












































Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking.
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs.
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs.


Breast screening with exceptional service can add families to the patient list.
An MRI Safety Officer is just one step in a series of steps when it comes to imaging safety for everyone.


Tamra Whitaker’s imaging career began after a chance encounter while visiting her mom at work.


X-ray market growth means a wide range of exciting products for healthcare professionals.
Find out the latest news from manufacturers and more.


Fear often gets mistaken for a lack of motivation.
President
Vice
Kristin
Vice
Jayme
Senior
Megan
Editorial
Beth
Kimberly
Megan
Dean
Senior
Art
Kristin
Digital
Cindy
Accounting
Diane



Pa ri V. Pandharipande, MD, MPH, FACR, a nationally renowned physicianscientist at The Ohio State University (OSU) College of Medicine and Wexner Medical Center, has been named Chair of the department of radiology at Penn Medicine, effective

“Dr. Pandharipande brings a wealth of experience in key leadership roles that uniquely position her to lead our ‘One Penn Medicine Radiology’ efforts at this critical time for health care,” said Kevin B. Mahoney, CEO of the University of Pennsylvania Health System. “As we continue to enhance care, enrich patient experience, increase efficiency, and standardize processes across our facilities, we are especially excited for her expertise in managing transformative clinical integration projects across other large health systems.”
Pandharipande has served as Chair
of Radiology at The OSU College of Medicine and Chief of Radiology Services at Wexner Medical Center since 2021. Under her leadership at OSU, the department has substantially grown its imaging infrastructure, volumes, and service line, and has significantly expanded its training program. In addition, the department is actively advancing a center of imaging excellence, with an emphasis on translational research and multidisciplinary science.
She previously spent 17 years at Massachusetts General Hospital (MGH) as a physician and researcher, studying topics ranging from imaging value to cancer screening, surveillance, and treatment selection.
Pandharipande also served as Associate Chair of Integrated Imaging and Imaging Sciences and as Executive Director of Clinical Enterprise Integration for Mass General Brigham Radiology, leading a transformative project for integration of imaging services across MGH, Brigham and Women’s Hospital and their community affiliates. She also served as the Director of the MGH Institute for Technology Assessment, a multidisciplinary health outcomes research institute, and led an NIH-funded research program centered in imaging and cancer outcomes, which continues at OSU.
“As we continue to enhance care, enrich patient experience, increase efficiency, and standardize processes across our facilities, we are especially excited for her expertise in managing transformative clinical integration projects across other large health systems.”
on the Advisory Board of the American College of Radiology’s Harvey L. Neiman Health Policy Institute. She also has served as Chair of the American Cancer Society’s Healthcare Outcomes, Policy, and Systems grant review committee and currently serves as a member of the NIH’s Organization and Delivery of Health Services study section. She is a past president of the Radiology Alliance for Health Services Research within the Association of Academic Radiology, and she has served on numerous local and national committees, including as a past, longtime Chair of the ACR’s Incidental Findings Committee.
Pandharipande earned both her undergraduate and medical degrees from Cornell University. She completed an internship at the New York Presbyterian Hospital-Cornell and her diagnostic radiology residency at New York University Medical Center. Her training continued with a cancer outcomes research fellowship and an abdominal imaging clinical fellowship, both at MGH, and earned a master’s degree in public health from the Harvard T.H. Chan School of Public Health.
— Kevin B. Mahoney, CEO of the University of Pennsylvania Health System
“Dr. Pandharipande has shown strong leadership in all our mission areas – research, clinical care, education, and community service – as well as in the field of radiology itself, which is rooted in everevolving technology,” said Jonathan A. Epstein, MD, Interim Executive Vice President of the University of Pennsylvania for the Health System and Dean of the Perelman School of Medicine. “We are fortunate for her guidance as Penn Medicine Radiology continues to set new standards for the role of imaging in health care delivery of the future.”
Pandharipande brings strong national leadership experience, currently serving on the Board of Directors for the Radiological Society of North America, where she oversees the Government Relations portfolio, and
Penn Medicine’s Department of Radiology is the first academic department of radiology in the world. Founded in 1898, it has eight divisions: abdominal, breast, and cardiothoracic imaging; community radiology; interventional radiology; musculoskeletal imaging; neuroradiology; and nuclear medicine and clinical molecular imaging. The department is comprised of more than 100 accomplished clinical and basic science faculty, and its imaging research spans four schools and more than 20 departments across Penn.
Pandharipande will succeed longtime department Chair Mitchell Schnall, MD, Ph.D., who now serves as Penn Medicine’s inaugural Senior Vice President for Data and Technology Solutions. William Stavropoulos, MD, an internationally recognized interventional radiologist, will continue to serve as interim Chair during the transition period before Pandharipande begins her new role. •

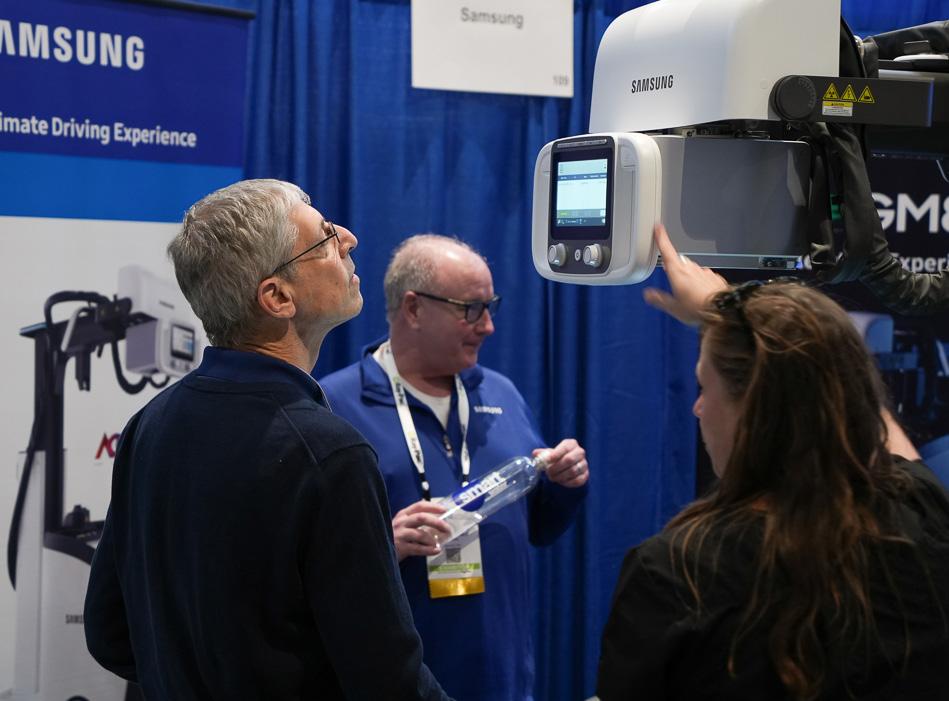
The 2025 Imaging Conference & Expo (ICE), held in Orlando, Florida, was a resounding success, drawing professionals from across the medical imaging industry. With more than 500 participants, the event created a vibrant hub for imaging directors, radiology administrators, and imaging engineers to network, learn, and explore the latest advancements in medical imaging technology.

Now in its 11th year, ICE has become a cornerstone event for the imaging community. The conference successfully combines accredited continuing education, a wide array of exhibitors, and valuable networking opportunities. This year, ICE met all the criteria for continuing education credits and was approved by AHRA: The Association for Medical Imaging Management for 25 Category A ARRT continuing education credits. Additionally, ICE 2025 was approved for 24 CEUs by the ACI, with approval code 0225IV-24 valid through February 22, 2026.
MD Publishing Vice President Kristin Leavoy, CMP, emphasized the event’s unique position within the medical
imaging industry.
“The Imaging Conference and Expo (ICE) is an event like no other that brings together the best minds in medical imaging,” she said. “As a dedicated space for imaging directors, radiology administrators, and imaging engineers, ICE provides invaluable insights into the latest industry trends, technologies, and best practices. The educational sessions are top-notch, offering CE credits that enhance professional growth, while the networking opportunities allow attendees to connect with industry leaders and peers. Whether you’re looking to expand your knowledge, discover cutting-edge solutions, or engage with experts, ICE is the premier conference to attend!”
Attendees participated in top-tier educational sessions addressing key topics such as the latest in imaging technologies, patient care advancements, and workflow optimization. In addition to the educational tracks, ICE offered numerous opportunities for networking and exploration of new products and services.
The conference kicked off with the Leadership Summit, an exclusive event by invitation only, followed by engaging

educational sessions. Attendees received continuing education credits as they explored the latest trends and solutions in imaging. This was followed by the ICE Break Networking Lunch, offering an informal space to connect with peers.
On Sunday afternoon, Fred Moore’s keynote address, “The Secrets to Time Management Magic,” provided valuable insights into personal and professional productivity, setting the stage for a packed afternoon of networking and exhibition. The Exhibit Hall Grand Opening took place later that evening, where exhibitors from leading industry companies displayed cutting-edge products and services aimed at enhancing imaging departments’ efficiency.
The exhibit hall showcased the latest technologies and tools to streamline imaging services and improve departmental efficiency. Vendors were on hand to present new products, allowing attendees to interact with the latest solutions shaping the future of medical imaging.
Networking was a key component of ICE 2025. Attendees had multiple opportunities to meet with industry leaders and peers, both formally and informally, throughout the event. One highlight was the Margaritaville at ICE Party, a fun-filled event that provided a relaxed setting to unwind and build relationships. •



Christopher Nowak, Senior Director at Community Health Systems, praised the event’s ability to bring the industry together.
“The first greatest medical imaging conference each year that provides education, technology showcasing, and camaraderie! Second-to-none!” Nowak said.
Wayne Kramer, President of W7 Global, LLC, highlighted ICE’s networking value.
“I like that it (ICE) brings a lot of relevant contacts that I can meet with in one place. Things like the networking lunch and exhibit hall are great for this,” Kramer said.
He also noted, “An intimate and relevant event that brings a lot of business opportunity to a single venue that generally feels relaxed, fun, and functional.”
Francis Vonder Haar, Vice President and General Manager-Imaging at PartsSource, shared,
“ICE 2025 was an excellent opportunity for imaging professionals to expand their networks, educate themselves on the latest trends, and explore new solutions to their challenges.”
Froedtert South Director, Imaging Services Carolyn Ruby summed up the conference best when asked to describe 2025 ICE in her own words she said,
“Amazing experience!”

The 2025 Imaging Conference & Expo (ICE) celebrated its 11th anniversary in Orlando, Florida, with imaging professionals from across the nation. More than 500 participants attended the event including imaging directors, radiology administrators and imaging engineers. ICE continues to be the conference for imaging professionals to network, learn, and explore the latest advancements in medical imaging technology. 1 2 3



1. Several attendees won door prizes in the ICE 2025 exhibit.
2. The ICE conference is a great place to network with peers.
3. The reverse expo is a special opportunity to make connections.
4. Women In Leadership (WIL) members pose for a group photo at ICE 2025.
5. The keynote address and continuing education sessions provided valuable insights for attendees.
6. The leadership summit provided a forum for idea sharing.
7. The exhibit hall brought attendees face-to-face with solutions to assist them do their jobs better.
8. The leadership breakfast brought decision makers together for meaningful conversations.
9. Everyone had a smile at the grand finale party capping off another wonderful conference.






10. Exhibitors provided information and hands-on experiences with equipment. 4 5 6 7 8 9 10

Imaging Supervisor Tamra Whitaker, RT(R)(M)(CT)(BD) (QM), helps maintain a smooth patient flow at Atrium Health Wake Forest Baptist Premier Imaging. Her imaging career began during a chance encounter while visiting her mom at work. ICE Magazine recently found out more about her start and her goals for the future.
Q: WHERE DID YOU GROW UP?
A: I grew up in a small town in North Carolina called Lewisville. I currently reside about 20 minutes from there in the rural town of Yadkinville.
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/ EDUCATION?
A: I graduated from Forsyth Technical Community College with an AAS in radiography in 1997 and completed my undergraduate in 2023 at Cabarrus College of Health Sciences. I hold a BS degree in medical imaging and am credentialed with ARRT in radiography, mammography, computed tomography, bone densitometry, and quality management.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: My mother worked as interior design coordinator at one of the larger hospitals in the Winston-Salem area. I was visiting her
for lunch one day and we happened to walk through the radiology department “line-up” area which was the hallway between fluoroscopy rooms. I happened to catch a glimpse into one of the rooms where they were performing a modified barium swallow and was immediately captivated. Thus began a lifelong passion and career path!
Q: WHAT IS THE MOST REWARDING ASPECT OF YOUR JOB?
A: The most rewarding aspect of being an imaging leader is seeing the difference we make in the lives and care of the patients we serve. Whether it is helping parents of a young child understand what is needed to obtain diagnostic images or holding the hand of an anxious lady who is undergoing a breast biopsy, this is the aspect I find most rewarding.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: Imaging leaders wear many hats, especially as a working supervisor. I enjoy making connections with people, both patients and teammates, who I am responsible for. Learning people and how to best inspire them through connections is important to me.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: EVERYTHING! I have transitioned through many technological advances since I entered the field of radiology 28 years ago. It never gets old to see emerging technology and how it will help technologists capture and radiologists interpret images and exams, knowing the advancements will make a difference in the lives of our patients! Artificial Intelligence has exploded onto the scene in the imaging world in recent years and is very exciting to learn about as it develops.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: My greatest accomplishment to date was completing my undergraduate degree while working fulltime with a family. I am incredibly blessed to have a great support system and am thankful to have had the opportunity to further my knowledge and earn a bachelor’s degree.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT FIVE YEARS?
A: In the next five years, I would like to continue to expand my knowledge in my current position. I have strong mentors in my manager and director who encourage and allow me to grow. Depending on opportunities that may arise, possibly advancing into a manager’s position. •


FAVORITE HOBBY: Hiking
FAVORITE SHOW: Who has time to watch TV?
FAVORITE FOOD: Tacos
FAVORITE VACATION SPOT: North Carolina mountains
1 THING ON YOUR BUCKET LIST: Drive a race car
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU: When I was in 7th grade, I won a writing contest in my school district which included a trip to Washington, D.C. and $250.
JENNIFER J. ALEXANDER,

BY MATT SKOUFALOS
Many healthcare professionals talk grandly about the need for continuing education and forming a lifelong commitment to learning. More than most, Jennifer J. Alexander has lived it.
Alexander, who cheerily sports the nickname “Dr. J,” is a registered X-ray and CT technologist and a Certified Radiology Administrator. She holds master’s degrees in business and healthcare administration and a doctorate in healthcare administration.
“I got my associates in my 20s, my bachelor’s in my 30s, two master’s degrees in my 40s, and my doctorate in my 50s,” she said.
At UT Southwestern Medical Center, Alexander has spent a decade as the operations manager for imaging services, and has made strengthening the medical imaging workforce pipeline her principal focus in that time.
The institution runs an MRI apprenticeship, which offers on-the-job training for employees to become MRI technologists; an imaging training assistance role for radiography students to bridge them from students to imaging professionals; and an advanced imaging fellowship to cross-train technologists into other imaging modalities.
“I spend a lot of my time getting this next generation ready for careers in imaging,” Alexander said. “I attend career and job fairs and speak at the local colleges about medical imaging to get them excited about a career pathway.”
The need for new talent is essential, she said. Medical
imaging plays a vital role in a patient’s journey, providing images to diagnose illness, guide treatment, and empower patients with options.
“Keeping the talent growing and learning by providing cross-training opportunities provides continued adaptation and critical thinking as they move to the next level of imaging.” Alexander said. “There are traditional ways to get into imaging by the college route, but there are other ways to upskill them by providing unique opportunities like the apprenticeship.”
Alexander views her efforts as “influencing the next generation” in closing education gaps for novice imaging professionals, and helping them learn through clinical experiences in a healthcare setting. She likens it to her own experience as a youngster, learning the electrician trade through practical training on the job site.
“Taking a frontline employee early in their career and investing in them by providing the opportunity to become a registered MRI tech is life-changing for them,” Alexander said.
“While it’s been challenging, I couldn’t have asked for a better profession,” she said. “I’m trying to stay ahead of the next generation to figure out how to motivate them, keep them, and grow them.”
Alexander focuses on helping imaging professionals hone their technical skills and education partly because her parents didn’t have a formal education to make their way in the world. Her mom, the oldest of 10 children, raised her own siblings while she was growing up herself. Due to life circumstances, both of her parents dropped out of high
school. Nonetheless, her parents made their way together and uplifted the people around them.
“The two of them together, without an education, were just hellacious,” Alexander said. “They could move product and people and truly raise people up. Each person my mom had working for her had an opportunity to unlock their true potential. She was always trying to improve everyone around her and upskill their talents.”
Alexander herself was early to enter the workforce. The Austin, Texas native spent 20 years growing up in New Mexico, where she rode dirt bikes at nine and 10 years old. She earned money working for an electrical contractor, plugging and switching for $2 an hour.
Alexander needed transportation when the family moved to a different high school district. At 14 years and nine months, she was eligible for a motorcycle license, and became the only girl in her high school who commuted to class on a Honda XL100.
“My mom bought me a pink jacket to wear,” Alexander remembers.
In school and outside of it, she hustled. Her mom helped her make breakfast burritos, which she sold off the back of the bike for $1 apiece. Alexander also spent six to eight hours a day working to make extra cash, whether at Stuffy’s Sopapillas, mowing lawns, or babysitting.
Winters were so cold that Alexander’s hands wouldn’t fully thaw from the commute until the final 15 minutes of her first-period class, which was typing. She became faster than her classmates when she had only the final few minutes of the period to complete her work.
“In New Mexico, we did fundraisers for paper,” Alexander said, a testament to some of the lower-resource regions.
“When I came to Texas and saw yard art, I had never seen that before. I didn’t see one car in North Dallas with chicken wire on it.”
At 15, Alexander got her first car, but she continued to ride her step-brother’s Honda motorcycle from time to time. Her riding habit “went dormant for a while,” but Alexander revived it around 2006 when a friend tried to impress her with his Harley Sportster 1200cc.
“He said, ‘Get on the back,’ and I said, ‘I’ll drive,’” Alexander said. “We went to Sturgis on that bike, did a lot of touring, and eventually got married.”
Alexander was the only mom to drop her son off at elementary school on a motorcycle. She had a Yamaha 1100cc, her husband had a Harley 1200cc, and the two rode together all through Texas; however, the trip to Sturgis, South Dakota, was where Alexander had “my favorite adult vacation.”
“It was the best time I had ever had on two wheels,” she said. “During that vacation, we put 3,000 miles on that bike. We went to Devils Tower National Monument, Wyoming; Mount Rushmore; and Deadwood. It was the most breathtaking landscape, and my most favorite vacation ever.”

For Alexander, driving in a car will never match the carefree feeling “of oneness with the world” that comes from riding a motorcycle.
“Nothing can get me in a better mood faster than being on a bike; nothing can improve my attitude more than the freedom of a motorcycle,” she said; “that fearless sense of ‘grab life by the horns and don’t be afraid.’”
“Dr. J” and her husband, John Alexander, a former U.S. Marine Corps helicopter mechanic and retired emergency room and critical care nurse, first encountered one another at work. She said that their comfort with the risks of riding motorcycles comes from their proximity to the life-anddeath circumstances that define their work.
“People are afraid of death because we’ve taken it out of the home and made it seem like it’s some kind of foreign thing, and it’s not,” Alexander said. “There are people who exist, but they’re not really alive.”
“My husband and I met on a code,” she said. “We’ve seen the worst, and we know what’s coming. We’re not strangers to what death looks like; the reality is, you have to have a strong faith, and we’re all heading in the same direction.”
“Work may get the best for now, but we still have a Harley Ultra Classic,” she said. •
Royal Philips has expanded its cloud-based radiology informatics solutions to Europe, including exploring the use of generative AI to enhance radiology reporting. After the successful migration of over 150 sites in North and Latin America to HealthSuite Imaging on Amazon Web Services (AWS), Philips will offer these innovative cloud services across Europe.
Philips HealthSuite Imaging is a comprehensive cloud-based solution for radiology departments, managed by Philips and hosted on AWS. As a pure software-as-a-service model (SaaS), it includes regular upgrades, security patches and compliance checks, enabling healthcare institutions to secure their data, while allowing clinicians to access the latest innovations from any location.
Within three years, 95% of health care providers plan to migrate over half of their applications to the cloud. With radiology exams available in the cloud, clinicians have secure, anytime, anywhere access to imaging studies and AI-enabled clinical and operational workflows, enhancing collaboration, speeding up clinical decisions, and improving patient care. In addition, remote access to scheduling, diagnostic reading and integrated reporting helps clinicians quickly adopt new capabilities, and health care organizations to improve operational efficiency and reduce IT management burdens.
“The availability of Philips’ cloud-based radiology solutions in Europe will be a game changer for healthcare providers, helping them to manage staff shortages, optimize workflows and drive better
outcomes”, said Shez Partovi, business leader enterprise informatics at Philips. “The scalability and security of enterprise imaging in the cloud will enable radiology departments to benefit from the transformative power of generative AI and allow clinicians to focus on the most important aspect, bringing better care to more people.”
One of the key benefits of cloud-based services is faster access to future innovations. Philips is exploring generative AI capabilities as part of its innovation strategy, focusing, for example, on conversational reporting to help health care providers face increased clinical demands and workforce shortages. These AI applications may reduce administrative burdens and time-consuming repetitive tasks, helping clinicians focus their expertise where it matters most – in critical decisionmaking. Philips aims to create robust and scalable generative AI applications that leverage state-of-theart foundation models from Amazon Bedrock and seamlessly integrate into clinical workflows.
“Ambient reporting in radiology is just the beginning of using large language models in reporting,” said Dr. J.J. Visser, Radiologist and CMIO at Erasmus Medical Center. “It’s not only about speed; with fewer distractions from the reporting tool, I can focus more on image details and produce higher-quality reports in less time. I anticipate even greater advancements in the coming years.”
Hologic Inc. recently announced that its Affirm Contrast Biopsy Software, which combines contrastenhanced diagnostic capabilities with accurate lesion targeting to help streamline workflow and accelerate biopsy procedures, is now CE-marked. The technology received clearance from the U.S. Food and Drug Administration in October 2020.
Designed from the ground up to integrate with the Selenia Dimensions and 3Dimensions systems, Hologic’s Affirm Contrast Biopsy Software enables clinicians to target and acquire tissue samples in lesions identified through contrast-enhanced mammography (CEM).
“At Hologic, we are committed to helping women live healthier lives everywhere, every day, including through innovative technologies that support the detection and diagnosis of breast cancer,” said Tanja Brycker, vice president of international strategic development for breast & skeletal health and gynecological surgical solutions at Hologic. “We understand the pressures that radiologists work under and the impact that the breast screening and diagnosis process can have on women. Our

new Affirm Contrast Biopsy solution is designed to support radiologists by maximizing workflow efficiencies while helping them to continue to deliver compassionate patient care.”
The software allows the targeting and acquisition of tissue samples in lesions identified on CEM where a correlation may not be found using tomosynthesis or ultrasound, offering an alternative to MRI-guided biopsy. In addition, for those patients who cannot tolerate MRI-guided biopsies, contrast-enhanced biopsy provides a smooth examination experience due to reduced noise and shorter examination time compared with MRI. Ultimately, contrast-enhanced biopsy has the potential to help save time, reduce costs and improve patient experience.
With Hologic’s powerful contrast mammography and biopsy portfolio – including the Affirm Upright Biopsy System, I-View 2.0 Contrast-Enhanced Mammography Software and Affirm Contrast Biopsy Software – the company provides solutions to confidently guide the clinical pathway from screening to diagnosis and biopsy.
Image One Medical is the only Engineer-Owned medical equipment service group that is fully dedicated to Florida’s amazing base of Imaging Centers, Hospitals, and Cancer Treatment Centers.
We have a mission: Self perform on every aspect of our business. Specialize on specific modalities: Pet CT, CT & MRI, and Focus in a key geographic region.
Fort Myers I Fort Lauderdale I Tampa I Orlando
Dealer and servicer of PET CT, CT and nuclear medicine
• Equipment service: full coverage plans
• Equipment sales: installation, relocation and project management
• Mobile coach construction, refurbishment, maintenance and management

and nuclear

Konica Minolta Healthcare Americas Inc. has announced publication of a case study by clinicians in the pulmonary and radiology departments at ASST Fatebenefratelli Sacco (Milan, Italy) demonstrating the use of Dynamic Digital Radiography (DDR) to help definitively diagnose diaphragm dysfunction. The study, published in the journal Diagnostics, highlights the clinical value of DDR through its unique ability to evaluate diaphragm movement in real time and integrate dynamic functional information with static anatomical data to provide a quantitative assessment of diaphragmatic movement, including excursion and speed.
DDR was used to evaluate a 46-year-old male with a past history of smoking and a 2021 SARS-CoV-2 infection for unexplained dyspnea and reduced exercise tolerance. Spirometry values were below predicted values and a standard chest radiograph depicted an elevated right hemidiaphragm that was not present on a prior CT examination during his SARS-CoV-2 infection.
With the dynamic functional imaging capability of DDR, the authors could visualize thoracic and pulmonary motion and track diaphragm movement. Additional post-processing of the DDR data using Konica Minolta’s Intelligent Workstation (IWS, also known as DI-X1) enabled the measurement of diaphragmatic motion and overall lung mobility, highlighting regional differences in ventilation of both lungs. As a result of the DDR examination, the patient was referred to a thoracic surgeon for possible plication of the right diaphragm.
“Diagnosing diaphragm dysfunction is challenging due to its varied symptoms and causes. While conventional chest X-rays and ultrasound can offer clues, additional imaging and tests are often needed for a precise diagnosis,” says Michaela Cellina, head of imaging research and a radiologist with ASST Fatebenefratelli Sacco. “Dynamic Digital Radiography is an innovative imaging technique that can be captured at the same time as a traditional static chest X-ray, providing valuable real-time insights for a quick and confident diagnosis.”
DDR is the only FDA-cleared radiography solution that enables visualization of anatomy in motion. It acquires up to 15 sequential radiographs per second and processes them as a cine loop, enabling clinicians to observe the physiological cycle as well as individual radiographs. No physician presence is required, radiation dose is lower than an average fluoroscopy exam and the dynamic images can be captured with the patient sitting, standing or on a table.
“Konica Minolta congratulates Dr. Michaela Cellina, Dr. Elisa Calabro and their colleagues on the publication of this case study that demonstrates the ability of one examination – DDR – to deliver a definitive diagnosis of the cause of dyspnea,” says John Sabol, Ph.D., clinical research manager, Konica Minolta Healthcare. “Adding DDR to a conventional chest X-ray, which is routinely acquired in these cases, may eliminate the need for additional tests or imaging studies, helping reduce costs to the patient and health system, and enable a more rapid diagnosis.”

Block Imaging recently announced the appointment of Mitch Foldi as executive vice president. With over nine years of leadership experience at Philips/AllParts, Foldi brings a wealth of knowledge and expertise that will be essential to the ongoing growth and expansion of Block Imaging’s parts and service business.
His deep industry experience, passion and strategic vision align with Block Imaging’s mission to extend the life of medical imaging equipment, empowering health care providers to extend the lives of patients. His leadership will be instrumental in enhancing
the company’s ability to deliver high-quality parts and services to its customers.
Jason Crawford, CEO of Block Imaging, expressed his enthusiasm for this new addition to the leadership team, stating, “Mitch’s leadership, industry expertise, and vision for the future of imaging service make him a tremendous asset to our team. His experience will be a key driver in our rapidly growing parts and service business, and we are confident he will help us reach new heights in serving the imaging industry.”
For more news like this, visit tinyurl. com/4ccbtnb4

FUJIFILM Healthcare Americas Corporation has been awarded a second, four-year contract for its innovative surgical C-arm systems by the Defense Logistics Agency (DLA). Under the contract, Fujifilm will outfit multiple U.S. military medical treatment facilities for the U.S. Army, Air Force, Navy and Marines with the company’s Persona C mobile fluoroscopy system, an advanced surgical C-arm designed for imaging across a broad range of diagnostic imaging and minimally invasive surgical procedures.
In December 2021, the company was awarded its first four-year from the U.S. Army and Defense Logistics Agency to deploy its surgical C-arm technology at multiple medical treatment facilities. The first C-arm system delivery and installation under the new contract is slated to begin in early Q1 of 2025, followed by additional installations throughout the next four years.
“Fujifilm is honored yet again to receive a multi-year federal award from the DLA, as it underscores the level of trust military officials place in our advanced technologies to treat our nation’s service men and women,” said Lou Cavallaro, senior director, federal government business group, FUJIFILM Healthcare Americas Corporation. “This esteemed achievement speaks volumes about Fujifilm’s
ongoing commitment to developing high quality diagnostic imaging solutions to improve patient outcomes.”
Fujifilm’s contract award valued more than $10 million was granted after a detailed evaluation of and comparison against numerous competitive C-arm technologies. Following a comprehensive assessment of each manufacturer’s system technology, functionality, adaptability, service support infrastructure and cybersecurity compliance, Fujifilm was selected as the singular vendor that best met or exceeded the U.S. Military’s exacting standards and demanding criteria.
Fujifilm has been awarded grants by various branches of the U.S. Federal Government. This latest contract follows Fujifilm’s announcement that its ASPIRE Cristalle Acquisition Workflow System (AWS), the workstation that is used in conjunction with the company’s 3D mammography system, has been granted a Risk Management Framework (RMF) and Authority to Operate (ATO) on U.S. Department of Defense (DoD) networks.
In November 2023, the DoD granted Fujifilm authority to operate Synapse 7x – the company’s next-generation enterprise imaging platform – on U.S. Department of Defense (DoD) networks.
SPONSORED BY: X-RAY AMERICA

X-RAY TUBES FOR RAD, R/F, MOBILES, C-ARMS
This month, the ICE Magazine roundtable discussion is focused on X-ray machine technology, management, and innovation.
Diagnostic imaging professionals participating in this roundtable discussion are:
• Angela Bosh, Director of Imaging and Cardiopulmonary Services, AdventHealth
• Chris Beasley, Imaging Director, MU Health Care
• Robert Hinton, Technical Director/Radiology Imaging Equipment Specialist, and Zachary Carr, Diagnostic Imaging Quality Lead Tech, The Ohio State University Wexner Medical Center
• Jill Jones, Associate Director of Medical Imaging, Banner Imaging
• Josh Miller, Manager of Technology, Manager, Technical Operations and Service Engineers, Corewell Health
Q: WHAT IS THE TYPICAL LIFESPAN OF AN X-RAY MACHINE IN YOUR FACILITY, AND HOW DO YOU DETERMINE WHEN IT’S TIME TO REPLACE IT?
Bosh: Within radiology, each imaging modality has a different useful life. Although manufactures provide endof-life (EOL) timelines for equipment, often parts and repairs extend years beyond that EOL timeline. EOL for equipment and equipment downtime frequency can be a key driver in prioritizing the replacement of equipment when it may be the only unit at your facility. Specific modalities within radiology require more frequent upgrades, updates or replacements to meet market demands. However, there are several other factors to
consider when determining when to replace equipment including:
• Downtime frequency
• Useful life
• Depreciation/book value
• Technology requirements for new service lines
• Upgrades/updates available for current system
• Lead time of equipment once ordered
• Construction timelines for updated code requirements
• Market needs and growth
• Efficiency in scan/exam time
• Security issues with current operating system of medical equipment
• Mobile or alternate location to provide services during construction
Beasley: Lifespans vary. In general, 10-15 years.
Hinton: The average lifespan of X-ray equipment across our facility is currently approximately 8.5 years. However, we have plans to replace older systems within the next 1-2 years, which will impact this figure. Over the past year, we have already replaced four systems as part of our ongoing modernization efforts. When evaluating equipment for replacement, we consider several key factors, including age, service history, maintenance costs, potential IT risks, and overall impact on operations.
Jones: The lifespan of the X-ray machines in our facilities are 15-20 years old. They are placed on an aging list to
be replaced once they become end of life for parts or upgrades.
Miller: We assign a 10-year useful life to all fixed X-ray assets. The average age of our fixed X-ray install base at Corewell West is 8 years. We evaluate equipment replacement based on the following elements: equipment risk, reliability, service support, life cycle stage, maintenance cost, patient safety, overall product quality, technology status and clinical staff productivity.
Q: WHAT FACTORS INFLUENCE YOUR DECISION TO REPLACE OR UPGRADE AN X-RAY MACHINE (E.G., COST, REGULATORY COMPLIANCE, TECHNOLOGICAL ADVANCEMENTS)?
Bosh: When equipment needs refreshed, it is my goal to upgrade equipment whenever possible to reduce overall cost and downtime. However, the exception to performing an upgrade versus full replacement is when there are limitations in feature/functionality.
Beasley: Replacements are often determined by a blend of several considerations. For example, utilization, downtime percentage, technology obsolesce, equipment age, end of service life status, and cost.
Hinton: The decision to replace or upgrade an X-ray machine is influenced by factors such as regulatory compliance, technological advancements, cost considerations, performance, and integration with existing systems (PACS and EHR). Ensuring compliance with evolving industry standards and leveraging new technology for improved imaging quality and efficiency are key drivers. Financial feasibility, service availability, and patient throughput also play crucial roles in the decision-making process. In recent years, a more evidence-based approach has been adopted, referencing data from organizations like ECRI and the American Hospital Association, consulting with vendors and clinical engineering teams, and considering end-of-life and end-of-support notifications. This strategic approach ensures that imaging infrastructure remains reliable, efficient, and aligned with industry best practices while optimizing patient care and operational sustainability.
Jones: Cost, Regulatory compliance, technological advancements and user friendliness are all factors that we consider when replacing X-ray equipment. Construction costs for floor mounted versus ceiling mounted units are a consideration as well.
Q: WHAT EMERGING X-RAY TECHNOLOGIES OR AI ARE YOU EXCITED ABOUT?
Bosh: I am very excited about the AI advances that provide enhanced imaging capabilities, advanced throughput and improved quality. I am also interested in the expansion of virtual capabilities that provide shared staffing models in certain modalities.
Beasley: We’ll continue to see the reading assistive technology to help streamline the radiologist’s workflow. This will include both diagnostic aids as well as reading prioritization assistance.






Hinton: There are several things. I guess we could break it down into a few categories: supporting technologies, system features, and benchmarking.
• Supporting technology would be things that support data analytics. If a department expects to keep track of things like repeat/reject rates, exposure trends, or technologist performance, they are going to need a robust system that can provide that information easily. EMRs can only do so much in terms of quality metrics, we’re going to need better software to manage these metrics. A lot of the large vendors have caught on and are building their platforms now. I look forward to seeing what they come up with.
• System features: Automation and safety features will probably have the largest impact on future X-ray systems. Things like barcode scanning patient wrist bands to bring up the patient on the modality screen. I’ve seen at least one company that can use facial recognition to ensure the correct patient is performed. A lot of large vendors are putting efforts into integrating automation features in their systems. Power driven tubes that line up with the correct detector, auto-selection of protocols based on order, etc. Detector technology will keep moving forward as well. Vendors are going to keep making their detectors lighter, more durable, better batteries with improved resolution and higher detector quantum efficiency so we can use less radiation to achieve the same image quality.
• Benchmarking: There are some projects from the American College of Radiology and the American Association of Physicists in Medicine to create benchmarks for exposure. This has been needed for a few years now, and I’m excited to see what they come up with. This will go a long way to help reduce overall patient dose for radiography.
Jones: Emerging AI technologies that excite me are the use of AI to assist radiologists with interpreting images. Using AI to analyze images and data to identify abnormalities and patterns will be very useful. Using VR for training can create immersive learning for technologists as they learn new equipment and procedures.
Miller: Advancements in solid state digital detectors. Specifically, the reliability and lower radiation dose.
Q: WHAT IS YOUR FACILITY’S APPROACH TO PREVENTIVE MAINTENANCE FOR X-RAY MACHINES? (DO YOU USE INHOUSE SERVICE ENGINEERS, THIRD-PARTY OR OEM?)
Bosh: At our facility, we have partnered with one company to support equipment via a third-party for a majority of our imaging equipment.
Beasley: All three can be a viable approach.
Hinton: Our facility employs a comprehensive preventive maintenance strategy for X-ray machines to ensure optimal performance, regulatory compliance, and patient safety. We utilize a combination of in-house service engineers and third-party service providers, depending on the specific needs of each system. Our clinical engineering team plays a central role in managing service contracts for all imaging equipment, ensuring that maintenance agreements align with operational and budgetary requirements. They also establish and oversee a planned routine maintenance and preventive maintenance schedule to proactively address potential issues, minimize downtime, and extend equipment lifespan. While our in-house team handles routine inspections and minor repairs, we collaborate with OEM service providers and authorized third-party vendors for specialized servicing, software updates, and complex repairs. This structured approach guarantees continuous system reliability, regulatory compliance, and the highest standard of patient care.
Jones: My facility has in-house service engineers that we work with for the preventative maintenance on the equipment. They do often send it out to third-party vendors based on service contracts or the makes and models of the equipment.
Miller: Corewell West uses a combination of in-house service engineers, OEM and third party. Our approach to service is influenced by the education/training level of our in-house engineering team, service contract costs, replacement part costs, end of service life status, etc. Our goal is to utilize the inhouse engineering team over service contracts when possible. We have a robust team that is well trained and brings a lot of experience. We are continually investing in the professional development of the team to ensure that we can maintain and repair the equipment in a timely manner. If we do not have the ability to maintain an X-ray system in house, we typically look first to the OEM to provide service. Third-party service providers are typically evaluated for equipment that is deemed end of service life by the OEM.
Bosh: Unexpected downtimes are a challenge for every leader especially in cases where you may only have one machine for that modality. To minimize the impact to patient care, we work closely with our service team to expedite the repair or issue that is causing the downtime. If extended downtimes occur due to delays in the repair, we work with our sister facilities to ensure patients are treated timely through a robust transfer process.
Beasley: Different units have different organizational and operation impacts. In critical places such as CT in the ED,
the redundancy of a second unit is important. Redundancy is a tactic that should be considered, however in some circumstances capital constraints makes this untenable. When unable to create redundancy, plans should be made in advance to determine alternate workflows. Other considerations to be considered would be to redirect off site, rescheduling, or choosing an alternate modality.
Hinton: We are actively working to analyze and refine our approach in this area. To minimize disruption to patient care during unexpected X-ray machine downtime, our facility has a structured contingency plan in place. Our clinical engineering team prioritizes rapid diagnostics and triaging, leveraging in-house expertise to quickly address minor issues. Given our focus on equipment standardization across our large institution, we primarily utilize Siemens imaging systems. For more complex failures, we engage vendorspecific service providers or authorized third-party vendors under pre-established service contracts to expedite repairs. Additionally, we maintain redundancy within our imaging fleet by designating backup units or reallocating patient cases to alternative imaging modalities when feasible. In high-volume areas, we implement proactive scheduling adjustments and closely coordinate with clinical teams to minimize patient impact. Regular preventive maintenance and system monitoring further help mitigate the risk of unexpected failures, ensuring consistent, reliable imaging services.
Jones: Most of our facilities only have one X-ray room per outpatient site. When we have the unexpected downtime, having the communication available to staff scheduling patients helps to get the patient scheduled at another close facility or for another day at our facility. Our service engineers work diligently to try to prevent an extended period of downtime.
Miller: From the radiology engineering standpoint, we always take first look to see if we can immediately troubleshoot and repair the asset to minimize downtime. If not, we engage the service supplier. The engineering team communicates with the clinical team/leadership team in downtime situations. This includes text, email, phone and in person conversations. Updates include equipment issues that were found, part delivery/arrival updates and overall updates on when the equipment will be returned to clinical use.
Q: WHAT ADVICE WOULD YOU GIVE TO RADIOLOGY DIRECTORS LOOKING TO OPTIMIZE THEIR X-RAY
Bosh: Why reinvent the wheel? Reach out to your vendors for the most up-to-date information. Also, reach out to peers to validate what the vendors suggest as value-ads when replacement equipment. Assess the financial impact of not having the technology and evaluate your market trends to remain competitive within your market.
Beasley: There are a lot of moving parts in any department. It’s difficult for any singular leader to know all the nuances of a given situation. So, learn to get into the details of your operations with your front line team members. They can help you understand where you do and do not have operational capacity. When capacity is exhausted, learn to work with administrators to make the case for expanding resources, such as equipment and staffing.
Hinton: I know imaging systems are expensive, and there is probably a desire to spend the least amount of money possible. Look for the best value, not the cheapest option. Some options are worth the cost like automation, and expert training on the equipment. The physics of X-ray exams hasn’t changed much, but the systems are getting more sophisticated. It’s worth it to spend the money to properly train your technologists to fully utilize these modern systems. Make sure your rooms are big enough! Small cramped X-ray rooms will limit your ability to adopt better systems and optimize throughput. Spend the money on supporting software that can help you analyze things like repeat rates and exposure trends. I have a feeling these are going to be reporting requirements in the future.
Jones: Outpatient imaging department X-ray volumes have increased in the past few years. Accurate staffing ensures that patients are in and out of the facility in a timely manner. If it is an option, having two technologists working together or a technologist with an assistant, as this helps to keep the workflow moving smoothly and timely.
Miller: Maximize your assets. The patient demand has changed as many patients expect second shift and weekend options. Pausing on capital and using your equipment 12-16 hours per day 7 days a week extends that request versus adding another incremental piece of equipment. •
This month’s article was sponsored by X-ray America. For more information on this company, visit x-rayamerica.com.


The global X-ray systems market size was estimated at $8.13 billion in 2023 and is projected to grow at a CAGR of 3.26% from 2024 to 2030, according to Grand View Research.
The major factor driving the market is the growing demand for early-stage diagnosis of chronic diseases. In addition, continuous technological advancements, improved funding and investments by the government, and a rise in product development along with business expansion by leading manufacturers, particularly in developing countries like India and China, are expected to contribute to the market growth.
For instance, in July 2024, Siemens Healthineers announced that the Multix Impact E digital radiography X-ray machine would be manufactured in India, marking a significant milestone in the company’s commitment to improving patient access to care in the country.
Medical imaging has experienced a significant transformation with advancements in digital radiology solutions. Diagnostic accuracy is at the core of the health care industry, and digital X-ray imaging plays a significant role in enhancing this precision. The high-resolution images produced by digital X-rays allow for more accurate and timely diagnoses, which are critical for effective treatment planning and patient outcomes. Furthermore, the integration of artificial intelligence (AI) in digital radiology systems has significantly contributed to market growth. AI algorithms can swiftly and accurately analyze images, identifying patterns and anomalies.
For instance, in October 2023, DeepTek.ai, India’s leading medical imaging artificial intelligence (AI) company, announced that it had received clearance from the U.S. Food and Drug
Administration (FDA) for its chest X-ray AI solution, the CXR Analyzer. This advanced technology utilizes deep learning algorithms to detect abnormalities in chest X-rays, automatically identifying, categorizing, and highlighting suspicious areas to assist clinicians in making accurate interpretations.
The increasing efficiency of X-ray technology in detecting various medical conditions is expected to contribute to overall market growth significantly. As advancements in digital radiography continue to improve image quality and diagnostic accuracy, X-rays are becoming a more reliable tool for identifying a wide range of health issues. Moreover, growing R&D activities in this field are further contributing to the market growth. For instance, in December 2023, An AI-enhanced chest X-ray reporting solution commenced trials in NHS Greater Glasgow and Clyde, aiming to enhance the early detection of lung cancer.
Fortune Business Insights also predicts market growth.
The global medical X-ray market size was valued at $14.24 billion in 2023, and is projected to grow from $14.99 billion in 2024 to $23.93 billion by 2032, exhibiting a CAGR of 6.0% during the forecast period, Fortune Business Insights reports.
North America dominated the global market with a share of 37.08% in 2023. Moreover, the U.S. medical X-ray market size is projected to grow significantly, reaching an estimated value of $6.09 billion by 2032, driven by increasing launches of technologically advanced medical X-ray systems by key players, Fortune Business Insights added.
Allied Market Research also predicts continued growth in the medical X-ray market. Allied Market Research predicts that the global X-ray market will eclipse $24 billion by the year 2032.•

Hologic’s Horizon DXA system is the latest in densitometry technology, with expanded capabilities beyond measuring bone density such as complete fracture risk assessment and more. It is lighter and smaller than previous generations and offers ultrafast, high-output, low-noise ceramic detectors that provide high-quality bone mapping and images. From vertebral fracture assessments to abdominal aortic calcifications, the system offers a variety of examination and assessment options to support providers in giving the best care to their patients. One of the options, the HD Instant Vertebral Fracture assessment, dramatically improves the detection of vertebral fractures by doubling the resolution of previously available techniques with a low dose, single energy image.1 Additionally, the HD Instant Vertebral Fracture assessment also allows for visualization of calcified plaque in the abdominal aorta, which may be a significant indicator of heart disease and stroke.2-4 This Hologic-exclusive feature provides vital information that may link coronary heart disease, the leading cause of death for women. Through its Dynamic Calibration system, the Horizon DXA system delivers real time pixelby-pixel calibration through bone and tissue equivalents for great long-term measurement and stability. Its OnePass single sweep scanning is designed to eliminate beam overlap errors and image distortion, offering an efficient and accurate experience to providers.
*Disclaimer: Products are listed in no particular order.
References:
1 F. Cosman, J. et al. Spine fracture prevalence in a nationally representative sample of US women and men aged 40 years: results from the National Health and Nutrition Examination Survey (NHANES) 2013 2014. Published online: 07 February 2017 International Osteoporosis Foundation and National Osteoporosis Foundation 2017
2 Wilson PWF, Kauppila LI, O’Donnell CJ, et al. Abdominal aortic calcific deposits are an important predictor of vascular morbidity and mortality. Circulation. 2001;103(11):1529 34.
3 Hollander M, Hak AE, Koudstaal PJ, et al. Comparison between measures of atherosclerosis and risk of stroke: the Rotterdam Study. Stroke. 2003;34(10):2367 2372.
4 van der Meer IM, Bots ML, Hofman A, del Sol AI, van der Kuip DAM, Witteman JCM. Predictive value of noninvasive measures of atherosclerosis for incident myocardial infarction: the Rotterdam Study. Circulation. 2004;109(9):1089-1094.

Ray-Pac offers a direct replacement for the Philips SRO 33100 ROT 360 X-ray tube. This high-performance glass tube is used for radiographic and fluoroscopic systems, surgery and other mobile applications. Ray-Pac currently offers 2 different options with the following focal spots 0.6/1.2 and 0.6/1.0. For this tube, Ray-Pac uses only the highest quality aftermarket parts and inserts from Varex. Every tube is built with precision by the best team in the industry. Then tested again before shipping to ensure that your customer experiences the least amount of downtime as possible. All of Ray-Pac’s tubes come with a full 18-month warranty. Both options of these units are available for overnight shipping.
GE HealthCare’s Definium Pace Select ST is the tool X-ray departments can use to conquer today’s challenges. This versatile, digital, floor-mounted system can produce consistent, high-quality images typically generated on premium systems at a value price point. This image quality can be easily achieved – even with novice technologists operating the system – thanks to a combination of hardware, software, and assistive technology. A high-powered X-ray generator and large, high-resolution FlashPad Select detectors are the key components that enable imaging of a complete range of anatomies and patient sizes. In addition, the system acts as a personal assistant for technologists to help with protocol and exposure factor selection, positioning of the system, and with making quality checks before images are sent to radiology. AI-driven Helix advanced image processing software provides consistent image quality despite variations in exam condition with customized image looks that radiologists demand. With a simple, easy-to-learn and operate design, the system can help prevent user errors and also help technologists efficiently deliver imaging exams that impart clinical confidence, helping to lower staffing burdens and reduce rejects and repeats.

The KDR Flex Overhead X-ray is the first system that can convert from manual to auto and assist mode that includes an intuitive and customizable user interface. It’s an integrated system for all conventional radiographic applications – with the patient sitting, standing, laying down or in a wheelchair – and includes a high-frequency generator, radiographic table and wall bucky. KDR Flex was designed for efficiency. The system automatically tracks the tube and moves to the detector’s center on the table or wall stand to ensure the alignment, SID and angulation. The motorized axes provide more than 5 meters/16 feet of travel and 3,600 angles. An integrated, tube-mounted 12-inch high-resolution touchscreen user interface allows the technologist to control the system and preview the images to reduce exam time. The capacitive handle in the tube head has internal sensors that release movements when touched by the operator. The KDR Flex is also Dynamic Digital Radiography (DDR) ready. DDR is a novel, low-dose X-ray imaging technique that acquires images at high speed, generating a cineloop that enables clinicians to visualize anatomical motion over time (cineradiography), enhancing the system’s diagnostic capabilities.

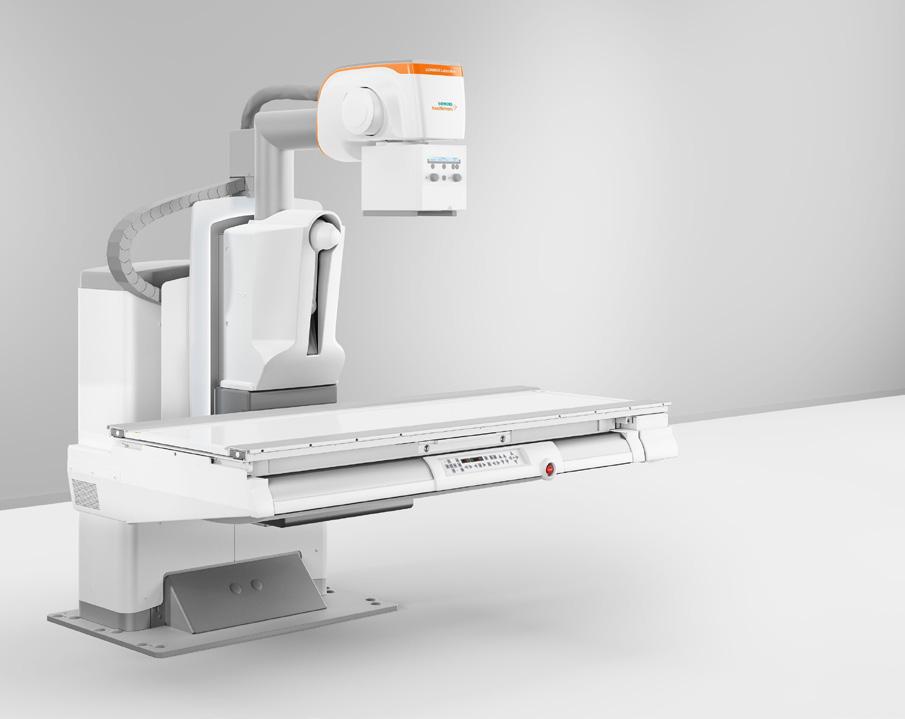
The LUMINOS Lotus Max, an advanced two-in-one fluoroscopy and radiography system from Siemens Healthineers, enhances system utilization and reduces the need for additional imaging systems and examination spaces. It features an integrated, remote-controlled design that delivers both dynamic and static images at a high level of quality with low radiation exposure for patients. Designed to accommodate a diverse range of examinations and patient types – including pediatric, bariatric and geriatric – the system allows for streamlined operations controlled via a single interface that is accessible from both the control and examination rooms. Enhanced with robust cybersecurity measures, the LUMINOS Lotus Max helps ensures top-tier protection against cyber threats.


In December 2025, we will announce the eight imaging directors or managers selected by our ICE audience for their outstanding contributions.
Do you know someone who exemplifies great leadership in imaging healthcare? Nominate a colleague—or yourself—to be recognized for their excellence!
Deadline for nominations ends MAY 16TH
Scan the QR code to place your nominations.








BY MATT SKOUFALOS
The conventional wisdom associated with magnetic resonance imaging (MRI) is that it’s a safer imaging modality than computed tomography (CT) or X-ray because it doesn’t rely on exposing human tissue to ionizing radiation. However, that doesn’t mean that MRI is a completely benign modality, or that there aren’t safety concerns and contraindications for patients prescribed an MR study.
Kimberly Love, vice president of the Nashville, Tennesseebased radiology consultancy Regents Health Resources, spoke about the variety of practical considerations associated with safely providing MR services. The principal resource for guidance managing those risks is provided by the American College of Radiologists (ACR) Manual on MR Safety.
The 2024 edition of the ACR Manual on MR Safety recommends establishing a well-defined organizational structure for MR safety, designating key positions within an imaging facility. Those include a Medical Director for MR Safety (MRMD), MR Safety Officers (MRSOs), which ACR notes “are often highly trained technologists,” MR Safety Experts (MRSEs), “who are typically highly trained medical physicists,” according to ACR. These roles ensure compliance with safety protocols, training, and risk mitigation strategies.
“If I were the MRI Safety Officer, my responsibilities would include ensuring that departmental policies and procedures align with ACR and FDA recommendations and guidelines,” Love said. “This would involve developing sitespecific protocols and screening procedures and keeping them consistently updated.”
Those procedures encompass onsite safety and training mechanisms, personnel education, including that of nonclinical staff as well as architects and engineers who design imaging facilities. More specifically, they also include the four ACR-designated safety zones in an imaging facility, their classification, meaning, and how to educate patients and visitors about their significance in context.
Maintaining rigorous screening protocols for patients,
staff, and visitors with ferromagnetic safety screenings and access restrictions involves creating proper signage, barriers and checkpoints, as well as maintaining MRI accessories so that they preserve their MRI safety performance characteristics.
“You need to ensure compliance with these protocols and establish a reporting mechanism for safety incidents. Additionally, an action plan must be in place to address and document these incidents effectively,” Love said.
“You need to coordinate an emergency protocol and what that would look like, and then you would have to have detailed records for the absolute and relative contraindications of patients for anything on or inside their body,” she continued. “If you set your information responsibly and correctly, I do believe you will cover all the protocols and safety procedures, adhering to those zones as they’re supposed to be.”
These precautions are established to mitigate risk of unnecessary exposure to radiofrequency (RF) fields and magnetic time-varying gradients, which are created during an MRI study, and can affect the body in different ways. Objects containing even small amounts of metal can be attracted by the magnetic fields, have induced electrical currents from the time-varying gradients, and radiofrequencies can heat them up to the point of damaging tissue.
Part of the challenge in conducting a rigorous screening process for mitigating patient risk lies in the number of unknown contraindications from materials that could have a negative interaction with the RF fields and magnetic gradients. Some of those items are more easily identifiable – removing piercings or body modification elements, keeping metallic items out of the magnetic field – and some are not.
“To me, there’s two types of contraindications,” Love said: “the absolute ones that can’t be removed, like implantable medical devices, and the relative ones that people do to themselves – foreign bodies, tattoos, fingernail polish. Beyond that, you have [gadoliniumbased] contrast injury.”
“The time spent screening a patient before an MRI is appropriately emphasized in these new safety codes,” she said. “Since the magnetic field can alter blood flow, it’s important to inform patients about potential side effects like dizziness, nausea, or rashes. Additionally, those sensitive to noise may require earplugs or noise-reducing headphones to prevent discomfort or adverse reactions.”
Francisco Rodríguez-Campos, Principal Project Officer I for Medical Imaging and Device Safety at the nonprofit ECRI of Plymouth Meeting, Pennsylvania, said that current best practices in MRI safety involve assessment tools to determine whether certain implantable medical devices can be scanned safely. Some manufacturers publicized this information in an organized fashion, but not all, Rodríguez-Campos said. Presently, however, most vendors have built in solutions in their scanning software to check for such elements.
“I am happy that almost all of them, if not all of them, have some sort of application that we’ve seen included as standard,” he said. “Since 2011, implant and device manufacturers should provide some information to you about what conditions made it an MR-conditional device; what are the magnetic field limits. That’s great because it’s an extra level of safety for the technician. It’s giving them more information that they can scan this patient safely.”
Rodríguez-Campos said that the safest point from which to begin contemplating MRI compatibility is to consider “anything that you put in your body” to be an implant, while noting that some are removable, and others are not. The list continues to grow beyond medical devices to cosmetics, augmented clothing fabrics, and even body art.”
“Something that nobody has thought about is fake eyelashes,” Rodríguez-Campos said. “I didn’t realize that some of those have magnets, or maybe some metal. There was one or two cases where they flew out.
“It’s a lot of stuff that you don’t think about,” he said.” “A bra underwire, you have to take it out. In the last couple years, many people are wearing leggings with copper in them, or silver. The metal won’t pull out, but it could warm up, and that’s why the recommendation is that if you have no idea about your clothing, the best thing to wear is a gown that you know is safe.”
Rodríguez-Campos also described less-common incidents that nonetheless have resulted in tragedy. In January 2023, a Brazilian lawyer and pro-gun advocate failed to disclose that he was carrying a concealed weapon into the MRI room. The magnetic field ripped the gun from his waistband, and it discharged into his midsection, fatally wounding him, The Independent reported. Something similar happened in June 2023,
when a 57-yearold woman did not disclose that she had a concealed firearm on her person during an imaging study.
“The list continues to grow beyond augmented clothing fabrics, and even body art.”
Francisco Rodríguez-Campos
According to a report filed with the U.S. Food and Drug Administration, the gun was pulled into the MRI magnet and fired a single round into her backside. In October 2023, a botched police raid on the Noho Diagnostic Center in Los Angeles, California led to a damaged MRI scanner when an officer ignored postage signage and took his rifle into an MRI suite, where it was pulled to the equipment, and damaged it, The Merced Sun-Star reported.

To safeguard against events like these, RodríguezCampos said, facilities are investing in door locks that won’t open if an embedded metal detector is triggered. Others are employing handheld wand detectors to make final checks of patients entering the study suite.
Still other guidance changes reflect the increasing strength of static MRI magnetic fields and their effect on implantable medical devices, namely, inadvertently activating them. Revised standards from the International Electrotechnical Commission (IEC) have changed the safe distance from an MRI magnet from a 5 to a 9-gauss standard, which means that patients can be closer to the magnet without fear of their devices malfunctioning.
“Magnet fabrication is better; shielding is better,” Rodríguez-Campos said. “Magnets are more homogenous; their fringe field is more stable. It may make an impact in new facilities.”
Rodríguez-Campos said there’s less information available about how implantable medical devices are affected by 7-Tesla magnets, which heretofore have been used mostly in research environments, but which slowly are gaining broader clinical application. Likewise, he foresees the increasing application of remote scanning environments as coming to the fore of future safety conversations.
“That’s another important thing, because remote scanning requires a lot of other considerations, not just about the capability of technicians, but you also have to have a very reliable connection onsite,” he said. “I’m glad a lot of places are adopting an MRSO onsite, and of course there are training requirements for personnel,
which are very high. This changes from state to state, too.”
Anticipating the future of MRI safety challenges involves more inclusive contemplation of patients and the accessibility of MRI, said MRI Safety Consultant Tobias Gilk, founder of Gilk Radiology Consultants of Overland Park, Kansas, and senior vice-president at Radiology Planning.
As of January 1, 2025, six new Current Procedural Terminology (CPT) codes for MRI safety services – 76014 through 76019 – offer enhanced reimbursement for providers who are taking extra MRI safety precautions for their patients. To certify that a patient with a pacemaker who is registered for an MRI study can undergo a scan safely, imaging teams might need to track down medical records from out-of-state or out-of-network institutions. They might need to contact the manufacturer of a specific device, or work with a radiologist to develop a patientspecific risk assessment or risk mitigation plan.
“These are not your meat-and-potatoes, everyday patients,” Gilk said. “These are patients who typically require more time, energy, and effort to be able to effectively scan. Previously, people were paid the same amount no matter what; now, if you’re doing extra work to be able to image this patient, there are extra dollars for you.”
Gilk also pushes back against the “bumper-sticker slogan” that MRI safety is a collective responsibility on the objection that it, perhaps counterintuitively, allows for the work to fall through the cracks.
“When we democratize safety to the point of saying it’s everybody’s responsibility, it becomes the world’s largest group project,” he said. “If you’re having a bad day, you can kind of check out because everybody else is going to cover you.”
“One of the critical elements of MR safety is that we name individuals who have specific responsibility and authority for patient care,” Gilk said. “We don’t do that to say ‘only these people need to worry about it,’ it’s a structural recognition that if we don’t have somebody specific in charge, we have nobody in charge.”
Related to that argument is Gilk’s critique that pointof-care-related MRI safety aspects are still fairly gently regulated. As important as the work of standards accreditation groups and credentialing organizations has been, those bodies either lack the authoritative capability for meaningful corrective action, or the nuance of appropriate responses to safety concerns.
“CMS (the Center for Medicare and Medicaid Services) has the power to do a bunch, but one of the problems is they have one ginormous stick to kick people out of reimbursements,” Gilk said.
“That is so impactful and disruptive to people’s ability to access healthcare that nobody wants to do that. You have these polite suggestions, and the nuclear option, and nothing in between, and it allows the cowboy providers to keep being cowboys.”

Moreover, the depth and complexity of potential patient contraindications for MRI has only broadened over time. Industry-wide, a rough calculation holds that between 30 and 50 percent of all MRI patients have a device, piercing, or tattoo that would be contraindicative of imaging or would complicate an imaging study.
“That has shifted the burden to technologists,” Gilk said. “Throughput has to be accelerated, and they have to identify and verify any of the things that is related to the workload of safely scanning MRI patients. Even if we hadn’t ramped up throughput and safety expectations, the safety-related workload has increased enormously for MRI technologists primarily, and it’s a blessing and a curse.”
“The blessing is there are all of these patients who for years were turned away from getting MRIs who can actually do this; the curse is, especially in a time of declining reimbursement, this is a case of do more with less,” he said. “It has been this Sisyphean task of rolling the boulder up the hill, and it just keeps getting harder each and every day based on the proliferation of implants and devices.”
Patients with complex medical needs who present for imaging studies would also benefit from greater coordination of their cases with other practitioners, Gilk said, but those “are difficult conversations to get started.
“The perfect metaphor for MRI safety is the frog in the boiling pot,”

Kimberly Love VP of the Nashville, Tennesseebased radiology consultancy Regents Health Resources,
he said. “It has been a very slow warm under the pot that the frog is in.”
“Everything that leads up to the act of putting the patient on the table and hitting the scan button has been changing around us,” Gilk continued: “imageguided biopsies, more pediatric patients, which means greater sedations; post-op checks for neurologists within six hours of a procedure. No one of these things is unreasonable, but you take these little things and start adding them together, and what we have done is create a more complicated risk environment.

the overall operation of a healthcare facility. Unless sites that deal with more complex patient-care setups are willing to rethink their processes holistically, those challenges will persist.
“How do we broach this subject about the need for an interdisciplinary approach that goes against the model that has been forever?” he asked. “There is an inherent resistance to building the collaborative structures that are really necessary to managing patients’ needs of today. It can be a real uphill battle, and it takes establishing buy-in.”
Beyond making small, immediate, tactical choices to resolve ongoing collaborative issues, Gilk said that imaging departments must partner with other specialty practitioners to find common solutions that affect

Francisco RodríguezCampos, Principal Project Officer Medical Imaging and Device Safety ECRI of Plymouth Meeting, Pennsylvania
“If all you ever make are tactical, putting-out-the-fire decisions, you will never have a system that is as safe as it could be in terms of delivering care,” Gilk said. “Because we’ve developed MRI organically, there’s never been an external thing that has happened that has really caused hospitals and imaging providers to completely reimagine how they provide service.”
“We’ve done it incrementally, but when you think systemically about MRI services and patient access and safety and those sorts of things, you can begin to build some remarkable systems.” •

Tobias Gilk Founder of Gilk Radiology Consultants, Senior VP of Radiology Planning
Finally, the features you love most about your favorite ride share app, food delivery app, Angi, UpWork, or TaskRabbit are available for medical imaging equipment maintenance and repair.
Enter a Trace Ticket with one tap to broadcast your repair needs to a network of qualified technicians.
Review Bids to find the best service option for improved repair outcomes with less equipment down time, resulting in a lower overall cost.
Track progress, issue payments and rate services all in a single dashboard.


Speed
Instantly blast your service request to every qualified and vetted service provider

Take Control of Tracking
From response times to uptime, you no longer have to rely on service companies to track their own activities and performance


Standardized Communication
Like your favorite personal apps, get in-app alerts when a service technician is on their way, arrived, waiting for a part, completed a job, etc.
Pay Through the App
Competitive bidding among service technicians allows you to get the best price and only pay and track one entity


X-ray imaging has been a cornerstone of diagnostic medicine for decades, providing a non-invasive way to visualize internal structures. From detecting fractures and foreign objects to monitoring diseases like pneumonia and cancer, X-ray systems play a vital role in patient care. Compared to other imaging modalities, X-ray offers unique benefits that make it indispensable in health care:
• Computed Tomography (CT): Provides detailed crosssectional images but requires more radiation and is more expensive, making it ideal for complex diagnostics.
• Magnetic Resonance Imaging (MRI): Offers superior soft tissue contrast but is less effective for bones and requires a longer, costlier process.
• Ultrasound: Radiation-free and widely used for soft tissue imaging but ineffective for bones or areas with significant gas interference.
X-ray’s versatility, cost-effectiveness, and speed make it a preferred choice for many diagnostic needs, particularly in emergency and outpatient settings.
X-ray systems are found in hospitals, outpatient clinics, and imaging centers. Their key components include:
1. X-ray tube: Generates X-rays by accelerating electrons into a target material.
2. Generator: Regulates energy and timing.
3. Detector: Captures images digitally or on film.
4. Software systems: Enhances, stores, and integrates images into patient records. Proper maintenance ensures reliable performance, making professional service training essential.
Maintaining and repairing X-ray systems requires technical expertise. Specialized training enables service professionals to:
• Diagnose and Repair Issues: Minimize downtime and ensure uninterrupted patient care.
• Perform Routine Maintenance: Extend equipment lifespan and maintain image quality.
• Ensure Regulatory Compliance: Meet radiation safety and operational standards.
For four decades, the Radiological Service Training Institute (RSTI) has trained thousands of professionals, ensuring the reliability of imaging systems worldwide. Our specialized programs offer both theoretical and hands-on training, equipping technicians with the skills needed for modern X-ray systems.
Key Offerings:
• Principles of Servicing Diagnostic X-Ray Systems (Phase 1): Covers X-ray operation, radiation safety, and troubleshooting.

• Advanced Digital Imaging System Maintenance: Focuses on servicing and calibrating digital X-ray systems.
• Custom Training Modules: Tailored courses for specific equipment models and emerging technologies. Our programs emphasize real-world applications, ensuring trainees gain practical skills that translate directly to their work environments.
As diagnostic imaging evolves, RSTI continuously updates its curriculum to incorporate the latest advancements, including:
• Digital Radiography Integration: Seamlessly connecting X-ray systems with hospital networks.
• Utilizing AI-Driven Diagnostics: Enhancing troubleshooting and system performance.
• Remote Monitoring Solutions: Reducing service response times and improving efficiency.
With 40 years of training excellence, RSTI remains dedicated to empowering service professionals with cutting-edge knowledge. In recognition of our
contributions, RSTI received two 2025 TechNation Tech Choice Awards, “The Wrenchies,” highlighting our industry leadership in imaging service education.
Health care facilities investing in well-trained professionals benefit from improved equipment reliability, reduced downtime, and enhanced patient outcomes. RSTI’s commitment to education ensures that X-ray systems continue to be the backbone of diagnostic medicine.
As medical imaging advances, X-ray systems remain fundamental to healthcare. The demand for skilled technicians has never been greater. Through comprehensive training programs, RSTI continues to advance the capabilities of imaging professionals and support the health care industry’s commitment to excellence. •
Scan QR code to visit RSTI’s website.


BY BETH ALLEN DIRECTOR’S CUT
Often a successful screening mammography program is the beacon of light for an imaging practice. For many patients it is the first encounter with imaging. It is our opportunity to make an outstanding first impression. These patients are judging our centers on cleanliness, friendliness and quality. It has been shown that women are likely to make health care decisions for the entire family. A well-run mammography program can lead patients through all the rest of our modalities as well as into our acute care facilities for their care.
Banner Imaging has several Breast Imaging Centers of Excellence as well as
several other sites offering mammography. Women’s imaging is complicated for many reasons. We have looked for ways to make our process quality driven and efficient, as well as compassionate and empathetic. Even women coming for their annual mammogram have that moment of dread when the voice in their head says, “What if they find something?” Not that this is any different than all our other patients having any exam for any reason. It is that this is a screening exam that you have every year, not ever expecting anything to be wrong. To create a more comprehensive program, Banner Imaging offers genetic testing through Ambry Genetics, a company that performs genetic testing for hereditary cancer. Through a health history form, patients are screened to determine who may benefit from the testing. Patients
that qualify submit a saliva sample and receive results through the Ambry portal. Results are also sent to their referring physician. We have partnered with the genetics program with Banner MD Anderson for continuum of care. Ambry Genetics also has a team of genetic counselors that can assist patients with understanding the results so they can make informed decisions.
Regardless of the technology within any successful mammography program, it is the people employed in the program that will make or break it.
Every area of imaging is short staffed. In order to cultivate the next generation of successful mammo techs, we have partnered with a local community college to create a mammography education program. This program is fairly new. Banner has worked to develop the curriculum with national mammography education leaders to ensure the program will produce skilled, welltrained technologists. Many techs find their passion in mammography because of a personal experience. This education will give them the tools they need to put their mark on women’s imaging.
This program will not only help Banner Imaging fill the gap in staffing mammography, but it will also help others in our community that provide this service. It may also allow technologists that have not had the opportunity

Premium Quality
Exceptional Value
Impressive Warranty

to move into a cross-training position be proactive and ready to achieve a career goal.
There are also non-technologists on our women’s imaging team that make a difference. We have interventional breast schedulers, medical imaging assistants, patient access representatives and other support staff that serve in our breast imaging centers. Our entire team has an impact on the patient experience. Those that need to return for additional views, an MRI or biopsy are even more anxious when they return. It is at this time that we can really go the extra mile, whether it is by the technologist or any other team member. Those soft skills are what make the difference.
I often see comments on our Medallia survey from patients that come back to our centers year after year to see the same technologist. Our patient trusts them and, in some cases, even look forward to seeing them, despite the fact that a mammogram is the reason to do so. It is a culture of caring that I see described in those comments. “We’ve got you; we are on your team,” is the message we are trying to convey.
Thanks for all you do! •
— Beth Allen, RT(R)(CT), CRA, is the director, clinical operations at Banner Imaging
• One-year-old company with 67 years of experience manufacturing and supplying X-ray tubes.
• High-quality components from IAE SpA, Europe’s premium X-ray tube manufacturer for 75 years.
Made in the USA with US and European components.
For a product list and prices contact us at:
Email: info@X-RayAmerica.com
Phone: 1.854.999.6888
Global: IAE.it
US Headquarters: X-RayAmerica.com




BY MARK WATTS
The COO sent me an email. “The turnaround times are inching up.” I reviewed the data and it showed 80 patients all with reports under one hour. Final signed reports, from a radiologist who stays up all night to read STAT cases to support a super busy emergency department, and one routine in patient KUB took 90 minutes to read. He has no idea how lucky we are to have good responsible radiologists. We in imaging understand and should appreciate the value a great radiologist brings to health care. We should also be prepared for the lack of great radiologists and find a way to provide services with less.
The field of radiology, crucial for diagnosing and treating a vast range of medical conditions, faces a growing challenge: a significant and
projected shortage of radiologists. This scarcity threatens patient care, increases workloads for existing professionals, and potentially delays critical diagnoses. While various factors contribute to this shortage, the increasing demand for imaging services, coupled with an aging workforce and the lingering effects of the COVID-19 pandemic, have created a perfect storm. However, emerging technologies, particularly artificial intelligence (AI), offer a beacon of hope, promising to alleviate the strain and reshape the future of radiology.
Recent studies paint a concerning picture of the radiologist workforce. A 2024 study, projecting the workforce to 2055, suggests that even with growth in residency positions, the radiologist workforce may only increase by 40%. If residency positions remain
stagnant, the increase shrinks to a mere 25%. Considering the anticipated increase in health care needs due to an aging population, these numbers are far from reassuring. Furthermore, the study highlighted the impact of attrition, particularly the increased rates observed post-COVID-19. This higher attrition, equivalent to a reduction of over 3,000 radiologists by 2055, underscores the fragility of the current workforce.
Several factors contribute to this dwindling supply. The demanding nature of the profession, coupled with long hours and increasing administrative burdens, can lead to burnout. An aging radiologist population is also a major concern, as experienced professionals retire, taking their expertise with them. The pandemic exacerbated these issues, pushing some radiologists into early retirement and further straining an already stretched system.
The consequences of a radiologist shortage are far-reaching. Longer wait times for crucial imaging procedures can delay diagnoses and treatment, potentially impacting patient outcomes. Overworked radiologists may experience increased stress and fatigue, potentially leading to errors. In rural areas, the shortage is often more acute, limiting access to specialized care and creating health care deserts. Ultimately, the shortage threatens to undermine the quality and accessibility of health care for all.
ENTER THE AI REVOLUTION: A POTENTIAL SOLUTION
Artificial intelligence is rapidly transforming various aspects of health care, and radiology is no exception. AIpowered tools offer the potential to address the radiologist shortage in several ways:
• Increased Efficiency: AI algorithms can analyze medical images faster and more accurately than humans in some cases. This can significantly reduce the workload on radiologists, allowing them to focus on more complex cases and improving overall efficiency. AI can also automate repetitive tasks, such as image
registration and segmentation, freeing up radiologists’ time.
• Improved Accuracy: AI algorithms can be trained to detect subtle patterns and anomalies in medical images that might be missed by the human eye. This can lead to earlier and more accurate diagnoses, improving patient outcomes. For example, AI systems are being developed to assist in the detection of lung nodules, breast cancer, and other critical conditions.
• Reduced Burnout: By automating routine tasks and increasing efficiency, AI can help reduce the workload and stress on radiologists, potentially mitigating burnout and improving job satisfaction. This, in turn, could contribute to retaining experienced professionals in the field.
• Expanding Access: AI-powered diagnostic tools can be deployed in remote areas where access to radiologists is limited. This can expand access to quality care for underserved populations and bridge the healthcare gap.
• Training and Education: AI can also play a role in training future radiologists. AI-powered platforms can provide interactive learning experiences and personalized feedback, accelerating the development of expertise.
While the potential of AI in radiology is immense, several challenges and considerations must be addressed:
• Data Bias: AI algorithms are trained on large datasets, and if these datasets are biased, the AI system may perpetuate or even amplify existing disparities in health care. Ensuring that training data is diverse and representative is crucial.
• Regulatory Framework: Clear regulatory pathways are needed to ensure the safety and efficacy of AIpowered diagnostic tools. Establishing standards and guidelines will be essential for responsible deployment of AI in clinical practice.
• Integration with Existing Systems: Integrating AI tools seamlessly into existing radiology workflows and electronic health record systems is crucial for maximizing their impact. This requires interoperability and collaboration
between technology developers and health care providers.
• Trust and Acceptance: Building trust in AI-powered diagnostic tools among radiologists and patients is essential for widespread adoption. Transparency in how AI algorithms work and clear communication about their capabilities and limitations are crucial.
• Ethical Considerations: The use of AI in health care raises ethical questions about data privacy, patient autonomy, and the potential for job displacement. Careful consideration of these ethical implications is necessary.
The radiologist shortage is a complex problem that requires a multifaceted solution. While AI offers a powerful tool to address this challenge, it is not a silver bullet. Other strategies, such as increasing residency positions, improving work-life balance for radiologists, and promoting the field to medical students, are also essential.
The future of radiology likely involves a collaborative approach, where AI augments the expertise of human radiologists, rather than replacing them. By embracing the potential of AI while addressing the associated challenges, we can ensure that patients receive timely and accurate diagnoses, and that radiologists are empowered to provide the best possible care. The looming shadow of the radiologist shortage can be mitigated with the bright promise of artificial intelligence, paving the way for a more efficient, equitable, and sustainable future for radiology.
Neurologists want CT perfusion on every headache patient, GI doctors want MRCP on every gallbladder patient before surgery, emergency room doctors want CT abdomen pelvis on each abdomen pain patient – the reliance on imaging is increasing at the same time the talent pool of radiologist is decreasing. Imaging AI safely applied may be the best option. •
— Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.

















































































































































































































































































BY ERIC MASSEY
According to a report by Business Wire, the global market for medical imaging equipment services was estimated at $20.9 billion in 2022 and is projected to reach a revised size of $29.7 billion by 2030.
Remote monitoring is not just about automation. It’s about empowering engineers with better information to deliver high-quality service. By integrating real-time data insights with hands-on problem-solving, hospitals can achieve greater reliability, efficiency, and cost savings. While predictive alerts help prevent some failures, skilled engineers remain essential for troubleshooting, repairs, and calibrations. Technology alone cannot replace the judgment, precision, and problem-solving capabilities of experienced professionals.
Strategically combining remote monitoring with onsite service allows hospitals and service providers to proactively address maintenance needs, optimize workforce utilization, and ensure uninterrupted imaging services. This balanced approach enhances equipment reliability, minimizes operational disruptions, and ultimately enables health care
providers to focus on delivering high-quality patient care.
• Enhancing Onsite Efficiency: Remote monitoring amplifies the effectiveness of onsite engineers by providing actionable insights before they arrive. While remote alerts help anticipate potential failures, final diagnosis and resolution still require hands-on expertise.
At a client location recently, remote access alerted us to a compressor failure in an MRI system over a long holiday weekend. The imaging center was closed, and without remote access, we wouldn’t have known until Monday. Remote monitoring detected the issue early, allowing us to order a new compressor and complete the repair over the weekend – preventing significant helium loss and avoiding extended downtime.
• Optimized Resource Allocation: By functioning as a triage system, remote monitoring helps service providers prioritize onsite interventions based on issue severity. This ensures engineers focus their efforts where they are most needed, minimizing downtime and improving operational efficiency.
• Stronger Collaboration Between Technology and Expertise: Together, these elements create a comprehensive strategy for imaging equipment reliability. While remote monitoring delivers precise diagnostics,
onsite engineers provide the critical thinking, adaptability, and hands-on expertise needed to implement effective solutions. By analyzing data to predict potential failures, remote monitoring helps reduce unplanned downtime and improve service operations efficiency.
• Operational Efficiencies Beyond Repairs: 83% of health care providers claim they do not have automated visibility into their fleet-wide utilization.
• Beyond failure prevention, remote monitoring improves operational efficiency:
- Systemwide Performance Optimization: Provides a comprehensive view of imaging equipment across multiple locations, allowing hospitals to benchmark performance, streamline maintenance processes, and ensure consistent service quality.
- Smart Maintenance Scheduling: By analyzing usage patterns, hospitals can strategically plan preventive maintenance during off-peak hours, minimizing disruptions to patient care.
- Better Resource Utilization: Monitoring data helps identify underperforming or underutilized assets, ensuring imaging systems are used effectively.
While remote monitoring offers significant advantages, it has limitations that necessitate onsite expertise.
• Insights Alone Aren’t Enough: While remote monitoring delivers real-time data and predictive insights, its value depends on skilled engineers to interpret the information and act. Without expert analysis and intervention, data alone cannot prevent failures or optimize equipment performance.
• Mechanical Failures Require Onsite Expertise: While remote solutions shine at diagnostics, onsite engineers remain essential for resolving mechanical issues, calibrations, or physical repairs, ensuring full functionality is restored.
• Cybersecurity Concerns: While remote monitoring systems can introduce potential entry points for unauthorized access, our approach prioritizes cybersecurity through strong encryption, multi-factor authentication, and strict access controls. These measures, combined with regular system audits, allow us to identify and address potential vulnerabilities.
Integrating Remote Monitoring with Onsite Expertise
• Remote monitoring is not a singular fix for imaging equipment downtime. While technology enhances how we work, it’s the insight, adaptability, and expertise of our people that ensure exceptional outcomes. By combining cutting-edge platforms with the insight and care of the service teams, we deliver solutions that go beyond expectations – driving reliability, efficiency, and better patient care.
We’re expanding our remote monitoring system’s functionality with planned CMMS integration. This will allow remote diagnostics to detect errors or failures, generate a work order, and assign it to the appropriate engineer based on service delivery plans, streamlining service coordination and improving response efficiency.
• Remote Monitoring as an Amplifier: Remote monitoring enhances onsite engineers’ efficiency by providing actionable insights before they arrive. For example, real-time diagnostics might detect a failing power cord allowing an engineer to prepare for a targeted repair bringing the correct replacement part and reduce repair time.
We’ve used remote access to detect tube failures in CT scanners and cath labs – repairs that typically take around eight hours. By identifying a failing tube early, we can replace it outside of business hours, ensuring imaging services remain uninterrupted.
• Tailored Resource Allocation: Hospitals can use remote monitoring to triage repairs, prioritizing onsite interventions based on issue severity. This approach ensures engineers focus their efforts where they are most needed, reducing downtime and improving operational efficiency.
• Collaborative Problem-Solving: Technology and human expertise must work together. Big data, AI, and human expertise each play a distinct yet complementary role in imaging equipment management. Big data serves as the vast pool of collected information, while AI and machine learning analyze patterns and predict potential failures. However, AI alone does not solve problems – it provides insights that require expert interpretation and action. By identifying subtle performance differences, AI-driven tools allow targeted interventions before failures occur, reducing downtime and improving efficiency. Yet, engineers remain essential for interpreting AI-generated insights, implementing repairs, and ensuring imaging systems function at peak performance. The synergy between analytics and hands-on service is key to creating a proactive maintenance strategy that enhances equipment reliability and patient care. Together, they create a comprehensive strategy for imaging equipment reliability.
As healthcare technology continues to evolve, maintaining the critical systems that support it demands adaptability and forward-thinking solutions. I’d love to hear how you are using remote monitoring or AI in your daily operations. To discuss how we’re integrating data-driven insights with hands-on service – or to share your perspective on the role of AI and machine learning in the industry – reach out to Eric Massey at eric.massey@crothall.com.
— Eric Massey is a Regional Director of Operations for Crothall Healthcare. To learn more about joining the Crothall team, contact Eric at eric.massey@crothall.com.


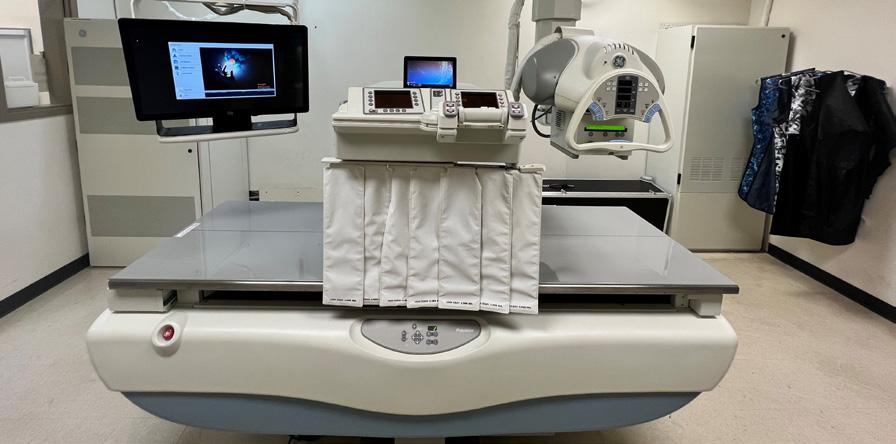




BY DANIEL BOBINSKI EMOTIONAL INTELLIGENCE
It ’s not uncommon for managers or supervisors to think that when someone’s performance is slipping, the person has lost motivation. However, the idea that people lack motivation is fundamentally flawed. In fact, it’s bad psychology. By definition, the word motivation means “a reason to move.” And everyone, at all times, has reasons to move. Therefore, everyone has motivation.
I have several topics to discuss regarding this. The first is about making connections. The key for managers and supervisors is to learn how to connect a person’s personal motivations with the goals of the organization.
Picture an employee who drags his feet all day at work but bolts out the door the moment his shift is over. Clearly, the person is motivated because he has reasons for picking up the pace as he leaves the building. So, rather than assuming a person is unmotivated, it’s more appropriate for managers or supervisors to explore what’s truly going on.
Think about our reasons for moving. Hunger motivates us to find food. Thirst compels us to drink. An itch leads us to scratch. Feeling cold drives us to turn up the heat, find a blanket or don a sweater. These are simple examples, but the same logic applies to larger aspects of our lives. If someone dreams of a beach vacation, they have a reason (motivation) to save money and plan a trip. When people want
promotions, they have a reason to take on extra work or learn new skills.
This brings me to the second topic: fear. After three decades of working with leaders and teams, I’ve observed a common pattern: people don’t slow down because of a lack of motivation. They slow down because something is blocking their forward progress, and it’s usually some kind of fear.
To illustrate the idea that fear gets mistaken for a lack of motivation, let me use a sales analogy. Here’s a truism I’ve stated for years. “Sales is one of the lowest paying easy jobs and one of the highest paying hard jobs.” Why? Because salespeople are often expected to make cold calls, and not everyone is cut out for the ongoing rejection that comes with that aspect of the sales process.
Let’s imagine a struggling new sales rep. His job depends on making sales or he can’t pay his bills, so he definitely has a reason (motivation) to make cold calls. However, when it comes to picking up the phone, this young man almost always stops. He stares at his phone and may even appear paralyzed. The reason is not a lack of motivation, but the presence of fear. The fear of rejection has taken up residence in the man’s head, and that fear has become larger than his motivation to make sales.
If this man’s manager buys into the ubiquitous myth that he simply lacks motivation, she might try offering an incentive. These often come in the form of a bonus, or perhaps tickets to a show or a sporting event, or some other reward for
“If you’re tired of over-inflating your tires, it might be beneficial to start clearing the road instead.”

closing more sales. Such carrots may produce short term results, but they do nothing when it comes to eliminating the underlying obstacle.
To help us understand this issue further, let’s think of motivation as tires on the salesperson’s car. The car’s tires (his motivation) allow him to move forward toward his goals. However, when he encounters an obstacle too large to roll over, such as a large amount of fear in front of him, stopping is a natural response.
Now let’s say the sales manager is rightly concerned, so she sends our sales rep to an inspirational sales seminar. At the seminar he’s encouraged to over-inflate his tires so he can roll over the obstacles. He returns, and filled with enthusiasm, he gets up the next morning and pumps extra air into his tires. With those over-inflated tires, he rolls over each obstacle with ease. For a few days, he’s having great success making cold calls and landing deals. Everyone is thrilled.
However, by the end of the week, all that extra air has leaked out, and his tires are back to their normal size. And the obstacle, which is really his fear of rejection, remains on the road in front of him.
When his boss looks at the situation, she assumes he simply lacks motivation, and considers replacing him.
Many motivational speakers and trainers emphasize the need to constantly pump up our motivation. As I said, that can work, but the effects are almost always temporary. What if we considered the problem from a different angle? What if, instead of a daily effort to pump up one’s motivation, we simply removed the obstacle that’s in the way?
From this perspective, we could imagine the sales rep working with someone to help him unwind his fear of rejection. Through some personalized assignments, our sales rep could rewire his thinking and build confidence. Then, without fear blocking his way, he wouldn’t need to rely on temporary motivation boosts. He would simply move forward naturally.
Naturally, we must acknowledge that some external obstacles are immovable. But when we encounter such obstacles, we are under no obligation to plow straight through them. We can go around immovable obstacles, find a different route, or even change our destination altogether. The key is understanding that it’s not a lack of motivation that’s slowing us down or bringing us to a complete stop, but obstacles.
Bottom line, the belief that success comes down to motivation alone is a myth. Everyone on the planet needs to identify hidden fears and remove or minimize them, or those fears remain obstacles that slow us down or keep us stuck. By identifying and removing these roadblocks, we free ourselves to make real progress.
So here’s something to think about. If you’re tired of over-inflating your tires, it might be beneficial to start clearing the road instead. •
— Daniel Bobinski, who has a doctorate in theology, is a best-selling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@protonmail.com or 208-649-6400.

BY FAMILY FEATURES
Stress, the physical or mental response to external causes like overwhelming work assignments or difficult life moments, can add unnecessary pressure to your day to day. While everyone feels stress from time to time, when left untreated or unrecognized, it can begin to wreak havoc in the form of anxiety.
In honor of National Stress Awareness Month, consider these strategies to combat stress from the National Institutes of Mental Health.
Different events and situations cause stress for different people. Knowing what triggers your stress to kick in –mounds of office paperwork, important financial decisions or hectic mornings, for example – can help you plan and prepare for stress-inducing moments.
Maintaining physical health can be beneficial for mental health, too. Find time to do exercises you enjoy like walking, jogging, yoga or playing a sport. Identifying activities that bring you joy can make it easier to fit 30-60-minute workouts into your schedule without adding even more stress. Complement your workout routine with nutritional meals that help you stay on track with your fitness goals.
Whether you find inner peace through journaling, breathing exercises, reading or some other form of slowing down, find what works for you and prioritize fitting it into your daily schedule. Relaxing activities help you slow down the pace of life, providing a chance to reset by doing something you enjoy.
A lack of quality sleep can add to stress. Creating a bedtime routine can increase your sleep habits and help you achieve the expert-recommended 7-9 hours per night. Put away electronics, which can interfere with your ability to calm your mind, and find an activity that puts you at ease like reading a book or listening to relaxing music. Ensure your bedroom is optimized for comfort by making it cool, dark and quiet.
Everyone experiences stress. Reach out to family members and close friends you can lean on in stressful and frustrating moments. Share your feelings and encourage others to do the same, which can increase trust and help everyone in your circle cope in a positive way.
Find more ways to combat stress and care for your mental health at eLivingtoday.com. •
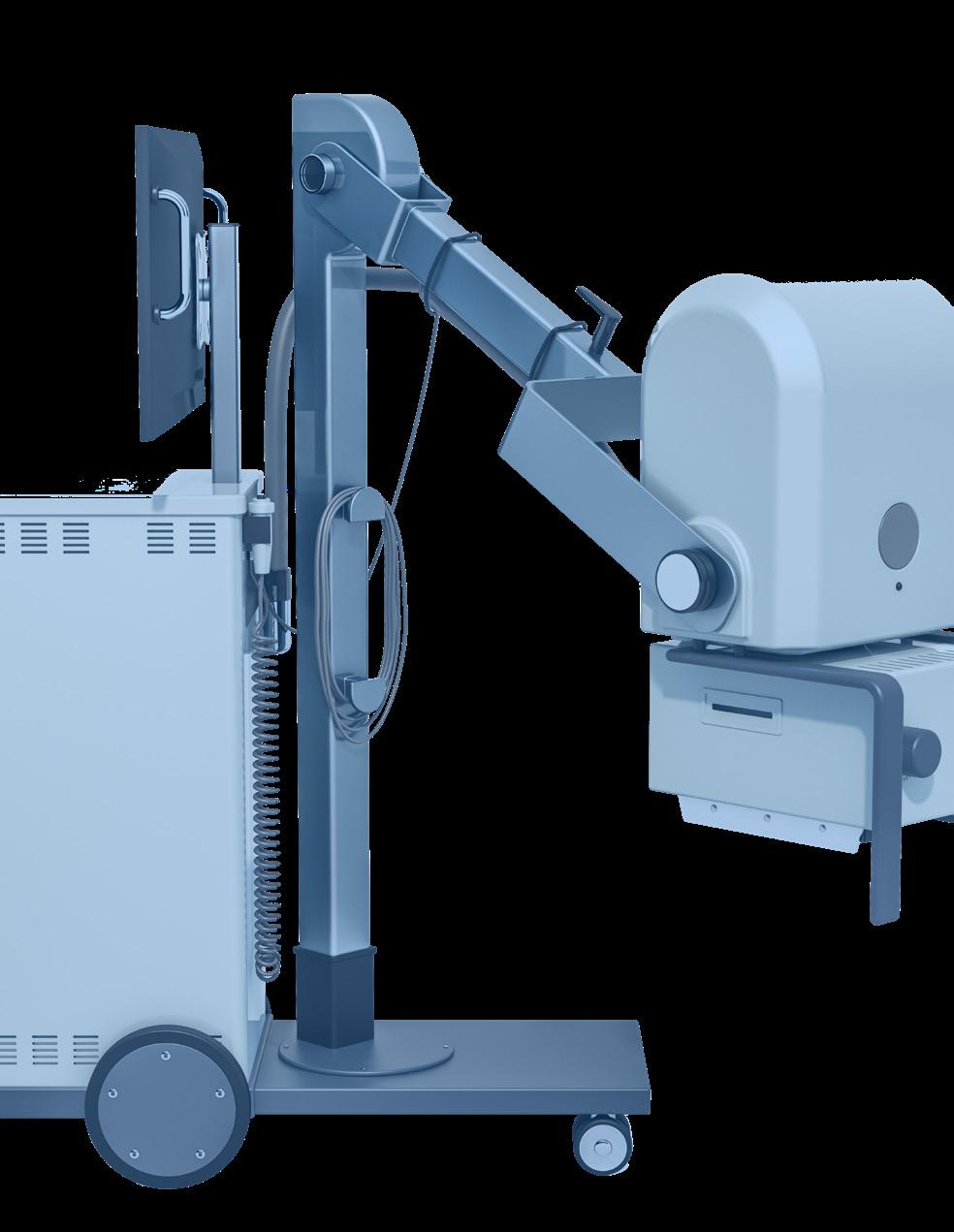


“ICE Webinars always provide great timely information in a well planned format.”
- Nancy Godby, Director of Radiology, Cabell Huntington Hospital - Marshall Health Network
“I attend ICE webinars because of the variety of topics and presenters.”
- John Beall, Regional Director, United Imaging Healthcare
“I attend ICE Webinars to learn more about other imaging styles and get CE credits.”
- Amanda Brunson, Manager of CT and MR Imaging Services, MUSC Health Orangeburg
“I participate in these webinars to enrich my professional knowledge and to be able to share the news in the field with my students. “
- Calin Corciova, Associate Professor, Medical Bioengineering Faculty

“I attend ICE Webinars to learn more information related to radiology and imaging technology.”
- Krista Andrews, Imaging Manager, BSHW
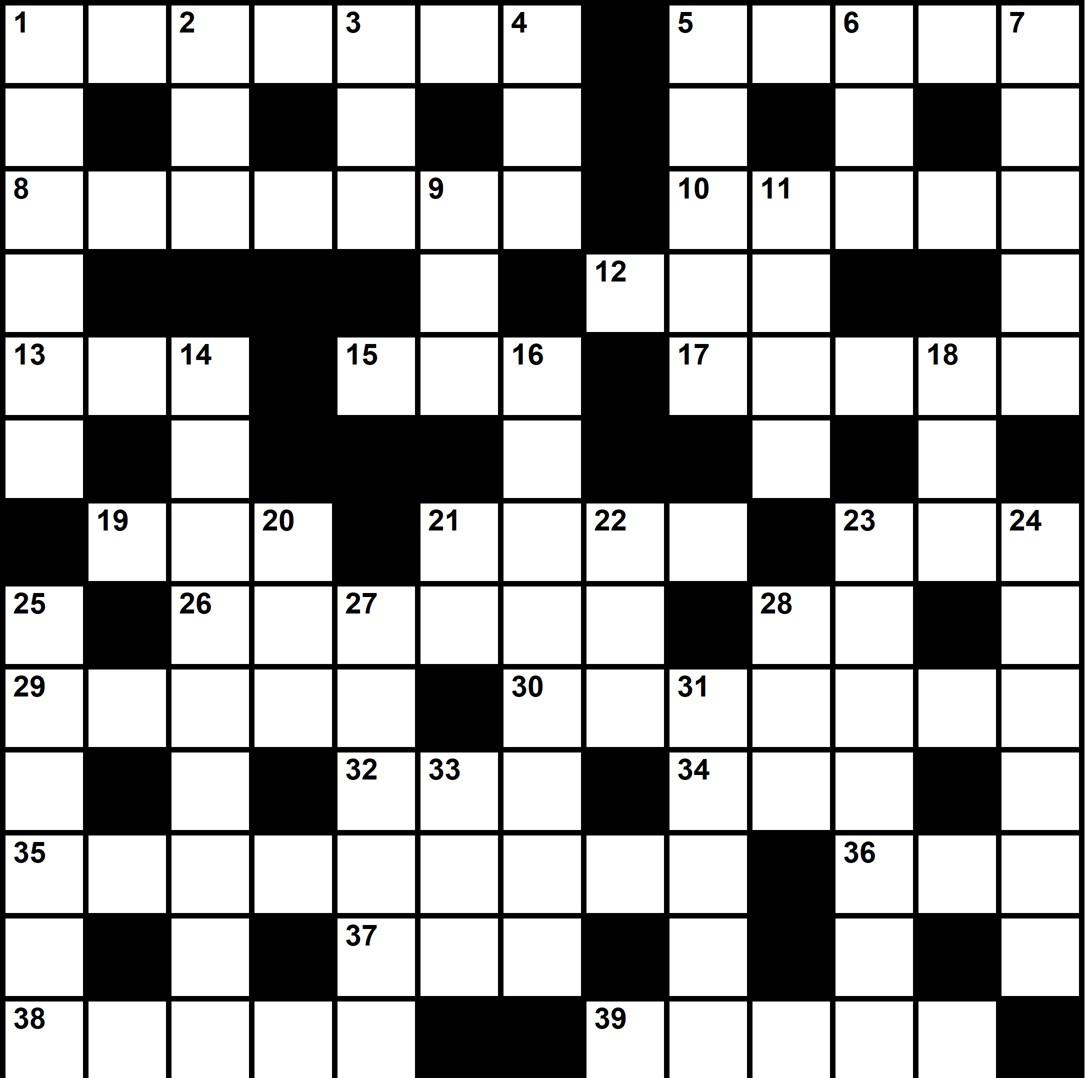

done by a series of small things brought together.” – Vincent van Gogh
Radon
CM Parts Plus cmpartsplus.com
image1group.com • 877-304-9000
KEI Medical Imaging Services keimedicalimaging.com • 512-477-1500
Metropolis International, LLC Metropolismedical.com • 718-371-6026
Managment
• $300 a month
• 1/6 page ad included in the marketplace
• Up to 5 categories in our ICEDEX
• Your company name, website and phone included in your ICEDEX listings
• Your company name in the alphabetical business index
• Appear in the print and digital magazine



















GE Elastomer Keypad
Extend the life of your GE LOGIQ Ultrasound with AIV’s Elastomer Lower Control Panel Keypad
120 Day Warranty
In Stock Ships Same Day Part Number: GE14205
The Elastomer Keypad is an AIV manufactured replacement keyboard silicone underlay compatible with GE LOGIQ OPIO S7 & S8 Ultrasound machines:






