good breast examination, encouraging them to talk to friends to improve breast and general health literacy and awareness, and guide them through the process to gauge their personal risk for breast cancer through evidenced-based online tool iPrevent.
This focus on the individual is what drives the Breast Clinic at Hollywood.
As private maternity services in WA face yet another blow, is it time private health insurers increase their rebates to support patients and practitioners?
Western Australia’s private maternity offerings have shrunk in recent years, with the closure of several maternity units in regional and metropolitan areas, sparking concerns about the viability of the service.
St John of God Hospital Mount Lawley, St John of God Hospital Bunbury and Glengarry Private Hospital have all seen closures in the past two years alone.
More recently, three experienced obstetricians working out of St John of God Subiaco left the field, prompting further concern for the State’s maternity services.
Among them was Dr Fiona Langdon who announced via social media that she would be closing her obstetric practice and joining Monash IVF in West Leederville from February this year.
AMA(WA) President Dr Michael Page said there were several reasons WA private maternity offerings had reduced, the main one being the cost of delivering the services.
“Private health insurance rebates are a big problem at the moment, private health insurers are not providing enough rebates, not keeping pace with the cost of providing services,” he told Medical Forum
“It has put private hospitals under a huge amount of pressure, and so they are needing to look at what services can actually keep them afloat and obstetrics is one of those things that, I think, suffered over the last few years.”
A shortage of staff and reduced demand for private maternity services were put forward as reasons for the recent closure of maternity services.

However, the Royal Australian and New Zealand College of Obstetricians and Gynaecologists has pointed the finger at private health insurance providers.
“Health funds frequently underpay private hospitals for obstetric and gynaecological services, failing to acknowledge the actual costs. As a result, when evaluating financial viability, private hospitals tend to favour more profitable specialist services over those focused on women’s health,” the College said in a statement.
The College acknowledged the number of women opting for private maternity care had reduced in recent years, and put this down to “rising premiums and out-ofpocket costs”.
It described obstetric and gynaecological services as being “under threat in Australia due to systemic gender bias”.
Dr Page added that difficulty attracting other healthcare practitioners such as midwives and anaesthetists was also contributing to the problem.
“The fact is, private obstetrics is too big to be allowed to fail, if the big private obstetric units in WA
were to be unviable, there is no way the public system could cope with the volume of obstetric work that would fall on it.”
Dr Langdon now heads up the State’s first private specialist-led early pregnancy service for women who have conceived after fertility treatment.
The new service aims to bridge the gap between fertility care and obstetrics.
Under the new model of care patients are monitored from six to 16 weeks and can access urgent appointments. They may choose to access the service weekly, monthly or at different intervals.
“After months, and sometimes years, of fertility treatment many patients are understandably highly anxious – even after finally achieving a much-wanted pregnancy,” Dr Langdon said.
“Yet there is often a significant gap in care between discharge from a fertility specialist at six to seven weeks gestation and the commencement of standard obstetric care at 18 to 20 weeks, leaving many women feeling anxious and stressed.”
Societal attitudes and policies relating to menstrual health have come a long way, but it’s not enough to ease the burden of ‘period poverty’. What still needs to be done?

By Suzanne Harrison
Each month, 14-year-old Charlotte endures heavy periods that can cause enough pain for her to miss school.
With her mother, Charlotte sought medical help and was lucky that her doctor made her feel supported and that her concerns were not being dismissed.
“I’m better at dealing with the pain now because I’ve had my period since I was nine and I’ve had to accept it. But the doctor says my normal is everyone else’s worst,” Charlotte told Medical Forum
The good news is, she can’t fault the availability of free period products at her school.
“All I have to do is visit the nurse and they’re really good about handing them out.”
Charlotte’s cycle started off as light but over the years her periods became heavier and more physically depleting.
“There are times when I have had to miss school because it’s too heavy, tiring or painful.
“I’m not the only one. Other girls have to travel further to get to school and it’s stressful for them on the bus, so sometimes they just stay at home to avoid leaking.”
Charlotte’s experience with seeking medical help is a sign times are changing, because until noise was made by those seeking to alleviate the reality of period poverty and menstrual issues, many felt their concerns were dismissed.
While stigma and misconceptions still abound, now free period products in schools are the norm and conversations are being had in the media.
Share the Dignity founder Rochelle Courtenay said a doctor once told her daughter – who was in immense pain –“You know periods can be painful”.
Unable to afford period products in the last 12 months
Source: Share the Dignity
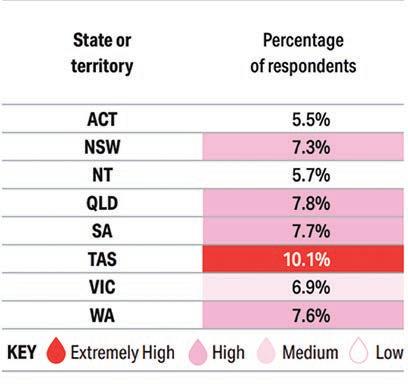
Missed out due to their period
Source: Share the Dignity

Share the Dignity defines period poverty as a lack of access to menstrual products, hygiene facilities, waste management, and education.
When people hit hard times, they sometimes have to choose between purchasing period products, buying food for their families or paying their rent, according to the charity.
People without fulltime employment and those who come from lower socioeconomic backgrounds are disproportionately impacted by this problem.

It was soon discovered her daughter had a twisted ovarian cyst, which needed immediate operation.
“That kind of comment was illinformed and wrong,” says Ms Courtenay.
The charity released a groundbreaking report in 2024, The Bloody Big Survey. The results show period poverty well and truly exists in Australia.
Students at schools, TAFEs and universities are struggling with the cost-of-living and being able to afford period products.
In WA, Brookton council – 100km from the Perth metropolitan area –
recorded high instances of period poverty, with 100% of respondents saying they had difficulty buying period products.
All respondents also said they had missed school due to periods.
More than 65% of WA respondents found it difficult to buy products, almost 8% were unable to afford them, and 20% had to improvise using materials like toilet paper due to the cost. The median spend was $50 per month on period products.
Some 55% of respondents have missed work due to their period, and one in three of these respondents said the reason was fear of leaking.
It’s costing the country economically too. Share the Dignity estimates $9.6 billion is attributed to missed working days per year due to periods.
“These figures are quite astonishing, and I hope will help shine a light on this issue in workplaces across the nation,” says Ms Courtenay.
Perth-based Dr Dani Barrington, senior lecturer in global health at UWA, said the concept of period poverty also encompasses issues surrounding societal expectations, cultural pressures and stigma.

It also relates to whether they can openly discuss, or feel comfortable, explaining their pain or be accepted within their community while menstruating.
Dr Barrington, a founding member of Share the Dignity and a public health engineer, has worked to improve people’s experiences with toilets, menstrual health and hygiene.
“Period poverty is not just about products and financials, but also about stigma and mental health,” she said.
“In Australia we do have people who can’t afford period products. But we also have quite poor
continued from Page 33
education around menstruation; there’s very little around the school curriculum and there’s not enough in the medical curriculum for GPs.”
Reducing the stigma and unnecessary embarrassment surrounding menstruation has long lagged behind other societal growth areas, she said.
And while there have been improvements when it comes to access, Dr Barrington is now
working on finding a better understanding of where this stigma comes from and how different cultural groups approach periods. That also involves doing work with men and boys.
RACGP Vice President and WA lead Dr Ramya Raman adds that people’s experiences with periods and menstrual issues are often shaped by their cultural backgrounds. In some cultures it is not discussed,

especially not outside the home. Therefore, the role of the GPs can be crucial in breaking down that barrier.
“That is one component that has not been touched on much in the articles I have seen,” said Dr Raman.

“In some cultures, a period is not to be talked about publicly. It’s taboo. So, they may not see it – menstrual pain or heavy bleeding – as an issue. And this is when the GP plays a role.”
Access to free or easily accessible period products in many Australian hospitals can be a challenge, both for patients and staff.
Unlike the move to provide vending machines and free products in State schools around the country, few hospitals have followed suit.
As part its Pad up Public Health campaign, Share the Dignity has called on the Federal Government to ensure free period products for all patients being cared for in public hospitals.
While some hospitals provide free products it is not mandatory for them to do so.
“In public hospitals across Australia, patients can get band-aids, bandages, painkillers, or incontinence aids, but not sanitary items when they need them,” the charity stated in an online petition.
“Some have been forced to bleed through their hospital gowns. Others have had to use unsuitable alternatives like dressings or adult nappies.
“When provision is managed at an individual hospital level, availability can be limited, and patients have relied on the kindness of doctors, nurses and staff who give pads of their own.”
The Federal Government has said responsibility for the provision of free period products in public health settings rests on State and Territory governments.
In Perth, a Dignity Vending Machine at Joondalup Health Campus has helped more than 6500 people each month since its installation. Some 12,000 period packs have been provided.
Goldfields Women's Health Care Centre also has a vending machine. At the time of going to print, no other WA hospitals are listed as offering this service.
The question begs, in hospitals without this service, how do medical staff deal with their own periods, especially when so time constrained?
Jodie, a Perth-based registered nurse, says nurses – the majority of whom are female – are already used to holding on to full bladders for as long as possible. So, in her experience when it comes to their periods, they rely on each other if they are caught short.
“Generally, you can find what you need or ask a colleague, but I think hospitals could actually provide a small array of products,” she told Medical Forum
“Hospitals should provide them to staff in the changing rooms. Even pads would be enough, or a vending machine. Then we don’t have to go fossicking for products.”
Building up that trust ensures women from diverse backgrounds have confidence in their doctor and also supports GPs to forge strong relationships over a patient’s lifetime.
“This is something patients should be empowered to talk about with their GP. It needs to be embraced and respected.”
Thankfully, Dr Raman added, there is a lot more information now available for girls and women, whether that’s through advertising, social media or even product placement in supermarkets. She hopes the more it is talked about the quicker the taboo will be broken.
In 2023, all Australian States and Territories implemented policies to provide free period products in public schools.
In WA, the State Government launched a program to provide free period products in 225 public high schools. It was later extended in 2024 to include more than 570 public primary schools.
This is a positive step, but is only part of the story. As Ms Courtenay explained: “I think we are about a quarter of the way there.”
For example, she said, what happens when girls can’t access period products during school holidays?
“We want vending machines in libraries. There should be period products everywhere,” Ms Courtenay said.
In some cultures, a period is not to be talked about. So, they may not see it – menstrual pain or heavy bleeding – as an issue. This is when the GP plays a role.
To that end, Share the Dignity hopes to work with local councils to encourage them to be part of the conversation.
The Victorian Government has recently announced plans to expand the initiative to also provide period products via vending machines in selected public spaces. Similarly, the ACT said it would make products available in some public health services, courts and child centres.
In June 2024, the Federal Government also announced it would provide free products to women and girls living in remote First Nations communities.
This initiative aims to help around 12,500 women and girls each year to access period products –
including pads, tampons, menstrual cups and period underwear.
Period products can be almost double the price in some remote communities, with people paying $15–$25 on average for a packet of pads, compared to an average of $10–$15 in metropolitan areas.
This inequity means women and girls in remote First Nations communities are often forced to miss out on school, work, community events and social activities when they have their period.
In May last year the Medical Journal of Australia cited a report from Dr Lauren Cameron and colleagues at Deakin University, that 90% of adolescents who menstruate experience period pain and
that for 21% this pain is severe (dysmenorrhoea).
They found that adolescents with dysmenorrhoea were “up to five times as likely to miss school and three times as likely to miss sporting or exercise for reasons related to their periods as female participants without dysmenorrhoea”.
The study makes clear that period and pelvic pain must be recognised, and evidence-based interventions provided to adolescents with persistent dysmenorrhoea.
“Understanding the trajectories of menstrual health throughout life is critical for developing effective public health interventions for optimising women's health,” the study found.
Ms Courtenay would like to see more training for health practitioners and the availability of products in healthcare settings.
“There’s no provision for period products in general practice or hospitals. We’ve got stories on our website of people being in hospital, getting their period and having to use such things as incontinence pads,” she said.


The Westin, East Perth Saturday 7th June 2025
The eighth annual GP Urology Masterclass offers comprehensive education to GPs, covering all aspects of urology to enhance their knowledge and skills in this broad field of practice.
Program Topics:
• Prostate cancer update – PSA, new treatments in WA
• Immunotherapy, ARPIs and radiopharmaceutical therapies – what GPs need to know
• LUTs, BPH and OAB – what’s new in 2025
• Incidental urological findings on imaging
• Haematuria and Recurrent UTIs
• Urology in the elderly
• Testosterone advances and PBS status
RACGP certificates will be issued with CPD hours. We expect between 5–6 hours in total split between educational and reviewing performance categories.
Launching in 2025, the PUC Foundation is a non-profit supporting excellence in urology research and education. THE PUC FOUNDATION
To secure your place, a $75 tax-deductible, non-refundable fee for the GP Urology Masterclass has been introduced with all proceeds going to the PUC Foundation.
Please book a place for the conference at https://gpurologymasterclass.com.au
Women’s health has had a strong national focus in recent months with new medications for endometriosis, menopause and IVF listed on the on the Pharmaceutical Benefits Scheme.
As of 1 May a new medication for endometriosis was listed on the PBS, alongside a progesteroneonly contraceptive pill.
Ryeqo, a new medication with Relugolix with estradiol and with norethisterone, is now available on the PBS for the treatment of endometriosis.
In Australia one in seven women suffer from endometriosis. Ryeqo is a new treatment option for patients who have experienced moderate to severe pain and cannot get adequate relief from other hormonal treatments and painkillers.
The Federal Government estimates around 8500 women will benefit from this listing each year, who without subsidy might pay more than $2700 for a year of treatment.
Alongside this, Drospirenone (Slinda) was also listed on the PBS from 1 May as a new contraceptive option.
Slinda is a progestogen-only-pill and may be used by women who cannot take contraceptives with oestrogens.
Earlier access to fertility treatment for women with specific low levels of reproductive hormones was also approved.
As of 1 April, Pergoveris (follitropin alfa with lutropin alfa) was made available at the earliest stage of an IVF journey. Previously it was only funded in later IVF cycles.
Additionally, double the maximum number of Pergoveris pens – four instead of two – per script were listed.
More than 6000 women access Pergoveris on the PBS each year, many of whom require four pens to

complete a cycle. They will now pay one patient co-payment for up to four pens as needed for their IVF cycle.
The PBS updates form part of a wider $793 million women’s health pledge. Further measures include:

• PBS listing of oral contraceptive pills Yaz and Yasmin – the first new listings in 30 years
• Better access to long-term contraceptives, with larger Medicare payments and more bulk billing for IUDs and birth control implants
• A new Medicare rebate for menopause health assessments, funding to train health professionals, and first-ever clinical guidelines
• PBS listings for new menopausal hormone therapies Prometrium, Estrogel and Estrogel Pro
• 11 new endometriosis and pelvic pain clinics
• Two national trials of pharmacies delivering contraceptives and treatment for uncomplicated UTIs for concession card holders.
The RACGP welcomed the updates as a crucial step towards women’s health equity.
RACGP Vice President and WA chair Dr Ramya Raman said:
“The women’s health package, which covers key initiatives such as increased rebates for intrauterine devices and implants, menopause health assessments, and more funding for endometriosis and pelvic pain, is a crucial step towards health equity.”
Part of the package also includes more training for GPs and other health professionals.
Speaking previously to Medical Forum Dr Raman said the funding and new PBS listings recognised the unique costs that female patients bore and provided greater choice for their healthcare.
“It’s an important announcement which does recognise the importance of supporting women’s health and also recognises the skills that our GPs have in providing care for patients.”

Whether they’re researching online or consulting with their GP for advice, patients and GPs alike should be able to easily identify a specialised, highly trained surgeon without having to navigate such a complex and uncertain process.
A new certification aims to help GPs and patients navigate the cosmetic surgery industry, writes Australasian Society of Aesthetic Plastic Surgeons President Dr Lily Vrtik.
The cosmetic surgery industry is growing, with Australians spending nearly $500 million on procedures per annum.
As demand continues to rise, a critical issue has come to the forefront: patients in Australia and New Zealand often struggle to identify which surgeons have the necessary qualifications, expertise, and ethical standards to provide a safe surgical experience.
Making the right choice in cosmetic surgery begins with having the right information. Misleading claims and lack of information transparency commonly result in poor decisions and sub-optimal patient outcomes.
Recognising the need for clear, trustworthy information, a new solution is now available to help patients and their GPs navigate the process of choosing a qualified cosmetic plastic surgeon.
The newly established Australian and New Zealand Board of Cosmetic Plastic Surgery (ANZBCPS) has introduced the Board Certified Program – a certification designed to give patients confidence in their choice of surgeon.
confusion
New research from the Board highlights the difficulties patients encounter when selecting a cosmetic plastic surgeon. The findings reveal that nearly three in five (58%) people considering cosmetic surgery face significant challenges in identifying a qualified surgeon, while 44% express distrust in online sources meant to guide them.
Additionally, 37% lack confidence in the available information and one in four (27%) are unsure about the legal regulations surrounding cosmetic surgery practitioners.
At best, this lack of confidence in verifying a surgeon’s expertise leaves patients feeling frustrated and confused. At worst, it compromises patient safety and surgical outcomes, which can have disastrous long-term effects on their physical and mental wellbeing.
Whether they’re researching online or consulting with their GP for advice, patients and GPs alike should be able to easily identify a specialised, highly trained surgeon without having to navigate such a complex and uncertain process.
The Board Certified Program aims to address these issues by providing a stringent certification process to distinguish surgeons who meet a high standard of training, expertise, and ethical practice.
This set of standards includes mandatory compliance with cosmetic surgeryspecific continuing professional development set by the Australian Health Practitioner Regulation Agency. ANZBCPS Board Certified surgeons must also commit to ongoing education to stay at the forefront of their field, ensuring patients receive the most up-to-date surgical care.

This initiative sets a new standard for cosmetic plastic surgery, differentiating and recognising surgeons who have undergone stringent specialist training and obtained the required qualifications for performing cosmetic plastic surgery.
One of the key benefit is its accessibility. Patients can now
search for surgeons through the ANZBCPS website, providing a reliable resource for those seeking safe and qualified professionals.
This development is particularly significant for GPs, who often play a crucial role in guiding their patients towards safe surgical options.
For GPs, recommending an ANZBCPS Board Certified surgeon ensures that their patients are in the

hands of a specialist who meets high safety and ethical standards.
Given the increasing number of patients seeking cosmetic surgery, it is more important than ever for medical professionals to provide guidance based on verifiable credentials that are relevant and recent.
Accurate and transparent information is essential to directly empower patients to make confident decisions and choices about their cosmetic surgery options. This is the foundation of informed consent, a crucial element in the statutory requirement of cosmetic surgery procedures.
The launch of the Board Certified Program marks a significant step towards empowering patients with the knowledge they need to make these informed decisions. Patients considering cosmetic surgery are encouraged to conduct thorough research and use the ANZBCPS certification as a benchmark for safety and expertise.
ED: More information can be found at boardcertified.org.au







People who eat a healthy Mediterranean diet may be less likely to develop Alzheimer's and depression, writes Dr Samantha Gardener, post-doctoral research fellow.
Depression and Alzheimer’s disease, the most common mental and neurological disorders among older adults, cause immense societal impact and financial burden.
One in six women and one in eight men will experience depression at some point in their lives. It can occur at any time and can lead to severe distress and disruption of life.
Alzheimer’s disease is the most common form of dementia. In 2021, the Australian Institute of Health and Welfare estimated there were between 386,200 and 472,000 Australians living with Alzheimer’s at that time, equivalent to 83 people per 1000 Australians aged 65 and over.
Alzheimer’s disease and depression are frequently comorbid; depression increases future risk of Alzheimer’s, and depression often accompanies an Alzheimer’s disease diagnosis.
A recent meta-analysis observed a 14.8% prevalence of major depression in Alzheimer’s disease. Approximately one-third of adults with depression have concomitant mild cognitive impairment, which often precedes Alzheimer’s disease.
Furthermore, depression, has been shown to promote the conversion of mild cognitive impairment into Alzheimer’s disease. The impact of depression on the clinical course of Alzheimer’s is as yet unclear.
A 2024 Lancet Commission into ‘Dementia prevention, intervention, and care’ identified 14 modifiable risk factors that are proposed to account for around 45% of dementia cases, worldwide.
Of these 14 modifiable risk factors, six can be positively impacted by a healthy diet – they are hypertension,
obesity, alcohol intake, type 2 diabetes, depression, and high lowdensity-lipoprotein cholesterol.
Moreover, certain dietary factors and dietary patterns have been proposed to modulate Alzheimer’s disease risk through direct effects on Alzheimer’s disease pathogenesis such as oxidative stress, inflammation, and cerebral amyloidbeta production and/or clearance – accumulation in the brain is a hallmark of Alzheimer's.
Studies show that certain nutrients may play an important role in the onset, severity and duration of depression as well as cognitive decline associated with Alzheimer’s disease.
The impact of diet on Alzheimer’s disease, depression and the relationship between these conditions may be explained by a complex set of pathways in which
dietary components interact with each other.
These interactions could reduce Alzheimer’s risk directly, via neuroprotective influences, or indirectly as protective factors against depression and cardiovascular disease, which are established risk factors for Alzheimer’s.
However, the specific dietary components that confer the greatest protection against depression and Alzheimer’s disease and impact the complex relationship between these conditions, requires further investigation.
Current evidence suggests that polyphenolic compounds, folate, B vitamins, polyunsaturated fatty acids, and adherence to dietary patterns like the Mediterranean diet are important.
The Mediterranean diet is a way of eating that is inspired by the traditional eating habits of people living in countries bordering the Mediterranean Sea. It's known for being heart-healthy and is rich in fruits, vegetables, whole grains, legumes, nuts, and seeds.
Recent research has advanced our understanding of the changes in levels of blood-based biomarkers over the course of Alzheimer’s disease.
Longitudinal studies have demonstrated that individuals with Alzheimer’s disease have elevated levels of Glial Fibrillary Acidic Protein, which increases as a response to injury or disease in the brain, and neurofilament light chain, a biomarker for neurodegeneration, compared to those who are cognitively unimpaired.
In addition, a lower ratio of Aβ42:Aβ40 and elevated GFAP, and NfL in cognitively unimpaired individuals are associated with future cognitive decline.
New research using a sample of 89 cognitively unimpaired
participants from the Australian Imaging, Biomarkers and Lifestyle study has shown that in males with a less healthy diet – average and below average Mediterranean diet adherence – depressive symptoms were associated with higher NfL levels.
In those with a healthier diet, depressive symptoms did not induce higher NfL levels.
Apolipoprotein E ε4 allele carriage is the strongest known genetic risk factor for Alzheimer’s disease, and in Apolipoprotein E ε4 non-carriers (those at lower risk of the disease) with a less healthy diet, depressive symptoms were associated with higher NfL and Aβ40 levels.
Elevated NfL levels, indicative of neurodegeneration, have been found in various neurological disorders like multiple sclerosis and Parkinson's disease.
This suggests that increased NfL levels in the results might not exclusively represent Alzheimer’s disease pathology but could also be influenced by other neurodegenerative processes.
The research shows that the
Mediterranean diet is potentially a moderator of the relationship between depressive symptoms and Alzheimer’s disease-related bloodbased biomarkers.
Overall, higher Mediterranean diet adherence potentially mitigates some of the negative impact depressive symptoms have on Alzheimer’s disease-related bloodbased biomarker alterations.
Based on these insights, further research into personalised dietary interventions, considering genotypes and sex-specific needs, is needed. This approach could lead to effective strategies in preventing or mitigating symptoms of depression and Alzheimer’s disease.
ED: Dr Gardener is a researcher at ECU and co-lead author on the study: The moderating effect of diet on the relationship between depressive symptoms and Alzheimer’s diseaserelated blood-based biomarkers.
Bulk-billed for three cycles
No out-of-pocket expenses for Medicare-eligible patients at Genea monitoring centres.
Easy online referrals
Simple referral process with full nursing support for your patients.
Ovulation reports sent directly to your practice
Receive detailed ovulation reports with hormonal status and cycle insights for informed fertility assessment and management.

Discover Genea’s ovulation tracking service
Scan the QR code to learn more and to download a referral pack.
Genea Perth
Level 2, 190 Cambridge Street, Wembley WA 6014
Genea Mandurah 29-31 Sholl Street, Mandurah WA 6210
HIV cases are increasing and health practitioners have a role to play in preventing the spread and encouraging the use of PrEP, writes Karina Reeves, Coordinator of Health Promotion at WAAC.
Recent data from the WA Department of Health show HIV notifications increased from 68 in 2023 to 77 in 2024. Between January and June 2024, 28 new diagnoses were reported, with the majority involving individuals born in South-East Asia and SubSaharan Africa.
People from culturally and linguistically diverse backgrounds are a priority group under both the Western Australian Sexual Health and Blood-borne Virus Strategy 2024–2030 and the Ninth National HIV Strategy 2024–2030.
Community consultations have revealed widespread gaps in knowledge about HIV risk, prevention, and treatment, particularly among migrants from Asia, Africa, and South America.
WA’s early HIV prevention success largely stemmed from communityled campaigns targeting gay, bisexual, and other men who have sex with men. These efforts were culturally relevant and resonated with the target population.
However, as HIV demographics shift to include more heterosexual individuals and those from CaLD backgrounds, prevention strategies must evolve accordingly.
The changing nature of HIV transmission highlights the importance of inclusive, adaptive approaches that address the specific needs of emerging at-risk groups.
Stigma remains a major barrier, especially around sexual health and HIV. Misconceptions persist in CaLD communities – such as the belief that PrEP is only for men.
These misunderstandings are sometimes reinforced by healthcare professionals, who may not perceive women in heterosexual relationships as being at risk.
A 2024 scoping review found many providers were unsure about prescribing PrEP to cisgender women, emphasising the need for improved education and awareness. PrEP is highly effective when taken as prescribed, preventing sexual transmission and reducing the risk of acquiring HIV from a partner who injects drugs.
For women, it offers a way to take control of their sexual health without relying on their partner's choices. Regular testing is also crucial, as delayed diagnoses lead to poorer health outcomes and increase the risk of further transmission.
Healthcare practitioners play a pivotal role in dispelling myths and initiating HIV-related conversations. In many cultural settings, patients expect providers to raise health concerns, including those related to HIV.
However, research shows clinicians may avoid such discussions for fear of offending patients from migrant backgrounds.
The Migrant and Refugee Blood Borne Virus Survey – a 2021 national study – found that most respondents would not be offended if offered an STI or BBV test by a doctor or nurse. Notably, only 41% of respondents knew that HIV is not automatically included in routine blood tests. This misconception can result in people wrongly believing they’ve already been tested.
When healthcare providers avoid

HIV discussions, opportunities for prevention and early detection are missed, further entrenching health disparities.
Language barriers, stigma, and limited healthcare engagement contribute to lower HIV testing rates in CaLD communities.
Addressing these requires promoting routine HIV testing –especially for women in high-risk situations or with partners from high-prevalence regions.
Early diagnosis and prompt pretreatment are essential to stopping transmission and improving health outcomes. It’s also critical to engage women of childbearing age to prevent vertical transmission to children.
Encouraging providers to initiate conversations about HIV risk, PrEP, and testing will help close the gap in service access and understanding. This proactive approach supports better health outcomes for CaLD women and ensures more equitable care.
Creating an environment where sexual health, HIV risk, and prevention are regularly discussed in clinical settings is essential to inclusive care.
The ASHM Decision Making in HIV tool and National PrEP Guidelines offer resources for clinicians.
ED note: WAAC’s ‘Even Me?” campaign aims to empower CaLD communities with the knowledge and tools to prevent HIV and improve public health outcomes for all Australians.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

In the same way frequent flyer points are not much use if you can’t access flights, free GP visits are not much use if there are no appointments when you need one.
We all like collecting frequent flyer points in a myriad of ways, most of which do not involve flying. Recently my bank invited me to apply for a new Visa card with a carrot of 100,000 points for doing so. I declined.
There is never such a thing as a free lunch. It is always much easier to accumulate points than to use them for holidays. Where am I going here?
As you read this, the Federal Election will likely be over and – unless we have a hung Parliament – we will know who the new government is.
Both major parties are committed to providing more ‘free’ GP visits, but in the same way frequent flyer points are not much use if you can’t access flights, free GP visits are not much use if there are no appointments when you need one.
The reality is that it is increasingly difficult for patients to access doctors.
There has been substantial population growth with negligible growth in doctor numbers. As of 31 December 2024, WA had 15,497 registered medical practitioners, of which 3800 were GPs.
Nationwide 23% of GPs are aged 65 or over, with 15% over the age of 70.
While the number of future GPs training in WA has risen 31% to 194 this year, the workforce still lags behind population growth.
Meanwhile, an interim report on the Federal Government’s Medicare Urgent Care Clinics found that each visit to a clinic costs $246.50, which is roughly six times the Medicare rebate for a standard consultation.
When I last checked, moving a doctor from point A to B does not increase doctor availability, thus urgent care clinics simply provide ribbon cutting opportunities for politicians.
Is there a solution? I am sure there is, but it requires lateral thinking and a willingness to concede what we are doing is not working. I don’t expect improvement anytime soon.

Sign up to our Wednesday clinical newsletter to get the latest updates from your local specialists.
Head to our website and click the subscribe button or scan the QR code
By Dr Sean Copson, Gynaecologist and AGES Advanced Laparoscopic Surgeon, West Perth
Endometriosis is a chronic inflammatory condition defined by the presence of endometrium-like tissue outside the uterine cavity.
Affecting approximately one in seven females, or those assigned female at birth, its hallmark symptoms include dysmenorrhoea, dyschezia, dyspareunia, dysuria, and non-cyclical pelvic pain.
While not all women with endometriosis are symptomatic, pain and infertility remain its most prominent clinical features.
Pain management strategies include analgesia, hormonal suppression, and surgery. All symptomatic women should be offered these options, with individualised care plans developed in partnership with the patient.
Surgery is an effective treatment option, particularly for patients with persistent pain despite medical management. It may also be appropriate as a first-line intervention in women who decline hormonal therapies or where a definite diagnosis is desired.
Laparoscopic surgery is the gold standard for endometriosis management. It is favoured over open surgery due to benefits such as reduced postoperative pain, shorter hospitalisation, faster
recovery, and improved cosmetic outcomes. Even in cases involving large endometriomas, laparoscopy should be the preferred approach.
Prior to surgery, all patients with suspected endometriosis should undergo a high-quality pelvic ultrasound by a dedicated women’s imaging service, as the accuracy of diagnosis is operator dependent.
Advanced imaging helps avoid ‘peek and shriek’ surgeries, where extensive disease is discovered unexpectedly intra-operatively, and no definitive treatment can be provided.
When treating superficial peritoneal endometriosis, clinicians may choose between excision and ablation. Meta-analysis of four RCTs showed no statistically significant difference between the two, although excision demonstrated a trend toward better outcomes for dysmenorrhoea and dyspareunia.
International guidelines recommend excision where possible, given its potential for greater symptom relief and the added benefit of obtaining tissue for histopathology.
Surgical excision is the preferred technique for deep infiltrating endometriosis (DIE), as ablative
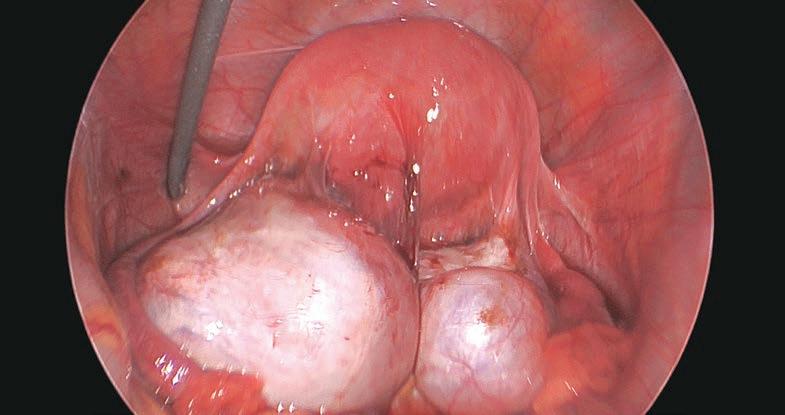

Laparoscopic surgery improves pain in 70–80% of patients with endometriosis. It is a suitable option when medical therapy fails, is declined, or in those preferring surgery as first line treatment
High-quality pelvic ultrasound detects almost all cases of severe endometriosis helping avoid ‘peek and shriek’ surgeries
Preoperative counselling is a key part of the process and allows for informed decision making.
methods may not achieve complete lesion removal. DIE requires careful preoperative planning and often necessitates referral to an advanced laparoscopic surgeon due to the complex anatomy involved.
Complete excision of lesions improves pain outcomes and reduces recurrence.
Up to 60% of patients with an ovarian endometrioma will have concurrent DIE. Pre-operative imaging with either a DIE ultrasound or, if not feasible, for example due to patients wanting to avoid a transvaginal ultrasound or rural patients where DIE ultrasounds are not available locally, MRI may be appropriate.
If DIE is confirmed, patients should be referred to a gynaecologist with formalised training in advanced laparoscopic surgery for reasons detailed above.
Management should involve cystectomy (cyst wall stripping) rather than simple drainage and coagulation. Cystectomy is associated with lower recurrence rates, improved pain control, and less ovarian damage. However, it also carries a risk of diminished ovarian reserve, and patients must be counselled accordingly.
Options for fertility preservation, including oocyte cryopreservation,
should be discussed, especially in cases where repeat surgery may be required on the same ovary as this is a major risk factor in infertility and failed IVF.
Postoperative hormonal suppression is recommended to reduce recurrence. Endometriomas greater than 5cm carry a small but notable malignancy risk (approximately 0.8%) and should be excised to obtain a histological diagnosis.
Surgical intervention provides significant pain relief in the majority of patients, with 70–80% experiencing a significant reduction in symptoms. However, 20-30% may have persistent symptoms postoperatively, and a small proportion (1–2%) report worsened pain. It is crucial to set realistic expectations and provide comprehensive preoperative counselling.
Persistent or worsening pain post-surgery may reflect other contributing factors, such as neuropathic pain, central sensitisation, myofascial dysfunction,

At the conclusion of surgery, all anatomy is normalised with the rectum mobilised free from the uterus and all endometriosis
or other gynaecological conditions like adenomyosis. Identifying and addressing these elements preoperatively can optimise the pain outcomes for patients.
Surgery is a valuable tool in the management of endometriosisassociated pain, particularly when conservative measures are ineffective or declined.
A high-quality preoperative assessment - including expert pelvic imaging - is essential to guide management, avoid unnecessary
There is no one-size-fits-all approach to vascular surgery. My team and I address patients’ individual needs with the most appropriate and best comprehensive management option.
diagnostic laparoscopies, and ensure optimal surgical planning.
Patients should be thoroughly counselled about the risks, benefits, and expected outcomes of surgery. A multidisciplinary approach that includes consideration of pain mechanisms beyond the disease itself will deliver the best outcomes for women living with endometriosis.
Author competing interests – nil



Dr Altaf alongside his colleagues – diagnostic sonographer Simon and clinical nurse Mel – provides a comprehensive diagnostic and therapeutic service of arterial and venous diseases including:
Abdominal aortic aneursyms
Peripheral artery disease
Varicose vein diagnosis & treatment
Carotid artery disease Leg ulcers & diabetic foot disease Renal access
Dr Altaf consults at Hollywood Medical Centre, SJOG Midland Private Hospital, SJOG Carine Specialist Centre and public appointments at RPH and SJOG Midland Public Hospital. Operates out of SJOG Midland Public and Private, Hollywood Hospital and SJOG Subiaco. Appointments are coordinated through practice manager Michelle Burrell and her team.

Hollywood Medical Centre Level 2 Suite 45/85 Monash Ave, Nedlands WA 6009
Phone: 6244 6215 | Fax: 6315 6423 | Healthlink ID: drnaltaf draltaf.com.au
By Dr Jana Combrinck GP & Dr Kym Jones, Gynaecologist, Joondalup
Attending the 19th Annual IMS Congress last year, we gained insights into the latest developments in menopause
Breast cancer risk is one of the most common concerns expressed by both patients and healthcare practitioners when discussing menopausal hormone therapy (MHT).
Professor Robert Langer, one of the principal investigators of the Women’s Health Initiative (WHI) trial, helped clarify several misconceptions about MHT. The WHI study, which contributed to widespread fear, suggested that oestrogen and progestin (CEE+MPA) increased breast cancer risk.
However, Professor Langer emphasised that the breast cancer outcomes in the study were not statistically significant, as breast cancer was a secondary outcome –not the primary outcome the study was designed to measure.
As breast cancer typically starts developing 7-12 years before a detectable mass, the increased rates of breast cancer three years into the WHI study cannot be directly attributed to MHT.
While synthetic progestins like MPA can mildly stimulate breast tissue, micronised progesterone –now the preferred option – has a neutral effect on breast cancer risk. Additionally, oestrogen, particularly when used alone, has been shown to reduce breast cancer risk.
For patients who are concerned about breast cancer, emphasise that lifestyle factors such as height, diet, and alcohol consumption have a greater impact on breast cancer risk than MHT.
Professor Steven Goldstein’s talk on bleeding in the menopausal transition emphasised the importance of using transvaginal



Concerns about breast cancer with menopausal hormone therapy have been overstated
DEXA scans can be offered to women under 65 to assess bone density
Genitoutrinary syndrome of menopause impacts quality of life but is under recognised.
ultrasound as the first step when investigating postmenopausal bleeding.
If the endometrial thickness is under 4mm, further investigation via endometrial biopsy is usually unnecessary and unreliable at excluding pathology. For women experiencing erratic bleeding during perimenopause, Goldstein suggested that a low dose
combined contraceptive pill may be more beneficial than MHT.
By suppressing ovarian function and providing a stable hormone level, it can improve psychosocial symptoms like irritability and brain fog, as well as provide effective contraception. Low-dose contraceptives can be used up to age 50 in low-risk women.
Professor Bronwyn Stuckey's presentation highlighted the critical role of oestrogen in bone health, describing it as "nature’s gift to bones”.
The menopausal transition represents a unique window of opportunity to use MHT to prevent bone loss and fractures, which significantly impact women’s quality of life. The maximal benefit from MHT occurs when started
early in the transition and continued for a prolonged period, offering gains of up to 20% improvement in BMD.
Dr Tobie De Villiers’ talk changed our approach to osteoporosis risk assessment. He argued FRAX is not particularly useful in women under 65 and that primary healthcare providers should feel confident offering DEXA scans to women in perimenopause to assess bone density.
Interest beyond treatment of hypoactive sexual desire disorder is growing. However, large studies have found no significant benefits for well-being, bone density, major depression, cognitive decline or lean mass.
When considering a diagnosis of HSDD we are encouraged to use the Decreased Sexual Desire Screening Questionnaire to exclude other factors which may contribute to decreased sexual desire.
MHT and the management of vaginal dryness is an important first step. Experts agree that total
serum testosterone should be used for screening and treatment is aimed at pre-menopausal female testosterone levels.
Androfeme 1 (testosterone 1% cream in 50ml) is the only approved testosterone formulation for women in Australia. A clear and concise guide to starting and maintaining treatment are available from the manufacturer on request.
Discontinue treatment if there has been no improvement at six months, assuming therapeutic levels. It does not need to be weaned.
All experts agreed that GSM is a prevalent yet under-recognised condition that significantly impacts quality of life. Topical oestrogen and DHEA therapy play key roles in symptom relief and vaginal health restoration.
While vaginal lubricants and moisturisers provide short-term symptom relief, the first-line treatment remains topical vaginal oestrogen. Topical oestrogen has not been found to improve prolapse or urge incontinence, nor have an
“Diabetes
effect on nerve-endings, but it has been shown to improve stress incontinence, prevent recurrent UTIs and reduce dyspareunia.
DHEA is synthesised by the adrenal glands and ovaries as an inactive precursor, then converted intracellularly to active hormones (oestrogens and androgens).
Relatively new to the market is the ‘biodentical’ DHEA vaginal pessary containing prasterone (6.5mg) that can lower the vaginal pH, improve dyspareunia and decrease vaginal dryness.
Vaginal DHEA is seen to provide targeted treatment without the systemic effects.
Other therapies for GSM, include vaginal laser such as fractionated CO2 laser and erbium laser, which works by causing microdamage in vaginal layers to promote collagen remodeling and neovascularization. It is seen as effective for vulvovaginal atrophy, but long-term safety and efficacy data is lacking.
Author competing interest – the authors were sponsored to attend the conference by Lawley Pharmaceuticals and Besins.



By Dr Amy Fitzgerald, Gynaecologist, Subiaco
The vulva comprises mostly of skin but is subject to a unique set of influences including reproductive hormones and its specific microbiome.
It is also affected by what can be a harsh physical environment, impacted by heat, friction and moisture. This can make managing vulval conditions and infections challenging.
The impact of vulval conditions on patients should not be underestimated. Wellbeing, sexual function, mood, self-esteem and body image, can all be affected.
Vulval conditions can be debilitating. The stigma associated with them often leads to late presentations contributing to delays in diagnosis and management.
Mainstays of vulval care include avoiding drying soaps by using a soap free wash, with a paraffinbased ointment and reducing exposure to irritants including heat, moisture, soaps, bleaches, dyes, urine and faeces.
This can be done by wearing lose cotton underwear, increasing underwear free time at night, using ‘leak proof’ or period underwear instead of pads or liners, limiting time in tight clothing, especially post workout or wet bathers, and treating and managing urinary and faecal incontinence.
Lichen Simplex (Chronicus) is characterised by localised well circumscribed thickened plaques typically affecting the labia majora and is the result of the itch-scratch cycle.
It can occur due to multiple dermatoses, for example allergic, contact or irritant dermatitis, systemic disease, and psychiatric conditions. Management centres around removing irritants, breaking the itch-scratch cycle, treating underlying conditions and reestablishing the normal skin barrier. Topical corticosteroid ointment and vulval care as described above
Lichen Sclerosus is a lifelong condition requiring steroid ointment suppression and follow up to prevent loss of vulvar architecture, dyspareunia and maligancy
Not all itching is thrush, consider alternative diagnosis particularly in post-menopausal women
Concurrently treating male and female partners to prevent BV recurrence is recommended.

Lichen Simplex. Characteristic bilateral erythematous thickened plaques on the labia majora with normal vulva architecture. Available at: https://dermnetnz.org/topics/vulvallichen-simplex-images
are mainstays of treatment. Steroid ointments is preferred. Tricyclic antidepressants may be used in severe refractory cases when simple measures fail.
Lichen Sclerosus is a lifelong autoimmune condition, which can occur at any age and has a bimodal distribution affecting premenarchal girls and more commonly peri and post-menopausal women.
Itch is the most common feature; however, some women are asymptomatic. The disease is


Characteristic appearance of Lichen Sclerosis with thin, crinkled, white areas commonly in a figure of eight distribution around the vaginal introitus and anus, accompanied by associated anatomical changes with fusion of the clitoral hood, labial resorption and narrowing of vaginal aperture.
Available at https://dermnetnz.org/ topics/vulval-lichen-sclerosus-images
characterised by periods of control with recurrent flares. Ultrapotent topical steroids, such as 0.05% betamethasone dipropionate ointment in optimised vehicle or compounded clobetasol propionate 0.05% ointment, are mainstays of treatment.
Apply daily or twice daily for twoto-four-weeks to induce remission before gradually weaning down to twice per week maintenance. A less potent steroid can be used for mild cases. Ideally use the least potent steroid that achieves control two to three times per week for lifelong maintenance.
Long term sequelae of LS include permanent changes in vulval architecture, narrowing of vaginal aperture, dyspareunia and approximately a 2-5% lifetime risk of progression to vulval intraepithelial neoplasia (VIN) and squamous cell carcinoma of the vulva.
Suppressive steroid treatment appears to reduce the risks. Unilateral lesions or ulcers should prompt suspicion of malignancy and early review for biopsy. LS requires lifelong steroid therapy and follow up, typically yearly with a gynaecologist or dermatologist.
Vulval infections
Symptoms of recurrent, chronic and difficult to treat vulvovaginal candidiasis include pruritus and burning, with resultant dysuria and dyspareunia. Vaginal discharge can be present but is often not the white cottage cheese like discharge of acute VVC.
Symptoms often worsen in the premenstrual phase of the cycle. Chronic VVC pathogenesis is thought to be a hypersensitivity reaction to candida.
It requires a well oestrogneised vagina and is rare in postmenopausal women without risk factors like diabetes and recent antibiotics.
Recurrent VVC is commonly defined as over four infections per year. Treatment regimens vary but commonly require induction with po
fluconazole 150mg daily every three days for three doses, then 150mg weekly for six months.
Speciation and sensitivities can be requested from vaginal swabs. Candida glabrata should be managed with boric acid pessaries 600mg PV nocte for 14 days.
If symptoms are not improving on usual management, consider:
• Swapping combined oral contraceptive pill to a low or non-oestrogen contraceptive
• Ceasing SGLT2 inhibitors (flozin) which cause glycosuria leading to contact irritant dermatitis and contribute to candidiasis
• 1% hydrocortisone ointment for co-existing dermatitis from topical antifungal cream bases which can be irritating
• Treating asymptomatic partners. Candida diets and probiotics lack evidence and are not recommended.
Bacterial vaginosis is the most common cause of vaginal discharge in women of reproductive age, commonly presenting with a thin grey, white, malodorous discharge.
It is due to vaginal microbiome dysbiosis with vaginal microbiota changing from lactobacilli dominating to increased anerobic bacteria numbers and diversity. BV is associated with increased risk of miscarriage, premature labour, chorioamnionitis, endometritis and pelvic inflammatory disease (PID) and is worth treating.
Options are Metronidazole 400mg PO bd for seven days, Clindamycin 2% intravaginal cream 5g nightly for seven nights, or Metronidazole gel 0.75% one applicator intravaginally nightly for five nights. These are considered safe in pregnancy.
Male partner treatment requires seven days of po Metronidazole and bd topical Clindamycin cream and can reduce BV recurrence. Treat male-female couples synchronously and advise avoiding sexual contact during treatment.
Condoms should be used if engaging in sexual contact during treatment, but Clindamycin cream can weaken latex condoms for 72 hours post the last dose.
Author competing interests – nil
Part one of major updates to antibiotics guidelines has been published by Therapeutic Guidelines, including updates to medicines for common infections and dosage amounts for both adults and children.
The multidisciplinary update contains more than 200 revised and new clinical topics.
The first release covers content updates on infections commonly managed in primary care, as well as information on serious infections often managed in hospitals, such as pneumonia and sepsis.
It also includes more than 1400 drug recommendations for treating conditions ranging from urinary tract infections to eye infections and sexually transmissible infections.
One major change is that nitrofurantoin is now recommended as the first-line treatment of acute cystitis in adults because of high

trimethoprim resistance among E-coli.
Another is that cefazolin is now recommended as an equal firstline alternative to flucloxacillin for the treatment of Staphylococcus aureus infections – for example bacteraemia, pneumonia, staphylococcal scalded skin syndrome.
Evidence suggests that cefazolin is equally effective for methicillinsusceptible S. aureus and it may
have a lower risk of acute kidney injury.
Changes to dosage options for children were also included in the update. Doxycycline recommendations are now included for the treatment of infections in children younger than eight years, provided the duration of therapy is less than 21 days, for example for the treatment of bronchiectasis exacerbations.
The update also includes targeted changes to infection-related content across other guidelines.
More updates are set to follow over the coming 12 months, including updates to surgical antibiotic prophylaxis, tropical and rare diseases, and infections in people with immune compromise.
For more information on the more than 200 clinical updates visit www.tg.org. au/products/therapeutic-guidelines/ updates/antibiotic
By Dr Mike Kamara, Obstetrician and Gynaecologist, Joondalup
Endometriosis is a debilitating disease that impacts every facet of life. It is defined by the presence of endometrial like tissue outside the uterine cavity and commonly causes pelvic pain and infertility.
In the last decade alone there has been an almost 40% increase in hospital admission due to endometriosis related ailments, with over 40,000 hospital admissions each year.
This condition impacts an estimated one in seven women and has been shown to take up to seven years before a diagnosis is made. Furthermore, endometriosis has significant impacts on fertility, with up to 30% of women undergoing IVF suffering from endometriosis and almost half of all women with endometriosis suffering infertility.
Laparoscopy plays a key role in the management of this disease, but symptoms commonly recur and repeat surgical exposure
comes with additional risk. Medical management, which is both hormonal and non-hormonal, is vital in managing painful symptoms.
All symptomatic women with suspected or confirmed endometriosis who are not desiring immediate fertility can be offered effective suppressive treatment to control symptoms and sometimes slow disease progression while preventing unwanted pregnancies.
Most guidelines recommend offering suppressive treatment to all women with suspected or confirmed endometriosis. The combined contraceptive pill and single agent progestogens currently remain first-line treatments.
A Cochrane meta-analysis showed significant improvements in dysmenorrhea, dyspareunia and dyschezia when compared with placebo. One prospective

study showed the use of 2mg dienogest/30microgram ethinyl oestradiol (Valette) when used in an extended regime in women with deep infiltrating endometriosis resulted in a significant reduction in non-menstrual pelvic pain and dysmenorrhoea over two years.
There was also a reduction in deep dyspareunia and dyschezia. This same cotreatment was assessed in an observational study of women with DIE and adenomyosis over 12 months, and these women also showed significant improvements in cyclical and non-cyclical pelvic pain and dyspareunia despite the presence of adenomyosis.
Oral progestins have been used in one form or another for over 50 years with several RCTs showing effectiveness in managing pain symptoms.
Dienogest is the most investigated progestogen in recent years leading to its listing on the PBS last year. It
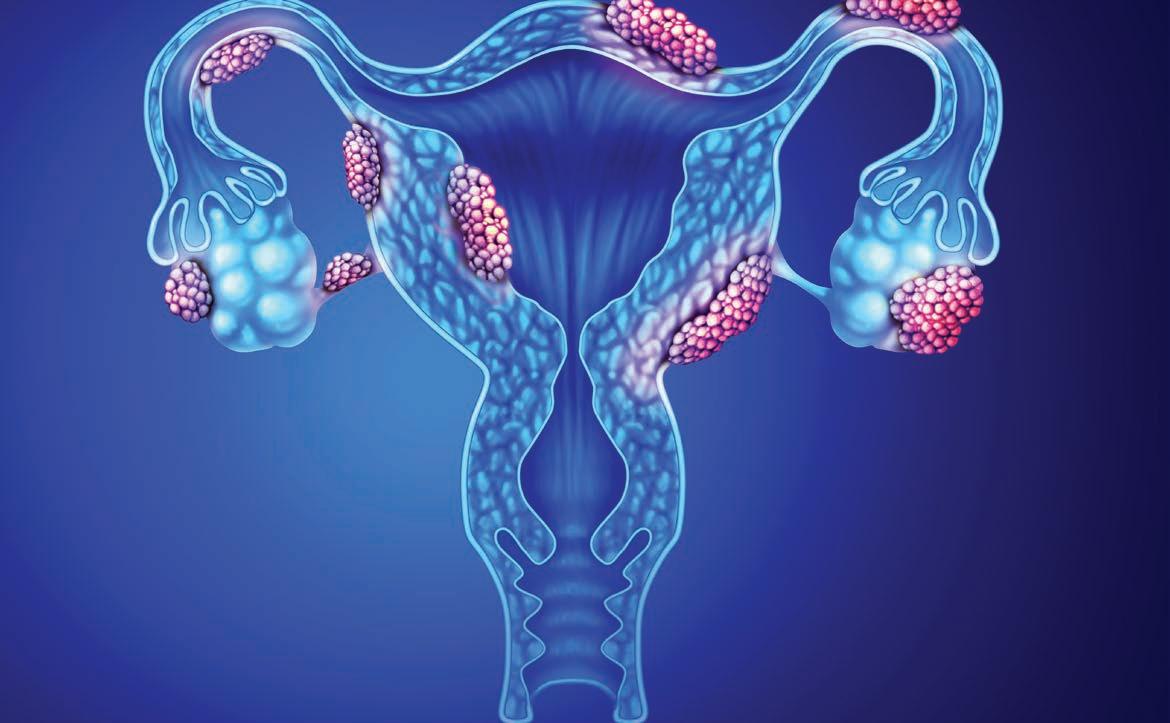
Consider the diagnosis of endometriosis in all young women with pelvic pain of any kind, including dyspareunia and dyschezia
Oral contraceptives, both combined and single agent progestogens, remain very effective treatments in women with proven or suspected endometriosis not desiring immediate fertility
Long-acting reversible progestogens may be associated with better tolerability and a reduced risk of repat surgical intervention and the use of second line agents.
is not, however, on its own licenced as a contraceptive.
More recently Drospirenone has been evaluated and now listed on the PBS as of May of this year. It has not been shown to be inferior to COCP and is well tolerated. It also provides a great alternative for women who cannot tolerate oestrogen.
Intrauterine levonorgestrel is associated with significant improvements in endometriosis related symptoms. Compared with Dienogest and the COCP, longterm use of the IUD was associated with significant decreases in NMPP, back pain, menstrual pain and dyspareunia and could be sustained for up to 10 years in post-surgical patients.
A Cochrane systematic review also showed significant improvements in dysmenorrhoea and overall quality of life when compared to expectant management. This treatment was also not shown to be inferior to the COCP.
The PRE-EMPT study compared long-acting progestogens (LAP) including medroxyprogesterone acetate to the COCP and showed a sustained, up to 40% reduction in endometriosis related symptoms. However it also showed that women in the LAP arm were less likely to undergo repeat surgical procedures or require second line treatments
Current evidence shows that simple first-line licenced contraceptives remain effective options for


women with proven or suspected endometriosis not desiring immediate fertility.
The choice of the first-line agent is personalised and will be driven by several factors such as the need to avoid estrogen, the desire to supress ovulation, compliance and convenience and when they are planning a pregnancy.
In the post-operative setting, women can be reassured that both short-and-long-acting contraceptives are effective, but LAP may be preferred due to a small reduction in re-operative risk and progression to second line treatments.
Author competing interests – nil

Modalis specialises in neuronavigation-guided Transcranial Magnetic Stimulation (TMS), improving treatment options in depression, OCD, PTSD, pain management & more.
Utilising MRI-guided targeting methods
Following evidence-based protocols
No lengthy waiting periods
No hidden fees
Easy referral process
Medicare and DVA support available for eligible patients receiving treatment for depression.



By Dr Veena Gilbert, Dr Fiona Chua & Dr Christabel Samy, General Practitioners, Rockingham
Australia’s fertility landscape has experienced substantial transformations in recent decades and we are confronted with the challenge of an aging population.
The persistent decline in fertility rates is coupled with increasing reliance on assisted reproductive technologies. This phenomenon significantly impacts the economy, social structure and labour market sustainability of the nation.
The decline in total fertility rate started exponentially since 1971. In 1976, it fell below the replacement rate and since then the drop has been gradual and perpetual. In 2023, Australia recorded its lowest birth rate of 1.5, far below the level of around 2.1 required to maintain population stability.
Meanwhile, Australia has one of the highest utilisations of assisted-reproduction technology. Every year, around 20,000 babies are born from IVF treatment in the country, representing one in 18 children. So, why are we still below the threshold required for population replacement?
Understandably, the decline is complex and interconnected. Reversing the low birth rate in Australia is an intricate challenge, but it is not entirely impossible. First and foremost, we must explore the factors leading to the downturn.
The average age of mothers has been rising over time, from 30 in 2010 to 31 in 2022. Societal norms have evolved.
Most individuals, especially women, emphasise career success and financial stability. They focus more on advancing their education, enhancing their career and travelling the world before starting a family. Cultural dynamics have transformed and there is less

societal pressure to build a family at a younger age, if at all, allowing individuals to prioritise other aspects of their lives.
Although the economy climate in Australia currently is characterised by modest growth, everyone is affected by inflationary pressures and external challenges arising from international trade tensions. Rising housing costs, job insecurity and childcare affordability considerably constrain reproductive choices. Individuals
with higher spending power have the upper hand, while those in lower socioeconomic standing may face challenges in obtaining adequate healthcare due to its cost, potentially impacting fertility outcomes. Hence, they might choose to not have children or maybe just one child suffices.
Despite Australia being a leader in ART, access to fertility services remains limited, particularly in rural areas. While rural regions typically have higher fertility rates, access to healthcare, including fertility treatments, is more limited.
Fertility rates in Australia have been declining since 1971and are well below replacement levels
Australia has high rates of assisted reproductive technologies
Fertility awareness programs are needed.
These areas frequently lack the infrastructure and specialised care found in urban centers, which can result in delayed diagnoses and treatments.
Long distances to urban fertility clinics impose both financial and emotional burdens on rural residents, and the shortage of healthcare professionals in remote areas can lead to underdiagnosis or delayed intervention for fertility concerns.
Contraception education is widely provided, beginning in middle school. Additionally, contraceptives are accessible and affordable. This



increased accessibility contributes declining birth rates.
Education in schools is actively promoted by the Australian Council of Natural Family Planning from year eight onwards. There is advice given to teachers on how to promote topics and services that are available, including assess to contraception.
In recent decades, family planning was heavily promoted. Campaigns highlighted its importance and benefits and government incentives encouraged adoption. This, however, led to a rise in infertility rates.
Modern diets often include unhealthy food with pesticides, antibiotics, and high mercury levels. This can result in infertility in women and reduced sperm counts in men.
There is currently no conclusive research evidence indicating that RF-EMF (Radio Frequency and Electromagnetic Frequency) emissions from commonly used devices adversely affect the reproductive organs in women and men.








There is a need for fertility awareness programs in schools and communities, covering family planning, genetics, menstrual cycles, menopause, and parenting fears.
Government support should include awareness initiatives, policies, digital health investments, and subsidies to make fertility support affordable and accessible.
Author competing interests – nil
ED: The GPs are from Samy Medical Practice

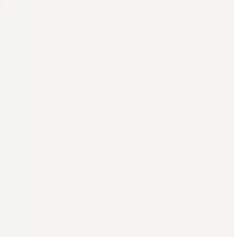
























By Dr Adeline Tan, Histopathologist and Cytopathologist, Osborne Park
The Australian Cervical Screening Program guidelines were updated in April this year to keep the program effective and relevant, with the goal of eliminating cervical cancer in Australia by 2035.
It’s an ambitious target, but one we’re all working towards.
You’ll be able to access the updated guidelines on the Cancer Council Australia website. They’re designed to be as user-friendly as possible, so you can quickly get the information you need to keep providing the best care to your patients.
Helpful resources
To make sure you’re ready to implement the new guidelines, there are some great training resources and sessions available.
Updated Education and Training Modules: There are updated modules on the Australian Centre for the Prevention of Cervical Cancer (ACPCC) website with five e-learning modules on the National Cervical Screening Program (NCSP) clinical education bundle. These modules are designed to walk you through the latest changes in an easy-to-understand way, so you can confidently apply them in your practice.
RACGP Webinars: The RACGP have hosted two webinars on the changes to the NCSP guidelines. On demand recordings are now available for free.
These resources are about making sure you’re supported as
Changes were made to cervical screening in April 2025 Resources and support are available
The aim remains to eliminate cervical cancer by 2035.
the guidelines evolve, and they cover important changes around both clinician-collected and selfcollected results.
Why and how are the guidelines changing?
The updates are part of an ongoing effort to refine the cervical screening process, especially since the introduction of the renewed screening test. After feedback from the Cervical Screening Expert Panel (CEP), there were certain identified areas that needed more clarity.
Plus, with new evidence emerging over time, it was time to update the guidelines to reflect the latest scientific data.
The Guidelines Working Party took a thorough approach, reviewing the latest evidence and gathering feedback from both experts and the public.
The result is a set of guidelines that reflect the most current evidence in cervical cancer prevention and help ensure the program stays effective as we move closer to our 2035 elimination goal.

These updated guidelines have the backing of some of the most respected medical organisations in Australia, including RACGP, Royal Australian and New Zealand College of Obstetricians and Gynaecologists, Royal College of Pathologists of Australasia, Australian Society for Colposcopy and Cervical Pathology and Australian Society of Gynaecologic Oncologists.
Key changes
Colposcopists now have guidelines for managing HPV (16/18) detection without visible lesions, including the possibility of endocervical curettage if appropriate. There is an option to defer re-referral for HPV (16/18) detected with negative LBC if follow-up testing remains HPVpositive.
Clarifications have also been made regarding the diagnostic excision of the transformation zone. Loop electrosurgical excision procedure (LEEP) is now recommended over cone biopsy due to lower postsurgical complications, as both procedures have similar effectiveness.
Patients with immune-deficiency have been separated into highly suppressive conditions (threeyearly testing) and moderately increased risk (five-yearly testing) categories.
Other important changes to “test of cure” and post hysterectomy follow-up are summarised in the table.
Author competing interests – nil



By Dr Sylvester Dodzi Nyadanu & Professor Gavin Pereira, Perinatal
Gestational age is a key factor in determining the health of a newborn, but could climate change influence when babies are born?
A new study suggests that exposure to air pollution and extreme weather conditions during pregnancy may not only trigger preterm birth but could also prolong pregnancy, with potential health risks for both mother and baby.
Pregnancy length and health implications
Preterm birth – born before 37 weeks – has been widely studied, with known risk factors including maternal health, socioeconomic status, and environmental factors such as heat and cold waves and poor air quality.
However, little attention has been given to prolonged pregnancy –born beyond 41 weeks – despite its own set of complications, including increased risk of stillbirth, birth trauma, caesarean delivery, pregnancy complications, postpartum haemorrhage, and childhood behavioural, emotional, and developmental disorders.
Climate exposure and prolonged pregnancy
The study looked at the association between climate-related exposures and prolonged pregnancy, analysing nearly 400,000 births in Western Australia between 2000 and 2015 using data from the Western Australian Midwives Notification System.
It also used satellite data to assess levels of fine particulate air pollution (PM2.5) and a biothermal stress index – a combined index of air temperature, radiant temperature, humidity, wind speed, and human physiology.
Climate change events such as air pollution and extreme weather impact pregnancy outcomes
Air pollution and extreme weather can lead to preterm or prolonged births
Climate actions across all levels – individual, community, government, and healthcare system – are essential to reduce related health risks.
After adjusting for maternal and fetal risk factors, it was found that exposure to higher levels of air pollution and extreme biothermal stress (heat and cold) during pregnancy was associated with an increased risk of prolonged pregnancy.
Certain groups were more vulnerable, including first-time mothers, those over 35-yearsold, women living in urban areas and those with pregnancy complications.
Out of 47,380 cases of prolonged pregnancy in the study, an estimated 2,085 cases (4.4%) were attributable to air pollution levels above the World Health Organization’s recommended annual limit of 5μg/m3, while 853 cases (1.8%) were attributed to high biothermal stress.
The exact mechanism explaining how climate-related exposures could affect health outcomes, including adverse pregnancy outcomes, is unknown. However, some of the direct ways by which climate-related exposures may influence pregnancy length are through factors such as oxidative stress, inflammation, disruptions to
endocrine or hormonal function, and epigenetic programming.
These could either trigger early labour, resulting in preterm birth, or extend gestation beyond the normal timeframe, resulting in prolonged pregnancy.
As climate change events increase in duration, frequency, and intensity, the findings, together with existing evidence, raise important questions about how healthcare systems can better support pregnant women in adapting to environmental risks.
Integrating climate-related health risks into prenatal care, particularly for vulnerable groups, and implementing public health interventions to build resilience against climate effects should be considered to promote a healthy pregnancy.
The findings also serve as a call to action for broader climate policies. Given the increasing pace of climate change and its effects on human health, ensuring pregnant women have access to clean air and protection from extreme weather should be a priority for policymakers.
This reinforces the need for climate action at every level – individual, community and government – to safeguard the health of present and future generations.
Author competing interests: Both authors were involved in the Curtin University study.
For more information visit: bit.ly/41WyqtO
By Dr Anitha Karunairajah, Breast Surgeon, Joondalup
Breast cancer remains one of the most prevalent cancers worldwide, affecting around one in seven women and ranking as the second most common cause of cancerrelated death among females.
However, the landscape of breast cancer treatment is evolving rapidly, bringing improved survival rates and better quality of life for patients.
One of the most significant advancements in breast cancer care is the move towards personalised treatment. Tumour profiling and precision medicine now allow for therapies tailored to the individual patient’s tumour biology, reducing treatment toxicity while improving efficacy, leading to prolonged survival and better quality of life.
Innovations in breast surgery
Surgical techniques have progressed significantly, offering patients more aesthetically favourable and functionally beneficial options.
Oncoplastic breast surgery techniques combine plastic surgery principles with breast-conserving surgery, allowing for better cosmetic outcomes. These techniques involve:
Volume displacement:
Repositioning breast tissue during tumour removal to maintain a natural shape.
Volume replacement: Using perforator flaps (fatty tissue with its own blood supply) to fill defects without requiring complex microvascular reconstruction.
Therapeutic mammoplasty: A technique where tumour removal is integrated with breast reduction, particularly beneficial for patients with larger breasts.
Skin and nipple sparing mastectomy: These advanced mastectomy techniques preserve the breast skin and, when appropriate, the nipple-areola complex, enabling immediate reconstruction with superior cosmetic and psychological outcomes.


in radiation therapy
Radiotherapy has also seen significant improvements, focusing on reducing treatment duration and side effects:
Partial breast radiation therapy: A technique delivering targeted radiation to the tumour bed rather than the entire breast – particularly useful for selected early-stage breast cancer patients, reducing radiation exposure and treatment duration while maintaining efficacy.
Hypofractionated radiation therapy: Delivers higher doses over fewer sessions, maintaining effectiveness while minimising patient burden.
Intraoperative radiation therapy: Administered during surgery, this technique reduces the need for postoperative radiation, particularly in elderly patients with early-stage cancer.
Systemic treatments and targeted therapies
HER2-positive breast cancer: Breakthrough therapies such as Trastuzumab, Pertuzumab, and Trastuzumab Deruxtecan have drastically improved patient outcomes.
CDK4/6 inhibitors: Drugs like Palbociclib, Ribociclib, and Abemaciclib are enhancing survival rates in hormone receptor-positive breast cancer.
PARP inhibitors: Used in BRCAmutated cancers, these drugs, such as Olaparib, exploit defective DNA repair mechanisms to kill cancer cells.
Immunotherapy and neoadjuvant therapy
Emerging as a promising option for triple-negative breast cancer, immunotherapy drugs like pembrolizumab (Keytruda) are
Breast cancer treatment is evolving rapidly
GPs play a vital role in early detection, screening, and lifestyle modification for breast cancer patients
They are essential in supporting and coordinating ongoing care, and a crucial member of the patient’s multidisciplinary team.
offering new hope in an area historically associated with poorer prognoses.
Preoperative treatments, including chemotherapy and targeted therapies, are increasingly being used to shrink tumours before surgery especially in HER-2 positive and triple negative breast cancers. This approach allows for more conservative procedures and facilitates response-guided surgical decisions.
Genomic tests such as OncotypeDX is used to assess the risk of recurrence in certain types of early-stage breast cancer and helps
avoid unnecessary chemotherapy for low-risk patients while ensuring high-risk patients receive appropriate treatment.
Genomic profiling is a cuttingedge approach in cancer treatment that analyses a tumour’s genetic mutations to guide personalised therapy, by identifying specific alterations in DNA, such as mutations in BRCA1/2, and is particularly valuable in metastatic breast cancer.
Multidisciplinary approach and the GP’s role
Breast cancer management requires a collaborative effort involving surgeons, oncologists, radiologists, pathologists, and other healthcare professionals. The GP plays an integral role in this multidisciplinary team.
1. During pre-diagnosis, screening and early detection, through clinical examination and imaging referrals. Identifying high-risk individuals and referring them for genetic counselling.
2. Post diagnosis and during treatment, by monitoring treatment side effects, including
chemotherapy or radiation induced toxicities. Providing emotional and psychological support, with referrals to mental health services when necessary. Direct patients to resources such as Cancer Council, Breast Cancer Care WA and Breast Cancer Network Australia for ongoing information and support.
3. Post-Treatment and Survivorship Care, through annual mammography and clinical exams for long term surveillance. Managing side effects of hormonal therapies, including osteoporosis monitoring for patients on aromatase inhibitors. Addressing lifestyle modifications to reduce recurrence risk.
When referring patients to breast surgeons, it is helpful to include relevant medical information or a summary, mammogram and ultrasound report of both breasts, core biopsy ± FNA report and, where applicable, full histopathology report including receptor status (ER/PR) and HER2 DISH.
Author competing interests – nil






By Dr William Ormiston & Dr Matthew Clifford, Interventional Radiologists, Nedlands
Uterine fibroids and adenomyosis are among the most common benign conditions affecting women in their reproductive years. While many cases are asymptomatic, others can cause heavy menstrual bleeding, pelvic pain, and pressure symptoms, significantly impacting quality of life.
For decades, the primary treatment options were medical therapy or surgery, particularly hysterectomy or myomectomy. However, for women seeking a uterus-sparing, nonsurgical alternative, uterine artery embolisation offers a compelling solution.
UAE is a minimally invasive procedure performed by an interventional radiologist. It involves the insertion of a thin catheter into the uterine arteries – typically via the wrist or groin – through which tiny particles are injected to block blood flow to the fibroids or areas of adenomyosis.
Deprived of blood supply, the abnormal tissue shrinks over time, resulting in symptom relief. The uterus, however, remains intact.
The procedure takes around 30-60 minutes and is usually performed with either twilight sedation or general anaesthesia. Most women experience pelvic cramping, fatigue, mild fever or nausea post procedure. These symptoms peak at four to six hours, lasting about two days and are usually well-managed with analgesia and antiemetics. Most patients are discharged within 24 hours and return to normal activities within seven to 14 days. The evidence
Multiple high-quality randomised trials (EMMY, FEMME, REST) have demonstrated that UAE is comparable to surgery in relieving symptoms and improving quality of life, with shorter recovery times and fewer perioperative complications.

Uterine artery embolisation is a minimally invasive, uterus-sparing treatment for symptomatic uterine fibroids and adenomyosis
It is safe and effective with comparable symptom relief to surgery, but fewer complications and faster recovery
The procedure is still underutilised in Australia despite NHMRC level one data and international endorsement of the procedure.
Most women – up to 90% – report a significant reduction in heavy bleeding, and approximately 70% report improvement in pressure symptoms or pain. UAE is associated with a small reintervention rate (~20–30% over 5–10 years), but the majority of women avoid further procedures, including hysterectomy.
While UAE is widely recognised for treating uterine fibroids, it is also an effective option for selected patients with adenomyosis – a condition where endometrial tissue infiltrates the uterine muscle, causing painful and heavy periods.

Evidence increasingly supports UAE as a safe and effective alternative to hysterectomy for women with symptomatic adenomyosis. UAE is most suitable for premenopausal women with symptomatic uterine fibroids or adenomyosis, especially those experiencing heavy menstrual bleeding or bulk-related symptoms who wish to avoid hysterectomy or myomectomy.
UAE has a favourable safety profile, but patients should be informed of potential risks, including postprocedural pain or fatigue (common but temporary), infection (<2.5%), fibroid expulsion – particularly with submucosal fibroids – and rare complications such as infection and need for emergency hysterectomy (<1%).
While pregnancy after UAE is possible, fertility outcomes are less predictable than with myomectomy, and UAE is generally not recommended for women actively trying to conceive.
UAE is increasingly accessible in Western Australia through the public
and private sectors, with streamlined referral pathways.
Interventional radiologists provide outpatient assessment, procedural care and follow-up imaging. Collaborative decision-making with gynaecologists ensures that patients are fully informed about all treatment options.
Despite strong clinical evidence and endorsement from organisations like NICE, ACOG, CIRSE, RANZCOG and IRSA, the procedure remains underutilised in Australia. Bridging this gap starts with increased awareness among GPs, gynaecologists and patients.
UAE represents a significant advancement in the management of fibroids and adenomyosis. For appropriately selected women, it provides effective symptom relief, a short recovery and the opportunity to preserve the uterus without the need for major surgery.
It’s time for UAE to be considered a first-line option alongside surgical and medical therapies in everyday gynaecological care.
Author competing interest – nil
Surgical intervention for endometriosis
Uterine fibroids and adenomysis
Menopause clinical insights
Referring to a cosmetic surgeon
Changes to the Cervical Screening Program
Management of common vulval conditions
Management of breast cancer patients
Hormonal treatments for endometriosis
Dietary advice for Alzheimer’s
Fertility concerns
HIV prevention in women
Podcasts Complete the self-reflection and claim your CPD time, please scan here

Alasdair Thompson started out studying molecular genetics, now he’s executive chef at Optus Stadium having mastered the science of cooking.
By Ara Jansen
Recently appointed executive chef at Optus Stadium, Alasdair Thompson now runs an almost small city behind the scenes which delivers food and drink to eager patrons.
He says no matter what’s on the menu, his goal is always to create food that resonates with people.
The chef first went to university and studied molecular genetics, planning a career in science because he was interested in how the body worked. There might have been some unconscious influence from his dad, retired renal surgeon Dr Ivan Thompson.
But Alasdair found himself becoming more interested in tactile and instant results – working in a lab wasn’t delivering that. Then, quite by chance, Alasdair met a chef and everything changed. At 21, he became a matureaged apprentice.
“Mum is a good cook,” Alasdair says. “Part of this journey started with her. She was always very family orientated and making sure everyone was happy with what they were eating and trying new recipes. That gave me a good grounding in good food.”
Now 77, she still loves to cook a family meal and Alasdair still loves to jump in and help.

Earlier this year, Optus Stadium announced Alasdair as the venue’s new Executive Chef – only the second person to hold the position since the stadium’s opening almost seven years ago.
He was part of the stadium’s original opening team, starting as chef de cuisine before becoming executive sous chef in January 2020. Prior to that, Alasdair was head chef at Crown Perth’s Italian fine dining restaurant Modo Mio and trained under Alain Fabregues, of much-loved and renowned classical French restaurant The Loose Box.
Working at Optus – which has won numerous awards for its food –Alasdair oversees 26 kitchens and a permanent staff of about 14, which can balloon to 200 casuals on busy event days, ranging from sous chefs right down to dish washers.
The Meeting and Special Events (MASE) side of Optus business contributes a significant amount of annual revenue. In addition to major events, the team also manage more than 600 other events a year ranging from small breakfast meetings, to launches, business events, large conferences and events of 1200 people.
“These happen on any day outside an event day like the cricket or footy. It gives us a lot of variety and I enjoy the challenge.”
These events require large amounts of food to be served, and Alasdair’s biology and molecular studies along with his childhood grounding remind him the food must not only look good on the plate but taste great.
These
events require large amounts of food to be served, and Alasdair’s biology and molecular studies along with his childhood grounding remind him
the food must not only look good on the plate but taste great.

The Optus kitchens use as much local produce as possible. They can serve up to 2000 plates at a MASE event and around 3000 bottles of wine. On the first day of a test match 700 kegs of beer slake fan thirst and over a year they use in excess of 25 tonnes of chicken.
Optus has become noted for their butter chicken, particularly popular during the cricket and seen to by the venue’s Indian cuisine specialist, sous chef Jinesh George.
Alasdair’s favourite cuisine is Asian and South East Asian for their flavours and aromatics. With the region on our doorstep, it’s easy to naturally integrate the flavours in WA cuisine.
His wife Hannah is Korean and has had a big impact on that, adding to his background in classical French and Italian cooking and what he learnt as a child. You’ll find pieces of these influences spread across the menus at Optus.
“I have three kids and my wife loves to experiment with Western food. She has learnt from me, and I have learnt from her. Now with this job I’m able to be home more often for family dinners and enjoy her food. It’s far more regular than when I used to run restaurants.”
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Chinese comedian He Huang usually pokes fun at her own life but has temporarily become a man for her latest show.

He Huang never knew comedy could be a job.
Born and raised in China, she studied politics in the United States so she could return home to be a public servant. During her first job for an American aid contractor, He realised she was never going to be able to change the world.
“Maybe it was my family, but I always looked towards public service,” say He. “It was just this sense I was born with. But after five years of working in that space I wanted to kill myself. There was so much unnecessary spending it made me question my decision.
“The system was too big to be changed as an individual and I didn’t want to be party to that. Some of my friends just sucked that up but I couldn’t be that person.”
Thoroughly disillusioned, He quit and promised her parents if she didn’t have success in the next two years exploring her newly found interest in stand-up comedy, she’d dutifully return home and become a teacher or a politician.
He moved to Melbourne and tried her hand at comedy, starting by sharply poking fun at her Chinese heritage, the confusion people have with her name (no, it’s not her pronoun) and other dry, deadpan gems from her life as a Chinese daughter and unmarried leftover lady.
In 2002 the unexpected happened, she went viral after appearing on Australia’s Got Talent. The clip racked up more than eight million views in less than a month and now has more than 60 million. It made her a viral sensation and scored her an agent in Los Angeles, launching her comedy career worldwide.
“I was almost ready to quit comedy and then then that happened.
By Ara Jansen

Suddenly I was getting bigger and more prestigious gigs.”
He has become part of a very small group of Chinese women succeeding at comedy in the West and quips she’s probably one of the few with a master’s as well. Now in her most ambitious show yet, the self-confessed low energy comedian has bought a suit and tie and has come out as a man for her show at the 2025 Perth Comedy Festival, White Man’s Burden
It’s a cultural satire where she reveals that white men have a lot to answer for but perhaps have also had a lot put on their shoulders.
“A year ago, I would not have dared make fun of white men, but now, things have changed. The idea of me doing this is absurd enough.
“It’s my first time trying something like this – taking on a character – and I thought it would be a challenge and something different. The hardest part is to keep my voice right and keep the energy up.”
He now travels constantly and performs all over the world as well as taking classes in voice coaching, character creation and acting. In her 30s she’s unmarried and while she’s still exploring Melbourne, she’s looking around for the city which inspires her the most creatively.
The Perth Comedy Festival runs from 21 April – 18 May. Tickets and full program from www.perthcomedyfestival.com

We’ve got five double passes to giveaway for the Perth Comedy Festival’s Best of the Fest show on Saturday, 17 May. The show takes place at The Rechabite in Northbridge.
We also have 10 double passes to see Karate Kid: Legends in cinemas from 5 June. And 10 double passes to see Materialists in cinemas from 12 June.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.
This page intentionally left blank



SHENTON PARK
Medical Rooms for Lease
98 Onslow Road, Shenton Park, WA 6008
Recently Refurbished
– Shenton Park Medical Centre
$79,000 + GST + Outgoings pa
Very rarely do you get the opportunity to lease a fully functioning centre in a sought after location.
Close to Major Hospitals within walking distance including;
• Perth Children’s Hospital
• St John of God
• Hollywood Private Hospital Main Features Include:
• 5 Suites / Rooms
• Reception / Waiting Room
• Ducted Air
• Alarm
• Ample Rear Parking (Corner location)
• Size 140sqm (Lettable area approx.)
• Close to Shenton Park & Daglish Train Stations
• Price: $79,000 p/a +GST + Outgoings For further information or to arrange a private inspection, please contact the Exclusive Letting Agent: Tino Bruzzese 0417 918 136



Contact Paul, paul@mforum.com.au or phone 9203 5222 to place your classified advert
MARGARET RIVER – GNARABUP
(DPA/MM4)
VR General Practitioner
– Full-time or Part-time
We’re looking for a VR GP to join our growing practice overlooking the ocean in idyllic Gnarabup.
Flexible working options are available to suit a new lifestyle Down South by the beach.
Vitality GP has been part of the community since 2022. Our fully accredited practice comes with onsite podiatrist, physiotherapy and nursing support, a friendly team, and brand-new, well-appointed facilities.
Please email resume to alison@vitalitygp.com.au
Contact: Dr Alison Lyons 9757 1022 www.vitalitygp.com.au

BURSWOOD
Earn 100% of Billings for the First 3 Months!
Join our well-established, accredited mixed-billing clinic in Burswood and earn 100% of billings for the first 3 months (75% thereafter).
Perfect for new VR GPs looking to establish themselves, with full-time/part-time options.
Work alongside 3 experienced GPs in a fully computerised clinic with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au

MOUNT LAWLEY
General Practitioner
$200 – $300 per hour 6-7 sessions available.
Excellent working environment, with modern facilities.
Quality nursing staff and an onsite non dispensing pharmacist.
Adjacent to the practice we have a pharmacy, and allied services, consisting of audiology, pathology, physiotherapy, podiatry, dental, and cardiology.
Visit our website: www.thirdavenuesurgery.com.au
If interested contact Practice
Manager Rachael Hadlow via email: rhadlow@3rdave.com.au

Come and join a practice that works around your life and family.
Palin Street Family Practice is seeking a new VR doctor for our well-established, fully accredited clinic in Palmyra, with easy access to Fremantle, Perth CBD and the Swan River foreshore.
There’s plenty of parking and you will be fully supported by an experienced nursing and admin team.
We are a small, privately owned General Practice, which has been continuously operating since 1923. Our mission is to provide the highest standard of patient care whilst incorporating a holistic approach towards diagnosis and management of illness.
We operate out of a converted house, creating a calm and welcoming space for patients, whilst still utilising the latest equipment and technology. Many of our patients have been coming to us for generations and you will have an immediate patient list on commencement. We are a close-knit team that meets regularly to collaborate, share our experience, and you’ll have access to some of Perth’s most experienced and respected GPs.
We’re looking forward to welcoming a new family friendly doctor into our team. For further information please contact Jackie our Practice Manager on 0403 343 401 or via email office@psfp.com.au

Spencer Road Family Practice is seeking an enthusiastic doctor, who thrives in a busy general practice. Avoid long commutes and work close to home in the foothills of Perth’s South-East.
Choose your days, set your own hours, and take home 65% of billings. We have room availability Monday – Saturday.
The practice is open from 8am to 6pm weekdays.
8am to 1pm Saturdays, 8am to 12pm Sundays and Public Holidays.
We only close on Good Friday and Christmas Day.
We currently have 10 GPs, 4 Nurses, a visiting Podiatrist & Dietitian and a Clinipath Pathology located within the practice.
Our patient’s range from the very young (we have an antenatal GP) to the elderly (some of our GPs have practised in this area for over 30 years)
For more information or to apply, please contact our Practice Manager, Paige on (08) 9493 8388 or send your resume to practicemanager@srfp.com.au
• 70% Mixed Billing or AUD
$180 per hour for the first 3 months
• Permanent, Full-Time
• VRGP
• Relocation allowance negotiable
• DPA MM1
Our small, friendly, accredited and wellestablished family practice is seeking an experienced VRGP who is ready for a challenging but satisfying full-time career that offers a great work-life balance.
Our GPs enjoy a loyal and varied patient base and have the opportunity to build long-term relationships with the patients and their families. Beckenham Medical Centre has easy access to public transport, private parking for the staff and has close proximity to allied health and hospitals.
• Permanent position
• Full-time
• 70% of Mixed billings or AUD $180 per hour for the first three months
• Large and varied patient base
• Full-time Nursing support
• Well-equipped Consult and Treatment room
• DPA MM1
• On-site Pathology & Pharmacy next door
• Relocation allowance negotiable for the right candidate
• Open hours: Monday to Thursday 8.30 am- 5.30 pm, Friday 8.30 am-5.00 pm and Saturday 9.00 am-12.30 pm
ELIGIBILITY CRITERIA
• Should hold General or Specialist Registration with AHPRA
• Unlimited working rights in Australia
• Must have competed FRACGP or FACRRM
For more information please contact our Office Manager, Shabana on 08 9451 2722 or alternatively, send through your resume to accounts@beckenhammedicalcentre.com.au

Full/Part Time VRGP
• GP Owned
• Fully Computerised
• Well-Equipped Treatment Room
• Full-time RN support
• Mixed Billing
• Centrally Located
• Long Established
• Accredited/Teaching Practice
We are a small, friendly, family orientated practice of four General Practitioners located in Wembley and we’ve been here for a long time! We are an accredited practice who takes pride in our reputation as a practice who looks after their patients and their staff.
We seek a VRGP to join a great bunch of people who are more like family than colleagues.
Our well-respected, experienced team can offer flexible sessions in a wellsupported environment.
Contact Cherie: 08 9387 5000 Email: office@wfmp.com.au
We are seeking a VR GP on an either full time or part time basis, who would love to join a great bunch of people whom are like family more than colleagues.
We would love to offer 90% of billings for the first 3 months and then 70% thereafter.
We are a small practice of General Practitioners located in South Perth. We take pride in our reputation as a practice who looks after their patient and staff. Our well-respected experienced team can offer flexible sessions in a wellsupported environment.
GP owned
Fully computerised
Well Equipped Treatment Room with RN support
Mixed Billing
Central location – 10 min from CBD
Accredited Practice
Please email docthet@gmail.com or call (Pat, the Practice Manager) on 0431 909 221 or call 9367 7840

General Practitioners wanted with a passion for older Australians’ health and wellbeing.
Are you the right doctor in the wrong placement, looking for a better fit? Sage Medical Consulting may just be where you belong.
We Offer:
• Flexible days and hours, work when you want
• Convenient location
• Competitive remuneration
• Relaxed and supportive work environment
We will work around your preferences to suit your goals and lifestyle and if your circumstances change, we’ll adapt to accommodate you. Please get in touch if you want to grow alongside Sage, and care for those who might otherwise slip through the cracks of the health system. About us:
Sage Medical Consulting comprises a group of General Practitioners who are committed to practicing “slow” medicine – medicine that is unrushed, quality and tailored to the patient in front of us. We have a particular soft spot for older Australians but we care for anyone - from pregnancy through to the end stages of life. No matter where you are in life, if you want a compassionate and thoughtful approach to your care - we are your partners to lifelong health.
Expressions of interest to admin@sagemed.com.au or call Practice Manager Jackie on 0401 681 495

MANDURAH
Falcon Grove Medical Centre is looking for a RACGP fellowed General Practitioner (or equivalent) to work at the practice on a full-time basis.
We offer:
• 70% of receipted billings.
• Guaranteed minimum earnings $180-$200K per year.
The practice has been operating in Mandurah for over 25 years. The practice has a supportive team of administration staff and nurses to support the GPs within the practice.
All aspects of GP services are provided such as skin cancer checks, women’s, men’s & child health, travel vaccinations, chronic disease management, mental health, emergency and the list goes on.
We have onsite Pharmacy, Pathology and Psychology.
Opening Hours:
Monday – Friday 8:00am till 5:00pm (No weekends)
The successful candidate will require:
• AHPRA registration
• RACGP fellowship or equivalent
• 1-3 years post graduate GP experience
For more information or to submit your resume, please contact Practice Manager Chelsea on (08) 9534 2380 or manager@falcongrove.com.au

SOUTH LAKE
VR GP Full time / Part time. DPA position.
South Lake Family Practice
70% billing and minimum guarantee $180/hr first 3 months.
Flexible hours. Opportunity to improve and develop special interests like skin cancer, cosmetic etc. Onsite pathology and Allied Health.
For further information please contact p.manager@southlakefamilypractice.com.au ph: 0499 404 043




your free copy delivered

EXCLUSIVE BOUTIQUE GENERAL PRACTICE
SERVICING THE PERTH WESTERN SUBURBS
The Age Less Clinic and General Practice Claremont has space available for a patient minded General Practitioner to be part of our vision for the very best, whole of patient care.
We want to work around your goals and lifestyle so this could be the opportunity you’ve been waiting for.
We are currently an independent solo practice with a fully booked functional GP, established medical and allied health referral base and experienced nursing support.
BENEFITS:
• Flexibility and support guaranteed for the right fit.
• Heritage building with generous consulting rooms, off street parking.
• Prized location.
Suitable for niche complimentary general practice fields. Practitioners in sports medicine, aesthetics, integrative, occupational and aviation medicine, hormone health, acupuncture, hypnotherapy, medicinal cannabis, weight loss would be complimentary to the current practice.
The Age Less Clinic would also welcome the interest of experienced mainstream general practitioners wanting a clinic within which to contribute to a unique culture and whole of patient focus.
For more information or to apply please contact Dr Aparna Hegde on 0408 888 790 or aparna.hegde@theagelessgp.com.au

A state of Art Skin cancer clinic with latest technology in total body mole mapping at Hillarys

What you can expect:
Boutique moder n Skin clinic in a busy Shopping centre
Fully private billing with a great income and a manageable workload
Working with state of art total body mole mapping machine and surgical equipments
For more infor mation or to apply, please contact the clinic on 08 6117 6300 or send your resume to info@skinscanwa.com.au
We are seeking General Practitioners to join the Curtin Health Services team! We offer flexibility, variety, and mixed billing opportunity in a highly supportive environment.
We are seeking General Practitioners that would like to expand their clinical scope in the provision of Adolescent & Young Adult Medicine (AYAM). We are investing in our services and looking to grow our team of General Practitioners.
We have a variety of contracting options available
We are seeking to expand our service by increasing available consultancy hours
Administrative, Mental Health Nursing Practitioner, Dietician, and Nursing support provided
We are recruiting a Medical Director to provide clinical oversight and support Centrally located at Curtin University Bentley campus
JOB REFERENCE
Join our friendly and collaborative team and help support the health needs of our diverse community of students, staff, families, alumni, and partners.
Our Medical Centre is a well-established, accredited and fully equipped practice with 7 consulting rooms, a procedure room, treatment room, and onsite pathology. Our team includes GPs, allied health professionals, Triage Nursing, Reception, Medical Director, Practice Manager, and Mental Health Nursing Practitioner. The Centre is open Monday to Friday between 8:30 am and 4:30 pm and is well-served by public transport and ample parking.
We offer full-appointment books with a large and diverse patient base offering lots of interesting work, plus walk-ins, opportunities for Healthcare Plans, Health Assessments, and procedures.
Mixed billing
Attractive service fees
Work full-time or part-time with flexible hours. You choose!
Excellent working conditions and room facilities
Walk into a full & immediate patient base, OR create your own, with walk-in presentations
Best Practice software in use throughout the practice
REQUIREMENTS
MBBS or equivalent
Current AHPRA registration as a General Practitioner
Vocationally Registered (VR)
No restrictions
To learn more about this opportunity, please contact Nandita Nadkar, Practice Manager on 08 9266 9348
TO APPLY: Send your CV to hsmanager@curtin.edu.au
For more information about our university, please visit www.curtin.edu.au



Every home we design and build starts with listening. We listen to your vision, your lifestyle and your budget. Then we translate that knowledge into thoughtful spaces that are beautifully crafted. By integrating architecture, interior design and construction, Humphrey Homes makes creating your forever home harmonious and stress-free
“We wanted the building process to be an enjoyable one, and Humphrey Homes made sure it was. They earned our trust early and never gave us a reason to question it. The outcome speaks for itself, but it’s the quality of the journey that sets them apart.”
- Simon and Deborah, City Beach
