I J S PT







LightForce® Therapy Lasers empower you to treat soft tissue with confidence. Harnessing photobiomodulation (PBM)—a powerful form of light therapy—our lasers stimulate cellular metabolism to help treat muscle and joint pain from acute and chronic conditions.
Equipped with smart features like dosing recommendations, real-time visual and haptic feedback, and convenient portability, our range of therapy lasers combines a fusion of power with intelligence to enhance the patient and user experience. With the ability to reach deep tissues, LightForce lasers can cut the time needed by clinicians to treat patients—making light work of pain.
TRUSTED GLOBALLY
More than 250 professional and collegiate sports teams around the world trust LightForce Therapy Lasers to provide rehabilitation and pain management.
Scan the QR code to request a demo, or visit https://learn.chattanoogarehab.com/ijspt-journal-2024.

of Directors / Business Advisory Board
Turner A Blackburn, APTA Life Member, AT-Ret, AOSSM-Ret President
Mary Wilkinson Executive Director
Michael Voight Executive Editor and Publisher
Joe Black, PT, DPT, SCS, ATC
Eric Fernandez
Jay Greenstein, DC
Skip Hunter, PT, ATC-Ret
Russ Paine, PT, DPT
Tim Tyler, PT, ATC
Sports Legacy Advisory Board
Turner A. Blackburn, PT, ATC
George Davies, PT, DPT, MEd, SCS, ATC, LAT, CSCS, PES, FAPTA
Terry Malone, PT, PhD
Bob Mangine, PT
Barb Sanders, PT, PhD
Tim Tyler, PT, ATC
Kevin Wilk, PT, DPT, FAPTA
Executive Editor/Publisher
Michael L. Voight, PT, DHSc, OCS, SCS, ATC, CSCS
Executive Director/Operations and Marketing
Mary Wilkinson
Editor in Chief
Barbara Hoogenboom, PT, EdD, SCS, ATC
Managing Editor
Ashley Campbell, PT, DPT, SCS
Manuscript Coordinator
Casey Lewis, PTA, ATC
NORTH AMERICAN SPORTS MEDICINE INSTITUTE
Publisher
Contact Information
International Journal of Sports Physical Therapy 6011 Hillsboro Pike Nashville, TN 37215, US, http://www.ijspt.org
IJSPT is a monthly publication, with release dates on the first of each month.
ISSN 2159-2896
Founding Sponsors
Enovis Exertools Hyperice Trazer Woodway
Platinum Sponsors ATI Elvation
Gold Sponsors Hawkgrips Kayezen Structure + Function Education Winback Partners
Northeast Seminars Academy of Human Movement
American Academy of Sports Physical Therapy
IJSPT is an official journal of the International Federation of Sports Physical Therapy (IFSPT). Countries with access to IJSPT as a member benefit. Reach us at www.ifspt.org.

IJSPT is an official journal of the ICCUS Society for Sports Rehabilitation. www.iccus.org






Stand out in your community with a diversified patient experience. Designed to improve outcomes, attract new patients, and increase revenue through insurance, cash-based services, and retail sales.


Gain access to a robust library of research, clinical education, and marketing tools including:
• On-demand clinical education courses
• Written treatment protocols
• Over 50 research studies specific to Hyperice technology
• Marketing tips and best practices including social media content, videos, and more
• Live trainings

Executive Editor/Publisher
Michael L. Voight, PT, DHSc, OCS, SCS, ATC, CSCS
Belmont University
Nashville, Tennessee – USA
Editor in Chief
Barbara Hoogenboom, PT, EdD, SCS, ATC
Grand Valley State University Grand Rapids, Michigan - USA
Managing Editor
Ashley Campbell, PT, DPT, SCS
Nashville Sports Medicine and Orthopaedic Center Nashville, Tennessee – USA
Manuscript Coordinator
Casey Lewis, PTA, ATC
Nashville Sports Medicine and Orthopaedic Center
Nashville, Tennessee – USA
Executive Director/Marketing
Mary Wilkinson
Indianapolis, Indiana – USA
Editors
Robert Manske PT, DPT, Med, SCS, ATC, CSCS
University of Wichita Wichita, KS, USA
Terry Grindstaff, PT, PhD, ATC, SCS, CSCS
Creighton University Omaha, NE, USA
Phil Page PT, PhD, ATC, CSCS
Franciscan University DPT Program Baton Rouge, LA, USA
Kevin Wilk PT, DPT, FAPTA
Clinical Viewpoint Editor Champion Sports Medicine Birmingham, AL, USA
International Editors
Luciana De Michelis Mendonça, PT, PhD UFVJM
Diamantina, Brazil
Colin Paterson PT, MSc PGCert(Ed), MCSP, RISPT, SFHEA
University of Brighton Brighton, England, UK
Chris Napier, PT, PhD
Clinical Assistant Professor
University of British Coumbia, Vancouver, BC, Canada
Nicola Phillips, OBE, PT, PhD, FCSP
Professor School of Healthcare Sciences Cardiff University, Cardiff, Wales, UK
Associate Editors
Eva Ageberg, PT, PhD
Professor, Lund University Lund, Sweden
Lindsay Becker, PT, DPT, SCS, USAW Buckeye Performance Golf Dublin, Ohio, USA
Keelan Enseki, PT, MS, OCS, SCS, ATC University of Pittsburgh Pittsburgh, PA, USA
John Heick, PT, PhD, DPT, OCS, NCS, SCS
Northern Arizona University
Flagstaff, AZ, USA
Julie Sandell Jacobsen, MHSc, PhD
VIA University
Aarhus, Denmark
RobRoy L. Martin, PhD, PT, CSCS
Duquesne University Pittsburgh, PA, USA
Andrea Mosler, PhD, FACP, FASMF
La Trobe Sport and Exercise Medicine Research Centre, School of Allied Health, Human Services and Sport, La Trobe University
Melbourne, Victoria, Australia
Brandon Schmitt, DPT, ATC
PRO Sports Physical Therapy Scarsdale, NY, USA
Barry Shafer, PT, DPT
Elite Motion Physical Therapy Arcadia, CA, USA
Laurie Stickler, PT, DHSc, OCS
Grand Valley State University
Grand Rapids, MI, USA
Editorial Board
James Andrews, MD
Andrews Institute & Sports Medicine Center
Gulf Breeze, AL, USA
Amelia (Amy) Arundale, PT, PhD, DPT, SCS
Red Bull/Ichan School of Medicine
Salzburg, Austria/New York, NY, USA
Gary Austin, PT PhD
Belmont University Nashville, TN, USA
Roald Bahr, MD
Oslo Sports Trauma Research Center Oslo, Norway
Lane Bailey, PT, PhD
Memorial Hermann IRONMAN Sports Medicine Institute
Houston, Texas, USA
Gül Baltaci, PT,Ph.D. Professor, CKTI, FACSM
Private Guven Hospital Ankara, Turkey
Asheesh Bedi, MD
University of Michigan
Ann Arbor, MI, USA
David Behm, PhD Memorial University of Newfoundland St. John's, Newfoundland, Canada
Barton N. Bishop, PT, DPT, SCS, CSCS Kaizo Clinical Research Institute Rockville, Maryland, USA
Mario Bizzini, PhD, PT Schulthess Clinic Human Performance Lab Zürich, Switzerland
Joe Black, PT, DPT, SCS, ATC Total Rehabilitation Maryville, Tennesse, USA
Turner A. "Tab" Blackburn, APTA Life Member, ATC-Ret, AOSSM-Ret NASMI Lanett, AL, USA
Lori Bolgla, PT, PhD, MAcc, ATC Augusta University Augusta, Georgia, USA
Matthew Briggs The Ohio State University Columbus, OH, USA
Tony Brosky, PT, DHSc, SCS Bellarmine University Louisville, KY, USA
Brian Busconi, MD UMass Memorial Hospital Boston, MA, USA
Robert J. Butler, PT, PhD St. Louis Cardinals St. Louis, MO, USA
Duane Button, PhD Memorial University St. Johns, Newfoundland, Canada
J. W. Thomas Byrd, MD Nashville Sports Medicine and Orthopaedic Center Nashville, TN, USA
Lyle Cain, MD Andrews Institute & Sports Medicine Center Birmingham, AL, USA
Gary Calabrese, PT, DPT Cleveland Clinic Cleveland, Ohio, USA
Meredith Chaput, PT, DPT, SCS Ohio University Athens, OH, USA
Rita Chorba, PT, DPT, MAT, SCS, ATC, CSCS United States Army Special Operations Command Fort Campbell, KY, USA
John Christoferreti, MD Texas Health Dallas, TX, USA
Richard Clark, PT, PhD Tennessee State University Nashville, TN, USA
Juan Colado, PT, PhD University of Valencia Valencia, Spain
Brian Cole, MD Midwest Orthopaedics at Rush Chicago, IL, USA
Ann Cools, PT, PhD
Ghent University Ghent, Belgium
Andrew Contreras, DPT, SCS Washington, DC, USA
George Davies, PT, DPT, MEd, SCS, ATC, LAT, CSCS, PES, FAPTA
Georgia Southern University Savannah, Georgia, USA
Pete Draovich, PT
Jacksonville Jaguars Footbal Jacksonvile, FL, USA
Jeffrey Dugas, MD Andrews Institute & Sports Medicine Center Birmingham, AL, USA
Jiri Dvorak, MD Schulthess Clinic Zurich, Switzerland
Todd Ellenbecker Rehab Plus Phoenix, AZ, USA
Carolyn Emery, PT, PhD University of Calgary Calgary, Alberta, Canada
Ernest Esteve Caupena, PT, PhD University of Girona Girona, Spain
Sue Falsone, PT, MS, SCS, ATC, CSCS, COMT Structure and Function Education and A.T. Still University Phoenix, Arizona, USA
J. Craig Garrison, PhD, PT, ATC, SCS Texas Health Sports Medicine Fort Worth, Texas, USA
Maggie Gebhardt, PT, DPT, OCS, FAAOMPT Fit Core Physical Therapy/Myopain Seminars Atlanta, GA and Bethesda, MD, USA
Lance Gill, ATC
LG Performance-TPI Oceanside, CA, USA
Phil Glasgow, PhD, MTh, MRes, MCSP Sports Institute of Northern Ireland Belfast, Northern Ireland, UK
Robert S. Gray, MS, AT Cleveland Clinic Sports Health Cleveland, Ohio, USA
Jay Greenstein, DC Kaizo Health Baltimore, MD, USA
Martin Hagglund, PT PhD
Linkoping University Linkoping, Sweden
Allen Hardin, PT, SCS, ATC, CSCS
University of Texas Austin, TX, USA
Richard Hawkins, MD
Professor of surgery, University of South Carolina
Adjunct Professor, Clemson University
Principal, Steadman Hawkins, Greenville and Denver (CU)
John D.Heick, PT, PhD, DPT, OCS, NCS, SCS
Northern Arizona University Flagstaff, AZ, USA
Tim Hewett, PhD
Hewett Consulting Minneapolis, Minnesota, USA
Per Hølmich, MD
Copenhagen University Hospital Copenhagen, Denmark
Kara Mae Hughes, PT, DPT, CSCS
Wolfe PT Nashville, TN, USA
Lasse Ishøi, PT, MSc
Sports Orthopedic Research Center
Copenhagen University Hospital Hvidovre, Denmark
Jon Karlsson, MD Sahlgrenska University Goteborg, Sweden
Brian Kelly, MD Hospital for Special Surgery New York, NY, USA
Benjamin R. Kivlan, PhD, PT, OCS, SCS Duquesne University Pittsburgh, PA, USA
Dave Kohlrieser, PT, DPT, SCS, OCS, CSCS
Ortho One Columbus, OH, USA
Andre Labbe PT, MOPT
Tulane Institute of Sports Medicine New Orleans, LA USA
Henning Langberg, PT, PhD University of Copenhagen Copenhagen, Denmark
Robert LaPrade, MD Twin Cities Orthopedics Edina, MN, USA
Lace Luedke, PT, DPT University of Wisconsin Oshkosh Oshkosh, WI, USA
Phillip Malloy, PT, PhD
Arcadia University/Rush University Medical Center Glenside, PA and Chicago, IL, USA
Terry Malone, PT, EdD, ATC, FAPTA University of Kentucky Lexington, KY, USA
Robert Mangine, PT University of Cincinnati Cincinnati, OH, USA
Eric McCarty, MD University of Colorado Boulder, CO, USA
Ryan P. McGovern, PhD, LAT, ATC Texas Health Sports Medicine Specialists Dallas/Fort Worth, Texas, USA
Mal McHugh, PhD
NISMAT
New York, NY, USA
Joseph Miller, PT, DSc, OCS, SCS, CSCS
Pikes Peak Community College Colorado Springs, CO, USA
Havard Moksnes, PT PhD
Oslo Sports Trauma Research Center Oslo, Norway
Andrew Murray, MD, PhD
European PGA Tour Edinburgh, Scotland, UK
Andrew Naylor, PT, DPT, SCS
Bellin Health
Green Bay, WI, USA
Stephen Nicholas, MD NISMAT New York New York, NY, USA
John O'Donnel, MD
Royal Melbourne Hospital Melbourne, Australia
Russ Paine, PT McGovern Medical School Houston, TX, USA
Snehal Patel, PT, MSPT, SCD
HSS Sports Rehabilitation Institute New York, NY, USA
Marc Philippon, MD
Steadman-Hawkins Clinic Vail, CO, USA
Kevin Plancher, MD, MPH, FAAOS
Plancher Orthopedics and Sports Medicine
New York, NY USA
Marisa Pontillo, PT, PhD, DPT, SCS
University of Pennsylvania Health System Philadelphia, PA, USA
Matthew Provencher, MD
Steadman Hawkins Clinic Vail, CO, USA
Charles E. Rainey, PT, DSc, DPT, MS, OCS, SCS, CSCS, FAAOMPT
United States Public Health Service Springfield, MO, USA
Alexandre Rambaud, PT PhD Saint-Etienne, France
Carlo Ramponi, PT Physiotherapist, Kinè Rehabilitation and Orthopaedic Center Treviso, Italy
Michael Reiman, PT, PhD Duke University Durham, NC, USA
Mark F. Reinking, PT, PhD, SCS, ATC Regis University Denver, CO, USA
Mark Ryan, ATC Steadman-Hawkins Clinic Vail, CO, USA
David Sachse, PT, DPT, OCS, SCS USAF San Antonio, TX, USA
Marc Safran, MD Stanford University Palo Alto, CA, USA
Alanna Salituro, PT, DPT, SCS, CSCS New York Mets Port Saint Lucie, FL, USA
Mina Samukawa, PT, PhD, AT (JSPO) Hokkaido University Sapporo, Japan
Barbara Sanders, PT, PhD, FAPTA, Board Certified Sports Physical Therapy Emeritus Professor and Chair, Department of Physical Therapy Texas State University Round Rock, TX, USA
Felix “Buddy” Savoie, MD, FAAOS Tulane Institute of Sport Medicine New Orleans, LA, USA
Teresa Schuemann, PT, DPT, ATC, CSCS, Board Certified Specialist in Sports Physical Therapy Evidence in Motion Fort Collins, CO, USA
Timothy Sell, PhD, PT, FACSM Atrium Health Musculoskeletal Institute Charlotte, NC, USA
Andreas Serner, PT PhD
Aspetar Orthopedic and Sports Medicine Hospital Doha, Qatar
Ellen Shanley, PT, PhD ATI Spartanburg, SC, USA
Karin Silbernagel, PT, PhD University of Delaware Newark, DE, USA
Holly Silvers, PT, PhD Velocity Physical Therapy Los Angeles, CA, USA
Lynn Snyder-Mackler, PT, ScD, FAPTA STAR University of Delaware Newark, DE, USA
Alston Stubbs, MD Wake Forest University Winston-Salem, NC, USA
Amir Takla, B.Phys, Mast.Physio (Manip), A/Prof
Australian Sports Physiotherapy The University of Melbourne Melbourne, Australia
Charles Thigpen, PhD, PT, ATC ATI
Spartanburg, SC, USA
Steven Tippett, PT, PhD, ATC, SCS Bradley University Peoria, IL, USA
Tim Tyler, PT, ATC NISMAT New York, NY, USA
Timothy Uhl, PT, PhD, ATC University of Kentucky Lexington, KY, USA
Bakare Ummukulthoum, PT University of the Witswatersrand Johannesburg, Gauteng, South Africa
Yuling Leo Wang, PT, PhD Sun Yat-sen University Guangzhou, China
Mark D. Weber, PT, PhD, SCS, ATC Texas Women’s University Dallas, TX, USA
Richard B. Westrick, PT, DPT, DSc, OCS, SCS US Army Research Institute Boston, MA, USA
Chris Wolfe, PT, DPT Belmont University Nashville, TN, USA
Tobias Wörner, PT, MSc Lund University Stockholm, Sweden
VOLUME 19, NUMBER 12
PAGE TITLE
SYSTEMATIC REVIEW/META-ANALYSIS
1509 Relationship Between Shoulder Pain, Trunk and Lower Limb Pain in Overhead Athletes –A Systematic Review With Meta-Analysis.
Leroux M, Lagniaus F.
SCOPING REVIEW
1521 Isokinetic Dynamometry for External and Internal Rotation Shoulder Strength in Youth Athletes: A Scoping Review.
Leahy I, Florkiewicz E, Shotwell MP.
ORIGINAL RESEARCH
1532 The Reliability and Validity of a Novel Clinical Test for Assessing Shoulder Rotation ROM in Collegiate Baseball Players: Functional Assessment of System Tension of the Shoulder (FAST-SHDR).
Dischiavi SL, Perry JM, Burk CL, et al.
1541 Let’s Swing it –The Interaction Between Participation-Related Shoulder Load and Pre-season Trunk Rotation Power on Shoulder Problems in Male Handball Players.
Arnason K, Agustsson A, Fredriksen H, et al.
1551 Changes in Shoulder and Lumbar Injury Incidence in Swimmers with Medical Check-up and Exercise Programs.
Takayama H, Nakamura M, Kataura S, et al.
1560 Injury and Illness Trends in the National Hockey League Following an Abrupt Cessation of Play. Pinkoski AM, Davies M, Sommerfeldt M, et al.
1569 Introduction of the “Blue Card” Concussion Policy to Semi-Elite Australian Football: Medical Staff Experiences and Perceptions.
Msando JR, Cowen G, Harris SA, et al.
1581 The Single Leg Bridge Test Does Not Measure the Isolated Hamstring Endurance in Healthy Men. Roberti LS, Franke RA, Robaina BQ, et al.
1589 The Patient-Physiotherapist Tango: a Personalized Approach to ACL Recovery -- a Qualitative Interview Study.
Piussi R, Brandt E, Johansson A, et al.
CLINICAL COMMENTARY
1600 Oh, My Quad: An Evidence-Based Framework for the Rehabilitation of Quadriceps Size and Strength after Anterior Cruciate Ligament Reconstruction.
Solie BS, Carlson MR, Doney CR, et al.
1629 Neurocognitive and Neuromuscular Rehabilitation Techniques after ACL injury - Part 2: Maximizing Performance in the Advanced Return to Sport Phase.
Thomas ZM, Lupowitz L, Ivey M, Wilk KE.
MSK ULTRASOUND BITES: TIPS AND TRICKS
1641 The Use of Diagnostic Musculoskeletal Ultrasound for the Evaluation of the Iliopsoas in the Anterior Hip: A Guide for Rehabilitation Providers.
Manske RC, Voight M, Wolfe C, Page P, Bardowski B.
EDITORIAL
1646 Beyond the Menstrual Cycle: Time for a Holistic Approach to Athlete Health and Performance. Stitelmann A, Gard S, Coen SE, et al.


Most Advanced Electrotherapy Device: Powerful, intuitive and user-friendly
Treat up to three body zones at once on all types of tissues
Effective in less than 10 minutes Enter A New Era of Therapy
TECAR
HIGH FREQUENCY
Metabolic Action at Cell Level
Hi-TENS
LOW FREQUENCY IN PULSED HIGH FREQUENCY
Ultimate Pain Management
Hi-EMS
MEDIUM FREQUENCY
Deep Muscle Contraction







Systematic Review/Meta-Analysis
Leroux M, Lagniaux F. Relationship between Shoulder Pain, Trunk and Lower Limb Pain in Overhead Athletes: A Systematic Review with Meta-analysis. IJSPT 2024;19(12):1509-1520. doi:10.26603/001c.125882
Marine Leroux1a , Franck Lagniaux1
1 SFMKS Lab
Keywords: back pain, kinetic chain, lower limbs pain, overhead sports, shoulder pain, subsequent injury https://doi.org/10.26603/001c.125882
International Journal of Sports Physical Therapy Vol. 19, Issue 12, 2024
Background
Forty-nine percent of overhead athletes suffer from shoulder pain. Throwing movements require the participation of all components of the kinetic chain to reduce risk for shoulder overuse. Thus, limited lower limb range of motion or weakness has been identified as a risk factor for shoulder pain in overhead athletes.
Purpose
This systematic review aims to evaluate the association between shoulder, trunk, and lower limb pain in overhead athletes.
Study Design
Systematic Review and Meta-analysis
Methods
A systematic review was conducted in the PubMed/MEDLINE, Science Direct and CENTRAL/Cochrane databases for observational studies. Search terms included sports-related terms (e.g., ‘overhead’, ‘baseball’, ‘volleyball’, ‘handball’) and injury-related terms (e.g., ‘injury history’, ‘shoulder pain’, ‘lower limb pain’, ‘hip pain’, ‘knee pain’, ‘ankle pain’, ‘foot pain’, ‘trunk pain’). Studies were considered for review if they met the following criteria: inclusion of overhead athletes, investigation of injury or pain in shoulder and lower limb or trunk, had data related to or could calculate the calculation of odds ratio (OR) or relative risk (RR), available in French or English. The ROBINS-E tool was used to assess the methodological quality of each article. The data were pooled in a random-effects meta-analysis, using odds ratios to estimate the strength of the association between shoulder pain and pain at other locations.
Results
Seven articles were included. Five of them were at moderate risk of bias and two were at high risk of bias. Shoulder pain was associated with low back pain (OR=5.51), hip pain (OR=4.32), knee pain (OR=3.03) and ankle/foot pain (OR=2.84).
Conclusion
This systematic review highlighted, with very low to low certainty, a significant association between shoulder pain and trunk/lower limb pain or injuries.
Level 3
Corresponding Author: Marine Leroux SFMKS Lab, Colombelles, France mar.leroux@hotmail.fr a
Shoulder pain is a common issue among overhead athletes participating in baseball, volleyball, tennis, swimming, and handball, with reported prevalence rates ranging from nine to forty-nine, depending on the sport and study 1‑3 The repetitive overhead movements and high biomechanical demands associated with these sports increase the risk of shoulder injury.4
Several risk factors for shoulder pain in overhead athletes have been identified, including male sex, a body mass index over 25, age between 20 and 25 years, training for more than 16 hours per week, limited shoulder range of motion, and strength deficits in rotator cuff muscles.1,3,5,6
In various overhead movements, such as a tennis serve, a volleyball spike, and a handball throw, the kinetic chain consists of a sequence of coordinated actions that contribute to the generation of velocity and force applied to the ball.4,7,8 The kinetic chain is initiated by the lower extremities with a push-off from the ground, engaging the muscles of the calves, quadriceps, and gluteal muscles, leading to the extension of the hips, knees, and ankles. The force produced by the lower limbs is then transferred to the core musculature. The core serves as a critical intermediary, stabilizing the trunk and facilitating efficient transfer of energy from the lower to the upper body The rotational movement of the trunk generates force that is transferred through the torso and into the arms amplifying the power of the overhead movement. The lower extremities and trunk are responsible for approximately 55% of the kinetic energy delivered during a baseball throw 4 Proper scapular control is essential for optimal shoulder mechanics, requiring coordinated motion of the scapulae with the arm. During overhead motion, the shoulder undergoes a combination of external then internal rotation, abduction and flexion. As the arm reaches the overhead position, the elbow extends, while the forearm muscles regulate the wrist’s position and motion, ensuring the hand is correctly aligned for the desired action.
Each segment in the kinetic chain must be functional to minimize the risk of shoulder injury and ensure optimal performance.4 A 20% reduction in energy production by the trunk can increase the load on the shoulder by up to 34% to maintain the same performance level.8 Such deficits may arise from poor technique, muscle weakness or imbalance, limited range of motion (ROM), or previous injury 4,8 Therefore, limitations in hip ROM, thoracic rotation, hamstring and quadriceps extensibility, and core neuromuscular control have been highlighted as factors leading to shoulder injuries.9‑11
Researchers have also suggested that injuries are interrelated across different regions of the body. For instance, Finch et al. reported that one in eight injuries in Australian Football players occurs as a subsequent injury, regardless of the initial injury’s location.12 Similarly, a systematic review by Toohey et al. identified an association between a history of anterior cruciate ligament (ACL) injuries and subsequent hamstring injuries. They also found that a previous muscle injury, involving the hamstrings, quadriceps,
adductors, or calves, was linked to an increased risk of subsequent injuries at different anatomical sites.13 These findings highlight the interconnected nature of injuries, particularly those originating in the lower limbs, suggesting that an initial injury can predispose athletes to additional injuries elsewhere in the body.
Even when an athlete is deemed fully recovered, initial injuries can result in tissue adaptations and neuromuscular alterations, which may predispose them to further injuries.14,15 Asker et al. have postulated that a history of shoulder or elbow injuries could serve as a potential risk factor for subsequent shoulder pain.1 However, the impact of pain within other regions of the kinetic chain on the risk of subsequent injuries has not been extensively studied. Therefore, the purpose of this systematic review was to evaluate the association between pain in the shoulder, trunk, and lower limb among overhead athletes.
This systematic review followed the COSMOS-E (Conducting Systematic Reviews and Meta-Analyses of Observational Studies of Etiology) and PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).16, 17 It was prospectively registered with PROSPERO, registered PROSPERO 2023 CRD42023398806. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023398806.
Studies were considered for review if they met the following criteria: 1) inclusion of overhead athletes (e.g., tennis, baseball, badminton, handball, volleyball, American football, javelin, water-polo, cricket, basketball) without age restrictions, 2) investigation of injury or pain in shoulder and lower limb or trunk, 3) had data related to or could calculate the calculation of odds ratio (OR) or relative risk (RR), 4) availability in French or English. Studies were excluded if they focused on interventions aiming to reduce the risk of shoulder pain.
A systematic search was conducted in July 2023 in the following databases: PubMed/MEDLINE, Science Direct and CENTRAL/Cochrane. The search terms included keywords and MESH (Medical Subject Heading) as shown in Appendix 1. Research review and review article filters were selected for Science Direct. Each column was combined with Boolean operators (AND and OR). Additionally, a hand search was conducted through the bibliography of relevant articles. See Appendix 2 for details.
All identified articles were added to the Rayyan® software which assisted in removing duplicates. Two independent
reviewers (ML and FL) screened and assessed the eligibility of studies based on title and abstract. Full-articles were then retrieved and read to determine whether they were to be included. Disagreement was resolved with a third reviewer
ML conducted data extraction which was subsequently verified by FL. Extracted data included metadata (author, publication date, country), population characteristics (number of persons included, age, sport, level and training load), study design, pain or injury locations, effect estimation and confidence interval. Authors were contacted in cases where data were missing.
The risk of bias was evaluated using Cochrane ROBINSE (Risk of Bias In Non-randomized Studies - of Exposure) tool.18 This tool assesses seven domains of bias: confounding, measurement of the exposure, selection of participants into the study, post-exposure interventions, missing data, measurement of the outcome and selection of the reported result. Each bias domain is addressed using a series of signaling questions judging the risk of bias of each domain (low risk, some concerns, high risk of bias, very high risk of bias).
Search results were illustrated in a flow diagram and the characteristics of each study, along with their results, were summarized in tables. A random-effect meta-analysis was performed when at least two studies evaluated the association between shoulder pain and pain in another joint. The analysis was conducted using RevMan 5.4 ® software. The meta-analysis used the inverse variance Der Simonian and Laird method. The overall odd-ratio (OR) with 95% confidence interval (CI) were calculated. An OR of 1,0 indicates that there is no difference in odds between the groups whereas an OR > 1,0 indicates an increase in odds among the exposed athletes.19 Heterogeneity was assessed using the I² statistic. It was considered high when I² was greater than 50%.19 A qualitative synthesis was performed when it wasn’t possible to pool the results due to high heterogeneity
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to rate the quality of each association. This tool evaluates risk of bias, inconsistency, indirectness, imprecision, publication bias, large effect, dose-response and antagonistic bias and delivers recommendations (high, moderate, low or very-low certainty of evidence).
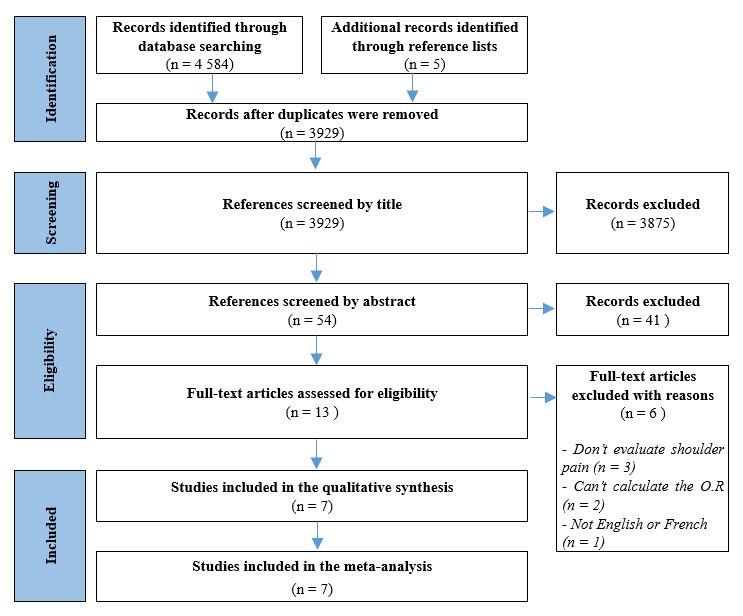
Overall, the search strategy identified 4 584 articles with an additional five studies were found by checking the references of other articles. After screening articles based on title and abstract, 13 articles were identified and thoroughly examined. Ultimately, seven articles met the inclusion criteria for the systematic review 20‑26 Of these, six studies were cross-sectional and one was a longitudinal study All studies were included in the meta-analysis. See Figure 1.
Overall, 5785 athletes were included in this review. Patients were aged between seven and 28 years old and played water-polo, basketball, baseball, softball, handball, tennis, badminton and volleyball. The play level was heterogenous, ranging from the last division to the international level. Every study assessed the association of shoulder pain with other body region. Five studies evaluated low back pain,21, 23‑26 two evaluated hip pain,20,23 three evaluated knee pain,23,24,26 and two evaluated ankle and foot pain.22,23 Every study used questionnaires for data collection. The characteristics of each study are detailed in Table 1.
Two studies were rated as having a high risk of bias while five were deemed to have some concerns. The poorer quality observed was primarily attributed to the lack of consideration for confunding factors, the subjective nature of outcome/exposure measurement through questionnaire, and issues related to the selection of participants. (Table 2)
The association between shoulder pain and back pain, hip pain, knee pain and ankle/foot pain were assessed through meta-analysis. Shoulder pain demonstrated a significant association with back pain (five studies, OR = 5.51, 95% CI [3.23-9.41], high heterogeneity), hip pain (two studies, OR = 4.32, 95%CI [2.10-8.88], high heterogeneity), knee pain (three studies, OR = 3.03, 95%CI [2.11-4.37], low heterogeneity), ankle/foot pain (two studies, OR = 2.84, 95%CI [1.97-4.11], low heterogeneity). (Figures 2)
The quality of evidence according to GRADE is presented in Table 3. Reasons for downgrading are cited in the table’s legend. The overall quality of evidence for the association of shoulder pain, back pain and knee pain was rated as low Additionally, the evidence was considered very low for the association between shoulder pain and hip pain as well as shoulder pain and ankle/foot pain.
The aim of this systematic review was to evaluate the association between shoulder pain and trunk/lower limb pain in overhead athletes. There is low to very low evidence of an association between trunk/lower limb pain and shoulder pain, but overhead athletes with trunk or lower limb pain appear to be two to five times more likely to also suffer from shoulder pain compared to those without pain in the kinetic chain.
The overhead movement is a sequential motion supposed to be initiated with the proximal segments and ending at maximum speed with the distal segments secondary to the summation of accelerative forces generated by the previous segments in the kinetic chain.4,7,8 A breakage, also known as a dysfunctional segment, in the kinetic chain increases the demand on the subsequent segments to maintain the functional ability or performance, a process known as the catch-up phenomenon.8,27 While this concept is well-known and described in numerous studies and reviews, the consequences of this catch-up have not been thoroughly studied.4,7,8
This systematic review suggests the existence of a relationship between shoulder pain and trunk/lower limb pain. Only two studies included in the systematic review evaluated the causal relationship between these pain.22,25 Yamaoka et al. showed that in the year following low back pain a baseball player was 2.31 times more likely to suffer from shoulder pain. According to the concept of the kinetic chain, functional factors such as poor lumbopelvic control have been brought out.9,28,29 However, not all studies generalized these conclusions. For example, Machado et al.
concluded in a meta-analysis of 65 studies in 2023 that there was low evidence of no association of trunk/lower limb strength, endurance, vertical jump or balance measures with shoulder pain. Yet, overhead athletes with shoulder pain were performing worse in trunk stability and endurance in tests like side bridge or trunk flexors/ extensors.30 This suggests that despite the lack of a direct association with shoulder pain in some measures, like vertical jump or balance, core stability remains a critical factor for performance and injury prevention in overhead athletes. Some authors have also emphasized the role of the anatomy of the latissimus dorsi—particularly its insertions to the thoracolumbar aponeurosis, iliac crest, scapula, and bicipital groove—as a contributing factor to shoulder pain following low back pain.21 Due to its attachments, the latissimus dorsi muscle is responsible for shoulder adduction, extension, internal rotation, as well as lumbar extension and lateral flexion.31 It is the only muscle that connects the upper body to the lower body Laudner and Williams have found that swimmers with a latissimus dorsi muscle that presented high resistance to deformation were more prone to have scapular movement dysfunction.32 Scapular movement is an integral part of the kinetic chain, and any disruption may reduce the efficiency of energy transfer 4 This systematic review indicates an association between shoulder pain and pain in distal body regions. While the results of the meta-analysis showed that the dysfunctional proximal segments had a higher probability of provoking shoulder pain, knee and ankle pain could also alter the kinetic chain dynamic. The ankle and foot play a significant role, as it has been recognized that foot arch posture is associated with shoulder and elbow surgeries.33 Liu et al. demonstrated that kinetic chain disruption can occur after an injury.22 However, the rehabilitation process following
Table 1. Characteristics of included studies
Study and Type Participants
Girdwood and al., 2021 Cross sectional
Hagiwara and al., 2020 Cross sectional
Liu and al., 2022 Cross sectional
Sekiguchi and al., 2016 Cross sectional
Sekiguchi and al., 2017 Cross sectional
Yamaoka and al., 2023 Longitudinal study
Zhou and al., 2021 Crosssectional
N=153
Water-polo F = 88 / M = 65
Age (median) = 23 y.o
N = 590 F = 259 / M = 331
Basketball
Age (median) = 13 y.o
N = 478
Badminton F = 267 / M = 211
Age (mean) = 7-12 y.o
N = 1582
Baseball F = 69 / M = 1513
Age (median) = 11 y.o
N = 2215
Baseball / Softball / Handball / Tennis / Badminton / Volleyball F = 632 / M = 1583
Age (median) = 11 y.o
N = 307
Baseball F= 0 / M = 307
Age (mean) = 15,8 y.o
N = 460
Badminton F = 266 / M = 194
Age (median) = 10 y.o
Girdwood et al. 2021
Hagiwara et al. 2020
Liu et al. 2022
Sekiguchi et al. 2016
Sekiguchi et al. 2017
Yamaoka et al. 2023
Zhou et al. 2021
Shoulder Hip Pain was evaluated through an online questionnaire and OSTRC
Shoulder Low back
Shoulder Ankle
Shoulder Knee Low back
Shoulder Knee
Low back Hip Foot
Exposition : Low back Outcome : Shoulder
Shoulder Knee Low back
Pain was evaluated through a selfreported questionnaire
Injury was evaluated through a self-reported questionnaire
Pain was evaluated through a selfreported questionnaire
Pain was evaluated through a selfreported questionnaire
Current shoulder pain was a risk factor for hip pain (RR = 1,99 [95%CI 1,27-3,12])
Current hip pain was also a risk factor for current shoulder pain (RR = 1,70 [95%CI 1,23-2,35])
Shoulder pain was significantly associated with LBP (adjusted OR 13,77 [95%CI 5,70-33,24], p < 0,001)
Previous ankle injury was significantly associated with subsequent shoulder injury (adjusted OR = 2,46[1,26-4,83], p<0,05)
Low back pain and knee pain were strongly associated with shoulder pain (adjusted ORlbp = 4,35[2,59-7,29], p < 0,001 and ORknee=3,31[2,17-5,06], p < 0,001)
Trunk and lower extremity pain were significantly associated with elbow/shoulder pain.
adjusted ORback: 5,52[3,51-8,69], p < 0,001 adjusted ORknee: 2,28[1,48-3,51] p < 0,001 adjusted ORhip: 6,13[3,35-11,22] p < 0,001 adjusted ORfoot: 3,03[1,95-4,72] p < 0,001
Self-completed questionnaire at baseline and 1 year follow up
Pain was evaluated through a selfreported questionnaire
LBP experienced during the last year at baseline and new onset of shoulder pain was identified adjusted OR = 2,31[1,29-4,12], p = 0,0049
The presence of shoulder pain was significantly associated with knee pain (adjusted OR 4,73[2,18-10,24] p < 0,001) and the presence of lower back pain was significantly associated with shoulder pain (adjusted OR = 9,87[4,02-24,21] p < 0,001
these injuries remains unclear. Secondary or subsequent injury can occur years after the initial injury/pain due to compensatory mechanisms. Even a well-rehabilitated injury can affect surrounding tissues in both the short and
long term, increasing the athlete’s susceptibility to further injury
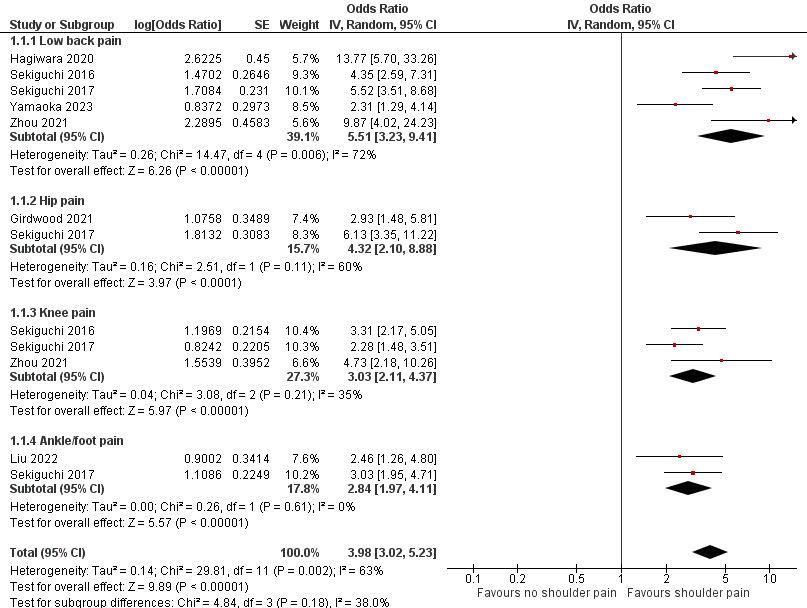
Figure 2. Forest plot for the association of shoulder pain and back pain, hip pain, knee pain and ankle/foot pain
Table 3. Quality of evidence according to GRADE
Shoulder pain - Ankle/foot pain
(3 studies)
(2
a. Subjective measurement of outcome (recall biais). No control population. Study design.
b. Heterogeneity is above 50%
c. Self-reported questionnaire isn’t a validated measurement tool.
d. No statistical adjustment of confounding factors. Subjective measurement of outcome (recall biais). No control population. Study design.
e. < 385 participants (Optimal Information Size)
CLINICAL IMPLICATIONS
There is evidence that a subsequent injury causes greater time loss and medical attention than a first injury.12,13 Therefore, it is essential to reduce the risk for subsequent injury by managing return-to-sport after a first injury and to treat any pain seriously the overhead athletes may feel while playing.
During the assessment of an injured overhead athlete, physiotherapists must consider every link in the kinetic chain. A shoulder injury can be the consequence of a modification in the motion pattern in the kinetic chain, just as lower limb or trunk pain/injury can lead to another injury if the kinetic chain has not been properly addressed. Shoulder ROM, rotator cuff strength, and functional test like the Closed Kinetic Chain Upper Extremity Stability Test
(CKCUEST) or the Upper Limb Rotation Test (ULRT) can be performed to assess shoulder function within the kinetic chain.27,35,36 The CKCUEST is designed to assess upper extremity strength, stability, endurance, and coordination in a closed kinetic chain, where the hands maintain contact with a fixed surface throughout the movement. It requires the coordinated activation of various upper body and core muscles, and its performance has been shown to correlate with shoulder function and injury risk, making it a valuable tool for both injury prevention and rehabilitation. Similarly, the ULRT evaluates dynamic shoulder mobility, stability, and coordination, with a specific emphasis on rotational movement of the upper limb. This test provides clinicians and coaches with insights into the functional rotational range of motion of the shoulder, enabling the identification
of movement limitations or asymmetries that may contribute to injury or dysfunction. It is also valuable to assess functional movement during the lunge test or leg squat test to identify any dysfunction in the kinetic chain.37 Nagamoto et al. evaluated the association between baseball players with a history of shoulder or elbow pain during or after playing baseball and their ability to deep squat. Although it may not be directly associated, their performance was adversely affected.38 This shows that after a shoulder injury the entire athlete has to be considered. Clinicians have to treat the injury, maintain or restore strength and mobility in the kinetic chain, and incorporate kinetic chain exercises as soon as possible in order to guide the athlete in returning to sport. As previously explained, it is essential to rehabilitate the entire movement to mitigate the risk of the catch-up phenomenon. Moreover, injury can lead to changes in the cortical areas of the brain, altering neuronal processing even after the patient has physically recovered.39 Consequently, incorporating motor imagery, gradual exposure to movement, and external cues during rehabilitation are crucial for addressing both the physical and neurological aspects of recovery.27
The Van Mechelen model is a widely adopted framework for injury prevention, consisting of a four-step approach: identification of the problem, determination of risk factors and injury mechanisms, implementation of a preventive intervention, and evaluation of the intervention’s effectiveness.36 However, the prevention of any injury in overhead athletes cannot be fully addressed with the Van Mechelen model, as its linear approach cannot capture the complexity of injuries with a single risk factor 36,40 This systematic review underscores the association between trunk and lower limb pain and shoulder pain in overhead athletes, reinforcing the concept that injuries arise from a combination of risk factors. As previously noted, potential risk factors for overhead athletes include training volume, BMI, age, ROM deficits, strength deficits, sport-specific techniques, core endurance deficits, muscle extensibility, and a history of shoulder or elbow injuries.1,3,5,6,9‑11 The presence of a single risk factor does not predict the occurrence of shoulder pain. Bittencourt et al. proposed a more “complex system approach” where all determinants (intrinsic, extrinsic, modifiable, non-modifiable) interact with each other in unpredictable and unplanned ways, creating a web of determinants.40 It enables the identification of patterns between determinants, the characteristics of the phenomenon and the emerging trends that arises from the web of determinants. This approach could facilitate the development of individualized risk profiles by evaluating each determinant throughout the rehabilitation process, leading to a better understanding of subsequent injuries. In line with the complex system approach, this systematic review proposed an initial interaction between lower limb/trunk pain and shoulder pain in overhead athletes. Thus, coaches or trainers should identify overhead athletes at risk for subsequent injuries when they first perceive any discomfort or pain. To detect injuries at an early stage, medical staff needs a re-
liable surveillance method that encourages athletes to disclose any discomfort. Surveillance programs usually define an injury using time-loss or medical attention criteria.41 In 2014, the Oslo Sports Trauma Research Center (OSTRC) questionnaire was created to declare all complaints, offering a better assessment of overuse injuries. Therefore, an all-complaint based surveillance method is a crucial tool for monitoring overuse injuries, allowing sports professionals to identify early signs of injury, assess severity, and develop strategies to prevent further complications.42
This systematic review presents several limitations. First, the included population is not representative of the overall overhead athlete population. The mean age of athletes is low and although age was assessed as a confounding factor and statistics were adjusted, the results might still be underestimated. Adolescents often exhibit a higher susceptibility to overuse injuries compared to younger children.43 Secondly, the definition of pain or injury may have differed between authors. In this systematic review, only Liu et al. and Zhou et al. defined pain or injury in the questionnaire, which introduces heterogeneity in exposure and outcome assessments. Additionally, the data were collected through self-reported questionnaires, which introduce the potential for recall bias, possibly affecting the accuracy of the responses. Also, while adjusted results were included in this study when available, the confounding factors taken in consideration were not consistent across studies. For the majority of the studies, gender, age, BMI, team level, hours of training per week and per weekend were considered. Furthermore, the study by Sekiguchi et al.23 included athletes with shoulder and elbow pain, which could have biased the results. Finally, due to the design of the included studies, it was not possible to determine a causal relationship between shoulder pain and trunk/lower limb pain; only associations between these factors can be concluded.
To establish a causal relationship between shoulder pain and trunk/lower limb pain, future longitudinal studies should be implemented with a clear definition of pain/ a painful event and assessment should be standardized using an all-complaint questionnaire.
This systematic review highlights, with very low to low certainty, a significant association between shoulder pain and trunk/lower limb pain. Overhead athletes with trunk or lower limb pain appear to be two to five times more likely to also suffer from shoulder pain compared to those without pain in the kinetic chain.
Submitted: May 12, 2024 CST, Accepted: September 17, 2024 CST
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Asker M, Brooke HL, Waldén M, et al. Risk factors for, and prevention of, shoulder injuries in overhead sports: a systematic review with best-evidence synthesis. Br J Sports Med 2018;52(20):1312-1319. doi:10.1136/bjsports-2017-098254
2. Kraan RBJ, Nobel D, Eygendaal D, Daams JG, Kuijer PPFM, Maas M. Incidence, prevalence, and risk factors for elbow and shoulder overuse injuries in youth athletes: A systematic review. Transl Sports Med 2019;2(4):186-195. doi:10.1002/tsm2.82
3. Mohseni-Bandpei MA, Keshavarz R, Minoonejhad H, Mohsenifar H, Shakeri H. Shoulder pain in Iranian elite athletes: The prevalence and risk factors. J Manipulative Physiol Ther 2012;35(7):541-548. doi:10.1016/j.jmpt.2012.07.011
4. Trasolini NA, Nicholson KF, Mylott J, Bullock GS, Hulburt TC, Waterman BR. Biomechanical analysis of the throwing athlete and its impact on return to sport. Arthrosc Sports Med Rehabil 2022;4(1):e83-e91. doi:10.1016/j.asmr.2021.09.027
5. Cools AM, Johansson FR, Borms D, Maenhout A. Prevention of shoulder injuries in overhead athletes: a science-based approach. Braz J Phys Ther 2015;19(5):331-339. doi:10.1590/bjpt-rbf.2014.0109
6. Reinold MM, Gill TJ, Wilk KE, Andrews JR. Current concepts in the evaluation and treatment of the shoulder in overhead throwing athletes, Part 2: Injury prevention and treatment. Sports Health. 2010;2(2):101-115. doi:10.1177/1941738110362518
7 Wagner H, Pfusterschmied J, Tilp M, Landlinger J, von Duvillard SP, Müller E. Upper-body kinematics in team-handball throw, tennis serve, and volleyball spike: Kinematic differences in overarm movements. Scand J Med Sci Sports. 2014;24(2):345-354. doi:10.1111/j.1600-0838.2012.01503.x
8. Lintner D, Noonan TJ, Kibler WB. Injury patterns and biomechanics of the athlete’s shoulder. Clin Sports Med 2008;27(4):527-551. doi:10.1016/ j.csm.2008.07.007
9. Cope T, Wechter S, Stucky M, Thomas C, Wilhelm M. The impact of lumbopelvic control on overhead performance and shoulder injury in overhead athletes: A systematic review. Int J Sports Phys Ther. 2019;14(4):500-513. doi:10.26603/ijspt20190500
10. Deal MJ, Richey BP, Pumilia CA, et al. Regional interdependence and the role of the lower body in elbow injury in baseball players: A systematic review. Am J Sports Med 2020;48(14):3652-3660. doi:10.1177/0363546520910138
11. Endo Y, Sakamoto M. Correlation of shoulder and elbow injuries with muscle tightness, core stability, and balance by longitudinal measurements in junior high school baseball players. J Phys Ther Sci. 2014;26(5):689-693. doi:10.1589/jpts.26.689
12. Finch CF, Cook J, Kunstler BE, Akram M, Orchard J. Subsequent injuries are more common than injury recurrences: an analysis of 1 season of prospectively collected injuries in professional australian football. Am J Sports Med. 2017;45(8):1921-1927. doi:10.1177/ 0363546517691943
13. Toohey LA, Drew MK, Cook JL, Finch CF, Gaida JE. Is subsequent lower limb injury associated with previous injury? A systematic review and metaanalysis. Br J Sports Med 2017;51(23):1670-1678. doi:10.1136/bjsports-2017-097500
14. Zügel M, Maganaris CN, Wilke J, et al. Fascial tissue research in sports medicine: from molecules to tissue adaptation, injury and diagnostics: consensus statement. Br J Sports Med 2018;52(23):1497-1497 doi:10.1136/bjsports-2018-099308
15. Nyland J, Klein S, Caborn DNM. Lower extremity compensatory neuromuscular and biomechanical adaptations 2 to 11 years after anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2010;26(9):1212-1225. doi:10.1016/ j.arthro.2010.01.003
16. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLOS Med. 2021;18(3):e1003583. doi:10.1371/ journal.pmed.1003583
17. Dekkers OM, Vandenbroucke JP, Cevallos M, Renehan AG, Altman DG, Egger M. COSMOS-E: Guidance on conducting systematic reviews and meta-analyses of observational studies of etiology. PLOS Med 2019;16(2):e1002742. doi:10.1371/ journal.pmed.1002742
18. ROBINS-E Development Group. Risk Of Bias In Non-randomized Studies - of Exposure (ROBINS-E). June 20, 2023. https://www.riskofbias.info/welcome/ robins-e-tool
19. Borenstein M, ed. Introduction to Meta-Analysis John Wiley & Sons; 2009. doi:10.1002/ 9780470743386
20. Girdwood M, Webster M. Quantifying the burden of shoulder and hip pain in water polo players across different playing levels. Int J Sports Phys Ther 2021;16(1). doi:10.26603/001c.18801
21. Hagiwara Y, Yabe Y, Sekiguchi T, et al. Upper extremity pain is associated with lower back pain among young basketball players: A cross-sectional study. Tohoku J Exp Med. 2020;250(2):79-85. doi:10.1620/tjem.250.79
22. Liu X, Imai K, Zhou X, Watanabe E. Influence of ankle injury on subsequent ankle, knee, and shoulder injuries in competitive badminton players younger than 13 years. Orthop J Sports Med 2022;10(5):232596712210974. doi:10.1177/ 23259671221097438
23. Sekiguchi T, Hagiwara Y, Momma H, et al. Coexistence of trunk or lower extremity pain with elbow and/or shoulder pain among young overhead athletes: a cross-sectional study Tohoku J Exp Med 2017;243(3):173-178. doi:10.1620/tjem.243.173
24. Sekiguchi T, Hagiwara Y, Momma H, et al. Youth baseball players with elbow and shoulder pain have both low back and knee pain: a cross-sectional study. Knee Surg Sports Traumatol Arthrosc 2018;26(7):1927-1935. doi:10.1007/ s00167-016-4364-y
25. Yamaoka H, Kato K, Otoshi K, et al. Impact of low back pain experience on future occurrence of shoulder pain in adolescent baseball players: A 1-year prospective cohort study J Orthop Sci Published online March 2023:S0949265823000829. doi:10.1016/ j.jos.2023.03.012
26. Zhou X, Imai K, Liu XX, Watanabe E. Epidemiology and pain in elementary school-aged players: a survey of Japanese badminton players participating in the national tournament. Sci Rep 2021;11(1):6459. doi:10.1038/s41598-021-85937-5
27. Schwank A, Blazey P, Asker M, et al. 2022 Bern consensus statement on shoulder injury prevention, rehabilitation, and return to sport for athletes at all participation levels. J Orthop Sports Phys Ther. 2022;52(1):11-28. doi:10.2519/jospt.2022.10952
28. Chaudhari AMW, McKenzie CS, Pan X, Oñate JA. Lumbopelvic control and days missed because of injury in professional baseball pitchers. Am J Sports Med 2014;42(11):2734-2740. doi:10.1177/ 0363546514545861
29. Pogetti LS, Nakagawa TH, Conteçote GP, Camargo PR. Core stability, shoulder peak torque and function in throwing athletes with and without shoulder pain. Phys Ther Sport. 2018;34:36-42. doi:10.1016/ j.ptsp.2018.08.008
30. Machado EDM, Haik MN, Ferreira JK, Da Silva Santos JF, Camargo PR, Mendonça LDM. Association of trunk and lower limb factors with shoulder complaints and sport performance in overhead athletes: A systematic review including GRADE recommendations and meta-analysis. Phys Ther Sport 2023;60:112-131. doi:10.1016/ j.ptsp.2023.01.012
31. Gerling ME, Brown SHM. Architectural analysis and predicted functional capability of the human latissimus dorsi muscle. J Anat. 2013;223(2):112-122. doi:10.1111/joa.12074
32. Laudner KG, Williams JG. The relationship between latissimus dorsi stiffness and altered scapular kinematics among asymptomatic collegiate swimmers. Phys Ther Sport 2013;14(1):50-53. doi:10.1016/j.ptsp.2012.02.007
33. Feigenbaum LA, Roach KE, Kaplan LD, Lesniak B, Cunningham S. The association of foot arch posture and prior history of shoulder or elbow surgery in elite-level baseball pitchers. J Orthop Sports Phys Ther 2013;43(11):814-820. doi:10.2519/ jospt.2013.4504
34. Shrier I, Steele RJ, Zhao M, et al. A multistate framework for the analysis of subsequent injury in sport (M-FASIS). Scand J Med Sci Sports 2016;26(2):128-139. doi:10.1111/sms.12493
35. Ellenbecker TS, Aoki R. Step by step guide to understanding the kinetic chain concept in the overhead athlete. Curr Rev Musculoskelet Med. 2020;13(2):155-163. doi:10.1007/s12178-020-09615-1
36. Cools AM, Maenhout AG, Vanderstukken F, Declève P, Johansson FR, Borms D. The challenge of the sporting shoulder: From injury prevention through sport-specific rehabilitation toward return to play. Ann Phys Rehabil Med. 2021;64(4):101384. doi:10.1016/j.rehab.2020.03.009
37 Brumitt J, Dale RB. Integrating shoulder and core exercises when rehabilitating athletes performing overhead activities. North Am J Sports Phys Ther NAJSPT 2009;4(3):132-138.
38. Nagamoto H, Muraki T, Takahashi S, et al. Relationship between a history of disabled throwing shoulder/elbow and the ability to perform the deep squat test among youth baseball players. J Orthop Rep 2023;2(4):100197 doi:10.1016/ j.jorep.2023.100197
39. Haller S, Cunningham G, Laedermann A, et al. Shoulder apprehension impacts large-scale functional brain networks. Am J Neuroradiol 2014;35(4):691-697. doi:10.3174/ajnr.A3738
40. Bittencourt NFN, Meeuwisse WH, Mendonça LD, Nettel-Aguirre A, Ocarino JM, Fonseca ST Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition—narrative review and new concept. Br J Sports Med. 2016;50(21):1309-1314. doi:10.1136/ bjsports-2015-095850
41. Clarsen B, Bahr R. Matching the choice of injury/ illness definition to study setting, purpose and design: one size does not fit all! Br J Sports Med. 2014;48(7):510-512. doi:10.1136/ bjsports-2013-093297
42. Clarsen B, Rønsen O, Myklebust G, Flørenes TW, Bahr R. The Oslo Sports Trauma Research Center questionnaire on health problems: a new approach to prospective monitoring of illness and injury in elite athletes. Br J Sports Med 2014;48(9):754-760. doi:10.1136/bjsports-2012-092087
43. Stracciolini A, Casciano R, Levey Friedman H, Meehan WP, Micheli LJ. Pediatric sports injuries: an age comparison of children versus adolescents. Am J Sports Med. 2013;41(8):1922-1929. doi:10.1177/ 0363546513490644
Download: https://ijspt.scholasticahq.com/article/125882-relationship-between-shoulder-pain-trunk-and-lower-limbpain-in-overhead-athletes-a-systematic-review-with-meta-analysis/attachment/ 253405.docx?auth_token=ViJa1CtXzpZ7HdQUgdnG
Download: https://ijspt.scholasticahq.com/article/125882-relationship-between-shoulder-pain-trunk-and-lower-limbpain-in-overhead-athletes-a-systematic-review-with-meta-analysis/attachment/ 253404.docx?auth_token=ViJa1CtXzpZ7HdQUgdnG

Scoping Review
Leahy I,
E,
MP. Isokinetic Dynamometry for External and Internal Rotation Shoulder Strength in Youth Athletes: A Scoping Review. IJSPT 2024;19(12):1521-1531. doi:10.26603/001c.125765
1a
Ian Leahy
, Erin Florkiewicz
1
, Mary P. Shotwell
2
1 Orthopedics, Rocky Mountain University of Health Professions, 2 Integrative Health Sciences, Rocky Mountain University of Health Professions
Keywords: Isokinetic dynamometry, shoulder, youth, overhead athlete, external rotation, internal rotation, strength, peak torque https://doi.org/10.26603/001c.125765
International Journal of Sports Physical Therapy
Vol. 19, Issue 12, 2024
Background
Accurately measuring shoulder strength in overhead athletes is critical, as sufficient strength is essential for safe and sustained performance during repetitive athletic movements. Isokinetic dynamometry (ID) offers dynamic strength assessments that surpass the capabilities of static methods, such as manual muscle testing and handheld dynamometry The dynamic assessment provided by ID may enhance upper extremity evaluation, aiding in the prediction of injury risk and the determination of return-to-sport criteria for overhead athletes.
Purpose
The purpose of this review was to examine the existing literature concerning the application of isokinetic shoulder strength testing in rehabilitation and clinical decision-making processes among youth athletes who perform repetitive overhead activities.
Study Design
Scoping review
Methods
A comprehensive literature search was conducted using PubMed and EBSCO Host databases, covering publications from 2000-2024. Search terms included “isokinetic dynamometry,” “shoulder,” and “youth athlete.” Inclusion criteria focused on youth athletes (<18 years) engaged in overhead sports, excluding those with neurological conditions or those designated as college or professional athletes. The PRISMA-ScR guidelines were followed.
Results
A total of 23 articles met the inclusion criteria. Volleyball and swimming were the most studied sports, with the most common testing position being the seated 90/90 position. Variations in testing speeds and outcome measures, such as peak torque and external rotation (ER) ratios, were identified.
Conclusions
Isokinetic dynamometry is a valuable tool for assessing shoulder strength in youth overhead athletes. It provides critical insights into muscle strength dynamics, aiding in injury prevention and rehabilitation. Further research is needed to optimize strength
a
Corresponding Author:
Ian Leahy, PT, DPT, OCS, SCS, CSCS, FAAOMPT 577 Washington Crossing Rd, Newtown PA 18940 267-226-5360 Leahydpt@gmail.com
assessment protocols and enhance clinical decision-making for safe return-to-sport practices.
Within a larger framework in the decision process for return to sports, recommendations for overhead athletes are reported considering normalized shoulder strength and scapular mechanics, range of motion (ROM), and successful completion of a plyometric program.1 However, many clinicians find it challenging to accurately measure shoulder strength due to limitations in equipment and expertise.
Shoulder strength assessment generally consists of isometric testing in neutral positions via manual muscle testing (MMT), handheld dynamometry (HHD), or isokinetic dynamometry (ID). Normative values for external rotation (ER) and internal rotation (IR) strength using HHD has been obtained in healthy adults,2,3 and physically active collegiate male and females.4 Studies indicate that HHD provides an assessment of shoulder IR/ER strength assessment that is highly correlated to assessments performed with ID.5 The concern, however, with MMT and HHD testing is that reliability of these methods is highly dependent on clinician size and strength.6 Additionally, because the testing position is static, HHD lacks the assessment of dynamic components associated with upper extremity movements required during overhead sports.7 In addition to torque output as a measure of strength, ID can capture endurance deficits and strength ratio imbalances which are predictors of shoulder injury 8 Ellenbecker demonstrated a significant difference in bilateral IR and ER strength measures between MMT grades and isokinetic dynamometry, widely recognized as the gold standard for measuring muscle strength and muscle endurance.9
Understanding the balance between the strength of agonist and antagonist muscles is crucial in evaluating and rehabilitating overhead athletes due to the intricate muscular activation patterns necessary for stability of the glenohumeral joint.7 One strategy for strength testing of the shoulder in multiple positions throughout the range of motion is ID Multiple authors have reported normative isokinetic strength assessment data for athletes involved in judo,10 tennis,11,12 badminton,13,14 and volleyball.15 In baseball, isokinetic strength testing has been performed in high school athletes,16 collegiate athletes,17,18 and professional athletes,19 yet limited information is available regarding normative values of isokinetic shoulder strength in youth athletes.
Gaps remain in the literature, particularly regarding the establishment of normative values for younger, skeletally immature athletes and how these values differ across various stages of development. The purpose of this review was to examine the existing literature concerning the application of isokinetic shoulder strength testing in rehabilitation and clinical decision-making processes among youth athletes who perform repetitive overhead activities.
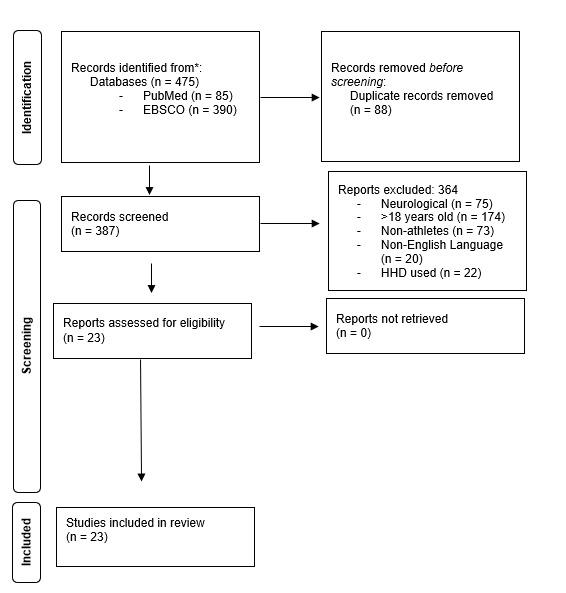
Figure 1. PRISMA flow diagram showing the literature search, screening, and eligibility results.
This literature review was conducted in accordance with the recommendations of the "Preferred Reporting Items for Systematic Reviews and Meta Analysis extension for Scoping Reviews (PRISMA-ScR).20
The literature review was performed with the databases PubMed, and EBSCO Host, which provides a range of databases, e-journals and e-books. Search terms included in the search strategies included phrases such as: “isokinetic dynamometry AND shoulder,” “isokinetic dynamometry AND shoulder AND youth athlete.” (See Appendix A for full search criteria). The search was limited to full-text available human research published between 2000-2024, including participants ages <18 years associated with an organized, overhead sport, and published in the English language. Exclusion criteria were articles pertaining to any neurological condition, and athletes designated as collegiate or professional.
Electronic database searches identified 475 total studies. The scoping review included 23 studies21‑43 after duplicate removal, title/abstract screen, and full text review
The PRISMA diagram (Figure 1) outlines the search process in its entirety
Table 1. Use of Isokinetic Dynamometry (ID) in Various Sports and ID Equipment Parameters
Author Sample / (Mean Age)
Batalha N21 25 males (13.28 yrs)
Batalha NM24 36 males (14.25 yrs)
Batalha N23 40 males (14.65 yrs)
Batalha NM25 40 males (14.65 yrs)
Batalha N22 49 males (14.48 yrs)
Clements AS26 18 males (13-16 yrs)
Sport
Swimming
Swimming
Swimming
Swimming
Swimming
Baseball
Volleyball
Type of Dynamometer
Biodex System-3
Biodex System-3
Biodex System-3
Biodex System-3
Biodex System-3
Biodex Multi-Joint Dynamometer
Biodex System-3
Position
Seated 90/90 position
Seated 90/90 position
Seated 90/90 position
Seated 90/90
Seated 90/90
Seated 90/90 de Lira CAB27 28 males (15.5 yrs)
Dupuis, C28 10 males (15.87 yrs)
Duzgun I29 24 athletes (14.5 yrs)
Eshghi S30 32 males (17.5 yrs)
Guney H31 65 athletes (16.1 yrs)
Lee DR32 23 males (18.2 yrs)
Mascarin NC33 26 females (15.3 yrs)
Mascarin NC34 39 females (15.3 yrs)
Mickevičius M35 14 boys (11-12 yrs)
Mohamed IW36 16 males (14.8 yrs)
Mulligan IJ37 39 males (15.36 yrs)
Pawlik D38 12 females (12-13 yrs)
Pontaga I39 14 males (14.6 yrs)
Saccol MF40 40 athletes (14 yrs)
van Cingel R41 40 females (17.6 yrs)
Vodička T42 20 males (13.23 yrs)
Yildiz Y43 40 males (17.2 yrs)
Baseball Kin-Com
Volleyball
Volleyball
Volleyball & Basketball
Baseball
Handball
Handball
Baseball
Weightlifting
Baseball
Volleyball
Handball
Tennis
Handball
Tennis
Volleyball, Handball, Tennis
Isomed 2000 Dynamometer
Biodex System-4
Isomed2000 D&R
Biodex Isokinetic Machine
Seated (angle not specified)
Seated 90/90
Seated 90/90 position
Seated position 90 degrees abduction / 30 degrees shoulder flexion
Seated 90/90
Seated 90/90 position
Biodex Isokinetic Machine Not Discussed
Biodex Isokinetic Dynamometer
Biodex System-3
Multi Joint System-3 Pro
Kin-Com Dynamometer
Multi-joint 4 Dynamometer Biodex
REV-9000
Cybex-6000
2-Humac Norm dynamometer
Human Norm CSMI
Cybex Norm
ISOKINETIC DYNAMOMETRY (ID) IN YOUTH REPETITIVE OVERHEAD ATHLETES
Of the included studies, volleyball was the most common overhead sport where ID was used for assessment.27,29‑31, 38,43 The second most common sport was swimming21‑25 followed by handball,33,34,39,41,43 baseball,26,28,32,37 tennis,40,42,43 weightlifting,36 and basketball.31 In the articles that fit the inclusion criteria, two pertained to symptomatic patients,31,35 whereas the remaining articles looked at isokinetic normative values, or the effects of repetitive sport specific movements. Table 1 describes the use of ID in various sports along with the variety of parameters used for testing ID
Seated 90/90
Seated 90/90
Seated 45/90 position
Repeat testing done @ 90/90
Seated: 90 degrees elbow flexion / 30 degrees abduction in scapular plane
Seated 90/90
Seated 90/90 position
Supine 90/90
Supine 90/90
Supine 90/90 position
Supine 90/90
Testing positions throughout studies varied, but trends are seen when testing the upper extremity (UE) of youth athletes with ID as illustrated in Table 1. The most utilized testing position for shoulder IR/ER is the seated position with the shoulder abducted to 90 degrees and the elbow flexed to 90 degrees, commonly known as the 90/90 position. It is postulated that this position, more than the arm at a neutral position, specifically addresses muscle function often required for an overhead athlete.44 The use of the 90/ 90 position also demonstrates strong intraclass coefficient for test/re-test reliability 45 Ellenbecker has discussed using a modified position of 30 degrees shoulder abduction, 30 degrees shoulder forward flexion, and 30 degrees diago-
nal tilt of the dynamometer to determine tolerance of the UE strength test prior to using the ID at a 90/90 position.7 Additional alterations to the 90/90 positions used in research are the seated 90/30 (90 degrees elbow flexion and 30 degrees shoulder abduction),37 seated 90/45 (90 degrees elbow flexion and 45 degrees shoulder abduction),36 seated 90/30 with 90 degrees of shoulder abduction and 30 degrees of shoulder flexion,30 and the 90/90 supine position.40‑43
Table 2 provides information regarding the variations in the speeds used for testing youth athletes. Most studies assessed participants at multiple speeds for different outcome measures or for different sports-related contexts. Common speeds for assessment of isokinetic peak torque both concentrically and eccentrically include 60 deg/sec,22‑25,27,29, 30,32‑34,38‑41 90 deg/sec,28,31,37,39,43 120 deg/sec,26,36,41 180 deg/sec,21‑25,28‑30,32,37,38,40,42 240 deg/sec,27,33,34,36,39 300 deg/sec,38,42 and 360 deg/sec.36
OBJECTIVE MEASURES FROM ISOKINETIC DYNAMOMETRY
PEAK TORQUE
In many studies pertaining to the use of ID in youth athletes, peak torque, normalized via body weight, was the primary objective measure.26,27,29,40 Peak torque is then used to compute measures of bilateral symmetry, using left and right values, and unilateral strength ratios using shoulder external and internal rotation strength values. Research indicates that repetitive sports-related movements lead to discernible discrepancies in peak torque between shoulder external rotation (ER) and internal rotation (IR) strength when comparing the dominant and non-dominant arms in athletes. Repetitive motions during youth sports such as volleyball,27,38,43 swimming,21‑25 and tennis40 result in increased IR peak torque in the dominant arm of the athlete. Variations exist among age groups within the same sport as evidenced by youth handball athletes demonstrating higher ER and IR peak torque in the dominant arm compared to non-dominant arm in athletes with a mean age of 17.6 years.41 Conversely, younger players (mean age of 14.6 years) showed no statistically significant difference between ER and IR peak torque.39 In a study of healthy teenage baseball players, Dupuis found greater concentric ER strength in the dominant arm at speeds of 90°/sec and 180°/sec.28 In contrast, Mickevičius observed decreased ER strength among younger baseball players (average age 11.6 years) who had a history of shoulder pain.35 It has been hypothesized that differences in peak torque output results in higher likelihood of overuse type injuries in youth athletes.24,27,41
Eight studies21‑25,35,40,42 used concentric external rotation to concentric internal rotation strength ratios during for their objective measurements whereas six studies28,30,31,34,
41,43 investigated various forms of eccentric to concentric ratios between ER and IR.
Comparison of shoulder agonist and antagonist muscle groups helps identify specific muscular imbalances.7 Variations in the dominant arm’s external rotation to internal rotation (ER:IR) ratios are frequently observed, particularly in cases where imbalances occur in the shoulder’s agonistantagonist muscle relationships. These imbalances can signify weaknesses that heighten athletes’ vulnerability to injury 24,40 Ideal ER:IR has been defined as 66%, which remains constant throughout the velocity spectrum46; however, this ratio is described in skeletally mature athletes.7
A common theme in youth overhead athletes is decreased ER:IR ratio in the dominant arm21‑24,34,40‑42 due to the theorized increase in IR peak torque because of sport specific repetitive motion. Although these imbalances do not result in changes in athletic performance, there is fear that if not addressed in the younger athlete they can result in overuse type injury.40
There are unique variations of the ER:IR used in ID assessment of youth athletes as evidenced by discussion of ER:IR acceleration and ER:IR deceleration described by Yildiz in youth volleyball players.43 The concept eccentric to concentric ER:IR is defined as the ratio of balance for muscle activity where the shoulder medial rotators eccentrically control external rotation, while lateral rotators eccentrically control internal rotation, ensuring optimal shoulder function.47 This explanation is similar to Dupuis’ definition of Dynamic Control Ratio (DCR) in youth baseball players.28 Both Yildiz and Dupuis investigate the eccentric and concentric relationship of the ER:IR ratio of the shoulder In each case, the ER:IR ratio into the acceleration phase (concentric ER to eccentric IR) was observed to be higher in the dominant arm,28,43 whereas the ER:IR ratio into the deceleration phase (eccentric ER to concentric IR) is lower in the dominant arm of the youth volleyball athlete,43 but no difference existed in the youth baseball athlete.28
This scoping review highlights the use of isokinetic dynamometry of the youth overhead athlete to obtain multiple objective measures. In adolescent overhead athletes, the repetitive nature of sport-specific movements imposes unique demands on the dynamic muscular control of the glenohumeral joint. This demand is highlighted by fluctuations in the external rotation to internal rotation peak torque ratio, a phenomenon hypothesized to significantly impact the vulnerability of the shoulder complex to injury.21‑25 Various studies support this hypothesis, including symptomatic athletes35 and those with glenohumeral internal rotation deficits.31
In sports like baseball, dynamic muscular control of the glenohumeral joint is essential, particularly given the substantial stress experienced across the upper extremity joints during pitching. The angular velocities of shoulder internal rotation and elbow extension can range from 1,000
Table 2. Isokinetic Dynamometry Testing Speed and Other Objective Measures
Author Testing Speed Objective Measures
Batalha N21 60 deg/sec 180 deg/sec
Batalha N24 60 deg/sec 180 deg/sec
Batalha N23 60 deg/sec 180 deg/sec
Batalha N25 60 deg/sec 180 deg/sec
Batalha N22 60 deg/sec 180 deg/sec
Clements AS26 120 deg/sec
de Lira CAB27 60 deg/sec 240 deg/sec
Dupuis, C28 90 deg/sec 180 deg/sec
Duzgun I29 60 deg/sec 180 deg/sec
Eshghi S30 60 deg/sec 180 deg/sec
Guney H31 90 deg/sec
Lee D32 60 deg/sec 180 deg/sec
Mascarin N33 60 deg/sec 240 deg/sec
Mascarin N34 60 deg/sec 240 deg/sec
Mickevičius M35 120 deg/sec
Mohamed IW36 120 deg/sec 240 deg/sec 360 deg/sec
Mulligan I37 90 deg/sec 180 deg/sec
Pawlik D38 60 deg/sec 180 deg/sec 300 deg/sec
Pontaga I39 60 deg/sec 90 deg/sec
• PT IR
• PT ER
• ER:IR ratio
• PT
• ER/IR ratio
• Max torque
• ER/IR ratio - norm is 66-75%
• PT
• ER/IR ratios
• PT
• ER/IR ratio
• PT/BW
• Absolute PT
• Relative PT (divided by BW)
• Absolute total work
• Relative total work (divided by BW)
• Conventional strength ratio
• Functional strength ratio
• PT
• IR con / ER ecc (performance ratio)
• ER con / IR ecc (cocking ratio)
• PT / BW
• Total work
• FDR
• EReccn:IRcon
• ER:IR
• Max eccentric ER torque / Max concentric IR torque
• PT
• PT and total work
• at 60 deg/sec:
• IR PT
• CR (ER con / IR con)
• at 240 deg/sec
• IR PT
• IR avg power
• FR (ER ecc / IR con)
• ER PT was measured at both speeds
• PT
• ER:IR ratio
• Relative PT
• Time to PT
• PT and Total work for both movements at both speeds
• Concentric IR PT
• PT
• Avg power
Author
Saccol M40 60 deg/sec
Vodička T42 180 deg/sec 300 deg/sec
Yildiz Y43 90 deg/sec
• PT / BW
• Total work / BW
• ER/IR ratio
• Peak torque
• ER/IR ratio
• ER ecc / IR con
• ER con / IR ecc
• Both in the late cocking phase of overhead motion and the deceleration phase
deg/sec to 7,200 deg/sec in youth and collegiate pitchers, respectively, from maximum external rotation through the acceleration phase.48,49 While ID testing velocities of 240 deg/sec do not fully replicate these speeds, they still yield valuable data on shoulder musculature function at higher isokinetic speeds.50 Table 3 provides a detailed breakdown of these different sport-specific findings.
ID studies of youth athletes skew towards specific sports such as volleyball and swimming. Limited information is available regarding the use of ID for assessment of athletes participating in youth baseball. In reviewing the ages of participants recruited for ID articles in youth athletes, the youngest subjects were 11 years old. However, pitching and repetitive throwing in baseball often begins as early as 6-7 years of age. Studies included in a systematic review suggest that starting repetitive pitching at 10 years of age or younger increases the risk of upper extremity-related injury 51 In most sports, children are playing and specializing in sport positions at a much younger age than captured in this review, but changes in shoulder IR strength between dominant and non-dominant arm has been seen in youth throwers under the age of 10 using HHD 52 Understanding dynamic strength values and muscular balance relationships with measurements from ID in skeletally immature athletes and the changes that occur with repetitive overhead motions can assist in developing injury prevention, rehabilitation programs, and return to sport decision making for youth throwing athletes.
Only studies in English languages were included in the review and the range of articles searched were between 2000-2024. Also, no quality assessment of the studies was performed, which may limit the impact of the findings.
Isokinetic dynamometry as an assessment in youth overhead athletes provides insights into shoulder strength
(torque) and strength ratios. There is variety in the assessment parameters utilized in the included studies of youth athletes in various sports. By precisely evaluating isokinetic strength, clinicians can gauge the shoulder’s dynamic control, facilitating the tailored design of training programs. Isokinetic assessments allow for detailed analysis of power and the balance between agonist and antagonist muscle groups during movement, enabling the identification of specific strength impairments and guiding targeted interventions to enhance upper extremity loading tolerance for repetitive overhead activities.
The authors declare that they have no conflicts of interest related to the content of this manuscript.
Submitted: June 19, 2024 CST, Accepted: September 17, 2024 CST
© The Author(s)
• Higher IR peak torque in dominant arm
• ER strength increased with weighted jump rope in dominant arm
• Functional Deceleration Ratio (eccentric to concentric strength of IR and ER) in dominant arm
• Increased ER:IR ratio after strengthening program
• Higher IR peak torque in dominant arm
• Higher IR peak torque in dominant arm
• Decreased ER:IR ratio in dominant arm in swimmers vs control
• Higher IR peak torque in swimmer dominant arm
• Decreased ER:IR ratio in dominant arm for swim only group
• Decreased ER:IR in dominant arm for swimmers-
• Higher IR peak torque in dominant arm for swimmers
• Decreased ER:IR in dominant arm for swimmers
• Training improved ER peak torque in dominant arm
• Peak torque of dominant arm not associated with throwing velocity
• Higher ER peak torque in dominant arm
• ER:IR lower in dominant arm
• ER concentric :IR eccentric in cocking phase was higher in dominant arm
• ER eccentric:IR concentric during deceleration was no different side to side
• IR and ER peak torque increased with CKC strengthening in dominant arm
• ER eccentric strength was weaker in baseball players dominant arm
• Decreased ER:IR in dominant arm for baseball players with pain
• IR eccentric: IR concentric – lower in dominant arm
• ER eccentric: IR concentric – lower in dominant arm
• ER concentric: IR eccentric – lower in dominant arm
• Decreased ER:IR ratio in the dominant arm
• No significant difference between eccentric and concentric peak torque between dominant vs non-dominant arm
• ER:IR lower in dominant arm
• ER eccentric : IR concentric was lower in dominant arm
• ER:IR ratio unchanged in dominant arm with strength training
• All participants demonstrated weak IR of the dominant arm
• ER:IR – 82.8 in experimental group vs 77.6 in control group
• Strength testing did not result in improvement in IR strength
• Strength training did not improve strength ratios
• Strength training improved average power
• No statistically significant differences between dominant and non-dominant arm peak torque
• Average power of IR was higher in dominant arm
• ER:IR lower in dominant arm of handball players
• Higher ER and IR peak torque in dominant arm
• Decreased ER:IR on dominant arm
• Higher ER strength in youth male tennis players
• Higher IR strength on dominant arm for both youth male and female athletes
• Decreased ER:IR ratio on dominant arm
• Higher ER strength in dominant arm
• Higher IR strength on dominant side
• ER:IR ratio of dominant arm improved with isokinetic strength program
• ER:IR ratio of dominant arm improved with isotonic strength program
• IR and ER peak torque of dominant arm increased in both training groups
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Sgroi TA, Zajac JM. Return to throwing after shoulder or elbow injury Curr Rev Musculoskelet Med 2018;11(1):12-18. doi:10.1007/s12178-018-9454-7
2. Bradley H, Pierpoint L. Normative values of isometric shoulder strength among healthy adults. Int J Sports Phys Ther. 2023;18(4):977-988. doi:10.26603/001c.83938
3. Harbin G, Leyh C, Harbin A. Upper extremity strength: Normative reference data among uninjured employees. Work 2020;67(4):979-991. doi:10.3233/ wor-203348
4. Westrick RB, Duffey ML, Cameron KL, Gerber JP, Owens BD. Isometric shoulder strength reference values for physically active collegiate males and females. Sports Health. 2013;5(1):17-21. doi:10.1177/ 1941738112456280
5. Chamorro C, Arancibia M, Trigo B, Arias-Poblete L, Jerez-Mayorga D Absolute reliability and concurrent validity of hand-held dynamometry in shoulder rotator strength assessment: systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(17). doi:10.3390/ijerph18179293
6. Nicholas JA, Sapega A, Kraus H, Webb JN. Factors influencing manual muscle tests in physical therapy J Bone Joint Surg Am. 1978;60(2):186-190. doi:10.2106/00004623-197860020-00008
7 Ellenbecker TS, Davies GJ. The application of isokinetics in testing and rehabilitation of the shoulder complex. J Athl Train 2000;35(3):338-350.
8. Bagordo A, Ciletti K, Kemp-Smith K, Simas V, Climstein M, Furness J. Isokinetic dynamometry as a tool to predict shoulder injury in an overhead athlete population: A systematic review Sports 2020;8(9). doi:10.3390/sports8090124
9. Ellenbecker TS. Muscular strength relationship between normal grade manual muscle testing and isokinetic measurement of the shoulder internal and external rotators. Isokin Exerc Sci 1996;6:51-56. doi:10.3233/IES-1996-6109
10. Marcondes FB, Castropil W, Schor B, Miana A, Vasconcelos R, Etchebehere M. Shoulder isokinetic performance in healthy professional judo athletes: normative data. Acta Ortop Bras. 2019;27(6):308-312. doi:10.1590/1413-785220192706223708
11. Niederbracht Y, Shim AL. Concentric internal and eccentric external fatigue resistanc of the shoulder rotator muscles in female tennis players. N Am J Sports Phys Ther 2008;3(2):89-94.
12. Ellenbecker T, Roetert EP Age specific isokinetic glenohumeral internal and external rotation strength in elite junior tennis players. J Sci Med Sport 2003;6(1):63-70. doi:10.1016/s1440-2440(03)80009-9
13. Zulfikri N, Selvanayagam VS, Yusof A. Evaluation of shoulder and knee isokinetic strength profile among elite adolescent badminton players. J Sport Rehabil. 2021;30(5):717-724. doi:10.1123/ jsr.2019-0483
14. Ng GY, Lam PC. A study of antagonist/agonist isokinetic work ratios of shoulder rotators in men who play badminton. J Orthop Sports Phys Ther 2002;32(8):399-404. doi:10.2519/jospt.2002.32.8.399
15. Hadzic V, Sattler T, Veselko M, Markovic G, Dervisevic E. Strength asymmetry of the shoulders in elite volleyball players. J Athl Train 2014;49(3):338-344. doi:10.4085/1062-6050-49.2.05
16. Trunt A, Fisher BT, MacFadden LN. Athletic shoulder test differences exist bilaterally in healthy pitchers. Int J Sports Phys Ther 2022;17(4):715-723. doi:10.26603/001c.35722
17 Lin HT, Ko HT, Lee KC, Chen YC, Wang DC. The changes in shoulder rotation strength ratio for various shoulder positions and speeds in the scapular plane between baseball players and non-players. J Phys Ther Sci 2015;27(5):1559-1563. doi:10.1589/ jpts.27.1559
18. Dodds FT, Knotts SS, Penrod MI, Scoggins WA, Conners RT Shoulder strength and range of motion between collegiate pitchers and position players in baseball. Int J Exerc Sci 2020;13(6):123-130.
19. Kim BG, Lim SK, Kong S. The Relationship between scapular upward rotation and shoulder internal and external rotation isokinetic strength in professional baseball pitchers. Healthcare 2021;9(6). doi:10.3390/healthcare9060759
20. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. doi:10.7326/m18-0850
21. Batalha N, Dias S, Marinho DA, Parraca JA. The effectiveness of land and water based resistance training on shoulder rotator cuff strength and balance of youth swimmers. J Hum Kinet. 2018;62:91-102. doi:10.1515/hukin-2017-0161
22. Batalha N, Marmeleira J, Garrido N, Silva AJ. Does a water-training macrocycle really create imbalances in swimmers’ shoulder rotator muscles? Eur J Sport Sci 2015;15(2):167-172. doi:10.1080/ 17461391.2014.908957
23. Batalha N, Raimundo A, Tomas-Carus P, Paulo J, Simão R, Silva AJ. Does a land-based compensatory strength-training programme influences the rotator cuff balance of young competitive swimmers? Eur J Sport Sci 2015;15(8):764-772. doi:10.1080/ 17461391.2015.1051132
24. Batalha NM, Raimundo AM, Tomas-Carus P, Barbosa TM, Silva AJ. Shoulder rotator cuff balance, strength, and endurance in young swimmers during a competitive season. J Strength Cond Res. 2013;27(9):2562-2568. doi:10.1519/ JSC.0b013e31827fd849
25. Batalha NM, Raimundo AM, Tomas-Carus P, Marques MA, Silva AJ. Does an in-season detraining period affect the shoulder rotator cuff strength and balance of young swimmers? J Strength Cond Res. 2014;28(7):2054-2062. doi:10.1519/ jsc.0000000000000351
26. Clements AS, Ginn KA, Henley E. Correlation between muscle strength and throwing speed in adolescent baseball players. Phys Ther Sport 2001;2(3):123-131. doi:10.1054/ptsp.2000.0025
27 de Lira CAB, Vargas VZ, Vancini RL, Andrade MS. Profiling isokinetic strength of shoulder rotator muscles in adolescent asymptomatic male volleyball players. Sports 2019;7(2). doi:10.3390/sports7020049
28. Dupuis C, Tourny-Chollet C, Delarue Y, BeuretBlanquart F. Influence of baseball practice on strength ratios in shoulder rotator muscles: A new position for isokinetic assessment. Isokin Exerc Sci 2004;12(2):149-157. doi:10.3233/IES-2004-0167
29. Duzgun I, Baltaci G, Colakoglu F, Tunay VB, Ozer D The effects of jump-rope training on shoulder isokinetic strength in adolescent volleyball players. J Sport Rehabil 2010;19(2):184-199. doi:10.1123/ jsr.19.2.184
30. Eshghi S, Zarei M, Abbasi H, Alizadeh S. The effect of shoulder injury prevention program on shoulder isokinetic strength in young male volleyball players. Res Sports Med. 2022;30(2):203-214. doi:10.1080/15438627.2020.1860050
31. Guney H, Harput G, Colakoglu F, Baltaci G. The effect of glenohumeral internal-rotation deficit on functional rotator-strength ratio in adolescent overhead athletes. J Sport Rehabil. 2016;25(1):52-57. doi:10.1123/jsr.2014-0260
32. Lee DR, Kim LJ. Internal- and external-rotation peak toque in little league baseball players with subacromial impingement syndrome: improved by closed kinetic chain shoulder training. J Sport Rehabil. 2016;25(3):263-265. doi:10.1123/ jsr.2014-0333
33. Mascarin NC, de Lira CAB, Vancini RL, da Silva AC, Andrade MS. The effects of preventive rubber band training on shoulder joint imbalance and throwing performance in handball players: A randomized and prospective study. J Bodyw Mov Ther. 2017;21(4):1017-1023. doi:10.1016/j.jbmt.2017.01.003
34. Mascarin NC, de Lira CAB, Vancini RL, de Castro Pochini A, da Silva AC, Dos Santos Andrade M. Strength training using elastic bands: improvement of muscle power and throwing performance in young female handball players. J Sport Rehabil. 2017;26(3):245-252. doi:10.1123/jsr.2015-0153
35. Mickevičius M, Rutkauskas S, Sipavičienė S, et al. Absence of bilateral differences in child baseball players with throwing-related pain. Int J Sports Med. 2016;37(12):952-957 doi:10.1055/s-0042-106297
36. Mohamed IW, Rahim MFA, Shaharudin S. Effects of isokinetic versus isotonic training on strength, power and muscular balance of rotator cuff muscles among advanced level of adolescent weightlifters. Int J Appl Sports Sci. 2017;29(2):143-154. doi:10.24985/ ijass.2017.29.2.143
37 Mulligan IJ, Biddington WB, Barnhart BD, Ellenbecker TS. Isokinetic profile of shoulder internal and external rotators of high school aged baseball pitchers. J Strength Cond Res 2004;18(4):861-866. doi:10.1519/14633.1
38. Pawlik D, Dziubek W, Rogowski Ł, Struzik A, Rokita A. Strength abilities and serve reception efficiency of youth female volleyball players. Appl Bionics Biomech 2022;2022:4328761. doi:10.1155/ 2022/4328761
39. Pontaga I, Zidens J. Shoulder rotator muscle dynamometry characteristics: side asymmetry and correlations with ball-throwing speed in adolescent handball players. J Hum Kinet. 2014;42:41-50. doi:10.2478/hukin-2014-0059
40. Saccol MF, Gracitelli GC, da Silva RT, et al. Shoulder functional ratio in elite junior tennis players. Phys Ther Sport 2010;11(1):8-11. doi:10.1016/j.ptsp.2009.11.002
41. van Cingel R, Habets B, Willemsen L, Staal B. Shoulder dynamic control ratio and rotation range of motion in female junior elite handball players and controls. Clin J Sport Med. 2018;28(2):153-158. doi:10.1097/jsm.0000000000000429
42. Vodička T, Zvonař M, Pačes J, Knjaz D, Ružbarský P, Zháněl J. Strength values of shoulder internal and external rotators in junior tennis players. Kinesiology. 2018;50(2):181-187 doi:10.26582/k.50.2.9
43. Yildiz Y, Aydin T, Sekir U, Kiralp MZ, Hazneci B, Kalyon TA. Shoulder terminal range eccentric antagonist/concentric agonist strength ratios in overhead athletes. Scand J Med Sci Sports 2006;16(3):174-180. doi:10.1111/ j.1600-0838.2005.00471.x
44. Bassett R, Browne A, Morrey B, An K. Glenohumeral muscle force and moment mechanics in a position of shoulder instability J Biomech 1990;23(5):405-415. doi:10.1016/ 0021-9290(90)90295-E
45. Durall CJ, Davies GJ, Kernozek TW, Gibson MH, Fater DC, Straker JS. The effects of training the humeral rotators on arm elevation in the scapular plane. J Sport Rehabil 2001;10(2):79-92. doi:10.1123/ jsr.10.2.79
46. Ivey FM Jr, Calhoun JH, Rusche K, Bierschenk J. Isokinetic testing of shoulder strength: normal values. Arch Phys Med Rehabil 1985;66(6):384-386.
47 Scoville CR, Arciero RA, Taylor DC, Stoneman PD End range eccentric antagonist/concentric agonist strength ratios: a new perspective in shoulder strength assessment. J Orthop Sports Phys Ther. 1997;25(3):203-207 doi:10.2519/jospt.1997.25.3.203
48. Tanaka N, Sakai Y, Maruyama Y, Hirayama T, Iwamoto W, Wagatsuma K. Throwing kinematics and elbow varus torque relative to ball size in junior baseball players. J Phys Ther Sci 2022;34(1):22-25. doi:10.1589/jpts.34.22
49. Hirashima M, Yamane K, Nakamura Y, Ohtsuki T. Kinetic chain of overarm throwing in terms of joint rotations revealed by induced acceleration analysis. J Biomech. 2008;41(13):2874-2883. doi:10.1016/ j.jbiomech.2008.06.014
50. Pawlowski D, Perrin DH. Relationship between shoulder and elbow isokinetic peak torque, torque acceleration energy, average power, and total work and throwing velocity in intercollegiate pitchers. Athl Train. 1989;24(2):129-132.
51. Agresta CE, Krieg K, Freehill MT Risk factors for baseball-related arm injuries: A systematic review Orthop J Sports Med. 2019;7(2):2325967119825557. doi:10.1177/2325967119825557
52. Nakaji RM, Ellenbecker TS, McClenahan KM, Roberts LM, Perez C, Dickenson SB. Descriptive strength and range of motion in youth baseball players. Int J Sports Phys Ther 2021;16(1):195-206. doi:10.26603/001c.18815
Download: https://ijspt.scholasticahq.com/article/125765-isokinetic-dynamometry-for-external-and-internalrotation-shoulder-strength-in-youth-athletes-a-scoping-review/attachment/ 253027.docx?auth_token=CtgDmsmn5AAoovfReD1B

Dischiavi S, Perry J, Burk C, Chiang J, Bleakley C. The Reliability and Validity of a Novel Clinical Test for Assessing Shoulder Rotation ROM in Collegiate Baseball Players: Functional Assessment of System Tension of the Shoulder (FAST-SHDR). IJSPT 2024;19(12):1532-1540. doi:10.26603/001c.126062
Steven Dischiavi1a , Jesse Perry1 , Connor Burk1 , Jeremy Chiang1 , Chris Bleakley2
1 Physical Therapy, High Point University, 2 Physical Therapy, University of Ulster
Keywords: Keywords: shoulder, range of motion, trunk rotation, rehabilitation, sports https://doi.org/10.26603/001c.126062
International Journal of Sports Physical Therapy
Vol. 19, Issue 12, 2024
Background
Traditional methods to measure rotational passive range of motion (PROM) in the throwing shoulder do not reflect the complexity of the throwing motion. Therefore, a sport specific shoulder rotation PROM test (FAST-SHDR) was developed and compared to traditional standard methods to measure shoulder internal and external rotational PROM in the throwing shoulder.
Purpose
The aim of this study was to determine the intra-rater reliability of the FAST-SHDR test in young, healthy, male Division 1 baseball players.
Study Design
Reliability and validity analysis
Methods
A study with 49 healthy participants (31 collegiate baseball players, 18 controls) examined a sport specific shoulder rotation PROM test (FAST-SHDR) and compared this to the standard supine 90/90 shoulder in a single session assessment. Intra-class correlation coefficient (ICC), standard error of measurement (SEM) and minimum detectable change (MDC) were calculated. Within and between group differences were based on t-tests (p<0.001), absolute differences and effect sizes (95% CIs).
Results
The novel test (FAST-SHDR) had good to excellent reliability with ICCs ranging from 0.95 (0.89 to 0.98) to 0.96 (0.92-0.98). MDC ranged from 7°-11° which is equivalent to 11-14% of mean PROM scores. In the dominant shoulder of baseballers, when FAST-SHDR IR/ER was compared to standard IR/ER testing the FAST-SHDR scores were lower for both IR (MD 23.3°; 95% CI 19.7-26.8) and ER (MD 50.7°; 95% 44.7 to 56.7). Comparing the shoulder rotation PROM in baseballers, the FAST-SHDR ER and IR measurements were significantly lower (p<0.0001) when compared to traditional standard PROM testing for shoulder IR and ER rotation.
a
Corresponding Author:
Steven L. Dischiavi, PT, PhD, DPT, MPT, SCS, ATC, COMT, Cert DN
High Point University
One University Parkway High Point, NC 27268
P: (336) 841-4606
F: (336) 888-5020
E: sdischia@highpoint.edu
FAST-SHDR testing shows good to excellent intra-rater reliability for measuring shoulder rotational PROM and demonstrates both face and discriminant validity
Level of Evidence
3
Upper extremity injuries are prevalent across all levels of baseball.1 Three quarters of adolescent baseball players report constant pain in their throwing arm, with injury incidence estimated at 0.86 and 1.39 per 10,000 athlete-exposures (AEs) respectively.2,3 Higher injury rates occur at collegiate level, with 1.85 to 5.75 upper limb injuries per 1000 AEs in game situations, with 25% requiring absence from play for 10 days.4 Major League Baseball (MLB) players are at greatest risk, with an average of 55 days of time loss due to shoulder injury5; this incurs substantial costs on MLB clubs, estimated at $400 million dollars each year 5
A commonly utilized metric in maintaining optimal performance in a baseball player’s dominant throwing shoulder, is to obtain passive range of motion (PROM) measurements of internal and external rotation (IR/ER). The traditional standard clinical assessment of shoulder rotation PROM involves placing the athlete in the supine position, lying completely flat on their back, with the lower extremities fully extended. A goniometer is then used to assess shoulder rotational PROM with the athlete’s test arm typically held in either 0° or 90° of humeral abduction during testing.6‑8 Although this standard method is reliable, it does not reflect the global torsional complexity of throwing mechanics.
It is important to recognize that the standard method to assess the rotational PROM of the throwing shoulder is to place the shoulder in a position of maximal tension locally at the shoulder, in combined abduction and external rotation. These combined motions do acknowledge the tissue tension that is occurring locally at the glenohumeral joint but neglects the potential impact on shoulder PROM once the torsion of the throw moves the trunk into contralateral rotation. For example, throwing a baseball encompasses movement throughout the kinetic chain at the shoulder, trunk, pelvis, hip joints, and lower extremities, and includes five phases of movement - wind up, cocking, acceleration, deceleration, and follow through.9
The transition from the early to late cocking phase is central to developing the torsion needed for throwing performance, as this rotation occurs and tissue elongation maximizes the length and tension on the musculoskeletal system, referred to as “system tension”. This release of stored elastic system tension transmits potential to kinetic energy at the ball release phase of throwing.9‑14
Musculoskeletal impairments at any point along the kinetic chain can have an impact on throwing performance and injury risk.9 Empirical data show that the recruitment of the scapulothoracic muscles during throwing is sensitive to changes in lower extremity and trunk position,15 and that the risk of shoulder and elbow injury is increased in
athletes with reduced hip extension on the same side as the throwing shoulder16 or internal rotation of the thrower’s stride leg.17 Increasingly, studies appear to support that the throwing shoulder is affected by the global kinetic chain, yet the currently utilized standard supine testing position used to assess shoulder rotational PROM does not capture any aspect of the sport specific throwing motion outside the shoulder
There is a precedent at the hip joint, for the idea that PROM assessments do not appear to reflect the task of the athlete that is being assessed. Sport specific testing positions have been developed for assessing lower limb hip PROM in the kicking athlete. Tak and Langhout developed a clinical test14 that recreates the system tension arc associated with kicking, using a combination of hip extension, abduction, adduction, and rotation, with contralateral rotation of the trunk and pelvis. The test has been reported to be reliable and can accurately differentiate asymmetries in kicking athletes with groin pain.18 As Tak, et al.19 observed, the standard traditional supine hip PROM testing position in soccer players lacks similar face validity, as does the standard traditional supine testing position of shoulder rotation PROM in baseball players. Neither of these traditional standard positions used to measure hip or shoulder PROM incorporate many of the key trunk and pelvic positions, and the accompanying torsional movements that occur during a maximal throw or kick.
Overhead throwing athletes should be assessed using a sports specific PROM test, which may better reflect the task specific global torsional positioning observed during throwing motion. This study proposes a novel clinical test to quantify shoulder rotational PROM in baseball players, which is underpinned by the global three-dimensional tension that is experienced during overhead throwing. The development of the FAST-SHDR test was built on the concept of interconnected muscle chains, connecting the lower to upper extremities via the trunk, which have been increasingly recognized in current literature.20,21
The key objectives were to determine the intra-rater reliability of the novel PROM test, and to establish reference values in throwing and non-throwing (control) populations. Construct and discriminant validity were also explored by comparing shoulder rotation PROM within (dominant vs non-dominant) and across populations (baseball vs control). It was hypothesized that the greatest variations to sport specific PROM would be seen in the dominant shoulders of baseball athletes.
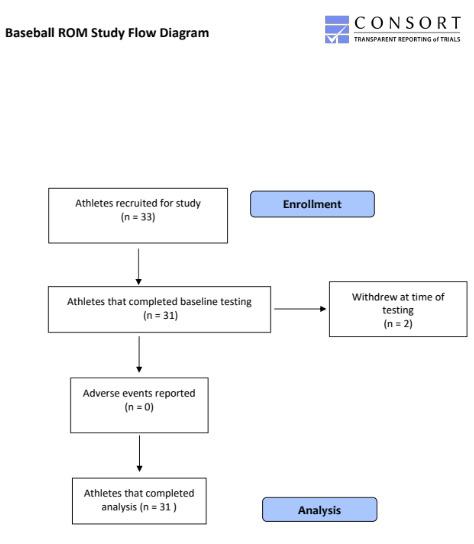
The study protocol was approved by the Institutional Review Board at High Point University (Protocol number 201508-387). Prior to any testing the potential risks of all experimental procedures were explained fully to all participants. Prior to participating in the study, all participants read and signed the informed consent form.
A sample of 31 collegiate male baseball players from the Division 1 baseball team were recruited during the preseason period of the 2018/19 playing season. The total number of roster players invited to participate was 33, and 33 total players volunteered (14 pitchers and 19 field players), but two were unable to participate on the day of testing secondary to pain from a previous weight room session (Figure 1).
The inclusion criteria in the study stated players must have been aged > 18years at the time of informed consent. The exclusion criteria included any current shoulder or elbow injury or shoulder or elbow injury in the previous 12 months, or pain reported during, or at the time of testing, that would not allow the participant to be assessed.
A convenience sample of 18 non-baseball research participants volunteered from a class of 66 physical therapy students from the same university (10 females and 8 males; age: 21.6 + 1.6). In an effort to allow the control participants to fully understand the aim of the study, all students were given a demonstration and thorough explanation of the procedure and why it was being performed, prior to giving their informed consent to participate in the study Participant recruitment and testing was undertaken by three final year High Point University Doctor of Physical Therapy

students (JMP, CLB, JAC), under the supervision of two experienced licensed physical therapists and clinical researchers (SLD, CMB).
TESTING PROCEDURES
FAST-SHDR PROM TESTING
A novel sport specific test (FAST-SHDR) was developed to quantify shoulder internal and external rotation. The FASTSHDR test is performed by having the athlete initially positioned in supine hook-lying, with the shoulder to be tested off the side of the plinth. While maintaining the supine hook lying position, the pelvis is passively rotated 90 degrees contralateral to the tested arm, which remains off the side of the plinth. Once the pelvis is rotated, the legs are secured by placing a strap around the knees, securing the legs to the plinth with a belt, while keeping the athlete flat on their back. The legs rest on the plinth when the strap is placed around the lower extremities, the strap serves to provide stability as the trunk is rotated and the arm is moved into horizontal abduction, thus, the strap does not force the legs to the table, rather, the strap holds the legs in position as tension is taken up more proximally (Figure 2).
Although the FAST-SHDR test could be performed by a single clinician, in this study the test was performed most efficiently by using two assessors. Assessor 1 positioned the test shoulder in 90 degrees of shoulder abduction, then into maximal passive horizontal abduction taking up spinal rotation slack as well, and then lastly rotated the shoulder to the passive end range testing direction (internal or external rotation). The end range of passive shoulder ROM was determined by soft tissue end-feels and all the available slack in the movement was taken up during the movement. As-

sessor 2 placed a bubble inclinometer on the distal styloid process of the ulna to determine shoulder angle. Assessor 1 was blinded to PROM angles for the duration of the testing process. The process was then repeated for the opposite shoulder with the testing order randomized (dominant vs non-dominant extremity) (Figure 3).
The standard testing position of shoulder rotation PROM began with the participants lying supine with the lower extremities in a fully extended and in a comfortable resting position. As participants were in the supine position the arm was brought passively into 90 degrees of shoulder abduction and 90 degrees of elbow flexion. A stabilizing hand was brought to the anterior shoulder with a slight posterior glide to maintain glenohumeral joint congruency. These steps were performed to fully replicate the current standard method of shoulder rotation PROM assessment used by the baseball athletic trainer at the university during pre-season screening (Figure 4). Reliability data were determined based on three repeated tests on both sides, during a single session, for each of the test conditions.
FAST-SHDR reliability was initially determined through ICCs, using a two-way, mixed effect model (absolute agreement).22 Standard Error of Measurement (SEM) was then calculated using the formula: SEM = SD √1-r (SD = standard deviation of sample scores; r = reliability of scores) and Minimum Detectable Change (MDC) was calculated using the formula: MDC = 1.96 X √2 X SEM.23 MDC was expressed both in absolute terms, and as a percentage of the grand mean.
Between and within group differences were assessed using relevant t-tests, effect sizes (Hedges g) and absolute

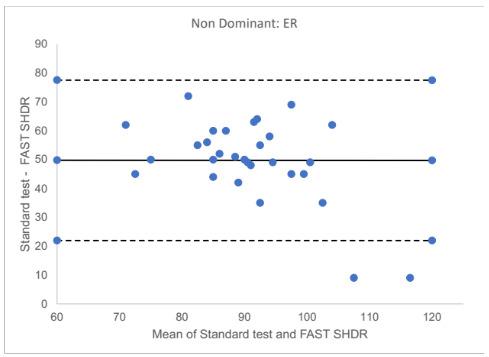
differences with 95% confidence intervals (CIs). Normality of data distribution was assessed visually using Q-Q, Box plots, and histograms. P values were set at 0.001 a priori due to the exploratory nature of the study, and all analyses were conducted in SPSS v21 (IBM, USA). ICCs were interpreted using the lower bound 95% confident interval of each estimate, as follows: <0.5 = poor, between 0.5 and 0.75 = moderate, between 0.75 and 0.9= good, and >0.90 =excellent reliability 22
On the day of testing, two baseballer players were unable to undergo the test procedure secondary to pain reported
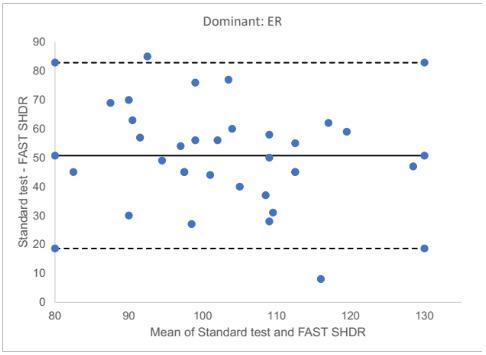
from a recent weight training session. Thus, 31 total baseball players completed the protocol on the day of testing. None of the 31 participants reported any pain or adverse effects because of the testing procedures.
The participant demographics were (M/SD): age: 19.2+ 1.2 y; weight: 86.1+ 7.7 kg; height: 185.5+ 5.39 cm. Intra-rater reliability and key clinimetrics of the sport specific FASTSHDR test are shown in Table 1 The test shows good to excellent reliability with ICCs ranging from 0.95 (0.89 to 0.98) to 0.96 (0.92-0.98). MDC for FAST- SHDR rotation ranged from 6.8° (IR) to 11.1° (ER), which represents 10.6% and 15.2% of mean scores respectively
Bland and Altman plots were used to visually examine the level of agreement between PROM when measured in non-dominant (Figure 5) and dominant (Figure 6) arms and across populations (baseball and controls). In both Figures 5 and 6 the solid black line represents the mean difference between the tests, while the dashed lines indicate the 95% limits of agreement. The largest differences were recorded for ER, with mean differences of 49.7° (95% CI 44.5 to 55.1)
and 50.7° (95% CI 44.7 to 56.7) at non-dominant (Figure 5) and dominant (Figure 6) shoulders respectively.
SPORT SPECIFIC ROTATION TESTING (FAST-SHDR) VS STANDARD ROTATION PROM TESTING
Normative testing data for the Division 1 baseball players is summarized in Table 2 Shoulder rotation PROM was normally distributed with no evidence of floor or ceiling effects. Sport specific FAST-SHDR IR was significantly lower in the dominant shoulder vs non-dominant (p <0.0001), however this pattern was reversed for ER (p <.0001).
The correlation between sport specific and standard test scores were weak to moderate for ER scores, and strong for IR scores (Table 2). Total arc shoulder rotation (Figure 7) was also consistently lower with sport specific testing compared to standard, at both dominant (MD 74.0°; 95% CIs 66.9 to 81.1 degrees; p<0.001) and non-dominant shoulders (MD 71.4°; 95% CIs 64.8 to 78.0 degrees; p<0.0001) (Table 2).
The study introduces a novel sport specific test (FASTSHDR) for assessing shoulder rotation PROM. The test was developed to acknowledge the multisegmented and torsional nature of throwing. The test demonstrated good to excellent intra-rater reliability, with MDC scores ranging from 6.8° to 11.1° for IR and ER respectively These figures compare favorably to traditional standard method of assessment of shoulder IR / ER (based on full supine lying, 90° shoulder abduction and 90° of elbow flexion), where MDC is estimated at 5 - 10°.24,25 The hypothesis of this study, that the greatest restrictions to sport specific rotation PROM (FAST-SHDR) would be seen in the dominant shoulders of baseball athletes was confirmed.
A key difference between traditional shoulder rotation PROM testing methods, and the new sport specific assessment, is that the FAST-SHDR test places the patient in a position that produces a similar “tension arc” position of the trunk and pelvis during the terminal phase of an overhead throw The sport specific PROM scores were consis-
(14.3)
(14.1) Test 3: 68.8 (12.1)
(14.2)
(20.6)
* P<0.0001; mean values, range, SEM, MDC, and SD values are all measurements in degrees.
Table 2. Sport Specific Testing (FAST-SHDR) vs Standard PROM Testing
Internal Rotation °
External Rotation °
Total arc of motion °
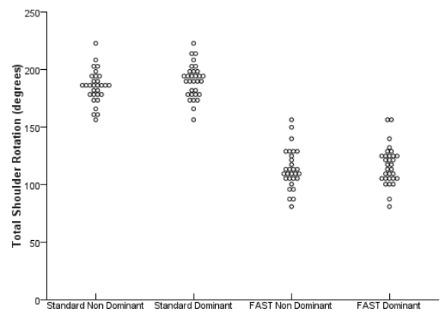
Figure 7. Total Arc of Motion
tently lower than standard assessment scores, in both isolated rotation and total arc of motion. The FAST-SHDR test is clearly measuring an independent construct compared to the standard testing methods. The authors suggest that shoulder PROM during sport specific testing is limited by a combination of local passive stabilizers (e.g. ligament and capsular tissue) and more global passive restraint from musculotendinous and fascial units across the shoulder, torso, and pelvic region (e.g. the anterior functional line, posterior functional line, and spiral line).14,20,26,27 The FAST-SHDR test specifically targets the anterior interconnected fascial muscle chain (pectoralis major, rectus abdominis, and adductor longus muscles) and the posterior fascial muscle chain (gluteus maximus, lumbodorsal fascia, and latissimus dorsi) which have both been reported via systematic review as having strong evidence to support their existence.20 In a 2018 consensus statement published in the British Journal of Sports Medicine, the authors stated that “improved assessment technology” would be needed to advance fascial system research.21 The FAST-SHDR assessment begins to contribute to this growing field of research targeting the interconnectedness of the musculoskeletal system and how it may inform future clinical practice.
In the traditional standard shoulder rotation PROM supine testing position, significantly more passive ER in the dominant throwing shoulder compared to the non-dominant shoulder is expected, which is what was observed in this study By rotating the pelvis in the opposite direction from the dominant throwing shoulder (FAST-SHDR), the soft tissue slack through the musculoskeletal system is taken up and system tension is created. During the FASTSHDR ER test the mean difference in passive shoulder ER was 50.7 less compared to the non-dominant shoulder This large of a difference in ER rotation finding may have consequences on performance or possible injury risk of the throwing shoulder of baseball athletes.
The within subject changes (sport specific vs standard testing) were normally distributed, suggesting that in some athletes, shoulder PROM was minimally affected by test position. Biomechanical properties of soft tissues such as stiffness,28 elasticity and fascial tension can vary across subjects. It may be that the athletes whose shoulder PROM did not change across test position have lower levels of stiffness or elasticity in the tissues beyond the shoulder complex, somewhere else in the kinetic linkage. This may be another variable to consider within their throwing mechanics and could potentially contribute to overworking the local soft tissue of the shoulder complex. For example, a baseball player who has less elastic stiffness in their interconnected musculoskeletal system, may compensate through active muscle force to generate the same throwing velocity; a compensation that is less efficient and more metabolically challenging.29 The differences in IR PROM recorded between baseball players and controls provides some further evidence of test validity. These between group differences were large and exceeded the MDC, with the largest differences recorded in the dominant shoulder, based on mean differences of 26°. The reduction in IR during FAST-SHDR testing also suggests there is some threedimensional interplay between the interconnected anterior and posterior muscle chains, and that the trunk and pelvis counterrotation potentially alters the body-wide tensegrity and muscle tension at the shoulder joint.
Throwing a baseball is a three dimensional task that requires the athlete to transfer ground reaction forces across
the kinetic chain, until the moment the ball leaves the hand.9 It has been reported that more than half of the kinetic energy that is transferred to the hand during throwing is maximized from the muscles of the core and lower extremities.30 As the kinetic energy moves through the kinetic chain, the thoracolumbar fascia transfers forces from the gluteus maximus to the latissimus dorsi.26 Currently, the posterior chain mechanism is not a consideration in the standard testing model for shoulder rotational PROM. Much of this clinical measurement of shoulder rotation is traditionally assessed at 90° of humeral abduction,6 where the end range is dictated primarily by local (glenohumeral) ligament and capsular restraints, thus, three-dimensional torsion is not captured in the traditional assessment techniques. Since throwing involves movement excursions at the trunk, pelvis and shoulder, over multiple planes, the new testing position was developed to capture how global musculoskeletal tension affects shoulder PROM. The current findings also support earlier research reports where a sport specific ROM assessment was developed for the hip joint in an effort to more accurately reflect assessment measures that replicate task specific sporting movements (throwing and kicking).14
The novel sport specific test procedure aims to recreate the tension arc position during the later phases of the overhead throw, and incorporate multiple kinetic links across the shoulder, torso, pelvis, and hip region. The authors acknowledge that the test position does not exactly replicate the mechanics of throwing, and it possibly captures a more task specific position related to external rotation, and that internal rotation maybe better suited with another novel test in the future. The FAST-SHDR test does acknowledge the value of the previous sport specific testing at the hip, which has provided useful clinical research. The test is also passive in nature and it may be that larger ranges of motion are achieved during an active and dynamic maximal throw, as tissue biomechanics are influenced by loading forces.9 Adopting a standing test position may be more specific, but it will be more difficult to stabilize the trunk during tests, and test reliability is likely to be reduced. Good to excellent intra-rater reliability was reported based on the collected data. Although two investigators were used in this study, the second assessor was only needed to hold the inclinometer since this device did not have a feature to “lock in the degree of inclination” before removing it from the subject. Had an inclinometer with this feature been used, the test could be performed by a single assessor, and reliability testing could be investigated with one assessor only in future studies. Further confirmatory research is required, and the findings cannot be extended to inter-observer agreement. There would be value in future testing to examine the FAST-SHDR for inter-rater reliability data. The test does have a level of subjectivity, particularly when passive hori-
zontal abduction is performed, which was limited as much as possible with stabilizing straps at the lower extremities. This subjectivity and “end-feel” was also acknowledged in the hip specific functional assessment by Tak and Langhout,14 and there is potential to limit the subjectivity of the measure by using pressure sensitive technology. Integrating more technology into the assessment would potentially allow the examiners to exert the same amount of force on each subject during the testing procedure.
There was not an a priori sample size calculation. The data reported in Table 2 can inform future sample size estimations. The results of the current study suggest that the true ICC for the new test is likely to be high e.g. around 0.95; if we set a minimal ICC value (null) of 0.90 (which equates to the lowest CI margin reported in Table 2), then n=62 participants is recommended in future studies (assuming two testing points, a significance level of .05 and power of 80%).31 Of note, the sample size for the current study was 31 which is still above average for reliability studies in the sports science field.31
A new sport specific assessment has been developed to quantify passive shoulder rotation ROM (FAST-SHDR) in the baseball population. The test is reliable and has been designed to reflect the global torsional soft tissue connectivity of throwing biomechanics when compared to the traditional supine standard method of measuring passive shoulder rotation. Traditional measures of shoulder PROM (taken from 90º of abduction) were consistently higher than those achieved with the new sport specific test. The magnitude of these differences were large (eg. 50° of difference for passive shoulder ER) and should be of relevance to clinicians working with these populations. The new test also consistently differentiated between athletes and controls, suggesting initial evidence of its discriminant validity The lower scores, which were consistently observed with the FAST-SHDR, support the hypothesis that adopting a sportspecific position engages relevant musculotendinous and fascial structures across the torso and pelvic region, influencing the available shoulder range of motion (ROM). Future research is needed to establish inter-rater reliability and to observe how these passive ROM limitations may affect performance and injury risk in baseball players.
The authors have no disclosures.
Submitted: February 23, 2024 CST, Accepted: September 21, 2024 CST
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Oberlander MA, Chisar MA, Campbell B. Epidemiology of shoulder injuries in throwing and overhead athletes. Sports Med Arthrosc Rev. 2000;8(2):115-123. doi:10.1097/ 00132585-200008020-00001
2. Makhni EC, Morrow ZS, Luchetti TJ, et al. Arm pain in youth baseball players: a survey of healthy players. Am J Sports Med 2015;43(1):41-46. doi:10.1177/ 0363546514555506
3. Saper MG, Pierpoint LA, Liu W, Comstock RD, Polousky JD, Andrews JR. Epidemiology of shoulder and elbow injuries among United States high school baseball players: School years 2005-2006 through 2014-2015. Am J Sports Med 2018;46(1):37-43. doi:10.1177/0363546517734172
4. Dick R, Lincoln AE, Agel J, Carter EA, Marshall SW, Hinton RY Descriptive epidemiology of collegiate women’s lacrosse injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train 2007;42(2):262-269.
5. Conte S, Camp CL, Dines JS. Injury trends in major league baseball over 18 seasons: 1998-2015. Am J Orthop. 2016;45(3):116-123.
6. Greene WB, Heckman JD. The Clinical Measurement of Joint Motion American Academy of Orthopaedic Surgeons; 1994.
7. Wilk KE, Reinold MM, Macrina LC, et al. Glenohumeral internal rotation measurements differ depending on stabilization techniques. Sports Health 2009;1(2):131-136. doi:10.1177/1941738108331201
8. Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med 2011;39(2):329-335. doi:10.1177/0363546510384223
9. Chu SK, Jayabalan P, Kibler WB, Press J. The kinetic chain revisited: New concepts on throwing mechanics and injury PM R 2016;8(3 Suppl):S69-77 doi:10.1016/j.pmrj.2015.11.015
10. Seroyer ST, Nho SJ, Bach BR, Bush-Joseph CA, Nicholson GP, Romeo AA. The kinetic chain in overhand pitching: its potential role for performance enhancement and injury prevention. Sports Health 2010;2(2):135-146. doi:10.1177/1941738110362656
11. Calabrese GJ. Pitching mechanics, revisited. Int J Sports Phys Ther. 2013;8(5):652-660.
12. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23(2):233-239. doi:10.1177/ 036354659502300218
13. Dischiavi SL, Wright AA, Hegedus EJ, Bleakley CM. Rethinking dynamic knee valgus and its relation to knee injury: Normal movement requiring control, not avoidance. J Orthop Sports Phys Ther. 2019;49(4):216-218. doi:10.2519/jospt.2019.0606
14. Tak IJ, Langhout RF, Groters S, Weir A, Stubbe JH, Kerkhoffs GM. A new clinical test for measurement of lower limb specific range of motion in football players: Design, reliability and reference findings in non-injured players and those with long-standing adductor-related groin pain. Phys Ther Sport 2017;23:67-74. doi:10.1016/j.ptsp.2016.07.007
15. Kaur N, Bhanot K, Brody LT, Bridges J, Berry DC, Ode JJ. Effects of lower extremity and trunk muscles recruitment on serratus anterior muscle activation in healthy male adults. Int J Sports Phys Ther. 2014;9(7):924-937
16. Scher S, Anderson K, Weber N, Bajorek J, Rand K, Bey MJ. Associations among hip and shoulder range of motion and shoulder injury in professional baseball players. J Athl Train 2010;45(2):191-197 doi:10.4085/1062-6050-45.2.191
17. Sekiguchi T, Hagiwara Y, Yabe Y, et al. Restriction in the hip internal rotation of the stride leg is associated with elbow and shoulder pain in elite young baseball players. J Shoulder Elbow Surg 2020;29(1):139-145. doi:10.1016/j.jse.2019.07.004
18. Tak IJR. Hip and groin pain in athletes: morphology, function and injury from a clinical perspective. Br J Sports Med 2018;52(16):1024-1025. doi:10.1136/bjsports-2017-098618
19. Tak I, Glasgow P, Langhout R, Weir A, Kerkhoffs G, Agricola R. Hip range of motion is lower in professional soccer players with hip and groin symptoms or previous injuries, independent of cam deformities. Am J Sports Med 2016;44(3):682-688. doi:10.1177/0363546515617747
20. Wilke J, Krause F, Vogt L, Banzer W. What is evidence-based about myofascial chains: A systematic review. Arch Phys Med Rehabil. 2016;97(3):454-461. doi:10.1016/j.apmr.2015.07.023
21. Zugel M, Maganaris CN, Wilke J, et al. Fascial tissue research in sports medicine: from molecules to tissue adaptation, injury and diagnostics. Br J Sports Med. 2018;52(93):1497-1506. doi:10.1136/ bjsports-2018-099308
22. Koo TK, Li MY A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-163. doi:10.1016/j.jcm.2016.02.012
23. Portney LG. Foundations of Clinical Research : Applications to Practice. Prentice Hall Health; 2000.
24. Mullaney MJ, McHugh MP, Johnson CP, Tyler TF. Reliability of shoulder range of motion comparing a goniometer to a digital level. Physiother Theory Pract. 2010;26(5):327-333. doi:10.3109/09593980903094230
25. Kolber MJ, Vega F, Widmayer K, Cheng MS. The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer Physiother Theory Pract 2011;27(2):176-184. doi:10.3109/09593985.2010.481011
26. Dischiavi SL, Wright AA, Hegedus EJ, Bleakley CM. Biotensegrity and myofascial chains: A global approach to an integrated kinetic chain. Med Hypotheses 2018;110:90-96. doi:10.1016/ j.mehy.2017.11.008
27 Myers TW Anatomy Trains : Myofascial Meridians for Manual and Movement Therapists. 3rd ed. Elsevier; 2014.
28. Langhout R, Tak I, van der Westen R, Lenssen T Range of motion of body segments is larger during the maximal instep kick than during the submaximal kick in experienced football players. J Sports Med Phys Fitness. 2017;57(4):388-395. doi:10.23736/ S0022-4707.16.06107-7
29. Manzi JE, Dowling B, Dines JS, Richardson A, McElheny KL, Carr JB. Increased shoulder distraction force and shoulder horizontal abduction in professional baseball pitchers with discordant torso rotation order. Am J Sports Med. 2021;49(13):3638-3646. doi:10.1177/ 03635465211041381
30. Kibler WB, Wilkes T, Sciascia A. Mechanics and pathomechanics in the overhead athlete. Clin Sports Med 2013;32(4):637-651. doi:10.1016/ j.csm.2013.07.003
31. Borg DN, Bach AJE, O’Brien JL, Sainani KL. Calculating sample size for reliability studies. PM R 2022;14(8):1018-1025. doi:10.1002/pmrj.12850

Arnason K, Agustsson A, Fredriksen H, Rafnsson ET, Briem K. Let´s Swing it –The Interaction Between Participation-Related Shoulder Load and Pre-season Trunk Rotation Power on Shoulder Problems in Male Handball Players. IJSPT 2024;19(12):1541-1550. doi:10.26603/001c.126187
Kari Arnason1a , Atli Agustsson2 , Hilde Fredriksen3 , Elis Thor Rafnsson4 , Kristin Briem1
1 Department of physical therapy - Research centre of movement science - Faculty of medicine, University of Iceland, 2 , Department of physical therapy - Research centre of movement science - Faculty of medicine, University of Iceland, 3 Olympiatoppen, Oslo, 4 Sjukratjalfun Islands
Keywords: Injury prevention, throwing mechanics, training load, overuse injury, lower body strength https://doi.org/10.26603/001c.126187
International Journal of Sports Physical Therapy
Vol. 19, Issue 12, 2024
Background
Little is known about the influence of kinetic chain strength and power on shoulder problems in handball players or the impact of participation-related shoulder load (PSL) during a season. Suboptimal activity of the kinetic chain during throwing might make the shoulder more vulnerable.
Purpose
The purpose of this study was to assess 1) the association between pre-season measurements and shoulder problems among handball players and 2) whether pre-season strength and power influence the association between PSL and severity of shoulder problems.
Study Design
Prospective observational cohort study
Methods
Pre-season measurements were done using the Isometric mid-thigh pull for lower body strength, a seated test for trunk rotation power (TRP) and isometric testing of external (ER) and internal rotation shoulder strength on 42 male players. Shoulder problems (prevalence, substantial prevalence, and severity score) were documented weekly through a season (31 weeks) with The Oslo Sports Trauma Research Center Overuse Questionnaire (OSTRC-O2) and PSL with the modified Borg rate of perceived exertion scale. Spearman´s correlation coefficient was applied to examine the association within the first aim, while a mixed model ANOVA was conducted to analyze the second aim.
A weak and negative correlation (rs=-0.34) was found between pre-season ER strength and the individual prevalence of shoulder problems (p=0.029). A main effect was found between PSL and the OSTRC-O2 severity score (p=<0.001) with higher severity scores observed with increased PSL. A significant interaction was found between PSL and pre-season TRP regarding their influence on the OSTRC-02 severity score (p=0.017). With higher PSL, a higher severity score was observed among players with pre-season TRP more than one standard deviation below the group’s mean.
a
Corresponding author:
Kari Arnason (KA), PT, Msc University of Iceland, Department of Physical Therapy - Research Centre of Movement Science - Faculty of Medicine 101 Reykjavik, Iceland kariarna@hi.is +3546978114
The results indicate that low TRP may make the throwing shoulder more vulnerable to an increase in load. Looking beyond shoulder strength and load may therefore be important.
Level of evidence 3
Handball is a vigorous team sport characterized by physical contact and collision between players, rapid change of direction, and powerful, repetitive throwing. Shoulder problems are common among handball players with a reported prevalence of 17-36% and most shoulder problems are defined as overuse injuries.1‑5 The prevalence of shoulder problems defined as substantial (causing moderate or severe reductions in sports performance or complete inability to participate6) has been reported to be 5-12%.3‑5
An increasing number of studies have attempted to identify possible risk factors for shoulder problems in handball, due to their high prevalence and impact on sports participation.1,3,7‑9 Their main findings have indicated that potential risk factors for shoulder problems include decreased strength of the external rotators1,3,7 (ER) and internal rotators1 (IR) in the throwing shoulder, scapular dyskinesis,1,3 and a low ER/IR strength ratio.7 The posterior rotator cuff (infraspinatus and teres minor) has been shown to be very active during the deceleration phase of the throwing motion, indicating the importance of ER strength and a high ER/IR ratio.10 Decreased total rotation range of motion and a sudden increase in training load have also been identified as possible risk factors.3,7,8 However, a study aiming to confirm previously identified risk factors for overuse shoulder problems was unable to do so regarding ER strength, total rotation range of motion, or scapular dyskinesis.9 Furthermore, a recent systematic review on risk factors for shoulder problems in overhead athletes showed limited or conflicting evidence for a variety of factors like participation level, sex, biomechanics, and external workload.11
Recent studies investigating the prevalence of shoulder problems and possible risk factors have primarily examined factors related to the shoulder girdle.1,3,4,7‑9,12 However, overhead throwing is a complex movement involving the whole body and the kinetic chain. The kinetic chain has been described as a linkage of multiple body segments that transfer forces and motion through the body and throwing velocity is generated via the acceleration provided through the lower extremity and the trunk muscles.13,14 Efficient force transmission from the lower extremities, through the pelvis and the trunk and to the upper extremity, called “the proximal to distal sequence”, is considered very important for throwing performance in sports.14‑16 Kibler´s biomechanical analysis of the tennis serve showed that 51% of the total energy production originates from the lower extremities and the trunk, while only 13% is generated at the shoulder 17 Furthermore, studies on baseball players have shown high levels of activity in the gluteus maximus and medius muscles and a positive association between gluteal activity and pelvic axial rotation during a pitching motion,
reflecting the importance of the kinetic chain for throwing performance.18 During throwing, deficits proximally in the kinetic chain may increase the loads on the more distal segments, such as the shoulder, which might lead to the development of shoulder problems.19
Without participation in a sport, however, non-participation-related risk factors like reduced strength or nonefficient force transmission through the kinetic chain may be of limited importance. A study by Moller et al. showed that a weekly increase of 20-60% in handball load (training and competition hours - described as a participation-related risk factor) led to increase of shoulder injury rate in players who had other underlying risk factors (non-participation-related) like diminished ER strength and scapular dyskinesis, indicating the contribution of sport participation towards increased injury risk.8 The complexity and the chaotic nature of the game of handball presents difficulties for monitoring participation-related shoulder load (PSL) such as the number of throws. A new way of monitoring PSL (number of throws, playing position etc.), was therefore introduced in the “2022 Bern Consensus Statement on Shoulder Injury Prevention, Rehabilitation, and Return to Sport for Athletes at All Participation Levels”. The consensus suggested the use of the modified Borg rate of perceived exertion scale to track the athlete´s weekly PSL in sports like handball.20
To the author’s knowledge, the influence of lower body strength and trunk rotation power (TRP) on shoulder problems in handball players has not previously been investigated. Moreover, the interaction between PSL and nonparticipation-related risk factors, like reduced lower body strength and TRP, has not been investigated in handball players. Hence, the aim of this study was to assess: 1) The association between pre-season lower body strength, TRP and shoulder strength measurements and shoulder problems among handball players, and 2) Whether pre-season strength and power measurements influence the association between PSL and severity of shoulder problems.
The hypotheses were that: 1) Handball players with low pre-season strength and power values would report more shoulder problems when followed through a regular season, and 2) Players with low pre-season strength and power values would report more severe shoulder problems as PSL increased through a regular season.
Seven clubs from the top Icelandic men’s handball division were approached in June 2022 and invited to participate in this prospective study Players 18 years and older were
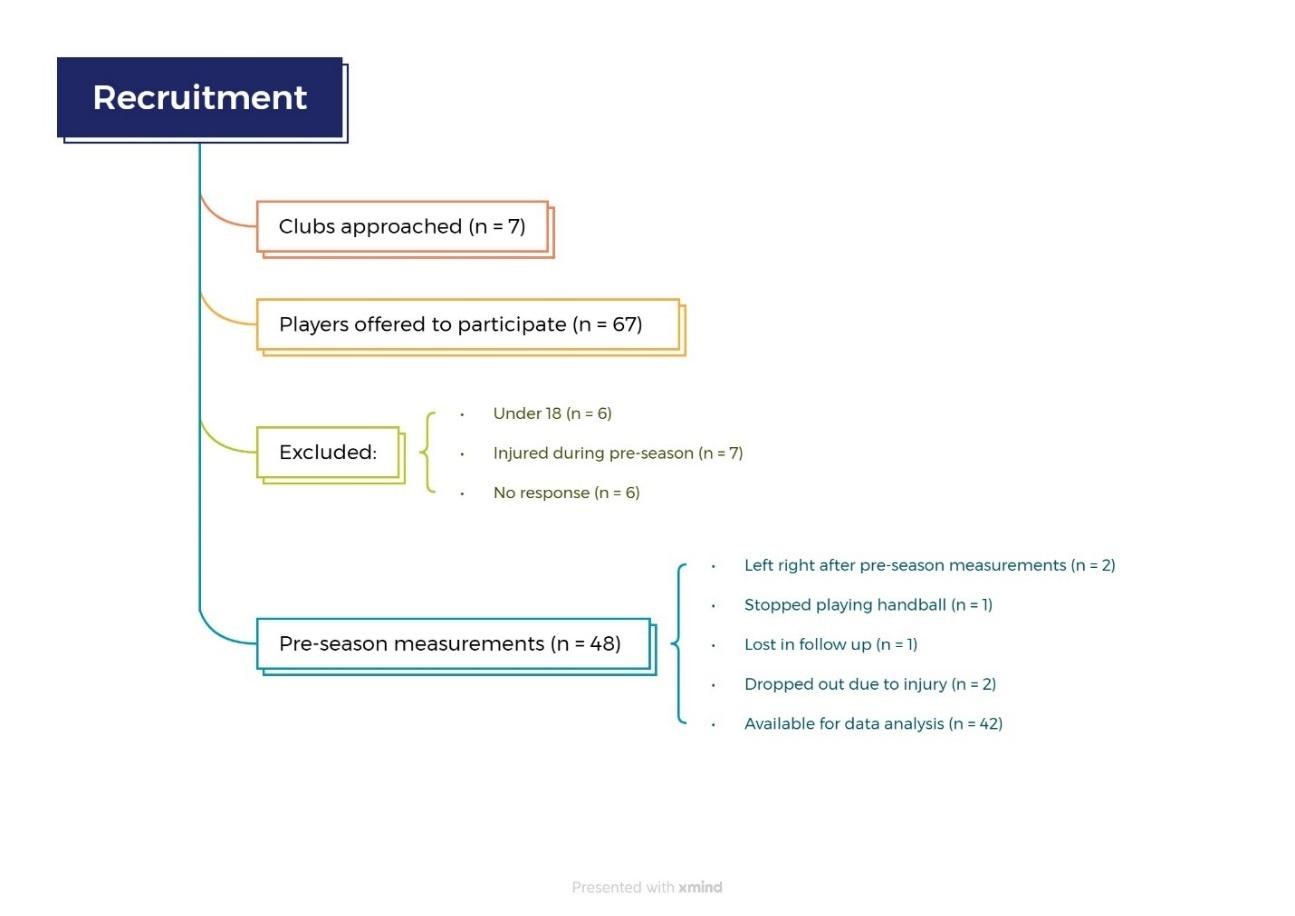
Figure 1. Flow chart of study recruitment and data collection
eligible for the study, irrespective of previous or current shoulder problems. Players who were away from full participation and training due to injuries during the pre-season data collection period were excluded from the study No other exclusion criteria were used. Pre-season strength and power measurements were conducted in August and September 2022. The measurements took place at the Research Center of Movement Science at the University of Iceland. A flowchart of the study recruitment and data collection is presented in Figure 1. Prior to data collection players received information about the study and signed a consent form. The study was approved by the National Bioethics Committee (VSN-22-084).
Lower body strength was measured with the Isometric midthigh pull (IMTP), a well-established and reliable test for lower body peak force measurements (Figure 2).21 Peak force of the IMTP has been shown to correlate highly with one repetition maximum squat and deadlift, indicating its appropriateness for measuring lower body strength in laboratory settings.22,23 Participants finished a standardized warm up routine and got three familiarization trials (at 50%, 75% and 90% subjective effort). During testing, knee and hip angles were standardized (between 125-145° and 140-145° respectively) as recommended by Comfort et al.24
Participants held a 20 kg weightlifting bar in a fixed position with their hands strapped to the bar with weightlifting straps to minimize the effect of their grip strength, while positioned on a force plate (AMTI, Watertown, Massachusetts, USA) to measure the vertical component of the ground reaction force, sampling at 100 Hz. Participants were encouraged to push as hard and as fast as possible
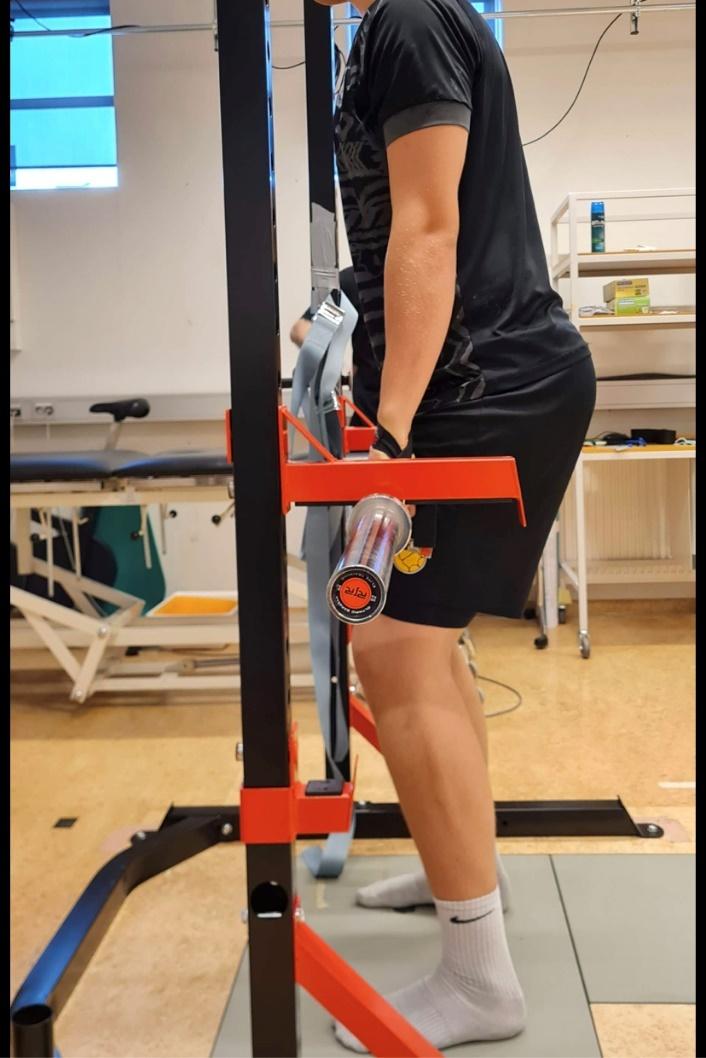
down into the force plate and all got verbal encouragement during each trial. Three trials were performed, and in cases where peak force (PF) values exhibited an increase between the second and third trial, extra trials were conducted until the PF values differed by less than 250 N.24 The trial with the highest absolute PF value, including participant´s body weight, was used for data analysis.

TRP was measured with a pulley machine in a seated position with the hips and knees in 90° flexion.25 Participants were instructed to keep the elbows straight in front of the body at shoulder height and the trunk in an upright position and to avoid all side bending motion, while rotating 5% of their body weight through 180° as fast as possible (Figure 3). Prior to conducting the measurements, participants completed a standardized warm-up routine and underwent two familiarization trials. A non-slip mat was placed under the participants´ feet and buttocks to prevent any sliding on the floor or on the plinth. Only left-side rotation was measured for right-handed players and right-side rotation for left-handed players. The acceleration of the weight was measured with inertial sensors (Movella dot, Henderson USA), placed on the top of the weights in the pulley machine and raw data were collected through the Movella dot app (Movella dot, Henderson USA). The acceleration values were then converted to power (W=(a+g)*t*F) (W=watt, a = acceleration, g = gravity, t = time, F = is the force, and represents the weight of the pulley). Three trials were performed and the trial with the highest absolute power value was used for data analysis.
A reliability analysis was done as this method differed slightly from the original version by Andre et al.25 Fourteen physiotherapy students were measured with 24-48 hours in between measurements to determine the test-retest reliability The results showed good reliability, an ICC (3,3) value of 0.874, standard error of measurement (SEM) of 5.17, coefficient of variation (CV) of 17% and MDD90 of 12.03.
An externally fixed handheld dynamometer (HHD) (Lafayette Instruments, USA) was used to measure maximal isometric IR and ER strength of the dominant shoulder in a supine position, with the shoulder in 90° abduction and 0° rotation (Figure 4).8,26 A towel was placed under the distal end of humerus to keep the upper arm in the horizontal plane. Participants finished a standardized warm up routine and got one familiarization trial.12 Participants were instructed to maintain stability in their torso, upper arm, and elbow and to avoid any substitution. They were given

instructions to exert maximum force upon cue and maintain it for a duration of three seconds. Stabilization was provided to the HHD and to the upper arm by the examiner (KA) and participants got verbal encouragement during each trial. The average value from the three trials was used for data analysis.26
Self-reported data were collected and managed using REDCap electronic data capture tools hosted at University of Iceland, with the Oslo Sports Trauma Research Center Overuse Injury Questionnaire (OSTRC-O2)27 emailed to all participants once a week throughout the regular season or for 31 weeks. An automatic reminder was sent to non-responders after two and four days. The OSTRC-O2 questionnaire has been widely used in handball related research and is specially designed to document the extent of overuse injuries in sports.3,4,6,9,27 The participants were asked about shoulder problems in their dominant shoulder with shoulder problems referring to any pain, ache, stiffness, clicking/ catching, swelling, instability/giving way, locking, or other complaints related to the dominant shoulder. The questionnaire included four questions about whether shoulder problems had affected participation, training/competition, or performance, and whether participants had experienced any pain in the dominant shoulder related to handball for the prior seven days. Each question had four response options, scored on the scale 0-8-17-25, 0 representing no problem and 25 maximum level. The scores from each of these four questions were then summed to calculate a weekly severity score on the scale 0-100. The average OSTRC-O2 severity score of each participant was calculated by dividing the total score from all the questionnaires answered throughout the season by the number of times answered. The group prevalence of shoulder problems was calculated by dividing the total number of times any participants reported any problem (anything but the minimum value in any of the four questions) with the total number of questionnaire respondents that week. The individual preva-
lence of shoulder problems was calculated by dividing the total number of times each participant reported a problem (anything but the minimum value in any of the four questions) by the total number of that participant´s questionnaire responses. The group and individual prevalence of substantial problems was calculated in the same way, respectively, for shoulder problems that had caused moderate or severe reduction (score 17 or 25 on questions no. 2 and/ or 3 on the OSTRC-O2) in training/competition or performance or total inability to participate (score 25 on question number 1 on the OSTRC-O2).27
Additionally, the authors added a question to the weekly questionnaire that asked the participants to rate the weekly PSL on a modified Borg rate of perceived exertion scale, by answering the question “On the scale 0-10, how hard was the recent week on your throwing shoulder?” as recommended by Schwank et al.20
The outcome measures were: 1) The association between the pre-season strength and power measurements and OSTRC-02 results (individual prevalence, individual substantial prevalence, and severity score); 2) The influence of pre-season strength and power measurements on the association between PSL and the OSTRC-O2 severity score.
All statistical work was done in Microsoft Excel and Jamovi statistical software (2023). The Shapiro-Wilk test was used to check the data for normality The Spearman´s rank correlation coefficient was applied to examine the association between variables in the first outcome measures, while a mixed model ANOVA was conducted to analyze the second outcome measure. An a-priori power analysis was conducted, indicating a sample size of minimum 46 participants to achieve 80% power for a correlation value of 0.4 for the association between the pre-season measurements and the OSTRC-O2 results. The p value was set at 0.05 for all analyses.
Participants were asked not to answer the questionnaire if they were away from regular training and/or competition because of an injury Some participants who got injured during the season nonetheless continued to answer the questionnaire while they were away They were contacted by one of the authors (KA) and information gathered about the type of injury and the time they were away, and appropriate questionnaire data removed from the data analysis.
PARTICIPANTS
A total of 42 male handball players participated in this study Participants’ demographics can be found in Table 1. Two players had a history of previous surgery of the throwing arm and 19 had a history of major lower limb injury, e.g., fracture, muscle tear, tendon rupture, ligament tear and meniscal injury
Table 1. Mean and standard deviation (SD) values for participants’ demographics, elite handball experience, prevalence of shoulder pain during previous season and hand dominance.
cm centimeters, kg kilograms, R=right, L=left, Elite handball experience number of years as a player in the first team squad
The average response rate for the OSTRC-02 questionnaire was 87%, with 16 players having 100% response rate,14 players having a response rate above 80% and 12 players below 80%. The average group prevalence of shoulder problems was 27% (95% CI 19.8-35.2, range 0-100%) and the average group prevalence of substantial shoulder problems was 4% (95% CI 1.75-7.77, range 0-52%). Fifteen players reported substantial shoulder problems at some point during the season. Of those, 12 players reported them less than five times. The average OSTRC-02 severity score was 7.58 out of 100 (95% CI 5.31-9.84, range 0-31). Forty-eight percent of the participants had an average OSTRC-O2 severity score <5 and 21% <1. The average PSL rated by players was 4.1/10 (95% CI 3.68-4.40, range 1.5-7.5).
PRE-SEASON MEASUREMENTS AND THEIR ASSOCIATION WITH THE OSTRC-O2 RESULTS
The average pre-season ER/IR ratio and the average absolute peak values for ER, IR and IMTP strength and TRP can be found in Table 2. The only strength variable that significantly correlated with OSTRC-O2 prevalence of shoulder problems was pre-season ER strength (rs = -0.34, p = 0.029). No significant association was found between any of the pre-season measurements and the average OSTRC-02 severity score (rs range: -0.22 to -0.11; p values range: 0.16 to 0.51) or between the pre-season measurement and prevalence of substantial shoulder problems (rs range: -0.01 to 0.12, p values range: 0.44 to 0.96).
INFLUENCE OF PRE-SEASON MEASUREMENTS ON THE ASSOCIATION BETWEEN PSL AND THE OSTRC-O2 SEVERITY SCORE
The mixed model ANOVA showed a main effect between the PSL and the OSTRC-O2 severity score (p<0.001). With higher PSL, a higher OSTRC-O2 severity score was observed. An interaction was found between the PSL and preseason TRP in terms of their influence on the OSTRC-O2 severity score (p=0.017). With higher PSL, a higher OSTRCO2 severity score was observed among players with pre-sea-
Table 2. Mean and 95% confidence intervals (CI) of pre-season strength and power measurements and ER/ IR ratio.
Measurements (unit) N=42
(kg)
(20.1-22.4)
(kg) 23.2 (21.8-24.8) IMTP (N) 3318 (3129-3486) TRP (W) 40.8 (35.6-42.8)
ER/IR ratio 0.94 (0.88-1)
ER external rotation, IR internal rotation, IMTP Isometric mid-thigh pull, TRP trunk rotation power, kg = kilograms, N = Newton, W = watts.
Note: IMTP values include participants’ body weight.
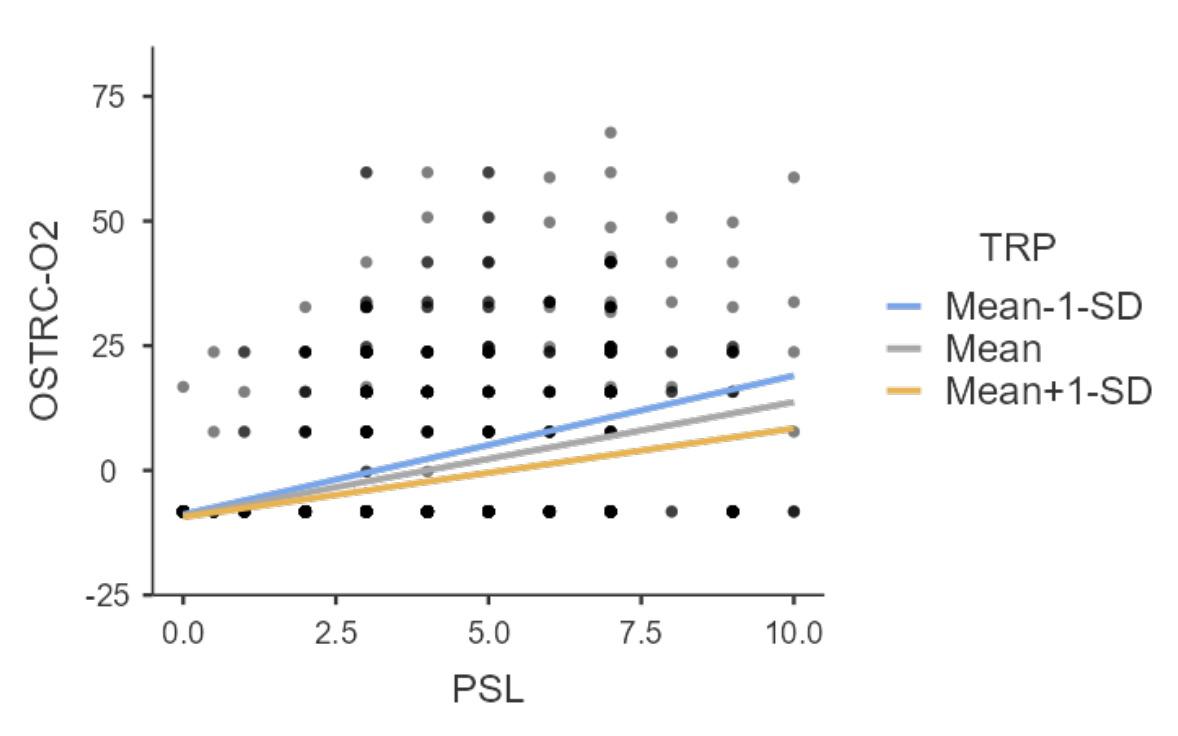
Figure 5. The interaction between the PSL and TRP in terms of their influence on the OSTRC-02 severity score.
PSL participation-related shoulder load, TRP trunk rotation power, OSTRC-O2 Oslo sports trauma research center overuse injury questionnaire, SD = standard deviation.
son TRP more than one standard deviation (SD) below the group’s mean. Conversely, with higher PSL, the OSTRC-O2 severity score was lower for players with greater pre-season TRP (Figure 5).
The main findings of this study indicate that the relationship between PSL and severity of shoulder problems through a regular season may be influenced by TRP, as low pre-season TRP might make the throwing shoulder more vulnerable for higher PSL during a season. Conversely, the findings indicate as well that high pre-season TRP might have a protective effect on the throwing shoulder when the PSL is high. A weak and significant negative correlation was also found between pre-season ER strength and the OSTRC-O2 prevalence of shoulder problems. This is, to the author’s knowledge, the first prospective study that shows that low pre-season TRP is linked to high severity of shoulder problems in handball players as the PSL is increased during the handball season.
The overall average OSTRC-O2 severity score of 7.58 is considerably lower than that of 29 and 35 (intervention and control group, respectively) reported by Andersson et. al.4 The group average prevalence of shoulder problems was 27%, which closely aligns with the 28% reported by Clarsen et al.3 but was higher compared to Andersson et al. who reported an average prevalence of 17% and 23% for their intervention and control group, respectively 4 The intervention group in the study by Andersson et al. had participated in a shoulder exercise program throughout the season aiming at reduced prevalence of shoulder problems which might explain the lower prevalence compared to results presented here.4 The group prevalence of substantial shoulder problems in this study was 4%, which is notably lower than the 12% reported by Clarsen et al.3 but similar with those found by Andersson et al.4
This is the first study to use the modified Borg rate of perceived exertion scale to monitor PSL in throwing athlete so no direct comparison to other studies is available but the average PSL throughout the season was rated 4/ 10 or “somewhat hard”.28 The authors of the “2022 Bern Consensus Statement on Shoulder Injury Prevention, Rehabilitation, and Return to Sport for Athletes at All Participation Levels” were not able to come to an agreement about whether monitoring internal vs external load was more important for risk or injury management for shoulder injuries.20 Monitoring factors like the number of throws, type of throws or throwing velocity is not practical because of the chaotic nature and unpredictability of the game of handball. In contrast, internal measures like the modified Borg rate of perceived exertion scale offer a simple but useful way to monitor PSL for handball players.
PRE-SEASON MEASUREMENTS AND THEIR ASSOCIATION WITH THE OSTRC-O2 RESULTS
The negative correlation found between the pre-season ER strength and the OSTRC-O2 prevalence of shoulder problems is consistent with previous studies linking reduced ER strength to shoulder problems in handball players.1,3,7 The angular velocity of the shoulder IR during a handball jump throw has been measured at 5039 °/s which underscores the importance of ER strength to absorb the load during the deceleration phase.29
The pre-season ER/IR shoulder strength ratio of 0.94 is higher than the cut off values of 0.75 and 0.89 that have been used to identify youth and adult handball players at increased risk of sustaining a shoulder injury 1,8,26,30 Moreover, the pre-season ER and IR absolute strength values were higher by more than 5 kg than the aforementioned reference values for adult handball players and pre-pitching ER strength in collegiate club baseball pitchers.30,31 This shows that this cohort as a whole had high shoulder strength, particularly for ER, at pre-season. These high strength values may reflect participants´ greater fatigue tolerance as ER strength measures have been shown to decrease immediately after intense throwing.31 Players with high ER strength may therefore be able to tolerate more
throwing load before fatiguing which might have a protective effect for overuse injuries.
This is the first study to use the IMTP to measure lower body strength in handball players, so no direct comparison is available. The pre-season IMTP PF in this study was higher by roughly 800 N than PF values reported for 33 senior male professional rugby players and higher by more than 200 N than PF values reported for u21 Academy rugby players,32,33 indicating high levels of lower body strength in this group of participants. High levels of lower body strength likely increase the athletes´ ability to utilize the more proximal segments in the kinetic chain during the throwing motion. Utilization of proximal segments might have a protective effect on the throwing shoulder as efficient force transmission from the more proximal segments to the distal segments has been shown to be very important for the throwing motion.14,16,17
Exercise interventions aimed at preventing sport injuries highlight the effectiveness of strength training in reducing overuse injuries in sports by nearly half.34 The high ER/ IR ratio and high absolute ER strength, IR strength and IMTP PF reported here might therefore explain the low average OSTRC-O2 severity score, low prevalence of substantial shoulder problems and lack of correlation between the pre-season measurement and the OSTRC-O2 severity score and prevalence of substantial shoulder problems.
INFLUENCE OF PRE-SEASON MEASUREMENTS ON THE ASSOCIATION BETWEEN PSL AND THE OSTRC-O2 SEVERITY SCORE
The influence of PSL on the OSTRC-O2 severity score throughout the season was affected, at least to an extent, by the pre-season TRP. These results are consistent with the previous findings showing an exacerbated effect of an increase in handball load on shoulder injury rate in players with low ER strength and scapular dyskinesis.8
The interaction between PSL and pre-season TRP in terms of their influence on the OSTRC-O2 severity score indicates the importance of the kinetic chain for shoulder health as the TR is believed to play a significant role in energy transfer to the throwing arm.35 A study on baseball pitchers showed that professional pitchers rotated their trunk significantly later within the pitching cycle compared to lower-level pitchers and had lower shoulder IR torque during throwing.36 Authors have speculated that the lower shoulder IR torque might be a function of that later trunk rotation timing, which makes professional pitcher able to use effective transfer of momentum from the larger, more proximal segments in a more efficient way as explained by the “proximal to distal sequence” 16,36 Hence, handball players with more TRP may need less time to generate the rotational energy needed for throwing. They may thereby be able to rotate the trunk later during the throwing motion and consequently minimize the load placed on the shoulder In contrast, to make up for lower TRP, or due to fatigue, players with lower TRP might initiate the TR earlier, causing higher contribution from the distal segments for throwing and lead to increased load on the shoulder. These speculations, however, need to be investigated further
This is the first study to use the seated TR test to measure TRP in any throwing athletes, so no direct comparison is available. No cut-off score calculation was done in the reliability analysis, so whether players with pre-season TRP one SD below the group´s mean really had a TRP deficit remains a speculation. However, the MDD90 for the test was 12.03 and the SD for the group´s mean was 12.3. The difference can therefore be considered a meaningful magnitude of TRP. As there was a weaker relationship between the PSL and the OSTRC-O2 severity score for players with TRP one SD above the mean, higher TRP can be considered to have a protective effect for shoulder problems. Further research is needed to investigate more detailed TRP reference values and appropriate cut-off scores in handball players. Until then our version can serve as a comparison for future research using the same testing and calculation methods.
The main limitation in this study is a small sample size which reduces statistical power Controlling the participants´ training load and intensity in the days leading up to the pre-season measurements was not feasible as each team had its own pre-season training schedule. Participants were allowed to make appointments for data collection when convenient, regardless of their training schedule. Therefore, some may have been fatigued, which might have influenced their capacity to generate maximum force and power during data collection. Some players reported mild discomfort during the ER strength measurements which might have influenced the absolute strength values. However, it is common for handball players to continue to throw despite mild discomfort3,4 and as those particular players did not indicate that this mild discomfort limited their ability to exert maximum force during testing, these values were included in the pre-season data analysis of the player´s shoulder profile. The shoulder isometric strength measurements done by Cools et. al, used for comparison earlier,30 were performed in a sitting position with the shoulder in 90° of abduction and neutral rotation. In this study the shoulder strength was measured in supine position while maintaining the same neutral rotation at the shoulder Different test positions have been used in research studies1,3,8,9,26,30 which may influence the outcome, so direct comparisons need to be made with that in mind. Despite different measurement positions the pre-season ER/IR ratio in this study was similar to the reference values for male handball players reported by Cools et. al.30
The OSTRC-O2 questionnaire and the PSL ratings inquired about the players’ subjective experience of shoulder problems and PSL over the preceding seven days, which introduces potential recall bias. Finally, the natural variation in the training and match load through the season might have had a lowering effect on the average OSTRC-O2 severity score, prevalence of shoulder problems and the PSL, but because of the total length of the follow up (31 weeks) that effect, if any, is believed to be minimal. Only one participant reported an acute injury to the shoulder during the season which influenced the average OSTRC-O2 score and the prevalence of shoulder problems for that player. The
overall score for that player was <8 so the effect of that acute injury on the overall score is believed to be minimal.
The results indicate that the overall high fitness state in this group of handball players might have had a protective effect on shoulder problems. However, while the results support the importance of TRP and ER shoulder strength in relation to shoulder problems in handball players, they also highlight the influence of shoulder load due to participation. Professionals working with handball players should monitor the PSL of their players and consider whether the key factor in maintaining a healthy shoulder might be to look beyond the shoulder
The authors declare no conflict of interest. The conduct of this study was approved by the National Bioethics Committee of Iceland and funded by the University of Iceland Research Fund.
Dr. Thorarinn Sveinsson for his assistance during the statistical analysis.
Submitted: May 09, 2024 CST, Accepted: October 20, 2024 CST
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Asker M, Walden M, Kallberg H, Holm LW, Skillgate E. Preseason clinical shoulder test results and shoulder injury rate in adolescent elite handball players: A prospective study J Orthop Sports Phys Ther 2020;50(2):67-74. doi:10.2519/jospt.2020.9044
2. Myklebust G, Hasslan L, Bahr R, Steffen K. High prevalence of shoulder pain among elite Norwegian female handball players. Scand J Med Sci Sport 2013;23(3):288-294. doi:10.1111/ j.1600-0838.2011.01398.xt
3. Clarsen B, Bahr R, Andersson SH, Munk R, Myklebust G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: A prospective cohort study. Br J Sports Med 2014;48(17):1327-1333. doi:10.1136/ bjsports-2014-093702
4. Andersson SH, Bahr R, Clarsen B, Myklebust G. Preventing overuse shoulder injuries among throwing athletes: A cluster-randomised controlled trial in 660 elite handball players. Br J Sports Med. 2017;51(14):1073-1080. doi:10.1136/ bjsports-2016-096226
5. Aasheim C, Stavenes H, Andersson SH, Engbretsen L, Clarsen B. Prevalence and burden of overuse injuries in elite junior handball. BMJ Open Sport Exerc. 2018;4(1):e000391. doi:10.1136/ bmjsem-2018-000391
6. Clarsen B, Myklebust G, Bahr R. Development and validation of a new method for the registration of overuse injuries in sports injury epidemiology: The Oslo sports trauma research centre (OSTRC) overuse injury questionnaire. Br J Sports Med. 2013;47(8):495-502. doi:10.1136/ bjsports-2012-091524
7. Achenbach L, Laver L, Walter SS, Zeman F, Kuhr M, Krutsch W Decreased external rotation strength is a risk factor for overuse shoulder injury in youth elite handball athletes. Knee Surg Sports Traum Arthrosc. 2020;28(4):1202-1211. doi:10.1007/ s00167-019-05493-4
8. Moller M, Nielsen RO, Attermann J, et al. Handball load and shoulder injury rate: A 31-week cohort study of 679 elite youth handball players. Br J Sports Med. 2017;51(4):231-237. doi:10.1136/ bjsports-2016-096927
9. Andersson SH, Bahr R, Clarsen B, Myklebust G. Risk factors for overuse shoulder injuries in a mixedsex cohort of 329 elite handball players: Previous findings could not be confirmed. Br J Sports Med 2018;52(18):1191-1198. doi:10.1136/ bjsports-2017-097648
10. DiGiovine NM, Jobe FW, Pink M, Perry J. An electromyographic analysis of the upper extremity in pitching. J Shoulder Elbow Surg. 1992;1(1):15-25. doi:10.1016/S1058-2746(09)80011-6
11. Asker M, Brooke HL, Walden M, et al. Risk factors for, and prevention of, shoulder injuries in overhead sports: A systematic review with best-evidence synthesis. Br J Sports Med 2018;52(20):1312-1319. doi:10.1136/bjsports-2017-098254
12. Fredriksen H, Cools A, Bahr R, Myklebust G. Does an effective shoulder injury prevention program affect risk factors in handball? A randomized controlled study Scand J Med Sci Sport 2020;30(8):1423-1433. doi:10.1111/sms.13674
13. Kibler BW. Understanding the kinetic chain in tennis performance and injury Aspetar Sports Med J Published online 2014:492-497
14. Chu SK, Jayabalan P, Ben Kibler W, Press J. The kinetic chain revisited: New concepts on throwing mechanics and injury PM &R 2016;8(3):S69-S77 doi:10.1016/j.pmrj.2015.11.015
15. Putnam CA. A segment interaction analysis of proximal-to-distal sequential segment motion patterns. Med Sci Sports Exer 1991;23(1):130-144. doi:10.1249/00005768-199101000-00019
16. Putnam CA. Sequential motions of body segments in striking and throwing skills - descriptions and explanations. J Biomech. 1993;26:125-135. doi:10.1016/0021-9290(93)90084-R
17 Kibler BW Biomechanical analysis of the shoulder during tennis activities. Clin Sports Med. 1995;14(1):79-85. doi:10.1016/ s0278-5919(20)30259-3
18. Oliver GD, Keeley DW. Gluteal muscle group activation and its relationship with pelvis and torso kinematics in high-school baseball pitchers. J Strength Cond Res. 2010;24(11):3015-3022. doi:10.1519/JSC.0b013e3181c865ce
19. Oyama S, Yu B, Blackburn JT, Padua DA, Li L, Myers JB. Improper trunk rotation sequence is associated with increased maximal shoulder external rotation angle and shoulder joint force in high school baseball pitchers. Am J Sports Med 2014;42(9):2089-2094. doi:10.1177/ 0363546514536871
20. Schwank A, Blazey P, Asker M, et al. 2022 Bern consensus statement on shoulder injury prevention, rehabilitation, and return to sport for athletes at all participation levels. J Orthop Sports Phys 2022;52(1):11-28. doi:10.2519/jospt.2022.10952
21. Brady CJ, Harrison AJ, Comyns TM. A review of the reliability of biomechanical variables produced during the isometric mid-thigh pull and isometric squat and the reporting of normative data. Sports Biomech 2020;19(1):1-25. doi:10.1080/ 14763141.2018.1452968
22. Wang R, Hoffman JR, Tanigawa S, et al. Isometric mid-thigh pull correlates with strength, sprint, and agility performance in collegiate rugby union players. J Strength Cond Res. 2016;30(11):3051-3056. doi:10.1519/Jsc.0000000000001416
23. De Witt JK, English KL, Crowell JB, et al. Isometric midthigh pull reliability and relationship to deadlift one repetition maximum. J Strength Cond Res 2018;32(2):528-533. doi:10.1519/ Jsc.0000000000001605
24. Comfort P, Dos’Santos T, Beckham GK, Stone MH, Guppy SN, Haff GG. Standardization and methodological considerations for the isometric midthigh pull. Strength Cond J. 2019;41(2):57-79. doi:10.1519/Ssc.0000000000000433
25. Andre MJ, Fry AC, Heyrman MA, et al. A reliable method for assessing rotational power. J Strength Cond Res 2012;26(3):720-724. doi:10.1519/ JSC.0b013e318227664d
26. Liaghat B, Bencke J, Zebis MK, et al. Shoulder rotation strength changes from preseason to midseason: A cohort study of 292 youth elite handball players without shoulder problems. J Orthop Sports Phys Ther 2020;50(7):381-387 doi:10.2519/ jospt.2020.9183
27. Clarsen B, Bahr R, Myklebust G, et al. Improved reporting of overuse injuries and health problems in sport: An update of the Oslo sport trauma research center questionnaires. Br J Sports Med. 2020;54(7):390-396. doi:10.1136/ bjsports-2019-101337
28. Borg G. Borg’s Perceived Exertion and Pain Scales Human kinetics; 1998.
29. Wagner H, Buchecker M, von Duvillard SP, Muller E. Kinematic description of elite vs. low level players in team-handball jump throw. J Sports Sci Med. 2010;9(1):15-23.
30. Cools AMJ, Vanderstukken F, Vereecken F, et al. Eccentric and isometric shoulder rotator cuff strength testing using a hand-held dynamometer: Reference values for overhead athletes. Knee Surg Sport Traum Arthrosc. 2016;24(12):3838-3847. doi:10.1007/ s00167-015-3755-9
31. Mirabito NS, Topley M, Thomas SJ. Acute effect of pitching on range of motion, strength, and muscle architecture. Am J Sports Med 2022;50(5):1382-1388. doi:10.1177/03635465221083325
32. Darrall-Jones JD, Jones B, Till K. Anthropometric and physical profiles of English academy rugby union players. J Strength Cond Res 2015;29(8):2086-2096. doi:10.1519/JSC.0000000000000872
33. Dobbin N, Hunwicks R, Jones B, Till K, Highton J, Twist C. Criterion and construct validity of an isometric midthigh-pull dynamometer for assessing whole-body strength in professional rugby league players. Int J Sports Physiol 2018;13(2):235-239. doi:10.1123/ijspp.2017-0166
34. Lauersen JB, Bertelsen DM, Andersen LB. The effectiveness of exercise interventions to prevent sports injuries: A systematic review and metaanalysis of randomised controlled trials. Br J Sports Med 2014;48(11):871-877 doi:10.1136/ bjsports-2013-092538
35. Fleisig GS, Barrentine SW, Escamilla RF, Andrews JR. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21(6):421-437 doi:10.2165/ 00007256-199621060-00004
36. Aguinaldo AL, Buttermore J, Chambers H. Effects of upper trunk rotation on shoulder joint torque among baseball pitchers of various levels. J Appl Biomech. 2007;23(1):42-51. doi:10.1123/jab.23.1.42

Takayama H, Nakamura M, Kataura S, et al. Changes in Shoulder and Lumbar Injury Incidence in Swimmers After Physical Examination and Exercise Programs. IJSPT 2024;19(12):1551-1559. doi:10.26603/001c.126189
Hiroki Takayama1a , Masatoshi Nakamura2 , Satoshi Kataura3 , Shinya Kazekami4 , Ryosuke Takane5 , Yosuke Mitomi6 , Shigeto Nakagawa7
1 Department of Physical therapy, Hanna Central College of Rehabilitation, 2 Faculty of Rehabilitation Sciences, Nishikyushu University, 3 PRO-motion, 4 Department of Rehabilitation, Uragami Internal Medicine Clinic, 5 Department of Rehabilitation, Japanese Red Cross Society Wakayama Medical Center, 6 Komatsu Ltd, 7 Sports Orthopedics, Yukioka Hospital
Keywords: Athlete exposure, Injury prevention, Low back pain, Shoulder pain, Swimming https://doi.org/10.26603/001c.126189
International Journal of Sports Physical Therapy
Vol. 19, Issue 12, 2024
Background
Previous injury and physical examination data collected by a physiotherapist were reviewed to investigate the causes of injury among competitive swimmers. Each swimmer received an injury improvement exercise program based on their injury history and physical examination findings.
Purpose
The purpose of this study was to identify trends in the number of shoulder and lumbar injuries and discern the effectiveness of exercise programs in swimmers. The authors hypothesize that these efforts would decrease injury rates.
Study Design
Observational Cohort study
Methods
Thirty-one male high school and college student swimmers underwent a physical examination. Previous injury was considered as pain that lasted for > three weeks or that caused the participant to stop practicing. A questionnaire was administered to all swimmers at the beginning of the study and one year later The questionnaire assessed the number of injuries sustained and the daily practice hours over the previous year The injury rate at the first examination and one-year followup was calculated as the number of injury incidents divided by the total number of player hours (1 h of practice is equivalent to 1) for one year, multiplied by 1,000 to obtain the injury rate per 1,000 hours (1000 player hours: 1,000 ph). Shoulder and hip exercise programs were prescribed based on measurement results and previous research.
Results
The numbers of injuries seen in the group were 12 shoulder and six lumbar at the first examination, and two shoulder and one lumbar at the one-year followup. The 1,000 ph (95% confidence interval) values were 0.32 (0.13–0.50) and 0.16 (0.03–0.29) at the first examination and 0.05 (0.00–0.12) and 0.03 (0.00–0.07) at the one-year followup for the shoulder and lumbar areas, respectively.
Corresponding Author: Hiroki Takayama: Department of Physical Therapy,Hanna Central College of Rehabilitation, 6-4-43 Tawaradai, Shijonawate, Osaka, 575-0013, Japan
Tel:+81-743-78-8711 E-mail:h.takayama@kuriokagakuen.ac.jp
The results indicates that exercise programs prescribed after a physical examination may reduce the incidence of injuries in male swimmers over the course of a year
Level of Evidence
Level 3
Overuse injuries demonstrate a high incidence in competitive swimmers.1 Studies on previous injuries in competitive swimmers revealed that shoulder and lumbar area injuries rank first and second overall, respectively 2‑4 Injury histories are obtained and physical examination is conducted in swimming and various other sports to investigate the occurrence of injuries.2‑7 The shoulder and lumbar injury rates per 1,000 practices (1,000 athlete exposures [AEs]) have been reported to be 0.51 and 0.24 for male and 0.29 and 0.60 for female swimmers, respectively.4 Specifically, shoulder impingement and joint capsular laxity, or lumbar intervertebral disc injuries are common causes of overuse injuries in swimmers.8 Strength training exercises for the rotator cuff, scapular stabilizers, and core muscle exercises have been demonstrated to be preventive for shoulder and lumbar injuries.8 Previous authors have examined the effects of exercise program prescriptions for competitive swimmers. They revealed a positive 14-year downward trend in disability occurrence in swimmers after an exercise program to prevent lumbar injury 2 However, other previous studies revealed that a six to eight-week shoulder injury prevention program caused physical function changes but no reduction in shoulder pain9,10 and that the effectiveness of exercise programs may differ between shoulder and lumbar injuries. Therefore, to further reduce injury risk, it is recommended that exercises tailored to individual injury histories and physical function be provided, in addition to general conditioning programs.
This study aimed to investigate the effects of implementing physical examination and providing an exercise program in reducing the occurrence of new shoulder and lumbar area injuries over one year Moreover, the authors hypothesize that these efforts would decrease injury rates.
METHODS
DESIGN
This cohort study investigated the effects of implementing exercise programs on competitive swimmers.
PARTICIPANTS
This study included 31 high school and college male swimmers. Swimmers who missed > one month of practice because of trauma or illness were excluded from this study. All participants were briefed under the declaration of Helsinki, and they signed written informed consent obtained by the team coach. For subjects under 18 years of age, written consent was obtained from a parent or guardian and the sub-
ject. The ethics committee of Hanna Central College of Rehabilitation approved this study (Registration number: HCCR-002).
Competitive swimmers under go an examination of physical function (the physical examination) and an interview is completed regarding their their injury history. The first measurements were taken at the start of the season in September and repeated a year later in September. Both measurements were carried out by 11 physiotherapists and 2 athletic trainers. We attempt to provide an exercise program based on the results. The team’s physiotherapist designed the exercise program. Swimmers were interviewed during the first physical examination about their injuries in the previous year An injury was considered “pain that lasted for > three weeks or that caused the patient to stop practicing.” Additionally, the hours of practice on weekdays and weekends were obtained.
The physical examination involved passive measurements of the lower limb (straight leg raise [SLR] and modified Thomas test) range of motion (ROM) and trunk function (modified Kraus–Weber test [M-KWT]11) (Figure 1). The participants were placed in a supine position in the SLR ROM measurements. One of the measurers flexed the hip joint with the knee joint in extension while another examiner measured ROM. The participant was positioned supine with the lower limb out over the edge of the bed for the modified Thomas ROM measurement. The participant holds the lower limb not being measured at the abdomen with both hands. The hip joint was in maximum extension while a measurer held the knee of the lower limb at 90 degrees of flexion and another assessed hip joint extension ROM. A 10% of body weight was loaded on the head (two hands grasp the weights and set them on the back of the head) or the end of the lower extremity (wrapping weights around the feet) for measurement to further load the normal M-KWT
The M-KWT was performed with 10% of the body weight loading.
Passive shoulder ROM was measured: external rotation at 90° shoulder abduction (Abd90°ER), internal rotation at 90° shoulder abduction (Abd90°IR), and internal rotation at 90° shoulder flexion (Flex90°IR).
Written and verbally-instructed exercise programs were provided to improve the physical function of each swimmer based on the injury history and the measurement results of swimmers with an injury history Details of the shoulder exercise (Figure 2) were as follows. (A) Lower trapezius strengthening exercises12 involved three sets of 10 with no load, twice a week, with a 1 kg weight for the second six
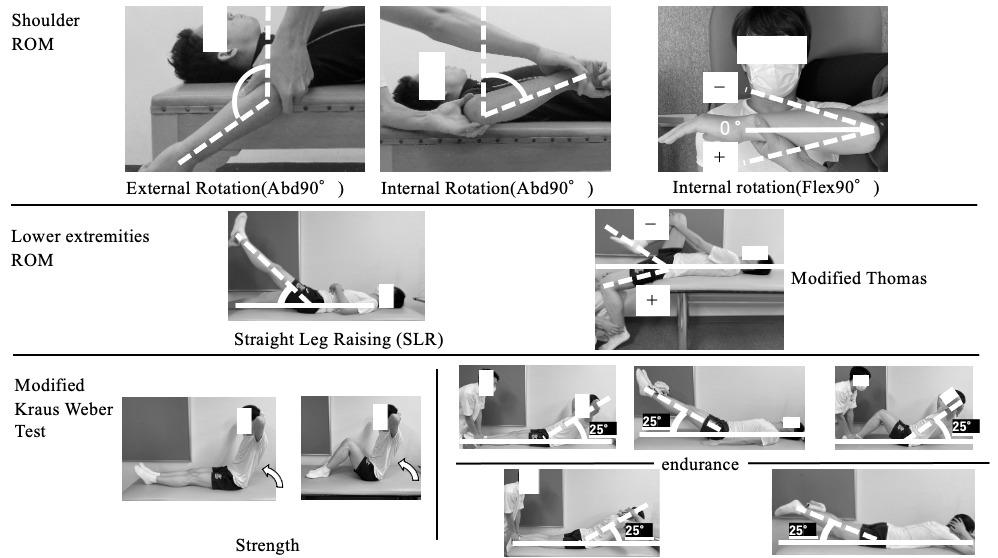
Figure 1. Physical examination items. ROM measurements were performed by two persons
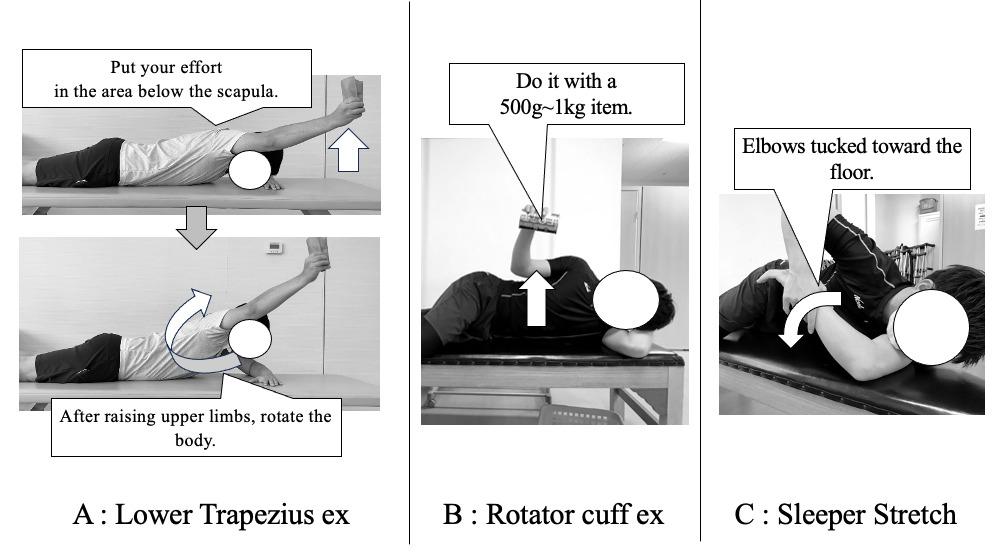
Figure 2. Program to address the shoulder
months. (B) Rotator cuff exercises13 involved three sets of 20 repetitions at a low load (1 kg), twice a week. (C) Modified sleeper stretches,14 three sets 30-s after every practice.
Details of the lumber exercise (Figure 3) are as follows: (D and E) Stretching of the spine and lower limb muscles, three 60-s held repetitions, with 30-s rest15 after every repetition. (F) Core exercise2 involved the front bridge while raising the upper and lower limbs on the diagonal 10 × 2 repetitions, twice a week. (G) Hip lift exercise2 involves
moving the lifting leg up and down during a single limb bridge, 10 × 2 repetitions, twice a week. During the year, the participants were interviewed weekly for pain and fatigue, and the team’s physiotherapist monitored their exercise program. Physical examination was repeated after one year, and an injury history was obtained.
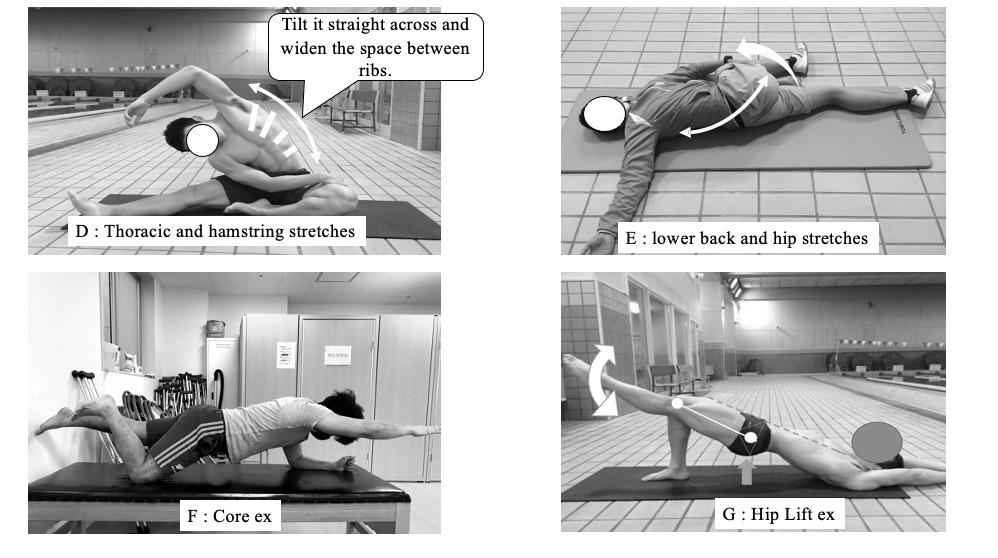
Figure 3. Program to address the lumbar region
The injury rate was calculated using 1,000 player h (1,000 ph). Here, 1,000 ph was calculated by dividing the number of injuries by the total number of hours that the athlete participated in practice and multiplying by 1,000. The 95% confidence interval (CI) for 1,000 ph was simultaneously calculated. Swimmers with shoulder and lumbar disabilities at the first physical examination were compared to asymptomatic athletes on each item with the Mann–Whitney Utest, and one-year measurements were compared. EZR version 1.5416 was utilized for statistical processing. A post hoc power analysis was conducted when the p-value was <0.05. A difference was considered significant if the study had sufficient statistical power (1-b ≧ 0.8).
The mean age of the participants was 17.0 ± 1.1 years, with a mean height of 172.5 ± 5.2 cm and a mean weight of 66.0 ± 7.4 kg. Table 1 presents the number of injuries and 1,000 ph (95%CI) results. The shoulder exhibited 1,000 ph of 0.32 (0.13–0.50) and 0.05 (0.00–0.12) at the first examination and one year thereafter, respectively. Swimmers who reported shoulder injuries in the prior year at the first examination demonstrated no shoulder injuries in the following year The lumbar area demonstrated 1,000 ph of 0.16 (0.03–0.28) and 0.03 (0.00–0.07) for the first examination and one year thereafter, respectively. The six swimmers with lumbar injuries reported no recurrences at the first ex-
amination, but one of the remaining 25 suffered a new injury
COMPARISON OF EACH MEASURED PARAMETER (THE SHOULDER AND LUMBAR AREA)
Swimmers who experienced shoulder pain at the first examination (n = 12) demonstrated a lower ROM of Flex90°IR (p = 0.003) and higher Abd90°ER (p = 0.034) compared to those without shoulder pain (n = 19). Post hoc power analysis revealed that Flex90°IR had high statistical power and was significantly different. All parameters exhibited no significant differences after one year (Table 2). The swimmers with lumbar injury at the first examination (n = 6) exhibited no significant difference in lower limb ROM and M-KWT compared with those without lumbar injury (n = 25), and the same was true after one year (Table 3).
This study consisted of the utilization of a physical examination and subsequent prescription of an exercise program based on the swimmers’ injury history and the measurement results of those with an injury history. The results revealed decreased shoulder and back injuries and improved Flex90°IR after one year.
A previous study on longitudinal survey implementation and disability incidence in competitive swimmers revealed no changes in disability incidence in males but decreased incidence in females.4 However, Kerr’s study included injuries other than those in the shoulder and lumbar area,
Table 1. Number of injuries and injury rates
Exam= examination. Two of 12 swimmers had a recurrent injury of the shoulder, and zero of six swimmers had a recurrence of a lumbar injury
Table 2. Comparison of shoulder joint ROM
(90° Flexion)
Exam= examination. Results are presented as medians (95%CI). Swimmers were divided into groups according to the presence or absence of shoulder injury at the time of the first examination and followed one year later Of the 12 swimmers with shoulder pain, seven had pain on the breathing side of the freestyle stroke and five on the dominant hand side. * p < 0.05; ROM showed a significant difference.
Exam= examination. Results are presented as medians (95%CI). Swimmers were divided into groups according to the presence or absence of lumbar joint injury at the time of the first examination and followed one year later
and the effects of physical examination on the lumbar and shoulder joints specifically remain unclear even after involving other sports. Longitudinal studies on swimmers undergoing medical check up (physical examination) and exercise programs have decreased lumbar injuries.2 However, 96% of swimmers have experienced shoulder pain at the end of the season, even when provided with a longitudinal examination and dryland exercise program provided by an athletic trainer 16 Some studies demonstrated that swimmers continue to practice even with lumbar or shoulder injuries if the injuries are minor,3 and swimmers do not consider minor injuries as important. However, preseason screening for shoulder ROM is useful in determining athletes at risk of disability,16 and the benefits of physical examination have been indicated. The current survey and interventions reduced the number of lumbar injuries from six to one and shoulder injuries from 12 to two within this cohort, with particularly favorable results for the shoulder. The provided intervention program was based on injury
history findings and physical examination results, and carried out with oversight from the physiotherapist regarding exercise content. Furthermore, participants were interviewed weekly for pain and fatigue, and the physiotherapist monitored their exercise program. Introducing exercise only with physical examination or without physical evaluation of target athletes may be unlikely to decrease the occurrence of injury. The current results indicate that a physical examination performed to determine the problematic areas and continuous exercise guidance afterward decreased the incidence of injuries.
The current study demonstrated that swimmers with shoulder pain at the first examination were characterized by decreased Flex90°IR ROM (Table 2). A previous study that investigated the ROM in swimmers with shoulder injuries revealed an external rotation ROM of <93° or >100° in the
90° shoulder abduction position as a predictor of shoulder disorders in swimmers with shoulder injuries.17 The median Abd90°ER ROM of the swimmers with shoulder disorders for the first time in this study was 101°, which is consistent with previous studies. However, the post hoc power analysis results revealed no significant difference between the two groups, and the incidence of disability decreased despite an increase in Abd90°ER ROM in both groups after one year. Factors, other than shoulder injury, may affect the magnitude of Abd90°ER ROM, as reports indicate that highperformance swimmers demonstrate greater Abd90°ER ROM18 and that competitive swimmers may also have acquired anterior shoulder tissue laxity.19 A previous study that investigated the shoulder internal rotation restriction in nonswimming athletes revealed that baseball players (pitchers) with glenohumeral internal rotation deficit are at approximately twice the risk of having a shoulder joint injury.20 Further, Takayama’s study reported reduced Flex90°IR ROM in swimmers with shoulder joint injuries.21 The Flex90°IR ROM may reflect posterior shoulder tightness. Posterior shoulder tightness may have caused the superior anterior displacement of the humeral head during shoulder flexion, thereby significantly increasing the contact pressure with soft tissues.22 Thus, improved internal rotation ROM may be associated with reduced incidence of shoulder joint disorders in swimmers.
The measured Flex90°IR position in this study is similar to that of the modified sleeper stretch position. Performance of the modified sleeper stretch has been associated with decreased tightness of the infraspinatus muscle which attaches to the posterior shoulder 14 Thus, swimmers with shoulder pain were instructed to perform modified sleeper stretch. Following a year-long modified sleeper stretch program, the shoulder pain group demonstrated significant improvements in Flex90°IR, and there were no significant differences between shoulder pain and the pain-free groups in one year later A previous study revealed that four weeks of modified sleeper stretching reduced the stiffness of the infraspinatus muscle.14 Therefore, long-term application of modified sleeper stretches that improved posterior shoulder flexibility (similar to the previous study14) may have contributed to the reduced incidence of shoulder joint injuries.
Posterior shoulder musculature reduced endurance23 and lower muscle activity in the lower trapezius during the crawl and backstroke24 has also been described, which may contribute to shoulder injuries among swimmers. Therefore, participants were instructed to perform low load, high-frequency exercises for the lower trapezius and external rotator muscles of the shoulder. The provision of these exercises contributed to reduced shoulder joint injury after one year. Moreover, some studies reported that a threeweek periscapular exercise prescription increased lower trapezius muscle thickness25 and decreased shoulder pain26 and that 16 weeks of training with the band elevated the external rotator muscle strength in competitive swimmers.27 These results indicate that exercises for the shoulder’s lower trapezius and external rotator muscles may help decrease the incidence of shoulder disorders.
Cejudo et al. revealed that hamstring flexibility deficits in male soccer and basketball players are related to low back pain.28 Iliopsoas elasticity and lumbar kyphosis angle have been shown to be greater during in-water movements in competitive swimmers with low back pain.29 However, the physical examination findings indicated that no difference in straight leg raise or modified Thomas ROM was present in the lumbar injury group compared with the nonlumbar injury group. The oblique abdominal muscles and erector spinae are constantly contracted in the butterfly stroke,30 and the endurance of the trunk muscles would be related to low back pain. However, the current study revealed no difference in M-KWT in swimmers with or without lumbar injury. On the other hand, lumbar spondylolysis and facet joint pain are possible causes of back pain in swimmers.31 This is believed to be due to a position of spinal hyperextension, which requires dynamic movement of the trunk for repeated flexion and extension of the spine.31 Another factor may be the scapulothoracic region, as patients with recurrent low back pain in sports with lumbar spondylolysis exhibit decreased flexibility of the scapulothoracic region/ thoracic cage.32 Further, elite diving athletes with low back pain demonstrated decreased scapulothoracic joint mobility 33 With these reports and guided by the exercise program2 used with the Japanese national team, the authors provided (1) thoracic stretching, (2) deep trunk muscle exercises (core stabilization), and (3) lower back and hip exercises. Hence, six swimmers who experienced back pain at the first examination reported no recurrence for one year, suggesting the effectiveness of exercise program based on the physical examination findings.
One limitation of the current study is that a few of the measures were not consistent with the prescribed exercise program. The exercise program included strengthening muscle endurance exercises around the shoulder, but the physical examination did not include a strength or muscle endurance variable in the assessment. Because the measurements of the physical examination were biased toward mobility In the future, investigating the association between force and injury in the upper and lower limbs and trunk using hand-held dynamometers will be necessary
Authors have suggested that decreased posterior shoulder muscle endurance, including the periscapular muscles, is seen in swimmers with shoulder pain23 and increased numbers (~ 50%) of swimmers displaying scapular dyskinesis after exercise.34 Thus, a longitudinal study on shoulder muscle endurance is warranted. The posterior shoulder endurance test has been measured in competitive swimmers,23 and the authors aim to include this in future research. Further, the authors plan to conduct a longitudinal study on the mobility of the thoracic cage and deep trunk muscles to identify the effectiveness of the exercise program utilized in the current study for the lumbar region. Finally, the number of participants is small and no control group was established; thus, the authors would like to re-
cruit more participants in the future. Additionally, conducting a survey that involves female athletes is imperative, as none were included among the participants in this study
This study prescribed an exercise program to swimmers with shoulder injuries after undergoing physical examination and obtaining injury history. None of the 12 injured
swimmers reported a history of shoulder injury recurrence, and none of the six injured swimmers exhibited a history of lumbar recurrence during the study period. These results indicate that using a prescribed exercise program subsequent to a physical examination reduces the incidence of injury over one year.
Submitted: February 09, 2024 CST, Accepted: September 21, 2024 CST
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. McMaster WC, Troup J. A survey of interfering shoulder pain in United States competitive swimmers. Am J Sports Med. 1993;21:67-70. doi:10.1177/036354659302100112
2. Matsuura Y, Hangai M, Koizumi K, et al. Injury trend analysis in the Japan national swim team from 2002 to 2016: Effect of the lumbar injury prevention project. BMJ Open Sport Exerc Med 2019;5:e000615. doi:10.1136/bmjsem-2019-000615
3. Nagano Y, Yamakawa KK, Higashihara A, Sukemoto HY Japanese translation and modification of the Oslo Sports Trauma Research Centre overuse injury questionnaire to evaluate overuse injuries in female college swimmers. PLoS One 2019;14(4):e0215352. doi:10.1371/journal.pone.0215352
4. Kerr ZY, Baugh CM, Hibberd EE, et al. Epidemiology of National Collegiate Athletic Association men’s and women’s swimming and diving injuries from 2009/2010 to 2013/2014. Br J Sports Med 2015;49(7):465-471. doi:10.1136/ bjsports-2014-094423
5. Mise T, Mitomi Y, Mouri S, et al. Hypomobility in males and hypermobility in females are risk factor for shoulder pain among young swimmers. J Sport Rehabil 2022;31(1):17-23. doi:10.1123/jsr.2020-0488
6. Habelt S, Hasler CC, Steinbrück K, Majewski M. Sports injures in adolescents. Orthop Rev. 2011;3(2):e18. doi:10.4081/or.2011.e18
7 McCall A, Carling C, Davison M, et al. Injury risk factors, screening tests and preventative strategies: a systematic review of the evidence that underpins the perceptions and practices of 44 football (soccer) teams from various premier leagues. Br J Sports Med. 2015;49(9):583-589. doi:10.1136/ bjsports-2014-094104
8. Khodaee M, Edelman GT, Spittler J, et al. Medical Care for Swimmers. Sports Med Open. 2016;2:27. doi:10.1186/s40798-016-0051-2
9. Hibberd EE, Oyama S, Spang JT, Prentice W, Myers JB. Effect of a 6-week strengthening program on shoulder and scapular-stabilizer strength and scapular kinematics in Division I collegiate swimmers. J Sport Rehabil. 2012;21(3):253-265. doi:10.1123/jsr.21.3.253
10. Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br J Sports Med 2010;44(5):376-381. doi:10.1136/bjsm.2009.066837
11. Morita E, Yokoyama H, Imai D, et al. Aerobic exercise training with brisk walking increases intestinal bacteroides in healthy elderly woman. Nutrients. 2019;11(4):868. doi:10.3390/nu11040868
12. Yamauchi T, Hasegawa S, Matsumura A, Nakamura M, Ibuki S, Ichihasi N. The effect of trunk rotation during shoulder exercises on the activity of the scapular muscle and scapular kinematics. J Shoulder Elbow Surg 2015;24(6):955-964. doi:10.1016/j.jse.2014.10.010
13. Bradley J, Kerr S, Bowmaker D MSc, Gomez JF. A swim-specific shoulder strength and conditioning program for front crawl swimmers. Strength Cond J. 2019;41(4):1-17 doi:10.1519/SSC.0000000000000457
14. Yamauchi T, Hasegawa S, Nakamura M, et al. Effects of two stretching methods on shoulder range of motion and muscle stiffness in baseball players with posterior shoulder tightness: a randomized controlled trial. J Shoulder Elbow Surg. 2016;25(9):1395-1403. doi:10.1016/j.jse.2016.04.025
15. Nakamura M, Ikezoe T, Nishihata S, Tanaka H, Umehara J, Ichihasi N. Static stretching duration needed to decrease passive stiffness of hamstring muscle-tendon unit. J Phys Fit Sports Med 2019;8(3):113-116. doi:10.7600/jpfsm.8.113
16. Tate A, Sarver J, DiPaola L, et al. Changes in clinical measures and tissue adaptations in collegiate swimmers across a competitive season. J Shoulder Elbow Surg. 2020;29(11):2375-2384. doi:10.1016/ j.jse.2020.03.028
17 Walker H, Gabbe B, Wajswelner H, Blanch P, Bennell K. Shoulder pain in swimmers: a 12-month prospective cohort study of in incidence and risk factors. Phys Ther Sport. 2012;13(4):243-249. doi:10.1016/j.ptsp.2012.01.001
18. Yoma M, Herrington L, Mackenzie T The effects of differing density of swim-training sessions on shoulder range of motion and isometric force production in national and university level swimmers. Int J Sports Phys Ther. 2023;18(2):375-387. doi:10.26603/001c.72717
19. Zemek MJ, Magee DJ. Comparison of glenohumeral joint laxity in elite and recreational swimmers. Clin J Sport Med 1996;6(1):40-47 doi:10.1097/00042752-199601000-00009
20. Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of glenohumeral internal rotation deficit and total rotation motion to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39(2):329-335. doi:10.1177/0363546510384223
21. Takayama H, Kataura S, Kazekami S, et al. Risk factors for shoulder injuries in male high school and college swimmers: with special attention to spine and shoulder range of motion. J Aqua Heal Med 2022;23(1):49-54.
22. Muraki T, Yamamoto N, Zhao KD, et al. Effects of posterior capsule tightness on subacromial contact behavior during shoulder motions. J Shoulder Elbow Surg 2012;21(9):1160-1167 doi:10.1016/ j.jse.2011.08.042
23. Feijen S, Struyf T, Kuppens K, Tate A, Struyf F. Prediction of shoulder pain in youth competitive swimmers: The development and internal validation of a prognostic prediction model. Am J Sports Med. 2021;49:154-161. doi:10.1177/0363546520969913
24. Matsuura Y, Matsunaga N, Akuzawa H, Oshikawa T, Kaneoka K. Comparsion of muscle coordination during front crawl and backstroke with and without swimmer’s shoulder pain. Sports Health 2024;16(1):89-96. doi:10.1177/19417381231166957
25. Park SH, Lee MM. Effects of lower trapezius strengthening exercises on pain, dysfunction, posture alignment, muscle thickness and contraction rate in patients with neck pain; Randomized controlled trial. Med Sci Monit 2020;26. doi:10.12659/MSM.920208
26. Seitz AL, Podlecki LA, Melton ER, Uhl TL. Neuromuscular adaptions following a daily strengthening exercise in individuals with rotator cuff related shoulder pain: A pilot case-control study. Int J Sports Phys Ther 2019;14(1):74-87 doi:10.26603/ijspt20190074
27 Batalha N, Raimundo A, Tomas-carus P, et al. Does a land-based compensatory strength-training programme influences the rotator cuff balance of young competitive swimmers? Eur J sport Sci. 2015;15(8):764-772. doi:10.1080/ 17461391.2015.1051132
28. Cejudo A, Centenera JMC, Medina FS. The potential role of hamstrings extensibility on sagittal pelvic tilt, sagittal spinal curves and recurrent low back pain in team sports players: Agender prespective analuysis. Int J Environ Res Public Health 2021;18(16):8654. doi:10.3390/ijerph18168654
29. Kitamura G, Tateuchi H, Ichihash N. Swimmers with low back pain indicate greater lumber extension during dolphin kick and psoas major tightness. J Sport Rehabil. 2019;29(6):716-722. doi:10.1123/ jsr.2018-0262
30. Matsuura Y, Matsunaga N, Akuzawa H, et al. Difference in muscle synergies of the butterfly technique with and without swimmer’s shoulder. Sci Rep 2022;12(1):14546. doi:10.1038/ s41598-022-18624-8
31. Hsu C, Krabak B, Cunningham B, Borg-Stein J. Swimming anatomy and lower back injuries in competitive swimmers: A narrative review Sports Health. 2024;16(6):971-981. doi:10.1177/ 19417381231225213
32. Yamasaki K, Kota S, Kawai H, et al. Physical characteristics of patients with symptomatic lumber spondylolysis who have recurrent low back pain after returning to sports. J Bodyw Mov Ther 2021;28:219-224. doi:10.1016/j.jbmt.2021.07.011
33. Narita T, Kaneoka K, Takemura M, et al. Critical factors for the prevention of low back pain in elite junior divers. Br J Sports Med. 2014;48(11):919-923. doi:10.1136/bjsports-2012-091875
34. Madsen PH, Bak K, Jensen S, Welter U. Training induces scapular dyskinesis in pain-free competitive swimmers: A reliability and observational study Clin J Sport Med 2011;21(2):109-113. doi:10.1097/ JSM.0b013e3182041de0

Pinkoski AM, Davies M, Sommerfeldt M, Eurich DT, Voaklander D. Injury and Illness
Adam M Pinkoski1 , Matthew Davies2 , Mark Sommerfeldt3 , Dean T Eurich1 , Don Voaklander1
1 Epidemiology, School of Public Health, University of Alberta, 2 Computer Science, University of Alberta, 3 Orthopedic Surgery, Department of Surgery, Faculty of Medicine and Dentistry, University of Alberta
Keywords: injury, COVID-19, NHL, ice hockey, epidemiology https://doi.org/10.26603/001c.125738
International Journal of Sports Physical Therapy
Vol. 19, Issue 12, 2024
Background
The National Hockey League (NHL) saw an unprecedented disruption to the competitive calendar due to the COVID-19 pandemic in March of 2020. Returning to play following an abrupt cessation of activity is a known risk factor for athletes.
Purpose
To analyze the occurrence and severity of events (injury and illness) in the NHL and to understand any differences in occurrence and severity between pre-pandemic seasons and seasons that immediately followed.
Study Design
Descriptive Epidemiology Study
Methods
Using a retrospective cohort inclusive of all players on active rosters in the NHL between 2016-2023, public access injury and illness data were collected. Outcome measures included event incidence, period prevalence, and severity (mean days lost; MDL), as well as incidence rate ratio (IRR) comparing pre- and post-pandemic seasons.
Results
IRR for illness peaked in December 2021 (IRR = 62.46; 95% CI 13.65 to 285.91). Incidence of upper body injuries was significantly higher in 2020-21 (IRR = 1.70, p = 0.001) and 2021-22 (IRR = 1.40, p = 0.044) compared to pre-pandemic seasons (Incidence = 17.58 injuries / 1000 player-hours). Injury incidence increased as the 2022-23 season progressed (p = 0.004); injury incidence was stable across all other seasons. Mean days lost (MDL) to injury was higher in 2020-21 (MDL = 18.12, p < 0.001), 2021-22 (MDL = 18.46, p = 0.015), and 2022-23 (MDL = 18.12, p < 0.001) compared to pre-pandemic seasons (MDL = 17.34).
Conclusion
Incidence of upper body injuries increased in the 2020-21 and 2021-22 NHL regular seasons while it decreased significantly in the 2022-23 regular season compared with the four pre-pandemic seasons. This suggests a need to examine if modifiable risk factors exist for determining optimal return to play strategies following an abrupt cessation of play.
Level of Evidence 3
INTRODUCTION
On March 12 2020, the National Hockey League (NHL) suspended regular season play due to the COVID-19 global pandemic.1 The following season (2020-2021) saw significant league-wide measures implemented to mitigate the risk of contraction and spread of COVID-19 including an extended off-season and a shortened regular season of 56 games.2 The 2021-2022 season returned to a standard com-
petitive calendar of 82 games with safety measures largely dictated by local, provincial/state, and federal regulations.3
There is strong historical evidence that abrupt disruptions to preparatory or competitive schedules in sport is linked with increased injury rates upon an athlete’s return to competition.4‑6 Several statements from health professionals and medical representatives from professional sporting organizations warned against rapid resumption to play from pandemic related disruptions and to allow for adequate re-conditioning time.7‑9 Increased musculoskeletal injury occurrence in professional baseball,10 American football,11 soccer,12,13 and basketball14 relative to pre-pandemic seasons have already been reported.
Injury is present across each level of ice hockey, with frequency tending to be highest at the most elite levels largely due to higher speeds and aggressive nature of play 15 Overall incidence in the NHL regular season between 2006 to 2012 has been reported to range from 39.4 to 41.3 injuries/ 1000 player game-hours, and 2.4 illnesses/1000 player game-hours.16 Limited rest between games (≤1 day of rest) has been observed to increase the rate and severity of injuries in the NHL.17
While several studies have investigated injury and illness incidence and severity in the NHL,16‑19 at the time of writing no study has described injury or illness in the NHL seasons following the declaration of the COVID-19 global pandemic. The purpose of this study was to analyze the occurrence and severity of events (injury and illness) in the NHL and to understand any differences in occurrence and severity between pre-pandemic seasons and seasons that immediately followed. Due to the schedule disruption and fixture congestion upon returning to play, we hypothesized that injury and illness occurrence and severity increased in the two seasons played since the COVID-19 pandemic was declared compared to pre-pandemic seasons. We further hypothesized that injury trends returned to pre-pandemic levels by the 2022-23 season.
This was a descriptive epidemiology study examining NHL injury and illness in the abbreviated 2020-2021 regular season (56 games), the 82 game 2021-2022 and 2022-23 regular seasons compared with a typical 82 game season in the pre-pandemic era (2016-2017 through to the 2019-2020 seasons).
Two examiners (AP and MD) extracted injury and illness (event) data logged between October 12 2016 and May 1 2023 from two online sources: www.prosportstransactions.com and www.sportsforecaster.com Event data included player name, player ID, date of event, date of return to lineup, and anatomical region (of injury). Basic descriptive player information and player-game exposure data was extracted at www.NHL.com, www.moneypuck.com, and
TheAHL.com All events that resulted in at least one day of lost time were collected for analysis.20 Only players who were injured during the NHL regular season calendar and were concurrently listed on the team’s active roster were included. Any event that was found in one source but not in the other, differed in anatomical region of injury (e.g., one source coded the injury as head, but the other coded as upper body), or listed an event as undisclosed, was cross referenced with media reports and game footage. Events that could not be corroborated between sources were excluded from further analysis. All data was obtained from the public-domain; therefore, ethics approval was not required.
Given the lack of standardized policy for publicly disclosing or categorizing injuries in the NHL,21,22 the available injury data were grouped into general anatomical regions: upper body, lower body, core, and head. Upper body injuries included any injury coded as upper body as well as those ranging from the sternoclavicular joint to the fingers, or the neck. Lower body injuries included any injury coded as lower body or those ranging from the pelvis to the toes. Core injuries included any injury coded in the torso or abdominal regions. Head injuries included any injury to the head or face, including facial lacerations and concussions. Illness included any non-injury events that resulted in time loss such as mental, flu, or COVID-19.3 As it is common practice for players to move between their NHL team and minor league affiliate, any event that occurred while a player was on the active roster of an NHL team and played at least one (1) game for the minor league affiliate after the event but before returning to the NHL, was excluded from analysis as time of event may have been overinflated due to uncertain time to return to play Analysis was conducted under the assumption that movement to the minors was not injury related.
Exposure was calculated using actual time on ice (TOI). Injury incidence rate, reported per 1000 player hours, was calculated as the quotient of number of injuries (numerator) and TOI summed for each player in the specified timeframe (denominator). Incidence rate was evaluated for overall injury and illness as well as for each general anatomical region. To account for variable season lengths between 2016-2023, injury and illness seasonal incidence was calculated using a standardized season length; each season was divided into ten equal sections, as defined by the first and last game of the respective season. Injuries that occurred during a given section were divided by TOI for each player in each game in the respective section. Period prevalence was calculated for each of the ten sections as the proportion of players with an injury (new injuries and those yet to return to play) out of all players in that given season. Period prevalence was calculated for each of the 2020-21, 2021-22, and 2022-23 seasons compared to pre-pandemic seasons. Injury/illness severity was calculated as the number of days the player was inactive due to the respective event.
Statistical analyses were conducted under the assumption of no difference in illness and injury incidence and severity for each (sub) category between pre-pandemic sea-
Table 1. Count data of event frequency and severity for each individual season. TOI reported in total ice time for all players in the season per 1000 player hours.
sons and the 2020-21, 2021-22, or 2022-23 seasons. Distributions were checked prior to statistical test selection and a positive skew was detected for each incidence and severity outcome. Incidence was thus assessed by fitting a Poisson regression model for each outcome category with incidence as the dependent variable, and season (pre-pandemic, 2020, 2021, or 2022), stage of season (1-10), the stage and season interaction, and COVID-related illness (COVID or not) as covariates. Overdispersion was checked for each incidence model; dispersion statistics for the Overall (13.74), Injury (1.33), Lower body injury (1.52), Head injury (1.27), and Illness (21.48) categories warranted use of negative binomial regression. Dispersion statistics for Upper body injury (0.88) and Core injury (0.86) categories warranted use of Poisson regression. Severity was assessed by fitting a Poisson regression model for each outcome category with severity (days lost) as the dependent variable and season as the independent variable. Dispersion statistics for Overall (23.6), Illness (10.8), Injury (23.8), Lower body injury (23.6), Upper body injury (23.0), Head injury (16.4), and Core (40.1) warranted use of negative binomial regression. Statistical significance was set at p < 0.05. Python version 3.10.4 (Python Software Foundation) was used for data collection, analysis, and visualization.
A total of 1872 individual players were active in the league between 2016-17 and 2022-23 with 83.44% (1562/1872) of all players missing at least one day due to injury or illness over that duration (Table 1).
SEASONAL INCIDENCE & PREVALENCE
Incidence of injury and illness across the season are shown in Figures 1 & 2. There was a notable spike in illness from December 12, 2021, to January 19 2022 (31-50% of season completion, peaking at an incidence of 331.36 illness per 1000 player-hours (IRR=33.79, 95% CI 5.21 to 219.21).
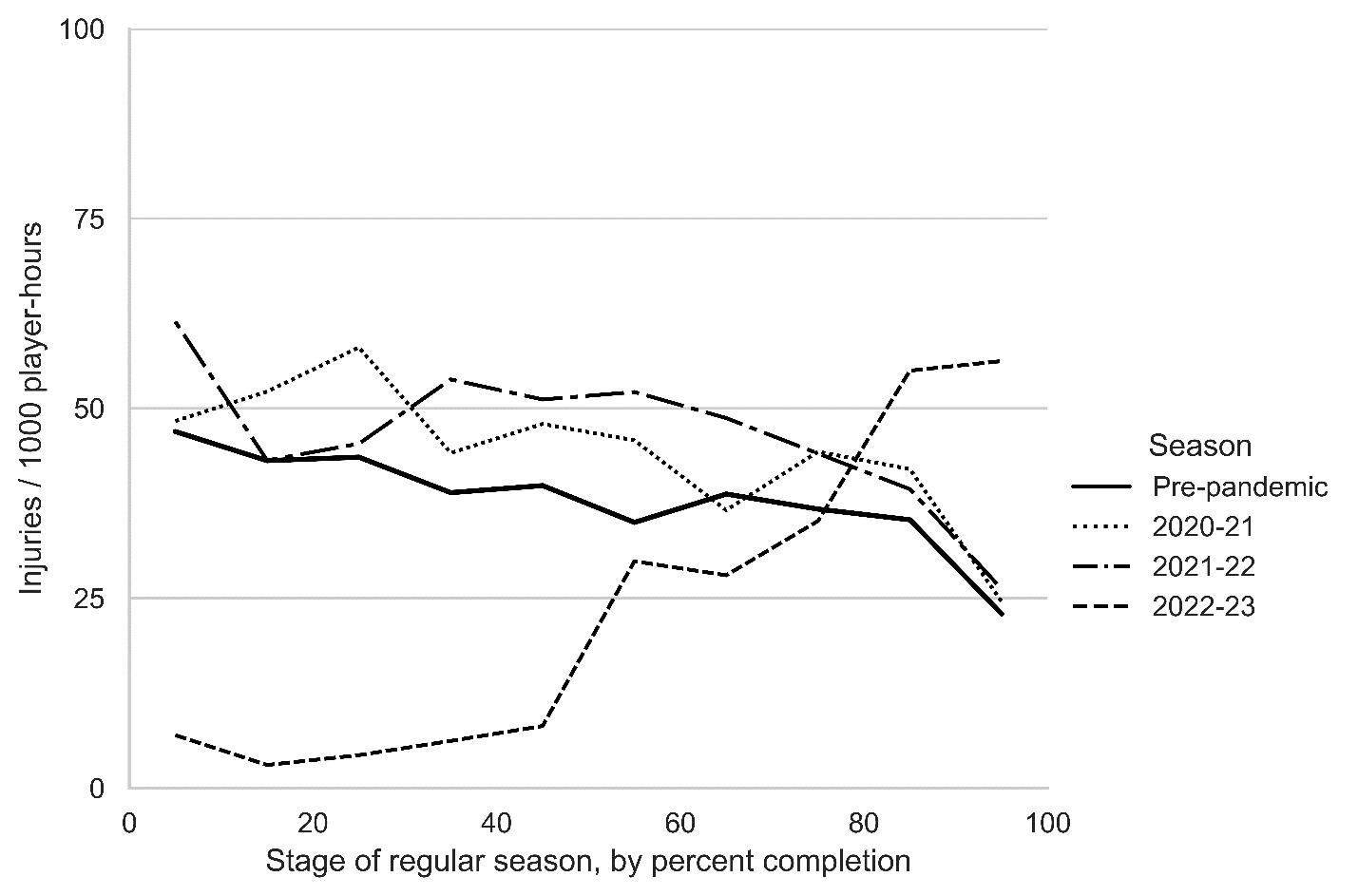
Figure 1. Incidence of injury over the duration of a regular season between pre-pandemic, 2020-21, 2021-22, and 2022-23 seasons. To account for variable season lengths, start and end dates, 0% stage of season corresponds to the first game and 100% to the last game of a given season.
Overall injury incidence did not differ significantly in the 2020-21 (IRR=1.19, 95% CI 0.26 to 5.40) or 2021-22 (IRR=1.22, 95% CI 0.27 to 5.55) seasons compared to the pre-pandemic seasons at any stage over the course of the season. Injury incidence was significantly lower in the 2022-23 season (IRR=0.05, 95% CI 0.01 to 0.27) relative to pre-pandemic seasons. IRR increased by 44.78% with each additional stage of the season in 2022-23 (p = 0.004). Period prevalence of injuries throughout the season can be seen in Figure 3. When adjusting for COVID-19 infection, incidence of non-COVID-19 related illness did not change in 2020-21 (0.95 illnesses / 1000 player-hours, p = 0.164), 2021-22 (6.63 illnesses / 1000 player-hours, p = 0.572), or 2022-23 seasons (0.49 illnesses / 1000 player-hours, p =0 .062) relative to pre-pandemic seasons (3.9 illnesses /1000 player-hours).
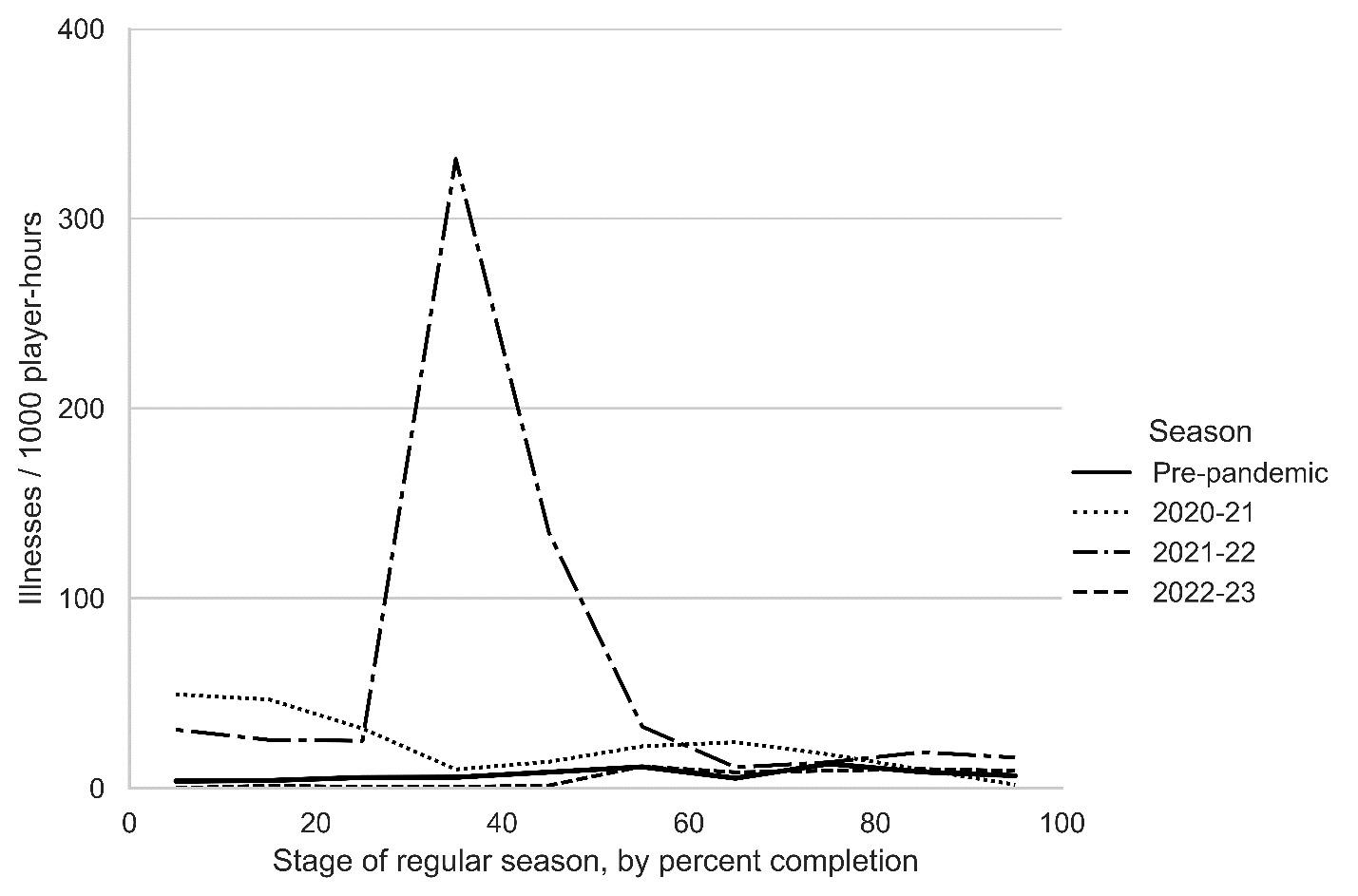
Figure 2. Incidence of illness over the duration of a regular season between pre-pandemic, 2020-21, 2021-22, and 2022-23 seasons.
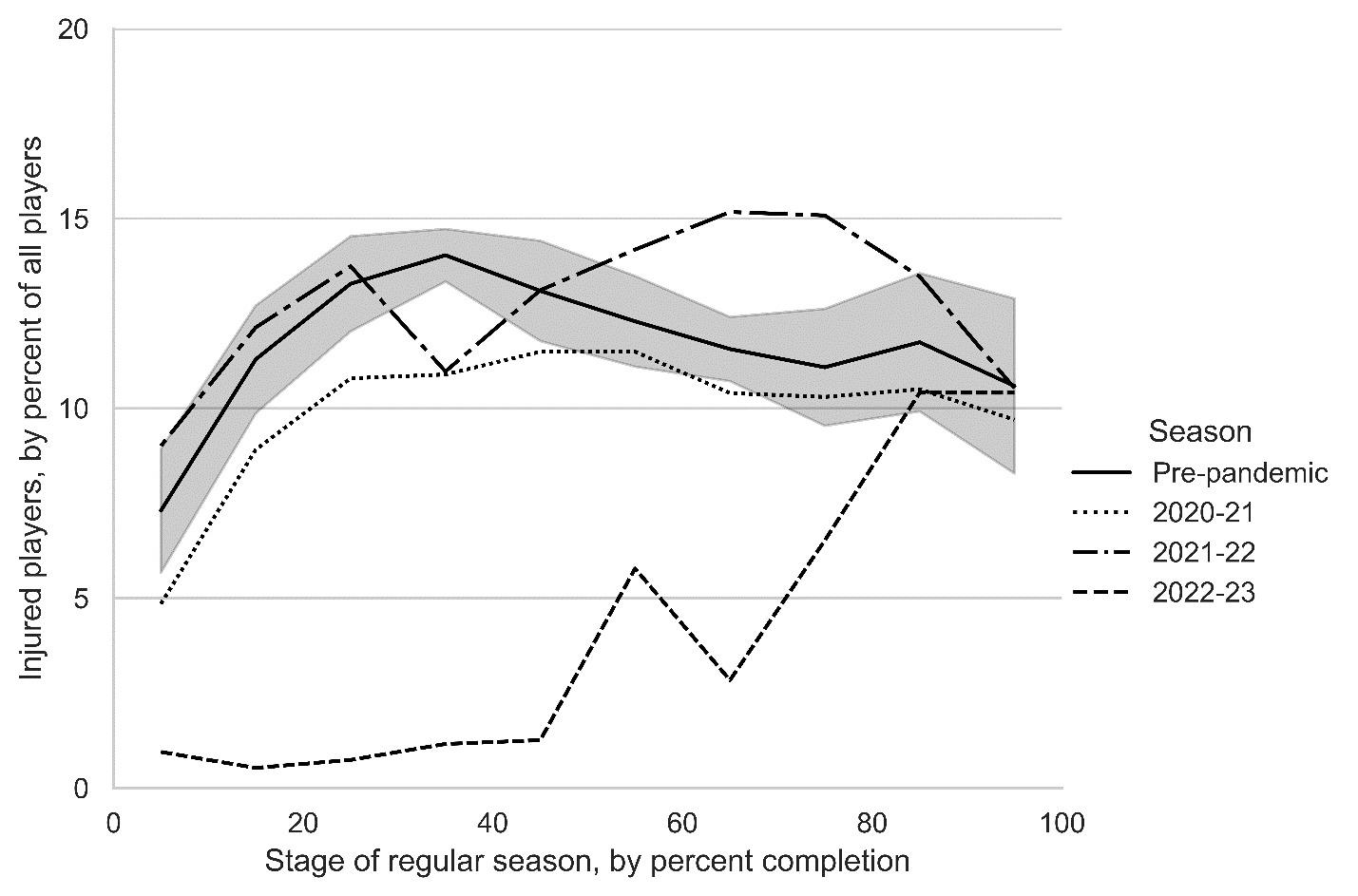
Figure 3. Period prevalence over the duration of the season. 95% confidence intervals for the pre-pandemic seasons shown by shaded area.
Incidence of overall injuries did not change across the 2020-21 and 2021-22 seasons while incidence decreased significantly in the 2022-23 season relative to pre-pandemic seasons (Table 2). Incidence of illness increased significantly in 2020-21 and 2021-22 though returned to prepandemic levels in the 2022-23 season. Upper body injuries were more frequent in 2020-2021 (29.95 vs 17.58 injuries / 1000 player-hours, p = 0.001) and 2021-22 seasons (24.65 vs 17.58 injuries / 1000 player-hours, p = 0.044) compared to pre-pandemic levels. In 2022-23, upper body injuries (1.64 vs 17.58 injuries / 1000 player-hours, p < 0.001) and lower body injuries (0.99 vs 23.03 injuries / 1000 player-hours, p = 0.001) decreased significantly compared to pre-pandemic values. Incidence of illness increased significantly during the 2020-21 season (IRR=16.40, 95% CI 3.53 to 76.19) and 2021-22 season (IRR=62.46, 95% 13.65 to 285.91) relative to pre-pandemic incidence of illness (3.67 illnesses / 1000 player-hours).
The average injury in 2020-21 was 0.78 days more severe than pre-pandemic seasons (18.12 vs 17.34 days lost, p < 0.001); the average injury in 2021-22 was 1.12 days more severe than pre-pandemic seasons (18.46 vs 17.34 days lost, p < 0.001); the average injury in 2022-23 was 1.29 more severe than pre-pandemic seasons (18.63 vs 17.34 days lost, p < 0.001) (Table 3). Increased severity of injury in 2020-21 can be accounted for by higher severity of lower body (0.74 days higher, p < 0.001) and upper body injuries (0.89 days higher, p < 0.001) compared to pre-pandemic seasons. Increased severity of injury in 2021-22 can be accounted for by higher severity of lower body (1.15 days higher, p < 0.001) and upper body injuries (1.15 days higher, p < 0.001) compared to pre-pandemic seasons. Increased severity of injury in 2022-23 can be accounted for by higher severity of upper body injuries (1.59 days higher, p < 0.001) compared to pre-pandemic seasons. There was no significant difference in severity of head or core injuries in post-pandemic seasons relative to pre-pandemic seasons. Severity of illness rose by 1.52 times in 2020-21 (7.35 vs 4.84 days lost, p < 0.001) and by 1.33 times in 2021-22 (7.35 vs 4.84 days lost, p < 0.001). Severity of illness in 2022-23 was no different from pre-pandemic seasons (5.88 vs 4.84 days lost, p = .0739).
The purpose of this study was to analyze the occurrence and severity of events (injury and illness) in the NHL and to understand any differences in occurrence and severity between pre-pandemic seasons and seasons that immediately followed. The incidence of upper body injuries was significantly higher in the 2020-2021 and 2021-2022 seasons compared to pre-pandemic seasons. Injury incidence in the 2022-23 season was significantly lower than pre-pandemic seasons but was the only season that had a notable increase in incidence as the season progressed. Severity of injury increased in the three seasons following the pandemic with upper and lower body injuries the most heavily impacted. The 2020-21 and 2021-22 seasons saw significant increases in illness incidence and severity while the 2022-23 saw illness incidence and severity return to prepandemic levels.
The increase in incidence of upper body injuries in the 2020-21 and 2021-22 seasons could in part be due to loss of sport-specific adaptations because of the interrupted competitive calendar 5 Shoulder checking is the most common mechanism of injury (MOI) in ice hockey, accounting for 29.8% of all man-games lost in the NHL.16 In addition, the 2020 offseason ranged from 10 months (for teams who did not make the adjusted playoffs) and < 5 months (for teams who did make the adjusted playoffs).23 During this window, State, Provincial and League mandates presented several barriers to normal off-season programming (e.g., social distancing, closures of weight rooms and ice), increasing the difficulty for performance staff to design and implement effective programs and for players to adhere to said pro-
Table 2. Model-adjusted incidence of injury and illness categories. IRR = Incidence rate ratio. Boldface p values indicate statistically significant difference between pre-pandemic and respective season (p < 0.05).
(1.19; 0.26 to 5.40)
(1.16; 0.25 to 5.32)
(0.05; 0.01 to 0.27) <
(0.04; 0.01 to 0.30) .001
(0.09;
(1.00; 0.31 to 3.23)
(16.40;
Table 3. Model-adjusted severity of injury and illness. Boldface p values indicate statistically significant difference between pre-pandemic and respective season (p < 0.05).
gramming. Without adequate stimulus for players to adapt to game-specific exposures, such as shoulder checking, and with extended and irregular time off, injury risk is likely to remain high without providing the necessary re-conditioning time needed to regain protective factors.5,24
Injury prevalence was highest in the first half of the season for pre-pandemic seasons (14.81% at 40% of season completion) and in the 2020-21 season (11.49% at 50% season completion). Injury prevalence in 2021-22 peaked at 70% of season completion (15.17%, between February
20, 2022, and March 12, 2022) and was associated with backlogging of games. 131 games were either postponed or rescheduled during the 2021-22 season, with 76.3% (100/ 131) rescheduled during the month of February 25 In a consensus statement from the International Olympic Committee on load and injury risk, it was emphasized that rapid increases in load, specifically, large week-to-week changes, are associated with placing athletes at significantly increased risk of injury 26 In addition, schedule congestion results in deliberate downregulation of training load, as the
focus of training turns toward recovery between competitive bouts.26 In a study focusing on NHL players exclusively, a condensed schedule and ≤1 day of rest between games were associated with increased injury risk.17
When adjusting for illnesses coded for COVID-19, there was no difference in incidence between pre-pandemic seasons and those that followed suggesting no impact of schedule disruption, abbreviated season, or schedule congestion on non-COVID-19 related illness. The incidence and severity of illness was significantly higher in the seasons following the pandemic compared to pre-pandemic seasons (2020-21: non-adjusted MDL=12.14; 2021-22: nonadjusted MDL=7.65). The increase in severity and difference between seasons following the pandemic is likely a reflection of the NHL’s COVID-19 policy changes in each of the seasons. At the beginning of the 2020-21 season (January 2021), players who tested positive for COVID-19 were required to isolate for ten days. Midway through the 2021-22 season (December 29 2021), the isolation period was reduced to five days for fully vaccinated players.27 Every notable change in incidence of illness in the seasons following the pandemic (Figure 2) was strongly correlated with patterns of disease transmission of COVID variants or revisions to the NHL’s COVID protocol. For example, the league introduced increased physical distancing and air flow requirements on February 4, 2021;28 incidence of illness for the 2020-21 season dropped shortly after (~25% of season completion) back to pre-pandemic levels of illness incidence. In December 2021 while the Omicron variant was spreading through North America,28 illness incidence spiked at 331.36 illnesses per 1000 player-hours (~35% of season completion). Following this surge, all games were suspended for a week.29 Illness incidence in the 2021-22 season returned to pre-pandemic levels around 55% of season completion (February 1, 2022); daily testing mandates for vaccinated players was removed on the same day,27 suggesting reported illnesses are likely underreported in the current study due to lack of available data.
An acknowledged limitation of the current study is the use of public access injury data. Although it poses an attractive option given its ease of access, its accuracy is often called into question, especially when used in isolation, or from a single source, resulting in missing or misreported data. While previous studies have used multiple sources to improve validity of injury data,^17, 19, 31^ this paper utilized a systematic approach to ensure injuries and illnesses were included or excluded through the cross-referencing of sources and corroboration of public access data with game footage and media reports. Given there are no known studies validating public access injury data against the NHL’s (gold standard) injury surveillance data, other means of validation are important for context and backing up the veracity of the claims. The non-model adjusted injury incidence between 2016 to 2019 (36.52 to 40.78 injuries per 1000 player-hours), was comparable to previous studies that utilized player-hours as a measure of exposure and utilized injury surveillance data directly from the respective
league. McKay et al. reported injury incidence in the NHL from 2008-2012 to be 39.4 to 41.3 injuries / 1000 playergame hours16; Tuominen et al. reported injury incidence in U20 World Juniors tournaments between 2006-2015 as 43.3 injuries / 1000 player-game hours.32 It should be noted that this task was time consuming, predominantly due to scrubbing through and watching days of game tape. With advances in motion detection and availability of vast historical footage it should be a realistic belief that artificial intelligence methods can be used in the future to replicate the methods presented in this paper for coding and classifying injuries.
Data inclusion involved the assumption that a movement of an injured player to a minor league affiliate was not injury related, though this is not always the case. Careful consideration was made as this would have likely overinflated injury severity In doing so however, may have underreported injury occurrence. Another notable limitation is that a player would return to play when healthy Return dates in the final month of the season often depend on the team’s position relative to the playoffs and is common practice for a player to be shut down if out of playoff contention, thus inflating the severity of injury in latter stages of the season. As a retrospective design, it was assumed that pre- and post-pandemic seasons differed only by the exposure to a disruptive competitive calendar, and that all pre-pandemic seasons were not significantly different from one another
Incidence of upper body injuries increased in the 2020-21 and 2021-22 NHL regular seasons while it decreased significantly in the 2022-23 regular season compared with the four pre-pandemic seasons. These effects lingered for the two seasons that immediately followed the abrupt disruption to the competitive calendar in the NHL. Although results show notable patterns and trends in injury and illness incidence and severity, the authors have been careful so as not to infer on the potential causal effects an abrupt cessation of play (due to the pandemic) has on injury occurrence and severity upon returning to play Future studies focusing on the nuances of offseason training program design and or adherence in the seasons immediately following the pandemic are of notable interest. In addition, studies adjusting for potential modifiable risk factors (e.g., schedule congestion, variable offseason length) and adjusting for current study limitations (e.g., via quasi-experimental designs) are warranted to help sports medicine professionals determine optimal injury prevention strategies following abrupt cessations of play
Submitted: April 04, 2024 CST, Accepted: September 17, 2024 CST
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Zucker J. Timeline of Coronavirus’ impact on sports. Turner Sports. March 11, 2020. Accessed June 21, 2022. https://bleacherreport.com/articles/ 2880569-timeline-of-coronavirus-impact-on-sports
2. National Hockey League. Arena Restart Protocols 2020/21: COVID-19 Protocol. Media.nhl.com. December 1, 2020. Accessed June 21, 2022. https:// media.nhl.com/site/asset/public/ext/2020-21/ 2020-21COVID19Protocol.pdf
3. National Hockey League. COVID-19 Protocol for the 2021-22 Season. Media.nhl.com. September 2, 2021. Accessed June 21, 2022. https://media.nhl.com/ site/asset/public/ext/2021-22/ 2021-22COVIDProtocol.pdf
4. Myer GD, Faigenbaum AD, Cherny CE, Heidt RS, Hewett TE. Did the NFL lockout expose the achilles heel of competitive sports? J Orthop Sports Phys Ther 2011;41(10):702-705. doi:10.2519/jospt.2011.0107
5. Stokes KA, Jones B, Bennett M, et al. Returning to play after prolonged training restrictions in professional collision sports. Int J Sports Med. 2020;41(13):895-911. doi:10.1055/a-1180-3692
6. Tak I, Rutten J, van Goeverden W, Barendrecht M. Sports participation and injury related to the COVID-19 pandemic: Will data support observations from clinicians and athletes? BMJ Open Sport Exerc Med. 2022;8(1). doi:10.1136/bmjsem-2022-001317
7. DiFiori JP, Green G, Meeuwisse W, Putukian M, Solomon GS, Sills A. Return to sport for North American professional sport leagues in the context of covid-19. Br J Sports Med. 2020;55(8):417-421. doi:10.1136/bjsports-2020-103227
8. Mulcahey MK, Gianakos AL, Mercurio A, Rodeo S, Sutton KM. Sports medicine considerations during the COVID-19 pandemic. Am J Sports Med 2020;49(2):512-521. doi:10.1177/0363546520975186
9. Paoli A, Musumeci G. Elite athletes and covid-19 lockdown: Future health concerns for an entire sector J Funct Morphol Kinesiol 2020;5(2):30. doi:10.3390/jfmk5020030
10. Platt BN, Uhl TL, Sciascia AD, Zacharias AJ, Lemaster NG, Stone AV Injury rates in Major League Baseball during the 2020 COVID-19 season. Orthop J Sports Med 2021;9(3):232596712199964. doi:10.1177/ 2325967121999646
11. Puga TB, Schafer J, Agbedanu PN, Treffer K. Covid-19 return to sport: NFL injury prevalence analysis. JMIRx Med. 2022;3(2). doi:10.2196/35862
12. Mazza D, Annibaldi A, Princi G, et al. Injuries during return to sport after the COVID-19 lockdown: An epidemiologic study of Italian professional soccer players. Orthop J Sports Med 2022;10(6):232596712211016. doi:10.1177/ 23259671221101612
13. Seshadri DR, Thom ML, Harlow ER, Drummond CK, Voos JE. Case report: Return to sport following the COVID-19 lockdown and its impact on injury rates in the German Soccer League. Front Sports Act Living Published online 2021:3. doi:10.3389/ fspor.2021.604226
14. Torres-Ronda L, Gámez I, Robertson S, Fernández J. Epidemiology and injury trends in the National Basketball Association: Pre- and per-covid-19 (2017–2021). PLoS One 2022;17(2). doi:10.1371/ journal.pone.0263354
15. Anderson GR, Melugin HP, Stuart MJ. Epidemiology of injuries in Ice Hockey Sports Health: A Multidisciplinary Approach 2019;11(6):514-519. doi:10.1177/1941738119849105
16. McKay CD, Tufts RJ, Shaffer B, Meeuwisse WH. The epidemiology of professional ice hockey injuries: A prospective report of six NHL seasons. Br J Sports Med. 2014;48(1):57-62. doi:10.1136/ bjsports-2013-092860
17 Blond BN, Blond JB, Loscalzo PJ. Game spacing and density in relation to the risk of injuries in the National Hockey League. Orthop J Sports Med 2021;9(4):232596712199940. doi:10.1177/ 2325967121999401
18. Donaldson L, Li B, Cusimano MD Economic burden of time lost due to injury in NHL hockey players. Injury Prevention. 2014;20(5):347-349. doi:10.1136/injuryprev-2013-041016
19. Longstaffe R, Leiter J, MacDonald P Anterior cruciate ligament injuries in the National Hockey League. Clin J Sport Med Published online 2018. doi:10.1097/jsm.0000000000000584
20. Clarsen B, Bahr R. Matching the choice of injury/ illness definition to study setting, purpose and design: One size does not fit all! Br J Sports Med 2014;48(7):510-512. doi:10.1136/ bjsports-2013-093297
21. Donskov AS, Humphreys D, Dickey JP What is injury in Ice Hockey: An integrative literature review on injury rates, injury definition, and athlete exposure in men’s Elite Ice Hockey. Sports. 2019;7(11):227 doi:10.3390/sports7110227
22. Kilgore A. Injury secrecy is an NHL tradition - and a dilemma for bookmakers. Washingtonpost.com. May 10, 2022. Accessed June 21, 2022. https:// www washingtonpost.com/sports/2022/05/09/nhlinjuries-gambling/
23. National Hockey League. NHL timeline of events since pause of 2019-20 season due to COVID-19. NHL.com. August 29, 2024. https://www.nhl.com/ news/nhl-timeline-of-events-since-pauseof-2019-20-season-due-to-covid-19-325500434
24. Jones CM, Griffiths PC, Mellalieu SD Training load and fatigue marker associations with injury and illness: a systematic review of longitudinal studies. Sports Med 2017;47(5):943-974. doi:10.1007/ s40279-016-0619-5
25. National Hockey League. 2021-22 Lists of Postponed and Rescheduled Games. Media.nhl.com. June 28, 2022. Accessed July 9, 2022. https:// media.nhl.com/public/news/15413
26. Soligard T, Schwellnus M, Alonso JM, et al. How much is too much? (part 1) International Olympic Committee Consensus statement on load in sport and risk of injury. Br J Sports Med. 2016;50(17):1030-1041. doi:10.1136/bjsports-2016-096581
27 National Hockey League. NHL, NHLPA issue update on COVID-19 protocol. www.nhl.com. January 31, 2022. Accessed July 8, 2022. https:// www.nhl.com/news/2021-22-nhl-covid-19-protocolupdates/c-330402034
28. Centers for Disease Control and Prevention. CDC Museum COVID-19 Timeline. August 16, 2022. Accessed January 28, 2023. https://www.cdc.gov/ museum/timeline/covid19.html#Late-2021
29. Siladitya R. NHL becomes first U.S. League to pause season amid covid-19 surge. Forbes. December 21, 2021. Accessed June 30, 2022. https:// www.forbes.com/sites/siladityaray/2021/12/21/nhlset-to-temporarily-halt-season-on-wednesday-amidcovid-19-surge/?sh=1e781e212c47

Jacob
R Msando1a , Gill
Cowen
2 , Sarah A
Harris
3 ,
Troy Kirkham
4 ,
Myles C Murphy
5
1 School of Health Sciences , The University of Notre Dame Australia, 2 Curtin Medical School, Curtin University, 3 Institute for Health Research, The University of Notre Dame Australia, 4 Western Australian Football Commission, 5 Nutrition and Health Innovation Research Institute, Edith Cowan University
Keywords: concussion, contact sport, injury prevention, umpire, football https://doi.org/10.26603/001c.125794
International Journal of Sports Physical Therapy Vol. 19, Issue 12, 2024
Background
The Western Australian Football League (WAFL) introduced a new umpire driven ‘blue-card rule’ for concussion, but its benefit to the sports medicine team is unknown.
Purpose
To determine the experiences and perceptions of medical staff within the 2022-2023 Men’s and Women’s WAFL competitions following the introduction of the ‘blue-card rule’
Study Design
Cross-sectional study.
Method
An online survey was delivered through Qualtrics to all WAFL medical staff (doctors, physiotherapists, head trainers). The survey contained four sections (demographics, concussion knowledge, concussion exposure and blue-card perceptions) with closed and multiple-answer questions. Standard methods for reporting descriptive data were applied, including mean ± standard deviation (SD) and proportions (%). Between-group differences were assessed using chi-square tests, and significance was accepted at p <0.05.
Results
Response rate was 48% (n=7 doctors, n=12 physiotherapists, n=12 head trainers). Most staff (70%) did not agree that the ‘blue-card rule’ was a helpful concussion policy or should remain within the WAFL. Staff also felt umpires are not qualified to identify suspected concussions on-field (67%). Over two-thirds of medical staff feel the Football Commission needs to provide education about concussion policies before the commencement of each season. Only 33% of medical staff felt completely confident in delivering a sideline assessment, and 17% felt completely confident in their diagnostic capabilities. Relationships between medical and other staff were not substantially impacted by the ‘blue-card rule’.
Conclusions
Medical staff within the WAFL reported the ‘blue-card rule’ as an ineffective concussion identification tool and did not support its continued use for future WAFL seasons. Staff
Corresponding author:
Email: jacob.msando@my.nd.edu.au a
Jacob Raymond Msando
School of Health Sciences, The University of Notre Dame Australia 32 Mouat St, Fremantle Western Australia 6160
suggested that the Football Commission needs to provide more education on concussion policies before the commencement of each season.
Sports-related concussions are becoming a growing concern in contact sports globally.1,2 However, while some data exist on concussion prevalence3 the incidence rate in semielite Australian football is largely unknown. This includes both West Australian Football League Men’s (WAFL-M) and WAFL Women’s (WAFL-W).4 However, almost half of WAFL (men’s and women’s) players included in a study on the prevalence of mental health complaints self-reported a concussion history.4 This is far more than the number diagnosed clinically within the WAFL-M,5 and no research has reported this for WAFL women (WAFL-W).
The ‘blue-card rule’ is a concussion identification program that aims to allow umpires to remove a player from the field of play for a medical review if they have sustained a suspected sports related concussion (SRC) from an onfield incident (WAFL Rules and Regulations, wafooty.com.au). Following this, medical staff perform their standard concussion assessment per WAFL guidelines.6 The rationale for the blue card includes improving the identification of concussive events and increasing safety of the game.
A study in Rugy Union explored referees’ perspectives on the ‘blue-card rule’ and found they were well prepared to be involved in on-field concussion recognition.7 Sullivan et al. also recommended investigating other stakeholders (i.e., medical staff, players, families) and their experiences with the ‘blue-card rule’.7 A similarly designed, larger study across multiple youth sports reported similar findings to the existing knowledge base.8 Thus, to improve implementation of the ‘blue-card rule’, in partnership with the WAFL, the authors sought to determine the perspectives of its introduction in match-day medical staff.
The purpose of this study was to report the experiences and perceptions of medical staff within the 2022-2023 Men’s and Women’s WAFL competitions following the introduction of the ‘blue-card rule’
A cross-sectional cohort study was performed, via an online survey of match-day medical staff (doctors, physiotherapists, head trainers), in the WAFL-M and WAFL-W between the 4th of April 2023 to the 6th of June 2023. This timeframe was following the conclusion of the 2022 WAFL-M and WAFL-W seasons and during the 2023 ‘in-season’ The final survey was distributed via the WAFC to WAFL-M and WAFLW staff using an email with a link to the online survey
The WAFL is a semi-elite Australian Football League comprising of the WAFL-M and WAFL-W competitions.9 The WAFL-M competition has nine clubs with three divisions (League, Reserves, Colts), while the WAFL-W competition has seven clubs with two divisions (League, Rogers). Each club within the WAFL-M and WAFL-W competition must have a qualified medical team (doctor, physiotherapist, and/or head trainer) to diagnose, assess and treat concussions on game day. The ‘blue-card rule’ allows umpires to remove a player from the field if the umpires believe that a player has a suspected SRC from an incident. That player is then sent to the medical team for a minimum 15-minute review, where a member of the match-day medical team assesses the player. This review involves completion of the SCAT (it was the SCAT 5 at the time of this study),6 and a judgement on whether the player is or is not concussed. At the same time, the offending player is also sidelined for 15 minutes before returning to the field of play.
In the WAFL-W, each club has a physiotherapist and/or doctor, and one head trainer Some clubs have the same one or two staff for both divisions, while other clubs may have an independent physiotherapist and/or head trainer for their Rogers team. In the WAFL-M competition, the league and reserves divisions require one doctor, physiotherapist, and head trainer. The Colts division has a minimum of a physiotherapist and/or head trainer Some clubs have the same three medical staff for all three divisions, or clubs may have an independent physiotherapist and head trainer for their Colts team.
Key medical staff (doctors, physiotherapists, and head trainers) from the WAFL-M and WAFL-W competitions in the 2022 and 2023 seasons were invited to participate. Participants contact details were obtained via emails, phone calls, and text messages through the research team and an industry partner (TK) from the Western Australian Football Commission (WAFC).
An online Qualtrics survey (Qualtrics, Provo, UT) was used to collect data and the survey was piloted with the final survey provided in Appendix A. Medical staff self-reported all answers in the survey, which consisted of four key sections addressing: demographics, concussion knowledge, concussion exposure and blue-card perceptions. Participants provided electronic consent via the online Qualtrics survey and participants were able to complete the survey in less than 30 minutes.
Key independent variables collated from the survey included age (years), gender (man, women, non-binary), competition (WAFL-M or WAFL-W or both), level of competition (Seniors or Colts/Rogers), and respondent’s experience in their respective role within the WAFL (years). Concussion exposure was self-reported using the following variables: concussions witnessed at training (n), and concussions witnessed in a game (n). Concussion knowledge was assessed on a five-point Likert scale (strongly agree, agree, neither agree nor disagree, disagree, strongly disagree) and included the capacity to perform a concussion assessment, referral of a potential concussion, and management of a concussion. The number of blue-cards witnessed per respondent was recorded (n). The opinions of the medical staff regarding the ‘blue-card rule’ were recorded with a five-point Likert scale (strongly agree, agree, neither agree nor disagree, disagree, strongly disagree). The ‘blue-card rule’ impact on the medical staff’s relationships with football personnel was assessed on a four-point scale (Positive effect, no effect, negative effect, prefer not to say).
The initial draft of survey questions was developed by a panel consisting of two concussion researchers (SAH and GC),10‑12 an expert in survey development and validation (MCM),13,14 a representative from the WAFC (TK), and a WAFL player (JRM). These experts also represent a former WAFL doctor, physiotherapist and sports trainer who are the target healthcare professions in the study
Once the panel developed the survey items, content and face validity of the items were assessed through a pilot survey that was distributed and reviewed by a small number of WAFL-M and WAFL-W medical team members (n=3) who worked as either a physiotherapist, head trainer or doctor within the WAFL for at least three seasons. This feedback was used to refine the survey’s relevance, comprehensiveness, and comprehensibility (as judged by medical team members and the research team, using a similar approach to the authors’ previous research).14
The process of ensuring the survey had adequate content validity (consisting of relevance, comprehensiveness, and comprehensibility), is the most important step in the validation of any self-reported data and improves accuracy.
Based on the WAFL-M and WAFL-W structure, in direct collaboration with the WAFC, it was assumed that each of the nine WAFL-M clubs had four key medical staff (doctor, physiotherapist, head trainer, and an additional physiotherapist/head trainer for Colts) (n=36) and each of the seven WAFL-W clubs had two key medical staff (head trainer, doctor and/or physiotherapist) (n= 14). Therefore, using a conservative estimate, the maximum sample was estimated to be 50 participants in the 2022 season, with an additional 14 staff (based off WAFC data) in the 2023 season due to turnover (e.g., a total sample of 66 medical staff). Finally, this study aimed for a >44% response rate, which is
reported as the average response rate in online surveys, to ensure diversity of the sample.15
All statistical analyses were performed using SPSS version 29.0 software (SPSS Inc., Chicago, IL, USA). Standard methods for reporting descriptive data were used, as appropriate. Between-group comparisons of medical team opinions (responses collapsed into agree OR did not agree) on the ‘bluecard rule’ were assessed using chi-square tests for three sub-groups of interest: Respondent profession (doctor, physiotherapist, trainer); competition (WAFL-M, WAFL-W); competition level [Seniors and Under 19’s (WAFL-M Colts/ WAFL-W Rogers)]. Statistical assumptions of chi-square test were met with a minimum of five responses per tabulation possible.16 Significance was set at p <0.05.
Ethical approval for this study was provided by the University of Notre Dame Australia Human Research Ethics Committee (Approval number: 2023-007F) and the WAFC. Participants were provided electronic consent, and all data were recorded in a de-identified format.
Sixty-four WAFL-M and WAFL-W medical team staff were sent the survey, and 40 commenced the survey (commencement rate 63%). A total of 31 (48%) completed the survey to the end (Figure 1), which exceeded the aim for an overall 44% response rate of all WAFL-M and WAFL-W medical team members.
Head trainers made up 38.7% of respondents (n=12), physiotherapists made up 38.7% of respondents (n=12), and doctors made up 22.6% (n=7). An equal split of men and women was observed, and a single participant reported being non-binary. ‘Australian’ was the most reported ethnicity (n=24, 80.0%), and participants were a mean (SD) of 36.7 (16.2) years old. About three-fourths (n=23, 79.3%) had tertiary qualifications. The majority of participants (n=22, 73.3%) reported having a history of playing contact sport, with 45.2% (n=14) of respondents reporting having had a concussion from contact sport. Ten (33.3%) participants reported being in their current role at their respective club for over five years. Complete participant characteristics can be found in Table 1.
The self-reported confidence of the medical team to assess, refer, and manage concussions varied substantially (Appendix B), with specific breakdowns by role presented in Table 2 Furthermore, most respondents (n=23, 74.2%) reported
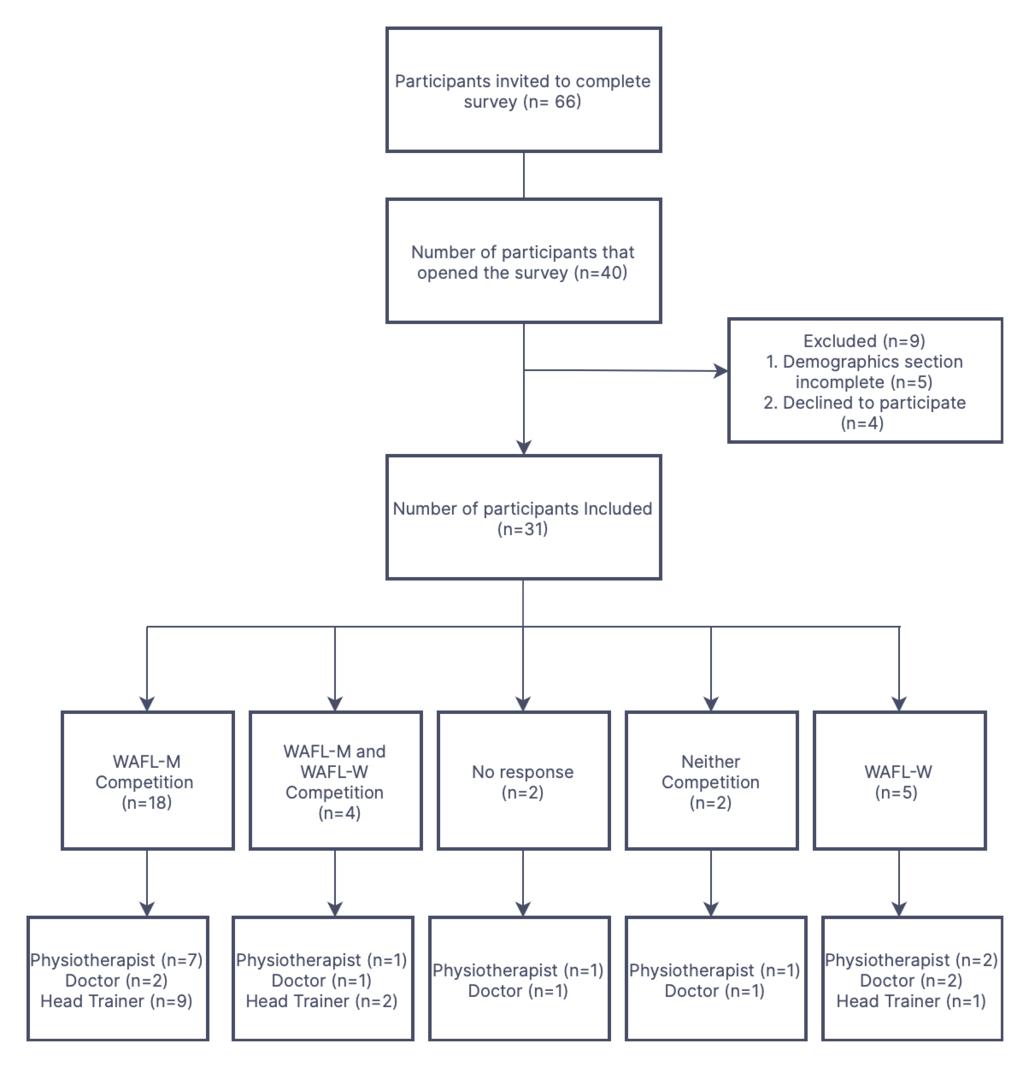
Figure 1. Strengthening the reporting of observational studies in epidemiology Flow Chart the need for the WAFL to provide specific concussion education.
The majority of respondents reported having witnessed a concussion during games (n=25, 83.3%) and/ or during training (n=17, 57%) (while the blue-card was in effect), with complete details per Appendix C. Seventeen participants (54.8%) reported being present when a ‘blue-card rule’ was enforced, 12 (38.7%) reported not having seen the ‘blue-card rule’ enforced, with two participants not responding. Of those participants who witnessed a ‘blue-card rule’ being enforced, 15 (86.7%) reported their player was the one with a suspected concussion, whereas eight (46.7%) reported their player was the offending player (respondents could select both options). For players who were assessed with suspected concussion via the ‘blue-card rule’, the majority were diagnosed with concussion either on the day or during the following two days (n=13, 75%). However, 69% (n=12) returned to play during the game [44% (n=5/ 12) of these were removed from play again during the same game].
VALUE OF THE ‘ BLUE-CARD RULE’
There was some diversity in opinions of medical staff about the ‘blue-card rule’ (Table 3). However, the majority of medical staff: did not agree that the ‘blue-card rule’ helps identify players with concussions (n=19/27, 70.4%); did not agree that the ‘blue-card rule’ assists medical staff in making a concussion diagnosis (n=19/27, 70.4%); did not agree that the ‘blue-card rule’ makes diagnosing a concussion easier (n=18/25, 72.0%); did not agree that the ‘blue-card rule’ should be for all concussions, not just reportable offenses (n=15/26, 57.6%); did not agree that the ‘blue-card rule’ is useful as it allows umpires (in addition to club staff) to identify concussions (n=18/27, 66.7%); and did not agree that the ‘blue-card rule’ should remain with the WAFL (n=19/27, 70.4%).
For those respondents who reported having witnessed the ‘blue-card rule’, there were mixed views on the effect of the rule on the relationship the respondent had with the player, medical team, coach, football manager, and umpire. However, less than 20% of medical staff reported any perceived negative effects concerning the player, coach or umpire, with no respondents reporting negative effects with
the medical team members or the football manager (Appendix D).
DIVERSITY OF RESPONSES TO THE VALUE OF THE ‘ BLUECARD RULE’ BASED ON PROFESSION
No significant between-group differences were detected for Medical Team Opinions on the ‘blue-card rule’ based on the respondent’s role for all items in Table 4 There was a trend that physiotherapists and doctors were in agreement, with differences usually due to head trainer responses, however this trend was not significant. A breakdown of medical staff responses to each item concerning their role can be found in Appendix E.
DIVERSITY OF RESPONSES TO THE VALUE OF THE ‘ BLUECARD RULE’ BASED ON COMPETITION TYPE
Significant between-group differences were detected for Medical Team Opinions on the ‘blue-card rule’ based on the ‘blue-card rule’ assists medical staff in making a concussion diagnosis (p=0.029), with WAFL-M staff feeling it
to be less helpful than WAFL-W staff Otherwise, no significant between-group differences were detected for competition type in all other items (Table 5). A breakdown of medical staff responses to each item concerning the competition they provide coverage at can be found in Appendix F.
DIVERSITY OF RESPONSES TO THE VALUE OF THE ‘ BLUECARD RULE’ BASED ON COMPETITION LEVEL
No significant between-group differences were detected for Medical Team Opinions on the ‘blue-card rule’ based on the respondent’s competition type for all items in Table 6 There was a trend that Colts/ Rogers respondents were more supportive of the ‘blue-card rule’, however this trend was not significant. A breakdown of medical staff responses to each item concerning their role can be found in Appendix G.
Table 2. Confidence in Concussion Assessment, Referral and Management by role.
Table 3. Medical Team Opinions on the Blue-card Rule
Table 4. Between-group comparisons for Medical Team Opinions on the Blue-card Rule based on the respondent role (doctor, physiotherapist, or head trainer)
This cross-sectional cohort study represents the first evaluation of ‘the blue-card rule’ in Australian Football. Moreover, it is the first study to distinctly quantify the medical staff’s viewpoint concerning the ‘blue-card rule’ in any sporting code to which it has been applied.^7 8^ This study reveals three primary findings: firstly, medical staff did not support that the ‘blue-card rule’ helped with concussion identification on gameday during the 2022-2023 WAFL season; secondly, there was not a substantial number of negative consequences for the relationships between the med-
ical team and football department staff due to the ‘blue-card rule’, and; lastly, the WAFC should provide more education to medical staff on concussion education (including the ‘blue-card rule’) in the pre-season.
In the context of rugby, two previous studies explored concussion knowledge, and the experiences of referees tasked with enforcing the ‘blue card rule’ Van Vuuren et al. (2020) evaluated a cohort of rugby stakeholders including medical staff and referees who participated in an online survey assessing their concussion knowledge.17 It was reported that referees attained a concussion knowledge score of 78%, comparable to the medical staff’s score of 79%, contrasting the perspectives of WAFL medical staff concern-
Table 5. Between-group comparisons for Medical Team Opinions on the Blue-card Rule based on the respondent’s league (WAFL-M or WAFL-W)
*Significant result with p<0.05
Table 6. Between-group Comparisons for Medical Team Opinions on the Blue-card Rule Based on the Respondent’s Competition Level (Seniors or Colts/Rogers)
ing concussion knowledge among WAFL umpires. However, the results need to be interpreted with caution due to the divergence in sporting codes the data were collected from and differing prior concussion education protocols. Additionally, Sullivan et al. (2017) explored referee’s experiences with implementing the ‘blue card rule’ within a New Zealand rugby union league.7 Two-thirds of the respondents felt the additional responsibility of the ‘blue card rule’ had no impact on their role performance. As differences in concussion management protocols between codes exist, and differences in the professional level exist (e.g., semi-elite versus elite Australia Football) the value of the ‘blue card rule’ is likely dependent on other concussion policies and procedures.
Medical staff in the current study disclosed that the WAFC needs to provide concussion education to medical staff in the pre-season. Previous literature has established the efficacy of this approach in referees. Notably, 95% of referees in Sullivan et al. reported having received education from their respective commissions for their expanded role.7 Moreover, King and Coughlan reported that referees with prior concussion education attained higher average scores in a general concussion knowledge survey in comparison to referees without education.8 Thus, reinforcing the potential effectiveness of the WAFC delivering concussion education to WAFL stakeholders.
Most of the blue cards issued were subsequently diagnosed with concussions, either on the day or within the following two days. Of specific concern, many players re-
turned to the field during the same game. Plausible explanations for this include: The likelihood that players may have experienced a delayed onset of symptoms18 or acute diagnostic and management skills of medical staff within the WAFL were inadequate compared to team physicians at higher levels of the sport.19 This is not necessarily surprising as this study was performed prior to the introduction of the SCAT 6,20 and the diagnostic accuracy of existing test batteries are known to be suboptimal.11,21
Considering this, Thomas et al. found that whilst doctors in their study were confident in making a diagnosis, they were not confident in concussion management.22 Similarly, in the current study only a small proportion of medical staff expressed that they ‘always’ felt confident in conducting a sideline assessment and believed in their diagnostic abilities, respectively. It’s important to note that the current dynamic nature of concussion protocols may be causing this uncertainty for medical staff This is of substantial concern when one of the primary roles of medical doctors on match day is to recognize and remove athletes from play when they have a concussion.
This study holds implications for the WAFL’s ‘blue-card rule’: 1) Based on the findings, the authors recommend that the WAFC provides concussion education to medical staff before the commencement of each season for the continued safeguarding of players. The authors recommend medical staff are consulted about what education is required to ensure it is appropriate for the league and addresses the concerns of medical staff, 2) The WAFC needs to con-
sider further research investigating umpire and player’s experiences with the ‘blue-card rule’ (e.g., do umpires even want responsibility for concussion) and, on top of that, reassess whether its continuation within the WAFL is beneficial when balanced against other potential positives of the blue-card rule (e.g., deterrent from rough conduct), and 3) Future amendments to concussion guidelines by the WAFC should be co-designed with medical staff to improve implementation.
To determine the effectiveness of the ‘blue card rule’ future research should evaluate how many concussive episodes are missed by medical team staff in semi-elite football, which would be picked up by ‘blue card rule’ Further, the sensitivity and specificity of the ‘blue card rule’ with actual concussions could be determined prospectively
This study had a low number of WAFL-W medical staff participants compared to WAFL-M. The key reason for this is that there were two fewer teams in the 2022 WAFL-W season and one less level within the competition compared to the WAFL-M. Consequently, achieving a balanced repre-
sentation of participants from both competitions was out of the authors’ control leading to sample size dissimilarity Furthermore, it was not anticipated that medical staff would be providing coverage across both competitions and multiple levels within the competition, potentially leading to participants witnessing and reporting the same concussions within the survey Another limitation was the potential for recall bias,23 because participants had to retrospectively report their past experiences with the ‘blue card rule’ from the previous year
Over two-thirds of medical staff did not support the continuation of the ‘blue-card rule’ into future WAFL seasons. It is recommended that the WAFC provide further education on concussion (including the ‘blue-card rule’) before the commencement of each season. These findings provide the WAFC additional information to assist with continued prioritisation of player well-being when implementing strategies to minimise concussion within the WAFL.
Submitted: April 09, 2024 CST, Accepted: September 25, 2024 CST
©
The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Patricios JS, Schneider KJ, Dvorak J, et al. Consensus statement on concussion in sport: the 6th International Conference on Concussion in SportAmsterdam, October 2022. Br J Sports Med 2023;57(11):695-711. doi:10.1136/ bjsports-2023-106898
2. Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019;53(4):213-225. doi:10.1136/ bjsports-2018-100338
3. Patterson B, King M, Cowan S, et al. Self-reported injuries in 2440 women and girls playing community Australian football: a cross-sectional study J Sci Med Sport. 2022;25:S39. doi:10.1016/j.jsams.2022.09.029
4. Henderson A, Harris SA, Kirkham T, et al. What is the prevalence of general anxiety disorder and depression symptoms in semi-elite Australian football players: A cross-sectional study Sports Med Open 2023;9(1):42. doi:10.1186/s40798-023-00587-3
5. Hecimovich M, King D, Dempsey AR, et al. The King-Devick test is a valid and reliable tool for assessing sport-related concussion in Australian football: A prospective cohort study. J Sci Med Sport. 2018;21(10):1004-1007 doi:10.1016/ j.jsams.2018.03.011
6. Echemendia RJ, Meeuwisse W, McCrory P, et al. The Sport Concussion Assessment Tool 5th Edition (SCAT5): Background and rationale. Br J Sports Med 2017;51(11):848-850. doi:10.1136/ bjsports-2017-097506
7 Sullivan J, Collins K, Grey A, et al. Blue card: referees’ perspectives of a rugby union concussion recognition and management programme. Br J Sports Med 2017;51(11):A80-A80. doi:10.1136/ bjsports-2016-097270.206
8. King C, Coughlan E. Blowing the whistle on concussion knowledge and education in youth sport referees. Open Access J Sports Med. 2021;12:109-117. doi:10.2147/oajsm.S324191
9. Hecimovich M, King D, Dempsey A, et al. Head impact exposure in junior and adult Australian football players. J Sports Med. 2018;2018:8. doi:10.1155/2018/8376030
10. Harris SA, Chivers PT, McIntyre FL, et al. Exploring the association between recent concussion, subconcussive impacts and depressive symptoms in male Australian Football players. BMJ Open Sport Exerc Med 2020;6(1):e000655. doi:10.1136/ bmjsem-2019-000655
11. Harris SA, Dempsey AR, Mackie K, et al. Do sideline tests of vestibular and oculomotor function accurately diagnose sports-related concussion in adults? A systematic review and meta-analysis. Am J Sports Med 2021:3635465211027946. doi:10.1177/ 03635465211027946
12. McCausland K, Thomas E, Bullen J, et al. Heads up on concussion: Aboriginal and Torres Strait Islander peoples’ knowledge and understanding of mild traumatic brain injury Health Promot J Austr Published online 2024. doi:10.1002/hpja.892
13. Murphy MC, McCleary F, Hince D, et al. TENDINopathy Severity assessment-Achilles (TENDINS-A): evaluation of reliability and validity in accordance with COSMIN recommendations. Br J Sports Med 2024;58(12):665-673. doi:10.1136/ bjsports-2023-107741
14. Murphy MC, Newsham-West R, Cook J, et al. TENDINopathy Severity Assessment - Achilles (TENDINS-A): Development and content validity assessment of a new patient-reported outcome measure for Achilles tendinopathy J Orthop Sports Phys Ther 2024;54(1):70-85. doi:10.2519/ jospt.2023.11964
15. Wu MJ, Zhao K, Fils-Aime F. Response rates of online surveys in published research: A metaanalysis. Comput Human Behav. 2022;7:100206. doi:10.1016/j.chbr.2022.100206
16. McHugh ML. The chi-square test of independence. Biochem Med (Zagreb). 2013;23(2):143-149. doi:10.11613/bm.2013.018
17 van Vuuren H, Welman K, Kraak W Concussion knowledge and attitudes amongst community club rugby stakeholders. Int J Sports Sci Coach. 2020;15(3):297-305. doi:10.1177/1747954120913175
18. Bunt SC, LoBue C, Hynan LS, et al. Early vs. delayed evaluation and persisting concussion symptoms during recovery in adults. Clin Neuropsychol. 2023;37(7):1410-1427. doi:10.1080/ 13854046.2022.2119165
19. Herring S, Kibler WB, Putukian M, et al. Selected issues in sport-related concussion (SRC|mild traumatic brain injury) for the team physician: a consensus statement. Br J Sports Med. 2021;55(22):1251-1261. doi:10.1136/ bjsports-2021-104235
20. Echemendia RJ, Brett BL, Broglio S, et al. Introducing the Sport Concussion Assessment Tool 6 (SCAT6). Br J Sports Med 2023;57(11):619-621. doi:10.1136/bjsports-2023-106849
21. Harmon KG, Whelan BM, Aukerman DF, et al. Diagnostic accuracy and reliability of sideline concussion evaluation: a prospective, case-controlled study in college athletes comparing newer tools and established tests. Br J Sports Med 2022;56(3):144-150. doi:10.1136/ bjsports-2020-103840
22. Thomas E, Chih H, Gabbe B, et al. A crosssectional study reporting concussion exposure, assessment and management in Western Australian general practice. BMC Fam Pract 2021;22(1):46. doi:10.1186/s12875-021-01384-1
23. Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol. 1990;43(1):87-91. doi:10.1016/ 0895-4356(90)90060-3
Download: https://ijspt.scholasticahq.com/article/125794-introduction-of-the-blue-card-concussion-policy-to-semielite-australian-football-medical-staff-experiences-and-perceptions/attachment/ 253146.docx?auth_token=35Izpik4URgBzsasf1bE
Download: https://ijspt.scholasticahq.com/article/125794-introduction-of-the-blue-card-concussion-policy-to-semielite-australian-football-medical-staff-experiences-and-perceptions/attachment/ 253147.docx?auth_token=35Izpik4URgBzsasf1bE
Download: https://ijspt.scholasticahq.com/article/125794-introduction-of-the-blue-card-concussion-policy-to-semielite-australian-football-medical-staff-experiences-and-perceptions/attachment/ 253144.docx?auth_token=35Izpik4URgBzsasf1bE
Download: https://ijspt.scholasticahq.com/article/125794-introduction-of-the-blue-card-concussion-policy-to-semielite-australian-football-medical-staff-experiences-and-perceptions/attachment/ 253145.docx?auth_token=35Izpik4URgBzsasf1bE
Download: https://ijspt.scholasticahq.com/article/125794-introduction-of-the-blue-card-concussion-policy-to-semielite-australian-football-medical-staff-experiences-and-perceptions/attachment/ 253143.docx?auth_token=35Izpik4URgBzsasf1bE
Download: https://ijspt.scholasticahq.com/article/125794-introduction-of-the-blue-card-concussion-policy-to-semielite-australian-football-medical-staff-experiences-and-perceptions/attachment/ 253142.docx?auth_token=35Izpik4URgBzsasf1bE
Download: https://ijspt.scholasticahq.com/article/125794-introduction-of-the-blue-card-concussion-policy-to-semielite-australian-football-medical-staff-experiences-and-perceptions/attachment/ 253141.docx?auth_token=35Izpik4URgBzsasf1bE

Roberti LS, Franke RA, Robaina BQ, Medeiros DM, Baroni BM. The Single Leg Bridge Test Does Not Measure Isolated Hamstring Endurance in Healthy Men. IJSPT 2024;19(12):1581-1588. doi:10.26603/001c.125763
Lucas S Roberti1 , Rodrigo A Franke1 , Bruno Q Robaina1 , Diulian M Medeiros1 , Bruno M Baroni1a
1 Universidade Federal de Ciências da Saúde de Porto Alegre
Keywords: hamstring, fatigue, strength https://doi.org/10.26603/001c.125763
International Journal of Sports Physical Therapy
Vol. 19, Issue 12, 2024
Background
The Single Leg Bridge Test (SLBT) is commonly described as a measure of ‘hamstring endurance’. Nevertheless, the relationship between the SLBT score and isolated hamstring endurance remains uncertain.
Purpose
This study aimed to investigate the correlation between SLBT scores and isolated hamstring endurance in healthy men. Additionally, the study aimed to assess the correlation between the limb symmetry index obtained from the SLBT and hamstring endurance test results.
Design
Cross-sectional study
Methods
Forty healthy and physically active men were evaluated at the research laboratory on two separate occasions, with a minimum interval of 48 hours between visits. During each visit, participants performed either the single-leg balance test (SLBT) or the hamstring endurance test on an isokinetic dynamometer, which involved 30 concentric knee flexion repetitions performed at maximum intensity, with an angular velocity of 120°/s and a range of motion of 90°. Correlations were analyzed between SLBT scores and hamstring fatigue indexes provided by peak torque and work outcomes.
Results
The SLBT score (27±7 reps) demonstrated no significant correlation with isolated hamstring endurance, as measured by isokinetic peak torque (52±9%; p=0.737, r=-0.038) or work (57±9%; p=0.489, r=0.078). Likewise, the limb symmetry index obtained from the SLBT (99±12%) did not significantly correlate with index from the hamstring endurance test: peak torque (107±26%; p=0.540, r=-0.100) and work (102±18%; p=0.849, r=0.031).
Conclusion
The SLBT does not appear to be a suitable tool for measuring isolated hamstring endurance in healthy men.
Corresponding Author:
Bruno Manfredini Baroni
E-mail: bmbaroni@yahoo.com.br a
Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA)
Rua Sarmento Leite, 245 – CEP 90050-170
Porto Alegre, Rio Grande do Sul, Brasil
Phone/fax +55 51 3303-8876
The hamstring strain injury (HSI) is a major concern in high-speed running-based sports. In football (soccer), for instance, a review including thirteen studies and 3,868 players with two million sport exposure hours demonstrated that HSI accounted from 4% to 13% of all injuries.1 Despite the advances in injury prevention by the scientific community over the last few decades, elite football teams have been unsuccessful in significantly reducing the incidence of HSI.2 This results in significant setbacks for both the teams’ performance and the financial health of the clubs.3 It is also noteworthy that around one in every five injured players experience a HSI recurrency, with more than two-thirds occurring within the initial two months of returning to sport.2 This underscores the importance of refining processes within injury rehabilitation and returnto-play stages, including the implementation of reliable measures for assessing hamstring function.
Diminished muscle strength has historically been considered a potential risk factor for HSI.4 Prospective cohort studies conducted in various sports have yielded inconsistent results,5 possibly because they correlate in-season injuries with muscular strength measured at a single point during the preseason.6 Despite the uncertainties provided by scientific literature, chief medical officers of elite football clubs recognize muscle strength-related deficits as playing a pivotal role in HSI,7 and hamstring strength assessments have been widely used to screen athletes with a higher injury risk.8 These assessments have also been esteemed in the context of HSI rehabilitation, with clinical practice guides recommending their utilization in decisionmaking regarding the patients’ progression.9 In addition, strength tests are the most common return-to-play criteria adopted following a HSI in elite athletes.10 Therefore, strength assessments have become a routine practice for prevention and rehabilitation of HSI.
Hamstring strength has been assessed through isokinetic dynamometry or specialized devices (e.g., Nordic curl test), as well as isometrically using handheld dynamometers and load cells. However, the expense associated with such equipment is a hindrance for professionals dealing with athletes at potential risk or in rehabilitation following an HSI. The Single Leg Bridge Test (SLBT) emerged as a portable and cost-effective option for assessing hamstring function in both the clinical setting and the field of play. Briefly, this test involves performing a unilateral bridge exercise with the tested leg supported on a 60 cm-high platform until the task failure (more details in the Methods section). The SLBT reliability enable its use in the sport context, with intratester intraclass correlation coefficient (ICC) values of 0.77–0.89 and intertester ICC values of 0.89–0.91.11 Furthermore, this test gained prominence since Freckleton et al.12 found that Australian football players who experienced in-season HSI exhibited lower preseason SLBT scores. From there, studies have used the SLBT
to assess hamstring function in healthy subjects,13‑15 as well as to help clinicians in decision-making on the athletes’ rehabilitation progress and return to sport following HSI.16,17
It is noteworthy that recent evidence does not support the SLBT as a valid tool for assessing the hamstring’s maximum strength.18‑20 Gasparin et al.18 were the first to document a lack of correlation between the SLBT score and hamstring concentric or eccentric isokinetic peak torques. This observation was echoed by Robaina et al.19 and Murakami et al.20 in their respective studies involving isometric and eccentric maximum strength tests. Thus, there is compelling evidence against the use of the SLBT as a surrogate for assessing maximum strength of the hamstring muscle group. Conversely, the SLBT has often been advocated as a measure of ‘hamstring endurance’.12,14,15 It seems plausible that muscular endurance (i.e., the ability to resist fatigue) is the dominant factor due to the nature of repetitions to failure in the SLBT However, the relationship between the SLBT score and hamstring endurance is still unknown. Therefore, the primary objective of the present study was to examine the correlation between the SLBT score and isolated hamstring endurance in healthy men. Secondly, this study aimed to examine the correlation between limb symmetry index (LSI) provided by the SLBT and hamstring endurance test results.
In this cross-sectional study, volunteers were evaluated at the research laboratory on two separate occasions, with a minimum interval of 48 hours between visits. During each visit, participants carried out either the SLBT or the hamstring endurance test on the isokinetic dynamometer The sequence of assessments was randomized. A single evaluator conducted all SLBT sessions while another conducted all isokinetic test sessions. Evaluators were blinded to the results of the test conducted by their colleague. This study was approved by the Federal University of Health Sciences of Porto Alegre ethics committee (#5.589.245) and all volunteers provided informed consent before starting study participation.
Volunteers were recruited through advertisements on social networks linked to the university community To be included in this study, the volunteers had to meet the following criteria: male subjects, aged between 18 and 35 years, who regularly participated in individual or team sports, or engaged in resistance training, with at least three sessions per week. Volunteers with history of knee or hip surgery, musculoskeletal injuries in the lower limbs in the three months prior to data collection (including hamstring strain
injury), or any contraindications to perform maximal strength tests and/or muscular endurance tests (e.g., heart failure, arterial hypertension, and physical disability of the lower limbs) were not included.
Participants were asked to avoid vigorous exercise 24 hours prior to tests and not to use analgesics and/or anti-inflammatory drugs 48 hours before the procedures. They were also instructed not to consume stimulant substances (e.g., caffeine) on testing days. Data collection sessions began with a standardized warm-up protocol, consisting of a fiveminute exercise on a cycle ergometer at a cadence of 60 to 80 rpm and a self-selected load corresponding to moderate intensity During the warm-up, participants received instructions about the tests, and all their questions were addressed. A minimum rest period of five minutes was provided between tests for each limb. The second limb was assessed only after the participant confirmed full recovery from the previous tests and indicated readiness to exert a new maximal effort.
Single Leg Bridge Test (SLBT): The SLBT (Figure 1-A) was conducted in accordance with the protocol described by Freckleton et al.12 After the standardized warm-up, participants were instructed to lie down on the ground, placing the heel of the limb being tested on a 60 cm high box. Employing a goniometer, the limb being tested was set to an approximate 20° knee flexion angle. Participants were directed to fold their arms across their chest and press the tested side heel on the top of the box, lifting their pelvis off the ground until their hip reached a fully extended position at 0°. A practice repetition was performed to familiarize participants with the proper execution and to establish the target height for the upward movement. This target height was measured using a one-meter scale and used for both limbs. During the SLBT execution, repetitions were considered valid if the volunteer performed the upright movement until the contact between their non-tested knee and the rater’s hand, positioned at the predetermined target height. Thereafter, they had to touch their buttocks to the ground with no noticeable pause before the next repetition. Additionally, the contralateral thigh was kept as perpendicular to the ground as possible to prevent any momentum from swinging. If the correct form was compromised, a warning was issued, and the test was finished at the next fault. Participants were encouraged to perform as many repetitions as possible until failure.
Hamstring endurance test: The isolated hamstring endurance was evaluated using an isokinetic dynamometer (Biodex System 4; Biodex Medical System, Shirley, NY). After the standardized warm-up, participants were positioned on the isokinetic dynamometer in accordance with the manufacturer’s guidelines (Figure 1-B). Considering the inevitable involvement of gluteal muscles in hip extension movements, the isolated hamstring endurance was tested through a maximum-intensity protocol of repeated knee flexion actions.21,22 For specific familiarization, the volunteer performed 10 submaximal concentric knee flexionextension repetitions at an angular velocity of 120°/s
throughout a 90° range of motion. Following a one-minute rest interval, participants completed the hamstring endurance test, which involved 30 concentric knee flexion repetitions performed at maximum intensity, with an angular velocity of 120°/s and a range of motion of 90°. After each repetition, the participant actively returned to the starting position (knee extended) using low-intensity quadriceps contractions. Throughout the test, participants were encouraged to exert their maximal strength from the first to the last repetition.
The ‘SLBT score’ was documented as the number of valid repetitions executed in each limb during the SLBT execution. The isolated hamstring endurance was assessed through two variables provided by the isokinetic dynamometry: peak torque and work. The ‘peak torque fatigue index’ was determined as the percentage reduction in peak torque along the endurance test. It was calculated by dividing the mean peak torque value obtained from the final five repetitions by the mean peak torque value from the initial five repetitions. The ‘work fatigue index’ was calculated as the percentage decline in work along the endurance test. It involved dividing the work executed during the last third (i.e., final 10 repetitions) by the work performed during the first third (i.e., initial 10 repetitions) of the endurance test. For both SLBT and hamstring endurance test, the LSI was calculated using the following equation: (left limb / right limb) x 100.
Descriptive statistics was used to describe the participants’ performance through mean, standard deviation (SD), 95% confidence intervals (CI), and minimum and maximum values. The Shapiro-Wilk normality test was used to analyze the distribution. Correlations between SBLT scores and isokinetic fatigue indexes were assessed through Pearson’s and Spearman’s correlation coefficients for normal and non-normal data, respectively A similar statistical approach was used to assess correlation between the LSI found in the SLBT and the hamstring endurance test. The following correlation criteria were adopted: 0.69 or less, poor correlation; 0.70 to 0.79, fair correlation; 0.80 to 0.89, good correlation; and 0.90 to 1.0, excellent correlation. Statistical significance was set at 5% (p<0.05).
Forty healthy, physically active men (mean age: 25 ± 2 years, mean weight: 83 ± 8 kg, mean height: 176 ± 1 cm) participated in this study, resulting in a total of 80 limbs evaluated. Fifteen participants were recreational athletes of a range of sports: running (n=6), soccer (n=2), crossfit (n=1), volleyball (n=1), basketball (n=3), Olympic weightlifting (n=1) and sport climbing (n=1). Some of these recreational athletes routinely practiced more than one sport. The other 25 volunteers were only engaged in resistance training.
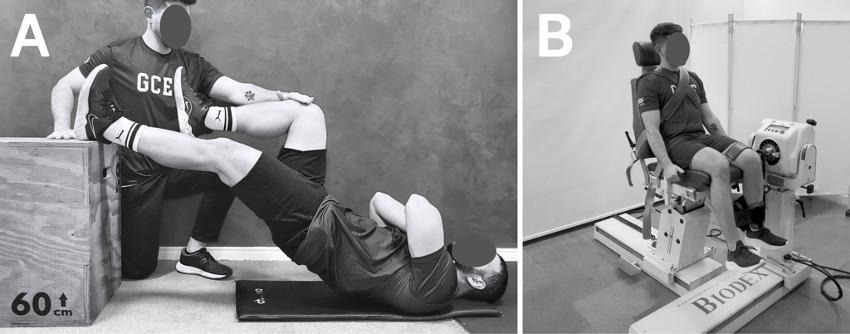
Figure 1. Single leg bridge test execution (A) and positioning adopted for the hamstring endurance test (B).
Table 1. Performance in the single leg bridge test and the hamstring endurance test (n=80 limbs).
Max, maximum; Min, minimum; PT, peak torque; SLBT, single leg bridge test.
Table 2. Limb symmetry index in the single leg bridge test and the hamstring endurance test (n=40 volunteers).
LSI, limb symmetry index; Max, maximum; Min, minimum; PT, peak torque; SLBT, single leg bridge test.
There was no significant correlation between the SLBT score and the hamstring fatigue indices provided by peak torque or work (p>0.05 for both; Table 1). Similarly, the LSI found in the SBLT was not significantly correlated with LSI found in hamstring endurance test (p>0.05; Table 2). Scatter plots on Figure 2 further demonstrate the failed association between the SLBT scores and the isolated hamstring endurance.
This study aimed to investigate the correlation between the SLBT score and isolated hamstring endurance. There was no significant correlation between the SLBT score and the fatigue indices provided by peak torque or work measurements. Additionally, the between-limb performance symmetry in the SLBT score, assessed through LSI, did not show
a significant correlation with those found in the hamstring endurance test.
The SLBT previously shown to be unable to represent hamstring maximum strength.18‑20 Conversely, considering the nature of repetitions to task failure in the SLBT, the hypothesis that this test would show an acceptable correlation with muscular endurance appeared reasonable. Hence, the current study used the gold standard tool to assess muscular strength-related variables and implemented a testing protocol under highly controlled conditions in a laboratory environment to evaluate isolated hamstring endurance.21,22 To broaden the scope of the analysis, the current study employed both torque and work as methods for measuring muscle endurance. In both instances, the protocol proved effective in inducing muscle fatigue, as indicated by average values of approximately 52% (95%CI 50% to 54%) and 57% (95%CI 55% to 58%) drop in torque and
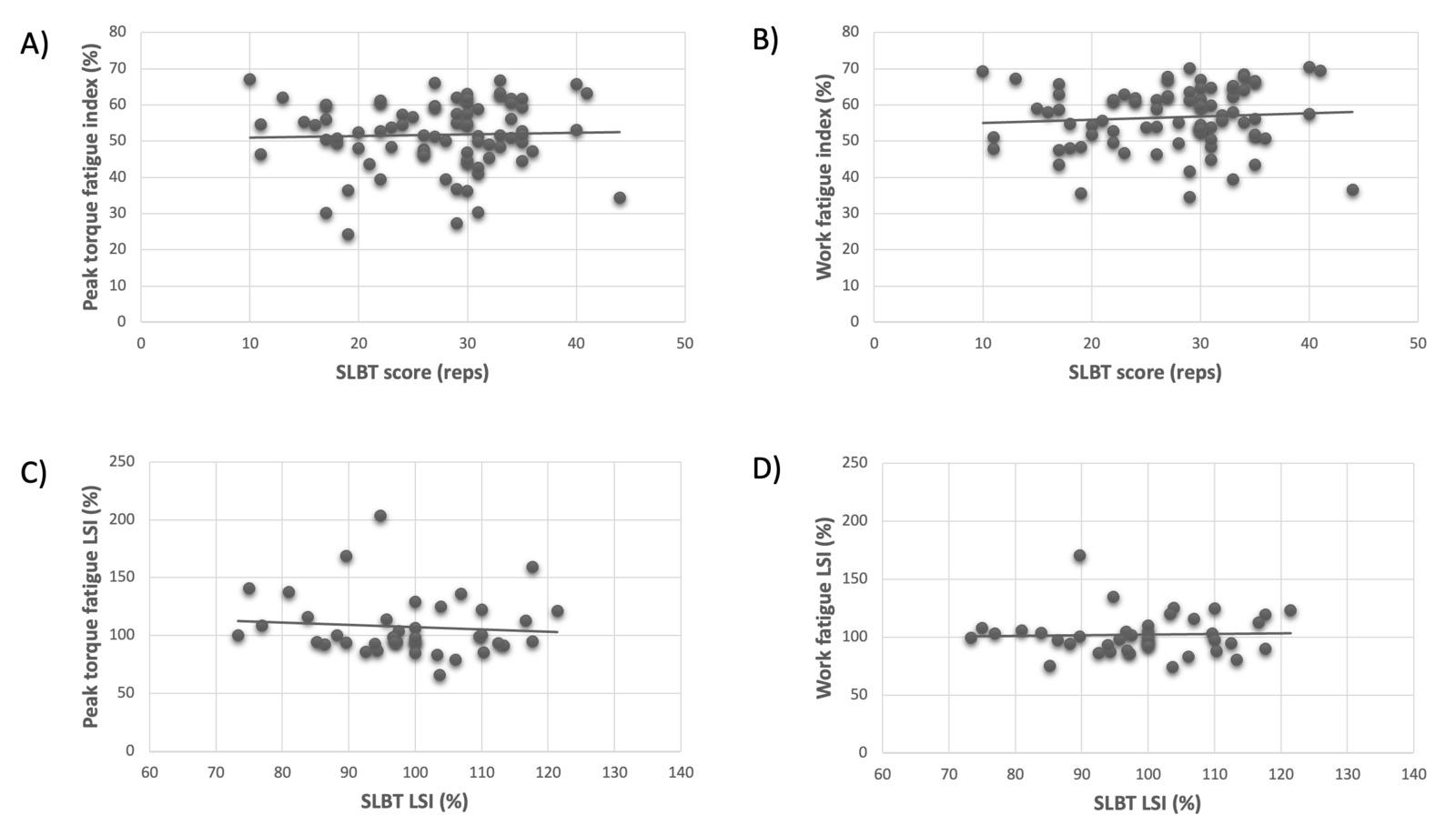
Figure 2. Scatter plots illustrating the relationship between the single leg bridge test (SLBT) and the hamstring endurance test. Panels A and B present the testing performance (n=80 limbs). Panels C and D present the limb symmetry index (LSI; n=40 volunteers).
work over the course of the 30 maximum-intensity repetitions, respectively
The results of the present study contradict those who promote the SLBT as a measure of hamstring endurance.12, 14,15 It is reasonable to consider some factors that may have played a role in these results. First, it should not be ignored that fatigue is a task-dependent phenomenon.23 Hence, a protocol involving a predetermined number of maximumintensity isokinetic contractions may elicit a different fatigue response compared to a protocol continuing until task failure in an exercise with fixed resistance (in the case of SLBT, using the volunteers’ body mass). The volunteers were acquainted with the tasks involved in the SLBT and the isokinetic endurance test, but they did not have the opportunity to undergo multiple assessments to refine their execution strategy for each test. The instructions and verbal stimuli were aimed to volunteers perform as many repetitions of SLBT as possible up to failure and to maximally contract their hamstring muscles in every isokinetic repetition throughout the endurance test. Nevertheless, the perception of discomfort and fatigue triggered by each test is individual-specific, influencing the volunteer’s responses during the execution of each test.
Concurrently, and possibly with a greater relevance to the results, the contribution of gluteal muscles to the hip extension movement during the SLBT should be highlighted. The gluteus maximus is considered the most relevant hip extensor.24 Specifically during unilateral bridge exercises, studies have found similar activation levels between gluteus maximus and hamstrings25 or higher activation for gluteus maximus compared to hamstrings.26 In addition, the middle segment of gluteus medius and the
posterior segment of gluteus minimus also exhibit high activation during the unilateral bridge.27 Therefore, gluteal muscles probably played a key role in the SLBT score, while they had no ability to contribute to the volunteers’ performance on the isokinetic endurance test, due to isolated knee flexion actions. In addition to the gluteal muscles, bridge exercises involve stabilizing muscles in the lumbopelvic region.25 Hence, these trunk muscles status may also influence the SLBT score.
Sprinting seems to place the highest demands on the hamstrings,28 and this muscle group is essential for horizontal force production during sprinting actions.29 Interestingly, in a situation of repeated sprint-induced fatigue, the gluteus maximus seems to assume a relatively more significant role than the hamstrings in horizontal force production.30 It has been hypothesized that gluteus maximus, as the primary hip extensor muscle, may compensate in a synergistic manner during sprinting for potentially altered hamstring muscle function due to fatigue.30 Applying this hypothetical scenario to the SLBT, the fatigue of the gluteal muscles would likely have a more decisive impact on the number of single-leg bridge repetitions before task failure than the hamstrings. This reinforces the notion that the current results might have varied if the isokinetic endurance test had incorporated repetitive hip extension movements instead of knee flexion. Conversely, since the SLBT has been described as a measure of hamstring endurance,12,14,15 the chosen protocol of repeated knee flexion actions emerged as the only way to assess hamstring endurance without involving other hip extensor muscles.
It is reasonable to speculate that the SLBT is likely a test assessing the endurance of the hip extensors. If this is
correct, the SLBT score should not be attributed solely to the condition of the hamstrings or gluteal muscles in isolation. From a practical perspective, an athlete with wellfunctioning hamstrings may still struggle with the SLBT if their gluteal muscles are unable to effectively perform the task. Therefore, implementing a hamstring strengthening program focused on knee-dominant exercises, such as Nordic curls, might not be an effective approach. Conversely, a satisfactory SLBT score for an athlete undergoing HSI rehabilitation does not necessarily indicate that hamstring function has fully recovered. The role of the gluteal muscles in hip extension may be a critical factor for satisfactory performance, making a return-to-play decision after HSI based solely on the SLBT premature. Therefore, even if future studies validate the potential association between the SLBT and the hip extensors’ endurance, practitioners should be aware that this test may not distinguish whether a low score is attributable to the gluteal or hamstring muscles.
The authors acknowledge some limitations of the present study First, these findings pertain to the performance of male recreational athletes, and caution should be exercised when extrapolating them to high-performance or female athletes. Second, none of the participants had previous experience with the SLBT or isokinetic testing, but the experience of some participants in specific sports may have positively influenced their performance in the SLBT due to their greater familiarity with the task. Third, conducting additional sessions to familiarize volunteers with each test was not feasible in this study Conversely, the same evaluators conducted all assessments, with one responsible for the SLBT and the other for the isokinetic test, ensuring that volunteers received consistent instructions and verbal stimuli. Lastly, the SLBT necessitates evaluators with the
ability to analyze technique, provide feedback, and count repetitions. Therefore, it is possible that some inherent errors in this assessment may have occurred in determining the test interruption due to task failure.
There was no significant correlation between the SLBT score and isolated hamstring endurance assessed isokinetically Similarly, the between-limb symmetry found in the SLBT was not significantly correlated with those found in the endurance test. Therefore, the SLBT does not appear to be a suitable tool for measuring isolated hamstring endurance in healthy men.
The authors have no conflicts of interest to declare.
BMB thanks CNPq-Brazil for the research productivity fellowship.
RAF and DMM thank CAPES-Brazil for scholarships.
Submitted: May 06, 2024 CST, Accepted: September 25, 2024 CST
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Diemer WM, Winters M, Tol JL, Pas H, Moen MH. Incidence of acute hamstring injuries in soccer: a systematic review of 13 studies involving more than 3800 athletes with 2 million sport exposure hours. J Orthop Sports Phys Ther 2021;51(1):27-36. doi:10.2519/jospt.2021.9305
2. Ekstrand J, Bengtsson H, Waldén M, et al. Hamstring injury rates have increased during recent seasons and now constitute 24% of all injuries in men’s professional football: the UEFA Elite Club Injury Study from 2001/02 to 2021/22. Br J Sports Med. 2022;57(5):292-298. doi:10.1136/ bjsports-2021-105407
3. Eliakim E, Morgulev E, Lidor R, Meckel Y
Estimation of injury costs: financial damage of English Premier League teams’ underachievement due to injuries. BMJ Open Sport Exerc Med 2020;(1):e000675. doi:10.1136/bmjsem-2019-000675
4. Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury Sports Med. 2012;42(3):209-226. doi:10.2165/ 11594800-000000000-00000
5. Green B, Bourne MN, van Dyk N, Pizzari T
Recalibrating the risk of hamstring strain injury (HSI): a 2020 systematic review and meta-analysis of risk factors for index and recurrent hamstring strain injury in sport. Br J Sports Med. 2020;54(17):1081-1088. doi:10.1136/ bjsports-2019-100983
6. Baroni BM, Oliveira Pena Costa L. Evidence-based prevention of sports injuries: is the sports medicine community on the right track? J Orthop Sports Phys Ther. 2021;51(1):91-93.
7. Ekstrand J, Ueblacker P, Van Zoest W, et al. Risk factors for hamstring muscle injury in male elite football: medical expert experience and conclusions from 15 European Champions League clubs. BMJ Open Sport Exerc Med 2023;9(1):e001461. doi:10.1136/bmjsem-2022-001461
8. Buckthorpe M, Wright S, Bruce-Low S, et al. Recommendations for hamstring injury prevention in elite football: translating research into practice. Br J Sports Med 2019;53(7):449-456. doi:10.1136/ bjsports-2018-099616
9. Martin RL, Cibulka MT, Bolgla LA, et al. Hamstring strain injury in athletes. J Orthop Sports Phys Ther. 2022;52(CPG1-CPG44). doi:10.2519/jospt.2022.0301
10. Valente HG, Oliveira RR, Baroni BM. How are hamstring strain injuries managed in elite men’s football clubs? A survey with 62 Brazilian physical therapists. Phys Ther Sport 2023;61:73-81. doi:10.1016/j.ptsp.2023.03.001
11. Hallett P. A Reliability Study Examining the Interand Intra-Observer Reliability of the Muscle Capacity Tests Included in the ECB Musculoskeletal Screening Protocol. Master’s thesis. University of Nottingham; 2010.
12. Freckleton G, Cook J, Pizzari T The predictive validity of a single leg bridge test for hamstring injuries in Australian Rules Football players. Br J Sports Med 2014;48(8):713-717 doi:10.1136/ bjsports-2013-092356
13. Rey E, Paz-Domínguez Á, Porcel-Almendral D, et al. Effects of a 10-week Nordic hamstring exercise and Russian belt training on posterior lower-limb muscle strength in elite junior soccer players. J Strength Cond Res 2017;31(4):1198-1205. doi:10.1519/JSC.0000000000001579
14. Macdonald B, O’Neill J, Pollock N, Van Hooren B. Single-leg Roman chair hold is more effective than the Nordic hamstring curl in improving hamstring strength-endurance in Gaelic footballers with previous hamstring injury J Strength Cond Res 2019;33(12):3302-3308. doi:10.1519/ JSC.0000000000002526
15. Mahnič N, Rauter S, Hadžić V, Šimenko J. The single leg bridge test (SLBT) as a field test to measure hamstring strength in young footballers. Science & Sports 2021;36(5):417.e411-417.e417 doi:10.1016/ j.scispo.2020.11.004
16. Jacobsen P, Witvrouw E, Muxart P, Tol JL, Whiteley R. A combination of initial and follow-up physiotherapist examination predicts physiciandetermined time to return to play after hamstring injury, with no added value of MRI. Br J Sports Med 2016;50(7):431-439. doi:10.1136/ bjsports-2015-095073
17 Mendiguchia J, Martinez-Ruiz E, Edouard P, et al. A multifactorial, criteria-based progressive algorithm for hamstring injury treatment. Med Sci Sports Exerc 2017;49(7):1482-1492. doi:10.1249/ MSS.0000000000001241
18. Gasparin GB, Ribeiro-Alvares JBA, Baroni BM. Single leg bridge test is not a valid clinical tool to assess maximum hamstring strength. Int J Sports Phys Ther 2022;17(4):613-621. doi:10.26603/001c.34417
19. Robaina BdQ, Medeiros DM, Roberti LdS, Franke RdA, Baroni BM. The single leg bridge test does not replace handheld dynamometer hamstring tests in a clinical setting. Phys Ther Sport. 2023;63:126-131. doi:10.1016/j.ptsp.2023.08.001
20. Murakami Y, Nishida S, Yoshida R, et al. Relationship between Nordic hamstring strength and single leg bridge test in university soccer players. J Sport Rehabil 2023;33(1):27-32. doi:10.1123/ jsr.2022-0451
21. O’Connor KM, Johnson C, Benson LC. The effect of isolated hamstrings fatigue on landing and cutting mechanics. J Appl Biomech 2015;31(4):211-220. doi:10.1123/jab.2014-0098
22. Samaan MA, Hoch MC, Ringleb SI, et al. Isolated hamstrings fatigue alters hip and knee joint coordination during a cutting maneuver. J Appl Biomech 2015;31(2):102-110. doi:10.1123/ JAB.2013-0300
23. Bigland-Ritchie B, Rice CL, Garland SJ, Walsh ML. Task-dependent factors in fatigue of human voluntary contractions. Adv Exp Med Biol 1995;384:361-380. doi:10.1007/ 978-1-4899-1016-5_29
24. Neto WK, Soares EG, Vieira TL, et al. Gluteus maximus activation during common strength and hypertrophy exercises: a systematic review J Sports Sci Med 2020;19(1):195-203.
25. Ekstrom RA, Donatelli RA, Carp KC. Electromyographic analysis of core trunk, hip, and thigh muscles during 9 rehabilitation exercises. J Orthop Sports Phys Ther. 2007;37(12):754-762. doi:10.2519/jospt.2007.2471
26. Youdas JW, Hartman JP, Murphy BA, et al. Electromyographic analysis of gluteus maximus and hamstring activity during the supine resisted hip extension exercise versus supine unilateral bridge to neutral. Physiother Theory Pract. 2017;33(2):124-130. doi:10.1080/09593985.2016.1271848
27 Moore D, Semciw AI, Pizzari T A systematic review and meta-analysis of common therapeutic exercises that generate highest muscle activity in the gluteus medius and gluteus minimus segments. Int J Sports Phys Ther. 2020;15(6):856-881. doi:10.26603/ ijspt20200856
28. van den Tillaar R, Solheim JAB, Bencke J. Comparison of hamstring muscle activation during high-speed running and various hamstring strengthening exercises. Int J Sports Phys Ther 2017;12(5):718-727. doi:10.26603/ijspt20170718
29. Morin JB, Gimenez P, Edouard P, et al. Sprint acceleration mechanics: the major role of hamstrings in horizontal force production. Front Physiol 2015;6:404. doi:10.3389/fphys.2015.00404
30. Edouard P, Mendiguchia J, Lahti J, et al. Sprint acceleration mechanics in fatigue conditions: compensatory role of gluteal muscles in horizontal force production and potential protection of hamstring muscles. Front Physiol 2018;9:1706. doi:10.3389/fphys.2018.01706

R, Brandt E, Johansson A, et al.
Ramana Piussi1,2a , Ella Brandt3 , Alicia Johansson3 , Thorkell Snaebjörnsson4 , Roland Thomeé1,3 , Kristian Samuelsson4 , Eric Hamrin Senorski1,2
1 Unit of Physiotherapy, Department of Health and Rehabilitation, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Box 455, SE-405 30 Gothenburg, Sweden, 2 Sahlgrenska Sports Medicine Center, Gothenburg, Sweden, 3 Sportrehab Sports Medicine Clinic, Stampgatan 14, SE-411 01 Gothenburg, Sweden, 4 Department of Orthopaedics, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
Keywords: person-centered care, qualitative, anterior cruciate ligament, acl, sport injury https://doi.org/10.26603/001c.126060
International Journal of Sports Physical Therapy
Vol. 19, Issue 12, 2024
Background
Person-centered care is a concept in healthcare that aims to promote the patient’s health and adapt resources and interventions based on the patient’s needs and wishes. Knowledge on what person-centered physiotherapy is for patients who rehabilitate after an anterior cruciate ligament (ACL) reconstruction, and how patients experience it within the context of sports injury rehabilitation, is lacking.
Purpose
The aim of this study was to explore how patients who were in a late rehabilitation stage (8-12 months) after ACL reconstruction experienced their rehabilitation from a person-centered perspective.
Study Design
Qualitative interview study
Methods
Fourteen patients (57% females), aged 18-57, treated with ACL reconstruction, were interviewed with semi-structured interviews 8-12 months after ACL reconstruction. Interviews were recorded, transcribed and analyzed with qualitative content analysis.
Results
One theme: all lights on me; be seen and heard, a cornerstone for patients, supported by three main categories: 1) rehabilitation: a roller coaster of physical and psychological challenges; 2) patient involvement; 3) the physiotherapist – stronger together; emerged from the collected data.
Conclusion
Patients in a late rehabilitation stage (8-12 months) after ACL reconstruction experienced that the rehabilitation process was person-centered when they felt to be the focus and were allowed to participate via open and constructive communication with the physiotherapists.
Corresponding author: Ramana Piussi,
Address: Sportrehab Sports Medicine Clinic, Stampgatan 14, SE-411 01 Gothenburg, Sweden ramana.piussi@gu.se, +46761677520
A rupture of the anterior cruciate ligament (ACL) annually affects approximately 8,000 people in Sweden.1 An ACL injury can negatively impact quality of life for several years, where common complaints include but are not limited to: persistent knee pain, the knee feeling different compared to before the ACL injury, and the adoption of a less active lifestyle.2‑4 Psychological barriers that patients can experience after ACL injury are fear of re-injury, and not trusting the knee.2 Patients who are physically and mentally prepared for an ACL reconstruction, that is, are optimistic, have greater quadriceps muscle strength, and have high knee self-efficacy have been reported with a better knee function and self-reported quality of life after ACL reconstruction.2 To enhance post-surgical outcomes it is therefore considered important that physiotherapists identify psychological factors that can be tailored to guide an individualized treatment.2
Person-centered care is a concept in healthcare that aims to promote the patient’s health and adapt resources and interventions based on the patient’s needs and wishes.5 Person-centered care is about seeing the individual behind the injury and making use of the patient’s and relatives’ knowledge and experience throughout care. A central concept in person-centered care is partnership, which aims for the care to be planned and carried out in agreement with the patient.5 Caregivers and patients create a partnership based on the patient’s story A mutual care plan is outlined with implementation strategies and follow-ups of goals.5 A collaboration between care recipient and care provider leads to the patient gaining greater influence in their rehabilitation, and has been reported to increase compliance and contribute to increased responsibility by the patient.5 This increased compliance and responsibility can in turn lead to improved perceived health, that is, the patient’s own perception of their health status as measured with patient reported outcome measures such as the short form health survey (SF-36), which can result in shorter care times.5 The implication in the field of ACL injury is that person-centered care could result in better knee-related outcomes as measured with patient reported outcome measures.
Previous qualitative studies have highlighted what patients experience as challenging during recovery after ACL reconstruction.4,6 One challenging period for patients who recover after ACL reconstruction is the period around the 12-month mark, where patients are commonly gradually discharged from rehabilitation and are supposed to resume unsupervised physical activity (for many patients, return to sport).7 The results indicate that a person-centered approach might improve mental and physical readiness to return to sports and that more and better information and communication between physiotherapist and patient with regard to realistic goal setting and expectations for rehabilitation is needed.4,6 Person-centered physiotherapy should have the characteristics of offering an individualized treatment, continuous communication, education during all aspects of treatment, and working with patient-defined goals together with a physiotherapist having social skills, being
confident, and showing specific knowledge.8 However, knowledge on what person-centered physiotherapy is for patients, and how patients experience it within the context of sports injury rehabilitation, is lacking.
Therefore, the aim of this study was to explore how patients who were in a late rehabilitation stage (8-12 months) after ACL reconstruction experienced their rehabilitation from a person-centered perspective.
The present study was conducted as a qualitative interview study Subjects were recruited from Project ACL, which is a local physiotherapy registry with the purpose to improve care and rehabilitation of patients who suffer an ACL injury Project ACL aims to improve care through regular muscle function tests as well as questionnaires at pre-defined follow-ups, with ACL injury or reconstruction as a baseline. Results from muscle function tests and questionnaires are shared with patients, treating surgeons, and physiotherapists. Project ACL has been previously described in detail.9 Ethical approval was obtained from the Swedish Ethical Review Authority (2020-02501). The experience of whether rehabilitation is person-centred can differ between every unique individual. Accordingly, the authors adopted an interpretive/constructivist epistemological approach, which is suitable for studying multiple realities, descriptions, and experiences in a population.10 An inductive approach was used, which aims to move from specific observation to broad generalizations. The Consolidated criteria for Reporting Qualitative research (COREQ)11 checklist, an extension of the Standards for Reporting Qualitative Research (SRQR) was used to report methodological information transparently
Patients aged 18-65, registered in Project ACL and who were between 8-12 months after ACL reconstruction at time of interview were eligible for inclusion. Patients registered with more than one ACL injury were excluded from the study. No exclusion criteria were applied for activity level at present time or pre-injury, associated injuries, or eventual complications during rehabilitation. From patients eligible for inclusion, a purposive sampling selection was used to select patients, ensuring representation across different age groups and sex. This approach aimed to capture the diversity typically seen in open-care physiotherapy settings, focusing on patients undergoing ACL reconstruction. Selected patients from Project ACL were contacted via email and informed about the purpose of the study, and asked whether they were interested in participating. A total of eighteen patients were contacted, of which four declined participations, and consequently, fourteen patients (Table 2) were included in the study, and fourteen interviews were scheduled. There were eight female (57%) and six male patients. Patients were aged 18-57, and for five patients, twelve months had passed from ACL reconstruction, while for nine patients, eight months had passed (Table 2).
Table 1. Interview guide
How did you sustain your ACL injury?
How was your rehabilitation after ACL reconstruction?
What did you experience as challenging during rehabilitation?
What did you experience as easy during rehabilitation?
What made you sad during rehabilitation?
What made you happy during rehabilitation?
What kind of support did you get during rehabilitation?
How often did you meet with your physiotherapist during rehabilitation?
What do you think about the amount of meetings you had with your physiotherapist?
*interviewer defines person-centered care*
How person-centered did you experience your rehabilitation?
What made your rehabilitation person-centered?
What kind of relation do you have with your physiotherapist?
What role has your physiotherapist had for you during rehabilitation?
Which characteristics of your physiotherapist did you appreciate?
Which characteristics of your physiotherapist did you not appreciate?
How did you and your physio set up goals during your rehabilitation?
What do you feel about the support you received from your physiotherapist?
Do you do any sport today?
What does your sport mean to you?
How has your ACL injury affected your life?
How do you feel in relation to your injury and recovery process today?
What would you change if you could go back in time?
In relation to person-centered care, is there anything else you would like to add?
An interview guide was created through discussion between authors RP, EB, AJ, and EHS (Table 1). Examples of openended questions included “were you involved in your rehabilitation?”; “what in your rehabilitation made it feel person-centered for you?”; “what kind of connection did/ do you have with your physiotherapist?” Before subjects received questions about person-centered care, the interviewer provided a definition of person-centered care, in order for patients to grasp the meaning of what the study aimed to understand. The provided definition of personcentered care was: “Patient-centered care is a health care process where you as a patient are involved in the process and an active part of the decision making process. The fundamental characteristics of patient-centered care are: patient involvement in care and the individualization of patient care”.12
Starting from the interview guide, eventual follow-up questions, such as “could you develop more on ” , or “what do you mean by … ” were posed when considered needed by the interviewer The interviews took place digitally via the communication platform ZOOM (ZOOM IncTM San José, California, USA). Verbal consent was recorded before commencing the interview. Data were collected during autumn 2022 by the first author (RP). The second (EB) or third author (AJ) of the study were present as a spectator. No field
notes were taken during or after the interviews and each informant was interviewed only once. No pilot interview was conducted. Interviews were recorded via the ZOOM recording function (mean length 24 minutes, range 18-35 minutes) and transcribed verbatim by the second and third authors (AJ, EB). The recorded files contained no information about the subjects and thus the data was anonymized in the analysis process.
The data were analyzed using qualitative content analysis based on Graneheim and Lundman.13,14 The authors acknowledge that researchers also play a role in the construction of the data, that is, there is no separation between researcher and the data. Since going through such a complicated process (i.e. ACL injury and rehabilitation) is a highly individual experience, the authors believe the choice of individual interviews to be justified. The first (RP), second (EB) and third (AJ) authors of the study were responsible for the analysis process, and the analysis was continuously triangulated with the senior author (EHS). Data were analyzed according to the following steps:
• Transcripts were first read thoroughly to obtain a general understanding of the collected data by all authors involved in the analysis process (RP, EB, AJ, EHS)
• Meaning units were identified, extracted and shortened to condensed meaningful units. Condensed meaning units were then abstracted in a Microsoft ExcelTM spreadsheet. This step was performed by RP, EB and AJ separately.
• Condensed meaning units were coded. This step was performed by RP, EB and AJ separately.
• Codes were grouped for similarities and differences in sub-categories. During the process of grouping codes in sub-categories transcripts were read again several times and sub-categories were validated against the transcripts, to ensure that data were not missed or erroneously included. The process of grouping codes into subcategories was performed by continuous discussions between RP, EB and AJ until consensus was reached. Up to this stage, authors made a strong effort to minimize interpretation and keep close to the text.
• Sub-categories were grouped for similarities and differences into main-categories. The process of grouping sub-categories into main categories was performed by continuous discussions between RP, EB, AJ and EHS until consensus was reached. At this stage, a minimal interpretation of the content of text was allowed.
• All authors involved in the analysis had extensive discussions to try to elaborate on the patients´ experiences of rehabilitation after ACL reconstruction from a patient-centred perspective. Interpretation of content at this stage was allowed, and finally consensus over a theme was reached.
REFLEXIVITY
Transparency and reflexivity (the process ongoing between the research data and the researchers analyzing the data) are important aspects of the qualitative research paradigm. To increase transparency, Table 3 presents an example of
codes and the grouping in sub-categories, as well as main categories. For reflexivity, we report background information concerning authors of the study: the first author (RP) is a male physiotherapist with seven years of clinical experience, and a PhD degree. The second (EB) and third (AJ) authors are female physiotherapists who have a great interest in sports medicine and who used part of the study data as a bachelor thesis. Both the second and third author have suffered an ACL injury, one treated with rehabilitation alone, and one treated with reconstruction. In terms of the other authors, one (RT) is a retired senior physiotherapist (professor) still active in the research field, while KS and TS are senior orthopedic surgeons within sports medicine and ACL reconstructions (professor and PhD degrees). Author KS has suffered two ACL injuries, both in the same knee. The senior author (EHS) is a male senior physiotherapist (associate professor) with over 10 years of clinical experience, and active within the research field. All authors except TS have been involved in Project ACL, either in the development of the project (RT; KS; EHS) or as test supervisors (RP; EB; AJ; EHS). No previous relationship between authors and subjects was present before the start of the study
One theme, supported by three main categories and eight sub-categories emerged from the collected data (Figure 1).
The rehabilitation experience of patients 8-12 months after ACL reconstruction, from a person-centered perspective, was summarized in one over-arching theme: “All lights on me – be seen and heard, a cornerstone for patients” The subjects that shared their experiences emphasized that personalized rehabilitation focused on them as individuals. They felt empowered to take part in their own recovery process, thanks to open and positive communication with their physiotherapists. The tailored rehabilitation plans aimed to restore their physical abilities contributed
Table 3. Examples of the analysis, from codes to main categories.
Main category
Rehabilitation: a roller coaster of physical and psychological challenges
Subcategory
Motivations, goals and feelings
Injury repercussions
Tailored treatment
Patient involvement
The Physiotherapist – stronger together
Factors giving satisfaction
Physiotherapist-patient alliance
Code
Tired of rehabilitation; Gave rehabilitation my everything; Having goals ahead gave motivation.
The injury affected my working ability;
Impact on social life Did not dare to use the knee.
Rehabilitation adapted to my needs; Try each exercise before implementing;
Continuous dialogue with physiotherapist
Reaching goals gives satisfaction; Regaining function gives happiness; Fun becoming strong again.
Connection with the physiotherapist; Friendly relationship with the physiotherapist;
Good cooperation with the physiotherapist.
Physiotherapist qualities Committed physiotherapist; Professional physiotherapist; Physiotherapist as a guide.
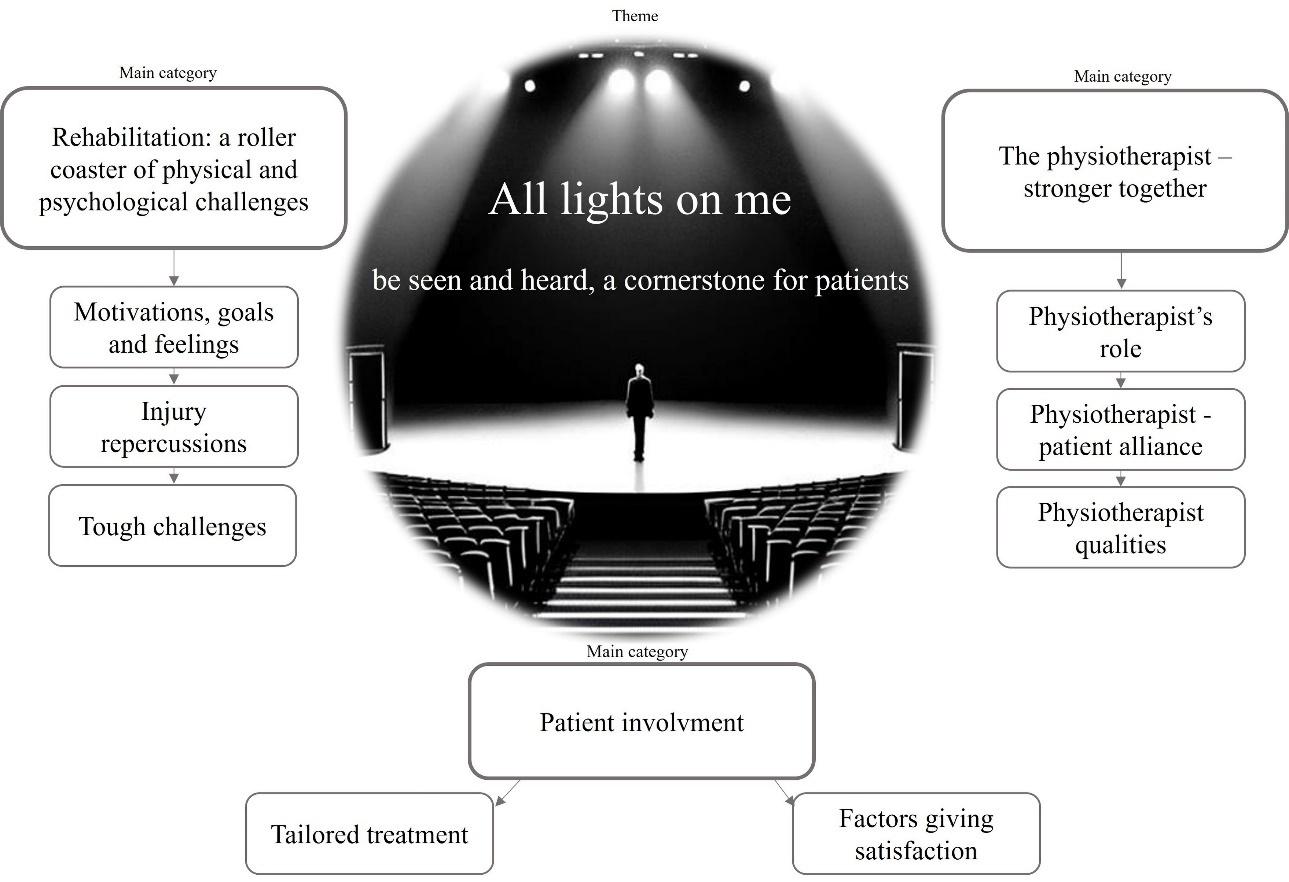
Figure 1. Study results comprising one theme, three main categories, and eight sub-categories. Image generated with https://getimg.ai/text-to-image
significantly to their sense of a personalized approach. They saw their physiotherapists as guides who provided both emotional and professional support, offered valuable information throughout their rehabilitation. Subjects highlighted the importance of a strong connection with their physiotherapists as a crucial aspect of feeling that rehabilitation was personalized. This ‘connection’ went beyond
the conventional therapeutic relationship and represented a deep human understanding and shared commitment between the subjects and their physiotherapists, which created an atmosphere of trust, open communication, and mutual support throughout the rehabilitation journey Another key factor was that subjects could actively engage in the rehabilitation journey Subjects valued the flexibility
and adaptability of the process, tailored to suit each person’s unique needs. Overall, personalized rehabilitation after ACL reconstruction was experienced with a high level of satisfaction.
The rehabilitation after ACL reconstruction was experienced by patients as a process filled with both physical and psychological challenges. One experienced challenge was not being able to participate in social activities due to knee symptoms, which consequently led patients to experience sadness and loneliness. Another challenge that was mentioned was the inability to cope with knee pain, especially early after ACL reconstruction. Some patients described that the pain reminded them that the knee was injured, which led to frustration. A feeling of frustration was also perceived in later stages of rehabilitation; however, it was described as not associated with pain, but rather with the experience that the knee was not as ‘good’ as it was before the ACL injury The experience oscillated between moments of frustration and loneliness, transforming into happiness when patients achieved milestones such as regaining knee-related physical abilities (e.g., squatting), reaching set goals, and receiving support from physiotherapists, family, or friends. Thus, this shift created a roller coaster of positive and negative feelings throughout the rehabilitation process.
A common goal for the majority of subjects was to be able to return to unlimited physical activity. To achieve goals designed together with the physiotherapist led patients to feel more motivated. Progression in rehabilitation and exercises perceived as fun to execute also contributed to give subjects more motivation. In the absence of clear goal setting or dialogue with the physiotherapist, subjects reported difficulties to find motivation. Some subjects reported that the rehabilitation was too unspecified, and that exercises and dosage were too much self-chosen. Subjects reported to sometimes experience an uncertainty about what subjects were allowed to do, restrictions regarding the knee, as well as unclear training instructions, such as the amount of training and which exercises were to be carried out, which diminished motivation towards rehabilitation. Quote 1, Table 4.
The major reported repercussions on life and rehabilitation were due to knee symptoms. Subjects reported that they felt that the knee as loose, had persistent knee pain, perceived weird feelings in the affected knee, and had to constantly move the knee in order to not perceive stiffness. Some subjects reported to feel fear of re-injury, which contributed to a limitation in that subjects did not dare to be as physically active as before their ACL injury Quote 2, Table 4
There was a variation among subjects about the feeling of loneliness: some subjects felt lonely during rehabilitation while others did not. Another feeling that emerged was an uncertainty about going to the gym to carry out rehabilitation, as the gym was by some experienced as a foreign environment which provided uncomfortable feelings. Overall, to cope with knee symptoms was mentioned as a major challenge. Quote 3, Table 4
One important factor mentioned by patients as a contributor to the experience of person-centered rehabilitation was to be involved in the rehabilitation. To be involved in rehabilitation was described as to be listened to, and foremost, the ability of the physiotherapist to adapt the rehabilitation to patients wishes, desires, and needs. To achieve preset goals led patients to feel involved in the rehabilitation process, and to be the main actor in the process.
One major action performed by physiotherapists, which led patients to perceive the rehabilitation as person-centered, was to tailor rehabilitation. Physiotherapists individually adapted rehabilitation according to subjects’ abilities and access to gyms or equipment. Several subjects reported the physiotherapists were flexible with exercises, dosage, and setting; something that made the rehabilitation experienced as fun to carry out. The fact that physiotherapists gave advice and informed patients about what was reasonable regarding rehabilitation were also appreciated contributions. Quote 4, Table 4.
To achieve goals, to become strong, to feel that the rehabilitation was moving forward, and to regain physical function were all reported by subjects to be experienced as strongly positive feelings. Patients experienced a great deal of joy and satisfaction when a goal was achieved or when they were physically able to do something that was perceived as “impossible”, e.g. hop for distance. Quote 5, Table 4
In this category, descriptions of experiences of patienttherapist interplay were summarized. Both concrete efforts that physiotherapists made, what the relationship with the physiotherapist was like, and which qualities the subjects appreciated or did not appreciate in their physiotherapist were presented. During interviews, concrete descriptions emerged from subjects about physiotherapists’ characteristics and ways of being. The physiotherapists were described as competent, educational, professional, problem-solving, and flexible by several subjects. A good relationship with the physiotherapist and a well-functioning communication
during rehabilitation were described by several subjects as a cornerstone in the physiotherapist-patient alliance. The relationship was described as professional and reasonable, and it was appreciated that subjects received professional answers to their questions.
The physiotherapist was described as a guidance, a mentor, and a support during the rehabilitation. Patients perceived the physiotherapist as somebody to follow in order to achieve the final goal with rehabilitation. Subjects experienced the rehabilitation person-centered, despite the physiotherapist having the role of a guidance to follow Quote 6, Table 4.
Several subjects expressed that their relationship with the physiotherapist evolved into a friendship. Subjects appreciated to share common interests and to engage in conversations about life beyond the scope of the ACL injury Negative aspects that were raised were that some subjects did not feel that they received enough support. Repeatedly, many subjects highlighted the pivotal and enduring role of the physiotherapist in their rehabilitation journey They emphasized that forming a strong alliance with the physiotherapist was crucial in shaping their perception of a person-centered rehabilitation experience. Quote 7, Table 4
PHYSIOTHERAPIST QUALITIES
In the description of physiotherapists qualities, subjects mainly reported positive qualities. Some qualities described were personality traits such as to be interested, engaged, reliable, reassuring and supportive. One informant who changed physiotherapists during rehabilitation experienced the first one as less competent and nonchalant. Quote 8, Table 4
The aim of this study was to explore how patients who were in a late rehabilitation stage (8-12 months) after ACL reconstruction experienced their rehabilitation from a person-centered perspective. The analysis resulted in a single theme, divided into three main categories. Overall, subjects articulated an overarching sense of person-centeredness in their experience of ACL reconstruction rehabilitation. Central to this narrative is the concept of being situated at the core of the rehabilitation process, actively engaged in its unfolding. Participants expressed a pronounced contentment with the rehabilitation post-ACL reconstruction, underscoring the pivotal role of the physiotherapist as a supportive figure throughout the recovery journey
In this main category the subjects’ experiences of the rehabilitation process were summarized. The rehabilitation after ACL reconstruction is long and it is not uncommon that the time period stretches over 12 months.15 The period between 8-12 months is important as patients approach resuming unrestricted activities and might face both mental and physical set-backs. Patients’ experiences during this period become an important piece to inform tailoring patient support strategies. Subjects reported to perceive this period like a roller coaster where some moments were experienced as positive, i.e. fun exercises to perform, while others as negative, i.e. feeling lonely due to the inability to participate in social activities. The experiences of subjects in the present study are consistent with other reported experiences of rehabilitation after ACL reconstruction. During rehabilitation patients have been reported to struggle with expectations of full recovery,4 fear of re-injury, and perceived inferior knee function.16,17 In addition, patients have been reported to have difficulty regaining both physical and mental balance.18
The rehabilitation after ACL reconstruction is a challenging period where patients go through both positive and negative loaded moments. In light of the rollercoaster-like nature of the rehabilitation process reported by subjects, clinicians working with individuals before and after ACL reconstruction should acknowledge and address the dynamic and fluctuating nature of their experiences. Recognizing that this rehabilitation journey extends over a prolonged period, often surpassing 12 months, clinicians can prepare patients for the emotional highs and lows inherent in the process. To prepare patients clinicians can stay up to date with current best evidence, provide realistic timelines, set achievable milestones, and foster open communication to manage expectations.19 Psychological support and realistic goal-setting during the 8-12 months period are important to maintain motivation and adherence to rehabilitation.20 It becomes important for healthcare professionals to accentuate the reported positive moments, such as enjoyment in engaging exercises, and concurrently, acknowledge the challenges, including feelings of isolation and frustration due to social limitations. Thus, insights provided in this study underscore the importance of tailoring support to the individual needs of patients during the extended rehabilitation period before and especially after ACL reconstruction. Using this information, clinicians can play a pivotal role to facilitate a more resilient and positive rehabilitation journey for their patients.
Subjects reported that being involved in rehabilitation was important to experience rehabilitation as person-centered. To be involved in rehabilitation was described as being listened to, and when the rehabilitation was adapted to a patient’s wishes. Even the achievement of goals made subjects experience rehabilitation as person-centered, and made subjects feel very satisfied. Physiotherapists working
Table 4. Quotes from each sub-category. Quote number within brackets.
Subcategory (quote number)
Motivations, goals and feelings during rehabilitation (1)
Injury repercussions on life and rehabilitation (2)
Tough challenges (3)
Tailored treatment (4)
Factors giving satisfaction (5)
Physiotherapist’s role (6)
Physiotherapistpatient alliance (7)
Physiotherapist qualities (8)
Quote
I noticed a difference pretty quickly. The right exercises made it easy, so it was good exercises that made the rehabilitation easier. And when rehabilitation got easy, I felt more motivated.
I was very sensitive and I had a lot of pain in my knee… And I still have pain in my knee. But it is getting better now. I have had quite a few problems with my knee after the operation. Because we have had to step back in my rehab to decrease pain. Then, we progressed again, but it did not work. And again… and it was like that, back and forth for a while.
It can hit you hard… when you cannot meet your friends who are going to the park because you cannot walk… You can feel so helpless.
We have adapted how much I train and what I do, type of exercises, to what I can do at home or what kind of equipment I have and then according to what I have access to… And then also how I, how I have started to go back to football training and how much I get to train there.
And then you have the progress… that all of a sudden I could jump sideways on one leg. If it had been before the operation, I would have collapsed like a house, right? So to jump sideways on one leg made me so happy… that I have been able to do, do things that I was not able to do for years before the surgery
I have of course done all the exercises, but he (the physiotherapist) has been the one who has been responsible for seeing the progress… and has pushed me as well. To actually challenge myself, and actually do what is required and not only the least possible. So I would say that he (the physiotherapist) has had a big role, that he has kind of pushed me to do the right things. And in the right amount.
It (the relationship with the physiotherapist) is very easy going and positive. I can ask any number of stupid questions like that, and still expect a professional answer. I have a good relationship with my physiotherapist.
I mean, he (the physiotherapist) is so interested (in me). He is very involved in…. I understand that he has a lot of patients, but he takes it very personally and seriously. It feels, sometimes it feels like I'm his only patient.
in a sport setting have reported goal-setting to be a helpful challenge, since reaching goals is believed to give patients motivation.21 Importantly, goal-setting, and goal achievement has an impact on outcomes such as muscle strength and is much appreciated by patients.22,23 There is low quality evidence with moderate effect that the goal-setting process in rehabilitation is better than no goal setting for improving health-related quality of life or self-reported emotional status.24 Consequently, the use of goal-setting within ACL reconstruction rehabilitation should be encouraged and implemented. In the 8-12 month time frame patient should be involved in sport-specific goal setting, as this is the period in which patients are supposed to transition back to sport or daily activities.
To enable participation and involvement in rehabilitation, the patient should be given relevant information about both care and treatment measures. In addition, patients need to be asked how they would want to be involved in rehabilitation. The rehabilitation needs then to be tailored based on the patient’s conditions and wishes. It is, however, highly individual how much influence a patient wants to have on his/her rehabilitation. Where some patients do have precise desires, others might want to leave all decisions up to the physiotherapist. Accordingly, it is important for physiotherapists to value patients’ own input: make patients a part of the rehabilitation and allow them to share their own beliefs and wishes towards the rehabilitation process.
Subjects reported that communication with the physiotherapist was important and allowed patients to build a relationship with the caregiver. Being clinically courageous has been described as an important characteristic needed to apply person-centered care.25 Clinically courageous means that the conversation is facilitated by the therapist through the use of open conversations, which can make it easier for the patient’s story to emerge. It is important that the therapist possesses certain qualities to tailor rehabilitation to be person-centered; technical expertise, emotional intelligence and personality, self-confidence and ability to inspire trust.25 A suggestion on how to effectively communicate with patients has been proposed.19 To effectively communicate, and to establish an environment where the patient feels cared for is one important part to increase the likelihood of positive outcomes of rehabilitation.26 Thus, it is important that there is an awareness of what qualities are required in a physiotherapist to tailor rehabilitation to be person-centered. Since good communication is a cornerstone of patient-centered care,25 it is important that physiotherapists reflect on their communication qualities, to create an awareness of their professional approach. In the 8-12 month time frame, patients begin to resume more challenging activities. Thus, maintaining a strong, communicative relationship with the physiotherapist is essential
for individualized adjustments and to address eventual concerns, such as fear of re-injury.27
To answer the research question, individual interviews were deemed to be a suitable data collection method. Qualitative content analysis was chosen, as this is suitable when it comes to providing access to each participant’s subjective experience of a certain event. Since we believe it impossible for the researcher to be completely detached from the data, the description according to Graneheim and Lundman was adopted.13,14 Accordingly, data are obtained through interactions between the researcher, the participants, and the analyzed text.
Within the description of Graneheim and Lundman13, 14 trustworthiness is a central notion. Trustworthiness is further divided into three core concepts: credibility, dependability and transferability. To establish credibility, the researchers must describe the research participants accurately, however, in a way that ensures confidentiality On the other hand, the researchers involved are described in accordance with the COREQ domains, to allow the reader to be able to assess how background information might have influenced the results. Dependability refers to the certainty of the analytical process and the stability of the data over time. To ensure dependability in this case, the interview guide was developed before the study started and not changed afterwards.
One important consideration in qualitative research if whether enough data has been collected to answer the study aim. To ensure enough data is collected, the researchers assessed whether new information (sub-categories) emerged from each interview as the analysis was performed. In the last three interviews, no new sub-categories emerged. Therefore, despite the relatively small sample (14 participants), authors believe the data was rich enough to describe patients´ experiences of person-centered care during rehabilitation after ACL reconstruction. Furthermore, a limitation is the variation in expectations regarding outcomes of late-stage rehabilitation based on age, as older patients may have different rehabilitation goals and timelines compared to younger patients. While age-related differences expectations are important, the aim was to capture the wide range of experiences that physiotherapists encounter in their daily practice. By including patients across diverse age groups, the authors sought to reflect the real-world variety in expectations and rehabilitation outcomes rather than focusing on a specific demographic. Another limitation can be the transferability of findings. Transferability refers to the potential for extrapolating the results to other groups and/or situations. Trans-
ferability is not always the aim with qualitative research and must be assessed by the reader. The current purpose was to explore how patients who were in a late rehabilitation stage after ACL reconstruction experienced their rehabilitation from a person-centred perspective, and results should be interpreted with caution.
The results highlight that patients felt most supported when actively involved in their rehabilitation, particularly through clear communication and individualized goals. Physiotherapists may consider fostering a partnership with patients by regularly discussion of progress, adaptation of exercises to suit individual needs, and to set personalized, achievable goals. While specific approaches may vary, this patient-centered strategy could help physiotherapists support patients during the challenging late-stage rehabilitation after ACL reconstruction. These practices may improve patient satisfaction and engagement, ultimately enhancing rehabilitation outcomes
Subjects in a late rehabilitation stage (8-12 months) after ACL reconstruction experienced that a rehabilitation process was person-centered when they were the focus of rehabilitation and were encouraged to participate via open and constructive communication with the physiotherapists. Physiotherapists working with patients who rehabilitate individuals after ACL reconstruction are encouraged to make patients an active part of the rehabilitation by using open and constructive communication.
Fundings for this study were received from the Research & Development Centre Gothenburg and Södra Bohuslän.
DISCLOSURE STATEMENT
Author KS is a board member for Getinge AB (publ), all other authors declare no conflicts.
Data is available from the corresponding author upon reasonable request.
Submitted: April 26, 2024 CST, Accepted: September 21, 2024 CST
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Felländer-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001-2009: incidence, treatment, and sex differences. Am J Sports Med 2012;40(8):1808-1813. doi:10.1177/0363546512449306
2. Filbay SR, Grindem H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract Res Clin Rheumatol 2019;33(1):33-47 doi:10.1016/ j.berh.2019.01.018
3. Ardern CL, Taylor NF, Feller JA, Webster KE. Fiftyfive per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014;48(21):1543-1552. doi:10.1136/ bjsports-2013-093398
4. DiSanti J, Lisee C, Erickson K, Bell D, Shingles M, Kuenze C. Perceptions of rehabilitation and return to sport among high school athletes with anterior cruciate ligament reconstruction: A qualitative research study. J Orthop Sports Phys Ther. 2018;48(12):951-959. doi:10.2519/jospt.2018.8277
5. Ekman I. Personcentrering inom hälso- och sjukvård: från filosofi till praktik. Liber; 2020.
6. Heijne A, Axelsson K, Werner S, Biguet G. Rehabilitation and recovery after anterior cruciate ligament reconstruction: patients’ experiences. Scand J Med Sci Sports 2008;18(3):325-335. doi:10.1111/ j.1600-0838.2007.00700.x
7. Lai CCH, Ardern CL, Feller JA, Webster KE. Eightythree per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med 2018;52(2):128-138. doi:10.1136/bjsports-2016-096836
8. Wijma AJ, Bletterman AN, Clark JR, et al. Patientcenteredness in physiotherapy: What does it entail? A systematic review of qualitative studies. Physiother Theory Pract 2017;33(11):825-840. doi:10.1080/ 09593985.2017.1357151
9. Hamrin Senorski E, Samuelsson K, Thomeé C, Beischer S, Karlsson J, Thomeé R. Return to kneestrenuous sport after anterior cruciate ligament reconstruction: a report from a rehabilitation outcome registry of patient characteristics. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1364-1374. doi:10.1007/s00167-016-4280-1
10. Denzin NK, Lincoln YS. The Sage Handbook of Qualitative Research. sage; 2011.
11. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int Jour Qual Health C 2007;19(6):349-357 doi:10.1093/ intqhc/mzm042
12. Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: Definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20(12):600-607. doi:10.1111/ j.1745-7599.2008.00360.x
13. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004;24(2):105-112. doi:10.1016/ j.nedt.2003.10.001
14. Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: A discussion paper. Nurse Educ Today. 2017;56:29-34. doi:10.1016/j.nedt.2017.06.002
15. Burgi CR, Peters S, Ardern CL, et al. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br J Sports Med 2019;53(18):1154-1161. doi:10.1136/ bjsports-2018-099982
16. Ivarsson A, Johnson U, Karlsson J, et al. Elite female footballers’ stories of sociocultural factors, emotions, and behaviours prior to anterior cruciate ligament injury. Int J Sport Exerc Psychol. 2019;17(6):630-646. doi:10.1080/ 1612197X.2018.1462227
17. Burland JP, Howard JS, Lepley AS, DiStefano LJ, Lepley LK, Frechette L. What are our patients really telling us? Psychological constructs associated with patient-reported outcomes after anterior cruciate ligament reconstruction. J Athl Train 2020;55(7):707-716. doi:10.4085/1062-6050-120-19
18. Karlström J, Wiklund M, Tengman E. Disrupted knee - disrupted me: a strenuous process of regaining balance in the aftermath of an anterior cruciate ligament injury. BMC Musculoskelet Disord. 2022;23(1):290. doi:10.1186/s12891-022-05252-6
19. Piussi R, Ivarsson A, Johnson U, Senorski EH. Psychological factors in sports injury rehabilitation: how can a sports rehabilitation practitioner facilitate communication? JOSPT Open 2024;2(1):1-3. doi:10.2519/josptopen.2023.0007
20. Brewer BW, Van Raalte JL, Cornelius AE, et al. Psychological factors, rehabilitation adherence, and rehabilitation outcome after anterior cruciate ligament reconstruction. Rehabil Psychol. 2000;45(1):20-37 doi:10.1037/0090-5550.45.1.20
21. Piussi R, Krupic F, Senorski C, et al. Psychological impairments after ACL injury - Do we know what we are addressing? Experiences from sports physical therapists. Scand J Med Sci Sports 2021;31(7):1508-1517. doi:10.1111/sms.13959
22. Johnson U. Short-Term Psychological Intervention: a study of long-term-injured competitive athletes. J Sport Rehabil. 2000;9(3):207-218. doi:10.1123/jsr.9.3.207
23. Johnson U, Ivarsson A, Karlsson J, Hagglund M, Walden M, Borjesson M. Rehabilitation after firsttime anterior cruciate ligament injury and reconstruction in female football players: a study of resilience factors. BMC Sports Sci Med Rehabil 2016;8(1):20. doi:10.1186/s13102-016-0046-9
24. Levack WM, Weatherall M, Hay-Smith JC, Dean SG, McPherson K, Siegert RJ. Goal setting and strategies to enhance goal pursuit in adult rehabilitation: summary of a Cochrane systematic review and meta-analysis. Eur J Phys Rehabil Med 2016;52(3):400-416.
25. Naylor J, Killingback C, Green A. What are the views of musculoskeletal physiotherapists and patients on person-centred practice? A systematic review of qualitative studies. Disabil Rehabil. Published online 2022:1-12. doi:10.1080/ 09638288.2022.2055165
26. Ekstrand J, Lundqvist D, Davison M, D’Hooghe M, Pensgaard AM. Communication quality between the medical team and the head coach/manager is associated with injury burden and player availability in elite football clubs. Br J Sports Med 2019;53(5):304-308. doi:10.1136/ bjsports-2018-099411
27. Little C, Lavender AP, Starcevich C, et al. Understanding fear after an anterior cruciate ligament injury: a qualitative thematic analysis using the common-sense model. Int J Environ Res Public Health 2023;20(4). doi:10.3390/ijerph20042920

Solie B, Carlson M,
C,
Oh, My Quad: A Clinical Commentary And Evidence-Based Framework for the Rehabilitation of Quadriceps Size and Strength after Anterior Cruciate Ligament Reconstruction. IJSPT. 2024;19(12):1600-1628. doi:10.26603/001c.126191
Braidy
Solie1 a , Mitchell Carlson2 , Christopher Doney1 , Michael
Kiely
3 , Robert LaPrade4
1 Physical Therapy, Twin Cities Orthopedics, 2 Bioengineering Lab, Twin Cities Orthopedics , 3 Sports Science, Twin Cities Orthopedics, 4 Orthopedic Surgery, Twin Cities Orthopedics
Keywords: ACL, exercise selection, hypertrophy training, muscle, physical therapy, strength training https://doi.org/10.26603/001c.126191
International Journal of Sports Physical Therapy
Vol. 19, Issue 12, 2024
Quadriceps weakness after anterior cruciate ligament reconstruction (ACLR) is a well-known phenomenon, with more persistent quadriceps weakness observed after ACLR with a bone-patellar tendon-bone or quadriceps tendon autograft than with a hamstring tendon autograft. Longstanding quadriceps weakness after ACLR has been associated with suboptimal postoperative outcomes and the progression of radiographic knee osteoarthritis, making the recovery of quadriceps size and strength a key component of ACLR rehabilitation. However, few articles have been written for the specific purpose of optimizing quadriceps size and strength after ACLR. Therefore, the purpose of this review article is to integrate the existing quadriceps muscle basic science and strength training literature into a best-evidence synthesis of exercise methodologies for restoring quadriceps size and strength after ACLR, as well as outline an evidence-informed quadriceps load-progression for recovering the knee’s capacity to manage the force-profiles associated with high-demand physical activity
Level of Evidence: 5
Anterior cruciate ligament (ACL) injuries are common within athletics,1 and ACL reconstruction (ACLR) is the preferred surgical procedure for treating knee instability after a complete ACL tear 2‑4 Regarding surgical technique, ACLR with a bone-patellar tendon-bone autograft (BPTB) may optimize ACL graft survivorship in select cohorts (e.g., athletes returning to Level-1 sports).5‑7 However, ACLR with the hamstring tendon autograft (HT) is the most popular surgical technique internationally,8,9 and the use of the quadriceps tendon autograft (QT) for ACLR is increasing in popularity 8,10
Partially due to arthrogenic muscle inhibition (AMI) from harvesting the quadriceps/patellar tendon autograft,11‑13 more persistent quadriceps weakness has been observed after ACLR with a BPTB or QT than with a HT 14‑18 Ongoing quadriceps weakness after ACLR has been associ-
ated with impaired knee biomechanics,19,20 a slower functional progression within rehabilitation,21 low return to sport rates and patient satisfaction scores,22‑27 and is correlated with the progression of radiographic knee osteoarthritis.28,29 Subsequently, recent literature has focused on improving postoperative strength outcomes,13, 30‑32 and therapeutic interventions prescribed to optimize the sensory/motor function of the surgical knee have shown efficacy for treating AMI after ACLR.12,31,32
Although the management/treatment of AMI is an important component of ACLR rehabilitation, prescribing exercise to stimulate improvements in muscle size and strength is also required to maximize performance-based outcomes, especially within cohorts returning to high-demand physical activities. Previous literature has explored the indications for various strengthening exercises and their ability to improve outcomes after ACLR,31,33‑35 but few articles have been written for the specific purpose of
Corresponding Author
ORCiD: 0000-0003-1747-327X a
Dr. Braidy Solie, DPT Training HAUS
2645 Viking Circle, Suite #200 Eagan, MN 55121
Cell Phone: (218) 289-3624
Email: BraidySolie@traininghaus.com
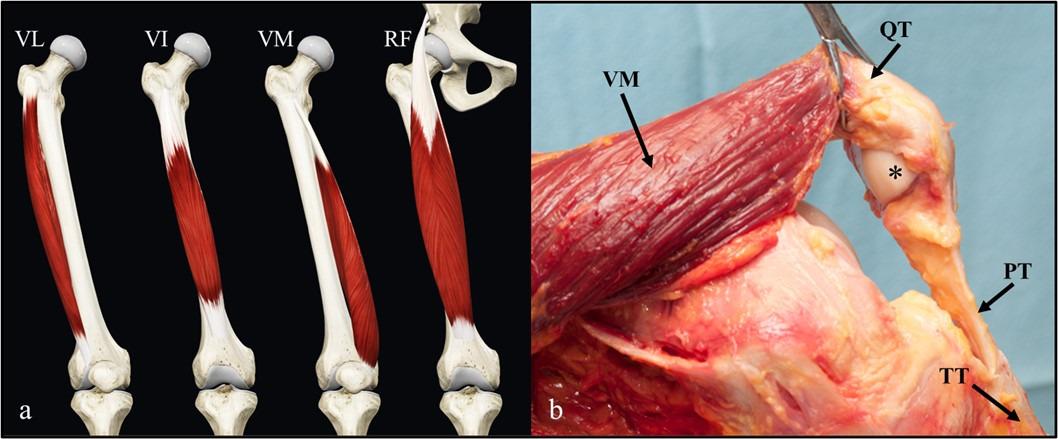
1. Quadriceps Anatomy.
optimizing quadriceps size and strength after ACLR.31 Moreover, few authors have integrated the existing muscle basic science and strength training literature into a review article.36,37 Therefore, the purpose of this commentary is to integrate the existing muscle basic science and strength training literature into a best-evidence synthesis of exercise methodologies for restoring quadriceps size and strength after ACLR.
QUADRICEPS ANATOMY
The quadriceps (i.e., quadriceps femoris) is typically divided into four muscles: (1) rectus femoris, (2) vastus lateralis, (3) vastus intermedius, and (4) vastus medialis (Figure 1a).38 All four muscles share a common insertion on the patella and tibial tuberosity (via the patellar tendon) and contribute to the primary action of knee extension (Figure 1b). Subsequently, exercises which isolate openkinetic-chain (OKC) and closed-kinetic-chain (CKC) knee extension will be highly-specific in activating/loading the quadriceps.
The rectus femoris originates on the anterior inferior iliac spine, making it the only biarticular quadriceps muscle (Figure 1a).38 It contributes to the primary action of hip flexion and knee extension and has an intramuscular tendon running longitudinally from its origin38‑40; the intramuscular tendon is utilized to store/transfer energy during the combined motion of hip flexion and knee extension (e.g., mid-swing phase of running).41,42 These anatomic features suggest optimal targeting of the rectus femoris should include exercises that isolate the combined motion of hip flexion with knee extension, such as the straight leg raise (SLR) exercise or high-velocity running/kicking,41‑43 whereas combining the primary actions of hip extension with knee extension (e.g., leg press exercise) can reduce
rectus femoris recruitment/involvement relative to the other quadriceps muscles.44,45
Motor branches from the femoral nerve produce regional innervation pathways within the anterior thigh, which facilitates selective motor unit recruitment within the quadriceps.38,46,47 For example, performing exercises at longer muscle lengths and with the primary action of knee extension can selectively activate the more distal regions of the quadriceps,47,48 whereas exercising with shorter muscle lengths and/or combining the primary action of hip flexion with knee extension may recruit the more proximal regions.46,47 Likewise, OKC tasks may recruit the more proximal regions of the quadriceps/rectus femoris, producing a proximal-to-distal sequence of muscle activity (e.g., OKC knee extensions, kicking, and the swing phase of gait),41‑43,45,49 whereas CKC tasks produce a more distalto-proximal sequence of quadriceps activation and demand less of the rectus femoris (e.g., squatting or a sagittal deceleration task).44,46,49 Altogether, the task-specific activation of the quadriceps exemplifies the need for a variety of OKC and CKC exercises to maximally stimulate quadriceps hypertrophy and strength.
ACTIVATION-THRESHOLD AND FIBERTYPE DISTRIBUTION
Compared to other muscles of the lower extremity, previous work has observed the quadriceps to possess a relatively high volitional recruitment threshold (Figure 2).50 While higher quadriceps recruitment thresholds may help produce larger knee extension torque-outputs,50 a higher baseline recruitment threshold makes volitional activation of the quadriceps a challenge after ACLR.13,51 Considering this, Boccia et al52 observed higher motor unit discharge
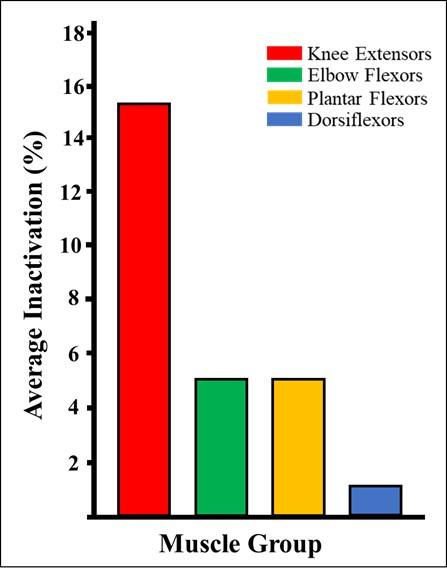
Figure 2. Average inactivation by muscle group.
Relative to other muscle groups within the human body, the knee extensors (i.e., quadriceps femoris) have the largest inactivation percentage.50 This higher inactivation percentage suggests maximal, volitional recruitment/activation of the quadriceps is a challenge at baseline (i.e., before knee injury or surgery). %, percentage.
rates and synaptic input to the vastus medialis and vastus lateralis with the use of resisted OKC knee extensions compared to the leg press exercise, suggesting OKC exercise may more specifically activate the quadriceps muscles.
The relative distribution of muscle fiber-type does not appear uniform within the quadriceps; the vastus lateralis is roughly 50% type-II muscle fiber,53 whereas the rectus femoris may be as much as 62%.54 These findings suggest the rectus femoris may experience more post-exercise fatigue and muscle damage than the vastus lateralis,55‑57 requiring more time to recover in between exercise bouts (e.g., 72-96 hours of recovery in between fatiguing exposures to high velocity running). The combination of a high volitional recruitment threshold and a relatively lower distribution of type-II fibers within the vastus lateralis may suggest a higher training frequency may be indicated for the single-joint quadriceps muscles (e.g., 48-72 hours of recovery in between exposures to resistance training on a leg press).53,58
Although a variety of training variables can be manipulated to improve muscle size and strength, exercising within a muscle’s ideal length-tension relationship may help stimulate a greater amount of mechanotransduction,59 and optimal muscle length-tension can improve the intramuscular force-output at any muscle activation level.60,61 Multiple studies have reported different muscular adaptations in response to the manipulation of exercise range-of-motion (ROM),62,63 to which superior improvements in muscular
hypertrophy have been observed with resistance training at longer muscle lengths64; this observation may be partially explained by a more optimal length-tension relationship within the muscle when resistance training is prescribed at relatively long muscle lengths.61 Considering the quadriceps consists of four separate muscles, the rehabilitation specialist should understand which hip/knee joint positions will optimize the length-tension properties within each muscle.
Previous work has outlined the sarcomere lengths of each quadriceps muscle (Figure 3).65,66 Due to its biarticular nature, the rectus femoris is the only quadriceps muscle that operates within the ascending limb of the length-tension curve (Figure 3a)65; loading the rectus femoris within higher degrees of hip flexion in combination with low levels of knee extension (e.g., OKC knee extensions between 0-40 degrees of knee flexion with the trunk positioned in 90+ degrees of hip flexion) may create a suboptimal length-tension relationship, producing active insufficiency and impaired force-output.60,61,63,65,67
At any degree of knee flexion, it appears the singlejoint quadriceps muscles have sarcomere lengths operating within the plateau to descending limb of the length-tension curve (Figure 3b-d).60 Therefore, active insufficiency considerations may only apply to the rectus femoris. Resistance training between 0-90 degrees of knee flexion may best activate/load the vastus intermedius,65 because greater regional hypertrophy has been observed within the vastus intermedius when performing the half squat exercise compared to the full squat.68 Inversely, resistance training at longer muscle lengths (i.e., 60-110+ degrees of knee flexion) may best facilitate regional hypertrophy within the distal vastus medialis and vastus lateralis by exercising within the descending limb of their length-tension curves48,65; the vastus medialis has a slightly longer sarcomere length than the vastus lateralis at 90 degrees of knee flexion (Figure 3c-d),66 suggesting resistance training within an even deeper level of knee flexion (i.e., a full squat to 140 degrees of knee flexion) may further facilitate regional hypertrophy within the distal vastus lateralis.48,68
Considering the quadriceps shares a common insertion on the patella (via the quadriceps tendon) and the tibial tuberosity (via the patellar tendon), it is important to consider the internal moment arm curve of each muscle as well as the quadriceps/patellar tendons. When analyzing each quadriceps muscle in isolation, previous literature has reported similar internal moment arm curves for all four muscles (Figure 4)69; the internal moment arm curve for the single-joint quadriceps muscles slightly increases and peaks from 0-30 degrees of knee flexion, then gradually decreases from 30-100 degrees.69 Similarly, the internal moment arm curve of the rectus femoris peaks at 20-30 degrees of knee flexion but has a slightly steeper moment arm curve (Figure 4).69,70
To best manage the graft harvest site after ACLR with the BPTB or QT autograft, the internal moment arms of the patellar and quadriceps tendons should also be con-
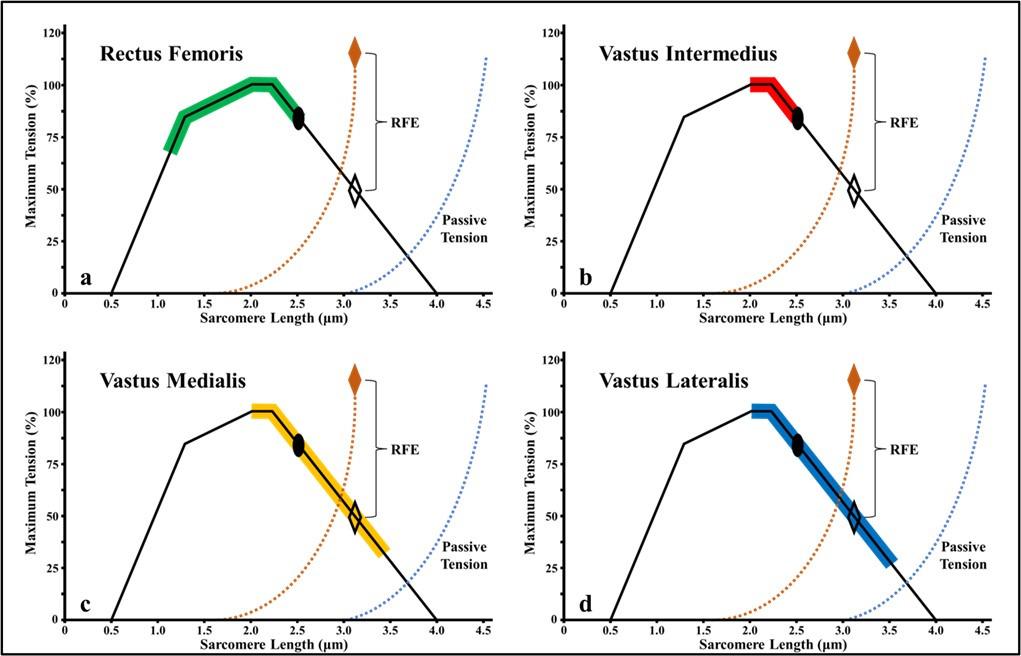
Figure 3. Length-tension properties of the quadriceps muscle group.
Previous work has outlined the sarcomere lengths of each quadriceps muscle throughout its functional operating range.65 66 The rectus femoris is the only quadriceps muscle that operates within the ascending limb of the length-tension curve. At any degree of knee flexion, the single-joint quadriceps muscles (i.e., vastus medialis, intermedius and lateralis) have sarcomere lengths that are working within the plateau to descending limb of the length-tension curve. %, percentage; μm, micrometers; RFE, residual force enhancement.
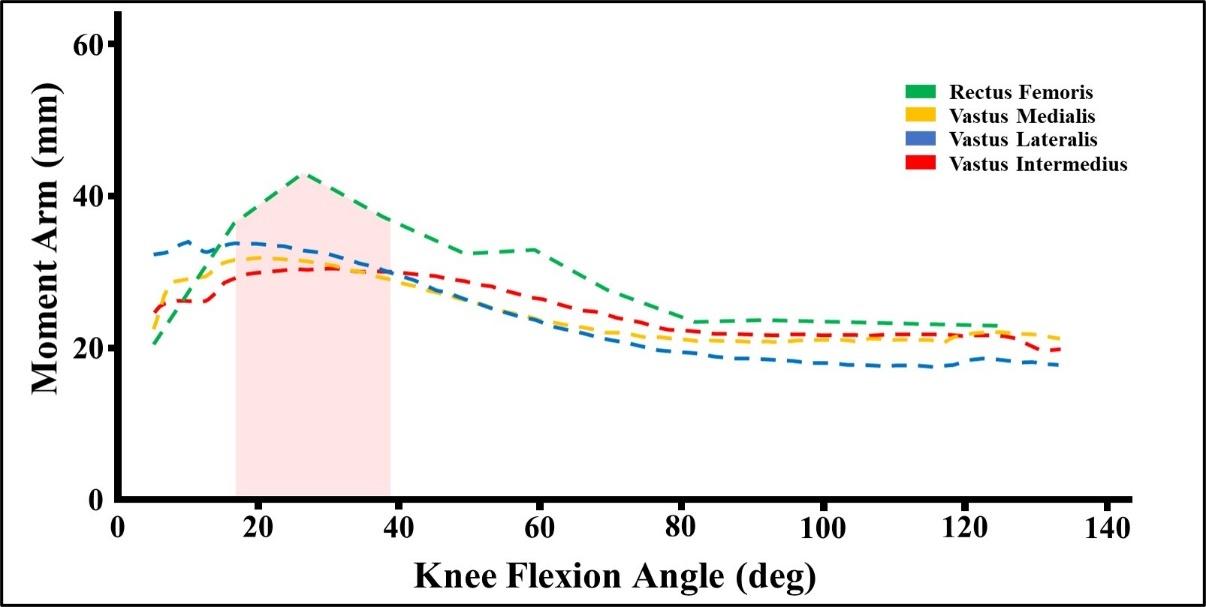
Figure 4. The internal moment arm curves of the quadriceps muscle group.
The internal moment arm curve for the single-joint quadriceps muscles slightly increases and peaks from 0-30 degrees of knee flexion, then gradually decreases from 30-100 degrees.69 Similarly, the internal moment arm curve of rectus femoris peaks between 20-30 degrees of knee flexion but has a slightly steeper moment arm curve.70 Deg, degrees; mm, millimeters; red shading, range of knee flexion associated with peak internal knee extension moment.
sidered.71 The internal moment arm of the patellar tendon rises and peaks from 0-30 degrees of knee flexion, then reduces from 30-100+ degrees.72 Therefore, exercises prescribed to preferentially load the patellar tendon may benefit from exercise prescriptions that initially emphasize low levels of knee flexion.71,73,74 The internal moment arm of the quadriceps tendon appears relatively constant between 0-25 degrees of knee flexion, with a peak moment greater than the patellar tendon at 20 degrees.75,76 As the knee moves into deeper flexion, force-transmission within the quadriceps tendon increases relative to the patellar tendon (Figure 5)74,77; this increase in quadriceps tendon force-
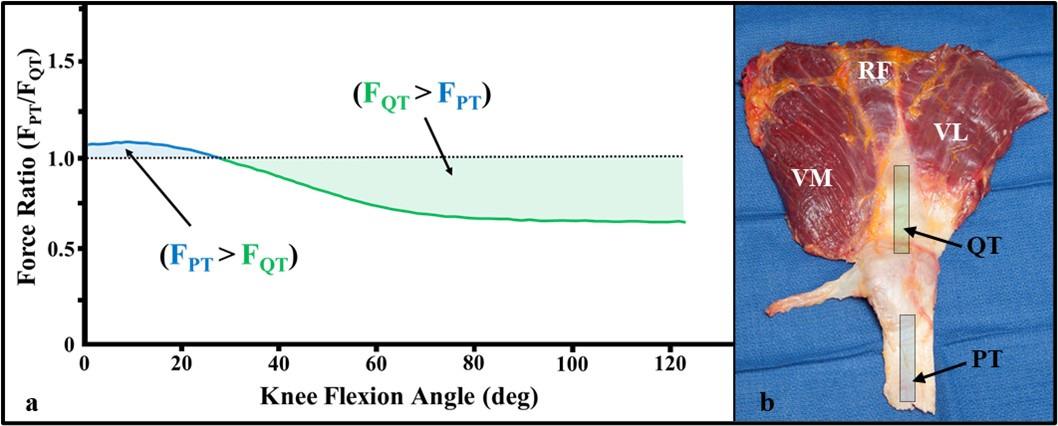
Figure 5. Force-ratio between the quadriceps and patellar tendons.
As the knee moves into deeper flexion, force transmission within the quadriceps tendon increases relative to the patellar tendon (a)74 77; this change in force-ratio is due to a decreasing quadriceps tendon internal moment relative to the patellar tendon (see Figure 6) with a concurrent increase in passive tension within the quadriceps muscle group (b). F, force; PT, patellar tendon; QT, quadriceps tendon; RF, rectus femoris; VL, vastus lateralis; VM, vastus medialis.
transmission is due to a decrease in internal moment with a concurrent increase in the amount of passive tension within the quadriceps (Figure 6).78 Subsequently, preferential loading of the quadriceps tendon relative to the patellar tendon can be achieved at deeper levels of knee flexion (i.e., 30-100+ degrees), but the rehabilitation specialist should also consider reducing the amount of knee flexion if quadriceps tendon pain is reported during exercise.71
Of the various parameters utilized to stimulate exerciseinduced adaptations within the neuromusculoskeletal system, muscle contraction mode appears highly influential.
Previous literature has observed specific neuromuscular adaptations from exposure to different contraction modes, to which the rehabilitation specialist should be able to effectively manipulate when designing rehabilitation programs. When prescribing the contraction mode, exercise prescriptions are commonly divided into isometric, eccentric and isotonic (i.e., exercises with concentric/eccentric phases) training programs.55,79‑84
Isometric training programs are traditionally implemented during the acute phase of rehabilitation.85 However, isometric resistance training is highly effective at improving muscle size and strength and can be prescribed within any rehabilitation phase.62 Studies examining the muscle’s response to isometric exercise have reported multiple types of isometric contractions86‑88; yielding/holding isometrics require the muscle to maintain a set joint position as external force is applied, whereas overcoming/pushing isometrics require the muscle to produce/transfer force into a fixed structure.88 Peripheral muscle activation and time to exhaustion may be increased with overcoming/ pushing isometrics,86,88 increasing motor recruitment relative to yielding/holding isometrics. Yielding/holding isometrics behave more like eccentric contractions,87 producing less peripheral muscle activation but a more synchronous motor plan; these observations suggest yielding/holding isometrics may require a more complex/specific mechanism of motor control and may accelerate volitional fatigue relative to overcoming/pushing isometrics.86,88 Collectively, overcoming/pushing isometrics may be best implemented when attempting to summate high volitional activation thresholds or mechanically stimulate a greater
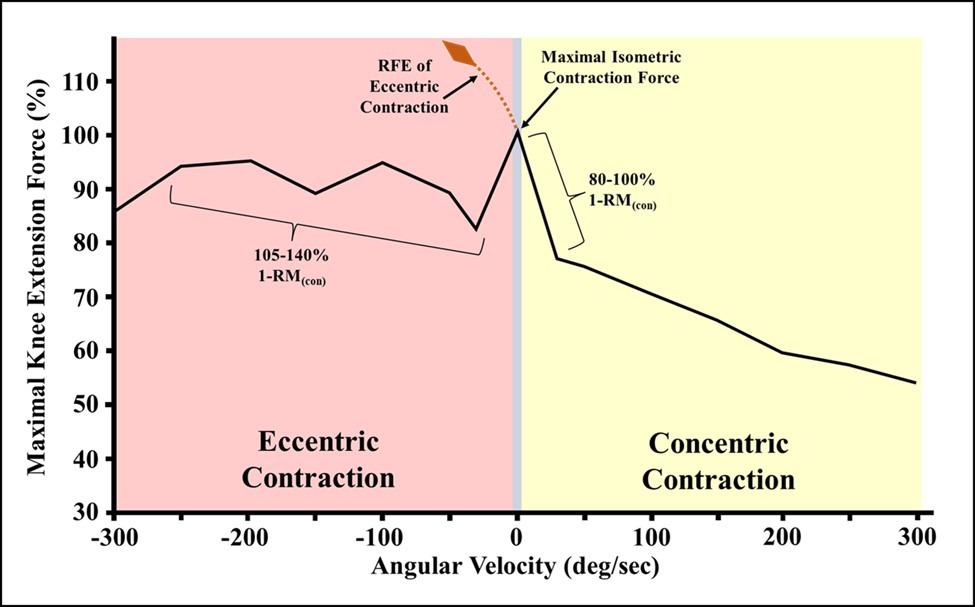
7. Depiction of the Knee Extensor ForceVelocity Relationship.
The force-velocity relationship for the quadriceps produces maximal concentric knee extension force/torque at slow contraction velocities (i.e., maximal effort pushing/overcoming isometric contractions or concentric contractions at < 60 degrees/second).93 Partially due to residual force enhancement during eccentric contractions (i.e., active muscle lengthening at maximal effort), maximal knee extension force/torque-output will be higher during eccentric than concentric contractions.94 %, percentage; 1-RM(con), 1-repitition maximum during a concentric contraction; deg, degrees; RFE, residual force enhancement; sec, second.
proportion of the recruited muscle fibers,86,88 whereas yielding/holding isometrics can be utilized to modulate tendon pain,89 manage/treat AMI and improve central motor excitability 90‑92
Partially due to residual force enhancement during eccentric contractions (Figure 7),95 the eccentric 1-repitition maximum (1-RM) for a given muscle/muscle group has
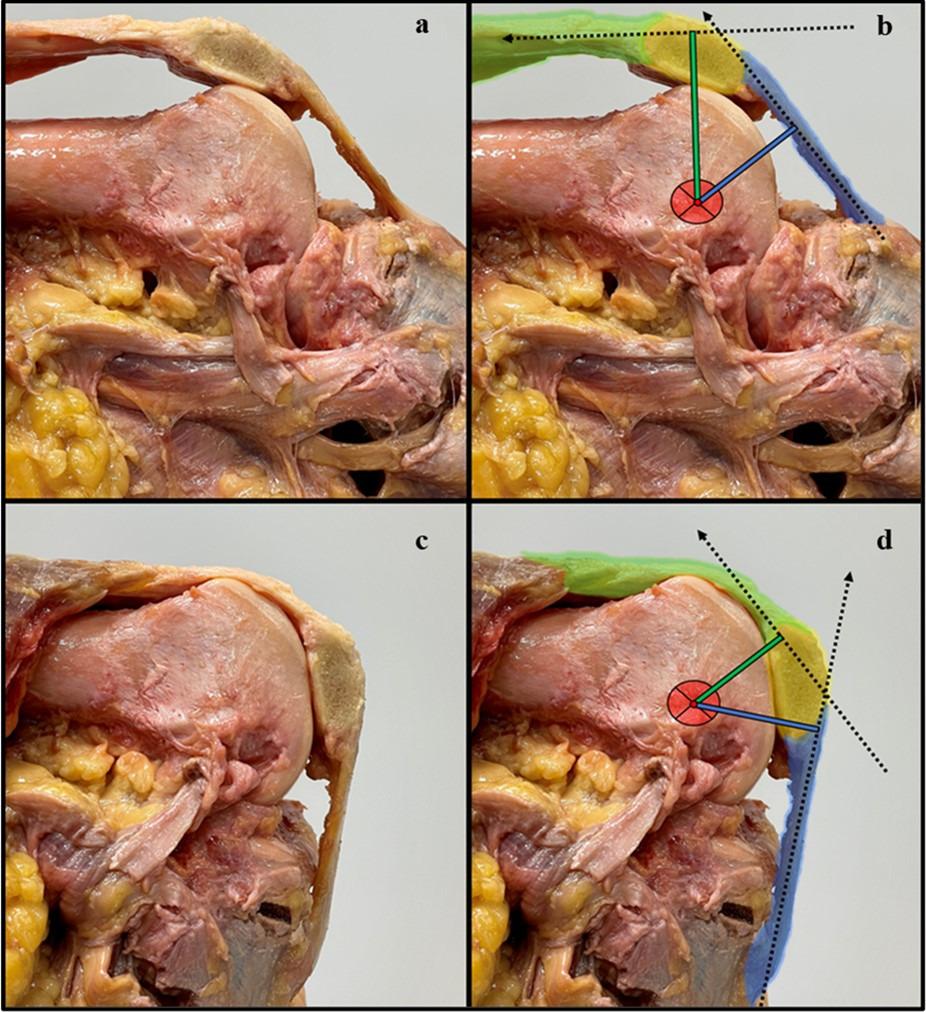
blue shading, patellar tendon; dotted black lines; resultant intratendinous
from a
quadriceps tendon internal moment arm; green shading, quadriceps tendon; red circle; estimated center of joint rotation; yellow shading, patella.
been observed to be around 41% greater than the concentric 1-RM.94 Eccentric contractions also produce less muscle activation than concentric contractions at any given force-output, making eccentric-specific exercise less metabolically demanding than isotonic/concentric exercise.96,97 Likewise, eccentric-specific training programs can enhance motor control and hypertrophy,51,90 improve strength outcomes,98 and facilitate injury-protective architectural adaptations within skeletal muscle.99,100 Therefore, any rehabilitation program designed to optimize quadriceps size and strength should gradually build the knee’s load-tolerance to a level that supports eccentric-specific training at loads greater than the concentric 1-RM.
More recently, eccentric quasi-isometric (EQI) contractions (i.e., a muscle contraction that involves maintaining a yielding/holding isometric contraction until task failure and eccentric muscle activity ensues) has been proposed as a novel stimulus for safely exposing the musculotendinous system to a large mechanical load.101,102 Eccentric quasi-isometric contractions produce similar architectural and neuromuscular adaptations as eccentric-specific contractions, but yield less post-exposure muscle soreness/fatigue.101 Theoretically, EQI resistance training should be prescribed after ACLR to stimulate favorable size, strength, and architectural adaptations within the surgical knee’s extensor mechanism, while concurrently protecting any desired postoperative structures within a predetermined ROM.
Recently, heavy-slow resistance training (HSRT) (i.e., high-load isotonic training at slow contraction velocities) has become popular for treating tendinopathy,103,104 and velocity-based training (i.e., a training method that monitors intraset muscle contraction/exercise velocity) has proven effective in eliciting desirable power/performance adaptations.105 Collectively, individuals with less resistance training experience may benefit from the use of isotonic/concentric training during the early phase of rehabilitation, when self-motivation is low, or when fatigue is high. To treat patellar/quadriceps tendinopathy at the autograft harvest site after ACLR, quadriceps HSRT should be prescribed at a load-intensity ≥ 70-100% of the concentric 1-RM,104 because this load-intensity will produce slow contraction velocities and maximize intramuscular force on the concentric side of the quadricep’s force-velocity relationship (Figure 7).93,106 Lastly, velocity-based training methods can be utilized throughout ACLR rehabilitation to optimize motor unit discharge-rates and quadriceps rate-of-force development.105,107
After ACLR, a needs analysis should be completed and modified throughout rehabilitation based on patient presentation and their objective progress.108 Information regarding the ACLR procedure (e.g., primary vs. revision ACLR); graft selection, composition, and fixation method; or any concomitant repairs/reconstructions should be considered.71 This information dictates the ACL graft ligamentization timeline,109‑112 the durability of the graft-bone tunnel con-
struct,113‑115 the amount of tissue trauma at the autograft harvest site and other areas,71,116 and the presence of quadriceps weakness related to BPTB or QT harvest from the extensor mechanism.14‑18,117 Lastly, non-modifiable risk factors for graft laxity and/or failure should be identified (e.g., knee hypermobility, allograft, hamstring autograft, meniscectomy, and high tibial slope),118‑122 because the rehabilitation specialist may elect to change/modify exercises when multiple risk factors are present (e.g., OKC quadriceps resistance training between 0-45 degrees of knee flexion produces more ACL strain than 45-100+ degrees).123,124
The quadriceps rehabilitation program should include both OKC and CKC exercise progressions,31,125 which should be prescribed in line with best-evidence recommendations for hypertrophy and strength training (Figure 8).126 Likewise, exercise prescriptions should consider the procedure specific ACLR technique, biological healing, joint homeostasis and patient preference.71 The sweep test and pain-monitoring model should be used throughout rehabilitation to objectively quantify knee irritability (Figure 8).71, 127 Lastly, ACLR rehabilitation should include best-practice strategies for managing AMI,32 and mitigating AMI after ACLR may improve the effectiveness of the quadriceps load-progressions.13,31,51,128
POSTOPERATIVE PHASE (WEEKS 0-3 AFTER ACLR)
The immediate postoperative exercise selection should restore active knee extension as soon as possible (Figure 8),129 because the slightest postoperative loss of knee extension can produce impaired knee arthrokinematics; provoke quadriceps inhibition130,131; and may increase the risk of developing knee osteoarthritis.129,132,133 Given the presence of AMI after ACLR and the high volitional recruitment threshold of the quadriceps (Figure 2),13,50 an OKC quadriceps training program may be more beneficial than a CKC program during the immediate postoperative phase.52 Lastly, high daily exercise-frequencies should be prescribed (Appendix A); high frequency/short duration exercise may work best when pain levels are high, knee motion is limited,134 exercise intensity is low,135 and neuroplastic improvements in quadriceps activation are desired (Appendix A).136
The OKC quadriceps load-progression should start with quadriceps setting (Figure 8) (Appendix A)71; quadriceps setting in low levels of hip flexion (i.e., a recumbent trunk position) may optimize length-tension of the rectus femoris.63 Likewise, positioning the knee in 20-45 degrees of flexion may be preferred when high levels of AMI are present (Figure 9A) (see Video, Supplemental Material 1, which demonstrates quadriceps setting), because this position will improve quadriceps length-tension and its internal moment arm(s).69,70,137 Prescribing yielding/holding quadriceps isometrics for longer durations (i.e., 45-90+ seconds) may be an effective strategy for improving motor re-
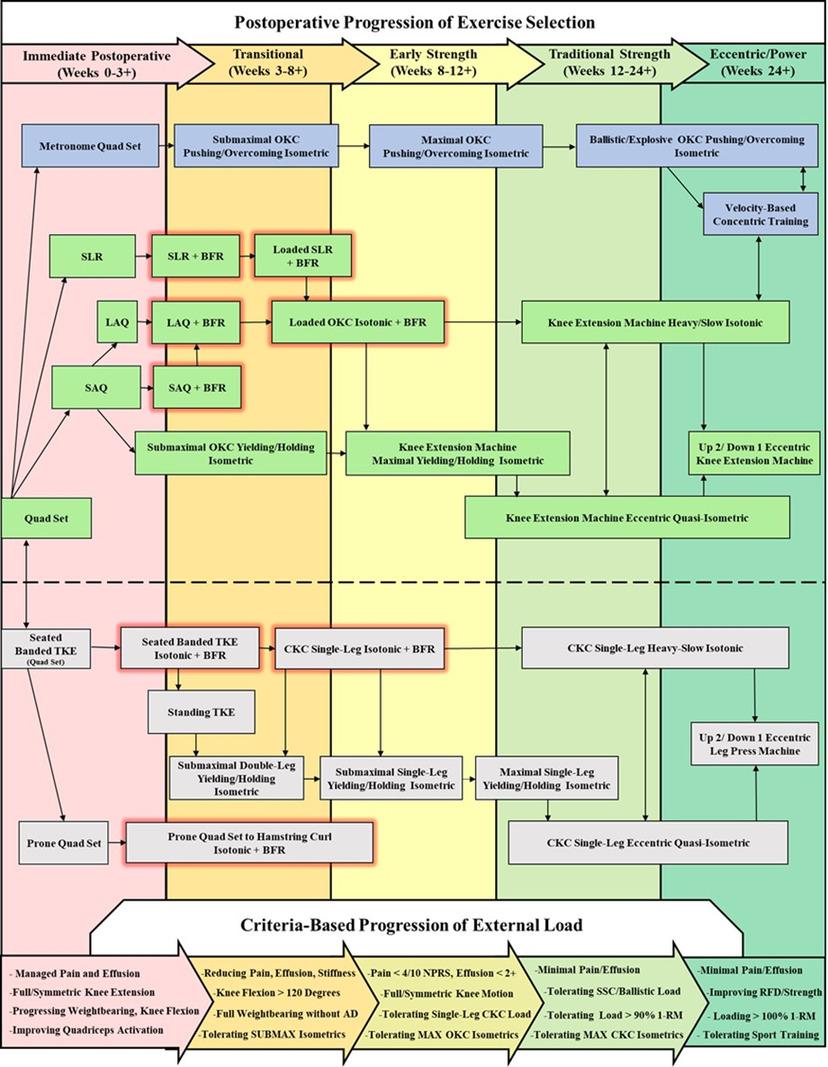
Figure 8. Overview of exercise selection for quadriceps training after anterior cruciate ligament reconstruction (ACLR).
After anterior cruciate ligament reconstruction, quadriceps training should begin with quadriceps setting and be developed onto both open and closed-kinetic-chain load progressions. Strength training load progressions should be primarily advanced through the progression of external load, and exercises that load the quadriceps close to volitional fatigue/task failure at relatively long muscle lengths should be prescribed to enhance muscular hypertrophy Lastly, a specific load progression to enhance quadriceps rate-of-force development should be prescribed throughout rehabilitation.
1-RM, concentric one-repetition maximum of the surgical limb; AD, assistive device; BFR, blood flow restriction; quad set, quadriceps setting exercise; black arrows, exercise progression pathway; blue boxes, exercise progression for quadriceps rate-of-force development; boxes with red glow, exercise with blood flow restriction; CKC, closed-kinetic-chain; green boxes, open-kinetic-chain exercise selection; grey boxes, closed-kinetic-chain exercise selection; LAQ, long-arc-quad exercise; MAX, maximal; NPRS, numeric pain rating scale; OKC, open-kinetic-chain; RFD, rate-of-force development; SAQ, short-arc-quad exercise; SCC, stretch-shortening cycle; SLR, straight leg raise exercise; SUBMAX, submaximal; TKE, terminal knee extension.
cruitment,86,88,138 and the superimposition of neuromuscular electrostimulation (NMES) during exercise may accelerate the recovery of quadriceps force-output (Appendix A) (see Video, Supplemental Material 2, which demonstrates quadriceps setting with NMES).139 The rehabilitation specialist should also consider advancing the tempo/ cadence of quadriceps setting (Appendix A), because higher-velocity quadriceps contractions (i.e., velocitybased training principles) may improve motor recruitment.107 A metronome can be used to advance the tempo/ cadence of quadriceps setting, and metronome training should be progressed onto higher cadence drills that challenge the capacity to quickly summate/regulate motor activity (Figure 8) (Appendix A) (see Video, Supplemental Material 3, which demonstrates high tempo quadriceps setting with a metronome).136,140,141
Once a volitional quadriceps contraction is achieved, exercise selection should include the SLR exercise (Figure 8) (Appendix A). To minimize knee flexion lag, cueing should reinforce the initiation of quadriceps setting into maximal superior patellar glide prior to the initiation of the SLR (see Video, Supplemental Material 4, which demonstrates proper straight leg raise technique); slight femoral external rotation with ankle dorsiflexion should be maintained throughout the SLR (Figure 9b), because this positioning can maximize force output from the quadriceps.142 The SLR exercise should start in tall sitting/standing and be progressed into the long-sitting position. Long-duration SLR isometrics and/or blood flow restriction (BFR) can be utilized to accelerate muscular fatigue,138,143‑145 and exercise intensity can be advance by adding external load distal to the knee joint (Figure 8).
Quadriceps setting can be progressed onto OKC knee extensions as soon as tolerated (Figure 8).146,147 The rehabilitation specialist may elect to first perform knee extensions between 0-45 degrees (see Video, Supplemental Material 5, which demonstrates the short-arc-quad exercise), because external knee moments are highest within this range.148 As knee flexion improves, full-arc knee extensions may best mechanically-stimulate the distal muscle fibers of the quadriceps and should be preferred to partial ROM exercise at shorter muscle lengths.41‑43,45,47‑49,61,149 Exercise with BFR can be utilized to accelerate muscular fatigue, and prescribing sets close to volitional fatigue/task failure may best stimulate muscular hypertrophy with low loads (Figure 8) (Appendix A).71,150,151 Lastly, submaximal OKC yielding/holding isometrics can be prescribed between 45-60 degrees of knee flexion to improve quadriceps activation and knee load-tolerance (Appendix A) (see Video, Supplemental Material 6, which demonstrates a submaximal OKC yielding/holding isometric)88; this ROM will preferentially target the quadriceps within the descending phase of the length-tension curve (Figure 3),65,66,137 improve the quadriceps’ internal moment arms relative to deeper knee flexion (Figure 4),69,70 optimize knee extension torque-output,137 decrease ACL graft strain relative to 0-45 degrees of knee flexion,123,152 and may downregulate patellar/quadriceps tendon pain after autograft harvest from the extensor mechanism.89
The CKC quadriceps load-progression should begin in sitting with the terminal knee extension (TKE) exercise (Figure 8) (Figure 9c-d),71 which should be utilized to preferentially activate the single-joint quadriceps muscles.44‑46,49 The sitting TKE exercise can be progressed by increasing the level of elastic band resistance (Appendix A),71 prescribing longer-duration yielding/holding isometrics,138 or the addition of BFR (Figure 8).143‑145 The rehabilitation specialist should also prescribe prone quadriceps setting (Appendix A), because this exercise omits visual feedback and may facilitate improvements in knee proprioception (see Video, Supplemental Material 7, which demonstrates prone quadriceps setting).136
As active knee ROM and volitional quadriceps activation have been recovered, the rehabilitation specialist should transition their quadriceps exercise prescription(s) from volume and variety-based load-progressions,135 onto more seminal load progressions that can be advanced throughout the remainder of the ACLR rehabilitation program.153 During this phase, joint irritability and a knee effusion are likely still present,35 and low-load exercise with BFR is indicated to recover joint homeostasis while mitigating atrophy/stimulating hypertrophy (Appendix A).71,154
Non-weightbearing quadriceps exercise with BFR should be prescribed 1-2x/day to maximize the anabolic response to exercise with very light loads (i.e., < 20% concentric 1-RM),155,156 and the use of higher individualized occlusion pressures may be recommended.157‑159 To specifically stimulate quadriceps hypertrophy, each BFR set (when possible) should be prescribed close to volitional fatigue/task failure (e.g., 0-2 repetitions in reserve) (Appendix A),126, 150,151 and combining OKC knee extension variations with the CKC seated TKE exercise may optimally stimulate all four quadriceps muscles in sitting (i.e., both the proximal and distal quadriceps) (Appendix A) (Figure 8) (see Video, Supplemental Material 8 and 9, which demonstrates the long-arc-quad and seated TKE exercise with BFR).45 The rehabilitation specialist should also consider prescribing the prone quad set to hamstring curl exercise (Figure 8); this exercise may improve mechanical signaling/regional hypertrophy within the distal quadriceps through the maximal lengthening of its sarcomeres (see Video, Supplemental Material 10, which demonstrates the prone quad set to hamstring curl exercise with BFR).48,65 Similarly, prescribing loaded inter-set stretching with the prone knee flexion stretch or reverse Nordic exercise can be utilized to therapeutically shear/mobilize the graft harvest site after ACLR with the QT autograft and can help stimulate stretch-mediated quadriceps hypertrophy/sarcomerogenesis (see Video, Supplemental Material 11 and 12, which demonstrates the prone knee flexion stretch and reverse Nordic exercise).71, 160,161
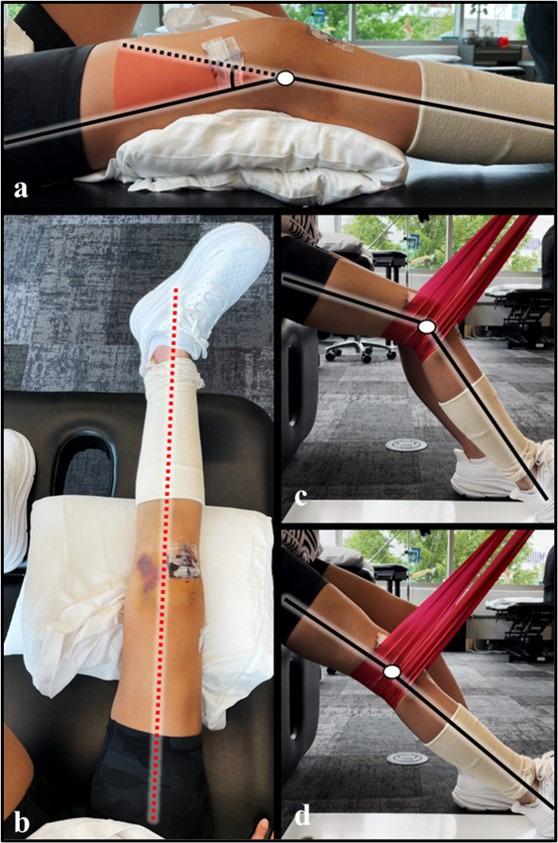
Figure 9. Exercise selection for the immediate postoperative phase.
Positioning the knee in 20-45 degrees of knee flexion prior to quadriceps setting will improve global quadriceps length-tension and its internal moment arm(s) (a). Slight femoral external rotation with active ankle dorsiflexion should be maintained throughout the straight leg raise exercise, as this position may maximize force output from the quadriceps (b). The CKC quadriceps load-progression should be initiated in sitting with the terminal knee extension exercise (i.e., isotonic, terminal knee extension with elastic band resistance); this exercise can be utilized to preferentially activate the distal / single-joint quadriceps muscles (c, d). Black lines, approximate tibial and femoral bone markers; dotted red line, midline/neutral hip rotation within the surgical limb; red shading, depiction of a knee flexion angle of 20-45 degrees; white circle; estimated center of joint rotation.
To enhance motor unit recruitment and/or manage tendon pain after ACLR with the BPTB or QT autograft, the OKC quadriceps load-progression should be advanced from yielding/holding quadriceps isometrics at 45-60 degrees of knee flexion, onto overcoming/pushing isometrics between 60-90 degrees of knee flexion (Appendix A) (Figure 8); overcoming/pushing isometrics will summate more motor activity than yielding/holding isometrics.88 Likewise, pro-
gressing the level of knee flexion during OKC overcoming/ pushing isometrics may help facilitate regional hypertrophy within the distal quadriceps,48,61,65,66 and the superimposition of NMES may improve quadriceps torque-output (see Video, Supplemental Material 13, which demonstrates an OKC overcoming/pushing isometric with NMES).139,162,163
CLOSED-KINETIC-CHAIN LOAD-PROGRESSION
Seated TKE contractions should be advanced onto the standing TKE exercise (Figure 8) (see Video, Supplemental Material 14, which demonstrates the standing TKE exercise)71; this exercise should be prescribed to recover TKE control in weightbearing and can be progressed through the addition of elastic band resistance (Appendix A). Due to the relatively large increase in the knee’s articular load when transitioning from non-weightbearing to weightbearing exercises,164,165 consideration should be given for the use of yielding/holding isometrics as the initial form of CKC resistance training; yielding/holding isometrics behave like eccentric contractions and stimulate muscle fatigue faster than overcoming/pushing isometrics.86‑88
The double-leg squat exercise can serve as the base regression for a CKC yielding/holding isometric program (Figure 8),71 and the non-surgical limb should be slightly posted to facilitate weight redistribution towards the surgical limb (Figure 10a).71,166 Prescribing submaximal yielding/holding isometrics from 45-60 degrees of knee flexion may be initially recommended, because this level of knee flexion will optimize knee extension torque-output and the internal moment arms of the quadriceps muscles (Figure 4) (Appendix A).69,70,137 Each exposure should include 3-6 sets of long-duration yielding/holding isometric contractions (e.g., submaximal contractions for 45-90 seconds), which are prescribed to improve motor unit recruitment86, 88,138; stimulate exercise-induced muscle fatigue138; facilitate stress relaxation of the quadriceps and patellar tendons167,168; and downregulate anterior knee/tendon pain.89 After ACLR with a BPTB or QT, CKC yielding/holding isometrics should be implemented at a frequency of 2 exposures/day (6-8+ hours apart) to optimally stimulate collagen synthesis/repair at the autograft harvest site (Appendix A).71,168,169 Double-leg yielding/holding isometrics should be progressed onto the split-squat position (Figure 10a-b),71 because this progression may mitigate the bilateral force deficit phenomenon as well as other inter-limb compensations.170,171 Lastly, the front-foot elevated splitsquat can be used to advance the level of knee flexion from the 45–60-degrees onto 60-90 degrees (see Video, Supplemental Material 15, which demonstrates the front-foot elevated split squat exercise).
Weeks 8-12 after ACLR, rehabilitation should focus on facilitating the resolution of any knee effusion/joint irritability while progressively loading the quadriceps.35,71 The rehabilitation specialist should consider increasing the level of knee flexion during resistance training before adding external load, because deeper flexion may optimize quadriceps hypertrophy (Figure 10d).48,61,149 However, knee flexion angle does effect the intratendinous force-ratio between the patellar and quadriceps tendons, making frequent monitoring of the autograft harvest site an important component of rehabilitation after ACLR with the BPTB or QT (Figure 5a).71
The OKC quadriceps load-progression should include resistance training between 45-100+ degrees of knee flexion (unless contraindicated by a concomitant procedure), because autograft harvest from the extensor mechanism appears to produce greater quadriceps weakness at deeper knee flexion angles (Figure 8).71,172‑174 Likewise, 45-100+ degrees of knee flexion produces low ACL graft strain (relative to 0-45 degrees) and provides a better length-tension position for facilitating regional hypertrophy within the distal quadriceps.61,123,149 Isometric and/or HSRT should be the preferred contraction mode for loading the quadriceps (especially after ACLR with the BPTB or QT) because the provocation of anterior knee pain with resistance training is still a concern.83,89,91,103,104 Submaximal yielding/ holding quadriceps isometrics should be advanced onto maximal effort isometric strength training through the addition of external load,126 and holding isometric contractions close to the point of volitional fatigue/failure may best-stimulate quadriceps hypertrophy 126 Once maximal OKC yielding/holding isometrics can only be sustained for 20-45 seconds in duration,138 resistance training with EQI contractions can be prescribed (Figure 8) (Figure 11).
EQI resistance training should be prescribed on a knee extension machine (Figure 11d-f) (see Video, Supplemental Material 16, which demonstrates an EQI contraction on a knee extension machine). It is advisable to begin EQI contractions between 45-70 degrees of knee flexion before progressing onto deeper flexion angles (Appendix A), because EQI contractions in deeper flexion (i.e., 70-120+ degrees of knee flexion) could theoretically trigger knee irritability if not progressed appropriately 101,102 This recommendation is based on the fact: (1) the internal moment arm of the quadriceps is reducing from 45-100+ degrees of knee flexion (Figure 4); (2) passive quadriceps tension will increase as knee flexion increases78; and (3) eccentric contractions will increase total force within the extensor mechanism (Figure 7).
The CKC load-progression should include unilateral exercises that optimize lower extremity stability, because high exercise stability can improve volitional quadriceps activation/force-output.175 Therefore, resistance training machines (e.g., leg press) or other weightbearing exercises with high stability are preferred to free-weight or compound exercises without external support/stability (Figure 10c-d). Similarly, a decline wedge/heel lift can be used to increase the relative contribution of the quadriceps during CKC exercise (Figure 10c).176,177 Submaximal to maximal CKC yielding/holding isometrics in 45-90+ degrees of knee flexion should be prescribed close to volitional fatigue/failure within 20-45 seconds (Appendix A), and task failure should be achieved more quickly as knee flexion/knee moment is increased.138 Once maximal effort CKC yielding/ holding isometrics are tolerated for 20-45 seconds in deeper knee flexion (Figure 10d), the addition of external load to the CKC quadriceps load-progression is indicated.
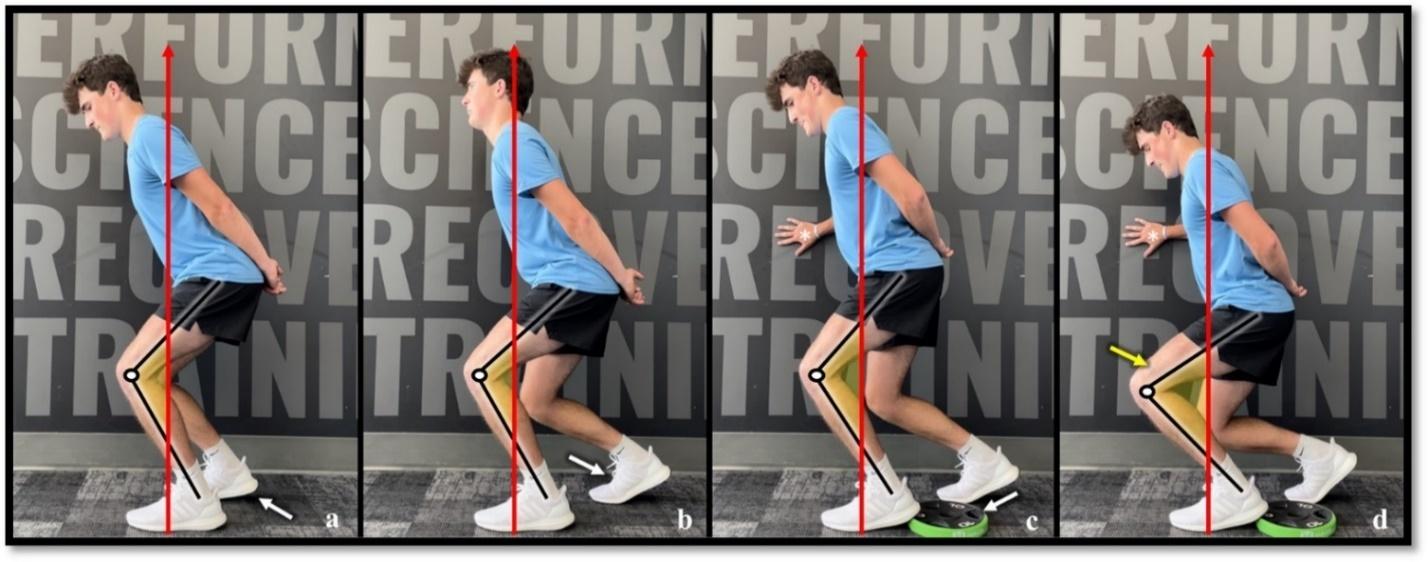
Figure 10. Closed-Kinetic-Chain Yielding/Holding Isometric Load-Progression.
The closed-kinetic-chain (CKC) yielding/holding isometric load progression should start with the double-leg squat exercise in low levels of knee flexion (a, non-surgical limb posted). Exercise selection can be advanced to include the split-squat exercise (b), and a heel wedge can be utilized to increase external knee flexion moment/load on the quadriceps (c). Submaximal yielding/holding isometric contractions should be advanced onto maximal effort contractions through increasing the degree of knee flexion/external knee flexion moment (d) or the progression of external load. Maximal effort CKC machine or weightbearing exercises with upper body stabilization (c, d) are preferred to free-weight or compound exercises prescribed without external support. Asterisk, use of wall support to stabilize the body during exercise (c, d); black lines, approximate tibial and femoral bone markers; red arrows; approximate ground reaction force-vector; white arrows, progression of knee/quadriceps load through the advancement of exercise position (a-c); white circle; estimated center of joint rotation; yellow arrow, progression of knee/quadriceps load by advancing the degree of knee flexion/external knee flexion moment (d); yellow shading; depiction of knee/ quadriceps-dominant loading with increasing external knee flexion moment (a-d).

Figure 11. Open and closed-kinetic-chain eccentric quasi-isometric quadriceps contractions.
Eccentric quasi-isometric (EQI) quadriceps resistance training can be completed on a leg press with a decline ankle-wedge (a-c) or knee extension machine (d-f) by (1) performing a concentric contraction to externally load the surgical knee/limb (a, d), (2) performing a yielding/holding isometric contraction to the point of volitional fatigue/failure (b, e), and (3) continuing to maximally resist the ensuing eccentric contraction throughout the prescribed range of knee motion. Black arrows, contraction direction; black lines, approximate tibial and femoral bone markers; green shading, concentric contractions; red shading, ensuing eccentric contractions as part of the EQI contraction; white asterisk, heel wedge; white circle, estimated center of joint rotation; yellow shading, depiction of large external knee flexion moment during yielding/holding isometric contractions
STRENGTHENING PHASE (WEEKS 12-24 AFTER ACLR)
Under normal healing conditions, most ACL grafts have integrated by 12-weeks after ACLR,178,179 and any autograft harvest-site within the extensor mechanism has remodeled with scar-like tendon tissue180; this objective increase in load-tolerance permits the full transition to maximal effort quadriceps loading.181 Subsequently, rest and recovery are important during this phase, and training schedules may need to be modified based on muscular soreness and/or the presence of fatigue. Lastly, exercise-intensity should be progressed with frequent monitoring of the knee for soreness/tissue irritability,127,182,183 and loading should be prescribed with graft/procedure-specific considerations in mind.71
For reasons previously mentioned, OKC resistance training between 45-100+ degrees of knee flexion should be continued during this phase.61,65,123,148,149,160,184 Eccentric quasi-isometric contractions on a knee extension machine can be prescribed to isometric failure within 20-45 seconds (Figure 11d-f),101,102,138 and more formal HSRT can be prescribed close to volitional fatigue/failure with an external load > 70-80% of the concentric 1-RM (Figure 8) (see Video, Supplemental Material 17, which demonstrates heavy-slow resistance exercise on a knee extension machine)104; these load-intensities will produce maximal effort concentric contractions at slow velocities (i.e., < 60 degrees/second), optimizing intramuscular force/mechanical tension within the quadriceps (Figure 7).
Single-leg CKC exercises with large external knee flexion moments should be prescribed during this phase (Figure 11b), because unilateral exercises may improve volitional motor unit recruitment/force-output relative to the use of bilateral exercises.170,185,186 To target the quadriceps more specifically, a decline wedge/heel lift should be used to increase knee flexion moment during CKC exercise,176,177 and maximal yielding/holding isometrics can be advanced by increasing the level of knee flexion44,149,160; this progression should be monitored because increasing knee flexion can provoke knee symptoms by increasing compression/ shear-forces within the quadriceps/extensor mechanism (Figure 4) (Figure 6d).69,70 As load-tolerance improves, surgical limb EQI contractions can be prescribed by holding a maximal yielding/holding isometric for 20-45 seconds and continuing to resist the ensuing eccentric contraction from 60-90+ degrees of knee flexion (Figure 11a-c) (see Video, Supplemental Material 18, which demonstrates surgical limb EQI contractions on a leg press).187 Likewise, HSRT can be prescribed between 45-120+ degrees of knee flexion with no more than 4-6 achievable repetitions per set (Figure 8) (Appendix A) (see Video, Supplemental Material 19, which demonstrates surgical limb HSRT on a leg press).104, 187
ECCENTRIC STRENGTHENING/POWER PHASE (WEEKS 24+ AFTER ACLR)
As the quadriceps develops the capacity to perform highload resistance training (i.e., >85% of the concentric 1-RM), the quadriceps load-progression should be advanced onto exercises with force-profiles similar to high-level functional tasks. For athletes returning to Level-1 sports, these loadprogressions should consider the forces associated with cutting/pivoting, to which peak patellofemoral forces have been reported to be as high as 13-18 times bodyweight.188 Considering this, previous studies have investigated the force-profiles associated with different exercise interventions165; a full squat (to 120 degrees of knee flexion) with a load-intensity of ≥85% of the concentric 1-RM produces a patellofemoral force-profile similar to cutting/pivoting,165, 189 but a maximal OKC overcoming/pushing knee extension isometric (at 90 degrees of knee flexion) may only produce a peak patellofemoral force of 7-8 times body weight.190 Collectively, these observations suggest CKC quadriceps resistance training should be progressed into 120+ degrees of knee flexion to best-replicate the force profiles associated with cutting/pivoting165,188,189; but to achieve a similar force-profile, submaximal depth CKC and OKC quadriceps resistance training should be progressed onto eccentricspecific training at a load-intensity > 100% of the concentric 1-RM.190
Due to the load-intensity for eccentric-specific training being greater than the concentric 1-RM, the surgical and nonsurgical limb should complete the concentric phase of each repetition, with the subsequent transition to the isolated use of the surgical limb during the eccentric phase (i.e., double-limb concentric, single-limb eccentric training) (Figure 12). Eccentric-specific CKC exercises should be prescribed between 0-110+ degrees of knee flexion and between 45-100+ degrees of knee flexion during OKC exercises (Figure 12) (see Video, Supplemental Material 20 and 21, which demonstrates the technique for both OKC and CKC eccentric-specific training).61,65,123,148,149,160,190 Eccentric-specific training should be integrated with progressive deceleration/change-of-direction tasks, because these tasks require the quadriceps to perform high-velocity eccentric contractions into large external knee flexion moments.44,46,49,71,188
The rehabilitation specialist should implement load-progressions with the specific intent of improving quadriceps rate-of-force development/knee power.191 Higher level evidence has observed longstanding impairments in quadriceps rate-of-force development after ACLR, and the use of a BPTB or QT autograft for ACLR may exacerbate these impairments.192 Velocity-based training can be utilized to improve quadriceps rate-of-force development,105 and the integration of these exercises with ballistic/plyometric exercise may enhance change-of-direction performance,193

Figure 12. Preferred exercise technique for eccentric-specific resistance training.
Eccentric-specific open and closed-kinetic-chain quadriceps resistance training should be progressed onto load-intensities > 100% of the surgical limb s concentric 1-repitition maximum. Eccentric-specific quadriceps training can be completed on a leg press with a decline ankle-wedge (a-d) or knee extension machine (e-h) by (1) performing a concentric contraction with both limbs from the machine’s bottom position (a, e) to the top position (b, f), (2) removing/moving the non-surgical limb to place all load on the surgical limb (c, g), and (3) eccentrically lowering the load through the desired range of knee motion. Green shading, concentric phase of exercise; red shading, eccentric phase of exercise; white asterisk, heel wedge; yellow asterisk; movement of the non-surgical limb throughout exercise.
improve knee biomechanics/motor control,194,195 and can mitigate the overall risk of ACL re-injury 196
Velocity-based quadriceps training may be most specifically prescribed utilizing a jump training machine and/or barbell equipped with a linear positioning transducer/accelerometer (Figure 13) (see Video, Supplemental Material 22 and 23, which demonstrate single and double-leg velocity-based training).197,198 To best stimulate improvements in peak quadriceps contraction-velocity/knee power, emphasis should be placed on the importance of a maximal effort/intent on each repetition, and working sets should be discontinued at a 10% velocity-loss threshold.198 Lastly, velocity-based quadriceps training should be integrated with ballistic/plyometric exercises, which may improve the function of the stretch-shortening cycle within the quadriceps (see Video, Supplemental Material 24, which demonstrates a plyometric exercise example).191,193,199
To prepare the proximal quadriceps/rectus femoris for sport, graded exposure to high-velocity running should be integrated into the power phase of rehabilitation.30,200 High-velocity running produces large angular velocities at the knee, requiring the quadriceps to perform repeated high-load eccentric contractions (see Video, Supplemental Material 25, which demonstrates high-velocity running on a curved treadmill).201 With this, load management is of extreme importance, and the rehabilitation specialist should gradually increase running volume and intensity. Likewise, an upwards of 3-4 days of recovery may be initially required in between fatiguing exposures to high-velocity running until the repeated bout effect of eccentric training on muscle soreness is reported,202 especially as the
rectus femoris appears to have a higher proportion of typeII muscle fibers relative to the other quadriceps muscles.54
Quadriceps weakness after ACLR is a well-known phenomenon.13,51,128 Although recent literature has investigated the best-practice methodologies for mitigating AMI after knee injury,31‑33 less has been published with respect to the use of exercise therapy to restore quadriceps size and strength after ACLR.31 By combining common ACLR rehabilitation principles with muscle basic science and strength training literature, this review article provides a rehabilitation framework that can be used to optimize the recovery of quadriceps size and strength after ACLR, as well as recover the knee’s ability to manage the force-profiles associated with high-demand physical activities (i.e., Level-1 sport). Lastly, this review article may serve as a foundational piece of literature for the further development of more robust ACLR rehabilitation programs, to which the rehabilitation specialist can use the exercise progressions outline within this article to organize any other loading exposures needed to optimize individualized outcomes after ACLR.
After ACLR, optimal quadriceps load-progressions can be derived from combining common rehabilitation principles with the existing muscle basic science and strength training literature. The anatomy, regional innervation, and taskspecific activation/sequencing of the quadriceps necessitates the rehabilitation specialist to utilize both OKC and CKC exercises to maximally stimulate quadriceps hyper-
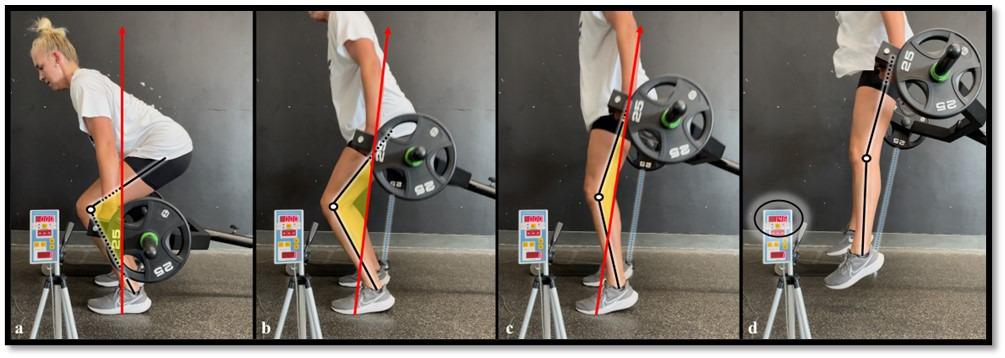
Figure 13. Example of velocity-based training with a linear positioning transducer/accelerometer.
Velocity-based training methods can be utilized after anterior cruciate ligament reconstruction to improve quadriceps motor recruitment and rate-of-force development (a-d). To best stimulate improvements in peak quadriceps contraction-velocity/knee power, emphasis should be placed on the importance of a maximal effort/intent on each repetition. Black lines, approximate tibial and femoral bone markers; black circle, feedback monitor from linear positioning transducer/accelerometer; blue lines, ripcord connecting the exercise bar to the linear positioning transducer/accelerometer; red arrows; approximate ground reaction force-vector; white circles; estimated center of joint rotation; yellow shading; depiction of external knee flexion moment.
trophy and strength. Graft-specific load progressions are also indicated after ACLR, and the rehabilitation specialist should consider the exercise type; muscle contraction mode; intensity of external load; and knee flexion angle when prescribing resistance training. To enhance the hypertrophic response to resistance training, exercise selection should include stable, single-limb exercises that load the quadriceps close to volitional fatigue/task failure at relatively long muscle lengths. Lastly, load-progressions for both OKC and CKC quadriceps strength training should be primarily advanced through the progression of knee flexion and external load.
The above authors have no conflicts of interest related to the development and publication efforts of this manuscript. The authors certify that they have no affiliations with or financial involvement in any organization or entity with a di-
rect financial interest in the subject matter or materials discussed in this manuscript.
We extend a special thank you to Hollis Fritz, MD; Jill Monson, MPT; and Jon Schoenecker, DPT, for their gift of time, mentoring, and teaching within the Twin Cities. We commemorate Chris Beardsley for his commitment to the dissemination and pragmatic translation of strength training research, which was the inspiration for this manuscript. Lastly, thank you to the physical therapists, licensed athletic trainers, sports scientists, and performance/strength coaches at Training HAUS for their ongoing teamwork and support, as well as the research department and bioengineering lab at Twin Cities Orthopedics for their support with ongoing research projects.
Submitted: June 10, 2024 CST, Accepted: September 17, 2024 CST
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Montalvo AM, Schneider DK, Webster KE, et al. Anterior cruciate ligament injury risk in sport: A systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train 2019;54(5):472-482. doi:10.4085/1062-6050-407-16
2. Lim HC, Yoon YC, Wang JH, Bae JH. Anatomical versus non-anatomical single bundle anterior cruciate ligament reconstruction: A cadaveric study of comparison of knee stability. Clin Orthop Surg. 2012;4(4):249. doi:10.4055/cios.2012.4.4.249
3. Eliya Y, Nawar K, Rothrauff BB, Lesniak BP, Musahl V, de SA D. Anatomical anterior cruciate ligament reconstruction (ACLR) results in fewer rates of atraumatic graft rupture, and higher rates of rotatory knee stability: a meta-analysis. Journal of ISAKOS. 2020;5:359-370. doi:10.1136/jisakos-2020-000476
4. Diermeier T, Rothrauff BB, Engebretsen L, et al. Treatment after anterior cruciate ligament injury: Panther Symposium ACL Treatment Consensus Group. Orthop J Sports Med 2020;8:232596712093109. doi:10.1177/ 2325967120931097
5. Carmichael JR, Cross MJ. Why bone-patella tendon-bone grafts should still be considered the gold standard for anterior cruciate ligament reconstruction. Br J Sports Med 2009;43:323-325. doi:10.1136/bjsm.2009.058024
6. Gifstad T, Foss OA, Engebretsen L, et al. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med 2014;42:2319-2328. doi:10.1177/ 0363546514548164
7. Sullivan JP, Huston LJ, Zajichek A, et al. Incidence and predictors of subsequent surgery after anterior cruciate ligament reconstruction: A 6-year follow-up study Am J Sports Med 2020;48:2418-2428. doi:10.1177/0363546520935867
8. Middleton KK, Hamilton T, Irrgang JJ, Karlsson J, Harner CD, Fu FH. Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc. 2014;22:1467-1482. doi:10.1007/s00167-014-2846-3
9. Arnold MP, Calcei JG, Vogel N, et al. ACL Study Group survey reveals the evolution of anterior cruciate ligament reconstruction graft choice over the past three decades. Knee Surg Sports Traumatol Arthrosc. 2021;29:3871-3876. doi:10.1007/ s00167-021-06443-9
10. Lubowitz JH. Editorial commentary: Quadriceps tendon autograft use for anterior cruciate ligament reconstruction predicted to increase. Arthroscopy. 2016;32(1):76-77 doi:10.1016/j.arthro.2015.11.004
11. Adams DJ, Mazzocca AD, Fulkerson JP Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft. Arthroscopy 2006;22(1):76-79. doi:10.1016/ j.arthro.2005.10.015
12. Rice DA, McNair PJ. Quadriceps arthrogenic muscle inhibition: Neural mechanisms and treatment perspectives. Semin Arthritis Rheum. 2010;40(3):250-266. doi:10.1016/ j.semarthrit.2009.10.001
13. Pietrosimone B, Lepley AS, Kuenze C, et al. Arthrogenic muscle inhibition following anterior cruciate ligament injury J Sport Rehabil 2022;31(6):694-706. doi:10.1123/jsr.2021-0128
14. Schuette HB, Kraeutler MJ, Houck DA, McCarty EC. Bone-patellar tendon-bone versus hamstring tendon autografts for primary anterior cruciate ligament reconstruction: A systematic review of overlapping meta-analyses. Orthop J Sports Med 2017;5(11):2325967117736484. doi:10.1177/ 2325967117736484
15. Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E. Anterior cruciate ligament reconstruction: a systematic review and metaanalysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstringtendon autografts. Am J Sports Med 2019;47:3531-3540. doi:10.1177/0363546518825340
16. Johnston PT, Feller JA, McClelland JA, Webster KE. Knee strength deficits following anterior cruciate ligament reconstruction differ between quadriceps and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc 2021;30(4):1300-1310. doi:10.1007/s00167-021-06565-0
17. Johnston PT, McClelland JA, Feller JA, Webster KE. Knee muscle strength after quadriceps tendon autograft anterior cruciate ligament reconstruction: systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2021;29(9):2918-2933. doi:10.1007/s00167-020-06311-y
18. Schwery NA, Kiely MT, Larson CM, et al. Quadriceps strength following anterior cruciate ligament reconstruction: normative values based on sex, graft type and meniscal status at 3, 6 & 9 months. Int J Sports Phys Ther 2022:17 doi:10.26603/ 001c.32378
19. Palmieri-Smith RM, Lepley LK. Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med 2015;43(7):1662-1669. doi:10.1177/ 0363546515578252
20. Ithurburn MP, Thomas S, Paterno MV, Schmitt LC. Young athletes after ACL reconstruction with asymmetric quadriceps strength at the time of return-to-sport clearance demonstrate drop-landing asymmetries two years later Knee 2021;29:520-529. doi:10.1016/j.knee.2021.02.036
21. Smith AH, Capin JJ, Zarzycki R, Snyder-Mackler L. Athletes with bone-patellar tendon-bone autograft for anterior cruciate ligament reconstruction were slower to meet rehabilitation milestones and returnto-sport criteria than athletes with hamstring tendon autograft or soft tissue allograft : secondary analysis from the ACL-SPORTS trial. J Orthop Sports Phys Ther 2020;50:259-266. doi:10.2519/jospt.2020.9111
22. Lepley LK. Deficits in quadriceps strength and patient-oriented outcomes at return to activity after ACL reconstruction. Sports Health 2015;7(3):231-238. doi:10.1177/1941738115578112
23. Lepley LK, Palmieri-Smith RM. Quadriceps strength, muscle activation failure, and patientreported function at the time of return to activity in patients following anterior cruciate ligament reconstruction: A cross-sectional study J Orthop Sports Phys Ther 2015;45(12):1017-1025. doi:10.2519/jospt.2015.5753
24. Zwolski C, Schmitt LC, Quatman-Yates C, Thomas S, Hewett TE, Paterno MV The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Am J Sports Med 2015;43(9):2242-2249. doi:10.1177/ 0363546515591258
25. Ithurburn MP, Altenburger AR, Thomas S, Hewett TE, Paterno MV, Schmitt LC. Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Knee Surg Sports Traumatol Arthrosc 2018;26. doi:10.1007/s00167-017-4678-4
26. Cristiani R, Mikkelsen C, Edman G, Forssblad M, Engström B, Stålman A. Age, gender, quadriceps strength and hop test performance are the most important factors affecting the achievement of a patient-acceptable symptom state after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2020:28. doi:10.1007/s00167-019-05576-2
27. Hetsroni I, Wiener Y, Ben-Sira D, et al. Symmetries in muscle torque and landing kinematics are associated with maintenance of sports participation at 5 to 10 years after ACL reconstruction in young men. Orthop J Sports Med 2020;8:27. doi:10.1177/2325967120923267
28. Wang LJ, Zeng N, Yan ZP, Li JT, Ni GX. Posttraumatic osteoarthritis following ACL injury Arthritis Res Ther. 2020;22:57. doi:10.1186/ s13075-020-02156-5
29. Arhos EK, Thoma LM, Grindem H, Logerstedt D, Risberg MA, Snyder-Mackler L. Association of quadriceps strength symmetry and surgical status with clinical osteoarthritis five years after anterior cruciate ligament rupture. Arthritis Care Res. 2022;74(3):386-391. doi:10.1002/acr.24479
30. Buckthorpe M. Optimising the late-stage rehabilitation and return-to-sport training and testing process after ACL reconstruction. Sports Med. 2019;49:30. doi:10.1007/s40279-019-01102-z
31. Buckthorpe M, La Rosa G, Della Villa F. Restoring knee extensor strength after anterior cruciate ligament reconstruction: A clinical commentary Int J Sports Phys Ther 2019;14(1):159. doi:10.26603/ ijspt20190159
32. Sonnery-Cottet B, Saithna A, Quelard B, et al. Arthrogenic muscle inhibition after ACL reconstruction: a scoping review of the efficacy of interventions. Br J Sports Med 2019;53(5). doi:10.1136/bjsports-2017-098401
33. Gokeler A, Bisschop M, Benjaminse A, Myer GD, Eppinga P, Otten E. Quadriceps function following ACL reconstruction and rehabilitation: implications for optimisation of current practices. Knee Surg Sports Traumatol Arthrosc 2014;22:1163-1174. doi:10.1007/ s00167-013-2577-x
34. Lepley LK, Wojtys EM, Palmieri-Smith RM. Combination of eccentric exercise and neuromuscular electrical stimulation to improve quadriceps function post-ACL reconstruction. Knee. 2015;22(3):270-277. doi:10.1016/j.knee.2014.11.013
35. Brinlee AW, Dickenson SB, Hunter-Giordano A, Snyder-Mackler L. ACL reconstruction rehabilitation: clinical data, biologic healing, and criterion-based milestones to inform a return-to-sport guideline. Sports Health 2022:19417381211056873. doi:10.1177/ 19417381211056873
36. Guex K, Millet GP Conceptual framework for strengthening exercises to prevent hamstring strains. Sports Med 2013;43:1207-1215. doi:10.1007/ s40279-013-0097-y
37. Bourne MN, Timmins RG, Opar DA, et al. An evidence-based framework for strengthening exercises to prevent hamstring injury Sports Med 2018;48:251-267. doi:10.1007/s40279-017-0796-x
38. Moore KL, Dalley AF II, Agur AM. Moore’s Clinically Oriented Anatomy Seventh ed. Lippincott Williams & Wilkins; 2021:545-546.
39. Hasselman CT, Best TM, Hughes C, Martinez S, Garrett WE. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med 1995;23(4):493-499. doi:10.1177/036354659502300421
40. Yang D, Morris SF. Neurovascular anatomy of the rectus femoris muscle related to functioning muscle transfer Plast Reconstr Surg 1999;104(1):102-106. doi:10.1097/00006534-199907000-00014
41. Jönhagen S, Ericson MO, Németh G, Eriksson E. Amplitude and timing of electromyographic activity during sprinting. Scand J Med Sci Sports. 2007;6(1):15-21. doi:10.1111/ j.1600-0838.1996.tb00064.x
42. Cerrah AO, Gungor EO, Soylu AR, Ertan H, Lees A, Bayrak C. Muscular activation patterns during the soccer in-step kick. Isokinet Exerc Sci 2011;19(3):181-190. doi:10.3233/ies-2011-0414
43. Soderberg GL, Cook TM. An electromyographic analysis of quadriceps femoris muscle setting and straight leg raising. Phys Ther 1983;63(9):1434-1438. doi:10.1093/ptj/63.9.1434
44. Ema R, Sakaguchi M, Akagi R, Kawakami Y Unique activation of the quadriceps femoris during single- and multi-joint exercises. Eur J Appl Physiol. 2016;116:1031-1041. doi:10.1007/s00421-016-3363-5
45. Stensdotter AK, Hodges PW, Mellor R, Sundelin G, Hager-Ross C. Quadriceps activation in closed and in open kinetic chain exercise. Med Sci Sports Exerc 2003;35(12):2043-2047 doi:10.1249/ 01.Mss.0000099107.03704.Ae
46. von Laßberg C, Schneid JA, Graf D, Finger F, Rapp W, Stutzig N. Longitudinal sequencing in intramuscular coordination: A new hypothesis of dynamic functions in the human rectus femoris muscle. PLoS One 2017;12(8):e0183204. doi:10.1371/ journal.pone.0183204
47 Watanabe K, Kouzaki M, Moritani T Non-uniform surface electromyographic responses to change in joint angle within rectus femoris muscle. Muscle Nerve. 2014;50(5):794-802. doi:10.1002/mus.24232
48. Pedrosa GF, Lima FV, Schoenfeld BJ, et al. Partial range of motion training elicits favorable improvements in muscular adaptations when carried out at long muscle lengths. Eur J Sports Sci. 2022;22(8):1250-1260. doi:10.1080/ 17461391.2021.1927199
49. Enocson AG, Berg HE, Vargas R, Jenner G, Tesch PA. Signal intensity of MR-images of thigh muscles following acute open- and closed chain kinetic knee extensor exercise - index of muscle use. Eur J Appl Physiol 2005;94:357-363. doi:10.1007/ s00421-005-1339-y
50. Behm DG, Whittle J, Button D, Power K. Intermuscle differences in activation. Muscle Nerve 2002;25(2):236-243. doi:10.1002/mus.10008
51. Lepley LK, Davi SM, Burland JP, Lepley AS. Muscle atrophy after ACL injury: Implications for clinical practice. Sports Health 2020;12(6):579-586. doi:10.1177/1941738120944256
52. Boccia G, Martinez-Valdes E, Negro F, Rainoldi A, Falla D Motor unit discharge rate and the estimated synaptic input to the vasti muscles is higher in open compared with closed kinetic chain exercise. J Appl Physiol 2019;127(4):950-958. doi:10.1152/ japplphysiol.00310.2019
53. Gouzi F, Maury J, Molinari N, et al. Reference values for vastus lateralis fiber size and type in healthy subjects over 40 years old: a systematic review and metaanalysis. J Appl Physiol 2013;115(3):346-354. doi:10.1152/ japplphysiol.01352.2012
54. Johnson MA, Polgar J, Weightman D, Appleton D Data on the distribution of fibre types in thirty-six human muscles. J Neurol Sci. 1973;18(1):111-129. doi:10.1016/0022-510x(73)90023-3
55. Mchugh MP, Tyler TF, Greenberg SC, Gleim GW Differences in activation patterns between eccentric and concentric quadriceps contractions. J Sports Sci 2002;20(2):83-91. doi:10.1080/026404102317200792
56. Brentano MA, Kruel MLF. A review on strength exercise-induced muscle damage: applications, adaptation mechanisms and limitations. J Sports Med Phys Fitness. 2011;51(1):1-10.
57. Jamurtas AZ, Theocharis V, Tofas T, et al. Comparison between leg and arm eccentric exercises of the same relative intensity on indices of muscle damage. Eur J Appl Physiol. 2005;95:179-185. doi:10.1007/s00421-005-1345-0
58. Chen TC, Yang TJ, Huang MJ, et al. Damage and the repeated bout effect of arm, leg, and trunk muscles induced by eccentric resistance exercises. Scand J Med Sci Sports 2019;29(5):725-735. doi:10.1111/sms.13388
59. Khan KM, Scott A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. Br J Sports Med. 2009;43(4):247-252. doi:10.1136/bjsm.2008.054239
60. Josephson RK. Dissecting muscle power output. J Exp Biol. 1999;202(23):3369-3375. doi:10.1242/ jeb.202.23.3369
61. Ottinger CR, Sharp MH, Stefan MW, Gheith RH, de la Espriella F, Wilson JM. Muscle hypertrophy response to range of motion in strength training: a novel approach to understanding the findings. Strength Cond J. 2023;45(2):162-176. doi:10.1519/ ssc.0000000000000737
62. Oranchuk DJ, Storey AG, Nelson AR, Cronin JB. Isometric training and long-term adaptations: Effects of muscle length, intensity, and intent: A systematic review Scand J Med Sci Sports 2019;29(4):484-503. doi:10.1111/sms.13375
63. Larsen S, Kristiansen BS, Swinton PA, et al. The effects of hip flexion angle on quadriceps femoris muscle hypertrophy in the leg extension exercise. SportRxiv Published online May 5, 2024. doi:10.51224/SRXIV.407
64. Wolf M, Androulakis-Korakakis P, Fisher J, Schoenfeld B, Steele J. Partial vs full range of motion resistance training: A systematic review and metaanalysis. Int J Strength Condit. 2023;3(1):2634-2235. doi:10.47206/ijsc.v3i1.182
65. Cutts A. The range of sarcomere lengths in the muscles of the human lower limb. J Anat 1988;160:79-88.
66. Son J, Indresano A, Sheppard K, Ward SR, Lieber RL. Intraoperative and biomechanical studies of human vastus lateralis and vastus medialis sarcomere length operating range. J Biomech 2018;67:91-97 doi:10.1016/j.jbiomech.2017.11.038
67 DiCarlo SE, Sipe E, Layshock PJ, Varyani S. Experiment demonstrating skeletal muscle biomechanics. Adv Physiol Educ 1998;275(6):59. doi:10.1152/advances.1998.275.6.S59
68. Kubo K, Ikebukuro T, Yata H. Effects of squat training with different depths on lower limb muscle volumes. Eur J Appl Physiol 2019;119:1933-1942. doi:10.1007/s00421-019-04181-y
69. Buford WL, Ivey MF, Malone D, et al. Muscle balance at the knee-moment arms for the normal knee and the ACL-minus knee. IEEE Trans Rehabil Eng 1997;5(4):367-379. doi:10.1109/86.650292
70. Spoor C, Van Leeuwen J. Knee muscle moment arms from MRI and from tendon travel. J Biomech. 1992;25(2):201-206. doi:10.1016/ 0021-9290(92)90276-7
71. Solie B, Monson J, Larson C. Graft-specific surgical and rehabilitation considerations for anterior cruciate ligament reconstruction with the quadriceps tendon autograft. Int J Sports Phys Ther. 2023;18(2):493. doi:10.26603/001c.73797
72. Dandridge O, Garner A, Amis AA, Cobb JP, Arkel RJ. Variation in the patellar tendon moment arm identified with an improved measurement framework. J Orthop Res 2022;40(4):799-807 doi:10.1002/jor.25124
73. Bell ZW, Dankel SJ, Mattocks KT, et al. An investigation into setting the blood flow restriction pressure based on perception of tightness. Physiol Meas 2018;39(10):105006. doi:10.1088/1361-6579/ aae140
74. Powers CM, Chen YJ, Scher IS, Lee TQ Multiplane loading of the extensor mechanism alters the patellar ligament force/quadriceps force ratio. J Biomech Engineer. 2010;132(2). doi:10.1115/1.4000852
75. Grood ES, Suntay WJ, Noyes FR, Butler DL. Biomechanics of the knee-extension exercise. Effect of cutting the anterior cruciate ligament. J Bone Joint Surg. 1984;66(5):725-734. doi:10.2106/ 00004623-198466050-00011
76. Im HS, Goltzer O, Sheehan FT The effective quadriceps and patellar tendon moment arms relative to the tibiofemoral finite helical axis. J Biomech 2015;48(14):3737-3742. doi:10.1016/ j.jbiomech.2015.04.003
77 Dan M, Parr W, Broe D, Cross M, Walsh WR. Biomechanics of the knee extensor mechanism and its relationship to patella tendinopathy: A review. J Orthop Res 2018;36(12):3105-3112. doi:10.1002/ jor.24120
78. Sprague A, Epsley S, Silbernagel KG. Distinguishing quadriceps tendinopathy and patellar tendinopathy: Semantics or significant? J Orthop Sports Phys Ther. 2019;49(4):627-630. doi:10.2519/ jospt.2019.0611
79. Maeo S, Saito A, Otsuka S, Shan X, Kanehisa H, Kawakami Y Localization of muscle damage within the quadriceps femoris induced by different types of eccentric exercises. Scand J Med Sci Sports 2018;28(1):95-106. doi:10.1111/sms.12880
80. Maeo S, Shan X, Otsuka S, Kanehisa H, Kawakami Y Neuromuscular adaptations to work-matched maximal eccentric versus concentric training. Med Sci Sports Exerc. 2018;50(8):1629-1640. doi:10.1249/ mss.0000000000001611
81. Yasuda T, Loenneke JP, Thiebaud RS, Abe T Effects of blood flow restricted low-intensity concentric or eccentric training on muscle size and strength. PLoS One 2012;7(12). doi:10.1371/ journal.pone.0052843
82. Franchi MV, Reeves ND, Narici MV Skeletal muscle remodeling in response to eccentric vs. concentric loading: morphological, molecular, and metabolic adaptations. Front Physiol 2017;8:82. doi:10.3389/fphys.2017.00447
83. Lim HY, Wong SH. Effects of isometric, eccentric, or heavy slow resistance exercises on pain and function in individuals with patellar tendinopathy: A systematic review. Physiother Res Int. 2018;23(4):e1721. doi:10.1002/pri.1721
84. Roig M, O’Brien K, Kirk G, et al. The effects of eccentric versus concentric resistance training on muscle strength and mass in healthy adults: A systematic review with meta-analysis. Br J Sports Med. 2009;43(8):556-568. doi:10.1136/ bjsm.2008.051417
85. Maestroni L, Read P, Bishop C, Turner A. Strength and power training in rehabilitation: underpinning principles and practical strategies to return athletes to high performance. Sports Med 2020;50(2):239-252. doi:10.1007/s40279-019-01195-6
86. Hunter SK, Ryan DL, Ortega JD, Enoka RM. Task differences with the same load torque alter the endurance time of submaximal fatiguing contractions in humans. J Neurophysiol 2002;88(6):3087-3096. doi:10.1152/jn.00232.2002
87. Garner JC, Blackburn T, Weimar W, Campbell B. Comparison of electromyographic activity during eccentrically versus concentrically loaded isometric contractions. J Electromyogr Kinesiol. 2008;18(3):466-471. doi:10.1016/j.jelekin.2006.11.006
88. Schaefer LV, Bittmann FN. Are there two forms of isometric muscle action? Results of the experimental study support a distinction between a holding and a pushing isometric muscle function. BMC Sports Sci Med Rehabil 2017;9:11. doi:10.1186/ s13102-017-0075-z
89. Rio E, van Ark M, Docking S, et al. Isometric contractions are more analgesic than isotonic contractions for patellar tendon pain. Clin J Sport Med. 2017;27(3):253-259. doi:10.1097/ jsm.0000000000000364
90. Lepley LK, Lepley AS, Onate JA, Grooms DR. Eccentric exercise to enhance neuromuscular control. Sports Health. 2017;9(4):333-340. doi:10.1177/ 1941738117710913
91. Rio E, Kidgell D, Purdam C, et al. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy Br J Sports Med 2015;49(19):1277-1283. doi:10.1136/ bjsports-2014-094386
92. Johnson AK, Palmieri-Smith RM, Lepley LK. Contribution of neuromuscular factors to quadriceps asymmetry after anterior cruciate ligament reconstruction. J Athl Train 2018;53(4):347-354. doi:10.4085/1062-6050-463-16
93. Seger T, Thorstensson T. Electrically evoked eccentric and concentric torque–velocity relationships in human knee extensor muscles. Acta Physiol Scand. 2000;169(1):63-69. doi:10.1046/ j.1365-201x.2000.00694.x
94. Nuzzo JL, Pinto MD, Nosaka K, Steele J. The eccentric: concentric strength ratio of human skeletal muscle in vivo: meta-analysis of the influences of sex, age, joint action, and velocity Sports Med 2023;53(6):1125-1136. doi:10.1007/ s40279-023-01851-y
95. Fukutani A, Herzog W Current understanding of residual force enhancement: cross-bridge component and non-cross-bridge component. Int J Molec Sci 2019;20(21):5479. doi:10.3390/ijms20215479
96. Peñailillo L, Blazevich AJ, Nosaka K. Factors contributing to lower metabolic demand of eccentric compared with concentric cycling. J Appl Physiol 2017;123(4):884-893. doi:10.1152/ japplphysiol.00536.2016
97 Peñailillo L, Guzmán N, Cangas J, Reyes A, Zbinden-Foncea H. Metabolic demand and muscle damage induced by eccentric cycling of knee extensor and flexor muscles. Eur J Sports Sci 2017;17(2):179-187. doi:10.1080/ 17461391.2016.1217278
98. Chen TCC, Tseng WC, Huang GL, Chen HL, Tseng KW, Nosaka K. Superior effects of eccentric to concentric knee extensor resistance training on physical fitness, insulin sensitivity and lipid profiles of elderly men. Front Physiol 2017;8. doi:10.3389/ fphys.2017.00209
99. Pollard CW, Opar DA, Williams MD, Bourne MN, Timmins RG. Razor hamstring curl and Nordic hamstring exercise architectural adaptations: Impact of exercise selection and intensity. Scand J Med Sci Sports 2019;29(5):706-715. doi:10.1111/sms.13381
100. Suskens JJM, Secondulfo L, Kiliç Ö, et al. Effect of two eccentric hamstring exercises on muscle architectural characteristics assessed with diffusion tensor MRI. Scand J Med Sci Sports 2023;33(4):393-406. doi:10.1111/sms.14283
101. Oranchuk DJ, Nelson AR, Storey AG, Diewald SN, Cronin JB. Short-term neuromuscular, morphological, and architectural responses to eccentric quasiisometric muscle actions. Eur J Appl Physiol. 2021;121:141-158. doi:10.1007/s00421-020-04512-4
102. Oranchuk DJ, Storey AG, Nelson AR, Cronin JB. Scientific basis for eccentric quasi-isometric resistance training: a narrative review J Strength Cond Res 2019;33(10):2846-2859. doi:10.1519/ jsc.0000000000003291
103. Beyer R, Kongsgaard M, Hougs Kjær B, Øhlenschlæger T, Kjær M, Magnusson SP Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy Am J Sports Med 2015;43(7):1704-1711. doi:10.1177/ 0363546515584760
104. Morrison S, Cook J. Putting “heavy” into heavy slow resistance. Sports Med 2022;52(6):1219-1222. doi:10.1007/s40279-022-01641-y
105. Włodarczyk M, Adamus P, Zieliński J, Kantanista A. Effects of velocity-based training on strength and power in elite athletes—a systematic review. Int J Environ Res Public Health 2021;18(10):5257 doi:10.3390/ijerph18105257
106. Rutherford OM, Purcell C, Newham DJ. The human force: velocity relationship; activity in the knee flexor and extensor muscles before and after eccentric practice. Eur J Appl Physiol. 2001;84:133-140. doi:10.1007/s004210000332
107 Del Vecchio A, Negro F, Holobar A, et al. You are as fast as your motor neurons: speed of recruitment and maximal discharge of motor neurons determine the maximal rate of force development in humans. J Physiol. 2019;597(9):2445-2456. doi:10.1113/ jp277396
108. Ratamess N. ACSM’s Foundations of Strength Training and Conditioning. 2nd ed. Lippincott Williams & Wilkins; 2021.
109. Scranton P, Lanzer W, Ferguson M, Kirkman T, Pflaster D. Mechanisms of anterior cruciate ligament neovascularization and ligamentization. Arthroscopy 1998;14(7):702-716. doi:10.1016/ s0749-8063(98)70097-0
110. Ma Y, Murawski CD, Rahnemai-Azar AA, Maldjian C, Lynch AD, Fu FH. Graft maturity of the reconstructed anterior cruciate ligament 6 months postoperatively: a magnetic resonance imaging evaluation of quadriceps tendon with bone block and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc 2015;23:661-668. doi:10.1007/ s00167-014-3302-0
111. Thaunat M, Fayard JM, Sonnery-Cottet B. Hamstring tendons or bone-patellar tendon-bone graft for anterior cruciate ligament reconstruction? Orthop Traumatol Surg Res. 2019;105(1):S89-S94. doi:10.1016/j.otsr.2018.05.014
112. Fukuda H, Ogura T, Asai S, et al. Bone-patellar tendon–bone autograft maturation is superior to double-bundle hamstring tendon autograft maturation following anatomical anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2022;30(5):1661-1671. doi:10.1007/ s00167-021-06653-1
113. Rodeo SA, Kawamura S, Kim HJ, Dynybil C, Ying L. Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft-tunnel motion? Am J Sports Med. 2006;34(11):1790-1800. doi:10.1177/ 0363546506290059
114. Michel PA, Domnick C, Raschke MJ, et al. Soft tissue fixation strategies of human quadriceps tendon grafts: A biomechanical study Arthroscopy 2019;35(11):3069-3076. doi:10.1016/ j.arthro.2019.05.025
115. Arakgi ME, Burkhart TA, Hoshino T, Degen R, Getgood A. Biomechanical comparison of three suspensory techniques for all soft tissue central quadriceps tendon graft fixation. Arthrosc Sports Med Rehabil. 2022;4(3):843-851. doi:10.1016/ j.asmr.2021.12.008
116. Strauss MJ, Miles JW, Kennedy ML, et al. Full thickness quadriceps tendon grafts with bone had similar material properties to bone-patellar tendonbone and a four-strand semitendinosus grafts: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 2022;30(5):1786-1794. doi:10.1007/ s00167-021-06738-x
117 Parrino RL, Adams W, Letter MI, et al. Impact of quadriceps tendon graft thickness on electromechanical delay and neuromuscular performance after ACL reconstruction. Orthop J Sports Med 2023;11(10):23259671231201832. doi:10.1177/23259671231201832
118. Heijne A, Werner S. Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study. Knee Surg Sports Traumatol Arthrosc 2007;15:472-473. doi:10.1007/s00167-007-0313-0
119. Dejour D, Pungitore M, Valluy J, Nover L, Saffarini M, Demey G. Tibial slope and medial meniscectomy significantly influence short-term knee laxity following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2019;27:3481-3489. doi:10.1007/s00167-019-05435-0
120. Sundemo D, Hamrin Senorski E, Karlsson L, et al. Generalised joint hypermobility increases ACL injury risk and is associated with inferior outcome after ACL reconstruction: a systematic review. BMJ Open Sport Exerc Med 2019;5:e000620. doi:10.1136/ bmjsem-2019-000620
121. Marmura H, Getgood AMJ, Spindler KP, Kattan MW, Briskin I, Bryant DM. Validation of a risk calculator to personalize graft choice and reduce rupture rates for anterior cruciate ligament reconstruction. Am J Sports Med 2021;49:1777-1785. doi:10.1177/03635465211010798
122. Zhao D, Pan J k., Lin F z., et al. Risk factors for revision or rerupture after anterior cruciate ligament reconstruction: a systematic review and metaanalysis. Am J Sports Med. Published online 2022:036354652211197 doi:10.1177/ 03635465221119787
123. Beynnon BD, Fleming BC. Anterior cruciate ligament strain in-vivo: A review of previous work. J Biomech 1998;31(6):519-525. doi:10.1016/ s0021-9290(98)00044-x
124. Wang C, Qiu J, Wang Y, et al. Loaded openkinetic-chain exercises stretch the anterior cruciate ligament more than closed-kinetic-chain exercises: In-vivo assessment of anterior cruciate ligament length change. Musculoskelet Sci Pract 2022;63:102715. doi:10.1016/j.msksp.2022.102715
125. Mikkelsen C, Werner S, Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc 2000;8(6):337-342. doi:10.1007/s001670000143
126. Morton RW, Colenso-Semple L, Phillips SM. Training for strength and hypertrophy: an evidencebased approach. Curr Opin Physiol 2019;10:90-95. doi:10.1016/j.cophys.2019.04.006
127. Solie B, Kiely M, Doney C, Schwery N, Jones J, Bjerke B. Return to elite-level basketball after surgical reconstruction of the anterior cruciate ligament and medial collateral ligament of the knee with meniscal repairs– it takes teamwork and time to restore performance: a case report. J Orthop Sports Phys Ther Cases 2022;2:1-22. doi:10.2519/ josptcases.2022.11103
128. Schilaty ND, McPherson AL, Nagai T, Bates NA. Arthrogenic muscle inhibition manifests in thigh musculature motor unit characteristics after anterior cruciate ligament injury. Eur J Sports Sci. 2022;23(5):1-11. doi:10.1080/17461391.2022.2056520
129. Cavanaugh JT, Powers M. ACL rehabilitation progression: where are we now? Curr Rev Musculoskel Med. 2017;10:289-296. doi:10.1007/ s12178-017-9426-3
130. Sengoku T, Nakase J, Mizuno Y, et al. Limited preoperative knee extension in anterior cruciate ligament reconstruction using a hamstring tendon affects improvement of postoperative knee extensor strength. Knee Surg Sports Traumatol Arthrosc. 2023;31(12):5621-5628. doi:10.1007/ s00167-023-07620-8
131. Hunnicutt JL, Xerogeanes JW, Tsai LC, et al. Terminal knee extension deficit and female sex predict poorer quadriceps strength following ACL reconstruction using all-soft tissue quadriceps tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2021;29:3085-3095. doi:10.1007/ s00167-020-06351-4
132. Shelbourne KD, Gray T Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37:471-480. doi:10.1177/0363546508326709
133. Driban JB, Vincent HK, Trojian TH, et al. Preventing osteoarthritis after an anterior cruciate ligament injury: an osteoarthritis action alliance consensus statement. J Athl Train 2023;58:193-197 doi:10.4085/1062-6050-0255.22
134. Biggs A, Jenkins W, Urch S, Shelbourne D. Rehabilitation for patients following ACL reconstruction: a knee symmetry model. N Am J Sports Phys Ther. 2009;4(1):2-12.
135. Wernbom M, Augustsson J, Thome R. The influence of frequency, intensity, volume and mode of strength training on whole muscle cross-sectional area in humans. Sports Med. 2007;37:225-264. doi:10.2165/00007256-200737030-00004
136. Machan T, Krupps K. The neuroplastic adaptation trident model: a suggested novel framework for ACL rehabilitation. Int J Sports Phys Ther 2021;16(3). doi:10.26603/001c.23679
137 Kannus P, Beynnon B. Peak torque occurrence in the range of motion during isokinetic extension and flexion of the knee. Int J Sports Med 1993;14(08):422-426. doi:10.1055/s-2007-1021203
138. Potvin JR, Fuglevand AJ. A motor unit-based model of muscle fatigue. PLoS Comput Biol 2017;13(6). doi:10.1371/journal.pcbi.1005581
139. Feil S, Newell J, Minogue C, Paessler HH. The effectiveness of supplementing a standard rehabilitation program with superimposed neuromuscular electrical stimulation after anterior cruciate ligament reconstruction. Am J Sports Med 2011;39(6):1238-1247 doi:10.1177/ 0363546510396180
140. Rio E, Kidgell D, Moseley GL, et al. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. Br J Sports Med 2016;50(4):209-215. doi:10.1136/ bjsports-2015-095215
141. Lee HK, Kim HJ, Kim SB, Kang N. A review and meta-analysis of interactive metronome training: Positive effects for motor functioning. Percept Mot Skills. 2022;129(5):1614-1634. doi:10.1177/ 00315125221110403
142. Mikaili S, Khademi-Kalantari K, Rezasoltani A, Arzani P, Baghban AA. Quadriceps force production during straight leg raising at different hip positions with and without concomitant ankle dorsiflexion. J Bodyw Mov Ther. 2018;22(4):904-908. doi:10.1016/ j.jbmt.2017.11.006
143. Lu Y, Patel BH, Kym C, et al. Perioperative blood flow restriction rehabilitation in patients undergoing ACL reconstruction: A systematic review Orthop J Sports Med 2020;8(3):232596712090682. doi:10.1177/ 2325967120906822
144. Hughes L, Paton B, Rosenblatt B, Gissane C, Patterson SD Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br J Sports Med 2017;51(13):1003-1011. doi:10.1136/ bjsports-2016-097071
145. Koc BB, Truyens A, Heymans MJLF, Jansen EJP, Schotanus MGM. Effect of low-load blood flow restriction training after anterior cruciate ligament reconstruction: A systematic review. Int J Sports Phys Ther 2022;17(3). doi:10.26603/001c.33151
146. Forelli F, Barbar W, Kersante G, et al. Evaluation of muscle strength and graft laxity with early open kinetic chain exercise after ACL reconstruction: A cohort study Orthop J Sports Med 2023;11(6):23259671231177594. doi:10.1177/ 23259671231177594
147 Noehren B, Snyder-Mackler L. Who’s afraid of the big bad wolf? Open-chain exercises after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2020;50(9):473-475. doi:10.2519/ jospt.2020.0609
148. McGinty G, Irrgang JJ, Pezzullo D. Biomechanical considerations for rehabilitation of the knee. Clin Biomech 2000;15(3):160-166. doi:10.1016/ s0268-0033(99)00061-3
149. Kassiano W, Costa B, Nunes JP, Ribeiro AS, Schoenfeld BJ, Cyrino ES. Which ROMs lead to Rome? A systematic review of the effects of range of motion on muscle hypertrophy J Strength Cond Res 2023;37(5):1135-1144. doi:10.1519/ jsc.0000000000004415
150. Cerqueira MS, Maciel DG, Barboza JAM, et al. Low-load blood-flow restriction exercise to failure and nonfailure and myoelectric activity: a metaanalysis. J Athl Train 2022;57(4):402-417 doi:10.4085/1062-6050-0603.20
151. Lorenz DS, Bailey L, Wilk KE, et al. Blood flow restriction training. J Athl Train 2021;56(9):937-944. doi:10.4085/418-20
152. Escamilla RF, Macleod TD, Wilk KE, Paulos L, Andrews JR. Anterior cruciate ligament strain and tensile forces for weight-bearing and non-weightbearing exercises: a guide to exercise selection. J Orthop Sports Phys Ther 2012;42(3):209. doi:10.2519/ jospt.2012.3768
153. Kakavas G, Forelli F, Malliaropoulos N, Hewett TE, Tsaklis P Periodization in anterior cruciate ligament rehabilitation: new framework versus old model? a clinical commentary. Int J Sports Phys Ther. 2023;18(2). doi:10.26603/001c.73035
154. Hughes L, Rosenblatt B, Haddad F, et al. Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK national health service randomised controlled trial. Sports Med 2019;49:1787-1805. doi:10.1007/ s40279-019-01137-2
155. Loenneke JP, Fahs CA, Rossow LM, Abe T, Bemben MG. The anabolic benefits of venous blood flow restriction training may be induced by muscle cell swelling. Med Hypotheses. 2012;78(1):151-154. doi:10.1016/j.mehy.2011.10.014
156. Caetano D, Oliveira C, Correia C, Barbosa P, Montes A, Carvalho P Rehabilitation outcomes and parameters of blood flow restriction training in ACL injury: A scoping review Phys Ther Sport 2021;49:129-137. doi:10.1016/j.ptsp.2021.01.015
157. Lixandrão ME, Ugrinowitsch C, Laurentino G, et al. Effects of exercise intensity and occlusion pressure after 12 weeks of resistance training with blood-flow restriction. Eur J Appl Physiol. 2015;115:2471-2480. doi:10.1007/s00421-015-3253-2
158. Cerqueira MS, Lira M, Mendonça Barboza JA, et al. Repetition failure occurs earlier during low-load resistance exercise with high but not low blood flow restriction pressures. J Strength Cond Res Published online 2021. doi:10.1519/jsc.0000000000004093
159. Li X, Li J, Qing L, Wang H, Ma H, Huang P Effect of quadriceps training at different levels of blood flow restriction on quadriceps strength and thickness in the mid-term postoperative period after anterior cruciate ligament reconstruction: a randomized controlled external pilot study. BMC Musculoskelet Disord 2023;24(1):360. doi:10.1186/ s12891-023-06483-x
160. Nunes JP, Schoenfeld BJ, Nakamura M, Ribeiro AS, Cunha PM, Cyrino ES. Does stretch training induce muscle hypertrophy in humans? A review of the literature. Clin Physiol Funct Imaging. 2020;40(3):148-156. doi:10.1111/cpf.12622
161. Alonso-Fernandez D, Fernandez-Rodriguez R, Abalo-Núñez R. Changes in rectus femoris architecture induced by the reverse nordic hamstring exercises. J Sports Med Phys Fitness 2018;59(4):640-647.
162. Doucet BM, Lam A, Griffin L. Neuromuscular electrical stimulation for skeletal muscle function. Yale J Biol Med. 2012;85(2):201-215.
163. Hauger AV, Reiman MP, Bjordal JM, Sheets C, Ledbetter L, Goode AP Neuromuscular electrical stimulation is effective in strengthening the quadriceps muscle after anterior cruciate ligament surgery Knee Surg Sports Traumatol Arthrosc 2018;26:399-410. doi:10.1007/s00167-017-4669-5
164. Van Rossom S, Smith CR, Thelen DG, Vanwanseele B, Van Assche D, Jonkers I. Knee joint loading in healthy adults during functional exercises: implications for rehabilitation guidelines. J Orthop Sports Phys Ther 2018;48(3):162-173. doi:10.2519/ jospt.2018.7459
165. Hart HF, Patterson BE, Crossley KM, et al. May the force be with you: understanding how patellofemoral joint reaction force compares across different activities and physical interventions—a systematic review and meta-analysis. Br J Sports Med 2022;56(9):521-530. doi:10.1136/ bjsports-2021-104686
166. Jean LMY, Chiu LZF. Elevating the noninvolved limb reduces knee extensor asymmetry during squat exercise in persons with reconstructed anterior cruciate ligament. J Strength Cond Res 2020;34(8):2120-2127 doi:10.1519/ jsc.0000000000003682
167. Atkinson TS, Ewers BJ, Haut RC. The tensile and stress relaxation responses of human patellar tendon varies with specimen cross-sectional area. J Biomech. 1999;32(9):907-914. doi:10.1016/ S0021-9290(99)00089-5
168. Baar K. Stress relaxation and targeted nutrition to treat patellar tendinopathy. Int J Sport Nutr Exerc Metab 2019;29(4):453-457 doi:10.1123/ ijsnem.2018-0231
169. Paxton JZ, Hagerty P, Andrick JJ, Baar K. Optimizing an intermittent stretch paradigm using ERK1/2 phosphorylation results in increased collagen synthesis in engineered ligaments. Tissue Eng. 2012;18(3-4):277-284. doi:10.1089/ten.tea.2011.0336
170. Nijem RM, Galpin AJ. Unilateral versus bilateral exercise and the role of the bilateral force deficit. Strength Cond J 2014;36(5):113-118. doi:10.1519/ SSC.0000000000000085
171. Sigward SM, Chan MS, Lin PE, Almansouri SY, Pratt KA. Compensatory strategies that reduce knee extensor demand during a bilateral squat change from 3 to 5 months following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2018;48(9):713-718. doi:10.2519/jospt.2018.7977
172. Hart LM, Izri E, King E, Daniels KA. Anglespecific analysis of knee strength deficits after ACL reconstruction with patellar and hamstring tendon autografts. Scand J Med Sci Sports. 2022;32(12):1781-1790. doi:10.1111/sms.14229
173. Xergia SA, Pappas E, Zampeli F, Georgiou S, Georgoulis AD. Asymmetries in functional hop tests, lower extremity kinematics, and isokinetic strength persist 6 to 9 months following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2013;43(3):154-162. doi:10.2519/jospt.2013.3967
174. Xergia SA, Pappas E, Georgoulis AD Association of the single-limb hop test with isokinetic, kinematic, and kinetic asymmetries in patients after anterior cruciate ligament reconstruction. Sports Health 2015;7(3):217-223. doi:10.1177/1941738114529532
175. Bampouras TM, Reeves ND, Baltzopoulos V, Maganaris CN. Interplay between body stabilisation and quadriceps muscle activation capacity J Electromyogr Kinesiol. 2017;34:44-49. doi:10.1016/ j.jelekin.2017.03.002
176. Pangan AM, Leineweber M. Footwear and elevated heel influence on barbell back squat: a review. J Biomech Engineer. 2021;143(9). doi:10.1115/ 1.4050820
177 Lu Z, Li X, Xuan R, et al. Effect of heel lift insoles on lower extremity muscle activation and joint work during barbell squats. Bioengineering 2022;9(7):301. doi:10.3390/bioengineering9070301
178. Baxter FR, Bach JS, Detrez F, et al. Augmentation of bone tunnel healing in anterior cruciate ligament grafts: application of calcium phosphates and other materials. J Tissue Eng. 2010;1(1):712370. doi:10.4061/2010/712370
179. Lu H, Chen C, Xie S, Tang Y, Qu J. Tendon healing in bone tunnel after human anterior cruciate ligament reconstruction: A systematic review of histological results. J Knee Surg 2019;32(05):454-462. doi:10.1055/s-0038-1653964
180. Yang G, Rothrauff BB, Tuan RS. Tendon and ligament regeneration and repair: Clinical relevance and developmental paradigm. Birth Defects Res C Embryo Today 2013;99(3):203-222. doi:10.1002/ bdrc.21041
181. Miyashita H, Ochi M, Ikuta Y. Histological and biomechanical observations of the rabbit patellar tendon after removal of its central one-third. Arch Orthop Trauma Surg. 1997;116:454-462. doi:10.1007/ bf00387577
182. Sturgill LP, Snyder-Mackler L, Manal TJ, Axe MJ. Interrater reliability of a clinical scale to assess knee joint effusion. J Orthop Sports Phys Ther 2009;39(12):845-849. doi:10.2519/jospt.2009.3143
183. Silbernagel KG, Thomeé R, Eriksson BI, Karlsson J. Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy. Am J Sports Med. 2007;35(6):897-906. doi:10.1177/0363546506298279
184. Patra SK, Narayan Nanda S, Prasad Patro B, Kumar Sahu N, Ranjan Mohnaty C, Jain M. Early accelerated versus delayed conservative rehabilitation protocol after anterior cruciate ligament reconstruction: a prospective randomized trial. Revista Brasileira de Ortopedia 2022;57:429-436. doi:10.1055/s-0042-1748970
185. Van Dieën JH, Ogita F, De Haan A. Reduced neural drive in bilateral exertions: a performancelimiting factor? Med Sci Sports Exerc 2003;35(1):111-118. doi:10.1097/ 00005768-200301000-00018
186. Herbert R, Gandevia S. Muscle activation in unilateral and bilateral efforts assessed by motor nerve and cortical stimulation. J Appl Physiol. 1996;80(4):1351-1356. doi:10.1152/ jappl.1996.80.4.1351
187. Ribeiro AS, Santos ED, Nunes JP, et al. A brief review on the effects of the squat exercise on lowerlimb muscle hypertrophy Strength Cond J 2023;45(1):58-66. doi:10.1519/ssc.0000000000000709
188. San Jose AJ, Maniar N, Whiteley R, Opar DA, Timmins RG, Kotsifaki R. Lower patellofemoral joint contact force during side-step cutting after return-tosports clearance following anterior cruciate ligament reconstruction. Am J Sports Med 2023;51(7):1777-1784. doi:10.1177/ 03635465231166104
189. Zavala L, Flores V, Cotter JA, Becker J. Patellofemoral joint kinetics in females when using different depths and loads during the barbell back squat. Eur J Sports Sci 2021;21(7):976-984. doi:10.1080/17461391.2020.1806935
190. Macdonald D, Hutton J, Kelly I. Maximal isometric patellofemoral contact force in patients with anterior knee pain. Bone Joint J. 1989;71-B(2):296-299. doi:10.1302/ 0301-620x.71b2.2925750
191. Tayfur B, Johnson AK, Palmieri-Smith R. Changes in quadriceps rate of torque development after anterior cruciate ligament reconstruction and association to single-leg hop distance. Sports Health. 2023;16(5):808-816. doi:10.1177/19417381231205295
192. Turpeinen JT, Freitas TT, Rubio-Arias JÁ, Jordan MJ, Aagaard P. Contractile rate of force development after anterior cruciate ligament reconstruction—a comprehensive review and meta-analysis. Scand J Med Sci Sports. 2020;30(9):1572-1585. doi:10.1111/ sms.13733
193. Asadi A, Arazi H, Young WB, de Villarreal ES. The effects of plyometric training on change-ofdirection ability: a meta-analysis. Int J Sports Physiol Perform 2016;11(5):563-573. doi:10.1123/ ijspp.2015-0694
194. Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med 2006;34(3):445-455. doi:10.1177/0363546505281241
195. Buckthorpe M, Della Villa F. Recommendations for plyometric training after ACL reconstruction – a clinical commentary Int J Sports Phys Ther 2021;16(3). doi:10.26603/001c.23549
196. Wong CY, Mok KM, Yung SH. Secondary anterior cruciate ligament injury prevention training in athletes: what is the missing link? Int J Environ Res Public Health. 2023;20(6):4821. doi:10.3390/ ijerph20064821
197 Weakley J, Morrison M, García-Ramos A, Johnston R, James L, Cole MH. The validity and reliability of commercially available resistance training monitoring devices: a systematic review Sports Med. 2021;51:443-502. doi:10.1007/ s40279-020-01382-w
198. Weakley J, Mann B, Banyard H, McLaren S, Scott T, Garcia-Ramos A. Velocity-based training: from theory to application. Strength Cond J 2021;43(2):31-49. doi:10.1519/ssc.0000000000000560
199. Read PJ, Pedley JS, Eirug I, Sideris V, Oliver JL. Impaired stretch-shortening cycle function persists despite improvements in reactive strength after anterior cruciate ligament reconstruction. J Strength Cond Res 2022;36(5):1238-1244. doi:10.1519/ jsc.0000000000004208
200. Buckthorpe M. Recommendations for movement re-training after ACL reconstruction. Sports Med. 2021;51(8):1601-1618. doi:10.1007/ s40279-021-01454-5
201. Kakehata G, Goto Y, Yokoyama H, Iso S, Kanosue K. Interlimb and intralimb coordination of rectus femoris and biceps femoris muscles at different running speeds. Med Sci Sports Exerc. 2023;55:945-956. doi:10.1249/ mss.0000000000003106
202. Penailillo L, Blazevich A, Numazawa H, Nosaka K. Metabolic and muscle damage profiles of concentric versus repeated eccentric cycling. Med Sci Sports Exerc. 2013;45(9):1773-1781. doi:10.1249/ MSS.0b013e31828f8a73
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254405.docx?auth_token=q0SMLgDk3ECnojaOLvim
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254406.mov?auth_token=q0SMLgDk3ECnojaOLvim
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254407.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254408.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 4: Optimal Straight Leg Raise
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254409.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 5: The Short-Arc-Quad Exercise | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254410.mov?auth_token=q0SMLgDk3ECnojaOLvim
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254411.mov?auth_token=q0SMLgDk3ECnojaOLvim
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/
254412.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 8: Long-Arc-Quad Exercise with BFR | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254413.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 9: Seated TKE Exercise with BFR | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254414.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 10: Prone Quad Set to Hamstring Curl with BFR | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254415.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 11: Prone Knee Flexion Stretch | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254416.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 12: Reverse Nordic Exercise | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254417.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 13: OKC Pushing/Overcoming Knee Extension with NMES | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254418.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 14: Standing TKE Exercise with Elastic Band Resistance | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254419.mov?auth_token=q0SMLgDk3ECnojaOLvim
Material
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/
254420.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 16: EQI Contraction on a Knee Extension Machine | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254421.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 17: Heavy-Slow Resistance Exercise on a Knee Extension Machine | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254422.mp4?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 18: EQI Contractions on a Leg Press | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254423.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 19: Heavy-Slow Resistance Exercise on a Leg Press | .mp4 file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254424.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 20: Eccentric-Specific Strength Training on a Leg Press | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254425.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 21: Eccentric-Specific Strength Training on a Knee Extension Machine | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254426.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 22: Velocity-Based Training on a Jump Training Machine | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254427.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 23: Velocity-Based Training with a Hex/Jammer Bar | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254428.mov?auth_token=q0SMLgDk3ECnojaOLvim
Material
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254429.mov?auth_token=q0SMLgDk3ECnojaOLvim
Supplemental Material 25: High Velocity-Running on a Curved Treadmill | .MOV file
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254430.mov?auth_token=q0SMLgDk3ECnojaOLvim
Download: https://ijspt.scholasticahq.com/article/126191-oh-my-quad-a-clinical-commentary-and-evidence-basedframework-for-the-rehabilitation-of-quadriceps-size-and-strength-after-anterior-cruciate-ligamen/attachment/ 254431.docx?auth_token=q0SMLgDk3ECnojaOLvim

Thomas ZM, Lupowitz L, Ivey M, Wilk KE. Neurocognitive and Neuromuscular Rehabilitation Techniques after ACL injury - Part 2: Maximizing Performance in the Advanced Return to Sport Phase. IJSPT. 2024;19(12):1629-1640.
doi:10.26603/001c.126270
Zachary M. Thomas, PT, DPT, OCS, SCS, CSCS1a , Lewis Lupowitz, PT, DPT, SCS, CSCS2 , Morgan Ivey, PT, DPT, SCS3 , Kevin E. Wilk, PT, DPT, FAPTA4,5
1 Piedmont Orthopedics and Sports Medicine, 2 Northwell Health, 3 Champion Sports Medicine, A Select Physical Therapy Clinic, 4 Associate Clinical Director, Champion Sports Medicine, Select Medical, 5 Director of Rehabilitative Research, American Sports Medicine Institute
Keywords: ACL injury, neurocognitive training, reactive testing, return to play https://doi.org/10.26603/001c.126270
International Journal of Sports Physical Therapy
Vol. 19, Issue 12, 2024
Background
Anterior cruciate ligament (ACL) injury and reinjury rates are on the rise, despite improved surgical techniques and prevention programs. ACL injuries also lead to a variety of neuroplastic and neuromuscular alterations. Emerging research highlights the importance of addressing neurocognitive deficits that can persist after injury including altered proprioception, impaired motor control, muscle recruitment and heightened reliance on visual feedback. This suggests a shift from subconscious movement, to movements that require increased volitional control, which may contribute to increased risk of re-injury and thus impede return to sport.
Given the neurophysiological changes associated with anterior cruciate ligament (ACL) injury that persistent into the late stages of rehabilitation, does the integration of neurocognitive training into mid to late stage rehabilitation protocols improve functional outcomes and reduce the risk of re-injury following ACL reconstruction (ACLR) in athletes?
The purpose of Part 2 of this clinical commentary is to offer strategies to implement neurocognitive training elements into the traditional ACLR rehabilitation (in weeks 9+) and review updated testing metrics that may better discern an athletes readiness to return to competition. A comprehensive rehabilitation framework incorporating both physical and neurocognitive components is proposed, aiming to improve both long-term outcomes and return to sport testing, as well as diminishing re-injury risk.
Conclusion
Updates to the traditional rehabilitation approach post ACLR, that include increased emphasis on neuroplastic, cognitive, and visual-motor capabilities exist. These help prepare athletes for the unpredictable and chaotic nature of the sporting environment and may facilitate a more effective return to sport for athletes, potentially mitigating the risk of re-injury
a
Corresponding Author: Dr. Zachary M. Thomas
1305 Jennings Mill Pkwy, Building 300 Watkinsville, GA 30677
Zachary.thomas1@piedmont.org (706) 552-1955
After ACLR, athletes often arrive a crossroads where they have “finished” their rehabilitation, but have not yet been cleared to return to sport. This commonly occurs due to insurance plan limitations, an inability to afford rehabilitation following the exhaustion of benefits, or self-discharge. Despite the abundance of evidence that suggests the importance of meeting specific return to play criteria, many athletes continue to exhibit strength deficits and poor results with functional testing including altered proprioception, impaired motor control and muscle recruitment, and heightened reliance on visual feedback.
Persistent efforts and countless time have been spent on research following ACLR, however the ability of an athlete to return to sport at their highest level of performance and reinjury rates continues to be a challenge to sports physical therapists.1‑3 Ardern et al. reported that current return to sports rates in elite athletes following ACLR is 81% to any sport, 65% to their preinjury level, and only 55% to their previous competition level.1 Athletes following ACLR are at increased risk for reinjury with documented rates as high as 30%, 21% occurring in the contralateral limb and 9% in the ipsilateral limb.3 Although time is not the only factor in return to sport decision making, delaying return until nine months after surgery can significantly reduce the reinjury rate by 51%4 and athletes that return prior to nine months post-operatively are at approximately a seven-fold increased rate of sustaining a second ACL injury.5 Strength continues to be a long-term concern following ACLR, with reports indicating that deficits in the hip, knee, and ankle musculature can persist for two-plus years following surgery 6,7 Deficits in deceleration performance and landing/jumping, both vital to reducing risk of ACL injury, may persiste for years following ACLR. Paterno et al demonstrated that biomechanical asymmetries exist during both landing and takeoff from a drop vertical jump two-plus years following ACLR.8 Asymmetries are also present during a 90-degree change of direction task in individuals following ACLR four-plus years following injury, demonstrating the need to address these biomechanical asymmetries in the later stages of rehab.9 Continued rehabilitation into the advanced/return to performance phases of ACL reconstruction is essential, however this begs the question; “Is there something missing from the traditional approach of ACL rehabiliation?”
While current training and testing metrics often fail to replicate the dynamic and unpredictable nature of sports, neurocognitive training offers a promising solution. Part 1 of this commentary advocates for early and consistent integration of neurocognitive rehabilitation in patients following ACLR. Incorporating these principles throughout ACL rehabilitation can better simulate the athletic environment, thus reducing the risk of re-injury, improving athletes’ confidence, and ultimately bridging the gap between rehabilitation and performance.
The overall goal of rehabilitation following ACLR is to return athletes back to sport safely. Continued neurocognitive rehabilitation and training into the advanced phases may be one of the missing links which helps bridge that gap from return to sport and return to performance at greater than or equal to an athlete’s prior level of competition. The purpose of this clinical commentary is to offer strategies to implement neurocognitive training elements into the traditional ACLR rehabilitation (in weeks 9+) and review updated testing metrics that may better indicate an athletes readiness to return to competition.
Neurocognitive deficits continue to persistent in the later stages of ACLR rehabilitation and have been shown to impact performance on traditional return to sport testing. Readiness to return to sport involves more than just the readiness of the musculoskeletal system and should also include psychological readiness, as well as adequate neuromuscular control. This is highlighted through the work by Swanik et al. found that amongst a cohort of NCAA athletes, those who sustained a non-contact ACL injury demonstrated slower reaction time, processing speed, and performed worse on verbal and visual memory tasks on IMPACT testing.10 Silvers-Granelli et al. demonstrated that in Division I and II men’s collegiate soccer players (1,500+ athletes), a warmup consisting of neuromuscular control and technique resulted in a reduction of injury rates by 46.1% and decreased time loss to injury by 28.6% in the competitive male collegiate soccer players.11 This data illustrates the importance of the continuation of neuromuscular/neurocognitive training into the advanced stages of ACLR rehabilitation and even as the athletes have been cleared for full competition to help minimize the risk of reinjury.
Simon et al. demonstrated that the addition of a neurocognitive and unanticipatory component to the traditional hop test series resulted in a significant difference in performance and may improve functional return to sport testing.12 This was further described by Smith et al. who demonstrated that reactive agility tasks that incorporate aspects of visual search, reactive decision making, working memory, and pathfinding, as well as the incorporation of visual perturbation resulted in a performance deficit.13
The authors propose that the traditional rehabilitation approach post ACLR, including the advanced stages progressing towards return to performance, should include increased emphasis on the neuroplastic, cognitive, and visual-motor capabilities that are impacted following injury to better prepare athletes for the chaotic nature of the sporting environment.
ACL Rehabilitation - Advanced Phase (Weeks 9-16)
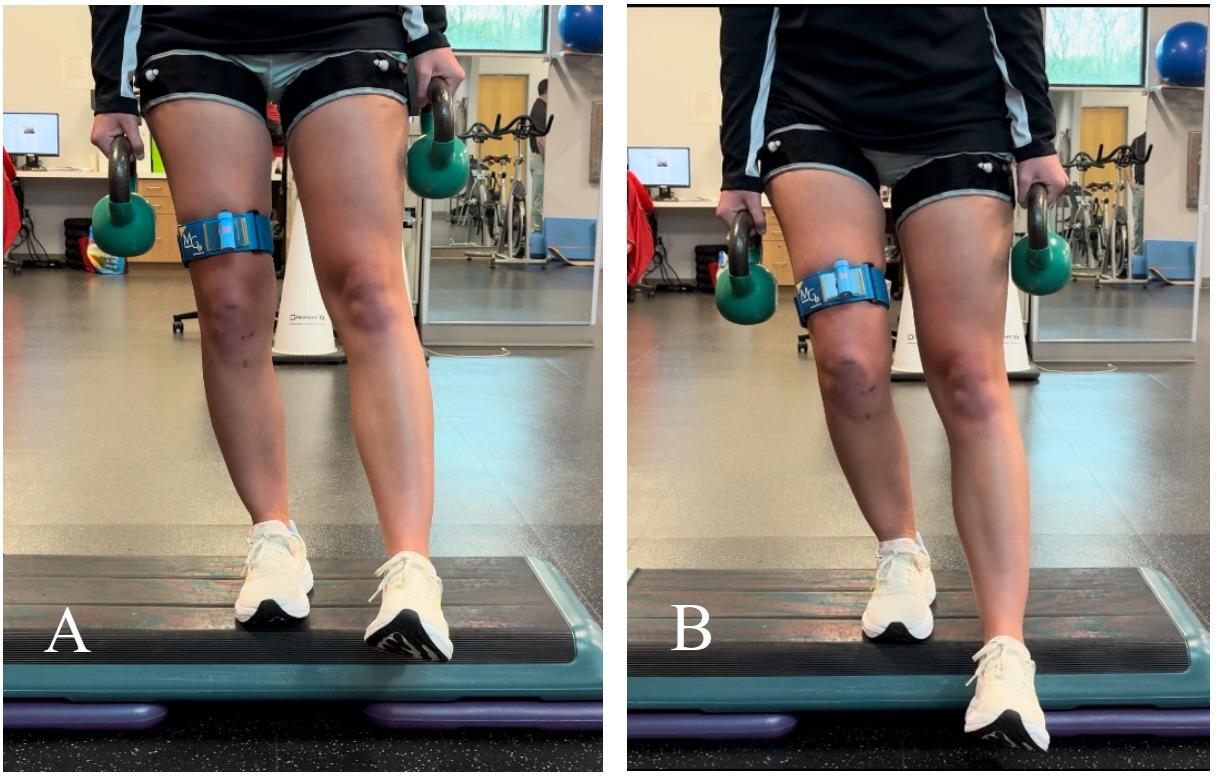
external
training
hypertrophy while minimizing muscle atrophy.
Part 1 of this clinical commentary, Optimizing Recovery in the Acute Post-Operative Phase, set the stage for goals to be achieved prior to starting this phase of rehabilitation. The advanced phase of ACLR rehabilitation focuses on traditional goals by continuing to restore full knee flexion PROM (heel to glute) and progressing the intensity of a strength training program (focusing on both double and single leg exercises). Additonally, the authors suggest implementing neuromuscular control drills which specifically target deficits that are common following ACLR. During this phase individuals may transition towards low level plyos (i.e. variety of double and single leg pogo hops) prior to a return to running progression. This progression will better prepare the athlete for the demands of running and assess their ability to generate and accept load. Lastly it is essential to begin assessing an athlete’s ability to decelerate because they must be able to “apply the brakes” (deceleration) prior to working on “hitting the gas” (acceleration).
In an effort to restore strength, blood flow restriction training can be an excellent adjunct as it respects the healing process by minimizing load on the tissue during this phase. It can be used in combination with heavy resistance training, to promote increased muscular strength and hypertrophy 14 Blood flow restriction can be coupled with neuromuscular control drills (such as an anterior step down) which are crucial prior to progressing towards higher level activities. The authors suggest utilizing a laser light system during exercise which provides an externally focused visual feedback mechanism to ensure proper lower limb alignment (Figure 1).
Once satisfactory mechanics, neuromuscular control, and strength (>65% of the contralateral limb via isokinetic or isometric hand held dynamometer) has been demonstrated, a gradual return to running progression may begin using the Alter-G or an underwater treadmill. This typically occurs at 10-12 weeks post-op, however the authors advise that objective criteria versus time alone should guide the decision as individuals who experience reactive symptoms during a return to running progression can experience significant setbacks.
Injury to the ACL often goes beyond injury to a soft tissue structure, resulting in joint damage and possibly contributing to early joint osteoarthritis. Bone bruising has been reported to occur in 98-100% of ACL tears.15,16 Byrd et al. assessed the prevalence of bone bruises in 208 patients (mean age: 23.8 years) who underwent ACL reconstruction with a median time from injury to MRI scan of 12 days.15 In this cohort, 59% of the athletes who suffered a non-contact injury with 98% (203/208) demonstrated evidence of a bone bruise, 79% at the medial tibial plateau, 83% in both the medial and lateral tibial plateau, and 46.6% demonstrating a bruise in all four locations (medial femoral condyle, lateral femoral condyle, medial tibial plateau, and lateral tibial plateau).15 This is important to consider in that it should guide the rehab professional towards a gradual return to impact progression in the advanced stages of rehab in order to preserve and maximize long term joint health.
Once the athlete demonstrates appropriate mechanics and tolerance through a gradual weight bearing progression, land-based running may begin typically around 14-16 weeks. The decision to return to running is based on a comprehensive evaluation by the rehabilitation specialist and is

Figure 2. (See Supplemental Video 1) Single leg balance on rocker board + external focus of demand/ selective attention via stroop test (athlete is instructed to recite either the color of the slide, the word itself (a specific color) or the color of the word on the slide.
informed by the athlete’s ability to tolerate the functional progression without an increase in pain and swelling, while demonstrating good hip and knee control.
During this phase, athletes should be progressing more towards the associative phase of motor learning, with increased task complexity and focusing on generating neuromuscular solutions that minimize error without focusing attention on the movement alone. This may include increased emphasis on visual distraction and/or working memory as well as perturbation training during a dynamic exercise such as ball toss, colored lights, or counting (Figure 2). The goal should be training both cognitive and motor function in an interactive manner to meet the demands of each individual sport. Examples of exercises that can be utilized during the phase are further described in Table 1
ACL Rehabilitation - Functional Sport Training Phase (Months 5-9)
During the functional sport training phase of ACLR rehabilitation the emphasis should be placed on continuing to progress athletes towards sport specific drills and later beginning to gradually progress towards return to practice participation. Athletes should be progressing towards the autonomous phase of motor learning performing multiplanar dynamic movements while simultaneously completing a high cognitively demanding challenge. Examples of exercises that can be utilized during the phase are further described in Table 2 By this point, athletes should have completed a return to straight line running progression and are continuing to progress plyometrics, agility drills, and sport specific training. Strength should not be forgotten at this stage, and athletes should be approaching 85-90% limb symmetry index (LSI) compared to their contralateral side. Overall, the goal of the functional sport training phase of ACLR rehabilitation should be to prepare athletes for the demands of sport by placing increased attention on reactive agility, multiplanar stability, power development, sprinting and jumping / landing capabilities.
Individuals entering this phase of rehabilitation will begin to participate in more advanced drills with the goal of progressing back into practice and later, competition. This phased approach to returning was proposed by the senior author in 2020.17 During the participation phase individuals are continuing to refine skills such as jumping, landing, single leg balance, and reaction time however it is imperative that they continue to be challenged. Figure 10 illustrates an individual performing a countermovement jump. They are given a variety of multi-step memory, counting, and verbal demands all while ensuring equal weight distribution is maintained. This can also be seen in Figure 11 where the individual has progressed from tradtional ladder drills. In this case they are given multiple commands, first to switch between two drills, occuring in two different planes of motion, second to change directions, and third to catch a ball with a specific hand. The goal is that the athlete can multitask without breaking stride and complete the cognitive challenge with minimal errors.
Once competent with these tasks in a clinic (closed) environment they can be returned to the practice (open) setting where sport specific progressions may take place. Communication among the entire team caring for the athlete are imperative as they may be spending more time with athletic trainers, strength and conditioning specialists, skills trainers, and coaches. The rehab provider must continue to ensure neurocognitive challenges are being imparted to the patient to combat potential long lasting deficits.
Deciding when to return to sport is a complex, multifactorial, and multidisciplinary decision not taken in isolation at the end of the recovery and rehabilitation process, but instead should be viewed as a continuum, paralleled with recovery and rehabilitation.18 Athletes’ struggles to return to play can be attributed to issues with the current return to sport testing procedures, or lack thereof In a 2011 systematic review of 264 articles, Noyes et al indicated that 40% (105) of studies discussing return to athletics following primary ACL reconstruction failed to provide any return to play criteria before sending ACL athletes back to sport.19 Of those that did provide criteria 32% (82) used time alone, while 15% (40) used time and subjective criteria. Only 13% (55) used objective criteria, without any consensus or agreement on the “best” tests. The importance of specific objective criteria, described by Kyritsis et al. as not achieving six specific markers (quadriceps deficit < 10% on isokinetic at 60°/s, LSI Single Hop >90%, LSI Triple Hop >90%, LSI Triple Crossover Hop >90%, completion of onfield drills, and a Running T-Test <11s) led to a four-fold increase in risk of re-rupture.20
Performing objective testing prior to returning athletes to sport is pivotal in ensuring positive outcomes, however, the authors suggest that there should be updates to our current practices. The criteria mentioned above is a good starting point, however flaws exist. The current tests place emphasis on limb symmetry and fail to respect the bilateral
deficits that commonly occur following injury, otherwise known as the “flat tire phenomenon”. This leads clinicians on a chase to achieve a moving target that is still below that of the athletes level of function prior to injury. More importantly these tests as traditionally completed are predictable in nature, which allows individuals the ability to practice the skill independently and may reflect a learning effect. Lastly it has been reported12 that there is a decrease in performance during functional tasks when a cognitive load is applied, and thus the authors suggest that modification be made to traditional hop testing when trying to replicate the demands of sport.
Based on the available knowledge pertaining to neurocognitive changes following ACLR a shift has begun related to return to sport testing. Schnittjer et al. aimed to understand how functional tasks were affected by cognitive challenge.21 They had individuals perform jump landing tasks under three conditions: no dual-task, “easy” dualtask, and “hard” dual-task. The authors concluded that with each increasing demand, movement quality was negatively affected.
Millikan et al. aimed to develop four clinical neurocognitive single-leg (SL) hop tests.22 Similarly Farraye et al. developed and tested the reliability of a Visual-Cognitive Reactive Triple Hop Test, and demonstrated excellent reliability for visual-cognitive reaction and moderate reliability for reaction time however, the maximum hop distance was significantly lower by 8.17%.23
Differences have also been described when comparing preplanned versus reactive agility or change of directions

Figure 3. Lateral slide test with numbered tape on the floor + perturbations.
Each target is 60 inches apart.
drills. Serpell et al. demonstrated a difference in mean reaction time between elite and subelite groups which they contributed to perceptual skills and/or reaction ability 24 When performing a reactive deceleration change of direction task in response to either a visual stimulus (i.e. light system)25 or an external object (i.e. soccer ball),26 changes were noted in a reduction of braking force at the penultimate step with an increase during the final step25 as well as a greater display of “high-risk” movement patterns.26 Both Grooms et al. and Wilk et al. have proposed frameworks for combining neurocognitive and functional tests to help improve re-
Exercise/Drill
Verbal/Visual Command
Step downs
Lateral slides (Figure 3)
Agility ladders
Low level plyos
Target Lights (Blaze Pod)
Lateral slides
4 corners (Figure 4)
SLB diamond
Single leg RDL
Weave dribble (basketball or soccer)
Target Lights (Quickboard)
Stagger step (L&R)
Array reactive foot fire (Figure 5)
Diagonal quick step
Foot fire Go/No Go
Visual Cognitive (Trazer)
Shuffle – Speed 3
Reaction – Speed 3
Box Drill – Speed 3
Get Back – Speed 3
Variables for Progression
Speed
Resistance
Dual task (i.e ball toss or HecoStix) Perturbations
Cognitive task (counting, memory, etc.)
Altered vision
Stroop Test
Speed
Resistance
Dual task (i.e ball toss or HecoStix) Perturbations
Cognitive task (counting, memory, etc.)
Altered vision # of distractions/colors
Speed
Resistance
Dual task (i.e ball toss or HecoStix) Perturbations
Cognitive task (counting, memory, etc.)
Altered vision # of distractions/colors
Speed
Resistance
Dual task (i.e ball toss or HecoStix) Perturbations
Cognitive task (counting, memory, etc.)
Altered vision
Neurocognitive Demand
Visual
Cognitive Decision making
Memory
Dual task
External focus of control Reaction time
Visual Cognitive Decision making
Memory
Dual task
External focus of control Reaction time
Visual Cognitive Decision making
Memory
Dual task
External focus of control
Reaction time
Visual Cognitive Decision making
Memory
Dual task
External focus of control
Reaction time

Figure 4. Four corner target light test (Blaze Pod, San Diego, CA).
Each light target is 21 feet apart.

5. (See Supplemental Video 2) Neurocognitive Training - Array Reactive Foot Fire to Target Color (QuickBoard, Memphis, TN)
This is a 20 sec drill in which the athlete is instructed to tap the target color as many times as possible while continuing rapid feet throughout the
turn to sport decision making following ACLR.27,28 Grooms et al. also aimed to understand the reliance on neurocognitive demand as it pertains to functional performance in an effort to improve return to play decisions following ACL reconstruction.27 They proposed the performance of four highly reliable tests both with and without neurocognitive augmentation in order assess for neurocognitive reliance.
Figure 12 Reactive Single Limb Cross Over Hop for Distance Test. The participant stands on one foot and hops outward – as the participant jumps, they are instructed which foot to land on and they must cross over the center tape. They will then complete the sequence by completing two more cross over hops on the same limb.
ACL Rehabilitation – Preventative Programs
Even following return to sport, research has demonstrated the importance of continuing a risk reduction program both in the preseason and throughout the season to help minimize the risk of reinjury These preventative programs (Sportsmetrics Program, FIFA 11, FIFA 11+, and


the Prevent Injury and Enhance Performance [PEP]) have shown that a session consisting of neuromuscular training including stretching, strengthening, plyometrics, and agility may have a direct benefit in minimizing the number of ACL injuries in male and female athletes.29‑32 The results of a recent systematic review indicate that a comprehensive program which includes plyometrics, strengthening, and neuromuscular training exercises led to a 50% reduction in the risk for all ACL injuries and 67% reduction for non-contact ACL injuries in female athletes.33 However these reviews also indicate an improvement in performance amongst organizations which were compliant to preventative programs due to the ability to keep more players healthy The authors suggest that when educating individuals that they not only promote the risk of injury reduction, but additionally the improvement in performance to improve compliance with these programs.
Table 2. ACLR Rehab Functional Sport Training Phase (5-9 months) Neurocognitive Drills
Exercise/Drill
Verbal/Visual Command
Reactive combo runs
Reactive acceleration/deceleration drills
Mirror Drill (Figure 7)
Target Lights (Blaze Pod)
Lateral slides
4 corners
Soccer retreat dribbles
Soccer kicks
QB reactive home base drops
Reactive 45 degree cutting (home base)
Target Lights (Quickboard)
Reactive vertical hops
Reactive lateral hops
Visual Cognitive (Trazer)
Box Drill – Speed 3
Get Back – Speed 3
Functional Tests
Reactive T-run (Figure 8)
Reactive L-run (Figure 9)
Reactive 3-cone drill
Reactive hop tests
Variables for Progression
Speed Resistance
Dual task (i.e ball toss or HecoStix) Perturbations
Cognitive task (counting, memory, etc.)
Altered vision
Speed Resistance
Dual task (i.e ball toss or HecoStix) Perturbations
Cognitive task (counting, memory, etc.)
Altered vision
Speed Resistance
Dual task (i.e ball toss or HecoStix) Perturbations
Cognitive task (counting, memory, etc.)
Altered vision
Speed Resistance
Dual task (i.e ball toss or HecoStix) Perturbations
Cognitive task (counting, memory, etc.)
Altered vision
Speed
Resistance
Dual task (i.e ball toss or HecoStix)
Perturbations
Cognitive task (counting, memory, etc.)
Altered vision
Neurocognitive Demand
Visual Cognitive Decision making
Memory
Dual task
External focus of control Reaction time
Visual Cognitive Decision making
Memory
Dual task
External focus of control Reaction time
Visual Cognitive Decision making
Memory
Dual task
External focus of control Reaction time
Visual Cognitive Decision making
Memory
Dual task
External focus of control Reaction time
Visual Cognitive Decision making
Memory
Dual task
External focus of control Reaction time
Visual Cognitive Decision making
Dual task
External focus of control Reaction time



Figure 10. Countermovement jump assessment with Force Plates (Vald Performance, Australia).
Analyzing symmetry bilaterally as well as concentric and eccentric forces compared to the uninvolved side.

Figure 11. (See Supplemental Video 5) Reactive agility ladders + dual tasking and external focus of demand/ selective attention via verbal commands and tennis ball toss.
Athlete is instructed to switch between drills and change direction as well as catch the tennis ball with a specific hand based on verbal command.
Further research must continue to test and implement reactive return to sport testing. As new tests develop clinicians must continue to ensure reliability and validity standards remain sufficient. Long term data collection and randomized control trials (RCTs) on athletes who have completed a reactive and neurocognitively challenged return to sport testing battery compared to traditional testing is needed to determine the effectiveness of such testing strategies regarding return to performance decisions and reinjury rates. Continued work is also needed to determine the impact on the uninvolved limb and whether or not neuromuscular training can help minimize the risk of contralateral injury as well. The authors’ recommendation for all sports physical therapists, athletic trainers, and/or strength and conditioning specialists is to think of an ACL injury as more than just a musculoskeletal injury and to understand/appreciate the importance of “training the brain” in order to best prepare our athletes for the chaotic and un-
predictable nature of the sporting environment they are returning to and testing accordingly.
Traditional ACLR rehabilitation has been well researched and progressed over the years, however the rates of return to prior level of performance and risk of reinjury continue to be less than optimal. It is important to understand that recovery following an ACL injury is not an isolated musculoskeletal issue, but also are accompanied by neuroplastic changes at the CNS. Recovery of the musculoskeletal impairments is only the minimum prerequisite for RTS, which does not fully ensure readiness to return. As rehab professionals, we gradually progress “chaos” from low to highly distractive environments to better prepare athletes for the demands of sport. Integrating neurocognitive challenges throughout the rehabilitation process, beginning during the acute post-operative phases and concluding with RTS testing, may allow clinicians to more confidently make decisions regarding returning individuals following ACLR to sports, not only at their same level of performance but at one that exceeds the level they were at prior to their injury.
The authors above are affliated with the organizations mentioned in this manuscript however there is no personal or financial gain from any of the organizations linked to this manuscript.
Kevin Wilk serves on the medical advisory board for BlazePods and receives educational grant from QuickBoard.
© The Author(s)
Measurements
Physician Clearance
Satisfactory Clinical Exam
Methods of Assessments
Pain (VAS/NPRS)
Range of motion (PROM & AROM)
Palpation
Special tests
Joint effusion (anthropometric measurements/Sweep Test)
Strength
Isokinetics
Patient Reported Outcomes (PROs) ACL-RSI
Balance/Proprioception
Gait/Running/ Movement Analysis
Functional Tests
Qualitative Analysis
Hop Tests
LE Y-Balance
T-run test
L-run test
Force Plates (Jump testing, isometric testing, etc.)
Reactive Agility Tests (T run, L run, Hop tests)
Objective Criteria – Goals
< 3 during & after exercise
Symmetrical & pain-free
No complaints of pain
Negative & no complaints of pain
< 1cm LSI
Quadriceps bilateral comparison: 90% or greater
Hamstrings bilateral comparison: 90% or greater
Q Peak Torque/BW: > 3Nm/kg
Hamstring/Quad ratio: M 66-75%, F >75%
Quadriceps bilateral comparison: 90% or greater
Hamstrings bilateral comparison: 90% or greater
Q Peak Torque/BW: M 60-65%, F 50-55%
Hamstring/Quad ratio: M 66-70%, F >75%
Accleration rate at 0.2 secs: >90%
>55 points
Controlled dynamic knee valgus Proper trunk alignment
< 10% LSI and/or Norms
T Run < 11s
< 10% Neurocognitive reliance (based on formula mentioned above)
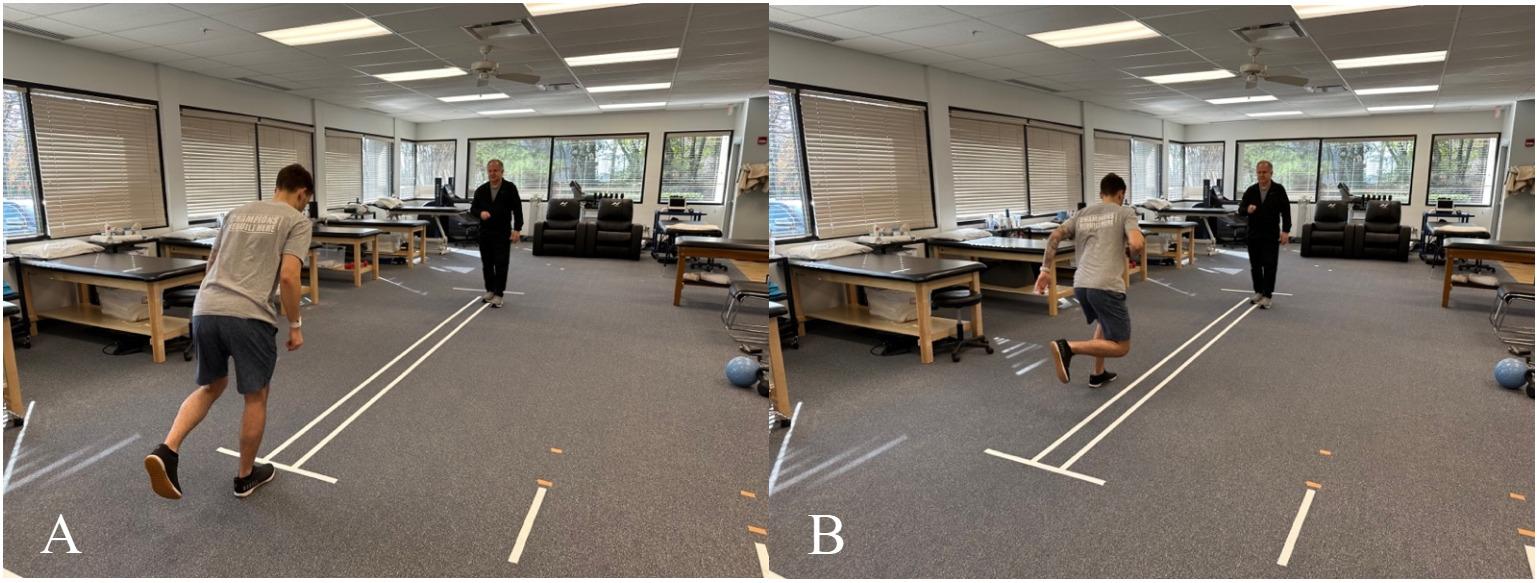
12. Reactive Single Limb Cross Over Hop for Distance Test.
The participant stands on one foot and hops outward – as the participant jumps, they are instructed which foot to land on and they must cross over the center tape. They will then complete the sequence by completing two more cross over hops on the same limb.
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Ardern CL, Taylor NF, Feller JA, Webster KE. Fiftyfive per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543-1552. doi:10.1136/ bjsports-2013-093398
2. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116-121. doi:10.1097/ JSM.0b013e318246ef9e
3. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567-1573. doi:10.1177/ 0363546514530088
4. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study Br J Sports Med 2016;50(13):804-808. doi:10.1136/ bjsports-2016-096031
5. Beischer S, Gustavsson L, Senorski EH, et al. Young athletes who return to sport before 9 months after Anterior Cruciate Ligament Reconstruction have a rate of new injury 7 times that of those who delay return. J Orthop Sports Phys Ther. 2020;50(2):83-90. doi:10.2519/jospt.2020.9071
6. Petersen W, Taheri P, Forkel P, Zantop T Return to play following ACL reconstruction: a systematic review about strength deficits. Arch Orthop Trauma Surg 2014;134(10):1417-1428. doi:10.1007/ s00402-014-1992-x
7 Buckthorpe M, La Rosa G, Villa FD Restoring knee extensor strength after Anterior Cruciate Ligament Reconstruction: A clinical commentary. Int J Sports Phys Ther 2019;14(1):159-172. doi:10.26603/ ijspt20190159
8. Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17(4):258-262. doi:10.1097/ JSM.0b013e31804c77ea
9. Mausehund L, Krosshaug T Knee Biomechanics during cutting maneuvers and secondary ACL injury risk: A prospective cohort study of knee biomechanics in 756 female elite handball and soccer players. Am J Sports Med 2024;52(5):1209-1219. doi:10.1177/03635465241234255
10. Swanik CB, Covassin T, Stearne DJ, Schatz P The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. Am J Sports Med 2007;35(6):943-948. doi:10.1177/ 0363546507299532
11. Silvers-Granelli H, Mandelbaum B, Adeniji O, et al. Efficacy of the FIFA 11+ injury prevention program in the collegiate male soccer player Am J Sports Med 2015;43(11):2628-2637. doi:10.1177/ 0363546515602009
12. Simon JE, Millikan N, Yom J, Grooms DR. Neurocognitive challenged hops reduced functional performance relative to traditional hop testing. Phys Ther Sport 2020;41:97-102. doi:10.1016/ j.ptsp.2019.12.002
13. Smith EM, Sherman DA, Duncan S, et al. Testretest reliability and visual perturbation performance costs during 2 reactive agility tasks. J Sport Rehabil. 2024;19:1-8. doi:10.1123/jsr.2023-0433
14. Patterson SD, Hughes L, Warmington S, et al. Blood flow restriction exercise: considerations of methodology, application, and safety. Front Physiol. 2019;15(10):533. doi:10.3389/fphys.2019.00533
15. Byrd JM, Colak C, Yalcin S, et al. Posteromedial tibial bone bruise after Anterior Cruciate Ligament injury: An MRI study of bone bruise patterns in 208 patients. Orthop J Sports Med. 2022;10(10):23259671221120636. doi:10.1177/ 23259671221120636
16. Filardo G, Andriolo L, di Laura Frattura G, Napoli F, Zaffagnini S, Candrian C. Bone bruise in anterior cruciate ligament rupture entails a more severe joint damage affecting joint degenerative progression. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):44-59. doi:10.1007/s00167-018-4993-4
17 Wilk KE, Bagwell MS, Davies GJ, Arrigo CA. Return to sport participation criteria following shoulder injury: A clincal commentary Int J Sports Phys Ther. 2020;15(4):624-642. doi:10.26603/ ijspt20200624
18. Ardern CL, Glasgow P, Schneiders A, et al. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med. 2016;50(14):853-864. doi:10.1136/bjsports-2016-096278
19. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy 2011;27(12):1697-1705. doi:10.1016/ j.arthro.2011.09.009
20. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med 2016;50(15):946-951. doi:10.1136/ bjsports-2015-095908
21. Schnittjer A, Simon JE, Yom J, Grooms DR. The effects of a cognitive dual task on jump-landing movement quality Int J Sports Med 2021;42(1):90-95. doi:10.1055/a-1195-2700
22. Millikan N, Grooms DR, Hoffman B, Simon JE. The development and reliability of 4 clinical neurocognitive single-leg hop tests: Implications for return to activity decision-making. J Sport Rehabil 2019;28(5):536-544. doi:10.1123/jsr.2018-0037
23. Farraye BT, Simon JE, Chaput M, Kim H, Monfort SM, Grooms DR. Development and reliability of a visual-cognitive reactive triple hop test. J Sport Rehabil. 2023;32(7):802-809. doi:10.1123/ jsr.2022-0398
24. Serpell BG, Ford M, Young WB, et al. The development of a new test of agility for rugby league. J Strength Cond Res 2010;24(12):3270-3277 doi:10.1519/JSC.0b013e3181b60430
25. Mulligan CMS, Johnson ST, Pollard CD, Hannigan KS, Athanasiadis D, Norcross MF. Deceleration profiles between the penultimate and final steps of planned and reactive side-step cutting. J Athl Train. 2024;59(2):173-181.
26. Needham C, Herrington L. Cutting movement assessment scores during anticipated and unanticipated 90-degree sidestep cutting manoeuvres within female professional footballers. Sports. 2022;10(9):128. doi:10.3390/sports10090128
27 Grooms DR, Chaput M, Simon JE, Criss CR, Myer GD, Diekfuss JA. Combining neurocognitive and functional tests to improve return-to-sport decisions following ACL reconstruction. J Orthop Sports Phys Ther. 2023;0(8):1-5. doi:10.2519/jospt.2023.11489
28. Wilk KE, Thomas ZM, Arrigo CA, Davies GJ. The need to change return to play testing in athletes following ACL injury: A theoretical model. Int J Sports Phys Ther. Published online 2023:272-281. doi:10.26603/001c.67988
29. Hewett TE, Di Stasi SL, Myer GD Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med 2013;41(1):216-224. doi:10.1177/ 0363546512459638
30. Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year followup. Am J Sports Med 2005;33(7):1003-1010. doi:10.1177/0363546504272261
31. Silvers-Granelli HJ, Bizzini M, Arundale A, Mandelbaum BR, Snyder-Mackler L. Does the FIFA 11+ injury prevention program reduce the incidence of ACL injury in male soccer players? Clin Orthop Relat Res 2017;475(10):2447-2455. doi:10.1007/ s11999-017-5342-5
32. Noyes FR, Barber-Westin SD, Tutalo Smith ST, Campbell T A training program to improve neuromuscular and performance indices in female high school soccer players. J Strength Cond Res 2013;27(2):340-351. doi:10.1519/ JSC.0b013e31825423d9
33. Webster KE, Hewett TE. Meta-analysis of metaanalyses of anterior cruciate ligament injury reduction training programs. J Orthop Res. 2018;36(10):2696-2708. doi:10.1002/jor.24043
Download: https://ijspt.scholasticahq.com/article/126270-neurocognitive-and-neuromuscular-rehabilitationtechniques-after-acl-injury-part-2-maximizing-performance-in-the-advanced-return-to-sport-phase/attachment/ 254806.mov?auth_token=F-Pfe56ZglLLvlzd60kx
Download: https://ijspt.scholasticahq.com/article/126270-neurocognitive-and-neuromuscular-rehabilitationtechniques-after-acl-injury-part-2-maximizing-performance-in-the-advanced-return-to-sport-phase/attachment/ 254807.mov?auth_token=F-Pfe56ZglLLvlzd60kx
Download: https://ijspt.scholasticahq.com/article/126270-neurocognitive-and-neuromuscular-rehabilitationtechniques-after-acl-injury-part-2-maximizing-performance-in-the-advanced-return-to-sport-phase/attachment/ 254808.mov?auth_token=F-Pfe56ZglLLvlzd60kx
Download: https://ijspt.scholasticahq.com/article/126270-neurocognitive-and-neuromuscular-rehabilitationtechniques-after-acl-injury-part-2-maximizing-performance-in-the-advanced-return-to-sport-phase/attachment/ 254809.mov?auth_token=F-Pfe56ZglLLvlzd60kx
Download: https://ijspt.scholasticahq.com/article/126270-neurocognitive-and-neuromuscular-rehabilitationtechniques-after-acl-injury-part-2-maximizing-performance-in-the-advanced-return-to-sport-phase/attachment/ 254810.mov?auth_token=F-Pfe56ZglLLvlzd60kx

Manske RC, Voight M, Wolfe C, Page P, Bardowski B. The Use of Diagnostic Musculoskeletal Ultrasound for the Evaluation of the Iliopsoas in the Anterior Hip: A Guide for Rehabilitation Providers. IJSPT. 2024;19(12):1641-1645.
doi:10.26603/001c.126334
Robert C. Manske, PT, DPT, MEd, SCS, ATC, CSCS, FAPTA, Michael Voight, PT, DHSC, SCS, OCS, ATC, CSCS, FAPTAa , Chris Wolfe, PT, DPT, OCS, Cert MDT, Phil Page, PT, PhD, ATC, CSCS, FACSM, Beth Bardowski, MSN, APN, ACNP-BC
Keywords: Musculoskeletal Ultrasound, Iliopsoas, Anterior Hip, Rehabilitation, Diagnostic Imaging https://doi.org/10.26603/001c.126334
International Journal of Sports Physical Therapy Vol. 19, Issue 12, 2024
Musculoskeletal ultrasound (MSK-US) has become an increasingly valuable tool in the evaluation and management of soft tissue and joint pathologies, particularly for rehabilitation providers. This article highlights the use of MSK-US for assessing the iliopsoas tendon and musculature in the anterior hip. The iliopsoas complex is often implicated in conditions such as tendinitis, snapping hip syndrome, and hip flexor strains, and accurate assessment can be challenging due to its deep anatomical location. MSK-US offers a safe, cost-effective, and dynamic modality for visualizing the iliopsoas, providing crucial insights into its morphology, pathology, and response to rehabilitation interventions. This paper discusses the anatomy of the iliopsoas, ultrasound scanning techniques, common findings, and the clinical relevance of MSK-US in rehabilitation settings. This paper explores the efficacy of MSK-US in the assessment of the iliopsoas muscle and tendon and underscores its utility in diagnosing iliopsoas-related abnormalities such as tendinopathy and bursitis.
The iliopsoas muscle complex plays a critical role in hip flexion and is involved in various activities, from daily movement to athletic performance. The iliopsoas consists of the psoas major and iliacus muscles, converging to form the iliopsoas tendon, which inserts at the lesser trochanter of the femur. Dysfunction or pathology of the iliopsoas can lead to anterior hip pain, which is commonly seen in athletes, dancers, and individuals with hip overuse injuries.1 Disorders of the iliopsoas, such as tendinopathy, bursitis, and snapping hip syndrome, are common sources of anterior hip and groin pain, particularly among athletes and individuals engaged in repetitive hip flexion activities. Recently, it has been felt that the psoas major may be representative of whole-body skeletal muscle mass, and a decrease in its cross-sectional area may be associated with a loss of motor function.2‑4
Traditional diagnostic modalities, such as magnetic resonance imaging (MRI), have limitations in accessibility and the ability to provide real-time, dynamic assessments. Diagnostic musculoskeletal ultrasound (MSK-US) is an excel-
lent modality for evaluating the iliopsoas complex due to its accessibility, cost-effectiveness, and ability to offer dynamic evaluation. This imaging technique enables practitioners to assess the iliopsoas during movement, evaluate muscle and tendon morphology, and identify abnormalities that may be contributing to hip pain or dysfunction. The purpose of this article is to provide an in-depth review of the use of diagnostic MSK-US in evaluating the iliopsoas muscle on the anterior hip. It outlines the relevant anatomy, scanning protocols, interpretation of findings, and discusses common iliopsoas-related pathologies detectable via ultrasound.
The iliopsoas is a complex muscle group that spans the lumbar spine to the anterior hip. The psoas major originates from the transverse processes and bodies of the T12 to L5 vertebrae, while the iliacus originates from the iliac fossa. Both muscles join to form the iliopsoas tendon, which passes deep to the inguinal ligament and inserts into
Corresponding Author:
Phone: 615.460.6174
Email: mike.voight@belmont.edu 1900 Belmont Boulevard | Nashville, TN 37212
the lesser trochanter of the femur The iliopsoas bursa, the largest bursa in the body, is located between the iliopsoas muscle and the hip joint capsule, reducing friction during muscle movement. The iliopsoas functions primarily as a hip flexor and also plays a role in stabilizing the lumbar spine and pelvis during movement. Given its deep location and proximity to important neurovascular structures, accurate imaging is essential for identifying pathology Common pathologies of the iliopsoas include:
• Iliopsoas Tendinopathy: Degenerative changes in the tendon due to repetitive overuse or acute injury
• Iliopsoas Bursitis: Inflammation of the iliopsoas bursa, often linked to overuse or mechanical irritation.
• Snapping Hip Syndrome (Coxa Saltans): Audible and palpable snapping during hip movements, caused by iliopsoas tendon impingement. Causes can be either extra- or intra-articular Extra- articular causes include iliopsoas tendon, iliofemoral ligament anteriorly and iliotibial band or gluteus maximus laterally Intra-articular causes include labral tears, chondral defects and loose bodies.5‑10
ADVANTAGES OF MSK ULTRASOUND FOR ILIOPSOAS EVALUATION
There are several advantages in using MSK-US to evaluate the iliopsoas in patients with anterior hip pain.
• Dynamic Imaging: Allows visualization of the iliopsoas during active movement, aiding in the diagnosis of snapping hip syndrome.
• Real-Time Guidance: Facilitates guided interventions such as injections or dry needling.
• Soft-Tissue Differentiation: Provides high-resolution imaging of tendons, muscles, and bursae.
• Cost-Effectiveness and Accessibility: Offers a less expensive and more readily available alternative to MRI.
DIAGNOSTIC MSK ULTRASOUND IN ILIOPSOAS EVALUATION
Proper patient positioning and transducer placement are crucial for visualizing the iliopsoas. The patient is typically positioned supine with the hip slightly externally rotated to improve access to the anterior hip region. A high-frequency linear transducer (7-12 MHz) is commonly used to visualize the iliopsoas complex. A curvilinear transducer may be necessary for deeper visualization.
The transducer is placed parallel to the inguinal ligament, just below the anterior superior iliac spine (ASIS), to identify the iliacus muscle, psoas major, and iliopsoas tendon. The psoas muscle has historically been divided into three sections during ultrasound scanning: 1) upper section from origin of muscle to lower pole of the kidney, 2) midsection from the lower pole of kidney to iliac crest, and 3) lower section from iliac crest to fusion with iliacus.11

Figure 1A: Patient Position
Patient is supine and instructed to allow their foot to rest in slight external rotation.
Figure 1B: Long Axis View (LAX) Transducer Placement
Orient the transducer in a longitudinal axis view, parallel to the femoral shaft. The femoral shaft will appear with a curved, echogenic surface. Gradually move the transducer proximally until both the greater and lesser trochanters are visualized. Once these landmarks are identified, rotate the transducer to align parallel with the femoral neck for optimal imaging. This angle is roughly 128 degrees in an oblique position. Position the transducer on the medial aspect of the femoral-acetabular joint to differentiate the psoas tendon from the hip capsule.
Figure 1C: Short Axis View (SAX) Transducer Placement
The transducer is placed in a transverse plane over the rectus femoris muscle belly at mid femur Sweep the transducer up proximally towards the origin of the rectus femoris. This transducer placement will be perpendicular to the femoral shaft. While sweeping please note the rectus femoris muscle belly is getting smaller in cross section. After locating the femoral head, then sweep slightly medially and superiorly
The scanning protocol for the iliopsoas includes 2 planes of transducer placement.
• Transverse Plane: The transducer is placed parallel to the inguinal ligament to identify the femoral vessels, then moved laterally to locate the iliopsoas muscle.
• Longitudinal Plane: The transducer is aligned along the muscle fibers to assess the muscle and tendon continuity.
By gradually moving the transducer distally, the practitioner can follow the iliopsoas tendon as it passes beneath the inguinal ligament to its insertion at the lesser trochanter. Dynamic assessment, such as asking the patient to flex the hip against resistance, can help visualize tendon movement and identify snapping or other abnormalities. Doppler imaging may be utilized to assess hyperemia, which can indicate active inflammation.
• Normal Anatomy: The iliopsoas muscle appears as a hypoechoic (darker) striated structure with internal echogenic (brighter) fibrous septa typical of a muscle.12 The tendon is more echogenic and is best visualized near its insertion on the lesser trochanter
• Dynamic Assessment: Active or passive movements can be performed to assess for snapping phenomena or to evaluate muscle function. MSK-US is ideally suited for dynamic assessment of muscles and tendons around the hip during motion and has been used to demonstrate correlation between abnormal iliopsoas tendon motion and painful snapping.13
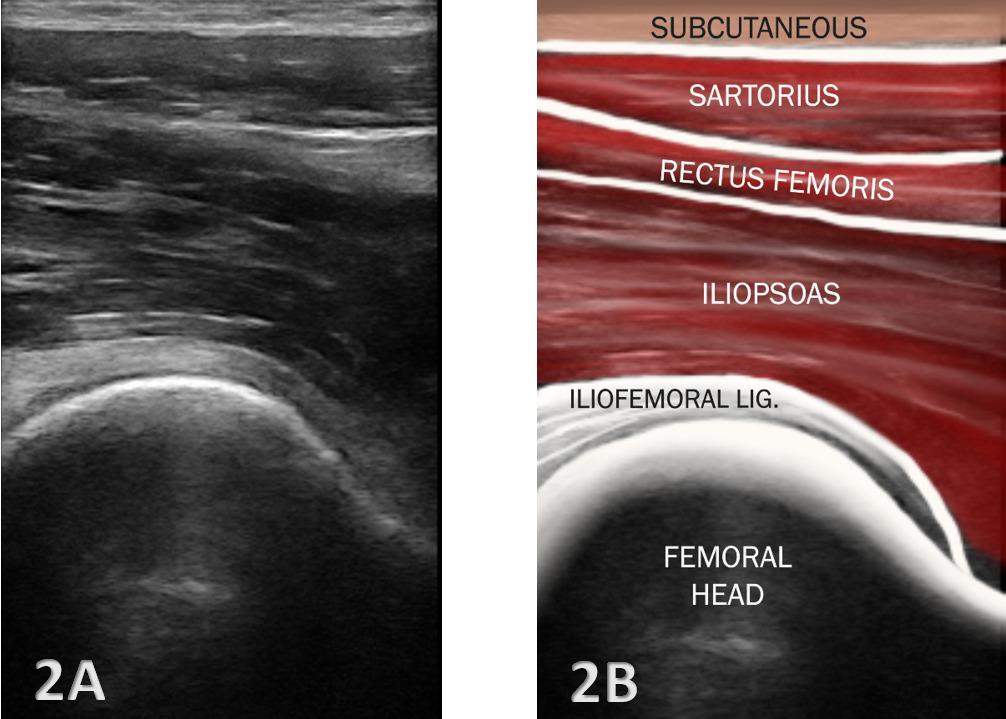
Figures: 2A and 2B
The bony landmark of the acetabulum is a linear cortical margin, as opposed to the sharp peak seen with the hip capsule image. The convexity of the femoral head is distal/ right of the acetabulum. The hip capsule/ligament complex is a hypoechoic interface following the bony contour The hyperechoic fibrous echotexture of the psoas tendon is superficial to the capsule. The hypoechoic muscle fibers of the psoas major and iliacus muscles are adjacent the hyperechoic tendon. The sartorius muscle is the most superficial interface.
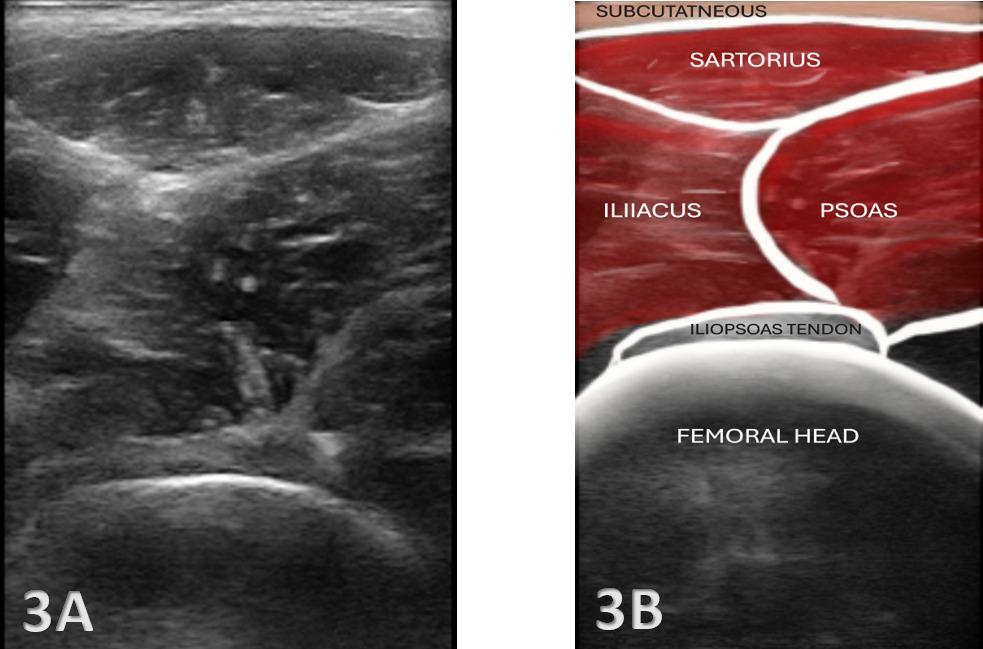
Figures: 3A and 3B
The iliopsoas region is evaluated by moving the transducer in the transverse plane over the femoral head. The anterior inferior iliac spine (AIIS) is visualized when moving superior The transducer can be moved inferiorly until the iliopsoas tendon comes into view and toggling the transducer may visualize the tendon as hyperechoic and sitting over the femoral head and acetabulum. Medial to the hip joint lies the femoral vasculature (nerve, artery, vein, empty space, lymphatic). The bony landmark of the hip bone is linear/scalloping cortical margin. The hyperechoic, bristle-like pattern of the psoas tendon is adjacent to the bony reflection. The hypoechoic muscles: psoas major and iliacus are superficial to the tendon. The sartorius can be visualized as the superior structure.
COMMON PATHOLOGICAL FINDINGS AND CLINICAL IMPLICATIONS
MSK-US is highly effective in identifying a range of iliopsoas pathologies, including:
• Tendinitis/Tendinopathy: Thickening of the iliopsoas tendon, hypoechoic changes, and increased Doppler signal may indicate tendinitis or tendinopathy Clinical implications focus upon the dentification of tendinopathy which guides the rehabilitation
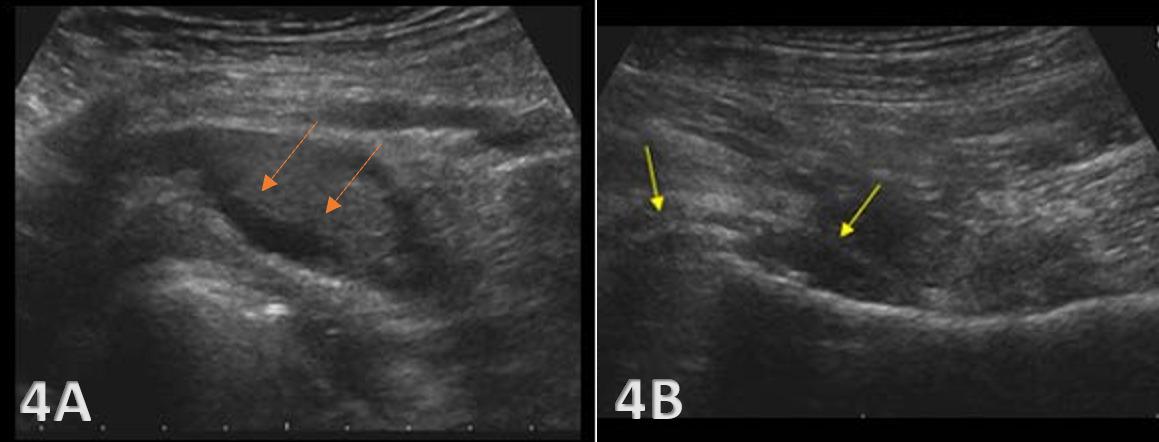
PATHOLOGY: Bursitis and Joint Effusion
Figures 4A and 4B: LAX View
Iliopsoas bursa filled with fluid and thickened
focused on eccentric strengthening and load management.
• Snapping Hip Syndrome: Dynamic ultrasound can capture the snapping of the iliopsoas tendon over the iliopectineal eminence, which is commonly seen in patients with internal snapping hip syndrome.5,6 The clinical implication for rehabilitation focuses on muscle flexibility, strength balance, and motor control exercises.
• Bursitis: Iliopsoas bursitis may present as an anechoic or hypoechoic fluid collection between the iliopsoas tendon and the hip joint capsule. The bursa originates at the level of the femoral head and typically extends medially and possibly deep to the psoas major tendon and iliopsoas tendon.13 An iliopsoas bursitis will present as hip and groin pain. Bursal distensions rarely produce compression neuropathy of the femoral nerve; however, large distensions may extend into the pelvis along the iliacus muscle and may displace the pelvis structures.14 Management includes anti-inflammatory strategies and ultrasoundguided bursal injections.
• Muscle Strain: Hypoechoic or mixed echogenic areas within the iliacus or psoas major may indicate muscle strain or partial tears, often associated with athletic overuse. Ultrasound findings can help tailor rehabilitation programs addressing muscle imbalances and joint mechanics. For example, changes in tendon thickness or echotexture can be tracked over time to assess the effectiveness of therapeutic interventions.
MSK-US findings should be integrated into a comprehensive rehabilitation plan including exercise, injections, and monitoring.
• Targeted Interventions: Use guided injections for bursitis or tendinopathy and implement specific therapeutic exercises to address biomechanical deficits.
• Progress Monitoring: Serial MSK-US assessments to evaluate the effectiveness of interventions.
• Collaborative Care: Enhance interdisciplinary collaboration by providing detailed imaging reports to referring providers.
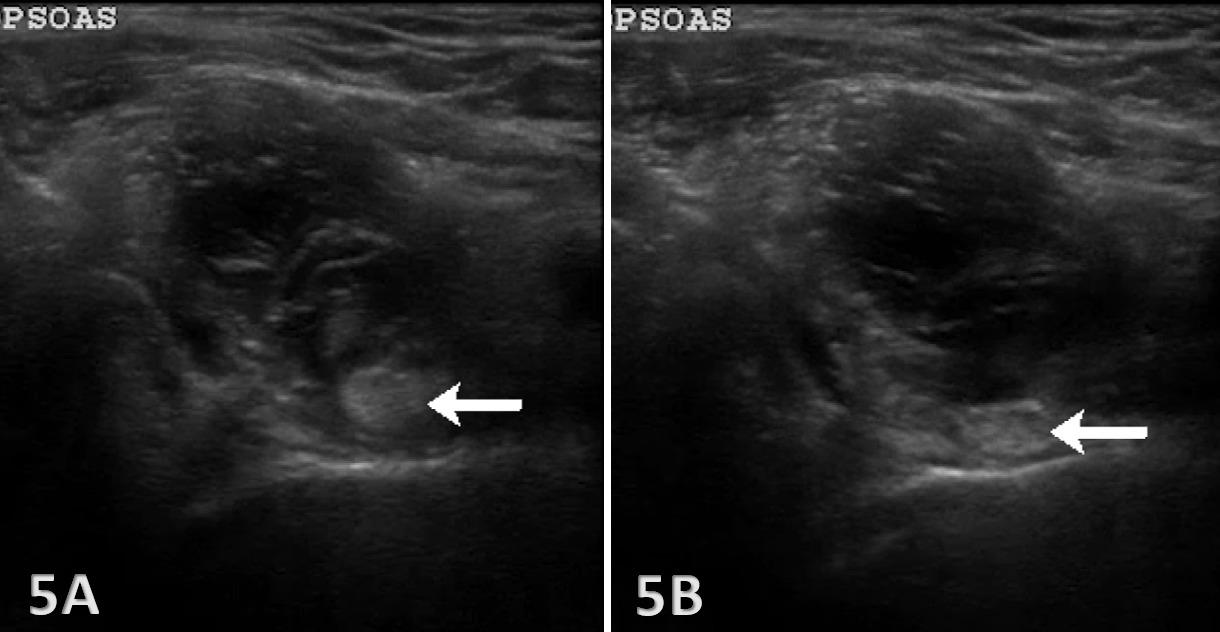
PATHOLOGY: Snapping Psoas Syndrome
Figures 5A and 5B: SAX View Snapping psoas syndrome, also known as internal snapping hip syndrome or Coxa Saltans, is a condition that occurs when the iliopsoas tendon in the hip snaps over bony structures in the hip joint. A dynamic assessment can be performed on the patient with the transducer held in a SAX position and the patient’s involved hip is moved from a flexed, externally rotated, and abducted position and returned to neutral. The hyperechoic psoas tendon, as shown above with the white arrows, is seen “snapping over” the anterior femoral head and moving abruptly from the elevated position (5A) to the lower position (5B).
Diagnostic MSK-US is a powerful, dynamic imaging modality for evaluating the iliopsoas complex in patients with anterior hip pain. Its ability to provide real-time visualization of soft tissue structures, evaluate tendon movement, and identify pathological changes makes it an ideal tool for rehabilitation providers. By integrating MSK-US into clinical practice, practitioners can enhance the accuracy of diagnosis, tailor rehabilitation interventions, and improve patient outcomes in individuals with iliopsoas-related hip pain. Ultrasound-guided interventions, such as dry needling or corticosteroid injections, can be performed with increased accuracy under direct visualization. MSK-US also facilitates the monitoring of treatment progress. Rehabilitation providers can use ultrasound findings to make informed decisions about progression through stages of rehabilitation, return to sport, or modifications in exercise prescription. As technology advances, further research is warranted to expand MSK-US applications and refine diagnostic criteria, potentially transforming rehabilitation practices focused on hip pathologies.
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Howse AJG. Orthopaedists aid ballet. Clin Orthop Relate Res 1972;89:52-63. doi:10.1097/ 00003086-197211000-00008
2. Yean C, Chao-Yin C, Chung LW, et al. Measurement of psoas major correlating with functional performance in asymptomatic adults - an MRI and ultrasound study Ex Sport Movement 2023;1(4):1-7 doi:10.1249/ESM.0000000000000016
3. Hamaguchi Y, Kaido T, Okumura S, et al. Proposal for a new diagnostic criteria for low skeletal muscle mass based on computed tomography imaging in Asian adults. Nutrition. 2016;31(11-12):1200-1205. doi:10.1016/j.nut.2016.04.003
4. Lawlor MA, Oliveto JM, Geske JA, Khandalavala BN. Computerized tomography derived psoas muscle indices in a healthy young population in the United States. J Frailty Sarcopenia Falls 2022;7(1):38-46. doi:10.22540/JFSF-07-038
5. Schaberg JE, Harper MC, Allen WC. The snapping hip syndrome. Am J Sports Med 1984;5:361-365. doi:10.1177/036354658401200504
6. Lyons CJ, Peterson LFA. The snapping iliopsoas tendon. Mayo Clin Proc 1984;59:327-365. doi:10.1016/S0025-6196(12)61428-1
7. Vaccaro JP, Sauser DD, Beals RD. Iliospoas bursa imaging: efficacy in depicting abnormal iliopsoas tendon motion in patients with internal snapping hip syndrome. Radiolgy. 1995;197:853-856.
8. King AD, Hine AL, McDonald C, Abrahams P The ultrasound appearance of the normal psoas muscle. Clin Rad. 1993;48(5):316-318. doi:10.1016/ S0009-9260(05)81238-3
9. Pelsser V, Cardinal E, Hobden R, Aubin B, Lafortune M. Extraarticular snapping hip: Sonographic findings. AJR Am J Roentgenol 2001;176:67-73. doi:10.2214/ajr.176.1.1760067
10. Cardinal E, Buckwalter KA, Capello WN, et al. Ultrasound of the snapping iliopsoas tendon. Radiology 1996;198:521-522. doi:10.1148/ radiology.198.2.8596860
11. Hashimoto BE, Green TM, Wiitala L. Ultrasonographic diagnosis of hip snapping related to iliopsoas tendon. J Ultrasound Med. 1997;16:433-435. doi:10.7863/jum.1997.16.6.433
12. Janzen DL, Partridge E, Logan M, Connell DG, Duncan CP The snapping hip: clinical and imaging findings in transient subluxation of the iliopsoas tendon. Can Assoc Radiol J 1996;47:202-208.
13. Jacobson JA. Fundamentals of Musculoskeletal Ultrasound. 3rd ed. Elsevier; 2018. doi:10.1016/ B978-1-4557-3818-2.00003-3
14. McNally E. Practical Musculoskeletal Ultrasound 2nd ed. Churchill Livingstone. Elsevier; 2014.

Editorial
Stitelmann A, Gard S, Coen SE, et al. Beyond the Menstrual Cycle: Time for
Anna Stitelmann1,2 , Suzanne Gard2,3,4 , Stephanie E. Coen5 , Joanne Parsons6 , Amy Arundale7 , Loic Bel8,9 , Florian Forelli4,10,11,12
1 Department of Orthopedic Surgery and Traumatology of the Musculoskeletal System, Geneva University Hospitals, 1205 Geneva, Switzerland, 2 Geneva School of Health Sciences, HES-SO University of Applied Sciences and Arts Western Switzerland, 1202 Geneva, Switzerland, 3 Centre SportAdo, Hospital of Lausanne, Lausanne, Switzerland, 4 International Federation of Sport Physical Therapy, Switzerland, 5 School of Geography, University of Nottingham, Nottingham, Nottinghamshire, UK, 6 College of Rehabilitation Sciences, University of Manitoba, Winnipeg, Manitoba, Canada, 7 Department of Rehabilitation, Icahn School of Medicine at Mount Sinai Health System, 8 Movare, Bulle, Switzerland, 9 Amsterdam Collaboration for Health and Safety in Sports, Department of Public and Occupational Health, Amsterdam Movement Sciences, Amsterdam University Medical Centers, Location VU University Medical Center, Amsterdam, The Netherlands, 10 Orthosport Rehab Center, Domont, France, 11 Orthopaedic Surgery Department, Clinic of Domont, Ramsay Healthcare, @OrthoLab, Domont, France, 12 SFMK Lab, Pierrefite sur seine, France https://doi.org/10.26603/001c.126285
Vol. 19, Issue 12, 2024
Gender differences in athlete performance and injury risk are often scrutinized through the narrow lens of the menstrual cycle. Basic research indicates that estrogen and progesterone levels may affect muscle function, energy metabolism, and thermoregulation1,2; however, results in vivo remain inconclusive.3‑5 While hormonal fluctuations may affect injury risk and performance for some women,6,7 we argue that it should not overshadow other important issues, such as socio-environmental or psychological factors. This article aims to broaden the awareness of the challenges faced by female athletes through an examination of the complex interplay of these factors and advocating for a more holistic approach to evaluating and supporting athlete health and performance.
Recently, the quantity of research into the menstrual cycle has increased. A recent meta-analysis suggested that the menstrual cycle may have a trivial effect on performance.5 However, the results of studies included in the meta-analysis were highly variable, and most of the included papers were of poor methodological quality, with menstrual cycle phases being estimated or assumed based on regular menstruations rather than accurately measured using validated methods for detecting ovulation and hormone levels.8,9 Therefore, even though the meta-analysis was performed, true, reliable conclusions on the effect of menstrual cycle on performance cannot be drawn.
To be clear, monitoring the menstrual cycle is a useful tool to assess the health of individual female athletes not using hormonal contraception. A regular cycle between 21 to 35 days with an ovulation and a menstrual bleeding is an indicator of good physiological function.10,11 Further, for some women menstrual cycle tracking can help them anticipate and mitigate symptoms associated with their menstrual cycle, which can improve their performance. Menstrual cycle tracking can also help identify the 50% of female athletes who experience menstrual disorders,12 which are often linked to relative energy deficiency, poor recovery, overtraining or gynecological issues. Although
the menstrual cycle itself is not conclusively associated with increased risk of injury, menstrual cycle disorders are associated with injury risk.13
It is clear that there is a lack of evidence to indicate the menstrual cycle has significant effects on the performance or injury risk of women athletes. Yet, the menstrual cycle remains a focal point in research and the media but is only one piece of the puzzle as injury risk and performance are driven by a multitude of other important factors.14,15 Focusing primarily on the menstrual cycle can result in us ignoring other critical socio-environmental and psychological factors that adversely affect women athletes.16
Female athletes operate within complex socio-environmental contexts that can profoundly impact their performance and well-being.16 For example, the lack of visibility and representation of female athletes in the media contributes to a cycle of inequality When female athletes receive less media coverage, they have fewer sponsorship opportunities, which limits their financial support and access to high-quality training resources.14,17 This disparity not only affects their current performance but also their longterm career prospects and post-retirement opportunities. It is essential to advocate for more equitable media coverage to highlight the achievements of female athletes and ensure they gain the tangible benefits from that exposure. Less funding and fewer sponsorship opportunities for women compared to men, limits their access to high-quality medical, training, and competition experiences.17,18 In football, women have less access to appropriate medical care, training and match facilities, as well as strength and conditioning support compared to their male peers.16,19 Less access to resources means less access to effective programs, such as anterior cruciate ligament injury prevention. Access to such prevention programming could have a major impact on an athlete’s entire career19; and if an injury does occur, treatment pathways can differ for women,
potentially affecting their recovery and long-term performance, independent of any physiological factors.20
Less funding and fewer resources in women’s sport has also contributed to significantly less research in women’s sport compared to men’s.21‑23 While there has been an increase in menstrual cycle research, there has not been a similar growth in training research. We need more research to understand differences between men and women in their physiological response to and experiences with training.24, 25 However, there is a drastic need for more strength and conditioning literature for female athletes.
Social support systems, including family, friends, and coaches, play a crucial role in an athlete’s career. Female athletes often juggle multiple roles, balancing their sporting ambitions with family responsibilities and gendered societal expectations.26 This juggling act can add significant stress and time constraints, which are rarely considered in performance evaluations or rehabilitation plans. Some organizations are beginning to build support systems such as on-site childcare or time for infant feeding or breast pumping, however these resources are still rare. The gendered attitudes and beliefs that remain pervasive in the sports world result in female athletes frequently facing sexism and unequal treatment27 compared to male athletes.28 These experiences not only limit the opportunities available to women but can undermine their confidence, motivation, and mental health, thereby impacting their injury risk and performance on the field.
Stakeholders, including coaches, organizations, and national governing bodies, need to be trained to recognize and address the unique challenges faced by female athletes, including the psychological and social pressures they encounter Creating a positive and supportive team culture can help female athletes feel valued and respected, enhancing their overall well-being and performance.29
Psychological well-being is critical for athlete health and performance. Female athletes are often subject to unique psychological stressors shaped by the gendered environments of sport and society For example, societal pressures regarding body image send strong messages about what women ‘should’ look like. The emphasis on physical appearance and the idealization of certain body types can lead to issues like eating disorders, which are more prevalent among female athletes.30 Female athletes recognize the benefits of resistance training for injury prevention and optimal performance, but for some the fear of being seen as “too muscular” or “too bulky” can interfere with how athletes adhere to their training program.31
In addition to body image concerns, female athletes often face psychological stressors related to balancing societal expectations about femininity and athleticism. Female athletes may feel pressured to conform to traditional gen-
der roles while also excelling in their sport, leading to a conflict of identity and increased mental strain.32
Gender discrimination, sexism, and harassment within sport present significant psychological stressors for female athletes. These stressors range from obvious forms, such as unequal pay and less media coverage, to more subtle forms, such as harassing comments/behavior or providing locker rooms with no toilets. Such experiences can diminish an athlete’s motivation and performance, as well as negatively impact their mental health.33
Moreover, the lack of female representation in coaching and leadership positions within sports organizations and governing bodies can exacerbate feelings of isolation and lack of support among female athletes. When female athletes do not see themselves represented in leadership roles, it can affect their self-confidence and aspirations.34 Mentorship from female coaches and role models can provide individual athletes with guidance, but a collective leadership effort is needed to change organizational and cultural attitudes as well as eliminate sexism and harassment.
To mitigate psychological stressors, it is important for sports organizations to implement comprehensive mental health support systems that are attuned to the gendered environments of sport. Access to sports psychologists can help athletes develop coping strategies and resilience.35 Additionally, creating a supportive team environment where female athletes feel valued and respected can significantly enhance their psychological well-being. Providing education and training for coaches, staff, and other stakeholders on the unique challenges faced by female athletes can also promote a more inclusive and supportive culture within sports.35
Looking beyond the menstrual cycle and providing interdisciplinary teams, including access to medical, strength and conditioning, sports psychologists, nutritionists, and sports trainers, who understand the gendered environments of sport, is vital to creating an equal playing field for women.
The injury risk and performance of female athletes are shaped by a multifaceted array of factors, including gendered sociocultural influences and psychological stressors. To fully support female athletes and help them achieve their highest potential, it is crucial to address these barriers head-on. Society, but especially the sporting community, must move past the narrow lens of focusing on the menstrual cycle as the key determinant of performance and injury risk in women. Embracing a comprehensive approach that considers social and psychological factors along with biological dimensions will ensure that female athletes receive the recognition and value they deserve, leveling the playing field so they can achieve the highest levels of success.
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Collins BC, Arpke RW, Larson AA, et al. Estrogen Regulates the Satellite Cell Compartment in Females. Cell Rep. 2019;28(2):368-381.e6. doi:10.1016/ j.celrep.2019.06.025
2. Oosthuyse T, Strauss JA, Hackney AC. Understanding the female athlete: molecular mechanisms underpinning menstrual phase differences in exercise metabolism. Eur J Appl Physiol 2023;123(3):423-450. doi:10.1007/ s00421-022-05090-3
3. Colenso-Semple LM, D’Souza AC, Elliott-Sale KJ, Phillips SM. Current evidence shows no influence of women’s menstrual cycle phase on acute strength performance or adaptations to resistance exercise training. Front Sports Act Living. 2023;5:1054542. doi:10.3389/fspor.2023.1054542
4. D’Souza AC, Wageh M, Williams JS, et al. Menstrual cycle hormones and oral contraceptives: a multimethod systems physiology-based review of their impact on key aspects of female physiology J Appl Physiol Bethesda Md 1985. 2023;135(6):1284-1299. doi:10.1152/ japplphysiol.00346.2023
5. McNulty KL, Elliott-Sale KJ, Dolan E, et al. The Effects of Menstrual Cycle Phase on Exercise Performance in Eumenorrheic Women: A Systematic Review and Meta-Analysis. Sports Med Auckl NZ. 2020;50(10):1813-1827 doi:10.1007/ s40279-020-01319-3
6. Hayward E, Akam L, Hunter D, Mastana S. Role of the Menstrual Cycle on Performance and Injury Risk: A Survey of Female Professional Rugby Players in the United Kingdom. Int J Environ Res Public Health. 2024;21(2):150. doi:10.3390/ijerph21020150
7 Legerlotz K, Nobis T Insights in the Effect of Fluctuating Female Hormones on Injury Risk—Challenge and Chance. Front Physiol 2022;13:827726. doi:10.3389/fphys.2022.827726
8. Burden RJ, Altini M, Ferrer E, et al. Measure do not guess: a call to action to end assumed and estimated menstrual cycle phases in research. BMJ Open Sport Exerc Med. 2024;10(2):e002095. doi:10.1136/ bmjsem-2024-002095
9. Elliott-Sale KJ, Minahan CL, de Jonge XAKJ, et al. Methodological Considerations for Studies in Sport and Exercise Science with Women as Participants: A Working Guide for Standards of Practice for Research on Women. Sports Med Auckl NZ. 2021;51(5):843-861. doi:10.1007/s40279-021-01435-8
10. Itriyeva K. The normal menstrual cycle. Curr Probl Pediatr Adolesc Health Care 2022;52(5):101183. doi:10.1016/j.cppeds.2022.101183
11. Popat VB, Prodanov T, Calis KA, Nelson LM. The Menstrual Cycle A Biological Marker of General Health in Adolescents. Ann N Y Acad Sci. 2008;1135:43-51. doi:10.1196/annals.1429.040
12. De Souza MJ, Toombs RJ, Scheid JL, O’Donnell E, West SL, Williams NI. High prevalence of subtle and severe menstrual disturbances in exercising women: confirmation using daily hormone measures. Hum Reprod Oxf Engl. 2010;25(2):491-503. doi:10.1093/ humrep/dep411
13. Mountjoy M, Ackerman KE, Bailey DM, et al. 2023 International Olympic Committee’s (IOC) consensus statement on Relative Energy Deficiency in Sport (REDs). Br J Sports Med 2023;57(17):1073-1097 doi:10.1136/bjsports-2023-106994
14. Martin D, Timmins K, Cowie C, et al. Injury Incidence Across the Menstrual Cycle in International Footballers. Front Sports Act Living. 2021;3:616999. doi:10.3389/fspor.2021.616999
15. Martínez-Fortuny N, Alonso-Calvete A, Da CuñaCarrera I, Abalo-Núñez R. Menstrual Cycle and Sport Injuries: A Systematic Review. Int J Environ Res Public Health 2023;20(4):3264. doi:10.3390/ijerph20043264
16. Parsons JL, Coen SE, Bekker S. Anterior cruciate ligament injury: towards a gendered environmental approach. Br J Sports Med 2021;55(17):984-990. doi:10.1136/bjsports-2020-103173
17. Fink JS. Female athletes, women’s sport, and the sport media commercial complex: Have we really “ come a long way, baby”? Sport Manag Rev 2015;18(3):331-342. doi:10.1016/j.smr.2014.05.001
18. Meier HE, Konjer MV, Krieger J. Women in International Elite Athletics: Gender (in)equality and National Participation. Front Sports Act Living. 2021;3:709640. doi:10.3389/fspor.2021.709640
19. Horan D, Delahunt E, Roe M, Hägglund M, Blake C, Kelly S. ‘More than likely the men come first. That’s just very frustrating’. A qualitative exploration of contextual factors affecting the implementation of injury prevention initiatives and the provision of effective injury management in elite-level women’s club football in Ireland. Br J Sports Med 2024;58(2):89-96. doi:10.1136/bjsports-2022-106548
20. Collins JE, Katz JN, Donnell-Fink LA, Martin SD, Losina E. Cumulative Incidence of ACL Reconstruction After ACL Injury in Adults: Role of Age, Sex, and Race. Am J Sports Med. 2013;41(3):544-549. doi:10.1177/0363546512472042
21. Cowan SM, Kemp JL, Ardern CL, et al. Sport and exercise medicine/physiotherapy publishing has a gender/sex equity problem: we need action now! Br J Sports Med 2023;57(7):401-407 doi:10.1136/ bjsports-2022-106055
22. Cowley ES, Olenick AA, McNulty KL, Ross EZ. “Invisible Sportswomen”: The Sex Data Gap in Sport and Exercise Science Research. Women Sport Phys Act J. 2021;29(2):146-151. doi:10.1123/wspaj.2021-0028
23. Smith ES, McKay AKA, Kuikman M, et al. Auditing the Representation of Female Versus Male Athletes in Sports Science and Sports Medicine Research: Evidence-Based Performance Supplements. Nutrients 2022;14(5):953. doi:10.3390/nu14050953
24. Bartolomei S, Grillone G, Di Michele R, Cortesi M. A Comparison between Male and Female Athletes in Relative Strength and Power Performances. J Funct Morphol Kinesiol. 2021;6(1):17. doi:10.3390/ jfmk6010017
25. Landen S, Hiam D, Voisin S, Jacques M, Lamon S, Eynon N. Physiological and molecular sex differences in human skeletal muscle in response to exercise training. J Physiol 2023;601(3):419-434. doi:10.1113/ JP279499
26. McGannon KR, McMahon J, Gonsalves CA. Juggling motherhood and sport: A qualitative study of the negotiation of competitive recreational athlete mother identities. Psychol Sport Exerc 2018;36:41-49. doi:10.1016/j.psychsport.2018.01.008
27. Biram MD. Mermaids in the land of the king: an ethnography of Santos FC women. Movimento 2021;27:e27005. doi:10.22456/1982-8918.109357
28. Cooky C, Messner MA, Musto M. “It’s Dude Time!”: A Quarter Century of Excluding Women’s Sports in Televised News and Highlight Shows. Commun Sport. 2015;3(3):261-287. doi:10.1177/ 2167479515588761
29. Banwell J, Kerr G. Coaches’ Perspectives on their Roles in Facilitating the Personal Development of Student-Athletes. Can J High Educ. 2016;46(1):1-18. doi:10.47678/cjhe.v46i1.185109
30. Sundgot-Borgen J, Torstveit MK. Prevalence of Eating Disorders in Elite Athletes Is Higher Than in the General Population. Clin J Sport Med 2004;14(1):25-32. doi:10.1097/ 00042752-200401000-00005
31. Roth RI, Knapp BA. Gender Negotiations of Female Collegiate Athletes in the Strength and Conditioning Environment. Women Sport Phys Act J. 2017;25(1):50-59. doi:10.1123/wspaj.2015-0049
32. Krane V, Choi PYL, Baird SM, Aimar CM, Kauer KJ. Living the Paradox: Female Athletes Negotiate Femininity and Muscularity Sex Roles 2004;50(5/ 6):315-329. doi:10.1023/B:SERS.0000018888.48437.4f
33. Cooky C, Messner MA, Hextrum RH. Women Play Sport, But Not on TV: A Longitudinal Study of Televised News Media. Commun Sport 2013;1(3):203-230. doi:10.1177/2167479513476947
34. Sartore-Baldwin M, Warner S. Perceptions of justice within intercollegiate athletics among current and former athletes. Journal of Issues in Intercollegiate Athletics 2012;5:269-282.
35. Reardon CL, Factor RM. Sport Psychiatry: A Systematic Review of Diagnosis and Medical Treatment of Mental Illness in Athletes. Sports Med. 2010;40(11):961-980. doi:10.2165/ 11536580-000000000-00000