

2025
IMF PATIENT AND FAMILY SEMINAR
BOCA RATON, FL

MARCH 14 & 15, 2025
Thank you to our sponsors!








IMF PATIENT AND FAMILY SEMINAR
BOCA RATON
FRIDAY AGENDA


Program Evaluations
Please be sure to complete your program evaluation today. If you are only attending the Friday Program, you can return your evaluations at the end of today. If you are returning for Saturday Program, please hold onto your survey, bring it back tomorrow and turn it in at the end of the program.
We greatly appreciate your time and feedback!

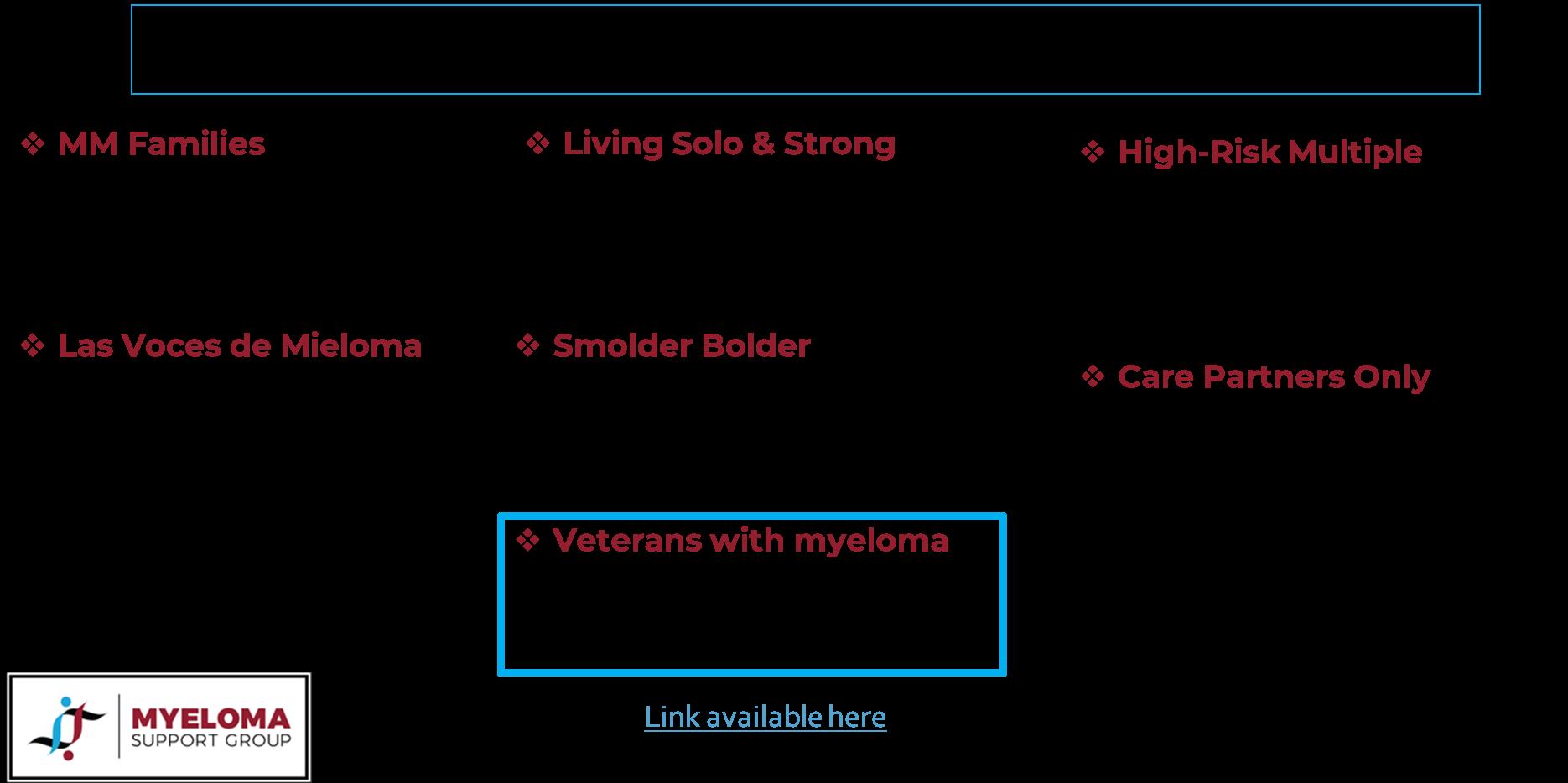
The IMF Support Group Team is Here





Melbourne Multiple Myeloma Support Group
Meets in-person on the 4th Monday of each month at 10:30AM
Maitland Multiple Myeloma Support Group
Meets in-person on the 2nd Monday of each month at 6:30pm
Ocala Multiple Myeloma Support Group
Meets in-person on the 3rd Saturday of each month at 11AM
Palm Beach County Multiple Myeloma Support Group
Meets in a hybrid format on the 1st nonholiday Monday of each month at 6:30PM
Fort Myers Multiple Myeloma Support Group
Meets in-person on the 3rd Tuesday of each month at 6pm
Hollywood Multiple Myeloma Support Group
Sarasota Multiple Myeloma Network & Education Group
Meets in-person on the 4th Friday of each month at 11AM

Meets virtually on the 2nd Tuesday of each month at 6PM
Jacksonville Multiple Myeloma Support Group
Meets in a hybrid format on the 2nd Wednesday of each month at 6PM
Palm Coast Multiple Myeloma Support Group
Meets in-person on the 2nd Thursday of each month at 3:30PM
Brooksville / Nature Coast
Multiple Myeloma Support Group
Meets virtually on the 3rd Wednesday of each month at 6PM
Tampa Bay/St Petersburg Multiple Myeloma Educational Group
Meets virtually on the 1st Saturday of each month at 10:30AM
Naples Multiple Myeloma Support Group
Meets hybrid on the 3rd Thursday of each month at 12pm
The Villages Multiple Myeloma Support Group
Meets in-person on the 1st Tuesday of each month at 1PM
North Tampa Multiple Myeloma Support Group
Meets hybrid on the 3rd Saturday of each month at 10:30AM
Tampa Central-Multiple Reasons Support Group
Meets virtually on the 2nd Thursday of each month at 11AM
Panama City Multiple Myeloma Support Group
Meets in-person on the 2nd Saturday of each month at 10AM
Sebring Multiple Myeloma Support Group
Meets virtually on the 3rd Thursday of each month at 6pm
Tallahassee Multiple Myeloma Support Group
Meets in-person on the 4th Monday of each month at 5:30PM

Myeloma Voices at ASH


In Person / 5 Virtual

Myeloma Voices


IMF InfoLine
Connecting Patients to Resources…
Shortening “Time to Hope” for Over 1,000 First-Time Callers Each Year
Assistance with understanding lab results, terminology and disease state
Preparing for medical visits
Access to medical providers
Access to medications
Financial resources
“Thank you so much for the informative conversation and all the time you spent listening and helping me decipher the MM lingo. What an amazing service!”


“Thank you for your response and excellent question suggestions for my hematology team.”







Written Education
Understanding Booklets
Tip Cards
Myeloma Minute Weekly Updates


Myeloma Today Quarterly News







































Live Patient Education
4 PATIENT & FAMILY SEMINARS including world-renowned experts
10 MYELOMA COMMUNITY WORKSHOPS including local myeloma experts

Locations



2025 Live Patient Education



Scan for Upcoming Events!






Hot Topics in Myeloma
Joseph Mikhael, MD, MEd, FRCPC, FACP, FASCO Chief Medical Officer, International Myeloma Foundation

Patient Empowerment: Shared Decision Making
Teresa Miceli, RN, BSN, OCN, InfoLine Advisor,
Nurse Leadership Board, Mayo Clinic - Rochester

Patient Empowerment: Participating in Shared Decision Making

Teresa Miceli, RN BSN OCN
International Myeloma Foundation - InfoLine Advisor, NLB Member, Support Group Leader (MMSS, Smolder Bolder)
Mayo Clinic – Myeloma Nurse Navigator
National Cancer Institute - Myeloma Patient Advocate


OUR VISION:
A world where every myeloma patient can live life to the fullest, unburdened by the disease.
OUR MISSION:
Improving the quality of life of myeloma patients while working toward prevention and a cure.


Goals
• Review Shared Decision Making (SDM) Concepts
• Identify Influencing Factors To Treatment Decision Making
• Discuss Strategies To Enhance Patient Empowerment & Promote Shared Decision Making


Patient-Centric Care
“The aim of shared decisionmaking is to ensure that:
• Patients understand their options and the pros and cons of those options.
• Patient's goals and treatment preferences are used to guide decisions.”

Image Credit: https://www.ahrq.gov/health-literacy/professional-training/shared-decision/index.html
Agency
for Healthcare Research and Quality (AHRQ)

https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/communication/strategy6i-shared-decisionmaking.html#6i1


Steps in the Shared Decision-Making Process
Identify that a decision is needed: The HCP informs the patient that a decision is to be made and that the patient's opinion is important (Choice talk).
Understand the options:
The HCP explains the evidence-based options and their pros and cons. The patient expresses their preferences, and the HCP supports the patient in decision-making (Option talk).
Come to a decision:
The HCP and patient discuss the patient's wish to take part in the decision making and incorporate the patient's values and preferences into the decision (Decision talk).
Follow-up:
Review and evaluate the decision, adjust as needed



Benefits of Shared-Decision Making
Patients, regardless of age, want to be a part of treatment decisionmaking
Reduces uncertainty and alleviates concerns
Decisions reflect personal and family values and preferences
Requires staying informed
Promotes patient and care partner engagement and sense of empowerment
Positive impact on QOL and continuation on therapy

“The 'efficacy' of treatment means different things to different patients, and treatment decision-making in the context of personalized medicine must be guided by an individual's composite definition of what constitutes the best treatment choice.” Terpos, et al.
https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/communication/strategy6i-shared-decisionmaking.html#6i1. Choon-Quinones, M. et al. 2022; Terpos, et al. 2021


Factors That Influence Shared-Decision Making
Disease-Derived
Biology: Risk stratification, Urgent intervention needed vs time to consider options

Patient-Derived

Treatment: Availability/access, effectiveness, toxicity, current research
Understanding complex treatment options
Physical and emotional wellness
Comfort in speaking up “Doctor knows best”
Financial, Cultural and Religious factors
Care partner & social network, transportation


Provider-Derived
Time limitations
Support for patient involvement
Provider bias and preference
https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/communication/strategy6i-shared-decisionmaking.html#6i1. Choon-Quinones, M. et al. 2022; Terpos, et al. 2021 https://www.valueinhealthjournal.com/action/showFullTableHTML?isHtml=true&tableId=tbl4&pii=S1098-3015%2822%2900198-X


STRATEGIES FOR PATIENT EMPOWERMENT & SHARED DECISION MAKING


Strategies: Stay Informed



















myeloma.org


Seek Information, Understand your options
Use caution considering stories of personal experiences
Your healthcare team members are resources
Use reliable and current sources of information
IMF Website: http://myeloma.org
• Publications
• Videos and Replays
• Future Events, both in-person & virtual




Strategies: Be Involved In Your Care

Consider your priorities
Consider your goals/values/preferences
Include your care partner/network in the discussion


Be a part of the conversation, create a dialog
Ask questions & express your goals/values/preferences
Ask for time to consider options, if needed
Arrive at a treatment decision together
Arrange follow up to review and adjust the plan, if needed





Strategies: Know The Members Of Your Team

Understand their different roles
Myeloma specialist and General Heme/Onc
Primary care: for health screening, general check ups, vaccinations
Sub-specialists: specialty needs
Stay connected
Keep a contact list of your providers
Know who to contact for more information








Allied

Strategies: Prepare for Medical Visits

Prepare
Medications: Bring a current list of prescribed and over-the-counter
Questions: Prioritize questions & concerns including financial issues
Paperwork needing medical signature (ex FMLA, prior authorizations)
Inform
Updates: Medical or life changes since your last visit
Symptoms: How have they changed (improved, worsened, stable)? Keep a symptom diary. Bring it along
Communicate effectively so your health care team can help
Follow Up
“Next Steps”: Future appointments, medication changes, plan of care. Ask for the information in writing or on your patient portal
Include a care partner, especially for pivotal appointments


Strategies: Prepare for Tele-Health Visits

Check with your healthcare team –
Is telemedicine an option?
What is the process and what technology is needed?
Are labs needed in advance? Do you need an order?
Preparation is similar for “in-person” appointment PLUS:
Location: quiet, well-lit location with strong Wi-Fi is best
Yourself: Do you need to show a body part - wear accessible clothing
Vital signs (blood pressure, temp, heart rate, weight) self-serve blood pressure cuff is available at many pharmacies and for purchase
Include a care partner, especially for pivotal appointments


Create a Care Network

Care partners assist in many ways

Myeloma causes the highest burden of symptoms, most commonly effecting people of older age with other medical issues. Care partner support is valuable in SDM

Attending medical appointments, being present to learn and discuss possible treatment options and alert the medical team of side effects to treatment
Some treatment options available only if care partner support exists
Care partners can be one person or a rotation of many people
Building a partnership is based in good communication
Finding the balance:



- helping the patient with needed activities while maintaining a sense of independence
- allowing the care partner to have time for good self-care



Key Take-Aways and Things to Think About

Over the next two days:
Evaluate where you are at in the process (What decisions need to be made?)
Absorb the information being presented (What are the options?)
Consider how the information impacts you and your family (What are your preferences?)
Create questions that will lead to better understanding (What more do I need to know before making a decision?)
Be an active member of your health care team
Shared Decision Making





Myeloma 101: The Big Picture Perspective with Q&A
Joseph Mikhael, MD, MEd, FRCPC, FACP, FASCO, Chief Medical Officer, International Myeloma Foundation
Teresa Miceli, RN, BSN, OCN, InfoLine Advisor,
Nurse Leadership Board, Mayo Clinic – Rochester, MN


MM101: The Big Picture Perspective

Joseph Mikhael, MD, MEd, FRCPC, FACP

• Professor, Applied Cancer Research and Drug Discovery, Translational Genomics Research Institute (TGen), City of Hope Cancer Center
• Chief Medical Officer, International Myeloma Foundation
• Consultant Hematologist and Director, Myeloma Research,
Phase 1 Program, HonorHealth Research Institute
• Adjunct Professor, College of Health Solutions, Arizona State University
Teresa S. Miceli RN BSN OCN
Mayo Associate, Assistant Professor of Nursing
Myeloma Research RN Navigator, Mayo Clinic, Rochester, MN
International Myeloma Foundation
InfoLine Advisor, Nurse Leadership Board, Support Group Leader
NCI Myeloma Steering Committee


How common is Myeloma in the US?








What
Causes Myeloma? How/Why Did I Get This?
Environmental Factors:
• Exposure to some chemicals
• Radiation exposure
Examples:
Agent Orange
Burn pits
Pesticides, Herbicides
Firefighter/First Responder exposures
Individual Factors:
• Age
• Family History of related disorders
• Personal History of MGUS or SMM
• Obesity
VA Study Documents Health Risks for Burn Pit Exposures
Leukemia and Multiple Myeloma Set to Be Added to List of Conditions Linked to Burn Pits
In most cases, the honest truth
WE DON’T KNOW



What is the Connection Between Bone Marrow & Myeloma ?






Photo Credit
Understanding (Mono)clonal Plasma Cells

Heavy Chain: G, A, M, D, E




Heavy Chain = M-Spike

65% IgG – most common
20% IgA – associated with AL Amyloid
5% to 10% light chain-only (kappa, lambda)
Less common: IgD, IgE, IgM



Is Myeloma the Only Protein Disorder?
• AL-Amyloid
• POEMS
• Light or Heavy Chain Deposition Disease
• MGCS = Clinical
• MGRS = Renal
• MGNS = Neuro
Condition
Clonal plasma cells in bone marrow
MGUS1-4 (Monoclonal Gammopathy of Undetermined Significance)
SMM1-5,8 (Smoldering Multiple Myeloma) Active Multiple Myeloma6-8
Presence of Myeloma
Defining Events
Likelihood

* In clinical trial






Testing For Myeloma: Blood & Urine
Test Name
CBC + differential
Complete metabolic panel
Beta-2 Microglobulin (B2M)
Lactate Dehydrogenase (LDH)
Serum Immunofixation and Protein
electrophoresis (SPEP+IFE)
Immunoglobulins (G, A, M, D, E)
Free light chain assay with kappa/lambda ratio
Urine immunofixation & protein electrophoresis (UPEP+IFE)
What it means
Hemoglobin, WBC, Platelets
Creatinine, Calcium, Albumin, Liver function
Part of staging and risk stratification
Measures the level of normal and clonal protein
Identifies the type of clonal protein

Measures the level of normal and clonal protein
Identifies the type of clonal protein




This Photo by Unknown Author is licensed under CC BY-SA-NC

Testing For Myeloma: Imaging
Imaging:
– Skeletal survey: Series of X-rays; less sensitive than other techniques
– Whole body low dose (CTWB-LD CT )
– Positron Emission Tomography (PET/CT)
– Magnetic Resonance Imaging (MRI)

Healthy bone versus myeloma bone disease




This Photo by Unknown Author is licensed under CC BY-NC-ND

Testing For Myeloma: Bone Marrow


Bone marrow biopsy & aspirate • Bone marrow plasma cells (%) • Congo Red staining if concern
Bone marrow genetics
• Cytogenetics
• Fluorescence in situ hybridization (FISH)
• Next generation sequencing (NGS)



This Photo by Unknown Author is licensed under CC BY-SA
What is the Myeloma Treatment Landscape?
Initial Therapy (a.k.a. Frontline, Induction)
Quad Therapy (ex. CD38+ MoAb + VRd)
HD-Melphalan + Stem Cell
Transplant (ASCT)
Maintenance
Treatment for Relapse
Supportive Care and Living Well
Relapse



Drug Class Overview

(thalidomide)
(lenalidomide)
(pomalidomide)
Rev, Len
or Pom
(daratumumab)
(isatuximab)


Drug Class Overview

Peptide Drug Conjugate* Pepaxto (Melphalan Flufenamide)
BCMA Targeted Antibody Drug
Conjugate (ADC)*
Blenrep (belantamab mafodotinblmf )
Abecma (idecabtagene vicleucel)
Belamaf, or B
Bispecific Antibodies
Carvykti (ciltacabtagene vicleucel)
Tecvayli (teclistimab)
Talvey (Talquetamab)
Elrexfio (Elranatamab)
Cevostamab, Iberdomide, Mezigdomide, Venetoclax Linvoseltamab, LCAR-B38M, ABBV-383

Measuring Disease Response: IMWG Response Criteria
























Negative by next generation flow (NGF) (minimum sensitivity 1 in 10-5 nucleated cells or higher)*
mCR AND normal Free Light Chain ratio, Bone Marrow negative by flow, 2 measures
CR AND negative PCR
Complete Response: Negative immunofixation (IFE); no more than 5% plasma cells in BM; 2 measures
Very Good Partial Response: 90% reduction in myeloma protein
Partial Response: at least 50% reduction in myeloma protein
Minimal Response
Stable Disease: Not meeting above criteria
Progressive Disease: At least 25% increase in identified myeloma protein from lowest level
MRD = Minimal Residual Disease
sCR = Stringent Complete Response; BM = Bone Marrow
Kumar, S., Paiva, B., Anderson, K. C., Durie, B., Landgren, O., Moreau, P., ... & Dimopoulos, M. (2016). International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. The lancet oncology, 17(8), e328-e346.


When Do I Need A New Treatment?
• Not every relapse requires immediate therapy
• Each case is different
Symptomatic or extramedullary disease


Asymptomatic biochemical relapse on 2 consecutive assessments

Asymptomatic high-risk disease or rapid doubling time or extensive marrow involvement Consider Observation Monitor Carefully Consider Treatment
Patient-/Disease-Specific Monitor Carefully
Initiate Treatment

Targets on the Myeloma Cell Surface and Therapeutic Antibodies

Bi-Specific Antibodies
Talvey (Talquetamab) CAR-T



Antibody Drug
Empliciti (Elotuzumab)
Bi-Specific Antibodies



Bi-Specific Antibodies
CAR-T






Monoclonal Antibodies
Daratumumab and Darzalex Faspro
Sarclisa (Isatuximab)
TAK-079 MOR202

Immune Therapies
Abecma (Ide-cel CAR-T)
Carvykti (Cilta-cel CAR-T)
Tecvayli (Teclistamab)
Elrexfio (Elranatamab)




Other CAR Ts



Other Bi Specific Antibodies



Antibody Drug Conjugates



How it works:
An antibody directed at a target (BCMA) combined with a cytotoxic agent (chemotherapy)
ADC = Antibody-Drug Conjugate
BCMA = B-Cell Maturation Antigen


ADCP/ADCC = Antibody-Dependent Cellular Cytotoxicity & Phagocytosis
Image Credit: https://creativecommons.org/licenses/by-nc/3.0/


Bispecific Antibodies: Mechanism of Action
• Incorporates 2 antibody fragments to target and bind both tumor cells and T cells
• Brings target-expressing MM cells and T cells into close proximity, enabling T cells to induce tumor-cell death
Targets of Bispecific Molecule Vary


FcRH5
“Off the Shelf” Advantage
• No manufacturing process, unlike CAR T-cell therapy (but like ADC/belantamab therapy)
• Thus, no delay between decision to treat and administration of drug ADC = Antibody-Drug Conjugate; BCMA = B-Cell Maturation Antigen; CD3 = Cluster of Differentiation 3; FcRH5 = Fc receptor-homolog 5; GPRC5D = G-protein coupled receptor family C group 5 member D


The Process of CAR T Cell Therapy
CAR T therapy recommended. Insurance approved and ready to move forward.













What about Disease Control and Cure in Myeloma?


Requiring Treatment Stable or Unmeasurable Disease, Receiving Treatment Control is the immediate priority with active disease Cure remains the overall goal
Defining “Cure” has many considerations:
Minimal Residual Disease Negative (MRD-)
Time Off Therapy
Functional Cure
Unmeasurable Disease, Receiving No Treatment Active Disease
https://seer.cancer.gov/statfacts/html/mulmy.html; dated 6.15.2024


The Evolution of Myeloma Therapy
VD
Rev/Dex
CyBorD
VTD
VRD
KRD
D-VMP
DRD
ASCT
Tandem ASCT (?)
Nothing
Thalidomide?
Bortezomib
Ixazomib
Lenalidomide
Combinations
Bortezomib
Lenalidomide
Carfilzomib
Pomalidomide
Selinexor
Panobinostat
Daratumumab
Ixazomib
Elotuzumab
Isatuximab
Belantamab mafodotin*
Melphalan flufenamide*
Idecabtagene autoleucel
Ciltacabtagene autoleucel
Teclistamab, Talquetamab
Elranatamab
D-VRD
Isa-VRD
D-KRD
Isa-VRD “More” induction?
Daratumumab?
Carfilzomib?
Lenalidomide + PI
ASCT, autologous stem cell transplant; CAR, chimeric antigen receptor; Cy, cyclophosphamide; d- daratumumab; D/dex, dexamethasone; isa, isatuximab; K, carfilzomib; M, melphalan; PD-L1, programmed death ligand-1; PI, proteasome inhibitor; Rev, lenalidomide; V, bortezomib.
Speaker’s own opinions.
CAR T Cell Therapy
Bispecific/Tri-specific
Antibodies
Cell Modifying Agents
Venetoclax
PD/PDL-1 Inhibition?
Small Molecules
* These agents are currently off the market but available through special programs
Anito-cel
Cevostomab
Linvoseltamab
Iberdomide, Mezigdomide
Sonrotoclax


















Advocacy Update: Myeloma Advocacy Priorities & How to Help
Danielle Doheny International Myeloma Foundation, Director of Public Policy & Advocacy
Advocacy Overview and Medicare Changes in 2025 & Beyond
Danielle Doheny IMF, Director of U.S. Policy & Advocacy



Introduction | Advocacy at the IMF
The Global Advocacy Team collaborates with multiple stakeholders to inform and influence decision-making on the critical healthcare issues that directly impact myeloma patients.

The U.S. Advocacy Team advocates for equitable access to timely diagnosis, innovative treatments and research funding on Capitol Hill and with key regulatory agencies.
The team advocates both alongside of and on behalf of the patient community that we serve.

Advocacy plays a critical role to educate policymakers about the issues important to our community and motivate them to act.
What Do We Advocate For?

The following policy principles are the foundation on which we prioritize our advocacy work.
1. Ensure Access to Care: We advocate for policies that ensure all myeloma patients have equitable, comprehensive, patient-centered care without insurance barriers that limit options or delay treatment initiation.
2. Eliminate Financial Barriers: We advocate for policies that allow myeloma patients access to treatments and supportive care interventions without facing financial hardships.
3. Advance Myeloma Research: We advocate for annual appropriations funding for myeloma research and the advancement of clinical trial eligibility and research protocols that ensure representation from diverse populations.


2025 U.S. Advocacy Priorities Snapshot

1. ENSURE ACCESS TO CARE
INSURANCE REFORM: DRUG ACCESS
Step Therapy Protocols Safe Step Act
INSURANCE REFORM: DRUG ACCESS PBM Reform PBM Reform Act
2. ELIMINATE FINANCIAL BARRIERS
3. ADVANCE MYELOMA RESEARCH
MEDICARE REFORM:
PHYSICIAN ACCESS
Tele-Health/Medicine
Telehealth Modern. Act
INSURANCE REFORM: COINSURANCE
Oral Parity Cancer Drug Parity Act
INSURANCE REFORM: COPAYS Copay Accumulators HELP Copays Act
FEDERAL FUNDING
Annual Appropriations
NIH: National Cancer Institute, National Institute on Minority Health, ARPAH

MEDICARE REFORM: ANNUAL COST LIMITS
ANNUAL APPROPS Inflation Reduction Act implementation Cap & Smoothing (MPPP), Drug Pricing, Drug Formularies
CDC: Comprehensive Cancer Control Initiative
DoD: Congressionally Directed Medical Research Program (CDMRP) for Myeloma.
CLINICAL TRIAL DIVERSITY
Primary care education, Focus on underserved, POC, rural settings and socioeconomically disadvantaged groups
Medicare Changes Detailed | A Phased Approach



No copays for vaccines under Part D
Insulin copays limited to $35/month

Expanded eligibility for the Extra Help Program (Federal Low-Income Subsidy) to help pay premiums, deductibles, coinsurance & other costs
$3,250 annual cap (approx.) on out-of-pocket spending for prescription drugs under Part D (eliminating 5% coinsurance in catastrophic phase)

$2,000 annual cap on out-of-pocket spending for prescriptions under Part D
Option for a monthly payment program to “smooth out” total out-of-pocket spending throughout the year, with an overall monthly maximum

• Patients will need to enroll in the program (opt-in)
• The earlier in the year you join the program, the more you can benefit
• Your monthly bill may fluctuate somewhat
• No one will pay more than $2000 for the year

Inflation Reduction Act (IRA) & Highlight of Changes to Medicare


What is Happening With Research Funding?





Addressing healthcare barriers for multiple myeloma patients depends on winning over the hearts and minds of policymakers. It is not enough to just identify an issue and have data-driven evidence/research to back it up. It is not even enough to work with coalition partners that agree with our point of view. We must convince policymakers to prioritize our issues, draft legislation and vote it into law. Join Us! Join the Advocacy Team and share Your Story.



Thank You



Understanding Clinical Trials
Joseph Mikhael, MD, MEd, FRCPC, FACP, FASCO, Chief Medical Officer, International Myeloma Foundation






Clinical Trials
Joseph Mikhael MD, MEd, FRCPC
Chief Medical Officer, International Myeloma Foundation
Professor, Translational Genomics Research Institute, City of Hope Cancer Center
Yelak Biru, MSc

President and CEO , International Myeloma Foundation

Objectives




Clinical Trials - Overview
Some Of The Important Principles Of Clinical Trials:

The drive of research has brought us to where we are
No one is expected to be a “guinea pig” with no potential benefit to them
Research is under very tight supervision and standards
Open, clear communication between the physician and the patient is fundamental Driving research forward!







MYTH: If I participate in a clinical trial, I might get a placebo, not active treatment
MYTH: If I participate in a clinical trial, I can’t change my mind
Clinical Trials: Myths
• Phase 1 and 2, everyone gets active treatment
• Phase 3 standard of care vs new regimen: often standard regimen with/without additional agent in MM trials
• Patients can withdraw their consent for clinical trial participation at any time
MYTH: Clinical trials are dangerous because they have new medicines and practices
• Some risk is involved with every treatment, but medicines are used in clinical trials with people only after they have gone through testing to indicate that the drug is likely to be safe and effective for human use
MYTH: Clinical trials are expensive and not covered by insurance
• Research costs are typically covered by the sponsoring company
• Standard patient care costs are typically covered by insurance
• Check with clinical trial team/insurers; costs such as transportation, hotel, etc may not be reimbursed and are paid by patient
website. Accessed March 25, 2024. https://phrma.org/-/media/Project/PhRMA/PhRMA-Org/PhRMA-Org/PDF/A-C/CLINICAL-TRIALS-MYTH-FACTPRINT.pdf?hsCtaTracking=f6689b95-1626-40d9-8c87-c6b8d31600a4%7C35221aa8-d487-4db3-9416-b9c3c35e3bac


Clinical Trials – Why Me??
Every patient is unique and must be viewed that way
Benefits of trials are numerous and include:
Early access to “new” therapy
Delay use of standard therapy
Contribution to myeloma world – present and future
Financial access to certain agents
Must be balanced with potential risks
“Toxicity” of side effects
Possibility of lack of efficacy


Overview of New Drug Development

Identify a target for therapy in the laboratory
Confirm the anticancer activity in laboratory and animal studies
Clinical trials (human studies) to determine safety, dosing and effectiveness
The whole process costs millions of dollars and years of effort!


Even Before Phase I
Most agents are tested in lab models
Various “myeloma cell lines”, also known as “in vitro”
Next step is animal model
We are more like mice than you think!!
Earliest study in Phase I is called “First in Human”
Often uses extremely low dose of drug to ensure safety


Phase 1 Clinical Trials
All patients receive the experimental therapy
Phase 1 trials find the optimal dose of a new drug or drug combination
Patients get higher doses as the study continues
Determine side effects of new drugs or combinations
Explore how the drug is metabolized by the body

Important for all stages of myeloma



Phase 2 Clinical Trials
Determine if a new drug or combination is effective against the cancer
May be added to a Phase 1 study once the ideal dose is found
Patients usually receive the experimental therapy
In some cases, the study may include two “arms” comparing either two different doses or a different treatment (another combination of drugs)



Phase 3 Clinical Trials
Highest form of clinical evidence. Typically, a large number of patients are required…usually required for full FDA approval
Patients receive either an experimental therapy (one or more drugs) or the current standard treatment
o The patient is randomly assigned to a treatment—a process called “randomization”
o Neither the physician or the patient can determine which treatment is given

May be placebo controlled, if no standard treatments are available
Very closely monitored for effectiveness and side effects


Preclinical

Clinical Trial Phases
ANIMAL STUDIES: Examine safety and potential for efficacy
PHASE 1
PHASE 2
FIRST INTRODUCTION OF AN INVESTIGATIONAL DRUG INTO HUMANS
• Determine metabolism and PK/PD actions, MTD, and DLT
• Identify AEs
• Gain early evidence of efficacy, studied in many conditions; typically, 20 to 80 patients; everyone gets agent
EVALUATION OF EFFECTIVENESS IN A CERTAIN TUMOR TYPE
• Determine short-term AEs and risks; closely monitored
• Includes up to 100 patients, typically
PHASE 3
GATHER ADDITIONAL EFFECTIVENESS AND SAFETY INFORMATION
COMPARED TO STANDARD OF CARE
• Placebo may be involved if no standard of care exists; hundreds to several thousand patients
• Often multiple institutions; single or double blind; sometimes open label
PHASE 4
APPROVED AGENTS IN NEW POPULATIONS OR NEW DOSE FORMS


Clinical Trials: Benefits of Participation
Possible Benefits:
• Patients will receive, at a minimum, the best standard treatment
• If the new treatment or intervention is proven to work, patients may be among the first to benefit
• Patients have a chance to help others and improve cancer care



Risks of Participation
Possible risks:
• New treatments or interventions under study are not always better than, or even as good as, standard care
• Even if a new treatment has benefits, it may not work for every patient
• Health insurance and managed care providers do not always cover clinical trials



Why Do So Few Cancer Patients Participate in Trials?
Patients may:
• Be unaware of clinical trials
• Lack access to trials
• Fear, distrust, or be suspicious of research
• Have practical or personal obstacles
• Face insurance or cost problems
• Be unwilling to go against their physicians’ wishes
• Not have physicians who offer them trials
• Have a disconnect with their healthcare team



Diversity in Clinical Trials
There has been a lack of diverse representation in clinical trials in myeloma.
In the U.S., approximately 20% of all myeloma patients are of African descent, but only 5%–8% of patients in myeloma clinical trials are of African descent.
This is significant for the following reasons:
All patients of all races and ethnicities should be able to benefit from clinical trials.
Diverse patient representation in clinical trials is required to ensure that the outcomes are applicable to all patients.
Reasons for underrepresentation in clinical trials are complex and include:
Systemic racism, accessibility of clinical trials, sensitivity to diversity by medical professionals
Misconduct in medicine in the past, the lack of trust in the system, and more.



Importance of Clinical Trial Participation by Diverse Populations
[P]eople from racial and ethnic minorities and other diverse groups are underrepresented in clinical research. This is a concern because people of different ages, races, and ethnicities may react differently to certain medical products.
– FDA

Leadership and commitment
Community engagement practices
Investigator hiring, training, and mentoring practices
Patient engagement practices
US Cancer Centers of Excellence: Strategies for Increased Inclusion of Racial and Ethnic Minorities in Clinical Trials


Commonly Asked Questions
How does the study work? How often will I need to see my doctor or visit the cancer center?
Will I need to undergo additional tests?
What is currently known about the new drug or combination?
What benefits can I expect?
What side effects should I expect? Who should I notify if I have side effects?




Can I take my vitamins or other medications?
Can I get the treatment with my local doctor?
Will my insurance pay for my participation in the clinical trial?






Is A Clinical Trial Right For Me?
Discuss with your physician if you are eligible for a clinical trial
Work with your physician to determine the best trial for you
Meet with the clinical research nurse or trials coordinator to discuss the trial
Carefully review the provided “Informed Consent”
Describes the study and any potential safety concerns related to the experimental medication







Accessed March 15, 2024. https://www.accccancer.org/home/attend/webinartemplate/2022/07/25/on-demand/just-askincreasing-diversity-in-cancer-clinical-research






Q&A WITH GUEST PANEL
Program Evaluations
Please be sure to complete your program evaluation today. If you are only attending the Friday Program, you can return your evaluations at the end of today. If you are returning for Saturday Program, please hold onto your survey, bring it back tomorrow and turn it in at the end of the program.
We greatly appreciate your time and feedback!

IMF PATIENT AND FAMILY SEMINAR
BOCA RATON
AGENDA
SATURDAY MORNING


IMF PATIENT AND FAMILY SEMINAR
BOCA RATON
AGENDA
SATURDAY
AFTERNOON


Thank you to our sponsors!








5:00 – 7:00 PM Welcome Reception



Royal Palm Ballroom
OUR VISION:
A world where every myeloma patient can live life to the fullest, unburdened by the disease.
OUR MISSION:
Improving the quality of life of myeloma patients while working toward prevention and a cure.

IMF Core Values:
These are the core values we bring to accomplishing our mission each day.
Patient Centric
The patient experience is the focus of everything we do. Every interaction is an opportunity to establish a personal connection built on care and compassion which is the basis for continued support.
Respect All
As a team, we value honesty and transparency while creating a culture of mutual respect. We foster a myeloma community built on sincerity, authenticity, and kindness.
Excellence and Innovation
We value accountability, personal responsibility, and a steadfast commitment to excellence. We respect the legacy and reputation of our organization while seeking new solutions and advancements to improve outcomes, quality of life, and access to the best available resources for everyone impacted by myeloma.
Honor differences
We recognize each team member's skills and talents through collaboration and cooperation. Our programs aim to celebrate and support the diversity of our patients and their communities.




