INSIDE
What Is Epigenetics and How Is It Relevant for Spine Surgeons?
Lateral Lumbar Interbody Fusion in the Prone Position: Where Do the Current Data Stand?
Static vs Expandable Interbody Cages for Minimally Invasive Transforaminal Lumbar Interbody Fusion
Emerging Management of Obesity in Spine Surgery
The Use of Radiolucent Technology in Spine Tumors
Robotic Spine Surgery: Current State and Future Outlook
Surgical Simulation in Spine Surgery
Vertebral COLUMNS
International Society for the Advancement of Spine Surgery
TRANSITIONING TO THE Ambulatory
Surgical Center
Part 2: Surgeon Perspective and Hurdles Faced
WINTER 2023
8
EDITORIAL
Transitioning to the Ambulatory Surgical Center, Part 2: Surgeon Perspective and Hurdles Faced
EPIGENETICS
What Is Epigenetics and How Is It Relevant for Spine Surgeons?
14
LUMBAR SPINE
Lateral Lumbar Interbody Fusion in the Prone
Position: Where Do the Current Data Stand?
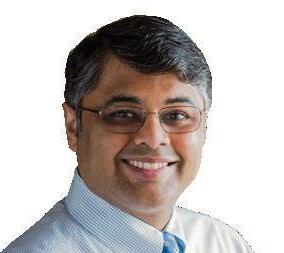
Editor in Chief
Kern Singh, MD
Editorial Board
Peter Derman, MD, MBA
Brandon Hirsch, MD
Sravisht Iyer, MD
20
LUMBAR SPINE
Static vs Expandable Interbody Cages for Minimally Invasive Transforaminal Lumbar Interbody Fusion
PATIENT OUTCOMES
Emerging Management of Obesity in Spine Surgery
24
INSTRUMENTATION
The Use of Radiolucent Technology in Spine Tumors
ROBOTICS
Robotic Spine Surgery: Current State and Future Outlook
TRAINING
Yu-Po Lee, MD
Sheeraz Qureshi, MD, MBA
Managing Editor
Audrey Lusher
Vertebral Columns is published quarterly by the International Society for the Advancement of Spine Surgery.
a member today
Become
©2023 ISASS. All rights reserved.
Opinions of authors and editors do not necessarily reflect positions taken by the Society.
This publication is available digitally at www.isass.org/news/vertebralcolumns-Winter-2023
17 isass.org Winter 2023 Vertebral Columns
3 30 26
Designer CavedwellerStudio.com
Surgical Simulation in Spine Surgery
https://www.isass.org/about/membership/
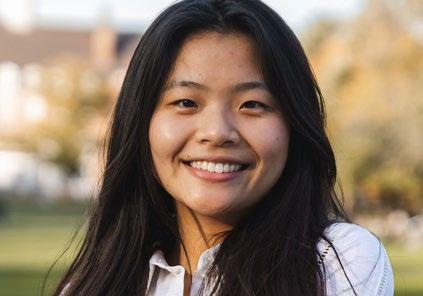
Transitioning to the Ambulatory Surgical Center, Part 2: Surgeon Perspective and Hurdles Faced




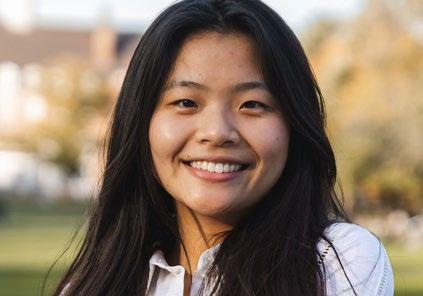


The first part of this series on ambulatory surgical center (ASC) utilization in spine surgery focused on the patient perspective. The article highlighted the myriad benefits that patients receive with regard to safety, surgical efficiency, cost efficacy, and additional conveniences that have affected the rising popularity of ASCs. As the concluding part of this two-piece series, the present article will examine the surgeon’s perspective. While many positive aspects of ASCs benefit both patients and surgeons alike, such as safety and surgical efficacy, this article will focus on those benefits and challenges exclusively accorded to and faced by the surgeon. These unique aspects include increased autonomy, greater surgical cost efficacy, and both technological and personnel efficiencies.
One of the largest draws in transitioning to ASCs for surgeons is the significant increase in managerial and surgical autonomy when compared to a hospital-based system. The majority of ASCs (approximately 65%)
are owned in entirety by physicians.1 From a managerial perspective, surgeons are able to control macro-level decisions with regard to insurance agreements, utilization of space, and efficient distribution of operating room time—factors that would generally be decided by administrative staff in the hospital setting. Furthermore, surgeons are in total control of hiring optimal staff that improve the flow of the surgical process from admission to discharge. As a result, the environment of the ASC is highly adaptable to meet the needs of the surgeons and thus optimize patient care. In the event surgeons would choose to defer the more mundane requirements of managing an ASC, surgeons are able to partner with experienced ASC companies for assistance with these tasks. In this model, physician-owners are able to prioritize the clinical environment and maintain autonomy while allowing the ASC company to interface with insurance and support staff contracting companies.1
3 isass.org Winter 2023 Vertebral Columns
EDITORIAL
From the Department of Orthopaedic Surgery at Rush University Medical Center in Chicago, Illinois.
Kern Singh, MD
Timothy J. Hartman, MD
James W. Nie, BS
Keith R. MacGregor, BS
Omolabake O. Oyetayo, BS
Eileen Zheng, BS
Arash Sayari, MD
In the previous article, the cost savings for patients was highlighted at approximately $3,000 per lumbar decompression procedure; however, this decrease in cost is highly reflective of downstream benefits from a surgeon-managed practice. 2–5 As part- or full-owners, surgeons are able to make small changes in the clinical setting, fine-tuning needs to the surgeon group to reduce inefficiencies. Two of these changes are (1) an increased proportion of operating room time per day as a result of improved room turnover rate and (2) decreased overhead through limiting unnecessary equipment purchases. Furthermore, in situations where inefficiencies are identified, surgeon-owners are able to make small changes to improve flow without bureaucratic delays or conflicts
with administrative staff. Thus, routine case-cost analyses can allow surgeons to quickly identify and adapt to improve the clinical setting, lowering costs for patients and surgeons alike. 6
In addition to constant adaptation of the clinical environment, ASCs allow spine surgeons to reduce overhead through technological efficiencies including radiological requirements, innovative intraoperative neuromonitoring techniques, and robotics and navigation. In ASC groups, it is important for surgeons to identify the necessary radiological equipment that meets the needs of the group without resulting in excess waste. By properly identifying this need, the right equipment can be shared without delays in patient care, increased operating room time,
4 isass.org Winter 2023 Vertebral Columns EDITORIAL
or overly idle devices that decrease cost efficacy. As indications for ASC care expand, surgeons also require technologies that allow for increasing productivity and safety in complicated cases.7–10 As an example, the lateral lumbar interbody fusion (LLIF) has been demonstrated to be a highly effective procedure for restoring sagittal parameters and achieving fusion with placement of a large interbody device.11–13 However, LLIF is performed via a transpsoas approach in which the identification of the femoral nerve is required in order to prevent injury.12
Currently, a variety of intraoperative neuromonitoring techniques, including a combination of electromyography and motor or somatosensory evoked potentials, are utilized in this process.14 Such techniques require additional staff, increased operative room setup time, and inherent equipment expenses. Newer technologies on the horizon, including real-time ultrasound devices that allow for quick identification of the vascular and neural elements, may further improve productivity and safety concurrently.14,15 Additionally, advances in robotics and intraoperative navigation have the potential to decrease operating room times and reduce complication rates.16 Utilization of these technologies in the ASC setting may vary depending on surgical group size, as the benefits of robotics may not be cost effective in smaller groups if not used routinely by multiple providers. While robotics have demonstrated significant benefits, ownership may not outweigh upfront purchasing and maintenance fees if not routinely utilized.
Additionally, the equipment requires a large amount of real estate even when not in use, further limiting utility in a smaller practice. As the final key to maintaining safety while optimizing productivity, the ASC setting offers surgeons a variety of personnel efficiencies. In order to be productive, surgeons rely on support staff, including circulating and scrub nurses, physician assistants, and medical assistants for rapid room turnover. Furthermore, anesthesiologists and their relevant support staff need to be reliable to safely induce and withdraw anesthesia in an efficient manner. Such consistent reliability requires a clear understanding between surgeons and anesthesiologists with regard to patient selection criteria and perioperative protocols. Patient selection criteria for ASCs generally include low comorbidity burden, lack of obstructive sleep apnea, manageable body mass index (i.e., ≤38), and a negative history of cardiac events. Additionally, multimodal analgesia protocols can minimize
5 isass.org Winter 2023 Vertebral Columns EDITORIAL
Surgeon autonomy allows for a reduction in redundancies while improving patient safety and access to care
anesthesia-related complications throughout the perioperative period.17–19 Outside of the clinical care setting, surgeons are also reliant on office personnel, including office assistants, case managers, and billing professionals. Appropriate hiring independently by surgeons or through experienced ASC companies may increase nonclinical efficiencies.
Overall, ASCs offer a substantial array of benefits to both patients and surgeons. Con-
References
1. Badlani N. Ambulatory surgery center ownership models. J Spine Surg. 2019;5(Suppl 2):S195-S203.
2. Malik AT, Xie J, Retchin SM, et al. Primary single-level lumbar microdisectomy/decompression at a free-standing ambulatory surgical center vs a hospital-owned outpatient department-an analysis of 90-day outcomes and costs. Spine J. 2020;20(6):882-887.
3. Lewandrowski KU. Incidence, management, and cost of complications after transforaminal endoscopic decompression surgery for lumbar foraminal and lateral recess stenosis: a value proposition for outpatient ambulatory surgery. Int J Spine Surg. 2019;13(1):53-67.
4. Pendharkar AV, Shahin MN, Ho AL, et al. Outpatient spine surgery: defining the outcomes, value, and barriers to implementation. Neurosurg Focus . 2018;44(5):E11.
5. Purger DA, Pendharkar AV, Ho AL, et al. Analysis of outcomes and cost of inpatient and ambulatory anterior cervical disk replacement using a state-level database. Clin Spine Surg. 2019;32(8):E372-E379.
6. Corporate SIS. ASC case costing: where should surgery centers start? Accessed January 19, 2023. https:// blog.sisfirst.com/asc-case-costingwhere-should-surgery-centers-start
cluding this two-part series, it is important to highlight the backbone of ASCs that underlie these efficiencies. Surgeon autonomy is paramount. Surgeon autonomy allows for a reduction in redundancies while improving patient safety and access to care. As the popularity of ASCs continues to rise, identifying other factors that lead patients and surgeons to choose the ambulatory setting is of great importance. n
7. Best MJ, Buller LT, Eismont FJ. National trends in ambulatory surgery for intervertebral disc disorders and spinal stenosis: a 12-year analysis of the National Surveys of Ambulatory Surgery. Spine . 2015;40(21):1703-1711.
8. Chin KR, Pencle FJR, Coombs AV, Packer CF, Hothem EA, Seale JA. Eligibility of outpatient spine surgery candidates in a single private practice. Clin Spine Surg. 2017;30(10):E1352-E1358.
9. Helseth Ø, Lied B, Halvorsen CM, Ekseth K, Helseth E. Outpatient cervical and lumbar spine surgery is feasible and safe: a consecutive single center series of 1449 patients. Neurosurgery 2015;76(6):728-737; discussion 737-738.
10. Basques BA, Ferguson J, Kunze KN, Phillips FM. Lumbar spinal fusion in the outpatient setting: an update on management, surgical approaches and planning. J Spine Surg. 2019;5(Suppl 2):S174-S180.
11. Teng I, Han J, Phan K, Mobbs R. A meta-analysis comparing ALIF, PLIF, TLIF and LLIF. J Clin Neurosci. 2017;44:11-17.
12. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18.
13. Salzmann SN, Shue J, Hughes AP. Lateral lumbar interbody fusion—outcomes and complications. Curr Rev Musculoskelet Med. 2017;10(4):539-546.
14. Singh K, Cha EDK, Lynch CP, et al. Device profile of SonoVision ultrasound system: efficacy and safety for lateral approach spinal surgery. Accessed October 20, 2022. https://journaloei. scholasticahq.com/article/27576.pdf
15. Carson T, Ghoshal G, Cornwall GB, Tobias R, Schwartz DG, Foley KT. Artificial intelligence-enabled, real-time intraoperative ultrasound imaging of neural structures within the psoas: validation in a porcine spine model. Spine . 2021;46(3):E146-E152.
16. D’Souza M, Gendreau J, Feng A, Kim LH, Ho AL, Veeravagu A. Robotic-assisted spine surgery: history, efficacy, cost, and future trends. Robot Surg. 2019;6:9-23.
17. Jenkins NW, Parrish JM, Nolte MT, et al. Multimodal analgesic management for cervical spine surgery in the ambulatory setting. Int J Spine Surg. 2021;15(2):219-227.
18. Bohl DD, Louie PK, Shah N, et al. Multimodal versus patient-controlled analgesia after an anterior cervical decompression and fusion. Spine . 2016;41(12):994-998.
19. Mathiesen O, Dahl B, Thomsen BA, et al. A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J. 2013;22(9):2089-2096.
6 isass.org Winter 2023 Vertebral Columns EDITORIAL
23RD ANNUAL CONFERENCE ISASS23

JUNE 1 – JUNE 3, 2023
MARRIOTT MARQUIS • SAN FRANCISCO, CA
• Interactive meeting led by world-class faculty
• Focused on new technologies and techniques





• AMA PRA Category 1 Credit(s)™ available
JOINTLY PROVIDED BY:
LEARN MORE: ISASS.ORG
Program Chair: Han Jo Kim, MD
Program Chair: Luis Tumialan, MD
Vice Chair: Praveen Mummaneni, MD
Vice Chair: Peter Passias, MD
President: Massimo Balsano, MD
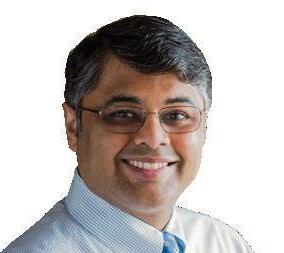
What Is Epigenetics and How Is It Relevant for Spine Surgeons?


Differential epigenomic markers have been associated with a number of spinal, musculoskeletal, and inflammatory conditions.1-3 Recently, epigenetic research has garnered considerable attention due to the multidirectional relationship between environmental exposures, genetic variables, epigenetic variables, and health/disease conditions. While the excitement has created considerable interest and hope for potential applications of this research, many are unaware of both the potential promises and pitfalls of epigenetic research. In this article, we introduce epigenetics as a concept, discuss challenges of epigenomic research, and apply this discussion to critically engage with research on osteoarticular diseases.
Understanding Epigenetics
The idea of an epigenomic landscape is not new. Waddington proposed the term epigenotype in the 1940s. Nanney subsequently reinterpreted epigenetics to include cellular memory in the 1950s, and Riggs and Holliday related DNA methylation with epigenetics in the 1970s.4 Recent technological advancements have allowed epigenetic studies to
flourish, and the applications of epigenetics for spine health and disease are just starting to be explored.

A basic understanding of epigenetics often starts by breaking down the etymology of the term: epi, which means over or beyond. As such, epigenetics is often described as above and beyond the genome. Epigenetics is more specifically defined as “the study of mitotically and/or meiotically heritable changes in gene function that cannot be explained by changes in DNA sequence.”5 The boundaries of genomic control that are encompassed within epigenetics are debated, but the mechanisms typically discussed are gene methylation, histone modification, and noncoding RNA.
Each of these epigenetic mechanisms affect genomic activity. We classically have taught about DNA as a fixed sequence— the nucleotide sequences an individual is born with generally does not change over an individual’s lifespan. We also often first introduce genomic sequences in a rather deterministic manner—this nucleotide sequence predicts this outcome. Studying the epigenomic landscape has the potential to shift this immutable and deterministic view as we learn more about the ways in which epigenetic mechanisms affect genetic activity and impact physiology, as well as how these mechanisms work in multidirectional
8 isass.org Winter 2023 Vertebral Columns
EPIGENETICS
From the Texas Back Institute in Plano, Texas.
Mary P. Rogers-LaVanne, PhD
Alexander M. Satin, MD
Peter B. Derman, MD, MBA
ways, with relationships explored between genomic, epigenomic, phenotypic, and environmental variables. 6,7
One of the keys to understanding epigenomics is to consider accessibility and readability of nucleotide sequences. Within the nucleus, DNA is compactly wrapped around histones. The more densely packed the DNA and histone proteins, the less likely transcription will occur. The more loosely packed, the more accessible it is for transcription. Enzymatic changes to histones with acetyl, methyl, or phosphate groups modify this accessibility, thereby affecting the potential transcription of specific regions of DNA. 8
Methyl groups can also be added to DNA nucleotides. Methylation typically occurs to cytosine nucleotide positionally followed by a
guanine (CpG). This is an enzymatic process that can be reversed, meaning methyl groups can be added or removed. Methylation at CpG islands (clusters of CpG dinucleotides located near gene promoter regions) is typically associated with gene silencing. While early research focused on DNA methylation at CpG islands, more contemporary work takes whole genome approaches, including intragenic regions, CpG islands, CpG shores, and CpG valleys. 9
Noncoding RNA (ncRNA) represent the majority of transcribed material.10 Some of what was once described as junk DNA is now known to produce ncRNA with regulatory and structural functions. Regulatory ncRNA often explored in epigenetics research include microRNAs (miRNAs), which are

9 isass.org Winter 2023 Vertebral Columns
EPIGENETICS
short ncRNAs typically 20–24 nucleotides in length, and long non-coding RNAs (lncRNAs), which are ncRNAs typically greater than 200 nucleotides in length. These ncRNAs can play a role in expression regulation at both the genetic and chromosomal level.10,11
In this article, we could repeat the sentence “differential epigenomic markers are associated with [insert spinal condition here],” as differential epigenomic markers have been associated with osteoarthritis, osteoporosis, ankylosing spondylitis, bone mineral density, spinal cord injury, adolescent idiopathic scoliosis, tumorous subtypes, aging, and more.1-3,12-23 However, the existence of an association only tells us so much. Thus, in the rest of this article, we will first discuss challenges of epigenomic research necessary for spine surgeons to be able to better critique the research they encounter. We follow this with a synthesis of data regarding osteoarticular diseases with a particular focus on applying these critiques.
Challenges in Epigenomic Research
Epigenetic mechanisms respond to and influence phenotypes and environmental variables, which is why epigenetic mechanisms are often seen as possible mechanistic links between exposures and health outcomes. There are nuances within epigenetic research that are critical to be aware of when interpreting the promises of this research.
Heijmans and Mill reviewed cautionary warnings for clinical epigenomics relevant for a nuanced understanding of epigenomic research results. They first emphasized that researchers often look first at gene methyl-
ation, rather than histone modification or non-coding RNA, while each mechanism may play a critical role in health and disease. 24 Additionally, similar to genome-wide association studies, epigenetic studies are identifying small differences in a number of CpG sites. 24 The meaning of methylated state for specific cytosines still needs to be explored; the existence of differential methylation tells us only part of the story. Learning what methylation or absence of methylation at each specific site signals for transcription will help fill in gaps. 24 Furthermore, while we have made strides in technological advancements, our tools are still imperfect. 9,24 Sample size and timing is a critical issue for mechanisms known to change over time and hypothesized to change in relation to health, disease, environment, treatments, etc. 2,24 Additionally, there is tissue-specificity in epigenetic markers, so the correlation may be low between the tissue of interest and the tissue available to measure (most often blood or saliva).
Existing biases in research, such as lack of diverse populations, sampling methods, and the misperceptions and biases of scientists affecting study design, cannot be ignored in epigenetic work. Just as in nongenomic epidemiological research, 25 studies have shown that scientists’ assumptions about sex, gender, sexuality, class, and social disparities can affect epigenetic research design and interpretation. 26 Randomized clinical trials in spine surgery are under scrunty for a lack of diverse representation, 27 which is an issue that should be scrutinized in spinal epigenetic research, too.
10 isass.org Winter 2023 Vertebral Columns
EPIGENETICS
Finally, multiple scholars warn that the high expectations and popular interest in medical epigenomics create a certain amount of hype that epigenetics may not be able to fully realize. 9,24
Epigenetics and Osteoarticular Diseases: Osteoarthritis, Osteoporosis, and Ankylosing Spondylitis
Epigenetic mechanisms have been implicated in osteoarticular diseases including osteoarthritis, osteoporosis, and ankylosing spondylitis.1-3 The site specificity observed in osteoarticular diseases has given rise to the hypothesis that epigenetic modifications may act as a mechanistic link between patients’ underlying genes and intrapersonal heterogenous diseases.1
One critique of epigenetic studies is the focus on DNA methylation in research, but epigenetic studies on osteoarthritis, osteoporosis, and ankylosing spondylitis have included research on DNA methylation, histone modification, and ncRNA activity.1,2
A related critique focuses on the meaning of epigenetic states: are these epigenetic states correlated with changes in gene expression or cellular physiology? In one study, articular cartilage sampled from the femoral head showcased differential DNA methylation between patients with and without osteoarthritis, and the differential methylation was correlated with changes in gene expression.16
A separate study reported that levels of a histone methyltransferase (SET-1A) increase in osteoarthritic cartilage and that the activity of this histone methyltransferase increases
expression of genes correlated with loss of chondrocytes and inhibition of collagen production.1,15
Similarly, differences in DNA methylation, histone acetylase and deacetylase activity, and miRNA expression have been observed in patients with ankylosing spondylitis compared to healthy controls.18-20 For example, one study compared methylation of a gene SOCS-1 in serum of 43 patients with ankylosing spondylitis to six control patients, reporting that methylation of SOCS-1 correlated with cytokine activity and severity of ankylosing spondylitis disease.18 Furthermore, a number of studies have reported a correlation between ncRNA and ankylosing spondylitis, specifically observing that miRNAs associated with ankylosing spondylitis have functional targets involved in regulation of T cell survival and bone remodeling (eg, osteoblast proliferation or osteoclasts activation).2 In epigenetic research on osteoarticular diseases, work is being conducted on multiple epigenetic mechanisms, and the potential meaning of these differential epigenetic states for gene expression and cellular physiology is being explored.
Another critique of epigenomic research in general relates to its reliance on imperfect samples and sample sizes—a critique that can be readily applied to epigenomic research of osteoarticular conditions. Whole blood, cartilage, and bone samples have all been used to identify differential epigenetic markers associated with either osteoarthritis or osteoporosis.1,14,16 Whole blood, peripheral blood mononuclear cells, and T cells, have all been used to identify differential epigenetic markers associated with ankylosing spondy-
11 isass.org Winter 2023 Vertebral Columns EPIGENETICS
EPIGENETICS
litis.1,2 Between these different sample types, there are differences in which epigenomic markers are correlated with osteoarticular conditions. Furthermore, most epigenetic work regarding osteoarthritis involves knee and hip studies rather than studies of the spine. Differences exist in epigenetic markers between similar tissues sampled from the hip and knee1; thus, there may be unique epigenetic markers associated with osteoarthritis and osteoporosis in the spine.
Further challenges in epigenomic research exist regarding the timing of sampling. DNA methylation is a stable marker, but it is also responsive to the environment. This means these epigenetic markers may change prior to disease onset, over the course of disease progression, or in response to treatments. Sampling pertinent tissue from humans across osteoarticular disease progression is unethical. 28 Yang et al also raise the possibility that treatments for ankylosing spondylitis such as nonsteroidal anti-inflammatory drugs (NSAIDs) also affect DNA methylation. 2 Studies comparing control patients to patients with ankylosing spondylitis need to address these potential confounding factors.
A final critique verges on managing the high expectations of epigenomic research promises. In osteoarticular conditions, more research is needed to fully understand the complex relationships observed. While therapeutic potentials have been explored, they show no benefit to osteoarthritis thus far.1 Roberts et al suggested that the most promising use for epigenetic markers is as a biomarker of disease.1 Understanding epigenetic changes over the course of os -
teoarticular disease progression may aid in staging the disease.1
Future Directions
It is an exciting time for the -omics world as technological breakthroughs allow for more efficient and less expensive sequencing. In this article, we reviewed some of the ways we should be critical of epigenomic studies in conditions affecting the spine. Specifically, we encourage understanding of the many epigenomic mechanisms and multidirectional relationships between genomic, epigenomic, condition, and environmental variables. We caution on the tissue specificity of epigenetic markers, epigenomic changes over the course of disease, and the potentially confounding variables that create challenges for designing sound research methodology. While more research is needed, there are promising applications of epigenetic research for the spine. Epigenetic research holds promise for risk screening, diagnostic screening, disease staging, and potential prognoses. 29 The use of epigenetic biomarkers is being explored to aid in the prognosis of spinal cord injury 21 and adolescent idiopathic scoliosis.12
Tumor subtypes are sometimes classified by DNA methylation patterns, such as in Ewing’s sarcoma, in which methylation patterns are associated with tumor aggression. 23
As more epigenomic research studies are conducted, it is important to be aware of the challenges inherent in epigenomic research. This will allow us to improve study designs, critique existing research, and analyze possible applications of epigenetic research related to the spine. n
12 isass.org Winter 2023 Vertebral Columns
References
1. Roberts SB, Wootton E, De Ferrari L, Albagha OM, Salter DM. Epigenetics of osteoarticular diseases: recent developments. Rheumatol Int . 2015;35(8):1293-305.
2. Yang H, Chen Y, Xu W, et al. Epigenetics of ankylosing spondylitis: Recent developments. Int J Rheum Dis . 2021;24(4):487-493.
3. Altorok N, Nagaraja V, Kahaleh B. Chapter 14: Epigenetics in bone and joint disorders. In: Tollefsbol TO, ed. Medical Epigenetics. 2nd ed. Academic Press; 2021:251-278.
4. Greally JM. A user’s guide to the ambiguous word ‘epigenetics’. Nat Rev Mol Cell Biol. 2018;19(4):207-208.
5. Russo VEA, Martienssen RA, Riggs AD. Epigenetic Mechanisms of Gene Regulation. Cold Spring Harbor Laboratory Press; 1996.
6. Non AL, Thayer ZM. Chapter 19: Epigenetics and human variation. In: O’Rourke ZM, ed. A Companion to Anthropological Genetics . Wiley; 2019:293-308.
7. Lappé M, Landecker H. How the genome got a life span. New Genet Soc . 2015;34(2):152-176.
8. Fischle W, Wang Y, Allis CD. Histone and chromatin cross-talk. Curr Opin Cell Biol. 2003;15(2):172-183.
9. Non AL, Thayer ZM. Epigenetics for anthropologists: an introduction to methods. Am J Hum Biol. 2015;27(3):295-303.
10. Kaikkonen MU, Lam MT, Glass CK. Non-coding RNAs as regulators of gene expression and epigenetics. Cardiovasc Res . 2011;90(3):430-440.
11. Wei JW, Huang K, Yang C, Kang CS. Non-coding RNAs as regulators in epigenetics [review]. Oncol Rep. 2017;37(1):3-9.
12. Perez-Machado G, Berenguer-Pascual E, Bovea-Marco M, et al. From genetics to epigenetics to unravel the etiology of adolescent idiopathic scoliosis. Bone . 2020;140:115563.
13. Horvath S, Raj K. DNA methylation-based biomarkers and the epigenetic clock theory of ageing. Nat Rev Genet . 2018;19(6):371-384.
14. Delgado-Calle J, Fernandez AF, Sainz J, et al. Genome-wide profiling of bone reveals differentially methylated regions in osteoporosis and osteoarthritis. Arthritis Rheum. 2013;65(1):197-205.
15. El Mansouri FE, Chabane N, Zayed N, et al. Contribution of H3K4 methylation by SET-1A to interleukin-1-induced cyclooxygenase 2 and inducible nitric oxide synthase expression in human osteoarthritis chondrocytes. Arthritis Rheum. 2011;63(1):168-179.
16. Kim KI, Park YS, Im GI. Changes in the epigenetic status of the SOX-9 promoter in human osteoarthritic cartilage. J Bone Miner Res. 2013;28(5):1050-1060.
17. Swingler TE, Wheeler G, Carmont V, et al. The expression and function of microRNAs in chondrogenesis and osteoarthritis. Arthritis Rheum. 2012;64(6):1909-1919.
18. Lai NS, Chou JL, Chen GC, Liu SQ, Lu MC, Chan MW. Association between cytokines and methylation of SOCS-1 in serum of patients with ankylosing spondylitis. Mol Biol Rep. 2014;41(6):3773-3780.
19. Lai NS, Yu HC, Chen HC, Yu CL, Huang HB, Lu MC. Aberrant expression of microRNAs in T cells from patients with ankylosing spondylitis contributes to the immunopathogenesis. Clin Exp Immunol. 2013;173(1):47-57.
20. Toussirot E, Abbas W, Khan KA, et al. Imbalance between HAT and HDAC activities in the PBMCs of patients with ankylosing spondylitis or rheumatoid arthritis and influence of HDAC inhibitors on TNF alpha production. PLoS One . 2013;8(8):e70939.
21. Zhang BY, Chang PY, Zhu QS, Zhu YH, Saijilafu. Decoding epigenetic codes: new frontiers in exploring recovery from spinal cord injury. Neural Regen Res . 2020;15(9):1613-1622.
22. Morris JA, Tsai PC, Joehanes R, et al. Epigenome-wide Association of DNA Methylation in Whole Blood With Bone Mineral Density. J Bone Miner Res . 2017;32(8):1644-1650.
EPIGENETICS
23. Fatema K, Luelling S, Kirkham M, Pavek A, Heyneman AL, Barrott J. Chapter 6: Epigenetics and precision medicine in bone and soft tissue sarcomas. In: García-Giménez JL, ed. Epigenetics in Precision Medicine Academic Press; 2022:147-191.
24. Heijmans BT, Mill J. The seven plagues of epigenetic epidemiology [commentary]. Int J Epidemiol. 2012;41(1):74-78.
25. van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA . 2011;306(9):995-996.
26. Kenney M, Müller R. Of Rats and Women: Narratives of Motherhood in Environmental Epigenetics. In: Meloni M, Cromby J, Fitzgerald D, Lloyd S, eds. The Palgrave Handbook of Biology and Society. Palgrave Macmillan UK; 2018:799-830.
27. Issa TZ, Lambrechts MJ, Canseco JA, et al. Reporting demographics in randomized control trials in spine surgery - we must do better [advance online publication November 17, 2022]. Spine J. doi:10.1016/j.spinee.2022.11.011
28. Housman G, Quillen EE, Stone AC. An evolutionary perspective of DNA methylation patterns in skeletal tissues using a baboon model of osteoarthritis. J Orthop Res . 2021;39(10):2260-2269.
29. Chaves P, Onieva JL, Barragán I. Chapter 7 - Epigenetic biomarkers of disease. In: Tollefsbol TO, ed. Medical Epigenetics. 2nd ed. Academic Press; 2021:117-141.
13 isass.org Winter 2023 Vertebral Columns
Lateral Lumbar Interbody Fusion in the Prone Position:
Where Do the Current Data Stand?

Lateral lumbar interbody fusion (LLIF) is a well-established technique for the surgical treatment of lumbar spine disorders. Lateral interbody approaches have many advantages, as they tend to be muscle-sparing, have high fusion rates, and can correct deformity in both the coronal and sagittal planes. One historical disadvantage of LLIF has been the prolonged operative time required to reposition patients to perform posterior decompression and/or instrumentation.
Single-position lateral lumbar interbody fusion (SP-LLIF), in which both portions of the procedure are performed without repositioning the patient, was developed in order to overcome this disadvantage. Early research has shown the technique to be effective, with multiple studies demonstrating reduction in operative time and length of stay with equivalent clinical outcomes compared to “two-position” LLIF.1,2 Traditional SP-LLIF has historically been performed with the patient in lateral decubitus. This requires posterior instrumentation and/ or decompression to be performed in a relatively unfamiliar position for the spine surgeon. Despite favorable outcome data, this technical disadvantage has limited the adoption of the procedure.
Prone lateral lumbar interbody fusion (P-LLIF) was developed to overcome this disadvantage and allows the surgeon to perform posterior approaches to the spine in a familiar position, while simultaneously allowing access to the anterior column via a retroperitoneal approach. The technique was first reported in the literature in February 2020 by Lamartina and Berjano. 3 In recent years, substantial interest has grown in performing lateral interbody approaches in the prone position. Surgery in the prone position comes with several advantages related to feasibility of performing decompression, revising posterior instrumentation for extension of fusion/pseudoarthrosis, performing posteriorly based osteotomies, and the ability for co-surgeons to perform simultaneous retroperitoneal and posterior surgery. Potential disadvantages associated with the prone position include difficulty in managing complications, technical/ ergonomic challenges in retroperitoneal retractor placement, and the potential for retractor migration during the procedure. Several published case series describe early clinical outcomes with P-LLIF. Lamartina and Berjano’s original article describing the technique contained 7 patients. 3 They reported a mean reduction in Oswestry Dis-
14 isass.org Winter 2023 Vertebral Columns
LUMBAR SPINE
From The CORE Institute in Phoenix, Arizona.
Brandon P. Hirsch, MD
ability Index (ODI) from 48.5 ± 21.0 to 14.6 ± 18.5 at an average postoperative follow-up of 6 months. Back and leg pain visual analog scale (VAS) scores were reduced from 7.7 ± 1.7 to 1.7 ± 2.9 and 8.5 ± 1.2 to 2.7 ± 3.3, respectively. In an 11-patient series, Godzik et al reported similar reductions in ODI (55.1 ± 30.4 to 28.5 ± 18.0) and back pain VAS (6.0 ± 2.3 to 1.6 ± 0.8).4 These data were collected relatively early in the postoperative period at an average follow-up of 2 months. The most recent clinical series of patients undergoing P-LLIF was published by Farber et al and included 28 patients with an average follow-up of 3 months. 5 In this series, ODI was reduced from 25.4 ± 9.0 to 12.3 ± 6.9.
VAS back (7.0 ± 2.9 to 3.3 ± 1.6) and VAS leg (6.2 ± 3.5 to 3.3 ± 3.0) scores also improved, albeit to a lesser extent than in other early case series.
Radiographic outcomes related to segmental and overall lumbar lordosis restoration appear favorable in P-LLIF. Pimenta et al
P-LLIF was developed to overcome the technical disadvantage of SPLLIF, which is traditionally performed in the lateral decubitus position. P-LLIF allows the surgeon to perform posterior approaches to the spine in a familiar position while simultaneously allowing access to the anterior column via a retroperitoneal approach.

reported on a series of 32 patients undergoing single and multilevel procedures. These authors reported an average increase in segmental lordosis from 8.7° to 14.8° postoperatively (P < 0.001).6 A large retrospective multicenter series that included 364 patients reported an average increase in overall lumbar lordosis of 4.8° (preoperative: 45.6°; postoperative: 50°; P < 0.001).
Two recent retrospective analyses have compared radiographic alignments following P-LLIF with that of traditional two-position LLIF.7,8 Walker et al found a greater improvement in segmental (5.1° vs 2.5°; P = 0.02) but not overall lumbar lordosis (6.3° vs 3.1°; P = 0.14) after P-LLIF when compared with two-position LLIF.7 In contrast, Soliman et al’s recent retrospective series found P-LLIF to have significantly greater improvement in overall lumbar lordosis when compared with two-position LLIF (9.9° vs 0.5°; P = 0.047). 8 Changes in segmental lordosis were not reported in this study.
15 isass.org Winter 2023 Vertebral Columns
LUMBAR SPINE
Image: © Clinics in Orthopedic Surgery 2016
LUMBAR SPINE
The complication profile of P-LLIF appears similar to traditional LLIF and includes sensorimotor deficits, psoas hematoma, anterior longitudinal ligament (ALL) rupture, and visceral or vascular injury. In Lamartina and Berjano’s original series of 7 patients, they reported 1 ALL rupture and 1 patient with persistent sensory loss in the thigh more than 3 months after surgery. 3 In Godzik et al’s 11-patient series, 1 patient had urinary retention and 2 patients had postoperative thigh pain that resolved by postoperative day 7.4 Pimenta et al reported 1 psoas hematoma and 4 transient unspecified neurological deficits in their initial series of 32 patients.6 In the 28-patient series by Farber et al, 2 ALL ruptures were reported. 5 Two patients had sensory deficits that persisted beyond 6 weeks. The authors reported 1 patient with an infection and 1 patient who required early return to surgery for direct decompression
References
1. Buckland AJ, Braly BA, O’Malley NA, et al. Lateral decubitus single position anterior posterior surgery improves operative efficiency, improves perioperative putcomes, and maintains radiological outcomes comparable with tradition anterior posterior fusion at minimum 2-year follow-up [advance online publication January 11, 2023]. Spine J. https:// doi.org/10.1016/j.spinee.2023.01.001
2. Keorochana G, Muljadi JA, Kongtharvonskul J. Perioperative and radiographic outcomes between single-position surgery (lateral decubitus) and dual-position surgery for lateral lumbar interbody fusion and percutaneous pedicle screw fixation: meta-analysis. World Neurosurg. 2022;165:e282–e291.
at postoperative day 8. No reports of great vessel or visceral injury exist in the early P-LLIF literature.
P-LLIF is a potentially powerful technique for minimally invasive lumbar fusion that offers advantages related to the familiarity of the prone position and straightforward access to the posterior spine. Early data suggest that the technique is clinically effective, capable of significant restoration of lumbar lordosis, and has a similar complication profile to that of traditional LLIF. Surgeons interested in adopting the technique should be aware that the literature to date includes only retrospective studies and that many authors reported conflicts of interest related to industry. Further prospective studies of P-LLIF are needed to evaluate long-term clinical and radiographic outcomes in comparison to well-established traditional techniques. n
3. Lamartina C, Berjano P. Prone single-position extreme lateral interbody fusion (Pro-XLIF): preliminary results. Eur Spine J. 2020;6–13.
4. Godzik J, Ohiorhenuan IE, Xu DS, et al. Single-position prone lateral approach: cadaveric feasibility study and early clinical experience. Neurosurg Focus . 2020;49:E15.
5. Farber SH, Naeem K, Bhargava M, et al. Single-position prone lateral transpsoas approach: early experience and outcomes. J Neurosurg Spine. 2022;36:358–365.
6. Pimenta L, Amaral R, Taylor W, et al. The prone transpsoas technique: preliminary radiographic results of a multicenter experience. Eur Spine J. 2021;30:108–113.
7. Walker CT, Farber SH, Gandhi S, et al. Single-position prone lateral interbody fusion improves segmental lordosis in lumbar spondylolisthesis. World Neurosurg. 2021;151:e786–e792.
8. Soliman MAR, Khan A, Pollina J. Comparison of prone transpsoas and standard lateral lumbar interbody fusion surgery for degenerative lumbar spine disease: a retrospective radiographic propensity score-matched analysis. World Neurosurg. 2022;157:e11–e21.
16 isass.org Winter 2023 Vertebral Columns
Static vs Expandable Interbody Cages for Minimally Invasive Transforaminal Interbody Fusion

Degenerative lumbar pathologies are common among the aging population and can often lead to pain, disability, and poor quality of life. Specifically, loss of lumbar lordosis (LL) is a common feature, and the literature suggests that restoration of sagittal alignment is associated with the best clinical outcomes. While decompression and stabilization of the spine have served as great surgical options, minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) has proven to be a safe and effective treatment for optimizing sagittal alignment.1 MI-TLIF requires a relatively small surgical corridor to access the disc space posteriorly and, traditionally, large static cages were inserted in the space to correct the sagittal alignment. However, the size of these static cages through the small opening posed a significant risk to injuring nearby nerve roots and violating the endplates.1 Thus, many spine surgeons hesitated to utilize static TLIF cages because of their limited ability to induce proper lordosis without complications.

Expandable TLIF cages were later developed and launched with the hope of optimizing the sagittal alignment dilemma and minimizing risks. 2 Expandable cages were


designed to be inserted in a low-profile, nonexpanded state into the relatively small disc space, and then expanded at the right time to the desired height. 2 The theoretical advantage of an expandable cage was to allow improved restoration of alignment through a small incision without injuring nearby nerve roots. However, it is not entirely clear how effective the cage expansion results are in disc space lordosis and distraction. In this article, we compare the literature regarding reported outcomes of expandable and static TLIF cages.
Static Cages
The first static cages implemented in MI-TLIF were inserted obliquely into the interbody space and have been shown to slightly decrease segmental lordosis (SL) through increased posterior disc height and unchanged anterior disc height. Thus, MI-TLIF with static cages has historically been considered a “kyphogenic” procedure. 3 More recently, static cages have provided
17 isass.org Winter 2023 Vertebral Columns
From the Hospital for Special
in
LUMBAR SPINE
Surgery
New York, New York.
Robert Kamil, BS
Omri Maayan, BS
Sravisht Iyer, MD
Pratyush Shahi, MBBS, MS (Ortho)
additional lordotic correction at the index level through increased anterior disc height at the potential cost of decreased foraminal height. 4 However, static cages have exhibited shortcomings, including an increased risk of pseudoarthrosis, subsidence, nerve root injuries, and lacerations of the dura. 5 Moreover, in a systematic review and meta-analysis by Calvachi-Prieto et al, patients who underwent minimally invasive lumbar fusion with static cages exhibited significantly longer hospital stays and smaller increases in postoperative disc height compared to patients with expandable cages. 6 The use of static cages in MI-TLIF necessitates extensive endplate preparation and testing, which may undermine biomechanical stability. 4
Expandable Cages
To account for the barriers presented by the narrow access corridor and the need to individualize lordotic correction for patients, cages with the capacity for multidirectional expansion were later developed. These cages are inserted into the interbody space in a collapsed, low-profile state prior to in-situ expansion. This design alleviates the possibility of retraction-induced nerve root injury and iatrogenic endplate damage due to decreased trialing and impaction during implantation. The capacity for in-situ expansion enhances the fit of the cage and therefore maximizes disc height, allowing for greater indirect decompression and lordotic correction, all while decreasing operative time.7 However, attempts to achieve optimal disc height via increased expansion
may also induce endplate damage that has the potential to compromise fusion and augment the risk of subsidence. 8 So, while expandable cages may have more power to induce lordosis, restore disc height, and save expenses by decreasing operative time, subsidence and endplate violation may negate any significant gains compared to static cages. Yet, one of the biggest drawbacks of expandable interbody fusion cages may be related to the increased implant cost. Further research will have to show whether the higher implant cost on the front end of a clinical treatment cycle are justified by perioperative cost savings on the back end due to shorter operative time, fewer complications, and fewer reoperations. 9
Comparisons
Many studies in the literature have retrospectively assessed direct comparisons between the two types of cages. One study found that there was a significant reduction in visual analog scale scores, numeric pain rating scale scores, and Oswestry Disability Index scores for both static and expandable cohorts, but the reductions were more pronounced in the expandable cohort. 3 Yet another study did the same assessments and found no statistical difference in the same scores for both cohorts.6 Further studies found significantly greater restoration of foraminal height in expandable cohorts and found that although both anterior/posterior disc height was achieved in both the static and expandable cohorts, the change was greater in the expandable cage cohort. 3,6 Expandable cages offered similar improvements in segmental lordosis
18 isass.org Winter 2023 Vertebral Columns
LUMBAR SPINE
at 6 weeks (static: 1.69° vs expandable: 2.81°; P = 0.243), but segmental lordosis was better maintained with expandable cages leading to significant differences at 1-year follow-up (static: 0.86° vs expandable: 2.45°, P = 0.001). 3 However, one study in patients undergoing single-level TLIF reported no difference in SL or LL improvement at 1 month or 1 year postoperatively between static and expandable cages.2 A separate study found that compared to static cages, expandable cages improve and maintain foraminal dimensions and disc height.8 While expandable cages have shown increased subsidence rates compared to static cages in some studies, others have also reported no difference or a decreased rate.6,7,10
Conclusion
The literature has shown expandable cages to induce good segmental lordosis, lumbar lordosis, disc height, and foraminal height comparable to static cages. Expandable cages have also been shown to reduce operative time and length of stay, but might not be overall cost effective, with rates of subsidence and endplate violations. While the use of expandable interbody devices leads to beneficial changes in the spine, this may not necessarily correlate with superior patient outcomes. As such, patients undergoing MITLIF can expect similar improvements in all patient-reported outcomes whether receiving static or expandable interbody devices. n
References
1. Chang CC, Chou D, Pennicooke B, et al. Long-term radiographic outcomes of expandable versus static cages in transforaminal lumbar interbody fusion [advance online publication November 13, 2020]. J Neurosurg Spine . https:// doi.org/10.3171/2020.6.SPINE191378
2. Yee TJ, Joseph JR, Terman SW, Park P. Expandable vs static cages in transforaminal lumbar interbody fusion: radiographic comparison of segmental and lumbar sagittal angles. Neurosurgery. 2017;81(1):69-74.
3. Woodward J, Koro L, Richards D, Keegan C, Fessler RD, Fessler RG. Expandable versus static transforaminal lumbar interbody fusion cages: 1-year radiographic parameters and patient-reported outcomes. World Neurosurg. 2022;159:e1-e7.
4. Gelfand Y, Benton J, De la Garza-Ramos R, Yanamadala V, Yassari R, Kinon MD. Effect of cage type on short-term radiographic outcomes in transforaminal lumbar interbody fusion. World Neurosurg. 2020;141:e953-e958.
5. Lin GX, Quillo-Olvera J, Jo HJ, et al. Minimally invasive transforaminal lumbar interbody fusion: a comparison study based on end plate subsidence and cystic change in individuals older and younger than 65 years. World Neurosurg. 2017;106:174-184.
6. Calvachi-Prieto P, McAvoy MB, Cerecedo-Lopez CD, et al. Expandable versus static cages in minimally invasive lumbar interbody fusion: a systematic review and meta-analysis. World Neurosurg. 2021;151:e607-e614.
7. Lin GX, Kim JS, Kotheeranurak V, Chen CM, Hu BS, Rui G. Does the application of expandable cages in TLIF provide improved clinical and radiological results compared to static cages? A meta-analysis. Front Surg. 2022;9:949938.
8. Boktor JG, Pockett RD, Verghese N. The expandable transforaminal lumbar interbody fusion—two years follow-up. J Craniovertebr Junction Spine . 2018;9(1):50-55.
9. Lewandrowski KU, Ferrara L, Cheng B. Expandable interbody fusion cages: an editorial on the surgeon’s perspective on recent technological advances and their biomechanical implications. Int J Spine Surg. 2020;14(s3):S56-S62.
10. Armocida D, Pesce A, Cimatti M, Proietti L, Santoro A, Frati A. Minimally invasive transforaminal lumbar interbody fusion using expandable cages: increased risk of late postoperative subsidence without a real improvement of perioperative outcomes: a clinical monocentric study. World Neurosurg. 2021;156:e57-e63.
19 isass.org Winter 2023 Vertebral Columns LUMBAR SPINE
Emerging Management of Obesity in Spine Surgery
The worldwide obesity rate has tripled since 1975, and current trends suggest rates will continue to rise. According to the World Health Organization, as of 2016, 650 million adults were estimated to be categorized as obese, with a body mass index (BMI) of 30 kg/m 2 or greater. Its relevance is front and center, as comorbidities such as type 2 diabetes, hypertension, heart disease, and stroke are among the leading causes of preventable death and are all linked to obesity.1 Furthermore, obesity places a strain on the healthcare system, incurring nearly $190 billion each year in healthcare expenditure. 2
Similarly, low back pain is a common complaint among obese patients and ranks as the fifth most common reason for a medical visit in the United States. 3 As such, obesity has been suggested to play a role in various spine disorders, including symptomatic degenerative disc disease, spondylolisthesis, and spinal stenosis.4 While increased biomechanical loads impart abnormal stresses to the spine, obesity and its correlation to spinal disorders is multifactorial and likely involves a component of chronic inflammation, reduced blood flow, and genetic and environmental factors. Studies have even suggested upregulation of adipokines such
as leptin, which is linked to osteoarthritis, disc degeneration, and radiculopathy. 5
Unfortunately, the literature is fraught with evidence suggesting inferior outcomes following spine surgery in obese patients. Aside from the added complexity of performing spine surgery, obesity has been linked to increased overall cost of surgery, blood loss, operative time, postoperative infections, risk of thromboembolism, narcotic consumption, and all-cause mortality.6–12 Minimally invasive techniques can often mitigate some of these risks, thus allowing obese patients to still benefit from spine surgery.13
Preoperative Optimization
Obesity is clearly a keystone surrogate for overall patient health and links to various comorbidities as previously mentioned. It is no surprise, therefore, that preoperative weight loss can significantly improve outcomes and reduce the risk of complications after surgery; thus, it should be at the forefront of preoperative optimization.14 Surgeons will often offer recommendations for weight loss leading up to surgery, such as providing online and in-print educational materials or recommending weight loss diets, but they are rarely successful in achieving meaningful weight reduction.15,16

20 isass.org Winter 2023 Vertebral Columns
From Rush University Medical Center in Chicago, Illinois.
PATIENT OUTCOMES
Arash J. Sayari, MD
More aggressive means of weight loss, such as bariatric surgery, have been well-studied in the literature. In patients with a BMI >30 kg/m 2 who are appropriate candidates, bariatric surgery has demonstrated cost effectiveness in patients undergoing elective spinal fusion.17 A meta-analysis of 183,570 obese patients undergoing elective spine surgery demonstrated a significant reduction in gastrointestinal, renal, neurologic, and thromboembolic complications, as well as all-cause mortality,18 though the risk of complications is still higher than in patients with a normal BMI.19
Emerging Medical Management
While weight loss undeniably can reduce the risks of postoperative complications, it may also improve axial low back pain and radiculopathy. 5 However, there are fewer published data evaluating the timeline in which rapid weight loss occurs. A database study by Rudy et al of 39,742 obese patients undergoing lumbar fusion evaluated a cohort of patients who had rapid weight loss leading up to surgery. The authors noted a significant increase in length of stay, surgical site infections, thromboembolism, and the need for transfusion. 20
While the study is intriguing, Rudy et al failed to evaluate the means of weight loss. Historically, bariatric surgery and incidental side effects from various medications were the only means of rapid weight loss. However, there has been a recent uptick in medications approved for weight loss, which may play a significant role in spinal surgery.
Saxenda (liraglutide) was the first medication approved by the US Food and Drug Administration (FDA) in December 2014 for the treatment of weight loss. However, its adoption was not widespread and there was stigma surrounding a medication solely approved for weight loss. Three years later, the FDA approved Novo Nordisk’s once-weekly Ozempic (semaglutide) for type 2 diabetes. During its use, increasing data began to suggest prolonged and maintained weight loss after initiation of therapy. A randomized controlled trial published in the New England Journal of Medicine evaluated 2.4 mg of semaglutide administered once-weekly in 1,961 patients and found an average weight loss of 15.3 kg at 68 weeks with only mild side effects. 21 Additional data supported using a similar dosage as well as a lower dosage of 1.7 mg weekly. Finally, a randomized controlled trial comparing liraglutide and semaglutide found the latter to be safe and effective in treating weight loss. 22
GLP-1 (glucagon-like peptide-1) is a hormone that is naturally produced by the body to regulate blood sugar levels. It works by stimulating the release of insulin and slowing down the rate at which food is emptied from the stomach. GLP-1 receptor agonists (GLP-1 RAs), like semaglutide, mimic the effects of GLP-1 by binding to GLP-1 receptors in the body and activating them.
Since its adoption, the use of semaglutide has skyrocketed, especially following public appraisal by billionaires such as Elon Musk. This “celebrity” medication quickly
21 isass.org Winter 2023 Vertebral Columns
PATIENT OUTCOMES
PATIENT OUTCOMES
made headlines and filled the homes of the public, raising controversy while creating a nationwide shortage. Therefore, variations in semaglutide and other GLP-1 RAs have flooded the FDA-approval queue. Wegovy (semaglutide) became the next medication approved by the FDA on June 4, 2021, with an indication for weight loss in both adults and adolescents older than 12 years. 23 The most recently approved medication, Mounjaro (tirzepatide, Eli Lilly), received accelerated approval on May 13, 2022, but it is being sold at a higher overall cost. In various clinical trials, tirzepatide was found to delay gastric emptying, lower fasting and postprandial glucose concentration, decrease food intake, and reduce body weight in patients with type 2 diabetes. Furthermore, tirzepatide was noninferior and superior to semaglutide at all doses. 24
Other classes of medications, such as sodium-glucose co-transporter 2 inhibitors, including canagliflozin, dapagliflozin, and empagliflozin, have been evaluated for their use in weight loss, though their effectiveness has not demonstrated to reach that of the GLP-1 RAs. 25
With literature reviews suggesting about 15% weight reduction at 1 year, 26,27 GLP-1 RAs may be a more effective alternative than bariatric surgery. Bariatric surgery induces a weight loss in the range of 5% to 16%, which can get as high as 30% of total body weight after 5 years. 28 However, such surgical interventions are fraught with complications and there is a long period of recovery, even with enhanced protocols. 24,29
This may preclude surgical intervention of the spine for months to years, furthering patients’ disability from spinal pathology. GLP-1 RAs have yet to be evaluated in patients undergoing spine surgery. However, with their increased use, providers will not only see more patients who are actively on these medications, they may be formulating algorithms and plans to initiate GLP-1 RA therapy leading up to surgery. In many cases, busy spine surgeons may have a lead time of weeks to months before a patient is scheduled to undergo surgery. In obese patients with comorbidities, a multidisciplinary approach to patient care improves postsurgical outcomes. Therefore, is it feasible to have patients visit their internist and/or endocrinologist to initiate medical management of obesity with a GLP-1 RA to not only begin weight loss leading up to surgery, but also improve the overall long-term health status of each patient, improving outcomes.
Additional Considerations
Overall, obesity is a complex, multifactorial medical condition associated with various comorbidities that are linked to poorer outcomes following spine surgery. As rates of obesity continue to rise, there may be a role for medical management over surgical management of obesity, both leading up to and following spine surgery. With appropriate patient education and intervention, we may be able to care for this patient population more expeditiously without compromising outcomes following spine surgery. n
22 isass.org Winter 2023 Vertebral Columns
PATIENT OUTCOMES
References
1. Smith KB, Smith MS. Obesity statistics. Prim Care . 2016;43(1):121-135, ix.
2. Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31(1):219-230.
3. Joseph JR, Farooqui Z, Smith BW, et al. Does clinical improvement of symptomatic degenerative lumbar disease impact obesity? J Neurosurg Spine . 2017;26(6):705-708.
4. Onyekwelu I, Glassman SD, Asher AL, Shaffrey CI, Mummaneni PV, Carreon LY. Impact of obesity on complications and outcomes: a comparison of fusion and nonfusion lumbar spine surgery. J Neurosurg Spine . 2017;26(2):158-162.
5. Jackson KL 2nd, Devine JG. The effects of obesity on spine surgery: a systematic review of the literature. Global Spine J. 2016;6(4):394-400.
6. Rihn JA, Radcliff K, Hilibrand AS, et al. Does obesity affect outcomes of treatment for lumbar stenosis and degenerative spondylolisthesis? Analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine . 2012;37(23):1933-1946.
7. Marquez-Lara A, Nandyala SV, Sankaranarayanan S, Noureldin M, Singh K. Body mass index as a predictor of complications and mortality after lumbar spine surgery. Spine . 2014;39(10):798-804.
8. Buerba RA, Fu MC, Gruskay JA, Long WD 3rd, Grauer JN. Obese Class III patients at significantly greater risk of multiple complications after lumbar surgery: an analysis of 10,387 patients in the ACS NSQIP database. Spine J. 2014;14(9):2008-2018.
9. Patel N, Bagan B, Vadera S, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine . 2007;6(4):291-297.
10. LeRoy TE, Moon AS, Gedman M, Aidlen JP, Rogerson A. Impact of body mass index on opioid consumption in lumbar spine fusion surgery. Spine J. 2021;6:100060.
11. Flippin M, Harris J, Paxton EW, et al. Effect of body mass index on patient outcomes of surgical intervention for the lumbar spine. J Spine Surg. 2017;3(3):349-357.
12. Seicean A, Alan N, Seicean S, et al. Impact of increased body mass index on outcomes of elective spinal surgery. Spine . 2014;39(18):1520-1530.
13. Cofano F, Perna GD, Bongiovanni D, et al. Obesity and spine surgery: a qualitative review about outcomes and complications. Is it time for new perspectives on future researches? Global Spine J. 2022;12(6):1214-1230.
14. Dowsey MM, Brown WA, Cochrane A, Burton PR, Liew D, Choong PF. Effect of bariatric surgery on risk of complications after total knee arthroplasty: a randomized clinical trial. JAMA Netw Open. 2022;5(4):e226722.
15. Lui M, Jones CA, Westby MD. Effect of non-surgical, non-pharmacological weight loss interventions in patients who are obese prior to hip and knee arthroplasty surgery: a rapid review. Syst Rev. 2015;4:121.
16. Pavlovic N, Boland RA, Brady B, et al. Effect of weight-loss diets prior to elective surgery on postoperative outcomes in obesity: a systematic review and meta-analysis. Clin Obes. 2021;11(6):e12485.
17. Paranjape CS, Gentry RD, Regan CM. Cost-effectiveness of bariatric surgery prior to posterior lumbar decompression and fusion in an obese population with degenerative spondylolisthesis. Spine . 2021;46(14):950-957.
18. Alhammoud A, Dalal S, Sheha ED, et al. The impact of prior bariatric surgery on outcomes after spine surgery: a systematic review and meta-analysis. Global Spine J. 2022;12(8):1872-1880.
19. Jain D, Berven SH, Carter J, Zhang AL, Deviren V. Bariatric surgery before elective posterior lumbar fusion is associated with reduced medical complications and infection. Spine J. 2018;18(9):15261532. doi:10.1016/j.spinee.2018.01.023
20. Rudy HL, Cho W, Oster BA, Tarpada SP, Moran-Atkin E. Rapid bodyweight reduction before lumbar fusion surgery increased postoperative complications. Asian Spine J. 2020;14(5):613-620.
21. Wilding JPH, Batterham RL, Calanna S, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384(11):989-1002.
22. O’Neil PM, Birkenfeld AL, McGowan B, et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet . 2018;392(10148):637-649.
23. Singh G, Krauthamer M, Bjalme-Evans M. Wegovy (semaglutide): a new weight loss drug for chronic weight management. J Investig Med. 2022;70(1):5-13.
24. Małczak P, Pisarska M, Piotr M, Wysocki M, Budzyński A, Pędziwiatr M. Enhanced recovery after bariatric surgery: systematic review and meta-analysis. Obes Surg. 2017;27(1):226-235.
25. Katsiki N, Dimitriadis G, Hahalis G, et al. Sodium-glucose co-transporter-2 inhibitors (SGLT2i) use and risk of amputation: an expert panel overview of the evidence. Metabolism. 2019;96:92-100.
26. Ojeniran M, Dube B, Paige A, Ton J, Lindblad AJ. Semaglutide for weight loss. Can Fam Physician. 2021;67(11):842.
27. Ghusn W, De la Rosa A, Sacoto D, et al. Weight loss outcomes associated with semaglutide treatment for patients with overweight or obesity. JAMA Netw Open. 2022;5(9):e2231982.
28. Wolfe BM, Kvach E, Eckel RH. Treatment of Obesity: Weight Loss and Bariatric Surgery. Circ Res . 2016;118(11):1844-1855.
29. Proczko M, Kaska L, Twardowski P, Stepaniak P. Implementing enhanced recovery after bariatric surgery protocol: a retrospective study. J Anesth. 2016;30(1):170-173.
23 isass.org Winter 2023 Vertebral Columns
The Use of Radiolucent Technology in Spine Tumors


Instrumentation is often used to stabilize the spine after resection of a spine tumor. Titanium is the most commonly used material for spine instrumentation because of its favorable modulus of elasticity, increased ability to bond with bone compared to other implant materials, and magnetic resonance imaging (MRI) compatibility. However, there are potential negatives with using titanium implants in patients with spine tumors. Titanium can create artifact and obscure or degrade the quality of MRIs, increasing the difficulty in evaluating patients for tumor recurrence. Titanium also creates radiation shielding from adjuvant radiotherapy treatments.1 Thus, it would be beneficial to identify a material lacking such limitations while maintaining spinal stability after implantation.
Polyetheretherketone (PEEK) cages have some advantages over titanium in tumor patients. Some benefits of PEEK cages include a modulus of elasticity more similar to cortical bone, less artifact on MRI, and less radiation shielding (Figure 1).1 Some studies have shown good results with PEEK and other carbon-based implants. Potential negatives of carbon-based implants may include potential difficulty visualizing screw placement on fluoroscopy and the inability to bend the
rods intraoperatively. The carbon-based pedicle screws are also more costly when compared to regular titanium pedicle screws. In a cohort study of 34 patients with operable spine tumors, Boriani et al examined the use of carbon fiber-reinforced PEEK implants. In this study, the authors noted that one intraoperative screw breakage occurred out of 232 implanted screws, and only two incidences of sacral screw loosening were found at long-term follow-up. However, 6 local recurrences were discovered, benefited by lack of implant artifact on follow-up imaging. Also, radiation oncologists reported better treatment planning on CT and lacking of scattering effect during the treatment. 2
Carbon fiber–reinforced cages have also been shown to have favorable results when used with spine tumors (Figure 2). In a separate study by Boriani et al, the authors evaluated the efficacy of carbon fiber reinforced PEEK cages in 42 patients with spine tumors. 3 At 24 months, 80% of the patients had radiographic evidence of a solid fusion and the remainder had probable fusions. There were no complications related to the carbon fiber–reinforced PEEK cages.
Biomechanical studies have been performed on PEEK and carbon fiber–reinforced implants. In a cadaveric study by Bruner et al., the authors performed biomechanical testing on titanium, PEEK, and carbon fiber–
24 isass.org Winter 2023 Vertebral Columns
INSTRUMENTATION
From UCI Health in Orange County, California (Dr. Lee) and Kaiser Permanente, Orange County in Anaheim, California (Dr. Hariri).
Yu-Po Lee, MD
Omid Hariri, DO
reinforced PEEK rods.4 All 3 constructs significantly limited range of motion in all planes in the destabilized cadaver spine except in axial rotation. All of the rods similarly restricted motion in all planes, except axial rotation (P < 0.05). In combined loading, rod stiffness was similar for each material. Rod strain was least in the titanium construct, intermediate in the carbon fiber reinforced PEEK construct, and maximal in the pure PEEK construct.
The radiolucency and lack of radiation shielding of PEEK and carbon fiber–reinforced implants have potentially large benefits for patients with spine tumors. More studies are needed to further evaluate the efficacy of these implants; however, initial data support the use of these implants in spine tumor patients. n


References
1. Ringel F, Ryang YM, Kirschke JS, et al. Radiolucent carbon fiber-reinforced pedicle screws for treatment of spinal tumors: advantages for radiation planning and follow-up imaging. World Neurosurg. 2017;105:294-301.
2. Boriani S, Tedesco G, Ming L, et al. Carbon-fiber-reinforced PEEK fixation system in the treatment of spine tumors: a preliminary report. Eur Spine J. 2018;27(4):874-881.
3. Boriani S, Bandiera S, Biagini R, De Iure F, Giunti A. The use of the carbon-fiber reinforced modular implant for the reconstruction of the anterior column of the spine. A clinical and experimental study conducted on 42 cases. Chir Organi Mov. 2000;85(4):309-335.
4. Bruner
N,
DJ,
Biomechanics of polyaryletherketone rod composites and titanium rods for posterior lumbosacral instrumentation. Presented at the 2010 Joint Spine Section Meeting. Laboratory investigation. J Neurosurg Spine . 2010;13(6):766-772.
25 isass.org Winter 2023 Vertebral Columns
INSTRUMENTATION
HJ, Guan Y, Yoganandan
Pintar FA, Maiman
Slivka MA.
Figure 1. Sagittal and axial MRI showing T6-T10 pedicle screw fixation with carbon fiber–reinforced PEEK pedicle screws for a T8 metastatic thyroid lesion with kyphoplasty at T8.
The radiolucency and lack of radiation shielding of PEEK and carbon fiber–reinforced implants have potentially large benefits for patients with spine tumors.
Figure 2 Sagittal and axial MRI showing pedicle screw fixation with carbon-fiber-reinforced pedicle screw for an extracavitary sarcoma for spinal cord compression.
From the Hospital for Special Surgery in New York, New York.
Robotic Spine Surgery:


Current State and Future Outlook
Minimally invasive spine surgery (MISS) is associated with inadequate visualization and palpation of anatomical landmarks and hence is reliant upon intraoperative imaging.1 Traditional fluoroscopy has been associated with high radiation exposure and low pedicle screw accuracy, resulting in the evolution of newer imaging modalities such as navigation and robotics over the past 2 decades. 2 Spinal robots were initially marred by limitations of lack of real-time visual feedback, difficulty with instrument localization, and unreliable depth gauging. However, with advancements of integrated 3-dimensional (3D) navigation, real-time visual feedback, better accuracy of registration, features to mitigate skiving, and rigid end-effectors, robotic platforms in spine surgery have seen a resurgence and are increasingly being adopted. 3 Recent studies have shown that the use of robotics in spine surgery leads to a decrease in intraoperative radiation exposure and an increase in pedicle screw accuracy.4,5 Although robotic platforms are mostly used for placing pedicle screws, they are now also being used for decompression, disc space preparation, and interbody placement. 3 This article aims to provide an overview of the emergence of
robotics in spine surgery, the current platforms being used, and the possible future advancements.


Current Stance: Where Are We at Present?
The current field of spine surgery is prospering with advancements in robotic techniques. Robotics in spine surgery has shown superior safety in various aspects of pedicle screw placement in spinal surgery. According to a recent meta-analysis,6 robotic navigation was found to have 2.3 times greater accuracy than conventional freehand techniques. Additionally, robotic screw placement was ranked as the most effective technique in terms of optimal placement, thereby reducing overall implant-related complications. 6 Before the advent of robotics and navigation technologies, patients, surgeons, and operating room personnel were frequently exposed to high doses of intraoperative radiation to attain technical safety.7 However, robotic navigation has the potential to reduce radiation exposure as well as provide high levels of safety during MISS. The skin-anchored spinal navigation system reduced intraoperative radiation exposure from 63.1 mGy with fluoroscopy to 28.3 mGy during a minimally invasive transforaminal

26 isass.org Winter 2023 Vertebral Columns
ROBOTICS
Nishtha Singh, MBBS
Tomoyuki Asada, MD
Sumedha Singh, MBBS, MD
Pratyush Shahi, MBBS, MS (Ortho)
Sheeraz Qureshi, MD, MBA
lumbar interbody fusion. 8 Furthermore, a more recent study demonstrated that even when compared to skin-anchored navigation, robotic screw placement appears to be secure and efficient at reducing fluoroscopy time.4 This technique has thus opened the possibility of performing MISS with reduced radiation exposure.
Currently, the U.S. Food and Drug Administration (FDA) has approved 5 robotic platforms for spinal surgery3: (1) Mazor X (Medtronic Spine, Memphis, TN, USA, approved in 2016) with Stealth Navigation (Medtronic Navigation Louisville, CO, USA), (2) ExcelsiusGPS (Globus Medical, Inc., Audubon, PA, USA, approved in 2017), (3) ROSA Spine (Zimmer Biomet, Montpellier, France, approved in 2019), (4) TiRobot (TINAVI Medical Technologies, Beijing, China, approved in 2020), and (5) Cirq with Loop-X (Brainlab, Munich, Germany, approved in 2021). Despite the benefits of increasing pedicle screw accuracy and reducing radiation exposure, these platforms share some drawbacks as well. One of the major issues is cost-effectiveness and affordability. Often, high installation costs, lack of affordability, and insufficient evidence make it difficult to justify the use of this technology. However, a study focusing on economic factors found that robotic spine surgery may be cost-effective based on factors such as a lower revision surgery rate, shorter hospital stays, and shorter operative times. 9 Additionally, robotics in spine surgery is not free from surgical pitfalls, wherein a technical guide might be required for all surgeons.10 Lack of haptic feedback and thereby skiving is a common issue when using navi-
gation-guided drills during surgery. This may require a learning curve to achieve a high level of safety even in robotic spine surgery. Previous research has suggested that it may take approximately 20 cases for a surgeon to become proficient in robotic spine surgery.11,12 To address the learning curve and improve safety, some platforms have added features such as an end effector that can detect excessive lateral forces generated by instrument skiving. Although newer robotic platforms are being developed to address the technical and economic challenges of current systems, they are still lacking sufficient clinical evidence. More platforms are expected to become available offering improved performance and cost-effectiveness. This opens the realm of future clinical studies in this ever-changing field of hardware and software.
Visionary Imagination: How the Future Unfolds?
The past few years have been instrumental in shaping the present and future of robotic spine surgery. Envisioning the successful use of robotics in spine will require a high volume of evidence-based studies reporting improved patient outcomes, patient satisfaction, surgeon expertise, and cost-effectiveness in the long run. 2,3 In addition, robust studies reporting reduced complications, morbidity, radiation, carbon footprint, and operative time are needed. 20
In the future, it is essential to explore the safety and efficiency of robotics in applications other than pedicle screw placement. The application of robotic technology in surgeries of decompression, decortication, rod place-
27 isass.org Winter 2023 Vertebral Columns
ROBOTICS
ment, deformity correction, and vertebral tumor resection is anticipated in the next few years.14 Although in infancy, the new idea suggests modification of the robotic software to include vertebral tumor classification systems to help with precise tumor resection, in turn helping with the reconstruction of the fibrosed parts following chemotherapy.15 Similarly, robotic-guided endoscopic spine surgery is an upcoming technology that requires higher quality evidence regarding puncture accuracy and fluoroscopy time.13 Hence, the future goal will be to tap into the potential of robotic navigation in treating a wide range of pathologies of spine.15
Furthermore, additional evidence and research are required in the field of ergonomic efficacy and efficiency of robotics in the spine, especially cervical, thoracic, and craniovertebral junction surgical procedures.20 Recently, Ueda et al have addressed the problem of autonomous collision in robotic spine surgery while working in closed spaces. Additionally, robotic surgery comes with the drawback of indirect visualization and a limited degree of freedom, which might pose a hazard in the field of MISS when the working spaces are narrow and deep. This often results in inevitable collision between the long arms of the robot with other instruments or soft tissues. With continued efforts and work on the robotic simulator and software, autonomous collisions can be avoided in the future using virtual fixtures and a well-thought artificial trajectory.19
In addition, the incorporation of virtual reality and augmented reality (AR) is expected to improve the learning curve and overall
performance of surgeons in training.17 The new school of thought builds on the idea of a semi-independent robot along with a wearable AR headset where a spine surgeon can visualize screw trajectories, review imaging, and operate with voice commands.18 One essential aspect of AR is projection overlay, which might be able to track the position and orientation of the operating field and personnel. This in turn will construct an accurate 3D picture and build communication between the operating surgeon and the machine. With the progress of digital optics, spatial measurements can be projected in the operation field along with the overlaying of high-resolution operative images. Hence, this will lend a helping hand to the surgeon performing spine surgery.16 Similarly, the addition of sensor gloves while operating with robotic spine surgery will help with natural hand motions and improved maneuverability, leading to a better sensory experience. Akin to this, the implementation of tactile stimulation can assist with outof-sight collisions. For the development of better haptic feedback, it is quintessential to improve the proprioception component of robotic navigation along with integration into the software to prevent any time lag in making decisions while performing life-saving procedures.18
The inclusion of artificial intelligence and the Internet of Skills in the field of robotics can revolutionize the way spine surgery is performed. With the combination of portability and machine learning, the Internet of Skills has the potential to utilize 5G connectivity with low latency in predicting surgical movements and allowing a surgeon to operate
28 isass.org Winter 2023 Vertebral Columns
ROBOTICS
remotely with precision.16 This will also help with real-time feedback to the surgeon when there is some evidence of deflection from a preplanned trajectory in a surgical procedure.
Conclusion
In a constant attempt to improve techniques in spine surgery, human efforts in the future will strive to achieve maximum precision along with high-functioning software in ro -
References
1. Virk S, Qureshi S. Navigation in minimally invasive spine surgery. J Spine Surg. 2019;5(S1):S25-S30.
2. Vaishnav AS, Othman YA, Virk SS, Gang CH, Qureshi SA. Current state of minimally invasive spine surgery. J Spine Surg. 2019;5(S1):S2-S10.
3. Kiran Alluri R, Sivaganesan A, Vaishnav AS, Qureshi SA. Robotic guided minimally invasive spine surgery. In: Perez-Cruet M, ed. Minimally Invasive Spine Surgery: Advances and Innovations. IntechOpen; 2022. Accessed January 11, 2023. http://dx.doi. org/10.5772/intechopen.97599
4. Shahi P, Vaishnav A, Araghi K, et al. Robotics reduces radiation exposure in minimally invasive lumbar fusion compared with navigation. Spine. 2022;47(18):1279-1286.
5. Fan Y, Du JP, Liu JJ, et al. Accuracy of pedicle screw placement comparing robot-assisted technology and the free-hand with fluoroscopy-guided method in spine surgery. Medicine. 2018;97(22):e10970.
6. Naik A, Smith AD, Shaffer A, et al. Evaluating robotic pedicle screw placement against conventional modalities: a systematic review and network meta-analysis. Neurosurg Focus. 2022;52(1):E10.
7. Rampersaud YR, Foley KT, Shen AC, Williams S, Solomito M. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine. 2000;25(20):2637-2645.
botic systems. Though our imagination can uncover only a part of future innovation in robotics, what matters the most is our relentless dedication to providing our patients with the best surgical treatment for all their needs. Hence, the futuristic model of robotics in spine surgery will comprise the current elements with a paradigm shift toward more independent, affordable, accessible, and optimizable software and machines. n
8. Vaishnav AS, Merrill RK, Sandhu H, et al. A review of techniques, time demand, radiation exposure, and outcomes of skin-anchored intraoperative 3D navigation in minimally invasive lumbar spinal surgery. Spine. 2020;45(8):E465-E476.
9. Menger RP, Savardekar AR, Farokhi F, Sin A. A cost-effectiveness analysis of the integration of robotic spine technology in spine surgery. Neurospine. 2018;15(3):216-224.
10. Torii Y, Ueno J, Iinuma M, Yoshida A, Niki H, Akazawa T. Accuracy of robotic-assisted pedicle screw placement comparing junior surgeons with expert surgeons: can junior surgeons place pedicle screws as accurately as expert surgeons? [advance online publication July 18, 2022]. J Orthop Sci. https:// doi.org/10.1016/j.jos.2022.06.012
11. Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res. 2014;472(6):1839-1844.
12. Khan A, Meyers JE, Siasios I, Pollina J. Next-generation robotic spine surgery: first report on feasibility, safety, and learning curve. Oper Neurosurg. 2018;17(1):61-69.
13. Liounakos JI, Basil GW, Urakawa H, Wang MY. Intraoperative image guidance for endoscopic spine surgery. Ann Transl Med. 2021;9(1):92.
14. Shafi KA, Pompeu YA, Vaishnav AS, et al. Does robot-assisted navigation influence pedicle screw selection and accuracy in minimally invasive spine surgery? Neurosurg Focus. 2022;52(1):E4.
15. Perfetti DC, Kisinde S, Rogers-LaVanne MP, Satin AM, Lieberman IH. Robotic spine surgery: past, present, and future. Spine. 2022;47(13):909-921.
16. D’Souza M, Gendreau J, Feng A, Kim LH, Ho AL, Veeravagu A. Robotic-assisted spine surgery: history, efficacy, cost, and future trends. Robot Surg. 2019;6:9-23.
17. Yoon JW, Chen RE, Kim EJ, et al. Augmented reality for the surgeon: systematic review. Int J Med Robot. 2018;14(4):e1914.
18. Madhavan K, Kolcun JPG, Chieng LO, Wang MY. Augmented-reality integrated robotics in neurosurgery: are we there yet? Neurosurgl Focus. 2017;42(5):E3.
19. Ueda H, Suzuki R, Nakazawa A, et al. Toward autonomous collision avoidance for robotic neurosurgery in deep and narrow spaces in the brain. Procedia CIRP. 2017;65:110-114.
20. Huang M, Tetreault TA, Vaishnav A, York PJ, Staub BN. The current state of navigation in robotic spine surgery. Annal Transl Med. 9(1):86-86.
29 isass.org Winter 2023 Vertebral Columns ROBOTICS
Surgical Simulation in Spine Surgery

Spine surgery is constantly evolving due to advancements in surgical techniques, such as minimally invasive surgery, and technological improvements, such as the advent of computer-assisted and robot-assisted navigation. Such advancements, in combination with the complex anatomy of the spine and the proximity of the spine to major neurovascular structures, makes mastering the many spine surgical techniques of utmost importance.1 Commonly used techniques such as anatomic placement of pedicle screws, if performed poorly, can have devastating consequences for patients. 2 A steep learning curve of at least 60-80 pedicle screws and 25 cases have been reported for spine surgery fellows to accurately place freehand pedicle screws in traditional open procedures. 3,4 Placing screws in a minimally invasive manner adds an additional layer of complexity and increases the learning curve. 5 The current method of spine surgical training through mentorship is effective but limited by the ever-changing nature of the field, short duration of residency and fellowship training, and workplace duty-hour restrictions. 2 Surgical simulation can supplement traditional surgical training and increase efficiency and performance in the operating
room while decreasing complications and errors.1,6 Surgical simulation with the use of cadaveric models, synthetic models, and virtual and mixed reality simulators have been used in spine surgery.1,2 Cadaveric models, especially fresh frozen cadavers, are the most realistic surgical simulation model because they most closely represent normal human tissue and haptics, as well as the normal relationships of the spine with adjacent neurovascular structures.1,2 They can be used to create a surgical experience similar to a real operating room. A team-based cadaveric training model has been shown to increase resident confidence in their surgical ability, understanding of anatomy, and satisfaction with training.1,7 It has also been shown to be more helpful than sawbones, web-based, or virtual-based training programs.7 Similarly, cadaveric models have been used to teach pedicle screw placement. A study comparing accuracy of thoracic pedicle screw placement by residents demonstrated an improvement in accuracy from 44% to 58% between 2 resident cadaver training sessions that were supplemented with didactics. 8 Despite these benefits, the use of cadaveric models is limited by the high cost and availability of cadavers, the costs of maintaining a cadaver laboratory, as well as the deterioration of tissues and differences in tissue quality. 9

30 isass.org Winter 2023 Vertebral Columns
SURGICAL TRAINING
From Rush University Medical Center in Chicago, Illinois.
Karan S. Patel, MD
Gregory D. Lopez, MD
Synthetic models, such as sawbones, plastic, or synthetic bone models, are an alternative to cadaveric models because of their low cost and wide availability.1 The low cost and availability of such models, especially sawbones, is offset by the lack of realistic anatomy and soft tissues. While sawbones can be used to teach anatomy and instrumentation, the haptic feedback necessary to mimic bone is lacking in such models. 9 Improvements in synthetic technology have enabled the creation of advanced spine models with synthetic skin, muscle, dura, and cerebrospinal fluid.10 Such models, can allow for a more realistic simulation when performing a variety of different techniques.10
Virtual reality simulators utilize computer software to create a 3-dimensional (3D) surgical environment. They can allow anatomy to be visualized in 3D and certain surgical techniques to be visualized and practiced without requiring cadavers or a surgical laboratory.1,11 Unlike cadaveric and

synthetic models, these simulators can be used repeatedly by multiple trainees. Whether repeated use can justify the cost of these simulators and their upkeep is still unknown. Virtual reality simulators can also be used to track a trainee’s progress and accuracy, and, depending on the program, they can be adjusted to a trainee’s level of training and ability.11 Multiple studies have reported on the use of virtual reality simulation in spine surgery. A systematic review of 19 articles that used virtual reality simulation to teach spine techniques such as pedicle screw placement, reported that despite variability in study designs, all studies reported that participants in the stimulator group outperformed those in the non-simulator group with respect to knowledge and skill. The impact of such simulators on trainee behaviors and any correlation to patient outcomes have not been studied.11
Mixed and augmented reality simulators combine virtual reality with synthetic or ca-
31 isass.org Winter 2023 Vertebral Columns
TRAINING
SURGICAL
SURGICAL TRAINING
daveric models to add an aspect of physical reality.11 Such simulators allow trainees to visualize 3D anatomy and experience haptic feedback simulataneously.10 A study of 15 orthopedic and neurosurgical trainees who were enrolled in a standardized curriculum consisting of lectures followed by two sessions on a mixed virtual reality and synthetic spine model reported improvements in resident proficiency and time with pedicle screw placement.12 Mixed reality models can also utilize computer-assisted navigation technology to stimulate spine surgery. A simulation training study for lateral mass cervical screw placement by 15 orthopedic residents reported that the addition of 3D computer-assisted navigation to cadaver and sawbones use improved accuracy in screw placement compared to groups that utilized
References
1. Wang Z, Shen J. Simulation training in spine surgery. J Am Acad Orthop Surg. 2022;30(9):400-408.
2. Sayari AJ, Chen O, Harada GK, Lopez GD. Success of surgical simulation in orthopedic training and applications in spine surgery. Clin Spine Surg. 2021;34(3):82-86.
3. Gonzalvo A, Fitt G, Liew S, et al. The learning curve of pedicle screw placement: how many screws are enough? Spine (Phila Pa 1976). 2009;34(21):E761-765.
4. Gang C, Haibo L, Fancai L, Weishan C, Qixin C. Learning curve of thoracic pedicle screw placement using the free-hand technique in scoliosis: how many screws needed for an apprentice? Eur Spine J. 2012;21(6):1151-1156.
5. Sharif S, Afsar A. Learning curve and minimally invasive spine surgery. World Neurosurg. 2018;119:472-478.
cadavers alone.13 Such studies suggest that mixed reality stimulators can improve resident technical skills by combining 3D or navigation imaging with physical models.
Spine simulators can be utilized to supplement spine training in residency and fellowship programs. They can allow for various techniques and procedures to be practiced and performed in a safe environment. While many different simulators exist, ranging from synthetic and cadaveric models to mixed reality models, they all have their benefits and limitations. An ideal spine simulator would be one that is low cost, easy to use, and replicable; would be able to monitor a trainee’s progress; and would provide accurate anatomic and haptic feedback. Such a simulator would greatly augment spine training and education. n
6. Satava RM. The revolution in medical education—the role of simulation. J Grad Med Educ . 2009;1(2):172-175.
7. Calio BP, Kepler CK, Koerner JD, Rihn JA, Millhouse P, Radcliff KE. Outcome of a resident spine surgical skills training program. Clin Spine Surg. 2017;30(8):E1126-E1129.
8. Tortolani PJ, Moatz BW, Parks BG, Cunningham BW, Sefter J, Kretzer RM. Cadaver training module for teaching thoracic pedicle screw placement to residents. Orthopedics . 2013;36(9):e1128-1133.
9. Atesok K, Mabrey JD, Jazrawi LM, Egol KA. Surgical simulation in orthopaedic skills training. J Am Acad Orthop Surg. 2012;20(7):410-422.
10. Coelho G, Defino HLA. The role of mixed reality simulation for surgical training in spine: phase 1 validation. Spine (Phila Pa 1976). 2018;43(22):1609-1616.
11. Pfandler M, Lazarovici M, Stefan P, Wucherer P, Weigl M. Virtual reality-based simulators for spine surgery: a systematic review. Spine J. 2017;17(9):1352-1363.
12. Gardeck AM, Pu X, Yang Q, Polly DW, Jones KE. The effect of simulation training on resident proficiency in thoracolumbar pedicle screw placement using computer-assisted navigation. J Neurosurg Spine . 2020:1-8.
13. Gottschalk MB, Yoon ST, Park DK, Rhee JM, Mitchell PM. Surgical training using three-dimensional simulation in placement of cervical lateral mass screws: a blinded randomized control trial. Spine J. 2015;15(1):168-175.
32 isass.org Winter 2023 Vertebral Columns