CPD: Overactive Bladder Continuing Professional Development
CPD 60 Second Summary Overactive bladder (OAB) is a common chronic condition associated with voiding dysfunction. The underlying OAB pathophysiology is overactivity of the detrusor muscle, which is a smooth muscle found in the wall of the bladder that contracts during urination. Because urinary urgency and incontinence symptoms can be difficult to objectively characterise for research and clinical purposes, many studies of OAB treatments have used other measures (number of daily micturitions or incontinence episodes) to enable quantification of treatment response. Often, patients have been living with OAB symptoms for substantial lengths of time, only seeking treatment when symptoms become particularly problematic. Diagnosis of OAB is made based on symptoms of daytime urinary frequency and urgency, potentially occurring with urge incontinence. Taking a clinical history is important, i.e. symptoms, aggravating/alleviating factors, 24 hour incontinence pad use. Physical examination of the genitourinary system, prostate assessment in men and vaginal examination in women should be performed. There are multiple guidelines for management of OAB such as those from the National Institute for Health and Care Excellence (NICE), European Association of Urology (EAU) and American Urological Association (AUA), which are generally in agreement with each other in terms of the type of stepwise approach to use. This stepwise approach should be tailored to the patient’s needs: they do not necessarily need to go through every step in the set order.
41
AUTHOR: Donna Cosgrove PhD MPSI Donna graduated with a BSc in Pharmacy from the Royal College of Surgeons in Ireland. She then returned to university to complete a MSc in Neuropharmacology. This led to a PhD investigating the genetics of schizophrenia, followed by a postdoctoral research position in the same area. Currently Donna works as a pharmacist in Galway, and as a clinical writer.
1. REFLECT - Before reading this module, consider the following: Will this clinical area be relevant to my practice?
knowledge gap - will this article satisfy those needs - or will more reading be required?
2. IDENTIFY - If the answer is no, I may still be interested in the area but the article may not contribute towards my continuing professional development (CPD). If the answer is yes, I should identify any knowledge gaps in the clinical area.
4. EVALUATE - Did this article meet my learning needs - and how has my practise changed as a result? Have I identified further learning needs?
3. PLAN - If I have identified a
5. WHAT NEXT - At this time you may like to record your learning for future use or assessment. Follow the
4 previous steps, log and record your findings. Published by IPN. Copies can be downloaded from www.irishpharmacytraining.ie Disclaimer: All material published is copyright, no part of this can be used in any other publication without permission of the publishers and author.
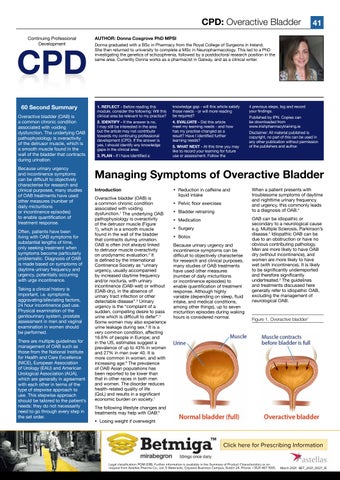
Managing Symptoms of Overactive Bladder Introduction Overactive bladder (OAB) is a common chronic condition associated with voiding dysfunction.1 The underlying OAB pathophysiology is overactivity of the detrusor muscle (Figure 1), which is a smooth muscle found in the wall of the bladder that contracts during urination. OAB is often (not always) linked to detrusor muscle overactivity on urodynamic evaluation.2 It is defined by the International Continence Society as “urinary urgency, usually accompanied by increased daytime frequency and/or nocturia, with urinary incontinence (OAB-wet) or without (OAB-dry), in the absence of urinary tract infection or other detectable disease”.3 Urinary urgency is the “complaint of a sudden, compelling desire to pass urine which is difficult to defer”.4 Some women may also experience urine leakage during sex.5 It is a very common condition, affecting 16.6% of people in Europe; and in the US, estimates suggest a prevalence of up to 43% in women and 27% in men over 40. It is more common in women, and with increasing age.6 The prevalence of OAB Asian populations has been reported to be lower than that in other races in both men and women. The disorder reduces health-related quality of life (QoL) and results in a significant economic burden on society.1
Reduction in caffeine and liquid intake Pelvic floor exercises Bladder retraining Medication Surgery Botox Because urinary urgency and incontinence symptoms can be difficult to objectively characterise for research and clinical purposes, many studies of OAB treatments have used other measures (number of daily micturitions or incontinence episodes) to enable quantification of treatment response. Although highly variable (depending on sleep, fluid intake, and medical conditions, among other things), up to seven micturition episodes during waking hours is considered normal.
When a patient presents with troublesome symptoms of daytime and nighttime urinary frequency and urgency, this commonly leads to a diagnosis of OAB.4 OAB can be idiopathic or secondary to a neurological cause e.g. Multiple Sclerosis, Parkinson’s disease.4 Idiopathic OAB can be due to an obstruction or have no obvious contributing pathology. Men are more likely to have OAB dry (without incontinence), and women are more likely to have wet (with incontinence). It is likely to be significantly underreported and therefore significantly undertreated.2 The guidelines and treatments discussed here generally refer to idiopathic OAB, excluding the management of neurological OAB.
Figure 1. Overactive bladder7
The following lifestyle changes and treatments may help with OAB:5 Losing weight if overweight
Click here for Prescribing Information Legal classification: POM (S1B). Further information is available in the Summary of Product Characteristics or on request from Astellas Pharma Co., Ltd, 5 Waterside, Citywest Business Campus, Dublin 24. Phone: +3531 467 1555.
March 2021 BET_2021_0027_IE