INTERNATIONAL JOURNAL OF SPORTS PHYSICAL THERAPY





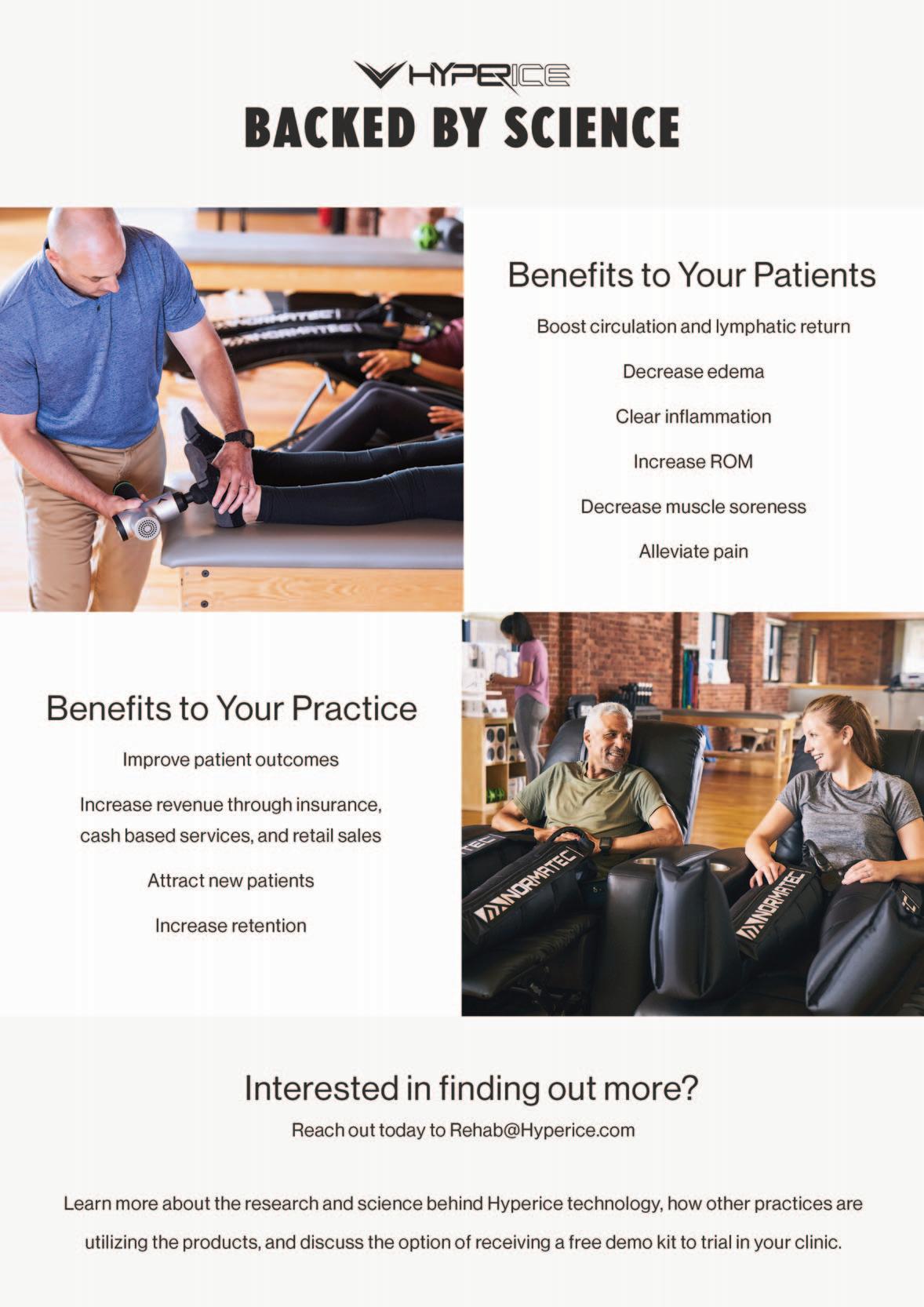
BOOST is a positive air-pressure off-weighting treadmill built on a WOODWAY slat-belt base. Learn more by visiting the link below.


the original. the best. | visit us at woodway.com

off-weighting has evolved, so have we.
Welcome to connected medicine. Butterfly brings the power of ultrasound into your injury assessment, diagnosis and treatment process.


Rx only (USA). For use by trained healthcare practitioners.
(For UK & EU countries) Butterfly iQ+™ is a Class IIa portable ultrasound system designed for ultrasound imaging by trained healthcare professionals. Carefully read and understand all cautions, warnings and operational instructions prior to use.
(For AUS) Butterfly iQ+™ is a Class IIa portable ultrasound system designed for ultrasound imaging by trained healthcare professionals. This product is not available for purchase by the general public. Carefully read and understand all cautions, warnings and operational instructions prior to use.
(For CAN) For healthcare professionals only. Réservé aux professionnels de santé. Not all presets, imaging modes and features are available everywhere. Check for availability in your country.980-22808-00 Rev A

Turner A Blackburn, APTA Life Member, AT-Ret, AOSSM-Ret President
Mary Wilkinson Executive Director
Michael Voight Executive Editor and Publisher
Joe Black, PT, DPT, SCS, ATC
Eric Fernandez
Jay Greenstein, DC
Skip Hunter, PT, ATC-Ret
Russ Paine, PT, DPT
Mike Reinold, PT, DPT, SCS, ATC, CSCS, C-PS
Tim Tyler, PT, ATC
Turner A. Blackburn, PT, ATC
George Davies, PT, DPT, MEd, SCS, ATC, LAT, CSCS, PES, FAPTA
Terry Malone, PT, PhD
Bob Mangine, PT
Barb Sanders, PT, PhD
Tim Tyler, PT, ATC
Kevin Wilk, PT, DPT, FAPTA
Staff
Executive Editor/Publisher
Michael L. Voight, PT, DHSc, OCS, SCS, ATC, CSCS
Executive Director/Operations and Marketing
Mary Wilkinson Editor in Chief
Barbara Hoogenboom, PT, EdD, SCS, ATC
Managing Editor
Ashley Campbell, PT, DPT, SCS, CSCS
Manuscript Coordinator
Casey Lewis, PTA, ATC
Publisher
Contact Information
International Journal of Sports Physical Therapy 6011 Hillsboro Pike Nashville, TN 37215, US, http://www.ijspt.org
IJSPT is a bimonthly publication, with release dates in February, April, June, August, October and December.
ISSN 2159-2896
Founding Sponsors
Arthrex Biodex
Butterly IQ Digitsole DJO Global Exertools
Foot Levelers Hydroworx Hyperice PT Genie Trazer Woodway Gold Sponsors Hawkgrips Squid
Structure + Function Education Winback
Greece Hong Kong Indonesia Ireland Israel Italy Japan Luxembourg
IJSPT is an official journal of the International Federation of Sports Physical Therapy (IFSPT) Countries with access to IJSPT as a member benefit: Argentina Australia Austria Belgium Bulgaria Brazil Cameroon Canada Chile Cyprus Denmark Finland France Germany
The Netherlands New Zealand Nigeria Norway Poland Portugal
Reach us at www.ifspt.org.
IJSPT is an official journal of the ICCUS Society for Sports Rehabilitation. www.iccus.org

Saudi Arabia Slovenia South Africa South Korea Spain Sweden Switzerland Thailand Turkey United Kingdom Zambia

Detailed reports track recovery and provide the medical team with quantitative data to help with the return-to-play decision





Michael L. Voight, PT, DHSc, OCS, SCS, ATC, CSCS
Belmont University Nashville, Tennessee – USA
Barbara Hoogenboom, PT, EdD, SCS, ATC
Grand Valley State University Grand Rapids, Michigan - USA
Ashley Campbell, PT, DPT, SCS, CSCS
Nashville Sports Medicine and Orthopaedic Center Nashville, Tennessee USA
Casey Lewis, PTA, ATC
Nashville Sports Medicine and Orthopaedic Center Nashville, Tennessee USA
Executive Director/Marketing
Mary Wilkinson Indianapolis, Indiana USA
Robert Manske PT, DPT, Med, SCS, ATC, CSCS
University of Wichita Wichita, KS, USA
Terry Grindstaff, PT, PhD, ATC, SCS, CSCS
Creighton University Omaha, NE, USA
Phil Page PT, PhD, ATC, CSCS
Franciscan University DPT Program Baton Rouge, LA, USA
Kevin Wilk PT, DPT, FAPTA
Clinical Viewpoint Editor
Champion Sports Medicine Birmingham, AL, USA
Luciana De Michelis Mendonça, PT, PhD UFVJM
Diamantina, Brazil
Colin Paterson PT, MSc PGCert(Ed), MCSP, RISPT, SFHEA
University of Brighton Brighton, England, UK
Chris Napier, PT, PhD
Clinical Assistant Professor
University of British Coumbia, Vancouver, BC, Canada
Nicola Phillips, OBE, PT, PhD, FCSP
Professor School of Healthcare Sciences Cardiff University, Cardiff, Wales, UK
Eva Ageberg, PT, PhD
Professor, Lund University Lund, Sweden
Lindsay Becker, PT, DPT, SCS, USAW Buckeye Performance Golf Dublin, Ohio, USA
Keelan Enseki, PT, MS, OCS, SCS, ATC University of Pittsburgh Pittsburgh, PA, USA
John Heick, PT, PhD, DPT, OCS, NCS, SCS Northern Arizona University Flagstaff, AZ, USA
Julie Sandell Jacobsen, MHSc, PhD VIA University Aarhus, Denmark
RobRoy L. Martin, PhD, PT, CSCS Duquesne University Pittsburgh, PA, USA
Andrea Mosler, PhD, FACP, FASMF La Trobe Sport and Exercise Medicine Research Centre, School of Allied Health, Human Services and Sport, La Trobe University Melbourne, Victoria, Australia
Brandon Schmitt, DPT, ATC PRO Sports Physical Therapy Scarsdale, NY, USA
Barry Shafer, PT, DPT Elite Motion Physical Therapy Arcadia, CA, USA
Laurie Stickler, PT, DHSc, OCS Grand Valley State University Grand Rapids, MI, USA
Editorial Board
James Andrews, MD Andrews Institute & Sports Medicine Center Gulf Breeze, AL, USA
Amelia (Amy) Arundale, PT, PhD, DPT, SCS Red Bull/Ichan School of Medicine Salzburg, Austria/New York, NY, USA
Gary Austin, PT PhD Belmont University Nashville, TN, USA
Roald Bahr, MD Oslo Sports Trauma Research Center Oslo, Norway
Lane Bailey, PT, PhD Memorial Hermann IRONMAN Sports Medicine Institute Houston, Texas, USA
Gül Baltaci, PT,Ph.D. Professor, CKTI, FACSM Private Guven Hospital Ankara, Turkey
Asheesh Bedi, MD University of Michigan Ann Arbor, MI, USA
David Behm, PhD
Memorial University of Newfoundland St. John's, Newfoundland, Canada
Barton N. Bishop, PT, DPT, SCS, CSCS Kaizo Clinical Research Institute Rockville, Maryland, USA
Mario Bizzini, PhD, PT Schulthess Clinic Human Performance Lab Zürich, Switzerland
Joe Black, PT, DPT, SCS, ATC Total Rehabilitation Maryville, Tennesse, USA
Turner A. "Tab" Blackburn, APTA Life Member, ATC-Ret, AOSSM-Ret NASMI Lanett, AL, USA
Lori Bolgla, PT, PhD, MAcc, ATC Augusta University Augusta, Georgia, USA
Matthew Briggs
The Ohio State University Columbus, OH, USA
Tony Brosky, PT, PhD Bellarmine University Louisville, KY, USA
Brian Busconi, MD UMass Memorial Hospital Boston, MA, USA
Robert J. Butler, PT, PhD St. Louis Cardinals St. Louis, MO, USA
Duane Button, PhD Memorial University St. Johns, Newfoundland, Canada
J. W. Thomas Byrd, MD
Nashville Sports Medicine and Orthopaedic Center Nashville, TN, USA
Lyle Cain, MD Andrews Institute & Sports Medicine Center Birmingham, AL, USA
Gary Calabrese, PT, DPT Cleveland Clinic Cleveland, Ohio, USA
Meredith Chaput, PT, DPT, SCS Ohio University Athens, OH, USA
Rita Chorba, PT, DPT, MAT, SCS, ATC, CSCS
United States Army Special Operations Command Fort Campbell, KY, USA
John Christoferreti, MD Texas Health Dallas, TX, USA
Richard Clark, PT, PhD Tennessee State University Nashville, TN, USA
Juan Colado, PT, PhD University of Valencia Valencia, Spain
Brian Cole, MD Midwest Orthopaedics at Rush Chicago, IL, USA
Ann Cools, PT, PhD Ghent University Ghent, Belgium
Andrew Contreras, DPT, SCS Washington, DC, USA
George Davies, PT, DPT, MEd, SCS, ATC, LAT, CSCS, PES, FAPTA Georgia Southern University Savannah, Georgia, USA
Pete Draovich, PT Jacksonville Jaguars Footbal Jacksonvile, FL, USA
Jeffrey Dugas, MD Andrews Institute & Sports Medicine Center Birmingham, AL, USA
Jiri Dvorak, MD Schulthess Clinic Zurich, Switzerland
Todd Ellenbecker Rehab Plus Phoenix, AZ, USA
Carolyn Emery, PT, PhD University of Calgary Calgary, Alberta, Canada
Ernest Esteve Caupena, PT, PhD University of Girona Girona, Spain
Sue Falsone, PT, MS, SCS, ATC, CSCS, COMT Structure and Function Education and A.T. Still University Phoenix, Arizona, USA
J. Craig Garrison, PhD, PT, ATC, SCS Texas Health Sports Medicine Fort Worth, Texas, USA
Maggie Gebhardt, PT, DPT, OCS, FAAOMPT Fit Core Physical Therapy/Myopain Seminars Atlanta, GA and Bethesda, MD, USA
Lance Gill, ATC LG Performance-TPI Oceanside, CA, USA
Phil Glasgow, PhD, MTh, MRes, MCSP Sports Institute of Northern Ireland Belfast, Northern Ireland, UK
Robert S. Gray, MS, AT Cleveland Clinic Sports Health Cleveland, Ohio, USA
Jay Greenstein, DC Kaizo Health Baltimore, MD, USA
Martin Hagglund, PT PhD
Linkoping University Linkoping, Sweden
Allen Hardin, PT, SCS, ATC, CSCS
University of Texas Austin, TX, USA
Richard Hawkins, MD
Professor of surgery, University of South Carolina Adjunct Professor, Clemson University Principal, Steadman Hawkins, Greenville and Denver (CU)
John D.Heick, PT, PhD, DPT, OCS, NCS, SCS
Northern Arizona University Flagstaff, AZ, USA
Tim Hewett, PhD Hewett Consulting Minneapolis, Minnesota, USA
Per Hølmich, MD
Copenhagen University Hospital Copenhagen, Denmark
Kara Mae Hughes, PT, DPT, CSCS Wolfe PT Nashville, TN, USA
Lasse Ishøi, PT, MSc
Sports Orthopedic Research Center
Copenhagen University Hospital Hvidovre, Denmark
Jon Karlsson, MD Sahlgrenska University Goteborg, Sweden
Brian Kelly, MD Hospital for Special Surgery New York, NY, USA
Benjamin R. Kivlan, PhD, PT, OCS, SCS
Duquesne University Pittsburgh, PA, USA
Dave Kohlrieser, PT, DPT, SCS, OCS, CSCS
Ortho One Columbus, OH, USA
Andre Labbe PT, MOPT
Tulane Institute of Sports Medicine New Orleans, LA USA
Henning Langberg, PT, PhD University of Copenhagen Copenhagen, Denmark
Robert LaPrade, MD Twin Cities Orthopedics Edina, MN, USA
Lace Luedke, PT, DPT University of Wisconsin Oshkosh Oshkosh, WI, USA
Lenny Macrina, PT, SCS, CSCS, C-PS Champion Physical Therapy and Performance Boston, MA, USA
Phillip Malloy, PT, PhD
Arcadia University/Rush University Medical Center Glenside, PA and Chicago, IL, USA
Terry Malone, PT, EdD, ATC, FAPTA University of Kentucky Lexington, KY, USA
Robert Mangine, PT University of Cincinnati Cincinnati, OH, USA
Eric McCarty, MD University of Colorado Boulder, CO, USA
Ryan P. McGovern, PhD, LAT, ATC Texas Health Sports Medicine Specialists Dallas/Fort Worth, Texas, USA
Mal McHugh, PhD NISMAT New York, NY, USA
Joseph Miller, PT, DSc, OCS, SCS, CSCS Pikes Peak Community College Colorado Springs, CO, USA
Havard Moksnes, PT PhD Oslo Sports Trauma Research Center Oslo, Norway
Michael J. Mullaney, PT, SCS NISMAT Mullaney & Associates Physical Therapy New York, NY and Matawan, NJ, USA
Andrew Murray, MD, PhD European PGA Tour Edinburgh, Scotland, UK
Andrew Naylor, PT, DPT, SCS Bellin Health Green Bay, WI, USA
Stephen Nicholas, MD NISMAT New York New York, NY, USA
John O'Donnel, MD Royal Melbourne Hospital Melbourne, Australia
Russ Paine, PT McGovern Medical School Houston, TX, USA
Snehal Patel, PT, MSPT, SCD HSS Sports Rehabilitation Institute New York, NY, USA
Marc Philippon, MD Steadman-Hawkins Clinic Vail, CO, USA
Kevin Plancher, MD, MPH, FAAOS Plancher Orthopedics and Sports Medicine New York, NY USA
Marisa Pontillo, PT, PhD, DPT, SCS University of Pennsylvania Health System Philadelphia, PA, USA
Matthew Provencher, MD Steadman Hawkins Clinic Vail, CO, USA
Charles E. Rainey, PT, DSc, DPT, MS, OCS, SCS, CSCS, FAAOMPT United States Public Health Service Springfield, MO, USA
Alexandre Rambaud, PT PhD Saint-Etienne, France
Carlo Ramponi, PT Physiotherapist, Kinè Rehabilitation and Orthopaedic Center Treviso, Italy
Michael Reiman, PT, PhD Duke University Durham, NC, USA
Mark F. Reinking, PT, PhD, SCS, ATC Regis University Denver, CO, USA
Mike Reinold, PT, DPT, SCS, ATC, CSCS, C-PS Champion Physical Therapy and Performance Boston, MA, USA
Mark Ryan, ATC Steadman-Hawkins Clinic Vail, CO, USA
David Sachse, PT, DPT, OCS, SCS USAF San Antonio, TX, USA
Marc Safran, MD Stanford University Palo Alto, CA, USA
Alanna Salituro, PT, DPT, SCS, CSCS New York Mets Port Saint Lucie, FL, USA
Mina Samukawa, PT, PhD, AT (JSPO) Hokkaido University Sapporo, Japan
Barbara Sanders, PT, PhD, FAPTA, Board Certified Sports Physical Therapy Emeritus Professor and Chair, Department of Physical Therapy Texas State University Round Rock, TX, USA
Felix “Buddy” Savoie, MD, FAAOS Tulane Institute of Sport Medicine New Orleans, LA, USA
Teresa Schuemann, PT, DPT, ATC, CSCS, Board Certified Specialist in Sports Physical Therapy Evidence in Motion Fort Collins, CO, USA
Timothy Sell, PhD, PT, FACSM
Atrium Health Musculoskeletal Institute Charlotte, NC, USA
Andreas Serner, PT PhD Aspetar Orthopedic and Sports Medicine Hospital Doha, Qatar
Ellen Shanley, PT, PhD ATI Spartanburg, SC, USA
Karin Silbernagel, PT, PhD University of Delaware Newark, DE, USA
Holly Silvers, PT, PhD Velocity Physical Therapy Los Angeles, CA, USA
Lynn Snyder-Mackler, PT, ScD, FAPTA STAR University of Delaware Newark, DE, USA
Alston Stubbs, MD Wake Forest University Winston-Salem, NC, USA
Amir Takla, B.Phys, Mast.Physio (Manip), A/Prof Australian Sports Physiotherapy The University of Melbourne Melbourne, Australia
Charles Thigpen, PhD, PT, ATC ATI Spartanburg, SC, USA
Steven Tippett, PT, PhD, ATC, SCS Bradley University Peoria, IL, USA
Tim Tyler, PT, ATC NISMAT New York, NY, USA
Timothy Uhl, PT, PhD, ATC University of Kentucky Lexington, KY, USA
Bakare Ummukulthoum, PT University of the Witswatersrand Johannesburg, Gauteng, South Africa
Yuling Leo Wang, PT, PhD Sun Yat-sen University Guangzhou, China
Mark D. Weber, PT, PhD, SCS, ATC Texas Women’s University Dallas, TX, USA
Richard B. Westrick, PT, DPT, DSc, OCS, SCS US Army Research Institute Boston, MA, USA
Chris Wolfe, PT, DPT Belmont University Nashville, TN, USA
Tobias Wörner, PT, MSc Lund University Stockholm, Sweden
ULTRASOUND BITES: TIPS AND TRICKS
1205 Long Head of the Biceps Tendon (LHBT) Manske RC, Voight M, Wolfe C, Page P.
1208 The Use of the Internal Brace to Repair the UCL Injury of the Elbow in Athletes. Wilk KE, Thomas ZM, Arrigo CA, Campbell AM, Shahien A, Dugas JR.
1219 The Efficacy of the Mulligan Concept to Treat Meniscal Pathology: A Systematic Review. Reep N, Leverett,S, Heywood R, et al.
1236 Application of Shear-Wave Elastography in the Evaluation of Hamstring Stiffness in Young Basketball Athletes. Bates N, Cummings P, Nagai T, et al.
1249 Sex-Specific Brain Activations during Single-Leg Exercise. Park-Braswell K, Grooms D, Shultz S, et al.
1259 Does the 2D Frontal Plane Projection Angle Predict Frontal Plane Knee Moments during Stepping, Landing, and Change of Direction Tasks? Straub R, Powers C.
1271 Lower Extremity Kinematic Waveform Analysis During A Single Leg Drop Task - A Single Subject Approach. Martonick N, Chun Y, Krumpl L, et al.
1282 Movement Competency Screen: Rethinking the Rating. Benoit-Piau J, Morin M, Guptill C, et al.
1290 An Updated Model Does Not Reveal Sex Differences in Patellofemoral Joint Stress during Running. Jacobson L, Vannatta CN, Schuman C, et al.
1298 Deficits in Dynamic Balance and Hop Performance Following ACL Reconstruction are not Dependent on Meniscal Injury History. VanZile A, Driessen M, Grabowski P, et al.
1307 Agreement Between Isokinetic Dynamometer and Hand-held Isometric Dynamometer as Measures to Detect Lower Limb Asymmetry in Muscle Strength After Anterior Cruciate Ligament Reconstruction. Ivarsson A, Cronström A.
1318 An Anterior Cruciate Ligament (ACL) Injury Risk Screening and Reduction Program for High School Female Athletes: A Pilot Study. Kuntz A, Peters O, Bello A, et al.
1330 Isometric Knee Strength Is Greater In Individuals Who Score Higher On Psychological Readiness To Return To Sport After Primary Anterior Cruciate Ligament Reconstruction. Sugarman B, Sullivan B, Le D, et al.
1340 Psychological Patient-reported Outcomes Cannot Predict a Second Anterior Cruciate Ligament Injury in Patients who Return to Sports after an Anterior Cruciate Ligament Reconstruction. Piussi R, Simonson R, Högberg J, et al.
1351 Correlational Study on Glenohumeral Instability and Arm Pain in Overhead Throwing Athletes. Wardell, M, Creighton, D, Kovalcik, C.
1358 Development of an Injury Burden Prediction Model in Professional Baseball Pitchers.
Bullock G, Thigpen C, Collins G, et al.
1372 Injuries and Illnesses Across 10 Years of Canada Games Competitions: 2009 – 2019.
Chimera N, Merasty D, Lininger M.
1383 Influence of High School Socioeconomic Status on Athlete Injuries during the COVID-19 Pandemic: An Ecological Study.
Bullock G, Prats-Uribe A, Thigpen C, et al.
1396 Understanding Youth Athlete Motivation, Training and Activity Progression During and After the COVID-19 Sports Interruption.
Greenberg E, Greenberg E, Lawrence JT, et al.
1404 Effects of Trigger Point Dry Needling on Strength Measurements and Activation Levels of the Gluteus Medius: A Quasi-Experimental Randomized Control Study.
Schneider E, Slaven E, Moore ES, et al.
1417 Barriers and Facilitators of Research in Pediatric Sports Medicine Practitioners: A Survey of the PRiSM Society.
Sugimoto D, Del Bel M, Butler L.
1430 Progressive Loading in a Strongman following Distal Biceps Repair: Re-Thinking Load Progression –A Case Report.
Lorenz D.
Robert
C. Manske, PT, DPT, Med, SCS, ATC, CSCSMichael Voight, PT, DHSC, SCS, OCS, ATC, CSCS, FAPTA
Chris Wolfe, PT, DPT, OCS, Cert Dip PT
Phil Page, PT, PhD, ATC, CSCS, FACSM
Pathology of the long head of the biceps brachii tendon (LHBT) is a common source of shoulder pain. While a careful history and a thorough physical examination are important steps in the assessment of LHBT pathology, it is still difficult to differentiate the type and severity of the pathology. Currently, the gold standard for confirming a diagnosis of LHBT pathologies is arthroscopic examination. Additionally, MRI is commonly ordered for diagnosis. Since an accurate diagnosis of pathology is critical for treat ment success, musculoskeletal ultrasound (MSK US) is an attractive adjunct to the diagnostic process due to it being safe, inexpensive and non-invasive. When used in combi nation with clinical special tests, MSK US can drastically increase the diagnostic accuracy of the clinical examina tion.
LHBT, a humeral head depressor, to be subject to overuse injury. Clinical success is always predicated upon an accu rate diagnosis and understanding of the pathological process. While a careful history and a thorough physical examination are important steps in the assessment of LHBT pathology, it is still difficult to differentiate the type and severity of the pathology. MSK US imaging has become an established tool to assist in and optimize the diagnostic process. While MSK US is very accurate in the diagnosis of rotator cuff tears, there is moderate to strong evidence to support the use of MSK US in diagnosis of LHBT pathology.8 MSK US can accurately help to diagnose partial and full-thickness tears, LHBT subluxation/disloca tion, and long head biceps (LHB) tendinopathy.8
Disorders of the long head of the biceps brachii tendon (LHBT) are a commonly recognized source of shoulder pain.1–5 It is not unusual to have LHBT pathology associat ed with rotator cuff tears and subacromial impingement.6-7 Rotator cuff deficiency increases superior translation of the humeral head in relation to the glenoid fossa, causing the
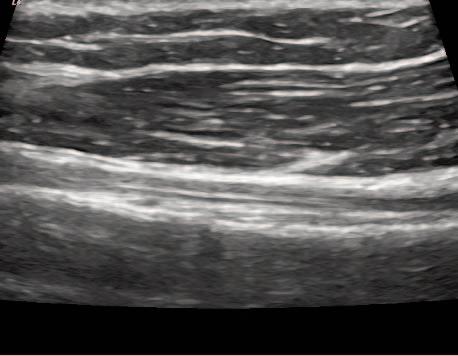
Figure 1a (left): Patient is seated with shoulder and elbow relaxed. Shoulder at 0 degrees of abduction, neutral rotation, elbow flexed and resting on leg or pillow with forearm supinated.
Transducer Placement: Short Axis (SAX). Probe placed transversely on the proximal anterior aspect of the shoulder, over the LHBT.
Figure 1b (right): Patient is seated with shoulder and elbow relaxed. Shoulder at 0 degrees of abduction, neutral rotation, elbow flexed and resting on leg or pillow with forearm supinated.
At times, MSK US can be a difficult diagnostic tool to use clinically and interpret the results. However, when used correctly, MSK US is a valuable tool to accurately diagnose a variety of LHBT pathologies. Therefore, its use should help to facilitate diagnosis and treatment of patients with shoulder pain due to suspected biceps tendon pathologies. The goal of this article is to provide a few tips and tricks to assist in using MSK US as a diagnostic tool for the assess ment of the LHBT. Figure 1a.


Transducer Placement: Long Axis View (LAX). Probe placed longitudinally on the proximal anterior aspect of the shoulder, over the LHBT.
Figure 1b.
Figure 2a: Normal Tendon-Short Axis View. LHBT is located deep within the inter-tubercular groove and viewed as a bright hyperechoic defined tendon. It is easily seen see between the bony greater and lesser tuber cles. The thin band of bright tissue overlying the top of the bicep’s tendon is the transverse humeral ligament.
TENDON PATHOLOGYFigure 3a: Effusion and edema are seen as an area of hypoechoic signal within the tendon sheath surrounding the LHBT. The anechoic ring is known as a “halo sign” on a SAX view. This edema could be either a tenosynovitis or a capsulitis. The LAX will be the differential view.
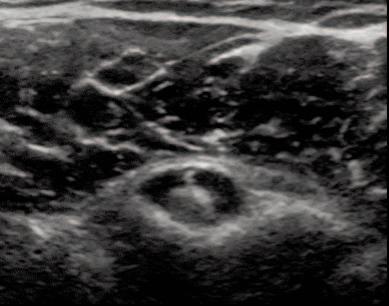
Figure 2b: Normal Tendon-Long Axis View.
LHBT is seen running parallel along the image running proximal to distal from left to right. It should be seen as a bright hyperechoic fibrous band of tissue.The deltoid is seen above as a linear tissue with darker muscle bundles.
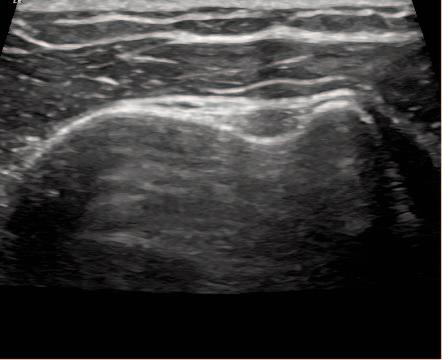

Figure 3b: Joint effusion within the tendon sheath seen here on the LAX. On the LAX views, it reveals presence of fluid distally indicating a tenosynovitis. A capsulitis would not show effusion in the biceps tendon sheath distally on the LAX view.
1. Ahrens P, Boileau P. The long head of biceps and associated tendinopathy. J Bone Joint Surg Br. 2007;89(8):1001-1009.
2. Boileau P, Ahrens PM, Hatzidakis AM. Entrapment of the long head of the biceps tendon: the hourglass biceps — a cause of pain and locking of the shoulder. J Shoulder Elbow Surg. 2004;13:249-257.
3. Desai S, Mata H. Long head of biceps tendon pathology and results of tenotomy in full-thickness reparable rotator cuff tear. Arthrosc J Arthrosc Relat Surg. 2017;33(11):P1971–P1976.
4. Skendzel J, Jacobson J, Carpenter J, et al. Long head of biceps brachii tendon evaluation: accuracy of preoperative ultrasound. Am J Roentgenol. 2011; 197(4):942-948.
5. Walch G, Nove-Josserand L, Boileau P, et al. Subluxations and dislocations of the tendon of the long head of the biceps. J Shoulder Elbow Surg. 1998; 7:100-108.
6. Dines D, Warren RF, Inglis AE. Surgical treatment of lesions of the long head of the biceps. Clin Orthop Relat Res.1982;164:165-171.
7. Chen CH, Hsu KY, Chen WJ, et al. Incidence and severity of biceps long head in tendon lesion in patients with complete rotator cuff tears. J Trauma. 2005 58:1189-1193.
8. Ostrowski JL, Beaumont A, Dochterman E. Diagnostic accuracy of musculoskeletal ultrasound on long head biceps tendon pathologies. J Sports Rehab. 2021;30: 1098-1101.
Kevin E Wilk, PT, DPT, FAPTA 1,2 , Zachary M Thomas, PT, DPT, OCS, CSCS 3 a , Christopher A. Arrigo, MS, PT, ATC 4 , Ashley M Campbell, PT, DPT, SCS 5,6 , Amir Shahien, MD 7 , Jeffrey R Dugas, MD 8
1 Vice President National Director Clinical Education & Research, Champion Sports Medicine, Select Medical, 2 Director of Rehabilitative Research, American Sports Medicine Institute, 3 Sports Physical Therapy Fellow, Champion Sports Medicine, 4 Advanced Rehabilitation, 5 Director of Rehabilitation, Nashville Hip Institute at TOA, 6 School of Physical Therapy, Belmont University, 7 Orthopaedic Surgeon, Fellow, American Sports Medicine, 8 Andrews Sports Medicine
Keywords: UCL, elbow, UCL repair https://doi.org/10.26603/001c.39614

The number of injuries to the ulnar collateral ligament (UCL) of the elbow are rising every year Several studies have reported increasing numbers of injuries, associated surgeries, and that patients affected by UCL pathology are gradually becoming younger. Hodgins et al reported a 193% increase in the number of UCL surgeries in the state of New York from 2002 to 2011.1 Erickson et al reported the age range for most UCL surgeries in the United States to be between 15-19.2 Conte et al noted in a survey of profes sional baseball teams, that 25% of all major league pitch ers have undergone UCL surgery, while only 14% of minor league pitchers have had UCL operations.3 Just four years later, the number of minor league pitches reporting prior UCL surgery increased by 5% to 19% and the number of ma jor league pitchers affected to 26%.4
The American Sports Medicine Institute (Birmingham, AL) has noted a shift in the majority of patients presenting with UCL injuries. Twenty-five years ago, that majority were college and professional aged baseball players, now the athletes sustaining UCL injuries are predominately younger than collegiate age. From 2001 to 2019 at the An drews Sports Medicine and Orthopaedic Center 4,606 UCL surgeries were performed with an average age of 17.6 years. This shift to younger patients being affected by UCL injury more often brought into focus the dilemma of athletes nearing the end of promising careers almost before they have even started. This also demonstrates the importance and the need to return to play as soon as safely possible. The internal brace repair for the UCL injured athlete ap pears to be a reasonable option to address these issues for the appropriate candidate.
Diagnosis of UCL tears is accomplished through a combi nation of physical exam and diagnostic imaging, in the con text of patient history.5 Non-operative management of UCL injury has historically been reserved for low to mediumgrade partial tears.6 Non-operative treatment is comprised of rest from throwing, rehabilitation to strengthen and im prove throwing mechanics, and a graduated return to
throwing program over a 3-4 month period of time. Addi tionally, the use of biologics such as platelet rich plasma (PRP) have the potential to augment the effectiveness of non-operative management in certain instances.7 For high demand throwing athletes that fail conservative manage ment, surgical intervention is warranted.
Since Dr. Frank Jobe’s initial description of the UCL re construction in 1974, it has been the gold standard for treatment of medial sided elbow pain and laxity in the throwing athlete.8,9 Reconstruction techniques have evolved over time with varied applications including dock ing, Jobe, and modified-Jobe techniques.10–12 Early com parisons of repair versus reconstruction revealed poor out comes, with less than 30% of repairs returning to the same or higher level of play, especially in a subset of Major League Baseball (MLB) overhead athletes.13,14 Although re turn to play rates are high with UCL reconstruction, be tween 85 -90%, the rehabilitation process which ranges be tween 12-18 months for pitchers is longer than desired.15
Newer technology and greater experience performing di rect repairs of the UCL have demonstrated return to play outcomes greater than 95%.16,17 Dugas et. al published two outcome studies first establishing the non-inferiority of UCL repair with internal brace to the modified Jobe recon struction and then reporting outcomes and return to play to the same or higher level in greater than 90% of patients, 92% of which returned to competition in a 6-7 month time frame.18,19
Although the potential for shorter rehabilitation and quicker return to play are attractive advantages of UCL repair with internal brace when compared with a recon struction, patient selection is crucial for success. There has been a trend toward an increasing number of adolescent and youth sport participants with UCL injury.16,17 These younger athletes typically have end-avulsions of the UCL or partial tears of the ligament in otherwise healthy ligament tissue. These types of injuries lend themselves well to re pair with internal brace. The UCL repair cannot augment a
preexisting tissue deficiency Patients with chronic UCL in sufficiency or adaptive changes such as ossification of the ligament are not repair candidates.
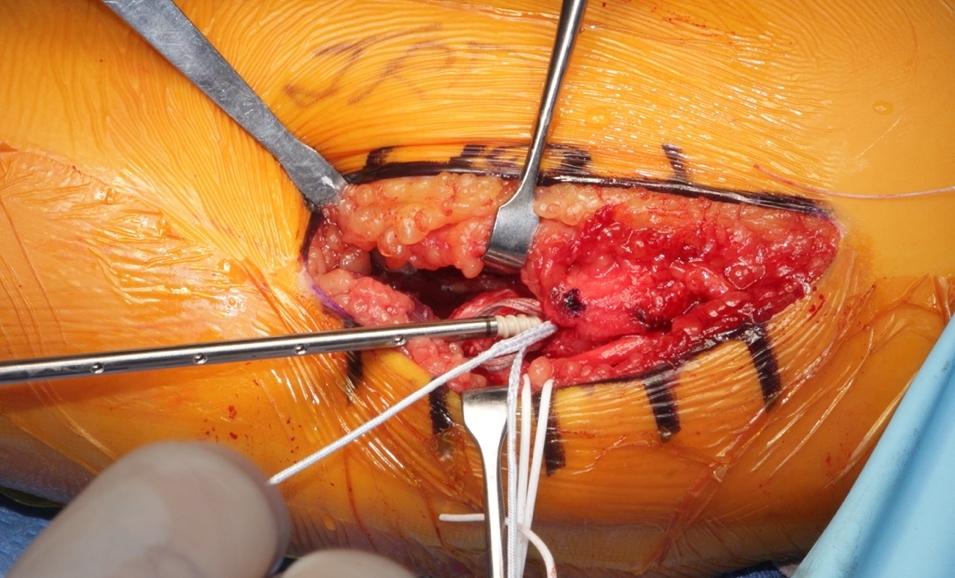
The authors’ current surgical approach to repair of the UCL includes the standard medial incision just posterior to the medial epicondyle (Figure 1). The cubital tunnel is exposed, and the ulnar nerve is dissected out both proximally and distally. The ulnar nerve is transposed to decrease the rate of post-operative ulnar neuritis.20 The sublime tubercle and medial epicondyle are then identified. For UCL expo sure, a muscle-elevating approach is used to elevate the flexor-pronator musculature off the anterior band of the UCL.13,21 With full exposure of the ligament, the anterior band is split in line with its fibers in order to access and de bride a proximal or distal avulsion. Once completed the in ternal brace, which was prepped on the back table, is placed through a 3.5 mm SwiveLock (Arthrex Inc, Naples, FL) with a 2-0 nonabsorbable suture for repair
The drill guide is then inserted either on the center of origin of the UCL at the medial epicondyle for proximal tears or the anterior aspect of the sublime tubercle for dis tal tears.22 The first anchor of the internal brace is placed appropriately and the limbs of the nonabsorbable suture are passed through the ligament’s anterior and posterior bands and tied in simple fashion to complete the repair The remaining FiberTape (Arthrex Inc, Naples, FL) is then loaded through a second 3.5 mm SwiveLock. A similar drilling and taping process is performed on either the re maining proximal or distal end of the ligament. The lon gitudinal split in the ligament is then closed with an in terrupted 0 vicryl. The FiberTape is tensioned as to not supersede the native tension of the ligament and the an chor is provisionally inserted as the arm is taken through a full range of motion to confirm reduction of the joint with adequate tensioning and isometry on the graft, ensur ing there is no non-physiologic constraint of the repaired UCL. The 3.5 SwiveLock is then inserted until the anchor is seated. Finally, interrupted 0 vicryl sutures are placed around the native ligament and around the internal brace to supplement fixation and prevent windshield wipering of the brace itself (Figure 2). The ulnar nerve is transposed an teriorly and secured under two fascial slings with 3-0 ticron and the internal brace is complete (Figure 3a/b).


In a cadaver study examining the UCL repair construct, UCL repair with internal bracing is more resistant to gap formation under fatigue loading than UCL reconstruc tion.22 Additionally, in cadaver specimens, contact me chanics of reconstructed and repaired specimens were not significantly different. Both reconstruction and repair pro cedures returned the overall resistance of the joint to valgus torsion to near-intact levels.23 Clinically, the authors have experienced good outcomes utilizing the described tech nique for UCL repair with Collagen-Dipped FiberTape aug mentation in Overhead-Throwing Athletes.
Rehabilitation following a UCL repair with internal brace (Table 1) begins on post-operative day 1 with an emphasis on shoulder and wrist passive range of motion (PROM), light voluntary muscle activation exercises for the shoulder, dressing/wound care, and ensuring that there is optimal communication between the rehabilitation team and ath
Figure 1. Medial elbow marked pre-operatively with standard UCL repair incision guideline. Figure 2. Intra-operative view of fixation of the internal brace. Figure 3a. Intra-operative ulnar nerve transposition.lete/patient. The goal of the rehabilitation process is to re turn the athlete to his or her previous functional level, or better, as quickly and safely as possible. Phase one (week 1) is intended to protect healing tissue, reduce pain and inflammation, minimize muscular atrophy, and regain full wrist/shoulder motion, while allowing early healing of the surgical repair. For the first week after surgery, the patient is placed in an adjustable ROM elbow brace (Figure 4), with the elbow immobilized at 90° of flexion to protect the heal ing of the UCL repair and ulnar nerve transposition. A pri mary focus in phase one is on voluntary muscle activa tion to help minimize muscular atrophy of the shoulder and scapulothoracic musculature, with all exercises performed isometrically, in a non-painful submaximal fashion with the elbow brace locked at 90° of flexion. Rhythmic stabiliza tion drills are also performed for the shoulder external and internal rotator muscles to begin re-establishing proprio ception and neuromuscular control of the upper extremity.
Phase two (weeks 2-5) focuses on gradually restoring el bow joint ROM (Figure 5), improving muscular strength and endurance, and normalizing joint arthrokinematics. On day 8 post-surgery, the elbow ROM brace is set to allow elbow motion from 30° to 110° of flexion. At the beginning of week 3 the brace is unlocked further progressing to 10° to 125° of motion. At this time the Throwers Ten program24 is usually initiated (Figure 6), based on the patient’s progres sion and signs and symptoms (Appendix A). By week 4 the elbow brace is unlocked to allow 0° to 145° of motion. Full elbow ROM is expected by the end of post-operative week 4. If everything improves as expected, the brace is discontin ued by week 6 and the athlete progresses to the Advanced Throwers Ten exercise program.25 (Appendix A) (Figure 7).

Phase three (6-8 weeks) of the rehabilitation process emphasizes maintaining (or fully restoring, if still limited) elbow and upper extremity mobility, improving muscular strength and endurance, reestablishing neuromuscular control of the elbow complex, and continuing with the pro gression of functional activity During this phase, 2-hand plyometric upper extremity exercises are initiated, begin ning with two hand plyometric chest pass (Figure 8). One hand plyometric throwing into a wall or rebounder with a light plyometric ball (1 & 2 pounds) is initiated at 8-10
Figure


weeks (Figure 9), depending on the patients progress and assessment. Dynamic stabilization drills such as ball on wall with stabilization (Figure 10), and one hand ball throws into the wall with end range stabilization (Figure 11) are also routinely performed in this timeframe.
Phase four begins at week 9 and goes through week 16 following surgery The goal of this phase is to gradually
Figure 3b. UCL internal brace in place. Figure 4. Elbow locked at 90° in adjustable elbow fixation brace 1 week post-operatively 5. Passive range of motion following UCL surgery.Figure
Figure 7. Seated on stability ball performing external rotation with resistance band and end range rhythmic stabilization, a component of the Advanced Throwers Ten program.

increase strength, power, endurance, and neuromuscular control to prepare the athlete for a gradual, progressive re turn to sports. The athletes exercise program is progressed to include more aggressive eccentric and plyometric move



Figure 8. Two hand plyometric chest pass off trampoline with 4lbs plyo ball.
Figure 9. One hand plyometric throw at 90-90 off trampoline with 1lb plyo ball.
ments during this phase. An interval hitting program is ini tiated at week 10, while an interval throwing program (ITP) for the overhead athlete is allowed to begin at week 12 after surgery, if the athlete is ready.24,26,27 In most cases, pitch ers will progress to throwing from a mound approximately 8 to 10 weeks after initiation of an ITP 28
6. Standing full can exercise being performed in forward lunge position, a component of the Throwers Ten programFigure 10. Ball on wall rhythmic stabilization in the scapular plane to enhance glenohumeral joint dynamic stabilization.
Figure 12. One of the functional tests we perform: single arm ball drops with shoulder at 90 degrees of abduction and palm down.


*This test utilizes a 2 Ib plyometric ball and is performed for 30 sec.*
The final phase (16+ weeks) of the rehabilitation process is the return-to-activity phase. During this phase, the goal is to allow the athlete to progressively return to full activity and competitive throwing. Gradual return to competitive throwing begins 5 months following UCL repair with inter nal brace, in contrast to 9 to 12 months following UCL re construction.15,29 During this return to competition phase, the athlete is instructed to continue the throwers ten +4 program to maintain ROM and strength for the entire body (Appendix A).
Figure 11. One hand plyometric wall throws at 90-90 (2lb plyo ball) with end range rhythmic stabilization.
A series of return to play tests is performed before ini tiating the ITP These tests include the following: 1)PROM testing for the entire upper extremity, 2) manual muscle testing for the entire upper extremity using a hand held dy namometer, 3) a satisfactory clinical exam of the elbow & shoulder, and the 4) the following functional tests: single arm prone ball drops (Figure 12), ball throws into the wall, ball throws into the plyoback from 20 ft away, single leg squats, and a prone plank test for time.

The outcomes demonstrated thus far using this proce dure and rehabilitation program have been encouraging. UCL repair with internal brace has been performed at our center since 2013 with approximately 527 procedures per formed to date. Dugas et. al examined outcomes in 111 overhead athletes, 92% (102/111) of those who desired to return to the same or higher level of competition were able to do so at a mean time of 6.7 months.19 Recently, Rothermich et al presented results of 40 non-throwing ath letes who had undergone UCL repair with a minimum fol low up of 2 years, the results indicated a 93% return to play rate with the average time to play occurring at 7.4 months.30 Based on our clinical observations, the success rate of 92-93% appear to be sustained for the long term (5-7 years and beyond).
The UCL is frequently injured in overhead athletes and these injuries continue to increase in number, particularly in youth athletes. Surgical repair of the UCL with internal brace is a viable option in athletes who meet specific find
ings at the time of surgery The rehabilitation of this unique surgical procedure has been presented based on the au thors’ experience treating more than 350 athletes over the past 3 years. The average time required for an athlete to return to participation in this cohort is 7 months which is approximately 5 months less than average return to play times after UCL reconstruction surgery Long-term results of this surgery and rehabilitation program are still needed but the initial experience is extremely promising. Long term studies are needed to determine the effectiveness and longevity of this procedure and rehabilitation program.
Submitted: September 01, 2022 CST, Accepted: October 22, 2022 CST
Table 1. UCL Repair with Internal Brace Rehabilitation Program
Long Term Goals:
• Full Elbow, Wrist, Shoulder
• Pain free ROM UE
Range of Motion Week 6
• Performing Shoulder, Arm & Entire Body Strengthening Program
• Improving Entire Body Strength & Flexibility
I. Initial Phase: (Week 1)
Goals: Full wrist ROM
Decrease swelling Decrease pain Prevent muscle atrophy Day of Surgery
Post op Day 1 and 2
• Return to Unrestricted Throwing 1. ROM Brace locked at 70 degrees to Elbow Joint for 7 days 2. PROM wrist & hand 1. Locked ROM Brace at 70 degrees flexion for 7 days
Immediate post-op hand, wrist, and hand exercises
Post-op Day 3 through 7
Hand gripping exercises
II. Acute Phase (Week 2-4)
Goals: Gradually restore Elbow Joint ROM Improve muscular strength and endurance Normalize joint arthrokinematics
Week 2, Day 8: Begin PROM & AAROM Elbow ROM 30-1100 Progress to Elbow ROM brace (30-1100) Elbow AAROM/PROM exercises
Initiate AROM elbow
Initiate AROM shoulder joint
Beginning Week 3: Progress Elbow ROM to 10-1250
III. Intermediate Phase: (Week 4-8)
Goals: Restore full Elbow ROM Progress UE strength Continue with functional progression
Week 4-6: Progress Elbow ROM to 0-1450
Beginning Week 7: Discontinue brace at end of week 6 Initiate 2 hand plyometric throws Prone planks Side plank on uninvolved side &ER on throwing side
The Use of the Internal Brace to Repair the UCL Injury of the Elbow in Athletes
Long Term Goals: Week 8: Continue with advanced thrower’s ten program Side planks with ER strengthening
IV. Advanced Phase: (Weeks 9-14)
*Criteria to progress to Advanced Phase:
1. Full nonpainful ROM 2. No pain or tenderness 3. Isokinetic test that fulfills criteria to throw 4. Satisfactory clinical exam
5. Completion of rehab phases without difficulty
Goals: Advanced strengthening exercises Initiate Interval Throwing Program Gradual return to throwing
Beginning Week 9: Continue all strengthening exercises Initiate 1 hand plyometric throws Advanced thrower’s ten program Plyometrics program (1 & 2 hand program)
Beginning Week 10: Seated machine bench press Initiate Interval Hitting Program (week10) Seated rowing machine Progress Biceps (dumbbell) strengthening Progress Triceps pushdowns
Beginning Week 11-16: Initiate Interval Throwing program week 12 (Long toss program) Phase I Continue all exercises as in week 9 – 10
Beginning Week 16-20: Initiate Interval Throwing Program Phase II (Off mound program) Initiate mound throwing when athlete is ready & completed ITP Phase I -Continue Advanced Thrower 10 exercise program -Continue plyometrics -Continue ROM & Stretching programs
V. Return to Play Phase: (weeks 20 >):
Goal: Gradual return to competitive throwing Continue all exercises & stretches
Week 20-24>: Initiate gradual return to competitive throwing Perform dynamic warm-ups & stretches Continue thrower’s ten program Return to competition when athlete is ready (Physician Decision)
Note: ** Each athlete may progress thru ITP at different rates/pace. Should complete 0-90 ft within 3 weeks of starting it & complete 120 ft within 8 weeks then begin mound program.
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of Medial Ulnar Collateral Ligament Reconstruction: A 10-Year Study in New York State. Am J Sports Med 2016;44(3):729-734. doi:10.1177/03 63546515622407
2. Erickson BJ, Nwachukwu BU, Rosas S, et al. Trends in Medial Ulnar Collateral Ligament Reconstruction in the United States: A Retrospective Review of a Large Private-Payer Database From 2007 to 2011. Am J Sports Med 2015;43(7):1770-1774. doi:10.1177/0363 546515580304
3. Conte SA, Fleisig GS, Dines JS, et al. Prevalence of Ulnar Collateral Ligament Surgery in Professional Baseball Players. Am J Sports Med 2015;43(7):1764-1769. doi:10.1177/036354651558079 2
4. Leland DP, Conte S, Flynn N, et al. Prevalence of Medial Ulnar Collateral Ligament Surgery in 6135 Current Professional Baseball Players: A 2018 Update. Orthop J Sports Med 2019;7(9):1-7
5. Erickson BJ, Harris JD, Chalmers PN, et al. Ulnar Collateral Ligament Reconstruction: Anatomy, Indications, Techniques, and Outcomes. Sports Health. 2015;7(6):511-517. doi:10.1177/194173811560 7208
6. Carr JB II, Camp CL, Dines JS. Elbow Ulnar Collateral Ligament Injuries: Indications, Management, and Outcomes. Arthroscopy. 2020;36(5):1221-1222. doi:10.1016/j.arthro.2020.02.0 22
7. Apostolakos JM, Lin KM, Carr JBI, Bedi A, Camp CL, Dines JS. The Role of Biologic Agents in the Nonoperative Management of Elbow Ulnar Collateral Ligament Injuries. Curr Rev Musculoskelet Med. 2020;13(4):442-448. doi:10.1007/s12178-020-09637-9
8. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am 1986;68(8):1158-1163. doi:10.2106/0000462 3-198668080-00004
9. Kerlan RK, Jobe FW, Blazina ME, et al. Throwing injuries of the shoulder and elbow in adults. Curr Pract Orthop Surg 1975;6:41-48.
10. Arner JW, Chang ES, Bayer S, Bradley JP. Direct Comparison of Modified Jobe and Docking Ulnar Collateral Ligament Reconstruction at Midterm Follow-up. Am J Sports Med. 2018;47(1):144-150. do i:10.1177/0363546518812421
11. Jensen AR, LaPrade MD, Turner TW, Dines JS, Camp CL. The History and Evolution of Elbow Medial Ulnar Collateral Ligament Reconstruction: from Tommy John to 2020. Curr Rev Musculoskelet Med 2020;13(3):349-360. doi:10.1007/s12178-020-09618-y
12. Watson JN, McQueen P, Hutchinson MR. A systematic review of ulnar collateral ligament reconstruction techniques. Am J Sports Med 2014;42(10):2510-2516. doi:10.1177/03635465135090 51
13. Azar FM, Andrews JR, Wilk KE, Groh D Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med 2000;28(1):16-23. doi:10.1177/03635465000280011401
14. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1):67-83. doi:10.2106/00004623-19927401 0-00009
15. Cain EL, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: Results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426-2434. doi:10.1177/03635465103781 00
16. Argo D, Trenhaile SW, Savoie FH, Field LD. Operative treatment of ulnar collateral ligament insufficiency of the elbow in female athletes. Am J Sports Med. 2006;34(3):431-437. doi:10.1177/0363546 505281240
17 Savoie FH III, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36(6):1066-1072. doi:10.1177/036354650831520 1
18. Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical Comparison of Ulnar Collateral Ligament Repair With Internal Bracing Versus Modified Jobe Reconstruction. Am J Sports Med 2016;44(3):735-741. doi:10.1177/036354651562 0390
19. Dugas JR, Looze CA, Capogna B, et al. Ulnar Collateral Ligament Repair With Collagen-Dipped FiberTape Augmentation in Overhead-Throwing Athletes. Am J Sports Med. 2019;47(5):1096-1102. do i:10.1177/0363546519833684
20. Rothermich MA, Fleisig GS, Lucas HE, et al. Early Complications of Ulnar Collateral Ligament Repair With Collagen-Coated Suture Tape Augmentation. Orthop J Sports Med. 2021;9(10):232596712110383. do i:10.1177/23259671211038320
21. Andrews JR, Jost PW, Cain EL. The ulnar collateral ligament procedure revisited: the procedure we use. Sports Health. 2012;4(5):438-441. doi:10.1177/194173 8112455318
22. Jones CM, Beason DP, Dugas JR. Ulnar Collateral Ligament Reconstruction Versus Repair With Internal Bracing: Comparison of Cyclic Fatigue Mechanics. Orthop J Sports Med 2018;6(2). doi:10.1177/23259671 18755991
23. Roth TS, Beason DP, Clay TB, Cain ELJ, Dugas JR. The Effect of Ulnar Collateral Ligament Repair With Internal Brace Augmentation on Articular Contact Mechanics: A Cadaveric Study Orthop J Sports Med 2021;9(4):1-7 doi:10.1177/23259671211001069
24. Wilk KE, Arrigo CA, Hooks TR, Andrews JR. Rehabilitation of the overhead throwing athlete: there is more to it than just external rotation/internal rotation strengthening. PMR. 2016;8(3S):S78-S90. do i:10.1016/j.pmrj.2015.12.005
25. Wilk KE, Yenchak AJ, Arrigo CA, Andrews JR. The Advanced Throwers Ten Exercise Program: a new exercise series for enhanced dynamic shoulder control in the overhead throwing athlete. Phys Sportsmed 2011;39(4):90-97 doi:10.3810/psm.2011.1 1.1943
26. Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR. Rehabilitation of the overhead athlete’s elbow. Sports Health 2012;4(5):404-414. doi:10.1177/194173 8112455006
27. Wilk KE, Reinold MM, Andrews JR. Rehabilitation of the thrower’s elbow Clin Sports Med 2004;23(4):765-801. doi:10.1016/j.csm.2004.06.006
28. Reinold MM, Wilk KE, Reed J, Crenshaw K, Andrews JR. Interval sport programs: guidelines for baseball, tennis, and golf J Orthop Sports Phys Ther 2002;32(6):293-298. doi:10.2519/jospt.2002.32.6.293
29. Erickson BJ, Gupta AK, Harris JD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med 2014;42(3):536-543. doi:10.1177/0363546 513510890
30. Rothermich MA. Paper 13: None: Clinical Outcomes of Ulnar Collateral Ligament Surgery in Non Throwing Athletes. Presented at: AOSSM Annual Meeting, Colorado Springs 2022.
Download: https://ijspt.scholasticahq.com/article/39614-the-use-of-the-internal-brace-to-repair-the-ucl-injury-ofthe-elbow-in-athletes/attachment/104076.pdf?auth_token=_Jc6N7GQum-FFpPtwcn_
Download: https://ijspt.scholasticahq.com/article/39614-the-use-of-the-internal-brace-to-repair-the-ucl-injury-ofthe-elbow-in-athletes/attachment/113648.pdf?auth_token=_Jc6N7GQum-FFpPtwcn_
Reep NC, Leverett SN, Heywood RM, Baker RT, Barnes DL, Cheatham SW. The Efficacy of the Mulligan Concept to Treat Meniscal Pathology: A Systematic Review. IJSPT Published online December 1, 2022:1219-1235.
Nathan C. Reep 1 a , Sydney N. Leverett 1 , Rebecca M. Heywood 1 , Russell T. Baker 1,2 , Darren L. Barnes 1 , Scott W. Cheatham 3
1 Department of Movement Sciences, University of Idaho, 2 WWAMI Medical Education, University of Idaho, 3 Department of Kinesiology, California State University Dominguez Hills
Keywords: lesion, manual therapy intervention, Mobilization with Movement (MWM), rehabilitation, knee injury https://doi.org/10.26603/001c.55540
Meniscal pathologies are common knee injuries and arthroscopic surgery is the current accepted gold standard for treatment. However, there is evidence to support the use of the Mulligan Concept (MC) Mobilization with Movement (MWM) for meniscal pathologies including the ‘Squeeze’ technique, tibial internal rotation (IR), and tibial external rotation (ER).
The purpose of this systematic review was to critically appraise the literature to investigate the effectiveness of MC MWMs for meniscal lesions on patient reported pain, function, and multi-dimensional health status in patients with clinically diagnosed meniscal pathologies.
A literature search was completed across multiple databases using combinations of the words “knee, function, mobilization with movement, MWM, mulligan concept, MC, meniscal pathology, meniscal derangement, and meniscal tear ” Studies written within the prior 10 years that examined MC MWM techniques to treat knee meniscal injury were included. Articles that met the inclusion criteria (used MC MWM ‘Squeeze’ technique, tibial IR, or tibial ER for treatment of clinically diagnosed meniscal pathologies; Patient reported outcome [PRO] measures had to be used in the assessment of knee pain or function) were analyzed for quality Randomized control trials were analyzed using the PEDro scale and the Downs & Black (D&B) checklist, case series were analyzed using the Joanna Briggs Institute (JBI) checklist, and case reports were analyzed using the CARES checklist.
Six articles met the inclusion criteria and were included in this review, two randomized controlled studies, two case series, and two case reports consisting of 72 subjects. All six papers included reports of improvements in pain and function that were either
a
Corresponding author:

Nathan R. Reep MAT, LAT, ATC, CSCS
Department of Movement Sciences
University of Idaho 875 Perimeter Drive Moscow, ID 83844
Fax: 765-677-1676 Email: reep2529@vandals.uidaho.edu Phone: 765-677-3034
statistically significant or met the minimal clinically important difference (MCID). Five studies reported the Disablement in the Physically Active (DPA) scale that also demonstrated statistically significant differences or met the MCID The MC MWM ‘Squeeze’ technique, tibial IR, or tibial ER demonstrated the ability to reduce pain, improve function, and improve patient perceived disability following treatment of a clinically diagnosed meniscal pathology. These studies demonstrated short term results lasting from one week to 21 weeks.
Treatment interventions incorporating MC MWM techniques demonstrated reduction of pain and improvement in function in the short term in patients with clinically diagnosed meniscal pathologies.
2a
Meniscal injuries are diagnosed through clinical evaluation, magnetic resonance imaging (MRI), or diagnostic arthroscopy.1,2 Arthroscopy, which is reported to have an accuracy of 90-95% and has the benefit of immediate surgi cal correction being able to be performed, is considered the gold standard diagnostic technique; however, arthroscopy has drawbacks such as unnecessary surgical costs and risks.1,3 The reported diagnostic accuracy of MRI has been as high as 88%,4 but MRI also has drawbacks, such as high prevalence of findings in asymptomatic uninjured knees,5 increased healthcare costs,6 and challenges with accessing imaging.7 Thus, accurate diagnosis with a physical exam is valuable; comprehensive physical examination and test ing batteries (i.e., positive McMurray’s, Thessaly’s, and Ap ley’s tests) have been associated with high diagnostic ac curacies of 90% and 81%, respectively 8 Similarly, a clinical prediction rule of a history of catching or locking, pain with forced hyperextension, pain with maximum knee flexion, joint line tenderness, and pain or clicking while performing McMurry’s test has been reported to have a positive predic tive value of 92.3% and a positive likelihood ratio of 11.45 when all five signs are present in a clinical exam.9
Once diagnosed, meniscal injuries are often treated sur gically in combination with conservative therapy or after conservative therapy has failed to produce the desired im provement.2,10,11 In fact, arthroscopic partial meniscec tomy (APM), which addresses meniscal injury by removing the damaged meniscal tissue, is one of the most commonly performed orthopedic surgeries.12,13 Surgical approaches, however, have often failed to have the desired result. For example, APM has not been found to outperform sham surgery or conservative management, and surgery has re sulted in patients who were more susceptible to developing osteoarthritis.11,12,14 Arthroscopic repair, which has a rep utation as the “gold standard” for meniscal injuries in cases where it is feasible to repair the specific meniscal tear pre sent,10,15 has high rates of failure (e.g., patients often redevelop symptoms, patients require additional corrective operations, etc.).16,17 When patient history, physical exam ination, current pain, and dysfunction or mechanical symp
toms indicate meniscal injury, non-operative or conserva tive treatment is recommended.2,18
Thus, there is a need to consider other treatment options for patients who present with the signs and symptoms of a meniscal pathology due to the prevalence of meniscal in juries, potential undesired surgical outcomes (e.g., adverse long-term outcomes), and recommendations for conserva tive care.2,12,19,20 The Mulligan Concept (MC), introduced by Brian Mulligan, is an innovative conservative treatment approach used to address common issues (e.g., joint pain, decreased ROM, movement dysfunction, etc.) associated with knee joint pathology.21,22 The MC incorporates move ment with mobilization by combining the patient’s active range of motion (AROM) with a clinician’s joint glides to at tempt to produce immediate changes in the patient’s com plaints and impairment measures. While consensus on the mechanism of action has not been reached, application of the MC is thought to alter the mechanoreceptive and noci ceptive responses to promote immediate improvements in the patient’s impairment.23,24
Specific MC mobilizations with movement (MWMs) techniques have been proposed as effective conservative non-surgical interventions for meniscal pathology.25 Re searchers have recently begun to examine the effects of the proposed MC MWM techniques (i.e., ‘Squeeze’ tech nique, tibial IR, and tibial ER) in patients with clinically di agnosed meniscal lesions.24,26–29 A synthesis of the avail able literature to assess the effectiveness of the proposed meniscal MC MWM techniques in the treatment of clini cally diagnosed meniscal lesions has not been conducted. Examining the effects of these MC MWMs in clinically diag nosed meniscal lesions would provide an update on the ev idence and help inform practitioners on an evidence-based method for incorporating MC MWMs ‘Squeeze’, tibial IR, and tibial ER into clinical practice. Therefore, the purpose of this systematic review was to critically appraise the lit erature to investigate the effectiveness of MC MWMs for meniscal lesions on patient reported pain, function, and multi-dimensional health status in patients with clinically diagnosed meniscal pathologies.
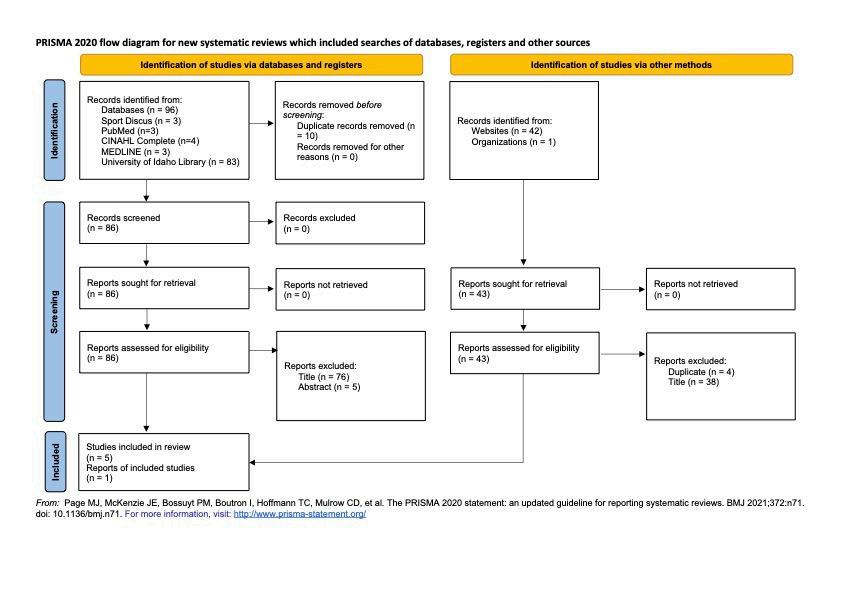
The systematic review was registered on the International Prospective Register of Systematic Reviews (PROSPERO), a database for tracking the quality of systematic reviews in health professions (CRD42021278025). The 13-item PROS PERO checklist for the creation of systematic reviews was followed for accuracy of study design and reporting.30 The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 27 item checklist was also used in the creation of the systematic review to ensure the quality of the study design.31
An electronic search of the literature was conducted in May 2022. The following databases were used for the lit erature search: PubMed, SportDiscus, CINHAL, MEDLINE, the University of Idaho library, and the indexed reference of published works listed on the Mulligan Concept website. The search was limited to the last ten years with an addi tional filter to specify academic articles or journal articles depending on the database. The search terms used were "menisc* AND mulligan AND pain (Figure 1). Other search terms (i.e., knee, function, mobilization with movement, MWM, mulligan concept, MC, meniscal pathology, menis cal derangement, and meniscal tear) were used to find ad ditional studies, but no additional studies were identified with these terms. A hand search of the references of iden tified articles was also performed; however, no additional studies were identified with this process, while one addi tional study was identified on the Mulligan Concept website that was published in the Journal of Sports Medicine and Allied Health Sciences, which is the official journal of the Ohio Athletic Trainers Association.
Each study had to meet the following inclusion criteria to be eligible for this review A clinical diagnosis of a menis cal pathology consisting of a minimum of three of the fol lowing items during the physical exam: 1) a positive test for McMurray’s, Thessaly’s, or Apley’s Compression tests; 2) pain at end range of knee flexion; 3) pain at end range of knee extension; 4) joint line tenderness; and 5) a history of painful popping or clicking (Table 1). Additionally, the use of the MC MWM ‘Squeeze’ technique, tibial IR, or tibial ER for treatment of clinically diagnosed meniscal pathologies had to be present. Finally, PRO measures had to be used in the assessment of knee pain or function. Studies were ex cluded if a non-MWM MC technique or alternative forms of manual therapy were utilized or if the included partic ipants had any other clinically diagnosed knee pathology, hyperalgesia, or a previous history of knee surgery Stud ies were also excluded if they were not published in Eng lish, not published within the last 10 years, or did not meet the expectations for blinded peer-review (e.g., disser tations, poster presentations,).
One author (NR) conducted the initial search, while a sec ond author (SL) repeated the search to ensure the accuracy and repeatability of the search results (Figure 1). The two search authors (NR and SL) were blinded to the initial re view of titles and abstracts and met to ensure final inclu sion was consistent. Four of the authors (NR, SL, RH, and DB) independently completed a full text review of the stud ies that met inclusion and exclusion criteria and met to reach consensus for inclusion; a fifth author (RB) was con sulted to confirm inclusion in the event of an impasse. All the authors agreed that the studies selected met the criteria for inclusion after review (Table 2).
The studies included were graded with the following scales to assess and measure the study quality (e.g., study type, internal validity, level of evidence; (Table 3). The PEDro scale was used to assess the internal validity of the random ized control trials (RCTs); scores of seven or higher were considered high methodological quality, five to six were fair quality, and zero to four were poor quality.32 The Downs and Black (D&B) Checklist for randomized studies exam ining health care interventions was also utilized to evalu ate included RCTs.33 The 27 item D&B Checklist was scored out of 32 total points where ranges of corresponding scores were given: excellent (26-32); good (20-25); fair (15-19); and poor (≤ 14).34 Any identified case series was assessed with the Joanna Briggs Institute (JBI) checklist for case se ries. A 6/10 or greater indicated a low risk of bias.35 Iden tified case studies were assessed with the CARES checklist and were scored out of twelve.36 The CARES checklist was scored on a 0-12 scale by giving a point to any question within a category when answered “yes” by the reviewer. The last question (Question 13) was not scored because it is in tended for the completion of a case study by the original author and is not always reported in the study Each study was assigned a level of evidence in accordance with the Ox ford Center of Evidence-Based Medicine.37 This system of assessment was designed to quickly assess the best liter ature based on the study’s design. Each study design falls within a specific level that can be graded up or down based on the quality of the study.37
The total number of participants and general demographic information were extracted from each qualified study The primary data extracted from each article were study charac teristics (e.g., publication data, study design, etc.), method ology (e.g., treatment protocol, inclusion/exclusion criteria, etc.), and results. Patient reported pain was assessed by the Numeric Pain Rating Scale (NRS). Patient-reported func tion was assessed by the Patient-Specific Functional Scale (PSFS), while multi-dimensional (e.g., impairment, quality of life, etc.) patient-reported assessment of health status was assessed with the Disablement in the Physically Active (DPA) and Knee Osteoarthritis Outcome Score (KOOS). The
The Efficacy of the Mulligan Concept to Treat Meniscal Pathology: A Systematic
Kasturi (2020)28
N=40 (32M, 8F)
Control (N=20)
Intervention (N=20)
Average age of all participants 28.87y (SD 7.09)
Hudson (2018)21
N=23 (11M, 12F)
Both athletic and general populations
Age range: 14-62 y
Average Age 24.91y (SD 12.09)
Control (N=11)
Acute: 3 | Chronic: 8 Intervention (N=12)
Acute: 6 | Chronic: 6 Generally healthy
Sanchez (2017)24 N=1 26-year-old physically active female
Hudson (2016)27 N=5 (4M, 1F)
All acute meniscal injury Age range: 15-24 years Average age: 19.6 (SD 3.2)
Brody (2015)26 N=2 (1M, 1F) Healthy college students and recreational athletes
Rhinehart (2015)29 N=1F 20-year-old female soccer player DX: lateral meniscus pathology
Lower Extremity Functional Scale (LEFS), Global Rating of Change (GRoC), Range of motion (ROM), and Client Spe cific Impairment Measures (CSIM) were assessed as sec ondary outcomes when reported. Lastly, follow-up results were collected to determine the long-term effectiveness of the treatment intervention.
Review
Each participant had all the following findings:
• Joint line tenderness
• Restricted AROM
• Pain with terminal knee flexion, knee extension, and internal/external rotation
• Feeling of locking and instability in the knee joint
Inclusion: Participants presented with at least three of the following findings:
• Positive McMurray’s test
• Pain with maximal knee flexion
• Pain with maximal knee extension
• Joint line tenderness
• History of clicking and/or popping
Positive finding on at least one of the following rotational tests:
• Apley’s compression and distraction
• Thessaly’s at 20°
• Insidious right knee stiffness and swelling
• History of locking and popping
• Pain with terminal knee extension and flexion
• Positive Thessaly’s test at 5º and 20º of knee flexion
• Positive Apley’s compression test
• Joint line tenderness
• Positive McMurray’s test
• Pain with terminal knee flexion
• Pain with terminal knee extension
• Joint line tenderness
• History of clicking and/or popping
Inclusion: Participants presented with at least three of the following: Positive finding on at least one of the following rotational tests:
• Apley’s compression and distraction
• Thessaly’s at 20°
Inclusion:
• Joint line knee pain
• History of catching or locking
• Pain with knee flexion or extension
Positive finding on at least one or more of the following orthopedic special tests:
• McMurray
• Apley’s
• Thessaly
• Inability to fully flex or extend knee
• Pain with stairs
• Sporadic giving out of knee
• Joint line tenderness
Clinical diagnosis of meniscal pathology due to the following examination findings: Moderate swelling at both medial and lateral joint lines
The NRS is an outcome measure designed to assess pain intensity.38 All six studies utilized the NRS, which is a single-item measure that ranges from 0 (no pain) to 10 (most severe pain) and is used to assess the best, current, and worst pain the patient has experienced over the past
Author (Year) Study Design Participants Intervention
Kasturi (2020)28 Experimental Randomized Control Trial
Hudson (2018)21 Experimental Randomized Control Trial
N=40 (32M, 8F) Control (N=20) Intervention (N=20)
N=23 (11M, 12F) Control (N=11) Intervention (N=12)
MC ‘Squeeze’ technique along with conventional therapy
Mulligan with Movement ‘Squeeze’ technique
Sanchez (2017)24 Case Study N=1F Tibial IR Mobilization with Movement And MC ‘Squeeze’ technique
Hudson (2016)27 Case Series N=5 (4M, 1F) MC ‘Squeeze’ technique
Brody (2015)26 Experimental Case Series N=2 (1M, 1F) MC ‘Squeeze’ technique
Rhinehart (2015)29
Case Study N=1F MC ‘Squeeze’ technique
NWB tibial IR
WB tibial IR glide
WB tibial IR glide combined with a distal anterior tibiofibular glide lateral tibial glide
MC tibial IR glide taping technique
Comparison Outcome Measures
Conventional Therapy NRS PSFS Knee ROM
Sham Mulligan Treatment NRS PSFS DPA KOOS
None DPA PSFS NRS
None NRS PSFS DPA KOOS
None DPA PSFS Knee ROM NRS
None DPA NRS LEFS GRoC PSFS CSIM Knee ROM
Study Author (Date) Study Design Scale Used Scale Score Level of Evidence
Kasturi (2020)28 RCT PEDro Scale / D&B 4/10 / 22/32 Level 2 Hudson (2018)21 RCT PEDro Scale / D&B 6/10 / 26/32 Level 2
Hudson (2016)27 Case Series JBI Checklist 8/10 Level 4
Brody (2015)26 Case Series JBI Checklist 9/10 Level 4
Sanchez (2017)21 Case Study CARES Checklist 10/12 Level 4
Rhinehart (2015)29 Case Study CARES Checklist 9/12 Level 4
24 hours.38,39 The minimal clinically important difference (MCID) on the NRS is 2 points or a 33% reduction indicating a “much better” improvement in symptoms.40
The PSFS was used to assess function. All six studies uti lized the PSFS, where patients choose and rate functional or personally important tasks from 0 (unable to perform activity) to 10 (able to perform activity at pre-injury level).34,35,41 The MCID for the PSFS is 3 points in orthope dic knee conditions.41
Five studies used the DPA scale to assess the patient’s per ception of disablement as a result of their injury 42 The DPA scale consists of 16 items scored from 1 (no problem) to 5 (the problem(s) severely affect me).42,43 The scores for each item are totaled and then 16 is subtracted from the to tal score to provide the DPA score; scores range from 0-64, with high scores indicating more severe disablement.42 The MCID value for the DPA scale is a change of 9 points in acute injuries and a change of 6 points in chronic injuries.42
Two studies used the KOOS, which is a self-administered outcome measure used to assess a patient’s perception of
M male; F female; MC-Mulligan Concept; NRS Numeric Pain Rating Scale; PSFS Patient-Specific Functional Scale; DPA Disablement in the Physically Active Scale; KOOS Knee injury and Osteoarthritis Outcomes Score; ROM Range of Motion; LEFS Lower Extremity Functional Scale; GRoC Global Rating of Change; CSIM Client Specific Impair ment Measure; NWB Non-weight bearing; WB Weight-bearing; IR Internal rotation RCT Randomized Control Trial; CARE Case Report guidelines; JBI Joanna Briggs Institute; PEDro Physiotherapy Evidence Database; D&B Downs and Black Checklisttheir knee injury and ability to complete usual activities.44 The KOOS assesses five different subscales specific to knee injury: pain, symptoms, activities of daily living, sport and recreational function, and knee-related quality of life over the past week.44 The KOOS includes 42 items across the five subscales with each item scored on a Likert scale from 0 (no problem or never) to 4 (extreme problem or always); the score is then converted to a 0-100 scale with a lower score representing more severe problems.44
One study used the LEFS to assess a patient’s perceived dis ablement with a 20-item questionnaire designed to assess a patient’s perceived level of difficulty completing different activities due to lower extremity injury 45 The LEFS items are scored on a Likert scale from 0 (extreme difficulty or un able to perform) to 4 (no difficulty) and the score for each is summed together for a total score; the maximum score on the LEFS is 80 points and indicates no functional limita tions.45
One study used the GRoC which is a single-item measure to assess the patient’s perceptions of their overall improve ment since the initial treatment.46 The GRoC is scored on a 15-point Likert Scale ranging from -7 (a very great deal worse) to +7 (a very great deal better).47 A change in score of 5 points or greater on the 15-point GRoC scale represents a clinically meaningful change.48
Three studies used range of motion (ROM) as a clinicianreported outcome measure used to assess joint motion. The normative ROM for knee flexion and extension ranges from 132.9° to 142.3° and 0.5° to 2.4° respectively 49
One study used the CSIM, which is a specific movement or muscle contraction that causes pain or is difficult for a patient to perform; the CSIM is rated on a scale from 0 (no difficulty or pain) to 10 (maximum difficulty or pain).50 The CSIM is used in the Mulligan Concept to identify what is painful for the patient and help the clincian use the ap propriate directional force or glide to relieve pain through out the previously painful movement. No validation of the CSIM has been done to date.
A total of 139 articles were initially identified from the search and 133 articles were excluded due to either being duplicates or not meeting the inclusion and exclusion cri teria (Figure 1). A total of six articles met the inclusion and exclusion criteria for full-text review and were included in the analysis (Table 2). All eligible articles yielded a total of 72 subjects (Male=48, Female=24) ranging in age from 14-62 years. All patients were clinically diagnosed with a meniscal pathology through a physical exam; participant demographics and physical exam diagnostic criteria are presented in Table 1
Six studies were included in the final analysis covering mul tiple designs and levels of evidence.21,24,26–29 Two RCTs, two case series, and two case studies were evaluated for quality using the appropriate measurements (Table 3). The two RCTs were graded down to Level 2 because of quality: both were scored as six or less on the PEDro scale indicating concerns with methodological quality. However, in the D&B checklist the Hudson RCT21 fell in the “excellent” range (26/32) while Kasturi28 fell in the “good” range (22/32). The case series were graded above a 6/10 demonstrating low risk of bias. Both case studies were assessed with the CARES checklist used for the reporting of a case study; both were able to answer “yes” to 75% or higher of the questions in the checklist. Table 1 details the assessment of each article included.
The total number of treatments used varied between stud ies. Kasturi28 was the only study without the total number of treatments reported; however, data was reported at three time points during the study The number of treatments reported in the other studies varied between two and six.21,24,26,27,29 The time between treatments varied across all six studies ranging from 24 hours to 14 days.21,26 The specific intervention protocols and study timelines are de scribed in Table 4.
Some of the patients were allowed to continue participa tion during treatment while other authors did not specify the amount of participation or restriction during treatment. Kasturi28 did not report on the level of activity before, dur ing, or after treatment. Hudson et al21 only reported on dis charge criteria and did not specify participation parame ters. Sanchez24 reported that all the patients returned to participation but did not describe participation during the intervention. In the case series, Hudson et al27 reported that the patients were able to continue participation throughout treatment and returned to previous levels of ac tivity. Brody et al26 and Rhinehart29 only reported that pa tients were able to return to previous levels of participation following the MC MWM treatment. No researcher reported any adverse reaction to the treatment or worsening of the symptoms following treatment.
Similar results were reported across the two RCTs.21,28 Kasturi28 reported both groups improved with rehabilita tion; however, the treatment group with MC MWM had a statistically significant improvement in comparison to the control group consisting of conventional rehabilitation. Hudson et al21 also demonstrated statistically significant results for those in the treatment group and crossover group compared to the sham treatment.
Author (Year)
Intervention Protocol Timeline
Kasturi (2020)28 IG: MC ‘Squeeze’ technique with conventional therapy
• 3x10 in one session
Conventional therapy:
• Static quadriceps, vastus medialis obliques, and hamstring strengthening
• Active hip, knee, ankle ROM exercises
• Seated multiple angle isometric exercises
• AROM and strengthening for the unaffected lower limb
• Gait training given on parallel bar in front of the mirror
• All exercises were repeated ten times with 10 sec hold and relaxed each time.
Control Group: conventional therapy only
Hudson (2018)21 Intervention Group: Control Group: Crossover Group:
• MWM: MC ‘Squeeze technique
• 3 x 10 with a minimum of 30 seconds of rest in be tween each set
• Used same protocol as IG, but with a sham Mulli gan using a different hand placement and amount of force
• No activity restriction
• Received MC ‘Squeeze’ treatment after not reach ing discharge criteria in the sham group
Sanchez (2017)24 Visit 1: Visit 2: Visit 3:
• MWM - MC ‘Squeeze’ technique
• Tibial IR MWM with squat 3 x 10
• MC ‘Squeeze’ 3 x 10
• MC ‘Squeeze’ 2 x 10
• Tibial IR MWM with terminal knee extension 3 x 10
Number of
Treatment was conducted for 6 weeks; frequency of treatment sessions (e.g., 1/week, 2/week) was not reported. Not provided
14-days 24-72 hours in between each Tx
Crossover group had an additional 14-day treatment period with the ‘Squeeze’ technique after the sham treatment if they had not recovered
≤ 6
Crossover group had an additional 1-6 treatments with the ‘Squeeze’ technique after the sham treatment
11-days 3
Author (Year)
Hudson (2016)27
• MC ‘Squeeze’ technique was administered accord ing to Mulligan Concept principles.
• All participants were treated until discharged
Average 14.2 days (SD = 5.68 days)
Ranged from 2 to 21 days
Ranged from 2 to 6 treatment sessions
Brody (2015)26 Patient 1: 21 days Patient 2: 15 days
• MC ‘Squeeze’ Tx given by same Mulligan trained clinician
• 3 sets of 10 reps in PWB during 1st Tx.
• 3 sets of 10 in squat during 2nd Tx.
• 3x10 NWB tibial IR MWM flexion/extension
• 3x10 WB tibial IR MWM knee flexion
• 3x10 WB tibial IR MWM with anterior tib/fib glide for dorsiflexion
• Taped the tibial IR glide using Coverall and Leuko tape
• 1x10 NWB tibial IR MWM flexion/extension
• 2x10 WB tibial IR MWM knee flexion
• 2x10 lateral tibial glide while walking up steps
• 2x10 tibial IR with lateral tibial glide while walking up steps
• 2x10 MC ‘Squeeze’ technique while walking up steps
• Taped the tibial IR glide using Coverall and Leuko tape
9-days 4
Both patients: 2 Rhinehart (2015)29 Visit 1: Visit 2: Visit 3: Visit 4:
• 2x10 MC ‘Squeeze’ technique while lunging 3x10 standing forward lunge with medial tibial glide
MWM Mobilization with Movement; MC Mulligan Concept; ROM Range of Motion; AROM Active Range of Motion; IG Intervention Group; Tx Treatment; CG Control Group; SD Standard Deviation; IR Internal Rotation; PWB Partial weight bearing; NWB Non-weight bearing; WB Weight bearingKasturi (2020)28
Hudson (2018)21
IG: 7.35 ± 1.18 CG: 7.2 ±0.15
IG: 2.64 ±0.89 CG: 3.67 ±2.50 COG: 3.40
IG: 1.1 ±0.79 CG 3.05 ±1.23
IG: 0.44 ± 0.44 CG 2.42 ±1.96 COG: 0.66
IG: 6.25 pt ↓* CG: 4.15 pt ↓*
IG: 2.2 pt ↓* CG: 1.25 pt ↓ COG: 2.73 pt ↓*
Sanchez (2017)24 3 (Worst score) 0 (worst) 3 pt ↓* Hudson (2016)27 4.32 (Average) 0.07 (average) 4.25 pt ↓* Brody (2015)26 Patient 1: 4 (average) Patient 2: 8 (average)
Both patients: 0 (average) Patient 1: 4 pt ↓* Patient 2: 8 pt ↓*
Rhinehart (2015)29 4.7 0.83 3.87 pt ↓
In the six included papers, the researchers reported de creases in pain that were either statistically significant or met the MCID of a two-point change on the NRS21,24,26–29,40All of the participants who received MC MWMs had a complete or near-complete resolution of pain (Table 5). Kasturi28 reported no significant difference after day one of treatment (p = 0.698) but a significant difference in NRS scores between the control group and the interven tion group at four weeks with a mean difference of 1.65 (p = < 0.001), six weeks post intervention with a mean difference of 1.95 (p = < 0.001). Both groups had a reduction in pain on the NRS that exceeded the MCID. In their RCT, Hudson et al.21 did not report a statistically significant difference be tween the sham-control group and the intervention group after the final treatment for pain; however, the interven tion group had over a two-point average reduction on the NRS and met the MCID, while the sham-control group did not meet the MCID for the NRS after the final treatment. Additionally, all the participants in the intervention group scored a two or less on the NRS scale following the final treatment.21
In the two included case series26,27 the researchers re ported decreases in pain in as little as two treatments26 to an average of five treatments.27 In both cases, pain was reduced to near zero at discharge on the NRS.26,27 The total number of patients treated between the two-case se ries was seven with five of them from the Hudson et al.27 study. Two additional patients have been reported in the literature through two case studies.27,29 Both patients re ported decreased pain in as few as three treatments.27,29 Both studies met the MCID with a greater than two-point change at discharge.27,29 In addition, both authors reported that the patients had less than 1/10 on the NRS at dis charge.27,29
Patient reported improvement in function was found on the PSFS (Table 6) in all six studies and the results were either
statistically significant or met the MCID.21,24,26–29 In both RCTs,21,28 a statistically significant difference in the PSFS scores of the participants in the intervention group com pared to the control group were found across each of the measured time points.21,28
Additionally, in a case series by Hudson et al.,27 each of the participants had an increase of at least 3 points on their PSFS by the time of discharge, meeting the MCID of 3.27,51 Furthermore, changes in patient reported function were reported to be statistically significant (p = 0.003) and a large effect size (d = 3.01) was reported.27,52 The other case series by Brody et al26 did not include inferential sta tistical analysis; however, both patients reported PSFS im provements which met the MCID value for the PSFS.
In a case study by Rhinehart,29 the participant had an in crease in their average PSFS score by 4.75 points from ini tial visit to discharge (nine days), which also met the MCID for the PSFS. In another case study,24 the participant im proved 2 points on their PSFS to reach the maximum 10 points from initial visit to discharge.
In each of the five studies that reported on the DPA scale, either the MCID was met or a statistically significant change in DPA scores was reported (Table 7) indicating the patient’s perceived disability improved with treat ment.21,24,26,27,29 The DPA scale was utilized in one RCT and a statistically significant difference (mean difference of 8.78 points; p = 0.013) was found between the MC MWM treatment group and the sham group.21 In the case series by Hudson et al.,27 each of the five participants had an im provement in their DPA scale at discharge: three of the five participants reported changes exceeding the MCID crite rion, while the other two participants reported DPA scale scores within the reported ranges of healthy people prior to starting treatment.27,42 Brody et al.26 reported that the DPA score increased from intake to discharge for one participant and noted that the increase was due to increased life stress. In the two case studies, both patients reported a decrease in their DPA score with each visit.24,29
* Denotes minimal clinically important difference; IG Intervention Group; CG Control Group; COG Crossover Group; pt pointKasturi (2020)28
Hudson (2018)21
IG: 3.39 ± 1.18 CG: 3.89 ±0.81
IG: 3.67 ±1.72 CG: 6.45 ±1.57 COG: 5.80
IG: 8.49 ± 0.61 CG 7.11 ±0.84
IG: 9.50 ±1.85 CG 7.00 ±2.07 COG: 9.00
IG: 5.1 pt ↑* CG: 3.22 pt ↑*
IG: 5.83 pt ↑* CG: 0.55 pt ↑ COG: 3.20 pt ↑*
Sanchez (2017)24 8 (average) 10.0 (average) 2 pt ↑ Hudson (2016)27 3.4 (average) 10.0 (average) 6.6 pt ↑* Brody (2015)26 Patient 1: 5.33 (average) Patient 2: 2.0 (average)
Patient 1: 8.67 (average) Patient 2: NT Patient 1: 3.34 pt ↑* Patient 2: N/A
Rhinehart (2015)29 4.0 8.75 4.75 pt ↑*
* Denotes minimal clinically important difference; IG Intervention Group; CG Control Group; COG Crossover Group; Tx treatment; pt point; NT not tested; N/A Not ap plicable
Kasturi (2020)28 N/A Hudson (2018)21
IG: 23.92 ±10.05 CG: 24.91 ±11.96 COG: 26.6
IG: 9.00 ±8.12 CG 18.55 ±14.05 COG: 10.4
IG: 14.92 pt ↓* CG: 6.36 pt ↓ COG: 16.2 pt ↓*
Sanchez (2017)24 16 6 10 pt ↓* Hudson (2016)27 25.6 (Average) 7.4 (average) 18.2 pt ↓* Brody (2015)26 Patient 1: 10 Patient 2: 40 Patient 1: 13* Patient 2: NT Patient 1: 3 pt ↑† Patient 2: N/A Rhinehart (2015)29 46 0 46 pt ↓*
* Denotes minimal clinically important difference; IG Intervention Group; CG Control Group; COG Crossover Group; Tx treatment; pt point; NT not tested; N/A Not ap plicable; † Increase in DPA score was attributed to other aspects of the patient’s life causing them stress
Two of the studies included the KOOS outcome measure to assess the patient’s perception of their knee injury and dys function.21,27 In a case series, Hudson et al.27 found the av erage change on the KOOS across participants was a 28.56 ± 5.68 point increase (i.e., improvement) from the initial exam to discharge, which was an average of 14.2 days across the five participants. In a randomized controlled trial, Hud son et al.21 observed an average increase (i.e., improve ment) of 13.82 ± 10.94 points on the KOOS in participants in the MC ‘Squeeze’ treatment group, while there was only a 9.07 ± 11.13 average increase in the sham group. Five participants crossed over and completed the MC ‘Squeeze’ treatment and reported a mean increase of 21.28 ± 11.38 from completion of sham trial to completion of MC ‘Squeeze’ trial.
The LEFS was included as an outcome measure in a single case report.29 Researchers reported the patient had an ini tial score of 55. After four treatment sessions over the course of 9 days, the patient had attained a score of 80
points, which is the highest score possible indicating no perceived functional limitations were identified by the pa tient on the LEFS.29 Additionally, this patient maintained this score at both the one-week and one-month follow up after discharge.29
The GRoC was used as an outcome measure in the case re port by Rhinehart.29 The patient reported a score of +6 (A great deal better) following the first treatment session.29 The discharge exam for this patient occurred nine days af ter initial treatment, and a GRoC score of +7 (A very great deal better) was reported. The GRoC score was maintained at both the one-week and one-month follow-up appoint ments.29
Three of the studies included knee ROM as an outcome measure (Table 8).26,28,29 In two of the studies, the patients had full knee range of motion by discharge.26,29 Addition ally, in their case report, Rhinehart29 found improvements in ROM were maintained through the one-month follow up. In an RCT, the researchers found a statistically signifi
Kasturi (2020)28
IG: Flexion: 99° CG: Flexion: 102.75°
Hudson (2018)21 N/A
Sanchez (2017)24 N/A
Hudson (2016)27 N/A
Brody (2015)26
Patient 1: Extension: lacking 2° Flexion: 143° Patient 2: Extension: 0° Flexion: 136°
*Rhinehart (2015)29
Extension: lacking 20° Flexion: 92°
IG: Flexion: 128.5° CG: Flexion: 121°
IG: 29.5° ↑ CG: 18.25° ↑
Patient 1: Extension: lacking 1° Flexion: 146° Patient 2: Extension: -2° Flexion: 152°
Patient 1: Extension: 1° ↑ Flexion: 3° ↑ Patient 2: Extension: 2° ↑ Flexion: 16° ↑
Extension: 0° Flexion: 135° Extension: 20° ↑ Flexion: 43° ↑
IG Intervention Group; CG Control Group; N/A Not applicable; * Type of ROM measured was not specified
cant mean difference of 7.5 (p = < 0.001) in ROM in the in tervention group compared to the control group.28
The Client Specific Impairment Measure (CSIM) outcome was included in a case report29 where the patient identified a body-weight squat and forward lunge as the motions causing pain and reported a 4 out of 10 for the squat and a 6 out of 10 for the lunge before treatment for pain/dif ficulty 29 Following the first treatment session, the CSIM scores improved to a 2; after the second treatment session, the reported CSIM scores were a 0 indicating no pain or dif ficulty with a body-weight squat or forward lunge. Scores of 0 on the CSIM were maintained through discharge, oneweek, and one-month follow up.29
Follow-up data collection post-discharge (Table 9) was only conducted in two26,29 of the included studies. In the case report by Rhinehart,29 the patient completed four treat ment sessions over the course of nine days and results were maintained or improved at follow-up. Brody et al26 ob tained follow-up results from one participant, 21 weeks (~5 months) post discharge. The participant received two treat ment sessions and was discharged three weeks after their initial evaluation, also reporting maintained or improved scores at follow-up.26
Researchers have reported that appropriate physical ex amination procedures can result in accurate diagnosis of meniscal pathology 6,7 Accurate identification of the con dition, as well as determining if the patient will respond to conservative therapy, is important for healthcare profes sionals and researchers. The MC includes MWMs such as the ‘Squeeze’ technique, tibial IR, and tibial ER proposed to rapidly restore pain-free, functional ROM for patients with suspected meniscal injury which could enhance conserva
tive care protocols and outcomes. The MWM techniques, however, have not been critically appraised via a systematic review. The purpose of this study was to evaluate the effec tiveness of MC MWMs on patient-reported pain, function, and multi-dimensional health status in patients with clini cally diagnosed meniscus pathologies.
Pain severity was assessed using the NRS in each of the in cluded studies21,24,26–29 The application of MWMs in cases of clinically diagnosed meniscal pathology produced sub stantial improvements in pain severity Improvements in cluded complete or near-complete resolution of pain in as little as one week of treatment26 or in as few as one or two treatment sessions.24,26 Asymptomatic meniscal tears are common among healthy people indicating that the dam aged meniscus may not need to be removed; thus, when pain is a primary complaint, conservative pain reduction therapies that successfully resolve this complaint may be sufficient.53 The use of MC MWMs, and specifically the MC ‘Squeeze’ technique, were found to be effective interven tions for pain reduction in clinically diagnosed meniscal pathology over shorter durations (e.g., one month-follow up) in the included literature. The included studies did not identify evidence to support the long-term effects of these interventions (e.g., length of pain resolution, relationship to OA development, etc.), patient-applied application of the techniques for symptom management, or outcomes of the techniques being applied as multimodal rehabilitation protocols. Thus, clinicians and researchers should consider measuring and assessing longer-term outcomes of these technique, outcomes from patient-application of the tech niques, and how the incorporation of other intervention or exercise protocols may influence patient outcomes.
The PSFS was used in all studies to assess patient-perceived functional improvements. The reported PSFS changes met the MCID and were statistically significant indicating the
Rhinehart (2015)29
Outcome Measure Initial Evaluation Discharge Follow-up Notes
NRS (0-10) 4.7 (Average) 0.83 0
Follow-up was conducted at both 1-week and 1-month after discharge and the patient had the same scores at both time points PSFS (0-10) 4 (average) 8.75 10
DPA 46 0 0
LEFS (0-80) 55 64 80 GRoC N/A +7 +7
CSIM (0-10) Squat; Lunge 4/10; 6/10 0/10; 0/ 10 0/10; 0/ 10
Brody (2015)26
NRS (0-10) 4 (Average) 0 0
• Squatting
• Knee extension
Follow-up was at 21 weeks and the patient did not require any additional treatments following discharge and was able to participate in their usual activities PSFS (0-10) 5 9 9 7 9 10 4 8 10
• Post-activity
technique not only provided a reduction in pain but also re stored function, as defined by the patient. The findings are valuable because pain and function are the primary symp toms for which patients seek treatment.11 In Kise et al,11 patients were divided into two groups following diagnosis of meniscal injury where one group was given exercise ther apy alone while the other group received surgery alone. The exercise therapy group and those who underwent meniscal repair showed no significant difference after two years in dicating a need for a treatment that will restore function and allow continued activity for otherwise healthy patients. While the MC ‘Squeeze’ technique seems promising to re store function in the short term, only two of the studies in cluded any long-term follow-up26,29 with the longest fol low-up point being 21 weeks post-discharge.26 Neither of the RCT’s21,28 did any long-term follow-up with the pa tients to see how long the treatment result lasted. The gold standard of surgical repair is not necessarily a longterm solution for the treatment of meniscal pathologies as some patients who have had surgery have needed ad ditional surgery in as few as two years, and in the event of a failed repair that is asymptomatic, it is advisable to leave the meniscus alone instead of performing resection or another repair 16 Therefore, alternative treatment ap proaches are needed, and the MC ‘Squeeze’ technique could be a valuable tool for the mitigation of symptoms to restore function when a meniscal pathology is suspected.
The DPA scale assesses physical impairment (e.g., pain, function) and quality of life in unique constructs. The in cluded studies provide evidence that the MC ‘Squeeze’ technique improved multidimensional health status as measured by the DPA scale. Four of the studies21,24,27,29
found a statistically significant change (i.e., improvement) in DPA scores following treatment. Brody,26 however, iden tified impaired quality of life (QOL) score on this outcome measure in her case study through the course of treatment. The case report design allowed patient questioning that revealed the QOL impairment was perceived to be due to other life-related stress independent of knee pain. The im plications of catching a change in life stress related to or independent of presenting pathologies could have longterm- treatment implications by informing future care de cisions.54 Overall, the MC ‘Squeeze’ technique restored physical and QOL impairments as measured by the DPA scale, which is expected because physical improvements (e.g., pain reduction, increased function) are likely to cor relate with improved QOL.55
The use of the KOOS could have addressed the lack of long-term follow-up data as it has been recommended as a long-term outcome measure for three months, six months, and a year 44 However, the researchers who included the KOOS did not collect discharge data further than 14 days after intake. The studies21,27 that used the KOOS revealed meaningful improvement in KOOS scores; however, KOOS data collected at wider intervals over a longer duration would have provided greater insight into long-term inter vention effectiveness.
The secondary outcome measures included in the different studies were the LEFS, GRoC, ROM, CSIM, and follow-up treatment. Only Rhinehart29 reported on the LEFS and GRoC, and both measurements revealed patient improve ment during the study These results were corroborated with other scales (e.g., DPA KOOS) also used in the study and revealed improvement in pain, function, and QOL. The
NRS Numeric Pain Rating Scale; PSFS Patient-Specific Functional Scale; DPA Disablement in the Physically Active Scale; LEFS Lower Extremity Functional Scale; GRoC Global Rating of Change; CSIM Client Specific Impairment MeasureThe Efficacy of
the Mulligan Concept to Treat Meniscal Pathology: A Systematic Review
Rhinehart29 study was the only study to include the CSIM; the CSIM data collected supported the PSFS and NRS data corroborating increased function and decreased pain fol lowing treatment. It is not known, however, if CSIM data provides unique or redundant information compared to other measures (e.g., NRS, PSFS).
Joint ROM was assessed in three of the articles26,28,29 in cluded in this review and was found to have increased fol lowing treatment. The increase in ROM was supported by patient-reported information found in other measures (e.g., NRS, PSFS, DPA scale) providing disease-oriented evidence supporting the patient-reported evidence. An advantage of assessing ROM in addition to patient reported outcomes is ROM provides quantifiable disease-oriented evidence sup porting improvement. The collection of disease-oriented outcomes, in addition to patient-oriented outcomes, should be considered for future studies to further understand the effects of the MC ‘Squeeze’ technique along with tibial IR and ER MWM’s.
Limitations are present in this review While all studies found positive findings for patients treated using the MC techniques, the quality of evidence should be considered. Only two RCTs were identified,21,28 and case reports and case series made up two-thirds of the studies included in this review. A meta-analysis was unable to be conducted due to the limited number of published studies and the het erogeneity of the included studies. The lack of long-term follow-up in the included studies is also a limitation, as only two studies26,29 included follow up visits with partic ipants’ post-discharge. The collection of longer-term out comes, including patient-oriented and disease-oriented, would be valuable in redetermining the effectiveness of MC MWM for the treatment of meniscal pathologies. Thus, fur ther high-quality RCTs are needed. The included studies generally lacked comparison to sham treatments, multi modal conservative treatment, diagnostic imaging, or sur gical intervention. Finally, the included studies generally included adolescent through middle aged adults of a phys ically active population. While other studies have success fully used the MC for other knee pathologies (e.g., os teoarthritis) in older populations,56 the findings of the
systematic review should be applied with caution across all populations.
Future research is needed on the MC ‘Squeeze’ technique along with other MC techniques as indicated by the patient case and their effectiveness in the treatment of clinically diagnosed meniscal pathologies. Long-term follow-up with patients from six months to three years would be helpful in better understanding how effective the treatment is at re ducing the need for surgery Higher level RCTs with a con trol or sham treatment group assessing a wider age range would also be beneficial. Lastly, studies using diagnostic imaging (e.g., MRI) or surgery to confirm the presence, type, and location of a meniscal pathology would help to further assess the effectiveness of the MC treatment for meniscal lesions and provide insight on types of meniscal pathology that may not respond to MC intervention.26,29
The results of this systematic review provide initial support for the use of MC MWM techniques for conservative treat ment of patients with a clinically diagnosed meniscal pathology. The MC MWMs reduced pain, increased func tion, increased knee range of motion, while decreasing pa tient reported symptoms of multidimensional health status impairment related to meniscus pathology Future research should focus on using the MC MWM techniques as adjunct or stand-alone interventions, in more diverse patient popu lations, in imaging confirmed meniscal pathology, and with longer-term follow-up to better understand the effective ness of the intervention.
All authors declare that they do not have any conflict of in terests with any of the topics discussed in this manuscript.
Submitted: July 15, 2022 CST, Accepted: September 12, 2022 CST
The Efficacy of the Mulligan Concept to Treat Meniscal Pathology: A Systematic Review
1. Brady MP, Weiss W Clinical assessment versus MRI diagnosis of meniscus tears. J Sport Rehabil 2015;24(4):423-427. doi:10.1123/jsr.2014-0182
2. Doral MN, Bilge O, Huri G, Turhan E, Verdonk R. Modern treatment of meniscal tears. EFORT Open Rev. 2018;3(5):260-268. doi:10.1302/2058-5241.3.170 067
3. Shekarchi B, Panahi A, Raeissadat SA, Maleki N, Nayebabbas S, Farhadi P. Comparison of Thessaly test with joint line tenderness and McMurray test in the diagnosis of meniscal tears. Malays Orthop J 2020;14(2):94-100. doi:10.5704/moj.2007.018
4. Yan R, Wang H, Yang Z, Ji ZH, Guo YM. Predicted probability of meniscus tears: comparing history and physical examination with MRI. Swiss Med Wkly. 2011;141:1-7 doi:10.4414/smw.2011.13314
5. Culvenor AG, Øiestad BE, Hart HF, Stefanik JJ, Guermazi A, Crossley KM. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta-analysis. Br J Sports Med. 2019;53(20):1268-1278. doi:10.1136/bjsports-2018-0 99257
6. Mather RC III, Garrett WE, Cole BJ, et al. Cost effectiveness analysis of the diagnosis of meniscus tears. Am J Sports Med 2015;43(1):128-137 doi:10.11 77/0363546514557937
7. Bor DS, Sharpe RE, Bode EK, Hunt K, Gozansky WS. Increasing patient access to MRI examinations in an integrated multispecialty practice. RadioGraphics 2021;41(1):E1-E8. doi:10.1148/rg.2021200082
8. McDermott I. Meniscal tears, repairs and replacement: their relevance to osteoarthritis of the knee. Br J Sports Med. 2011;45(4):292-297. doi:10.113 6/bjsm.2010.081257
9. Lowery DJ, Farley TD, Wing DW, Sterett WI, Steadman JR. A clinical composite score accurately detects meniscal pathology J Arthrosc Rel Surg 2006;22(11):1174-1179. doi:10.1016/j.arthro.2006.0 6.014
10. Fox AJS, Wanivenhaus F, Burge AJ, Warren RF, Rodeo SA. The human meniscus: a review of anatomy, function, injury, and advances in treatment. Clin Anat 2015;28(2):269-287 doi:10.100 2/ca.22456
11. Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ 2016;354:i3740. doi:10.1136/bmj.i3740
12. Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy for a degenerative meniscus tear: a 5 year follow-up of the placebosurgery controlled FIDELITY (Finnish Degenerative Meniscus Lesion Study) trial. Br J Sports Med 2020;54(22):1332-1339. doi:10.1136/bjsports-2020-1 02813
13. Hall MJ, Schwartzman A, Zhang J, Liu X. Ambulatory surgery data from hospitals and ambulatory surgery centers: United States, 2010. Natl Health Stat Report 2017;102:1-15.
14. Paradowski PT, Lohmander LS, Englund M. Osteoarthritis of the knee after meniscal resection: long term radiographic evaluation of disease progression. Osteoarthritis Cartilage. 2016;24(5):794-800. doi:10.1016/j.joca.2015.12.002
15. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762-769. d oi:10.1177/0363546518755754
16. Ronnblad E, Barenius B, Engstrom B, Eriksson K. Predictive factors for failure of meniscal repair: a retrospective dual-center analysis of 918 consecutive cases. Orthop J Sports Med 2020;8(3):2325967120905529. doi:10.1177/232596712 0905529
17 Nepple JJ, Dunn WR, Wright RW Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am 2012;94(24):2222-2227 doi:10.2106/jbjs.k.01584
18. Farha N, Spencer A, McGervey M. Outpatient evaluation of knee pain. Med Clin North Am. 2021;105(1):117-136. doi:10.1016/j.mcna.2020.08.017
20. Roemer FW, Kwoh CK, Hannon MJ, et al. Partial meniscectomy is associated with increased risk of incident radiographic osteoarthritis and worsening cartilage damage in the following year. Eur Radiol. 2017;27(1):404-413. doi:10.1007/s00330-016-4361-z
21. Hudson R, Richmond A, Sanchez B, et al. Innovative treatment of clinically diagnosed meniscal tears: a randomized sham-controlled trial of the Mulligan concept ‘squeeze’ technique. J Manual Manip Ther. 2018;26(5):254-263. doi:10.1080/106698 17.2018.1456614
22. Varghese JG, Dilakshana S, Ganesh SD, Varshini L. A study to analyze the effectiveness of mobilization with movement in OA knee dysfunction: a quasi experimental study Res J Pharm Technol 2019;12(5):2279-2282. doi:10.5958/0974-360x.2019.0 0380.9
23. Hing W, Hall T, Mulligan B. The Mulligan Concept of Manual Therapy 2nd ed. Elsevier Australia; 2020.
24. Sanchez BJ, Baker RT. Conservative management of possible meniscal derangement using the Mulligan concept: a case report. J Chiropr Med 2017;16(4):308-315. doi:10.1016/j.jcm.2017.08.005
25. Hing W, Hall T, Rivett DA, Vicenzino B, Mulligan B. The Mulligan Concept of Manual Therapy: Textbook of Techniques. 1st ed. Churchill Livingstone; 2015.
26. Brody K, Baker RT, Nasypany A, Seegmiller J. Treatment of meniscal lesions using the mulligan “Squeeze” technique: a case series. Int J Athl Ther Train 2015;20(6):24-31. doi:10.1123/ijatt.2014-0135
27 Hudson R, Richmond A, Sanchez B, et al. An alternative approach to the treatment of meniscal pathologies: a case series analysis of the Mulligan concept “Squeeze” technique. Int J Sports Phys Ther 2016;11(4):564-574.
28. Kasturi S, Jampa NSK, Mohan L. Effectiveness of Mulligan’s Squeeze technique as an adjunct to conventional therapy to decrease pain and improve range of motion in meniscal tear-a randomized controlled trial. Int J Physio 2020;7(1):20-25. doi:10.1 5621/ijphy/2020/v7i1/193669
29. Rhinehart A. Effective treatment of an apparent meniscal injury using the Mulligan concept. J Sports Med Allied Health Sci 2015;1(2):1-5. doi:10.25035/jsm ahs.01.02.04
30. Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L. Establishing a minimum dataset for prospective registration of systematic reviews: an international consultation. PLoS One 2011;6(11):e27319. doi:10.1371/journal.pone.002731 9
31. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021;372:1-9. do i:10.1136/bmj.n71
32. PEDro scale PEDro. Published June 21, 1999. Accessed October 11, 2021. https://pedro.org.au/engli sh/resources/pedro-scale/
33. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52(6):377-384. doi:10.1136/j ech.52.6.377
34. Hooper P, Jutai JW, Strong G, Russell-Minda E. Age-related macular degeneration and low-vision rehabilitation: a systematic review Can J Ophthalmol 2008;43(2):180-187. doi:10.3129/i08-001
35. Moola S, Munn Z, Tufanaru C, et al. JBI Critical Appraisal Checklist for Case Reports. In: Aromataris E, Munn Z, eds. Joanna Briggs Institute Reviewer’s Manual The Joanna Briggs Institute; 2017:1-7 htt p://www.joannabriggs.org
36. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D The CARE guidelines: consensus-based clinical case reporting guideline development. Glob Adv Health Med. 2013;2(5):38-43. doi:10.7453/gahm j.2013.008
37 OCEBM Levels of Evidence Centre for EvidenceBased Medicine (CEBM), University of Oxford. Published 2011. Accessed October 12, 2021. https://w ww.cebm.ox.ac.uk/resources/levels-of-evidence/oceb m-levels-of-evidence
38. Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth 2008;101(1):17-24. doi:10.1093/bja/aen103
39. Boonstra AM, Stewart RE, Köke AJA, et al. Cut-off points for mild, moderate, and severe pain on the numeric rating scale for pain in patients with chronic musculoskeletal pain: variability and influence of sex and catastrophizing. Front Psychol 2016;7(1466):1-9. doi:10.3389/fpsyg.2016.01466
40. Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Europ J Pain. 2004;8(4):283-291. doi:10.1016/j.ejpain.2003.09.004
41. Kowalchuk Horn K, Jennings S, Richardson G, van Vliet D, Hefford C, Abbott JH. The patient-specific functional scale: Psychometrics, clinimetrics, and application as a clinical outcome measure. J Orthop Sports Phys Ther 2012;42(1):30-42. doi:10.2519/josp t.2012.3727
42. Vela LI, Denegar CR. The disablement in the physically active scale, part II: the psychometric properties of an outcomes scale for musculoskeletal injuries. J Athl Train. 2010;45(6):630-641. doi:10.408 5/1062-6050-45.6.630
43. Vela LI, Denegar C. Transient disablement in the physically active with musculoskeletal injuries, part I: a descriptive model. J Athl Train. 2010;45(6):615-629. doi:10.4085/1062-6050-45.6.615
44. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and osteoarthritis outcome score (KOOS) development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998;28(2):88-96. doi:10.2519/jospt.1998.28.2.88
45. Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther 1999;79(4):371-383. doi:10.10 93/ptj/79.4.371
46. Kamper SJ, Maher C, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. Austral J Physio 2009;55(4):289. doi:10.1016/s0004-9514(09)70015-7
47 Lauridsen HH, Hartvigsen J, Korsholm L, Grunnet Nilsson N, Manniche C. Choice of external criteria in back pain research: Does it matter? Recommendations based on analysis of responsiveness. Pain 2007;131(1-2):112-120. doi:1 0.1016/j.pain.2006.12.023
48. Stratford PW, Binkley J, Solomon P, Gill C, Finch E. Assessing change over time in patients with low back pain. Phys Ther. 1994;74(6):528-533. doi:10.109 3/ptj/74.6.528
49. Soucie JM, Wang C, Forsyth A, et al. Range of motion measurements: reference values and a database for comparison studies. Haemophilia 2011;17(3):500-507. doi:10.1111/j.1365-2516.2010.02 399.x
50. Vicenzino B, Hing W, Rivett DA, Hall T Mobilisation with Movement: The Art and the Science Churchill Livingstone/Elsevier; 2011.
51. Chatman AB, Hyams SP, Neel JM, et al. The patient-specific functional scale: measurement properties in patients with knee dysfunction. Phys Ther 1997;77(8):820-829. doi:10.1093/ptj/77.8.820
52. Stratford PW, Gill C, Westaway M, Binkley J. Assessing disability and change on individual patients: a report of a patient specific measure. Physiother Canada 1995;47(4):258-263. doi:10.3138/p tc.47.4.258
53. Matar HE, Duckett SP, Raut V Degenerative meniscal tears of the knee: evaluation and management. Br J Hosp Med. 2019;80(1):46-50. doi:1 0.12968/hmed.2019.80.1.46
54. Nippert AH, Smith AM. Psychologic stress related to injury and impact on sport performance. Phys Med Rehabil Clin N Am 2008;19(2):399-418. doi:10.1016/ j.pmr.2007.12.003
55. Casanova MP, Nelson MC, Pickering MA, et al. Disablement in the physically active scale short form-8: psychometric evaluation. BMC Sports Sci Med Rehabil. 2021;13(1):1-18. doi:10.1186/s13102-021-00 380-3
56. Tsokanos A, Livieratou E, Billis E, et al. The efficacy of manual therapy in patients with knee osteoarthritis: a systematic review. Medicina. 2021;57(7):696. doi:10.3390/medicina57070696
Paige Cummings 1,2 , Nathan D. Schilaty 1,3,4 , Takashi Nagai 5 , Luca Rigamonti 6 , Ryo Ueno 8 , Nathaniel A. Bates 1,7 a
1 Department of Orthopedic Surgery, Mayo Clinic, 2 Alix School of Medicine, Mayo Clinic, 3 Center for Neuromusculoskeletal Research, University of South Florida, 4 Department of Neurosurgery & Brain Repair, University of South Florida, 5 United States Army Research Institute of Environmental Medicine, 6 School of Medicine and Surgery, University of Milano-Bicocca, 7 Department of Orthopaedics, The Ohio State University Wexner Medical Center, 8 Department of Sport Science, University of Innsbruck
Keywords: hamstring stiffness, shear wave elastography, targeted neuromuscular training, hamstring quadriceps ratio, ultrasonography https://doi.org/10.26603/001c.55757
Previous literature has postulated a relationship between greater hamstring stiffness and a higher risk of sustaining injury. Shear wave elastography (SWE) presents a relatively new means for non-invasive evaluation of soft tissue elasticity pre- and post injury or intervention.
(1) To establish baseline hamstring stiffness measures for young competitive athletes and (2) determine effect of targeted neuromuscular training (TNMT) on shear wave stiffness of the hamstring.
Un-blinded, prospective, non-randomized, cohort study
Six-hundred forty-two lower extremities from 321 high school and collegiate basketball athletes (177 F: 139 M) were examined for hamstring stiffness prior to the start of their competitive basketball season. Teams were cluster assigned to either the control or intervention (TNMT) group. Subjects in the control group underwent regular season activities as directed, with no influence from the research team. For the TNMT group, the research team introduced a hamstring targeted dynamic warm-up program as an intervention focused on activating the hamstring musculature.
Collegiate status was significant to hamstring stiffness for both sexes (p ≤ 0.02), but hamstring stiffness did not correlate to age or sex (r2 ≤ 0.08). Intervention was a significant factor to hamstring stiffness when the hip was positioned in extension (p ≤ 0.01), but not in deeper flexion (p = 0.12). This effect was sex-specific as TNMT influenced hamstring stiffness in females (p = 0.03), but not in males (p ≥ 0.13). Control athletes suffered three HAM injuries; TNMT athletes suffered 0 hamstring injuries.

Higher SWE measurements correlated with increased risk of injury, male sex, and collegiate athletics. TNMT intervention can lessen muscle stiffness which may reduce relate to injury incidence. Intervention effectiveness may be sex specific.
a
Corresponding Author: Nathaniel Bates 410 W 10th Ave Columbus, OH 43210 nate.bates@osumc.edu
Hamstring strain injuries are among the most prevalent in juries sustained by basketball athletes.1 Previous epidemi ological studies show the most common type of injury sus tained by professional basketball athletes is a strain, with the hamstring muscle group being the most frequently strained muscle.1 An evaluation of injuries of the National Basketball Association showed strains comprised up to 57% of reported injuries.1 Of these strain injuries, 23% related to the hamstring muscle group. Universally, hamstring in juries are one of the most prevalent non-contact injuries in sports with approximately 96% of hamstring injuries occur ring in non-contact situations.2,3 Although hamstring in juries are common, they can result in a substantial loss of playing time and an increased re-injury rate.2 The average number of days missed for basketball players who sustained a strain was 7.4 days, with nearly one-third of hamstring strains recurring within the first year of returning to play1,4 High rates of re-injury (12-14% within two years)5–7 cause more concern for athletes as re-injuries present with wors ening severity and more lost play time upon re-injury 2 Pre vious authors have shown a near doubling of play time lost after hamstring re-injury 8
Many variables may play a role in an athlete’s suscepti bility to initial hamstring injury and re-injury Previous lit erature has postulated a relationship between greater ham string stiffness and a higher risk of sustaining a hamstring injury 9 More recent literature has established a connection between increased hamstring stiffness and injury with male sex and past hamstring strain history 10,11 Male athletes routinely exhibit greater hamstring stiffness overall when compared to their female counterparts.10 Hamstring stiff ness measurements (kPa) in male athletes are nearly double that of females on both the athlete’s dominant and nondominant leg.10 Increased hamstring stiffness is a risk fac tor in male athletes as it associates with higher hamstring injury rates and a greater proportion of recurrent hamstring injuries.7 Compared to female athletes, male athletes par ticipating in intercollegiate soccer are 64% more likely to sustain a hamstring injury and are nearly twice as suscep tible to hamstring re-injury 4,12 In addition, initial ham string injury can alter the length-tension relationship of the hamstring muscle group, which increases hamstring stiffness.9 On average, athletes with hamstring injury ex hibit 11% higher hamstring stiffness than uninjured coun terparts. This mechanical change places greater tension on the hamstring muscle group and may increase the re-injury rate after initial hamstring injury 9 Additionally, hamstring muscles in a lengthened state exhibit reduced strength and returning to sport without engaging eccentric strengthen ing in a lengthened muscle state predisposes secondary in jury 13 In correlation with this increased stiffness, athletes with previous hamstring injury are also two to three times more likely to encounter a future hamstring strain than non-injured counterparts.8,14 However, increased ham
string stiffness is not universally observed after injury 15 Apart from associating with injury, muscle stiffness is also modifiable as dynamic stretching, which is known to de crease soft tissue injuries, has also been shown to decrease hamstring stiffness.16
Despite this data, findings that correlate injury preven tion with hamstring stiffness based on sex are not unilat eral. Female college basketball athletes suffer hamstring strains at higher rate than their male counterparts7 and, as noted, demonstrate decreased hamstring stiffness com pared to their male counterparts. Decreases in passive stiff ness are unfavorably associated with peak knee flexion torque generation,17 and knee flexion torque is subse quently associated with injury prevention.17 Indeed, greater hamstring stiffness has been associated with re duced knee ligament loading and reduced ligament injury risk18,19 Further, patients experiencing back pain exhibit reduced hamstring stiffness compared to matched con trols.20 Accordingly, insufficient muscle stiffness can affect the stability of the surrounding joints. Thus, there is meri torious data to support injury prevention through both in creased and decreased hamstring stiffness, but excessive hamstring stiffness is directly related to increased risk of injury to the muscle itself
In addition to sex differences and hamstring injury his tory, increasing age and competition level correlate with in creased hamstring injury incidence.9 Previous authors have found that in both football and soccer, surpassing 23 years of age was associated with a higher risk of hamstring injury in athletes compared to their younger counterparts.3,21 An estimated 1.78 increase in risk of hamstring injury is asso ciated with every year increase in age after an athlete turns 23.22 The variation in hamstring injury rate by age is asso ciated with an overall decrease in hamstring strength as in dividuals age resulting in a muscle imbalance between the quadriceps and hamstring muscle groups, ultimately lead ing to an increased risk of hamstring injury 6,23 Recently Alfuraih et al. showed decreasing hamstring shear-wave elastography (SWE) stiffness associated with aging in which elderly participants (77-94 years) had on average 16.5% lower hamstring stiffness compared to their young coun terparts (20-35 years).24 Changes in SWE stiffness correlate with muscle weakness associated with aging.23,24 The epi demiology of collegiate injuries versus high school injuries shows a more drastic increase in injury rate than those as sociated with age.25 The rate of overuse injury in college athletes is 3.28 times higher than in high school athletes.25 In both high school and college athletes, muscle strain is the most common injury 25
The mechanisms of hamstring injury are essential start ing points for developing injury prevention programs. Pre ventative biomechanical techniques are an increasingly popular means of decreasing the risk and incidence of mus culoskeletal injuries.26 Targeted neuromuscular training (TNMT) is a preventative biomechanical technique that consists of exercises designed to activate deficient muscle
Application
of Shear-Wave Elastography in the Evaluation of Hamstring Stiffness in Young Basketball Athletes
groups and encourage muscle co-activation that may be re lated to injury through movements that mimic those expe rienced during sport.26,27 Monajati el al. demonstrated that hamstring-based neuromuscular training increases ham string strength and flexibility over time.28 As a prevention technique, TNMT addresses muscle stiffness and hamstring to quadriceps strength ratio (H:Q) as plausible risk factors for hamstring injury 28 This biomechanical technique ac complishes neuromodulation using motor learning princi ples to focus on optimal control of 3D body positions and movement symmetry.27 Ultimately, re-establishing connec tions between nerves and muscles after injury leads to a reduced risk of re-injury.27 Accordingly, extrapolation of TNMT to non-contact hamstring injuries may prove effica cious in decreasing hamstring strain prevalence and sever ity by altering baseline biomechanics.
Commonly, hamstring injury is evaluated and diagnosed via dynamic ultrasonography. Classic clinical implementa tion of ultrasonography, relative to musculoskeletal injury, provides high-resolution imaging of fluid collection around an injured muscle or tendon.11 These images are highly ac curate in the determination of the location and extent of a hamstring injury Beyond diagnosis and localization, these images have limited use for risk prevention as they fail to provide feedback on mechanical properties or quality of in dividual muscle.10 Shear wave elastography (SWE) is a rel atively new ultrasound technology that can provide a noninvasive evaluation of soft tissue elasticity 29 Accordingly, interest in musculoskeletal applications for SWE has grown in the past several years.10,11,29 Ultrasound SWE uses vari ation in wave propagation to create images that provide an objective measure of tissue elasticity with anatomic speci ficity 29 Past researchers have used SWE to evaluate and provide an initial characterization pathologic conditions and injuries of the musculoskeletal system, including, but not limited to, the hamstring muscle group, neck/back muscles, the Achilles’ tendon, and the anterior cruciate lig ament.10,11,24,29,30 SWE can be used to assess hamstring stiffness at the time of injury, pre, and post-injury provid ing feedback on injury risk associated with increased stiff ness and decreased hamstring stiffness post injury preven tion facilitation.27,28 Sex differences in SWE for adolescent basketball athletes have previously been explored,10 but further study into the relationship between hamstring stiff ness and injury rate is necessary to determine whether hamstring stiffness is a primary causal factor for increased injury rate by age and competition level. It is known that in creased stiffness at the muscle-tendon unit correlates with greater work absorption, muscle force, and power during countermovement jumps.31,32 As muscle stretch is neces sary to induce injury and muscle failure occurs at forces greater than maximal isometric contractions,33 it remains that excessive passive muscle stiffness may predispose muscle tissue to injury. Subsequently, viscoelastic muscle stiffness can be reduced through passive and active stretch ing which increases both the force and energy absorption till failure.33 Additional investigation may also elucidate whether alteration of hamstring stiffness is a primary mechanism for injury prevention techniques such as TNMT
Finally, strong correlation between hamstring stiffness and injury may provide data that suggests that SWE is an opti mal tool for determining injury risk and intervention effi cacy.
This study’s objectives were to (1) To establish baseline hamstring stiffness measures for young competitive ath letes and (2) determine effect of targeted neuromuscular training (TNMT) on shear wave stiffness of the hamstring. Regarding the first objective, it was hypothesized that ham string stiffness would increase with age in high school bas ketball and college basketball athletes. Finally, it was hy pothesized that TNMT intervention would decrease SWE stiffness in basketball athletes.
Six hundred forty-two lower extremities from 321 high school and collegiate basketball athletes (177 F: 139 M; Table 1) were examined for hamstring stiffness across a range of passive hip and knee flexibility prior to the start of their competitive basketball season. Two subjects were ex cluded from this cohort due to a lack of demographic data. The subject population was a cohort of convenience, re cruited from high school and college basketball teams that compete near Rochester, MN, USA. Teams were contacted via a clinical coordinator and offered the opportunity to participate in research with no remuneration. Teams who agreed to participate in the study were cluster assigned to either the Control or intervention (TNMT) group prior to arriving for their first data collection. In this manner, all individuals from the same team were assigned to the same group, intended to reduce potential for data crosscontamination. This design has previously been employed for other training intervention studies.34–36 Group assign ments occurred in a predetermined order and were assigned to a team based on when they accrued into the investi gation. Subject recruitment spanned a three-year period. The current investigation was unblinded to both investi gator and participant. Subjects knew they would either re ceive a targeted training intervention during regular prac tice warmups or that they would proceed through their season activities unchanged. Pre-season data collection was completed after the start of team activities, but prior to the first competitive game. Post-season testing was com pleted after the last competitive game. All activities in this study were approved by the institution’s Institutional Re view Board (IRB 17-003905). Informed consent was ob tained for all subjects over 18 years old. Informed consent and parent/guardian assent were obtained for all subjects under 18 years old.
1.
N 450 192
Female 270 92 Male 180 100
Average Age 16.18 15.5
Collegiate Lower Extremities 60 0
HS Lower Extremities 390 192
*N total number of lower extremities
an intervention focused on activating the hamstring mus culature. This intervention was substituted in place of each team’s regular warm-up activities for 15 minutes twice weekly. Intervention dynamic warm-ups were initiated at the start of the season immediately following the preseason evaluation session and continued until the team was elim inated from playoff contention. As multiple teams were training at the same time, warm-up sessions were overseen either by the lead athletic trainer on the research team (TN) or by additional athletic training staff assigned to the par ticipating schools. These additional staff received instruc tion from the lead athletic trainer prior to enacting the interventional dynamic warm-up protocol. For the TNMT group, the intervention period lasted approximately 10 weeks in duration for each team. Selection of dynamic warm-up activities were orchestrated by the lead athletic trainer and the program was designed to incorporate ele ments known to positively affect the hamstring muscula ture.37–40 Specifically, the dynamic warm-up was designed around the incorporation of elements of stretching, skip ping/hopping, lunging, jumping/landing, concentric/eccen tric hamstring loading, balance, and dynamic range of mo tion at the core, hip, and knee (APPENDIX 1). Static stretching remains controversial relative to its efficacy for injury prevention; however, multiple studies have indicated that static stretching aides in the reduction of hamstring injuries.41–45 Warm-up drills are known to improve neuro muscular control during running.40 While the value of flex ibility and dynamic range of motion remain controversial to hamstring injury prevention, incorporation of eccentric hamstring loading has shown efficacy due to its’ ability to affect hamstring to quadricep (H:Q) muscle deficits.38,39,41 Lumbopelvic exercises were incorporated as they have demonstrated importance to lower extremity neuromuscu lar control and injury recovery 39
Ultrasound SWE was used to measure shear wave velocity (kPa) of the biceps femoris muscle at three leg positions (40%, 60%, and 80%) of the maximum passive 90-90 straight-leg raise position for each leg as previously de scribed.10 Briefly, hamstring flexibility was assessed by a
clinician who used a passive knee extension test and a dig ital inclinometer. Neutral position was considered to be ipsilateral hip and knee flexion both positioned at 90°.46 The three leg positions (40%, 60%, and 80%) were subject specific and calculated from the maximum flexibility ob served by the clinician. The greater trochanter and femoral condyle were then marked, and the midpoint was identified by the clinician for repeatable placement of the ultrasound transducer both within and between subjects. While lying supine, an assistant moved and held the athlete’s leg at each position for the clinician to measure the biceps femoris stiffness using ultrasound SWE at each position (GE Logiq E9, 9L-D transducer, GE Healthcare, Wauwatosa, WI). Ultrasound SWE captures the Young’s Modulus of soft tis sues in kPa based on displacements of the shear wave beam the propagation across the tissue. The Young’s Modulus equation is as follows:
where is the density of the medium, is the Gaussian profile of the beam, is a dimensionless diffraction pa rameter, and is the rising time.47 Three SWE images were acquired at each position for average values. Prior to lower limb manipulation, each subject was instructed to fully relax their muscles and allow the assistant to fully support the leg. To ensure that passive muscle stiffness was being obtained, random subjects were selected to be monitored by surface electrodes placed on the medial ham string muscle. These electrodes would provide real-time audio feedback to ensure the subject did not actively en gage the hamstring muscles and that the ultrasound SWE measurements were of passive muscle stiffness. Electrode subject selection was randomized based on the availability of the sensors as several subjects could be undergoing eval uation simultaneously Throughout pilot testing and the first year of randomly selected subjects, electrodes con firmed that the hamstrings musculature was maintained in a passive state. Beyond this, electrode monitoring was de termined to be redundant and ceased. Copious ultrasound gel and minimal pressure was applied to the ultrasound transducer probe to minimize tissue compression and arti fact error in tissue stiffness induced from externally applied pressure. Muscle stiffness (kPa) was measured using shear wave velocities from the SWE elastogram calculated via custom designed MATLAB software.10 Following comple tion of preseason testing, 103 athletes (206 lower extremi ties) returned for post-season evaluations that repeated the identical process. Post-season evaluations were conducted within two weeks following each team’s playoff elimina tion. Whether or not an athlete returned for post-season testing, the Mayo Clinic athletic training staff embedded at each school tracked participants for occurrence of ham string strain during the basketball season.
For statistical analysis, data were separated by sex and a one-way ANOVA was used to assess hamstring stiffness dif ferences between ages (14-18 years) with a Tukey’s post hoc test to assess individual differences within each age
Application of Shear-Wave Elastography in the Evaluation of Hamstring Stiffness in Young
Females
Males
Basketball Athletes
Age (Years) 80% Orientation 60% Orientation 40% Orientation
14 37.0 (26.3) 43.4 (28.2) 37.0 (20.7) 15 52.4 (35.7) 58.5 (35.8) 50.0 (28.8) 16 53.5 (38.8) 52.2 (32.0) 44.2 (26.5) 17 35.8 (22.9) 44.3 (30.2) 43.2 (26.7) 18 46.5 (38.3) 45.0 (27.7) 44.3 (28.9)
14 71.3 (37.3) 73.1 (39.2) 55.3 (33.0) 15 71.6 (38.4) 80.3 (37.7) 59.5 (32.2) 16 63.0 (39.5) 60.1 (34.0) 47.1 (27.3) 17 53.9 (33.1) 52.6 (31.0) 50.8 (29.7) 18 64.9 (37.6) 69.8 (37.6) 62.4 (31.7)
year. A Student’s t-test was used to assess differences in hamstring stiffness relative to competitive level (high school vs. collegiate). Pearson correlations were used to as sess association between age and stiffness at each orien tation. A 2x2 ANOVA of Intervention (TNMT, Control) vs. Time (Pre-, Post-Season) was used to assess for statisti cal differences among these groups. Individual differences within groups were assessed via Tukey’s post-hoc test. All statistical analyses were performed in JMP Pro (version 14, SAS Institute, Cary, NC, USA). Significance was set a priori at < 0.05.

Of the 321 total athletes recruited into this investigation, 103 athletes returned for post-season testing. Of these 103 athletes who completed both preseason and post-season evaluations, 22 athletes were assigned to the Control group and 81 athletes were assigned to the TNMT group (Table 1).
Age was a significant factor for hamstring stiffness in fe males at all three orientations (p ≤ 0.03) and in males at the 60% extended orientation (p < 0.01). However, there was no significant linear correlation between age and hamstring stiffness for either sex at any orientation (r2 ≤ 0.08). In fe males, hamstring stiffness peaked at ages 15 and 16 for the 80% orientation and age 15 for the 60% and 40% orienta tions (Table 2). In males, hamstring stiffness decreased by age 17 relative to age 14 and 15 in the 80% and 60% orien tations (Table 2). Collegiate status was significant to ham string stiffness for females at all orientations and for males at the 80% and 60% orientations. In each of these orienta tions, the collegiate athletes had significantly greater ham string stiffness than their high school counterparts (Figure 1).
TNMT intervention was a significant factor at the 80% and 60% flexibility orientation (p ≤ 0.01), but not at the 40% orientation (p = 0.12). Time was not a significant factor when sampled across the whole cohort (p ≥ 0.28). However, within the TNMT group, Time was significant for the 80% and 60% orientation (p ≤ 0.05). In all cases where Time was significant, the TNMT group exhibited a decrease in
Figure 1. Hamstring stiffness as recorded by SWE at orientations of 80% (blue), 60% (red), and 40% (green) of peak passive flexion.
At the 80% and 60% position, collegiate basketball players have significantly increased hamstring stiffness relative to their high school counterparts.
hamstring stiffness from pre-season to post-season testing (Table 3, Figure 2). Despite being measured with the same SWE machine with the same collection settings, pre-season SWE stiffness was higher in the TNMT group than the con trol group (p < 0.01).
For female athletes, intervention was a significant factor as hamstring stiffness at the 60% flexibility orientation de creased after TNMT (p = 0.04). TNMT intervention with fe male athletes approached significance at the 80% flexibility orientation (p = 0.07). TNMT intervention in male athletes did not show a significant change in hamstring stiffness at any orientation (p ≥ 0.13; Table 4).
Table 3. SWE stiffness of hamstring (mean ± SD) by Intervention and Time
Flexibility Targeted Neuromuscular Training Control
Pre Post Flexibility p-value Time pvalue Pre Post Flexibility p-value Time pvalue
80% 69.4 ± 35.4† 62.0 ± 33.4†* <0.01 0.05 43.3 ± 31.4 45.5 ± 29.4 0.96 0.79 60% 67.7 ± 32.4† 60.2 ± 33.4†* <0.01 0.04 54.3 ± 31.3 53.5 ± 34.4 0.41 0.73 40% 56.1 ± 29.4 50.8 ± 27.3 --- 0.12 48.8 ± 25.7 47.9 ± 25.9 --- 0.95
† Significant difference (α < 0.05) from 40% flexibility orientation
* = Significant difference (α < 0.05) from pre-season evaluation
Figure 2. Hamstring stiffness at 80% of peak passive flexion (top) and 40% of peak passive flexion (bottom).
TNMT reduced hamstring stiffness at the 80% orientation but exhibited no effect at 40%.
Table 4. SWE stiffness of hamstring (mean ± SD) Pre- and Post-Season for the TNMT Group separated by Sex
Position Males Females
Pre Post p-value Pre Post p-value
80% 70.8 ± 35.2 66.5 ± 32.5 0.60 57.6 ± 36.0 51.5 ± 32.3 0.07 60% 66.7 ± 32.3 63.8 ± 34.5 0.55 63.2 ± 32.8 54.4 ± 32.5* 0.04 40% 54.5 ± 30.2 48.2 ± 24.8 0.13 54.6 ± 27.6 52.0 ± 28.7 0.58
* Significant difference (α < 0.05) from pre-season evaluation
juries, while 93 athletes assigned to the TNMT group suf fered zero hamstring injuries. All three injured athletes were female (age = 16.7 ± 1.5 years; height = 173.0 ± 2.2 cm; mass = 79.4 ± 13.3 kg). The mean pre-season SWE ham string stiffness among the three injured athletes was 27.1 ± 15.7 kPa at the 40% flexibility orientation, 26.9 ± 16.1 kPa at the 60% flexibility orientation, and 18.8 ± 5.1 kPa at the 80% flexibility orientation.
Within the baseline stiffness measures, there were signifi cant sex differences in hamstring stiffness.10 Males showed significantly greater hamstring stiffness than females for all three flexibility orientations across all ages, 14-18. Nei
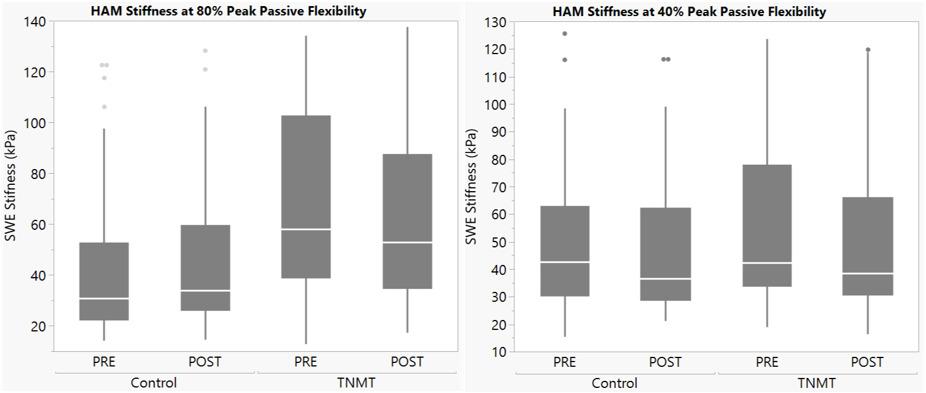
ther males nor females showed linear correlation between age and hamstring stiffness. This data rejects the hypoth esis that hamstring stiffness would increase with age in high school basketball athletes. Based on this data, ham string stiffness does not appear to be directly associated with maturational or athletic development.
Researchers have determined that SWE muscle stiffness decreases with ageing from 20 to 94 years along with changes in muscle composition and dysfunction in extra cellular fibers24,48; however, hamstring stiffness in adoles cent athletes has not previously been disseminated. While neuromuscular efficiency muscle size and contractile force has been shown to increase as adolescents age, data regard ing changes in elastic properties remains scarce.49–51 Past findings measuring musculotendinous stiffness, joint stiff
Application of
Shear-Wave Elastography in the Evaluation of Hamstring Stiffness in Young Basketball Athletes
ness, and series elastic component (SEC) stiffness show dif ferences in development and changes to muscle stiffness between the lower and upper extremities in adoles cence.49,52,53 Previous data showed knee extensor stiffness decreasing as children age and identical measures for elbow flexor stiffness between children and adults.49,52,53 Similar studies have yet to be conducted using SWE stiffness as the primary measure of muscle stiffness in adolescence during development. The lack of association between hamstring stiffness and age during adolescence likely indicates a lim ited influence of pubertal status on muscle stiffness; how ever, pubertal status was not assessed in the present inves tigation and further validation is warranted.49,54 Likewise, strength was not directly assessed in this study, so it was not possible to determine if SWE stiffness was directly cor related with athlete strength.
Unlike age, level of competition was a significant indica tor for increased hamstring stiffness in both sexes. The pre sent data supports the hypothesis that collegiate athletes would have greater hamstring stiffness than high school athletes. In conjunction with increased hamstring stiffness, musculoskeletal injury incidence and sport-specific perfor mance attributes also associate with higher levels of com petition.25,55 Accordingly, muscle stiffness may be relevant to both injury prevention and sports performance as data from the current study demonstrated that hamstring stiff ness is modifiable in female athletes through a minimal regimen of TNMT Despite these fiindings, further investi gation is warranted to determine whether muscle stiffness has a causal influence on injury prevention within sports as musculoskeletal injuries increase dramatically between high school and collegiate levels.27,55
The present data indicates that a TNMT hamstring warm-up program is likely to decrease hamstring stiffness. The results of the study show lower postseason hamstring stiffness compared to the control group. This supports the hypothesis that TNMT intervention would decrease shear wave stiffness in basketball athletes. Throughout this study three hamstring injuries occurred. Each reported injury oc curred in a female high school athlete who was not assigned to the TNMT group. Further investigation is necessary to determine whether dynamic warm-ups targeted to specific muscle groups can offer prevention against soft-tissue in juries in females during athletic participation.
Further, regarding the three injured subjects, the SWE hamstring stiffness in this sub-cohort was different than the whole study cohort, as the three injured athletes indi vidual SWE values were below the cohort mean. This fact remained true regardless of what age bracket the injured subjects were compared against. Relative to the position and limb where SWE was measured, the first injured subject was between 0.12-1.09 standard deviations below the co hort mean, the second injured subject was 0.44-1.02 devi ations below the mean, and the third injured subject was 1.12-1.40 deviations below the mean. While this granular data demonstrates that injuries only occurred in athletes with hamstring stiffness deficiencies, the current results are unable to conclusively prove that hamstring stiffness is
a primary cause of predisposing athletes to injury during a competitive season.
Optimal hamstring stiffness for basketball athletes is likely to lie along a Bell curve where extremes of extremes of high and low stiffness increase injury risk. It is also in teresting to note that overall subject population increased hamstring stiffness with increased extension in the pas sively manipulated straight leg extension (Table 3), but the injured cohort did not exhibit this trend. Additional inves tigation is necessary to determine whether these functional mechanics have clinical implications. Further study is also warranted due to preseason differences in the Control and TNMT groups. Measurements were recorded with identical methodology between groups, so it remains unknown as to why the control group was initially less stiff than the TNMT group. It is possible that the TNMT group would have been more susceptible to influence due to their higher initial stiffness.
The current intervention program, TNMT, included ec centric resistance exercise such as Nordic hamstring (NH) eccentric strength training which is associated with re duced injury.56–58 However, studies show while NH strength training lowered future hamstring strain injury post-intervention, data showed no significant changes to muscle fascicle length, stiffness, or eccentric hamstring strength occur 56 The results of this study compliment these previous data and demonstrate that mechanical vari ables outside increased strength or muscle length56–58 may contribute to muscle strain prevention. Thus, further stud ies are warranted to determine if the decrease in injury rate related to TNMT is directly associated with changes in mus cle stiffness or occurs through other biomechanical modifi cations.9
Data from this study support past literature that indi cates TNMT effectively reduces injury rate and muscle stiff ness.27,28 Furthermore, the present data demonstrates that the magnitude of response to TNMT varies by sex. Com pared to female athletes, hamstring stiffness in males re sponded less significantly to TNMT at all flexibility orien tations. Reduced stiffness response seen in male athletes is exacerbated by a substantially higher risk of hamstring in jury and re-injury 4,12 Thus, additional study into the util ity of injury prevention programs for male athletes may be warranted. More research is needed to determine the cause for sex differences associated with TNMT effectiveness. Fu ture studies may look at TNMT intervention in male and female college athletes who show higher overall hamstring stiffness than their high school counterparts, to elucidate whether the magnitude of hamstring stiffness plays a role in TNMT effectiveness while isolating sex differences.
that multiple schools underwent TNMT training simultane ously, a single universal athletic trainer could not be used for this study This introduces potential variation in facil itation of TNMT intervention, but improved generalizabil ity To combat any variations in administration of inter vention across trainers, all schools implemented the same program, each school trainer was taught by the same in terventionalist, and a written protocol was provided. While the population cohort for this study encompassed athletes between ages 13-22 years, data was captured on an insuffi cient number of athletes aged 13 (n = 3), 19 (n = 9), 20 (n = 3), 21 (n = 8), and 22 (n = 3) to include them as separate groups within the age-based statistical analysis.
In addition, this investigation experienced limitations in the collection of post-season data that accounts for the large number of athletes unable to be tested at follow-up. Post-season data collection was deterred by two events: 1) teams that were assigned to the control group felt a lack of investment in the investigation and subjects were reluc tant to return for post-season testing, 2) government man dated shutdowns due to the COVID pandemic prevented the capture of post-season data in Spring 2020. These unfor tunate events contributed to substantial attrition in par ticipants in postseason data collection, limiting the inter nal validity of the study Unfortunately, this limitation was unavoidable, but the captured cohort was deemed accept able for statistical analysis as each group had a minimum of 21 athletes that completed full analysis. This outbreak also impeded the planned implementation of collegiate TNMT groups for the 2020-2021 basketball season, which resulted in zero collegiate TNMT subjects (Table 1). Lastly, the GE Logiq E9 had a ceiling of SWE of 120 kPa. As hamstring elastic modulus exceeds 2500 kPa,59 even in a passively flexed state, many SWE stiffness values for the hamstring stiffness were saturated during imaging, which likely in creased variability and standard deviations observed in this study Future studies should incorporate SWE technology with a larger range of measurement for improved precision. Finally, the clinical significance of SWE stiffness measure ments remain undescribed. SWE measurements on muscle tissue are reliable within a session but lack precision and offer substantial variability within a whole population,61 as is herein observed with the standard deviations. Intra-ses
sion standard error of the mean for SWE stiffness on lower extremity muscles are between 8-12 kPa,61 which should be considered when accounting for clinical applicability of sta tistical findings.
Higher SWE measurements have been correlated with in creased risk of injury and groups at higher risk of hamstring injury (i.e., males and collegiate athletes). As such, poten tial exists to utilize SWE stiffness as a surrogate for in jury risk; however, further study is necessary to substanti ate these claims. Age did not factor into hamstring stiffness or injury The current findings contradicted previous re search citing correlation between increased hamstring in jury and decreased stiffness with increased age and may be indicative of a separate trend in adolescent cohorts. Data from this study reiterated that TNMT intervention can lessen muscle stiffness and incidence of re-injury However, the current data uniquely exhibited that females showed greater response to TNMT, and that intervention effective ness can be sex specific.
The authors have no financial disclosures or conflicts of in terest.
This investigation was funded by and NBA / GE Collabo rative Grant, as well as National Institute of Health grants from National Institute of Arthritis and Musculoskeletal and Skin Diseases R01-AR055563 and L30-AR070273 and the National Institute of Children and Human Development K12-HD065987 We also acknowledge the contributions of Rena F. Hale, PhD, to the early stages of data collection for this project.
Submitted: November 05, 2021 CST, Accepted: August 09, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Jackson TJ, Starkey C, McElhiney D, Domb BG. Epidemiology of hip injuries in the National Basketball Association: A 24-year overview. Orthop J Sports Med 2013;1(3):2325967113499130. doi:10.117 7/2325967113499130
2. Liu H, Garrett WE, Moorman CT, Yu B. Injury rate, mechanism, and risk factors of hamstring strain injuries in sports: A review of the literature. J Sport Health Sci. 2012;1(2):92-101. doi:10.1016/j.jshs.201 2.07.003
3. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med 2011;39(6):1226-1232. doi:10.1177/ 0363546510395879
4. Erickson LN, Sherry MA. Rehabilitation and return to sport after hamstring strain injury J Sport Health Sci 2017;6(3):262-270. doi:10.1016/j.jshs.2017.04.001
5. Malliaropoulos N, Isinkaye T, Tsitas K, Maffulli N. Reinjury after acute posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med 2011;39(2):304-310. doi:10.1177/0363546510382857
6. Lee JWY, Mok KM, Chan HCK, Yung PSH, Chan KM. Eccentric hamstring strength deficit and poor hamstring-to-quadriceps ratio are risk factors for hamstring strain injury in football: A prospective study of 146 professional players. J Sci Med Sport 2018;21(8):789-793. doi:10.1016/j.jsams.2017.11.017
7. Dalton SL, Kerr ZY, Dompier TP. Epidemiology of hamstring strains in 25 NCAA sports in the 2009-2010 to 2013-2014 academic years. Am J Sports Med. 2015;43(11):2671-2679. doi:10.1177/036354651 5599631
8. Brooks JHM, Fuller CW, Kemp SPT, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med 2006;34(8):1297-1306. doi:10.1177/036354650528602 2
9. Watsford ML, Murphy AJ, McLachlan KA, et al. A prospective study of the relationship between lower body stiffness and hamstring injury in professional Australian rules footballers. Am J Sports Med 2010;38(10):2058-2064. doi:10.1177/03635465103701 97
10. McPherson AL, Nagai T, Schilaty ND, Hale R, Hewett TE, Bates NA. High school male basketball athletes exhibit greater hamstring muscle stiffness than females as assessed with shear wave elastography Skeletal Radiol 2020;49(8):1231-1237 d oi:10.1007/s00256-020-03397 w
11. McPherson AL, Bates NA, Haider CR, Nagai T, Hewett TE, Schilaty ND Thigh musculature stiffness during active muscle contraction after anterior cruciate ligament injury BMC Musculoskelet Disord 2020;21(1):320. doi:10.1186/s12891-020-03342-x
12. Cross KM, Gurka KK, Saliba S, Conaway M, Hertel J. Comparison of hamstring strain injury rates between male and female intercollegiate soccer athletes. Am J Sports Med. 2013;41(4):742-748. doi:1 0.1177/0363546513475342
13. Tyler TF, Schmitt BM, Nicholas SJ, McHugh MP Rehabilitation after hamstring-strain injury emphasizing eccentric strengthening at long muscle lengths: Results of long-term follow-up. J Sport Rehabil. 2015;26(2):131-140. doi:10.1123/jsr.2015-00 99
14. Brockett CL, Morgan DL, Proske U. Predicting hamstring strain injury in elite athletes. Med Sci Sports Exerc 2004;36(3):379-387 doi:10.1249/01.ms s.0000117165.75832.05
15. Kawai T, Takahashi M, Takamoto K, Bito I. Hamstring strains in professional rugby players result in increased fascial stiffness without muscle quality changes as assessed using shear wave elastography. J Bodyw Mov Ther 2021;27:34-41. doi:10.1016/j.jbmt.2 021.03.009
16. Chen CH, Xin Y, Lee KW, Lin MJ, Lin JJ. Acute effects of different dynamic exercises on hamstring strain risk factors. PLoS ONE 2018;13(2):e0191801. d oi:10.1371/journal.pone.0191801
17. Nishida S, Tomoto T, Kunugi S, Miyakawa S. Effect of change in passive stiffness following low-intensity eccentric hamstring exercise on peak torque angle. J Phys Ther Sci. 2018;30(12):1434-1439. doi:10.1589/jpt s.30.1434
18. Blackburn JT, Pamukoff DN. Geometric and architectural contributions to hamstring musculotendinous stiffness. Clin Biomech 2014;29(1):105-110. doi:10.1016/j.clinbiomech.201 3.10.011
19. Blackburn JT, Norcross MF, Cannon LN, Zinder SM. Hamstrings stiffness and landing biomechanics linked to anterior cruciate ligament loading. J Athl Train. 2013;48(6):764-772. doi:10.4085/1062-1050-4 8.4.1
20. Tafazzoli F, Lamontagne M. Mechanical behaviour of hamstring muscles in low-back pain patients and control subjects. Clin Biomech. 1996;11(1):16-24. doi:10.1016/0268-0033(95)00038-0
21. Woods C, Hawkins RD, Maltby S, Hulse M, Thomas A, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football--analysis of hamstring injuries. Br J Sports Med. 2004;38(1):36-41. doi:10.1136/bjsm.2 002.002352
22. Henderson G, Barnes CA, Portas MD Factors associated with increased propensity for hamstring injury in English Premier League soccer players. J Sci Med Sport 2010;13(4):397-402. doi:10.1016/j.jsams.2 009.08.003
23. Orchard J, Steet E, Walker C, Ibrahim A, Rigney L, Houang M. Hamstring muscle strain injury caused by isokinetic testing. Clin J Sport Med. 2001;11(4):274-276. doi:10.1097/00042752-20011000 0-00011
24. Alfuraih AM, Tan AL, O’Connor P, Emery P, Wakefield RJ. The effect of ageing on shear wave elastography muscle stiffness in adults. Aging Clin Exp Res. 2019;31(12):1755-1763. doi:10.1007/s4052 0-019-01139-0
25. Roos KG, Marshall SW, Kerr ZY, et al. Epidemiology of overuse injuries incollegiate and high school athletics in the United States. Am J Sports Med 2015;43(7):1790-1797 doi:10.1177/0363546515 580790
26. Hewett TE, Bates NA. Preventive Biomechanics: A paradigm shift with a translational approach to injury prevention. Am J Sports Med. 2017;45(11):2654-2664. doi:10.1177/0363546516686080
27 Di Stasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury J Orthop Sports Phys Ther 2013;43(11):777-792, a1-11. doi:10.2519/jospt.2 013.4693
28. Monajati A, Larumbe-Zabala E, Goss-Sampson M, Naclerio F. The effectiveness of injury prevention programs to modify risk factors for non-contact anterior cruciate ligament and hamstring injuries in uninjured team sports athletes: A systematic review PLoS One. 2016;11(5):e0155272. doi:10.1371/journa l.pone.0155272
29. Taljanovic MS, Gimber LH, Becker GW, et al. Shear-wave elastography: Basic Physics and musculoskeletal applications. Radiographics 2017;37(3):855-870. doi:10.1148/rg.2017160116
30. Nagai T, Schilaty ND, Krause DA, Crowley EM, Hewett TE. Sex differences in ultrasound-based muscle size and mechanical properties of the cervical-flexor and -extensor muscles. J Athl Train. 2020;55(3):282-288. doi:10.4085/1062-6050-482-18
31. Ito M, Kawakami Y, Ichinose Y, Fukashiro S, Fukunaga T. Nonisometric behavior of fascicles during isometric contractions of a human muscle. J Appl Physiol 1998;85(4):1230-1235. doi:10.1152/japp l.1998.85.4.1230
32. Gesel FJ, Morenz EK, Cleary CJ, LaRoche DP Acute effects of static and ballistic stretching on muscle-tendon unit stiffness, work absorbtion, strength, power, and vertical jump performance. J Strength Cond Res 2020;36(8):2147-2155. doi:10.151 9/jsc.0000000000003894
33. Garrett WE Jr Muscle strain injuries: clinical basic aspects. Med Sci Sports Exerc 1990;22(4):436-443. doi:10.1249/00005768-19900800 0-00003
34. Hewett TE, Ford KR, Xu YY, Khoury J, Myer GD Effectiveness of neuromuscular training based on the neuromuscular risk profile. Am J Sports Med 2017;45(9):2142-2147 doi:10.1177/036354651770012 8
35. Foss KDB, Thomas S, Khoury JC, Myer GD, Hewett TE. A school-based neuromuscular training program and sport-related injury incidence: A prospective randomized controlled clinical trial. J Athl Train 2018;53(1):20-28. doi:10.4085/1062-6050-173-16
36. Hewett TE, Ford KR, Xu YY, Khoury J, Myer GD. Utilization of ACL injury biomechanical and neuromuscular risk profile analysis to determine the effectiveness of neuromuscular training. Am J Sports Med 2016;44(12):3146-3151. doi:10.1177/036354651 6656373
37. Rogan S, Wüst D, Schwitter T, Schmidtbleicher D. Static stretching of the hamstring muscle for injury prevention in football codes: A systematic review Asian J Sports Med. 2013;4(1):1-9.
38. Mjolsnes R, Arnason A, Osthagen T, Raastad T, Bahr R. A 10-week randomized trial comparing eccentric vs. concentric hamstring strength training in well-trained soccer players. Scand J Med Sci Sports 2004;14(5):311-317 doi:10.1046/j.1600-0838.2003.36
7.x
39. Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. J Orthop Sports Phys Ther. 2010;40(2):67-81. doi:10.2519/jospt.2010.3047
40. Cameron ML, Adams RD, Maher CG, Misson D Effect of the HamSprint Drills training programme on lower limb neuromuscular control in Australian football players. J Sci Med Sport 2009;12(1):24-30. do i:10.1016/j.jsams.2007.09.003
41. Arnason A, Andersen TE, Holme I, Engebretsen L, Bahr R. Prevention of hamstring strains in elite soccer: an intervention study Scand J Med Sci Sports 2008;18(1):40-48. doi:10.1111/j.1600-0838.2006.0063 4.x
42. Dadebo B, White J, George KP A survey of flexibility training protocols and hamstring strains in professional football clubs in England. Br J Sports Med 2004;38(4):388-394. doi:10.1136/bjsm.2002.000 044
43. Ekstrand J, Gillquist J, Liljedahl SO Prevention of soccer injuries. Supervision by doctor and physiotherapist. Am J Sports Med. 1983;11(3):116-120. doi:10.1177/03635465830110030 2
44. Weldon SM, Hill RH. The efficacy of stretching for prevention of exercise-related injury: a systematic review of the literature. Man Ther 2003;8(3):141-150. doi:10.1016/s1356-689x(03)00010-9
45. Verrall GM, Slavotinek JP, Barnes PG. The effect of sports specific training on reducing the incidence of hamstring injuries in professional Australian rules football players. Br J Sports Med 2005;39(6):363-368. doi:10.1136/bjsm.2005.018697
46. Reurink G, Goudswaard GJ, Oomen HG, et al. Reliability of the active and passive knee extension test in acute hamstring injuries. Am J Sports Med 2013;41(8):1757-1761. doi:10.1177/036354651349065
0
47 Bercoff J, Tanter M, Fink M. Supersonic shear imaging: A new technique for soft tissue elasticity mapping. IEEE Transactions on Ultrasonics 2004;51(4):396-409. doi:10.1109/tuffc.2004.1295425
48. Masaki M, Aoyama T, Murakami T, et al. Association of low back pain with muscle stiffness and muscle mass of the lumbar back muscles, and sagittal spinal alignment in young and middle-aged medical workers. Clin Biomech 2017;49:128-133. do i:10.1016/j.clinbiomech.2017.09.008
49. Lambertz D, Mora I, Grosset JF, Pérot C. Evaluation of musculotendinous stiffness in prepubertal children and adults, taking into account muscle activity. J Appl Physiol. 2003;95(1):64-72. do i:10.1152/japplphysiol.00885.2002
50. Davies CT, White MJ, Young K. Muscle function in children. Eur J Appl Physiol Occup Physiol 1983;52(1):111-114. doi:10.1007/bf00429036
51. McComas AJ, Sica RE, Petito F. Muscle strength in boys of different ages. J Neurol Neurosurg Psychiatry 1973;36(2):171-173. doi:10.1136/jnnp.36.2.171
52. Cornu C, Goubel F. Musculo-tendinous and joint elastic characteristics during elbow flexion in children. Clin Biomech. 2001;16(9):758-764. doi:10.10 16/s0268-0033(01)00076-6
53. Cornu C, Goubel F, Fardeau M. Stiffness of knee extensors in Duchenne muscular dystrophy. Muscle Nerve 1998;21(12):1772-1774. doi:10.1002/(sici)109 7-4598(199812)21:12
54. Lloyd RS, Oliver JL, Hughes MG, Williams CA. The influence of chronological age on periods of accelerated adaptation of stretch-shortening cycle performance in pre and postpubescent boys. J Strength Cond Res 2011;25(7):1889-1897 doi:10.151 9/jsc.0b013e3181e7faa8
55. Clifton DR, Hertel J, Onate JA, et al. The first decade of web-based sports injury surveillance: Descriptive epidemiology of injuries in us high school girls’ basketball (2005-2006 through 2013-2014) and National Collegiate Athletic Association women’s basketball (2004-2005 Through 2013-2014). J Athl Train. 2018;53(11):1037-1048. doi:10.4085/1062-605 0-150-17
56. Seymore KD, Domire ZJ, DeVita P, Rider PM, Kulas AS. The effect of Nordic hamstring strength training on muscle architecture, stiffness, and strength. Eur J Appl Physiol 2017;117(5):943-953. do i:10.1007/s00421-017-3583-3
57. Ribeiro-Alvares JB, Marques VB, Vaz MA, Baroni BM. Four weeks of Nordic hamstring exercise reduce muscle injury risk factors in young adults. J Strength Cond Res 2018;32(5):1254-1262. doi:10.1519/jsc.0000 000000001975
58. Bourne MN, Timmins RG, Opar DA, et al. An evidence-based framework for strengthening exercises to prevent hamstring injury Sports Med 2018;48(2):251-267. doi:10.1007/s40279-017-0796-x
59. Blackburn JT, Bell DR, Norcross MF, Hudson JD, Kimsey MH. Sex comparison of hamstring structural and material properties. Clin Biomech 2009;24(1):65-70. doi:10.1016/j.clinbiomech.2008.1 0.001
60. Hochman M, McCormick D Endpoint selection and relative (versus absolute) risk reporting in published medication trials. J Gen Intern Med. 2011;26(11):1246-1252. doi:10.1007/s11606-011-181 3-7
61. McPherson AL, Nagai T, Schilaty ND, Hale R, Hewett TE, Bates NA. High school male basketball athletes exhibit greater hamstring muscle stiffness than females as assessed with shear wave elastography Skeletal Radiol 2020;49(8):1231-1237 d oi:10.1007/s00256-020-03397 w
Download: https://ijspt.scholasticahq.com/article/55757-application-of-shear-wave-elastography-in-the-evaluationof-hamstring-stiffness-in-young-basketball-athletes/attachment/120358.docx?auth_token=QTSbsl5u0oul8q6gR1E0
Park-Braswell K, Grooms D, Shultz S, Raisbeck L, Rhea C, Schmitz R. Sex-Specific Brain Activations during Single-Leg Exercise. IJSPT. Published online December 1, 2022:1249-1258.
Kyoungyoun Park-Braswell 1 a , Dustin Grooms 2,3 , Sandra Shultz 4 , Louisa Raisbeck 4 , Christopher Rhea 4 , Randy Schmitz 4,5
1 Division of Health & Human Performance, Indiana Wesleyan University, 2 Division of Physical Therapy & Division of Athletic Training, College of Health Sciences and Professions, Ohio University, 3 Ohio Musculoskeletal & Neurological Institute, Ohio University, 4 Department of Kinesiology, University of North Carolina at Greensboro, 5 Gateway MRI Center, University of North Carolina at Greensboro
Keywords: neuromuscular control, neuroscience, neuroplasticity, fMRI, Musculoskeletal injuries risk, ACL injury risk https://doi.org/10.26603/001c.40367
Females have an increased incidence of musculoskeletal injuries compared to males. Sex differences in neuromuscular control has been widely studied regarding the dynamics and muscle activity during preplanned movements. While muscle activation patterns and movement biomechanics are understood to differ between sexes, it is not well understood how sex influences brain activity for lower extremity movement. Since the brain plays a vital role for voluntary movement and joint stability, it is important to understand the sex differences in brain function in order to better understand neuromuscular control associated with increased musculoskeletal injury risk in female.
The purpose of this study is to understand the differences in brain activation patterns between sexes during a simple active knee extension-flexion movement. It was hypothesized that females would demonstrate higher cortical activation in the somatosensory areas compared to males as a compensatory strategy
Thirteen males and seventeen females who were healthy and physically active participated in this study (Male: 23.7±3.8 years, 74.5±13.5 kg, 172.3±6.4 cm; Female: 20.6±1.6 years, 65.4±12.8 kg, 163±6.1 cm). Functional magnetic resonance imaging data were obtained during a simple left knee extension-flexion exercise with their own leg weight while lying on the MRI table. The blood oxygen level dependent (BOLD) signals were compared between sexes.
There was significantly greater activation in the visual cortices and premotor cortex in females compared to males during the studied movement. Males demonstrated significantly greater activation in the right cerebellum.

The results revealed sex differences in BOLD signal during simple knee extension-flexion movement. The results suggest that sex may be a biological factor in understanding brain activity associated with knee motor control.
a
Corresponding Author: Kyoungyoun Park-Braswell, Ph.D., ATC 144B Recreation and Wellness Center, Indiana Wesleyan University, 4201 South Washington Street Marion, IN, 46953, Email: anne.park-braswell@indwes.edu Phone: 605-592-6598
Sex differences related to neuromuscular control have been widely studied due to higher musculoskeletal injuries in cident rates, such as anterior cruciate ligament (ACL) in jury,1 ankle instability,2 and shoulder instability,3 in fe males compared to males. Females are two to four times more likely than males to sustain ACL injury when account ing for sport and activity level.4 Sex differences in anatom ical structure, hormones, and neuromuscular control have been described to contribute to ACL injury risk.5 It has been widely reported that movement biomechanics and as sociated neuromuscular factors differ between sexes.6 Fe males show greater knee valgus,7 less knee flexion at initial ground contact,8 less muscle stiffness,9 and larger quadri cep activation10 during jump landing tasks. One of the pos sible contributors to sex differences in neuromuscular con trol is proprioception. Proprioception, the sensory information arising from peripheral areas, influences neu romuscular control through its modulation of postural con trol, joint stability, and conscious sensation.11 Females are generally known to have diminished proprioception in comparison to males,12 especially when measured by kines thesia (one’s ability to detect motion and direction).13 However, the underlying mechanisms responsible for the observed sex differences in movement patterns are poorly understood.
While much of the ACL literature has considered sex as a biological variable influencing dynamic movement and knee neuromuscular control,14 sex differences have only been documented peripherally using such tools as biome chanical analyses and electromyography.7 However, less is known about cortical contributions to sex differences for knee motor control. As the brain has an essential role in processing and integrating the sensory signals that arise from the peripheral areas to generate appropriate motor responses,15 sex differences in cortical activity may play a role in neuromuscular control variability Neuroimaging techniques provide an avenue to identify brain function during movement to better understand neuromuscular con trol mechanisms. Functional magnetic resonance imaging (fMRI) is a neuroimaging technique that allows noninvasive measurement of human brain structure and function with high spatial resolution.16 Over the past few decades, upper limb fine motor control movement tasks have been widely studied with fMRI methods to better understand mech anisms of neuromotor control.17 However, fewer studies have observed brain function while performing gross lower leg movement tasks due to technical difficulties, including the need to minimize head motion. These studies have ex amined knee extension-flexion movements,18 pedaling,19 and unilateral leg presses,20 finding that brain regions in cluding sensorimotor area, supplementary motor area, pre motor cortex, cerebellum were highly activated during lower extremity movement tasks. Despite this research on brain activation during lower extremity motor tasks, less is
known regarding whether males and females have differ ential cortical activity during lower extremity movements. There is only one previous study examining sex differences in brain activation during isometric ankle dorsiflexion in men and women.21 While Yoon et al.21 reported that young men and women have similar cortical activation of motor areas, this was limited to an isometric contraction. It is un known if any studies have investigated sex differences in brain activity during dynamic knee joint actions. Therefore, the purpose of this study is to understand the differences in brain activation patterns between sexes during a sim ple active knee extension-flexion movement. Since females are reported to have poorer knee joint proprioception rela tive to males,12 It is hypothesized that females would have higher activation in the somatosensory areas as a com pensatory strategy to sustain the same knee motor perfor mance.
Twelve males and seventeen females age eighteen to twenty eight, physically active at least two to three times a week, and right-handed/footed were recruited from a uni versity population. Participants participated in running or cutting/pivoting activity as demonstrated on the Marx scale22 at least once a week. Participants were excluded if they had: a previous history of significant lower leg injuries and surgeries, any neurologic disorders, were currently un dergoing a neuromuscular training program or had any contradictions to MRI assessment (any metal or implanted medical device in the body or claustrophobic, etc.). All par ticipants read and signed an informed consent form ap proved by a University’s Institutional Review Board for the Protection of Human Subjects.
All MRI data were obtained using a 3T Siemens MRI scan ner with a 16-channel head coil (Siemens Tim Trio; Erlan gen, Germany). Participants were placed on the MR scan ner table headfirst and in a supine position. Head motions generated by lower extremity movement tasks can induce unwanted artifacts that interfere with fMRI data.23 There fore, we spent considerable effort to minimize head motion by using a variety of restraints. Participants were stabilized with straps around their hips and chest, then sandbags and multiple sizes of pads were placed around the participant’s head within the head coil to minimize head motion. A mir ror was placed on the head coil so that participants were able to see both their own leg and the researchers posi tioned in the adjacent operator room during the entire MRI scan.
Figure
Participants
While obtaining functional MRI data, participants are re quired to perform knee extension flexion movement task. A bolster was placed underneath the participant’s leg to allow approximately 45 degrees of knee extension flexion (Figure 1). An ankle immobilizer was positioned on the left ankle to ensure isolated knee extension-flexion movements dur ing the functional imaging tasks (Figure 1). Instruction was given to participants to perform left leg knee extensionflexion movements with a metronome (1.2 HZ) following the auditory cue from the researcher to “start” and “stop”. During the movement task, participants relaxed for 30 sec onds then performed 30 seconds of continuous knee ex tension-flexion exercise of the left leg followed by 30 sec onds of relaxation. The participants complete four cycles of movement and relaxation. The auditory metronome was heard by the participant during the entire duration of fMRI scan to control rate of knee extension-flexion movements. The participants performed the task with only the weight of their own limb. There was a familiarization session prior to the scan.

The structural and functional neuroimaging were collected following the methodology of a previous fMRI study by Raisbeck et al.24 Structural images were initially obtained (repetition time = 2000 ms; echo time = 4.58 ms, matrix field of view = 256 mm; voxel size = 1 mm x 1 mm x 1 mm; scan time=6.5 mins). Then, functional magnetic resonance images were measured to attain the blood oxygen level-de pendent (BOLD) signals during knee extension-flexion ex ercise. Functional image data (fMRI) were obtained (repe tition time = 3000 ms; echo time = 28 ms, Flip angle = 78 deg; phase encoding direction = anterior to posterior; ma trix field of view = 220 mm; voxel size = 2.5 mm x 2.5 mm x 2.5 mm) during the movement tasks.
A block design was used for the experimental tasks that in clude rest and knee movement blocks. It measured 10 fullbrain datasets for each 30 seconds block, which resulted in 40 full-brain images for knee extension-flexion movements
(4 blocks) and 50 full-brain images for rest (5 blocks); a to tal of 90 full brain images, congruent with previous work.24 MRI data were analyzed using the fMRI of the brain (FM RIB) software library (FSL: The Oxford Centre for Func tional MRI of the Brain, Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, United King dom).25 Standard processing was completed for each sub ject’s data, including image format converting, reorienta tion, and brain extraction (using FSL BET).
Then, FEAT (sub-component of the FSL software) was used to perform pre-processing. The pre-process includes motion correction (MCFLIRT), interleaved slice timing cor rection, spatial smoothing at 6 mm full width at half maxi mum (FWHM), 4D mean intensity normalization.25 The In dependent Component Analysis-based Automatic Removal of Motion Artifacts (ICA-AROMA) was used to remove mo tion-related noise and increase sensitivity to group-level activation.26 Then, the first-level analysis was performed for subject-level contrast (rest vs knee movements) using a cluster-based threshold with z threshold at 2.3 and p threshold at 0.05.25 This process also includes temporal fil tering (90s).25
Finally, the higher-level analyses were performed with FLAME stage 1+2 using unpaired samples t-test to contrast between sexes (Female > Male; Male > Female) with a z threshold of 2.3 and p<.05 Gaussian random field cluster corrected.27 To avoid possible differences in brain structure between sexes that may can lead to misinterpretation of functional results, voxel-wise gray matter volumes were in cluded as covariates during the higher-level analysis.28 Re gions of brain activity were identified based on FSL tool atlasquery with Juelich Histological Atlas, Harvard-Oxford Cortical Structural Atlas, and Cerebellar Atlas in MNI152 space after normalization with FNIRT. Featquery was used to calculate a mean percentage signal change for each indi vidual’s FEAT results within a cluster mask images from the higher-level analysis.
Demographics of the female and male groups are presented in Table 1 There were no significant differences between sexes in BMI (p=0.77) and Marx (p=0.32) physical activity scales (Table 1). Additionally, there was no significant dif ference in absolute (p=0.52) and relative (p=0.94) head mo tion between sexes during the experimental tasks (Table 1).
The fMRI comparisons between sexes are reported in Table 2 During repetitive knee flexion-extension move ments, females demonstrated higher BOLD signals in right premotor cortex (p=0.008; Table 2; Figure 2A), the visual cortices right V3, V4 (p=0.011; Table 2; Figure 2B) and Left V1, V2 (p=0.004; Table 2; Figure 2C) Juelich Histological Atlas among the entire brain. The same regions also rep resent precentral gyrus, lateral occipital cortex, and intra calcarine cortex in the Harvard-Oxford Cortical Structural Atlas. Males demonstrated significantly greater activation in the right cerebellum compared to females with the peak voxel right VIIIa and VIIb (p <0.001; Table 2; Figure 2D).
performed left leg extension flexion movements with a bolster and an ankle immobilizerstandard deviation)
Female Male p-value Effect size (Cohen’s d)
Age (year) 20.6±1.6 23.7±3.8 0.004 1.06
Mass (kg) 65.4±12.8 74.5±13.5 0.076 0.69
Height (cm) 163±6.1 172.3±6.4 0.000 1.49
BMI (kg/m2) 24.6±4.5 25.1±4.6 0.767 0.11
Marx Activity 14.0±2.9 15.3±4.2 0.320 0.36
Absolute Head Motion (mm) 0.39±0.2 0.35±0.1 0.516 0.26
Relative Head Motion (mm) 0.11±0.1 0.11±0.1 0.935 0.00
Given the importance of sex as a biological variable in the study of neuromuscular control, the differences in brain activation between sexes associated with a simple knee flexion-extension task was examined. The results demon strated that females had greater activation in the premotor cortex and the visual cortices compared to males during a voluntary knee extension-flexion task. Males had signifi cantly greater activation in cerebellum.
The premotor cortex plays an essential role in the planning or programming of voluntary movements.15 It has been re ported that neurons in the premotor cortex begin firing about 800ms prior to voluntary movement.29 The premotor cortex also activates when receiving an instruction to move.30 During the experimental tasks in the current study, participants were given the auditory cues to begin lower limb movements and relax. Higher activation in the pre motor cortex in females may indicate that females required greater resources dedicated to the planning of movement for even simple leg extension and flexion movement com pared to males.
Activation in the premotor cortex also correlates with increasing complexity of targeted movements,31 especially the complex sequential movements.32 The current study movement task is involved with sequential knee extensionflexion exercise with rhythmic timing. Since females typ ically have a lower hamstring to quadriceps muscular ra tio33,34 and decreased muscle strength of the lower extremity,35 potentially indicating a lower capacity for the knee extension-flexion movement task resulting in it being relatively more complex to regulate for females than males.
activity in males: D (blue)=right cerebellum (VIIIa, VIIb). R=right, S=superior, P=poste rior
The results also demonstrated that females had signifi cantly higher activation in their visual cortices. The visual cortex has a primary role in visual processing.15 The visual system is crucial to execute desired physical movements, especially in coordination, regulation, and control of move ments.36 The finding of visual cortex activation was likely related to the ability of participants to see their leg during the tasks through the mirror located on the head coil. How
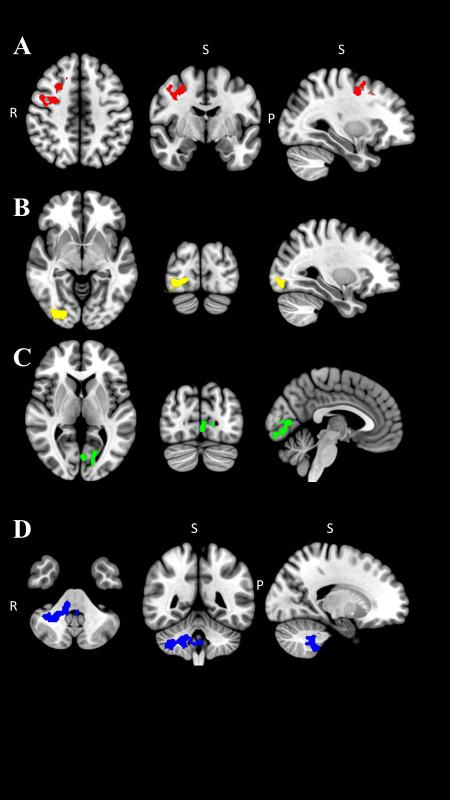 Figure 2. Cluster masks from the higher-level analysis (A,B,C: Females > Males, D: Males > Females) in transverse, frontal, and sagittal view. The region was identified through binarized the z-stat cluster mask (z> 2 3). Brain re gions with higher activation in females: A (red)= right premotor cortex, B (yellow)= right visual cortices (V3, V4), C (green)= left visual cortices (V1, V2). Brain regions with higher
Figure 2. Cluster masks from the higher-level analysis (A,B,C: Females > Males, D: Males > Females) in transverse, frontal, and sagittal view. The region was identified through binarized the z-stat cluster mask (z> 2 3). Brain re gions with higher activation in females: A (red)= right premotor cortex, B (yellow)= right visual cortices (V3, V4), C (green)= left visual cortices (V1, V2). Brain regions with higher
Atlas Regions
F>M Juelich
Voxels p-value Z max Peak MNI Coordinate (mm) MRI mean(m) Signal Change (%)
Female Male x y z m SD m SD
R premotor cortex 553 0.008 5.65 2 -92 -6 0.09 0.08 -0.09 0.12
R Visual cortex V3, V4 523 0.011 5.38 42 -80 -18 0.17 0.24 -0.19 0.25
L Visual cortex V1, V2 408 0.044 4.06 42 0 44 0.19 0.18 -0.13 0.29
M>F Cerebellar R cerebellum VIIIa, VIIb, 928 0.000 4.18 -2 -44 -40 -0.17 0.14 0.17 0.23
ever, this activation was significantly higher in females compared to males. Previous work had reported that fe males demonstrated diminished postural stability com pared to males, especially when visual perception was im paired.37 In addition, females show decreased proprioception compared to males.11,12 This may suggest that females rely more on using visual information in order to execute lower extremity motor tasks, potentially sec ondary to increased visual cortex activity to generate pos tural corrective knee movements.
Specifically, the results revealed significantly more ac tivation in visual cortices V1, V2, V3, and V4 in females when compared to males. The primary visual cortex (V1) is the first stage of processing visual information that receives visual input from the retina.38 The secondary visual cor tex (V2) processes visual stimuli and illusory contours.39 V3 plays a critical role in transmitting visual information, es pecially processing motion, from the primary visual cortex to parietal and temporal cortices.40 V4 is interconnected with the higher-order cortex transferring object and spatial visual information.40
The Harvard-Oxford Cortical Structural Atlas also re ports that subregions in the visual cortex includes the in tracalcarine cortex, lingual gyrus, occipital fusiform gyrus, and lateral occipital cortex. The intracalcarine cortex and lingual gyrus are a part of the primary visual cortex,41 and they contribute to the process of visual stimuli.38 The oc cipital fusiform gyrus is located in the occipital lobe, and is associated with perceiving body parts and their actions.42 The lateral occipital cortex is also responsible for visual shape processing.43 The lingual gyrus also known as the cross-modal cortex has a high capacity for neuroplasticity when experiencing loss of sensory input.44 Sensory infor mation, including vision, proprioception, and vestibular systems, all have a demonstratable impact on proper motor system function.45 When proprioceptive information is de ficient, vision and vestibular systems may become more highly engaged in order to carry out motor function. There fore, impaired proprioception in females may alter the cor tical function in order to increase neural activity in the visual cortices as a potential compensatory strategy This compensatory strategy may contribute to females relying more heavily on visual information to perform motor tasks and contribute to sex differences in neuromuscular control. Since the findings suggest that females may rely more on utilizing visual information during physical movement, vi sual-motor training additions to injury prevention training may be particularly efficacious for females.
Males displayed higher cerebellar activation in lobule pri marily VIIIa and VIIb as well as VIIIb and IX of the right cerebellum compared with females. The cerebellum coor dinates voluntary movements, motor control, muscular co ordination, and executive function.15 The lobule VIIIa re ceives projections from the primary motor cortex,46 and the lobule VIIIa and VIIIb represent sensorimotor function.47 With regard to lobule VIIIa and VIIIb function, previous work has demonstrated increased activation of these areas
in the upper limb compared to lower limb motion in a fe male only population.47 The lobules VIIb and IX are associ ated with executive functions, including working memory, planning, organizing, and visual divergent thinking.48 The cerebellum is also engaged with voluntary movement with event timing.49 O’Reily et al.49 showed a significant cere bellum activation during perceptual prediction task when only temporal information (velocity) is involved to predict, but not spatial information (direction). During movement task used in the current study, there was a metronome to assist participants in performing extension-flexion move ment with the same timing. Thus, the results of higher activation in the cerebellum in males may indicate that males have a heavier cortico-cerebellar strategy during mo tor control than females, especially when the task was in volved with precise timing. However, the relation to poten tial injury risk is unknown at this time.
According to the best-known available data, there is limited research of sex differences in brain activation during lower limb motor tasks. Yoon et al. assessed brain activation pat terns in males and females during isometric ankle dorsi flexion with various force control.21 They discovered that most of the motor cortex areas were activated similarly, with the exception of the right inferior temporal gyrus hav ing greater activity in males at 70% of maximal voluntary isometric contraction. The inferior temporal gyrus plays a primary role in visual stimuli processing, objects recogni tion as well as biological motion processing.15 While this previous finding does not support current results, signif icant differences in task (isometric vs. isotonic), intensity (70% MVIC vs. body weight), and joint (ankle vs. knee) may confound direct comparisons to current work that the vi sual cortex area was highly activated in females than males.
While sex differences in brain function during lower limb motor control is not well studied, investigations into sex differences during the upper limb fine motor tasks have been reported.17 Females demonstrated generally higher cortical activation than males during finger tapping tasks.17 These highly activated regions included the parietal, supe rior temporal, motor, and somatosensory regions, in addi tion to the middle occipital cortex. Males displayed higher cortical activation of the caudate nucleus and basal ganglia, as well as the fronto-parietal and temporal regions.17 Lis sek et al.17 suggested that there may be a different aspect of the motor-related cortical process between sexes. Thus, a sex-specific functional cerebral organization may be used to achieve the same motor skills. Sex differences in brain structure and structural connectivity are also well under stood and may contribute to differences in functional activ ity Gur et al.50 found that males have increased white mat ter size and spinal fluid. Males also have relatively larger cerebrum and ventricle volumes, whereas females were found to have larger overall cortical volumes.51 Moreover, males reveal higher communication within the hemisphere, and females show higher interhemispheric communica tion.52 Even though brain function and brain structure are
measured differently, the previous and current results sup port the differences in the brain between sexes. Thus, while work is limited in scope, there is support for sex to be con sidered as a biologic variable when performing research in volved in understanding central activation during motor tasks.
The current study results revealed that females showed higher activation in the premotor cortex and visual cortices. This may be due to the fact that females require greater cor tical resources to plan and execute motor movement and exhibit less proprioception than males. Furthermore, males demonstrate heavier cortico-cerebellum strategies than fe males, especially when precise timing is involved with the movement task. These findings may help practitioners and clinicians develop training and rehabilitation methods that improve the efficacy of using visual and sensory informa tion in females. There are a few studies utilizing a visual resources, such as virtual reality system and visual biofeed back to train neuromuscular control in order to induce movement adaption to decrease injury risks.53–55 Thus, re habilitation methods using visual resources may help train female athletes to rapidly pre-plan/program movements in response to changing stimuli, thereby decreasing the risk of injury
Limitations must be considered when interpreting the current study There was a relatively low sample size (N=29, male=12; female=17) in this study. In addition, there was a significant age difference between groups (male=22.8±2.2; female=20.6±1.6, p=0.004). However, age was controlled in this study by limiting participants age to between 18-28 years old. Despite well know effects of aging on brain func tion,56 an age difference of just a few years would likely have a minimal effect on the results, thus the impact of the age difference to our results was not a major concern. It is also important to note that the cortical activation differ ences may not be due to sex differences but instead other factors that may inherently differ by sex (structural differ ences). To that end, physical activity level was controlled in this study by recruiting only participants who were physi
cally active in order to minimize the impact of confounding variables. In addition, the movement task was standardized to individual’s body size by performing knee flexion-exten sion movements with participants’ own limb weight.
Results of the current study revealed that females have higher neural activation in the premotor cortex and visual cortices compared to males during active knee extensionflexion movements. Males demonstrated significant higher activation in the cerebellum than females. The results, as well as previous work17 reporting sex differences in brain activity during motor tasks suggests the need to include sex as a biologic variable in neuroimaging studies involving motor tasks. Understanding sex-specific brain function dur ing an equivalent lower limb motor task may shed further light on sex differences in lower extremity neuromuscular control.
The results of this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. There are no conflicts of interest or funding associated with the present study.
The authors declare no significant competing financial, professional or personal interests that might have influ enced the presentation of the work described in this manu script.
Submitted: March 13, 2022 CST, Accepted: August 16, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: A review of the literature part 1: neuromuscular and anatomic risk. Sports Health 2012;4(1):69-78. doi:10.1177/19417381 11428281
2. Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123-140. doi:10.1007/s40279-013-0102-5
3. Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy Am J Sports Med 2007;35(7):1168-1173. doi:10.1177/036354650629517 9
4. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 2014;42(10):2363-2370. doi:10.1177/03635465145427 96
5. Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: A review of the literature-Part 2: Hormonal, genetic, cognitive function, previous injury, and extrinsic risk factors. Sports Health 2012;4(2):155-161. doi:10.1177/194173 8111428282
6. Carson DW, Ford KR. Sex differences in knee abduction during landing: a systematic review Sports Health. 2011;3(4):373-382. doi:10.1177/19417381114 10180
7 Holden S, Boreham C, Delahunt E. Sex differences in landing biomechanics and postural stability during adolescence: A systematic review with metaanalyses. Sports Med 2016;46(2):241-253. doi:10.100 7/s40279-015-0416-6
8. Chappell JD, Creighton RA, Giuliani C, Yu B, Garrett WE. Kinematics and electromyography of landing preparation in vertical stop-jump: Risks for noncontact anterior cruciate ligamentinjury. Am J Sports Med 2007;35(2):235-241. doi:10.1177/0363546 506294077
9. Demirbüken I, Yurdalan SU, Savelberg H, Meijer K. Gender specific strategies in demanding hopping conditions. J Sports Sci Med. 2009;8(2):265-270.
10. Shultz SJ, Schmitz RJ. Effects of transverse and frontal plane knee laxity on hip and knee neuromechanics during drop landings. Am J Sports Med 2009;37(9):1821-1830. doi:10.1177/0363546509 334225
11. Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability J Athl Train 2002;37(1):71-79.
12. Muaidi QI. Does gender make a difference in knee rotation proprioception and range of motion in healthy subjects? J Back Musculoskelet Rehabil 2017;30(6):1237-1243. doi:10.3233/bmr-169613
13. Lephart SM, Warner JJP, Borsa PA, Fu FH. Proprioception of the shoulder joint in healthy, unstable, and surgically repaired shoulders. J Shoulder Elb Surg 1994;3(6):371-380. doi:10.1016/s10 58-2746(09)80022-0
14. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study Am J Sports Med 2005;33(4):492-501. doi:10.1177/0363546504269591
15. Kandel ER, Schwartz JH, Jessell TM. Principles of Neural Science. 3rd ed. Appleton & Lange; 1991.
16. Scott H, Allen S, McCarthy G. Functional Magnetic Resonance Imaging 3rd ed. Sinauer; 2014.
17. Lissek S, Hausmann M, Knossalla F, et al. Sex differences in cortical and subcortical recruitment during simple and complex motor control: An fMRI study. Neuroimage. 2007;37(3):912-926. doi:10.1016/ j.neuroimage.2007.05.037
18. Kapreli E, Athanasopoulos S. The anterior cruciate ligament deficiency as a model of brain plasticity. Med Hypotheses. 2006;67(3):645-650. doi:1 0.1016/j.mehy.2006.01.063
19. Mehta JP, Verber MD, Wieser JA, Schmit BD, Schindler-Ivens SM. A novel technique for examining human brain activity associated with pedaling using fMRI. J Neurosci Methods. 2009;179(2):230-239. doi:1 0.1016/j.jneumeth.2009.01.029
20. Grooms DR, Diekfuss JA, Ellis JD, et al. A novel approach to evaluate brain activation for lower extremity motor control. J Neuroimaging. 2019;29(5):580-588. doi:10.1111/jon.12645
21. Yoon T, Vanden Noven ML, Nielson KA, Hunter SK. Brain areas associated with force steadiness and intensity during isometric ankle dorsiflexion in men and women. Exp Brain Res. 2014;232(10):3133-3145. doi:10.1007/s00221-014-3976-z
22. Cameron KL, Peck KY, Thompson BS, Svoboda SJ, Owens BD, Marshall SW Reference values for the marx activity rating scale in a young athletic population: History of knee ligament injury is associated with higher scores. Sports Health. 2015;7(5):403-408. doi:10.1177/1941738115576121
23. Ogawa S, Lee TM, Nayak AS, Glynn P Oxygenation-sensitive contrast in magnetic resonance image of rodent brain at high magnetic fields. Magn Reson Med 1990;14(1):68-78. doi:10.100 2/mrm.1910140108
24. Raisbeck LD, Diekfuss JA, Grooms DR, Schmitz R. The effects of attentional focus on brain function during a gross motor task. J Sport Rehabil 2019;29(4):441-447. doi:10.1123/jsr.2018-0026
25. Smith SM, Jenkinson M, Woolrich MW, et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23(Suppl 1):S208-S219. doi:10.1016/j.neuroima ge.2004.07.051
26. Pruim RHR, Mennes M, van Rooij D, Llera A, Buitelaar JK, Beckmann CF. ICA-AROMA: A robust ICA-based strategy for removing motion artifacts from fMRI data. Neuroimage. 2015;112:267-277. doi:1 0.1016/j.neuroimage.2015.02.064
27 Beckmann CF, Jenkinson M, Smith SM. General multilevel linear modeling for group analysis in FMRI. Neuroimage 2003;20(2):1052-1063. doi:10.101 6/s1053-8119(03)00435-x
28. Oakes TR, Fox AS, Johnstone T, Chung MK, Kalin N, Davidson RJ. Integrating VBM into the General Linear Model with voxelwise anatomical covariates. Neuroimage. 2007;34(2):500-508. doi:10.1016/j.neuroi mage.2006.10.007
29. Deecke L, Scheid P, Kornhuber HH. Distribution of readiness potential, pre-motion positivity, and motor potential of the human cerebral cortex preceding voluntary finger movements. Exp Brain Res 1969;7(2):158-168. doi:10.1007/bf00235441
30. Wise SP. The primate premotor cortex: past, present, and preparatory Annu Rev Neurosci 1985;8(1):1-19. doi:10.1146/annurev.ne.08.030185.00 0245
31. Harrington DL, Rao SM, Haaland KY, et al. Specialized neural systems underlying representations of sequential movements. J Cogn Neurosci. 2000;12(1):56-77. doi:10.1162/08989290051 137602
32. Schubotz RI, von Cramon DY A blueprint for target motion: fMRI reveals perceived sequential complexity to modulate premotor cortex. Neuroimage 2002;16(4):920-935. doi:10.1006/nimg.2 002.1183
33. Hannah R, Folland JP, Smith SL, Minshull C. Explosive hamstrings-to-quadriceps force ratio of males versus females. Eur J Appl Physiol 2015;115(4):837-847. doi:10.1007/s00421-014-3063-y
34. Andrade MDS, De Lira CAB, Koffes FDC, Mascarin NC, Benedito-Silva AA, Da Silva AC. Isokinetic hamstrings-to-quadriceps peak torque ratio: the influence of sport modality, gender, and angular velocity J Sports Sci 2012;30(6):547-553. doi:10.108 0/02640414.2011.644249
35. Behan FP, Maden-Wilkinson TM, Pain MTG, Folland JP Sex differences in muscle morphology of the knee flexors and knee extensors. PloS one. 2018;13(1):e0190903. doi:10.1371/journal.pone.0190 903
36. Warren WH Jr, Kay BA, Zosh WD, Duchon AP, Sahuc S. Optic flow is used to control human walking. Nat Neurosci 2001;4(2):213-216. doi:10.1038/84054
37. Blaszczyk JW, Beck M, Sadowska D. Assessment of postural stability in young healthy subjects based on directional features of posturographic data: vision and gender effects. Acta Neurobiol Exp. 2014;74(4):433-442.
38. Morris AP, Krekelberg B. A stable visual world in primate primary visual cortex. Curr Biol. 2019;29(9):1471-1480.e6. doi:10.1016/j.cub.2019.03.0 69
39. Orban GA. Higher order visual processing in macaque extrastriate cortex. Physiol Rev. 2008;88(1):59-89. doi:10.1152/physrev.00008.2007
40. Arcaro MJ, Kastner S. Topographic organization of areas V3 and V4 and its relation to supra-areal organization of the primate visual system. Vis Neurosci 2015;32:E014. doi:10.1017/s0952523815000 115
41. Wandell BA, Dumoulin SO, Brewer AA. Visual field maps in human cortex. Neuron 2007;56(2):366-383. doi:10.1016/j.neuron.2007.10.01 2
42. Peelen MV, Downing PE. Selectivity for the human body in the fusiform gyrus. J Neurophysiol. 2005;93(1):603-608. doi:10.1152/jn.00513.2004
43. Kourtzi Z, Erb M, Grodd W, Bülthoff HH. Representation of the perceived 3-D object shape in the human lateral occipital complex. Cereb Cortex 2003;13(9):911-920. doi:10.1093/cercor/13.9.911
44. Palejwala AH, Dadario NB, Young IM, et al. Anatomy and white matter connections of the lingual gyrus and cuneus. World Neurosurg 2021;151:e426-e437. doi:10.1016/j.wneu.2021.04.050
45. Kandel ER, Schwartz JH, Jessell TM. Principles of Neural Science 4th ed. McGraw-Hill, Health Professions Division; 2000.
46. Balsters JH, Cussans E, Diedrichsen J, et al. Evolution of the cerebellar cortex: The selective expansion of prefrontal-projecting cerebellar lobules. Neuroimage 2010;49(3):2045-2052. doi:10.1016/j.neu roimage.2009.10.045
47 Ashida R, Cerminara NL, Edwards RJ, Apps R, Brooks JCW. Sensorimotor, language, and working memory representation within the human cerebellum. Hum Brain Mapp. 2019;40(16):4732-4747. doi:10.1002/hbm.24733
48. Stoodley CJ, Schmahmann JD Functional topography in the human cerebellum: a metaanalysis of neuroimaging studies. Neuroimage. 2009;44(2):489-501. doi:10.1016/j.neuroimage.2008.0 8.039
49. O’Reilly JX, Mesulam MM, Nobre AC. The cerebellum predicts the timing of perceptual events. J Neurosci 2008;28(9):2252-2260. doi:10.1523/jneurosc i.2742-07.2008
50. Gur RC, Turetsky BI, Matsui M, et al. Sex differences in brain gray and white matter in healthy young adults: correlations with cognitive performance. J Neurosci. 1999;19(10):4065-4072. do i:10.1523/jneurosci.19-10-04065.1999
51. Goldstein JM, Seidman LJ, Horton NJ, et al. Normal sexual dimorphism of the adult human brain assessed by in vivo magnetic resonance imaging. Cereb Cortex 2001;11(6):490-497 doi:10.1093/cercor/ 11.6.490
52. Ingalhalikar M, Smith A, Parker D, et al. Sex differences in the structural connectome of the human brain. Proc Natl Acad Sci USA 2014;111(2):823-828. doi:10.1073/pnas.1316909110
53. Diekfuss JA, Grooms DR, Bonnette S, et al. Real time biofeedback integrated into neuromuscular training reduces high risk knee biomechanics and increases functional brain connectivity: A preliminary longitudinal investigation. Psychophysiology. 2020;57(5):e13545. doi:10.1111/psy p.13545
54. Rausch M, Simon JE, Starkey C, Grooms DR. Smartphone virtual reality to increase clinical balance assessment responsiveness. Phys Ther Sport 2018;32:207-211. doi:10.1016/j.ptsp.2018.05.017
55. Grooms DR, Kiefer AW, Riley MA, et al. Brainbehavior mechanisms for the transfer of neuromuscular training adaptions to simulated sport: initial findings from the train the brain project. J Sport Rehabil 2018;27(5):1-5. doi:10.1123/jsr.2017-02 41
56. Damoiseaux JS. Effects of aging on functional and structural brain connectivity Neuroimage 2017;160:32-40. doi:10.1016/j.neuroimage.2017.01.07 7
Straub RK, Powers CM. Does the 2D Frontal Plane Projection Angle Predict Frontal Plane Knee Moments during Stepping, Landing, and Change of Direction Tasks? IJSPT Published online December 2, 2022:1259-1270.
Rachel K Straub , Christopher M Powers a
Keywords: 2D video, movement screening, knee biomechanics
https://doi.org/10.26603/001c.39612
Although dynamic knee valgus can be visually identified using the 2D frontal plane projection angle (FPPA), the validity of the FPPA in terms of predicting frontal plane knee kinematics has been questioned. The biomechanical utility of the FPPA may lie in its ability to predict frontal plane knee moments.
The purpose of the current study was to comprehensively evaluate the ability of the FPPA to predict the frontal plane knee kinetics (peak moment, average moment, and moment at peak knee flexion) across a wide range of tasks (stepping, landing, and change of direction).
Crossover Study Design.
Three-dimensional lower-extremity kinetics and 2D video were obtained from 39 healthy athletes (15 males and 24 females) during execution of six tasks (step down, drop jump, lateral shuffle, deceleration, triple hop, side-step-cut). Linear regression analysis was performed to determine if the 2D FPPA at peak knee flexion predicted frontal plane knee moment variables during the deceleration phase of each task (peak moment, average moment, moment at peak knee flexion).
The FPPA was found to significantly predict the peak frontal plane knee moment for two tasks (deceleration and side-step-cut, R2 = 12% to 25%), average frontal plane knee moment for five tasks (drop jump, shuffle, deceleration, triple hop, side-step-cut, R2 = 15% to 40%), and frontal plane knee moment at peak knee flexion for five tasks (drop jump, shuffle, deceleration, triple hop, side-step-cut, R2 = 16% to 45%).

An increased FPPA (medial knee collapse) predicted increased knee valgus moments (or decreased knee varus moments) during landing and change of direction tasks (but not stepping). However, the predictive ability of the FPPA was weak to moderate.
a
Corresponding author:
Christopher M. Powers, PT, PhD, FACSM, FAPTA
USC Division of Biokinesiology & Physical Therapy
1540 E. Alcazar St. CHP-155 Los Angeles, CA 90089-9006
Phone: 323.442.1928
Fax: 323.442.1515
Email: powers@usc.edu
The frontal plane projection angle (FPPA) is a two-dimen sional (2D) clinical measure that was developed to identify knee valgus during dynamic tasks.1,2 Although the FPPA has been questioned in terms of being able to predict noncontact ACL injury,3,4 this measurement has been shown to distinguish between persons with and without patellofemoral pain5–7 and predict acute lower-extremity injuries (hip, groin, thigh, knee, lower leg, ankle, or foot).8
Given the potential clinical usefulness of the FPPA, there has been interest in understanding its biomechanical utility in relation to traditional laboratory based measures of frontal plane knee kinematics.
To date, several studies have compared FPPA measure ments and 3D knee kinematics during various tasks. Across studies, the association (R2) between the FPPA and 3D knee valgus angle has been reported to range from 0% to 64% across a wide range of tasks (i.e., single limb squat, drop jump, single leg hop, single leg land, lateral jump, and cutting).1,5,9–15 Although some authors have found that the FPPA and 3D knee valgus are correlated, the reported agreement between these angular measures is poor.16 More specifically, the FPPA has been shown to overestimate true frontal plane knee motion during a single leg squat,11 drop jump,10 and single leg hop,10 with the 95% limits of agree ment ranging from -30° to 17°.10,11
The poor agreement between the FPPA and 3D frontal plane knee valgus can be explained by previous research that has shown that what appears as knee valgus on 2D video actually is a combination of sagittal, frontal, and transverse motions at the hip and knee.5,17,18 For example, studies have reported that individuals who exhibit poor frontal plane knee alignment based on visual assessment during a step down or single leg squat have increased hip adduction,17 hip flexion,17 knee external rotation,17 and hip internal rotation.18 Furthermore, an increased FPPA has been found to be correlated with increased hip adduc tion, knee external rotation, and hip external rotation dur ing a single leg squat.5
While it is readily apparent that out-of-plane motions at the hip and knee compromise the ability of the FPPA to accurately represent frontal plane knee kinematics, these frontal and transverse rotations of the thigh and tibia seg ments may influence variables used to calculate the frontal plane knee joint moment using inverse dynamic equations (e.g., joint center location, joint angular velocities, segment accelerations, etc.). To date, two studies have evaluated the relationship between the FPPA and knee valgus moments with mixed results.12,14 Herrington et al. reported a strong relationship between the FPPA and peak knee valgus mo ment during the single leg step down (R2 = 42%) but not the single leg landing (R2 = 13%).12 Similarly, Mizner et al. re ported a strong association between the FPPA and knee val gus moment at peak knee flexion during a double-leg drop jump (R2 = 35%).14 To date, the ability of the FPPA to pre dict frontal plane knee moments during tasks that involve pivoting and/or change of direction is not known. This is important as such movements have been shown to result in
high knee valgus moments when compared to tasks that are more linear in nature.19
The purpose of the current study was to comprehen sively evaluate the ability of the FPPA to predict the frontal plane knee kinetics (peak moment, average moment, and moment at peak knee flexion) across a wide range of tasks (stepping, landing, and change of direction). The authors hypothesized that an increased 2D FPPA would be predic tive of frontal plane knee moments (i.e., increased knee valgus moments or decreased knee varus moments). In formation gained from this study will advance knowledge about the clinical utility of the FPPA in characterizing movement behavior that may expose individuals to lower extremity injury
The present study included a sample of 39 healthy athletes from prior studies with different study aims, as previously described.20–22 Athletes between the ages of 13 and 40 years participated (15 males: age = 23.8 (7.3) yrs., height = 1.81 (0.08) m, mass = 78.9 (16.2) kg; 24 females: age = 17.3 (6.3) yrs., height = 1.65 (0.08) m, mass = 56.1 (11.3) kg). All participants were currently partaking in a sport with high levels of jumping, cutting, or lateral movements (such as soccer, basketball, volleyball, lacrosse, football, netball, or tennis). Participants were excluded if they had current lower-extremity pain, any history of ACL reconstruction, lower-extremity injuries/surgeries in the prior six months or indicated any medical condition that would impair their ability to perform the athletic tasks.
A sample size calculation was performed in G*Power (Version 3.1) based on pilot data to determine the number of participants needed to assess the relationship between the FPPA and frontal plane knee moment across six tasks. Using a 5% significance level, 90% power, R2 value of 0.30 (based on pilot data), and 1 predictor, a minimum of 27 par ticipants was deemed necessary.
Three dimensional and 2D kinematic data were collected at 120 Hz using a video-based 8-camera motion analysis system (Simi Reality Motion Systems GmbH, Unterschleis sheim, Germany). One of the eight cameras was positioned 80 cm off the ground (perpendicular to the force plate) and was used to collect the required frontal plane images for the 2D analysis.
Ground reaction forces were collected at 1200 Hz (Model #BP600900-2000, Advanced Mechanical Technology, Inc, Watertown, MA, USA) and synchronized with the motion capture system. The force plate was embedded into the floor and was used for five out of the six tasks evaluated. For the step-down task described below, a portable force plate was integrated into a 22 cm step (Model #O60-7000, Ad vanced Mechanical Technology, Inc, Watertown, MA, USA).
Table 1. Description of the Tasks Evaluated.
Step Down Participants were instructed to lower themselves from a 0.22 m step, tap the opposite heel to the floor, then return to the starting position. This motion was repeated five times without stopping.
Drop Jump Participants stood on a 0.46 m box and were instructed to drop from the box, land with only the tested limb on the force plate, then jump as high as possible.
Lateral Shuffle
Participants were instructed to shuffle to the side as quickly as possible (4.6 m runway), plant only the tested limb on the force plate, then switch directions and shuffle back to the start. This motion was repeated two times without stopping.
Deceleration Participants were instructed to run forward as quickly as possible (4.6 m runway), plant only the tested limb on the force plate, then backpedal to the starting position. This motion was repeated two times without stopping.
Triple Hop Participants were instructed to perform three consecutive maximal forward hops on the tested limb and stick the landing on the force plate. The starting distance was 90% of the maximal hop length, measured from the center of the force plate. Maximal hop length was established prior to biomechanical testing.
Side-StepCut
Participants were instructed to run forward as quickly as possible (4.6 m runway), plant only the tested limb on the force plate, then turn 90°
Prior to data collection, participants were informed about the nature of the study and written consent was obtained as approved by the Institutional Review Board of the Health Sciences Campus at the University of Southern California. Once informed consent was obtained, participants warmed up on a stationary bike for 5-10 minutes. For all data proce dures outlined below, data were obtained on the right limb.
Participants were instrumented with 17 reflective mark ers (10 mm diameter) on the right lower extremity, as pre viously described.21,22 Two-dimensional video and 3D mo tion analysis were collected during the following tasks: 1) Step Down, 2) Drop Jump, 3) Lateral Shuffle, 4) Decelera tion, 5) Triple Hop, and 6) Side-Step-Cut. Details regard ing the instructions provided to participants for each of the tasks can found in Table 1 20–22 These tasks were selected based on current knowledge of movements thought to be associated with various sport injuries. A trial was consid ered successful if all markers remained visible and only the foot of tested limb fully contacted the force plate. Partici pants were permitted to practice until comfortable with the performance of each task. One to two trials were obtained for each of the tasks.
The first successful trial was selected for each task and used for data analysis. Marker position data were labeled in Simi Motion and then exported with the force data to Visual3D software (C-Motion, Inc, Germantown, MD, USA). Marker trajectory and analog force plate data were low-pass filtered at 12 Hz, using a fourth-order Butterworth filter 23 Joint an gles were calculated using a X-Y-Z (sagittal-frontal-trans verse) Cardan sequence.
Inverse dynamics equations were used to calculate net joint moments (external) at the knee. Moment data were normalized to body mass and height. Three frontal plane knee moment variables were extracted (peak moment, av erage moment, and moment at peak knee flexion). The peak and average frontal plane knee moments were calculated
during the deceleration phase of all tasks (initial contact to peak knee flexion). In addition, the frontal plane knee mo ment at peak knee flexion was identified. For the step down, the peak and average frontal plane knee moments were cal culated during the lowering phase (initiation of the move ment to the time at which the heel touched the ground). For calculation of the peak moment for trials in which a valgus moment was not present, the minimum varus moment was identified and used for statistical analysis.
For the 2D video analysis, the image containing peak knee flexion was identified. For the step down, the image at which the contralateral heel touched the ground was used for analysis. Images were uploaded into ImageJ software (Version 1.50i, National Institute of Health, USA) for 2D angle assessments. The FPPA was measured as the angle formed by three points (ASIS, knee joint center, ankle joint center). This value was subtracted from 180 to represent the anatomical frontal plane alignment of the knee.10 A positive value represented knee valgus (knee joint center medial to a line formed from the ankle and ASIS) and a neg ative represented knee varus (knee joint marker lateral to a line formed from the ankle and ASIS) (Figure 1). All 2D measurements were obtained by a single investigator who demonstrated excellent intra-rater reliability for all tasks prior to the start of the study (ICCs ranging from 0.91 to 1.0).
Linear regression analysis was used to assess the ability of the 2D FPPA angle (independent variable) to predict the frontal plane knee moment (dependent variable). This analysis was repeated for each task and was run separately for each dependent variable (peak frontal plane knee mo ment, average frontal plane knee moment, and frontal plane knee moment at peak knee flexion). R2 values were interpreted as strong (>= 0.50), moderate (0.25-0.49), weak (0.10-0.24), and negligible (0.0-0.09).24 All statistical analyses were performed using SPSS Version 27 (Chicago, Illinois, USA) and a custom MATLAB script (The Math works, Inc., Natick, MA) with alpha set at 0.05.
Figure 2. Average FPPA and moment variables for the six tasks evaluated. Error bars represent one SD
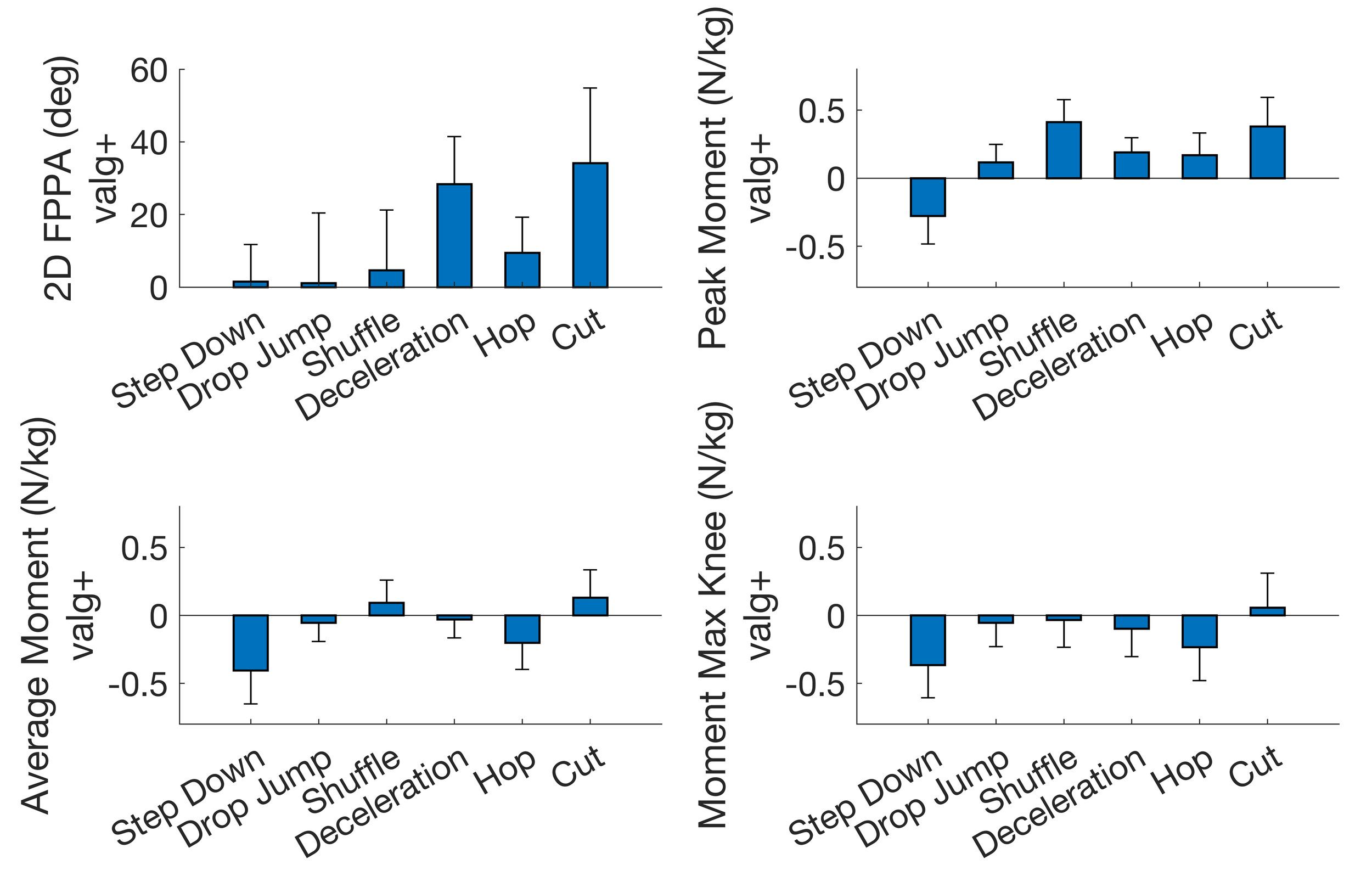
Due to technical issues with the force plate, ground reac tion force data were not available for one subject during the drop jump and eight participants during the step-down task. Descriptive statistics for the FPPA, peak frontal plane knee moment, and average frontal plane knee moment for each task are presented in Figure 2 Time series data for the frontal plane knee moment are presented in Figure 3.
The FPPA was found to significantly predict the peak frontal plane knee moment for deceleration (R2 = 0.12, p = 0.032) and side-step-cut (R2 = 0.25, p = 0.001), with a
larger FPPA predicting increased knee valgus moments (or decreased knee varus moments). However, the FPPA did not predict the peak frontal plane knee moment for step down, drop jump, lateral shuffle, and triple hop (Figure 4).
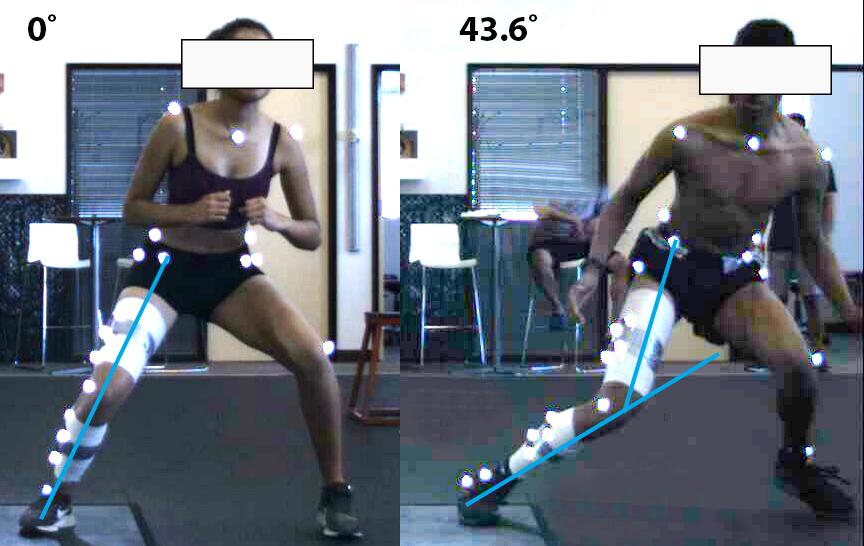
RELATIONSHIP BETWEEN FPPA AND AVERAGE FRONTAL PLANE KNEE MOMENT
The FPPA was found to significantly predict the average frontal plane knee moment for drop jump (R2 = 0.25, p = 0.001), shuffle (R2 = 0.40, p < 0.001), deceleration (R2 = 0.20, p = 0.004), triple hop (R2 = 0.15, p = 0.015), and side-stepcut (R2 = 0.31, p < 0.001), with a larger FPPA predicting increased knee valgus moments (or decreased knee varus moments). However, the FPPA did not predict the average frontal plane knee moment for step down (R2 = 0.0, p = 0.775) (Figure 5).
The FPPA was found to significantly predict the frontal plane knee moment at peak knee flexion for drop jump (R2 = 0.39, p < 0.001), shuffle (R2 = 0.45, p < 0.001), decelera tion (R2 = 0.16, p = 0.013), triple hop (R2 = 0.17, p = 0.008), and side-step-cut (R2 = 0.27, p < 0.001), with a larger FPPA predicting increased knee valgus moments (or decreased knee varus moments). However, the FPPA did not predict the frontal plane knee moment at peak knee flexion for step down (R2 = 0.02, p = 0.41) (Figure 6).
Figure 1. Measurement of the FPPA obtained at peak knee flexion from 2D video. Positive values indicate knee valgus.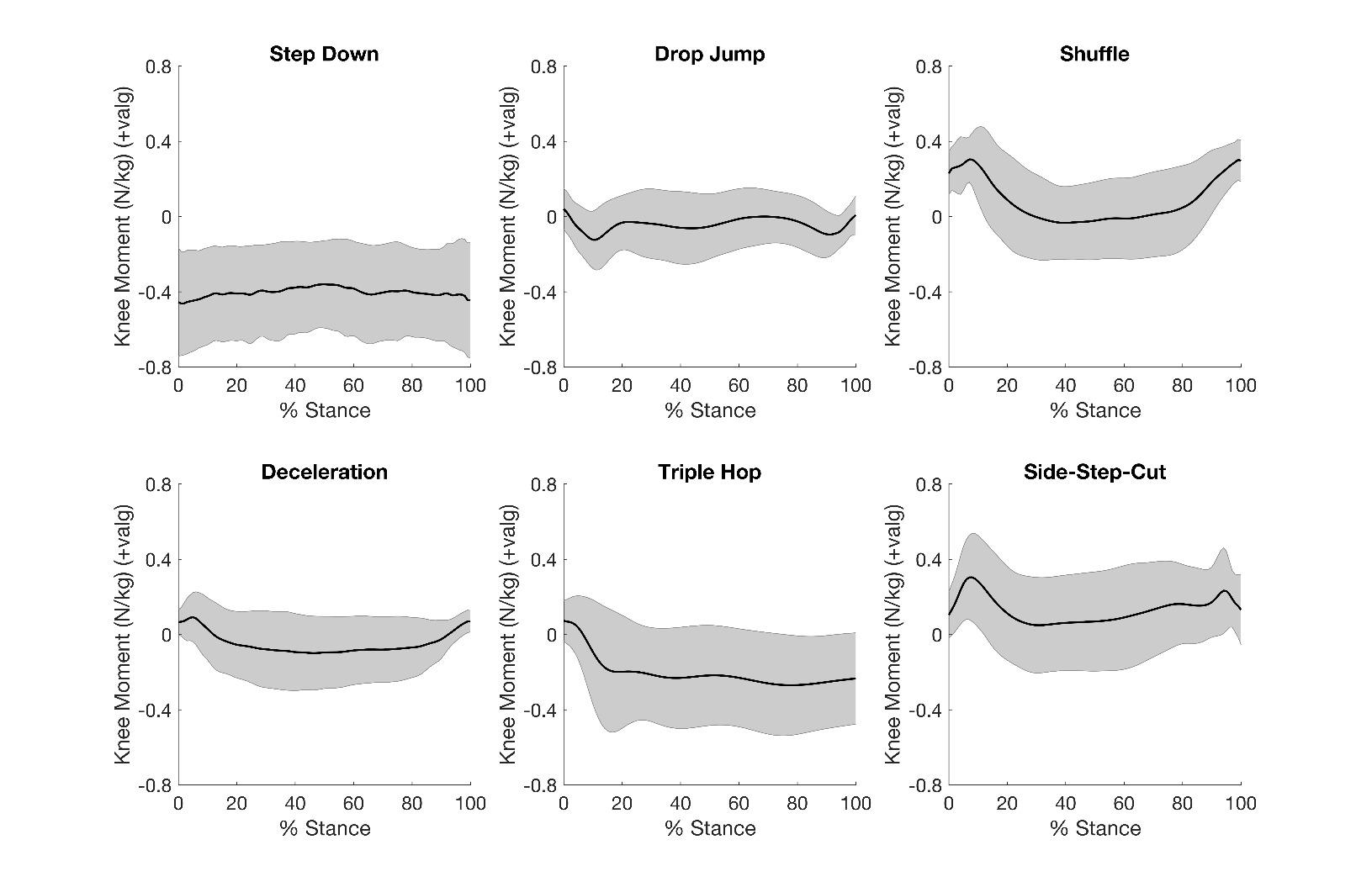
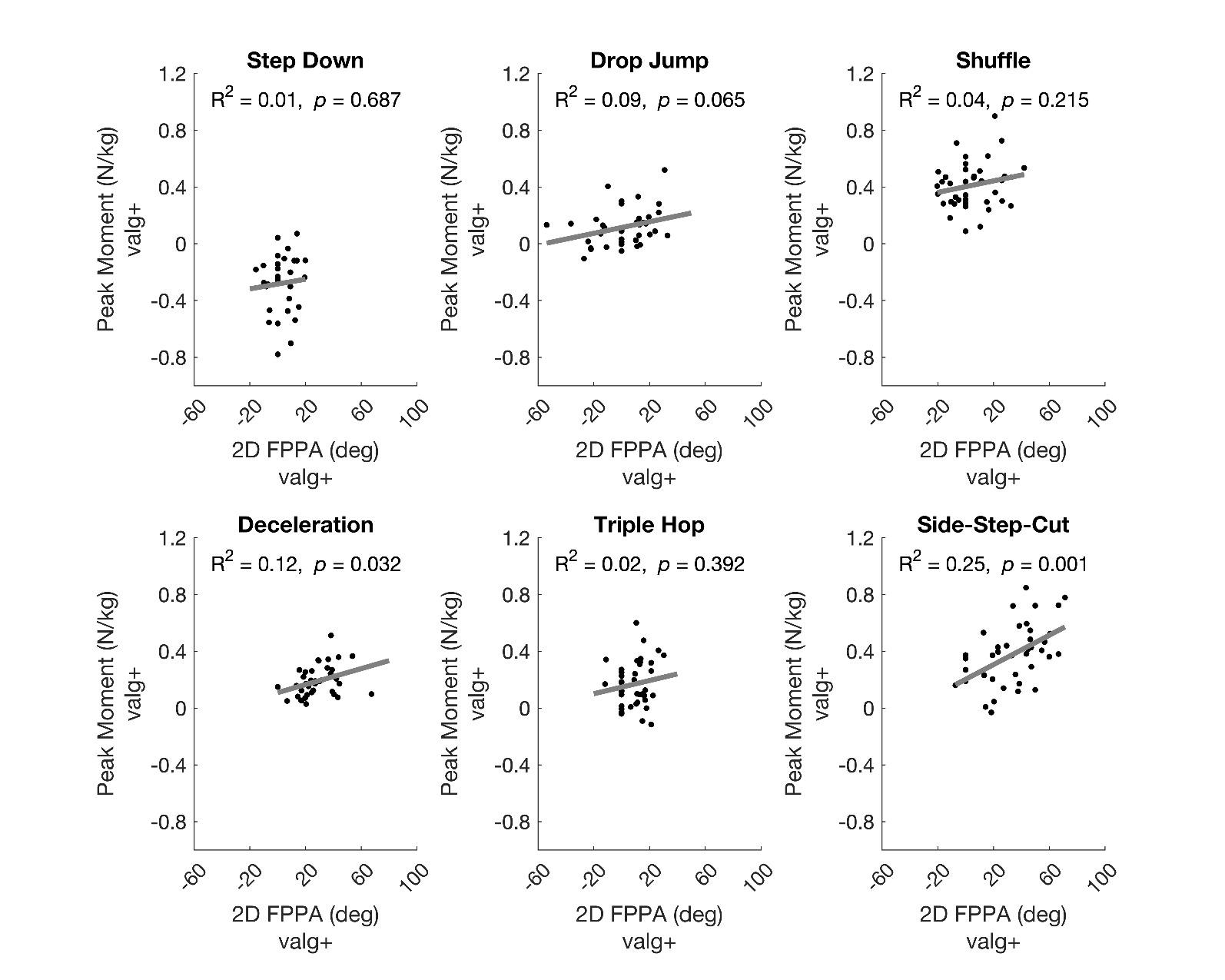 Figure 4. Linear regression models to predict the peak frontal plane knee moment for each task.
Figure 4. Linear regression models to predict the peak frontal plane knee moment for each task.
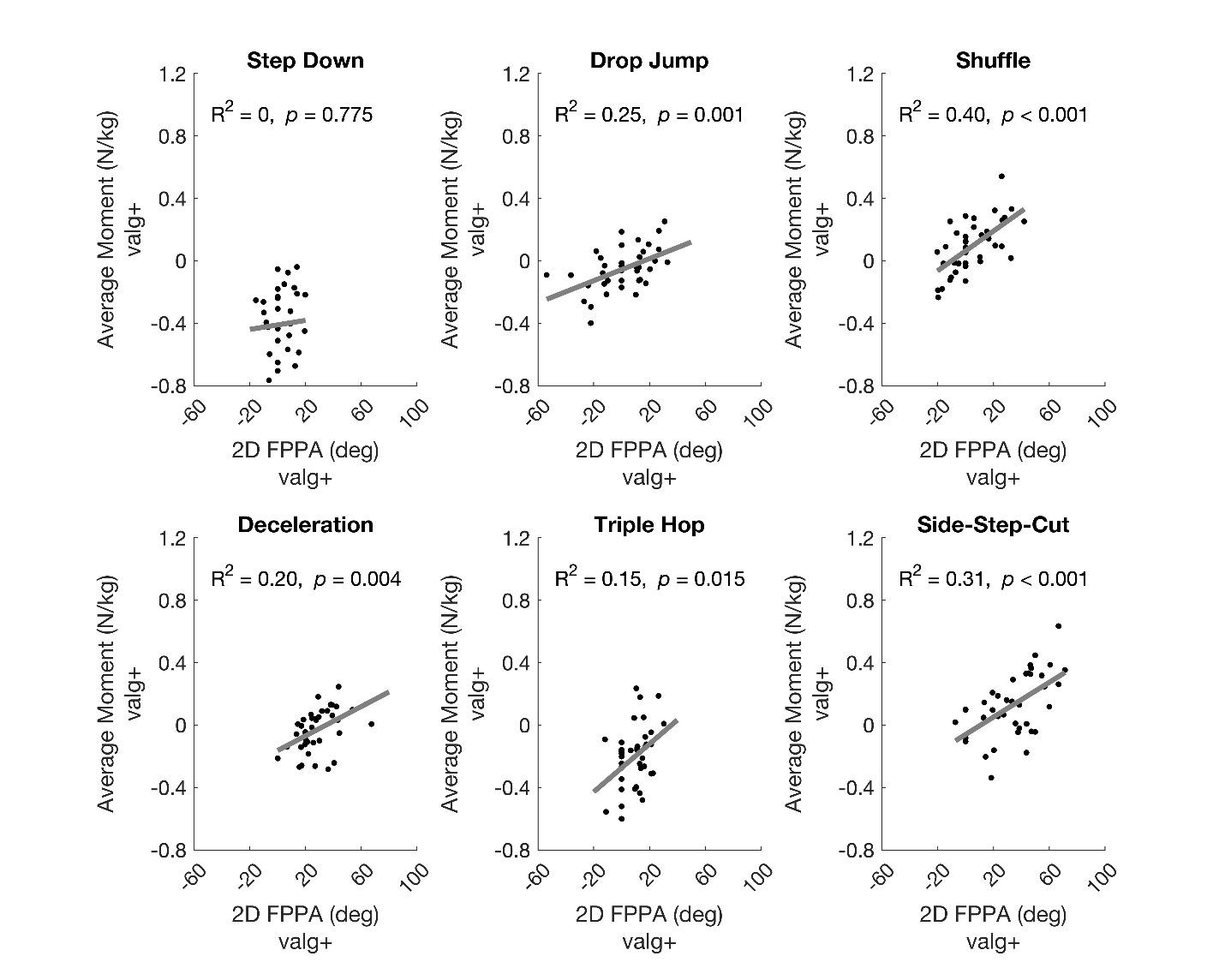 Figure 5. Linear regression models to predict the average frontal plane knee moment for each task.
Figure 5. Linear regression models to predict the average frontal plane knee moment for each task.
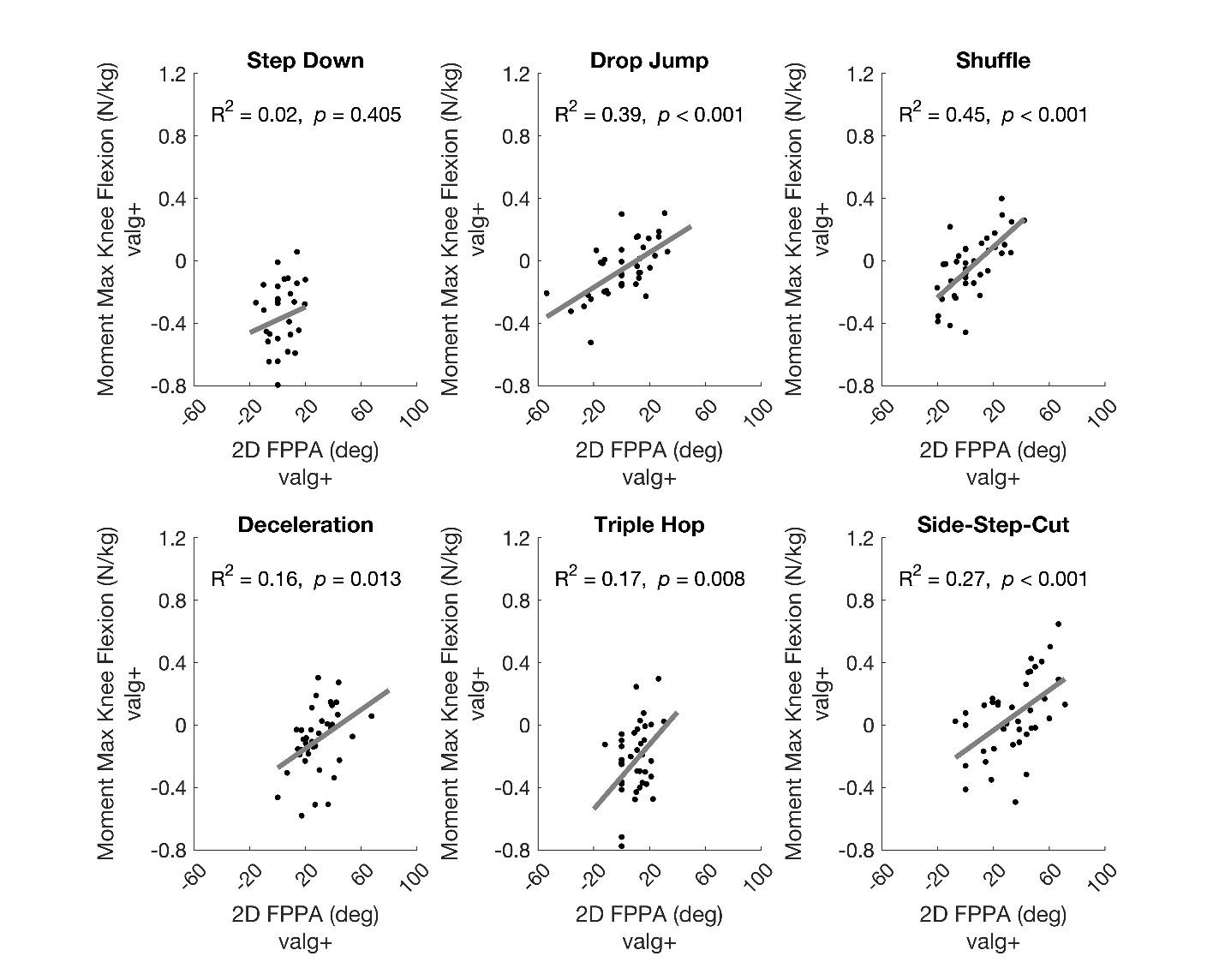 Figure 6. Linear regression models to predict the frontal plane knee moment at maximum knee flexion for each task.
Figure 6. Linear regression models to predict the frontal plane knee moment at maximum knee flexion for each task.
The purpose of the current study was to comprehensively evaluate the ability of the FPPA to predict the frontal plane knee kinetics (peak moment, average moment, and mo ment at peak knee flexion) across a wide range of tasks (stepping, landing, and change of direction). In general, the FPPA was a better predictor of the average frontal plane knee moment (five out of six tasks) and frontal plane knee moment at peak knee flexion (5 of 6 tasks) compared to the peak frontal plane knee moment (two out of six tasks).
For all significant models, an increased FPPA predicted in creased knee valgus moments (or decreased knee varus mo ments) during landing and change of direction tasks (but not stepping). However, the strength of the predictive mod els was weak to moderate (R2 = 12% to 45%), highlighting that the utility of the FPPA as an indicator of frontal plane knee moments during landing and change of direction tasks is limited.
The current results are in general agreement with the findings of Herrington et al.12 and Mizner et al.,14 both of whom examined the ability of the FPPA to predict knee val gus moments during various tasks. Mizner et al. reported that an increased FPPA predicted the knee valgus moment at peak knee flexion during a drop jump task (R2 = 35%),14 which is comparable to our moment results at peak knee flexion for the drop jump (R2 = 39%). Herrington et al. re ported that an increased FPPA did not predict the peak knee valgus moment during a single leg landing from a box (R2 = 13%),12 which agrees with our finding for the peak frontal plane knee moment during the triple hop (R2 = 2%). How ever, Herrington et al. reported that an increased FPPA pre dicted the peak knee valgus moment during a single leg squat (R2 = 42%),12 which is in contrast with our findings for the step down for the peak frontal plane knee moment (R2 = 1%). However, the step down and single leg squat dif fer in a number of kinematic variables,25 which makes di rect comparisons difficult.
Across tasks, the highest R2 values were found for the average frontal knee moments and frontal plane knee mo ments at maximum knee flexion. Given that the FPPA was measured at peak knee flexion, it is logical that the FPPA was predictive of the frontal plane knee moment at that point in time. Additionally, the fact that peak knee flexion was used to indicate the end of the deceleration phase for each task may explain why the FPPA predictive models for the average moment during the deceleration phase were similar to those observed for the frontal plane knee mo ment at peak knee flexion. The ability of the FPPA to pre dict the peak frontal plane knee moment was limited to two of the six tasks (deceleration and cutting), with R2 val ues being lower than the other two variables examined. The limited ability of the FPPA to predict the peak frontal plane knee moments may be explained by the fact that the peak moment did not always occur at the same time point at which the FPPA was measured (Figure 3). As such, the tim ing of the kinetic variables of interest should be considered when measuring the FPPA at a single point in time.
With respect to the strength of the predictions across tasks, the step down exhibited non-significant results for all three frontal plane knee moment variables (R2 = 0-2%) ( Figure 4 6). This finding may be related to the fact that 100% of participants exhibited average knee varus mo ments during this movement, and this task had the lowest average frontal plane knee moment (Figure 2, Figure 5). In contrast, the strongest significant relationship was ob served for the shuffle task, which had the second highest average frontal plane knee moment and a relatively large prevalence of average knee valgus moments (69% of partic ipants) (Figure 2, Figure 5). It appears that the FPPA may be a stronger predictor of frontal plane knee kinetics when a knee valgus moment is present, with the strength of the predictability contingent on the observed frequency and magnitude of knee valgus moments. This is logical as the FPPA is indicative of inward collapse of the knee and there fore would be expected to be indicative of the variables that would be related to a knee valgus moment (i.e., medial po sitioning of the knee joint center, etc.).
Previous studies have reported that the FPPA is an in consistent predictor of frontal plane knee kinemat ics1,5,9–15 and that the general agreement between 2D and 3D frontal plane knee angles is poor 16 Based on the current study and the work of previous authors who have evaluated the ability of the FPPA to predict frontal plane knee mo ments,12,14 it appears that the FPPA may be a better indi cator of knee kinetics as opposed to knee kinematics. It is possible that the clinical utility of the FPPA as a predictor of injury8,26 or the ability of the FPPA to differentiate between healthy and clinical populations5–7 may lie in the fact that this measure is a predictor of frontal plane knee moments. An argument could be made that the frontal plane knee moment is more suggestive of knee loading as opposed to frontal plane knee motion.
Regarding clinical application, the current results sug gest that obtaining measures of the FPPA from hand-held mobile devices (i.e.., phones, tablets, etc.) may be of value. However, it is important to note that the 2D video data obtained in the current study were captured from a fixed camera that was aligned perpendicular to the force plate. As with all measurements obtained from 2D video, there is potential for parallax error owing to the camera being po sitioned at an angle to the patient. Such error would in fluence the measurement of the FPPA and the ability to in fer frontal plane knee moments as described in the current study.
There are several limitations within the current study that warrant discussion. First, these data were obtained from healthy individuals. As such, our results may not be applicable to those with specific knee conditions (i.e., patellofemoral pain, ACL injury, etc.). Second, only the de celeration or lowering phase of each task was considered in our moment analysis. Therefore, our results may not apply to the acceleration phase of the tasks evaluated. Third, the current study was cross-sectional in nature. The current re sults cannot be interpreted to suggest that increased FPPA angles are predictive of knee injury Lastly, for all regres sion models, only a single predictor (FPPA) was examined.
The R2 values reported could be improved by including other 2D measurements such as frontal plane motion at the hip, pelvis, or trunk.27
In summary, the results of the current study suggest that the FPPA is a predictor of frontal plane knee loading during landing and change in direction tasks, specifically when the frontal plane knee moment is calculated as the average mo ment or the moment at peak knee flexion. For all signifi cant models, an increased FPPA (indicative of medial knee collapse) predicted increased knee valgus moments (or de creased knee varus moments) during landing and change of direction tasks (but not stepping). However, the ability of the FPPA to predict frontal plane knee kinetics appears to be task dependent, with the strength of the prediction
improved with increased frequency and magnitude of ob served knee valgus moments. In addition, the strength of the prediction was weak to moderate, highlighting that the validity of the FPPA as a predictor of frontal plane knee mo ments during landing and change of direction tasks is lim ited.
The authors have no conflicts of interest to disclose.
Submitted: March 04, 2022 CST, Accepted: August 15, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. McLean SG, Walker K, Ford KR, Myer GD, Hewett TE, van den Bogert AJ. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury Br J Sports Med 2005;39(6):355-362. doi:10.1136/bjs m.2005.018598
2. Willson JD, Ireland ML, Davis I. Core strength and lower extremity alignment during single leg squats. Med Sci Sports Exerc. 2006;38(5):945-952. doi:10.124 9/01.mss.0000218140.05074.fa
3. Petushek E, Nilstad A, Bahr R, Krosshaug T Drop jump? Single-leg squat? Not if you Aim to predict anterior cruciate ligament injury from real-time clinical assessment: A prospective cohort study involving 880 elite female athletes. J Orthop Sports Phys Ther 2021;51(7):372-378. doi:10.2519/jospt.202 1.10170
4. Nilstad A, Petushek E, Mok KM, Bahr R, Krosshaug T Kiss goodbye to the ‘kissing knees’: no association between frontal plane inward knee motion and risk of future non-contact ACL injury in elite female athletes. Sports Biomech Published online April 28, 2021:1-15. doi:10.1080/14763141.2021.1903541
5. Willson JD, Davis IS. Utility of the frontal plane projection angle in females with patellofemoral pain. J Orthop Sports Phys Ther 2008;38(10):606-615. doi:1 0.2519/jospt.2008.2706
6. Herrington L. Knee valgus angle during single leg squat and landing in patellofemoral pain patients and controls. Knee. 2014;21(2):514-517. doi:10.1016/j.kne e.2013.11.011
7 Gwynne CR, Curran SA. Two-dimensional frontal plane projection angle can identify subgroups of patellofemoral pain patients who demonstrate dynamic knee valgus. Clin Biomech 2018;58:44-48. d oi:10.1016/j.clinbiomech.2018.06.021
8. Räisänen AM, Pasanen K, Krosshaug T, et al. Association between frontal plane knee control and lower extremity injuries: a prospective study on young team sport athletes. BMJ Open Sport Exerc Med 2018;4(1):e000311. doi:10.1136/bmjsem-2017-0 00311
9. Scholtes SA, Salsich GB. A dynamic valgus index that combines hip and knee angles: Assessment of utility in females with patellofemoral pain. Int J Sports Phys Ther. 2017;12(3):333-340.
10. Kingston B, Murray A, Norte GE, Glaviano NR. Validity and reliability of 2-dimensional trunk, hip, and knee frontal plane kinematics during single-leg squat, drop jump, and single-leg hop in females with patellofemoral pain. Phys Ther Sport 2020;45:181-187. doi:10.1016/j.ptsp.2020.07.006
11. Schurr SA, Marshall AN, Resch JE, Saliba SA. Two-dimensional video analysis is comparable to 3d motion capture in lower extremity movement assessment. Int J Sports Phys Ther 2017;12(2):163-172.
12. Herrington L, Alenezi F, Alzhrani M, Alrayani H, Jones R. The reliability and criterion validity of 2D video assessment of single leg squat and hop landing. J Electromyogr Kinesiol. 2017;34:80-85. doi:10.1016/j.j elekin.2017.04.004
13. Alahmari A, Herrington L, Jones R. Concurrent validity of two-dimensional video analysis of lower extremity frontal plane of movement during multidirectional single-leg landing. Phys Ther Sport 2020;42:40-45. doi:10.1016/j.ptsp.2019.12.009
14. Mizner RL, Chmielewski TL, Toepke JJ, Tofte KB. Comparison of 2-dimensional measurement techniques for predicting knee angle and moment during a drop vertical jump. Clin J Sport Med 2012;22(3):221-227 doi:10.1097/jsm.0b013e31823a46 ce
15. Belyea BC, Lewis E, Gabor Z, Jackson J, King DL. Validity and intrarater reliability of 2-dimensional motion analysis using a handheld tablet compared to traditional 3-dimensional motion analysis. J Sport Rehabil 2015;24(4). doi:10.1123/jsr.2014-0194
16. Lopes TJA, Ferrari D, Ioannidis J, Simic M, Mícolis de Azevedo F, Pappas E. Reliability and validity of frontal plane kinematics of the trunk and lower extremity measured With 2-dimensional cameras during athletic tasks: A systematic review with metaanalysis. J Orthop Sports Phys Ther 2018;48(10):812-822. doi:10.2519/jospt.2018.8006
17. Rabin A, Portnoy S, Kozol Z. The association between visual assessment of quality of movement and three-dimensional analysis of pelvis, hip, and knee kinematics during a lateral step down test. J Strength Cond Res 2016;30(11):3204-3211. doi:10.151 9/jsc.0000000000001420
18. Ageberg E, Bennell KL, Hunt MA, Simic M, Roos EM, Creaby MW. Validity and inter-rater reliability of medio-lateral knee motion observed during a singlelimb mini squat. BMC Musculoskelet Disord. 2010;11(1):265. doi:10.1186/1471-2474-11-265
19. Cortes N, Onate J, Van Lunen B. Pivot task increases knee frontal plane loading compared with sidestep and drop-jump. J Sports Sci. 2011;29(1):83-92. doi:10.1080/02640414.2010.523087
20. Straub RK, Horgan A, Powers CM. Estimation of vertical ground reaction force parameters during athletic tasks using 2D video. Gait Posture 2021;90:483-488. doi:10.1016/j.gaitpost.2021.09.175
21. Straub RK, Horgan A, Powers CM. Clinical estimation of the use of the hip and knee extensors during athletic movements using 2D video. J Appl Biomech. 2021;37(5):458-462. doi:10.1123/jab.2021-0 055
22. Straub RK, Powers CM. Utility of 2D video analysis for assessing frontal plane trunk and pelvis motion during stepping, landing, and change in direction tasks: A validity study Int J Sports Phys Ther. 2022;17(2):139-147. doi:10.26603/001c.30994
23. Tomescu SS, Bakker R, Beach TAC, Chandrashekar N. The effects of filter cutoff frequency on musculoskeletal simulations of high-impact movements. J Appl Biomech. 2018;34(4):336-341. do i:10.1123/jab.2017-0145
24. Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69-71.
25. Lewis CL, Foch E, Luko MM, Loverro KL, Khuu A. Differences in lower extremity and trunk kinematics between single leg squat and step down tasks. PLoS One 2015;10(5):e0126258. doi:10.1371/journal.pon e.0126258
26. Dingenen B, Malfait B, Nijs S, et al. Can twodimensional video analysis during single-leg drop vertical jumps help identify non-contact knee injury risk? A one-year prospective study. Clin Biomech. 2015;30(8):781-787 doi:10.1016/j.clinbiomech.2015.0 6.013
27. Weir G, Alderson J, Smailes N, Elliott B, Donnelly C. A reliable video-based ACL Injury screening tool for female team sport athletes. Int J Sports Med 2019;40(3):191-199. doi:10.1055/a-0756-9659
Nickolai JP Martonick 1 a , Youngmin Chun 2 , Lukas Krumpl 1 , Joshua P Bailey 1
1 Department of Movement Sciences, University of Idaho, 2 Department of Kinesiology, Sonoma State University
Keywords: Drop Landing, Single Subjects, Statistical Parametric Mapping, Lower Limb Asymmetry https://doi.org/10.26603/001c.55538
Lower limb asymmetries may be associated with increased injury risk in an active female population. However, an appropriate method for determining these asymmetries has not been established.
The purpose of the present study was to examine the single leg drop landing (SLD) kinematic waveforms of female recreational athletes for the pelvis, hip, and knee using statistical parametric mapping (SPM). It was hypothesized that individual bilateral differences would be masked by the group analysis.
Descriptive Laboratory Study
The current study examined the sagittal and frontal plane pelvis, hip, and knee kinematics of nine physically active females during a SLD. To better elucidate whether asymmetries were present between right and left limbs throughout the landing phase, data were analyzed with SPM. The time-series data were comprised from initial contact to the bottom of the landing. A single subject design was also included to account for potential interindividual variability.
At the group level there were no statistical differences between the right and left limbs of participants for all variables. The single subject design yielded at least two significant asymmetries for all participants. Six out of the nine participants had bilateral differences for all six kinematic time-series.
The lack of significant differences at the group level may have been masked by movement variability amongst participants. For example, when considering participants with significant differences for hip flexion, four participants had greater values on the left limb and three on the right. A similar observation was made for knee flexion where three participants had significantly greater kinematic values on the left versus four on the right. Until a method is developed to adequately dichotomize lower extremities during the SLD task, a single subject design strategy be used with group analysis when making bilateral comparisons.
a
Corresponding author: Nickolai JP Martonick University of Idaho, Department of Movement Sciences, Moscow ID 83843 nmartonick@uidaho.edu

Landing on a single leg is a common movement in sports such as basketball, volleyball, and soccer When this move ment is not adequately controlled by the neuromuscular system, non-contact anterior cruciate ligament (ACL) in jury may occur.1,2 It is well established that female athletes are more likely to suffer non-contact ACL injuries than male counterparts participating in the same sports.3 Fe male athletes have also been shown to have an increased propensity to experience ACL injury on their non-dominant limb which was defined as the stance limb when kicking a ball.4,5 However, minimal differences in mechanical vari ables have been reported between dominant and non-dom inant limbs during a cutting task in female soccer athletes.6 Thus, it is unclear whether the reported increase in injury rate between dominant and non-dominant limbs are linked to bilateral mechanical differences.
Mechanisms for non-contact ACL injury consist of dy namic joint angles that result in excessive tensile forces on the ligament. For example, excessive knee abduction, and internal rotation have been shown to increase ACL strain during cadaveric modeling.7 Video analysis of ACL injury incidents has identified combined knee abduction and in ternal rotation as a mechanism of injury.8 Investigators have also demonstrated an increased lateral pelvic tilt is related to increased knee abduction moments, which may increase the risk of non-contact ACL injury 1,9,10 Alterna tively, studies using 3D modeling and magnetic resonance imaging suggest that the ACL is under greatest strain dur ing knee extension during dynamic and static loading.11,12 In addition to the various mechanisms of ACL injury, re searchers have also hypothesized that lower extremity kinematic differences (asymmetry) can increase the risk for injury due to an increased loading and reliance on one limb, combined with an inability to maintain stability on the other 13
The single leg drop-landing (SLD) task is often used to assess lower limb kinematic symmetry.14–16 Other tasks that are more functionally related to sport movements, in cluding cutting maneuvers, single leg hop for distance, and single leg jumps, have also been used to analyze lower limb symmetry.17–20 However, these tasks may require greater coordination and training to achieve or perform within the limits of a study design.16 Thus, the relatively limited com plexity of the SLD may make it advantageous for the analy sis of intrinsic bilateral asymmetries across individuals with varied training backgrounds.
Previous studies that have used a SLD task to examine potential bilateral lower extremity asymmetries have re ported mixed results. Recently, Wang and Fu demonstrated an increased total hip and knee range of motion in the sagittal plane in the dominant limb of female soccer play ers.21 Other researchers16 did not find bilateral kinematic hip and knee differences in recreationally active females. The differences between populations may explain the con
flicting findings. However, another possible reason for the discrepancies between these studies is the classification of lower extremities by either dominant limb or non-dominant limb when performing a group analysis.
When using a group analysis for the examination of bi lateral differences, problems may arise from the difficulty of classifying a dominant lower limb. While several studies have defined the dominant lower limb as the leg used to kick a ball,5,6,14–16 limb dominance is likely task specific.22 If limb dominance is task-specific, grouping participants’ limbs based on what would be an arbitrary question, may generate misleading results. These factors have led re searchers to contend that single subject design data should be reported in addition to group analysis when making bi lateral comparisons.23 Thus, reducing the potential for ap plicable findings to be masked by interindividual variability between dominant or non-dominant limbs.
Another potential reason for discrepancies between the aforementioned studies is the interpretation of variables at discrete time points which may lead to analysis of less than 5% of the data.24 Discrete analysis of biomechanical variables may not always be comparable across participants or within participants due to temporal variations in move ment traces.18,25 These potential inconsistencies may limit the interpretation of a temporal component, and how kine matics temporally relate to other biomechanical factors within the same movement. Thus, a more robust method may be required when examining a movement related to ACL injury risk that does not have a clear mechanism and timing. A proposed solution to this problem is statistical parametric mapping (SPM) which can be used to statisti cally analyze the kinematic waveform of the complete task cycle.25
Bilateral asymmetries during a SLD have not been an alyzed with a SPM analysis at the group or single subject level. Thus, the purpose of the present study was to ex amine the SLD kinematic waveforms of female recreational athletes for the pelvis, hip, and knee using SPM. By includ ing a group analysis and single subject design, the current study sought to identify the potential of inter-participant variability to influence group bilateral asymmetries. It was hypothesized that bilateral differences of the waveforms at the single subject design level would occur but not at the group level due to inter-participant variability
Nine female participants who were free from lower limb surgery, disease, or current injury volunteered for this study Participants had a mean [SD] age of 22.4 [3.5] years, height of 1.68 [0.57] m, mass of 61.0 [6.7] kg. All partici pants were defined as physically active and performed ply ometric activities at least once per week. Physically active was defined as performing at least 30 minutes of low-in
tensity exercise five times per week, 20 minutes of high-in tensity exercise three times per week, or participants who ran at least five miles per week. For descriptive purposes, all participants were asked which limb they preferred to kick a ball with. All reported that their right limb was their pre ferred kicking limb. Prior to participation, all participants signed an informed consent form approved by the Univer sity’s internal review board.
Three-dimensional marker trajectories were collected with an eight-camera motion capture system (250 Hz; VICON, Oxford Metric Ltd., Oxford, UK). Participants were equipped with 73 retro-reflective markers (14mm) used to create a custom cluster-based model for the upper extremities, torso, pelvis, and lower extremities (Figure 1).
A force-platform (1000 Hz; ORG-6, AMTI Inc., Water town, MA, USA) time synchronized with the motion capture system was used to collect ground reaction forces (GRFs).
Prior to performing the SLD, participants performed a fiveminute warm-up on a stationary bicycle. Participants were then asked to perform the SLD task from a 60 cm platform after completing two practice trials on each leg. The plat form was positioned behind the force platform with a min imum distance that allowed participants to vertically land on the center of the force platform to minimize GRF in the anteroposterior direction. Participants were asked to place the limb they would land on off the step and then drop down onto the force plate with minimal assistance from their stance limb to drop off the box. No restrictions were
placed on the positioning of the arms. Participants per formed 10 successful trials on each leg with a maximum of 15 attempts. Participants were given as much time as they needed between trials and the starting limbs were coun terbalanced to reduce the potential effect of fatigue. Tri als were considered successful if the participant was able to drop off the box without lowering themselves with the stance leg and maintain balance upon landing as deter mined by the researcher. All participants wore their own ac tivity shoes, which was done to remove any perturbation caused by novel footwear

Angular kinematics and center of mass were computed us ing a Cardan (X-Y-Z) rotation sequence with Visual 3D soft ware (v6, C-Motion Inc., Germantown, MD, USA). Pelvis segment angles were calculated using a Z-Y-X sequence of rotations to be consistent with the conventional clinical understanding of pelvic tilt and pelvic drop. The pelvis was modeled as a using the anterior and posterior superior iliac spines and pelvis segment angles were calculated relative to the global coordinate system. Pelvic drop was defined as the angle in the frontal plane and pelvic tilt was defined as the segment’s rotation in the sagittal plane. Negative val ues in the frontal plane were represented as a contralateral pelvic drop and anterior pelvic tilt was represented by posi tive values. Marker trajectories were filtered using a fourthorder Butterworth filter at 8 Hz and kinetic data were fil tered at 20 Hz respectively Vertical GRF data was used to define initial contact (IC) at the beginning of the deceler ation phase. The IC was defined as the moment when the vertical GRF threshold of 20 N was surpassed. To define the end of the deceleration phase, we used the minimum ver
Figure 1. Custom cluster based model with calibration markers included.Mean values are represented by dashed lines with the solid lines indicating standard deviations. The right limb is shown as black, and the left shown as red. Positive and negative val ues indicate the direction of the variable (e.g., (+) values indicate hip adduction and (-) values indicate hip abduction.
tical height of the center of mass (minCOM).26 Joint (hip and knee) and segment (pelvis) temporal data were ana lyzed between IC and minCOM using MATLAB (MathWorks, Natick, MA, USA). Temporal data were interpolated to 101 data points (100% of cycle) for the SPM analysis.
All SPM analyses were conducted in MATLAB using an open-source software package spm1D 0.4.27 Multiple paired t-tests (p < 0.05) were performed with Bonferroni corrections to compare the grouped kinematic data of lower extremity limbs for all participants at each percentage of the cycle. For group analysis the mean trajectories of each participant’s twenty trials (10 on each leg) were used. Addi tionally, paired t-tests were performed comparing the limbs for each individual participant that was calculated using 10 trials from each limb. The significance level for all sta tistical tests after the alpha corrections was (p = 0.006). The null hypothesis was rejected if the computed t value exceeded the critical threshold. In SPM the t value is cal culated across the temporal region of interest (i.e., IC to minCOM). Whereas, the critical threshold is a product of random field theory that can be used to determine a thresh old where equivalently smooth Gaussian random fields would cross at the specified alpha level when the null hy pothesis is true.28
The group SPM analysis with paired t-tests did not reveal any significant differences between the dominant and nondominant limbs for all kinematic variables (Figure 2).
Individual SPM analysis with paired t-tests revealed sig nificant kinematic differences between the right and left limbs for all participants. At the hip in the sagittal plane, seven participants had a significant difference between their two limbs. During the phase when the difference be tween lower limbs exceeded the critical threshold, four of
those seven participants had a relative increase in hip flex ion on the right limb (Figure 3).
Conversely, the remaining three with significant differ ences were shown to have increased hip flexion on their left limb. At the knee in the sagittal plane, seven participants had a significant relative difference between their two limbs (Figure 4).
Four of those participants increased knee flexion on the left limb and three increased knee flexion on the right limb. Anterior pelvic tilt was greater when landing on the left limb in five participants, and in three participants when landing on their right limb (Figure 5).
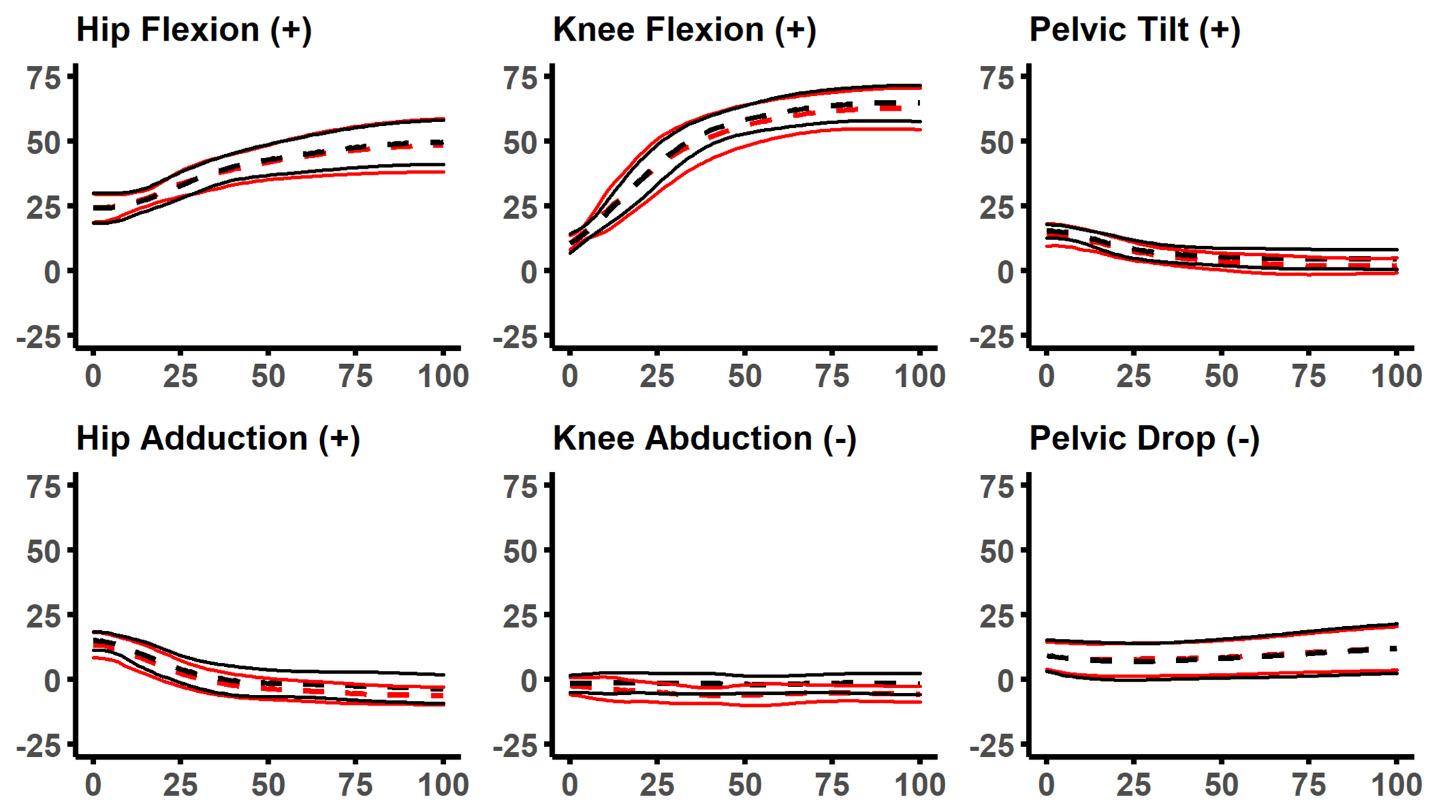
For frontal plane hip motion, six participants had in creased hip adduction on the right limb and three partic ipants had relatively increased adduction on the left limb (Figure 6).
At the knee, two participants had increased knee abduc tion on the right limb, 4 had relative increases on the left limb, and participants six and eight had relative differences between limbs in both directions (Figure 7).
Significant differences for pelvic drop occurred in eight of the nine participants (Figure 8).
Six of those participants had a relative decrease in pelvic drop when landing on their right limb.
The aim of this study was to examine physically active fe males for potential bilateral differences in pelvis, hip, and knee kinematics during a SLD task. A group analysis (com parison of mean data between right and left limbs) and a single subject design was used to ascertain the findings of potential bilateral differences among the population stud ied. The findings indicated that there were no significant differences for kinematic variables between the right and left limbs when analyzed at a group level. However, this was not indicative that bilateral differences were not preva lent among the study’s population. For instance, each of
Figure 2. Group kinematics from initial contact to the minimum height of the center of mass.Figure 3. Hip sagittal plane kinematics for each participant from initial contact to the minimum height of the center of mass.
Positive values indicate hip flexion. Mean values are represented by dashed lines with the solid lines indicating standard deviations. The right limb is shown as black, and the left shown as red. Shaded areas represent significant differences as determined from the statistical parametric mapping.
the participants demonstrated at least two asymmetries out of the six variables in question and six out of the nine par ticipants had bilateral differences for all kinematic time-se ries. Thus, the hypothesis that bilateral differences would be observed at the single subject design level, but not at the group level was accepted. The consequence of group analy sis concealing individual differences is not novel to the cur rent study 29–31
The data were grouped by right and left limbs because there is currently not a clear metric for determining limb dominance during a SLD task. However, the selection of comparing right and left limbs was not an adequate method for homogenizing participant data to describe the observed differences between limbs. Therefore, the approach of in cluding a single subject design allowed us to look at bilat eral differences without defining the criteria of which leg was dominant during the task. It should be noted that all participants reported that they preferred kicking a ball with their right limb. Thus, grouping limbs by this metric would not have affected the outcome of the data.
The absence of significant group findings may be ex plained by not all participants displaying similar movement patterns with their right or left limb. For example, partic ipants (4, 5, 9) had a significant relative increase for hip flexion angles on their right limbs when compared to their left (Figure 3). Conversely, participants (1, 2, 6, 8) demon strated greater hip flexion on their left limb (Figure 3). Sim ilar participant variability was also observed in the other variables of interest. Thus, it appears that in this sample
population of uninjured participants, the heterogeneous movement patterns influenced the findings at a group level and provided support for the use of single subject analysis.
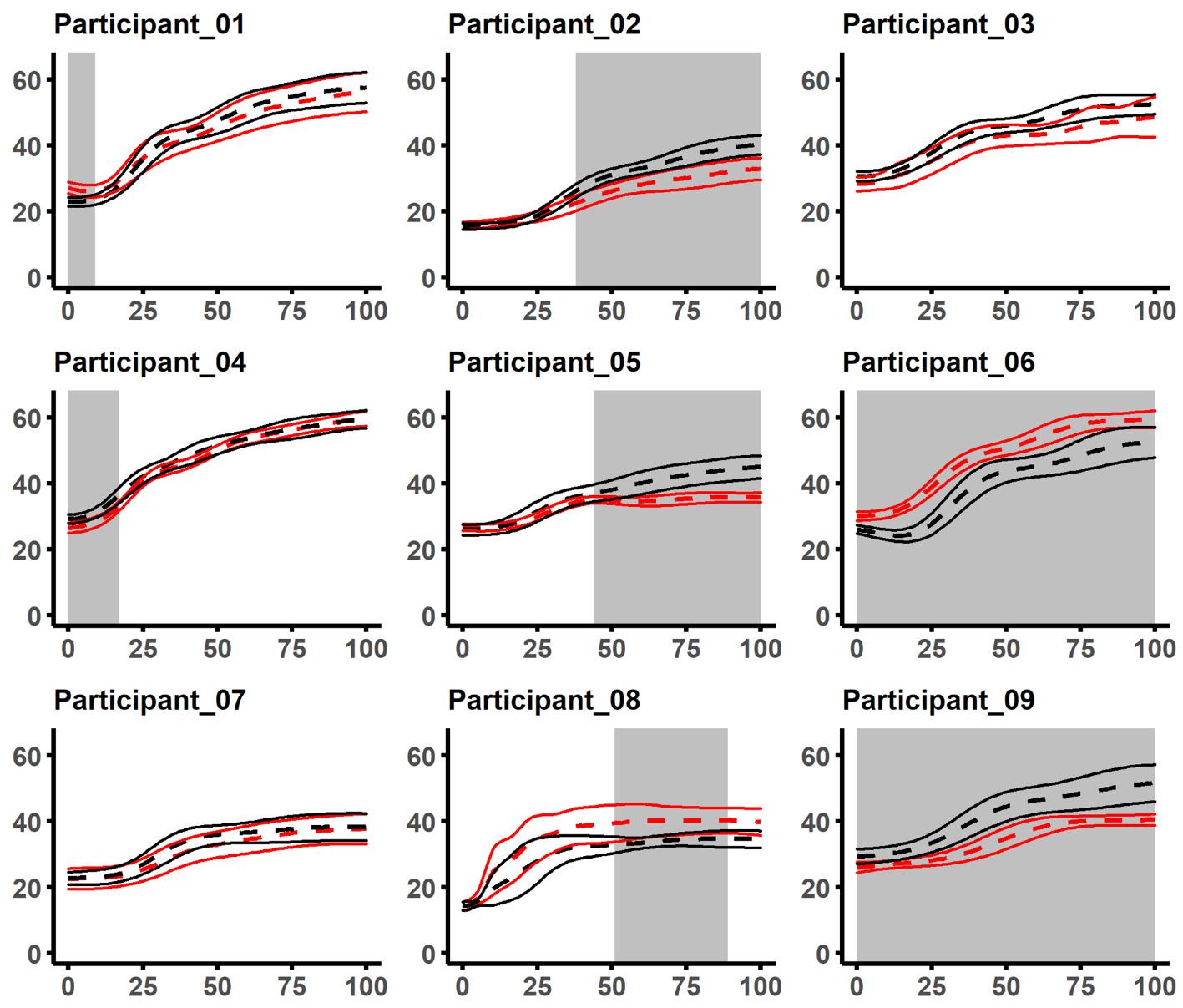
The current study’s group findings in recreational female athletes are similar with those of Wang and Fu21 who found no bilateral differences in female soccer players at IC. How ever, the researchers15 did not include a single subject de sign which may have limited their interpretation of their results. For instance, when considering this study, four of the participants (1, 4, 6, 9) had a significant difference for hip and knee flexion at IC (Figure 3, 4). Interestingly, for hip frontal plane motion all but one of the participants (8) demonstrated a significant difference at IC (Figure 6). At the knee in the frontal plane, all but two of the partici pants (4, 8) had statistically similar waveforms at IC (Figure 7). Another difference between the two studies methods is the fact that the female soccer players dropped from a box 20cm shorter than what was used for the current study’s participants (60cm).
It has been shown that increasing the height of the SLD task may result in greater bilateral kinematic differences.16 In a study where participants landed from the same height for the SLD task as the current study, the researchers16 also reported that no bilateral differences were observed for hip and knee flexion between the limbs of recreationally ac tive females. However, the researchers16 analyzed the kine matic data at the moment of peak vertical GRF because it was thought to be related to the timing of injury. As dis crete time points were not considered in the current analy
Figure 4. Knee sagittal plane kinematics for each participant from initial contact to the minimum height of the center of mass.
Positive values indicate knee flexion. Mean values are represented by dashed lines with the solid lines indicating standard deviations. The right limb is shown as black, and the left shown as red. Shaded areas represent significant differences as determined from the statistical parametric mapping.
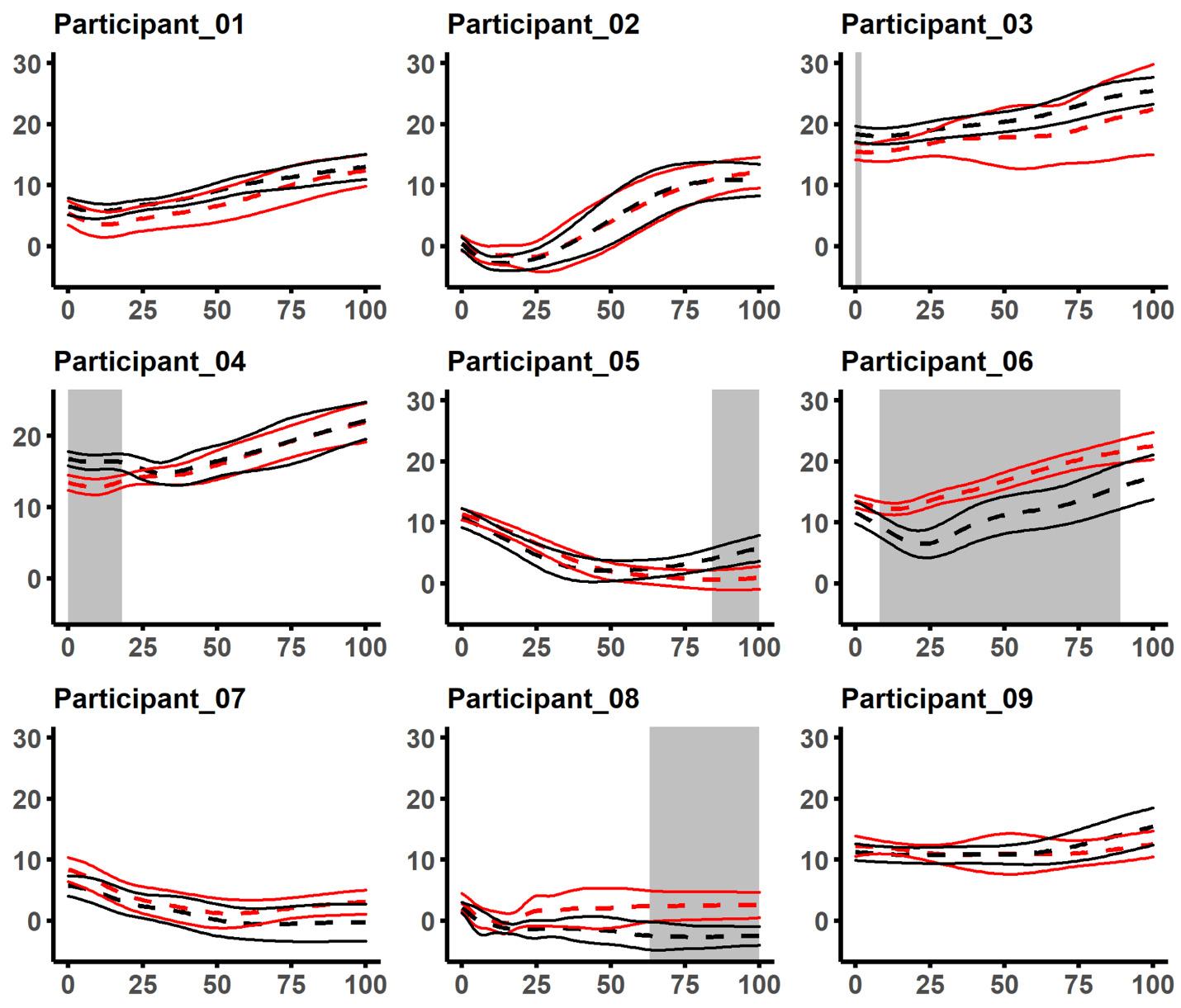
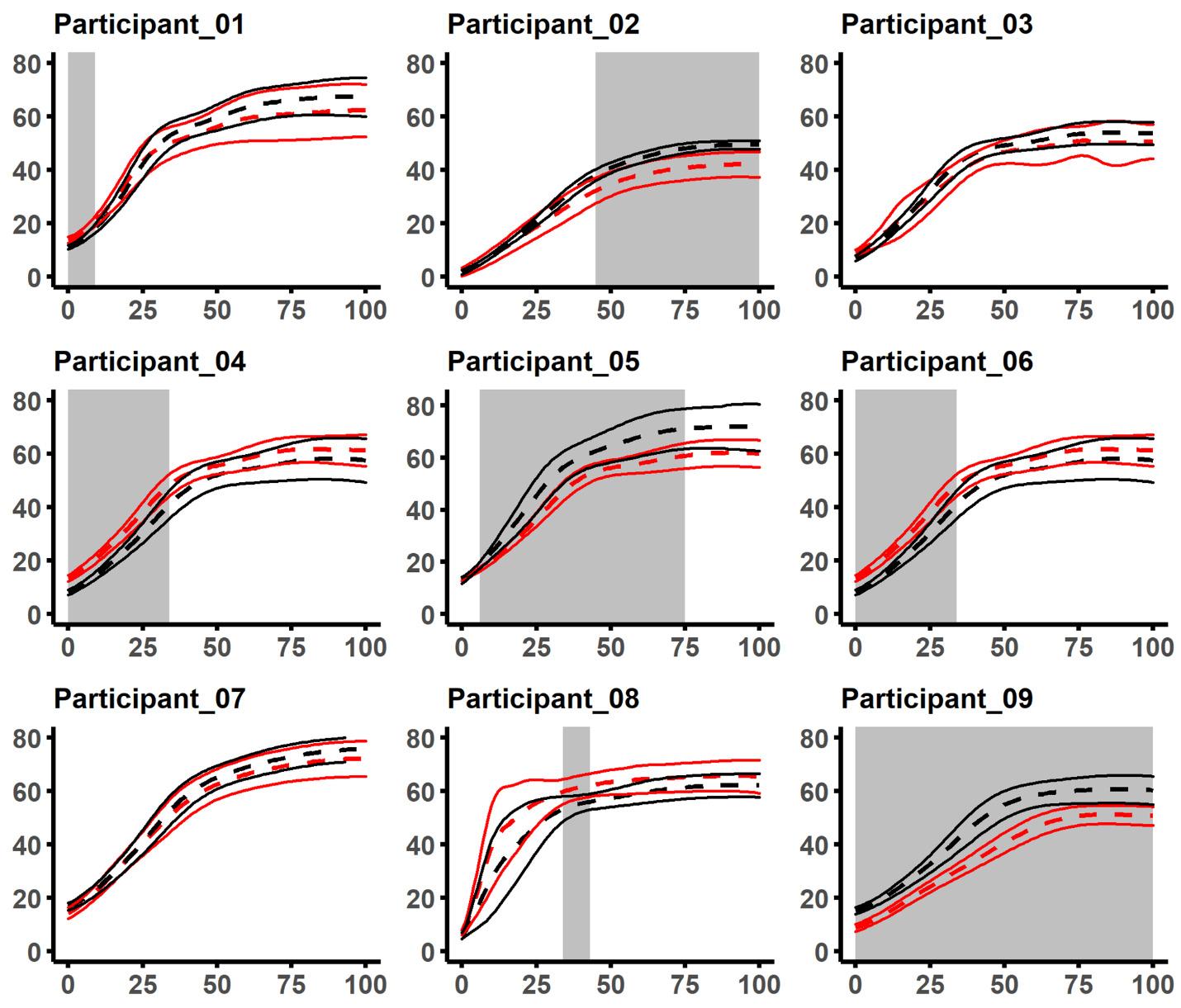
Figure 5. Pelvis sagittal plane kinematics for each participant from initial contact to the minimum height of the center of mass.
Positive values indicate anterior pelvic tilt. Mean values are represented by dashed lines with the solid lines indicating standard deviations. The right limb is shown as black, and the left shown as red. Shaded areas represent significant differences as determined from the statistical parametric mapping.
sis (other than to determine the beginning and end of the movement) it is difficult to draw comparisons with their kinematic data. The discrepancies between cadaveric7,32 and model simulated ACL strain11,12 is conflicting for re searchers looking to identify the optimal time or joint angle for assessing risky lower extremity movement patterns. Re search from cadaveric modeling has been used to suggest that peak ACL strain occurs simultaneously with peak knee abduction angles.33,34 Thus, there is a potential advantage of using a wave form analysis technique as it limits the bias of researchers when selecting discrete time points for analysis.
To the best of the authors’ knowledge, this is the first study to include pelvic kinematics with bilateral compar ison during a SLD task in females. Bilateral pelvic imbal ances may be relevant to injury prevention as increased pelvic kinematics have been shown to result in amplified torque at the knee in the frontal plane during a SLD jump.35 Only three of the participants (Figure 8) displayed mean pelvic drop angles below 0° (neutral). However, these find ings may be more indicative of the SLD methods than the ability of the participants to stabilize their pelvis in the frontal plane. For example, each of the participants landed with a negative pelvic drop (i.e., their hip on their landing limb was lower). This is likely due to asking them to step off the box with the same limb that they landed on. If the participants had landed in a more neutral position, greater pelvic drop angles may have been observed. Nonetheless, all but one of the participants (8) demonstrated a bilateral
difference. Interestingly, six of the participants (1, 2, 3, 5, 7, 9) who landed in a more neutral pelvic position (closer to 0°) had increased knee abduction angles on the same limb (Figure 7, 8). This suggests that pelvic and knee kinematics may be linked during a SLD task. However, a causative rela tionship cannot be established with the current evidence.
When examining anterior pelvic tilt, most of the partic ipants (3-9) demonstrated a significant bilateral difference. Although the purpose of the current study was not to de scribe the ideal anterior pelvic tilt during the movement task, it may be that not all participants with bilateral differ ences possess inadequate pelvic control. For instance, par ticipants 7, 8, and 9 either maintained a relatively neutral pelvis, or decreased the amount of pelvic tilt throughout the motion (Figure 5). In contrast, participants 1 and 2 did not present with bilateral differences but increased their degree of anterior pelvic tilt from initial contact to the end of the movement.
Although the results of this single subject analysis in dicated that each of the participants had kinematic imbal ances during the SLD task, it is still unclear whether these asymmetries were suggestive of poor movement patterns (on one or both limbs) that may facilitate an increased risk of injury It may be that the observed bilateral differ ences were simply a result of performance variability be tween the two limbs. In short, performance variability is a natural biologic phenomenon that adapts for desired out comes based on force distribution mechanisms, develop ment or skill level, and environmental factors.23 Inter-indi
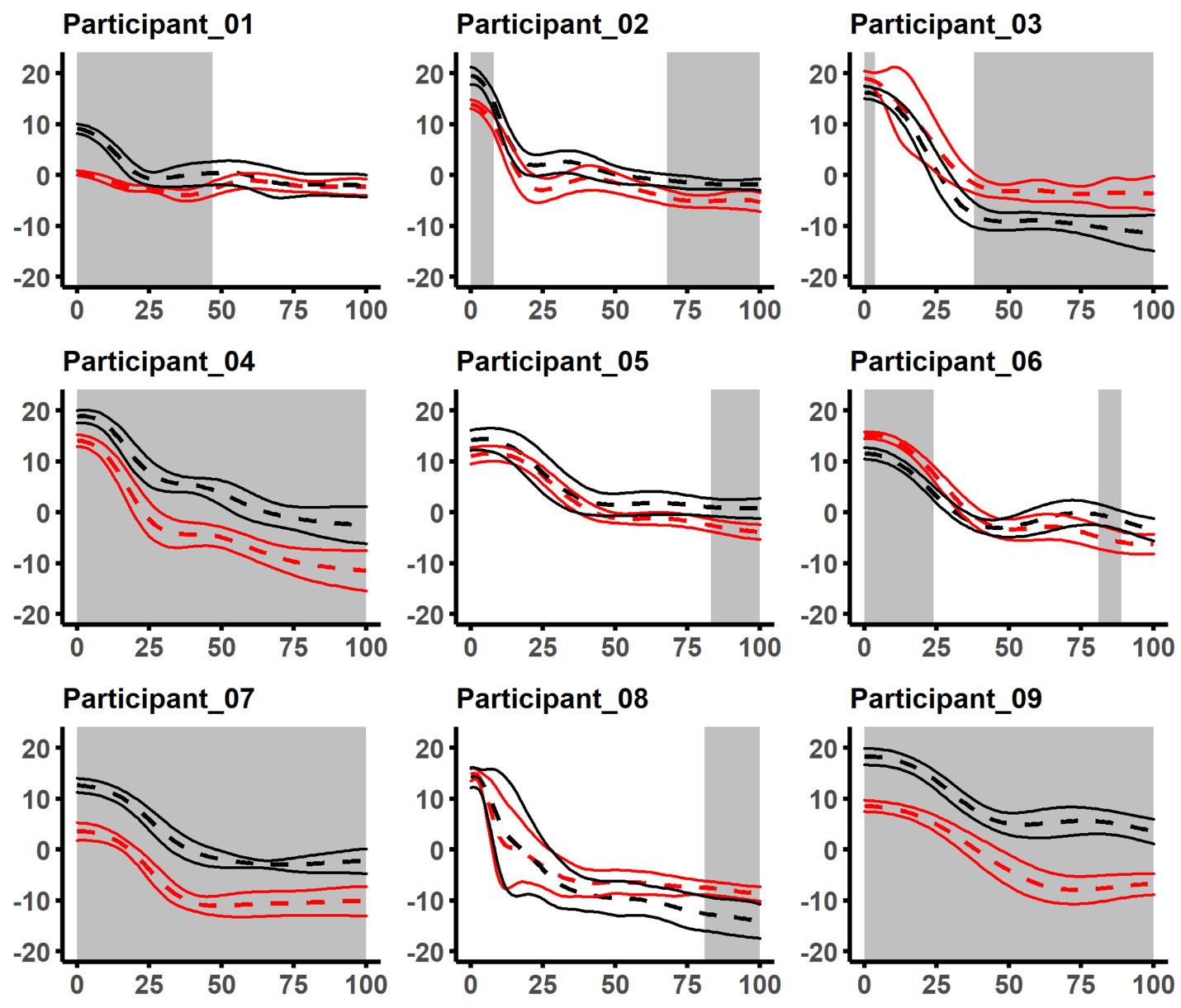 Figure 6. Hip frontal plane kinematics for each participant from initial contact to the minimum height of the center of mass.
Positive values indicate hip adduction. Mean values are represented by dashed lines with the solid lines indicating standard deviations. The right limb is shown as black, and the left shown as red. Shaded areas represent significant differences as determined from the statistical parametric mapping.
Figure 6. Hip frontal plane kinematics for each participant from initial contact to the minimum height of the center of mass.
Positive values indicate hip adduction. Mean values are represented by dashed lines with the solid lines indicating standard deviations. The right limb is shown as black, and the left shown as red. Shaded areas represent significant differences as determined from the statistical parametric mapping.
vidual variability has been shown to occur in professional athletes during basketball shooting and elite javelin throw ers,30 as well as in recreational athletes while running and performing a SLD 23,30 The participants’ bilateral kinematic differences in the current study may have been compensa tions that occurred due to muscular strength imbalances, prior training, or possibly structural/anatomical asymme tries. Thus, the observed imbalances may have been nec essary to complete the task. Further research is needed to examine the circumstances in which movement compensa tions and bilateral differences are beneficial or detrimental.
This study has several limitations. First, the current study only collected data on a small sample of physically active female participants. Group findings may have been apparent if participants had more homogeneous training backgrounds. A larger sample size may also have provided a greater probability of observing differences at the group level. Second, participants were only stratified based on their right or left limb. Future research might examine the potential for task specific methods to dichotomize limbs. For example, participants may self-identify their preferred landing limb. Lastly, due to the method participants dropped off the box (i.e., stepping), there may have been differences in the distance they fell onto the force plate, ei ther between legs, or participants.
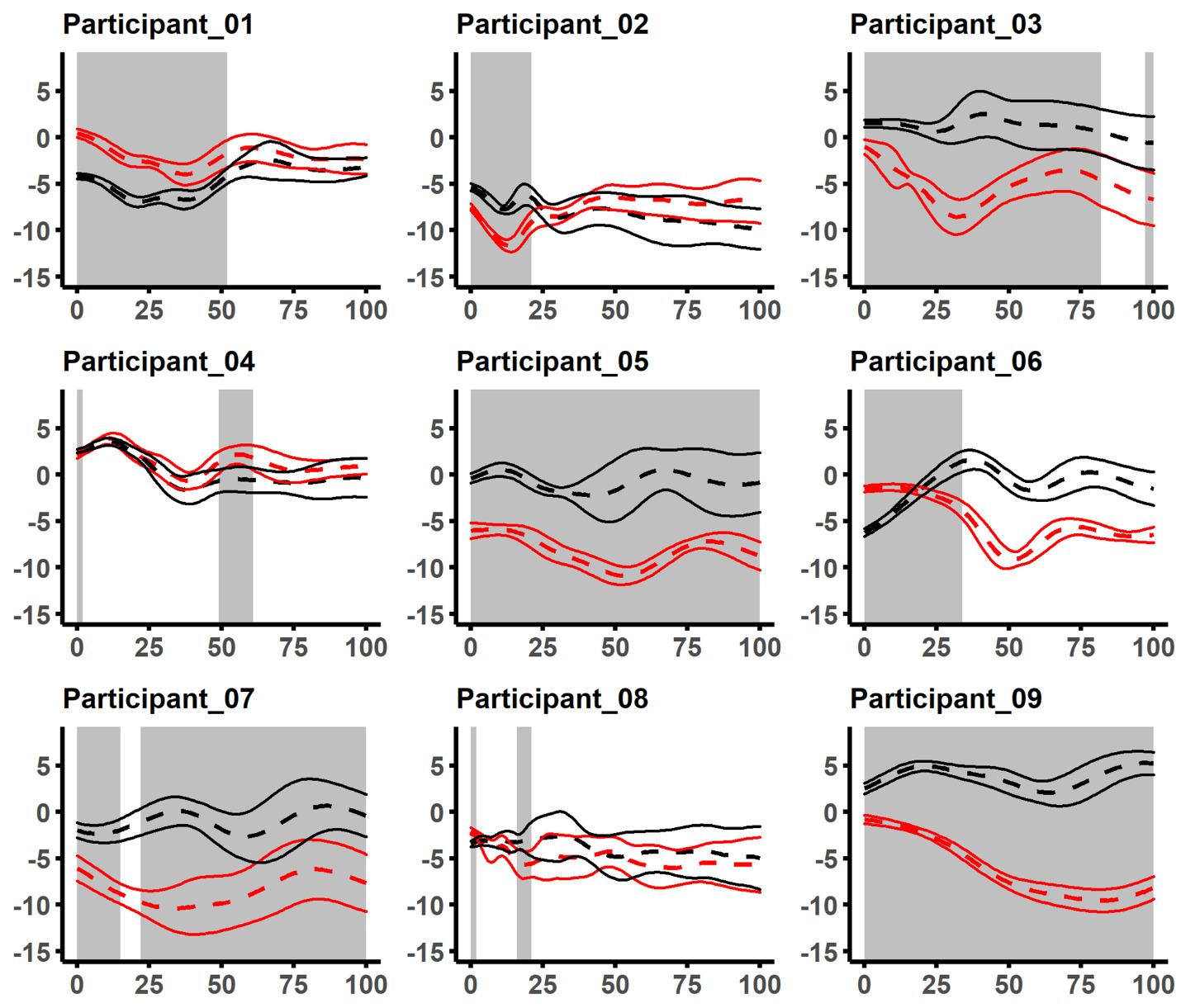
At the single subject analysis level, participants were asym metrical regarding their kinematic time-series. However, these differences were not observed in any of the wave forms for the group analysis. The authors recommend that until an accepted method for dichotomizing right and left limbs for bilateral comparisons is accepted, single subject design should be included with any group analysis where bilateral differences are examined.
This study was approved by the University of Idaho Institu tional Review Board, irb@uidaho.edu
The authors did not have any financial or personal rela tionships with people or organizations that may have inap propriately influenced or biased their work.
Submitted: May 11, 2022 CST, Accepted: September 12, 2022 CST
Figure 7. Knee frontal plane kinematics for each participant from initial contact to the minimum height of the center of mass. Positive values indicate knee abduction. Mean values are represented by dashed lines with the solid lines indicating standard deviations. The right limb is shown as black, and the left shown as red. Shaded areas represent significant differences as determined from the statistical parametric mapping.Figure 8. Pelvic frontal plane kinematics for each participant from initial contact to the minimum height of the center of mass.
Positive values indicate pelvic drop. Mean values are represented by dashed lines with the solid lines indicating standard deviations. The right limb is shown as black, and the left shown as red. Shaded areas represent significant differences as determined from the statistical parametric mapping.
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
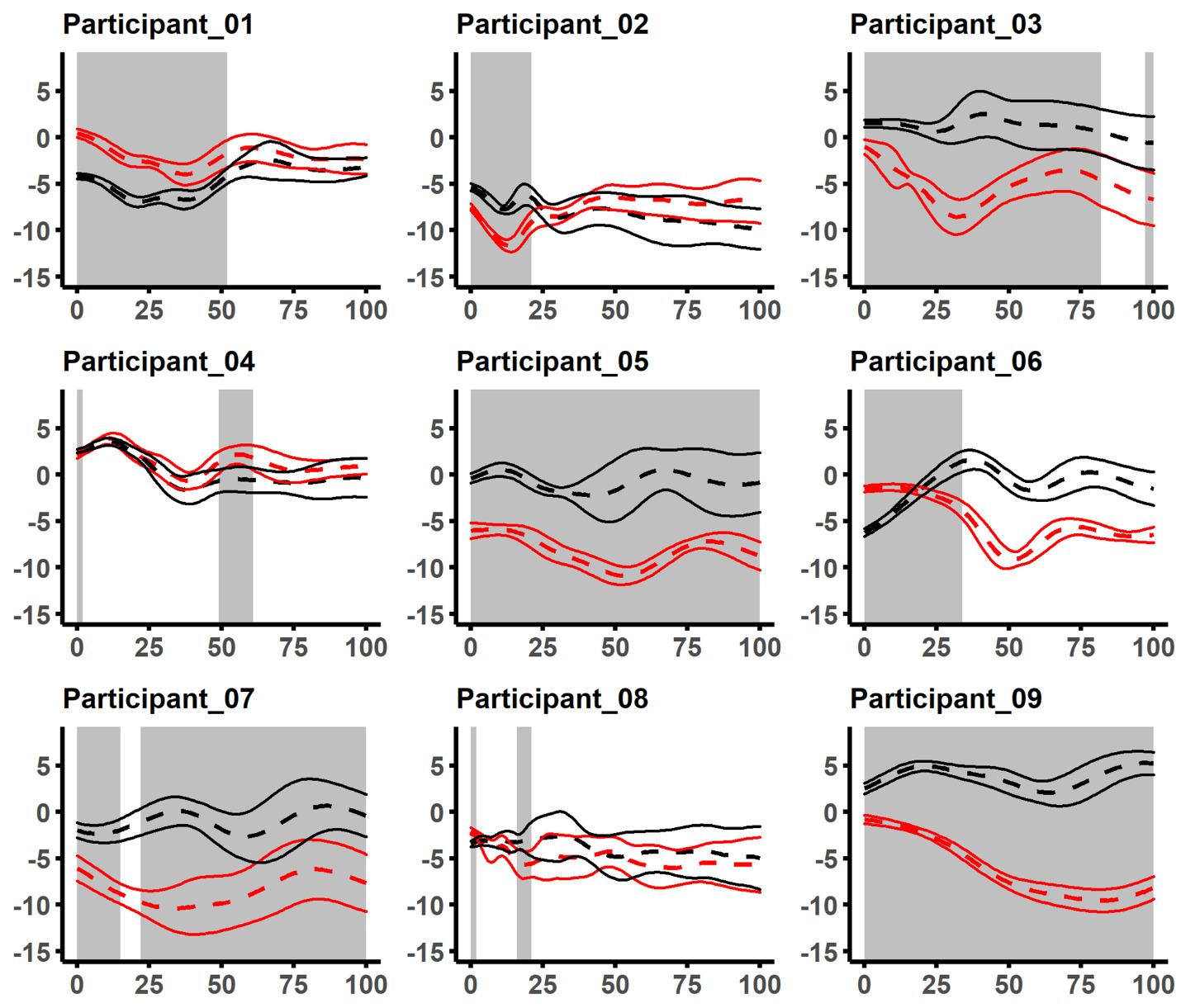
1. Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: A prospective biomechanical-epidemiologic study Am J Sports Med 2007;35(7):1123-1130. doi:10.1177/036354650730158
5
2. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes A prospective study Am J Sports Med 2005;33(4):492-501. doi:10.1177/036354 6504269591
3. Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34(2):86-92.
4. Ruedl G, Webhofer M, Helle K, et al. Leg dominance is a risk factor for noncontact anterior cruciate ligament injuries in female recreational skiers. Am J Sports Med 2012;40(6):1269-1273. doi:1 0.1177/0363546512439027
5. Brophy R, Silvers HJ, Gonzales T, Mandelbaum BR. Gender influences: the role of leg dominance in ACL injury among soccer players. Br J Sports Med 2010;44(10):694-697. doi:10.1136/bjsm.2008.051243
6. Greska EK, Cortes N, Ringleb SI, Onate JA, Van Lunen BL. Biomechanical differences related to leg dominance were not found during a cutting task. Scand J Med Sci Sports. 2016;27(11):1328-1336. doi:1 0.1111/sms.12776
7 Kiapour AM, Demetropoulos CK, Kiapour A, et al. Strain response of the anterior cruciate ligament to uniplanar and multiplanar loads during simulated landings. Am J Sports Med. 2016;44(8):2087-2096. do i:10.1177/0363546516640499
8. Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38(11):2218-2225. doi:10.1177/036354651 0373570
9. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study Am J Sports Med. 2005;33(4):492-501. doi:10.1177/03 63546504269591
10. Boden BP, Sheehan FT, Torg JS, Hewett TE. Noncontact ACL injuries: mechanisms and risk factors. J Am Acad Orthop Surg. 2010;18(9):520-527. doi:10.543 5/00124635-201009000-00003
11. Utturkar GM, Irribarra LA, Taylor KA, et al. The effects of a valgus collapse knee position on in vivo ACL elongation. Ann Biomed Eng 2013;41(1):123-130. doi:10.1007/s10439-012-0629-x
12. Englander ZA, Baldwin EL III, Smith WAR, Garrett WE, Spritzer CE, DeFrate LE. In vivo anterior cruciate ligament deformation during a single-legged jump measured by magnetic resonance imaging and highspeed biplanar radiography Am J Sports Med 2019;47(13):3166-3172. doi:10.1177/03635465198760 74
13. Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35(10):1745-1750. doi:10.1249/01.mss.0000089 346.85744.d9
14. Pappas E, Carpes FP. Lower extremity kinematic asymmetry in male and female athletes performing jump-landing tasks. J Sci Med Sport 2012;15(1):87-92. doi:10.1016/j.jsams.2011.07.008
15. Wang J, Fu W. Asymmetry between the dominant and non-dominant legs in the lower limb biomechanics during single-leg landings in females. Adv Mech Eng. 2019;11(5):1-8. doi:10.1177/16878140 19849794
16. Mokhtarzadeh H, Ewing K, Janssen I, Yeow CH, Brown N, Lee PVS. The effect of leg dominance and landing height on ACL loading among female athletes. J Biomech. 2017;60:181-187. doi:10.1016/j.jb iomech.2017.06.033
17 van der Harst JJ, Gokeler A, Hof AL. Leg kinematics and kinetics in landing from a single-leg hop for distance. A comparison between dominant and non-dominant leg. J Clin Biomech 2007;22(6):674-680. doi:10.1016/j.clinbiomech.2007.0 2.007
18. Whyte EF, Richter C, O’Connor S, Moran KA. Investigation of the effects of high-intensity, intermittent exercise and unanticipation on trunk and lower limb biomechanics during a side-cutting maneuver using statistical parametric mapping. J Strength Cond Res. 2018;32(6):1583-1593. doi:10.151 9/jsc.0000000000002567
19. Sugiyama T, Kameda M, Kageyama M, Kiba K, Kanehisa H. Asymmetry between the dominant and non-dominant legs in the kinematics of the lower extremities during a running single leg jump in collegiate basketball players. J Sport Sci Med 2014;13:951-957
20. Brown TN, Palmieri-Smith RM, Mclean SG. Sex and limb differences in hip and knee kinematics and kinetics during anticipated and unanticipated jump landings: implications for anterior cruciate ligament injury Br J Sport Med 2009;43(13):1049-1056. doi:1 0.1136/bjsm.2008.055954
21. Wang J, Fu W Asymmetry between the dominant and non-dominant legs in the lower limb biomechanics during single-leg landings in females. Adv Mech Engin. 2019;11(5):168781401984979. doi:1 0.1177/1687814019849794
22. Mcgrath TM, Waddington G, Scarvell JM, et al. The effect of limb dominance on lower limb functional performance a systematic review. J Sport Sci 2015;34(4):289-302. doi:10.1080/02640414.201 5.1050601
23. Schot PK, Bates BT, Dufek JS. Bilateral performance symmetry during drop landing: a kinetic analysis. Med Sci Sport Exerc 1994;26(9):1153-1159. d oi:10.1249/00005768-199409000-00013
24. Richter C, O’Connor NE, Marshall B, Moran K. Comparison of discrete-point vs. dimensionality reduction techniques for describing performancerelated aspects of maximal vertical jumping. J Biomech 2014;47(12):3012-3017 doi:10.1016/j.jbiom ech.2014.07.001
25. Pataky TC. Generalized n-dimensional biomechanical field analysis using statistical parametric mapping. J Biomech. 2010;43(10):1976-1982. doi:10.1016/j.jbiomech.201 0.03.008
26. Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am J Sports Med 2015;43(11):2727-2737 doi:10.1177/0363 546515602016
27 Pataky TC. One-dimensional statistical parametric mapping in Python. Comput Methods Biomech Biomed Engin. 2012;15(3):295-301. doi:10.10 80/10255842.2010.527837
28. Pataky TC. rft1d: Smooth one-dimensional random field upcrossing probabilities in python. J Stat Soft 2016;71(7). doi:10.18637/jss.v071.i07
29. Scholes CJ, Mcdonald MD, Parker AW Singlesubject analysis reveals variation in knee mechanics during step landing. J Biomech 2012;45(12):2074-2078. doi:10.1016/j.jbiomech.201 2.05.046
30. Bartlett R, Wheat J, Robins M. Is movement variability important for sports biomechanists? Sport Biomech. 2007;6(2):224-243. doi:10.1080/1476314070 1322994
31. Õunpuu S, Winter DA. Bilateral electromyographical analysis of the lower limbs during walking in normal adults. Electro Clin Neurophysiol 1989;72(5):429-438. doi:10.1016/001 3-4694(89)90048-5
32. Kiapour AM, Quatman CE, Goel VK, Wordeman SC, Hewett TE, Demetropoulos CK. Timing sequence of multi-planar knee kinematics revealed by physiologic cadaveric simulation of landing: Implications for ACL injury mechanism. Clin Biomech 2014;29(1):75-82. doi:10.1016/j.clinbiomech.2013.1 0.017
33. Kiapour AM, Demetropoulos CK, Kiapour A, et al. Response of the anterior cruciate ligament to uniplanar and multiplanar loads during simulated landings: implications for injury mechanism. Am J Sports Med. 2016;44(8):2087-2096. doi:10.1177/03635 46516640499
34. Kiapour AM, Quatman CE, Goel VK, Wordeman SC, Hewett TE, Demetropoulos CK. Timing sequence of multi-planar knee kinematics revealed by physiologic cadaveric simulation of landing: Implications for ACL injury mechanism. J Clin Biomech 2014;29(1):75-82. doi:10.1016/j.clinbiomec h.2013.10.017
35. Chijimatsu M, Ishida T, Yamanaka M, et al. Landing instructions focused on pelvic and trunk lateral tilt decrease the knee abduction moment during a single-leg drop vertical jump. Phys Ther Sport 2020;46:226-233. doi:10.1016/j.ptsp.2020.09.0 10
Benoit-Piau J, Morin M, Guptill C, Fortin S, Gaudreault N. Movement Competency Screen: Rethinking the Rating. IJSPT. Published online December 1, 2022:1282-1289.
Justine Benoit-Piau 1 , Mélanie Morin 1 , Christine Guptill 2 , Sylvie Fortin 3 , Nathaly Gaudreault 1 a
1 Faculté de médecine et des sciences de la santé, Université de Sherbrooke, 2 School of Rehabilitation Sciences, University of Ottawa, 3 Danse, Université du Québec à Montréal
Keywords: movement competency, dance, athlete, pre-season screening, musculoskeletal disorder https://doi.org/10.26603/001c.55531
Dancers are at high risk of musculoskeletal disorders. There has been a growing interest in the last few years in pre-season screening using tools to evaluate movement competency, among which is the Movement Competency Screen (MCS). It is currently scored using a categorical 3-level rating system, but this method does not seem to take into account the load level of movements. A 5-level scoring system could potentially alleviate this problem.
For each scoring system, to investigate (1) the internal consistency, and (2) the association with transversus abdominis activation (TrA), hip muscle strength and with Functional Movement screen (FMSTM) total score.
Secondary analyses of a prospective cohort study
One hundred and eighteen professional and preprofessional dancers evolving in ballet or contemporary dance were recruited. The MCS was performed and was scored according to the 3- and 5-level scoring systems. The key variables for movement competency that were considered for convergent validity were the activation ratio of the TrA evaluated with ultrasound imaging and hip strength assessed with a handheld dynamometer. Movement competency was also measured with the FMSTM
Internal consistency was higher for the 5-level scoring of the MCS items ( =0.548) compared to the 3-level scoring system ( =0.494). Multiple linear regressions showed that TrA activation, hip adductor strength, and FMSTM could significantly explain 24.0% of the variance for the 5-level scoring system of the MCS whereas hip internal rotator strength and FMSTM could explain only 16.4% of the variance for the 3-level scoring system.

The 5-level scoring system showed better metrologic properties in terms of internal consistency and concurrent validity and therefore, should be preferred over the 3-level scoring system in future research.
Corresponding author:
Nathaly Gaudreault, PT, Ph.D
Faculty of Health Medicine and Science
Université de Sherbrooke 3001 12e avenue N Sherbrooke QC Canada J1H5N4
Tel : 819-821-8000 P.15216
Nathaly.gaudreault@usherbrooke.ca
Musculoskeletal injuries among dancers represent a major concern.1–4 In addition to being associated with serious physical and psychological disabilities in athletes, injuries can represent an extensive financial burden on health care systems.5 In order to better understand the underlying pathokinesiology of non-traumatic injuries among dancers, researchers have focused on specific, segmental impair ments identified as potential risk factors in other athlete populations.6–9 These risk factors include lower or delayed activation of the transversus abdominis muscle (TrA),6–8 as well as reduced hip and knee muscle strength.9 However, with prevention of injuries in mind, there has been a con tinued interest in the evaluation of movement competency in recent years, as opposed to specific segmental impair ments assessments.10 This shift in approach has given rise to the development of movement competency screening tools.11–14 Movement competency can be defined as the ability to achieve fundamental movements without any functional deficits.15 Strength and motor control are key to preventing faulty movement patterns. For instance, the ac tivation of the TrA and having stronger lower limb muscles have been linked to movement competency 16 The evalu ation of movement competency using screening tools has enabled the identification of athletes and workers at risk of injuries.17,18
Among the multiple movement competency screening tools that have been developed, the Functional Movement Screen (FMSTM) and the Movement Competency Screen (MCS) have been investigated.16–21 The MCS was devel oped and validated for athletes and dancers.16,17,21 It has the interesting characteristic of evaluating different load levels during the performance of movements used in re habilitation and training programs. Out of 11 movement competency assessment tools reported in the literature, the MCS was identified among the most promising to assess performance capabilities in terms of applicability and the rigor with which it was developed.22 In the original version of the MCS, Kritz described load grades as being scored us ing a 5-level scoring system : (1) assisted loading, (2) body weight loading, (3) external loading, (4) eccentric loading, and (5) plyometric loading.21 According to the currently ac cepted method for scoring the MCS, those five levels are re grouped into three levels as follows : (1) assisted and body weight loading, (2) external and eccentric loading, and (3) plyometric loading.21
The 3-level scoring system thus collapses the five levels into three levels. For example, a movement performed with certain compensations could be rated as a 3 or a 4 on the 5-level system, while on the 3-level scoring system it would be rated as a 2. This appears to be less than optimal since the merging of load levels results in a loss of detailed in formation. The 5-level scoring system would allow greater precision and, as a result, would more accurately character ize movement competency The strength of the MCS com
pared to other movement competency screening tools is the use of load levels. It should therefore be accounted for in detail in the scoring method.
The aim of this technical note was to investigate, in a sample of dancers, and for each MCS scoring system (1) the internal consistency between items and (2) their asso ciation with TrA activation, hip strength, and FMSTM to tal score. It was hypothesized that the 5-level scoring sys tem would show better psychometric properties in terms of internal consistency and concurrent validity as assessed by association with key components of movement competency and another validated movement competency tool.
Data for this study were gathered at one time point prior to the beginning of the 2018-2019 and 2019-2020 dance sea son and were derived from a prospective cohort study in volving 118 dancers, varying in dance style (ballet and con temporary) and status (professional and pre-professional). Dancers were recruited following a presentation of the re search project in multiple dance schools and companies. This study was approved by the institutional review board and each participant gave written informed consent. Par ticipants had to be at least 16 years old and had to dance professionally or pre-professionally for at least 10 hours per week. They were excluded if they were pregnant because of the impact on the lumbopelvic muscles, or if they had a musculoskeletal disorder that restricted dancing at the time of the evaluation. Participants underwent an assessment conducted by an experienced physiotherapist who has been a dancer for 17 years, a dance educator for eight years and who treats dancers in her regular practice. The assessment included the evaluation of TrA activation, hip strength, and movement competency The evaluation was done on-site in dance schools or companies, either in a dance studio or in a physiotherapist’s office if one was available.
The preferential activation ratio of the TrA was evaluated using ultrasound imaging (GE LOGIQ E, GE Healthcare, Milwaukee, Wisconsin, 13 MHz linear probe in B-mode) in a standardized position.23–25 Dancers were in a supine po sition with both knees at a 90° flexion. The probe was po sitioned between the axillary and mamillary lines, at middistance between the iliac crest and 12th rib in a transverse plane. The preferential activation ratio is calculated to take into account the activation of the internal and external obliques. This method thus considers the possible compen sations of these muscles. Both sides were assessed three times and a mean value was obtained.
The strength of the hip flexors, extensors, abductors, ad ductors, and external and internal rotators were measured in a standardized position using a handheld dynamometer secured with straps.26 The exact positions used are de scribed in a previous study 16 Both sides were assessed three times with a 30 second break in between each mea surement. A mean value was obtained and used for analy sis.
Movement competency was screened using two distinct instruments, the FMSTM and the MCS.17–21 The MCS is composed of five tasks designed to assess global movement competency: (1) squat, (2) lunge and twist, (3) bend and pull, (4) push-up and (5) single-leg squat. The lunge and twist, and the bend and pull are subdivided into the indi vidual components of each movement. Therefore, there are seven items to be evaluated. Each item has a set of pos sible primary and secondary compensations. The scoring is completed by evaluating the number of compensations observed. More frequent compensations result in a lower score. Additionally, primary compensations are more detri mental to the score than secondary compensations. The tasks of the MCS can be completed with multiple load lev els, according to the evaluator’s judgement. The movement can be completed slowly, rapidly, or using plyometrics. As per the accepted scoring system, the 3-level score is attrib uted only according to the compensations observed, with no discrimination between assisted and bodyweight load ing or external and eccentric loading. The MCS was scored using both the 5-level scoring system that uses separate load levels (assisted, bodyweight, external, eccentric, and plyometric) and the 3-level scoring system in which they are grouped as described above. The FMSTM does not in clude different load levels. Each movement is done at a slow pace. Figure 1 shows a comparison between the movements from the MCS and the FMSTM
Statistical analyses were conducted in SPSS 28.0. Cron bach’s alpha was first calculated for items scored with the 5-level system and then, for items scored with the 3-level system, to assess internal consistency. To identify the scor ing system that best suited the variables, simple linear re gressions were first used for the 5-level and then for the 3-level scoring system. FMS scores, TrA activation, and hip strength were used as independent variables. Each inde pendent variable’s association with movement competency was examined, as well as the proportion of variance for the total MCS score that they each explained. A multiple re gression model was built which included the variables sig nificantly associated with the MCS score for each scoring system. Therefore, a different model was built for the 5-level and 3-level systems since the results from the sim ple regression analyses identified different variables as be ing associated with the dependent variables. Since dance hours could be a potential confounder in the analyses, each linear regression was controlled for this variable. The level of significance for all statistical analyses was set at p≤0.05. Statistical assumptions were met for each linear regression completed.
The sample was composed of 118 preprofessional and pro fessional dancers. Table 1 presents demographic informa tion. No adverse events occurred during the evaluations. Table 2 presents the results of separate linear regres sions between each independent variable and the MCS total score, where each item was scored using either the 5-level system or the 3-level system.
The internal consistency assessed with Cronbach’s alpha for the seven items of the MCS scored with the 5-level system was 0.548. It was found using simple linear re gressions that TrA activation, hip extensor, abductor, ad ductor, and external rotator strength, as well as FMSTM to tal score (β=0.455, p<0.001) were statistically significantly associated with the MCS total score as measured by the 5-level scoring system. Given multicollinearity between hip strength variables in the multiple linear regression model, only hip adductor strength was introduced in the model. This variable was chosen since it was the most significantly and strongly associated with the MCS total score. As seen in Table 3, the multivariate model accounted for 24% of the variance for the MCS scored on the 5-level system (F=13.324, p<0.001).
3-LEVEL SCORING SYSTEM AS THE DEPENDENT VARIABLE
Regarding the internal consistency, Cronbach’s alpha for the seven items of the 3-level scoring system was 0.494. Simple linear regression analyses revealed significant asso ciations with hip internal rotator strength and FMSTM to tal score (β=0.250, p=0.006) with the MCS total scored on a 3-level system. Results showed that the multiple linear re gression model built accounted for 13.3% of the variance for the MCS on a 3-level scoring system (F=9.959, p<0.001).
The purpose of this study was to examine the internal con sistency for the items scored with each system and to ex plore if the association of TrA activation, hip muscle strength, and FMS score was higher with the 5-level scoring system, as opposed to the 3-level scoring system.
Although both point systems did not have a Cronbach’s alpha that exceeded the generally accepted value of 0.7 as acceptable internal consistency,27 the 5-level system showed a moderate internal consistency (≥0.5) and the 3-level scoring system showed a poor internal consistency (<0.5).28 This supports the hypothesis that the 5-level scor ing system would show higher internal consistency than the 3-level scoring system.
Findings from a previous study on the correlations be tween the MCS total score (3-level scoring) and TrA acti vation, hip strength, and FMS showed significant associa
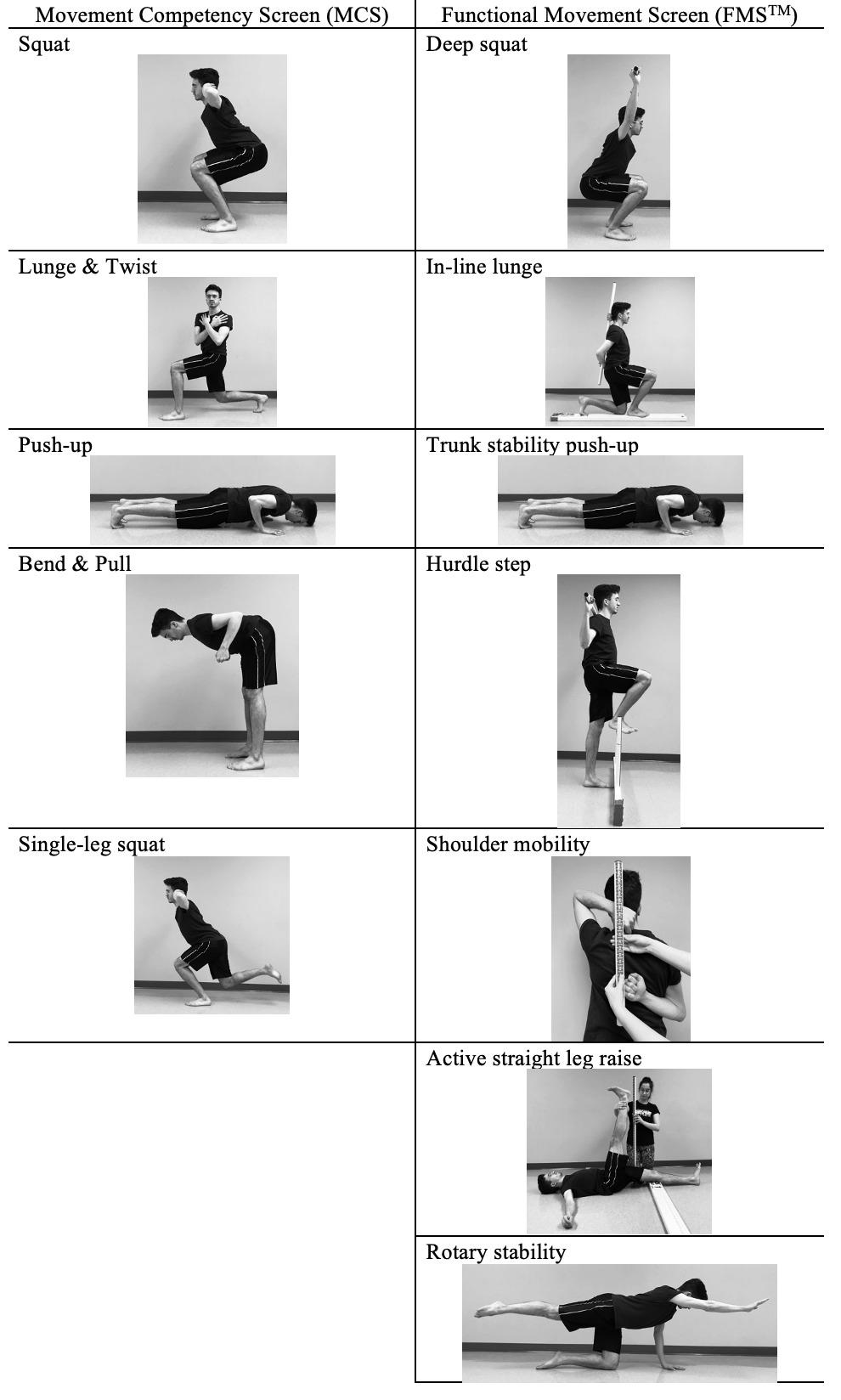
N(%) or Mean ± SD
Sample 118 (100)
Age (years) 21.6 ± 5.2
Gender (female / male / nonbinary) 92 (78) / 24 (20) / 2 (2)
Style (contemporary / ballet) 66 (57) / 49 (43) Status (preprofessional / professional) 91 (78) / 25 (22)
MCS total score /5 as dependent variable
Independent variables
Adjusted R2 Standardized β 95% C.I. p
TrA activation Dominant side 0.033 0.203 [0.281, 4.800] 0.028
Hip flexor strength Non dominant side 0.024 0.180 [-0.001, 0.168] 0.052
Hip extensor strength Non dominant side 0.081 0.301 [0.029, 0.136] 0.003
Hip abductor strength Non dominant side 0.075 0.288 [0.035, 0.146] 0.002
Hip adductor strength Non dominant side 0.084 0.303 [0.039, 0.145] 0.001
Hip external rotator strength Non dominant side 0.038 0.215 [0.022, 0.250] 0.019
Hip internal rotator strength Non dominant side -0.009 0.010 [-0.083, 0.093] 0.913
FMSTM total score 0.200 0.455 [0.758, 1.610] <0.001
MCS total score /3 as dependent variable
Independent variables
Adjusted R2 Standardized β 95% C.I. p
TrA activation Dominant side 0.005 0.116 [-0.433, 1.936] 0.211
Hip flexor strength Non dominant side -0.005 0.063 [-0.029, 0.059] 0.498
Hip extensor strength Non dominant side -0.001 0.098 [-0.015, 0.42] 0.342
Hip abductor strength Non dominant side -0.005 0.063 [-0.020, 0.040] 0.499
Hip adductor strength Non dominant side -0.008 0.031 [-0.024, 0.034] 0.738
Hip external rotator strength Non dominant side 0.001 -0.098 [-0.092, 0.028] 0.293
Hip internal rotator strength Non dominant side 0.037 -0.214 [-0.097, -0.008] 0.020
FMSTM total score 0.054 0.250 [0.096, 0.575] 0.006
tions.16 However, linear regressions for the 3-level scoring system in the current study did not reveal significant asso ciation with TrA activation or hip strength, with the excep tion of internal rotators.16 In the present study, the model with the 3-level system as the dependent variable explained only 13.3% of the variance. In a previous model using the 3-level system, similar independent variables could explain only 10.8% of the variance.16 In the current study, it was found that 24% of the variance for the total MCS score using
the 5-level system could be explained by the independent variables selected. These results are of particular interest because they show that the variance of the 5-level scoring system is explained in a greater proportion by components that have been identified as key to movement competency This supports the assumption that the 5-level scoring sys tem shows higher concurrent validity
This study is not the first to reconsider the MCS scoring. Instead of using the common 3-level scoring for only the
MCS : Movement Competency Screen; FMSTM : Functional Movement Screen; TrA : transversus abdominisMCS total score /5 as dependent variable
Independent variables
TrA activation
Dominant side
Adjusted R2 Standardized β 95% C.I. p
0.115 [-0.595, 3.482] 0.163
Hip adductor strength Non dominant side 0.195 [0.009, 0.109] 0.021
0.240
FMSTM total score 0.389 [0.582, 1.446] <0.001
MCS total score /3 as dependent variable
Independent variables
Adjusted R2 Standardized β 95% C.I. p
Hip internal rotator strength Non dominant side 0.133 -0.303 [-0.118, -0.031] <0.001
FMSTM total score 0.332 [0.208, 0.684] <0.001
weaker side, Lee et al. used the 3-level scoring system for both sides and added up the points, giving a 6-level score for each task.17 The reasoning behind this choice is unfor tunately not explained in the article. Considering both sides when evaluating each MCS item could lead to a higher score and to an overestimation of the athlete’s physical abilities when one side scores higher than the other. This method using the 3-level scoring system still presents the problem of grouping the five initial load levels. Results from the cur rent study support the use of a 5-level scoring system to ob tain more precise measurement of movement competency Taking both sides into account when evaluating athletes could be considered; but to group this information in a to tal score could also mean overestimation of the athlete’s movement competency Future research should consider the benefits and risks associated with an inflated movement competency score when considering both sides.
The main limitation of this study is the inclusion of dancers practicing various types of dance. Indeed, the in clusion of ballet and contemporary, as well as preprofes sional and professional dancers could lead to increased het erogeneity in the dancers’ characteristics that are inherent to dance style and/or level of experience. The sample size could not allow analysis of these subgroups. However, this heterogeneity increased external validity.
The items scored with the 5-level system showed higher in ternal consistency of the test scores than with the 3-level system. Simple and multiple linear regressions used in the present technical note indicate that a 5-level system is more representative of the essential components of move ment competency than the commonly used 3-level system because of its higher and more significant association with TrA activation, hip strength, and FMSTM score. For these reasons, health professionals and researchers should con sider using the 5-level scoring system of the MCS in future clinical settings and research.
The authors report no conflicts of interest.
This study was funded by a partnership between the Insti tut de recherche Robert-Sauvé en santé et sécurité du tra vail (IRSST) and REPAR (03SNT007).
Submitted: June 23, 2022 CST, Accepted: September 12, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
MCS: Movement Competency Screen; TrA : transversus abdominis; FMSTM : Functional Movement Screen.1. Caine D, Bergeron G, Goodwin BJ, et al. A survey of injuries affecting pre-professional ballet dancers. J Dance Med Sci. 2016;20(3):115-126. doi:10.12678/108 9-313x.20.3.115
2. Ekegren CL, Quested R, Brodrick A. Injuries in preprofessional ballet dancers: Incidence, characteristics and consequences. J Sci Med Sport 2014;17(3):271-275. doi:10.1016/j.jsams.2013.07.013
3. Yau RK, Golightly YM, Richardson DB, Runfola CD, Waller AE, Marshall SW Potential predictors of injury among pre-professional ballet and contemporary dancers. J Dance Med Sci. 2017;21(2):53-63. doi:10.12 678/1089-313x.21.2.53
4. Mainwaring LM, Finney C. Psychological risk factors and outcomes of dance injury: a systematic review J Dance Med Sci 2017;21(3):87-96. doi:10.126 78/1089-313x.21.3.87
5. Lehr ME, Plisky PJ, Butler RJ, Fink ML, Kiesel KB, Underwood FB. Field-expedient screening and injury risk algorithm categories as predictors of noncontact lower extremity injury. Scand J Med Sci Sports. 2013;23(4):e225-e232. doi:10.1111/sms.12062
6. Roussel NA, Nijs J, Mottram S, Van Moorsel A, Truijen S, Stassijns G. Altered lumbopelvic movement control but not generalized joint hypermobility is associated with increased injury in dancers. A prospective study. Man Ther. 2009;14(6):630-635. do i:10.1016/j.math.2008.12.004
7 Roussel N, De Kooning M, Schutt A, et al. Motor control and low back pain in dancers. Int J Sports Med. 2013;34(2):138-143.
8. Gildea JE, Hides JA, Hodges PW Morphology of the abdominal muscles in ballet dancers with and without low back pain: a magnetic resonance imaging study J Sci Med Sport 2014;17(5):452-456. doi:10.101 6/j.jsams.2013.09.002
9. Moita JP, Nunes A, Esteves J, Oliveira R, Xarez L. The relationship between muscular strength and dance injuries: a systematic review Med Probl Perform Art. 2017;32(1):40-50. doi:10.21091/mppa.20 17.1002
10. Cook G, Burton L, Hoogenboom B. Preparticipation screening: the use of fundamental movements as an assessment of function part 1. N Am J Sports Phys Ther 2006;1(2):62-72.
11. Culhane PeM. Proposed model to assess an athlete’s physical competency and capacity J Aust Strength Cond. 2019;27(7):38-61.
12. Zoellner A, Whatman C, Read P, Sheerin K. The association between sport specialisation and movement competency in youth: a systematic review. Int J Sports Sci Coach 2021;16(4):1045-1059. doi:10.1 177/1747954121998456
13. Kibler WB, Chandler TJ, Uhl T, Maddux RE. A musculoskeletal approach to the preparticipation physical examination. Preventing injury and improving performance. Am J Sports Med. 1989;17(4):525-531. doi:10.1177/03635465890170041 3
14. Conley KM, Bolin DJ, Carek PJ, Konin JG, Neal TL, Violette D National athletic trainers’ association position statement: preparticipation physical examinations and disqualifying conditions. J Athl Train 2014;49(1):102-120. doi:10.4085/1062-6050-4 8.6.05
15. Myer GD, Kushner AM, Brent JL, et al. The back squat: A proposed assessment of functional deficits and technical factors that limit performance. Strength Cond J. 2014;36(6):4-27. doi:10.1519/ssc.00000000000 00103
16. Benoît-Piau J, Morin M, Fortin S, Guptill C, Gaudreault N. Does the Movement Competency Screen correlate with deep abdominals activation and hip strength for professional and pre-professional dancers? Int J Sports Phys Ther. 2021;16(1):31-40. do i:10.26603/001c.18792
17 Lee L, Reid D, Cadwell J, Palmer P Injury incidence, dance exposure and the use of the Movement Competency Screen (MCS) to identify variables associated with injury in full-time preprofessional dancers. Int J Sports Phys Ther. 2017;12(3):352-370.
18. Bonazza NA, Smuin D, Onks CA, Silvis ML, Dhawan A. Reliability, validity, and injury predictive value of the functional movement screen: a systematic review and meta-analysis. Am J Sports Med. 2017;45(3):725-732. doi:10.1177/036354651664 1937
19. Moran RW, Schneiders AG, Mason J, Sullivan SJ. Do Functional Movement Screen (FMS) composite scores predict subsequent injury? A systematic review with meta-analysis. Br J Sports Med 2017;51(23):1661-1669. doi:10.1136/bjsports-2016-0 96938
20. Bardenett SM, Micca JJ, DeNoyelles JT, Miller SD, Jenk DT, Brooks GS. Functional Movement Screen normative values and validity in high school athletes: can the FMSTM be used as a predictor of injury? Int J Sports Phys Ther 2015;10(3):303-308.
21. Kritz M. Development, Reliability and Effectiveness of the Movement Competency Screen (MCS) Doctorate Thesis. AUT University; 2012.
22. Bennett H, Davison K, Arnold J, Slattery F, Martin M, Norton K. Multicomponent musculoskeletal movement assessment tools: a systematic review and critical appraisal of their development and applicability to professional practice. J Strength Cond Res. 2017;31(10):2903-2919. doi:10.1519/jsc.0000000 000002058
23. Mangum LC, Sutherlin MA, Saliba SA, Hart JM. Reliability of ultrasound imaging measures of transverse abdominis and lumbar multifidus in various positions. PM&R 2016;8(4):340-347 doi:10.1 016/j.pmrj.2015.09.015
24. Hodges PW, Pengel LHM, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve 2003;27(6):682-692. doi:10.1002/mus.10375
25. Koppenhaver SL, Hebert JJ, Parent EC, Fritz JM. Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub-maximal contractions: a systematic review Aust J Physiother 2009;55(3):153-169. doi:1 0.1016/s0004-9514(09)70076-5
26. Krause DA, Neuger MD, Lambert KA, Johnson AE, DeVinny HA, Hollman JH. Effects of examiner strength on reliability of hip-strength testing using a handheld dynamometer. J Sport Rehab. 2014;23(1):56-64. doi:10.1123/jsr.2012-0070
27 Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53-55. doi:1 0.5116/ijme.4dfb.8dfd
28. Hinton PR, McMurray I, Brownlow C. SPSS Explained. 1st edition. Routledge; 2004.
Jacobson L, Vannatta CN, Schuman C, Kernozek TW. An Updated Model Does Not
Reveal Sex Differences in Patellofemoral Joint Stress during Running. IJSPT. Published online December 2, 2022:1290-1297.
1 Family Medicine, Gundersen Health System, 2 Department of Sports Physical Therapy, Gundersen Health System; La Crosse Institute for Movement Science, University of Wisconsin – La Crosse, 3 La Crosse Institute for Movement Science, University of Wisconsin – La Crosse; Department of Health Professions, University of Wisconsin - La Crosse
Keywords: knee, kinetics, patellofemoral pain, biomechanics
https://doi.org/10.26603/001c.39608
Structure-specific loading may have implications in understanding the mechanisms of running related injury As females demonstrate a prevalence of patellofemoral pain twice that of males, this may indicate differences in patellofemoral loads between males and females. Previous works investigating differences in patellofemoral joint stress have shown conflicting results, but the models employed have not used estimates of muscle forces or sex specific contact areas.
The aim of this study was to examine sex differences in patellofemoral joint stress using an updated model to include estimates of quadriceps muscle force and sex-specific patellofemoral contact area.
Forty-five healthy recreational runners ran at a controlled speed down a 20-meter runway. Kinetic and kinematic data were utilized to estimate muscle forces using static optimization. Quadriceps muscle force was utilized with sex-specific patellofemoral joint contact area in a two-dimensional patellofemoral joint model to estimate patellofemoral joint stress. Multivariate tests were utilized to detect sex differences in patellofemoral loading and hip and knee kinematics.
No differences were found between sexes in measures of patellofemoral loading or quadriceps force. Females displayed a reduced knee extension moment and greater hip adduction and internal rotation than males.

The inclusion of static optimization to estimate quadriceps muscle force and sex-specific contact area of the patellofemoral joint did not reveal sex differences in patellofemoral joint stress, but differences in non-sagittal plane hip motion were detected. Therefore, two-dimensional patellofemoral models may not fully characterize differences in patellofemoral joint stress between males and females. Three-dimensional
a
Corresponding author:
C. Nathan Vannatta, PT, DPT, SCS
Department of Sports Physical Therapy
Mail Stop: NC1-002 3111 Gundersen Drive Onalaska, WI 54650 Phone: 608.775.8986 Email: cnvannat@gundersenhealth.org
patellofemoral models may be necessary to determine if sex differences in patellofemoral joint stress exist.
Level of Evidence 3b
Structure-specific loading has become of interest, espe cially pertaining to overuse running injuries.1,2 This premise seeks to understand how elements of running bio mechanics, such as different kinematic and kinetic features of running, may lead to stresses on tissues that predispose those structures to injury 2 This has implications to under standing common running injuries such as patellofemoral pain (PFP). Patellofemoral pain has been reported as the most common running related injury accounting for 16.5% of all injuries presenting to a running clinic.3 More re cently, a systematic review and meta-analysis has esti mated an incidence rate of 1080.5/1000 person-years in amateur runners.4 As increased patellofemoral joint stress (PFJS), patellofemoral bone stress, and cartilage strain have been implicated in PFP and certain running kinematics and kinetics may increase structure-specific loading (i.e. PFJS), understanding differences in structure-specific loading be tween sexes may be relevant to the development of this common injury 5–7
As PFP is two times more prevalent in females,8 it has been proposed that females may demonstrate increased PFJS leading to greater structure-specific load. Although the theoretical link is clear, studies investigating sex differ ences in PFJS have shown mixed findings.9–11 Almonroeder & Benson9 reported males had greater PFJS and patellofemoral joint reaction force (PFJRF) during running, while there were no differences between sexes in knee ex tension moments or knee flexion. Sinclair & Selfe10 re ported females had greater patellofemoral contact force, PFJS, and peak knee extension moment compared to males, while Willson et al.11 did not demonstrate sex differences in PFJS, PFJRF, or knee extensor moment.
To understand these discrepancies, important differ ences should be noted in the musculoskeletal modeling ap proaches employed. First, two studies9,10 utilized estimates of PFJS based on inverse dynamics methods that calculate joint stress directly using the knee extension moment. This may not account for any potential muscle co-contraction. Therefore, inverse dynamics approaches alone may lead to underestimation of PFJS.12
Willson et al.11 adjusted their model to account for the force of the knee flexors but how this method compares to other approaches estimating quadriceps force is unknown. Static optimization based methods used to estimate muscle forces yield different values of PFJS compared with inverse dynamic approaches.12 Therefore, estimates of PFJS from musculoskeletal models utilizing muscle forces may pro vide a more robust estimate of quadriceps loading for esti mates of PFJS.
Methods used to estimate patellofemoral joint contact area (PFJCA) is another factor that may explain the dif
Table 1. Demographic factors reported as means (SD).
Age (yrs) 21.8 (1.5) 21.1 (2.2)
Height (cm) 167.6 (6.4) 179.1 (8.2)
Mass (kg) 62.0 (8.1) 74.6 (10.3)
Tegner Scale 6 (5-7) 6 (5-9)
Tegner scale is reported as the median (range).
ferent findings associated with PFJS based on sex. Al monroeder & Benson used in vivo measurements in females obtained via MRI to estimate PFJCA despite testing a mixed sex sample.9 Willson et al.11 used similar data that were sex-specific while Sinclair & Selfe10 used data from cadav eric, non-sex specific samples. As PFJCA differences have been reported between sexes,13 it seems imperative to uti lize sex-specific contact areas in attempts to elucidate dif ferences in PFJS.
A combination of utilizing quadriceps muscle force esti mates from static optimization and sex-specific PFJCA may help to clarify inconsistencies reported in previous studies examining sex differences in PFJS, lead to further under standing of tissue stresses imposed on the patellofemoral joint during running, and help guide future research.
The purpose of this study was to examine sex differences in patellofemoral joint stress using an updated model to in clude estimates of quadriceps muscle force and sex-specific patellofemoral contact area. It was hypothesized that fe males would demonstrate increased PFJS when quadriceps muscle force and sex-specific contact area were considered.
Using the peak patellofemoral joint stress differences from Willson et al.,11 an alpha = 0.05, a correlation between scores of 0.5 to determine a power of 0.8, a sample size of 18 subjects was calculated. Twenty-four healthy females and 21 males participated (Table 1). Inclusion criteria: self-re ported running routine of greater than 16 km/week, rear foot strike pattern (first ground contact made with the heel) while running, score of ≥5 on the Tegner scale, and no reported injuries limiting regular running participation within the prior 12 months. Exclusion criteria: pregnancy, reported cardiovascular pathology, and surgery to either lower extremity within the prior 12 months. All subjects provided informed consent approved by the Institutional Review Board at the university
A static trial was completed to calibrate the musculoskele tal model. Then after a minimum of three practice running trials, participants ran down a 20-m runway using their typ ical rearfoot running pattern. Pattern was verified using the foot strike index where the center of pressure at ground contact was located in the rear third.14
Speed was restricted to a range of 3.52-3.89 m/s using photocells interfaced with a digital clock. Range was chosen to ensure comparable running speeds were present between groups. Running pattern was observed and no targeting of the force plate was allowed. A minimum of five successful right leg trials were completed.
Prior to running, participants were prepped for motion analysis. Forty-seven retroreflective markers were applied to each participant’s skin, tight fitted clothing, or footwear as previously described.15 Markers were left in place during data collection and data were captured at 180 Hz via 15 Mo tion Analysis cameras (Motion Analysis Corporation, Santa Rosa, CA, USA) surrounding the runway. Ground reaction forces were collected with a force platform (Model 4080, Bertec Corporation, Columbus, OH, USA) flush with the runway. Analog data were sampled at 1800 Hz. Both analog data from force platforms and kinematic data were processed through a low-pass Butterworth filter at 12 Hz.
The Human Body Model (HBM, Motek Medical, Amsterdam, Netherlands) was used to calculate muscle forces using a 44 degree of freedom (DOF) musculoskeletal model with 16 rigid segments.16 The hip joint was treated as a ball-insocket joint based on Bell et al.17 The knee joint was mod eled as a single DOF hinge where any tibio-femoral trans lations and non-sagittal rotations were constrained as a function of knee flexion. Limb segments and inertial char acteristics were sex-specific.18 From estimates of hip joint center from the standing neutral trial and estimates of the of sacroiliac joint center,19 the HBM creates pelvic geome try for each participant.
Eighty-six muscles were modeled in the lower extremi ties where the muscle insertion points and wrapping points were from Delp.20 A kinematic solver within HBM used global optimization to determine skeletal model kinemat ics.21,22 Joint moments were then obtained from equations of motion and estimated by minimizing a static cost func tion where the sum of squared muscle activations is related to maximum muscle strengths at each time step.20 A recur rent neural network was used to solve the static optimiza tion problem.23
The muscle forces from the HBM were then used to quantify the total quadriceps force (QF) by summing the muscle forces of the rectus femoris, vastus medialis, vastus lateralis, and vastus intermedius. PFJS is calculated by di viding PFJRF by the PFJCA. To determine the PFJRF, a con version factor (k) was estimated from Brechter & Powers24:
where x is the knee joint angle in the sagittal plane. This represented the portion of the quadriceps force acting di rectly on the patellofemoral joint. Both knee angle and the orientation of the quadriceps muscle affect force imposed on the patellofemoral joint. Therefore,
Sex-specific PFJCA was calculated as a function of knee an gle using the data reported from Besier et al.13 to formulate predictive equations:
PFJS was then calculated as follows:
A multivariate analysis of variance (MANOVA) was used to examine any sex differences in peak PFJS, PFJRF, QF, knee extensor moment, peak knee flexion, peak hip adduction, and internal rotation during the stance phase of running (α=0.05). Follow up univariate tests were performed to as sess sex differences in these same kinetic and kinematic data. A Bonferonni correction was employed. Statistical cal culations were performed in SPSS 24.0 (IBM, Armonk, NY, USA). Effect sizes were calculated using partial eta squared (η2) where a small effect size was considered as η2<0.06, a medium effect size 0.06≤ η2 <0.14, and a large effect size η2 ≥0.14.
Multivariate differences were shown on sex (Wilk’s lambda = 0.456; p =0.000). From follow up univariate tests, there were no differences between the sexes in peak PFJS (Figure 1), PFJRF, QF, or knee flexion angle shown during running (Table 2). Females showed 11.7% less knee extensor mo ment compared to males (p = 0.049). Effect sizes for peak PJFS, PFJRF, QF and knee flexion angle were small while a medium effect size was present for knee extensor moment (Table 2).
Follow up univariate tests showed hip adduction (Figure 2A) and internal rotation (Figure 2B) were different be tween sexes. Females demonstrated 111% greater peak value for hip internal rotation (absolute difference: 3.62°). Females also demonstrated 48.5% greater hip adduction (absolute difference: 4.80°) than males. A large effect size was present for hip adduction and medium effect size was present for hip internal rotation (Table 2).
The aim of this study was to examine sex-related differ ences in patellofemoral joint loads. Even with static op timization and sex-specific contact areas, no differences in PFJS, PFJRF, or QF were shown between sexes during running. However, females demonstrated less knee exten
Figure 1. Ensemble average of patellofemoral joint stress over the stance phase of running.
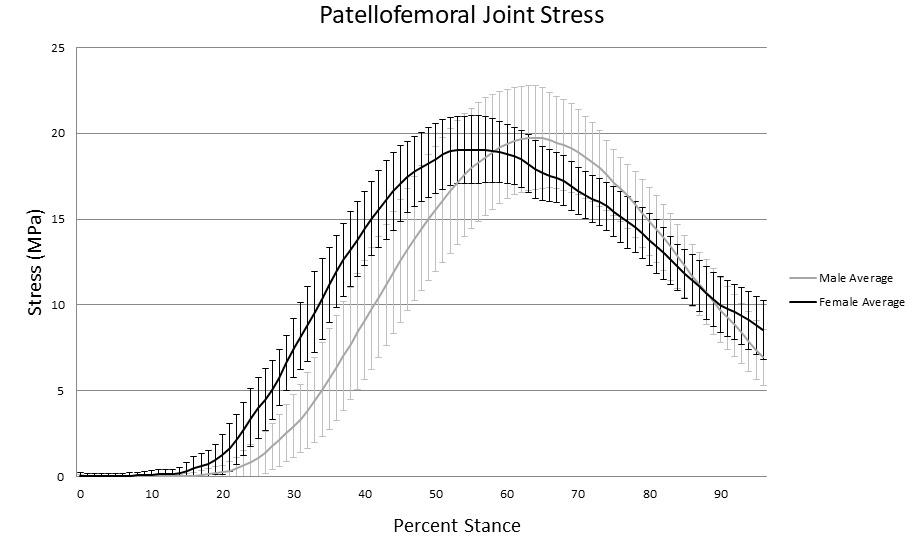
Table 2. Peak values of selected variables.
Females Males p value Effect Size (η2)
PFJS (MPa) 9.20 (1.65) 9.32 (2.22) 0.829 0.001 PFJRF (BW) 6.89 (1.22) 7.24 (1.52) 0.391 0.017 QF (BW) 7.82 (1.17) 8.28 (1.50) 0.249 0.031
Knee extensor moment (N•m/kg) 0.869 (0.136) 0.984 (0.239) 0.049 0.087 Knee flexion (degrees) 48.4 (5.00) 46.6 (5.20) 0.244 0.031 Hip adduction (degrees) 14.7 (4.07) 9.90 (4.20) 0.000 0.259 Hip internal rotation (degrees) 6.89 (5.71) 3.26 (5.28) 0.034 0.101
Values are presented as group averages with standard deviations. Bold type indicates statistically significant differences.
sion moment and greater transverse and frontal plane hip motion than males. The presence of a sex difference in knee extension moment and lack of a sex difference be tween QF may indicate that the use of muscle force es timates could be important in describing sex differences in PFJS. Further, as hip motion may affect loads at the patellofemoral joint,25,26 more comprehensive models of the patellofemoral joint may be needed to account for these motions. Since muscle force estimates to derive PFJRF and sex-specific contact areas did not detect sex differences in PFJS, a consideration of frontal and transverse plane con tributions to PFJCA in conjunction with muscle force esti mates may be necessary to detect such differences. Further characterization of PFJS with the use of 3D patellofemoral joint models may be a necessary step in understanding structure-specific load based on sex.
Results were contrary to what was hypothesized. This study and previous work on sex differences in patellofemoral joint loading have had inconsistent find ings.9–11 Several aspects of approaches used within previ
ous models could have contributed to these inconsistencies that attempts were made to account for in the current in vestigation. This was an attempt to build on previous ef forts by improving on the available 2D models to see if in clusion of muscle forces and a sex-specific PFJ model could support the hypothesis that females demonstrate greater PFJS. Yet, even with these additions, no differences in peak PFJS were detected. Based on a qualitative assessment of the average ensemble PFJS time series data, it appears that males had a later peak in PFJS during stance (65% of stance vs. 57% of stance). However, in both males and females, peak QF seemed to occur at nearly the same time as peak PFJS during stance (65% and 60%, respectively) whereas knee flexion occurred only slightly later in stance for males (69% of stance) but a larger difference in the timing of peaks was seen in females (peak knee flexion occurred at 67% of stance in females). This may depict that males are displaying a peak PFJS and QF closer to the time of peak knee flexion where PFJCA is increased as the knee is more flexed. Therefore, this might indicate that males may be
demonstrating peak QF during stance when the knee is in a more desirable position to distribute these patellofemoral contact forces across the patellofemoral joint. However, this hypothesis needs further examination. In addition, the lack of differences in peak patellofemoral forces shown here may indicate that 2D models may be insufficient to fully characterize PFJS based on sex.
Estimates of PFJS from static optimization are higher as inverse dynamics does not account for co-contraction of muscles crossing the same joint.12 In the present study, peak knee extension moment during stance was similar to previous studies.9,11 In previous work, Almonroeder et al.9 reported females had 12.9% less knee extension moment than males, whereas Sinclair & Selfe10 reported females demonstrating 14.1% greater knee extension moment than males, and Willson et al.11 reported no differences between sexes. Differences may be related to how individuals cocontract their knee flexors and extensors to control knee motion during running. These results from the current study showed differences between sexes in knee extension
moment, but not in QF. This may indicate differences be tween sexes in the muscle force production of the knee flex ors during stance may affect the net knee moment. Consid eration of muscle forces from static optimization may be an important in portraying PFJS.
As PFJS is the quotient of PFJRF and PFJCA, differences in either of these can also explain study differences. De spite sex-specific estimates of PFJCA, no differences in PFJS between males and females was identified. However, con sistent with previous studies,9,27,28 peak hip adduction and internal rotation during the stance phase of running were greater in females. Although statistical differences were de tected in non-sagittal plane hip motions, the meaningful ness of these small differences is uncertain. However, the reported differences appear consistent with previously re ported literature where females display more non-sagittal hip motion during running than males.27–30
Hip positioning has been demonstrated as impacting PFJCA and, thus, measures of PFJS in individuals with and without PFP 25,26 This occurs as frontal and transverse
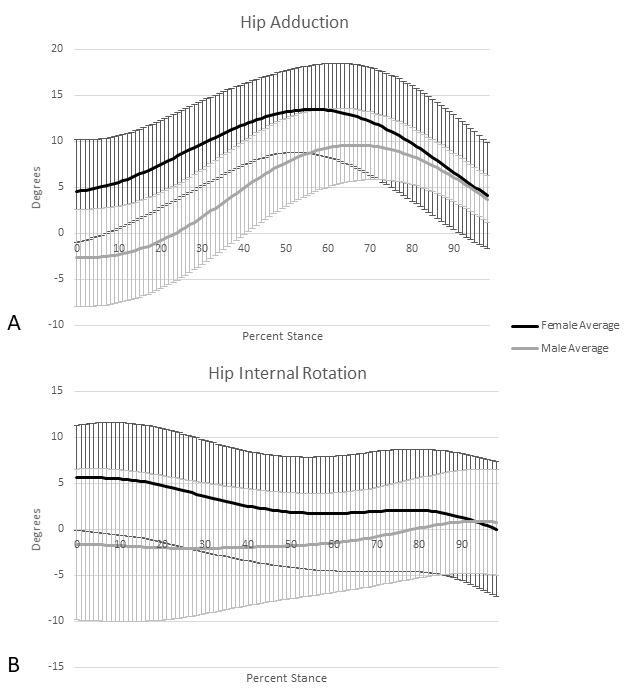 Figure 2. Ensemble averages of hip adduction (A) and hip internal rotation (B) over the stance phase of running.
Figure 2. Ensemble averages of hip adduction (A) and hip internal rotation (B) over the stance phase of running.
plane rotations at the hip can position the femur and the patella in a way that the location and contact area is either increased or decreased. Liao & Powers26 reported that the location and magnitude of peak patella cartilage stress did not differ between runners with and without PFP These authors did find, however, that tibiofemoral rotations in both the transverse and frontal planes explained 45% and 26% of the variance in patellar cartilage stress, respectively Further, when investigating the isolated role of tibial and femoral rotations on patellar cartilage stress, it has been re ported that increased femoral internal rotation of 4°, 6°, 8°, and 10° yielded increases in patellar cartilage stress rang ing from 41-77%.25 Similarly, increases in 10° of femur ad duction produced increases in patellar cartilage stress of 43%.25
Therefore, even small changes in femoral rotation may have a notable impact on PFJS. Since there was nearly a 4-5° difference shown between males and females in both femoral internal rotation and adduction, it is likely that these differences in hip kinematics here would have influ enced the magnitude of PFJS in participants. As the model used in this study did not utilize frontal or transverse plane knee motion to determine PFJS, sex differences in patellofemoral joint loads may have gone undetected. Therefore, the lack of observed differences between sexes even with quadriceps muscle force estimates supports the notion that if sex differences in PFJS exist it may be related to differences in frontal and transverse plane kinematics at the patellofemoral joint. If contributions from the frontal and transverse planes can be characterized and quantified, this may assist clinicians in assessing when increased hip motion may be a contributing factor to a patient’s presenta tion. Further research characterizing the effects of femoral orientation on patellofemoral joint loads by sex in running appears warranted.
Despite the attempts to build on the work of previous authors, several limitations to the approach used should be noted. First, the patellofemoral model was limited to two-dimensions and was incapable of capturing frontal and transverse plane motions. This was largely due to the limi tations of the musculoskeletal model constraining the knee to one degree of freedom. However, this model attempted to build upon previous work using 2D models by including muscle force estimates and sex-specific 2D estimates of PFJCA in the model. Next, all musculoskeletal models uti lize numerous anatomical assumptions to yield estimates of muscle force. As these do not necessarily reflect the anatomy of the included participants, there is an amount of error inherent to this approach. Therefore, the degree to
which these estimates reflect the actual physiological loads is still questionable and therefore may not fully reflect the true patellofemoral joint loading present. Thirdly, running speed was controlled for all participants to assist with com parisons between groups. As joint kinematics and muscle forces change with running speed,31,32 the patellofemoral joint loading estimated here may not reflect the loads reg ularly imposed on the individual participants during their typical training runs. Additionally, only rearfoot strike run ners were examined as forefoot striking appears to alter patellofemoral joint stress.15,33 To what extent sex differ ences in PFJS is present in those who employ a non-rearfoot strike pattern is unknown. Because only healthy runners were investigated, these findings may not be applicable to injured runners. Finally, differences in running experience were not accounted for As aspects of running mechanics can differ with greater experience,34 how these results may differ in novice versus experienced runners is uncertain.
The results of the current study indicate that there was no difference between sexes in PFJS during the stance phase of running despite the use of quadriceps muscle force and sex-specific contact area estimates in a 2D patellofemoral joint model. Differences were noted between sexes in knee extension moment yet not in quadriceps force. This indi cates that the methods employed to estimate PFJRF should be considered when comparing modeling approaches uti lized. Further, peak hip adduction and internal rotation an gles during running were greater in females compared to males. Since quadriceps muscle force estimates did not re veal sex differences in PFJS, it is plausible that, if these dif ferences exist, they may be related to frontal and transverse plane kinematics. Utilization of 3D models that incorpo rate transverse and frontal plane kinematics of the patellofemoral joint in conjunction with estimates of quadriceps muscle force may be necessary to characterize potential differences in PFJS between sexes and may help clinicians identify risk factors for PFP.
The authors have no financial conflicts of interest to de clare.
Submitted: April 26, 2022 CST, Accepted: July 24, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Bertelsen ML, Hulme A, Petersen J, et al. A framework for the etiology of running-related injuries. Scand J Med Sci Sports. 2017;27(11):1170-1180. doi:10.1111/sms.12883
2. Nielsen RO, Bertelsen ML, Møller M, et al. Training load and structure-specific load: applications for sport injury causality and data analyses. Br J Sports Med 2018;52(16):1016-1017 doi:10.1136/bjsports-20 17-097838
3. Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD A retrospective casecontrol analysis of 2002 running injuries. Br J Sports Med 2002;36(2):95-101. doi:10.1136/bjsm.36.2.95
4. Smith BE, Selfe J, Thacker D, et al. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS One 2018;13(1):e0190892. doi:10.1371/journal.pone.0190 892
5. Ho KY, Keyak JH, Powers CM. Comparison of patella bone strain between females with and without patellofemoral pain: A finite element analysis study. J Biomech 2014;47(1):230-236. doi:10.1016/j.jbiomec h.2013.09.010
6. Liao TC, Keyak JH, Powers CM. Runners with patellofemoral pain exhibit greater peak patella cartilage stress compared with pain-free runners. J Appl Biomech. 2018;34(4):298-305. doi:10.1123/jab.20 17-0229
7 Farrokhi S, Keyak JH, Powers CM. Individuals with patellofemoral pain exhibit greater patellofemoral joint stress: A finite element analysis study. Osteoarthr Cartil 2011;19(3):287-294. doi:10.1016/j.j oca.2010.12.001
8. Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725-730. doi:10.1111/j.160 0-0838.2009.00996.x
9. Almonroeder TG, Benson LC. Sex differences in lower extremity kinematics and patellofemoral kinetics during running. J Sports Sci 2017;35(16):1575-1581. doi:10.1080/02640414.2016.1 225972
10. Sinclair J, Selfe J. Sex differences in knee loading in recreational runners. J Biomech 2015;48(10):2171-2175. doi:10.1016/j.jbiomech.201 5.05.016
11. Willson JD, Loss JR, Willy RW, Meardon SA. Sex differences in running mechanics and patellofemoral joint kinetics following an exhaustive run. J Biomech. 2015;48(15):4155-4159. doi:10.1016/j.jbiomech.201 5.10.021
12. Kernozek TW, Vannatta CN, van den Bogert AJ. Comparison of two methods of determining patellofemoral joint stress during dynamic activities. Gait Posture. 2015;42(2):218-222. doi:10.1016/j.gaitp ost.2015.05.017
13. Besier TF, Draper CE, Gold GE, Beaupré GS, Delp SL. Patellofemoral joint contact area increases with knee flexion and weight-bearing. J Orthop Res 2005;23(2):345-350. doi:10.1016/j.orthres.2004.08.00 3
14. Cavanagh PR, Lafortune MA. Ground reaction forces in distance running. J Biomech 1980;13(5):397-406. doi:10.1016/0021-9290(80)9003 3-0
15. Vannatta CN, Kernozek TW Patellofemoral joint stress during running with alterations in foot strike pattern. Med Sci Sports Exerc 2015;47(5):1001-1008. doi:10.1249/mss.0000000000000503
16. Van Den Bogert AJ, Geijtenbeek T, Even-Zohar O, Steenbrink F, Hardin EC. A real-time system for biomechanical analysis of human movement and muscle function. Med Biol Eng Comput. 2013;51(10):1069-1077. doi:10.1007/s11517-013-107 6-z
17 Bell AL, Pedersen DR, Brand RA. A comparison of the accuracy of several hip center location prediction methods. J Biomech 1990;23(6):617-621. doi:10.1016/ 0021-9290(90)90054-7
18. De Leva P. Adjustments to zatsiorsky-seluyanov’s segment inertia parameters. J Biomech 1996;29(9):1223-1230. doi:10.1016/0021-9290(95)001 78-6
19. Reynolds H, Snow C, Young J. Spatial Geometry of the Human Pelvis Oklahoma City; 1982.
20. Delp SL, Loan JP, Hoy MG, Zajac FE, Topp EL, Rosen JM. An Interactive Graphics-Based Model of the Lower Extremity to Study Orthopaedic Surgical Procedures. IEEE Trans Biomed Eng. 1990;37(8):757-767 doi:10.1109/10.102791
21. Lu TW, O’Connor JJ. Bone position estimation from skin marker co-ordinates using global optimisation with joint constraints. J Biomech 1999;32(2):129-134. doi:10.1016/s0021-9290(98)0015 8-4
22. Press WH, Teukolsky S a, Vetterling WT, Flannery BP Numerical Recipes 3rd Edition: The Art of Scientific Computing.; 2007. doi:10.1137/1031025
23. Xia Y, Feng G. An improved neural network for convex quadratic optimization with application to real-time beamforming. Neurocomputing. 2005;64:359-374. doi:10.1016/j.neucom.2004.11.009
24. Brechter JH, Powers CM. Patellofemoral stress during walking in persons with and without patellofemoral pain. Med Sci Sports Exerc 2002;34(10):1582-1593. doi:10.1097/00005768-20021 0000-00009
25. Liao TC, Yin L, Powers CM. The influence of isolated femur and tibia rotations on patella cartilage stress: a sensitivity analysis. Clin Biomech. 2018;54:125-131. doi:10.1016/j.clinbiomech.2018.0 3.003
26. Liao TC, Powers CM. Tibiofemoral kinematics in the transverse and frontal planes influence the location and magnitude of peak patella cartilage stress: An investigation of runners with and without patellofemoral pain. Clin Biomech 2019;62:72-78. do i:10.1016/j.clinbiomech.2019.01.003
27. Chumanov ES, Wall-Scheffler C, Heiderscheit BC. Gender differences in walking and running on level and inclined surfaces. Clin Biomech 2008;23(10):1260-1268. doi:10.1016/j.clinbiomech.20 08.07.011
28. Ferber R, Davis IM, Williams DS III. Gender differences in lower extremity mechanics during running. Clin Biomech 2003;18(4):350-357 doi:10.10 16/s0268-0033(03)00025-1
29. Willson JD, Petrowitz I, Butler RJ, Kernozek TW. Male and female gluteal muscle activity and lower extremity kinematics during running. Clin Biomech 2012;27(10):1052-1057. doi:10.1016/j.clinbiomech.20 12.08.008
30. Phinyomark A, Hettinga BA, Osis ST, Ferber R. Gender and age-related differences in bilateral lower extremity mechanics during treadmill running. PLoS One 2014;9(8):e105246. doi:10.1371/journal.pone.01 05246
31. Schache AG, Blanch PD, Dorn TW, Brown NAT, Rosemond D, Pandy MG. Effect of running speed on lower limb joint kinetics. Med Sci Sports Exerc. 2011;43(7):1260-1271. doi:10.1249/mss.0b013e31820 84929
32. Dorn TW, Schache AG, Pandy MG. Muscular strategy shift in human running: dependence of running speed on hip and ankle muscle performance. J Exp Biol. 2012;215(11):1944-1956. doi:10.1242/jeb.0 64527
33. Kulmala JP, Avela J, Pasanen K, Parkkari J. Forefoot strikers exhibit lower running-induced knee loading than rearfoot strikers. Med Sci Sports Exerc 2013;45(12):2306-2313. doi:10.1249/mss.0b013e3182 9efcf7
34. Hafer JF, Peacock J, Zernicke RF, Agresta CE. Segment Coordination Variability Differs by Years of Running Experience. Med Sci Sports Exerc. 2019;51(7):1438-1443. doi:10.1249/mss.00000000000 01913
VanZile A, Driessen M, Grabowski P, Cowley H, Almonroeder T. Deficits in Dynamic Balance and Hop Performance Following ACL Reconstruction Are Not Dependent on Meniscal Injury History. IJSPT. Published online December 1, 2022:1298-1306.
1 Optimum Performance Therapy, 2 Department of Health Professions, University of Wisconsin - La Crosse, 3 College of Health Professions, Trine University
Keywords: anterior cruciate ligament reconstruction, knee, rehabilitation, return to sport, meniscus https://doi.org/10.26603/001c.55542
Athletes often exhibit persistent deficits in dynamic balance and hop performance in their involved limb following ACL reconstruction. However, it is unclear how meniscal injury history affects inter-limb asymmetry
The purpose of this study was to compare inter-limb asymmetry in dynamic balance and hop performance in athletes with and without a history of concomitant meniscal injury
Cross-sectional study
Dynamic balance and hop test data were analyzed for 34 adolescent athletes who had undergone ACL reconstruction; 19 athletes had sustained an isolated ACL tear, while 15 had sustained an ACL tear along with a meniscus injury. Athletes who had sustained a meniscus injury were sub-divided into those who underwent a meniscal repair (n = 9) versus a partial meniscectomy (n = 6). Dynamic balance was assessed using the Y-Balance Test, while hop performance was assessed using the single and triple hop tests. Data were recorded at the time of return-to-sport testing (5-11 months post-surgery). For each variable, mixed-model analysis of variance, with a between-subjects factor of group (isolated ACL tear, meniscal repair, partial meniscectomy) and a within-subjects factor of limb (involved, uninvolved), was conducted.
The groups exhibited similar degrees of inter-limb asymmetry in dynamic balance and hop test performance, as there was not a group-by-limb interaction effect for the Y-Balance Test distances (p ≥ 0.43) or hop test distances (p ≥ 0.96). However, there was a main effect of limb for the anterior and posteromedial Y-Balance Test distances and the single and triple hop test distances (p ≤ 0.004). For each variable, performance was worse for the involved limb, compared to the uninvolved limb.
a
Corresponding author:

Thomas G. Almonroeder, DPT, PhD
Assistant Professor
College of Health Professions
Doctor of Physical Therapy Program Trine University 1819 Carew St., Fort Wayne, IN, USA, 46805
E-mail: almonroedert@trine.edu Phone: 608-738-6174
It appears that deficits in dynamic balance and hop performance among adolescent athletes who have undergone ACL reconstruction are not dependent on meniscal injury/ surgery history.
Level of Evidence 3
Anterior cruciate ligament (ACL) tears are common among high school age athletes who participate in sports that in volve frequent single-leg landing, cutting, and pivoting.1,2 Athletes who have sustained an ACL tear typically undergo ACL reconstruction and then complete extensive post-op erative rehabilitation.3 Approximately one in five of these athletes will go on to sustain a second ACL injury shortly after returning to sport.4 This alarmingly high injury rate highlights the urgent need to examine factors that may in fluence an athlete’s ability to safely return to sport follow ing ACL reconstruction.
Athletes who have undergone ACL reconstruction often demonstrate deficits in postural stability and dynamic bal ance for their involved limb (vs. their uninvolved limb), even after completing post-operative rehabilitation.5–7 This is concerning since deficits in postural stability and dynamic balance are associated with an increased risk for ACL injury/re-injury.8,9 Athletes who have undergone ACL reconstruction also tend to exhibit persistent (12+ months post-surgery) deficits in single leg hop performance for their involved limb,10–12 which is likely due, at least in part, to limitations in lower extremity strength and power gen eration.11 These types of persistent neuromuscular deficits may contribute to re-injury and/or limit an athlete’s ability to return to their prior level of sport performance.
Factors such as quadriceps weakness13,14 and kinesio phobia15,16 have been studied extensively and appear to contribute to the persistent deficits in dynamic balance and hop performance commonly exhibited by athletes follow ing ACL reconstruction. However, one potential factor that has not been thoroughly examined is an athlete’s meniscal injury history At this time, only one previously published study has compared dynamic balance for athletes with and without a history of concomitant meniscal injury13 and no studies have examined how meniscal injury status affects inter-limb symmetry in hop performance. It is important to further examine the influence of meniscal injury his tory since more than half of all ACL tears are accompa nied by a meniscus tear,17–19 with 56% of tears involving the lateral meniscus and 44% of tears involving the me dial meniscus.17 It is also important to examine whether neuromuscular performance is affected by how an athlete’s meniscal tear was managed. While surgeons typically at tempt to repair the meniscus if possible, in some cases they must debride the injured part of the meniscus (par tial meniscectomy). This could potentially negatively im pact knee control, since the menisci serve as a source of mechanical stability for the knee.20–22
Therefore, the purpose of this study was to compare in ter-limb asymmetry in dynamic balance and hop perfor mance for athletes with and without a history of concomi tant meniscal injury. It was hypothesized that the degree of interlimb asymmetry in dynamic balance and hop perfor mance would be similar for athletes with isolated ACL tears, compared to athletes with concomitant meniscal injuries, regardless of whether they had undergone meniscal repair or partial meniscectomy
Clinical outcomes for 34 adolescent athletes were analyzed as part of this cross-sectional study; 19 (9 males, 10 fe males) of these athletes had sustained an isolated ACL tear, while 15 (8 males, 7 females) had sustained an ACL tear along with a partial meniscus tear. All athletes were com peting at the high school level at the time of injury and were between 14-19 years of age at the time of testing. This age range aligns with the World Health Organization’s definition of adolescence.23 To be included in this study, athletes needed to have undergone successful primary uni lateral ACL reconstruction (either bone-patellar tendonbone autograft or hamstring tendon autograft), completed conventional post-operative rehabilitation, participated in facility-standard return to sport testing (which included testing of dynamic balance and hop performance), and ex pressed an intention to return to competitive sports. Data were excluded for athletes with a history of major injury or surgery for their uninvolved limb, a history of major injury or surgery for their involved limb (aside from their ACL in jury/reconstruction), or a concomitant ligament injury (e.g. medial collateral ligament tear). ACL reconstruction surg eries were performed by one of a group of five orthopedic surgeons. All athletes had completed post-operative reha bilitation (see Rehabilitation Protocol sub-section for de tails) with the same physical therapist who is a board-cer tified sports clinical specialist through the American Board of Physical Therapy Specialists. The athletes had resumed high-level dynamic activities, such as landing and jump ing, but had not been cleared to return to sport at the time of testing. At the time of testing, none of the athletes had notable limitations in knee range of motion (beyond what could be attributed to measurement error) or visible signs of effusion for their involved knee. The athletes who had sustained a meniscus injury had either undergone a menis cal repair (n = 9) or a partial meniscectomy (n = 6). Study data were obtained through retrospective chart review This
study protocol was approved by the Institutional Review Board at Lutheran Hospital (Fort Wayne, IN, USA).
The athletes’ rehabilitation generally progressed through four phases (a copy of the protocol is included as supple mentary material). Phase 1 focused on controlling swelling/ effusion, increasing knee motion, maintaining patellar mo bility, facilitating quadriceps activation and strength, and initiating and progressing weight-bearing. Phase 2 focused on regaining full knee range of motion, improving quadri ceps and hamstring strength, normalizing walking gait, promoting knee control during functional tasks, general lower body strengthening, and aerobic conditioning. Phase 3 focused on more advanced strengthening and condition ing, initiation and progression of running, jumping, and cutting, and sport-related training. Phase 4 focused on more advanced strengthening and training to promote sport-specific skills (e.g. sprinting, agility drills). Rehabili tation followed this general protocol for all athletes; how ever, athletes progressed through the stages at different rates, depending on a variety of factors (e.g. surgical fac tors, rate of recovery). Return-to-sport testing was con ducted once athletes exhibited full knee motion (based on goniometric measurements), minimal pain/effusion, sym metrical strength for their involved limb (within 90% of the uninvolved limb, based on standardized testing with a handheld dynamometer), and no major movement faults (e.g. quadriceps avoidance, excessive knee valgus) during dynamic activities such as landing, jumping, and cutting (based on visual observation by the therapist). At the time of testing all athletes had successfully “completed” rehabil itation from the standpoint of they had met the criteria for formal return-to-sport testing.
The data analyzed as part of this study were recorded at the time of the athletes’ return-to-sport testing session (within a range of 5-11 months after surgery). To promote con sistency, testing was standardized and administered by the same physical therapist who has extensive experience in administering the tests used in this study. Subjects wore their own athletic shoes during testing.13
All athletes completed the single hop test and triple hop test, which are both common performance-based outcome measures used to assess knee-related function and lower extremity strength/power following ACL reconstruc tion.24,25 For each hop test, the athlete was given a demon stration, performed a practice trial with each limb, and then completed two successful trials per limb, with the unin volved limb tested first.24,25 Successful trials were defined as trials where the athlete was able to maintain single-limb stance for at least two seconds upon the final landing.25 Unsuccessful trials, such as when an athlete was unable to maintain single-limb stance for at least two seconds, were
repeated (up to two repeat trials per limb). The average of the two successful trials was recorded as the outcome of in terest. No restrictions were placed on arm movement dur ing hop testing.25 Hop testing was performed in a field house with artificial field turf
For the single hop test, the athletes initiated the test in single-limb stance (test limb) with their toes behind a marked line. They then hopped forward for maximal dis tance, landing on their test limb. Hop distances were mea sured in centimeters using a tape measure affixed to the turf. Measurements were taken at the point of the heel of the athlete’s shoe for the test limb. The triple hop test was completed in the same manner, except the athlete com pleted three consecutive maximal hops with their test limb.
Performance on both the single hop test and triple hop test have been shown to demonstrate excellent test-retest reliability, are sensitive to changes for the involved limb over the course of rehabilitation, and correlate with per ceived lower extremity function in athletes with a history of ACL reconstruction.25,26
Similar to the hop tests, the athletes completed the Lower Quarter Y Balance Test (also referred to as the modified Star Excursion Balance Test) with both their involved and unin volved limbs. A Y-Balance Test kit was used to record test performance (Functional Movement System; Danville, VA, USA). The Y-Balance Test is a commonly used clinical test to assess single leg dynamic balance. As part of the test, athletes must maintain their balance on a single limb (test limb) while reaching as far as possible in the anterior, pos teromedial, and posterolateral directions with their con tralateral limb, while a sliding indicator is used to mark their reach distance (Figure 1). Athletes completed three trials per limb in each direction. An examiner recorded the single farthest distance reached (centimeters) for each direction. As recommended, the athletes were given a demonstration of the test and completed practice trials in each direction prior to formal testing.27 Athletes completed three trials with their right limb and then three trials with their left limb in the anterior direction.27 The same test ing procedures were then completed in the posteromedial and posterolateral directions. As recommended,28 athletes where required to maintain their hands on their hips when completing the Y-Balance Test in order to limit their abil ity to use their upper extremities to assist in maintaining stability 29,30 This allows for a more direct assessment of lower body neuromuscular control, since it limits an ath lete’s ability to stabilize themselves with their upper ex tremities.28 Trials were considered invalid if the athlete failed to maintain single-leg stance throughout the trial, failed to maintain foot contact with the indicator when reaching, used the indicator for support, or removed their hands from their hips during a trial.13,27
The Y-Balance Test has been shown to demonstrate ex cellent intrarater and interrater reliability 31 In addition, relatively poor Y-Balance Test performance has been found to be associated with an increased risk of sport-related noncontact lower extremity injury, including ACL tears.9,31
Figure 1. Example of an individual completing the Y-Balance Test in the anterior (left panel), posteromedial (middle panel), and posterolateral (right panel) directions. In this case, the dynamic balance of the individual’s left limb is being assessed.
The dependent variables of interest were the reach dis tances for the Y-Balance Test (anterior, posteromedial, and posterolateral directions) and the hop distances for the sin gle hop test and triple hop test. For each variable, a twoway, mixed-model analysis of variance with a between-sub jects factor of group (isolated ACL tear, meniscal repair, partial meniscectomy) and a within-subjects factor of limb (involved, uninvolved) was conducted. An alpha level of 0.05 was used for each test of statistical significance. In ad dition, 95% confidence intervals (CI95%) were generated to supplement the results of the null hypothesis significance tests.
A limb symmetry index (LSI) was also generated for each variable by dividing the distance for the involved limb by the distance for the uninvolved limb and then multiplying by 100 to express as a percentage.6,24,25 An LSI equal to 100% reflects perfect inter-limb symmetry, an LSI less than 100% reflects poorer performance for the involved limb, and an LSI greater than 100% reflects poorer performance for the uninvolved limb. SPSS software was used for statis tical analysis (Version 28; IBM Corp., Armonk, New York, USA).
Table 1 describes the characteristics of the athletes whose data were analyzed as part of this study
There was not a group-by-limb interaction effect for the anterior [F (2, 31) = 0.26; p = 0.77], posteromedial [F (2, 31) = 0.86; p = 0.43], or posterolateral [F (2, 31) = 0.41; p = 0.67] Y-Balance Test reach distances, or the single hop test [F (2, 31) = 0.04; p = 0.96] or triple hop test distances [F (2, 31) = 0.03; p = 0.97], which indicates that the groups ex hibited similar degrees of inter-limb asymmetry in dynamic balance and hop test performance.
There was a main effect of limb for the anterior [F (1, 31) = 16.52; p < 0.001] and posteromedial [F (1, 31) = 9.76; p =
0.004] Y-Balance Test reach distances; however, there was not a main effect of limb for the posterolateral direction [F (1, 31) = 1.56; p = 0.22] (Figure 2). On average, Y-Balance Test reach distances were 2.7 cm less in the anterior direc tion [CI95% = (-3.8 cm, -1.6 cm)] and 3.3 cm less in the pos teromedial direction [CI95% = (-5.1 cm, -1.5 cm)] for the in volved limb, compared to the uninvolved limb.
There was also a main effect of limb for the single hop test [F (1, 31) = 15.55; p < 0.001] and triple hop test [F (1, 31) = 20.92; p < 0.001] distances (Figure 3). Single hop test distances were 19.2 cm less for the involved limb [CI95% = (-27.5 cm, -10.8 cm)] and triple hop test distances were 57.5 cm less for the involved limb [CI95% = (-80.1 cm, -34.9 cm)], compared to the uninvolved limb.
There was not a main effect of group for any of the vari ables of interest (p ≥ 0.12).
The purpose of this study was to compare inter-limb asym metry in dynamic balance and hop performance for athletes with and without a history of concomitant meniscal injury As hypothesized, the degree of interlimb asymmetry in dy namic balance and hop performance was similar among athletes with isolated ACL tears and athletes with concomi tant meniscal injuries who had undergone meniscal repair or partial meniscectomy. Each group of athletes (isolated ACL tear, meniscal repair, partial meniscectomy) exhibited deficits in dynamic balance and hop performance for their involved limb, vs. their uninvolved limb (main effect of limb). In general, it appears that deficits in dynamic bal ance and hop performance following ACL reconstruction are not dependent on meniscal injury history
A previous study by Clagg et al.13 also compared Y-Bal ance Test performance at the time of return to sport (av erage of 6.7 months after ACL reconstruction) for athletes with isolated ACL tears vs. those with concomitant menis cal injuries. Although the investigators did not examine in ter-limb symmetry, their results were generally consistent
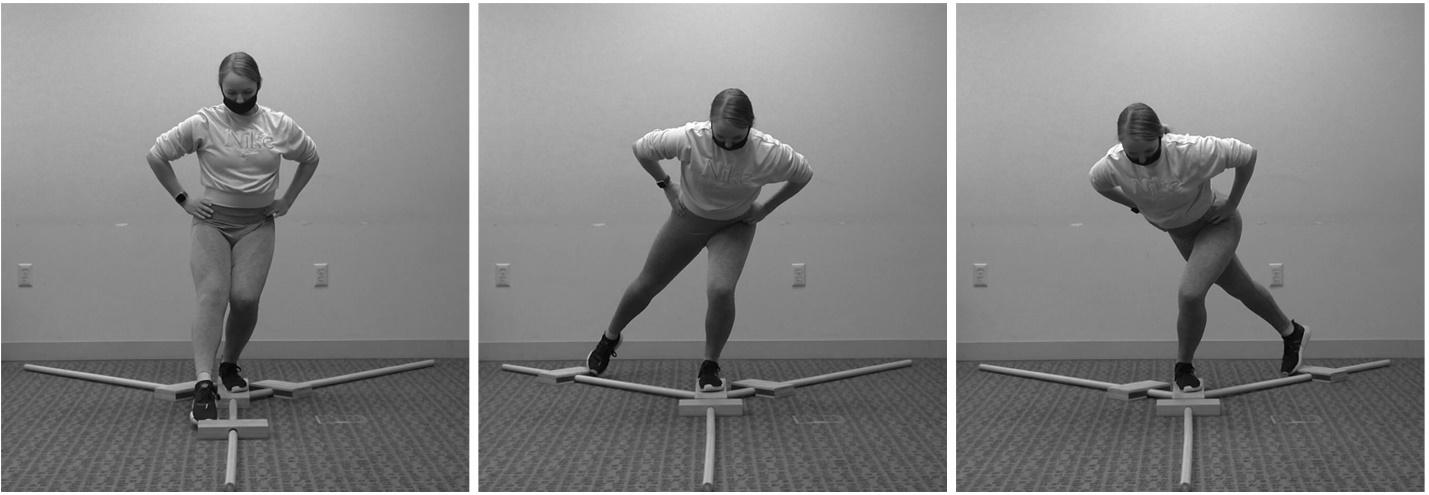
Table 1. Characteristics of the athletes in the isolated ACL tear, meniscal repair, and partial meniscectomy groups.
Isolated ACL tear Meniscal Repair Partial Meniscectomy
Number of athletes 19 9 6
Injured limb (right/left) 8/11 4/5 4/2
Gender (male/female) 9/10 4/5 4/2 Age (years) 16.7 ± 1.5 16.3 ± 1.0 16.5 ± 0.6
Days since surgery 196 ± 41 (151-315) 233 ± 58 (166-327) 164 ± 8 (156-174)
Mean ± standard deviation for age and days since surgery Minimum and maximum number of days since surgery is also reported (minimum-maximum)
Figure 2. Mean (± 95% confidence interval) limb symmetry index values based on the Y-Balance Test distances (anterior, posteromedial, and posterolateral directions) for the athletes in the isolated ACL tear (black), meniscal repair (grey), and partial meniscectomy (white) groups. Limb symmetry index values less than 100% reflect worse performance for the involved limb, compared to the uninvolved limb.
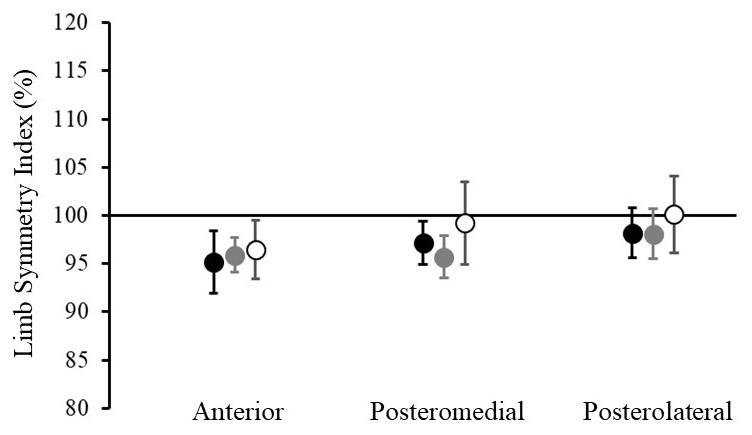
with those of the current study, as they found no signifi cant differences in involved-limb anterior, posteromedial, or posterolateral Y-Balance Test reach distances for ath letes with isolated ACL tears vs. those with concomitant meniscal injuries. Considering the results reported by Clagg et al.,13 as well as those of the current study, it does not appear that deficits in dynamic balance differ for athletes with and without a history of concomitant meniscal in jury While Clagg et al.13 reported the average single hop test and triple hop test distances for their entire cohort of athletes, they did not compare hop performance based on meniscal injury history They also did not differentiate between athletes who had undergone meniscal repairs vs. those who had undergone partial meniscectomies, as they grouped these athletes together in their analysis.
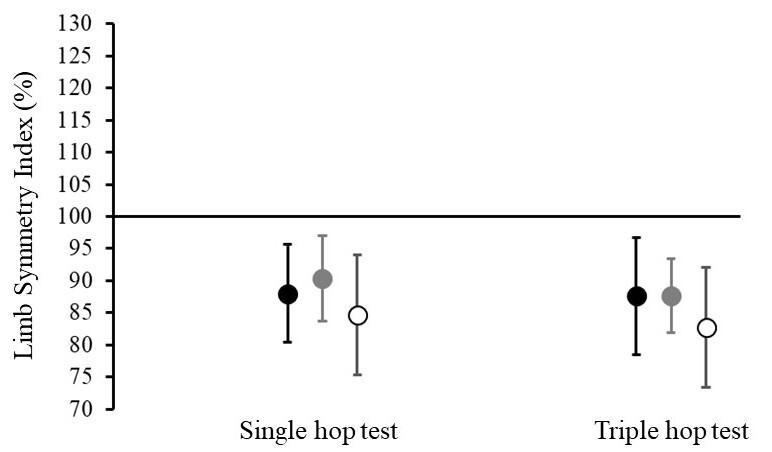
Figure 3. Mean (± 95% confidence interval) limb symmetry index values based on the hop test distances for the athletes in the isolated ACL tear (black), meniscal repair (grey), and partial meniscectomy (white) groups. Limb symmetry index values less than 100% reflect worse performance for the involved limb, compared to the uninvolved limb.
The results of this study suggest that athletes who have undergone ACL reconstruction exhibit deficits in dynamic balance at the time of return-to-sport testing, regardless of their meniscal injury history. In addition to their role in distributing axial joint loads, the menisci provide passive mechanical stability to the knee, contributing secondary re straint to tibial translations both anteriorly and posteri orly 20–22 The lack of an association between meniscal in jury history and dynamic balance impairments in this study suggests these deficits may be related more to general neu romuscular factors than residual mechanical insufficiency of the involved limb. It has long been known that detri ments to neuromuscular performance and limb asymme tries persist for years after ACL reconstruction and con tribute to risk of future injury 11,32 However, the addition of rehabilitation techniques targeting these neuromuscular factors, such as perturbation training, has not resulted in consistent/significant improvements in functional out comes or return to sport success rates.33 While a longer course of rehabilitation may be effective in mitigating in jury risk and improving achievement of evidence-based re turn to sport criteria,34 an extended return-to-sport time line may not be a satisfactory solution to many athletes. Thus, further research into emerging/novel surgical and rehabilitation techniques that specifically preserve or en hance neuromuscular function is needed. For example, transcranial direct current stimulation has the potential to impact corticospinal activity and may provide a means to maintain or improve neuromuscular function over the course of recovery after injury or surgical intervention.35
Additionally, surgical repair techniques that seek to pre serve native ACL tissue, and potentially the neural ele ments of the ligament, may allow for greater natural restoration of neuromuscular function. Early studies of techniques such as the bridge-enhanced ACL reconstruc tion36 or other similar approaches have shown promise in the short term.37
While these techniques continue to develop, it is im portant to recognize there are long-standing treatment ap proaches with strong evidence that could be examined within a broader neuromuscular context. For instance, elec trical stimulation is strongly recommended to enhance quadriceps strength in the latest clinical practice guidelines from the Orthopedic Section of the American Physical Therapy Association.38 However, studies of patients with neurologic disorders have demonstrated the value of func tional electrical stimulation to enhance the neural repre sentation of a limb within the central nervous system.39 Given that similar neurophysiologic and neurocognitive deficits have been demonstrated in individuals with ACL in jury,40 use of electrical stimulation, in combination with more conventional rehabilitation components (e.g. tar geted strengthening, active isometric muscle contraction), should be considered as a standard of care for more than restoration of simple muscular strength. In addition to aug mented sensorimotor stimulation, the environmental con text and cognitive-attentional demands of functional and sport-specific tasks should be considered in the rehabilita tion plan. A graded exposure approach to the neurophys iologic and neurocognitive demands of patients’ activities may prove to be the most salient, cost-effective means to restoration of multi-system neuromuscular function.41
As with any study, it is important to consider the limi tations of this work. First, it should be noted that the cur rent study did not consider the extent or location of menis cal injury. This was also a limitation noted by Clagg et al.13 Future studies should examine how the nature/extent of meniscal injury affects neuromuscular performance. In ad dition, the effect of graft type was not examined as part of this study. Previous studies have compared neuromuscular performance among athletes who received different types of grafts6,13; however, the findings from these studies have been somewhat inconsistent. Also, it is important to note that clinical measures of dynamic balance and hop distance may not be sensitive to subtle differences in postural stabil ity and movement performance. Future studies should con sider applying more advanced instrumentation to identify more subtle differences in postural stability and movement control/performance. The relatively low number of athletes (n = 6) who underwent partial meniscectomy should also be considered as a limitation. Although not necessarily sur
prising, since surgeons typically aim to repair the meniscus when possible, the low number of athletes in this group may have limited our ability to detect subtle between-group differences in dynamic balance and/or hop performance.
Finally, it is worth noting the variability in when athletes were tested (ranging from 5-11 months post-surgery). Dy namic balance and hop test data were recorded at the point of return-to-sport testing, which is typical for studies of this nature.13 Since athlete’s progress through rehabilita tion at different rates, this resulted in significant variability in the time from surgery to return-to-sport testing. The reason for comparing performance at the point of returnto-sport testing was to ensure that athletes were at a sim ilar stage of recovery, even though they were not neces sarily at the same time post-surgery An alternative would have been to compare performance at a consistent time point (e.g. five months post-surgery); however, this would be problematic since athletes would be at different phases in their rehabilitation (e.g. some would be preparing to re turn-to-sport, while others would be just beginning to ini tiate landing/jumping tasks). Regardless, it is interesting to note the variability among athletes with respect to their re turn-to-sport timeline.
The results of this study indicate that adolescent athletes who have undergone ACL reconstruction exhibit deficits in dynamic balance and hop performance for their involved limb, even after completing post-operative rehabilitation. The results of this study also suggest that the magnitude of the inter-limb asymmetries in dynamic balance and hop performance are not dependent on meniscal injury history
The authors have no conflicts of interest to report.
The authors would like to thank their partners at Lutheran Hospital and Optimum Performance Therapy for supporting this work.
Submitted: March 02, 2022 CST, Accepted: September 12, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139(3):e20161877 doi:10.1542/peds.2016-1877
2. Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and metaanalysis. Am J Sports Med. 2016;44(10):2716-2723. do i:10.1177/0363546515617742
3. Carey JL, Shea KG. AAOS Clinical practice guideline: Management of anterior cruciate ligament injuries evidence-based guideline. J Am Acad Orthop Surg 2015;23(5):e6-e8. doi:10.5435/jaaos-d-15-00095
4. Barber-Westin S, Noyes FR. One in 5 athletes sustain reinjury upon return to high-risk sports after ACL reconstruction: a systematic review in 1239 athletes younger than 20 years. Sports Health. 2020;12(6):587-597 doi:10.1177/1941738120912846
5. Cervenka JJ, Decker MN, Ruhde LA, Beaty JD, Ricard MD. Strength and stability analysis of rehabilitated anterior cruciate ligament individuals. Int J Exerc Sci 2018;11(1):817-826.
6. Sugimoto D, Heyworth BE, Brodeur JJ, Kramer DE, Kocher MS, Micheli LJ. Effect of graft type on balance and hop tests in adolescent males following anterior cruciate ligament reconstruction. J Sport Rehabil. 2019;28(5):468-475. doi:10.1123/jsr.2017-0244
7 Sugimoto D, Howell DR, Micheli LJ, Meehan WP Single-leg postural stability deficits following anterior cruciate ligament reconstruction in pediatric and adolescent athletes. J Pediatr Orthop B 2016;25(4):338-342. doi:10.1097/bpb.0000000000000 276
8. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968-1978. doi:10.1177/03635465103760 53
9. Stiffler MR, Bell DR, Sanfilippo JL, Hetzel SJ, Pickett KA, Heiderscheit BC. Star excursion balance test anterior asymmetry is associated with injury status in division I collegiate athletes. J Orthop Sports Phys Ther. 2017;47(5):339-346. doi:10.2519/jospt.201 7.6974
10. Mohammadi F, Salavati M, Akhbari B, Mazaheri M, Mohsen Mir S, Etemadi Y Comparison of functional outcome measures after ACL reconstruction in competitive soccer players: a randomized trial. J Bone Joint Surg Am 2013;95(14):1271-1277. doi:10.2106/jbjs.l.00724
11. Orishimo KF, Kremenic IJ, Mullaney MJ, McHugh MP, Nicholas SJ. Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2010;18(11):1587-1593. doi:10.1007/s00167-010-118 5-2
12. Thomeé R, Neeter C, Gustavsson A, et al. Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2012;20(6):1143-1151. doi:10.1007/s00167-012-191 2-y
13. Clagg S, Paterno MV, Hewett TE, Schmitt LC. Performance on the modified star excursion balance test at the time of return to sport following anterior cruciate ligament injury J Orthop Sports Phys Ther 2015;45(6):444-452. doi:10.2519/jospt.2015.5040
14. Myers H, Christopherson Z, Butler RJ. Relationship between the lower quarter Y-Balance Test scores and isokinetic strength testing in patients status post ACL reconstruction. Intl J Sports Phys Ther 2018;13(2):152-159. doi:10.26603/ijspt2018015 2
15. Norte GE, Solaas H, Saliba SA, Goetschius J, Slater LV, Hart JM. The relationships between kinesiophobia and clinical outcomes after ACL reconstruction differ by self-reported physical activity engagement. Phys Ther Sport 2019;40:1-9. doi:10.1016/j.ptsp.2019.08.0 02
16. Paterno MV, Flynn K, Thomas S, Schmitt LC. Self reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Sports Health. 2018;10(3):228-233. doi:10.1177/1941738117745806
17 Christino M, Willimon SC, Perkins C, Schaafsma B, Busch M. The rate of meniscus tears in association with anterior cruciate ligament injuries increases with age. Orthop J Sports Med 2019;7(3).
18. Hagino T, Ochiai S, Senga S, et al. Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg 2015;135(12):1701-1706. d oi:10.1007/s00402-015-2309-4
19. Mitchell JJ, Cinque ME, Dornan GJ, et al. Primary versus secondary revision anterior cruciate ligament reconstruction: patient demographics, radiographic findings, and associated lesions. Arthroscopy. 2018;34(3):695-703. doi:10.1016/j.arthro.2017.08.305
20. Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SLY Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res 2000;18(1):109-115. doi:10.1002/jor.1100180116
21. Flandry F, Hommel G. Normal anatomy and biomechanics of the knee. Sports Med Arthrosc Rev. 2011;19(2):82-92. doi:10.1097/jsa.0b013e318210c0aa
22. Masouros SD, McDermott ID, Amis AA, Bull AM. Biomechanics of the meniscus-meniscal ligament construct of the knee. Knee Surg Sports Traumatol Arthrosc 2008;16(12):1121-1132. doi:10.1007/s0016 7-008-0616-9
23. Adolescent Health. World Health Organization. ht tps://www who.int/health-topics/adolescent-health#t ab=tab_1
24. Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med 1991;19(5):513-518. doi:10.1177/0363546 59101900518
25. Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides and reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87(3):337-349. doi:10.2522/ptj.20060143
26. Reinke EK, Spindler KP, Lorring D, et al. Hop tests correlate with IKDC and KOOS at minimum of 2 years after primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2011;19(11):1806-1816. doi:10.10 07/s00167-011-1473-5
27. Plisky PJ, Gorman PP, Butler RJ, et al. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther. 2009;4(2):92-99.
28. Picot B, Terrier R, Forestier N, Fourchet F, McKeon PO The star excursion balance test: an update review and practical guidelines. Int J Athl Ther Train 2021;26(6):285-293. doi:10.1123/ijatt.2020-010
6
29. Cuğ M. Stance foot alignment and hand positioning alter star excursion balance test scores in those with chronic ankle instability: what are we really assessing? Physiother Theory Pract. 2017;33(4):316-322. doi:10.1080/09593985.2017.1302 028
30. Hébert-Losier K. Clinical implications of hand position and lower limb length measurement methods on Y-Balance Test scores and interpretations. J Athl Train. 2017;52(10):910-917. do i:10.4085/1062-6050-52.8.02
31. Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study Sports Health 2013;5(5):417-422. doi:10.1177/ 1941738113498703
32. Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med 2008;27(3):405-424. doi:10.1016/j.csm.2008.02.001
33. Arundale AJH, Cummer K, Capin JJ, Zarzycki R, Snyder-Mackler L. Report of the clinical and functional primary outcomes in men of the ACL SPORTS trial: similar outcomes in men receiving secondary prevention with and without perturbation training 1 and 2 years after ACL reconstruction. Clin Orthop Relat Res 2017;475(10):2523-2534. doi:10.100 7/s11999-017-5280-2
34. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804-808. doi:10.1136/bjsports-2016-096 031
35. Rush JL, Lepley LK, Davi S, Lepley AS. The immediate effects of transcranial direct current stimulation on quadriceps muscle function in individuals with a history of anterior cruciate ligament reconstruction: a preliminary investigation. J Sport Rehabil. 2020;29(8):1121-1130. doi:10.1123/js r.2019-0179
36. Murray MM, Fleming BC, Badger GJ, et al. Bridgeenhanced anterior cruciate ligament repair is not inferior to autograft anterior cruciate ligament reconstruction at 2 years: results of a prospective randomized clinical trial. Am J Sports Med. 2020;48(6):1305-1315. doi:10.1177/036354652091353 2
37 Goto S, Hannon JP, Singleton SB, Dietrick L, Garrison C. Twelve week post operative joint loading between individuals with anterior cruciate ligament reconstruction vs repair. J Orthop Sports Phys Ther. 2022;52(1):CSM25-CSM54.
38. Logerstedt DS, Scalzitti D, Risberg MA, et al. Knee stability and movement coordination impairments: knee ligament sprain revision 2017. J Orthop Sports Phys Ther 2017;47(11):A1-A47 doi:10.2519/jospt.201 7.0303
39. Hoffman L, Field-Fote E. Effects of practice combined with somatosensory or motor stimulation on hand function in persons with spinal cord injury Top Spinal Cord Inj Rehabil. 2013;19(4):288-299. doi:1 0.1310/sci1904-288
40. Piskin D, Benjaminse A, Dimitrakis P, Gokeler A. Neurocognitive and neurophysiological functions related to ACL injury: a framework for neurocognitive approaches in rehabilitation and return-to-sports tests. Sports Health. 2021:19417381211029264.
41. Gokeler A, McKeon PO, Hoch MC. Shaping the functional task environment in sports injury rehabilitation: a framework to integrate perceptualcognitive training in rehabilitation. Athl Train Sports Health Care 2020;12(6):283-292. doi:10.3928/194258 64-20201016-01
Ivarsson A, Cronström A. Agreement Between Isokinetic Dynamometer and Hand-held Isometric Dynamometer as Measures to Detect Lower Limb Asymmetry in Muscle Torque After Anterior Cruciate Ligament Reconstruction. IJSPT. Published online November 1, 2022:1307-1317.
Angelica Ivarsson 1 a , Anna Cronström 1,2
1 Department of Health Sciences, Lund University, 2 Department of Community Medicine and Rehabilitation, Umeå University, Umeå, Sweden
Keywords: agreement, anterior cruciate ligament reconstruction, hand-held dynamometer, isokinetic dynamometer, limb symmetry index. https://doi.org/10.26603/001c.39798
Two commonly used instruments to assess muscle strength after anterior cruciate ligament reconstruction are the isokinetic dynamometer, which measures isokinetic torque and the hand-held dynamometer, which measures isometric torque. Isokinetic dynamometers are considered superior to other instruments but may not be commonly used in clinical settings. Hand-held dynamometers are small, portable, and more clinically applicable devices.
The purpose of this study was to assess agreement between a hand-held dynamometer and an isokinetic dynamometer, used to assess lower limb symmetry in knee muscle torque one year after anterior cruciate ligament (ACL) reconstruction.
Cross-sectional measurement study
Seventy-two participants who had undergone ACL reconstruction (35 men, 37 women; age= 25.8 ± 5.4 years) were included. Isokinetic muscle torque in knee flexion and extension was measured with an isokinetic dynamometer. Isometric flexion and extension knee muscle torque was measured with a hand-held dynamometer Bland & Altman plots and Cohen’s Kappa coefficient were used to assess agreement between measurements obtained from the instruments.
Bland & Altman plots showed wide limits of agreement between the instruments for both flexion and extension limb symmetry index. Cohen´s Kappa coefficient revealed a poor to slight agreement between the extension limb symmetry index values (0.136) and a fair agreement for flexion limb symmetry index values (0.236). Cross-tabulations showed that the hand-held dynamometer detected a significantly larger number of participants with abnormal flexion torque limb symmetry index compared to the isokinetic dynamometer.

The wide limits of agreements and Cohen’s Kappa coefficients values revealed insufficient agreement between the measurements taken with the two instruments,
a
Corresponding author: Angelica Ivarsson Department of Health Sciences, Lund University, Lund, Sweden angelica.ivarsson@skane.se, +4676 82 84 887
indicating that the instruments should not be used interchangeably The hand-held dynamometer was more sensitive in detecting abnormal limb symmetry index in flexion torque, which promotes the option of use of hand-held dynamometers to detect differences between the injured and uninjured leg after ACL reconstruction.
3b
Anterior cruciate ligament (ACL) injury is common in ath letes, and it is often followed by ACL reconstructions (ACLR). An ACLR is followed by an extensive rehabilitation period and one of the most important rehabilitation goals is to reach symmetric function and strength in the lower limbs.1,2 Limb asymmetry in strength and function after ACLR can predict an increased risk of reinjury, which in turn increases the risk of early post-traumatic knee os teoarthritis.3–6 Further, knee extensor muscle weakness has also been suggested to be associated with an increased risk of knee osteoarthritis development and progression.7,8 Thus, the results of limb symmetry tests are of great impor tance for clinicians in determining if a patient is fully reha bilitated or ready to return to sport (RTS). Limb symmetry index (LSI) is calculated by dividing the test scores of the injured limb with the uninjured limb multiplied by 100. LSI is typically used to calculate the level of symmetry between the two legs. A LSI >90% is considered satisfactory and is often a criterion before letting a patient RTS.9,10
There are a number of functional tests that can be con ducted to assess limb symmetry after ACLR. Hop tests, one of the most commonly used functional tests, assess differ ences in various hopping tasks between the injured and un injured leg.11,12 However, LSI measured with hop tests can be overestimated. Barford et al. confirmed this by deter mining that satisfactory LSI was reached significantly faster with hop tests than with knee extensor muscle symmetry tests.13 In another study Nagai et al. suggest that mus cle strength tests are a better method to evaluate LSI af ter ACLR since hop tests often result in higher LSI values compared to leg press tests and isokinetic muscle strength tests.14
To assess LSI in muscle strength, different measurement instruments can be used. Hand-held dynamometers (HHD) and isokinetic dynamometers (IKD) are commonly used. IKDs are advanced computerized machines measuring iso kinetic muscle torque (as a proxy for strength) and HHDs are small portable devices used to measure isometric mus cle torque (also as a proxy for strength).15,16
IKDs are considered superior compared to other instru ments to assess muscle strength, however they are both space-consuming and expensive, therefore are not very common in clinics. HHDs, on the other hand are cost-ef fective, small, and clinically applicable. Previous authors have established the reliability and validity of IKDs and HHDs.16–19 In a systematic review and meta-analysis Chamorro et al. established the reliability and concurrent validity of a HHD and IKD in measuring muscle strength in the knee, hip, and ankle joint. Their results revealed
low reliability for knee extension and ankle plantar flexion strength when measured with an HHD. Additionally, the re sults showed a high correlation between the measurements from the instruments for hip strength values and a moder ate correlation for knee and ankle strength values.16 Lesnak et al. assessed the agreement between the two instruments measuring isometric quadricep strength in a healthy popu lation. Their results showed that the HHD produced higher peak torque strength values as compared to those from the IKD 17 In a more recent study, Hirano et al. established high validity (r=0.78) and intra-rater reliability comparing the results of knee extension muscle strength measured with a belt stabilized HHD to an IKD (ICC1,1≥0.75).18 However, Toonstra et al. concluded that significant differences were found in peak torque strength values observed between iso metric knee flexion and extension measured using IKD and HHD 19
To the knowledge of the authors, no previous studies have assessed agreement or sensitivity in detection of ab normal LSI between LSI values calculated from isokinetic strength tests measured with an IKD and isometric strength tests measured with an HHD. Isokinetic strength measures are commonly used in research while HHDs are more com monly used clinically, highlighting the importance of com paring these instruments. In addition, the instruments should be studied in subjects who have undergone ACLR, as this a patient group where lower limb strength tests are fre quently used to assess both progress in rehabilitation and to make clinical decisions regarding RTS. Thus, the purpose of this study was to assess agreement between a hand-held dynamometer and an isokinetic dynamometer, used to as sess lower limb symmetry in knee muscle torque one year after ACLR. In addition, the authors investigated which of these two instruments was superior in detecting limb asym metry It was hypothesized that the agreement between the two types of strength measurements is low and that the IKD would be superior in detecting individuals with an LSI <90.
A cross-sectional study assessing agreement between two different measurement instruments adhering to the STROBE guidelines (https://www.strobe-statement.org/).
This study is an explorative analysis of baseline data from an ongoing prospective cohort study aiming to assess the correlation between lower limb function and early post traumatic osteoarthritis after ACLR.20 Participants were
consecutively recruited from the department of orthope dics, Skåne University Hospital. All patients who had un dergone an ACLR during the time period January 2017 Feb ruary 2019 were asked to participate via letter. Inclusion criteria were i) one year (10-16 months) after ACLR, with or without associated injuries to other knee structures, ii) age between 18-35 years. Exclusion criteria were i) previous se rious injury or surgery to either knee, ii) other diseases or disorders affecting lower extremity function (e.g., hernia). The present study has received ethical approval from the Swedish Ethical Review Board (Dnr 2017/916). The partic ipants received a letter with information of the study and gave their written consent before participating in the study. All participants were informed that they were allowed to cancel their participation in the study at any time.
Baseline data for the prospective cohort study was collected between March 2018 and March 2020. One physiotherapist (AC) collected all data. Demographic data (age, height, weight, type of ACL graft) was collected prior to the testing. Before executing the tests, all participants performed a five-minute warm up on an ergometer bicycle. The HHD torque measures were performed first and then the IKD as sessments for all participants, allowing for a rest period of at least five minutes in between.
Isometric knee extension torque was measured with a HHD (Power Track II Commander Echo; JTECH Medical, Salt Lake City, Utah, USA) with the participants sitting on a treat ment table with their knee in 90° flexion and their thighs fixated to the treatment table with a strap. Another strap was used around the leg of the treatment table and the HHD, which was placed on the anterior side of the partic ipants’ distal tibia. The participants were asked to extend their knee with maximal effort.
Isometric knee flexion torque was tested with the par ticipants laying on their stomach on a treatment table with their knee in 90° flexion. The examiner was sitting on the end of the table with a strap around the pelvis and around the HHD placed on the posterior side of the participants’ distal tibia. The pelvis and the leg that was not being tested were fixated to the treatment table with two straps. The participants were asked to flex their knee with maximal ef fort. When testing isometric extension and flexion torque with the HHD each test was repeated three times and the participants were asked to hold each maximal contraction for five seconds with 15 seconds of recovery between the contractions. The peak torque (N) of three measurements with each leg was collected and then normalized to body mass (N/kg*100). To randomize and avoid learning affects the right leg was always tested first.20
Isokinetic concentric torque in knee flexion and knee ex tension was measured in 60 degrees/sec with a Biodex
(Medical Systems, Shirley, New York) with the participants in a sitting position with their arms across their chest. The chest, pelvis and thigh were secured with straps. The Biodex was calibrated before each test and the starting po sition of the knee was 90° flexion. The test was performed in a range of motion of 0-90° knee flexion. Four trial repe titions were performed with submaximal effort. After this, the participants performed five maximal contractions with each leg, starting with the non-injured leg. The peak value of the five trials for each leg was recorded. The measure ments were presented as peak torque, expressed in New ton-meters (Nm) and then normalized to body mass, (peak torque divided by the participants’ body weight in kg (Nm/ kg)).
Descriptive statistics with mean and standard deviation was used for presentation of demographic data such as weight, height, age, and body mass index (BMI). Analysis of agree ment was performed in The Statistical Package for Social Sciences (SPSS), (Version 26.0 IBM Corp). Normalized peak torque values of extension and flexion strength of the in jured and uninjured leg were used to calculate LSI.
Bland & Altman plots with 95% limits of agreement (LOA) (average difference between measurement instru ments ± 1.96 x SD of the difference) and Cohen’s Kappa co efficient were used to assess agreement between the two measurement methods. The results of Bland & Altman plots give a visual representation of the difference between the mean of two different measurement methods used on the same subject, which in this case is the IKD and HHD, and shows systematic differences.21 The following thresh olds for Cohen’s Kappa coefficient were used; <0.00 no agreement, 0.00-0.20 poor to slight agreement, 0.21-0.40 fair agreement, 0.41-0.60 moderate agreement, 0.61-0.60 substantial agreement, 0.81-1.00 almost perfect agree ment.22
To measure which instrument was superior in detecting lower limb asymmetry in muscle strength the participants were divided into two different groups. One group included the participants with a LSI≥90% and the other group in cluded participants with a LSI<90%. After this, cross tab ulations with abnormal LSI (LSI<90%) and normal LSI (LSI≥90%) were constructed. McNemars’s test was used to test the proportion of participants with normal versus ab normal LSI values for the HHD and IKD in flexion and ex tension strength. Statistical significance was set at p≤0.05.
Seventy-two (37 women; age= 25.8 ± 5.4 years), were in cluded in this study (Table 1 and Figure 1).
Of the 73 participants originally included, one of the participants experienced discomfort during the extension strength test with the HHD and did not proceed with this test but performed all flexion strength tests. Data for an other participant were lost for both knee flexion and exten sion strength due to technical problems with the Biodex,
Table 1. Participant characteristics (n=72)
Age (y), mean (SD) 25.8 (5.4)
Women (n), (%) 37 (51.4)
Height (cm) 174.0 (8.7)
Weight (kg) 75.7 (14.3)
BMI (kg/m2), mean (SD) 24.9 (4.0)
Injured knee n (%)
Left Right 22 (31) 50 (69)
Associated injuries n (%) Meniscal Cartilage Collateral ligament
Hamstring Patella Other
62 (86) 52 (69) 14 (18) 21 (28)
62 (86) 9 (13) 1 (1)
Time since ACLR (months), mean (SD) 12.3 (1.4)
y years, SD standard deviation, n number of participants, BMI body mass index
leaving 72 (flexion strength) and 71 (extension strength) participants, respectively, for the analysis.
Overall, the participants had a higher mean peak torque value in their uninjured leg compared to their injured leg in both isokinetic and isometric strength. Generally, the peak torque value measured with the IKD was higher than the peak torque value measured with the HHD The mean LSI measured with the HHD was 75.3 % for flexion and 94,6% for extension. The mean LSI measured with the IKD was 91.3% for flexion and 87,7% for extension (Table 2).
The Bland & Altman plots for both extension and flexion LSI-values revealed wide limits of agreement (Figures 2 and 3). Cohen’s Kappa coefficient was low for both extension Figure 1. Flow chart of participants
LSI values (0.136) and for flexion LSI values (0.236) indicat ing a poor to slight respectively a fair agreement between the instruments.
The cross tabulations showed that the HHD detected sig nificantly more participants with abnormal flexion torque LSI compared to the IKD (59 vs 35, p<0.001) (Table 3) whereas there was no statistically significant difference for extension torque LSI (HHD 29, IKD 38, p=0.150) (Table 4).
The purpose of this explorative analysis was to assess mea surement agreement between an IKD and a HHD, used to detect lower limb asymmetry in flexion and extension knee muscle torque after ACLR. In addition, the aim was to in vestigate which of these two instruments was superior in detecting lower limb asymmetry In support of the hypoth esis, the results of this study showed that the measurement agreement between the instruments is low, indicating that the HHD and IKD should not be used interchangeably. In addition, contrary to the hypothesis, the HHD detected a significantly larger number of participants with abnormal flexion LSI than the IKD
The different types of strength, at different angles that the instruments measure may explain the low agreement between the LSI values. As previously mentioned, the IKD measures isokinetic torque whereas the HHD measures iso metric torque. Isokinetic torque is assessed during a con traction of the muscles at a constant speed in a specific ROM, implying that the muscle length is changing. Isomet ric torque is a static strength assessment inferring that the muscle remains contracted at specific joint angle and the length of the muscle does not change.15,16,23 Since peak torque (strength) values were the values used to calculate

Table 2. Mean peak torque value (SD/SE) (% of body weight) for injured leg (inj) and uninjured leg (uninj), mean difference (diff) in peak torque value (with 95% CI) between injured and uninjured leg. Mean of limb symmetry index (LSI, %) of torque measured with HHD and IKD, mean difference between HHD LSI-values and IKD LSIvalues.
Peak torque HHD Inj
Mean (SD/SE)
Peak torque HHD Uninj Mean (SD/SE)
Peak torque IKD Inj Mean (SD/SE)
Peak torque IKD Uninj Mean (SD/SE)
Injured vs uninjured HHD Mean diff (95% CI)
Injured vs uninjured IKD Mean diff (95% CI)
LSI% HHD Mean (SD/SE)
LSI% IKD Mean (SD/SE)
HHD vs IKD (%) Mean diff (95% CI)
Flexion 62.8 (21.6/ 2.5) 83.0 (18.7/ 2.2) 111.0 (29.6/ 3.5) 121.4 (26.5/ 3.2) -45.3 (-61.4;-31.2) -10.4 (-19.6;-1.2) 75.3 (17.1/ 2,0) 91.3 (12.5/ 1.5) -16.0 (-21.0;11.1)
Extension 182.0 (54.3/ 6.4) 197.3 (64.7/ 7.6) 194.7 (58.1/ 6.8) 222.1 (58.1/ 6.8) -29.7 (-75.4;16.1) -30.3 (-49.4;-11.2) 94.6 (18.8/ 2.2) 87.7 (20.9/ 2.5) 6.9 (0.3;13.5)
SD standard deviation, SE standard error, CI confidence interval, HHD hand-held dynamometer, IKD isokinetic dynamometer
Figure 2. Bland and Altman plot with 95% limits of agreement (LOA) for limb symmetry index (LSI) of extension muscle torque.
The differences in LSI between muscle torque measured with a HHD and an IKD plotted against their mean LSI. Mean difference 6.92 (95% LOA -42.60 to 56.44).
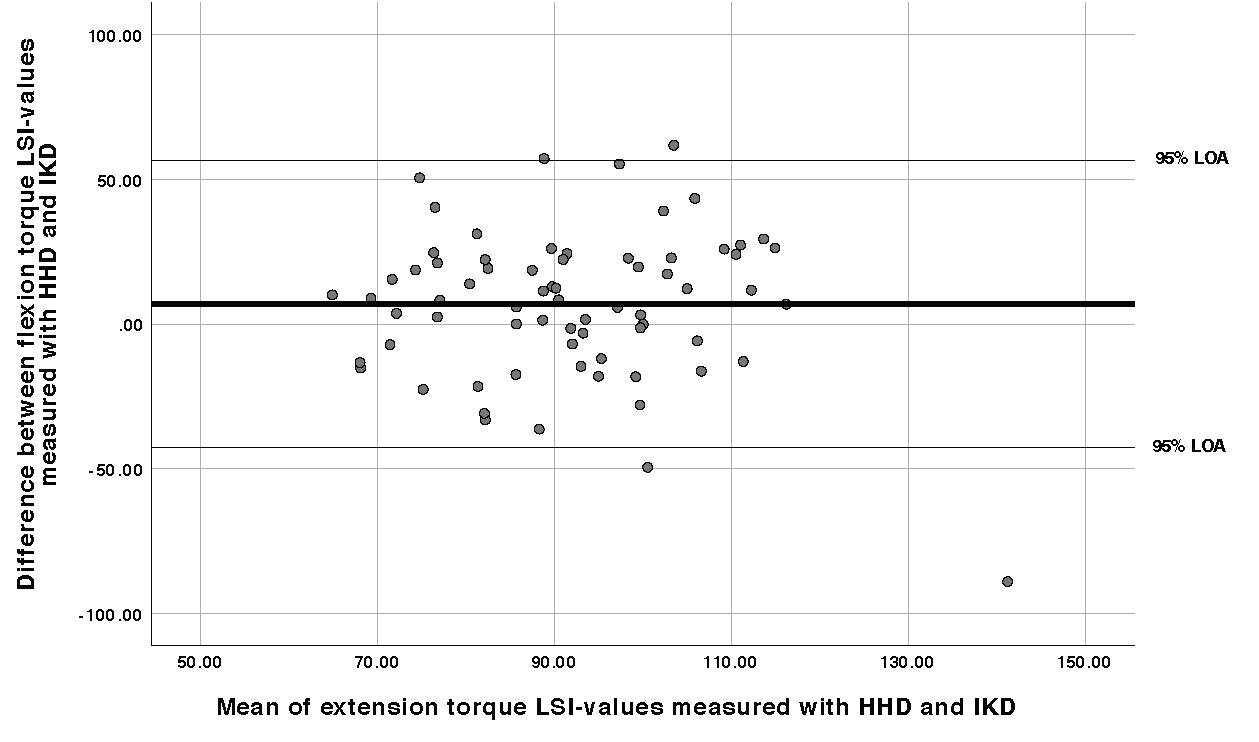
LSI in this study, it is most likely that the isokinetic mus cle torque peak torque value was reached at different joint angles (between 0-90° flexion) in the knee joint. On the contrary, the isometric flexion and extension torque was only tested at 90° of flexion in the knee joint. Emami et al. found that isometric flexion torque measured at 90° and 100° of flexion was significantly reduced (compared prior to surgery) one year after ACLR. The same study showed that flexion torque was not significantly reduced at 20° and 45° of flexion.24 This is also supported by the mean peak torque value presented in this study, since the HHD measurements reveled generally lower peak torque value in both flexion and extension strength. This may imply that if the isomet ric torque would have been tested at different angles and the highest peak torque value across the range would be used in the data analysis of this study it could have affected the LSI value and thus, also the agreement between the in struments.
In this study, agreement and sensitivity for both knee flexion and knee extension torque were assessed. Several studies and systematic reviews have concluded that weak ness in extensor muscles is associated to development of osteoarthritis, reduced quality of life and functional dis abilities, highlighting the importance of regaining extensor strength after ACLR.7,25,26 In Sweden the majority of pa tients undergoing ACLR receive a hamstring tendon graft.27 Studies show that patients who receive a hamstring graft have a remaining weakness in flexion strength two years af ter ACLR.28–30 Taken together, this emphasizes the impor tance of detecting both knee extension and flexion strength deficits after ACLR. The results of this study revealed that the HHD detected almost twice as many participants with
abnormal flexion strength LSI compared to the IKD, whereas there was no significant difference between the in struments for extension strength LSI. These results high light the potential use of isometric measurement instru ments to assess knee flexion torque asymmetries in ACLR patients
As discussed above, the IKD is popular, especially in sports medicine and research.16 One reason that the IKD is considered superior to the HHD is that IKDs are not af fected by the strength differences between the patient and the examiner holding the dynamometer 31 Further, the IKD has been criticized since patients do not always reach max imum strength performance in the IKD if they are not fa miliar with the equipment and know how it works.32 Other limitations with the IKD include the costs and the limited availability in clinics.33 However, although both instru ments have limitations, the high incidence of ACL re-in juries imply that the functional tests are not sufficient to assure readiness to RTS. Muscle strength tests could thus be a good complement to the functional tests.34,35 The re sults of the current study showed that the HHD at 90° of knee flexion identified more patients with abnormal flex ion LSI one year after ACL and promote the clinical use of HHDs. Further studies may reveal if there are any strength measures that are superior in detecting deficits in knee ex tension LSI.
One of the strengths of this study is the large sample which increases the chance of accurate results.20 Another strength of this study is that the same researcher performed
Figure 3. Bland and Altman plot with 95% limits of agreement (LOA) for limb symmetry index (LSI) of flexion muscle torque.
The differences in LSI between muscle torque measured with a HHD and an IKD plotted against their mean LSI. Mean difference -16.01 (95% LOA -51.19 to 19.17)

Table 3. Cross tabulation of the proportion of normal LSI (LSI>90%) and abnormal LSI (LSI<90%) between the two measurement methods (HHD and IKD) measuring flexion torque.
LSI Flexion torque IKD Total LSI<90% LSI>90%
LSI Flexion torque HHD LSI<90% LSI>90% 33 2 26 11 59 13
Total 35 37 72
LSI Limb symmetry index, HHD hand-held dynamometer, IKD isokinetic dynamometer
Table 4. Cross tabulation of the proportion of normal LSI (LSI>90%) and abnormal LSI (LSI<90%) between the two measurement methods (HHD and IKD) measuring extension torque.
LSI Extension torque IKD Total LSI<90% LSI>90%
LSI Extension torque HHD LSI<90% LSI>90% 18 20 11 22 29 42
Total 38 33 71
LSI Limb symmetry index, HHD hand-held dynamometer, IKD isokinetic dynamometer
all data collection to avoid inter-rater variability Further, in contrast to other studies, the current study compared muscle strength LSI values in injured subjects who went through ACLR. Previous studies have only compared peak torque strength values in healthy subjects. To assess which instruments should be used clinically for strength assess ment in ACLR rehabilitation it is important that they have been tested in participants who have undergone ACLR.
One major limitation of this study is that agreement between two instruments that measures different types of strength (isometric vs. isokinetic) was assessed. This may imply that there may not be a good agreement between the two instruments. However, in this study LSI values were used in the data analysis for agreement. The LSI values are independent of both demographic factors and what type of strength that is tested since the variable is a ratio between the participants’ injured and uninjured leg. This means that
it is not the instruments per se that are compared against each other, but the LSI values. Also, to avoid bias associated with gravitational forces,36,37 only isometric torque at 90° of knee flexion was assessed, which may have contributed to the poor agreement between measurements. It may fur ther be argued that 90° of knee flexion is not a functional position with regards to knee injury risk.38 Although, in a recent study Beere et al. confirmed that testing isomet ric quadriceps strength with a dynamometer is dependent on the angle of the knee joint and that quadricep strength should be tested in either 90° or 30° of flexion to detect asymmetries similar to the IKD,39 future studies investi gating if strength deficits, assessed in 90° of knee flexion, are associated with relevant outcomes, such as RTS and risk of second injuries are warranted. Due to practical reasons, isometric knee flexion torque was assessed in a prone po sition, whereas the isokinetic knee flexion torque was as sessed in a seated position, according to the IKD standard ization. Although a prone position is proposed to be more functional,40 the difference in testing position may consti tute another reason for the lack of agreement in the current study.
Furthermore, LSI presumes that the strength and func tion in the uninjured leg corresponds to the patient’s strength and function in the injured leg before the ACL in jury However, the ACL injury may also affect the strength and function of the uninjured limb due to general decon ditioning and/or arthrogenic muscle inhibition.41,42 It is therefore possible that the LSI is overestimated when as sessing lower limb muscle strength. However, studies show that patients who return to sport before they have reached a satisfactory LSI have an increased risk of early develop
ment of osteoarthritis and lower self-perceived function in the knee, implying that LSI, despite criticism, is a useful measure.43,44 Finally, since this was an exploratory analysis of an ongoing longitudinal trial, no a priori power calcula tion was performed. However, since the sample size in the current study is more than twice the recommended sample size of 32 participants for agreement studies,45 the sample should be adequate for the purpose of this study
The wide limits of agreements and low Cohen’s Kappa co efficients in this study, indicate a poor agreement between IKD and HHD implying that the instruments should not be used interchangeably for measurements of strength after ACLR. The hand-held dynamometer at 90° of knee flexion was more sensitive in detecting abnormal limb symmetry index in knee flexion strength. However, future research is needed to determine which type of instrument is superior in detecting deficits in knee extension strength and if strength deficits in 90° of knee flexion are associated with relevant ACLR outcomes, such as RTS and re-injury risk.
The authors report no conflicts of interest related to this manuscript
Submitted: May 06, 2022 CST, Accepted: September 11, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Kruse LM, Gray B, Wright RW Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(19):1737-1748. doi:10.2106/jbjs.k.01246
2. Hughes G, Musco P, Caine S, Howe L. Lower limb asymmetry after anterior cruciate ligament reconstruction in adolescent athletes: A systematic review and meta-analysis. J Athl Train 2020;55(8):811-825. doi:10.4085/1062-6050-0244-19
3. Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc 2015;47(7):1426-1434. doi:10.1249/mss.00000000000 00560
4. Shimizu T, Samaan MA, Tanaka MS, et al. Abnormal biomechanics at 6 months are associated with cartilage degeneration at 3 years after anterior cruciate ligament reconstruction. Arthroscopy 2019;35(2):511-520. doi:10.1016/j.arthro.2018.07.033
5. Tourville TW, Jarrell KM, Naud S, Slauterbeck JR, Johnson RJ, Beynnon BD Relationship between isokinetic strength and tibiofemoral joint space width changes after anterior cruciate ligament reconstruction. Am J Sports Med 2014;42(2):302-311. doi:10.1177/0363546513510672
6. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and metaanalysis. Am J Sports Med 2016;44(7):1861-1876. do i:10.1177/0363546515621554
7. Øiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23(2):171-177 doi:10.1016/j.joca.2014.10.008
8. Dell’isola A, Wirth W, Steultjens M, Eckstein F, Culvenor AG. Knee extensor muscle weakness and radiographic knee osteoarthritis progression. Acta Orthop 2018;89(4):406-411. doi:10.1080/17453674.2 018.1464314
9. Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc 2000;8(2):76-82. doi:10.1007/s00 1670050190
10. Lawrence S, Killian C, Rundquist P, Jenkins W Measures of limb symmetry used for injury risk identification: What is normal? Br Journal Sports Med. 2017;51:347 doi:10.1136/2016097372162
11. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: A systematic review Orthop J Sports Med 2014;2(1):2325967113518305. doi:10.1177/2325 967113518305
12. Barber-Westin SD, Noyes FR. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review Phys Sportsmed 2011;39(3):100-110. doi:10.3810/psm.2011.09.1926
13. Barfod KW, Feller JA, Hartwig T, Devitt BM, Webster KE. Knee extensor strength and hop test performance following anterior cruciate ligament reconstruction. Knee. 2019;26(1):149-154. doi:10.101 6/j.knee.2018.11.004
14. Nagai T, Schilaty ND, Laskowski ER, Hewett TE. Hop tests can result in higher limb symmetry index values than isokinetic strength and leg press tests in patients following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):816-822. doi:1 0.1007/s00167-019-05513-3
15. Osternig LR. Isokinetic dynamometry: implications for muscle testing and rehabilitation. Exerc Sport Sci Rev. 1986;14:45-80. doi:10.1249/00003 677-198600140-00005
16. Chamorro C, Armijo-Olivo S, De la Fuente C, Fuentes J, Javier Chirosa L. Absolute reliability and concurrent validity of hand held dynamometry and isokinetic dynamometry in the hip, knee and ankle joint: Systematic review and meta-analysis. Open Med (Wars) 2017;12(1):359-375. doi:10.1515/med-20 17-0052
17. Lesnak J, Anderson D, Farmer B, Katsavelis D, Grindstaff TL. Validity of hand-held dynamometry in measuring quadriceps strength and rate of torque development. Intl J Sports Phys Ther. 2019;14(2):180-187 doi:10.26603/ijspt20190180
18. Hirano M, Katoh M, Gomi M, Arai S. Validity and reliability of isometric knee extension muscle strength measurements using a belt-stabilized handheld dynamometer: a comparison with the measurement using an isokinetic dynamometer in a sitting posture. J Phys Ther Sci 2020;32(2):120-124. d oi:10.1589/jpts.32.120
19. Toonstra J, Mattacola CG. Test-retest reliability and validity of isometric knee-flexion and -extension measurement using 3 methods of assessing muscle strength. J Sport Rehabil. 2013;22(1). doi:10.1123/jsr.2 013.tr7
20. Cronström A, Risberg MA, Englund M, et al. Is good muscle function a protective factor for early signs of knee osteoarthritis after anterior cruciate ligament reconstruction? The SHIELD cohort study protocol. Osteoarthr Cartil. 2020;2(4):100102. doi:1 0.1016/j.ocarto.2020.100102
21. Altman DG, Bland JM. Measurement in medicine: The analysis of method comparison studies. J Stat 1983;32(3):307-317. doi:10.2307/2987937
22. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas 1960;20(1):37-46. doi:10.1 177/001316446002000104
23. Huang H, Guo J, Yang J, et al. Isokinetic anglespecific moments and ratios characterizing hamstring and quadriceps strength in anterior cruciate ligament deficient knees. Sci Rep 2017;7(1):7269. doi:10.1038/ s41598-017-06601-5
24. Emami Meybodi MK, Jannesari M, Rahim Nia A, Yaribeygi H, Sobhani Firoozabad V, Dorostegan A. Knee flexion strength before and after ACL reconstruction using hamstring tendon autografts. Trauma Mon 2013;18(3):130-133. doi:10.5812/traum amon.12813
25. Palmieri-Smith RM, Lepley LK. Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med 2015;43(7):1662-1669. doi:10.1177/ 0363546515578252
26. Morrissey MC, Hooper DM, Drechsler WI, Hill HJ. Relationship of leg muscle strength and knee function in the early period after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2004;14(6):360-366. doi:10.1046/j.1600-0838.2003.36 6.x
27. Persson A, Gifstad T, Lind M, et al. Graft fixation influences revision risk after ACL reconstruction with hamstring tendon autografts. Acta Orthop 2018;89(2):204-210. doi:10.1080/17453674.2017.1406
243
28. Nakamura N, Horibe S, Sasaki S, et al. Evaluation of active knee flexion and hamstring strength after anterior cruciate ligament reconstruction using hamstring tendons. Arthroscopy 2002;18(6):598-602. doi:10.1053/jars.2002.32868
29. Adachi N, Ochi M, Uchio Y, Sakai Y, Kuriwaka M, Fujihara A. Harvesting hamstring tendons for ACL reconstruction influences postoperative hamstring muscle performance. Arch Orthop Trauma Surg. 2003;123(9):460-465. doi:10.1007/s00402-003-0572-2
30. Elmlinger BS, Nyland JA, Tillett ED Knee flexor function 2 years after anterior cruciate ligament reconstruction with semitendinosus-gracilis autografts. Arthroscopy 2006;22(6):650-655. doi:10.1 016/j.arthro.2006.03.010
31. Martin HJ, Yule V, Syddall HE, Dennison EM, Cooper C, Aihie Sayer A. Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? A comparison with the gold standard Biodex dynamometry Gerontology 2006;52(3):154-159. doi:10.1159/000091824
32. Lee SEK, Lira CAB, Nouailhetas VLA, Vancini RL, Andrade MS. Do isometric, isotonic and/or isokinetic strength trainings produce different strength outcomes? J Bodyw Mov Ther. 2018;22(2):430-437. do i:10.1016/j.jbmt.2017.08.001
33. Impellizzeri FM, Bizzini M, Rampinini E, Cereda F, Maffiuletti NA. Reliability of isokinetic strength imbalance ratios measured using the Cybex NORM dynamometer Clin Physiol Funct Imaging 2008;28(2):113-119. doi:10.1111/j.1475-097x.2007.00 786.x
34. Davies WT, Myer GD, Read PJ. Is it time we better understood the tests we are using for return to sport decision making following ACL reconstruction? A critical review of the hop tests. Sports Med 2020;50(3):485-495. doi:10.1007/s40279-019-01221-7
35. Losciale JM, Bullock G, Cromwell C, Ledbetter L, Pietrosimone L, Sell TC. Hop testing lacks strong association with key outcome variables after primary anterior cruciate ligament reconstruction: A systematic review Am J Sports Med 2020;48(2):511-522. doi:10.1177/0363546519838794
36. Hartog J, Dijkstra S, Fleer J, van der Harst P, Mariani MA, van der Woude LHV A portable isometric knee extensor strength testing device: test retest reliability and minimal detectable change scores of the Q-Force ӀӀ in healthy adults. BMC Musculoskelet Disord. 2021;22(1):966. doi:10.1186/s12 891-021-04848-8
37 van der Leeuw GH, Stam HJ, van Nieuwenhuyzen JF. Correction for gravity in isokinetic dynamometry of knee extensors in below knee amputees. Scand J Rehabil Med 1989;21(3):141-145.
38. Stuelcken MC, Mellifont DB, Gorman AD, Sayers MGL. Mechanisms of anterior cruciate ligament injuries in elite women’s netball: A systematic video analysis. J Sports Sci. 2016;34(16):1516-1522. doi:10.1 080/02640414.2015.1121285
39. Beere M, Ebert JR, Joss B, Ackland T Isometric dynamometry, dependent on knee angle, is a suitable alternative to isokinetic dynamometry when evaluating quadriceps strength symmetry in patients following anterior cruciate ligament reconstruction. Knee 2022;34:124-133. doi:10.1016/j.knee.2021.11.00
7
40. Worrell TW, Perrin DH, Denegar CR. The influence of hip position on quadriceps and hamstring peak torque and reciprocal muscle group ratio values. J Orthop Sports Phys Ther. 1989;11(3):104-107 doi:10.2519/jospt.1989.11.3.104
41. Wellsandt E, Failla MJ, Snyder-Mackler L. Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. J Orthop Sports Phys Ther 2017;47(5):334-338. doi:10.2519/jos pt.2017.7285
42. Larson D, Vu V, Ness BM, Wellsandt E, Morrison S. A multi-systems approach to human movement after ACL reconstruction: The musculoskeletal system. Int J Sports Phys Ther. 2022;17(1):27-46. doi:1 0.26603/001c.29456
43. Logerstedt D, Grindem H, Lynch A, et al. Singlelegged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study Am J Sports Med. 2012;40(10):2348-2356. doi:10.117 7/0363546512457551
44. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538-543. doi:10.1177/0363546510384798
45. Liao JJZ. Sample size calculation for an agreement study Pharm Stat 2010;9(2):125-132. doi:10.1002/ps t.382
Kuntz A, Peters O, Bello A, Perkins R, Monti R, Murray L. An Anterior Cruciate Ligament (ACL) Injury Risk Screening and Reduction Program for High School Female Athletes: A Pilot Study. IJSPT. Published online December 1, 2022:1318-1329.
Allison Kuntz 1 , Olivia Peters 1 , Andrew Bello 1 , Ryan Perkins 1 ,
1 Physical Therapy, Walsh University, 2 Physical Therapy, Graceland University
Keywords: anterior cruciate ligament, female athletics, injury, screening https://doi.org/10.26603/001c.40370
1 a ,
a
Anterior cruciate ligament (ACL) injury causes physical, mental, and financial burdens. Therefore, it is imperative to screen, identify, and educate athletes who are at high-risk. The combination of screening and education could identify those at risk and potentially reduce future injuries.
The purpose was to conduct a feasible community pre-season screening program for high school female athletes for the presence of known modifiable risk factors that predispose them to sustaining a non-contact ACL injury.
Non-experimental prospective study
A convenience sample of 15 healthy female athletes were recruited from local high schools, consisting of 11 soccer players and four basketball players. A pre-season screening program was designed encompassing four stations that addressed modifiable neuromuscular and biomechanical risk factors including range of motion (ROM), jump-landing technique, strength, and balance. Athletes were categorized into high-risk versus low-risk groups based on cutoff scores previously established in the literature.
Every athlete met the high-risk cutoff score for at least one extremity during the ROM screening, and some met high-risk cutoff scores for more than one ROM. Out of all four categories tested, lower extremity ROM demonstrated the greatest deficits.

This study identified athletes as having multiple modifiable risk factors that can be addressed with training and exercises. This supports implementing a pre-season program aimed at screening for injury risk factors.
Level 3
Corresponding Author:
Ryan Monti, PT, DPT, SCS
Walsh University Physical Therapy Program, 2020 East Maple Street, North Canton, OH 44720
Phone Number: (330) 307-8648 Fax Number: (330) 490-7371 Email: Ryanmontipt@gmail.com
The anterior cruciate ligament (ACL) connects the femur to the tibia and plays a key role in stabilizing the knee in both the sagittal and transverse planes which include an terior tibial translation and rotational loads, respectively 1 Approximately 70% of ACL injuries occur by noncontact mechanisms, such as when the athlete is changing direc tions, slowing down at near or full knee extension, or land ing from a jump.1,2 There is an estimated 200,000 ACL-re lated injuries a year with 100,000 requiring reconstructive surgery 3 The average cost of ACL reconstruction is $24,707, making the total annual cost approaching $2.5 billion.4 ACL injuries are common in adolescent female athletes often re sulting in long-term physical, mental, and financial bur dens.5
Female adolescents participating in jumping and pivot ing sports have a two to nine time greater chance of ex periencing an ACL injury versus male athletes of the same age and sport.2 In female high school athletes, knee injuries are the most common disability accounting for nearly 91% of season-ending injuries.3 Additionally, year-round female soccer and basketball athletes have a 5% chance of tearing their ACL every year they participate in sports.3 ACL inci dence rate for soccer athletes ranges from 0.06 to 3.7 per 1000 hours of active play including practice and games.2 Approximately 50% of ACL injuries have associated con comitant injuries which include the medial collateral liga ment (MCL) and medial meniscus.5
ACL injury risk factors are multifactorial, including nonmodifiable and modifiable factors. Non-modifiable anatom ical and hormonal factors, such as a wider Quadriceps-an gle (Q-angle) or the release of estrogen and relaxin, cannot be influenced by physical therapy intervention. Although non-modifiable factors cannot be addressed by exercise in tervention, they provide further insight and create an en compassing profile of at-risk athletes. For example, an in creased Q-angle could result in altered biomechanical hip internal rotation (IR) and knee valgus, which could increase patellofemoral joint stress and instability 6 However, bio mechanical abnormalities and neuromuscular recruitment, such as poor postural positioning or proximal stability, can be modified with appropriate training and provide the greatest impact on reducing the risk of noncontact ACL in juries.2
Abnormal positioning and irregular movement patterns, as well as strength imbalances, can predispose an athlete to a higher risk of ACL injury A movement pattern known as dynamic valgus, is an associated biomechanical risk fac tor during performance of agility and plyometric physical activities such as planting, cutting, or jumping.1,5 Dynamic valgus includes hip adduction and internal rotation (IR), tibial external rotation (ER), and ankle eversion, which re sult in increased joint reaction force in the lateral com partment of the knee and increased strain on the MCL. Hip abductor weakness is a contributing factor to dynamic val gus biomechanics at the knee.1,5 A stronger lateral quadri ceps and weaker medial hamstring (HS) strength leads to quadriceps dominance. This neuromuscular imbalance pre
disposes the risk of ACL injury due to increased stress placed on the ACL.7
Since the passage of Title IX, the number of female ath letes participating in high school and college sports has increased 10- and five-fold, respectively 3 Over the past twenty years, the speed, power, and aggressiveness of fe male athletes have drastically increased which has resulted in a greater number of musculoskeletal injuries.3 Overall, ACL injury risk is multifactorial which includes non-mod ifiable anatomical and hormonal risk factors, as well as modifiable biomechanical and neuromuscular risk factors that can be positively affected by appropriate screening and conditioning.
Physical therapists (PTs) have a role in injury prevention and should design and develop screening programs aimed at preventing injury as a part of a wellness-focused initia tive for community health.8 Additionally, PTs should fo cus on engaging with the community and offer preventative and screening services to reduce the need for costly man agement following an injury.9 The cost of potential screen ing programs has been found to range from $2.00 to $15.00 per player, depending on the equipment and personnel used; whereas, the cost of an ACL reconstruction can cost upwards of $17,000.10 Screening programs have been esti mated to reduce the incidence of ACL injury by an average of 40%, resulting in an improvement of health outcomes.10 In the literature, the majority of ACL screening programs focus on one risk factor in isolation, such as range of mo tion.11,12 Currently, there are no existing protocols that combine several modifiable risk factors into an all-inclusive ACL injury screening program. The purpose was to conduct a feasible community pre-season screening program for high school female athletes for the presence of known mod ifiable risk factors that predispose them to sustaining a non-contact ACL injury
The study was approved by the Institutional Review Board of Walsh University prior to completion and data collection (#2021007).
This study was a non-experimental, prospective pilot study of high school female soccer and basketball athletes. In clusion criteria were female soccer and basketball athletes, aged 13-18 years old. None of the participating athletes had undergone knee surgery nor were recovering from any lower extremity injury A convenience sample was utilized by contacting local coaches through email to provide in formation regarding the screening program and to inquire about volunteer recruitment. All athletes completed a med ical history form prior to starting the program. All athletes and parents were informed of the purpose and components of the program, and all athletes and parents provided as sent and consent, respectively, for participation in the pro gram due to the study involving minors.
Each athlete progressed through the pre-season screening program in the following order: range of motion, jump landing assessment, strength testing, and dynamic balance testing. The sequencing of performing the screening mea sures promoted reliability of testing procedures and limited the effects on performance for subsequent tests.13 Because of test sequencing, rest in between each station was not deemed necessary, allowing for increased efficiency of the screening program. All screening measures were performed by student physical therapists (SPT’s), who were previously educated on the below measures. Ten SPTs completed 30-minutes of instruction, training, and practice for their respective measures. Throughout the entire program, all outcomes were assessed by the same SPTs. The screening program and educational presentation provided to the coaches were reviewed and supervised by licensed PTs. Prior to completing the screening stations, athletes com pleted a five-minute warm-up on an upright exercise bike.
The primary outcomes of this program included range of motion, jump landing strategy, muscle strength, and sin gle-leg dynamic balance.
A goniometer was used to measure the passive range of mo tion (PROM) of hip IR, hip ER, weight-bearing ankle dor siflexion (DF), and the Q-angle. The reliability of PROM goniometric measurements for the lower extremity is con sidered good to excellent.14 The standard error of measure (SEM) reported in the literature for the four measurements utilizing a goniometer are as follows: 2.42 degrees for hip IR, 2.53 degrees for hip ER, 1.8-2.8 degrees for weight-bear ing ankle DF, and 1.02 degrees for Q-angle.15–17 The same testing positions described below were the same testing positions utilized in the articles where the SEMs were re ported.15–17 However, the populations of the articles where the SEMs were reported were different from the target pop ulation of female high school athletes. For hip IR and hip ER, the population was comprised of individuals with femoral acetabular impingement compared to healthy con trols.15 For weight-bearing ankle DF, the population was healthy young adults with an average age of 24 years old.16 For Q-angle, the population consisted of females and males between the ages of 21-50 years.17 Currently, there is a lack of literature on reporting SEM for the female adolescent population.


To measure hip IR and ER PROM, the athlete was supine on the treatment table with the hip and knee of the mea sured leg flexed to 90° and the non-measured leg fully ex tended on the table.11 The examiner lined up the stationary arm of the goniometer with the tibial tuberosity and then passively took the flexed hip into both IR and ER.11 The ex aminer moved the moveable arm of the goniometer to align with the tibial tuberosity while keeping the stationary arm in its vertical position (Figures 1 and 2).11 This was com
Figure 2. Measurement of supine hip external rotation range of motion.
pleted three times on each lower extremity and the average of each side was recorded.
To measure weight-bearing ankle DF, the athlete was asked to stand with the ankle being measured perpendic ular to the wall with the second toe and midline of the foot placed directly on a piece of tape placed on the floor.12 The athlete was then instructed to lunge the knee towards
Figure 1. Measurement of supine hip internal rotation range of motion.the wall until their maximal ankle DF was reached, which was indicated when the heel lifted off the ground.12 If the athlete’s knee contacted the wall before maximal DF was achieved, their foot was moved posteriorly.12 The axis of the goniometer was placed below the lateral malleolus, the stationary arm was in line with the 5th metatarsal, and the moveable arm was in line with the fibular head. This was completed three times on each lower extremity and the av erage of each side was recorded (Figure 3).
To measure the Q-angle, the athlete stood in anatomical position without shoes and socks. The examiner placed the axis of the goniometer at the center of the patella and aligned the stationary arm of the goniometer with the ip silateral ASIS.18 Next, the examiner aligned the moveable arm of the goniometer with the tibial tuberosity (Figure 4). The intersection of the line drawn from the ASIS to the cen ter of the patella and the line drawn from the center of the patella to the tibial tuberosity is considered the Q-angle.18 This was completed three times on each lower extremity and the average of each side was recorded.
Jump landing was analyzed using the Landing Error Scoring System (LESS). The athlete stood on a 30 cm (12 in) box. A taped line that marked 50% of their height was positioned in front of the box. The athlete began the test standing on the box and was instructed to jump in front of the taped line followed by jumping as high as they could immedi ately upon landing. The test was repeated for a second trial with a minute-long break in between. Each trial was video taped using iPads (Apple, Cupertino, CA) in both frontal and sagittal views and analyzed with the Hudl applica
tion (Hudl, Lincoln, NE). Hudl allowed for slowing down the videos and applying virtual angles to each frame. This test utilizes a 17-category scoring system to rate jump landing characteristics.19 Quality of jump landing mechanics are classified into four categories: ≤ 4 errors is rated as excel lent, > 4 to ≤ 5 errors is rated as good, >5 to ≤ 6 errors is rated as moderate, and > 6 errors is rated as poor.20 Females commonly score lower than males, with one study find ing that only 14% of the female participants were classified in the excellent category, compared to 29% of males scor ing within the excellent category 20 College-aged athletes have been found to have lower scores on the LESS compared to their high school-aged counterparts (4.42 and 5.36 re spectively); however, these reported scores combined both males and females.21 There are currently no studies re porting youth female LESS scores in isolation to deter mine normative values for this population. Research has demonstrated adequate interrater and intrarater reliability of the LESS test with intraclass correlation coefficient val ues of 0.84 and 0.91 respectively 20 Validity of the LESS was item-dependent when comparing the results with the “gold standard” of three-dimensional motion analysis and ranged from poor (10%) to excellent (100%).22
A handheld dynamometer (HHD; Hoggan Scientific Micro FET2, Salt Lake City, UT) utilizing stabilization belts was used to assess hip ER, hip abduction, knee flexion, and knee extension strength. Proximal body segments were stabi lized using external support via stabilization belts. For each strength measurement, the athlete was prompted to per form a make-contraction which consisted of a two-second ramp-up time followed by a five-second maximal contrac
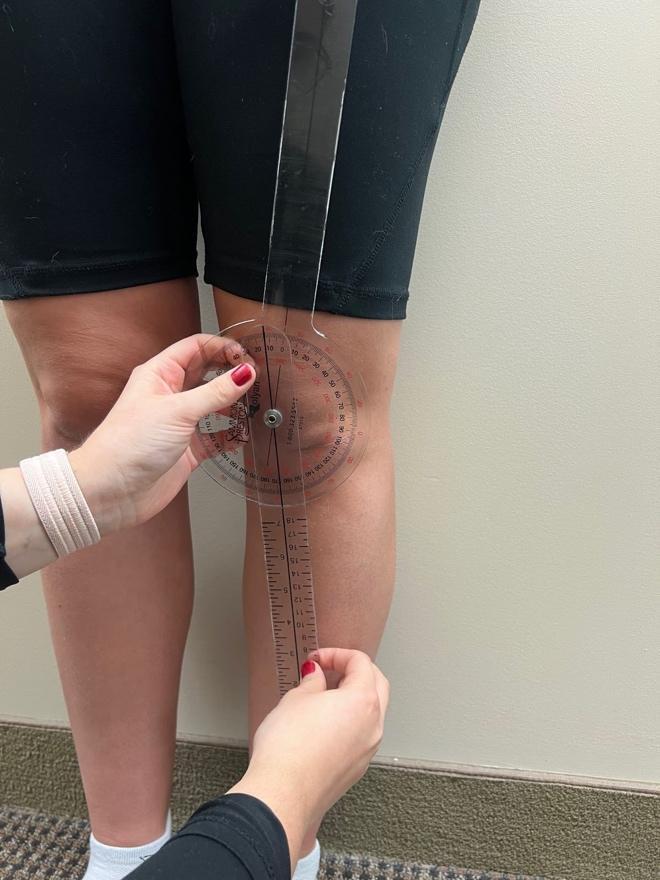
 Figure 3. Measurement of weighted ankle dorsiflexion range of motion.
Figure 4. Measurement of Q-angle.
Figure 3. Measurement of weighted ankle dorsiflexion range of motion.
Figure 4. Measurement of Q-angle.
tion.23 After five seconds, the athlete relaxed, and data was recorded. This was completed three times on each lower extremity and the average of each side was recorded. The belt stabilized HHD displayed moderate to excellent intraexaminer reliability for measuring hip and knee muscle groups and was moderately to highly correlated with the isokinetic dynamometer 24 While the ideal method would be to use an isokinetic dynamometer, it is expensive, lacks portability, and requires expert training. An HHD has proven to be an appropriate alternative that is inexpensive, portable, and easy to use.24
To measure hip ER strength, the athlete sat at the edge of a treatment table and a belt was positioned at the prox imal thighs and secured around the table to stabilize the legs.25 The knees were bent to 90o , and the HHD was placed proximal to the medial malleolus.25 The examiner stood medial to the test extremity when measuring strength (Fig ure 5).25 Hip ER strength measures were recorded in kilo grams (kg) and expressed as a percentage of body weight (BW).
To measure hip abduction strength, the athlete was side lying on a treatment table, and a belt was positioned around the waist proximal to the iliac crest and secured around the table to stabilize the pelvis.25 The hips were in neutral meaning no forward or backward rotation, neutral lumbopelvic positioning, and no hip extension or flexion.25 The HHD was placed 10 cm proximal to the lateral femoral epicondyle.25 The examiner stood posteriorly to the athlete when testing to ensure neutral alignment of the pelvis (Fig ure 6).25 Hip abduction strength measures were recorded in kg and expressed as a percentage of BW.

To measure knee flexion strength, the athlete was prone on a treatment table and two blue foam pads (Airex,
Switzerland) were placed underneath their stomach to pro mote hip flexion for more optimal HS length-tension.26 With increased hip flexion, there is a greater knee flexion torque and a better replication of stride position in gait.26 A belt was positioned proximal to the iliac crest and se cured around the table to stabilize the pelvis.26 The HHD was placed proximal to the Achilles tendon, and the exam iner stood at the end of the table in line with the athlete.26 The make-contraction was performed into knee flexion of approximately 60o (Figure 7). Knee flexion strength mea sures were recorded in kg and expressed as a hamstring to quadriceps (H:Q) strength ratio.

To measure knee extension strength, the athlete was sit ting at the edge of a treatment table and a belt was po sitioned at the proximal thighs.27 The knees were bent to 90o , and the HHD was placed at the anterior lower leg prox imal to the ankle.27 The examiner held the HHD in posi tion by placing their elbows in their abdomen with their back against the wall to provide a more stable barrier (Fig ure 8).27 Knee extension strength measures were recorded in kg and expressed as an H:Q strength ratio.
Dynamic balance was measured by assessing the quality of movement during a lateral step-down test (LSD). Athletes performed the LSD from a 6-inch step and quality of move ment was visually assessed using a scale with scores rang ing from 0 to 6.28 Using this scale, a total score of 0 or 1 is classified as “good” quality of movement, 2 or 3 is “mod erate” quality, and 4 or above is “poor” quality.29 Scoring was based on five criteria: 1) Arm strategy If the subject re moved a hand off their waist during the test, 1 point was added; 2) Trunk movement. If the trunk leaned to any side,
Figure 5. Measurement of hip external rotation strength. Figure 6. Measurement of hip abduction strength.1 point was added; 3) Pelvis plane. If the pelvis rotated or elevated one side compared with the other, 1 point was added; 4) Knee position. If the knee deviated medially and the tibial tuberosity crossed an imaginary vertical line over the 2nd toe, add 1 point, or, if the knee deviated medi ally and the tibial tuberosity crossed an imaginary vertical line over the medial border of the foot, add 2 points, and; 5) Maintain steady unilateral stance. If the subject stepped down on the non-tested side, or if the subject’s tested limb


Characteristic Soccer (n=11) Basketball (n=4)
Age 14.46 ± 0.92 15.75 ± 0.96
Height (in) 64.36 ± 2.94 66.5 ± 1.73
Weight (kg) 58.06 ± 11.03 64.66 ± 8.15
Values shown as mean ± standard deviation Abbreviations: in, inches; kg, kilograms
became unsteady (i.e. wavers from side to side on the tested side), add 1 point.28
Using the previously mentioned scale of measurement, several studies have found the interrater reliability to be substantial (Kappa Coefficient (K) = 0.67 & K = 0.81)28,29 for the LSD in females diagnosed with patellofemoral pain syn drome and moderate (K = 0.59)30 for healthy females. These values indicate a moderate to excellent level of agreement which is considered suitable for use in clinical practice. Validity has not been specifically mentioned in the litera ture for the LSD; however, studies have shown that altered movement patterns that lead to excessive knee valgus alignment, as measured by the LSD, have been implicated as a risk factor for lower extremity injuries including non contact ACL injuries.30,31 There is an association between decreased quality of movement on the LSD and decreased ankle dorsiflexion ROM.30 Females who demonstrate de creased dorsiflexion during the LSD exhibit other altered movement patterns associated with ACL injury: increased frontal plane hip motion, increased transverse plane knee motion, and decreased sagittal plane knee motion.31
Athletes were asked to remove shoes and socks prior to the test, and a sticker was placed on the athlete’s tibial tuberosity to help with visualization during the test.28 A second sticker was placed on the step just under the ath lete’s second toe once they assumed the starting position to aid examiners with scoring.28 A verbal explanation of the procedure was given to the athlete, followed by a demon stration. Athletes performed five practice repetitions, fol lowed by five consecutive test repetitions that were scored.28 The LSD was evaluated by two examiners simul taneously, and after scoring the test, both examiners came to a consensus on the final score that was recorded. This process was then repeated for the contralateral leg.
A total of 15 female athletes participated in the screening program (Table 1). Athletes were considered to be at a higher risk of injury when meeting the cutoff score on at least one lower extremity. Group means were calculated for each variable, excluding the measurements for hip ER and abduction strength (Figure 9). These measures were ex cluded due to the normalization of the data based on each individual athlete’s weight.
Figure 7. Measurement of knee flexion strength. Figure 8. Measurement of knee extension strength.Figure 9. Group means and standard deviation for range of motion, jump landing, strength, and single-leg dynamic balance measures.
Abbreviations: DF, dorsiflexion; ER, external rotation; H, hamstring; IR, internal rotation; L, left; LESS, landing error scoring system; LSDT, lateral step-down test; Q, quadriceps; R, right
Hip ER below 30° or a combined measurement of hip IR and ER below 75° is correlated with a higher risk of ACL in jury.11 In this sample, 13/15 athletes would be considered at a higher risk of injury due to lack of internal rotation; and when examined for total hip rotation, 11/15 athletes would be considered at a higher risk of injury (Table 2). Weighted ankle DF below 41° has been correlated with a higher risk of ACL injury 12 This measure was most preva lent in the sample with every athlete meeting the high-risk cutoff score in at least one lower extremity (Table 2). Qangle of greater than 19° has also been correlated with a higher risk of ACL injury.18 Only one athlete was found to have met this cutoff score (Table 2).
A score of five or greater on the LESS has been correlated with an increased risk of ACL injury (sensitivity = 86%, specificity = 64%).19 The LESS results indicate that 10/15 athletes met the high-risk cutoff score (Table 3). The most common suboptimal landing characteristics were lack of adequate knee flexion at initial contact and excessive me dial knee displacement at both initial contact and at the point of maximal knee flexion.
Hip ER strength of ≤20.3% of body weight or a hip abduc tion strength of ≤35.4% of body weight has been correlated with an increased risk of ACL injury 25 For hip ER strength,
13/15 athletes met the high-risk cutoff score (Table 4). For hip abduction strength, 5/15 athletes met the high-risk cut off score (Table 4).
Previous authors have suggested that a H:Q strength ra tio of less than 60% was linked with a higher risk of ACL in jury 32 For H:Q ratio, 10/15 athletes met the high-risk cut off score with a higher prevalence of imbalance in the right extremity versus the left extremity (Table 4).
Quality of movement categories were determined by the score on the LSD test good, moderate, and poor.28 Based on prior research, scores between two and six were utilized as the cut off for increased risk of ACL injury.30
A majority of the sample fell into the “moderate” cat egory The remainder of the sample was split evenly be tween the “good” and “poor” quality of movement cate gories, with four athletes in each. For the LSD test, 11/15 athletes met the high-risk cutoff score with two athletes scoring the maximal score of 6 which signifies altered movement patterns, poor balance, and a higher risk of in jury Furthermore, only 1/15 athletes scored a perfect score of 0 (Table 3).
The purpose of this study was to screen female high school soccer and basketball athletes for the presence of modifi able risk factors that predispose them to increased risk of sustaining a non-contact ACL injury that have been identi

Table 2. Range of Motion.
Subject R Hip IR (deg) L Hip IR (deg)
R Hip IR+ER (deg)
L Hip IR+ER (deg)
R Q-angle (deg)
L Q-angle (deg)
R Ankle DF (deg) L Ankle DF (deg) 1 26* 20* 62* 54* 10 7 35* 27* 2 29* 28* 64* 68* 5 5 37* 37* 3 24* 27* 62* 65* 10 10 32* 25* 4 27* 25* 66* 55* 13 15 31* 24* 5 27* 20* 70* 60* 6 6 21* 21* 6 29* 25* 61* 61* 13 11 20* 16* 7 28* 28* 72* 72* 11 12 30* 28* 8 18* 15* 61* 64* 15 15 38* 39* 9 16* 15* 53* 50* 11 12 31* 30* 10 38 38 86 95 15 15 36* 34* 11 21* 15* 72* 69* 20* 19 18* 17* 12 27* 30 79 80 10 12 31* 24* 13 32 36 87 95 10 12 43 39* 14 27* 30 77 80 11 12 27* 30* 15 26* 23* 68* 68* 15 12 23* 22* Mean (± SD) 26.33 (±5.33) 25 (±7.15) 69.33 (±9.68) 69.07 (±13.56) 11.67 (±3.74) 11.67 (±3.68) 30.2 (±7.23) 27.53 (±7.35) * Met cutoff score
Abbreviations: deg, degrees; DF, dorsiflexion; ER, external rotation; IR, internal rotation; L, left; R, right; SD, standard deviation
Table 3. Measures of Dynamic Motor Control. Subject LESS (points) LSDT (points) 1 6* 3* 2 6* 0 3 6* 3* 4 4.5 6* 5 4.5 1 6 5* 2* 7 5.5* 6* 8 3 3* 9 5.5* 1 10 3.5 4* 11 6.5* 5* 12 5* 1 13 4.5 2* 14 5.5* 2* 15 6.5* 2* Mean (± SD) 5.17 (±1.03) 2.73 (±1.83) * Met cutoff score
Abbreviations: LESS, landing error scoring system, LSDT, lateral step-down test; SD, standard deviation
fied in the research. Numerous studies have demonstrated screening methods that have the capability to identify ath letes who demonstrate many of the known anatomical, bio mechanical, or neuromuscular risk factors associated with
an ACL injury 11,12,18,19,25,30,32 Several of these studies have focused on screening only one or two of these risk fac tor components in isolation.11,12,18,19,25,30,32 There were no studies found in the literature that completed a battery of tests to identify if a female athlete was at increased risk for a non-contact ACL injury.11,12,18,19,25,30,32
Currently, many authors have focused on identifying ACL injury risk using expensive, high-technology equip ment that requires extensive experience, training, and time to use, which would be difficult to implement in a commu nity program.14,20,26,31 Radiographic measurement is con sidered more precise than goniometric measurements; however, this method is expensive, exposes subjects to ra diation, and is not readily accessible in the environment where most screening programs would be held.14 Force plates with electromagnetic tracking systems for 3-D analy sis is the ideal method to assess jump landing and ground reaction force; however, not all clinics would be able to im plement the equipment utilized for analysis due to their expense and spatial requirements.20 An isokinetic dy namometer is the gold standard to assess strength, but it is expensive and space-consuming.26 Kinematic motion and quality of movement during the LSD is best visualized us ing 3-D motion analysis; however, this method requires training and expertise to use properly, is expensive, and is time-consuming, which makes it not ideal for use in a screening program.31 For the program to be feasible, the chosen screening methods utilized readily accessible equip ment and materials that were easy to implement by SPTs. This allowed the program to be conducted in an organized and timely manner.
Table 4. Muscle Strength. Subject R Hip ER (% bw) L Hip ER (% bw) R Hip Abd (% bw) L Hip Abd (% bw) R H:Q Ratio (%) L H:Q Ratio (%) 1 15.02 15.02 32.92 28.95 60 60 2 9.57* 9.93* 16.03* 14.81* 66 60 3 7.15* 8.16* 21.51 20.09 60 64 4 9.87* 9.7* 22.76 21.22 56* 68 5 11.22* 12.17 22.21 23.87 91 79 6 8.13* 10.2* 23.29 18.9* 65 54* 7 7.32* 9.85* 27.85 23.26 41* 49* 8 6.99* 6.55* 13.19* 10.09* 44* 68 9 9.25* 10.41* 19.53 19.34 40* 54* 10 10.63* 13.83 25.05 28.55 36* 53* 11 7.89* 7.12* 12.57* 12.72* 44* 44* 12 16.38 18.32 32.93 28.31 56* 51* 13 12.23 11.61* 23.67 21.19 59* 70 14 10.71* 11.81* 26.58 25.15 43* 35* 15 13.85* 13.16* 22.58* 23.97* 42* 52* Mean (± SD) N/A∮ N/A∮ N/A∮ N/A∮ 53.53 (±14.37) 57.4 (±11.25)
bodyweight; ER, external rotation; H, hamstring; Q, quadriceps; N/A, not applicable; SD, standard deviation
Biomechanical and neuromuscular components are risk factors that can be identified and modified with appropriate screening and interventions.6,33 The screening methods and interventions utilized in this program have been shown to identify and address these types of modifiable risk fac tors which can be easily applied to clinical prac tice.11,12,18,19,25,30,32 After completion of the screening program, all 15 of the participating athletes demonstrated at least four of the eight modifiable risk factors that were measured. This demonstrates that there are likely several components that each athlete could improve upon, in order to help decrease the risk of an ACL tear
There are several limitations with the present study that need to be considered. First, the small sample size utilized in this study is a limitation. Thus, this is described as a pilot study. Due to the population under study, proximity to the testing facility was needed to participate in data collection. In addition, coordination of transportation presented as a barrier for the parents of the subjects participating in this study. Planning in accordance with sport seasonal demands and personal time away appeared to also challenge partici pant recruitment. Suggestions for future research would be to plan testing in accordance with practice schedules and at a facility that is easily accessible to the athlete, such as their practice location. A second limitation is the lack of long-term follow-up with at-risk athletes to assess if an ACL injury occurred, and whether that correlated to the findings of the athletes being identified as high-risk for in
jury or not. It is possible that players who were identified as a higher risk for ACL injuries completed the whole sea son without an injury or vice versa. Future research would benefit to follow the at-risk athletes through seasonal play to determine which factors in combination predict the out come of injury and if there is a correlation to leg domi nance. This would allow researchers to determine if there is a relationship between the quantity of identified risk fac tors and the rate of injury risk.
The screening program utilized was feasible to implement and identified potential risk factors for injury in the cohort of female athletes studied. Prior researchers have analyzed impairments in ROM, landing mechanics, strength, and balance that increase the likelihood of ACL injuries in fe male athletes; however, no screening programs have inves tigated these categories together to identify female athletes at elevated risk for an ACL tear All the studied athletes were found to have at least one factor that could lead to risk of ACL injury. This pilot study provides clinicians with a battery of tests and measures that are quick to perform, inexpensive, and do not require extensive experience.
This study protocol was approved by the Institutional Re view Board of Walsh University (#2021007). The authors re
port no conflicts of interest or financial compensation in the completion of this study.
The authors would like to thank the additional SPT volun teers that assisted in the completion of this program.
Submitted: January 06, 2022 CST, Accepted: September 12, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. ACL injury Mayo Clinic. Published March 10, 2021. Accessed October 20, 2021. https://www.mayoclinic.o rg/diseases-conditions/acl-injury/symptoms-causes/s yc-20350738
2. Thompson JA, Tran AA, Gatewood CT, et al. Biomechanical effects of an injury prevention program in preadolescent female soccer athletes. Am J Sports Med 2017;45(2):294-301. doi:10.1177/036354 6516669326
3. Heckman M. Female ACL injuries epidemic in the US. San Antonio Sports Medicine. Published April 14, 2019. Accessed October 20, 2021. https://sanantonios portsmedicine.com/female-acl-injuries-epidemic/
4. Bokshan SL, Mehta S, DeFroda SF, Owens BD What are the primary cost drivers of anterior cruciate ligament reconstruction in the United States? A cost minimization analysis of 14,713 patients. Arthroscopy. 2019;35(5):1576-1581. doi:10.1016/j.arth ro.2018.12.013
5. Joyner DC. The Effectiveness of an 8-Week Sport Specific Intervention Program on Improving Proprioception, Balance, and Function in Adolescent Female Soccer Players Dissertation. California State University; 2017.
6. Pagare V. “Q” angle. Physiopedia. Published 2021. Accessed October 20, 2021. https://www.physio-pedi a.com/%27Q%27_Angle
7. Zebis MK, Andersen LL, Brandt M, et al. Effects of evidence-based prevention training on neuromuscular and biomechanical risk factors for ACL injury in adolescent female athletes: a randomised controlled trial. Br J Sports Med 2016;50(9):552-557. doi:10.1136/bjsports-2015-09477
6
8. American Physical Therapy Association. Physical therapists’ role in prevention, wellness, fitness, health promotion and management of disease and disability Published 2019. Accessed October 20, 2021. https://www.apta.org/apta-and-you/leadershipand-governance/policies/pt-role-advocacy
9. Sullivan KJ, Wallace JG Jr, O’Neil ME, et al. A vision for society: physical therapy as partners in the national health agenda. Phys Ther. 2011;91(11):1664-1672. doi:10.2522/ptj.20100347
10. Swart E, Redler L, Fabricant PD, Mandelbaum BR, Ahmad CS, Wang YC. Prevention and screening programs for anterior cruciate ligament injuries in young athletes. J Bone Joint Surg 2014;96(9):705-711. doi:10.2106/jbjs.m.00560
11. VandenBerg C, Crawford EA, Sibilsky Enselman E, Robbins CB, Wojtys EM, Bedi A. Restricted hip rotation is correlated with an increased risk for anterior cruciate ligament injury. Arthroscopy. 2017;33(2):317-325. doi:10.1016/j.arthro.2016.08.014
12. Wahlstedt C, Rasmussen-Barr E. Anterior cruciate ligament injury and ankle dorsiflexion. Knee Surg Sports Traumatol Arthrosc 2015;23(11):3202-3207 do i:10.1007/s00167-014-3123-1
13. McGuigan M. Principles of test selection and administration. In: Haff G, Triplett NT, eds. Essentials of Strength Training and Conditioning Fourth. Human Kinetics; 2016:255-257.
14. Ore V, Nasic S, Riad J. Lower extremity range of motion and alignment: A reliability and concurrent validity study of goniometric and three-dimensional motion analysis measurement. Heliyon 2020;6(8):e04713. doi:10.1016/j.heliyon.2020.e04713
15. Nussbaumer S, Leunig M, Glatthorn JF, Stauffacher S, Gerber H, Maffiuletti NA. Validity and test-retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskelet Disord 2010;11(1). doi:10.1186/1471-2 474-11-194
16. Konor MM, Morton S, Eckerson JM, Grindstaff TL. Reliability of three measures of ankle dorsiflexion range of motion. Int J Sports Phys Ther. 2012;7(3):279-287.
17 Roush J, Bustillo K, Low E. Measurement error between a goniometer and the NIH ImageJ program for measuring quadriceps angle. Internet J Allied Health Sci Pract 2008;7 doi:10.46743/1540-580x/200 8.1195
18. Mohamed E, Useh U, Mtshali B. Q-angle, pelvic width, and intercondylar notch width as predictors of knee injuries in women soccer players in South Africa. Afr Health Sci. 2012;12(2):174-180. doi:10.431 4/ahs.v12i2.15
19. Padua DA, DiStefano LJ, Beutler AI, de la Motte SJ, DiStefano MJ, Marshall SW. The landing error scoring system as a screening tool for an anterior cruciate ligament injury–prevention program in elite-youth soccer athletes. J Athl Train 2015;50(6):589-595. doi:10.4085/1062-6050-50.1.10
20. Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE Jr, Beutler AI. The landing error scoring system (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics. Am J Sports Med 2009;37(10):1996-2002. doi:10.1177/0363 546509343200
21. Smith HC, Johnson RJ, Shultz SJ, et al. A prospective evaluation of the landing error scoring system (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med. 2011;40(3):521-526. doi:10.1177/0363546511429776
22. Hanzlíková I, Hébert-Losier K. Is the landing error scoring system reliable and valid? A systematic review. Sports Health. 2020;12(2):181-188. doi:10.117 7/1941738119886593
23. Jackson SM, Cheng MS, Smith ARJr, Kolber MJ. Intrarater reliability of hand held dynamometry in measuring lower extremity isometric strength using a portable stabilization device. Musculoskelet Sci Pract 2017;27:137-141. doi:10.1016/j.math.2016.07.010
24. Martins J, da Silva JR, da Silva MRB, BevilaquaGrossi D Reliability and validity of the belt-stabilized handheld dynamometer in hip- and knee-strength tests. J Athl Train 2017;52(9):809-819. doi:10.4085/1 062-6050-52.6.04
25. Khayambashi K, Ghoddosi N, Straub RK, Powers CM. Hip muscle strength predicts noncontact anterior cruciate ligament injury in male and female athletes: A prospective study. Am J Sports Med. 2016;44(2):355-361. doi:10.1177/0363546515616237
26. Ogborn DI, Bellemare A, Bruinooge B, Brown H, McRae S, Leiter J. Comparison of common methodologies for the determination of knee flexor muscle strength. Int J Sports Phys Ther 2021;16(2):350-359. doi:10.26603/001c.21311
27 Katoh M, Hiiragi Y, Hirano M, et al. Isometric knee muscle strength measurement using a belt stabilized hand-held dynamometer and an isokinetic dynamometer with and without trunk fixation: investigation of agreement of measurement values and factors influencing measurement. J Phys Ther Sci 2019;31(11):878-883. doi:10.1589/jpts.31.878
28. Piva SR, Fitzgerald K, Irrgang JJ, et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskelet Disord 2006;7(1):33. doi:10.1186/1471-2474-7-33
29. Rabin A, Kozol Z. Measures of range of motion and strength among healthy women with differing quality of lower extremity movement during the lateral step-down test. J Orthop Sports Phys Ther 2010;40(12):792-800. doi:10.2519/jospt.2010.3424
30. Rabin A, Kozol Z, Moran U, Efergan A, Geffen Y, Finestone AS. Factors associated with visually assessed quality of movement during a lateral stepdown test among individuals with patellofemoral pain. J Orthop Sports Phys Ther 2014;44(12):937-946. doi:10.2519/jospt.2014.5507
31. Rabin A, Portnoy S, Kozol Z. The association of ankle dorsiflexion range of motion with hip and knee kinematics during the lateral step-down test. J Orthop Sports Phys Ther. 2016;46(11):1002-1009. doi:10.251 9/jospt.2016.6621
32. Kim D, Hong J. Hamstring to quadriceps strength ratio and noncontact leg injuries: A prospective study during one season. Isokinet Exerc Sci 2011;19(1):1-6. doi:10.3233/ies-2011-0406
33. Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. Mechanisms, prediction, and prevention of ACL injuries: Cut risk with three sharpened and validated tools. J Orthop Res. 2016;34(11):1843-1855. doi:10.1002/jor.23414
Sugarman BS, Sullivan ZB, Le D, et al. Isometric Knee Strength is Greater in Individuals Who Score Higher on Psychological Readiness to Return to Sport After Primary Anterior Cruciate Ligament Reconstruction. IJSPT. Published online December 1, 2022:1330-1339.
Barrie S. Sugarman 1 a , Zach B. Sullivan 2 , Daniel Le 3 , Carolyn Killelea 4 , Mallory S. Faherty 5 , Lee H. Diehl 4 , Jocelyn R Wittstein 4 , Jonathan C. Riboh 6 , Alison P. Toth 4 , Annunziato Amendola 4 , Dean C. Taylor 4 , Timothy C. Sell 7
1 Orthopaedic Surgery, University of Michigan, 2 Radiology, Boston Medical Center, 3 School of Medicine, University of North Carolina, 4 Orthopaedic Surgery, Duke University Medical Center, 5 Ohio Health Research Institute, 6 OrthoCarolina, 7 Atrium Health Musculoskeletal Institute
Keywords: anterior cruciate ligament reconstruction, psychological readiness, return to sport https://doi.org/10.26603/001c.39737
Anterior cruciate ligament (ACL) injury is extremely common among athletes. Rate of second ACL injury due to surgical graft rupture or contralateral limb ACL injury is approximately 15-32%. Psychological readiness to return to sport (RTS) may be an important predictor of successful RTS outcomes. Psychological readiness can be quantified using the ACL Return to Sport after Injury (ACL-RSI) questionnaire, with higher scores demonstrating greater psychological readiness.
The purpose of this study was to investigate differences in functional performance and psychological readiness to return to sport among athletes who have undergone primary ACL reconstruction (ACLR).
Eighteen athletes who had undergone primary ACLR were tested at time of RTS clearance. The cohort was divided into two groups, high score (HS) and low score (LS), based on median ACL-RSI score, and performance on static and dynamic postural stability testing, lower extremity isokinetic and isometric strength testing, and single leg hop testing was compared between the groups using an independent samples t-test.
The median ACL-RSI score was 74.17 The average ACL-RSI score was 83.1±6.2 for the HS group and 61.8±8.0 for the LS group. High scorers on the ACL-RSI performed significantly better on isometric knee flexion as measured via handheld dynamometry (22.61% ±6.01 vs. 12.12% ±4.88, p=0.001) than the low score group.

The findings suggest that increased knee flexion strength may be important for psychological readiness to RTS after primary ACLR. Further research is indicated to
a
Barrie S. Sugarman
University of Michigan Department of Orthopaedic Surgery
Attn: Sheila Menna
1500 E Medical Center Drive TC2912, SPC5328 Ann Arbor, MI 48109 sugarmab@med.umich.edu
explore this relationship, however, a continued emphasis on improving hamstring strength may be appropriate during rehabilitation following ACLR to positively impact psychological readiness for RTS.
Anterior cruciate ligament (ACL) injury is common among athletes.1,2 Rate of second injury due to surgical graft rup ture or contralateral limb injury is approximately 15-32%, with increased risk during the first two years postopera tively 3–7 Known factors associated with successful return to sport (RTS) include delay of return until at least nine months postoperatively, symmetric quadriceps strength measured as a ratio of knee extensor torque normalized to body mass, lower levels of pain and knee joint effusion, lower levels of kinesiophobia, and extended preoperative rehabilitation.4,6,8–10 Successful return to sport is primarily defined as avoidance of second injury, but can also include return to pre-injury activity levels or avoidance of pain with activity Despite the identification of these predictors, ACL reinjury rates remain high, suggesting that other factors may play an important role in successful RTS. One of these additional factors may be psychological readiness to RTS, which includes fear of reinjury, anxiety, anger, and stress, and lack of confidence to return to sport.11 Approximately 40-63% of athletes return to their preinjury level of sport after primary ACL injury,12–14 and among athletes who do not return, fear of injury is the most common reason they cite for this decision.15 Lack of psychological readiness is a major barrier for return to preinjury level of sport after ACL reconstruction (ACLR).13,16–18 Psychological factors, in ad dition to physical readiness, are important to consider in RTS evaluation.8,11,15
Several authors have indicated that psychological readi ness predicts successful RTS.13,14,19–23 Psychological readiness to return to sport may be quantified using a ques tionnaire known as the ACL Return to Sport after Injury (ACL-RSI) scale.24 Webster et al. developed this 12-item questionnaire in 2008 to assess the psychological impact of returning to sport after ACLR.10,24 The scale measures psychological readiness to RTS after an ACL injury in three main categories: emotions, confidence, and risk appraisal, and a higher score suggests greater psychological readiness for return to sport.21,24,25 The ACL-RSI has been shown to be a good indicator of successful RTS.10,11,23 Sadeqi et al. describes that ACL-RSI score improves throughout the re habilitation process, and that higher ACL-RSI score is cor related with an athlete’s return to sport.25 Athletes who re turn to sport after ACLR have higher ACL-RSI scores than athletes who do not return to their sport even after being medically cleared to do so.10,13 Importantly, young athletes (<20 years of age) who sustain a second ACL injury after RTS had lower psychological readiness scores at 12 months af ter ACLR and a smaller change in their ACL-RSI score from preoperative evaluation to 12 months postoperative evalu ation than their counterparts who do not sustain a second
injury.21,22 ACL-RSI score indicates psychological readiness for successful RTS, and therefore may be a useful tool in RTS evaluations for athletes.
Although there is strong evidence demonstrating that psychological readiness plays a significant role in successful RTS, the predictors of psychological readiness remain largely unknown. The purpose of this study was to inves tigate differences in functional performance and psycho logical readiness to return to sport among athletes who have undergone primary ACLR. Predictors of high ACL-RSI scores will be determined based on single leg functional performance in single leg hop for distance, quadriceps strength testing, and single leg static postural stability and Dynamic Postural Stability Index (DPSI). Because athletes with higher ACL-RSI scores are shown to have greater suc cess in RTS, it was hypothesized that subjects in this study with higher ACL-RSI scores will perform better in func tional testing at time of RTS than athletes with lower ACL RSI scores. Findings from this study may guide clinicians when determining how psychological factors contribute to functional performance. These results may also affect both physical and psychological rehabilitation for athletes after ACLR to improve RTS outcomes.
This descriptive cohort study utilized individuals who had undergone a primary ACLR at a single academic institution. Subjects were recruited to participate if they were 12 years or older and had undergone primary ACL reconstruction with a contributing author orthopaedic surgeon. A total of 18 participants enrolled in the study voluntarily. All sub jects were cleared by their orthopaedic surgeon to return to their previous level of activity prior to participation in the study
Subjects were included in this study if they participated in a sport at any level prior to their injury, and intended to return back to sport after being cleared to do so. Subjects were excluded if they had a history of any prior major lower extremity injuries, prior lower extremity or back surgery, any medical diagnosis that could affect balance, or any multi-ligamentous injury Concurrent meniscal injury was not an exclusion criterion. Subject demographics for the co hort are outlined in Table 1 All subjects read and signed an informed consent form prior to participating in the study
Ground reaction forces (GRF) for static and dynamic pos tural stability testing were collected at 1000 Hz with an AMTI force plate (Advanced Mechanical Technologies, Inc.,
Age (years) Range: 13-36
Height (cm) Mass (kg) Tegner Activity Level
Mean ±SD Mean ±SD Mean ±SD Mean ±SD
Females (n=8)
19.4 5.73 165.88 7.38 76.33 25.82 6.75 1.58
Males (n=10) 20.8 7.04 178.97 8.02 76.89 10.74 7.70 1.25
Total (n=18) 20.2 6.35 173.15 10.06 76.64 18.32 7.28 1.44
Watertown, MA, model BP600900). Knee isokinetic strength was measured using an isokinetic dynamometer (Biodex Medical Systems, Inc., Shirley, NY), and knee iso metric strength was measured using a handheld dy namometer (Lafayette Instrument Company, Lafayette, IN).
Participants completed the ACL Return to Sport after Injury (ACL-RSI) 12-item questionnaire at time of RTS clearance, as previously described. Several studies have used the ACL RSI, and the questionnaire shows high internal consistency (Cronbach alpha = 0.96).14,15,20,21,23,26–28
Subjects also completed the Tegner Activity Scale prior to functional performance testing. The Tegner Activity Scale is a scored assessment from zero to ten that assesses the activity level in daily life and sport or recreation that a participant can comfortably complete.29–31 Participants may only achieve a score of five or greater if they participate in recreational or competitive sports.29 The activity scale has been shown to have high test-retest reliability.29,31 Av erage Tegner Activity Level for the cohort at time of RTS testing is reported in Table 1.
Static postural stability testing was assessed under eyes open (EO) and eyes closed (EC) conditions. Participants as sumed a single-leg stance on their injured leg on the force plate with their hands on their hips and were asked to fo cus on a marker at eye level approximately ten feet in front of them for a total of ten seconds in EO condition. Sub jects assumed the same stance with their eyes closed for EC condition. Subjects completed one practice trial for each condition before three ten second trials were collected for data analysis. Trials were repeated if the subject shifted their standing foot on the force plate or touched down with their opposite foot off of the force plate. This protocol has been previously described and found to have excellent in ter-session reliability.32–37 The standard deviation of the GRF were calculated for each trial in the anterior-posterior, medial-lateral, and vertical directions. In addition, an over all composite GRF was calculated for each trial. These val ues were averaged across the three trials for the eyes open and eyes closed conditions following data reduction.
For dynamic postural stability testing, participants were instructed to jump forward from a two-legged stance over a 30.5 cm hurdle to a force plate that was positioned at a dis tance of 40% of their height. Subjects were asked to land on their injured leg on the force plate and hold the stance for at least five seconds after landing. Trials were discarded if
the subject did not land with one foot entirely on the force plate or if they were unable to hold a single leg stance after landing for at least five seconds. This procedure has been previously described in the literature and has good inter session reliability 8,35–39 The dynamic postural stability in dex (DPSI) for each GRF component was calculated for the anterior-posterior, medial-lateral, and vertical directions, as well as an overall composite index following data reduc tion.40
Knee strength was first assessed using an isokinetic dy namometer with concentric testing at 60° per second. Sub jects were positioned on the isokinetic dynamometer ac cording to manufacturer specifications. Participants were tested for average peak torque for knee flexion and knee ex tension. Strength was tested on the injured limb. Subjects performed three practice trials of knee flexion and exten sion at 50% of their maximum strength, followed by three practice trials at maximum strength. Following one minute of rest, participants proceeded with five consecutive repe titions of flexion and extension at maximum strength. This protocol has been previously described in the literature, and has been shown to have good between-group and sideto-side reliability 34,41 Average peak torque for knee flexion and knee extension were calculated and normalized to body mass in kilograms.
A handheld dynamometer was also used to assess iso metric knee flexion and extension strength. For knee flex ion testing, participants were in the prone position on an exam table with their injured knee in 30-45° of flexion. The subject then accelerated into full flexion strength while the examiner resisted the subject’s flexion using a handheld dy namometer placed on the distal one-third of the calf For knee extension, participants sat on the edge of the exam table with their legs hanging off in 30-45° of flexion. Us ing a gait belt strap, the dynamometer was secured on the distal one-third of the tibia of the injured leg, participants accelerated into maximum extension. Each trial with the handheld dynamometer was repeated three times. Hand held dynamometry has been previously described and val idated for intra-rater, inter-rater, and inter-device reliabil ity, especially for proximal muscle testing.42–44 Peak force was averaged over the three trials and normalized to body mass in kilograms. One tester performed all of the hand held strength testing. Intra-rater reliability of this tester using the protocol employed in the current study was 0.94 or greater
Hop distance was assessed for both triple hop and crossover hop. For each hop test, individuals were asked
to complete three consecutive hops on the affected foot, jumping as far as possible along a ¾" tape measure on the ground. For the triple hop, all three jumps were made on the same side of a tape measure secured to the floor. For the crossover hop, participants alternated on which side of the tape they jumped with each hop in a lateral-medial-lateral pattern. Trials were discarded if participants landed on the tape or if participants did not stick the landing on their fi nal hop. This procedure has been described previously,45,46 with intraclass correlation coefficients of 0.82-0.93.47 Par ticipants performed a practice trial for each hop test, and data were recorded for two test trials, with the results aver aged and normalized to the participant’s height in centime ters.
Custom MATLAB (Mathworks, v7.0.4, Natick, MA) scripts were used for filtering and processing data for static and dy namic postural stability testing. The data was filtered with a low-pass Butterworth filter using a cutoff frequency of 20 Hz. For static postural stability, the GRF from each of the three successful trials were normalized to body mass in kilograms and averaged. The standard deviation of the GRF in the anterior-posterior, medial-lateral, and vertical directions were calculated, as well as a combined measure from all three directions. For dynamic postural stability, a stability index in the anterior-posterior, medial-lateral, and vertical directions was calculated, in addition to a compos ite score from all three directions. These values were cal culated using the first three seconds after initial contact on the force plate, as determined by the time in which ver tical GRF was recorded at greater than five percent of the subject’s body mass. The calculations are based on a mean square standardization around a zero point, with lower val ues for all variables indicating a better score.39
The median ACL-RSI score was calculated across the co hort. Participants were divided into two groups of equal participants based on the median score. Groups were des ignated as “high score” or “low score” ACL-RSI group, rela tive to the median.
The data for each variable (height, mass, age, ACL-RSI score, time to RTS, static and dynamic postural stability testing, isokinetic knee flexion/extension, isometric knee flexion/extension, triple/crossover hop) was assessed for normality using a Shapiro-Wilk test. Trial data from the participant’s injured limb was assessed. Data from the noninjured limb was not included in this study An independent samples t-test was used to compare the functional perfor mance, strength, and postural stability testing between the high and low score ACL-RSI groups for each variable, and a Mann-Whitney U test was used if the data did not meet normality criteria. All statistical analysis was performed us ing IBM SPSS Statistics (IBM SPSS, Version 24). Statistical significance was set a priori at p < 0.05.
The Shapiro-Wilk normality test showed that the data was normally distributed for all variables tested except for age. There was no significant difference in age between the two groups (mean age 18.67±5.17 years and median 17 years in the high-score ACL-RSI group vs. mean age 21.67±7.33 years and median age 18 in the low-score ACL-RSI group, p=0.331). The height, body mass, and age demographics be tween the two groups are presented in Table 2
The median ACL-RSI score was 74.17. The average ACL RSI score was 83.1±6.2 for the “high score” group (HS) and 61.8±8.0 for the “low score” group (LS). There was a significant difference in ACL-RSI score between groups (HS= 83.06, LS=61.76, p<0.001). The distribution of scores is shown in Figure 1.
The means, standard deviations, and p-values for the HS and LS group for static and dynamic postural stability tasks are presented in Table 3 None of the comparisons between groups achieved statistical significance. The means, stan dard deviations, and p-values between groups for strength testing are presented in Table 4 High scorers on the ACL RSI had statistically significant greater isometric knee flex ion strength normalized to body mass as measured via handheld dynamometry (36.6±11.4 vs. 32.9±11.8, p=0.001). There were no other statistically significant findings in iso metric and isokinetic strength testing. The means, standard deviations, and p-values for hop testing between groups are presented in Table 5. There were no statistically significant differences in performance between the HS and LS groups for hop testing.
The purpose of this study was to evaluate if greater psy chological readiness for RTS was associated with better per formance on strength, postural stability, and hop testing at time of RTS clearance among athletes who had under gone primary ACL reconstruction. It was hypothesized that participants with greater psychological readiness, as de termined by ACL-RSI score, would have greater strength, static and dynamic postural stability, and greater hop dis tance than participants with lower ACL-RSI scores. The hy pothesis was partially supported by the finding that par ticipants with greater psychological readiness for RTS had greater mean isometric knee flexor strength. However, no other statistically significant differences were found be tween groups in any other performance test measured.
Both psychological readiness to RTS and return of knee flexor strength have been shown to be an important predic tor of successful RTS outcomes. Athletes with greater ACL RSI scores, a marker of psychological readiness, are more likely to return to sport after injury recovery 13,25 Further, athletes with lower ACL-RSI scores and a smaller improve ment in ACL-RSI score throughout postoperative rehabil itation are more likely to experience a second ACL injury upon returning to sport.21 Knee flexor strength deficits af ter ACLR have been associated with an increased second in jury risk.48,49
HS Group (n= 9)
LS Group (n = 9) p-value Mean ± SD Mean ± SD
Height (cm) 176.43 10.77 169.87 8.66 0.173
Mass (kg) 74.48 11.68 78.80 23.80 0.631 Age (yrs) 18.67 5.17 21.67 7.33 0.331
ACL-RSI Score 83.06 6.22 61.76 8.00 <0.0001*
Mean time to RTS clearance (months) 8.74 1.54 9.50 2.75 0.475
*denotes statistically significant difference HS= high score ACL-RSI group, LS = low score ACL-RSI group
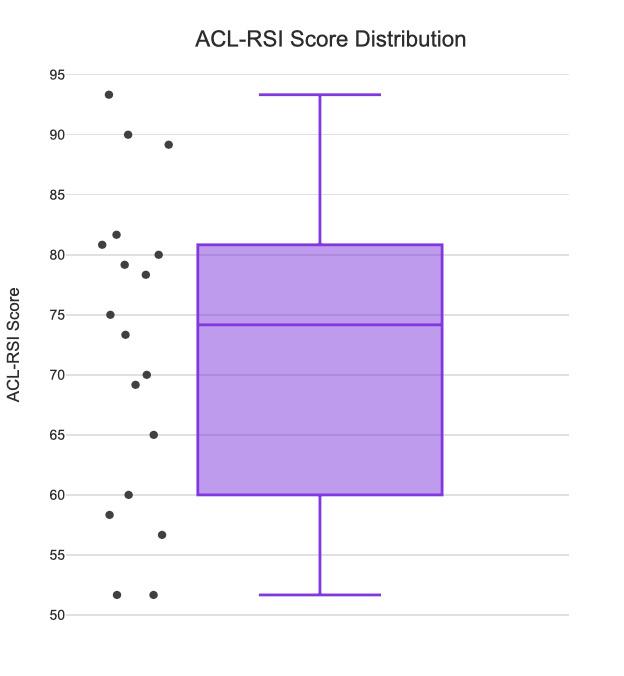
Previous studies have also identified relationships be tween strength and functional performance testing with psychological readiness to return to sport. Paterno et al identified that athletes with greater fear, a component of psychological readiness, were less likely to return to previ ous levels of activity and were more likely to have isometric knee extensor strength asymmetry and hop testing asym metry between legs at time of RTS, and were more likely to experience second ACL injuries.50 Lepley et al. observed that lower levels of presurgical pain and greater knee exten sor strength in both the injured and uninjured limbs at time of RTS clearance were associated with greater psychologi cal readiness to return to sport.27 Burland et al found that greater isometric and isokinetic extensor strength were as sociated with higher ACL-RSI scores at three and six months postoperative in adolescent patients.26 Meierbach tol et al. and Muller et al. found a positive correlation be tween ACL-RSI score and triple hop for distance.20,28
The time before recovery of static and postural stability skill after ACLR remains controversial,51–54 but has been shown to improve upon training and is often trained in
postoperative rehabilitation programs.55–58 Balance deficits may persist six months to three years after ACL in jury 54 It is possible that no difference was observed be tween the high and low score groups on static and postural stability testing because all athletes had been exposed to balance testing throughout rehabilitation and had ade quately recovered their balance at time of return to sport testing.
There are several limitations to this study First, there was a relatively small enrollment size. Generalization of these findings should be done with caution, given the small sample size and small age range of athletes enrolled. Par ticipants volunteered to enroll in the study, so enrollment was limited by their willingness to complete testing leading to selection bias. Additionally, the type of surgical graft used intraoperatively, and postoperative rehabilitation pro grams were not controlled among participants. Athletes may have exhibited reduced hamstring strength if they re ceived a hamstring autograft, which would be unrelated to psychological readiness. Graft type for each participant was not recorded for this study, therefore we were unable to stratify results based on this finding. Postoperative reha bilitation protocols are not standardized after ACLR,57,59,60 which could contribute to varying levels of familiarity or preparation for the test battery used in this study However, because participants were tested after RTS clearance by their clinicians, it is assumed that all subjects had demon strated some level of competency with strength, balance, and functional performance testing prior to enrollment in this study
This study demonstrated an association between greater isometric knee flexor strength and ACL-RSI score, a surro gate of psychological readiness to RTS, partially supporting the hypothesis. We found no association between greater psychological readiness to RTS and knee extensor strength, static or dynamic postural stability, or hop testing among the cohort. Findings from this study indicate that improv ing hamstring strength may contribute to greater psycho logical readiness to return to sport, both of which may help reduce second ACL injury rates. Given that psychological readiness has been shown to be related to successful RTS outcomes and lower second injury rates, future research
Figure 1. Distribution of ACL-RSI scores.HS Group (n= 9) LS Group (n = 9) p-value Mean ± SD Mean ± SD
Static Balance GRF - AP, EO 2.68 0.73 2.71 1.10 0.947
Static Balance GRF - ML, EO 3.53 1.29 3.53 1.73 0.993
Static Balance GRF - V, EO 5.64 1.68 5.17 2.34 0.630
Static Balance GRF - Combined, EO 7.20 2.15 6.85 3.05 0.780
Static Balance GRF - AP, EC 5.33 1.53 6.29 4.02 0.510
Static Balance GRF - ML, EC 9.09 4.39 10.80 7.02 0.545
Static Balance GRF - V, EC 12.48 5.09 12.85 7.02 0.898
Static Balance GRF - Combined, EC 16.42 6.65 17.99 10.59 0.711
DPSI 0.35 0.05 0.36 0.04 0.479
APSI 0.14 0.01 0.14 0.01 0.303
MLSI 0.03 0.00 0.03 0.01 0.950
VSI 0.32 0.05 0.33 0.04 0.505
GRF= ground reaction forces, EO= eyes open, EC eyes closed, AP= anterior-posterior, ML= medial-lateral, V= vertical, HS= high score ACL-RSI group, LS low score ACL-RSI group
HS Group (n= 9) LS Group (n = 9) pvalue Mean ± SD Mean ± SD
Isokinetic Knee flexion avg peak torque/ BM *100 124.98% 25.87 102.03% 46.49 0.214 Isokinetic Knee extension avg peak torque / BM * 100 189.06% 45.63 192.68% 67.99 0.896
Handheld dynamometry knee flexion avg peak force/ BM * 100 22.61% 6.01 12.12% 4.88 0.001*
Handheld dynamometry knee extension avg peak force/ BM *100 36.55% 11.37 32.90% 11.82 0.528
*denotes statistical significance HS= high score ACL-RSI group, LS = low score ACL-RSI group, BM = body mass (kg)
HS Group (n= 9) LS Group (n = 9) p-value Mean ± SD Mean ± SD
Triple hop distance / height 265.19 55.65 209.74 65.66 0.071 Crossover hop distance / height 238.94 54.17 187.58 73.91 0.112 HS= high score ACL-RSI group, LS = low score ACL-RSI group
should explore ways to train and optimize psychological readiness in additional to functional strength prior to an athlete’s return to sport.
None
IRB PROTOCOL Pro00088033 DUHS IRB
Submitted: August 11, 2021 CST, Accepted: August 16, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am J Sports Med 2016;44(6):1502-1507 doi:10.1177/0 363546516629944
2. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 2014;42(10):2363-2370. doi:10.1177/03635465145427 96
3. Wiggins ME, Fadale P, Barrach H, Ehrlich M, WW Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sport Med 2016;44(7):1861-1876. doi:10.1177/036354651562155 4.Risk
4. Lentz TA, Zeppieri G Jr, Tillman SM, et al. Return to preinjury sports participation following anterior cruciate ligament reconstruction: Contributions of demographic, knee impairment, and self-report measures. J Orthop Sports Phys Ther. 2012;42(11):893-901. doi:10.2519/jospt.2012.4077
5. Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger Am J Sports Med 2016;44(2):384-392. doi:10.1177/0363546515623032
6. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules reduce reinjury risk after anterior cruciate ligament reconstruction: The Delaware-Oslo ACL cohort study Br J Sports Med 2016;50(13):804-808. doi:10.1136/bjs ports-2016-096031.SIMPLE
7. Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury J Bone Jt Surg Am Vol 2017;99(11):897-904. doi:10.2106/jbj s.16.00758
8. Ross CA, Clifford A, Louw QA. Factors informing fear of reinjury after anterior cruciate ligament reconstruction. Physiother Theory Pract. 2017;33(2):103-114. doi:10.1080/09593985.2016.1271 847
9. Failla MJ, Logerstedt DS, Grindem H, et al. Does extended preoperative rehabilitation influence outcomes 2 years after ACL reconstruction? Am J Sports Med. 2016;44(10):2608-2614. doi:10.1177/0363 546516652594
10. Müller U, Krüger M, Schmidt M, Rosemeyer B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery Knee Surg Sports Traumatol Arthrosc 2015;23(12):3623-3631. doi:10.1007/s0016 7-014-3261-5
11. Ardern CL, Kvist J, Webster KE. Psychological aspects of ACL injuries. Oper Tech Sports Med 2015;24(1):77-83. doi:10.1053/j.otsm.2015.09.006
12. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play Br J Sports Med 2011;45(7):596-606. doi:10.1136/bjsm.2010.076364
13. Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sport Med. 2009;43(5):377-381. doi:10.11 36/bjsm.2007.044818
14. Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48(22):1613-1619. doi:10.1136/bjsports-2014-0 93842
15. Nwachukwu BU, Adjei J, Rauck RC, et al. How much do psychological factors affect lack of return to play after anterior cruciate ligament reconstruction? A systematic review. Orthop J Sport Med. 2019;7(5):1-7 doi:10.1177/2325967119845313
16. Webster K, Nagelli C, Hewett T, Feller J. Factors associated with psychological readiness to return to sport after an anterior cruciate ligament reconstruction surgery Am J Sports Med 2019;46(7):1545-1550. doi:10.1177/036354651877375
7.Factors
17 Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery Am J Sports Med. 2013;41(7):1549-1558. doi:10.1177/0363546513 489284
18. Czuppon S, Racette B, Klein S, Harris-Hayes M. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review Br J Sport Med 2014;48(5):356-364. doi:10.1136/bjsports-2012-0917 86.Variables
19. Burgi CR, Peters S, Ardern CL, et al. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review Br J Sports Med. 2019;53(18):1154-1161. doi:10.1136/ bjsports-2018-099982
20. Müller U, Krüger-Franke M, Schmidt M, Rosemeyer B. Predictive parameters for return to preinjury level of sport 6 months following anterior cruciate ligament reconstruction surgery Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3623-3631. do i:10.1007/s00167-014-3261-5
21. Mcpherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med 2019;47(4):857-862. doi:1 0.1177/0363546518825258
22. Mcpherson AL, Feller JA, Hewett TE, Webster KE. Smaller change in psychological readiness to return to sport is associated with second anterior cruciate ligament injury among younger patients. Am J Sports Med 2019;47(5):1209-1215. doi:10.1177/0363546519 825499
23. Rosso F, Bonasia DE, Cottino U, Cambursano S, Dettoni F, Rossi R. Factors affecting subjective and objective outcomes and return to play in anterior cruciate ligament reconstruction: A retrospective cohort study Joints 2018;6(1):23-32. doi:10.1055/s-0 038-1636931
24. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport 2008;9(1):9-15. doi:10.1016/j.ptsp.20 07.09.003
25. Sadeqi M, Klouche S, Bohu Y, Herman S, Lefevre N, Gerometta A. Progression of the psychological ACL-RSI score and return to sport after anterior cruciate ligament reconstruction. Orthop Jounral Sport Med 2018;6(12):1-7 doi:10.1177/232596711881 2819
26. Burland JP, Kostyun RO, Kostyun KJ, Solomito M, Nissen C, Milewski MD Clinical outcome measures and return-to-sport timing in adolescent athletes after anterior cruciate ligament reconstruction. J Athl Train 2018;53(5):442-451. doi:10.4085/1062-6050-30 2-16
27. Lepley AS, Pietrosimone B, Cormier ML. Quadriceps function, knee pain, and self-reported outcomes in patients with anterior cruciate ligament reconstruction. J Athl Train. 2018;53(4):337-346. do i:10.4085/1062-6050-245-16
28. Meierbachtol A, Yungtum W, Paur E, Bottoms J, Chmielewski TL. Psychological and functional readiness for sport following advanced group training in patients with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2018;48(11):864-872. doi:10.2519/jospt.2018.8041
29. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 1985;198:42-49. doi:10.1097/00003086-198 509000-00007
30. Briggs KK, Steadman JR, Hay CJ, Hines SL. Lysholm score and tegner activity level in individuals with normal knees. Am J Sports Med 2009;37(5):898-901. doi:10.1177/0363546508330149
31. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form. Arthritis Care Res 2011;63(0 11):208-228. doi:10.1002/acr.20632.Measures
32. Goldie PA, Evans OM, Bach TM. Steadiness in one-legged stance: development of a reliable forceplatform testing procedure. Arch Phys Med Rehabil 1992;73(4):348-354. doi:10.1016/0003-9993(92)9000 8-k
33. Goldie PA, Bach TM, Evans OM. Force platform measures for evaluating postural control: reliability and validity Arch Phys Med Rehabil 1989;70(7):510-517
34. Abt JP, Sell TC, Laudner KG, et al. Neuromuscular and biomechanical characteristics do not vary across the menstrual cycle. Knee Surg Sports Traumatol Arthrosc. 2007;15(7):901-907. doi:10.1007/s00167-00 7-0302-3
35. Sell TC, Lovalekar MT, Nagai T, Wirt MD, Abt JP, Lephart SM. Gender differences in static and dynamic postural stability of soldiers in the Army’s 101st airborne division (air assault). J Sport Rehabil 2018;27(2):126-131. doi:10.1123/jsr.2016-0131
36. Sell T, House A, Abt J, Lephart S. An examination, correlation, and comparison of static and dynamic measures of postural stability in healthy, physically active adults. Phys Ther Sport 2012;13(2):80-86. doi:1 0.1016/j.ptsp.2011.06.006
37 Akins JS, Longo PF, Bertoni M, et al. Postural stability and isokinetic strength do not predict knee valgus angle during single-leg drop-landing or single-leg squat in elite male rugby union players. Isokinet Exerc Sci 2013;21(1):37-46. doi:10.3233/ies-2 012-0469
38. Ross S, Guskiewicz K. Time to Stabilization: A Method for Analyzing Dynamic Postural Stability. Int J Athl Ther Train 2003;8(3):37-39.
39. Sell TC, Pederson JJ, Abt JP, et al. The addition of body amor diminishes dynamic postural stability in military soldiers. Mil Med 2013;178(1):76-81. doi:1 0.7205/milmed-d-12-00185
40. Wikstrom EA, Tillman MD, Smith AN, Borsa PA. A new force-plate technology measure of dynamic postural stability: The dynamic postural stability index. J Athl Train. 2005;40(4):305-309.
41. Sell TC, Clark NC, Abt JP, Lovalekar M, Lephart SM. Isokinetic strength of fully operational U.S. Navy Seals with a previous history of shoulder and knee injury Isokinet Exerc Sci 2016;24(4):349-356. doi:10.3 233/ies-160637
42. Jackson SM, Cheng MS, Smith AR Jr, Kolber MJ. Intrarater reliability of hand held dynamometry in measuring lower extremity isometric strength using a portable stabilization device. Musculoskelet Sci Pract. 2017;27:137-141. doi:10.1016/j.math.2016.07.010
43. Mentiplay BF, Perraton LG, Bower KJ, et al. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: A reliability and validity study PLoS One 2015;10(10):1-19. doi:1 0.1371/journal.pone.0140822
44. Hébert LJ, Maltais DB, Lepage C, Saulnier J, Crête M, Perron M. Isometric muscle strength in youth assessed by hand-held dynamometry: A feasibility, reliability, and validity study: A feasibility, reliability, and validity study Pediatr Phys Ther 2011;23(3):289-299. doi:10.1097/pep.0b013e318227cc ff
45. Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Jt Surg 1984;66-A(3):344-352. doi:10.2106/00004623-198466030-00005
46. Haitz K, Shultz R, Hodgins M, Matheson GO. Test retest and interrater reliability of the functional lower extremity evaluation. J Orthop Sports Phys Ther. 2014;44(12):947-954. doi:10.2519/jospt.2014.4809
47 Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther 2007;87(3):337-349. doi:10.2522/ptj.20060143
48. Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: A review of the Hunt Valley II Meeting, January 2005. Am J Sports Med. 2006;34(9):1512-1532. doi:10.1177/036354650628686 6
49. Kellis E, Galanis N, Kofotolis N. Hamstring-toquadriceps ratio in female athletes with a previous hamstring injury, anterior cruciate ligament reconstruction, and controls. Sports. 2019;7(10):214. doi:10.3390/sports7100214
50. Paterno MV, Flynn K, Thomas S, Schmitt LC. Self reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study Sports Health 2018;10(3):228-233. doi:10.1177/1941738117745806
51. Ferdowsi F, Rezaeian ZS. Evaluating equilibrium in anterior cruciate ligament reconstruction. J Phys Ther Sci 2018;30(5):726-729. doi:10.1589/jpts.30.726
52. Fischer-Rasmussen T, Jensen PE. Proprioceptive sensitivity and performance in anterior cruciate ligament-deficient knee joints. Scand J Med Sci Sport 2000;10(2):85-89. doi:10.1034/j.1600-0838.2000.0100 02085.x
53. Clagg S, Paterno MV, Hewett TE, Schmitt LC. Performance on the modified star excursion balance test at the time of return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015;45(6):444-452. doi:10.2519/jospt.201 5.5040
54. Delahunt E, Chawke M, Kelleher J, et al. Lower limb kinematics and dynamic postural stability in anterior cruciate ligament-reconstructed female athletes. J Athl Train 2013;48(2):172-185. doi:10.408 5/1062-6050-48.2.05
55. Taubert M, Mehnert J, Pleger B, Villringer A. Rapid and specific gray matter changes in M1 induced by balance training. Neuroimage. 2016;133:399-407. d oi:10.1016/j.neuroimage.2016.03.017
56. Garrison JC, Bothwell JM, Wolf G, Aryal S, Thigpen CA. Y Balance TestTM anterior reach symmetry at three months is related to single leg functional performance at time of return to sports following anterior cruciate oigament reconstruction. Int J Sports Phys Ther 2015;10(5):602-611.
57 Saka T Principles of postoperative anterior cruciate ligament rehabilitation. World J Orthop. 2014;5(4):450-459. doi:10.5312/wjo.v5.i4.450
58. Cavanaugh JT, Powers M. ACL Rehabilitation progression: where are we now? Curr Rev Musculoskelet Med 2017;10(3):289-296. doi:10.1007/s 12178-017-9426-3
59. Simoneau GG, Wilk KE. The challenge of return to sports for patients post-ACL reconstruction. J Orthop Sports Phys Ther 2012;42(4):300-301. doi:10.2519/jos pt.2012.0106
60. Wright R, Preston E, Fleming B, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation part II: open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. J Knee Surg 2008;21(3):225-234. doi:10.1055/s-0030-1247823
Piussi R, Simonson R, Högberg J, Thomeé R, Samuelsson K, Hamrin Senorski E.
Psychological Patient-reported Outcomes Cannot Predict a Second Anterior Cruciate Ligament Injury in Patients who Return to Sports after an Anterior Cruciate Ligament Reconstruction. IJSPT. Published online December 1, 2022:1340-1350.
Ramana Piussi 1,2,3 a , Rebecca Simonson 1,3 , Johan Högberg 1,2,3 , Roland Thomeé 1,2 , Kristian Samuelsson 3,4 , Eric Hamrin Senorski 1,2,3,5
1 Sportrehab Sports Medicine Clinic, Gothenburg, Sweden, 2 Unit of Physiotherapy, Department of Health and Rehabilitation, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden, 3 Sahlgrenska Sports Medicine Center, Gothenburg, Sweden, 4 Department of Orthopaedics, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden, 5 Swedish Olympic Committee (SOC), Stockholm, Sweden
Keywords: anterior cruciate ligament, knee self efficacy scale, pateient reported outcomes, psychological outcomes, return to sport, return to sport after injury scale
https://doi.org/10.26603/001c.55544
Psychological patient-reported outcomes (PROs) are recommended for use in test batteries to aid in decision-making, regarding whether patients are well prepared to return to sports (RTS) after anterior cruciate ligament (ACL) reconstruction. However, the values that should be regarded as “pass” or “fail” are still unclear
This study aimed to identify cut-off values for three commonly used psychological PROs that could differentiate patients who suffer a second ACL injury from patients who do not within two years of RTS in patients after ACL reconstruction with respect to recovery of symmetrical quadriceps strength.
Demographic data, isokinetic strength test data for quadriceps, as well as results for the ACL-Return to Sport after Injury scale (ACL-RSI), Knee Injury and Osteoarthritis Outcome Score (KOOS) Quality of Life, and Function in Sport and Recreation sub-scales, and the 18-item version of the Knee Self-Efficacy Scale (K-SES18) were extracted from a registry. Receiver operating characteristic (ROC) curves were calculated for each PRO. Accuracy of the cut-offs was presented with two summary measures for the ROC: the area under the curve (AUC) and Youden index.
In total, 641 (355 men, 61%) patients (24.8 [SD 7.6] year old at ACL reconstruction) were included. The cut-off values were not able to differentiate patients who suffered a second ACL injury up to 24 months after RTS and ACL reconstruction from patients who did not. Additionally, achieving symmetrical quadriceps strength did not improve the cut-off psychometric properties.
a

Corresponding author: Ramana Piussi
Sportrehab Sports Medicine Clinic, Stampgatan 14, SE-411 01 Gothenburg, Sweden Ramana.piussi@gu.se +46761677520
Since cut-off values could not differentiate between patients who suffered a second ACL injury and those who did not, clinicians should not rely only on cut-off values or a single PRO of those analyzed in this study when making decisions on which patients are at risk of experiencing a second ACL injury when returning to sports after ACL reconstruction.
Level of Evidence Level 3
Anterior cruciate ligament (ACL) injury is most commonly treated with rehabilitation, and about 50% of patients un dergo surgical reconstruction of the ruptured ligament.1 To sustain a second ACL injury after ACL reconstruction can be devastating; and this further increases the risk for longterm consequences, such as osteoarthritis and lower levels of physical activity and perceived quality of life.2–5 A com mon goal for patients treated with rehabilitation and ACL reconstruction is to return to sport (RTS).6,7 As participat ing in sports is associated with a risk of sustaining a second ACL injury,8 a primary concern is to evaluate the patients readiness for RTS, i.e. returning to sports with minimal risk for suffering a second ACL injury
Responses to psychological patient-reported outcomes (PROs) can differ between patients who suffer a second ACL injury and those who do not, as patients who suffer a sec ond ACL injury have reported greater scores, that is, better responses, on validated PROs.9,10 Collected evidence, in cluding the results from systematic reviews on psychologi cal outcomes after ACL reconstruction and clinical practice guidelines,11–13 as well as patients’ experiences,14 suggest that psychological PROs should be used in test batteries to help identify whether patients are well prepared for RTS af ter ACL reconstruction.
An issue related to the use of PROs in RTS test batteries is, which cut-off values best identify whether patients “pass” (patients can be cleared to RTS) or “fail” (patients should be advised against RTS)? Different cut-offs for dif ferent PROs and outcomes have been proposed.15,16 No tably, some cut-offs commonly used in the decision-making if the patient can RTS have not been anchored against a second ACL injury,15 but are instead based on responses from PROs that were collected several months prior to pa tients suffering a second ACL injury 16 It is important to acknowledge that the reasons for a second ACL injury are multifactorial and include genetic, physical, psychological, trauma, and surgical factors.17–20 Recovery of symmetrical quadriceps strength has been proposed as a possible pro tective factor that can reduce the risk of a second ACL in jury in high-level athletes with RTS.21 However, the results are inconclusive.22,23
There is a need to better understand which cut-offs for PROs best predict a second ACL injury in patients treated with ACL reconstruction, especially regarding protective factors for a second ACL injury, such as the recovery of sym metrical quadriceps strength. This study aimed to identify cut-off values for three commonly used psychological PROs that could differentiate patients who suffer a second ACL
injury from those who do not within two years of RTS after ACL reconstruction with respect to recovery of symmetrical quadriceps strength.
Following the guidelines from the Enhancing the Quality and Transparency of Health Research (EQUATOR) network, the Standards for Reporting Diagnostic Accuracy (STARD) statement was used as a checklist to report this study.24 Data for the present study were prospectively collected from a rehabilitation outcome registry, the Project ACL. The registry was established in 2014, which aims to im prove the care of patients with ACL injuries. Data in the Project ACL consists of results from muscle function tests and PROs collected prospectively before the surgery (in case of ACL reconstruction), at 10 weeks, 4, 8, 12, 18, and 24 months, and every five years with ACL injury/reconstruc tion as a baseline.25 Prior to participation in the Project ACL, written consent was collected. Ethical approval was obtained from the Swedish Ethical Review Authority (regis tration number:2020-02501).
All consecutive patients registered in the Project ACL with one ACL injury treated with reconstruction with or without sustaining a subsequent second ACL injury within two years from RTS [Tegner Activity Scale (Tegner)26 ≥6] were eligible for inclusion. The patients included in this study were fol lowed up for two years after RTS. Patients were excluded if one of the following criteria were fulfilled: age <16 or >50 years; not participating in knee-strenuous sports prior to index ACL injury, i.e. reporting a Tegner Activity Scale26 of <6; sustaining a second ACL injury before surgical re construction; or not participating in any of the follow-ups of project ACLs. Second ACL injuries are reported by pa tients themselves, responsible physical therapists, or the test leader at follow-up in Project ACL.
The PROs used in this study were the ACL-Return to Surgery after Injury scale (ACL-RSI),27 Knee Injury and Os teoarthritis Outcome Score subscale Quality of Life (KOOS QoL),28 and Function in sport and recreation (KOOS Sports), the 18-item version of the Knee Self-Efficacy Scale (K-SES18),29 and Tegner Activity Scale.26
The ACL-RSI aims to measure patients’ emotions, confi dence, and risk appraisal of RTS after an ACL injury Herein,
the validated 12-item short version was used.27 Each item was graded from 0 to 10, where 10 is the highest response, representing the best possible psychological response to RTS (highest confidence and emotion, and lowest risk ap praisal). The final score is calculated by summing the total score of all items (highest score 120), and then normalizing the score to a 0-100 scale as proposed in the original pa per 27
The K-SES18 aims to evaluate knee-related self-effi cacy,29 that is, the belief in one’s ability to perform a phys ical task, such as running or jumping. The K-SES18 com prises 18 items divided into two subscales: present (14 items) and future (four items) knee self-efficacies. Each item was graded from 0 to 10, with 10 being the most pos itive response, representing the greatest belief in carrying out a given physical task. The results from each item were added and divided by the number of items to generate a mean value for the subscales.
The KOOS QoL and KOOS Sports were used in the as sessment of patients with ACL injury.28 They comprise four (QoL) and five (Sports) items, respectively The KOOS QoL assess how often patients are reminded of their knee prob lems, whether patients can trust their knee function, have to make life changes due to knee function, and whether pa tients experience problems related to the knee. The KOOS Sports comprises five items assessing a patient’s perceived difficulty in performing different tasks, such as running and jumping during the last week. Each item is rated from 0 to 4 on a 5-point Likert scale, and a normalized score from 0 to 100 is calculated for each subscale, where 0 indicates the most severe symptoms, and 100 indicates no symptoms.
The Tegner Activity Scale (Tegner)26 aims to measure strenuous knee activity Patients grade their activity based on work and sports activities on a scale from 1 to 10, where one represents disability because of knee problems and 10 represents, for example, national or international level soc cer From level 6 on the Tegner, only sports activities are registered, and therefore when patients rate Tegner ≥6, it is assumable patients are active in a knee strenuous sport.
Strength tests for unilateral concentric knee extension and flexion were performed according to a standardized pro tocol,30 with an isokinetic dynamometer [Biodex System 4 (Biodex Medical Systems, Shirley, New York, USA)]. The testing procedure started with a standardized warm-up of 10 minutes on a stationary bike and sub-maximum trials on each test. The injured leg was tested first, followed by the uninjured leg. Isokinetic testing was performed at an angu lar velocity of 90°/s with the patients in a seated position. Three maximum repetitions with approximately 40 s of rest between each repetition were performed, and the greatest peak torque was recorded in the Project ACL database. For this study, the results from the unilateral knee extension test were extracted for analysis.
In this study, demographic data, results from PROs, and strength tests for the quadriceps were extracted for analysis from the Project ACL in November 2021.
Time frame for returning to knee-strenuous sports typ ically varies between 6-13 months31 after primary ACL re construction. Results of the PROs and strength tests from the follow-up closest in time to RTS (Tegner Activity Scale, level ≥6) were selected for the included patients as the “in dex test.”
Primary outcomes of this study were the cut-off values with sensitivity and specificity for predicting a second ACL injury for each of the included PROs. Therefore, patients who did not go on to suffer a second ACL injury were treated as a reference, and patients who suffered a second ACL injury were treated as having the outcome of interest. Clinical reference standard was not applicable, as the analysis aimed to predict the outcome of interest. In order to account for the recovery of symmetrical quadriceps strength as a protective factor,21,32 sensitivity analyses were performed with regard to patients who had and had not recovered ≥90% of their quadriceps strength in the in jured limb compared to the uninjured limb.33 Symmetrical quadriceps strength was presented with the limb symmetry index (LSI), where result from the injured limb was divided with result from the uninjured limb and multiplied by 100.
Receiver operating characteristics (ROC) were calculated for each PRO at available follow-ups within two years of RTS (Tegner ≥6). The ROC is a graphical method of display ing the discriminatory accuracy of a marker (in this case, responses to PROs) for separating two populations, or dis tinguishing between patients affected by an outcome, that is, suffering a second ACL injury within two years after RTS (return to Tegner ≥6), and individuals not affected by the outcome of interest, that is, patients who did not suffer a second ACL injury within two years after RTS. A patient was assessed as “positive” if the tested PRO value was greater than a given threshold value; otherwise, the patient was assessed as negative.34 The accuracy of any given thresh old value was measured by the probability of a true positive (sensitivity) and true negative (specificity), and presented with two summary measures for ROC: the area under the curve (AUC) and Youden index. The area under the curve (AUC) is a measure of the ability of a classifier to distin guish between outcomes and is used as a summary of the ROC curve. The higher the AUC, the better the performance of the model in distinguishing between positive and neg ative outcomes. When AUC is comprised between 0.5 and 1, there is a chance that the classifier can be able to dis tinguish the positive class values from the negative class values, depending on the AUC value, according to the fol lowing rule of thumb: 0.5 = no discrimination, with the same value of a coin flip; 0.5-0.7 = poor discrimination, not much better than a coin flip; 0.7-0.8 = acceptable dis crimination; 0.8-0.9 = excellent discrimination; and >0.9 = outstanding discrimination.35 Therefore, when interpret
Figure 1. Flowchart on inclusion and exclusion.
ACL = Anterior Cruciate Ligament; RTS = Return to Sport (return to Tegner Activity level ≥6); n = number
ing the AUC; values between 0.7 to 0.8 were considered to reflect acceptable accuracy 36 The Youden Index is a fre quently used summary measure of the ROC and it measures the effectiveness of a diagnostic marker and enables the selection of an optimal threshold value (cut-off point) for the marker 34 The Youden index value ranges from 0 to 1,37 where 0 means that a diagnostic test gives the same pro portion of positive results for groups with and without the disease, i.e. the test is useless, while a value of 1 indicates that there are no false positives or false negatives, i.e. the test is perfect.
Statistical analyses were performed using Statistical Analysis System (SAS) software version 9 (SAS Institute Inc., Cary, North Carolina, USA). Mean values with stan dard deviations (SD) or medians with minimum and maxi mum are presented for the demographic data. Significance level was set at 0.05.
In total, 641 patients (355 men, 61%) were included in the present study Figure 1 shows the inclusion and exclusion process. Table 1 presents the demographic characteristics of the patients.
Figure 2 presents the frequency of a second ACL injury stratified by months from return to knee-demanding activ ity (Tegner ≥6).
Table 2 presents the Youden index with specificity and sensitivity, as well as the model AUC for all assessed PROs.
The cut-offs that best differentiated patients who suf fered a second ACL injury after ACL reconstruction from patients who had not were: ≥71.7 for the ACL-RSI, <56 for the KOOS QoL, ≥96.0 for the KOOS Sports, ≥9.4 for the K SES18 present and ≥7.0 for the K-SES18 future. The AUC and Youden index for each cut-off were below acceptable val ues, indicating the inability of the cut-offs to properly dif ferentiate between patients who suffered a second ACL in jury after ACL reconstruction and those who did not. Table 3 presents the number of patients who suffered a second
ACL injury in relation to the achievement of the cut-off val ues for the different PROs.
Table 4 presents the cut-off analysis stratified according to patients who had and had not achieved an LSI of ≥90% in the quadriceps strength test at the time of RTS.
Stratifying patients based on achieved symmetrical quadri ceps strength (≥90% LSI) or not at the time of RTS did not lead to cut-off values with better psychometric properties, i.e., the Youden index or AUC compared with the cut-offs determined for the entire cohort. In the current results, the best Youden index was 0.24, and the best AUC was 0.613, which is well below acceptable levels.36,37 Therefore, the calculated cut-offs appear unable to separate the two out comes, with or without a second ACL injury.
Table 5 presents the number of patients who suffered a second ACL injury in relation to the achievement of the cut offs for the different PROs in patients who achieved sym metrical quadriceps strength at the time of RTS.
The main finding from this registry study was that the de termined cut-off values for different PROs were not able to differentiate patients who suffered a second ACL injury up to 24 months after RTS following ACL reconstruction from patients who did not. Additionally, achieving symmet rical quadriceps strength, i.e., ≥90% LSI did not improve the cut-offs’ psychometric properties. Regardless of recov ering symmetrical quadriceps strength, patients with either a higher or lower knee perceived quality of life, knee-re lated self-efficacy, confidence, emotions, and risk appraisal appear as likely to suffer a second ACL injury. Therefore, it can be assumed that passing the calculated cut-off for PROs
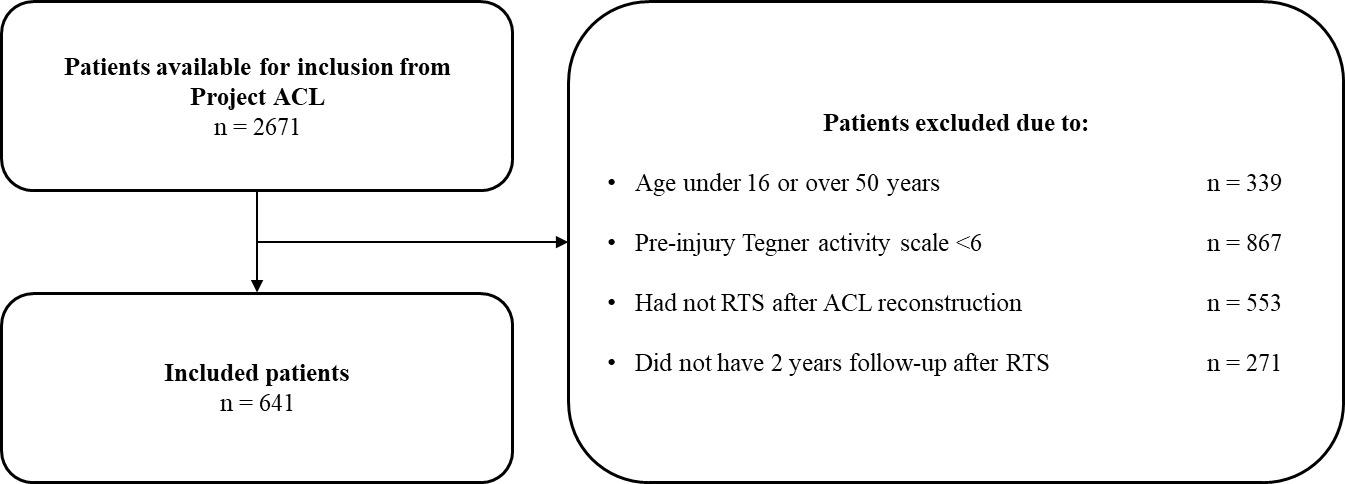
Table 1. Demographic data, mean values, standard deviations (SD), count (n) and proportions (%).
All patients; n=641 Men; n=355 Women; n=286
Age at reconstruction, years 24.8 (7.6) 25.8 (7.4) 23.5 (7.6)
Height, cm 175.7 (9.3) 181.7 (6.4) 168.2 (6.5) Weight, kg 73.5 (12.7) 80.9 (10.2) 64.2 (8.9)
BMI 23.7 (2.8) 24.5 (2.6) 22.7 (2.7)
Time to RTS, months 11.8 (15.1) 10.3 (13.8) 13.6 (16.4) Tegner pre-injury level, n (%)
6 44 (6.9%) 20 (5.6%) 24 (8.4%) 7 108 (16.8%) 66 (18.6%) 42 (14.7%) 8 158 (24.6%) 69 (19.4%) 89 (31.1%) 9 213 (33.2%) 129 (36.3%) 84 (29.4%) 10 118 (18.4%) 71 (20.0%) 47 (16.4%)
Returned to pre-injury Tegner Yes, n (%) 442 (69.0%) 248 (69.9%) 194 (67.8%)
Returned to pre-injury Tegner Months from index reconstruction
4 108 (24.4%) 79 (31.8%) 29 (15%) 5-8 75 (17%) 45 (18.1%) 30 (15.5%) 9-12 128 (29%) 61 (24.6%) 67 (34.5%) 12-24 70 (15.8%) 35 (14.1%) 35 (18.0%) >24 61 (13.8%) 28 (11.3%) 33 (17%)
Graft choice
Hamstring graft, n (%) 465 (72.5%) 260 (73.2%) 205 (71.7%) Patellar graft, n (%) 77 (12.0%) 43 (12.1%) 34 (11.9%) Other graft, n (%) 6 (0.9%) 2 (0.6%) 4 (1.4%)
Unknown n (%) 93 (14.5%) 50 (14.1%) 43 (15.0%)
Second ACL injury within 24 months from RTS
Yes n (%) 64 (10.0%) 31 (8.7%) 33 (11.5%)
Ipsilateral second ACL injury n (%) 43 (67.2%) 22 (71.0%) 21 (63.6%)
Contralateral second ACL Injury n (%) 21 (32.8%) 9 (29.0%) 12 (36.4%)
used in the present study is not sufficient for safe RTS. Cau tion must thus be taken if patients are cleared to RTS based on the cut-off values used in the present study, regardless, if they achieve ≥90% LSI in quadriceps strength or not.
The used cut-off values for PROs in this study could not generate an acceptable AUC value (0.7-0.8),36 indicating that the cut-off values are no better than ‘flipping a coin’ when used to assess the risk of suffering a second ACL in jury The poor discriminative ability of the cut-offs can be partly explained by the specificity and sensitivity values. The sensitivity ranged between 0.19-0.59 for all the cut-offs except for the K-SES18 future (0.78). Using the ACL-RSI as an example, a sensitivity of 0.50 means that half of the pa tients who suffered a second ACL injury had a score above 71.7. Further, when a patient scores above 71.7 on the ACL RSI, there is approximately a 50% chance to correctly guess if the patient will go on to suffer a second ACL injury (AUC = 0.553); therefore, the psychometric value for the cut-off is very low (Youden index = 0.13). Since the cut-offs that best
differentiated patients who suffered a second ACL injury from patients who did not have low AUC values,36 there is a possibility that the PROs used in this study are not suit able for identifying patients who are at increased risk of a second ACL injury at the time of RTS.
One issue related to the inability of PROs to identify pa tients who will continue to suffer a second ACL injury can be related to the development of the PROs used in this study The ACL-RSI was developed to assess confidence, emotion, and risk appraisal of RTS after ACL injury,27 which are three different psychological domains (constructs). However, the ACL-RSI is summarized into a single score, ranging between to 0-100; this may be questionable be cause the scale comprises three domains,38 which can lead to limitations as it induces indirectness towards the out come when interpreting the PRO as a single score.
When assessing the KOOS, using a stringent psychome tric method, i.e. the Rasch analysis, criteria for one-dimen sionality are respected only in two out of the five subscales,
ACL = Anterior Cruciate Ligament; BMI = Body Mass Index; cm = centimeters; kg = kilograms; n = number; RTS= Return to Sport; Tegner = Tegner Activity ScalePsychological Patient-reported Outcomes Cannot Predict a Second Anterior Cruciate Ligament Injury in Patients who Return.
Figure 2. Frequency of a second ACL injury for every month after RTS.
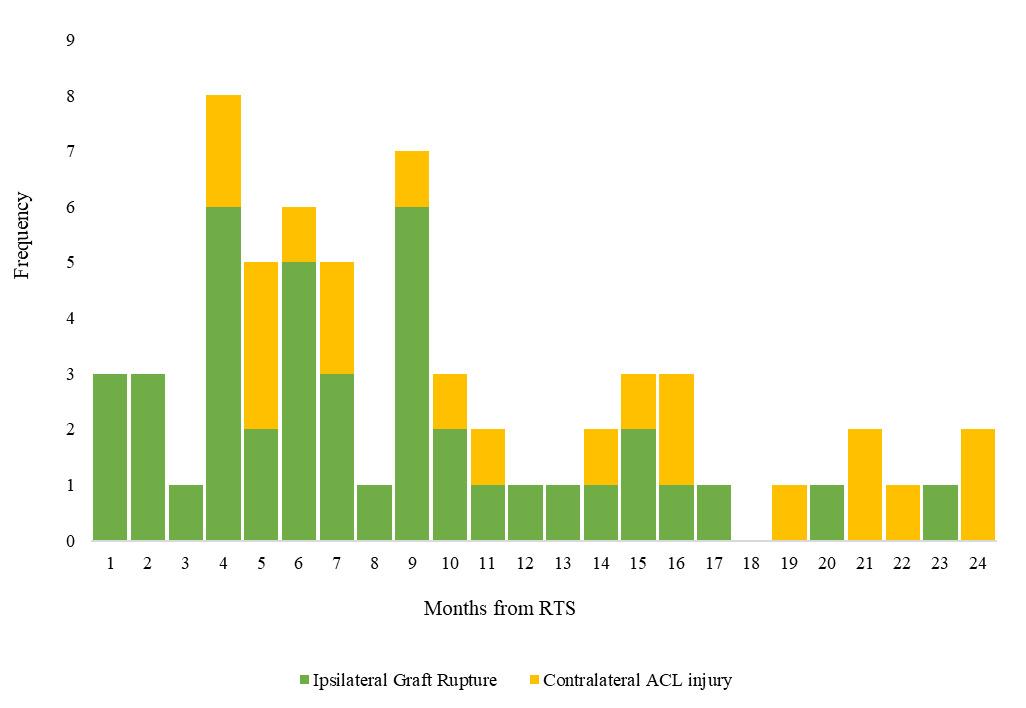
ACL Anterior Cruciate Ligament; RTS Return to Sport (defined as return to Tegner Activity level ≥6); n number
Table 2. Cut-off values, Youden index, and specificity and sensitivity for the included PROs in the analysis. n Cut-off Youden Index 1 - Specificity Sensitivity Model AUC
ACL-RSI 382 71.7 0.13 0.37 0.50 0.553 KOOS QoL 627 56.0 0.12 0.47 0.59 0.531 KOOS Sports 627 96.0 0.12 0.07 0.19 0.557 K-SES18 present 630 9.4 0.09 0.26 0.34 0.520 K-SES18 future 630 7.0 0.08 0.70 0.78 0.511
PROs = Patient Reported Outcomes; n = number i.e., patients responding (please note ACL-RSI is not administered at all follow-ups); ACL-RSI = Anterior Cruciate Ligament Return to Sport after Injury Scale; KOOS Knee injury and Osteoarthritis Outcome Score; QoL subscale Quality of Life; K-SES Knee Self-Efficacy Scale; AUC Area Under the Curve
Table 3. Proportion and number of patients above or below cut-offs who suffered a second ACL injury.
PROs Cut off Second ACL injury, % (n) 95% CI ACL RSI ≥71.7 14% (19) 8.4% 20.5% <71.7 9% (21) 5.4% 12.9%
KOOS QoL ≥56 10% (40) 7.2% 13.2% <56 11% (24) 7.0% 15.6%
KOOS Sports ≥96 23% (12) 12.5% 36.8% <96 9% (52) 6.8% 11.7%
K-SES present ≥9.4 23% (12) 12.5% 36.8% <9.4 9% (52) 6.8% 11.7% K-SES future ≥7 23% (12) 12.5% 36.8% <7 9% (52) 6.8% 11.7%
PROs = Patient Reported Outcomes; ACL = Anterior Cruciate Ligament; n = number i.e., patients responding; CI = Confidence Interval; ACL-RSI = Anterior Cruciate Ligament Return to Sport after Injury Scale; KOOS Knee injury and Osteoarthritis Outcome Score; QoL subscale Quality of Life; K-SES Knee Self-Efficacy Scale
Table 4. Cut-off values, Youden index, and specificity and sensitivity for the included PROs in the analysis, stratified by whether patients achieved symmetrical quadriceps strength or not
Patients with LSI of ≥90% (n=308)
n Cut-off Youden Index 1 - Specificity Sensitivity Model AUC
ACL-RSI 220 71.7 0.22 0.35 0.57 0.591
KOOS QoL 307 56.0 0.24 0.35 0.59 0.580
KOOS Sports 307 96.0 0.18 0.09 0.27 0.600
K-SES18 present 308 9.4 0.17 0.34 0.51 0.569
K-SES18 future 308 8.3 0.05 0.62 0.68 0.495
Patients with LSI of ≤90% (n=181)
ACL-RSI 87 46.7 0.23 0.77 1.00 0.561
KOOS QoL 179 38.0 0.13 0.81 0.94 0.537
KOOS Sports 179 55.0 0.24 0.61 0.84 0.613
K-SES18 present 180 6.1 0.21 0.74 0.95 0.537
K-SES18 future 180 8.0 0.22 0.57 0.79 0.523
PROs Patient Reported Outcomes; n number, i.e., patients responding (please note that ACL-RSI is not administered at all
Table 5. Proportion and number of patients above or below the determined cut-offs who suffer a second ACL injury were stratified, depending on whether the patients achieved symmetrical quadriceps strength or not at the time of RTS.
PROs Cut off Second ACL injury, % (n) 95% CI
ACL-RSI
≥71.7 18.7% (15) 10.9% 29.0% <71.7 9.3% (13) 5.0% 15.4%
KOOS QoL ≥56 11.6% (27) 7.8% 16.5% <56 13.3% (10) 6.6% 23.2%
Patients with LSI of ≥90% (n=308)
KOOS Sports ≥96 29.4% (10) 15.1% 47.5% <96 9.9% (27) 6.6% 14.1%
K-SES18 present ≥9.4 29.4% (10) 15.1% 47.5% <9.4 9.9% (27) 6.6% 14.1%
K-SES18 future
ACL RSI
≥8.3 29.4% (10) 15.1% 47.5% <8.3 9.9% (27) 6.6% 14.1%
≥46.7 7.2% (9) 3.3% 13.2% <46.7 8.1% (3) 1.7% 21.9%
KOOS QoL ≥38 9.1% (24) 5.9% 13.3% <38 5.3% (3) 1.1% 14.6%
Patients with LSI of ≤90% (n=181)
KOOS Sports
≥55 8.9% (19) 5.5% 13.6% <55 7.4% (8) 3.3% 14.1%
K-SES18 present ≥6.1 8.9% (19) 5.5% 13.6% < 6.1 7.4% (8) 3.3% 14.1%
K-SES18 future ≥8.0 8.9% (19) 5.5% 13.6% <8.0 7.4% (8) 3.3% 14.1%
follow-ups); LSI Limb Symmetry Index; ACL-RSI Anterior Cruciate Ligament Return to Sport after Injury Scale; KOOS = Knee injury and Osteoarthritis Outcome Score; QoL = subscale Quality of Life; K-SES = Knee Self-Efficacy Scale; AUC Area Under the Curvei.e. KOOS Sports and KOOS Quality of life.39 Furthermore, the KOOS´s development quality has been rated as “inad equate,” and the KOOS´s psychometric properties with re gard to patients with an ACL injury have been reported to be “poor,” “insufficient,” and “inconsistent”, but the au thors opinions are based on that studies evaluating the psy chometric properties are lacking.38,40 The inconsistency re ported in the psychometric properties of the KOOS with regard to patients with an ACL injury can be due to issues during scale development, since no patients who suffered an ACL injury participated in the development and were asked whether the items were relevant.
As for the K-SES18, a recent publication reported that it has acceptable reliability and validity for measuring self efficacy in patients with ACL injury 41 However, no Rasch analysis has yet been performed on the K-SES18, and good psychometric values can be obtained by correlating the K SES18 with other scales of debatable psychometric prop erties, such as the KOOS, leading to possible misinterpre tation of results. Finally, the inability of PROs to identify patients who would suffer a second ACL injury is likely re lated to the fact that patients with a second ACL injury were not taken into account when developing PROs.
One limitation of this study was the relatively small num ber of patients in the second ACL injury group (n=64), which could have influenced the statistical power A post hoc power calculation was performed, which showed that 33 patients in each group were needed to detect an AUC of 0.7 with a 90% power and an alpha of 0.05. Due to the heterogeneity in the population of patients who suffered an ACL injury, 33 patients per group might still not be suffi cient for the statistical power; therefore, the results should be appreciated with caution. Another limitation of the pre sent study could be its conceptual character. A second ACL injury is multifactorial, and both high and low values on PROs can be risk factors for a second ACL injury 20 Assum ing that both too high and too low knee related self-efficacy could induce a greater risk for a second ACL injury, using only one cut-off value (reflecting a greater risk for a sec ond ACL injury) for one single scale could be conceptually wrong. If a PRO is sensitive in predicting a second ACL in
jury, future studies might need to use two different cut-off values: taking K-SES as an example, one cut-off reflecting an extremely high knee-related self-efficacy, and one cut off reflecting an extremely low knee-related self-efficacy. Notably, some patients returned to the pre-injury Tegner level as early as four months after the ACL reconstruction. It is unclear how this might have affected the results. A fur ther possible limitation of this study concerns age as the ACL-RSI has been reported to be more sensitive for change in younger patients (≤ 20 years) who go on to suffer a sec ond ACL injury.16 Patients in this cohort were on average 24.8 years, and it is not known whether the calculated cut offs are influenced by age, and if age-specific cut-offs may be better to predict second ACL injuries.
The determined cut-off values for three commonly used psychological PROs could not differentiate patients who suffered a second ACL injury from those who did not within two years from RTS, regardless of whether the patients achieved symmetrical quadriceps strength or not, in a co hort of patients who had undergone with ACL reconstruc tion. Therefore, clinicians are recommended to not only rely on cut-off values or a single PRO of those analyzed in this study when making decisions on which patients are at risk of experiencing a second ACL injury when returning to sports after ACL reconstruction.
We would like to thank Editage (www.editage.com) for Eng lish language editing, and Bengt Bengtsson at Statistiska Konsultgruppen for the help with statistical analysis.
Authors declare no conflict of interest.
Submitted: May 20, 2022 CST, Accepted: October 10, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Bogunovic L, Matava MJ. Operative and nonoperative treatment options for ACL tears in the adult patient: a conceptual review. Phys Sportsmed. 2013;41(4):33-40. doi:10.3810/psm.2013.11.2034
2. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and metaanalysis. Am J Sports Med. 2016;44(7):1861-1876. do i:10.1177/0363546515621554
3. Svantesson E, Hamrin Senorski E, Kristiansson F, Alentorn-Geli E, Westin O, Samuelsson K. Comparison of concomitant injuries and patient reported outcome in patients that have undergone both primary and revision ACL reconstruction—a national registry study J Orthop Surg Res 2020;15(1):9. doi:10.1186/s13018-019-1532-z
4. Levy YD, Hasegawa A, Patil S, Koziol JA, Lotz MK, D’Lima DD Histopathological changes in the human posterior cruciate ligament during aging and osteoarthritis: correlations with anterior cruciate ligament and cartilage changes. Ann Rheum Dis 2013;72(2):271-277 doi:10.1136/annrheumdis-201 2-201730
5. Kvist J, Ek A, Sporrstedt K, Good L. Fear of reinjury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2005;13(5):393-397 doi:1 0.1007/s00167-004-0591-8
6. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med 2015;43(4):848-856. doi:10.1177/0363546514563282
7 Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play Br J Sports Med 2011;45(7):596-606. doi:10.1136/bjsm.2010.076364
8. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL Injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567-1573. doi:10.1177/03635 46514530088
9. Paterno MV, Thomas S, VanEtten KT, Schmitt LC. Confidence, ability to meet return to sport criteria, and second ACL injury risk associations after ACL reconstruction. J Orthop Res Published online 2021.
10. Piussi R, Beischer S, Thomeé R, et al. Greater psychological readiness to return to sport, as well as greater present and future knee-related self-efficacy can increase the risk for an ACL re-rupture: a matched cohort study. Arthroscopy. 2022;38(4):1267-1276.e1. doi:10.1016/j.arthro.2021.0 8.040
11. Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review Knee Surg Sports Traumatol Arthrosc. 2015;23(3):752-762. d oi:10.1007/s00167-013-2699-1
12. te Wierike SC, van der Sluis A, van den Akker Scheek I, Elferink-Gemser MT, Visscher C. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports. 2013;23(5):527-540.
13. Andrade R, Pereira R, van Cingel R, Staal JB, Espregueira-Mendes J. How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II). Br J Sports Med 2020;54(9):512-519. doi:10.1136/bjsp orts-2018-100310
14. DiSanti J, Lisee C, Erickson K, Bell D, Shingles M, Kuenze C. Perceptions of rehabilitation and return to sport among high school athletes with anterior cruciate ligament reconstruction: A qualitative research study J Orthop Sports Phys Ther 2018;48(12):951-959. doi:10.2519/jospt.2018.8277
15. Muller B, Yabroudi MA, Lynch A, et al. Defining thresholds for the patient acceptable symptom state for the IKDC subjective knee form and KOOS for patients who underwent ACL reconstruction. Am J Sports Med 2016;44(11):2820-2826. doi:10.1177/0363 546516652888
16. McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med. 2019;47(4):857-862. doi:1 0.1177/0363546518825258
17 Maletis GB, Inacio MCS, Funahashi TT Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am J Sports Med. 2015;43(3):641-647 doi:10.1177/0363546514561745
18. Kaeding CC, Pedroza AD, Reinke EK, et al. Risk Factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583-1590. doi:10.1177/036354651557883 6
19. Schilaty ND, Nagelli C, Bates NA, et al. Incidence of second anterior cruciate ligament tears and identification of associated risk factors from 2001 to 2010 using a geographic database. Orthop J Sports Med 2017;5(8):2325967117724196. doi:10.1177/2325 967117724196
20. Fältström A, Kvist J, Bittencourt NFN, Mendonça LD, Hägglund M. Clinical risk profile for a second anterior cruciate ligament injury in female soccer players after anterior cruciate ligament reconstruction. Am J Sports Med 2021;49(6):1421-1430. doi:10.1177/036354652199910 9
21. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study Br J Sports Med 2016;50(13):804-808. doi:10.1136/bjsports-2016-096 031
22. Webster KE, Hewett TE. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med 2019;49(6):917-929. doi:10.1007/s40279-019-01093-x
23. Losciale JM, Zdeb RM, Ledbetter L, Reiman MP, Sell TC. The association between passing return-tosport criteria and second anterior cruciate ligament injury risk: A systematic review with meta-analysis. J Orthop Sports Phys Ther 2019;49(2):43-54. doi:10.251 9/jospt.2019.8190
24. Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. Br Med J 2015;351:h5527.
25. Hamrin Senorski E, Samuelsson K, Thomeé C, Beischer S, Karlsson J, Thomeé R. Return to kneestrenuous sport after anterior cruciate ligament reconstruction: a report from a rehabilitation outcome registry of patient characteristics. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1364-1374. do i:10.1007/s00167-016-4280-1
26. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 1985(198):43-49.
27 Webster KE, Feller JA. Development and validation of a short version of the anterior cruciate ligament return to sport after injury (ACL-RSI) scale. Orthop J Sports Med 2018;6(4):2325967118763763. do i:10.1177/2325967118763763
28. Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi:10.1186/1477-7525-1-64
29. Beischer S, Hamrin Senorski E, Thomeé P, Thomeé R. Validation of an 18-item version of the Swedish Knee Self-Efficacy Scale for patients after ACL injury and ACL reconstruction. J Exp Orthop 2021;8(1):96. doi:10.1186/s40634-021-00414-2
30. Neeter C, Gustavsson A, Thomeé P, Augustsson J, Thomeé R, Karlsson J. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg Sports Traumatol Arthrosc 2006;14(6):571-580. d oi:10.1007/s00167-006-0040-y
31. Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with metaanalysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52(2):128-138. doi:10.1136/bjsports-2016-0968 36
32. King E, Richter C, Daniels KAJ, et al. Can biomechanical testing after anterior cruciate ligament reconstruction identify athletes at risk for subsequent ACL injury to the contralateral uninjured limb? Am J Sports Med 2021;49(3):609-619. doi:10.11 77/0363546520985283
33. Lynch AD, Logerstedt DS, Grindem H, et al. Consensus criteria for defining ‘successful outcome’ after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2015;49(5):335-342. doi:10.1136/bjsports-2013-0922 99
34. Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biom J 2005;47(4):458-472. doi:10.1002/bimj.200410135
35. Lemeshow H. Assessing the Fit of the Model. In: Applied Logistic Regression ; 2013:153-225.
36. Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010;5(9):1315-1316. doi:10.1097/jto.0b013e3181ec1 73d
37. Youden WJ. Index for rating diagnostic tests. Cancer 1950;3(1):32-35. doi:10.1002/1097-0142(195 0)3:1
38. Gagnier JJ, Shen Y, Huang H. Psychometric properties of patient-reported outcome measures for use in patients with anterior cruciate ligament injuries: A Systematic Review. J Bone Joint Surg Rev. 2018;6(4):e5.
39. Comins J, Brodersen J, Krogsgaard M, Beyer N. Rasch analysis of the Knee injury and Osteoarthritis Outcome Score (KOOS): a statistical re-evaluation. Scand J Med Sci Sports. 2008;18(3):336-345. doi:10.11 11/j.1600-0838.2007.00724.x
40. Hansen CF, Jensen J, Odgaard A, et al. Four of five frequently used orthopedic PROMs possess inadequate content validity: a COSMIN evaluation of the mHHS, HAGOS, IKDC-SKF, KOOS and KNEESACL. Knee Surg Sports Traumatol Arthrosc. Published online 2021.
41. Beischer S, Hamrin Senorski E, Thomeé P, Thomeé R. Validation of an 18-item version of the Swedish Knee Self-Efficacy Scale for patients after ACL injury and ACL reconstruction. J Exp Orthop 2021;8(1):96. doi:10.1186/s40634-021-00414-2
Max Wardell 1 , Doug Creighton 2 , Carter Kovalcik 1
1 Overhead Athletic Institute, 2 Physical Therapy, Oakland University
Keywords: Glenohumeral, instability, hypermobility, overhead throwing athletes, baseball pitchers, Load and Shift Assessment, FAST, KJOC, pain https://doi.org/10.26603/001c.39800
The overhead activity of throwing a baseball is arguably the most demanding athletic endeavor placed on the glenohumeral (GH) joint. Previous studies illustrate that 75-80% of baseball players will experience some degree of upper extremity (UE) pain. GH instability is thought to play a role.
The purpose of this study was to investigate the relationship between GH joint hypermobility and instability with measures of arm pain and performance in overhead throwing athletes.
Actively competing baseball pitchers were recruited and evaluated once with the anterior-posterior Load and Shift examination procedure, the Kerlan-Jobe Orthopedic Clinic Shoulder and Elbow Questionnaire (KJOC), and the Functional Arm Scale for Throwers (FAST). Multivariate analysis was performed to identify correlation between severe GH capsular laxity (GH instability), mild capsular laxity (GH hypermobility), no capsular laxity (GH normal), and presence of shoulder pain when pitching.
Cross-sectional Study.
Forty-five pitchers were evaluated, 62.2% of throwing shoulders were classified normal stability, 26.7% were classified hypermobile, and 11.1% were classified unstable. Average KJOC scores for pitchers with the three mobility categories were 66.1 (normal), 59.7 (hypermobile), and 45.0 (unstable). Average FAST scores among the pitchers were 19.9 (normal), 34.2 (hypermobile), and 32.2 (unstable). Pitchers with GH instability and GH hypermobility demonstrated increased arm pain compared to athletes with normal GH joints; KJOC scores of 3.2, 5.5, and 7.4 (p = 0.0007), respectively.

Pitchers with GH instability and hypermobility demonstrated significantly increased ratings of arm pain compared to pitchers with no capsular laxity.
Level of Evidence
3b
Prevention of baseball throwing-related injuries and identi fication of potential risk factors for pain and injury in over head throwing athletes is a topic of interest for physical therapists, athletic trainers, physicians, and other medical providers involved in the care and treatment of these ath
letes. Prevention of throwing related injuries is imperative considering current trends in injury and the incidence of surgery to the shoulder and elbow in young athletes. Up to 50% of youth pitchers between nine and 14 years old expe rience arm pain.1 Analysis of 241 shoulder injuries and 150 elbow injuries in high school baseball players revealed that 93.5% and 88.0% of shoulder and elbow injuries, respec tively, were throwing related injuries.2 In addition, the risk
of injury increases with increasing levels of competition.3,4 Youth throwing-related injuries pose problems to partici pation and competitiveness in sport, and may also result in long-term pain and increased incidence of degenerative change to the throwing shoulder and elbow 5
Both translatory and angular motion changes occur in the shoulders of throwing athletes.6,7 The dominant shoul ders of pitchers have been shown to demonstrate greater amounts of anterior and posterior translation than the nondominant shoulders.7 Additionally, angular range of motion changes occur in the dominant shoulder of pitchers with increased external rotation of 5 to 15 degrees and de creased internal rotation of 5 to 20 degrees compared to the nondominant shoulder 7–9 These changes have been observed in athletes younger than 12 years old, and occur secondary to humeral retrotorsion, soft tissue changes, and other joint-related adaptations such as glenoid retroversion or labral tearing.6–10
It has been shown that glenohumeral (GH) instability contributes to shoulder pain and injury in athletes of var ious sports.1,11,12 Chronic instability plays a role in de generative conditions at the shoulder, including the de velopment of osteochondral defects, capsuloligamentous enlargement and tearing, labral deformation, and tendinopathy 13–15 Currently, it is not fully understood how the presence of GH instability or hypermobility in the throwing shoulders of baseball players influences ratings of pain or the role it may play in throwing arm function The purpose of this study was to investigate the relationship between GH joint hypermobility and instability with mea sures of arm pain and performance in overhead throwing athletes.
IRB approval was received in the Fall of 2019. Prior to recruiting participants, a categorical inter-rater reliability test of the load and shift assessment was conducted on a cohort of thirty physical therapy students (n=30). This test was to substantiate the researchers’ ability to perform and reliably assess shoulder stability with the Load and Shift test. The results of this test were compared to the results of a board-certified, fellowship-trained orthopedic physical therapist who has been a practicing clinician and educa tor for 37 years. The ICC value for the two researchers who later conducted the Load and Shift test on the participants in this study was found to be .81 and .85 in comparison to the aforementioned clinician, demonstrating good reliabil ity
Baseball pitchers (n=45) trained at the Overhead Athletic Institute were recruited to participate in this study All par ticipants met the inclusion criteria of being male and cur rently competing in baseball. Participants were excluded from this study if they reported having undergone surgery within the prior 12 months, were under the age of 13 or over the age of 30 years old or were not currently competing due
to injury Participants were asked to report any history of previous arm injury.
Prior to participation, subjects and/or their parents/ guardians (for those under 18 years old) were informed about the aim of this study and that their consent would be necessary to participate. Pitchers under 18 years old re quired parent/guardian permission as well as personal as sent. All participants and/or their parents/guardians were provided informed written consent prior to testing. This study was approved by the Oakland University Institutional Review Board: IRB Protocol # 1902.004.
Following obtaining informed consent, a consistent testing procedure was performed. Each participant first was pro vided the KJOC questionnaire, upon its completion the FAST survey was provided. When the FAST survey was com pleted the Load and Shift test was conducted on the par ticipant’s throwing shoulder The Load and Shift test was conducted with the participant seated on a treatment table, the participant was instructed to gently lift their chest as to be positioned in a more erect posture and to relax their throwing arm, allowing it to hang by their side. The re searcher, standing in front of the participant, then stabi lized scapula posteriorly and clavicle anteriorly with one hand and while grasping humeral head with the other hand by gradually compressing through the soft tissues (Figure 1). Mid-range anterior and posterior translatory oscilla tions of the humeral head were performed followed by an terior translation and posterior translation into tissue re sistance. No surveys, KJOC or FAST, were analyzed by the researchers prior to the application of the Load and Shift test.
To quantify arm pain and dysfunction, participants com pleted the Kerlan-Jobe Orthopedic Clinic Shoulder and El bow Questionnaire (KJOC), which is a Patient-Reported Outcomes (PRO) Scale. The KJOC scale evaluates the func tional status of the upper extremity (UE) in overhead ath letes. It includes 10 items divided into three categories: im pact of injury on function and athletic performance (five items), UE symptoms (four items), and interpersonal rela tionships related to performance (one item). The responses are recorded using a visual analog scale, where a mark is placed along a 10-cm line indicating the athlete’s current level of physical function. The KJOC’s scores range from 0-100 with lower scores indicating greater disability. The KJOC demonstrated excellent reliability and can distinguish between athletes with or without shoulder or elbow pain.16,17 The KJOC has been used as an effective means of assessing arm pain and injury in collegiate and profes
sional throwing athletes and shows good correlation with the Youth Throwers Scale in adolescents.18–22
To further investigate the functional status of the partic ipants arm, a second PRO scale, the FAST, was also col lected. The FAST is a 22-item PRO scale that includes five subscales: pain ( (six items), throwing (10 items), ADL (five items), psychological impact (four items), and advancement (three items). There is also an additional nine-item module specifically for pitchers. Higher FAST scores indicated greater disability The FAST demonstrated excellent test retest reliability (ICC, 0.91-0.98), acceptable correlation with the DASH (ICC = .49-.82) and KJOC (ICC = 0.62-0.81) scores and classified 85.1% of players into the correct injury group. The FAST has been validated as an effective PRO scale in adolescent and adult throwing athletes.23,24 For UE injury status, the FAST proved 91% sensitivity and 75% specificity The FAST is a valid and reliable tool for as sessing reported health care outcomes in throwing athletes with injury.24
The Load and Shift (L-S) test has proven to be a valid and reliable means of assessing GH joint mobility 25 The accu racy of the L-S test has been validated in comparison to MRI arthrograms of the shoulder by van Kampen et al.26 The L-S test has been demonstrated to be 84% accurate in diagnosis of labral tearing and shoulder instability com pared to MRI arthrogram.26
To assess the degree of shoulder instability present in the participants of this study, the L-S test was performed on all participants, as shown in Figure 1 The researcher graded the participant as normal, hypermobile, or unstable. During the L-S assessment, the GH joint was classified nor mal if it displayed minimal anterior and posterior transla tion with an immediate firm capsular end feel. The GH joint was classified as hypermobile if it displayed a great amount of anterior or posterior translation and the capsular end feel was less firm, with no immediate stop in translatory motion. Finally, the GH joint was classified unstable if the head of the humerus could be easily subluxed over the edge of the glenoid labrum, in either an anterior or posterior di rection, during the L-S assessment.27
Mean and variance values were calculated for age, total score of the KJOC and FAST (the cumulative result of all survey questions for both the KJOC and FAST), and arm pain. One-way Analysis of Variance (One-way ANOVA) was performed to identify any correlation between GH classi fication of unstable, hypermobile, or normal and self-re ported measures of shoulder and elbow performance and discomfort. Question 2 on the KJOC, “How much arm pain do you experience in your throwing shoulder or elbow?” was used to assess arm pain from the KJOC questionnaire. Question 2 on the FAST, “How painful is your arm during
Figure 1. Load and Shift test being performed.
‘game-speed’ throwing?” was used to assess arm pain from the FAST survey
Independent t-tests with unequal variances were used to test for differences in total KJOC and total FAST scores be tween baseball pitchers with unstable and normal shoul ders and between athletes with and without a history of in jury, which was recorded by the participant as part of the KJOC questionnaire. Statistical analyses were performed using Microsoft Excel Statistics Data Analysis ToolPak (Mi crosoft, Albuquerque, NM), alpha level of p ≤ 0.05.
Forty-five baseball pitchers, ages 13-25 years old, mean age of 15.98 ± 2.82 were included in this cross-sectional study. Distribution of participants by age ranged from 13-25 years old. Arm dominance was recorded, with n=36 for right handed throwers and n=9 for left-handed throwers. These descriptive statistics are presented in Table 1.
Eleven percent (n=5) of throwing shoulders were found to be unstable, 26.7% (n=12) were found to be hypermobile, and 62.2% (n=28) were found to be normal. Total KJOC score means were found to be 66.1 ± 18.4, 59.7 ± 18.0, and 45.0 ± 20.1 for normal, hypermobile, and unstable shoul ders, respectively. Total FAST score means were found to be 19.9 ± 14.6, 34.2 ± 18.1, and 32.1 ± 11.2 for normal, hypermobile, and unstable shoulders, respectively. Pitchers with normal shoulders exhibited significantly higher levels of function than pitchers with unstable and hypermobile shoulders when measured with the FAST, as demonstrated in Table 2. Pitchers with normal shoulders exhibited sig nificantly higher levels of function than pitchers with un stable shoulders when measured with the FAST and KJOC, as demonstrated in Table 3. Pitchers with normal shoulders exhibited significantly less arm pain than pitchers with un stable and hypermobile shoulders in both the FAST and KJOC, as demonstrated in Table 4

Table 1. Descriptive Demographics Baseball Pitchers (total n=45, all were male, 36 were right hand dominant while 9 were left hand dominant) Age N 13 9 14 7 15 4 16 11 17 5 18 4 19 1 20 1 21 1 22 1 24 1 25 1 Total 45
A previous history of injury was noted in 80% (n=36) of the participants in the study. When comparing total KJOC scores of pitchers with a history of arm injury to pitchers with no history of arm injury, healthy pitchers scored 71.9, while pitchers with a history of injury scored 59.6 (p=0.029). These scores indicate reduced subjective ratings of function in pitchers with a history of arm injury When FAST scores of pitchers with a history of injury were com pared to pitchers with no history of injury, there was no statistically significant difference (p=0.095); healthy pitch ers scored 16.6 while athletes with a history of injury scored 27.2.
The aim of this study was to determine if there is a correla tion between measures of GH hypermobility and subjective reports of arm pain and impairment during pitching. Cur rent literature suggests that baseball pitchers have greater GH translation and greater angular motion in their throw ing shoulder compared to the non-throwing shoulder 7 Hy permobility and instability have correlated with increased reports of pain and impairment in other sports.1,12 The presence of joint instability and angular hypermobility has also been correlated to the development numerous ortho
pedic conditions including capsular strains, labral tears, in ternal impingement, tendinopathy, and other degenerative conditions such as osteochondral defects.14,28,29
Examination for excessive capsular laxity and labral in stability is possible with the application of the L-S test.25–27 Given this, the authors’ believe there is a need for greater player and parental awareness of this examination procedure and the potential adverse effects of GH hyper mobility on the throwing shoulder. Perhaps athletic train ers and physical therapists trained in the application of the L-S procedure could offer optional pre-season screening ex ams at facilities where private pitching lessons occur and at local high schools and colleges. If capsular laxity or insta bility is found, therapeutic advice regarding joint hypermo bility, pitch count limits, the benefits of stabilization exer cise, or perhaps referral to an orthopedist could be provided to that athlete.
The shoulder undergoes massive loading during the ac celeration phase of the throw and immediately after ball re lease. Fleisig and colleagues found that in adult pitchers’ shoulders undergo 380N of anterior force during accelera tion and 400N of posterior force and 1080N of compressive force immediately after ball release.30 GH instability or ex cessive joint translation in the presence of these large loads has the potential to damage stabilizing structures of the shoulder such as the labrum and the capsule. Excessive an gular motion during the late cocking phase of the throw has been shown to increase the likelihood of capsular strains, SLAP lesions, and internal impingement.28,31 At present, the literature does not address changes in glenohumeral translatory motion and the role this may play in shoulder pain and performance during overhead throwing. This cur rent study examined the potential importance of this type of passive joint motion in evaluation overhead throwing athletes. The results demonstrated an association between increased passive joint translation (GH hypermobility and instability) and increased pain perception and throwing performance impairment.
This study evaluated overhead throwing athletes (baseball pitchers) with a mean age of 15.98 years of age, as such, the current findings may not apply to more physically ma ture collegiate and professional baseball pitchers. The au thors believe that this study should be replicated on a larger number of older baseball pitchers such as those competing at the professional and collegiate levels. Additionally, the number of subjects (n=45), may impact the generalizability of the findings.
Parameter
Mobility, reported as mean ± SD,
FAST Total 19.9 ± 14.6 34.2 ± 18.1 32.1 ± 11.2 0.025 KJOC Total 66.1 ±18.4 59.7 ± 18.0 45.0 ± 20.1 0.075
Outcomes are reported in units used by the questionnaire (0-100 for KJOC where higher score indicates better function and less pain and 0-100 for FAST where higher number indi cates more pain and less function).
Glenohumeral Instability and Arm Pain in Overhead Throwing Athletes: A Correlational Study
Table 3. Comparison of Normal and Unstable Shoulder Total FAST and KJOC Scores, reported as mean ± SD
Parameter Normal Unstable t p-value
FAST Total 19.9 ± 14.6 32.1 ± 11.2 -2.14 0.035 KJOC Total 66.1 ± 18.4 45 ± 20.1 2.19 0.04
Outcomes reported in units used by the questionnaire (0-100 for KJOC where higher score indicates better function and less pain and 0-100 for FAST where higher number indicates more pain and less function) utilizing paired t testing.
Table 4. Analysis of Variance of Arm Pain Scores in KJOC and FAST and Glenohumeral Mobility, reported as mean ± SD
Parameter Normal Hypermobile Unstable p-value
Arm Pain FAST 2 ± 1.2 3 ± .8 3 ± 1 0.019 Arm Pain KJOC 7.4 ± 2.2 5.5 ± 2.3 3.2 ± 2.1 0.0007
Outcomes reported in units used by the questionnaire (0-10 for KJOC where lower score indicates more pain, and 0-5 for FAST where higher number indicates more pain).
The results of this study indicate that baseball pitchers who exhibit greater amounts of passive anterior and posterior translation of the GH joint as demonstrated by the L-S as sessment report higher levels of arm pain and discomfort. Pitchers who demonstrate increased passive humeral head translation at the GH joint also report lower levels of func tion and performance. Pitchers who showed the greatest amount of instability at the GH joint, as evidenced by man ual subluxation of the humeral head during the load and shift assessment, demonstrated the worst overall scores for function and pain. Additional research is needed to deter mine the association between increased passive humeral head translation, shoulder pain, and throwing performance in other age groups.
The authors of this paper declare that they have no conflicts of interest.
The authors of this study would like to acknowledge the late Ed Martel III PT, former professional baseball pitcher, and owner of the Overhead Athletic Institute, and Marcee Wardell Barbatano, MFA.
Submitted: January 07, 2022 CST, Accepted: August 16, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Lyman S, Fleisig GS, Andrews JR, Osinski ED Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med 2002;30(4):463-468. doi:1 0.1177/03635465020300040201
2. Saper MG, Pierpoint LA, Liu W, Comstock RD, Polousky JD, Andrews JR. Epidemiology of shoulder and elbow injuries among united states high school baseball players: School years 2005-2006 through 2014-2015. Am J Sports Med 2018;46(1):37-43. doi:1 0.1177/0363546517734172
3. Han KJ, Kim YK, Lim SK, Park JY, Oh KS. The effect of physical characteristics and field position on the shoulder and elbow injuries of 490 baseball players: Confirmation of diagnosis by magnetic resonance imaging. Clin J Sport Med 2009;19(4):271-276. doi:1 0.1097/jsm.0b013e3181aad7b1
4. Oberlander MA, Chisar MA, Campbell B. Epidemiology of shoulder injuries in throwing and overhead athletes. Sports Med Arthrosc Rev 2000;8(2):115-123. doi:10.1097/00132585-20000802 0-00001
5. Bullock GS, Nicholson KF, Waterman BR, et al. Persistent joint pain and arm function in former baseball players. JSES International 2021;5(5):912-919. doi:10.1016/j.jseint.2021.05.001
6. Nakaji RM, Ellenbecker TS, McClenahan KM, Roberts LM, Perez C, Dickenson SB. Descriptive strength and range of motion in youth baseball players. Int J Sports Phys Ther. 2021;16(1):195-206. do i:10.26603/001c.18815
7 Sethi PM, Tibone JE, Lee TQ Quantitative assessment of glenohumeral translation in baseball players: A comparison of pitchers versus nonpitching athletes. Am J Sports Med 2004;32(7):1711-1715. do i:10.1177/0363546504263701
8. Chant CB, Litchfield R, Griffin S, Thain LMF. Humeral head retroversion in competitive baseball players and its relationship to glenohumeral rotation range of motion. J Orthop Sports Phys Ther. 2007;37(9):514-520. doi:10.2519/jospt.2007.2449
9. Polster JM, Bullen J, Obuchowski NA, Bryan JA, Soloff L, Schickendantz MS. Relationship between humeral torsion and injury in professional baseball pitchers. Am J Sports Med. 2013;41(9):2015-2021. do i:10.1177/0363546513493249
10. Pennock AT, Dwek J, Levy E, et al. Shoulder MRI abnormalities in asymptomatic little league baseball players. Orthop J Sports Med. 2018;6(2):2325967118756825. doi:10.1177/232596711 8756825
11. Kvitne RS, Jobe FW, Jobe CM. Shoulder instability in the overhand or throwing athlete. Clin Sports Med 1995;14(4):917-935. doi:10.1016/s0278-5919(20)3018 8-5
12. Patel DR, Breisach S. Evaluation and management of shoulder pain in skeletally immature athletes. Transl Pediatr. 2017;6(3):181-189. doi:10.21037/tp.20 17.04.06
13. Woertler K, Waldt S. MR imaging in sports-related glenohumeral instability. Eur Radiol. 2006;16(12):2622-2636. doi:10.1007/s00330-006-025 8-6
14. Omoumi P, Teixeira P, Lecouvet F, Chung CB. Glenohumeral joint instability. J Magn Res Imag. 2011;33(1):2-16. doi:10.1002/jmri.22343
15. Laudner K, Meister K, Noel B, Deter T Anterior glenohumeral laxity is associated with posterior shoulder tightness among professional baseball pitchers. Am J Sports Med 2012;40(5):1133-1137 do i:10.1177/0363546512437522
16. Alberta FG, ElAttrache NS, Bissell S, et al. The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. Am J Sports Med 2010;38(5):903-911. doi:10.1177/0363546509355642
17. Kraeutler MJ, Ciccotti MG, Dodson CC, Frederick RW, Cammarota B, Cohen SB. Kerlan-jobe orthopaedic clinic overhead athlete scores in asymptomatic professional baseball pitchers. J Shoulder Elbow Surg 2013;22(3):329-332. doi:10.101 6/j.jse.2012.02.010
18. Faherty MS, Plata A, Chasse P, Zarzour R, Sell TC. Upper extremity musculoskeletal characteristics and the kerlan-jobe orthopaedic clinic questionnaire score in collegiate baseball athletes. J Athl Train. 2019;54(9):945-952. doi:10.4085/1062-6050-81-18
19. Franz JO, McCulloch PC, Kneip CJ, Noble PC, Lintner DM. The utility of the KJOC score in professional baseball in the united states. Am J Sports Med 2013;41(9):2167-2173. doi:10.1177/0363546513 495177
20. Holtz KA, O’Connor RJ. Upper extremity functional status of female youth softball pitchers using the kerlan-jobe orthopaedic clinic questionnaire. Orthop J Sports Med. 2018;6(1):2325967117748599. doi:10.1177/232596711 7748599
21. Cain EL Jr, Liesman WG, Fleisig GS, et al. Clinical outcomes and return to play in youth overhead athletes after medial epicondyle fractures treated with open reduction and internal fixation. Orthop J Sports Med 2021;9(2):2325967120976573. doi:10.117 7/2325967120976573
22. Ahmad CS, Padaki AS, Noticewala MS, Makhni EC, Popkin CA. The youth throwing score: Validating injury assessment in young baseball players. Am J Sports Med. 2017;45(2):317-324. doi:10.1177/0363546 516667503
23. Sauers E, Shimozawa Y, Bay R, Snyder Valier A, Huxel Bliven K. Test-retest reliability and concurrent validity of a region-specific patient self-report scale in baseball and softball players: The functional arm scale for throwers, FAST. J Athl Train. 2014;49:143.
24. Huxel Bliven KC, Snyder Valier AR, Bay RC, Sauers EL. The functional arm scale for throwers (FAST)—Part II: Reliability and validity of an upper extremity region-specific and population-specific patient-reported outcome scale for throwing athletes. Orthop J Sports Med. 2017;5(4):2325967117700019. do i:10.1177/2325967117700019
25. Kolber M, Carrao M. The interrater reliability of the load and shift test for anterior shoulder instability: A technical report. Inter J Allied Health Sci Pract 2010;8(2). Accessed May 10, 2021. https://nsuw orks.nova.edu/ijahsp/vol8/iss2/10
26. van Kampen DA, van den Berg T, van der Woude HJ, Castelein RM, Terwee CB, Willems WJ. Diagnostic value of patient characteristics, history, and six clinical tests for traumatic anterior shoulder instability J Should Elbow Surg 2013;22(10):1310-1319. doi:10.1016/j.jse.2013.05.006
27 DeFroda SF, Owens BD Arthroscopic load-shift technique for intraoperative assessment of shoulder translation. Arthrosc Techn 2018;7(3):e211-e214. do i:10.1016/j.eats.2017.08.071
28. Rizio L, Garcia J, Renard R, Got C. Anterior instability increases superior labral strain in the late cocking phase of throwing. Orthopedics 2007;30(7):544-550. doi:10.3928/01477447-2007070 1-03
29. Mihata T, Safran MR, McGarry MH, Abe M, Lee TQ. Effect of humeral rotation on elbow valgus laxity: A cadaveric study Japanese Soc Surg Hand 2004:S70-S70.
30. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med 1995;23(2):233-239. doi:10.1177/03635465950230021 8
31. Mihata T, McGarry MH, Kinoshita M, Lee TQ Excessive glenohumeral horizontal abduction as occurs during the late cocking phase of the throwing motion can be critical for internal impingement. Am J Sports Med. 2010;38(2):369-374. doi:10.1177/0363546 509346408
Bullock
Garrett Bullock 1,2 a , Charles Thigpen 3,4 , Gary Collins 5,6 , Nigel Arden 1,2 , Thomas Noonan 7,8 , Michael Kissenberth 9 , Ellen Shanley 3,4
1 Department of Orthopaedic Surgery & Rehabilitation, Wake Forest University School of Medicine, 2 Centre for Sport, Exercise and Osteoarthritis Research Versus Arthritis, University of Oxford, 3 University of South Carolina Center for Rehabilitation and Reconstruction Sciences, 4 ATI Physical Therapy, 5 Centre for Statistics in Medicine, University of Oxford, 6 Oxford University Hospitals NHS Foundation Trust, 7 Department of Orthopaedic Surgery, University of Colorado School of Medicine, 8 University of Colorado Health, Steadman Hawkins Clinic, 9 Steadman Hawkins Clinic of the Carolinas
Keywords: Prognostic Model, Shoulder, Elbow, Humeral Torsion, Pitch Load https://doi.org/10.26603/001c.39741
Baseball injuries are a significant problem and have increased in incidence over the last decade. Reporting injury incidence only gives context to rate but not in relation to severity or injury time loss.
The purpose of this study was to 1) incorporate both modifiable and non-modifiable factors to develop an arm injury burden prediction model in Minor League Baseball (MiLB) pitchers; and 2) understand how the model performs separately on elbow and shoulder injury burden.
The study was conducted from 2013 to 2019 on MiLB pitchers. Pitchers were evaluated in spring training arm for shoulder range of motion and injuries were followed throughout the season. A model to predict arm injury burden was produced using zero inflated negative binomial regression. Internal validation was performed using ten-fold cross validation. Subgroup analyses were performed for elbow and shoulder separately Model performance was assessed with root mean square error (RMSE), model fit (R2), and calibration with 95% confidence intervals (95% CI).
Two-hundred, ninety-seven pitchers (94 injuries) were included with an injury incidence of 1.15 arm injuries per 1000 athletic exposures. Median days lost to an arm injury was 58 (11, 106). The final model demonstrated good prediction ability (RMSE: 11.9 days, R2: 0.80) and a calibration slope of 0.98 (95% CI: 0.92, 1.04). A separate elbow model demonstrated weaker predictive performance (RMSE: 21.3; R2: 0.42; calibration: 1.25 [1.16, 1.34]), as did a separate shoulder model (RMSE: 17.9; R2: 0.57; calibration: 1.01 [0.92, 1.10]).
a

The injury burden prediction model demonstrated excellent performance. Caution should be advised with predictions between one to 14 days lost to arm injury Separate elbow and shoulder prediction models demonstrated decreased performance. The inclusion of both modifiable and non-modifiable factors into a comprehensive injury burden model provides the most accurate prediction of days lost in professional pitchers.
Level of Evidence 2
Baseball injuries are a significant problem with increased incidence over the last decade.1–3 The greatest injury in cidence is to the elbow and shoulder,1,4 with orthopaedic surgery signifying a significant proportion of injuries.5 These injuries have a substantial medical,6 financial,7 and psychological burden5 on the individual and team.8 Due to the significance of these injuries,6,7 individual physical risk factors have been recognized to assist clinicians in identi fying baseball players at risk for arm injury.9–12 However, these methods are limited by their simplicity, without ac counting for the complex interrelated nature of modifiable and non-modifiable relationship to baseball injuries.13,14
While identifying individuals at risk for injury can im prove athlete injury outcomes,9 this does not give a com plete clinical perspective. Reporting injury incidence only gives the rate but not injury severity or associated time loss.8 For example, the professional baseball shoulder and elbow injury incidence is 1.4 and 0.9 injuries per 1000 ath lete exposures, respectively,15 but elbow injuries have over six times more days missed compared to shoulder in juries.16 Simply identifying baseball players at risk for in jury would give equal weight to shoulder and elbow injuries and additionally would not distinguish between minor and severe injuries.8 Severity and site of injury will relate to the requirement for surgical interventions, including re construction, and hence time loss, highlighting the need to assess these parameters.17
Further, considerations must be given to the unbalanced nature of injury data, as the majority of athletes will report no injuries (i.e., no days lost), with a sparse number sus taining severe injuries, providing greater complexity to in jury burden data.18 Pinpointing potential high injury bur den athletes (pitchers) would allow for improved resource consolidation.8 Due to the continued rise in pitching in juries,1,2 and the incomplete clinical context of the iden tified injury risk factors,16 there is a need to distinguish pitchers at increased risk for greater comprehensive arm in jury burden.
Pitching is a series of coordinated movements that in volve the entire body 19 The interplay between modifiable and non-modifiable intrinsic and extrinsic factors in de termining injury risk and burden signify the intricacies of this problem.13 The complex nature of pitching injuries require in depth examination, reasoning, and clinical de cisions.20 However, while sports medicine clinicians have advanced skills and reasoning,21 there continues to be am biguity in determining true risk.22 A more complex ap
proach to identify at risk athletes has been proposed,23 in volving the assessment of modifiable and non-modifiable factors as a whole.23–25 One method that incorporates this approach is via risk prediction models.26 Prediction models are statistical models that combine multiple predictors to estimate an individual’s risk of an event.27–29 These tools are not designed to supersede clinical experience and de cisions; rather, assist in determining the best actions (or inaction) for patients.26 Prediction models have been used extensively in clinical medicine, such as whether to pre scribe of cholesterol lowering therapies through the Fram ingham cardiovascular risk score.30
Quantifying complex systems through prediction models is needed to enumerate injury burden.24 These predictions can be used by clinicians and other healthcare professionals to better identify baseball players at risk for a high injury burden,31 and subsequently improve injury identifica tion.32 Therefore, the purpose of this study was to 1) in corporate both modifiable and non-modifiable factors to develop an arm injury burden prediction model in Minor League Baseball (MiLB) pitchers; and 2) understand how the model performs separately on elbow and shoulder in jury burden.
A prospective longitudinal study was conducted from 2013 to 2019 on MiLB pitchers in one Major League Baseball (MLB) organization. Prior to testing, the risk and benefits of participation were explained in verbal and written form to all participants. Participants were tested at the beginning of spring training (pre-season). All test administrators were blinded to hand dominance.33 Participants were tested for shoulder range of motion (ROM) and humeral torsion (HT). Following testing, participants were followed for the entire season for total athletic exposures and arm injuries. Each pitcher was incorporated into each individual season. If a pitcher played multiple seasons, each season was an in dividual observation. If a pitcher sustained an injury, the pitcher was no longer included in observation for the next season. All participant information was de-identified and coded into an encrypted centralized database. This investi gation received favorable ethics approval from the Univer sity Institutional Review Board.
Sports medicine clinicians, performance professionals, and coaches within the organization were included in deter mining the variables to be collected. Presentations were performed for organizational stakeholders throughout data collection and prediction model development.
Participants were included if they were able to participate in all practices and competitions and were under a MiLB contract. Participants were excluded if they were currently injured or not participating in all spring training activities, participating in MLB spring training at time of data collec tion, or signed a professional contract in the middle of the season (e.g., draft, free agent, or international signing).9
Shoulder external (ER), internal (IR), horizontal adduction (HA) range of motion (ROM) was measured using previously described methods.34–37 Internal reliability testing demon strated excellent reliability for shoulder ER (intraclass cor relation coefficient (ICC) (2,1) =0.99; Standard error of measure (SEM) = 2.0; ICC (2,K) = 0.99; SEM= 0.95), IR (ICC (2,1)= 0.97; SEM = 2.5; ICC (2,K) = 0.97 SEM= 2.6), and HA (ICC (2,1) = 0.99; SEM =2.59; ICC (2,K) =0.97; SEM = 1.2). Shoulder ER and IR were summed to measure shoulder total ROM (TROM). Humeral torsion (HT) were measured with a 5-MHz transducer (Sonosite Inc., Bothell, WA, USA) with previously described methods.10 HT testing demonstrated excellent reliability (ICC (2,1) = 0.97; SEM = 2.5; ICC (2,K) = 0.97 SEM= 2.6). Two data collection trials were performed per shoulder and the data collection trials were averaged for analyses.38 For further explanation of the methods, please refer to the Appendix 1.
Baseball (i.e., athlete) exposure was defined as number of days participating in training, practice, or games in a sea son.39 Pitching exposure was defined as the total number of pitches within a season.39
An injury was defined as an injury to a tendon, ligament, nerve, muscle, or bone that occurred during any baseball team sponsored activity or event and was followed by at least one day of missed practice or baseball games.33 If a player was unavailable to play for injury prevention reasons (i.e., has reached league or individually determined pitch or innings count limits), then their absence was not con sidered as an injury Injuries were defined by the Orchard Sports Injury Classification system and arms injuries strati fied by shoulder/clavicle, upper arm, elbow, and forearm.40 All other injuries and illness were also recorded, and time loss was not taken into account for overall exposure, nor included in the injury burden analyses. Arm injury burden
was defined as the product of incidence and severity 8 Arm injury burden was quantified as the total number of days lost to arm injury in one baseball season.8
Residual inspection demonstrated model instability above 90 days lost to arm injury Following research team and MLB organizational discussion, time loss to arm injury was truncated to 90 days. In other words, if a player sus tained an injury of 120 days, within the model, this would be included at 90 days.
All data were investigated for missingness prior to analyses using the R package naniar Missing data was low (3% of en tire cohort had one or more missing values), thus complete case analyses were performed. Participant characteristics were described using mean (standard deviation) for contin uous normally distributed variables, median (interquartile range) for non-normally distributed continuous variables, and frequencies and percentages for categorical variables. Arm injury incidence was calculated by sum of arm injuries divided by sum of baseball (i.e., athlete) exposures (AE) multiplied by 1000. For expanded statistical analyses de scription, please refer to Appendix 2.
Linearity was not assumed, and prior to model develop ment, continuous variables were assessed for non-linearity in relation to the outcome of days lost to arm injury All predictors were observed to have linear relationships.
An a priori sample size calculation was performed prior to model development.41 It should be noted that this sample size method does not explicitly cover zero inflated models. During the study period, a total of 297 pitchers met inclu sion criteria, therefore a maximum of 26 parameters (i.e., the number of degrees of freedom) could be included in the development of the injury burden prediction model. The R package pmsampsize was used to calculate the required sample size.
To predict the number of days lost (up to 90 days) to arm in jury in professional pitchers a zero inflated negative bino mial regression model was utilized.42 An alternative model, a hurdle model was developed, to demonstrate similar pre diction performance (Appendix 3). Predictor variables in cluded were chosen based on the baseball injury prevention literature and included: 1) age, 2) BMI, 3) pitching role (starter versus reliever), 4) seasonal number of pitches, 5) number of pitching appearances in a season, 6) HT differ ence between dominant and nondominant shoulder (in de grees), 7) dominant shoulder TROM (in degrees), 8) dom inant HA (in degrees), 9) lower extremity or trunk injury in the same year, 10) any previous arm injury history, 11) years played professionally, 12) received individualized in jury prevention programs, 13) continent of origin, and 14) days practiced and competed in the season (expo sure).9,43–52 Variable selection was performed using elastic
net penalization, using ten-fold cross-validation.53 Inter nal validation of the model was performed using ten-fold cross validation.53 Prediction model performance was as sessed by calculating the root mean square error (RMSE), explained variation (R2), and calibration. Calibration is the agreement between predicted and actual risk.32 Calibration was assessed by calculating the calibration slope with 95% confidence intervals and graphically plotting the observed values against the predicted values. Subgroup analyses were performed for elbow and shoulder separately A sen sitivity analysis was performed with the inclusion of only modifiable predictors to assist clinicians in understanding risk and treatment options including: (1) seasonal number of pitches, 2) number of pitching appearances in a season, 3) dominant shoulder TROM (in degrees), 4) dominant HA (in degrees), 5) received individualized injury prevention programs, 6) days practiced and competed in the season (exposure). All analyses were performed in R version 3.5.1 (R Core Team (2013). The R package pscl was used for zero inflation modelling and mpath for elastic net. For full code, please see Appendix 4.
Reporting of this study followed the transparent report ing of a multivariable prediction model for individual prog nosis or diagnosis (TRIPOD) recommendations.54
A total of 297 pitchers were included (age: 23.0 (2.2) years, BMI: 24.8 (2.2), left handed: 21%). A total of 84 pitchers re ported an arm injury during data collection. Overall arm in jury incidence was 1.15 arm injuries per 1000 AE’s, 0.5 el bow injuries per 1,000 AE’s, and 0.8 shoulder injuries per 1,000 AE’s (Table 1). Median days lost to an arm injury was 58 (11, 106).
Model development following tenfold internal validation demonstrated a RMSE of 11.9 days, 0.80 R2 , and a calibra tion slope of 0.98 (95% CI: 0.92, 1.04); Figure 1). Full model equation is reported in Table 2
The zero-inflated negative binomial model incorporates two models (count and zero) into one comprehensive model. As such, the count and zero model should be con sidered one model
Elbow injury burden model development demonstrated a RMSE of 21.3 days, 0.42 R2 , and a calibration slope of 1.25 (95% CI: 1.16, 1.34; Figure 2).
Shoulder injury burden model development demonstrated a RMSE of 17.9 days, 0.57 R2 , and a calibration slope of 1.01 (95% CI: 0.92, 1.10; Figure 3).
The inclusion of only modifiable predictors within the pre diction model decreased performance compared to the original model (RMSE: 21.2, R2: 0.42, Calibration: 1.12 (95% CI: 0.99, 1.25).
This prediction model demonstrated excellent perfor mance, as demonstrated by the high R2 and calibration slope. Due to the model error of 12 days, predictions of one to 14 days should be interpreted with caution. Strat ifying by predicting individual elbow or shoulder burden decreased prediction model performance. Including only modifiable predictors demonstrated decreased prediction performance.
Clinicians integrate a plethora of skills, tools, and expe rience to keep athletes on the field.55 The complexity as sociated with examination and performance, including ad vances in technology,56 load monitoring,57 and rehabilitation and performance testing,23 necessitates the need employ these tools and information. Within baseball, athletes are physically examined in spring training and tra ditionally this information is used to assess each individual risk factor.9 This prediction model incorporated multiple predictors into one cohesive model to calculate a predicted number of days lost to arm injury, ranging from 0 to 90. These individual injury burden predictions are meant to help reduce complexity of a difficult issue through clarify ing prognosis,58 to improve a clinician’s ability to care for their patients.
This model reported an RMSE of 12 days. What this means clinically is that for any predicted days of injury bur den, the actual number of days lost to injury will be within 12 days of the predicted value. While an error rate of 12 days for higher burden injuries (i.e., >30 days) may not alter clinical interpretation, a difference between 0 and 14 days could affect clinical decisions. To give an example, if the model predicted 3 days lost to injury, the days lost could be between one and 15 days. This would be clinically in terpreted as a minor to moderate arm injury On the other hand, if a pitcher was predicted to have 60 days lost to injury, a 12 day difference (48 to 72 days) would not af fect clinical decisions. The pitcher would still be identified as a pitcher who could sustain a serious arm injury during the season. These findings suggest that this injury burden model can help identify pitchers who are at risk for sustain ing a high injury burden during the season. However, these models should be interpreted with caution for predicted in jury burden for one to 14 days.
Table 1. Characteristics of the pitchers included in the study. Values are percentages unless stated otherwise.
All Pitchers (n = 297)
Non-Arm Injured Pitchers (n = 203)
Arm Injured Pitchers (n = 94)
Elbow Injury (n = 40)
Shoulder Injury (n = 64)
Mean (SD) Age (years) 23.0 (2.2) 22.8 (2.2) 23.2 (2.0) 23.2 (2.4) 22.8 (2.1)
Left Right 14% 86% 19% 81% 22% 78% 16% 84% 16% 84%
Mean (SD) BMI (kg/m2) 24.8 (2.2) 24.6 (2.3) 24.8 (2.1) 25.1 (2.3) 24.9 (2.3)
Starting Pitcher Relief Pitcher 55% 45% 52% 48% 62% 38% 52% 48% 58% 42%
Continent of Origin North America Latin America 71% 29% 66% 34% 83% 17% 68% 32% 80% 20%
Years within Professional Baseball 1-2 years 3-4 years 5+ years
73% 22% 5%
80% 3% 1%
57% 33% 11%
42% 46% 12%
58% 32% 10%
Mean (SD) Seasonal Pitch Load 900 (657) 991 (643) 548 (615) 468 (594) 572 (609)
Mean (SD) Dominant Total Range of Motion in degrees 160 (13) 159 (13.2) 159 (11.8) 162 (12) 159 (14)
Mean (SD) Dominant Horizontal Adduction in degrees -2.3 (12.2) -2.8 (11.9) -1.1 (14.6) -1.4 (12.6) -0.2 (13.2)
Mean (SD) Humeral Torsion Difference in degrees 18.2 (13.7) 18.5 (13.5) 16.2 (11.9) 17.3 (13.4) 15.9 (12.8)
Kinematic Chain Injury 15% 3% 11% 5% 13%
Elbow and shoulder injury burden models demonstrated decreased performance compared to the primary model and had reduced sample sizes therefore, should be interpreted with caution. The discrepancies between elbow and shoul der injury burden may decrease the performance of these models. Elbow and shoulder injuries can have different risk factors,9,10,59 with mechanisms of injury occurring during different points within the pitching motion.19,60 Different clinical interventions may be required to reduce shoulder verses elbow injury risk.61,62 The contrasting injury burden risk factors between shoulders and elbows may decrease the prediction precision of individual shoulder or elbow mod els. Future research is required to develop separate shoul der and elbow burden prediction models.
Including only modifiable predictors demonstrated de creased injury burden prediction compared to the inclusion of modifiable and non-modifiable predictors. Previous work14 has called for the inclusion of both modifiable and non-modifiable predictors to improve understanding and ultimately decrease sports injuries. However, while this has been proposed for many years,14 the majority of current ev
idence only includes isolated modifiable factors when as sessing injury risk.9 As these results suggest, without the inclusion of non-modifiable predictors, clinicians are in hibited from having an improved understanding of current injury risk. While it may seem from a clinical perspective that including non-modifiable predictors does not improve how a clinician will treat a patient, a more comprehensive injury risk examination allows the clinician to better iden tify athletes at risk for sustaining an injury 63 These pre diction models are not recommended to be used to identify which specific interventions or factors should be the focus of care.28,29 Prediction models are not causal, as such, if a particular predictor is “significant” with a specific athlete, this does not mean that particular predictor should be in tervened upon. A thorough physical exam and clinical rea soning should be used to identify which tests and measures to intervene on.
This study utilized a seven-year prospective cohort that was specifically designed to assess arm injuries in professional baseball players. All data collectors were physical thera pists, specifically trained and evaluated for reliability in the physical examination techniques, improving the consis tency and reliability of these data. Only a small proportion
Total range of motion Sum of shoulder external and internal rotation range of motion Humeral torsion difference is calculated as dominant nondominant shoulderFigure 1. Calibration Plot of the Arm Injury Burden Prediction Model.
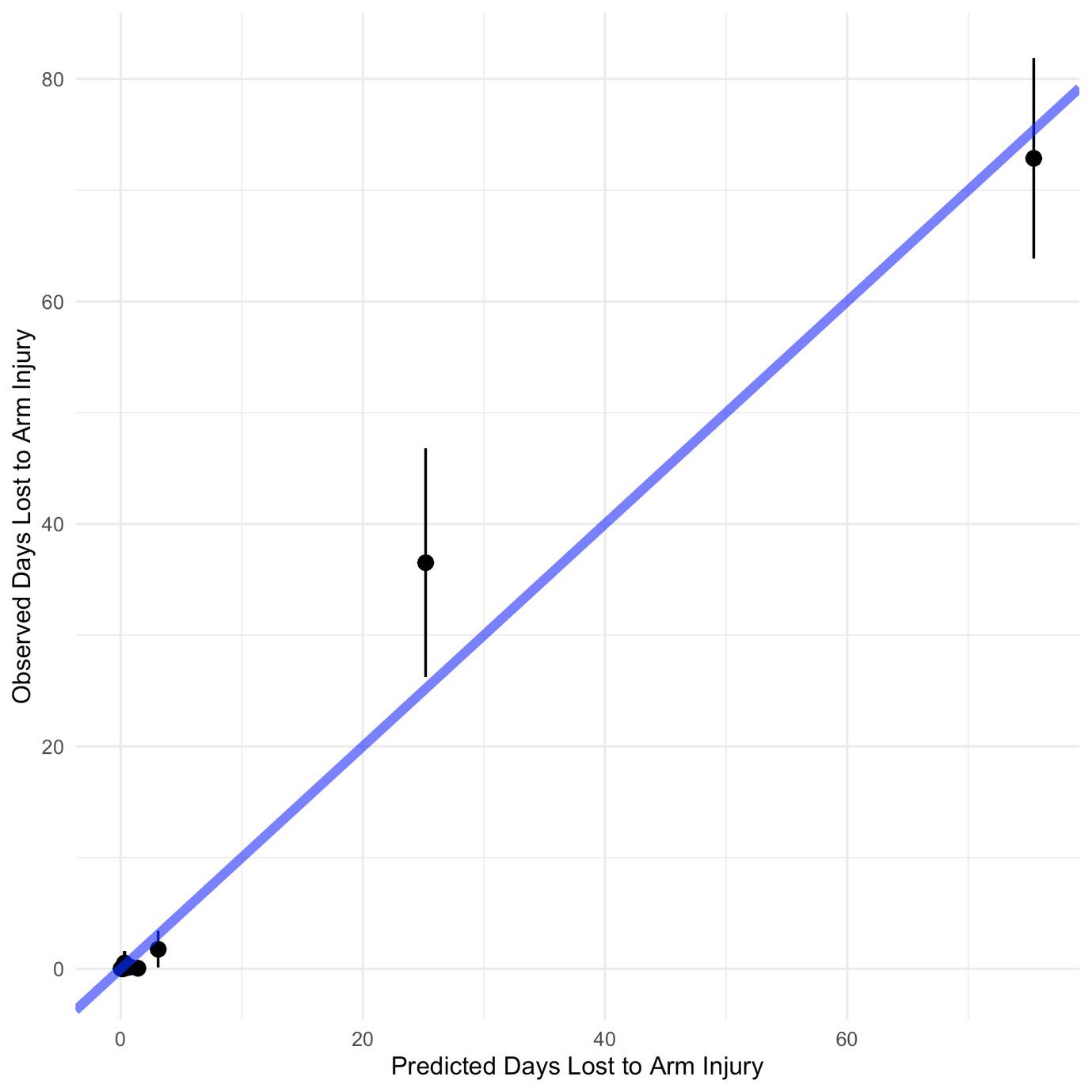
Calibration is the relationship between predicted and actual probability of the event. Perfect calibration would be a 45-degree line. A calibration line below the blue line is over-pre dicting risk. A calibration line above the blue line is under-predicting risk.
of data were missing, allowing for a complete case analysis, increasing the validity of these findings. An a priori sample size calculation was performed to create a stable prediction model, increasing the utility of these findings. Internal val idation was performed in order to shrink optimism, increas ing the generalizability of these results. The full model is reported, increasing transparency and usefulness for future validation.64 Time lost to injury was truncated at 90 days. Pitchers may be placed on the injured list longer than 90 days; however, truncation was performed at 90 days due to the paucity of players sustaining time loss greater than this time period and the organizational significance of this time period. A small proportion of pitchers were excluded due to participating MLB spring training during data col lection. These pitchers were predominantly at the AAA or AA level, decreasing the generalizability of these results to high MiLB players. Injury history was limited to profes sional baseball seasons and orthopaedic surgery prior to signing a professional baseball contract. As pitchers may sustain arm injuries that last only a few days or a week, there is the potential for residual confounding. All impair ment data were collected prior to the season. As predic tors can change throughout the season, this decreases the clinical utility of these results. Player salary and signing
bonuses were not included in these analyses. As MLB or ganizational investment may influence time loss to injury, this decreases the precision in these models. This model was not externally validated. It is recommended that exter nal validation should be performed prior to integrating in a clinical setting. This prediction model should be used with caution without further validation.
This professional baseball injury burden model may have clinical utility in predicting pitchers that are at risk for sus taining a high injury burden within the season. However, caution should be advised with predictions between 1 to 14 days lost to arm injury as this is below the prescribed model error. The inclusion of modifiable and non-modifi able predictors demonstrated improved prediction perfor mance, suggesting that prediction models should include both types of predictors when evaluating injury risk. Sep arate elbow and shoulder prediction models demonstrated decreased performance and should be interpreted with cau tion due to low sample size. Further research is required to externally validate this model to understand the generaliz ability of these findings.
Table 2.
Arm Injury Burden Prediction Model.
Coefficient *95% CI
Intercept 1.62 0.11, 210
Age -0.02 0.89, 1.05
Body Mass Index 0.05 0.99, 1.16
Right Arm Dominance ø 0.04 0.68, 1.72 Starting Pitcher¥ 0.08 0.76, 1.38
Number of Pitching Appearances -0.02 0.97, 0.99
Dominant Shoulder Total Range of Motion 0.01 1.00, 1.03
Dominant Shoulder Horizontal Adduction -0.01 0.98, 0.99
Previous Arm Injury History 0.07 0.61, 1.47 2 to 4 Years Played Professionally‡ -0.37 0.45, 0.83
5+ Years Played Professionally‡ 0.08 0.60, 2.03
Received Individualized Injury Prevention Program -0.11 0.55, 1.01 Continent of Origin§ 0.06 0.76, 1.08 Exposure Days -0.006 0.98, 0.99
Intercept -5.82 0.00, 8.99
Right Arm Dominanceø -0.21 0.01, 1.87 Starting Pitcher¥ -0.06 0.15, 1.78
Number of Pitching Appearances 0.01 0.97, 1.08 Kinematic Chain Injury 0.86 2.12, 73 Continent of Origin§ 0.07 0.74, 11.16 Exposure Days 0.05 1.03, 1.07 The zero-inflated
øReference is Left
¥Reference is relief pitcher
‡Reference is 0 to 1 years played professionally
§Reference is North America
GSC was supported by the NIHR Biomedical Research Cen tre, Oxford, and Cancer Research UK (programme grant: C49297/A27294).
All authors declare no conflicts of interest.
Submitted: June 13, 2022 CST, Accepted: August 16, 2022 CST
Figure 2. Calibration Plot of the Elbow Injury Burden Prediction Model.
Calibration is the relationship between predicted and actual probability of the event. Perfect calibration would be a 45-degree line. A calibration line below the blue line is over-pre dicting risk. A calibration line above the blue line is under-predicting risk.
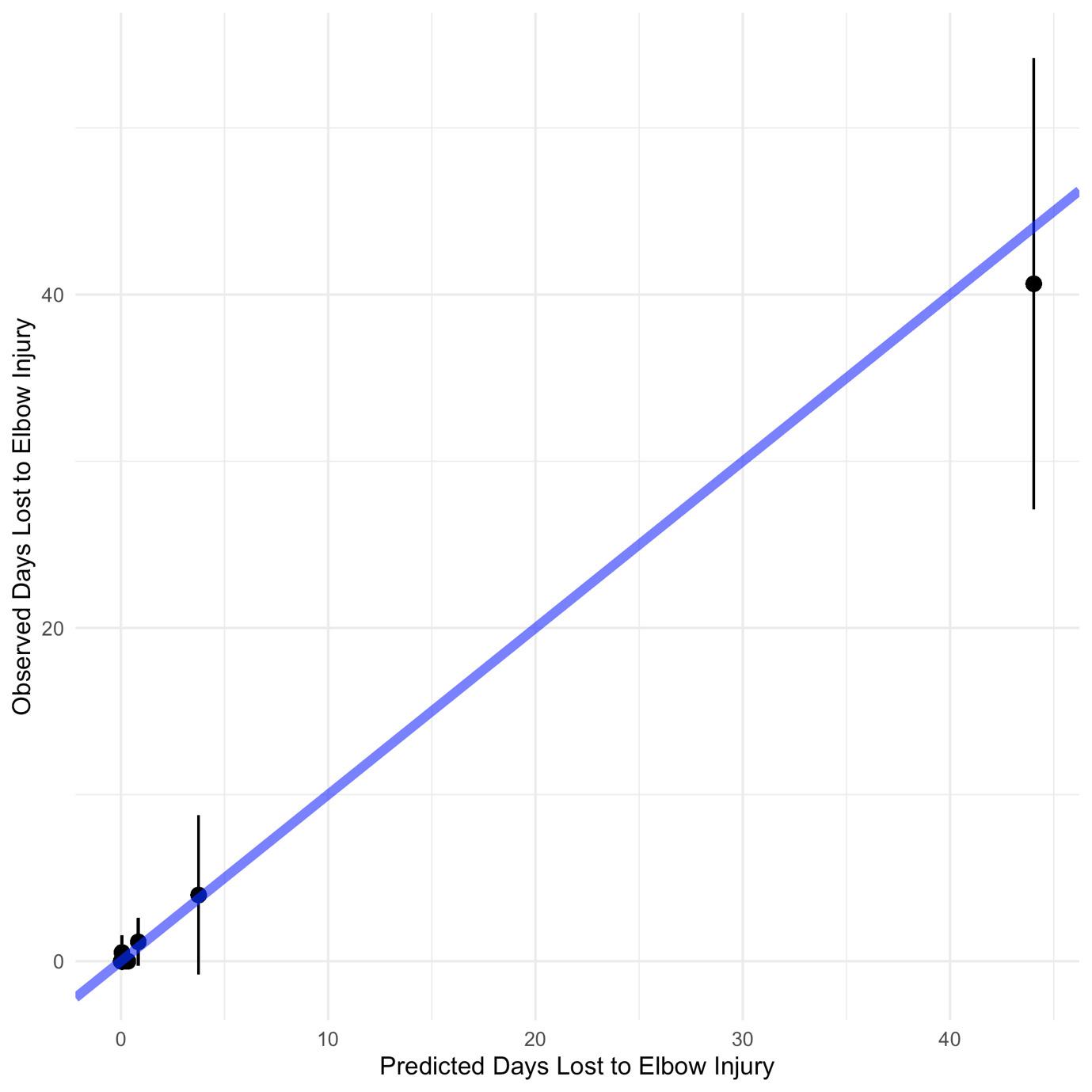
Figure 3. Calibration Plot of the Shoulder Injury Burden Prediction Model.
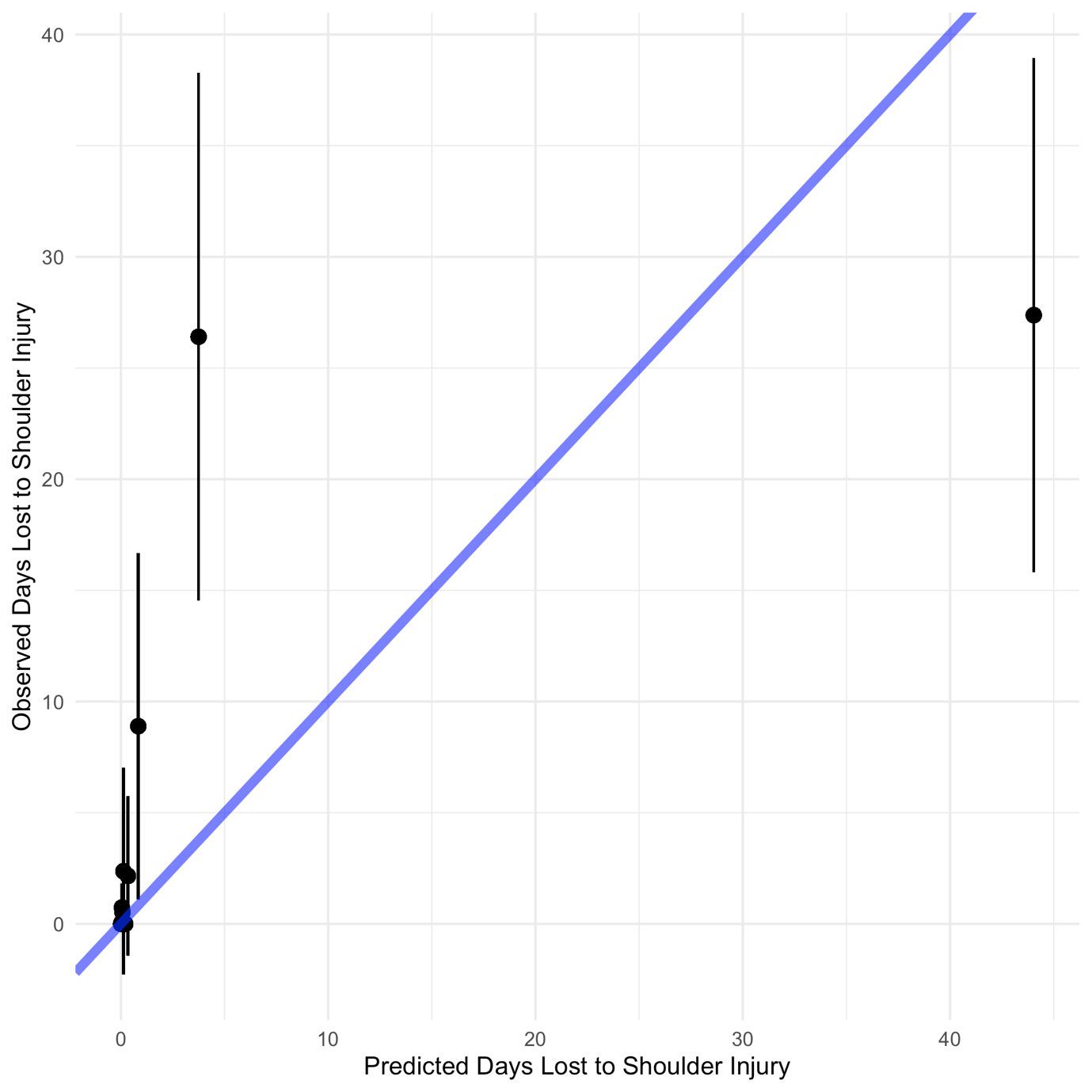
Calibration is the relationship between predicted and actual probability of the event. Perfect calibration would be a 45-degree line. A calibration line below the blue line is over-pre dicting risk. A calibration line above the blue line is under-predicting risk.
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Camp CL, Conte S, D’Angelo J, Fealy SA. Epidemiology of ulnar collateral ligament reconstruction in Major and Minor League Baseball pitchers: comprehensive report of 1429 cases. J Shoulder Elbow Surg 2018;27(5):871-878. doi:10.101 6/j.jse.2018.01.024
2. Conte S, Requa RK, Garrick JG. Disability days in major league baseball. Am J Sport Med 2001;29(4):431-436. doi:10.1177/03635465010290040 801
3. Camp CL, Dines JS, van der List JP, et al. Summative report on time out of play for Major and Minor League Baseball: an analysis of 49,955 injuries from 2011 through 2016. Am J Sport Med 2018;46(7):1727-1732. doi:10.1177/036354651876515 8
4. Conte SA, Fleisig GS, Dines JS, et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sport Med 2015;43(7):1764-1769. doi:10.1177/036354651558079 2
5. Bullock GS, Uhan J, Harriss EK, Arden NK, Filbay SR. The Relationship Between Baseball Participation and Health: A Systematic Scoping Review. J Orthop Sport Phys Ther 2020;50(2):55-66. doi:10.2519/josp t.2020.9281
6. Knowles SB, Marshall SW, Miller T, et al. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj Prevent 2007;13(6):416-421. doi:10.1136/ip.2006.014720
7. Conte S, Camp CL, Dines JS. Injury Trends in Major League Baseball Over 18 Seasons: 1998-2015. Am J Orthop (Belle Mead NJ). 2016;45(3):116-123.
8. Bahr R, Clarsen B, Ekstrand J. Why we should focus on the burden of injuries and illnesses, not just their incidence. Br J Sport Med 2018;52(16):1018-1021. do i:10.1136/bjsports-2017-098160
9. Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: a prospective study Am J Sport Med 2014;42(9):2075-2081. doi:10.1177/036354651453839 1
10. Noonan TJ, Thigpen CA, Bailey LB, et al. Humeral torsion as a risk factor for shoulder and elbow injury in professional baseball pitchers. Am J Sport Med. 2016;44(9):2214-2219. doi:10.1177/036354651664843 8
11. Lyman S, Fleisig GS, Andrews JR, Osinski ED Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sport Med 2002;30(4):463-468. doi:10.1177/03635465020300040 201
12. Garner JC, MacDonald C, Wade C, Johnson A, Ford MA. The influence of body composition on youth throwing kinetics. Ped Ex Sci. 2011;23(3):379-387 doi:10.1123/pes.23.3.379
13. Karakolis T, Bhan S, Crotin RL. An inferential and descriptive statistical examination of the relationship between cumulative work metrics and injury in Major League Baseball pitchers. J Strength Cond Res 2013;27(8):2113-2118. doi:10.1519/jsc.0b013e318278 5059
14. Meeuwisse WH. Assessing causation in sport injury: a multifactorial model. Clin J Sport Med. 1994;4(3):166-170. doi:10.1097/00042752-19940700 0-00004
15. Saper MG, Pierpoint LA, Liu W, Comstock RD, Polousky JD, Andrews JR. Epidemiology of shoulder and elbow injuries among United States high school baseball players: school years 2005-2006 through 2014-2015. Am J Sport Med 2018;46(1):37-43. doi:1 0.1177/0363546517734172
16. Li X, Zhou H, Williams P, et al. The epidemiology of single season musculoskeletal injuries in professional baseball. Orthop Rev 2013;5(1):3. doi:1 0.4081/or.2013.e3
17. Ciccotti MG, Pollack KM, Ciccotti MC, et al. Elbow injuries in professional baseball: epidemiological findings from the Major League Baseball Injury Surveillance System. Am J Sport Med. 2017;45(10):2319-2328. doi:10.1177/03635465177069 64
18. Philp F, Al-Shallawi A, Kyriacou T, Blana D, Pandyan A. Improving predictor selection for injury modelling methods in male footballers. BMJ Open Sport Exerc Med. 2020;6(1):e000634. doi:10.1136/bmjs em-2019-000634
19. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sport Med 1995;23(2):233-239. doi:10.1177/03635465950230021 8
Development of an Injury Burden Prediction Model in Professional Baseball Pitchers
20. Erikkson E. Sports injuries of the knee ligaments: their diagnosis, treatment, rehabilitation, and prevention. Med Sci Sport 1976;8(3):133-144. doi:1 0.1249/00005768-197600830-00001
21. Cleland J, Koppenhaver S, Su J. Netter’s Orthopaedic Clinical Examination: An Evidence-Based Approach Elsevier Health Sciences; 2015.
22. Bahr R. Why screening tests to predict injury do not work—and probably never will…: a critical review Br J Sport Med 2016;50(13):776-780. doi:10.1136/bjsp orts-2016-096256
23. Hughes T, Sergeant JC, van der Windt DA, Riley R, Callaghan MJ. Periodic health examination and injury prediction in professional football (Soccer): theoretically, the prognosis is good. Sport Med 2018;48(11):2443-2448. doi:10.1007/s40279-018-092 8-y
24. Bittencourt NFN, Meeuwisse WH, Mendonça LD, Nettel-Aguirre A, Ocarino JM, Fonseca ST Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition—narrative review and new concept. Br J Sport Med. 2016;50(21):1309-1314. doi:10.1136/bjspo rts-2015-095850
25. Galea S, Riddle M, Kaplan GA. Causal thinking and complex system approaches in epidemiology. Int J Epidemiol 2010;39(1):97-106. doi:10.1093/ije/dyp29
6
26. Moons KGM, Royston P, Vergouwe Y, Grobbee DE, Altman DG. Prognosis and prognostic research: what, why, and how? BMJ 2009;338(feb23 1):b375-b375. do i:10.1136/bmj.b375
27. Moons KGM, Kengne AP, Woodward M, et al. Risk prediction models: I. Development, internal validation, and assessing the incremental value of a new (bio)marker Heart 2012;98(9):683-690. doi:10.1 136/heartjnl-2011-301246
28. Bullock GS, Hughes T, Sergeant JC, Callaghan MJ, Riley R, Collins G. Methods matter: clinical prediction models will benefit sports medicine practice, but only if they are properly developed and validated. Br J Sport Med 2021;55(23):1319-1321. do i:10.1136/bjsports-2021-104329
29. Bullock GS, Hughes T, Sergeant JC, Callaghan MJ, Riley RD, Collins GS. Clinical prediction models in sports medicine: A guide for clinicians and researchers. J Orthop Sport Phys Ther. 2021;51(10):517-525. doi:10.2519/jospt.2021.10697
30. Kannel WB, McGee D, Gordon T A general cardiovascular risk profile: the Framingham Study. Am J Cardiol 1976;38(1):46-51. doi:10.1016/0002-914 9(76)90061-8
31. Quatman CE, Quatman CC, Hewett TE. Prediction and prevention of musculoskeletal injury: a paradigm shift in methodology Br J Sport Med 2009;43(14):1100-1107. doi:10.1136/bjsm.2009.06548 2
32. Van Calster B, Vickers AJ. Calibration of risk prediction models: impact on decision-analytic performance. Med Decis Making 2015;35(2):162-169. doi:10.1177/0272989x14547233
33. Shanley E, Kissenberth MJ, Thigpen CA, et al. Preseason shoulder range of motion screening as a predictor of injury among youth and adolescent baseball pitchers. J Shoulder Elbow Surg. 2015;24(7):1005-1013. doi:10.1016/j.jse.2015.03.012
34. Lintner D, Mayol M, Uzodinma O, Jones R, Labossiere D. Glenohumeral internal rotation deficits in professional pitchers enrolled in an internal rotation stretching program. Am J Sport Med 2007;35(4):617-621. doi:10.1177/0363546506296736
35. Meister K, Day T, Horodyski M, Kaminski TW, Wasik MP, Tillman S. Rotational motion changes in the glenohumeral joint of the adolescent/Little League baseball player Am J Sport Med 2005;33(5):693-698. doi:10.1177/0363546504269936
36. Laudner KG, Stanek JM, Meister K. Assessing posterior shoulder contracture: the reliability and validity of measuring glenohumeral joint horizontal adduction. J Athl Train. 2006;41(4):375-380.
37. Myers JB, Oyama S, Wassinger CA, et al. Reliability, precision, accuracy, and validity of posterior shoulder tightness assessment in overhead athletes. Am J Sport Med 2007;35(11):1922-1930. do i:10.1177/0363546507304142
38. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sport Med 2011;39(9):1997-2006. doi:10.1177/0 363546511408876
40. Rae K, Orchard J. The Orchard sports injury classification system (OSICS) version 10. Clin J Sport Med 2007;17(3):201-204. doi:10.1097/jsm.0b013e318 059b536
41. Riley RD, Ensor J, Snell KIE, et al. Calculating the sample size required for developing a clinical prediction model. BMJ 2020;368:m441. doi:10.1136/b mj.m441
42. Simning A, Orth J, Temkin Greener H, Li Y Patients discharged from higher quality skilled nursing facilities spend more days at home. Health Services Res 2021;56(1):102-111. doi:10.1111/1475-6 773.13543
43. Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sport Med. 2011;39(2):329-335. doi:10.1177/0363546510384223
44. Reinold MM, Wilk KE, Macrina LC, et al. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sport Med 2008;36(3):523-527 doi:10.1177/036354650730 8935
45. Noonan TJ, Thigpen CA, Bailey LB, et al. Humeral Torsion as a Risk Factor for Shoulder and Elbow Injury in Professional Baseball Pitchers. Am J Sport Med 2016;44(9):2214-2219. doi:10.1177/0363546516 648438
46. Helmkamp JK, Bullock GS, Rao A, Shanley E, Thigpen C, Garrigues GE. The Relationship Between Humeral Torsion and Arm Injury in Baseball Players: A Systematic Review and Meta-analysis. Sports Health 2020;12(2):132-138. doi:10.1177/1941738119 900799
47. Polster JM, Bullen J, Obuchowski NA, Bryan JA, Soloff L, Schickendantz MS. Relationship between humeral torsion and injury in professional baseball pitchers. Am J Sport Med. 2013;41(9):2015-2021. doi:1 0.1177/0363546513493249
48. Takeuchi S, Yoshida M, Sugimoto K, Tsuchiya A, Takenaga T, Goto H. The differences of humeral torsion angle and the glenohumeral rotation angles between young right-handed and left-handed pitchers. J Shoulder Elbow Surg. 2019;28(4):678-684. d oi:10.1016/j.jse.2018.09.002
49. Sciascia A, Thigpen C, Namdari S, Baldwin K. Kinetic chain abnormalities in the athletic shoulder. Sports Med Arthrosc 2012;20(1):16-21. doi:10.1097/js a.0b013e31823a021f
50. Bullock GS, Thigpen CA, Noonan TK, Kissenberth MJ, Shanley E. Initial Kinematic Chain Injuries Increase Hazard of Subsequent Arm Injuries in Professional Baseball Pitchers. J Shoulder Elbow Surg. 2022;31(9):1773-1781. doi:10.1016/j.jse.2022.04.016
51. Bullock GS, Thigpen CA, Collins GS, et al. Starting pitchers demonstrate a greater hazard of arm injury compared to relief pitchers. J Athl Train. 2022;57(1):65-71. doi:10.4085/1062-6050-0262.21
52. Bradbury JC, Forman SL. The impact of pitch counts and days of rest on performance among major-league baseball pitchers. J Strength Cond Res 2012;26(5):1181-1187 doi:10.1519/jsc.0b013e31824e 16fe
53. Zou H, Hastie T Regularization and variable selection via the elastic net. J Royal Statistical Soc B 2005;67(2):301-320. doi:10.1111/j.1467-9868.2005.00 503.x
54. Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 2015;350:g7594. doi:10.1136/bmj.g7594
55. Levy AS, Lintner S, Kenter K, Speer KP Intra-and interobserver reproducibility of the shoulder laxity examination. Am J Sport Med. 1999;27(4):460-463. do i:10.1177/03635465990270040901
56. Osborne B. Legal and Ethical Implications of Athletes’ Biometric Data Collection in Professional Sport. Marq Sports L Rev 2017;28:37
57 Gabbett TJ, Jenkins DG. Relationship between training load and injury in professional rugby league players. J Sci med Sport. 2011;14(3):204-209. doi:10.1 016/j.jsams.2010.12.002
58. Wynants L, Collins G, Van Calster B. Key steps and common pitfalls in developing and validating risk models. BJOG 2017;124(3):423-432. doi:10.1111/147 1-0528.14170
59. Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in glenohumeral passive range of motion increase risk of shoulder injury in professional baseball pitchers: a prospective study. Am J Sport Med. 2015;43(10):2379-2385. doi:10.1177/03635465155943 80
60. Werner SL, Guido JA Jr, Stewart GW, McNeice RP, VanDyke T, Jones DG. Relationships between throwing mechanics and shoulder distraction in collegiate baseball pitchers. J Shoulder Elbow Surg. 2007;16(1):37-42. doi:10.1016/j.jse.2006.05.007
61. Reinold MM, Gill TJ, Wilk KE, Andrews JR. Current concepts in the evaluation and treatment of the shoulder in overhead throwing athletes, part 2: injury prevention and treatment. Sports Health. 2010;2(2):101-115. doi:10.1177/1941738110362518
62. Wilk KE, Reinold MM, Andrews JR. Rehabilitation of the thrower’s elbow Clin Sport Med 2004;23(4):765-801. doi:10.1016/j.csm.2004.06.006
63. Shanley E, Thigpen CA, Collins GS, et al. Including modifiable and non-modifiable factors improves injury risk assessment in professional baseball pitchers. J Orthop Sport Phys Ther. 2022(0):1-42.
64. Bullock GS, Hughes T, Arundale AAJH, Ward P, Collins GS, Kluzek S. Black Box Prediction Methods in Sports Medicine Deserve a Red Card for Reckless Practice: A Change of Tactics is Needed to Advance Athlete Care. Sports Med. Published online October 14, 2022:1-7 doi:10.1007/s40279-022-01771-3
Download: https://ijspt.scholasticahq.com/article/39741-development-of-an-injury-burden-prediction-model-inprofessional-baseball-pitchers/attachment/103300.docx?auth_token=vKBsrPbUbkIqryKTab8e
Download: https://ijspt.scholasticahq.com/article/39741-development-of-an-injury-burden-prediction-model-inprofessional-baseball-pitchers/attachment/103301.docx?auth_token=vKBsrPbUbkIqryKTab8e
Download: https://ijspt.scholasticahq.com/article/39741-development-of-an-injury-burden-prediction-model-inprofessional-baseball-pitchers/attachment/103302.docx?auth_token=vKBsrPbUbkIqryKTab8e
Download: https://ijspt.scholasticahq.com/article/39741-development-of-an-injury-burden-prediction-model-inprofessional-baseball-pitchers/attachment/103303.docx?auth_token=vKBsrPbUbkIqryKTab8e
Chimera NJ, Merasty D, Lininger MR. Injuries and Illnesses Across 10 Years of Canada Games Competitions: 2009 – 2019. IJSPT. Published online December 1, 2022:1372-1382.

Nicole J Chimera 1 a , Danielle Merasty 1 , Monica R Lininger 2
1 Department of Kinesiology, Brock University, 2 Department of Physical Therapy and Athletic Training, Northern Arizona University
Keywords: athlete, epidemiology, incidence, odds of injury https://doi.org/10.26603/001c.39743
The Canada Games are a national level competition held every two years alternating between Summer and Winter Games. Participation in elite level athletics, like the Canada Games, have an inherent risk of injury and illness.
To analyze the incidence and characteristics of injuries and illnesses during Canada Games competitions from 2009-2019 (primarily) and to understand sex differences in odds of musculoskeletal injury for Summer and Winter Canada Games athletes (secondarily).
Study
Using a retrospective cohort, data were abstracted from medical incident reports generated during Canada Games from 2009 2019. Data were coded for body part injured and injury type or illness system; injuries were also categorized as acute or chronic.
Across all 10 years of competition, 3160 injuries reported in 8710 male athletes and 3272 injuries reported in 8391 female athletes. Injury incidence was 362.8 and 389.9 and illness incidence was 47.8 and 64.5 per 1000 male and female athletes, respectively. Female athletes had a 1.12 (95% CI: 1.06; 1.19) greater odds of injury and 1.37 (95% CI: 1.20; 1.57) greater odds of illness compared to male athletes. Overall, injury (399.31 vs. 360.31; p < 0.001) and illness (68.67 vs. 47.30; p < 0.001) incidences were higher in Winter Games, compared to Summer Games, per 1000 athletes. When comparing male and female athletes participating in similar sports, sex specific differences exist in odds of both injury and illness.
Male and female athletes competing in Canada Games competitions demonstrate differences in injury and illness incidence and odds of injury This suggests a need to examine if additional modifiable risk factors may exist, which could contribute to prevention strategies to reduce injury and illness during Canada Games competition.
a
Corresponding author: Nicole J. Chimera, PhD, CAT(C), ATC, CSCS
Department of Kinesiology
Brock University 1812 Sir Isaac Brock Way St. Catharines, ON L2S 3A1 Phone: 905-688-5550 x6755 nchimera@brocku.ca
The Canada Games, which are the highest level of national competition for Canadian athletes, were first held in 1969 and occur every two years, alternating between Summer and Winter games.1 Participation in elite level competi tions, such as the Canada Games, encourages large scale participation in multiple sports over the course of a set time period. While athletic participation of this magnitude and level is desirable for many athletes, there are inherent risks of injury for participants. Following the Sequence of Prevention model, in order to prevent injuries, researchers must first identify and describe the injury problem(s).2
To better understand the injury problem, surveys were first conducted during international sports competition in 2004 and included injury data from the Olympic Games and International Federation of Association Football tour naments held between 1998-2001.3 Injury surveillance pro grams are now used widely at the organizational level4–6; while numerous studies of injury/illness incidences are re ported at both the national level7–9 and interna tional3,10–13 levels of competition. Epidemiological assess ments of sport injury can provide direction for injury prevention programs and, when assessed over multiple years, provide insight on how injury patterns/frequencies may change over time. Based on epidemiological data, it has been suggested that athletes participating in athletics should have preventative injury intervention focused on overuse injuries, proper rehabilitation of previous injuries, and be sex specific.10,14,15
Researchers have reported differences in injury inci dence and risk of injury between male and female athletes in international track and field competitions16 and in col legiate athletes17,18; however, incidence proportions were similar between male and female international athletics championships.19 To date, one recent study successfully implemented an injury surveillance protocol in Canadian varsity athletes.20 However, there is a paucity of literature regarding injury and illness incidence during the Canada Games with only one study reporting dental injuries during a single Canada Games competition held over 30 years ago.21 Therefore, the primary purpose of this study was to analyze the incidence and characteristics of injuries and ill nesses during Canada Games competitions from 2009-2019. The secondary purpose of this study was to understand sex differences in odds of musculoskeletal injuries for Summer and Winter Canada Games athletes.
This research utilized a retrospective cohort for a descrip tive epidemiological design to assess injury and illness pat terns in 10 years of Canada Games participants.
From 2009 2019, 17101 (8710 male; 8391 female) athletes participated in Canada Games competitions held in various cities across Canada. 10169 (5457 male; 4712 female) ath letes competed in the Summer Canada Games, which were held in the years 2009, 2013, and 2017 and 6932 (3253 male; 3679 female) athletes competed in Winter Canada Games, which were held in the years 2011, 2015, and 2019. Ath letes completed a consent for treatment form; a release for Canada Games to use anonymous medical information was acquired starting in 2015.
Following ethics approval for Secondary Analysis of Data through Brock University Research Ethics Board, data were abstracted and de-identified by the Canada Games Council for any individual seeking medical attention during their participation in the Canada Games. Medical attention/en counters were recorded in an electronic medical record (EMR) by various clinicians (i.e., athletic therapist, phys iotherapist, chiropractor, physician) working with Canada Games events. Medical attention was defined as assessment of a participant’s medical condition by a qualified medical/ healthcare practitioner 22 Abstracted data, for those seek ing medical attention, included the following: subjective information on injury, objective information on injury, in jury assessment, type of injury, injury diagnosis, further treatment of injury, action taken, place of treatment, and incident status, as well as participant sex, contingent (province), sport, chief complaint, and assessment date. Data were inclusive of Canada Games from 2009 and 2019. For this study, only the first report of an injury/illness were recorded from the medical incident report. There were re ports for follow up (linked through incident numbers), but follow ups were not counted as a new injury In some in stances, there was a medical incident that was linked to an earlier incident report but had an additional or new injury in the follow up incident report. In this case both the initial injury as well as the additional (new) injury reported were included for this analysis.
Using initial and follow up medical incident reports from Canada Games, data were organized based on the Interna tional Olympic Committee Injury Surveillance System for categorizing affected injury location, injury type, and ill ness affected system (Table 1).12 Given the data set and the way injuries were reported within the Canada Games EMR, there were three additional injury type categories included beyond those from the International Olympic Committee Injury Surveillance System; these included patellofemoral pain syndrome (PFPS), compartment syndrome, and pos tural. Injuries were also categorized as acute or overuse (Table 1). Acute sports injury was defined as “loss or abnor mality of bodily structure or functioning resulting from an isolated exposure to physical energy during sports training
Abdomen
Achilles tendon
Arm (Upper)
Ankle
Back (Full)
Cervical spine/Neck Elbow
Face (including eye, ear, nose)
Finger Forearm Foot/toe Groin Hand Head
Hip Knee Leg (Full)
Leg (Lower)
Lumbar spine/lower back Organs
Patellofemoral joint Pelvis/sacrum/buttock Shoulder/clavicular Sternum/ribs
Thigh Thoracic spine/upper back Unknown Wrist
Arthritis/synovitis/bursitis Compartment syndrome
Concussion
Contusion/haematoma/bruise Dental injury/broken tooth Fracture (trauma, stress, other bone injuries)
Impingement
Laceration/abrasion/skin lesion Other (including nerve, spinal cord, fasciitis)
Sprain (dislocation, subluxation, ligamentous rupture)
Strain (muscle rupture, tear, tendon rupture)
Meniscus/cartilage Muscle cramps/spas Patellofemoral pain syndrome
Postural
Tendinosis/tendinopathy
or competition that following examination is diagnosed by a clinical professional as a medically recognized injury” 23 Overuse sports injury was defined as: “loss or abnormality of bodily structure or functioning resulting from repeated bouts of physical load without adequate recovery periods in association with sports training or competition that follow ing examination is diagnosed by a clinical professional as a medically recognized disease or syndrome”.23 Illness was defined as “ a physical or psychological complaint or man ifestation by an athlete not related to injury, regardless of whether it received medical attention or its consequences with respect to impairments in connection with competi tion or training” 10,11 In addition to the categories of af fected system as classified by the International Olympic Committee Injury Surveillance System, we also added a standalone category for cardiovascular and used symptom clusters to identify affected illness system based on the 2020 International Olympic Committee Consensus State ment (Table 1).24
Following data categorization, participants were separated male and female by sport to determine injury and illness frequency, incidence, and odds of injury and illness, with 95% confidence intervals, for male and female athletes across and between sports. Frequency of injury/illness types and locations were calculated as percentages. Injury/ illness incidence was calculated as the total number of in juries/illnesses per 1000 registered athletes using registra tion numbers (numbers of athletes registered for compe tition per sport) provided by Canada Games Council.
Allergic Cardiovascular Dermatologic Endocrinological Environmental Gastrointestinal Immunological Metabolic Other (including urogenital, gynaecological, neurological, psychiatric, musculoskeletal, dental)
Respiratory
Incidence was calculated by first determining the total number of injuries/illnesses reported in all male and female athletes as well as separating out the total numbers of in juries/illnesses reported based on sport and sex. Once in jury/illness totals were counted, the registration numbers were used to calculate incidence of injury in all athletes, male athletes, female athletes, and further subdivided to calculate incidence of injury in male or female athletes based on sport. Registration numbers were divided by 1000 to indicate the total number of participants per 1000. Con sistent with previous research,12,13 incidence was then cal culated as the total number of injuries/illnesses divided by the total number of athletes registered for competition in each sport (using the equation below).
Odds ratios (from 2 x 2 contingency tables) were calculated to determine odds of injury/illness between male and fe male athletes and when comparing between similar sports. Additionally, 95% confidence intervals (95% CIs) were cal culated to determine precision. Data were analyzed in Ex cel; the 95% CI (interval exclusion of null of 1.0) was used to indicate statistical significance in odds of injuries/ill nesses between males and females competing in Canada Games. MedCalc (https://www.medcalc.org/; v.20.113) was used to determine statistically significant differences (p < 0.05) in incidence of injury/illness (overall and in Summer vs. Winter Games) between male and females athletes com peting in Canada Games.
Table 2. Injury location for male and female participants across all 10 years of Canada Games competitions.
Injury Location (n; % of total injuries) Male Female
Abdomen 17; 0.5% 15; 0.4%
Achilles Tendon 29; 0.9% 37; 1.1%
Ankle 243; 7.4% 232; 6.8%
Arm (Upper) 41; 1.2% 30; 0.9%
Back (Full) 21; 0.6% 18; 0.5%
Cervical Spine/Neck 156; 4.7% 228; 6.7%
Elbow 88; 2.7% 85; 2.5%
Face 93; 2.8% 61; 1.8%
Finger 91; 2.8% 60; 1.8%
Forearm 43; 1.3% 37; 1.1%
Foot/Toe 144; 4.4% 131; 3.8% Groin 70; 2.1% 55; 1.6%
Hand 43; 1.3% 32; 0.9%
Head 112; 3.4% 96; 2.8%
Hip 128; 3.9% 125; 3.6%
Knee 215; 6.5% 288; 8.4%
Leg (Full) 7; 0.2% 9; 0.3%
Leg (Lower) 178; 5.4% 213; 6.2%
Lumbar Spine/Low Back 350; 10.6% 378; 11.0%
Organs 6; 0.2% 0
Patellofemoral Joint 38; 1.2% 68; 2.0%
Pelvis/Sacrum 163; 4.9% 188; 5.5%
Sternum/Ribs 61; 1.8% 87; 2.5%
Shoulder/Clavicle 373; 11.3% 405; 11.8%
Thoracic Spine/Upper Back 237; 7.2% 247; 7.2%
Thigh 302; 9.1% 234; 6.8%
Unknown 0 1; 0.03%
Wrist 52; 1.6% 68; 2.0%
Total number of athletes across all 10 years of Canada Games: 8710 male; 8391 female
Across all 10 years of Canada games, 3160 injuries reported in 8710 male athletes (n = 5457 in Summer Games; 3253 in Winter Games) and 3272 injuries reported in 8391 female athletes (n = 4712 in Summer Games; 3679 in Winter Games). Injury incidence was 362.8 and 389.9 (p = 0.004) and illness incidence was 47.8 and 64.5 (p< 0.001) per 1000 male and female athletes, respectively Injuries to the shoulder (Table 2) and muscle strains (Table 3) were the most common regardless of sex.
The respiratory system was most often affected illness system for male and female athletes (Table 4). Female, compared to male, athletes had a 1.12 (95% CI: 1.06; 1.19) significantly greater odds of injury and 1.37 (95% CI: 1.20; 1.57) significantly greater odds of illness.
Assessing Summer and Winter Canada Games competi tions separately, the overall injury and illness incidences were significantly higher in Winter, compared to Summer, Canada Games when all athletes were combined and in male athletes (Figure 1). Overall incidence of illness was significantly higher in females competing in Winter com pared to Summer Games; however, there was no difference in overall incidence of injuries in females competing in Winter compared to Summer Games (Figure 1).
Female freestyle skiing participants had the highest in jury incidence while female target shooting participants had the highest illness incidence (Tables 5 and 6). Female athletes competing in softball, canoe-kayak, rowing, sail ing, swimming, tennis, triathlon, fencing, alpine skiing, biathlon, judo, snowboarding, and wheelchair basketball had a significantly increased odds of injury compared to males competing in similar sports (Tables 5 and 6). Female athletes competing in athletics, softball, soccer, and speed skating had a significantly increased odds of illness com pared to males competing in similar sports; while females competing in diving had a significantly decreased odds of illness compared to male participants (Tables 5 and 6).
Strains were most common across all athletes in Summer and Winter games (Table 7); thigh and shoulder were the most frequently injured in male Summer and Winter par ticipants, respectively; shoulder was most frequent in fe male Summer and Winter participants (Table 7). Male Sum mer and Winter participants reported more acute injuries; female Summer and Winter participants reported more chronic injuries (Table 7). In Summer Games, participants reported highest illness in other category (urogenital, gy naecological, neurological, psychiatric) (Table 7) and in Winter games respiratory system was most often affected system for illness (Table 7).
The purpose of this study was to analyze the incidence and characteristics of injuries and illnesses during Canada Games competitions from 2009-2019 and to understand sex differences in odds of musculoskeletal injury for Summer and Winter Canada Games athletes. The Canada Games oc cur every two years and alternate between Summer and Winter Games. Overall, there were similarities in types of injuries and illnesses as well as area of the body commonly injured, however; incidence and odds of injury and illness differed between male and female athletes.
When considering all 10 years of Canada Games competi tions, strains, sprains, and contusions/hematomas/bruises were most common; demonstrating that approximately 70% of all injuries during 10 years of Canada Games com petitions were of one of three injury type categories. These findings are similar to those reported in the 2008 and 2010 Olympic Games with contusions (26 46%), sprains (11 20%), and strains (8 16%) being most common.12,13,25
Table 3. Injury type for male and female participants across all 10 years of Canada Games competitions.
Injury Type (n; % of total injury types)
Male Female
Arthritis/Synovitis/ Bursitis 21; 0.7% 34; 1.0%
Compartment Syndrome 5; 0.2% 9; 0.3%
Concussion 80; 2.5% 74; 2.3% Contusion/ Hematoma/Bruise 386; 12.2% 299; 9.1%
Dental/Tooth 3; 0.1% 3; 0.1%
Fracture 110; 3.5% 107; 3.3%
Impingement 40; 1.3% 56; 1.7% Laceration/Abrasion/ Skin 228; 7.2% 173; 5.3%
Meniscus/Cartilage 32; 1.0% 51; 1.6% Muscle Cramp/Spasm 139; 4.4% 143; 4.4%
Other 51; 1.6% 64; 2.0% Patellofemoral Pain Syndrome 35; 1.1% 61; 1.9%
Postural 9; 0.3% 12; 0.4% Sprain 674; 21.3% 770; 23.5% Strain 1149; 36.4% 1236; 37.8%
Tendinopathy 198; 6.3% 180; 5.5% Acute 1716; 54.3% 1534; 46.9% Chronic 1444; 45.7% 1738; 53.1%
Total number of athletes across all 10 years of Canada Games: 8710 male; 8391 female
Affected System (n; % of total illnesses) Male Female
Allergic 6; 1.4% 24; 4.4%
Cardiovascular 14; 3.4% 14; 2.6%
Dermatologic 63; 15.1% 61; 11.3%
Endocrinological 0 2; 0.4%
Environmental 18; 4.3% 19; 3.5%
Gastrointestinal 70; 16.8% 76; 14.0% Immunological 0 1; 0.2% Metabolic 0 0
Other 114; 27.4% 153; 28.3%
Respiratory 131; 31.5% 191; 35.3%
Total number of athletes across all 10 years of Canada Games: 8710 male; 8391 female
Overall, the shoulder was the most commonly injured body area in all participants. However, when considering injured body area in male and female participants in Summer and Winter Canada Games separately, the thigh was most com monly injured in male participants in Summer Games. Pre
vious findings suggest that male athletes sustained signifi cantly more injuries to the thigh region (Relative Risk [RR]= 1.64; 95% CI 1.32; 2.05) with a 1.66 (95% CI 1.25; 2.19) increased risk of thigh strains compared to female partic ipants during International Athletics Competitions.16 Al though the measure of RR is different from the odds ra tios presented in this current study, both measures are used to describe an association between a variable and an out come. However, there are distinct differences between mea suring RR and OR. Relative risk assesses the probability of an injury occurring and requires participants at risk to con sider the frequency of a risk while OR primarily consider the rate of injury.26,27 In a retrospective design, which was used in this current study, because the total number of partici pants at risk is not known, RR cannot be calculated. There fore, OR were used in this current study to measure the strength of association between variables (males and fe males or Summer and Winter Games) and the outcomes of interest (injury types, locations, etc.).
When considering male and female participants across all 10 years of Canada Games competitions, in addition to the shoulder and thigh, the ankle and knee were the also commonly injured body areas. These findings are more consistent with previous literature suggesting that lower extremity injuries occur most commonly (at least half of all injuries) as reported in previous Olympic competi tions,12,13,25 in Olympic athletes on the British World Class Performance Programme,28 and Youth Olympic Games.29 Additionally, across all 10 years of Canada Games com petitions as well as when comparing specifically between Summer and Winter Canada Games, males had more acute injuries while females had more chronic injuries. These findings are directly in line with previous reports from a Di vision I collegiate institution in the United States indicat ing female athletes had a greater rate of chronic injuries per 10000 athlete exposures (AEs) across three years of compe tition while males athletes had a higher rate of acute in juries per 10000 AEs in the same time frame.18 Perhaps these combined findings suggest a need to investigate mit igating risk of injury differently between male and female athletes with greater focus on prevention of chronic injury in female and acute injury in males.
Across all 10 years of Canada Games competitions, the respiratory system was the most often affected system in illness while the category of ‘other’ was the second most affected system. Together these two systems represented more than 50% of all illness in both male and female partic ipants. This is consistent with previous literature indicating the respiratory system was the most commonly reported system affected (19 62% of all reported illnesses) in Sum mer and Winter Olympics, International Athletics Competi tions, Rugby, and Youth Olympic Games.11,12,19,29–31 Risk factors for respiratory illness can include stress (mechan ical/dehydration) to the airway as well as airborne pollu tants, irritants, and allergens that can be inhaled by the athlete during exercise.32 Given the demands of sport there are inherent stresses to the respiratory system that may be further exacerbated by air quality, which cannot be pre vented.
Incidence was calculated by first determining the total number of injuries in all athletes, in male athletes, and in female athletes for both Winter and Summer Games. The number of registered athletes (based on the categories of total, male, female, winter, and summer) were divided by 1000 and used as the denominator whereby total number of injuries/illnesses were divided by
* Significant difference in Winter compared to Summer Games for total and male injury incidence and total, male, and female illness incidence; p < 0.001
! Significant difference in Winter compared to Summer Games for female illness incidence; p 0.004
Injury incidence was higher in female, compared to male, athletes across all 10 years of Canada Games competitions. When considering differences specific to participation in Summer versus Winter Canada Games, incidence of injury was higher in Winter than Summer Games across all ath letes. When looking at participation in specific sports, fe male athletes had a higher incidence of injury, per 1000 athletes, in the majority of Summer and Winter Canada Games sports. Interestingly, incidence of injury was nearly identical between in females competing in Summer and Winter Games, while males competing in Winter Games had higher incidence of injury than males competing in Summer Games. This may suggest more consistency in fe male athlete’s reporting of injury across all Games.
Similar to injury incidence reports from the 2008 Sum mer Olympic Games,13 the lowest overall incidence of in jury per 1000 Summer Canada Games participants in swim
ming, canoe-kayak, and sailing. In Winter Canada Games, the highest overall incidence of injury per 1000 athletes was observed in freestyle skiing and women’s snowboard ing. These findings are similar to those reported from the 2010 and 2014 Winter Olympic Games with alpine skiing and snowboarding having high injury risk12 and injury in cidence.30 Additionally, similar to the current findings, in cidence of injury (per 1000 athletes) was lowest in men’s archery, previous research suggests low injury rates or in cidences in archery and table tennis during Olympic com petition.11,13 Collectively, these Canada Games injury in cidence findings are in support of suggestions that sports with jumping, cutting, sprinting, and pivoting have higher risk of injury.33
Female athletes had a significantly increased odds of in jury when combining all athletes together; however, odds of injury varied when also considering specific sport partic ipation. In Canada Winter Games, female alpine skiers had a 2.6 greater odds of injury compared to male alpine skiers.
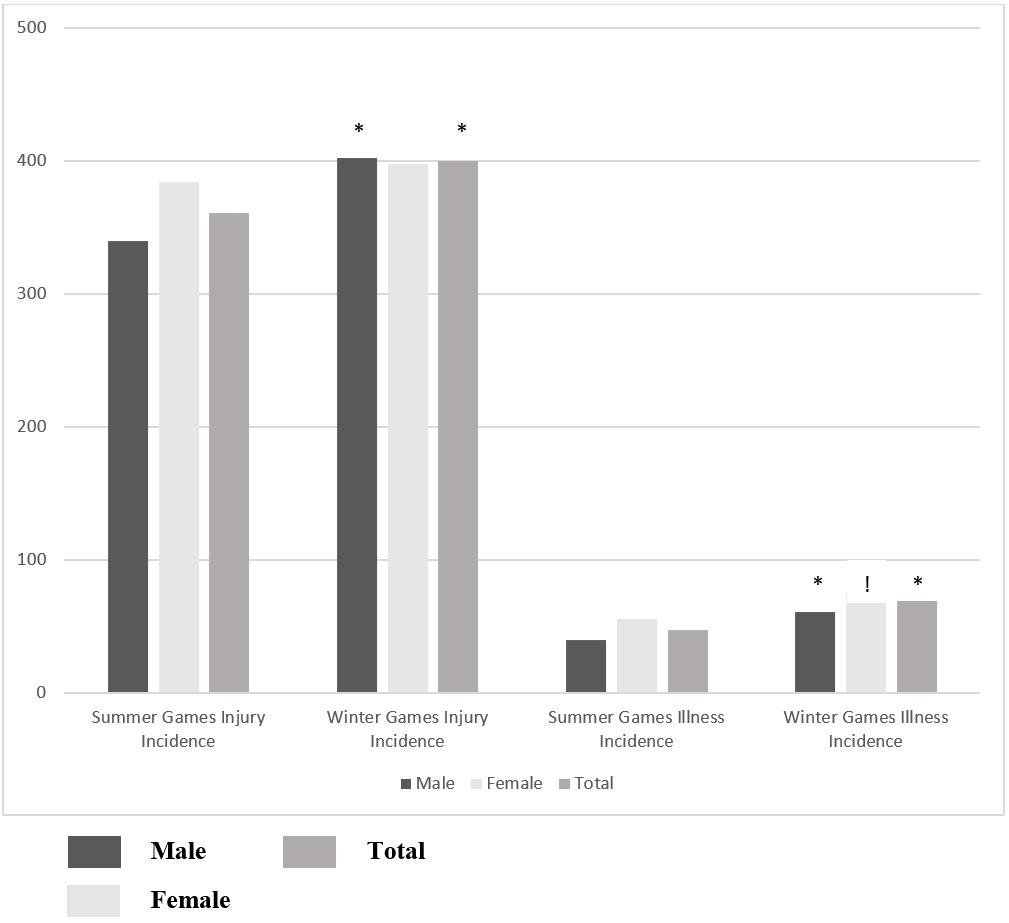
Injury Incidence OR [95% CI]
Male Female
Illness Incidence OR [95% CI]
Male Female
Athletics ♂ = 824; ♀ = 796 349.1 355.7 1.0 [0.8;1.3] 30.0 60.0 2.1 [1.3;3.4]
Baseball/Softball ♂ = 586; ♀ = 448 188.9 473.3 3.8 [2.9;5.1] 16.9 40.2 2.4 [1.1;5.3]
Basketball ♂ = 416; ♀ = 384 448.1 414.9 0.9 [0.7;1.2] 39.2 38.9 1.0 [0.5;2.1]
Canoe-Kayak ♂ = 229; ♀ = 217 153.7 301.7 2.4 [1.5;3.8] 44.8 74.0 1.7 [0.8;3.9]
Cycling ♂ = 209; ♀ = 143 291.2 330.1 1.2 [0.8;1.9] 31.1 55.9 1.7 [0.6;4.8]
Diving ♂ = 93; ♀ = 86 441.8 336.6 0.6 [0.3;1.1] 116.7 22.2 0.2 [0.0;0.8]
Golf ♂ = 102; ♀ = 91 234.8 260.6 1.2 [0.6;2.2] 0 109.3 N/A
Fencing* ♂ = 53; ♀ = 42 301.9 904.8 22.0 [6.7;71.9] 0 95.2 N/A
Rowing ♂ = 326; ♀ = 337 177.6 329.6 2.2 [1.5;3.2] 36.9 53.0 1.5 [0.7;3.1]
Rugby* ♂ = 250; ♀ = 0 728.0 N/A N/A 60.0 N/A N/A
Sailing ♂ = 90; ♀ = 91 164.8 529.9 5.6 [2.8;11.1] 86.9 96.0 1.1 [0.4;3.1]
Soccer ♂ = 642; ♀ = 620 523.0 433.0 0.7 [0.6;0.9] 26.3 66.1 2.6 [1.5;4.6] Swimming ♂ = 483; ♀ = 493 89.0 144.8 1.7 [1.2;2.6] 39.1 44.5 1.1 [0.6;2.1]
Tennis ♂ = 129; ♀ = 125 344.8 554.1 2.3 [1.4;3.8] 85.5 57.1 0.6 [0.2;1.7]
Triathlon ♂ = 89; ♀ = 89 271.8 581.9 3.8 [2.0;7.1] 100.1 46.2 0.4 [0.1;1.4]
Volleyball ♂ = 470; ♀ = 472 353.8 412.4 1.3 [1.0;1.7] 34.4 21.3 0.6 [0.3;1.4]
Wrestling ♂ = 317; ♀ = 278 537.7 495.4 0.8 [0.6;1.2] 94.1 111.5 1.2 [0.7;2.0]
OR odds ratio for odds of injury or illness
There are limited reports of differences in odds of injury be tween male and female athletes competing in high levels of competition; one study reported findings similar to ours suggesting that female athletes competing in slopestyle skiing were at greater risk of injury compared to male ath letes (RR=3.00; 95% CI: 1.04; 8.63).30 Additionally, female fencers had 22 times greater odds of injury compared to their male counterparts. It has been previously reported that male fencers have higher relative risk (RR=1.42, 95% CI 1.05 to 1.94) of time loss injury compared to female fencers34; perhaps the difference in our findings from those previously reported are that we included all injuries rather than only those that resulted in time loss. It has been sug gested that as much as 90% of overuse injuries may be missed when using time loss in defining injury 35 The nor
malization of continuing to participate at all costs, even when injured,36 can limit the understanding of injury epi demiology in large scale events such as Canada Games if in jury definitions only include time loss injuries. Further, in juries sustained in sport can impact both preparation for, and performance in, future sport participation.37 Therefore, previous literature has advocated for the use of more inclu sive injury definitions.38
Similar to injury incidence, illness incidence was higher in female, compared to male, athletes across all 10 years of Canada Games competitions. This is similar to the re ports that women competing in the 2010 Vancouver, 2012 London, and 2014 Sochi Olympics had higher reports of illnesses compared to male athletes.11,12,30 Previous liter ature has indicated female athletes had 1.5 times greater
if female compared to male athlete competing in similar sport. N/A odds of injury/illness not calculated based on no participants or in juries/illnesses being recorded in male or female participants. OR were calculated from 2 x 2 contingency tables with 95% CIs calculated for precision and statistical significance. To tal number of male and female athletes registered for competition per sport are indicated under each sport in the sport column. *data are from one year of competition only due to change in sport inclusion in Canada Games.Injury Incidence OR [95% CI]
Illness Incidence OR [95% CI]
Male Female Male Female
♂ = 200; ♀ = 186 267.5 460.9 2.3 [1.5;3.5] 42.3 100.9 2.3 [1.0;5.2]
Alpine Skiing
Archery ♂ = 59; ♀ = 59 139.2 188.3 1.5 [0.5;3.9] 33.3 103.8 3.2 [0.6;16.7]
Badminton ♂ = 172; ♀ = 163 548.2 456.4 0.7 [0.4;1.1] 58.4 86.2 1.5 [0.7;3.5]
Biathlon ♂ = 120; ♀ = 119 356.8 633.3 3.1 [1.8;5.2] 34.3 84.0 2.7 [0.8;8.7]
Boxing ♂ = 108; ♀ = 0 646.7 N/A N/A 14.9 N/A N/A
Cross Country Skiing ♂ = 193; ♀ = 182 247.6 330.1 1.5 [0.9;2.3] 124.0 143.5 1.2 [0.6;2.1]
Curling ♂ = 140; ♀ = 143 198.9 252.2 1.4 [0.8;2.4] 56.2 53.1 1.0 [0.4;2.7]
Figure Skating
♂ = 130; ♀ = 191 197.0 141.9 0.7 [0.4;1.2] 55.3 68.4 1.3 [0.5;3.3]
Freestyle Skiing ♂ = 107; ♀ = 72 774.2 1015.2 N/A 7.6 53.3 6.2 [0.7;57.0]
Gymnastics ♂ = 211; ♀ = 235 717.4 539.0 0.5 [0.3;0.7] 40.9 44.2 1.1 [0.4;2.9]
Ice Hockey ♂ = 741; ♀ = 697 337.2 310.2 0.9 [0.7;1.1] 76.3 54.5 0.7 [0.5;1.1]
Judo ♂ = 198; ♀ = 167 464.2 621.5 1.8 [1.2;2.8] 77.8 81.6 1.1 [0.5;2.4] Ringette ♂ = 0; ♀ = 468 N/A 439.8 N/A N/A 71.0 N/A
Snowboarding ♂ = 134; ♀ = 107 524.7 732.7 2.6 [1.5;4.5] 45.7 36.8 0.8 [0.2;3.0]
Speed Skating ♂ = 246; ♀ = 231 417.5 356.6 0.8 [0.5;1.1] 40.5 91.8 2.4 [1.1;5.1]
Squash ♂ = 136; ♀ = 130 490.3 473.0 0.9 [0.6;1.5] 72.2 101.4 1.6 [0.6;3.8]
Synchronized Swimming ♂ = 0; ♀ = 288 N/A 205.6 N/A N/A 38.2 N/A
Table Tennis ♂ = 101; ♀ = 94 174.0 175.9 0.9 [0.5;2.0] 50.3 97.1 2.0 [0.7;6.3]
Target Shooting ♂ = 70; ♀ = 74 262.3 373.6 1.8 [0.9;3.6] 85.8 192.7 2.5 [0.9;6.9]
Wheelchair Basketball ♂ = 187; ♀ = 73 607.7 888.4 4.1 [2.2;7.7] 121.1 168.0 2.3 [1.0;5.1]
relative risk for developing an illness compared to male ath letes.30 When considering differences specific to participa tion in Summer versus Winter Canada Games, incidence of illness was higher in Winter than Summer Games. This may not be surprising given that exposure to cold during win ter months increases the risk of developing respiratory ill ness, which may be due to vasoconstriction in the respi ratory tract mucosa and suppression of immune responses that occur with inhaling cold air.39
It is important to acknowledge that boxing and rugby had only male participants while synchronized swimming
and ringette had only female participants. Both fencing and golf had no illnesses reported by male participants during any years of Canada Games so a comparison could not be directly assessed between male and female illness incidence or odds; to the researcher’s knowledge this does not repre sent an error in reporting but rather a lack of illness being reported by any member of these teams. Further, rugby and fencing were only included in Canada Games competitions in only 2009 and 2013 respectively; therefore, for each of these sports, only one year of data are available. Finally, ex posure and time loss data were not collected, therefore in
Table 7. Most common injury type, body area, chronic/acute, affected system (illness) in male and female athletes across 10 years of Summer and Winter Canada Games
Winter Games Male Female Male Female
Injury Type Strain n = 603 (32.5%) Strain n = 616 (34.0%) Strain n = 546 (41.8%) Strain n = 620 (42.4%)
Body Area Thigh n = 215 (11.0%) Shoulder n = 204 (10.8%) Shoulder n = 192 (14.3%) Shoulder n = 200 (13.0%)
Chronic/ Acute Acute n = 1019 (55.0%) Chronic n = 975 (53.9%) Acute n = 697 (53.4%) Chronic n = 763 (52.2%)
Affected System Other n = 69 (31.7%) Other n = 73 (27.8%) Respiratory n = 85 (42.9%) Respiratory n = 131 (47.1%)
cidence rate cannot be calculated, and the incidence of in jury/illness data cannot be dichotomized into time loss vs. no time loss. To give a frame of reference to the number of injuries/illnesses, we used athlete registration numbers to report incidence per 1000 athletes registered for competi tion. These are limitations to the data set as well as the ret rospective design of the secondary analysis of data; how ever, this is the first report of the epidemiology of injury and illness during Canada Games and therefore provides an understanding to the differences that exist in male and fe male athletes competing in Canada Games competitions.
Although injured body area and type of injury were similar between males and females competing in Canada Games, female athletes had a significantly greater overall odds of both injury and illness. Differences exist in injuries and ill nesses between Summer and Winter Canada Games and be tween male and female participants in like sports. Given these differences, there may be an interest in future explo ration of modifiable risk factors as this may help to clini cians to target strategies to reduce injuries that occur dur ing Canada Games competitions.
Chimera Brock University Canada Games Grant provided support for hiring a research assistant and for conference registration fees
Merasty paid research assistant through Chimera’s Brock University Canada Games Grant funding
Lininger none
The authors wish to thank and Canada Games Council for providing de-identified data for this analysis. This work was supported by a Brock University Canada Games Grant.
Submitted: April 07, 2022 CST, Accepted: September 11, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Canada Games. Accessed July 25, 2022. https://ww w.canadagames.ca/
2. van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med 1992;14(2):82-99. d oi:10.2165/00007256-199214020-00002
3. Junge A, Dvorak J, Graf-Baumann T, Peterson L. Football injuries during FIFA tournaments and the Olympic Games, 1998-2001: development and implementation of an injury-reporting system. Am J Sports Med 2004;32(1 Suppl):80S-89S. doi:10.1177/0 363546503261245
4. Allen AN, Wasserman EB, Williams RM, et al. Epidemiology of secondary school boys’ and girls’ basketball injuries: National Athletic Treatment, Injury and Outcomes Network. J Athl Train 2019;54(11):1179-1186. doi:10.4085/1062-6050-33 0-18
5. Mack CD, Meisel P, Herzog MM, et al. The establishment and refinement of the National Basketball Association Player Injury and Illness Database. J Athl Train 2019;54(5):466-471. doi:10.40 85/1062-6050-18-19
6. Dick R, Agel J, Marshall SW National Collegiate Athletic Association injury surveillance system commentaries: introduction and methods. J Athl Train. 2007;42(2):173-182.
7. Solis-Mencia C, Ramos-Álvarez JJ, Murias-Lozano R, Aramberri M, Saló JC. Epidemiology of injuries sustained by elite under-18 rugby players. J Athl Train. 2019;54(11):1187-1191. doi:10.4085/1062-605 0-510-18
8. Micieli JA, Zurakowski D, Ahmed IIK. Impact of visors on eye and orbital injuries in the National Hockey League. Can J Ophthalmol 2014;49(3):243-248. doi:10.1016/j.jcjo.2014.03.008
9. Gulbrandsen M, Hartigan DE, Patel KA, Makovicka JL, Tummala SV, Chhabra A. Ten-year epidemiology of ankle injuries in men’s and women’s collegiate soccer players. J Athl Train. 2019;54(8):881-888. doi:1 0.4085/1062-6050-144-18
10. Alonso JM, Tscholl PM, Engebretsen L, Mountjoy M, Dvorak J, Junge A. Occurrence of injuries and illnesses during the 2009 IAAF World Athletics Championships. Br J Sports Med 2010;44(15):1100-1105. doi:10.1136/bjsm.2010.07803 0
11. Engebretsen L, Soligard T, Steffen K, et al. Sports injuries and illnesses during the London Summer Olympic Games 2012. Br J Sports Med. 2013;47(7):407-414. doi:10.1136/bjsports-2013-09238 0
12. Engebretsen L, Steffen K, Alonso JM, et al. Sports injuries and illnesses during the Winter Olympic Games 2010. Br J Sports Med 2010;44(11):772-780. d oi:10.1136/bjsm.2010.076992
13. Junge A, Engebretsen L, Mountjoy ML, et al. Sports injuries during the Summer Olympic Games 2008. Am J Sports Med. 2009;37(11):2165-2172. doi:1 0.1177/0363546509339357
14. Alonso JM, Edouard P, Fischetto G, Adams B, Depiesse F, Mountjoy M. Determination of future prevention strategies in elite track and field: analysis of Daegu 2011 IAAF Championships injuries and illnesses surveillance. Br J Sports Med. 2012;46(7):505-514. doi:10.1136/bjsports-2012-0910 08
15. Edouard P, Depiesse F, Branco P, Alonso JM. Analyses of Helsinki 2012 European Athletics Championships injury and illness surveillance to discuss elite athletes risk factors. Clin J Sport Med. 2014;24(5):409-415. doi:10.1097/jsm.0000000000000 052
16. Edouard P, Feddermann-Demont N, Alonso JM, Branco P, Junge A. Sex differences in injury during top-level international athletics championships: surveillance data from 14 championships between 2007 and 2014. Br J Sports Med 2015;49(7):472-477 d oi:10.1136/bjsports-2014-094316
17. Covassin T, Moran R, Elbin RJ. Sex differences in reported concussion injury rates and time loss from participation: An update of the National Collegiate Athletic Association Injury Surveillance Program from 2004-2005 through 2008-2009. J Athl Train 2016;51(3):189-194. doi:10.4085/1062-6050-51.3.05
18. Yang J, Tibbetts AS, Covassin T, Cheng G, Nayar S, Heiden E. Epidemiology of overuse and acute injuries among competitive collegiate athletes. J Athl Train 2012;47(2):198-204. doi:10.4085/1062-6050-47.2.198
19. Edouard P, Junge A, Sorg M, Timpka T, Branco P. Illnesses during 11 international athletics championships between 2009 and 2017: incidence, characteristics and sex-specific and disciplinespecific differences. Br J Sports Med 2019;53(18):1174-1182. doi:10.1136/bjsports-2018-1 00131
20. Gamble ASD, Mountjoy ML, Bigg JL, Spriet LL. Implementation of injury and illness surveillance protocols in varsity athletes. Clin J Sport Med Published online May 2, 2018. doi:10.1097/jsm.00000 00000000587
21. Lee-Knight CT, Harrison EL, Price CJ. Dental injuries at the 1989 Canada games: an epidemiological study. J Can Dent Assoc. 1992;58(10):810-815.
22. Timpka T, Alonso JM, Jacobsson J, et al. Injury and illness definitions and data collection procedures for use in epidemiological studies in Athletics (track and field): consensus statement. Br J Sports Med 2014;48(7):483-490. doi:10.1136/bjsports-2013-0932 41
23. Timpka T, Jacobsson J, Bickenbach J, Finch CF, Ekberg J, Nordenfelt L. What is a sports injury? Sports Med 2014;44(4):423-428. doi:10.1007/s40279-014-01 43-4
24. International Olympic Committee Injury and Illness Epidemiology Consensus Group, Bahr R, Clarsen B, et al. International Olympic Committee
Consensus Statement: Methods for Recording and Reporting of Epidemiological Data on Injury and Illness in Sports 2020 (Including the STROBE Extension for Sports Injury and Illness Surveillance (STROBE-SIIS)). Orthop J Sports Med 2020;8(2):2325967120902908. doi:10.1177/232596712 0902908
25. Junge A, Langevoort G, Pipe A, et al. Injuries in team sport tournaments during the 2004 Olympic Games. Am J Sports Med. 2006;34(4):565-576. doi:1 0.1177/0363546505281807
26. Ranganathan P, Aggarwal R, Pramesh CS. Common pitfalls in statistical analysis: Odds versus risk. Perspect Clin Res 2015;6(4):222-224. doi:10.410 3/2229-3485.167092
27. Ruddy JD, Cormack SJ, Whiteley R, Williams MD, Timmins RG, Opar DA. Modeling the risk of team sport injuries: A narrative review of different statistical approaches. Front Physiol. 2019;10:829. do i:10.3389/fphys.2019.00829
28. Kelly S, Pollock N, Polglass G, Clarsen B. Injury and illness in elite athletics: A prospective cohort study over three seasons. Int J Sports Phys Ther 2022;17(3):420-433. doi:10.26603/001c.32589
29. Nabhan D, Walden T, Street J, Linden H, Moreau B. Sports injury and illness epidemiology during the 2014 Youth Olympic Games: United States Olympic Team Surveillance. Br J Sports Med. 2016;50(11):688-693. doi:10.1136/bjsports-2015-095 835
30. Soligard T, Steffen K, Palmer-Green D, et al. Sports injuries and illnesses in the Sochi 2014 Olympic Winter Games. Br J Sports Med 2015;49(7):441-447. doi:10.1136/bjsports-2014-09453 8
31. Buchholtz K, Barnes C, Burgess TL. Injury and illness incidence in 2017 Super Rugby Tournament: A surveillance study on a single South African team. Int J Sports Phys Ther 2022;17(4):648-657 doi:10.26603/ 001c.35581
32. Kippelen P, Fitch KD, Anderson SD, et al. Respiratory health of elite athletes preventing airway injury: a critical review Br J Sports Med 2012;46(7):471-476. doi:10.1136/bjsports-2012-0910 56
33. Emery CA. Risk factors for injury in child and adolescent sport: a systematic review of the literature. Clin J Sport Med 2003;13(4):256-268. doi:1 0.1097/00042752-200307000-00011
34. Harmer PA. Epidemiology of time-loss injuries in international fencing: a prospective, 5-year analysis of Fédération Internationale d’Escrime competitions. Br J Sports Med. 2019;53(7):442-448. doi:10.1136/bjsp orts-2018-100002
35. Richardson A, Clarsen B, Verhagen E a. LM, Stubbe JH. High prevalence of self-reported injuries and illnesses in talented female athletes. BMJ Open Sport Exerc Med 2017;3(1):e000199. doi:10.1136/bmjs em-2016-000199
36. Wiese-Bjornstal DM. Psychology and socioculture affect injury risk, response, and recovery in highintensity athletes: a consensus statement. Scandinavian Journal of Medicine & Science in Sports 2010;20(s2):103-111. doi:10.1111/j.1600-0838.2010.0 1195.x
37 Chen Y, Buggy C, Kelly S. Winning at all costs: a review of risk-taking behaviour and sporting injury from an occupational safety and health perspective. Sports Med Open 2019;5(1):15. doi:10.1186/s40798-0 19-0189-9
38. Hodgson L, Gissane C, Gabbett TJ, King DA. For debate: consensus injury definitions in team sports should focus on encompassing all injuries. Clin J Sport Med. 2007;17(3):188-191. doi:10.1097/jsm.0b01 3e3180547513
39. Mourtzoukou EG, Falagas ME. Exposure to cold and respiratory tract infections. Int J Tuberc Lung Dis. 2007;11(9):938-943.
G, Prats-Uribe A, Thigpen C, Martin H, Loper B, Shanley E. Influence of High School Socioeconomic Status on Athlete Injuries during the COVID-19 Pandemic: An Ecological Study. IJSPT. Published online December 2, 2022:1383-1395.
Garrett Bullock 1 a , Albert Prats-Uribe 2 , Charles Thigpen 3 , Heather Martin 4 , Beverly Loper 4 , Ellen Shanley 3
1 Department of Orthopaedic Surgery & Rehabilitation, Wake Forest School of Medicine; Centre for Sport, Exercise and Osteoarthritis Research Versus Arthritis, University of Oxford, 2 Pharmaco-Device Epidemiology, University of Oxford, 3 ATI Physical Therapy; University of South Carolina Center for Effectiveness Research in Orthopedics, 4 ATI Physical Therapy
Keywords: Household Income, Collision Sport, Incidence, Socio-determinants of Health https://doi.org/10.26603/001c.39610
It is presently unclear how the cessation of high school sport has affected injury incidence at different socioeconomic levels. The COVID-19 pandemic may have disproportionately affected athletes of lower socioeconomic status, potentially increasing injury risk in this population.
To 1) Describe athlete injury incidence prior to and during the 2019-2020 and 2020-2021 school years in high school athletes by socioeconomic status; 2) Investigate the association between socioeconomic status and injury incidence in high school athletes.
High schools were matched between the 2019-2020 and 2020-2021 school years. All athletes from all sports were included. High school socioeconomic status was determined by the school district median household income. Socioeconomic strata were defined as <$30,000, $30,000-50,000, $50,001-100,000, and >$100,000. Injury incidence proportion with 95% confidence interval (95% CI) was calculated for each academic year. Mixed effects negative binomial models with robust errors were performed to assess the association between the incidence proportion ratio and high school median household income. Six states and 176 high schools were included (2019-2020: 98,487 athletes; 2020-2021: 72,521 athletes).
Injury incidence increased in three of four socioeconomic strata during the 2020-2021 year (<$30,000: 2019-2020: 15.6 (13.1-18.1), 2020-2021: 26.3 (23.1-29.6); $30,000-50,000: 2019-2020: 7.8 (7.1-8.6), 2020-2021: 14.9 (13.8-15.9); $50,001-100,000: 2019-2020: 15.1 (14.7-15.4), 2020-2021: 21.3 (20.9-21.8); >$100,000: 2019-2020: 18.4 (18.1-18.8), 2020-2021: 17.3 (16.8-17.7)). An association was observed between injury incidence ratio and log median high school household income in 2019-2020 [1.6 (1.1-2.5)] but not 2020-2021 [1.1 (0.8-1.6)] school years.
a

Corresponding Author: Garrett S. Bullock PT, DPT, DPhil Department of Orthopaedic Surgery
Wake Forest School of Medicine 475 Vine St Winston-Salem, NC 27233 (336) 716-4264 gbullock@wakehealth.edu
Athletes from lower socioeconomic high schools reported increased injury incidence compared to higher socioeconomic high schools during the 2020-2021 academic school year. These results highlight the increased COVID-19 pandemic vulnerability in athletes from lower socioeconomic high schools. High school sport stakeholders should consider how abrupt sport stoppage can affect lower socioeconomic athletes.
Level of Evidence 2
There are over 15 million high school students in the United States, with over eight million participating in high school sports yearly 1,2 High school sports play a pivotal role in student health and wellbeing, including cardiovas cular fitness,3,4 psychological wellbeing,5,6 academic per formance,7–9 and quality of life.10–12 However, participat ing in high school sport poses inherent risk. High school athletes suffer an estimated 1.4 million injuries per year and sustain as high as 4.6 injuries and 0.7 severe injuries per 1000 athletes exposures.13,14 These injuries result in 2.5 million high school athletes eliciting emergency depart ment services,15 and costing $44.7 million in human capital and $144.6 million in comprehensive costs annually as re ported in 2007.16
Abrupt cessation of practice and game play can increase injury risk in high school athletes.17,18 This increased in jury risk is related to decreased cardiovascular fitness and conditioning, reductions in strength, and decreased sport specific training.18–20 During the spring and summer of 2020, the SARS-CoV-2 coronavirus and the resultant dis ease, coronavirus disease (COVID-19) pandemic stemmed an abrupt stoppage of high school sport training, practice, and competition.21,22 The prolonged cessation from high school training and sport resulted in overall decreases in physical activity, running, and individual sport specific practice.23–26 The return to high school sport during the subsequent academic school year may have exposed high school athletes to abrupt increases in training and competi tion load,18–20 predisposing these athletes to increased in jury incidence and subsequent medical burden.24,25
There is a distinct relationship between an individual’s living environment and physical activity.27 Availability and access to parks, running trails, and sport and recreational facilities have demonstrated improved physical activity habits, sport participation, and overall physical health in adolescents and adults.28–31 However, socioeconomic sta tus can influence access to recreational and park facilities, with cost, safety, weather, and quality and density of recre ational facilities identified as potential barriers.28,32–34 In dividuals and families of lower socioeconomic status have also demonstrated decreased physical activity habits, irre spective of race or urban or rural settings.35,36 Further, high school athletes from lower socioeconomic levels reported decreased weekly organized practice hours and months training compared to higher socioeconomic level ath letes.37 During the COVID-19 pandemic, people of lower socioeconomic status were disproportionately affected by
infection prevalence38 and less healthcare resources.39 High school athletes of lower socioeconomic may also have been disproportionately affected.26 In a survey of 13,000 high school athletes, male and female athletes from lower socioeconomic backgrounds reported decreased physical activity and higher anxiety and depression compared to athletes of higher socioeconomic status.26 This highlights a clinical and research gap concerning the current under standing of the impact of socioeconomic status on athlete injury risk when returning to sport following high school sport cessation.
It is presently unclear how the cessation of high school practice and game play has affected injury incidence in ado lescent athletes. Socioeconomic status can influence phys ical activity,35,36 and recreational and leisure re sources.28,32–34 Further, the COVID-19 pandemic may have disproportionately affected athletes of lower socioeco nomic status,26,38,39 potentially increasing injury risk in this population. These data can inform sports medicine clinicians, educators, and policy makers on understanding the secondary effects of the COVID-19 pandemic, specifi cally high school injury burden at different socioeconomic strata. Therefore, the purpose of this study was to 1) De scribe athlete injury incidence prior to and during the 2019-2020 and 2020-2021 school years in high school ath letes by socioeconomic status; 2) Investigate the associa tion between socioeconomic status and injury incidence in high school athletes.
An ecological study investigating the influence of high school socioeconomic status on athlete injury incidence over an academic year was performed, with the high school level used as the unit of analyses. The Strengthening the Reporting of Observational Studies in Epidemiology for Sport Injury and Illness Surveillance (STROBE-SIIS) were followed.40 Informed consent was not required as this was a retrospective study This investigation was approved by the University Institutional Review Board.
Athletes presenting with any illness or injury reported to their school athletic trainer (AT) and were documented as presenting with a time-loss problem during a team-spon sored practice or game. AT sport coverage was based on the school’s sport participation population, not on socioeco
nomic status. Internal validity data checks were performed by the regional athletic trainer supervisor and the regional and national quality control supervisors on a quarterly ba sis.
High school athletes, from six states (Alabama (AL); Delaware (DE); Illinois (IL); Maryland (MD); Michigan (MI); Pennsylvania (PA)) were included in this study High schools were matched between the 2019-2020 and 2020-2021 academic school years. Matching was based on the high school participating in athletics during the 2020-2021 academic school year. If the high school did not report or participate in high school athletics during the 2020-2021 year, they were excluded from the analyses (Fig ure 1). This resulted in 176 high schools rostered in the Players Health Rehab System for participating sports over the two-year study Athlete health was monitored by the full-time athletic trainer assigned to each school by ATI Physical Therapy
The main exposure was year of the pandemic, defined as athlete participation training, practices, or games on acad emic year 2020-2021. An athlete-exposure (AE) was defined as one athlete participating in one practice or competition where a player was at risk of sustaining an injury.41,42
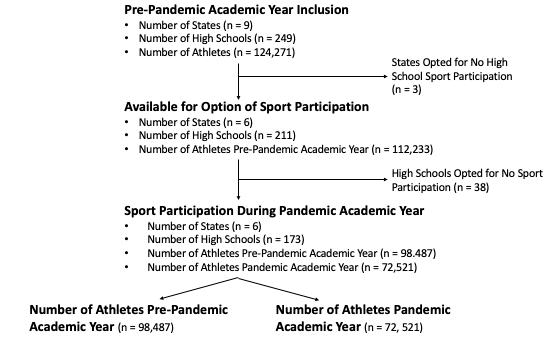
An injury was defined as tissue damage or other derange ment of normal physical function occurring during any training session or competition that resulted in at least one
day lost to training and/or competition and that required medical attention.40,43 Athlete complaints that resulted in cessation of a competition or training session but the ath lete returned to training or competition the same session or following day were recorded as zero days of time loss and did not result in a recorded injury 40 Injured body segments and body parts were defined by the Orchard Sports Injury Classification System.44 Injury severity calculated as over all time loss, with further injury severity stratified by 7-28 (moderate) and 28+ (severe) days.40 The AT documented the injury or illness in the Players Health Rehab system. The documentation included the injury or illness date, ath lete sex, sport of participation, body part, problem type, the participation status of the athlete, athlete phase of recovery and days until return to sport. Total data missingness was 3%, for a more complete description of missingness, please refer to the statistical analyses section.
High school socioeconomic status was determined by the median household income for the school district. Median household income was determined through federal public reports on National Center for Education Statistics. For epi demiological calculations, median household income was stratified into <$30,000, $30,000 to $50,000, $50,001 to $100,000, and >$100,000 based on previous public health research.45
Self-identified gender, state, and sport were identified as confounders. Due to the large number of sports played, sport was collapsed into four categories: collision (Amer ican football, lacrosse, wrestling, ice hockey, rugby), field
and court (basketball, field hockey, soccer, tennis, volley ball, gymnastics, softball, baseball), individual (track and field, swimming, mixed rifle, mixed skiing, golf, dance, div ing, cross country, bowling, archery, rowing, cheerleading), and other These sport collapsed categories are also al ternatively known as collision, contact, and non-contact sports. Other was utilized for non-descript sport records.
All data were assessed for missingness prior to analyses (Gender: 0%; Age: 0%; Date of Injury: 3%; Sport: 1.7%; Body Part: 1.6%; Return to Play: <0.1%; Pain: <0.1%) with data demonstrating minimal missingness. Complete case analyses were performed. Participant statistics were de scribed using mean (standard deviation) for continuous normally distributed variables, median (25th quartile, 75th quartile) for non-normally distributed continuous vari ables, and frequencies and percentages for categorical vari ables. Distributions were assessed through visual inspec tion and normal plots. Injury incidence proportion (also known as cumulative incidence) with 95% confidence in terval (95% CI) was calculated as new injuries per 100 ath letes for each academic year, overall and by state, gender, severity, sport, and body part.46 A mixed effects negative binomial model with robust errors were performed to assess the association between the incidence proportion ratio and high school median household income. Random effects were modeled at the high school level. Model fixed effects were controlled for gender, state, and percentage of male and female high school athletes compared to male and fe male school population. An offset of the log of male and female high school athlete participation was included. Due to the changes in injury incidence between the academic school years, academic school years were stratified. Sensi tivity analyses included: 1) Including only severe injuries; 2) Including socioeconomic status as an ordinal variable, with $50,000 to $100,000 set as the reference; 3) Stratified by state. All analyses were performed in R version 4.01 (R Core Team (2013). R: A language and environment for sta tistical computing. R Foundation for Statistical Comput ing, Vienna, Austria. URL http://www.R-project.org/), using the naniar package for missingness assessment47 and the GLMMadaptive package for mixed effects negative binomial modelling.48
A total of 98,487 athletes (Female: 43,250; Male: 55,239) participated in high school sport in the pre-pandemic aca demic year and 72,521 athletes (Female: 32,968; Male: 39,554) in the pandemic academic year The median high school family income was $92,143 ($70,596, $113,692) with a range of $25,500 to $193,100. A total of three (2%) high schools reported a median high school family income of <$30,000, 10 (6%) $30,000 to $50,000, 99 (57%) $50,001 to $100,000, and 61 (35%) > $100,000.
A total of 15,477 injuries were reported in the pre-pan demic academic year compared to 14,057 injuries during
the pandemic academic year Median injury time loss strat ified by socioeconomic status is reported in Table 1. For in jury incidence stratified by socioeconomic status, gender, severity, sport, and state, please refer to Table 2, Table 3, and Table 4
Unadjusted [2.3 (95% CI: 1.4, 3.7)] and adjusted [1.6 (95% CI: 1.1, 2.5)] injury incidence increased for every unit of log median high school household income in the 2019-2020 academic school year Unadjusted injury incidence de creased by a ratio of 0.7 (95% CI: 0.5, 1.0) for every increase of log median high school household income in the 2020-2021 academic school year. Adjusted injury incidence demonstrated no association between injury incidence ra tio of 1.1 (95% CI: 0.8, 1.6) log median high school house hold income in the 2020-2021 academic school year. For full models refer to Appendix A. For results of actual and predicted injury counts, please refer to Table 4.
No relationship was observed between severe injury inci dence and log median high school household income for the 2019-2020 academic school year 1.1 (95% CI: 0.8, 1.6) nor the 2020-2021 academic school year 0.7 (95% CI: 0.5, 1.0). Moderate injury incidence increased by a ratio of 1.6 (95% CI: 1.1, 2.4) for an increase of log median high school household income in the 2019-2020 academic school year No relationship was observed between moderate injury in cidence and log median high school household income for the 2020-2021 academic school year [1.1 (95% CI: 0.7, 1.6)]. When stratifying by median high school household income, no relationship was observed for the 2019-2020 academic school year When stratifying by state, Alabama, and Penn sylvania demonstrated similar results, while Delaware, Illi nois, Maryland, and Michigan observed no relationship for the 2019-2020 and 2020-2021 academic school years.
The main findings of this study were that while there was an overall 26% reduction in high school sport participation, different socioeconomic strata demonstrated different par ticipation reductions, with lower socioeconomic strata demonstrating a smaller decrease in participation (<$30,000: 11%; $30,000 to $50,000: 5%; $50,001 to $100,000: 40%; >$100,000: 24%). Lower socioeconomic strata reported greater increases in pandemic injury in cidence, ranging from 69% to 91%, compared to higher socioeconomic strata ranging from 41% increase to a 6% decrease in injury incidence. Athletes of lower socioeco nomic status that participated in collision sports demon strated an increase in injury incidence ranging from 159% to 213%, with the highest socioeconomic strata demon strating only a 10% increase in injury incidence during the pandemic academic school year. A unit increase in me dian high school household income was associated with a
Injury IP Identified Gender IP
Injury Severity IP
Male Female Minor Moderate Severe
19-20 20-21 19-20 20-21 19-20 20-21 19-20 20-21 19-20 20-21 19-20 20-21
Overall 19-20: n: 98,487 20-21: n: 72, 521
<$30,000 19-20: n: 806 20-21: n: 717
$30,000 to $50,000 19-20: n: 5,114 20-21: n: 4,882
$50,001 to $100,000 19-20: n: 49,079 20-21: n: 34,310
>$100,000 19-20: n: 40,882 20-21: n: 31,226
IP = Incidence Proportion
15.7 (15.5, 15.9) 19.4 (19.1, 19.7) 17.0 (16.7, 17.3) 23.4 (23.0, 23.8) 14.0 (13.7, 14.4) 14.5 (14.2, 14.9) 4.1 (3.9, 4.2) 4.9 (4.7, 5.0) 4.9 (4.7, 5.0) 7.8 (6.6, 8.0) 6.8 (6.6, 6.9) 6.5 (6.3, 6.6)
15.6 (13.1, 18.1) 26.3 (23.1, 29.6) 17.8 (14.3, 21.4) 41.9 (36.9, 46.9) 12.7 (9.2, 16.2) 9.4 (6.3, 12.4) 5.0 (3.5, 6.5) 5.9 (4.1, 7.6) 3.5 (2.2, 4.7) 7.1 (5.2, 9.0) 7.2 (5.4, 9.0) 13.1 (10.6, 15.6)
7.8 (7.1, 8.6) 14.9 (13.8, 15.9) 7.2 (6.5, 8.0) 16.2 (14.9, 17.5) 4.0 (3.3, 4.8) 12.2 (10.6, 13.9) 1.6 (1.3, 2.0) 3.3 (2.8, 3.9) 1.7 (1.2, 3.0) 5.8 (5.1, 6.5) 4.6 (4.0, 5.1) 5.7 (5.0, 6.3)
15.1 (14.7, 15.4) 21.3 (20.9, 21.8) 16.0 (15.5, 16.4) 25.2 (24.5, 25.8) 13.9 (13.5, 14.4) 15.3 (14.7, 15.8) 4.1 (3.9, 4.2) 5.5 (5.3, 5.8) 4.6 (4.4, 4.8) 8.6 (8.3, 8.9) 6.4 (6.2, 6.6) 7.0 (6.8, 7.3)
18.4 (18.1, 18.8) 17.3 (16.8, 17.7) 20.0 (19.5, 20.5) 20.2 (19.6, 20.8) 15.5 (15.0, 16.0) 13.3 (12.7, 13.8) 4.6 (4.4, 4.8) 4.1 (3.9, 4.3) 6.0 (5.7, 6.2) 7.1 (6.8, 7.4) 7.9 (7.6, 8.1) 5.7 (5.5, 6.0)
Incidence proportion is per 100 athletes
All incidence proportion is reported with 95% confidence intervals
19-20 = Pre-pandemic academic school year 20-21 = Pandemic academic school year
Collision Field & Court Individual Other 19-20 20-21 19-20 20-21 19-20 20-21 19-20 20-21
Overall 19-20: n: 98,487 20-21: n: 72, 521
5.4 (5.2, 5.5 8.7 (8.5, 8.9) 5.3 (5.1, 5.4) 8.1 (7.9, 8.3) 2.5 (2.4, 2.6) 3.2 (3.1, 3.4) 2.9 (2.8, 3.0) 0.5 (0.4, 0.6)
<$30,000 19-20: n: 806 20-21: n: 717
$30,000 to $50,000 19-20: n: 5,114 20-21: n: 4,882
$50,001 to $100,000 19-20: n: 49,079 20-21: n: 34,310
>$100,000 19-20: n: 40,882 20-21: n: 31,226
IP = Incidence Proportion
Incidence proportion is per 100 athletes
5.7 (4.1, 7.3) 15.6 (13.0, 18.3) 5.3 (3.8, 6.9) 8.6 (6.6, 10.7) 2.3 (1.3, 3.4) 2.0 (0.9, 2.9) 2.2 (1.2, 3.3) 0.1 (0.0, 0.4)
3.0 (2.5, 3.4) 6.4 (5.7, 7.1) 2.9 (2.4, 3.3) 5.3 (4.7, 6.0) 0.9 (0.6, 1.1) 2.3 (1.9, 2.8) 1.1 (0.8, 1.4) 0.8 (0.5, 1.1)
5.0 (4.8, 5.2) 9.4 (9.1, 9.7) 5.3 (5.1, 5.5) 21.3 (20.9, 21.8) 2.1 (1.9, 2.2) 2.9 (2.8, 3.1) 2.8 (2.6, 2.9) 0.3 (0.2, 0.4)
6.2 (6.0, 6.4) 6.8 (6.5, 7.1) 5.6 (5.4, 5.9) 6.6 (6.3, 6.9) 3.3 (3.2, 3.5) 3.4 (3.2, 3.6) 3.3 (3.1, 3.5) 0.5 (0.4, 0.6)
All incidence proportion is reported with 95% confidence intervals
19-20 = Pre-pandemic academic school year 20-21 = Pandemic academic school year
Alabama Delaware Illinois Maryland Michigan Pennsylvania
19-20 20-21 19-20 20-21 19-20 20-21 19-20 20-21 19-20 20-21 19-20 20-21
Overall 19-20: n: 98,487 20-21: n: 72, 521
7.4 (7.0, 7.8) 30.6 (29.9, 31.2) 22.4 (21.7, 23.2) 16.2 (15.4, 17.2) 11.0 (10.7, 11.4) 21.2 (20.5, 21.9) 29.0 (28.2, 29.7) 7.2 (6.7, 7.7) 18.0 (17.4, 18.7) 17.6 (17.0, 18.3) 15.6 (14.9, 16.3) 14.3 (13.7, 15.0)
<$30,000 19-20: n: 806 20-21: n: 717
$30,000 to $50,000 19-20: n: 5,114 20-21: n: 4,882
$50,001 to $100,000 19-20: n: 49,079 20-21: n: 34,310
>$100,000 19-20: n: 40,882 20-21: n: 31,226
IP = Incidence Proportion
Incidence proportion is per 100 athletes
8.2 (5.8, 10.6) 22.1 (18.7, 25.5) 28.4 (23.3, 33.5) 44.7 (35.5, 51.8)
29.7 (26.7, 32.7) 21.2 (18.8, 23.4) 16.2 (13.8, 18.6) 13.5 (11.2, 15.8) 5.8 (5.0, 6.6) 12.3 (11.0, 13.6)
4.7 (4.3, 5.1) 30.2 (29.4, 30.9) 22.9 (22.0, 23.7) 17.0 (16.1, 18.0) 9.3 (8.8, 9.7) 25.2 (23.8, 26.6) 34.4 (33.2, 35.6) 9.3 (8.5, 10.2) 13.4 (12.5, 14.3) 12.9 (12.0, 13.9) 22.6 (21.1, 24.1) 17.0 (15.6, 18.4)
15.7 (14.5,16.9) 30.4 (28.9, 32.0) 15.1 (14.5, 15.6) 22.4 (21.4, 23.5) 25.5 (24.6, 26.4) 5.8 (5.2, 6.4) 21.4 (20.5, 22.4) 20.7 (19.7, 21.6) 14.7 (13.9, 15.6) 14.3 (13.6, 15.1)
All incidence proportion is reported with 95% confidence intervals
19-20 = Pre-pandemic academic school year 20-21 = Pandemic academic school year
Table 4. Injury Incidence Proportion by Stratified by State and Socioeconomic Status.
Actual Injury Count 19-20
Predicted Injury Count 19-20 (95% CI)
Actual Injury Count 20-21
Predicted Injury Count 20-21 (95% CI)
Overall 15,477 15,376 (11,096, 22,099) 14,057 12,096 (9,640, 17,533)
Severe Injuries 6,665 6,597 (4,877, 9,078) 4,690 4,426 (3,092, 6,341)
Moderate Injuries 4,784 4,744 (3,402, 6,560) 5,655 5,056 (3,510, 7,286)
Stratified household income 15,477 15,375 (10,720, 22,381) 14,057 13,255 (9,401, 18,975)
Alabama 1,191 1,186 (698, 2,039) 5,843 5,478 (4,492, 6,796)
Delaware 2,347 2,331 (1,767, 3,067) 1,153 1,048 (492, 3,258)
Illinois 3,783 3,775 (1,931, 8,762) 2.522 2,497 (1,613, 4,109)
Maryland 4,302 4,149 (2,663, 6,408) 806 788 (478, 1,288)
Michigan 2,178 2,173 (1,654, 2,973) 2,126 2,125 (1,610, 2,902)
Pennsylvania 1,191 1,186 (698, 2,039) 1,607 1,622 (1,073, 2,472) 95% CI
60% increase in injury incidence in the 2019-2020 academic school year; but no association was observed for the pan demic academic school year.
Lower socioeconomic strata demonstrated increased in jury incidence during the 2020-2021 academic school year, with the highest socioeconomic strata of $100,000+ median household income demonstrating similar injury incidence between school years. Further, lower socioeconomic males demonstrated the greatest increase in injury incidence. These differences in injury incidence may be related to recreational and sport facility access. Lower socioeconomic people have less access and quality of recreational and sport facilities.28–31 People from lower socioeconomic strata generally have increased fear of violence28,32–34 and increased barriers to performing physical activity and ex ercise.35,36 Concerning high school athletes, athletes from lower socioeconomic strata have demonstrated reduced training time per week.37 During the prolonged cessation of high school sport, athletes from lower socioeconomic strata may have had reduced access and time to train and practice sport compared to higher socioeconomic athletes, provid ing increased deconditioning and loss of sport specific skill, subsequently increasing injury incidence.
Lower socioeconomic collision sport participants demonstrated a two to three times increase in injury in cidence during the 2020-2021 academic school year, while the highest socioeconomic strata demonstrated similar col
lision injury incidence between the 2019-2020 and 2020-2021 academic school years. High school collision sports such as football, lacrosse, and wrestling have pre viously demonstrated the greatest injury incidence, com pared to field and court and individual sports.13,14 Collision sports also require further physical preparation beyond general fitness and strength, due to athlete to athlete colli sions.49–51 The repetitive physical trauma involved in colli sion sport requires physical adaptations to handle the high impact forces involved in tackles and blocking.49,50 This supports previous research where decreased off season and preseason training demonstrated greater injury incidence in collision sports,51,52 suggesting a truncated preseason predisposes an athlete to greater musculoskeletal injury risk in this population compared to other sports.
A proportional association was observed between injury incidence and median high school household income in the 2019-2020 academic school year after controlling for con founders. These results support previous research concern ing socioeconomic status and injury incidence.53,54 One study observed that low material wealth was a protective effect against sport injuries.55 However, this study exam ined adolescent injuries in 35 countries, and specific com parisons of sport participation was not performed. As many countries do not provide school sponsored sports, socioeco nomic status can be a barrier to sport participation in many countries.56,57 However, in this study, sport participation
95% Confidence Intervalin relation to overall high school population was controlled for, and these athletes solely participated in sport within the United States, decreasing the transferability of this lit erature to this study’s findings. A possible explanation is that lower socioeconomic high school athletes are more prone to decreased injury reporting compared to higher socioeconomic high school athletes.37,58 Lower socioeco nomic athletes may have greater fear of losing playing time, differences in self-regulation, or health care access outside of school athletics.37 However, injury under reporting may be for only minor or moderate injuries. Within the sensi tivity analyses, severe injury incidence ratios were similar between socioeconomic strata. The similar severe injury in cidence between strata may be due to the nature of severe injuries, which can cause greater limits on sports perfor mance and function compared to moderate or minor in juries.40 These greater physical and sport specific limita tions may be associated with a greater propensity of lower socioeconomic status high school athletes to report these injuries. However, further research is needed to investigate these potential discrepancies.
No association between median household income and injury incidence was observed for the 2020-2021 academic school year As stated previously, higher socioeconomic strata demonstrated similar injury incidence between the academic school years; however, lower socioeconomic strata reported an increased in injury incidence. The con flicting findings between socioeconomic status and injury incidence ratios between the pre-pandemic and pandemic academic school years may be related to secondary effects related to COVID-19 vulnerability.38,39 The increased in jury incidence in lower socioeconomic strata may have negated the injury underreporting effect during the pan demic academic school year. Further qualitative and quan titative research into barriers and facilitators of injury re porting and risk are needed within these populations to understand potential solutions to socioeconomic athlete injury discrepancies.
Due to the nature of high school sport and resource avail ability, it was not possible to collect more granular expo sure data such as practice or competition minutes. This precludes injury rate calculations, decreasing the clinical usefulness of these incidence and model results. COVID-19 infection rates changed throughout the reporting period, and were different for the included states, decreasing the precision of these results. The included states reported dif ferent prevalence of high school socioeconomic strata, bi asing the results towards the null. Recruitment was based on athlete coverage by the sports medicine organization and sport participation during the 2020-2021 academic year, increasing risk of recruitment bias and non-response bias. There are inherent yearly fluctuations in injuries at the high school and state level. This study only had access
to one year of injury data prior to the COVID-19 pandemic, decreasing the precision of these results. Due to the ecolog ical nature of this study, individual injury history, strength, range of motion, balance, and sport experience were not available, resulting in unmeasured confounding that could bias these results. Causality cannot be inferred from these data, with future causal study design required to under stand the cause and effect of abrupt prolonged sport stop page.
Lower socioeconomic high schools reported increased in jury incidence compared to higher socioeconomic high schools during the 2020-2021 academic school year. This relationship was most pronounced in males and within col lision sports. The highest socioeconomic high school strata reported similar injury incidence between academic school years, suggesting greater access and time to exercise, train ing, and sport practice during the abrupt high school sport stoppage. Increased high school socioeconomic status was associated with a statistically significant increased injury incidence within the 2019-2020 but not the 2020-2021 aca demic school years. These results highlight the secondary downstream COVID-19 pandemic associations and the in creased potential pandemic vulnerability in lower socioe conomic high school athletes. Sports medicine clinicians, high school administrators, and policy makers need to con sider the magnified effect abrupt stoppage from high school sport practice and competition can incur in lower socioeco nomic high school athlete injuries when designing return to sport protocols. Expanded preseason and inquiries into pre vious training and practice habits may be required for more vulnerable high school athletes when returning to sport.
The authors would like to thank Chris Le, PT, PhD for her helpful editorial comments.
This research did not receive any specific grant from fund ing agencies in the public, commercial, or not-for-profit sectors.
None
Submitted: March 02, 2022 CST, Accepted: August 09, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Child Trends Website. Participation in school athletics. Accessed August 19, 2021. https://www.chil dtrends.org/indicators/participation-in-school-athlet ics
2. K-12 school enrollment & student population statistics. General secondary school enrollment trends. Accessed September 9, 2021. https://educatio ndata.org/k12-enrollment-statistics
3. Shull ER, Dowda M, Saunders RP, McIver K, Pate RR. Sport participation, physical activity and sedentary behavior in the transition from middle school to high school. J Sci Med Sport. 2020;23(4):385-389. doi:10.1016/j.jsams.2019.10.017
4. Marques A, Ekelund U, Sardinha LB. Associations between organized sports participation and objectively measured physical activity, sedentary time and weight status in youth. J Sci Med Sport 2016;19(2):154-157. doi:10.1016/j.jsams.2015.02.007
5. Easterlin MC, Chung PJ, Leng M, Dudovitz R. Association of team sports participation with longterm mental health outcomes among individuals exposed to adverse childhood experiences. JAMA Peds 2019;173(7):681-688. doi:10.1001/jamapediatric s.2019.1212
6. Ashdown-Franks G, Sabiston CM, Solomon-Krakus S, O’Loughlin JL. Sport participation in high school and anxiety symptoms in young adulthood. Mental Health Phys Act. 2017;12:19-24. doi:10.1016/j.mhpa.2 016.12.001
7 Rees DI, Sabia JJ. Sports participation and academic performance: Evidence from the national longitudinal study of adolescent health. Econ Educ Rev. 2010;29(5):751-759. doi:10.1016/j.econedurev.20 10.04.008
8. Dyer AM, Kristjansson AL, Mann MJ, Smith ML, Allegrante JP Sport participation and academic achievement: A longitudinal study. Am J Health Behav 2017;41(2):179-185. doi:10.5993/ajhb.41.2.9
9. Lumpkin A, Favor J. Comparing the academic performance of high school athletes and non-athletes in Kansas 2008-2009. J Appl Sport Manag 2013;4(1):31.
10. Baciu C, Baciu A. Quality of life and students’ socialization through sport. Procedia-Social Behav Sci 2015;209:78-83. doi:10.1016/j.sbspro.2015.11.260
11. Houston MN, Hoch MC, Hoch JM. Health-related quality of life in athletes: a systematic review with meta-analysis. J Athl Train. 2016;51(6):442-453. doi:1 0.4085/1062-6050-51.7.03
12. Lam KC, Valier ARS, Bay RC, McLeod TCV A unique patient population? Health-related quality of life in adolescent athletes versus general, healthy adolescent individuals. J Athl Train 2013;48(2):233-241. doi:10.4085/1062-6050-48.2.12
13. Rechel JA, Yard EE, Comstock RD An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train 2008;43(2):197-204. doi:10.4085/1062-6050-4 3.2.197
14. Darrow CJ, Collins CL, Yard EE, Comstock RD. Epidemiology of severe injuries among United States high school athletes: 2005-2007 Am J Sport Med 2009;37(9):1798-1805. doi:10.1177/036354650933301 5
15. Simon TD, Bublitz C, Hambidge SJ. Emergency department visits among pediatric patients for sports-related injury: basic epidemiology and impact of race/ethnicity and insurance status. Ped Emerg Care. 2006;22(5):309-315. doi:10.1097/01.pec.000021 5139.29039.5c
16. Knowles SB, Marshall SW, Miller T, et al. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj Prev. 2007;13(6):416-421. doi:10.1136/ip.2006.014720
17 Bloemers F, Collard D, Paw MCA, Van Mechelen W, Twisk J, Verhagen E. Physical inactivity is a risk factor for physical activity-related injuries in children. Br J Sport Med. 2012;46(9):669-674. doi:10.1 136/bjsports-2011-090546
18. Caterisano A, Decker D, Snyder B, et al. CSCCa and NSCA joint consensus guidelines for transition periods: safe return to training following inactivity. Strength Cond J 2019;41(3):1-23. doi:10.1519/ssc.000 0000000000477
19. Courson R, Goldenberg M, Adams KG, et al. Inter association consensus statement on best practices for sports medicine management for secondary schools and colleges. J Athl Train. 2014;49(1):128-137. doi:1 0.4085/1062-6050-49.1.06
20. Gabbett TJ. The training—injury prevention paradox: should athletes be training smarterandharder? Br J Sport Med 2016;50(5):273-280. doi:10.1136/bjsports-2015-0957 88
21. Hash PM. Remote learning in school bands during the COVID-19 shutdown. J Res Music Educ 2021;68(4):381-397. doi:10.1177/0022429420967008
22. Dorn E, Hancock B, Sarakatsannis J, Viruleg E. COVID-19 and student learning in the United States: The hurt could last a lifetime. McKinsey & Company. 2020;1.
23. Jagim AR, Luedke J, Fitzpatrick A, et al. The impact of COVID-19-related shutdown measures on the training habits and perceptions of Athletes in the United States: a brief research report. Frontier Sport Active Living. 2020;2:208. doi:10.3389/fspor.2020.623 068
24. Constandt B, Thibaut E, De Bosscher V, Scheerder J, Ricour M, Willem A. Exercising in times of lockdown: an analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. Int J Environ Res Public Health. 2020;17(11):4144. doi:10.3390/ijerph17114144
25. McGuine TA, Biese KM, Hetzel SJ, et al. High school sports during the CoVID-19 pandemic: The impact of sport participation on the health of adolescents. J Athl Train 2021;57(1):51-58. doi:10.40 85/1062-6050-0121.21
26. McGuine TA, Biese KM, Petrovska L, et al. Mental health, physical activity, and quality of life of US adolescent athletes during COVID-19–related school closures and sport cancellations: a study of 13 000 athletes. J Athl Train 2021;56(1):11-19. doi:10.4085/1 062-6050-0478.20
27 Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science 1998;280(5368):1371-1374. doi:10.1126/science.280.5 368.1371
28. Henderson KA, Neff LJ, Sharpe PA, Greaney ML, Royce SW, Ainsworth BE. “It takes a village” to promote physical activity: the potential for public park and recreation departments. J Park Rec Admin 2001;19(1):23-41.
29. Jackson LE. The relationship of urban design to human health and condition. Landscape Urban Planning. 2003;64(4):191-200. doi:10.1016/s0169-204 6(02)00230-x
30. Humpel N, Owen N, Leslie E. Environmental factors associated with adults’ participation in physical activity: a review Am J Prevent Med 2002;22(3):188-199. doi:10.1016/s0749-3797(01)0042 6-3
31. Brownson RC, Baker EA, Housemann RA, Brennan LK, Bacak SJ. Environmental and policy determinants of physical activity in the United States. Am J Public Health 2001;91(12):1995-2003. doi:10.2105/ajph.91.1 2.1995
32. Moore LV, Roux AVD, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prvent Med. 2008;34(1):16-22. doi:10.1016/j.amepre.2 007.09.021
33. Wilson DK, Kirtland KA, Ainsworth BE, Addy CL. Socioeconomic status and perceptions of access and safety for physical activity Ann Behav Med 2004;28(1):20-28. doi:10.1207/s15324796abm2801_4
34. Powell LM, Slater S, Chaloupka FJ. The relationship between community physical activity settings and race, ethnicity and socioeconomic status. Evidence-Based Prevent Med. 2004;1(2):135-144.
35. Parks SE, Housemann RA, Brownson RC. Differential correlates of physical activity in urban and rural adults of various socioeconomic backgrounds in the United States. J Epidemiol Comm Health. 2003;57(1):29-35. doi:10.1136/jech.57.1.29
36. Giles-Corti B, Donovan RJ. Socioeconomic status differences in recreational physical activity levels and real and perceived access to a supportive physical environment. Prevent Med 2002;35(6):601-611. doi:1 0.1006/pmed.2002.1115
37. Jayanthi NA, Holt DB Jr, LaBella CR, Dugas LR. Socioeconomic factors for sports specialization and injury in youth athletes. Sports Health 2018;10(4):303-310. doi:10.1177/1941738118778510
38. Hatef E, Chang HY, Kitchen C, Weiner JP, Kharrazi H. Assessing the impact of neighborhood socioeconomic characteristics on COVID-19 prevalence across seven states in the United States. Frontiers Public Health 2020;8. doi:10.3389/fpubh.202 0.571808
39. Khalatbari-Soltani S, Cumming RG, Delpierre C, Kelly-Irving M. Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J Epidemiol Community Health 2020;74(8):620-623. doi:10.1136/j ech-2020-214297
40. International Olympic Committee Injury and Epidemiology Consensus Group, Bahr R, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sports 2020 (including the STROBE extension for sports injury and illness surveillance (STROBE-SIIS)). Orthop J Sport Med 2020;8(2):2325967120902908.
41. Powell JW, Barber-Foss KD Injury patterns in selected high school sports: a review of the 1995-1997 seasons. J Athl Train 1999;34(3):277
42. Powell JW, Barber-Foss KD Sex-related injury patterns among selected high school sports. Am J Sport Med. 2000;28(3):385-391. doi:10.1177/03635465 000280031801
43. Ljungqvist A, Jenoure P, Engebretsen L, et al. The International Olympic Committee (IOC) Consensus Statement on periodic health evaluation of elite athletes March 2009. Br J Sport Med 2009;43(9):631-643. doi:10.1136/bjsm.2009.064394
44. Rae K, Orchard J. The Orchard Sports Injury Classification System (OSICS) version 10. Clin J Sport Med. 2007;17(3):201-204. doi:10.1097/jsm.0b013e318 059b536
45. Krishnan S, Cozier YC, Rosenberg L, Palmer JR. Socioeconomic status and incidence of type 2 diabetes: results from the Black Women’s Health Study Am J Epidemiol 2010;171(5):564-570. doi:10.1 093/aje/kwp443
46. Knowles SB, Marshall SW, Guskiewicz KM. Issues in estimating risks and rates in sports injury research. J Athl Train. 2006;41(2):207.
47. Tierney N, Cook D, McBain M, et al. Naniar: Data structures, Summaries, and Visualizations for Missing Data. R Package. Published online 2019.
48. Rizopoulos D. GLMMadaptive: generalized linear mixed models using adaptive Gaussian quadrature. R package version 05–1 Published online 2019.
49. Gabbett TJ. Physiological characteristics of junior and senior rugby league players. Br J Sport Med 2002;36(5):334-339. doi:10.1136/bjsm.36.5.334
50. Gabbett TJ. Physiological and anthropometric characteristics of amateur rugby league players. Br J Sport Med 2000;34(4):303-307 doi:10.1136/bjsm.3 4.4.303
51. Gabbett TJ, Domrow N. Risk factors for injury in subelite rugby league players. Am J Sport Med 2005;33(3):428-434. doi:10.1177/0363546504268407
52. Upton P, Roux C, Noakes TD. Inadequate preseason preparation of schoolboy rugby players-a survey of players at 25 Cape Province high schools. South Afr Med J. 1996;86(5).
53. Cubbin C, LeClere FB, Smith GS. Socioeconomic status and the occurrence of fatal and nonfatal injury in the United States. Am J Public Health. 2000;90(1):70-77 doi:10.2105/ajph.90.1.70
54. Williams JM, Currie CE, Wright P, Elton RA, Beattie TF. Socioeconomic status and adolescent injuries. Soc Science Med 1997;44(12):1881-1891. do i:10.1016/s0277-9536(96)00297-3
55. Pickett W, Molcho M, Simpson K, et al. Cross national study of injury and social determinants in adolescents. Inj Prevent 2005;11(4):213-218. doi:10.1 136/ip.2004.007021
56. Amusa L, Toriola A, Onyewadume I, Dhaliwal H. Perceived barriers to sport and recreation participation in Botswana. Afr J Phys Health Educ, Rec Dance. 2008;14(2):115-129. doi:10.4314/ajpherd.v14i 2.24797
57 Thibaut E, Eakins J, Vos S, Scheerder J. Time and money expenditure in sports participation: The role of income in consuming the most practiced sports activities in Flanders. Sport Manag Rev 2017;20(5):455-467. doi:10.1016/j.smr.2016.12.002
58. Kroshus E, Rivara FP, Whitlock KB, Herring SA, Chrisman SPD Disparities in athletic trainer staffing in secondary school sport: implications for concussion identification. Clin J Sport Med 2017;27(6):542-547 doi:10.1097/jsm.0000000000000 409
Download: https://ijspt.scholasticahq.com/article/39610-influence-of-high-school-socioeconomic-status-on-athleteinjuries-during-the-covid-19-pandemic-an-ecological-study/attachment/102921.docx?auth_token=3Ql3L3ZTJInPYyc8WOF
Greenberg E, Greenberg E, Lawrence JT, Ganley T. Understanding Youth Athlete Motivation, Training, and Activity Progression During and After the COVID-19 Sports Interruption. IJSPT. Published online December 1, 2022:1396-1403.
Greenberg 1 a , Eric Greenberg 2 , J. Todd Lawrence 1,3 , Theodore Ganley 1,4
1 Sports Medicine and Performance Center, Children’s Hospital of Philadelphia, 2 Department of Physical Therapy, New York Institute of Technology, 3 Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia, 4 Department of Orthopaedic Surgery, University of Pennsylvania
Keywords: Covid-19, exercise, training, pandemic, youth athlete
https://doi.org/10.26603/001c.40372
COVID-19 restrictions created a period of disrupted sports participation for youth athletes. The physical conditioning, sports training habits, and patterns of sports activity resumption upon returning to normal sports activity are currently unknown.
This study aimed to determine the extent to which youth athletes maintained their training levels during the early stages of the COVID-19 pandemic and understand the strategies that enhanced motivation and adherence to a training regimen while in isolation. A secondary aim was to analyze how youth athletes returned to activity and identify injuries associated with prolonged sports interruption.
A survey designed to determine activity changes, type of organized instruction, and athlete preferences for training support were distributed by email using snowball sampling methodology to athletes 14-21 years old who were involved in competitive sports when pandemic restrictions were enacted. As sports activities resumed, a follow-up survey was distributed to the same respondents to identify feelings of preparedness, training habits, and injuries.
Of the155 subjects (mean age 16.1 ± 2 years, 64.5% female) that completed the initial survey, 98% reported a stoppage of in-person sports participation and 70% decreased their exercise/training volume, with 41% (n=63) reporting > 50% reduction. Most athletes (86%) received instruction from coaches, with written workouts (70%) being most common; however, most athletes (70%) preferred instructor-led, group training sessions. Of the 43 subjects that completed the follow-up survey (34% response rate), there was an increase in athletic exposures compared to mid-pandemic levels, and 25% reported sustaining a sports-related injury shortly after resuming sports activities.
a
Corresponding author: Elliot M. Greenberg, PT, PhD
Sports Medicine and Performance Center at The Children’s Hospital of Philadelphia Pediatric and Adolescent Specialty Care Center Bucks County 500 W. Butler Ave. Chalfont, PA 18914
Email: greenberge@chop.edu

Pandemic-related sports restrictions resulted in a significant reduction in youth athlete training and conditioning. Coaches attempted to maintain training via the use of written workouts; however, athletes preferred instructor-led, group training sessions. There was a rapid resumption of sports activities, which may have contributed to the high rate of injuries in this study.
Level of Evidence 3
The SARS-CoV-2 coronavirus and COVID-19 pandemic reached epic proportions at the start of the Spring and Summer sports seasons in 2020. In attempts to limit the spread of disease, intermediate schools, high schools, and colleges across the United States transitioned to remote learning strategies and suspended any formal interscholas tic sports activities and extracurricular events.
The Center for Disease Control recommends that chil dren participate in at least 60 minutes of vigorous activity daily 1 The maintenance of fitness and skill development is crucial for sports performance and injury risk reduction.2 However, in the Fall of 2020, six months following the sports shutdown, only 14 US states allowed full Fall sports participation, while the remaining states permitted either modified or no athletics due to the COVID-19 restrictions.3 Prolonged decreases in physical activity levels can result in adverse physiological consequences across multiple body systems, including the cardiovascular, respiratory, muscu loskeletal, and endocrine systems.2 Recent evidence further highlight the adverse psychological consequences associ ated with the COVID -19 restrictions in both adult and youth athlete populations.4–6 Thus, enriching athlete mo tivation and adherence to prescribed training programs are of utmost importance to maintain physical activity, en hance emotional and mental health, and decrease injury risk.7 Currently, there is limited understanding of how youth athletes train while away from the traditional team environment during the COVID-19 sports interruption.
Additionally, the specific factors that increased motiva tion to maintain physical fitness and athletic performance during this time are currently unknown. This study aimed to determine the extent to which athletes maintained their training levels during the COVID-19 pandemic and under stand the strategies that enhanced motivation and adher ence to a training regimen while in physical isolation. A secondary aim was to further understand how youth ath letes returned to activity and identify any secondary effects of the prolonged sports interruption as they resumed ath letic activities.
A team of two physical therapists and two orthopedic sur geons specializing in the treatment of youth athletes de veloped a two-part electronic survey in REDCap, hosted by The Children’s Hospital of Philadelphia. The initial survey
aimed to determine activity changes, the current level of organized instruction, and athlete preferences for ongoing training support during the pandemic-related stoppage of in-person sports activity in the spring/summer of 2020. The initial survey contained six components: eligibility screen ing, general and sports demographics, current and previous training volumes, type of instruction received, individual training preferences, and perceptions of a future return to activity (Appendix A). After sports activities had resumed, a follow-up survey was distributed to the same cohort to un derstand athlete perceptions and experiences of sports re sumption after the prolonged period of forced reduction in team-based activities (Appendix B).
The development of each survey instrument followed a similar process. Initial development identified key topics and consensus regarding survey structure and question for mat. The survey was pilot-tested and refined after consulta tion with a small group of youth athletes representing the population of interest. The final surveys consisted of mul tiple-choice questions and took approximately four to six minutes to complete.
To be eligible for this study, subjects needed to be be tween 14 and 21 years old and actively engaged in com petitive sports at the onset of the pandemic-restricted inperson sports activities. The initial survey was distributed directly to athletes by email, using a snowball sampling methodology starting with the primary team of authors’ personal, professional, and community connections. The survey period began in June 2020 and remained open for eight weeks. The secondary survey was distributed in Octo ber 2020 to those individuals who consented to follow-up questioning while completing the initial survey The sub jects received a single email invitation and one reminder email to complete the follow-up survey This survey re mained open for a period of four weeks. This study was re viewed and approved by the Institutional Review Board at The Children’s Hospital of Philadelphia.
The survey was accessed a total of 266 times. Ninety-eight individuals accessed the survey consent and/or eligibility screening portions but did not complete the survey Thus, a total of 168 subjects met eligibility and were included in Phase I of this study The mean age of the sample was 16.3 ± 2.1 years. Subjects were 62% female, predominantly white (95%), and mainly from Pennsylvania (54%), New Jersey
Age, years (mean ± SD)
16.3 ± 2.1
16.3 ± 2.0
Sex, n (%) Female, 104(62%) Female, 28(65%)
Race, n (%) White, 160(95%) White, 42(98%)
Type of School Attended, n (%)
Type of Sport played, n (%)
Team Type, n (%)
Public, 114 (68%) Private, 24 (14%) College or University, 32 (19%)
Soccer, 63(38%) Lacrosse, 34(20%) Track & Field, 28(17%)
School Based, 54 (32%) Club or Private, 46 (27%) Both, 68 (40%)
(19%), and New York (10%). While subjects reported partic ipating in a total of 22 different sports, the majority of sub jects participated in soccer (38%), lacrosse (20%), and track and field (17%) (Table 1).
Nearly all (98%) of subjects reported that in-person practices and sports-related activities were canceled due to the COVID-19 pandemic. Most athletes (86%) reported receiving sports-related training instructions from their coaching or training staff during this time. Written work outs represented the most common method of instruction (70%). However, “live” online sessions via Zoom or similar platforms represented 53% of instructions, and prerecorded videos accessed through YouTube or other plat forms were also commonly utilized modes (33%) (Figure 1). A large proportion of athletes (73%) reported supple menting team-based training recommendations with indi vidually designed workouts, most frequently jogging (62%), strength training (54%), and sports-specific drills (51%). Despite team-based training suggestions and individual supplemental workouts, only 21% of the sample reported their weekly training hours remained similar to their prepandemic levels. Most subjects (67%) reported a decrease in their overall weekly training volumes, with 40% of ath letes reporting their training volumes decreased by more than half of their pre-pandemic levels. Along with reduced training volumes, many youth athletes (40%) indicated they would not feel physically prepared to resume in-person sports-related activities.
Improving athletic skill and performance was the pri mary motivator (66%) to independently train while not par ticipating in in-person activities, followed by being healthy (50%), and improving their physical appearance (30%). In terestingly, a small number of athletes indicated they trained due to coaches’ (18%) or parents’ (6%) expectations.
When asked about their preferred remote training meth ods, a large majority of athletes felt their performance was best when training in an online “live” group setting led by a coach or trainer (70%). Only a small subset of athletes felt at their best while training with a written-guided workout (25%) or independently designing their workouts (5%) (Fig ure 2).
Public, 28 (65%) Private, 6 (14%) College or University, 9 (21%)
Soccer, 18(42%) Swimming, 6(14%) Lacrosse, 4(9%)
School Based, 11 (26%) Club or Private, 8 (19%) Both, 24 (56%)
One hundred forty-four subjects indicated consent to par ticipate in Phase II of this study A total of 49 subjects (re sponse rate 34%) accessed the follow-up survey Six ath letes had not resumed in-person sports activities yet, leaving 43 subjects who completed the follow-up survey
The demographics and subject characteristics were sim ilar between the initial and secondary survey participants (Table 1). A majority of athletes felt either moderately (60%) or extremely prepared (21%) for in-person sports ac tivities. Approximately 30% of athletes reported initially resuming in-person activities with more than one sports team. When practices initially resumed, athletes indicated a nearly even split of practice frequency between 1-2 days per week (35%), 3-4 days per week (30%), and 5-7 days per week (35%), however at the time of survey completion, the frequency of practices increased to 5-7 days per week for 63% of the sample (Figure 3). Despite this increase in practice frequency, 63% of the sample reported they still supplemented team-based practices with jogging (51%), sports-specific skill work (47%), and strength training (40%) on an individual basis. A return to competitive game activities was reported to occur within the first month of re suming in-person practices for 34% of the sample.
Since the resumption of in-person sports activity, 28% of the sample reported experiencing “aches or pains that lim ited their ability to participate in sports.” Notably, nearly 25% of the sample reported they sustained an injury re quiring them to visit a doctor, urgent care, or another med ical provider, with muscle strains (70%) and torn ligaments (20%) making up most of the diagnoses.
Infection mitigation precautions adopted in response to the COVID-19 pandemic created a rapid change in the sports environment for youth athletes. The results of this study are the first to present specific information related to ac tivity changes, athlete perception of training effectiveness, and self-reported injuries during the period of organized
sports restriction and following return to in-person sports activities.
There was a substantial reduction in youth athlete train ing and sports conditioning amidst COVID-19-related sports restrictions, with nearly 40% of the sample reporting participating in less than half of pre-pandemic weekly hours of sports activity These data expand upon previously published reports demonstrating decreased physical activ ity due to social distancing prevention protocols in re

sponse to the COVID-19 pandemic across various popu lations. The reduction in training volumes experienced during the pandemic poses an interesting situation. Exces sive sports volumes, competition congestion, and limited rest intervals have all been suggestive of creating an in creased risk of musculoskeletal injury in youth athletes.8,9 Therefore, the reduction in training volume brought about by the pandemic may have served as a much-needed break from sports-specific training for these young athletes. This
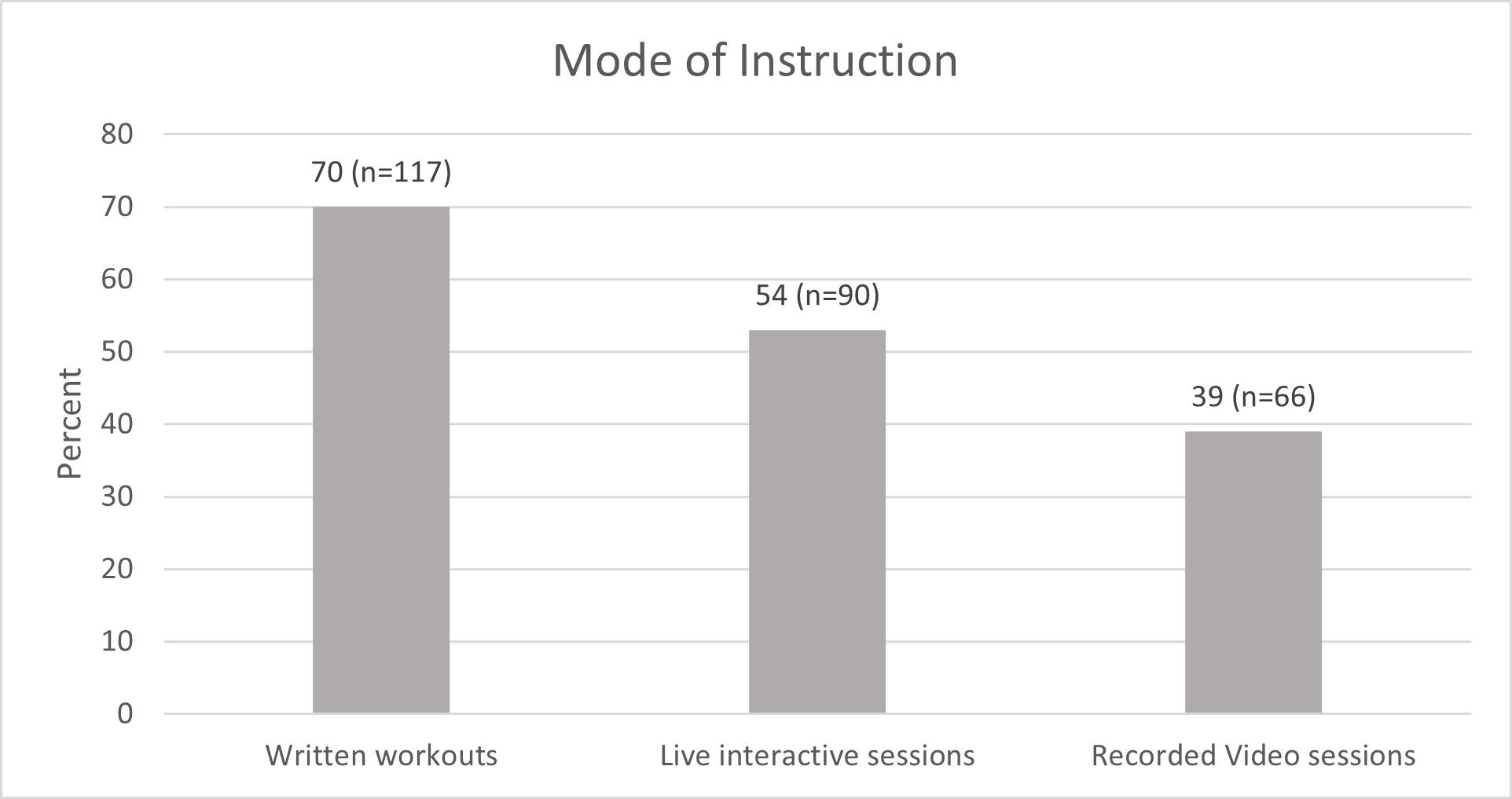 Figure 1. Mode of sports-related instruction provided to athletes during the COVID-19 sports shutdown
Figure 2. Athlete training preferences during the COVID-19 sports shutdown
Figure 1. Mode of sports-related instruction provided to athletes during the COVID-19 sports shutdown
Figure 2. Athlete training preferences during the COVID-19 sports shutdown
suggestion is further supported by data from a multi-center study finding a decrease in sports-related musculoskeletal injuries amongst youth athletes during the COVID-19 pan demic.10 Though this change in activity may have been protective in the short term, these behaviors may become problematic as COVID-related sports restrictions decline. While this survey cannot quantify specific relationships be tween acute and chronic workloads, the subjects indicated a significant decrease in overall training hours during socially distant sports protocols, followed by a rapid resumption of in-person athletic activity (Figure 3). In addition, approxi mately 30% of subjects reported immediately returning to play for more than one sports team, which may contribute to overall increased sports-related workloads. Several stud ies have demonstrated an increased risk of injury with acute spikes or rapid alterations in an athlete’s acute workload compared to their chronic workloads and current fitness levels.11–13 This concept may help explain why 25% of the sample required medical attention for an injury within a mean time of 79 days after resuming in-person sports activ ity While a small number of follow-up respondents limits the strength of these conclusions, these findings are con sistent with previous studies that found an increased rate of injuries and earlier time to injury within older groups of athletes upon returning to competitive sports after COVIDrelated sports interruptions.14–16 Though it is unknown whether maintenance of physical activity workloads during time away from organized sports could have mitigated this injury risk, future studies should seek to evaluate these fac tors more specifically This information could help inform more effective youth fitness programs during ongoing and future pandemic mitigation strategies. These findings may also inform coaches, parents, athletes, and healthcare prac
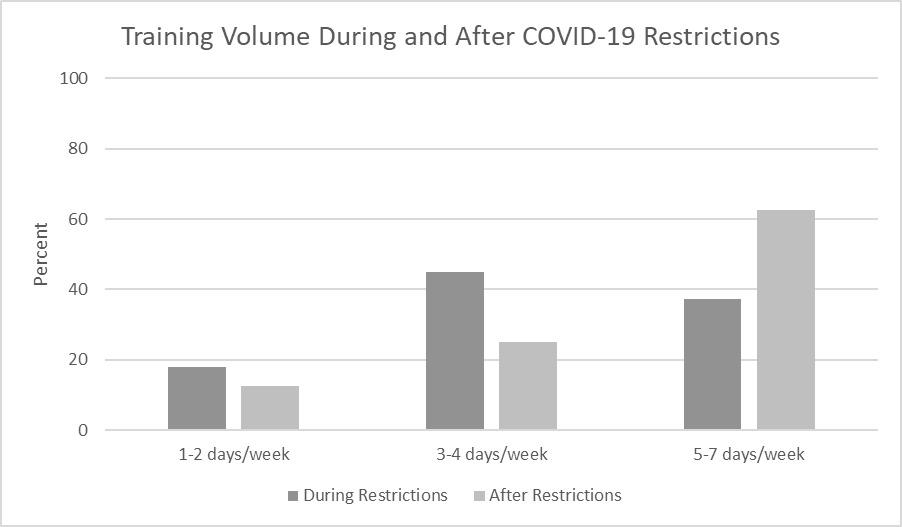
titioners about injury prevention efforts after a prolonged absence from team-based sports activity, such as after re covering from significant injury, surgery, or other circum stances necessitating a particularly inactive period between sports seasons.
In addition to the potential role in mitigating injury risk, the direct relationship between physical activity and mental health is well established.17–19 Recent studies have highlighted the adverse consequences on mental health and quality of life for youth athletes during this pan demic.6,20,21 Collectively, the data from the current study and these previous reports highlight the relationship be tween exercise and training in maintaining an athlete’s physical and psychological well-being.
To maximize youth athlete compliance with recom mended training activities, athlete preferences of instruc tion mode should be considered. While coaches and train ing staff attempted to maintain physical activity using various methods, the primary means was via written hand outs. While this instruction method offers several benefits regarding ease of administration and adaptability, it did not match athlete preferences for virtual “live” or recorded instruction. Exercise instruction that matches athlete or patient preferences may improve maintenance of physical activity through enhanced motivation and exercise partic ipation. Issues of compliance with recommended physical activity levels or home-exercise prescriptions are problem atic amongst healthy and injured populations.22 Inade quate exercise amongst children may contribute to suboptimal athletic performance and future health consequences.7,23 Thus, the utilization of effective and mo tivational exercise communication strategies should be of high priority. Previous studies have shown improved com
Figure 3. Training Volume (days/week) of participants during the COVID-19 sports shutdown and following the resumption of in-person activitiespliance to prescribed exercises using video-based exercise instruction.24,25 Youth athletes in the current world are technologically savvy and highly digitally connected through smartphones and other devices and, not surpris ingly, indicated a preference for synchronous and asynchro nous web-based exercise instruction. In addition, youth athletes indicated they were most motivated to exercise or train to improve their athletic performance and health. Though future studies examining instruction mode on compliance are needed, coaches, healthcare practitioners, and other sports-related professionals should consider em ploying the more preferred video-based exercise instruc tion.
Approximately 75% of youth athletes indicated they sup plemented coach-supplied training instructions with inde pendent workouts during the forced hiatus of in-person ac tivities. While this was not unexpected, the authors found it surprising that 63% of athletes continued to supplement in-person sports with their routines once in-person activi ties had resumed. Coaches and medical staff typically base exercise or training volume progression decisions on the assumption that they understand their athletes’ current training volumes. The data from this survey suggests that a large proportion of youth athletes are pursuing further training than what is provided during monitored training sessions. Medical staff and coaches should consider ques tioning their athletes about independent training habits or use automated technology-based workload monitoring methods to understand their athletes’ training habits more accurately This information would help guide prescriptive workload decisions and may help reduce the potential for overuse injuries among youth athletes.
There are several limitations to this study that should be recognized. The survey questionnaires were not previously validated, and although efforts were made to ensure clarity and accurate interpretation during development and pilot testing, individual variations in the interpretation of ques tions may exist. Nearly all of the sample came from the Northeastern United States and were predominately white; thus, the results of this study may not be generalizable to a broader population. The sample size for the follow-up survey was smaller than the original survey and may cre ate bias thus, the results of the follow-up survey should be taken with caution. Finally, the snowball, electronic sam
pling methodology could have led to a sampling bias by sharing this survey within groups of athletes with similar social, demographic, or physical characteristics, which may limit the generalizability of these results.
In-person sports activity restrictions brought about by the mitigation efforts to reduce the spread of Covid-19 created an acute decrease in youth athlete training and exercise volumes. Athletes preferred using online video platforms to engage in remote training instruction. Though most ath letes supplemented training activities with individualized training, many significantly declined physical activity dur ing the time of pandemic-related sports restrictions. These reported changes in training habits and volumes may have contributed to a high injury rate among study participants following the resumption of organized sports activities. By understanding youth athlete training preferences, the re sults of this study can help professionals working with youth athletes maximize compliance with home-based ex ercise instruction, enhance youth physical fitness, and mit igate the adverse physical and psychological health seque lae of inactivity
We, the authors, affirm that we have no financial or com mercial affiliations related to the performance or outcome of this manuscript.
This research did not receive any specific grant from fund ing agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board of The Children’s Hospital of Philadelphia approved this study Protocol #: 20-017595
Submitted: February 04, 2022 CST, Accepted: September 11, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for americans. JAMA 2018;320(19):2020-2028. doi:10.1001/jama.2018.1485 4
2. Mulcahey MK, Gianakos AL, Mercurio A, Rodeo S, Sutton KM. Sports medicine considerations during the COVID-19 pandemic. Am J Sports Med 2021;49(2):512-521. doi:10.1177/0363546520975186
3. National Federation of State High School Associations. Sports Seasons Modifications Update. Published 2021. Accessed May 2021. https://www.nfh s.org/articles/sports-seasons-modifications-update/
4. Czeisler MÉ, Board A, Thierry JM, et al. Mental health and substance Use among adults with disabilities during the COVID-19 pandemic United States, February-March 2021. MMWR Morb Mortal Wkly Rep 2021;70(34):1142-1149. doi:10.15585/mmw r.mm7034a3
5. Gassman-Pines A, Ananat EO, Fitz-Henley J II. COVID-19 and parent-child psychological well-being. Pediatrics. 2020;146(4). doi:10.1542/peds.2020-00729 4
6. McGuine TA, Biese KM, Petrovska L, et al. Mental health, physical activity, and quality of life of US adolescent athletes during COVID-19-related school closures and sport cancellations: a study of 13 000 athletes. J Athl Train. 2021;56(1):11-19. doi:10.4085/1 062-6050-0478.20
7 Hägglund M, Atroshi I, Wagner P, Waldén M. Superior compliance with a neuromuscular training programme is associated with fewer ACL injuries and fewer acute knee injuries in female adolescent football players: secondary analysis of an RCT. Br J Sports Med. 2013;47(15):974-979. doi:10.1136/bjsport s-2013-092644
8. Jayanthi N, Kleithermes S, Dugas L, Pasulka J, Iqbal S, LaBella C. Risk of injuries associated with sport specialization and intense training patterns in young athletes: a longitudinal clinical case-control study. Orthop J Sports Med. 2020;8(6):2325967120922764. do i:10.1177/2325967120922764
9. Jayanthi NA, LaBella CR, Fischer D, Pasulka J, Dugas LR. Sports-specialized intensive training and the risk of injury in young athletes: a clinical casecontrol study. Am J Sports Med. 2015;43(4):794-801. d oi:10.1177/0363546514567298
10. Johnson MA, Halloran K, Carpenter C, et al. Changes in pediatric sports injury presentation during the COVID-19 pandemic: a multicenter analysis. Orthop J Sports Med 2021;9(4):23259671211010824. doi:10.1177/23259671 211010826
11. Bowen L, Gross AS, Gimpel M, Bruce-Low S, Li FX. Spikes in acute:chronic workload ratio (ACWR) associated with a 5–7 times greater injury rate in English Premier League football players: a comprehensive 3-year study Br J Sports Med 2020;54(12):731-738. doi:10.1136/bjsports-2018-099 422
12. Gabbett TJ. The training—injury prevention paradox: should athletes be training smarterandharder? Br J Sports Med 2016;50(5):273-280. doi:10.1136/bjsports-2015-0957 88
13. Hulin BT, Gabbett TJ, Caputi P, Lawson DW, Sampson JA. Low chronic workload and the acute:chronic workload ratio are more predictive of injury than between-match recovery time: a twoseason prospective cohort study in elite rugby league players. Br J Sports Med. 2016;50(16):1008-1012. do i:10.1136/bjsports-2015-095364
14. Seshadri DR, Thom ML, Harlow ER, Drummond CK, Voos JE. Case report: return to sport following the COVID-19 lockdown and its impact on injury rates in the German soccer league. Front Sports Act Living. 2021;3:604226-604226. doi:10.3389/fspor.202 1.604226
15. Mannino BJ, Yedikian T, Mojica ES, Bi A, Alaia M, Gonzalez-Lomas G. The COVID lockdown and its effects on soft tissue injuries in Premier League Athletes. The Physician and Sportsmedicine Published online September 20, 2021:1-5. doi:10.1080/0091384 7.2021.1980746
16. Bailey EP, Goodloe JB, McNeely RA, Traven SA, Woolf SK, Slone HS. COVID-19 modifications of offseason and preseason training for NFL athletes are associated with increased risk of regular season injuries. Physician Sportsmed. Published online September 8, 2021:1-5. doi:10.1080/00913847.2021.1 976602
17. Lubans D, Richards J, Hillman C, et al. Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics 2016;138(3). doi:10.1542/peds.2016-1642
18. Schuch FB, Vancampfort D, Firth J, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry 2018;175(7):631-648. doi:10.1176/appi.ajp.2018.1711 1194
19. White RL, Babic MJ, Parker PD, Lubans DR, Astell-Burt T, Lonsdale C. Domain-specific physical activity and mental health: a meta-analysis. Am J Prev Med 2017;52(5):653-666. doi:10.1016/j.amepr e.2016.12.008
20. Bazett-Jones DM, Garcia MC, Taylor-Haas JA, et al. Changes in motivation, socialization, wellness and mental health in youth long-distance runners during COVID-19 social distancing restrictions. Front Sports Act Living 2021;3:696264. doi:10.3389/fspor.2021.696 264
21. McGuine TA, Biese KM, Hetzel SJ, et al. High school sports during the COVID-19 pandemic: the impact of sport participation on the health of adolescents. J Athl Train. 2021;57(1):51-58. doi:10.40 85/1062-6050-0121.21
22. Faigenbaum AD, Myer GD Exercise deficit disorder in youth: play now or pay later. Curr Sports Med Rep 2012;11(4):196-200. doi:10.1249/jsr.0b013e 31825da961
23. Della Villa F, Andriolo L, Ricci M, et al. Compliance in post-operative rehabilitation is a key factor for return to sport after revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2020;28(2):463-469. doi:10.1007/ s00167-019-05649-2
24. Kingston G, Gray MA, Williams G. A critical review of the evidence on the use of videotapes or DVD to promote patient compliance with home programmes. Disabil Rehabil Assist Tech. 2010;5(3):153-163. doi:10.3109/17483101003671709
25. Kingston GA, Williams G, Gray MA, Judd J. Does a DVD improve compliance with home exercise programs for people who have sustained a traumatic hand injury? Results of a feasibility study Disabil Rehabil Assist Tech. 2014;9(3):188-194. doi:10.3109/1 7483107.2013.806600
Eric Schneider, PT, MPT, DHSc, OCS 1 a , Elizabeth S. Moore, PhD 2 , Rob Stanborough, PT, DPT, MHSc, FAAOMPT 3 , Emily Slaven, PT, PhD, OCS, FAAOMPT 4
1 Department of Physical Therapy, Mount St Joseph University, 2 College of Health Sciences, University of Indianapolis, 3 Department of Physical Therapy, First Coast Rehabilitation, 4 Krannert School of Physical Therapy, University of Indianapolis
Keywords: gluteus medius, latent trigger points, muscle activation levels, muscle strength, trigger point dry needling, myofascial trigger points https://doi.org/10.26603/001c.55536

Latent trigger points have been identified as a source of impaired muscle function giving rise to a reduction in force production and alterations in muscle activation patterns and movement efficiency. There is limited investigation into the effectiveness of a treatment in reducing these clinical manifestations.
To investigate whether the application of trigger point dry needling (TDN) to latent trigger points within the gluteus medius musculature affected strength measurements and muscle activation levels immediately following intervention.
Quasi experimental, single group, pretest-posttest, randomized control study
A control and an intervention side were randomly assigned for each participant (N = 39). Hand held dynamometer (HHD) force measurements and raw surface electromyography (sEMG) amplitude readings were recorded during maximal volitional isometric contractions of the gluteus medius in two separate positions before and after application of TDN. Comparison of within and between group data were conducted.
A statistically significant interaction between time (pre-TDN to post TDN) and groups (intervention side and control side), p < 0.001 was found for HHD measurements in both positions. Post hoc analysis revealed a statistically significant difference (p < 0.001) for all comparisons in the side lying neutral (SL0) position, while statistically significant differences (p < 0.001) were found for pre and post TDN measurements within intervention side as well as between the intervention and control side for post TDN measurements in the side lying internal rotation (SLIR) position. For sEMG amplitude measurements, statistically significant differences were found only in the SL0 position for within group comparisons on the intervention side (p = 0.009) and for between group comparisons for post TDN measurements (p = 0.002).
Corresponding Author: Eric Schneider, PT, MPT, DHSc, OCS
Department of Physical Therapy, Mount St Joseph University Cincinnati, OH, 45233 (513) 244-4826, eric.schneider@msj.edu
Application of TDN to latent trigger points within the gluteus medius can significantly increase gluteus muscle force production immediately following intervention while reducing the level of muscle activation required during contraction.
Level 2
Myofascial trigger points (MTrPs) have been identified as a potential source of musculoskeletal dysfunction.1–5 My ofascial trigger points have been defined as hyperirritable and palpable nodules within a taut band of muscle and are classified as either active trigger points or latent trigger points.6 Active trigger points can cause localized pain that is spontaneous in nature,4,5 while latent trigger points are not spontaneously painful and will only elicit pain when palpated.3–5 Some authors have argued that latent trigger points have the same pathophysiology as active trigger points, just to a lesser extent,3–5,7 which may explain a reduction in nociceptive input without mechanical stimu lus.8–10
Most of the research on MTrPs has focused on active trigger points due to their ability to generate spontaneous pain without being palpated, even though latent trigger points are more commonly found in muscle tissue.11,12 De spite a lack of attention in the literature, latent trigger points are not without clinical significance. Regarding function, they have been found to increase muscle fatiga bility,13 decrease muscle strength,14 and alter muscle acti vation patterns.1,15 Furthermore, latent trigger points may have the potential to transition into active trigger points if left untreated.7
Trigger point dry needling (TDN) has become an increas ingly popular intervention among physical therapists to re verse the effects of MTrPs.16,17 Authors of previous studies have demonstrated a reduction in substance P and calci tonin related peptide levels, while blood flow and subse quent tissue oxygenation increased following the applica tion of TDN to MTrPs.8,18 However, there is still debate surrounding the effectiveness of TDN provided by physical therapists as a viable treatment option for musculoskeletal dysfunction as compared to other physical therapy inter ventions.19
A potential cause for the formation of MTrPs has hy pothesized to be repetitive or unaccustomed eccentric load ing of muscle tissue.4,5,7,20–22 Musculature such as the glu teus medius must eccentrically control motion of the pelvis within the frontal plane during the gait cycle23 or during other functional activities where single limb support is re quired.24 Subtle alterations in frontal plane gait kinematics may lead to excessive loading of the gluteus medius muscu lature, which in turn may lead to the formation of MTrPs. If latent trigger points are able to affect muscle function, then an asymptomatic individual may have altered stability of the pelvis and the hip during loading response of the gait and running cycles, which then has the potential to alter the alignment of the lower limb relative to the ground.
Despite the increased demand for eccentric control dur ing functional activities, such as ambulation, there are no studies that have investigated the effects of latent trigger points on the strength of the gluteus medius. Furthermore, studies that have investigated changes in strength of lower extremity musculature following the application of dry needling to MTrPs report conflicting results.25–32 The pur pose of this study was to investigate whether the appli cation of TDN to latent trigger points within the gluteus medius musculature affected strength measurements and muscle activation levels immediately following interven tion.
This quasi-experimental study used a single group, pretest posttest, randomized control design (ww.ClinicalTrials.gov, ID NCT03580200). The study was approved by the Human Research Protections Program at the University of Indi anapolis and a reliance agreement was enacted with Mount St Joseph University in Cincinnati, OH where data were col lected.
A convenience sample of males and females age 18 to 50 years old were recruited provided they were asymptomatic at the time of screening and data collection. Asymptomatic was defined as experiencing no pain in the lumbar spine, sacroiliac region, pelvis, or bilateral lower extremities while at rest or with activity Participants were excluded if they had one of the following: were pregnant or attempting to become pregnant; pain intensity greater than 0 out of 10 on the visual analogue scale in the lumbar spine, sacroiliac re gion, pelvis, and bilateral lower extremities at rest or with activity; positive Flexion Adduction Internal Rotation test (FADIR)33 on either the left or right hip; presented with signs and symptoms consistent with hip osteoarthritis dur ing clinical screening using the criteria proposed by Altman et al.34; diagnosed with a progressive neurological disorder, a chronic pain condition such as fibromyalgia or myofascial pain syndrome, a connective tissue disorder, or osteoarthri tis of the hip joint; history of hip dysplasia or Legg Calve Perthes disease.
Informed consent was obtained following eligibility screening but immediately prior to data collection. The pri mary investigator (PI), a licensed physical therapist with 13 years of clinical experience was responsible for data collection and the application of TDN for all participants throughout the study.
A simple randomizing method of flipping a coin was used to assign each participant an intervention side, which was the side of the body that received TDN, and a control side, which was the side of the body that did not receive TDN.
Strength of the gluteus medius muscle was defined as the amount of force output measured by a handheld dy namometer (HHD) during a maximal volitional isometric contraction (MVIC) break test.35–37 Force output was mea sured in kilograms (kg) using a microFET2 HHD (Hoggan Scientific, LLC, Salt Lake City, UT) on both the control and intervention sides. The HHD is commonly used to assess force production and has been shown to be a reliable and valid measurement tool for assessing strength of the lower extremity musculature.36,38–40
Surface electromyography (sEMG) amplitude readings of the gluteus medius were recorded at the same time as HHD measurements on both the control and intervention sides. Raw sEMG data were collected using a two-channel sEMG recording system (MP36R, Biopac, Goleta, CA) and were measured in millivolts (mV). Parameters for recording the raw sEMG data included a rejection ratio of > 110 dB at 60 Hz, a gain of 1000 Hz, band pass filtered at 20-450 Hz, and a sampling rate of 2000 Hz.37,41,42 Recorded sEMG ampli tude readings can be used as a direct measure of the ac tivation level of a muscle during a contraction43–45 and is a common method of assessing the activation level of the gluteus medius muscle during a MVIC as well as dynamic movements.37,41,42,46–48
Prior to the start of data collection, intrarater and test retest reliability was established for the PI’s HHD and sEMG measurements during MVIC break testing of the gluteus medius. Ten participants with characteristics consistent with the study’s sample were recruited. A 10-minute break was given between measurements. All calculated ICCs (3, 1) were greater than .75 indicating acceptable intrarater and test-retest reliability49 (Table 1).
Bipolar sEMG electrodes were placed 2 cm apart in a posi tion distal to the iliac crest, midway between the anterior and posterior superior iliac spines and in line with the prox imal tip of the greater trochanter 41,42 A reference electrode was placed on the greater trochanter (Figure 1). Electrode placement on the intervention side was marked by a sterile surgical pen as electrodes needed to be removed during the application of TDN.
To ensure that the participant understood the position of testing, the leg to be tested was passively moved in to the testing position with verbal cueing. The pelvis was kept from rotating backwards by a manual stabilization force placed on the posterior and lateral iliac crest.35,36 The par ticipant was then asked to assume the testing position without assistance, but with standardized verbal cueing from the PI. After the participant successfully achieved the
proper position for testing without compensation on three consecutive attempts, a trial MVIC break test was per formed.
Application of TDN to the gluteus medius was not lim ited to one specific region of the muscle. As such, all sub divisions of the gluteus medius muscle needed to be active during each MVIC break test. Using the recommendations of Otten et al.37 the hip was placed in two separate testing positions that were found to have the highest sEMG activa tion levels for all three subdivisions of the gluteus medius. Participants were positioned in side lying with their bottom or stabilization leg in a position of approximately 30 de grees of hip flexion and 90 degrees of knee flexion. The first testing position had the hip on the side being tested in a neutral or zero starting position (SL0) at the hip with the knee fully extended. Neutral or zero starting position was defined as a position where the hip is in neutral position with respect to hip flexion and extension, abduction and adduction, as well as internal rotation and external rotation (Figure 2). The second testing position had the hip in a po sition of neutral hip flexion and extension as well as abduc tion and adduction, but the hip was maximally internally rotated (SLIR) with the knee fully extended (Figure 3).
The resistance applied during each MVIC break test was applied gradually until maximal resistance was provided for a total of five seconds, or until the participant could no longer hold the testing position.35 To standardize the re sistance applied for each trial as well as each participant, the entire body weight of the PI was placed 4 cm proximal to the lateral malleolus.35,36 The exact position of where the pressure should be placed was measured and marked on both the control and intervention sides.
Three MVIC break tests were performed first on the con trol side and then the intervention side. One minute of rest was given in between each test for both the SL0 and SLIR positions in an attempt to reduce the effects of muscular fatigue.47 If compensatory movements were observed dur ing the recording of a strength measurement, the measure obtained was not recorded, the form was corrected and an other test was performed. Once three valid tests were per formed on the control and intervention each side, the HHD values were averaged.14,36 Following application of TDN, the same procedure for measuring strength and muscle ac tivation levels of the gluteus medius was repeated.
Following the pre-TDN measurement of gluteus medius strength and muscle activation levels, latent trigger points were identified in the gluteus medius musculature on both the control and intervention sides using the methods pro posed by Simons et al.20 Each participant was positioned in side lying with the hip on the side that was assessed in a slightly adducted position so normal muscle fibers were still on slack while the taut bands of muscle were placed under tension, which made them more easily palpa ble.11,12,14,15
Participants needed at least two latent trigger points in the gluteus medius muscle on the intervention side in or der to receive TDN.14 Trigger point dry needling was ap
Reliability of HHD and sEMG measurements within trials
Pre 10 min break ICC* (95% CI)
Post 10 min break ICC* (95% CI)
SL0 on R 0.96 (0.89 - 0.99) 0.96 (0.89 - 0.99)
SLIR on R 0.92 (0.79 - 0.98) 0.98 (0.95 - 0.99)
SL0 on L 0.94 (0.84 - 0.98) 0.95 (0.85 - 0.99)
SLIR on L 0.95 (0.87 - 0.99) 0.95 (0.87 - 0.99)
SL0 on R 0.83 (0.60 - 0.95) 0.94 (0.83 - 0.98)
SLIR on R 0.92 (0.78 - 0.98) 0.93 (0.80 - 0.98)
SL0 on L 0.96 (0.88 - 0.99) 0.91 (0.76 - 0.97)
SLIR on L 0.93 (0.81 - 0.98) 0.81 (0.55 - 0.94)
Test retest reliability of HHD and sEMG measurements prior to and following 10 min break
HHD measurements ICC *(95% CI)
sEMG measurements ICC* (95% CI)
SL0 on R pre and post
0.91 (0.80 - 0.97) 0.85 (0.69 - 0.95)
SLIR on R pre and post 0.91 (0.80 - 0.97) 0.92 (0.82 - 0.98)
SL0 on L pre and post 0.94 (0.87 - 0.98) 0.90 (0.80 - 0.97)
SLIR on L pre and post 0.93 (0.85 - 0.98) 0.87 (0.74 - 0.96)
Abbreviations: HHD = hand held dynamometer; sEMG = surface electromyography; ICC = interclass coefficient; CI = confidence interval; SL0 = side lying neutral position; SLIR = side lying internal rotation position; R = right; L = left lying internal rotation position; R right; L left *(3, 1) model was used for ICC calculation
LTR was elicited, the needle was manipulated either fur ther into the muscle tissue or at a different angle until no more LTRs were elicited, or if the participant verbally re quested the intervention to stop. Once the needle was re moved, manual pressure was held at the site of needle in sertion for a total of 30 seconds to achieve hemostasis.25,29 The same process was repeated for all identified latent trig ger points within the gluteus medius muscle. The applica tion of TDN was stopped when no more LTR were elicited and there were no more palpable latent trigger points.
Following the application of TDN, each participant was asked to stand up and walk for two minutes in an attempt to assess each participants’ level of soreness with func tional movement. Time was managed by the PI for stan dardization purposes. Following the two minutes, partici pants were asked to rate their level of soreness on a 0 to 10 scale with a response of 0 representing, “No soreness at all” and a response of 10 representing, “The worst soreness imaginable”

Abbreviations: EMG electromyography
plied to each of the identified latent trigger points in an attempt to elicit a localized twitch response (LTR). Once a
Biopac Student Lab software (Biopac, Goleta, CA) was used to analyze the recorded sEMG data. Raw sEMG readings were visually inspected and the peak amplitude that oc curred during each MVIC was identified. Readings were then transformed using a root mean square calculation. Data were smoothed over 1000 points representing a 500 ms window around the identified peak amplitude, 250 ms prior to the peak and 250 ms following the peak.43 If the
500 ms window included readings that were not part of the MVIC, the next closest peak within the MVIC was identified and used. The mean amplitude within the 500 ms window was recorded for each trial.
Once a mean sEMG amplitude was found for each trial, the three trials in the SL0 and SLIR positions were averaged and recorded for both the intervention and control sides. The recorded HHD force measurements for all three trials in each position were also averaged and recorded for both sides. This process was performed for all measurements recorded prior to and following the application of TDN. The averaged values for the sEMG and HHD measurements were used for statistical analysis.
In order to be compared between trials or between in dividuals, sEMG readings must be normalized.44,45 The method of normalization has been debated, but normaliza tion using a MVIC is a widely used44 and reliable method47 of comparing sEMG readings of the gluteus medius. The re sultant sEMG data for measurements recorded prior to the application of TDN were used as the 100% MVIC reference for both the intervention and control sides. Averaged sEMG measurements recorded following the application of TDN were expressed as a percentage of the 100% MVIC.
An a priori sample size estimation was conducted based on using a repeated measures ANOVA, analyzing the betweenwithin interaction effect of four measurements between two groups and the following parameters, two-tailed test, alpha of 0.05, power of 0.80, a moderate effect size of 0.20. A minimum sample size of 36 participants was needed. To
account for a potential participant dropout rate of 10% as well as individuals not presenting with latent trigger points in the gluteus medius when palpated, 40 participants were recruited.


All data were analyzed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp., Armonk, NY). Normality of the data was determined using the Shapiro-Wilk test. All comparisons were two-tailed and an alpha level of less than 0.05 was considered statistically significant unless other wise noted. Effect sizes were interpreted using the recom mendations of Cohen.50 Descriptive statistics were used to describe the baseline characteristics of the sample.
A two-way repeated measures ANOVA was used to assess if there was a significant interaction between time (preTDN and post-TDN) and groups (intervention side and con trol side) for HHD force measurements for the SL0 and SLIR positions. Post hoc analysis using paired t tests with a Bon ferroni correction (alpha level of p < 0.013) were used to identify which pairs had a significant difference. Effect size of the interaction between time and groups were calculated (partial eta squared).
To assess whether there was a significant difference in sEMG measurements within the intervention side and the control side over time as well as between sides prior to and following the application of TDN, pairwise tests were con ducted for both the SL0 and SLIR positions. Since sEMG data were not normally distributed, Wilcoxon signed-ranks tests with Bonferroni correction (alpha level of p < 0.013) were conducted. Effect sizes for the results of the Wilcoxon signed-ranks test were calculated (Cohen’s d) using the rec ommendations of Field.51
Forty participants were recruited and met the inclusion cri teria for the study. One participant’s results were excluded due to the protocol for data collection not being followed (Figure 4). Therefore, the total sample size for the study was 39 participants. Descriptive statistics for the baseline char acteristics of the sample can be found in Table 2.
Hand held dynamometer measurements of force for the in tervention and control sides for both the SL0 and SLIR po sitions are presented in Table 3 and Figure 5. There was a statistically significant interaction between the time (preTDN to post-TDN) and groups (intervention side and con trol side) for both positions, SL0 position, F(1,38) = 107.89, p < 0.001 and SLIR position, F(1,38) = 93.37, p < 0.001. The overall effect sizes were large for the interactions in the SL0 position (partial eta squared = 0.74) and the SLIR position (partial eta squared = 0.71).
Pairwise post hoc analyses were statistically significant (p < 0.001) for all comparisons in the SL0 position: preTDN to post-TDN within and between the intervention side and the control side for both time periods. For the SLIR po sition, there was a statistically significant difference (p <
Figure 2. Side lying neutral position for MVIC testing Figure 3. Side lying internal rotation position for MVIC testingFigure 4.
Abbreviations: MVIC = maximal volitional isometric contraction
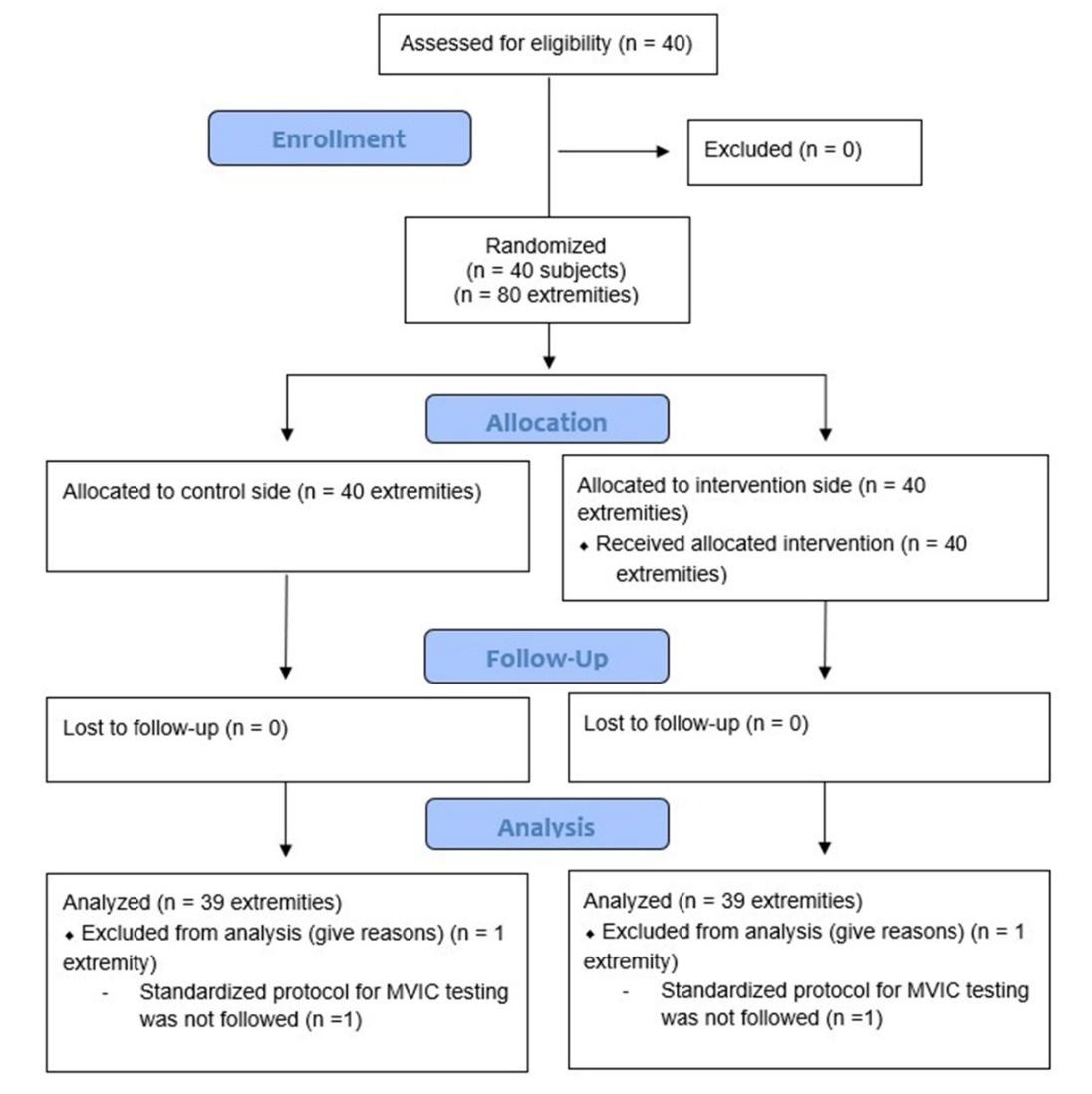
0.001) for pre-TDN and post-TDN measurements within the intervention side and between the intervention and control side for the post-TDN measurements. There was no signif icant difference (p = 0.146) within the control side when comparing pre-TDN and post TDN measurements, or when comparing pre-TDN measurements between the interven tion and control sides (p = 0.074).
Hand held dynamometer measurements for the control side in the SL0 position decreased by 1.31 kg following the application of TDN. Three separate paired t tests were used to assess differences between the three trials of HHD mea surements taken on the control side following the appli cation of TDN. Significant differences were found for the measurements recorded between trial 1 and trial 2 (mean difference = -0.71, t(38) = -2.42, p = 0.020) and trial 1 and trial 3 (mean difference = -0.97, t(38) = -3.60, p = 0.001). No significant difference was found between measurements recorded for trial 2 and trial 3 (mean difference = -0.26, t(38) = -1.08, p = 0.287).
Surface EMG measurements of amplitude for the interven tion and control sides for both positions are presented in Table 4 and Figure 6 Within group analysis revealed a sta
tistically significant difference between pre-TDN and post TDN sEMG amplitude measurements on the intervention side in the SL0 position Z(39) = 2.60, p = 0.009 with a medium effect size (Cohen’s d = 0.62). There were no sta tistically significant differences between pre-TDN and post TDN sEMG amplitude measurements in the SL0 position on the control side, Z(39) = -1.46, p = 0.145. For the SLIR posi tion, there was no statistically significant difference within either the intervention side, Z(39) = -2.09, p = 0.037 or the control side, Z(39) = -1.00, p = 0.317.
Between TDN group comparisons for the SL0 position revealed there was not a statistically significant difference in pre-TDN sEMG amplitude measurements between the intervention side and control side, Z(39) = -1.17, p = 0.241. However, there was a statistically significant difference in post-TDN sEMG amplitude measurements between the in tervention side and control side in the SL0 position, Z(39) = -3.08, p = 0.002 with a medium effect size (Cohen’s d = 0.74). In the SLIR position, the difference between the in tervention side and control side at pre-TDN and post-TDN was not statistically significant, Z(39) = -0.27, p = 0.786 and Z(39) = -0.20, p = 0.042, respectively.
Table 2. Descriptive statistics for demographic information of sample (n=39)
Mean (SD) Minimum Maximum
Age (years) 28.72 (5.47) 19.00 41.00
Height (inches) 67.18 (3.76) 58.00 74.00
Weight (pounds) 167.67 (27.89) 107.00 232.00 Hours of weekly activity 7.00 (5.00)* 0.00 40.00
Number of trigger points
Intervention side‡ 4.00 (1.00)* 3.00 8.00 Control side 4.97 (1.65) 2.00 9.00
Number of needles used 7.00 (2.00)* 5.00 10.00
Level of soreness post TDN 3.00 (2.00)*† 0.00† 8.00† N %
Gender
Male 16 41.03% Female 23 58.97%
Side of lower extremity dominance Right 33 84.62% Left 6 15.38%
Abbreviations: TDN = trigger point dry needling; SD = standard deviation
*Was not normally distributed. Results are reported as median and interquartile range †Soreness was measured on a scale of 0 to 10 ‡ Denotes the side that received TDN
Table 3. Descriptive statistics for HHD measurements, reported in kilograms
SL0 Position (n = 39) Mean (SD)
SLIR Position (n = 39) Mean (SD)
Intervention*
Control
Pre-TDN 18.86 (4.20) 17.92 (4.56) Post-TDN 21.39 (4.77) 21.49 (4.71)
Pre-TDN 20.56 (5.27) 18.49 (4.47) Post-TDN 19.25 (4.77) 18.77 (4.58)
Abbreviations: HHD hand held dynamometer; TDN trigger point dry needling; SLO side lying neutral position; SLIR side lying internal rotation position *Denotes the side that received TDN
The purpose of this study was to investigate whether the application of TDN to latent trigger points within the glu teus medius musculature affected strength measurements and muscle activation levels immediately following inter vention. Participants within this study had to be asympto matic to ensure that the latent trigger points themselves were the sole reason for muscle weakness, not pain or ar ticular dysfunction. Furthermore, to specifically assess the effect that TDN had on strength measurements, it had to be completed in isolation of any other therapeutic interven tion. As such, this is the first study to investigate the effects of TDN in isolation on strength measurements of the glu teus medius in asymptomatic individuals.
Results reported from previous research assessing the effect of TDN to latent trigger points in the gastrocnemius found no significant difference in strength measurements
as measured by a HHD immediately following interven tion.25,26 In contrast, participants within this study demon strated a statistically significant increase in HHD measure ments of gluteus medius force production immediately following the application of TDN in both testing positions. While the minimal clinically important difference for HHD measurements of the gluteus medius muscle has not been established,52,53 a large treatment effect size was found for interactions in the SL0 position (partial eta squared = 0.74) and the SLIR position (partial eta squared = 0.71) fol lowing the application of TDN suggesting a strong rela tionship between intervention and the difference in HHD measurements over time as well as between groups. These results are consistent with previous studies that investi gated immediate changes in force production of hip muscu lature measured by a HHD following the application of dry needling to MTrPs in the lower extremities for both symp
Abbreviations: HHD hand held dynamometer; SL0 side lying neutral; SLIR side lying internal rotation; TDN trigger point dry needling; kg kilograms
Table 4. Descriptive statistics for sEMG amplitude readings, reported in millivolts
SL0 Position (n = 39)
SLIR Position (n = 39) Median (IQR) % MVIC Median (IQR) % MVIC Intervention*
Pre-TDN 0.23 (0.19) 100% 0.22 (0.19) 100% Post-TDN 0.18 (0.15) 78.17% 0.20 (0.13) 90.32% Control
Pre-TDN 0.24 (0.14) 100% 0.20 (0.15) 100% Post-TDN 0.23 (0.12) 95.89% 0.21 (0.14) 107.07%
tomatic29,30 and asymptomatic individuals when combined with other interventions.31
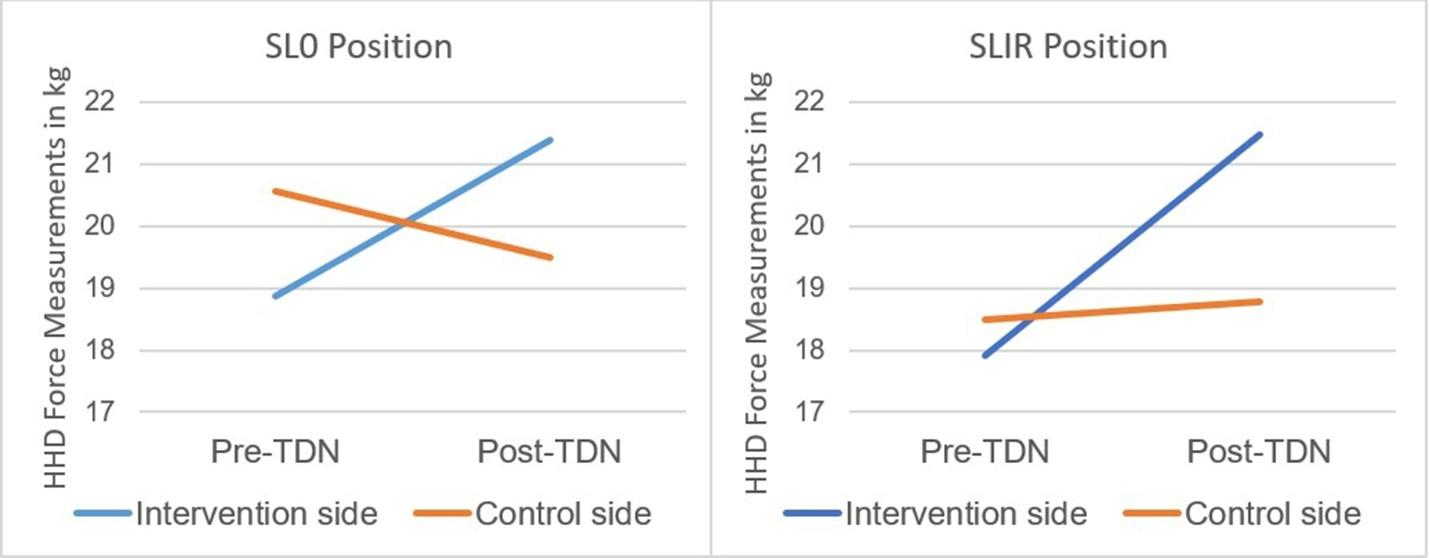
Strength as measured by HHD force measurements was not the only outcome measure utilized in this study Par ticipants demonstrated a statistically significant decrease (78.17% of pre-TDN readings) in sEMG amplitude readings on the intervention side following the application of TDN even though HHD force measurements increased by 2.52 kg in the SL0 position. While not statistically significant, sEMG amplitude readings in the SLIR position also de creased (90.32% of pre-TDN readings) on the intervention side, while HHD force measurements increased by 3.38 kg. Recorded sEMG amplitude readings can be used as a direct measure of the activation level of a muscle during a con traction.43–45 Both Dwyer et al54 and Penney et al41 found an increase in sEMG amplitude readings recorded during functional activities for individuals who demonstrated weakness of the gluteus medius muscle during baseline testing. These results suggest individuals who present with weakness of a muscle will require an increased level of muscle activation during a contraction, which may be a compensatory mechanism used to increase the amount of motor unit recruitment in order to achieve a given force
output.55 As such, the inverse relationship of HHD force measurements and sEMG amplitude readings found in this study suggests a more efficient gluteus medius muscle con traction following the application of TDN, as participants required less motor unit recruitment to achieve greater lev els of force production.
Based on the results of this study, latent trigger points can be identified as a potential source for impaired muscle function of the gluteus medius muscle resulting in a weak and inefficient muscle contraction. Authors of previous re search have stressed the importance of eliciting a LTR dur ing TDN to ensure that the myofilament needle has come in contact with a myofascial trigger point.56,57 While it is still unclear if the elicitation of one or multiple LTRs during the application of dry needling is essential for reductions in pain and disability in various patient populations,58,59 the purpose of this study was to investigate the effects of TDN specifically to latent trigger points within the glu teus medius muscle. As such, it was critical that a LTR was elicited during the application of TDN to ensure that the needle had in fact come in contact with a latent trigger point.25,26,32 All of the study participants demonstrated a
sEMG surface electromyography; TDN trigger point dry needling; MVIC maximal volitional isometric contraction; IQR interquartile range; SLO side lying neutral position; SLIR = side lying internal rotation position *Denotes the side that received TDN
Abbreviations: sEMG = surface electromyography; TDN = trigger point dry needling; MVIC = maximal volitional isometric contraction
palpable LTR and subjectively reported feeling a LTR during the application of TDN.
The exact mechanism of how TDN can reverse the effects of MTrPs is still unknown.5 Following the application of dry needling as well as the elicitation of a LTR, an increase in blood flow and subsequent tissue oxygenation have been found, along with a reduction of the biochemicals associ ated with pain and a localized muscle contraction within the milieu of a myofascial trigger point.8,18 Increases in lo calized blood flow and biochemical changes within the tis sue itself may explain the increase in force production fol lowing the application of TDN observed during this study. Specifically, a reduction of calcitonin gene related peptide may allow for improved overlap of actin and myosin pro teins through elimination of the localized muscle contrac ture22 which has the potential to improve cross bridge for mation within the sarcomere unit, thereby improving muscle force production. Furthermore, Lucas1 argued that a reduction of group III and IV afferent input to second or der neurons could potentially reverse alpha motor neuron inhibition, thereby improving neuromuscular control which may further explain the inverse relationship between HHD force measurements and sEMG amplitude readings found in this study following the application of TDN. Similarly, changes in neuromuscular function including a reduction in resting muscle tone25,26 as well as a decrease in muscle contraction time25 have been found following the elicita tion of a LTR during the application of TDN to latent trigger points within the gastrocnemius.
An unexpected outcome of the study was that there was also a statistically significant difference in HHD measure ments for the control side in the SL0 position as force mea surements decreased by 1.31 kg. A possible explanation for this result could be found in the order in which the strength measurements were recorded and the level of soreness ex perienced following the application of TDN. Post-TDN strength assessments were completed first on the control side and then the intervention side. Participants reported an increased level of soreness in the gluteus medius muscle
on the intervention side during the first MVIC break test trial on their control side while in the SL0 position. Even though strength was being assessed on the control side, participants reported an increased level of soreness on the side that they were lying on potentially due to the need for stabilization during testing. Post needling soreness is com monly reported following the application of TDN58 and may have affected the participants’ ability to generate force dur ing their first MVIC break test trial on the control side in the SL0 position.
To support this explanation, post-TDN HHD force mea surements of all three trials in the SL0 position on the con trol side were analyzed for differences. Significant differ ences for the measurements recorded between trial 1 and trial 2 and trial 1 and trial 3, while no significant differ ence was found between measurements recorded for trial 2 and trial 3. It is plausible that the level of soreness ex perienced in the gluteus medius musculature following the application of TDN reduced with each subsequent MVIC break test trial. This phenomenon may explain why there was no significant difference found between measurements recoded for trial 2 and trial 3 in the SL0 position as well as no significant difference between any of the measurements recorded in the SLIR position on the control side, which were collected following the measurements in the SL0 posi tion. Clinically, TDN is rarely performed in isolation and as such, clinicians should be aware of the possibility for post needling soreness and its potential effect on force produc tion. Results of this analysis suggest that it may be benefi cial to perform isolated gluteus medius contractions in an open chain position prior to any functional strengthening activities. This may reduce the effects that post-needling soreness may have on force production, thereby potentially reducing the risk for compensatory movement patterns during strengthening activities.
Effects of Trigger Point Dry Needling on Strength Measurements and Activation Levels of the Gluteus Medius: A.
The PI, who collected all of the data and applied the inter vention to each of the study’s participants, was not blinded to which side received TDN and which side was the control. Even with standardized protocols, the risk of inadvertent bias during MVIC testing cannot be eliminated.
During the informed consent process, participants were instructed that the purpose of the study was to assess the effects of TDN on strength measurements of the gluteus medius, whether that be an increase or decrease in strength in an attempt to reduce the risk of performance bias. How ever, since participants were not blinded to which side re ceived TDN and which side was the control side, perfor mance bias cannot be completely ruled out.
Sham needles have been utilized in studies that have in vestigated the effects of dry needling to account for a po tential placebo effect.27 When it comes to TDN studies, participants are able to feel the difference in needle depth penetration between the sham and TDN needles, as well as the elicitation of a LTR. Furthermore, if study participants have previously received TDN they may be able to realize the difference between the placebo and actual intervention. Future research on this topic could include other types of dry needling including superficial dry needling techniques, which may make it easier to include sham needles as a true placebo, while also reducing the potential for post needling soreness.58
While the side of dominance was recorded for each of this study’s participants, it was not considered during sta tistical analysis outside of descriptive statistics for demo graphic information of the sample. Future studies may con sider if side of dominance has an effect on the number of MTrPs found in the muscle tissue as well as study out comes.
This study only assessed the outcome measures imme diately following the application of TDN. Future studies should assess the effects of TDN on muscle strength at dif ferent post-treatment time intervals. Furthermore, TDN’s effect on muscle force production or activity during func tional movements should also be investigated as this may have a more direct clinical application to improving perfor mance during activities of daily living.
Application of TDN to latent trigger points within the glu teus medius musculature was able to significantly increase gluteus muscle force production immediately following in tervention while reducing the level of electromyographic muscle activation required during force production testing. These results suggest that latent trigger points may have a negative impact on gluteus medius muscle strength as well as the efficiency of contraction. Clinically, latent trig ger may be considered as a potential source of impaired muscle function.
ClinicalTrials.gov, ID NCT035802000
The authors report no conflicts of interest
Submitted: June 29, 2022 CST, Accepted: September 12, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Lucas KR. The impact of latent trigger points on regional muscle function. Curr Pain Headache Rep 2008;12(5):344-349. doi:10.1007/s11916-008-0058-6
2. Ge HY, Arendt-Nielsen L. Latent myofascial trigger points. Curr Pain Headache Rep 2011;15(5):386-392. doi:10.1007/s11916-011-0210-6
3. Celik D, Kaya Mutlu E. Clinical implication of latent myofascial trigger point. Curr Pain Headache Rep. 2013;17(8):353-360. doi:10.1007/s11916-013-03 53-8
4. Dommerholt J, Bron C, Franssen J. Myofascial trigger points: an evidence-informed review J Man Manip Ther. 2006;14(4):203-221. doi:10.1179/106698 106790819991
5. Shah JP, Thaker N, Heimur J, Aredo JV, Sikdar S, Gerber L. Myofascial trigger points then and now: A historical and scientific perspective. PM R 2015;7(7):746-761. doi:10.1016/j.pmrj.2015.01.024
6. Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual Vol 1. Williams & Wilkins; 1983.
7. Hong CZ, Simons DG. Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points. Arch Phys Med Rehabil 1998;79(7):863-872. d oi:10.1016/s0003-9993(98)90371-9
8. Shah JP, Danoff JV, Desai MJ, et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. 2008;89(1):16-23. doi:10.1016/j.apmr.2007.10.018
9. Shah JP, Gilliams EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: An application of muscle pain concepts to myofascial pain syndrome. J Bodyw Mov Ther. 2008;12(4):371-384. doi:10.1016/j.jbmt.2008.06.006
10. Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J Appl Physiol 2005;99(5):1977-1984. doi:10.1152/jappl physiol.00419.2005
11. Çelik D, Kaya Mutlu E. The relationship between latent trigger points and depression levels in healthy subjects. Clin Rheumatol 2012;31(6):907-911. doi:1 0.1007/s10067-012-1950-3
12. Lucas KR, Rich PA, Polus BI. How common are latent myofascial trigger points in the scapular positioning muscles. J Musculoskelet Pain. 2009;16(4):279-286. doi:10.1080/10582450802479800
13. Ge HY, Arendt-Nielsen L, Madeleine P Accelerated muscle fatigability of latent myofascial trigger points in humans. Pain Med 2012;13(7):957-964. doi:10.1111/j.1526-4637.2012.01 416.x
14. Celik D, Yeldan İ. The relationship between latent trigger point and muscle strength in healthy subjects: a double-blind study. J Back Musculoskelet Rehabil. 2011;24(4):251-256. doi:10.3233/bmr-2011-0302
15. Lucas KR, Polus BI, Rich PA. Latent myofascial trigger points: their effects on muscle activation and movement efficiency J Bodyw Mov Ther 2004;8(3):160-166. doi:10.1016/j.jbmt.2003.12.002
16. Caramagno J, Adrian L, Mueller L, Purl J. Analysis of Competencies for Dry Needling by Physical Therapists: Final Report Federation of State Boards of Physical Therapy; 2015.
17. Dommerholt J. Dry needling: peripheral and central considerations. J Man Manip Ther 2011;19(4):223-227 doi:10.1179/106698111x1312972 9552065
18. Cagnie B, Barbe T, De Ridder E, Van Oosterwijck J, Cools A, Danneels L. The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. J Manipulative Physiol Ther 2012;35(9):685-691. doi:10.1016/j.jmpt.2012.10.005
19. Gattie E, Cleland JA, Snodgrass S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: a systematic review and meta-analysis. J Orthop Sports Phys Ther 2017;47(3):133-149. doi:10.2519/jospt.201 7.7096
20. Simons DG, Travell JG, Simmons L. The Trigger Point Manual 2nd ed. Williams and Wilkins; 1999.
21. Hoyle JA, Marras WS, Sheedy JE, Hart DE. Effects of postural and visual stressors on myofascial trigger point development and motor unit rotation during computer work. J Electrormyogr Kinesiol 2011;21(1):41-48. doi:10.1016/j.jelekin.2010.04.006
22. Gerwin RD, Dommerholt J, Shah JP. An expansion of Simons’ integrated hypothesis of trigger point formation. Curr Pain Headache Rep 2004;8(6):468-475. doi:10.1007/s11916-004-0069-x
23. Neumann DA. Kinesiology of the hip: A focus on muscular actions. J Orthop Sports Phys Ther. 2010;40(2):82-94. doi:10.2519/jospt.2010.3025
24. Ward SR, Winters TM, Blemker SS. The architectural design of the gluteal muscle group: Implications for movement and rehabilitation. J Orthop Sports Phys Ther 2010;40(2):95-102. doi:10.25 19/jospt.2010.3302
25. Pérez-Bellmunt A, Casasayas-Cos O, López-deCelis C, et al. Effects of dry needling of latent trigger points on viscoelastic and muscular contractile properties: preliminary results of a randomized within-participant clinical trial. J Clin Med 2021;10(17):3848. doi:10.3390/jcm10173848
26. Albin SR, Koppenhaver SL, MacDonald CW, et al. The effect of dry needling on gastrocnemius muscle stiffness and strength in participants with latent trigger points. J Electrormyogr Kinesiol 2020;55:102479. doi:10.1016/j.jelekin.2020.102479
27. Mansfield CJ, Vanetten L, Willy R, di Stasi S, Magnussen R, Briggs M. The effects of needling therapies on muscle force production: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2019;49(3):154-170. doi:10.2519/jospt.2019.8270
28. Mayoral O, Salvat I, Martín MT, et al. Efficacy of myofascial trigger point dry needling in the prevention of pain after total knee arthroplasty: a randomized, double-blinded, placebo-controlled trial. Evid Based Comp Alternat Med. 2013;2013:1-8. doi:1 0.1155/2013/694941
29. Ceballos-Laita L, Jiménez-Del-Barrio S, MarínZurdo J, et al. Effectiveness of dry needling therapy on pain, hip muscle strength, and physical function in patients with hip osteoarthritis: A randomized controlled trial. Arch Phys Med Rehabil. 2021;102(5):959-966. doi:10.1016/j.apmr.2021.01.077
30. Rossi A, Blaustein S, Brown J, et al. Spinal and peripheral dry needling versus peripheral dry needling alone among individuals with a history of lateral ankle sprain: a randomized control trial. Int J Sports Phys Ther. 2017;12(7):1034-1047. doi:10.2660 3/ijspt20171034
31. Haser C, Stöggl T, Kriner M, et al. Effect of dry needling on thigh muscle strength and hip flexion in elite soccer players. Med Sci Sports Exerc 2017;49(2):378-383. doi:10.1249/mss.0000000000001 111
32. Janowski JA, Phelan-Smith DML, Kroat Brady MN, et al. Acute effects of dry needling on myofascial trigger points in the triceps surae of ballet dancers: a pilot randomized controlled trial. Int J Sports Phys Ther 2021;16(2):418-430. doi:10.26603/001c.21475
33. Maslowski E, Sullivan W, Forster Harwood J, et al. The diagnostic validity of hip provocation maneuvers to detect intra-articular hip pathology PM R 2010;2(3):174-181. doi:10.1016/j.pmrj.2010.01.014
34. Altman R, Alarcón G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505-514. doi:10.100 2/art.1780340502
35. Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA. Muscles Testing and Function With Posture and Pain 5th ed. Lippincott Williams & Wilkins; 2005.
36. Mastenbrook MJ, Commean PK, Hillen TJ, et al. Hip abductor muscle volume and strength differences between women with chronic hip joint pain and asymptomatic controls. J Orthop Sports Phys Ther. 2017;47(12):923-930. doi:10.2519/jospt.2017.7380
37 Otten R, Tol JL, Holmich P, Whiteley R. Electromyography activation levels of the 3 gluteus medius subdivisions during manual strength testing. J Sport Rehabil 2015;24(3):244-251. doi:10.1123/jsr.2 013-0149
38. Arnold CM, Warkentin KD, Chilibeck PD, Magnus CRA. The reliability and validity of handheld dynamometry for the measurement of lower extremity muscle strength in older adults. J Strength Cond Res 2010;24(3):815-824. doi:10.1519/jsc.0b013e 3181aa36b8
39. Hébert LJ, Maltais DB, Lepage C, Saulnier J, Crête M, Perron M. Isometric muscle strength in youth assessed by hand-held dynamometry: a feasibility, reliability, and validity study Pediatr Phys Ther 2011;23(3):289-299. doi:10.1097/pep.0b013e318227cc ff
40. Ieiri A, Tushima E, Ishida K, Inoue M, Kanno T, Masuda T Reliability of measurements of hip abduction strength obtained with a hand-held dynamometer Physiother Theory Pract 2015;31(2):146-152. doi:10.3109/09593985.2014.9605 39
41. Penney T, Ploughman M, Austin MW, Behm DG, Byrne JM. Determining the activation of gluteus medius and the validity of the single leg stance test in chronic, nonspecific low back pain. Arch Phys Med Rehabil 2014;95(10):1969-1976. doi:10.1016/j.apmr.2 014.06.009
42. Semciw AI, Neate R, Pizzari T A comparison of surface and fine wire EMG recordings of gluteus medius during selected maximum isometric voluntary contractions of the hip. J Electrormyogr Kinesiol 2014;24(6):835-840. doi:10.1016/j.jelekin.20 14.08.015
43. Bamman MM, Ingram SG, Caruso JF, Greenisen MC. Evaluation of surface electromyography during maximal voluntary contraction. J Strength Cond Res 1997;11(2):68-72.
44. Burden A. How should we normalize electromyograms obtained from healthy participants? What we have learned from over 25years of research. J Electrormyogr Kinesiol. 2010;20(6):1023-1035. doi:1 0.1016/j.jelekin.2010.07.004
45. Soderberg GL, Knutson LM. A guide for use and interpretation of kinesiologic electromyographic data. Phys Ther 2000;80(5):485-498. doi:10.1093/ptj/ 80.5.485
46. Boren K, Conrey C, Le Coguic J, Paprocki L, Voight M, Robinson TK. Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Int J Sports Phys Ther. 2011;6(3):206-223.
47 Bolgla LA, Uhl TL. Reliability of electromyographic normalization methods for evaluating the hip musculature. J Electrormyogr Kinesiol 2007;17(1):102-111. doi:10.1016/j.jelekin.20 05.11.007
48. Claiborne TL, Timmons MK, Pincivero DM. Test–retest reliability of cardinal plane isokinetic hip torque and EMG. J Electrormyogr Kinesiol. 2009;19(5):e345-e352. doi:10.1016/j.jelekin.2008.07.0
05
49. Portney LG, Watkins MP. Foundations Of Clinical Research: Applications To Practice 2nd ed. Prentice Hall Health; 2000.
50. Cohen J. A power primer Psychol Bull 1992;112(1):155-159. doi:10.1037/0033-2909.112.1.1
55
51. Field A. Discovering Statistics Using IBM SPPS Statistics. 4th ed. SAGE; 2013.
52. Bohannon RW Considerations and practical options for measuring muscle strength: A narrative review Biomed Research Int 2019;2019:8194537-8194537. doi:10.1155/2019/81945 37
53. Romney W, Weisbach C, Anderson H, Yoshida R. Hand held myometry/dynamometry Published 2016. https://www.sralab.org/rehabilitation-measures/han d-held-myometry-dynamometry
54. Dwyer MK, Stafford K, Mattacola CG, Uhl TL, Giordani M. Comparison of gluteus medius muscle activity during functional tasks in individuals with and without osteoarthritis of the hip joint. Clin Biomech. 2013;28(7):757-761. doi:10.1016/j.clinbiome ch.2013.07.007
55. Ling SM, Conwit RA, Talbot L, et al. Electromyographic patterns suggest changes in motor unit physiology associated with early osteoarthritis of the knee. Osteoarthritis Cartilage 2007;15(10):1134-1140. doi:10.1016/j.joca.2007.03.02 4
56. Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil 1994;73(4):256-263. doi:10.1097/00002060-19940700 0-00006
57 Rha D wook, Shin JC, Kim YK, Jung JH, Kim YU, Lee SC. Detecting local twitch responses of myofascial trigger points in the lower-back muscles using ultrasonography Arch Phys Med Rehabil 2011;92(10):1576-1580.e1. doi:10.1016/j.apmr.2011.0 5.005
58. Perreault T, Dunning J, Butts R. The local twitch response during trigger point dry needling: is it necessary for successful outcomes? J Bodyw Mov Ther. 2017;21(4):940-947 doi:10.1016/j.jbmt.2017.03.008
59. Hakim IK, Takamjani IE, Sarrafzadeh J, Ezzati K, Bagheri R. The effect of dry needling on the active trigger point of upper trapezius muscle: Eliciting local twitch response on long-term clinical outcomes. J Back Musculoskelet Rehabil. 2019;32(5):717-724. do i:10.3233/bmr-181286
Dai Sugimoto 1,2 a , Michael Del Bel 3 , Lauren Butler 4
1 The Micheli Center for Sports Injury Prevention, 2 Faculty of Sport Sciences, Waseda University, 3 School of Rehabilitation Science, University of Ottawa, 4 Department of Rehabilitation, Nicklaus Children's Hospital
Keywords: Evidence-based medicine, clinician-scientists, education, mentorship https://doi.org/10.26603/001c.39739
Barriers and facilitators to research in sports medicine (SM) by physicians and allied health (AH) professions such as physical therapists and athletic trainers are understudied. The purpose of this research was to examine and compare research barriers, facilitators, and other research related facets including interests, comfort, knowledge, and resources among SM physicians and AH practitioners.
The survey was sent to Pediatric Research in Sports Medicine (PRiSM) members. The survey was designed to ask respondents to identify their top barrier and facilitator to conducting research. Research interest (binary), self-rated comfort reading research articles (0-100 scale), self-rated knowledge conducting research independently (0-100 scale), and available research resources were evaluated. Descriptive statistics, chi-square, and t-tests were used to compare the responses between SM physicians and AH practitioners. The value of p<0.05 was set as a statistically significant criterion.
The response rate was 35.7% (N=100). For both SM physicians and AH practitioners, the greatest research barrier was a lack of time. However, the leading research facilitators differed in the two professions. The top research facilitator for SM physicians was availability of research personnel, while availability of research mentoring was selected as a prime facilitator by AH practitioners. There were no differences in research interest between SM physicians (87.0%) and AH practitioners (95.5%, p=0.267). However, self-rated comfort reading research articles was higher in SM physicians (75.6±20.6) than AH practitioners (60.6±28.3, p=0.018). There were no differences in self-rated knowledge conducting research independently between SM physicians (70.2±18.6) and AH practitioners (63.4±24.6, p=0.163).

Lack of time was the top research barrier for both SM physicians and AH practitioners. Regarding research facilitators, having available time was the main facilitator for SM physicians while availability of mentoring was the leading facilitator in AH practitioners.
a
Corresponding author: Dai Sugimoto, PhD, ATC Waseda University 2-7-5, Higashifushimi, Nishi-Tokyo city, Tokyo 202-0021, Japan Telephone: 042-420-2304 Email: dai.sugimoto.007@gmail.com
Evidence-based practice (EBP) was developed with the aim to translate the most updated, appropriate evidence to clin ical practices.1 The EBP model consists of three compo nents: scientific evidence from empirical research, clinical experience of healthcare providers, and fundamental values of an individual patient. A combination of the these three pillars is considered an important aspect in decision mak ing.2 To enhance the EBP initiative, it was recommended to conduct research studies in the clinical setting where pa tients are present.3 Several studies reported positive clini cal outcomes utilizing this approach.4,5 In this model, med ical providers, also referred to as clinician-scientists, play an integral role as point personnel to translate research evidence to clinical practice. Although clinician-scientists are considered key personnel in the EBP model, they are also recognized as an “endangered species.”6,7 According to Roberts et al., there has been a decrease in the number of clinician-scientists as well as reduction in the research ac tivity time among physicians.8
Several studies have been performed to identify reasons for the downward trend in research activities in clinicianscientists.3,9,10 According to the literature, a lack of avail able time, research knowledge, and administrative support were frequently reported.11–13 Additionally, some authors found that overall priorities for the research activities were different between physicians and allied healthcare (AH) practitioners.14,15 In summary, there are several known barriers to a clinician-scientist’s participation in research and the perception of research activities differs between physicians and AH practitioners.
In contrast, factors that facilitate research activities are understudied compared to research barriers. Moreover, studies that focused on research barriers and facilitators specifically in the field of sports medicine (SM) are limited. Identifying barriers and facilitators to research is an impor tant first step to help optimize the research engagement of clinician-scientists in the SM community. Furthermore, as previous research identified differences in research en gagement between physicians and AH practitioners,14,15 it is important to examine the research barriers and facilita tors between the two healthcare professions in SM com munity Therefore, the purpose of this study was to exam ine and compare research barriers, facilitators, and other research related components including interests, comfort, knowledge, and resources among SM physicians and AH practitioners.
A cross-sectional survey study design was employed. The recruitment strategy and the survey were reviewed and ap proved by the research ethics board of the host institution
(Boston Children’s Hospital) prior to the initiation of this study.
The survey, which consisted of research interests, percep tions, resources, barriers and facilitators, was developed by one clinician-scientist, a doctoral student, and a full-time researcher all who specialize in SM. The survey was re viewed by several SM physicians and AH practitioners prior to the dissemination. The survey was updated several times based on their feedback. The Pediatric Research in Sports Medicine (PRiSM) community was targeted as an initial source of participants to complete the survey The main reason for selecting the PRiSM was that this organization is known as a multidisciplinary group in north America, mainly US, with members consisting of SM physicians (MD, DO) and SM specific AH practitioners including physical therapists (PTs) and athletic trainers (ATs). In this study, SM physicians were defined as those who held a Doctor of Medicine (MD) and/or a Doctor of Osteopathic Medi cine (DO) degree, and individuals who held a physical ther apy and/or athletic training license as AH practitioners. For analyses of the data from PRiSM members as a whole, all collected responses were included. For comparisons be tween SM physicians and AH practitioners, responses from those who did not have clinical duties, described as “oth ers” were excluded from analyses.
Following approval from the PRiSM board, the on-line survey was disseminated to the PRiSM members via email in May 2020. To capture the survey responses, research electronic data capture (REDCap, Vanderbilt University, Nashiville, TN, USA) was utilized. After an initial email, a total of three reminder emails were subsequently sent to the PRiSM members to encourage participation. All emails were sent from the PRiSM headquarters to ensure that the survey was only delivered to the PRiSM members. An access to the survey link was available for three months (closed in August 2020). The REDCap system was programmed to compute binary variables, multiple choices, and propor tional ratios such as percentages (%).
Respondents were asked to identify and rank three bar riers and three facilitators that contributed most to their participation in research activities from 10-11 distinctively unique choices. Additionally, respondents were instructed to rate each component of the 10-11 choices with four scales, 1) to no extent, 2) to a little extent, 3) to a moderate extent, and 4) to a great extent, and an option of no opin ion/not applied. Respondents were asked whether they were interested in research or not with binary manner (yes or no), and for those who answered “yes,” specific areas of research interests and actual research involvement were subsequently sought. Also, respondents were asked to give a self-rating of comfort reading research articles and their knowledge regarding conducting research independently with a 0-100 scale. For research resources, there were nine
choices including 1) graduate students, 2) facilities for re search, 3) residents, 4) research coordinator, 5) research technician, 6) biostatistician, 7) statistical/analytical soft ware, 8) none, and 9) other, and respondents were re quested to pick available resources.
Primary outcome measures were barriers and facilitators of research activities. Secondary outcome measures were re search interests, self-rated comfort reading research article, self-rated knowledge conducting research independently, and resources associated with research activities.
Descriptive statistics including mean, standard deviation, and 95% confidence interval (95%CI) was used to analyze participants’ demographics. T-tests were used to compare continuous variables related to research perceptions be tween SM physicians and AH practitioners. Frequency of certain categories and ranks were expressed as percentages (%). For binary categorical variables such as research inter ests, 2 x 2 chi-square (x2) analyses were employed to ex amine proportional differences between SM physicians and AH practitioners. The a priori statistical significance level was set as p<0.05 for all analyses. The top three parame ters of the primary outcome variables, barriers and facili tators, were selected and stratified between SM physicians and AH practitioners. IBM SPSS statistical software (Ver sion 26, SPSS Inc, Chicago, IL) was used for all analyses.
There were 100 responses (57 males and 39 females, miss ing sex responses: N=4). Response rate from PRiSM was 35.7%. Mean ages of participants were 42.5±10.7 (95%CI: 40.3, 44.7) years. Mean ages of males were 45.0±10.9 (95%CI: 42.1, 48.0) years, while females were slightly younger 38.9±9.5 (95%CI: 35.8, 42.0). About 86.6% of re spondents reported spending 10 hours or more per week providing direct patient care. Also, 89.6% worked more than 15 hours per week at their primary medical care set tings. Other demographics of the respondents including primary occupation, medical care settings, and geographic regions are presented in Table 1.
Furthermore, medical care settings of SM physicians and AH practitioners were examined. Medical care settings of SM physicians consisted of hospital (33.3%), hospital-based outpatient center (42.0%), private practice (15.9%), univer sity (7.3%), and others (1.5%). Breakdown of care provision settings of AH practitioners were hospital (12.5%), hospi tal-based outpatient center (66.6%), university (12.5%), fit ness center (4.2%), and others (4.2%).
Results of the 10-11 choices related to research barriers with the four rating scales were listed in Table 2
Frequency (%)
Professional Credentials: Doctor of Medicine (MD) 3 (3.0%) Doctor of Osteopathic Medicine (DO) 66 (66.0%) Physical Therapy (PT) 17 (17.0%) Athletic Trainer (AT) 7 (7.0%) Other* 7 (7.0%)
Primary Practice Settings:† Hospital 26 (26.8%) Hospital based outpatient center 45 (46.4%)
Private practice 11 (11.3%) University 11 (11.3%) School 0 (0.0%) Fitness/Training facility 1 (1.0%) Other 3 (3.1%)
Geographic Locations:‡ Mid-Atlantic 4 (4.7%) Mid-West 17 (19.8%) North East 14 (16.3%) North West 4 (4.7%) South East 17 (19.7%)
South West 11 (12.8%) West 13 (15.1%) Others 6 (7.0%)
* Others: professional credentials of these individuals are PhD and MSc.
† Primary practice setting: three responses were missing.
‡ Geographic locations: fourteen responses were missing.
Among the 11 choices, the greatest barrier for research activity was a lack of time (28.3%). The research barriers were further stratified by SM physicians and AH practition ers. The top selection of the research barriers was the same between the two medical professions: a lack of time (Fig ures 1, 2). However, other reported barriers differed be tween SM physicians and AH practitioners (Figures 1, 2).
Similarly, 10 choices related to research facilitators were assessed by four rating scales and the outcomes were found in Table 3
In the 10 choices, the leading research facilitator was available time (18.5%). Moreover, research facilitators were analyzed separately between SM physicians and AH prac titioners (Figures 3, 4). The top research facilitator for SM physicians was availability of research personnel, while availability of research mentoring was selected as the top facilitator in AH practitioners (Figures 3, 4).
About 88.7% of respondents expressed an interest in re search, while 11.3% chose no research interest (missing re sponses, N=3). AH practitioners showed higher research in terest (95.5%) compared with SM physicians (87.0%), but
Table 2. Ratings of research barriers
To No Extent
To a Little Extent
1. As a clinician, I feel I do not have enough authority or ability to implement research into a clinical setting to improve patient care
To a Moderate Extent
To a Great Extent
No Opinion / Not Applied
Overall 32 (39.0%) 23 (28.0%) 17 (20.7%) 5 (6.1%) 5 (6.1%)
SM physicians 27 (49.1%) 16 (29.1%) 10 (18.2%) 2 (3.6%) 0 (0.0%)
AH practitioners 6 (27.3%) 6 (27.3%) 6 (27.3%) 1 (4.5%) 3 (13.6%)
2. Facilities
Overall 15 (18.3%) 29 (35.4%) 20 (24.4%) 16 (19.5%) 2 (2.4%)
SM physicians 9 (16.4%) 22 (40.0%) 12 (21.8%) 12 (21.8%) 0 (0.0%)
AH practitioners 6 (27.3%) 4 (18.2%) 7 (31.8%) 3 (13.6%) 2 (9.1%)
3. Coworkers and/or leadership is not supportive of research
Overall 39 (47.6%) 15 (18.3%) 15 (18.3%) 9 (11.0%) 4 (4.9%)
SM physicians 30 (54.5%) 8 (14.5%) 10 (18.2%) 5 (9.1%) 2 (3.6%)
AH practitioners 9 (40.9%) 5 (22.7%) 4 (18.2%) 2 (9.1%) 2 (9.1%)
4. Lack of perceived benefit to my own professional career
Overall 46 (56.1%) 15 (18.3%) 15 (18.3%) 4 (4.9%) 2 (2.4%)
SM physicians 32 (58.2%) 11 (20.0%) 11 (20.0%) 1 (1.8%) 0 (0.0%)
AH practitioners 12 (54.5%) 4 (18.2%) 4 (18.2%) 1 (4.5%) 1 (4.5%)
5. Limited or no funding
Overall 8 (9.8%) 23 (28.1%) 27 (32.9%) 20 (24.4%) 4 (4.9%)
SM physicians 6 (10.9%) 18 (32.7%) 16 (29.1%) 14 (25.5%) 1 (1.8%)
AH practitioners 2 (9.1%) 5 (22.7%) 8 (36.4%) 5 (22.7%) 2 (9.1%)
6. Limited access to a regulatory team
Overall 31 (37.8%) 26 (31.7%) 12 (14.6%) 10 (12.2%) 2 (3.7%)
SM physicians 23 (41.8%) 20 (36.4%) 6 (10.9%) 6 (10.9%) 0 (0.0%)
AH practitioners 8 (36.4%) 5 (22.7%) 6 (27.3%) 2 (9.1%) 1 (4.5%)
7. Limited access to research coordinator
Overall 22 (26.8%) 21 (25.6%) 16 (19.5%) 20 (24.4%) 3 (3.7%)
SM physicians 17 (30.9%) 11 (20.0%) 11 (20.0%) 16 (29.1%) 0 (0.0%)
AH practitioners 5 (22.7%) 8 (36.4%) 3 (13.6%) 4 (18.2%) 2 (9.1%)
8. Limited access to biostatistician
Overall 19 (23.2%) 22 (26.8%) 16 (19.5%) 20 (24.4%) 5 (6.1%) SM physicians 14 (25.5%) 13 (23.6%) 11 (20.0%) 15 (27.3%) 2 (3.6%)
AH practitioners 5 (22.7%) 8 (36.4%) 3 (13.6%) 3 (13.6%) 3 (13.6%)
9. Difficulty recruiting participants
Overall 21 (25.6%) 33 (40.2%) 20 (24.4%) 6 (7.3%) 2 (2.4%)
SM physicians 15 (27.3%) 24 (43.6%) 14 (25.5%) 2 (3.6%) 0 (0.0%)
AH practitioners 5 (22.7%) 8 (36.4%) 7 (31.8%) 1 (4.5%) 1 (4.5%)
10. Lack of time
Overall 2 (2.4%) 15 (18.3%) 27 (32.9%) 36 (43.9%) 2 (2.4%)
SM physicians 1 (1.8%) 8 (14.5%) 21 (38.2%) 24 (43.6%) 1 (1.8%)
AH practitioners 1 (4.5%) 6 (27.3%) 5 (22.7%) 9 (40.9%) 1 (4.5%)
11. Restrictive privacy law
Overall 31 (37.8%) 29 (35.4%) 12 (14.6%) 4 (4.9%) 6 (7.3%)
To No Extent
To a Little Extent
To a Moderate Extent
To a Great Extent
No Opinion / Not Applied
SM physicians 21 (38.2%) 23 (41.8%) 6 (10.9%) 2 (3.6%) 3 (5.5%) AH practitioners 8 (36.4%) 6 (27.3%) 5 (22.7%) 1 (4.5%) 2 (9.1%)
Note: Eighteen responses were missing from overall (fourteen responses from SM physicians, two responses from AH practitioners, and two responses from others).
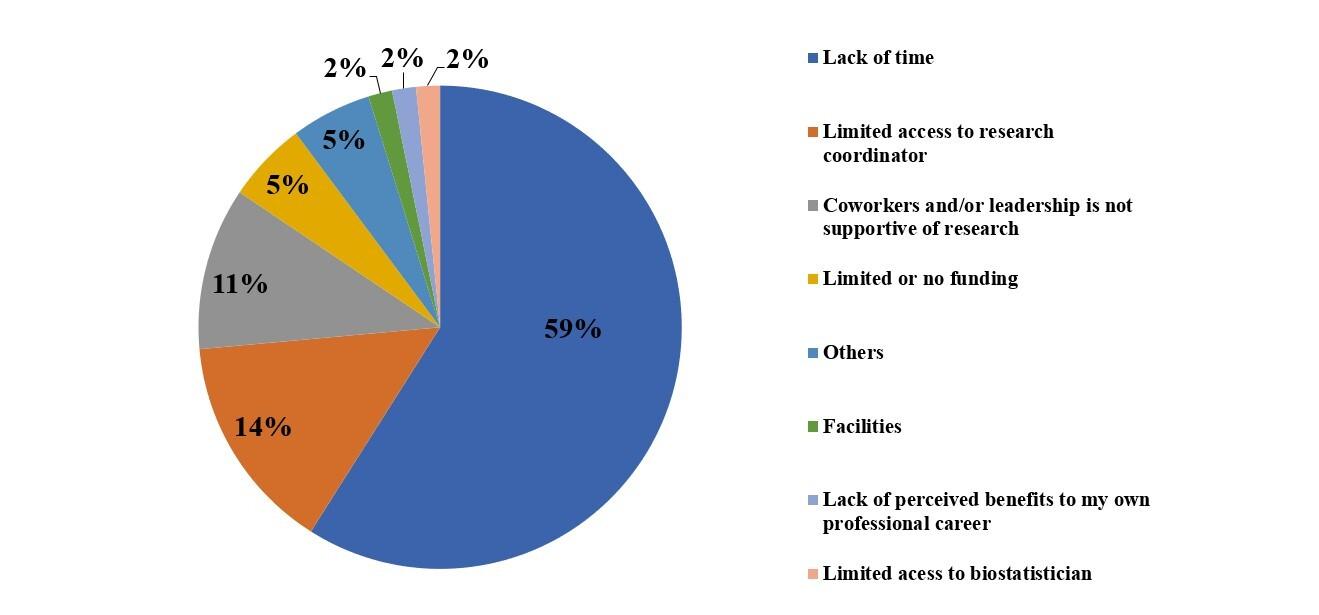
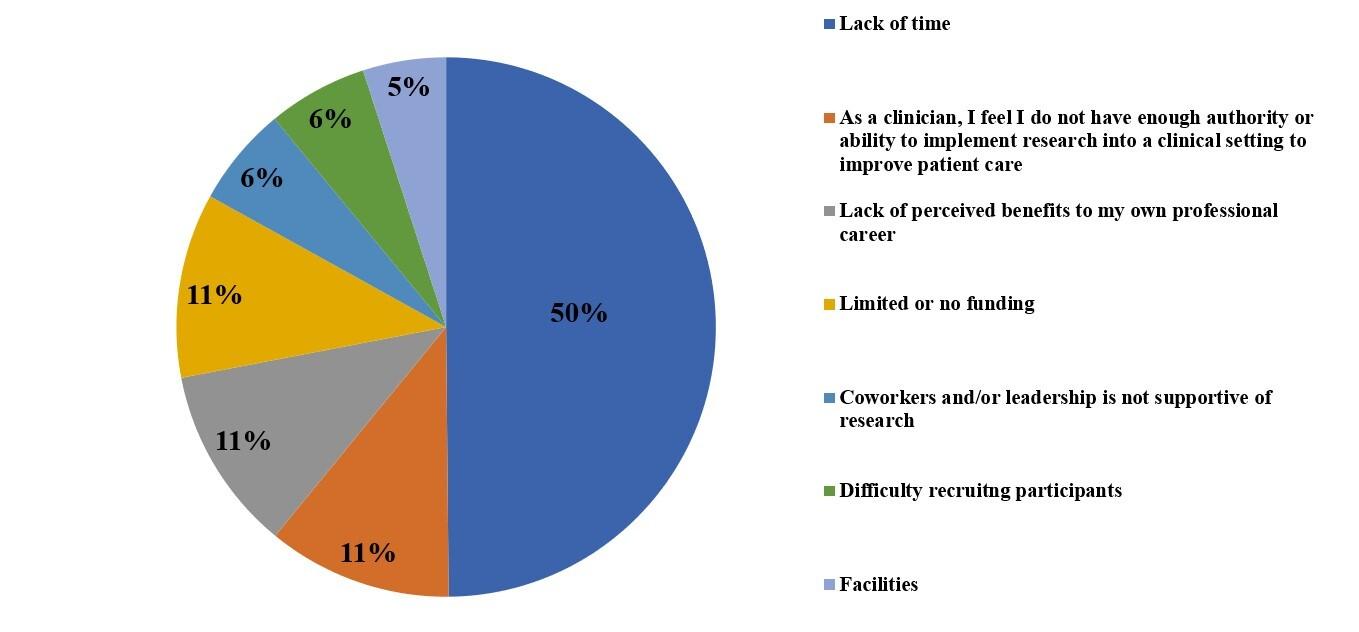
Note: no SM physicians chose “As a clinician, I feel I do not have enough authority or ability to implement research into a clinical setting to improve patient care,” “Limited access to a regulatory team,” Difficulty recruiting participants, and “Restrictive privacy law ”
Note: no AH practitioners selected “Limited access to a regulator team,” “Limited access to research coordinator,” “Limited access to biostatisticians,” “Restrictive privacy law,” and “Other ”
1. Membership in professional organization(s)
To No Extent
To a Little Extent
To a Moderate Extent
To a Great Extent No Opinion / Not Applied
Overall 3 (3.5%) 20 (23.5%) 29 (34.1%) 33 (38.8%) 0 (0.0%)
SM physicians 1 (1.8%) 14 (24.6%) 18 (31.6%) 24 (42.1%) 0 (0.0%)
AH practitioners 1 (4.5%) 5 (22.7%) 8 (36.4%) 8 (36.4%) 0 (0.0%)
2. Participation in special research interest group(s)
Overall 1 (1.2%) 13 (15.3%) 22 (25.9%) 46 (54.1%) 3 (3.5%)
SM physicians 1 (1.8%) 6 (10.5%) 14 (24.6%) 34 (59.6%) 2 (3.5%) AH practitioners 0 (0.0%) 5 (22.7%) 6 (27.3%) 10 (45.5%) 1 (4.5%)
3. Availability of research mentorship
Overall 0 (0.0%) 10 (11.8%) 30 (35.3%) 42 (49.4%) 3 (3.5%)
SM physicians 0 (0.0%) 6 (10.5%) 20 (35.1%) 29 (50.9%) 2 (3.5%)
AH practitioners 0 (0.0%) 3 (13.6%) 8 (36.4%) 11 (50.0%) 0 (0.0%)
4. Funding
Overall 5 (5.9%) 17 (20.0%) 22 (25.9%) 38 (44.7%) 3 (3.5%)
SM physicians 3 (5.3%) 13 (22.8%) 15 (26.3%) 24 (42.1%) 2 (3.5%)
AH practitioners 1 (4.5%) 4 (18.2%) 6 (27.3%) 11 (50.0%) 0 (0.0%)
5. Support from leadership/colleagues
Overall 2 (2.4%) 4 (4.7%) 28 (32.9%) 48 (56.5%) 3 (3.5%)
SM physicians 1 (1.8%) 2 (3.5%) 22 (38.6%) 30 (52.6%) 2 (3.5%)
AH practitioners 1 (4.5%) 1 (4.5%) 6 (27.3%) 13 (59.1%) 1 (4.5%)
6. Available time
Overall 6 (7.1%) 13 (15.3%) 9 (10.6%) 55 (64.7%) 2 (2.4%)
SM physicians 4 (7.0%) 10 (17.5%) 5 (8.8%) 37 (64.9%) 1 (1.8%) AH practitioners 1 (4.5%) 3 (13.6%) 3 (13.6%) 14 (63.6%) 1 (4.5%)
7. Research seen as beneficial to patient care
Overall 4 (4.7%) 5 (5.8%) 27 (31.8%) 45 (52.9%) 4 (4.7%)
SM physicians 2 (3.5%) 4 (7.0%) 17 (29.8%) 32 (56.1%) 2 (3.5%) AH practitioners 1 (4.5%) 2 (9.1%) 5 (31.8%) 11 (50.0%) 1 (4.5%)
8. Research training and education
Overall 1 (1.2%) 12 (14.1%) 36 (42.3%) 36 (42.3%) 0 (0.0%) SM physicians 1 (1.8%) 8 (14.0%) 25 (43.9%) 23 (40.4%) 0 (0.0%) AH practitioners 1 (4.5%) 3 (13.6%) 9 (40.9%) 9 (40.9%) 0 (0.0%)
9. Access to research resource (equipment, laboratory, software, etc)
Overall 5 (5.9%) 16 (18.8%) 30 (35.3%) 34 (40.0%) 0 (0.0%)
SM physicians 3 (5.3%) 14 (24.6%) 20 (35.1%) 20 (35.1%) 0 (0.0%)
AH practitioners 1 (4.5%) 3 (13.6%) 8 (36.4%) 10 (45.5%) 0 (0.0%)
10. Availability of research personnel (statisticians, research assistants, coordinators, etc)
Overall 3 (3.5%) 15 (17.8%) 17 (20.0%) 47 (55.3%) 3 (3.5%)
SM physicians 2 (3.5%) 8 (14.0%) 9 (15.8%) 36 (63.2%) 2 (3.5%)
AH practitioners 1 (4.5%) 4 (18.2%) 7 (31.8%) 9 (40.9%) 1 (4.5%)
Note: Fifteen responses were missing from overall (twelve responses from SM physicians, two responses from AH practitioners, and one response from others).
this difference was not statistically significant (p=0.267). The specific areas of research interests were presented in
Table 4 Additionally, actual research involvement is also displayed in Table 4.
Note: no SM physicians chose “Access to resources,” and “Other ”
Note: no AH practitioners selected “Membership in professional organization(s),” “Funding,” “Access to resources,” “Availability of research personnel,” and “Other ”
Regarding self-rated comfort in reading research articles, overall mean was 72.0±23.6 (95%CI: 67.2, 76.8) using a 0-100 scale (missing responses, N=5). In comparison be tween SM physicians and AH practitioners, the mean value was higher in SM physicians [75.6±20.6 (95%CI: 70.6, 80.6)] compared with AH practitioners [60.6±28.3 (95%CI: 47.0, 74.3)] (p=0.018). Additionally, overall mean score of self rated knowledge regarding conducting a research study in dependently was 68.4±20.5 (95%CI: 64.2, 72.5) using a 0-100 scale (missing responses, N=6). The mean value of the self-rated knowledge conducting research in SM physi
cians was 70.2±18.6 (95%CI: 65.7, 74.7), while AH practi tioners demonstrated a score of 63.4±24.6 (95%CI: 51.5, 75.2) (p=0.163). Available resources to perform research ac tivities as a whole and by each profession are shown in Table 5
The current study investigated barriers and facilitators to research, as well as other research related components in cluding interests, comfort, knowledge, and resources among SM physicians and AH practitioners. According to
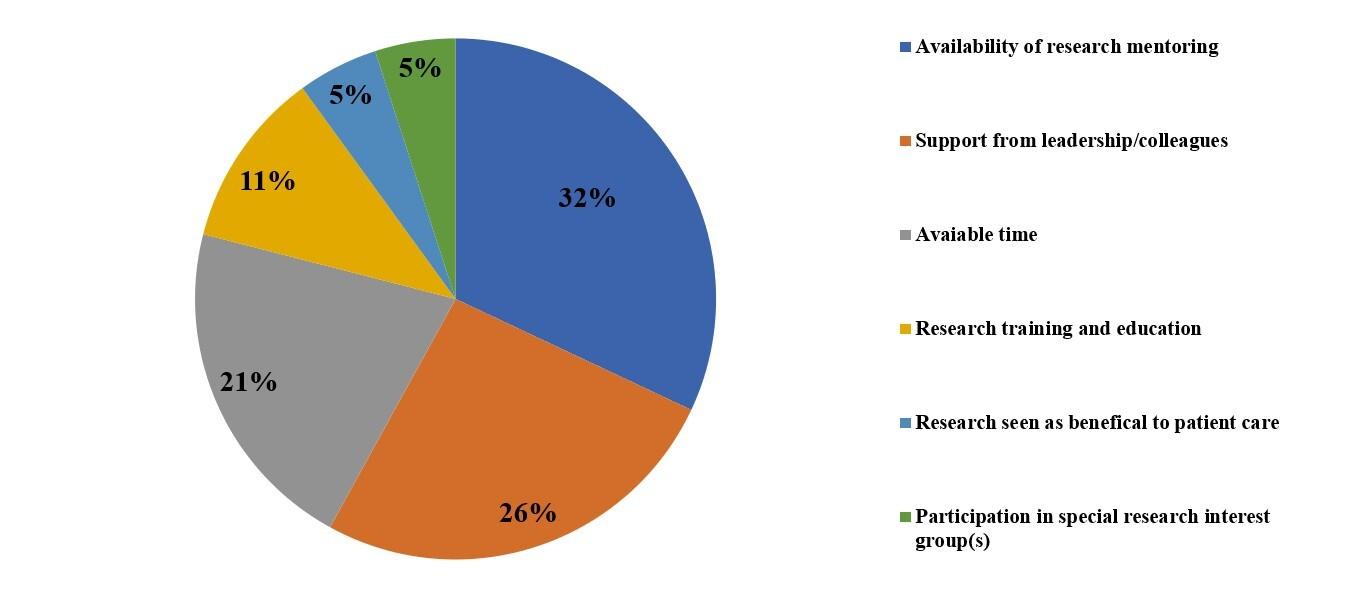
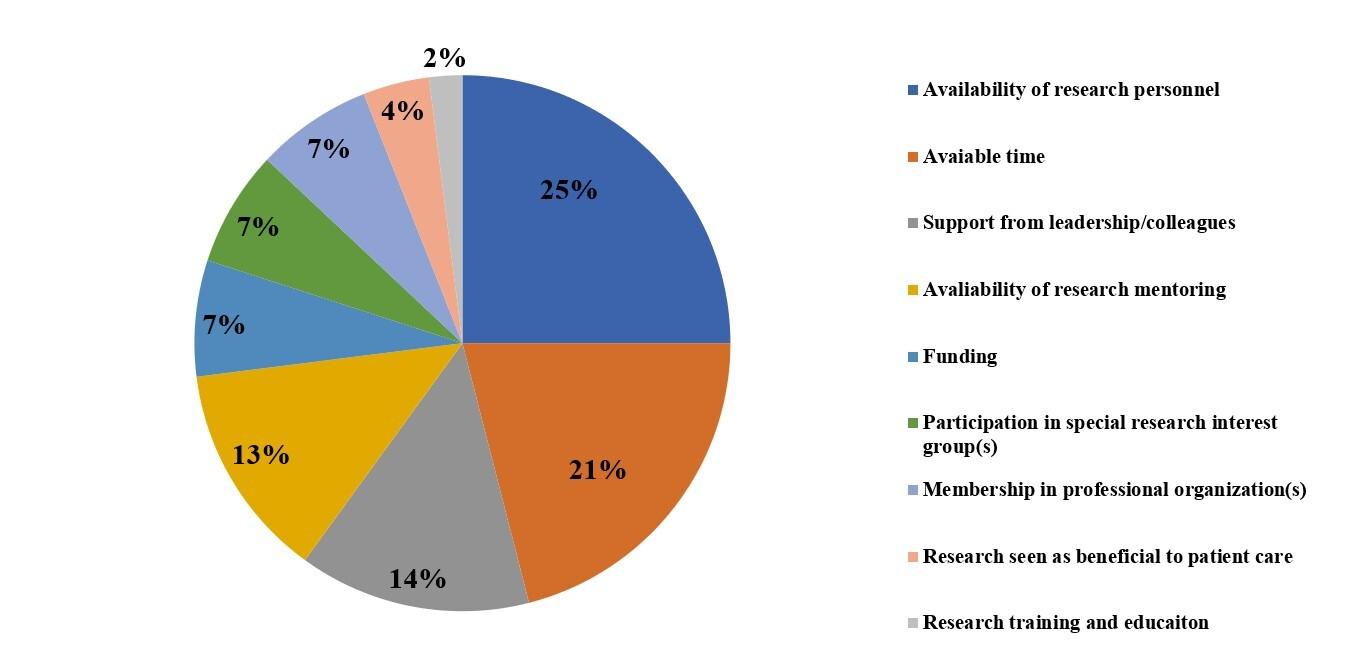 Figure 3. Research facilitators of SM physicians.
Figure 4. Research facilitators of AH practitioners.
Figure 3. Research facilitators of SM physicians.
Figure 4. Research facilitators of AH practitioners.
Interests:
Overall (N=92) SM Physicians (N=63) AH Practitioners (N=22)
Grant writing/editing 24 (26.1%) 16 (25.4%) 4 (18.2%) Manuscript writing/editing 62 (67.4%) 48 (76.2%) 11 (50.0%) Consultation 45 (48.9%) 35 (55.6%) 6 (27.3%) Supervision 41 (44.6%) 35 (55.6%) 3 (13.6%)
Research design/protocol development 54 (58.7%) 34 (54.0%) 16 (72.7%)
Data Collection 53 (57.6%) 33 (52.4%) 15 (68.2%) Data Analyses 43 (46.7%) 27 (42.9%) 12 (54.5%) Peer Review 54 (58.7%) 44 (69.8%) 7 (31.8%)
Others 1 (1.1%) 1 (1.6%) 0 (0.0%)
Involvement:
Grant writing/editing 41 (44.6%) 30 (47.6%) 6 (27.3%) Manuscript writing/editing 70 (76.1%) 55 (87.3%) 11 (50.0%) Consultation 40 (43.5%) 32 (50.8%) 5 (22.7%) Supervision 53 (57.6%) 43 (68.3%) 7 (31.8%)
Research design/protocol development 72 (78.3%) 52 (82.5%) 16 (72.7%) Data Collection 78 (84.8%) 55 (87.3%) 18 (81.8%)
Data Analyses 63 (68.5%) 48 (76.2%) 11 (50.0%) Peer Review 62 (67.4%) 49 (77.8%) 9 (40.9%) Others 0 (0.0%) 0 (0.0%) 0 (0.0%)
Resources:
Overall (N=90) SM Physicians (N=62)
AH Practitioners (N=21)
Graduate students (PhD, Masters) 34 (37.8%) 21 (33.9%) 9 (42.9%)
Facilities for research (equipment, space) 58 (64.4%) 38 (61.3%) 16 (76.2%)
Residents 67 (74.4%) 54 (87.1%) 8 (38.1%)
Research coordinator 62 (68.9%) 45 (72.6%) 13 (61.9%)
Research technician 18 (20.0%) 15 (24.2%) 1 (4.8%)
Biostatistician 45 (50.0%) 38 (61.3%) 5 (23.8%)
Statistical/Analytical software 43 (47.8%) 29 (46.8%) 11 (52.4%)
None 8 (8.9%) 8 (12.9%) 0 (0.0%)
Other 4 (4.4%) 4 (6.5%) 0 (0.0%)
Note: Ten responses were missing (seven responses from SM physicians and three responses from AH practitioners).
our data, both SM physicians and AH practitioners identi fied a lack of time as the top barrier to research partici pation (Figures 1, 2). However, the remaining top research barriers were different between the two professions. The second and third most common research barrier identified from SM physicians were limited access to a research co ordinator and having co-workers or leadership that is not supportive of research. This finding indicated the impor tance, for SM physicians, of having access to valuable re
search staff as well as support from peers and leadership. Conversely, the second and third barriers in AH practition ers were apparently related to a negative mindset/outlook toward research.
AH practitioners who participated in the current study were PTs and ATs. Since investigations related to research barriers and facilitators of PTs and ATs were understudied, available studies related to another group of AH practition ers, nurses, were synthesized.16–19 A few studies indicated
Note: Eight responses were missing (six responses from SM physicians and two responses from AH practitioners).that the negative mindset/outlook toward research activi ties may stem from a clinical hierarchy between physicians and nurses.16–18 The authors of these studies described that nurses were not ranked or positioned to change clinical practices within the clinical setting.16–18 They postulated that a lack of autonomy in the clinical setting may neg atively influence research interests and activities.16,18,19 This description aligns well with the current study findings (Figure 2). About 11% of respondents from the AH practi tioners in the current study showed disbeliefs and/or doubt of having enough authority or ability to implement re search into a clinical setting to improve patient care. Ad ditionally, another 11% of respondents from the AH prac titioners did not perceive research as being beneficial to their own professional career This may be related to an other barrier, coworkers and/or leadership is not supportive of research, among the AH practitioners (6%). In fact, one study discussed that an underlying major research barrier was a lack of research support from leadership.3 This lack of research support from leadership stemmed from the culture of the AH practitioners work environment.3 According to this report,3 direct patient care is usually perceived as a pri mary responsibility, and research activity was often viewed as secondary or as a non-essential task in AH practition ers.3 The primary job of both PTs and ATs is, indeed, di rect patient care, and therefore, if research is perceived as a non-essential task, this will likely contribute to the per ceived lack of benefit that PTs and ATs feel toward spending time engaging in research activities.
Research facilitators were distinctively different and unique in each profession (Figure 3, 4). Among SM physi cians, availability of research personnel was the top facil itator (25%) followed by available time (21%). Underlying reasons of these facilitators may stem from a special role a few SM physicians often take. One unique role of SM physicians is to work as a local sports team doctor.20,21 The responsibility of working as a team doctor is consid erably comprehensive, especially for a collision sport such as American football,22,23 and for some high-profile teams, traveling with the team is also a part of the job.24 In short, serving a team physician to local sports teams is a timeconsuming commitment, which explains the reason why availability of research personnel to facilitate research ac tivities is extremely important. Furthermore, SM physicians reported being are more comfortable reading research arti cles than AH professionals and reported a higher self-per ceived ability to conduct research independently (although not statistically different) as compared to AH practition ers. Therefore, having access to available research person nel may be a key factor to the promotion of research activi ties within their limited time.
Unlike selections of SM physicians, availability of re search mentoring (32%) and support from leadership/col leagues (26%) were chosen as leading facilitators from AH practitioners. The importance of available time as a re search facilitator has been previously documented by var ious authors.3,25–27 However, the availability of mentoring and support from leadership/colleagues as primary facili tators expressed by PTs and ATs has not been previously
reported. This alone is an important finding to highlight, indicating the current lack of mentorship or support from leadership among AH professionals. This concept should be considered moving forward when evaluating and dis cussing barriers and facilitators in SM research. Yet, it is essential to recognize that this finding may also be unique to the field of SM, given the prevalence of PTs and ATs in this community Furthermore, although not statistically significantly different, AH practitioners showed greater re search interests (95.5%) than SM physicians (87.0%), espe cially with regards to research design/protocol development and data collections, while having less access to a research technician and a biostatistician. These findings emphasize the importance of providing support to further facilitate re search activities in AH professionals.
A potential solution to overcome the identified barriers and nurture the facilitators may be to develop those who have a role as researcher associates. In this study, 7% of the survey respondents did not have clinical duties and were la beled “others”, and their primary responsibilities were as sociated with research activities. Since a lack of time was the top barrier for both SM physicians and AH practitioners, collaborating with research associates (others) may help save time and facilitate participation. For instance, pivotal research activities such as preparing IRB documents, an alyzing collected data, and drafting scientific manuscripts often take substantial time. However, research associates may be able to optimize these steps and shorten the time in each step. Additionally, availability of research person nel was found as a leading facilitator in SM physicians, and research associates are an ideal candidate to fill their needs. Furthermore, availability of research mentoring was selected as the greatest facilitator in AH practitioners. De veloping a mentor-mentee relationship with established re searchers may help enhance research productivity of AH practitioners. In summary, leadership and/or administra tors should investigate promoting and solidifying a collabo rative relationship among SM physicians, AH practitioners, and research associates.
Several limitations need to be stated, with a main limita tion being that the current study data were obtained solely from the PRiSM membership. Clinicians and practition ers who are in societies such as PRiSM, are likely to al ready have positive perspectives on research, and thus in troduce a potential bias in the study findings, especially as involvement is typically on a volunteer basis. Regardless, this preliminary assessment into barriers and facilitators is an important first step in capturing the current state of research participation among members in the SM commu nity. Furthermore, although the current study had accept able response rate (35.7%), an overall number of survey re spondents was 100, which is a relatively small sample size. Also, nearly all members were geographically located in the US and Canada. Thus, the results may not be general ized to other regions or continents of SM physicians and AH practitioners. Additionally, responses from AH practi tioners (24%) were lower than SM physicians (69%). More
over, approximately 9% of respondents had additional de grees such as a Doctor of Philosophy (PhD), Masters of Public Health (MPH), and Masters of Science (MSc). Some respondents may be using those degrees as their primary responsibility/function in their institutions. Lastly, the sur vey was programmed to be sent to each of the PRiSM mem bers only once. To avoid confusion and errors, the survey was directly delivered from the PRiSM headquarters to all PRiSM members. The collected responses were rigorously checked. However, the possibility of responses from nonmembers and potential duplicates (multiple responses from one member) could not be eliminated.
The results of this study indicate that a lack of time was the top research barrier for both SM physicians and AH prac titioners. Research facilitators were different between SM physicians and AH practitioners. Having available person nel was the main facilitator for SM physicians, while avail
ability of mentoring was the leading facilitator in AH prac titioners. Those who take a leadership position in a SM department may need to be aware these findings, especially if enhancement of research productivity is priority. Future studies are warranted to investigate other parameters to optimize evidence-based practices.
All authors have no conflict of interest to disclose.
Submitted: January 28, 2022 CST, Accepted: August 16, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71-72. doi:1 0.1136/bmj.312.7023.71
2. Guyatt G. Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992;268(17):2420. doi:10.1001/jama.1992.03490170 092032
3. Paget SP, Caldwell PHY, Murphy J, Lilischkis KJ, Morrow AM. Moving beyond ‘not enough time’: factors influencing paediatric clinicians’ participation in research. Intern Med J. 2017;47(3):299-306. doi:1 0.1111/imj.13351
4. Gelijns AC, Gabriel SE. Looking beyond translation--integrating clinical research with medical practice. N Engl J Med 2012;366(18):1659-1661. doi:10.1056/nejmp1201850
5. Ozdemir BA, Karthikesalingam A, Sinha S, et al. Research activity and the association with mortality. PLoS ONE 2015;10(2):e0118253. doi:10.1371/journa l.pone.0118253
6. Munk-Jørgensen P, Blanner Kristiansen C, Uwawke R, et al. The gap between available knowledge and its use in clinical psychiatry Acta Psychiatr Scand 2015;132(6):441-450. doi:10.1111/acps.12512
7 Yin HL, Gabrilove J, Jackson R, Sweeney C, Fair AM, Toto R. Sustaining the Clinical and Translational Research Workforce: Training and Empowering the Next Generation of Investigators. Acad Med 2015;90(7):861-865. doi:10.1097/acm.0000000000000 758
8. Roberts SF, Fischhoff MA, Sakowski SA, Feldman EL. Perspective: Transforming science into medicine: how clinician-scientists can build bridges across research’s “valley of death.” Acad Med 2012;87(3):266-270. doi:10.1097/acm.0b013e3182446 fa3
9. Bookey-Bassett S, Bianchi A, Richards J, Kelly H. Overcoming Challenges to Support ClinicianScientist Roles in Canadian Academic Health Sciences Centres. Health Q 2019;22(1):60-66. doi:1 0.12927/hcq.2019.25834
10. Yoon S, Koh WP, Ong MEH, Thumboo J. Factors influencing career progress for early stage clinicianscientists in emerging Asian academic medical centres: a qualitative study in Singapore. BMJ Open. 2018;8(3):e020398. doi:10.1136/bmjopen-2017-02039 8
11. Bonner A, Sando J. Examining the knowledge, attitude and use of research by nurses. J Nurs Manag 2008;16(3):334-343. doi:10.1111/j.1365-2834.2007.00 808.x
12. Grimmer-Somers K, Lekkas P, Nyland L, Young A, Kumar S. Perspectives on research evidence and clinical practice: a survey of Australian physiotherapists. Physiother Res Int 2007;12(3):147-161. doi:10.1002/pri.363
13. Higgins I, Parker V, Keatinge D, et al. Doing clinical research: the challenges and benefits. Contemp Nurse. 2010;35(2):171-181. doi:10.5172/con u.2010.35.2.171
14. Eller LS, Kleber E, Wang SL. Research knowledge, attitudes and practices of health professionals. Nurs Outlook 2003;51(4):165-170. doi:10.1016/s0029-655 4(03)00112-x
15. Roberts R, Perry N, Phillips A, Richardson D, Soni S. Clinical research should be a priority in the NHS but what do genito-urinary medicine clinic staff think? Int J STD AIDS. 2015;26(2):107-112. doi:10.117 7/0956462414531241
16. Parahoo K. Barriers to, and facilitators of, research utilization among nurses in Northern Ireland. J Adv Nurs. 2000;31(1):89-98. doi:10.1046/j.1 365-2648.2000.01256.x
17 Funk SG, Champagne MT, Wiese RA, Tornquist EM. Barriers to using research findings in practice: the clinician’s perspective. Appl Nurs Res 1991;4(2):90-95. doi:10.1016/s0897-1897(05)80062-x
18. Walsh M. Perceptions of barriers to implementing research. Nurs Stand 1997;11(19):34-37 doi:10.7748/ ns.11.19.34.s46
19. Solomons NM, Spross JA. Evidence-based practice barriers and facilitators from a continuous quality improvement perspective: an integrative review J Nurs Manag. 2011;19(1):109-120. doi:10.1111/j.136 5-2834.2010.01144.x
20. Miller TL, Jones GL, Hutchinson M, Vyas D, Borchers J. Evolving Expectations of the Orthopedic Team Physician: Managing the Sidelines and Landmines. Curr Sports Med Rep 2021;20(10):553-561. doi:10.1249/jsr.0000000000000 896
21. Tayne S, Hutchinson MR, OʼConnor FG, Taylor DC, Musahl V, Indelicato P. Leadership for the Team Physician. Curr Sports Med Rep 2020;19(3):119-123. doi:10.1249/jsr.0000000000000696
22. Wojtys EM. Team Physician Quagmire. Sports Health 2018;10(3):203-204. doi:10.1177/1941738118 768271
23. West R. Back to Basics: The Role of the Team Physician. Am J Orthop (Belle Mead, NJ) 2016;45(6):338.
24. Jenoure P. The travelling sports physician. Rev Med Suisse 2016;12(525):1267-1270.
25. Hommelstad J, Ruland CM. Norwegian nurses’ perceived barriers and facilitators to research use. AORN J 2004;79(3):621-634. doi:10.1016/s0001-209 2(06)60914-9
26. Carroll DL, Greenwood R, Lynch KE, Sullivan JK, Ready CH, Fitzmaurice JB. Barriers and facilitators to the utilization of nursing research. Clin Nurse Spec 1997;11(5):207-212. doi:10.1097/00002800-19970900 0-00009
27 Abrahamson KA, Fox RL, Doebbeling BN. Facilitators and barriers to clinical practice guideline use among nurses. Am J Nurs 2012;112(7):26-35; quiz 46,36. doi:10.1097/01.naj.0000415957.46932.bf
Download: https://ijspt.scholasticahq.com/article/39739-barriers-and-facilitators-of-research-in-pediatric-sportsmedicine-practitioners-a-survey-of-the-prism-society/attachment/ 103276.pdf?auth_token=AHw9Y-94PbmydYX5aS5R
Lorenz D. Progressive Loading in a Strongman Following Distal Biceps Repair: ReThinking Load Progression – A Case Report. IJSPT. Published online November 1, 2022:1430-1441.
Daniel Lorenz, DPT, PT, ATC, CSCS 1 a
1 Physical Therapy, Lawrence Memorial Hospital/OrthoKansas
Keywords: distal biceps rupture, shared decision making strongman, blood flow restriction, ischemic preconditioning https://doi.org/10.26603/001c.39796
Rupture of the distal biceps is relatively rare and post-operative protocols are typically vague and are used on many patients, regardless of pre-morbid status. The primary objective is to share the progressive loading strategy used in the rehabilitation of a strongman athlete following a surgical repair of the distal biceps. An additional objective is to highlight the need for individualized protocols and progressions with respect to patient goals and sport demands, as well as the need for shared decision making (SDM) between the medical doctor, patient, and rehabilitation provider.
The subject is a 39-year-old strong man competitor who suffered a distal biceps rupture while doing a tire flip during training. After having it repaired, the post-operative recovery was unremarkable. The focus of the described intervention was establishing load during rehabilitation exercises that were unique to this individual based on his pre-morbid level of strength and training history as well as the unique demands of his sport.
The patient achieved symmetrical isokinetic strength of the elbow flexors at 60°/second in supine at six months post-operative.
The case highlights a successful outcome in a strongman competitor with a distal biceps rupture repair Typically, protocols are vague and lack specific standards for establishment of load for exercises. Often starting points and progressions are arbitrary and lack rationale tailored to individual needs and/or pre-morbid status. The case offers a framework for establishing and progressing load while also discussing how a shared decision-making model can lead to positive outcomes.
Avulsion of the distal biceps brachii tendon represents about 3% of bicep tendon injuries.1 The typical mechanism of these injuries occurs in a flexed elbow and supinated forearm position,1,2 which may be associated with acute tensile overload.3 Patients frequently report a history of an audible pop and acute pain at the antecubital fossa after an eccentric contraction of the biceps caused by unexpected
extension force applied to a flexed elbow with the forearm in a supinated position.3,4 The majority of patients with distal bicep tendon ruptures are males in the fourth to fifth decade of life, and 52-86% occur in their dominant extrem ity.2,5,6 Common risk factors include increased body mass index (BMI), use of anabolic steroids, smoking, weightlift ing, and bodybuilding.1,4–7 Distal biceps rupture (DBR) can result in functionally significant loss of supination and el bow flexion strength, as well as decreased resistance to
a

Corresponding Author: Dan Lorenz
6265 Rock Chalk Dr. Suite 1700, Lawrence, KS 66049
Phone: 785-838-7812
Email: danielslorenz@gmail.com
fatigue.1–8 Immediate surgical repair is the recommended course of treatment, but delaying surgery for a few weeks after diagnosis has been found to be equally beneficial com pared to patients who have early surgical intervention within a week of injury.9 In other words, immediate repair is advocated in ideal circumstances but a short delay may not necessarily lead to worse outcomes.
Strongman is a competitive sport where athletes perform a variety of tasks with very high loads to test physical strength and stamina. The first World’s Strongest Man com petition took place in 1977 Most strongman competitions consist of six to eight events. Contestants are awarded points for each event based on their position in stand ings.10 Strongman competitions typically have four key components the overhead or push press, the deadlift, grip strength, and anaerobic capacity.11 Strongman has some nuances in competition compared to other weightlifting sports. Contrary to powerlifting and weightlifting where only a loaded bar is used, strongman events often have im plements like logs (Figure 1 ), atlas stones (Figure 2), axles, sandbags, or devices that allow high loads to be carried over distances, like the farmer’s walk (Figure 3) or the yoke walk (Figure 4). Tire flips (Figure 5) and pushing/pulling high loads like sleds, vehicles or trucks (Figure 6) or sustaining isometric contractions with high loads such as the “Her cules Hold” (Figure 7) are also often a part of strongman competitions. Strongman competitors face a high relative risk of bicep injury due to their body mass coupled with lift ing high loads.



Among strongman competitors, in a retrospective re view12 of 213 strongman athletes, 82% reported injuries. Most (24%) common were in the low back, followed by bicep and knee (11% each), with most being strains of muscle (38%) and tendon (23%). 68% of the injuries were acute.12
There were significantly more competition injuries for those under 30 years of age compared to those over the age of 30.12 Training with implements almost doubled the in juries compared to traditional weight training methods us ing barbells, dumbbells, or universal weight training ma chines.12 Ninety-one percent of those injured sustained injuries when lifting loads 90% of 1RM or greater. The inci dence of bicep injury in the strongman athlete was higher than for weightlifting,13 powerlifting,13,14 and bodybuild ing.15 Events like the tire flip and stone lifts suggest that bicep weakness or fatigue may limit the transfer of force produced from the larger muscle groups about the shoulder and torso and increase bicep injury risk.12 Deadlifting has also been implicated as a mechanism of bicep rupture. A study evaluating mechanisms of distal bicep found that all ruptures occurred in the supinated arm in “mixed grip” lifters when the elbow was in extension (“mixed grip” is when one hand is supinated and the other is pronated). As such, researchers proposed that eccentric loading on an ex tended and supinated elbow may be an alternative mecha nism of injury.4




Due to the nature of the sport, the extreme loads lifted, as well as the pre-morbid strength levels of these athletes, adjusting rehabilitation protocols to accommodate the physical capabilities of the athlete is warranted. Alterna tively, there may be implications for healing rate and strength of repair due to pre-morbid status. A published post-operative protocol limited loading to 5-10 pounds for the first several weeks and limited biceps isotonics till 12 weeks,8 but protocols vary among surgeons. The reattach ment site is at the greatest risk for failure during the first one to two weeks after surgery.8 Normal tension of the bi cep with the elbow at 90° against gravity is about 50 New tons.8,15 Mazzocca et al.16 evaluated four different distal bicep repair techniques and cyclical load to failure varied from 232 Newtons to 440 Newtons. Kettler and others17 evaluated the linear load to failure strength of thirteen dif ferent methods for distal biceps tendon repair and found
that the EndoButton had a significantly higher failure load than other techniques (259 +/- 28 N), with a mean failure rate of 180 N among all methods. The transosseous suture technique, used for the subject in this case, showed a mean failure of 210 +/- 29 N. In Kettler et al.,17 no tendon failure was seen in any transosseous or suture anchor repair when using an Ethibond No. 2 suture. Of note, the subject in this case was fixated with FiberWire, rather than Ethibond. A previous study by Miller et al.18 comparing orthopedic su tures found that FiberWire had higher ultimate load to fail ure and resisted the greatest number of cycles to failure compared to Ethibond and other suture types. The clinical utility of cadaveric study information is questionable how ever because the Mazzocca et al16 study was in “much older” elbows with low bone density and it included cyclic loading at 3600 cycles with 50 Newtons. In contrast, the Kettler et al.17 study was linear load to failure, but also in cadaveric elbows with an age range of 79 +/- 13 years. Older, cadaveric elbows with low bone density are arguably not a proper comparison with the patient in this case.
From a rehabilitation perspective, it has been suggested that unrestricted or early range of motion may begin earlier since repair strength is greater than the force of an un weighted forearm in a splint or brace.19–21 Restrictions typ
Figure 4. Yoke Walkically include lifting no more than five pounds and no supination against resistance. At six weeks, gradual strengthening of the upper extremity and aerobic condi tioning may begin.8 Strength training commences usually about two to three months post-operative.22 Return to heavy lifting is allowed at three to six months after surgery. The reader is referred to rehabilitation plans that have been outlined previously 23–25
Given that each patients’ demands are unique, should this same loading restriction in the initial phases be used for a strongman as it would be for a recreational athlete? In Srinivasan et al.,8 return to heavy lifting is suggested at three to six months after surgery. What defines “heavy?” A heavy load for one patient may be maximal for another, and a general warm-up for yet another Therefore, the pur pose of this case report is twofold. The primary objective of this case report is to share the progressive loading strat egy used in the rehabilitation of a strongman athlete fol lowing a DBR repair An additional objective is to highlight the need for individualized protocols and progressions with respect to patient goals and sport demands, as well as the need for shared decision making (SDM) between the med ical doctor, patient, and rehabilitation provider 24
The subject (age = 39 years old, height= 187 cm, weight= 125kg) is a right-hand dominant male who ruptured his right distal bicep tendon doing a tire flip. The subject un derwent successful surgical repair (DBR) approximately 14 days later. Post-operatively, he was placed in a splint at 90° flexion with the forearm supinated. Per the physician pro tocol for this subject, the first two weeks required the el bow brace to be locked at 90° when not performing reha bilitation activities. Exercises included elbow extension to 45° with the forearm supinated, passive elbow flexion to tolerance, passive forearm pronation and supination with the elbow flexed to 90°, and maintenance of range of mo tion of the shoulder, wrist, and hand. From two to six weeks post-operative, the elbow brace was to remain locked at 90° when not doing rehabilitation exercises. Exercises during this time frame included elbow active extension and pas sive flexion. Extension was allowed to be increased by 15° per week. While braced, the protocol advised light progres sive resistance exercise for the musculature of the shoul der and grip strength exercises, but no active or resisted bi ceps work. From weeks six to eight, he was to wean from the brace and begin active elbow flexion without resistance. If needed, more aggressive treatments to get full extension could be utilized. From weeks 8-12, resisted bicep isotonic exercises could be initiated, and at twelve weeks post-op erative, the protocol indicated that sport-specific activities could commence.
The subject’s first physical therapy visit was approxi mately three weeks post-operatively The subject presented to physical therapy with his brace at 90° flexion. The wound was healed, wrist and hand motion were symmetrical and pain free. Left elbow range of motion was 0-150°, while the right was 11-142° passively (note, lacking 11 degrees
from full extension).There were no other objective mea sures performed on this date because a lengthy discussion commenced about his displeasure with what he felt was a generic protocol that didn’t suit his needs. He felt that he should not be doing the same protocol as the typical pa tient would. The subject was very frustrated with his med ical provider and the lack of guidance he received, and he was dismayed by the fact that the protocol read “updated in 2015,” about six years before his injury. Further, he felt like advances had to have been made since then. He struggled with compliance as he believed there had to be more cur rent knowledge and subsequently adjustments or updates to treatment protocols. As the discussion progressed, he revealed that he was doing some active flexion out of his brace in the early phases and had not been very compli ant with his brace. The subject was educated on the need for compliance with brace use and avoiding active flexion range of motion to protect his repair and healing until told otherwise. The potential adverse effects of non-compliance were highlighted by discussing graft failure. The physical therapist also talked about long-term planning and goals and a timeline was discussed for getting back into his de sired level of high loading activities necessary for training for strongman events. The physical therapist also made it clear that in order to continue working together, there had to be some mutual respect and compromise on progression of activities.
On the second visit three days later, gentle isometrics of the bicep at 90° flexion using two-fingers of resistance mid-forearm and multi-angle tricep isometrics were initi ated. Even though the protocol at the time called for no ac tive bicep work, gentle two-finger isometrics with a short lever arm at mid forearm was used due to the patient’s premorbid status and to retard muscle atrophy.
Blood flow restriction (BFR) training (Delfi Medical, Van couver, BC) with supine tricep extension to 30° of extension utilizing a resistance band was performed to help accom modate the subject’s desire to “somehow get some arm work in.” He was pre-occupied with the level of atrophy compared to his uninvolved arm already. Given the sub ject’s typical workout routine and level of effort he was ac customed to, BFR to the triceps was a reasonable compro mise to simultaneously protect the repair and potentially provide some psychological benefit to the patient by en hancing low-load training. BFR is a training modality that utilizes low loads to promote hypertrophy and strength gains in muscle when higher loads are not appropriate.26 Sessions closed with neuromuscular electrical stimulation (NMES) to the bicep with the arm resting at his side in approximately 90° flexion, followed by ischemic precondi tioning (IPC) to the involved arm inferior to the deltoid tuberosity. Contrary to BFR being performed with exercise at a percentage of arterial occlusion pressure for three to five sets of an exercise, IPC is performed with full occlusion at rest for three to five minutes followed by reperfusion for three to five minutes, and this cycle is repeated three times. IPC has been shown to increase muscle perfusion,27,28 oxy gen uptake and force in strength-trained athletes,26,27 in crease microvascular blood flow,28 provide an ergogenic
benefit,29 increase muscle performance when performed prior to resistance training,30 and help with recovery.31 IPC was used in this case after the session to potentially help with recovery and the muscle physiology benefits listed above, but also to maximize individualized patient care time. While the benefit of IPC for this subject is debatable, he was grateful for the progressive approach to his reha bilitation that went beyond the general protocol. For his home program, he was also encouraged to perform highload isolated biceps isotonics to his uninvolved side to po tentially realize the benefit of cross-education. Cross-edu cation is the use of unilateral resistance training to increase the strength of the contralateral non-trained side.32 Sato et al.32 found that progressive eccentric or concentric elbow flexor activity performed twice a week for five weeks showed strong cross-education effects on involved side maximum voluntary isometric contraction (MVIC) and one-repetition maximum (1RM).
The subject was seen only once a week due to his sched ule and the distance he travelled for his appointments. Ses sions involved soft tissue and scar mobilization, passive range of motion, elbow joint mobilizations, isometrics, and exercises and modalities described previously At week six, despite the initial protocol limiting resisted bicep activities till eight weeks, he was cleared by his physician to begin resisted exercise at week six with a five-pound restriction and was “released to his PT.” The physical therapist was unable to reach the provider for confirmation. The subject was again frustrated by the minimal guidance received by his medical provider, stating that he was only told not to “ go too heavy too fast.” For this subject in particular, “too heavy” for him would far exceed a maximal attempt for a typical patient. For rehabilitation professionals in a num ber of settings, there is a delicate balance between tailoring protocols to individual histories and physical qualities prior to injury or surgery and respecting the healing process. Arbitrary guidelines are provided (such as the statement above) with no sound progression or template for patients or their rehabilitation providers.
At this physical therapy visit, the subject’s range of mo tion was 2-141° actively, and 0-145° passively Bicep strength was measured with a hand-held dynamometer (HHD) in sitting with elbow flexed to 90°. The subject was instructed to push to comfort without pain or pulling sen sation over the repair site. Testing consisted of three, fivesecond flexion tests against a rigid dynamometer placed in his hand. His uninvolved side averaged 48 pounds while the involved side averaged 26 pounds. The rationale for per forming HHD testing at 90° because the bicep is more vul nerable the closer the lifting load is to extension based on previously discussed mechanisms of injury The test was not intended to be a maximum force assessment but rather a test of force to tolerance without pain. Interestingly, the uninvolved side values seemed rather low given his premorbid status. These lower-than-expected values may be due to the position of the elbow during testing or a decline in strength due to limited resistance training of the un involved side since the surgery At this time frame, sled pushes were added with the elbow was locked in extension
and the movement was driven by the legs. Additionally, iso metric mid-thigh pull (IMTP) (Figure 8) was added with the involved side in pronation due to previous studies showing the supinated grip position has been implicated in DBR.4 The IMTP is a useful exercise in rehabilitation because it has been correlated to athletic capabilities of strength, maximal sprint speed, countermovement jump, and change of direction tests.33–35
Bench press as well as barbell military press were initi ated at six weeks post-op due to the subject’s previous ex perience and desired goals as well as the limited involve ment of the bicep in these activities. Saeterbakken and colleagues36 previously found that that flat bench press resulted in 48.3%-68.7% less bicep activity than incline bench position and that a narrow grip (biacromial distance) elicited lower bicep loads than a wide grip (50% more than biacromial distance). For the military press, Saeterbakken and Fimland37 found similar EMG of the biceps during seated barbell and dumbbell shoulder press, and about 16% greater bicep activation in standing barbell versus dumbbell shoulder presses. Loads used were either 30% of previous one-repetition maximum (1RM), 30% bodyweight, or com fort, whichever came first. The American College of Sports Medicine (ACSM) has previously stated38 that for muscular endurance training, the loads should be about 50% of 1RM and this was supported by Schoenfeld et al39 in a later re view These guidelines are in the healthy general popula tion. 30% was used because it is about half of the load used in the healthy population as suggested by the ACSM.38 The rationale here was to establish a load that was pain free and that the subject felt comfortable/confident with while facilitating proper technique. For this subject, previ ous best on the bench press was close to 400 pounds. He worked up to 185 pounds on the first day after initial sets

of five repetitions each at 95, 135, and 165 pounds. Pre vious military press 1RM was 270 pounds, and the sub ject worked up to 95 pounds in the first training session. Given the subject’s extensive training experience, he was given the freedom to load within a subjectively comfortable range on these specific lifts with the guidelines of limiting to no more than 50% of previous 1RM. This approach al lowed the subject to have input into his progression limited by his subjective analysis of limb confidence, comfort, and pain or pulling sensation at the distal bicep during the lifts (had to be absent). It was theorized that using pain, a sub jective increase in “pulling sensation” at the location of the repair, or breakdown in exercise technique would be an adequate clinical basis for judgment of load tolerance. In this case, the subject’s pre-morbid status along with sur rounding healthy tissue stress shielding the bicep as well as these being multi-joint, total body lifts made this a plau sible guideline. Additionally, almost all the exercises per formed were not bicep exercises in isolation or where the bicep is the prime mover, as would be the case in bicep curls or pull-ups. In the exercises performed, the biceps acted as stabilizers or synergists.
When isolated bicep isotonics commenced at week six, BFR was used due to the ability to improve strength and hypertrophy with low loads. The use of BFR enabled the physical therapist to load the bicep in isolation but miti gating risk of injury by using heavier loads without BFR. An initial load of five pounds was used due to it being the physician recommendation. The subject performed the sug gested repetition scheme of 30/15/15/15 with 45 seconds rest between sets and the cuff remaining inflated. If the subject did not achieve failure or close to it on the final set, weight was increased one to two pounds for subsequent sessions.
At week eight, seated rows with a pronated grip were added, along with hammer curls using a rope with the fore arm pronated at the start and ending the concentric phase in a neutral forearm position. Barbell snatch was also added at 30% of previous military press best. Chen and others40 found that bicep activity in the snatch increases with greater loads and velocities. Olympic lifts are typically per formed at maximal velocities. Due to the low loads for this subjects and low speed/effort of performance, it was not ex pected that the bicep load would be too high for this point in time.
From weeks 10-12, a neutral forearm grip was used for all lifts including seated rows, trap bar deadlifts, and ham mer curls, for example. The subject’s previous 1RM on the straight-bar deadlift was 900 lbs. Load was established to 30% of that for the first day, up to 270 lbs. At week 12, a supinated grip was used for more exercises, including the deadlift. Additionally, a front dumbbell carry was added to the routine, similar to the atlas stone carry position. His in volved side HHD at 90° flexion averaged 46 pounds of force and 67 pounds on the uninvolved at the twelve-week as sessment. Based on these HHD values, a 55-pound dumb bell was used as his target starting load due to the shared bilateral bicep load for the exercise and was increased 10% till the subject felt the load was comfortable Also at 12
Table 1. Proposed grip progression for weight training following distal biceps rupture and repair.
Involved side pronated 8-10 Neutral 10-12 Involved side supinated 12+
weeks, farmer walks with a trap bar were added. The farmer walk load commenced up to 30% of previous deadlift best. For all lifts, load was increased 20% per week as tolerated. Interestingly, the subject inquired about doing pull-ups at a previous visit and was advised against doing so, then came to his following visit with studies showing very high bicep EMG activity during pull-ups.41,42 These were avoided at this time. The reader is referred to Table 1 for the exercise grip progression used in this case.
At 16 weeks, the first isokinetic test was performed in supine and he had an 11% deficit at 60°/second in elbow flexion. It was performed at this point due to the subject having approximately eight weeks of strength training completed. On his 15th visit at six months post-op, his iso kinetic testing was symmetrical and he was released to re sume training as tolerated with the addition of implements and he was cleared for progression to pull-ups at this time, starting with assisted pull-ups using elastic bands. The sub ject was strongly advised to obtain full clearance from his physician.
This case highlights two primary concerns in establishing resistance with load in the post-operative patient. First of all, this case highlights the call for medical and rehabili tation professionals to be more specific regarding progres sions and loading rather than speaking in vague descrip tions such as “don’t go to heavy,” “don’t go too fast,” “don’t push it,” “ go slowly,” or “ resume heavy lifting.” Obviously, these statements are non-specific and are entirely subjec tive. Furthermore, they provide no structure for decisions to be made by patients or rehabilitation providers. Compli cating this are varying personality types and degrees of mo tivation. Any of the above statements could be interpreted completely different by two different patients.
There are established interval return to sport programs for a number of different sports that outline both volume and intensity progressions, but there is little guidance for medical or rehabilitation professionals on what best prac tices are regarding establishing the proper load for indi vidual patients based on their injury, surgical intervention, and prior experience. Establishing load is often arbitrary or a “best guess,” and often lacks precision regarding loading for each patient specifically Complicating matters further
is the lack of data on ultimate load to failure on repaired or reconstructed tissues in non-cadaveric subjects. Because of that, extrapolating this information to patients is highly questionable.
Secondly, the case presents various potential methods to establish resistance including based on a percentage of bodyweight, a percentage of previously known 1RM, or a percentage of HHD values when appropriate. Subjective re ports of pain, atypical feelings at the repair site, or break down in exercise technique may also help the rehabilitation provider in establishment of appropriate load. The subject in this case was accustomed to lifting extremely high loads, atypical for a great majority of patients.
The author proposes starting loads be at 30% of known previous 1RM or 30% of bodyweight with the understand ing that the patient can load comfortably and with no pain or apprehension for multi-joint lifts. For isolated, single joint movements, it is suggested that the subject begin with 20-30% of their average HHD value for that exercise. Warmup sets with up to five repetitions leading up to the tar get weight can be utilized for familiarization and instill ing confidence. Certainly, if pain or discomfort occurs prior to achieving the 30% goal with the first few months, no further progression would be advised. Pain or discomfort may be more acceptable in later stages once equal strength has been achieved or it is short-lived and decreases and/ or is eliminated after five to six repetitions are completed. Furthermore, due to the subject’s experience lifting in this case, he had a good “feel” for the weight and safety in exe cution of the lift. He was provided guidelines to work within and he complied with them. Once the loads were estab lished on core lifts, load was increased about 20% per week. Previous guidelines38 from the ACSM have established a 2-10% increase between sessions in the same week if the individual can perform the current workload for one to two repetitions over the desired number on two consecutive training sessions. Given the subject’s pre-morbid status, up to 20% was a reasonable target increase with the ability to adjust based on specific lifts and subjective comfort with the load prescribed.
Obviously in this case, the pre-morbid loads this subject lifted far exceeded what a majority of patients could lift safely. Two hundred seventy pounds on a deadlift for the first day might be a maximal attempt for some patients, but in this case, it was a weight that was easily lifted for him. The deadlift is primarily lifted with the legs and the biceps are isometrically contracted. This case highlights the need to be more individualized in loading progressions as well as establishing resistance for a given session. To the author, using 50% of the suggested loads in the healthy population was a reasonable anchor to begin with. Without establish ment of appropriate loading, there is an opportunity cost to the subject in losing valuable sessions with under-loading. In other words, why lift in three or four weeks what can be lifted today safely and appropriately?
This case also highlights how shared decision making can be used during rehabilitation planning.43 While the ef fect of shared decision making (SDM) on the outcome in this case is not known, the subject’s confidence in the phys
ical therapist and his optimism on the course of treatment likely changed for the better once the rules were established but his previous lifts and experience were considered in the progressions. Plus, more modern modalities such BFR and were well-received, along with cross-education exer cise. SDM is a collaborative approach in clinicians and pa tients integrate the best available evidence for managing health care problems with patients’ experiences and pref erences.43 It has been recognized for its potential to im prove care and outcomes, and has been used to individ ualize evidence-based recommendations, improve patient adherence and clinical outcomes, increase patient’s knowl edge of treatment options, engagement in health care de cision making, satisfaction with treatment decisions, and overall care.43 The reader is referred to Table 2 for more in formation on shared decision making.
The process of SDM is in three phases: preparing for collaboration, exchanging information about options inclu sive of patients’ values and preferences, and affirming and implementing the decision or plan. In this case, preparing for collaboration entailed a discussion about how decisions about his plan needed to be made, what options he had, and allowing the patient to help participate in the plan of care. The method for establishment of load made sense to the patient and considered his level of pre-morbid strength, but also with the understanding that the patient needed to work within limitations for healing and protection of the repair He needed to understand that although he was frus trated, the protocol that the physician provided was what the physical therapist needed to adhere to, it unless told otherwise. Next, the exchange of information involved dis cussions about blood flow restriction training, something the patient did not know much about but was interested in. Talking about blood flow restriction then led to a discus sion about ischemic preconditioning and cross-education, additional treatment methods he was not familiar with but was receptive to the progressive nature of the approach and the evidence associated with it. Treatment options also in volved providing a list of potential exercises and activities he could do within restrictions, but also a list of activities and exercises that should not be performed based on recov ery timelines. In this phase, patients are equally valued as experts regarding their own values, preferences, and abil ities to adhere to options.43 The subject did his own re search not only on EMG activation of the bicep during ex ercises, but he also researched pull-out strength of various bicep tendon repairs. It was evident that he wanted to re spect the repair and healing process but have some evi dence to support exercise selection. In the final stage, the physical therapist and the patient agree to the plan set forth as well as compliance with the restrictions suggested. The key of this phase is to both summarize the plan and confirm mutual understanding, ensure congruence with the subject’s priorities and goals, and the subject’s understand ing of the condition and its consequences.43 Obviously the subject’s goal was to be able to train and compete in the future, but he felt five and ten-pound restrictions were not the way to get to the desired outcome based on his premorbid status. At the same time, the subject was educated
Shared Decision Making Model43
Stage 1: Preparing for Collaboration Comfortable partnering with patients
• Invite patient to participate
• Determine decisions to be made
• Negotiate priorities
Be empathetic
Actively listen
Able to manage time constraints
Stage 2: Exchange information on Options Is knowledgeable of options, benefits, and risks
• Identify patient knowledge, concerns, val ues
• Value the expertise of the patient and PT
• Outline options with benefits and risks
• Deliberation between PT and patient about options
• Clarify and correct perceptions on op tions
• Determine congruence between patient and priorities and available options
Translates information to patient in nonbiased understandable manner
Communication skills
Health literacy
Past experiences
Cultural norms on health care
Desire for information
Desire to participate in decisionmaking
Identifies and communicates priorities and values
Ability and willingness to share potential barriers to options
Stage 3: Affirm and implement decision Active listening and concise summarizing
• PT summarizes the plan
• Confirm congruence with patient priori ties and goals
• Patient summarizes the plan and relates concerns and confidence about plan
• Document decision-making process and plan
• Document implementation and outcomes of plan.
Negotiation comfort to finalize the plan and accept patient’s preferences
Measurement and documentation skills
Ability to summarize back to PT
Ability and willingness to accurately report implementation
Identifies outcomes and their measures
Self-reflection as values or concerns change during implementation
about potential adverse reactions, including failure of the surgical repair, if he abdicated his responsibility to perform exercises and activities as prescribed within the guidelines provided. Indeed, there were some compliance concerns in the early phases, but once a positive, open relationship was established with clear expectations as well as an appeal for responsible progressions, the subject was more compliant and willing to follow the plan set forth.
The subject had a positive outcome in this case. Not only was range of motion fully restored, but he had symmetrical bicep strength at 60° degrees/second on isokinetic testing, and only an 11% deficit at four months. Given that resisted bicep activities had only been done for eight weeks previ ously, this case highlights how proper loading may have led to the positive subjective and objective outcomes achieved. The case potentially underscores the potential benefit as well of cross-education, BFR and IPC as adjunctive treat ments, but given there was no control, benefits of these modalities is speculative.
This case report describing successive loading in a strong man with a distal bicep rupture and subsequent surgical re
pair highlights the need for clear expectations and com munication between providers and patients using a SDM model. The potential to adjust treatment protocols to suit individual patient needs, goals, and preferences (as appro priate within healing constraints) is stressed. Finally, the importance of establishing of possible reference standard to promote loads appropriate for individual patients is high lighted.
The author offers a continuing education course regarding Blood Flow Restriction Therapy, for which he is compen sated. This does not affect the content or presentation of this case report.
Submitted: April 05, 2022 CST, Accepted: September 12, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://cre ativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. D’Alessandro DF, Shields CLJ, Tibone JE, Chandler RW Repair of distal biceps tendon ruptures in athletes. Am J Sports Med. 1993;21(1):114-119. doi:1 0.1177/036354659302100119
2. Thomas JR, Lawton JN. Biceps and triceps ruptures in athletes. Hand Clin. 2017;33(1):35-46. doi:10.1016/ j.hcl.2016.08.019
3. Lin TW, Cardenas L, Soslowsky LJ. Biomechanics of tendon injury and repair. J Biomech. 2004;37(6):865-877 doi:10.1016/j.jbiomech.2003.11.0 05
4. Kapicioglu M, Bilgin E, Guven N, Pulatkan A, Bilsel K. The role of deadlifts in distal biceps brachii tendon ruptures: an alternative mechanism described by YouTube videos. Orthop J Sports Med. 2021;9(3):1-6. d oi:10.1177/2325967121991811
5. Kelly MP, Perkinson SG, Ablove RH, Tueting JL. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med 2015;43(8):e2012-e2017 doi:10.1177/036 3546515587738
6. Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Rel Res 2002;404:275-283. do i:10.1097/00003086-200211000-00042
7 Visuri T, Lindholm H. Bilateral distal biceps tendon avulsions with use of anabolic steroids. Med Sci Sports Exerc. 1994;26(8):941-944. doi:10.1249/000057 68-199408000-00002
8. Srinivasan RC, Pederson WC, Morrey BF. Distal biceps tendon repair and reconstruction. J Hand Surg Am 2020;45(1):48-56. doi:10.1016/j.jhsa.2019.09.014
9. Rantanen J, Orava S. Rupture of the distal biceps tendon: a report of 19 patients treated with anatomic reinsertion, and a meta-analysis of 147 cases found in the literature. Am J Sports Med 1999;27(2):128-132. doi:10.1177/03635465990270020 201
10. Accessed March 2, 2022. https://www.topendsport s.com/sport/list/strongman.htm
11. Introduction to strongman competitions. Accessed November 21, 2021. http://wwwxbodyconce pts.com/introduction-to-strongman-competitions/
12. Winwood PW, Keogh JWL, Hume PA, Cronin JB. Retrospective injury epidemiology of strongman athletes. J Strength Cond Res. 2014;28(1):28-42. doi:1 0.1519/jsc.0b013e3182986c0c
13. Raske Å, Norlin R. Injury incidence and prevalence among elite weight and powerlifters. Am J Sports Med 2002;30(2):248-256. doi:10.1177/0363546 5020300021701
14. Keogh J, Hume P, Pearson SJ. Retrospective injury epidemiology of one hundred competitive Oceania powerlifters: the effects of age, body mass, competitive standard, and gender. J Strength Cond Res 2006;20:672-681.
15. Nordin MF. Biomechanics of the Elbow: Basic Biomechanics of the Musculoskeletal System. Lippincott Williams & Wilkins; 2001.
16. Mazzocca AD, Burton KJ, Romeo AA, Santangelo S, Adams DA, Arciero RA. Biomechanical evaluation of 4 techniques of distal biceps brachii tendon repair. Am J Sports Med 2007;35(2):252-258. doi:10.1177/03 63546506294854
17. Kettler M, Lunger J, Kuhn V, Mutschler W, Tingart MJ. Failure strengths in distal biceps tendon repair Am J Sports Med 2007;35(9):1544-1548. doi:10.1177/ 0363546507300690
18. Miller T, Feinblatt J, Craw J, et al. Evaluation of high-strength orthopedic sutures: a head-to-head comparison. Orthopedics. 2010;33(9).
19. Chebli C. Upper extremity: an upate on distal biceps tendon ruptures. Curr Orthop Pract 2015;26(2):119-125. doi:10.1097/bco.0000000000000 210
20. Sethi PM, Rubin E, Radler K. Upper extremity: distal biceps tendon ruptures and repairs: current trends. Curr Orthop Pract. 2017;28(2):168-172. doi:1 0.1097/bco.0000000000000485
21. Spencer EE Jr, Tisdale A, Kostka K. Is therapy necessary after distal biceps tendon repair? Hand. 2008;3(4):316-319. doi:10.1007/s11552-008-9129-8
22. Cheung EV, Lazarus M, Taranta M. Immediate range of motion after distal biceps tendon repair. J Shoulder Elbow Surg 2005;14(5):516-518. doi:10.101 6/j.jse.2004.12.003
23. Wentzell M. Post-operative rehabilitation of a distal biceps tendon reattachment in a weightlifter: a case report. J Can Chiropr Assoc 2018;62(3):193-201.
24. Logan CA, Shahien A, Haber D, Foster Z, Farrington A, Provencher MT. Rehabilitation following distal biceps repair Int J Sports Phys Ther 2019;14(2):308-317 doi:10.26603/ijspt20190308
25. Horschig A, Sayers S, LaFontaine T, Scheussler S. Rehabilitation of a surgically repaired rupture of a distal biceps tendon in an active middle aged male: a case report. Int J Sports Phys Ther. 2012;7(6):663-671.
26. Lorenz DS, Bailey L, Wilk KE, et al. Blood flow restriction training. J Ath Train 2021;56(9):937-944. doi:10.4085/418-20
27. Deschênes-Paradis P, Joanisse DR, Billaut F. Ischemic preconditioning increases muscle perfusion, oxygen uptake, and force in strength-trained athletes. Appl Physiol Nutr Metab 2016;41(9):938-944. doi:10.1139/apnm-2015-0561
28. Jeffries O, Waldron M, Pattison JR, Patterson SD Enhanced local muscle oxidative capacity and microvascular blood flow following 7-day ischemic preconditioning in healthy humans. Front Physiol. 2018;9:1-12. doi:10.3389/fphys.2018.00463
29. Cheung CP, Slysz JT, Burr JF. Ischemic preconditioning: improved cycling performance despite nocebo expectation. Int J Sports Physiol Perform 2020;15(3):354-360. doi:10.1123/ijspp.201 9-0290
30. Novaes J, Telles LG, Monteiro ER, et al. Ischemic preconditioning improves resistance training session performance. J Strength Cond Res 2021;35(11):2993-2998. doi:10.1519/jsc.00000000000 03532
31. Patterson SD, Swan R, Page W, Marocolo M, Jeffries O, Waldron M. The effect of acute and repeated ischemic preconditioning on recovery following exercise-induced muscle damage. J Sci Med Sport. 2021;24(7):709-714. doi:10.1016/j.jsams.2021.0 2.012
32. Sato S, Yoshida R, Kiyono R, et al. Crosseducation and detraining effects of eccentric vs. concentric resistance training of the elbow flexors. BMC Sports Sci Med Rehabil 2021;13(1):105. doi:10.1 186/s13102-021-00298-w
33. Mason L, Kirkland A, Steele J, Wright J. The relationship between isometric mid-thigh pull variables and athletic performance measures: empirical study of English professional soccer players and meta-analysis of extant literature. J Sports Med Phys Fitness 2021;61(5):645-655. doi:10.23736/s002 2-4707.20.11205-2
34. Townsend JR, Bender D, Vantrease WC, et al. Isometric mid-thigh pull performance is associated with athletic performance and sprinting kinetics in Division I men’s and women’s basketball players. J Strength Cond Res 2019;33(10):2665-2673. doi:10.151 9/jsc.0000000000002165
35. West DJ, Owen NJ, Jones MR, et al. Relationships between force-time characteristics of the isometric mid-thigh pull and dynamic performance in professional rugby league players. J Strength Cond Res 2011;25(11):3070-3075. doi:10.1519/jsc.0b013e3 18212dcd5
36. Saeterbakken AH, Mo DA, Scott S, Andersen V. The effects of bench press variations in competitive athletes on muscle activity and performance. J Hum Kin 2017;57(1):61-71. doi:10.1515/hukin-2017-0047
37 Saeterbakken AH, Fimland MS. Effects of body position and loading modality on muscle activity and strength in shoulder presses. J Strength Cond Res. 2013;27(7):1824-1831. doi:10.1519/jsc.0b013e318276 b873
38. American College of Sports Medicine. American College of Sports Medicine position stand: progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41(3):687-708. do i:10.1249/mss.0b013e3181915670
39. Schoenfeld BJ, Grgic J, Van Every DW, Plotkin DL. Loading recommendations for muscle strength, hypertrophy, and local endurance: a re-examination of the repetition continuum. MDPI Sports 2021;9(32):1-25. doi:10.3390/sports9020032
40. Chen SK, Wu MT, Huang CH, et al. The analysis of upper limb movements and EMG activation during the snatch under various loading conditions. J Mech med Biol 2013;1(13):1-13.
41. Youdas JW, Amundson CL, Cicero KS, Hahn JJ, Harezlak DT, Hollman JH. Surface electromyographic activation patterns and elbow joint motion during a pull-up, chin-up, or perfect pull-up rotational exercise. J Strength Cond Res. 2010;24(12):404-414. do i:10.1519/jsc.0b013e3181f1598c
42. Dickie JA, Faulkner JA, Barnes MJ, Lark SD Electromyographic analysis of muscle activation during pull-up variations. J Electromyogr Kinesiol 2017;32:30-36. doi:10.1016/j.jelekin.2016.11.004
43. Moore CL, Kaplan SL. A framework and resources for shared decision making: opportunities for improved physical therapy outcomes. Phys Ther 2018;98(12):1022-1036. doi:10.1093/ptj/pzy095
Stimulates the body’s natural repair mechanisms with our non-invasive current. The unique combination of Winback energy & manual treatments offers great rehabilitation results and a faster recovery of muscle and joint functions.









Needling (SFDN) is a system of dry needling developed by Sue Falsone, utilizing the most recent science and evidence in dry needling, as well as, her vast experience with rehabilitation and performance of the professional athlete




Her philosophy includes looking at each athlete a a whole, working with th entire body to create an optimal environment for healing and performance training.















Reference
1.
InternalBrace surgical technique is intended only to support the primary repair and is not intended as a replacement for the standard of care using biologic augmentation in a primary repair. InternalBrace surgical technique is intended only for soft-tissue-to-bone fixation and is not cleared for bone-to-bone fixation.
© 2022 Arthrex, Inc. All rights reserved. AD1-000347-en-US_A
u Patients and athletes who walk in a HydroWorx pool are better equipped to transfer what they learn to land than their counterparts who engage in self-directed shallow water walking.

u Aquatic therapy is bene昀cial to achieve threshold-intensity training while lowering the stress on the joints that is caused by land running.
u The bene昀ts of water therapy on the underwater treadmill included reduced soreness, body fat and in昀ammation while also improving muscle mass and strength performance.
u Clinical results show that athletes who participate in water rehabilitation and land-based post rehabilitation have better scores on postural sway, indicating better balance and fewer episodes of re-injury.
u Bene昀ts of hydrotherapy exercises included a lean body mass increase with underwater treadmill training, with gain seen mainly in the legs.