State
44






44





Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking.
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering. This helps maximize uptime and minimize repair costs.





Kenneth Saltrick, President of Engineering Services in Twinsburg, Ohio, knows from his long experience that C-arm machines themselves are absolute workhorses.
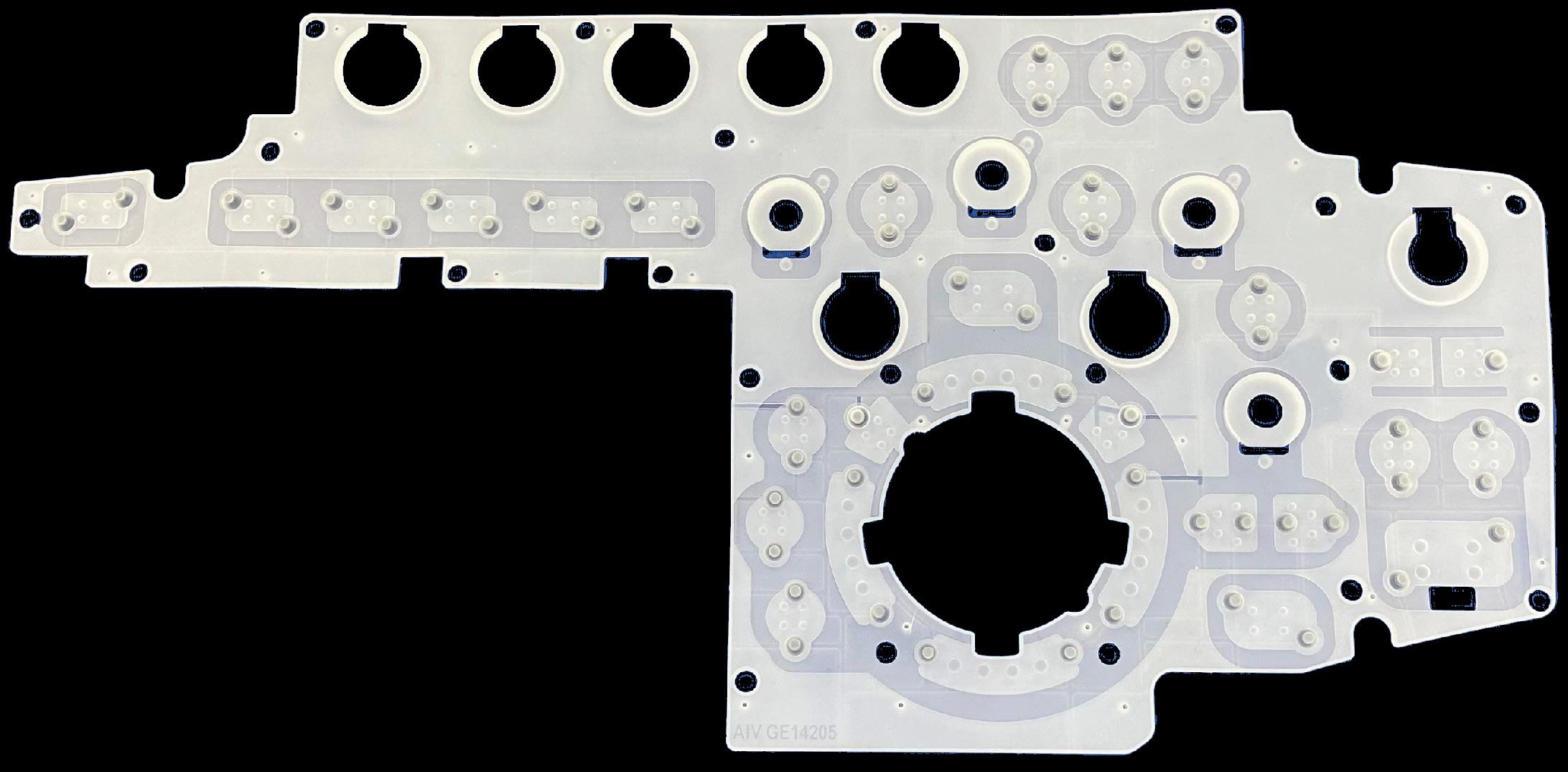
For customers looking to blend the gap between expensive OEM and unreliable used assemblies, WE have your solution.
Our complete repair contains a new cable assembly, utilizing all OEM cable and components with a harvested plate and connector housing as they are proprietary items. These completely repaired products will have a significant cost savings with build quality above new OEM products and carry a warranty of 180 days, which is untouchable in the market.




You can’t be an effective leader if you’re exhausted, reactive, and constantly running damage control. This isn’t about just “self-care.” This is about taking back control of your time, energy and sanity.
A look at the state of imaging including personalized medicine, particularly in the fields of oncology and neurology, where surgeries, therapies, and radiopharmaceuticals are all guided by diagnostic and interventional imaging studies.

Raleigh Radiology’s Christina Allen, RT (R)(MR), is a Rising Star in the diagnostic imaging community.
JULY 2025

Catch up on the latest news from around the diagnostic imaging world.


This month ICE Magazine looks at imaging training options.
Stress is part of life. Whether you’re leading a team, raising a family, or managing a project, stress finds its way into the equation. But is stress always a villain?
MD
President
Vice
Kristin
Vice
Jayme
Senior
Megan
Editorial
Editorial
Beth
Senior
Art
Kristin
Digital
Cindy
Accounting

Ra leigh Radiology Associate Director of Compliance and Regulatory Affairs Carmen Geerlings nominated C hristina Allen, RT (R)(MR), as a Rising Star.
“Christina is an asset to our team and takes on far more than typical supervisor duties. As our organization has moved from 3rd party MRI management and services to bring MRI in-house, she has launched our MRI safety program and has worked as a primary point of contact for the installation of two new MRI units in our outpatient offices. Even with all she does, she makes sure that all her team members are taken care of and works tirelessly for the patient’s best interest.
Christina holds a bachelor’s in healthcare science and currently serves as an MRI supervisor with Raleigh Radiology. ICE Magazine took some time to find out more about Christina via a Q&A session.
Q: WHERE DID YOU GROW UP?
A: Philadelphia, Pennsylvania
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/ EDUCATION?
A: I completed a radiologic technology program at Tower Health Hospital in Reading, Pennsylvania, where I began gaining hands-on experience early by working as
a student X-ray technologist in the evenings following clinical shifts. After graduation, I spent two years working in emergency and operating room settings before transitioning to the MRI department at Reading Hospital. There, I had the privilege of working alongside some of the most skilled MRI technologists in my career. They were instrumental in mentoring me and shaping my technical expertise. I earned my bachelor’s degree from Alvernia University while balancing fulltime work.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: In high school, I developed a passion for photography. I loved capturing images, experimenting with exposure, and learning how to develop film. At the same time, anatomy was one of my favorite subjects. Combining these two interests felt like a natural fit.
Q: WHAT IS THE MOST REWARDING ASPECT OF YOUR JOB?
A: I’m passionate about helping others, whether it’s working as a technologist scanning a day of scheduled patients, mentoring students, or developing policies and procedures to improve our organization. I find great fulfillment in being someone people can rely on, especially when they need support the most.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: What I enjoy most about my position is the ability to develop and implement policies and procedures that not only enhance patient workflow but also keep MRI safety and patient care as top priorities within our organization.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: What interests me most about the imaging field is the strong sense of teamwork across the entire organization. Providing the best care to our community isn’t the work of just one department or individual; it requires collaboration among many highly skilled and trained professionals working together toward a common goal.
Q: WHAT IS YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: My greatest accomplishment has been developing a deep expertise in the complexity of MRI and having the knowledge to develop policies and procedures that others utilize in their day-to-day workflow. This has allowed me to confidently and effectively lead my department of MRI technologists in delivering exception -
al care with strong fundamentals. I’m also proud of the role we play in mentoring students, helping them build a strong foundation of skills early in their careers, and being an example of what it looks like to take extra effort for our patients.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: In the next five years, I hope to lead process improvement initiatives on a broader scale, with the goal of developing standardized MRI safety and patient preparation criteria that can be adopted across the industry. •
FAVORITE HOBBY: Throwing on the pottery wheel
FAVORITE SHOW: “Schitt’s Creek”
FAVORITE FOOD: Asian Fusion
FAVORITE VACATION SPOT: The beach
1 THING ON YOUR BUCKET LIST: Eat homemade pasta in Italy
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU: I lived in Japan.
BY JOHN WALLACE
Banner Imaging Associate Director Angela Naylor’s resume is what every hiring manager dreams of when looking for an imaging leader. She has 33 years of clinical experience as a registered radiologic technologist, 18 years of clinical experience as registered mammographer and 20 years of experience in a lead/supervisory role. Add to that her proven ability to be a good team player with excellent work habits and leadership skills and you have an ideal hire.
Banner Imaging Director of Clinical Operations Beth Allen suggested Angela for the In Focus feature in ICE Magazine.
“She is one of our associate directors and has been a part of our team for decades! She has been very influential in the creation of our team over the years, and I am excited for her to share her insights,” she wrote.
Interestingly enough, Angela did not start her higher education seeking a career in diagnostic imaging.
“My original plan was to go to nursing school,” Angela recalls. “I had a wonderful professor in college ask if I ever thought about radiology, he gave me some information on the radiology program at Gateway Community College. I did some research and decided to apply to both programs. I was placed on a waiting list for the nursing program and was accepted into Gateway’s Radiologic Technology Program and 33 years later here I am.”
It is an opportunity that continues to pay dividends.
“For me, it’s making a difference every day,” Angela explains as to why she loves her job. “From our teams to the patients we serve, our partners within Banner and outside of
Banner and our community. It’s the people part I really love and being part of our leadership team.”
As for leadership, Angela’s goal is to serve as a catalyst for others.
“I aim to inspire and motive others, I enjoy partnering with our leaders, building trust and meaningful relationships,” Angela says. “Prioritizing time to build those connections, being a reliable resource and maintaining a good balance for coaching and support are important to me. I also try to adapt and fit the specific needs of a circumstances and/or individual to meet goals.”

She adds that working with a mentor helps her meet her goals and grow as a leader. She also loves it when she is able to assist a colleague.
“Kara Mayeaux has been a mentor to many of us here and she has guided me through my career. Her ability to connect with others, making it a point to really understand processes, digest the information to be able to come to decisions with a clear intent and her overall integrity are qualities I really respect,” Angela says. “I have gained a greater ability to navigate challenges and make those harder calls working alongside with her. Kara has a gift of sharing the vision and this has helped me broaden my mindset and how our overall actions impact us and basically being able to keep the bigger picture in mind.”
“I work with a group of managers myself and hope to

inspire them just as Kara has and continues to enrich my journey,” Angela adds. “The best part of my day is working with other leaders and being able to support their growth journey. Over the years, it brings joy to me to see team members’ development that I hired. Whether that be continued schooling, cross training or moving into a leadership role.”
Away from work is where you can find Angela’s greatest accomplishment.
“Being a mom,” is what Angela lists as her greatest accomplishment. “Seeing your kids become good-hearted, thriving, honest adults is the greatest feeling. My parents were hard working role models, and my goal was to provide that same foundation to my kids. Second would be around the 33 years with initially the same organization, step by step evolving and supporting outpatient imaging through change, challenges and our growth.”
Speaking of 33 years with the same organization … “I have been married for 33 years, we have built a great life together including two incredible kids along with multiple family pets through the years. Currently, we have two very spoiled dogs. We are very proud of our kids’ paths and the adults they have become, we love watching their growth and life experiences.” •
1. What is the last book you read? “The Women,” and currently reading, “Be The Unicorn”
2. Favorite movie? Oh my gosh, so many … “The Breakfast Club,” “16 Candles,” “Thelma and Louise,” “Stand By Me” are a few that never get old, even as old as they may be!
3. What is something most of your coworkers don’t know about you? I’m afraid of heights, a true crime junkie and passionate about supporting animal shelters locally and one in Rocky Point.
4. What is one thing you do every morning to start your day? I like to start my day with a nice brisk walk, then coffee!



5. Best advice you ever received? Work hard, stay humble.
6. Who has had the biggest influence on your life? I have been very blessed to surround myself with many amazing people in my life, but my mom must be at the top by showing resilience and inner strength even when things are hard.
7. What would your superpower be? Flying, to overcome my fear of heights!
8. What are your hobbies? Hiking, gardening, attending music festivals and supporting animal shelters.
9. What is your perfect meal? Can’t pick one, but between tacos and good seafood.

BY MATT SKOUFALOS
For the next eight years, the U.S. Bureau of Labor Statistics anticipates significant opportunity in the imaging field for MRI and rad techs: a need to add 16,000 professionals annually to meet the growing demand for medical imaging services across a variety of patient populations.
At Children’s Wisconsin, Imaging Manager Jennifer Peterson took a look at those numbers and saw an opportunity to push back against the deficit. For the past 18 months, she’s spearheaded the development of a dedicated pediatric imaging technologist training program, creating just the second such school in the United States. It’s intended to help address the ongoing shortfall of radiologic technologists in the field, especially in a specialty that’s traditionally lacked the same level of attention as others.
“Typical to other service lines, we’re experiencing an imbalance between the number of qualified applicants for a job and the number of jobs posted,” Peterson said.
“Before COVID, we’d seen this spike in vacancy rates, with a declining supply of certified exam-takers versus the job vacancy rate of radiographers over time,” she said. “We want to educate pediatric technologists in the workforce, and develop a pipeline for the imaging workforce.”
The program, which was created in partnership with the Joint Review Committee on Education in Radiologic Technology (JCERT), should receive its first cohort of 10 students in September 2026. They will be taught by four faculty members – a program director, clinical coordinator, and two clinical instructors – from Children’s Wisconsin. Additional affiliations are being explored with institutions located in Wisconsin, Michigan
and Minnesota.
To certify their education, the Children’s Wisconsin pediatric imaging training program will endeavor to have 85 percent of its graduates successfully complete the American Registry of Radiologic Technologists (ARRT) credentialed exam on their first attempt, and 100 percent of graduates complete it within two attempts. Peterson said the program aims to place 80 percent of its students on a jobsite within one year of graduation, and maintain an annual attrition rate of less than 30 percent.
“You set that bar, you re-evaluate, you continue to push yourself,” she said. “How can we continue to align within our own department, and push forward and be a contributor at a different level?”
Students’ education will be delivered through online coursework and virtual learning as well as in-person schooling at a dedicated learning environment housed within Children’s Wisconsin. JCERT helped craft the course by identifying faculty to support that program and their levels of education, a manageable class size based on the number of techs, equipment, didactic policies and procedures; and ASRT guidelines for coursework.
Applicants will be admitted through a direct process, which requires them to have completed a minimum of an associate degree, college-level anatomy and physiology I and II, medical terminology, and algebra.
A second “two plus two” pathway would be available for students at colleges and universities with which Children’s Wisconsin has formed affiliation agreements. Students at these institutions would attend them their freshman and sophomore year, and then, once accepted, complete their junior and senior schoolwork at the hospital within their schools.
“[JCERT has] a really well laid-out structure for you to
follow to make sure that you’re having your students graduate,” Peterson said. “We want people operating at the top of their licenses; certified technologists that are well-versed in what they do and what they need to do.”
Peterson said that creating the program reflected her efforts to make an impact on the vocational vacancies in pediatric imaging. She credited the “overwhelming support and excitement” of her colleagues, “from the start to where we are now,” in its development. It launched April 22.
Peterson said she was grateful “to have the support of our executive team to do things differently, look at process improvement, and focus on education.”
“The awesome thing about pediatric institutions and imaging as a whole is everybody wants you to win – on behalf of the program, on behalf of the profession,” she said. “It’s a really tight-knit group, and with support all around, has really been an incredible thing to be a part of.”
The importance of professionally trained technologists isn’t just underscored in the quality of images that they’re obtaining, Peterson said; it also lies in learning how to work with board-certified pediatric radiologists, how to position young patients, and how to manage safe radiation doses for the most medically vulnerable kids they may encounter at Children’s.
“In an adult imaging program, they don’t have that dedicated patient population of pediatrics, [but this training] sets them up for more success,” Peterson said. “This education can be transferred and helpful to those patients you’re seeing in adult institutions or in a rural area.”
At work, Peterson is thinking about how to develop the next generation of talented caregivers for children, while at home, she is raising Arthur, 4, and Aggie, 2, together with her husband of nine years, Trevor. Peterson is also a lifelong equestrian, who’s competed in dressage at the amateur level; sadly, last year, she lost her lifelong partner, a 29-year-old horse named Zu.
“You always are trying to do something with purpose, and your competitor is yourself,” Peterson said. “We joke that you don’t know true partnership until your partner is 1,200 pounds and has a mind of their own.”
These days, she keeps active with a Milwaukee group called Team Phoenix, through which women who have survived cancer train together for a sprint triathlon – a 500-meter swim, 15K bike, and 5K run. A 2018 survivor of Hodgkins lymphoma, Peterson said the experience of training with people who understand what she’s been through is “rejuvenating.”
“Health is important, well-being is important; as a cancer survivor, your life depends on it,” Peterson said. “You do much better when you stay active, so it’s a really important thing to keep in focus.” •



Finally, the features you love most about your favorite ride share app, food delivery app, Angi, UpWork, or TaskRabbit are available for medical imaging equipment maintenance and repair.
Enter a Trace Ticket with one tap to broadcast your repair needs to a network of qualified technicians.
Review Bids to find the best service option for improved repair outcomes with less equipment down time, resulting in a lower overall cost.
Track progress, issue payments and rate services all in a single dashboard.


Speed
Instantly blast your service request to every qualified and vetted service provider

From response times to uptime, you no longer have to rely on service companies to track their own activities and performance


Like your favorite personal apps, get in-app alerts when a service technician is on their way, arrived, waiting for a part, completed a job, etc.
Competitive bidding among service technicians allows you to get the best price and only pay and track one entity




BY JOHN WALLACE
Steve Cannon, 68, passed away May 11, 2025. He served his country in the U.S. Air Force and worked in healthcare for 45 years. When he wasn’t working, he loved to ride his motorcycle and work on his farm. He is survived by his wife, Becky Cannon; son, Preston Cannon; daughter, Amber (Steven) Guarino; and four grandchildren –Phoenix, Rocco, Allie, and Vinny.
Dave Francoeur, president of medical equipment service at Downtime Trace, shared news of Steve’s passing with colleagues in a heartfelt email.
“It is with a heavy heart that I let you know our dear friend Steve Cannon passed away on May 11, 2025. His loss is felt deeply by all of us who were lucky enough to know him,” Francoeur wrote. “Steve was more than a colleague or a friend – he was a true companion, a confidant, and a constant source of light. His kindness, his humor, and the genuine care he brought to every relationship left a lasting impact on all of us. I will forever cherish the memories we shared and carry his spirit with me.”
“Words can’t fully express the influence Steve had on my life – both personally and professionally. He challenged me to think more deeply about who I am and how I contribute to the growth of others. He reminded me that writing isn’t just a task – it’s a powerful way to communicate intent and shape how others see us,” he continued.
“Steve was an incredible sounding board. He listened, offered feedback, and helped me shape ideas that I believed could change the professional world we live in. He was supportive, but never afraid to offer a reality check – and always encouraged me to push beyond what felt

comfortable,” Francoeur added.
Steve enjoyed a long and distinguished career in the healthcare technology and the asset management industry. He held executive leadership positions at Sun Health and Premier, one of the nation’s largest GPOs. He served as the inaugural president at AllParts Medical, and held executive leadership roles at Aramark, Philips Healthcare, Sodexo and Althea U.S. MD Publishing President and Founder John Krieg says the world lost a leader and gentleman who inspired everyone he met.
“Having known Steve for over 25 years, it is easy to see the love and outpouring of support for him and his family. His presence was felt immediately when he entered a room. He was a man of great strength, morals and fiercely loyal. His handshake is all you needed to know about the quality of the man he was,” Krieg said. “He was a pillar in our industry, someone who helped forge the path for so many great people and companies. He touched lives in more ways than one could count, anyone who spent time with him was better off, and he will be deeply missed.”
Tim Riehm, executive vice president with U.S. Medical Equipment Consultants Inc. (USMEDIC), first met Steve in 2002 and soon thereafter moved to North Carolina where the two men worked together to create an Aramark training center.
“Steve was very detail focused and always put 100% into everything he did. There were no short answers when you asked Steve a question. He always provided a well thought out and super detailed response because he truly cared,” Riehm said.
Lexicon MedParts CEO Scott Kinkade also first met Steve in the early 2000s.
“The first time I met Steve was in 2003 when he was a vice president at Aramark and I was a sales rep for ReMedPar calling on Aramark,” Kinkade said. “I had the privilege of working for Steve two different times. The first time was in 2006 when
AllParts Medical was founded and the second time was in 2018 at Althea. Both times were a blessing and I learned a great deal from a great man.”
Tri-Imaging Senior Vice President of Business Development Wanda Legate met Steve when he was the president of Aramark.
“Steve was a great person and would help anyone in need of help or guidance,” Legate said. “Steve will be missed by all. I personally will miss the text messages with songs and words of wisdom.”
“Steve was a man among men. He was a great friend and I will miss him dearly. Some people in our lives will never be replaced, but their presence never leaves us either,” Trust Medical President Chad Fowlkes said. “I hope to give love and offer friendship like Steve did. I am truly blessed to have had him in my life. He will be greatly missed!”
Rick Staab, CHTM, met Steve when he was with AllParts and then Aramark.
“I will always remember how open Steve was with me and honest about the industry and his thoughts,” Staab said. “I will also always think kindly about Steve and images that include motorcycles, cows, and big equipment at his farm.”
Eric Wright, CEO and co-founder at Tri-Imaging Solutions met Steve in 2009 when he became president of AllParts Medical.
“The thing I remember most about Steve is how he could control a room and a meeting. When Steve spoke, the room became quiet and people focused on him,” Wright said. “One thing that Steve said multiple times that I will always remember is, ‘Hope is not a strategy.’ ”
“Steve and I traveled together during our time at All-
Here are some words from Steve’s wife Becky Cannon.
Forever in our hearts
Steve was a lot of things to a lot of people – husband, dad, brother, papaw, uncle, and friend.
But to all of us, he was simply The Boss.
Not just because he spent his life leading big companies, but because he had a presence you couldn’t miss, a voice you listened to, and a heart big enough to carry us all.
He loved the open road on his motorcycle. He wore his Native American heritage with pride.
He had a soft spot for farm overalls as he did the farm chores and the tree work.
He loved classic country music.
He’d never let you go without always saying yes to one more drink, a little more food, or building the fire just a little higher.
Steve had a giving soul. If you needed help, he was already there.
If you needed advice, he had it.
If you needed a friend, he showed up no matter how hard things were.
He loved me beyond measure. If I wished for something, Steve made it happen.
Steve wasn’t a man of many apologies, but he showed
Parts, and we shared many dinners and rounds of golf,” Wright added. “He was always someone I enjoyed being around, and I will cherish the conversations we shared, both professionally and personally.”
“I met Steve Cannon for the first time at an AMSP meeting that was being held at AllParts just following the Phillips acquisition in 2011,” AMSP Business Operation Manager John Snyder said. “Being his generous self, Steve allowed us to have our meeting at his facility. I will always remember how professionally he carried himself. Despite working for a big OEM, Steve, believed in the value independents (ISOs) brought to the diagnostic imaging service industry. Honesty and concise communication were his trademarks!”
Snyder also shared examples of Steve’s unselfish nature and the impact he had on his career.
“Steve was a man of unique character and I’m forever grateful to him for what he did for me,” Snyder added.
Steve was a force in the HTM industry and, more importantly, a trusted friend to many.
“While Steve was initially a great leader and mentor to me it will always be his friendship that I cherished the most,” Riehm said.
“Steve was a cornerstone of the industry, well connected and respected by all. He always treated me like a little brother offering guidance and support with genuine kindness and a sincere desire to help,” Staab shared.
“Steve will always be remembered for his work in our industry. However, I will remember him as a family-loving, Harley-riding, and farming man! He cherished his family the most, and my thoughts, prayers, and best wishes go out to Becky, Preston, and Amber,” Wright said. •
his love and his gratitude in the only way he knew which was through action, loyalty, and showing up.
And he showed up for me always.
He adored our children, Amber and Preston, and extended that love without hesitation to Amber’s husband, Steven and Phoenix’s mother, Shannon.
He became that father figure – steady, generous, and fiercely protective – to everyone that was in his circle.
Our grandchildren – Phoenix, Rocco, Allie and Vinny were his pride and joy.
Steve wasn’t always easy – he was the boss, after all. But he loved fiercely and loyally.
And when you were part of his circle, you knew it.
So, if you knew Steve, I invite you to honor him in your own way.
Maybe with a ride down a winding road, a glass raised in the summer sun, a fire lit a little higher than usual, or even plant something in his memory.
Remember him when the wind blows just right and the sun warms your back.
That’s where he’ll be.
And just know, when we finally see him again, he will have his arms open and a list of stuff for you to do.
The Association for Medical Imaging Management (AHRA) is gearing up for its highly anticipated 2025 Annual Meeting, slated for August 3-6 at the Paris Las Vegas Hotel & Casino. This flagship event for medical imaging professionals promises to deliver a blend of top-tier education, leadership development, industry insight, and invaluable networking – all set against the vibrant backdrop of the Las Vegas Strip.
Whether you’re a first-time attendee or a seasoned AHRA member, this year’s meeting offers something for everyone looking to stay ahead in the rapidly evolving world of imaging administration.
The AHRA Annual Meeting is not just another industry conference – it’s a premier gathering for leaders in imaging management. Each year, hundreds of radiology directors, imaging supervisors, operations managers, and administrators come together to share best practices, explore innovations, and learn strategies to drive clinical and operational excellence. This year, AHRA is taking feedback seriously by designing a program that maximizes impact while minimizing the time attendees are away from their departments. With tailored content tracks, a restructured schedule, and new networking opportunities, the 2025 meeting is more focused and efficient than ever.
To kick off the event, AHRA will host several deep-dive workshops on Saturday, August 2, allowing participants to gain certification prep or leadership insights without missing a minute of the general conference. These include:
• CRA Exam Workshop: Ideal for those preparing to earn their Certified Radiology Administrator (CRA) credential, this comprehensive review will help candidates navigate key topics and exam strategies.
• Executive Leadership Workshop: Targeted at senior professionals and those aspiring to C-suite roles, this session focuses on high-level leadership skills, strategic planning,
and healthcare transformation.
• Imaging Negotiation Workshop: A newer addition to the lineup, this session helps attendees develop negotiation techniques for vendor contracts, internal budget discussions, and interdepartmental collaboration.
These workshops are designed not only to educate but to empower imaging leaders to return to their organizations with actionable knowledge.
The heart of the Annual Meeting lies in its robust educational programming. AHRA 2025 will feature dozens of breakout sessions and keynotes across a variety of critical focus areas, including:
• Leadership and Professional Development
• Operational Efficiency
• Quality and Safety
• Finance and Budgeting
• Technology Trends and Innovation
Each session is led by experienced professionals and subject matter experts, ensuring that attendees leave with evidence-based tools to implement change and drive performance improvements.
In keeping with AHRA’s commitment to inclusivity and development, many sessions will also be eligible for continuing education credits, including those needed for CRA and ARRT renewals.
No AHRA Annual Meeting is complete without compelling keynote speakers. While the full speaker lineup will be announced closer to the event, past years have featured prominent voices in healthcare leadership, motivational speakers, and industry disruptors. Attendees can expect to hear from experts who will challenge them to think differently about leadership, resilience, and the future of imaging.
The keynote sessions are often standing-room only, as they set the tone for each day and ignite the energy for the rest of the program.
The Gathering Place serves as the central hub of the Annual Meeting – a dynamic space where attendees can interact with exhibitors, network with peers, and explore emerging technologies. With extended hours in 2025, including Sunday access and earlier daily openings, attendees will have more time to:
• Demo cutting-edge imaging equipment and software
• Meet with vendors and service providers
• Discover innovative solutions for clinical and operational challenges
• Participate in sponsored learning labs and mini-sessions
This year’s exhibit hall is expected to host over 100 exhibitors, offering attendees a unique chance to evaluate products and services that can enhance performance and patient care.
One of the standout features of the AHRA Annual Meeting is its focus on meaningful connection. From structured networking events to informal gatherings, the 2025 conference will include:
• New Member and First-Time Attendee Reception: A welcoming environment for those new to AHRA or attending their first meeting, providing a chance to connect with leadership and peers early in the event.
• Drinks on ICE at Beer Park is set for Sunday, August 3 from 7 to 8 p.m. The event is sponsored by IAC. RSVP online at theicecommunity.com/ ahra-rsvp
• Regional Meetings: A space for attendees to connect with others from their geographic area, fostering local networks that last long after the conference ends.
• Women in Imaging Leadership: A growing initiative that highlights the contributions of women in the field and creates space for mentorship and dialogue.
• The Closing Party: Scheduled for Tuesday evening, August 5, from 7 to 10 p.m., this signature celebration features food, music, and fun in a relaxed setting – perfect for unwinding and reflecting on the week’s learnings.
The Paris Las Vegas Hotel & Casino offers a central, luxurious venue for this year’s event. Attendees can book within the official AHRA room block to enjoy discounted rates and convenient access to all meeting events. Staying at the host hotel also enhances networking opportunities and makes it easier to participate fully in the experience.
Conference programming will end by 12:30 p.m. on Wednesday, August 6, allowing ample time for travel home – a thoughtful adjustment designed with East Coast participants and those with tight schedules in mind.
With so much to offer, the AHRA 2025 Annual Meeting promises to be a transformative experience for imaging professionals at every stage of their careers. Registration is now open, and early sign-ups are encouraged to take advantage of hotel discounts and secure spots in limited-capacity workshops.
To learn more and register, visit ahra.org.
Join your peers in Las Vegas and be part of shaping the future of medical imaging leadership. •



As attendees of the 2025 AHRA Annual Meeting gather at the Paris Las Vegas Hotel this July, the City of Light meets the city of neon. While the annual radiology conference will be packed with sessions, networking and exhibits, there’s no reason not to indulge in a little leisure between professional obligations. Whether you have an
1
Take in the View from the Eiffel Tower Viewing Deck
One of the most iconic features of the Paris Las Vegas Hotel is its half-scale replica of the Eiffel Tower. Visitors can ride a glass elevator 46 stories up to the Eiffel Tower Viewing Deck, which offers panoramic views of the Las Vegas Strip and beyond. Day or night, it’s a must-see attraction. After dark, the tower even sparkles with lights in homage to its Parisian counterpart.
Stroll the ‘Streets’ of Paris Indoors
Even if you don’t have time to leave the hotel, you can still enjoy the ambiance of a Parisian street. Inside the resort, the cobblestone walkways, wrought-iron details and painted ceilings create a charming faux-France experience. Boutiques, bakeries and wine bars line the promenade, making it ideal for a leisurely afternoon stroll or spontaneous shopping trip.
hour or a whole evening, the Paris Las Vegas Hotel and its immediate surroundings offer a variety of experiences that extend far beyond the meeting agenda. Here are seven things to do in and around the Paris Las Vegas Hotel that will make your stay even more memorable.

See a Show at the Theater des Arts
Paris Las Vegas frequently hosts live performances at its Theater des Arts, featuring a rotating lineup of comedians, musicians and variety acts. Check the schedule ahead of time for performances during your stay. A night out at the theater is a perfect way to unwind after a day of learning and networking.
Explore the Strip from a Central Location
Enjoy Fine Dining at the Eiffel Tower Restaurant
3 5 7 2 4 6 BONUS TIP:
Paris Las Vegas is centrally located on the Las Vegas Strip, offering easy access to nearby attractions. Just across the street, the Fountains of Bellagio offer dazzling water shows set to music every 30 minutes in the evening. The LINQ Promenade, with its High Roller observation wheel, is a short walk away and provides shopping, dining and entertainment options.
Perched within the Eiffel Tower, the Eiffel Tower Restaurant delivers an elegant dining experience with unbeatable views. The French-inspired menu includes favorites like beef Wellington, foie gras and a renowned Grand Marnier soufflé. Make reservations early, as this is a hotspot for visitors looking to enjoy a romantic or upscale meal just steps from their hotel room.
Unwind at Voie Spa & Salon
For attendees in need of relaxation, the Voie Spa & Salon provides a luxurious escape. The spa draws inspiration from wellness traditions across France, offering a full menu of massages, facials and salon services. Whether you’re recovering from a red-eye flight or simply seeking a break from the conference grind, a spa session can rejuvenate both body and mind.
Whether you’re a seasoned gambler or just feeling lucky, the Paris Las Vegas Casino offers an elegant gaming floor beneath a simulated Parisian sky. Table games, slot machines and poker tournaments run throughout the day and night. Grab a cocktail and test your luck, or simply enjoy the atmosphere, which feels more like a European plaza than a typical casino.
If you’re short on time, grab a café au lait and a croissant from Café Belle Madeleine, located right inside the Paris Las Vegas Hotel. It’s the perfect fuel for a busy conference day – or a quick morning treat before heading to a session.

Wh o better to ask about AHRA and the annual meeting than AHRA President Mario Pistilli? ICE Magazine Editor John Wallace reached out for information leading into the annual meeting and Pistilli graciously made time to share his thoughts.
Q: THIS YEAR’S AHRA ANNUAL MEETING IS RETURNING TO LAS VEGAS. WHAT MAKES THIS LOCATION AND THE PARIS LAS VEGAS HOTEL & CASINO THE RIGHT FIT FOR 2025?
Pistilli: Very excited to be returning the AHRA to Las Vegas which has been a highly attended location in the past. What will make the Paris so great is that it can house all attendees within the same hotel and offer easy access from the room to all conference events. We also got access to some really exciting spaces to hold our receptions that I know attendees will love. We will also be located right in the middle of the strip so easy access in either direction to all of the properties on the strip.
Q: AHRA IS KNOWN FOR LISTENING TO ITS MEMBERS. WHAT FEEDBACK FROM PAST MEETINGS HELPED SHAPE THE EXPERIENCE WE’LL SEE THIS AUGUST?
Pistilli: We heard from members how much they loved the Ambassador program and how much new members and first-time attendees are included to make sure their first experience is as easy and meaningful as possible. We also moved the closing party so that more people could attend and still head home to get back to family or work obligations timely – as in the past to attend the party you had to stay past the conference end. This should open up the experience to everyone attending and this year’s party will be epic and I am really excited to try the specialty Mario-themed cocktail.
Q: CAN YOU HIGHLIGHT A FEW EDUCATIONAL OR KEYNOTE SESSIONS THAT YOU’RE PERSONALLY EXCITED ABOUT? WHAT THEMES DO YOU EXPECT TO RESONATE MOST THIS YEAR?
Pistilli: I always love the keynotes and this year will feature Alex Sheen. He is the founder of because I said I would, a social movement and nonprofit dedicated to bettering humanity through promises made and kept. Sparked by the loss of his father, Alex and his organization send “promise cards” to anyone anywhere in the world at no cost.

Alex is someone who truly honors commitment. He once walked over 240 miles across the entire state of Ohio in 10 days to fulfill a promise. In just two years, because I said I would has sent over 9.81 million promise cards to over 153 different countries. The promises written on these cards have made headlines around the world.
His charitable work has been featured on ABC World News with Diane Sawyer, CNN, The Today Show, NPR, The Los Angeles Times and many other programs We will also have plenty of sessions to help us all navigate the ever-changing healthcare financial and regulatory landscape, manage our staffs, and take care of ourselves.
Q: THE GATHERING PLACE IS A MAJOR ATTRACTION FOR ATTENDEES AND VENDORS ALIKE. WHAT CAN PARTICIPANTS EXPECT FROM THIS YEAR’S EXHIBIT HALL EXPERIENCE?
Pistilli: The exhibit hall is already at capacity and we have many first-time exhibitors along with our long-
term valued partners that we love to see each year. The design team has worked hard to make the exhibit hall a great place to gather and will incorporate some fun events for members. One thing I want to stress is that it is so important for attendees to engage with the vendors. Even if you do not intend on buying right now, take time to network and learn what’s new and our vendor partners also want to hear what your pain points are and the things you are working on. This is a great way for vendors to get the voice of the customer which helps inform future development. Visiting vendors is also a great way for you to help the AHRA mission as the more engaged members connecting with our vendors, the more vendors are excited to engage and support AHRA which turns into more products and services for all of you.
Q: AHRA HAS MADE GREAT STRIDES IN COMMUNITY-BUILDING INITIATIVES. HOW WILL NETWORKING OPPORTUNITIES — ESPECIALLY FOR NEW MEMBERS — BE ELEVATED THIS YEAR?
Pistilli: We are bringing back and expanding the Ambassador program and making sure that there are not many competing things going on so that more people can focus on meeting and welcoming new members and first-time attendees. Also moving the party will help more people participate. There will be an elevated President’s reception which offers a great kick-off networking event. The location being near so many fun things to do will also help networking tremendously.
Q: AS AHRA PRESIDENT, HOW DO YOU SEE THE ORGANIZATION EVOLVING TO MEET THE NEEDS OF IMAGING LEADERS IN TODAY’S COMPLEX HEALTHCARE LANDSCAPE?
Pistilli: The organization continues evolving and one major area of growth is in our collaboration with many other industry professional organizations to share ideas and support each other in advocating for policy change and in raising awareness of the profession of imaging nationwide. We also have so many methods of content delivery including webinars, podcasts, on-demand sessions, and the largest number of local area meetings in AHRA history. Coming soon will be enhancements to the educational web platform and more content on data and benchmarking.
Q: WHAT MESSAGE WOULD YOU SHARE WITH SOMEONE CONSIDERING ATTENDING THE AHRA ANNUAL MEETING FOR THE FIRST TIME?
Pistilli: I would say do whatever you have to do to get to the annual meeting and make it a priority for your personal and professional growth. Your eyes will be opened to the rich variety of support and resources
that will carry forward well beyond the annual meeting. If you put yourself out there you will gain tons of new colleagues and friends that will be invaluable as we all try and do our best for our patients and our teammates.
Q: FINALLY, WHAT ARE YOU MOST LOOKING FORWARD TO PERSONALLY AT THIS YEAR’S ANNUAL MEETING?
Pistilli: I always most look forward to seeing many long-time treasured friends and in meeting new ones. I love helping other leaders grow and prosper in their careers and I usually connect with a few new folks that I can collaborate with to get them more involved in AHRA. To me the AHRA annual is my family reunion and is the oxygen for my soul to carry me through when times are tough. •


Be sure to visit these exhibitors!

AHRA
ahra.org/home
Booth # 436

Beekley Medical beekley.com
Booth # 529
Guerbet guerbet.com Booth # 537

HealthLevel healthlevel.com
Booth #603
ICE Magazine theicecommunity.com
Booth #644

Intersocietal Accreditation Commission (IAC) intersocietal.org
Booth #445

Marketlab marketlab.com
Booth #646

Medical Technology Management Institute (MTMI) mtmi.net
Booth #626

RTI Group North America rtigroup.com
Booth #422
AllParts Medical, a Philips company, announced two key leadership updates that will strengthen the organization’s growth trajectory and operational excellence. Kelly Feist has joined the company as vice president of sales, and James Akins has been promoted to vice president of operations.
The announcement was shared by Richard Gerler, newly appointed CEO of AllParts at Philips and former vice president of operations for AllParts Medical.
“We’re entering a pivotal time for AllParts Medical as we continue to scale our impact across the healthcare service ecosystem,” said Gerler. “I’m incredibly excited to welcome Kelly to the team and to celebrate James’s well-earned promotion. Both bring outstanding experience, leadership, and vision to our organization.”
Kelly Feist officially joined AllParts Medical on May 19, bringing with her over a decade of experience in healthcare technology and service leadership. She most recently served as managing director of Ascom Inc., where she led transformational initiatives in healthcare information and communications systems.
Previously, Kelly held multiple leadership roles at Philips, including overseeing North America customer service and serving as business leader for patient care and monitoring solutions, where she expanded market share and achieved consistent double-digit growth in service revenue.
Feist holds an MBA from Vanderbilt University and a post-graduate certificate in Healthcare IT Leadership
from the Harvard School of Public Health.
“Kelly’s ability to align strategy with customer value is unmatched,” added Gerler. “She’s not only a proven leader – she’s also someone who deeply understands the challenges and opportunities within our space.”
In her new role, Feist will oversee the national sales team, focusing on growth, innovation, and maintaining AllParts Medical’s industry-leading customer satisfaction.
AllParts Medical also announced the promotion of James Akins to vice president of operations. Since joining the company in 2014, Akins has served in key roles across sourcing, logistics, technical operations, and supply chain management.
Starting as a Sourcing Specialist III, Akins advanced into operational leadership roles including logistics manager and, most recently, senior manager of repair operations. Under his leadership, the company’s repair and refurbishment services have seen significant improvements in quality, efficiency, and scalability.
“James is a leader who leads with precision,” said Gerler. “He knows our business inside and out, and his steady hand has helped us continuously raise the bar on performance. This promotion is not only well-deserved – it’s critical to our ongoing success.”
In his new role, Akins will lead operations across AllParts Medical’s facilities, ensuring seamless execution, supply chain efficiency, and continued excellence in customer delivery.


Simplifying The Imaging Equipment Ownership Experience
Image One Medical is the only Engineer-Owned medical equipment service group that is fully dedicated to Florida’s amazing base of Imaging Centers, Hospitals, and Cancer Treatment Centers.
We have a mission: Self perform on every aspect of our business. Specialize on specific modalities: Pet CT, CT & MRI, and Focus in a key geographic region.
Fort Myers I Fort Lauderdale I Tampa I Orlando
FLORIDA BASED
Dealer and servicer of PET CT, CT and nuclear medicine
• Equipment service: full coverage plans
• Equipment sales: installation, relocation and project management
• Mobile coach construction, refurbishment, maintenance and management


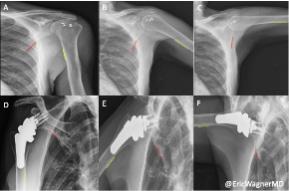
Emory Healthcare researchers published a study using Dynamic Digital Radiography (DDR) to compare shoulder biomechanics in patients after two widely accepted surgical interventions for massive irreparable rotator cuff tears (MIRCTs). Reverse shoulder arthroplasty (RSA) and arthroscopically assisted lower trapezius tendon (aLTT) transfer are often used to repair these tears, however, quantifying shoulder function post-operatively has remained difficult to assess. However, with the use of novel DDR imaging, it provided the ability to examine in-vivo kinematics by measuring scapulohumeral rhythm (SHR), the ratio of the glenohumeral and scapulothoracic contributions to shoulder motion, non-invasively in patients. The authors also aimed to design an objective methodology for selecting the appropriate intervention that will maximize the patient’s shoulder mobility with the help of DDR. The study is available online in the Journal of Shoulder and Elbow Surgery.
DDR is a novel, low-dose X-ray imaging technique available on Konica Minolta Healthcare DR Systems that captures both static images and cinegrams, providing an innovative way to obtain detailed images of complex joints like shoulders while in motion. By acquiring a series of images at high speed, DDR generates a cineloop that enables clinicians to visualize anatomical motion over time (cineradiography), enhancing the system’s diagnostic capabilities. Utilizing DDR to characterize scapulohumeral rhythm both pre- and post-operative and evaluate for precise changes in SHR, Sameer R. Khawaja, MD, and collaborators, including the leadership of Eric R. Wagner, MD, MSc, and his research lab, demonstrate that Dr. Wagner’s patients undergoing aLTT yields superior restoration of shoulder biomechanics for patients suffering from MIRCTs than his
patients undergoing RSAs. The study highlights how aLTT transfer enhances shoulder stability and improves functional mobility. In contrast, RSA is a very successful treatment of MIRCTs and other pathologies but fails to restore the same level of native biomechanics as the aLTT.
“Using the dynamic radiography provided by Konica Minolta’s DDR imaging enables us to change the clinical algorithms for both preoperative decision making and postoperative evaluations of surgical outcomes,” says Dr. Wagner.
“It’s often difficult to decide whether we should do a RSA or aLTT for these patients with massive rotator cuff tears. These are very different treatments,” says Zaamin Hussain, MD, Orthopedic Surgery Resident, Emory Healthcare. “Not only can the DDR images help make that decision preoperatively, but the results of this study suggest there is potential for improved overall coordination of the shoulder with aLTT, which is only possible to assess with in vivo dynamic imaging!”
“Konica Minolta congratulates the team at Emory Healthcare on the publication of their study demonstrating the clinical utility of DDR in comparing post-surgical outcomes in patients undergoing reconstructions for MIRCTs,” says John Sabol, PhD, Clinical Research Manager, Konica Minolta Healthcare. “DDR is an FDA cleared radiography solution that provides valuable insight into the dynamic relationship of bones and soft tissue through their full range of motion. As the Emory team has demonstrated in this work, DDR overcomes the historical challenges in evaluating biomechanics in clinical patient populations. This will enable improvements in the quality of care and patient outcomes.”
A type of artificial intelligence called fine-tuned large language models (LLMs) greatly enhances error detection in radiology reports, according to a new study. Researchers said the findings point to an important role for this technology in medical proofreading.
Radiology reports are crucial for optimal patient care. Their accuracy can be compromised by factors like errors in speech recognition software, variability in perceptual and interpretive processes and cognitive biases. These errors can lead to incorrect diagnoses or delayed treatments, making the need for accurate reports urgent.
LLMs like ChatGPT are advanced generative AI models that are trained on vast amounts of text to generate human language. While they offer great potential in proofreading, their application in the medical field, particularly in detecting errors within radiology reports, remains underexplored.
To bridge this gap in knowledge, researchers evaluated fine-tuned LLMs for detecting errors in radiology reports during medical proofreading. A fine-tuned LLM is a pre-trained language model that is further trained on domain-specific data.
“Initially, LLMs are trained on large-scale public data to learn general language patterns and knowledge,” said study senior author Yifan Peng, Ph.D., from the Department of Population Health Sciences at Weill Cornell Medicine in New York City. “Fine-tuning occurs at the next step, where the model undergoes additional training using smaller, targeted datasets relevant to particular tasks.”
To test the model, Peng and colleagues built a dataset with two parts. The first consisted of 1,656 synthetic reports, including 828 error-free reports and 828 reports with errors. The second part comprised 614 reports, including 307 error-free reports from MIMIC-CXR, a large, publicly available database of chest X-rays, and 307 synthetic reports with errors.
The researchers used the synthetic reports to boost the amount of training data and fulfill the data-hungry needs of LLM fine-tuning.
“Synthetic reports can also increase the coverage
and diversity, balance out the cases and reduce the annotation costs,” said the study’s first author, Cong Sun, Ph.D., from Peng’s lab. “In radiology, or more broadly, the clinical domain, synthetic reports allow safe data-sharing without compromising patient privacy.”
The researchers found that the fine-tuned model outperformed both GPT-4 and BiomedBERT, a natural language processing tool for biomedical research.
“The LLM that was fine-tuned on both MIMIC-CXR and synthetic reports demonstrated strong performance in the error detection tasks,” Sun said. “It meets our expectations and highlights the potential for developing lightweight, fine-tuned LLM specifically for medical proofreading applications.”
The study provided evidence that LLMs can assist in detecting various types of errors, including transcription errors and left/right errors, which refer to misidentification or misinterpretation of directions or sides in text or images.
The use of synthetic data in AI model building has raised concerns of bias in the data. Peng and colleagues took steps to minimize this by using diverse and representative samples of real-world data to generate the synthetic data. However, they acknowledged that synthetic errors may not fully capture the complexity of real-world errors in radiology reports. Future work could include a systematic evaluation of how bias introduced by synthetic errors affects model performance.
The researchers hope to study fine-tuning’s ability to reduce radiologists’ cognitive load and enhance patient care and find out if fine-tuning would degrade the model’s ability to generate reasoning explanations.
“We are excited to keep exploring innovative strategies to enhance the reasoning capabilities of finetuned LLMs in medical proofreading tasks,” Peng said. “Our goal is to develop transparent and understandable models that radiologists can confidently trust and fully embrace.”


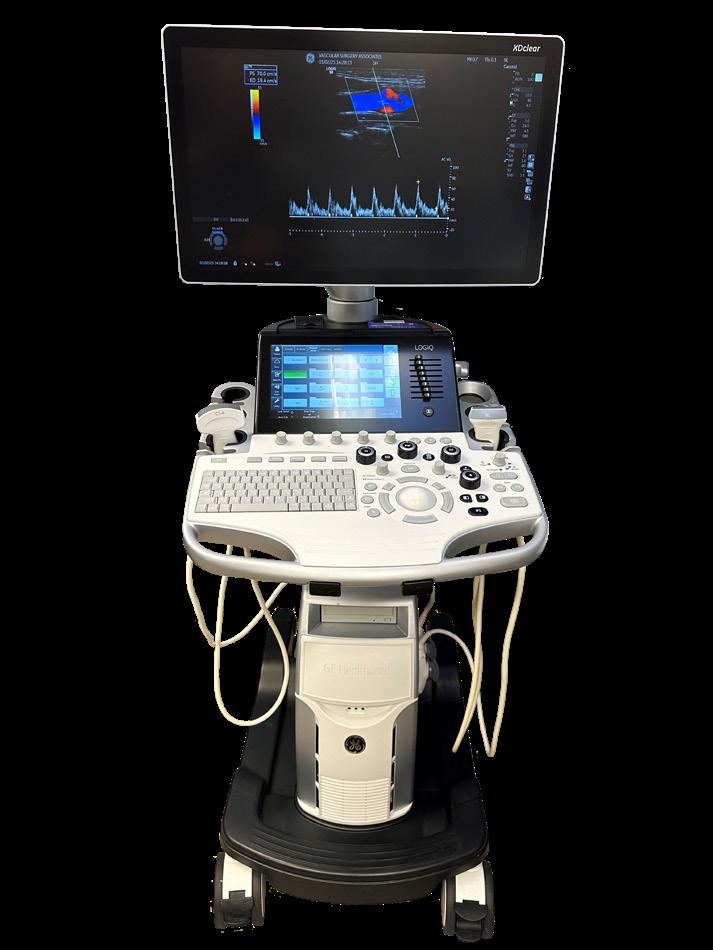
The U.S. Food and Drug Administration (FDA) has approved a pediatric indication for GE HealthCare’s Optison (Perflutren Protein-Type A Microspheres Injectable Suspension, USP) ultrasound enhancing agent (UEA). This approval will help improve the clarity and diagnostic accuracy of echocardiograms in pediatric patients, giving cardiologists a fuller picture of ventricular function when assessing possible heart abnormalities or disease.
“In some pediatric patients, standard echocardiography cannot produce sufficiently clear images of the heart, potentially hindering cardiologists’ ability to accurately diagnose underlying conditions,” said Jit Saini, MD, chief medical officer of the pharmaceutical diagnostics (PDx) segment of GE HealthCare. “This regulatory approval is a significant milestone that affirms the safety and efficacy of Optison in pediatric patients of all ages and expands our ability to offer this advanced imaging solution to a broader patient population. By facilitating more accurate measurement of left ventricular function, Optison enhances diagnostic capabilities, ultimately improving patient outcomes and providing greater value to healthcare providers and their patients.”
Optison contains gas-filled microbubbles that reflect ultrasound waves more effectively than surrounding tissues or blood, making the heart chambers and endocardial borders more visible, which is necessary for assessing heart conditions. Optison has a proven safety profile established over decades and
is the only UEA available in the U.S. that does not contain polyethylene glycol (PEG). This allows it to be safely used by patients with PEG hypersensitivity, as PEG carries the potential to trigger anaphylaxis or hypersensitivity reactions in some patients.
“Ultrasound enhancing agents have significantly advanced diagnostic quality in adult echocardiography over the years, and we are now seeing promising research supporting their safe and effective use in pediatric patients,” said Arash Sabati, MD, FACC, pediatric cardiologist and non-invasive imaging specialist at Phoenix Children’s. “The availability of agents like Optison will further enhance diagnostic imaging for pediatric patients, helping to ensure the best possible care.”
Optison is currently indicated for use in patients with suboptimal echocardiograms. The FDA approved Optison for adults in 1997, and healthcare professionals have administered Optison to more than 5 million patients in the U.S. As the first of the second generation of UEAs to be approved by the FDA, the approval for the pediatric indication follows GE HealthCare’s Phase IV, prospective open-label multicenter study to evaluate the efficacy of Optison for contrast-enhanced echocardiograms in patients. The study found that the use of intravenous Optison optimized endocardial border delineation, improved the visualization of left ventricular wall segments and reduced the number of suboptimal echocardiogram images in pediatric patients.

Siemens Healthineers has announced the first mobile stroke unit (MSU) featuring the Somatom On.site head computed tomography (CT) scanner in the United States. The technology has been deployed at UCLA Health of Southern California. The MSU is a specialized ambulance designed to quickly deliver advanced stroke care directly to patients to improve their chances of recovery. At the core of UCLA’s MSU is the Somatom On.site, which is integrated into the ambulance to streamline workflow, enhance diagnostic accuracy, and empower MSU teams to deliver timely, life-saving care. When a 911 call indicates a potential stroke, an MSU is dispatched alongside or instead of a standard ambulance. Upon arrival, the MSU care team conducts an on-scene CT scan to determine whether the stroke is ischemic or hemorrhagic. The care team consults with a stroke specialist via telemedicine to guide immediate treatment decisions.
“The phrase ‘time is brain’ is used frequently when discussing stroke. The Somatom On.site head CT scanner at the heart of our mobile stroke unit empowers MSU teams to make informed decisions sooner and potentially improve patient outcomes,” said Matthew Dedman, head of computed tomography at Siemens Healthineers North America. “This innovative CT solution will help stroke care teams improve access to care and reduce the critical time from symptom onset to diagnosis and treatment.”
“Advancements in mobile stroke imaging represent
a significant step forward in pre-hospital stroke care,” said May Nour, MD, Ph.D., FSVIN, medical director of the Arline and Henry Gluck Mobile Stroke Rescue Program at UCLA Health, Los Angeles. “Our commitment to innovative approaches in emergency medicine aims to improve patient outcomes through rapid assessment and treatment when every minute counts.”
Every 40 seconds, someone in the United States has a stroke, with many patients experiencing long-term disabilities due to delayed treatment, and fatal strokes occur every 3 minutes and 11 seconds. To save critical time and improve this situation, MSUs allow pre-hospital diagnosis of suspected stroke patients. These units can help reduce time to treatment by an average of 30 minutes compared with conventional stroke pathways, and 65% more patients recover without health issues.
The Somatom On.site mobile head CT scanner in the MSU delivers a high level of image quality comparable to stationary CT scanners, aiding in reliable detection of ischemia or brain bleeding. Integrated patient- support accessories, including the isocentered head holder and customized shoulder board, promote efficient workflow and easy patient positioning. The self-shielded telescopic gantry supports high-quality imaging for greater diagnostic confidence. The intuitive touch user interface and myExam Companion workflow, which is guided by artificial intelligence, help CT technologists acquire and automatically reconstruct high-quality images.


On May 20, the ICE webinar “Finally, an App for Medical Equipment Services” was eligible for 1.0 ARRT Category A CE credit by the AHRA. Sponsored by Downtime Trace, the webinar explored a new app for the imaging service community. A recording of the webinar is available for continuing education credit via on-demand viewing at ICEwebinars.live.
On May 20, the ICE webinar “Finally, an App for Medical Equipment Services” was eligible for 1.0 ARRT Category A CE credit by the AHRA. Sponsored by Downtime Trace, the webinar explored a new app for the imaging service community. A recording of the webinar is available for continuing education credit via on-demand viewing at ICEwebinars.live.
Whenever your imaging equipment breaks, how do you ensure that you are connected to all of the qualified service providers (vendors) as quickly and efficiently as possible? There have been very recent and significant advancements in the medical imaging equipment service industry that allow radiology technologists and equipment operators to buy services like they would order transportation on Uber, food from their favorite food delivery app, or help with household repairs (TaskRabbit and Angi).
Dave Francoeur, president of medical equipment service at Downtime Trace, advised and educated
attendees on how to reduce downtime for medical imaging equipment.
Approximately 100 people registered for the informative webinar that included a question-and-answer session with subject matter experts from Downtime Trace.
Sarah Kaul, a radiation safety specialist with Froedtert Hospital in Wisconsin, won an ICE gym bag during the webinar.
The webinar received positive feedback via a survey sent out to attendees.
One question attendees answered was, “Why do you read ICE magazine ?”
“I like the blend of industry leaders being focused, along with imaging technology news,” said Devin Dixon, radiology business affairs manager, UCSF Health.
“ICE Magazine always contains the most relevant and updated information in the world of imaging,” said Angela Harris, mammography care coordinator, Harris Health.
“Information on cutting edge imaging technology and topics,” said Kathryn Zenerovitz, HIM services manager, STAR Medical Auditing LLC. •

ICE Magazine looks at training in this month’s Director’s Circle roundtable article. ICE Magazine invited several healthcare organizations to participate in an effort to share best practices, trends, tips and sage advice from throughout the diagnostic imaging realm.
Participants in the Director’s Circle on training are:
• AdventHealth University Director of Radiography and Advanced Imaging Jena Heflin, DSL, MBA, RT(R);
• Scripps Health Manager of Imaging Services Matthew Hill; and
• Corewell Health Clinical Education Specialist-Imaging Laura Holstege, BS, RT(R).
Q: WHAT FOUNDATIONAL SKILLS OR CERTIFICATIONS DO YOU CONSIDER ESSENTIAL FOR SOMEONE STARTING OUT IN RADIOLOGIC TECHNOLOGY OR IMAGING?
Heflin: Starting a career in radiologic technology or medical imaging requires a strong foundation in patient
care, anatomy and radiation safety. New professionals should be comfortable with medical terminology, imaging equipment operation and optimal patient positioning techniques. American Registry of Radiologic Technologists (AART) certifications are essential, along with any applicable state licensure and HIPAA training. Possessing skills in communication, critical thinking, and attention to detail are just as important as technical know-how. For those planning to specialize, additional training in venipuncture and gaining credentials in the advanced imaging modalities can be valuable steps toward a thriving and rewarding career in this fast-growing healthcare field.
Hill: American Registry of Radiologic Technologists (ARRT) is the nationally recognized license standard. In California, the Radiologic Health Branch (RHB) issues a license for certified radiologic technologist (CRT) and is an additional requirement. For someone starting out as a new radiology technologist, I look for a candidate that demonstrates both empathy and an ability to multitask as these are important qualities for a technologist.


Holstege: For someone beginning their imaging career, I believe foundational skills like critical thinking, empathy, and emotional intelligence are essential. While technical proficiency is crucial, so much of our daily work centers around direct patient interaction. We constantly give instructions and guide patients through procedures, often when they’re anxious or in pain. Critical thinking allows us to adapt to each unique situation and make appropriate decisions under pressure. Empathy and emotional intelligence help us connect with patients, understand their concerns, and communicate clearly and compassionately. These qualities are equally important in our interactions with colleagues. Imaging departments thrive on teamwork, and strong interpersonal skills help promote trust and collaboration.
Q: WHAT DOES YOUR DEPARTMENT DO TO SUPPORT ONGOING TRAINING AND DEVELOPMENT FOR TECHNOLOGISTS OR RADIOLOGISTS?
Heflin: While I currently serve in the capacity of program director of an A.S. radiography, B.S. imaging sciences, and advanced imaging certificate programs, I believe it is critical to support ongoing training and development by offering access to continuing education courses, hands-on workshops with current and emerging imaging technology, and opportunities to earn specialty certifications. Encouraging professional growth through mentorship programs, participation in conferences, and partnerships with fellow industry leaders ensures technologists and radiologists remain at the forefront of advancements in medical imaging.
Hill: Scripps Imaging supports CEU for our staff by offering financial support to continuing education.
Holstege: Our department organizes and hosts its Radiology Virtual Professor Presentation Series where we invite radiologists to speak to imaging team members on radiology related topics for 1 hour and offer CE credit for these lectures. The residents meet with the

same speaker for 3 hours afterwards for a board review session. We recently added physicist lectures for CE credit where our physicists educate on radiation safety. Our team has also created an internal MRI technologist training program and CT and MRI apprenticeship opportunities.
Q: WHAT ROLE DO CERTIFICATIONS (E.G., ARRT, SPECIALTY CREDENTIALS) PLAY IN ADVANCEMENT?
Heflin: Certifications like those offered by the American Registry of Radiologic Technologists (ARRT) play a crucial role in career advancement for imaging professionals. They not only validate a technologist’s expertise and commitment to high standards of care but also open doors to specialized fields such as MRI, CT, mammography, and nuclear medicine. Employers often look for certified professionals when hiring for advanced or leadership roles, making these credentials essential for those seeking long-term growth and professional recognition in the imaging sciences.
Hill: Certifications and licensures confirm that an individual meets national standards in their field. Technologists who obtain advanced credentials show proven expertise, which can lead to greater career mobility, increased earning potential, and opportunities for leadership roles.
Holstege: Specialty credentials allow our imaging technologists the ability to work independently in additional modalities. Experience in multiple modalities and the addition of a higher degree can give you an edge when applying for formal leadership opportunities in imaging and other departments across the hospital system.
Q: WHAT ARE THE BIGGEST BARRIERS TO CAREER GROWTH THAT YOU SEE IMAGING PROFESSIONALS FACE?
Heflin: One of the biggest barriers to career growth for imaging professionals is limited access to advanced training and certification opportunities. With the cur -
rent workforce labor needs, institutions may grapple with advancing existing team members into advanced modalities without having new hires to fill vacancies. Balancing full-time work with continuing education can also be challenging, and some professionals face a lack of mentorship or clear pathways for advancement. This creates a great opportunity for academic institutions to work with hospital and imaging leaders to identify pathways for entrance into their high demand workforce models.
Hill: One barrier I have seen is an unwillingness to go outside your comfort zone or change facilities. Throughout my career, I have accepted additional responsibilities and moved to different facilities within the same company to seek career growth.
Holstege: Time and fear. We get comfortable with our roles and if we dare to think of something different, we feel we don’t have time to get it done and fear the new beginning. We fear the fresh start because we may no longer be that “go-to person” others seek out but rather the one who needs a go-to person. It’s OK. It’s growth. You miss 100% of the chances you don’t take (Wayne/Walter Gretzky).
Q: ARE YOU SEEING CHALLENGES IN RECRUITING OR RETAINING TALENT IN ANY PARTICULAR IMAGING SPECIALTIES?
Heflin: Many colleges and universities saw a decrease in imaging applicants during the pandemic. This created a challenge for imaging departments to recruit talent for existing vacancies and future growth needs. The tide is turning as many higher education institutions are seeing an increase in applicant pools. Additionally, we’re seeing notable challenges in recruiting and retaining talent in specialized areas such as MRI, CT, and sonography. These fields require advanced training and certification, and the demand often outpaces the supply of qualified professionals. Factors like workforce burnout and limited clinical training sites contribute to staffing shortages, making it difficult to maintain full coverage in high-demand specialties.
Hill: MRI and nuclear medicine are two modalities that come to mind. To address this challenge, Scripps now accepts ARMRIT MRI certification. This certification is unique in that it does not require a traditional X-ray background.
Holstege: Yes, MRI and CT. The market is quite competitive, so our team is implementing apprenticeship opportunities in both these modalities. Apprenticeship programs range from about 3 to 6 months. The organization pays for them to cross-train in that modality and purchases all their materials/online modules to best set them up for success. Our senior imaging specialist and physicists also have live system lectures to support the new employee.
Q: WHAT ADVICE WOULD YOU GIVE TO SOMEONE LOOKING TO MOVE FROM A TECHNOLOGIST ROLE INTO LEADERSHIP?
Heflin: For technologists aiming to move into leadership, my advice is to seek out opportunities for professional development beyond clinical skills – such as courses in management, communication and healthcare administration. Many times, imaging departments “home grow” their leadership through advancement opportunities. This makes it even more critical for the team member to seek opportunities to grow their leadership toolbox to ensure they are an effective and respected leader in their department. Additionally, building strong relationships with mentors, taking initiative on department projects, and staying informed about industry trends can also demonstrate one’s readiness for leadership. Arguably, the most important piece is to develop a mindset focused on collaboration, problem-solving and supporting the growth of others.
Hill: Seek out more responsibility and additional roles to demonstrate your abilities. At each step of my career, I took on responsibilities on the next role above me to demonstrate I was ready for a promotion.
Holstege: Research and choose a best-selling leadership book and put the information you learn into practice the next day. Seek opportunities like superuser roles or hospital committee involvement to lead from the middle. You can lead from anywhere and you should practice your leadership skills wherever you are. You will stumble as you go, but learning from your mistakes is one of the ways you move forward. •
LOCATED AT PARIS HOTEL
Join ICE Magazine for our 5th Drinks on ICE Party, sponsored by IAC, at AHRA 2025!
RSVP and pick up your wristband on Sunday during AHRA's gathering place hours at IAC's booth #445 or ICE Magazine's booth #644. See you there!


The U.S. Bureau of Labor Statistics reports that overall employment of radiologic and MRI technologists is projected to grow 6 percent from 2023 to 2033, faster than the average for all occupations.
About 16,000 openings for radiologic and MRI technologists are projected each year, on average, over the decade. Many of those openings are expected to result from the need to replace workers who transfer to different occupations or exit the labor force, such as to retirement.
Radiologic technologists perform diagnostic imaging examinations on patients. MRI technologists operate magnetic resonance imaging (MRI) scanners to create diagnostic images. Radiologic and MRI technologists work in healthcare facilities, and more than half work in hospitals. Most radiologic and MRI technologists work full time.
Radiologic technologists and MRI technologists typically need an associate’s degree. MRI technologists also typically need several years of related work experience. Most states require radiologic technologists to be licensed or certified, but few states require licensure for MRI technologists. Regardless of state requirements, employers typically require or prefer to hire technologists who are certified.
Grand View Research reports that the global online radiology education platforms market size was estimated at $2.15 billion in 2024 and is projected to grow at a CAGR of 7.72% from 2025 to 2030.
This growth is attributed to the increasing demand for specialized training, technological advancements, flexible and accessible learning options, and the growing emphasis on continuous professional development. In addition, market players are collaborating with universities to provide online learning platforms to enhance the knowledge and skills of radiologists. For instance, in January 2023, King Saud University and DetectedX announced a joint project to improve radiologic image quality assessment. The collaboration explored the impact of an interactive and innovative self-assessment platform accessi-
ble all the time to clinicians and students worldwide.
Grad View Research adds that, “The increasing demand for flexible learning options is a primary driver, as online platforms offer unparalleled convenience for healthcare professionals with busy schedules. These platforms enable radiologists to access expert-led case reviews and lectures in short, accessible videos, allowing them to master new subspecialties or improve their reading skills in minutes each day from any location. Modern platforms combine multiple learning modalities, such as virtual reality simulations, 3D anatomical models, real-time case studies, interactive assessment tools, and peer collaboration features, catering to different learning styles and preferences.”
The report also states that technological advancements in education delivery are vital, with AI playing a transformative role in radiology education and practice. AI tools create new opportunities for learning, diagnostics, and patient communication. Emerging generative AI techniques summarize complex medical records, generate radiology reports from images, and simplify explanations of reports for patients in clear terms.
The rising need for specialized medical training is another significant driver, as rapid technological advancements and the increasing complexity of clinical cases demand that radiologists stay updated with the latest knowledge and skills. The online environment supports digital upskilling and continuous learning as technology advances. The global expansion of online radiology education reflects varying levels of healthcare infrastructure development and digital transformation across regions.
MarketsandMarkets reports that “The global diagnostic imaging services market size is projected to reach $702.6 billion by 2027, at a CAGR of 5.1%. Major factors such as high chronic diseases coupled with growing geriatric patient population, increasing awareness about the different imaging procedures, rapid expansion of new imaging diagnostic centers with state-of-the art imaging technologies are playing major fueling the diagnostic imaging services market growth during the forecast period.”
The growth in these markets is an indicator that the imaging service and repair training market will also see growth in coming years.•

The Certified Radiology Administrator (CRA) designation is the gold standard for medical imaging leaders. This certification validates key skills, knowledge, and competencies required and expected of leaders in medical imaging and demonstrates a commitment to quality and value. For those interested in preparing for the CRA exam, AHRA: The Association for Medical Imaging Management, offers the CRA Exam Workshop. This course is available online and on demand to prepare for the CRA exam anywhere, anytime. It helps identify areas of strength and opportunities for improvement. Watch the videos all at once or a little bit at a time and replay as often as you like.
Over 1,000 medical imaging professionals hold the CRA credential and gain a competitive edge. Learn more about the CRA at crainfo.org, and the CRA Exam Workshop at onlineinstitute.ahra.org/products/virtual-cra-exam-workshop.
*Disclaimer: Products are listed in no particular order.


Advanced Ultrasound Systems has built a robust training program that meets a variety of student needs. Students have access to dozens of ultrasound systems and the expertise of AUS techs and engineers.
AUS proudly offers multiple options for training:
• In-house “hands-on” training: Come visit our dedicated training facility in Tulsa, OK. Our hands-on training course includes an Introduction to Diagnostic Ultrasound Service, as well as advanced systems training on different OEM makes and models. The students are then presented with hands-on instructions that include the system back up procedure, system tear down and software reloads. We successfully end each class with a troubleshooting exercise and a test to confirm their familiarity with the system.
• “House Call” training: We travel to your facility and provide training at your facility to your biomedical engineers. We offer customizable class size and system types. This maximizes the training time by using the same models of systems they are maintaining at their facility without the customer having to have multiple people travel to remote locations.
AUS supports biomedical associations and colleges that offer a biomedical engineering career path nationwide. We have offered training to over 1,000 students through these different programs designed to benefit our customers and students entering the imaging/HTM industry.
Maull Biomedical Training is an independent training company specializing in service training on contrast injectors since 2008 and have trained over 2,400 BMETs in that time. The owner and instructor, Steve Maull, was an Air Force BMET and BMET instructor. His company provides service training on contrast injectors manufactured by Bayer/Medrad, LF/Guerbet and Bracco. Maull Biomedical Training also provides tech support, PM kits and toolkits.
*Disclaimer: Products are listed in no particular order.
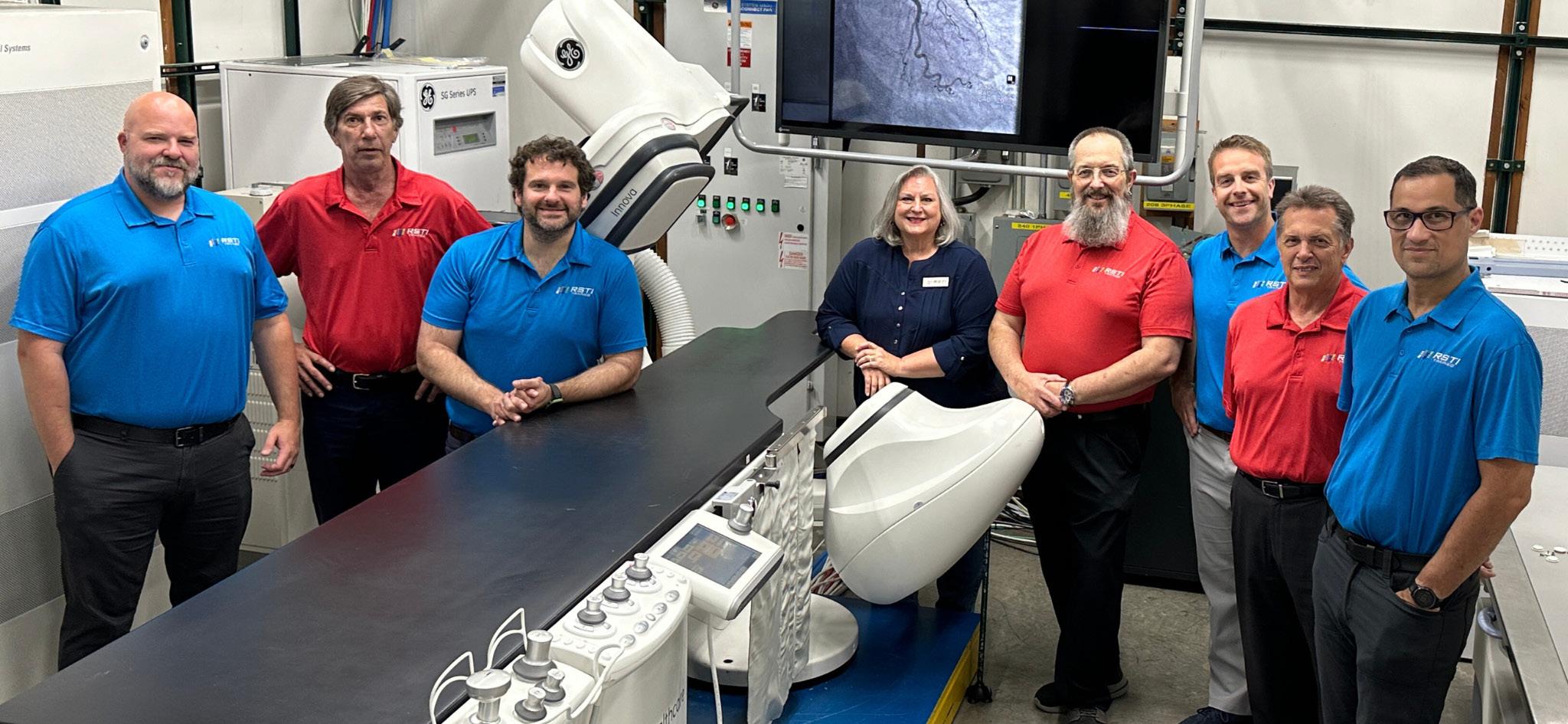
Meet the instructors behind the brand, RSTI’s team representing over 187+ combined imaging experience for a 23+ year average tenure. Radiological Service Training Institute – training the industry since 1985!

The SmartSimulator from Siemens Healthineers is a cloud-based educational tool that enables staff to virtually train and practice on a simulated version of a Siemens Healthineers medical device’s interface. This simulated environment can help staff fully leverage system capabilities from day one and reduce ramp-up times for new imaging equipment, features, and workflows by allowing them to train on complex cases at any time – without impacting daily operations. SmartSimulator provides individual education and practice for an interactive learning experience anytime, anywhere, on a computer or tablet. It supports various education methods and environments, including classroom training, onsite workshops, and virtual formats. The SmartSimulator simulates the interfaces of Siemens Healthineers computed tomography, magnetic resonance imaging, positron emission tomography, single-photon emission computed tomography, radiography, and angiography systems. •
• The fastest growing HTM talent network in the country.
• 350+ open opportunities throughout the United States.
» A variety of posting options ranging from single-job postings to 12-month unlimited memberships.
“My HR department advertised on various government sites and our web site but we did not get a single applicant in over 120 days. Fairbanks Alaska is hard to recruit for but I took out an ad on HTM Jobs and got two good applicants in less than 30 days. I am hiring them both. Thanks HTM Jobs.”
- D. Anderson, Tanana Chiefs Conference
Featured Employers: Agiliti, Renovo Solutions, TRIMEDX, Erbe USA, Incorporated, ISS Solutions, Banner Health, Althea, and more!
By Matt Skoufalos
If the landscape for diagnostic imaging demand in the United States were depicted as a topographical map, it might resemble nothing less than a steep, sharp peak, climbing skyward into a cloud bank.
A February 2025 study published in the Journal of the American College of Radiology (JACR) by Eric W. Christensen, et al., which sampled 348 million medical records, projected utilization rates for medical imaging in the United States to increase as much as 45 percent over current levels by 2030, if
recent trends hold. Although population aging accounts for as much as 12 to 27 percent of that figure, population growth accounts for three-quarters to 88 percent of it.
To that end, the industry is left to determine how to manage these demands, which are on the increase, even
as the workforce to manage them is on the decline.
Murat Gungor, senior vice-president and head of diagnostic imaging North America at Siemens Healthineers of Malvern, Pennsylvania, observes three primary, overarching trends shaping medical imaging demand at present and into the near future. Foremost among these is a growing demand for imaging driven by increasingly medically complex patients burdened by chronic diseases.
In September 2024, an American Hospital Association (AHA) analysis of clinical data from more than 1,300 hospitals showed that inpatient discharges at the end of 2024 are still up 1.6 percent over fourth-quarter baseline data from the end of 2019, while patient acuity is up 3 percent over data from that same period four-and-a-half years ago. Nonetheless, the same study showed that risk of mortality in the first quarter of 2024 was down nearly a quarter from 2019 levels.
This data, AHA reported, showed that “while caring for sicker patients, hospitals’ efforts to improve safety led to 200,000 Americans hospitalized between April 2023 and March 2024 surviving episodes of care they wouldn’t have in 2019.”
In part, that survivability itself points to the greater demands placed upon imaging services, as the same study showed that expanded access to screenings for breast, cervical, and colon cancer has qualified more people for earlier testing, thereby allowing for earlier life-saving interventions into their care needs.
“Increasing efforts to promote and facilitate screenings has further boosted participation rates, emphasizing the importance of early detection and its role in improving cancer care and outcomes,” the study reported.
Parallel to that experience is another dominant trend in the medical imaging space, Gungor said: the advancement of personalized medicine, particularly in the fields of oncology and neurology, where surgeries, therapies, and radiopharma-
ceuticals are all guided by diagnostic and interventional imaging studies.
“That’s a massive trend we’re following,” he said. “Innovations in that field impact the landscape of the imaging space.”
A study on the diagnostic imaging of brain tumors published in the January 2024 issue of Advances in Neuro-Oncological Imaging enumerated the various applications of MRI technologies to specific strategies, including perfusion, spectroscopy, elastography, intra-operative ultrasound, and fingerprinting techniques.
“These advancements have not only improved the accuracy of tumor diagnosis but have also addressed challenging clinical scenarios, including the evaluation of treatment-related changes, responses to novel therapies like immunotherapy, and the early detection of disease progression.”
- Paniz Sabeghi
Alongside those, researchers pointed out advancements in PET/MRI, PET tracers, and radiomics as “delineat[ing] the pivotal role of imaging within the field of neurology,” significantly in “the diagnosis, prognostication, and evaluation of treatment responses for central nervous system (CNS) tumors.”
“These advancements have not only improved the accuracy of tumor diagnosis but have also addressed challenging clinical scenarios, including the evaluation of treatment-related changes, responses to novel therapies like immunotherapy, and the early detection of disease progression,” study authors Paniz Sabeghi, et al, wrote.
“The knowledge of both the capabilities and limitations of these emerging imaging technologies is essential for providing a higher level of personalized care to patients with neuro-oncological conditions.”
Successes like these, or like the recent disease-modifying drug therapies for Alzheimer’s disease and theranostics treatments for patients with prostate cancer, thyroid cancer, and neuroendocrine tumors, push OEMs like Siemens Healthineers “to innovate continuously for better treatments,” Gungor said, “because providers are pushing us to think differently.”
“Drug therapies are making us be partners in the field and provide the blended treatments to the customers that drive this business,” he said. “We’re trying to align our portfolio with this in the back of our mind.”
To that end, he highlighted investments in photon-counting CT technologies, which support “the ambitions of personalized treatment and how we can make an impact,” whether through dose reduction, better image capture, or limiting unnecessary interventions. Eventually, Gungor said, elements of these technologies, no matter how novel, should make their way throughout the roster of diagnostic imaging technologies.
“The goals of improving the diagnosis and the treatment of patients are driving all our investments,” Gungor said. “Ultimately, all this technology will trickle down the portfolio.”
How it gets there, however, is itself another state-of-the-union issue; namely, that of access, which can involve various barriers to clear, be they issues of technology portability, innate dependency, or facility construction.
MR “is not a very installation-friendly modality,” Gungor said, so manufacturers can focus on ways to make it easier to situate in a facility.
“How can you make it easier to install, available in every location, more affordable, more compact?” he said. “Maybe even eliminate certain
dependencies – like helium-based magnet-cooling technologies – to simplify the installation all over the place.
“Being able to make scanners more autonomous, more user-friendly, will all help our customers,” Gungor said. “You have to be able to install the box and train customers how to use it.”
So, too, will advances in elements of the patient experience that improve health outcomes by addressing environmental concerns like atmospherics and comfort, whether in a pediatric setting, in which the scanning experience is improved by creating better audio-visual experiences, or wider-bore scanners that accommodate adult patients who might be obese or claustrophobic.
“All these things are changing the dynamics, improving access to the technology, and increasing the number of patients who can benefit from the technology,” Gungor said. “Better image capture leads to better diagnosis and treatment.”
In general, technological improvements lead to gains in operational efficiency, and eventually, greater productivity. In an environment of increasing demand, hardware innovations can take many forms, from mobile scanners to high-end patient tables that support bedside imaging, or modular upgrades that allow base model systems to be tailored to specific institutional needs.
Advancements like these add up wherever they are found in an overall health system, and reflect how manufacturers are forever pushing themselves to improve upon existing processes, Gungor said.
“As an industry, we need to raise the awareness of the radiologist’s value and why it’s important for them to provide the interpretation at those kind of facilities.
In radiology, there’s actionable findings. If a radiologist finds something that needs action, and that may not have been in the normal course of the patient’s care, we do not yet have strong systems to make sure that patient is properly flagged and followed up on.”
- Jason Theadore
“We are re-inventing ourselves as an organization,” he said. “How we can adapt our identity to help our customers and make a bigger impact in the marketplace? We have to be there continuously because the needs are changing, and we have to understand our customers and speak their language.”
Another fundamental challenge for the medical imaging space remains its ongoing workforce shortage, a confluence of several compounding factors, including the effects of the post-novel coronavirus (COVID-19) pandemic “Great Recession” and a failure to cultivate a pipeline of radiologists, technologists, and other related professionals to replenish the depleted workforce.
Parag Paranjpe is the founder and CEO of HealthLevel, a software company in Mountain View, California that produces the radiology business platform, Foundations. It’s designed to drive operational efficiencies throughout the imaging life cycle by alleviating a confluence of issues that are showing up in the imaging space, from workforce shortfalls to reimbursement challenges to revenue recapture.
“Investment and cost pressures are always going to be there,” Paranjpe said. “We are seeing more and more customers saying, ‘Is there technology we can adopt that improves efficiency but also improves the revenue? Can we find effective technology solutions, get up and running quickly?’”
“That’s where we’ve been able to help our customers,” he said. “That helps the cost basis, helps them on their margins. They’re also finding ways to improve the revenue to get all the money they’re worth.”
At the same time as improving workflow and throughput efficiencies, Paranjpe sees opportunities for imaging entities that are willing to support patient services while they’re shoring up operational challeng-
es on the back end of the business. He observes challenges in the unevenness of some patient experience issues; to wit, he said, they may be able to get an appointment quickly, but not the results of the scan.
As imaging utilization rates for Americans dwarf those in other countries – 245 CT scans per 1,000 people and 118 MR scans per 1,000 people, according to Ohad Oren of the Mayo Clinic, Electron Kebebew of the Stanford University School of Medicine, and John P.A. Ioannidis of Stanford University in the Journal of the American Medical Association –the question of value derived from all that diagnostic imaging becomes more salient.
“We are doing more imaging than the rest of the world,” Paranjpe said. “Do we need to do so much imaging? If we’re more efficient, we may need to do less.”
Moreover, if the systems that gather imaging data don’t work in concert with those which host and manage it, HealthLevel foresees a business opportunity solving interoperability challenges – or at least removing barriers to them – in order to generate insights that improve functionality and, hopefully, recapture revenues.
“The entire world [of consumer devices] operates on plug-and-play solutions; for family healthcare, it is maddening to have these interoperability issues,” Paranjpe said. “It’s doing the customers a disservice. The clinical application may be very good, but if it is not talking to anyone else, it is not as good. We can reduce healthcare costs significantly through technology efficiency.”
One of the biggest hurdles HealthLevel works to clear is the siloing of information. Paranjpe said that he frequently sees organizations limit their partners’ access to data, primarily because of perceived concerns related to security or loss of patients. He points to proven technology standards that provide a secure approach
to data management that can drive operational efficiency and derive better health outcomes. Paranjpe traces much of it back to interoperability issues across best-of-breed systems, and across the industry itself.
“What we should be thinking about is, if I want to grow my business, I want to be at an interoperability standard to make it easier for my customers to make a better hospital, a better imaging center, to increase the margins for everyone in radiology,” Paranjpe said. “If you give them information at once place, that helps them make decisions, it’s a massive time-saver, and it increases their actual revenue.”
Jason Theadore, vice president and chief operating officer, radiology, at AdventHealth Medical Group Central Florida, said that he observes one of the most significant challenges in imaging as being related to its inadequate labor force. As practitioner burnout from short staffing gives way to turf wars between non-radiologists and non-physicians, specialists are expanding their scopes of practice, and advance practice providers (APPs) try to help absorb the increasing workload – not always successfully.
“The need for APPs in our space has drastically increased as we don’t have enough radiologists to handle the current workload,” Theadore said. “In various organizations, we have non-radiologists providing exam interpretations: NPs, radiological assistants, physician assistants. They’ve begun to provide interpretation, and I’m not sure if that’s a good thing or a bad thing yet.”
According to the Christensen study from JACR, researchers observed office-based diagnostic imaging interpretations by non-physician practitioners (NPPs) in Medicare environments up 9 percent annually from 2013 to 2022, across all modalities.
“In various organizations, we have non-radiologists providing exam in-
terpretations: NPs, radiological assistants, physician assistants,” Theadore said. “I think it actually decreases the value of the radiologist at the local and national level.”
“As an industry, we need to raise the awareness of the radiologist’s value and why it’s important for them to provide the interpretation at those kind of facilities,” he said. “In radiology, there’s actionable findings. If a radiologist finds something that needs action, and that may not have been in the normal course of the patient’s care, we do not yet have strong systems to make sure that patient is properly flagged and followed up on.”
As patient volumes move from inpatient to outpatient environments, physician-owned imaging practices still command high levels of investment, but differences in ownership and owner priorities may be exacerbating that scope-of-practice concern.
Even as advancements in technology can help radiologists provide care and push back against burnout or exhaustion, Theadore is most concerned with how institutions like his are managing the changes implicit in offloading these challenges to automated software solutions.
“I think of going from paper charts to EMR; we went through PACS. Now we’re going from no AI (artificial intelligence) to lots of AI,” Theadore said. “We need to have a lot of strong change-management processes for that, both institutionally and as individual entities.”
The bottom line, he said, is that “it’s just going to be so important for us all to make sure that we have the agility and adaptability and accountability to adjust as it evolves.
“If we miss this, things can get offtrack,” Theadore said. “But if we’re agile, we can have the best interests of all involved.” •






































This immersive experience offers:
· Meaningful Connections –Engage with peers facing similar challenges and goals




· Leadership Growth – Discover new tactics to enhance your leadership approach and problem-solving abilities

Step into the spotlight at AHRA’s 2025 Annual Meeting and take your leadership skills to the next level. This isn’t just a conference — it’s an all-encompassing experience designed to give you the tools, strategies, and connections you need to thrive in the ever-evolving medical imaging field.
· Technology in Action –Experience live demos and hands-on interactions with cutting-edge equipment
· Expert Insights – Learn from top industry leaders













BY NICOLE DHANRAJ
As a radiology leader, you make decisions every day that affect your team and the patients you serve.
But have you ever considered whether unconscious bias about disability is shaping those decisions? Ableism – the belief that people with disabilities are less capable – often creeps into leadership practices without us realizing it. It might show up in hiring, promotions, or even the way workplace policies are written.
The problem with hidden bias is that it’s just that – hidden. It’s not always obvious, and most leaders don’t intentionally discriminate.
But assumptions about what a person with a disability can or cannot do can hold back talented employees and create barriers to inclusion.
The good news? Once you recognize these biases, you can start making real, impactful changes to foster a more equitable and high-performing department.
One of the most common biases in leadership is assuming that a person with a disability can’t handle certain tasks. Let’s say
you’re hiring an administrative assistant for the radiology department, and one of the top candidates has multiple sclerosis (MS). They have years of experience and excellent references, but during the interview, you find yourself wondering:
• Will they be able to keep up with the fast pace of the office?
• What if they need extra breaks? Will that disrupt the workflow?
Before you even realize it, you’ve shifted the focus from their qualifications to their medical condition. Instead of seeing their skills, professionalism, and experience, you’re worrying about things that might not even be an issue.
The reality is that many professionals with MS effectively manage their workload, and if accommodations are needed, they’re often minimal – like an ergonomic workstation or flexible scheduling.
A simple way to combat this bias? Ask, don’t assume. Instead of ruling someone out because of what you think might be a problem, ask them, “What would help you succeed in this role?” You’ll likely find that the solution is much simpler than you expected.
Bias doesn’t just show up in hiring – it also affects who gets promoted and who doesn’t. Imagine you have a radiologic technologist who has dyslexia.
They’re one of the best techs on your team, known for their strong patient care, ability to train new hires, and leadership skills. But when it comes time to promote a new lead tech, they’re overlooked because:
• “They struggle with reading orders quickly.”
• “Would they have a harder time keeping up with training materials?”
Rather than evaluating their actual leadership potential, the decision is based on assumptions about dyslexia and paperwork. The truth is, small accommodations – like speech-to-text software, templates for structured reports, or voice recording tools – could make documentation a non-issue.
By assuming they wouldn’t be able to handle leadership responsibilities, the department misses out on a great leader who could bring valuable skills to the team.
If someone is excelling in their role, look at their strengths rather than making assumptions about challenges. Leadership isn’t about how fast someone reads a report – it’s about how well they guide a team, solve problems, and create a positive work environment.
Another common ableist assumption is that hiring people with disabilities will be costly or disruptive because of workplace accommodations. In reality, most accommodations cost very little or nothing at all.
For example, a radiologic scheduler who has attention-deficit/hyperactivity disorder (ADHD) may benefit from structured digital tools with automatic reminders, task management features, which can help them with organization. They can also benefit from noise-canceling headphones or a quieter workspace to reduce distractions in a busy office. A technologist with arthritis might benefit from an ergonomic chair or voice-command software. None of these adjustments disrupt workflow or impact productivity – in fact, many of them can improve overall efficiency.
According to data from the Job Accommodation Network (JAN), most workplace accommodations cost less than $500, and many are free.
A lot of the time, the biggest adjustment isn’t money – it’s a shift in leadership mindset.
1. Rethink How You Hire and Promote
When reviewing applications or considering promotions, ask yourself:
• Am I making assumptions about what this person can or can’t do?
• Am I evaluating their skills and potential fairly?
• Are there simple accommodations that could help them succeed rather than excluding them?
If a job description automatically disqualifies someone with a disability, question whether it’s truly necessary. For example, does an administrative assistant really need to be able to lift 50 pounds, or was that just copied from an old job listing?
Many employees don’t disclose disabilities because they fear discrimination or negative assumptions.
Instead of waiting for employees to ask for accommodations, create a culture where support is the norm. Ask, “What do you need to do your best work?” rather than waiting until someone struggles.
Even the most inclusive leaders have unconscious biases, and that’s OK – as long as you work to recognize and challenge them.
Consider taking disability bias training or having discussions with employees about what barriers they face.
Take a walk through your department and ask:
• Are workstations, breakrooms, and imaging rooms physically accessible?
• Are policies flexible enough to support employees who need adjustments?
• Is technology available to make documentation and communication easier for people with disabilities?
Hidden bias isn’t always intentional – but its effects are real. When we assume that a qualified candidate won’t be able to do the job, or that an existing employee can’t handle leadership responsibilities, we create barriers that don’t need to exist.
The best way to lead adaptively? Ask, listen, and be willing to adapt. The strongest teams are diverse, and the best leaders recognize that talent comes in all forms.
When radiology leaders commit to breaking down ableist assumptions, they don’t just create a more inclusive department – they build a stronger, more effective workforce.
Are you ready to start making changes?
Small steps – like reviewing hiring policies, updating job descriptions, and having open conversations – can make a world of difference.
Let’s start breaking down barriers together. •
Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, RT(R)(CT)(MR), is an experienced imaging director.
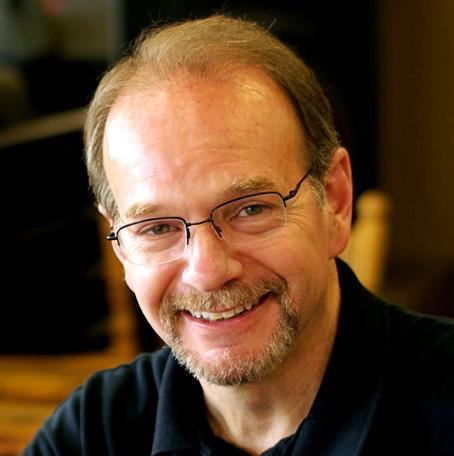
BY DANIEL BOBINSKI
tress is part of life. Whether you’re leading a team, raising a family, or managing a project, stress finds its way into the equation. But is stress always a villain?
Like most things in life, the answer is nuanced. Stress can be both a catalyst for growth and a recipe for disaster, depending on how we manage it.
THE UPSIDE: STRESS ISN’T ALWAYS BAD
First, let’s acknowledge that not all stress is harmful. In fact, stress can be downright beneficial. If we want to become stronger or get toned up, our muscles must experience some level of stress. Pushups, pullups, running and walking all create stress on our muscles, but the result is better health.
Also, to become responsible adults, children must learn to deal with deadlines and established standards, lest they become lazy and spoiled. In the workplace, obstacles before us can be considered stressful, but those situations serve as catalysts for becoming inventive and resourceful. And, learning from mistakes helps us build confidence and adaptability, enabling us to tackle future challenges.
THE DOWNSIDE: WHEN STRESS BECOMES DESTRUCTIVE
On the other hand, chronic or excessive stress can wreak havoc on both our physical and mental health. Prolonged exposure to stress hormones can suppress our immune systems, disrupt our sleep and even lead to an increased risk of heart disease. Mentally, stress can lead to burnout and anxiety, plus other issues that sap our motivation and cloud our judgment.
In the workplace, stress can erode morale and fracture team cohesion, and stress-filled workplaces often experience high turnover and reduced productivity. Left unchecked, stress creates a toxic environment that stifles innovation.
Thus, with stress having both pros and cons, our goal should not be to eliminate stress, but to manage it.
In reality, when we use the word “stressed,” what we really mean is we sense our control starting to slip away. Think about it:
• We can’t get the computer software to do what we want. We’re losing control of our workday, but we say we’re stressed.
• We have employees with clashing personalities who are causing workplace problems. We sense we’re losing control, but we say the employees are causing us stress.
• We have burdensome new state regulations for our industry and work now seems overwhelming. Privately, we’re sensing a loss of control, but publicly we say we’re stressed.
In other words, we use the word “stressed” because saying we’re experiencing a loss of control doesn’t exactly inspire confidence or command respect.
Before I continue, I want to emphasize that differences exist among the categories of stress. We can experience basic stress, chronic stress, and depression. As I mentioned, a modicum level of stress in our lives is healthy, but left unchecked, chronic stress can really take its toll. And if “stress” is the publicly acceptable way to say we’re feeling a loss of control, “depression” occurs when we sense we’ve lost control altogether.
That’s an overly simplistic description, but I wanted to point out that unmanaged chronic stress is a common path to depression. I used to believe that sheer willpower was enough to overcome depression, but speaking from personal experience of 20 years ago, I found that depression often requires a time of medication to address the reuptake of dopamine and norepinephrine in the brain.
Therefore, if you think you’re dealing with chronic stress or depression, a visit to a doctor about the issue is definitely recommended. There is no shame in it. There is nothing wrong with you. The real you is fine. It’s just that if chronic stress has you bordering on depression, it’s the switches in our brains that need attention, that’s all. Full blown depression can be accompanied by feelings of overwhelming helplessness, and nobody needs that.

The above being said, let’s return to addressing the issue of regular stress. Allow me to lean on the writings of the late Dr. William Glasser. In his writings on “Control Theory,” Glasser said our actions affect our thoughts, our thoughts affect our feelings, and our feelings affect our physiology. Therefore, to head off reaching a level of chronic stress or depression (a physiological response to feeling out of control), when stress starts to emerge, we can prevent unnecessary problems if we can catch hold of our thought patterns early enough.
To do that, it helps to know that everything in our lives can be placed in one of four zones.
1. Things happening about which we have no concern
2. Things about which we have concern, but no influence or control
3. Things we are concerned about and have some influence over, but little direct control
4. Things over which we have both control and influence plus a great deal of control
Organizational psychologist Elaine Pulakos supports this categorization through her research on adaptive performance. She says, “Employees who can distinguish between controllable and uncontrollable aspects of challenging situations demonstrate greater resilience and lower stress levels.”
This begs the question: What do you have control over? Why should we find the answer to this question? Because to
minimize unhealthy stress, we should direct our energy onto things over which we have control. For example:
• When facing tight deadlines, rather than focusing on an immovable end date (no control), we can direct our energy toward optimizing our workflow and communication (control).
• During organizational restructuring, instead of stressing about decisions coming from the ivory tower (no control, we can concentrate on maintaining quality work and strengthening key relationships (control).
Thus, the key to managing stress is not trying to control everything, but simply identifying those things over which we have direct control and finding satisfaction in focusing our energy on those activities.
Bottom line, the next time you sense your tension levels rising, pause and ask: “In what aspect of this situation can I exercise influence and control?” Our goal should not be to have a stress-free life, but a life in which stress is a tool, not a tyrant. •
Daniel Bobinski, Th.D. is the author of the best-selling book “Creating Passion-Driven Teams” and the owner of Workplace Excellence. Also a certified behavioral analyst, Daniel consults and conducts training on workplace effectiveness and leadership development. He can be reached at danielbobinski@protonmail.com or eqfactor.net.


BY MARK WATTS PACS/IT/AI
Early in a career as a system leader you are asked to make decisions that seem like a 50/50 bet at best. I was in the process of crafting a corporate imaging data retention guideline for a 19-hospitals system. The question was: “Do we save the CAD overlay box on mammogram studies or not?” I said, “No, let the radiologists see them in the moment but delete them from permanent storage.” What would you have done?
For the better part of a decade, the field of radiology has been abuzz with the promise of artificial intelligence. We’ve seen presentations, read the early papers, and marveled at the algorithms that can, in controlled settings, outperform human experts at specific, narrow tasks. The vision is seductive: an AI co-pilot that never tires, flagging subtle nodules on a chest CT, quantifying white matter hyperintensities on a brain MRI with perfect repro-
ducibility, and prioritizing the acute stroke case on a worklist of hundreds of studies. This is the future we were promised – a future of augmented intelligence, reduced burnout and superhuman accuracy.
Yet, in the quiet, low-lit reading rooms where the real work of diagnosis happens, a different conversation is taking place. It’s a conversation laced with a healthy dose of professional skepticism, born from decades of experience. The central question is not “Can AI be accurate?” We know it can. The more pressing, more nuanced question is: “What happens when it’s wrong?”
An AI model is not a seasoned colleague with whom one can debate the finer points of a case. It is, for now, largely a black box. It presents its findings with an unblinking, uncalibrated confidence. And in that confident assertion lies a hidden danger – the potential for cognitive capture, for the human expert to be swayed by a fallible machine. This is not a failure of the radiologist, but a fundamental
challenge of human-computer interaction.
The true frontier of AI in radiology is not just building more accurate algorithms, but designing systems that gracefully account for their own inevitable imperfections. It is a human factors problem. A recent study1 has shed a powerful light on this very issue, offering compelling evidence that how we present AI findings to radiologists is just as important as the findings themselves. The study reveals that simple changes to the user interface and workflow can either amplify or mitigate the influence of an incorrect AI, with profound implications for patient safety.
I want to unpack the findings of this pivotal research and explore what it means for our profession. This isn’t just an academic exercise; it’s a roadmap for responsibly integrating these powerful tools into our clinical lives.
Before we dive into the study’s solutions, we must first intimately understand the problem. The core psychological phenomenon at play is automation bias. This is the well-documented tendency for humans to over-rely on automated systems, often trusting their output more than their own judgment. We see it in our daily lives: the driver who follows their GPS into a lake, the writer who accepts a grammatically correct but nonsensical suggestion from their word processor.
In the high-stakes environment of a radiology reading room, the conditions are ripe for this bias to take hold. A radiologist may interpret dozens, sometimes hundreds, of complex studies in a single day. The pressure for speed and efficiency is immense. Amidst this torrent of data, an automated tool that offers a definitive-seeming shortcut is incredibly alluring.
When an AI flags a 4mm lung nodule, the radiologist is primed to agree. Finding that same nodule de novo might take minutes of careful scrolling and windowing. The AI offers it up instantly. This is a tremendous benefit when the AI is correct.
But what happens when the AI flags a confluence of pulmonary vessels and calls it a nodule? The study we’re discussing confirmed our deepest anxieties: incorrect AI results can, and do, influence radiologists to make a wrong decision. In the study’s control group, when an AI was wrong, the human radiologist was more likely to be wrong, too. The AI’s error became the radiologist’s error. This is the cognitive siren song: a beautiful, alluring call that can lead the unwary clinician onto the rocks of misdiagnosis. It’s a silent pull, a subtle suggestion that plants a seed of confirmation bias, prompting the radiologist to find evidence to support the AI’s claim rather than approaching the area with a neutral, diagnostic mindset.
To simply deploy AI tools into this environment without guardrails is to ignore decades of human factors research. It is an invitation for error. The study’s brilliance lies not in identifying this problem, but in testing practical, elegant solutions to solve it.
The first major insight from the study is as profound as it is subtle. Researchers tested two different psychological framings for the AI’s output.
1. The “Keep” Condition: One group of radiologists was told that the AI’s findings – whether they agreed with them or not – would be permanently saved as part of the patient’s imaging record.
2. The “Delete” Condition: The other group was told that the AI’s findings were merely suggestions. If the radiologist disagreed with the AI, its output would be completely deleted, leaving no trace in the patient’s file.
The results were striking. Radiologists in the “Delete” condition were significantly less likely to be swayed by an incorrect AI suggestion. They were more willing to overrule the machine and trust their own expertise.
Why would such a seemingly small change in workflow have such a large effect on diagnostic judgment? The answer lies in the psychology of accountability and professional friction.
When an AI’s finding is destined for the permanent record, it takes on an air of officialdom. For a radiologist to disagree with it creates a recorded conflict. The final report would essentially say, “I, the human expert, saw this case and made my determination, but a permanent part of this record is an algorithm that disagrees with me.” This creates a cognitive dissonance. It introduces a layer of professional friction and a potential medico-legal shadow. A future physician, or worse, a lawyer in a malpractice suit, could point to that permanent AI finding and ask, “The computer saw something, doctor. Why did you ignore it?”
Conversely, in the “Delete” condition, the AI is framed as what it truly should be: a consultative, ephemeral input. It is a junior resident whispering a suggestion in your ear. You can consider it, accept it, or dismiss it without ceremony. If you dismiss it, it vanishes. The final report is yours and yours alone. The signature at the bottom carries the full weight of your professional judgment, unencumbered by a dissenting digital ghost.
This finding has massive implications for AI vendors and hospital IT departments. The prevailing wisdom might be to save everything, to create a complete data trail. But this study suggests that, from a human factors perspective, the ephemerality of AI suggestions can be a powerful safety feature. The best systems may be those that allow a radiologist to easily and completely dismiss an incorrect finding, empowering them to remain the ultimate arbiter of truth for that patient’s diagnosis without creating a confusing and potentially hazardous permanent record of disagreement.
The second, and arguably more powerful, finding from this research centers on the presentation of the AI’s results. The
study showed that when the AI provided a simple bounding box – a visual outline drawn around the suspicious region – it fundamentally changed the dynamic between the human and the machine for the better.
This may sound obvious. Of course, showing the radiologist where the finding is located would be helpful. But the true genius of the box emerged when the researchers analyzed its effect in both scenarios: when the AI was right, and when the AI was wrong.
When the AI correctly identified a pathology (like a lung nodule) and drew a box around it, the benefit was clear and expected. Radiologist performance improved. The box acts as a powerful attentional cue. It slashes search time, reduces the risk of perceptual errors (so-called “satisfaction of search,” where finding one abnormality makes you less likely to find others), and provides instant visual confirmation. This is the classic value proposition of Computer-Aided Detection (CADe) and it works splendidly.
SCENARIO
This is where the paradigm-shifting insight lies. The study found that even when the AI was wrong, providing a bounding box for its incorrect finding still improved the radiologist’s overall performance.
Let that sink in for a moment. An AI making a mistake – for instance, drawing a box around a benign vessel crossing and calling it a nodule – made the human radiologist better. How is this possible? This counter-intuitive result is the key to understanding how to build a truly synergistic human-AI partnership. There are a few complementary hypotheses for why this occurs.
• The Focused Scrutiny Hypothesis: Without a box, an incorrect AI finding might be a vague text alert, like “Suspicious nodule in the right upper lobe.” The radiologist then has to re-search a large anatomical area, a task prone to error. With a box, however, the cognitive task is transformed. The question is no longer “Is there a nodule somewhere in this lobe?” but rather, “Is the thing inside this specific box a nodule?” This is a much simpler, more constrained question. The radiologist can zoom in, change the window and level settings, and apply their expert knowledge to that precise location. They can more easily and confidently conclude, “No, that is not a nodule; it is clearly a vessel.” The box forces a micro second-look, turning a passive search into an active, focused process of confirmation or rejection. It allows the radiologist to kill the bad idea quickly and definitively.
• The “Intelligent Second Look” Heuristic: The bounding box acts as a prompt for re-evaluation, much like a colleague pointing to a film and asking, “What do you make of this spot here?” Even if your colleague is mistaken, their query forces you to engage with that specific area of the image with a higher level of scrutiny than you might have during a routine
sweep. The AI, even in its error, is essentially flagging an area of anatomical complexity or ambiguity that might warrant a closer look anyway. In rejecting the AI’s specific hypothesis (nodule), the radiologist might notice a different, more subtle finding nearby (e.g., a faint area of ground-glass opacity) that they might have otherwise missed.
• Reducing Cognitive Load for Rejection: The act of rejecting a hypothesis is a cognitive task in itself. The bounding box makes this task easier. By localizing the “threat,” the AI allows the radiologist to neutralize it efficiently. This may prevent the lingering doubt or the need for time-consuming re-scans of the entire study that a vague, non-localized alert might trigger.
In essence, the bounding box turns the AI from a would-be oracle into a focused searchlight. Sometimes the searchlight illuminates the treasure. Other times, it illuminates a pile of rocks, but in doing so, it allows you to quickly identify them as rocks and move on, confident that you’ve thoroughly examined that spot. This is the definition of augmentation: the tool makes the human expert more efficient and more confident, both when it is right and when it is wrong.
This study is more than an interesting academic paper; it is a direct call to action. The findings provide a clear, evidence-based mandate for how we must proceed with the integration of AI into clinical practice. This responsibility is shared among three key groups.
1. For Radiology Practices and Hospital Administrators: The implementation of AI is not just a software purchase; it is a clinical pathway redesign. You are not just buying an algorithm; you are buying a human-computer interface that will directly impact patient care.
• Prioritize Human-Centered Design: When evaluating AI vendors, scrutinize the user interface (UI) and user experience (UX) with the same rigor you apply to the algorithm’s accuracy metrics. How are findings displayed? Is there a bounding box or segmentation mask? How easily can a radiologist dismiss, edit, or accept a finding?
• Embrace the “Delete” Principle: Work with vendors to create workflows where AI suggestions are treated as non-permanent, consultative inputs. The radiologist’s final signed report should be the single source of truth. The AI’s “opinion” should not haunt the patient’s record unless it has been explicitly validated and incorporated by the human expert.
• Pilot and Observe: Before a department-wide rollout, conduct pilot studies within your own environment. Observe how your radiologists interact with the tool. Gather feedback. The interaction in a controlled demo is very different from the reality of a high-volume Tuesday afternoon.
2. For Radiological Societies (RSNA, ACR, ESR, and others): As the professional bodies that guide our specialty, we have a duty to lead. The wild west of AI implementation must be tamed with thoughtful, evidence-based guidance.
The future is a radiologist, armed with decades of experience and nuanced judgment, working in a seamless, intelligent partnership with tools designed to augment their strengths and guard against their weaknesses.

• Formulate Clinical Practice Guidelines: We need to move swiftly to develop and disseminate guidelines for the clinical use of AI. These should address best practices for interaction, how to handle AI-human disagreements, and standards for the user interface.
• Standardize Reporting of AI Usage: A major debate is brewing: should the use of an AI tool be documented in the final radiology report? If so, how? Standardizing this language is essential for clinical clarity, legal protection, and patient communication.
• Develop AI Literacy Curricula: We must define and promote “AI literacy” for all radiologists – not just an understanding of the statistics, but a deep, practical knowledge of these human-factors principles, including automation bias and the importance of interface design. This should become a core part of residency training and continuing medical education.
3. For Every Practicing Radiologist: Ultimately, the responsibility for the final diagnosis rests with us. We are the final line of defense for our patients.
• Cultivate “Informed Skepticism”: We must learn to treat AI tools as we would a first-year resident: enthusiastic and often correct, but requiring constant supervision and verification. Never accept an AI finding without personally verifying it from the source data.
• Understand Your Tool’s Weaknesses: Demand more than a sales pitch from vendors. Ask for data on their algorithm’s failure modes. Where does it struggle? Does it perform poorly on certain patient populations or with certain scanner protocols? Knowing your tool’s limitations is as important as knowing its strengths.
• Be an Active Participant in Design: You are the end-user. Your feedback is invaluable. Advocate for better interfaces. If a tool’s workflow is clumsy or its presentation of findings is ambiguous, speak up. You are not just a consumer of this technol-
ogy; you are a critical partner in its development.
The integration of artificial intelligence into radiology represents a monumental shift in the history of medicine. But its ultimate success will not be measured by the cleverness of our algorithms, but by the wisdom of our implementation.
The study reminds us that the human in the loop is not a bug to be engineered out, but the central feature of a safe and effective system. It proves that simple, thoughtful design choices – a bounding box to focus attention, a workflow that empowers the radiologist’s final judgment – can transform AI from a potential source of error into a robust tool for augmentation.
The future is not a radiologist replaced by a machine. The future is a radiologist, armed with decades of experience and nuanced judgment, working in a seamless, intelligent partnership with tools designed to augment their strengths and guard against their weaknesses. By focusing on the human factors, by building systems that are forgiving of the AI’s flaws and respectful of the human’s expertise, we can deliver on the promise of AI and elevate the standard of care for every patient we serve. •
(1) European Radiology https://doi.org/10.1007/s00330-023-09747-1 CHEST Can incorrect artificial intelligence (AI) results impact radiologists, and if so, what can we do about it? A multireader pilot study of lung cancer detection with chest radiography Michael H. Bernstein1,2,3 · Michael K. Atalay1,3 · Elizabeth H. Dibble1 · Aaron W. P. Maxwell1,3 · Adib R. Karam1 · Saurabh Agarwal1 · Robert C. Ward1 · Terrance T. Healey1 · Grayson L. Baird1,2,3 Received: 9 December 2022 / Revised: 16 April 2023 / Accepted: 18 April 2023
Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.








































































































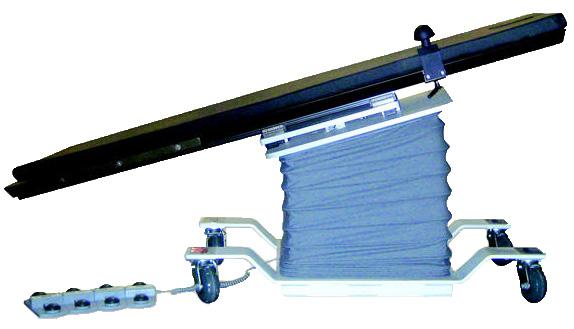


DIRECTOR’S CUT
BY NICOLE DHANRAJ
Being an imaging leader isn’t just about running a department. It’s about holding everything together.
You’re the go-to person for late-night calls, staff issues, physician demands, and administrative pressures.
You’re expected to be available, responsive, and on top of everything 24/7. But at what cost?
Maybe you feel like you’re running on fumes. Maybe you check emails at midnight. Maybe you’ve had days where you couldn’t even step away for lunch. You tell your staff to take care of themselves, but do you ever take your own advice?
You can’t be an effective leader if you’re exhausted, reactive, and constantly running damage control.
This isn’t about just “self-care.” This is about taking back control of your time, energy and sanity.
Burnout for leaders isn’t just about feeling tired – it shows up in different ways. You might find yourself as the first call for every problem, big or small.
You may be constantly firefighting
instead of focusing on strategic improvements. Perhaps you’re stretched so thin that personal time feels like a luxury. You may even feel guilty stepping away, even when you desperately need to. You’re not alone. Many imaging leaders feel trapped in a cycle of overwork, fearing that if they unplug, everything will fall apart. But the truth is, it won’t. And you need to start leading in a way that’s sustainable for you and your team. Here are some strategies to unplug without guilt:
• Set a Personal No-Call Window and Enforce It: You don’t need to be available every second. If you don’t set boundaries, your team won’t either. Set a two-hour window daily where you are completely unreachable, except for true emergencies. Communicate this clearly to your team so they understand that this is your recharge time. Delegate smaller issues so that others can step in when needed. I did this and saw a 25% drop in after-hours calls because staff learned to handle non-urgent problems independently.
• Stop Micromanaging and Coach Your Team Instead: Your job isn’t to solve every single problem – it’s to lead a team

that can handle things without you. When someone comes to you with a problem, ask them first, “What do you think we should do?” Encourage your team to think critically rather than defaulting to you for answers. Empower a second-in-command so you’re not the only decision-maker. Leaders who shift from problem-solver to mentor build stronger teams and reclaim their time in the process.
• Treat Your Time Off as Sacred: Would you expect your techs to work 14 days straight with no break? Then why do you hold yourself to that standard? When you’re off, you’re off. No emails, no “just checking in.” Train your team to handle daily decisions without you. If necessary, start with baby steps – take a half-day off without checking your phone and build from there.
An imaging director who was fully unplugged during a vacation later admitted, “I was terrified to step away, but when I came back, nothing had fallen apart. It was all in my head.”
• Push Back on Unrealistic Expectations: Sometimes, the real pressure comes from above. Admins expect more productivity with fewer resources, leaving you stuck in the middle. Use data to set boundaries. Instead of saying, “We can’t do this,” show them why with staffing ratios, patient load trends, and overtime costs. Offer solutions, such as automation tools or adjusted workflows. Document everything. If leadership won’t listen, having a record of workload data can protect you and your department. Leaders who negotiate with facts rather than frustration get taken more seriously.
• Build a Support System: Leadership can be isolating, but trying to handle everything yourself is a fast track to burnout. Find a leadership buddy – I had many – it could be another imaging manager or someone outside your department – to vent to and seek advice from. Join an industry group for fresh perspectives and problem-solving ideas. Hold a monthly leader huddle with your colleagues, even if it’s just 30 minutes, to exchange strategies and support.
Every great leader has a circle of trusted advisors –don’t try to do this solo.
• Lead by Example, Not Exhaustion: Your team is watching you. If they see you running yourself into the ground, always on call, and never taking breaks, they’ll assume that’s what leadership looks like. But if they see you setting boundaries, prioritizing your well-being, and delegating effectively, they’ll follow suit.
You don’t need to be available 24/7 – train your team to manage without you. Set clear boundaries and protect your time so you can lead better.
Negotiate with data and push back on unrealistic demands. Build your network – you don’t have to carry this alone.
Your department needs a leader, not a martyr. What’s one small change you can make today to reclaim your time and energy? •
Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, RT(R)(CT)(MR), is an experienced imaging director.

X- ray imaging has been a cornerstone of diagnostic medicine for decades, providing a non-invasive way to visualize internal structures. From detecting fractures and foreign objects to monitoring diseases like pneumonia and cancer, X-ray systems play a vital role in patient care. Compared to other imaging modalities, X-ray offers unique benefits that make it indispensable in health care:
• Computed Tomography (CT): Provides detailed cross-sectional images but requires more radiation and is more expensive, making it ideal for complex diagnostics.
• Magnetic Resonance Imaging (MRI): Offers superior soft tissue contrast but is less effective for bones and requires a longer, costlier process.
• Ultrasound: Radiation-free and widely used for soft tissue imaging but ineffective for bones or areas with significant gas interference.
X-ray’s versatility, cost-effectiveness, and speed make it a preferred choice for many diagnostic needs, particularly in emergency and outpatient settings.
X-ray systems are found in hospitals, outpatient clinics, and imaging centers. Their key components include:
1. X-ray tube: Generates X-rays by accelerating electrons into a target material.
2. Generator: Regulates energy and timing.
3. Detector: Captures images digitally or on film.
4. Software systems: Enhances, stores, and integrates images into patient records.
Proper maintenance ensures reliable performance, making professional service training essential.
Maintaining and repairing X-ray systems requires technical expertise. Specialized training enables service professionals to:
• Diagnose and Repair Issues: Minimize downtime and ensure uninterrupted patient care.
• Perform Routine Maintenance: Extend equipment lifespan and maintain image quality.
• Ensure Regulatory Compliance: Meet radiation safety and operational standards.
For four decades, the Radiological Service Training Institute (RSTI) has trained thousands of professionals, ensuring the reliability of imaging systems worldwide. Our specialized programs offer both theoretical and hands-on training, equipping technicians with the skills needed for modern X-ray systems.
Key Offerings:
• Principles of Servicing Diagnostic X-Ray Systems (Phase 1): Covers X-ray operation, radiation safety, and troubleshooting.
• Advanced Digital Imaging System Maintenance: Focuses on servicing and calibrating digital X-ray systems.
• Custom Training Modules: Tailored courses for specific equipment models and emerging technologies. Our programs emphasize real-world applications, ensuring trainees gain practical skills that translate di -

rectly to their work environments.
As diagnostic imaging evolves, RSTI continuously updates its curriculum to incorporate the latest advancements, including:
• Digital Radiography Integration: Seamlessly connecting X-ray systems with hospital networks.
• Utilizing AI-Driven Diagnostics: Enhancing troubleshooting and system performance.
• Remote Monitoring Solutions: Reducing service response times and improving efficiency.
With 40 years of training excellence, RSTI remains dedicated to empowering service professionals with cutting-edge knowledge. In recognition of our contributions, RSTI received two 2025 TechNation Tech Choice
Awards, “The Wrenchies,” highlighting our industry leadership in imaging service education.
Health care facilities investing in well-trained professionals benefit from improved equipment reliability, reduced downtime, and enhanced patient outcomes. RSTI’s commitment to education ensures that X-ray systems continue to be the backbone of diagnostic medicine.
As medical imaging advances, X-ray systems remain fundamental to healthcare. The demand for skilled technicians has never been greater. Through comprehensive training programs, RSTI continues to advance the capabilities of imaging professionals and support the health care industry’s commitment to excellence.
Learn more at rsti-training.com.

BY FAMILY FEATURES
Sweet-tasting foods and drinks may be beloved by many, but a new survey from the International Food Information Council (IFIC) reveals a mounting tension between consumers’ enjoyment and health goals when it comes to sweetness in the diet.
According to the IFIC Spotlight Survey: Americans’ Perceptions of Sweetness in Their Diets, nearly 6 in 10 Americans (58%) prefer sweet as their favorite taste – more than savory/umami (49%), salty (45%), sour (24%), or bitter (21%). Yet despite their fondness for sweet flavors, 8 in 10 Americans (78%) believe it is important to reduce the overall sweetness of their diet, primarily to eat healthier, manage blood sugar or diabetes, manage body weight, and support dental health.
“From a biological perspective, our love of sweet taste makes sense – it’s thought to be an ancient survival mechanism that signaled safe, energy-rich food, like glucose from plants” said IFIC Senior Director of Research & Consumer Insights Kris Sollid, RD. “As we’ve evolved, navigating our innate preferences and health goals has become more complicated.”
When asked what comes to mind first when they think about sweet-tasting foods or drinks, most Americans mentioned a specific food (39%) or beverage (23%) – while far fewer thought of an ingredient or feeling. But their attitudes toward that sweetness are nuanced. While 59% agree that sweet-tasting foods and drinks can be part of a healthy diet, many still support scaling back the overall sweetness of their diets (78%).
Among those who think it is important to reduce sweetness, the most common reasons include eating healthier (49%), managing blood sugar or diabetes








(43%), managing weight (41%), and improving dental health (36%). Notably, women were more likely than men to cite each of these as top reasons for cutting back on sweet-tasting foods.































The survey asked respondents what they would ex pect if they reduced the sweetness of their current diet. The top expectations? Improvements in overall health (64%) and the healthfulness of their diet (64%), fol lowed by lower calorie intake (58%) and reduced body weight (55%).
But when it comes to cravings, Americans are split. One-third (36%) believe reducing sweetness would increase their cravings, while an equal number think cravings would decrease.


“This kind of cognitive dissonance shows how emo tionally and biologically complex our relationship with sweetness is,” said Wendy Reinhardt Kapsak, MS, RDN, IFIC President & CEO. “There is a deep-rooted tension between enjoying food and aspiring to eat what we think of as ‘healthier.’ We need more tools and strategies that help people strike a balance.”
When asked why they think sugar is added to foods and drinks, the leading reason is sweetness, according to 77% of respondents. Far fewer recognized its other functional roles, such as texture (24%), shelf-life (21%), or fermentation (13%).
The foods and beverages Americans believe contribute the most sweetness to their diets? Desserts and sweet snacks (53%) and candy (49%) topped the list, followed by fruit (41%) and sugar-sweetened beverages (36%).
Sweetness, whether from added sugars or low- and no-calorie sweeteners, plays a powerful role in how we experience and enjoy food. But as this survey shows, Americans are increasingly looking for balance.
“Sweetness alone is not always a reliable marker of poor diet quality. Context matters – especially when high levels of sweetness can contribute to overconsumption of less nutrient dense foods that are high in calories from added sugars and saturated fat,” said Sollid.
“There is no one-size-fits-all approach to dietary sweetness,” added Reinhardt Kapsak. “Science does not necessarily support the idea that simply reducing sweetness automatically leads to better health outcomes. What we need is thoughtful innovation, consumer education, and supportive environments that honor both health and enjoyment.” •














































































































































































































































1 Imaging machine connections 4 _____ camera: medical imaging device 9 Below 10 Ultra-low-field MR _____: popular subject of a recent ICE webinar
12 Friend
13 Retrieving lost data in a computer system 15 Light metal symbol
18 ____ speckle contract imaging
19 Company working with GE Healthcare to create an innovative imaging system, SonoSAMTrack
21 Put into position
22 Training institute for radiology professionals, abbr. 24 Imaging technology, abbr.
25 Medical imaging system used during surgical procedures 28 Specialist suffix
Recommended practice
Solidify 31 They’re used for holding and manipulating imaging equipment
1 They measure continuing education progress, abbr. 2 Financial plans 3 Otologist’s concern 5 Detailed examination 6 Principal 7 Tube for conveying fluids or gases 8 Able to adapt to new challenges
Damage 14 Shrek, for example
16 Warning of a non-optimum situation
17 Metal used in MRI machines 19 Kind of acid 20 Twelfth month of the year, abbr. 23 ____ body irradiation
Is introduced to
Close tightly
• $300 a month
• 1/6 page ad included in the marketplace
• Up to 5 categories in our ICEDEX
• Your company name, website and phone included in your ICEDEX listings
• Your company name in the alphabetical business index
• Appear in the print and digital magazine
































“ICE Webinars always provide great timely information in a well planned format.”
- Nancy Godby, Director of Radiology, Cabell Huntington Hospital - Marshall Health Network
Register to view the webinars each month
Watch recorded webinars on-demand
3.EARN
ARRT Category A CE credits pending approval

Ray-Pac proudly reintroduces the INTERAY name to the x-ray tube replacement industry. Our direct replacements for Canon / Toshiba diagnostic tubes are now available from the country’s leading manufacturer of aftermarket x-ray tubes. Trust the best to deliver “When Quality Counts”

