







Dr Ushma Narsai Avant member

anddeductions for








With general practice becoming more expensive, public hospitals under strain and workforce pressures showing no sign of abating, one thing is for certain, the State Government cannot afford to get it wrong.
Andrea Downey | Managing Editor
We’re one election down for the year and WA Labor have had another landslide victory, but now the hard work begins.
Health is clearly high on the re-elected Cook Government’s agenda with the creation of two new health portfolios and the appointment of a new Minister for Health, Meredith Hammat.
But will it be enough? Some have voiced concerns about Ms Hammat’s inexperience as a minister, while others are more confident she can deliver given her trade union background.
The election campaign saw some big promises for health, including diagnostic support for GPs, revamped hospitals and new GP prescribing powers.
With general practice becoming more expensive, public hospitals under strain and workforce pressures showing no sign of abating, one thing is for certain, the State Government cannot afford to get it wrong.
WA doctors need to see action now. Big promises come with big expectations.
On a lighter note from me, I want to hear from you.
We’re asking Medical Forum readers for their thoughts on our content, what they like to read and what they want more of as part of our two-minute 2025 Readership Survey.
One lucky reader will win a $1000 Luxury Escapes voucher by completing the survey – that’s quite the penny for your thoughts.
We want to deliver more of what you like. Call it our big promise to you.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.




A new approach to autism care
20 Close-up: Professor Livia Hool 24 Cystic fibrosis: new treatments, new challenges
52 Art by the sea – what’s on at this year’s Sculpture at Bathers
53 Read all about it: Margaret River Readers & Writers Festival

want to hear from you – take part in Medical Forum’s readership
A breath of fresh air – Dr Joe Kosterich
Our popular competitions have seen Medical Forum readers enjoy a trip to the movies, a night of culture at the Alliance Française French Film Festival and a glass of Fermoy’s delightful wine. The lucky winner of our February wine giveaway was Dr Penny Wilson of Grove Medical in Victoria Park.
She received her delivery Fermoy Wines this month. We hope you enjoy a well-deserved glass.
Over the coming months we’re giving one lucky reader a chance to win a $1000 Luxury Escapes getaway, all you have to do is take part in our 2025 Readership Survey.
To enter scan the QR code and fill out the survey. Additional entries available if you update your contact details at the end.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Classifieds Manager
Paul Riessen 08 9203 5222 paul@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
















Australia’s first durable heart transplant has been hailed a clinical success after the patient was the first in the world to be discharged from hospital with the innovative device.
During a six-hour operation at St Vincent’s Hospital Sydney last November, a man in his forties had a BiVACOR Total Artificial Heart implanted, a titanium mechanical blood pump capable of providing high flows of over 12 litres per minute.
The device is a treatment option for patients with endstage biventricular HF who need support while on a heart transplant waiting list. While it is not currently used as a permanent solution, BiVACOR is designed to one day be a permanent replacement for a failing heart.
The surgery was performed by cardiothoracic and transplant surgeon Dr Paul Jansz and post-surgery observation led by heart failure and transplant cardiologist Professor Chris Hayward.
After a few weeks in ICU followed by ward observation overseen by Dr Hayward, the man was discharged from hospital in February 2025.
The patient received their donor heart transplant in March and is recovering well. At 105 days, it is the longest a BiVACOR transplant patient has gone between the implant surgery and receiving their donor heart.
Professor Hayward said the procedure ushers in “a whole new ball game for heart transplants”.
“Within the next decade we will see the artificial heart becoming the alternative for patients who are unable to
Nine new Distribution Priority Areas (DPA) have been named in Western Australia as GP service levels remain a concern.
The Federal Government has updated the DPA classifications of 17 localities across Australia, the majority in WA.
Joondalup is now a partial DPA having previously not been a DPA, and the three localities of Cockburn, Gosnells and Mundaring-Swan View have gone from being non-DPA to full DPA.
Armadale, Byford, Kalamunda and Swan have all moved from a partial DPA to full DPA.
Two WA locations also had their level of remoteness increased under the Modified Monash Model.


wait for a donor heart or when a donor heart is simply not available.”
The first BiVACOR Total Artificial Heart implant was performed in the US in July 2024. The Australian implant was the first to take place outside of the US and the sixth in the world.
Green Head and Leeman, both of which had previously been considered small town rural, or MM5, are now considered remote, or MM6.
AMA (WA) President Dr Michael Page said lifting incentives for rural and outer metropolitan general practice was important to address some of the “distribution-related inequalities in access to primary care in WA”.
However, he said changing the classification of areas was only part of the solution and other factors affecting GP clinics needed to be considered.
“Many of these practices are smaller with significant running costs to contend with despite lacking scale, and depend on private billing,” he said.
RACGP Rural Chair Dr Michael Clements said lessons must be
learned from the last round of DPA changes, which the College said “drained doctors from rural and remote communities to more desirable locations.”
“While this latest announcement is good news for some, it will not help communities where the need is greatest. If everywhere is a priority, the system doesn’t work,” he said.
Six new urgent care clinics are set to open in Western Australia as part of a national expansion of the program, but the RACGP has warned it cannot come at the cost of mainstream general practice.
Federal Labor has committed $644 million to open a further 50 Medicare Urgent Care Clinics across Australia, if re-elected.
In WA clinics are earmarked for Bateman, Ellenbrook, Geraldton, Mirrabooka, Mundaring and Yanchep.
RACGP Vice President and WA Chair Ramya Raman said urgent care clinics were an expensive model of care and there had been no clear evaluation on their impact.
“The clinics can be an important addition to the health infrastructure, but the concern we have is whether it is coming at the expense of mainstream general practice,” she told Medical Forum
“This is not about dismissing urgent care clinics or doctors who are working there – we support our GPs who are working in urgent care centres – but equally we would like to see some of this funding going into existing infrastructures to enable more efficient care to be delivered.
“We want to make sure the urgent care clinic model is not shifting funding and the workforce from our existing general practices and then making them less viable.”
Dr Raman said putting the funding towards existing general practice instead would support after hours care to ensure GPs could assist with urgent care needs.
AMA (WA) has welcomed seven new members to its Council:
Dr Paddy Glackin –Chair, Rural Doctors Practice Group
Dr Mary Wyatt –Chair, GP Practice Group
The new clinics will open during the 2025/26 financial year. The Department of Health and Aged Care claimed the expansion would ensure four in five Australians will live within a 20-minute drive of a clinic, but it was unclear if that included people living in rural and remote areas.
The clinics are in addition to the 87 currently operational across Australia and the eight in Western Australia.
The largest ever funding round for MS Australia in terms of the number of projects being supported was made possible thanks to investment from MSWA.
In addition to its normal contribution to MS Australia research, MSWA contributed a further $2.4 million dollars into this grant round which allowed for the funding of an additional 10 of the 35 funded projects.
The additional funding, part of $5.7 million in research investment, guaranteed important MS research would commence, not just in Western Australia, but throughout the country.
The grants enable a diverse array of projects, from novel studies to multiyear investigations of MS through fields such as neurobiology, genetics, epidemiology, immunology, and social and applied research.

Dr Rebecca Anglin –Head of Medical School, University of Notre Dame
Dr Helen Wilcox –Interim Dean, UWA Medical School
Sanjeev Singh –President, Medical Students’ Council of WA
Ollie Smith –President, Medical Students Associate Notre Dame
Shreya Salunkay –President, Curtin Association Medical Students
MSWA chief executive Melanie Kiely thanked the WA community for their ongoing support of the charity’s work.
“Ultimately this investment is about getting us closer to cures, closer to better treatments and ensuring Australians living with MS can maintain their ability to do what matters to them for longer.”
A team from the Harry Perkins Institute of Medical Research and UWA is using new technology to create a detailed map of chromosomes in the hope of preventing miscarriages.
The Optical Genome Mapping research will analyse these maps to identify changes in chromosomes that could explain reproductive issues.
Professor Gina Ravenscroft, Group Leader Rare Disease Genetics and Functional Genomics Group at the Institute and Senior Research Fellow at UWA is leading the research.
Her team is recruiting couples of reproductive age who have experienced two or more unexplained miscarriages. The miscarriages do not need to be consecutive.
Professor Andrew Whitehouse has been appointed Deputy Director of Research at The Kids Research Institute Australia.
The Council of Presidents of Medical Colleges has appointed Jodie Long as its new chief executive.

Former Victorian Premier John Brumby has been appointed Independent Chair of Private Healthcare Australia.
WA Primary Health Alliance has appointed Bernadette Kenny as its new CEO. She will take on the role in early April, succeeding Learne Durrington.

At Hollywood Private Hospital, we offer quality heart and lung care provided by our dedicated team of cardiologists, cardiothoracic and vascular surgeons, and allied health professionals. Patients benefit from the latest advancements in medical technology, ensuring top-tier treatment and support.
Our comprehensive Cardiac services
• Advanced diagnostics: Cutting-edge cardiovascular diagnostics.
• 24/7 care: Around-the-clock interventional cardiology and emergency services.
• Expert team: Access to top cardiothoracic surgeons and specialists.
• Specialised units: ICU, Acute Cardiac Unit, and Cardiology/Cardiothoracic ward and Coronary Care Unit.
• Holistic rehabilitation: Comprehensive postprocedural care and tailored rehab programs.
Join us in providing exceptional Cardiac Care
• Refer your patients to Hollywood Private Hospital for comprehensive, cutting-edge cardiac services.
• In a cardiac emergency, patients can call 000 and ask to go to the Hollywood Private Hospital Emergency Department.
Contact us today to discuss how we can support your patients’ heart health. Call (08) 9346 6174
continued from Page 6
“Our DNA works best when it is packaged correctly in our chromosomes in the right order and right amount. Sometimes, though we do not know it, we are born with our chromosomes mixed up and rearranged,” Prof Ravenscroft said.
“It is not something that affects our day to day lives, but it can affect our ability to fall pregnant or carry
a baby to term. Our research study aims to test a new technology to look for structural changes in your DNA that could be affecting your reproductive health.
“Conservatively, 2% of couples experience recurrent miscarriage and at least 10% of these have an underlying genetic cause.”
Once the underlying chromosomal abnormality is identified, couples can have IVF and pre-implantation
genetic diagnosis. Embryos without the chromosomal abnormality are implanted, minimising the risk of future miscarriage.
The research is being funded by a Medical Research Future Fund grant of more than $4.8m.
Western Australia’s unique healthcare system was discussed with AMA National President Dr Danielle McMullen during her recent visit to the State.
Dr McMullen spent a week in Perth and regional areas at the end of March, visiting doctors and specialists at Fiona Stanley Hospital, St John of God Hospital in Murdoch and local general practices.
“It was back-to-back member and site visits to really get across the issues in WA and talk with doctors about what’s happening,” she told Medical Forum
“The issues discussed were similar, but sometimes different amplifications from what we get everywhere.
“Private practice was a really hot topic – we’ve seen the closure of maternity services in Hobart and Darwin make big news, but there’s also been closures of maternity services in WA.
“More broadly in the private sector it really shone through that the private health system is under strain.
“When visiting the emergency departments, ramping was visible. These EDs were full and overcrowded and the doctors and nurses in there were working as hard as they possibly could.
“It’s like an unending tide of patients. In the meantime, GPs are also flat out and so are our private practitioners, so everyone is under strain and we’ve seen that across the country.”
Dr McMullen also met with the Royal Flying Doctor Service to hear about their work supporting regional Western Australians.

“We were able to discuss the provision of healthcare in some really remote parts of WA and understand the geography of rural health there a bit better.”
But it was a visit to Pramana Medical Centre in Gosnells that stuck out as a highlight of the trip.
“I was blown away by the commitment to the community that the practice had,” Dr McMullen said.
“Their doctors and whole healthcare team are just so committed to serving the disadvantaged population that they do. It was a really inspiring practice to visit.
“But it was all highlights, it really was a fantastic visit and every interaction and conversation I had was really valuable.”
Practice and hospital visits aside, Dr McMullen said her walk along the Swan River on a sunny Saturday morning was “pretty amazing”.


Western Australia has a new Minister for Heath as the re-elected Labor Government looks to make health a bigger priority over the next four years.
First-time minister Meredith Hammat has been given the health and mental health portfolio, replacing Amber-Jade Sanderson who has held the portfolio since December 2021.
Ms Sanderson will be moving to the portfolio of Energy and Decarbonisation.
Ms Hammatt was Secretary of UnionsWA prior to being elected for the first time in 2021, and Assistant Secretary of the Australian Services Union before that.
This is the first time she has held a ministerial position, taking on a notoriously difficult portfolio.
The State Government also announced two new health portfolios: Health Infrastructure and Preventative Health, meaning responsibility for health will be scattered across three ministers and four portfolios.
John Carey will take on the role as Minister for Health Infrastructure, responsible for increasing bed capacity and revamping hospitals, while Sabine Winton becomes Minister for Preventative Health.
A new portfolio of Aged Care and Seniors will aim to deliver more aged care places in a bid to free up beds in the under-strain hospital system.
Premier Roger Cook said the new portfolios will reduce demand on hospitals over the long-term and ensure Western Australians continue to live in the healthiest state in Australia.
AMA (WA) President Dr Michael Page said the new portfolios were a good opportunity to refresh thinking on health policy.
“The responsibilities for health don’t just fall under one minister, and we hope that works well in terms of spreading the load and enabling enough resource to be allocated to health,” he told Medical Forum
“Ultimately, someone has got to be accountable for bringing our health system into the 21st century and building it out for the next couple of generations of Western Australians, or beyond a single election cycle.”
Two GPs also retained their seats in the recent State Election. The Labor Party’s Dr Jags Krishnan retained his seat of Riverton, while Dr Brian Walker of the Legalise Cannabis Party retained his seat on the Legislative Council.
Health formed a major pillar in the Labor Government’s election campaign, with millions in funding promised to

improve general practice, public hospitals and patient care.
The party promised $8.2 million for its GP ASK pilot program, which would allow GPs to securely message five medical specialists in paediatrics, immunology, respiratory medicine, spinal surgery and geriatrics to advise on a patient’s care.
It formed part of a wider $254 million health pledge, which includes $104.8m to transform Midland Health Campus’ emergency department, $36.3m to expand the WA Virtual Emergency Department program and $104.4m for Royal Perth Hospital, including a new emergency department.
The party also pledged to expand GPs scope of practice to allow them to diagnose and treat ADHD.
A new book In a Heartbeat aims to shine a light on cardiovascular disease, with the help of cardiologists including Dr Kushwin Rajamani. Heart is at the centre of this book, in more ways than one.
By Andrea Downey
Compassion, gratitude and love are all matters of the heart, so it’s especially fitting that these are cardiologist Dr Kushwin Rajamani’s main motivators.
From studying and training abroad, setting up his own clinic here in Perth, to humanitarian work, the Associate Professor can now add literature to his list of achievements after contributing to a new book about cardiovascular disease.
In a Heartbeat, by Rachel Jayne Cassidy, details in-depth stories from experts, survivors and medical professionals. The book seeks to shine a light on the experiences of those working in the field of cardiovascular disease, as well as that of patients and their loved ones.
Cardiovascular disease is a leading cause of death in Australia, claiming the lives of one in four people. On average, 120 Australians die from cardiovascular disease every day.
With such stark figures in mind, it’s a safe bet to say most of us will be affected by CVD at some point in our lives, whether that’s reflected in our own health or the health of a loved one.
Rachel penned the book after her own near-death experience. Had it not been for a chance visit from her son, Rachel – who was otherwise fit and healthy – may not have survived her heart attack.
The poignant and often inspiring stories in each chapter serve as a reminder that life is fragile and can change in a heartbeat, while championing the important work underway here in Perth, and nationally, to improve outcomes.
For Dr Rajamani – the only WAbased cardiologist featured in the book – he hopes it will spread the message of heart health to wider audiences.
“As a clinician, I can have a reach of about 10,000 patients a year, but what this book can do is reach millions of people,” he told Medical Forum
“Being part of this book was important to me. This is the first time that a publication of this nature has come forward where you have patient and clinical perspectives in the same book, presented with valuable information from which patients can take away from.

“This is also an important resource for general practitioners and other doctors to give them an understanding of where a lot of the misconceptions of care or gaps in understanding come from in the general population, and to help identify where these gaps could be addressed both in primary care and in the cardiology space.”
With an increase in public awareness of different cardiac conditions, Dr Rajamani is also hoping for increased patient engagement and ownership of their health.
“What we are attempting to do in this journey is increase public awareness of heart conditions. We want to engage patients holistically and also enable them to take ownership of their own heart condition,” he adds.
“The more patients understand their condition, the more likely they will be to be engaged and compliant with medications, as well as their necessary lifestyle changes.”
Born in Sri Lanka, Dr Rajamani did his medical degree at Ireland’s Royal College of Surgeons before moving to Australia. He completed basic and advanced physician training in cardiology at Royal Prince Alfred Hospital in 2011 and has a PhD from the University of Sydney. He also spent two years at the Cleveland Clinic in Ohio.
In 2018 he set up his practice Omni Corde, with a focus on heart rhythm disorders and atrial fibrillation. He has clinics in three Perth locations and in York.
“I’ve always loved reading ECGs since medical school and that’s one of the things that attracted me to cardiology and heart rhythm conditions.
“Atrial fibrillation is the most common heart rhythm condition we deal with. For me the physiology of arrhythmias is fascinating and what we can offer patients procedurally – because I like doing things hands on – is a major appeal.”
In the book Dr Rajamani details the enormous strides that have been made in the treatment and prevention of AF, which fuel his desire to work.
For 50 years the anticoagulant warfarin has been the mainstay in treating the clot and stroke risk associated with AF, but there are new therapies emerging.
While warfarin is effective, it requires regular assessment and blood tests to ensure levels in the body are kept at a healthy level – regulated by measuring the International Normalised Ratio.
New blood thinners, known as Novel Oral Anticoagulants (NOACs) have been available for 10 years and are not only more effective than warfarin, but do not require blood tests.
But blood thinners are only part of the picture. If medications for AF do not work, then a minimally invasive catheter ablation can be provided.
This allows cardiologists, like Dr Rajamani, to access the heart


Prime Claremont location with the above pictured river views!

Prime Claremont location with the above pictured river views! Located on the lower ground floor.
Located on the lower ground floor.
86 sqm and 75 sqm spaces available.
86 sqm and 75 sqm spaces available.
Fitted to warm shell - enabling the tenant to design internals to fit individual requirements.
Fitted to warm shell - enabling the tenant to design internals to fit individual requirements.
For more information, please contact Neale Fong on (08) 9340 6396.
For more information, please contact Neale Fong on (08) 9340 6396.
continued from Page 11
through the femoral vein. A small part of the heart is scarred using radiofrequency energy to maintain a normal heart rhythm. The surgery has a 60-90% success rate and only takes around two to three hours.
It’s the impact these advancements have on patients that stick with Dr Rajamani. He recalls a patient from several years ago who woke up in the middle of the night unable to move.
“This patient was worried about her husband who was breathing erratically during sleep, but she found she couldn’t move to wake him up and then recognised that she was having a stroke,” he says.
She made it to the hospital in time and the clot was extracted successfully from her brain. At the time her heart rhythm was normal, but further testing revealed that she had AF.
The patient was started on anticoagulants and made a full recovery.
“This was a situation where a patient did not have any warning signs and, thanks to the advanced medical care, we extracted the clot in her brain and avoided long-term disability, plus detected the cause to prevent a future event.”
In a Heartbeat is full of patient stories like this, alongside the incredible work of cardiologists, researchers and advocates across Australia.
There’s the story of Andrew, a 64-year-old fit and healthy accountant who survived a major heart attack, and the story of Greg Page, the original Yellow Wiggle, who survived ventricular fibrillation that led to cardiac arrest, among other cardiac conditions.
Then there’s the story of Arlo who was born with half a heart and had his first cardiology appointment at six days old, his first surgery at 10 days old, and went on to have numerous emergency surgeries.
While advances in research and treatment are often known within the medical community, the patient journey is always at the heart of it.
Both are important, but combining the two in this book makes it more impactful.
Dr Rajamani has grasped every opportunity afforded to him through his own hard work and dedication, but he has never lost sight of his desire to give back to the community.
His father has no formal education and can only write numbers, while his mother only went to primary school. Educating their children was a huge priority for them and gave Dr Rajamani his drive to make them proud.
It’s a drive that has given him energy to undertake humanitarian work alongside his cardiology work, regularly traveling to Sri Lanka on medical missions to to implant pacemakers in patients living in remote regions with limited medical facilities through his work with charity The Goodness Foundation. He also fundraises for The Orangutan Project which aims
to protect 100,000 hectares of Indonesia’s Leuser Ecosystem, where critically endangered orangutans, elephants, rhinos and tigers coexist in the wild.
“I like to think our role is as ‘custodians of this planet’ and my goal is to make the biggest difference possible in this short time of life,” he says.
“I feel it is my duty to give back and it’s a fulfilling journey for me to know that I have done the best I could to make the biggest difference I can in this life.
“For me the three things that drive me are gratitude, passion and love.
“Everything is seen through that, that is the fundamental driver for me. Through that I feel like I have boundless energy for my work.”
In a Heartbeat can be found online and in all major book retailers.
Western Australia is seen as a leader in autism care, but there is still a way to go to improve diagnosis and access to services. The National Autism Strategy aims to support that, but what will it look like in practice?

By Andrea Downey
It is not understating it to say early diagnosis of autism alongside access to early interventions can have a profound impact on a child’s development.
But referral delays and lengthy waitlists are having a combined impact on autism care across the country.
Waitlists to see a specialist can be more than a couple of years and some parents have reported feeling as though their GP – through no fault of their own – was unaware of how best to support them during the diagnosis process.
For Perth-based Stacey Green, her son Harry’s diagnosis was the key to unlocking a wealth of support that has seen him start pre-primary this year as a happy, sociable boy.
But that was not always the case and without early intervention, which Harry received through CliniKids at The Kids Research Institute of Australia among others, his story would be different.
The experiences of the almost 300,000 people with autism across Australia vary and can heavily depend on their health practitioner’s understanding of autism, timely access to specialists – which differs between private and public services – and other support systems within education and communities.
Autistic people experience more barriers to healthcare than nonautistic people, they are 2.5 times more likely to experience depression, and they have a life expectancy of 20–36 years shorter than the general population.
To address these stark numbers, the Federal Government has developed a seven-year National Autism Strategy which aims to create “a safe and inclusive society where all autistic people are supported and empowered to thrive”.
A National Roadmap to Improve the Health and Mental Health of Autistic People is also being developed and will provide a more in-depth look at the changes needed.
Until then, the strategy sets out key areas for consideration including better diagnosis, identification and assessment of autism.
GPs are often the first point of contact for people at the beginning of their diagnosis, but the strategy
“The sooner we can empower GPs with knowledge the sooner they can change lives,”
– Professor Andrew Whitehouse
notes that often autistic people, their families and carers “can experience difficulties at all stages of the identification, assessment, and diagnosis process”.
To mitigate this, the strategy commits to the development of standardised co-designed training and professional development materials to support those involved in the diagnosis of autism, and exploring ways to make diagnosis and assessment more affordable.
Consideration will also be given to early screening and developmental monitoring, and improved access to health and other professionals.
Dr Andrew Whitehouse, Director of Clinikids and Professor of Autism Research, says the strategy notes all the right things, but there are also large gaps.
“Things such as early diagnosis and high-quality support, education, housing, ageing – these are, when I speak to families, the most pressing issues they are talking about,” he told Medical Forum
“WA knows how to do this, and I suspect it will be the first state that will find it easier to get diagnostic and early intervention supports back on track for small children.”
To name just some of the good work underway in WA, the Autism Association of Western Australia has delivered training to improve patient experience in emergency healthcare settings at Fiona Stanley Hospital and Perth Children’s Hospital.
The Association also has an ongoing partnership with Curtin University Oral Health Therapy Clinic, providing autism-specific training to oral health students in their final year of training.

CliniKids is also renowned for its work in this space, with its Early Start Denver Model therapy and JASPER – Joint Attention, Symbolic Play, Engagement and Regulation therapy providing early intervention support for children as young as 12 months.
While more must be done to improve care in this space, Western Australia is broadly seen as a national leader in autism care, with several experts in the field pointing to the State’s success in early intervention.
“If you were going to be in any place to have a child diagnosed with autism, or be autistic yourself, you’d choose WA. We really are doing things as well as anyone in the world, which is a huge pat on the back, but that’s not to say that we can’t do better,” Professor Whitehouse adds.
Autism Awareness Australia chief executive Nicole Rogerson says that WA is “without a doubt” ahead of some of the eastern states.
“Western Australia has always been seen as a leader in the early intervention space,” she told Medical Forum
While positive work in this space should be applauded, WA is not immune to the issues seen nationwide. Workforce shortages across the board are resulting in lengthy waitlists and difficulty accessing specialists.
“One of the things we do know is that we have large waiting lists to receive assessment services, which means kids can be on a waitlist for two to three years before they are able to access these services,” Professor Whitehouse says.
“The demand for services has outstripped the supply of clinicians multiple fold, and we’re at the point now where it’s difficult to see how we could ever train the amount of clinicians we would require to meet the demand for assessment services.
“For many people, achieving a diagnosis has been the gateway
continued on Page 17
22 clinics across Perth!
Discover unparalleled cardiac imaging excellence with our specialised team of cardiac reporting experts and dedicated radiographers, united in delivering superior medical imaging and exceptional patient care.

Experience comprehensive cardiac imaging at PRC
• Remarkably low radiation doses • Complete CT coronary angiograms in a single heartbeat
• Suitable for patients with arrhythmic and high heart rates • Exceptional image quality.
Services include: MRI Cardiac • MPS • CTCA • CT Calcium Score.
Doctor Priority Line for urgent bookings and enquiries
continued from Page 15
to getting support, which is why waitlists have been driven so high. We all realise the flaw in that, so we need systems to provide services to kids based on their needs and their level of functional impact, not necessarily the presence or absence of a diagnosis.”
Joan McKenna Kerr chief executive of AAWA, said the importance of a diagnosis cannot be understated as it provides a “shorthand to others on how best to support that person”.

“We know that when you work with people with autism you need structure, you need routine, you need predictability, you know they have sensory difficulties,” she tells Medical Forum
“If you manage those sensory difficulties, you can manage their anxiety. You know that if you present information in a particular way then that child will cope better than if you provide it in a more conventional way.”
One area the strategy aims to improve is training and professional development for those involved in the diagnosis of autism. Ms Rogerson says reluctance to refer to specialists too early can be a barrier to care.
“If the warning signs are there, you’re not doing anyone a favour by putting it off. We know that intervention is better when it’s early,” she says.
“If a GP is not sure, referring them on to have an assessment or to see somebody that will know a bit more is critical.”
While a child is waiting for a formal diagnosis, referral to support services should also be considered.
“Don’t wait, if you have an inkling then it’s worth investigating that straight away. The earlier we can identify kids and provide them with the support they need the better,” Professor Whitehouse adds.
Harry with his mum Stacey, dad Sam and sister Schyler

Stacey Green suspected her son Harry might have autism when he was just six months old. With a brother who received a late diagnosis at 26, she was aware of the signs and knew the importance of early intervention.
While she knew all children develop differently, she also knew she wanted health practitioners to take her concerns seriously.
“There were little milestones he wasn’t quite hitting – my nephew is the same age, and it made it really obvious when Harry wasn’t hitting those milestones,” she told Medical Forum
“He was avoiding eye contact, he had started developing ‘mum’ and ‘dad’, but really that was it language wise, he wasn’t progressing in his speech.
“In the first six months of my own feelings, I just had it in the back of my mind that it could be autism… but I felt quite brushed off.”
When Harry was around 12 months old Stacey knew something was not right and began her own research into the supports her son might need. She reached out to AAWA for support and visited her family GP.
But that’s where the challenge began. Not only did Stacey feel she had to advocate for her son, she also struggled to get an appointment with a specialist and was told there was a two-and-a-half-year wait to see a paediatrician.
“I remember when we were starting that process, we knew we had to see a speech therapist, psychologist and a paediatrician. It would have been when Harry was about 14 months, so we’d been to see the GP, done some reading and got more information,” she says.
“I sat with a list of about 30 paediatricians and just phoned one after the other to be told I’d have to call back at the end of the year, or that waitlists were full. At that point I remember just sitting on the bathroom floor crying.
“From a mum’s point of view, it was quite a frustrating process because we knew we needed to see these three specific healthcare professionals to get the diagnosis, but we couldn’t even get that.”
Stacey also visited her GP three times before those referrals were made.
“I never felt judged or anything like that, I just think there was more of a focus on speech delay. There were a couple of times when we were told children develop differently.
“I definitely had to advocate for Harry a lot more than I thought I would in those sessions.”
Stacey and her husband chose to go down the private route, which meant they could get Harry to specialists sooner.
continued on Page 19
continued on Page 18
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
continued from Page 17
“Diagnosis is an important step, but it doesn’t necessarily need to be the first step. Your referral to a speech pathologist, not for an assessment or a diagnosis but for support, can actually be more important than that diagnosis.
“If we can empower primary practitioners within the bounds and confines in which they work, then they have the ability to change the lifelong trajectories of autistic kids by identifying differences early on, by understanding where to refer and who families need to speak to. This is the stuff that changes lives.
“Just like how we’re starting to embed knowledge of autism and how to support autistic kids within teacher training, this absolutely has to be a core part of GP training.”
Time spent with a GP can also create an unnecessary barrier. Through their work with families, the AAWA has found longer consultations help empower patients and allow them time to understand their care.
“When you know an autistic person has booked an appointment,
continued from Page 17
make sure you diary in a longer consultation,” Ms McKenna Kerr says. Diagnostic overshadowing
“The one thing that people with autism still do experience is diagnostic overshadowing, meaning that if you have autism then everything is explained through autism rather than considering other issues.
“For example, we can still experience a situation where someone presents with a behavioural change to a GP and it can be immediately put down to their autism, whereas there are a number of things that need to be considered in regards to this population.
“We know they have higher rates of anxiety and depression. All behavioural change is not explained by autism, there are several things we need to look at when someone presents with qualitative changes.”
Professor Whitehouse is hopeful that better understanding of autism and changes in care, like earlier referral to specialists, will go some way to improving the health outcomes of those with autism.
He began weekly occupational therapy in July 2021. He also took part in Early Start Denver Model therapy and JASPER therapy through CliniKids and sees a speech therapist. He started pre-primary this year and is enjoying being at school.
While Harry was seeing specialists before his diagnosis, the eventual diagnosis was life changing. For the now happy, sociable five-year-old, diagnosis and early intervention was everything.
“If we hadn’t had that intervention, where would he be now? He went from being non-verbal to now using four-to-five-word sentences. What we saw from Harry was a really frustrated little boy and, through that early intervention, he’s turned into this really sociable, happy kid.
“Early intervention, for him, has been life changing because he has that ability to interact with the communities around him.”
If there’s one thing Stacey wants healthcare professionals to consider, it is that a parent’s instincts should not be overlooked – and that providing relevant information can make a difference.
“A mother’s instinct can sometimes hold as much weight to it. It’s about really listening and hearing when someone is coming in with those concerns,” she says.
“I know that GPs are already doing this, but I think supporting parents and giving them the information that’s relevant to them, and the right resources to give them a really clear understanding of the journey ahead of them, would be really helpful.”
“There is nothing inherent in the biology of autistic people that means they are more prone to illness and disease,” he says.
“What the statistics indicate is that those social determinants of health are being affected – the lifestyle factors ranging from what people eat, all the way through to social connection and loneliness.
“It is also around health seeking behaviour – do we have systems that encourage and embrace autistic people when they do seek out health practitioners?”
For now, it is a case of wait and see whether the National Autism Strategy delivers change. The devil will be in the detail of the National Roadmap to Improve the Health and Mental Health of Autistic People but, as is so often the case in healthcare, it will need to be backed by workforce investment and practitioner training.


Professor Livia Hool is a champion of research and advocacy which aims to impact the global leading cause of death – cardiac disease.
By Ara Jansen
As a cardiovascular researcher, Professor Livia Hool certainly likes to get to the heart of the matter.
“I’m passionate about what I do,” says Livia. “Passionate about building a strong research community. I’m passionate about discovery research, which is ultimately what is essential for successful translation into clinical benefits.”
Livia loves the thrill of discovery. When she discovers something, she’s the first to find it and that really gives her a buzz.
“Then you have to clarify it and test it many different ways. If you are able to reproduce it under different conditions and confirm it, then that’s really exciting,” she says.
“People who come into this type of work are dedicated to finding something special. I think most people get involved in biomedical research because they want to make a difference.”
While details remain confidential, Livia’s team have helped develop a drug protocol which is heading into clinical trials. She has designed a protein that prevents an inherited heart disease from progressing.
Born and raised in Sydney, she has called Perth home for 26 years and has degrees in science, molecular biology and a PhD in cellular electrophysiology. She’s also the first woman to be awarded the Cardiac Society of Australia and New Zealand RT Hall Prize.
Livia’s mother was a pathology technician and spoke of her experience enthusiastically.
“She gave me a foundation for what it would be like to work in a hospital. Since I was young, I was fascinated by cardiovascular diseases as the leading cause of death. Later, I remember seeing people dying from breathlessness and thinking it was terrible. That sparked an interest in undertaking research in the area.”
She knew a number of doctors working in the field of blood pressure regulation and initially thought that what they were doing was interesting. After starting work in the field, she realised it wasn’t for her.
In 1991 German physiologist Bert Sakmann and German biophysicist Erwin Neher won the Nobel Prize for Physiology or Medicine. The prize was awarded for “their discoveries concerning the function of single ion channels in cells” and development of the patch-clamp
technique, a laboratory method now widely used in detecting tiny electrical currents in cell membranes.
This has revolutionised our understanding of the electrical activity responsible for the heartbeat and contraction of the heart muscle.
“When this came from Europe to Sydney, I saw it and thought I just had to have some of it. I literally crossed the corridor in the Cardiology Department and left my previous research work in this area, learning the patch-clamp technique and becoming one of the first researchers in the country to use it in my research.
“My interest in translational cardiovascular research came later. I have always loved physiology and in my undergraduate years I had some excellent lecturers who inspired me to learn about how the healthy body functions and what goes wrong with disease processes.”
Livia’s father died from a brain tumour when she was in Year 12. The positive to come from this was that it added to her curiosity at a scientific level and helped shape her interest in physiology.
“The heart is fascinating and once I found out about the patchclamp technique I thought ‘I have to do this’. It was purely instinct. Here I was in Australia with the opportunity to learn about and use technology from Europe that had won a Nobel Prize.”
She decided to pursue a career

in heart research after seeing how quickly heart attack patients deteriorated into heart failure.
Livia was the Gaston Bauer Cardiovascular Research Fellow in the Cellular Electrophysiology Laboratory at Sydney’s Royal North Shore Hospital from 1991-1995. Then she spent two years at Case Western Reserve University in Ohio as an American Heart Association Postdoctoral Fellow.
She’d already been fortunate to have travelled and presented her work at various conferences and was keen to widen her knowledge. She strongly advocates for researchers to travel, present their work, expand their knowledge, learn and live in other cultures for a while.
“When I came back to Australia it was quite usual thinking that the next step would be to use this knowledge in industry or in pharmaceuticals. Or establish a career as a research fellow.”
Livia took the research fellow path and has been raising money and funding her own position and that of her team for 30 years. She has raised more than $25 million towards her work understanding the excitation and contraction of the heart.
In that time too, success rates for grant funding have dropped from around 24% to 10%. Most grants or fellowships last five years, so typically in the fourth year she’s back applying for more funding, championing the feasibility of the work and its value.
Her team – eight to 10 researchers –is working on more than one project at a time as well, which offers diversity for funding opportunities.
Her lab is at UWA and in 2013 she joined the Victor Chang Cardiac Research Institute. For the last three years, Livia has held an endowed chair at UWA, supported by the university and Wesfarmers. She still has to raise money to fund her work and the team.
As a passionate advocate for medical research funding, she was a founding director and secretary of the Australian Cardiovascular Alliance. In 2019 she also established and chairs the Western Australian Cardiovascular Research Alliance (WACRA).

MEDICAL FORUM HAS BEEN PART OF THE WA MEDICAL COMMUNITY FOR ALMOST 25 YEARS, DELIVERING LOCAL INDEPENDENT HEALTH JOURNALISM DIRECT TO YOU.
Complete our short survey to help us understand your reading habits and how we can better deliver the content you want to read.
By completing this survey, you have the chance to win a $1000 Luxury Escapes voucher, additional entries available if you update your postal address or email address at the end of the survey.
Scan the QR code to enter and be in running to win!
mforum.com.au



continued from Page 21
The alliance advocates for increased awareness of cardiovascular disease and funding for cardiovascular research to stem the loss of capacity in research expertise as researchers leave the field.
“We don’t have an institute for cardiovascular research in WA, but researchers work across the five universities and research institutions, so WACRA has united researchers as a single voice to advocate.
“There is a lot still unknown about how cardiovascular disease occurs. For example, one in 100 babies are born with a congenital heart defect and we still don’t really know how that occurs. Also, we really are only just starting to understand the DNA and genetics related to the heart.
“With the inherited heart disease I study, one in 200 people carry a genetic mutation responsible for developing the disease. That’s shocking – it’s a lot of people. And we don’t know why some develop this disorder while others remain healthy but still carry the mutation.”

“Inherited cardiac disease is the leading cause of sudden cardiac death in five-to-15-year-olds – it’s more common than you think.”
These are some of the reasons Livia is known as a passionate educator and advocate to government for heart disease awareness and research, and has come to have a significant media presence.
Livia has found advocacy work fascinating and was involved in a WACRA submission to last year’s WA Parliamentary Inquiry about declining levels of health and medical investment in the State.
“I do a lot of advocacy and leadership. I want researchers in the field to feel they have a powerful and significant voice.”
She also sits on a number of committees and councils nationally and internationally.
The married mum of two universityaged children loves the coastline on this side of the country. A fan of the outdoors, she’s a regular swimmer, both in the pool and the ocean, and does a lot of walking and hiking in

the South West. In colder climes she enjoys skiing – Japan is a favourite spot.
Livia travels regularly to deliver papers, speak at conferences and attend meetings interstate and overseas. Occasionally there’s the time and opportunity to discover new places. She says travelling to such events can pose a challenge for researchers from WA because of the distance, time and cost. Livia encourages her team to broaden their horizons this way.
Preferring to work with her team in her lab rather than working from home, Livia goes in to UWA every day, something she and her team kept up during COVID.
“Our techniques require us to work on site, but it also meant we could focus as a team on the research which was good for morale. We were a rare group in that regard.”
The professor has been described as having a no-nonsense, down-toearth approach. Livia says while she wouldn’t necessarily say that about herself, her science and research mind certainly helps her say what she means.
“There are times when you have to be very clear about what you stand for particularly with advocacy. You have some money and you have to decide what to do with it, you have to put it to the best use for the benefit of the community. People often assume academics are very competitive and automatically assume we’re doing it for ourselves.
“I love working with people. You can’t be an introvert doing what I do. I love working with people who share their stories about their lived experience. It’s a privilege to work to improve the lives and health of others.
“Even though everyone is trying to get money, with advocacy you can’t be in it for yourself, you have to be in it for everyone. Sometimes you just have to be very clear about that.”
Livia is also very clear that there’s plenty of work to do and she has plenty more questions to research for the rest of her already awarded career.
Once upon a time doctors could only give children with cystic fibrosis a slim chance of surviving past young adulthood. Thanks to new treatments and more holistic care, the prognosis has changed, but that is presenting new challenges.

Cathy O’Leary reports
For people born with cystic fibrosis before 1989 it was a grim prognosis, with survival past their 30s considered rare. Even 20 years ago, the average age of death for someone with the condition was only 27.
Understandably, much of the research and medical focus was traditionally on extending life rather than improving symptoms or treating side effects.
But the advent of new treatments, such as the genetic modulator drug Trikafta, means a baby diagnosed with cystic fibrosis now can be offered a very different future to that of someone born in the 1990s – with a good chance of living to middleage and beyond.
Cystic fibrosis is a complex, multisystem condition caused by one of several genetic alterations that can be passed down through family bloodlines or occur spontaneously. The mutations affect the CFTR gene, which manages the flow of water and chloride in and out of cells lining many of the body’s soft organs, including the respiratory, digestive and reproductive tracts.
The result is a build-up of sticky mucus, leading to recurrent respiratory infections, difficulties absorbing nutrients from food, damage to the pancreas and an increased risk of diabetes, and fertility problems.
Modulator therapies are considered the biggest change in the CF world in more than 50 years, after years of only small incremental improvements. Although not a cure, they have the potential to move CF from being a debilitating, chronic disease to something much more manageable.
In the past, the focus was largely on CF’s respiratory issues, as those
symptoms were the most obvious, but now the approach is more holistic and addresses other systems in the body, such as nutrition, cardiac care and endocrinology.
But with more people with CF living longer it is creating new challenges for health services, which need to be resourced and equipped to support them.
There has been a recent injection of money into the local CF efforts, including the State Government late last year pledging $1 million from the Future Health Research and Innovation Fund towards new WAbased research projects this year.
With co-funding from the charities Conquer Cystic Fibrosis and Cystic Fibrosis WA (CFWA), more than $2 million will be used to explore therapies and treatment options for the 430 cystic fibrosis sufferers in the State, addressing critical issues such as antimicrobial resistance.
But experts argue that with no cure for CF, and its trajectory still hard to predict, medical support for the growing adult CF population needs better resourcing.
Even among those born with cystic fibrosis decades ago, there are some who have defied the odds to live beyond their predicted life expectancy, including 64-year-old Perth man Mitch Messer
When he was born, he was not expected to live long enough to go to school, because the treatments were very limited.
Last year, Mr Messer was honoured as West Australian of the Year in the community category for his leadership and achievements.
His parents, who lost two sons to CF, were among the founders of CFWA more than 50 years ago.
Following in their path, Mr Messer took on leadership roles within CFWA and the national group Cystic Fibrosis Australia, driving advocacy, research and clinical trial efforts.
His day job is working at The Kids Research Institute as a community involvement coordinator, which is a good fit for his voluntary work with CF.
Mr Messer said the recent State Government funding would help to speed progress so people with CF could plan their lives without the constant shadow of the condition hanging over their heads.
A few years ago Mr Messer was facing the prospect of needing a lung transplant when the drug Trikafta came along, which he credits for saving his life, giving him more energy and improving his lung function.
While he still needs treatment for chest infections, takes medication daily and his lungs are still damaged, the rate of it advancing has slowed.

He is now one of the oldest people with CF in Australia and has packed much into those years.
With co-funding from the charities Conquer Cystic Fibrosis and Cystic Fibrosis WA (CFWA), more than $2 million will be used to explore therapies and treatment options for the 430 cystic fibrosis sufferers in the State, addressing critical issues such as antimicrobial resistance.
He told Medical Forum that his health had significantly improved since he started taking Trikafta about four years ago.
“I was looking at having a lung transplant probably within a year or two, and now they’ve told me they will give me a call in a year to see how I’m going,” he said.
“It’s great than I can get on with my life these days, but like all new drugs they don’t work for everyone, and they can cause issues.”
Mr Messer said modulators did not stop someone having CF, but helped their body to function much closer to how it should.
“And that’s especially good for young people because they haven’t had the damage caused by CF yet so it will keep them healthy,” he said.
“But we still need to understand what happens to older people like me, or those in their 30s and 40s
continued on Page 27



Capital Partners proudly supports our greater community as part of creating a better world.
Capital Partners proudly supports our greater community as part of creating a better world.
Capital Partners proudly supports our greater community as part of creating a better world.
Creating wealth is important, but without a purpose to guide us, all the money in the world won’t lead to a richer, happier life.
Creating wealth is important, but without a purpose to guide us, all the money in the world won’t lead to a richer, happier life.
Creating wealth is important, but without a purpose to guide us, all the money in the world won’t lead to a richer, happier life.
Find your purpose, and your true prosperity with us.
Find your purpose, and your true prosperity with us.
Find your purpose, and your true prosperity with us.



continued from Page 25
who’ve got residual damage that’s been caused by CF. While these drugs slow it down, they’re not going to stop it because the damage has already been done.”
Mr Messer said the modulators could take some getting used to as they can affect the presentation of symptoms.
“I know when I’m unwell now, but the symptoms are different to when I was unwell before I started the treatment, so it’s harder to recognise when you’re having an exacerbation,” he said.
“In the old days you would cough a lot more, and cough a lot more gunk up, but because the drugs are stopping that cycle, it sort of sneaks up on you – you start getting a bit tired and breathless and realise you’re actually unwell, so you’re sort of learning how to live in a new body.”
Mr Messer said the risk of infection was always looming over people with CF, and with antimicrobial resistance it was getting harder to get antibiotics that could treat all the bugs.
That meant researchers needed to find new ways to treat infections using options such as phage therapy, which enlists viruses to kill bacterial infections.
Mr Messer said that while better drug treatments had resulted in less in-patient care, it had in turn increased the need for more care on an outpatient basis.
Sir Charles Gairdner Hospital houses WA’s adult CF centre, with a multidisciplinary team including CF doctors, nurses, physiotherapists, dieticians, pharmacists and a social worker. It also liaises with the paediatric CF team at Perth Children’s Hospital, helping patients transition to the adult unit.
Mr Messer said it needed to be able to provide comprehensive care to meet the complex healthcare needs of adults with CF.
“The treatment model is shifting, and we’re talking to the State Government to say that we need to ensure the facility that provides

that outpatient care, the CF clinic, is actually fit for purpose,” he said.
“It was developed in the 1990s and the number of people with CF going to the hospital was about 100, whereas we now have well over 200 people with CF going there.
“But it hasn’t really kept pace, so it’s not up to standard and we’re saying you will lose the benefits that have been achieved if we don’t keep the standards and services, and we don’t have that in WA.
“That will require extra funding. If you don’t provide good care there’s no point in providing people with new drugs because they will end up being unwell because they couldn’t get access to an appropriate facility, and then the only way is to go into hospital as an in-patient which is much more expensive.”
Lisa Bayakly, chief executive of CFWA, the peak advocacy group in the State, agreed that the course of CF had changed and needed to be factored into the health services required.
“We’ve been funding research for about 30 years and a lot of the earlier work was around how we treat the inflammation in the lungs, treating infections to extend life, and what sort of exercise and physio people should be doing to stay healthy and alive as long as possible,” she said.
“And now people are living longer with the new treatments and new modulator therapy, it’s very much about how we improve the quality of that life and deal with some of the complications that CF adds to a person’s daily load.
“The focus has shifted from keeping people alive to helping them live as healthy as possible. One of the fears people still have is getting a resistant infection, or if they’ve already got resistant infection that it exacerbates and becomes problematic and leads to long hospital stays.

continued from Page 27
“We still need to look at how we better prevent that, and how we know quickly when someone is at risk, but we also need other options, things like bacterial phages.”
Ms Bayakly told Medical Forum another concern was that as people with CF age, they become more prone to other conditions.
“For example, we have CF-related diabetes, which is a whole other form of diabetes, presenting differently to other forms,” she said.
“What it means is that people are living with two chronic conditions. It’s related to how CF affects the function of the pancreas.
“There is also a high prevalence of liver disease in the CF community, as the CF takes its toll on the liver over time, with successive medications. And unfortunately, having advanced liver disease can make people with CF ineligible for some of the more contemporary gold standard treatments.
“The focus has shifted from keeping people alive to helping them live as healthy as possible. One of the fears people still have is getting a resistant infection, or if they’ve already got resistant infection that it exacerbates and becomes problematic and leads to long hospital stays.”
– Lisa Bayakly
“We’re currently funding some research to better understand liver disease because historically a lot of the research has been focussed on the lungs.
“The liver is not well-studied, nor is the CF-related diabetes, and with new treatments people are also having babies, so we need to better understand fertility and the impact of medications on the child.”
The cardiovascular health of people with CF also needed attention because the legacy CF diet was a high-fat diet to help the pancreas function, she explained.
“In many people on the new treatments the pancreas function might not be returning to normal but it is improving, so now there are concerns about the potential impact on their cardiovascular health.





“We’re also conscious that there are some people who aren’t eligible to take the new modulator therapy, or they’ve had to come off them because they can’t tolerate them, so we have to keep progressing alternatives.
“We support babies through to those in their early 60s who would have had one or more organ

transplants. And we’ve had some people diagnosed later in life as adults. Obviously, it is genetic so you are born with it, but some only get a diagnosis as adults.”
Ms Bayakly says that our healthcare system must adapt to change, with the CF adult population growing 20%


in three years and set to continue on that trajectory.
“With less people being in-patient, some of that funding needs to be redirected to outpatient clinic because it’s so important to keep on top of the disease and it can be quite harmful to pick up an infection and not get onto it quickly.
“Preventative care is vital, and we’re in discussion with the State Government about the need for a redevelopment or expanded CF clinic.
“Every part of the health ecosystem which is supporting individuals is affected by the dramatic changes we’ve seen, but where it probably needs to change the most is in the adult outpatient care because that’s where the numbers are growing so dramatically.
“The clinic is under a lot of pressure, and something needs to change.”
ED: For more information visit www.cysticfibrosis.org.au/wa


An integrated approach to fertility care with Dr Lucy Williams
Working together to enhance our patients' fertility outcomes
Dr Lucy Williams
Fertility in primary care and how specialist care c an help our patients to reach their goals
Dr Babak Shakeri
Office Gynaecology, what is it and how can it benef it your patients?
Fertility Nurses Corry Moore & Chantelle Trower
The important role of the Fertility Nurse
(08) 9382 2388 conceptfertility.com.au marketing@conceptfertility.com.au
RSVP via the QR code
GPs earn CPD points
Join us for a complimentary three-course dinner & drinks 21 May 2025
6pm arrival for a 6.30pm start Event concludes at 9pm Cooee Next Door 171-173 Mounts Bay Rd, Perth



Addressing the decline in medical students specialising in general practice requires student and GP involvement, writes Kei Hsieh, National Chair, General Practice Students Network.
One of the biggest questions medical students ask themselves throughout their training is: “What type of doctor will I be?”
While some students enter medical school with a clear vision of their future specialty, for most this decision is something we explore throughout our training.
However, the latest National Data Report by the Medical Deans of Australia and New Zealand highlights a worrying trend – fewer students are choosing general practice as their preferred career.
In 2023, only 10.5% of final-year medical students selected general practice as their first-choice specialty, down from 13% the previous year.
Adding to this challenge, the RACGP reports that 32% of the current GP workforce intends to retire within the next five years, further worsening the GP shortage.
This raises a critical question – why are fewer medical students choosing general practice, and what needs to change to reverse this trend?
Despite being the cornerstone of Australia's healthcare system, general practice remains undervalued and underrepresented in medical training.
Medical students receive limited and often delayed exposure to the specialty, with GP placements typically occurring later in their studies, by which time many have already developed preferences for other specialties.
These placements are often brief and offer only a superficial glimpse into the breadth and complexity of general practice. In contrast, hospital rotations are longer and more immersive, exposing students to a broader range of complex cases.
This imbalance skews perceptions, leading many to overlook the intellectual challenge, diversity, and impact of general practice. Therefore, given that most healthcare is delivered in the community, should undergraduate medical training be restructured to better reflect this reality?
Simply increasing the number of GP placement days is not enough. The quality of teaching and student involvement during these placements is equally important.
Medical students want to actively participate in consultations but also be part of the broader aspects of community healthcare. To provide a comprehensive understanding of primary care, we encourage GP practices to offer students opportunities to work alongside nurses, administrative staff, and allied health professionals, gaining insight into the full scope of community-based healthcare.
The General Practice Students Network is a national, student-led organisation connecting more than 5,000 medical students across more than 20 Australian medical schools.
The Network is one of a kind in the world. As a grassroots initiative, it fosters peer-to-peer learning and direct engagement with practising GPs and pre-vocational doctors to inspire and support the next generation of general practitioners.
Local clubs host various events to prepare students for GP placements. The events range from hands-on workshops that build essential clinical skills, such as suturing, injections, and breaking bad news training, to career nights where students gain unfiltered insights into GP training pathways.
These events offer unique insights into training pathways, professional
Earlier GP placements: Introducing GP rotations in the early years of medical school would allow students to explore general practice before forming biases toward hospital-based specialties.
Enhanced student involvement: Placements should encourage active participation in patient care, including procedural skills and patient communication, rather than limiting students to passive observation.
Funded holiday placements: Providing opportunities for students to undertake holiday placements in GP clinics would give them additional clinical exposure and insights into the day-to-day realities of general practice.

development, and diverse opportunities within general practice. They also serve as valuable networking opportunities, helping students connect with mentors to maximise their GP placement experience.
Mentorship is a key focus, bridging the gap between students and GPs at various career stages. Events like GP speaker nights, networking speed-dating, and registrar rounds connect students with consultants, registrars, and pre-vocational doctors who share career advice.
Studies by the RACGP underscore the power of near-peer mentoring, where students benefit from guidance from those just ahead of them in training.
Reversing the declining interest in general practice requires systemic changes, including earlier and higher-quality GP placements, increased student involvement, and financial support for additional training opportunities.
This approach ensures that medical students are well-prepared to maximise their GP placements.
By advocating for and facilitating these experiences, the GPSN hopes to play a crucial role in shaping the future of Australia's GP workforce. Together, these changes are key to securing Australia’s future GPs.
ED: For more information visit: gpsn.org.au



Medical Forum podcasts bring you key insights to new treatment options available in WA from local specialists.
Join our clinical editor Dr Joe Kosterich as he interviews specialists across disciplines to keep you abreast of developments that could improve outcomes for your patients.
Perfect for a spot of CPD on your drive to work.
Topics covered this series:
Holistic approaches to bariatric surgery
How to approach ventricular tachycardia in primary care
The painful knee
Aortic stenosis diagnosis, surveillance and treatment.
Listen on your favorite podcast platform – scan the QR code to follow us!


Practitioner awareness of low iron among infants will support early intervention to improve outcomes, writes Dr Jamie Tan, Head of Paediatrics at Joondalup Health Campus.
One of the most surprising findings so far from ORIGINS is that one in three Western Australian children at 12 months, and nearly two in three at three years, can be classified as having low iron.
The big question we are now asking is: why are we seeing such low iron levels in this cohort of patients?
The IRON Child ORIGINS subproject was born from the need to make sense of this data. It seeks to investigate the reasons for low iron levels and provide information and advice to parents and clinicians on early intervention measures.
This is critical as we know iron is crucial for infants and toddlers, including for immunity and oxygen transport through to the blood.
Low iron can affect eating habits, sleep and speech and may result in infants and toddlers presenting as lethargic or grumpy. If left untreated, low iron and anaemia may also lead to neurocognitive and behavioural issues.
One area of focus includes the investigation of possible links between iron deficiency and childhood mental health, behaviour, and neurodevelopmental conditions, including ADHD.
For practitioners, being aware of the levels of prevalence that we have found may allow them to either prescribe further tests to look for low iron or anaemia, or to provide education on simple, low-cost, and effective ways of improving iron intake in children. These changes include boosting iron-rich foods in the diet and potentially decreasing milk consumption alongside eating those foods.
One of the benefits of the way the ORIGINS study is being conducted is that millions of data points are being made accessible


to researchers both locally and globally. Co-Directors Professor Desiree Silva and Dr Jackie Davis also decided to incorporate realtime feedback, giving parents nearimmediate access to data, including test results.
This information equips parents and caretakers with the ability to act – whether through consultation with their general practitioner, paediatrician, or other specialists or allied health professionals.
We know first-hand from parents in Joondalup, that this was one of the key drivers of them signing up for the study and one of the benefits they most value.
While long-term outcomes will take time to emerge, the knowledge that has already come to light gives us scope to intervene. So far, more than 800 children across the two projects have been identified as being low in iron, with parents or caretakers notified and provided with nutritional advice.
The IRON Child team is also harnessing the power of artificial intelligence to help analyse data, with the ultimate aim to prevent and treat issues caused by iron deficiency before they become clinically significant.
The work being done will also shape appropriate WA guidelines and provide data for national and international review via the World Health Organisation 2025 Anaemia Policy Brief.
ED: The ORIGINS study is a longitudinal cohort study following the health of 10,000 babies born at Joondalup Health Campus in collaboration with The Kids Research Institute Australia.
Dr Tan is part of the ORIGINS study.

A simple screening tool gave emergency department staff confidence in identifying at-risk children, writes Dr Marshall Makate from the School of Population Health at Curtin University.
Paediatric physical abuse is tragic and heartbreaking. Emergency departments (EDs) are often the first point of contact with the health system for children with nonaccidental injuries.
Only some cases are identified early and the consequences of missing these can be devastating.
Undetected abuse can lead to repeated harm, long-term trauma, and even death. ED staff often face difficult decisions with limited time and information, making it essential to have tools that help them recognise when a child may be at risk.
Recent research in a rural Australian hospital tested a simple screening tool and education program to help staff recognise possible abuse. The results show that small changes can make a big difference in child safety, if adequately resourced.
The problem we face
In Australia’s busy hospitals, missing the warning signs of possible non-accidental injury could mean discharging patients back to an unsafe environment.
Non-verbal children cannot explain their history, so subtle red flag signs and patterns for staff to recognise are important.
Specific bone injuries, unexplained bruising, historical inconsistencies with a child’s observed milestones or an unreasonable delay to seek care can all be subtle signs that staff need to be aware of when assessing paediatric injuries, burns and poisonings.
Without tools and training, we may not always know when or how to act. This is particularly true in rural hospitals, where resources may be limited. In these settings, there may be fewer paediatricians and staff must rely heavily on their clinical judgment.
Researchers from Curtin University introduced a screening tool to help clinicians assess potential physical abuse cases. The tool used an abridged version of a checklist developed at Perth Children’s Hospital for all paediatric patients presenting with injuries, burns or poisonings.
The goal was to identify and document red flags so clinicians could take the next steps suggested by the tool, such as making a referral to child protection services.
The research was supported by local leadership who funded regular safety net multidisciplinary team meetings, ensuring no cases were missed. Evidence was triangulated with multiple sources to confirm concerns for physical abuse.
Over 16 months, 1,469 cases were studied before and after the tool was introduced. The results were striking:
• Better documentation – doctors were almost eight times more likely to record detailed notes about injuries, making it easier to track concerns over time
• Cases less likely to be missed – cases that needed further investigation were five times more likely to be referred to child protection services
• Fewer unnecessary hospital admissions – doctors felt more confident in their decisions, ensuring that children received the right care without unnecessary hospital stays. Children were less likely to be admitted
• No increase in re-presentations –the number of children returning to the hospital within 30 days stayed about the same.
One of the most important findings was that the tool helped guide medical decision-making without

overwhelming the system. ED staff felt more confident in identifying children at risk knowing they had a structured process to follow.
This study reminds us that when combined with whole-of-staff education, a simple, evidencebased tool can improve child safety.
The project highlighted the need for ongoing training and support for ED staff, who play an important role in protecting Western Australian children. Additional resources and interagency communication would help strengthen the impact of this project.
EDs have a unique opportunity to prevent harm from paediatric physical abuse. A well-designed screening tool, combined with training and support, can improve outcomes.
Every child in the ED deserves to be discharged to a safe environment. If we want to protect children, we must give ED staff the tools and resources they need to act with confidence.
ED: Dr Marshall Makate is a co-author of the study How useful was a paediatric physical abuse screening project in a rural Australian emergency department? published in Emergency Medicine Australasia.







Science, including medical science, has historically begun from a stance of not knowing and needing to be convinced, rather than we know and want to confirm. Science advances by being questioning.
This quote from George Orwell has never been more apt: “During times of universal deceit, telling the truth becomes a revolutionary act.”
This came to my mind watching the confirmation proceedings for Dr Jay Bhattacharya as new head of the National Institutes of Health (NIH).
Bhattacharya was one of the authors of the Great Barrington Declaration in 2020, which called for focussed protection of the vulnerable in place of lockdowns.
Science, including medical science, has historically begun from a stance of not knowing and needing to be convinced, rather than we know and want to confirm. Science advances by being questioning.
Dr Bhattacharya’s statements are worth reflecting on.
“NIH-supported science should be replicable, reproducible and generalisable. Unfortunately, much modern biomedical science fails this basic test. I will establish a culture of respect for free speech in science and scientific dissent at the NIH,” he stated.
This is a breath of fresh air.
Some may wonder what this has to do with Australia. Firstly, a large amount of research is done in the USA and its priorities affect the rest of the world, including us.
Also, whether we care to admit it or not, we follow the lead of the USA in many aspects of life.
We live in interesting times, which is variably described as a blessing and a curse.
I am optimistic that the 2020's will end well. Time will tell.


By Dr Joey Kaye, Endocrinologist, and Dr Paul Maggiore, Cardiologist, Osborne Park
Cardiovascular disease remains the primary cause of premature death in Australian adults. Patients with metabolic dysfunction –such as diabetes or obesity – and renal disease remain exposed to elevated risk.
The underlying complex pathophysiology is referred to as the cardio-metabolic renal syndrome (CMRS). Excess adiposity has multiple negative physiological effects including insulin resistance, inflammation and endothelial dysfunction.
The result is an accelerated risk of cardiovascular events, heart failure, kidney failure, and premature mortality. Patients often require recurrent hospitalisations, with reduced quality of life, while the healthcare system bears the burden of chronic disease management.
Evolving therapeutic strategies
Whilst insulin resistance is a feature of CMRS, traditional glucose-
Cardiovascular disease remains the leading cause of premature death in Australia
Despite effective therapies, barriers to treatment remain A multidisciplinary model can improve outcomes.
centric treatment approaches have been largely ineffective at improving outcomes.
New therapies initially developed for diabetes – SGLT2 inhibitors and incretin-based agents – are demonstrating cardiac and renal benefits, largely independent of glucose lowering.
CMRS management is shifting to addressing broader cardiometabolic and renal risks, though is limited by differing treatment priorities across specialties as well as complexities of Australia’s
Pharmaceutical Benefits Scheme (PBS) prescribing restrictions.
Sodium-glucose co-transporter-2 (SGLT2) inhibitors have both glycemic and non-glycemic effects, with resultant cardiovascular and renal benefits.
Heart failure hospitalisations are lower, CKD progression delayed, and survival improved. This has led to widespread use and incorporation into multiple guidelines. However, in practice, their use is constrained by competing priorities across specialties, for example heart failure benefits vs renoprotective effects vs glucose lowering, complex PBS eligibility criteria, important drug-interactions and side-effects such as hypoglycaemia with insulin, electrolyte disturbance and dehydration with diuretics, limited evidence for use in type 1 diabetes, limited trial evidence for efficacy and safety of specific combinations like SGLT2 inhibitors and GLP-1 analogues.

Emerging evidence suggests glucagon-like peptide-1 receptor agonists (GLP-1RAs) reduce major adverse cardiovascular events, promote weight loss, and may offer renal protection.
However, PBS restrictions limit access to those with type 2 diabetes, excluding many with weight-related co-morbidities who might benefit from these therapies based on cardiovascular or renal indications alone.
Furthermore, shortages of GLP1RAs, driven in part by off-label use for obesity, have created inequities in access. As highlighted with SGLT2i’s above, competing priorities across specialities may limit adaptation of incretin-based therapies.
Despite the availability of new and effective therapies, several barriers hinder optimal CMRS management in Australia, including:
• Fragmented care across specialties – patients with CMRS ideally require input



from GP’s, cardiologists, nephrologists, endocrinologists, hepatologists and various allied health professionals. However, siloed care often results in delays, inconsistent prescribing practices, and missed opportunities for holistic management.
• Competing treatment priorities –clinicians may focus on different aspects of CMRS management, leading to therapeutic inertia, adverse drug effects or conflicting recommendations.
• PBS restrictions, access, supply and evidence limitations –Australia’s PBS listing criteria, while based on best available evidence and cost considerations, still creates barriers to early intervention and adds to the complexities of clinical decision making and individualising care.
• Allied health underutilisation –while GPs and specialists focus on medical management, allied health professionals, including dietitians, exercise physiologists, diabetes educators, and pharmacists, play a crucial role in lifestyle modification, medication adherence, and patient
education. However, access to these services is often limited by Medicare restrictions, funding constraints and a system that rarely provides all the care in one place.
Reducing cardiovascular disease and premature mortality in the setting of a complex condition such as the cardio-metabolic renal syndrome, requires dedicated management strategies across multiple specialties.
To overcome the barriers outlined in this article, a shift towards multidisciplinary, patient-centred and coordinated care is needed.
A cardiometabolic clinic, which delivers evidence-based therapy whilst integrating GPs, specialists and allied health professionals in one service, is a proposed solution to improving outcomes.
Author competing interests – both authors have served on advisory boards and received honoraria for education events regarding therapeutics referred to in this article
We are delighted to announce the expansion of our services at St John of God Murdoch Hospital

Dr. Helen Ballal and Dr. Lee Jackson are joining Dr. Wen Chan Yeow in delivering state of the art breast surgery.
Our well-established unit is dedicated to providing exceptional, patient-focused care through a compassionate and evidence-based approach. We coordinate the entire patient journey with a multidisciplinary team of highly regarded and qualified specialists and a broad range of allied health professionals.
Our comprehensive services include:
Management of malignant and benign breast conditions
Level 1,2 and 3 oncoplastic breast resections
Breast reconstruction
Breast reduction and mastopexy
Assessment and care for individuals with high-risk family histories or lesions
Healthlink EDI: perthsbc | drwcyeow (Dr Yeow only)
Appointment bookings: Phone 9382 4622 | Fax 9382 4611
With regular consulting and theatre sessions at SJOG Murdoch, we ensure that patients are treated in an extremely timely manner.
We are pleased to inform you that Dr. Lee Jackson will also continue to offer consultations in Joondalup.
At Perth Specialist Breast Care, we are committed to guiding you and your patients through every step of the journey with expertise, care, and compassion.
For referrals and appointments, please contact us today.
Murdoch St John of God Medical Clinic Suite 37, Level 1, 100 Murdoch Drive
Joondalup Genesis Care, Shenton House, 57 Shenton Ave
By A/Prof Kushwin Rajamani, Cardiologist & Cardiac Electrophysiologist, Nedlands
The incidence of atrial fibrillation (AF) in Australia is among the highest in the world. Atrial fibrillation has major implications with a five-fold increase in heart failure and two-fold increase in cardiovascular death.
Across Australia, AF related hospital admission is now the most common cause of cardiovascular hospitalisation, contributing up to a five-fold increase in stroke risk and responsible for 20% of stroke incidence.
The economic impact of atrial fibrillation annually is $1.25 billion and for stroke it is more than $15 billion. These are astounding figures both clinically and economically, creating a national emergency for early detection, intervention and treatment.
Advancing research is key to developing targeted treatment modalities. In vitro models using 3-dimensional engineered tissue models of varying cell types such as fibroblasts, endothelial cells, neurons and immune cells could offer a more realistic assessment of the microenvironment related to arrhythmogenicity.
The use of animal models has provided critical knowledge about mechanism, substrate and molecular differences.
Certain gaps including the biological pathways that lead to the atrial triggers and substrate, mechanism of atrial remodelling and clot formation, sex differences and outcomes based on comorbidities are to be determined.
Gene testing or genotyping at this stage is largely undertaken in research settings and there is potential for early detection of AF risk and early preventive strategies with pre-emptive genotyping.
The underlying pathophysiologic mechanism that results in the onset, maintenance and progression of atrial fibrillation can be classified into ‘triggers’ and ‘substrate’.


Triggers are fundamentally referred to as the electrical ectopic activity from the pulmonary veins and substrate pertains to the structural remodelling of the atrium characterised by fibrosis, fatty infiltration, and inflammation leading to conduction abnormalities and re-entry resulting in AF.
The prospect of machine learning using ECG data including P wave duration, amplitude and dispersion, along with electrical biomarkers may hold promise for prediction of AF.
The value of atrial imaging specifically using cardiac MRI to quantify fibrosis need to be evaluated further to be considered as a measure to guide therapy.
There have been significant advancements in the options for rhythm control over the past
three decades. Catheter ablation for AF is now considered a Class IA recommendation in clinical guidelines to reduce the risk of recurrence of atrial fibrillation and symptoms.
Radiofrequency ablation has been the mainstay thus far and, to a lesser extent, cryoablation. There is rapidly emerging use of Pulse Field Ablation technology to achieve pulmonary vein isolation. AF ablation is more effective than antiarrhythmic therapy, however, there remains a high burden of recurrent AF after PVI.
This leads to the focus on aggressive lifestyle modifications and addressing biological mechanisms that contribute to AF.
There is strong evidence that lifestyle changes alone can influence the incidence, maintenance and progression of AF.
Atrial fibrillation is an important healthcare priority with increasing burden
Primary prevention is the key Addressing atrial fibrillation requires a collaborative effort with engagement of the public, healthcare providers, researchers, industry, government, policy makers, patient advocates and campaigners.
Australian-led research has proven that weight loss with aggressive risk factor reduction, exercise training, management of sleep apnoea and alcohol abstinence can result in reduction in AF burden and symptoms.
Primary prevention
Primary prevention is key. Developing improved risk assessment tools employing polygenic risk score, electrical or blood-based biomarkers and cardiac imaging indicators may allow for targeted intervention for high-risk individuals.
The value of managing hypertension, diabetes, obesity and physical inactivity in reducing AF cannot be underestimated. The advent of AI driven tools may accelerate the ability to identify high-risk individuals across various demographics allowing for education, risk factor reduction, early identification and treatment.
Population based screening may help detect AF early to reduce the progression of AF, hospital admissions and perhaps the prevention of stroke.
Patient education and empowerment is a key priority to achieve self-management, compliance, reduction in hospital admissions and improved quality of life.
Education programs need to enhance the understanding of AF, the symptoms, management, compliance to therapy and possible complications. These initiatives would particularly assist asymptomatic patients to take the condition more seriously.
Shared decision making with a patient-centric approach allows patients to actively participate
in their care. The technological advancements with smart watches and self-monitoring tools provide real time data and help patients to monitor their own heart rate and trends so they can be empowered to participate in the process.
Support groups, online communities and phone applications could provide useful information, shared experiences and offer emotional support.
Health information integration between hospitals, primary care physicians and cardiologists will certainly optimise the delivery of care and improve outcomes. Both rural and indigenous populations who tend to have worse outcomes will additionally benefit from all these initiatives.
Author competing interests - nil
‘In the last decade, there’s been a big leap in technology and skills that has seen the introduction of game changing endovascular surgery. Our work is constantly evolving making a real difference in people’s lives.’

Dr Altaf and his team provide a comprehensive diagnostic and therapeutic service of arterial and venous diseases including:
Abdominal aortic aneursyms
Carotid artery disease
Peripheral artery disease
Leg ulcers & diabetic foot disease
Varicose vein diagnosis & treatment
Renal access
Dr Altaf consults at Hollywood Medical Centre, SJOG Midland Private Hospital, SJOG Carine Specialist Centre and public appointments at RPH and SJOG Midland Public Hospital. Operates out of SJOG Midland Public and Private, Hollywood Hospital and SJOG Subiaco.
Appointments are coordinated through practice manager Michelle Burrell and her team.

Hollywood Medical Centre Level 2 Suite 45/85 Monash Ave, Nedlands WA 6009
Phone: 6244 6215 | Fax: 6315 6423 | Healthlink ID: drnaltaf draltaf.com.au
By Pragnesh Joshi, Cardiothoracic Surgeon, Nedlands
True incidence and prevalence of aortic root aneurysm is not exactly known. Pooled incidence and prevalence of thoracic aortic aneurysm was reported to be 5.3 per 100,000 individuals per year.
The aortic root replacement is considered a standard of care when surgery is indicated and includes replacement of native aortic valve, aortic sinuses and ascending aorta along with re-implantation of native main coronary arteries.
Aortic aneurysm affects mainly the aortic wall and aortic sinuses. Quite often, native aortic valve is not diseased or, at most, there is aortic regurgitation. Aortic valve replacement in this situation can be avoided by re-using a patient’s native valve. However, in most cases even when the aortic valve is normal, it is replaced with artificial mechanical or tissue prosthesis while performing aortic root replacement due to lack of expertise.
David’s procedure is an aortic root replacement operation where in patients’ native aortic valve is used and re-implanted instead of a mechanical or tissue valve. This operation was introduced by Dr Tiorne David from Canada. Also known as Valve Sparing Aortic Root Replacement (VSARR), it allows patients to retain their native valve, avoiding the associated lifetime complications of an artificial valve.
Indications
Indications for David’s procedure overlaps with indications of aortic root replacement. Current threshold to advise aortic replacement surgery is 5.5 cm diameter. However, the indications need to be tailored to a patient’s medical background.
Candidates for David’s procedure need good quality, native valve and a surgeon experienced in performing the procedure. It can be considered in:
• patients with high-risk features
• at diameter of 4.5-5.0cm in patients with connective tissue disorders and high-risk features
• at diameter of 4.5 in patients with family history of dissection of aorta.
Aortic replacement surgery can be considered at 5.0cm in diameter if performed by an experienced aortic surgeon. While evaluating patient for aortic root surgery, indexed aortic diameter and cross-sectional area ratio should be taken into consideration.
The aortic valve must be of good or reasonable quality for consideration of reimplantation. Those who are not suitable include patients with aortic stenosis, infective endocarditis with features of valve destruction, aortic valve with signs of advanced degeneration such as calcification or retraction of leaflets, quadricuspid or unicuspid aortic valve, and multiple large fenestrations in leaflets.
A bi-cuspid valve can be reimplanted as long as they are of good quality and devoid of calcification. The long-term results are very good.
Most David surgeons should be experienced aortic root surgeons, which requires close to 70 aortic root replacement surgeries. From published data one can say that the risk of valve related reoperations, bypass time and cross clamp time tends to be better after 30-40 cases per surgeon.
This means that the surgeons who should perform David’s operation should be proficient in aortic root surgeries and should be undertaking this operation on a regular basis.
How is the procedure performed?
The standard approach is via median sternotomy under general anaesthesia. Highly experienced surgeons may be able to offer this operation via mini sternotomy. The procedure requires cardiopulmonary bypass and requires the heart to be stopped. Native ascending aorta and aortic root tissues are excised while leaving native aortic valve attached to aortic annulus.

Native aortic valve can be reused in patients undergoing aortic root aneurysm surgery with David’s procedure
Native aortic valve has lower risk of endocarditis and eliminates need for anticoagulation
David’s procedure should be performed by experienced aortic root surgeons.
Left and right main coronary arteries are separated, the aortic root and ascending aorta are reconstructed using a polyester tube graft. The native aortic valve is reimplanted within this graft along with coronary arteries.
Valve is tested for symmetry and function using aortoscopy. Prior to closing the chest, transoesophageal echocardiography is performed to check the form and function of the valve repair. The post operative course is the same as any other cardiac surgery.
The long-term results of this operation are excellent, both in terms of survival and freedom from valve related reoperations. Freedom from reoperation is close to 90% at 10 years and 85% at 15 years. This closely matches with conventional aortic root replacement with artificial heart valves, however eliminates the risk of bleeding or thromboembolism which is more with artificial heart valves.
Another advantage of native aortic valve is lifelong lower risk of endocarditis compared to artificial heart valves. Every artificial heart valve comes with lifelong risk of endocarditis and thromboembolism.
The mechanical valve comes with added risk of bleeding. Native aortic valve does not require anticoagulation and risk of stroke from the valve would be no different to anyone else with native valve.
Author competing interests – nil
By Dr Faith Njue, Cardiologist, Subiaco
Cardiovascular disease complicates 1-4% of pregnancies and accounts for up to 15% of maternal mortality. It is the leading cause of maternal mortality in Australia.
The risk during pregnancy depends on the specific cardiac condition and current clinical status of the woman. Risk stratification guides management in pregnancy. There are several classifications or risk scores for assessing maternal cardiovascular risk in pregnancy, the most wellestablished risk assessment for acquired disease is CARPREG (Cardiac Disease in Pregnancy) and the modified WHO Classification. The ZAHARA risk score is well validated for congenital heart disease.
Some of the identified risk factors include advanced maternal age, obesity, hypertension, smoking and diabetes, which all have increasing prevalence in Australia’s pregnant population.
The associated morbidity and mortality is even higher with Aboriginal and Torres Strait Islander
Cardiovascular disease in pregnancy: The need for cardioobstetrics teams
Cardiovascular disease is the leading cause of maternal mortality in Australia.
Adverse pregnancy outcomes significantly increase the risk of subsequent cardiovascular issues.
Cardio-obstetrics and multidisciplinary care of women with cardiac disease in pregnancy improves outcomes.
women – between 2012 and 2018 the maternal mortality ratio of these women was 20.2 per 100,000 women giving birth.
In the same period, the MMR for non-Indigenous women was 5.5 per 100,000 women giving birth. This is likely related to the higher prevalence of valvular heart disease due to rheumatic heart disease.
Research is also uncovering more evidence of long-term cardiovascular risk in women related to adverse pregnancy outcomes like pre-eclampsia and gestational hypertension, with some evidence of long-term risk to the child.
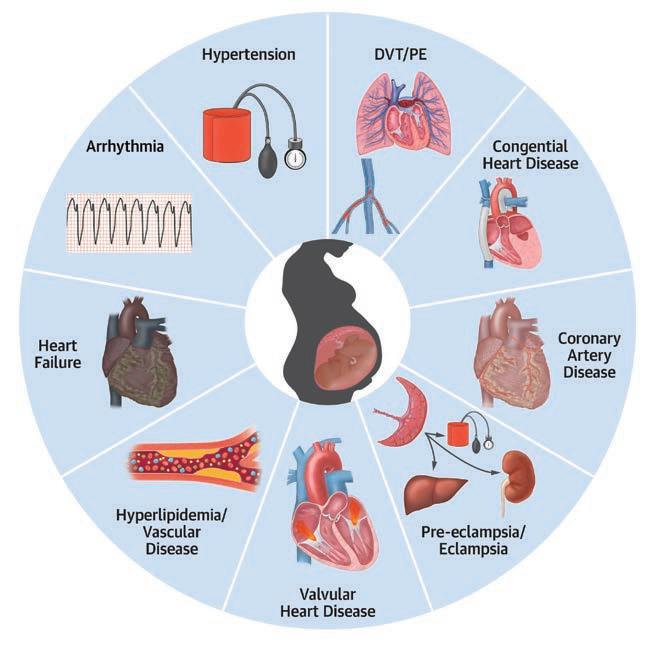
Emerging data shows that preterm birth –less than 37weeks – is also associated with short-tolonger-term cardiovascular disease risk in the mother and long-term cardiovascular disease risk in the child. Although the exact pathophysiology is uncertain, APOs are likely caused by underlying metabolic or vascular abnormalities that originate with defective

Management of adverse pregnancy outcomes or underlying risk factors is essential. Cardiovascular risk is increased almost 2-4-fold in women who have had an APO.
This has significant implications for individuals and wider society as this is risk identified in a relatively young population. North American data demonstrated that cardiovascular mortality rates among women aged 35 to 44 years of age have been increasing on average since 1997.
Women who have experienced adverse pregnancy outcomes are at high risk for several types of cardiovascular disease including heart failure with preserved ejection fraction (HFpEF) later in life.
The development of cardioobstetrics and multidisciplinary care of women with cardiac disease in pregnancy has been shown to improve outcomes. Cardio-obstetrics is an expanding subspecialty within cardiology that focuses on the prevention, early detection, and appropriate management of cardiovascular disease in pregnancy.
Patients with known cardiac conditions should be referred for pre-conception counselling. This is particularly important for women with high-risk conditions like cardiomyopathy, aortopathy or prosthetic valves. It should also ideally be offered for women with significant cardiovascular risk factors. This also extends to patients being offered, or undergoing, assisted reproduction. Pre-conception counselling would also involve a review of cardiac medications to avoid those associated with teratogenicity.
Currently, cardio-obstetric services are offered at Fiona Stanley Hospital with multidisciplinary involvement of cardiology, obstetrics, maternalfoetal medicine specialists and anaesthetists. It is also available in the private sector.
Author competing interests- nil
By


The recent Australian burden of health review revealed ‘back pain and problems’ to be the second most recorded cause of disease burden. Cervical degenerative disease (CDD) has been shown to affect over 50% of those aged 40 and over.
Patients with CDD generally present with either neck pain, radiculopathy, myelopathy or a combination. While many patients improve with conservative measures alone, those with unremitting symptoms, progressive neurology or significant neurological compromise often require surgical intervention.
Historically anterior cervical discectomy and fusion (ACDF) has been the go-to gold standard surgical option. Accessing the cervical spine from the front of the neck allows excision of the target cervical disc and underlying osteophytes, thereby relieving the identified neural compression.
An iliac crest bone, polyether ether ketone (PEEK) or 3D-printed titanium cage can be placed into the cleared disc space, aiming to achieve fusions between the two adjacent vertebrae. Despite the fact ACDF has been demonstrated to be efficacious, development of compressive adjacent level degenerative disease has been observed in up to 10% of individuals five years post-operatively and up to 40% at 10 years.
The concept of a cervical disc replacement (CDR) was pioneered by Dr Ulf Fernstrom in the 1960’s. This ultimately aimed to retain mobility of the cervical spine, reduce the stress on neighbouring cervical levels, and subsequently reduce the progression of neighbouring level disease. Unfortunately, early attempts were plagued with both surgical

and device-related complications, including dysphagia, implant migration and cervical instability. Marked improvements in arthroplasty devices have been made with several devices on the market.
Not everyone with CDD is a candidate for cervical disc arthroplasty, with several contraindications frequently cited. These include patients with cervical instability, severe facet disease/ spondylosis or osteoporosis. Indications for cervical disc replacement generally include adults with radiculopathy or myelopathy resulting from either one- or two-level spondylosis –between C3-C7 – who have failed at least six weeks of conservative management.
Long-term data is now available for disc replacement, with the Byran disc device offering 20-year data from a RCT against ACDF. There is a 10% reoperation rate compared to the 41% reoperation rate of ACDF.
Further randomised control trials, with 2–10-year followup, comparing cervical disc


replacement to ACDF support these findings.
The reduced reoperation rate after CDR is due to its potential to reduce the incidence of adjacent segment disease (ASD). Meta analyses assessing the long-term CDR outcomes have demonstrated significantly lower rates of symptomatic ASD and subsequent re-operations at adjacent levels compared to ACDF.
Rates of reoperation at the operated level provide another comparison between CDR and ACDF. In this case, ACDF typically has a lower rate of revision likely due to the static nature of a fusion.
A mobile disc replacement, like any joint replacement, can lead to issues such as implant wear, loosening or subsidence and continued abnormal bone growth around the prosthesis. Each of these may potentially require revision surgery.
While higher revision rates have been observed at the index level, long term data still suggests higher total rates of second cervical procedures in ACDF patients.
CDR offers outcomes at least equivalent to ACDF, with advantages in motion preservation, reduced ASD, and fewer adjacent-level surgeries
Both procedures effectively alleviate symptoms, but CDR may provide more function for some candidates
Continued surveillance beyond the current follow-up, and assessment of additional indications, will enable further assessment of the lifespan and utility of CDR implants.
The major aim of disc replacements is to mimic normal movements of the native disc, retaining mobility at the operated segment.
Post-operative studies show CDR effectively maintains range of
movement at the operated level, with longer term studies confirming that the preserved cervical kinematics are maintained in a high percentage of patients.
CDR as a result has also been demonstrated to be as effective, if not more so, at achieving improvements in recognised outcomes scores, such as the Neck Disability Index (NDI), visual analog scale (VAS) for neck and arm pain, with CDR patients experiencing sustained improvements typically superior to those undergoing ACDF at 5-10-year follow up. Patient satisfaction and quality of life measures also tend to favour CDR in these mid-to-long-term assessments.
Cervical disc replacement appears to have cemented a place in the management of cervical degenerative disease, generally performing best in younger, active individuals with one or two level
Weight loss drug Wegovy has been approved to also treat cardiovascular disease in overweight and obese patients.
The Therapeutic Goods Administration has approved semaglutide 2.4mg – sold as Wegovy – to be used as a complementary therapy for reducing major adverse cardiovascular events, including cardiovascular death, non-fatal myocardial infarction and non-fatal stroke.
Wegovy is indicated as an adjunct to standard of care therapy to reduce the risk of major adverse cardiovascular events in adults with established cardiovascular disease, with a BMI higher than 27kg/m2, and without established type 1 or type 2 diabetes, the TGA guidance states.
It is the first time a weight loss drug has been approved for such a use in Australia.
The approval follows findings from the SELECT trial, which showed Wegovy reduced cardiovascular events by 20% in people with preexisting heart disease who were
disease who have minimal preoperative degeneration.
Over recent years a number of groups have reported on its potential use in multilevel disease. A seven-year review of patients with three or four level cervical disc arthroplasty observed high rates of patient satisfaction and retained long-term improvements in outcome scores, suggesting this may be a future avenue.
Additionally, a recent increase in reporting of the use of hybrid constructs in which multilevel cervical degenerating is managed with a combination of disc arthroplasty and fusion has occurred, with future randomised control trials planned.
Author competing interests - nil

overweight or obese but did not have diabetes.
SELECT is an international study involving more than 17,000 participants across 41 countries, including Australia.
Director of the Victorian Heart Institute at Monash University Professor Stephen Nicholls, who led the Australian part of the trial, said it demonstrated that the cardiovascular benefits of semaglutide extend beyond weight loss.
“This approval highlights the critical role of overweight and obesity as major drivers of heart disease—on
par with cholesterol, blood pressure, diabetes and smoking. It reinforces that these risks can be actively reduced with targeted therapies,” he said.
“This drug also positively impacts inflammation, blood lipids and blood pressure, which are all crucial in preventing heart attacks and strokes.
“What this tells us is that if you have heart disease and are overweight or obese, not only are you at a higher risk of another cardiovascular event, but that risk can now be significantly reduced. This is a groundbreaking result for patients.”
By Dr Susan Kurvilla, Cardiologist, Nedlands
Cardiovascular disease remains the leading cause of mortality and is responsible for a significant number of death and disabilities that are largely preventable. It kills one in every four Australians.
Breakthrough therapies and advanced risk prediction tools offer remarkable possibilities of prevention, yet basic proven interventions often fail to reach many who need them most. Addressing the challenges we face in delivering proven preventive care is as crucial as identifying new treatments.
Achieving the promise of cardiovascular disease prevention requires solving the problem of translating what we know into tangible benefits for patients and populations.
High systolic blood pressure remains the leading modifiable risk factor globally for attributable premature cardiovascular deaths – 10.8 million cardiovascular deaths and 11.3 million deaths overall in 2021 – particularly linked to ischaemic heart disease and stroke-related death. Intensive blood pressure control is projected to extend life expectancy by up to three years when initiated in middle age.
Dietary risks accounted for 6.58 million cardiovascular deaths and 8 million deaths overall in 2021. This estimate included food types that are under consumed globally –fruits, vegetables, legumes, whole grains, nuts and seeds, milk, fibre calcium, omega-3 fatty acids from seafood, and polyunsaturated fatty acids – or overconsumed like red meat, processed meat, sugarsweetened beverages, trans-fatty acids, and sodium.
Excess dietary sodium is a major driver of hypertension in many countries and modest dietary sodium restriction by 3g per day has been projected to avert cardiovascular events and reduce deaths in a cost-saving manner.
High LDL-C has persisted as a


Cardiovascular disease is the leading cause of mortality globally
Attention to delivering proven preventive care is as crucial as development of new therapies.
leading modifiable risk factor and is one of the most closely linked markers of atherosclerotic CVD. In 2021, 3.81 million cardiovascular deaths and 3.81 million deaths overall were attributed to elevated LDL-C levels.
Exposure to lower cumulative LDL-C levels in young and middle-aged adults has been associated with reduced long-term cardiovascular risk. Statins are the cornerstone of primary and secondary prevention
of CVDs. Sequential advances have identified other effective classes of lipid-lowering therapies that lower LDL-C and positively affect cardiovascular health, for example ezetimibe, PCSK9 inhibitors and Inclisiran.
Air pollution in the form of ambient particulate matter with an aerodynamic diameter smaller than 2.5 μm and household air pollution from cooking fuels represents the leading environmental risk factor for premature CVD and mortality. In 2021, 4.75 million cardiovascular deaths and 8.54 million deaths overall were attributable to air pollution.
Tobacco is the fifth leading actual cause of cardiovascular death, with 3.01 million cardiovascular deaths and 7.61 million deaths overall attributable to tobacco use in 2021.
Obesity is closely associated with multiple health risks and directly contributes to the pathogenesis and progression of CVD. In 2021, 1.95 million cardiovascular deaths and 3.7 million deaths overall were attributable to elevated BMI. Changing the trajectory
Community-based health promotion and intensive lifestyle management interventions may have durable impact on cardiometabolic health long-term. Early, comprehensive programs that can be embedded in schools have been demonstrated to influence childhood behaviours and cardiovascular health trajectories.
High fasting plasma glucose tracks closely with high burden of prediabetes, diabetes, and obesity worldwide. In 2021, 2.30 million cardiovascular deaths and 5.4 million deaths overall were attributable to elevated fasting plasma glucose.
Population strategies to improve glycaemic risk overlap substantially with approaches to other primary risk factors, including low physical activity and adverse dietary profiles.
Two therapeutic classes, SGLT2 inhibitors and the glucagonlike peptide-1 receptor agonists, can prevent cardiovascular complications and kidney disease progression in patients with diabetes. Continuous glucose monitoring has been introduced to minimize glycaemic excursions and improve precision of glycaemic control.
In 2021, 1.87 million cardiovascular deaths and 3.47 million deaths overall were attributable to reduced kidney function. Patients who ultimately progress to end-stage kidney disease requiring dialysis face reduced health-related quality of life and heightened risk of death while contributing substantially to increased health system costs.
Lead exposure remains a silent but major contributor to CVD mortality and health loss. Lead is an under recognised environmental factor linked with hypertension, stroke, coronary artery disease, peripheral artery disease, and other CVDs.
Low physical activity levels represent an important threat to cardiovascular health. In 2021, 0.397 million cardiovascular deaths and

0.686 million deaths overall were estimated as being attributable to inadequate physical activity. There is clear evidence of substantial years of life lost and reduction in life expectancy with heavy alcohol use, especially as alcohol consumption exceeds 100g weekly. Cardiovascular risks associated with increased blood pressure and arrhythmias are seen with higher alcohol use.
The COVID-19 pandemic has had a profound impact on health worldwide. Patients with CVDs faced among the highest risks of mortality and complications when infected.
COVID-19 may trigger acute cardiovascular events, such as myocardial infarctions or strokes and the longer-term cardiovascular health implications of COVID-19 infection are increasingly recognised.
Author competing interests – nil






By Prof Mario Siervo, School of Population Health, Curtin University
Dietary nitrate should not be confused with organic nitrates, which are pharmacological compounds used primarily for the management of coronary heart disease.
Dietary nitrate is an essential nutrient for plant and animal physiology. In plants, dietary nitrate plays a key role in the nitrogen cycle and ensure their optimal growth. In humans, dietary nitrate not only contributes to the regulation of nitrogen balance but also participates in several physiological functions including vascular tone regulation, immune response, and gut microbiota health.
Dietary nitrate significantly contributes to the generation of nitric oxide. NO is a soluble gas primarily produced by endothelial cells through the classical, enzymatic L-arginine-nitric oxide synthase (NOS) pathway. However, an alternative non-enzymatic pathway called nitrate-nitrite-NO pathway also exists that converts dietary nitrate into NO through a two-step reduction process, helping maintain optimal NO production.
Dietary nitrate represents a natural and accessible approach to improve cardiovascular health Promotion of the consumption of nitrate-rich foods should be considered part of comprehensive cardiovascular health management
As research evolves, dietary nitrate may become an important component of both primary and secondary cardiovascular disease prevention strategies.
When ingested, dietary nitrate is rapidly absorbed in the upper gastrointestinal tract and enters the bloodstream. While approximately 75% is excreted by the kidneys, the remaining 25% is actively concentrated in saliva by the salivary glands. The oral microbiome is crucial in this process, as bacteria on the tongue reduce salivary nitrate to nitrite.
Upon swallowing, some nitrite converts to NO in the acidic stomach environment. The

remaining nitrite enters circulation, serving as a reservoir for NO generation, particularly when the oxygen-dependent NOS pathway is compromised during hypoxic or ischemic conditions.
Dietary nitrate therefore represents an important alternative source of NO. Recently, it has emerged as a promising nutritional compound with significant cardiovascular benefits.
This naturally occurring molecule, abundant in green leafy and root vegetables like rocket, lettuce, spinach, beetroot and turnip, demonstrates potential for improving vascular function, reducing blood pressure, and enhancing skeletal muscle performance through its conversion to NO in the body.
The most well-documented cardiovascular effect of dietary nitrate is its ability to reduce blood pressure. Meta-analyses of randomised controlled trials have shown that dietary nitrate supplementation, typically through beetroot juice supplementation, can reduce systolic blood pressure

by approximately 4 to 5 mmHg and diastolic blood pressure by 2 to 3 mmHg, with greater effects seen in individuals with elevated blood pressure.
Dietary nitrate supplementation has been linked to improved endothelial function, as measured by flowmediated dilation (FMD), a marker of vascular health. Additional beneficial effects of dietary nitrate supplementation include a reduction of arterial stiffness, a key predictor of cardiovascular risk and inhibition of platelet aggregation.
Emerging evidence also suggests that dietary nitrate may improve cardiac efficiency by reducing oxygen consumption without compromising cardiac output, with potential benefits in patients with heart failure.
Several prospective cohort studies have also provided strong epidemiological evidence that higher vegetable nitrate intake is associated with reduced cardiovascular disease incidence and mortality.
These studies found that moderate vegetable nitrate consumption – approximately 60-140 mg/day –
was associated with 15-27% lower risk of cardiovascular diseases, with benefits observed for ischemic heart disease, heart failure, stroke, and peripheral artery disease.
These protective effects appear to be independent of other lifestyle factors and partly mediated through blood pressure reduction, supporting the clinical findings from randomised controlled trials.
The evidence for cardiovascular benefits has increased interest in dietary nitrate supplementation as a complementary approach to cardiovascular health management.
Current data suggests that a daily nitrate intake of approximately 300-400 mg, equivalent to approximately 300ml of beetroot juice or about 200-300g of nitrate-rich vegetables, may be sufficient to achieve meaningful cardiovascular benefits.
Plant-rich dietary patterns such as the Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets are widely recommended by authoritative associations and incorporated
into clinical guidelines for both the prevention and management of cardiovascular diseases.
The cardiovascular benefits of these dietary patterns could be partly attributable to their high nitrate content as they can provide approximately 1000mg of nitrate, depending on vegetable choices.
Doctor’s orders
Health professionals and clinicians involved in the prevention and management of cardiovascular diseases could consider recommending increased consumption of nitrate-rich foods, particularly leafy greens like spinach, rocket, kale and lettuce, as well as beetroot as part of a hearthealthy diet.
This recommendation aligns with existing dietary guidelines that emphasise plant-based foods. For patients with established hypertension or cardiovascular disease, structured dietary approaches incorporating nitraterich foods may potentially serve as an adjunct to pharmacological therapy.
Author competing interests – nil
The eighth annual GP Urology Masterclass offers comprehensive education to GPs, covering all aspects of urology to enhance their knowledge and skills in this broad field of practice.
Program Topics:
• Prostate cancer update – PSA, new treatments in WA
• Immunotherapy, ARPIs and radiopharmaceutical therapies – what GPs need to know
• LUTs, BPH and OAB – what’s new in 2025
• Incidental urological findings on imaging
• Haematuria and Recurrent UTIs
• Urology in the elderly
Please book a place for the conference at gpurologymasterclass.com.au or rsvp to events@perthurologyclinic.com.au Limited seats available
Launching in 2025, The PUC Foundation is a non-profit to promote excellence in urology research and education. To support this initiative, a $75 tax-deductible, non-refundable fee has been introduced for the GP Urology Masterclass with all proceeds going to the foundation. THE PUC FOUNDATION
By Dr Sanjay Sharma, Cardiothoracic Surgeon, Perth
Rib and chest wall fractures are common. Rib fracture is associated with 15% of all trauma admission while 30% of all rib fractures develop chronic pain six months post-injury.
Factors associated with increased risk of chronic pain include pretrauma smoking history, two or more rib fractures, oxygen saturation less than 95% on admission, osteoporosis and prolonged opiate requirement. Sternal fracture is present in 4-8% of all blunt trauma injuries and can be painful chronically.
Traditional management has been conservative based on analgesia and physiotherapy. However, increased patient demand for earlier return to work and sport, intolerance of long-term analgesics and chronic pain has led to a push for early fixation.
Technology has also improved, with a large array of rib and sternal specific plates now available. Rib plates are designed for each rib with their own individual angulation and spiral, which allows for stronger, more minimally invasive fixation often with earlier discharge, return to work and sport and decreased opioid use.

A 51-year-old female teacher fell down some stairs five months ago. Ongoing opioid requirements left her unable to return to work or exercise. The patient had fibrous non-union of sternum on CT. Patient had plating.


Three weeks post fixation, the patient was on intermittent Panadol and able to return to work and exercise.
2:
A 67-year-old female driver with an acute sternal fracture. She was discharged with an opioid prescription but was later readmitted with pain, productive sputum and sepsis.

The patient underwent a sternal fixation two days post IV antibiotics for pneumonia. She returned to work three weeks post fixation with occasional Panadol.
3:
An elite sportsman fractured their rib. They were unable to train and sleep due to pain with clicking. CXR showed fibrous non-union of the left 10th rib fracture.
The patient received a rib-specific plate and was able to return to professional sport in four weeks.
4:
A 54-year-old policeman was left injured after being attacked at work. They were only able to sleep in an upright position because of severe pain.
Key messages
Rib fractures are common
Historically management has been conservative
Surgical fixation can speed recovery and improve outcomes.
They had displaced fractures of right 5th,6th and 7th ribs. The ribs were plated and the patient returned to light duties three weeks post-op and full duties eight weeks post-plating.
Positive results
Due to higher patient expectations and advanced plating systems, rib and sternal fixation greatly decreases pain and morbidity and accelerates return to work and sport in selected patients.
Patients are advised not to lift more than 5kg for at least three weeks post plating. Procedures are relatively low risk with a low rate of bleeding, infection and plate migration.
Author competing interests - nil
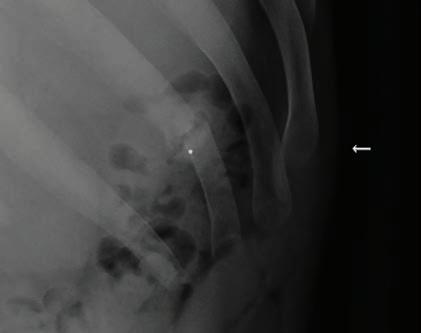

Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy
Surgery can be open or endoscopic.

The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.



Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare.


St John of God Medical Centre Suite 10, 100 Murdoch Drive, Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301 www.murdochorthopaedic.com.au Murdoch

Get up close to the art as you explore Sculpture at Bathers when it returns to Fremantle’s Bathers Beach this month.
There are many reasons why it’s fabulous living on the west coast.
One of them is a daily sunset over the ocean, another is being able to watch that sunset surrounded by sculptures and watching the light play on them.
Experience that across this month at Sculpture at Bathers at the Bathers Beach Art Precinct in Fremantle.
“Seeing the work is so special and particularly rewarding at sunset,” says Sandra Murray, S@B artistic director and lead curator, about one of her favourite parts of the event.
“People walking around the sculptures, getting up close or sitting on the grass with a picnic, it’s a perfect way to enjoy the work and the beautiful setting. It’s always such a friendly vibe here.”
This year marks the sixth instalment of the much-loved WA outdoor sculpture exhibition. Held roughly every three years, it started in 2013 as a grassroots event and Sandra says it has very much remained so.
The artists involved are of all ages and range from new and emerging through to established.
In an attempt to avoid the summer heat, this year’s S@B runs from April 4-21 and also shares its closing
By Ara Jansen
weekend with the always colourful 2025 Fremantle International Street Arts Festival.
This exhibition spreads across three spaces – Bathers Beach/Manjaree, inside the WA Shipwrecks Museum and a satellite exhibition at Old Customs House.
The work inside the museum comprises smaller and more delicate pieces like ceramics and those that won’t tolerate the outdoors. All work is for sale.
“There’s a wonderful sense of achievement once all the work is installed, we’ve had the opening and people are experiencing it. There’s also a genuine sense of satisfaction for the artists and the crew seeing everything in situ.”
The exhibition features a number of free public tours – artist-led tours, family friendly ones and artist talks, all of which are free. There are also paid twilight tours led by the artists.
More than 55 WA artists, from Perth and regional, have work on display and exhibitors include Tony Davis, Kevin Draper, Jill Paynter-O’Meehan, Adam Hisham Ismail, Yuko Takahashi and Eileen Cunningham to name a few.
This year, the exhibition pays tribute to founder and creative patron Tony
Jones and features six pieces of his work. Known for his statue of Eliza in Crawley Bay and the bronze of C.Y. O’Connor on his horse in North Coogee, Tony was named a State Cultural Treasure late last year.
“Bathers Beach is such a picturesque location for this event, it’s family friendly and the scale of the outdoor space is intimate,” Sandra says.
Sandra also loves that such a variety of materials are used for the works, from recycled elements, to clay, plastic, granite, wool and aluminium. Some are delicate, some tactile, others robust and with kinetic elements which move in the wind.
“We assess the applications largely from submitted images and accompanying text, so when you get to see them in the flesh it’s impressive – the scale, the materials and the colour. There’s even a sculpture that will sit at the tideline and interact with the water.
“We’ll also have lights on the works each evening, so you’ll be able to see the pieces from a different perspective. That’s always very lively.”
For more information, bookings and tours tickets, visit www.sculptureatbathers.com.au

From big ideas to comforting thoughts, the Margaret River Readers & Writers Festival offers an entertaining weekend for bookworms of all ages.
When Sian Baker first visited Busselton, she fell in love with the beaches and the energy of the locals.
This year the UK native celebrates five years as artistic director of the Margaret River Readers & Writers Festival – and there’s nowhere else she’d rather be.
By Ara Jansen

Running from May 2-4 in Margaret River and Busselton, the festival features Australian and international writers and thinkers.
This year’s list of guests includes Stan Grant, Peter Grayling, Marian Keyes, Marcus Zusak, Jane Caro, Dr Anita Heiss, Tasma Walton, Charlotte Wood and Lee Constable. The festival also has a fun and interactive children’s program.
“Creating a program for a festival like this is a big jigsaw,” says Sian. “The challenge of programming is balancing what the audience wants to see with what you have access to.
“I often have a good idea of areas to highlight, or I know the audience want to discuss or know about this topic.
“Creating opportunities for WA authors is in our DNA. We support
South West authors and both groups don’t always get opportunities at bigger festivals like this.
“You also never know when the alchemy is going to happen when you put two people together or a group on stage, something clicks and the magic happens. Then offstage they made a new connection and that’s pretty special.”
Sian continues to foster closer ties to other writers’ festivals around the country and believes they are stronger working together rather than considering each other competition. That collaboration gives everyone access to a wider collection of authors.
With free and paid events, there’s also a distinct difference between the interests of the Busselton and Margaret River audiences, which allows her to program a wideranging mix of popular fiction through to thought leaders.
“Margaret River likes the big thinkers and the challenging conversations, while the Busselton program leans
a little more commercial. They like people they have heard of or seen on television.”
The army of festival volunteers are a big part of its heart. Last year the 65-strong group logged more than 5000 hours. While the group has a large number of retirees, Sian says more and more young people are volunteering.
“I’m blown away by how much time, energy and passion the volunteers give to the festival. The festival feels like a family and a community –and that’s also the feedback we’ve received.
“I feel like I have found my tribe of people. We all love books and big ideas and love being made to think about things in a different way. We’re all on the journey together.
“It always feels special looking out on an audience enjoying an event. Being in a room with 500 other people having this beautiful moment and enjoying the story.”
For more information, sessions and tickets visit www.mrrwfestival.com
MARGARET RIVER – GNARABUP
(DPA/MM4)

Medical/Consulting for Lease in Dunsborough
Commonage Road Frontage
•Building: 275-275m2
•Land: 302m2
1/88 Commonage Road offers a unique opportunity to lease a prominently located, modern building that will suit medical, allied health or other professional pursuits.
Total available space of 275m2 is split over the ground floor and an expanded mezzanine floor, construction of which will be completed in March 2025.
There is a current fit-out which can be retained or modified depending on your requirements for consulting rooms, office, reception or break out space and an expanded mezzanine which can be partitioned according to the spaces you require.
The premises has a kitchen space, toilets, A/C, an attractive façade facing Commonage Road and is located next door to Dental 88, a prominent local Dental Practice.
1/88 Commonage Road is ideally suited for a single tenant with the bonus of being able to sub lease some of the building or provide reception either now or in the future.
Convenient parking available for clients/ customers at your front door and great exposure to the passing parade on Commonage Road for signage.
The premises will be available in February with annual rental from $75,000pa + GST + outgoings estimate of $19,250pa. To view the plans and discuss the possibilities contact John Reid 0418 931 100 / john.reid@raywhite.com or Michelle Pownall 0438 913 570 / michelle.pownall@raywhite.com
VR General Practitioner
– Full-time or Part-time
We’re looking for a VR GP to join our growing practice overlooking the ocean in idyllic Gnarabup.
Flexible working options are available to suit a new lifestyle Down South by the beach.
Vitality GP has been part of the community since 2022. Our fully accredited practice comes with onsite podiatrist, physiotherapy and nursing support, a friendly team, and brand-new, well-appointed facilities.
Please email resume to alison@vitalitygp.com.au
Contact: Dr Alison Lyons 9757 1022 www.vitalitygp.com.au

BURSWOOD
Earn 100% of Billings for the First 3 Months!
Join our well-established, accredited mixed-billing clinic in Burswood and earn 100% of billings for the first 3 months (75% thereafter).
Perfect for new VR GPs looking to establish themselves, with full-time/part-time options.
Work alongside 3 experienced GPs in a fully computerised clinic with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au
Contact Paul, paul@mforum.com.au or phone 9203 5222 to place your classified advert


MOUNT LAWLEY
General Practitioner
$200 – $300 per hour 6-7 sessions available.
Excellent working environment, with modern facilities.
Quality nursing staff and an onsite non dispensing pharmacist.
Adjacent to the practice we have a pharmacy, and allied services, consisting of audiology, pathology, physiotherapy, podiatry, dental, and cardiology.
Visit our website: www.thirdavenuesurgery.com.au
If interested contact Practice Manager Rachael Hadlow via email: rhadlow@3rdave.com.au

Come and join a practice that works around your life and family.
Palin Street Family Practice is seeking a new VR doctor for our well-established, fully accredited clinic in Palmyra, with easy access to Fremantle, Perth CBD and the Swan River foreshore.
There’s plenty of parking and you will be fully supported by an experienced nursing and admin team.
We are a small, privately owned General Practice, which has been continuously operating since 1923. Our mission is to provide the highest standard of patient care whilst incorporating a holistic approach towards diagnosis and management of illness.
We operate out of a converted house, creating a calm and welcoming space for patients, whilst still utilising the latest equipment and technology. Many of our patients have been coming to us for generations and you will have an immediate patient list on commencement. We are a close-knit team that meets regularly to collaborate, share our experience, and you’ll have access to some of Perth’s most experienced and respected GPs.
We’re looking forward to welcoming a new family friendly doctor into our team. For further information
please contact Jackie our Practice Manager on 0403 343 401 or via email office@psfp.com.au

Doctor Opportunity at The Woods Medical Centre
We are looking for an enthusiastic and experienced GP to join our growing team.
The Ideal Candidate:
Strong General Practice Skills:
•Proven experience in providing highquality patient care across a diverse range of medical conditions
•Excellent clinical skills and a commitment to preventative healthcare
•Experience in managing chronic diseases effectively
•A keen interest in skin cancer management preferred but not essential. We offer a unique opportunity to combine comprehensive general practice duties with an opportunity to develop skin cancer screening and procedures for that candidate with skin cancer management interest.
Team Player and Communicator:
•Ability to collaborate effectively with a supportive team of healthcare professionals
•Excellent interpersonal and communication skills to build rapport with patients.
Essential Requirements:
•FRACGP qualification
•Vocational Registered
•AHPRA registration.
What We Offer:
•Supportive and friendly work environment with a focus on work-life balance
•Nursing support
•No weekends or afterhours work
•Modern facilities and equipment
•Best Practice software
•Mentorship and training opportunities should you wish to develop skin cancer management skills
•Opportunity to work alongside experienced practitioners in a collaborative setting
•A location that is not far from the beach.
For more information or a confidential chat, please contact our Practice Manager at 0478 021 910 or email practicemanager@thewoodsmedical.com.au


Queens Road Surgery is a busy GP owned general practice located in Mount Pleasant looking for VR GP to join our well established practice. We offer a supportive team based culture, quality full time nursing support and experienced administrative staff. We have an upcoming opportunity from July this year with one of our long term doctors retiring.
Queens Road Surgery is a fully equipped accredited practice.
For a confidential discussion please contact our Practice Manager Narelle 0412 113 584 or narelle@queensroadsurgery.com.au

VR General Practitioners, Specialists, Allied Health – Full time or Part time
Join us in our newly built clinic based in the inner city of East Perth, only a short distance from the centre of Perth’s CBD. Next Practice East Perth aims to redefine patient care and allows you to practice medicine in your own way. By joining the clinic, you’ll experience a range of benefits such as:
Innovative Technology - We utilise cloudbased software to easily manage EHRs and appointments
New Modern Clinic – Our clinic has been designed to be inviting and calming for both patients and practitioners
Doctor Managed and Owned - As a doctor-run clinic, we understand your needs and don’t dictate strict KPIs that impact the way you practice
Ongoing Support – We have a friendly and dedicated administrative and nurse support team so you can focus on providing patients with the upmost care
Flexible Scheduling - We are able to offer flexible scheduling and work around your desired days and hours
Negotiable Terms – With flexible rates and contracts that are fully negotiable, our long-term opportunities are designed to align with your professional goals
About Next Practice
Next Practice is a network of medical centres across Australia that offers a new kind of healthcare experience for Health care providers, doctors, and patients. With innovative clinic designs, cloudbased practice software, and a dedicated support team, we aim to revolutionise the healthcare industry. Our network of doctors and practitioners collaborate to make a lasting impact on healthcare. Join us in East Perth, WA, 6004 and be part of this exciting journey.
If you’d like more information, please contact us at info@nextpracticehealth.com and we will be in touch.

Silver Sands General Practice
Exciting Opportunity for a Full-Time or Part-Time VR General Practitioner in Mandurah!
Are you a passionate and dedicated VR General Practitioner looking for a rewarding opportunity in a familyfriendly environment? Look no further!
Silver Sands General Practice is one of the longest standing medical centres in Mandurah, and we are actively seeking a talented GP to join our dynamic team on a contract basis.
Our practice is committed to providing high-quality, patient-centred care to individuals and families. Our team is supportive, collaborative and dedicated to creating a positive work environment. Requirements:
•MBBS
•Current general / specialist registration with the Australian Health Practitioner Regulation Agency (AHPRA)
•FRACGP or FACRRM qualifications or active enrolment with the training program
•Medical Indemnity Insurance
•Commitment to providing high quality patient care
•ABN as an independent GP Benefits:
•Competitive remuneration package at 70% of billings (30% service fee)
•Supportive and collaborative team environment
•Flexible working hours. Ideally 4-5 days per week +/- nursing home visits if desired
•Mixed billing
•Replacing outgoing GP with full books
•Large existing patient base with great billing potential and rewarding continuity of care
To apply, please submit your resume and cover letter to office@silversandsgp.com.au

SOUTH LAKE
GP Opportunity at South Lake Family Practice.
We are looking for an enthusiastic VR GP to join our team.
Full time / Part time VR GP.
Flexible hours. 75% and minimum guarantee for first 3 months.
Onsite pathology & Allied Health.
Day and after hours shifts available. Ability to do Women’s health and procedures preferred.
For further information please contact p.manager@southlakefamilypractice.com.au ph: 08 9417 1009

General Practitioner MM2 location
Full-Time or Part-Time
We take pride in our patient-centred approach and are seeking a passionate and dedicated GP to join our team. We have a compounding pharmacy onsite with an interest in Medicinal cannabis.
Serpentine medical Centre is a wellestablished medical practice dedicated to providing high-quality healthcare services to our community. We take pride in our patient-centred approach and are seeking a passionate and dedicated General Practitioner to join our team. We have a compounding pharmacy onsite with an interest in Medicinal cannabis.
Role & Responsibilities:
•Provide comprehensive primary healthcare to patients of all ages.
•Diagnose and manage a wide range of medical conditions.
•Perform routine examinations, preventive care, and chronic disease management.
•Collaborate with other healthcare professionals to ensure optimal patient outcomes.
•Maintain accurate and up-to-date patient records.
•Offer guidance on lifestyle, diet, and preventive healthcare measures.
Requirements:
•Medical degree and full registration with AHPRA, supervision unavailable
•Strong communication and interpersonal skills.
•Ability to work independently and as part of a multidisciplinary team.
•Commitment to delivering highquality patient care.
Benefits:
•Competitive salary package.
•Flexible working hours, the ability to work from home doing telehealth
•Supportive and friendly work environment.
•Opportunities for professional development and training
•Modern, well-equipped facilities.
For more information or to apply, please contact our Practice Manager Krystal on 08 9525 3934 or send resume to practicemanager@serpmedical.com.au

Spencer Road Family Practice is seeking an enthusiastic doctor, who thrives in a busy general practice. Avoid long commutes and work close to home in the foothills of Perth’s South-East.
Choose your days, set your own hours, and take home 65% of billings.
We have room availability Monday – Saturday.
The practice is open from 8am to 6pm weekdays.
8am to 1pm Saturdays, 8am to 12pm Sundays and Public Holidays.
We only close on Good Friday and Christmas Day.
We currently have 10 GPs, 4 Nurses, a visiting Podiatrist & Dietitian and a Clinipath Pathology located within the practice.
Our patient’s range from the very young (we have an antenatal GP) to the elderly (some of our GPs have practised in this area for over 30 years)
For more information or to apply, please contact our Practice Manager, Paige on (08) 9493 8388 or send your resume to practicemanager@srfp.com.au
paul@mforum.com.au (08) 9203 5222
www.mforum.com.au
Contact Paul, paul@mforum.com.au or phone 9203 5222 to place your classified advert



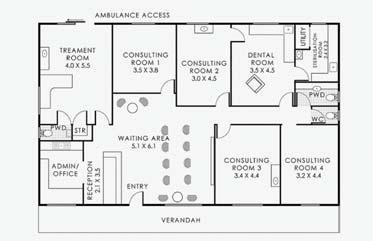
WARWICK MEDICAL CENTRE FOR LEASE
Modern Reception area
Treatment Room with own WC, basin & Ambulance access
Various Consulting Rooms plus Treatment Room available to choose from
Dental plumbing ready in two rooms & able to connect to others (Category 1 ready)
Rooms with medical curtains & wash basin set up
2 common WCs
21 car bays
Consulting Rooms from $15,000 p.a. + VO approx. $4,450 p.a. + GST Whole Premise $68,500 p.a. + VO approx. $17,810 p.a. + GST
Contact Leasing Agent Kong Wai WONG on 0421 883 338 / kongwai@jardimproperty.com.au to secure your exciting new business premise

We are seeking General Practitioners to join the Curtin Health Services team! We offer flexibility, variety, and mixed billing opportunity in a highly supportive environment.
We are seeking General Practitioners that would like to expand their clinical scope in the provision of Adolescent & Young Adult Medicine (AYAM). We are investing in our services and looking to grow our team of General Practitioners.
We have a variety of contracting options available
We are seeking to expand our service by increasing available consultancy hours
Administrative, Mental Health Nursing Practitioner, Dietician, and Nursing support provided
We are recruiting a Medical Director to provide clinical oversight and support Centrally located at Curtin University Bentley campus
JOB REFERENCE
Join our friendly and collaborative team and help support the health needs of our diverse community of students, staff, families, alumni, and partners. Our Medical Centre is a well-established, accredited and fully equipped practice with 7 consulting rooms, a procedure room, treatment room, and onsite pathology. Our team includes GPs, allied health professionals, Triage Nursing, Reception, Medical Director, Practice Manager, and Mental Health Nursing Practitioner. The Centre is open Monday to Friday between 8:30 am and 4:30 pm and is well-served by public transport and ample parking.
We offer full-appointment books with a large and diverse patient base offering lots of interesting work, plus walk-ins, opportunities for Healthcare Plans, Health Assessments, and procedures.
Mixed billing
Attractive service fees
Work full-time or part-time with flexible hours. You choose!
Excellent working conditions and room facilities
Walk into a full & immediate patient base, OR create your own, with walk-in presentations Best Practice software in use throughout the practice
REQUIREMENTS
MBBS or equivalent
Current AHPRA registration as a General Practitioner
Vocationally Registered (VR) No restrictions
To learn more about this opportunity, please contact Nandita Nadkar, Practice Manager on 08 9266 9348
TO APPLY: Send your CV to hsmanager@curtin.edu.au
For more information about our university, please visit www.curtin.edu.au


























