









Dr Ushma Narsai Avant member

anddeductions for








Nothing can replace the years of training and expertise held by a GP, but it’s also becoming harder for patients to see a GP when they need one. Something must change for the system to survive.

Complete the self-reflection and claim your CPD time, please scan here
Andrea Downey | Managing Editor
You can’t mention scope of practice without it ruffling a few feathers – some want to see changes while others are more cautious.
Pharmacists and nurses want to work more. Some States have permanently expanded pharmacists’ scope to include prescribing for some medications without the need for a GP consultation.
Soon registered nurses will also be able to prescribe certain medicines in partnership with an authorised health practitioner.
Understandably, this causes alarm among doctors with many concerned about patient safety.
Nothing can replace the years of training and expertise held by a GP, or the continuity of care that comes with general practice.
But, at the same time, workforce pressures are increasing, burnout is prevalent, and it’s becoming harder for patients to see a GP when they need one.
We’re also facing a GP shortage in many areas, with official figures predicting a national shortage of 8900 by 2048.
Something must change for the system to survive, and that’s about the one thing practitioners agree on.
As for what the answer is, I don’t know. Having watched the drama around physician associates unfold while reporting on the NHS, I can sympathise with where doctors are coming from.
But having also been a patient who has sometimes struggled to get a GP appointment, I’m more receptive to being able to see a different practitioner when I need one.
In this edition we took a closer look at the recent Scope of Practice Review and whether its time, now the Federal election is over, for a rethink.
It’s a fascinating topic that I can’t make my mind up on. I’m keen to hear your thoughts, you can email a letter to the editor at editor@mforum.com.au.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.



The cost of doctor burnout
Taking the pressure off wounds
Close Up: A lived experience
Time for a scope of practice revamp?
54 Suspended in art 56 Belle of the ball


Editorial: Scope for change
Andrea Downey
Fit your own oxygen mask first – Dr Joe Kosterich
Our popular competitions have seen Medical Forum readers enjoy a trip to the Perth Comedy Festival, a night of culture at the Alliance Française French Film Festival and a glass of Fermoy’s delightful wine.
Now we’re giving you the chance to win more movie tickets.
See our lifestyle section for more details.
Enter our competitions by using the QR code or go to www.mforum.com.au and hit the competitions tab.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Classifieds Manager
Paul Riessen 08 9203 5222 paul@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au


















St John of God Subiaco Hospital has scrapped its plans for a family birthing centre, in what was described as another blow to maternity services in Perth.
Stage three of the $311 million expansion of the hospital is set to progress to tender soon but will no longer include what was promised to be a “world-class mother and baby centre”.
Chief executive Tina Chinery told Medical Forum: “The clinical building will be two storeys less than the original eight storey design and will no longer include a family birthing centre.”
National Association of Specialist Obstetricians and Gynaecologists (NASOG) WA representative Dr Hannah Sylvester told Medical Forum that demand for services was going up due to other recent closures of maternity services in Mount Lawley, Geraldton and Bunbury.
Dr Sylvester, an obstetrician at St John of God Murdoch, said: “A significant proportion of my patients drive from Bunbury, Esperance, Albany, the whole Wheatbelt and Goldfields to come here to birth in Murdoch, because there isn’t anywhere else.
“It’s incredibly clear that the problem lies within the funding from the private health insurers.”
St John of God Subiaco Hospital experienced a 52% increase in births in 2024 compared to the previous year.
When the closure of maternity services in Mount Lawley was announced in 2023, St John of God Health Care
Almost 500 WA GPs are set to be contacted by the Department of Health and Aged Care over Medicare claims made for services provided while they are believed to have been overseas.
A spokesperson for the department told Medical Forum more than 5800 letters were being sent to health practitioners around the country regarding “potential noncompliance”. Some 488 of those letters are destined for WA GPs.
The potential cases of noncompliance related to the treating doctor being overseas at the time of the consult.
The GPs identified by the department are expected to receive a letter encouraging them to “review their billing processes and take any necessary action, including returning any incorrectly received government benefits, and ensure future services

chief executive Bryan Pyne said maternity services would transfer to Subiaco under what was branded a “new maternity model of care for Perth”.
Ms Chinery said while it was disappointing that the initial plans for maternity within the hospital were no longer going ahead, she was confident the needs of our maternity patients would be met.
She said the decision not to press ahead with the mother and baby centre was made with consideration of the maternity infrastructure already available to patients and the ability to expand on that in the future.
St John of God Health Care has invested more than $280 million in the first two stages of the major redevelopment project, with stage two understood to be on-track for completion in 2026.
Concerns have been raised about the viability of private maternity services in Perth amid a spate of closures in recent years, with some suggesting could not continue without a change in funding models from private health insurers.
are not billed to their provider number while they are overseas”.
In addition to paying back compliance debt, GPs could also face penalties of up to 20% of the recoverable debt amount.
A spokesperson for the department said: “While telehealth provides more flexible access to care for many patients, it is a priority that high standards of care are maintained, and patient safety is supported.”
They pointed to the Health Insurance Act 1973 which requires services, including telehealth, to be rendered in Australia.
Overseas billing was a focus at the recent six-monthly general practice compliance roundtable attended by the RACGP, along with other primary care and medical indemnity providers to discuss emerging compliance issues.
Letters were being sent to GPs from May.
UWA has developed an Australianfirst program specifically for pharmacists to deliver more specialised services, but doctors remain concerned.
The university will offer Australia’s first Doctor of Pharmacy Practice, a one-year online program designed for registered pharmacists seeking to enhance their qualifications and expand their scope of practice.
The launch of the program follows the Federal Government’s November 2024 announcement that pharmacy graduates completing an Australian Qualifications Framework Level 9 standard (extended) course could use the title Doctor of Pharmacy from 1 January 2025.
Both the RACGP and AMA have warned of risks to patient safety if patients were confused about where to seek medical advice.

AMA (WA) President Dr Michael Page told Medical Forum: “There are concerns about members of the public not understanding the enormous difference between a pharmacy graduate who has completed a one-year crash course in diagnostics and therapeutics, and a doctor who has completed a decade-long supervised clinical apprenticeship.”
The Federal Government’s call on the Doctor of Pharmacy title came just a few months after WA expanded the role of community pharmacists.
Senior lecturer at UWA and 2024 Pharmacist of the Year Dr Amy Page said the university’s new program would address a critical need in the pharmacy profession.
“Pharmacists are evolving beyond traditional dispensing roles,” she said. “This qualification will equip the existing workforce with advanced skills to improve medicine safety and deliver patient-centred care, particularly for older Australians with complex medication needs.”
The course will be delivered from 2026, with enrolments due to open later in 2025.
The Federal Government claimed GPs who offer universal bulk billing will earn more than $400,000 a year under its election pledge to update Medicare bulk billing rebates.
At the moment, a fully bulk billing GP earns less than their mixed billing or privately billing colleagues for providing the same number of services.
Ahead of May’s Federal election Labor promised $8.5b in Medicare funding, which it said would deliver an additional 18 million bulk billed GP appointments each year.
It said a GP who currently bulk bills one in four patients could earn $371,390 a year, while a GP who bulk bills all of their patients would be earning about $45,000 less than that.
But from 1 November its new measures would close that earnings gap, with the government claiming a city GP who bulk bills all of their patients could earn up to $403,805, and a GP who bulk billed one in four of their patients could earn up to $398,448 a year.
But AMA (WA) President Dr Michael Page and GP West founder Dr Kiran Puttappa say it’s not as simple as that.
Dr Page said: “For most GPs, in the city in particular, it’s more likely to reduce their take home income if they go ahead and bulk bill all patients.
“The average fee for each patient will decrease rather than increase, so there’s no way, with a decreasing fee paid per patient, you can increase your income.”
The decreasing fee Dr Page refers to is the rate at which the government is proposing to pay for a standard consult under bulk billing arrangements.
While the AMA’s suggested fee for such a consult is $102, the government is proposing to provide a little less than $70 for a standard consult when it is bulk billed.
Dr Puttappa said many factors came into individual GP wages but he estimated the average take home salary of full time GP in Australia was between about $200,000 and $320,000.
Nominations are now open for the 2025 WA Health Excellence Awards, acknowledging excellence and innovation in healthcare.
The 10 award categories open for nominations include Excellence in Mental Health, Person-Centred Care, Safety and Quality, Workplace Wellbeing and Culture, Research and Innovation, Sustainability, Aboriginal Health, Preventive Health, Rural and Remote Health Care, and Primary Health Care Integration.
The 7NEWS Health Heroes category will also return this year, inviting the community to nominate a standout frontline healthcare worker.
Nominations close on Friday, 4 July and winners will be announced at a gala dinner on Tuesday, 25 November. To enter, visit:
However, it is standard for about 30% of a GP’s earnings to be paid as a practice fee to cover clinic operating costs.
There was also confusion over a promised additional 12.5% loading payment on fully bulk billing GP’s Medicare rebates.
‘It’s not very clear who gets it, because they also said that there will be a split between the practice and the practitioner,” Dr Puttappa said.
Labor said the payment split would be determined in consultation with the sector prior to the program’s launch.
Researchers at Perth’s Harry Perkins Institute of Medical Research have developed a genetic test for heart failure – potentially transforming early intervention and personalised care for patients.
In Australia, more than 400,000 people develop heart failure each year, and in 2021 heart failure or cardiomyopathy contributed to 26,000 deaths.
Heart failure results from the heart pumping blood around the body less effectively. It cannot be cured due to irreversible damage to the heart muscle.
New research published in the International Journal of Molecular Science, led by Perkins researcher in genetics of complex disease and Director of the Centre for Diabetes Research Professor Grant Morahan, found 41 genetic variants indicative of heart failure risk.
Prof Morahan said: “Until now, it has only been possible to predict health outcomes for rare mutations which cause rare single-gene diseases.
“There are no approved clinically useful genetic tests for the common diseases affecting our society, such as heart diseases, diabetes, cancer, dementia and so on.
“Our breakthrough now allows us to identify people who are at risk of these common diseases because they have certain patterns of these interacting genetic variants.
“People can now be identified as at risk of heart failure before they develop symptoms, years – even decades – earlier, allowing preventive treatments before irreversible damage occurs.”
The decision to change the way a GP clinic operates, or the services offered, are not made lightly.
Not only are there financial implications, but it is important to know that by doing things differently the needs of patients will be met better.
Murdoch-based GP Emilie Pitter is confident in the recent changes made at her workplace, Garden Family Medical Clinics, because she had data to back them up.
In 2023 she began planning for a data collection initiative at her clinic and its sister clinic in Piara Waters.
“The idea came because we thought we’d like to better understand what conditions and presentations our patients were coming with, and more about who our patients were in terms of their demographics and what they were presenting with,” she told Medical Forum
The project saw de-identified details about patients and the conditions they were presenting with collected and analysed.
Patients were provided written information about the project ahead of the appointment, as well as

being asked for their verbal consent during their appointment.
Data was collected via a secure, custom-built survey, which GPs were able to complete in less than a minute.
Seventeen out of the 24 GPs across the clinics opted to take part in the project.
Dr Pitter said analysis of the data found there was a “very high proportion of mental health presentations” at the Murdoch clinic.
Members of the West Australian medical community who worked with Dr Barry Hopkins have fondly remembered the well-known cardiologist.
The co-founder of Western Cardiology passed away in late April. He taught and influenced many in the industry.
Dr Philip Cooke from Western Cardiology trained under Dr Hopkins at Sir Charles Gairdner Hospital.
“He was knowledgeable, had a good sense of humour and was really well respected and loved by staff who worked with him because he was very approachable,” he said.
Born in Midland in 1938, Dr Hopkins grew up in the area before going on to study pharmacy and then medicine at UWA.
Dr Hopkins then went on to do a PhD, which focused on aortic regurgitation and was awarded an overseas fellowship to research at Harvard, Massachusetts, where he became an associate professor of cardiology.
Upon returning to WA in the 1970s, Dr Hopkins spent time as a professor at UWA’s medical school, and as a consultant physician, instituted echocardiography services in WA and directed what was the new cardiac catheterisation unit at Sir Charles Gairdner Hospital.
“We innately knew from our consults, but the data was able to confirm that,” she said.
She said this was “a reinforcing reason” that led to the practice employing two new psychologists, who have now been contracted to the clinic since late 2024.
It also allowed GPs to see that they mostly saw a younger demographic of patients, more of which were female than male.
“The data also highlighted common conditions and that the number one thing that we saw was actually immunisations, which was fantastic because that reflects on our preventative health for our patients.
“There was feedback from the GPs who participated that they would like to be doing this more regularly. That way we would get information on seasonal presentations of our patients as well... it would be really interesting to see how things vary throughout the year.”
Dr Pitter was awarded the 2024 RACGP Peter Mudge Medal.

After establishing a private practice with Dr Brian Lloyd in the late 1970s, in 1988 they relocated their private cardiology consulting rooms to St John of God Healthcare in Subiaco, founding St John of God Cardiology, which is now Western Cardiology.
His daughter Lara Hopkins said while not at work “he loved flying and gliding, accumulating thousands of hours in the air and teaching many glider students”.
Dr Hopkins leaves behind six children and eleven beloved grandchildren.
To coincide with the commencement of the National Lung Cancer Screening Program, ChestRad is bringing their sub-specialist service to Mandurah

ChestRad are specialists in Cardiac CT, Chest CT and Lung Cancer Screening
Cardiologists – Dr Edmund Brice, A/Prof Abdul Ihdayhid, A/Prof Chris Judkins, Dr Sam Tayeb, Dr Justin Teng and Dr Tashi Zhaxiduojie
Cardiothoracic radiologists – Dr Conor Murray and Dr Shriv Srigandan
ChestRad's rooms are at the Mandurah Specialist Centre on Minilya Parkway, Greenfields (near the Peel Health Campus) All Medicare rebated services BULK BILLED! www.chestrad.com.au

With work on the first clinical practice guidelines for the appropriate use of MDMA to treat post-traumatic stress disorder underway, Medical Forum spoke to psychiatrist Jonathan Laugharne about how the treatment has progressed at his Perth clinic.
By Aleisha Orr

Two years on from authorised psychiatrists in Australia being given the greenlight to prescribe MDMA for patients with PTSD, work is underway on clinical guidelines for its appropriate use beyond current arrangements.
At the Empax Centre in Perth more than 30 patients have been treated using MDMA-assisted psychotherapy.
Co -founder and Consultant
Psychiatrist Jonathan Laugharne said while standard treatments for PTSD, such as psychotherapy and medication, have about a 60% success rate, about 30-40% of patients are considered treatmentresistant. It is those people who his clinic considers for treatment using MDMA.
“Really, they’re the toughest group, and we’re seeing substantial improvements,” Dr Laugharne told Medical Forum
He said about 50% of patients who had taken part in the MDMA therapy no longer met the criteria for PTSD treatment after completing the program.
“That’s quite remarkable,” he said. That level of improvement in PTSD symptoms was not the general outcome when using other medication in combination with therapy, he added.
While the use of the drug in Australia for any purpose had previously been illegal, its rescheduling by the Therapeautic Goods Administration in 2023 from a Schedule 9 prohibited substance to a Schedule 8 controlled substance allowed authorised prescribers to administer the drug for the treatment of PTSD.
At the same time the same change was also made for psilocybin, a chemical found in certain mushrooms, to allow it to be used
for treatment-resistant depression outside of clinical trials.
Patients undergoing MDMA therapy generally spend the whole day at Dr Laugharne’s clinic, with therapy sessions held following the administration of the medication.
He said the brain’s increased neuroplasticity as a result of the administration of MDMA had assisted many patients to make quick progress in their therapy.
“You see a lot of progress with therapy because the person is much more open to ideas and conceiving things and taking in new perspectives,” he said.
“We’ve had patients come through who have done a lot of regular therapy with us over several years and they do this drug-assisted therapy and just make so much progress so quickly compared to having previously been very stuck.”
Dr Laugharne said while neuroplasticity of the brain would not be a long-term effect of the MDMA, the progress made in the window in which it lasted provided a springboard for continued improvement following the medication-assisted treatment.
He said a very controlled and supportive environment was put in place for the administration of the drug, which took place following several sessions.
While use of illegal, unregulated MDMA may at times be associated with antisocial behaviour, Dr Laugharne said the preparation leading up to administration, the setting involved, and the fact that the MDMA was clinical grade, were all contributing factors to how the treatment was received.
During treatment, blood pressure and temperature are measured at the start of the day, before a second supplementary dose, and at the end of the day to ensure safety.
“The psychiatrist has to walk with them and check their vital signs. They have to go home with a trusted person, they can’t drive for 48 hours, and that trusted person has to stay with them overnight,” he said.
The treatment can cost patients about $25,000 to $30,000. It’s not the medication itself that makes the treatment so expensive, but the hours of psychotherapy and support involved.
It generally consists of three dosing days of about seven or eight hours each, followed by another nine integration sessions.
Dr Laugharne said some patients seen at his clinic had shown improvements doing fewer dosing sessions and some required more.
Private health insurance generally does not cover the treatment.
Mind Medicine Australia created a support fund to assist patients to access the treatment, which several Empax Centre patients have used.
The Department of Veterans Affairs also funds psychedelic assisted psychotherapy for eligible veterans, including MDMA for PTSD and psilocybin for treatment resistant depression.
A Monash University study on the safety and efficacy of MDMA treatment compared to psychotherapy alone will inform the new clinical practice guidelines in combination with the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) process.
The study, published in the Australian & New Zealand Journal of Psychiatry, assessed the current evidence regarding the safety and efficacy of MDMA-AP compared to psychotherapy alone among adults with PTSD.
Researchers found evidence of improved PTSD outcomes, however the evidence was considered to be of low to very-low certainty.
A ketamine-type nasal spray treatment for depression was added to the PBS in May.
Esketamine, sold under the brand name Spravato, can be prescribed to adults with treatment-resistant depression.
This means Australians living with depression that has not been relieved with the use of antidepressant tablets will have more affordable access to this medicine.
Esketamine is a version of the anesthetic drug ketamine and works by increasing glutamate levels in the brain to stimulate and restore message transmission. The nasal spray is used in conjunction with an oral antidepressant.
It is the first new type of medicine for major depression to be funded by the government in 30 years.
Up to 30,000 Australians are expected to receive Spravato through the PBS at a cost of $31.60, or $7.70 for those with a pensioner or concession card.
Clinical psychologist Dr Rob Schütze, of Curtin University’s School of Population Health and Royal Perth Bently Group, said many people did not respond to traditional clinical interventions like CBT, antidepressants and lifestyle interventions.
“Those who don’t respond to two conventional treatments are classified as having treatment-resistant depression (TRD). Evidence suggests less than 15% of people with TRD recover,” he told Medical Forum
“Listing esketamine on the PBS will make it accessible to more people with TRD, although it will be some time before there are enough doctors

with the training and facilities to provide this supervised treatment.”
Dr Schütze said it would be important to integrate eskatamine into a comprehensive treatment plan, rather than relying on the medicine alone.
“It should ideally be combined with lifestyle interventions focusing on exercise, sleep and diet in order to get lasting benefits. For those who can access a psychologist, combing ketamine with psychotherapy will also give it the best chance of relieving depression in the long-term,” he added.
To be eligible for a prescription a patient will need a diagnosis of treatment-resistant depression.
Prescribers will need to pay particular attention to harms associated with drug interactions, Dr Schütze said.
More information on the clinical use of esketamine can be found on page 40.

It takes a lot to shake Dr Angela Alessandri. She’d previously gone through breast cancer and losing her sister, but after the most stressful year in her clinical paediatric haematology and oncology career, she finally decided she could not continue with her workload as it was.
One in seven GPs experience it and WA junior doctors report it at moderate-to-high levels – what is causing burnout among doctors and how can it be fixed?
By Aleisha Orr

The chest pains she had a week prior when walking away from a parent of one of her patients who was screaming at her had still not subsided when she met with the hospital’s management.
She told them she was not functioning as she should be and was not willing to continue in her head of department role at that same capacity.
As she waited at the lift afterwards, a senior colleagues said: “I have to say you don't look like you're a woman on the edge.”
Dr Alessandri told Medical Forum that she replied: “What you don't understand is, I will look like this in my coffin, just because I look like this doesn't mean I'm well.”
Many doctors may be able to relate, she was burnt out.
This may have been more than a decade ago in a Perth hospital that no longer exists, but burnout continues to be an issue for physicians in Western Australia.
Burnout, recognised by the World Health Organisation in the 1990s and classified an “occupational phenomenon” in 2019, manifests in energy depletion, increased mental distance from one's job, and reduced professional efficacy.
It results from chronic workplace stress that has not been successfully managed.
Almost 61% of Australian workers were estimated to have experienced burnout, and doctors have been found to be particularly vulnerable.
According to a 2024 RACGP survey, one in seven GPs experienced burnout and a survey of 1100 junior doctors in WA’s hospitals last year found what it described as moderate-to-high levels of burnout.
The highest levels were recorded among women and newborn health (83%) and child and adolescent mental health (80%) services, however even in hospitals with more moderate rates one in five practitioners reported it.
Recent research from Ahpra also found burnout and feeling undervalued were contributing to health practitioners leaving their profession – with one in 10 either considering quitting within a year or unsure about their future.
Long hours and high stress are common when it comes to working as a doctor.
In Dr Alessandri’s case, she was on call 24/7 apart from two of three weekends and she had what she describes as her most difficult set of families.
Doctors Health Advisory Service WA (DHASWA) assistant director Sarah Newman says many factors impact stress levels of practitioners.
“Not being able to get your leave, having your roster turn up with only twoweeks’ notice and not being able to plan your life, and then there’s stress of unpaid overtime,” she told Medical Forum

“You might feel inefficient or weighed down a lot by administration and then you don't feel you are able to connect with the patients, and not being able to connect can bring feelings of cynicism, and present as sarcasm and resentment against these people for presenting for healthcare.”
and 29% of IMGs said they had witnessed discrimination compared to 22% of other doctors.

Dr Newman said such feelings are not conducive with providing a good standard of care.
“The hours and structures make it difficult in terms of self-care and to do things we all know we should do, even the basics like eating, having breaks to drink, or go to the toilet.”
Dr Newman said those who most often become doctors are perfectionists with a great deal of resilience, but this often means they push on until almost breaking point.
“We hold ourselves to very high account in the quality of our work,” she said.
“In medicine we highly stigmatise ourselves for having issues with ‘coping’ and especially for mental health issues.”
A Beyond Blue survey from 2013 highlighted the stigmatising attitudes within the industry around the competence of doctors with mental health conditions, and their opportunities for career progression.
The results may be from 12 years ago, but it was a landmark study with relevance in the current landscape.
About 40% of doctors surveyed felt medical professionals with a history of mental health issues were perceived as less competent and 48% felt those doctors were less likely to be appointed roles.
Weighed down by workplace pressures
Dr Newman said in a way burnout “is the antithesis of being professionally fulfilled” and can lead to a lack of professional efficacy.
She explained that while most come to medicine wanting to help people, poorly managed workplace stress often makes them lose that drive.
“We know there's more medical errors, there's more patient deaths when doctors are not well, and when they're not able to look after themselves.”
AMA (WA) President Dr Michael Page said burnout can be directly traced back to the inadequacies of the health system.
“Whilst we absolutely support hospitals doing what they can to treat the symptoms of burnout, the root cause needs to be addressed,” he said.
Dr Alessandri says this was the case in 2014, when her burnout peaked.
“We were really struggling to cover the workload,” she said.
When Dr Alessandri eventually raised her concerns about the level of pressure staff in her department were under and received media attention, she recalled how her working environment became unwelcoming.
"People who I knew pretty well were ignoring me in the corridor,” she added.
Workplace culture has also been found to be an issue, with a third of medical trainees reported having witnessed bullying, harassment, discrimination, sexual harassment, or racism in 2024.
The impact is even higher on international medical graduates (IMG). This year's AMA (WA) Hospital Health Check report found IMGs were more likely to experience bullying, discrimination or harassment.
A total of 23% of IMG respondents reported experiencing discrimination compared to 12% of other doctors,
Dr Ashwita Siri Vanga, DHASWA’s international medical graduate (IMO) wellbeing representative, left the State after being repeatedly overlooked for roles she said she was more than qualified for.
She remembers seeking support via her employee assistance program after experiencing racism at work.
“The person on the line was not comfortable talking to me, they said ‘I am a white Caucasian male… I don't know much about your cultural background or what happens in your life, and I don't think I'm the right person, but I'm still happy to continue and have another session’.”
She adds that IMOs were often more reluctant than the average doctor to seek support.
“They don't want to complain and isolate themselves further.”
While burnout may not be considered a medical condition, GPs can provide support for it, including to their peers. However, many doctors are often reticent to see a GP.
The Beyond Blue study also found 59% of doctors felt being a patient themselves causes embarrassment.
Dr Newman estimates about 50% of Australian doctors have a regular GP compared to almost 80% of the general population.
While doctors in WA can selfprescribe, Dr Newman said they should have a GP for matters “requiring an objective assessment”.
Dr Newman says doctors often fear being reported.
A spokesperson for the Medical Board of Australia confirmed mandatory reporting about health impairment does not apply in WA.
The spokesperson said that it was only in very rare cases that treating doctors may decide to make a voluntary notification about a





continued from Page 13
doctor-patient if they were refusing care and putting patients at risk.
welfare concerns in staff and DHASWA provides a confidential 24/7 telephone advice line.


Surveys repeatedly show levels of stress are most severe in junior doctors and it can begin before a medical student graduates.
Changing the culture
Medical Students' Association of Notre Dame (MSAND) vice president Yoveena Brian explained that rosters vary, but some senior students would be doing 40-hour weeks on top of their studies.
Ms Brian said role modelling and culture are important for those entering the profession.
“Students look to those ahead of them to understand what is normal and acceptable when it comes to managing stress,” she told Medical Forum
“However, everyone is facing pressure from the system, as such, system level support is key.”
She admits the attitude of ‘just getting on with it’ still exists among students but is hopeful this is shifting.
“When asking current junior doctors about recommendations for internship, they often mention the amount of overtime, ease of taking leave/sick days and pastoral care/ support as key points to consider.”
MSAND wellbeing chair Jay Caruso says there is growing awareness among students that “it is okay not to be okay”.
However, the structure of the course can reinforce the ‘pushing through’ mentality.
“When some clinical rotations are only two weeks long it can be hard to take time off, as it either means missing valuable hospital time or having to make up for it with longer days or weekends,” Mr Caruso said.
As well as some universities having clinical psychologists that medical students can access confidentially, many also have core curriculum components that seek to embed skills to prevent burnout.
There is support available to practitioners through wellbeing officers in hospitals to address
“Doctors usually call when they are at a crisis point where they can no longer manage themselves, and this can mean their health needs are urgent,” Dr Newman added.
Those responding have a variety of doctors representing different interest groups, who they can put callers in touch with.
“You're talking to a colleague who understands the strains and stresses of being a doctor.”
DHASWA has a list of GPs and clinical psychologists willing to see doctors and medical students as a priority.
In 2024, 55% of callers expressed concerns about workplace stressors including medico-legal and Australian Health Practitioner Regulation Agency issues, worklife balance, bullying, harassment discrimination, or racism, physical health and the ability to access care.
With almost a fifth of WA’s medical specialists due to reach retirement age in a decade and lost productivity from burnout in doctors costing the national economy billions annually, the issue requires attention at all stages.
Dr Alessandri, who now works part-time as a clinical paediatric haematologist at Perth Children's Hospital, said she is encouraged by the stronger focus on work-life balance from younger doctors.
Dr Helen Wilcox, head of UWA’s medical school, said while medicine may have once been dominated by ‘type-A’ personalities, universities were increasingly looking for diversity in their medical student cohorts.
“We find there may be students who are studying medicine who do have that more driven, high stress, perfectionist personality, but by spending time with other students that have a more measured approach to workload, that helps them regulate, and that's the power of community.
“There's a role for all personas, all approaches, those with the more
perfectionistic approach, who place a sense of urgency in study, they're often quite motivating for the students who have a steadier, lower paced approach. They balance each other.”
In an effort to provide supportive work settings, the national branch of Doctors Health Services has released the Every Doctor, Every Setting Framework.
It provides a comprehensive strategy to support the mental health and wellbeing of Australian doctors and medical students, and it focuses on practical implementation.
The plan outlines actionable items across primary, secondary, and tertiary prevention as well as mental health promotion and leadership.
While the AMA (WA)’s most recent Hospital Health Check, released in May, shows a welcome reduction in burnout rates among junior doctors in WA hospitals, Dr Page told Medical Forum that burnout in doctors “won’t be addressed until the need to significantly expand our health infrastructure and medical training is taken seriously by governments”.
The report noted it was encouraging to see notable improvement across the majority of employers, which is likely linked to the significant improvements in access to leave this year.
While the Women and Newborn Health Service again recorded the greatest level of burnout, it decreased by 13% since 2024, to 70%.
The WA Government’s Health Workforce Strategy in place until 2034 acknowledges that due to increased demands on health staff in the public system “introducing mechanisms to manage workrelated stress is a priority”.
But as workforce pressures, doctor shortages, difficult shifts and increasing patient demand continues, so too does the risk of losing valuable doctors to burnout.
By David Rossbach

In the words of former US Secretary of Defence Don Rumsfeld, there are “known knowns, known unknowns, and unknown unknowns”. Sequencing risk falls into the "known unknowns" category – we know market fluctuations will happen, but we can't predict their timing or severity.
This uncertainty is especially relevant for doctors transitioning from a stable, high-income career to the unpredictability of retirement.
Sequencing risk, or the risk of poor investment returns early in retirement, can significantly affect the longevity of retirement savings. For medical professionals nearing retirement, understanding and addressing this risk is essential to maintaining financial security.
By recognising the potential impact of early negative returns and planning accordingly, doctors can better safeguard their savings and enjoy a more stable retirement.
This article explores sequencing risk, its implications for retirement planning, and strategies to help retiring doctors navigate this financial challenge.
What is sequencing risk?
Sequencing risk refers to the danger that the order and timing of
withdrawals from your retirement account will negatively affect the overall rate of return on your investments.
This risk is particularly relevant during the initial years of retirement when you start withdrawing funds from your portfolio. If the market experiences a downturn during this period, the value of your investments can be significantly reduced, leading to long-lasting impacts on your retirement savings.
Sequencing risk at play
To illustrate sequencing risk, let's consider two hypothetical retirees, Dr Smith and Dr Jones, both with a retirement portfolio of $5 million.
They each plan to withdraw $250,000 annually, adjusted for 2.5% inflation each year.
• In the first two years of retirement, Dr Smith's portfolio experiences a 15% decline each year, followed by a 6% annual return for the next 16 years. After 18 years, Dr Smith's portfolio is reduced to $62,671.
• Dr Jones enjoys a 6% annual return for the first nine years, followed by a 15% decline in the 10th and 11th years, and then a 6% return for the remaining years. After 18 years, Dr Jones's
portfolio still has a significant balance of $1,926,018.
After 18 years, Dr Smith's portfolio is essentially depleted, while Dr Jones still has a significant balance.
This example highlights how early losses can severely impact the longevity of a retirement portfolio, while mid-retirement downturns may be less detrimental if the portfolio has already grown.
In this scenario, Dr Brown and Dr Green both start with a retirement portfolio of $4 million. They each plan to withdraw $175,000 annually, adjusted for 2.5% inflation each year.
• In addition to the annual living expenses, Dr Brown incurs a big European trip costing $100,000 in the first year and financial support of $300,000 for their children in years two and four. Their portfolio experiences a 10% decline in the first year and an 8% decline in the second year, followed by a 6% annual return for the next 16 years. After 18 years, Dr Brown's portfolio is reduced to $328,392.
• Dr Green has the same additional expenses but funds them at a later stage – years 11, 12, and 14. Dr Green enjoys a 6% annual

return for the first nine years, followed by a 10% decline in the 10th year and an 8% decline in the 11th year, and then a 6% return for the remaining years.
After 18 years, Dr Green's portfolio still has a balance of $2,010,797.
This example highlights how the timing of additional expenses, combined with the sequence of returns, can severely impact the longevity of a retirement portfolio.
Early losses and early additional expenses can drastically reduce the portfolio's value, while delaying these expenses can help preserve the portfolio's balance.
Sequencing risk can have profound implications for your retirement planning, including:
• Depletion of savings: As seen in the examples, an early market downturn can lead to a faster depletion of your retirement savings. This is because you are withdrawing funds from a shrinking portfolio, leaving less capital to recover when the market rebounds.
• Reduced financial security: The risk of running out of money can lead to financial insecurity, forcing retirees to adjust their
lifestyle or spending habits unexpectedly. This can cause emotional stress and anxiety, undermining the peace of mind that should accompany retirement.
• Impact on withdrawal strategies: Fixed withdrawal strategies, where a set amount is withdrawn annually, can be particularly vulnerable to sequencing risk. Retirees may need to adopt more flexible withdrawal strategies that adjust based on market performance to mitigate this risk.
While sequencing risk cannot be entirely eliminated, there are strategies to mitigate its impact:
• Ensure your investments are spread across various asset classes to reduce risk. A welldiversified portfolio can help cushion the impact of market downturns. Including a mix of stocks, bonds, and other assets can provide stability and reduce the overall risk to your retirement savings.
• Continuously review and adjust your asset allocation to ensure it aligns with your risk tolerance and retirement goal.
• Plan around lump sum expenses.
• Adjust withdrawal rates – be flexible with your withdrawal rates, reducing them during
market downturns to preserve capital.
• Maintain a cash reserve –having a cash reserve can help cover expenses during market downturns, allowing your investments time to recover.
For medical professionals nearing retirement, understanding and planning for sequencing risk is crucial.
By being aware of this risk and implementing strategies to mitigate its impact, you can better ensure the longevity and security of your retirement savings. Remember, the key to a successful retirement is not just about accumulating wealth but also about managing risks effectively.
Does your investment strategy need a financial check-up? If so, reach out to drossbach@capital-partners.com.au
Once referred to as bed sores, pressure injuries can have a profound impact on health, even leading to death, as well as costing billions of dollars to treat. Now there is new expert advice on how to prevent and manage them.
By Cathy O’Leary

It is unsurprising that the sores that plagued patients and elderly people lying in bed for many hours of the day were once blamed on the bed itself – hence the term ‘bed sores’.
But clinical understanding of the pathways that lead to these common and costly wounds now recognises that many factors can lead to what are more appropriately called pressure injuries.
And while primary prevention is the main goal, careful management of early-stage damage to the skin also reduces the chance of them developing into more serious, even life-threatening, invasive wounds.
Now, an industry consortium led by Wounds Australia – the national peak body for chronic wound advocacy and education – has released updated international advice on the prevention and management of pressure injuries.
Key objectives are to update busy clinicians with easy-to-navigate standards for identification and clinical management, better support patients at risk of pressure injuries, and reduce unnecessary and costly hospitalisations.
The resource is of particular importance in regional areas due to the distances people often travel to access healthcare. If wounds are left untreated, the health consequences can snowball.
While the new guideline is aimed at a broad range of health professionals as well as carers in the home, the role of primary care and acute care clinicians is recognised.
The definition and grading system for pressure wounds has also become more nuanced over time. Pressure injuries are defined as localised damage to the skin or underlying tissue, because of pressure or pressure in combination with shear.
Shearing wounds occur when skin and underlying tissues move in opposite directions, compounding the injury created by pressure and damaging skin at a more invasive level.
Pressure injuries usually occur over a bony prominence but may also be related to a medical device or object.
While bed sores were once seen as the domain of the elderly and infirmed, pressure injuries are a potential risk for anyone whose mobility is compromised.
If a person is so unwell or physically disabled that they stop moving for prolonged periods of time, there is a serious risk of pressure injuries.
This includes people with spinal cord injuries, as well as patients of all ages temporarily immobilised or needing to wear monitoring or breathing
equipment which causes pressure on the skin.
Wounds Australia, which has more than 18,000 stakeholders including doctors, nurses, pharmacists, researchers, allied health and aged care professionals, estimates that each year more than 450,000 Australians are faced with a chronic wound.
It defines chronic wounds as sores that have not progressed through normal healing stages within 30 days. They may heal very slowly, partially or reoccur. Warning signs include pain and heat, odour, excess fluid and excess healing time.
Leg ulcers and pressure sores are the most common types.
The group co-launched the new advice – The Prevention and Management of Pressure Ulcers/ Injuries: Clinical Practice Guideline: The International Guideline 4th Ed –in March this year.
Considered the gold standard in evidence-based care for common and costly wounds, the guideline was produced by an international consortium of leading wound experts from more than 40 countries.
Wounds Australia chief executive Jeff Antcliff said the launch
represented an important opportunity for healthcare workers and carers to proactively adopt leading practices for preventing and managing pressure injuries.
Pressure injuries affect 13% of the world’s population, causing physical pain and distress to individuals and costing Australian public hospitals $9 billion a year to treat.
Co-hosts of the guideline launch, Forward Ability Support (FAS), operates Sydney’s Ferguson Lodge, a high-level residential personal and clinical care facility for people living with spinal cord injury.
FAS clinical advisor Dr Dinesh Palipana shared his personal experiences living with quadriplegia.
A Gold Coast emergency medicine doctor, he was the first quadriplegic medical intern in Queensland.
While studying medicine at Griffith University, Dr Palipana was in a catastrophic car accident in 2010 which left him paralysed from the chest down.
“Guidelines are a critical tool, especially for clinicians to provide good care for their patients, and with this guideline there's even a quick reference guide for people who are busy.”
A key speaker at the launch was Curtin University Professor Keryln Carville, who has worked with Silver Chain for 35 years, and is a leading pressure injury expert and chair of guideline co-publisher the Pan Pacific Pressure Injury Alliance.

“I nearly died in that car accident, so I've come to learn that life is short,” he said at the launch.
“For a human being, a wound is a huge thing, and if a wound gets out of control, it can stop life for a month, two, three, maybe longer. Some people need surgery, and some people end up in hospital for a long period of time.
“Pressure injuries are not just a physical problem for a person. There can be a life-threatening issue or a limb-threatening issue.
Stage 1:
• Intact skin with non-blanchable redness, usually over a bony prominence
• Darkly pigmented skin may not have visible blanching
• The area may be painful, firm, soft, warmer or cooler compared to adjacent tissue
Stage 4:
• Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound.
• As with stage 3, the depth varies by anatomical location.
• Stage 4 injuries can extend into muscle and/or supporting structures making osteomyelitis possible. Exposed bone/ tendon is visible or directly palpable.

She noted that insufficient wound care education for primary health and aged care workers in non-metropolitan regions could lead to poorer patient outcomes and higher treatment costs.
Pressure injuries were the number one reported or penalised hospitalacquired complication in public hospitals, but they also impacted on individuals, increasing morbidity and mortality.
Prof Carville told Medical Forum that the new edition of the guideline would offer the most contemporary evidence for prevention and treatment.
“Anybody who has a mobility issue is potentially at risk of pressure injury, so that means anyone for whatever reason who is unable to reposition themselves,” she said.
“That presents challenges for people who have spinal cord injuries, people who are unconscious due to surgery or trauma, or people who have cognition difficulties such as advanced dementia and are not able to reposition.
“You know yourself that if you sit in a place for too long you can get a numb backside or a tight elbow, so you wriggle to get off that position.
“That’s the normal physiological response that comes to you day and night, even when you’re sleeping. You probably reposition every 20 or 30 minutes, moving something even slightly.
“But if you’re in a position because of a change in your condition such as trauma, surgery, being under anaesthetic, some cognitive difficulty that affects your mental ability to focus on what you’re doing, then you can’t do that.”
Prof Carville said the change in terminology for pressure injuries over the past 30 years was very deliberate. Australia had led the way in calling them injuries rather than sores or ulcers because it reminded everyone that they were largely preventable.
Pressure injuries have been around since the ancient Egyptian times, with scientists putting mummies through MRI scanners able to see them.
• Partial loss of dermis presenting as a shallow open ulcer with a red/pink wound bed, without slough
• May also present as an intact or open/ ruptured serum-filled blister
• Presents as a shiny or dry shallow ulcer without slough or bruising.
• The depth varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and so ulcers can be shallow but areas of significant adiposity can develop extremely deep pressure ulcers. 1 4 2 3
Stage 2 should not be used to describe skin tears, tape burns, perineal dermatitis, maceration or excoriation.
Stage 3:
• Full thickness tissue loss. Subcutaneous fat may be visible, but bone, tendon or muscle not exposed. Slough may be present but does not obscure the depth of tissue loss.
Expand your treatment options for clients who have plateaued in their healing journey

Since January 2024, Empax Centre has delivered comprehensive, evidence-based MDMA and psilocybin-assisted treatment programs for individuals with PTSD and treatment-resistant depression, who have experienced limited success with traditional interventions.
To learn more, including details on funding support, request an information pack
empaxcentre.com
+61 (0) 8 9455 5889
info@empaxcentre.com

Empax Centre Medical Director, Dr Jonathan Laugharne

continued from Page 19
“The bed was often perceived to be the problem and if you think about the early 1800s era, particularly around the period time of Florence Nightingale, unless you were extremely wealthy, if you had a mattress it was probably made of horse hair or straw so it was very hard,” Prof Carville said.
“Because the bed was seen as the problem, people did all sorts of things like cut doughnut shapes in the mattress to try to relieve pressure. Today we know that’s the last thing you want to do because you just concentrate pressure outside the doughnut.
“We know that what causes pressure injuries is unrelieved pressure –perpendicular or direct force – but the other thing is shear – parallel –force.
“If you’re sitting on a hard spot and nothing’s relieving it, that’s pressure, but if the person was to be dragged up a chair or slide down a bed or chair then that’s shear.
“And then under the heels you get rubbing where the person moves their heels up and down to reposition in the bed and that’s friction. So, pressure, shear and friction all impact on the skin, and the type of force and duration are important.”
Prof Carville said another critical factor in pressure injury development was a person’s skin tolerance.
“If a person is in good health, they’re well hydrated and nourished and their skin is clean and dry then they’ll be able to tolerate more pressure, shear and friction than if they’re malnourished and in a poor health state, or if their skin is wet because of sweat, or urine or faeces.”
A prevailing belief was that pressure injuries only affected the bed-bound elderly, however they impact across all populations.
“We get pressure injuries in neonates, infants and children but in hospitals they’re related to the devices we use with them, so things like catheters,” she added.
“Neonates, because of their light weight, don’t have so much of a
problem with pressure but they have significant pressure injuries because of the devices attached to their skin.
“Often in the frail elderly, whether they be in the community or nursing homes or hospitals, they turn their chairs into their world.
“They often sleep in their chairs, and they have what I call bed clutter –the TV remote, the telephone, the cutlery that they missed from lunch – and they lie on these objects.”
Pressure injuries are now classified according to four stages and two other conditions.
“The first stage is intact skin which is damaged, it’s red, so it’s technically not an ulcer because there’s no break in the skin,” Prof Carville explained.
“With a stage one, when you turn the person over the skin is red, and if you press on it, normal skin blanches, and the skin is still intact. If you get them off that point 50% will resolve, while 50% will go on to become deeper wounds.
“Stage one, which is intact skin, and stage two, which is superficial skin loss, are the most common pressure injuries in Australia, but a large portion go on to become deeper stage three and four, or another condition we call unstageable because it’s covered in dead tissue so we can’t see the depth.”
Prof Carville said that while superficial wounds were more common, they had the potential to become significant wounds that could increase co-morbidities and even lead to death.
“And that’s the reason why we have prevention strategies, first and foremost to do anything we can do to encourage mobility and repositioning, so that could be prompts or asking families in the home or the hospital staff to turn them frequently if they can’t do it themselves.
“Repositioning is number one, but of course you must keep the skin clean and dry, and then you have to make sure they’re well-nourished. Being overweight or underweight can lead to changes in the skin, and that can mean the skin is more vulnerable to pressure shear.”
Education is key
Prof Carville recognised that as more elderly people wanted to stay in their homes, family members were needing to take on some of the role with pressure injury prevention. And staffing constraints in facilities like hospitals and aged care could not be ignored.
“The important thing is that we educate the individual who is potentially affected, and their carers, and we need a good education program for our health professionals too,” she said.
“I teach undergraduate nurses that every time we turn someone, we’re checking their skin and it’s their responsibility to make sure they don’t have any pressure injury or are at risk of injury, such as finding something in the bed that shouldn’t be there, like their phone.”
Prof Carville said the guideline was research driven and updated about every five years.
The key difference with the latest guideline was that it was a living document that would allow new evidence to be added as it became available rather than waiting for five years.
Everyone’s responsibility
She added that it was important to keep challenging the notion that pressure injuries were inevitable. While it was often nurses or other staff doing the moving, it was something that doctors needed to be across.
“Every health professional – the physio, the OT, doctors – everyone needs to be aware that a pressure injury is a problem, because with every injury you cannot reposition the person that increases their risk for more pressure injuries.
“So it’s every health practitioner’s goal, I’d like to say responsibility, to stay abreast of the evidence and how best we can intervene to avoid these preventable wounds.
“If you look at the cost – $9 billion spent on pressure injury treatment in public hospitals in Australia in a year – just think what you could do with that money?
“The important message is that prevention is the best cure, and it’s the cheapest cure.”
We are please to announce Dr Sheldon Moniz joining Orthopaedics WA
MBBS, FRACS (Ortho), FA Orth A
Dr Sheldon Moniz is a dedicated orthopaedic surgeon with expertise in arthroplasty, sports medicine and trauma surgery.
His subspecialty interests include:
Upper Limb Surgery:
Hand, wrist, elbow, and shoulder procedures.
Arthroplasty:
Shoulder, elbow, wrist, knee and hip joint replacements.
Sports Medicine:
Arthroscopic reconstructive surgeries.
General Trauma: Comprehensive care for fractures and workplace injuries.

Dr Moniz was awarded Fellowship of the Royal Australasian College of Surgeons (FRACS) and the Australian Orthopaedic Association (FAOrthA) on completion of orthopaedic training in Western Australia. He completed an AOA-accredited fellowship at the Orthopaedic Research Institute of Queensland and also gained international experience with renowned orthopaedic surgeons in Ireland, the UK, France, Switzerland and Italy.
His subspecialty interests include:
Upper Limb Surgery: Hand, wrist, elbow, and shoulder procedures. Arthroplasty: Shoulder, elbow, wrist, hip and knee joint replacements.
Sports Medicine: Arthroscopic reconstructive surgeries.
General Trauma: Comprehensive care for fractures and workplace injuries.
Dr Moniz continues to maintain an academic role at UWA as a clinical lecturer and mentor to medical students. He is an active contributor to orthopaedic research, with academic interests in enhanced recovery after surgery and the use of assistive technologies, including patient-specific implants, artificial intelligence and robotic technologies.
Dr Moniz is committed to combining proven techniques with professional and personalised care to support his patients in achieving the best possible outcomes. Whether you are seeking treatment for an injury or considering surgery, Dr Moniz will guide you through the process with care and understanding.
Outside of work, Dr Moniz enjoys playing the piano, saxophone, and guitar. Most importantly, he values spending quality time with his young family.








Tel: 08 9312 1135
e : reception@orthopaedicswa.com.au

PROF PIERS YATES
Hip, Knee & Trauma
Primary & Revision
Arthroplasty
Hip Resurfacing
Fax: 08 9332 1187
w : www.orthopaedicswa.com.au


MR BENJAMIN WITTE
Knee Surgery
ACL & Sports Injuries
Knee & Hip Replacement
Medico Legal
MR THOMAS BUCHER
Hip & Knee - Primary & Revision
ACL and Trauma
Gluteal Tendon Reconstruction


MR ANDREW MATTIN
Shoulder, Elbow & Wrist
Knee, Shoulder Replacement
Sports injuries
Trauma
MR SIMON WALL
Hip & Knee-Primary & Revision
ACL and Trauma
Ilizarov Frames


A/PROF GARETH PROSSER
Hip, Knee & Trauma
Primary & Revision
Young Adult Hip
Hip Resurfacing

MR SATYEN GOHIL
Knee & Shoulder
ACL & Sports Injuries
Arthroplasty & Trauma
MR LI-ON LAM
Knee, Shoulder & Hip
Uni Compartmental Knee
Knee and Shoulder
Arthroscopy
ACL and Trauma
A/PROF CHRISTOPHER JONES
Hip & Knee Replacement
-Primar y & Revision
Computer assisted Surgery
Hip Resurfacing Trauma
MR DANIEL MARSHALL
Hip, Knee, Foot & Ankle
Ankle Replacement
Robot Assisted Arthroplasty
Trauma
DR SHELDON MONIZ
Hand & wrist surgery
Shoulder arthroscopy & replacement
Knee arthroscopy & replacement
Peripheral nerve surgery
Rooms located at: Murdoch, Perth, Albany and Denmark
Matt O’Shea’s experience as a military medic inspired him to open a holistic and integrated practice for veterans and first responders.

By Ara Jansen
As a young person Matt O’Shea knew he wanted to be more involved in serving the community than the average person.
Migrating to Perth from the UK when he was 10, Matt got to the end of Year 12 and didn’t know what he wanted to do with his life. Most of his uncles had served in the army and his grandparents had served in the navy in World War II.
“I looked up to them and their stories and the things they had done,” says Matt. “At the same time, as a teen, I was rebelling and didn’t sit any of my final exams, which my parents weren’t happy about. I decided the men in my family had turned out alright, so I decided to join the military and see what it had to offer.”
Matt spent 30 years in the Australian Defence Forces working here and overseas. He started with basic training and became a junior medic at 18, alongside training in specialist skills such as underwater medicine, army-qualified diving, weapons training, counter terrorism and added training for the Sydney Olympics, insertion, parachuting and trained with the US Marines.
During his career Matt has worn different hats and parlayed his skills and training in numerous ways. He served in Special Air Services Regiment (SASR) and Special Operations Headquarters (SOHQ) and the 6th Battalion Royal Australian Regiment (6 RAR), a mechanised infantry battalion with a history of serving in various overseas deployments.
Matt has served on various operations and deployments domestically and in the Middle East and Asia, including East Timor and Afghanistan. While deployed his primary function was to provide medical care to personnel.
He has also been an instructor at the Army School of Health in

I would regularly scrub in on a surgery and sometimes we’d be there all night.
When Matt was stationed in Afghanistan in 2006, he had a bad fall and hurt his back.
“I was lying on the ground thinking ‘I need to get another job’. We were doing a night move, I was holding onto the back of a truck, I lost my grip and fell off. The next day I could hardly move.
“That incident was the catalyst to think ‘what am I doing here?’ Even while we were on base myself and the Australian doctor would help out with the nearby US surgical team.
“The Taliban would engage at dark and all the casualties would arrive a little later, so we’d go and backfill in the theatre or emergency theatre.
“I was an extra set of hands for the surgeons. It was intense, we did some crazy things and I learnt a lot.”
“I was an extra set of hands for the surgeons. It was intense, we did some crazy things and I learnt a lot.”
After his time in Afghanistan, Matt retuned to Perth, took long service leave and, wanting to do something different, completed a graduate certificate in business at Curtin.
“I was probably still in the prime of my career and still very deployable. I probably could have continued for another five to 10 years, but I decided not to.”
Instead, he transferred to become a Reservist and spent some time working in mining and gas as a medic in the State’s north-west and later started a registered training organisation which revolved around first responder care before getting to hospital.
He worked for CareFlight, an aeromedical charity and is currently manager of emergency strategy at St John WA. He’s on the board of Richmond WA and was a volunteer member of the SAS Association Advocacy and Welfare Team.
Now a Major in the Reserves, Matt is Army Reserve Company

Located within the Murdoch Health & Knowledge Precinct, this clinic offers easy access to advanced imaging services. With three PRC clinics within 5km including PRC Wexford Medical Centre, Booragoon and the brand new Murdoch Square - we provide a complete network of diagnostic imaging solutions.
Murdoch Square services include:

continued from Page 25
Commander of 7 Health Support Company based in Perth. The company is made up of mostly medical people whose day jobs are in places like GP surgeries, hospital emergency departments or the Royal Flying Doctor Service, and some with army training.
Married with two boys and living in Perth, in 2015 Matt found himself in the middle of a mental health crisis. What was challenging him were the incidents he’d responded to overseas that involved children.
While he “did a lot of work on blokes” in the field, it was the memories of children and noncombatants that followed him home.
“It didn’t cause me an issue until I had my own kids, and I started rerunning all the medical incidents involving kids whilst in country. I was getting really worked up around a couple of things and blaming myself. I started drinking a lot.
“I decided I needed to sort it out. I’d had three knee surgeries and my back is still not great. I knew I needed to get to the gym, see my GP, a psychologist and a physio. I hadn’t been paying enough attention to my own health.
“I also wanted to put some time in and finish my MBA in business administration.”
He also did a PTSD course, which he credits as being one of the best things he has ever done.
“It helped me clear up so many things in my head. I felt completely reset. I was definitely mentally heading in the wrong direction,” he says.
“Most of the issues were related to my time overseas, and that affected everything. It affects family and work. Realising it was a problem and then taking action was crucial.”
On his healing journey, having to see different people in different practices, make separate appointments and travel to them all, gave Matt an idea. What if he could put these services for veterans, first responders and those currently serving all in one place?

“What if you could see an advocate and get all the paperwork done and your team can collaborate around your care? What if you could get the doctor and the psychologist in the same room, at the same time, to agree on care?”
That’s exactly what Matt has done as owner and volunteer veteran care coordinator of the recently opened West Coast Health Alliance in Joondalup.
Instead of clients having to go to several different places to access different services, Matt wanted a place where someone could see a psychologist, a GP, pharmacist, exercise physiologist, physio and DVA advocate under one roof.
This allied health model also allows staff to work together to deliver comprehensive, integrated and holistic care for patients – veterans and their families.
“A lot of work has gone into the layout of the space and the kind of staff we have. All of the staff have worked as first responders or in the military and know what kind of issues are common to both groups. They get it, they are well-informed –and they may well have been there themselves.”
The clinic’s Enhanced Veteran Allied Care (EVAC) Program has been designed by veteran clinicians
for veterans and comprises of collaborative care, personalised wellness plans and opportunities for community and connection to “build a healthier, brighter future – one that honours your past and strengthens your future”.
Matt’s plan is to have three clinics like Joondalup over the next few years.
They’ve already started working on clinics in Ellenbrook and Rockingham. Subtle touches include bigger consulting rooms for those who might be triggered by small spaces and more space between equipment in the gym.
You’ll also find a number of allied health and helpful groups located there – Soldiers & Sirens and Buddy Up Australia provide mental health and mindfulness programs and there’s an RSL advisory team.
One of the challenges they have come up against is finding GPs who want to deal with the Department of Veterans Affairs paperwork. Matt is keen to meet and collaborate with those who do.

When the Scope of Practice review was published last year, dissenting views were heard loud and clear – some groups were keen to expand their scope while doctors had some reservations. We take a closer look at the ever-changing landscape of scope of practice.
By Suzanne Harrison
Everyone agrees that collaboration, communication and integration are imperative to sustaining the healthcare workforce and system.
But at the time of its release last October, a review led by Professor Mark Cormack – Unleashing the Potential of our Health Workforce – resulted in more disagreement rather than consensus.
The year-long independent review examined the system changes needed to support health practitioners to work to their full scope of practice. It found that almost all health professions in Australia faced restrictions and barriers to their work.
Among its 18 recommendations to address this was the implementation of new direct referral pathways to improve access to some non-GP specialists.
It also called for changes to some prescribing powers and the establishment of a primary care workforce development program to support the retention of skilled staff.
Both the AMA and RACGP urged the government to tread with caution when considering the recommendations. They warned that they could result in a costlier health system, more delays to care, and higher out-of-pocket costs for patients.
The RACGP said the review did little to allay their long-held concerns around task substitution, and had a lack of risk assessment, costing and evaluation of direct referrals.
Conversely, nurses and pharmacy groups were welcoming of the report having campaigned to expand their scope of practice.
Now some months and a Federal election later, what has been the impact of the review and is it time to redefine different practitioners’ scope of practice?
Collaboration is key
One of the biggest concerns GPs had was around direct referral pathways. Under the recommendation, non-GP specialists would be able to refer patients needing further treatment, for example a physiotherapist could refer to an orthopaedic surgeon, or a dietitian could refer to gastroenterologist.
GPs raised concerns about this creating inappropriate referrals, fragmenting care and increasing out-of-pocket costs for patients.
RACGP Vice President and WA Chair Dr Ramya Raman said working collaboratively across different professions underpins general practice, but any changes to scope of practice must ensure quality and safety of care.

is well coordinated and there is a good communication pathway.”
Dr Raman said the less fragmentation there was across primary care, the better that was for the patient.
“When there is better continuous co-ordinated care from a GP, it means a reduced cost for both State and Federal health and, ultimately, the patient.”
Professor of General Practice and Co-Lead Doctor of Medicine at Bond University Dr Mark Morgan also warned of the risk of fragmenting care and instead suggested more funding was part of the solution.
“Funding longer GP consults, supported by a complementary multidisciplinary team, seems the only way to efficiently support the health of Australians,” he said.
“Rather than creating systems of competition, it seems much more reasonable to recognise complementary skill sets. Working under the same roof, with the same medical record, allows patients to get the best mix of advice and allows the clinical team to learn continuously about each other and from each other.”
Multidisciplinary care, not expanded practice
This ‘under one roof’ approach has been received more positively and has brought about change since the review was published.

“The one thing we always have to remember is that accessibility is really important, and the quality and safety of care is really important,” she told Medical Forum
“Our approach is to always ensure patient safety, and patient care is foremost, so that’s one of the reasons we say there is no substitute for the quality of care provided by a GP.
In May this year, the RACGP and Pharmaceutical Society of Australia (PSA) joined forces to call for funding of general practice-based pharmacists to work with specialist GPs to support high-quality prescribing.
Funding for more nondispensing pharmacists, nurses, psychologists, and other health professionals in practice teams is part of the RACGP plan for accessible and affordable care released earlier this year.
Multidisciplinary care is already underway in some general practice teams, but it needs secure funding and strong relationships with GPs to leverage the full benefits, according to the PSA.
medicine reviews. They are also on hand to help patients understand their medicines, any changes to those medicines, and to ensure safe and effective medicine use.
RACGP President Dr Michael Wright said the move would enable general practices to expand their teams to have “immediate and long-term benefits” for patients and the healthcare system.
“People with chronic illness get the best care when their specialist GP works with pharmacists and other health professionals in multidisciplinary care teams,” he said.
“Most practices provide multidisciplinary care, and most GPs want to grow their teams to better serve our patients.”
Dr Raman agreed that increased funding for a multidisciplinary approach was needed, especially for chronic disease.
“Chronic disease is the most prevalent and, given the changing demographics in our population, that automatically increases the risk of hospitalisation,” she said.
“Targeting funding towards a multidisciplinary team approach that is GP-led will ultimately mean there is a collaborative approach that will work for better outcomes for the patient.”
Despite concerns about fragmentation of care, pharmacists are already operating under an expanded scope of practice in various places across the country – a move that has caused some controversy among doctors but proved popular with patients.
In WA late last year the State Government announced expanded roles for community pharmacists. The expansion allowed pharmacists to provide care for a range of conditions including mild to moderate shingles, acne, dermatitis, musculoskeletal pain and inflammation, nausea and vomiting, urinary tract infections and wound management.
In Queensland, the government has announced its pharmacy pilot program will be made permanent –allowing registered pharmacists the ability to diagnose and prescribe
“A GP-led multidisciplinary team approach would ensure that care continued on Page 30
Non-dispensing pharmacists in general practice answer queries, monitor prescribing, and conduct
continued from Page 29
medication for a variety of health issues.
While in Victoria a 2023 pharmacy prescribing pilot was made permanent in last month’s State budget, with pharmacists also handed greater powers to prescribe medications for a range of complex conditions including high blood pressure without the need for a specialist GP consultation.
It prompted warnings from the RACGP that patient care would be compromised.
Pilot programs around Australia will inform the next steps for WA.
GP concerns have focused on the risk of misdiagnosis and that it could result in a less connected doctorpatient model – within the same vein as direct referral pathways.
WA GP and founder of the Perth Weight Clinic Dr Mark Mellor said there was clearly a need to expand scope of practice in some areas –especially as GP shortages continue – but there were some instances where it would not be appropriate.
“There are pockets where it looks like it’s going a little bit too far, a good example would be whether pharmacists will be able to prescribe weight loss medication,” he told Medical Forum

got a UTI and it’s actually something very different. So I’m a bit concerned about that patient falling through the cracks.

“Are pharmacists’ experts in providing prescriptions? Or experts in medicine and medication? That’s where the concern from doctors comes from. It’s not about being divisive and against each other.”
Dr Mellor said some health practitioners could do a bit more work beyond their current scope but any decision needed to ensure safe healthcare was at the forefront.
“That could be really dangerous. At the same time you’ve got telemedicine providers that are staffed by medical practitioners and nurse practitioners that are dishing these drugs out… it’s a bit of a wild west and we always have to have patient safety as the focus here.”
Dr Mellor gives another example of pharmacists being able to prescribe for UTIs.
“A person could turn up to a pharmacy thinking they’ve got a UTI and the pharmacist does some screening that determines it’s a UTI and it needs antibiotics.
“But do you know how often a GP sees a patient that thinks they’ve
Perhaps the most closely linked with GPs are nurses, who were largely welcoming of Professor Cormack’s review.
The Australian College of Nursing (ACN) urged the government to accept the recommendations.
ACN Chief Executive Professor Kathryn Zeitz said the review acknowledged the restrictions, barriers, and inconsistencies that prevent nurses, nurse practitioners, and midwives from working to their full capability.
Soon after, in December 2024, the Federal Government approved a new registration standard, paving the way for qualified RNs
to prescribe certain medicines in partnership with an authorised health practitioner. This change will take effect mid-2025.
Ken Griffin, chief executive of the Australian Primary Health Care Nurses Association (APNA), told Medical Forum that progress since the Cormack review was delayed by the recent Federal election, but the Labor Government had been clear it intends to pursue scope of practice reform.
“Not allowing nurses to work to their full scope of practice is a significant waste of the skills, experience and capability of the largest workforce in primary health care.”
But the devil lies in the detail. Some groups remain concerned about the impact any changes will have on various practitioners.
In the lead up to the Federal election nine of Australia’s peak nursing and midwifery groups called for reforms to allow nurses and midwives to provide specialist referrals, prescribe medicines and order diagnostic testing.
They said this reflects the recommendations of the Scope of Practice Review, adding that patients and communities – especially those in rural and regional areas – would benefit when they can work to their full scope.
But it was met with concern from
the RACGP, which took the stance that care is best delivered when GPs and nurses work together rather than if nurses were able to make some standalone care decisions.
The College has reiterated that nursing colleagues complement GPled care based on a relationship of trust and collaboration.
Its latest Health of the Nation report found 88% of responding GPs agreed practice nurses benefit patient health when embedded in general practice teams.
As it stands, health practitioners remain divided on the best way forward for expanding scope of practice and improving access to care.
Understandably, doctors are concerned about any impact changes may have on patient care, but other professions want to help more.
It begs the question – do we need to accept that change amidst a healthcare system that is showing signs of struggling to keep up with patient demand?
If not, what is the best way to alleviate current workforce problems and ensure the best outcome for all primary care and allied health workers?
“I think we all appreciate that the current model of healthcare in Australia isn’t working,” Dr Mellor said.
“We do need to expand the workforce and therefore the government is looking to introduce top of scope practice for pharmacists and nurses. That’s all understandable, but it looks like it’s out of scope from a GP perspective.”
To that end, Dr Mellor added: “We need more GPs and to incentivise junior doctors to go into general practice.”
For Dr Raman, the bottom line is patient care and increased GP funding.
“As a GP who’s in the community, I work with allied health staff and pharmacists and the only thing we have in our mind is the outcome for the patient,” Dr Raman said.
“These allied practitioners are all
touch points, but you also have to look at the concept of keeping general practice central.”
However, Mr Griffin concludes that a system based on GPs being the primary point of call for care may not work in some areas.
“We need to realise that our health system is designed around the assumption that people have a GP or a hospital which provides them access to the best of the health workforce,” he said.
“We know this is not always the case. We need to utilise the workforce that is in place to provide in-scope care when a hospital or GP are not accessible.”
One thing we can say for certain is that the healthcare system is changing. There’s increased patient demand coupled with workforce shortages, higher prevalence of chronic disease and an ageing population.
New ways are needed to ensure the best possible patient care and a safe workplace for GPs and other practitioners, so we will need to find an agreed path to move forward.

Proudly hosted by the Autism Association of Western Australia, the Asia Pacific Autism Conference brings you face-to-face with some of the most influential thinkers and researchers in Autism today.







Rates of dementia in Australia are expected to double in the next 30 years without a significant intervention, so it is vital that Australians have immediate, ongoing and flexible access to early intervention supports.
Allied health professionals play an important role in supporting patients with dementia, writes Professor Tanya Buchanan, Chief Executive of Dementia Australia.
People living with dementia need access to appropriately funded pathways to allied health support and services.
We know that early intervention can help delay the progression of dementia, and allied health services provide significant benefits by helping people to maintain their physical and cognitive health, independence and wellbeing for as long as possible.
There are an estimated 433,300 Australians who live with dementia in 2025. In Western Australia, there are an estimated 42,000 people living with all forms of dementia. This figure is projected to increase 107% to an estimated 87,000 by 2054.
Rates of dementia in Australia are expected to double in the next 30 years without a significant intervention, so it is vital that Australians have immediate, ongoing and flexible access to early intervention supports.
Challenges faced post-diagnosis
Receiving a diagnosis of dementia can be a distressing experience for the person and their family members and carers. They are often left to process their diagnosis and identify appropriate supports on their own and can encounter challenges in navigating healthcare, specialist, disability and aged care systems, including referral and access to allied health services.
For many people impacted by dementia, including carers and family members, it can be a confusing and overwhelming experience.
These challenges can impact a person’s ability to understand their diagnosis and what support is available to them, and as a result can delay timely access to allied health services and supports.
People tell us that they are relieved when they find our services. They also tell us that they need greater levels of assistance to navigate the health, disability and aged care systems to access the care and support they need.
A network of trusted specialist dementia care coordinators would directly address these commonly faced challenges, and help people get the right support at the right time, which is critical to ensuring better outcomes for everyone involved. It is one of the key asks Dementia Australia has of the 48th Parliament as they return after the election.
Early intervention can enable people living with dementia to maintain their independence and functional capacity for as long as possible.
Allied health professionals play a key role in this and provide interventions to support the maintenance of current strengths and capacities, improve skill acquisition and promote recovery, enablement and rehabilitation.

People living with dementia can experience changes that impact their ability to perform tasks such as driving, managing finances, and everyday tasks such as showering and getting dressed.
Occupational therapists can implement strategies to support people to continue to participate in activities. Evidence shows that working with an occupational therapist can help to maintain independence, reduce the impact of changes in behaviour and improve



quality of life for people living with dementia.
People can also experience changes to their communication, eating, drinking and swallowing. Speech pathology plays an important role in supporting people to continue to maintain independence and communicate their needs, an essential part of living well with dementia.
Speech pathology and occupational therapy are examples of the very significant benefits provided by allied health professionals in supporting daily activities and








maintaining skills and strengths. Allied health is an essential part of a multidisciplinary approach for a person living with dementia to support wellbeing and independence.
Greater awareness for better outcomes
Improving awareness and understanding of dementia, and the importance of timely access to allied health services and supports, will lead to better outcomes for people living with dementia, their families, carers and communities.
Dementia Australia has a number of resources on allied health and dementia including position statements on physiotherapy, occupational therapy and speech pathology.
For dementia information and support you can contact the National Dementia Helpline on 1800 100 500 or visit www.dementia.org.au/ get-support/national-dementiahelpline
ED: Dementia Australia’s position statements are available at dementia. org.au/about-us/publications/positionstatements


























As vaccine hesitancy and misinformation drive a surge in illness, new tactics are needed to restore trust in vaccinations, writes Curtin University Professor of International Health Jaya Dantas.
Health practitioners are bracing for a horror flu season in 2025 amid falling immunisation rates. Vaccine apathy and misinformation is driving a drop in vaccinations, raising concerns as we approach winter and peak flu season.
Post-COVID-19 there has been a decrease in flu vaccination uptake in Australia from 9.3 million in 2023 to 8.8 million in 2024. This is a cause for concern, especially as we head into winter and we have the simultaneous risks of influenza, COVID-19 and RSV in the population.
The elderly, children, those who are immune-compromised and people with co-morbidities are especially vulnerable.
Data from the National Centre for Immunisation Research and Surveillance Australia shows WA has the lowest vaccination rates among all the age groups, with immunisation rates dropping across all age groups in Australia since 2022.
Cases of measles are surging in several states in the US with over 800 cases, including three deaths and over 700 hospitalisations. Over 65% of the hospitalisations were among those who were unvaccinated.
Australians aren’t as protected against measles as they should be, which is a significant problem given the disease is one of the most contagious in the world.
We also have an outbreak of the measles virus in WA with 19 cases in WA recorded since 19 March 2025, so it is especially important that vaccinations are up to date.


Outbreaks are usually a result of too low vaccination rates due to misinformation and hesitancy.
We need childhood vaccination rates of 95% for herd immunity but currently only 92.21% of twoyear-old children in Australia are vaccinated against measles – with some regions at much lower rates. We need to keep reenforcing that vaccines do make a difference and protect us from infectious diseases that can be debilitating or cause death. Most people globally, especially those in middle-to high-income countries, have never witnessed the devastating effects of diseases like polio or measles, which once caused widespread illness and death.
Prior to the introduction of the measles vaccine in 1963, hundreds of thousands of cases occurred each year. However in the decade following the vaccine’s rollout infection rates dropped by over 88%.
Overall, childhood vaccination programs over the past 50 years are estimated to have saved approximately 154 million lives.
Vaccine misinformation, apathy, hesitancy and a lack of understanding of side effects are some of the reasons for poor vaccine uptake.
While some people believe that abstaining from vaccination keeps
Community immunity is not a personal choice, it is a collective responsibility.
them healthier or more resistant to diseases, the reality is that their immunity has, until now, been borrowed from their vaccinated neighbours.
This collective shield, known as herd immunity, is not automatic or enduring, it has been built over decades through high vaccination rates.
Unfortunately, this protection is now eroding due to rising vaccine scepticism and many who have unwittingly benefited from herd immunity in the past are now at greater risk.
Social media has also been weaponised to spread
misinformation, with a recent study suggesting that its algorithms fuel scepticism and vaccine hesitancy by creating echo chambers that reinforce users existing beliefs and perpetuate inaccurate public health messaging.
There is also limited fact-checking of misinformation since Facebook disabled the fact checking tab.
So, what can be done by the government, the Department of Health and GPs who are the first port of call for the public?
We need a more coordinated approach to address the growing scepticism. Standard behavioural approaches such as mandatory vaccines, incentives, and public health campaigns should continue to be implemented alongside more contemporary approaches like fact-checking on social media, improving digital literacy, and using social media to actively counter misinformation and reinforce the global success of vaccines.
These efforts must be grounded in trust and transparency as history has shown these elements are
essential for the success of public health initiatives.
Other measures should include launching public education campaigns, ensuring vaccine access, and working with local officials to restore trust in immunisation programs.
The ability of a minority to remain unvaccinated always depends on the decisions of a vast community to protect them. Today, in our global world of conflict, migration and mobility we confront more outbreaks, one message is uncontested: community immunity is not a personal choice, it is a collective responsibility.
For the sake of our public health, our children, our elderly and those most vulnerable it is critical to note that vaccines and immunisation are one of the great public health success stories of the past century.

Compassion fatigue is common in caring professions – from GPs to unpaid carers. Supporting and understanding each other through difficult times is vital, writes Adam Birch, Carers WA Manager Counselling Team.
One of the greatest challenges we face working in a caring profession is what we do with the build-up of emotional fatigue engendered by exposure to other peoples’ emotional pain and suffering. How does one handle the compassion fatigue as we see client after client? Some say that’s what we are remunerated for, others encourage the need for regular breaks and attending to a healthy lifestyle.
Some professions, like mine, can have clinical standards for supervision to ensure that, at minimum, someone else is checking in.
While compassion fatigue is not a new concept, legislation around psychosocial hazards at work is now applicable. It indicates responsibilities in the workplace around psychological stressors and management of exposure to hazards that can have an impact on our health acutely and chronically.
As a counsellor and manager, I’m encouraged by the focus on stressors impacting health outcomes. What we see here is a shift and acknowledgment away from behaviours that glorify overwork and acknowledge the often unseen and unheard impact of what we do.
Regardless of remuneration or field of work, caring for people takes a toll.
Keeping in mind this toll, when is your next break? Is it after your next run of patients? Your lunch break? Maybe you skip that because there is another patient to see.
Finally, the end of the day, you hope you were able to help. You wrote that mental health treatment


plan, a patient thanked you, another walked out forlornly after difficult news. You finally get to breathe at day’s end.
Some who provide care don’t always get that. There are some in the community who take on challenges of this profession, without the protections of legislation and remuneration. It’s the plight of the unpaid carer. I would guarantee that you have met
an unpaid carer. Maybe you are one, additional to your professional role.
Statistically that’s likely. After your shift at work, there is someone waiting for you when you are ‘offthe-clock’, yet not really. A child with disability, or a loved one with a chronic physical or mental illness, or an elderly parent?
With over 3.04 million carers across Australia (roughly 12% of the population nationally), over 320,000 in WA, and estimations at
What about you? Do you take five when a patient receives unwelcome news, and you feel the heartache with them? What if you’re fully booked and people are still waiting?
When demands, appointments and waitlists expand, it can feel like there is no space to stop and think about our own wellbeing. That’s what it’s like for unpaid carers.
There are two main reasons I wanted to write this. First, it’s for every unpaid carer out there who has spoken about a challenging experience with a GP or other health professional.
Second, for every GP and other health professional who has found themselves in front of a challenging unpaid carer.
an hourly rate of $36.12 per hour equating to roughly $77.9 billion nationally to replace that unpaid care, it is not insignificant.
What’s an unpaid carer to do? For the love of their loved one, they must care day in, day out, due to lack of services, finances or various other reasons, putting their own health at risk.
Perhaps you’ve seen them, informing them they have carer burnout, and advised them to seek supports or to focus on themselves. How many take the advice? Or do



they come back with high blood pressure, disrupted sleep, erratic eating, anxiety and depression?
What about you? Do you take five when a patient receives unwelcome news, and you feel the heartache with them? What if you’re fully booked and people are still waiting?
After nearly eight years watching the carer community, we ourselves can be notorious for wanting to do more and not taking the time to look after ourselves.
One thing that we could do for you, as a potentially fatigued health professional, or for unpaid carers, is to be mindful of relentless expectations that we should somehow be perfect or always have the answer.
Perhaps rather than a statement of expectation, we could offer a reflection and acknowledgement of how hard it is, and how valuable what we are doing is.



While burnout rates in our State’s hospital system have improved in the last couple of years, it remains a problem. A similar scenario is seen in general practice.
We are all familiar with safety demonstrations on planes – if oxygen is required, we’re advised to fit our own masks before helping others. The reason is obvious: how can you help anyone else if you are not getting oxygen yourself?
This principle applies in life in general but it is widely ignored, and doctors are no exception.
As recently reported by Medical Forum, one third of junior doctors in WA have experienced bullying and harassment, according to AMA (WA)’s Hospital Health Check 2025.
A similar number said they were concerned that reporting bullying could adversely impact them.
While burnout rates in our State’s hospital system have improved in the last couple of years, it remains a problem.
In fact, burnout remains a significant issue across the board in medicine. To quote AMA (WA) President Dr Michael Page: “Our doctors are burning out from the relentless workloads pushed onto them by perpetually over-full hospital wards and emergency departments.”
Substitute full waiting rooms and a lack of doctors and you have a similar scenario in private practice. Burnout rates may be lower, but we do not know.
Politicians make promises of ‘free’ healthcare and somehow doctors are supposed to deliver on that promise.
The workload and stress on doctors is, by nature of our work, considerable. We do not work a typical 9-5 job with scheduled lunch breaks and the option to work from home.
While we cannot change the system, we can change ourselves. What can we do to make sure our own oxygen masks are on?
Practice saying no. Get some regular exercise, prioritise sleep, diarise in some down/relaxation time.
As the old adage goes: you can’t pour from an empty cup.

By Dr Mathew Samuel, Psychiatrist, Nedlands
Depression, specifically major depressive disorder (MDD), is a widespread mental health condition that affects hundreds of millions globally.
In Australia, over 1.3 million individuals – 5.9% of the population – are affected.
MDD is characterised by a persistent low mood and loss of interest or pleasure in most activities, accompanied by a range of somatic and cognitive symptoms.
These can include sleep disturbances (insomnia or hypersomnia), changes in appetite or weight, fatigue, poor concentration, psychomotor changes, feelings of worthlessness or excessive guilt, and recurrent thoughts of death or suicide. The impact of these symptoms often extends to daily functioning, relationships, and overall quality of life.
Treatment for MDD can be challenging with many not responding to initial therapies. Remission rates decrease with each successive treatment attempt (31% after a second treatment to 13% after a fourth).
Delays in finding effective treatment can prolong suffering and increase the risk of suicide –people with MDD have a suicide risk up to 20 times higher than the general population.
Early identification of inadequate treatment response and timely adjustments in therapy are crucial to improving outcomes.
Around one third of those with MDD develop treatment-resistant depression (TRD), defined as depression that does not improve after at least two adequate trials of antidepressants.
It is associated with a longer duration of depressive episodes, greater functional impairment, higher rates of comorbid conditions, and a substantially increased risk of suicide attempts.


This underscores the urgent need for more effective therapeutic strategies for TRD.
Esketamine for treatmentresistant depression
Esketamine nasal spray has emerged as a novel third-line treatment for adults with TRD. Esketamine acts as a glutamate receptor modulator, with evidence suggesting it may help restore synaptic connections in the brain affected by depression.
Multiple randomised clinical trials have demonstrated its efficacy
and tolerability when used in conjunction with a newly initiated oral antidepressant. Esketamine has been approved by regulatory authorities in Australia and New Zealand for use in individuals with TRD, offering hope for those who have not benefited from traditional antidepressant therapies. It was made available on the PBS from 1 May.
Esketamine, the S-enantiomer of racemic ketamine, is an antidepressant with a novel mechanism of action. It is a non-selective, non-competitive,
MDD is a prevalent and disabling condition with a substantial proportion of patients experiencing inadequate response to standard treatments
TRD represents a particularly severe and burdensome form of depression
Innovative treatments such as esketamine nasal spray can improve patient outcomes and quality of life.
antagonist of the N-methyl-Daspartate (NMDA) receptor, an ionotropic glutamate receptor.
Putative aetiological contributors of depression, including stress and other conditions, are known to cause structural and functional impairment of synapses in brain regions involved with the regulation of mood and emotional behaviour.
Evidence within the literature suggests that through NMDA receptor antagonism, esketamine produces a transient increase
in glutamate release leading to increases in α-amino-3-hydroxy5-methyl-4-isoxazolepropionic acid receptor (AMPAR) stimulation and subsequently to increases in neurotrophic signalling that restore synaptic function in these brain regions.
Esketamine comes as a single-use device delivering a total of 28mg in two actuations – one actuation per nostril. To prevent loss of medication, the device should not be primed before use.
Administration is by the patient under the supervision of a psychiatrist, using one device for a 28mg dose, two devices for a 56mg dose, or three devices for a 84mg dose, with a five-minute rest between use of each device.
This is followed by post administration observation under the supervision of a psychiatrist.
During and after administration at each treatment session, patients should be monitored until the patient is stable based on clinical judgment.
Before administration, patients’ blood pressure should be assessed and patients instructed not to engage in potentially hazardous activities, such as driving a motor vehicle or operating machinery until the next day after a restful sleep.
After administration blood pressure should be reassessed at approximately 40 minutes and subsequently as clinically warranted. Due to the possibility of sedation, dissociation and elevated blood pressure, patients must be monitored by a healthcare professional until the patient is considered clinically stable and ready to leave the healthcare setting.
Since some patients may experience nausea and vomiting, advise not to eat for at least two hours before administration and not to drink liquids at least 30 minutes prior to administration.
Author competing interests – the author was a member of the Janssen-Cilag Advisory panel.
Refer to Jeff.
Alcohol and drug clinical assessment and pathway navigation. Brighter patient outcomes with Lumera.
Complement your care with clinical insight, personalised treatment plans and immediate availability.
Led by Clinical Nurse Specialist Jeff Butterfield, our approach to AOD care is confidential and free of judgement.
Why refer to Lumera?
• Excellence in clinical assessment.
• 20+ years in ethical AOD care.
• Collaborative approach.
• Personalised treatment plans
• Seamless referral process.
• Flexible consult options.
• No waitlists.

Scan to learn more

We work with you to enable the best possible recovery pathway for your patients.
By Dr Sheldon Moniz, Orthopaedic Surgeon, Murdoch & Albany
The shoulder is one of the most complex and versatile joints in the human body, allowing for a remarkable range of motion. However, this complexity makes it particularly vulnerable to a variety of injuries and degenerative conditions.
The shoulder is made up of three main joints or spaces - the acromioclavicular joint (ACJ), the subacromial space and glenohumeral joint.
In clinical discussions, the shoulder joint typically refers to the glenohumeral joint. There are multiple sources that can contribute to pain within the shoulder.
Identifying specific areas is crucial for targeted injections. For example, if suspecting subacromial bursitis – a targeted injection into the glenohumeral joint may be of limited benefit to the patient.
Presenting complaint is key
Diagnostic approach for shoulder disorders is structured around four key clinical domains. Systematically assessing pain, instability, weakness, and stiffness allows clinicians to effectively narrow a differential diagnosis and identify the most relevant underlying pathology within a patient age group.
Shoulder problems often correlate with a patient's age. One of the most common age-related conditions is degenerative rotator cuff tears.
Studies show that 70% of individuals aged 70 and above will have some degree of rotator cuff degeneration, though only 5% of these patients will progress to cuff-related arthropathy. Recognising the natural history of these conditions can help guide treatment decisions and patient expectations.
Understanding of diagnostic clues can help differentiate between various shoulder pathologies. Some key conditions to recognise include:
ACJ Disruption: Often resulting from trauma, this condition presents with localised pain and deformity at the acromioclavicular joint.


Biceps Rupture: Patients may report a "pop" followed by pain and a noticeable bulge in the upper arm –Popeye sign.
Shoulder Dislocation: Anterior dislocations are the most common and require immediate reduction and referral.
Impingement Syndrome: Caused by compression of the rotator cuff tendons and bursa, often leading to pain with overhead movements.
Instability: Can be due to repetitive microtrauma or acute dislocation, leading to shoulder subluxation or persistent laxity.
Glenohumeral Osteoarthritis (OA): Characterised by progressive pain, stiffness, and loss of external rotation.


Capsulitis): Marked by progressive stiffness and pain, often idiopathic or associated with diabetes.
Blood tests are useful for detecting infections and systemic conditions such as rheumatoid arthritis or diabetes.
Plain film X-Ray remains a crucial first-line investigation that is often underutilised. Ultrasound can diagnose rotator cuff tears, bursitis, and other soft tissue injuries.
MRI is considered the gold standard for assessing soft tissue structures, including the rotator cuff, labrum, and biceps tendon.
However, findings should always be correlated with clinical symptoms, and it is not a first-line investigation.
Certain shoulder conditions require immediate referral to an orthopaedic specialist or emergency department. These include fractures, infections, tumours, acute rotator cuff tears and unreduced dislocations.
Prompt recognition and referral of these conditions are crucial to preventing complications and ensuring the best possible patient outcomes.
Conservative management is often effective and includes rest, physical therapy, and anti-inflammatory medications.
A structured approach that incorporates patient age and symptoms aids in narrowing the differential diagnosis and guiding appropriate management strategies
Know your target – injections can be a useful tool for both diagnostic and therapeutic purposes and are often more judicious than MRI to guide management
Early diagnosis, appropriate investigations, and timely referrals can significantly improve patient outcomes.
However, some conditions may require surgical intervention, including:
• Rotator cuff repair for significant tears, especially in younger or active patients
• Shoulder stabilisation surgery for recurrent dislocations or instability
• ACJ excision for painful ACJ arthritis
• Subacromial decompression for
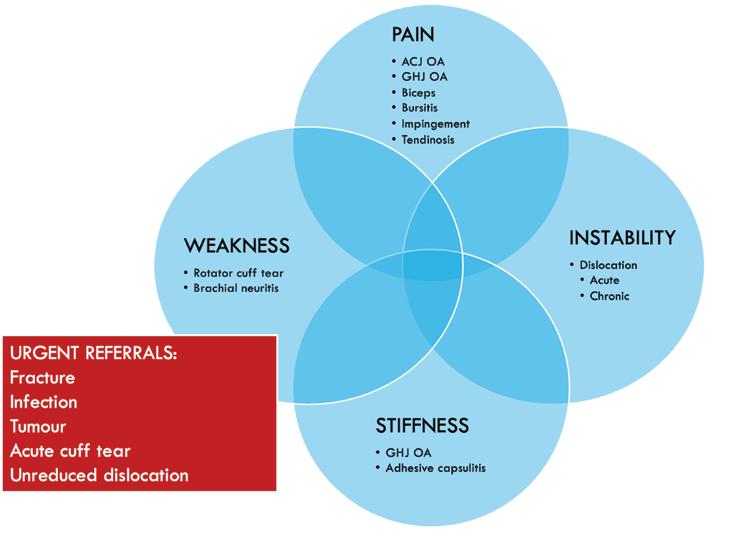
impingement syndrome to relieve pain and improve function
• Biceps tenotomy or tenodesis for symptomatic biceps tendon pathology
• Shoulder arthroplasty – a total or reverse shoulder replacement is considered for severe osteoarthritis or irreparable rotator cuff tears.
General practitioners play a crucial role in the early diagnosis and
management of shoulder conditions. Referral to an orthopaedic specialist is warranted in cases of persistent pain despite conservative treatment, functional limitations affecting daily activities, suspected structural damage requiring surgical intervention and urgent conditions (fractures, dislocations, infections, or tumours).
Author competing interests – Nil




By Dr Kim White, Senior Occupational Therapy Practitioner, Osborne Park
Emotional dysregulation is strongly related to adult attentiondeficit/hyperactivity disorder (AuDHD) along with paediatric ADHD, even when controlling for comorbid disorders.
While emotional dysregulation is significantly linked to other ADHDassociated neuropsychological deficits, it has been shown that when these deficits are controlled for, emotional dysregulation has an independent deleterious effect upon ADHD
Emotional dysregulation and social interaction skills can act as barriers or enablers to occupational engagement and participation.
People interact during activities of daily living, whether it be productivity, self-care or leisure occupations, and supporting occupational engagement, participation and performance is the overarching purpose of occupational therapy.
Emotional regulation is a series of processes through which individuals modulate their emotions, utilising different strategies toward goal-directed behaviour, for example cognitive reappraisal, emotional suppression or avoidance.
People with emotional dysregulation and AuDHD are likely to experience lower levels of functional capacity and social-emotional occupational performance than those with AuDHD and no emotional regulation difficulty.
Occupational performance in the social-emotional domain requires attention and problem-solving skills, appropriate functional cognition, and various socialemotional learning skills.
Often there are limited opportunities available beyond elementary and secondary schooling to access programs that


support social-emotional learning and development of associated skills and competencies. Patients with difficulties in this regard can be supported as adults through occupational therapy.
Comprehensively assessing emotional regulation when working with adults experiencing ADHD is important to understand specific emotional regulation difficulties and create individualised occupational therapy intervention plans.
Contemporary research in the fields of interoception and mindfulness informs the progression and development of social-emotional support and intervention in adult occupational therapy.
Multi-dimensional consideration of emotional regulation capacity will support appropriate intervention planning, and the relatively recent CERI (Comprehensive Emotion Regulation Inventory) is a good clinical choice designed for AuDHD, enabling insight into emotion regulation strategies, difficulties implementing emotion regulation strategies, effect of poor emotion regulation upon activities of daily living (ADLs), and emotional reactivity.
Interacting socially with other humans requires, among many things, modulation of our own cognitive processes and emotions
Occupational therapy can support development of emotional regulation and social interaction skills, which are essential for successful occupational engagement and participation
Emotional dysregulation has an independent and significant negative impact on adults with ADHD, affecting their functional capacity and social-emotional occupational performance
Mindfulness and interoceptive intervention can support emotional regulation in AuDHD, as this can help to build selfawareness, self-other distinction, and support social-emotional health.
whilst attempting to form an impression of others’ affect and emotional state.
The ability to successfully complete and differentiate this determination is essential for achieving occupational performance across the variety of social complexities that humans encounter in their
environments and day-to-day lives.
The ability to distinguish between self and other, both in a physical and narrative sense is necessitated by this determination and is largely dependent upon our interoceptive and exteroceptive sensory capacity, processing and integration abilities.
Interoception is critical for forming our realities and understanding of the world, holding subjectivity within our physical selves, that is embodiment. Interoception is emerging as a crucial determinant of mental and physiological health, and we know that interoception is closely linked to emotional awareness and emotional regulation.
Mindfulness, or self-awareness, is necessary for social-emotional health and the ability to distinguish between self-other boundaries.
The fourth edition of the Occupational Therapy Practice Framework specifically references social interaction skills as a subset of performance skills, which directly influence occupational
engagement, performance and participation.
Utilising person-centred intervention plans that incorporate mindfulness, interoceptive awareness and attention can help occupational therapy practitioners to support social interaction, emotional regulation and development of social-emotional health and capacity in this group of patients.
In summary, occupational therapy can support social-emotional health, occupational performance and overall functional capacity through assessing and intervening appropriately for emotional dysregulation in AuDHD.
Author competing interests – nil
‘In the last decade, there’s been a big leap in technology and skills that has seen the introduction of game changing endovascular surgery. Our work is constantly evolving making a real difference in people’s lives.’

Dr Altaf and his team provide a comprehensive diagnostic and therapeutic service of arterial and venous diseases including:
Abdominal aortic aneursyms
Carotid artery disease
Peripheral artery disease
Leg ulcers & diabetic foot disease
Varicose vein diagnosis & treatment
Renal access
Dr Altaf consults at Hollywood Medical Centre, SJOG Midland Private Hospital, SJOG Carine Specialist Centre and public appointments at RPH and SJOG Midland Public Hospital. Operates out of SJOG Midland Public and Private, Hollywood Hospital and SJOG Subiaco.
Appointments are coordinated through practice manager Michelle Burrell and her team.

Hollywood Medical Centre Level 2 Suite 45/85 Monash Ave, Nedlands WA 6009
Phone: 6244 6215 | Fax: 6315 6423 | Healthlink ID: drnaltaf draltaf.com.au
By Miss Rebecca Ong, Perron Institute & UWA, and Professor John Reynolds, University of Otago
A recent study expanded on the current understanding of noninvasive brain stimulation and its application in modulating various neural circuits and neurological processes across the brain.
The knowledge gained from this research could help optimise the application of non-invasive brain stimulation to promote neural plasticity in targeted regions of the brain that may be affected in neurological disorders.
Specifically, this preclinical study explored the effects of repetitive transcranial magnetic stimulation (rTMS), a form of non-invasive brain stimulation currently approved by the TGA in Australia as a treatment for people with treatment-resistant depression.
It involves the delivery of a rapidly changing magnetic field which induces an electrical current in the underlying tissue, thereby stimulating cells within the targeted region.
Currently, a number of different rTMS protocols exist, with each thought to induce different effects on neural activity and neural plasticity in the brain. Given its ability to noninvasively induce changes in the brain, several studies have looked into the potential of using rTMS in the treatment of neurological disorders where neural plasticity is impaired, for example in stroke and dementia.
However, the molecular and cellular changes that occur following different rTMS protocols and how these effects may differ between brain regions is still unknown. By characterising within specific brain regions the different cellular processes that rTMS is able to modulate, it provides a greater evidence base to guide the selection and use of different rTMS protocols for the treatment of neurological conditions.
The method
In this study, the research team used two common protocols – intermittent theta burst

New research provides an understanding of how different brain regions respond to rTMS and which protocols may be best suited to target different neurological conditions
Multiple neural plasticity mechanisms induced by rTMS were found to be specific to each layer of the cortex and subcortical structures
By mapping what rTMS is changing in the brain and in which neural circuits, we have a clearer understanding of how to apply and interpret effects of rTMS.
stimulation and continuous theta burst stimulation. They revealed that rTMS targeted towards the primary motor cortex not only induced multiple neural plasticity mechanisms in the targeted cortical region, but also in several subcortical regions outside the direct stimulation site.
These rTMS-induced changes varied depending on the rTMS protocol that was applied to the brain and differed between each brain region, even down to individual cortical layers.


It is well understood that rTMS is capable of altering processes relating to the strength of communication between neurons, better known as synaptic plasticity. However, increasing evidence has shown that rTMS can also affect other plasticity processes beyond the synapse.
For example, it may alter the neuron’s ability to generate action potentials, known as intrinsic plasticity, or may affect cells that produce and maintain myelin, the insulating fatty sheath around the axons of neurons, in the brain.
This research was the first to show that rTMS induces multiple neural plasticity mechanisms simultaneously across various regions of the brain but again varied depending on the stimulation protocol that was applied.
The results of this study are exciting. Mapping out how various non-invasive brain stimulation protocols affect different regions of the brain provides a foundation to optimise TMS with a more targeted approach in both clinical and nonclinical applications.
It uncovers some of the specific effects that rTMS protocols can have on various neural circuity, and considered together with existing rTMS literature, provides new insights into the molecular mechanisms underlying the therapeutic effects of rTMS.
Author competing interests – Miss Ong was directly involved in the study and Prof Reynolds provided critical input to the research.
By Dr Vash Singh, Psychiatrist, Subiaco
During the Federal election campaign promises to expand mental health services were front and centre, yet many proposed initiatives are not firmly anchored in evidence, nor have they demonstrated real value in improving long-term patient outcomes.
In a system already strained, it is critical that new investments prioritise models of care that are innovative, integrated, and genuinely value based. Without such focus, we risk perpetuating the very cycle we seek to escape.
There is currently a gap in mental health care. Demand for mental health services has surged in recent years, exacerbated by the pandemic, economic pressures, and social isolation. Yet, traditional inpatient admissions often function as short-term crisis interventions rather than part of a broader therapeutic continuum.
Inpatient teams frequently disengage after discharge, leaving GPs to manage patients who are still at high risk and require significant support.
This abrupt handover – often described by GPs as the hospital having “washed their hands” of the patient – places enormous pressure on primary care without the necessary backup.
Moreover, many patients require more intensive intervention than standard outpatient models can offer, but not the full containment of a hospital bed.
This is where current services fall short – there is a large and growing gap between acute inpatient care and outpatient community management.
Innovative, integrated day hospital models provide a critical bridge across this divide. These programs deliver daily, multidisciplinary care for several weeks, allowing patients to stabilise without severing ties to their families, jobs, and communities.

Once acute symptoms improve, patients can transition to lowerintensity outpatient therapy within the same service, offering a seamless step-down pathway.
In effect, a single service can offer multiple tiers of care – from intensive to maintenance – tailored to patient needs at different stages of recovery.
Evidence supports the effectiveness of such models. A randomised controlled trial published in The Lancet Psychiatry (2020) found that day hospital care for adolescents with eating disorders was as effective as inpatient treatment in reducing symptom severity, while enabling patients to maintain crucial social and familial connections.
A review in Psychiatric Services (2019) further highlighted that step-down day hospital programs significantly reduced hospital readmissions and improved continuity of care.
The concept of value-based healthcare has become central to discussions about the future of health service delivery.
Applying this framework to mental health care demands that we:
• Prioritise services that deliver measurable, patient-centred

There is a gap in mental health care between hospitals and primary care
Innovative, integrated day hospital models can bridge this divide
Future mental health reform must be value-based and evidenceinformed.
outcomes, not just activity or throughput
• Invest in models that reduce reliance on acute crisis admissions by providing early, intensive intervention
• Integrate tiers of care under one service umbrella, allowing for flexibility, continuity, and personalised step-down care.
Day hospital programs embody this value-based approach. They are less costly than prolonged inpatient stays, reduce burden on emergency services, and offer outcomes that match or exceed traditional models.
Yet, despite their strong evidence base, these programs remain underfunded and under-recognised in policy discussions.
With any new funding pledges, policymakers must look beyond short-term political wins and invest in models of care that are truly innovative and sustainable.
Integrated intensive day programs should be scaled up and incorporated as a core part of Australia's mental health service landscape.
Failing to do so risks continuing a reactive, fragmented system that leaves vulnerable patients – and their GPs – without the support they need.
If we are serious about changing mental health outcomes in Australia, it is time to build bridges, not just hospital beds.
Author competing interests – nil

By Caitlin Chase and Mike Pappas, Exercise Physiologists, Osborne Park
Within WA if a motor vehicle accident was another driver’s fault, reasonable treatment for injuries is covered by the Insurance Commission of Western Australia.
Whiplash-associated disorders (WAD) are a result of rapid acceleration-deceleration forces, affecting up to 83% of all patients involved in motor vehicle accidents. WAD’s can lead to a spectrum of severity of psychological and physiological injuries.
Recent studies have advocated for a multidisciplinary active management approach to improve long-term patient outcomes.
Recent statistics outlined that 50% of individuals who have sustained WAD’s fully recover, 30% have persisting mild to moderate pain and disability, and the other 20% continue to have moderate to severe pain and disability.
Whiplash-associated disorders are classified into five grades based on the severity of symptoms and clinical findings:
• Grade 1 involves neck pain, stiffness, or tenderness without any positive findings on physical examination
• Grade 2 is characterised by musculoskeletal signs such as reduced range of motion and point tenderness
• Grade 3, patients also present with neurological symptoms, which may include sensory deficits, decreased deep tendon reflexes, and muscle weakness
• Grade 4 involves evidence of a fracture
• Grade 5 represents more severe or multiple fractures.

Importantly, with appropriate management and early intervention, patients with grades one to three WAD can expect near full recovery within 18-24 weeks.
There can be varying physiological changes in the cervical region in individuals who have sustained a WAD.
Under the surface, muscle behaviour and motor control impairment can arise between the fine muscle groups and the gross muscle groups. The musculature can undergo morphological changes such as loss of endurance at different contraction intensities, muscle atrophy, and loss of feed forward response.
This can consequently lead to impaired function, posture and movement. Additionally,

Whiplash associated disorder has a spectrum of severity of psychological and physiological injuries
Early active management with exercise improves outcomes
Multidisciplinary collaboration is encouraged.
psychological injuries can be commonly associated with motor vehicle accidents, and this can impact physiological recovery.
Individuals involved in an accident can often experience symptoms of anxiety, depression and stress.
Active exercise rehabilitation prioritises safe early mobilisation and patient involvement in management of their injuries. This strategy aligns with the biopsychosocial model of care, which recognises the interplay of physical, psychological, and social factors in recovery.
In WAD of grades between one to three, proactive referral to an
accredited exercise physiologist is a crucial part of the multidisciplinary treatment plan. Utilising experts in active rehabilitation to restore the physiological changes whilst also addressing the biopsychosocial flags.
An effective exercise rehabilitation protocol typically includes:
• Gentle range of movement (ROM) exercises that are completed early following a WAD injury, allowing for a reduction in muscle guarding and increased mobility
• Isometric exercises of the neck and surrounding structures allow for gentle dynamic strengthening and stability in the initial phases of the rehabilitation programme, targeting the muscle group imbalances
• Following this, dynamic movements involving resistance should be introduced to further build upon general functional movement.
Postural correction, ergonomic advice, and education on certain postures and movements that may contribute to symptoms and delay recovery. Additionally, providing

education on the benefits of staying active and continuing to self-manage their rehabilitation ongoing.
Aerobic conditioning plays a vital role in conjunction with increasing strength and ROM of the neck as it can assist in enhancing overall function, improve psychological wellbeing, and aid in a return to work or recreational activities.
Recent best practice guidelines advocate for early, active intervention. Progression of the rehabilitation program should be based on symptom severity, functional capacity, and psychosocial factors, tailoring to individual responses.
Multidisciplinary collaboration is encouraged, referring to required specialists and allied health professionals, to address all impairments and maximise the recovery for the patient.
Author competing interests- nil








By Malina Kelly and Alison Wroth, Physiotherapists, Guildford
Pain is an integral part of human experience and serves the purpose of a vital protective function.
Persistent pain may be thought of as overprotection – pain can be experienced in the body, with no real threat of damage or disease.
Health professionals sit with patients daily, listening to their experience of persistent pain. Many patients have faced difficulty accessing sustainable and effective management for persistent pain, while some have unhelpful beliefs about the generators of their pain and feel helpless in their own management.
Modern pain neuroscience offers a current evidence-based model of pain, utilising a biopsychosocial approach. Current scientific understanding views pain as an
emergent and dynamic process influenced by many factors, including individual beliefs, emotions, life stressors, trauma, nutrition, sleep, inflammation, movement and social connection. Thus, pain is an output from the central nervous system.
Pain is always real; it is felt in the body tissues. Pain occurs due to a complex interplay of multiple systems, including musculoskeletal, neuroimmune and endocrine systems.
When explained to patients effectively via this updated model, individuals can understand their pain through a more accurate, holistic lens.
Being complex and multifactorial means there are many ways that
pain can be changed. Changing any contributing system, can change the experience of pain.
Persistent pelvic pain affects one in four women and one in 12 men in Australia.
Common treatments, including medication, surgery and hormonal intervention, are often unsuccessful.
While modern pain science teaches that persistent pelvic pain results from multiple interacting systems, including psychological and social factors, biomedical treatments continue as the mainstay.
Biomedical-focused treatments reinforce the patient’s belief that there must be something wrong, and that they require

Pain is an emergent and dynamic process, with many contributing factors
The pelvic floor muscles often tighten in response to pain and high energy emotions
Modern pain science and a biopsychosocial approach offers hope for patients with persisting pain conditions.
pharmacological and/or surgical treatments to fix whatever is wrong.
The pelvic floor muscles (PFM) are found in men and women, at the base of the pelvis. PFM have an important role to play in bladder and bowel continence. PFM contract to allow control of continence and relax to allow effective bladder and bowel emptying.
PFM provide support to the organs of the pelvis; they are important for sexual function in men and women.
What is less commonly known about PFM is that these small muscles are responsive to emotions. PFM are often the first muscles in the body to tighten in response to high energy emotions such as anxiety, fear, excitement and anger. PFM
often tighten when humans are in pain or feeling unsafe.
In persisting pelvic pain conditions in both men and women, PFM are often tense and overactive. PFM tension contributes to symptoms such as sexual pain, cyclical pelvic pain in women, bladder pain, urinary urgency, urinary incontinence, pain with defaecation, anal fissures, bowel urgency, constipation and genital pain.
Often overlooked in a biomedical approach to pain, the role of the PFM may not be identified as a contributing factor to a patient’s symptoms.
Pelvic health physiotherapists provide individual PFM assessment and training using a range of biofeedback techniques. In patients with persistent pelvic pain, PFM training typically involves a ‘downtraining’ approach.
This begins with providing feedback for individuals to feel their muscles, move them, and finally to learn to relax them – unwinding tension in the pelvis over the longer term.
This becomes a vital tool in changing their pain experience. As patients learn to feel their tension, they are empowered with the ability
to change tension, and ultimately their pain experience.
A biopsychosocial approach forms the foundation of pelvic health physiotherapy. Patients are often surprised by the comprehensive nature of assessment and the time taken to investigate the multiple potential contributing systems to their pain.
Postgraduate training incorporates updated pain science as such pelvic health physiotherapists are well placed to help patients better understand and explore their pain.
As part of holistic management, pelvic health physiotherapists address PFM dysfunction, physical activity, hydration, nutrition, sleep, emotional health and social factors – referring on to more suitable practitioners as required.
Modern pain science teaches that pain is a changeable experience. Many factors contribute to pain and there are many ways to connect to pain and promote recovery. Current pain science is very hopeful, it is now up to practitioners to integrate this hope into our practice.
Author competing interests – nil
Untreated atrial fibrillation has been linked to one in 10 deaths, with some 45% of high-risk patients missing out on potentially life-saving anticoagulant therapy, new research suggest.
The research, published in the Australian Journal of General Practice, coincides with the launch of a free, comprehensive program designed to improve atrial fibrillation treatment and stroke prevention through better anticoagulant use.
It forms part of the work of the Quality Use of Medicines Alliance.
Atrial fibrillation is an irregular, fast heartbeat that increases stroke risk. It accounts for more than 200,000 hospitalisations each year, yet nearly half of high-risk patients are not prescribed anticoagulants and
43% stop their therapy within twoand-a-half years.
Prof Nigel Stocks, Head of Discipline of General Practice at the University of Adelaide and RACGP spokesperson contributed to the program.
“It is in the realm of GPs to identify and manage patients with atrial fibrillation which can be missed, particularly if it is intermittent or doesn’t cause symptoms,” he said.
“GPs should take any opportunity to screen for AF in at risk populations. Once diagnosed, patients may be reluctant to take anticoagulants, so it is important that they fully understand their individual stroke and bleeding risk so they can make informed decisions about future care.”
The program aims to increase
awareness of atrial fibrillation and stroke and encourage patients to take preventative action.
It provides GPs with the tools to assess stroke and bleeding risks, support shared decision-making, and manage complex situations. Resources include:
• Educational visits and peer group learning
• Interactive webinars and online clinical cases
• Practice audits and point-of-care tools.
It has been welcomed by the Stroke Foundation, Heart Foundation, Heart Support Australia and Hearts4heart.
By Dr Marek Garbowski, Vascular Surgeon, Subiaco
Abdominal vascular compression syndromes are a group of rare conditions in which blood vessels in the abdomen and/or pelvis become compressed by surrounding structures, leading to a range of symptoms.
These syndromes can cause significant discomfort, digestive issues, and even organ dysfunction if left untreated.
The four main types of abdominal vascular compression syndromes are Median Arcuate Ligament Syndrome (MALS), Superior Mesenteric Artery Syndrome (SMAS), Nutcracker Syndrome (NCS), and May-Thurner Syndrome (MTS).
Each has distinct causes, symptoms, and treatment approaches.
Median Arcuate Ligament
MALS occurs when the median arcuate ligament, a fibrous band of the diaphragm, compresses the coeliac artery and the surrounding nerve plexus.
This compression may lead to decreased blood flow to the abdominal organs and irritation of the coeliac plexus, causing significant pain and other gastrointestinal symptoms.
Symptoms include chronic abdominal pain, particularly after eating, weight loss due to food avoidance, nausea and vomiting and early satiety.
It is often diagnosed through imaging techniques like duplex ultrasound, CT angiography (CTA), or magnetic resonance angiography (MRA), which reveal extrinsic compression of the coeliac artery.
A diagnostic coeliac plexus block can also help confirm MALS if it provides temporary pain relief.
The primary treatment for MALS is surgical decompression of the coeliac artery. This typically involves laparoscopic median arcuate ligament release to relieve the compression.

In some cases, additional procedures like coeliac artery angioplasty and stenting may be necessary to restore normal blood flow.
SMAS is a rare disorder in which the superior mesenteric artery (SMA) compresses the third part of the duodenum, leading to partial or complete obstruction of this part of small intestine.
The condition is often associated with rapid weight loss, which reduces the fat cushion around the SMA, making compression more likely.
Symptoms include severe postprandial after eating abdominal pain, nausea and vomiting, sometimes bilious, early satiety,
significant weight loss, bloating and reflux.
SMAS is diagnosed using contrastenhanced CT scans, upper gastrointestinal (GI) series, or endoscopy, which reveal narrowing of the duodenum and delayed gastric emptying.
Treatment starts with conservative management, including nutritional support to regain weight and increase retroperitoneal fat, small, frequent meals and nasogastric feeding or total parenteral nutrition in severe cases.
If conservative measures fail, surgical options such as open or laparoscopic duodenojejunostomy or gastrojejunostomy may be necessary to bypass the compressed portion of the duodenum.
Abdominal vascular compression syndromes are rare but potentially serious conditions that can significantly impact patient’s quality of life. Consider them in unexplained abdominal/pelvic pain, gastrointestinal symptoms, haematuria, or leg oedema
Early diagnosis and appropriate management are crucial for preventing complications and improving patient outcomes
While conservative measures may help in some cases, surgical or endovascular interventions are often necessary to relieve vascular compression and restore normal function.
This occurs when the left renal vein is compressed between the superior mesenteric artery and the aorta, leading to impaired venous return from the left kidney. This condition can cause symptoms related to increased venous pressure in the kidney and pelvic venous network.

Symptoms include haematuria without UTI, flank or abdominal pain, especially on the left side, pelvic pain and pressure related discomfort, orthostatic proteinuria, vaginal/labial varicose veins, pelvic varicosities seen during laparoscopy and varicocoele.
Diagnosis is made through duplex ultrasound, CTA, or venography combined with intravascular ultrasound (IVUS), which demonstrate stenosis of the left renal vein and increased pressure. Mild cases are managed conservatively with analgesia and trial of micronised purified flavonoid fraction (MPFF) supplements.
Endovascular stenting of the left renal vein to restore normal blood flow remains a controversial option requiring more evaluation. Surgical options include renal vein bypass or renal or left ovarian vein transposition if symptoms persist.
May-Thurner Syndrome (MTS) occurs when the left common iliac vein is compressed by the overlying right common iliac artery against the sacrum, leading to reduced
blood flow and an increased risk of deep vein thrombosis.
Symptoms include swelling and pain in the left leg, varicose veins in the pelvic and left lower limb, chronic venous insufficiency and deep vein thrombosis in severe cases
MTS is diagnosed through venous duplex ultrasound, CT venography, or MR venography, which reveal compression of the left common iliac vein and possible DVT.
Treatment includes anticoagulation therapy for established DVT, endovascular treatment using stenting to keep the left common iliac vein open and thrombectomy or thrombolysis if clinically indicated (percutaneous mechanical suction thrombectomy provides improved results and lesser complications rates).
Graduated compression stockings manage lower limb symptoms and minimise the risk of postphlebitic syndrome in DVT patients.
Author competing interests – nil
Esketamine for depression
Innovative models of mental health care
Whiplash-associated disorders
Abdominal vascular compression syndromes
Shoulder joint injuries
Emotional dysregulation and adult ADHD
Physiotherapy for persistent pelvic pain
Managing compassion fatigue
Allied health for dementia care
Tackling vaccine hesitancy
TMS in treatment-resistant depression
Managing acute and chronic knee pain

The subject of a documentary film, Australian performance artist Stelarc is considered an icon for, among other works, his nude suspensions.
By Ara Jansen
As a young man, Richard Moore witnessed something which has stayed with him for decades. Now he’s made a documentary about the artist he saw.
Between 1976 and 1989 a performance artist named Stelarc staged two dozen suspension events where his nude body was pierced with hooks and hung from various locations.
His Prepared Tree Suspension, where Stelarc was hung from a tree in October 1982 in Canberra, was what Richard had seen.
“At some point,” says Richard, “he asked everyone to leave. And when they brought him down and removed the hooks, they wrapped him in a shroud and took him away.
“He chose this beautiful gumtree, and it conjured up images of a hanging, a public crucifixion and ritual sacrifice.”
The film maker said it reminded him of the 1970 Western movie A Man Called Horse when they hung actor Richard Harris by the nipples.

“Sometimes you see something or someone in your life that just shakes you to your core. It was that image of someone suspended from a tree and the whole ritual of it.”
Richard, a festival artistic director, a curator, executive producer and documentary film maker, will be screening his Stelarc Suspending Disbelief doco at July’s Revelation International Perth Film Festival.
“When we were doing research for the film we came across other footage around the world of suspensions in several different cultures, like in Sri Lanka. But Stelarc has definitely become a bit of a grandfather of great suspensions.”

Stelarc is a Cyprus-born Australian from Melbourne. The 78-year-old performance artist has visually probed and amplified his body as art for decades. Notable events include a moving suspension high above New York in 1984 and attaching a real ear to his arm in 2015, with the idea of people being able to hear what it hears.
In a 2016 work at PICA in Northbridge, Stelarc spent six hours a day across five days encased in a mechanised body where he could only see with the eyes of someone in London, hear with the ears from someone in New York but anyone, anywhere could remotely access his right arm.
He also spent some time at Curtin as a visiting professor around a decade ago.
Over the years, Stelarc’s work has morphed from performance pieces like suspensions to exploring the intersection between a human, technology and robotics. His work often expressing his mantra “the body is obsolete”.
Stelarc Suspending Disbelief is Richard’s salute to this extraordinary Australian artist. Be warned though, there’s plenty of full-frontal nudity and some moments which might make you look away.
The documentary – which has been six years in the making – pulls together archive footage from across Stelarc’s career, interspersed with cuts from a new interview filmed in his car as Stelarc drives around Melbourne.
An artist of international standing, Stelarc continues to work around the world and the documentary runs right up to the opening of a recent exhibition.
“Filming him in his car was a way to get him relaxed. He’s cracking jokes and has an interesting laugh. It’s very endearing. There’s lots of loopy people in the world, but everything with Stelarc comes from science, is extremely well researched and they are not flights of fancy.
“His work has a serious intent. He explores what it is to be human and he uses his body as his medium.
“The good thing about him is that he keeps on exploring and keeps pushing boundaries. He’ll still be doing things into his 80s. There’s definitely a toughness to him, and you need that level of toughness, especially when you are trying to raise money to make this kind of art.
“Apart from telling a story on screen, we also wanted to challenge, tease and surprise people. Also, the change in attitudes in recent times towards aspects of body art such as piercings and tattoos might also draw an audience to this film.”
Stelarc Suspending Disbelief is part of the Revelation International Perth Film Festival from July 2 – 13. See www.revelationfilmfest.org for session info.

Do you want to see Stelarc Suspending Disbelief, or any of the other films at this year’s Revelation International Perth Film Festival?
We’ve got five double passes to give away to lucky Medical Forum readers.
From outrageous animation and genre-defining horror, this year’s program delves into diverse narratives, innovative storytelling and cinematic artistry.
Showcasing the works of both established and emerging filmmakers, the festival is one of the most daring and diverse film festivals down under.
The festival runs from July 2-13.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.
Disney’s Beauty and the Beast the Musical comes to Perth, promising a dazzling and colourful spectacular.

By Ara Jansen
The last time Shubshri Kandiah performed in Perth was about six years ago. Now she returns to her hometown as a Disney princess – complete with a set of gorgeous gowns to prove it.
The Brisbane-based singer, dancer and actor is playing the female lead in Beauty and the Beast the Musical, based on the 1991 animated film. The original production played for more than 13 years on Broadway, remaining to this day one of the top 10 longest running shows in Broadway history. It has toured 37 countries and the last time it played in Australia was 30 years ago, only in Sydney and Melbourne.
In the story of Beauty and the Beast a wicked enchantress turns an arrogant prince into a beast until he learns to love and be loved. Belle –played by Shubshri – a headstrong village girl helps draw the cold-hearted beast from his isolation.

Compared to the original Belle, the musical’s character is much stronger and more empowered, as shown by subtle but noticeable changes to the script from, ‘dance with me?’ to ‘dance with me’.
This Belle is a young woman who makes active choices and doesn’t rely on her looks, her charm or a sword to fulfill her aspirations. She is an avid reader who wears glasses, and what she wears shows her in a more modern light – no aprons for this Belle.
As a musical, the production prides itself on being a spectacular of Disney proportions which includes 300 costumes and 119 wigs, made
of a combination of synthetic hair, human hair and yak hair in each one.
Belle’s yellow ballgown design was based on Elizabeth II’s coronation dress. Each petal on the dress is made of around 300-600 crystals, pearls and beads.
Shubshri has been performing as Belle since last year and says she has loved being able to play the same character over and over, each time finding something new or different about the character she can tease out or the way she can play her.
“You can take what you discover and run with it,” says Shubshri. “At
her core, the character is the same, but I get to grow with her. Because of these little things I still find this wonderful joy each night.
“I really enjoy being able to do all the things in the show. I love telling a story through song and though movement. I think the thing I love most about musicals is the storytelling.”
Shubshri says playing a Disney princess is definitely a challenge but she revels in the character changes Belle goes through and finds it satisfying to experience that emotion every night.
“It’s a really beautiful arc through the story and it’s fun to share that. Plus, I feel like in their own way so many people go through that journey of finding a relationship and falling in love, even if it’s unexpected or happens in an unusual way.”
Beauty and the Beast the Musical is at Crown Theatre from July 24 – October 12. Tickets from Ticketmaster.


Our podcasts bring you the latest updates and key insights into new treatment options available.
Join our clinical editor Dr Joe Kosterich in conversation with WA specialists to learn more about developments to improve patient outcomes. Our podcasts are now CPD verified. Look for the CPD logo to complete your self-reflection and claim your time.
Topics covered in this series:
Holistic management of osteoarthritis with Dr Arash Taheri
Diagnosing ventricular tachycardia with Dr Ben King
Holistic approaches to bariatric surgery with Dr Harsha Chandraratna
Management of childhood leukemia with Prof Cathy Cole
Advances in lung cancer management with A/Prof Tim Clay
Listen on your favorite podcast platform – scan the QR code to follow us!

General Practitioner
$200 – $300 per hour 6-7 sessions available.
Excellent working environment, with modern facilities.
Quality nursing staff and an onsite non dispensing pharmacist.
Adjacent to the practice we have a pharmacy, and allied services, consisting of audiology, pathology, physiotherapy, podiatry, dental, and cardiology. Visit our website: www.thirdavenuesurgery.com.au
If interested contact Practice Manager Rachael Hadlow via email: rhadlow@3rdave.com.au
•70% Mixed Billing or AUD
$180 per hour for the first 3 months
•Permanent, Full-Time
•VRGP
•Relocation allowance negotiable
•DPA MM1
Our small, friendly, accredited and wellestablished family practice is seeking an experienced VRGP who is ready for a challenging but satisfying full-time career that offers a great work-life balance. Our GPs enjoy a loyal and varied patient base and have the opportunity to build long-term relationships with the patients and their families. Beckenham Medical Centre has easy access to public transport, private parking for the staff and has close proximity to allied health and hospitals.
OFFER DETAILS
•Permanent position
•Full-time
•70% of Mixed billings or AUD
$180 per hour for the first three months
•Large and varied patient base
•Full-time Nursing support
•Well-equipped Consult and Treatment room
•DPA MM1
•On-site Pathology & Pharmacy next door
•Relocation allowance negotiable for the right candidate
•Open hours:
Monday to Thursday 8.30 am- 5.30 pm, Friday 8.30 am-5.00 pm and Saturday 9.00 am-12.30 pm
ELIGIBILITY CRITERIA
•Should hold General or Specialist Registration with AHPRA
•Unlimited working rights in Australia
•Must have competed FRACGP or FACRRM
For more information please contact our Office Manager, Shabana on 08 9451 2722 or alternatively, send through your resume to accounts@beckenhammedicalcentre.com.au

We are seeking a VR GP on an either full time or part time basis, who would love to join a great bunch of people whom are like family more than colleagues. We would love to offer 90% of billings for the first 3 months and then 70% thereafter.
We are a small practice of General Practitioners located in South Perth. We take pride in our reputation as a practice who looks after their patient and staff.
Our well-respected experienced team can offer flexible sessions in a wellsupported environment.
GP owned
Fully computerised
Well Equipped Treatment Room with RN support
Mixed Billing
Central location – 10 min from CBD
Accredited Practice
Please email docthet@gmail.com or call (Pat, the Practice Manager) on 0431 909 221 or call 9367 7840

Doctor Opportunity at The Woods Medical Centre
We are looking for an enthusiastic and experienced GP to join our growing team.
The Ideal Candidate:
Strong General Practice Skills:
•Proven experience in providing high-quality patient care
•Excellent clinical skills and a commitment to preventative healthcare
•Experience in managing chronic diseases effectively
•A keen interest in skin cancer management preferred but not essential. A unique opportunity to combine comprehensive general practice duties with an opportunity to develop skin cancer screening and procedures.
Team Player and Communicator:
•Ability to collaborate effectively
•Excellent interpersonal and communication skills to build rapport with patients.
Essential Requirements:
•FRACGP qualification
•Vocational Registered
•AHPRA registration.
What We Offer:
•Supportive work environment with a focus on work-life balance
General Practitioner
(Full-time or Part-time)
Immediate start, $200/hour minimum guarantee (first 3 months), then 68% of billings.
We are a busy, GP-owned, non-corporate practice seeking a motivated and caring GP to join our friendly and supportive team. Whether you’re looking for full-time or part-time work, we offer flexibility, excellent earning potential, and a positive team environment. You’ll be stepping into a practice with full books, and we’ll open to new patients once you start.
Key Features:
•Pathology onsite
•Excellent nursing and administrative support
•Wide variety of patients and strong demand
•Family-friendly, flexible working hours
•Practice is happy to support special interests
•Team-building activities and supportive culture
•Opportunity for your own consulting room if full-time
About You:
Vocationally Registered (FRACGP or equivalent), AHPRA registration, Strong communication skills and a collaborative mindset.
Please email your CV to Debi practicemanager@balcattafamilypractice.com.au or call 6478 3955 for a confidential discussion.

Spencer Road Family Practice is seeking an enthusiastic doctor, who thrives in a busy general practice.
Avoid long commutes and work close to home in the foothills of Perth’s South-East. Choose your days, set your own hours, and take home 65% of billings.
We have room availability Monday
– Saturday.
The practice is open from 8am to 6pm weekdays.
8am to 1pm Saturdays, 8am to 12pm Sundays and Public Holidays.
We only close on Good Friday and Christmas Day.
We currently have 10 GPs, 4 Nurses, a visiting Podiatrist & Dietitian and a Clinipath Pathology located within the practice.
Our patient’s range from the very young (we have an antenatal GP) to the elderly (some of our GPs have practised in this area for over 30 years)
For more information or to apply, please contact our Practice Manager, Paige on (08) 9493 8388 or send your resume to practicemanager@srfp.com.au

Eastern Perth Metro GP Practice looking for FT or PT GPs
•Nursing support
•No weekends or afterhours work
•Modern facilities and equipment
•Best Practice software
•Mentorship and training opportunities should you wish to develop skin cancer management skills.
Contact our Practice Manager at 0478 021 910 or email practicemanager@thewoodsmedical.com.au

GPs and Nurse Practitioners with a passion for older Australian’s health and wellbeing wanted.
We Offer:
•Flexible days and hours
•Convenient location
•Competitive remuneration
•Relaxed and supportive environment
We will work around your preferences to suit your goals / lifestyle, if your circumstances change, we’ll adapt.
About us:
Sage Medical Consulting is a group of GPs who are committed to practicing “slow” medicine – that is unrushed, quality and tailored to the patient. No matter where you are in life, if you want a compassionate and thoughtful approach to your care - we are your partners to lifelong health.
Expressions of interest to admin@sagemed.com.au or call Practice Manager Jackie on 0401 681 495
What we can offer You:
•DPA location – suitable for doctors under the 10-year moratorium
•Experienced and well-trained staff
•VERY Competitive service fee rates
•Agreed Guarantee period. 70% Tops of Mixed Billing
•Supportive GPs
•Family friendly culture, with great community links
•Reliable clinical software
•Potential Pathway to equity options. What we want from You:
•Current AHPRA registration and right to work in Australia
•FRACGP (or equivalent), VR General Practitioner. Non-VR on pathway to achieving VR registration are welcome to apply
•Current medical indemnity insurance.
Please forward your CVs to practice. manager@swanviewfp.com.au

COMO
Opening for VR GP - F/time or P/time
Full Private List Available
FRACGP essential
Up to 70% private billings
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs.
Enjoy working for a doctor-owned, non-corporate, well support, and accredited practice.
Please contact the Practice Manager on 6165 2444 or email: reception@comogp.com.au




Positioned in the heart of Mandurah, this purpose-built 505sqm Medical Center offers an exceptional opportunity for healthcare providers seeking a prime location.
THE SUBJECT PROPERTY OFFERS:
11, 000 cars per average on weekdays
2 level with lift access
Reverse Cycle Air-Conditioning
Independent treatment rooms
22 exclusive parking bays
High quality office and separate reception area
Kitchenette, shower and disabled toilet
Good natural lighting
With its spacious layout, modern amenities, and patient-friendly design, this facility is ideal for a range of medical, allied health, or specialist services. Contact Con Passaris or Jonathan Kilborn to arrange an inspection.
Building Area: 505sqm Approx.
Current Rent:
$220,000.00 pa net + GST
Outgoings: $50,000.00 pa + GST
Available: January 2026



The Age Less Clinic and General Practice Claremont has space available for a patient minded General Practitioner to be part of our vision for the very best, whole of patient care.
We want to work around your goals and lifestyle so this could be the opportunity you’ve been waiting for.
We are currently an independent solo practice with a fully booked functional GP, established medical and allied health referral base and experienced nursing support.
BENEFITS:
• Flexibility and support guaranteed for the right fit.
• Heritage building with generous consulting rooms, off street parking.
• Prized location.
Suitable for niche complimentary general practice fields. Practitioners in sports medicine, aesthetics, integrative, occupational and aviation medicine, hormone health, acupuncture, hypnotherapy, medicinal cannabis, weight loss would be complimentary to the current practice.
The Age Less Clinic would also welcome the interest of experienced mainstream general practitioners wanting a clinic within which to contribute to a unique culture and whole of patient focus.
For more information or to apply please contact Dr Aparna Hegde on 0408 888 790 or aparna.hegde@theagelessgp.com.au
































