
61 minute read
FEATURE: MEDICATION IN PREGNANCY
The Maternity-Pharmacy Axis- Caring for women before, during and after pregnancy

Written by Dr Claire McCarthy, Consultant Obstetrician/ Gynaecologist, Rotunda Hospital
Over 1 million women of child-bearing age live in the Republic of Ireland and at any point could be planning to conceive, be pregnant or in the postnatal period. While pregnancy and childbirth are normal physiological events, some women do require extra care to optimise their pregnancy outcomes. During a woman’s reproductive years, there are increased opportunities to engage and educate women on their healthcare priorities, as well as those of their families. It is thus imperative that all healthcare providers use any of these interactions for health promotion and protection. At the heart of the community, a pharmacy and its’ staff are in the valuable position of being able to provide care to women and their families for both minor ailments and illnesses, but also provide advice, support and dispensing of medication to service users. Therefore, there can be innumerable opportunities to provide advice and support
Dr Claire McCarthy is a Consultant Obstetrician/Gynaecologist with a special interest in managing medical conditions in pregnancy. Dr McCarthy is also involved with the Irish Medicines in Pregnancy Service (IMPS), a multidisciplinary service based at the Rotunda Hospital, which provides information and expertise to support safe and effective use of medicines before, during and after pregnancy and in lactation.
for those pregnant or considering pregnancy. Some of these elements are outlined in the Health Service Executive document “Healthy Ireland, the Framework for Improved Health and Wellbeing 2013-2025”, which underlines that early intervention before birth is as critical as ongoing early years support. The National Maternity Strategy was formally launched in 2016 as a ten-year plan, with the aim to support the implementation of National Standards of Care. The National Maternity Strategy, along with the National Standards represent the essential building blocks to provide a consistently safe and high-quality maternity service. This is both hospital and community based, with input from the multidisciplinary team. The National Women and Infants Health Programme provides oversight and governance of maternity services nationally, with the aim to further improve the quality and standard of care that is received. From a pre-conceptual perspective, it is advised that women have a healthy balanced diet, minimise alcohol consumption and take folic acid (0.4mg once daily) for at least three months pre-conceptually. Some women (e.g. those with Diabetes Mellitus, family or personal history of a neural tube defect, taking anti-seizure medication or those with a Body Mass Index over 30kg/m2) should be prescribed higher dose folic acid (5mg) supplementation. Vitamin D supplementation is also recommended for women who are deficient, or at risk of being deficient. Women who are entering pregnancy with a medical condition can sometimes benefit from pre-conceptual counselling. This can provide an opportunity to optimise medication, achieve disease control and allow counselling on potential pregnancy complications or outcomes that may arise owing to their condition, or indeed medications that they are taking. It is essential that women who are taking prescribed medication do not suddenly cease or discontinue taking medication on finding out they are pregnant, as in some cases this can lead to a deterioration in their health, putting themselves and their pregnancy at a greater risk. It is essential that these women undertake a risk-benefit discussion with their
prescriber and evaluate whether continuing to take the medication is of a greater benefit than the actual or theoretical risks that taking the medication might pose. Smoking during pregnancy additionally is noted to be detrimental to the health of both the mother and the fetus. The national tobacco control policy document “Tobacco Free Ireland” provides specific recommendations for smoking cessation both in pregnancy, but also pre-pregnancy. It notes that frontline healthcare professionals should have formalised and documented training in smoking cessation. Women may attend their community pharmacy for support in accessing nicotine replacement therapy if non-pharmacological methods have failed, which required a detailed discussion on the risks, benefits and alternatives. MBRRACE-UK (Mothers and Babies: Reducing Risk through Audits and Confidential Enquires across the UK) is a report published annually which examines maternal deaths and morbidities over a rolling three-year period, critically analysing and evaluating care given to women and their families. It provides healthcare providers with essential information to allow us to continually strive for improved care in our maternity services. Closer to home, the NPEC (National Perinatal Epidemiology Centre) based in University College Cork also publishes reports documenting Ireland’s maternal morbidity and mortality findings. It has been noted in many of these reports that there is a rising cultural bias to medication use in pregnancy, particularly in the context of older mothers, and those with increasingly complex medical conditions. Recommendations from these reports can be seen to take a pattern over the years. Specifically, with respect to medication, the 2018 MBRRACE report noted that the “decision on continuing, stopping or changing medication in pregnancy should be made only after careful review of the benefits and risks of doing so, to both mother and infant”. Antenatally, the National Maternity Strategy aims is to create three dedicated pathways for women to access care. The Supported Care pathway is intended for normal-risk mothers and babies with midwives leading and delivering care within the multi-disciplinary framework. The Assisted Care pathway is intended for mothers/babies considered to be at medium risk, and for those who chose obstetricled care. This care is provided by obstetricians and midwives, as part of a multi-disciplinary team. For those women who are high-risk, the Specialised Care pathway provides obstetricled care, with input from other medical specialities, again delivered in partnership with midwifery services. These women may require a multi-disciplinary, multi-speciality approach to care and care planning. Currently, from an obstetric perspective, families can opt for consultant-led care, or combined care. This is facilitated through the Maternity and Infant Care Scheme, available to every woman who is pregnant and ordinarily resident in Ireland, sharing care between the family doctor and hospital service. A number of maternity units also provide a suite of midwifery-led care, as well as midwifery-led units, a DOMINO (Domiciliary In and Out) service, Early Transfer Home and homebirth services. The HSE also facilitates a homebirth service through a number of registered selffree contraception scheme for women aged 17-25 years of age. From 2023, this will be extended to 16 to 30 year olds. The community pharmacy will be at the crux of the provision and dispensing of medications, along with the primary care teams. Going forward, it may be possible for women to access some hormonal contraceptive options in the community pharmacy, which will continue the precedence set by the successful provision of emergency contraception in the pharmacy setting. While this is a significant undertaking by the community pharmacy sector, it has revolutionised contraception provision, underpinning the centrality of the role of the community pharmacist and their team in the community. Finally, it is known that one in six couples may experience difficulties in conceiving and may attend for advice both prior to attending for assessment, as well as during treatment. The community pharmacy can again play a key role in the support of couples through their subfertility journey, as well as the supply of medications that may be prescribed during this period of time. The Assisted Reproductive Technology journey can be fraught with emotional challenges, and can pose financial difficulties to couples which is important to acknowledge and help support as much as possible.
employed community midwives. Community pharmacists are an important resource during the antenatal period. Women may need support and resources in the management of both pregnancy-related and pre-existing complications. It is essential that pharmacists are empowered and supported in providing this, but also referring to the patients’ primary care or maternity care provider where necessary. Postnatally, women are eligible for postnatal care both in hospital, but also in the community. Ideally, this should be a seamless transfer, either through hospital follow-up (i.e. community midwifery, early transfer home schemes), or through public health nurses and community care, in liaison with a primary care service. In this period, women may access the pharmacy for postnatal medications, or medical equipment/devices to support their recovery and rehabilitation. Vaccination is also a key public health innovation to afford protection from severe forms of a condition but also to prevent disease. Some pharmacies offer vaccination against a variety of diseases to their communities, and thus knowledge on vaccination during pregnancy is important. The Irish Immunisation Guidelines for Pregnant Women recommend that all rubella seronegative women of childbearing age should be offered a dose of the MMR postnatally. All pregnant women should be offered the influenza vaccine throughout the influenza season. The pertussis vaccine should be offered between 16 and 36 weeks gestation in order to allow passage of antibodies to the fetus. More recently, vaccination against COVID has predominated healthcare advice. It is essential that pharmacists and their staff are proactive in supporting and recommending vaccination. There are helpful Decision Aids and Infographics available through the Royal College of Physicians of Ireland website to support and assist women in their decisionmaking surrounding COVID vaccination. Breastfeeding is important for the health of both mothers and infants. From the maternal perspective, it reduces risk of cardiovascular disease, breast and ovarian cancer, as well as more short term conditions such as postpartum depression. For infants, breastmilk provides improved protection from acute infections and respiratory illnesses, as well as reduced childhood obesity. Despite this, breastfeeding rates in Ireland are amongst the lowest in the OECD. Public consultations have noted that some of the factors in these low rates are lack of breastfeeding supports in the hospital, community and home setting, as well as inconsistent and contradictory poor quality information on breastfeeding. In that context, support from all healthcare professionals, including pharmacists, is essential to improve our breastfeeding rates and support mothers who wish to successfully breastfeed. This can include on medication use in lactation, but also the provision of correct knowledge and support surrounding challenges women may experience and attend for advice (such as thrush, painful feeding, low supply) for both medical reasons, but assistance with medical supplies such as nipple shields and breast pump supports. It would be remiss not to mention contraception when discussing women’s health and maternity services. In July 2022, the Minister for Health announced the introduction of a The community pharmacy as a location at the hub of a community has the unique ability and position to influence and promote positive healthcare changes in their clientele. Their knowledge of both their patients, but the wider factors surrounding prenatal, antenatal and postnatal care will be crucial going forward in the success of the National Maternity Strategy but also the healthcare of the population at large. Through continued engagement with education and increased provision of funding to the sector, the community pharmacy will continue to remain an essential part of the multidisciplinary healthcare team caring for generations of pregnant women.
References
Health Service Executive. Healthy Ireland, the Framework for Improved Health and Wellbeing 2013-2025. Department of Health/Health Service Executive. National Maternity Strategy: Creating a Better Future Together 2016-2026 Health Information and Quality Authority. National Standards for Safer Better Maternity Services. 2016. Department of Health. Tobacco Free Ireland: Report of the Tobacco Policy Review Group. Oct 2013. Knight M, Bunch K, Tuffnell D, Jayakody H, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ (Eds.) on behalf of MBRRACE-UK. Saving Lives, Improving Mothers’ Care - Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2014-16. Oxford: National Perinatal Epidemiology Unit, University of Oxford 2018 https://www.hse.ie/eng/health/immunisation/ pubinfo/pregvaccs/ https://www.rcpi.ie/news/releases/informationfor-women-who-are-pregnant-or-breastfeedingabout-the-covid-19-vaccine-update/

United Drug Documentary: United We Stand
United Drug have been waiting to tell a very special story, one that will be a remembered forever as one of their greatest achievements in the history of their business. Finally, after a long and challenging period of lockdown, the business has been able to produce an incredible documentary called; United We Stand.

The documentary details the unprecedented time in history and through a series of intimate interviews with some of the company’s senior leaders, coupled with behind-the-scenes footage, the viewer will learn first-hand what it took to set up the operation for the storing, handling, and distribution of the COVID-19 vaccine across Ireland.
All McKesson Ireland staff were invited to the United Drug HQ on September 15th for a premiere style event, to not only watch the first showing of the “United We Stand” documentary but also to finally stand together in one room after 3 years, united in celebrating their colleague’s success and this incredible achievement. Managing Director Paul Reilly and Catherine Cummins, Operations Director addressed the audience before the showing to reiterate how proud they were of their teams and all involved. The energy was electric! “We are all extremely proud of what we have achieved, and our efforts and commitment has helped to save lives.” - Catherine Cummins, Operations Director of United Drug The collaboration and trojan work of the United Drug teams during the Covid Crisis has proven to impact not just their business but the entire nation. Their tireless efforts, including long days and nights, and commitment to an incredibly complex project has benefitted nearly each and every individual in our country. Not all heroes wear capes, and they are thrilled to finally be able to share their story. If you haven’t had a chance to see the Covid-19 Documentary, you can view it on the United Drug website or check it out directly here by scanning the QR code below:
David Keyes, Distribution and Hospitals Director
Paul Reilly, Managing Director

www.united-drug.com
McKesson and United Drug are shortlisted with the Irish Pharma Awards 2022
Health & Safety Award:
McKesson Ireland are delighted to have been shortlisted for the Health & Safety Award in the Pharma Industry Awards. In February 2019, the McKesson Ireland Health and Safety team began their discussions around the potential dangers of Covid19 to the business. Because McKesson plays such a pivotal role in the Irish Healthcare system, it was absolutely critical that whatever challenges lay ahead with Covid19, would not impact the supply of vital medicines across the Irish Health system and that every Pharmacy would where possible remain operational. With this in mind, the Covid19 Task Force Team was formed. The main objectives were to proactively put measures and processes in place to minimize risk to employees, customers, and most importantly patients.
COVID-19 Crisis Response
Award: United Drug were also shortlisted for the COVID-19 Crisis Response Award. As the global pandemic placed continuous and relentless pressures on the Health care sector, United Drug set about to prepare their business and teams for the challenges to come. They critically evaluated the risk at hand and implemented innovative processes, and protocols to receive, store, handle and distribute Covid19 Vaccinations. Their efforts ensured that vital medications, vaccines, and services could continue to be provided and maintained to the Irish Public throughout the entire Pandemic.
Wishing the McKesson and United Drug teams all the best in the upcoming awards! Shortlists can be viewed on the Pharma awards website:
www.pharmaawards.ie.



Budget 2023: Huge Help for Cancer Patients
The abolition of hospital charges announced in the Government Budget will be a huge help for patients at a tough time financially, according to the Irish Cancer Society.

Each time a patient without a medical card attends hospital for treatment they are currently charged ¤80 per visit, up to an annual cap of ¤800. Irish Cancer Society Director of Advocacy Rachel Morrogh said, “After many years of campaigning to reduce the costs carried by cancer patients, the Irish Cancer Society welcomes today’s momentous announcement that hospital in-patient charges are to be abolished. This will come as a huge relief to patients who are struggling to make ends meet in the current cost of living crisis. “This has been a central plank of our advocacy and we thank every patient who shared their story about how charges levied by the Government was adding to their financial misery. We will write to Minister Donnelly in the coming days to thank him for successfully negotiating this important measure, alongside his Government colleagues who supported it.
Rachel Morrogh, Irish Cancer Society Director of Advocacy “The Irish Cancer Society is pleased that the National Cancer Strategy has been funded for the third successive year and that money has been made available to reduce waiting times. We will stay engaged with patients and clinicians over the winter period to monitor this and to ensure the funding is making a measurable difference.
“Finally, Government’s commitment to funding a catch-up programme for HPV (human papillomavirus) vaccinations for boys and girls in secondary school and for women up to the age of 25 who may have missed vaccinations, as campaigned for by the Irish Cancer Society and other groups, is further welcome news.
“We will continue to campaign on the measures that did not get funded in Budget 2023, such as reductions in the cost of hospital car parking and the entitlement of every cancer patient to a medical card.”
cpmire.com
If you need a world class partner for sales and brand execution... Come and talk to us.

Pharmacy & Medical Detailing Technical Sales & Service Solutions Field Sales & Merchandising Shopper Marketing
CPM is Ireland’s longest established and largest Field Marketing Agency and is 36 years in business here this year. Part of the Omnicom Group, a global Top 4 media conglomerate. CPM operates internationally across Ireland, UK, Europe, India & Australia, providing outsourced Sales & Field Marketing Teams.
We grow brands and drive sales for our clients by providing integrated sales solutions that increase profitability. Our client offering is expansive & constantly evolving across sales & merchandising, customer care, experiential, technical service & maintenance, call centre and sampling as we capitalise on new opportunities and the latest technology.
We are ‘People, People’– understanding what makes our team and our clients tick is the key to our success.
Contact our team at sales@cpmire.com or visit us at cpmire.com Data Analysis & Insights
Product Sampling & Demonstrations
We inspire and influence human behaviour.

Cold and Flu Film-Coated Tablets contain:

Professionally recommended for:

Colds and Flu Runny Nose Pain Relief Congestion
A triple combination of antihistamine, analgesic and stimulant Caffeine strengthens the analgesic and antipyretic effects of Paracetamol* A therapy for the management of the symptoms of upper respiratory tract infections
Please consult the summary of product characteristics or contact the marketing authorisation holder for full product information. Name of product: Ilvico Cold and Flu film-coated tablets. Active Ingredient: Paracetamol 325 mg, Caffeine 30 mg, Brompheniramine maleate 3 mg. Supply classification: For supply through pharmacies only. Name and address of the marketing authorisation holder: P&G Health Germany, GmbH, Sulzbacher Strasse 40, 65824 Schwalbach am Taunus, Germany Licence Number: PA22703/001/001. Indication: For the relief of symptoms associated with the common cold, influenza and upper respiratory tract infections. Method of administration: For oral use. Adults and children older than 12 years: One or two tablets taken orally with water three times daily and the maximum dose of 6 tablets daily should not be exceeded. Not recommended for children under the age of 12 years. Please refer to the SmPC for posology instructions for the elderly or those with renal or hepatic impairment. Potential Side effects: thrombocytopenia, leucopenia, agranulocytosis, pancytopenia, haemolytic-anaemia, palpitations, arrhythmia, ventricular depression, bradycardia, hypertention, hypotension, transient vasodepression, sedation, drowsiness, ataxia, headache, restlessness, insomnia, somnolence, impairment of cognition, tremor, dizziness, mydriasis, blurred vision, dry eyes, bronchospasms, dyspnoea, nausea, dry mouth, fatigue, increased level of aminotransferase, jaundice, urinary retention, urinary hesitation, erectile dysfunction, skin reactions, quinke’s oedema, sweating, acute generalised exanthematous pustulosis (AGEP), stevens-johnson syndrome (SJS), toxic epidermal necrolysis (TEN). Special warnings and precautions: Paracetamol should be administered with caution under the following circumstances: hepatic impairment; chronic alcoholism; renal impairment (GFR≤50ml/min); gilbert’s Syndrome (familial non-haemolytic jaundice); concomitant treatment with medicinal products affecting hepatic function; glucose-6-phosphate dehydrogenase deficiency; haemolytic anaemia; glutathione deficiency; dehydration; chronic malnutrition; weight less than 50kg; the elderly. Contraindications: Must not be used if patient: has hypersensitivity to the active substances or to any of the excipients listed in section 6.1; has the presence of narrow-angle glaucoma; has brain damage or epilepsy; is less than 12 years old; has tachyarrhythmias; has peptic ulcers; has severe renal impairment; has severe hepatic impairment (including viral hepatitis); has haemophilia; has vesical neck obstruction, symptomatic prostatic hypertrophy or urinary retention. Reviewed: November 2021.
*Summary of Product Characteristics, Ilvico Cold and Flu film-coated tablets.
P&G Health Germany GmbH, Sulzbacher Strasse 40, 65824, Schwalbach am Taunus, Germany
84 Erectile Dysfunction
Management and Treatment of Erectile Dysfunction
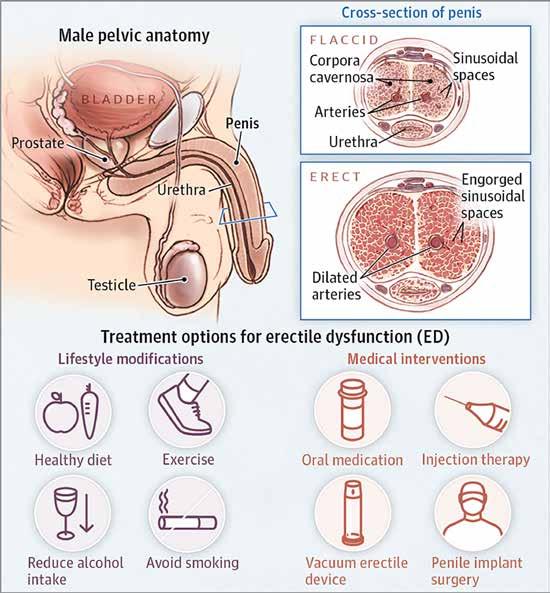
Erectile dysfunction (ED) is a common condition occurring in males over 40 years of age, although it can occur earlier. It is estimated that at least 150 million men globally have ED. It is difficult to obtain accurate values for the true prevalence of erectile dysfunction however, as many patients fail to seek medical attention, and many clinicians are reluctant to ask patients about their sexual health.

We recently spoke to Theresa Lowry Lehnen, RGN, GPN, RNP, BSc, MSc, M. Ed, PhD Clinical Nurse Specialist and Associate Lecturer South East Technological University to understand more about this condition and its impact on males in Ireland. ED can have a substantial negative impact on a man’s quality of life, Theresa reflects. She says, “Erectile dysfunction is the inability to achieve or maintain an erection for satisfactory sexual performance, and affects a considerable proportion of men at least occasionally. It is often treatable, however, if left untreated, ED can be a source of severe emotional stress for both the man and their partner.” Theresa notes that erectile dysfunction is often an under recognised, yet important, cardiovascular risk factor. She says, “Owing to its strong association with metabolic syndrome and cardiovascular disease, cardiac assessment is warranted in men with symptoms of ED.”
Aetiology of Erectile Dysfunction
Although most men will experience periodic episodes of erectile dysfunction, it tends to become more frequent with advancing age. “Many factors can contribute to sexual dysfunction in older men, including physical and psychological conditions, comorbidities and polypharmacy,” she adds. “Aspects of an ageing man’s lifestyle behaviour and androgen deficiency, most often decreasing testosterone levels, can affect sexual function.
“Studies have shown that the percentage of men who engage in some form of sexual activity, decreases from 73% in men aged 57–64 years to 26% for men aged 75–85 years. The aetiology for this decline in male sexual activity is multifactorial, and is in part related to female partners menopause at approximately 52 years of age, leading to a significant decline in female libido and desire to engage in sexual activity.” While ED is associated with ageing, many studies and largescale surveys have concluded that ED is a major health concern among young men. Theresa adds, “One study in 2013 reported that 1: 4 men seeking medical help for erectile dysfunction in the real-life setting, is < 40 years of age. Another study in 2016 concluded that 22.1% of men < 40 years of age had low (<21) Sexual Health Inventory for Men (SHIM) scores. “In the past, erectile dysfunction was almost always considered a psychogenic disorder. However, evidence now suggests that more than 80% of cases have an organic aetiology. While most patients with ED have organic disease, some do have a primary psychological cause, particularly younger men. Even when ED is organic in nature, there are almost always psychological consequences regarding relationship issues, cultural norms and expectations, loss of self-esteem, shame, and anxiety and depression related to sexual performance.” Erectile dysfunction is multidimensional in nature, and Theresa says it can be broadly divided into endocrine and nonendocrine causes.
“The condition can be caused by any disease process which affects penile arteries, nerves, hormone levels, smooth muscle tissue, corporal endothelium, or tunica albuginea. It is closely related to cardiovascular disease, diabetes mellitus, hyperlipidaemia, hypertension, and endothelial dysfunction,” she explains. “Erectile dysfunction and vascular disease are thought to be linked at the level of the endothelium. Endothelial dysfunction, results
An interview with Theresa Lowry- Lehnen (PhD), CNS, GPN, RNP, South East Technological University in the inability of smooth muscle cells lining the arterioles to relax and prevents vasodilatation. The endothelial cell is known to affect vascular tone and impact the process of atherosclerosis and impacting ED, CVD and peripheral vascular disease. Cardiovascular disease and hypertension are very significant risk factors for erectile dysfunction.” Besides cardiovascular disease, there are strong correlations between ED and hyperlipidaemia, diabetes, hypogonadism, obesity, smoking, alcoholism, benign prostatic hyperplasia (BPH) with lower urinary symptoms (LUTS), depression, and premature ejaculation. Diabetes is a common aetiology of sexual dysfunction, because it can affect both the blood vessels and the nerves that supply the penis. Men with diabetes are four times more likely to experience erectile dysfunction, and on average, experience it 15 years earlier than men without diabetes.
“Obesity is also correlated to the development of several types of dysfunction, including a decrease in sex drive and an increase in episodes of ED,” she


Sexual Health Inventory for Men (SHIM)
continues. “Neurogenic erectile dysfunction is caused by a deficit in nerve signalling to the corpora cavernosa. Such deficits can be secondary to spinal cord injury, multiple sclerosis, Parkinson disease, lumbar disc disease, traumatic brain injury, radical pelvic surgery and diabetes. Men being treated for prostate cancer with treatments such as radical prostatectomy, radiation therapy or the use of lutenising hormonereleasing hormone (LHRH) agonists and antagonists often experience ED.” Numerous medications are listed with erectile dysfunction and/ or a decreased libido as a side effect. Drugs that can cause ED include hydrochlorothiazide’s and beta-blocking agents. Medications used to treat depression, particularly the SSRIs such as citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine and sertraline, can also contribute to ED. The severity of erectile dysfunction is often described as mild, moderate or severe according to the five-item International Index of Erectile Function (IIEF-5) questionnaire, with a score of 1–7 indicating severe, 8–11 moderate, 12–16 mild–moderate, 17–21 mild and 22–25 no erectile dysfunction.
The International Index of Erectile Function (IIEF-5) Questionnaire
The IIEF is a multidimensional validated questionnaire with 15 questions in the five domains of sexual function (erectile and orgasmic functions, sexual desire, satisfaction with intercourse and overall sexual satisfaction), and there is also an abbreviated format of five questions in the Sexual Health Inventory for Men (SHIM).
Investigations and Diagnosis
Theresa continues, “A thorough medical history, detailed sexual history, and physical examination are required before commencing treatment or further investigations. It is important to distinguish between psychological and organic causes of ED, as well as to ensure that the patient has erectile dysfunction and not another disorder. History that points towards a psychological aetiology include, sudden onset of erectile dysfunction especially if it is related to a new partner or a major life-changing event, situational ED, normal erections with masturbation or a different partner, presence of morning erections and high daily variability in erectile rigidity. “The main differential diagnosis for erectile dysfunction is hypogonadism, loss of libido, depression with low mood, and other psychological conditions. It may also be the first manifestation of diabetes or cardiovascular disease as well as depression. It is important to differentiate between true erectile dysfunction and other sexual disorders such as premature ejaculation, and this is usually assessed by obtaining a good sexual history. “A complete medication list including supplements should be checked with the patient. ED can be a result of prescription or other medications. Prescription drugs that can cause ED include, antidepressants especially SSRIs, cimetidine, ketoconazole, spironolactone, sympathetic blockers, thiazide diuretics, and other antihypertensives. ACE inhibitors and calcium channel blockers are the least likely to cause ED. Beta-blockers are only a minor contributor, while alpha-blockers can improve erectile function.” Vascular risk factors such as hypertension and diabetes and lifestyle factors such as smoking, activity level, alcohol intake, and the use of any recreational drugs should be assessed, Theresa adds. A full general and cardiovascular examination should be undertaken, as erectile dysfunction can be the first symptom of underlying vascular disease. Peripheral pulses should be checked and blood pressure measured. The genitalia should be carefully inspected for hypogonadism, signs of infection, the presence of penile fibrosis or plaques, and phimosis. Theresa continues, “The role of testosterone replacement therapy (TRT) as a potential to improve erectile function in ED remains an issue for clinicians who are comfortable treating androgen deficiency. Androgens are known to have a significant impact on the function of the smooth musculature within the corpus spongiosum. “Testosterone supplementation is more effective as a treatment for low libido than for ED. For most men with both ED and hypogonadism, oral PDE5 inhibitors alone are recommended as the initial therapy. Testosterone supplementation is reasonable in men with proven hypogonadism and ED who have already failed PDE5 inhibitor therapy or who also have low libido. Hypogonadal patients with borderline erectile rigidity are most likely to benefit from testosterone supplementation. “Testosterone replacement therapy may cause increased levels of haemoglobin or haematocrit which is associated with an increased risk of heart attack, stroke and blood clots. Testosterone treatment can also cause an enlarged prostate or other prostate disorders. During TRT treatment, the prostate specific antigen (PSA) will be measured to monitor for any changes and this is particularly important in men over 45 years of age. “As a result of using testosterone replacement, natural production of testosterone may be reduced. This may lead to a reduction in sperm production and fertility. Other side effects of TRT include: weight gain, increased appetite, hot flushes, acne, depression, restlessness, irritability, aggression, tiredness, general weakness and excessive sweating. Lifestyle modifications are considered first-line therapy for ED, and men should be encouraged to make the necessary changes to benefit both their sexual function and their overall health.
“PDE5 inhibitors are highly effective and have an overall success rate of up to 76%. PDE5 inhibitors are contraindicated in patients taking nitrates, but otherwise are safe and effective. When PDE5 inhibitors are co-administered with nitrates, pronounced systemic vasodilation and severe hypotension can occur. “PDE5 inhibitors and α-adrenergic
1. How do you rate your confidence that you could get and keep an erection?
2. When you had erections with sexual stimulation, how often were your erections hard enough for penetration?
3. During sexual intercourse, how often were you able to maintain your erection after you had penetrated (entered) your partner?
4. During sexual intercourse, how difficult was it to maintain your erection to completion of intercourse?
5. When you attempted sexual intercourse, how often was it satisfactory for you?
Over the past 6 months:
Very low 1 Low 2 Moderate 3 High 4 Very high 5
Almost never/never 1
Almost never/never 1
Extremely difficult 1 A few times (much less than half the time) 2 Sometimes (about half the time) 3 Most times (much more than half the time) 4
A few times (much less than half the time) 2 Sometimes (about half the time) 3 Most times (much more than half the time)4
Very difficult 2 Difficult 3 Slightly difficult 4 Almost always/always 5
Almost always/always 5
Not difficult 5
Almost never/never 1 A few times (much less than half the time) 2 Sometimes (about half the time) 3 Most times (much more than half the time) 4 Almost always/always 5
IIEF-5 scoring:
The IIEF-5 score is the sum of the ordinal responses to the 5 items. 22-25: No erectile dysfunction 17-21: Mild erectile dysfunction 12-16: Mild to moderate erectile dysfunction 8-11: Moderate erectile dysfunction 5-7: Severe erectile dysfunction
Total Score __________
receptor blockers, often used for treatment of BPH, need to be taken at least 4 hours apart. Among second-line therapies, external vacuum devices (VCDs) are a good, non-surgical option for patients with ED. VCDs are clear plastic chambers placed over the penis, tightened against the lower abdomen with a mechanism to create a vacuum inside the chamber. This directs blood into the penis. If an adequate erection occurs inside the chamber, the patient slips a small constriction band off the end of the VCD and onto the base of the penis. An erection beyond 30 minutes is not recommended. While cumbersome, these devices are considered safe.
“Other second-line therapy includes the use of either intracavernosal injection (ICI) or intraurethral suppositories (IUS). A small needle is used to inject the ICI medication into the lateral aspect of the penis through a small-gauge needle. These vasoactive agents include prostaglandin E1, papaverine and phentolamine and sometimes atropine, which work alone or in combination to elicit an erection. Response is dose related, usually occurs within 10– 15 minutes, and does not require stimulation. A concern with ICI use is priapism, and if this occurs the patient will need to seek urgent medical attention. Bruising can also occur, due to it being an injected medication. The intraurethral suppository consists of a tiny pellet of prostaglandin E1 inserted into the urethral meatus. Response is dose related, and onset usually occurs within 10–15 minutes. Patients need to be trained on the technique of the IUS before use, and should be advised that pain or burning may occur with this medication.
“In men who fail to respond to first or second-line therapy, or who are not interested in conservative therapies, penile prosthesis implantation is available. Penile implants include malleable and inflatable devices, although most implants used are of the inflatable variety. Adverse effects including malfunction and infection are rare, and patient satisfaction is high.”
Outlook
Theresa told us that future Therapies for ED Clinical studies in gene therapy are looking towards replacing proteins that may not be functioning properly in the penile tissue of men with erectile dysfunction. She says, “Replacement of these proteins may result in improvement in ED. Experimental animal models have demonstrated improvement in erectile function with gene therapy. Human studies may demonstrate success with this therapy in the future, however, gene therapy in humans is controversial, and can take a long time for regulatory approval and public acceptance. “Stem cell studies may also provide advancements in the treatment of ED in the future. The mechanism of action of stem cells is to generate angiogenesis with subsequent increase in cavernosal smooth muscle cells within the corporal bodies. “The clinical studies published to date provide encouraging results, with improvement of sexual function reported with no side effects. Although pioneering, stem cell studies to date are small scale, with a short follow up period, various aetiologies of ED and without a control group. Melanocortin activators are drugs that act through the central nervous system, and have been shown in animal studies to produce an erection. Initial studies in humans suggest that the drug (PT-141) can be effective if given intranasally in men with psychological rather than physical causes, and mild to moderate ED.
“Larger studies are necessary, however, to demonstrate the safety and overall effectiveness of these drugs. Another potential new treatment for ED, is penile low intensity shock wave lithotripsy. This consists of 1500 shocks twice a week for 3–6 weeks. The purpose is to stimulate neovascularisation to the corporal bodies with improvement in penile blood flow and endothelial function. The use of low-intensity shock wave lithotripsy may convert PDE5 inhibitor non-responders to responders.”
Pharmacy Role in ED Care
Background of ED
Erectile dysfunction is defined as the persistent inability to attain and maintain an erection sufficient to permit satisfactory sexual performance. Erectile dysfunction is one of the most common health conditions affecting men. EAU guidelines from 2020 indicate a prevalence of 52% of men aged 40-70 years with erectile dysfunction (ED).4 ED is very common in Ireland, one in 5 Irish men experience this regularly.
Causes of ED
There are many causes of ED which can result from both physical and psychological conditions
Physical Causes • Conditions such as heart disease, atherosclerosis, high blood pressure diabetes, metabolic syndrome, parkinson’s disease and multiple sclerosis • Obesity • Certain Prescription medication (10-25% of ED causes are drug induced)* • Treatment for prostate cancer • Tobacco Use • Excessive substance abuse such as alcoholism • Sleep Disorders • Low Testosterone Psychological Causes • Depression, anxiety or other mental health conditions • Stress
• Relationship problems * Common medicines that cause ED are antidepressants, antihistamines, high blood pressure medicines and diuretics of which thiazides are the most common cause of ED following by beta blockers. Other classes of medications include Parkinsons disease medicines, chemotherapy and hormonal medicines, opiate analgesics and recreational drugs. We would always advise men who are unsure of the reason behind their ED to speak confidentially to their pharmacist, we always recommend a visit to a GP to ascertain underlying conditions that might cause this.
Lifestyle changes
Modifiable risk factors that can help improve symptoms of ED include losing weight, exercise daily, stop smoking, eat a healthy diet and reduce stress and anxiety.
Written by Lisa Byrne, Superintendent Pharmacist, McCabes Pharmacy Group
Treatment of ED
Sildenafil has been licensed for the treatment of ED since 1998 and is available in three different strengths on prescription. Sildenafil 50mg (Viagra Connect) is available without a prescription to those over 18 from the pharmacy, following consultation with a pharmacist which can be done in the privacy of a consultation room.
Studies have reported that patients sought out online platforms for accessing ED treatments citing convenience, shame and discretion as treatment barriers.2 Pharmacists have a key role to allow customers access to medication in an environment that encourages them to seek treatment, be afforded counselling, and thus building a trusting relationships.3 At McCabes Pharmacy there is the option to Click & Collect. The customer completes an online consultation form on the website and collects their medication in store from the pharmacist, after answering a few questions to ascertain if it is indeed the most appropriate medication for their needs. This has proved to be a very popular service, by nature of its discretion.

88 Lithium Management
Lithium Therapy: a national patient safety and quality improvement initiative 1. BACKGROUND AND CLINICAL INFORMATION: Lithium Indications:
• Bipolar Disorder: mania, hypomania and prophylaxis of
Bipolar Disorder • Recurrent Depressive
Disorder: used to augment antidepressants • Reduction of intentional selfharm and suicidality.
Switching lithium products:
Priadel tablets are recommended for routine use. The tablets have score- lines therefore they can be divided accurately to provide smaller dosage requirements. If a patient is unable to swallow tablets a liquid may be prescribed. It is essential that a switch from tablets to liquid is prescribed by their Doctor, and calculation confirmed by Pharmacist.
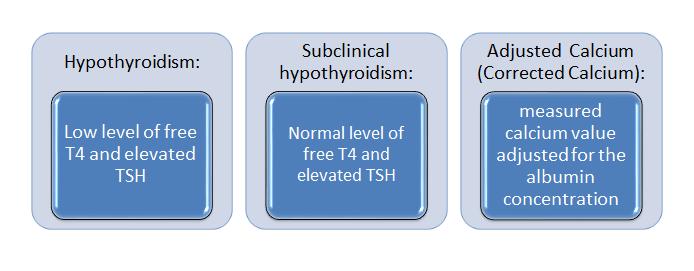
Written by Audrey Purcell B(Sc) Pharm. MPSI. MSc. Psych Pharm. Chief 2 Pharmacist, Saint John of God Hospital, Stillorgan, Co Dublin. Honorary Senior Clinical Lecturer, Royal College of Surgeons in Ireland. Example: Switching patient from • Serum Creatinine+/-estimated Priadel tablet (Carbonate) 800mg Glomerular Filtration Rate (eGFR) nocte to Priadel liquid (Citrate) = 400mg (10ml) BD morning and • Adjusted Calcium night. Lithium level to be checked 5-7 days post- switch. • Thyroid Function Tests (TFTs): include Free T4 and Thyroid Baseline work-up: Stimulating Hormone (TSH). • ECG : if cardiac history, risk factors for QTc prolongation, Patient should be euthyroid before initiation concomitant medicines that • Full Blood Count prolong QTc • Weight and height • Pregnancy test and review of contraception (in women of • Urea and Electrolytes childbearing age).
Product: Formulation: Recommended dosing: Prescribing:
Starting dose may usually range from 400mg-800mg OD (nocte) in adults, depending on indication. Elderly patients, those with renal impairment or those below 50kg in weight, often require lower starting dose (eg 200mg), and maintenance doses.
Plasma levels:
Lithium plasma level should be checked 5-7 days after starting, after every dose change, and after addition/discontinuation of medication that can affect level.
Lithium level sampling time: Priadel Tablets:
200mg+400mg (200mg tablet may be halved to facilitate 100mg dose )
Lithium Carbonate. 400mg tablet contains 10.8mmol/L Lithium.
Once daily:
at night-time (Prolonged Release) 12 hours post-dose (acceptable 10-14 hours) Camcolit tablet EMP 400mg EMP: Exempt Medicinal Product
Lithium Carbonate Once daily: at night-time (Prolonged Release) 12 hours post-dose (acceptable 10-14 hours) Priadel Liquid EMP 520mg/5ml
204mg/5ml (calculate as 200mg/5ml) Twice daily:
Li-Liquid EMP 509mg/5ml Lithium Citrate 509mg/ml: equivalent to Lithium Carbonate
200mg/5ml (calculate as 200mg/5ml) Twice daily:
morning and night (Immediate Release)
(ACEI) Angiotensin Receptor Blockers (ARBs)
Switching lithium products:
accurately to provide smaller dosage requirements. If a patient is unable to swallow tablets a liquid may be prescribed. It is essential that a switch from tablets to liquid is prescribed by their Doctor, and calculation confirmed by Pharmacist. Example: Switching patient from Priadel tablet (Carbonate) 800mg nocte to Priadel liquid (Citrate) = 400mg (10ml) BD morning and night. Lithium level to be checked 5-7 days post- switch.
Baseline work-up:
• ECG : if cardiac history, risk factors for QTc prolongation, concomitant medicines that prolong QTc • Weight and height • Urea and Electrolytes • Serum Creatinine+/-estimated Glomerular Filtration Rate (eGFR) • Adjusted Calcium • Thyroid Function Tests (TFTs): include Free T4 and Thyroid Stimulating Hormone (TSH).Patient should be euthyroid before initiation • Full Blood Count • Pregnancy test and review of contraception (in women of childbearing age).
N: Non- Steroidal Antiinflammatories (NSAIDs)
OTC NSAIDs and use Paracetamol if
OTC analgesic required.
T: Thiazide Diuretics
Unpredictable Up to fourfold increase in lithium level. Thiazides reduce renal clearance of lithium and levels can rise within a few days Usually apparent in the first 10 days Any effect will be apparent in the first month. Thiazide diuretics should only be used where unavoidable and with strict monitoring Loop diuretics may be safer.
S: Sodium
Excess Sodium can reduce lithium levels Sodium restriction can lead to lithium toxicity. Consider high Sodium content OTC preparations and recommend suitable alternatives Care with Sodium content in effervescent formulation Refer to SPS Pharmacy NHS

Target levels:
The minimum effective plasma level for prophylaxis in adults is 0.4mmol/L; optimal range is 0.60.8 mmol/L. A level of 0.4mmol/L may be effective in unipolar depression; 0.6 -1 mmol/L in Bipolar Disorder, and levels at the higher end of the range in mania (0.8-1mmol/L).
Name: Magnitude: Timescale: Additional Information: Name: Magnitude: Timescale: Additional Information: A:
A: ACE Inhibitors (ACEI) ACE InhibitorsAngiotensin (ACEI) Receptor Angiotensin Blockers (ARBs)Receptor Blockers (ARBs)
Unpredictable
Consider alternative anti-hypertensive
Unpredictable Up to fourfold increase in lithium level. Develops over several weeks Most likely to cause lithium toxicity within a month of starting. Sevenfold increased risk of hospitalisation for lithium toxicity in the elderly Consider alternative anti-hypertensive If combination necessary, increased monitoring of lithium level and renal function required.
N: Non Anti Steroidal Non- Steroidal inflammatories Anti(NSAIDs) inflammatories (NSAIDs) T:
T: Thiazide Diuretics Thiazide Diuretics
S: Sodium Sodium
Unpredictable
OTC NSAIDs and use Paracetamol if
OTC analgesic required.
Diclofenac: up to 23% increase in lithium level Ibuprofen: up to 25% increase in lithium level Patients should be advised to avoid OTC NSAIDs and use Paracetamol if Unpredictable OTC analgesic required. Up to fourfold increase in lithium level. Thiazides reduce renal clearance of lithium and levels can rise within a few days Usually apparent in the first 10 days Any effect will be apparent in the first month. Thiazide diuretics should only be used where unavoidable and with strict monitoring Loop diuretics may be safer. Furosemide is probably the safest diuretic to use with lithium but frequent monitoring required.
Unpredictable Up to fourfold increase in lithium level. Thiazides reduce renal clearance of lithium and levels can rise within a few days Usually apparent in the first 10 days Any effect will be apparent in the first month. Thiazide diuretics should only be used where unavoidable and with strict monitoring Loop diuretics may be safer.
Excess Sodium can reduce lithium levels Consider high Sodium content OTC preparations and recommend suitable Sodium alternatives restriction can lead to lithium Care with Sodium content in toxicity. effervescent formulation Refer to SPS Pharmacy NHS “Considering Sodium content of medicines”; particular care with products > 17mmol Sodium in maximum daily dose https://www.sps.nhs.uk/articles/consi dering-sodium-content-of-medicines/ Example: Sodium Bicarbonate in antacids (Gaviscon); recommend Maalox instead.
Monitoring frequency:
TFTs, renal function, Calcium level, and weight check, recommended every 6 months; or every 3 months in at-risk patients.
Once stable, serum lithium levels recommended every 3 months for the first year, then every 6 months; or every 3 months in at-risk patients.
At risk patients include:
• Elderly (> 65 years)
• Have received less than 12 months treatment • Renal impairment (eGFR<60ml/min)
• Impaired Thyroid function at last test
• Raised Calcium level (adjusted) at last test
• Poor symptom control or suspected poor adherence
• Significant change in patient’s sodium or fluid intake
• Last serum lithium level >0.8mmol/L • Interacting medicines. Key interacting medicines include:
ACEI, ARBs, NSAIDs and
Thiazide diuretics. (See summary below and BNF/Stockley’s for exhaustive list).
Discontinuation:
If a decision is made to discontinue lithium, the risk of relapse may be reduced by reducing the dose gradually. It is recommended to reduce the dose slowly over at least 4 weeks or longer, and preferably up to 3 months in Bipolar Disorder; except in medical emergency or overdose.
ALARM BELL INTERACTIONS: THINK “ANTS” (SEE TABLE LEFT) ADVERSE EFFECTS : ( NOT AN EXHAUSTIVE LIST)
Cardiac: Lithium may cause cardiac arrhythmia, including bradycardia, sinoatrial dysfunction (SA block), abnormal T waves on ECG (T-wave inversion), and STsegment depression. Dermatological: Lithium may cause acne vulgaris and/or psoriasis (including exacerbation of both) in patients with and without either condition at baseline.
GI: Lithium may cause dyspepsia, diarrhoea, nausea, vomiting, dysgeusia (metallic or salty taste), gastritis and abdominal pain. Some effects (e.g. nausea) may occur early in treatment. Other effects may take longer to develop. Supratherapeutic lithium levels should be suspected with severe nausea, vomiting and diarrhoea. Hypothyroidism: Lithium has varied effects on Thyroid Hormone production and regulation, including inhibition of Iodine uptake in the Thyroid, inhibition of Thyroid Hormone synthesis and release, and hepatic conversion of free Thyroxine. Patient may present with typical hypothyroidism symptoms including lethargy, impaired cognition, weight gain, dry skin, and cold intolerance. Risk factors include females, older adults, family history of hypothyroidism, and presence of anti-thyroid antibodies. Hyperparathyroidism and hypercalcaemia: Hypercalcaemia has been reported with Lithium therapy, which may or may not be related to drug-induced hyperparathyroidism. While lithium has been observed to affect Parathyroid Hormone levels after a single dose, long -term exposure is likely required to observe clinically relevant alterations in Calcium homeostasis.
Polydipsia and polyuria: Common adverse effects associated with lithium. Patients may notice increased urinary frequency (> 3 L in 24 hours) due to poor urine concentration; and increased thirst, which is independent of dry mouth effects of lithium.
Renal effects: Up to one-third of patients may develop some degree of decreased kidney function during the course of lithium therapy, with approximately 5% developing significant kidney impairment/failure. Sexual dysfunction: Studies report rates of the various effects of 5-40 %. Effects can include decreased libido, impaired sexual arousal, and
About this booklet
There are two parts to this booklet: • an information section, and • a record book.
The Lithium Record book is on page 19.
Information section
Page number 1. What is lithium and what is it used for?................................3 2. What checks are needed before starting lithium? ................4 3. How do I take lithium?..........................................................5 4. What blood tests do I have when I take lithium?..................8 5. What side effects can lithium cause?.................................10 6. What happens if lithium level in my blood is too high?.......13 7. What can make lithium blood levels too high? ...................14 8. Pregnancy and lithium: what do I need to know?...............16 9. Alcohol and lithium: what do I need to know? ....................17
6. What happens if lithium level in my blood is too high?
If you have too much lithium in your blood, this is called lithium toxicity (or lithium poisoning). This can make you very ill.
Read the following list very carefully. If you get one or more of these problems at any time, talk to your doctor straight away.
Symptoms if there is too much lithium in your system
• Severe hand shake (tremor). • Vomiting or severe nausea and persistent diarrhoea. • Muscle weakness. • Being unsteady on your feet. • Muscle twitches. • Slurring of words so that it is difficult for others to understand what you are saying. • Blurred vision. • Confusion. • Feeling unusually sleepy.
A small number of people may not have any immediate symptoms of toxicity when the lithium in their blood is too high. This is why it is important to have regular checks. Regular checks can prevent long-term problems.
2 13 Lithium therapy record book – your healthcare
Date Daily Dose
(mg):
Example 1: 2/3/22
Example 2: 2/3/22 600mg
600mg Lithium blood level
(mmol/L)
0.8
0.8 Kidney Checks
(eGFR/ Creatinine) + Ref Range
eGFR 85 Thyroid checks
TSH
(mlU/L): + Ref Range
2.59 (0.27-4.2) Thyroid checks
Free T4
(pmol/L): + Ref Range
13 (12-22) Adjusted Calcium
(mmol/L): + Ref Range
Weight/ BMI:
2.25 (2.1-2.6) 67kg
67kg Date of next blood test:
6/6/22
6/6/22
erectile dysfunction. Sexual dysfunction can negatively impact a patient’s quality of life. Tremor: Lithium can cause tremor in up to 25% of patients, making it one of the most common adverse effects. This is commonly a bilateral, symmetrical hand tremor, which may spontaneously decrease over time as compensatory mechanisms develop within the patient. Course tremor and muscle twitching may be observed in lithium toxicity. Tremor commonly begins early in treatment, but can develop later in treatment, with or without a dose increase. Risk factors include: 6 higher doses/serum levels, medicines that can increase lithium level, medicines known to induce tremor (e.g. antipsychotic, antidepressants), caffeine and older adults. Weight gain: Increases of 4 to 7 Kg within the first year have been reported in the literature. Effects on central mechanisms related to weight gain, satiety and metabolism are possible. Increased consumption of highcalorie, sugary beverages from increased thirst with lithium could contribute.
Symptoms of toxicity:
For patients with symptoms of toxicity (eg diarrhoea, vomiting, coarse tremor, mental state changes or falls): Withhold lithium, refer to GP/Clinic/Hospital for urgent lithium level and U+Es, and seek specialist advice. Referral to secondary care may be required depending on the severity of symptoms.
LITHIUM THERAPY : A BLUE BOOK FOR SAFETY
• The national patient information booklet has been produced by Audrey Purcell, Chief 2
Pharmacist, Saint John of God Hospital, and supported by Professor Dolores
Keating, Chief Pharmacist, and Saint John of God Drug and Therapeutics Committee. • This initiative is intended to provide and promote safer lithium therapy, and empower patients to engage with their Healthcare
Professional to discuss all aspects of lithium therapy, monitoring, and side-effects.
Appropriate information and monitoring is imperative to ensure best outcomes for patients on lithium therapy and reduce likelihood of harm. • The booklet has been reviewed and endorsed by Ciara Kirke, HSE Clinical Lead,
National Medication Safety Programme, and the national print supported by the
HSE’s National Quality and Patient Safety
Directorate. • It has been edited and reviewed by the
National Adult Literacy Agency and has successfully been awarded the plain English mark by NALA. • It has been reviewed and endorsed by
Saint John of God Hospital Drug and
Therapeutics Committee, Irish Medication
Safety Network, Irish Pharmacy Union, and the College of Psychiatrists.
The Lithium booklet contains:
• Essential clinical and safety information for patients • Information on side-effects and signs of toxicity • Advise on appropriate OTC medicines and contra-indications • A programme of monitoring to ensure safe and appropriate monitoring • A record book to record lithium levels and essential blood test results.
3 4 5 7 8
Healthcare Professionals provide essential support and are recommended to:
• Ensure patients have a lithium booklet • Reinforce essential information verbally • Refer patient to the booklet to be aware of potential side-effects and signs of toxicity • Ensure the patient understands their own programme of monitoring • Support patients to engage in appropriate blood test monitoring: keep their record book up to date, and have available at consultations with GP, Consultant,
Pharmacist, Nurse.
National launch of the Lithium booklet:
• Saint John of God Hospital, the HSE National
Medication Safety Programme and the
Irish Pharmacy Union have collaborated to implement a national launch of the booklet. • Lithium booklets will be distributed from the
HSE directly to Hospital Pharmacies, and to
Community Pharmacies via the IPU Review.
GPs may sign-post patients to Community
Pharmacists to avail of a booklet.
• Booklets can be ordered from Saint John of
God Hospital: hospital.pharmacy@sjog.ie
Acknowledgements:
Many thanks to Aoife Carolan, Senior Pharmacist, Saint John of God Hospital, and Ciara Kirke, HSE Clinical Lead, for article peer-review.
References available on request
Exercise for Bone Health in Women
Osteoporosis and Fracture Risk: Osteoporosis is a disease characterised by low bone mass which affects both men and women but with a higher prevalence among women. It is estimated that 1 in 3 women over age 50 will experience fractures due to osteoporosis, as will 1 in 5 men. With people living longer, the lifetime risk of a fracture related to bone fragility is heightened.

Bone Health across the Lifespan
Childhood and adolescence represent a critical period for the development of strong healthy bones with peak bone mass usually achieved between age 25 to 30. Bone density remains relatively stable until age 50 but begins to decline thereafter. Adopting and sustaining healthy lifestyle behaviours including exercise, a healthy diet (adequate calcium, Vitamin D, Protein intake) and getting sufficient sun exposure (Vitamin D) are advocated to promote bone health across the lifespan. At menopause bone loss may accelerate significantly in women due to the reduction in oestrogen, a key regulator of bone metabolism. Women should actively seek a DXA scan at that time. Where bone loss issues are identified, pharmacological therapy may be required which is based on a number of factors including DXA findings, prior fragility fracture and the risk of future fracture.
Exercise and Bone Health
Exercise for bone health should start in the childhood years with the goal of optimising peak bone mass. In the middle years maintaining bone mass is the goal and in later life, the emphasis is more on slowing down bone loss. As for all exercise programmes achieving an effective exercise dose is critical with consideration of frequency, intensity, type and time (FITT). Some bone health exercise programmes aim to prevent Caitriona Cunningham is an Associate Professor at UCD School of Public Health, Physiotherapy and Sports Science. A Chartered Physiotherapist, she and colleagues at UCD cofounded UCD’s Better Bones programme in 2012, which focused on empowering individuals (age 55+) to adopt positive bone building and fracture prevention behaviours
osteoporosis in healthy populations whereas exercise prescription for individuals with osteoporosis requires risk stratification.
What type of exercise is optimal to build bone?
Bone responds to mechanical stimuli with adjustment of skeletal mass and architecture in response to changing mechanical environments. The best types of exercise to build bone (osteogenic exercise) are impact (involves running, hopping and jumping) and resistance (strength) training with a combination of both the most effective. Strength training is also critical to slow down age related loss of muscle mass and function. Walking is a form of impact exercise but higher impact, more unusual activity will likely induce an even better bone formation response. Recent research places more emphasis on the need for higher loads to enhance bone when engaging in resistance training. Most of the studies regarding exercise interventions focusing on enhancing bone have been conducted in post -menopausal women. Mixed loading programmes (impact+ resistance training) conducted two to three times per week for approximately one hour for over six to nine months have shown positive changes in bone mineral density (BMD) on DXA scan. However, the minimal effective exercise dose to enhance BMD has not been established to date.
Exercising if have osteoporosis
Maintaining an active lifestyle is always positive and it is important that individuals with osteoporosis do not become fearful about exercise participation but adapt their exercise as required. ‘Bone building’ may continue to be a key goal of exercise for people with osteoporosis. However, when osteoporosis is more severe the main focus switches to improving muscle strength and balance to maintain and enhance function and reduce the risk of a fall and fracture, rather than aiming for an improvement in bone density. For example, where a person has severe osteoporosis of the spine and/or a history of a fragility fracture, exercises which involve lifting heavier weights with twisting of the spine are to be avoided, consistent with manual handling principles. In addition, higher impact exercises may not be appropriate. A risk benefit assessment and exercise prescription by a physiotherapist is recommended, bearing in mind that maintaining cardiovascular fitness through exercise is always important for health.
Key Messages
• Exercise for bone health should start in the childhood years and continue through all life stages • A combination of strength and impact exercise is optimal for building bone • A DXA scan is recommended for women around the time of menopause, with repeat scans thereafter.
• Consultation with healthcare professionals is critical to decide on the need for initiation of pharmacological therapy to enhance bone, a decision which is based on a number of factors including DXA findings, prior fragility fracture and the risk of future fracture.
• Exercise continues to be very important for women with osteoporosis and consultation with a physiotherapist is recommended

Migraine in Women
Introduction: Migraine is a neurological disorder characterised by recurrent bouts of severe headaches with autonomic and neurological symptoms. Scientific advances in recent decades have provided us with a clear understanding of the pathophysiology of migraine and enabled the development of migraine specific acute and preventative therapies. Migraine occurs in 10-12% of the population and there is a 3:1 female to male ratio. It is particularly common, in women of all ages, and female preponderance begins around the time of the menarche. The World Health Organisation Global Burden of Disease study ranked migraine as the 2nd leading cause of disability and the leading cause in women under the age of 50 years.
Diagnosis: The International Headache Society has standardised the diagnosis of migraine using universally accepted diagnostic criteria (ICHD3) and these guidelines have provided us with a uniform approach to diagnosis in clinical practice (Fig 1,2,3,4).
Migraine Without Aura: 1.1
A. At least 5 attacks fulfilling criteria B-D B. Headache attacks lasting 4-72 hours (untreated or unsuccessfully treated) C. Headache has > 2 of the following characteristics 1. Unilateral Location 2. Pulsating Quality 3. Moderate or severe pain intensity 4. Aggravated by or causing avoidance of routine physical activity. D. During Headache > 1 of the following. 1. Nausea and or vomiting 2. Photophobia and Phonophobia E. Not better accounted for by another ICHD-3 diagnosis Fig: 1
Migraine With Typical Aura: 1.2.1
A. At least 2 attacks fulfilling B and C B. Aura of visual, sensory and /or speech /language symptoms, each fully reversible, but no motor, brainstem or retinal symptoms. C. > 2 of the following 4 characteristics 1. > aura symptom spreads gradually over 5 minutes and /or > 2 symptoms occur in succession. 2. Each individual aura symptom lasts 5-60 minutes 3. > 1 aura symptom is unilateral 4. Aura accompanied by or followed in < 60 minutes by headache D. Not better accounted for by another ICHD-3 diagnosis, and
TIA excluded. Fig: 2
Chronic Migraine: 1.3
A. Headache (TTH-like and /or
Migraine-like on >15 d/mo for > 3 month and fulfilling criteria
B and C.
B. In a patient who has had > 5 attacks of fulfilling criteria B-D
For 1.1 Migraine Without Aura and /or criteria B and C for 1.2
Migraine With Aura C. On > 8 d/month for > 3 month fulfilling any of the following: 1. Criteria C and D for Migraine Without Aura
2. Criteria B and C for Migraine With Aura
3. Believed by the patient to be migraine at onset and relieved by a triptan or ergot derivative D. Not better accounted for by another ICHD-3 diagnosis Fig: 3
Hemiplegic Migraine: 1.2.3
A. Attacks fulfilling criteria for 1.2 Migraine With Aura and criterion B below.
B. Aura consists of both of the following 1. Fully reversible motor weakness
2. Fully reversible visual, sensory, and or speech / language symptoms Fig: 4 Many migraine patients also experience other symptoms which are disabling but are not incorporated into the diagnostic guidelines. These symptoms vary and include vertigo, dizziness, cutaneous alloydynia, tiredness and psychomotor slowing. The natural history of migraine in women is that it begins around the time of the menarche and early teenage years, peaks in the 30’s and declines rapidly in the post-menopausal years. The average patient gets 2-3 attacks per month and for 10% of sufferers migraine is a progressive disorder leading to Chronic Migraine (>15 days per month) at a time in life when individual demands and commitments are greatest. Migraine and Women: Throughout a woman’s life hormonal factors have a significant influence in the threshold, susceptibility, risks, and management of migraine (Fig:5). 1. Migraine and the menstrual cycle 2. Migraine and the oral contraceptive 3. Migraine and Pregnancy 4. Migraine and HRT / Menopause Fig:5
1. Migraine and Menstrual
Cycle: Women are vulnerable to migraine attacks at the time of menses and less commonly around the time of ovulation. Attacks, however, are not exclusive to these times and many other migraines may occur either spontaneously or on exposure to a trigger (e.g. diet factors, alcohol, stress and lifestyle factors). Menstrual migraines most frequently occur between days -2 to + 3 of menses. Attacks are more likely to be migraine without aura and are longer in duration (> 72 hours). It is also considered more disabling and more difficult to treat. In the perimenstrual period, and to a lesser extent at the time of ovulation, oestrogen levels decline and fluctuate. This decline activates the trigeminovascular system resulting in an acute attack. Many patients are able to anticipate menstrual migraines enabling them to treat early, particularly with longer acting triptans (e.g. frovatriptan 2.5mg or naratriptan 2.5mg) with or without an NSAID (e.g. naproxyn 500mg).
2. Migraine and Oral
Contraceptive: The combined oral contraceptives are ethinyloestradiol / progestogen preparations (COCP). The newer versions contain lower doses of the oestrogen component. The combined pill is a risk factor for cardiovascular and cerebrovascular disease and careful consideration needs to be given when prescribing in migraine patients. Migraine With Aura is an independent risk factor for stroke as are the COCP, cigarette smoking and hypertension. This risk is accumulative and migraine patients need to be advised to stop smoking. The use of a headache diary is invaluable in this supervision as the pill is known to:
Written by Dr Edward M. O’ Sullivan, Clinical Director Headache Migraine Clinic Department of Neurology Cork University Hospital General Practitioner in Cork
Medical advisor to the Migraine Association of Ireland


• Trigger headache and first attack of migraine without aura. • Trigger aura symptoms for the first time in patients already diagnosed with migraine without aura.
• Worsen and increase the frequency of migraine in patients with an established diagnosis. • It can improve migraine or in others it has no impact on the frequency, severity and duration attacks.
• Continuation of the pill without break through 3 cycles may prevent menstrual migraine attacks. In patients with an established diagnosis of Migraine With Aura the combined pill is contraindicated and patients who develop aura symptoms after commencing the COCP need to discontinue the pill immediately due to stroke risk. The headache diary will identify those patients in whom the COCP worsens their migraine and for whom it must be stopped or is contraindicated in the first place. The diary, paradoxically, will also demonstrate those patients in whom the COCP has benefited their migraine and reduced the frequency of attacks. The protestrogen-only-preparations are an alternative in women for whom the COCP is contraindicated. The POP’s are safe and do not trigger or worsen migraine.
3. Migraine and Pregnancy:
Pregnancy is a positive time for migraine patients and up to 6070% of migraneurs improve during pregnancy, particularly after the first trimester, with many achieving a remission. This is due to the sustained high levels of oestrogen, which no longer fluctuate, providing a preventative benefit to triggering attacks. After childbirth the migraine pattern tends to re-emerge within the first month. Breast-feeding may delay the re-emergence in the puerperium. 7% of women, however, experience their first migraine attack during pregnancy and women who present with new onset headache may have other causes such as cerebral venous thrombosis (CVS), preeclampsia or subarachnoid haemorrhage. Many of the acute and preventative therapies are contraindicated during pregnancy due to their potential for harm. These include the triptans, paracetamol / codeine preparations, topiramate, sodium valproate and the latest preventative therapies the CGRP monoclonal anti-body antagonists. Patients are limited to the use of simple analgesics such as paracetamol combined with metoclopramide for the treatments of acute attacks.
4. Migraine HRT and the
menopause: The perimenopausal years frequently sees a rise in the frequency and disability of migraine attacks with many women progressing to chronic migraine (> 15 headache days per month) along with the vasomotor symptoms of the menopause. This can be a very challenging time and it is due to the fluctuating and erratic oestrogen levels during this time.
The use of hormone replacement therapy (HRT) is NOT contraindicated in either Migraine With Aura or Without Aura . Oestrogen replacement therapy administered transdermally (with progestogen) in physiological doses can be very efficacious as a preventative migraine therapy and also for the troublesome menopausal vasomotor symptoms. The natural history of history of migraine is that migraine prevalence goes into a rapid decline after the menopause. It is rare, but not unheard of, for the elderly to continue to complain of migraine in their advancing years.
Management of Migraine:
The guiding principles in the management and treatment of migraine are outlined in fig:6. 1. Use of a Headache Diary. 2. Acute Therapies. 3. Preventative Therapies. 4. Non Drug Therapies. Fig:6
1.Use of a Headache Diary:
Migraine is a recurrent disorder and a headache diary is a useful guide and aid memoir in chronicling the frequency, severity, duration and impact of attacks. It helps identify trigger factors and evaluate the efficacy of acute and preventative therapies. 1. Acute Therapies: One third of migraine patients can effectively manage their acute attacks with over-the-counter simple analgesics such as soluble aspirin, paracetamol or ibuprofen. Prescribed medications, the triptans, are now the gold standard in the management of the acute attack and these include: sumatriptan, zolmitriptan, almotriptan, eletriptan, frovatriptan and naratriptan. Ideally patients should get meaningful relief from their headache and most bothersome symptoms within 2 hours. These medications can be combined with anti-nausea medication and NSAIDS (e.g. naproxyn) which may enhance efficacy. Acute therapies which provide no relief within 4 hours are deemed to be lacking in efficacy. Compound analgesics (e.g. paracetamol / codeine, tramadol) should be avoided or prescribed with caution due to risk of developing Medication-OveruseHeadache.
Newer treatments, the small molecule ‘’gepants’’, CGRP antagonists, are on the horizon and soon to be approved. They will add to armamentarium for the treatment of acute attacks and also as a preventative therapy.
2. Preventative Therapies:
Preventative therapies are indicated when patients experience 4 or more migraine days per months, and are poor responders to acute therapies. The conventional preventative therapies are listed in fig:7 1. B-blockers: propranolol, metoprolol, atenolol. 2. Anti-depressants: amitriptyline, venlafaxine.
3. Anti-epileptics: topiramate, sodium valproate. 4. Anti-hypertensives: candesartan.
5. Flunarizine.
6. Pizotifen.
7. Botulinun Toxin. Fig: 7 The benchmark in evaluating the efficacy of preventative therapies is the achievement of at least a 50% reduction in the frequency of headaches in 50% of patients. To determine this end point patients need to remain on their medication for 3 months before a determination is made. Many patients in clinical practice discontinue their preventative therapy within weeks either due to side-effects or a perceived lack of efficacy.
New Preventative Therapies:
C.G.R.P. (Calcitonin Gene Related Peptides) Monoclonal Antibody Antagonists: The CGRP monoclonal antibody antagonists are the first specifically developed migraine preventative therapies targeting the underlying mechanisms of migraine (Fig:8). 1. Erenumab 70mg or140mg s.c monthly injection. 2. Fremanezumab 225mg s.c monthly or 3 monthly 3. Galcanezumab s.c monthly 4. Eptinezumab 100mg or 300mg IV every 3 months (awaiting approval) Fig: 8 Erenumab, fremanezumab and galcanezumab are approved by the HSE on the Hi-Tech hub for patients who have Chronic Migraine (>15 headache days per month) and have failed to benefit from 3 previously prescribed conventional preventative therapies. They are licenced for patients aged between 18 and 65 years. In clinical trials benefits and efficacy are seen within 1 week and 25% of patients achieve up to 75% reduction in the frequency of headaches. Conclusions: Migraine is a common disabling disorder which significantly impacts on the quality of life of women at pivotal times throughout their adult lives. In the past, it has traditionally been underdiagnosed and undertreated. Many patients have fatalistic expectations regarding the management of migraine as they have had to endure migraine attacks for many years. Others may have witnessed a family member such as a parent or aunt or uncle suffer and endure a similar fate.
Today we are much better at diagnosing, understanding and treating migraine. Migraine specific acute and preventative are now available enabling us to better manage migraine. On going research is developing additional treatments (small molecule ‘gpants’ and ditans) which will further advance our ability to manage migraine and improve the quality of life for many migraneurs.










