











Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking.
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering. This helps maximize uptime and minimize repair costs.
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering. This helps maximize uptime and minimize repair costs.

Finally, the features you love most about your favorite ride share app, food delivery app, Angi, UpWork, or TaskRabbit are available for medical imaging equipment maintenance and repair.
Enter a Trace Ticket with one tap to broadcast your repair needs to a network of qualified technicians.
Review Bids to find the best service option for improved repair outcomes with less equipment down time, resulting in a lower overall cost.
Track progress, issue payments and rate services all in a single dashboard.


Speed
Instantly blast your service request to every qualified and vetted service provider

From response times to uptime, you no longer have to rely on service companies to track their own activities and performance


Like your favorite personal apps, get in-app alerts when a service technician is on their way, arrived, waiting for a part, completed a job, etc.
Competitive bidding among service technicians allows you to get the best price and only pay and track one entity








DEI
By understanding different models of disability, radiology leaders can create a more inclusive department.
COVER STORY
Right to repair continues to be an unresolved issue with imaging equipment, especially amid tighter budgets.


RISING STAR
Maria Nunez is a Multimodality Breast Imaging Specialist-Lead Technologist and QC Specialist with a bright future.


Catch up on the latest news from around the diagnostic imaging world.

Technological innovations are driving the global MRI.

MEDICINE FOR THE SOUL
A walk isn’t just good for your body; it’s a simple, powerful way to care for your mind and soul.


Ma ria Nunez, RT (R) (M), ARRT Breast Sonographer, holds an Associate In Applied Science and serves as a Multimodality Breast Imaging Specialist-Lead Technologist and QC Specialist at Jackson Memorial Hospital, Taylor/Chaplin Breast Center, in Miami, Florida.
ICE Magazine recently found out more about this Rising Star after she was nominated by Associate Director Kathryn Fields.
Q: WHERE DID YOU GROW UP? OR, WHERE ARE YOU FROM?
A: Asuncion – the capital of Paraguay. Moved to the USA 23 years ago.
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/ EDUCATION? WHAT DEGREES/CERTIFICATIONS DO YOU HAVE?
A: Miami Dade College in Miami. I started in radiology and transitioned into mammography right after graduation. I was offered a full-time mammography position at an outpatient imaging facility at Miami Lakes Radiology.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: Originally started off as a journalist in Paraguay. I
was attending seminars for work in Miami. During my work trips I met my husband. For a while I was going back and forth from my home county to the U.S. and finally, I decided to stay in the Miami and change my career path. While searching for jobs, I discovered that healthcare had a lot of growth and opportunities especially in radiology. It was a stable and reliable field that was in high demand. It was challenging and I started out from zero. I took English classes since my primary language was Spanish and I remember I got permission to take my two-year-old daughter with me to the English classes so I could finish.
Q: WHAT IS THE MOST REWARDING ASPECT OF YOUR JOB?
A: Breast imaging plays an important part in saving lives when it comes to breast cancer. The care depends on mammography and what is seen.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: The interaction with the patients. I have an opportunity to add positive things to the care that is offered to patients, the center, and my colleagues. I enjoy sharing my expertise with the team to improve patient experience, workflows, and produce better outcomes. I think it’s really important to work as a team.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: Breast sonography
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: Working at Jackson. I still remember my first day of clinicals in X-ray school, I was at a local community hospital and the first exam I shadowed was a barium enema. I was like, “What did I get myself into?” I went home and cried. I felt like I had made a huge mistake. Now, I can look back and laugh. I’ve come such a long way in my career. I feel like if you’re going to do something in life you should really enjoy it. I’m at that place in my life now. When you see patients so grateful for the care you just provided, its reassurance that you achieved your goals in life.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: I want to be in a position where I know my work is valuable, and value, whether that’s a direct progression of this role or something I don’t even know about yet. •
FAVORITE HOBBY: Reading – Fiction/Romance Novels
FAVORITE SHOW: “Friends”
FAVORITE FOOD: Asados (BBQ)
FAVORITE VACATION SPOT: Italy
1 THING ON YOUR BUCKET LIST: Travel to London
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU: I’m very shy

Wh en Jose E. Rodriguez graduated high school, he wasn’t sure what career path to follow. A trip overseas to live with his sister and brotherin-law in Germany helped set his course toward what would become a distinguished career in medical imaging.
“I knew I wanted to work in healthcare,” Rodriguez said. “I walked through the local clinic and asked staff members for advice. Ten out of 11 people pointed me to radiology.”
After speaking with a radiologic technologist, he was convinced. Rodriguez entered the field by enlisting in the U.S. Army as an E-1 Radiology Specialist, a decision that launched what would become a 25-year journey dedicated to clinical excellence, leadership and advocacy.
Today, Rodriguez serves as director of radiology clinical operations at the University of Kansas Health System and as an adjunct instructor for Southwest Universi -
ty at El Paso, where he helps train the next generation of radiology leaders.
Rodriguez holds a master’s degree in healthcare administration with a concentration in quality management, a bachelor’s in radiologic sciences, and numerous advanced certifications, including Certified Radiology Administrator (CRA), Certified Healthcare Finance Professional (CHFP), and Certified Professional in Healthcare Quality (CPHQ). He is also ARRT-registered in radiography, computed tomography, and quality management.
Throughout his career, Rodriguez has held leadership roles in numerous professional organizations, including the American Society of Radiologic Technologists (ASRT), the American Healthcare Radiology Administrators (AHRA), and the Radiology Administration Certification Commission (RACC), where he currently serves as a commissioner, secretary, and co-chair of the CRA Job Task Analysis Committee. He is also a past president of the Texas Society of Radiologic Technologists.
Rodriguez counts his advocacy efforts as his greatest professional accomplishment.
“My greatest accomplishment is every current and future technologist, leader, and policy I’ve influenced,” he said. “Even when there’s no direct recognition, knowing that I’ve helped shape the profession is what matters most.”
Rodriguez’s leadership philosophy was shaped early during his Army leadership training, where he learned that integrity, accountability, and hard work are the cornerstones of success. His approach centers around mentorship, growth, and creating a cohesive, patient-centered culture.
“I believe in leading by example and building a team that feels valued and supported,” he said. “Every discussion, whether it’s with a 40-year veteran or a new graduate, is a learning opportunity.”
Rodriguez is passionate about mentoring but notes the biggest challenge is being asked. “There are so many experienced leaders willing to mentor if someone would just ask,” he said.
He volunteers his time mentoring through platforms like
the AHRA Mentor Program, milmentor.com, and alumni networks, encouraging new leaders to believe in themselves even when self-doubt creeps in.
“No one feels completely ready for the next role,” he said. “Trust in your decisions, learn from your mistakes, and remember – you know more than you think you do.”
Rodriguez’s commitment to patient-centered care deepened following a personal tragedy in 2020 when one of his twin daughters passed away after a car accident.
“Sitting in the ICU, making life-altering decisions while trying to hold it together, I experienced firsthand the impact of compassionate healthcare,” he said. “Every physician, nurse, housekeeper, technologist – every role mattered. That experience reaffirmed why we must give our best to patients and families at their most vulnerable.”
His daughter’s organ donation saved two lives that day, a testament to the values of service and sacrifice that Rodriguez carries with him both personally and professionally.
Rodriguez sees artificial intelligence (AI) and innovation as critical tools to address the growing staffing shortages facing the imaging field.
“AI will reshape education, workflows, and clinical processes to meet patient needs more efficiently,” he said.
He’s also inspired by the rising leaders in the field, mentioning several names as future stars, including Brooke Lockridge, David Poon, Jose Melendez, Leah Hudkins, Lisa Welch, and Rachel Thiesse-Yount.
Rodriguez balances his professional passion with family life, hobbies, and self-care. He’s a devoted husband and father, a Marvel movie enthusiast, and starts every morning with a necessary dose of caffeine. He also credits much of his leadership approach to the influence of mentors, family, and spiritual leaders who instilled in him the values of compassion, patience, and humility.
Asked for the best advice he ever received, Rodriguez doesn’t hesitate: “Always lead with integrity, humility, and a heart for others.” •
3. What is your morning routine? Caffeinate first – brain function second
Director of Radiology Clinical Operations at
the University of Kansas Health System
& Adjunct Instructor
1. What is the last book you read? “The 21 Irrefutable Laws of Leadership” by John C. Maxwell
2. What is your favorite movie? Any Marvel Cinematic Universe film
4. What is the best advice you have recieved? Always lead with integrity, humility, and compassion.
5. What isyour biggest life influence? Unwavering examples of compassion and patience


BY MATT SKOUFALOS
When he’s not reviewing medical images for his role as the medical director for MRI and radiology at Nebraska Orthopedic Hospital in Omaha, radiologist Derek Burdeny is out studying images in the field – quite literally.
Burdeny has spent most of his life in the North American Midwest. Born in Winnipeg, Manitoba, Canada, he graduated medical school at the University of Manitoba before moving to Sioux Falls, South Dakota to work in private practice as a radiologist. He met his wife there, and after completing an imaging fellowship at the University of North Carolina, relocated to Omaha, Nebraska, where the couple have remained for nearly 30 years.
“I grew up in the middle of Canada, where it’s brutally cold,” Burdeny said. “When I moved to Sioux Falls, I figured why not? It was straight south for me, and it had to be better. Sure enough, the winters were actually much warmer than I was used to in Canada.”
“Moving to Omaha was warmer still,” he said, “and it can get really hot in the summertime; pretty miserable in July and August. You’ve got extreme heat and cold.”
Nebraska also gets tornado warnings, which were novel to Burdeny. Being raised in the prairies exposed him to storms and extreme weather, but never tornados. Natural phenomena fascinate him, from the change of the seasons to the habits of wildlife, but tornados first grabbed his attention as a younger man, visiting a farmer in southwest Manitoba.
“I remember in his kitchen, he had a picture of a tornado coming towards his house,” Burdeny said. “I said, ‘Where’d you get that picture? He said, ‘That’s my house.’”
“When I first moved to Sioux Falls, South Dakota, I heard the sirens going off in the city, and I had no idea what that meant,” he said. “I realized later on that it was a tornado warning, and I’d slept right through it.”
The next best thing to experiencing extreme weather from a safe distance is capturing it on film. For Burdeny, photography is a hobby he traces directly to his days after medical school, when a friend with a good camera inspired him to pursue the subject. Burdeny has never received any formal photography training, but has built skill on his own through the years by reading and practice.
Much as his professional career in medical imaging evolved from the study of film into manipulating images with software, Burdeny’s expertise grew expansively in the age of the digital camera.
“In the old days, a tech would give you a film, and whatever they exposed, what you see is what you get,” he said, “whereas, when things went digital, I could take pictures on the edge of a film that was not the best exposure, window and level them, and see all the things there.”
“If you use PhotoShop or shoot in RAW, [the unprocessed data communicated directly from a camera lens], it captures all the information on that picture without any loss of compression,” Burdeny said, “so it’s like the same thing every day when I’m reading MRIs.”
Advanced digital cameras on cellular phones have nearly made point-and-shoot cameras obsolete altogether, with the exception of photographers whose specialty is film work, Burdeny said. Any novice today will start with the advanced functionality on their phone camera, and then maybe push into a semi-professional camera as their interest – and budget – grows.
“The entry-level cameras don’t exist anymore,” he said. “You can even adjust your pictures in RAW on your iPhone.”
All Burdeny’s favorite subjects are found in the natural world. Photography and travel go hand-in-hand, and Burdeny has already amassed a gallery replete with studies of landscapes, wildlife, and weather phenomena, from eclipses and auroras to supercell storms and tornados.
“I think it’s fascinating,” he said. “Nature can be beautiful. You can go to Vermont and New Hampshire and see the maple trees turning color. Snowcapped mountains are beautiful, rocks on beaches and the waves; birds and wildlife, moose and loons. Getting outside is beautiful, if you really focus on it.”
“I’ve been to Arizona in the desert trying to shoot lighting,” Burdeny said. “I’ve been through the slot canyons in Utah. I’ve been to Africa eight times and always taken cameras with me. I’ve got some great iceberg pictures from Greenland. I’m heading to Newfoundland this summer, and going to Antarctica in November.”
In North America, it’s nothing for Burdeny to put in 25,000 miles in a month and a half of driving to chase a storm. The

farther off he’s traveling – say, from Omaha to southwest Texas – the more he’ll want to follow a system that will remain in an area for a few days, as disappointment is part of the process.
“When you go out, you don’t know if it’s going to be a successful day or not,” Burdeny said. “If it is, it’s a bonus. You’ll go someplace and figure it’s going to be a great day, and it doesn’t turn out, or you see the storm, and someone else gets the tornado.”
Storm chasing is also difficult to do alone. Burdeny brings a friend, Rick, who drives while he previews road networks, Internet maps, and satellite programs to see how the storm is shaping up. Catching up with a storm enough to photograph it inevitably requires finding a way to avoid its path as well as an awareness of how to flee in any scenario. His advice: keep your distance if the local road network is unreliable or hard to identify.
“Tornados usually move from west to east, so if you’re approaching from the east, that means you’ve got a chance that the storm’s coming at you,” Burdeny said. “You’ve got to make sure that you’ve got a safety escape route. You don’t want to cross a tornado’s path. If

you’ve got a tornado coming towards you and a road ends, or you’ve got a bridge to cross, you can be in trouble. Going down gravel roads can be a little dangerous unless you’ve been on them.”
Of course, the drive out in pursuit of a storm invites observation of its own sort of beauty. Burdeny enjoys experiencing new and unfamiliar countryside, like the Oklahoma farm hills that move like waves in a green ocean when the wind hits, or the creek bed that cuts through them in orange slices.
“If we get a big, good picture, you feel good; it’s a success, especially if it’s a severe storm in the middle of nowhere,” Burdeny said. “It’s nice to see these things, but then you’ve got to realize that what’s happening is someone else’s worst nightmare, destroying their buildings and hurting people.”
“I don’t like going out to Eastern Texas, Oklahoma, Arkansas, Louisiana, Kentucky,” he said; “there’s a lot of trees, people, more chance of damage, and people getting hurt. I just want to see these things when they’re beautiful and not any chance of hurting anybody.” •
To see more of Derek’s work, visit derekburdenyphotography.com.


“I think it’s fascinating. Nature can be beautiful. You can go to Vermont and New Hampshire and see the maple trees turning color. Snow-capped mountains are beautiful, rocks on beaches and the waves; birds and wildlife, moose and loons. Getting outside is beautiful, if you really focus on it.”




Nanox Imaging LTD, an innovative medical imaging technology company, has received 510(k) clearance from the U.S. Food and Drug Administration (FDA) for the Nanox. ARC X, its new multi-source digital tomosynthesis system. The FDA 510(k) clearance was received in less than 30 days from the date of submission and covers the production of tomographic images for general use, including the human musculoskeletal system and pulmonary, intra-abdominal and paranasal sinus indications, adjunctive to conventional radiography on adult patients.
The Nanox.ARC X maintains the Nanox.ARC’s proprietary digital Nanox.SOURCE and advanced tomosynthesis technology with a cold cathode, which enables it to create a more comprehensive, sliced three-dimensional view of the body, enhance visualization with multiple layers of images, and reduce the super-imposition of structures often seen in 2D X-rays. The Nanox. ARC X introduces a fully integrated, single-unit system with a streamlined design that significantly reduces the physical footprint. The system features “plug and play” one-day installation capability, making advanced tomosynthesis technology more accessible to diverse
healthcare settings with space constraints.
“The FDA clearance of the Nanox.ARC X marks an important evolution in our imaging technology,” said Erez Meltzer, chief executive officer and acting chairman of Nanox. “By integrating our proprietary digital technology in this new imaging system, we’re making it easier for healthcare providers to adopt digital 3D imaging. This milestone advances our mission to expand access to essential medical imaging technology to more patients, regardless of their location. We look forward to introducing further capabilities to the Nanox.ARC X in the future and making them available through remote and immediate upgrades.”
The Nanox.ARC X is designed to be installed in any standard X-ray shielded room with minimal infrastructure requirements. The system operates on standard power (110v/230v 16A) and features a cables-free design for enhanced user and patient safety, ease of cleaning, and maintenance. Nanox will offer the Nanox.ARC X system, later this year, alongside the current Nanox.ARC, expanding the company’s product portfolio to meet diverse customer needs and use cases.
ScreenPoint Medical showcased innovative new capabilities of its Breast AI, Transpara, at the 2025 Society of Breast Imaging Symposium. The most clinically validated AI for breast cancer detection on the market, Transpara provides radiologists with a “second pair” of eyes to help detect cancers earlier and reduce recall rates.
ScreenPoint will highlight its latest advancements, including Transpara 2.1, an update and improved breast cancer detection algorithm that further refines Transpara’s industry-leading performance. This includes compatibility with options for breast density (BI-RADS like and volumetric) and temporal comparison with multiple prior exams. This robust temporal

Simplifying The Imaging Equipment Ownership Experience
comparison capability will be the first of its kind in the market and will allow suspicious areas on a current study to be analyzed against up to 3 priors over 6 years. The Transpara 2.1 algorithm is both CE-marked and FDA cleared.
“We are excited about the significant improvement of Transpara performance when priors are used, especially when more priors with a longer time interval are included, which is in line with radiologists’ experience. Our solution is designed for screening and diagnostic use to truly improve clinical workflow,” said Professor Nico Karssemeijer, Ph.D., co-founder and chief scientific officer of ScreenPoint Medical.
Image One Medical is the only Engineer-Owned medical equipment service group that is fully dedicated to Florida’s amazing base of Imaging Centers, Hospitals, and Cancer Treatment Centers.
We have a mission: Self perform on every aspect of our business. Specialize on specific modalities: Pet CT, CT & MRI, and Focus in a key geographic region.
Fort Myers I Fort Lauderdale I Tampa I Orlando
Dealer and servicer of PET CT, CT and nuclear medicine
• Equipment service: full coverage plans
• Equipment sales: installation, relocation and project management
• Mobile coach construction, refurbishment, maintenance and management

Self performing team of in-house engineers
High level problem solving for Siemens and GE PET CT, CT and nuclear medicine • In-house inventory of 40+ systems and parts for repair
• 24 hour service with quick uptime guarantee

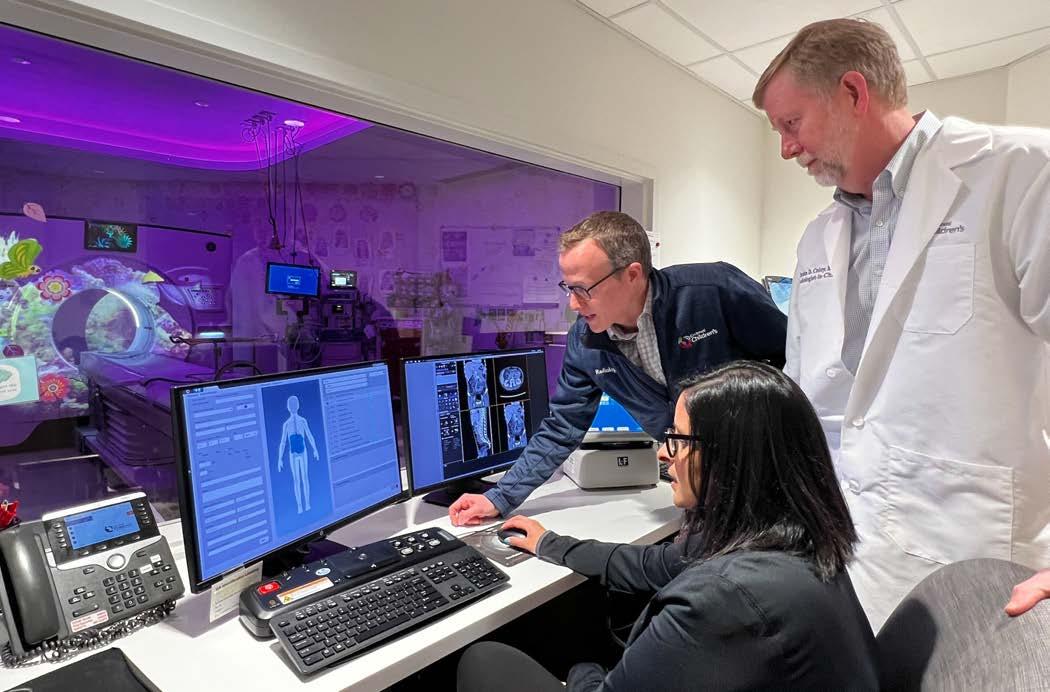
Cincinnati Children’s and GE HealthCare will form a strategic research program focused on driving clinical and technical research to advance innovation for pediatric care delivery across modalities, including magnetic resonance imaging (MRI), ultrasound, molecular imaging (MI), and computed tomography (CT). The research program will establish the first pediatric Care Innovation Hub nationwide, representing a new model established by GE HealthCare and Cincinnati Children’s to combine their talents and resources to accelerate the impact of innovation and scientific activities for the benefit of pediatric patients.
Ranked as one of America’s best children’s hospitals by U.S. News & World Report, Cincinnati Children’s brings clinical and research excellence to pair with GE HealthCare’s leading global medical technology expertise. The findings and new technologies realized between the organizations could be utilized by care providers globally who serve pediatric populations to help improve clinical and patient care.
“This collaboration with GE HealthCare is an opportunity to increase our ability to impact and improve how children are imaged far beyond our own health system,” said Andrew Trout, MD, Director of Clinical Re-
search at Cincinnati Children’s department of Radiology and Medical Imaging.”
“Collaborating with GE HealthCare is an opportunity to leverage Cincinnati Children’s clinical and research capabilities and participate in technology development with a global imaging leader. Rather than having to adapt techniques created for adults to pediatric use as is usually necessary, access to the latest technology at earlier stages of development will allow us to create pediatric-focused imaging technology from the beginning,” said Brian Coley, MD, Radiologist-in-Chief at Cincinnati Children’s. “Once developed, this partnership will foster translation into the broader pediatric healthcare ecosystem, bringing these advances to pediatric imaging worldwide and making the impact that Cincinnati Children’s, as a research powerhouse, is known for.”
With a ‘built for kids’ mission, this collaborative, multi-modality approach aims to further help build understandings and innovations for diagnostic imaging beyond pediatric use cases, as children are often the most challenging patients due to their wide range of sizes and unique positioning challenges.
“Pediatric research and increasing access to
precision care technologies are priorities for GE HealthCare. We are thrilled to partner with the renowned Cincinnati Children’s to develop this Care Innovation Hub,” said GE HealthCare Vice President of Research & Scientific Affairs Erin Angel. “When we think of diagnostic imaging, we may be predisposed to think of aging populations who are experiencing serious illness or disease, but we also need to consider pediatric patients and how to improve the healthcare experience for all populations based on our learnings. That is what this Care Innovation Hub is about. It is a chance to do better and be better for all who may need diagnostic imaging whether it is for themselves or a loved one.”
• Developing pediatric excellence in MRI
This partnership aims to build and test prototypes of high-density MR coil arrays sized appropriately for children, which can help both increase patient comfort and enable more precise images in smaller patients. Additionally, there will be an emphasis on developing imaging techniques that address the challenges of imaging a child, such as highly accelerated and motion robust methods that enable rapid, high-quality exams in body, neurologic, cardiovascular, and musculoskeletal applications.
• Unlocking solutions in clinical challenges of ultrasound
Ultrasound projects developed will focus on engaging with radiology and cardiology departments at Cincinnati Children’s to collaborate on product development and ensure early clinical feedback specific to pediatric use to shape the future of GE HealthCare features and devices, including AI algorithms. GE HealthCare and Cincinnati Children’s will also work together to improve the use of ultrasound to gather measurable data, including development of new technology and clinical evidence for liver imaging techniques.
• Evaluating Molecular Imaging in pediatrics
Cincinnati Children’s and GE HealthCare teams hope to evaluate new and emerging technologies in positron emission tomography (PET) and single photon emission computed tomography (SPECT) imaging, including the personalization of treatment plans based on optimized software workflows. Cincinnati Children’s and GE HealthCare intend to collaborate on optimizing and improving image reconstruction and developing evidence showing the utility of PET and SPECT imaging in pediatric imaging.
• Optimizing, evaluating Computed Tomography for pediatrics
Cincinnati Children’s and GE HealthCare scientists plan to work together to further optimize and automate CT workflows for pediatric patients and the clinicians that serve them. Researchers will do this by evaluating new CT technology in a pediatric context and will disseminate best practices to health providers globally that administer pediatric care.
Check out our YouTube channel for more information and exclusive content!
Medicine for the Soul
Go LIVE with ICE
ICE Webinars
ICE Breaks
Testimonials
Education From ICE Conference

Probo Medical has announced a new distribution relationship with GE HealthCare. This relationship signifies a major milestone for Probo and reinforces its dedication to offering customers advanced medical imaging technology in the industry.
In this relationship, Probo will offer new GE HealthCare ultrasound machines in the Vivid, LOGIQ, Versana, Venue and Vscan Air product lines. This new relationship enables Probo to bring these premium products and solutions to its customers nationwide.
GE HealthCare’s ultrasound systems are globally recognized for their exceptional quality, cutting-edge technology, and ability to meet the diverse needs of medical professionals and patient populations. GE HealthCare has been producing innovative ultrasound machines for decades, and today it offers a wide variety of available diagnostic ultrasound machines.
“This relationship takes Probo to a new level,” said Mike Dilick, Probo’s president and chief commercial officer. “I couldn’t be more excited about this relationship, it brings significant benefits to us, GE HealthCare, and, above all, the healthcare community. At Probo, we are committed to providing exceptional products and resources to help our customers achieve their goals. GE HealthCare’s advanced ultrasound technology perfectly aligns with Probo’s vision to empower healthcare professionals with the tools to deliver exceptional patient care.”
This new relationship promotes Probo’s mission of delivering high-quality medical equipment while supporting healthcare providers with personalized sales, expert services, comprehensive training, and more. As a GE HealthCare distributor, Probo is making greater strides in simplifying healthcare delivery and equipping medical professionals with the tools they need to deliver compassionate, high-quality care.





The American Society of Radiologic Technologists has named Diane Kosenko, R.T.(R)(CT)(CV), of Bristol, Connecticut, as the winner of the 2025 ASRT Individual Award for Advocacy and the Minnesota Society of Radiologic Technologists as the affiliate award winner.
The ASRT Award for Advocacy recognizes and acknowledges achievements in advocacy efforts, including overall growth and development of individual and affiliate grass-roots involvement. ASRT members recommend award nominees, and the ASRT Committee on R.T. Advocacy selects the winners. The 2025 Award for Advocacy recognizes efforts that took place between Oct. 1, 2023, and Sept. 30, 2024.
Diane Kosenko, R.T.(R)(CT)(CV), has been an active advocate for more than 30 years. She has served as a computed tomography technologist at Radiology Associates of Hartford, in Connecticut, for 26 years, and throughout that time she has been active with the Connecticut Society of Radiologic Technologists. Her roles include board chair, president, president-elect, vice president, treasurer, delegate, legislative contact and senior board member. She served as chair of the Ambassadors for R.T. Advocacy for five years and is a graduate of the ASRT Leadership Academy.
In 2024, when a House bill was introduced that would allow advanced practice registered nurses to practice fluoroscopy independently without proper radiation safety training and a credentialed professional present, Kosenko joined forces with other medical imaging and radiation therapy professionals to oppose the bill. They testified at a public health hearing and encouraged technologists, educators and radiologists affected by this bill to submit testimony using the language she helped draft. She and her colleagues were successful in amending the bill to prohibit APRNs from independently performing fluoroscopy without proper supervision.

Kosenko has advocated that the CSRT hold a day at the capitol for students to learn about the legislative process. In addition, she has presented to CSRT members on how bills are passed, where to find their legislative contacts and what legislative committees most affect members. She also presented at the Missouri Society of Radiologic Technologists annual conference on the topic of advocacy. Kosenko continues to encourage others in the profession to take an active role and has mentored members of the CSRT Board of Directors on how to advocate for the profession.
The Minnesota Society of Radiologic Technologists is highly engaged with its members, community and state elected officials. The MSRT has created a way for members to share ideas and collaborate with other affiliate and advocacy leaders through a web forum called 50 States, 50 Standards: A State-By-State Guide to Licensure. When two encroachment bills surfaced in Minnesota, the MSRT worked with sonographers and midwifery groups to hold discussions on advocacy issues. MSRT advocacy committee members met with Medi-Sota – a nonprofit health care consortium of 35 rural health care providers in Minnesota – to discuss licensure and the role of limited x-ray machine operators.
Community is a priority for MSRT, and its members participated in the American Cancer Society Breast Cancer Walk and virtually in the ASRT Invisible Heroes 5k event to recognize the vital role medical imaging and radiation therapy professionals perform in health care. The MSRT also appeals to educators to allow their students to participate in conference open forums and lectures.
Additionally, the MSRT advocacy chair met with local state representatives and has obtained a bill sponsor as it prepares for a 2025 full licensure bid.
United Imaging, a global manufacturer of modern medical imaging technology, will feature its uMI Panorama at a state-of-the-art new facility in Jupiter, Florida.
Focused on patient-centered and precision medicine, Florida Theranostics is committed to establishing a high-quality level of personalized patient care and an emphasis on a comprehensive treatment experience for the surrounding communities. They celebrate their grand opening today, just one short year after achieving the Radiopharmaceutical Therapy Center of Excellence designation from SNMMI (Society of Nuclear Medicine and
Molecular Imaging), the only one in South Florida, according to their website.
A special introduction at today’s grand opening in Jupiter is the digital positron emission tomography/computed tomography (PET/CT) scanner from United Imaging. A PET/CT scan is a non-invasive imaging technique that combines the functional information of a PET scan with the detailed anatomical data of a CT scan. This powerful combination allows physicians to detect and monitor a wide range of medical conditions including cancer.

Th e ICE webinar “Tips, Tricks and Tools for Improving Quality and Safety” by Nancy Davis was popular with more than 100 individuals registering for the session. Amanda Hedges, a lead mammo tech with Sutter Health won an ICE gym bag during the webinar.
Nancy Davis, BS, RT(R)(M)(CT), director of accreditation, IAC CT, asked the questions:
• Do you feel lost in your quality and safety efforts?
• Does it seem like you are solely responsible for making quality improvement a reality in your practice?
• Not sure how to navigate choosing engineers and physicists that best suit your needs?
• Does the thought of accreditation make you anxious?
She then invited attendees to learn how to navigate these challenges explaining that it is easier than you think when you know where to look for help and what to look for in stakeholders.
Her objectives included:
1. Evaluate outside quality and safety stakeholders to choose the best options for your practice.
2. Choose team members who will strengthen your quality and safety efforts.
3. Use the four “Cs” to improve quality and safety in your practice.
4. Identify tools and resources that assist with quality and continuous improvement in your practice.
She also answered questions during a Q&A session with attendees.
ICE Webinars would like to thank webinar sponsor Intersocietal Accreditation Commission. Since 1991 IAC has operated as a nonprofit, accrediting facilities that provide vascular testing, echocardiography, nuclear/PET, MRI, diagnostic CT and intervention-based procedures under its mission of Improving health care through accreditation. More than 14,000 IAC-accredited sites have implemented standardized and optimized processes, experienced cost reductions and, most importantly, continuously improved their patient outcomes. To learn more about IAC, visit intersocietal.org.
Attendees were asked, “What do ICE webinars provide the industry?”
“Up to date and relevant information and training,” said Richard Sherry, MR Manager, Barrow Neurological Institute.
“A great source for information on our industry. It is appreciated,” Francisco De La Garza, Clinical Specialist, Agiliti Health.
“Continuing Education and the ability to stay current with trends and technology,” added Kenneth Repking, Practice Associate Radiation Safety Services, Landauer.
“ICE allows industry professionals to keep up with new standards and best practices to meet the needs of their organizations,” said Cindy Winter, Director of Radiology and Patient Transportation, JPS.
For more information, visit ICEwebinars.live.
Ea ch month, ICE Magazine reaches out to healthcare systems, imaging centers and vendors to garner the latest insights, tips and advice regarding an imaging modality. MRI is the modality in the spotlight in this issue of ICE Magazine .
Participants in this roundtable-style Director’s Circle article on MRI are:
• University Hospitals MRI Supervisor Martin Ayres, RT(R) (MR), MRSO(MRSC);
• Banner Imaging Associate Director Michelle Brady;
• Crothall Healthcare Imaging Director Gulf Coast Region Brian Howell; and
• Scripps Clinic Imaging Manager Toni Anne Serna, ARDMS
Q: WHAT EMERGING TRENDS IN MRI ARE YOU MOST EXCITED ABOUT?
Ayres: The emergence of AI in MRI is very exciting. This technology not only allows for faster acquisition times, but it can also be used to improve both image sharpness and resolution.
Brady: There are so many exciting trends in MRI right now. AI, remote scanning, increase in number of implants that can be scanned, new air coils are just a few examples. I am most excited about the use of AI in the newer versions of software that are being released by vendors. This allows the ability to maximize throughput without sacrificing image quality. This equates to less time in the scanner for patients, which is a big win for claustrophobic patients. Howell: I’m particularly excited about MRI systems
with reduced helium requirements. These systems are not only more economical, but also require a smaller footprint and have lower installation costs. Additionally, larger bore sizes enhance the patient experience and make it easier for facilities to transition away from traditional Open MRI systems.
Serna: Specifically in cardiac MRI, we are excited about faster imaging sequences, AI-assisted motion correction, and improved tissue characterization techniques. These advances are making cardiac scans more accurate, efficient and accessible for a broader range of patients.
Q: HOW DO YOU PRIORITIZE UPGRADES OR INVESTMENTS IN MRI SYSTEMS WITHIN YOUR DEPARTMENT?
Ayres: Our system prioritizes system upgrades largely based on the age of the overall unit. Older units often lack the ability to match the quality and speed of the newer magnets and must be retrofitted with new hardware and software or be fully replaced to do so.
Brady: We have 22 scanners in our fleet. We prioritize our upgrades by the age of the scanner, tracked downtime, cost of repairs and maintenance, appointment availability, as well as community needs of both patients and providers.
Howell: We prioritize upgrades by collaborating with our partners to evaluate system performance, operating costs, and emerging technologies that enhance diagnostic capabilities and patient satisfaction. We also rely on replacement priority scores that factor in equipment




age, utilization, and clinical impact – helping us make objective, data-driven decisions. By reviewing this data alongside peer insights from across the country, we ensure our recommendations align with both clinical goals and long-term value.
Serna: We prioritize upgrades based on feedback from our technologists and radiologists – they’re the ones using the systems every day and know where improvements are needed. We also consider patient experience and clinical demand when making investment decisions.
Q: WHAT ROLE DOES SERVICE AND MAINTENANCE SUPPORT PLAY IN YOUR LONG-TERM PLANNING?
Ayres: MRI machines, just like all pieces of machinery, require preventive maintenance at routine intervals to ensure peak performance. It is important to have a pre-existing service contract in place so unexpected repairs can be resolved in a timely manner. Our sites rely heavily on our field service engineers to keep our machines running smoothly. This relationship and support is crucial to our current and future success. Afterall, what good is a non-working MRI machine?
Brady: Given how expensive MRI systems are to operate and maintain, service and maintenance support play a vital role in the long-term planning. Service and maintenance determine how quickly you get back up and running so it is very important to choose vendors and contracts wisely. Support equipment should also be considered, such as chillers and injectors.
Howell: Service and maintenance support are essential to both operational performance and long-term planning. By tracking system uptime, repair history, and total cost of ownership, we can identify performance issues early and plan replacements before they impact care. This data-driven approach helps align equipment decisions with broader capital planning and clinical goals.
Serna: Service and maintenance are essential to our long-term planning. They minimize downtime, keep our schedule running smoothly, and ensure consistent, high-quality imaging. A responsive service team helps us avoid costly delays, maintain patient trust, and extend the life span of our equipment – making it a smart investment as well as a clinical necessity.
Q: ARE YOU USING OR EVALUATING ANY AI OR MACHINE LEARNING TOOLS WITH YOUR MRI SYSTEMS? HOW ARE THEY IMPACTING WORKFLOW OR DIAGNOSIS?
Ayres: AI is currently being used on a few select MRI machines/exams within our system. The technology is being closely analyzed and compared against conventional acquisitions to confirm both quality and accuracy. We do utilize machine learning tools within the University Hospitals system for offline processing of stroke, tumor, dementia, as well as other exams. These machine learning tools allow for faster and more thorough evaluations for our patients.
Brady: We are fortunate to have systems that are utilizing the AI software to scan. This has had a positive impact on our workflows. We are able to utilize shorter scan times without sacrificing image quality. Having the shorter scan times has been a huge patient satisfier for our claustrophobic patients, as well as allowing us to get through any backlog of volume all while maintaining exceptional image quality. Everyone can appreciate less time in an MRI scanner.
Howell: AI and machine learning are becoming key tools in how we service MRI systems. These technologies help us detect irregular performance patterns earlier, prioritize service response, and even predict failures before they occur. It’s allowing our teams to shift from reactive repairs to more proactive, targeted support that keeps systems running more reliably.
Serna: Yes, our GE 3T MRI system uses Deep Learning software. It enhances image reconstruction, reduces scan times and improves workflow efficiency without compromising diagnostic quality.
Q: HOW DO YOU MANAGE SCAN TIME EFFICIENCY WHILE MAINTAINING IMAGE QUALITY?
Ayres: Our site has prebuilt protocols that take full advantage of conventional, non-AI acceleration techniques. The sequences within the protocols have been fine-tuned and allow for just the right balance of signal and resolution with parameters that meet or exceed ACR standards and are acquired within an acceptable time frame. That being said, it is really the skill and understanding of the technologist behind the scanner that makes this possible. They must be in tune with the patient and the task at hand and know when to prioritize speed, resolution or sometimes both.
Brady: Safety and quality are our top priority. Although it is wonderful to be able to scan faster, we have ensured that image quality has not been sacrificed. We have continued to work the vendors, radiologists, and technologist to optimize the software for the protocols that we utilize. We have also implemented a variety of workflows to help ensure our quality is maintained, such as a QC program, technologist assistants so the techs can focus on the patient, as well as MRSO personnel to help the technologists clear their patients with implants. All of these tools allow for the technologists to focus on the images and patient in front of them, and limiting the distractions around them.
Howell: With our newer systems, AI has really assisted in these areas. Both in scan time and post-processing image analysis.
Serna: We focus on clear communication and setting expectations before the scan begins. Taking a little extra time to make patients comfortable upfront helps us maintain both efficiency and image quality.
Q: WHAT ADVICE WOULD YOU GIVE TO OTHER IMAGING CENTERS LOOKING TO INVEST IN NEW MRI SYSTEMS?
Ayres: I would suggest investing in a machine with a fully capable package of software licenses and MRI
coils. The features I would look for are as follows: powerful gradients, high channels, acceleration and reconstruction techniques including AI, large scan range without coil repositioning and a dockable table. All of these elements combined will help result in the fastest, most comfortable exam experience for the patient.
Brady: I would advise anyone looking to invest in a new MRI system to know what you want/ need out of the system. Maybe you specialize in ortho cases, or the need is for breast imaging? Know what you need from the system and then explore all vendors. Get radiologist feedback regarding image quality and scan optimization opportunities. There are great advancements with software, coils, etc. I would also recommend that you work closely with an MRI lead technologist, so you have a clear understanding of how to optimize the department workflow as well as protocols. This will allow you to be as efficient as possible while maintaining quality and safety.
Howell: Build a strong partnership with your imaging service team. Their expertise provides valuable insights into system performance and life cycle planning, helping you make more informed, cost-effective investment decisions tailored to your department’s needs.
Serna: Understand your patient demographics and which types of imaging drive your business. Invest in MRI systems that align with both your current needs and future goals – wide bore systems are a must for patient comfort and versatility. •

LOCATED AT PARIS HOTEL
Join ICE Magazine for our 5th Drinks on ICE Party, sponsored by IAC, at AHRA 2025!
RSVP and pick up your wristband on Sunday during AHRA's gathering place hours at IAC's booth #445 or ICE Magazine's booth #644. See you there!


The global magnetic resonance imaging (MRI) market is experiencing significant growth, driven by technological advancements, an aging population, and the increasing prevalence of chronic diseases. Valued at $7.1 billion in 2024, the market is projected to reach $10.29 billion by 2030, growing at a compound annual growth rate (CAGR) of 6.5%, according to Grand View Research.
Technological innovations are central to this expansion. Recent developments include the integration of artificial intelligence (AI) in MRI systems, enhancing image reconstruction and diagnostic accuracy. For instance, in August 2023, FUJIFILM Healthcare Americas Corporation received U.S. FDA clearance for its 1.5 Tesla MRI system, the ECHELON Synergy, which utilizes Synergy DLR, a deep learning reconstruction technology that improves image sharpness and accelerates scanning.
The market is also witnessing a shift in MRI system architecture preferences. Closed MRI systems held the largest share of over 75% in 2023 due to their superior image quality. However, open MRI systems are gaining traction, especially among claustrophobic patients and pediatric cases, and are expected to grow at a CAGR of 7.7% during the forecast period.
Field strength is another critical factor influencing the market. Mid-field MRI systems (1.5T to 3T) accounted for 47.7% of the market share in 2023, favored for their balance between image quality and cost. High-field MRI systems (>3T) are anticipated to experience the fastest growth rate of 7.9%, driven by their enhanced imaging capabilities, particularly in neurological and musculoskeletal applications.
The rising prevalence of chronic diseases such as cancer, cardiovascular disorders, and neurological conditions is a significant driver of MRI market growth. According to the International Agency for Research on Cancer, over 19.2 million new cancer cases were recorded globally in 2020. MRI plays a crucial role in the early detection and monitoring of these diseases, thereby increasing its demand, according to Grand View Research.
Regionally, North America dominated the global MRI market with a share of over 36.74% in 2023, attributed to the high prevalence of chronic diseases and advanced healthcare infrastructure. Asia Pacific is expected to exhibit the fastest growth rate of 7.4% during the forecast period, driven by an increasing geriatric population, rising healthcare expenditures, and growing medical tourism in countries like India, China, and Japan, according to Grand View Research MarketsandMarkets and Grand View Research agree that despite the positive outlook, the MRI market faces challenges such as the high cost of MRI systems, which can range from $1 million to $5 million depending on the system’s features and field strength. Additionally, the shortage of trained professionals to operate advanced MRI systems poses a barrier to adoption in some regions.
Key players in the MRI market include Siemens Healthineers, GE Healthcare, Koninklijke Philips N.V., and Canon Medical Systems. These companies are investing in research and development to introduce innovative technologies that enhance imaging quality and patient comfort.
In conclusion, the global MRI market is poised for substantial growth, driven by technological advancements, an aging population, and the increasing prevalence of chronic diseases. While challenges such as high equipment costs and a shortage of trained professionals persist, the integration of AI and the development of more patient-friendly MRI systems present significant opportunities for market expansion.•

*Disclaimer: Products are listed in no particular order.
GE HealthCare’s SIGNA 3.0T MRI scanner can help support providers with even the most demanding cases. It offers unmatched productivity due to a 70cm patient bore, award-winning AIR Coils for a more comfortable experience, and a comfortable detachable patient table. This productivity, combined with the latest in deep learning technology for speed and quality, allows SIGNA Hero to help improve patient outcomes, reduce clinician burden, and simplify MRI exams. Its next-generation, low-helium magnet is also built for sustainability, and the GE HealthCare SIGNA Continuum upgrade program also makes it built for the future.

The Magnetom Free.Max MR scanner from Siemens Healthineers extends access to severely obese and claustrophobic patients with the first and only 80cm open-bore system while offering every patient an improved experience. The most lightweight, compact whole-body MR scanner ever offered by Siemens Healthineers at under 3.5 tons and less than 80 inches high, the Magnetom Free.Max has a novel magnet design that requires less than 1 liter of helium, contributing to reduced infrastructure and total cost of ownership. Deep Resolve Boost employs deep learning to deliver sharper, higher-resolution images while reducing acquisition times. The myExam Companion workflow solution incorporates artificial intelligence to help the user navigate the examination more efficiently. Features such as the Contour Knee Coil and BioMatrix Contour Large Coil with embedded respiratory sensors enable seamless patient setup with consistent results. The scanner’s unique field strength of 0.55 Tesla can improve implant imaging, reduce susceptibility challenges and enable new clinical opportunities in imaging.

Philips BlueSeal is the company’s most sustainable MRI scanner containing its most advanced technology. A helium-free operating system that reduces operational costs and eliminates the need for helium refills. A fully AI-enabled scanner that delivers unmatched performance, integrating SmartSpeed Precise’s1 Dual AI2 technology for ultimate precision at maximum speed by optimizing
image quality with better signal-to-noise ratio and up to 65% higher sharpness3 and increasing your imaging speed by up to a factor of 3.4 •
BY MATT SKOUFALOS
In the medical equipment manufacturing space, proprietary information is powerful.
The investments required to bring a life-saving technology to market are often measured in the hundreds of thousands or millions of dollars, and the opportunity to profit from those investments isn’t always guaranteed in a free-market economy, or at least, not for long.
When it comes to extending the functional, useful life of those products, whether through preventive maintenance or repair, there’s a secondary revenue-generation opportunity. The skilled professionals who administer the repairs

must be highly trained in not only the general modality of the equipment, but the specific device models themselves. The former skill set may be developed with an aftermarket or third-party business, often referred to as an independent service organization (ISO), whereas the latter increasingly can only be delivered by the original equipment manufacturer (OEM).
That’s because, as the budgets of healthcare organizations are increasingly stretched, they’re seeking any opportunity they can find to conserve costs, including contracting with ISOs for their medical device servicing and maintenance. For years, this wasn’t a fight that OEMs pursued particularly relentlessly; it wasn’t uncommon for a veteran
OEM service professional to find a second career as an ISO, working on the same kinds of equipment they’d maintained for years under their own banner.
However, as customers’ purse-strings tightened, OEMs sought to recapture market share they’d relinquished to the ISOs they hadn’t previously regarded as competition. But they didn’t seek to compete on price; instead, they took the tack that the proprietary ownership of their intellectual property was being undermined in contravention of their legal rights. That set up a battle for the courts and the legislatures over whether ISOs were competent to do the work of fixing OEM equipment without risking patients’ lives, or whether ISOs were filling a necessary role in repairing devices that OEMs either couldn’t support, or declined to do at a rate healthcare organization could afford.
The question central to the conflict is still unresolved. It distills to the fundamental issue of whether the owner of a piece of technology has the right to repair it after purchasing it, and secondarily, what role the OEM might be obligated to play in facilitating that repair when the technology in question is a life-saving medical device.
Nathan Proctor, senior director of the Campaign for the Right to Repair at the Public Interest Research Group (PIRG), said that the battle for medical device owners to legally repair and maintain their own equipment seems to have produced different messaging around the issue.
Previously, OEMs had painted a picture for lawmakers and the courts that third-party servicing of medical equipment is dangerous, and that anything less than repair or maintenance provided by the manufacturer constitutes negligence or ineptitude representing serious patient risks. When the data didn’t support that contention, the OEM argument shifted to the claim that all servicing should be regulated through the U.S. Food and Drug Administration, Proctor said.
“Because GE, Philips, and Siemens are paying fees to the FDA, and they’re regulated as manufacturers, they’re saying they’re safe, but those who aren’t regulated should not be allowed to make repairs,” he said. “It’s basically outlawing third-party repair.”
“To me, there’s an obvious incentive from the manufacturers to completely eliminate competition from service,” Proctor said. “There’s huge money stakes here, just like everything in American healthcare.”
As the manufacturing businesses “have completely organized their money” and rely on “brass-knuckle tactics,” Proctor believes the ISO sector must comparably rally its institutions to push back on the issue. Thus far, however, the Right to Repair movement hasn’t found its federal legislative champion.
“We started pushing for Right to Repair for the military,” Proctor said. “I interviewed several military biomeds
talking about being at field hospitals in Afghanistan and not being able to get service keys from manufacturers. They had Marines coming in, and they needed a CT scan to save their lives, just to be told that they have the wrong [service] contract.”
Proctor believes that there may be inroads to be made in convincing the U.S. Department of Defense and Congress that supporting Right to Repair in cases such as these is necessary, and from that foothold, build a case that the broader issue doesn’t just exist under battlefield conditions.
“People should be able to fix the stuff they’ve purchased,” he said; “that includes hospitals and the U.S. military. There’s nothing magical or special about what manufacturers can do. They hire the same kinds of people doing the same kinds of work, and competition is beneficial. You don’t have to run a good company to compete in a monopolized environment.”
Although there’s been little appetite to develop a federal law around Right to Repair, the concept has gained traction for consumer products at the state level. Right to Repair legislation has been introduced in all 50 states as of February 2025, but so far, only five states – New York, Colorado, Minnesota, Oregon, and Colorado – have passed them, and those laws don’t specifically include provisions for medical devices.
To Proctor, that means there’s more room for ISOs to step up and rally support for the cause from other stakeholder groups, including healthcare organizations. What could help, he said, is whether they’re ready to step forward with data that can illustrate the extent of their maintenance challenges in terms of service failures, costs, and down time — precisely the kinds of information that hospitals track internally but
“By OEMs not allowing us to service that equipment, that’s really affecting patient care. The hospital owns that equipment, and I feel it should be up to the hospital who services that device.”
- Eric Massey, regional director of field service operations for Crothall Healthcare
are reluctant to present to the public.
“It’s very challenging to share data,” Proctor said; “I don’t know anyone who’s willing to talk about this stuff publicly. We need the healthcare organizations to support this thing because ultimately, they’re the customers. If they’re letting the manufacturers steer them into uncompetitively priced service contracts, that’s what’s going to make or break longterm efforts to expand medical device servicing.”
Proctor relayed an anecdote involving a healthcare technology management professional who defended switching to an ISO for device maintenance because it lowered his parts failure rate and halved the cost of his repairs. The OEM challenged that decision as risky to patient health; instead the institution’s CFO responded that the ISOs were outperforming the OEM contract in terms of equipment uptime and maintenance costs.
“Lawmakers need to understand that hospitals are making deliberate decisions about what is best in a very challenging operation to service medical needs,” Proctor said. “[Healthcare organizations] can’t even choose to save money if they want to, even if it means improving the quality of the healthcare that they’re delivering.”
Eric Massey, regional director of field service operations for Crothall Healthcare, an ISO headquartered in Wayne, Pennsylvania, said his personnel are more than capable of repairing and maintaining the medical devices they’re tasked with servicing. Their greatest hurdle is often getting access to the manufacturer-controlled parts, software keys, and technical manuals that are necessary to effectuate the work. OEMs are required by the FDA to provide basic service documentation to ISOs working on equipment repairs; what they get beyond that varies by manufacturer.
“I have very little need to reach out to the OEMs on old technology, but there’s certain things that we’re locked out,” Massey said. “The thing that’s frustrating is that I have OEMtrained engineers who can work on these systems, and they won’t give us that access.”
Massey said he’s familiar with OEMs using what he described as “scare tactics” to denigrate the quality of technicians employed by independent service organizations and the work that they perform. He agreed that there can be a gulf between a veteran, qualified service professional and an amateur who doesn’t have the requisite level of skill to do the work. But when every technician in the same field is lumped in with one another as an excuse to run down their qualifications collectively, he bristles at the implications.
“My techs get proper training and are more than capable on their own,” Massey said. “We have a large, national support system, and remote access [technical support] has made it easier. We work with our part vendors to for-
ward-stock parts; we’re fixing these systems, most of them, in the same day.”
“We teach our techs to troubleshoot at the component level,” he said. “If they left and went to GE and now, they get the special service key, they’re better equipped because of the training they got from us. At GE, they learn how to use the service key that tells them what parts to replace. Our techs know the schematics, the service manual, everything. They have our national support to help them understand these systems.”
“By OEMs not allowing us to service that equipment, that’s really affecting patient care,” Massey said. “The hospital owns that equipment, and I feel it should be up to the hospital who services that device.”
ISOs like Crothall typically save healthcare organizations anywhere from 15 to 20 percent over OEM service contracts, but Massey offered that their true value lies in providing high-quality professionals to do the work of equipment maintenance. In a field where talent is stretched thin, and reinforcements are difficult to source, not only are both business entities competing for the same customers, they’re also pooling talent from the same sources.
“We’re going head-to-head against [the OEMs],” Massey said. “A lot of people like working for us better because there’s more opportunity with us than the OEM, because we do everything from biomed up to imaging.”
“They train in specific CTs and MRI, whereas we train our engineers on multiple modalities,” he said. “I feel our programs are a lot better. We have a lot better engineers; we compete very well against them. They’re losing a lot of business to us, and they’ve dropped their prices considerably over the last two years to compete against us.”
Nonetheless, Massey said, he’d prefer to be in a hybrid service arrangement – or something more cooperative than exists currently – which would leverage the strengths of both ISOs and OEMs in service to healthcare organizations and their patients. Rather than competing to reinforce or challenge a monopoly, he said it would be more efficient to leave service on newer technologies to the manufacturers and allow ISOs to facilitate onsite repairs in places where OEMs aren’t able to be present physically.
“We’re all for working with the OEM; they’re not for working with us,” Massey said. “I believe a hybrid model is good; newer technology should be serviced by them, older by us. I think right now government is the best bet to getting the stuff quickly. We need service keys and anything to fix this at a reasonable cost.”
Another critical consideration for the Right to Repair issue involves what’s to be done with devices that OEMs regard as “end of life” as far as their obligation to support
such equipment past a certain amount of time. Some well-maintained medical devices may have lifespans measured in a decade or longer, but OEMs may decline to service them or provide replacement parts for most of them any longer than seven years after their release.
“They’re bringing the end-of-life down, and I think that’s backfiring,” Massey said. “We can service these systems for 12 to 15 years.”
Just as AdvaMed is the advocacy arm of OEM interests, the International Association of Medical Equipment Remarketers and Servicers (IAMERS) represents the ISO world and its constituent businesses. Attorney Rob Kerwin, who serves as counsel for IAMERS, believes that the issue of Right to Repair has both never been more timely, and yet is not a legislative priority in Congress.
“While it may be important for OEMs, ISOs, and healthcare organizations, it’s challenging to get the legislators to focus on this area because of the many other matters on Congress’ plate,” Kerwin said.
Kerwin points out that, in its decision on the Digital Millennium Copyright Act (DMCA), the Librarian of Congress has exempted access and use of medical equipment servicing manuals; however, that exemption is being challenged in the courts, and ISOs are following closely along. The European Data Act contains some relevant parallels that similarly have yet to be interpreted on the issue of Right to Repair.
“Could we have a situation where the multinational medical device companies are required to share service access information in Europe, but are permitted to restrict access to ISOs?” Kerwin asked.
“Will legislators and regulators take note that, for all the hyperbole, there has been no real uptick in the reporting of adverse events? If OEM positions are truly about patient safety, why would some of the manufacturers not readily share equipment manuals with the hospitals and the servicers the hospitals choose?”
Moreover, Kerwin said, the industry of medical equipment repair has been defined by consolidation, not just within each business apparatus, but with OEMs purchasing ISOs. To him, that raises the question: “If independent servicers were so unreliable, why are they being bought by the major device owners?”
“The reality of the marketplace is that many hospitals can’t afford new equipment with struggling budgets, post-COVID financial challenges, challenging CMS reimbursement,” Kerwin said. “Therefore, legacy medical equipment is still very attractive.”
When purchasing medical devices, hospitals want a turnkey solution, Kerwin said. They often measure total cost of ownership against functional concerns including cyber-security, compatibility with existing systems, and residual value at the point of sale or retirement from active use. He believes that manufacturers that restrict access to their technologies for the purposes of maintenance may well face “diminished interest” in hospital and group medical practice purchases.
“All of this should send an economic message that it makes business sense to let hospitals chose their own servicing paths without such restrictions,” Kerwin said.
“We have very sophisticated buyers who know the lay of the land, and if the only ones who can repair the equipment are the OEMs, that’s a cost that has to be figured,” he continued. “The market situation remains challenging, and the sophistication of all the parties is great. We are still making the case that we need fundamental, level playing fields, because healthcare and hospitals deserve choices.” •






BY NICOLE DHANRAJ
Radiology is a fast-paced field where precision and efficiency are critical. But have you ever considered how the way we define disability influences not only patient care but also hiring practices, workplace policies and team culture? Many leaders still operate under a medical model of disability, focusing on individual limitations rather than examining the environmental barriers that exclude people from fully participating in the workplace.
By understanding different models of disability, radiology leaders can create a more inclusive department – one that supports employees at all levels while also enhancing the patient experience. Let’s explore the four key models of disability and how shifting perspectives can break down barriers in radiology.
The medical model treats disability as a condition inherent to the person, viewing it as a deficit that needs correction. This perspective is useful in clinical care, where diagnosing and treating conditions is essential. But when this model is applied to workplace policies, it often leads to exclusion, missed opportunities, and hiring biases.
For example, consider a CT technologist
who has hearing loss. If viewed solely through a medical model lens, leadership might assume they can’t function efficiently in a fast-moving environment because they won’t hear verbal instructions or alarms.
This assumption overlooks simple accommodations, such as captioning software, visual alert systems, and designated communication protocols, that would allow them to perform just as effectively as any other team member.
The problem isn’t the disability – it’s the lack of flexible systems that allow people to work at their full potential. When radiology leaders broaden their perspective, they move beyond outdated assumptions and find real solutions that benefit both employees and the department.
The social model of disability shifts the focus from the individual to the barriers within the environment. Instead of seeing disability as the issue, this model recognizes that the way workplaces are designed determines how accessible they are to everyone.
For instance, let’s take a patient who uses a wheelchair and struggles to access a radiology exam table. The issue isn’t their disability – it’s that the department lacks height-adjustable tables and proper transfer equipment.
The solution? Investing in accessible imaging equipment, training staff on patient mobil-
ity needs, and designing facilities with accessibility in mind.
But these barriers aren’t just limited to patient care. They exist within hiring practices and everyday workplace policies as well.
Imagine your department is hiring a radiology front desk coordinator, and one of the most qualified candidates uses a wheelchair. During the hiring process, the leadership team raises concerns:
• “Will they be able to move around the front desk efficiently?”
• “Can they retrieve files and supplies when needed?”
• “Wouldn’t it be easier to hire someone without mobility challenges?”
These questions reveal an unconscious bias rather than an actual barrier to job performance. The reality is, most front desk tasks are desk-based, and any mobility concerns can often be solved with simple adjustments, like lowered shelves, an adjustable desk, or digital file management systems.
If the best candidate is overlooked because of assumptions about what they “can’t do,” rather than focusing on what they bring to the role, the department loses out on valuable skills and diversity. The social model teaches us that the real issue isn’t the disability – it’s how we design our workspaces and policies.
This model combines medical and social perspectives, recognizing that both personal health conditions and environmental factors shape disability experiences.
In radiology, where staff are often required to stand for long periods, lift patients, and perform repetitive movements, this model is particularly relevant.
Consider a sonographer who develops chronic wrist pain from years of scanning. If treated solely through a medical model, the focus might be on pain management or surgery. However, the biopsychosocial model encourages leaders to look deeper:
• Are ergonomic transducers available to reduce strain?
• Are there scheduled breaks to minimize repetitive stress?
• Could the workload be redistributed to prevent longterm injuries?
By addressing both the individual’s needs and workplace design, radiology leaders not only support their employees but also reduce turnover and increase job satisfaction.
The Human Rights Model: Ensuring Equal Access for All
The human rights model emphasizes that people with disabilities have the right to equal opportunities and full participation in society, including in the workplace.
While the medical and social models help identify challenges and solutions, the human rights model ensures that these solutions become the standard, not just accommoda-
tions made on a case-by-case basis.
Let’s revisit the secretary who uses a wheelchair. Under the human rights model, the conversation shifts from “Should we hire them?” to “How do we ensure they have what they need to succeed?”
Instead of debating whether a candidate with mobility challenges can navigate the front desk area, the focus should be on:
• Ensuring an accessible workspace – Adjustable desks, wider pathways, and digitized systems that eliminate unnecessary movement.
• Setting inclusive hiring policies – Focusing on skills and qualifications rather than assumptions about limitations.
• Creating a culture of accessibility – Making sure team members understand disability etiquette and fostering a workplace where everyone feels valued.
When radiology leaders adopt this mindset, inclusion becomes a leadership priority, not just a compliance requirement.
Disability inclusion doesn’t require overhauling your entire department – it starts with small but impactful changes that create an accessible, supportive work environment.
• Assess department accessibility – Are front desks, control rooms, and patient care areas designed with inclusion in mind?
• Address unconscious bias – Are hiring and promotion decisions based on skills, not assumptions about disability?
• Invest in workplace accommodations – Simple tools like ergonomic equipment, captioning software, and flexible schedules can make all the difference.
• Train your team – Disability etiquette and inclusion workshops help build awareness and foster a more inclusive culture.
By shifting away from outdated perspectives and embracing modern disability models, radiology leaders do more than comply with regulations – they create a workplace where all professionals can thrive.
Disability inclusion isn’t about charity – it’s about creating a workforce that reflects the real world.
When leaders understand the different ways disability is framed, they stop seeing it as a problem to solve and start recognizing it as an opportunity to build stronger, more inclusive teams.
In radiology, where technology and patient care are constantly evolving, accessibility should be a core part of leadership strategy, not an afterthought. •
Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, R.T(R)(CT)(MR), is an experienced imaging director.


BY JIM RICKNER
In the past several years the trend has been moving toward simplifying the hardware used in ultrasound systems. Clearly, advances in technology have aided in the endeavor. From a electromechanical perspective, ultrasound systems have become much easier to troubleshoot and maintain. However, one area that has not become easier to work is the software. Manufacturers are now making software reload a tedious task for everyone but their own engineers. In the past, software reloads were commonplace as hard drives fail, and software becomes corrupt. Today, OEMs are adding levels of security, requiring service dongles, hiding/ encrypting options keys to keep owners from maintaining and fixing their systems. There are, however, several things that we can do to safeguard our ultrasound systems such as cloning the hard drive, making a bit-by-bit copy or using a hard drive disk duplicator. Let’s discuss these in detail. Let’s begin with using a hard drive disk duplicator. These are inexpensive tools that are probably the easiest and often the fastest of the methods we will discuss. There are many different brands,
but I am familiar with the StarTech Hard Drive Duplicator. A disk duplicator copies the file structure on one hard drive and places it on another. This works on some ultrasound systems such as the Philips iU22 and iE33. This process can usually be completed in under 2 hours. After completion, either hard drive can be put in the system and work. Unfortunately, a disk duplicator simply copies the files leaving behind the system data and boot information some systems require to boot or function properly.
This brings us to cloning. Cloning uses software that allows us to create an exact replica of the hard drive, including the operating system and all hidden files, which ensures a functional duplicate. Cloning should not be confused with imaging a hard drive. Imaging a hard drive creates a compressed image file that contains the data on the drive. Imaging can also be slower than cloning. For the purpose of creating a new hard drive that is identical to the one installed in the ultrasound system, cloning is the best option. We recommend EaseUS Todo Backup or HDD Raw Copy to use as a cloning software solution. Finally, let’s discuss a bit-by-bit copy of the hard drive. Although cloning and bit-by-bit copies are often considered the same there is a subtle difference. Bit-by-bit duplicates every single bit on the source drive, regardless


of whether it’s used or unused. It creates an exact, sector-by-sector replica of the drive. Cloning, on the other hand, focuses on replicating the data structure and contents of the drive, rather than every single bit. Although the slowest of the options, this makes bitby-bit the best option when creating a new identical bootable hard drive.
As we discuss ways to maintain our ultrasound systems, we need to be aware of other considerations. One consideration is patient data located on these cloned hard drives. If we are cloning hard drives with patient data on them, we need to follow HIPAA practices to safeguard them. Some systems have patient data on separate hard drives while some are all on one. Make sure you are aware of the configuration of your system. If able, delete patient data on the hard drive prior to cloning, this can also speed up the process. Another consideration is that some OEMs are adding a CDFS partition to the hard drive. CDFS stand for Compact Disc File System, and they are often used to load software or boot files that need to be accessed as if they were on a CD, and it helps protect those files from being overwritten. This creates a problem when cloning a hard drive as this partition may not be copied over. To determine if your hard drive contains this partition go to the hard drive
properties and it will define the file systems present. If you are unsure whether your system uses this CDFS partition, make sure to test your newly cloned drive in your system. Lastly, make sure to clone your system hard drive while the unit is operating normally. If you wait until there are issues with the hard drive or software, cloning will not solve your problem.
I have discussed some of the issues surrounding the maintenance of your ultrasound systems. Many systems come without software and others provide it but lock you out of being able to reload it. I’ve provided some alternate methods of capturing your system software and settings that can work if executed while the system is fully functional. After cloning a hard drive make sure to install it into your system to make sure it is functional. Make sure to safeguard any patient data that might be on the cloned hard drive as it is HIPAA data. Taking these steps can save you substantial expenses in software and service costs. •
Jim Rickner is the Director of Service and Training with Advanced Ultrasound Systems (AUS).
For more information about Advanced Ultrasound Systems (AUS) visit advancedultrasound.com.
Recently, I have been doing some research on how our leaders can assist our team members focus on the important tasks they have to do as a part of their job. Each position is critical. If we could eliminate a step in our process and not require a person to perform that task, we would eliminate it. If we are asking people to do something, it needs to be done accurately.
Unfortunately, as humans sometimes we lose focus. We are easily distracted. We are asked to do more and given less time to do it. Some of us have developed a habit of multitasking, which really doesn’t work as well as we think it does. When we try to do more than one thing at a time, it is just not possible give it our full concentration. It also decreases productivity, even though multitasking sounds like it does the opposite. It takes much longer to complete a task if we are trying to do something else at the same time.
In a medical imaging department, lack of focus can cause errors which can lead to harm to our patients. While this is never intentional, it is reckless behavior.
I learned a few things about focus. Getting a grip on our ability to focus can reduce stress and help us avoid mistakes. Focusing on one task allows for more time to understand the details resulting in more effective solutions. We need to be intentional about being accurate.
This also all relates to time management skills. I ask techs to plan the day. Run that schedule of patients, don’t let it run you. This is easier said than done.
After reviewing several resources regarding focus, I determined that they all pretty much said the same thing.
I discovered that most information included lists that looked something like this:
1. Be self-aware. Is your focus scattered or directed?
2. Avoid distractions.
3. Take care of your body.
4. Practice concentration.
5. Make concentration a daily habit.
6. Prioritize time to unstimulate your brain.
7. Take regular breaks.
Attention drifts are going to happen, and we need to be prepared for them. The number one distraction is our cellphones. We need to put them away where we cannot be tempted to be distracted by them. This is a no brainer. To

BY BETH ALLEN DIRECTOR’S CUT
reduce the chance of making an error that could cause a patient harm, which could not only lead to a poor outcome for the patient, but it could also lead to corrective action or loss of an imaging license, it seems smart to put the phone away. That phone can drain our mental energy, having less to spend on the details that are required to do our jobs correctly.
Concentration is a skill that can be learned. You can train for it like you would a sport. Elite athletes plan their nutrition, rest and physical activity. As we are people with important jobs taking care of other people, we should do the same. I have read in multiple places that under 7 hours of sleep per night can make it more difficult to concentrate. Food choices and hydration also contribute to our mental focus. A diet high in sugar can lead to brain fog. Exercise is important because it releases neurotransmitters that stimulate our ability to concentrate. We don’t have to run a marathon. Even a short walk will help our brains.
If we practice concentration and focus regularly, we will get better at it. One technique is to set a timer and concentrate on something for that amount of time, then take a short break and start over again. The more we practice, the more skilled we will become. We can make it a habit.
This is easier in the morning before our brain has had time to become distracted by too many things. To be able to carry our attention into the afternoon, we need to unstimulate our brains. That can happen over a lunch break, which is a great time to take a short walk. Some people may be able to meditate for a few minutes. It does not mean it is a good time to take out our phones and scroll for 30 minutes. That is not a mental break.
This is all great advice that I need to use myself. It all makes sense. We don’t allow our brains to become bored anymore. For me, I find that solutions to problems come to me in the shower. This is likely because that is a time and place where my mind is not being distracted and my thoughts can just wander. There is a lot of creativity that can happen when my brain has time to rest.
Our jobs are too important to go about our routines on auto pilot. Our patients deserve our focus and concentration. We can flex that muscle and reduce our own stress at the same time. It is a win-win. Thanks for all you do. •
Beth Allen, RT(R)(CT), CRA, is the director, clinical operations at Banner Imaging






























This immersive experience offers:
· Meaningful Connections –Engage with peers facing similar challenges and goals





· Leadership Growth – Discover new tactics to enhance your leadership approach and problem-solving abilities

Step into the spotlight at AHRA’s 2025 Annual Meeting and take your leadership skills to the next level. This isn’t just a conference — it’s an all-encompassing experience designed to give you the tools, strategies, and connections you need to thrive in the ever-evolving medical imaging field.
· Technology in Action –Experience live demos and hands-on interactions with cutting-edge equipment
· Expert Insights – Learn from top industry leaders












BY MARK WATTS PACS/IT
’ m always on the lookout for opportunities to help you elevate your expertise and connect with the brightest minds in our field. Mark your calendars because SIIM 2025 in Portland, Oregon, from June 11-14, is shaping up to be an unmissable event! Beyond the beautiful scenery and fantastic food that Portland offers, my hometown. SIIM is bringing together a powerhouse of presenters ready to share their invaluable insights.
Let me give you a sneak peek at some of the luminaries you’ll have the chance to learn from:
• Paul Nagy: A true visionary in medical imaging informatics, Dr. Nagy consistently pushes the boundaries of what’s possible. His sessions are always thought-provoking, offering a glimpse into the future of our field. Why attend his presentation? Expect to gain a deeper understanding of cutting-edge technologies and strategic approaches that can transform your practice.
• Dawn Cram: With her extensive experience in clinical informatics, she brings a practical and insightful perspective to the challenges and opportunities we face daily. Why attend her presentation? Look forward to actionable strategies and best practices that you can implement immediately to improve workflow and efficiency.
• Woojin Kim: Dr. Kim is a leading expert in artificial intelligence and its application in medical imaging. His presentations demystify complex AI concepts and showcase their real-world impact. Why attend his presentation? Prepare to be inspired by the potential of AI to revolutionize diagnostics and patient care, and gain clarity on how to navigate this rapidly evolving landscape.
• Teri Sippel Schmidt: Sippel Schmidt’s expertise in imaging informatics leadership and education is un-
paralleled. She has a knack for empowering individuals and teams to excel. Why attend her presentation? You’ll gain valuable insights into effective leadership strategies and practical approaches to fostering growth and innovation within your department.
• Nina Kottler: Dr. Kottler is a renowned radiologist and researcher with a deep understanding of the clinical applications of imaging informatics. Her presentations bridge the gap between technology and patient care. Why attend her presentation? Expect to learn about the latest clinical advancements and how informatics plays a crucial role in delivering optimal patient outcomes.
Judy Gichoya: Dr. Gichoya is a passionate advocate for addressing bias and promoting equity in AI and medical imaging. Her work is critical in ensuring that technological advancements benefit all patient populations. Why attend her presentation? Be prepared for an eye-opening discussion on the ethical considerations of AI and how we can build more inclusive and equitable imaging systems.
SO,
Because these aren’t just lectures; they are opportunities to learn from the best, engage in stimulating discussions, and gain knowledge that can directly impact your work and your patients’ lives. You’ll walk away with fresh perspectives, practical tools, and a renewed sense of purpose in your vital role in the healthcare ecosystem.
Don’t miss out on this incredible chance to learn, connect, and grow at SIIM 2025 in Portland. The topic I would recommend concentrating on is the importance of Pre-Determined Change Control Plans by the FDA in Medical Imaging Artificial Intelligence.
Following our discussion on the importance of Pre-Determined Change Control Plans (PCCPs), let’s now focus
on how the FDA’s approach to PCCPs specifically for imaging artificial intelligence (AI) differs significantly from current practices for traditional medical devices and even earlier AI implementations. This shift reflects the unique dynamic and adaptive nature of AI algorithms.
Currently, the traditional FDA pathway for medical devices, including software, often operates on a “lockand-key” principle. Once a device receives clearance or approval, significant changes, especially those affecting performance or intended use, typically require a new premarket submission (e.g., a 510(k) supplement or a new De Novo application). This model can be cumbersome and slow the iterative improvement that is inherent to AI development.
Here’s how FDA’s PCCP framework for imaging AI marks a departure from this traditional approach:
1. Embracing Adaptability and Continuous Improvement
• Current Practice: Traditional devices and even early “locked” AI algorithms are largely static after-market authorization. Updates often necessitate a new review cycle.
• PCCP for Imaging AI: The FDA recognizes that AI algorithms, particularly machine learning-based ones, are designed to learn and improve over time with new data. PCCPs provide a mechanism to prospectively outline anticipated modifications to the AI model (e.g., retraining with new datasets, adjusting model parameters) within pre-defined boundaries, without requiring a new submission for each change. This fosters a life cycle approach to regulation.
2. Prospective Review of Planned Changes
• Current Practice: Changes are typically reviewed after they are developed and implemented (or planned for implementation), often triggering a regulatory hurdle.
• PCCP for Imaging AI: Manufacturers are now encouraged to submit a detailed PCCP as part of their initial premarket submission. This plan outlines the types of modifications they foresee, the protocols for evaluating these changes (including validation and testing metrics), and the criteria for determining if a modification falls within the pre-approved scope. The FDA reviews and authorizes this plan upfront.
3. Risk-Based Approach to Change Management
• Current Practice: All significant changes might trigger a similar level of regulatory scrutiny, regardless of the potential risk.
• PCCP for Imaging AI: The PCCP framework emphasizes a risk-based approach. Manufacturers need to
clearly articulate the potential impact of planned modifications on the device’s safety and effectiveness. The level of detail and rigor required in the PCCP will likely be proportional to the potential risk associated with the anticipated changes.
4. Focus on Transparency and Labeling
• Current Practice: Device labeling typically describes the device’s functionality at the time of market authorization.
• PCCP for Imaging AI: The FDA emphasizes the need for clear labeling that informs users about the AI’s adaptive nature and the existence of an authorized PCCP. This ensures users are aware that the device’s performance or outputs may evolve over time through software updates.
5. Emphasis on Performance Monitoring and Validation Protocols
• Current Practice: Post-market surveillance often relies on adverse event reporting and periodic reviews.
• PCCP for Imaging AI: PCCPs require manufacturers to define robust protocols for monitoring the AI’s performance in the real world and validating the effectiveness and safety of any implemented changes according to the pre-approved plan. This signifies a more proactive approach to ensuring ongoing safety and efficacy.
In essence, PCCPs for imaging AI represent a shift from a static, reactive regulatory model to a more dynamic, proactive, and life cycle-oriented approach. This framework aims to balance the need for innovation in this rapidly evolving field with the FDA’s mandate to ensure the safety and effectiveness of medical devices. It requires manufacturers to think ahead, plan for change, and demonstrate a robust understanding of how their AI algorithms will be managed and monitored throughout their life cycle.
This evolution in regulatory strategy is crucial for realizing the full potential of AI in medical imaging while maintaining the highest standards of patient care. As we learn more at SIIM 2025, understanding these shifts will be paramount for all stakeholders in the imaging AI ecosystem. •
Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.

BY DANIEL BOBINSKI
he workplace seems to be spinning faster these days. We live in a hyper-connected world of instant messaging, video calls, and digital paper trails. But one thing hasn’t changed much, and that’s the impulse to point the finger of blame as soon as possible when something goes wrong.
Granted, some person or some department may ultimately need to be identified as being at fault for a problem, but simply identifying who gets the blame and stopping there does not solve the problem. In fact, placing a spotlight on who’s to blame and making a big deal of it often creates more problems than it solves.
This blame game is as old as time. In the book of Genesis, when God asked Adam if he ate the forbidden fruit, Adam immediately blamed Eve. When God questioned Eve, she promptly blamed the serpent. This is the first story we have of something going wrong and blame was everyone’s first choice!
If you’re a parent or you’ve spent time around children, you know this tendency seems to be hardwired in our genetic makeup. Ask any young child about something that went wrong and they’ll instantly tell us someone else is to blame. It’s remarkable how humans of all ages deflect personal responsibility. It’s even more interesting that nobody teaches us this behavior. It comes naturally.
Let’s consider someone who’s been promoted into management but practices the blame game. You’ve probably seen it. A project deadline is missed, and the manager immediately opens up the project management program to learn which person or team is the guilty party. That’s reasonable enough, but if all the manager does is contact that person or department and gets on their case, the manager isn’t making progress for improving the team.
Another situation might be managers spending too much time in meetings talking about why mistakes are bad. We
know these things. A better use of time is discussing ways to prevent a mistake from happening again.
In other words, pointing only to who caused a problem does nothing. However, if true solutions are discussed and implemented, the likelihood of similar future problems occurring is greatly diminished.
I hope the blame game isn’t an issue at your workplace, but if you see it happening – whether in-person or through emails or text messages – I urge you to work toward changing it. Having consulted across numerous industries, I’ve observed how a culture in which blame runs rampant leads to lower commitment levels and reduced effectiveness, as well as plummeting morale.
In fact, over the past decade, you’ve probably noticed an increase in people feeling it’s OK to be snide and snippy in their digital communications. I am regularly appalled as I see people say things digitally that they would never say to someone’s face. This is particularly dangerous because the absence of face-to-face interaction makes restoration of trust even more challenging.
To err is human, so it really helps if us humans have a way to get past the blame game. A structured approach helps, and the following four-step plan creates an easy-to-remember framework:
1. Analyze and define the problem. For larger problems that have complex situations, I strongly recommend conducting a “root cause analysis” (an online search will reveal several methodologies). Without a clearly defined target, it’s impossible to develop solutions that address the actual problem rather than just putting bandages on its symptoms.
2. Identify viable solutions. Too many people think good leadership means solving problems quickly. Sometimes that’s absolutely necessary, but more
often, an effective solution developed over time is better than a quick, efficient one.
3. Evaluate and implement a solution. This means working collaboratively, even if it’s over distances. More than one set of eyes should evaluate potential solutions to ensure the best chances for longterm success, and with phones and video conferencing readily available anyplace and anytime, take advantage of those communication avenues.
4. Determine prevention strategies. Identify which systems, training, or changes can be implemented to prevent similar issues in the future.
One effective technique when going through these steps is examining what’s known as the four P’s: People, Products, Policies, and Procedures. For each category, we can ask –and answer – some direct questions:
People: Do team members have adequate training? Are communication problems occurring? (This is especially important in remote settings where nonverbal cues may be missed.) Are the right people in the right roles? What feedback do those closest to the problem have about preventing recurrence? Is management willing to make necessary adjustments?
Products: Did the problem result from using incorrect tools or platforms? Was the right technology used incorrectly? Are better tools available? Is there a system for regularly evaluating and updating our technology and resources?
Policies: Do clear policies exist for both in-office and
remote work? Are they documented or just assumed? Who creates them? How are they communicated and enforced across different work environments? How can policies be reviewed more effectively?
Procedures: Do procedures exist for the circumstances surrounding the problem? If not, can they be created? How are procedures taught, especially to remote team members? Is there a better way to document and share procedures in your digital workplace?
The list of questions above is not exhaustive, but notice one thing. Nowhere do you see, “Who screwed up?” If we’ve hired someone not suited to the job and that person is the cause of multiple problems, it’s one thing to blame that person. However, in reality, we have another root issue to solve, and it likely involves our hiring process, our training or our onboarding procedures.
The bottom line is that the blame game is shortsighted and should be avoided by those who consider themselves professionals. A better approach is to first ask the right questions, identify what caused the problem in the first place, and then take corrective actions. •
Daniel Bobinski, Th.D. is the author of the best-selling book “Creating Passion-Driven Teams” and the owner of Workplace Excellence. Also a certified behavioral analyst, Daniel consults and conducts training on workplace effectiveness and leadership development. He can be reached at danielbobinski@protonmail.com or eqfactor.net.




BY FAMILY FEATURES
Awalk isn’t just good for your body; it’s a simple, powerful way to care for your mind and soul. Physical activity, like walking, reduces stress, boosts mood and promotes overall well-being. Yet physical activity levels in the United States continue to decline, a trend threatening both mental and physical health.
Less than half of adults and fewer than 1 in 5 children in the U.S. get the recommended amount of physical activity needed for heart health, according to the American Heart Association’s 2025 Heart & Stroke Statistical Update.
National recommendations call for children to get at least one hour of physical activity each day, but the latest statistics show less than 19% of children in the U.S.
achieve that target. Meanwhile, less than half of adults get the recommended 150 minutes or more of weekly physical activity.
What’s more, according to data from a National Health and Nutrition Examination Survey, 1 in 4 U.S. adults sits for longer than eight hours each day, which can have negative consequences on physical and mental health.
For decades, the American Heart Association has championed the importance of physical activity in communities across the country. These tips and information can help you understand how a brisk walk can make a world of difference for heart health and mental clarity.
Staying active is one of the best ways to keep your mind and body healthy.
The physical health benefits may be obvious, but
research suggests physical activity can also help bring more joy to your life. According to the 2019 Physical Activity Guidelines for Americans, people who get the recommended amount of physical activity are less likely to experience depression.
Regular physical activity enhances your mood, sharpens your mind, improves sleep and boosts overall well-being, all while reducing the risk of disease and depression and increasing the quality and longevity of life.
Exercise as simple as a brisk walk can put a major spring in your step. It can even energize you to finish other tasks at hand, whether it’s cooking or running errands. Give your daily physical activity level a boost with these tips:
• Exercising outdoors is a great way to get moving. Spending time outdoors has been shown to reduce stress, promote a sense of belonging and improve mood. It’s even better if you can enjoy the sunshine outside, which can improve mood, boost your immunity and help you get some vitamin D.
• Invite a family member or friend along with you.
It’s good for them, it’s good for you and it’s good company all around.
• Instead of wondering if you’ll move today, explore how you’ll move. A walk, a dance or a stretch all count.
Pets are part of your family, and they can help you get healthy together. Pets provide a fun reason to spend more time outside and get the exercise needed to reduce the risk of disease later in life.
Getting moving along with your pet adds more exercise to your routine, which means living longer, reducing risk of dying from heart attack or stroke, reducing risk of diabetes, reducing stress and even boosting your overall happiness and well-being.
Exercising with your pet can also mean enjoying more socializing. You may find yourself meeting other dog owners in your area on a walk or at the dog park. •
Learn more about how simple habits like walking can support your overall health at heart.org/MoveMore.
























































































































































































































































































































































The Association of Medical Service Providers (AMSP) recently held its winter meeting in Florida. AMSP is a national association of independent medical service providers whose common goal is a dedication to the support and improvement of the member organizations by providing process
1. AMSP Business Manager John Snyder welcomes Medical Imaging Systems President Marc Schaefer from Birmingham, Alabama.
2. The rooftop ocean terrace provided a great view as AMSP members Brian Doak and Chuck Lambert with Radon Medical chatted with Adam Tiberius and Steffan Mortimer from Zenopa Inc.
3. A golf outing provided another opportunity for AMSP members to network. Among those hitting the links are Brian Doak with Radon Medical, Billy Luety with TI-BA Enterprises and Dave Francoeur with Downtime Trace.


improvement, revenue growth initiatives, expertise sharing and regulatory compliance. Today, membership exists across the United States. This extensive membership has developed a strategy that allows AMSP to effectively negotiate and compete with the OEMs and national ISOs.
4. AMSP Members network at two large tables during the member dinner.
5. AMSP networking events are a popular aspect of the winter meeting. John Snyder is seen with the hotel’s event coordinator, Mike Halsey with Chesapeake Medical Systems Inc., Associate Member Maritza Jones with PaxeraHealth and AMSP Treasurer Bill Laird with Brandywine Imaging.
6. AMSP vendor presentations like this one from Zenopa Inc. provide insights and tips for members to take back to their businesses following the annual meeting. 1 2 3 6 5 4




Radon
Maull


• $300 a month
• 1/6 page ad included in the marketplace
• Up to 5 categories in our ICEDEX
• Your company name, website and phone included in your ICEDEX listings
• Your company name in the alphabetical business index
• Appear in the print and digital magazine






















Register to view the webinars each month
Watch recorded webinars on-demand
3.EARN
ARRT Category A CE credits pending approval
Ray-Pac proudly reintroduces the INTERAY name to the x-ray tube replacement industry. Our direct replacements for Canon / Toshiba diagnostic tubes are now available from the country’s leading manufacturer of aftermarket x-ray tubes. Trust the best to deliver “When Quality Counts”

