







Dr Ushma Narsai Avant member

anddeductions for








There’s a darker side to social media that GPs and other health practitioners must contend with – its detrimental impact on people’s mental health.

Complete the self-reflection and claim your CPD time, please scan here
Andrea Downey | Managing Editor
The rise of social media has its perks; people are more connected, it’s a useful marketing tool and, if you’re like me, a great way to switch off your brain.
But there’s a darker side to social media that GPs and other health practitioners are increasingly having to contend with – it is having a detrimental impact on people’s mental health.
I may need to preface this with an apology, but I think I’m safe in saying that many of Medical Forum ’s readers did not grow up in the age of social media, so this is new territory.
I also didn’t grow up in the age of social media as we know it now. I had MSN and MySpace, but I was still playing snake on a Nokia 3315 in maths. I’m glad I didn’t grow up with it.
These days social media feels inescapable and the rise of the influencer is giving way to new ways of sharing information –good and bad.
A recent report from Movember found so-called ‘masculinity influencers’ are having a profound impact on young men’s mental health.
Higher levels of worthlessness, nervousness and sadness were reported among men who consume this content. Meanwhile, male suicide rates remain significantly higher.
As a woman who grew up in the era of “nothing tastes as good as skinny feels” I can too easily imagine how this type of content is impacting men.
Does social media need to be added to the long list of things GPs and other health practitioners consider when dealing with men’s mental health?
In this edition we take a deeper look at the impact of social media on young men and the role GPs have to play.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.




Is enough being done?

Are you in need of a luxury winter getaway complete with wine tasting and a gorgeous vineyard setting?
Inside this issue we’ve got an incredible competition to win a two-night stay at Ampersand Estate’s most luxury property, The Homestead.
Worth $4600, the stay comes with a locally sourced breakfast hamper and a sit-down wine tasting experience at the Estate’s cellar door.
We’ve also got more movie tickets to give away, this time to the Hurtigruten Scandinavian Film Festival running from 24 July – 13 August.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Classifieds Manager
Rita Murphy 08 9203 5222 rita@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au





















A number of West Australian doctors and medical professionals were among the 830 Australians on this year’s King’s Birthday Honours list.
Professor Richard Prince, consultant physician in the Department of Endocrinology and Diabetes at Sir Charles Gairdner Hospital and senior honorary research fellow within the UWA Medical School, was named an Officer (AO) of the Order of Australia.
Another WA person to add an AO behind their name is Dr Michael Repacholi, who has worked as a radiation protection physicist around the world.
A number of WA medical figures were also named as Members (AM) of the Order of Australia.
Professor Timothy William Jones, co-director of diabetes and obesity research at the Kids Research Institute Australia, got a nod for his significant service to paediatric endocrinology and diabetes.
Draft clinical guidelines for the early detection of prostate cancer have been released, with significant changes to how GPs approach screening.
The draft guidelines aim to support early detection of prostate cancer on a national scale.
Key changes include offering men who are not at high-risk an initial prostate-specific antigen (PSA) test from 40, a recommendation for GPs to initiate conversations about PSA testing, and offering testing every two years to all men aged 50-69.
Current guidelines state men with
Professor Britta Regli-von Ungern-Sternberg , paediatric anaesthetist at Perth Children’s Hospital, received a Member (AM) of the Order of Australia for her significant service to medicine and related research.
Professor Regli-von Ungern-Sternberg said she was grateful to be honoured in this way – not just for herself, but for her colleagues.
“They play such important roles in the teamwork that makes any research possible,” she said.
“I am proud that my research has led to innovative, pragmatic and highly implementable solutions to common problems experienced by children having surgery.”
For more on this story visit mforum.com.au and hit the news tab.
an average risk of prostate cancer should be screened every two years from the ages of 50 to 69, while only men with a high-risk should be offered testing from the age of 40.
The RACGP flagged risks of overdiagnosis if all men over 40 are offered routine testing without adequate discussion on the risks and benefits of PSA testing. It also recommended cutoff limits for some patient groups, particularly men who are at average risk of prostate cancer.
The College recommended earlier and more frequent testing start at 40 for men at higher risk, including those with a family history or of
sub-Saharan ancestry, and for Aboriginal and Torres Strait Islander men to be tested every two years from age 40.
GP clinics will need to be prepared come 1 July when changes to Medicare chronic disease management items are enacted. Items for preparation of GP management plans, team care arrangements and reviews will be replaced with a GP chronic condition management plan (GPCCMP).
According to the Department of Health and Aged Care the changes
aim to simplify arrangements, promote continuity of care and encourage regular reviews of chronic condition management plans.
Currently the rebate for preparation of a GP management plan is $164.35, preparation of team care arrangements is $130.25, and a review is $82.10.
Under the new framework, those items will be simplified so there is one item that covers plan preparation and another for plan review.
The Medicare fee will be $156.55 for GPs when preparing and reviewing a plan, and $125.30 for prescribed medical practitioners.
Changes to the way Medicare handles chronic disease management were flagged in 2024 with the expectation they would come into place late that year, but they were delayed.
The RACGP criticised the delay and lack of notice about the major changes coming into play in July.
New research from the Prostate Cancer Foundation of Australia has found men are delaying GP visits and cutting back on medication to save money.
The charity’s annual Men’s Health Report found 51% of the 1,300 respondents had avoided seeing a healthcare practitioner due
A GP Urology Masterclass, hosted by Perth Urology Education and Research, was held on 7 June, covering topics such as prostate cancer, immunotherapy, ARPIs and radiopharmaceutical therapies.
Speakers included Perth Urology Clinic urologists, endocrinologists, radiation oncologists, radiologists and nuclear medicine physician. Attendees said the day included “superb, informative, relevant sessions”.
to cost, one in 10 had skipped prescribed medication to make it last longer and 57% said healthcare is ‘expensive’ or ‘very expensive’.
PCFA chief executive Anne Savage said: “For too many men, cost is becoming a barrier to care – and that has real consequences.
“When men put off seeing a GP or stretch their medications just to get by, we increase the risks of delayed diagnosis of a range of serious illnesses and disease, including prostate cancer.
“Access to affordable, timely healthcare is not a luxury — it’s a life-saving necessity.”
WA’s Minister for Health Meredith Hammat has confirmed training for GPs to provide increased support to those with ADHD is currently being formulated.
Ms Hammat confirmed to Medical Forum that the Department of Health was working with the RACGP on the rollout of a GP ADHD training certification program.
While a date has not been announced for the training to begin, Ms Hammat said it would be rolled out “as soon as possible”.
The State Government committed to expanding GP’s scope of practice to provide support, diagnosis and treatment of ADHD ahead of the State election.
Dr Tim Leahy, who is part of the RACGP WA ADHD working group and the ADHD WA professional advisory body, said not all GPs would do the training, but for those who want to diagnose and initiate treatment of ADHD he expected the training to be compulsory.
“Every doctor throughout their professional career needs to read the sign of the times, and one of the clear shifts in the last five to 10 years is a growing awareness of people young and old living with neurodevelopmental disorders including ADHD, autism, dyslexia,” he said.
“Now there are new guidelines and new regulations, so it’s appropriate that GPs embrace the opportunities, embrace the requests and the demands of their patients, and offer a better service than we did in the past.”
More on Ms Hammat's plans for WA, see page 8
For more on these stories visit mforum.com.au and hit the ‘news’ tab.

To coincide with the commencement of the National Lung Cancer Screening Program, ChestRad is bringing their sub-specialist service to Mandurah

ChestRad are specialists in Cardiac CT, Chest CT and Lung Cancer Screening
Cardiologists – Dr Edmund Brice, A/Prof Abdul Ihdayhid, A/Prof Chris Judkins, Dr Sam Tayeb, Dr Justin Teng and Dr Tashi Zhaxiduojie
Cardiothoracic radiologists – Dr Conor Murray and Dr Shriv Srigandan
ChestRad's rooms are at the Mandurah Specialist Centre on Minilya Parkway, Greenfields (near the Peel Health Campus) All rebatable Mandurah services BULK BILLED! www.chestrad.com.au

We need to plan wisely, manage resources responsibly, and keep reforming so the system can keep up with the growing demand.
Meredith Hammat was appointed Minister for Health following this year’s State election, taking on her first ministerial portfolio in the re-elected Cook Government.
Speaking to Medical Forum on a wide range of issues, Ms Hammat said while there was work to do to improve the health system, the government had put in place a system that would allow a sharper focus on priority areas.
MF: What are your top three priorities for your first year within the health portfolio?
MINISTER: I’ve spent the first few months in the job listening closely to clinicians, patients and staff across our system to understand what’s working, and where we need to improve.
My top three priorities are clear. First is improving access, whether it's getting into an emergency department, receiving elective surgery in a timely way, or getting care closer to home in our communities. I want every West Australian to feel supported, no matter where they live.
Second is building a strong, stable health workforce.
If we want to maintain world-class care, we need to invest in the people delivering it.
And third is long-term sustainability.
We need to plan wisely, manage resources responsibly, and keep reforming so the system can keep up with the growing demand.
MF: With responsibility for health scattered across multiple ministers and portfolios in the current cabinet, how have you found the team approach working so far? Is there a clear understanding of where each portfolio starts and another begins?
MINISTER: It’s a fresh and innovative approach and it's working well. We’ve got a dynamic team and division of responsibilities is clear.
As lead Health Minister, I keep us coordinated and focused on delivering accessible healthcare to all West Australians.
John Carey is handling infrastructure; his job is to upgrade and build the hospitals we need.
Simone McGurk will lead efforts to reduce pressure on hospitals by improving access to aged care beds and supporting timely discharge of our largest cohort of patients.
Sabine Winton will drive long-term initiatives to keep people well and to keep them out of our hospitals.
And Medical Research Minister Stephen Dawson will continue to lead health and medical research and innovation.
It’s a smart, whole-of-government approach, and it’s helping us focus more sharply on priority areas.
MF: You have not only been appointed to the significant portfolio of health but also mental health, do you see advantages to having both portfolios sitting with the same minister?
MINISTER: Mental health should be treated with the same urgency and care as physical health.
Having both portfolios together means we can take a more holistic approach.
I’m proud to be driving and delivering our election commitment to provide a multimillion-dollar expansion of our mental health services, including a new residential eating disorder recovery centre, expanded care for struggling new parents and strengthened mental health support in the workplace.
MF: With WA becoming the first State to create a dedicated preventative health portfolio, is there a lot of expectation on your colleague Sabine Winton to make measurable change within the WA health landscape?
Now
that the Federal election is over, I look forward to engaging with the reappointed Federal Health Minister Mark Butler to advocate strongly that WA receives its fair share of funding commitments, including the expansion of GP training places, junior doctor rotations in primary healthcare, and an increase in Commonwealth Supported Places.
MINISTER: There’s pressure, sure, but it’s the good kind. Sabine and I talk all the time, our offices are just down the hall from one another.
We’re both particularly proud of our nation leading RSV vaccination program, which has kept hundreds of newborns and children out of hospital since it started last year.
And at the start of June we got our free flu shots together.
This is a really important program to keep West Australians healthy in the winter months.
MF: For months we’ve heard warnings that the already stretched public hospital system would struggle even further if the private system continues to come under pressure. What can be done within WA (and nationally too) to ensure private services are viable and remain part of the broader health system?
MINISTER: The private system handles around 41% of hospital admissions in WA, it’s a crucial part of our system.
We’re supporting reforms proposed by the Federal Health Minister to assist the sector and we’ll continue to work with the Federal Government to keep private health viable.
We need both systems to be strong.
MF: What are you doing to address GP deserts across WA?
MINISTER: This is a serious challenge, especially in regional, remote, and outer suburban areas.
The Federal Government is responsible for funding primary care and it holds the key policy levers
to address GP shortfalls in WA and elsewhere, including Commonwealth Supported Places for medical students, GP training and the Medicare Benefits Schedule.
Now that the Federal election is over, I look forward to engaging with the reappointed Federal Health Minister Mark Butler to advocate strongly that WA receives its fair share of funding commitments, including the expansion of GP training places, junior doctor rotations in primary healthcare, and an increase in Commonwealth Supported Places.
MF: With WA projected to be short 720 fulltime equivalent GPs by 2028, and 1350 by 2048, what steps will the government be taking to boost the workforce in the short term, but also to encourage more individuals into the profession and to support medical students?
MINISTER: The department engages regularly with key medical colleges and training providers including the RACGP, Australian College of Rural and Remote Medicine, WA Primary Health Alliance and other stakeholders to support strategies that enhance GP attraction, retention and equitable distribution in WA.
We’ve partnered with stakeholders to implement programs that promote general practice and strengthen GP training, including the GP Hospital Training Pathway that optimises hospital training for junior doctors with GP intent.
Other programs include the Community Residency Program, and Commonwealth-funded John
continued on Page 11

Perth Radiological Clinic offers a comprehensive range of men’s imaging services including:
• Multi-parametric MRI for early detection and staging of prostate cancer
• MRI guided prostate biopsy
• PET-CT PMSA studies
• Penile ultrasound
• Scrotal ultrasound—adult and paediatric
• Urethrograms
• Scrotal interventional procedures
• Cross sectional imaging including MRI for diagnosis and staging of male genitourinary malignancy
• All imaging reported by PRC’s expert sub-specialist urogenital and nuclear medicine reporting teams. Doctor
continued from Page 9
Flynn Prevocational Doctor Program that provides junior doctors with exposure to general practice, and the Rural Generalist Pathway WA.
That means more training opportunities, better support in rural areas, and initiatives to give doctors hands-on experience. We're also helping overseas GPs get registered faster because we need them now, and into the future.
MF: Allowing GPs to diagnose and treat ADHD was an election commitment. What steps are yet to be taken for GPs in WA to begin diagnosing ADHD and prescribing associated medication, and when do you see GPs being able to start delivering this service?
MINISTER: We’re proud of our commitment to allow families to access ADHD care without needing to go to a psychiatrist or paediatrician, especially at a time when we’re working to ease the demands on our Child Development Services waitlists.
The Department of Health is working with the RACGP to roll out a GP ADHD Training Certification Program as soon as possible.
It’s practical, it’s timely, and it will help ease pressure on the whole system.
MF: What progress has been made on the implementation of the GP ASK program and when will it be operational?
MINISTER: GP ASK is another exciting initiative. It’s all about supporting GPs so more care can be delivered outside hospitals to ease growing pressures on our system.
The ASK project team is continuing planning with GPs with rollout starting mid-year. It’ll begin with immunology and expand from there.
MF: There have been calls to make Meningococcal B immunisations free, do you have plans to expand the State’s immunisation schedule to include this vaccination?
MINISTER: The Minister for Preventative Health and I continue to be guided on this by the National Immunisation Program, which currently provides free
We’re proud of our commitment to allow families to access ADHD care without needing to go to a psychiatrist or paediatrician, especially at a time when we’re working to ease the demands on our Child Development Services waitlists. The Department of Health is working with the RACGP to roll out a GP ADHD Training Certification Program as soon as possible.
Meningococcal B immunisations to Aboriginal and Torres Strait Islander children, and other children and adults with certain medical conditions.
However, we will work closely with the Department of Health to consider a State-funded Meningococcal B vaccination program should the number of reported cases significantly escalate beyond the annual average of seven.
MF: How would you rate the WA health system as it is today?
MINISTER: I’d say we have a health system we should be incredibly proud of. It’s staffed by some of the
most dedicated professionals you’ll find anywhere.
However, we know there are areas that we need to work on, and challenges we’ll face in the future.
We’re expanding emergency departments, adding hospital beds, performing record numbers of elective surgeries, and using smart tech like the Virtual ED and the State Health Operations Centre to work smarter.
We’ve got work to do, but I’m optimistic. And I’m in this to make a real difference.

In light of the increasing influence of toxic 'masculinity influencers' and a rise in male suicide rates, how can GPs better identify and support men at risk of experiencing poor mental health?
By Suzanne Harrison
In 2018 friends Leighton Bradfield and Lockie O'Donoghue lost two mates to suicide. Prior to this, Leighton had gone through his own battles with depression when he was at school and university.
“I didn’t even know it was depression. I didn’t know what to do, where to go. All of my friends were suffering,” says Perth-based Leighton, now 27 and cofounder of 20Talk, a preventative mental health organisation.
“Then we lost our friends, the second one having been at the funeral of the first. Lockie and I got together around a fire and we said, ‘We can’t let this happen again’. I have a saying of, ‘If not us, then who?’.
“The problem then came from who we could speak with. At that point in time, we didn’t know what we were doing. We just knew something needed to change.”
At the age of 20, he and Lockie – recognising what they saw as a lack of relatable, preventative mental health support for young people – founded 20Talk.
Their flagship free one-day course called Mental Health Maintenance is offered at universities, TAFEs and to the public in WA. It’s based on Dr Bill Hettler’s Six Dimensions of Wellbeing.
GPs are also encouraged to recommend 20Talk to young people who they feel may benefit from mental health support. They can refer patients directly to 20Talk’s website or encourage them to engage with the charity’s social media channels on Instagram and TikTok.
The charity has also worked with mental health campaigner and founder of The Cloud GP, Dr Shiromi, to develop resources for patients on preparing for their first GP appointment.
Leighton and Lockie’s determination to make change is desperately needed. The current state of men’s mental health is dire not only in Australia, but around the world.
In 2023, the Australian Bureau of Statistics reported that more than
three-quarters (75.3%) of people who died by suicide were male, a statistic made starker after the deaths of twins Adam – a former West Coast Eagles footballer – and Troy Selwood to suicide this year. According to Beyond Blue, death from suicide amongst men is nearly double the national road toll, with 43% experiencing anxiety or depression at some stage in their lives and 26% admitting to delaying seeing their GP for help when they needed it.
Increasingly intertwined within this issue is the rising power of social media influencers and the so-called ‘manosphere’, a concept explored in the recent explosive TV show Adolescence, in which a young boy is accused of murder after being influenced by online ‘incel’ culture. What once was a fringe community is reportedly now becoming mainstream. At the apex of this are digital male influencers, such as controversial Andrew Tate and Jordan Peterson, among a multitude of others globally.
For Leighton Bradfield, co-founder of mental health charity 20Talk, the rise of social media ‘masculinity influencers’ and their impact on young men is the result of a lack of relatable mentors for younger people.
“I feel that a lot of men have felt pushed away by third wave feminism, in that they feel they’ve been targeted, and that’s why these Andrew Tate figures have come to light, and that’s been quite destructive,” he tells Medical Forum
“We’re seeing that a lot of men don’t really have mentors or community anymore to give them direction. They feel victimised, they’re given a direction by influencers – which is not the right direction – and that’s why it’s amplifying.”
Leighton believes that lack of mentorship stems from men being put in the “bad box”, even good men, so they feel discouraged from standing up and tackling the narrative of poor role models.
He believes many middle-aged men in his community don’t want to stand up, for fear of being criticised.
“They feel their voice doesn’t mean anything anymore, and then the destructive influencers step in and fill that void.”
Recently, The Movember Institute of Men’s Health in Australia released a groundbreaking new study, Young Men’s Health in a Digital World. It found that popular socalled ‘masculinity influencers’ are captivating millions of young men across YouTube, TikTok, and Instagram, offering them advice on everything from self-improvement and fitness to relationships, finances, and career success.
The first-of-its-kind report gathered insights from more than 3000 young men aged 16-25 across Australia, the United Kingdom and the United States.
It explored why young men are turning to these online figures and what they think about the content they consume.
“While many young Australian men turn to these figures for motivation and inspiration, a groundbreaking new study reveals that the long-term effects of this online influence may
continued on Page 15

Introducing the recently launched not-for-profit association, Perth Urology Education and Research, established to enhance healthcare professionals’ expertise in urology through comprehensive medical training and innovative research. We invite you to join us in advancing patient outcomes and raising healthcare standards in the field of urology. foundation@perthurologyclinic.com.au

expert care for men to achieve their best health.
Dr Shane La Bianca
Dr Andrew Tan
Dr Jeff Thavaseelan
Dr Trent Barrett
Dr Matt Brown
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
With the largest partnership of Urologists in Western Australia, Perth Urology Clinic can manage all urological conditions, offering a wide range of treatment options. For urgent referrals or queries, use our GP Hotline on 1800 487 656 (Press 9). refer@perthurologyclinic.com.au
Healthlink: puclinic Hollywood Clinic | Wexford Clinic

continued from Page 13
be far more complex,” the charity said in a statement.
One major finding is particularly worrisome – young men watching these influencers regularly reported significantly higher levels of worthlessness, nervousness and sadness.
They were also less likely to prioritise their mental health (45%) compared with young men who did not actively engage with these influencers (55%).
And they were significantly more likely to use performance-enhancing or body modifying substances including steroids, nootropics or supplements, and diet pills.
Specifically, 23% had taken or considered taking steroids, 22% had used or were considering testosterone injections, and 24% had taken or were contemplating diet pills.
A 23-year-old male interviewed by Medical Forum said: “While most men in that 18-30 bracket are smart enough to dismiss these influencer types as brain-dead fools, many are still subconsciously affected.
“A quiet voice of insecurity can form in their minds. Worse, the glorification of performanceenhancing drugs continues to spread the fitness epidemic.
“Young men take substances that temporarily enhance their physiques but eventually suffer the long-term mental and physical consequences of steroid use.”
Unchartered territory
It was no doubt timely that during International Men’s Mental Health Week in June the central theme was ‘See your GP’.
No one wants to send that message more than Dr Lloyd Evans, a Perth-based GP and the founder of MAN Health, which focuses on men’s health and wellbeing.
Dr Evans said he has seen an increase in men’s mental health cases and believes the drivers are loneliness, financial pressures, and social media.
more men present with mental health symptoms, and in one way maybe that’s a positive,” Dr Evans said.
“Is it that men’s mental health is getting worse or is it that we’re encouraging more men to seek help? It’s a bit of both probably.”
Dr Evans is aware of the influx of social media that young men in particular are being exposed to, especially teens.
“They’re seeing so much of that perfectionist approach to life and I wonder if many are feeling that they can’t live up to that.”
He believes that it’s the years after a young man leaves school, around 18-25, that they are particularly susceptible.
“At school, you have an identity,” he said. “There are teachers, sport and a routine you’re familiar with, you’re part of that camaraderie.
“And then after school, there’s this new place, a big open world and they have to find themselves. They’re at risk, trying to find their place, and they can get information that is maybe toxic or takes them on that path.
“They’re bombarded with information, then algorithms come in and that narrows it down to say three or four influencers, and they may not be the right ones.”
To that end, Dr Evans has taken steps to be a positive influencer, creating a podcast titled In My World. It is the antithesis of the manosphere approach, with subjects such as ‘Men need to feel safe to talk’ and ‘Learning to be honest’.
Dr Stephen Adams, a semi-retired GP formerly with West End Medical and Integrated Sexual Health in Fremantle, said the increasingly complex situation for men now was unprecedented.

“I’ve worked in the field of men’s health for many years now, and there have been different crises or problems over the years. But this one I think is quite unique,” Dr Adams said.
people’s social and academic interactions and the rise of the ‘manosphere’ – where some men seek to reclaim traditional masculine roles – have all combined to create a perfect storm for men young and old.
“Young men are described as ‘lost’, dealing with biological drives, confusing societal expectations and inconsistent role models,” says Dr Adams.
When it comes to the role of GPs and men’s mental health, it is fundamental.
“GPs are vital in identifying and supporting mental health issues among young men but system barriers still exist, including bureaucracy around the ability for more direct referrals by a wider group of professionals,” Dr Adams said.
Healthcare providers generally “should be encouraged to initiate open, empathetic conversations with men about mental health at every opportunity”.
For example, Dr Adams said, healthcare providers – and not just GPs – should be able to refer people to mental health services.
“It could come from a social worker, a school nurse or a counsellor. The mental health plan is there as a barrier to over-servicing, but instead it ends up adding to the whole problem with unnecessary bureaucracy.”
In Dr Adams experience, anxiety and depression remain the most common diagnosis, often presenting through physical symptoms like panic attacks, erectile dysfunction and unexplained tiredness, rather than clear declarations of mental distress.
He also stresses the importance of communication when it comes to the role of GPs, with more welcoming and easier access to care also needed.
“It’s important that we have systems in place. GPs need to instil trust and an environment that men are comfortable to walk into, maybe with more flexible hours and even weekends, or video consults.
“From a GP perspective, I’m seeing
He said that toxic social media content, the advent of the #MeToo movement, COVID-19 limiting


continued from Page 15
“I worry that there’s young men who don’t even know how to book a GP, or the name of their local practice. They don’t build that trust with their doctor.
“We need to make GP practices more welcoming for men. They see their mechanic regularly, but not a GP.”
As for mental health specifically, Dr Evans is a great believer in the close relationship between physical and mental health. That is, looking at the whole man – is he getting enough sleep, is he eating well?
“I can’t emphasise enough how much that impacts mental health. There are more complex conditions that can’t be dealt with by eating better or sleeping more, but good physical health can really help with good mental health,” he said. By creating a safe space for men without judgement and asking the right questions, GPs can then better delve in and ask about relationships, drugs and pressures.
“In my day-to-day life as a GP, I see so many guys with issues that need to be discussed but they book 10 minutes and they want a quick fix. I can tell they need more,” Dr Evans adds.
“We need to offer follow-up appointments and go out of our way to recognise that this guy needs to talk about it. It’s about the whole man.”
The good news is, change is afoot, and there are some wonderful charities and initiatives, such as Movember, Lifeline, ManUp WA and Menshed, that are dedicated to supporting men’s mental health.
During Men’s Health Week, Movember launched Men in Mind, a workforce training program for healthcare practitioners to transform the way that men experience mental health care.
According to the charity, Men in Mind helps practitioners better grasp the complexities of men's health and masculinity to deliver care that engages, motivates and connects with male clients.
Movember – among other groups

– has also lobbied governments for increased funding to support and promote men’s mental health initiatives.
In April, the Federal Government made a $1 billion mental health commitment, which includes:
• $225 million for 31 new and upgraded Medicare Mental Health Centres
• More than $200 million for 58 new, upgraded or expanded headspace services
• $500 million for 20 Youth Specialist Care Centres for young people with complex needs
• $90 million for more than 1200 training places for mental health professionals and peer workers.
However, specific funding packages targeting men’s mental health were lacking.
Prevention is key
For Leighton and Lockie’s organisation, it’s all about prevention.
“To give you some context, only 2% of government funding goes into preventative mental health. So, our whole thing is how do we connect this existing, evidence-based education to young people in a way that they actually want to learn about and understand?” Leighton said.
20Talk is now expanding into the Eastern States, and its ‘20 Hours for 20Talk ’ challenge, where participants raise a minimum of $1000, is a key fundraising component that Leighton said is “blowing up” in terms of signups.
A bit like the 40-hour famine concept, participants spend 20 hours in a two-by-two metre space with no talking or technology, symbolising the challenges of mental health and the need for support.
Such initiatives and programs can’t come soon enough. It was reported in June that more than one in three Australian men (35%) aged 18-65 years have used intimate partner violence in their lifetime, according to data from Ten to Men – the Australian Institute of Family Studies longitudinal study of boys and men.
Of those, men with moderate or severe depressive symptoms were 62% more likely to use intimate partner violence, compared to men without these symptoms.
There is no doubt that there is now more awareness and conversations when it comes to men’s mental health, but actioning that as a society is the next major step.
As Dr Adams concludes: “Everyone is talking about it and that is definitely a good thing, a good way to make change. People need to discuss it, and they’re now realising this is an issue.”
ED: More information on 20Talk can be found at www.20talk.com.au

Damian Collins is the Founder and CEO of Westbridge Funds Management and a leading voice in the Australian property investment landscape. With over two decades of experience in finance and real estate, he is also a former President and Chair of the Real Estate Institute of Western Australia (REIWA). Drawing on his extensive background in property strategy, fund management and investor education, Damian shares his insights into building diversified, income-generating property portfolios.
Property has always been a cornerstone of Australian wealth creation. With its strong longterm performance, incomeproducing potential, and relative stability compared to other asset classes, it’s no surprise that over two million Australians have chosen to invest in real estate.
Yet despite our strong affinity for property, many investors still overlook one of the fundamental principles of successful investing – diversification.
In my experience working with a wide range of investors, I’ve seen first-hand the importance of spreading risk to build a more resilient and higher-performing portfolio. And when it comes to
property, diversification doesn’t just mean mixing asset classes like shares, bonds and real estate. It can – and should – be applied within property itself.
For those of us with a strong property focus, diversification can take many forms. It might involve investing across different geographic locations to take advantage of varied residential market cycles, or diversifying across property types, such as houses, villas or townhouses.
But there’s another powerful way to diversify that many overlook: balancing your portfolio across
different wealth creation strategies – namely, combining both residential and commercial property.
Residential property is often the first step for investors – and rightly so. It’s accessible, familiar, and offers strong capital growth over time. But as your portfolio grows and your investment goals shift, residential property may not always be enough on its own.
For example, investors heading into retirement often begin prioritising stable income over long-term growth. This is where commercial property can play a strategic role.
By Damian Collins, CEO –Westbridge Funds Management
While residential properties typically offer solid capital growth with modest rental returns, commercial properties are known for their strong income potential. This is largely due to longer lease terms and lease structures where many property outgoings are covered by tenants.
In fact, these complementary characteristics make residential and commercial property powerful partners within a diversified portfolio. When combined strategically, they can help deliver both consistent income and longterm value growth.
I understand that for many investors, commercial property can feel unfamiliar – but it’s not as complex as it may seem. It does require a different mindset, however.
Unlike residential, commercial tenants are businesses. So instead of focusing on features like ocean views, the emphasis

shifts to proximity to transport routes, employment hubs, and infrastructure. Lease lengths are generally longer too, which helps deliver stable income – but it also means tenant quality and professional property management become even more important.
One of the biggest hurdles for investors is the high capital outlay often required to purchase commercial property. Quality assets can easily start from $5 million, limiting direct ownership opportunities and concentrating risk in just one or two properties.
But there’s a smarter, more accessible solution – managed property funds.
Managed property funds offer investors the ability to access large-scale commercial assets with a much lower entry point, often from just $25,000. These pooled investments allow you to share in
both the income generated and capital gains from a professionally managed portfolio.
They also open the door to greater diversification – across asset types like retail, industrial or healthcare, and across geographic markets – without the stress or capital burden of direct ownership.
A well-balanced portfolio does more than reduce risk – it aligns with your financial goals at every stage of your journey.
By combining residential and commercial assets, and considering professionally managed funds as part of your strategy, investors can benefit from both long-term growth and ongoing income.
At Westbridge, we help investors build portfolios that are not only diversified, but also adaptable to evolving objectives.
Whether you’re just starting out or planning for retirement, the key is balance – and a strategy that works as hard as you do.
An advocate for men’s health, Dr Tom Shannon likes to set a good example for his patients and encourage self-care for the prevention of illness.

By Ara Jansen
Urologist and prostate cancer surgeon Dr Tom Shannon aims to be in his patient’s lives for the shortest time possible.
“I love the fact that I can be important to a patient for a very short period of time. The goal is not to need me and to get on with their lives, free of cancer, which is such a privilege to be part of. Our team makes a difference,” he says.
Tom has been a urologist for more than 25 years, specialising in prostate cancer diagnosis and treatment. He still loves his profession as much today, if not more than when he started.
From a young age Tom knew he wanted to be a doctor, even though it wasn’t something that was in his family. Fascinated with the human body, he was drawn to books about how the body worked.
Tom was also very clear he was going to be a physician during medical school, but exposure to some great surgical bosses in early years changed his view. As a young intern at Hollywood Hospital he had his own theatre list, developing a love for surgery.
“Hollywood was a great place to be a junior doctor. I had a great boss who gave true one-on-one mentoring. I learnt so much. When I finished my internship, I just started studying for surgery.”
“I was really interested in cardiothoracics but after a year realised it wasn’t for me. I was sent to do urology for a rotation and remember complaining loudly. I was given great advice – the only way to know if I liked it was to approach it like I would be doing that job every day for the rest of my career.
“I discovered urology was a rare specialty where you can be both a physician and a surgeon and threw myself into it. I’m still madly in love with it. Urology has been challenging and rewarding, always changing and progressing with technology.”
A UWA graduate, Tom finished his Fellowship in Urology in 1999 and did training in the UK, with additional training in minimally invasive surgery in Edinburgh and prostate brachytherapy in Seattle.
Throughout his career Tom has sought out and trained with pioneers in the field all over the world and been part of prostate

surgery’s evolution from open surgery, to laser use, and now robotic assistance in laparoscopic surgeries.
Recognising the importance of patient education and support, he championed the role of the prostate cancer specialist nurse and a multidisciplinary team.
“Our care is now holistic, routinely involving weight loss and lifestyle changes to enhance physical and mental health.”
A pioneer of minimally invasive urological surgery in WA, Tom was amongst the first surgeons in Australia to perform keyhole surgery for kidney cancer, reconstruction, transplantation and partial kidney excision for small tumours. During several visits, Tom was mentored by the Cleveland Clinic’s Dr Indiber Gill, one of the world leaders in keyhole surgery. In 2005 Tom brought the expert to Perth to teach other urologists.
Among other accomplishments, in 2004 Tom operated in WA with the pioneering French surgeon Professor Claude Abbou for the first demonstration of a laparoscopic radical prostatectomy. To date, the urologist has cared for more than 10,000 men and performed more than 3,000 open, laparoscopic and robotic surgeries.
A big advocate of self-care and the prevention of illness, Tom actively advocates for men’s health and prostate cancer. He has been involved with the Prostate Cancer Foundation of Australia since inception and holds an adjunct associate professor role with Edith Cowan University in exercise medicine.
With around 26,400 cases diagnosed in 2024, prostate cancer is estimated to account for 28% of the cancers to be diagnosed in males for the year. Because prostate cancer survival rates are high, Tom says it’s a rewarding field to be working in.
He says there’s still work to do to bring equality to early detection. There’s excellent data showing the benefits of Prostate-Specific Antigen (PSA) testing and new Australian guidelines advocate men start testing at 40 and at regular intervals after, depending on personal risk. Tom argues that we could achieve significant gains with simple, but uniform changes.
“The goal is to find significant cancers early and cure them. Cures are achieved by complete surgical resection, which is a challenge, because you get one chance to





continued from Page 21


do it really well. There are minimal margins for the cancer. To cure and retain continence and sexual function, you must be precise. The trifecta is the goal. Cure avoids needing testosterone suppression, which can be devastating.
“Technology has helped us be more consistent and have better outcomes. Integrated team management minimises risks and maximises health, sexual and urinary functional recovery. Outcomes today are much better as a result.
“It’s an exciting time with technology because we don’t know what’s humanly possible. AI and robotics are allowing us to cure more patients, even when cancers are found later.
“We try and empower men to get involved in their self-care. Most of my patients have not taken care of themselves to date and commonly have obesity, diabetes or cardiovascular risk factors. The cancer is a big wakeup call, but also a teachable moment.
“Men rarely stop and pay attention unless they are so sick they cannot function. By integrating self-care into the cancer pathway, men learn to retain good health as they age and simply just feel much better. If you get can 20kg off them and get them exercising every day, they are going to live longer and minimise future disease risk.”
Tom says that’s a rewarding thing to be able to do. Partners often join in the new health kick and you’ll often see a couple grow closer as they approach the challenge together. This passion for wellness has led to published research in weight loss and exercise medicine and a wellness retreat in the Maldives.
You’ll always hear music in Tom’s operating rooms. He says it puts him in the zone and allows him to be hyper-focussed on and immersed in what he’s doing. His choice of music is usually funk, soul or something flowing.
If it’s a particularly tricky surgery, something newer by Rufus might make an appearance. There’s no death metal here and he enjoys

it when people recommend something he’s not heard before. Sometimes there is even singing. These days, Tom does most of his operating with one of the $2 million Da Vinci robots at Hollywood Hospital. The technology offers better vision and dexterity that makes surgery safer, with consistent results, but it is still just a tool.
Seated, Tom places his head into a small booth and uses his hands and feet to operate multiple robotic arms. There are little speakers next to his ears and a microphone to communicate with staff.
“When we first got this machine, I would go in on weekends and sit on the machine for six hours at a time using the in-built simulator. It’s a fascinating use of so many skills – co-ordination, sight, hearing, using hands and feet, the mental component. I think the best thing to learn is something you can never fully master.
“You cannot do live animal training in Australia as yet, so there have been trips to California and Korea to learn, as well as watching many others through video. We video all our surgeries and continue to refine techniques.”
While he did plenty of training on the machine before working on
his first patient, Tom also keeps his hands and brain supple with a racing SIM at home.
“There’s a natural competition in me that I have to find an outlet for. Playing computer games allows you to be competitive without any risk. I like to cycle, but I do it more socially now, rather than competitively.”
Robotics may not be the best choice for everyone but Tom is a convert. New technologies such as the NanoKnife allow treatment of just the cancer in select patients, effectively destroying the cancer using high-voltage pulse electricity, with minimal side effects. There are now 10-year data that shows the NanoKnife destroys cancer cells without affecting surrounding tissue in more than 95% of cases.
“Medicine has been a great choice for me, and I don’t ever regret it. It can be hard to find the perfect work/life balance sometimes, but doing something meaningful and rewarding is not something everyone gets in life – and I’m grateful for that. Finding the challenge in the everyday and expanding broadly have kept me excited and passionate about what we get to do.”
Rates of overweight and obesity in Australians since the 1990s have skyrocketed – and men have been leading the charge. Cathy O’Leary looks at how doctors are using a more nuanced approach with anti-obesity medications to help turn the tide.
Australians – young and old – have stacked on the weight in the past few decades and the reasons why are part of a complex web of evolutionary, physiological, environmental and societal changes.
According to the most recent data from the Australian Institute of Health and Welfare, two-thirds of adults – about 13 million people –were overweight or obese in 2022, a significant increase from 56% in 1995.
Men in particular have become a lot bigger – with a staggering 71% of them carrying too much weight in 2022 compared to 61% of women. It comes at a hefty cost to individuals as well as public health. Overweight and obesity are red flags for a range of diseases and chronic conditions, including cancer, cardiovascular disease, type 2 diabetes and musculoskeletal disorders.
Men are more likely than women to die prematurely of heart disease and cancer, and weight is often a key factor.
At the pointy end of the weight crisis are the 32% of Australian adults who are obese and therefore potential targets for anti-obesity medications

such as the semaglutides Ozempic and Wegovy and the newer kid on the block tirzepatide (Mounjaro).
watershed moment
Many doctors believe healthcare has reached a watershed moment, where the undeniable results from these blockbuster drugs have changed forever the way obesity is viewed and managed – with it no longer seen and approached purely as a lifestyle choice.
But how best to use them, to get the biggest bang for their buck, is now attracting big interest from scientists, doctors and the government bean counters under pressure to fund the medicines on the Pharmaceutical Benefits Scheme (PBS).
And there could be other benefits from anti-obesity medications beyond weight loss, with research presented at the European Congress on Obesity in Spain in May this year finding that first-generation weightloss medications like liraglutide and exenatide appear to have anticancer benefits.
Ozempic (semaglutide) is probably the best-known name among the group of medicines known as
glucagon-like peptide-1 receptor agonists (GLP-1RAs), which mimic the naturally occurring hormone GLP-1 to tell the brain that the stomach is full.
But like many of the new antiobesity drugs, it is approved on the PBS only as a diabetes treatment, so patients using them only for weight loss have to pay hundreds of dollars for each private script.
It is a sore point with them and the GPs who are increasingly being asked to prescribe these popular medicines.
The RACGP recently called for effective obesity management medication to be subsidised on the PBS to address what it says are big health inequities – with the medicines currently only available to those who can afford them.
The change in the peak body for GPs’ position on medication for weight loss follows the RACGP’s release of a new position statement on obesity prevention and management in February this year.
The College said more government funding for longer GP consults was also essential in supporting people who were overweight or obese.
Management Chair Dr Terri-Lynne South said there was growing evidence that semaglutide medicines were an effective way for patients to reduce their risk of developing complex and chronic conditions that were linked to overweight and obesity.
She said manufacturers had drawn “exceptional profits” from these medications and they needed to invest in reducing costs for patients.
“If a medicine is effective and safe, and the cost of a condition to the health system outweighs the cost of treating it with a medicine, there’s also a strong case to subsidise that medicine,” she said.
“The evidence for semaglutide and similar GLP-1 receptor agonists as effective weight loss medicines is if not at, then approaching, that point.”
While Ozempic captures most of the headlines, the newer drug tirzepatide is garnering growing interest. Since last year, Australian GPs have been able to prescribe it to patients for obesity.
It is available to adults with an initial body mass index of ≥ 30 kg/m2 or ≥ 27 kg/m2 in the presence of at least one weight-related comorbid condition such as hypertension, dyslipidaemia, obstructive sleep apnoea, cardiovascular disease, prediabetes or type 2 diabetes.
Tirzepatide has been likened to a master key that unlocks two important doors in the body’s weight control system, by mimicking
the hormones GLP-1 and GIP (glucose-dependent insulinotropic polypeptide), whereas semaglutide only acts on GLP-1.
Both drugs trick the brain into making people feel full, so they eat less and instead burn fat stored in the body.
Some research suggests tirzepatide (Mounjaro) may have the edge over Ozempic and Wegovy, affecting feelings of hunger and fullness, as well as changing how the body processes food.
The first head-to-head trial of two blockbuster weight loss drugs –undertaken in the US recently – concluded that Mounjaro is more effective than rival Wegovy.
Perth research deep dive In Perth, UWA researchers are taking a strong interest in tirzepatide, but with an important add-on which they believe makes it a better and safer weight loss treatment.
Their current study is investigating how to maximise the benefits of the new blockbuster anti-obesity medication by combining it with a tailored exercise program to address a potential downside of significant weight loss –a decrease in muscle or lean mass.

Both drugs led to substantial weight loss, but Mounjaro's 20% weight reduction after 72 weeks of treatment exceeded the 14% from Wegovy, according to the trial's findings.
Researchers who led the trial at the Comprehensive Weight Control Center at Weill Cornell Medicine in New York said both drugs had a role, but Mounjaro might help those with the most weight to lose.
In the UK, private sales of tirzepatide are now reportedly well ahead of those of semaglutide, but the huge amount of global research into weight loss drugs means it is a dynamic field of medicine, and more pharmaceuticals are already in the pipeline.
71% of men carry too much weight, compared to 61% of women Australia's obesity stats
13 million adults are overweight or obese
*Based on Australian Institute of Health and Welfare 2022 data.
32% of Australians are considered obese
They have recently been trying to recruit more men to sign up for the study, known as T-REX.
Led by Professors Bu Yeap and Daniel Green, the research examines whether combining tirzepatide with structured exercise gives better outcomes for cardiovascular health, compared to medication alone.
Already they are urging doctors who are prescribing anti-obesity medications to be aware of the need for resistance exercise to combat changes in body composition such as muscle loss.

Prof Green, from UWA’s School of Human Sciences, said all participants in the randomised study were receiving 40 weeks of free treatment with Mounjaro and half of them also had the chance of getting a free state-of-the-art exercise program supervised by a specialised exercise physiologist at the UWA gym.
“The medication being studied has shown remarkable effectiveness in clinical trials, exceeding that of Ozempic, and produces weight reduction of 15-to-20% over a 40week period,” he said.
“However, questions remain about how to optimise their health benefits beyond weight loss alone.”
The researchers had already recruited more than 100 women and men when Medical Forum spoke to them but still had openings for more male participants.

Our podcasts bring you the latest updates and key insights into new treatment options available.
Join our clinical editor Dr Joe Kosterich in conversation with WA specialists to learn more about developments to improve patient outcomes. Our podcasts are now CPD verified. Look for the CPD logo to complete your self-reflection and claim your time.
Topics covered in this series:
Advances in lung cancer management with A/Prof Tim Clay
Holistic management of osteoarthritis with Dr Arash Taheri
Diagnosing ventricular tachycardia with Dr Ben King
Holistic approaches to bariatric surgery with Dr Harsha Chandraratna
Difficult-to-treat depression with Dr Kyle Hoath
Listen on your favorite podcast platform – scan the QR code to follow us!
continued from Page 25
Prof Yeap said several of the men who had already completed the treatment course had described their experience as “life-changing”.
The study allowed men and women to receive a highly effective treatment in a carefully supervised environment.
As part of the study researchers are testing heart and artery function, so they need people who are not on blood pressure or cholesterollowering medication and have not previously been on Ozempic or other weight loss drugs.
Prof Yeap, an endocrinologist with UWA’s Medical School, told Medical Forum that with both semaglutide and tirzemide people could get decent weight loss in the obesity setting.
“But what we also now realise is that you lose a bit of lean mass as well, and a big chunk of that is muscle, and that might not be so good in the longer term,” he said.
“If you lose muscle, you’re losing a site where a lot of glucose is consumed, and if you lose muscle then it may increase your risk of becoming frail and having sarcopenia (progressive muscle disorder) frailty, so what we want to do is look at that in more depth.
“We also want to know whether if you’re going to use tirzepatide or semaglutide, or any of the other ones that are going to be coming up soon, is the best way to do it with a resistant exercise program that will protect your muscle mass?
“And apart from protecting the muscle mass, you maybe even lose more fat.”
Prof Yeap said the exercise needed to be weight-bearing resistance types – with upper and lower body exercises – and in the study it was being done in the gym at UWA so it could be monitored.
“We’re also going to look at the cardiovascular side of things in a lot more detail, so we’ll be looking at vascular and cardio function using echocardiograms, looking at what happens when you lose a lot of weight with these anti-obesity medications, and how is that affected when you’re combining it
right from the onset with a resistant exercise program.
“So we should be getting some really good data on vascular function and cardio function.”
The researchers believe the scale of lean mass loss associated with some incretin therapies for diabetes could be greater than that seen during 10 years of ageing, while preserving lean mass in obesity treatments could also prevent rebound fat gain when people stop their pharmacotherapy.
“We know these drugs work, they’re really effective, and losing a huge amount of fat is very beneficial, but what we’re trying to figure out is the best way to use them with a proper resistance exercise program, as opposed to simply telling people to maintain their protein intake and exercise,” Prof Yeap said.
“In terms of overweight and obesity, in the past 20 years the figures have got worse, so if we’re looking at the early 1990s to 2018 across the Australian population, the average BMI has really gone up.
“It’s a problem that’s been getting worse in the past couple of decades, and we now have the chance to treat it effectively medically, so it’s exciting times but what we want to know is whether you get the best effect by having an exercise program as well as medications.”
Prof Yeap said they had a strong hypothesis, after canvassing the use of incretin therapy for type 2 diabetes in a paper published in Diabetes Care last year.
“We think there is a very sound rationale behind this, but we have to prove it scientifically. We have to get high quality evidence and the only way to do it is through a randomised trial, so everyone in the study is getting background medications, and the randomisation is for the exercise intervention versus the usual.”
Although the study is yet to finish, there was already some advice to share with GPs and other health professionals.
“It's probably not a bad idea to draw to everyone’s attention that this is a possible concern – losing lean muscle mass – and obviously we’re
looking at it very carefully,” Prof Yeap said.
“But it wouldn’t hurt when doctors are talking to patients about to start this treatment for them to discuss things like protein intake and resistance exercise and encourage all of them to take it onboard.
“We really should be recommending everyone in the Australian population do resistant exercise, but probably more so in this scenario.”
Meanwhile, Monash University researchers recently cautioned that while the new anti-obesity medications were seen as wonder drugs, the approach to managing patients needed to be nuanced.
Their review in the Medical Journal of Australia said key considerations included funding models, prescribing pathways, and guidelines for treatment duration, including prevention of rebound weight gain after patients stop using the drugs.
“Because of how these new medications work, they’re transforming the way we view obesity as a condition,” Associate Professor Suong Le, a gastroenterologist at Monash University’s School of Clinical Sciences wrote.
“It’s clear that obesity is not just a lifestyle choice but should be regarded as a chronic inflammatory disease with links to cancer, brain function and autoimmune conditions.
“In Australia, we need to focus on researching more niche, specific-use cases where these medications can make a meaningful difference in our clinical practice while also developing a greater understanding on how exactly they lead to improved cardiovascular health, kidney function and neuroprotection.
“This will help us develop a more nuanced and scientifically comprehensive understanding of obesity as a condition and a risk factor for other diseases.”
ED: For more details of UWA’s T-REX study email the research team at trexstudy-shs@uwa.edu.au

Mental health is not so clear-cut. The warning signs can be subtle or mistaken for something else. A man who becomes withdrawn or irritable might be seen as just having a bad day, when in fact he’s experiencing the early stages of a mental health decline.
For many men, talking about mental health is incredibly difficult but new technologies like smartwatches offer a new window of opportunity, writes Dr Michael Kyron, Interim Director, Suicide Prevention and Resilience Research Centre.
Stigma, social expectations, and a reluctance to appear vulnerable often mean that men’s emotional struggles go unspoken.
As a result, symptoms of depression, anxiety, or stress can go unnoticed until they become much more serious. But what if there was a way to spot signs of mental strain early, without requiring someone to speak up first?
When it comes to physical health, we tend to be much more responsive. Think about chest pain or shortness of breath, most people know these are warning signs of a heart problem and would encourage someone to seek medical help straight away.
Doctors have clear tests they can run, like ECGs or blood work, to confirm whether something is wrong. The symptoms are visible, measurable, and familiar.
Mental health is not so clear-cut. The warning signs can be subtle or mistaken for something else. A man who becomes withdrawn or irritable might be seen as just having a bad day, when in fact he’s experiencing the early stages of a mental health decline.
Without clear markers, and without someone saying they need help, it can be difficult to know when to step in.
That’s why finding practical, consistent markers of mental health is so important. Checking in with someone directly can be meaningful, but doing so every day over long periods isn’t always realistic. We need other ways to keep an eye on wellbeing, methods that don’t rely entirely on self-reporting but still give valuable insight.
Spotting mental health through physical health
Physical and mental health are closely linked, often affecting each other in subtle but significant ways.
When someone is experiencing emotional distress, it often shows up physically. Disrupted sleep, reduced physical activity, or even changes in heart rate or breathing can all be signs that something deeper is going on. These are not just side effects of poor mental health, they can be early indicators that something is beginning to shift.

Today, we’re better equipped than ever to notice these changes –smartwatches and fitness trackers mean many people are already collecting data about their sleep and movement. This opens the door to a powerful opportunity: using everyday physical health data to spot early signs of mental strain, especially for those who may not be ready to talk.
But to turn this potential into reliable support, we need to explore how these physical indicators map onto mental health with enough accuracy and consistency to be clinically meaningful.
New WA research is focused on young men currently receiving psychiatric care, and is exploring how physiological data can be used to detect early signs of mental health deterioration, thereby facilitating timely and targeted interventions.
So far, the study has found that poor sleep quality and increases in resting heart rate often show up before other symptoms become noticeable. This makes it a valuable signal for early intervention.
By combining objective physiological data, with personal insights such as mood tracking or life events, the research team is building a smarter and more responsive way to support mental health.
The next step is turning these insights into practical support, both for individuals managing their own wellbeing and for professionals delivering timely care.
Advances in artificial intelligence (AI) can help detect subtle patterns across sleep, activity, and physiological data that may signal early signs of mental strain.
When these changes are flagged, care providers can choose to check in or adjust support before things escalate. This early detection opens the door for more targeted, preventative interventions rather than waiting for a crisis.
At the same time, AI can empower individuals with tailored insights about their own health. Simple prompts or personalised strategies can help people make small adjustments to their sleep, movement, or routines – changes that can have real benefits for mental wellbeing.
This approach respects privacy while still enabling meaningful support. This balance between space and connection can make care feel safer and more accessible. AI is not a replacement for human connection, it’s a tool that can enhance clinical care by providing earlier, more targeted insight.
Not every man is ready to talk about how he’s feeling, so it’s essential to bring mental health support into daily life in subtle but powerful ways.
Just as we treat early signs of physical illness, we can use realworld data and AI to support mental wellbeing proactively. Through this we can help men before they reach a breaking point, and offering tools that genuinely fit into how they live.
ED: The research is funded by The Hospital Research Foundation Group and led by the Suicide Prevention and Resilience Research Centre at UWA.






Understanding where patients’ knowledge gaps are can empower GPs to ask important fertility questions, writes Dr Jesse Clifford
From prescribing contraception and treating sexually transmitted infections, to arranging referrals to fertility specialists and obstetricians, reproductive health appointments are common in primary care.
However, given the timepressured nature of consultations, it can be challenging for a GP to delve deeply into a patient’s understanding and knowledge of fertility.
A new initiative could help GPs provide more holistic care that meets their patients’ overall reproductive goals.
The Fertility Insights Index is an annual research project that aims to uncover valuable and ongoing information on what Australian men and women – including those living in the West – really think, know, feel and do when it comes to their fertility and reproductive health.
It provides important insights into fertility attitudes, awareness, knowledge and behaviours among those aged 18-44 and is a source of data that can help those in healthcare and policy better understand what’s driving fertility trends, and what education, services and government support programs are needed to support fertility needs and goals.
Four in 10 West Australians rated fertility as highly important to them at this point in their life, but just one third feel comfortable talking to their GP about fertility.
While it’s difficult to cover multiple health concerns in a short consultation, this finding should encourage more GPs to initiate these important conversations.
Governments could also consider supporting longer consultations


that would allow patients the time and space for deeper fertility discussions with a general practitioner.
Asking women of any reproductive age about their menstrual and sexual symptoms is essential in understanding more about their reproductive health. In the presence of symptoms, access to a good quality pelvic ultrasound will help to gain important clarity about their pelvic health.
Four in 10 West Australians are not aware being over 40 can pose a major challenge to conceiving a pregnancy, while six in 10 are unaware irregular menstrual cycles might make conception challenging.
Knowledge gaps like these highlight potential lost opportunities for couples to reach their reproductive goals.
The importance of both men's and women's fertility knowledge should not be underestimated. Fertility is a time sensitive issue, biologically speaking, and addressing issues early gives those who want to start a family the best possible chance to do so.
It’s clear we need to do more to better educate people about their fertility, especially if they plan to have children. However, fertility isn’t just about having babies – it’s also about making informed choices about our bodies.
Misconceptions and myths can lead to late diagnosis of serious conditions and overall poorer health outcomes.
These findings highlight significant gaps in knowledge in the general community and provide all healthcare professionals with a great opportunity to educate patients about reproductive health. It also provides us with an opportunity to advocate to governments for improved support for our patients.
Closing these gaps should empower more individuals to take control of their fertility, to ask the right questions and, if they need to, to seek a timely referral to a fertility specialist to optimise their reproductive success.
ED: Fertility Insights Index is an initiative by Monash IVF.
For patients who may not feel ready to see a psychologist, GPs should consider referring to a mental health OT, writes Michelle Oliver.
When a patient sits across from you, grappling with their mental health, your role as a GP is to guide them toward the right support.
In most cases, that means initiating a Mental Health Treatment Plan and referring them to a psychologist. But with psychologist waitlists growing and some patients hesitant to engage in traditional therapy due to stigma, past experiences, or personal preference, that pathway isn’t always the best fit.
With one in five Australians experiencing mental illness, it’s clear that mental health care can’t be a one-size-fits-all model. For patients who would benefit from a more hands-on, practical approach, there’s another option that many GPs might not know about: endorsed mental health occupational therapists (OTs). Under the same Mental Health Treatment Plan, patients can access up to ten subsidised sessions with a mental health OT. For many, this type of support can be the key to regaining stability, rebuilding confidence, and managing daily life with more ease.
Mental health OTs bring a different lens to care. Rather than focusing solely on talking therapies, they support people to re-engage with daily life by helping them rebuild routines, connect with their communities, and regain a sense of identity and purpose.
This approach can be particularly effective for patients whose distress is deeply tied to everyday functioning, like a new mum overwhelmed by her changing role, or a young person finding it hard to engage in the classroom or with peers.
While psychologists play a vital role in the mental health system, mental health OTs offer a complementary service that’s often underutilised simply due to a lack of awareness.


By considering OTs in your mental health referral toolkit, you can:
• Offer more diverse and personcentred care options to your patients
• Reduce the pressure on psychologists so they can focus on higher-intensity therapeutic cases
• Support patients who might be resistant to seeing a psychologist, whether due to stigma or personal preference.
An OT’s approach is often seen as less intimidating, which can be a vital step in helping someone begin their mental health recovery journey.
There are many scenarios where a referral to a mental health OT can be particularly beneficial, especially for patients who are struggling to function day-to-day but may not need, or want, traditional therapy.
For example, a new mother experiencing postnatal anxiety may feel overwhelmed by her shifting identity, disrupted sleep, and the demands of caregiving. While she may not feel ready to speak to a psychologist, a mental health OT can support her to build structure into her day, reconnect with meaningful activities, and gradually
regain her confidence in her new role.
Similarly, a young person finding it difficult to participate in school due to anxiety or social isolation might benefit from the practical, strengths-based approach of an OT.
An OT can work with them to develop real-world strategies for managing the school environment, improving concentration, and reengaging with peers in a way that feels safe and achievable.
Mental health OTs can also play an important role in the ongoing care plan for people living with chronic health conditions. In addition to their physical health challenges, many of these people experience mental health difficulties as a result of long-term pain, fatigue, or isolation.
Referring these patients to a mental health OT can assist with goal setting, pacing strategies, and environmental modifications that empower the person to manage both their physical and mental health more effectively.
What sets mental health OTs apart is their ability to provide tailored



What sets mental health OTs apart is their ability to provide tailored strategies that promote mental wellbeing through practical change for people of all ages, abilities and stages of life.
strategies that promote mental wellbeing through practical change for people of all ages, abilities and stages of life. For patients who might not feel ready for traditional therapy, or who need support that bridges the gap between mental and functional health, mental health OTs are a great option.
The healthcare system thrives when professionals work together. Just as you might refer to a physiotherapist for physical rehab or a dietitian for nutritional guidance, OTs should be considered an essential part of the mental health care ecosystem.









Incorporating mental health OTs into your mental health referral network not only provides your patients with more options, but it ensures more people get the right help at the right time.
With the growing need for mental health care in Australia, tapping into this underutilised resource allows GPs to provide practical, compassionate care to those who need it most.
ED: Michelle Oliver is the Chief Occupational Therapist at Occupational Therapy Australia.
























Helping you deliver Better Mental Health care
Scan to learn more or visit blackdoginstitute.org.au/hp-training We're proud to be an RACGP CPD Provider in the 2023-2025 Triennium


as patient compliance of >71% over 42 months with Testogel2
PBS Information: Authority required. Refer to PBS Schedule for full information.
Please review Product Information before prescribing. The Product Information can be accessed at www.besins-healthcare.com.au/PI or telephone 1800 BESINS (237 467).
Testogel is 1% testosterone gel. INDICATIONS: Testosterone replacement therapy for male hypogonadism when testosterone deficiency has been confirmed by clinical features and biochemical tests. CONTRAINDICATIONS: known or suspected prostatic cancer/breast carcinoma; known hypersensitivity to testosterone or any other ingredient, use in women or children. PRECAUTIONS: Regular monitoring of the prostate gland and breast, hypercalcaemia, severe cardiac, hepatic or renal insufficiency, ischaemic heart disease, hypertension, diabetes, epilepsy and migraine. Risk of sleep apnoea. Effect on doping tests. Must not be used in women. Testosterone transfer to others via skin contact. Must not be used in pregnant women. Must not be used in breast-feeding women. INTERACTIONS WITH OTHER MEDICINES: Oral anticoagulants, ACTH or corticosteroids, oxyphenbutazone, insulin requirements, buproprion, cyclosporine. In general, any substance which affects liver function should not be taken with testosterone. ADVERSE EFFECTS: Reaction at the application site, erythema, acne, dry skin, changes in laboratory tests, headache, prostatic disorders, gynaecomastia, mastodynia, dizziness, paraethesia, amnesia, hyperaesthesia, mood disorders, hypertension, diarrhoea, alopecia, urticarial. DOSAGE AND ADMINISTRATION: Adult Men: 5g of gel applied once daily at about the same time, preferably in the morning. Depending on clinical/ laboratory response, the dose may be adjusted by 2.5 g steps to a maximum 10g of gel per day. REFERENCES: 1. Testogel Australian Approved Product Information, 31 March 2021. 2. Wang C et al. J Clin Endocrinol Metab 2004;89:2085–98. 3. Bhasin S et al. J Clin Endocrinol Metab 2018;103:1–30. 4. Pexman-Fieth C, et al. Aging Male 2014;17(1):1-11.

Of these deaths, 2419 (75%) were men. This is a significant gap. The deaths of Adam and Troy Selwood this year has brought it closer to home for many.
Last month saw a challenge to do 3214 push-ups in 23 days. The unusual number caught my eye – it represented one push-up for every death by suicide in Australia in 2023.
Of these deaths, 2419 (75%) were men. This is a significant gap.
The deaths of Adam and Troy Selwood this year has brought it closer to home for many. There are calls for the AFL to focus more on mental health, with the Think Mental Health Round recently held.
The State Government committed $960,000 in its recent budget to continue to delivery of mental health initiatives in the sport, including Talk to a Mate barbeques.
In medicine it can be hard to navigate. We are unlikely to achieve response to treatment if we have not got the diagnosis correct.
Estimates vary, but around 40% of those who die by suicide have no record of any mental health illness.
The elephant in the room when it comes to football – and other sports – is acquired brain damage, and chronic traumatic encephalopathy (CTE) in particular.
There is currently a class action against the AFL involving more than 100 former players who claim to have acquired a brain injury.
It is becoming more evident that there are behaviour patterns which emerge over time in those who have a history of head injury.
There is also no treatment, which in usual circumstances would prompt research into finding a treatment.
That said, prevention is key. Following the death of Richmond footballer Shane Tuck in 2020, a coroner made recommendations to the AFL that contact training sessions be limited and an independent doctor be employed at all matches to assess players after a knock to the head.
But as suicide remains prevalent among men, the difficult question arises: are we doing enough to prevent male suicide?

By Dr Matt Clifford & Dr Will Ormiston , Interventional Radiologists, Nedlands
Benign prostatic hyperplasia (BPH) is the most common cause of lower urinary tract symptoms (LUTS) in older men, significantly impacting quality of life.
While pharmacotherapy and surgical options such as transurethral resection of the prostate (TURP) remain mainstays of treatment, a growing cohort of patients are now turning toward minimally invasive, lower risk therapies that preserve sexual function and reduce recovery time.
Prostate artery embolisation (PAE) has emerged as an endovascular alternative. With mounting highlevel evidence, including multiple randomised controlled trials and long-term follow-up studies, PAE is now formally included in the British National Institute for Health and Care Excellence (NICE) guidelines and the latest American Urological
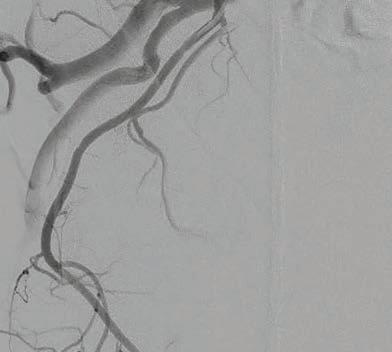
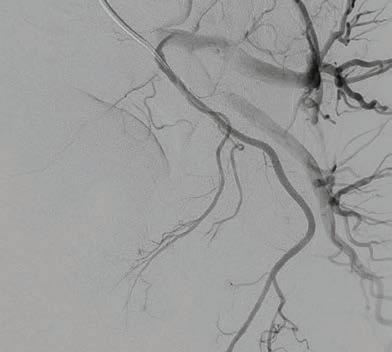
Association (AUA) guidelines for the management of BPH-related LUTS.
PAE involves selective embolisation of the prostatic arteries via a femoral or radial arterial approach, using microspheres to induce ischemia, volume reduction, and ultimately symptom relief.
Unlike transurethral approaches, PAE is performed by interventional radiologists in an angiographic suite, typically as a day procedure without the need for general anaesthesia or catheterisation.
Appropriate patient selection is critical. PAE is best suited to men with moderate-to-severe LUTS due to BPH, particularly those wishing to avoid surgery or preserve ejaculatory function.
PAE is also a valuable option for

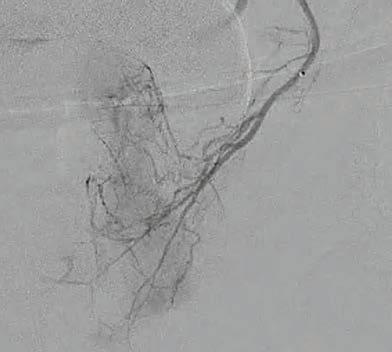


patients intolerant of medications or poor surgical candidates, including factors such as age, comorbidities, or anticoagulation status.
Severe pelvic atherosclerosis can complicate the embolisation procedure, so pre-procedural imaging may be warranted.
Generally, patients with prostate volumes over 60cc achieve more predictable outcomes. There is no upper gland size limit for PAE efficacy; the bigger the better.
Over 20 prospective studies and six RCTs – including head-tohead comparisons with TURP, pharmacotherapy, and sham controls – have been published.
These consistently show a significant reduction in symptom burden, typically a 9-21 point drop in International Prostate Symptom Score, or IPSS, alongside improvements in quality of life and preservation of sexual function.
While PAE offers a less pronounced increase in maximum urinary flow rate compared to TURP – 5–7mL/s versus 10–13mL/s – it results in fewer adverse events, very low rates of urinary incontinence and better preservation of erectile and ejaculatory function.
Post-PAE MRI findings typically show a 20-30% reduction in central gland volume and decreased vascular enhancement.
Long-term data suggest durability, with symptomatic improvement maintained in most patients at five years. Recurrence requiring retreatment occurs in approximately 20% of cases.
Repeat PAE or transition to surgical management remains a viable pathway for these patients.
the trials say
Recent high-quality randomised trials have challenged the traditional stepwise management of
PAE is an evidence-based, minimally invasive treatment for BPH-related LUTS endorsed in British and American guidelines. Trials show it is more effective than medication in improving symptoms, quality of life, and urinary function in BPH
Ideal candidates are men with large prostates and moderate-tosevere LUTS who are not surgical candidates, or seek to preserve sexual function
Effective implementation requires close collaboration between GPs, urologists and interventional radiologists.
BPH, suggesting that PAE may be considered as an early intervention, even in treatment-naïve patients.
The PARTEM trial, a multicentre phase three French RCT, demonstrated that in men with BPH ≥ 50mL unresponsive to alpha-blocker monotherapy, PAE resulted in a significantly greater improvement in IPSS, quality of life, and erectile function compared to
combined medical therapy with dutasteride and tamsulosin.
Similarly, the Australian P-EASY ADVANCE trial showed that in treatment-naïve men with moderate-to-severe LUTS and urodynamic obstruction, PAE provided superior symptom relief, improved urodynamic parameters, greater prostate volume reduction, and fewer sexual side effects than medication.
These results support considering PAE as a first-line, non-surgical alternative to long-term pharmacotherapy for appropriately selected men with symptomatic BPH.
PAE is generally well tolerated. The most common side effects are mild and self-limiting and include dysuria, urinary frequency, haematospermia and low-grade post-embolisation syndrome.
Major complications such as nontarget embolisation to bladder, rectum, or penis are rare (<1%) when performed by experienced operators using cone-beam CT and advanced microcatheter techniques.
Radiation exposure is a frequently cited concern. Contemporary studies place the effective dose at the equivalent of two to three abdominal CT scans.
While PAE is well established in Europe and North America, access in Australia remains variable, often dependent on local interventional radiology expertise and the strength of referral networks with GP's and urologists.
Local demand is growing for the procedure with most PAE centres around Australia seeing a rapid uptick in frequency, often with prior patients promoting the procedure in their social circles.
Interventional radiologists must work closely with GPs and urologists to identify suitable candidates, ensuring patients are informed of all available options and their respective trade-offs. PAE can offer patients a safe, effective and durable alternative to medication and surgery.
Author competing interests – nil




By Professor Fraser Brims, Curtin Medical School & Institute for Respiratory Health
Lung cancer accounts for approximately 9% of all new cancer diagnoses and nearly 18% of all cancer-related deaths.
The National Lung Cancer Screening Program (NLCSP) will roll out nation-wide on 1 July 2025, targeting individuals at high risk of developing lung cancer.
Lung cancer screening saves lives. Studies have demonstrated that low dose CT scan (LDCT) screening can improve lung cancer-related mortality by at least 20% when targeting a high-risk population.
LDCT identifies potential earlystage lung cancer while minimising radiation exposure. The NLCSP will target a population at high risk for developing lung cancer using LDCT to identify lung cancer at an early stage, when lobectomy may offer a chance of cure.
The NLCSP eligibility criteria include those aged between 50 to 70 years old who have more than a 30-pack year smoking history in current tobacco users, or in former tobacco users who quit less than 10 years ago.
Screening CTs will be free for participants and there are two new Medicare item numbers for the NLCSP.
Key features of the NLCSP include:
• Bi-annual screening: eligible participants undergo a LDCT scan every two years
• Primary care will play a key role in recruitment into the NLCSP and follow up of the results, with integration with the National Cancer Screening Register (NCSR)
• Risk-based assessment of nodules: most LDCTs in high-risk populations will demonstrate a nodule, but most nodules are not a lung cancer. The NLCSP will risk-assess the likelihood of malignancy of screen detected

nodules and base recommended follow up accordingly
• Integrated smoking cessation support is a critical component to realise the full health impacts of the NLCSP
• To accompany the NLCSP roll-out, the Thoracic Society of Australia and New Zealand (TSANZ) recently published guidelines for clinicians managing incidental and screen detected nodules.
Who will follow up the LDCT findings?
The medical practitioner who requested the original LDCT will remain responsible for follow up and requesting the interval CTs.
The NCSR will write to the participant and their requesting medical practitioner with the LDCT results. The NLCSP LDCT report will be synoptic – clearly stating recommended actions, both for nodule follow up and any actionable additional findings.
It is estimated that around 70% of participants screened will simply stay under bi-annual screening. Further, not all additional findings will require action or further investigations.
Using the direct experience from studies in Australia and the riskbased nodule follow up protocol, it is anticipated that only around 3% of all LDCT scans will have a high or very high nodule risk requiring further investigation by an expert lung cancer multidisciplinary team.
All other remaining nodules will have interval CTs within the NLCSP program at three, six or 12 months.
While the NLCSP is a groundbreaking initiative and the first national screening program in Australia for 19 years, its implementation is not without challenges.
Ensuring equitable access to screening across to the hardest
NLCSP eligibility criteria: 50-70 years old, 30-pack year history in current tobacco users, or former tobacco users who quit less than 10 years ago. LDCT scans will be free for eligible participants
Most LDCT scans will detect a nodule, but most nodules are not a lung cancer
An early-stage screen detected lung cancer may be suitable for lobectomy and cases should be discussed in multidisciplinary teams.
to reach populations, including Aboriginal communities and those in rural areas, is a key priority for Cancer Australia.
This will be achieved in part by the commissioning of mobile LDCT trucks, which will serve regional and remote Australian communities. WA will be the first State to have access to this service in late 2025.
unnecessary treatments is critical and, therefore, the NLCSP protocol states that patients with high-risk nodules should be referred to respiratory teams linked to a cancer multidisciplinary team.
Accurate staging of lung cancer is critical to ensure an appropriate management plan.
The complexity of investigating and staging lung cancer has increased significantly in the last 10 years. Early-stage patents may require endobronchial ultrasound bronchoscopy as FDG-PET scans have a low sensitivity with most screen detected nodules.
Therefore, a multidisciplinary approach is required to ensure appropriate investigations and accurate interpretation of results.
The recent TSANZ guidelines recommend patients are discussed at dedicated nodule multidisciplinary meetings.
Community and patient education will be essential to ensure uptake within eligible populations and
and managing expectations will be important, with simple, positive messaging.
The NLCSP is expected to have a transformative impact on lung cancer in Australia. By shifting the focus to early detection, the program aligns with broader efforts to reduce the burden of cancer, aligned with a continuing strong tobacco control policy.
Continuous evaluation of the program will be crucial to refine the protocols, optimising and expanding eligibility criteria as new insights emerge.
Advances in imaging technology and biomarker development may further enhance the efficacy and precision of a future screening program, ensuring maximum impact for Australia’s leading cause of cancer death.


Proudly hosted by the Autism Association of Western Australia, the Asia Pacific Autism Conference brings you face-to-face with some of the most influential thinkers and researchers in Autism today.







By Associate Professor Jonathan Hallett , Dr Jenny McCloskey & Dr Daniel Vujcich , Curtin University
Despite Australia's world-leading initiatives in HPV prevention, a critical gap remains in our healthcare approach that requires urgent attention. This is the disproportionate burden of anal cancer among gay, bisexual, and other men who have sex with men (GBMSM).
The incidence of anal cancer in Australia has increased significantly, rising by an average of 3.4% annually since 2010. GBMSM experience up to 20 times higher risk compared to the general population – comparable to cervical cancer rates in women prior to the implementation of screening programs.
For GBMSM living with HIV, this risk is further elevated to more than 60 times higher than the general population.
HPV infection constitutes the primary cause of anal cancer, with significantly higher prevalence among GBMSM compared to heterosexual men. Research demonstrates that persistent HPV infection, particularly with HPV16, is strongly associated with reduced clearance of high-grade anal intraepithelial neoplasia.
A study reported that HIV-positive GBMSM exhibited significantly lower HPV clearance rates compared to HIV-negative GBMSM across multiple HPV genotypes. Evidence indicates that treatment of highgrade anal intraepithelial neoplasia can reduce anal cancer incidence.
The protection gap Australia pioneered HPV vaccinations with school-based programs for girls commencing in 2007 and boys in 2013-14. While these initiatives have dramatically reduced HPV prevalence in younger cohorts, they created a significant protection gap for adults who were beyond school age when the programs were implemented.
Although vaccination against HPV
There is a disproportionate burden of anal cancer among gay, bisexual and other men who have sex with men (GBMSM)
Expanding vaccination access, improving education, and implementing systematic and innovative screening approaches, can prevent suffering and save lives
GBMSM patients deserve comprehensive attention to this preventable cancer burden.
is recommended for GBMSM up to age 45 in Australia's immunisation guidelines, it is not funded through the National Immunisation Program for individuals over 26 years.
In WA, certain healthcare providers have administered HPV vaccination "off-label" to GBMSM aged over 35 years, creating a natural experiment to evaluate vaccine effectiveness in this population.
Current evidence on HPV vaccine efficacy in adults with prior HPV exposure remains limited, though studies examining vaccination in non-HPV naive GBMSM have shown promising results.
Knowledge deficits further compound this issue. In 2019 it was reported that most HIV-positive (51.8%) and HIV-negative (68.1%) GBMSM underestimated their risk of anal cancer, with only 12.5% reporting ever having discussed anal cancer with their healthcare provider.
Understanding of the relationship between HPV infection and anal cancer remains generally poor.
Late-stage detection exacerbates poor outcomes. Factors contributing to delayed diagnosis include the absence of formal screening

programs, stigma surrounding anal symptoms, and negative experiences with healthcare providers.
Healthcare professionals need to address these gaps with urgency. Several evidence-based approaches warrant immediate attention:
• Expansion of funded access to HPV vaccination for adult GBMSM irrespective of age is necessary. Current age-based funding restrictions create an artificial barrier to prevention unsupported by clinical evidence.
• Implementation of targeted education campaigns would increase awareness among both GBMSM and healthcare providers. Many practitioners may be inadequately informed about elevated risk factors or uncomfortable discussing anal health, perpetuating knowledge gaps.
• Implementation of the recently Released Anal Cancer Screening Guidelines for people living with HIV (2025) from the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM). These provide a crucial framework for systematic screening and recommend that gay, bisexual and other men who have sex with men and trans women living with HIV over age 35, as well as other people living with HIV over age 45, should be offered primary high-risk HPV testing with cytology triage every three years for those who test negative for high-risk HPV.
• Self-sampling methods for HPV testing demonstrates significant potential. Recent research has validated that self-collection of anal specimens shows high concordance with cliniciancollected samples.
Author competing interests – nil
By Dr Talia Steed, Holistic Author, Perth
Patient, problem, investigation, diagnosis, treat and repeat. Our conditioning to operate within the context of western medicine is a model operating from an outdated framework.
The pendulum shifted from the preenlightenment era from mysticism to rationalism – over-emphasising biology over our psyche and soul.
The human body, our biology, is not just influenced by the foods we eat, our genetics, DNA, or by whether we smoke or drink alcohol. While relevant, these are only part of the puzzle of symptoms and illnesses that affect us.
Perhaps it is time to reflect on the notion that if we are getting the same outcome, it is foolish to keep taking the same action.
When we take a glimpse into life around us, we see how much people are suffering, sick and facing health battles of the body and mind. From serious diagnoses like cancer and those deemed incurable, to chronic relentless symptoms like gut issues or non-specific lower back pain.
A healthcare revolution
People are crying out for something different, a revolution in healthcare.
Surely with our preoccupation with evidence bases, to assess just how well our current model is serving us, the evidence is something we need to pay attention to.
It may be the deeper questions that we need to start asking patients, those without a quick fix solution. For instance:
• Do you feel connected and seen within your relationships?
• Do you feel valued for the contribution you are making, whether in your vocation or life situation as a parent, partner, child or friend?
• Do you feel chronically lonely, isolated or disconnected from yourself or those around you?
• How do you feel about yourself as a person?
• Are the people in your life aligned with you?
• Are you holding on to any hurts or regrets from the past or anger towards yourself or another?
• When was the last time you experienced pure joy?
For these are what truly impact our health and wellbeing. Would that gene turn on if we felt connected rather than isolated? Would the chronic symptoms continue, if we


When we can walk alongside our patients as equal human beings, we can awaken their ability to uncover the healer within
It is the deeper questions related to our experience of life, that are far more connected to our state of health and wellbeing.
felt at peace rather than constantly on hyper-alert?
Would our system be able to settle, if we slowed down the pace of our lives, rather than living as if we were running an Olympic 100m sprint?
Beyond Western medicine
There is so much more to health and healing than what we have been conditioned to consider.
Many outside of Western medicine have been turning to other avenues like reiki, acupuncture, Chinese medicine and Indigenous wisdom.
If you asked an Aboriginal elder what might be affecting our health and wellbeing, they may encourage you to consider the impact of spirit or unseen forces at play.
Wouldn’t it be far more helpful as doctors to educate and support patients to discover whatever tool or modality would be most helpful, with an attitude of open-minded discernment?
There are polarities within all professions, all modalities have the good and the bad. It is not someone's professional standing that dictates the behaviour of a person, but rather the qualities of their character beyond status or role.
And so, it is time to open our eyes to this reality. To let go our collective ego attachment to being at the top of some illusory health and healing pyramid, and to find our humility to support society to find the middle ground.
Author competing interests – nil
By Mr Kaushalendra Rathore, Cardiothoracic Surgeon, Nedlands, and Dr Manju Rathore, GP, East Victoria Park
Infective endocarditis (IE) is an uncommon but fatal infection that targets the endocardium, especially around the inlet-outlet cardiac valves.
In 90-95% of patients aetiology is bacterial and the rest can be a fungal organism. Often severe IE is seen in high-risk patients with a history of various systemic co-morbidities. These cases are managed with the highest suspicion and often get early referral for further evaluation.
However, there is a sizable subset of the patient population at low risk who may get inappropriately delayed diagnosis.
A 21-year-old male patient presents with night sweats, weight loss –15kg in the last couple of months –and low grade fever.
Patient was non-alcoholic, non-smoker with no history of recreational drug use. Initial working diagnosis was haematological malignancy and he was admitted under medicine ward.
Trans-thoracic echocardiogram (TTE) showed large aortic root abscess with fistula from aortic valve leaflet to anterior mitral leaflet with severe aortic regurgitation (Figure 1).
Blood cultures were positive for Streptococcus Paragenisus and intra-venous antibiotics were started as per culture sensitivity. Although there was no clinical feature of stroke, multi slice computed tomography (MSCT) angiogram revealed multiple mycotic cerebral aneurysms (5mm) with embolic manifestation in right middle cerebral artery and left parieto-occipital artery.
Abdominal scans showed renal and splenic infarcts. Mycotic aneurysms were managed with endovascular coiling and the patient was taken for an early high-risk cardiac surgery.



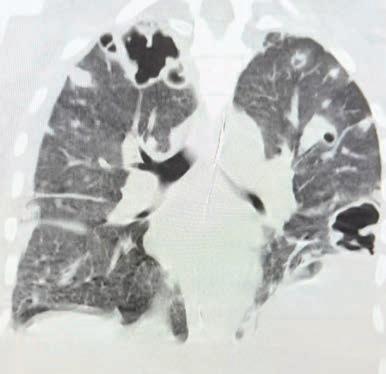
With improving healthcare and overall social awareness, nosocomial microbe (Staphylococcus and Streptococcus) associated infections are down trending, but healthcare associated infections from prosthetic implants, cardiology interventions, haemodialysis, chemotherapy ports, for example, and intra venous drug user-related IE is on the rise (Figure 2).
Even asymptomatic patients undergoing dental procedure (7.9%), gastrointestinal intervention
(3.4%), colonoscopy (3.3%), and urogenital intervention (2.8%) in the last six months are at risk of bacterial colonisation and IE.
The most common site of infection is the aortic valve (49.5%) followed by the mitral (42.0%), tricuspid (11.4%), and pulmonary (2.4%).
A white cell count of >10535/ mm3, CRP of >85mg/dl and procalcitonin of ≥ 0.4ng/mL should be considered red flags.
There is a 27-fold higher risk of inhospital mortality in undiagnosed patients with high biomarkers. Thus, keep a high clinical suspicion when a low-risk patient presents.
Serology: 10-20% of patients have negative blood culture and reported long-term mortality is higher compared to culture positive patients.
Two thirds of the culture negative cases can be diagnosed with steadfast refining serology –indirect immunofluorescence assays, indirect fluorescent antibody tests [IFAT], enzymelinked immunosorbent assays [ELISA], complement fixation tests and molecular techniques (PCR). The first step is ruling out zoonotic organisms, such as Q fever, Bartonella species, Mycoplasma species, Legionella species, using serological testing, followed by
running a PCR test to find a specific microbe.
If all these tests are negative then focus can be placed on autoimmune diseases – marantic endocarditis – and antinuclear antibodies or rheumatoid factor should be assessed.
Newer procedures like molecular techniques such as fluorescence in situ hybridisation (FISH), Quorum sensing detection, 16S rRNA PCR and metagenomic sequencing can be useful.
Echocardiography: TTE have very high sensitivity and specificity to diagnose IE and should be used as the first line. Echocardiogram not only shows mechanical complications such as large vegetations, destructive lesions, valve aneurysm, prolapse, chordae rupture, abscess, pseudoaneurysm, and/or fistula formation, but can also assess cardiac functions.
However, it is not so specific in slow growing infections and may require further investigations.
Radiology and nuclear imaging: MSCT and nuclear imaging –18F-fluorodeoxyglucose positron
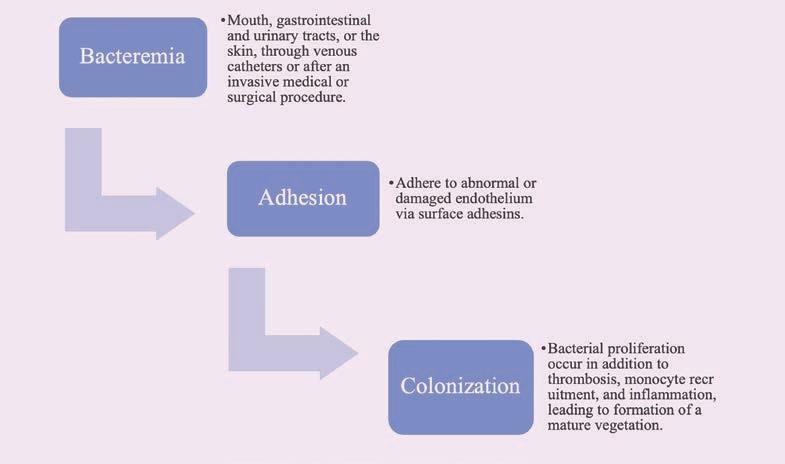
emission tomography/computed tomography [FDG-PET/CT] –and leucocyte scintigraphy with single-photon emission computed tomography/low-dose CT are other modalities to assist in decision making.
FDG-PET/CT is good for the patients with prosthetic valve endocarditis and patients with extra cardiac infectious complications. A positive signal at the site of
prosthetic valve, if implanted less than 3 months back, is highly suspicious of IE.
When to involve a specialist?
Multi-disciplinary consensus should be made by involving a cardiologist, infectious disease physician and surgical team in any patient with persistent signs and symptoms of IE.
Author competing interests – nil

By Matt Tilley, Curtin University & Clinical Psychologist, West Leederville
ADHD has rightly gained much attention in recent years, with around one in 20 Australians receiving a diagnosis. Presentation is marked by a persistent pattern of hyperactivity/impulsivity and/ or inattention negatively impacting the persons executive function and day-to-day experiences.
In adults, disruptions and difficulties are typically seen with the person's personal relationships and work experiences.
There are three types of ADHD – hyperactive/impulsive type, inattentive type, and combined type (a mixture of both).
Impact ranges from mild to severe. Although research is inconclusive with no absolutes, men seem to be more likely to exhibit externalising symptoms and be diagnosed with the hyperactive/impulsive type, and women seem to be more likely to exhibit internalising symptoms and be diagnosed with the inattentive type.
Research into transgender and non-binary people is even less clear.
Typically, the hyperactive/ impulsive type is characterised by constant fidgeting, restlessness, a tendency to talk excessively, and impulsive behaviours like interrupting and acting on thoughts or feelings without consideration. These symptoms are often more noticeable, making diagnosis easier.
While women are more likely to be diagnosed with the inattentive type, men can also experience these difficulties. This ADHD type is characterised by disruptions with cognitive focus and attention (distractibility), listening skills, and difficulties with organisation.
The combined type is most prevalent, characterised by a mixture of the symptoms discussed above, a combination of hyperactivity and impulsivity symptoms plus inattention and distractibility.
Although ADHD is usually associated with hyperactive

behaviour, an adult can still have ADHD without being hyperactive.
As ADHD is a childhood-onset disorder, people would have had symptoms when they were younger, even if not diagnosed or realising it. Consequently, it’s common for men to report feelings of shame, embarrassment, and inadequacy which can foster beliefs about their abilities as adults which may not be true.
These feelings and experiences may be further intensified if he was undiagnosed.
For example, we know that children with ADHD can experience disruption in attention and impulsivity. The impact on their schooling can be significant; commonly represented by disorganisation and forgetfulness, poor academic achievements, and experiences of behavioural misconduct.
These experiences are often met with negative attention from both parents and schools, for example frustration, scolding, messages of inadequacy, and even punishment.
It is not uncommon for people with ADHD to report beliefs about themselves representing an internalisation of these experiences, thus shaping their adult beliefs and experiences.
Men with ADHD are more likely to experience low frustration tolerance or irritability; frequent mood fluctuations/dysregulation; forgetfulness/often losing things; heightened distractibility; time management difficulties; often ‘on the go’ acting as if ‘driven by a motor’; excessive talking and interrupting; stimming behaviours (dopamine seeking); masking (acting in socially expected ways to fit in); rejection sensitivity dysphoria; negative self-image; hyper-focus; object constancy; sleep disruptions; and fatigue.
An adult can still have ADHD even if they’re not hyperactive
Not everyone with ADHD was diagnosed as a child, and a late ADHD diagnosis can be positively life changing
There are many symptoms that can highlight an undiagnosed ADHD presentation; the ASRS-v1.1 psychometric test (free online) can offer clarity.
In addition to well documented issues with relationship disruption and work or career stress, research indicates that compared to the general population men living with ADHD may be more likely to experience a higher number of sexual partners; more STI diagnoses; potentially risky hyper-sexual activities like sexual compulsivity and addiction; increased experiences of online risk behaviours; premature ejaculation; and Male Hypoactive Sexual Desire Disorder.
Of course it’s not all negative, and it’s important to remember that there are also some common



ADHD ‘superpowers’ like being empathetic, enthusiastic, spontaneous, creative, intuitive, imaginative, innovative, problem solvers, adventurous, and hyper focus on interests.
Despite these reported difficulties, many men with ADHD thrive and learning about their ADHD can be positively life changing. Having ADHD does not define the person’s intelligence, strengths, capabilities, nor achievements.
Diagnosis, treatment, and support for men with ADHD can assist them to manage their symptoms, build and maintain healthy relationships, and achieve their work and career goals.
A multimodal approach is the most effective way to manage everyday life and behaviours associated with ADHD, with an aim to improve the management and experiences of the core symptoms, improve functioning, and increase wellbeing. Therefore, consider a combination of psychoeducation, psychotherapy, and pharmacotherapy.
Psychoeducation assists to increase understanding of ADHD symptoms and experiences, and improve communication skills and time management, for example.
Evidence based psychological therapies like Cognitive Behavioural Therapy, Dialectical Behavioural Therapy, and potentially EMDR, can assist men to process their experiences of living with ADHD. There are several types of pharmacotherapies used to help manage ADHD symptoms. Stimulants are the most widely used and can work quickly but have side effects and finding the most effective regimen can be trial and error.
Although a good option for many, medication does not necessarily address all ADHD symptoms, and not everyone responds well to them.
Author competing interests – nil
By Dr Arpita Ghosh, Gynaecologist & Fertility Specialist, Nedlands
Historically, women have carried the stigma of infertility alone on their shoulders. However, men and women are just as likely to contribute to a couple’s infertility and male infertility needs to be investigated right from the very outset.
Sperm count from seminal fluid analysis is a crucial indicator of male reproductive health. When couples seek conception or face fertility challenges, sperm count is often the first parameter evaluated in males.
Although it is possible to conceive naturally, a reduced sperm count means there is statistically less chance to become pregnant. Numerous studies suggest a decline in sperm counts among men in Western and other countries over the past decades, with proposed contributing factors including environmental pollutants, lifestyle changes, and rising obesity rates.
But how robust is the evidence? What are its implications?
Although spermatogenesis naturally decreases with age, evidence clearly shows that even young adult males have been greatly affected by declining sperm counts.
Environmental and lifestyle factors emerge as primary culprits in the reported declines, including:
• Exposure to endocrine-disrupting chemicals (EDCs) such as phthalates, pesticides, and bisphenol.
• Longstanding stress and mental health issues – studies indicate chronic stress can disrupt testosterone and other hormone levels, negatively impacting spermatogenesis. Unhealthy coping mechanisms like smoking, excessive alcohol consumption, or poor dietary habits and stress can amplify negative health outcomes, causing further decline. High BMI and sedentary lifestyle also impact fertility.


• Chronic disease such as diabetes mellitus, hypertension, hyperlipidaemia and complications related to cancer treatments are linked to lower sperm counts. Some medications can also impair sperm function.
• Sexually Transmitted Infections – according to World Health Organisation (WHO), the number of STIs around the world is increasing, with chlamydia, gonorrhoea, syphilis and trichomoniasis being responsible for more than one million infections daily in adults aged 15-49 years. Men with leukocytospermia from STIs can have significantly decreased semen volume, concentration, total motility, progressive motility and abnormal morphology.
Male infertility, closely tied to sperm count, incurs rising social
and economic costs. From an environmental standpoint low sperm counts correlate with conditions like cryptorchidism, hypospadias, and testicular cancer, suggesting that prenatal exposures and environmental factors can have prolonged effects on male health.
Geographic and lifestyle disparities further highlight how urbanisation, environmental degradation, and socioeconomic conditions shape reproductive trends.
As natural conception becomes more challenging, the demand for assisted reproductive technologies (ART), including in vitro fertilisation (IVF), has risen. This shift not only places emotional strain on couples but also raises financial burdens.
Despite mounting evidence, some researchers challenge the extent of sperm decline due to potential biases in volunteer selection
A significant global decline in sperm counts over the past four decades has global implications for male reproductive health
Assisted reproductive technologies have helped address infertility, a more definitive solution involves prevention with public health strategies, policy changes, and individual behavioural modifications
Future studies should focus on identifying causative mechanisms and evaluating intervention efficacy to safeguard reproductive health for future generations.
criteria, differences in laboratory standards, and heterogeneity in study designs.
Another key debate revolves around the role of environmental

and declining sperm quality means ongoing research is needed to clarify the extent, causes, and long-term consequences of this phenomenon.
A multifaceted approach is urgently required to mitigate the reported sperm count decline. Five main strategies can help address declining sperm counts:
Education: including incorporation of reproductive health topics into school curricula, emphasising the impact of environmental and behavioural risks, highlighting prevention and early treatment of chronic diseases and encouraging healthy habits like regular exercise, balanced nutrition, avoiding smoking and excessive alcohol.
Public health campaigns: including awareness campaigns on lifestyle and environmental risks, promoting healthier habits and raising awareness of the reproductive risks associated with occupations involving EDCs.
Medical interventions: including advocating for routine screenings
for metabolic and reproductive health, addressing male factor infertility earlier, and diagnosing potential issues before couples spend years trying to conceive.
Policy and environmental regulations: Advocating for statutory restriction of exposure to harmful chemicals in occupational and consumer settings and for safer workplace practices for men in high-risk professions.
Fertility preservation: Promoting sperm cryopreservation for individuals at risk.
Author competing interests - nil
Prostate
Infective
Referring to a mental health
Addressing fertility knowledge gaps
Weight loss drugs and obesity in men
Social media and men’s mental health
Holistic Approach to bariatric surgery
Managing ventricular tachycardia
Bangarra Dance Theatre’s latest work explores light in the Kimberley through movement.
By Ara Jansen
The light and night sky of the Dampier Peninsula is the focal point around which Bangarra Dance Theatre has created their latest work.
Titled Illume, it is the world premiere of Australia’s leading Indigenous performing arts company's first-ever visual arts collaboration. Illume will be staged at the Heath Ledger Theatre from July 10-13.
Illume’s WA connection is that it’s a collaboration with Goolarrgon Bard visual artist Darrell Sibosado, who hails from the Djarindjin/Lombadina community on the Dampier Peninsula. Darrell is known for his prints and installations, including large scale LED light works.
Illume draws together music, visual arts and dance to explore


the ways light has captivated and sustained Indigenous cultural existence for millennia. Alongside Bangarra artistic director Frances Rings, the company worked with Darrell exploring this theme alongside how artificial light has disrupted ecosystems and obscures the darkness of the night sky, devastating First People’s connection to sky country.
Bangarra dancer Maddison Paluch says it’s the biggest show the company has ever staged and one that the whole company has been involved in from conception through to the first performance.
“Darrell has done dance and has a beautiful understanding of and a care for us as dancers,” Maddison says. “He worked with us, and it has been special to hear his point of view and how important he believes our role is in the space.”
While creating Ilume, the company’s rehearsal room was covered in research – photos of Lombadina, notes, drawings, writings. Maddison says this helped connect with country as they worked on the other side of Australia.
“It helped us see and feel all these different elements, get a new sense of the world and a feel on country while exploring different stories from a different part of the country.”
The sets and images from Illume are a fiery red, which Maddison says pay homage to our pindan red dirt, sometimes echoed in the sky at sunset.
“I’ve always had a sense of country on stage with the designs because there are always elements of it.
“With this show the light is really impactful in telling the story and connecting to Darrell’s artwork which draws us into country, taking us to a whole new level.
“It has been interesting to watch him interpret things to show us how country has its own rhythms and
that human forms should adapt to that rhythm rather than trying to change it. We just kept going back to that as the work is evolving.
“Light can be harsh or healing. There’s a section in the piece called Light Pollution and it explores the impact on the rhythm of country when the light isn’t clear.
“As a dancer it was exciting to connect with different mobs and hear their stories and to find places we could connect.”
A life-long dancer, Maddison says one of the joys of dancing with Bangarra is that she is constantly learning and connecting with new aspects of culture and country.
“It has challenged me on perspective and has opened my eyes to a wider view. I’ve been inspired to continue growing and keeping my eyes wide open to be educated and understand better.”
Illume is at the Heath Ledger Theatre from July 10-13. Tickets from www.artsculturetrust.wa.gov.au

A new film following a neurologist on a shift that will change her life forever will show at this year’s Hurtigruten Scandinavian Film Festival. Second Victims is a Danish-set medical drama starring Trine Dyrholm that offers a timely reflection on the challenges faced by healthcare professionals today.
The film explores the weight of guilt and the power of compassion. We’ve got five double passes to giveaway. The Scandinavian Film Festival runs from 24 July – 13 August at Palace Cinemas Raine Square, Luna Leederville and Luna on SX.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.

Are you in need of a luxury winter getaway complete with wine tasting and a gorgeous vineyard setting?
Ampersand Estates in Pemberton is giving one lucky Medical Forum reader the chance to win a two-night stay in the winery’s most luxurious property, The Homestead.
Worth $4600, the stay comes with a locally sourced breakfast hamper and a sit-down wine tasting experience at the Estate’s cellar door.
Rated the top winery to stay at in WA by Australian Traveller and Business Traveller last year – and one of the top nationally –the South West gem offers award-winning wines, gourmet food and unique spirits.
The Homestead, situated alongside the Donnelly River, offers five bedrooms with a king-sized bed and ensuite, as well as a cosy lounge and library.
Unwind in the peace and quiet of your own home away from home, or venture out to some of the nearby attractions including the Karri Valley, Pemberton Town, Yeagurup Dunes and Beedelup Falls.
To enter scan the QR code or go to mforum.com.au and hit the competitions tab.







It is always exciting to review new wines and indeed a pleasure to experience the wines from Ampersand Estates.
The first thing that intrigued me was their name. Ampersand is the name of the symbol we use for ‘and’ (&). To quote co-owner Corrie Scheepers “and is much more acceptable than ‘or’ or ‘but’.” Their philosophy is we shouldn’t have to choose – we should have it all.
The Estate is located between Pemberton and Nannup amongst the magnificent Karri forests and the Donnelly River. Originally Donnelly River Wines, the property has been revitalised by Corrie and co-owner Melissa Bell.
The 20 hectares of vineyards focus on Sauvignon Blanc, Chardonnay and Pinot Noir – varieties for which the region has become well known. They also lease another Pemberton vineyard and source fruit from Frankland River, which offers varieties like Syrah, or Shiraz, which are not as suited to the Pemberton region.
Wine making is contracted out to the skilled hands of Rob Mann.
The Pemberton Estate offers wine tasting, accommodation, and hosts events and weddings. On-site the Rainfall Distillery produces Gin and Vodka and soon the addition of a Gin Botanicals garden will add a further unique dimension.
My next visit to Pemberton will certainly include Ampersand.

Ampersand Estates, Pemberton, Sauvignon Blanc 2024 (RRP $36)
A vibrant wine, the aromatics are amazing. Fresh guava, herbaceous green pea and tropical pineapple leap from the glass, backed by minerality and crisp acidity. A fresh 12% alcohol and easy drinking style, this will give pleasure for another year or two.
Ampersand Estates, Pemberton, Esperluette 2022 (RRP $80)


Esperluette is French for ampersand. This is a limited release wine, only produced in 2022 and 2024. The 2022 is an interesting blend of Merlot – just dominant at 53% – Petit Verdot and Cabernet Sauvignon, just 5%. It displays a ruby colour with a purple meniscus. The palate is harmonious, supple and mellow. Merlot adds velvet fruitcake characters and herbal elements, while Petit Verdot, often called the winemakers spice, adds tannic structure. The touch of Cabernet gives a bit more weight. A great food wine that will drink well for eight or 10 years.
Ampersand Estates, WA, Pinot Noir 2022 (RRP $56)
Ampersand Estates, Pemberton, Pinot Noir 2024 (RRP $60)
The 2024 vintage was warm, dry and early. The berry size was smaller, giving great flavour concentration. This is a terrific Pinot. It shows a brilliant beetroot red colour, the nose gives fresh vibrant red fruits of cherries, strawberries and plum. A lighter, fresher, brighter style when compared to the 2022 Pinot. Wonderful drinking now and will be good for three or four years.
Ampersand Estates, Frankland River, Syrah 2024 (RRP $50)
From Shiraz sourced from Frankland River, this wine displays a youthful deep garnet colour, the nose is spicy and shows cardamon and blackcurrant. The palate, sweet fruited and supple, include flavours of spices, black olive and mulberry. Very enjoyable and will reward for a further six-to-eight years.
A wet winter and spring resulted in moderate fruit set and lower yields, A cooler summer and late vintage gave good acid levels, fine tannins and wines of elegance. This wine has an attractive deep crimson-purple colour, the nose is exotic, spicy and ethereal. More complex than the 2024, the palate is elegant with black cherry and cranberry, alongside background flavours of cinnamon and bramble. Tannins are fine and elegant, firm acidity binds this wine together structurally. This is a very complete Pinot, drinking beautifully now and with the structure to give quite a few more years.


Seven strangers use boxing and writing to heal their life-long trauma in a confronting and moving Australian documentary.
Seven survivors of childhood sexual abuse respond to a call-out to take part in an experimental recovery program.
Designed by Melbourne boxing coach, academic and survivor Donna Lyon, a program called Left Write Hook addresses both the physical and emotional impacts of trauma through a unique combination of the physical release of boxing and the emotional outlet of creative writing. What began as an eight-week plan for female and gender diverse participants becomes much more. Then over 18 months, with intimate and privileged access, filmmaker Shannon Owen documented the journey and the bonds this group forged that led to unexpected transformations.
The program aims to provide survivors of sexual abuse with a unique space to both physically and verbally tap into repressed memories and the associated impacts of trauma, allowing them to begin reclaiming their bodies and minds, and imagine new lives for themselves.
The witnessing documentary, also named Left Write Hook and now on Netflix, is a powerful and timely exploration of resilience, expression and healing that redefines what it means to be a survivor of childhood sexual abuse in Australia.
By Ara Jansen
Nikki, Dove, Pixie, Gabby, Claire, Julie and Lauren respond to the call to break their silence. Despite different life journeys, they all share the experience of living as adult survivors. Most have never disclosed their abuse outside of a therapy session, let alone with other survivors. When they arrive to start Donna’s program, they are presented with a unique opportunity for recovery but also a huge risk. Fear and shame initially unite them, uncertain of where the process will take them.
Documentary maker Shannon says Left Write Hook is motivated by opportunities for bearing witness and re-storying experiences rather than excavating trauma memories for evidence sake.
“It was a corridor conversation with Donna – we’re colleagues at the University of Melbourne – where she started telling me about the workshop program,” says Shannon. “The boxing came from her own history as something that helped her in her own struggles. I really loved boxing as a way to process trauma and the writing part appealed to the storyteller in me and my creative background.”
While largely done in documentary style, there are some interestingly creative moments where Shannon
and her team have translated each of the women’s journeys in a way which helps them take back a piece of their power.
One woman sings, another tromps through a miniature city like Godzilla reclaiming her power, while a third transcribes her words onto a black wall with white marker. Video diaries are used as a stark insight into what it’s like to live with trauma for those with no experience of it.
“There’s definitely something profound happening for these women and I was keen to figure out how to capture that on screen. I’m also interested in the potential of film as a transformative tool in and of itself, rather than just bearing witness. How do you take filmmaking and push it somewhere positive?
“These women are different people to when I first met them. To do that in front of an audience is pretty radical. There’s something amazing about the lived experience and the healing that happened in that space. I’ve seen the scenes so many times and I’m still moved by it.”
WEMBLEY
Full/Part Time VRGP
•GP Owned
•Fully Computerised
•Well-Equipped Treatment Room
•Full-time RN support
•Mixed Billing
•Centrally Located
•Long Established
•Accredited/Teaching Practice
We are a small, friendly, family orientated practice of four General Practitioners located in Wembley and we’ve been here for a long time! We are an accredited practice who takes pride in our reputation as a practice who looks after their patients and their staff. We seek a VRGP to join a great bunch of people who are more like family than colleagues.
Our well-respected, experienced team can offer flexible sessions in a wellsupported environment.
Cherie:
Phone 08 9387 5000
Email office@wfmp.com.au
WINTHROP
Full-Time General Practitioner
Full-time GP position in Winthrop
To replace departed Male GP and long-established GP also reducing hours
Private Billing Practice
(BB children under 16)
Well established small but busy General Practice of over 30 years in ideal location.
Individual large room available in comfortable and relaxed setting
Fully Accredited
Appreciative Patients
Full Nursing Support with well equipment treatment rooms
On site Pathology.
Please contact Sharon at Hatherley Medical on 08 9310 4400 or email admin@hatherleymedical.com.au for further queries.

COMO
Opening for VR GP - F/time or P/time
Full Private List Available
FRACGP essential
Up to 70% private billings
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs.
Enjoy working for a doctor-owned, non-corporate, well support, and accredited practice.
Please contact the Practice Manager on 6165 2444 or email: reception@comogp.com.au

General Practitioner
$200 – $300 per hour
6-7 sessions available.
Excellent working environment, with modern facilities.
Quality nursing staff and an onsite non dispensing pharmacist.
Adjacent to the practice we have a pharmacy, and allied services, consisting of audiology, pathology, physiotherapy, podiatry, dental, and cardiology.
Visit our website: www.thirdavenuesurgery.com.au
If interested contact Practice Manager Rachael Hadlow via email: rhadlow@3rdave.com.au
BECKENHAM
•70% Mixed Billing or AUD
$180 per hour for the first 3 months
•Permanent, Full-Time
•VRGP
•Relocation allowance negotiable
•DPA MM1
Our small, friendly, accredited and wellestablished family practice is seeking an experienced VRGP who is ready for a challenging but satisfying full-time career that offers a great work-life balance. Our GPs enjoy a loyal and varied patient base and have the opportunity to build long-term relationships with the patients and their families. Beckenham Medical Centre has easy access to public transport, private parking for the staff and has close proximity to allied health and hospitals.
OFFER DETAILS
•Permanent position
•Full-time
•70% of Mixed billings or AUD
$180 per hour for the first three months
•Large and varied patient base
•Full-time Nursing support
•Well-equipped Consult and Treatment room
•DPA MM1
•On-site Pathology & Pharmacy next door
•Relocation allowance negotiable for the right candidate
•Open hours:
Monday to Thursday 8.30 am- 5.30 pm, Friday 8.30 am-5.00 pm and Saturday 9.00 am-12.30 pm
ELIGIBILITY CRITERIA
•Should hold General or Specialist Registration with AHPRA
•Unlimited working rights in Australia
•Must have competed FRACGP or FACRRM
For more information please contact our Office Manager, Shabana on 08 9451 2722 or alternatively, send through your resume to accounts@beckenhammedicalcentre.com.au

We are seeking a VR GP on an either full time or part time basis, who would love to join a great bunch of people whom are like family more than colleagues. We would love to offer 90% of billings for the first 3 months and then 70% thereafter.
We are a small practice of General Practitioners located in South Perth. We take pride in our reputation as a practice who looks after their patient and staff. Our well-respected experienced team can offer flexible sessions in a wellsupported environment.
GP owned
Fully computerised
Well Equipped Treatment Room with RN support
Mixed Billing
Central location – 10 min from CBD
Accredited Practice
Please email docthet@gmail.com or call (Pat, the Practice Manager) on 0431 909 221 or call 9367 7840

GPs and Nurse Practitioners with a passion for older Australian’s health and wellbeing wanted.
We Offer:
•Flexible days and hours
•Convenient location
•Competitive remuneration
•Relaxed and supportive environment
We will work around your preferences to suit your goals / lifestyle, if your circumstances change, we’ll adapt. About us:
Sage Medical Consulting is a group of GPs who are committed to practicing “slow” medicine – that is unrushed, quality and tailored to the patient. No matter where you are in life, if you want a compassionate and thoughtful approach to your care - we are your partners to lifelong health.
Expressions of interest to admin@sagemed.com.au or call Practice Manager Jackie on 0401 681 495
General Practitioner
(Full-time or Part-time)
Immediate start, $200/hour minimum guarantee (first 3 months), then 68% of billings.
We are a busy, GP-owned, non-corporate practice seeking a motivated and caring GP to join our friendly and supportive team. Whether you’re looking for full-time or part-time work, we offer flexibility, excellent earning potential, and a positive team environment. You’ll be stepping into a practice with full books, and we’ll open to new patients once you start.
Key Features:
•Pathology onsite
•Excellent nursing and administrative support
•Wide variety of patients and strong demand
•Family-friendly, flexible working hours
•Practice is happy to support special interests
•Team-building activities and supportive culture
•Opportunity for your own consulting room if full-time
About You:
Vocationally Registered (FRACGP or equivalent), AHPRA registration, Strong communication skills and a collaborative mindset.
Please email your CV to Debi practicemanager@balcattafamilypractice.com.au or call 6478 3955 for a confidential discussion.

Spencer Road Family Practice is seeking an enthusiastic doctor, who thrives in a busy general practice.
Avoid long commutes and work close to home in the foothills of Perth’s South-East. Choose your days, set your own hours, and take home 65% of billings.
We have room availability Monday – Saturday.
The practice is open from 8am to 6pm weekdays.
8am to 1pm Saturdays, 8am to 12pm Sundays and Public Holidays. We only close on Good Friday and Christmas Day.
We currently have 10 GPs, 4 Nurses, a visiting Podiatrist & Dietitian and a Clinipath Pathology located within the practice.
Our patient’s range from the very young (we have an antenatal GP) to the elderly (some of our GPs have practised in this area for over 30 years)
For more information or to apply, please contact our Practice Manager, Paige on (08) 9493 8388 or send your resume to practicemanager@srfp.com.au
Contact Rita, rita@mforum.com.au or phone 9203 5222 to place your classified advert









The Age Less Clinic and General Practice Claremont has space available for a patient minded General Practitioner to be part of our vision for the very best, whole of patient care.
We want to work around your goals and lifestyle so this could be the opportunity you’ve been waiting for.
We are currently an independent solo practice with a fully booked functional GP, established medical and allied health referral base and experienced nursing support.
BENEFITS:
• Flexibility and support guaranteed for the right fit.
• Heritage building with generous consulting rooms, off street parking.
• Prized location.
Suitable for niche complimentary general practice fields. Practitioners in sports medicine, aesthetics, integrative, occupational and aviation medicine, hormone health, acupuncture, hypnotherapy, medicinal cannabis, weight loss would be complimentary to the current practice.
The Age Less Clinic would also welcome the interest of experienced mainstream general practitioners wanting a clinic within which to contribute to a unique culture and whole of patient focus.
For more information or to apply please contact Dr Aparna Hegde on 0408 888 790 or aparna.hegde@theagelessgp.com.au





MURDOCH WEXFORD MEDICAL CENTRE –CONSULTING ROOMS AVAILABLE FOR SESSIONAL RATE
Fully fitted including sink
Includes use of waiting area, staffroom/kitchen $250 per half day session
Reception/patient check-in support available for additional fee.
For further information or to arrange inspection please contact: admin@wocwexford.com.au




Development Approved for Medical Centre
Estimated completion August 2026
Excellent street frontage exposure
27 Parking Bays
We are seeking Expressions of Interest from experienced medical operators for:
Medical Centre 495m2
Pharmacy 200m2
This exciting site offers plenty of traffic exposure and convenience making it a key location at the northern entry to the growing communities of Anketell, South Wandi and surrounding areas.


Prime City Medical/Consultancy Space* – established since 1898! Take advantage of the character of the Boladeras Building, built 1898 & just a short distance from the Murray St Mall.
With plenty of pharmacies, medical centres, dentists, physios, and allied health services, this office would suit a medical business well, bringing you into the heart of the City* (subject to council approval).
Full
Double French doors onto balcony provide
Onsite parking
GP, Physio and Psychology in same building
Includes use of waiting area, kitchen
$200 half day; $300 full day
Admin support available for additional fee Please

Set up now to take advantage of the City Centre University campuses & Student Accommodation soon to open (estimated 1st Semester 2026). 180sqm (approx), set over 2 floors with large open display room, service area & 2 separate appointment rooms downstairs.
1st floor has an office and open plan area with male & female toilets. Designated parking for 1 car off private, gated laneway adjacent to the building.
Plenty of foot traffic passing by, client parking available in nearby Wilson & CPP Parking.
East End revival is happening! Make this space your own (STCA if required).
Rent from $300psqm + GST = $54,000p.a + GST
Budget Outgoings = $26,000p.a + GST
Parking $300 per bay/pcm + GST * Subject to council change of use approval
to arrange private inspection

























Every home we design and build starts with listening. We listen to your vision, your lifestyle and your budget. Then we translate that knowledge into thoughtful spaces that are beautifully crafted. By integrating architecture, interior design and construction, Humphrey Homes makes creating your forever home harmonious and stress-free
“We wanted the building process to be an enjoyable one, and Humphrey Homes made sure it was. They earned our trust early and never gave us a reason to question it. The outcome speaks for itself, but it’s the quality of the journey that sets them apart.”
- Simon and Deborah, City Beach