I J S PT






so have we.







so have we.

Deep Tissue Laser Therapy™ is used to treat painful muscles and joints associated with acute and chronic soft tissue injuries. It is also indicated for helping relieve pain and stiffness associated with osteoarthritis.

DEEP TISSUE LASER THERAPY™ HAS BEEN CLINICALLY STUDIED TO HELP IN THE TREATMENT OF: •
Request a Demo Today at learn.chattanoogarehab.com/ijspt-feb-23-journal-quote

Deliver precise care. Engage patients with real-time injury monitoring and biofeedback assessment, and guide interventions for accuracy.
Learn more
Rx only (USA). For use by trained healthcare practitioners.
(For UK & EU countries) Butterfly iQ+ is a Class IIa portable ultrasound system designed for ultrasound imaging by trained healthcare professionals. Carefully read and understand all cautions, warnings and operational instructions prior to use.
(For AUS) Butterfly iQ+ is a Class IIa portable ultrasound system designed for ultrasound imaging by trained healthcare professionals. This product is not available for purchase by the general public. Carefully read and understand all cautions, warnings and operational instructions prior to use.
(For CAN) For healthcare professionals only. Réservé aux professionnels de santé. Not all presets, imaging modes and features are available everywhere. Check for availability in your country.

Board of Directors / Business Advisory Board
Turner A Blackburn, APTA Life Member, AT-Ret, AOSSM-Ret President
Mary Wilkinson Executive Director
Michael Voight Executive Editor and Publisher
Joe Black, PT, DPT, SCS, ATC
Eric Fernandez
Jay Greenstein, DC
Skip Hunter, PT, ATC-Ret
Russ Paine, PT, DPT
Mike Reinold, PT, DPT, SCS, ATC, CSCS, C-PS
Tim Tyler, PT, ATC
Sports Legacy Advisory Board
Turner A. Blackburn, PT, ATC
George Davies, PT, DPT, MEd, SCS, ATC, LAT, CSCS, PES, FAPTA
Terry Malone, PT, PhD
Bob Mangine, PT
Barb Sanders, PT, PhD
Tim Tyler, PT, ATC
Kevin Wilk, PT, DPT, FAPTA
Staff
Executive Editor/Publisher
Michael L. Voight, PT, DHSc, OCS, SCS, ATC, CSCS Executive Director/Operations and Marketing
Mary Wilkinson
Editor in Chief
Barbara Hoogenboom, PT, EdD, SCS, ATC Managing Editor
Ashley Campbell, PT, DPT, SCS, CSCS Manuscript Coordinator
Casey Lewis, PTA, ATC
Publisher
Contact Information
International Journal of Sports Physical Therapy 6011 Hillsboro Pike Nashville, TN 37215, US, http://www.ijspt.org
IJSPT is a bimonthly publication, with release dates in February, April, June, August, October and December.
ISSN 2159-2896
Founding Sponsors
Arthrex
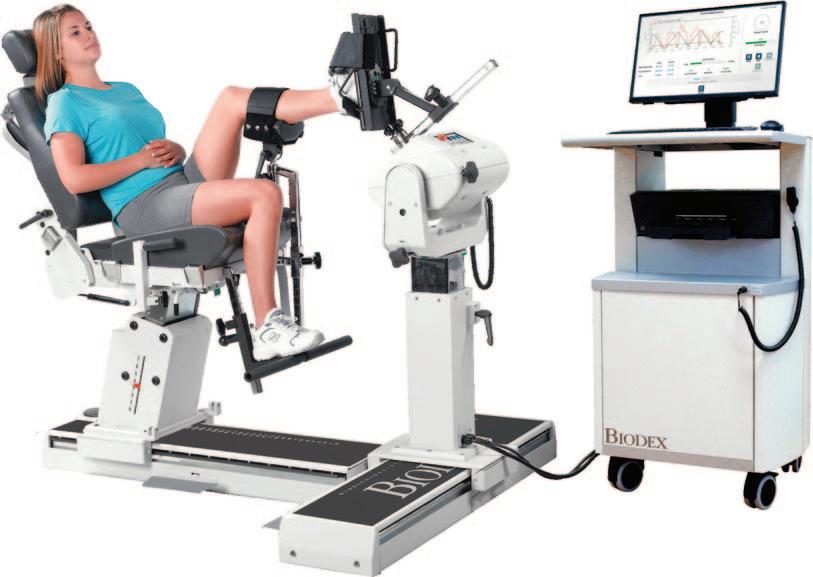
Biodex
Butterly IQ
Digitsole
DJO Global Exertools
Foot Levelers
Hydroworx
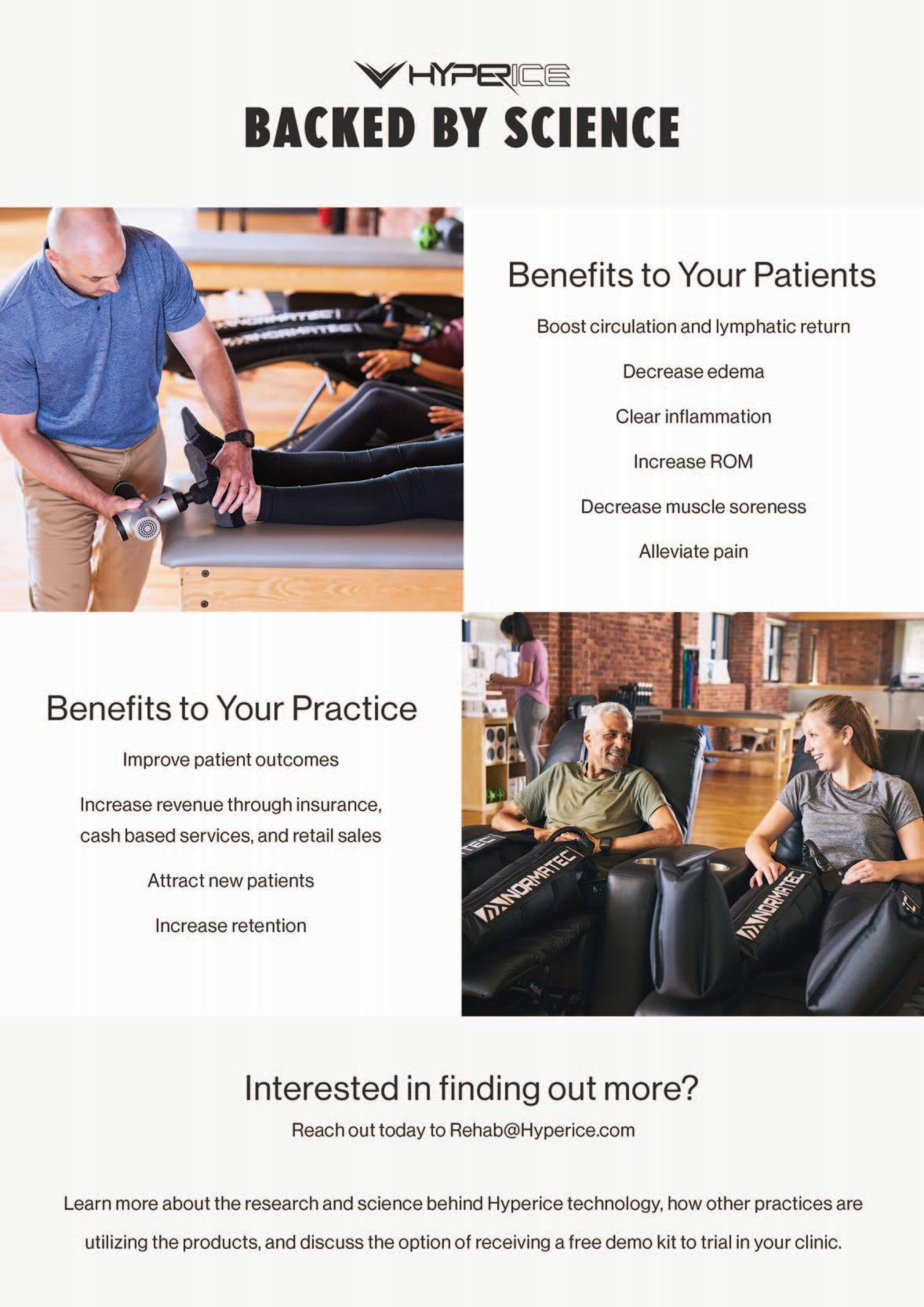
Hyperice
PT Genie
Trazer
Woodway
Gold Sponsors
Hawkgrips
Squid
Structure + Function Education
Winback
IJSPT is an official journal of the International Federation of Sports Physical Therapy (IFSPT) Countries with access to IJSPT as a member benefit:
Argentina
Australia
Austria
Belgium
Bulgaria
Brazil
Cameroon
Canada
Chile
Cyprus
Denmark
Finland
France
Germany
Greece
Hong Kong
Indonesia
Ireland
Israel
Italy
Japan
Luxembourg
The Netherlands
New Zealand
Nigeria
Norway
Poland
Portugal
Reach us at www.ifspt.org.
Saudi Arabia
Slovenia
South Africa
South Korea
Spain
Sweden
Switzerland
Thailand
Turkey
United Kingdom
Zambia
IJSPT is an official journal of the ICCUS Society for Sports Rehabilitation. www.iccus.org


The IJSPT Editorial Board is pleased to announce the winners of the 2022 awards.
The selection process: All 2022 published papers in each category are considered, and the award is determined by a jury of IJSPT editorial board members. These awards were established to encourage submission of high-quality manuscripts that ultimately add to our current body of knowledge.
Awards will be presented at the Hyperice/IJSPT booth, number 1307, at APTA
Combined Sections
Meeting on Friday, February 24, from 1:30 to 2:00 PM.
Arthrex®-IJSPT Best MD-PT Collaboration Manuscript

Isometric Knee Strength is Greater in Individuals who Score Higher on Psychological Readiness to Return to Sport after Primary Anterior Cruciate Ligament Reconstruction. Sugarman BS, et al. Volume 17, Number 7
IJSPT Best Case Report
The Effect of Blood Flow Restriction Therapy on Shoulder Function Following Shoulder Stabilization Surgery: A Case Series.
McGinniss JH, et al (series). Volume 17, Number 6.
IJSPT Best Original Research
Don’t Peak Too Early: Evidence for an ACL Injury Prevention Mechanism of the FIFA-11+ Program.
Sigurosson HB, et al. Volume 17, Number 5.
IJSPT Best Systematic Review / Meta-Analysis
Effective Interventions for Improving Functional Movement Screen Scores Among “High-Risk” Athletes: A Systematic Review.
Clark SC, et al. Volume 17, Number 2
Lee H. Diehl, MD; Jocelyn R. Wittstein, MD; Jonathan C. Riboh, MD; Alison P. Toth, MD; Annunziato Amendola, MD; Dean C. Taylor, MD. Duke and OrthoCarolina
New prospective, randomized trial data confirm that patients with InternalBrace ligament repair can participate in an accelerated rehabilitation protocol with an average return to pre-injury level of play of 13.3 weeks versus 17.5 weeks with standard repair.1
The InternalBrace procedure gives patients the flexibility to move freely while protecting the primary repair by limiting abnormal or excessive lateral movement during the healing process.

InternalBrace surgical technique is intended only to support the primary repair and is not intended as a replacement for the standard of care using biologic augmentation in a primary repair. InternalBrace surgical technique is intended only for soft-tissue-to-bone fixation and is not cleared for bone-to-bone fixation.






Executive Editor/Publisher
Michael L. Voight, PT, DHSc, OCS, SCS, ATC, CSCS
Belmont University
Nashville, Tennessee – USA
Editor in Chief
Barbara Hoogenboom, PT, EdD, SCS, ATC
Grand Valley State University
Grand Rapids, Michigan - USA
Managing Editor
Ashley Campbell, PT, DPT, SCS, CSCS
Nashville Sports Medicine and Orthopaedic Center
Nashville, Tennessee – USA
Manuscript Coordinator
Casey Lewis, PTA, ATC
Nashville Sports Medicine and Orthopaedic Center
Nashville, Tennessee – USA
Executive Director/Marketing
Mary Wilkinson
Indianapolis, Indiana – USA
Editors
Robert Manske PT, DPT, Med, SCS, ATC, CSCS
University of Wichita
Wichita, KS, USA
Terry Grindstaff, PT, PhD, ATC, SCS, CSCS
Creighton University
Omaha, NE, USA
Phil Page PT, PhD, ATC, CSCS
Franciscan University DPT Program
Baton Rouge, LA, USA
Kevin Wilk PT, DPT, FAPTA
Clinical Viewpoint Editor
Champion Sports Medicine
Birmingham, AL, USA
International Editors
Luciana De Michelis Mendonça, PT, PhD
UFVJM
Diamantina, Brazil
Colin Paterson PT, MSc PGCert(Ed), MCSP, RISPT, SFHEA
University of Brighton
Brighton, England, UK
Chris Napier, PT, PhD
Clinical Assistant Professor
University of British Coumbia, Vancouver, BC, Canada
Nicola Phillips, OBE, PT, PhD, FCSP
Professor School of Healthcare Sciences
Cardiff University, Cardiff, Wales, UK
Associate Editors
Eva Ageberg, PT, PhD
Professor, Lund University
Lund, Sweden
Lindsay Becker, PT, DPT, SCS, USAW
Buckeye Performance Golf
Dublin, Ohio, USA
Keelan Enseki, PT, MS, OCS, SCS, ATC
University of Pittsburgh
Pittsburgh, PA, USA
John Heick, PT, PhD, DPT, OCS, NCS, SCS
Northern Arizona University
Flagstaff, AZ, USA
Julie Sandell Jacobsen, MHSc, PhD
VIA University
Aarhus, Denmark
RobRoy L. Martin, PhD, PT, CSCS
Duquesne University
Pittsburgh, PA, USA
Andrea Mosler, PhD, FACP, FASMF
La Trobe Sport and Exercise Medicine Research
Centre, School of Allied Health, Human Services and Sport, La Trobe University
Melbourne, Victoria, Australia
Brandon Schmitt, DPT, ATC
PRO Sports Physical Therapy
Scarsdale, NY, USA
Barry Shafer, PT, DPT Elite Motion Physical Therapy
Arcadia, CA, USA
Laurie Stickler, PT, DHSc, OCS
Grand Valley State University
Grand Rapids, MI, USA
Editorial Board
James Andrews, MD
Andrews Institute & Sports Medicine Center
Gulf Breeze, AL, USA
Amelia (Amy) Arundale, PT, PhD, DPT, SCS
Red Bull/Ichan School of Medicine
Salzburg, Austria/New York, NY, USA
Gary Austin, PT PhD
Belmont University
Nashville, TN, USA
Roald Bahr, MD
Oslo Sports Trauma Research Center
Oslo, Norway
Lane Bailey, PT, PhD
Memorial Hermann IRONMAN Sports Medicine Institute
Houston, Texas, USA
Gül Baltaci, PT,Ph.D. Professor, CKTI, FACSM
Private Guven Hospital
Ankara, Turkey
Asheesh Bedi, MD
University of Michigan
Ann Arbor, MI, USA
David Behm, PhD
Memorial University of Newfoundland
St. John's, Newfoundland, Canada
Barton N. Bishop, PT, DPT, SCS, CSCS
Kaizo Clinical Research Institute
Rockville, Maryland, USA
Mario Bizzini, PhD, PT
Schulthess Clinic Human Performance Lab
Zürich, Switzerland
Joe Black, PT, DPT, SCS, ATC
Total Rehabilitation
Maryville, Tennesse, USA
Turner A. "Tab" Blackburn, APTA Life Member, ATC-Ret, AOSSM-Ret
NASMI
Lanett, AL, USA
Lori Bolgla, PT, PhD, MAcc, ATC
Augusta University
Augusta, Georgia, USA
Matthew Briggs
The Ohio State University
Columbus, OH, USA
Tony Brosky, PT, PhD
Bellarmine University
Louisville, KY, USA
Brian Busconi, MD
UMass Memorial Hospital
Boston, MA, USA
Robert J. Butler, PT, PhD
St. Louis Cardinals
St. Louis, MO, USA
Duane Button, PhD
Memorial University
St. Johns, Newfoundland, Canada
J. W. Thomas Byrd, MD
Nashville Sports Medicine and Orthopaedic Center
Nashville, TN, USA
Lyle Cain, MD
Andrews Institute & Sports Medicine Center
Birmingham, AL, USA
Gary Calabrese, PT, DPT
Cleveland Clinic
Cleveland, Ohio, USA
Meredith Chaput, PT, DPT, SCS
Ohio University
Athens, OH, USA
Rita Chorba, PT, DPT, MAT, SCS, ATC, CSCS
United States Army Special Operations Command
Fort Campbell, KY, USA
John Christoferreti, MD
Texas Health
Dallas, TX, USA
Richard Clark, PT, PhD
Tennessee State University
Nashville, TN, USA
Juan Colado, PT, PhD
University of Valencia
Valencia, Spain
Brian Cole, MD
Midwest Orthopaedics at Rush
Chicago, IL, USA
Ann Cools, PT, PhD
Ghent University
Ghent, Belgium
Andrew Contreras, DPT, SCS
Washington, DC, USA
George Davies, PT, DPT, MEd, SCS, ATC, LAT, CSCS, PES, FAPTA
Georgia Southern University
Savannah, Georgia, USA
Pete Draovich, PT
Jacksonville Jaguars Footbal
Jacksonvile, FL, USA
Jeffrey Dugas, MD
Andrews Institute & Sports Medicine Center
Birmingham, AL, USA
Jiri Dvorak, MD
Schulthess Clinic
Zurich, Switzerland
Todd Ellenbecker
Rehab Plus
Phoenix, AZ, USA
Carolyn Emery, PT, PhD
University of Calgary
Calgary, Alberta, Canada
Ernest Esteve Caupena, PT, PhD
University of Girona
Girona, Spain
Sue Falsone, PT, MS, SCS, ATC, CSCS, COMT
Structure and Function Education and A.T. Still University
Phoenix, Arizona, USA
J. Craig Garrison, PhD, PT, ATC, SCS
Texas Health Sports Medicine
Fort Worth, Texas, USA
Maggie Gebhardt, PT, DPT, OCS, FAAOMPT Fit Core Physical Therapy/Myopain Seminars
Atlanta, GA and Bethesda, MD, USA
Lance Gill, ATC
LG Performance-TPI
Oceanside, CA, USA
Phil Glasgow, PhD, MTh, MRes, MCSP
Sports Institute of Northern Ireland
Belfast, Northern Ireland, UK
Robert S. Gray, MS, AT
Cleveland Clinic Sports Health
Cleveland, Ohio, USA
Jay Greenstein, DC
Kaizo Health
Baltimore, MD, USA
Martin Hagglund, PT PhD
Linkoping University
Linkoping, Sweden
Allen Hardin, PT, SCS, ATC, CSCS
University of Texas
Austin, TX, USA
Richard Hawkins, MD
Professor of surgery, University of South Carolina
Adjunct Professor, Clemson University
Principal, Steadman Hawkins, Greenville and Denver (CU)
John D.Heick, PT, PhD, DPT, OCS, NCS, SCS
Northern Arizona University
Flagstaff, AZ, USA
Tim Hewett, PhD
Hewett Consulting
Minneapolis, Minnesota, USA
Per Hølmich, MD
Copenhagen University Hospital
Copenhagen, Denmark
Kara Mae Hughes, PT, DPT, CSCS
Wolfe PT
Nashville, TN, USA
Lasse Ishøi, PT, MSc
Sports Orthopedic Research Center
Copenhagen University Hospital
Hvidovre, Denmark
Jon Karlsson, MD
Sahlgrenska University
Goteborg, Sweden
Brian Kelly, MD Hospital for Special Surgery
New York, NY, USA
Benjamin R. Kivlan, PhD, PT, OCS, SCS
Duquesne University
Pittsburgh, PA, USA
Dave Kohlrieser, PT, DPT, SCS, OCS, CSCS
Ortho One
Columbus, OH, USA
Andre Labbe PT, MOPT
Tulane Institute of Sports Medicine
New Orleans, LA USA
Henning Langberg, PT, PhD
University of Copenhagen
Copenhagen, Denmark
Robert LaPrade, MD
Twin Cities Orthopedics
Edina, MN, USA
Lace Luedke, PT, DPT
University of Wisconsin Oshkosh
Oshkosh, WI, USA
Lenny Macrina, PT, SCS, CSCS, C-PS
Champion Physical Therapy and Performance
Boston, MA, USA
Phillip Malloy, PT, PhD
Arcadia University/Rush University Medical Center
Glenside, PA and Chicago, IL, USA
Terry Malone, PT, EdD, ATC, FAPTA
University of Kentucky
Lexington, KY, USA
Robert Mangine, PT
University of Cincinnati
Cincinnati, OH, USA
Eric McCarty, MD
University of Colorado
Boulder, CO, USA
Ryan P. McGovern, PhD, LAT, ATC
Texas Health Sports Medicine Specialists
Dallas/Fort Worth, Texas, USA
Mal McHugh, PhD
NISMAT
New York, NY, USA
Joseph Miller, PT, DSc, OCS, SCS, CSCS
Pikes Peak Community College
Colorado Springs, CO, USA
Havard Moksnes, PT PhD
Oslo Sports Trauma Research Center
Oslo, Norway
Michael J. Mullaney, PT, SCS
NISMAT
Mullaney & Associates Physical Therapy
New York, NY and Matawan, NJ, USA
Andrew Murray, MD, PhD
European PGA Tour
Edinburgh, Scotland, UK
Andrew Naylor, PT, DPT, SCS
Bellin Health
Green Bay, WI, USA
Stephen Nicholas, MD
NISMAT New York
New York, NY, USA
John O'Donnel, MD
Royal Melbourne Hospital
Melbourne, Australia
Russ Paine, PT
McGovern Medical School
Houston, TX, USA
Snehal Patel, PT, MSPT, SCD
HSS Sports Rehabilitation Institute
New York, NY, USA
Marc Philippon, MD
Steadman-Hawkins Clinic
Vail, CO, USA
Kevin Plancher, MD, MPH, FAAOS
Plancher Orthopedics and Sports Medicine
New York, NY USA
Marisa Pontillo, PT, PhD, DPT, SCS University of Pennsylvania Health System
Philadelphia, PA, USA
Matthew Provencher, MD
Steadman Hawkins Clinic
Vail, CO, USA
Charles E. Rainey, PT, DSc, DPT, MS, OCS, SCS, CSCS, FAAOMPT
United States Public Health Service
Springfield, MO, USA
Alexandre Rambaud, PT PhD
Saint-Etienne, France
Carlo Ramponi, PT Physiotherapist, Kinè Rehabilitation and Orthopaedic Center
Treviso, Italy
Michael Reiman, PT, PhD
Duke University
Durham, NC, USA
Mark F. Reinking, PT, PhD, SCS, ATC Regis University
Denver, CO, USA
Mike Reinold, PT, DPT, SCS, ATC, CSCS, C-PS Champion Physical Therapy and Performance
Boston, MA, USA
Mark Ryan, ATC
Steadman-Hawkins Clinic
Vail, CO, USA
David Sachse, PT, DPT, OCS, SCS USAF
San Antonio, TX, USA
Marc Safran, MD
Stanford University
Palo Alto, CA, USA
Alanna Salituro, PT, DPT, SCS, CSCS
New York Mets
Port Saint Lucie, FL, USA
Mina Samukawa, PT, PhD, AT (JSPO) Hokkaido University
Sapporo, Japan
Barbara Sanders, PT, PhD, FAPTA, Board Certified Sports Physical Therapy Emeritus Professor and Chair, Department of Physical Therapy Texas State University
Round Rock, TX, USA
Felix “Buddy” Savoie, MD, FAAOS
Tulane Institute of Sport Medicine
New Orleans, LA, USA
Teresa Schuemann, PT, DPT, ATC, CSCS, Board Certified Specialist in Sports Physical Therapy Evidence in Motion
Fort Collins, CO, USA
Timothy Sell, PhD, PT, FACSM
Atrium Health Musculoskeletal Institute
Charlotte, NC, USA
Andreas Serner, PT PhD Aspetar Orthopedic and Sports Medicine Hospital
Doha, Qatar
Ellen Shanley, PT, PhD ATI
Spartanburg, SC, USA
Karin Silbernagel, PT, PhD University of Delaware
Newark, DE, USA
Holly Silvers, PT, PhD Velocity Physical Therapy
Los Angeles, CA, USA
Lynn Snyder-Mackler, PT, ScD, FAPTA STAR University of Delaware
Newark, DE, USA
Alston Stubbs, MD
Wake Forest University
Winston-Salem, NC, USA
Amir Takla, B.Phys, Mast.Physio (Manip), A/Prof
Australian Sports Physiotherapy
The University of Melbourne
Melbourne, Australia
Charles Thigpen, PhD, PT, ATC ATI
Spartanburg, SC, USA
Steven Tippett, PT, PhD, ATC, SCS
Bradley University
Peoria, IL, USA
Tim Tyler, PT, ATC NISMAT
New York, NY, USA
Timothy Uhl, PT, PhD, ATC University of Kentucky
Lexington, KY, USA
Bakare Ummukulthoum, PT University of the Witswatersrand
Johannesburg, Gauteng, South Africa
Yuling Leo Wang, PT, PhD
Sun Yat-sen University
Guangzhou, China
Mark D. Weber, PT, PhD, SCS, ATC
Texas Women’s University
Dallas, TX, USA
Richard B. Westrick, PT, DPT, DSc, OCS, SCS
US Army Research Institute
Boston, MA, USA
Chris Wolfe, PT, DPT
Belmont University
Nashville, TN, USA
Tobias Wörner, PT, MSc
Lund University
Stockholm, Sweden
VOLUME 18, NUMBER 1
EDITORIAL
MSK Ultrasound and Introduction of IJSPT Ultrasound Bites Feature. Manske R, Page P, Voight M, Wolfe C
INVITED CLINICAL COMMENTARY
1 MSK Ultrasound - An IJSPT Perspective. Page P, Manske R, Voight M, Wolfe C.
INTERNATIONAL PERSPECTIVE
11 Leadership Practice in Sport and Exercise Medicine – from Diagnosis to Dialogue. Glasgow P.
CLINICAL VIEWPOINT
14 My Top Five Concepts for Selecting Lower Extremity Exercises For Cruciate Ligament and Patellofemoral Rehabilitation.
Escamilla R.
SYSTEMATIC REVIEW
26 The Effectiveness of Physical Therapy Interventions for Athletes Post-Concussion: A Systematic Review.
Hassen-Miller A, Art K, Ridenour C, et al.
28 Are Exercise Therapy Protocols for the Treatment of Hip-related Pain Adequately Described? A Systematic Review of Intervention Descriptions. Estberger A, Kemp J, Thorborg K, et al.
SCOPING REVIEW
55 Examining the Peer-reviewed Published Literature Regarding Low Back Pain in Rowing: A Scoping Review.
Athy V, Hach S, Anderson H, et al.
ORIGINAL RESEARCH
70 A Preliminary Investigation into the Neural Correlates of Knee Loading during a Change of Direction Task in Individuals after Anterior Cruciate Ligament Reconstruction.
Culiver A, Grooms D, Edwards N, et al.
81 Adding A Structured Educational Session to the Rehabilitation Program of Soccer Players Following Anterior Cruciate Ligament Reconstruction: A Feasibility Study.
Almuhaya A, Albarati A, Ahowimel A, et al.
92 The Comparison of Psychological Barriers Between Individuals with a History of Anterior Knee Pain, Anterior Cruciate Ligament Reconstruction, and Healthy Individuals.
Zuk E, Kim S, Burland J, et al.
102 Differences in Thigh Muscle Activation Between Standing and Landing Exercises for Knee Injury Prevention and Rehabilitation.
Bencke J, Strøm M, Curtis D, et al.
113 The Association Between Functional Movement Screen™ Scores and Knee Valgus Moments During Unplanned Sidestep Cutting in Netball.
Boey D, Lee M.
122 Video Analysis of 26 Cases of Second ACL Injury Events in Collegiate and Professional Sports. Bates N, Vargas M, Chaney G, et al.
132 Signs of Nervous System Sensitization in Female Runners, with Chronic Patellofemoral Pain. Eckenrode BJ, Kietrys DM, Brown A, et al.
VOLUME 18, NUMBER 1
PAGE TITLE
145 Confirmatory Factor Analysis of the Hip Disability and Osteoarthritis Outcome Score (HOOS) and Associated Sub-scales.
Miley E, Casanova M, Cheatham S, et al.
169 Effectiveness of Spinal Stabilization Exercises on Movement Performance in Adults with Chronic Low Back Pain.
Alkhathami K, Alshehre, Brizzolara K, et al.
173 Effectiveness of Spinal Stabilization Exercises on Dynamic Balance in Adults with Chronic Low Back Pain.
Alshere Y, Alkhathami K, Brissolara K, et al.
188 Bodyblade™ Training in Athletes with Traumatic Anterior Shoulder Instability. Pulido V, Alvar B, Behm D.
199 Survey of Knowledge, Use, and Diagnostic Applicability of Special Tests for Rotator Cuff Involvement in Clinical Practice.
Bandy W, Forbush S, Back-Kremers G, et al.
208 Flexor-Pronator Mass Training Exercises Selectively Activate Forearm Musculature. Tyler T, Fukunaga T, Fedge C, et al.
CASE SERIES
215 Physical Therapists Use of Diagnostic Ultrasound Imaging in Clinical Practice: A Review of Case Reports.
Manske R, Podoll K, Markowski A, et al.
CASE REPORT
228 The “Mother Load” and Return to Sport: A Case Report of Returning to Professional Netball Following Cesarean Section. Diggles A.
240 Novel Orthobiologic Preparation and Regenerative Rehabilitation of a Complex Shoulder Injury in a Competitive Female Athlete. Young I, Escaloni J, Mazloomdoost D.
CLINICAL COMMENTARY
253 Personalized Injury Reduction Strategies in Sports Medicine: Lessons Learned from Advances in Breast Cancer Treatment.
Bullock G, Collins G, Adams R, et al.
262 A Clinically-Reasoned Approach to Manual Therapy in Sports Physical Therapy. Short S, Tuttle M, Youngman D.
CLINICAL SUGGESTION/UNIQUE PRACTICE TECHNIQUE
272 The Need To Change Return to Play Testing in Athletes Following ACL Injury: A Theoretical Model.
Wilk KE, Thomas ZM, Arrigo CA.
ULTRASOUND BITES
The Use of MSK Ultrasound with Quadriceps Muscle Injury.
Manske R, Voight M, Wolfe C, Page P.
 Chris Wolfe, PT, DPT, OCS, Cert Dip PT
Chris Wolfe, PT, DPT, OCS, Cert Dip PT
 Phil Page, PT, PhD, ATC, CSCS, FACSM
Phil Page, PT, PhD, ATC, CSCS, FACSM


Point of care ultrasound (POCUS), musculoskeletal ultrasound (MSK-US), and rehabilitation ultrasound imaging (RUSI) are similar procedures that use a non-ionizing imaging and is becoming more inexpensive, portable, safe, and able to be used quickly.1-4 These modalities are commonly used in various medical disciplines to assess musculoskeletal tissues (bones, muscles, tendons, ligaments, nerves) as well as structures such as the heart, lungs, and bladder just to name a few. MSK-US primarily focuses on the structural integrity or characteristics of the neuromuscular system. This would include viewing soft tissues for assessment of normalcy or abnormality. For example, viewing the supraspinatus for signs of swelling or a rotator cuff tear, or assessing the median nerve to measure swelling or size differences in those with carpal tunnel syndrome are commonly performed using MSK-US. RUSI is similar but includes the evaluation of muscle and soft tissue during exercise or movement dynamically including its use for biofeedback.5-6 An example of RUSI include realtime observation of spinal muscle (lumbar multifidus and transverse abdominus) activation patterns during exercise to facilitate improved neuromotor control.6
The use of MSK-US in clinical practice has nearly quadrupled since the early 2000’s, mainly due to its use with non-radiologists.3,7,8 Its surge in popularity parallels research suggesting that MSK-US is accurate and cost effective, with patients reporting greater satisfaction with MSK-US compared to magnetic resonance imaging (MRI).9-11
Ultrasound is becoming more widely recognized in rehabilitation as a valuable tool to objectively assess musculoskeletal structures and guide rehabilitation.6,12 The appropriate use of imaging is essential in all healthcare professions for accurate patient diagnosis and management as well as optimizing the use of healthcare resources.13 It should
also be stressed that mistakes made by inadequately trained operators could jeopardize a patients’ wellbeing by delaying treatment for life threatening conditions.14 Because of this, the International Journal of Sports Physical Therapy (IJSPT) Editorial Board thought it important to educate readership with common tips to view various musculoskeletal structures. Starting with the long head of biceps tendon in our last issue,15 subsequent issues of IJSPT will include a section entitled “MSK Ultrasound Bites: Tips and Tricks.” Each month, a new structure that can be assessed with MSK-US will be thoroughly described, including normal and pathological structure findings with clear and concise guidelines describing probe placement and findings. As can be seen in a corresponding study in this issue, many therapists are utilizing MSK-US clinically.16 In addition, our clinical commentary
Robert Manske Michael Voight Phil Page Chris Wolfethis month provides an overview and introduction to the clinical use of MSK-US for rehabilitation, diagnosis, interventions and research. We believe that its use will continue to evolve as physical therapists become more adept at using this skill to propagate care beyond the traditional examination.16
1. Backhaus M, Burmester G, Gerber T, et al. Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis. 2001; 60(7): 641-649.
2. Jacobson JA. Musculoskeletal ultrasound and MRI: Which do I choose? In: Seminars in Musculoskeletal Radiology: 2005. New York, New York. Thieme Medical Publishers, Inc. 2005; 135-149.
3. Klauser AS, Tagliafico A, Allen GM, et al. Clinical indications for musculoskeletal ultrasound: A Delphi-Based consensus paper of the European Society of Musculoskeletal Radiology. Eur Radiol. 2012;22(5):1140-1148.
4. Nazarian LN. The top 10 reasons musculoskeletal sonography is an important complementary or alternative technique to MRI. Am J Roentgenol. 2008;190(6):1621-1626.
5. Koppenhaver SL, Hebert JJ, Parent EC, et al. Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub-maximal contractions: A systematic review. Aust J Physiother. 2009;55(3):153-169.
6. Whittaker JL, Teyhen DS, Elliott JM, et al. Rehabilitative ultrasound imaging: understanding the technology and its applications. J Orthop Sports Phys Ther. 2007; 37(8):434-449.
7. Kanesa-Thasan RM, Nazarian LN, Parker L, et al. Comparative trends in utilization of MRI and ultrasound to evaluate nonspine joint disease 2003-2015. J Am Coll Radiol. 2018;15(3 pt A): 402-407.
8. Sharpe RE, Nazarian LN, Parker L, et al. Dramatically increased musculoskeletal ultrasound utilization from 2000-2009, especially by podiatrists in private offices. J Am Coll Radiol. 2012;9(2):131-146.
9. Roy JS, Braen C, Leblond J, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterization of rotator cuff disorders: a systematic review and metaanalysis. Br J Sports Med. 2015;49:1316-1328.
10. Parker L, Nazarian LN, Carrino JA, et al. Musculoskeletal imaging: Medicare use, costs, and potential for cost substitution. J Am Coll Radiol. 2008;5:182-188.
11. Middleton WD, Payne WT, Teefey SA, et al. Sonography and MRI of the shoulder: comparison of patient satisfaction. Am J Roetngen. 2004;183:1449-1452.
12. Pillen S, van Alfen N. Skeletal muscle ultrasound. Neurological Res. 2011;33:1016-1024.
13. Henderson REA, Walker BF, Young KJ. The accuracy of diagnostic ultrasound imaging for musculoskeletal soft tissue pathology of the extremities: a comprehensive review of the literature. Chiropractic Man Ther. 2015;23:3. DOI: 10.1186/s12998-015-0076-5.
14. Edwards H. Let’s all jump on the ultrasound bandwagon. Ultrasound. 2010;18:4-7.
15. Manske RC, Voight M, Wolfe C, Page P. Long head of the biceps tendon (LHBT). Int J Sports Phys Ther. 2022;17(7) doi.org/10.26603/001c.55786
16. Manske RC, Podoll KR, Markowski A, et al. Physical therapist use of diagnostic ultrasound imaging in clinical practice: A review of case reports. Int J Sports Phys Ther. 2023. Ahead of print.

Keywords: MSK ultrasound, PT imaging https://doi.org/10.26603/001c.68184
MSK ultrasound is a valuable imaging technique which has become increasingly popular in recent years. This efficient technique proves beneficial in a variety of ways. MSK ultrasound effectively streamlines the process by enabling practitioners to securely and accurately image and assess structures all in one simple step. By allowing healthcare providers to access critical information quickly and conveniently, MSK ultrasound can help identify conditions early when interventions are most effective. Moreover, it may be able to shorten diagnostic times and reduce costs through more cost-effective use of resources such as imaging and laboratory testing. Furthermore, MSK ultrasound can provide additional insights into musculoskeletal anatomy and help improve patient care and outcomes. In addition, utilizing this method reduces exposure to radiation and provides enhanced patient comfort with its quick scan duration. MSK ultrasound has a high potential to provide quick and accurate diagnosis of MSK disturbances when used correctly. As clinicians become more comfortable and familiar with this technology, we will continue to see its use expand for various MSK assessments. In this commentary we’ll explore how ultrasound can be used in physical therapy, specifically for musculoskeletal assessment. We’ll also look at some of the potential benefits and limitations of using ultrasound in PT practice.
Point of Care Ultrasound (POCUS) is commonly used in various medical disciplines to assess structures quickly and conveniently such as the heart, lungs and bladder Musculoskeletal (MSK) ultrasound (US) is quickly growing as a non-invasive and safe manner of assessing musculoskeletal structures (bones, muscles, tendons, ligaments) without the need for expensive or potentially harmful studies such as radiograph or MRI.
MSK-US provides clinicians with a “window” through the skin to examine different tissues including muscle, bone, tendon, and ligament. In addition to structural integrity, visualizing inflammation using MSK-US may support a physical therapy diagnosis and guide appropriate physical therapy interventions. While physical therapists (PTs) are familiar with “therapeutic” ultrasound, MSK-US is not widely used by PTs. The earliest publications of MSK-US use by PTs were in the 1980s, focusing on the quadriceps muscle to describe its size.1,2 In the 1990’s, researchers and clinicians at the University of Queensland identified the activity of the deep multifidus and transverse abdominus muscles in relation to other abdominal muscles in patients
with lower back pain.3,4 They discovered that the multifidus was atrophied and the transverse abdominus muscle was delayed in activation in patients diagnosed with lower back pain; they subsequently used MSK-US to provide visualization of patients for real-time feedback during rehabilitation.5 More recently, researchers reported high levels of agreement when PTs using MSK-US were compared with radiologists on 40 cadaveric shoulders.6
“Rehabilitative” ultrasound imaging (RUSI) was the term initially used to describe its use in evaluating soft tissue structures during tasks.7 Since then, 4 categories of ultrasonography have been identified in physical therapy: diagnostic, rehabilitation, interventional, and research ultrasound.8 Because these categories were only recently described, the terminology used in the literature may not be consistent; therefore, this review will follow the descriptions provided by Whittaker et al.8 In general, POCUS consists of diagnostic, rehabilitative, and interventional US; research US is used for scientific purposes:
Diagnostic US: diagnosis and monitor pathology (haemarthrosis, sprains, strains, healing stage, lesions, disease) Corresponding
Phil Page, PT, PhD, ATC, CSCS, FACSM 1 a , Robert C Manske, PT, DPT, Med, SCS, ATC, CSCS 2 , Michael Voight, PT, DHSC, SCS, OCS, ATC, CSCS, FAPTA 3 , Chris Wolfe, PT, DPT, OCS, Cert MDT 3Rehabilitative US: evaluate muscle and other soft tissue structure and function (including biofeedback) during physical tasks
Interventional US: guide percutaneous procedures involving ‘dry’ (acupuncture) or ‘wet’ needling (injection)
Research US: measurement; explore muscle and soft tissue structure and function; develop and evaluate screening tools and interventions
Although PTs do not make medical diagnoses, they evaluate pathoanatomic structures in making a physical therapy diagnosis. Identifying structural lesions beyond the physical therapy scope of practice (such as a fracture) allows the PT to refer patients to appropriate providers if needed quickly MSK-US has been shown to be a cost-effective measure in diagnosing structural pathologies.9,10
For some MSK conditions ultrasound has been proven to be equal to or better than MRI for accurate diagnosis of meniscal injuries,11 ACL and PCL injuries,12 Achilles tendinopathy,13 peripheral nerve injuries,14 lateral epicondylitis,15 thumb ulnar collateral ligament injuries,16–27 identifying rotator cuff tears,16–27 and supraspinatus lesions.28,29 There are several types of MSK injuries that US may not be comparable to MRI that include distal biceps tendon avulsions,30 plantar plates.31 MSK-US has also been used for the evaluation of acute athletic injury 32,33
Interest is gaining in US’s ability to view muscles both statically and dynamically 34–40 Dynamic US protocols have been published by an international group of experts to help clinicians evaluate structures while recording video during real-time patient examination to improve their understanding of their diagnosis.41–44 Dynamic ultrasound allows for real-time visualization of structures as they move in relation to other structures. For example, the movement of adjacent fascial layers can be evaluated during active muscle contraction to assess fascial mobility. Muscle architecture can be examined under contraction or relaxation for deficits.
One of the more unique properties of MSK-US that can be used to assess musculoskeletal pathology is use of Doppler imaging of blood flow. This utilizes the Doppler effect which describes the change in frequency of the sound wave that is seen as an object moves closer to (toward) or farther (away) from the transducer The amount of movement can be seen as the Doppler shift that can be picked up on an US image using color enhancement. In diagnostic US this is usually used to determine the presence or absence of blood flow, seen with issues like deep venous thrombosis after musculoskeletal injury to the lower,45–48 and upper extremities,49 or even vascular supply to joints).50 Color Doppler imaging is also useful in detecting effusions51 and musculoskeletal inflammation such as soft tissue hyperemia.52,53
RUSI is used to provide real-time feedback for physical therapy patients. As mentioned previously, real-time US can be used for patient feedback in re-training activation of the transverse abdominus muscle in patients with lower back pain.5 RUSI has been used to assess muscle function in screening athletes for injury risk (Hides 2016, 2017).54,55 Other rehabilitation applications include pelvic health for urinary incontinence.56,57
Physical therapists can integrate MSK-US into their interventions to guide treatment. Silleves et al.58 reported a case of a runner with plantar fasciitis managed with MSK-US imaging to guide decision-making for optimal treatment location and progress. As dry needling has increased in popularity among PTs, the use of MSK-US to assist with needle placement has slowly grown59,60; however, the authors of one study suggested there is no additional benefit to using US-guided dry needling with PT in chronic neck pain patients.61
Typically, interventional MSK-US is performed by practitioners giving injections. While outside the scope of practice for most PTs, MSK-US provides for accurate placement of needles for injection of anti-inflammatory medication or during prolotherapy Recently, the technique of “hydrodissection” has been introduced in musculoskeletal medicine.62–64 During hydrodissection, MSK-US is used to guide hypodermic needles into muscle and fascia to inject saline while breaking-up adhesions and facilitating fascial mobility
MSK-US is also used as a measurement tool for soft tissues in research. In the past, instruments to measure muscle mass included bioelectrical impedance, dual X-ray absorptiometry, computed tomography, and magnetic resonance imaging. The use of MSK-US appears to be a simple, fast, safe, valid and reliable way to measure both muscle and tendon length and thickness.65–71 In addition to length and thickness, MSK-US can also be utilized to assess fascicle or pennation angles.72
Muscle thickness can be quantified to represent muscle contraction. A systematic review in 200973 suggested that MSK-US was a valid measure of trunk muscle activation and size during submaximal isometric contractions. Recently, fascia muscle thickness has been measured with MSKUS.74–76 Tissue stiffness can be measured as well, including tendon stiffness and overall tissue tension. Shear wave elastography, for example, has been shown to be a useful measure of quadriceps tendon and muscle stiffness.77–81 Pressure applied with the transducer is compared to the movement of the tissue on the ultrasound, and the tissue stiffness is quantified with a color map.
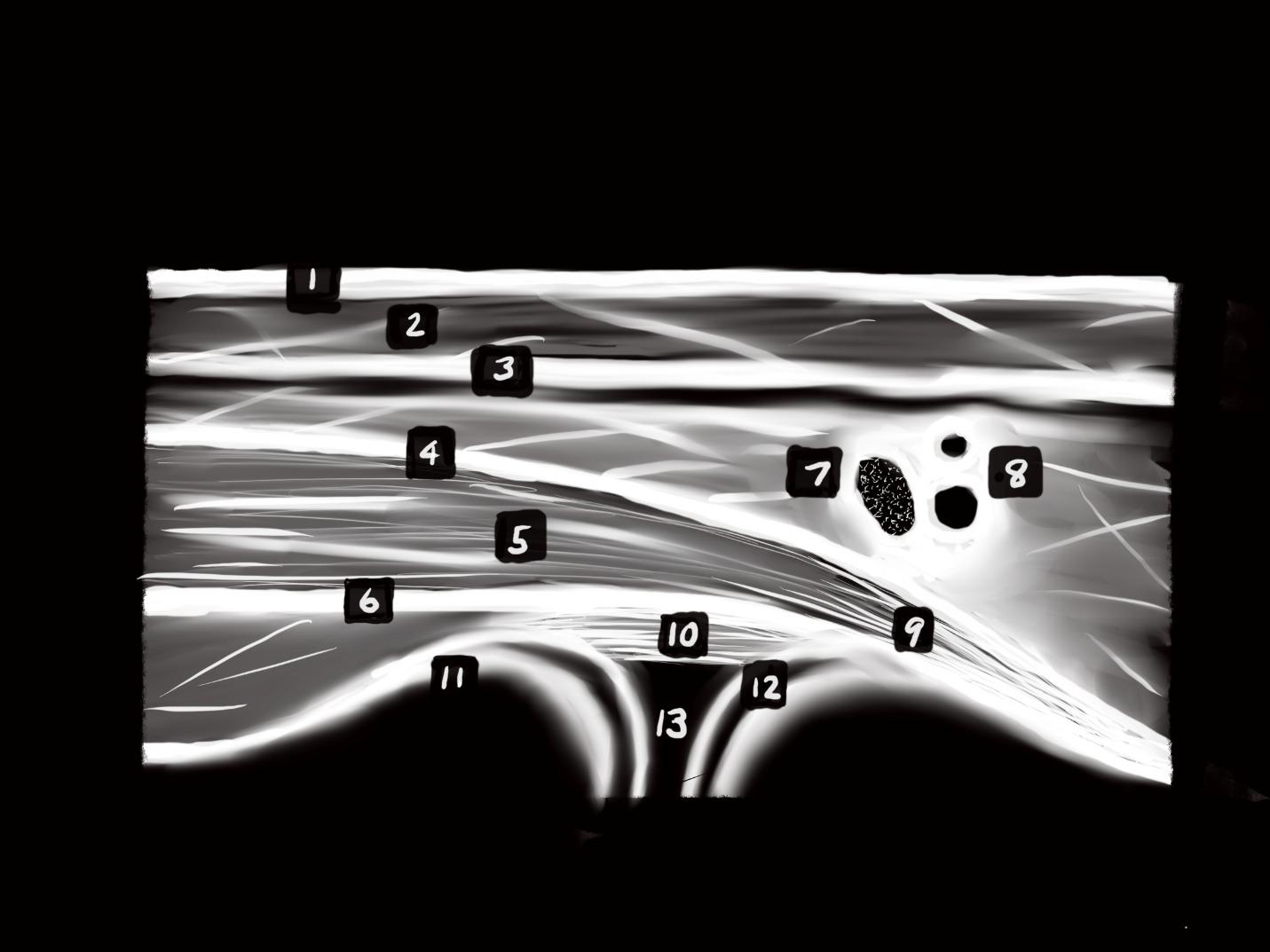
Anechoic Black Fluid
Hyaline Cartilage
Blood vessels or swelling/inflammation
At end of long bones, surrounded by bright white periosteum
Fat Hazy streaks below skin
Hypoechoic Grayscale
Muscle Fasciculated/ speckled hypoechoic with hyperechoic striations, encased by bright fascia
Tendon Linear striated hyperechoic at ends of muscle inserting into bone (fibrillated in long-axis)
Nerve Hyperechoic “starry night” appearance
Ligament Linear Striated hyperechoic surrounding ends of bones at joints
Cartilage Articular cartilage at end of bones includes anechoic periosteum Fascia Bright white, surrounding muscles
Hyperechoic White
Bone Bright white line with acoustic shadow at bottom of image
As stated previously, MSK-US can be used to quantify blood flow in arteries and resultant hyperemia of tissues. Many physical therapy interventions purport to increase blood flow to the treated area. Arterial blood flow can be quantified with MSK-US by vessel diameter and pulse flow during exercise or after interventions.82,83
To perform musculoskeletal ultrasound, the therapist will require an ultrasound sonography device that includes an appropriate transducer Generally, US transducers are classified as linear or curvilinear for superficial and deep tissue sonography, respectively
Some devices such as the Butterfly IQ (Burlington, MA) use a single transducer capable of both superficial and deep sonography. The transducer is the component that converts electrical energy into sound waves. Piezoelectric crystals within the transducer produce the piezoelectric effect that allows ultrasound waves to produce an image on the screen of the device. A soundwave is created that is sent to the tissue, which is returned to the transducer
Various frequencies of sound waves are used depending on the depth of the tissue of interest. Most diagnostic US devices have pre-modulated settings depending on the target tissue. Musculoskeletal tissues are generally more superficial, thus using higher frequencies, while deeper structures, such as the abdominal organs require lower frequencies for best visualization. The sound waves are either reflected to the transducer, absorbed by the tissue, or refracted. Ultrasound waves that are reflected from tissue create an “echo” that returns to the transducer, where the echoes are electronically transformed into digital images at various shades of black and white. The level of reflection (and thus color) is known as “echogenicity”
Ultrasonography measures the amount of echo from sound waves produced by the transducer at specific frequencies.
Ultrasound “echogenicity” is defined as how bright musculoskeletal structures appear on an ultrasound image relative to other structures. Musculoskeletal tissues viewed on US will be either normal or pathologic tissues, and each displays a varying level of echogenicity Structures run the gamut from hyperechoic (brighter) or hypoechoic (less bright) on imaging. Structures that are viewed as hyperechoic or echogenic are high in collagen content such as bones, normal healthy tendons, or certain calcifications in soft tissues. Nerves are hyperechoic and appear as a ‘starry night’ pattern on cross-section. A hypoechoic structure is one where the viewed structures appear darker (less white than hyperechoic structures). These structures could include fat, masses, cysts, or inflammation. A structure that is totally black is termed anechoic and usually represents fluid. For example, blood vessels appear as round, black circles in cross-section. Lastly, a structure is termed isoechoic when used to describe similar echogenicity of surrounding tissue. Table 1 provides an ‘echogenicity’ scale of tissues and Figure 1 is a general schematic of different layers of tissue viewed with ultrasound.
Generally, a gel is used to promote transmission of sound waves to and from the tissues. This is done to couple the transducer with the body part so that air is not located between the skin and device. When air is introduced between the patient and the transducer the sound waves are more easily reflected away from the structures of importance resulting in a poorer image. Ultrasound gel pads can also be used as an interface between the transducer and bony prominences to minimize artifact.
Clinicians must have a keen knowledge of regional anatomy and palpation skills to ensure proper position of the transducer over the target tissue. The transducer should be held perpendicular to the skin with the indicator directed proximal and/or lateral; this standard positioning orients the examiner with the image. Most commonly, MSUS views can be viewed in either a short axis (transverse)
or long axis (longitudinal). The short axis (SAX) is performed through the transverse plane of the intended tissue, while the long axis (LAX) is performed along the longitudinal length of the tissue (See Figure 2). When possible, it is best to visualize both to get an accurate representation of the entire tissue.
Proper technique and adequate technology are essential for an accurate diagnosis. Improper technique can lead to artifacts, which can lead to an inaccurate diagnosis. A unique artifact in MSK-US is “anisotropy” where tissues of fibrillar structure, such as tendons and ligaments, have reduced ecogenicity based on the angle of the transducer. This can result in mistaken interpretation of pathological defects.
Although access to diagnostic ultrasound equipment has improved in cost and convenience, the ability to perform and interpret MSK-US requires training and experience. The use of MSK-US in PT practice is supported by the American Physical Therapy Association (APTA) and is generally not prohibited by state regulations; however, reimbursement may be denied unless the PT is credentialed to perform diagnostic ultrasound as a certified and registered MSK sonography practitioner (RSMK-certified).
Several companies provide education and training on MSK-US including virtual and hands-on courses, while some manufacturers such as Butterfly IQ (Burlington, MA) provide instructional videos. SonoSim (Santa Monica, CA)
 Figure 1. Schematic representation of echogenicity of various structures with musculoskeletal ultrasound.
Figure 2. Ultrasound transducer position in the transverse short axis (left image) and in the longitudinal long axis (right image)
Figure 1. Schematic representation of echogenicity of various structures with musculoskeletal ultrasound.
Figure 2. Ultrasound transducer position in the transverse short axis (left image) and in the longitudinal long axis (right image)
provides an affordable and portable POCUS simulation that includes a ‘dummy’ transducer to provide both didactic and psychomotor skills needed for MSK-US. Several excellent textbooks are available specific to MSK-US as well.84–86
Physical therapists have an opportunity to embrace technology and integrate MSK-US into their practice. Emerging research continues to support its use in PT for a variety of patients, including diagnosis, treatment, and research.
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0
International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Young A, Hughes I, Russell P, Parker MJ, Nichols PJR. Measurement of quadriceps muscle wasting by ultrasonography. Rheumatology. 1980;19(3):141-148. doi:10.1093/rheumatology/19.3.141
2. Stokes M, Young A. Measurement of quadriceps cross–sectional area by ultrasonography: a description of the technique and its applications in physiotherapy Physiother Pract 1986;2(1):31-36. do i:10.3109/09593988609027039
3. Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/ subacute low back pain. Spine 1994;19(2):165-172. d oi:10.1097/00007632-199401001-00009
4. Hodges PW, Richardson CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. J Spinal Disord. 1998;11(1):46-56. doi:10.1097/0000251 7-199802000-00008
5. Hides JA, Richardson CA, Jull GA. Use of real-time ultrasound imaging for feedback in rehabilitation. Man Ther 1998;3(3):125-131. doi:10.1016/s1356-689 x(98)80002-7
6. Duijn EAHD, Roy van S, Karel YHJM, Provyn S, Pouliart N. An interexaminer agreement and reliability study on cadavers with musculoskeletal ultrasound of the shoulder performed by physiotherapists and radiologists compared with dissection. Musculoskelet Sci Pract 2022;60:102569. d oi:10.1016/j.msksp.2022.102569
7. Teyhen D. Rehabilitative Ultrasound Imaging Symposium San Antonio, TX, May 8-10, 2006. J Orthop Sports Phys Ther. 2006;36(8):A1-3. doi:10.251 9/jospt.2006.0301
8. Whittaker JL, Ellis R, Hodges PW, et al. Imaging with ultrasound in physical therapy: What is the PT’s scope of practice? A competency-based educational model and training recommendations. Br J Sports Med. 2019;53(23):1447-1453. doi:10.1136/bjsports-20 18-100193
9. Acebes C, Rubio L, Román A, Herrero A, Arcos J. Cost-effectiveness of on-site musculoskeletal ultrasound in an outpatient rheumatology clinic. Rheumatology 2021;60(4):1832-1838. doi:10.1093/rhe umatology/keaa678
10. Bureau NJ, Ziegler D. Economics of musculoskeletal ultrasound. Curr Radiol Rep 2016;4(8):44. doi:10.1007/s40134-016-0169-5
11. Elshimy A, Osman AM, Awad MES, Abdel Aziz MM. Diagnostic accuracy of point-of-care knee ultrasound for evaluation of meniscus and collateral ligaments pathology in comparison with MRI. Acta Radiol Published online December 1, 2021:2841851211058280. doi:10.1177/028418512110 58280
12. Lee SH, Yun SJ. Efficiency of knee ultrasound for diagnosing anterior cruciate ligament and posterior cruciate ligament injuries: a systematic review and meta-analysis. Skeletal Radiol 2019;48(10):1599-1610. doi:10.1007/s00256-019-032 25-w
13. Gatz M, Bode D, Betsch M, et al. Multimodal ultrasound versus mri for the diagnosis and monitoring of achilles tendinopathy: a prospective longitudinal study Orthop J Sports Med 2021;9(4):23259671211006824. doi:10.1177/23259671 211006826
14. Nischal N, Gupta S, Lal K, Singh JP Performance evaluation of high-resolution ultrasound versus magnetic resonance imaging in diagnosing peripheral nerve pathologies. Indian J Radiol Imaging 2021;31(1):43-48. doi:10.1055/s-0041-1729130
15. Bachta A, Rowicki K, Kisiel B, et al. Ultrasonography versus magnetic resonance imaging in detecting and grading common extensor tendon tear in chronic lateral epicondylitis. PloS One 2017;12(7):e0181828. doi:10.1371/journal.pone.0181 828
16. Abd-ElGawad EA, Ibraheem MA, Fouly EH. Evaluation of supraspinatus muscle tears by ultrasonography and magnetic resonance imaging in comparison with surgical findings. Egypt J Radiol Nucl Med 2013;44(4):829-834. doi:10.1016/j.ejrnm.2013.0 8.001
17 Al-Shawi A, Badge R, Bunker T The detection of full thickness rotator cuff tears using ultrasound. J Bone Joint Surg Br. 2008;90(7):889-892. doi:10.1302/0 301-620x.90b7.20481
18. Day M, Phil M, McCormack RA, Nayyar S, Jazrawi L. Physician training ultrasound and accuracy of diagnosis in rotator cuff tears. Bull Hosp Jt Dis (2013) 2016;74(3):207-211.
19. de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. Am J Roentgenol. 2009;192(6):1701-1707. doi:10.2214/ ajr.08.1241
20. Farooqi AS, Lee A, Novikov D, et al. Diagnostic accuracy of ultrasonography for rotator cuff tears: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(10):23259671211035104. doi:10.1177/23 259671211035106
21. Elmorsy A, Keightley A, Flannery M. Accuracy of ultrasonography (US) and magnetic resonance imaging (MRI) in detection of rotator cuff tears in district general hospital. Pol J Radiol 2017;82:634-637. doi:10.12659/pjr.903004
22. Iannotti JP, Ciccone J, Buss DD, et al. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am 2005;87(6):1305-1311. doi:10.2106/jbjs.d.02100
23. Okoroha KR, Mehran N, Duncan J, et al. Characterization of rotator cuff tears: Ultrasound versus magnetic resonance imaging. Orthopedics. 2017;40(1):e124-e130. doi:10.3928/01477447-201610 13-04
24. Rutten MJCM, Spaargaren GJ, van Loon T, de Waal Malefijt MC, Kiemeney LALM, Jager GJ. Detection of rotator cuff tears: the value of MRI following ultrasound. Eur Radiol. 2010;20(2):450-457. doi:10.10 07/s00330-009-1561-9
25. Sabharwal T, Khanduri S, Khan S, et al. A comparative assessment between high-resolution ultrasonography and field magnetic resonance imaging in supraspinatus tear cases and its arthroscopic correlation. Cureus. 2019;11(9):e5627. d oi:10.7759/cureus.5627
26. Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am 2004;86(4):708-716. doi:1 0.2106/00004623-200404000-00007
27. van Holsbeeck MT, Kolowich PA, Eyler WR, et al. US depiction of partial-thickness tear of the rotator cuff Radiology 1995;197(2):443-446. doi:10.1148/rad iology.197.2.7480690
28. Yazigi Junior JA, Nicolao FA, Matsunaga FT, Archetti Netto N, Matsumoto MH, Tamaoki MJS. Sensitivity and specificity of ultrasonography in diagnosing supraspinatus lesions: a prospective accuracy diagnostic study Sao Paulo Med J 2018;136(4):292-297. doi:10.1590/1516-3180.2018.00 69170418
29. Dinnes J, Loveman E, McIntyre L, Waugh N. The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review Health Technol Assess 2003;7(29):iii,1-166. doi:10.3310/hta7290
30. Lynch J, Yu CC, Chen C, Muh S. Magnetic resonance imaging versus ultrasound in diagnosis of distal biceps tendon avulsion. Orthop Traumatol Surg Res. 2019;105(5):861-866. doi:10.1016/j.otsr.2019.0 1.021
31. Duan X, Li L, Wei DQ, et al. Role of magnetic resonance imaging versus ultrasound for detection of plantar plate tear. J Orthop Surg Res. 2017;12(1):14. d oi:10.1186/s13018-016-0507-6
32. Bailowitz Z, Visco CJ, Christen K, Ahmad CS. Diagnostic musculoskeletal ultrasound for the acute evaluation and management of soccer players. Curr Sports Med Rep 2021;20(10):525-530. doi:10.1249/js r.0000000000000890
33. Robotti G, Draghi F, Bortolotto C, Canepa MG. Ultrasound of sports injuries of the musculoskeletal system: gender differences. J Ultrasound. 2020;23(3):279-285. doi:10.1007/s40477-020-00438-x
34. Flavell CA, Marshman LG, Gordon SJ. Measurement of transversus abdominis activation in chronic low back pain patients using a novel standardized real-time ultrasound imaging method. Ultrasound. 2019;27(1):31-37. doi:10.1177/1742271x1
8785403
35. Hodges PW, Pengel LHM, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve 2003;27(6):682-692. doi:10.1002/mus.10375
36. Reeves ND, Maganaris CN, Narici MV. Ultrasonographic assessment of human skeletal muscle size. Eur J Appl Physiol 2004;91(1):116-118. d oi:10.1007/s00421-003-0961-9
37. Maganaris CN, Baltzopoulos V, Sargeant AJ. Human calf muscle responses during repeated isometric plantarflexions. J Biomech. 2006;39(7):1249-1255. doi:10.1016/j.jbiomech.2005.0
3.011
38. Sosnowska AJ, Vuckovic A, Gollee H. Automated semi-real-time detection of muscle activity with ultrasound imaging. Med Biol Eng Comput 2021;59(9):1961-1971. doi:10.1007/s11517-021-0240
7-w
39. Zhou Y, Li JZ, Zhou G, Zheng YP Dynamic measurement of pennation angle of gastrocnemius muscles during contractions based on ultrasound imaging. Biomed Eng Online 2012;11(1):63. doi:10.11 86/1475-925x-11-63
40. Zheng YP, Chan MMF, Shi J, Chen X, Huang QH. Sonomyography: monitoring morphological changes of forearm muscles in actions with the feasibility for the control of powered prosthesis. Med Eng Phys. 2006;28(5):405-415. doi:10.1016/j.medengphy.2005.0 7.012
41. Ricci V, Chang KV, Güvener O, et al. EUROMUSCULUS/USPRM Dynamic ultrasound protocols for shoulder Am J Phys Med Rehabil 2022;101(3):e29-e36. doi:10.1097/phm.000000000000 1833
42. Ricci V, Güvener O, Chang KV, et al. EUROMUSCULUS/USPRM Dynamic ultrasound protocols for elbow. Am J Phys Med Rehabil. 2022;101(6):e83-e92. doi:10.1097/phm.000000000000 1915
43. Mezian K, Ricci V, Güvener O, et al. EUROMUSCULUS/USPRM Dynamic ultrasound protocols for (adult) hip. Am J Phys Med Rehabil 2022;101(11):e162-e168. doi:10.1097/phm.000000000 0002061
44. Mezian K, Ricci V, Güvener O, et al. EUROMUSCULUS/USPRM Dynamic ultrasound protocols for wrist and hand. Am J Phys Med Rehabil 2022;101(9):e132-e138. doi:10.1097/phm.0000000000 002005
45. Garcia JVDC, Takata V, Diaz LEP, Dada Neto F, Santana MVF, Dobashi ET Efficiency of deep venous thrombosis prevention in proximal femur fractures. Acta Ortop Bras 2022;30(6):e256947 doi:10.1590/141 3-785220223006e256947
46. Schafer K, Goldschmidt E, Oostra D, Kaminski B, Mattin M, Lurie F. Defining the role of risk stratification and duplex ultrasound in the diagnosis of acute lower extremity deep vein thrombosis. J Vasc Surg Venous Lymphat Disord 2022;10(5):1021-1027 d oi:10.1016/j.jvsv.2022.02.017
47. Yang W, Wang H, Wei Q, et al. Preoperative incidence and risk factors of deep vein thrombosis in patients with an isolated patellar fracture. BMC Musculoskelet Disord. 2022;23(1):204. doi:10.1186/s12 891-022-05163-6
48. Xiong X, Cheng B. Preoperative risk factors for deep vein thrombosis in knee osteoarthritis patients undergoing total knee arthroplasty J Orthop Sci 2023;28(1):180-187 doi:10.1016/j.jos.2021.09.016
49. Tan G, Ng M. Emergency department point-ofcare ultrasound for upper extremity deep venous thrombosis ED POCUS for upper extremity DVT Int J Emerg Med. 2021;14(1):66. doi:10.1186/s12245-021-0
0391-4
50. Baksa G, Czeibert K, Sharp V, et al. Vascular supply of the metacarpophalangeal joint. Front Med. 2022;9:1015895. doi:10.3389/fmed.2022.1015895
51. Cushman DM, Ross B, Teramoto M, English J, Joyner JR, Bosley J. Identification of knee effusions with ultrasound: a comparison of three methods. Clin J Sport Med 2022;32(1):e19-e22. doi:10.1097/jsm.000 0000000000823
52. Newman JS, Adler RS, Bude RO, Rubin JM. Detection of soft-tissue hyperemia: value of power Doppler sonography. Am J Roentgenol. 1994;163(2):385-389. doi:10.2214/ajr.163.2.8037037
53. Breidahl WH, Newman JS, Taljanovic MS, Adler RS. Power Doppler sonography in the assessment of musculoskeletal fluid collections. Am J Roentgenol 1996;166(6):1443-1446. doi:10.2214/ajr.166.6.863346 0
54. Hides JA, Mendis MD, Franettovich Smith MM, Miokovic T, Cooper A, Low Choy N. Association between altered motor control of trunk muscles and head and neck injuries in elite footballers – An exploratory study Man Ther 2016;24:46-51. doi:10.1 016/j.math.2016.05.001
55. Hides JA, Stanton WR. Predicting football injuries using size and ratio of the multifidus and quadratus lumborum muscles. Scand J Med Sci Sports. 2017;27(4):440-447 doi:10.1111/sms.12643
56. Dietz HP, Wilson PD, Clarke B. The use of perineal ultrasound to quantify levator activity and teach pelvic floor muscle exercises. Int Urogynecol J 2001;12(3):166-168; discussion 168-169. doi:10.1007/ s001920170059
57. Gu X, Yang M, Liu F, Liu D, Shi F. Effects of adding ultrasound biofeedback to individualized pelvic floor muscle training on extensibility of the pelvic floor muscle and anterior pelvic organ prolapse in postmenopausal women. Contrast Media Mol Imaging. 2022;2022:4818011. doi:10.1155/2022/48180 11
58. Sillevis R, Shamus E, Mouttet B. The management of plantar fasciitis with a musculoskeletal ultrasound imaging guided approach for instrument assisted soft tissue mobilization in a runner: a case report. Int J Sports Phys Ther. 2020;15(2):274-286. doi:10.26603/ij spt20200274
59. Bağcıer F, Tufanoğlu FH. A new treatment modality in piriformis syndrome: Ultrasound guided dry needling treatment. Agri J Turk Soc Algol 2020;32(3):175-176. doi:10.14744/agri.2019.92170
60. Vas L. Ultrasound guided dry needling: Relevance in chronic pain. J Postgrad Med. 2022;68(1):1-9. doi:1 0.4103/jpgm.jpgm_710_21
61. Stieven FF, Ferreira GE, Wiebusch M, de Araújo FX, da Rosa LHT, Silva MF. Dry needling combined with guideline-based physical therapy provides no added benefit in the management of chronic neck pain: a randomized controlled trial. J Orthop Sports Phys Ther 2020;50(8):447-454. doi:10.2519/jospt.202 0.9389
62. Courseault J, Kessler E, Moran A, Labbe A. Fascial hydrodissection for chronic hamstring injury Curr Sports Med Rep 2019;18(11):416-420. doi:10.1249/js r.0000000000000650
63. Kaga M, Ueda T Effectiveness of hydro-dissection of the piriformis muscle plus low-dose local anesthetic injection for piriformis syndrome: a report of 2 cases. Am J Case Rep 2022;23:e935346. doi:10.12 659/ajcr.935346
64. Kaga M. First case of occipital neuralgia treated by fascial hydrodissection. Am J Case Rep 2022;23:e936475. doi:10.12659/ajcr.936475
65. Cronin K, Foley S, Cournane S, De Vito G, Delahunt E. Hamstring muscle architecture assessed sonographically using wide field of view: A reliability study. PloS One. 2022;17(11):e0277400. doi:10.1371/j ournal.pone.0277400
66. Hammond K, Mampilly J, Laghi FA, et al. Validity and reliability of rectus femoris ultrasound measurements: Comparison of curved-array and linear-array transducers. J Rehabil Res Dev 2014;51(7):1155-1164. doi:10.1682/jrrd.2013.08.0187
67. Hogenbirk RNM, Viddeleer AR, Hentzen JEKR, et al. Thickness of biceps and quadriceps femoris muscle measured using point-of-care ultrasound as a representation of total skeletal muscle mass. J Clin Med 2022;11(22):6606. doi:10.3390/jcm11226606
68. Madden KM, Feldman B, Arishenkoff S, Meneilly GS. A rapid point-of-care ultrasound marker for muscle mass and muscle strength in older adults. Age Ageing. 2021;50(2):505-510. doi:10.1093/ageing/afaa1 63
69. Nijholt W, Scafoglieri A, Jager-Wittenaar H, Hobbelen JSM, van der Schans CP The reliability and validity of ultrasound to quantify muscles in older adults: a systematic review J Cachexia Sarcopenia Muscle. 2017;8(5):702-712. doi:10.1002/jcsm.12210
70. Park J, Kim YH, Choi WJ, et al. The value of the peroneus brevis tendon cross-sectional area in early diagnosing of peroneus brevis tendinitis: The peroneus brevis tendon cross-sectional area. Medicine (Baltimore) 2022;101(43):e31276. doi:10.1097/md.00 00000000031276
71. Yoshimura A, Kunugi S, Hirono T, et al. Association of muscle strength with muscle thickness and motor unit firing pattern of vastus lateralis muscle in youth athletes. Int J Sports Physiol Perform. 2022;17(12):1725-1731. doi:10.1123/ijspp.2022-0094
72. Pinto MD, Pinto RS, Nosaka K, Blazevich AJ. Do intramuscular temperature and fascicle angle affect ultrasound echo intensity values? Med Sci Sports Exerc Published online November 9, 2022. doi:10.124 9/mss.0000000000003082
73. Koppenhaver SL, Hebert JJ, Parent EC, Fritz JM. Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub-maximal contractions: a systematic review Aust J Physiother 2009;55(3):153-169. doi:1 0.1016/s0004-9514(09)70076-5
74. Pirri C, Pirri N, Guidolin D, Macchi V, De Caro R, Stecco C. Ultrasound imaging of the superficial fascia in the upper limb: arm and forearm. Diagnostics 2022;12(8):1884. doi:10.3390/diagnostics12081884
75. Pirri C, Guidolin D, Fede C, Macchi V, De Caro R, Stecco C. Ultrasound imaging of brachial and antebrachial fasciae. Diagnostics. 2021;11(12):2261. d oi:10.3390/diagnostics11122261
76. Pirri C, Pirri N, Porzionato A, Boscolo-Berto R, De Caro R, Stecco C. Inter- and intra-rater reliability of ultrasound measurements of superficial and deep fasciae thickness in upper limb. Diagnostics 2022;12(9):2195. doi:10.3390/diagnostics12092195
77 Coombes BK, Ziegenfuss B, David M, et al. Heterogeneity of passive elastic properties within the quadriceps femoris muscle–tendon unit. Eur J Appl Physiol 2018;118(1):213-221. doi:10.1007/s00421-01 7-3763-1
78. Ebihara B, Mutsuzaki H, Fukaya T. Relationships between quadriceps tendon elasticity and knee flexion angle in young healthy adults. Med Kaunas Lith. 2019;55(2):53. doi:10.3390/medicina55020053
79. Mannarino P, Matta TT da, Oliveira LF de. An 8-week resistance training protocol is effective in adapting quadriceps but not patellar tendon shear modulus measured by Shear Wave Elastography PloS One 2019;14(4):e0205782. doi:10.1371/journal.pon e.0205782
80. Ozcan ANS, Tan S, Tangal NG, et al. Real-time sonoelastography of the patellar and quadriceps tendons: pattern description in professional athletes and healthy volunteers. Med Ultrason. 2016;18(3):299-304. doi:10.11152/mu.2013.2066.18
3.ays
81. Zardi EM, Franceschetti E, Giorgi C, Palumbo A, Franceschi F. Reliability of quantitative point shearwave ultrasound elastography on vastus medialis muscle and quadriceps and patellar tendons. Med Ultrason 2019;21(1):50-55. doi:10.11152/mu-1712
82. Li S, McDicken WN, Hoskins PR. Blood vessel diameter measurement by ultrasound. Physiol Meas 1993;14(3):291-297. doi:10.1088/0967-3334/14/3/007
83. Rådegran G. Ultrasound Doppler estimates of femoral artery blood flow during dynamic knee extensor exercise in humans. J Appl Physiol 1997;83(4):1383-1388. doi:10.1152/jappl.1997.83.4.13
83
84. Bradley M, O’Donnell P Atlas of Musculoskeletal Ultrasound Anatomy 2nd ed. Cambridge University Press; 2010. doi:10.1017/cbo9780511691782
85. Rawat M. Atlas of Musculoskeletal Ultrasound of the Extremities SLACK Incorporated; 2020.
86. Strakowski JA. Introduction to Musculoskeletal Ultrasound: Getting Started Demos Medical; 2016. do i:10.1891/9781617052309

Leadership advice is everywhere. Across social media platforms, in formal teaching environments, and a large number of industries we are bombarded with courses, podcasts, books, and conferences telling us how to be a great leader. But what does it mean to lead well in sport and exercise medicine? How can we demonstrate leadership in inter-disciplinary teams to support athlete performance and promote wellbeing? What skills are required to lead complex discussions on athlete availability?
Models of leadership often describe expert leaders and provide an inventory of competencies. The inference is that if we can just develop these competencies, we too can be great leaders. Is accumulation of competencies the key to leadership development or is this approach missing important elements of what it means to lead?
We are all familiar with the Diagnostic Approach to patient management. The expert practitioner assesses the patient, diagnoses the issue, and prescribes a particular intervention. Here the focus is firmly on the expertise of the practitioner with little attention given to the role of the patient. Similar trends are seen in popular leadership literature; the expert leader with unique insight is able to identify problems and “fix” failing teams or companies. The problem with such leadership (and practitioner) hagiography is that it belies what we all know intuitively – it’s not that simple.
While deterministic models of thinking that reduce uncertainty and promote greater consistency of approach can be attractive, they are less applicable when dealing with complex issues.1 In an increas-
ingly VUCA (Volatile, Uncertain, Complex, and Ambiguous) world it is necessary to interact with and respond to our environment rather than trying to impose our views. As leaders we are often faced with complex decisions involving personal, physical, social, and cultural factors.
The Gestalt proposition that ‘the whole is more than (or something altogether different to) the sum of parts’ succinctly expresses the concept that it is not possible to describe leadership purely in terms of the performative aspects of certain skills but rather as a phenomenon in and of itself that occurs as a consequence of the interactions of a group of people within a specific setting. Decontextualising leadership competencies from the specific interpersonal situation is like removing individual clinical skills from the clinic. Expert leaders are not an agglomerate of physical or mental traits, as noted by Araújo and Davids,2 but “active individuals engaged in ongoing dynamical transactions with their functionally defined environments.”
Just as accurate performance of a clinical skill in and of itself does not constitute the individual as a healthcare practitioner, so the presence of certain leadership skills doesn’t make you a leader. Rather, it is the ability to execute this skill in concert with a range of other skills in the moment (i.e., with the patient or team) that determines its effectiveness. When executed out of context and without the accompanying expression of other components, a skill ceases to be of any inherent value. It is possible to have a specific skill and be unable to use it; as Harrison observes, “possession does not equal use.”3
I propose that the Diagnostic Approach to leadership is better replaced with a Dialogic Approach that views leadership as an ongoing interaction within a given socioecological context.4 This important shift makes leadership less about the leader and more about the team. Where the leader seeks to better understand the individuals, the issue, and the context while working collaboratively to identify and enact the best solution; all the time enabling and empowering those in their team. For example, leading a performance team to agree how best to support an athlete’s preparation for a major championship will require a nuanced understanding of the athlete’s injury history, performance goals, and playing style as well as an appreciation of the skills of each team member, the prior experience of the athlete, and the effectiveness of previous models of support. The role of the leader here is to ensure all the relevant information is shared, key points highlighted, and to facilitate discussion that achieves consensus on how the plan will be implemented.
Leaders have been described leaders as sensemakers who help teams frame and facilitate responses.5 The best leaders I have worked with have consistently demonstrated the ability to blend science and art to embody expert practice that works “in the moment.” Rather than focusing solely on developing a list of so-called leadership competencies, leaders are encouraged to consider how they might enhance the quality of dialogue with their environment. This includes taking time to reflect more deeply and discuss relevant factors. Sharing stories and learning to attend to what is really going on will help us respond to, and lead more effectively in, an increasingly complex world.
1. Kjellström S, Stålne K, Törnblom O. Six ways of understanding leadership development: An exploration of increasing complexity. Leadership. 2020;16(4):434-460.
2. Araújo D, Davids K. The (sport) performerenvironment system as the base unit in explanations of expert performance. J Expertise. 2018;31:1(3).
3. Harrison RT. “Leadership, leadership development and all that jazz.” Leadership. 2017;13(1):81–99.
4. Bushe GR, Marshak RJ. The dialogic organization development approach to transformation and change. Practicing organization development. 2016;4:407-418.
5. Ancona D, Malone TW, Orlikowski WJ, et al. In praise of the incomplete leader. Harv Bus Rev. 2007;85(2):92-100.

Keywords: cruciate rehab, patellofemoral rehab, knee loading https://doi.org/10.26603/001c.65896
This clinical commentary will address five key concepts that can be used by clinicians as criteria for selecting lower extremity weight bearing exercises (WBE) and non-weight bearing exercises (NWBE) employed for cruciate ligament and patellofemoral rehabilitation. The following will be discussed for both cruciate ligament and patellofemoral rehabilitation: 1) Knee loading varies between WBE and NWBE; 2) Knee loading varies with technique variations within WBE and NWBE; 3) Knee loading varies between different WBE; 4) Knee loading varies as a function of knee angle; and 5) Knee loading increases with increased knee anterior translation beyond toes.
WEIGHT BEARING EXERCISE (WBE) AND NONWEIGHT BEARING EXERCISE (NWBE)
CRUCIATE LIGAMENT REHABILITATION
Regarding ACL loading between WBE and NWBE, peak ACL strain and tensile loading is greater in NWBE seated knee extension than most WBE.1–11 For example, performing stair climbing, forward lunging, and a leg press type exercise with 40% bodyweight resistance all produced less ACL strain compared with performing a seated knee extension with no external resistance.4,9,10 Interestingly, performing a NWBE seated knee extension with no external resistance, produced the same amount of ACL strain compared with performing a one leg sit-to-stand or stair climbing WBE, with WBE being more effective in recruiting important hip and thigh musculature that help stabilize the knee and protect the ACL.4,10 For NWBE, peak ACL loads have been reported to be 158 N at 15º knee angle for the 12-RM isotonic seat knee extension and 254-396 N at 35-40º knee angles for the isometric and isokinetic seated knee extension.4,11 These are higher than peak ACL loads during WBE, including 0-28 N at 25º knee angle for the bodyweight squat and 12-RM barbell squat, 0 N for the 12-RM leg press, 59-142 N at 30º knee angle for the bodyweight and 12 repetition maximum (12-RM) dumbbell one-leg squat, and 253 N at 33-48º for a two-feet drop landing stepping off a 60 cm high
platform.1–8,11–13 As a reference, peak ACL load during level walking is 303 N at 15-20º knee angles.14 Therefore, WBE minimizes ACL strain or tensile loading to a greater extent compared with the seated knee extension NWBE. Moreover, WBE are more functional multi-joint, multimuscle exercises effective in developing important hip and thigh musculature, such as the gluteals, hamstrings, quadriceps, adductors and abductors, whereas the seated knee extension only targets the quadriceps.
Since most ACL injuries are not isolated injuries and often involve bone bruises and cartilage damage, menisci damage, or collateral ligament injury, tibiofemoral compressive loads also need to be considered when selected lower extremity exercises after an ACL injury, repair, or reconstruction. For example, performing 12-RM squatting and lunging exercises, or performing a two-leg drop jump from a 60 cm platform height, all resulted in tibiofemoral compressive loads between 4-8 times body weight, which could be injurious to the healing bone, cartilage, or meniscus.1–3,6–8,13 Performing squatting or lunging type exercises with bodyweight only should be first performed and then progress to external resistance secondary to less tibiofemoral compressive knee loading occurring using bodyweight only as resistance compared to using an external load.15,16 Therefore, lower-intensity resistance and plyometric exercises should precede higher intensity resistance or plyometric exercises, such as the single-leg drop jump or 12-RM squatting and lunging. The rate of deceler-
Corresponding author:
Rafael Escamilla, Ph.D., P.T., C.S.C.S., F.A.C.S.M. ProfessorCalifornia State University, Sacramento
Department of Physical Therapy
6000 J Street; Sacramento, CA 95819-6020 916-278-6930 (office); 916-278-5053 (fax) rescamil@csus.edu (e-mail)
ation should also be considered when performing plyometric exercises, as a higher deceleration rate results in greater ACL loading. A peak ACL load of 1294 N at 25-30º knee angles has been reported during rapid deceleration during running to a stop.17
Regarding PCL loading between WBE and NWBE, peak PCL tensile forces were greater in the seated knee flexion isometric and isokinetic NWBE (2701-3330 N at 90º knee ankle) compared to WBE, including 12-RM barbell squat (1868-2212 N at 63-77º knee angles), 12-RM leg press (1726-1866 N at 88-95º knee angles), 12-RM one leg dumbbell squat (414 N at 90º knee angle), 12-RM wall squat (757-786 N at 80-90º knee angle), 12-RM forward and side lunge (612-765 N at 60-90º knee angles), and the bodyweight forward and side lunge (317-334 N at 60-80º knee angles).2,4–8,11 PCL loading during the knee extension NWBE is less than the knee flexion NWBE but greater than most WBE, with the 12-RM isotonic seated knee extension producing a peak PCL force of 959 N at 79º knee angle,2,4,5 which was greater than all the aforementioned WBE except the 12-RM barbell squat and 12-RM leg press. As a reference, the peak PCL load during level walking is 160 N at 15-20º knee angles.14 As a general rule, NWBE and WBE should first begin with no external resistance (resulting in less ACL and PCL loading) and progress to increasing amounts of external resistance (resulting in more ACL and PCL loading).
When comparing WBE (12-RM squat and 12-RM leg press) to NWBE (12-RM seated knee extension), patellofemoral force and stress was greater in WBE than NWBE for 85-95º knee angles, but greater in NWBE than WBE for 15-57º knee angles.2
Forward and side lunge exercises can be performed with varying technique variations using bodyweight only or external resistance, such as a 12-repetition maximum (12-RM) load, and the amount of resistance used does affect cruciate ligament loading. As shown in Figures 1A-1D, the forward lunge can be performed on either a flat surface (Figures 1A and 1B) or up to a platform (Figures 1C and 1D), and by taking a long step (results in lead knee being over lead ankle at maximum knee flexion), which is referred to as forward lunge long (Figures 1B and 1D), or by taking a short step (results in knees moving forward over toes approximately 8-10 cm), which is referred to as forward lunge short (Figures 1A and 1C).
Using a 12-RM load, mean PCL forces were significantly greater (p < 0.001) between 0-80° knee flexion angles in the forward lunge long with a stride (step forward and push back to starting position) compared to the forward lunge short with a stride (Figure 2).7 Moreover, between
0-20° knee flexion angles mean PCL forces were significantly greater (p < 0.001) without a stride (lunging up and down with feet stationary) compared to with a stride.7 Mean ACL forces were generated (0-50 N range between 0-10° knee flexion angles) only in the forward lunge short with a stride (Figure 2).7
Peak ACL strain was not significantly different between squatting with or without 136 N of external resistance, or between stair climbing at slower versus faster rates.10,18,19 It can be concluded from these WBE data that increasing resistance during the squat, or increasing the rate of stepping during stair climbing, may not increase ACL strain; however, the technique employed during the squat will influence ACL loading. This may occur because adding resistance or stepping faster may affect muscle recruitment patterns, such as recruiting the hamstrings to a greater extent (perhaps owing to changes in technique, such as a greater forward trunk tilt). Muscle force from the hamstrings helps unload the ACL owing to their posterior directed force on the leg. This finding during WBE (eg, squatting and lunging), is different compared with the seated knee extension NWBE, in which ACL strain increased from 2.8% without external resistance to 3.8% with adding only 45 N (10 lbs) of external resistance.9 One possible explanation for this is that technique variations typically do not occur during the seated knee extension exercise (and the hamstrings are not recruited to unload the ACL), but techniques variations do occur during WBE, such as with the squat and lunge, because trunk position may change, such as the trunk being more vertical (more quads, less hamstrings) or more horizontal (more hamstrings, less quadriceps).
If technique variations do occur during the seated knee extension NWBE, ACL tensile force can also be affected. For example, when a constant external torque is being applied at the knee, ACL force decreases when the resistance pad is moved more proximal up the leg towards the knee compared to when the resistance pad is moved more distal down the leg towards the ankle.20 When a constant external torque was applied at the knee at 30º knee angle, the ACL tensile force was approximately twice as great when the resistance pad was positioned near the ankle (approximately 400 N) compared with when the resistance pad was positioned near the middle of the leg (approximately 200 N).20 Also, ACL loading decreased progressively from 15º knee angle (approximately 500 N when the resistance pad was near the ankle and approximately 325 N when the resistance pad was placed near the middle of the leg) to 60º knee angle (approximately 100 N when the resistance pad was near the ankle and approximately 0 N when the resistance pad was positioned near the middle of the leg), with no ACL loading at knee angles greater than 60º.20 Wilk and Andrews21 have reported that in ACL-deficient knees during isokinetic exercises, anterior tibial translation can be reduced by utilizing a proximal resistance pad position and performing higher knee angular velocities (e.g. 180 º/s and 300º/s) compared to using slower knee angular velocities (e.g. 60 º/s).
Performing the forward and side lunge by stepping forward or sideways and then pushing back to the upright
starting position produced significantly greater PCL tensile force compared to performing the forward and side lunge while keeping both feet stationary and simply lunging up and down by flexing and extending the lead knee.8 Therefore, there are different progressions within the forward and side lunge that can be employed during PCL rehabilitation.
Technique variations during the leg press can also affect PCL loading. During the 12-RM leg press, mean PCL force was 11-13% greater in the wide stance leg press than the narrow stance leg press between 33-85º knee angles.2 No significant differences in PCL loading were found between the narrow and wide stance squat.2
Technique variations within WBE has also been shown to affect patellofemoral loading. While performing the bodyweight forward lunge exercise with step length and step
height variations (Figures 1A-1D), patellofemoral joint loading changed according to step length, step height, and knee angle.16 Specifically, patellofemoral force and stress in the lead knee were greater with a long step forward lunge (forward lunge long) compared to a short step forward lunge (forward lunge short) between 10°–40° knee angles, and greater with the forward lunge short than the forward lunge long between 50°–100° knee angles (Figure 3).16
For the 12-RM forward lunge, patellofemoral force and stress in the lead knee were greater with the forward lunge short than the forward lunge long between 70°–90° knee angles (Figure 4).22 Interestingly, performing forward lunge with bodyweight only (Figure 3) compared to with a 12-RM load (Figure 4) did change the overall pattern of patellofemoral loading as a function of knee angles.
Comparing step height variations in the bodyweight forward lunge, patellofemoral loads were greater lunging at ground level compared to lunging up to a 10-cm platform
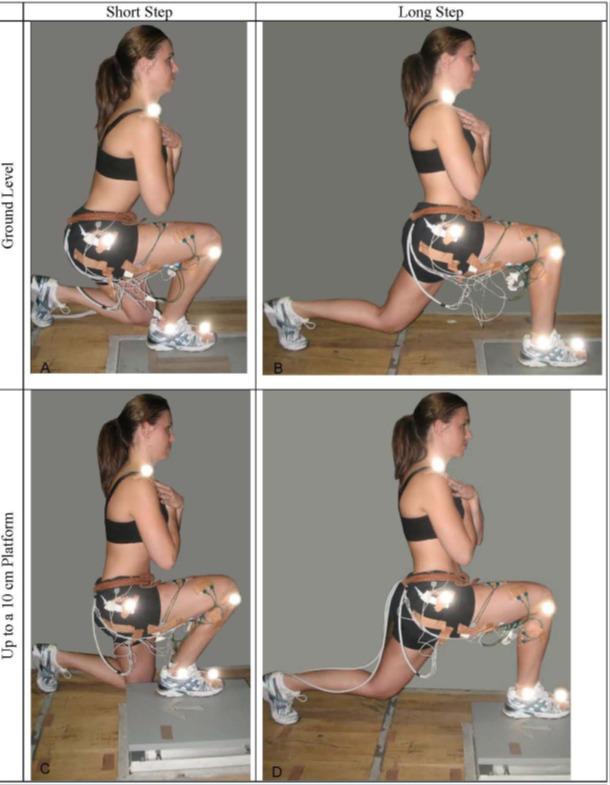 Figure 1. Forward lunge with (A) a short step at ground level, (B) a long step at ground level, (C) a short step up to a 10 cm platform, and (D) a long step up to a 10 cm platform.
Figure 1. Forward lunge with (A) a short step at ground level, (B) a long step at ground level, (C) a short step up to a 10 cm platform, and (D) a long step up to a 10 cm platform.
Figure
(SD) ACL and PCL tensile force between forward lunge long and short with a stride (step forward and push back to starting position) using a 12-repetition maximum load (12-RM). Significant differences (p < 0.001) occurred between 0°–80° knee angles.7
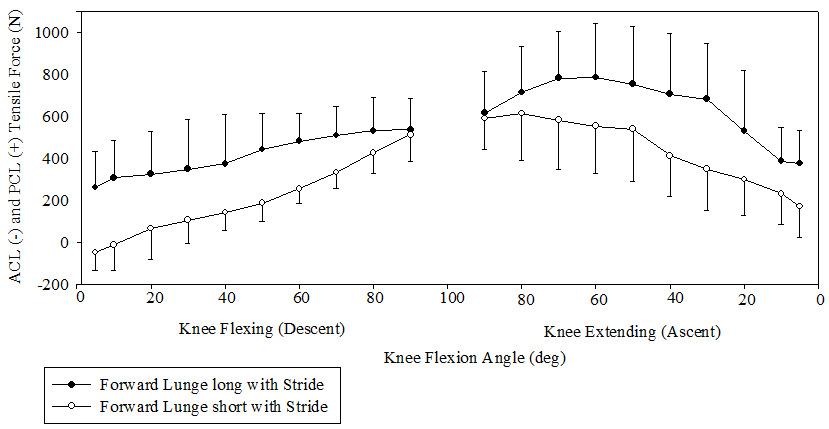
Figure
patellofemoral compressive force in lead knee for forward lunge with a long step and forward lunge with a short step with a stride (step forward and push back to starting position) using bodyweight only.16
Note: Mean (SD) patellofemoral stress followed a similar pattern and results as patellofemoral force.
between 40°–100° knee angles (Figure 5).16 A similar pattern was also observed while performing the side lunge at ground level versus up to a 10-cm platform.15 These data show a progression in patellofemoral rehabilitation, sug-
gesting that lunging up to a 10-cm platform should precede lunging at ground level when the goal is to minimize patellofemoral joint loading.
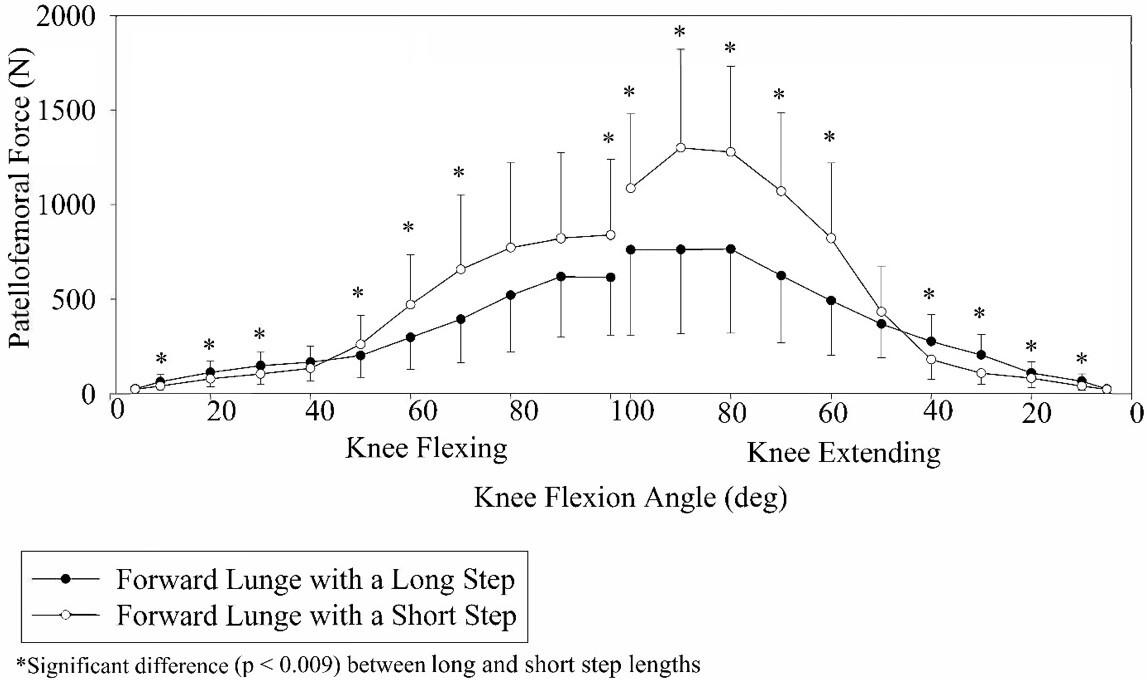 2. Mean
3. Mean (SD)
2. Mean
3. Mean (SD)
Note: Mean (SD) patellofemoral stress follows a similar pattern and results as patellofemoral force.
Note: Mean (SD) patellofemoral stress follows a similar pattern and results as patellofemoral force.
When comparing patellofemoral force and stress with a stride to without a stride during the forward lunge, between 10°-50° knee angles of the knee flexing phase and between 50°-20° knee angles of the knee extending phase

patellofemoral force and stress were significantly greater with a stride than without a stride (Figure 6),23 and a similar pattern was also observed during the side lunge exercise.23 These data show a progression in patellofemoral re-
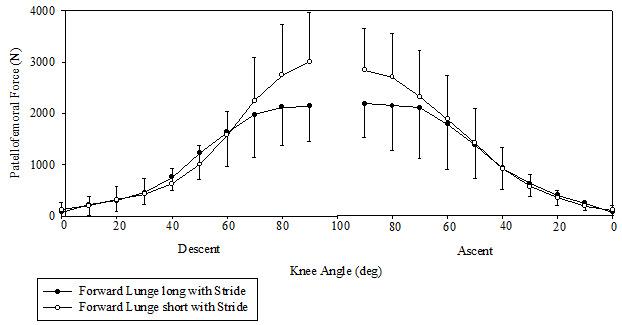 Figure 4. Mean (±SD) patellofemoral joint compressive force in lead knee for the forward lunge long and short with a stride (step forward & push back to starting position) using a 12-repetition maximum load (12-RM).22 Significant differences (p < 0.009) occurred between 70°–90° knee angles.
Figure 5. Mean (SD) patellofemoral compressive force in lead knee for forward lunge at ground level and forward lunge up to a 10 cm platform with a stride (step forward and push back to starting position) using bodyweight only.16
Figure 4. Mean (±SD) patellofemoral joint compressive force in lead knee for the forward lunge long and short with a stride (step forward & push back to starting position) using a 12-repetition maximum load (12-RM).22 Significant differences (p < 0.009) occurred between 70°–90° knee angles.
Figure 5. Mean (SD) patellofemoral compressive force in lead knee for forward lunge at ground level and forward lunge up to a 10 cm platform with a stride (step forward and push back to starting position) using bodyweight only.16
Note:
habilitation, suggesting that stationary lunging (without a stride) should precede lunging by stepping forwards/sideways and pushing back (with a stride) when the goal is to minimize patellofemoral joint loading.
There are several conclusions from examining the forward lunge data from Figures 3-6 when the goal is to initially minimize patellofemoral joint force and stress and then gradually progress loading: 1) initially employ a more functional knee flexion range between 0-50º; 2) then, progress to higher knee angles (0°–100°); (3) then employ a long step and higher knee angles (0°–100°) up to a 10-cm platform; and (4) finally, employ a long step and higher knee angles (0°–100°) at ground level.
Technique variations within squatting techniques can also affect patellofemoral loading. Patellofemoral force and stress were significantly greater at 90º knee angle in the 12-RM wall squat with the feet a short distance from the wall (causing the knees to translate anteriorly beyond the toes - referred to as wall squat short), with a peak force of approx. 3650 N, compared to the 12-RM wall squat with feet farther away from the wall (allowing the knees to stay over the feet - referred to as wall squat long), with a peak force of approx. 2900 N.24 During the 12-RM barbell squat, peak patellofemoral force and stress were greater with a wide stance squat (4313-4674 N at 80-90º knee angles) compared to a narrow stance squat (3958-4246 N at 80-90º knee angles), and mean patellofemoral force and stress was 15% greater in the wide stance squat than the narrow stance squat between 21-79º knee angles.2
Technique variations during the leg press can also affect patellofemoral loading. During the 12-RM leg press, peak
patellofemoral force and stress were greater with a narrow stance leg press (4316-4809 N at 80-90º knee angles) compared to a wide stance leg press (3761-4389 N at 80-90º knee angles), and mean patellofemoral force and stress was 18% greater in the narrow stance leg press than the wide stance leg press between 19-91º knee angles.2
CRUCIATE LIGAMENT REHABILITATION
For PCL loading between different WBE, peak force was highest in the two-leg 12-RM barbell squat (1868-2212 N at 63-77 º knee angles), followed by the 12-RM leg press (1690-1726 N at 88-95 º knee angles), 12-RM wall squat (757-786 N at 80-90º knee angles), 12-RM forward and side lunges (641-765 N at 80-90º knee angles), 12-RM one-leg squat (414 N at 90º knee angle), bodyweight forward and side lunges (279-328 N at 70-80º knee angles), and level ground walking (160 N at 15-20º knee angles).1–8,11–14

PCL loading was greater in the 12-RM wall squat (259-757 N) compared to the 12-RM one leg squat (64-414 N) between 0-90º knee angles, while in contrast ACL loading was greater in the 12-RM one leg squat (22-59 N) than the 12-RM wall squat (0 N) between 0-40º knee angles.6 PCL loading was greater in the 12-RM barbell squat than the 12-RM leg press between 27-79º.2
Cruciate ligament differences were also observed between the forward lunge and side lunge exercises performed both with bodyweight and with a 12-RM external
Figure 6. Mean (SD) patellofemoral compressive force in lead knee between forward lunge with a stride (step forward and push back to starting position) and without a stride (lunging up and down with feet stationary).23 Patellofemoral force was significantly greater (p<0.009) between 10°-50° knee angles of the knee flexing phase and between 50°-20° knee angles of the knee extending phase. Mean (SD) patellofemoral stress follows a similar pattern and results as patellofemoral force.Figure 7 Mean (SD) PCL tensile force during forward and side lunges with a stride (step forward and push back to starting position) using a 12-repetition maximum load (12-RM).8 Significant differences (p < 0.009) occurred between 40°–80° knee angles.
load.8 PCL loading was greater in the 12 RM forward lunge than the 12-RM side lunge between 40-80º knee angles (Figure 7).8

Differences in patellofemoral joint loading also occurred between the bodyweight forward and side lunge exercises when performed with step height variations, such as performing the forward and side lunge exercises at ground level versus performing the forward and side lunge exercises up to a 10-cm high platform (Figure 8).15,16
As shown in Figure 9 for the bodyweight forward and side lunge, at 10° knee angle during the lunge descent and at 10° and 30° knee angles during the lunge ascent, patellofemoral force and stress were significantly greater in the forward lunge compared to the side lunge.15 In contrast, at 40°, 50°, 60°, 70°, 80°, 90°, and 100° knee angles during the lunge descent and at 50°, 60°, 70°, 80°, and 90° knee angles during the lunge ascent patellofemoral joint force and stress were significantly greater in the side lunge compared to the forward lunge.15
In contrast to the bodyweight forward and side lunge, during the 12-RM forward and side lunge the only significant differences found were between 80°-90° knee angles during the lunge descent and at 90° knee angle during the lunge ascent, in which patellofemoral force and stress were greater in the side lunge compared to the forward lunge (Figure 10).23
Patellofemoral force and stress were greater while performing the bodyweight side lunge (252-1302 N) compared to the bodyweight forward lunge (167-766 N) between 40-100° knee angles.15 When external resistance was ap-
plied, patellofemoral compressive force and stress magnitudes were greater during the 12-RM side lunge (2493-2668 N) compared to the 12-RM forward lunge (2161-2191 N) between 80-90º knee angles.
Peak forces for the 12-RM squat and 12-RM leg press were between 4500-5000 N at 90º knee angle, and not significantly different between each other.2 Patellofemoral force and stress were greater in the 12-RM wall squat (approx. 2100-3650 N) than the 12-RM one leg squat (approx. 1800-2800 N) between 60-90º knee angles.24
If we arbitrarily use a 0-100º knee angle range (0º = full knee extension), which is a common knee angle range of motion for most lower extremity WBE and NWBE, this range can roughly be divided in half for anterior cruciate ligament (ACL) loading (0-50º knee angles) and posterior cruciate ligament (PCL) loading (50-100º knee angles). However, for many WBE and NWBE, PCL loading can occur throughout the entire 0-100º knee angle range of motion. Peak PCL loading was generally greater at the higher knee angles (50-100º) than lower knee angles (0-50º), with peak PCL loading typically occurring at knee angles around 70-90º.2,4–8,11 In contrast, peak ACL strain/tensile force typically occurs at lower knee angles between 10-30º for both WBE and NWBE.2,6,10 For example, ACL strains during the isometric seated leg extension using a 30 Nm torque as resistance were 4.4% at 15º knee angle, 2% at 30º knee angle, and no ACL strain at 60º and 90º knee angles.10 More-
over, when tested at 30º, 50º, and 70º knee angles, squatting, lunging and step-up and step-down exercises had the greatest ACL strain at 30º knee angle.10 Moreover, it should be emphasized that peak ACL loading from both NWBE and WBE are of relatively small magnitudes, typically less than 150 N or 3.7% ACL strain (which is roughly the same as a 150 N Lachman test) for WBE, but higher (150-350 N) for NWBE,1–8,10,25,26 Therefore, if the rehabilitation goal is to minimize ACL or PCL loading, such as during the early phases after ACL or PCL reconstruction surgery, training with both NWBE and WBE would be appropriate starting with lower knee angles (e.g. 0-50º) for PCL rehabilitation and higher knee angles (e.g. 50-100º) for ACL rehabilitation.
In general, for both WBE and NWBE, patellofemoral force and stress increase as knee angle increases and decrease as knee angle decreases. Therefore, when the goal is to minimize patellofemoral force and stress, performing exercise at lower knee angles (eg, 0-50º) is desirable, and progression
to higher knee angles (eg, 50-100º) as more patellofemoral force and stress can be tolerated later in the rehabilitation process.
For ACL rehabilitation, anterior knee movement of 8-10 cm or more beyond the toes may increase ACL loading during squatting, lunging, leg press, and other WBE.4,6–8 Moreover, squatting with the heels off the ground, which typically results in increased anterior knee movement beyond the toes, resulted in over three times ACL loading compared with squatting with the heels on the ground.4,11
ACL loading was significantly greater in the one-leg squat, in which the knees moved forward beyond the toes 10±2 cm, compared to performing the wall squat long with the knees positioned over the feet.6 ACL loading was significantly greater in the 12-RM forward lunge short (using
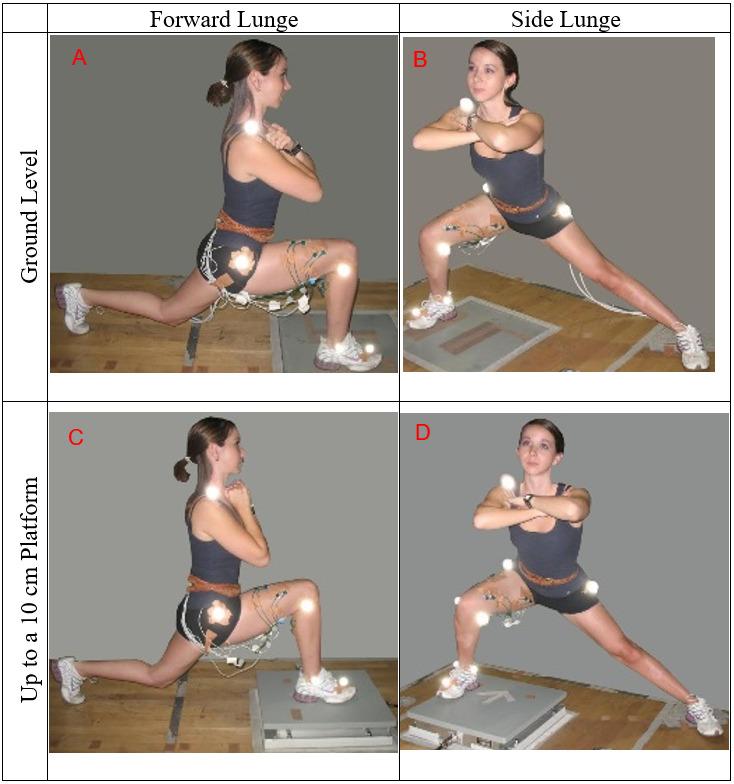 Figure 8. Forward lunge at ground level (A), side lunge at ground level (B), forward lunge up to a 10 cm platform (C), and side lunge up to a 10 cm platform (D).
Figure 8. Forward lunge at ground level (A), side lunge at ground level (B), forward lunge up to a 10 cm platform (C), and side lunge up to a 10 cm platform (D).
Figure 9. Mean (SD) patellofemoral compressive force in lead knee between forward lunge and side lunge with bodyweight and a stride (step forward and push back to starting position) collapsed across step height.15
Significant differences (p < 0.009) occurred at 10° during the lunge descent,10° and 30° during the lunge ascent, 40°-100° during the lunge descent, and 50°-90° during the lunge ascent.
Note: Mean (SD) patellofemoral stress follows a similar pattern and results as patellofemoral force.
Figure 10. Mean (SD) patellofemoral compressive force in lead knee between forward and side lunges with a stride (step forward and push back to starting position) using a 12-repetition maximum load (12-RM).23
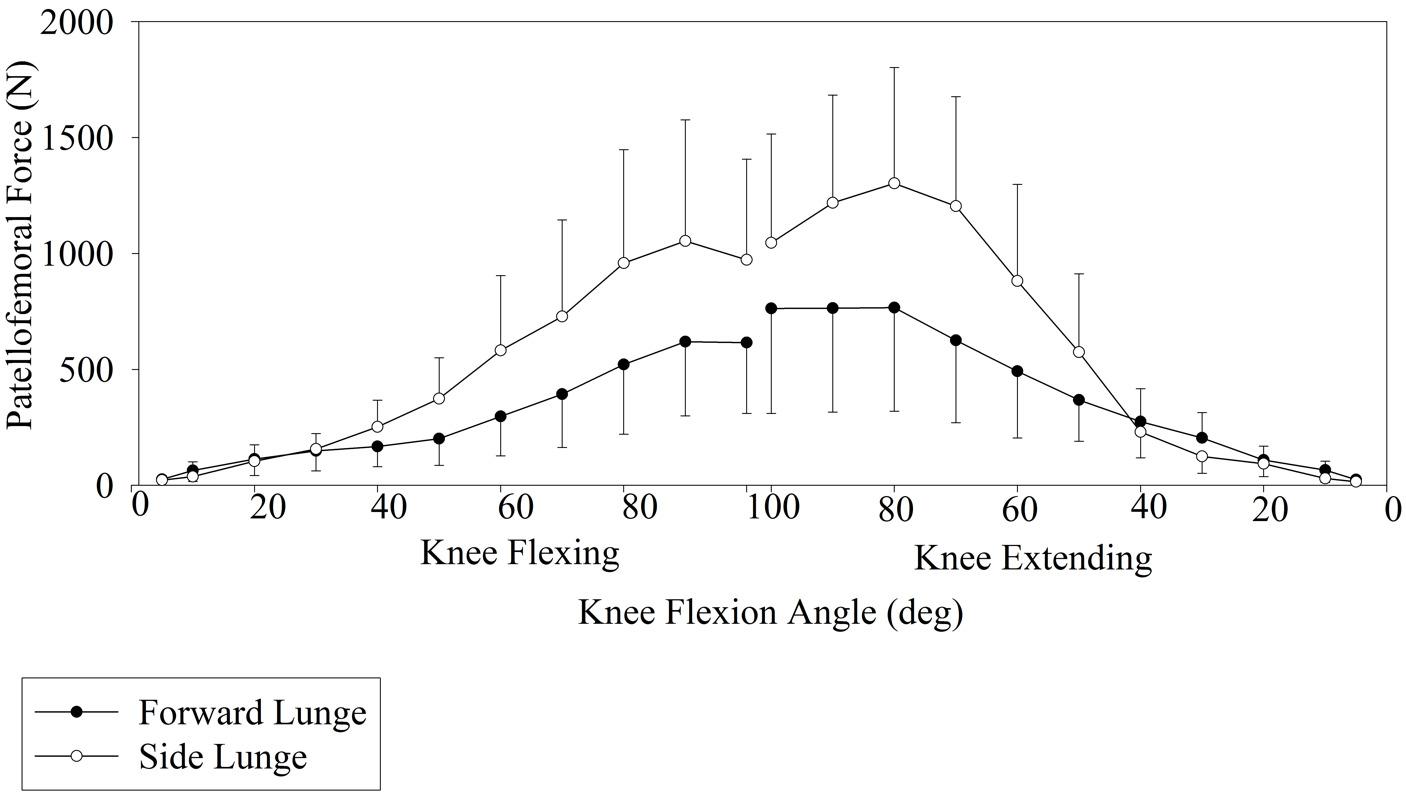
Significant differences (p < 0.009) occurred between 80°-90° during the lunge descent and at 90° during the lunge ascent.
Note: Mean (SD) patellofemoral stress follows a similar pattern and results as patellofemoral force.
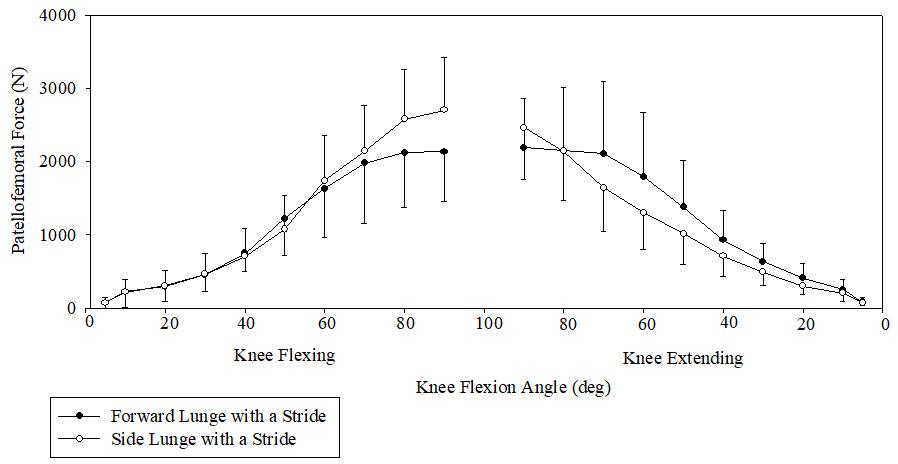
a short step, in which the knees moved forward beyond the toes 9±2 cm), compared to the 12-RM forward lunge long (using a long step, in which the knees stay over the feet throughout the movement).4,5,7 Moreover, squatting with a more erect trunk position compared with squatting with a 30-40º forward trunk tilt position tends to cause more anterior translation of the knees beyond the toes, as well as greater quadricep activation (which increases ACL tensile force at lower knee angles) and less hamstring activation (which results in less unloading of the ACL).2,6
Patellofemoral force and stress were significantly greater at 90º knee angle in the wall squat short (knees translate anteriorly beyond the toes), with a peak force of ~3650 N, compared to the wall squat long (knees stay over the feet), with a peak force of ~2900 N.24 At the lowest position of the wall squat short (90º knee angle), the knees translated beyond the toes 9±2 cm, compared to the knees being above the ankles and over the feet for the wall squat long.24
It has been demonstrated that both cruciate ligament loading and patellofemoral loading varies between WBE and NWBE, varies with technique variations within WBE and NWBE, varies between different WBE, and varies as a function of knee angle. Understanding how varying techniques within and between WBE and NWBE affect cruciate ligament and patellofemoral loading may help clinicians better prescribe WBE and NWBE in a safe and effective manner during cruciate ligament and patellofemoral rehabilitation.
The author of this manuscript affirm we have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript. The authors of this manuscript also affirm they have no conflict of interest of any kind.
Submitted: October 31, 2022 CST, Accepted: December 01, 2022 CST This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Escamilla RF. Knee biomechanics of the dynamic squat exercise. Med Sci Sports Exerc 2001;33:127-141. doi:10.1097/00005768-200101000-00020
2. Escamilla RF, Fleisig GS, Zheng N, Barrentine SW, Wilk KE, Andrews JR. Biomechanics of the knee during closed kinetic chain and open kinetic chain exercises. Med Sci Sports Exerc 1998;30(4):556-569. d oi:10.1097/00005768-199804000-00014
3. Escamilla RF, Fleisig GS, Zheng N, et al. Effects of technique variations on knee biomechanics during the squat and leg press. Med Sci Sports Exerc 2001;33(9):1552-1566. doi:10.1097/00005768-200109 000-00020
4. Escamilla RF, Macleod TD, Wilk KE, Paulos L, Andrews JR. Cruciate ligament loading during common knee rehabilitation exercises. Proc Inst Mech Eng H 2012;226(9):670-680. doi:10.1177/0954411912 451839
5. Escamilla RF, Macleod TD, Wilk KE, Paulos L, Andrews JR. Anterior cruciate ligament strain and tensile forces for weight-bearing and non-weightbearing exercises: a guide to exercise selection. J Orthop Sports Phys Ther 2012;42(3):208-220. doi:10.2 519/jospt.2012.3768
6. Escamilla RF, Zheng N, Imamura R, et al. Cruciate ligament force during the wall squat and the one-leg squat. Med Sci Sports Exerc. 2009;41(2):408-417. doi:1 0.1249/mss.0b013e3181882c6d
7 Escamilla RF, Zheng N, Macleod TD, et al. Cruciate ligament forces between short-step and long-step forward lunge. Med Sci Sports Exerc. 2010;42(10):1932-1942. doi:10.1249/mss.0b013e3181 d966d4
8. Escamilla RF, Zheng N, MacLeod TD, et al. Cruciate ligament tensile forces during the forward and side lunge. Clin Biomech (Bristol, Avon) 2010;25(3):213-221. doi:10.1016/j.clinbiomech.200 9.11.003
9. Fleming BC, Beynnon BD, Renstrom PA, et al. The strain behavior of the anterior cruciate ligament during stair climbing: an in vivo study Arthroscopy 1999;15(2):185-191. doi:10.1053/ar.1999.v15.015018
10. Heijne A, Fleming BC, Renstrom PA, Peura GD, Beynnon BD, Werner S. Strain on the anterior cruciate ligament during closed kinetic chain exercises. Med Sci Sports Exerc. 2004;36(6):935-941. d oi:10.1249/01.mss.0000128185.55587.a3
11. Toutoungi DE, Lu TW, Leardini A, Catani F, O’Connor JJ. Cruciate ligament forces in the human knee during rehabilitation exercises. Clin Biomech (Bristol, Avon) 2000;15(3):176-187 doi:10.1016/s026 8-0033(99)00063-7
12. Shelburne KB, Pandy MG. A dynamic model of the knee and lower limb for simulating rising movements. Comput Methods Biomech Biomed Engin 2002;5(2):149-159. doi:10.1080/10255840290010265
13. Pflum MA, Shelburne KB, Torry MR, Decker MJ, Pandy MG. Model prediction of anterior cruciate ligament force during drop-landings. Med Sci Sports Exerc 2004;36(11):1949-1958. doi:10.1249/01.mss.00 00145467.79916.46
14. Shelburne KB, Torry MR, Pandy MG. Muscle, ligament, and joint-contact forces at the knee during walking. Med Sci Sports Exerc 2005;37(11):1948-1956. doi:10.1249/01.mss.0000180404.86078.ff
15. Escamilla R, Zheng N, MacLeod TD, et al. Patellofemoral Joint Loading During the Performance of the Forward and Side Lunge with Step Height Variations. Int J Sports Phys Ther 2022;17(2):174-184. doi:10.26603/001c.31876
16. Escamilla RF, Zheng N, MacLeod TD, et al. Patellofemoral Joint Loading in Forward Lunge With Step Length and Height Variations. J Appl Biomech 2022;38(4):210-220. doi:10.1123/jab.2021-0313
17. Shin CS, Chaudhari AM, Andriacchi TP. The influence of deceleration forces on ACL strain during single-leg landing: a simulation study J Biomech 2007;40(5):1145-1152. doi:10.1016/j.jbiomech.2006.0 5.004
18. Beynnon BD, Fleming BC, Johnson RJ, Nichols CE, Renström PA, Pope MH. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. Am J Sports Med 1995;23(1):24-34. doi:10.1177/ 036354659502300105
19. Beynnon BD, Johnson RJ, Fleming BC, Stankewich CJ, Renström PA, Nichols CE. The strain behavior of the anterior cruciate ligament during squatting and active flexion-extension. A comparison of an open and a closed kinetic chain exercise. Am J Sports Med 1997;25(6):823-829. doi:10.1177/03635465970250061 6
20. Pandy MG, Shelburne KB. Dependence of cruciate-ligament loading on muscle forces and external load. J Biomech 1997;30(10):1015-1024. do i:10.1016/s0021-9290(97)00070-5
21. Wilk KE, Andrews JR. The effects of pad placement and angular velocity on tibial displacement during isokinetic exercise. J Orthop Sports Phys Ther. 1993;17(1):24-30. doi:10.2519/josp t.1993.17.1.24
22. Escamilla RF, Zheng N, MacLeod TD, et al. Patellofemoral joint force and stress between a shortand long-step forward lunge. J Orthop Sports Phys Ther 2008;38(11):681-690. doi:10.2519/jospt.2008.26 94
23. Escamilla RF, Zheng N, MacLeod TD, et al. Patellofemoral compressive force and stress during the forward and side lunges with and without a stride. Clin Biomech (Bristol, Avon). 2008;23(8):1026-1037 doi:10.1016/j.clinbiomech.200
8.05.002
24. Escamilla RF, Zheng N, Macleod TD, et al. Patellofemoral joint force and stress during the wall squat and one-leg squat. Med Sci Sports Exerc 2009;41(4):879-888. doi:10.1249/mss.0b013e31818e7 ead
25. Beynnon BD, Fleming BC. Anterior cruciate ligament strain in-vivo: a review of previous work. J Biomech. 1998;31(6):519-525. doi:10.1016/s0021-929 0(98)00044-x
26. Wilk KE, Escamilla RF, Fleisig GS, Barrentine SW, Andrews JR, Boyd ML. A comparison of tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am J Sports Med. 1996;24(4):518-527. doi:10.1177/036354659602
400418
Kylie Art 1 ,
Courtney Ridenour1 ,
Stephanie Durbin1 , Max
Bauer1 , Amy
Hassen-Miller1 a 1
Physical Therapy, Walsh UniversityKeywords: athlete, adolescent, concussion, exercise, physical therapy intervention https://doi.org/10.26603/001c.68071
Sports-related concussions are the most common cause of head injury in adolescents and young adults. Typical treatment methods for this injury include cognitive and physical rest. Evidence suggests that physical activity and physical therapy interventions can be beneficial to decrease post-concussion symptoms.
The aim of this systematic review was to investigate the effectiveness of physical therapy interventions for adolescent and young adult athletes post-concussion.
The following databases were utilized for the search: PubMed, CINAHL, Proquest, MEDLINE, SPORTDiscus, and SCOPUS. The search strategy focused on athletes, concussions, and physical therapy interventions. Data extraction from each article included: Authors, subjects, gender, mean age, age range, specific sport, acute or chronic concussion, first or recurrent concussion, treatments for intervention and control group, and outcomes measured.
Eight studies met the inclusion criteria. Six of the eight articles scored seven or higher on the PEDro Scale. Physical therapy intervention(s), such as an aerobic intervention or a multimodal approach, show improvements in time to recovery and reduction of post-concussion symptoms in patients who have had a concussion. Physical activity and physical therapy as early as a couple days following injury, is beneficial at decreasing post-concussion symptoms, allows for earlier return to play, and/or shorter days to recovery, and is considered safe for treating post-concussion symptoms.
This systematic review demonstrates that physical therapy interventions including aerobic exercise and multimodal approaches have been found to be beneficial in treating adolescent and young adult athletes post-concussion. Utilizing aerobic or multimodal interventions for this population allows for a quicker symptom recovery and return to sport than traditional treatment of physical and cognitive rest. Future research should investigate the superior intervention for adolescents and young adults with
Corresponding Author:
Dr. Amy Hassen-Miller Associate Professor Walsh University2020 E. Maple St. North Canton, OH, 44702
E-Mail: ahassenmiller@walsh.edu

post-concussion syndrome and determine if a single treatment or a multimodal approach is more beneficial.
Concussion is a mild traumatic brain injury. Concussion occurs as a result of direct trauma, whiplash, or blast injury that causes the brain to move forward and backward. Symptoms associated with concussion include headache, dizziness, vertigo, nausea, fatigue, light and noise sensitivity, as well as altered mental status.1,2 The leading cause of head injury in adults occurs from car accidents, whereas in the younger population (15-24 years old), injury occurs from a sport related accident. Of the forty-four million children involved in various sports-related activities, around 3.8 million experience a concussion related to sport each year 2 Emergency department visits due to sport-related concussions increased by more than double between 2001-2012.1,3 The most common cause of sport-related concussion is player to player contact and happens frequently in football and ice hockey Female athletes have a higher incidence of concussion compared to male athletes. Athletes who have had a prior concussion also have a higher rate of experiencing additional concussions.2,4 Adolescent athletes are at higher risk of suffering a concussion than adults and may also require a longer period of time to recover.5 If an athlete is diagnosed with a concussion, they must be cleared by a health care professional before returning to play
Traditional treatment for concussion includes physical and cognitive rest.6,7 Unfortunately, individuals prescribed with rest can demonstrate withdrawal from life activities, deconditioning, and mental health issues.8 Research is emerging that shows the benefit of exercise and early physical activity after a concussion.2 Specifically, early physical activity is advantageous and lower rates of post-concussive symptoms are associated with higher levels of physical activity and this research states that patients suffering from concussion should be encouraged to exercise as tolerated 1-2 days after concussion and initial rest.2 Individuals with a concussion present with varying symptoms and presentations requiring patient-specific intervention strategies. According to a clinical practice guideline, recommended frequency, intensity, timing, and type(s) of intervention is dependent on the severity of a patient’s concussion, their level of irritability, and how they respond to treatment. Patients should also be educated on symptom reporting so that interventions can be adjusted resulting in earlier return to sport.9
Existing literature suggests that cervical and vestibular interventions as well as sub-symptom threshold exercise may be beneficial for individuals 24-48, hours after concussion. Aerobic exercise has been shown to improve autonomic nervous system function suggesting that subthreshold exercise treatment could be a beneficial treatment for concussion. Systematic reviews have shown that exercise post-concussion can improve symptom scores after concussion and that sub-symptomatic aerobic exercise programs can be more effective in reducing post-con-
cussion syndrome symptoms than traditional standard of care.10
There is a gap in the current literature regarding sportsrelated concussions in adolescent and young adult athletes and the appropriate interventions for treatment. The aim of this systematic review was to investigate the effectiveness of physical therapy interventions for adolescent and young adult athletes post-concussion.
This systematic review was registered with Prospero and completed using guidelines from Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). PRISMA is a 27-item checklist based on evidence that focuses on reporting the impact of interventions in systematic reviews and meta-analysis.11 Prospero provides the opportunity to determine if a similar review already exists or is in the process of being published to prevent unwanted duplication.12 The registration ID for Prospero for this systematic review is CRD42021256465.
In order to be included in this systematic review, articles had to meet the following inclusion criteria: be original research, a randomized controlled-trial, include participants that were athletes under the age of thirty, have an acute or chronic sport-related concussion, and include physical therapy intervention(s). Randomized controlled-trial articles were chosen due to high placement on the hierarchy of evidence and to strengthen the results of this systematic review Articles were excluded if they were not of a randomized controlled-trial study design, not reported in English, or did not fit the inclusion criteria stated.
The following databases were utilized for the search: PubMed, CINAHL, Proquest, MEDLINE, SPORTDiscus, and SCOPUS. The search strategy focused on three key concepts: athletes, concussions, and physical therapy interventions. After these concepts were identified, similar terms were noted, defined, and used in the searches. These terms were then utilized in each database and any database-specific terms such as Subject Heading (SH) or Medical Subject Heading (MESH) when relevant. Appendix 1 provides the specific search strategies utilized in this search. A hand search was completed by looking through the references of articles included in this systematic review The initial search was started in March 2021 and the final search concluded in January 2022.
The total number of abstracts, titles, and full texts from the search strategy were divided in half and allocated to
Balance Error Scoring System (BESS)
Beck Depression Inventory for Youth
Post-Concussion Symptom Inventory (PCSI)
Post-Concussion Symptom Scale (PCSS)
Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT)
BORG CR 10 RPE
Description
Measures postural stability and vestibular dysfunction related to return to play.15 Used primarily in youth, athletes, and patients with a traumatic brain injury 15
Self-reported outcome measure with 21 items ranked on a four point scale to assess depression.16 Score >10 is positive for depression which is common in athletes.16 Used commonly for Parkinson’s Disease, stroke, spinal cord, and nonspecific populations.
26 item self-reported outcome measure for individuals aged 5-18.17 Assess cognition, sleep, emotions, and physical domains.
21 item self-reported outcome measure using a 7 point likert scale. Used to determine whether athletes have a concussion or not.17
Online computerized neuropsychological series including patient demographics, determine if any of the 22 listed concussion symptoms are present and at what severity, and neuropsychological modules to assess attention, memory, processing speed, reaction time, sequencing, and learning. Used primarily with the athlete population.17
Measures exercise intensity perceived by the patient during exercise and used primarily with patients with breathlessness, angina, and musculoskeletal pain.18
Post Ride Symptom Change Rating Experiential likert scale that ranks perceived exertion after biking.19
two teams of two authors. Each title, abstract, and full text for each article was assessed independently and screened by two separate authors to be reviewed for inclusion in the systematic review. If a tie breaker was needed due to a disagreement between team members, then a third author would serve as a tie breaker Any duplicates found during the search were removed. Cohen’s unweighted Kappa was calculated for agreement during the title, abstract, and full text review. “Kappa is a measurement that is used to determine agreement among raters when scores are repeated.”13 Recommended values for Kappa include: <0.00 is poor agreement, (0.01-0.20) is slight agreement among raters, (0.21-0.40) is considered fair agreement, (0.41-0.60) is moderate, (0.61-0.80) is considered substantial agreement among raters, and (0.81-1.0) is almost perfect agreement."13
Risk of bias assessment for included studies was performed by two authors independently and was reviewed for each of the articles. If a disagreement was present, a third author would serve as a tiebreaker to reach consensus. Risk of bias assessment in the included studies was assessed using the PEDro scale. The PEDro scale is an appropriate tool to assess the quality of randomized controlled trials. A higher score on the PEDro scale indicates a lower risk of bias in an article, with the highest score possible being a 10 and lowest score of a 0. The PEDro scale has 11 criterion but is only scored using 10, thus has a score out of 10. One item, the item on eligibility, is not counted towards the score because it is related to external validity The PEDro scale does not assess external validity or effect size of treatment.14
Two authors performed data extraction independently. Consensus was reached after independent extraction. Data
extraction included: Authors, subjects, gender, mean age, acute or chronic concussion, treatment for intervention group versus control group, and outcomes measured.
The initial search results produced 7,034 titles. There were 3,253 titles found after all duplicates were removed. Two authors screened titles and abstracts and 3,193 articles were excluded. A hand search was completed, and two additional randomized controlled trials were included. After title and abstract review, 60 articles were chosen for full-text review with an observed kappa value of one and confidence interval of one to one demonstrating perfect agreement between reviewers. Non-randomized control trials were excluded as well as one ongoing study, which resulted in eight articles that fit the inclusion criteria to be included in the systematic review. Details of the study selection can be seen in Figure 1
Aerobic intervention for the treatment groups was used for four of the eight articles, and multimodal intervention for the treatment groups was used for the remaining four articles. The control groups for each of the articles either participated in education, rest, sub-therapeutic exercise, placebo, or sham treatment. The outcome measures varied throughout the eight studies and included: days from injury to recovery, PCSS, PCSI, Health Related Quality of Life, Beck Depression Inventory for Youth, Pediatric Quality of Life Multidimensional Fatigue Scale, the BESS, ImPACT, time to return to play, health and demographic questionnaires, Borg CR10, Rate of Perceived Exertion (RPE), and Post Ride Symptom Change Rating. See Table 1 for a description of the outcome measures that were used in the
articles included in this systematic review In total, there were 375 subjects that participated in the eight studies with 163 females and 212 males. The age range of participants included was 11.2-21.2 years old. Four articles included subjects who had acute post-concussion symptoms, one article included participants with chronic post-concussion symptoms, two articles included participants with both acute and chronic post-concussion symptoms, and one article did not indicate severity of concussion. Six of the eight articles included participants who have had one concussion or a recurrence of concussions while the other two articles did not indicate occurrence of concussion. Study characteristics can be found in Table 2
Two reviewers assessed the risk of bias of the eight articles included in this systematic review using the PEDro Scale. Each of the articles was given a PEDro Scale score, shown in Table 3. To evaluate the level of agreement between the two reviewers, an unweighted kappa was calculated totaling one, (CI = 1:1), which demonstrates perfect agreement. Five of the eight articles were of a higher quality relating to risk of bias compared to the other three included articles, with scores ranging from a 5 to a 10 out of 10 items. Three of the five higher quality articles found sig-
nificant improvements in the treatment groups compared to the control groups.20,21,24 Although only three articles demonstrated statistically significant results for the treatment group compared to the control group, all articles demonstrated improved symptoms with time and there were no adverse effects reported with early physical activity and therapy. Three of the eight articles had a lower quality relating to risk of bias scoring a 3 to 4 out of 10 items.19,25,26 Criterion 1, 2, 4 and 10 were met by all articles included in this study
Four of the eight studies included in the systematic review used aerobic interventions for the treatment group.19–21,26 Leddy et al.20 included aerobic exercise on a stationary bike or treadmill if available, or walking/jogging outdoors if they did not have access to exercise equipment. The aerobic exercise would last 20 minutes or until their symptoms increased by two or more points from their pre-exercise symptom level (based on a 10-point Visual Analogue Scale). Participants in the aerobic exercise group recovered in a median of 13 days compared to the control group who recovered in 17 days (p = 0.009). Leddy et al.21 included aer-
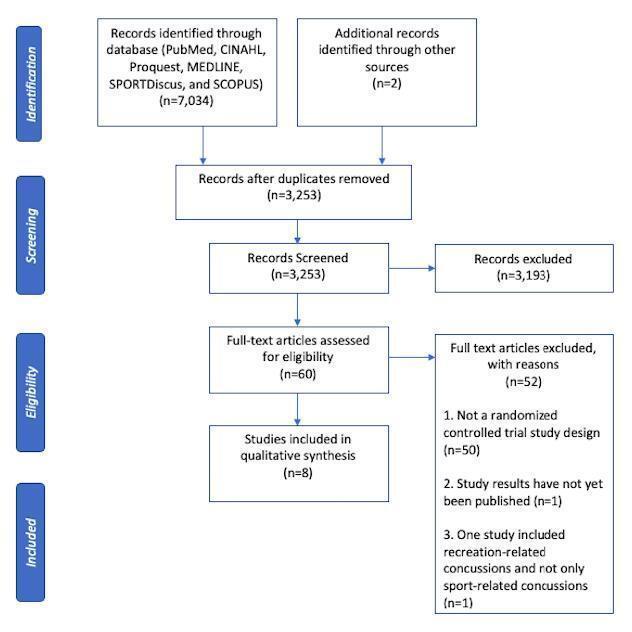 Figure 1. Study Selection.
Figure 1. Study Selection.
Leddy20 Aerobic Exercise on bike or treadmill
Placebo-like stretching regimen
Leddy, Master21
Aerobic exercise: walking, jogging, or stationary bike
Chan22
Reneker23
Aerobic Training: coordination exercises and visualization/imagery techniques
Pragmatically designed individualized and progressive treatment plan
Schneider24
Postural education, range of motion exercises and cognitive and physical rest, until asymptomatic followed by a protocol of graded exertion. Along with cervical spine and vestibular rehab
Days from injury to recovery; symptom severity score, proportion of participants with delayed recovery
Placebo-like stretching regimen PSCI, days to recovery, development of post-concussive symptoms
Usual Treatment (education about symptom management, school consultation with a hospital affiliated teacher who facilitated return to school, physician consult for medication and referral for community therapy)
sham, subtherapeutic, and non-progressive therapeutic techniques to minimally progressive therapy
PCSS, health-related quality of life, beck depression inventory for youth, pediatric quality of life, multidimensional fatigue scale, balance error scoring system, immediate post-concussion assessment
>/= 1
PCSS, time to return to play
Same as the intervention group except the cervical spine and vestibular rehab. Return to play (days)
Both, but more chronic than acute
Dobney25
Maerlender19
4 components: (1) aerobic activity, (2) coordination/skill practice, (3) visualization, and (4) education beginning 2 weeks post injury
Exertion: Stationary bike ride for 20 min unless uncomfortable for 0-6 on RPE scale (mild to moderate exertion)
Micay26
Aerobic exerciseprogressive intensity/ duration on cycle ergometer;
4 components: (1) aerobic activity, (2) coordination/skill practice, (3) visualization, and (4) education beginning at the standard 4 week post injury
No physical exertion other than walking to school or daily activities.
Recovery length-symptom free from bike ride, IMPACT, neurocognitive test battery, BORG CR10 RPE.
usual care-rest followed by physician advised progressions of activity
Intervention feasibility: symptom status pre-post exercise sessions and completion of intervention; Clinical recovery: symptom status at weeks 1,2,3, and 4 post injury and medical clearance date using self reported symptom severity scores on PCSS and days to clearance
The Effectiveness of Physical Therapy Interventions for Athletes Post-Concussion: A Systematic Review
1. Eligibility criteria were specified. 2. Subjects were randomly allocated to groups. 3. Allocation was concealed. 4. The groups were similar at baseline regarding the most important prognostic indicators. 5. There was blinding of all subjects.
6. There was blinding of all therapists who administered the therapy. 7. There was blinding of all assessors who measured at least one key outcome. 8. Measures of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups. 9. All subjects for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome was analyzed by “intention to treat.” 10. The results of between group statistical comparisons are reported for at least one key outcome. 11. The study provides both point measures and measures of variability for at least one key outcome.
obic exercise such as walking, jogging, or stationary biking. The aerobic group would exercise for 20 minutes and up to 90% of their maximum heart rate achieved on the Buffalo Concussion Treadmill Test. They were instructed to stop when reaching 90% of their maximum heart rate or when they experienced concussion-like symptoms. Median days to recovery for the aerobic exercise group was 14 days compared to 19 days for the stretching group. Four out of 43 participants in the aerobic exercise group (9%) had persistent post-concussive symptoms, compared to 12 out of 39 participants in the stretching group (31%), (p=0.014 with Fisher’s exact test). Maerlender et al19 had participants ride on a stationary bike with an RPE of 0 - 6 for 20 minutes or until they felt uncomfortable. There was no significant difference between groups for days of recovery, with a median of 13 days to recovery for the standard group, and 15 days to recovery for the exertion group. Micay et al26 had participants complete eight sessions that progressed with duration and intensity using a stationary bike that was connected to a heart rate monitor. Each session started with a five-minute warm up and ended with a five-minute cool down. If symptoms worsened, intervention was terminated. The aerobic exercise group showed greater symptom resolution compared to the control group over time, however there was not a significant difference between groups. Independent t-tests were performed for or between-group difference in mean time to medical clearance which was 36.1±18.5 days for the aerobic exercise group and 29.6±15.8 days for the control group (t(13)=0.03; p=0.87).
Four of the eight studies included in the systematic review used multimodal intervention for the intervention provided to the treatment group.22–25 Chan et al.22 utilized an active rehabilitation program including submaximal aerobic training, light coordination, sport-specific exercises, visualization and imagery techniques, and a home exercise program. The active rehabilitation group had a mean ± SD change of -24.7±19.1 on the PCSS from baseline to followup. The control group had a mean ± SD change of -15.8±12.5 on the PCSS from baseline to follow-up. These results were associated with a significant difference between groups with a Cohen’s d treatment medium effect size of 0.55. Reneker et al.23 study’s treatment group received manual techniques including soft tissue release, mobilizations, and thrust manipulations, and vestibular rehabilitation techniques including habituation, adaptation, oculomotor control, neuromotor control, and balance exercises. The interventions provided were tailored to each specific patient’s needs and progressed over time as the patient’s symptoms would allow The median number of days to post-concussion syndrome (PCS) recovery for the experimental group was 13.5 days and 17 days for the control group, with a log-rank of 0.13 representing no statistical significance between groups. Schneider et al.24 had participants in the treatment group receive cervical spine physical therapy interventions and vestibular rehabilitation accompanied by non-provocative range of motion exercises, stretching, and postural education. The cervical spine
physical therapy interventions included manual therapy of the thoracic and cervical spine and therapeutic exercises including cervical neuromotor retraining exercises. The vestibular rehabilitation was individualized to each person and consisted of habituation, gaze stabilization, adaptation exercises, standing and dynamic balance exercises, as well as canalith repositioning maneuvers. There was a greater number of participants that were medically cleared to return to sport within eight weeks of treatment in the treatment group (11 of the 15 individuals), compared to the control group (one out of the 14 individuals). Individuals in the treatment group were 10.27 (95% CI 1.51 to 69.56) times more likely to be medically cleared to return to sport within eight weeks than the participants in the control group (p<0.001). Dobney et al25 had participants in both the treatment group and control group complete 15 minutes on a stationary bike or treadmill, 10 minutes of coordination and skill practice related to sport preference, 5 to 10 minutes of visualization related to sport preference, and education about recovery, coping with post-concussion symptoms, and the process of returning to school or sport. The only difference between groups was that the treatment group started two weeks post-concussion and the control started treatment four weeks post-concussion. Participants were instructed to discontinue activity if symptoms increased. Post-concussion symptoms improved over time for both groups, with no significant difference between the two groups.
When looking at physical therapy interventions, whether it be aerobic interventions or a multimodal approach, the included studies show improvements in outcomes of time to recovery and reduction of post-concussion symptoms in patients who have had a concussion. Four of the studies had significant between-group differences. The other four did not have significant between group differences but did show improvements overall with no significant adverse effects.
The aim of this systematic review was to investigate the effectiveness of physical therapy interventions for athletes post-concussion. There is a gap in the current literature regarding sports-related concussions in athletes and appropriate interventions for treatment. This review aims to reveal physical therapy interventions to address post-concussive symptoms. Overall, this review demonstrates decreased time to recovery and reduced post-concussion symptoms when patients receive active physical therapy interventions post-concussion. None of the studies demonstrated any significant adverse effects from early physical activity and physical therapy intervention, indicating that this treatment approach is safe for adolescent and young adult athletes post-concussion. Physical therapists should incorporate physical activity and physical therapy interventions earlier to optimize post-concussion recovery
One limitation of this systematic review is that three articles were at high risk of bias according to PEDro, including Maerlender,19 Micay,26 and Dobney 25 Another limitation is that all studies included a small sample size that ranged from 15 to 118 total participants. This could result in larger effect sizes, decrease the power of the data, and be unrepresentative of the population. One article included only male participants decreasing the generalizability of the results.26 Another limitation of this systematic review is that the articles reviewed incorporated both acute and chronic concussions. By including both, the variation in time to resolve symptoms and return to play following the concussion may impact the overall validity and generalizability of the results. Because some of the articles included a combination of treatment interventions for athletes post-concussion, this made determining which treatment was most
effective and beneficial for the participant difficult to determine.
One strength of this systematic review is that only randomized control trials were included. Kappa statistics were calculated among authors and resulted in perfect or near perfect agreement and this review was conducted following PRISMA guidelines. Lastly, available articles for this systematic review are from the year 2014 to present, and attempt to provide the most up to date research on athletes with post-concussion syndrome.
A weakness of this review is the results from the search strategy captured physical therapy interventions that were similar in nature being either aerobic or multimodal, as opposed to a broader spectrum of potential interventions. Also, limited evidence is available regarding athletes postconcussion resulting in only eight randomized control trials available for this review.
There are multiple published systematic reviews that present similar findings. One included 14 articles comparing rest and exercise and concluded that exercise was beneficial at improving PCSS score, decreasing symptoms, and decreasing the duration of lingering post-concussion symptoms.27 A systematic review that included five articles assessing athletes post-concussion with aerobic training demonstrated improvements in post-concussion symptoms.3 Along with these, a systematic review by Makdissi et al28 also found evidence supporting the importance of including physical therapy and aerobic exercise in the treatment of a sports related concussion. This review specifically assessed athletes with persistent symptoms, but they found evidence that treating the patient’s specific persistent symptoms that was beneficial and safe. Lastly, a systematic review that assessed mode and intensity of treatment post sport-related concussion found that light, moderate, and high-intensity levels of exercises can be safe and beneficial for patients during treatment.
The results of this systematic review suggest that physical therapists should incorporate early physical activity and physical therapy interventions into their treatment for adolescent and young adult athletes with post-concussion syndrome. Practicing therapists should determine the individualized impairment(s) present, treat the impairment(s), and use symptom reporting as a guideline to return the athlete to sport to ensure proper timing of interventions.8,9 Due to limitations of this current study, future research should investigate the impact of physical therapy interventions for adolescent and young adult athletes status post chronic versus acute concussion rather than mixing the two and research should be conducted with a larger sample size to allow for a more accurate effect size to be calculated. Future research should also investigate the superior interven-
tion for adolescents and young adults suffering from postconcussion syndrome and determine if single treatment is more beneficial or if multimodal approach is more beneficial to the participants’ recovery. Lastly, future research should include more randomized controlled trials to improve validity and enhance professional decision making.
The results of this systematic review indicate that there is evidence supporting the use of physical therapy interventions including aerobic or multi-modal treatments in the treatment of adolescent and young adult athletes post concussion. The evidence included in this systematic review suggests that aerobic exercise or multi-modal interventions may lead to quicker recovery and return to sport in adolescent and young adult athletes with post-concussive symptoms when compared to traditional treatments such as physical and cognitive rest. Physical therapists should consider incorporation of these interventions into their plan of care for this population to allow for quicker recovery and return to sport.
The authors indicate no conflicts of interest in the reporting of this systematic review
Submitted: April 20, 2022 CST, Accepted: November 30, 2022
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Baker B, Koch E, Vicari K, Walenta K. Mode and intensity of physical activity during the postacute phase of sport-related concussion: a systematic review J Sport Rehabil 2020;30(3):492-500. doi:10.11 23/jsr.2019-0323
2. Mullally WJ. Concussion. Am J Med. 2017;130(8):885-892. doi:10.1016/j.amjmed.2017.04.0 16
3. Powell C, McCaulley B, Scott Brosky Z, Stephenson T, Hassen-Miller A. The effect of aerobic exercise on adolescent athletes post-concussion: a systematic review and meta-analysis. Int J Sports Phys Ther. 2020;15(5):650-658. doi:10.26603/ijspt20200650
4. Reneker JC, Babl R, Flowers MM. History of concussion and risk of subsequent injury in athletes and service members: a systematic review and metaanalysis. Musculoskelet Sci Pract 2019;42:173-185. do i:10.1016/j.msksp.2019.04.004
5. Kimbler DE, Murphy M, Dhandapani KM. Concussion and the adolescent athlete. J Neurosci Nurs. 2011;43(6):286-290. doi:10.1097/jnn.0b013e318 23858a6
6. Leddy J, Hinds A, Sirica D, Willer B. The role of controlled exercise in concussion management. PM R 2016;8(3 Suppl):S91-S100. doi:10.1016/j.pmrj.2015.1 0.017
7 Silverberg ND, Iverson GL. Is rest after concussion “the best medicine?”: recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil. 2013;28(4):250-259. doi:10.1097/ht r.0b013e31825ad658
8. Sawyer Q, Vesci B, McLeod TC. Physical activity and intermittent postconcussion symptoms after a period of symptom-limited physical and cognitive rest. J Athl Train 2016;51(9):739-742. doi:10.4085/10 62-6050-51.12.01
9. Quatman-Yates CC, Hunter-Giordano A, Shimamura KK, et al. Physical therapy evaluation and treatment after concussion/mild traumatic brain injury J Orthop Sports Phys Ther 2020;50(4):CPG1-CPG73. doi:10.2519/jospt.2020.030
10. Leddy JJ, Wilber CG, Willer BS. Active recovery from concussion. Curr Opin Neurol 2018;31(6):681-686. doi:10.1097/wco.0000000000000 611
11. Prisma. PRISMA. Accessed July 28, 2021. http://pr isma-statement.org/
12. Register a review. PROSPERO. Accessed July 28, 2021. https://www.crd.york.ac.uk/PROSPERO/
13. Jewell DV Guide to Evidence-Based Physical Therapist Practice Jones & Bartlett Learning; 2018.
14. Pedro scale. PEDro. Published September 9, 2020. Accessed August 29, 2021. https://pedro.org.au/englis h/resources/pedro-scale/
15. Balance error scoring system. Shirley Ryan AbilityLab. Accessed July 1, 2021. https://www.srala b.org/rehabilitation-measures/balance-error-scoringsystem
16. Beck depression inventory. Shirley Ryan AbilityLab. Accessed July 1, 2021. https://www.srala b.org/rehabilitation-measures/beck-depression-inven tory
17 Graham R, Rivara FP, Ford MA, Committee on Sports-Related Concussions in Youth; Board on Children, Youth, and Families; Institute of Medicine. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. National Academies Press (US); 2014.
18. Borg rating of perceived exertion. Physiopedia. Accessed July 15, 2021. https://www.physio-pedia.co m/Borg_Rating_Of_Perceived_Exertion
19. Maerlender A, Rieman W, Lichtenstein J, Condiracci C. Programmed physical exertion in recovery from sports-related concussion: a randomized pilot study Dev Neuropsychol 2015;40(5):273-278. doi:10.1080/87565641.2015.1067 706
20. Leddy JJ, Haider MN, Ellis MJ, et al. Early subthreshold aerobic exercise for sport-related concussion: a randomized clinical trial. JAMA Pediatr. 2019;173(4):319-325. doi:10.1001/jamapediatrics.201 8.4397
21. Leddy JJ, Master CL, Mannix R, et al. Early targeted heart rate aerobic exercise versus placebo stretching for sport-related concussion in adolescents: a randomised controlled trial. Lancet Child Adolesc Health 2021;5(11):792-799. doi:10.101 6/s2352-4642(21)00267-4
22. Chan C, Iverson GL, Purtzki J, et al. Safety of active rehabilitation for persistent symptoms after pediatric sport-related concussion: a randomized controlled trial. Arch Phys Med Rehabil. 2018;99(2):242-249. doi:10.1016/j.apmr.2017.09.108
23. Reneker JC, Hassen A, Phillips RS, Moughiman MC, Donaldson M, Moughiman J. Feasibility of early physical therapy for dizziness after a sports-related concussion: a randomized clinical trial. Scand J Med Sci Sports. 2017;27(12):2009-2018. doi:10.1111/sms.1 2827
24. Schneider KJ, Meeuwisse WH, Nettel-Aguirre A, et al. Cervicovestibular rehabilitation in sport-related concussion: a randomised controlled trial. Br J Sports Med 2014;48(17):1294-1298. doi:10.1136/bjsports-20
13-093267
25. Dobney DM, Grilli L, Beaulieu C, et al. Feasibility of early active rehabilitation for concussion recovery in youth: a randomized trial. Clin J Sport Med 2020;30(6):519-525. doi:10.1097/jsm.0000000000000 671
26. Micay R, Richards D, Hutchison MG. Feasibility of a postacute structured aerobic exercise intervention following sport concussion in symptomatic adolescents: a randomised controlled study. BMJ Open Sport Exerc Med 2018;4(1):e000404. doi:10.113 6/bmjsem-2018-000404
27 Lal A, Kolakowsky-Hayner SA, Ghajar J, Balamane M. The effect of physical exercise after a concussion: a systematic review and meta-analysis. Am J Sports Med. 2018;46(3):743-752. doi:10.1177/036354651770
6137
28. Makdissi M, Schneider KJ, Feddermann-Demont N, et al. Approach to investigation and treatment of persistent symptoms following sport-related concussion: a systematic review Br J Sports Med 2017;51(12):958-968. doi:10.1136/bjsports-2016-097 470
Appendix
Download: https://ijspt.scholasticahq.com/article/68071-the-effectiveness-of-physical-therapy-interventions-forathletes-post-concussion-a-systematic-review/attachment/135447.docx?auth_token=eGjfGIMkoD83hA13KcHS
1
August Estberger 1 a , Joanne L Kemp 2 , Kristian Thorborg 1,3 , Anders Pålsson 1 , Eva
Ageberg1 Department of Health Sciences, Lund University, Lund, Sweden, 2 La Trobe Sport and Exercise Medicine Research Centre, School of Allied Health, Human Services and Sport, La Trobe University, 3 Sports Orthopedic Research Center – Copenhagen (SORC-C), Departement of Orthopedic Surgery, Amager-Hvidovre Hospital, Institute for Clinical Medicine, Copenhagen University, Copenhagen, Denmark
Keywords: Hip, femoroacetabular impingement, groin pain, exercise therapy, rehabilitation https://doi.org/10.26603/001c.68069
Hip-related pain is an umbrella term encompassing pain from non-arthritic hip joint pathologies, such as femoroacetabular impingement syndrome, hip dysplasia, and labral tears. Exercise therapy is commonly recommended for these conditions, but the reporting completeness of these interventions is currently unclear
The aim of this systematic review was to assess the reporting completeness of exercise therapy protocols for people with hip-related pain.
Systematic review according to PRISMA guidelines.
A systematic search was conducted, searching the MEDLINE, CINAHL, and Cochrane databases. The search results were independently screened by two researchers. Inclusion criteria were studies using exercise therapy in people with non-arthritic hip-related pain. Two independent researchers used the Cochrane risk of bias tool version 2 to analyze risk of bias, and the Consensus on Exercise Reporting Template (CERT) checklist and score (1-19) to synthesize reporting completeness.
Fifty-two studies used exercise therapy for hip-related pain, but only 23 were included in the synthesis as 29 studies had no description of the intervention. CERT scores ranged from 1 to 17 (median 12, IQR 5-15). The most well-described items were tailoring (87%), and the least well-described items were motivation strategies (9%) and starting level (13%). Studies used exercise therapy alone (n=13), or in combination with hip arthroscopy (n=10).

Only 23 of 52 eligible studies reported sufficient details to be included in the CERT synthesis. The median CERT score was 12 (IQR 5-15), with no study reaching the maximum score of 19. Lack of reporting makes it difficult to replicate interventions in future research, and to draw conclusions on efficacy and dose-response to exercise therapy for hip-related pain.
Corresponding author:
August Estberger
Mail: august.estberger@med.lu.se
Phone: +46703384147
Address: Health Science Centre, Box 157, 22100, Lund, Sweden
Hip-related pain is an umbrella term encompassing pain arising from non-arthritic hip joint pathologies in three categories: 1) femoroacetabular impingement syndrome (FAIS), 2) acetabular dysplasia and/or instability, and 3) hip joint problems without distinct morphology (such as labral and chondral lesions).1 Hip-related pain is associated with significant burden in young and middle-aged adults, leading to poor function and low quality of life.2
Exercise therapy for musculoskeletal pain is an effective, low-cost intervention with few adverse events,3,4 and is recommended in high quality clinical practice guidelines for diagnoses such as osteoarthritis, low back pain, neck pain and rotator cuff disorders.5 Exercise therapy is also suggested as a key component of treatment for hip-related pain, whether or not surgical intervention is undertaken.6,7
Physical therapist-led interventions that mainly include exercise therapy, have moderate positive effects compared to sham/control interventions.8 However, the optimal content and delivery of exercise therapy is unclear.9
To establish best practice, the details of exercise therapy interventions must be described. Complete reporting of the details of an intervention is an important aspect of study quality. Incomplete reporting of the intervention details within a study limits the ability to inform future research,10 and lowers the clinical applicability of the research findings.11 With the aim to increase the reporting completeness of complex interventions, the CONSORT statement extension for non-pharmacological trials,10 and the Template for intervention description and replication (TIDieR) guidelines,12 were developed. The Consensus for Exercise Reporting Template (CERT) was developed to guide and facilitate reporting completeness of exercise therapy interventions.13 The CERT checklist can also be used to evaluate completeness of reporting of exercise therapy protocols. It is unknown whether reporting completeness of exercise therapy interventions for hip-related pain has improved since the publication of the CERT guidelines (i.e., 2016). It is also unclear whether any relationship exists between reporting completeness of exercise therapy interventions and other factors related to study quality, such as risk of bias.
Some studies have examined the reporting completeness of exercise therapy interventions for pain around the hip and groin.14–16 Systematic reviews have described incomplete reporting in studies using exercise therapy as treatment for extra-articular groin pain (i.e. adductor-related, inguinal-related or pubic-related groin pain)15 and hip OA.14 A recent scoping review examined specific exercises for FAIS, and how these relate to proposed pathomechanics, in people treated with a non-operative approach.16 The authors used CERT as a secondary measure and a proxy for study quality, but did not report any detailed CERT synthesis or description of the intervention content.16
To the authors knowledge, there are no systematic reviews examining the completeness of the reporting of exercise therapy interventions with/without concurrent surgical intervention for people with hip-related pain. Such knowledge can inform understanding of efficacy of exercise therapy for this patient population, as well as improve future research. Therefore, the main aim of this study was to assess the reporting completeness of exercise therapy protocols for people with hip-related pain. In addition, the aim was also to provide a summary of the content of the exercise therapy protocols included in the study, as well as compare CERT scores between i) studies published before and after publication of CERT, and ii) studies with different levels of risk of bias.
This systematic review, adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement, was preregistered in the PROSPERO database (CRD42020154139).
A systematic search in the MEDLINE, CINAHL, and Cochrane databases was conducted by a research librarian for research studies from earliest available to 31 October 2019 and updated February 19, 2021. The following key words were used:
Population-based terms: ‘hip’, ‘hip pain’, ‘femoroacetabular impingement’, ‘ non arthritic hip pain’, ‘acetabular labrum’, ‘dysplas*’, ‘hip chondral’, ‘hip instability’
Intervention-based terms: ‘exercis*’, ‘training’, ‘physiotherap*’, ‘therap*’, ‘physical therap*’, ‘rehabilitat*’, ‘ manual therap*’, ‘mobilization’, ‘patient education’, ‘ conservative’, ‘ non operative’
The search strategy was adapted to the different databases (Appendix A). Reference lists of included studies were screened for further relevant studies.
Studies were eligible for inclusion if they were randomized controlled trials, cohort studies, case control studies, or published study protocols that included:
• People with non-arthritic hip-related pain, as defined by the International Hip-related Pain Research Network, Zurich 20181
• People with persistent pain (>3 months duration)
• Aged 18 to 50 years
• A description of exercise therapy, including details such as treatment modality, prescription, type and/or duration.
Review studies and clinical commentaries were not eligible for inclusion. Studies were also excluded if they included:
• People with verified osteoarthritis (Tönnis grade >1)
• People with total hip replacement
• People with acute hip injury, such as a fracture of the neck of the femur
• People with extra-articular pain, such as adductor-related groin pain
• Interventions including treatment (e.g., therapeutic injection therapy or manual therapy) without exercise therapy
After the initial search performed by a research librarian, all records were imported into the Covidence software, and duplicates were removed. Two researchers (AE, AP) conducted independent screening of titles and abstracts and eligible studies were read in full text (Figure 1). Any disagreements on inclusion were resolved in a consensus meeting, with a third researcher (EA) acting as deciding vote if necessary
Descriptive details of included studies were extracted by a single researcher and included author, publication year, patient population, sample size, participant age, intervention type (exercise therapy alone or in combination with surgery), outcome measures and results.
The CERT checklist17 was used to extract and assess the reporting completeness of the included studies. The CERT consists of 16 items over seven domains; what (materials); who (provider); how (delivery); where (location); when, how much (dosage); tailoring (what, how); and how well (compliance/planned and actual). Each item was scored as a 0 (not described), 1 (described) or NA (not applicable). The score ranges from 0 to 19 with higher numbers indicating better description. If any studies compared exercise therapy to surgery and exercise therapy, the treatment protocol for the group receiving exercise therapy only was examined. If a study had multiple exercise therapy treatment groups, the treatment protocol hypothesized to be superior was selected for analysis. Data from each study and any related sources (i.e., appendices, supplemental material, published study protocols, development descriptions and feasibility studies) was independently extracted and assessed by two researchers with experience treating hip-related pain with exercise therapy. The Explanation and Elaboration statement to the CERT was used to guide scoring.17 The reason for any items being considered ‘not described’, were recorded. The details and location of each item response was recorded for each study (Appendix B). To evaluate if completeness of reporting has improved since the publication of CERT (December 2016), studies published 2019 or later were considered likely to have had access to the tool during planning and conducting of their study
Data related to risk of bias was also independently extracted and assessed by two researchers (AE, AP) using the Cochrane risk of bias tool version 2 (RoB 2).18 Any disagreements on CERT or RoB 2 scores were resolved in a consen-
sus meeting, with a third researcher (EA) acting as deciding vote if necessary.
Cohen’s kappa was used to measure agreement between raters on the CERT score and RoB 2 tool, and median and inter-quartile ranges (IQR) were used to describe the data. The item responses from the included studies were synthesized by a single researcher, to provide an overview of the contents of the interventions. Mann-Whitney U test was used to compare the CERT scores of studies published before and after the publication of the CERT checklist, and studies with different levels of bias.
In total, 5444 records were identified, and 234 studies were screened in full text. While 52 studies used exercise therapy as part of their intervention, only 23 studies19–41 (44%) reported any details. The remaining 29 studies were not included in the CERT synthesis (Figure 1). Twenty-five of these 29 studies were surgical trials, using exercise therapy as part of post-operative rehabilitation (Appendix C). Study characteristics and CERT scores are described for the 23 studies that could be included in the synthesis.
Of the 23 studies, three were randomized controlled trials (RCTs),23,27,30 four pilot RCTs,19,25,29,34 four RCT study protocols,21,36,37,41 five prospective case series,20,22,24,26,32 one feasibility study,28 and six retrospective case series.31,33,35,38–40 Sample size ranged from 15 to 348. The studies used exercise therapy alone,19–29,40,41 or in combination with hip surgery 30–39
The studies reported mean ages ranging from 23-43 years and included participants with a diagnosis of FAIS,19–25,27,29,30,34–38 dysplasia,26,28,41 FAIS and borderline dysplasia,33,39 hip-related pain,31,40 and chondrolabral pathology 32
The studies included in the synthesis reported effects of interventions on hip-specific and/or generic patient-reported outcome measures, as well as tests of physical function (Table 1).
None of the studies referred to CERT in their methods section. CERT scores ranged between 1 and 17, with a median of 12 (IQR 5-14). Five21,25,28,30,36 studies reported on 15 or
Casartelli et al 2018 Prospective case series High FAIS 34 (35) / NA 25 (5) / NA
arthroscopy and rehabilitation (ROM ex., stretching, isolated hip muscle ex., functional ex., running progressions, sport specific drills)
Hip arthroscopy and rehabilitation consisting of ROM ex., soft tissue therapy, isometric ex., gradual progression to proprioceptive, functional ex., and running.
Hip abductor exercises and core exercises compared to hip abductor exercises alone.
Incidence of postoperative iliopsoas tendinoapthy
60 (24%) of patients developed post-op iliopsoas tendinopathy 47% resolved symptoms with physical therapy, 53% required an injection.
Iliopsoas tedinopathy is an under-reported complication after hip arthroscopy
Primary: Not described
Secondary: HOS-ADL, satisfaction, frequency and duration of physical therapy sessions, perceived importance of home program
Primary: Not described
Secondary: Hip ROM, hip strength, trunk endurance, iHOT-12, mHHS, Vail hip score
HOS-ADL and satisfaction level was correlated with frequency and duration of physical therapy visits as well as perceived importance of home exercise program.
No between group differences in hip ROM or strength at 8 weeks, Vail and iHOT-12 significant improvement in trunk training group, mHHS no difference
Hip arthroscopy and rehabilitation consisting of joint mobilisations, core ex., gait training, functional exercises
Hip arthroscopy and rehabilitation consisting of motor control ex. of hip rotators, aquatic ex., ROM ex., functional ex., jogging and sport specific drills
Isolated hip muscle ex., isometric trunk training, balance ex., stretching & functional ex.
Primary: Not described
Secondary: HOS-ADL, HOS-SS, mHHS, VAS.
Patient perception and the length and frequency of individual physical therapy sessions are important factors in self-reported outcomes after hip arthroscopy for FAIS.
The addition of trunk stabilisation exercises improves short-term outcomes
Success rates 5 years after arthroscopy for FAIS were not significantly different between patients with borderline dysplasia and normal acetabular coverage.
Primary: iHOT-33, HOSSport
Secondary: HAGOS, Tegner activity scale, GRC
Primary: Not described Secondary: Global treatment outcome questionnaire (GTO), HOS-ADL, HOS-Sport, EQ-5D VAS, hip strength, dynamic pelvic control
Post-operative physical therapy performed better in primary outcome in the short term, compared to controls.
52% responders to therapy (GTO). PROMs, abduction strength, pelvic control higher in responders, nonresponders had more severe cam
Coppack et al 2016 RCT study protocol Some concerns FAIS 50 / 50 (planned) 18-50 (inclusion)
Motor control ex. of hip rotators and trunk/pelvis, isolated hip muscle ex., functional ex., stretching
International Journal of Sports Physical Therapy
NA NA
Secondary: NAHSphysical function, EQ5D,
HADS, 6-minute walk test, Y-balance test, Hip ROM, hip strength, SIRBS, adherence
Stretching, activity modification Primary: not described Secondary: HHS, NAHS, Hip ROM
Hip arthroscopy and rehabilitation (ROM ex., isometric ex., isolated hip muscle ex., functional ex., plyometrics, running, sports specific training)
Hip arthroscopy and rehabilitation (ROM ex., isometric contractions, aquatic therapy stretching, isolated hip muscle ex., functional ex., trunk ex., running, power and plyometrics)
Hip arthroscopy and pre- and rehabilitation (circulation, muscle activation, ROM ex., motor control ex. for trunk/ pelvis hydrotherapy, balance, isolated hip muscle ex., functional ex., running drills)
Motor control ex. for the trunk and pelvis, isolated hip muscle ex., functional ex.
Isolated hip muscle ex., isometric trunk training, balance, functional ex.
Primary: Not described
Secondary: Hip ROM and isometric hip strength
Significant improvements in HHS and NAHS, no change in hip ROM
ROM and strength improved after arthroscopy and rehabilitation, but some strength and ROM variables remained lesser than matched controls
Primary: not described
Secondary: mHHS, SF-12, HOS
Patients with FAIS and borderline dysplasia reported improvements in all PROMs after arthroscopy and rehabilitation.
Primary: not described
Secondary: NAHS, EQ5D-5L, hip muscle strength
Pre-operative exercise therapy and postarthroscopy rehabilitation compared to just arthroscopy and rehabilitation resulted in better outcomes in muscle strength and EQ5D
Primary: iHOT-33
Secondary: EQ5D-5L, SF12, adverse events, health care cost
Primary: not described
Secondary: Isometric hip muscle strength, HOOS, GRC
Significant improvement in primary outcome in both arthroscopy and physical therapy groups, with more improvement in arthroscopy
Significant improvement in HOOS, and isometric strength in abduction, internal rotation and adduction.
Conservative treatment of FAIS achieved good early results.
By 6 months after arthroscopy, strength in all directions and flexion and rotation ROM are significantly improved in both limbs.
FAI and labral pathology can be successfully managed using hip arthroscopy, with capsular management, in patients with borderline dysplasia.
Patients undergoing hip arthroscopy for FAI, may improve their pain, function and muscle power pre- and post-operatively using specific exercises
Offering hip arthroscopy to patients with FAIS led to better patient-assessed function 12 months compared with best conservative care.
An exercise programme could be safely completed and statistically significant changes in strength, function, and self-reported clinical outcomes were achieved.
Isolated hip muscle ex., isometric trunk training, functional ex., plyometrics, cardiovascular training
Isometric abduction
Mobility ex., isolated hip muscle ex., isometric trunk training, functional ex.
Primary: Feasibility
Secondary: iHOT-33, HOOS, isometric hip muscle strength, hip ROM, functional task performance
Primary: not described Secondary: Hip instability, isometric hip abduction strength, VAS
Primary: HOS
Secondary: iHOT-33, GRC
A full scale study is feasible. FAIS-specific physical therapist intervention performed better than standard physical therapy
Improvement in hip instability and VAS after abductor training, no significant increase in abductor strength.
Significant improvement in primary outcome in both groups, no significant differences between groups.
A FAIS specific physical therapy intervention may have a positive effect on improving hip adductor strength, reducing pain, and improving function.
Abductor muscle strengthening exercises can significantly improve patient pain levels and muscle strength
Most patients perceived little to no change in status at 2 years, and one-third of military patients were not medically fit for duty at 2 years.
Reimer et al 2021 RCT study protocol Some concerns Hip dysplasia 48 / 48 (planned)
18-40 (inclusion)
Individualized supervised and home-based exercise therapy mainly using functional ex.
VAS, HOS-ADL HOS-SS 30 out of 46 improved their functional performance tests and these patients also reported better improvements in PROMs.
Isolated hip muscle machinebased training, functional ex.
Primary: Feasibility (VAS, adherence, drop-out)
Secondary: HAGOS, hop tests, isokinetic hip strength
The treatment had good adherence and few adverse events, and showed improvement in HAGOS, hop tests and strength.
Progressive resistance training using cable machines and dumbbells/barbells, with gradual increase in intensity
Riff et al 2018 Retrospective case series High FAIS 32 (41) / NA 34.7 (6.7) / NA Hip arthroscopy and rehabilitation consisting of isometric ex., functional ex., plyometrics, running, trunk isometric training
Risberg et al 2018 RCT study protocol Low FAIS 70 / 70 (planned)
18-50 (inclusion)
Hip arthroscopy and rehabilitation consisting of isolated hip muscle ex., functional ex. plyometric ex.,
Primary: HAGOS
Secondary: HAGOS sub scales, single leg hop for distance, adverse events and medications
Primary: Not described
Secondary: Return-toHIIIT questionaire, mHHS, HOS
Primary: iHOT-33
Secondary: HOOS, Arthritis Self-Efficacy Scale, Tampa Scale of
Patients that improved their functional movement control following rehabilitation are likely to report less pain and greater functional ability in their daily and sports-related activities.
Supervised progressive resistance training is feasible and may improve pain, PROMs, functional performance and hip flexion muscle strength.
NA NA
A high rate of patients returned to high-intensity training at the same level after arthroscopy and rehabilitation
Patients participating in HIIT returned to sport 88% of the time at a mean 9.86 5.7 months after hip arthroscopic surgery for FAIS.
NA NA
Tijssen
trunk isometric training, aerobic training
Hip arthroscopy and rehabilitation consisting of ROM ex., stretching, aerobic training, isolated hip muscle ex.), functional ex., sport specific ex.
Supervised training (stretching, isolated hip muscle ex., functional ex., trunk muscle training) and manual therapy.
Kinesiophobia, HSAS, PSFS, GRC, hip ROM, isometric hip strength, functional task performance
Primary: Feasibility
Secondary: iHOT-33, functional task performance, hip ROM, isometric hip strength, HSAS, GRC
Primary: HOS, VAS
Secondary: Lower extremity functional scale (LEFS), GRC, functional task performance
Improvement in pain and PROM in both groups, no significant difference between groups
Physical therapy interventions provide significant, clinically important improvements in pain for patients with FAI.
more CERT items (75%), 1420,21,23–30,34,36,37,41 reported on 10 (50%) or more and 18 studies19–21,23–30,32–34,36,37,40,41 reported on five (25%) or more items. No study had the maximum score of 19. The most reported items were tailoring (14a and 14b), which was reported in 2019–34,36,37,40,41 of 23 studies. The lowest score was observed for motivation strategies (item 6) and starting level (item 15), which was reported in two23,37 and three21,28,41 studies, respectively Details regarding scores are provided in Table 2, and protocol content in Appendix B. The agreement for CERT scores between the two raters was K=0.72, representing a substantial agreement.
Eighteen (78%) studies19,21–30,32–34,36–39 described equipment used. Commonly used materials were resistance bands, weight cuffs, stationary bicycles, and unstable surfaces. While most studies described the equipment used (e.g., leg press), the specific type of equipment (e.g. model of machine) or resistance level was rarely described.
Six (26%) studies21,25,29,30,34,36 sufficiently described the title and qualifications of the prescriber Of the studies that did not report this item, eleven studies20,23,24,26–28,32,37,38,40,41 described the professional title (primarily physical therapists) but not qualifications or experience, while six studies19,22,31,33,35,39 provided no details about the prescribers.
Eleven (48%) studies20,21,23–27,29,30,34,37 provided detail whether exercise therapy was conducted in individual or group settings, with all 11 studies using individual training sessions.
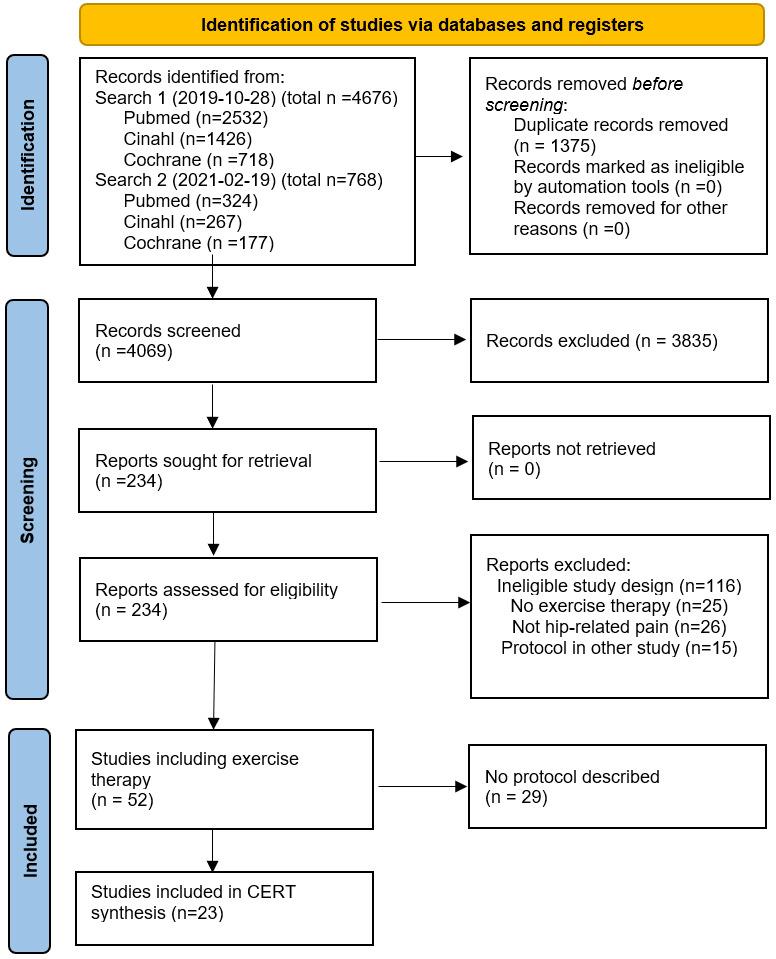
Sixteen (70%) studies20,21,23–30,34,36–38,40,41 reported on supervision. Fourteen of these20,21,23–25,27,29,30,34,36–38,40,41 used a combination of supervised (ranging from 5-24 sessions) and non-supervised exercise. One study28 had supervision on every train-
Are Exercise Therapy Protocols For The Treatment of Hip-Related Pain Adequately Described? A Systematic Review of
ing session (20 sessions), and one study26 had no supervision.
Twelve (52%) studies20,21,23–26,28,30,34,36,37,41 reported adherence tracking. Eight studies20,21,23–25,34,36,37 used a training diary or app, two studies21,30 a Likert scale, two studies19,26 used verbal confirmation of adherence, and three studies28,30,41 recorded the number of attended sessions.
Two (9%) studies23,37 reported any motivation strategies used. This consisted mainly of education on the importance of adherence to the exercise therapy
Eight (35%) studies24,28,30,32–34,36,41 reported criteria for progression of exercise. The criteria varied, with studies reporting the use of time frames,41 pain free range of motion and ambulation,32–34 pain free exercise execution,30,32–34 a rate of perceived exertion24,36 and/or VAS pain cut-off,36 being able to complete >2 repetitions above prescribed on last set,28,41 and/or force production limb symmetry index32–34 as markers for progression.
Ten (43%) studies21,24–26,28–30,36,41 described how the program was progressed. Most studies used concurrent means of progression, including: i) increased exercise volume (repetitions and/or sets performed),21,25,26,41 ii) increased intensity, targeting heavier loads,25,28,29,36,41 iii) progression from isolated muscle exercises to more complex motions, such as compound functional movements, single leg work or unstable surfaces,21,24,25,29,30,36 iv) addition of more exercises over time,27 v) faster loading rates, such as plyometric training.25,36
Seventeen (74%) studies19,21,23–30,32–34,36,37,40,41 reported the exercises used. These included isolated non-weightbearing exercises (such as side lying hip abduction),19,21,23–30,32–34,36,37,41 isometric trunk training (such as planks),19,24,25,27,29,33,36 compound lower extremity exercises (such as squats and lunges),21,23–25,27–30,32–34,36,37,40,41 cardiovascular training (with exercise bikes, elliptical machines or running),25,30,32–34,36 stretching/mobility,21,27,29,30,32–34,37 and/or plyometrics (jumping and landing drills, running progressions).25,32–34,36
HOME COMPONENT (ITEM 9)
Fourteen (61%) studies20,21,23–26,28–30,34,36,37,40,41 reported on any home component to their exercise program. Twelve studies20,21,23–25,29,30,34,36,37,40,41 primarily provided participants with a home-based program, with supervised sessions to check exercise technique and progression. One study26 used a home program only as the intervention, and one study28 used no home component.
Seventeen (74%) studies19–23,25,27–30,33–39 described any non-exercise component. Manual therapy (such as soft-tissue treatment and/or mobilizations) was performed in 13 studies21,23,25,27,29,30,33–39 and 8 studies19–23,25,30,34 used patient education, commonly concerning hip anatomy and activity modification.
Twelve (52%) studies20,21,23–26,28–30,36,37,41 described adverse events related to their exercise intervention. No serious adverse events related to exercises were reported, though 4 studies23,24,28,30 reported participants experiencing muscle soreness and a transient increase in pain after exercise therapy One study reported approximately 25% of patients dropping out of the intervention due to increases in pain or fatigue related to the exercises.26
Seventeen (74%) studies20,21,23–30,34,36–41 included descriptions of the study setting, with exercise therapy interventions mostly being performed at outpatient physical therapy clinics.
Fourteen (61%) studies19–21,24–30,34,36,37,41 reported on intervention dosage. The duration ranged from three weeks to six months, and frequency ranged between daily training to three sessions weekly. Six studies21,24,28,30,36,41 provided dosage anchored against a measure of intensity, such as rate of perceived exertion or a percentage of repetition maximum (RM).28,36,41
Twenty (87%) studies19–34,36,37,40,41 reported whether the program was tailored to the individual, of which 15 used an individualized approach20,21,23–25,27,29–34,36,37,40 and five a generic program.19,22,26,28,41 The treating physical therapist tailored the program based on the patient impairment, pain-free range of motion surgical procedure, and desired activity levels and sport-specific demands. Three studies (13%)21,28,41 reported the patients’ starting level, two of which RM-based starting levels,28,41 and one where the treating physical therapist adapted the starting dose based on patient presentation.21
Eight (35%) studies21,23,25,29,30,34,36,37,41 reported on intervention fidelity To increase fidelity, physical therapists delivering the intervention were given written instruction21,23,30,34,36 and physical training21,23,25,29,30,36 in application of the protocol. Two studies used follow up sessions with the researchers.23,36 The authors of two studies were also treating clinicians.25,37 Seven studies (54%)20,23–25,27,28,30 reported whether the interventions
were delivered according to plan, primarily using reports of adherence and attended sessions to describe the applied intervention. The included RCT study protocols21,36,37,41 were not applicable for this item as the intervention had not been completed.
Studies published before 201921–31,33–37 had higher (better) CERT scores (n=16, median 14, IQR 7.25-15) compared to those published 2019 or later19,20,32,38–41 (n=7, median 6, IQR 3-11) (p=0.034).
Risk of bias was high in 14 studies,19,20,22,24,26–28,31–33,35,38–40 some concerns in 8 studies21,23,25,29,30,34,37,41 and low in one study36 (Table 1, Appendix D). Studies with some concerns or low risk of bias were analyzed together (n=9), and had higher CERT scores (median 14, IQR 14-16) compared to those with high risk of bias (n=14) (median 6, IQR 3-11) (p<0.001). Agreement for risk of bias was substantial (K=0.69).
Fifty-two studies used exercise therapy as part of their intervention to treat hip-related pain, but 29 studies provided no details beyond mentioning the use of exercise therapy and could not be included in the CERT synthesis. Of the 23 studies included in the synthesis, the median CERT score was 12 (IQR 5-14) and none reached the maximum score of 19. The results suggest that studies using exercise therapy to treat hip-related pain did not report protocols in sufficient detail to allow replication in future studies or clinical practice.
In line with the results of the present study, previous systematic reviews have reported median CERT scores ranging from 5-15 in exercise therapy studies for diagnoses such as rotator cuff disorders,42 achilles rupture,43 low back pain,44 and hip OA.14 In the present study, the most described item was tailoring (item 14a and 14b, described by 87%), while the least reported items were motivation strategies (item 6, 9%) and starting level (item 15, 13%). Motivation is a key factor in adherence to rehabilitation,45 and behavior change related to physical activity.46 A lack of describing motivational strategies could imply this aspect has not been considered, which could in turn limit the effectiveness of otherwise well designed and described protocols. People with hip-related pain is a heterogenous group with varying levels of functional impairments.2,47 Therefore, the appropriate starting level may be unique to the individual, and a lack of criteria description may lead to a starting level that is too challenging for some, and not sufficiently demanding for others. Also, less than half of the studies described progression criteria (item 7a, 35%), or how progression was performed (item 7b, 43%), and 14 of 23 (61%) studies had descriptions of dosage, such as repetitions, sets and frequency (item 13). This is in ac-
cordance with previous systematic reviews where the commonly unreported items were motivation strategies, starting levels, progression criteria and fidelity 14,42–44 Based on our results and similar reviews, important aspects of exercise therapy protocols are consistently unreported in the literature. Improvement of reporting completeness may better our understanding of exercise therapy for this patient population, as well as allow for replication in further studies and implementation into clinical practice.
As the optimal exercise therapy for people with hip-related pain is currently unknown, a clinical focus on impairments related to the disorder, such as reduced hip muscle strength, has been suggested.7 Without complete reporting in research trials, the strategies to best address these impairments are unclear Also, results from trials comparing exercise therapy to other interventions, such as hip arthroscopy, need to be analyzed with completeness of reporting in mind, as exercise therapy may encompass a wide range of treatment strategies.
In the present study, CERT scores were significantly lower (worse) in studies published 2019 or later compared to those published earlier. One reason for this result could be that only six studies were published in the later time frame, whereof three were retrospective. Complete reporting requires thorough planning which is less likely achieved in a retrospective compared to a prospective design. Although the goal of reporting guidelines, such as CERT, is to improve reporting completeness, a recent systematic review using TIDieR found that reporting on physical therapy interventions had not meaningfully improved in a sample of trials from 2000 and 2018.48 This, and the fact that no studies in our review referred to CERT in their methods section, indicate of a lack of implementation of guidelines by the research community. In our review, studies with lower risk of bias had significantly higher CERT scores than those with higher risk of bias. While the RoB 2 tool was designed to assess risk of bias in RCTs, the authors used it as a secondary measure for all included studies to provide a broad picture of the risk of bias, although this tool may not be the most appropriate for all study designs. While CERT and the RoB 2 measure different constructs, their association may reflect that a more thoroughly designed and planned study address factors related to risk of bias as well as intervention transparency Increasing the overall scientific rigor of the published literature by raising awareness and implementation of relevant guidelines, and addressing important aspects of risk of bias, may also affect reporting completeness.
CERT has been suggested to be used as a checklist when planning an exercise therapy protocol, and as a measure of reporting completeness in systematic reviews on exercise therapy.17 There are some challenges in using CERT in systematic reviews. First, there is no consensus on what is to be considered a good or sufficient score. Charlton et al used a classification of CERT scores based on percentage of items described; high (>75% of items reported), moderate (60-74%) and poor (<60%) levels of reporting standard.15 However, these values were chosen based on cut-offs from the Downs and Black scale, and not on recommendations
or evaluation of data specific to CERT Second, the maximum score of 19 was not met by any studies included in the current study or in any of the other reviews using CERT,15,16,42–44 apart from one study in the systematic review on hip osteoarthritis.14 Further research into what constitutes a realistic and relevant score might be needed. Third, the use of a composite overall score may not be appropriate, as some items may be of greater importance to allow replication. For example, the type and goal of exercises performed (for example: isolated hip muscle strength, functional performance), the dosage prescribed (volume, intensity), progression and adherence might be considered the basis of an exercise therapy protocol, with other items providing additional details. Further research on the relative importance of items or domains in the CERT may enhance its interpretability, and potentially lead to weighting of different items.
Strengths of this study include adherence to established guidelines and good agreement between raters. Both raters were experienced in using exercise therapy for hip-related pain, which may be valuable for understanding the nuance of the protocols. Also, the inclusion of a comprehensive description of the exercise therapy protocol content may serve as a summary to researchers and clinicians. There are limitations to the current study To be included in the CERT synthesis, the inclusion criteria required some form of exercise therapy description. For this reason, most studies (29 of 52) that had used exercise therapy could not be included in the CERT synthesis, due to no description of their intervention. As such, these results may paint an overly positive picture of the state of reporting completeness for this patient population and should be viewed in combination
with the other 29 studies. It should be noted that 25 of the 29 studies not included in the CERT synthesis were surgical studies using exercise therapy as part of post-operative care, highlighting a lack of reporting in these trials.
Less than half of the studies (23 out of 52) using exercise therapy to treat hip-related pain reported sufficient details to be included in the CERT synthesis. Of the 23 studies included in the synthesis, the median CERT score was 12 (IQR 5-15), with no study reaching the maximum CERT score of 19. Interestingly, studies with less risk of bias had better CERT scores. Furthermore, the publication of CERT did not yield better scores. Taken together this seems to suggest that study rigor may drive better overall exercise intervention reporting. The lack of reporting completeness of exercise therapy protocols makes it difficult to replicate interventions in future research as well as in clinical practice, and to draw conclusions on efficacy and dose-response to such interventions.
The authors declare no conflict of interest.
Submitted: June 28, 2022 CST, Accepted: December 23, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0
International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Reiman MP, Agricola R, Kemp JL, et al. Consensus recommendations on the classification, definition and diagnostic criteria of hip-related pain in young and middle-aged active adults from the International Hip-related Pain Research Network, Zurich 2018. Br J Sports Med. 2020;54(11):631-641. doi:10.1136/bjsport s-2019-101453
2. Kierkegaard S, Langeskov-Christensen M, Lund B, et al. Pain, activities of daily living and sport function at different time points after hip arthroscopy in patients with femoroacetabular impingement: a systematic review with meta-analysis. Br J Sports Med 2017;51(7):572-579. doi:10.1136/bjsports-201 6-096618
3. Babatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J. Effective treatment options for musculoskeletal pain in primary care: A systematic overview of current evidence. PloS One. 2017;12(6):e0178621. doi:10.1371/journal.pone.0178 621
4. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database of Systematic Reviews. 2017;2020(2). doi:10.1002/14651858.cd011279.pub3
5. Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from highquality clinical practice guidelines: systematic review Br J Sports Med. 2020;54(2):79-86. doi:10.1136/bjspor ts-2018-099878
6. Griffin DR, Dickenson EJ, O’Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016;50(19):1169-1176. doi:10.1136/bjsports-2016-0 96743
7 Kemp JL, Risberg MA, Mosler A, et al. Physiotherapist-led treatment for young to middleaged active adults with hip-related pain: consensus recommendations from the International Hip-related Pain Research Network, Zurich 2018. Br J Sports Med. 2020;54(9):504-511. doi:10.1136/bjsports-2019-1014 58
8. Kemp JL, Mosler AB, Hart H, et al. Improving function in people with hip-related pain: a systematic review and meta-analysis of physiotherapist-led interventions for hip-related pain. Br J Sports Med 2020;54(23):1382-1394. doi:1 0.1136/bjsports-2019-101690
9. Kemp JL, King MG, Barton C, et al. Is exercise therapy for femoroacetabular impingement in or out of FASHIoN? We need to talk about current best practice for the non-surgical management of FAI syndrome. Br J Sports Med 2019;53(19):1204-1205. d oi:10.1136/bjsports-2018-100173
10. Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P, CONSORT NPT Group. CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts. Ann Intern Med. 2017;167(1):40-47. doi:1 0.7326/m17-0046
11. Glasziou P, Chalmers I, Altman DG, et al. Taking healthcare interventions from trial to practice. BMJ. 2010;341:c3852. doi:10.1136/bmj.c3852
12. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687 doi:10.1136/bmj.g1687
13. Slade SC, Dionne CE, Underwood M, et al. Consensus on Exercise Reporting Template (CERT): Modified Delphi Study Phys Ther 2016;96(10):1514-1524. doi:10.2522/ptj.20150668
14. Burgess LC, Wainwright TW, James KA, von Heideken J, Iversen MD The quality of intervention reporting in trials of therapeutic exercise for hip osteoarthritis: a secondary analysis of a systematic review Trials 2021;22(1):388. doi:10.1186/s13063-02 1-05342-1
15. Charlton PC, Drew MK, Mentiplay BF, Grimaldi A, Clark RA. Exercise Interventions for the Prevention and Treatment of Groin Pain and Injury in Athletes: A Critical and Systematic Review. Sports Med. 2017;47(10):2011-2026. doi:10.1007/s40279-017-074 2-y
16. Wright AA, Tarara DT, Gisselman AS, Dischiavi SL. Do currently prescribed exercises reflect contributing pathomechanics associated with femoroacetabular impingement syndrome? A scoping review Phys Ther Sport 2021;47:127-133. doi:10.101 6/j.ptsp.2020.11.034
17. Slade SC, Dionne CE, Underwood M, Buchbinder R. Consensus on Exercise Reporting Template (CERT): Explanation and Elaboration Statement. Br J Sports Med. 2016;50(23):1428-1437. doi:10.1136/bjsp orts-2016-096651
18. Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. doi:1 0.1136/bmj.d5928
19. Aoyama M, Ohnishi Y, Utsunomiya H, et al. A Prospective, Randomized, Controlled Trial Comparing Conservative Treatment With Trunk Stabilization Exercise to Standard Hip Muscle Exercise for Treating Femoroacetabular Impingement: A Pilot Study. Clin J Sport Med. 2019;29(4):267-275. doi:10.1097/jsm.0000000000000
516
20. Casartelli NC, Bizzini M, Maffiuletti NA, et al. Exercise therapy for the management of femoroacetabular impingement syndrome: preliminary results of clinical responsiveness. Arthritis Care Res (Hoboken) 2019;71(8):1074-1083. d oi:10.1002/acr.23728
21. Coppack RJ, Bilzon JL, Wills AK, et al. A comparison of multidisciplinary team residential rehabilitation with conventional outpatient care for the treatment of non-arthritic intra-articular hip pain in UK Military personnel – a protocol for a randomised controlled trial. BMC Musculoskelet Disord. 2016;17(1):459. doi:10.1186/s12891-016-130
9-z
22. Emara K, Samir W, Motasem EH, Ghafar KAE. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong) 2011;19(1):41-45. doi:10.1177/230949901101900109
23. Griffin DR, Dickenson EJ, Wall PDH, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet 2018;391(10136):2225-2235. doi:10.1016/s0140-6736(18)31202-9
24. Guenther JR, Cochrane CK, Crossley KM, Gilbart MK, Hunt MA. A Pre-Operative Exercise Intervention Can Be Safely Delivered to People with Femoroacetabular Impingement and Improve Clinical and Biomechanical Outcomes. Physiotherapy Canada 2017;69(3):204-211. doi:10.3138/ptc.2016-34
25. Kemp JL, Coburn SL, Jones DM, Crossley KM. The Physiotherapy for Femoroacetabular Impingement Rehabilitation STudy (physioFIRST): A Pilot Randomized Controlled Trial. J Orthop Sports Phys Ther 2018;48(4):307-315. doi:10.2519/jospt.2018.794
26. Kuroda D, Maeyama A, Naito M, et al. Dynamic hip stability, strength and pain before and after hip abductor strengthening exercises for patients with dysplastic hips. IES. 2013;21(2):95-100. doi:10.3233/i es-130480
27 Mansell NS, Rhon DI, Meyer J, Slevin JM, Marchant BG. Arthroscopic Surgery or Physical Therapy for Patients With Femoroacetabular Impingement Syndrome: A Randomized Controlled Trial With 2-Year Follow-up. Am J Sports Med 2018;46(6):1306-1314. doi:10.1177/036354651775191
28. Mortensen L, Schultz J, Elsner A, et al. Progressive resistance training in patients with hip dysplasia: A feasibility study. J Rehabil Med. 2018;50(8):751-758. doi:10.2340/16501977-2371
29. Wright AA, Hegedus EJ, Taylor JB, Dischiavi SL, Stubbs AJ. Non-operative management of femoroacetabular impingement: A prospective, randomized controlled clinical trial pilot study J Sci Med Sport. 2016;19(9):716-721. doi:10.1016/j.jsams.2 015.11.008
30. Bennell KL, Spiers L, Takla A, et al. Efficacy of adding a physiotherapy rehabilitation programme to arthroscopic management of femoroacetabular impingement syndrome: a randomised controlled trial (FAIR). BMJ Open. 2017;7(6):e014658. doi:10.113 6/bmjopen-2016-014658
31. Adib F, Johnson AJ, Hennrikus WL, Nasreddine A, Kocher M, Yen YM. Iliopsoas tendonitis after hip arthroscopy: prevalence, risk factors and treatment algorithm. J Hip Preserv Surg 2018;5(4):362-369. do i:10.1093/jhps/hny049
32. Freke MD, Crossley K, Sims K, et al. Acute and Subacute Changes in Hip Strength and Range of Movement After Arthroscopy to Address Chondrolabral Pathology. Am J Sports Med. 2019;47(8):1939-1948. doi:10.1177/036354651985081 6
33. Fukui K, Briggs KK, Trindade CAC, Philippon MJ. Outcomes After Labral Repair in Patients With Femoroacetabular Impingement and Borderline Dysplasia. Arthroscopy. 2015;31(12):2371-2379. doi:1 0.1016/j.arthro.2015.06.028
34. Grant LF, Cooper DJ, Conroy JL. The HAPI ‘Hip Arthroscopy Pre-habilitation Intervention’ study: does pre-habilitation affect outcomes in patients undergoing hip arthroscopy for femoro-acetabular impingement? J Hip Preserv Surg. 2017;4(1):85-92. do i:10.1093/jhps/hnw046
35. Riff AJ, Ukwuani G, Clapp I, Movassaghi K, Kelly DM, Nho SJ. High Rate of Return to High-Intensity Interval Training After Arthroscopic Management of Femoroacetabular Impingement Syndrome. Am J Sports Med. 2018;46(11):2594-2600. doi:10.1177/0363 546518776638
36. Risberg MA, Ageberg E, Nilstad A, et al. Arthroscopic Surgical Procedures Versus Sham Surgery for Patients With Femoroacetabular Impingement and/or Labral Tears: Study Protocol for a Randomized Controlled Trial (HIPARTI) and a Prospective Cohort Study (HARP). J Orthop Sports Phys Ther. 2018;48(4):325-335. doi:10.2519/jospt.201
8.7931
37 Tijssen M, van Cingel REH, Staal JB, Teerenstra S, de Visser E, Nijhuis-van der Sanden MWG. Physical therapy aimed at self-management versus usual care physical therapy after hip arthroscopy for femoroacetabular impingement: study protocol for a randomized controlled trial. Trials 2016;17(1):91. do i:10.1186/s13063-016-1222-7
38. Amar E, Martin RL, Tudor A, Factor S, Atzmon R, Rath E. Midterm Outcomes and Satisfaction After Hip Arthroscopy Are Associated With Postoperative Rehabilitation Factors. Orthop J Sports Med. 2021;9(1):2325967120981888. doi:10.1177/232596712
0981888
39. Beck EC, Drager J, Nwachukwu BU, et al. Patients With Borderline Hip Dysplasia Achieve Clinically Significant Improvement After Arthroscopic Femoroacetabular Impingement Surgery: A CaseControl Study With a Minimum 5-Year Follow-up. Am J Sports Med 2020;48(7):1616-1624. doi:10.1177/0363 546520916473
40. McGovern RP, Martin RL, Phelps AL, Kivlan BR, Nickel B, Christoforetti JJ. Conservative management acutely improves functional movement and clinical outcomes in patients with pre-arthritic hip pain. J Hip Preserv Surg 2020;7(1):95-102. doi:10.1093/jhps/ hnz075
41. Reimer LCU, Jakobsen SS, Mortensen L, et al. Efficacy of periacetabular osteotomy followed by progressive resistance training compared to progressive resistance training as non-surgical treatment in patients with hip dysplasia (PreserveHip) – a protocol for a randomised controlled trial. BMJ Open 2019;9(12):e032782. doi:1 0.1136/bmjopen-2019-032782
42. Major DH, Røe Y, Grotle M, et al. Content reporting of exercise interventions in rotator cuff disease trials: results from application of the Consensus on Exercise Reporting Template (CERT). BMJ Open Sport Exerc Med 2019;5(1):e000656. doi:1 0.1136/bmjsem-2019-000656
43. Christensen M, Zellers JA, Kjær IL, Silbernagel KG, Rathleff MS. Resistance Exercises in Early Functional Rehabilitation for Achilles Tendon Ruptures Are Poorly Described: A Scoping Review. J Orthop Sports Phys Ther 2020;50(12):681-690. doi:1 0.2519/jospt.2020.9463
44. Davidson SRE, Kamper SJ, Haskins R, et al. Exercise interventions for low back pain are poorly reported: a systematic review J Clin Epidemiol 2021;139:279-286. doi:10.1016/j.jclinepi.2021.05.020
45. Chan DK, Lonsdale C, Ho PY, Yung PS, Chan KM. Patient Motivation and Adherence to Postsurgery Rehabilitation Exercise Recommendations: The Influence of Physiotherapists’ Autonomy-Supportive Behaviors. Arch Phys Med Rehabil 2009;90(12):1977-1982. doi:10.1016/j.apmr.2009.05.0 24
46. Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and selfdetermination theory: a systematic review. Int J Behav Nutr Phys Act 2012;9(1):78. doi:10.1186/147 9-5868-9-78
47. Pålsson A, Kostogiannis I, Ageberg E. Physical impairments in longstanding hip and groin pain: Cross-sectional comparison of patients with hiprelated pain or non-hip-related groin pain and healthy controls. Phys Ther Sport 2021;52:224-233. d oi:10.1016/j.ptsp.2021.09.011
48. McCambridge AB, Nasser AM, Mehta P, Stubbs PW, Verhagen AP Has Reporting on Physical Therapy Interventions Improved in 2 Decades? An Analysis of 140 Trials Reporting on 225 Interventions. J Orthop Sports Phys Ther 2021;51(10):503-509. doi:10.2519/jo spt.2021.10642
Appendix A
Download: https://ijspt.scholasticahq.com/article/68069-are-exercise-therapy-protocols-for-the-treatment-of-hiprelated-pain-adequately-described-a-systematic-review-of-intervention-descriptions/attachment/ 135442.docx?auth_token=-XnpyB6AB1H-3DFyCk_t
Download: https://ijspt.scholasticahq.com/article/68069-are-exercise-therapy-protocols-for-the-treatment-of-hiprelated-pain-adequately-described-a-systematic-review-of-intervention-descriptions/attachment/ 135580.xlsx?auth_token=-XnpyB6AB1H-3DFyCk_t
Download: https://ijspt.scholasticahq.com/article/68069-are-exercise-therapy-protocols-for-the-treatment-of-hiprelated-pain-adequately-described-a-systematic-review-of-intervention-descriptions/attachment/ 135581.xlsx?auth_token=-XnpyB6AB1H-3DFyCk_t
Download: https://ijspt.scholasticahq.com/article/68069-are-exercise-therapy-protocols-for-the-treatment-of-hiprelated-pain-adequately-described-a-systematic-review-of-intervention-descriptions/attachment/ 135582.xlsx?auth_token=-XnpyB6AB1H-3DFyCk_t
Veronica Athy 1 a , Sylvia Hach 1 , Helen Anderson 1 , Jesse Mason 1
1 Unitec Institute of Technology
Keywords: low back pain, low back ache, rowing, athlete, back injury, sports injury https://doi.org/10.26603/001c.67836
International Journal of Sports Physical Therapy
Background
Low back pain (LBP) is highly prevalent in the rowing population. The body of existing research variously investigates risk factors, prevention, and treatment methods.
The purpose of this scoping review was to explore the breadth and depth of the LBP literature in rowing and to identify areas for future research.
Scoping review
PubMed, Ebsco and ScienceDirect were searched from inception to November 1, 2020. Only published, peer-reviewed, primary, and secondary data pertaining to LBP in rowing were included for this study Arksey and O’Malley’s framework for guided data synthesis was used. Reporting quality of a subsection of the data was assessed using the STROBE tool.
Following the removal of duplicates and abstract screening, a set of 78 studies were included and divided into the following categories: epidemiology, biomechanics, biopsychosocial, and miscellaneous. The incidence and prevalence of LBP in rowers were well mapped. The biomechanical literature covered a wide range of investigations with limited cohesion. Significant risk factors for LBP in rowers included back pain history and prolonged ergometer use.
Conclusion

A lack of consistent definitions within the studies caused fragmentation of the literature. There was good evidence for prolonged ergometer use and history of LBP to constitute risk factors and this may assist future LBP preventative action. Methodological issues such as small sample size and barriers to injury reporting increased heterogeneity and decreased data quality. Further exploration is required to determine the mechanism of LBP in rowers through research with larger samples.
Low back pain (LBP) is a common complaint in the general population all over the world and often persists beyond the
Corresponding Author:
Veronica AthyUnitec Institute of Technology
139 Carrington Road, Mount Albert, Auckland 1025, New Zealand
E-mail: vathy214@gmail.com
acute stage.1,2 It is commonly associated with sedentary occupations and lifestyles, obesity and smoking.1 Throughout the general population, research regarding epidemiology of LBP has been well established.3 Physical activity has
been suggested to have a protective effect against LBP,4 and it is well documented that participation in sport has a positive effect on health in general.5 However, there is an inverse relationship between LBP risk in sedentary and in active people.6 There is an absence of information regarding the ideal dose-effect relationship of physical activity.3 Back pain is common among athletes and regularly influences sport performance and participation.3 A consensus statement published in 20217 examined the management and prevention of LBP in rowing. Their findings corroborated those in this study.
Intense physical activity may create a greater risk of LBP,6 particularly in demanding sports such as rowing.8 In New Zealand, the Accident Compensation Corporation (ACC) identifies the back/spine to be the most commonly injured area in rowing.9 The literature has covered a variety of different aspects of LBP, but its value is limited due to its heterogeneity. Epidemiological investigation has observed the widespread nature of the condition. Furthermore, various mechanical factors have been investigated to examine their impact on LBP in the rower and finally, a biopsychosocial approach to management has tentatively been explored.
A LBP definition has not been precisely determined, potentially due to a lack of definition within the literature.10 The heterogeneous data sets and wide variety of topics explored through the literature make a scoping review the best-suited study methodology to systematically map and appraise all the available literature and identify areas for further research. Therefore, the aim of this scoping review was to investigate and collate the available literature regarding LBP in rowing to inform athletes, coaches, and further research.
The original methodological framework for scoping reviews published by Arksey and O’Malley11 and amended by Levac et al12 along with the reporting checklist developed by Tricco et al13 were utilized to synthesize relevant information available within the peer-reviewed literature. Updated guidance for scoping reviews was provided by Peters et al.14
The current scoping review was directed by using the following broad research question: What is the current peer-reviewed literature that has examined low back pain in rowing?
The objectives of the review were: (1) to complete a scoping review on the current literature available on low back pain (LBP) in rowing, (2) to investigate the breadth and depth of research regarding LBP within the rowing population, (3) to elucidate areas where research may be lacking to inform future research, and (4) to undertake a critical appraisal to assess the quality of research within a clinically or scientifically important section of the total literature reviewed.
The search strategy was developed by the first author with input from a knowledge specialist, amended by the second author and applied to PubMed, ScienceDirect, and Ebsco health database (final search: 01.11.2020). Combinations of the following search terms were used on each database: “low back pain” OR “low back injury” OR “lumbar injury” AND “rowing” OR “rower”.
Eligibility criteria were drafted prior to conducting the search, and in accordance with the process described by Arksey and O’Malley,11 any modifications required were applied throughout the progress of the review The inclusion criteria were the following: (1) includes combinations of search terms within the title and/or abstract, (2) is on LBP in the context of the sport rowing, (3) full text available online, (4) no date restriction, (5) peer-reviewed published data. Exclusion criteria were as follows: (1) studies relating to similar water sports not specified to be rowing, (2) studies not relating to the region of the low back, and (3) grey literature.
The selection process comprised two screening levels: (1) a title/abstract/keyword review and (2) full-text review During the initial screen, the first author reviewed titles and abstracts of the identified articles. Each citation from the electronic bibliographic database were entered into a Microsoft ® Excel (version 2002) spreadsheet, screened through the eligibility criteria and then concluded to be either included or excluded. Throughout this initial level of screening, it was clear that the search terms were not broad enough and were expanded from “low back pain” to include “low back injury” and “lumbar injury”
During the second level of review, the full texts of studies were reviewed by the first author to establish their eligibility. Additionally, reference lists of included studies were searched manually to identify further pertinent studies (Figure 1). Each study picked up during the full-text review to meet the inclusion criteria were collated in Mendeley Desktop (version 1.19.4).
Three papers identified in the search were not published in English. Submitting these texts to Google Translate, resulted in significant translation errors and they were excluded.
Throughout the initial screening level, studies reviewed by the primary author were reviewed by the second and third authors and a consensus as to eligibility was obtained. The inclusion and exclusion criteria were checked against a sample of the papers found through the first search (28 papers) by the second author and ‘substantial’ agreement, Fleiss Kappa = 0.625,15 was found between the authors’ decisions on inclusion of the subset of papers. Any discrepancies were resolved with the help of the third author until a consensus was reached.
Data were extracted from the pertinent studies with the use of a standardized data charting form (where relevant) on the ensuing features: (1) Citation details, (2) sample size, (3) study aim, (4) results, and (5) definition given (Appendix 1).
The remaining 78 studies were examined for similarities and differences once the primary author had established familiarity with the data. The papers were then categorized into four main themes as follows: (1) epidemiology, (2) biomechanics, (3) biopsychosocial, and (4) miscellaneous. Each theme was subsequently divided into further sub-categories (Table 1).
Agreement on study selection of the papers into the themes created by the primary author was attained and finalized through verification of 5% of the total number of articles (four of the total 78 papers) by the second and third authors. One paper from each of the four themes was picked out at random for verification. Any discrepancies found throughout the verification process were talked through by the authors until a final decision was reached.
Data were analyzed by sorting the extracted data concerning the research question and objective of the review. The results were displayed in accordance with the four themes and their individual categories, using an illustrative outline of the key findings, summarized, and displayed in table format (Appendix 1).
A total of 12 papers with primary data within the epidemiology category were appraised using The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) tool.16 This tool was created to assist authors when producing analytical observational studies and “…to facilitate critical appraisal and interpretation of results” 16,17(p1)
Overall, the search yielded 1,002 studies, of which 501 were screened after the elimination of duplicates (Figure 1). First level (title and abstract) screening eliminated 414 studies. Thirteen further studies were eliminated during the second level (full text) review (Figure 1). Four additional studies were found to be relevant during manual searching of reference lists, resulting in a total of 78 studies included in this study. Included studies were allocated into one or several of four main themes, epidemiology, biomechanics, biopsychosocial, and miscellaneous, and studies were classified to a specific category within the theme (Table 1). In five instances, papers were identified into two categories.18–22
 Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) flow diagram of the search strategy and study selection.13
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) flow diagram of the search strategy and study selection.13
used custom-made rowing-specific questionnaires.21,33,34,37 One study adapted the Rugby Injury and Performance Project questionnaire44 along with interviews.24 Ten did not specify the questionnaire utilized.20,22,23,25,26,28,32,35,38,39
The low back was reported as the most commonly injured site for rowers in sixteen of the included studies.3,10,21,28,30,33,34,37,38,42,45–50 The low back injury rate was reported to be 53% of total injuries for rowers.41 Thus, many studies investigated risk factors for LBP in rowers. The rowing stroke requires repetitive actions that place an increasing load on the lumbar spine.10 Wilson et al10 identified the most significant risk factors for LBP onset to be a history of lumbar spine injury and volume of ergometer training (Appendix 1). Stationary ergometers were suggested to increase the risk of LBP onset or exacerbation10,21,23,24,28,32 with many papers identifying use for more than 30 minutes to increase risk. Trease et al29 reported dynamic ergometers to be positively associated with a lower incidence and burden of low back injury compared to stationary ergometers. It must be noted here that the majority of studies observing prolonged ergometer use do not specify the type of ergometer It may be inferred that for most articles, stationary ergometers are discussed as these are the more widely used models since their invention in 1981.51 In contrast, dynamic ergometers are a more recent innovation being created in 2010.51 Moreover, none of the studies included in the present review have commented specifically on the effects of prolonged dynamic ergometer use.
Only 21% (27) of the total papers mentioned a definition of either low back pain (LBP), back pain or injury (Appendix 1). Definitions were most commonly given within the epidemiology category (18 of 27).
Low back pain (LBP) in rowers was explored through peerreviewed literature and included the incidence and prevalence of LBP, aggravating factors, sex differences, previous injury, and time off training or competition.
Incidence of LBP was reported as 1.5-3.7 per 1000 hours of rowing training and competition,21,23,24 and LBP prevalence was observed to be between 6% and 66% over 12 months.8,21 Seventeen papers reported incidence,8,20,21,24–37 the number of people developing LBP during one time, while nine papers reported prevalence,3,22,23,27,38–42 the number of people who have LBP at one time. Three papers employed a prospective design with both incidence and prevalence reported.8,21,29
Throughout the primary data sources, many papers utilized retrospective questionnaires.eg, 32,33,38 Of the 19 papers employing questionnaires, four adapted the standardized Nordic Musculoskeletal Questionnaire43 with additional rowing-specific questions.8,27,40,41 Four papers
Training in winter was associated with higher rates of LBP development potentially due to increased volumes of land-based training,10,24,35 including the use of free weights and weight machines.28,29,32,39 Additional factors suggested to contribute to LBP in rowers included on-water rowing28,29 and long rowing sessions.23 Results regarding frequency of injuries by sex were inconsistent and inconclusive.21,27–29,33,35,37,38
Arend et al39 identified higher LBP intensity when training between seven to 16 hours per week compared with lower training volumes. Additionally, Newlands et al21 found a positive correlation between LBP and total training hours (on- and off-water) as well as with kilometers rowed per month (Appendix 1).
Previous history of LBP was positively associated with further LBP episodes.8,10,21,25,26,32 O’Kane et al25 observed that rowers with previous back pain had a higher risk of further episodes than rowers without. However, rowers with preexisting back pain had less time off training while individuals without were more likely to end their rowing career due to back pain.25
Finlay et al38 observed 39.2% of their cohort reported more than 21 days off training or competition while Teitz et al32 found 72% lost one month or less due to pain. One paper suggested that time lost due to pain was a poor indicator of injury severity as injured rowers in their study were able to complete a larger mean training volume than noninjured athletes.24 High injury rates have prompted investigation of the utility of pre-participation evaluation tools
in individuals without pre-existing back pain without success.21,22
Epidemiological investigation is important in mapping the influence of LBP on the rowing population. Examining incidence and prevalence found that LBP was seen as the most common injury in the rowing population. Some consensus has been reached regarding training volume, the use of the ergometer, and a history of LBP constituting risk factors. Exploration of sex differences and risk assessment tools have not yet yielded any statistically significant results.
Studies in this theme assess the movement involved in the rowing stroke. Sub-categories include spinal mobility, muscular contribution, pre-participation evaluation tools, and force produced by the lower extremity Spinal mobility assesses the amount of movement accessed through the rowing stroke. Wilson et al47 compared lumbar spine kinematics when rowing on-water with ergometer rowing (Appendix 1). Both the ergometer and on-water rowing resulted in larger ranges of sagittal lumbar flexion by the final round of the step test compared to a full standing flexion test.47 Moreover, ergometer rowing showed a greater range of lumbar flexion and maximum angle compared to rowing on-water 47 Ng et al52 observed rowers experiencing LBP spent more time in increased flexion in the upper lumbar spine during the drive phase compared with rowers without LBP Lumbopelvic movement has shown varying results between studies. Due to limited study numbers, no agreement has been found.50,53,54
Prolonged rowing caused greater ranges of spinal motion to achieve the same start and finish positions.55 Wilson et al46 found that as stroke rate increased, so did lumbar spine frontal plane angular displacement. These studies suggest that deterioration of technique due to fatigue may contribute to LBP 55
Muscular contribution describes muscles involved in the rowing stroke and assesses factors such as activation, symmetry between either side of the body and trunk flexor/ extensor ratios. Electromyography has been used to assess muscle activation in rowers and Martinez-Valdes et al56 observed inefficient recruitment of erector spinae muscles in rowers with a previous history of LBP Caldwell et al57 found that increased activity of lumbar extensor muscles (multifidus, iliocostalis lumborum, longissimus thoracis) may suggest muscular fatigue contributes to increased levels of lumbar flexion.
Additional muscles are suggested to affect the low back. Shortened hamstrings are suggested to alter the hip and low back mechanics resulting in pain or injury, however, this has not been demonstrated as a significant relationship.58
The epidemiology theme did not find utility of pre-participation evaluation tools. Clay et al49 utilized a functional movement screen (FMSTM) and found rowers with a higher risk of injury were significantly more likely to experience LBP during the rowing season.49 In contrast, Gonzalez et al59 cautioned against the use of the FMSTM to identify an
increased risk of back pain due to the small effect and large variability observed in their study. Overall, these tools have not yet shown utility in assessing risk of injury in the rowing population.
The impact of asymmetry in the stroke motion on the lower limb has been the focus of a small number of investigations.60,61 While there was a measurable lack of symmetry in sweep rowing,61 there has been no evidence of this being a causal factor for LBP.62
In the biomechanics grouping, investigation into movement of the lumbar spine has suggested increasing angles of flexion are achieved with increased rowing speed and time spent rowing. Fatigue has been suggested to contribute to the deterioration of technique seen with prolonged rowing. Tools used to assess potential risk of LBP and lower extremity force have proved inconclusive.
Five of the 78 articles explored the biopsychosocial influence of LBP Wilson et al63 investigated the lived experience and impact of LBP on rowers. A culture of injury concealment was documented, influenced by fear and isolation63 (Appendix 1). McNally et al64 further suggested a lower rate of symptom reporting by rowers. Wilson et al63 discussed the complex condition athletes face when experiencing LBP and suggested that factors outside of the physical domain need to be addressed.
Ng et al18 utilized an individualized cognitive functional approach with adolescent rowers compared to a control group. Participants undergoing the cognitive functional approach had larger reductions in pain during ergometer rowing and reduced disability.18 Similarly, Thorpe et al65 demonstrated a 24% (pre-post-season) decrease in LBP following a back pain education session.
These papers observed some positive influence when considering a biopsychosocial approach to LBP in rowers. Although limited in number, these papers provided information on the use of back pain education and additional support required for athletes experiencing LBP.
A final small set of six studies were found to satisfy the inclusion criteria but did not fit the above categories and these were grouped under the miscellaneous heading. For example, Smoljanovic et al,66 described adaptive rowing at the Paralympic level advocating for an increase in racing distance. Injuries to adaptive rowers including the low back region are briefly mentioned, however, this is not the focus and there is no elaboration on LBP 66
Further although peer-reviewed, four of the six papers were identified as promotional pieces or using relatively older dataeg 67–69 and do not add to the present review
The ‘aggravating factors’ grouping within the epidemiology category was chosen for appraisal as this category may provide the greatest value to rowers and coaches when assess-
ing preventative measures for LBP that may be considered. Using The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) tool, it was found that the abstracts and introductions of the papers provided relevant information (Table 2). Details of study characteristics and boundaries (such as participants, variables, measurement, and study size) were described including diagnostic criteria in the methods sections of the appraised studies. Results were commonly missing some of the STROBE recommended items although provided accurate information regarding participants, descriptive data, and outcomes of the study Finally, the majority of information required by the STROBE process in the discussions was present, however, some did not discuss generalizability of the results (Table 2).
Eight STROBE items were missing in two-thirds of papers. These included representation of missing data and aspects of statistical analyses such as relative risk estimate and sensitivity analyses. None of the papers met all 22+ criteria.
The purpose of this study was to systematically map and investigate the currently available literature relating to low back pain (LBP) in rowing to inform athletes and coaches, and to identify gaps for future research.
In the general population, LBP has been associated with poor health, heavy physical work, obesity, smoking and low socioeconomic status.70 Athletes may, at first sight, be unlikely to be affected by these factors. However, athletes may be impacted by stress, anxiety, fatigue and reduced sleep and mood,71,72 factors that have been associated with increased risk of LBP. Furthermore, exercise and LBP have been expressed as a U-shaped curve where exercise reduces risk while simultaneously, high levels of physical activity can predispose to LBP 73 Elite athletes in one study were shown to have a higher prevalence of back pain in comparison with a physically active control group.27 Elite athletes may undergo a higher level of stress on the musculoskeletal system which may account for a higher back pain prevalence.27 Elite rowers were well represented as participants in the research reviewed in this study (23 of the 78 papers).
Many risk factors for LBP were identified, most notably, prolonged ergometer use and previous back pain history. Prevention may be a significant factor in avoiding the first back pain episode to decrease the chance of future LBP.74,75 Prevention has been investigated through the use of preparticipation evaluation tools, however, these have not yet shown utility in rowers. Prolonged ergometer use (particularly for more than 30 minutes) has been identified throughout the literature as a risk factor for LBP in rowers.7,10,21,23,24,28,32 The statement “prolonged ergometer use” has not been clarified further in the literature as to whether this pertains to stationary ergometer rowing or dynamic ergometer rowing, it may be useful in future to clarify this. This risk may be interpreted through biomechanical analysis of rowing technique on- and off-water, where it has been observed that technique seems to deteriorate
with prolonged ergometer use and rowing at higher-intensities.46,50,53,55 During on-water rowing, the rower is required to maintain balance, through activation of hip and trunk flexors, particularly during the recovery phase to create a smooth stroke.76 Balance is not required in the same way while using the stationary ergometer as it would be when rowing on water which means the sensory feedback is also altered. This has been observed through the literature where some studies have shown that increasing angles of lumbar spine flexion may be the result of fatigue. Prolonged ergometer use and back pain history were the only significant risk factors agreed upon within the literature. Furthermore, many of the studies assessing rowing technique observed the rower while on the ergometer10 and results may not generalize to on-water rowing.
The present study found that a LBP definition was not well established, in line with previous studies.10 The terms low back injury and low back pain were used interchangeably by many authors.35,38,39,41 The authors of the Global Burden of LBP define LBP as “pain in the area on the posterior aspect of the body from the lower margin of the twelfth ribs to the lower gluteal folds with or without pain referred into one or both lower limbs that lasts for at least one day” 77(p968) In total, only 21% (27) of the papers included in the present review mentioned a definition of either LBP, back pain or injury (Appendix 1). Definitions were most commonly given in the epidemiology category (18 of 27). This has been reflected in the critical appraisal as 11 of the 12 papers appraised reported a definition (Table 2). Without effective defining of terms within the study or in using incompatible definitions, a comparison between studies is difficult to make. It has also been observed that a lack of common definition may affect prevalence data.3 Furthermore, this decreases the ability to build a literature base that adds evidence to create clarity and consistency of findings. Future research should include definitions of significant terms such as LBP to provide understanding for the readers as well as for quality reporting.
The literature within the present study contained many limitations concerning methods employed. These issues include low injury reporting, minimal prospective studies, low participant numbers and a lack of randomized controlled trials (RCTs).
With regard to low injury reporting, prevalence has been well mapped to highlight the widespread nature of LBP, however, the figures produced may vary considering the lack of reliable injury reporting mentioned in some papers.63,64 Decreased injury reporting was referenced in a 2020 systematic review of athletes stating that some may be reluctant to highlight their condition due to fear of repercussions.75 Some papers are calling for a more comprehensive view of pain management.71 This has been explored within the studies included in the biopsychosocial category of the present study. Specifically, these studies bring to light the importance of understanding and supporting the athlete by people around them. However, family and other people in an athlete’s circle may directly or indirectly pressure the athlete to ignore, not report pain or treat an injury with short-term remedies that may create
Examining the Peer-Reviewed Published Literature Regarding Low Back Pain in Rowing: A Scoping Review
Table 2. Critical Appraisal of ‘aggravating factors’ in the Epidemiology Category using the STROBE tool16
A value of 1 in this table indicates meeting the criterion whereas 0 indicates not meeting the criterion. Percentages represent the number of papers that met the criteria and are rounded to the nearest whole number
long term negative consequences so that they can continue their sport.71,78 There seems to be a broad sporting culture that promotes playing through pain and injury and lessen its significance.79 This may create future episodes of back pain for the athlete. This culture of concealment seems to be common throughout many sporting disciplines75 and breaking this down may help to allow athletes to disclose pain earlier resulting in prompt rehabilitation and potentially less time taken off training and competition.63 Wilson et al63 recommended education for athletes, coaches and medical staff around appreciating the complexity of LBP, the significance of early disclosure, and the negative effect of concealment. Removing the stigma would allow athletes to disclose LBP which would additionally produce more accurate research data. Moreover, generating further prospective studies may produce more useful results.
A retrospective design was common in the epidemiological category (18 papers)20,22,23,25–28,30,32–41 with only four papers adopting a prospective design.8,21,24,29 Recall bias may have been an impact for study participants in remembering previous episodes of back pain and the factors associated with it.80 One study discusses their retrospective cross-sectional design as “ a survey of the survivors” whereby only the athletes who continued their sport have been surveyed and others who may have left were not accessible, therefore, introducing bias.41(p452) This is a consideration for the remaining retrospective papers as to whether they have included rowers who left the sport. Prospectively designed papers with adequate sample sizes are needed to accurately survey risk factors for LBP 10,40
The epidemiological category has provided some conclusions when considering risk factors for LBP on the rower However, conclusions are difficult to make from the biomechanical category due to a lack of cohesiveness and smaller study sizes. Increasing study sizes and using repeat methods will help to allow a more confident conclusion as to the effect of factors such as stroke rate, optimal lumbopelvic position and muscular activation. Additionally, for the results set of the present study, only one RCT was included.18 Conducting more RCTs would increase the understanding of and confidence in this literature. Further, critical appraisal of (a subset of) the literature can work to increase confidence in the findings to date.
For the present study, the subset of articles investigating aggravating factors was assessed against the STROBE tool to advance critical analysis of current knowledge of LBP in rowing. This subsection of data was chosen as it contained the most cohesive information and, therefore, conclusions have been easier to draw. The critical appraisal revealed significant strengths in reporting quality with some gaps around thorough reporting within the results. When read critically, the appraised literature is informative in providing epidemiological data. Researchers can view this subsection of data to highlight gaps in the literature such as a lack of definition. Additionally, this section of data highlights risk factors such as prolonged ergometer use and history of LBP that may be useful to coaches and athletes in thinking about LBP prevention.
Injury prevention is an important aspect of LBP in rowing. A six-staged process developed by Finch81,82 called The Translating Research into Injury Prevention Practice (TRIPP) has been developed whereby injury surveillance leads to implementation of preventative measures. Due to the methodological issues described earlier, this study may not inform injury surveillance in the first step of the TRIPP model.81,82 However, this scoping review may work to inform subsequent studies in highlighting areas for further investigation.
A 2021 consensus statement corroborated the findings of this study That is risk factors such as a history of LBP and ergometer use (longer than 30 minutes) were highlighted similar to the present findings.7 Furthermore, the contributors to the consensus statement recognized the need for increased research in this area.7 Although methodologically less rigorous than the present scoping review, the consensus statement provided pertinent information regarding management of LBP in rowers that is in line with the present review and the quality appraisal contained herein and may be useful for rowers, coaches and health practitioners.7
This study highlights the importance of prevention of the first LBP episode for athletes and coaches. Prolonged ergometer use should be approached with caution as it was the most commonly agreed upon risk factor. The rigorous methods used in this study including the use of a critical appraisal create increased confidence in the conclusions found.
Underreporting by rowers and retrospectively designed studies may result in imprecise epidemiological findings and affect the validity of the study outcomes. Use of a strong definition such as that by the Global Burden of Disease77 would strengthen the data. There is a need to consider ways to decrease emotional and physical stress on athletes and break down the culture of concealment with regard to injury reporting.
Undertaking a larger critical appraisal to assess the reporting quality of all of the included papers would have given greater weight to the findings of the study
This scoping review identified a body of literature that showed good quality epidemiological information to document the widespread effect of LBP on rowers. Many risk factors were highlighted, most significantly, back pain history and prolonged ergometer use. Issues of method within the literature were present including, a lack of LBP definition, issues with injury reporting, and small sample sizes. Avenues of investigation within the literature covered a range of topics e.g., spinal mobility, muscular contribution, pre-
participation evaluation tools, lower extremity force, and biopsychosocial effect. These showed some promise, however, need further investigation. The widespread prevalence of LBP in rowers observed in this study shows the significance of the injury on this population. Previous back pain history and prolonged ergometer use have been recognized to be significant risk factors. Future research should include LBP definitions and ideally be undertaken prospectively. This would help to support coaches and athletes to consider ways to prevent LBP, increase injury reporting and early rehabilitation for rowers.
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
The scoping review protocol was registered prospectively with the open science framework on 7 April 2021. Reference: Athy, V (2021, April 7). Examining the peer-reviewed literature regarding low back pain in rowing: A scoping review.
Retrieved from osf.io/b6ydj
Submitted: May 24, 2022 CST, Accepted: November 30, 2022
CST
The study protocol was approved by the Ethics Committee of Unitec Institute of Technology, Auckland, New Zealand.
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Vos T, Abajobir AA, Abbafati C, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211-1259. doi:10.1016/s014 0-6736(17)32154-2
2. Institute for Health Metrics and Evaluation. Findings from the Global Burden of Disease Study 2017 Published 2018. http://www.healthdata.org/site s/default/files/files/policy_report/2019/GBD_2017_Boo klet.pdf
3. Trompeter K, Fett D, Platen P Prevalence of back pain in sports: A systematic review of the literature. Sport Med. 2017;47(6):1183-1207. doi:10.1007/s4027 9-016-0645-3
4. National Health Committee. Low Back Pain: A Pathway to Prioritisation. Published 2015. https://ww w.health.govt.nz/system/files/documents/publication s/nhc-lbp-pathway-to-prioritisation.pdf
5. Heneweer H, Staes F, Aufdemkampe G, van Rijn M, Vanhees L. Physical activity and low back pain: A systematic review of recent literature. Eur Spine J 2011;20(6):826-845. doi:10.1007/s00586-010-1680-7
6. Heuch I, Heuch I, Hagen K, Zwart JA. Is there a Ushaped relationship between physical activity in leisure time and risk of chronic low back pain? A follow-up in the HUNT Study. BMC Public Health. 2016;16(1):1-9. doi:10.1186/s12889-016-2970-8
7 Wilson F, Thornton JS, Wilkie K, et al. 2021 consensus statement for preventing and managing low back pain in elite and subelite adult rowers. Br J Sports Med. 2021;55(16):893-899. doi:10.1136/bjsport s-2020-103385
8. Foss IS, Holme I, Bahr R. The prevalence of low back pain among former elite cross-country skiers, rowers, orienteerers, and nonathletes: A 10-year cohort study Am J Sports Med 2012;40(11):2610-2616. doi:10.1177/03635465124584 13
9. Accident Compensation Corporation. [GOV-004839]. [Unpublished Raw Data] 2020
10. Wilson F, Gissane C, McGregor A. Ergometer training volume and previous injury predict back pain in rowing; strategies for injury prevention and rehabilitation. Br J Sports Med. 2014;48(21):1534-1537 doi:10.1136/bjsports-2014-09 3968
11. Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol 2005;8(1):19-32. doi:10.1080/1364557032000119616
12. Levac D, Colquhoun H, O’Brien KK. Scoping studies: Advancing the methodology Implement Sci 2010;5(69):1-9. doi:10.1186/1748-5908-5-69
13. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169(7):467-473. doi:10.7326/m18-0850
14. Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119-2126. doi:1 0.11124/jbies-20-00167
15. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. doi:10.2307/2529310
16. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med 2007;4(10):1628-1654. doi:1 0.1371/journal.pmed.0040297
17. Da Costa BR, Cevallos M, Altman DG, Rutjes AWS, Egger M. Uses and misuses of the STROBE statement: Bibliographic study. BMJ Open. 2011;1(1):1-6. doi:1 0.1136/bmjopen-2010-000048
18. Ng L, Cañeiro JP, Campbell A, Smith A, Burnett A, O’Sullivan P. Cognitive functional approach to manage low back pain in male adolescent rowers: A randomised controlled trial. Br J Sports Med 2015;49(17):1125-1131. doi:10.1136/bjsports-2014-0 93984
19. Perich D, Burnett A, O’Sullivan P, Perkin C. Low back pain in adolescent female rowers: A multidimensional intervention study. Knee Surg Sport Traumatol Arthrosc 2011;19(1):20-29. doi:10.1007/s0 0167-010-1173-6
20. Howell DW. Musculoskeletal profile and incidence of musculoskeletal injuries in lightweight women rowers. Am J Sports Med. 1984;12(4):278-282. doi:1 0.1177/036354658401200407
21. Newlands C, Reid D, Parmar P The prevalence, incidence and severity of low back pain among international-level rowers. Br J Sports Med. 2015;49(14):951-956. doi:10.1136/bjsports-2014-093 889
22. Stutchfield BM, Coleman S. The relationships between hamstring flexibility, lumbar flexion, and low back pain in rowers. Eur J Sport Sci 2006;6(4):255-260. doi:10.1080/17461390601012678
23. Ng L, Perich D, Burnett A, Campbell A, O’Sullivan P Self-reported prevalence, pain intensity and risk factors of low back pain in adolescent rowers. J Sci Med Sport. 2014;17(3):266-270. doi:10.1016/j.jsams.2 013.08.003
24. Wilson F, Gissane C, Gormley J, Simms C. A 12-month prospective cohort study of injury in international rowers. Br J Sports Med 2010;44(3):207-214. doi:10.1136/bjsm.2008.048561
25. O’Kane JW, Teitz CC, Lind BK. Effect of preexisting back pain on the incidence and severity of back pain in intercollegiate rowers. Am J Sports Med 2003;31(1):80-82. doi:10.1177/0363546503031001250
26. Teitz CC, O’Kane JW, Lind BK. Back pain in former intercollegiate rowers. Am J Sports Med. 2003;31(4):590-595. doi:10.1177/03635465030310041 901
27. Fett D, Trompeter K, Platen P. Back pain in elite sports: A cross-sectional study on 1114 athletes. PLoS One 2017;12(6):1-17 doi:10.1371/journal.pon e.0180130
28. Socratis K, Eleni D, Kostas D, Vasilios D. Injuries of Greek rowers participating on different competitive categories. Biol Exerc. 2013;9(2):29-39. d oi:10.4127/jbe.2013.0068
29. Trease L, Wilkie K, Lovell G, Drew M, Hooper I. Epidemiology of injury and illness in 153 Australian international-level rowers over eight international seasons. Br J Sports Med 2020;54(21):1288-1293. do i:10.1136/bjsports-2019-101402
30. Verrall G, Darcey A. Lower back injuries in rowing national level compared to international level rowers. Asian J Sports Med 2014;5(4):1-5. doi:10.5812/asjs m.24293
31. Arumugam S, Ayyadurai P, Perumal S, Janani G, Dhillon S, Thiagarajan KA. Rowing injuries in elite athletes: A review of incidence with risk factors and the role of biomechanics in its management. Indian J Orthop 2020;54(3):246-255. doi:10.1007/s43465-02
0-00044-3
32. Teitz CC, O’Kane JW, Lind BK, Hannafin JA. Back pain in intercollegiate rowers. Am J Sports Med 2002;30(5):674-679. doi:10.1177/03635465020300050 701
33. Smoljanovic T, Bojanic I, Hannafin JA, Hren D, Delimar D, Pecina M. Traumatic and overuse injuries among international elite junior rowers. Am J Sports Med. 2009;37(6):1193-1199. doi:10.1177/0363546508 331205
34. Smoljanović T, Bohaček I, Hannafin J, Nielsen HB, Hren D, Bojanić I. Sport injuries in international masters rowers: A cross-sectional study. Croat Med J. 2018;59(5):258-266. doi:10.3325/cmj.2018.59.258
35. Bernardes F, Mendes-Castro A, Ramos J, Costa O Musculoskeletal injuries in competitive rowers. Acta Med Port 2015;28(4):427-434. doi:10.1016/s0025-619 6(12)61906-5
36. Hickey GJ, Fricker PA, McDonald WA. Injuries to elite rowers over a 10-yr period. Med Sci Sports Exerc 1997;29(12):1567-1572. doi:10.1097/00005768-19971 2000-00004
37 Smoljanovic T, Bohacek I, Hannafin JA, et al. Acute and chronic injuries among senior international rowers: A cross-sectional study. Int Orthop 2015;39(8):1623-1630. doi:10.1007/s00264-0 14-2665-7
38. Finlay C, Dobbin N, Jones G. The epidemiology of injuries in adult amateur rowers: A cross-sectional study Phys Ther Sport 2020;41:29-33. doi:10.1016/j.p tsp.2019.11.001
39. Arend M, Akel J, Haabpiht L, Jürgenson J. Selfreported prevalence of low back pain in Estonian rowers. Acta Kinesiol Univ Tartu. 2016;22:82-92. doi:1 0.12697/akut.2016.22.07
40. Maselli F, Ciuro A, Mastrosimone R, et al. Low back pain among Italian rowers: A cross-sectional survey. J Back Musculoskelet Rehabil. 2015;28(2):365-376. doi:10.3233/bmr-140529
41. Bahr R, Andersen SO, Løken S, Fossan B, Hansen T, Holme I. Low back pain among endurance athletes with and without specific back loading - A crosssectional survey of cross-country skiers, rowers, orienteerers, and nonathletic controls. Spine. 2004;29(4):449-454. doi:10.1097/01.brs.0000096176.9 2881.37
42. Farahbakhsh F, Rostami M, Noormohammadpour P, et al. Prevalence of low back pain among athletes: A systematic review J Back Musculoskelet Rehabil 2018;31(5):901-916. doi:10.3233/bmr-170941
43. Crawford JO The Nordic musculoskeletal questionnaire. Occup Med 2007;57(4):300-301. doi:1 0.1093/occmed/kqm036
44. Waller AE, Feehan M, Marshall SW, Chalmers DJ. The New Zealand rugby injury and performance project: I. design and methodology of a prospective follow-up study. Br J Sports Med. 1994;28(4):223-228. doi:10.1136/bjsm.28.4.223
45. MacManus C, Dankaerts W, O’Sullivan K. Using wireless technology to monitor lumbo-pelvic kinematics in rowing. Physiother Pract Res. 2013;34(2):113-121. doi:10.3233/ppr-130021
46. Wilson F, Gormley J, Gissane C, Simms C. The effect of rowing to exhaustion on frontal plane angular changes in the lumbar spine of elite rowers. J Sports Sci 2012;30(14):1481-1489. doi:10.1080/02640 414.2012.711486
47 Wilson F, Gissane C, Gormley J, Simms C. Sagittal plane motion of the lumbar spine during ergometer and single scull rowing. Sport Biomech. 2013;12(2):132-142. doi:10.1080/14763141.2012.7266 40
48. Pollock CL, Jenkyn TR, Jones IC, Ivanova TD, Garland SJ. Electromyography and kinematics of the trunk during rowing in elite female rowers. Med Sci Sports Exerc. 2009;41(3):628-636. doi:10.1249/mss.0b 013e31818c1300
49. Clay H, Mansell J, Tierney R. Association between rowing injuries and the Functional Movement ScreenTM in female collegiate Division I rowers. Int J Sports Phys Ther 2016;11(3):345-349. http://www.pu bmedcentral.nih.gov/articlerender.fcgi?artid=PMC488 6802
50. McGregor AH, Bull AMJ, Byng-Maddick R. A comparison of rowing technique at different stroke rates: A description of sequencing, force production and kinematics. Int J Sports Med 2004;25(6):465-470. doi:10.1055/s-2004-820936
51. Concept2 inc. Timeline. https://www.concept2.co m/company/about-concept2/timeline
52. Ng L, Campbell A, Buernett A, Smith A, O’Sullivan P. Spinal kinematics of adolescent male rowers with back pain in comparison to matched controls during ergometer rowing. J Appl Biomech. 2015;31(6):459-468. doi:10.1017/cbo978110741532
4.004
53. McGregor AH, Patankar ZS, Bull AMJ. Spinal kinematics in elite oarswomen during a routine physiological ‘step test.’ Med Sci Sports Exerc 2005;37(6):1014-1020. doi:10.1249/01.mss.00001716
18.22263.58
54. McGregor AH, Anderton L, Gedroyc W The assessment of intersegmental motion and pelvic tilt in elite oarsmen. Med Sci Sports Exerc 2002;34(7):1143-1149. doi:10.1097/00005768-200207 000-00015
55. Holt PJE, Bull AMJ, Cashman PMM, McGregor AH. Kinematics of spinal motion during prolonged rowing. Int J Sports Med. 2003;24(8):597-602. doi:10.1 055/s-2003-43273
56. Martinez-Valdes E, Wilson F, Fleming N, McDonnell SJ, Horgan A, Falla D. Rowers with a recent history of low back pain engage different regions of the lumbar erector spinae during rowing. J Sci Med Sport. 2019;22(11):1206-1212. doi:10.1016/j.j sams.2019.07.007
57 Caldwell JS, McNair PJ, Williams M. The effects of repetitive motion on lumbar flexion and erector spinae muscle activity in rowers. Clin Biomech 2003;18(8):704-711. doi:10.1016/s0268-0033(03)0011 7-7
58. Özdinçler AR, Kaya BK, Yazgan EA, Yanıkoğlu Ö, Bakırel T, Çam E. Comparison of acute effects of ballistic stretching and kinesiotaping in rowers with hamstring tightness. J Rom Sport Med Soc 15(2):3126-3132. https://www.researchgate.net/profil e/Beguem-Kara-Kaya/publication/338108354_Compar ison_of_Acute_Effects_of_Ballistic_Stretching_and_Kin esiotaping_in_Rowers_with_Hamstring_Tightness/link s/5dff2b6aa6fdcc2837352c01/Comparison-of-Acute-E ffects-of-Ballistic-St
59. Gonzalez SL, Diaz AM, Plummer HA, Michener LA. Musculoskeletal screening to identify female collegiate rowers at risk for low back pain. J Athl Train. 2018;53(12):1173-1180. doi:10.4085/1062-605 0-50-17
60. Mattes K, Wolff S. Asymmetry of the stretcher force during symmetrical ergometer rowing and leg press test of scullers and sweep rowers. Biol Exerc. 2019;15(2):23-37 doi:10.4127/jbe.2019.0160
61. Mattes K, Wolff S. Asymmetry of the leg stretcher force high-performance female and male juniors in sweep rowing. Int J Perform Anal Sport 2019;19(5):737-748. doi:10.1080/24748668.2019.1651 085
62. An WW, Wong V, Cheung RTH. Lower limb reaction force asymmetry in rowers with and without a history of back injury. Sport Biomech. 2015;14(4):375-383. doi:10.1080/14763141.2015.1061 047
63. Wilson F, Ng L, O’Sullivan K, et al. ‘You’re the best liar in the world’: A grounded theory study of rowing athletes’ experience of low back pain. Br J Sports Med. 2021;55(6):327-335. doi:10.1136/bjsport s-2020-102514
64. McNally E, Wilson D, Seiler S. Rowing injuries. Semin Musculoskelet Radiol 2005;9(4):379-396. doi:1 0.1055/s-2005-923381
65. Thorpe A, O’Sullivan P, Burnett A, Cañeiro J. Assessing the efficacy of a specific physiotherapy intervention for the prevention of low back pain in female adolescent rowers: A field study New Zeal J Sport Med 2009;36(2):38-46.
66. Smoljanovic T, Bojanic I, Hannafin JA, et al. Complete inclusion of adaptive rowing only 1000m ahead. Br J Sports Med 2013;47(13):819-825. doi:10.1 136/bjsports-2013-092157
67 Devereaux MD, Lachmann SM. Athletes attending a sports injury clinic - A review Br J Sports Med 1983;17(4):137-142. doi:10.1136/bjsm.17.4.137
68. Boland AL, Hosea TM. Rowing and sculling and the older athlete. Clin Sports Med 1991;10(2):245-256. doi:10.1016/s0278-5919(20)3063
0-x
69. Reid DA, McNair PJ. Factors contributing to low back pain in rowers. Br J Sports Med 2000;34(5):321-322. doi:10.1136/bjsm.34.5.321
70. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356-2367. doi:10.1016/s014 0-6736(18)30480-x
71. Hainline B, Turner JA, Cañeiro JP, Stewart M, Lorimer Moseley G. Pain in elite athletes—neurophysiological, biomechanical and psychosocial considerations: a narrative review Br J Sports Med. 2017;51(17):1259-1264. doi:10.1136/bjsp orts-2017-097890
72. O’Sullivan K, O’Sullivan PB, Gabbett TJ. Pain and fatigue in sport: Are they so different? Br J Sports Med 2018;52(9):555-556. doi:10.1136/bjsports-201 7-098159
73. Heneweer H, Vanhees L, Picavet HSJ. Physical activity and low back pain: A U-shaped relation? Pain 2009;143(1-2):21-25. doi:10.1016/j.pain.2008.1 2.033
74. Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol 2010;24(6):769-781. doi:10.1016/j.berh.20 10.10.002
75. Wilson F, Ardern CL, Hartvigsen J, et al. Prevalence and risk factors for back pain in sports: A systematic review with meta-analysis. Br J Sports Med 2021;55(11):601-607 doi:10.1136/bjsports-202 0-102537
76. Fleming N, Donne B, Mahony N. A comparison of electromyography and stroke kinematics during ergometer and on-water rowing. J Sports Sci 2014;32(12):1127-1138. doi:10.1080/02640414.2014.8 86128
77 Hoy D, March L, Brooks P, et al. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study Ann Rheum Dis 2014;73(6):968-974. doi:10.1136/annrheumdis-201
3-204428
78. Ommundsen Y, Roberts GC, Lemyre PN, Miller BW Parental and coach support or pressure on psychosocial outcomes of pediatric athletes in soccer. Clin J Sport Med 2006;16(6):522-526. doi:10.1097/01.j sm.0000248845.39498.56
79. Weinberg R, Vernau D, Horn T. Playing through pain and injury: Psychosocial considerations. J Clin Sport Psychol 2013;7(1):41-59. doi:10.1123/jcsp.7.1.4
80. Althubaiti A. Information bias in health research: Definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211-217. doi:10.2147/jmd h.s104807
81. Finch C. A new framework for research leading to sports injury prevention. J Sci Med Sport 2006;9(1-2):3-9. doi:10.1016/j.jsams.2006.02.009
82. Finch CF, Talpey S, Bradshaw A, Soligard T, Engebretsen L. Research priorities of international sporting federations and the IOC research centres. BMJ Open Sport Exerc Med 2016;2(1):1-8. doi:10.113 6/bmjsem-2016-000168
Download: https://ijspt.scholasticahq.com/article/67836-examining-the-peer-reviewed-published-literatureregarding-low-back-pain-in-rowing-a-scoping-review/attachment/134506.pdf?auth_token=ElBwiL6ZK7uLCkbKgy7j
Adam Culiver 1,2 a , Dustin Grooms 3,4,5 , Nathan Edwards 1,2 , Laura Schmitt 2,6 , James Oñate 2,7
1 School of Health and Rehabilitation Sciences, Ohio State University, 2 Jameson Crane Sports Medicine Research Institute, Ohio State University, 3 Division of Physical Therapy, School of Rehabilitation and Communication Sciences, College of Health Sciences and Professions, Ohio University, 4 Division of Athletic Training, School of Applied Health Sciences and Wellness, College of Health Sciences and Professions, Ohio University, 5 5. Ohio Musculoskeletal and Neurological Institute, Ohio University, 6 Division of Physical Therapy, School of Health and Rehabilitation Sciences, Ohio State University, 7 Division of Athletic Training, School of Health and Rehabilitation Sciences, Ohio State University
Keywords: anterior cruciate ligament reconstruction (ACLR), functional magnetic resonance imaging (fMRI), blood oxygen level dependent (BOLD) response, peak internal knee extension moment, neurologic activity, change of direction, biomechanics https://doi.org/10.26603/001c.57782
Central nervous system (CNS) function after ACLR, quantified by the blood oxygen level dependent (BOLD) response, is altered in regions of sensory function during knee movement after ACLR. However, it is unknown how this altered neural response may manifest in knee loading and response to sensory perturbations during sport specific movements.
To investigate the relationship among CNS function and lower extremity kinetics, under multiple visual conditions, during 180° change of direction task in individuals with a history of ACLR.
Eight participants, 39.3 ± 37.1 months after primary, left ACLR performed repetitive active knee flexion and extension of their involved knee during fMRI scanning. Participants separately performed 3D motion capture analysis of a 180° change of direction task under full vision (FV) and stroboscopic vision (SV) conditions. A neural correlate analysis was performed to associate BOLD signal to knee loading of the left lower extremity
Involved limb peak internal knee extension moment (pKEM) was significantly lower in the SV condition (1.89 ± 0.37 N*m/Kg) compared to the FV condition (2.0 ± 0.34 N*m/Kg) (p = .018). Involved limb pKEM during the SV condition was positively correlated with BOLD signal in the contralateral precuneus and superior parietal lobe (Voxels: 53; p = .017; z-stat max: 6.47; MNI peak: 6, -50, 66).

There is a positive association between involved limb pKEM in the SV condition and BOLD response in areas of visual-sensory integration. Activation of contralateral
Corresponding author: Adam Culiver, PT, DPT, SCS
School of Health and Rehabilitation Sciences, Ohio State University
Sports Medicine Research Institute
2835 Fred Taylor Dr. Suite 3120
Columbus, OH 43202
Adam.culiver@osumc.edu
precuneus and superior parietal lobe brain regions may be a strategy to maintain joint loading when vision is perturbed.
Level 3
Anterior cruciate ligament (ACL) injury poses a significant risk to individuals participating in cutting and pivoting sports.1 ACL injury is debilitating as it often requires reconstructive surgery, intense rehabilitation, and a time loss from sport of nine months or greater.2 Despite completion of rehabilitation, 20% to 30% of individuals returning to sport will sustain a second ACL injury.3,4 Traditional measures of motor function (i.e., strength and hop performance) may not accurately predict patient function,5 warranting the investigation of other systems, such as the central nervous system (CNS).6 Individuals after ACL reconstruction (ACLR) have alterations in the brain’s blood oxygen level dependent (BOLD) response within sensorimotor regions of the brain during basic knee movement.7–9
The BOLD response is a hemodynamic function which measures the oxygen consumption in a given brain region, and directly reflects the neurologic activity occurring due to local input and processing.10,11 This BOLD response has been associated with patient reported functional outcome measures after ACLR9 but has yet to be linked with other aspects of patient function, such as biomechanical performance. Restoration of functional movement patterns is an aspect of patient function vital to recovery following ACLR.2 Movement patterns are often quantified with biomechanical analysis and abnormal biomechanics are a key indicator of dysfunctional motor control within the CNS.12,13 Resolving movement pattern dysfunction through neuromuscular training is a high priority for individuals following ACLR,2 yet movement patterns remain dysfunctional for years.14,15 Determining an association between CNS activity and more dynamic movement control may provide insight on the neurologic mechanisms underlying prolonged movement dysfunction following ACLR.
The BOLD response in bilateral motor cortex (M1), ipsilateral secondary somatosensory area, and lingual gyrus is altered in individuals who are on average three years following ACLR.8 Researchers have prospectively identified connectivity patterns in the brain’s BOLD response which differentiate high school athletes who sustain a future ACL injury and those who do not.16,17 Despite the growing body of literature to support altered CNS function in association with future ACL injury16,17 and ACLR,8,18 there is a missing link between the brain’s BOLD response and biomechanical performance. Evidence indicates that musculoskeletal indicators of function, such as strength, may not fully explain the loading deficits in an individual’s involved knee which start immediately after surgery, continue throughout rehabilitation, and remain years after returning to full activity 19,20 The negative biomechanical consequences of ACLR have been reported through systematic reviews evaluating gait,21 running,22 and landing biomechanics.23 These tasks
are functionally relevant but lack a targeted application to cutting and pivoting sports where ACL injuries are most prevalent.1 A recent narrative review24 highlighted the need to increase testing for change of direction (CoD) movements following ACLR due to their frequent performance in sports such as football, soccer, and basketball, among others.24–26 The long-term negative impact to knee joint loading biomechanics after ACLR is well documented, but less is known about how manipulating sensory information (i.e., visual) during movement affects joint loading in sports-relevant tasks.
ACL injury impairs mechanoreceptor function inherent to the ligament, disrupting afferent input to the primary somatosensory cortex (S1).27 Restoration of this somatosensory signaling to S1 after ACLR, and the CNS’s ability to interpret the signal, is unclear 28,29 Vision and somatosensory input are complementary sources of sensory information used to support motor control.30 Vision may be more heavily relied upon when somatosensory input is dampened as vision is able to adapt more quickly to changes in stimuli than vestibular input.31 For individuals with altered somatosensory input after ACLR, the addition of a visual perturbation reduces available sensory information which may negatively impact the brain’s ability to regulate motor control. Disrupting visual sensory information can be accomplished with stroboscopic goggles which intermittently restricts vision and is known to impact landing biomechanics.32 The effect of stroboscopic perturbation on CoD movements is unknown and determining its impact on biomechanics will provide insight on how vision influences key indicators of knee and lower extremity function during highly dynamic, sport relevant movement.
The purpose of this study was to investigate the relationship among CNS function and lower extremity kinetics, under multiple visual conditions, during 180° change of direction task in individuals with a history of ACLR. The primary hypothesis was that there would be distinct neural correlates of sagittal and frontal plane limb loading in the motor cortices during FV and in regions within the parietal and occipital cortices during the SV condition. The secondary hypothesis was that limb loading strategies would differ between the FV and SV conditions.
Eight individuals after primary, unilateral, left ACLR participated in this specific study as part of a larger crosssectional investigation.8 Individuals signed informed consent prior to participation and the study was approved by Ohio State University Institutional review board. Individuals were screened for participation with the following inclusion criteria: primary left ACLR, Tegner level of activity ≥ 5,
cleared for return to full activity, no lower extremity injury in the prior six months, no history of lower extremity injury besides primary ACLR, and normal or corrected to normal vision. Participants were cleared for return to full activity by their surgeon, but neither objective return to activity testing nor time-based discharge criteria were controlled for in this study. Injury was defined as anything causing a time loss from activity for at least one day Individuals were excluded for the following reasons: multiligament injury, prior orthopedic surgery besides ACLR, known neurologic condition, pregnancy, and right ACLR. Movement from one side of the body can elicit a negative BOLD response in ipsilateral sensorimotor cortex and a positive response in contralateral sensorimotor cortex, therefore participants were excluded based on ACLR laterality to avoid confounding BOLD response across hemispheres.33 Participant demographics can be viewed in Table 1
Participants performed three-dimensional (3D) motion analysis testing and a functional magnetic resonance imaging (fMRI) scan within one week, a majority of participants performed both testing sessions within two days of one another. Lower extremity kinematic and kinetics were captured during performance of a run-pivot task. Kinematic data were tracked with a 10-camera 3D motion analysis system, at 240Hz (Vicon model MX-F40; Los Angeles, CA). Retroreflective markers were placed directly over the skin on specific anatomic locations, including the pelvis, thigh, shank, and foot, consistent with the point cluster marker set.32,34,35 Ground reaction force data were simultaneously captured using three embedded 40cm x 60cm platforms (Bertec Corporation, Columbus, OH; 1500 Hz). For the change of direction (CoD) task, participants began 5.5 to 6.5 meters away from the force platforms and the starting distance was modified to accommodate each individual’s stride length so contact with force platforms occurred at the same stride number for each participant (Figure 1). Participants performed all trials in full vision (FV) first, followed by trials under stroboscopic visual (SV) perturbation (SPARQ Vapor stroboscopic goggles, Nike, Inc, Beaverton OR) until 3 successful trials were captured on each lower extremity The SV goggles oscillated between opaque (lasting 43ms) and transparency (lasting 100ms). Participants were aware of which lower extremity would make contact with the force plate target, but were unaware of whether to perform a 45° or 180° CoD until the directional indicators illuminated. The directional indicator illuminated when participants were halfway between the start line and force
plate target. Up arrow indicated a 180° CoD, horizontal arrows indicated a 45° CoD towards the side opposite of the foot contacting the force plate target (right arrow = 45° CoD to the right, planting on the left foot). The average of three pivot trials, in both the FV and SV condition, were used for subsequent analysis.
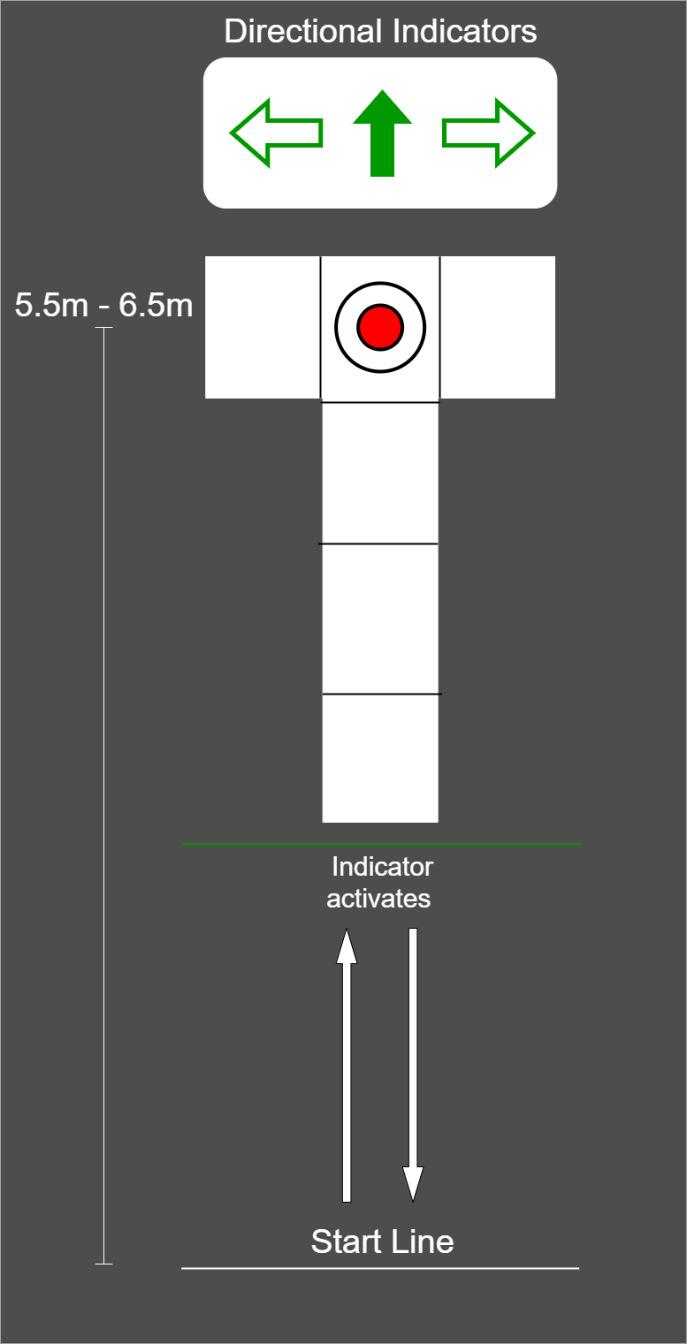
Biomechanical data analysis was performed in Visual 3D (v6.03.3 Professional, C-Motion, Inc., Germantown, MD). Variables of interest [peak vertical ground reaction force (vGRF), peak internal knee adduction moment (pKAM), peak internal knee extension moment (pKEM), peak knee flexion angle (PKFA)] were extracted using a custom MATLAB code (R2021b, MathWorks, Natick, MA, USA) and were body weight normalized. Data were analyzed during the
weight acceptance phase only, defined as initial contact (IC) to peak knee flexion angle of the ACLR limb. A matched low-pass Butterworth filter was applied at 15Hz to filter both kinematic and kinetic data, methods that have been used previously 32 To determine the influence of the stroboscopic condition on biomechanical performance, a strobe effect change score was calculated by the following equation:
where = strobe vision performance, = full vision performance, and = absolute value. Three values (FV performance, SV performance and strobe effect change score) for each variable of interest were demeaned and included as explanatory variables in the follow-up neural correlate analysis. Three paired samples t-tests were conducted using STATA (StataCorp LLC, College Station, TX) to determine if group average vGRF, pKEM, or pKAM were statistically different across visual conditions. Two followup paired t-tests were performed to compare pKEM of the involved and uninvolved limbs. Other biomechanical variables are provided for reference in the results section and reported as descriptive, but statistical testing was not performed.
A 3 Telsa MAGNETOM scanner (Siemens AG, Munich, Germany) with a 12-channel head coil was used for fMRI data collection. A T1 weighted anatomical scan was collected at TR = 2000ms, TE = 4.58ms, field of view (FoV) = 256mm, slice thickness = 1mm for a total of 176 slices. BOLD signal was captured during functional data collection using 90 whole brain gradient echo scans (TR = 3000ms, TE = 30ms, 2.5mm slice thickness, 55 total transverse slices, voxel size = 2.5mm3 , FoV = 256mm). Participants performed a repetitive active knee flexion/extension task from full knee extension to approximately 45° of flexion, at a 1.2 Hz frequency or roughly 36 cycles per 30 second block, while in the scanner Each movement block was separated by 30 seconds of rest, participants performed four blocks of movement and five blocks of rest.8
Pre-processing steps were performed in FSL (5.6.0, FMRIB, Oxford, UK) including brain extraction using BET, MCFLIRT motion correction,36,37 Gaussian kernel 5mm spatial smoothing, and high-pass temporal filtering at 90 Hz.38,39 Denoising and reduction of signal variation secondary to motion was completed using an Independent Component Analysis for Automatic Removal of Motion Artifacts (ICAAROMA).40,41 Functional images were registered to the high resolution anatomical image for each participant and structural normalization to Montreal Neurological Institute template 152 was performed using 12 degrees of freedom. Whole brain images were collected during the functional run and BOLD signal during the movement block was contrasted against the rest block using fixed effects at the subject level. A one sample t-test was used to determine group
level BOLD signal exceeding a z-statistic threshold of 3.1 and cluster corrected to p = .05 using Gaussian Random Field Theory A binarized mask was then created from the group average voxels identified as significantly active during the movement vs. rest contrast. This step was performed to include only voxels significantly active during the task in our subsequent neural correlate analysis. General linear models (GLM) were created using FMRIB’s Local Analysis of Mixed Effects (FLAME) 1 + 2 with biomechanical variables entered into the model as explanatory variables. Nine GLMs were performed, with a separate de-meaned biomechanical variable entered in each iteration of the GLM (Model 1: FV pKEM, Model 2: SV pKEM, Model 3: pKEM SECS, etc.). Each GLM creates a parameter estimate which fits the biomechanical variable to BOLD signal in each voxel. Parameter estimates are transformed into z-statistics and the correlate analysis identifies associated fluctuations in BOLD signal and the biomechanical variable. A z-statistic threshold of 3.1 and voxels cluster corrected at p = .05 using Gaussian Random Field Theory was again applied for each GLM.
LOWER EXTREMITY BIOMECHANICAL PERFORMANCE
vGRF, pKAM and PKFA were not different between visual conditions (Table 2). pKEM was lower in the SV condition compared to the FV condition (Table 2, p=0.018). When comparing the involved to uninvolved limb performance, pKEM was not different in either the FV or SV conditions (Table 4). Kinetic and kinematic values for the uninvolved limb are provided to characterize cohort performance (Table 3).
There were no significant associations among task relevant BOLD response and FV biomechanical variables of interest. There was a significant positive correlation between pKEM and task relevant BOLD signal in the contralateral (right) precuneus and superior parietal lobe [53 voxels; p = .017; zstat max = 6.47; MNI Coordinates (6, -50,66), figure 2]. There were no significant correlations among task relevant BOLD response and vGRF or pKAM in the SV condition and no significant associations with any variable’s SECS and BOLD response.
The purpose of our study was to investigate the relationship between BOLD response during repetitive knee movement and lower extremity biomechanics during a run to pivot task, under multiple visual conditions. The primary hypothesis was partially supported as involved limb pKEM in the SV condition was positively correlated with BOLD response in the contralateral precuneus and superior parietal lobe. However, there were no associations among any biomechanical variables of interest in the FV condition and task relevant BOLD response. Our secondary hypothesis
vGRF = vertical ground reaction force. pKAM = peak internal knee adduction moment. pKEM = peak internal knee extension
m = meter, kg = kilogram, deg = degree. Values are body mass normalized and reported separately for each visual condition and strobe effect change score. The strobe effect change score is calculated within subject, then averaged. Negative indicates a lower value in the SV condition. ªPaired t-test comparing FV to SV performance.
vGRF = vertical ground reaction force. pKAM = peak internal knee adduction moment. pKEM = peak internal knee extension moment. PKFA = peak knee flexion angle. N = Newtons, m meter, kg kilogram, deg degree. Values are body mass normalized and reported separately for each visual condition.
Negative values indicate the involved limb had a lower value than the uninvolved limb: vGRF = vertical ground reaction force. pKAM = peak internal knee adduction moment. pKEM = peak internal knee extension moment. PKFA peak knee flexion angle. N Newtons, m meter, kg kilogram, deg degree. Values are body mass normalized and reported separately for each visual condition. ªPaired t-test comparing involved limb to uninvolved limb performance.
was partially supported as well; involved limb pKEM was significantly lower in the SV condition compared to the FV condition.
This cohort had a significant reduction in pKEM during the SV condition compared to FV, representing an underloading of their involved knee in response to visual perturbation. Visual disruption in individuals after ACLR has previously caused reduced knee velocity and knee displacement during a change of direction task.42 The authors concluded that the small change to the overall movement pattern may be due to task design as participants were static prior to the CoD task and vision was only disrupted for one second while participants were actively changing direction.42 This could have allowed participants ample time to plan their movement prior to visual disruption, leading to only minor changes in movement performance. The task design of the current study consisted of continuous intermittent visual perturbation as participants were running and changing direction which may account for the different results. Other work has reported greater knee flexion excursion but
no change in knee moments comparing SV to FV during a drop vertical jump.32 Greater knee flexion excursion in the SV condition was deemed to be a clinically important alteration in neuromuscular control32 as the condition elicited a similar effect to a laterally directed physical perturbation delivered mid- jump,43 a situation common to various sports. This finding related to pKEM may be attributable to the different requirements of the run-pivot task evaluated here. The CoD task in this study is a highly dynamic, multi-planar, single limb and unpredictable task whereas the drop vertical jump, used in previous work,32 is bilateral and linear The complexity of this CoD task may be difficult enough to induce changes in knee joint loading in response to the SV perturbation, whereas the bilateral and linear nature of a drop vertical jump may not be complex enough to create this effect.
There were no statistically significant differences in pKAM or vGRF between visual conditions, despite a trend towards greater vGRF in the SV condition compared to FV This corroborates prior work reporting no effect of SV perturbation on frontal plane knee kinetics during a drop vertical jump32 or vGRF during CoD.42 When evaluating this cohort’s pKEM performance across limbs, there was a trend
Neural correlate statistical testing results and location of the identified cluster towards lower involved limb pKEM in FV compared to their uninvolved limb. Albeit just a trend, this supports numerous publications reporting individuals after ACLR underload their involved knee across many tasks compared to their contralateral limb and healthy controls.21–23 This includes a 90° CoD task as individuals exhibit lower pKEM compared to healthy controls, despite no difference in timed performance.44 Previously reported normative data for pKEM during a CoD task is 2.3 ± 0.6 N*m /kg45 whereas this cohort’s involved limb pKEM performance was 2.0 ± 0.34 N*m /kg (FV) and 1.90 ± 0.37 N*m /kg (SV). This may represent a clinically meaningful difference in pKEM,46 however, the difference in this cohort’s involved limb pKEM across visual conditions (0.11 ± 0.16 N*m/kg) is between the minimum detectable change (0.10 N*m/kg) and minimal clinically important difference (0.12 N*m/kg).46 Therefore, the difference in performance between FV and SV conditions reported here is statistically different but may not represent a clinically meaningful difference.
The association of greater pKEM in the SV condition and increased BOLD response in contralateral precuneus and superior parietal lobe during knee extension-flexion suggests a potential sensory activation strategy in the CNS to maintain joint loading when vision is perturbed. The precuneus and superior parietal lobe have been associated with motor imagery,47,48 cross modal sensory matching tasks,49 visuomotor mapping,50 and coordinated motor behaviors that connect cognition with action.51 Following

ACLR, it has been theorized that the CNS undergoes an adaptive re-organization which may occur to integrate sensory information differently,52–54 likely due to the disruption in somatosensory signaling to spinal cord and S1 after ACLR.28,29 Identification of precuneus and superior parietal lobe as neural correlates of biomechanical performance during visual perturbation suggest these regions play an important role in sensorimotor function for individuals after ACLR. Prior work has established a greater BOLD response in bilateral precuneus during combined hip and knee flexion compared to rest,18 and greater BOLD response in superior parietal lobe18 and lingual gyrus8,18 in those with ACLR compared to healthy controls. Greater BOLD response in the superior parietal lobe has shown significant connectivity with primary motor cortex, primary and secondary somatosensory cortices, and regions of the frontal lobe associated with executive function and attention.18 Although a connectivity analysis was not performed with the cluster identified here, the previous association of superior parietal lobe to areas within the frontal lobe may warrant further investigation as the BOLD response in multiple areas of the frontal lobe decrease from 2 to 10 weeks after ACLR.9 However, this cohort was on average 3.5 years post ACLR and thus may not require the same level of attentional cognitive resources to perform basic knee flexion/ extension as individuals weeks after surgery, potentially indicating a sensory neuroplasticity, separate from cognition, as time from injury increases.
Results from this work suggest that greater neurologic activity within the precuneus is positively associated with sagittal plane knee loading in situations of visual perturba-
Figure 2. Cluster Configurationtion. Visual perturbations occur frequently in sport related activity and vision training is recommended during rehabilitation following ACLR55,56 to improve anticipatory timing during high-velocity movement and to re-weight sensorimotor processing.56,57 With the results presented here, and due to the known cross-modal functionality of the precuneus,49 clinicians may consider incorporating interventions which manipulate visual and somatosensory stimuli simultaneously during late phase rehabilitation. Targeting multiple sensory systems may help CNS processing of stimuli simultaneously which, in theory, may improve neural efficiency throughout the sensorimotor network. Future work should investigate sensory re-weighting interventions to determine their impact on precuneus and other regions of the sensorimotor network since it is unclear which sub-regions within the network are impacted by reweighting interventions. Future work should also seek to determine a causal relationship between sensorimotor network activation and biomechanical performance during sport related tasks to determine which brain regions are critical to knee sensorimotor control after ACLR.
This was a preliminary analysis of the neural correlates of biomechanical performance including only eight participants, and thus a larger sample is needed to draw definitive conclusions. This work included individuals from a wide range of time points following ACLR which may have influenced the results due to a lack of control for their physical activity since completion of rehabilitation. No control group was included which limits the ability to interpret this data as a beneficial or negative adaptation in the ACLR population. Statistical testing for all biomechanical interactions was not considered due to the small sample and the correlational approach limits the ability to establish a cause-and-effect relationship of these results.
Another consideration when interpreting these results is the attentional demand of the SV paradigm. Attentional demands and visual-spatial memory requirements are increased under SV conditions, due to the lack of visual monotony, but the amount of time an individual can maintain a higher level of attention and visual memory performance
without cognitive fatigue is uncertain.58 Participants performed numerous trials on both lower extremities, requiring a prolonged period of time under the SV condition. Neither visual memory nor visual attention were recorded in this study, but it is an important factor to consider which may have influenced the results.
From previous work, BOLD response during basic knee movement is altered in active individuals years after ACLR and is associated with patient reported knee function and visual performance. This study evaluated the correlation between BOLD response during basic knee movement and knee loading during a dynamic sports maneuver in an ACLR population. In this preliminary analysis, there was a positive association between involved limb sagittal plane knee loading during perturbed vision and BOLD response in areas of visual-sensory integration. Activation of visual-sensory integration brain regions may be a strategy to maintain joint loading when vision is perturbed. Clinicians may consider incorporating interventions which manipulate visual and somatosensory stimuli simultaneously to target cross-modal processing within the sensorimotor network for individuals after ACLR. However, the correlational statistical approach limits a cause-and-effect interpretation of the results presented here. Further investigation is warranted to identify which patients could most benefit from multi-sensory interventions and understand potential sensory related neural activity variation after ACLR.
All authors report no relevant financial disclosures to the submitted work.
Submitted: April 08, 2022 CST, Accepted: November 03, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and metaanalysis. Am J Sports Med 2016;44(10):2716-2723. do i:10.1177/0363546515617742
2. Melick N van, Cingel REH van, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med 2016;50(24):1506-1515. doi:10.1136/bjsports-2015-0 95898
3. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med 2014;42(7):1567-1573. doi:10.1177/03635 46514530088
4. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and retaanalysis. Am J Sports Med 2016;44(7):1861-1876. do i:10.1177/0363546515621554
5. Losciale JM, Zdeb RM, Ledbetter L, Reiman MP, Sell TC. The association between passing return-tosport criteria and second anterior cruciate ligament injury risk: a systematic review with meta-analysis. J Orthop Sports Phys Ther 2019;49(2):43-54. doi:10.251 9/jospt.2019.8190
6. Chaput M, Ness BM, Lucas K, Zimney KJ. A multisystems approach to human movement after ACL reconstruction: the nervous system. Int J Sports Phys Ther 2022;17(1):47-59. doi:10.26603/001c.30020
7 Criss CR, Onate JA, Grooms DR. Neural activity for hip-knee control in those with anterior cruciate ligament reconstruction: a task-based functional connectivity analysis. Neurosci Lett 2020;730:134985. doi:10.1016/j.neulet.2020.134985
8. Grooms DR, Page SJ, Nichols-Larsen DS, Chaudhari AMW, White SE, Onate JA. Neuroplasticity associated with anterior Cruciate Ligament reconstruction. J Orthop Sports Phys Ther 2016;47(3):180-189. doi:10.2 519/jospt.2017.7003
9. Lepley AS, Grooms DR, Burland JP, Davi SM, Kinsella-Shaw JM, Lepley LK. Quadriceps muscle function following anterior cruciate ligament reconstruction: systemic differences in neural and morphological characteristics. Exp Brain Res 2019;237(5):1267-1278. doi:10.1007/s00221-019-054 99-x
10. Logothetis NK. What we can do and what we cannot do with fMRI. Nature. 2008;453(7197):869-878. doi:10.1038/nature06976
11. Logothetis NK, Pauls J, Augath M, Trinath T, Oeltermann A. Neurophysiological investigation of the basis of the fMRI signal. Nature 2001;412(6843):150-157 doi:10.1038/35084005
12. Silfies SP, Vendemia JMC, Beattie PF, Stewart JC, Jordon M. Changes in brain structure and activation may augment abnormal movement patterns: an emerging challenge in musculoskeletal rehabilitation. Pain Med 2017;18(11):2051-2054. do i:10.1093/pm/pnx190
13. Shanahan CJ, Hodges PW, Wrigley TV, Bennell KL, Farrell MJ. Organisation of the motor cortex differs between people with and without knee osteoarthritis. Arthritis Res Ther. 2015;17(1):164. doi:10.1186/s1307 5-015-0676-4
14. Ithurburn MP, Paterno MV, Thomas S, et al. Change in drop-landing mechanics over 2 years in young athletes after anterior cruciate ligament reconstruction. Am J Sports Med 2019;47(11):2608-2616. doi:10.1177/03635465198646 88
15. Slater LV, Hart JM, Kelly AR, Kuenze CM. Progressive changes in walking kinematics and kinetics after anterior cruciate ligament injury and reconstruction: a review and meta-Analysis. J Athl Train. 2017;52(9):847-860. doi:10.4085/1062-6050-5 2.6.06
16. Diekfuss JA, Grooms DR, Yuan W, et al. Does brain functional connectivity contribute to musculoskeletal injury? A preliminary prospective analysis of a neural biomarker of ACL injury risk. J Sci Med Sport. 2019;22(2):169-174. doi:10.1016/j.jsams.2 018.07.004
17 Diekfuss JA, Grooms DR, Nissen KS, et al. Alterations in knee sensorimotor brain functional connectivity contributes to ACL injury in male highschool football players: a prospective neuroimaging analysis. Braz J Phys Ther. 2020;24(5):415-423. doi:1 0.1016/j.bjpt.2019.07.004
18. Criss CR, Onate JA, Grooms DR. Neural activity for hip-knee control in those with anterior cruciate ligament reconstruction: a task-based functional connectivity analysis. Neurosci Lett. 2020;730:134985. doi:10.1016/j.neulet.2020.134985
19. Roper JA, Terza MJ, Tillman MD, Hass CJ. Adaptation strategies of individuals with anterior cruciate ligament reconstruction. Orthop J Sports Med 2016;4(2):232596711562761. doi:10.1177/23259 67115627611
20. Rocchi JE, Labanca L, Laudani L, Minganti C, Mariani PP, Macaluso A. Timing of muscle activation is altered during single-leg landing tasks after anterior cruciate ligament reconstruction at the time of return to sport. Clin J Sport Med 2020;30(6):e186-e193. doi:10.1097/jsm.00000000000 00659
21. Hart HF, Culvenor AG, Collins NJ, et al. Knee kinematics and joint moments during gait following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Br J Sports Med 2016;50(10):597-612. doi:10.1136/bjsports-2015-0947 97
22. Pairot-de-Fontenay B, Willy RW, Elias ARC, Mizner RL, Dubé MO, Roy JS. Running biomechanics in individuals with anterior cruciate ligament reconstruction: a systematic review Sports Med Auckl NZ. 2019;49(9):1411-1424. doi:10.1007/s40279-019-0
1120-x
23. Lepley AS, Kuenze CM. Hip and knee kinematics and kinetics during landing tasks after anterior cruciate ligament reconstruction: a systematic review and meta-Analysis. J Athl Train 2018;53(2):144-159. doi:10.4085/1062-6050-334-16
24. Marques JB, Paul DJ, Graham-Smith P, Read PJ. Change of direction assessment following anterior cruciate ligament reconstruction: a review of current practice and considerations to enhance practical application. Sports Med Auckl NZ 2020;50(1):55-72. d oi:10.1007/s40279-019-01189-4
25. Lipps DB, Wojtys EM, Ashton-Miller JA. Anterior cruciate ligament fatigue failures in knees subjected to repeated simulated pivot landings. Am J Sports Med. 2013;41(5):1058-1066. doi:10.1177/0363546513
477836
26. Chen J, Kim J, Shao W, et al. An anterior cruciate ligament failure mechanism. Am J Sports Med. 2019;47(9):2067-2076. doi:10.1177/036354651985445
27 Valeriani M, Restuccia D, Lazzaro VD, Franceschi F, Fabbriciani C, Tonali P. Central nervous system modifications in patients with lesion of the anterior cruciate ligament of the knee. Brain. 1996;119(5):1751-1762. doi:10.1093/brain/119.5.1751
28. Ochi M, Iwasa J, Uchio Y, Adachi N, Sumen Y The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 1999;81-B(5):902-906. doi:10.130 2/0301-620x.81b5.0810902
29. Zandiyeh P, Küpper JC, Mohtadi NGH, Goldsmith P, Ronsky JL. Effect of stochastic resonance on proprioception and kinesthesia in anterior cruciate ligament reconstructed patients. J Biomech. 2019;84:52-57 doi:10.1016/j.jbiomech.2018.12.018
30. Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability J Athl Train 2002;37(1):71-79.
31. Toth AJ, Harris LR, Zettel J, Bent LR. Vision can recalibrate the vestibular reafference signal used to re-establish postural equilibrium following a platform perturbation. Exp Brain Res 2017;235(2):407-414. doi:10.1007/s00221-016-4801-7
32. Grooms DR, Chaudhari A, Page SJ, Nichols-Larsen DS, Onate JA. Visual-Motor control of drop landing after anterior cruciate ligament reconstruction. J Athl Train 2018;53(5):486-496. doi:10.4085/1062-6050-17 8-16
33. McGregor KM, Sudhyadhom A, Nocera J, Seff A, Crosson B, Butler AJ. Reliability of negative BOLD in ipsilateral sensorimotor areas during unimanual task activity. Brain Imaging Behav. 2015;9(2):245-254. do i:10.1007/s11682-014-9302-3
34. Andriacchi TP, Alexander EJ, Toney MK, Dyrby C, Sum J. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. J Biomech Eng 1998;120(6):743-749. doi:10.1115/1.283 4888
35. Jamison ST, Pan X, Chaudhari AMW. Knee moments during run-to-cut maneuvers are associated with lateral trunk positioning. J Biomech. 2012;45(11):1881-1885. doi:10.1016/j.jbiomech.201 2.05.031
36. Jenkinson M, Bannister P, Brady M, Smith S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. NeuroImage. 2002;17(2):825-841. doi:10.100 6/nimg.2002.1132
37 Smith SM. Fast robust automated brain extraction. Hum Brain Mapp 2002;17(3):143-155. do i:10.1002/hbm.10062
38. Woolrich MW, Ripley BD, Brady M, Smith SM. Temporal autocorrelation in univariate linear modeling of fMRI Data. NeuroImage 2001;14(6):1370-1386. doi:10.1006/nimg.2001.0931
39. Smith SM, Jenkinson M, Woolrich MW, et al. Advances in functional and structural MR image analysis and implementation as FSL. NeuroImage 2004;23:S208-S219. doi:10.1016/j.neuroimage.2004.0 7.051
40. Pruim RHR, Mennes M, van Rooij D, Llera A, Buitelaar JK, Beckmann CF. ICA-AROMA: A robust ICA-based strategy for removing motion artifacts from fMRI data. NeuroImage 2015;112:267-277 doi:1 0.1016/j.neuroimage.2015.02.064
41. Pruim RHR, Mennes M, Buitelaar JK, Beckmann CF. Evaluation of ICA-AROMA and alternative strategies for motion artifact removal in resting state fMRI. NeuroImage 2015;112:278-287 doi:10.1016/j.n euroimage.2015.02.063
42. Bjornaraa J, Di Fabio RP. Knee kinematics following acl reconstruction in females; the effect of vision on performance during a cutting task. Int J Sports Phys Ther. 2011;6(4):271-284.
43. Yom JP, Simpson KJ, Arnett SW, Brown CN. The effects of a lateral in-flight perturbation on lower Extremity biomechanics during drop landings. J Appl Biomech 2014;30(5):655-662. doi:10.1123/jab.2013-0 331
44. King E, Richter C, Franklyn-Miller A, et al. Biomechanical but not timed performance asymmetries persist between limbs 9 months after ACL reconstruction during planned and unplanned change of direction. J Biomech 2018;81:93-103. doi:1 0.1016/j.jbiomech.2018.09.021
45. Leppänen M, Parkkari J, Vasankari T, et al. Change of direction biomechanics in a 180-degree pivot turn and the risk for noncontact knee injuries in youth basketball and floorball players. Am J Sports Med 2021;49(10):2651-2658. doi:10.1177/036354652
11026944
46. Arundale AJH, Silvers-Granelli HJ, Marmon A, Zarzycki R, Dix C, Snyder-Mackler L. Changes in biomechanical knee injury risk factors across two collegiate soccer seasons using the 11+ prevention program. Scand J Med Sci Sports 2018;28(12):2592-2603. doi:10.1111/sms.13278
47. Hanakawa T, Immisch I, Toma K, Dimyan MA, Van Gelderen P, Hallett M. Functional properties of brain areas associated with motor execution and imagery J Neurophysiol. 2003;89(2):989-1002. doi:10.1152/jn.00
132.2002
48. Ogiso T, Kobayashi K, Sugishita M. The precuneus in motor imagery: a magnetoencephalographic study. NeuroReport 2000;11(6):1345-1349. doi:10.1097/0000 1756-200004270-00039
49. Huang J, Reinders AATS, Wang Y, et al. Neural correlates of audiovisual sensory integration. Neuropsychology 2018;32(3):329-336. doi:10.1037/ne u0000393
50. Haar S, Donchin O, Dinstein I. Dissociating visual and motor directional selectivity using visuomotor adaptation. J Neurosci. 2015;35(17):6813-6821. doi:1 0.1523/jneurosci.0182-15.2015
51. Wenderoth N, Debaere F, Sunaert S, Swinnen SP The role of anterior cingulate cortex and precuneus in the coordination of motor behaviour Eur J Neurosci 2005;22(1):235-246. doi:10.1111/j.1460-956 8.2005.04176.x
52. Ageberg E, Fridén T Normalized motor function but impaired sensory function after unilateral nonreconstructed ACL injury: patients compared with uninjured controls. Knee Surg Sports Traumatol Arthrosc 2008;16(5):449-456. doi:10.1007/s00167-00 8-0499-9
53. Friden T, Roberts D, Movin T, Wredmark T Function after anterior cruciate ligament injuries: Influence of visual control and proprioception. Acta Orthop Scand 1998;69(6):590-594. doi:10.3109/17453 679808999261
54. Ageberg E, Roberts D, Holmström E, Fridén T. Balance in single-limb stance in patients with anterior cruciate ligament injury: relation to knee laxity, proprioception, muscle strength, and subjective function. Am J Sports Med 2005;33(10):1527-1537 doi:10.1177/03635465052749 34
55. Kakavas G, Malliaropoulos N, Pruna R, Traster D, Bikos G, Maffulli N. Neuroplasticity and Anterior Cruciate Ligament Injury. Indian J Orthop. 2020;54(3):275-280. doi:10.1007/s43465-020-00045-2
56. Gokeler A, Neuhaus D, Benjaminse A, Grooms DR, Baumeister J. Principles of motor learning to support neuro-plasticity after ACL injury: implications for optimizing performance and reducing risk of second ACL injury. Sports Med. 2019;49(6):853-865. doi:10.10 07/s40279-019-01058-0
57 Wohl TR, Criss CR, Grooms DR. Visual perturbation to enhance return to sport rehabilitation after anterior cruciate ligament injury: a clinical commentary Int J Sports Phys Ther 2021;16(2):552-564. doi:10.26603/001c.21251
58. Ballester R, Huertas F, Uji M, Bennett SJ. Stroboscopic vision and sustained attention during coincidence-anticipation. Sci Rep 2017;7(1). doi:10.1 038/s41598-017-18092-5
Keywords: Education, ACLR, Return To Play, Fear, psychological readiness https://doi.org/10.26603/001c.68141
While a lack of psychological preparedness and fear of movement may be linked with the anterior cruciate ligament (ACL) re-injury, these variables are rarely addressed throughout the therapy stages via educational sessions. Unfortunately, in terms of reducing fear, increasing function, and returning to play, no research has been done yet on the efficacy of adding organized educational sessions to the rehabilitation programs of soccer players post-ACL reconstruction (ACLR). Therefore, the study’s aim was to assess the feasibility and acceptability of adding organized educational sessions to the rehabilitation programs post-ACLR.
A feasibility randomized controlled trial (RCT) was conducted in a specialized sports rehabilitation center Participants post ACL reconstruction were randomized to either usual care with a structured educational session (intervention group) or usual care alone (control group). This feasibility study investigated three aspects: recruitment, intervention acceptability and randomization, and retention. The outcome measures included Tampa Scale of Kinesiophobia, ACL-Return to Sport after Injury, and International Knee Documentation Committee for knee function. Measurements were done at baseline and one week after the intervention.
All of the 36 players who were undergoing rehabilitation post-ACLR at the center at the time of the study were invited to participate in the study Thirty-five players (97.2%) agreed to participate in the study The participants responded to some questions about the acceptability of the intervention and randomization and most of them thought they were appropriate. 30 (85.7%) participants completed the follow-up questionnaires one week after the randomization.

This feasibility research found that adding a structured educational session to the rehabilitation program for soccer players after ACLR is feasible and acceptable. Full-scale RCTs with longer follow-ups and multiple locations are recommended.
Corresponding author:
ABDULLAH ALMUHAYA, PT, MSc.
Sport Rehabilitation center, PhysioTrio clinic, 2622 - marqan Al Yarmuk Dist. Unit Number : 2635
Telephone: 00966541407447
Email: abdullahalmuhaya@gmail.com
RIYADH-13251- 7956 Kingdom of Saudi Arabia
The anterior cruciate ligament (ACL) injury is among the most frequent injuries in competitive games.1 The prevalence of ACL injury in Saudi Arabia is calculated at 31 injuries per 100,000 people.2 ACL injuries account for around 53% of all knee injuries and affect 60% of young active participants.2
ACL injury is usually managed surgically by ACL reconstruction (ACLR) followed by rehabilitation. As the ACL rehabilitation program progresses, determining the appropriate return to play (RTP) time is difficult and somewhat complicated.3 The RTP has to be strongly individualized to train the knee for competition and prepare the whole body for the next step.4 For optimal neuromuscular patterning and biomechanics, the knee needs to be stable and solid.5 The athlete, however, needs to be psychologically prepared for RTP.6
Psychological issues frequently are at play during both the acute and recovery phases following surgery and might be present for many years after the ACLR.7 Although an assessment of psychological readiness following ACLR was developed to predict the time of RTP, this has not been formally integrated in the rehabilitation protocols and has not been studied adequately.8 Moreover, the fear of movement might also contribute to re-injury and has been shown to affect RTP.9 Indeed, a lower psychological readiness and a higher score of fear of movement might be among the most relevant factors associated with re-injury after ACL, yet they are still not consistently considered during the rehabilitation phases.10
Some authors have examined psychosocial intervention and its effectiveness in improving RTP outcomes after ACLR.8 A systematic review was done by Coronado et al.,8 looking for the role of psychosocial intervention with regard to improving patient-reported clinical outcomes after ACLR. Their review suggests that there is limited evidence on the reduction of the fear of re-injury. Besides, there is little evidence of the effectiveness of psychosocial approaches in the post-surgical phase to improve functional rehabilitation following ACLR.8 In order to apply a highquality experimental design in the conduct of research assessing the effectiveness of any novel intervention, first and foremost the assessment of the feasibility and acceptability of such investigation should be examined. Therefore, this study aimed to examine the feasibility and acceptability of adding a structured educational session to the rehabilitation program for soccer players post ACLR.
Ethical approval was obtained from the Research Ethics Committee of the Faculty of Rehabilitation and Health Science at Prince Sattam University in Kharj, Saudi Arabia (IRB: RHPT/021/006). The study was registered in the Research Registry (ResearchRegistry.com) with registration number 6634.
A feasibility double-blind randomized controlled study was conducted in collaboration with the sport rehabilitation center in Riyadh, from March 28, 2021 until April 6, 2021. Participants were randomly allocated to either the intervention group (Group A: usual care with a structured educational session) or the control group (Group B: usual ACL rehabilitation program).
Soccer players undergoing ACLR rehabilitation were invited to participate in the study All the players included had to satisfy the inclusion criteria.
Soccer players (professional and amateurs) were invited to participate if they satisfy these inclusion criteria:
• Aged between 18 and 45 with an ACL injury
• Have undergone ACLR (any graft type; patellar or hamstring) and were at any rehabilitation phase of ACLR rehabilitation.
• Were able and willing to give informed consent.
Players with any additional surgical procedures other than ACLR and/or undergoing prevention programs (discharge phase from rehab services) were excluded.
A convenience sample of soccer players was recruited from the center Potential participants were invited to participate. Information on the participant’s demographics (height, weight), dominant leg (as described by which side they preferred to kick a ball), average number of hours spent in a week for rehabilitation was collected. In addition, Tampa Scale of Kinesiophobia (TSK-17), ACL-Return to Sport after Injury (ACL-RSI), and International Knee Documentation Committee (IKDC) were completed electronically by all participants using google forms (https://docs.google.com/forms).
To minimize bias, the study was double-blinded. Thus, the outcome assessor and the clinicians involved in the rehabilitation had no information on group assignment.
Each player had an equal chance of being assigned to either one of the study groups. The allocation was concealed, and the sequentially generated numbers were placed into opaque sealed envelopes.
After randomization, participants in the control group continued their usual care in the same clinic. After one week, they were asked to answer the final survey.
Participants in intervention group received the same rehabilitation protocol as the control group, and attended a virtual interactive structured educational session via ZOOM platform. The educational session included a series of topics related to the surgery and the rehabilitation process as well as simple answers to some frequently asked questions among players undergoing ACLR rehabilitation.
The structured educational topics were prepared and supplemented with graphs and pictures to ensure the clarity and understandability of the materials. The educational session materials were based on recent evidence, available literature, and advice from five expert sport physiotherapists.
After one week, the participants were asked to answer the final follow-up survey. In addition, they were asked to answer whether “the intervention and the randomization were acceptable”, with optional choice to add more details using open-ended questions (by both players and clinicians) regarding the acceptability of the intervention and randomization.
The sample size was based on the number of patients with ACLR attending the center In the three months prior to recruitment, 45 ACLR players visited the center The percentage of consenting eligible players was expected to be 50%, resulting in eight players randomized per month. This translated into an expected total of at least 24 players over the proposed three months of recruitment. Therefore, this feasibility study aimed to recruit at least 24 participants.
The TSK was originally employed to evaluate the fear of movement in patients with low back pain. It has also been used to assess fear of re-injury and pain in patients with different conditions, such as ACL injuries.11,12 It consists of a self-report checklist of seventeen domains using a Likert scale of four items. Total values from 17 to 68 indicate a high degree of kinesiophobia. The cut-off score has also been established by Vlaeyen et al.13 The Arabic version of the TSK showed high test-retest reliability between repeated measurements. It demonstrated an intraclass correlation coefficient (ICC) of 0.86 and a Cronbach alpha value of 0.87 for low back pain patients.14 For post-ACLR patients it showed an ICC of 0.93 and a Cronbach alpha value of 0.90, which represent strong internal consistency.15
The ACL-RSI scale was developed to assess a number of psychological factors associated with return to sports, such as fear and frustration, confidence, and self-efficacy.9 Twelve elements are tested on a scale of zero to 100, measuring three psychological frameworks: emotion, confidence, and risk perception.9 Higher ratings reflect a more optimistic view on RTP, 56 or more reflect the ability to RTP, and 76 and more indicate a return to maximum performance.9 The test-retest reliability of the Arabic ACL-RSI was high (ICC = 0.93).
IKDC consists of 18 questions in the regions of symptoms, working during everyday life, current function of the knee, and involvement in work and sport.16 The Arabic IKDC showed an excellent test-retest reliability between repeated measurements, as the ICC in patients post ACLR was 0.95.15
• Recruitment number:
◦ Set goal: 24 players
• Acceptability rate
◦ Set goal: at least 65% of eligible participants consent to participate in the trial.
◦ In addition, if most participants and clinicians reported that intervention and randomization were acceptable (open-ended questions).
• Retention rate
◦ Set goal: ≥ 80% at the follow-up survey
The mean, Standard deviation (SD), absolute and relative frequency, were used to describe the data.
Chi-square test was used to examine the significant difference between the two groups.
There were 36 players rehabilitating post-ACLR at the center at the time of the study They were screened and all 36 (100%) satisfied the inclusion criteria. One participant (2.7%) of these 36 did not wish to participate in the study, providing the reason he did not have time to participate. The remaining 35 (97.2%) consented to participate and agreed to be randomized. Of these, 30 (85.7%) completed the study (the one-week follow-up).
After randomization, the 35 participants were randomly assigned to one of the two groups: the intervention group (n=18 at baseline, with two losses to follow up; n=16) and
the control (n=17 at baseline, with three losses to follow up; n=14).
The intervention group received the online educational session (either live or recorded), with eleven (61.1%) of the intervention group receiving the educational session synchronously at the same time that the instructor performed it. The other seven (38.9%) could not attend the live educational session, therefore they watched the recorded lecture later on the same day The latter group was instructed to ask and comment on any information needed. The progress of the RCT phases is depicted in Figure 1 (Flow Diagram).
The 35 participants included were ACLR male players with a mean (SD) age of 26 years (±6), an average mass of 78.6 kg (±13.8), and an average BMI of 25.8 (±3.8). Of these, 27 (77.1%) had suffered from an ACL injury in the right knee, and eight (22.8%) in the left knee. Additionally, 14 (40%) had received patellar tendon graft reconstruction for the ACL, ten (28.6%) had received hamstring tendon grafts, three (8.5%) had received allografts, and eight (22.8%) were unsure about the graft type.
Participants in both groups had similar physical characteristics (p>0.05). The intervention group had more patellar tendon-bone grafts than the control group (72.2% to 5.88%, respectively; X2 [2, n=35]=13, p= 0.0002).
The average time to rehabilitation start post ACLR was 3.1 days, ranging from zero to 14 days, with six (17.1%)
starting their rehab immediately after the surgery Table 1 presents the demographic and clinical characteristics of the participants in both the intervention and control groups.
In this study, the feasibility indicators were:
RECRUITMENT NUMBER
• Set goal: 24 players
Overall, 36 players were screened over the one-day recruitment period. Of these, 36 satisfied the inclusion criteria. All the participants completed the questionnaire, and there was no missing data. The questionnaire completion typically took five to fifteen minutes, and according to the participants, none of the items were said to be complicated.
• Set goal: at least 65% of eligible participants consent to participate in the trial. In addition, most of the participants and clinicians report acceptability of the intervention and randomization.
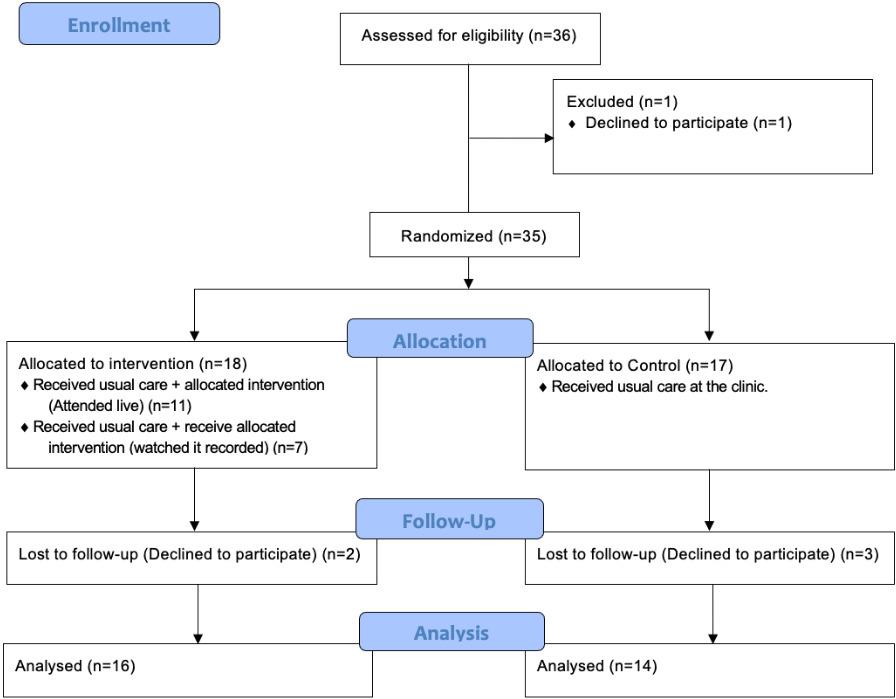
One participant (2.7%) did not wish to participate in the study while 35 (97.2%) agreed to join the trial.
All the participants responded to the yes/no questions about the acceptability of the intervention and randomiza-
Figure 1. Flow Diagramtion, which were found to be acceptable by 100% of the participants. However, only two players and one clinician agreed to give a more detailed statement with regard to the intervention.
The participants’ responses suggest that an educational session at the beginning of the rehab is helpful regarding the awareness of the process; additionally, it might help players to overcome fear, thus enhancing psychological readiness post-ACLR.
Among the responses collected, we report the following representative ones:
• “If I had received such an intervention from the beginning, it would have helped me understand more about my situation and have a reasonable expectation regarding RTP timing and readiness.” A23
• “This is a unique way of helping ACLR patients with their understanding of the plan of treatment; my clini-
cian had discussed the information provided in the lecture with me before, but not in an organized and structured way like the one we had in the lecture. I think it will be a great addition to the rehabilitation plan. Still, I think it will be much better if it provided onsite, rather than online, so it will be easier to interact with the lecturer and participate.” A35
One of the clinicians also responded as follows:
• “The lecture is a great way to help the patients wonder and answer most of their questions. However, I think it will be of great value for the patients to have it at the beginning of their rehab and also to have a repeated section addressing their current phase, at the end of each phase.” Clinician 1
In the follow-up (one week after the randomization), 30 (85.7%) participants completed the questionnaires, and five (14.3%) declined to participate in the reassessment, two reported they were not interested to participate in the follow up, and three reported that they did not have time to answer the survey
The baseline measurements showed similar levels of fear of re-injury in both groups based on TSK-17 scores (mean of 41.7 for the intervention and 41.8 for the control). However, ACL-RSI was slightly higher in the intervention group at baseline (mean of 65.3; SD ± 23.7) compared to the control (63.7; SD ± 20.4). Similarly, this was also the case with the IKDC measure (73.2; SD ± 14.3 for the intervention compared to 68.7; SD ± 15.6 for the control). Table 2 shows the outcome measurement scores of the participants in both the intervention and control groups.
In the follow-up measurement, the intervention group shows improvement from the educational session after one week with a lower TSK-17 mean score ( =37.6; SD ± 4.8), and an improvement in readiness as shown by an increased ACL-RSI mean score ( =83.4; SD ± 15.8). However, there was no change in knee function as measured by the IKDC.
This study indicates that conducting an RCT examining the effectiveness of adding a structured educational session to the rehabilitation program for soccer players post ACLR is both feasible and acceptable. This was based on achieving the recruitment number, acceptability, and retention rate indicators.
Patient education is an essential part of physical therapy intervention. It is widely used in most musculoskeletal conditions, such as back pain,17 and shoulder pain.18 In addition, patient education is considered to have some psychological aspects when treating the patient.19–21 Besides, no known adverse events are associated with education in physical therapy interventions. All of this makes education an important constituent to be included in other parts of the intervention.
In the intervention and control groups, the ACLR players were healthy, active men undergoing rehabilitation postACLR. Participants in both groups were mostly similar in terms of age, weight, height, BMI, and injured leg. However, the results showed more patellar tendon-bone grafts in the intervention group than in the control group (72.2%:5.88%). Nevertheless, the results regarding the strength outcomes and patient experience were similar after patellar tendon-bone grafts or hamstring autograft bone, and both exceeded the strength outcome following other types of surgeries for ACLR.22,23 Additionally, the question on the surgery type was self-reported; thus, it could be affected by recall bias. Indeed, almost half of the
participants in the control group reported they did not know or could not remember the surgery type. Therefore, it is recommended that surgery type data be gathered in future studies directly from the medical/surgical record for each player
The study’s main goal was to examine the feasibility of conducting an RCT to examine the effectiveness of adding a structured educational session to the ACLR rehabilitation.
Several indicators were set in this study to assess the feasibility of conducting a full-scale RCT
The initial objective was to recruit at least 24 players with ACLR. This was calculated based on 45 ACLR players having visited the center in the previous three months (August to October 2020). The expected percentage of consenting eligible players was 50%, suggesting eight players could be randomized per month. This would result in at least 24 players over the three months, as proposed for the recruitment. This study was able to recruit and randomize up to 35 participants. This was possibly due to the fact that recruitment took place in a major private center specialized in rehabilitating such cases.
The second index addressed in this feasibility study was the acceptability of the intervention and randomization. The goal was to have at least 65% of the eligible soccer players willing to participate, in addition to the acceptability of the study by most of the participating players and clinicians involved. Only one player (2.7%) declined to participate in the study, thus ending up with 35 (97.2%) willing to participate in the study and to be randomized.
Furthermore, all participants responded they found both the intervention and the randomization as acceptable. In addition, the responses to the open-ended questions suggest that adding a structured educational session at the beginning and after each phase is also thought to enhance the awareness of the player about the rehabilitation process. Raising rehabilitation process awareness and covering most of the rehab phases is expected to help with the players’ fear of re-injury and their psychological readiness post ACLR.
Further, this study shows that it might be helpful to deliver the educational part through online recorded educational sessions, since 38.4% of the study participants in the intervention group could not attend the live online educational session and they had to watch it recorded. Sending the recorded lecture to be watched by every participant in the experimental group will help in standardizing the intervention and examining the effect. Despite some responses indicated that an onsite lecture would help in terms of better communication and interaction, future studies could include a special live event to discuss the educational session after watching it recorded. In the end, it is still an acceptable way to go further with a full RCT, and it should be remembered that the inclusion of patient satisfaction indicators is encouraged into the complete RCT, if this is to be conducted.
The third dimension addressed by this feasibility study was follow-up. In the study, 80% of the included players were maintained in the follow-up until the final assessment. The loss of follow-up in this study was 14.3% (n=5).
Adding A Structured Educational Session to the Rehabilitation Program of Soccer Players Following Anterior Cruciate.
A follow-up loss of 5% or less is typical.24 Conversely, a loss of 20% or more suggests that researchers should be worried about the risk of bias.25 Since 14.3% is closer to 20% we should be concerned and this should be looked at in future studies and intention to treat analysis may be considered to avoid any potential bias.
The study’s outcome measure results suggest that adding a structured educational session to the rehabilitation program for soccer players post ACLR might help reduce the fear of re-injury (using the TSK-17) and improve the level of psychological readiness (using the ACL-RSI) for players one week following the intervention. According to Ardern et al.,10 lower psychological readiness and a higher fear of movement score might be among the most important factors associated with re-injury Yet, they are still disregarded during the rehabilitation process.
The results also showed no change in knee function in both groups one week after baseline as assessed by IKDC in patients post ACLR. This might be due to the short study’s follow-up and more theoretical intervention, with no change in the exercise program provided to the participants. Other studies used and observed an IKDC difference for knee function, when reassessed at a follow-up of more than six weeks.26,27
In conclusion, the main results of this study provided support for the feasibility of a novel RCT examining the addition of a structured educational session to the rehabilitation plan for players post-ACLR. In addition, multiple factors emerged from the players’ and clinicians’ responses to the open-ended questions that could improve the efficiency of future studies.
A variety of factors limited the findings in this study and need to be taken into account when interpreting the results.
The significant differences observed in the two outcomes (TSK-17 and ACL-RSI) are questionable since this study was not powered to examine the significance of this difference. It is important to acknowledge the limited sample size (less than 35 per group is not ideal) when thinking of such difference in the outcome measures.28 Moreover, some factors may introduce confounding bias related to the participants’ characteristics and surgical type. It was also surprising that seven of the participants from the control group reported not knowing or remembering their surgi-
cal procedure, while none from the intervention group reported this. However, after looking back at the data collection procedure, we found a standard procedure regardless of the group assignment and therefore this can be only attributed to random error In future studies, this can be mitigated using stratified sampling techniques and collecting information on the type of surgery directly from the medical/surgical files of the participants. Moreover, the relatively short follow-up of the study might have affected its results.
While the intervention was a live online version, more than a third of the target participants could not watch it synchronously, but had to watch it recorded; this may have impacted the standardization of the educational session.
Furthermore, using only one center to recruit the study sample is inherently linked with selection bias. A larger trial with multiple recruitment centers and on a larger sample would ensure more diverse groups and more robust results.
The results of this study indicate that conducting an RCT examining the effectiveness of adding a structured educational session to the rehabilitation program of soccer players post ACLR is both feasible and acceptable. However, several factors need to be considered before conducting a full-scale RCT, such as, longer follow-up time, multiple recruiting centers, larger sample size, and stratified sampling techniques to ensure similar groups. Finally, using recorded educational sessions would provide more standardized intervention, which is also deemed to be preferable.
The authors have no conflict of interest to declare.
We would like to thank the Researchers Supporting Project number (RSPD2023R647), King Saud University, Riyadh, Saudi Arabia, for supporting this research.
Submitted: March 01, 2022 CST, Accepted: November 30, 2022
CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Arundale AJH, Bizzini M, Giordano A, et al. Exercise-based knee and anterior cruciate ligament injury prevention. J Orthop Sports Phys Ther. 2018;48(9):A1-A42. doi:10.2519/jospt.2018.0303
2. Alshewaier S. Developing a Standardised Preoperative Physiotherapy Programme to Improve the Outcomes of Patients Undergoing Anterior Cruciate Ligament Reconstruction in Riyadh (KSA) PhD thesis. 2016.
3. Ardern CL. Anterior cruciate ligament reconstruction—not exactly a one-way ticket back to the preinjury level: A review of contextual factors affecting return to sport after surgery Sports Health 2015;7(3):224-230. doi:10.1177/1941738115578131
4. Burgi CR, Peters S, Ardern CL, et al. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review Br J Sports Med. 2019;53(18):1154-1161. doi:10.1136/bjsp orts-2018-099982
5. Rambaud AJM, Ardern CL, Thoreux P, Regnaux JP, Edouard P. Criteria for return to running after anterior cruciate ligament reconstruction: A scoping review Br J Sports Med 2018;52(22):1437-1444. doi:1 0.1136/bjsports-2017-098602
6. Webster KE, Hewett TE. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med. 2019;49(6):917-929. doi:10.1007/s40279-019-01093-x
7 Tripp DA, Stanish W, Ebel-Lam A, Brewer BW, Birchard J. Fear of reinjury, negative affect, and catastrophizing predicting return to sport in recreational athletes with anterior cruciate ligament injuries at 1 year postsurgery. Sport Exerc Perf Psychol 2011;1(S):38-48. doi:10.1037/2157-3905.1.s.3 8
8. Coronado RA, Bird ML, Van Hoy EE, Huston LJ, Spindler KP, Archer KR. Do psychosocial interventions improve rehabilitation outcomes after anterior cruciate ligament reconstruction? A systematic review Clin Rehabil 2018;32(3):287-298. d oi:10.1177/0269215517728562
9. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport 2008;9(1):9-15. doi:10.1016/j.ptsp.20
07.09.003
10. Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med 2014;48(22):1613-1619. doi:10.1136/bjsports-2014-0 93842
11. Chmielewski TL, Zeppieri G Jr, Lentz TA, et al. Longitudinal changes in psychosocial factors and their association with knee pain and function after anterior cruciate ligament reconstruction. Phys Ther 2011;91(9):1355-1366. doi:10.2522/ptj.20100277
12. Lentz TA, Zeppieri G Jr, George SZ, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of re-injury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med 2015;43(2):345-353. doi:10.1177/0363546514559707
13. Vlaeyen JWS, Kole-Snijders AMJ, Boeren RGB, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain 1995;62(3):363-372. doi:10.1016/0304-3959(9 4)00279-n
14. Yangui N, Yahia A, Ghroubi S, Habib Elleuch M. Translation and validation of the Tampa Scale of Kinesiophobia Arabic version in chronic low back pain. Ann Phys Rehabil Med. 2017;60:e20. doi:10.101 6/j.rehab.2017.07.145
15. Almalki H. Functional Recovery at Discharge from Rehabilitation Following Anterior Cruciate Ligament Reconstruction PhD thesis. 2019.
16. Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee subjective knee evaluation form: Normative data. Am J Sports Med 2006;34(1):128-135. doi:10.1177/0363546505280214
17. Furlong B, Aubrey-Bassler K, Etchegary H, et al. Patient education materials for non-specific low back pain and sciatica: a protocol for a systematic review and meta-analysis. BMJ Open. 2020;10(9):e039530. d oi:10.1136/bmjopen-2020-039530
18. Burke K, Ellrodt AS, Levine J, et al. Exploring the use of educational material about shoulder dysfunction: A quality improvement project in people with Amyotrophic Lateral Sclerosis. Am J Phys Med Rehabil. 2018;97(5):379-382. doi:10.1097/phm.00000
00000000885
19. Claus D, Coudeyre E, Chazal J, Irthum B, Mulliez A, Givron P. An evidence-based information booklet helps reduce fear-avoidance beliefs after first-time discectomy for disc prolapse. Ann Phys Rehabil Med. 2017;60(2):68-73. doi:10.1016/j.rehab.2015.10.008
20. de Jong JR, Vlaeyen JWS, Onghena P, Goossens MEJB, Geilen M, Mulder H. Fear of movement/(re)injury in chronic low back pain: Education or exposure in vivo as mediator to fear reduction? Clin J Pain. 2005;21(1):9-17. doi:10.1097/0 0002508-200501000-00002
21. Guck TP, Burke RV, Rainville C, Hill-Taylor D, Wallace DP A brief primary care intervention to reduce fear of movement in chronic low back pain patients. Translat Behav Med 2015;5(1):113-121. do i:10.1007/s13142-014-0292-x
22. Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: A prospective study of hamstring and patellar tendon grafts. Am J Sports Med 2012;40(3):595-605. doi:10.1177/0363546511430375
23. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database of Systematic Reviews. 2011;9. do i:10.1002/14651858.cd005960.pub2
24. Fergusson D, Aaron SD, Guyatt G, Hébert P Postrandomisation exclusions: The intention to treat principle and excluding patients from analysis. Br Medical J. 2002;325(7365):652-654. doi:10.1136/bmj.3 25.7365.652
25. Dumville JC, Torgerson DJ, Hewitt CE. Reporting attrition in randomised controlled trials. Br Medical J 2006;332(7547):969-971. doi:10.1136/bmj.332.7547.9 69
26. Bregenhof B, Jørgensen U, Aagaard P, et al. The effect of targeted exercise on knee-muscle function in patients with persistent hamstring deficiency following ACL reconstruction – study protocol for a randomized controlled trial. Trials. 2018;19(1):75. do i:10.1186/s13063-018-2448-3
27 Maddison R, Prapavessis H, Clatworthy M. Modeling and rehabilitation following anterior cruciate ligament reconstruction. Ann Behav Med 2006;31(1):89-98. doi:10.1207/s15324796abm3101_13
28. Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: A simulation study. Trials 2014;15(1):264. doi:10.1186/1745-6215-15-264
Download: https://ijspt.scholasticahq.com/article/68141-adding-a-structured-educational-session-to-therehabilitation-program-of-soccer-players-following-anterior-cruciate-ligament-reconstruction-a-feasibi/attachment/ 135714.docx?auth_token=_NHyDLWzr4z3vMDr062d
Download: https://ijspt.scholasticahq.com/article/68141-adding-a-structured-educational-session-to-therehabilitation-program-of-soccer-players-following-anterior-cruciate-ligament-reconstruction-a-feasibi/attachment/ 135991.docx?auth_token=_NHyDLWzr4z3vMDr062d
Keywords:
 knee injury, fear avoidance, kinesiophobia, pain catastrophizing
knee injury, fear avoidance, kinesiophobia, pain catastrophizing
https://doi.org/10.26603/001c.68045
Psychological barriers due to anterior knee pain (AKP) and anterior cruciate ligament reconstruction (ACLR) may have a direct impact on an individual’s return to physical activity. A comprehensive understanding of these psychological barriers in individuals with AKP and ACLR may help clinicians to develop and implement better treatment strategies to address deficits that may exist in these individuals.
The primary purpose of this study was to evaluate fear-avoidance, kinesiophobia, and pain catastrophizing in individuals with AKP and ACLR compared with healthy individuals. The secondary purpose was to directly compare psychological characteristics between the AKP and ACLR groups. It was hypothesized that 1) individuals with AKP and ACLR would self-report worse psychosocial function than healthy individuals and 2) the extent of the psychosocial impairments between the two knee pathologies would be similar.
Eighty-three participants (28 AKP, 26 ACLR, and 29 healthy individuals) were analyzed in this study. Fear avoidance belief questionnaire (FABQ) with the physical activity (FABQ-PA) and sport (FABQ-S) subscales, Tampa scale of Kinesiophobia (TSK-11) and pain catastrophizing scale (PCS) assessed psychological characteristics. Kruskal-Wallis tests were used to compare the FABQ-PA, FABQ-S, TSK-11, and PCS scores across the three groups. Mann-Whitney U tests were performed to determine where group differences occurred. Effect sizes (ES) were calculated with the Mann-Whitney U z-score divided by the square root of the sample size.
Individuals with AKP or ACLR had significantly worse psychological barriers compared to the healthy individuals for all questionnaires (FABQ-PA, FABQ-S, TSK-11, and PCS) (p<0.001, ES>0.86). There were no differences between the AKP and ACLR groups (p≥0.67), with a medium ES (-0.33) in the FABQ-S between AKP and ACLR groups.
Corresponding author:
Emma Zuk, MS, ATC
2095 Hillside Rd, Unit 1110
Storrs, CT 06269
Emma.Zuk@uconn.edu
Conclusion
Greater psychological scores indicate impaired psychological readiness to perform physical activity Clinicians should be aware of fear-related beliefs following knee-related injuries and are encouraged to measure psychological factors during the rehabilitation process.
2
The knee is the most commonly injured joint in both male and female adults, accounting for 19% to 23% of all orthopedic injuries.1 Two of the most frequent musculoskeletal knee conditions are anterior knee pain (AKP), which incorporates patellofemoral pain, patellar subluxation, and patella dislocations, and anterior cruciate ligament injuries (ACL).2–4 AKP has an annual prevalence of 22.7%5 while over 250,000 ACL injuries occur each year.6 AKP is a multifactorial pathology linked to increase stress on the patellofemoral joint, resulting in pain,7 and recurrent or chronic symptoms.3 ACL injuries are often the result of direct or indirect trauma to the knee, often leading to surgical intervention (e.g., reconstruction) to restore stability and function of the knee.8 While the mechanism of injury between conditions differs, both present with similar clinical impairments. Individuals with AKP and ACL reconstruction (ACLR) often present with decreased self-reported function,7 lower extremity muscle weakness,7 reduced physical activity level7,9,10 and poor health-related quality of life.11,12 Additionally, both AKP13 and ACLR14 are suggested to result in increased risk for the development of knee osteoarthritis.
Although therapeutic interventions and surgical procedures aim to enhance physical function in individuals with AKP and ACLR, many individuals still report long-term disability.8,15 Restoration of functional outcomes and patientreported satisfaction is one of the primary criteria for medical clearance for return to daily activities following knee pathologies.16–18 Unfortunately, many patients exhibit psychological impairments during their rehabilitation that can act as barriers to successful recovery 19 Both individuals with AKP and ACLR present with injury-related fear-avoidance, kinesiophobia, and pain catastrophizing.20–22 Greater psychological barriers in both patient populations has been associated with inability to resume pre-injury levels of sport, decreased physical activity engagement, and decreased health- or knee-related quality of life.8,23 Fearavoidance is based off a psychiatric model that describes how individuals develop and maintain musculoskeletal pain as a result of avoiding behavior based on past pain experiences.24 Kinesiophobia is generally defined as fear of movement due to the pain experience25 whereas pain catastrophizing is depicted as magnifying pain and feeling helpless in the face of pain.26
Self-reported questionnaires to quantify psychological barriers have emerged as an important component for AKP11 and ACLR27 rehabilitation. These tools are frequently integrated into return to play testing with psy-
chological barriers being predictive of athletes success in returning to sport17,28 and regaining optimal physical function.29 In recent literature, the decision to return to sport after ACLR has been strongly influenced by psychosocial factors.30 Additionally, elevated fear-avoidance beliefs and fear of reinjury are associated with increased risk of injury, impaired return to prior levels of performance, and reduced physical activity level.9,31–34 Over time psychological barriers and physical performance improve; however, the improvements do not exceed clinical thresholds and still present years following injury and treatment.35–37 This reinforces that physical performance should not be the lone post-operative outcome and that consideration of psychological consequences in those with knee pathologies should also be accounted for 30 Psychological characteristics amongst AKP and ACLR patient populations have been reported separately; however, it is unknown if similar psychological responses exist between two common knee conditions.
A comprehensive understanding of the psychological features in individuals with AKP and ACLR would help clinicians to develop and implement better treatment strategies to address deficits that may exist in these individuals. Therefore, the primary purpose of this study was to evaluate fear-avoidance, kinesiophobia, and pain catastrophizing in individuals with AKP and ACLR compared with healthy individuals. The secondary purpose was to directly compare psychological characteristics between the AKP and ACLR groups. We hypothesized that 1) individuals with AKP and ACLR would self-report worse psychosocial function than healthy individuals and 2) the extent of the psychosocial impairments between the two knee pathologies would be similar
A survey was used to examine the influence of AKP and ACLR on fear-avoidance beliefs, kinesiophobia, and pain catastrophizing. Independent variables include each group: AKP, ACLR, and a no injury history group. Dependent variables include the fear-avoidance belief questionnaire (FABQ) with the physical activity (FABQ-PA) and sport (FABQ-S) subscales, Tampa scale of Kinesiophobia (TSK-11) and pain catastrophizing scale (PCS) scores. The reporting of the study adhered to the CHERRIES guidelines recommendations.38 The study was approved by each university’s Institutional Review Board (University of Connecticut and University of Toledo) and all participants provided in-
formed consent via an online consent process. Participants were provided information regarding study purpose, estimated time for study completion, management of identifiable data, and contact information for the research team. Cookies or timestamps were not used in this study but duplicate IP addresses were extracted.
Data were collected over an eight-month period from two large public universities (one in the Midwest and one in the Northeast) from college-aged students as part of a larger study evaluating musculoskeletal injury history Recruitment for the study was conducted electronically via email, social media platforms, and research announcements at each university A total of 502 participants between the two universities completed a survey, 83 participants met the purpose of this study and were included in this analysis.
Participants completed a self-reported injury history questionnaire. The injury history questionnaire was derived from previously reported measures and included 15 categories of sports-related injuries.39 Participants were asked to self-report if they had previously sustained any musculoskeletal conditions The questionnaire also collected basic demographic information (e.g., height, weight) and if participants were currently experiencing an injury that was resulting in pain. Participants who reported a previous musculoskeletal condition were also asked to indicate additional demographic information about the type and severity of injury, whether surgery was required, the number of times the injury occurred, and time since injury/ surgery All participants, regardless of injury status, then completed three previously validated patient reported outcome metrics developed to capture psychological function after musculoskeletal injury. The included the FABQ-PA, FABQ-S, TSK-11, PCS in an online data management system (Qualtrics). We adhered to previously described methods that no time restrictions were instituted for either AKP or ACLR history and included any self-reported knee injuries.40 Finally, the last question of the survey inquired about fear surrounding the COVID-19 pandemic.
The FABQ was developed as a 16-item dimension specific questionnaire that originally measured fear-avoidance beliefs related to physical activity and work in individuals with low back pain.41 A modified FABQ was utilized that replaced “low back” with “knee” in order to be joint specific in addition to modifying the work subscale to the sport subscale.18 The physical activity subscale (FABQ-PA) includes six questions that are scored out of 30 points while the sport subscale (FABQ-S) includes 10 questions that are scored out of 60 points. Greater scores reflect increased fear-avoidance beliefs related to physical activity and sport. The modified FABQ physical activity and sport subscales have acceptable internal consistency in individuals with a history of knee injuries.42
The TSK-11 is an 11-item dimension specific questionnaire that is used to measure kinesiophobia. The TSK-11 ranges from 11 to 44, with greater scores reflecting greater fear of movement and reinjury due to movement. The TSK-11 has demonstrated acceptable internal consistency
(0.79) and reliability (0.81) in a chronic low back pain population.43 The TSK-11 has also been reported across various knee injury populations, including ACLR.44
Pain catastrophizing was measured with the PCS, which is a 13-item dimension specific questionnaire. The PCS ranges from 0 to 52, with greater scores representing greater catastrophic pain. The PCS has good to excellent test-retest reliability (ICC=0.88-.90), adequate validity (0.40-0.42) and excellent internal consistency (0.92).45 A total score above 30 indicates clinically relevant level of catastrophizing.
Participants were extracted based off who previously reported history of either AKP and/or ACLR and then extracted a third group of individuals without a history of musculoskeletal injury AKP was defined as patellofemoral pain, history of patella subluxation / dislocation, or patella maltracking, but did not include patellar or quadriceps tendinopathy. Participant responses were excluded for missing data of the health history form or questionnaires. A total of 83 participants were included: 28 participants (13 males and 15 females) with a history of AKP, 26 participants (11 males and 15 females) with a history of ACLR and 29 participants (11 males and 18 females) without a history of musculoskeletal injury (i.e., healthy individuals).
SPSS software (V.22; IBM Corporation, Armonk, NY) was used for all statistical analyses. We assessed normality of data with a Kolmogorov-Smirnov test, which identified non-normally distributed data. Separate Kruskal-Wallis tests were used to compare the FABQ-PA, FABQ-S, TSK-11, and PCS scores across the three groups (AKP, ACLR, Healthy). Mann-Whitney U tests were performed to determine where group differences occurred. We calculated nonparametric effect sizes to determine the magnitude of difference between groups for all questionnaires. Effect sizes were calculated with the Mann-Whitney U z-score divided by the square root of the group size. Effect sizes were interpreted as small (|0.10-0.29|). medium (|0.30-0.49|), and large (|≥0.50|).46 Descriptive statistics for all four questionnaires (FABQ-PA, FABQ-S, TSK-11, and PCS) were reported as medians, along with 25% and 75% interquartile ranges. Alpha for all analyses was set a priori as p≤0.05 meaning there is a 5% chance that the significant findings were due to error
Descriptive demographics between groups are reported in Table 1, and there were no differences in age or sex across the three groups, p=0.72. The AKP group included 15 cases of patellofemoral pain, 10 cases with history of patella subluxation (n=7) or dislocation (n=3) and one case of patella maltracking. There was a significant interaction effect between injury history and questionnaire (FABQ-PA, FABQ-S, TSK-11, and PCS) interaction effect present, p<0.001 (Table 2). Participants with a history of AKP or ACLR had significantly worse scores compared to the healthy group for all
*7 cases of AKP (all self-reported as patellofemoral pain, reported they were not pain free)
* Kruskal-Wallis test demonstrated significant differences, p<.05
FABQ-PA: Fear-Avoidance Belief Questionnaire-Physical Activity, FABQ-S: Fear-Avoidance Belief Questionnaire-Sport, TSK: Tampa Scale of Kinesiophobia, PCS: Pain Catastrophizing Scale, AKP: Anterior Knee Pain, ACLR: Anterior Cruciate Ligament Reconstruction, Z: Z-Score, ES: Effect Size
questionnaires; however, there were no differences between the AKP or ACLR groups (Figure 1).
There were large magnitude effect sizes with the healthy versus AKP (ES= -1.20 to -0.94) and healthy versus ACLR (ES= -1.06 to -0.86) group comparisons. There was a medium effect size (ES= -0.33) in the FABQ-S between the AKP and ACLR groups, but small effect sizes for the remaining questionnaires (ES= -0.27 to -0.08).
College-aged individuals with a history of AKP or ACLR report elevated fear-avoidance, kinesiophobia, and pain catastrophizing compared to healthy individuals. There were no statistical or clinically meaningful differences in fearavoidance, kinesiophobia, or pain catastrophizing between AKP and ACLR groups; however, there was a medium effect
that individuals with AKP had a greater FABQ-S score compared to the individuals with ACLR.
AKP and ACLR groups exhibited greater scores in the FABQ-PA, FABQ-S, TSK-11 and PCS compared to the healthy group, which is consistent with previous literature. The findings emphasize the importance of assessing psychological factors in patients with knee pathologies, as various constructs may be present throughout the rehabilitation process.28,47 Both the AKP and ACLR groups had elevated scores across the four questionnaires but did not differ statistically between groups; however, there were small-to-moderate clinical differences in the FABQ-PA, FABQ-S and PCS scores.
There was a wide range in scores across the AKP and ACLR groups for all four psychological scales (Figure 1). Clinical thresholds have been established for three of the four included questionnaires to identify individuals with elevated fear-avoidance beliefs, kinesiophobia, and pain cat-
astrophizing. A threshold score of 15 on the FABQ-PA47 is used to identify individuals with elevated fear-avoidance beliefs while a score of 30 on the PSC26 quantifies pain catastrophizing. The TSK-11 has been divided into four subgroups: minimal (≤22), low (23-28), moderate (29-35) and high (≥36). Fourteen individuals (50%) with AKP exceeding the threshold for having elevated fear-avoidance beliefs, but more interestingly, no individual with AKP scored below a 9 on the FABQ-PA (Figure 1). This differs from the ACLR group who did not exceed threshold values fearavoidance beliefs on the physical activity scale, suggesting that fear-avoidance beliefs might be more common in individuals with AKP. The fear-avoidance model may help explain these findings, as the recurring chronic pain may provide individuals with AKP more opportunities to confront or develop fear of their pain. However, it is difficult to determine if the fear-avoidance model contributes to this phenomenon without longitudinal data exploring severity and frequency of pain, physical activity level, return to sport or other factors that may contribute to fear of pain. Similar trends in the other scales were observed, with a greater number of individuals with AKP demonstrating moderate to high kinesiophobia (eight individuals with AKP compared to three ACLR individuals) (Figure 1c) and exceeding pain catastrophizing (eight individuals with AKP compared to four ACLR individuals) (Figure 1d). The smallto-moderate clinical differences in fear-avoidance beliefs and pain catastrophizing scores in the AKP group may be due to the included cohort. The AKP cohort mainly included individuals with patellofemoral pain, which results in pain during functional tasks that require knee flexion and lasts for years after initial diagnosis.23,48 Additionally, almost half of our AKP cohort were still experiencing pain at the time of survey completion, which may explain why they had greater psychological barriers.
Although both groups reported greater fear related beliefs compared to the healthy group, there was no statistical differences between AKP and ACLR groups. Therefore, regardless of knee pathology, individuals may benefit from psychological interventions to combat increased fearavoidance, kinesiophobia, and catastrophic pain. Despite the lack of differences between groups, interventions are essential to minimize secondary consequences and poor long-term implications associated with elevated psychological domains. The fear-avoidance model shows the longitudinal influence of psychological status on outcome where elevated pain catastrophizing and fear of movement or reinjury led to a more chronic disability.49 Individuals with increased fear-avoidance may also be at an increased risk for physical inactivity by adapting strategies to minimize painful stimuli.7 Additionally, greater levels of fear-avoidance are associated with stiffened movement patterns, reduced knee, hip and trunk flexion,50 that may predispose individuals to secondary injuries and readiness to return to sport.51 To address the long-term consequences and improve outcomes, clinicians must assess psychological domains and integrate appropriate interventions for patients suffering from injury regardless of injury type. There are various interventions that clinicians may prescribe when treating psychological impairments in their patients, such as relaxation therapy, guided imagery, goal-setting, and cognitive behavioral therapy 52,53 Psychologically informed interventions have been beneficial at reducing FABQ-PA, TSK-11, and pain catastrophizing in adolescents with PFP,54 while in vivo exposure therapy reduces injury related fear in ACLR cohort.55 Additionally, pain neuroscience education for chronic musculoskeletal conditions reduces psychosocial factors and improved movement impairments.56 While there is limited research directly comparing interventions across AKP and ACLR groups, the lack of differ-
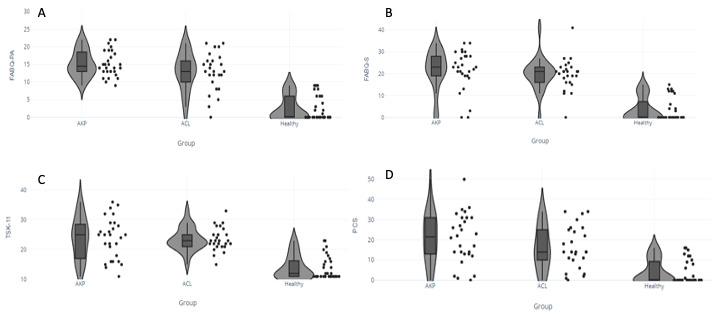 Figure 1.
Figure 1a: FABQ-PA; Figure 1b: FABQ-S; Figure 1c: TSK-11; Figure 1d: PCS between AKP, ACL and Health Individuals. FABQ-PA: Fear Avoidance Belief Questionnaire – Physical Activity; FABQ-S: Fear Avoidance Belief Questionnaire – sport; TSK-11: Tampa Scale of Kinesiophobia; PCS: Pain Catastrophization Scale; AKP: Anterior Knee Pain; ACL: Anterior Cruciate Ligament
Figure 1.
Figure 1a: FABQ-PA; Figure 1b: FABQ-S; Figure 1c: TSK-11; Figure 1d: PCS between AKP, ACL and Health Individuals. FABQ-PA: Fear Avoidance Belief Questionnaire – Physical Activity; FABQ-S: Fear Avoidance Belief Questionnaire – sport; TSK-11: Tampa Scale of Kinesiophobia; PCS: Pain Catastrophization Scale; AKP: Anterior Knee Pain; ACL: Anterior Cruciate Ligament
ence in psychological variables from our data suggests multiple interventions may be beneficial to patients with knee related injuries.
Interestingly, the healthy group had individuals who responded to some questions, resulting in scores above zero on the FABQ-PA, FABQ-S and PCS, and greater than 11 on the TSK-11. While individuals responded to some questions across the scales, most did not exceed the threshold scores that signify clinical classification. No healthy individuals exceeded the threshold for elevated fear-avoidance belief on the FABQ-PA.47 Two healthy participants would be classified as low kinesiophobia, scoring a 23 on the TSK-11, while the remaining 27 healthy participants would be classified as minimal kinesiophobia.57 Finally, no healthy participants exceeded the clinical threshold on PCS. Another possible explanation would be that the study was administered during the COVID-19 pandemic, which could account for the responses within the healthy individuals.58 Fear and stress are common responses when individuals are exposed to perceived threats or during uncertainty, which were common due to the pandemic. Fear and stress increased during the pandemic,59 which may impact both our pathological and healthy groups when completing fear-based questionnaires such as those included in our study The final question in the survey inquired if participants had increased anxiety levels or depression due to COVID-19; however, there were significant differences depending on question responses.
While some relationships exist across psychological domains, fear-avoidance beliefs, kinesiophobia and pain catastrophizing are distinct constructs. Similar scores were observed in the FABQ, TSK-11 and PCS between both the AKP and ACLR groups; however, the selection of questionnaires may be specific to the type of pathology.60,61 Decreasing fear-avoidance beliefs specifically on the FABQ-PA, predicts function and pain of a standard intervention program in individuals with AKP Additionally, lower pain catastrophizing four-weeks after ACLR were associated with better knee function 12-weeks post-surgery,35 while greater kinesiophobia increased the odds of identifying patients at risk for delayed progression in their rehabilitation program. The integration of psychological questionnaires in clinical practice may be a viable approach to predict success of traditional intervention programs or identify patients who warrant psychological interventions.62 These findings provide a baseline look into fear-avoidance beliefs, kinesiophobia, and pain catastrophizing; however further investigations are needed to determine if the scales selected correlate with responses from various intervention programs.
This study is not without limitations. Due to the perceptual scales and injury history questionnaire being self-
reported, there is a risk of missing injuries or recall bias. We also did not acquire detailed data regarding pain severity or time since pain/injury which may influence these results. Patient reported outcome measures selected in this study may have been influenced by time since surgery and recurrent bouts of pain. Differences exist between the clinical presentation and duration of impairments between AKP and ACLR. Patients experiencing AKP have pain for years after diagnosis, suggesting greater duration of pain may provide more opportunities for the development of fearavoidance behaviors. Additionally, within the ACLR group time since injury also may have influenced the results along with comorbidities associated with an ACL injury. Frequency of injuries was not controlled, which may have a compounding effect on the reported scores. Current physical activity was also not assessed, which may influence symptoms or psychological impairments in the included populations. Injury history within our participant recruitment was also not accounted for, which reduces the interval validity. However, this choice improves the external validity, as clinicians often treat individuals with ACLR or AKP that have experienced previous musculoskeletal conditions. Similarities in the number of participants with previous conditions between each group were not analyzed. Finally, there should be some caution with the generalizability of the findings, due to the cohort only including college aged individuals and the participants self-reporting their injury history
College-aged individuals with a history of AKP or ACLR demonstrated greater fear-avoidance beliefs, kinesiophobia, and pain catastrophizing than healthy controls. There were no differences across the four questionnaires between individuals with AKP or ACLR, suggesting that despite the difference in the knee pathologies, psychological responses may be similar. Clinicians should be aware of fear-related beliefs following knee-related injuries and are encouraged to measure psychological factors during the rehabilitation process.
The authors have no conflicts of interest to disclose.
Submitted: February 28, 2022 CST, Accepted: November 03, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Hootman JM, Macera CA, Ainsworth BE, Addy CL, Martin M, Blair SN. Epidemiology of musculoskeletal injuries among sedentary and physically active adults. Med Sci Sports Exerc 2002;34(5):838-844. do i:10.1097/00005768-200205000-00017
2. Weiss K, Whatman C. Biomechanics associated with patellofemoral pain and ACL injuries in sports. Sports Med 2015;45(9):1325-1337 doi:10.1007/s4027 9-015-0353-4
3. Bolgla LA, Boling MC, Mace KL, DiStefano MJ, Fithian DC, Powers CM. National athletic trainers’ association position statement: management of individuals with patellofemoral pain. J Athl Train 2018;53(9):820-836. doi:10.4085/1062-6050-231-15
4. Padua DA, DiStefano LJ, Hewett TE, et al. National athletic trainers’ association position statement: Prevention of anterior cruciate ligament injury J Athl Train. 2018;53(1):5-19. doi:10.4085/1062-6050-99-16
5. Smith BE, Selfe J, Thacker D, et al. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS One. 2018;13(1):e0190892. doi:10.1371/journal.pone.0190 892
6. Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34(9):1512-1532. doi:10.1177/036354650628686 6
7 Kim S, Kim D, Park J. Knee joint and quadriceps dysfunction in individuals with anterior knee pain, anterior cruciate ligament reconstruction, and meniscus surgery: A cross-sectional study. J Sport Rehabil. 2021;30(1):112-119. doi:10.1123/jsr.2018-04 82
8. Sepúlveda F, Sánchez L, Amy E, Micheo W Anterior cruciate ligament injury: Return to play, function and long-term considerations. Curr Sports Med Rep. 2017;16(3):172-178. doi:10.1249/jsr.000000 0000000356
9. Glaviano NR, Baellow A, Saliba S. Physical activity levels in individuals with and without patellofemoral pain. Phys Ther Sport. 2017;27:12-16. doi:10.1016/j.pt sp.2017.07.002
10. Bell DR, Pfeiffer KA, Cadmus-Bertram LA, et al. Objectively measured physical activity in patients after anterior cruciate ligament reconstruction. Am J Sports Med 2017;45(8):1893-1900. doi:10.1177/03635 46517698940
11. Coburn SL, Barton CJ, Filbay SR, Hart HF, Rathleff MS, Crossley KM. Quality of life in individuals with patellofemoral pain: A systematic review including meta-analysis. Phys Ther Sport. 2018;33:96-108. doi:1 0.1016/j.ptsp.2018.06.006
12. Filbay SR, Ackerman IN, Russell TG, Macri EM, Crossley KM. Health-related quality of life after anterior cruciate ligament reconstruction: a systematic review Am J Sports Med 2014;42(5):1247-1255. doi:10.1177/036354651351277
13. Crossley KM. Is patellofemoral osteoarthritis a common sequela of patellofemoral pain? Br J Sports Med 2014;48(6):409-410. doi:10.1136/bjsports-201 4-093445
14. Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: A 14-year follow-up study of a randomized controlled trial. Am J Sports Med 2014;42(5):1049-1057 doi:10.1177/0363 546514526139
15. Lankhorst NE, van Middelkoop M, Crossley KM, et al. Factors that predict a poor outcome 5–8 years after the diagnosis of patellofemoral pain: a multicentre observational analysis. Br J Sports Med. 2016;50(14):881-886. doi:10.1136/bjsports-2015-094 664
16. Baez SE, Hoch MC, Hoch JM. Psychological factors are associated with return to pre-injury levels of sport and physical activity after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):495-501. doi:10.1007/s00167-019-05696-9
17 Fones L, Kostyun RO, Cohen AD, Pace JL. Patientreported outcomes, return-to-sport status, and reinjury rates after anterior cruciate ligament reconstruction in adolescent athletes: Minimum 2-year follow-up. Orthop J Sports Med. 2020;8(11):2325967120964471. doi:10.1177/23259671 20964471
18. Piva SR, Fitzgerald GK, Irrgang JJ, et al. Associates of physical function and pain in patients with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2009;90(2):285-295. doi:10.1016/j.apmr.200 8.08.214
19. Sullivan MJL, Adams H, Thibault P, Corbière M, Stanish WD. Initial depression severity and the trajectory of recovery following cognitive-behavioral intervention for work disability. J Occup Rehabil. 2006;16(1):60-71. doi:10.1007/s10926-005-9013-0
20. Baez SE, Hoch MC, Hoch JM. Psychological factors are associated with return to pre-injury levels of sport and physical activity after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2020;28(2):495-501. doi:10.1007/s00167-019-05696-9
21. Louw QA, Leibbrandt DC. Patients’ perceptions of recovery following a 6-week exercise intervention for the treatment of patellofemoral pain: A mixed methods study. South African Journal of Physiotherapy. 2019;75(1):1-8.
22. Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review Knee Surg Sports Traumatol Arthrosc 2015;23(3):752-762. d oi:10.1007/s00167-013-2699-1
23. Lankhorst NE, van Middelkoop M, Crossley KM, et al. Factors that predict a poor outcome 5–8 years after the diagnosis of patellofemoral pain: a multicentre observational analysis. Br J Sports Med 2016;50(14):881-886. doi:10.1136/bjsports-2015-094
664
24. Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317-332. doi:10.101 6/s0304-3959(99)00242-0
25. Kori S. Kinesiophobia: a new view of chronic pain behavior. Pain Manage. 1990;3:35-43.
26. Sullivan MJ. The Pain Catastrophizing Scale: User Manual McGill University; 2009.
27 Filbay SR, Culvenor AG, Ackerman IN, Russell TG, Crossley KM. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. Br J Sports Med 2015;49(16):1033-1041. doi:10.1136/bjsports-2015-0
94864
28. Carolan D, King E, Richter C, Franklyn-Miller A, Moran R, Jackson M. Differences in strength, patientreported outcomes, and return-to-play rates between athletes with primary versus revision ACL reconstruction at 9 months after surgery. Orthop J Sports Med 2020;8(9):2325967120950037 doi:10.117 7/2325967120950037
29. Roe C, Jacobs C, Kline P, et al. Correlations of single-leg performance tests to patient-reported outcomes after primary anterior cruciate ligament reconstruction. Clin J Sport Med. 2020;31(5):e265-e270. doi:10.1097/jsm.00000000000 00780
30. Burland JP, Toonstra J, Werner JL, Mattacola CG, Howell DM, Howard JS. Decision to Return to Sport After Anterior Cruciate Ligament Reconstruction, Part I: A Qualitative Investigation of Psychosocial Factors. J Athl Train 2018;53(5):452-463. doi:10.408 5/1062-6050-313-16
31. Filbay SR, Crossley KM, Ackerman IN. Activity preferences, lifestyle modifications and re-injury fears influence longer-term quality of life in people with knee symptoms following anterior cruciate ligament reconstruction: a qualitative study Journal of Physiotherapy 2016;62(2):103-110. doi:10.1016/j.jp hys.2016.02.011
32. Kvist J, Ek A, Sporrstedt K, Good L. Fear of reinjury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2005;13(5):393-397 doi:1 0.1007/s00167-004-0591-8
33. Flanigan DC, Everhart JS, Pedroza A, Smith T, Kaeding CC. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy 2013;29(8):1322-1329. doi:10.1016/j.arthro.2013.05.0 15
34. Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med 2014;48(22):1613-1619. doi:10.1136/bjsports-2014-0 93842
35. Chmielewski TL, George SZ. Fear avoidance and self-efficacy at 4 weeks after ACL reconstruction are associated with early impairment resolution and readiness for advanced rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):397-404. doi:1 0.1007/s00167-018-5048-6
36. Chmielewski TL, Zeppieri G Jr, Lentz TA, et al. Longitudinal changes in psychosocial factors and their association with knee pain and function after anterior cruciate ligament reconstruction. Physical Therapy. 2011;91(9):1355-1366. doi:10.2522/ptj.2010 0277
37 Filbay S, Kvist J. Fear of reinjury following surgical and nonsurgical management of anterior cruciate ligament injury: An exploratory analysis of the NACOX multicenter longitudinal cohort study. Physical Therapy 2021;102(2). doi:10.1093/ptj/pzab27
38. Bryson GL, Turgeon AF, Choi PT The science of opinion: survey methods in research. Can J Anesth. 2012;59(8):736-742. doi:10.1007/s12630-012-9727-3
39. Houston MN, Hoch JM, Van Lunen BL, Hoch MC. The impact of injury on health-related quality of life in college athletes. J Sport Rehabil 2017;26(5):365-375. doi:10.1123/jsr.2016-0011
40. Hoch JM, Houston MN, Baez SE, Hoch MC. Fearavoidance beliefs and health-related quality of life in post-ACL reconstruction and healthy athletes: A case–control study. J Sport Rehabil. 2019;29(6):772-776. doi:10.1123/jsr.2018-0491
41. Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability Pain 1993;52(2):157-168. doi:10.1016/0304-3959(93)9012 7-b
42. Swinkels-Meewisse EJCM, Swinkels RAHM, Verbeek ALM, Vlaeyen JWS, Oostendorp RAB. Psychometric properties of the Tampa Scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Man Ther. 2003;8(1):29-36. doi:10.1054/math.2002.0484
43. Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain 2005;117(1-2):137-144. doi:10.1016/j.pain.2005.05.02 9
44. George SZ, Lentz TA, Zeppieri G Jr, Lee D, Chmielewski TL. Analysis of shortened versions of the Tampa Scale for Kinesiophobia and Pain Catastrophizing Scale for patients following anterior cruciate ligament reconstruction. Clin J Pain 2012;28(1):73-80. doi:10.1097/ajp.0b013e31822363f4
45. Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O’Neill E. Factor structure, reliability, and validity of the Pain Catastrophizing Scale. J Behav Med 1997;20(6):589-605. doi:10.1023/a:10255705089 54
46. Cohen J. The effect size. In: Statistical Power Analysis for the Behavioral Sciences ; 1988:77-83.
47 George SZ, Stryker SE. Fear-avoidance beliefs and clinical outcomes for patients seeking outpatient physical therapy for musculoskeletal pain conditions. J Orthop Sports Phys Ther. 2011;41(4):249-259. doi:1 0.2519/jospt.2011.3488
48. Glaviano NR, Bazett-Jones DM, Boling MC. Pain severity during functional activities in individuals with patellofemoral pain: A systematic review with meta-analysis. Journal of Science and Medicine in Sport. 2022;25(5):399-406. doi:10.1016/j.jsams.2022.0 1.004
49. Leeuw M, Goossens MEJB, Linton SJ, Crombez G, Boersma K, Vlaeyen JWS. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 2007;30(1):77-94. doi:10.1007/ s10865-006-9085-0
50. Trigsted SM, Cook DB, Pickett KA, CadmusBertram L, Dunn WR, Bell DR. Greater fear of reinjury is related to stiffened jump-landing biomechanics and muscle activation in women after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2018;26(12):3682-3689. doi:10.1007/s00167-018-495 0-2
51. Hart HF, Culvenor AG, Guermazi A, Crossley KM. Worse knee confidence, fear of movement, psychological readiness to return-to-sport and pain are associated with worse function after ACL reconstruction. Phys Ther Sport. 2020;41:1-8. doi:10.1 016/j.ptsp.2019.10.006
52. Levack WM, Weatherall M, Hay-Smith JC, Dean SG, McPherson K, Siegert RJ. Goal setting and strategies to enhance goal pursuit in adult rehabilitation: summary of a Cochrane systematic review and meta-analysis. Eur J Phys Rehabil Med. 2016;52(3):400-416.
53. Johnson U. Short-term psychological intervention: A study of long-term-injured competitive athletes. J Sport Rehabil. 2000;9(3):207-218. doi:10.1123/jsr.9.3.207
54. Selhorst M, Fernandez-Fernandez A, Schmitt L, Hoehn J. Effect of a psychologically informed intervention to treat adolescents with patellofemoral pain: A randomized controlled trial. Arch Phys Med Rehabil. 2021;102(7):1267-1273. doi:10.1016/j.apmr.2 021.03.016
55. Baez S, Cormier M, Andreatta R, Gribble P, Hoch JM. Implementation of In vivo exposure therapy to decrease injury-related fear in females with a history of ACL-Reconstruction: A pilot study Phys Ther Sport. 2021;52:217-223. doi:10.1016/j.ptsp.2021.09.00
56. Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract. 2016;32(5):332-355. doi:10.1080/09593985.2016.1194 646
57 Chimenti RL, Post AA, Silbernagel KG, et al. Kinesiophobia severity categories and clinically meaningful symptom change in persons with achilles tendinopathy in a cross-sectional study: Implications for assessment and willingness to exercise. Front Pain Res 2021:57
58. Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr: Clin Res Rev 2020;14(5):779-788. doi:10.1016/j.dsx.2020.05.0 35
59. Peng X, Liu L, Liang S, Chen J, Zhao J. Longitudinal changes in fear and anxiety among Chinese college students during the COVID-19 pandemic: a one-year follow-up study. Curr Psychol. 2022;2022:1-10. doi:10.1007/s12144-022-03487-z
60. Van Wyngaarden JJ, Jacobs C, Thompson K, et al. Quadriceps strength and kinesiophobia predict longterm function after ACL reconstruction: a crosssectional pilot study. Sports Health. 2021;13(3):251-257 doi:10.1177/1941738120946323
61. Chmielewski TL, Jones D, Day T, Tillman SM, Lentz TA, George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther. 2008;38(12):746-753. doi:1 0.2519/jospt.2008.2887
62. Bay S, Kuster L, McLean N, Byrnes M, Kuster MS. A systematic review of psychological interventions in total hip and knee arthroplasty. BMC Musculoskelet Disord 2018;19(1):1-11. doi:10.1186/s12891-018-212
Bencke J, Strøm M, Curtis DJ, Bandholm T, Zebis MK. Differences in Thigh Muscle Activation Between Standing and Landing Exercises for Knee Injury Prevention and Rehabilitation. IJSPT. Published online February 1, 2023:102-112.
Jesper Bencke 1 a , Mark Strøm 2 , Derek J. Curtis 1,3 , Thomas Bandholm 4 , Mette K. Zebis 5,6
1 Human Movement Analysis Laboratory, Dept. of Orthopaedic Surgery, Copenhagen University Hospital, Amager-Hvidovre, Denmark, 2 Clinic of Sports Physiotherapy and Rehabilitation, Denmark, 3 Child Centre Copenhagen, The Child and Youth Administration, Denmark, 4 Department of Clinical Research, Copenhagen University Hospital, Amager and Hvidovre, Denmark, 5 Department of Physiotherapy and Occupational Therapy, University College Copenhagen, Denmark, 6 Institute of Sports Medicine Copenhagen, Copenhagen University Hospital–Bispebjerg and Frederiksberg, Denmark
Keywords: EMG, exercises, injury prevention, m. semitendinosus, sex difference, knee https://doi.org/10.26603/001c.67829
In injury prevention or rehabilitation programs, exercises that facilitate enhanced hamstring activity may be beneficial when aiming to enhance knee joint stability during movements in sports with higher risk of acute knee injury Information about neuromuscular activation of the hamstring muscles in commonly used exercises may improve exercise selection and progression in programs for knee injury prevention or rehabilitation.
To investigate (1) how balance devices with progressing degrees of instability influence the activity of muscles controlling the knee joint in typical balance exercises with different demands on postural control, and (2) if any between-sex differences exist.
Cross-sectional study
Twenty habitually active healthy adults (11 males) participated in this cross-sectional study Single-leg stance, single-leg squat and single-leg landing were performed on the floor and two different balance devices imposing various levels of challenge to postural control. Three-dimensional motion analysis was used to obtain hip and knee joint angles, and as primary outcomes, and peak normalized EMG activity from the hamstrings and quadriceps muscles was measured for comparison between exercises.
The more challenging in terms of maintaining stable balance the devices were, the higher hamstring muscle activity levels were observed. There was a clear progression across balance devices from single-leg stance to single-leg squat and further to single-leg landing displaying increasing hamstring activity levels. The change in medial hamstring activity across all devices when changing from single-leg squat to single-leg landing was significantly higher for the female participants than for the males reaching a higher level of activity

The muscle activity of the hamstrings and quadriceps increased when the motor task was more dynamic. Specifically, single-leg landings were effective in increasing the hamstring
Corresponding author:
Jesper Bencke, Dept. of Orthopaedic Surgery, Copenhagen University Hospital, Amager-Hvidovre, Kettegård alle 30, 2650 Hvidovre, Denmark
Mail: jesper.bencke@regionh.dk, tel: +45 38626932
muscle activity over the single-leg stance to single-leg squat exercises, and muscle activity was significantly increased with the most unstable device. Increases in hamstring muscle activation was greater in female subjects than males with increasing instability of the balance devices. Trial identifier
The risk of sustaining a serious acute knee injury, especially injury to the anterior cruciate ligament (ACL), is elevated in ball and racket sports that involve abrupt changes of direction (i.e. landing, turning, and sidecutting).1–4 The incidence rate may be as high as 2.0 per 10,000 exposures in female football5 and 3.1 per 10,000 player hours in female handball.6 However, when looking at incidence rate during game play incidence rate rises to 16 ACL injuries per 10,000 hours in female handball.6 The individual long term consequences may be substantial, as the knee injury may increase the risk of early osteoarthritis7 and reduce the quality of life.8
Many studies examining anatomical, physiological, biomechanical and neuromuscular risk factors have been carried out to investigate various mechanisms potentially influencing injury risk.9–13 It is shown in a case study that an ACL injury may occur after landing with little knee flexion and displaying rapid changes of knee abduction and knee rotation angles during the very early phase (<40 ms) after initial contact, thus emphasizing the importance of proper knee joint stability at landing.14 Also, anatomical studies show that quadriceps muscle contraction forces, as observed during the initial landing phase, may result in an anterior translation of tibia, thus increasing strain in the ACL.15–17 These tranaslational forces would best be counteracted by the hamstring muscles,18–20 and prospective studies have also shown that reduced medial hamstring activity at initial contact during a sidecutting maneuver significantly increased the risk of ACL injury.12,13 Exercises for increasing the medial hamstring activity may be especially important for females, as studies have shown less medial hamstring activity in female athletes during sidestep cutting.21
Although multi-exercise prophylactic training, including exercises on different balance devices, is estimated to be able to reduce the risk of ACL injury by 50% or more,22 few studies have examined the effect of such training regimes on the hamstring activation level during ACL injury risk movements. Zebis et al.23 found increased hamstring preactivation during sidestep cutting after a prevention training program24 which consisted of both standing and landing balance exercises on floor and unstable surfaces. To understand which exercises may be the most effective in increasing hamstring activation levels during risk movements like sidestep cutting, greater knowledge about the muscular activation, e.g. hamstring muscle activity, during the differ-
ent specific exercises may be helpful. Further, such information may assist in planning the optimal progression and designing the most efficient prevention program or rehabilitation program.
Previously, studies investigating lower leg muscle activity during balance exercises showed gradually increased activation of the ankle joint stabilizing muscles when moving from standing balance on the floor to balancing on an Airex® mat and BOSU-ball®, respectively 25 Few studies have investigated if these increased activity patterns are also true for the knee joint muscles during such balance exercises. Thus, performing exercises that facilitate enhanced hamstring activity – and knowing how to progress them –may be a promising approach both in prevention and clinical rehabilitation, when aiming to enhance knee joint stability during vigorous movements seen in many ball and racket sports.
Therefore, the purpose of the present study was: Firstly, to investigate how knee muscle activation levels and knee and hip joint kinematics were influenced by exercises with increasing levels of postural control demands, progressed as either increasing the instability of the surface and/or increasing the demands of the balance task from standing exercises to landing exercises. Secondly, post-hoc analyses were made for analyzing possible effects of sex on muscle activation patterns and knee and hip joint kinematics within the different exercise modalities and balance devices.
The study used an exploratory, cross-sectional design in which a cohort of 20 healthy subjects (11 males) were examined for sagittal plane hip and knee kinematics and muscle activation while performing different exercises challenging postural stability with increasing difficulty in a 3-dimensional (3D) movement analysis laboratory. There was no pre-defined weighting of study outcomes or outcome hierarchy, but given the described potential importance of the hamstring muscles as knee joint stabilizers, particular the medial hamstrings,12,13,21 the primary focus was on identifying exercises with high medial hamstring activation. Data for ankle muscle activity and ankle kinematics during balance exercises in the same cohort have been reported previously 25
A convenience sample of twenty healthy subjects, 11 male and nine females, volunteered to participate in the study
Mean age (± SD) was 28.8 ± 2.3 yrs, mean weight was 71.9 ± 11.5 mean height 177 ± 11 cm. All the participants were active in different sports, on average 5.2 ± 3.0 hours per week (range 1-13.5 hours per week). Subjects were excluded if they had any history of an injury in the lower extremity in the preceding six months. An injury was defined as an injury occurring during a scheduled game or practice, causing the player to miss the next game, practice session or to participate with considerable discomfort. Furthermore, subjects were excluded if they had performed any specific proprioceptive training during the same period or had performed any strength training sessions within a period of 48 hours before testing. None of the subjects reported any history of neurological or vestibular impairments. The local ethics committee did not need to perform a full ethics review, because the exercises were all commonly used in standard training programs and the non-invasive character of the experimental procedures, and furthermore only healthy participants were included. All participants gave their informed consent, according to the Helsinki Declaration, before entering the study.
The test session comprised three types of exercises commonly used in prevention programs or rehabilitation regimes: 1) single-legged standing balance, 2) singlelegged squatting, and 3) single-legged landings. The singleleg stance exercise demanded 15 seconds of quiet standing balance, while the single-leg squat test was a starting from straight leg position performing a single knee flexion to approximately 90 degrees followed by full extension, in a 2-second up and 2-second down steady rhythm. The singleleg landing tests were performed as one-legged hop from a distance of 80 % of the subject’s leg length, and the subject was required to maintain balance after landing for five seconds.
Each exercise was performed on three different surfaces of varying degrees of instability, one stable and two unstable, in this way a total of nine different tests were performed. The stable reference surface was solid floor, and the two unstable balance devices were a foam pad (Airex-mat®, Sins, CH) and the convex side of a BOSU-ball® (OH, USA), henceforth called Airex and BOSU, respectively Both balance devices are commonly used in rehabilitation or injury prevention training programs.24,26,27
The BOSU exercises were considered to challenge the postural balance more than the Airex. Subjects were instructed to maintain balance as steady as possible with no restrictions or instructions on leg and arm positioning. Subjects were permitted three familiarization trials before single-leg landing and one to two familiarization trials before single-leg squat and single-leg stance tests. Three trials were collected for each test and used for analysis. The test protocol ensured that all exercises were performed in a randomized order with a 30 second rest between trials and
two minutes rest between different tests to avoid musclefatigue and maintain a high level of focus. A trial was discarded if the subject could not stand for 15 seconds during the single-leg stance test, lost balance during the squatting movement, or could not maintain balance during the first five seconds after landing in single-leg landing. Lost balance was defined as the subject requiring any correction such as re-positioning their foot or touching the floor/balance device with the opposite foot during the test.
Kinematic differences in knee and hip joint angles between exercises and balance devices were determined using 3D motion analysis (Vicon 612 Vcam motion capture system, Vicon Motion Systems., Oxford, UK). Before testing, sixteen reflective markers were placed over anatomical landmarks according to a modified Helen Hayes marker setup,28 except for the thigh markers, which were substituted by markers attached over the patella, to reduce soft tissue artefacts.29 Knee and hip joint angles were calculated using inherent Vicon plug-in-gait software, including Woltring cubic spline filtering of marker trajectories. The tests were performed with the balance devices placed on a force platform (AMTI OR6-7, MA, USA). The single-leg stance test was a static standing exercise, therefore mean hip and knee flexion angles during the duration of the test were obtained for comparison with the two dynamic exercises. Hip and knee flexion angles were obtained for both the initiation of the movement and the maximal hip and knee flexion angles displayed during the single-leg squat and single-leg landing, respectively The initiation of the movement was defined as the start of the downwards movement during the single-leg squat and the time of initial contact during the single-leg landing, recorded as the instant the vertical ground reaction force exceeded 20 N.
Electromyographic (EMG) recordings were used to measure the activity of the muscles controlling the knee joint during all tests. EMG signals were recorded using rectangular (20 mm x 30 mm) bipolar surface electrodes (DE-2.1, Delsys, Boston, MA, USA). The electrodes were attached to the quadriceps muscle over two vastii, the vastus medialis (VM) and the vastus lateralis (VL), the hamstrings, the semitendinosus (ST) and the biceps femoris (BF) according to standard guidelines.30 All electrodes were placed on the dominant leg determined as the preferred kicking leg. Skin surfaces were shaved, abraded, and cleansed with alcohol to improve the conductivity of the EMG signal.21 All EMG signals were pre-amplified and sampled with a frequency of 1000Hz by a device (Myomonitor IV, Delsys, Boston, MA, USA) carried on the back of the subject. Data was wirelessly transmitted to a computer with a fixed delay of 200 ms and recorded synchronously with the kinematic recordings by inherent software in the Motion Analysis system (Vicon 612 Workstation, Vicon Motion Systems, Oxford, England). Prior to dynamic exercises, three trials with five seconds of maximum voluntary contractions (MVC) were performed to
obtain maximal EMG-levels for each muscle. The maximal activation of the quadriceps muscle was obtained in a sitting position with 60° of knee flexion, and the hamstring maximal activation levels were obtained during prone lying with neutral hip and 20 degrees of knee flexion.
The fixed transmission delay was adjusted to have the EMG data synchronized with the kinematic data. The raw EMG-signals were filtered first using a fourth-order highpass filter with a cutoff at 10 Hz, and subsequently filtered using a root-mean square (RMS) sliding windows of 30 ms with 29 ms overlap. Similar filtering procedures were applied to the MVC-trials over the five second period. Peak values from each muscle during the MVC-trials were used for normalization of EMG data during the exercise trials.
To compare the level of muscle activity between three dynamically different exercises the peak amplitude obtained during the trial was chosen as primary output parameter. During the single-leg stance test, only the mid-10 seconds of the 15 second trial were used to exclude postural adjustments at the beginning and to avoid muscle-fatigue at the end of the balance trial.31 For the single-leg squat the peak amplitude in the period from the beginning of the descending motion to the end of the ascending motion was obtained. During single-leg landing, the peak amplitude recorded from 100 ms before landing to one second after landing was obtained.
Because this study used an exploratory design, no a priori sample size estimation was performed.
Peak normalized EMG amplitudes for the four muscles and joint angles of the hip and knee joints were averaged across the three trials for each of the test conditions. A mixed-design ANOVA was applied for the data defining test modalities (single-leg stance, single-leg squat and singleleg landing tests) and balance devices (floor, Airex and BOSU) as within-subjects random effects factors, and sex was defined as between-subjects fixed effects factor The level of significance was set at p < 0.05, and partial Eta squared (η2) was used as effect size estimate. If significant differences were found in muscle activation levels across exercises and/or levels of balance stability, a Bonferroni adjusted post-hoc analysis of differences between each condition was performed. The statistical analyses were performed in SPSS version 22.0.0.
Knee flexion and hip flexion at initiation of the exercise varied significantly between the different exercises showing a larger degree of flexion with increased dynamic intensity of the task (knee: F(2,36)=12.39, p<0.001, η2=0.41; hip: F(2,36)=111.60, p<0.001, η2=0.86). Likewise, the maximal knee and hip flexion angle were affected by the specific exercise performed (knee: F(2,36)=577.71, p<0.001, η2=0.97; hip: F(2,36)=228.62, p<0.001, η2=0.93) showing a larger degree of flexion during the single-leg squat exercise com-
pared to both single-leg standing (knee: p<0.001, η2=0.98; hip: p<0.001, η2=0.95) and single-leg landing (knee: hip: p<0.001, η2=0.96; hip: p<0.001, η2=0.72).
The choice of balance device also significantly affected kinematics. The knee and hip flexion at initiation of the task increased with the increased postural challenge induced by the balance device with the floor offering the least challenge and the BOSU inducing the most postural challenge (knee: F(2,36)=52.22, p<0.001, η2=0.74; hip: F(2,36)=37.40, p<0.001, η2=0.68). The maximal knee flexion was not affected by the choice of balance device, but the maximal hip flexion increased with increased postural challenge (knee: F(2,36)=4.48, p=0.018, η2=0.20; hip: F(2,36)=11.38, p<0.001, η2=0.39).
Overall, female subjects displayed across all tests less maximal joint angle flexion compared with male subjects (Table 1) and a tendency to have less flexion at the initiation of the exercise. However, no significant difference between sexes was found in the change in kinematics with between balance devices or between exercises (p>0.05 for all kinematic parameters).
In general, the hamstring activity increased significantly with each level of test modality, from very low peak activity during single-leg stance to medium activity during singleleg squat (ST: F(1,18)=14.106, p<0.001, η2=0.44; BF: F(1,18)=34.108, p<0.001, η2=0.66), and from medium activity during single-leg squat to highest activity during singleleg landing activities (ST: F(1,18)=64.040, p<0.001, η2=0.78; BF: F(1,18)=42.744, p<0.001, η2=0.70) (Figures 1 and 2, and Tables 2-3).
The quadriceps activity was very low during the singleleg stance exercises, but increased four-fold during the single-leg squat (VM: F(1,18)=83.103, p<0.001, η2=0.82; VL: F(1,18)=151.515, p<0.001, η2=0.89). No difference in activity levels of either VM or VL was seen when performing single-leg landing exercises compared to single-leg squat (F(1,18)< 2.8) (Tables 4 and 5).
When comparing the different balance devices across exercise modalities, the BOSU induced significantly higher hamstring activity levels than the Airex (ST: F(1,18)=24.216 , p<0.001, η2=0.57; BF: F(1,18)=25.245, p<0.001, η2=0.58). No difference in hamstring activity was found between exercises on the floor and on an Airex (F(1,18)<0.5) (see tables 2-3). Also for the two quadriceps vastii, there was no difference between exercises on the floor and on the Airex (F(1,18)<1.9), but the VL-activity increased significantly when exercising on the BOSU (F(1,18)=6.993,p=0.016, η2=0.28). The increase in activity of VM from Airex to BOSU was minor and non-significant (F(1,18)=3.828, p=0.066, η2=0.18) (Tables 4 and 5).
Based on post-hoc independent pairwise comparison among the estimated marginal means. KF and HF indicates knee flexion and hip flexion respectively Ini indicates mean values recorded at initial contact and max as the mean maximal angle recorded during the test modalities.
Figure 1. Knee joint angles and raw, rectified muscular activation levels of the semitendinosus from a representative subject during the three types of exercises; SLS (top two graphs), SLSq (middle two graphs) and SLL (lower two graphs) using a BOSU balance device.
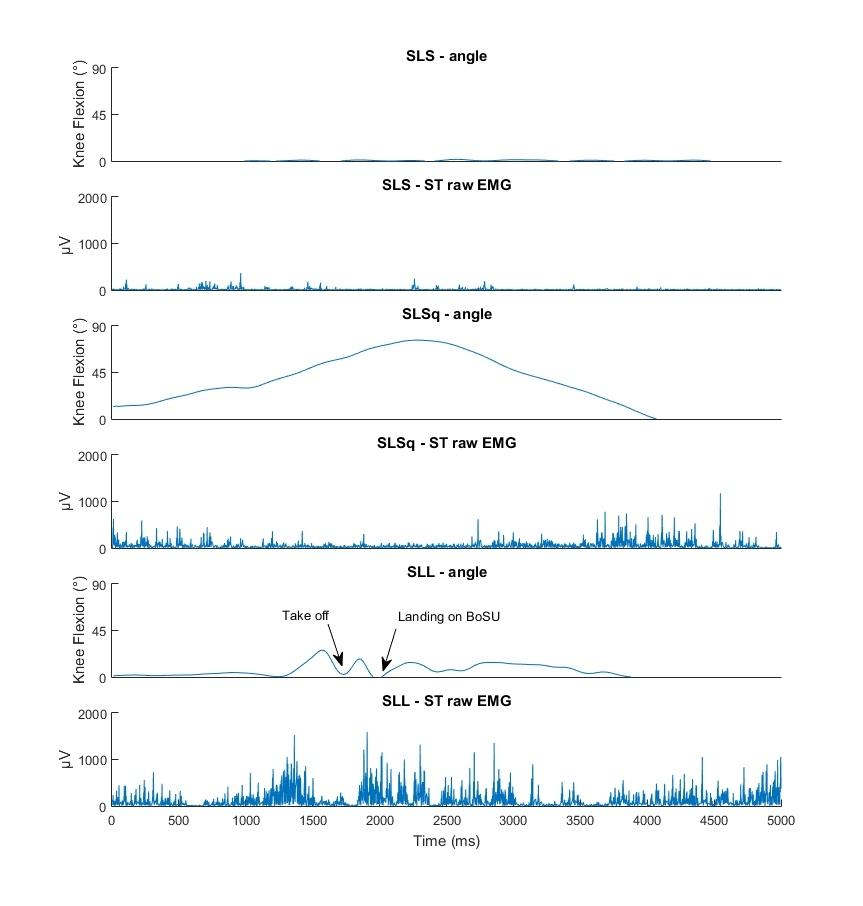
Differences in Thigh Muscle Activation Between Standing and Landing Exercises for Knee Injury Prevention and Rehabilitation
normalized mean peak activation level.
Abbreviations. ST: semitendinosus; SLS: single-legged stance; SLSq: single-legged squat; SLL: single-legged landing; Air: Airex; Fl: floor
mean peak activation level
ST: semitendinosus; SLS: single-legged stance; SLSq: single-legged squat; SLL: single-legged landing; Air: Airex; Fl: floor
medialis normalized mean peak activation level
Abbreviations. ST: semitendinosus; SLS: single-legged stance; SLSq: single-legged squat; SLL: single-legged landing; Air: Airex; Fl: floor
normalized mean peak activation level
Abbreviations. ST: semitendinosus; SLS: single-legged stance; SLSq: single-legged squat; SLL: single-legged landing; Air: Airex; Fl: floor
No overall differences in muscle activity across all test modalities and devices were found between sexes, however when including sex as a between-subjects effect, small but significant differences in activity level changes from singleleg squat to single-leg landing were observed for the medial hamstring. The increase in ST activity across all devices
when changing from single-leg squat to single-leg landing was larger for the female participants than for the males reaching a higher level of activity (F(1,18)=4.335, p=0.038, η2=0.19) (Figure 2). This sex-specific increase in activity was most apparent for exercises on the BOSU (Figure 2). No changes were observed for the other muscles as an effect of sex.
Black filled symbols: male subjects; Grey open symbols: female subjects, diamonds denote exercises on floor, squares denote exercises on Airex mattress and circles denote exercises on BOSU. Error bars denote ±standard error
The main results of the present study were that the more challenging, i.e. unstable, the balance devices were, the higher the hamstring muscle activity levels, with a clear progression from standing balance exercises to standing dynamic exercises to dynamic landing exercises. Thus, dynamic exercises on an unstable surface are superior to static exercises in terms of increased hamstring activation. Interestingly, the data furthermore indicate that this increase in hamstring activation is especially pronounced in female athletes when progressing from single-leg squat to singleleg landing exercises (Figure 2).
As mentioned earlier, a high level of muscle activity around the knee joint, including high activity of especially the medial hamstrings, seems important for prevention of ACL injuries.12,13,18–21 Therefore, specific attention was given to how different exercises with three levels of progression would affect hamstring activation levels.
The present data show little activity in any of the examined muscles during the single-leg stance exercise. This corresponds to other studies also showing low levels of activity in the thigh muscles during standing balance exercises.32,33 Considering the lack of loaded movement around the hip and knee joint this may not be surprising, however increasing the demand on postural control may also induce an increase in the degrees of hip and knee flexion significantly for the most challenging device, i.e. the BOSU as a compensation for the reduced ability of the ankle to control postural stability. These changes in the need for stabilisation and slight increase in hip and knee joint flexion

increase the external moment, and as such place more demand on force production in the knee and hip extensors, thereby explaining the small, yet significantly increased levels of muscle activation in the hamstrings and quadriceps during single-leg stance on the BOSU. Furthermore, no difference in thigh muscle activation was observed during standing balance, between the firm floor surface and the less stable Airex. It should be noted that the present study was conducted with healthy subjects and that standing on an Airex may possibly be more challenging and induce greater muscle activation with subjects in the early phase of rehabilitation after an ACL injury
Performance of single-legged squats are extensively investigated as an exercise for knee injury prevention or rehabilitation exercise.32,34–39 The present data corroborate previous studies in showing highly increased levels of quadriceps activity for all balance devices, compared to single-leg stance, but a more moderate increase in mean peak hamstring activity Although the increase in hamstring activity relative to single-leg stance was significant for the Airex and the floor, single-leg squat on BOSU still required larger levels of hamstring activation compared to the less demanding devices. None of the tested devices, however, produced hamstring activation above 40% during single-leg squat. This emphasises, as also shown by other studies, that the single-leg squat may not be optimal if the purpose is to induce high levels of hamstring activation in co-contraction with quadriceps activation.32,35,39 This may be an important consideration when designing prevention programs or rehabilitation programs after ACL-reconstruction. In contrast, during the dynamic landing exercises much higher
Figure 2. Normalized mean activity levels of semitendinosus (ST) depending on test category (x-axis) and sex and balance devicelevels of activity in both hamstring and knee extensor muscles were present around the time of initial contact, regardless of the type of landing surface. No studies have compared the activity levels of dynamic landings to standing balance exercises, but studies on landing show peak values of knee muscle activity very similar to the present study 40–42 Although muscular activity levels above 40-60% are considered necessary for inducing strength gain,43 the high activation levels of the hamstrings during dynamic single-leg landing exercises may not be in increasing hamstring strength, due to the short duration of the activity bursts. However, optimizing the neuromuscular coordination in terms of increasing medial hamstring activation during injury risk situations, like side-cutting, has also been shown to be important.12,13 Studies on motor learning have shown that a consistent perturbation of the muscle synergies involved in an existing motor program, e.g. the motor program used during landing, may be the fastest way to make consistent changes in a motor program.44 It is therefore likely that the increased hamstring activity observed in the single-leg landing exercises may indicate that single-leg landing is more efficient in altering the motor programs during landing or cutting movements and as such suggest that dynamic landing exercises may be more suitable for injury prevention programs and probably also late phase rehabilitation after ACL-reconstruction. The importance of dynamic exercises for improving joint control is also highlighted in a review of effectiveness of ankle stability exercises, which concluded that dynamic landing exercises were particular beneficial for increasing the anticipatory adjustments stabilising the ankle joint.45 And also, addressing knee joint stability, a recent meta-analysis showing that prevention programs consisting of balance exercises alone were less successful in ACL injury prevention compared to programs consisting of a variety of dynamic exercises, and this effect may be partly due to a more effective alteration of hamstring activation after dynamic exercises.46 The results of the present study also showed that the dynamic landing exercises investigated increased the medial hamstring activation more in female subjects than male subjects, indicating that such exercises might be even more beneficial for female athletes (Figure 2). The results further suggest that exercises on the BOSU device may potentially be most effective.
When designing injury prevention or rehabilitation programs, different training devices designed to challenge a subject’s balance may be selected. Information about the
effect of the different devices may be very useful to guide an optimal training progression, and the results of the present study may offer such guidance. Some care should be taken in the interpretation of the results, as the number of subjects was low Furthermore, subjects in this study were healthy persons without previous injuries affecting their performance, and some of the tests may be too challenging early in ACL rehabilitation. Also, when designing injury prevention programs, these results may help in selecting exercises, however the subjects were a randomly selected group of physically active young, adult subjects, and the neuromuscular response to the selected exercises may be different in other populations e.g. highly trained athletes or adolescent subjects. In addition, the implementation of these results may be a challenge in some sports, as the instable surfaces may be less accessible in outdoor settings. Given these limitations, the results of the present study indicate how increasing the instability with balance devices and increasing the dynamics of the exercise may influence the neuromuscular control of the knee joint in young, physically active men and women.
In this explorative trial in healthy, physically active male and female subjects, the neuromuscular activity of the quadriceps and hamstrings increased when the motor task became more dynamic. Specifically jump landings were effective in increasing the hamstring muscle activity. Also increasing the instability introduced by the balance device increased muscle activity, however only when progressing from the Airex to the BOSU. The data also indicated that female subjects increase hamstring muscle activation more than males when using the most unstable balance device. This information may be useful when selecting exercises for knee injury prevention or rehabilitation.
The authors report no conflicts of interest.
Submitted: January 18, 2022 CST, Accepted: December 23, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Faude O, Junge A, Kindermann W, Dvorak J. Risk factors for injuries in elite female soccer players. Br J Sports Med. 2006;40(9):785-790. doi:10.1136/bjsm.20 06.027540
2. Myklebust G, Maehlum S, Engebretsen L, Strand T, Solheim E. Registration of cruciate ligament injuries in Norwegian top level team handball. A prospective study covering two seasons. Scand J Med Sci Sports 1997;7(5):289-292. doi:10.1111/j.1600-0838.1997.tb0 0155.x
3. Pasanen K, Hietamo J, Vasankari T, et al. Acute injuries in Finnish junior floorball league players. JSciMedSport 2017;1878-1861.
4. Waldén M, Krosshaug T, Bjørneboe J, Andersen TE, Faul O, Hägglund M. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases. Br J Sports Med 2015;49(22):1452-1460. doi:10.1136/bjsp orts-2014-094573
5. Montalvo AM, Schneider DK, Silva PL, et al. ‘What’s my risk of sustaining an ACL injury while playing football (soccer)?’ A systematic review with meta-analysis. Br J Sports Med. 2019;53(21):1333-1340. doi:10.1136/bjsports-2016-0 97261
6. Myklebust G, Maehlum S, Holm I, Bahr R. A prospective cohort study of anterior cruciate ligament injuries in elite Norwegian team handball. Scand J Med Sci Sports. 1998;8(3):149-153. doi:10.111 1/j.1600-0838.1998.tb00185.x
7 Molloy MG, Molloy CB. Contact sport and osteoarthritis. Br J Sports Med. 2011;45(4):275-277. d oi:10.1136/bjsm.2011.083956
8. Filbay SR, Ackerman IN, Russell TG, Crossley KM. Return to sport matters-longer-term quality of life after ACL reconstruction in people with knee difficulties. Scand J Med Sci Sports 2017;27(5):514-524. doi:10.1111/sms.12698
9. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med 2005;33(4):492-501. doi:10.1177/036354 6504269591
10. Bencke J, Curtis D, Krogshede C, Jensen LK, Bandholm T, Zebis MK. Biomechanical evaluation of the side-cutting manoeuvre associated with ACL injury in young female handball players. Knee Surg Sports Traumatol Arthrosc 2013;21(8):1876-1881. do i:10.1007/s00167-012-2199-8
11. Simonsen EB, Magnusson SP, Bencke J, et al. Can the hamstring muscles protect the anterior cruciate ligament during a side-cutting maneuver? Scand J Med Sci Sports 2000;10:78-84.
12. Zebis MK, Andersen LL, Bencke J, Kjær M, Aagaard P. Identification of athletes at future risk of anterior cruciate ligament ruptures by neuromuscular screening. Am J Sports Med 2009;37(10):1967-1973. d oi:10.1177/0363546509335000
13. Zebis MK, Aagaard P, Andersen LL, et al. Firsttime anterior cruciate ligament injury in adolescent female elite athletes: a prospective cohort study to identify modifiable risk factors. Knee Surg Sports Traumatol Arthrosc 2021;30(4):1341-1351. doi:10.100 7/s00167-021-06595-8
14. Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med 2010;38(11):2218-2225. doi:10.1177/036354651 0373570
15. Chappell JD, Yu B, Kirkendall DT, Garrett WE. A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med 2002;30(2):261-267 doi:10.1177/0363546 5020300021901
16. Shultz SJ, Nguyen AD, Leonard MD, Schmitz RJ. Thigh strength and activation as predictors of knee biomechanics during a drop jump task. Med Sci Sports Exerc. 2009;41(4):857-866. doi:10.1249/mss.0b013e31 81e3b3f
17 Sell TC, Ferris CM, Abt JP, et al. Predictors of proximal tibia anterior shear force during a vertical stop-jump. J Orthop Res. 2007;25(12):1589-1597. do i:10.1002/jor.20459
18. Solomonow M, Baratta R, Zhou BH, et al. The synergistic action of the anterior cruciate ligament and thigh muscles in maintaining joint stability Am J Sports Med. 1987;15(3):207-213. doi:10.1177/0363546 58701500302
19. Baratta R, Solomonow M, Zhou BH, Letson D, Chuinard R, D’Ambrosia R. Muscular coactivation. The role of the antagonist musculature in maintaining knee stability. Am J Sports Med. 1988;16(2):113-122. doi:10.1177/03635465880160020
20. Li G, Rudy TW, Sakane M, Kanamori A, Ma CB, Woo SL. The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J Biomech. 1999;32(4):395-400. doi:10.101 6/s0021-9290(98)00181-x
21. Bencke J, Zebis MK. The influence of gender on neuromuscular pre-activity during side-cutting. J Electromyogr Kinesiol. 2011;21(2):371-375. doi:10.101 6/j.jelekin.2010.10.008
22. Webster KE, Hewett TE. Meta-analysis of metaanalyses of anterior cruciate ligament injury reduction training programs. J Orthop Res 2018;36(10):2696-2708. doi:10.1002/jor.24043
23. Zebis MK, Bencke J, Andersen LL, et al. The effects of neuromuscular training on knee joint motor control during sidecutting in female elite soccer and handball players. Clin J Sport Med. 2008;18(4):329-337 doi:10.1097/jsm.0b013e31817f3e 35
24. Myklebust G, Engebretsen L, Brækken IH, Skjølberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med 2003;13(2):71-78. doi:10.10 97/00042752-200303000-00002
25. Strom M, Thorborg K, Bandholm T, et al. Ankle joint control during single-legged balance using common balance training devices. IntJSports PhysTher. 2016;11:388-399.
26. Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ 2005;330:449. doi:10.1136/bmj.38330.632801.8f
27 Walden M, Atroshi I, Magnusson H, Wagner P, Hagglund M. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ 2012;344:e3042. do i:10.1136/bmj.e3042
28. Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8(3):383-392. doi:1 0.1002/jor.1100080310
29. Wren TAL, Do KP, Hara R, Rethlefsen SA. Use of a patella marker to improve tracking of dynamic hip rotation range of motion. Gait Posture 2008;27(3):530-534. doi:10.1016/j.gaitpost.2007.07.00 6
30. Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol 2000;10(5):361-374. doi:10.1016/s1050-641 1(00)00027-4
31. Wahl MJ, Behm DG. Not all instability training devices enhance muscle activation in highly resistance-trained individuals. J Strength Cond Res 2008;22(4):1360-1370. doi:10.1519/jsc.0b013e318175 ca3c
32. Harput G, Soylu AR, Ertan H, Ergun N, Mattacola CG. Effect of gender on the quadriceps-to-hamstrings coactivation ratio during different exercises. J Sport Rehabil 2014;23(1):36-43. doi:10.1123/jsr.2012-0120
33. Donath L, Kurz E, Roth R, Zahner L, Faude O. Leg and trunk muscle coordination and postural sway during increasingly difficult standing balance tasks in young and older adults. Maturitas. 2016;91:60-68. do i:10.1016/j.maturitas.2016.05.010
34. Dedinsky R, Baker L, Imbus S, Bowman M, Murray L. Exercises that facilitate optimal hamstring and quadriceps co-activation to help decrease acl injury risk in healthy females: a systematic review of the literature. Int J Sports Phys Ther. 2017;12:3-15.
35. Youdas JW, Hollman JH, Hitchcock JR, Hoyme GJ, Johnsen JJ. Comparison of hamstring and quadriceps femoris electromyographic activity between men and women during a single-limb squat on both a stable and labile surface. J Strength Cond Res 2007;21(1):105-111. doi:10.1519/00124278-20070200 0-00020
36. McCurdy K, O’Kelley E, Kutz M, Langford G, Ernest J, Torres M. Comparison of lower extremity EMG between the 2-leg squat and modified single-leg squat in female athletes. J Sport Rehabil 2010;19(1):57-70. doi:10.1123/jsr.19.1.57
37 Zeller BL, McCrory JL, Kibler WB, Uhl TL. Differences in kinematics and electromyographic activity between men and women during the singlelegged squat. Am J Sports Med 2003;31(3):449-456. d oi:10.1177/03635465030310032101
38. Graham VL, Gehlsen GM, Edwards JA. Electromyographic evaluation of closed and open kinetic chain knee rehabilitation exercises. J Athl Train. 1993;28:23-30.
39. Begalle RL, DiStefano LJ, Blackburn T, Padua DA. Quadriceps and hamstrings coactivation during common therapeutic exercises. J Athl Train 2012;47(4):396-405. doi:10.4085/1062-6050-47.4.01
40. Shultz R, Silder A, Malone M, Braun HJ, Dragoo JL. Unstable Surface Improves Quadriceps:Hamstring Co-contraction for Anterior Cruciate Ligament Injury Prevention Strategies. Sports Health. 2015;7(2):166-171. doi:10.1177/1941738114565088
41. Nagano Y, Ida H, Akai M, Fukubayashi T Gender differences in knee kinematics and muscle activity during single limb drop landing. Knee 2007;14(3):218-223. doi:10.1016/j.knee.2006.11.008
42. Nagano Y, Ida H, Akai M, Fukubayashi T. Effects of jump and balance training on knee kinematics and electromyography of female basketball athletes during a single limb drop landing: pre-post intervention study Sports Med Arthrosc Rehabil Ther Technol 2011;3(1):14. doi:10.1186/1758-2555-3-14
43. Andersen LL, Magnusson SP, Nielsen M, Haleem J, Poulsen K, Aagaard P. Neuromuscular activation in conventional therapeutic exercises and heavy resistance exercises: implications for rehabilitation. Phys Ther 2006;86(5):683-697 doi:10.1093/ptj/86.5.6 83
44. d’Avella A. Modularity for Motor Control and Motor Learning. In: Laczko J, Latash ML, eds. Progress in Motor Control: Theories and Translations Springer International Publishing; 2016:3-19.
45. Calatayud J, Borreani S, Colado JC, Flandez J, Page P, Andersen LL. Exercise and Ankle Sprain Injuries: A Comprehensive Review Phys Sportsmed 2014;42(1):88-93. doi:10.3810/psm.2014.02.2051
46. Sugimoto D, Myer GD, Foss KD, Hewett TE. Specific exercise effects of preventive neuromuscular training intervention on anterior cruciate ligament injury risk reduction in young females: meta-analysis and subgroup analysis. Br J Sports Med 2015;49(5):282-289. doi:10.1136/bjsports-2014-0934
Keywords: functional movement screen, knee valgus moments, netball, unplanned sidestep cut https://doi.org/10.26603/001c.57678
Regular employment of three-dimensional (3D) motion analyses to assess and monitor knee valgus moments; a contributor to non-contact anterior cruciate ligament (ACL) injury; during unplanned sidestep cutting (USC) is costly and time-consuming. An alternative quick-to-administer assessment tool to infer an athlete’s risk for this injury could allow prompt and targeted interventions to mitigate this risk.
This study investigated whether peak knee valgus moments (KVM) during weight-acceptance phase of an unplanned sidestep cut were correlated with composite and component scores of the Functional Movement Screen (FMS™).
Cross-sectional, Correlation
Thirteen female national-level netballers performed six movements of the FMS™ protocol and three trials of USC. A 3D motion analysis system captured lower limb kinetics and kinematics of each participant’s non-dominant leg during USC. Averages of peak KVM across USC trials were calculated and examined for correlations with composite and component scores of the FMS™.
No correlations were found between FMS™ composite or any of its component scores with peak KVM during USC.
The current FMS™ did not show any correlations with peak KVM during USC on the non-dominant leg. This suggests that the FMS™ has limited utility in screening for non-contact ACL injury risks during USC.
Level of Evidence

3
Corresponding author: Lee J.C. Marcus Sport Biomechanics, Singapore Sport Institute, Sport Singapore, Singapore 3 Stadium Drive, Singapore 397630, Singapore marcusleejc@gmail.com
Non-contact anterior cruciate ligament (ACL) injuries make up 70% of all ACL injuries,1 with rapid deceleration, singleleg landing and sidestep-cutting movements being the main contributors.1,2 Females who display poor neuromuscular control of the lower body when performing these high-risk movements resulting in high knee valgus and knee internal rotation moments that could strain the ACL are 4-6 times more susceptible to ACL injury than males.3 While several factors combined may incite an ACL injury,4 high knee valgus moments (KVM) during unplanned sidestep-cutting (USC) can rupture the ACL.3,5 KVM was reported to predict ACL injuries with 73% specificity, 78% sensitivity and an r2 of 0.88.3 Video-based studies have also reported that most ACL ruptures occur during initial foot contact during the weight-acceptance phase of USC when the knee goes into valgus.6–9 USC reportedly results in larger peak frontal knee moments in comparison to a single-leg landing.10
Netball, a team ball-sport with high female participation rates and over 20 million participants globally, involves multiple repetitions of single-leg landing and USC and accounts for many non-contact ACL injuries.11,12 Not only is recovery from ACL injury costly, full return to sport postACL reconstruction can take up to twelve months.13,14
Knee injuries were reported to be the most disabling injury in netball.15 The identification of non-contact ACL injury risk through periodic screening is therefore crucial.
The current gold standard for assessing knee moments during sporting maneuvers involves the use of three-dimensional (3D) motion analysis systems that are costly, time-consuming to operate and often inaccessible to the masses. Consequently, simple-to-administer screening tools are increasingly sought after to replace these sophisticated laboratory-based tests that can be used to infer sporting performance and injury risk. Examples of which include the Landing Error Scoring System and Tuck Jump Assessment that have been used to quickly recognize injurious postures such as knee flexion and valgus angles during double-legged landing that may injure the ACL.16,17 Relating to sport-specific maneuvers such as sidestep-cutting and single-leg landing, where unilateral balance, lateral hip and trunk control, and proper alignment of the lower extremity all contribute to ACL strain,5–7,18,19 a screening tool assessing these elements may be more relevant. An example of this includes the quick and simple-to-administer Y-Balance Test, which is performed unilaterally, replicating the stance after a single-leg landing. Correlations were found between the posteromedial and anterior reach distances with knee flexor and internal rotation moments, respectively, during single-legged jump-landing, and was suggested to be a useful screening tool for inferring knee moments contributing to non-contact ACL injury risk.20 No correlations between the Y-Balance Test and KVM during USC were found. Another screening tool, the Functional Movement Screen (FMS™),21,22 did however show potential to illuminate non-contact ACL injury risks.21,22
The FMS™ assesses seven fundamental movement patterns that require mobility and stability of the body and limbs.20,21 These seven movements include the 1) Deep squat (DS) 2) Hurdle step (HS) 3) In-line lunge (IL) 4) Active straight leg raise (ASLR) 5) Trunk push-up (TP) 6) Rotary stability (RS) and 7) Shoulder mobility. Each movement in the FMS™ is rated by an assessor from 0 to 3 based on their ability to perform the movements without compensatory actions.23,24 A composite score of 14 and below out of the maximum 21 has been associated with high injury risk,25–29 but has also been reported by some studies to be limited in predicting injury 29–32 Notably, when the shoulder mobility test is removed from the seven movements, a stronger correlation was shown to exist between the scores of the other six movements and lower extremity injury 26
While the majority of studies assessed lower extremity injury incidences post-testing, two were able to link the FMS™ scores to injury mechanism. In one study, it was reported that higher composite scorers displayed less spine and frontal plane knee movement during performance of the FMS™ than lower scorers22; both contributing factors to high KVM during the sidestep cut. In another study, clinical measures used to identify knee abduction(valgus) moment probability during a drop jump landing, albeit a proxy measure of actual KVM, found an increased risk for noncontact ACL and lower extremity injuries when FMS™ composite scores were lower than 14.21 Could the FMS™ scores also be used to identify participants who demonstrate high KVM during the sport-specific maneuver of USC and by means of inference indicate risk of non-contact ACL injury?
The purpose of this study was to investigate whether externally applied peak KVM during weight-acceptance phase of USC were correlated with the composite and component scores of the FMS™. The presence of correlations may present a screening tool that can be used to infer KVM, a contributor to non-contact ACL injury, during USC in netball.
Fifteen well-trained female netballers (age: 24.6 ± 2.5 y; height: 1.75 ± 0.1 m; mass: 63.2 ± 7.4 kg) from the Singapore National Open’s team participated in the study. A minimum of eleven participants were required for this study, according to G*power analysis (v3.1.9.2, HeinrichHeine University, Düsseldorf, Germany), to detect a Pearson’s correlation coefficient of r = 0.75 (β = 0.80, α = 0.05, two-tailed). This effect size of r = 0.75 was set based on correlations found in a study by Chorba and colleagues (2010).26 All participants had no pre-existing lower limb injury and were proficient in performing USC on either leg. Participants were briefed that they would perform both the USC and FMS™ with the order randomized to eliminate sequencing effects. In addition, participants were asked to indicate if they were menstruating at the time of testing as it can affect ligament laxity 33 All procedures and forms were approved by the Singapore Sport Institute Institutional Review Board, and all participants provided their informed written consent before data was collected.
Participants performed bilateral USC (Figure 1) at a cut angle of 45o ± 10o toward the left or right by reacting to an arrow presented on a screen in front of them.34 The arrow direction sequence was randomized but counterbalanced in order to minimize anticipation, bias or sequencing effects. Participants were required to perform this task with an approach speed of 4.5 ± 0.5 m/s that was monitored by two pairs of customized timing gates, and react immediately with a sidestep cut in the direction of the arrow displayed on a screen upon passing through the second pair of gates. The 45º ± 10º cut angle was ensured by requiring participants to pivot on the force plate and then run through either pair of cones placed 45º to the left and right from the middle of the force plate. To avoid force plate targeting, participants were instructed to focus on the screen ahead of them during the approach run. Further, a cone was placed in a participant-specific position to demarcate the starting location of each participant, determined during familiarization, so that running with their natural cadence resulted in foot contact on the force plate. Eight familiarization trials were provided for USC.5 For the actual test, a trial was deemed successful when
1) the participant’s entire foot landed completely within the designated force plate and 2) the participant ran through the correct pair of cones after performing USC. Demonstration and familiarization were done prior to testing. Unfortunately, due to logistical reasons and the positioning of the force plate, only data from USC to the right side (i.e., left foot ground contact) could be obtained and analyzed. A total of three successful trials were required from each participant on their left leg. The prior decision was made to assess the left leg, between the two, as it was the non-dominant leg for majority (13 out of 15) of the participants. Females have been reported to suffer from non-contact ACL injuries more frequently on their non-dominant leg.35,36 Participants verbally indicated which leg they would perform a single-leg jump push-off with. This leg was determined as the participants’ dominant leg while the other leg was determined as their non-dominant leg. Consequently, data of only 13 out of 15 participants’, whose left legs were their non-dominant legs, were presented and discussed.

Three-dimensional body kinematics during the USC were captured using twelve 3D opto-reflective motion capture cameras (Vicon Industries Inc., Edgewood, NY, USA) at a sampling rate of 250 Hz. A single 0.6 m by 0.9 m Kistler force plate (Kistler 9287CA Piezoelectric, Winterthur, Switzerland) captured ground reaction forces synchronously at 1000 Hz. Thirty-two retro-reflective markers, following the University of Western Australia (UWA) Lower Limb Model and Marker Set, were affixed to selected anatomical landmarks on each participant to facilitate 3D motion analysis.37 Detailed description of data collection with this marker set set-up and calibration can be found from previous research by Besier and colleagues.37
Captured kinematic and kinetic data were analyzed in Vicon Nexus (version 2.3, Oxford Metric Group, Oxford, UK). Knee moments were calculated, through inverse dynamics, during the weight-acceptance phase of the USC where the peak of KVM occurred, and when the ACL load is high.9 Output moments calculated were externally applied and indicated as “+” for valgus and “-” for varus. Marker trajectories and force plate data were filtered with a lowpass (4th order, zero-lag) Butterworth digital filter at a cutoff frequency of 20 Hz after residual analysis and visual inspection of the data.38 Final KVM value for each participant was presented as the mean of peaks from three successful trials and normalized to their respective heights and masses.
Participants performed the six movements (Figure 2), 1) Deep squat (DS) 2) Hurdle step (HS) 3) In-line lunge (IL) 4) Rotary stability (RS), 5) Active straight leg raise (ASLR), 6) Trunk push-up (TP), of the FMS™ in a randomized sequence, with the shoulder mobility test removed. Demonstration was provided prior to each movement test according to the standardized procedures and verbal instructions described by Cook and colleagues.23,24 Two familiarization trials; necessary in order to eliminate any possible learning effects39; and three test trials per side were required for each movement. An adapted half-point scoring from 0 to 3, in 0.5 increments, was adopted as the original wholenumber scoring had been critiqued to be of low sensitivity where a score of 2 can be achieved in multiple ways.22 Zero point was awarded for participants who experienced any pain while performing any of the movements, and 3 points was awarded for participants who could perform the movements in accordance to the FMS™ guide.23,24 For movements that were performed bilaterally, the scores on the left side were used as only the left KVM, during sidestep cutting to the right, were recorded. Composite scores were obtained by summing the six movement scores, providing a maximum of 18 points. Both appraisers of the FMS™ were trained through a minimum of three weeks of pilot testing and were familiar with the half-point scoring criteria for each movement prior to data collection for the research.
All statistical analyses were done using SPSS (IBM Corp., SPSS Version 22.0, Armonk, NY, USA) with significance level set at p ≤ 0.05. Intra-class correlation coefficients (ICC) (model 2,1) were used to establish interrater and intrarater reliability for the FMS™ composite. Both raters appraised the three participants performing the six move-
Figure 1. Unplanned Sidestep-Cutting (USC)ments of the FMS, that was recorded on video, and repeated this appraisal of the same videos on another separate occasion. Each rater’s score on both occasions were used to assess the intrarater reliability, while both their scores for the second round of appraisal were compared to assess interrater reliability Cohen’s Kappa (κ) was used to determine the interrater reliability of the component (individual movements) scores.25 Kendall’s tau-b (τb) was used to assess the associations between normalized peak KVM with FMS™ composite score and its six component scores; this statistical analysis was chosen due to the small sample size and its ability to compare between continuous and ordinal data (i.e. KVM and FMS™ component scores).40 Means ± standard deviations (SD) are also presented for each variable. All variables were tested for outliers.
ICC displayed good to excellent intra- and inter-rater reliability with single measures ranging from 0.62 to 0.84 at 95% confidence interval, for the FMS™.41 Cohen’s κ displayed a moderate agreement between both raters, κ = 0.50 (95% CI, 0.31 to 0.68), p < 0.01.42 Table 1 details the mean ± SD of KVM and FMS™ composite score, τb and significance level for the various FMS™ scores and peak KVM during USC.
Figure 3 displays the frequency of scores for each movement. No significant correlations were found between peak KVM and any of the seven scores (0.09 < p < 0.95) (Table 1).
The present study examined the correlation between FMS™ scores and peak KVM during USC in well-trained female netballers. The USC tasks were performed on the left leg, corresponding to the non-dominant legs of all participants. While past studies have reported on the FMS™’ ability to predict generic musculoskeletal injury predisposition retrospectively,26–28,43 the current study attempted to identify the relationship between FMS™ scores and peak KVM, a contributor to non-contact ACL injury, during USC, to assess the FMS™ diagnostic utility.30 Neither the composite nor component scores of the FMS™ showed any significant correlations with peak KVM.
To understand why the FMS™ composite score may be able to predict lower extremity injuries in general but has thus far not been able to predict specific injuries, the nature and type of movements tested in the FMS™ need to be examined. The FMS™ requires individuals to perform a series of movements that are meant to illuminate issues with stability, mobility and motor control dysfunction.23 However, the FMS™ is limited in its utility to predict specific sporting injury risks as many athletic movements encompass elements such as power, endurance, and change of direction; elements that differ considerably in nature from the movements tested in the FMS™.23,24,44 Several authors have, however, reported correlations between the composite scores and lower extremity injury risks.25–29 Afterall, the FMS™ component movements test elements of
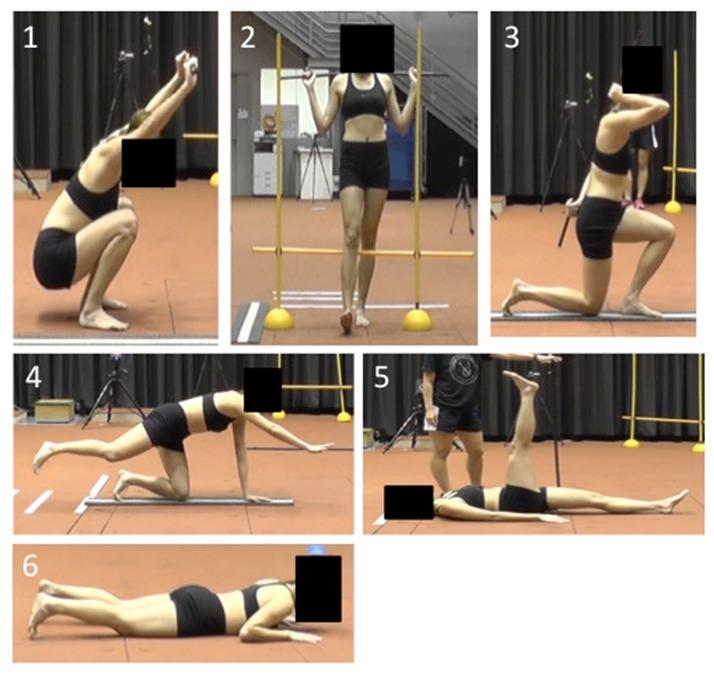 Figure 2. Tested Movements of Functional Movement Screen (FMS™)
Figure 2. Tested Movements of Functional Movement Screen (FMS™)
strength, posture and movement capacities that are related to performance of the lower limb. For example, core strength affects lumbo-pelvic stability, which in turn has a cascading effect on alignment, structural loading, and injury implications of more distal lower limb segments and joints. This is assessed through the TP and RS movements.23,45 Postural stability, an indication of neuromuscular control and contributor to intersegmental joint forces that can strain the lower extremity soft tissue structures, is assessed through the HS and IL.23,46 The lack of hip, knee and ankle range of motion and strength, associated with dysfunctional lower limb biomechanics during sporting movements and increased injury risk, are assessed by the DS, ASLR, HS and IL.23,24,46–48 As a result, when assessing an individual’s ability to perform these various tasks using a composite score, it represents the cumulative propensity for which this individual may be subjected to any or all of the abovementioned risks linked to lower extremity injuries.
Considering the abovementioned, the past authors that found correlations between FMS™ composite scores and lower extremity injury rates assessed injury incidences retrospectively, over a period after the FMS™ was performed.26–28,43 One reason for the correlations found could be that overuse injuries arise from poor movement patterns that are repeatedly performed.23 In which case, it is possible that the poor scores on the FMS™ may associate with eventual injury incidences when these compensatory movement patterns are repeated over time. Another reason could simply be due to an increased exposure to confounding effects in the period between the conducting of FMS™ test and time of injury occurrence.30
In the current study, the FMS™ was investigated specifically for its correlations with peak KVM during USC. With the above explanation regarding the composite score and its higher sensitivity but lower specificity, component scores were also assessed in order to investigate if specific FMS™ movements showed correlations with peak KVM. Amongst the six movements tested, the HS was the most
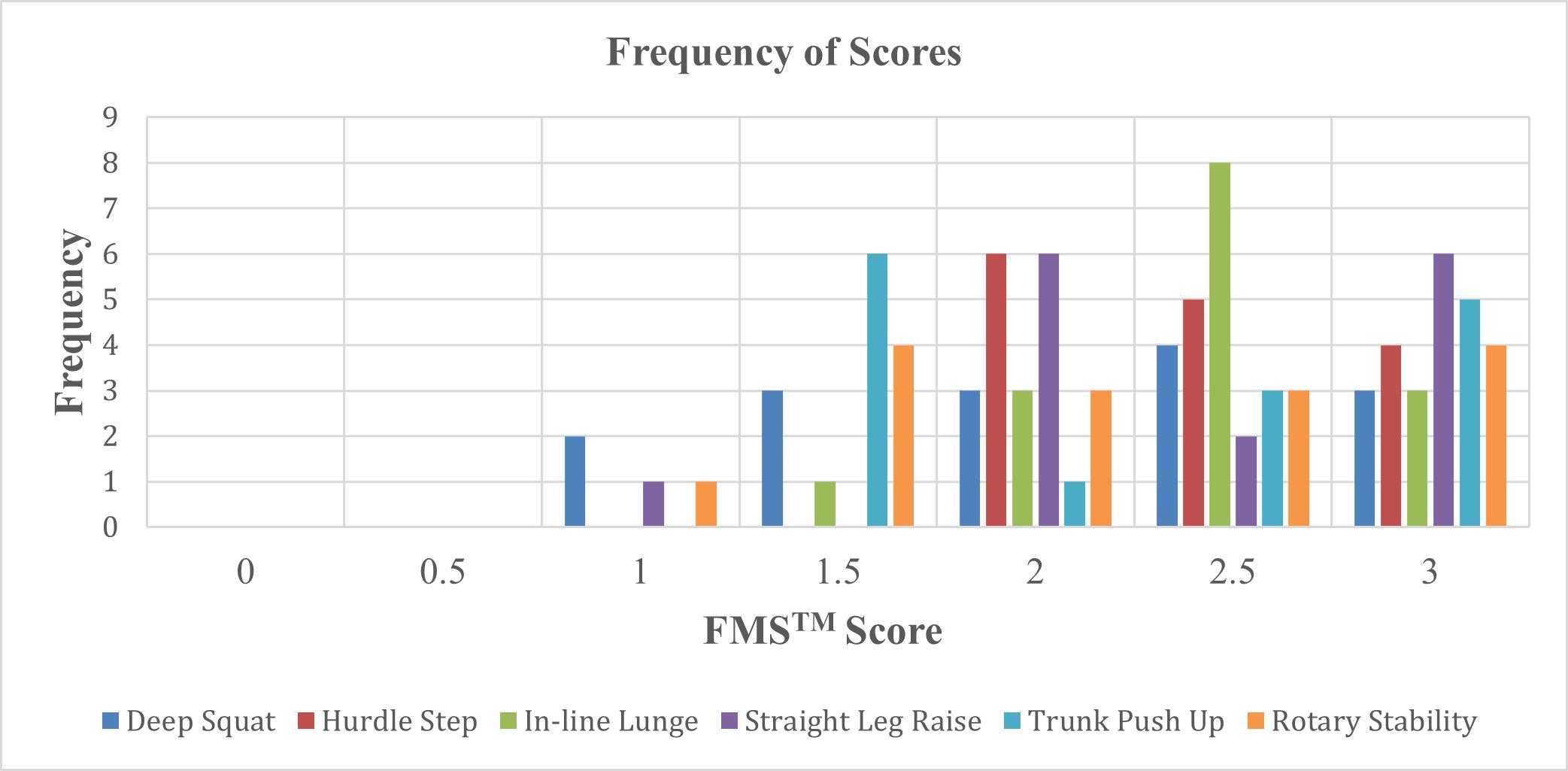
replicable in its posture to that of USC; unsurprisingly, it was also the only component test that showed correlation that approached statistical significance (τb = - 0.39, p = 0.09). Both are performed with an upright single-leg stance where emphasis is on trunk and pelvic stability to maintain dynamic stability, with proper lower extremity alignment while lifting the opposite leg.23 Despite the similarities in posture, neither the HS, nor any other movements displayed significant correlations.
What may be lacking in the FMS™ movements compared with movements in a sport-specific context are the conditions in which these postures are executed. In unplanned scenarios such as USC, the knee can be loaded up to twice that of planned scenarios.49 This raises the utility of the planned FMS™ movements in assessing injury risk during unplanned scenarios. Boey and Lee echoed this supposition when they found correlations between reach distances in the planned Y-Balance Test with knee moments during a planned forward single-leg jump-landing task but not with an USC.20 Additionally, other instances when high KVM were recorded during single-leg stance, participants had either landed from a lateral or diagonal jump50 and/or in the presence of perturbations,51 and/or landed with high velocities such as a running take-off landing.52 It is therefore important that the movement tasks within the selected screening tests encompass some of these aforementioned conditions in order to make it more specific for assessing non-contact ACL injuries. Tran et al. suggested the Landing Error Scoring System to be a better predictor of ACL injury than the FMS™ due to its faster and higher-impact movements; elements present during ACL injury occurrences; assessed compared to the slower controlled movements of the FMS™.53 Alternatively, advanced methods utilizing two-dimensional video to reliably predict 3D knee moments during unplanned sidestepping could be considered most specific in identifying injury risk as the movement assessed is that performed during the sport and can comprise the sport-specific conditions such as an unplanned scenario.54 It is postulated that in order for a screening test to be specific to non-contact ACL injury risk during USC, one or more of the following conditions in the movement task assessed needs to be included: 1) performed in singleleg stance, 2) replicate a similar motor pattern, 3) executed in an unplanned scenario, 4) include a weight-absorption phase, 5) approached from high velocity, and 6) movement in a lateral or diagonal direction.
Unlike a typical exploratory study assessing correlation between a screening test and subsequent injury occurrence, this study investigated if there was a correlation between the FMS™ scores and peak KVM during USC in the lab with the aim of preventing the onset of injury in the first place. Unfortunately, the six-movement version of the FMS™ protocol did not show any such relationships. To identify non-
contact ACL injury risk during specific sporting maneuvers, the FMS™ movements may need to be modified or supplemented to account for the maneuver-specific mechanisms and conditions under which they are performed.
Firstly, the sample size of 15 in this study is small despite our power analysis reporting that 11 was enough to yield a power of 0.8. Secondly, due to logistical reasons, only the left leg; the non-dominant leg for majority of the participants; reflected as USC towards the right, could be assessed. The relationship between FMS™ scores and peak KVM on the dominant leg during USC should also be explored to expand the current findings.
Future research utilizing the FMS™ should consider supplementing it with additional tests to accurately assess dynamic movements. In addition, exploration of the knee flexor and internal rotation moments, that can also contribute to strain of the ACL, during the USC with FMS™ scores may provide new insights on its utility Finally, a larger sample size comprising athletes from more variety of team sports would better confirm any results and allow generalizability to participants of team sports.
The results of this study indicate that there are no significant correlations between six-movement FMS™ scores and peak KVM during USC. The FMS™ as used in past studies may be able to identify generic risk of lower extremity injury due to compensated mechanics which should be corrected promptly before an injury eventually occurs. However, in order to screen for non-contact ACL injury risk during USC, movement tasks within the screening assessment may need to be more similar in mechanism and conditions to that of the maneuver that puts an individual at risk of that injury.
The authors declare no funding resources and no conflict of interest in the authorship and publication of this contribution.
Submitted: February 20, 2022 CST, Accepted: October 10, 2022
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Boden BP, Dean GS, Feagin JA, Garrett WE. Mechanisms of anterior cruciate ligament injury Orthopedics. 2000;23(6):573-578. doi:10.3928/0147-7 447-20000601-15
2. Besier TF, Lloyd DG, Cochrane JL, Ackland TR. External loading of the knee joint during running and cutting maneuvers. Med Sci Sports Exerc 2001;33(7):1168-1175. doi:10.1097/00005768-200107 000-00014
3. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study Am J Sports Med 2005;33(4):492-501. doi:10.1177/03 63546504269591
4. Quatman CE, Hewett TE. The anterior cruciate ligament injury controversy: is “valgus collapse” a sex-specific mechanism? Br J Sports Med. 2009;43(5):328-335. doi:10.1136/bjsm.2009.059139
5. McLean SG, Huang X, van den Bogert AJ. Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: Implications for ACL injury Clin Biomech. 2005;20(8):863-870. doi:10.1016/j.clinbiome ch.2005.05.007
6. Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: Video analysis of 39 cases. Am J Sports Med 2007;35(3):359-367 doi:10.1177/036354650629 3899
7. Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: A systematic video analysis. Am J Sports Med. 2004;32(4):1002-1012. do i:10.1177/0363546503261724
8. Boden BP, Torg JS, Knowles SB, Hewett TE. Video analysis of anterior cruciate ligament injury: Abnormalities in hip and ankle kinematics. Am J Sports Med. 2009;37(2):252-259. doi:10.1177/0363546 508328107
9. Dempsey AR, Lloyd DG, Elliott BC, Steele JR, Munro BJ, Russo KA. The effect of technique change on knee loads during sidestep cutting. Med Sci Sports Exerc 2007;39(10):1765-1773. doi:10.1249/mss.0b013
e31812f56d1
10. Chinnasee C, Weir G, Sasimontonkul S, Alderson J, Donnelly C. A biomechanical comparison of singleleg landing and unplanned sidestepping. Int J Sports Med 2018;39(8):636-645. doi:10.1055/a-0592-7422
11. IFNA. About IFNA. Published 2011. Accessed September 6, 2017. https://web.archive.org/web/2011 0308132327/http://www.netball.org/IFNA.aspx
12. Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national populationbased study J Sci Med Sport 2009;12(6):622-627 do i:10.1016/j.jsams.2008.07.005
13. Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: Risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141-150. doi:10.5435/00124635-20000500 0-00001
14. Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer: NCAA data and review of literature. Am J Sports Med 1995;23(6):694-701. doi:10.1177/03635465950230061
15. McKay GD, Payne WR, Goldie PA, Oakes BW, Stanley JJ. A comparison of the injuries sustained by female basketball and netball players. Aust J Sci Med Sport 1996;28(1).
16. Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE Jr, Beutler AI. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: The jump-ACL Study. Am J Sports Med. 2009;37(10):1996-2002. doi:10.1177/03635465093432 00
17. Myer GD, Ford KR, Hewett TE. Tuck jump assessment for reducing anterior cruciate ligament injury risk. Hubbard TJ, ed. Athl Ther Today 2008;13(5):39-44. doi:10.1123/att.13.5.39
18. Cochrane JL, Lloyd DG, Buttfield A, Seward H, McGivern J. Characteristics of anterior cruciate ligament injuries in Australian football. J Sci Med Sport 2007;10(2):96-104. doi:10.1016/j.jsams.2006.0 5.015
19. Dempsey AR, Lloyd DG, Elliott BC, Steele JR, Munro BJ. Changing sidestep cutting technique reduces knee valgus loading. Am J Sports Med 2009;37(11):2194-2200. doi:10.1177/03635465093343 73
20. Boey D, JC Lee M. The relationship between ybalance test scores and knee moments during singleleg jump-landing in netball. Intl J Sports Phys Ther 2020;15(5):722-731. doi:10.26603/ijspt20200722
21. Landis SE, Baker RT, Seegmiller JG. Non-contact anterior cruciate ligament and lower extremity injury risk prediction using functional movement screen and knee abduction moment: An epidemiological observation of female intercollegiate athletes. Intl J Sports Phys Ther. 2018;13(6):973-984. doi:10.26603/ij spt20180973
22. Frost DM, Beach TAC, Campbell TL, Callaghan JP, McGill SM. An appraisal of the Functional Movement ScreenTM grading criteria – Is the composite score sensitive to risky movement behavior? Phys Ther Sport 2015;16(4):324-330. doi:10.1016/j.ptsp.2015.0
2.001
23. Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: The use of fundamental movements as an assessment of function ‐ part 1. Int J Sports Phys Ther 2014;9(3):396.
24. Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: The use of fundamental movements as an assessment of function‐part 2. Int J Sports Phys Ther. 2014;9(4):549.
25. Schneiders AG, Davidsson Å, Hörman E, Sullivan SJ. Functional movement screenTM normative values in a young, active population. Int J Sports Phys Ther 2011;6(2):75.
26. Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther 2010;5(2):47-54. Accessed December 20, 2021. https://pubmed.ncbi.nl m.nih.gov/21589661/
27 Shojaedin SS, Letafatkar A, Hadadnezhad M, Dehkhoda MR. Relationship between functional movement screening score and history of injury and identifying the predictive value of the FMS for injury Int J Inj Contr Saf Promot 2014;21(4):355-360. doi:1 0.1080/17457300.2013.833942
28. Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? N Am J Sports Phys Ther 2007;2(3):147
29. Bonazza NA, Smuin D, Onks CA, Silvis ML, Dhawan A. Reliability, validity, and injury predictive value of the Functional Movement Screen: A systematic review and meta-analysis. Am J Sports Med. 2017;45(3):725-732. doi:10.1177/036354651664 1937
30. Moran RW, Schneiders AG, Mason J, Sullivan SJ. Do Functional Movement Screen (FMS) composite scores predict subsequent injury? A systematic review with meta-analysis. Br J Sports Med. 2017;51(23):1661-1669. doi:10.1136/bjsports-2016-0 96938
31. Krumrei K, Flanagan M, Bruner J, Durall C. The accuracy of the Functional Movement Screen to identify individuals with an elevated risk of musculoskeletal injury. J Sport Rehabil. 2014;23(4):360-364. doi:10.1123/jsr.2013-0027
32. Dorrel BS, Long T, Shaffer S, Myer GD Evaluation of the Functional Movement Screen as an injury prediction tool among active adult populations: A systematic review and meta-analysis. Sports Health 2015;7(6):532-537. doi:10.1177/1941738115607445
33. Myer GD, Ford KR, Paterno MV, Nick TG, Hewett TE. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med. 2008;36(6):1073-1080. do i:10.1177/0363546507313572
34. Lee MJC, Lloyd DG, Lay BS, Bourke PD, Alderson JA. Effects of different visual stimuli on postures and knee moments during sidestepping. Med Sci Sports Exerc 2013;45(9):1740-1748. doi:10.1249/mss.0b013e 318290c28a
35. Ruedl G, Webhofer M, Helle K, et al. Leg dominance is a risk factor for noncontact anterior cruciate ligament injuries in female recreational skiers. Am J Sports Med 2012;40(6):1269-1273. doi:1 0.1177/0363546512439027
36. Brown SR, Wang H, Dickin DC, Weiss KJ. The relationship between leg preference and knee mechanics during sidestepping in collegiate female footballers. Sports Biomech. 2014;13(4):351-361. doi:1 0.1080/14763141.2014.955047
37 Besier TF, Sturnieks DL, Alderson JA, Lloyd DG. Repeatability of gait data using a functional hip joint centre and a mean helical knee axis. J Biomech 2003;36(8):1159-1168. doi:10.1016/s0021-9290(03)00 087-3
38. Winter DA. Biomechanics and Motor Control of Human Movement John Wiley & Sons, Inc.; 2009. do i:10.1002/9780470549148
39. Okada T, Huxel KC, Nesser TW. Relationship between core stability, functional movement, and performance. J Strength Cond Res. 2011;25(1):252-261. doi:10.1519/jsc.0b013e3181b22b 3e
40. Khamis H. Measures of association: How to choose? J Diagn Med Sonogr. 2008;24(3):155-162. do i:10.1177/8756479308317006
41. Smith CA, Chimera NJ, Wright NJ, Warren M. Interrater and intrarater reliability of the Functional Movement Screen. J Strength Cond Res 2013;27(4):982-987 doi:10.1519/jsc.0b013e3182606df 2
42. Altman DG. Practical Statistics for Medical Research 1st ed. Chapman and Hall/CRC; 1990. doi:1 0.1201/9780429258589
43. Duke SR, Martin SE, Gaul CA. Preseason Functional Movement Screen predicts risk of timeloss injury in experienced male rugby union athletes. J Strength Cond Res 2017;31(10):2740-2747 doi:10.15 19/jsc.0000000000001838
44. Pfeifer CE, Sacko RS, Ortaglia A, et al. Functional Movement ScreenTM in youth sport participants: Evaluating the proficiency barrier for injury Intl J Sports Phys Ther 2019;14(3):436-444. doi:10.26603/ij spt20190436
45. Chuter VH, Janse de Jonge XAK. Proximal and distal contributions to lower extremity injury: A review of the literature. Gait Posture. 2012;36(1):7-15. doi:10.1016/j.gaitpost.2012.02.001
46. Murphy DF, Connolly DAJ, Beynnon BD Risk factors for lower extremity injury: A review of the literature. Br J Sports Med 2003;37(1):13-29. doi:10.1 136/bjsm.37.1.13
47 Kaufman KR, Brodine SK, Shaffer RA, Johnson CW, Cullison TR. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999;27(5):585-593. doi:10.1177/03 635465990270050701
48. Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19(1):76-81. doi:10.1177/036354659101900113
49. Besier TF, Lloyd DG, Ackland TR, Cochrane JL. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33(7):1176-1181. doi:10.1097/00005768-200107 000-00015
50. Sinsurin K, Vachalathiti R, Jalayondeja W, Limroongreungrat W Altered peak knee valgus during jump-landing among various directions in basketball and volleyball athletes. Asian J Sports Med. 2013;4(3):195-200. doi:10.5812/asjsm.34258
51. Stuelcken MC, Mellifont DB, Gorman AD, Sayers MGL. Mechanisms of anterior cruciate ligament injuries in elite women’s netball: A systematic video analysis. J Sports Sci 2016;34(16):1516-1522. doi:10.1 080/02640414.2015.1121285
52. Daneshjoo A, Abu Osman NA, Sahebozamani M, Yusof A. Analysis of jumping-landing manoeuvers after different speed performances in soccer players. Baur H, ed. PLoS One 2015;10(11):e0143323. doi:10.1 371/journal.pone.0143323
53. Tran AA, Shen J, Wernecke C, Gatewood CT, Harris AHS, Dragoo JL. A comparison of the Functional Movement ScreenTM and the Landing Error Scoring System: A cohort study. Curr Orthop Pract 2020;31(1):8-12. doi:10.1097/bco.00000000000 00822
54. Weir G, Alderson J, Smailes N, Elliott B, Donnelly C. A reliable video-based ACL injury screening tool for female team sport athletes. Int J Sports Med 2019;40(3):191-199. doi:10.1055/A-0756-9659/ID/R69 00-0040
1
Biomedical Engineering, Universidad EIA, 2 Department of Orthopedic Surgery, Mayo Clinic, 3 Sports Medicine Center, Mayo Clinic, 4 Alix School of Medicine, Mayo Clinic, 5 United States Olympic & Paralympic Committee, 6 Orthopaedics, The Ohio State UniversityKeywords: ACL injury, sports injury, video review, secondary injury, kinematics https://doi.org/10.26603/001c.67775
Significant effort has gone into the identification and quantification of the underlying mechanisms of primary ACL injury. Secondary ACL injury is observed in approximately 1/4 to 1/3 of athletes who return to sport following ACL reconstruction. However, little has been done to evaluate the mechanisms and playing circumstances surrounding these repeat injuries.
The purpose of this study was to characterize the mechanisms of non-contact secondary ACL injuries using video analysis. It was hypothesized that in video recordings of secondary ACL injury, athletes would exhibit greater frontal plane hip and knee angles, but not greater hip and knee flexion, at 66 ms following initial contact (IC) as compared to at IC and 33ms following IC.
Twenty-six video recordings of competitive athletes experiencing secondary ACL ruptures via noncontact mechanisms were analyzed for lower extremity joint kinematics, playing situation, and player attention. Kinematics were assessed at IC as well as 33 ms (1 broadcast frame) and 66 ms (2 broadcast frames) following IC.
Knee flexion and knee frontal plane angles were greater at 66 ms than IC (p ≤ 0.03). Hip, trunk, and ankle frontal plane angles were not greater at 66 ms than IC (p ≥ 0.22). Injuries were distributed between attacking play (n=14) and defending (n=8). Player attention was most commonly focused on the ball (n=12) or an opponent (n=7). A single-leg landing accounted for just over half of the injuries (54%), while a cutting motion accounted for the remainder of the injuries (46%).

Secondary ACL injury was most likely to occur during landing or a sidestep cut with player attention external to their own body. Knee valgus collapse combined with limited hip motion was identified in the majority of secondary injuries.
Corresponding author:
Nathaniel Bates
Email: batesna@gmail.com
Address: Mayo Clinic 200 First St SW Rochester MN, 55902
Anterior cruciate ligament (ACL) tears present a challenging injury for athletes to recover from and return to sport. While the mechanisms of primary injury have been well defined,1 risk factors and mechanisms for contact and noncontact secondary ACL injury continue to be investigated.
2,3 Risks for both primary and secondary ACL tears occur during sports that involve cutting, pivoting, and landing maneuvers such as basketball, football, rugby, and soccer 4–6 Although surgical treatment and rehabilitation protocols have improved over past few decades thanks to increased research investigation,7 only 63% of athletes, across levels of competition, have been reported to return to pre-injury sports participation level and only 44% returned to competitive sport level following primary ACL reconstruction at a mean follow up of 41.5 months.8 Moreover, with the increasing rate of athletes who return-to-play (RTP) after primary ACL injury, the incidence of secondary ACL injury has become a more prominent topic of interest. Recent studies have reported rates of secondary ACL injury to be between 5-34% of athletes following RTP.9–11
Secondary ACL injuries include both ACL graft ruptures and contralateral (uninjured) side ACL tears. Factors that have been identified that increase the risk of non-contact secondary ACL injury include age, sex, rehabilitation time after primary ACL injury, graft type, biomechanical deficits, lower limb kinematics and muscle strength.10,12 Regarding biomechanical deficits, prospective screening after ACL reconstruction revealed transverse plane hip kinematics and frontal plane knee kinematics during landing, sagittal plane knee moments at landing, and postural stability deficits predict secondary ACL injury (C statistic = .94) with excellent sensitivity (0.92) and specificity (0.88).2,3 More specifically, using the Biodex stability system, Capin et al. found an increase in total frontal plane (valgus) movement, greater asymmetry in internal knee extensor moment at initial contact, and a deficit in single-leg postural stability of the involved limb, to be predictive of secondary ACL injury. In a separate investigation of gait mechanics after primary ACL injury, despite the absence of clinical or gait impairments, athletes who returned to sport sooner were at a greater risk for secondary ACL injury 5 Although identification of functional joint biomechanics during an injury screening movement can provide important information for injury prevention and training, it may not be sufficient to identify athletes at risk for second injury due to biological considerations such as graft maturation, religamentization, and proprioceptive compensation.4,5
In addition to the intrinsic factors and biomechanical mechanisms that contribute to an injury mechanism, player behaviors and the playing situation have also been reported to influence the overall injury mechanism and are important factors to consider in a comprehensive model of injury causation.13 Previously, researchers have used publically
available video footage of injury situations in collegiate and professional basketball games to identify factors such as kinematics, playing situation, and player behavior involved in primary ACL injury mechanisms.14,15 Significant differences were observed in both frontal and sagittal plane kinematics between male and female athletes as measured from video captured during a play where ACL injury occurred.14,15 In addition, analysis of the playing situation and playing behavior indicated that although 72% of the injuries were classified as non-contact, perturbations in the playing environment may have influenced the movement patterns leading to injury 14 However, similar quantifications of scenario and behavior have not been described for secondary ACL injury events.
Publically available high quality video footage of secondary ACL injuries can similarly be evaluated for comprehensive secondary ACL injury mechanism analysis. Therefore, purpose of this study was to characterize the mechanisms of non-contact secondary ACL injuries using video analysis. It was hypothesized that during secondary ACL videos athletes would exhibit greater frontal plane hip and knee angles, but not greater hip and knee flexion, at 66 ms following IC than they would at IC and 33 ms following IC.
An exhaustive google search for news articles was completed using the search terms “ACL injury” AND “Basketball” OR “Soccer” OR “Football” OR “Rugby” OR “AFL” AND “secondary” OR “second”. News articles were used to identify athletes who suffered secondary ACL injury Videos of these injuries were then obtained by searching through publicly available records, highlights, news reports and game replays available from January 2010 through April 2017. A total of 78 videos of non-contact secondary ACL injuries suffered by male and female collegiate and professional athletes across various sports that incorporate jumping and cutting maneuvers were identified and 26 (10 contralateral and 16 graft rupture) were included for analysis (Table 1). From the initial search, 52 videos were excluded due to poor video quality in the frontal or sagittal planes at IC or thereafter. Poor video quality was determined by direct obstruction of the knee or hip during the targeted landing or change of direction event. Furthermore, as this investigation was targeted to non-contact secondary ACL ruptures, contact injuries that were incurred by a direct blow of force to the knee were excluded.
Videos were analyzed in both the frontal and sagittal planes dependent on the camera angles available for each athlete. Out of 26 videos, six allowed for complete angle measurement of the hip and knee joints in both planes, eight were restricted to frontal plane analysis, and twelve were restricted to the sagittal plane. For trunk angles, six
Table 1. Injury breakdown by sport, country, and league.
9 American Football USA NFL
1 American Football USA College
2 Basketball USA NBA
3 Soccer Spain La Liga
1 Rugby Australia NRL
1 Baseball USA MLB
9 Australian Rules Football Australia AFL
NFL= National Football League, NBA= National Basketball Association, MLB= Major League Baseball, NRL=National Rugby League, AFL= Australian Football League
videos allowed for both frontal plane and sagittal plane measurements, eight were restricted to frontal plane only, and twelve were restricted to sagittal plane only
Videos obtained from the internet were recorded using Screencast-O-Matic (free version, Big Nerd Software, Seattle, WA). Full screen recordings were made from broadcast footage and saved in MP4 format and imported to Kinovea (v0.8.15, Kinovea, France). Inter and intrarater reliability of the assessment of angular measurements was established with a subcohort from the total sample of this investigation. Twenty videos were randomly selected to comprise this cohort. Two investigators determined the initial contact (IC) frame for the injured leg in each video and used this as the reference frame for analysis. Initial contact frame was selected as the instant where the athlete’s whole foot had come in contact with the ground. A second set of angular measurements was collected at 33 ms (one broadcast frame) following IC. A third set of angular measurements was collected at 66 ms (two broadcast frames) following IC. Any disagreements between the two investigators were resolved by the senior author Interrater reliability was excellent for frontal and sagittal plane knee (ICC ≥ 0.975), hip (ICC ≥ 0.973), trunk (ICC ≥ 0.977), and ankle dorsiflexion (ICC ≥ 0.973) angle measurements each at IC as well as 33 ms and 66 ms following IC. Once interrater reliability was established, one investigator completed angular analysis of all 26 included videos.
In previous video analysis and simulation-based studies, ACL injury was thought to occur promptly following IC.16,17 More recent literature, however, has shown that an ACL injury event is expected to occur between 0 and 61 ms after IC, with mean time to peak strain roughly 53 ms after IC.18,19 Common media capture frame rate is 30 Hz, therefore, two broadcast frames are expected to be recorded in the injury event period following IC. Because the authors were unable to manipulate the playback rate of publically available video footage, IC as well as 33 ms and 66 ms fol-
lowing IC were examined, which corresponds to one and two frames following IC.
A kinematic joint analysis protocol was designed to extract frontal plane angles (knee valgus-varus, hip abduction-adduction, trunk left-right sway) and sagittal plane angles (knee flexion-extension, hip flexion extension, ankle flexion and trunk flexion; Figure 1). All angle measurements for the kinematic joint analysis protocol (see supplemental file) were completed using Kinovea software. Knee flexion-extension angle was measured as the angle between a line that started immediately superior to the greater trochanter and passed through the femoral epicondyle at the knee and a second line that started at the anterior-posterior midpoint of the ankle and passed through the center of the femoral epicondyle at the knee. Hip flexion-extension angle was measured as the angle between a line that started at the acromion and stopped immediately superior to the greater trochanter and a second line that started immediately superior to the greater trochanter and passed through the center of the femoral epicondyle. Trunk flexion angle was measured as the angle between a vertical line passing through the hip joint and a second line that started at the acromion and ended immediately superior to the greater trochanter Knee varus-valgus angle was measured as the angle between a line that passes through the middle of the femoral shaft and the second line through the middle of the tibial shaft. The femoral shaft was determined by drawing a line perpendicular to the long axis of the thigh, selecting the midpoint of that line, then drawing a second line perpendicular to the first that passes through this midpoint. In the same manner, the tibial shaft was located relative to the shank. The hip abduction-adduction angle was measured as the angle between the femoral shaft line and a second line that was drawn perpendicular to an axis formed between the right and left ASIS or PSIS (dependent on a primarily ventral or dorsal view). Frontal plane trunk angle was measured as the angle between the line perpendicular to the ASIS or PSIS axis and a second line that started at the midpoint of the ASIS or PSIS axis and passed through either C7 or the manubrium (dependent on a primarily ventral or dorsal view). In adherence to previous convention, hip flexion, hip adduction, knee extension, knee adduction, and ankle dorsiflexion were represented as positive values.20 Frontal plane trunk angle was treated as an absolute magnitude of deviation from center.
In addition to angular measurements, several categorical variables were independently assessed from each video by the rater Playing situation was categorized as attacking, defending, or celebrating. Player action was categorized as single-leg landing, double-leg landing, cutting, or pivoting. Player attention was selected based on where the player’s focus appeared to be immediately prior to injury and was categorized as on the ball, on an opponent, on the objective, or on landing.14 Player attention was then considered to be external if it was categorized as on the ball, on an opponent, or on the objective. Internal player attention was determined if the players focus was immediately directed at their feet or foot placement instead of being directed at the playing environment. If the categorical variable was
unclear, that variable was scored as indeterminate for the given video. In addition, each video was classified as a contralateral tear, or a graft rupture based on each athlete’s searchable injury history
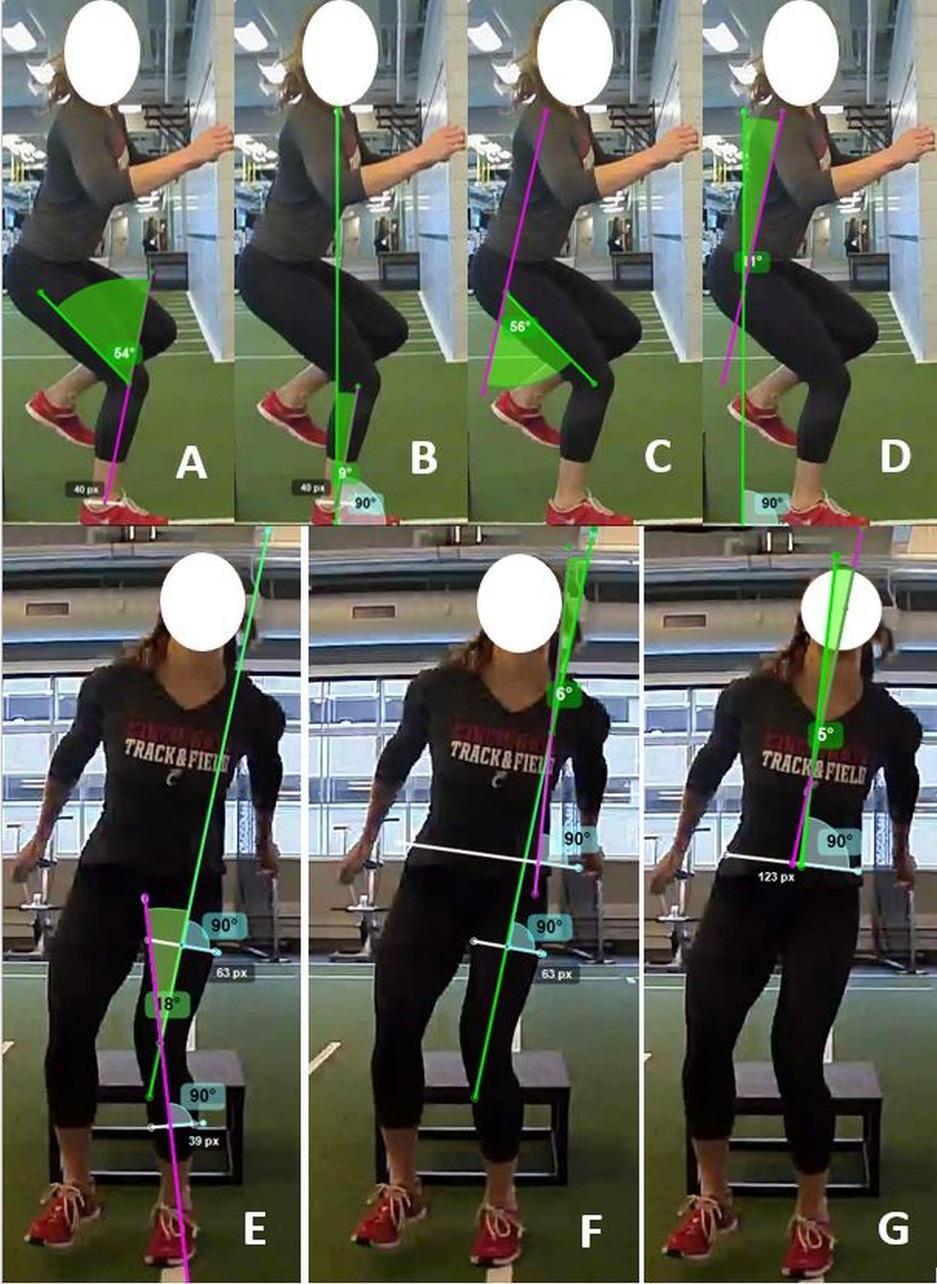
Dependent variables were reported as angles in degrees. Statistical calculations were performed in JMP Pro (version 10, SAS Institute, Inc., Cary, NC, USA) and significance was assessed with a 2x3 ANOVA between contralateral tear and graft rupture as well as between IC, 33 ms, and 66 ms time points. Significance was determined at α < 0.05. A Tukey’s Test was used for time point post-hoc testing between pairs. Interrater reliability was assessed in MATLAB (version 2021b, The MathWorks, Inc., Natick, MA, USA) and was assessed separately for each dependent variable via in-
terclass correlation coefficient (ICC 2-1). ICC values were scored based on previous literature where ICC < 0.4 was poor, 0.4 < ICC < 0.75 was fair-to-good, and ICC > 0.75 was excellent.20–22 A Fisher’s Exact Test was used in order to analyze trends in player characteristics in both the contralateral tear and graft rupture groups.
Of the 26 second injury cases analyzed, 10 cases were contralateral tears and 16 were graft ruptures. Fourteen second injuries occurred while the player was attacking, eight occurred while defending, and the remaining four were a celebration or indeterminate (Table 2). For the present cohort, there were no statistically significant differences between the contralateral tear and graft rupture groups for playing
Figure 1. Examples of kinematic joint angle measurements as dictated by the written protocol (see supplemental file). Sagittal plane measurements: A) knee flexion extension B) hip flexion-extension C) trunk flexion D) ankle flexion. Frontal plane measurements: E) knee varus-valgus F) hip abduction-adduction G) trunk right-left swaysituation, player action, player attention, or ball possession (p ≥ 0.57). However, the raw percentage of athletes in possession of the ball was larger for the contralateral tear group (five cases, 50%) than graft rupture group (seven cases, 44%), while the raw percentage of athletes without the ball was lower in the contralateral group (one case, 14%) than in the graft rupture group (five cases 38%). In two cases in the contralateral group (28%) and three cases for the graft rupture group (23%), injury occurred while the ball was in transition. Sidestep cutting was responsible for just under half of all second injuries observed (Table 1), while single-leg landing constituted the other remaining injuries. Single-leg landing injuries made up 50% of contralateral tears (five cases) and 50% of graft ruptures (eight cases).
Knee valgus collapse was identified in 18 of 26 cases, adduction collapse in one case, no collapse was readily evident in four cases, and three cases could not be accurately judged. The mean knee flexion angle at IC was 40± 17°, while the mean knee abduction angle at IC was 14 ± 8° (Table 3). There were no statistically significant differences between the contralateral and graft rupture groups in frontal or sagittal plane knee angles (p ≥ 0.19). Time point had a significant effect on sagittal and frontal plane knee angle (p = 0.04) as knee flexion angle and knee abduction angle were greater at 66 ms than at IC (p ≤ 0.03).
The mean hip flexion angle at IC was 53 ± 26°, while the mean hip abduction angle at IC was 35 ± 13° (Table 4). Tear type (contralateral, graft rupture) was a significant factor to sagittal plane hip angles (p < 0.01), as the graft rupture group exhibited greater hip flexion than the contralateral
tear group (p = 0.02). There were no statistically significant differences between the two groups in frontal plane hip angles (p = 0.25). Timing was not a significant factor in frontal or sagittal plane hip angles (p ≥ 0.88).
The mean trunk flexion angle at IC was 20 ± 13°, while the mean trunk frontal plane angle at IC was 16 ± 14°, away from center (Table 5). There were no statistically significant differences between the two groups in frontal or sagittal plane trunk angles (p ≥ 0.22). Time point was also not a statistically significant factor (p ≥ 0.82).
The mean ankle dorsiflexion angle at IC was 18 ± 13° (Table 6). Tear type (contralateral, graft rupture) was not a significant factor to ankle dorsiflexion (p = 0.95). Time was also not a significant factor to ankle dorsiflexion (p = 0.39).
The purpose of the current study was to characterize the mechanisms of non-contact secondary ACL injuries using publically available video of the injury event. Joint kinematics, playing situation, and player attention were analyzed to provide comprehensive analysis of the injury mechanism. It was hypothesized that athletes would exhibit greater frontal plane hip and knee angles, but not greater hip and knee flexion, at 66 ms following IC than at IC and 33 ms following IC. No change was observed between IC and 33 ms for any variables of interest. Knee frontal plane motion did support the hypothesis that knee abduction would increase over the observed time period. Additionally, sagittal plane hip angles supported the hypothesis as they did not change over the observed time pe-
*IC = Initial contact
riod. However, contrary to our hypothesis, frontal plane hip angles did not change over the observed time period. In addition, knee flexion at 66 ms following IC did not support the stated hypothesis that athletes would exhibit less knee flexion over the observed time period. Therefore, the initial hypothesis was not fully accepted due to the mixed nature of these results.
In the present study, a clear increase in frontal knee angle from IC to 66 ms following IC was found. This finding supports existing literature, which suggests abduction drives the ACL toward injury 23,24 Hewett et al. previously reported that athletes with ACL injury display up to 2.5 times greater knee abduction moments and 20% higher ground reaction force than uninjured atheltes.24
In addition to increased knee abduction, reduced sagittal plane motion was observed which has been found to be linked to ACL injury 1,25 Previous kinematic analysis has shown there to be greater sagittal plane motion in healthy landings as compared to ACL injury events. Using a threedimensional analysis system, sagittal plane angles at the hip and knee during the first and second landings of a drop vertical jump were evaluated in a cohort of healthy female basketball athletes.26 In these landings, the healthy athletes demonstrated approximately 30° and 60° of change in the sagittal plane at the hip and knee, respectively, from IC to the lowest center of mass position in the first landing. In the second landing of the drop vertical jump, the same athletes demonstrated approximately 20° and 50° change in the sagittal plane at the hip and knee, respectively.26 Analysis of total joint excursion during a drop vertical jump in healthy male elite athletes demonstrated an average of
15.4° and 43.4° change in hip and knee flexion, respectively, for the dominant leg in the first landing.27 In the current analysis of injury events, the average change in sagittal plane angles were 4° and 29° at the hip and knee. In comparison to the joint excursions previously reported during healthy landings, the average joint excursions for hip and knee flexion from IC to 66 ms during an injury event were significantly lower It is important to acknowledge that previous research has reported mixed results for the agreement and correlation between two-dimensional video analysis and three-dimensional kinematics.16,28,29 However, recent research by Schurr et al. demonstrated moderate to strong relationships between two-dimensional analysis and three-dimensional motion capture in lower extremity investigation.30 Additionally, a drop vertical jump does not take into account potential player distraction and cannot be fully compared to an athletic task.
In addition to the combination of increased knee abduction and reduced sagittal motion, lateral trunk motion has been shown to further increase the load on the ACL.31 Lateral trunk movement shifts the ground reaction force vector lateral to the knee, which increases the potential for knee valgus loading and thus ACL strain. Knee valgus motion is a predictor in both primary and secondary ACL injury risk models.1,2 Neuromuscular training studies have identified strategies to modify athletes’ landing techniques to lessen lateral trunk and knee valgus motions to reduce injury risk.32–34
The results of the current investigation did not reveal statistically significant differences between IC and 33 ms; however, a trend toward significance occurred after the 33 ms time point. Knee flexion angle was greater at 66 ms than at IC (p ≤ 0.03). In addition, frontal plane angles trended toward reduced hip adduction at 66 ms. This trend may indicate that the injury occurs somewhere between the 33 ms and 66 ms time points following IC; however, additional studies are necessary to determine the exact timing of an injury event.
In previous primary injury analysis, player attention was most commonly on the basket rim (the objective) (38%), the opponent (28%), or the ball (23%).14 In the present secondary injury analysis, player attention was found to be primarily split between the ball (46%) or an opponent (27%). Rehabilitation programming and future studies should consider the incorporation of diverse training environments and playing situations which challenge player attention (via “distraction” exercises) to assist with secondary ACL injury prevention. Additionally, in comparison to primary injury video analysis, different trends for secondary ACL injury regarding player action and playing situation were observed.14 In the present study, 54% (14/26) of secondary injury events occurred during a single-leg landing while the remaining 46% (12/26) of events occurred during a cutting or pivoting movement. Comparable to the findings of the present study, Krosshaug et al. reported a substantial percentage (26%) of ACL injury events occurred during a single-leg landing. However, they did not
4 ACL injury events involving a direct blow to the knee, the present study only examined non-contact secondary ACL injury events.
*Krosshaug et al. cohort comprised primary 39 ACL injury events
**Vargas et al. (current study) comprised 26 secondary ACL injury events
find a substantial percentage (10%) of ACL injury events which occurred following a cutting or pivoting movement. Furthermore, in primary analysis, 33% of injuries occurred in double-leg landings, while in secondary analysis of the present study 0% of injury events involved a double-leg landing. In both analyses, a larger percentage of injuries occurred while the player was attacking compared to defending. In addition to the inclusion of “distraction” training, which would challenge an athlete’s ability to divide their attention across multiple tasks, preventative programs should include exercises which involve unanticipated landing and cutting movements. Comparisons of player attention, action, and playing situation in primary ACL and secondary ACL injury can be found in Table 7.
While 26 videos of secondary ACL were analyzed in the current study, this does not give a true representation of the prevalence of secondary ACL injuries that occur in these sports. An average of 200,000 ACL injuries occur annually in the United States, and meta-analysis of recent literature
reported that secondary ACL injury rate for athletes younger than 25 is 23%.9,35 Few videos of secondary ACL injuries are publically available. Additional videos of secondary ACL injuries would help strengthen the analysis of secondary ACL injury mechanisms, playing situations, and player behaviors.
Although the use of videos allows for insight into an injury mechanism, previous authors have reported mixed results for the agreement and correlation between two-dimensional video analysis and three-dimensional kinematics.16,28,29 In addition, the publically available video camera angles are not directly aligned with the subject in the frontal or sagittal plane, which may skew video measurements and limit comparison across videos. Furthermore, due to the presence of protective equipment and/or other sport clothing, identification of anatomical landmarks used for joint angle measurements were not exact. Unfortunately, true three-dimensional kinematics or perfectly aligned videos of injury-inducing plays do not exist. Despite the inconsistencies in camera angles, there was excellent reliability of measurement for each of the frontal and sagittal plane angles considered in this analysis. Although an exhaustive search of publically available records was conducted, this study had a limited sample size and small cohort due to poor camera quality and/or angles which could influence the study results. Additionally, it is important to note the inability to account for ground reaction forces in video analysis, as a result, how forces and loads propagated through the closed kinetic chain could not be evaluated. We were unable to appreciate how forces and loads propagated through the closed kinetic chain. Finally, knowledge of the athletes’ injury history as well as the de-
tails of athletes’ primary ACL injury, rehabilitation time, and RTP time were unknown.
Secondary ACL injuries occurred most frequently during single-leg landing and cutting movements. Injuries occurred in both attacking and defensive plays, and most commonly the player was determined to have an external focus, such as the ball or an opponent. Knee valgus collapse was identified in the majority of cases at the time of injury, with knee flexion angle increasing from IC to 66 ms. Additionally, at time of injury, most athletes exhibited a stiff landing in the hip, with no significant changes in hip frontal or sagittal angles from IC to 66 ms. Athletes experiencing secondary ACL injury exhibit frontal and sagittal plane angle deviations in knee kinematics but not hip kinematics following IC. These patterns were consistent whether the secondary injury was on the contralateral limb or a graft rupture. Secondary injury prevention intervention should focus on restricting frontal plane knee motion while mobilizing sagittal plane hip motion. Furthermore, preventative and rehabilitation programming should consider the inclusion of “distraction” training to mimic the athlete’s playing environment.
This investigation was supported by funding from NIH grant R01-AR055563.
Submitted: February 16, 2022 CST, Accepted: October 10, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study Am J Sports Med 2005;33(4):492-501. doi:10.1177/03 63546504269591
2. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 2010;38(10):1968-1978. doi:10.1177/03635465103760 53
3. Paterno MV, Schmitt LC, Ford KR, et al. Dynamic hip rotation deficits predict second anterior cruciate ligament injury after ACL reconstruction and return to sport. Am J Sports Med 2010;38(10):1968-1978. do i:10.1177/0363546510376053
4. Nagelli CV, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and Functional Considerations. Sports Med 2017;47(2):221-232. do i:10.1007/s40279-016-0584-z
5. Capin JJ, Khandha A, Zarzycki R, Manal K, Buchanan TS, Snyder-Mackler L. Gait mechanics and second ACL rupture: Implications for delaying return-to-sport. J Orthop Res. 2017;35(9):1894-1901. doi:10.1002/jor.23476
6. Erickson BJ, Harris JD, Cvetanovich GL, et al. Performance and return to sport after anterior cruciate ligament reconstruction in male major league soccer players. Orthop J Sports Med 2013;1(2):232596711349718. doi:10.1177/2325967113
497189
7 Liukkonen RJ, Ponkilainen VT, Reito A. Revision Rates After Primary ACL Reconstruction Performed Between 1969 and 2018: A Systematic Review and Metaregression Analysis. Orthop J Sports Med 2022;10(8):23259671221110190. doi:10.1177/2325967 1221110191
8. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play Br J Sports Med 2011;45(7):596-606. doi:10.1136/bjsm.2010.076364
9. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and metaanalysis. Am J Sports Med 2016;44(7):1861-1876. do i:10.1177/0363546515621554
10. Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med 2016;44(10):2492-2498. doi:1 0.1177/0363546516648439
11. Wright RW, Magnussen RA, Dunn WR, Spindler KP Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93(12):1159-1165. doi:10.2106/jbjs.j.00898
12. Bates NA, Schilaty ND, Nagelli CV, Krych AJ, Hewett TE. Novel mechanical impact simulator designed to generate clinically relevant anterior cruciate ligament ruptures. Clin Biomech 2017;44:36-44. doi:10.1016/j.clinbiomech.2017.03.00 5
13. Bahr R, Krosshaug T Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med 2005;39(6):324-329. doi:1 0.1136/bjsm.2005.018341
14. Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359-367. doi:10.1177/036354650629 3899
15. Hewett TE, Torg JS, Boden BP Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med 2009;43(6):417-422. doi:10.1136/bjsm.2009.059 162
16. McLean SG, Walker K, Ford KR, Myer GD, Hewett TE, van den Bogert AJ. Evaluation of a twodimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. Br J Sports Med 2005;39(6):355-362. doi:10.1136/bjs m.2005.018598
17. Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002-1012. do i:10.1177/0363546503261724
18. Bates NA, Schilaty ND, Ueno R, Hewett TE. Timing of strain response of the ACL and MCL relative to impulse delivery during simulated landings leading up to ACL failure. J Appl Biomech. 2020;36(3):1-8. doi:10.1123/jab.2019-0308
19. Kiapour AM, Quatman CE, Goel VK, Wordeman SC, Hewett TE, Demetropoulos CK. Timing sequence of multi-planar knee kinematics revealed by physiologic cadaveric simulation of landing: implications for ACL injury mechanism. Clin Biomech. 2014;29(1):75-82. doi:10.1016/j.clinbiomech.2013.1
0.017
20. Ford KR, Myer GD, Hewett TE. Reliability of landing 3D motion analysis: implications for longitudinal analyses. Med Sci Sports Exerc 2007;39(11):2021-2028. doi:10.1249/mss.0b013e3181
49332d
21. Fleiss JL. The Design and Analysis of Clinical Experiments Wiley; 1986.
22. Myer GD, Wordeman SC, Sugimoto D, et al. Consistency of clinical biomechanical measures between three different institutions: implications for multi-center biomechanical and epidemiological research. Int J Sports Phys Ther 2014;9(3):289-301.
23. Bates NA, Schilaty ND, Nagelli CV, Krych AJ, Hewett TE. Multiplanar loading of the knee and its influence on anterior cruciate ligament and medial collateral ligament strain during simulated landings and noncontact tears. Am J Sports Med. 2019;47(8):1844-1853. doi:10.1177/036354651985016 5
24. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study Am J Sports Med 2005;33(4):492-501. doi:10.1177/0363546504269591
25. Pollard CD, Sigward SM, Powers CM. Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments. Clin Biomech. 2010;25(2):142-146. doi:10.1016/j.clinb iomech.2009.10.005
26. Bates NA, Ford KR, Myer GD, Hewett TE. Kinetic and kinematic differences between first and second landings of a drop vertical jump task: Implications for injury risk assessments. Clin Biomech 2013;28(4):459-466. doi:10.1016/j.clinbiomech.201 3.02.013
27 McPherson AL, Dowling B, Tubbs TG, Paci JM. Sagittal plane kinematic differences between dominant and non-dominant legs in unilateral and bilateral jump landings. Phys Ther Sport. 2016;22:54-60. doi:10.1016/j.ptsp.2016.04.001
28. Maykut JN, Taylor-Haas JA, Paterno MV, DiCesare CA, Ford KR. Concurrent validity and reliability of 2D kinematic analysis of frontal plane motion during running. Int J Sports Phys Ther 2015;10(2):136-146.
29. Schurr SA, Marshall AN, Resch JE, Saliba SA. Two-dimensional video analysis is comparable to 3D motion capture in lower extremity movement assessment. Int J Sports Phys Ther 2017;12(2):163-172.
30. Schurr SA, Marshall AN, Resch JE, Saliba SA. Two-Dimensional video analysis is comparable to 3D motion capture in lower extremity movement analysis. Int J Sports Phys Ther 2017;12(2):163-172.
31. Hewett TE, Myer GD The Mechanistic connection between the trunk, knee, and ACL injury. Exerc Sport Sci Rev 2011;39(4):161-166. doi:10.1097/jes.0b013e3 182297439
32. Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med 2013;41(1):203-215. doi:10.1177/03 63546512460637
33. Sugimoto D, Myer GD, McKeon JM, Hewett TE. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a critical review of relative risk reduction and numbers-needed-to-treat analyses. Br J Sports Med 2012;46(14):979-988. doi:10.1136/bjspo rts-2011-090895
34. Di Stasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther 2013;43(11):777-792, A771-711. doi:10.2519/jos pt.2013.4693
35. Marshall SW, Covassin T, Dick R, Nassar LG, Agel J. Descriptive epidemiology of collegiate women’s gymnastics injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train 2007;42(2):234-240.
Keywords: patellofemoral pain, running, central sensitization, peripheral sensitization, pressure pain threshold https://doi.org/10.26603/001c.57603
Patellofemoral pain (PFP) is a common overuse injury among runners, affecting females at a higher rate than males. PFP can often become chronic, with evidence suggesting it may be linked to both peripheral and central sensitization of the nervous system. Sensitization of the nervous system can be identified through quantitative sensory testing (QST).
The primary objective of this pilot study was to quantify and compare pain sensitivity as identified through QST measures, in active female runners with and without PFP
Cohort Study
Twenty healthy female runners and 17 female runners with chronic PFP symptoms were enrolled. Subjects completed the Knee injury and Osteoarthritis Outcome Score for Patellofemoral Pain (KOOS-PF), University of Wisconsin Running Injury and Recovery Index (UWRI), and the Brief Pain Inventory (BPI). QST consisted of pressure pain threshold testing to three local and three distant sites to the knee, heat temporal summation, heat pain threshold, and conditioned pain modulation. Data was analyzed utilizing independent t-tests for comparison of between-group data, effect sizes for QST measures (Pearson’s r), and Pearson’s correlation coefficient between pressure pain threshold values at the knee and functional testing.
The PFP group exhibited significantly lower scores on the KOOS-PF (p<0.001), BPI Pain Severity and Interference Scores (p<0.001), and UWRI (p<0.001). Primary hyperalgesia, identified through decreased pressure pain threshold at the knee, was detected in the PFP group at the central patella (p<0.001), lateral patellar retinaculum (p=0.003), and patellar tendon (p=0.006). Secondary hyperalgesia, a sign of central sensitization, was observed via differences in pressure pain threshold testing for the PFP group at the uninvolved knee (p=0.012 to p=0.042), involved extremity remote sites (p=0.001 to p=0.006), and uninvolved extremity remote sites (p=0.013 to p=0.021).
Corresponding author:

Brian J. Eckenrode
Phone: 215-572-2097
Fax: 215-517-2342
eckenrodeb@arcadia.edu
Compared to healthy controls, female runners with chronic PFP symptoms exhibit signs of both peripheral sensitization. Despite actively participating in running, nervous system sensitization may contribute to continued pain in these individuals. For female runners with chronic PFP, physical therapy management may need to include interventions which address signs of central and peripheral sensitization.
Level 3
Overuse injuries of the lower extremities are common in runners,1 with patellofemoral pain (PFP) reported as the most frequently occurring condition.2 Females have been found to be more than two times more likely to develop PFP when compared to males.3 Multiple theories for the development of PFP have been proposed, including motor performance deficits, movement coordination deficits, mobility impairments, and over-training, but PFP is likely the result of multifactorial contributions.4,5 PFP can often become chronic, with up to 91% of individuals reporting continued pain 4-18 years after the initial diagnosis.6
Sensitization of the nervous system has been proposed as a mechanism to explain chronic musculoskeletal pain.7–10 Both peripheral and central sensitization mechanisms may contribute to enhanced nociceptive drive beyond that seen with typical tissue injury.11 Peripheral sensitization is described as the increased responsiveness and reduced threshold of nociceptive neurons in the periphery to the stimulation of the of their receptive fields; whereas central sensitization is defined as the increased responsiveness of nociceptive neurons in the central nervous system to normal or subthreshold afferent input.12 The chronicity of PFP symptoms may be, in part, explained by changes in sensitization of the nervous system in some individuals.
Pain is highly subjective and is influenced by individual differences in pain perception, and typically assessed clinically through a pain intensity scale.13 One limitation to using a pain intensity scale includes the variability of patient interpretation of pain measurement.14 Quantifying pain is challenging due to the subjective nature of each individual’s pain experience.15 Objective assessment of nervous system sensitivity can be conducted through quantitative sensory testing (QST) via thermal or mechanical measures. QST is a noninvasive way of assessing and quantifying sensory nerve function.16 QST can objectively measure the central and peripheral components of pain, and can detect the facilitation and inhibition of pain.15
Numerous QST measurement tools have been described17–21 including pressure pain threshold, heat pain threshold, temporal summation, and conditioned pain modulation. Mechanical pressure pain threshold is utilized to assess the functioning of A-delta fibers.22 Both local and remote structures can be tested, with primary hyperalgesia determined through increased sensitivity at the site of the injury, and secondary hyperalgesia determined through increased sensitivity at sites remote from the site of injury The presence of widespread mechanical hyperalgesia is
suggestive of a centrally-mediated facilitation mechanism of chronic pain.23 Heat pain threshold testing is also utilized to assess the functioning of A-delta fibers.24 Temporal summation is used to assess the functioning of C-fibers and is a measure of pain facilitation.24 Conditioned pain modulation paradigms are designed to assess for an impairment in pain inhibition.18,22,25 Central nervous system sensitization can be inferred through QST by the presence of secondary hyperalgesia26 or enhanced pain facilitation.18
Several authors have reported signs of central sensitization in individuals with PFP as assessed through QST.27–34
The QST measurement method utilized in a majority of these studies utilized mechanical pressure pain threshold testing. Of these, only Holden et al.27 included temporal summation and conditioned pain modulation (through cuff pressure algometry), and two studies included heat pain threshold and cold pain threshold testing.28,29 No identified studies reported on the QST measures of pressure pain threshold (for the presence of primary and secondary hyperalgesia), heat pain threshold (for the presence of primary hyperalgesia), temporal summation (for the presence of impaired central pain facilitation), and conditioned pain modulation (for the presence of impaired descending inhibition) in patients with PFP. Additionally, of these identified studies, only Pazzinatto et al.32 controlled for the activity level of subjects and found evidence for lower local and remote pressure pain threshold values in female runners with PFP In female runners with chronic PFP, heat pain threshold, temporal summation, and conditioned pain modulation findings have not previously been investigated, nor compared with healthy controls.
The relationship between pain and functional performance remains poorly understood. Individuals with greater localized hyperalgesia (due to peripheral sensitization) from chronic lower extremity conditions have been shown to exhibit impaired lower extremity mechanics that are believed to be related to increased nociceptive input.30 It has been proposed that movement changes which persist beyond the original protective phase of injury may lead to changes in function and further affect recovery.35 A lack of evidence exists for the association of functional performance with measures of primary hyperalgesia in female runners with chronic PFP
The primary objective of this pilot study was to quantify and compare pain sensitivity as identified through QST measures, in active female runners with and without PFP This information will help clinicians and researchers understand which of these QST procedures may be more sensitive to differences in pain between groups. A secondary
objective was to determine if there was an association between a dynamic lower extremity functional performance measure and measures of pain sensitization.
Twenty healthy, pain-free female runners and 20 female runners with chronic PFP symptoms were enrolled for this pilot research study from April 2017 through January 2018. No formal power analysis was performed for this pilot study. Twenty subjects in each group were selected based on similar studies which compared pressure pain threshold values in patients with PFP.32,36 A convenience sample of subjects were recruited from the university community, local running clubs, and local running shoe stores via advertisement flyers and social media postings. The study protocol was approved by the Institutional Review Boards of Arcadia University and Rutgers, The State University of New Jersey All subjects gave informed consent to participate in this study.
Inclusion criteria for all subjects included female sex, age between 18-45 years, and a self-reported involvement in running activity for a minimum of one hour per week. A time-based criterion for running activity was selected to standardize a minimal amount of joint loading time, versus a distance-based criterion. The upper age limit of 45 is consistent with the typical clinical presentation of patients with PFP, and to control for possible effects of degenerative joint disease.37 Inclusion criteria for both groups also included intact skin (no cuts or abrasions to the lower legs that would interfere with the testing), intact sensation via verbal self-report by the subject, and the ability to converse, read, and write in English. Subjects were excluded if they reported a recent musculoskeletal injury that limited participation in running over the prior two weeks, a history of any neurological condition that may affect sensory perception, the presence of any other acute or chronic pain conditions, and use of prescription medication for pain or psychological conditions, as such medications may affect pain perception. Subjects were instructed to not take any over-the-counter pain medication for 24 hours prior to testing.
For the PFP group, inclusion criteria included unilateral or bilateral knee pain of at least 3/10 (during running), pain for at least six weeks prior to enrollment, and clinical examination findings indicative of PFP (e.g., anterior, retropatellar, or peripatellar pain, pain reproduction with knee loading activities or prolonged knee flexion, atraumatic onset, exclusion of other knee pathologies).5 Subjects were initially screened by phone to confirm their anterior knee or retropatellar pain was of an insidious onset for a minimum of six weeks. Additional screening included the presence of knee pain symptoms provoked by at least two of the following activities: prolonged sitting or kneeling, squatting, running, hopping, or stair climbing; and pain intensity with running in the previous week of at least a 3/10 on the Numeric Pain Rating Scale (NPRS). Prior to the initial testing session, subjects in the PFP group underwent a physical examination by a physical therapist to rule out other knee
joint injuries such as ligamentous, tendon or meniscal injury, and to confirm the presence of PFP. Presence of PFP was confirmed if pain was reproduced or worsened with any activities that served as diagnostic criteria for PFP.5
All subjects completed the Knee injury and Osteoarthritis Outcome Score for Patellofemoral Pain and Osteoarthritis (KOOS-PF), the Brief Pain Inventory short-form (BPI), and the University of Wisconsin Running Injury and Recovery Index (UWRI). The KOOS-PF has been shown to be a valid and reliable self-report measure for patients with PFP 38 This is an 11-item knee-specific outcome scale, with a high score of 100 indicating no limitation with daily function and sport activity in addition to the absence of symptoms, and 0 indicating extreme limitations. The KOOS-PF has good test-retest reliability38 and has a published minimally important change of 14.2 points.39
The BPI has been shown to be valid and reliable for measuring pain severity and impact on function.40 It is a nine item self-report questionnaire, which is scored in two parts: pain severity and pain interference. Both parts of the BPI are calculated out of a maximum of 10 points. For pain severity, a 0 indicates no pain and a 10 indicates pain “ as bad as you can imagine”. For pain interference, a 0 indicates no interference and a 10 indicates that pain completely interferes with activity. The minimum clinically important difference (MCID) for the pain severity score has been found to be 2.2 points in patients with fibromyalgia.41 No published MCID for BPI interference score has been identified in the literature.
The UWRI has been shown to be a valid and reliable patient-reported outcome measure to assess issues related to injury recovery, frustration, and training progression following a running related injury 42,43 It is a nine question self-report measure, with a maximum possible score of 36 which indicates no deficit in running ability, with lower scores indicating a greater limitation in running ability The MCID for the UWRI has been found to be eight points.43
Quantification of lower extremity functional performance was conducted via the Y-Balance Test-Lower Quarter (YBTLQ) utilizing the YBT testing kit (Move2Perform, Evansville, IN). Testing of the YBT-LQ was performed following procedures previously published utilizing this measure.44 The YBT-LQ has been described as integrating strength, flexibility, neuromuscular control, stability, range of motion, balance, and proprioception.45 A significant positive correlation has been shown between the YBT-LQ and hip abduction strength.46 The YBT-LQ has demonstrated excellent inter- and intra-rater reliability in healthy individuals.47
All QST measurements were performed by the primary investigator For pressure pain threshold testing, subjects
were positioned supine on a plinth with the knee in full extension, and a handheld pressure algometer with a 1 cm2 tip (Wagner Instruments, Greenwich, CT) was used to apply increasing amounts of pressure (~1kg/sec) to each testing site bilaterally The force was withdrawn as soon as the subject reported that the sensation changed from pressure to pain. Two trials were performed at each location with a minimum of 30 secs of rest in between, with the mean of the two trials used for data analysis. At the knee, two sites were tested: the center of the patella and lateral retinaculum.33 The location of the center of the patella was determined by measuring the midpoint in the mediallateral and superior to inferior direction and determining the center For the lateral patella retinaculum, a point 2 cm lateral to the lateral border of the patella was used. Two sites along the medial aspect of the tibia were also tested. Tibial sites were determined from a measurement from the distal tip of the medial malleolus to the medial tibial condyle. The length of the tibia was divided into thirds, with the distal third and proximal third measurement utilized for pressure pain threshold testing. Additionally, pressure pain threshold testing was performed at the mid-portion of the patellar tendon (mid-point between the inferior pole of the patella and tibial tubercle) and at midquadriceps muscle belly (midline of the anterior thigh, midway between the iliac crest and the superior border of the patella). The patella tendon pressure pain threshold measurement was performed with the subject’s knee flexed to 90 degrees. Pressure pain threshold testing order was performed in the following standardized sequence: right distal tibia, left distal tibia, right central patella, left central patella, right proximal tibia, left proximal tibia, right patellar lateral retinaculum, left patellar lateral retinaculum, right mid-quadriceps, left mid-quadriceps, right patella tendon, left patella tendon. This order was chosen to alternate between extremities to allow adequate time for washout between pain testing, and to provide for separation of potential cutaneous dermatome overlap.
Thermal heat testing was performed using a computercontrolled contact thermode (TSA-II Neurosensory Analyzer, Medoc, Ramat Yishai, Israel) which was fastened to the anterolateral aspect of the knee at the tibiofemoral joint line. The subject was seated in a chair with the dominant (healthy group) or most painful leg (PFP group) extended, facing away from the computer monitor. The temporal summation test consisted of 10 heat pulses which rise rapidly from 42-51°C at 10°C/second at a rate of one pulse every three seconds. During this test, the participant rated their perception of pain intensity for each of the 10 heat pulses using a rating scale following prompts by the investigator This scale consists of a 100mm line with descriptor anchors attached (0mm = no pain, 20mm = pain threshold, 100mm = worst pain imaginable) which was adapted from Staud et al.48 For the heat pain threshold test, the thermode temperature started at 35°C and increased at a rate of 0.5°C/second until the participant indicated a change from perception of warmth to the perception of pain by clicking a mouse to stop the test; or when the temperature reached a maximum of 51°C, whichever came first. Follow-
ing a 60-second rest the test was repeated.49 The mean value of the two trials was used for data analysis.
For the conditioned pain modulation test, subjects were seated with both feet on the floor. A cold water bath with a circulating pump was maintained at a temperature of 6° C and monitored by a digital thermometer. An initial pressure pain threshold rating was recorded at the tibialis anterior on the dominant (healthy group) or most painful lower extremity (PFP group). The anterior tibialis location was the midpoint distance as measured from the medial malleolus to the lateral joint line of the knee. Subjects then placed their dominant hand into the cold water bath for one minute, with subsequent pressure pain threshold measurements recorded at the tibialis anterior 30 and 60 seconds while the was hand submerged. The subject was also asked to report the pain rating at its worst in their hand while submerged at 60 seconds on a 10cm visual analog scale. A standardized video of ocean waves was shown to subjects on a separate computer monitor during the conditioned pain modulation test. This was to provide the subjects with something to look at for distraction from the discomfort while their hand was submerged in the cold water bath.50,51
Statistical analysis was performed with SPSS version 26 (IBM Corporation, Armonk, NY). Means, standard deviations, and/or confidence intervals were calculated for each outcome variable and examined for normality using graphical approaches. Comparison of between-group data were performed with independent t-tests. The most painful knee was utilized for data collection for those in the PFP group with bilateral symptom complaints (n=4). For the healthy control group, no significant difference was found between extremities for the healthy control group for all pressure pain threshold sites, so the dominant extremity was utilized for comparison with the involved extremity of the PFP group. For all statistical calculations, a p value < 0.05 was considered significant. Effect sizes for QST measures (Pearson’s r) from the independent t-tests were calculated, with the following interpretation: ≥ 0.1 a small effect, ≥ 0.3 a medium effect, and ≥ 0.5 a large effect. Correlations between pressure pain threshold values at the knee and functional testing were assessed via Pearson’s correlation coefficient.
From September 2017 through June 2018, a total of 40 subjects (20 with PFP and 20 healthy controls) participated in the study Three subjects with PFP were excluded from data analysis, as they had reported a past knee surgery (two with a prior anterior cruciate ligament reconstruction and one with a medial meniscus repair). A total of 17 subjects with PFP and 20 healthy controls were included in the final analysis (Table 1). The participant characteristics are presented in Table 1. There were no significant differences between groups for age (t(35)= -1.735, p=0.091), BMI (t(35)=
Table 1. Subject characteristics, presented as mean ± standard deviation
BMI, body mass index; cm, centimeters; kg, kilograms; m, meters; N, number; PFP, patellofemoral pain a Values are mean (95% confidence interval) (Independent t-test)
Table 2. Between-group comparison of pain and self-reported measures.
BPI, Brief Pain Inventory; KOOS-PF, Knee injury and Osteoarthritis Outcome Score for Patellofemoral Pain and Osteoarthritis; n, number; NPRS, numeric pain rating scale; PFP, patellofemoral pain; UWRI, University of Wisconsin Running Injury and Recovery Index Boldface indicates large effect, r≥.5 a Values are mean (95% confidence interval) (Independent t-test)
1.208, p=0.235), years of running (t(35)= -.599, p=0.553), and average weekly running mileage (t(35)= -.933, p=0.357).
Table 2 presents the between group comparison of pain and self-reported function. There was a significant difference between groups for worst pain (t(35)=4.655, p<0.001), pain severity score (t(35)=5.064, <0.001), and pain interference score (t(35)=3.365, p=0.002), with a large effect for worst pain (r=.619) and pain severity score (r=.650) and medium-to-large effect for pain interference score (r=.495). Significant and very large differences were found for the self-report functional outcomes of KOOS-PF (t(35)=12.676, p<0.001, r=.906)) and UWRI (t(35)=-7.882, <0.001, r=.800).
For QST testing, a significant difference was found at all sites tested for pressure pain threshold between the PFP group and healthy controls (Table 3). A lower value on pressure pain threshold is indicative of an increase in sensitivity of the tested structure. Both local (patellar retinaculum, patellar tendon, and central patella) and remote sites (midportion quadriceps, distal tibia, and proximal tibia) were significantly different between groups with a medium to large effect sizes. No significant difference was detected for heat pain threshold (t(35)=-12.69, p=0.213), temporal summation (t(35)=-.544, p=0.590), or conditioned pain modulation (t(35)=.230, p=0.819) between groups (Table 3).
In terms of lower extremity functional performance as assessed via the YBT-LQ, no significant difference was found between groups for anterior reach distance, posteromedial reach distance, posterolateral reach distance, or
composite score (Table 4). A weak and non-significant relationship was found for YBT-LQ composite score and pressure pain threshold at the central patella for the involved knee (r=-.310, p=0.227) and uninvolved knee (r=-.161, p=0.538). Additionally, a weak and non-significant relationship was found for YBT-LQ composite score and pressure pain threshold at the central patella for the dominant knee (r=.292, p=0.211) and non-dominant knee (r=.253, p=0.281). A scatterplot summarizes the correlation results in Figure 1 and 2
Compared to healthy controls, female runners with chronic PFP symptoms exhibit signs of both peripheral sensitization, via reduced pressure pain threshold to sites local to the knee, and central sensitization, as determined through reduced pressure pain threshold to remote sites in the lower extremities. These widespread findings of hypersensitivity at remote sites from the involved knee is commonly interpreted as resulting from central sensitization.18,52,53 The additional QST measures of heat pain threshold, temporal summation, and conditioned pain modulation were not found to be significantly different between those with and without PFP symptoms.
Primary hyperalgesia, a sign of peripheral sensitization, was indicated through the reduced pressure pain threshold at local structures of the involved knee, which in this study
Table 3. Between-group comparison of pressure pain threshold values, heat pain threshold, temporal summation, and conditioned pain modulation.
(Note: Dominant extremity used for comparison with involved extremity; non-dominant extremity used for comparison with uninvolved extremity)
Key: C, Celsius; kg, kilograms; n, number; PPT, pressure pain threshold
a Values are mean (95% confidence interval) (Independent t-test)
b Defined as the pain rating difference between the last and first heat stimuli.
Key: cm, centimeters; n, number
a Values are mean (95% confidence interval) (Independent t-test)
included the central patella, patella retinaculum, and patella tendon. Additionally, secondary hyperalgesia, a sign of central sensitization, was determined through the reduced pressure pain threshold values at remote sites from the involved knee, which included the involved and uninvolved distal tibia, proximal tibia, and mid-portion quadriceps, and uninvolved central patella, patella retinaculum, and patella tendon. Pressure pain threshold values were found to be significantly lower at all locations tested in both the involved and uninvolved lower extremities of the
PFP group when compared to the healthy control group. This widespread hyperalgesia suggests that central sensitization may contribute to the chronic pain state in females with patellofemoral pain. Such nervous system sensitization has been demonstrated in other lower extremity musculoskeletal conditions such as osteoarthritis,54 patellar tendinopathy,55 and Achilles tendinopathy 56
The results of this study are similar to findings from two recent systematic reviews and meta-analyses which found the presence of pain sensitization in patients with PFP as
kg,
kg,
assessed with pressure pain threshold.57,58 A medium to large effect was found for decreased pressure pain threshold at all sites, both local and remote, in female runners with chronic PFP. Conclusions from Bartholomew et al.57

similarly noted a medium effect for pressure pain threshold local to the knee and small effect distal to the knee. Contrary to these findings, Rathleff et al.51 did not find evidence for an impaired pain state in individuals with PFP
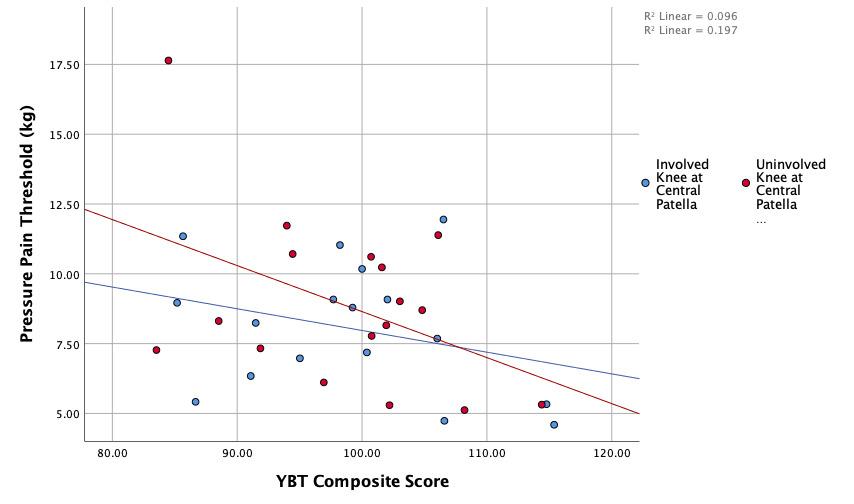 Figure 1. Scatterplot of pressure pain threshold measures at the central patella versus the YBT-LQ composite score for subjects in the PFP group.
kilograms; PFP, patellofemoral pain; YBT-LQ, Y balance test-lower quarter
Figure 2. Scatterplot of pressure pain threshold measures at the central patella versus the YBT-LQ composite score for subjects in the healthy control group.
kilograms; PFP, patellofemoral pain; YBT-LQ, Y balance test-lower quarter
Figure 1. Scatterplot of pressure pain threshold measures at the central patella versus the YBT-LQ composite score for subjects in the PFP group.
kilograms; PFP, patellofemoral pain; YBT-LQ, Y balance test-lower quarter
Figure 2. Scatterplot of pressure pain threshold measures at the central patella versus the YBT-LQ composite score for subjects in the healthy control group.
kilograms; PFP, patellofemoral pain; YBT-LQ, Y balance test-lower quarter
with pressure pain threshold measures. Rathleff et al51 included both males and females in their study which may have affected their findings as females have been shown to exhibit lower pain thresholds (thermal and mechanical) as compared to males.59,60 Increased pain sensitivity in females may be suggestive of a less efficient endogenous pain mechanisms in females.61 More research is needed to help understand the link between sex and increased pain sensitivity.
Regarding heat pain threshold, temporal summation, and conditioned pain modulation, there were no significant differences found for these measures between females with chronic PFP symptoms and healthy controls. QST measures can provide information about the processing of sensory inputs and the facilitation or inhibition of the nervous system.15 While differences were found in pressure pain threshold, a mechanical stimulus which targets A-delta fibers,24 the other QST measures did not achieve statistical significance between groups. Different QST tools are often used to assess different pain pathways. The lack of significant findings, aside from pressure pain threshold, between groups may be explained by the lack of disability (via KOOS-PF scores) in the current study population or the fact that PFP symptoms may not necessarily affect all pain pathways.
Heat pain threshold was not found to be different between groups in this study. This result is similar to two studies that compared heat pain threshold at the involved knee of subjects with PFP to both the uninvolved knee and healthy controls.28,29 Hence, differences in heat pain threshold may not be present in individuals with chronic PFP symptoms. Thermal sensory deficits in the painful region are commonly found in patients who present with neuropathic pain,62 and the lack of difference with thermal testing in this study may indicate that neuropathic pain symptoms were not prevalent in the this group of subjects with PFP
Temporal summation is another potential sign of central sensitization.48,63 Impaired temporal summation of pain levels have previously been demonstrated in individuals with fibromyalgia,48 osteoarthritis,64 temporomandibular disorder,65 and migraine headache.66 No significant difference was found between groups in temporal summation in this study Two previous studies assessed temporal summation via cuff pressure in patients with PFP but reported conflicting results.27,67 Rathleff et al.67 found no between group difference in female subjects with PFP compared to pain-free controls, whereas Holden et al.27 reported a significant difference in elevated temporal summation pain levels (effect sizes were not reported in either study). Similar to this study, Rathleff et al.67 included subjects with PFP of which 80% were currently involved in sports despite their pain. Perhaps maintaining an individual’s activity level may help to modulate this measure of central facilitation. Additionally, the elevated temporal summation levels reported by Holden et al.27 may be attributed to the high chronicity rate of subjects with PFP (subjects with a mean of 8 years duration of symptoms) compared to this study and Rathleff
et al.67 Facilitated central pain mechanisms have been shown to worsen with a greater duration of symptoms.68 Impaired conditioned pain modulation is indicative of impaired descending inhibition of pain. The inability of a noxious conditioning stimulus to increase pain thresholds may signify a potential deficiency in the body’s endogenous pain modulation system.67 No significant difference was found for conditioned pain modulation using cold water immersion between groups in this study. These findings are similar to those published on individuals with PFP by Rathleff et al.51 who also used cold water immersion for the conditioned stimulus, but in contrast to the results of Rathleff et al.67 and Holden et al.27 who did find impaired conditioned pain modulation utilizing cuff pressure as the conditioned stimulus. The differences in methodology of the noxious conditioning stimulus may explain the inconsistent findings for impaired conditioned pain modulation in patients with PFP. Oono et al.69 found that conditioned pain modulation paradigms with different noxious stimuli may yield different results.51 Less efficient conditioned pain modulation has been reported in other chronic musculoskeletal pain conditions such as chronic low back pain,70 neck pain,71 and temporomandibular disorders.72 This study found no difference in conditioned pain modulation, which may have been offset by the high level of physical activity of the participants with PFP Engagement in cardiovascular exercise and knee-loading activity may help minimize impairments in descending pain inhibition.
There was a significant difference in pain rating between a group of healthy controls and subjects with chronic PFP, which was expected as the inclusion criteria consisted of a minimum pain rating at worst of 3/10 on the NPRS. Additionally, the BPI pain severity score and BPI pain interference score were significantly worse in the PFP group. These differences between groups suggest indirect evidence of a relationship between subjective pain rating and functional scores. Both the KOOS-PF and UWRI, subjective measures of functional ability, demonstrated significant differences between groups. Even though the subjects with chronic PFP symptoms continued to engage in running activity, their scores on these scales reflect measurable impaired function. A large effect for KOOS-PF and UWRI were found between groups.
A secondary objective of this study was to determine if there is an association between a dynamic lower extremity functional performance measure and quantitative measures of pain. The YBT-LQ was included as a measure of functional performance due to its ease of application, good test-retest reliability, and applicability to the athletic population, in addition to being positively correlated with hip abduction strength.46 Decreased hip force production, including hip abduction) has been demonstrated in individuals with PFP 5 Since the only significant measure between groups was pressure pain threshold, functional performance on the YBT-LQ was compared with pressure pain threshold values at the central patella. The central patella location was the predominant location of pain in the PFP group and exhibited the largest effect size. No significant association was found between YBT-LQ anterior reach and
pressure pain threshold values at the center patella in either group. For correlation between pressure pain threshold at the central patella and YBT-LQ scores, there was a negative correlation for subjects in the PFP group and a positive correlation for the subjects in the heathy group. The YBT-LQ may not be effective in identifying movement dysfunction in subjects with chronic PFP symptoms. Further research is need to better understand the influence of pain on movement.
There was also no significant difference in reach distance or composite score between the PFP and healthy control groups. Although the YBT-LQ was designed to predict lower extremity injury,73 this test was not able to discriminate between female runners with and without PFP symptoms. For the anterior reach portion on the YBT-LQ, there was a lack of significant difference between groups. In addition, the mean anterior reach difference between sides was less than 3cm for both groups in this study. The lack of a significant difference and clinically meaningful difference in the anterior reach portion of the YBT between the PFP group and healthy control may be explained by the fact that the knee pain may not have been high enough to contribute to alterations in lower extremity functional movement.
Limitations of this study include the small sample size and lack of pressure pain threshold assessment outside of the lower extremity Three subjects with PFP were excluded from data analysis due to a history of prior knee surgery, which affected the overall sample size in this study Due to the potential structural changes from the surgery and possibility that their knee symptoms may be related to their surgery, it was determined post hoc to exclude them from analysis. Heat pain threshold was not assessed outside of the local site of pain. A standardized temperature for temporal summation testing was utilized for all subjects, whereas an individually determined value for peak temperature in the temporal summation test may have provided different results. Formally assessing strength of the lower
extremity via hand held dynamometry or isokinetics, may have yielded better insight on the strength of the lower extremity musculature as opposed to the YBT-LQ Other functional performance tools should be considered in future investigations to help determine if subjects with chronic musculoskeletal present with impaired movement patterns.
The findings of this study provide additional evidence for the use of pressure pain threshold to help determine the presence of signs of peripheral and central sensitization in individuals with chronic PFP. Physical therapy management may need to consider interventions which address the signs of central sensitization in order to achieve optimal outcomes and recovery Future studies should focus on investigating what interventions may lead to favorable changes in nervous system sensitization specifically for runners with chronic knee pain complaints.
Female runners with chronic PFP exhibit signs of both peripheral and central sensitization through pressure pain threshold testing. However, the presence of impaired central pain facilitation and descending pain inhibition were not evident in a population of active female runners with chronic PFP symptoms. Thus, interventions to address the nervous system sensitization may be needed in some patients in order to achieve optimal outcomes.
The authors have no conflicts of interest to disclose.
Submitted: July 22, 2022 CST, Accepted: October 10, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD A retrospective casecontrol analysis of 2002 running injuries. Br J Sports Med 2002;36(2):95-101. doi:10.1136/bjsm.36.2.95
2. Francis P, Whatman C, Sheerin K, Hume P, Johnson MI. The proportion of lower limb running injuries by gender, anatomical location and specific pathology: a systematic review J Sports Sci Med 2019;18(1):21-31.
3. Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725-730. doi:10.1111/j.160 0-0838.2009.00996.x
4. Davis IS, Powers CM. Patellofemoral pain syndrome: proximal, distal, and local factors, an international retreat, April 30-May 2, 2009, Fells Point, Baltimore, MD J Orthop Sports Phys Ther 2010;40(3):A1-16. doi:10.2519/jospt.2010.0302
5. Willy RW, Hoglund LT, Barton CJ, et al. Patellofemoral pain. J Orthop Sports Phys Ther 2019;49(9):CPG1-CPG95. doi:10.2519/jospt.2019.030
6. Stathopulu E, Baildam E. Anterior knee pain: a long-term follow-up. Rheumatology 2003;42(2):380-382. doi:10.1093/rheumatology/keg09
7 Coronado RA, Simon CB, Valencia C, George SZ. Experimental pain responses support peripheral and central sensitization in patients with unilateral shoulder pain. Clin J Pain 2014;30(2):143-151. doi:1 0.1097/ajp.0b013e318287a2a4
8. Plinsinga ML, Brink MS, Vicenzino B, van Wilgen CP Evidence of nervous system sensitization in commonly presenting and persistent painful tendinopathies: a systematic review J Orthop Sports Phys Ther 2015;45(11):864-875. doi:10.2519/jospt.20
15.5895
9. Rees JD, Maffulli N, Cook J. Management of tendinopathy Am J Sports Med 2009;37(9):1855-1867. doi:10.1177/036354650832428
11. Skou ST, Simonsen O, Rasmussen S. Examination of muscle strength and pressure pain thresholds in knee osteoarthritis: test-retest reliability and agreement. J Geriatr Phys Ther 2015;38(3):141-147 d oi:10.1519/jpt.0000000000000028
12. Terminology. International association for the study of pain. Published April 19, 2022. Accessed September 12, 2022. https://www.iasp-pain.org/resou rces/terminology/
13. Birnie KA, McGrath PJ, Chambers CT When does pain matter? Acknowledging the subjectivity of clinical significance. Pain. 2012;153(12):2311-2314. d oi:10.1016/j.pain.2012.07.033
14. Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94(2):149-158. doi:10.1016/s0 304-3959(01)00349-9
15. Uddin Z, MacDermid JC. Quantitative sensory testing in chronic musculoskeletal pain. Pain Med 2016;17(9):1694-1703. doi:10.1093/pm/pnv105
16. Siao P, Cros DP. Quantitative sensory testing. Phys Med Rehabil Clin N Am 2003;14(2):261-286. doi:10.10 16/s1047-9651(02)00122-5
17. Arendt-Nielsen L, Graven-Nielsen T. Translational musculoskeletal pain research. Best Pract Res Clin Rheumatol 2011;25(2):209-226. doi:10.1016/j.berh.20 10.01.013
18. Arendt-Nielsen L, Morlion B, Perrot S, et al. Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur J Pain 2018;22(2):216-241. doi:10.1002/ejp.1140
19. Arendt-Nielsen L, Yarnitsky D Experimental and clinical applications of quantitative sensory testing applied to skin, muscles and viscera. J Pain. 2009;10(6):556-572. doi:10.1016/j.jpain.2009.02.002
20. Rolke R, Magerl W, Campbell KA, et al. Quantitative sensory testing: a comprehensive protocol for clinical trials. Eur J Pain 2006;10(1):77-88. doi:10.1016/j.ejpain.2005.02.003
10. Rio E, Moseley L, Purdam C, et al. The pain of tendinopathy: physiological or pathophysiological? Sports Med 2014;44(1):9-23. doi:10.1007/s40279-01 3-0096-z
21. Yarnitsky D. Conditioned pain modulation (the diffuse noxious inhibitory control-like effect): its relevance for acute and chronic pain states. Curr Opin Anaesthesiol. 2010;23(5):611-615. doi:10.1097/aco.0b 013e32833c348b
22. Sluka K. Central pain mechanisms. In: Sluka K, ed. Mechanisms and Management of Pain for the Physical Therapist IASP Press; 2009:41-72.
23. Woolf CJ, Salter MW Neuronal plasticity: increasing the gain in pain. Science. 2000;288(5472):1765-1769. doi:10.1126/science.288.5 472.1765
24. Sluka KA. Mechanisms and Management of Pain for the Physical Therapist 2nd ed. Wolters Kluwer; 2016.
25. Staud R. The important role of CNS facilitation and inhibition for chronic pain. Int J Clin Rheumtol. 2013;8(6):639-646. doi:10.2217/ijr.13.57
26. Heales LJ, Lim EC, Hodges PW, Vicenzino B. Sensory and motor deficits exist on the non-injured side of patients with unilateral tendon pain and disability—implications for central nervous system involvement: a systematic review with meta-analysis. Br J Sports Med 2014;48(19):1400-1406. doi:10.1136/ bjsports-2013-092535
27 Holden S, Straszek CL, Rathleff MS, Petersen KK, Roos EM, Graven-Nielsen T. Young females with long-standing patellofemoral pain display impaired conditioned pain modulation, increased temporal summation of pain, and widespread hyperalgesia. Pain 2018;159(12):2530-2537 doi:10.1097/j.pain.000
0000000001356
28. Jensen R, Hystad T, Kvale A, Baerheim A. Quantitative sensory testing of patients with long lasting patellofemoral pain syndrome. Eur J Pain. 2007;11(6):665-676. doi:10.1016/j.ejpain.2006.10.007
29. Jensen R, Kvale A, Baerheim A. Is pain in patellofemoral pain syndrome neuropathic? Clin J Pain. 2008;24(5):384-394. doi:10.1097/ajp.0b013e318
1658170
30. Noehren B, Shuping L, Jones A, Akers DA, Bush HM, Sluka KA. Somatosensory and biomechanical abnormalities in females with patellofemoral pain. Clin J Pain 2016;32(10):915-919. doi:10.1097/ajp.000
0000000000331
31. Pazzinatto MF, de Oliveira Silva D, Barton C, Rathleff MS, Briani RV, de Azevedo FM. Female adults with patellofemoral pain are characterized by widespread hyperalgesia, which is not affected immediately by patellofemoral joint loading. Pain Med. 2016;17(10):1953-1961. doi:10.1093/pm/pnw06
32. Pazzinatto MF, de Oliveira Silva D, Pradela J, Coura MB, Barton C, de Azevedo FM. Local and widespread hyperalgesia in female runners with patellofemoral pain are influenced by running volume. J Sci Med Sport 2017;20(4):362-367 doi:10.1 016/j.jsams.2016.09.004
33. Rathleff MS, Roos EM, Olesen JL, Rasmussen S, Arendt-Nielsen L. Lower mechanical pressure pain thresholds in female adolescents with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2013;43(6):414-421. doi:10.2519/jospt.2013.4383
34. van der Heijden RA, Rijndertse MM, BiermaZeinstra SMA, van Middelkoop M. Lower pressure pain thresholds in patellofemoral pain patients, especially in female patients: a cross-sectional casecontrol study. Pain Med. 2018;19(1):184-192. doi:10.1 093/pm/pnx059
35. Butera KA, Fox EJ, George SZ. Toward a transformed understanding: from pain and movement to pain with movement. Phys Ther. 2016;96(10):1503-1507 doi:10.2522/ptj.20160211
36. Rathleff MS, Roos EM, Olesen JL, Rasmussen S, Arendt-Nielsen L. Self-reported recovery is associated with improvement in localized hyperalgesia among adolescent females with patellofemoral pain: results from a cluster randomized trial. Clin J Pain. 2016;32(5):428-434. doi:10.1097/ajp.00000000000002 75
37. Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12-19. do i:10.2519/jospt.2009.2885
38. Crossley KM, Macri EM, Cowan SM, Collins NJ, Roos EM. The patellofemoral pain and osteoarthritis subscale of the KOOS (KOOS-PF): development and validation using the COSMIN checklist. Br J Sports Med. 2017;52(17):1130-1136. doi:10.1136/bjsports-20 16-096776
39. Crossley KM, Macri EM, Cowan SM, Collins NJ, Roos EM. The patellofemoral pain and osteoarthritis subscale of the KOOS (KOOS-PF): development and validation using the COSMIN checklist. Br J Sports Med. 2018;52(17):1130-1136. doi:10.1136/bjsports-20 16-096776
40. Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess 1995;7(4):524-532. doi:10.1037/104 0-3590.7.4.524
41. Mease PJ, Spaeth M, Clauw DJ, et al. Estimation of minimum clinically important difference for pain in fibromyalgia. Arthritis Care Res 2011;63(6):821-826. doi:10.1002/acr.20449
42. Nelson EO, Ryan M, AufderHeide E, Heiderscheit B. Development of the University of Wisconsin running injury and recovery index. J Orthop Sports Phys Ther. 2019;49(10):751-760. doi:10.2519/jospt.20 19.8868
43. Nelson EO, Kliethermes S, Heiderscheit B. Construct validity and responsiveness of the University of Wisconsin running injury and recovery index. J Orthop Sports Phys Ther 2020;50(12):702-710. doi:10.2519/jospt.2020.9698
44. Smith CA, Chimera NJ, Warren M. Association of Y Balance Test reach asymmetry and injury in division I athletes. Med Sci Sports Exerc 2015;47(1):136-141. doi:10.1249/mss.0000000000000 380
45. Gonell AC, Romero JA, Soler LM. Relationship between the Y Balance Test scores and soft tissue injury incidence in a soccer team. Int J Sports Phys Ther 2015;10(7):955-966.
46. Wilson BR, Robertson KE, Burnham JM, Yonz MC, Ireland ML, Noehren B. The relationship between hip strength and the Y Balance Test. J Sport Rehabil 2018;27(5):445-450. doi:10.1123/jsr.2016-0187
47 Powden CJ, Dodds TK, Gabriel EH. The reliability of the Star Excursion Balance Test and lower quarter Y-Balance Test in healthy adults: a systematic review. Intl J Sports Phys Ther 2019;14(5):683-694. doi:10.26 603/ijspt20190683
48. Staud R, Vierck CJ, Cannon RL, Mauderli AP, Price DD Abnormal sensitization and temporal summation of second pain (wind-up) in patients with fibromyalgia syndrome. Pain. 2001;91(1-2):165-175. d oi:10.1016/s0304-3959(00)00432-2
49. Stackhouse SK, Taylor CM, Eckenrode BJ, Stuck E, Davey H. Effects of noxious electrical stimulation and eccentric exercise on pain sensitivity in asymptomatic individuals. Phys Med Rehabil 2015;8(5):415-424. doi:10.1016/j.pmrj.2015.07.009
50. Graven-Nielsen T, Vaegter HB, Finocchietti S, Handberg G, Arendt-Nielsen L. Assessment of musculoskeletal pain sensitivity and temporal summation by cuff pressure algometry: a reliability study Pain 2015;156(11):2193-2202. doi:10.1097/j.pa in.0000000000000294
51. Rathleff MS, Rathleff CR, Stephenson A, et al. Adults with patellofemoral pain do not exhibit manifestations of peripheral and central sensitization when compared to healthy pain-free age and sex matched controls – an assessor blinded crosssectional study. PLoS One. 2017;12(12):e0188930. do i:10.1371/journal.pone.0188930
52. Smart KM, Curley A, Blake C, Staines A, Doody C. The reliability of clinical judgments and criteria associated with mechanisms-based classifications of pain in patients with low back pain disorders: a preliminary reliability study J Man Manip Ther 2010;18(2):102-110. doi:10.1179/106698110x1264074 0712897
53. Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain 2011;152(3 Suppl):S2-S15. doi:10.1016/j.pain.2010.09.030
54. Bajaj P, Bajaj P, Graven-Nielsen T, Arendt-Nielsen L. Osteoarthritis and its association with muscle hyperalgesia: an experimental controlled study Pain 2001;93(2):107-114. doi:10.1016/s0304-3959(01)0030 0-1
55. van Wilgen CP, Konopka KH, Keizer D, Zwerver J, Dekker R. Do patients with chronic patellar tendinopathy have an altered somatosensory profile? - a Quantitative Sensory Testing (QST) study Scand J Med Sci Sports. 2013;23(2):149-155. doi:10.1111/j.160 0-0838.2011.01375.x
56. Eckenrode BJ, Kietrys DM, Stackhouse SK. Pain sensitivity in chronic Achilles tendinopathy. Intl J Sports Phys Ther 2019;14(6):945-956. doi:10.26603/ij spt20190945
57. Bartholomew C, Lack S, Neal B. Altered pain processing and sensitisation is evident in adults with patellofemoral pain: a systematic review including meta-analysis and meta-regression. Scand J Pain. 2019;20(1):11-27 doi:10.1515/sjpain-2019-0079
58. de Oliveira Silva D, Rathleff MS, Petersen K, Azevedo FM, Barton CJ. Manifestations of pain sensitization across different painful knee disorders: a systematic review including meta-analysis and metaregression. Pain Med. 2018;20(2):335-358. doi:1 0.1093/pm/pny177
59. Chesterton LS, Barlas P, Foster NE, Baxter DG, Wright CC. Gender differences in pressure pain threshold in healthy humans. Pain 2003;101(3):259-266. doi:10.1016/s0304-3959(02)003
30-5
60. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL III. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain 2009;10(5):447-485. doi:10.1016/j.jpain.2008.1
2.001
61. Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choinière M. A systematic literature review of 10 years of research on sex/ gender and experimental pain perception – part 1: are there really differences between women and men? Pain 2012;153(3):602-618. doi:10.1016/j.pain.2011.1
1.025
62. Bowsher D, Leijon G, Thuomas KA. Central poststroke pain: correlation of MRI with clinical pain characteristics and sensory abnormalities. Neurology 1998;51(5):1352-1358. doi:10.1212/wnl.51.5.1352
63. Yarnitsky D, Granot M, Granovsky Y. Pain modulation profile and pain therapy: between proand antinociception. Pain 2014;155(4):663-665. doi:1 0.1016/j.pain.2013.11.005
64. Arendt-Nielsen L, Nie H, Laursen MB, et al. Sensitization in patients with painful knee osteoarthritis. Pain. 2010;149(3):573-581. doi:10.101 6/j.pain.2010.04.003
65. Sarlani E, Grace EG, Reynolds MA, Greenspan JD Evidence for up-regulated central nociceptive processing in patients with masticatory myofascial pain. J Orofac Pain 2004;18(1):41-55.
66. Weissman-Fogel I, Sprecher E, Granovsky Y, Yarnitsky D Repeated noxious stimulation of the skin enhances cutaneous pain perception of migraine patients in-between attacks: clinical evidence for continuous sub-threshold increase in membrane excitability of central trigeminovascular neurons. Pain. 2003;104(3):693-700. doi:10.1016/s0304-3959(0 3)00159-3
67 Rathleff MS, Petersen KK, Arendt-Nielsen L, Thorborg K, Graven-Nielsen T. Impaired conditioned pain modulation in young female adults with longstanding patellofemoral pain: a single blinded crosssectional study. Pain Med. 2016;17(5):980-988. doi:1 0.1093/pm/pnv017
68. Arendt-Nielsen L, Skou ST, Nielsen TA, Petersen KK. Altered central sensitization and pain modulation in the CNS in chronic joint pain. Curr Osteoporos Rep. 2015;13(4):225-234. doi:10.1007/s11 914-015-0276-x
69. Oono Y, Nie H, Matos RL, Wang K, Arendt-Nielsen L. The inter- and intra-individual variance in descending pain modulation evoked by different conditioning stimuli in healthy men. Scand J Pain 2011;2(4):162-169. doi:10.1016/j.sjpain.2011.05.006
70. Neelapala YVR, Bhagat M, Frey-Law L. Conditioned pain modulation in chronic low back pain: a systematic review of literature. Clin J Pain 2020;36(2):135-141. doi:10.1097/ajp.00000000000007
78
71. Zabala Mata J, Lascurain-Aguirrebeña I, Dominguez López E, Azkue JJ. Enhanced pronociceptive and disrupted antinociceptive mechanisms in nonspecific chronic neck pain. Phys Ther. 2021;101(3). doi:10.1093/ptj/pzaa223
72. La Touche R, Paris-Alemany A, Hidalgo-Pérez A, López-de-Uralde-Villanueva I, Angulo-Diaz-Parreño S, Muñoz-García D. Evidence for central sensitization in patients with temporomandibular disorders: a systematic review and meta-analysis of observational studies. Pain Pract. 2018;18(3):388-409. doi:10.1111/ papr.12604
73. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther 2006;36(12):911-919. doi:1 0.2519/jospt.2006.2244
1 Department of Orthopaedic Surgery and Sports Medicine, University of Florida, 2 Department of Movement Sciences, University of Idaho, 3 WWAMI Medical Education Program, University of Idaho, 4 Movement Sciences, University of Idaho, 5 University of Idaho
Keywords: hip osteoarthritis, hip disability, physically active, patient outcomes https://doi.org/10.26603/001c.67938
Background
Hip Disability and Osteoarthritis Outcome Score (HOOS), HOOS-Joint Replacement (JR), HOOS Physical Function (PS), and HOOS-12 item scale have been suggested as reliable and valid instruments for assessing hip disability However, factorial validity, invariance across subgroups, and repeated measures of the scale across different populations have not been well supported in the literature.
Purpose
The primary study objectives were to: (1) assess model fit and psychometric properties of the original 40-item HOOS scale, (2) assess model fit of the HOOS-JR, (3) assess model fit of the HOOS-PS, and (4) assess model fit of the HOOS-12. A secondary objective was to perform multigroup invariance testing across physical activity level and hip pathology subgroups for models that met recommended fit indices.
Cross-Sectional Study
Methods
Individual confirmatory factor analyses (CFAs) were conducted for the HOOS, HOOS-JR, HOOS-PS, and HOOS-12. Additionally, multigroup invariance testing (i.e., activity level, injury type) was conducted on the HOOS-JR and HOOS-PS.
Model fit indices did not meet contemporary recommendations for the HOOS and the HOOS-12. Model fit indices for the HOOS-JR and the HOOS-PS met some, but not all, contemporary recommendations. Invariance criteria was met for the HOOS-JR and HOOS-PS.

The scale structure of the HOOS and HOOS-12 were not supported; however, preliminary evidence to support the scale structure of the HOOS-JR and HOOS-PS was found. Clinicians and researchers who utilize the scales should do so with caution due to their limitations and untested properties until further research establishes the full psychometric properties of these scales and recommendations for their continued use.
Corresponding Author:
Emilie N. Miley
3450 Hull Road, Gainesville, FL 32607 (352) 273-7361
mileyen@ortho.ufl.edu
Hip osteoarthritis (OA) is a debilitating degenerative joint disorder that leads individuals to experience a multitude of symptoms including pain, disability in daily activity, reduced independence and quality of life (QoL).1,2 With the multifaceted nature of hip OA on the rise, there is a need for a valid multidimensional (i.e., not specific to body location or injury) scale to adequately assess constructs across varied sub-populations.3–6 Although several region-specific instruments (e.g., Lower Extremity Functional Scale) exist,3,4 the majority of patient-reported outcome (PRO) measures for the hip joint primarily measure recovery following a total hip arthroplasty (THA) due to hip OA. Thus, many scales may not sufficiently assess all the relevant dimensions associated with OA (e.g., QoL), other pathologies, nor may be applicable to certain sub-populations (e.g., individuals who have not had a total hip replacement, younger active individuals, etc.). Additionally, some scales place an excessive response burden on patients and clinicians due to item redundancy, excessive number of items, or inclusion of items with inappropriate difficulty 7 To adequately address these concerns, the Hip Disability and Osteoarthritis Score (HOOS) scale was developed.8–11
The HOOS consists of 40 items used to assess five dimensions: pain (10 items); other symptoms (five items); function in daily living (activities of daily living [ADL]; 17 items), function in sport and recreation (Sport/Rec; four items); and hip-related QoL (four items).7,10,12 The HOOS can be used over both short-term and long-term intervals. For example, the HOOS can be used to evaluate changes from week-to-week, as produced by treatments such as medication, operation, or physical therapy, or to evaluate changes over years as a result of the primary injury or posttraumatic OA.7,12 The HOOS is primarily intended to evaluate functional limitations and symptoms related to hip pathology or disability, with or without OA.7 The HOOS has been studied in relatively small sample sizes (n < 200) of adults aged 42-85,1,7,10,13 and in patients who have either been diagnosed with hip OA or who have received a THA due to OA.7,14 The HOOS, has not been extensively studied in healthy or younger populations, or in patients without hip OA. Additionally, the psychometric properties of the HOOS have not been established between groups (e.g., sex, different pathologies) or across patient visits (e.g., intake, discharge) using invariance testing.
In addition to the original 40-item HOOS, there have been several short-form versions created: the HOOS-JR (Joint Replacement), multiple HOOS-PS versions (Physical Function Short-Form), and the HOOS-12 item scale. The short-form versions were developed using items from different subdimensions of the original 40-item HOOS instrument, and have been studied in patients who have undergone THA.10,15,16 The HOOS-JR includes six items from the original HOOS: two items from pain subscale, and four items from the function in daily living subscale.16 One version of the HOOS-PS includes three items from the subscale function in daily living and two items from the Sport/Rec subscale10; whereas, other versions of the HOOS-PS in-
clude additional items (i.e., as many as seven items).13 Because the HOOS-JR and HOOS-PS only provide a summary score and assess a single dimension,10,17 the HOOS-12 short-form was developed to assess multiple dimensions.15,17
The HOOS-12 was created by developing an item bank using item response theory modeling, confirmatory factor analysis (CFA) procedures, and computerized adaptive test (CAT) simulations.17 The item bank consisted of a set of items, taken from the original HOOS questions, that were identified to measure the same domain and parameters.17 Individual CFAs were then performed on the individual constructs (i.e., pain, function, QoL) to verify that each item was unidimensional.17 Following development of the item bank, CAT simulations were used to reduce the bank to include the fewest, yet most informative, items measuring each domain.17 The final version of the HOOS-12 consisted of three constructs (pain, function, and QoL), that include four items from each of the subscales of the original HOOS.15,17
Psychometric examination of the HOOS and short-form versions have primarily focused on the construct validity, reliability, and responsiveness of the instrument. Construct validity has been established by correlating scores (i.e., Spearman’s Correlation Coefficient) on the HOOS with the Short Form (SF)-36, which was intended to measure similar constructs within the HOOS (i.e., physical function vs. ADLs, physical function vs. sport and recreation, and bodily pain vs. pain), where low to moderate correlations (r = 0.49-0.66) were found.7,18 Lower correlations were identified among the HOOS and SF-36 constructs measuring mental health, whereas higher correlations were found between physical health constructs.7,19 Internal consistency, or the assessment of homogeneity of the items, was assessed by interpreting Cronbach’s alpha values, values ranging from > .70 to ≤ .90 have been recommended.20–22 For the HOOS, Cronbach’s alpha values have ranged from 0.75 to 0.98 across multiple studies13,18,23; high values (i.e., >.90) may be indicative of potential issues (e.g., of item redundancy, construct underrepresentation, inclusion of too many items, etc.).21,24–26 Test-retest reliability has also been assessed and values found have ranged from good to excellent (ICC = 0.75 to 0.97).13,18,23 Finally, responsiveness to the 40-item HOOS has been assessed using the standardized response mean (SRM); researchers report a high response rate (SRM = > .80) when compared to the Western Ontario and MacMaster Universities Osteoarthritis Index LK 3.0.7
The HOOS-JR and HOOS-12 have been reported to have acceptable internal consistency (0.70-0.92),15,16 and high responsiveness (0.80).16 External validity assessed using Spearman’s Correlation Coefficient of the HOOS-JR has been reported to be acceptable with moderate to high correlations with the HOOS subscales (0.60-0.94)15,16 and the HOOS-PS (0.81-0.86).16 The HOOS-12 was also highly correlated with the HOOS (r = 0.75-0.94).15 The HOOS-JR, HOOS-PS, and HOOS-12 are all considered to be reliable (Cronbach’s alpha = 0.77-0.92).15
Although the HOOS, HOOS-JR, HOOS-PS, and HOOS-12 have been suggested as reliable and valid instruments, factorial validity, invariance across subgroups, and repeated testing of the scales across different time points (i.e., longitudinal invariance) have not been well supported in the literature. Additionally, complete psychometric analysis of the HOOS and the short-form versions of the scale to ensure the instrument can be used in clinical practice and research have not been completed. Conducting a CFA to examine the factor structure of the proposed scales (i.e., HOOS, HOOS-JR, HOOS-PS, HOOS-12) and conducting CFA-based invariance testing to explore measurement properties of the scale across subgroups of the population (e.g., sex, physical activity levels, etc.), stages or types of musculoskeletal injury (i.e., healthy, acute, sub-acute, persistent, and chronic), and across time (i.e., intake, discharge) are warranted prior to adoption of a model for practice and research.26,27 Establishing measurement properties through invariance testing ensures that the interpretations between groups or across time are valid and reliable.20,27 Additionally, identifying a meaningful factor structure via CFA procedures enhances the rigor of psychometric examination of an instrument’s measurement properties.20,27
Researchers have performed CFAs on the individual constructs (i.e., pain, function) proposed in the original HOOS17: some model fit recommendations for the pain and function constructs were met (CFI = 0.97-0.99, TLI = 0.97-0.98), while other construct fit indices did not meet recommendations (i.e., RMSEA = 0.14-0.19).17 However, no assessment of the complete model structure, nor results from invariance testing have appeared in the literature to date. Thus, there exists need for additional assessment of the measurement properties of the HOOS and the proposed short form versions of the scale. Therefore, the primary purposes of this study were to: (1) assess the model fit of the original HOOS scale using a diverse sample to examine its psychometric properties, (2) assess the model fit of the HOOS-JR, (3) assess the model fit of the HOOS-PS, and (4) assess the model fit of the HOOS-12. The secondary purpose, if model fit held, was to perform multigroup invariance testing of the scale across physical activity level and hip pathology subgroups.
After institutional review board approval (19-142), informed consent was obtained from all participants prior to data collection. Participants between the ages of 18 and 65 were recruited through social media (i.e., Facebook), email, and ResearchMatch. Participants self-reported their physical activity (i.e., inactive, low-, moderate-, high-activity), injury status (e.g., healthy, acute injury), and athlete level (e.g., competitive athlete, recreational athlete) classification (Table 1).
Social media recruitment was performed by providing study information (e.g., purpose of the study, inclusion/exclusion criteria, estimated survey duration) and a link to
the survey on multiple Facebook pages.28 Email recruitment was performed by emailing the same study details from the social media recruitment and a separate survey link to a convenience sample of coaches (NCAA and recreational sports teams), athletic trainers, and ROTC officers across different higher education institutions, requesting the survey email to be shared with their athletes, patients, or cadets.
ResearchMatch was utilized as an additional online email recruitment tool. Searches of the ResearchMatch database were performed to identify potential participants (i.e., participants that were healthy, diagnosed with hip osteoarthritis, individuals who had undergone a THA, and those who had sustained a lower extremity musculoskeletal injury). Members of the database who fit the search criteria were recruited for this study per ResearchMatch protocol. Potential participants were identified and emailed invitations for study participation. If the participant voluntarily consented to participate, a follow-up email was sent to the individual containing a link to the survey.
Qualtrics (Qualtrics, LLC, Provo, UT) software was utilized to create an electronic survey via a weblink. The survey responses were collected directly into Qualtrics. Information collected included demographic information (e.g., age, sex, physical activity level) and responses to the items of the HOOS.
The HOOS asks participants to rate how frequently they engaged in the behaviors over the past week using a 5-point Likert scale (1 = none/not at all/never, 2 = rarely/mild/ monthly, 3 = sometimes/moderately/weekly, 4 = often/severe/daily, and 5 = extreme/always). Items were summed to create a score for each subscale, and global HOOS score, where 0 indicated extreme problems and 100 indicated no problems.7,12
Data were exported from the Qualtrics software and downloaded using Statistical Package for Social Sciences Version 24.0 (IBM Corp., Armonk, NY). Missing data were treated conservatively and any participant’s data missing more than 10% of the responses on the HOOS (i.e., four or more missing responses) was removed from the data set.26 Individuals missing less than 10% (i.e., three items or less) of the items within the HOOS were replaced with the mean score of the respective item for analysis purposes.26 Participants with missing demographic data were not excluded from analysis and were left as missing values. Data were assessed for normality using z-scores, skewness, and kurtosis values. Multivariate outliers were also identified using descriptive statistics and Mahalanobis distance, the cut-off value was for 5 degrees of freedom at a p-value of 0.001, was 15.089.26,29 This methodology generated the final data set used for analysis.
Physically Active4
Injury
Classification4
“An individual who engages in athletic, recreational, or occupational activities that require physical skills and who uses strength, power, endurance, speed, flexibility, range of motion, or agility at least 3 days/week.”
Healthy “Free from musculoskeletal injury and fully able to participate in sport or activity”
Acute Injury “A musculoskeletal injury that precludes full participation in sport or activity for at least 2 consecutive days (0–72 hours post-injury).”
Subacute Injury “A musculoskeletal injury that precludes full participation in sport or activity for at least 2 consecutive days (3 days to 1-month post-injury).”
Persistent Pain
“A musculoskeletal injury that has been symptomatic for at least 1 month.”
Chronic Pain "Pain that consistently does not get any better with routine treatment or nonnarcotic medication.”
Athlete Level4
Competitive athlete
Recreational athlete
Occupational athlete
Physically active in ADLs
"A participant who engages in a sport activity that requires at least 1 preparticipation examination, regular attendance at scheduled practices and/or conditioning sessions, and a coach who leads practices and/or competitions."
"A participant who meets the criteria for physical activity and participates in sport but does not meet the criteria for competitive status."
"A participant who meets the criteria for physical activity for occupation or recreation but does not meet the criteria."
"A participant who does not meet the criteria for any athlete category but who is physically active through daily activities (e.g., physically active for at least 30 min/day for 3 days/week)."
The final data set was used to conduct a CFA using Analysis of Moment Structures (AMOS) software (IBM Corp., Armonk, NY) on the 40-item HOOS and associated subscales. Consistent with the original proposed model, the HOOS scale was specified as a five factor, 40-item model.12 Additionally, the HOOS-JR was specified as a one factor, 6-item model, the HOOS-PS was specified as a one factor, 5-item model, and the HOOS-12 was specified as a three factor, 12-item model. Given the subscales were created using items from the 40-item HOOS, the original item number labels were retained from the HOOS during the CFA procedures.10,15–17 Full Information Maximum Likelihood Estimation was used to generate the parameter estimates. Model fit statistics included the likelihood ratio statistic (CMIN), Goodness of Fit Index (GFI), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Bollen’s Incremental Fit Index (IFI), and Root Mean Square Error of Approximation (RMSEA).26 Model fit was evaluated based on a priori values: GFI ≥ 0.95, CFI ≥ 0.95, TLI ≥ 0.95, RMSEA ≤ 0.06, IFI; ≥ 0.95.26,30 Latent construct correlations and path coefficient values with R2 ≥ 0.90 were used to identify potential multicollinearity among the latent constructs, which indicates that item removal within a potential dimension might be beneficial to prevent model misspecification.31,32
Confirmatory factor analysis invariance testing was conducted if recommended model fit criteria were met to determine if the association between the latent constructs
(i.e., symptoms, pain, function, QoL) and the respective items were stable and equal across groups.26,31,33 This was accomplished using a set of hierarchical procedures with an increasing level of constraint.26,31,33 Individual CFAs were first conducted by subgroup category (i.e., activity level, injury type), ensuring the construct and factors (e.g., pain, function, symptoms) were measuring what was intended.31,33 The model then underwent configural, metric, and scalar invariance testing.31–33 First, the configural invariance test placed all groups in the same model to ensure the same factors have similar items across subgroups. Secondly, the metric model then tested if factor loadings were equal across subgroups.32 If the model met metric invariance requirements, equal variances (i.e., group differences) between groups were then assessed.32 Lastly, the scalar invariance test ensured that item intercepts were equal across groups, which indicated the means were not determined or altered by external factors.32 If the model met scalar invariance requirements, equal mean models (i.e., score differences) were tested between groups.32
Model fit was compared using the CFI difference test (CFIDIFF) and the chi-square difference test (χ2 DIFF), with a p-value cut-off of 0.01.30,33 Given the sensitivity of the χ2 DIFF test to sample size,30 the CFIDIFF test held greater weight in decisions regarding invariance testing model fit. If a model exceeded the χ2 DIFF test, but met the CFIDIFF test, invariance testing continued. Specifically, the HOOSPS and HOOS-JR underwent invariance testing across physical activity level (i.e., inactive, low, medium, high) and injury type (i.e., hip OA and THA pathology, no hip pathology).
ADL Activities of daily livinga The sum does not equal 100% because percentages were rounded
Among the total responses (ResearchMatch = 487; social media = 370; total = 857), 149 participants were missing responses to more than 10% of the HOOS items and most of the demographic items. Thus, information could not be verified (e.g., sex, injury status) and these responses were removed from the dataset. Three individuals were missing responses to less than 10% of the HOOS; the missing values for those participants were replaced with the rounded mean for each item missing. Additionally, 53 (6.18%) participants reported scores that were identified as univariate (z scores ≥ 3.4) or multivariate (Mahalanobis distance ≥ 15.089) outliers and were removed from the dataset.29,34 Of the participants removed, all injury categories (i.e., healthy, acute, persistent, chronic) and both sexes were represented. A total of 655 participants (i.e., social media/email: n= 247 [37.7%]; ResearchMatch: n = 408 [62.3%]) were included in the final data set (mean age = 38.93 ± 15.05 yrs.; mean weight = 165.42 ± 41.99 lbs.; Table 2). Participants self-reported their injury status and level of activity. The sample primarily included healthy participants (i.e., free of musculoskeletal injury; n = 453, 69%; Table 2), and the largest physically active response group indicated a level of moderate activity (n = 276, 42.1%; Table 2). Respondents reported participation in a variety of sports (Table 3) and a variety of injury locations (Table 4).
The proposed CFA model of the HOOS did not meet contemporary fit recommendations (CFI = 0.847; TLI = 0.836; IFI = 0.847; RMSEA = 0.098; Figure 1). Correlations between the first-order latent constructs (e.g., symptoms and pain) were high (0.80-0.96; Figure 1). Modification indices indicated a number of meaningful cross-loadings between several items (e.g., item 6 and item 37 [134.58]) were present.26 Additionally, modification indices revealed the incorporation of error correlations amongst several items (e.g., item 24 [putting on socks/stockings] and 26 [taking off socks/stockings; 344.25]) would improve model fit (CFI = 0.934; TLI = 0.927; IFI = 0.934; RMSEA = 0.065).
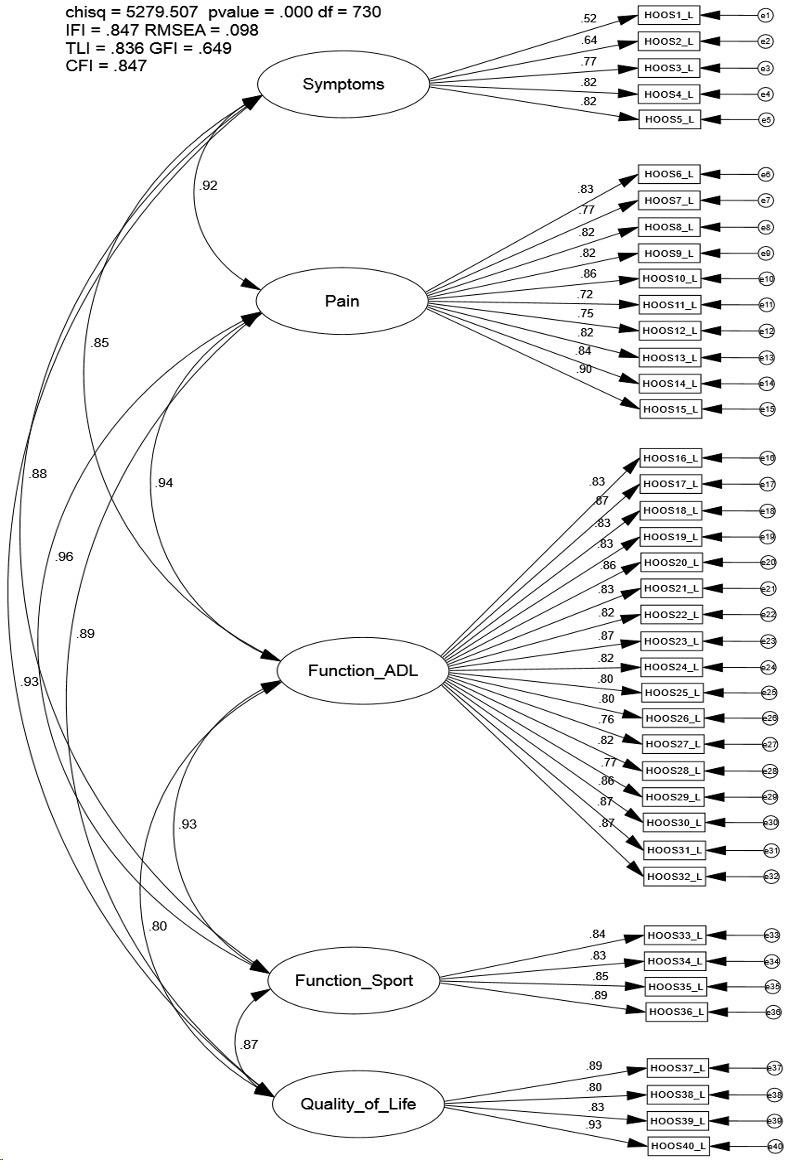
The CFA model fit indices of the HOOS-JR met some, but not all contemporary recommendations (CFI = 0.965; TLI = 0.941; IFI = 0.965; RMSEA = 0.133; Figure 2); however, CFI and IFI values exceeded recommendations and loadings were statistically significant (p < 0.001; Figure 2). Modification indices revealed the incorporation of error correlations between two items (i.e., item 10 [going up or down stairs] and 15 [walking on an uneven surface; 69.57] would improve model fit (CFI = 0.994; TLI = 0.988; IFI = 0.994; RMSEA = 0.059).
The CFA model fit indices of the HOOS-PS met some, but not all, contemporary recommendations (CFI = 0.967; TLI = 0.933; IFI = 0.967; RMSEA = 0.137; Figure 3); loadings were statistically significant (p < 0.001; Figure 3). Modification indices revealed that the incorporation of error correlations between two items (i.e., item 16 [descending stairs] and 15 [getting in and out of the bath; 28.90] would improve model fit (CFI = 0.986; TLI = 0.966; IFI = 0.986; RMSEA = 0.098).
The CFA model fit indices of the HOOS-12 did not meet contemporary recommendations (CFI = 0.906; TLI = 0.878; IFI = 0.906; RMSEA = 0.147; Figure 4). Correlations between the first-order latent constructs (e.g., pain and function) were particularly high (0.84-0.98) (Figure 4). Modification indices indicated meaningful cross-loadings between several items (e.g., item 6 and item 37; 57.77) and constructs (e.g., error 37 and pain; 43.34).26 Additionally, modification indices revealed the incorporation of error correlations between several items (i.e., item 6 [how often is your hip pain] and 37 [how often are you aware of your hip problem;
218.42]) would improve model fit (CFI = 0.976; TLI = 0.965; IFI = 0.976; RMSEA = 0.079).

Given that several model fit indices met recommended fit criteria for the HOOS-JR (i.e., CFI, IFI) and the HOOSPS (i.e., CFI, TLI), multigroup invariance testing was performed across two subgroups: a hip pathology group (i.e., those diagnosed with hip OA and/or those who underwent a THA) and a non-hip pathology group. The analyses were conducted on the hip pathology group (n = 48; CFI = 0.940), along with a random sample of those who had no self-reported hip pathology (n = 94; CFI = 0.954).
For the HOOS-JR, the initial model (configural) met some recommended model fit indices (CFI = 0.95; χ2 = 48.01; TLI = 0.914; IFI = 0.95; RMSEA = 0.067; Table 5), indicating equal form between groups on the one factor, 6-item model. The metric model (i.e., equal loadings) passed both the CFIDIFF and the χ2 DIFF tests, which warranted testing of equal latent variances. After constraining the variances to be equal, the metric model did not pass the CFIDIFF or the χ2 DIFF test, indicating variances were not equal between groups. When variances were not constrained to be equal, the hip pathology group reported scores with more variance compared to the group without a hip pathology The scalar model (i.e., equal loadings and intercepts) also passed both the CFIDIFF and the χ2 DIFF tests (Table 5), which warranted assessment of the equal means. When the means were constrained to be equal, the model did not pass the CFIDIFF or the χ2 DIFF tests (Table 5), which indicated differences in means between scores. When means were not constrained to be equal, the hip pathology group reported higher mean scores (i.e., more hip dysfunction) than the group without a hip pathology.
Figure 2. The HOOS-JR scale hierarchical confirmatory factor analysis measurement model with standardized loadings (n = 656).For the HOOS-PS, the initial model (configural) met some, but not all, model fit indices (CFI = 0.948; χ2 = 48.01; TLI = 0.88; IFI = 0.942 RMSEA = 0.13; Table 6). The metric model (i.e., equal loadings) did not pass the CFIDIFF or the
χ2 DIFF tests, which indicated that the meaning of the items was not the same across groups. As such, further exploration of the multigroup invariance testing procedures was not warranted on the HOOS-PS.
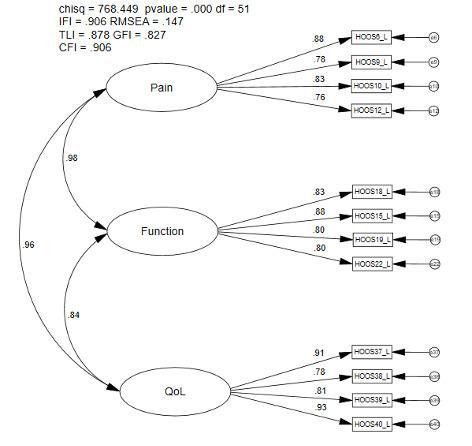
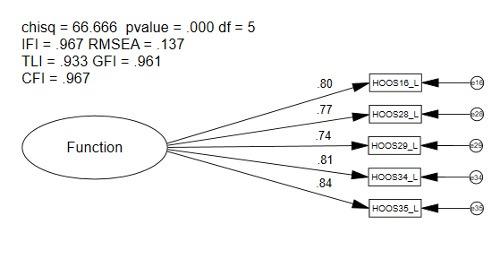 Figure 3. The HOOS-PS hierarchical confirmatory factor analysis measurement model with standardized loadings (n = 656).
Figure 4. The HOOS-12 item scale hierarchical confirmatory factor analysis measurement model with standardized loadings (n = 656).
Figure 3. The HOOS-PS hierarchical confirmatory factor analysis measurement model with standardized loadings (n = 656).
Figure 4. The HOOS-12 item scale hierarchical confirmatory factor analysis measurement model with standardized loadings (n = 656).
For the HOOS-JR, the initial model (configural) met some recommended model fit indices (0.95; χ2 = 171.91; TLI = 0.92; IFI = 0.95; RMSEA = .076; Table 7), which indicated equal form between groups on the one factor, 6-item model. The metric model (i.e., equal loadings) passed both the CFIDIFF and the χ2 DIFF tests, which warranted testing of equal latent variances. After constraining the variances to be equal, the metric model did not pass the CFIDIFF or the χ2 DIFF test which indicated variances were not equal between groups. When variances were not constrained to be equal, the inactive group reported scores with more variance compared to the other three groups. The scalar model (i.e., equal loadings and intercepts) also passed both the CFIDIFF and the χ2 DIFF tests (Table 7), which warranted assessment of the equal means. When the means were constrained to be equal, the model did not pass the CFIDIFF or the χ2 DIFF tests (Table 7), which indicated differences in means between scores. When means were not constrained to be equal, the inactive group reported higher mean scores (i.e., more hip dysfunction) than the active groups.
For the HOOS-PS, the initial model (configural) met model fit indices (CFI= 0.97; χ2 = 79.03; TLI = 0.93; IFI = 0.97; RMSEA = 0.067; Table 8), which indicated equal form of the one factor, 5-item model between groups. The metric model (i.e., equal loadings) passed both the CFIDIFF and the χ2 DIFF test, which warranted testing of equal latent variances. After constraining the variances to be equal, the
model did not pass the CFIDIFF or the χ2 DIFF test, which indicated differences in variance between groups. When variances were not constrained to be equal, the inactive group reported more variance in scores than the active groups (i.e., low-, moderate-, and high activity). The scalar model (i.e., equal loadings and intercepts) also passed both the CFIDIFF and the χ2 DIFF tests (Table 8), which warranted assessment of the equal means model. When means were constrained to be equal, the model did not pass the CFIDIFF or the χ2 DIFF tests (Table 8); when means were not constrained to be equal, individuals in the inactive group reported higher mean scores (i.e., more hip dysfunction) than the active groups.
The purpose of this study was to examine the psychometric properties of the published 40-item HOOS, HOOS-PS, HOOS-JR, and HOOS-12 scales by using contemporary CFA and multigroup invariance testing procedures in a larger and more diverse physically active sample. Confirmatory factor analysis procedures were used as an approach to examine these scales for use in clinical practice and research, while invariance testing procedures helped assess for itemlevel bias and substantive differences between groups.27 Previous literature demonstrated good model fit of individual constructs (i.e., pain, function, and QoL)17; however, previous researchers failed to provide model fit of the full latent variable scale model as recommended26,31 to assess scale properties for use in practice and research.26,31,33 The
current results indicate the original HOOS and HOOS-12 do not meet recommended measurement criteria for this sample of physically active participants. Therefore, caution is warranted if using results from either measure for research or clinical practice. The HOOS-JR and the HOOS-PS demonstrated stronger evidence supporting their use given the CFA and multigroup invariance findings. Further exploration to determine when to use the scales and when the measurement properties may not be sufficient for assessing group differences in larger samples of physically active patients with and without hip pathology is warranted to confirm or refute our findings.
The original five factor, 40-item HOOS scale structure was not supported in our study 26,33 Poor model fit indices, along with high correlation values between latent constructs, indicates potential multicollinearity and a lack of unique constructs. Additionally, the modification indices revealed that model fit could be substantially improved if numerous modifications in the model (e.g., error-terms were correlated) were instituted.26,33 Assessment of the error-term cross-loadings revealed that most of the items shared commonalities.26,35 Correlation of the error terms
may indicate the presence of overlapping items, or items that are perceived to ask similar questions.26 Further, there were concerns with Cronbach’s alpha values; in our sample, the high values (0.84-0.98) were similar to previously reported levels (0.75-0.98)13,18,23 and may be indicative of potential item redundancy 20,36 The high correlation values between constructs and items, along with high Cronbach’s alpha values, re-affirmed multicollinearity as a concern and may indicate respondents are unable to differentiate between the items used to measure different constructs.20,36
The current findings suggest the model may be improved by re-writing items or by removing items from the original model.26,31 Furthermore, the results make it difficult to conclude that items in the constructs are measuring unique phenomena.26,31,33 Also, exploration may be warranted to determine if the correlated errors are theoretically justified and to determine when the inclusion of those correlations are warranted in research.26,35 Thus, the instrument may be improved through exploratory procedures (i.e., EFA procedures) to help determine if a more concise instrument can be identified from the originally developed item.20,26,31 However, given the design of the HOOS items, further modification may be necessary. For example, many HOOS items are double-barreled questions (i.e., asking more than one question in an item), which may result in analysis complications because the respondent may not know which as-
pect of the item to respond to for their scored response and may cause confusion and generate inconsistent results.37 As such, it would be prudent for researchers to rewrite items or provide fewer overlapping examples which may result in improved model fit and more precise assessment of the patient experience.37
The current CFA analysis approach on the full HOOS scale provides insight where previous studies separated the dimensions to conduct CFAs on individual dimensions of the scale (i.e., the development of the HOOS-12).17 To the authors knowledge, this study is the first to perform CFA procedures on the full HOOS reflective latent variable model. Analyses examining psychometric properties of a scale should first examine the full model prior to conducting exploratory procedures and item removal.26,31,33 The model fit indices found in our study were substantially lower than those previously reported for the pain and function dimensions when the constructs were examined individually 17 These results demonstrate the importance of testing the full model before recommending a multi-dimensional scale for use in practice or research.30,31
The HOOS-JR met recommended CFI and IFI values26,33; model fit concerns (e.g., high item cross-loadings) may have contributed to a reduced overall model fit. Additionally, the modification indices revealed that model fit could be substantially improved if modifications in the model were instituted.26,33 Assessment of the error term crossloadings identified in the modification indices indicated two items (i.e., item 10 [going up or down stairs] and item 15 [walking on an uneven surface]) shared commonalities, which may warrant further exploration as including the error term covariances may be appropriate in certain analysis situations.26,35 Similar to the HOOS, another potential explanation for poor model fit indices could be item design. It may be beneficial to address double-barreled questions and overlapping items to improve model fit and reduce response burden for respondents.15,37
The HOOS-JR was subjected to multigroup invariance testing by injury type and activity level as certain model fit criteria (i.e., CFI, IFI) thresholds were met. The multigroup invariance findings across injury type provide some evidence for scale validity As the model met criteria for measurement invariance, group differences for variances and latent means could be assessed as these differences could be considered true differences as opposed to differences due to item bias or measurement error.26,31 If the HOOSJR was valid scale, it would be expected that respondents who had hip OA or previous history of a THA would report higher mean scores with greater variances if the scale is measuring the intended phenomenon. A higher score on the HOOS-JR construct indicates those respondents have more difficulty related to pain and function,16,17 while a finding of more score variance and higher mean scores for impaired function and pain in the injured group would be expected because hip OA is one of the leading causes of decreased function due to pain.10 Our results indicate the individuals with hip pathology reported larger amounts
of variance and higher mean scores compared to the no hip pathology group. These substantive findings provide support that the HOOS-JR is capturing valid group differences among those who are suffering from a hip injury/ dysfunction and those who are not. Thus, clinicians and researchers could assess score differences between these groups on the HOOS-JR.
Multigroup invariance testing was then performed by activity level subgroups. Group differences for variances and means were also found between activity level subgroups, which also support the validity of the HOOS-JR. A higher score on the HOOS-JR constructs indicates those respondents have greater difficulty related to pain and function16,17 and it could be theorized that individuals with higher levels of hip dysfunction (e.g., pain) would be less active than those with lower levels of dysfunction. The current findings reveal individuals who were classified as inactive reported larger amounts of variance in their scores and exhibited higher mean scores (i.e., more pain and decreased function) compared to those who were more active (i.e., low-, moderate-, and high-activity). The findings indicate the group differences likely represent true score differences as opposed to measurement error; thus, our results provide substantive support for scale validity, given that the HOOS-JR identified higher dysfunction in inactive patients who likely alter activity levels due to hip pain and dysfunction. Further analysis of the inactive group supports this theory as 42% (N = 17) of theses participants reported a current physical injury, and 20% (N = 8) reported a previous injury to their hip. Thus, the findings support the HOOSJR is capturing valid group differences in those who are less active and suffering from a hip injury/dysfunction as compared to healthy, active respondents.
The one factor, 5-item HOOS-PS met the recommended levels for CFI, GFI, and TLI26,33; however, additional model fit concerns such as item cross-loadings may have contributed to reduced overall model fit. Like the HOOS and the HOOS-JR, a potential explanation for poor model fit indices could be item design. Assessment of cross-loadings identified through the modification indices was performed; review of the items did not indicate a theoretical justification for the shared commonalities.26,35 Thus, sound rationale for further exploration of the correlation of error terms was not identified.26,35 However, it may be beneficial to address double-barreled questions and overlapping items to improve model fit.15,37
Next, the HOOS-PS was subjected to multigroup invariance testing by injury type. As model fit indices for the metric invariance model were not met,26 the use of this scale may not be appropriate for examining group differences and differences in scores between respondents who have a hip pathology and those who do not in its current form.
Without meeting multigroup invariance testing recommendations, it should not be assumed that score differences between healthy or injured respondents are true differences and not measurement error 26 Multigroup invariance test-
ing should be performed again in a larger sample of healthy and hip injured respondents to confirm or refute our findings.
Lastly, when performing invariance testing by activity level subgroups, evidence was found to support scale structure with the configural, metric, and scalar results.26 Group differences in variances and means for function were found between activity levels. Individuals who were classified as being inactive had more variance in their responses compared to those who were classified as active. A higher score on the HOOS-PS constructs indicates those respondents have more difficulty related to physical function.10,38 A finding of more score variance and higher mean scores in physical function of the inactive group would be expected, as some participants in this sample were more likely to have difficulties pertaining to their hip while performing physical activity Thus, the substantive findings provide support that the HOOS-PS is capturing valid group differences between activity levels in our sample, which provides theoretical support for the HOOS-PS.
As the HOOS-12 model did not meet the recommended model fit indices in our sample26,33; a number of concerns regarding model fit were present. First, a high correlation values between latent constructs indicate potential multicollinearity and an inability of the items to measure unique constructs. The modification indices also revealed model fit could be substantially improved if modifications in the model (e.g., error terms were correlated) were made.26,33 Additionally, concerns with Cronbach’s alpha values were present; the values were high (0.88-0.91), which are similar to previously reported levels (0.77-0.95)15 indicates potential item redundancy 20,36 Lastly, assessment of cross-loadings identified through the modification indices revealed that some, but not all, of the items shared commonalities which could be justified.26,35 As such, further exploration may be warranted to determine if and when the correlated errors should be included in a model.26,35 High correlation values between constructs and items, coupled with high Cronbach’s alpha values, reiterate the concern regarding the presence of multicollinearity bordering on singularity and the potential need to remove items, alter items to improve clarity, or to develop new items which better measure the intended construct.26,31
While the present study identified concerns regarding the factorial validity in the HOOS, the HOOS-JR, the HOOSPS and the HOOS-12, there are still limitations to consider The current sample was larger than those used for most studies on the HOOS, but this sample was comprised mostly of self-reported healthy individuals. Moreover, the sample used included few participants who had been diagnosed with hip OA, THA, or injury to their hip. Of note,
a sub-sample of the healthy participants was used in the multigroup invariance testing due to the limited sample of injured participants. Utilizing such a small sample size may impact the statistical power of the test and result in model misspecification, which is why larger sample sizes are recommended.26 As such, further exploration is warranted using larger, more evenly distributed and diverse samples. Also, due to the limited sample size and the current clinical application of the scale, invariance testing using the HOOS-JR was limited to the originally proposed model; however, future research should explore the validity of including the error term correlation identified and how it influences findings.
The sample of participants also responded to all 40-items of the HOOS. Thus, it is possible that responses to the short forms were influenced by the additional items not on the scale. Therefore, future research should be completed on a sample of participants who only responded to the items on the instrument. The authors also did not conduct long-term follow-up nor compare the results of the modified scale with another criterion scale. Due to study design (i.e., collection at one time point), we could not perform test-retest reliability, assess the minimal detectable change, assess responsiveness (e.g., the minimal clinically important differences [MCIDs]), or perform longitudinal invariance testing. Future research should aim to assess longitudinal invariance and measures of instrument precision (e.g., MCIDs) to fully establish the psychometric properties of each scale and to provide guidance for use of the scales in clinical practice and research.
In conclusion, the scale structure of the original HOOS and HOOS-12 were not supported in the current study Analyses found preliminary evidence to support the use of the HOOS-JR and HOOS-PS as psychometrically sound instruments and multigroup invariance testing results provided substantive support for these scales measuring the intended phenomenon and ability to assess true group differences in certain situations. Clinicians and researchers who utilize the scales, should do so with caution regarding their limitations or untested properties (e.g., longitudinal invariance testing). Thus, more research is warranted to establish the full psychometric properties of these scales and identify an improved version which meets contemporary recommendations to measure the multi-dimensional experience of patient disability following hip pathology
The authors report no conflicts of interest
Submitted:
This is an open-access article distributed under the terms of the Creative Commons
Attribution 4.0
International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Ruyssen-Witrand A, Fernandez-Lopez C, Gossec L, Anract P, Courpied J, Dougados M. Psychometric properties of the OARSI/OMERACT osteoarthritis pain and functional impairment scales: ICOAP, KOOS-PS and HOOS-PS. Clin Exp Rheum-Incl Supplements. 2011;29(2):231.
2. Botha‐Scheepers S, Watt I, Rosendaal FR, Breedveld FC, Hellio le Graverand MP, Kloppenburg M. Changes in outcome measures for impairment, activity limitation, and participation restriction over two years in osteoarthritis of the lower extremities. Arthrit Care Res. 2008;59(12):1750-1755. doi:10.1002/ art.24080
3. Jette AM. Outcomes research: shifting the dominant research paradigm in physical therapy. Phys Ther 1995;75(11):965-970. doi:10.1093/ptj/75.1
1.965
4. Vela LI, Denegar CR. The disablement in the physically active scale, part II: The psychometric properties of an outcomes scale for musculoskeletal injuries. J Athl Train. 2010;45(6):630-641. doi:10.408 5/1062-6050-45.6.630
5. Vingård E, Alfredsson L, Malchau H. Osteoarthrosis of the hip in women and its relationship to physical load from sports activities. Am J Sports Med 1998;26(1):78-82. doi:10.1177/0363 5465980260013101
6. Felson DT, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum. 1998;41(8):1343-1355.
7 Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS) – validity and responsiveness in total hip replacement. BMC Musculoskelet Disord 2003;4(1):10. doi:10.1186/1471-2474-4-10
8. Ryser L, Wright BD, Aeschlimann A, Mariacher‐Gehler S, Stucki G. A new look at the Western Ontario and McMaster Universities Osteoarthritis Index using Rasch analysis. Arthrit Care Res 1999;12(5):331-335.
9. Davis AM, Badley EM, Beaton DE, et al. Rasch analysis of the western ontariomcmaster (WOMAC) osteoarthritis index: results from community and arthroplasty samples. J Clin Epidemiol. 2003;56(11):1076-1083. doi:10.1016/s0895-4356(03)0 0179-3
10. Davis AM, Perruccio AV, Canizares M, et al. The development of a short measure of physical function for hip OA HOOS-Physical Function Shortform (HOOS-PS): an OARSI/OMERACT initiative. Osteoarthr Cartil Open 2008;16(5):551-559. doi:10.10 16/j.joca.2007.12.016
11. Sun Y, Sturmer T, Gunther KP, Brenner H. Reliability and validity of clinical outcome measurements of osteoarthritis of the hip and knee a review of the literature. Int J Rheum Dis 1997;16(2):185-198. doi:10.1007/bf02247849
12. Nilsdotter A, Bremander A. Measures of hip function and symptoms: Harris hip score (HHS), hip disability and osteoarthritis outcome score (HOOS), Oxford hip score (OHS), Lequesne index of severity for osteoarthritis of the hip (LISOH), and American Academy of orthopedic surgeons (AAOS) hip and knee questionnaire. Arthrit Care Res. 2011;63(S11):S200-S207 doi:10.1002/acr.20549
13. Ornetti P, Parratte S, Gossec L, et al. Crosscultural adaptation and validation of the French version of the Hip disability and Osteoarthritis Outcome Score (HOOS) in hip osteoarthritis patients. Osteoarthr Cartil Open. 2010;18(4):522-529. doi:10.10 16/j.joca.2009.12.007
14. Nilsdotter A, Petersson I, Roos EM, Lohmander L. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study Ann Rheum Dis 2003;62(10):923-930. doi:10.1136/ar d.62.10.923
15. Gandek B, Roos EM, Franklin PD, Ware JE Jr A 12-item short form of the Hip disability and Osteoarthritis Outcome Score (HOOS-12): tests of reliability, validity and responsiveness. Osteoarthr Cartil Open 2019;27(5):754-761. doi:10.1016/j.joca.2 018.09.017
16. Lyman S, Lee YY, Franklin PD, Li W, Mayman DJ, Padgett DE. Validation of the HOOS, JR: a short-form hip replacement survey. Clin Orthop Relat Res. 2016;474(6):1472-1482. doi:10.1007/s11999-016-471 8-2
17. Gandek B, Roos EM, Franklin PD, Ware JE Jr. Item selection for 12-Item short forms of the knee injury and osteoarthritis outcome score (KOOS-12) and hip disability and osteoarthritis outcome score (HOOS-12). Osteoarthr Cartil Open 2019;27(5):746-753. doi:10.1016/j.joca.2018.11.011
18. De Groot IB, Reijman M, Terwee CB, et al. Validation of the Dutch version of the Hip disability and Osteoarthritis Outcome Score. Osteoarthr Cartil Open. 2007;15(1):104-109. doi:10.1016/j.joca.2006.0
6.014
19. Hinkle DE, Wiersma W, Jurs SG. Applied Statistics for the Behavioral Sciences Vol 663. Houghton Mifflin College Division; 2003.
20. Leech NL, Barrett KC, Morgan GA. IBM SPSS for Intermediate Statistics: Use and Interpretation Routledge; 2014.
21. Streiner DL. Starting at the beginning: an introduction to coefficient alpha and internal consistency. J Pers Assess. 2003;80(1):99-103. doi:1 0.1207/s15327752jpa8001_18
22. Taber KS. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ 2018;48(6):1273-1296. doi:10.1007/s11165-016-960
2-2
23. Klässbo M, Larsson E, Mannevik E. Hip disability and osteoarthritis outcome scoreAn extension of the Western Ontario and McMaster Universities Osteoarthritis Index. Scand J Rheumatol 2003;32(1):46-51. doi:10.1080/03009740310000409
24. Panayides P Coefficient alpha: interpret with caution. Eur J Psychol. 2013;9(4):687-696. doi:10.596 4/ejop.v9i4.653
25. Pesudovs K, Burr JM, Harley C, Elliott DB. The development, assessment, and selection of questionnaires. Optom Vision Sci 2007;84(8):663-674. doi:10.1097/opx.0b013e318141fe
75
26. Kline RB. Principles and Practice of Structural Equation Modeling Guilford publications; 2015.
27. Bryant FB, Yarnold PR. Principal-components analysis and exploratory and confirmatory factor analysis. In: Grimm LG, Yarnold PR, eds. Reading and Understanding Multivariate Statistics. American Psychological Association; 1995:99-136.
28. Whitaker C, Stevelink S, Fear N. The use of Facebook in recruiting participants for health research purposes: a systematic review J Med Internet Res. 2017;19(8):e290. doi:10.2196/jmir.7071
29. Tabachnick BG, Fidell LS. Using Multivariate Statistics 4th ed. Allyn & Bacon; 2001.
30. Grimm LG, Yarnold PR. Reading and Understanding Multivariate Statistics. American Psychological Association; 1995.
31. Brown TA. Confirmatory Factor Analysis for Applied Research. Guilford publications; 2015.
32. Byrne BM. Structural equation modeling with AMOS: basic concepts, applications, and programming (multivariate applications series). New York: Taylor & Francis Group. 2010;396(1):7384.
33. Byrne BM. Structural Equation Modeling with Mplus: Basic Concepts, Applications, and Programming Routledge; 2013. doi:10.4324/9780203807644
34. Aguinis H, Gottfredson RK, Joo H. Best-practice recommendations for defining, identifying, and handling outliers. Organ Res Methods. 2013;16(2):270-301. doi:10.1177/1094428112470848
35. Nachtigall C, Kroehne U, Funke F, Steyer R. Pros and cons of structural equation modeling. Methods Psychological Research Online 2003;8(2):1-22.
36. Lohr KN, Aaronson NK, Alonso J, et al. Evaluating quality-of-life and health status instruments: development of scientific review criteria. Clin Ther. 1996;18(5):979-992. doi:10.1016/s0149-2918(96)8005 4-3
37. Dillman DA, Smyth JD, Christian LM. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method John Wiley & Sons; 2014.
38. Davis AM, Perruccio AV, Canizares M, et al. Comparative, validity and responsiveness of the HOOS-PS and KOOS-PS to the WOMAC physical function subscale in total joint replacement for osteoarthritis. Osteoarthr Cartil Open 2009;17(7):843-847 doi:10.1016/j.joca.2009.01.005
Keywords: functional movement screen, pain intensity, disability level, lumbar spine, movement impairments, movement system https://doi.org/10.26603/001c.68024
Low back pain (LBP) is a musculoskeletal disorder that affects more than 80% of people in the United States at least once in their lifetime. LBP is one of the most common complaints prompting individuals to seek medical care. The purpose of this study was to determine the effects of spinal stabilization exercises (SSEs) on movement performance, pain intensity, and disability level in adults with chronic low back pain (CLBP).
Forty participants, 20 in each group, with CLBP were recruited and randomly allocated into one of two interventions: SSEs and general exercises (GEs). All participants received their assigned intervention under supervision one to two times per week for the first four weeks and then were asked to continue their program at home for another four weeks. Outcome measures were collected at baseline, two weeks, four weeks, and eight weeks, including the Functional Movement ScreenTM (FMSTM), Numeric Pain Rating Scale (NPRS), and Modified Oswestry Low Back Pain Disability Questionnaire (OSW) scores.
There was a significant interaction for the FMSTM scores (p = 0.016), but not for the NPRS and OSW scores. Post hoc analysis showed significant between-group differences between baseline and four weeks (p = 0.005) and between baseline and eight weeks (p = 0.026) favor SSEs over GEs. Further, the results demonstrated that all participants, regardless of group, had significant improvements in movement performance, pain intensity, and disability level over time.

The results of the study favor SSEs over GEs in improving movement performance for individuals with CLBP, specifically after four weeks of the supervised SSE program.
Low back pain (LBP) is a musculoskeletal disorder that affects more than 80% of people in the United States at least once in their lifetime.1,2 LBP is considered to be one of the most common complaints prompting individuals to seek medical care. It is a very costly condition as the total direct and indirect medical spending for LBP is estimated between
Corresponding author:
Khalid Alkhathami PT, PhD
$100 and $200 billion a year.2 In addition, LBP is a leading cause of disability, contributing to work absenteeism and loss of productivity worldwide.3,4 Clinically, aberrant movement patterns such as a painful arc, lateral shifting, or Gower’s sign are associated with lumbar instability or movement coordination impairment.5,6 Furthermore, patients with CLBP often develop compensatory movement patterns to complete functional tasks, such as stepping over an obstacle and squatting.7 Therefore, observation and
Address: Department of Health Rehabilitation, College of Applied Medical Sciences, Shaqra University, Shaqra 11961, Kingdom of Saudi Arabia
E-mail: kalkhthami@su.edu.sa
Phone: +966566343732
analysis of movement quality may be key elements in LBP management, particularly for patients with subacute and chronic LBP 8
The quality of movement has been measured in different ways, including the use of self-reported measures, impairment measures, and movement performance measures. Self-reported questionnaires are commonly administered because they are based on the patients’ own evaluation of their pain and function.9 However, these self-reported questionnaires do not always distinguish whether or why a specific task is performed properly.10 The self-reported questionnaires lack the description of movements and how the patient will perform the specific task and only address whether the patient is able to do it or not. Therefore, to address the inadequacy of self-reported questionnaires, functional performance measures that are capable of assessing the patient’s ability to perform specific functional tasks, as well as the ease and efficiency of performing these tasks, may be more appropriate to determine the quality of movement.
The Functional Movement ScreenTM (FMSTM) is a quantitative assessment tool that was developed to assess movement performance by identifying limitations and restrictions of movement patterns and to determine whether abnormal movements are present.11,12 Individuals or athletes with lower FMSTM scores also have been found to be associated with a higher risk of musculoskeletal injury 13–16 Because of its ability to evaluate and treat patients with injuries, the FMSTM has been advocated as a tool to be incorporated in rehabilitation.11 The FMSTM has been used as an outcome measure to examine the effects of an exercise program on healthy people and was found to be capable of capturing the improvement of functional movement patterns after an exercise program.17,18 Moreover, a recent study found that patients with CLBP demonstrated lower FMSTM scores as compared to healthy controls.7 Therefore, the FMSTM appears to be a useful functional assessment measure to identify movement deficits in patients with CLBP 7
A variety of treatments have been used by physical therapists for treating CLBP, including manual therapy, exercise programs (e.g., trunk coordination, strengthening, and endurance exercises), lower quarter nerve mobilization, traction, and patient education.19,20 Given the high prevalence of CLBP and high recurrence of LBP and the associated costs, clinicians have been advised to place a priority on interventions which can prevent recurrences and transitions of acute and subacute to CLBP 20 Among conservative treatments, therapeutic exercises are the most widely used for the management of LBP 21 A plethora of evidence has shown that therapeutic exercises are moderately effective for CLBP.22 A meta-analysis of exercise therapy for the treatment of LBP reported that therapeutic exercise was effective in decreasing pain in patients with CLBP.23 However, debates continue regarding what specific type of exercise may be most effective. More recently, spinal stabilization exercises (SSEs) have been advocated as the optimal choice in the rehabilitation of LBP because SSEs have a positive effect on supporting and stabilizing the lumbar spine, re-
ducing pain, and enhancing proprioception as a result of LBP.24,25 In addition, SSEs were found to be more effective than GEs in decreasing pain and improving physical function in patients with LBP and were more effective than a placebo intervention in lumbar segmental instability in patients with LBP.26,27
However, the FMSTM has not yet been used to examine the effectiveness of physical therapy interventions in the LBP population. Although SSEs have been shown to be effective in treating patients with LBP, it is not known if SSEs would improve movement performance. To date, no study has been conducted for assessing the effects of SSEs on the quality of movement performance. Therefore, a randomized clinical trial was warranted to examine whether or not SSEs would have a favorable outcome on movement performance assessed by the FMSTM The purpose of this study was to determine the effects of SSEs on movement performance, pain intensity, and disability level in adults with CLBP.
This study was a double-blinded randomized clinical trial, comparing two exercise programs: SSE vs. GE. Approval from the investigators’ institutional review board was obtained prior to participant enrollment and data collection. To determine adequate sample size for this study, an a priori power analysis was performed using G*Power 3.1.9.28 Using a small-to-medium effect size of 0.20 and an alpha level of 0.05, a sample size of 40 participants was needed to ensure an adequate power level of 0.80 for a mixed-model 2 x 4 analysis of variance (ANOVA) test. Participants of any ethnicity, sex, or race who did not receive physical therapy at the time and within the prior three months, were recruited for this study from the local communities through flyers, word-of-mouth marketing, emails, and direct mail advertisements. Participants were adults of 18 to 65 years of age with LBP for a duration of more than 12 weeks.29 In addition, the eligible participants must have the ability to understand and speak English and had a minimum pain score of 2/10 in the past week using the NPRS. Participants who met inclusion criteria and agreed to participate in the study were asked to sign a written informed consent form.
Participants were excluded if they had (1) serious spinal conditions, such as fracture, infection, or tumor, (2) signs of nerve root compression, (3) a history of the lower extremity or lumbar spine surgery, (4) a history of hip, knee, or ankle pain in the previous two years, (5) current pregnancy by self-report, (6) systemic joint disease (e.g., rheumatologic or neurological disorders), (7) vestibular or other balance disorders, (8) ongoing treatment for the inner ear, sinus, or upper respiratory infection, (9) a history of falls or fear of falling, or (10) a need for any form of walking aids (e.g., cane or walker). A neurological examination was performed to further screen for each participant’s eligibility Once the participants were deemed to be eligible for this study, their demographic characteristics (i.e., age, sex, height, weight, leg dominance) and pain history (e.g., pain duration, pain intensity) were collected. In addition, partic-
ipants completed two questionnaires, the Fear-Avoidance Beliefs Questionnaire (FABQ) and Patient-Reported Outcomes Measurement Information System®-29 (PROM-29), which were used to describe the participants of this study.
Two investigators were responsible for data collection for this study The principal investigator, investigator #1, was the treating therapist who was responsible for group allocation and intervention administration and was blinded to the results of the FMSTM , NPRS, and OSW Investigator #2 was responsible for collecting outcome measures and was blinded to each participant’s group assignment.
The FMSTM Test Kit (Functional Movement Systems Inc., Chatham, VA) was used to assess the movement performance of seven different movement patterns for this study
The FMSTM Test Kit consists of a two-inch by six-inch board, one four-foot-long dowel, two shorter dowels, and an elastic cord.30 The FMSTM includes seven test components: the deep squat, hurdle step, in-line lunge, shoulder mobility, active straight-leg-raise, trunk stability push-up, and rotary stability Additionally, there are three clearance screens, including the impingement-clearing test, pressup clearing test, and posterior-rocking clearing test. These three clearance screen tests are used to determine the presence of pain associated with internal rotation and flexion of the shoulder, spinal flexion, and spinal extension. However, because this study focused on the LBP population, the impingement-clearing test was excluded (Appendix A).
In the original FMSTM scoring system, each of the seven test components is scored on a scale of 0 to 3: 3 when the test component is performed correctly without compensations, 2 when completion of the test component required compensatory movement, 1 when the participant is unable to perform the test component as required, and 0 when there is an occurrence of pain during the test component. However, as all of the participants had LBP in this study, the FMSTM scores were modified so that a zero score was given only when the participant reported an increase in the LBP, not simply for the presence of LBP The validity and reliability of this modified FMSTM scoring system have been established previously with excellent inter-rater reliability in those with LBP (ICC = 0.99).31 Lastly, a composite score ranging from 0 to 21 is calculated to indicate the overall quality of movement performance, with a higher score indicating higher quality of movement performance. A score of 14 or lower on the original FMSTM scoring system indicates that the participant could have a higher risk for future injury 11,13
Each participant was asked to complete the two clinical outcome measures, the NPRS and the OSW, prior to the FMSTM test. During the FMSTM , each participant performed all seven test components in the same order as described
by Cook et al. (2010). No warm-up was required before the start of the measurement. Each participant performed three trials for each of the seven FMSTM test components, and the best score from the three trials was recorded. However, the participants performed the two clearance screens only once. Therefore, when a participant had no pain with a clearance screen, the screen was considered negative. If there was an increase in LBP, not simply the presence of LBP with a clearance screen, the screen was considered positive, and the associated test was scored zero. Two FMSTM test components are associated with a clearance screen: the push-up test with the press-up clearance screen and the rotator stability test with the posterior rocking clearance screen. Five of the seven FMSTM test components were performed bilaterally: hurdle step, in-line lunge, shoulder mobility, active straight leg raise, and rotary stability test. Each participant performed these five tests first on the right side and then on the left side. For movements that were scored on both limbs simultaneously, the lower score was used to compute the composite score. The total score of the seven test components was added together to obtain a composite score of the FMSTM .
For each participant, the FMSTM , NPRS, and OSW measurements scores were collected at baseline and then two weeks, four weeks, and eight weeks after the initiation of treatment. Additionally, NPRS measurements were collected at the beginning of each session, before and after each test, and any aggravation of LBP was recorded throughout the entire testing procedure.
Once the participants completed the FMSTM , they were assigned randomly into either the SSE group or the GE group. Participants in the SSE group were instructed in the SSEs, which were modeled on the SSE program designed by Hicks et al. (Appendix B).32 The SSE program of this study targeted the spinal stabilizer muscles, including the transversus abdominus, erector spine, lumbar multifidus, quadratus lumborum, and oblique abdominal muscles. The SSEs consisted of four categories. The exercises in the first category were abdominal bracing exercises, which were designed primarily to target the transversus abdominus muscle. The participant performed each abdominal bracing exercise up to 30 repetitions with a target hold time of eight seconds. The SSEs in the second category were quadruped exercises, which were designed to target both the erector spinae and multifidus. The participant performed each quadruped exercise up to 30 repetitions with a target hold time of eight seconds. The SSEs in the third category were prone-plank exercises, which were designed to primarily target the quadratus lumborum muscle. The participant performed each prone plank exercise up to 30 repetitions with a target hold time of eight seconds. Lastly, the SSEs in the fourth category were side-plank exercises, which were designed to train the oblique abdominal muscle. The participant performed each side-plank exercise up to 30 repetitions with a target hold time of eight seconds.
The GE program consisted of ROM and flexibility exercises of low back and lower extremities (Appendix C). There
were four exercise categories, including knee-to-chest, lower trunk rotation, prone press-ups, and hamstring stretch. Each participant in this group was asked to perform each exercise up to 20 times with a target hold time of 10 seconds. The participants were instructed to perform all of the four exercises within a pain-free range.
At the initial treatment session, all participants were instructed to perform four exercises, one from each category The exercise intensity progressed to the next level when the participant could perform the exercise with proper form and for the required repetitions and hold time. Once they progressed to the next level of the exercise, they discontinued the previous level of the exercise.
On the first visit, all participants were instructed in the exercises at a level that they were able to perform without pain. All participants were given an exercise log based on the assigned group to report their exercise compliance (Appendix D). In addition, all participants were given an exercise handout, which illustrated the exercises and listed the required exercise repetitions and holds time. All participants were asked to return one to two times per week for four weeks for exercise progression and to ensure that they were performing the exercises properly The intervention frequency and duration were chosen to reflect common physical therapy practice. However, each participant was asked to perform their assigned exercise program at least five times per week, and exercises during the on-site visits were counted toward the required exercise frequency After the four-week intervention, all participants were asked to continue their exercise program at home five times a week for another four weeks until their final follow-up visit at week 8. In addition, the participants were instructed on how to progress their exercises at home.
All statistical analyses were performed using SPSS Statistics, Version 25 (IBM Corp., Armonk, NY, USA). Descriptive statistics, including frequency, means, and standard deviations, were calculated for the demographic data of the participants, including age, gender, height, weight, body mass index (BMI), the participants’ characteristics (e.g., duration of pain, distribution of pain, FABQ scores, and PROMIS scores), and the results of outcome measures (i.e., FMSTM , NPRS, and OSW scores). Independent t-and chisquare tests were used to determine if there was a difference in participants’ characteristics at baseline. Three separate 2 (group) x 4 (time) repeated measure (RM) ANOVAs were used to analyze the three outcome measures collected over four different time points. Post hoc analysis was performed if there was a significant interaction. The α level was set at 0.05 for all statistical analyses.
A total of 40 participants met the inclusion criteria and completed the eight-week exercise program (Figure 1).
The characteristics of the participants and baseline outcome measurements are summarized in (Table 1).
In general, the participants had mild LBP with an average NPRS score of 3.5 ± 1.6. There was no significant difference (p < 0.05) in any of the baseline participants’ characteristics, and outcome measurements between participants in the SSE group and those in the GE group (Table 1). Therefore, the two groups were considered similar at the beginning of the study
The means and standard deviations of all three outcome measurements at all four-time points are shown in (Table 2).
The ANOVA results showed a significant interaction of group by time, F (3, 114) = 3.599, p = 0.016, indicating that there was a significant difference in the modified FMSTM scores between groups over eight weeks. Next, separate 2 x 2 RM ANOVAs followed to examine the between-group differences between each two-time point. Consequently, significant between-group differences were found between baseline and four weeks (p = 0.005) and between baseline and eight weeks (p = 0.026) favor SSEs over GEs. In addition, there was a significant main effect of time. Post-hoc pairwise comparisons showed that all participants made significant improvements in the modified FMSTM scores between the two adjacent time points: from baseline to two weeks (p = 0.011), from two weeks to four weeks (p = 0.001), and from four weeks to eight weeks (p = 0.008) (Figure 2).
The RM ANOVA for the NPRS and OSW scores showed no significant interaction of group by time: F (3, 114) = 1.185, p = 0.319 and F (3, 114) = 0.538, p = 0.605, respectively.
However, there was a significant main effect of time (p < 0.001) for both the NPRS and OSW scores. Post-hoc pairwise comparisons showed significantly lower NPRS scores from baseline to two weeks (p = 0.007), from two weeks to four weeks (p < 0.001), but no significant difference from four weeks to eight weeks (p = 0.818) (Figure 3).
Similarly, post-hoc pairwise showed significantly lower OSW scores from baseline to two weeks (p = 0.017), from two weeks to four weeks (p = 0.047), but no significant difference from four weeks to eight weeks (p = 0.117) (Figure 4).
There were no significant differences between the two groups in the supervised phase and the unsupervised phase. However, both groups had significantly better exercise compliance in the supervised phase (first four weeks) than they did in the unsupervised phase (last four weeks) (p = 0.044 for the SSE group, p = 0.025 for the GE group) (Table 3).
The modified FMSTM scores showed that participants who received SSEs had made significantly greater improvement on movement performance than those who received a GE
program. The results suggest that the exercises prescribed to the individuals with CLBP should be specific to and target spinal stabilizers in order to improve quality of movement as compared to GEs, such as ROM and flexibility exercises. There is no published evidence regarding the effectiveness of the SSE program on movement performance in patients with LBP However, this finding is in agreement with a previously published study by Bagherian et al., who demonstrated that the SSE program enhanced functional movement patterns in healthy, pain-free collegiate athletes, particularly for those who had low baseline FMSTM scores (i.e., ≤ 14).17 In contrast to the participants in the Bagherian et al. study, the participants in this study were those with CLBP Although the participants in this study had low disability levels, the SSEs designed in this study were at a low level of difficulty and intensity as compared to those in the Bagherian et al. study, which included high-level exercises, such as back extension and sit-ups. Considering the improvement made by the participants in the SSE group, the dosage and progression of the SSEs seemed to be appropriate for this patient population.
The SSE group demonstrated a significantly greater improvement than the GE group in movement performance at
the conclusion of the supervised phase (i.e., 4 weeks), and the differential effects were maintained at the end of the study period (i.e., 8 weeks). This finding is consistent with other studies which also found that a four-week SSE program was effective for enhancing stability and functional capabilities, as well as for reducing pain intensity in patients with CLBP 33,34 It was hypothesized that four weeks were necessary to alter neuromuscular control of the spinal column, and therefore improve inter-segmental spinal stability 34 Further examination of each of the seven test components at baseline, week 4, and week 8 revealed that the SSE group appeared to have greater improvement on the rotary stability test and the trunk stability push-up test than the GE group. Not surprisingly, these two test components were designed specifically to assess an individual’s spinal stability, which is consistent with the goal of the SSE program.12
The results of this study support that SSEs were effective in enhancing the spinal stabilizers, thus improving movement performance. Deficits in the spinal stabilizers are considered to be the primary cause of spinal instability leading to LBP.35 Specifically, the TrA and LM muscles are considered to play an essential role in lumbopelvic stabilization.
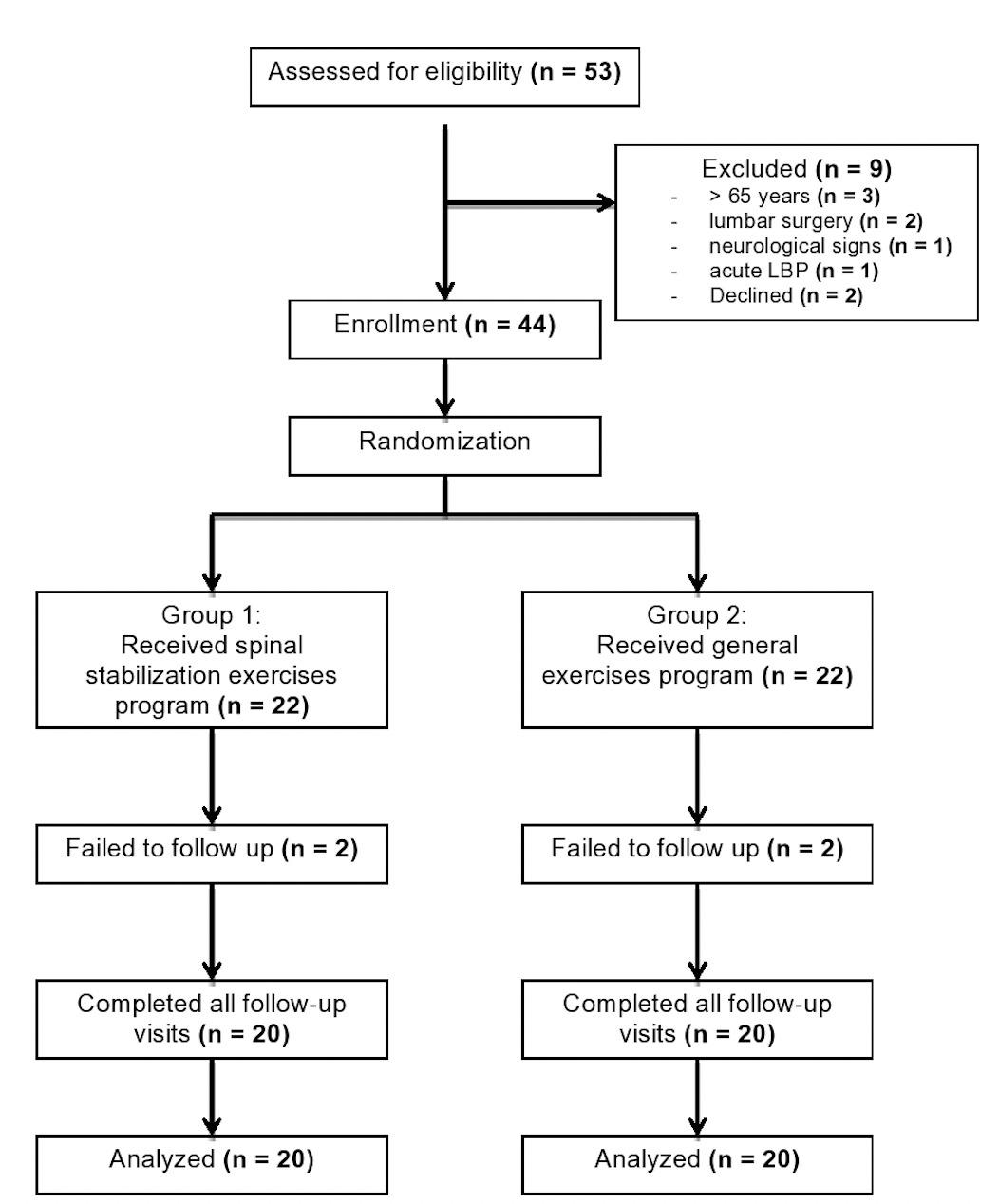 Figure 1. Consort diagram of participants’ screening, enrollment, and randomization.
Figure 1. Consort diagram of participants’ screening, enrollment, and randomization.
Impairments inactivation and coordination of the TrA and LM muscles have been identified in patients with CLBP and are believed to contribute to their poor movement coordination.36–38 Therefore, strength and proper activation of these muscles are necessary for the stability of the lumbar spine in order to restore proper functional movements for this patient population, as indicated by the results of this study 37–41 Furthermore, the literature supports the use of SSEs for individuals with LBP for improving neuromuscular control and endurance, retraining and strengthening deep spinal muscles, reducing pain, and enhancing proprioception related to the dysfunction.24,25,42
At eight weeks, the SSE group had a reduction in NPRS score of 1.4 points from baseline, and the GE group had a
reduction in NPRS score of 1.6 points from baseline. Neither group demonstrated a clinically meaningful change in pain intensity that exceeded the minimal detectable change (MDC) or minimal clinically important change (MCID) score of 2 for the NPRS in individuals with LBP.43 Although there was no difference in pain between groups, there were differences in the modified FMSTM scores between groups. For individuals with CLBP who have low levels of pain, the NPRS may not be a useful outcome measure to examine treatment effects. Instead, a high functional level test, such as the FMSTM , may be necessary to detect different treatment effects.
Similar to the result of the NPRS scores, the results of the study indicated no significant differences in disability reduction between the SSE program and the GE program over eight weeks. This result implies that both exercise interventions had an equivalent effect on functional improve-
ment and disability reduction. Both groups were considered to have a minimal disability level at baseline (OSW score:18.2 for the SEE group and 18.1 for the GE group). Although the participants in this study reported minimal disability levels at baseline, all participants demonstrated significant improvement in disability levels, in the first four
weeks. Although neither group demonstrated a clinically meaningful change in their disability level that exceeded the MDC of 10.5 for the OSW in individuals with LBP, only the SSE group’s disability improvement (OSW score: 6.2 points) exceeded the MCID of 6 points.6,44 The minimal pain intensity and disability levels at baseline could have
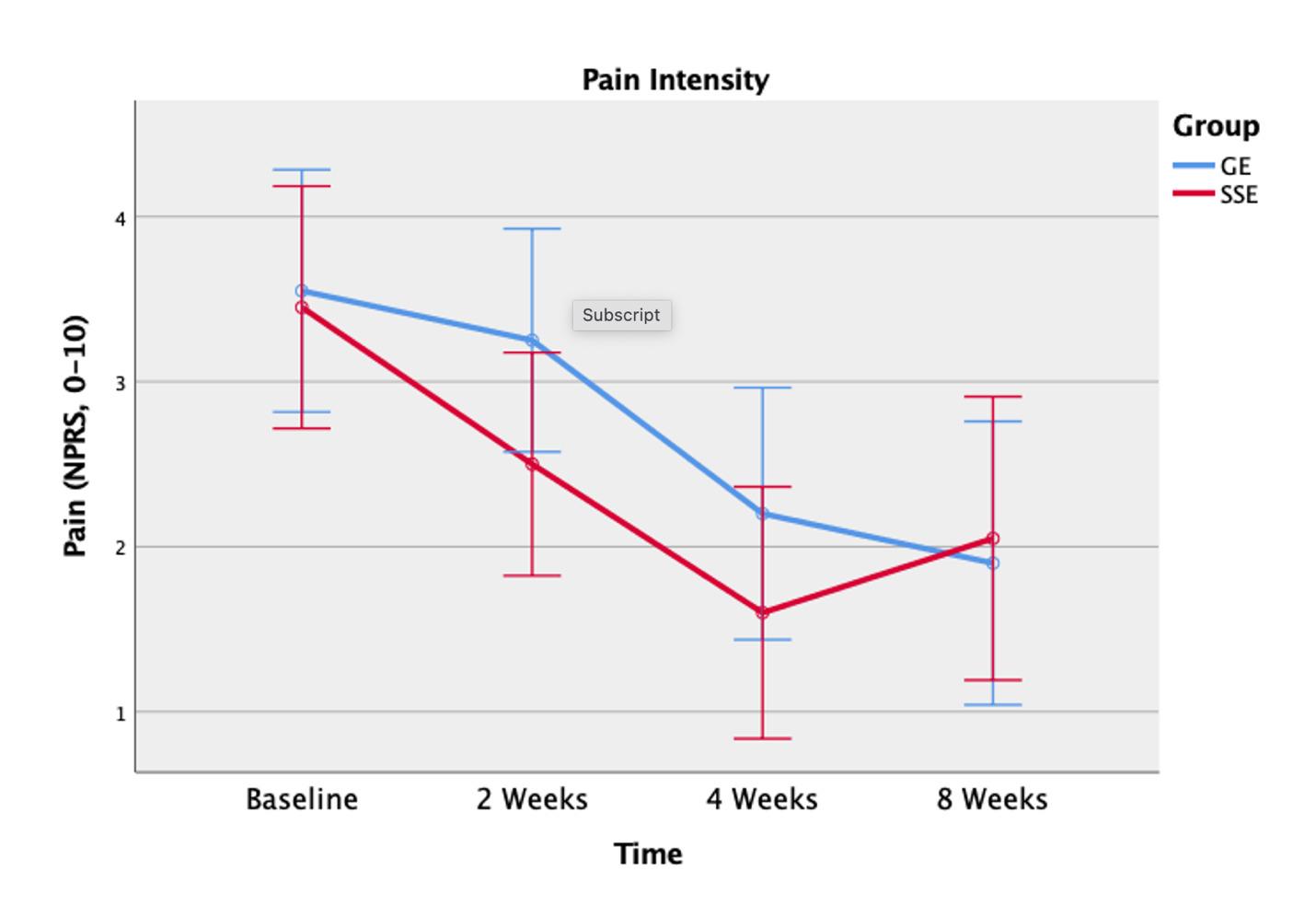
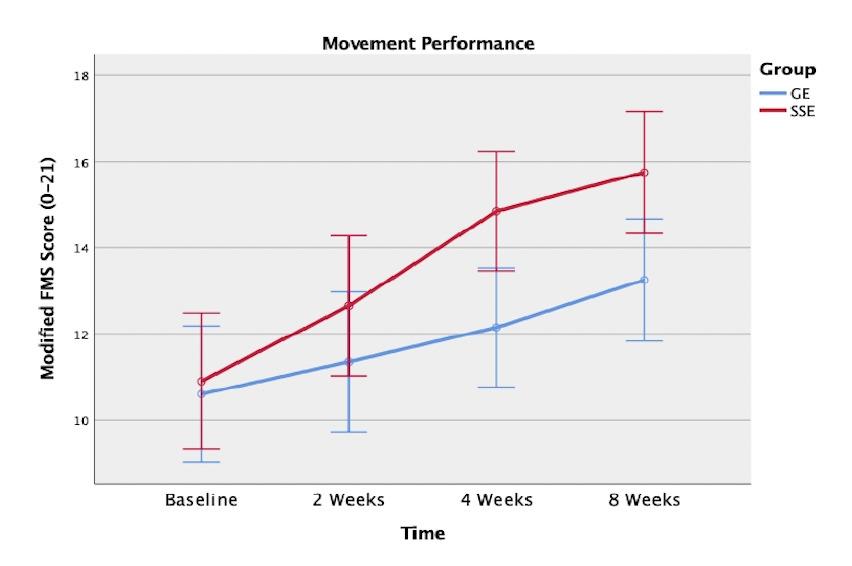 Figure 2. Movement performance using the modified Functional Movement Screen scoring system between the spinal stabilization exercise (SSE) group and the general exercise (GE) group at baseline, 2 weeks, 4 weeks, and 8 weeks.
Figure 3. Pain intensity using the Numeric Pain Rating Scale (NPRS) between the spinal stabilization exercise (SSE) group and the general exercise (GE) group at baseline, 2 weeks, 4 weeks, and 8 weeks.
Figure 2. Movement performance using the modified Functional Movement Screen scoring system between the spinal stabilization exercise (SSE) group and the general exercise (GE) group at baseline, 2 weeks, 4 weeks, and 8 weeks.
Figure 3. Pain intensity using the Numeric Pain Rating Scale (NPRS) between the spinal stabilization exercise (SSE) group and the general exercise (GE) group at baseline, 2 weeks, 4 weeks, and 8 weeks.
contributed lack of clinically meaningful changes. However, participants with high pain and disability levels may not be able to complete the FMSTM
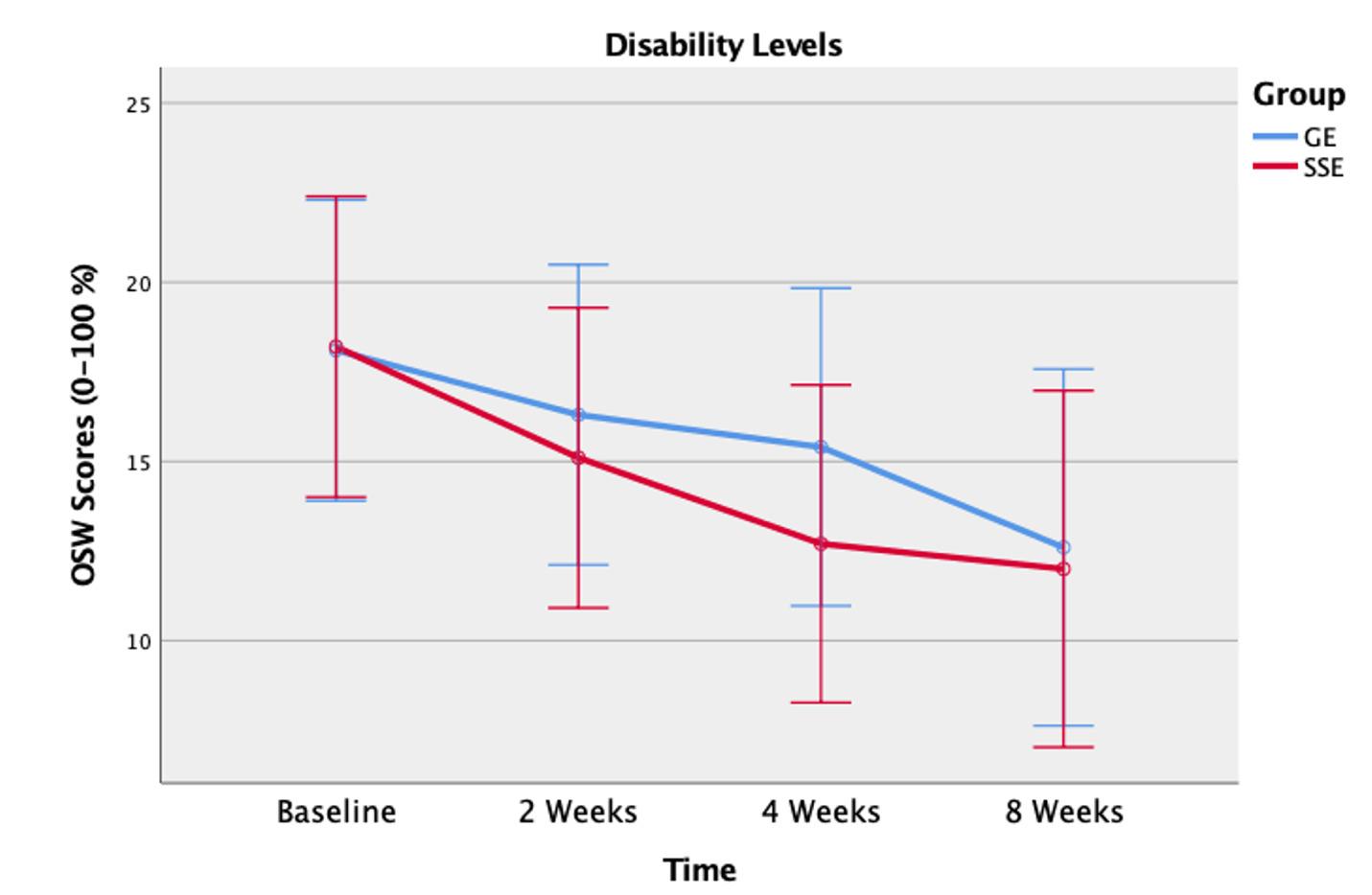
The FMSTM with the modified scoring system may be a useful outcome measure for assessing the quality of movement, specifically in adults with LBP Identification and quantification of abnormal movement patterns may allow therapists to address movement impairments in their plan of care.
There were limitations in this study The participants in this study had low NPRS and OSW scores. Therefore, the results of this study only can be generalized to those indi-
viduals with CLBP with low pain intensity and mild disability levels. However, participants with a moderate or moderate-to-high level of pain may not be able to complete or perform the FMSTM tests or SSE program. Furthermore, this study was conducted on participants between 18 and 65 years old. Therefore, this study might not be generalized to patients over 65 years old. The other limitation is that the participants were not restricted from other physical activities although participants were advised not to engage in any activity that might increase their LBP However, the randomization procedure may have minimized this uncontrolled factor Lastly, medication use was not controlled in this study in order to reflect the current clinical practice collected at baseline. However, at each follow-up visit, all participants were asked if they had taken any medication because of their LBP. Future studies should examine the effects of eight-week supervised treatments (e.g., SSEs) in or-
Figure 4. Disability levels using the Modified Oswestry Low Back Pain Disability Questionnaire (OSW) between the spinal stabilization exercise (SSE) group and the general exercise (GE) group at baseline, 2 weeks, 4 weeks, and 8 weeks.der to achieve better outcomes and maximize the benefits of the treatment. In addition, it is recommended that future studies should examine the effectiveness of SSEs on the movement performance of individuals who have moderate and higher pain intensity of LBP and disability levels. Furthermore, longer-term follow-ups are recommended for future studies to examine the effects of physical therapy interventions on movement performance in patients with CLBP.
The results of this study suggest that SSEs are more effective in enhancing movement performance than GEs over a period of eight weeks in individuals with CLBP. In addition, all participants in both groups demonstrated a significant reduction in pain intensity and disability level while attending supervised PT sessions in the first four weeks of the study. However, these significant improvements seemed to be diminished during the unsupervised PT sessions for the last four weeks when the participants stopped meeting regularly with the investigators. Moreover, this study demon-
strated that supervised SSE sessions seemed to maximize the benefits of this treatment including improving the quality of movement and reducing the aberrant movement that is associated with CLBP.
The authors would like to thank the Texas Physical Therapy Foundation for funding this project.
The authors declare that there is no conflict of interest. In addition, the results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation, and the statement that the results of the present study do not constitute an endorsement by ACSM.
Submitted: June 03, 2022 CST, Accepted: December 23, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons
Attribution 4.0
International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet 2012;379(9814):482-491. doi:10.1016/s0140-6736(1 1)60610-7
2. Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med 2009;169(3):251-258. doi:10.1001/archint ernmed.2008.543
3. Fitzmaurice C, Dicker D, Pain A, et al. The global burden of cancer 2013. JAMA Oncol 2015;1(4):505-527 doi:10.1001/jamaoncol.2015.0735
4. Marini M, Bendinelli B, Assedi M, et al. Low back pain in healthy postmenopausal women and the effect of physical activity: A secondary analysis in a randomized trial. PloS One. 2017;12(5):e0177370. do i:10.1371/journal.pone.0177370
5. Biely SA, Silfies SP, Smith SS, Hicks GE. Clinical observation of standing trunk movements: What do the aberrant movement patterns tell us? J Orthop Sports Phys Ther 2014;44(4):262-272. doi:10.2519/jos pt.2014.4988
6. Davidson M, Keating JL. A comparison of five low back disability questionnaires: Reliability and responsiveness. Phys Ther 2002;82(1):8-24. doi:10.10 93/ptj/82.1.8
7 Ko MJ, Noh KH, Kang MH, Oh JS. Differences in performance on the functional movement screen between chronic low back pain patients and healthy control subjects. J Phys Ther Sci 2016;28(7):2094-2096. doi:10.1589/jpts.28.2094
8. van Dijk MJH, Smorenburg NTA, Visser B, Nijhuis–van der Sanden MWG, Heerkens YF. Description of movement quality in patients with low back pain: A qualitative study as a first step to a practical definition. Physiother Theory Pract 2017;33(3):227-237 doi:10.1080/09593985.2017.1282 998
9. Reiman MP, Manske RC. The assessment of function: How is it measured? A clinical perspective. J Man Manip Ther. 2011;19(2):91-99. doi:10.1179/106 698111x12973307659546
10. Simmonds MJ. Measuring and managing pain and performance. Man Ther. 2006;11(3):175-179. doi:10.1 016/j.math.2006.03.002
11. Gray Cook LB, Hoogenboom BJ, Voight M. Functional movement screening: The use of fundamental movements as an assessment of function‐part 1. Int J Sports Phys Ther 2014;9(3):396.
12. Gray Cook LB, Hoogenboom BJ, Voight M. Functional movement screening: The use of fundamental movements as an assessment of function‐part 2. Int J Sports Phys Ther 2014;9(4):549.
13. Butler RJ, Contreras M, Burton LC, Plisky PJ, Goode A, Kiesel K. Modifiable risk factors predict injuries in firefighters during training academies. Work. 2013;46(1):11-17.
14. Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther 2010;5(2):47
15. Clay H, Mansell J, Tierney R. Association between ROWING injuries and the functional movement SCREENTM in female collegiate division I ROWERS. Int J Sports Phys Ther. 2016;11(3):345.
16. Kiesel K, Plisky P, Butler R. Functional movement test scores improve following a standardized offseason intervention program in professional football players. Scand J Med Sci Sports 2011;21(2):287-292. d oi:10.1111/j.1600-0838.2009.01038.x
17. Bagherian S, Ghasempoor K, Rahnama N, Wikstrom EA. The effect of core stability training on functional movement patterns in college athletes. J Sport Rehabil. 2019;28(5):444-449. doi:10.1123/jsr.20 17-0107
18. Stanek JM, Dodd DJ, Kelly AR, Wolfe AM, Swenson RA. Active duty firefighters can improve functional movement screen (FMS) scores following an 8-week individualized client workout program. Work. 2017;56(2):213-220. doi:10.3233/wor-172493
19. Amatya B, Young J, Khan F. Non-pharmacological interventions for chronic pain in multiple sclerosis. Cochrane Database Syst Rev. 2018;2018(12). doi:10.10 02/14651858.cd012622.pub2
20. Delitto A, George SZ, Van Dillen LR, et al. Low back pain: Clinical practice guidelines linked to the international classification of functioning, disability, and health from the Orthopaedic section of the american physical therapy association. J Orthop Sports Phys Ther 2012;42(4):A1-A57 doi:10.2519/jos pt.2012.42.4.a1
21. Lizier DT, Perez MV, Sakata RK. Exercises for nonspecific low back pain treatment. Rev Bras Anestesiol 2012;62(6):842-846. doi:10.1590/s0034-70 942012000600008
22. Chou R, Huffman LH. Medications for acute and chronic low back pain: A review of the evidence for an american pain society/american college of physicians clinical practice guideline. Ann Intern Med. 2007;147(7):505-514. doi:10.7326/0003-4819-147-7-2 00710020-00008
23. Hayden J, van Tulder MW, Malmivaara A, Koes BW Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev 2005;2005(3). doi:10.1002/14651858.cd000335.pub2
24. Bliss LS, Teeple P Core stability: The centerpiece of any training program. Curr Sports Med Rep 2005;4(3):179-183. doi:10.1097/01.csmr.000030620 3.26444.4e
25. Panhale VP, Gurav RS, Nahar SK. Association of physical performance and fear-avoidance beliefs in adults with chronic low back pain. Ann Med Res 2016;6(6):375-379.
26. Wang XQ, Zheng JJ, Yu ZW, et al. A meta-analysis of core stability exercise versus general exercise for chronic low back pain. PloS One 2012;7(12):e52082. doi:10.1371/journal.pone.0052082
27. Kumar SP. Efficacy of segmental stabilization exercise for lumbar segmental instability in patients with mechanical low back pain: A randomized placebo controlled crossover study N Am J Med Sci 2011;3(10):456-461. doi:10.4297/najms.2011.3456
28. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-191. doi:10.3758/bf0319 3146
29. Marin TJ, Van Eerd D, Irvin E, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. Cochrane Database Syst Rev. 2017;2017(6). doi:10.1002/14651858.cd002193.pub2
30. Cook G. Movement: Functional Movement Systems: Screening, Assessment. Corrective Strategies. 1st ed. On Target Publications; 2010.
31. Alkhathami K, Alshehre Y, Wang-Price S, Brizzolara K. Reliability and validity of the functional movement screenTM with a modified scoring system for young adults with low back pain. Int J Sports Phys Ther 2021;16(3):620-627 doi:10.26603/001c.23427
32. Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil 2005;86(9):1753-1762. doi:10.1016/ j.apmr.2005.03.033
33. Inani SB, Selkar SP Effect of core stabilization exercises versus conventional exercises on pain and functional status in patients with non-specific low back pain: A randomized clinical trial. J Back Musculoskelet Rehabil 2013;26(1):37-43. doi:10.3233/ bmr-2012-0348
34. Salavati M, Akhbari B, Takamjani IE, Bagheri H, Ezzati K, Kahlaee AH. Effect of spinal stabilization exercise on dynamic postural control and visual dependency in subjects with chronic non-specific low back pain. J Bodyw Mov Ther 2016;20(2):441-448. do i:10.1016/j.jbmt.2015.10.003
35. Jeong UC, Sim JH, Kim CY, Hwang-Bo G, Nam CW The effects of gluteus muscle strengthening exercise and lumbar stabilization exercise on lumbar muscle strength and balance in chronic low back pain patients. J Phys Ther Sci 2015;27(12):3813-3816. do i:10.1589/jpts.27.3813
36. Cho KH, Beom JW, Lee TS, Lim JH, Lee TH, Yuk JH. Trunk muscles strength as a risk factor for nonspecific low back pain: A pilot study Ann Rehabil Med. 2014;38(2):234-240. doi:10.5535/arm.2014.3
8.2.234
37 Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain: A motor control evaluation of transversus abdominis. Spine 1996;21(22):2640-2650. doi:10.109 7/00007632-199611150-00014
38. Panjabi MM. Clinical spinal instability and low back pain. J Electromyogr Kinesiol 2003;13(4):371-379. doi:10.1016/s1050-6411(03)0004 4-0
39. Chang WD, Lin HY, Lai PT Core strength training for patients with chronic low back pain. J Phys Ther Sci. 2015;27(3):619-622. doi:10.1589/jpts.27.619
40. Gardner-Morse MG, Stokes IA. The effects of abdominal muscle coactivation on lumbar spine stability. Spine. 1998;23(1):86-91. doi:10.1097/000076 32-199801010-00019
41. Haladay DE, Denegar CR, Miller SJ, Challis J. Electromyographic and kinetic analysis of two abdominal muscle performance tests. Physiother Theory Pract 2015;31(8):587-593. doi:10.3109/095939 85.2015.1062945
42. Grenier SG, McGill SM. Quantification of lumbar stability by using 2 different abdominal activation strategies. Arch Phys Med Rehabil 2007;88(1):54-62. d oi:10.1016/j.apmr.2006.10.014
43. Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 2005;30(11):1331-1334. doi:10.109 7/01.brs.0000164099.92112.29
44. Fritz JM, Irrgang JJ. A comparison of a modified oswestry low back pain disability questionnaire and the quebec back pain disability scale. Phys Ther 2001;81(2):776-788. doi:10.1093/ptj/81.2.776
Download: https://ijspt.scholasticahq.com/article/68024-effectiveness-of-spinal-stabilization-exercises-onmovement-performance-in-adults-with-chronic-low-back-pain/attachment/ 135993.pdf?auth_token=Cvo9Er3SzcY8hask1cal
Download: https://ijspt.scholasticahq.com/article/68024-effectiveness-of-spinal-stabilization-exercises-onmovement-performance-in-adults-with-chronic-low-back-pain/attachment/ 135994.pdf?auth_token=Cvo9Er3SzcY8hask1cal
Download: https://ijspt.scholasticahq.com/article/68024-effectiveness-of-spinal-stabilization-exercises-onmovement-performance-in-adults-with-chronic-low-back-pain/attachment/ 135995.pdf?auth_token=Cvo9Er3SzcY8hask1cal
Download: https://ijspt.scholasticahq.com/article/68024-effectiveness-of-spinal-stabilization-exercises-onmovement-performance-in-adults-with-chronic-low-back-pain/attachment/ 135996.pdf?auth_token=Cvo9Er3SzcY8hask1cal
Keywords: Instability, Lumbar spine, Movement impairment, Postural stability, Supervised exercises https://doi.org/10.26603/001c.68075
Dynamic balance is a vital aspect of everyday life. It is important to incorporate an exercise program that is useful for maintaining and improving balance in patients with chronic low back pain (CLBP). However, there is a lack of evidence supporting the effectiveness of spinal stabilization exercises (SSEs) on improving dynamic balance.
To determine the effectiveness of SSEs on dynamic balance in adults with CLBP Study Design
A double-blind randomized clinical trial.
Forty participants with CLBP were assigned randomly into either an SSE group or a general exercise (GE) group, which consisted of flexibility and range-of-motion exercises. Participants attended a total of four to eight supervised physical therapy (PT) sessions and performed their assigned exercises at home in the first four weeks of the eight-week intervention. In the last four weeks, the participants performed their exercises at home with no supervised PT sessions. Participants’ dynamic balance was measured using the Y-Balance Test (YBT) and the normalized composite scores, Numeric Pain Rating Scale and Modified Oswestry Low Back Pain Disability Questionnaire scores were collected at baseline, two weeks, four weeks, and eight weeks.
A significant difference between groups from two weeks to four weeks (p = 0.002) was found, with the SSE group demonstrating higher YBT composite scores than the GE group. However, there were no significant between-group differences from baseline to two weeks (p =0.098), and from four weeks to eight weeks (p = 0.413).
Supervised SSEs were superior to GEs in improving dynamic balance for the first four weeks after initiating intervention in adults with CLBP However, GEs appeared to have an effect equivalent to that of SSEs after 8-week intervention.
1b.
Corresponding author:
Yousef Alshehre PT, M.S., PhD
Consultant Physical Therapist and Assistant Professor, Physical Therapy Department, Faculty of Applied Medical Sciences, University of Tabuk, Tabuk, Saudi Arabia.
Address: 71491 University of Tabuk, Tabuk, Saudi Arabia 47713
E-mail: Yalshehre@ut.edu.sa
Phone: +966500095626

Low back pain (LBP) is the leading cause of disability and a primary contributor to work absenteeism and loss of productivity globally 1–4 Over 50% of individuals with chronic LBP (CLBP) may not recover until one year later 2 Impairments from LBP include mobility deficits,5 physical disabilities,6 and balance disturbances.7–10 Several studies have identified alterations in muscle recruitment and movement patterns as potential pathomechanisms which further lead to spinal instability.6–9,11 Recently, evidence revealed that dynamic balance is reduced in individuals with CLBP and in individuals with a history of LBP as compared to asymptomatic controls.7,8 The reduced use of the lumbopelvic movement to maintain balance has been reported to be due to the reduced motion of the lumbar spine and hip.12 Furthermore, once individuals with LBP lose their balance, they have more difficulty regaining it, and balance deficits can persist even after their LBP has subsided.8 Although pain is a major factor in CLBP, pain is not the only impairment present in CLBP populations. Balance abnormalities and pain-avoiding compensations could further contribute to an individual’s increased re-injury risk and chronicity 2,8,9 Moreover, individuals with LBP can be fearful of performing dynamic tasks because of a fear of additional pain and injury in response to the movement.2,8,9
Uncertainty remains regarding the best treatment approach for LBP Evidence suggests that exercise therapy is a moderately effective intervention for treating LBP.6,13 A systematic review found that therapeutic exercises were associated with small-to-moderate effects on pain and with an increased likelihood of return-to-work for patients with LBP 13 Spinal stabilization exercise (SSE) programs are widely used by physical therapists for rehabilitation of patients with LBP 14–17 Evidence has shown that recruitment of spinal stabilization muscles (e.g., transversus abdominis and lumbar multifidi) may be altered in patients with LBP as compared to healthy controls. It has been proposed that SSEs are used to retrain proper activation and coordination of the trunk musculature to increase spinal stability and reduce pain.14–18 SSEs also have been shown to be effective for improving pain, disability, and physical performance in patients with LBP.4,16–18 Systematic reviews have indicated that SSEs were more effective than general exercises for decreasing pain and improving disability in patients with LBP 4,16,18 Furthermore, recent research reports showed that some forms of SSEs have promising outcomes on postural control in patients with LBP 19,20
Although balance has been used as an outcome measure to examine the effects of SSEs on patients with LBP, the balance measures commonly used in the literature consist of only static postural control assessments and lack dynamic component assessments.21,22 For instance, force plates and the NeuroCom Balance Master® measure ground reaction forces and center of pressure (CoP) displacement, and both provide quantified measures of static or semi-dynamic postural control, but do not measure an individual’s ability to maintain balance while performing a purposeful maneuver.8,21,22 Moreover, these static balance tests usually are
used in a laboratory setting, are expensive and time-consuming, and often are impractical for use in clinical settings.8,21
In recent years, several tests have been used to investigate dynamic balance in LBP populations, such as the Star Excursion Balance Test (SEBT),7,10,23,24 the Y-Balance Test (YBT),8,25 and the functional reach test.26,27 Of these dynamic tests, the reliability and validity of the YBT has been established specifically for the CLBP population. In addition, the YBT is a shorter version of the SEBT, and is more feasible for clinical practice. The YBT evaluates single-legbalance, dynamic neuromuscular control, proprioception, and strength of an individual while simultaneously moving the non-stance limb in anterior (ANT), posteromedial (PM), and posterolateral (PL) directions.21,28,29 The YBT is portable and easy to administer, and it requires little training, making it practical to use in multiple settings.8,25,28,29 Recently, a relaiblity and validity study aimed to determine the inter-rater reliability of the YBT and to compare dynamic balance between young adults with CLBP and an asymptomatic group found that the YBT had an excellent inter-rater reliability, with intraclss correlation coefficients ranging from 0.99 to 1.0. In addition, the CLBP group had a significantly lower composite score (p < 0.001) and shorter reach distances in the ANT (p = 0.023), PM (p < 0.001), and PL (p = 0.001) directions than the asymptomatic group.25
Initial evidence regarding the effect of SSEs on postural control in patients with LBP has been encouraging; however, balance measures used in these studies primarily assessed static postural control and did not have dynamic components, which are imperative for performing daily functional activities. Additionally, these static balance tests are impractical for use in clinical settings. Given that dynamic balance is a vital aspect of everyday life and that diminished balance is a well-recognized impairment in individuals with LBP, including athletic patients with CLBP who are physically active, it is important to routinely include a relatively quick and cost-effective balance test in physical therapy (PT) practice, and to incorporate an exercise program that is useful for maintaining and improving balance in LBP populations. However, there is a lack of evidence supporting the effectiveness of SSEs on improving dynamic balance. To date, no randomized clinical trials have been conducted to assess the effectiveness of SSEs on dynamic balance in adults with CLBP using the YBT. Therefore, the primary purpose of this study was to determine the effectiveness of SSEs on dynamic balance in adults with CLBP. The secondary purpose of this study was to examine whether or not the participants who received an SSE program (treatment group) would have greater improvement in pain intensity and disability level than those who received a general exercise (GE) program (placebo group). The GE program consisted of general range-of-motion (ROM) and flexibility exercises.
This study was a double-blinded randomized clinical trial, to compare two exercise programs: SSE vs. GE on dynamic balance, pain intensity, and disability level in adults with CLBP The two independent variables were group, which was a between-subject factor, and time, which was a within-subject factor. The independent variable of group had two levels: (1) the treatment group which received SSEs, and (2) the placebo group, which received general ROM and flexibility exercises. The independent variable of time had four levels: baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention. The three dependent variables were: (1) dynamic balance measured by the YBT, (2) pain intensity measured by the Numeric Pain Rating Scale (NPRS), and (3) disability level measured by the Modified Oswestry Low Back Pain Disability Questionnaire (OSW).
The sample size for this study was determined based on a priori power analysis using G*Power version 3.1.9 using a small-to-medium effect size of 0.20 and an alpha level of 0.05.30 Based on the analysis, 40 participants were needed to ensure an adequate power level of 0.80 for a mixedmodel analysis of variance (ANOVA) test. Participants were recruited regardless of ethnicity, sex, or race through flyers, word of mouth marketing, and emails. Approval from the Texas Woman’s University institutional review board was obtained for the study, and it was registered with ClinicalTrials.gov (NCT03597191). Once the participant agreed to participate in the study, the participant signed a written informed consent form. Consenting participants were screened for their eligibility, and those who qualified were assigned randomly to one of the two groups. Eligible participants were individuals who had CLBP (back pain for a duration of more than 12 weeks).2 Additional inclusion criteria included: (1) age of 18 to 65 years; (2) ability to understand, speak, and follow verbal instructions in English; and (3) a minimum pain intensity score of 2/10 using the NPRS in the past week.
Participants were excluded from the study if they have had or reported any of the following: (1) serious spinal conditions, such as fracture, infection, or tumor; (2) signs of nerve root compression; (3) a history of lower extremity or lumbar spine surgery; (4) a history of hip, knee, or ankle pain in the previous two years; (5) current pregnancy; (6) systemic disease (e.g., rheumatologic or neurological disorders); (7) vestibular or other balance disorders; (8) ongoing treatment for inner ear, sinus, or upper respiratory infection; (9) a concussion within the previous three months; (10) a history of falls or fear of falling; and (11) a need for any form of walking aids (cane, walker). Participants were screened with neurological tests, which included reflexes, sensation, strength, and the straight-leg-raise (SLR) test for the lower extremities to further assess their eligibility for the study. The SLR test was considered positive when pain referred below the knee was present during passive SLR
testing and was used to rule out participants with lumbar radiculopathy. These neurological tests are parts of a standard PT examination used in clinics for assessing neurological signs and symptoms. In addition, a physical examination was performed based on the test procedures described by Hicks et al.14
The Y-Balance Test Kit (Functional Movement Systems, Inc. Chatham, VA) was used to assess dynamic balance in this study This kit contains a single central stance platform with three moveable reach indicators arranged in the ANT, PM, and PL directions. Dynamic balance of an individual is quantified by measuring how far the individual places the reach indicator relative to the stance platform while maintaining a unilateral stance. A farther reach distance is indicative of a greater dynamic balance.28 The YBT has been shown to be a reliable measure of dynamic balance, with intraclass correlation coefficients (ICCs) ranging from 0.85 to 0.91 for intra-tester reliability, and from 0.99 to 1.00 for inter-tester reliability.28 The reliability of composite reach scores has been reported to be good-to-excellent, with the ICCs being 0.91 for intra-tester and 0.99 for inter-tester reliability The YBT has a minimal detectable change of 8.62 centimeters.28 The reach distances were measured in centimeters and were averaged and normalized to the participant’s leg length. Leg length was measured twice for each leg, and the two measurements were averaged. In particular, participants’ leg length was measured to the nearest millimeter using a tape measure from the inferior tip of the anterior superior iliac spine to the distal border of the ipsilateral medial malleolus with the participant lying supine on an examination table.25 The composite score was calculated by taking the average between the right and the left reach distances for all three directions and then summing the averages of the three reach directions. The score was then divided by three times the average leg length and multiplied by 100.31 The YBT composite scores were used for statistical analysis and collected at baseline, two weeks, four weeks, and eight weeks after intervention was initiated.
Two investigators participated in this study. Investigator #1, the primary investigator (PI) was blinded to participants’ group assignment and intervention and performed the eligibility screening and standard PT examination for all participants. In addition, the PI collected the pre- and post-intervention measurements of dynamic balance using the YBT, pain scores using the NPRS, and disability level using the OSW. Investigator #2 was blinded to participants’ pre- and post-intervention measurements and was responsible for group allocation and administering the intervention, either an SSE program or a GE program, to participants in both groups.
Eligible participants filled out an intake form, including questions about demographic data (age, sex, height, weight, occupation, limb dominance), duration of symptoms, painful side of the LBP, and physical activity level (minutes per week). The leg dominance was determined by asking the participants to report their preferred leg used when kicking a ball.32 In addition, participants completed the Fear-Avoidance Beliefs Questionnaire (FABQ) and Patient-Reported Outcomes Measurement Information System®-29 (PROMIS-29), which were used to describe the participants of this study All participants were asked to rate their average pain intensity in the low back in the past week and to rate their current pain level using NPRS. Next, participants were asked to complete the OSW. The FABQ, PROMIS-29, NPRS, and OSW have been reliable and valid tools for assessing LBP-related fear-avoidance beliefs, participants’ traits, pain intensity, and perceived disability, respectively 33–38
Next, the YBT was used to assess participants’ dynamic balance. Each participant’s leg length was measured bilaterally in centimeters and was used to normalize reach distances because leg length has been shown to be a factor affecting YBT performance.39 Next, each participant was asked to slide a reach indicator along a pipe in the three testing directions: ANT, PM, and PL on both legs as described in details by Alshehre et al.25 The PI was responsible for giving verbal instructions and visual demonstrations of the YBT, as well as recording the YBT measures. The trial was discarded and retried when the participant (1) moved the foot of the stance leg from the platform or crossed the marked line, (2) kicked, pushed, or stepped on the reach indicator, (3) touched the floor with the reaching leg, or (4) lost balance before returning to the standing position. To reduce fatigue, participants were given a rest of a minimum 10 seconds between each reach and 30 seconds between each direction of testing.40 The reach distance was measured to the nearest centimeters by reading the line at the proximal edge of the reach indicator Three successful test trials in each direction (ANT, PM, and PL) on each leg were recorded and normalized to the leg length and the composite score was used for data analysis.
Participants in the treatment group were instructed in the SSEs, modeled after the SSE program designed by Hicks et al.14 Each participant was instructed to perform four exercises in total, one exercise from each of the following four categories: (a) abdominal bracing, (b) quadruped, (c) prone plank, and (d) side plank exercises. Each exercise was progressed and advanced in difficulty by increasing repetitions, hold times, and/or extremity movements. For the SSEs, the progression of exercises was based on the participants’ performance at each supervised PT session based on pre-established criteria by Hicks et al.14 The SSE program and criteria for progression are listed in Appendix A.
The placebo group performed a GE program, consisting of ROM and flexibility exercises for the low back and lower
extremities. Each participant was instructed to perform four exercises in total, one exercise from each of the following four categories: (a) knee to chest, (b) lower trunk rotation, (c) prone press-ups, and (d) hamstring stretch exercises. These exercises were progressed by increasing repetitions and pain-free ROM. The exercise programs and criteria for progression are listed in Appendix B.
On the first visit, the participants in both groups were instructed in the exercises at a level that they could perform without pain. All participants were provided exercise handouts and also were asked to fill out an exercise log form to track the frequency of their home exercise sessions and to determine their compliance. In both groups, Investigator #2 instructed and corrected performance when necessary, and progressed the exercise program for each participant. As such, when participants performed the exercise with proper technique and without any rest breaks, they were instructed to progress to the next level of the exercise and were asked to discontinue the previous level of that exercise from their program. The proper technique was achieved by instructing the participants to tighten their abdominal muscles while breathing normally and maintaining a steady continuous muscle contraction with no recruitment of accessory muscles.41 Participants were instructed to perform the most updated exercises at home once a day at least five times a week.
The participants were asked to attend a total of four to eight supervised PT sessions and one follow-up session after the four-week intervention was completed for exercise progression and to ensure that they performed the exercises properly. Each session took about 30 to 45 minutes for exercise progression or an hour for collection of outcome measures and exercise progression. The intervention frequency and duration were chosen to reflect common PT practice. Each participant also was asked to perform their assigned exercise program at least five times per week, and the on-site visits were counted toward the required exercise frequency. After the 4-week intervention, each participant was asked to continue their exercise program at home five times a week for another four weeks. On their follow-up visit at week eight, the participants were instructed on how to progress their exercises.
All participants were instructed to bring the exercise log to each visit and to submit it to the investigators at the eight-week follow-up in order to determine compliance with the program. The average compliance was calculated using the completed exercise sessions divided by the prescribed exercise sessions. This equals to the number of exercise sessions completed out of the total possible exercise sessions. For this study, the average compliance for completing the prescribed home exercise program for the first four weeks (supervised PT sessions), the last four weeks (unsupervised PT sessions), and the total compliance for the duration of the study for both groups was calculated.
All statistical analyses were performed using SPSS Statistics, Version 25 (IBM Corp., Armonk, NY, USA). Descriptive statistics, including frequencies, means, and standard de-
viations, were calculated for the demographic data of the participants and the outcome measures (YBT composite score, NPRS, and OSW). Independent t-tests were used for ratio data to determine if there was a difference between groups at baseline, including demographic data, such as age, weight, height, body mass index, and duration of symptoms, and baseline outcome measures. Chi-square analysis was used for non-ratio data to determine betweengroup differences for non-parametric baseline data, such as sex, onset of symptoms, pain distribution. Three separate 2 (group) x 4 (time) analyses of variance (ANOVAs) with repeated measures were used to determine any differences in the three outcome measures between groups. Follow-up analysis was performed if there was a significant interaction. The alpha level was set at 0.05 for all statistical analyses.
Fifty-three participants were recruited for the study and were also assessed for other outcomes. The CONSORT diagram in Figure 1 summarizes the screening, enrollment, randomization, and analysis of participants for this study
The 40 participants who completed this study were generally young with an average age of 39.9 ± 12.5 years and a range of 21 to 64 years. Both groups had lower physical activity levels (99.7 ± 145.1) than the recommended weekly minutes by the 2008 guidelines for adults, which is a minimum of 150 minutes per week.42 All participants had CLBP without signs of lumbar radiculopathy, with symptoms averaging for 95.2 ± 87.5 months. In addition, the participants had an average NPRS score of 3.5 ± 1.6 and an average OSW score of 18.1 ± 9.1, indicating that participants, in general, had relatively low pain intensity and a mild disability level. Table 1 describes the characteristics of the participants who completed the study.
Table 2 displays the means and the standard deviations for the YBT, NPRS, and OSW at each time point. All three outcome measurements showed no significant differences between groups at baseline, except in the YBT composite scores. There was a significant difference in the dynamic balance between groups (t = -2.575, p = 0.014), with a lower YBT composite score in the GE group (72.9 ± 14.0) than in the SSE group (82.1 ± 7.7). Therefore, 2 x 4 ANCOVA with repeated measures was performed with the baseline YBT composite scores of all participants were used as covariates. The ANCOVA results revealed a statistically significant interaction of group by time for dynamic balance (F = 7.146, p < 0.001, partial η2 = 0.162), which indicates that there was a difference between the GE and SSE groups in dynamic balance over eight weeks as presented in Figure 2 Six separate 2 x 2 ANCOVAs with repeated measures were used to test for between-group differences in dynamic balance. A significant difference was found between groups from four weeks (p < 0.001) and eight weeks (p = 0.007) compared to baseline, and from two weeks to four weeks (p = 0.002), with
the SSE group demonstrating higher YBT composite scores than the GE group. However, there were no statistically significant differences from baseline to two weeks (p = 0.098), two weeks to eight weeks (p = 0.107), and four weeks to eight weeks (p = 0.413) between groups. In addition, a significant main effect of time on the dynamic balance was found. Both groups demonstrated a significant improvement in dynamic balance from baseline to two weeks (p < 0.001), 2 weeks to 4 weeks (p = 0.023), and two weeks to eight weeks (p = 0.004), but there was no statistically significant difference from four weeks to eight weeks (p = 0.144) (Figure 2).
The ANOVA with repeated measures for the NPRS and OSW scores revealed no statistically significant interaction of group by time (F = 1.185, p = 0.319, partial η2 = 0.030), (F = 0.538, p = 0.605, partial η2 = 0.014), respectively However, there was a significant main effect of time (p < 0.001) for both the NPRS and OSW scores. However, a significant main effect of time (p < 0.001) for both the NPRS and OSW scores was found. Post-hoc pair-wise comparisons showed significantly lower NPRS scores from baseline to two weeks (p = 0.007), from two weeks to four weeks (p < 0.001), but there was no statistically significant difference from four weeks to eight weeks (p = 0.818) (Figure 3). Similarly, post-hoc pair-wise reveled that both groups demonstrated a significant reduction in disability level from baseline to two weeks (p = 0.017), from two weeks to four weeks (p = 0.047), but there was no statistically significant difference from four weeks to eight weeks (p = 0.117) (Figure 4).
Table 3 lists the means, the standard deviations, and the compliance rates for home exercise compliance for both groups. No significant differences in compliance between the two groups for the duration of the study However, paired t-tests for within-group differences revealed that the home exercise compliance was significantly higher during the first four weeks after initiating the intervention as compared to the last four weeks of intervention for both groups (t = 2.456, p = 0.024 for GE group, t = 2.163, p = 0.044 for SSE group). This indicates that all participants regardless of group performed their home exercises more often in the first four weeks, which included supervised PT sessions than they did in the last four weeks, which had no supervised PT sessions.
The results of this study show that four-week supervised SSEs were superior to GEs in improving dynamic balance in adults with CLBP after eight weeks of intervention. This implies that the SSE group was able to demonstrate better dynamic balance than the GE group for the first four weeks after initiating intervention, which included home exercises and supervised PT sessions. Then, the SSE group maintained the improvement of the first four weeks but showed no improvement in dynamic balance during the last four weeks, which included the participants performing ex-
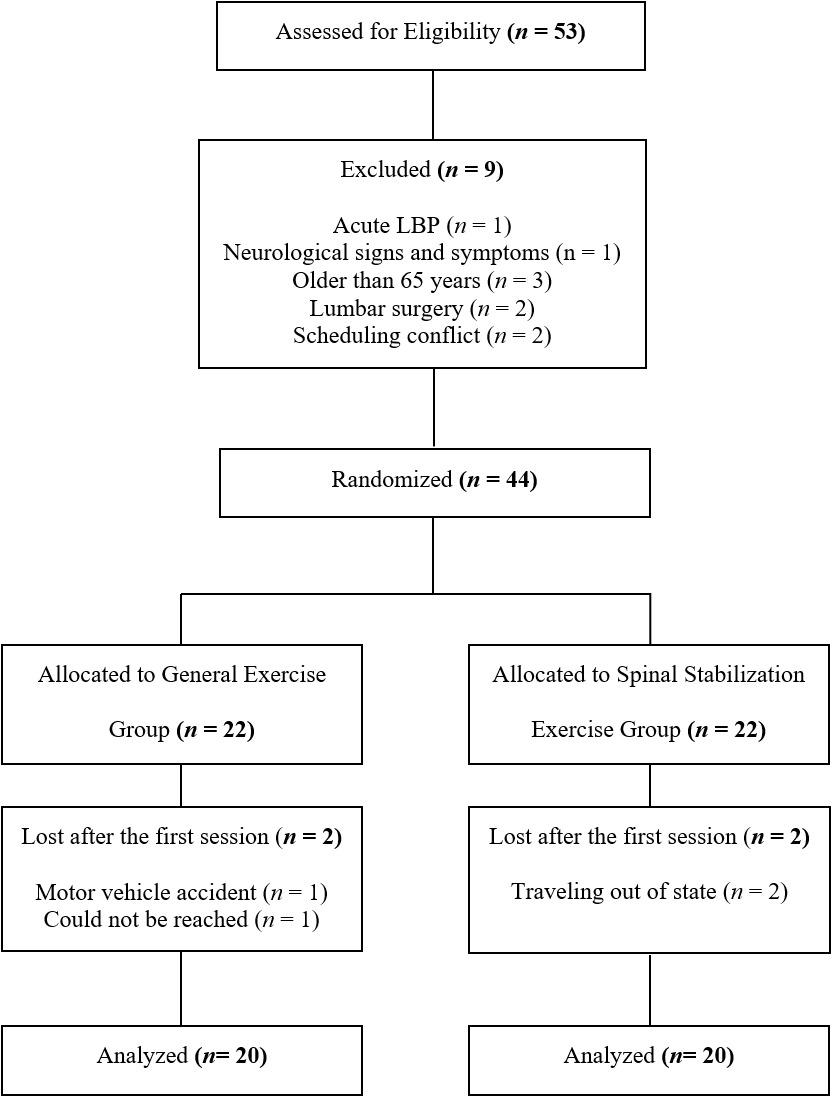
ercises at home with no supervised PT sessions. However, there was no difference between the GE and the SSE groups in dynamic balance during the last four weeks of the intervention. These results support previous studies,19,20 which have shown that those with LBP who received SSEs for four weeks had significantly improved balance as compared to a control group. However, these two studies utilized different methods than the method used in the current study to assess balance, as Kim et al.19 and Rhee et al.20 used a pressure platform and force plates, respectively, to measure CoP excursions for balance ability. The authors of the prior studies hypothesized that SSEs might have improved neuromuscular responses to compensate for postural control deficits in patients with LBP 19,20
Given that balance is a motor control process which regulates movement quality and creates stability; improved neuromuscular control in this patient population can be achieved in part through strength from the lumbar spinal stabilizer muscles.43 Previous evidence has shown a delay in the firing of the deep abdominal muscles and decreased recruitment of the transversus abdominus and lumbar multifidus muscles in patients with CLBP as compared to asymptomatic individuals.14–17 Evidence also suggests that
altered lumbar proprioception in those with LBP may cause reweighting of visual and vestibular sensory inputs to compensate for impaired proprioception in order to maintain an individual’s balance.44 An SSE program is a motor control intervention which has been used to retrain proper activation and coordination of the trunk musculature to increase spinal stability and reduce pain.14,18 In particular, spinal stabilization muscles, such as transversus abdominis and lumbar multifidi have been reported to play a major role in maintaining postural stability Proper activation of these muscles in a feedforward mechanism reduces displacement of the body’s center of gravity 15 Based on these findings, it is speculated that SSEs may minimize faulty movement strategies and compensatory muscle contractions by properly coordinating abdominal and back musculature during functional tasks in the SSE group, which possibly led to better dynamic balance performance following the SSE program.
In contrast, a previous study reported that four weeks of SSEs combined with usual PT care (hot pack, ultrasound, and transcutaneous electric nerve stimulation) compared to usual PT care alone did not show greater improvement in postural control in patients with CLBP 45 However, bal-
Figure 1. Consort diagram of participants’ screening, enrollment, randomization, and analysis.Effectiveness of Spinal Stabilization Exercises on Dynamic Balance in Adults with Chronic Low Back Pain
Table 2. Outcome Measurements (Mean ± Standard Deviation) at Baseline, 2 Weeks, 4 Weeks, and 8 Weeks after initiating intervention
GE general exercise program, SSE spinal stabilization exercise program, p-values for between-group differences were determined by independent t-tests. YBT Y-Balance Test, %LL = Composite score normalized to leg length expressed as a percentage, NPRS = Numeric Pain Rating Scale, OSW = Modified Oswestry Low Back Pain Disability Questionnaire. * indicates statistically significant, p < 0.05.
Figure 2. Dynamic balance as measured by the Y-Balance Test (YBT) at baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention was initiated, for both the general exercise (GE) group and the spinal-stabilization exercise (SSE) group.

ance was assessed differently between the studies. Salavati et al.45 assessed postural control using a Biodex Balance System®. In the current study, balance was measured using the YBT, which could be considered a more challenging bal-
ance task. It also could be argued that the two studies measured different constructs related to balance.
After the four-week supervised intervention, there was a trend that the GE group improved in dynamic balance during the last four weeks of the study The GEs were de-
signed to be similar to the SSEs in terms of frequency, duration, and number of one-on-one supervised PT sessions as well as contact time with the treating physical therapist. It is likely that the GEs, which consisted of ROM and flexibility exercises for the low back and lower extremities,
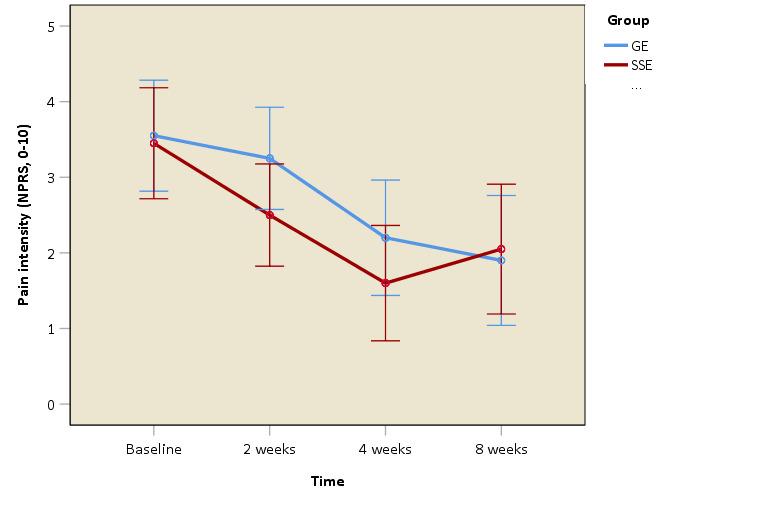
could be learned more easily and performed independently at home by the participants, whereas SSEs may require supervised PT training. The SSEs could be considered a more complex exercise regimen and may require higher cognitive skills to be learned and performed as compared to the
 Figure 3. Pain intensity as measured by the Numeric Pain Rating Scale (NPRS) at baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention was initiated, for both the general exercise (GE) group and the spinalstabilization exercise (SSE) group.
Figure 4. Disability level as measured by the Modified Oswestry Low Back Pain Disability Questionnaire (OSW) at baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention was initiated, for both the general exercise (GE) group and the spinal-stabilization exercise (SSE) group.
Figure 3. Pain intensity as measured by the Numeric Pain Rating Scale (NPRS) at baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention was initiated, for both the general exercise (GE) group and the spinalstabilization exercise (SSE) group.
Figure 4. Disability level as measured by the Modified Oswestry Low Back Pain Disability Questionnaire (OSW) at baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention was initiated, for both the general exercise (GE) group and the spinal-stabilization exercise (SSE) group.
GE general exercise program, SSE spinal stabilization exercise program, p-values were determined by independent t-tests for between-group differences and paired t-tests for within-group differences. The within-group difference for both groups was determined by comparing the compliance of the first four weeks with the last four weeks.* indicates statistically significant, p < 0.05.
GEs. In addition, in terms of exercises intensity, it could be argued that level three of the GEs could be easier to perform, whereas level three of the SSEs could be considered more difficult, requiring more effort and PT supervision to perform correctly. Therefore, it is possible that the SSE group did not show continued improvements on dynamic balance because the effort needed to perform the SSEs was not to the same level of intensity it was for the first four weeks, which included PT supervision. However, it is also not certain whether the SSE group used proper exercise form during the unsupervised portion of the intervention. In addition, evidence has demonstrated that lower-extremity flexibility could affect YBT performance in healthy populations.46,47 Therefore, the GE group could have potentially increased lower-extremity flexibility after eight weeks of intervention and therefore could have been able to reach farther distances during the YBT However, lower-extremity ROM was not assessed after implementing the intervention in this study, so it was not certain whether the improvement on the YBT performance is the result of increased lower-extremity flexibility.
The results of this study also indicate that all participants, regardless of intervention, made significant improvement in dynamic balance after eight weeks. A point of discussion here is that it is apparent that YBT performance may require both spinal stability and ROM/lower-extremity flexibility since both exercise programs seemed to help improve dynamic balance performance after eight weeks. It is also important to note that the small magnitude of change observed in dynamic balance in this study during the last four weeks may be due to the unsupervised nature of the exercises. In this study, home exercise compliance was significantly higher during the first four weeks after initiating the intervention as compared to the last four weeks for both groups. This indicates that all participants performed their home exercises more often in the first four weeks, which included supervised PT sessions, than they did in the last four weeks, which had no supervised PT sessions. Evidence has shown that PT supervised SSEs were shown to be more effective than the unsupervised PT SSEs in patients with LBP.41
All participants regardless of the intervention they received showed significant improvements in pain intensity and disability level over eight weeks. However, the decrease in pain intensity and disability level did not exceed the MCID or MDC, which is 2 points for the NPRS and 10 points for the OSW in patients with CLBP 36,48 This finding agrees
with a pooled analysis that reported no significant benefits for pain or disability between SSEs versus other forms of active exercises. The authors indicated that improvements were minimal and not regarded as clinically significant.49 In addition, Salavati et al.45 reported that four weeks of SSEs combined with usual PT care as compared to usual PT care alone resulted in no significant improvement in pain and disability ratings in patients with CLBP The trend toward better results in pain intensity and disability level suggests that significant changes may take longer than eight weeks to become detectable.
The current study is unique because it is the first to assess the effectiveness of SSEs on dynamic balance in adults with CLBP using the YBT. This study evaluated dynamic balance in a multi-planar manner while performing dynamic tasks that considerably challenged the stability of the spine. This study also demonstrates that the YBT is able to detect change in dynamic balance over time, suggesting that the YBT may be a useful tool for clinicians to assess dynamic balance deficits in patients with CLBP and monitor treatment progression. A better understanding of impairments associated with LBP would assist clinicians in developing personalized intervention programs and individualizing exercise prescription to address those identified at high risk for recurrent LBP.
Strengths of this study include the implementation of a double blinded, concealed allocation randomized clinical trial design in which the participants and the investigators were blinded. Specifically, one investigator was fully blinded to the participants’ group allocation and intervention while the other investigator was blinded to the participants’ pre- and post-intervention measurements. All participants were not informed whether they were assigned to the placebo or to the treatment group. Therefore, the design of the study provided control over potentially important sources of bias, so that the observed effects of the implemented interventions were less likely to be due to chance. However, there are limitations in this study. First, participants were recruited by means of advertisements; therefore, it is possible that individuals seeking medical care for their LBP are different from those responding to an advertisement, thus limiting the generalizability of the study results. In addition, only individuals with CLBP were enrolled in the study. Therefore, the findings are not ap-
plicable for individuals with acute or subacute LBP Another possible limitation is that participants reported low pain intensity, mild disability level, and low physical activity level which limits the generalizability of findings to nonathlete individuals with mild pain and disability levels. Lastly, although efforts were made to control the potential influence of confounding factors that may affect YBT performance, factors such as knee and ankle strength and joint ROM were not investigated.
Future studies are warranted with supervised SSEs and long-term follow-up to examine the effectiveness of these exercises on dynamic balance in individuals with LBP. In addition, future studies should consider measuring participants’ lower-extremity ROM across the study. Lastly, future research is needed to determine which directions of the YBT are the most sensitive to dynamic balance changes in LBP populations.
The results of this study show SSEs to be more effective than GEs in improving dynamic balance, but not pain intensity nor disability level in adults with CLBP. Specifically, four weeks of supervised SSEs along with a home exercise
program is more effective in improving dynamic balance than GEs in participants with CLBP in four weeks. However, GEs appeared to have an effect equivalent to that of SSEs after four weeks of supervised intervention and another four weeks of unsupervised intervention. In addition, all participants had reduction in pain intensity and disability level over eight weeks after the intervention. However, no differences were found between groups, and the decrease in pain intensity and disability level did not exceed the MCID or MDC. The results of the study provide evidence for clinicians to include SSEs for improving dynamic balance in the management of patients with CLBP
The authors would like to thank the Texas Physical Therapy Foundation for funding this study.
No conflicts of interest were present in this study.
Submitted: July 28, 2022 CST, Accepted: December 23, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356-2367. doi:10.1016/s014
0-6736(18)30480-x
2. Marin TJ, Van Eerd D, Irvin E, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. Cochrane Database of Syst Rev 2017;2017(6). doi:10.1002/14651858.cd002193.p ub2
3. Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1211-1259. doi:10.1016/s014
0-6736(17)32154-2
4. Wang H, Naghavi M, Allen C, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1459-1544. doi:10.1016/s0140-673 6(16)31012-1
5. Laird RA, Gilbert J, Kent P, Keating JL. Comparing lumbo-pelvic kinematics in people with and without back pain: A systematic review and meta-analysis. BMC Musculoskelet Disord. 2014;15(1):1-13.
6. Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514-530. do i:10.7326/m16-2367
7 Ganesh GS, Chhabra D, Mrityunjay K. Efficacy of the star excursion balance test in detecting reach deficits in subjects with chronic low back pain. Physiother Res Int 2015;20(1):9-15. doi:10.1002/pri.1 589
8. Hooper TL, James CR, Brismée JM, et al. Dynamic balance as measured by the Y-balance test is reduced in individuals with low back pain: a cross-sectional comparative study Phys Ther Sport 2016;22:29-34. d oi:10.1016/j.ptsp.2016.04.006
9. Etemadi Y, Salavati M, Arab AM, Ghanavati T. Balance recovery reactions in individuals with recurrent nonspecific low back pain: Effect of attention. Gait Posture. 2016;44:123-127. doi:10.101 6/j.gaitpost.2015.11.017
10. Tsigkanos C, Gaskell L, Smirniotou A, Tsigkanos G. Static and dynamic balance deficiencies in chronic low back pain. J Back Musculoskelet Rehabil. 2016;29(4):887-893. doi:10.3233/bmr-160721
11. Panjabi MM. A hypothesis of chronic back pain: Ligament subfailure injuries lead to muscle control dysfunction. Eur Spine J 2006;15(5):668-676. doi:10.1 007/s00586-005-0925-3
12. Mok NW, Brauer SG, Hodges PW. Hip strategy for balance control in quiet standing is reduced in people with low back pain. Spine 2004;29(6):E107-E112. do i:10.1097/01.brs.0000115134.97854.c9
13. Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain: A systematic review for an american college of physicians clinical practice guideline. Ann Intern Med 2017;166(7):493-505.
14. Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil 2005;86(9):1753-1762. doi:10.1016/ j.apmr.2005.03.033
15. Akuthota V, Ferreiro A, Moore T, Fredericson M. Core stability exercise principles. Curr Sports Med Rep 2008;7(1):39-44. doi:10.1097/01.csmr.000030866 3.13278.69
16. Haladay DE, Miller SJ, Challis J, Denegar CR. Quality of systematic reviews on specific spinal stabilization exercise for chronic low back pain. J Orthop Sports Phys Ther. 2013;43(4):242-250. doi:10.2 519/jospt.2013.4346
17 Brumitt J, Matheson JW, Meira EP Core stabilization exercise prescription, part 2: A systematic review of motor control and general (global) exercise rehabilitation approaches for patients with low back pain. Sports Health. 2013;5(6):510-513. doi:10.1177/1941738113502634
18. Byström MG, Rasmussen-Barr E, Grooten WJA. Motor control exercises reduces pain and disability in chronic and recurrent low back pain: A metaanalysis. Spine 2013;38(6):E350-E358. doi:10.1097/br s.0b013e31828435fb
19. Kim JH, Kim YE, Bae SH, Kim KY The effect of the neurac sling exercise on postural balance adjustment and muscular response patterns in chronic low back pain patients. J Phys Ther Sci 2013;25(8):1015-1019. doi:10.1589/jpts.25.1015
20. Rhee HS, Kim YH, Sung PS. A randomized controlled trial to determine the effect of spinal stabilization exercise intervention based on pain level and standing balance differences in patients with low back pain. Med Sci Monit 2012;18(3):CR174-CR181. doi:10.12659/msm.882522
21. Fullam K, Caulfield B, Coughlan GF, Delahunt E. Kinematic analysis of selected reach directions of the star excursion balance test compared with the Ybalance test. J Sport Rehabil. 2014;23(1):27-35. doi:1 0.1123/jsr.2012-0114
22. Sell TC. An examination, correlation, and comparison of static and dynamic measures of postural stability in healthy, physically active adults. Phys Ther Sport 2012;13(2):80-86. doi:10.1016/j.pts p.2011.06.006
23. Ganesh GS, Chhabra D, Pattnaik M, Mohanty P, Patel R, Mrityunjay K. Effect of trunk muscles training using a star excursion balance test grid on strength, endurance and disability in persons with chronic low back pain. J Back Musculoskelet Rehabil 2015;28(3):521-530. doi:10.3233/bmr-140551
24. Hemmati L, Rojhani-Shirazi Z, Malek-Hoseini H, Mobaraki I. Evaluation of static and dynamic balance tests in single and dual task conditions in participants with nonspecific chronic low back pain. J Chiropr Med 2017;16(3):189-194. doi:10.1016/j.jcm.2 017.06.001
25. Alshehre Y, Alkhathami K, Brizzolara K, Weber M, Wang-Price S. Reliability and validity of the Ybalance test in young adults with chronic low back pain. Int J Sports Phys Ther. 2021;16(3):628. doi:10.26 603/001c.23430
26. Hlaing SS, Puntumetakul R, Wanpen S, Boucaut R. Balance control in patients with subacute nonspecific low back pain, with and without lumbar instability: A cross-sectional study J Pain Res 2020;13:795-803. doi:10.2147/jpr.s232080
27 Young KJ, Je CW, Hwa ST Effect of proprioceptive neuromuscular facilitation integration pattern and swiss ball training on pain and balance in elderly patients with chronic back pain. J Phys Ther Sci 2015;27(10):3237-3240. doi:10.1589/jpts.27.3237
28. Plisky PJ, Gorman PP, Butler RJ, et al. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther. 2009;4(2):92-99.
29. Shaffer SW, Teyhen DS, Lorenson CL, et al. Ybalance test: a reliability study involving multiple raters. Mil Med. 2013;178(11):1264-1270. doi:10.720 5/milmed-d-13-00222
30. Faul F, Erdfelder E, Lang A, Buchner A. G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-191. doi:10.3758/bf0319 3146
31. Chimera NJ, Kremer K. SportsmetricsTM training improves power and landing in high school rowers. Int J Sports Phys Ther. 2016;11(1):44.
32. Alonso AC, Brech GC, Bourquin AM, Greve JMD. The influence of lower-limb dominance on postural balance. Sao Paulo Med J 2011;129(6):410-413. doi:1 0.1590/s1516-31802011000600007
33. Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther 2002;82(10):973-983. doi:10.1093/ptj/82.1 0.973
34. Swinkels-Meewisse EJ, Swinkels RA, Verbeek AL, Vlaeyen JW, Oostendorp RA. Psychometric properties of the Tampa scale for kinesiophobia and the fearavoidance beliefs questionnaire in acute low back pain. Man Ther 2003;8(1):29-36. doi:10.1054/math.2 002.0484
35. Deyo RA, Ramsey K, Buckley DI, et al. Performance of a patient reported outcomes measurement information system (PROMIS) short form in older adults with chronic musculoskeletal pain. Pain Med 2015;17(2):314-324. doi:10.1093/pm/ pnv046
36. Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 2005;30(11):1331-1334. doi:10.109 7/01.brs.0000164099.92112.29
37. Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 2002;82(1):8-24. doi:10.10 93/ptj/82.1.8
38. Fritz JM, Irrgang JJ. A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Phys Ther. 2001;81(2):776-788. doi:10.1093/ptj/81.2.776
39. Gribble P, Hertel J, Plisky P Using the star excursion balance test to assess dynamic posturalcontrol deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47(3):339-357. doi:10.4085/1062-6050-4 7.3.08
40. Kwon YU, Blaise Williams DS. The effect of variable rest intervals and chronic ankle instability on triplanar ankle motion during performance of the star excursion balance test. Hum Mov Sci. 2017;52:143-150. doi:10.1016/j.humov.2017.01.013
41. Zapata KA, Wang-Price SS, Sucato DJ, Thompson M, Trudelle-Jackson E, Lovelace-Chandler V Spinal stabilization exercise effectiveness for low back pain in adolescent idiopathic scoliosis: A randomized trial. Pediatr Phys Ther. 2015;27(4):396-402. doi:10.1097/p ep.0000000000000174
42. Kay MC, Carroll DD, Carlson SA, Fulton JE. Awareness and knowledge of the 2008 physical activity guidelines for americans. J Phys Act Health. 2014;11(4):693-698. doi:10.1123/jpah.2012-0171
43. Hertel J, Miller SJ, Denegar CR. Intratester and intertester reliability during the star excursion balance tests. J Sport Rehab 2000;9(2):104-116. doi:1 0.1123/jsr.9.2.104
44. Berenshteyn Y, Gibson K, Hackett GC, Trem AB, Wilhelm M. Is standing balance altered in individuals with chronic low back pain? A systematic review Disabil Rehabil. 2019;41(13):1514-1523. doi:10.1080/0 9638288.2018.1433240
45. Salavati M, Akhbari B, Takamjani IE, Bagheri H, Ezzati K, Kahlaee AH. Effect of spinal stabilization exercise on dynamic postural control and visual dependency in subjects with chronic non-specific low back pain. J Bodyw Mov Ther 2016;20(2):441-448. do i:10.1016/j.jbmt.2015.10.003
46. Gribble PA, Hertel J, Plisky P Using the star excursion balance test to assess dynamic posturalcontrol deficits and outcomes in lower extremity injury: A literature and systematic review. J Athl Train 2012;47(3):339-357 doi:10.4085/1062-6050-4
7.3.08
47 Overmoyer GV, Reiser RF. Relationships between lower-extremity flexibility, asymmetries, and the Y balance test. J Strength Cond Res 2015;29(5):1240-1247. doi:10.1519/jsc.000000000000 0693
48. Hägg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12-20. doi:10.1007/s00586-002-0464-0
49. Smith BE, Littlewood C, May S. An update of stabilisation exercises for low back pain: A systematic review with meta-analysis. BMC Musculoskelet Disord 2014;15(1):1-21. doi:10.1186/1471-2474-15-416
Download: https://ijspt.scholasticahq.com/article/68075-effectiveness-of-spinal-stabilization-exercises-on-dynamicbalance-in-adults-with-chronic-low-back-pain/attachment/135463.docx?auth_token=uJm7vEPVFJFqm8zN1nAn
Download: https://ijspt.scholasticahq.com/article/68075-effectiveness-of-spinal-stabilization-exercises-on-dynamicbalance-in-adults-with-chronic-low-back-pain/attachment/135772.docx?auth_token=uJm7vEPVFJFqm8zN1nAn
2
Human Kinetics and Recreation, Memorial University of NewfoundlandKeywords: glenohumeral, instability, subluxation, upper quarter y-balance test, Western Ontario Shoulder Index https://doi.org/10.26603/001c.65900
The Bodyblade™ has the potential of enhancing conservative management of Traumatic Anterior Shoulder Instability (TASI).
The purpose of this study was to compare three different protocols: Traditional, Bodyblade™, and Mixed (Traditional & Bodyblade™) for shoulder rehabilitation on athletes with TASI.
Randomized-controlled longitudinal training study

Thirty-seven athletes (age = 19.9±2.0 years) were allocated into Traditional, Bodyblade™, and Mixed (Traditional/Bodyblade™) training groups (3×week for 8-weeks). The traditional group used resistance bands (10-15 repetitions). The Bodyblade™ group transitioned from classic to the pro model (30-60-s repetitions). The mixed group converted from the traditional (weeks 1-4) to the Bodyblade™ (weeks 5-8) protocol. Western Ontario Shoulder Index (WOSI) and the UQYBT were evaluated at baseline, mid-test, post-test, and at a three-month follow-up. A repeated-measures ANOVA design evaluated within and between-group differences.
All three groups significantly (p=0.001, eta2: 0.496) exceeded WOSI baseline scores (at all timepoints) with training (Traditional: 45.6%, 59.4%, and 59.7%, Bodyblade™: 26.6%, 56.5%, and 58.4%, Mixed: 35.9%, 43.3% and 50.4% respectively). Additionally, there was a significant (p=0.001, eta2: 0.607) effect for time with mid-test, post-test and follow-up exceeding baseline scores by 35.2%, 53.2% and 43.7%, respectively The Traditional and Bodyblade™ groups (p=0.049, eta2: 0.130) exceeded the Mixed group UQYBT at post-test (8.4%) and at three-month follow-up (19.6%). A main effect (p=0.03, eta2: 0.241) for time indicated that WOSI mid-test, post-test and follow-up exceeded the baseline scores by 4.3%, 6.3% and 5.3%.
All three training groups improved their scores on the WOSI. The Traditional and Bodyblade™ groups demonstrated significant improvements in UQYBT inferolateral reach scores at post-test and three-month follow-up compared to the Mixed group. These
Corresponding author: Dr. David G Behm
School of Human Kinetics and Recreation, Memorial University of Newfoundland, St. John’s, Newfoundland and Labrador, Canada, A1C 5S7
Email: dbehm@mun.ca
findings could lend further credibility to the role of the Bodyblade as an early to intermediate rehabilitation tool.
3
The glenohumeral joint requires the coordinated neuromuscular interaction of several cooperative joints, balancing its contrasting roles of mobility and stability The increased mobility can contribute to shoulder instability-related injuries1,2 such as traumatic anterior shoulder instability (TASI). TASI generally occurs when excessive forces during a traumatic event displace the humeral head anteriorly, out of the shoulder socket, resulting in the joint surfaces completely losing contact3 and may lead to recurrent anterior shoulder instability
The shoulder is the most frequently dislocated joint; occurring in 8.2-23.9 per 100,000 people per year 3 Following TASI, there is a higher risk (39%) of experiencing recurrent anterior shoulder dislocation.4 Estimates of TASI in various countries reported incidences per 100,000 of 23.9 (USA), 23.1 (Canada), 27.5 (Sweden), 56.3 (Norway), and 12.3 (Denmark). TASI incidence is highest in the late teens and early twenties (15-20 years, proportion of recurrent instability: 51%), and is attenuated with increasing age (21-40 years, proportion of recurrent instability: 36%) with higher incidence in males (71.8%) and in athletes.5–7
Within the National Collegiate Athletic Association, glenohumeral instability occurs 12% per 1000 athlete exposures with the time lost to the sport on average greater than 10 days,8 with a return to normal activity ranging from five days to six months.9
Traditional rehabilitation for shoulder dislocation has a success rate of only 20%.10 Commonly, the treatment for TASI is surgical intervention followed by rehabilitation.11,12 However, 20% of surgeries after an initial TASI event, even amongst athletes, are unnecessary and an additional 14% of surgeries are unsuccessful,13 and there is an estimated pooled failure rate of 13.7% (7.7%-19.6%) for arthroscopic repair of shoulder dislocation.14 Hence, more effective non-invasive treatment modalities would be a benefit to this population.
The comprehensive conservative management approach to TASI requires several months to complete. Conservative management typically involves three to four weeks or up to six weeks of immobilization15 followed by a variation of rehabilitation timelines.9 During the management of athletes with TASI, the demands to return to play are much higher than non-athletes and an accelerated program would be more fitting for this population. Buss et al.16 examined 30 in-season athletes with TASI and found that they returned to play within 10.2 days. Consequently, ten athletes sustained a recurrent instability episode, and 16 eventually underwent surgical stabilization during the subsequent offseason. Furthermore, this expeditious return to play protocol appeared to center around allowing athletes to return to play faster instead of considering the long-term ef-
fects. Alternative tools that could be effective in accelerating recovery would be a valuable addition to the health professional’s tool box of rehabilitation implements.
An oscillation tool such as the Bodyblade™ has the potential to improve efficiency and efficacy in a rehabilitation program.17 Bodyblade™ has been shown to produce kinetic chain movement for the upper and lower body 18 Additionally, it has also been found in a number of studies to produce higher electromyography (EMG) activity than traditional rehabilitation tools,19–21 which may enhance the traditional conservative management approaches to TASI. The primary rationale for the high EMG activity could be due to the higher movement velocity required to oscillate the Bodyblade™. The increased velocity incurs enhanced concentric activity and decreased eccentric activity. The same concept occurs when slowing down the Bodyblade™, eccentric activity enhances, and concentric movement decreases.22,23 In comparison to dumbbell exercises, the Bodyblade™ reaches greater EMG activity exceeding 50% of maximum voluntary isometric contraction (MVIC)20 and can activate multiple muscle groups compared to other traditional rehabilitation tools. These factors lend further credibility to the exploration of effective and efficient oscillation devices to accelerate recovery.
There is limited research available on the benefits of this tool in rehabilitation. A case study10 reported on treatment of an individual with a shoulder dislocation using a Bodyblade™ over 11 visits. Following the Bodyblade™ treatment, pain rating scales reduced from 4 to 0, range of motion measures returned within normal range with the exception of external rotation, strength returned and exceeded contralateral limb strength and the Western Ontario Shoulder Index (WOSI) decreased from 482 to 46. Oliver et al.21 had participants perform common shoulder rehabilitation exercises with the Bodyblade™ and reported moderate to moderately strong activation of upper and lower extremity muscles suggesting that these Bodyblade™ exercises may be utilized for a shoulder rehabilitation program. While current tools used for shoulder rehabilitation include elastic resistance bands, weighted balls, medicine balls, cuff weights, and dumbbells,19,22 Bodyblade™ has been found to achieve high EMG activity in the scapular stabilizers,22 shoulder,20 and core musculature.18,20 Hence, there is a dearth of research investigating the effectiveness of the Bodyblade™ as a major component of a sustained rehabilitation training program
Bodyblade™ recommends that an individual resist oscillation for up to 60 seconds to improve strength, pain relief, attain aerobic benefits, and improve proprioception.17 However, these claims have not been validated. The exploration of this multifaceted oscillation tool has the potential to improve traditional shoulder rehabilitation guidelines. Therefore, the purpose of this study was to compare three
BB: basketball, FB: football, SB: softball, WP: water polo
different protocols: Traditional, Bodyblade™, and Mixed (Traditional & Bodyblade™), for shoulder rehabilitation on athletes with TASI.
Thirty-seven student-athletes were recruited from five community colleges (Table 1). Five of the 37 participants were left hand dominant and 14/37 had injured their left shoulder The mean time since injury was 4.77±4.78 months with a range of one week to 12 months. Using controlled randomization, participants were randomly allocated regarding sport, training group, sex, type of athlete and time since injury The sample size was justified by a priori power analysis (α= .05, β= .80 and meaningful effect size (ES) difference of 0.50: moderate magnitude), which indicated a minimum of 22 participants. Participants were considered to participate in the study if they had a history of TASI episode(s) and actively enrolled in an athletics class at their college. Researchers were blinded to the group allocation.
The inclusion criteria consisted of the participant indicating a TASI episode which was defined as a shoulder instability event in the prior 12 months based on the Shoulder History Questionnaire, cleared to participate in the demands of their respective sport by an orthopedic surgeon based on pre-participation physical examinations, or was cleared with recommended exercises supervised by a certified athletic trainer at selected colleges. The mechanisms of injury were shoulder abduction with external rotation with 18 participants, shoulder abduction and external rotation with external force with 15 participants, three participants fell onto an outstretched hand and one participant was injured swinging a baseball bat. Participants were excluded from the study if they had a surgical repair for shoulder instability, upper or lower extremity amputation, vestibular disorder, recent fractures (<6 months) to the involved upper extremity (clavicle, scapula, humerus, ulna, radius, metacarpals, or carpals), injury to the neck, elbow, hand; tendinitis, sprain or strain, undergone any treatment for the inner ear, sinus or upper respiratory tract infection, or concussion in the prior three months, undergone nonsurgical rehabilitation or under any care for their shoulder with an orthopedic surgeon, physical therapist, or athletic trainer The participants were not undergoing any rehabil-
itation from a physical therapist or athletic trainer during the study.
The study design consisted of a randomized-controlled longitudinal training study (pre-test, mid-test [4 weeks], post-test [8 weeks], and a three-month follow-up). Participants were placed in one of three experimental groups. The Traditional (elastic resistance) protocol was designed to activate scapulothoracic musculature and promote optimal scapular positioning (n = 12).21 The Bodyblade™ protocol intended to activate scapulothoracic musculature at various movement planes (n = 13).18–20,22–26 The Mixed group was designed to include a combination of both Traditional and Bodyblade™ protocols (n = 12). Approval for the study was obtained from the Institutional Review Board (IRB) at Rocky Mountain University (IRBNet ID # 889924-10 – Protocol # 160443-03). The informed consent forms were obtained from all participants before the beginning of the study.
The study was an eight-week intervention performed three times a week with a three-month follow-up under the guidance of supervising athletic trainers. An eight-week duration was chosen as both neural and morphological changes, which contribute to the objective of increased strength are reported to occur in an eight-week training program,27,28 and the duration would be reasonable to ensure participant retention. Each group progressed weekly by either progressively adding resistance, repetitions, or increasing time and intensity. Participants needed to attend at least two sessions per week and were instructed that they would be removed from the study if they missed more than four sessions overall.
The Traditional protocol included four elastic resistance band exercises: 1) shoulder adduction, 2) shoulder extension, 3) shoulder abduction and 4) bilateral row (Figure 1). Based on prior research by Kibler et al.,24 expectations were that the serratus anterior (SA) and lower trapezius (LT) would be activated between 15% and 30% in all four exercises and the upper trapezius (UT) activation between 21% and 36% in the dynamic exercises (Shoulder Abduction and Bilateral Row). The anterior deltoid (AD), and posterior deltoid (PD), which act as both mobilizers and stabilizers would also be expected to be moderately active.20 The moderate activation levels found in these exercises are consistent with physiologic activation sequences and restoration
Shoulder IR/ER: internal and external rotation 65º, flexion 90°, abduction 90° and flexion 180°.
of shoulder function and are effective for asymptomatic and symptomatic populations.19–21,24 This protocol followed strengthening exercise guidelines that limit atrophy and allow for pain-free movement.29
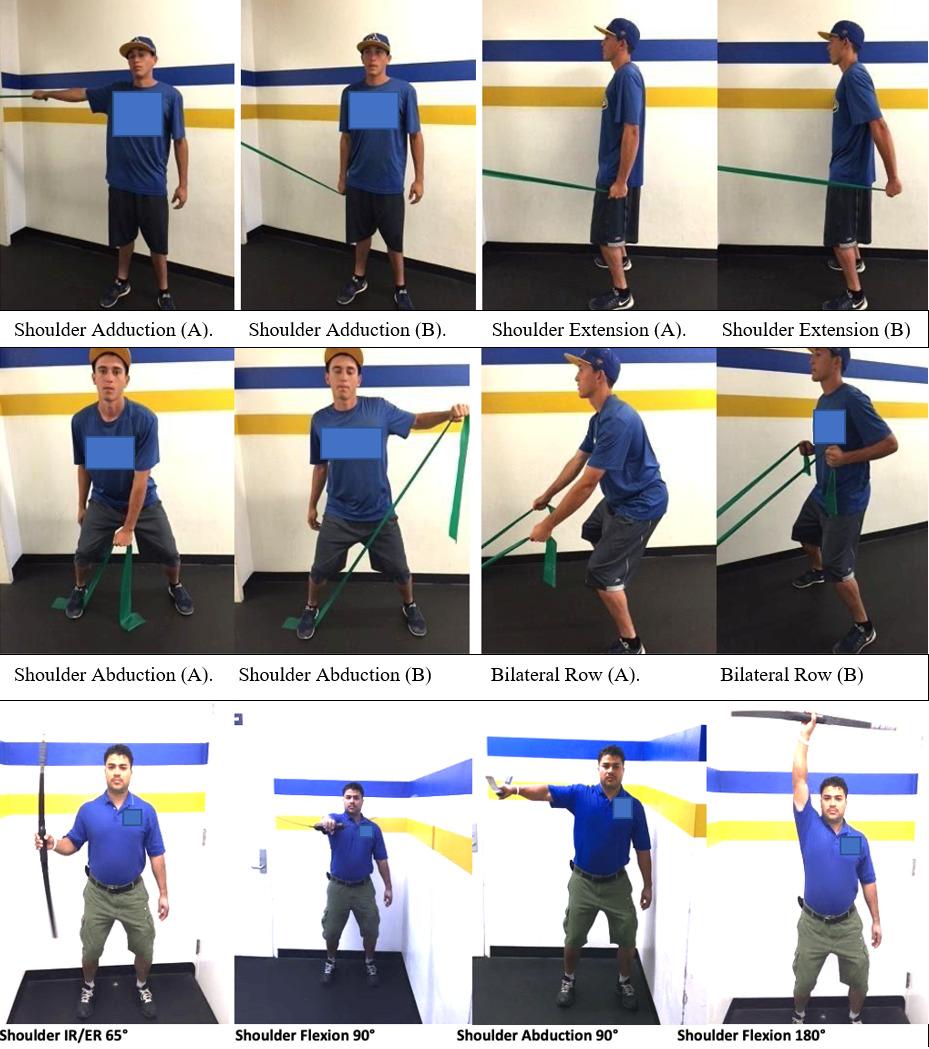
The Traditional group trained three sessions per week (Table 2). The guidelines followed were based on the Essentials of Strength and Conditioning textbook.30 Supervising athletic trainers documented progression using the Traditional Elastic Resistance Checklist.
The Bodyblade™ exercise protocol consisted of shoulder internal and external rotation (IR/ER) at 65° (transverse plane: longitudinal axis), shoulder flexion at 90° (sagittal plane: mediolateral axis), shoulder abduction at 90°
(frontal plane: anteroposterior axis), and shoulder flexion at 180° (sagittal plane: mediolateral axis) (Figure 1). The exercises and the modified progression were based on prior studies.18–26 Supervising athletic trainers provided participants with a demonstration of Bodyblade™ exercise protocols using verbal and tactile cues to maintain a neutral pelvis, athletic position, and shoulder retraction throughout the selected exercises. Participants practiced with the selected tool until the principal investigator felt confident that the participant was proficient. Supervising athletic trainers continued to provide feedback to participants as instructed at the start of the study The Bodyblade™ exercises were proposed to challenge scapulothoracic muscula-
Figure 1. Traditional elastic resistance exercises (first two rows) and Bodyblade™ exercises (third row).Table 2. Traditional elastic resistance exercises and training parameters
Exercises
1. Shoulder
2. Shoulder Extension
3. Shoulder
4.
Table 3. Bodyblade™ exercises and training parameters: Shoulder Internal Rotation / External Rotation: internal and external rotation 65º, flexion 90°, abduction 90° and flexion 180°.
1. Shoulder IR/ER 65º
2. Shoulder Flexion 90º
3. Shoulder Abduction 90º
4. Shoulder Flexion 180º
Pro 40-s, 40-s rest, each
Week 7 Pro 50-s, 50-s rest, each
Week 8 Pro 60-s, 60-s rest, each
ture at various planes of movement and promote joint stability.19–22,24–26 Prior research indicated moderate muscle activation (≥20%MVIC) of the UT, LT, and GM for all four exercises.21 The Bodyblade™ (polycarbonate flexible oscillating blade with a handgrip in the center) intervention started with participants using the Classic model (0.68 kg and 122 cm) for the first four weeks. Three sessions per week were performed to maintain consistency throughout each group. On week 1, sessions started at 30-seconds and progressed weekly in 10-second increments to 60 seconds. At weeks 5–8, participants transitioned to the Pro model (1.13 kg and 152.4 cm). The rest between each set equaled the time spent performing the exercise (30-60-seconds, 1:1 work to rest ratio) to minimize the effects of fatigue27 (Table 3). The supervising athletic trainers documented progression using the Bodyblade™ Checklist.
The Mixed exercise protocol group utilized both Traditional and Bodyblade™ exercise protocols (Table 4). The protocol alternated weekly starting with the Traditional on odd-numbered weeks and continuing with the Bodyblade™ on even-numbered weeks. The Mixed group’s progression allowed the participants to only advance to the halfway point from each protocol (Table 4). The supervising athletic
trainers documented progression using the Mixed Checklist.
There were six supervising athletic trainers from five colleges that participated in the study (31-51 yrs., all master’s degrees with 8-27 yrs. of experience). Supervising athletic trainers-initiated participation in the study by submitting a letter of support and completing research training. Research efforts began by identifying potential participants in the respective athletic programs. The principal investigator provided supervising athletic trainers and participants with a brief demonstration of exercise protocols using verbal and tactile cues to maintain pelvic neutral, athletic position, and shoulder retraction throughout the selected exercises. Participants practiced with the selected tool until the principal investigator felt confident that the participant was proficient. Throughout the intervention, supervising athletic trainers continued to provide feedback to participants as instructed at the start of the study. There was a 30-60 second rest between sets and exercise tools to minimize the effects of fatigue.27 Exercise log checklists were
Exercises Elastic Resistance / Bodyblade™
Week
Week
Week
Week
Week
Week
Week 7
Week
submitted to the principal investigator via electronic mail or fax no later than Friday of each week. Any questions, concerns, or data collection issues that arose supervising athletic trainers immediately contacted the principal investigator
Researchers performing the testing were blinded to the group allocation. Demographic information was obtained before taking baseline measures (age, sex, sport, and arm dominance) followed by anthropometric measures (height, weight, and upper limb length). Arm dominance was determined as the arm used to throw a ball. The measurement of upper limb length was taken by instructing the participant to stand with their back against a wall, feet together, shoulders and arms in 90° abduction, and back of hand flat against the wall: this position limited trunk movement and scapular tilting. A cloth tape measure was used to determine arm length by placing the stationary end of the tape on the spinous process of the 7th cervical vertebrae and the loose end at the tip of the hand’s middle finger.
The WOSI (web-based) 21 item questionnaire evaluates outcomes occurring after interventions for patients with shoulder instability 31 WOSI consists of four domains; a) physical symptoms (10 items), b) sport/recreation/work function (4 items), c) lifestyle function (4 items), and d) emotional function (3 items). Participants used a visual analog scale that ranged from no complaints (0) to severe complaints (100). The WOSI was conducted before the start of the intervention, during the 4th week, after the intervention (8th week), and at the three-month follow-up. The total score from the four domains and each domain individually were used to perform statistical analyses.
Following WOSI, the UQYBT, (Move2Perform, Evansville, IN) was conducted. The UQYBT was developed to identify upper extremity and trunk mobility in the reaching limb’s open kinetic chain as well as midrange limitations, asymmetries, core stability in the closed kinetic chain on the stabilizing limb.32 To complete the analysis, each direction’s maximum score was extracted to represent the end range of the athlete’s performance. The average maximum reach from the three directions was calculated to record a
1 set per exercise, 3 × week
Repetitions (reps)
between sets
composite score for each participant. The assessment progresses in the following order: a) medial, b) inferolateral and c) superolateral directions. Before official testing, participants watched an instructional video entitled “Y Balance Test Upper Quarter – Client Instruction” Once participants watched the video, they removed their shoes and began warming up by reaching in all three directions two times on each arm. After warming up, participants began three official trials. The trials were acceptable if they maintained the following criteria: 1) three points of contact to the floor with involved arm and feet, 2) participant did not use momentum to move the reach box (i.e., push the box), 3) participant did not let the reaching hand touch the ground during the trial, 4) participant did not use the top of the reach box or testing equipment to help stabilize their body Participants did not experience any pain or discomfort during trials that would inhibit any further testing.
The three reach directions were named based on the arm placed on base during the trial. For example, the righthanded stance was labeled; (right) medial, (right) inferolateral, and (right) superolateral and the left-handed stance followed the same procedure (left) medial, (left) inferolateral, and (left) superolateral. Each trial was performed without stopping between the three reach directions. Subsequently, participants returned to their starting position after each reach direction in a controlled manner The principal investigator recorded the greatest distance from each direction and averaged those numbers to attain a composite score.29 Measures were taken before the intervention (pretest), at the 4th week (mid-test), at the conclusion of the 8th week (post-test), and at the three-month follow-up.
Descriptive statistics included means and standard deviations for all tests and measures. Kolmogorov–Smirnov tests of normality were conducted for all dependent variables. Significance was defined as p<0.05. If the assumption of sphericity was violated, the Greenhouse−Geiser correction was employed. A mixed model, repeated measures 4x3 ANOVA design was used to evaluate UQYBT and WOSI score differences within tests (pre-test, mid-test, post-test, and three-month follow-up), and between groups (Traditional,
Bodyblade™, and Mixed) interactions (SPSS Version 20.0). The modified Bonferroni post-hoc analysis controlled for Type 1 error rate across multiple comparisons and was used to find significant differences between and within groups. Eta-squared (eta2) was utilized as a measure of effect size with ratios interpreted as 0.01: small, 0.06: medium, and >0.14: large magnitude. Cronbach alpha intraclass correlation coefficients (ICCs) were measured for the pre-test trials of each condition to assess consistency of these data. Based on Koo and Li,33 ICC between 0.75 – 0.9 were classified as good, and over 0.9 was considered excellent.
There was nearly full (97.3%) participation and adherence throughout the study, except for one participant in the Mixed group who could not complete the three-month follow-up on the UQYBT due to surgery on the involved shoulder Demographic, anthropometric characteristics and the average time since the last injury were not significantly different between groups with no initial differences during baseline measures.
Reliability (ICC) for the WOSI was classified as good (ICC: 0.85). There were no significant differences between participants and multiple comparisons composite score findings (Table 5). There were main effects for time demonstrating improvements for WOSI physical symptoms (F(3,102)=32.4, p<0.0001, eta2: 0.488), WOSI Sports, Recreation, Work (F(3,102) =16.53, p<0.0001, eta2: 0.327), WOSI Lifestyle Output (F(3,102) =10.21, p<0.0001, eta2: 0.231) and WOSI Emotion (F(3,102) =16.16, p<0.0001, eta2: 0.322). Hence, with the WOSI composite score, there was a significant, large magnitude (F(3,102) =21.61, p=0.001, eta2: 0.61) main effect for time with mid-test (4 weeks), post-test (8 weeks), and three month follow-up exceeding the baseline scores by 35.2% (p=0.01), 53.2% (p=0.004), and 43.7% (p=0.005), respectively. There were significant (p=0.001, eta2: 0.496), large magnitude, composite WOSI scores for within-participants interaction effect for the time and group. All groups (Traditional, Bodyblade™, and Mixed) improved over the three measurement points (mid-test (4 weeks), post-test (8 weeks), and three-month follow-up) exceeding baseline scores by; Traditional: 45.6% (p=0.002), 59.4% (p=0.01), and 59.7% (p=0.07), Bodyblade™: 26.6% (p<0.05), 56.5% (p=0.01), and 58.4% (p=0.01), Mixed: 35.9% (p=0.03), 43.3% (p=0.01) and 50.4% (p=0.008) respectively (Table 5). There were minimally clinically important differences between the pre-test and mid-test (4 weeks) with all three groups, as well as between the mid-test and post-test (8 weeks) for the Traditional and Bodyblade™ groups
Reliability for the UQYBT was also classified as good (ICC: 0.81). The composite scores for between-participants and within-participants effects showed no significant findings
(Table 5). There was a significant, large magnitude (F(3,102) =16.84, p=0.03, eta2: 0.24) main effect for time with midtest (4 weeks), post-test (8 weeks), and three-month followup exceeding the baseline scores by 4.3% (p<0.05), 6.3% (p=0.03), and 5.3% (p<0.05), respectively The inferolateral reach was the only direction with a significant, large magnitude, between-participants effect (F(3,102) =14.64, p=0.042; eta2: 0.17). Additionally, the Bodyblade™ group exceeded (p=0.038) the Mixed group at post-test (8 weeks) and threemonth follow-up by 10.7% and 24.5% (Table 5). There were minimally clinically important differences with the composite scores between the pre-test and mid-test (4 weeks) with the mixed group, as well as between the post-test (8 weeks) and three-month follow up for the Bodyblade™ and mixed groups. With the inferolateral scores, minimally clinically important differences were detected between the pretest and mid-test (4 weeks) with the Bodyblade™ group and between the post-test (8 weeks) and three-month follow up for the Bodyblade™ and mixed groups.
A major finding in this study was that all three training groups demonstrated significant improvements over time in the WOSI composite scores. However, there was no significant difference between any of the groups. The UQYBT demonstrated improvement only during the inferolateral reach at post-test (8 weeks) and three-month follow-up. The Bodyblade™ and Traditional groups outperformed the Mixed group, with the Mixed group demonstrating decreased UQYBT performance towards the latter duration of the study
The WOSI (scores range from no complaints: 0, to severe complaints:100) demonstrated significant improvements in the composite scores (physical symptoms (10 items), sport/ recreation/work functions (4 items), lifestyle functions (4 items), and emotional functions (3 items)) during all the three testing periods for all groups (Table 5). The current study reported reliability as excellent (ICC: 0.85), which is consistent with previous reports of ICC 0.88-0.92.31 The eight-week intervention performed three times a week provided consistent supervision, design, and compliance amongst participants for all three treatment groups and these factors may have contributed to the significant findings in the WOSI. The present findings are contrary to Eshoj et al.34 who reported no significant differences when comparing 12-week treatment protocols for shoulder instability utilizing a self-managed at-home exercise protocol versus a physical therapist-led semi-supervised exercise protocol. Although both at-home and semi-supervised exercise attempted to provide their participants with sound training progression throughout the protocols, there were major differences in the design of protocols which varied in sets, repetitions, and types of exercises. At-home exercise used general strengthening exercises compared to semi-supervised exercise that used more shoulder instability-specific exercises. Supervision for at-home exercise was limited to only the initial physical therapy session and the remaining sessions were self-reported. Alternatively, the semi-super-
Table 5. Western Ontario Shoulder Index (WOSI) and Upper Quarter Y-Balance test (UQYBT) composite mean (± standard deviation) scores. Minimal clinically important difference (MCID = >1.96) in relation to the following test (i.e., pre- vs. mid-test (4 weeks), mid-test vs. post-test (8 weeks), post-test (8 weeks) vs. 3 month follow-up)
vised group received supervised sessions twice a week for the first two weeks and then once a week for the remaining 10 weeks. Compliance for both at-home and semi-supervised exercise was set at 66%.
Kirkley et al.12 compared participants that received shoulder surgery for instability to those that chose conservative management and found that at the 32-month followup period, the surgical group had 16% (p=0.03) greater improvement than the conservative group. At the 72-month follow-up, the surgical group did not change in score. However, the conservative group reduced the difference to 11% (p=0.17). These delayed improvements at the 32- and 72-month periods may have influenced this tool’s utility. Earlier and more frequent testing may have better illustrated potential differences.
Furthermore, previous UQYBT studies to date suggests the need to develop rehabilitation protocols for those with shoulder instability and continue to expand the knowledge into different types of athletes to increase normative data and allow to screen for those at risk of injury
32,35,36
The utilization of the Bodyblade - Classic and Pro models used in this study are in accord with UQYBT authors’ recommendations in developing rehabilitation protocols for TASI. All four Bodyblade™ exercises used in this study have been shown to elicit moderate to moderately strong muscle activation levels between 20% - 46% MVIC of the infraspinatus, upper trapezius, lower trapezius, and gluteus maximus.21,37 These levels are considered to be effective for moderate muscle strengthening.21 Furthermore, Escamilla et al.37 utilized the Bodyblade™ Classic (0.68 kg, 119.38 cm) and Pro (1.13 kg, 152.4 cm) in two of the four exercises used in this study However, Oliver et al.21 utilized the Bodyblade™ CxT model (0.68 kg, 102 cm), which weighs less than the Pro and is shorter in length compared to the Classic and Pro models. These factors may have to be further explored to determine their effect on muscle activation levels. Nevertheless, the whole-body kinetic-chain patterns found by Oliver et al.21 are favorable for rehabilitation and could explain why the Bodyblade™ group was the only group to obtain significant findings during the inferolateral reach direction.
32,35,36
The Bodyblade™ group demonstrated significant improvements in the UQYBT during the inferolateral reach, outperforming the Mixed group at post-test (8 weeks) and three-month follow-up. This finding could have been due to the Mixed group only performing 50% of the Traditional and Bodyblade™ protocols. The Mixed group did not progress beyond the green resistance band or get to advance to the Bodyblade™ pro model. Hence, the progressive training stimulus did not reach the intensity of the Bodyblade™ or the Traditional training protocols and thus may have been insufficient. Previous UQYBT studies only used healthy participants to help establish reliability and sex differences in performance.32 No participants in previous studies exhibited pre-existing shoulder instability conditions. Nonetheless, the UQYBT foundational studies provide insight into how normal values can be utilized to determine performance without an intervention.
The inferolateral reach demands its participants to maintain a prone three-point stance position while supporting themselves on the involved arm. The arm must maintain a stationary position of approximately 90° of shoulder flexion. Basset et al.38 reported that the pectoralis major, the short head of the biceps brachii, coraco-
brachialis, anterior deltoid, and subscapularis were the primary restraints in anterior shoulder instability when the shoulder is in a flexed position. Furthermore, Kronberg et al.39 identified decreased muscle activity of the anterior deltoid, subscapularis, pectoralis major, latissimus dorsi, and serratus anterior in participants with shoulder instability Thus, Parry et al.19 in examining the utilization of the Bodyblade™ Pro in shoulder flexion reported the anterior deltoid, serratus anterior, and pectoralis major and infraspinatus all elicited 50% MVIC, which may have been the reason for the greater improvement in the UQYBT inferolateral reach direction.
It can only be speculated that the improved Bodyblade™ group performance during the UQYBT inferolateral direction resulted from greater muscle activation based on previous studies. The interventions performed in this study required participants to perform the exercises while in an athletic stance position. However, the UQYBT is performed in a prone three-point stance. The transferability of the interventions onto the UQYBT reach directions may have affected the potential for significant outcomes. There could have been different outcomes if the interventions were also performed prone similarly to the demands of the UQYBT Behm & Sale28 suggested that task-specific resistance training will exhibit optimal gains with a similar testing training method. In accordance with the SAID (Specific Adaptation to Imposed Demands) principle, when training methods deviate from testing measures, there will be decreased improvements.
However, it is unknown whether the benefits of the Bodyblade and Traditional groups were from strength gains or motor control, or possibly a combination of both. The timing of muscle activation (motor control) is an important component of neuromuscular efficiency, which can be affected by shoulder conditions compared to healthy patients.40 The late improvements during the eight-week intervention allow clinicians to understand the delayed benefits of using the Bodyblade™ and help educate patients on its utility These findings are further supported by the Sugimoto & Blanpied25 study that found participants reported the Bodyblade™ more challenging at the start of the 5th week of intervention. Additionally, these findings could lend further credibility to the role of the Bodyblade as an early to intermediate phase rehabilitation tool.
The study participants were cleared by an orthopedic surgeon during pre-participation physical examinations and satisfied the inclusion criteria based on the shoulder history questionnaire. However, the severity of shoulder instability was unknown amongst each participant. Participants
may have had pre-existing conditions that could have contributed to decreased performance. Only through diagnostic imaging would the participant’s level of shoulder instability be fully determined. Nonetheless, if this component would have been added to the study, it may have presented several challenges with the imaging findings and their clinical relevance. This challenge could have potentially reduced the number of participants included in the study if the structural abnormalities exceeded the orthopedic recommendations for conservative management. These potential factors were carefully considered during the development of the inclusion, exclusion criteria, and assessment strategies. Based on the limited resources available for this study, a practical training and testing approach was taken. Future research on the Bodyblade™ to manage TASI may perform manual orthopedic assessments, instead of imaging to confirm anterior shoulder instability
The main significant findings were demonstrated in the Bodyblade™ group during the UQYBT inferolateral reach at the post-test (8 weeks) and at the three-month follow-up. Conversely, the Mixed group had deleterious effects during the post-test and three-month follow-up. This could have been due to the Mixed group performing only 50% of the Traditional and Bodyblade™ protocols, preventing participants from obtaining high enough stimulus for positive benefits.
The stepwise progressions discovered in each of the three groups during the WOSI measurement points allow clinicians to provide their patients with the option of choosing the Traditional or the Bodyblade™ protocols. However, choosing the Mixed protocol has no additional benefit and may decrease performance based on the UQYBT post-test and three-month follow-up findings. Finally, it is not recommended to use the WOSI as a standalone outcome measure for shoulder instability rehabilitation. The WOSI should be accompanied by a functional outcome measure such as the UQYBT to make a sound clinical decision.
The authors declare no conflicts of interest with the contents of this manuscript.
Submitted: April 02, 2022 CST, Accepted: October 10, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Good CR, MacGillivray JD Traumatic shoulder dislocation in the adolescent athlete: advances in surgical treatment. Curr Opin Pediatr. 2005;17(1):25-29. doi:10.1097/01.mop.0000147905.9 2602.bb
2. Dala-Ali B, Penna M, McConnell J, Vanhegan I, Cobiella C. Management of acute anterior shoulder dislocation. Br J Sports Med 2014;48(16):1209-1215. doi:10.1136/bjsports-2012-091300
3. Brownson P, Donaldson O, Fox M, et al. BESS/BOA patient care pathways: traumatic anterior shoulder instability. Shoulder Elbow. 2015;7(3):214-226. doi:1 0.1177/1758573215585656
4. Eshoj H, Rasmussen S, Frich LH, Jensen SL, Søgaard K, Juul-Kristensen B. Patients with nonoperated traumatic primary or recurrent anterior shoulder dislocation have equally poor self-reported and measured shoulder function: a cross-sectional study BMC Musculoskelet Disord 2019;20(1):59-63. d oi:10.1186/s12891-019-2444-0
5. Cameron KL, Mauntel TC, Owens BD. The epidemiology of glenohumeral joint stability: incidence, burden, and long-term consequences. Sports Med Arthroscopy Rev. 2017;25(3):144-149. do i:10.1097/jsa.0000000000000155
6. Olds M, Ellis R, Donaldson K, Parmar P, Kersten P Risk factors which predispose first-time traumatic anterior shoulder dislocations to recurrent instability in adults: a systematic review and meta-analysis. Br J Sports Med. 2015;49(14):913-922. doi:10.1136/bjsport s-2014-094342
7 Zacchilli MA, Owens BD Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92(3):542-549. doi:10.2106/jbjs.i.00450
8. Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med 2009;37(9):1750-1754. doi:10.1177/036354650933459 1
9. Karatsolis K, Athanasopoulos S. The role of exercise in the conservative treatment of the anterior shoulder dislocation. J Bodywork Mvmt Ther. 2006;10(3):211-219. doi:10.1016/j.jbmt.2005.10.008
10. Buteau JL, Eriksrud O, Hasson SM. Rehabilitation of a glenohumeral instability utilizing the body blade. Phys Theory Prac 2007;23(6):333-349. doi:10.1080/09 593980701247337
11. Jakobsen BW, Johannsen HV, Suder P, Søjbjerg JO Primary repair versus conservative treatment of firsttime traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy 2007;23(2):118-123. doi:10.1016/j.arthr o.2006.11.004
12. Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: longterm evaluation. Arthroscopy. 2005;21(1):55-63. doi:1 0.1016/j.arthro.2004.09.018
13. McLaughlin HL, Cavallaro WU. Primary anterior dislocation of the shoulder. Am J Surg. 1950;80(6):615-621. doi:10.1016/0002-9610(50)9058
1-2
14. Adam M, Attia AK, Alhammoud A, Aldahamsheh O, Al Ateeq Al Dosari M, Ahmed G. Arthroscopic Bankart repair for the acute anterior shoulder dislocation: systematic review and meta-analysis. Int Orthop 2018;42(10):2413-2422. doi:10.1007/s0026 4-018-4046-0
15. Itoi E, Hatakeyama Y, Kido T, et al. A new method of immobilization after traumatic anterior dislocation of the shoulder: A preliminary study J Shoulder Elbow Surg. 2003;12(5):413-415. doi:10.1016/s1058-2746(0 3)00171-x
16. Buss DD, Lynch GP, Meyer CP, Huber SM, Freehill MQ. Nonoperative management for in-season athletes with anterior shoulder instability Am J Sports Med 2004;32(6):1430-1433. doi:10.1177/03635 46503262069
17. Bodyblade® Website. Accessed March 21, 2020. ht tp://www.bodyblade.com
18. Moreside JM, Vera-Garcia FJ, McGill SM. Trunk muscle activation patterns, lumbar compressive forces, and spine stability when using the bodyblade. Phys Ther. 2007;87(2):153-163. doi:10.2522/ptj.20060 019
19. Parry JS, Straub R, Cipriani DJ. Shoulder-and back-muscle activation during shoulder abduction and flexion using a Bodyblade pro versus Dumbbells. J Sport Rehabil 2012;21(3):266-272. doi:10.1123/jsr.2
1.3.266
20. Arora S, Button DC, Basset FA, Behm DG. The effect of double versus single oscillating exercise devices on trunk and limb muscle activation. Int J Sports Phys Ther. 2013;8(4):370-380.
21. Oliver GD, Sola M, Dougherty C, Huddleston S. Quantitative examination of upper and lower extremity muscle activation during common shoulder rehabilitation exercises using the bodyblade. J Strength Cond Res 2013;27(9):2509-2517 doi:10.151 9/jsc.0b013e31827fd4c2
22. Lister JL, Rossi GD, Ma F, et al. Scapular stabilizer activity during Bodyblade®, cuff weights, and Theraband® use. J Sport Rehabil 2007;16(1):50-67 doi:10.1 123/jsr.16.1.50
23. Kang JI, Park JS, Jeong DK, Choi HH, Moon YJ, Choi HH. Effects on muscle activities according to the type of bodyblade exercise in quadruped position. J Phys Ther Sci 2018;30(6):862-865. doi:10.1589/jpts.3 0.862
24. Kibler WB, Sciascia AD, Uhl TL, Tambay N, Cunningham T Electromyographic analysis of specific exercises for scapular control in early phases of shoulder rehabilitation. Am J Sports Med. 2008;36(9):1789-1798. doi:10.1177/036354650831628
25. Sugimoto D, Blanpied P. Flexible foil exercise and shoulder internal and external rotation strength. J Athl Train 2006;41(3):280-285.
26. Kim EK, Kang JH, Lee HT. The effect of the shoulder stability exercise using resistant vibration stimulus on forward head posture and muscle activity. J Phys Ther Sci. 2016;28(11):3070-3073. doi:1 0.1589/jpts.28.3070
27 Behm DG. Neuromuscular implications and applications of resistance training. J Strength Cond Res 1995;9(4):264-274.
28. Behm DG, Sale DG. Velocity specificity of resistance training. Sports Med 1993;15(6):374-388. doi:10.2165/00007256-199315060-00003
29. Wilk KE, Macrina LC, Reinold MM. Non-operative rehabilitation for traumatic and atraumatic glenohumeral instability. N Am J Sports Ther. 2006;1(1):16-31.
30. Baechle TR, Earle RW Essentials of Strength Training and Conditioning. 3rd ed. Human Kinetics; 2008.
31. Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability. The Western Ontario Shoulder Instability Index (WOSI). Am J Sports Med 1998;26(6):764-772. d oi:10.1177/03635465980260060501
32. Westrick RB, Miller JM, Carow SD, Gerber JP Exploration of the y-balance test for assessment of upper quarter closed kinetic chain performance. Int J Sports Phys Ther. 2012;7(2):139-147.
33. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15(2):155-163. doi:10.1016/j.jcm.2016.02.012
34. Eshoj HR, Rasmussen S, Frich LH, et al. Neuromuscular exercises improve shoulder function more than standard care exercises in patients with a traumatic anterior shoulder dislocation: a randomized controlled trial. Orthop J Sports Med 2020;8(1):1-12. doi:10.1177/2325967119896102
35. Butler R, Arms J, Reiman M, et al. Sex differences in dynamic closed kinetic chain upper quarter function in collegiate swimmers. J Athl Train. 2014;49(4):442-446. doi:10.4085/1062-6050-49.3.17
36. Gorman PP, Butler RJ, Plisky PJ, Kiesel KB. Upper quarter y balance test: reliability and performance comparison between gender in active adults. J Strength Cond Res 2012;26(11):3043-3048. doi:10.151 9/jsc.0b013e3182472fdb
37 Escamilla RF, Yamashiro K, Dunning R, et al. An electromyographic analysis of the shoulder complex musculature while performing exercises using the Bodyblade® classic and bodyblade® pro. Int J Sports Phys Ther 2016;11(2):175-189.
38. Bassett RW, Browne AO, Morrey BF, An KN. Glenohumeral muscle force and moment mechanics in a position of shoulder instability J Biomech 1990;23(5):405-415. doi:10.1016/0021-9290(90)9029 5-e
39. Kronberg M, Broström LÅ, Németh G. Differences in shoulder muscle activity between patients with generalized joint laxity and normal controls. Clin Orthop Relat Res 1991;269:181-192. doi:10.1097/000 03086-199108000-00026
40. Myers JB, Lephart SM. The role of the sensorimotor system in the athletic shoulder J Athl Train. 2000;35(3):351-363.
66. May S, Chance-Larsen K, Littlewood C, Lomas D, Saad M. Reliability of physical examination tests used in the assessment of patients with shoulder problems: a systematic review. Physiotherapy. 2010;96(3):179-190. doi:10.1016/j.physio.2009.12.002
67 Pierce J, Anderson M. Update on diagnostic imaging of the rotator cuff. Clin Sports Med. 2023;42(1):25-52. doi:10.1016/j.csm.2022.08.009
68. CARE Case Report Guidelines. What are the CARE guidelines? https://www.care-statement.org
Keywords: rotator cuff, special tests, shoulder https://doi.org/10.26603/001c.67934
Background
Recently, researchers have commented that shoulder special tests cannot identify the structure causing rotator cuff symptoms and should only be considered pain provocation tests. Others have disagreed, reporting that special tests were able to accurately detect the presence of rotator cuff involvement.
The purpose of this study was to determine the knowledge, use, and perceived effectiveness of 15 selected special tests utilized to examine patients with possible rotator cuff dysfunction.
Study Design
Descriptive study using survey
An electronic survey was returned by 346 members of the Academies of Orthopedic and Sports Physical Therapy through list serves. Descriptions and pictures for 15 special tests of the shoulder were included in the survey Information regarding years of clinical experience and American Board of Physical Therapy Specialties (ABPTS) specialist certification in Sports or Orthopedics was collected. Respondents were asked if they could identify and use the special tests to evaluate dysfunction of the rotator cuff - and how confident they were in ability of the tests to diagnose dysfunction of the rotator cuff
The four tests most readily known by respondents included the empty can, drop arm, full can, and Gerber’s tests, and the four tests used regularly by the respondents included the infraspinatus, full can, supraspinatus, and champagne toast tests. The infraspinatus, champagne toast, external rotation lag (ERLS), and the belly-off tests were found to be the be most useful for establishing a diagnosis of the muscle-tendon complex involved. Years of experience and clinical specialization was not relevant to knowledge or use or these tests.
Corresponding author:
 William D. Bandy PT, PhD, SCS, FAPTA Department of Physical Therapy
William D. Bandy PT, PhD, SCS, FAPTA Department of Physical Therapy
University
ofCentral Arkansas
201 Donaghey Ave, PTC Suite 300
Conway, Arkansas 72035
Phone: (501) 450-5547
Fax: (501) 450-5822
billb@uca.edu
This study will allow clinicians and educators to understand which special tests are easily identified, regularly used, and perceived as helpful for the diagnosis of muscles involved in a rotator cuff dysfunction.
3b
Physical examination of any joint in the body is extremely important to evaluate the presence, location, and extent of problems or dysfunction that may exist in a person. One joint that may be a challenge for practitioners to examine and diagnose is the shoulder, due to the highly complex architecture of bony and soft-tissue anatomy which allows for the greatest range of motion of any joint of the body. As a result of the complexity of the shoulder joint, difficulty exists when conducting an appropriate clinical examination, especially the examination of rotator cuff involvement in the shoulder.1,2
Recently, McFarland et al3 wrote a clinical commentary and stated that shoulder special tests cannot identify the structure causing rotator cuff symptoms and should only be considered pain provocation tests. The authors suggested that use of special tests to inform individuals of the specific source of their symptoms, and then recommend surgical or nonsurgical intervention for that structure is not the best practice. Furthermore, the authors suggested that a comprehensive clinical interview and physical examination without special tests can be used to determine a working diagnosis to implicate a rotator cuff pathology.
Salamh and Lewis4 wrote in an editorial that special tests do not impart diagnostic information and should not be an important part of the physical therapist examination.
Requejo-Salinas et al5 used a group of international expert physical therapists to come to a consensus statement suggesting that resistive testing, response to overhead loading, and reported symptoms were more effective at creating a diagnostic impression than any of the special tests. Van Kampen et al6 stated in a systematic review, that predictive values of special tests are low After additional systematic reviews, Gismervik et al7 and Hegedus et al8 reported no support for most special tests of the shoulder but both groups of authors found some benefit of using the Jobe’s supraspinatus test with reasonable sensitivity and specificity
Cadogan et al9 disagreed with the McFarland group and related research, reporting that using special tests for the shoulder allows for accurate diagnosis in identifying rotator cuff involvement. Tennent et al10 stated that “careful examination of the shoulder is an essential component in forming a diagnosis of problems in this area and special testing is an important tool in this arsenal.” These authors suggested the discrepancy in the use of special testing is due to the number of tests available and the lack of knowledge of how to properly perform the tests.
Other published manuscripts reviewed the sensitivity and specificity for specific rotator cuff special tests with a
variety of results – pro and con - for including special tests for the shoulder as part of an examination. After researching sensitivity and specificity of multiple rotator cuff tests, Yuen et al11 found only the Jobe (empty can) test had good sensitivity at 0.89 when compared to MRI, but found that only 37% of practitioners in their study correctly diagnosed the impairments using the gauntlet of tests available. Zou et al12 also found that the Jobe and Hug-up tests had favorable positive likelihood values of 2.58 and 2.3 respectively Similarly, Liu et al13 found the Hug-up test to have a 0.94 sensitivity and a 0.77 specificity Bak et al14 researched the external rotation lag sign (ERLS) as a diagnostic tool compared to arthroscopic surgery findings and found sensitivity of 0.91 and specificity of 0.86 in full thickness tears of the rotator cuff. Additionally, Sgroi et al15 also found favorable diagnostic ability with the same test (ERLS) and reported resisted external rotation to have some diagnostic precision depending on the extent of the rotator cuff tear The same authors found that the combination of resisted external rotation combined with the Patte test was the most effective in comparison with surgical findings.
Yazigi et al16 researched the use of the empty can, full can, drop arm, Patte, and infraspinatus tests in an article published in 2021 and found good sensitivity of the empty can (0.81) and good specificity of the drop arm and Patte tests (0.98). They also suggested prediction of diagnosis of injury at 58% for the empty can test. Finally, Dinnes et al17 suggest the opposite of Salalm and Lewis4 and stated that using rotator cuff special tests, a practitioner can rule out tears because of overall high sensitivity as indicated previously.
A problem that exists when discussing special tests of the shoulder for detecting rotator cuff involvement is that over 70 special tests have been described to examine patients with shoulder injuries.18 Because of the vast array of tests, clinicians and educators in health care curricula are challenged to decide which tests should be used and taught, respectively. Therefore, the purpose of this study was to determine the knowledge, use, and perceived effectiveness of 15 selected special tests utilized to examine patients with possible rotator cuff dysfunction.
Following a review of the literature, 15 special tests used for the musculoskeletal examination of the shoulder complex were chosen to be included in a survey. The tests chosen were the most common found in the literature in several data searches and were described in textbooks.
ER resistance at 0 degrees abduction (Appendix- Figure 1)
a. Purpose: Assess for infraspinatus muscle-tendon complex tears and dysfunction.
b. Positioning: Patient seated with elbow flexed at 90 degrees and shoulder adducted to their trunk. Patient asked to externally rotate the arm while the therapist applies resistance.
c. Interpreting results: Test is positive if patient reports pain or is unable resist motion.
d. Sensitivity and Specificity not reported.
Hug up test13 (Appendix- Figure 2)
a. Purpose: Assess for supraspinatus muscle-tendon complex tears and dysfunction.
b. Positioning: Patient seated or standing and places hand of involved arm on opposite shoulder. Therapist applies a downward force perpendicular to elbow while patient resists the motion.
c. Interpreting results: Test is positive if patient reports pain or is unable to resist motion.
d. Sensitivity 94.1%, Specificity 76.6%.
Drop arm sign15 (Appendix- Figure 3)
a. Purpose: Asses for full thickness rotator cuff tears, especially for supraspinatus muscle-tendon complex tears.
b. Positioning: Patient seated. Therapist abducts the involved arm to 90 degrees and externally rotates the arm, while supporting the arm at the elbow. The therapist releases the arm, and the patient slowly lowers the arm down.
c. Interpreting results: Test is positive if patient suddenly drops arm or struggles to maintain arm position.
d. Sensitivity 73%, Specificity 77%.
Subscapularis test (Appendix- Figure 4)
a. Purpose: Assess for subscapularis muscle-tendon complex tears or dysfunction.
b. Positioning: Patient seated with elbow flexed at 90 degrees. Patient pushes hand into chest (contracts as internally rotates) as therapist resists.
c. Interpreting results: Test is positive if patient reports pain or is unable resist motion.
d. Sensitivity and Specificity not reported.
Belly press off19 (Appendix- Figure 5)
a. Purpose: Assess for subscapularis muscle-tendon complex tears or dysfunction. This test is often used when a patient is unable to perform the Gerber lift off test due to pain or limited internal rotation ROM.
b. Positioning: Patient seated with elbow flexed at 90 degrees with palm facing the chest (hand should be placed right below xyphoid process). Patient pushes hand into chest (contracts as internally rotates) as therapist resists.
c. Interpreting results: Test is positive if patient compensates (common compensations seen are wrist flex, shoulder adduction, and shoulder extension).
d. Sensitivity 34% , Specificity 92%.
Infraspinatus test (Appendix- Figure 6)
a. Purpose: Assess for infraspinatus muscle-tendon complex tears and dysfunction.
b. Positioning: Patient side-lying with elbow flexed at 90 degrees and shoulder adducted to their trunk. Therapist applies force to resist external rotation
c. Interpreting results: Test is positive if patient reports pain or is unable resist motion.
d. Sensitivity and Specificity not reported.
Patte test20 (Appendix- Figure 7)
a. Purpose: Assess for teres minor muscle-tendon complex dysfunction.
b. Positioning: Patient either sitting or standing. The involved arm is placed in 90 degrees of shoulder abduction in the scapular plane with elbow also at 90 degrees. Patient asked to externally rotate the arm while the therapist applies resistance.
c. Interpreting results: Test is positive if pain with resisted external rotation.
d. Sensitivity 93%, Specificity is 72%.
Champagne toast (and pour) test21 (Appendix- Figure 8)
a. Purpose: Assess for supraspinatus muscle-tendon complex dysfunction and injury
b. Positioning: Patient seated and puts shoulder at 30 degrees abduction, 15 degrees ER, and 30 degrees flex, with elbow flexed to approx. 90 degrees. Therapist applies downward force along elbow
c. Interpreting results: Test is positive if patient reports pain or weakness occurs during movement.
d. Sensitivity and Specificity not reported.
Empty can22 (Appendix- Figure 9)
a. Purpose: Assess for supraspinatus muscle-tendon complex and tendon pathology.
b. Positioning: Patient can be seated or standing. Involved arm is elevated to 70 degrees. With elbow at full extension, the shoulder is held in internal rotation, and pronation (thumbs-down position). Therapist applies downward force through arm.
c. Interpreting Results: Test is positive if patient reports pain or weakness with resistance.
d. Sensitivity 88.6%, Specificity 58.8% for tendon tears.
Full can22 (Appendix- Figure 10)
a. Purpose: Assess for dysfunction of supraspinatus muscle-tendon complex.
b. Positioning: Patient standing or seated and holds involved arm at 70 degrees in scapular plane with hand in the "thumbs up " position. Therapist applies downward force at the mid-forearm.
c. Interpreting Results: Test is positive if patient reports pain or weakness with resistance.
d. Sensitivity 70%, Specificity 81%.
Hornblower’s test20 (Appendix- Figure 11)
a. Purpose: Assess for teres minor muscle-tendon complex dysfunction.
b. Positioning: Patient is supine with involved arm placed in 90 degrees of shoulder abduction with elbow also at 90 degrees. Patient asked to externally rotate the arm while the therapist applies resistance.
c. Interpreting results: Test is positive if pain with resisted external rotation.
d. Sensitivity 93%, Specificity is 72%.
Gerber lift off test23 – Also called lift off test (AppendixFigure 12)
a. Purpose: Assess for rupture of the subscapularis muscle-tendon complex.
b. Positioning: Patient standing, and places involved arm behind the back. Patient then lifts hand off the back (performs IR) while therapist applies pressure against the hand (utilizes an external rotation force).
c. Interpreting results: Test is positive if patient cannot resist external rotation force, lift hand off the back, or compensates.
d. Sensitivity 35%, Specificity 98%.
ER lag sign24 Also called the Infraspinatus Spring Back Test. (Appendix- Figure 13)
a. Purpose: Assess for teres minor and infraspinatus muscle-tendon complex involvement.
b. Positioning: Patient seated with elbow flexed at 90 degrees and shoulder at 20 degrees elevation in scapular plane. Therapist externally rotates arm just short of maximal external ROM.
c. Interpreting results: Test is positive if patient cannot maintain position or arm springs anterior
d. Sensitivity 97%, Specificity 93% for infraspinatus involvement. Sensitivity 100%, Specificity 93% for teres minor involvement.
Horizontal adduction25 (Appendix- Figure 14)
a. Purpose: Assess the integrity of the supraspinatus muscle-tendon complex.
b. Positioning: Patient seated and holds arm horizontally adducted across the chest in full external rotation and with elbow extended. Subject is asked to pull the arm into horizontal abduction (away from the chest).
c. Interpreting results: Observation is made as to whether the humeral head engages into the glenoid which can only occur when the supraspinatus is active and viable.
d. Sensitivity and Specificity were not reported.
Bear hug test26 (Appendix- Figure 15)
a. Purpose: Assess the integrity of the supraspinatus muscle-tendon complex.
b. Positioning: Patient seated and holds arm horizontally adducted across the chest in full external rotation and with elbow remaining extended. Subject is asked to pull the arm into horizontal abduction (away from the chest).
c. Interpreting results: Observation is made as to whether the humeral head engages into the glenoid which can only occur when the supraspinatus is active and viable.
d. Sensitivity and specificity were not reported.
Along with the descriptions, pictures for each test were provided in the survey so participants could identify the test visually. For each test, respondents were asked a) if they could identify each of the 15 special tests, b) regarding their use of the tests to evaluate dysfunction of the rotator cuff, and c) how confident they were in the ability of the special tests to identify the rotator cuff muscle-tendon complex involved. In addition, the survey included questions about years of clinical experience, as well as whether the participants were certified specialist by the American Board of Physical Therapy Specialties (ABPTS).
After receiving approval from the Institutional Review Board at the University of Central Arkansas, the survey was sent electronically using the list serves of both the Academy of Orthopedic Physical Therapy and the American Academy of Sports Physical Therapy As part of the survey instructions, the respondents were notified that completing and submitting the survey was considered their informed consent.
The participant ranked each of the 15 special tests on a 7-point Likert scale. Rating possibilities ranged from 1 “strongly disagree” to 7 “strongly agree” for each of the following areas: a) knowledge of the test, b) use of the test clinically, and c) ability of the test to determine if the rotator cuff was involved.
Results of the survey were tallied using the Likert score in each of the three categories for each test. To determine if years of experience made a difference as to whether the special tests were utilized clinically, the years were divided into quartiles. Quartiles were formed by review of the frequencies of the years of experience and forming four groups where natural divisions occurred. A one-way ANOVA was then performed on these rankings related to years of experience. A t-test was used to compare rankings between clinical specialists and non-specialists.
Three hundred forty-six surveys were returned from active members of the Academies. The average years of experience among the respondents was 15.41 (+/- 13.02) years. One hundred twenty-four were ABPTS Orthopedic or Sports Specialists and 225 respondents were not.
Results indicated that the four tests most readily known by respondents included the empty can test, drop arm test, full can test, and Gerber’s test. The top four tests used regularly by the respondents were the infraspinatus test, full can test, supraspinatus test and the champagne toast test. Finally, the infraspinatus test, champagne toast test, external rotation lag (ERLS) test, and the belly-off test were re-
ported by respondents to be the be most useful for establishing a diagnosis of the muscle-tendon complex involved.
Those respondents with more years of experience had significantly higher determination or diagnosis (most useful) using only one special test, the belly-off test. Years of experience made no difference in the knowledge or used regularly categories for any other special test. In addition, no difference existed between those who were clinical specialists and those with no specialization for any of the tests or categories.
This study attempted to discern the knowledge of and use of defined rotator cuff special tests and the perceptions regarding the use of these tests as diagnostic tools. The results suggest that several tests exist that are well known and used frequently by those that responded to the survey, but did not assist in determining the structure involved. However, other tests used by the respondents to come to clinical conclusions were used less often. No test was noted in all of the categories of interest: “known,” “used,” and “most useful in diagnosis.” For example, the infraspinatus (ER at 0° of abduction) and the champagne toast tests (a test for supraspinatus function) were both “used” and most “useful in diagnosis.” But, the full can and empty can tests were both “known” and “used” but were not the most “ useful in diagnosis.”
Prior to further discussion of results of this study, a review of the concepts of sensitivity and specificity may be in order. Sensitivity and Specificity describe the accuracy of a test which reports the presence or absence of a condition. For the purposes of this study, sensitivity is the ability of a special test of the shoulder to correctly identify those with rotator cuff dysfunction (true positive rate), whereas specificity is the ability of the shoulder special test to correctly identify those without the rotator cuff problem (true negative rate). As an example, if 100 patients known to have rotator cuff problems were evaluated using a particular special test, and 43 test positive, then that special test has 43% sensitivity If 100 with no rotator cuff involvement are assessed and 96 return a completely negative test result, then that shoulder special test has 96% specificity.27 For purposes of this study, the authors have operationally defined sensitivity and specificity of 70% and greater as the determination that the special test was important in the diagnostic interpretation of rotator cuff injuries.
As indicated in the previous literature review included in this manuscript, some editorial comments and research articles suggest none of the special tests for rotator cuff pathology are helpful in the diagnosis of the rotator cuff4,5,7 - while others reported that using special tests for the shoulder allows a more accurate diagnosis in identifying rotator cuff involvement.9,10
The present survey reinforces previous research by finding that many of the respondents believed some special tests were helpful in the clinical setting in coming to an accurate diagnosis involving the rotator cuff In reviewing the 15 special tests used in this study, five tests (Hug-up, Patte,
Full can, Hornblowers, and ERLS) had sensitivity and specificity above 70%. For the other tests, sensitivity above 70% was found for one test (Empty can); and specificity above 70% was found for three tests (Belly off, Gerber lift, and the Bear hug).
Reviewing the result of this study and comparing the four tests {infraspinatus, champagne toast, ERLS, and the belly-off tests} identified in the survey as the most useful to the diagnosis of rotator cuff dysfunction, the ERLS and belly off tests were among those tests identified in the literature of being accurate test for the examination of the rotator cuff problems. Of note, two of these tests that the respondents said were helpful in the diagnosis of the rotator cuff muscles (Champagne toast and Infraspinatus tests) have had no research performed to determine their sensitivity and specificity The suggestion by Salahm et al, and others, that special tests for the shoulder are not helpful in the diagnosis of rotator cuff injuries was disputed by the results of this study Many of the tests reviewed for this study show substantial specificity or sensitivity and should be considered as diagnostic tools.
No information was gathered on why the responding therapists chose the special tests that were favored or why physical therapy entry-level programs chose the special tests they are teaching in their educational programs. Information regarding where the respondents learned a specific special test may provide information as to the “knowledge” of these special tests reported to be used in the survey. For instance, the Champagne Toast test for the supraspinatus is a relatively new test (described in 2016) and, therefore, may not be taught in many entry-level programs.21 The Champagne Toast test has been explored in some manuscripts but has not been reviewed in most systematic reviews or in comparison to other rotator cuff tests.21,28
Many of the common rotator cuff tests were not known or used by a percentage of the respondents though some had support for their use in the literature. No studies were found that suggested the choice or usage of special tests in physical therapy educational programs would lead to a possible increase in the “known” category in this survey
A study was performed by Sciascia et al29 that surveyed orthopedic surgeons on special tests performed to come to diagnostic conclusions for potential rotator cuff injuries or pathology. The authors suggested the choice of tests were dictated by their fellowship training and their graduate studies. Physical therapists might have a similar diversity in the training and use of certain special tests for diagnosing rotator cuff pathologies leading to a lack of usage of these same tests across the country More studies exploring which of the rotator cuff special tests are taught in physical therapy entry-level programs are needed to understand the paucity of knowledge concerning certain special tests.
Experience and specialization might be expected to make a difference in the knowledge, use, and application of special tests for the rotator cuff. However, based on the results of this survey, no differences existed in the knowledge of, and the use of, the special tests selected for this study based on years of experience (even between the least and
most experienced therapists) or being specialized. Larger numbers of respondents may demonstrate more stratification of experience and greater statistical difference between more and less experienced physical therapists.
The survey was sent to members of the Orthopedics Academy and Sports Academy of the American Physical Therapy Association and no method of recording the contact or opening rate of the survey was able to be determined. Therefore, the actual response rate could not be determined. Of the thousands of members of the Academies with the opportunity to participate, 346 surveys were received. The researchers do not know if members responding to the survey may be the most motivated by the question, or reflect the actual make-up of the physical therapy community within the Academies, or represent the responses from the licensees in Physical Therapy in the United States.
As previously indicated, the literature contains numerous tests for use in rotator cuff examination. The researchers on this study picked a group of 15 tests they reviewed reflected the most frequently used tests. A different body of researchers may have chosen a different group of rotator cuff tests or may not include tests more easily recognized or utilized. The researchers believed a survey using all the possible rotator cuff tests would be too numerous to allow an effective review.
Some of the special tests mentioned in these articles reviewed were not listed as the top four tests in the current survey for diagnostic assistance. This lack of agreement between authors could suggest that many of the practitioners surveyed were not comfortable in use of certain tests or did not perform them as frequently in evaluations. Some less-known tests (diagonal horizontal abduction, external rotation with adduction, etc) have been noted by other re-
searchers as effective at isolating specific rotator cuff musculature, and were noted by respondents as effective in diagnosis, but did not have the same weight of response as the other tests measured.25 The authors behind the creation and interpretation of this survey would suggest more research needs to be added to the literature pool for all of the specific tests with validation against gold standard testing such as MRI and arthroscopy
The results of this survey revealed the most known (the empty can, drop arm, full can, and Gerber’s tests), used (the infraspinatus, full can, supraspinatus, and champagne toast tests), and diagnostically relevant (the infraspinatus, champagne toast, external rotation lag [ERLS], and the belly-off tests) rotator cuff tests from selected tests among a sample of physical therapists. Common knowledge of tests and use of tests did not vary by years of experience, nor by having an ABPTS Clinical Specialization. These data may allow clinicians and educators to understand which special tests are easily identified, regularly used, and helpful for the diagnosis of muscles involved in rotator cuff dysfunction.
The authors of this manuscript have no Conflicts of Interest related to reviewers, editor, editorial board member – nor any financial or personal relationships with other individuals or organizations that could inappropriately influence our actions in a way that creates bias.
Submitted: July 11, 2022 CST, Accepted: November 03, 2022
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Dutton M. Dutton’s Orthopaedic Examination, Evaluation, and Intervention 5th ed. McGraw Hill; 2020.
2. Jain NB, Luz J, Higgins LD, et al. The diagnostic accuracy of special tests for rotator cuff tear: The ROW cohort study. Am J Phys Med Rehabil. 2017;96(3):176-183. doi:10.1097/phm.000000000000 0566
3. McFarland EG, Kibler WB, Murrell GAC, Rojas J. Examination of the shoulder for beginners and experts: An update. Instr Course Lect 2020;69:255-272.
4. Salamh P, Lewis J. It is time to put special tests for rotator cuff-related shoulder pain out to pasture. J Orthop Sports Phys Ther. 2020;50(5):222-225. doi:10.2 519/jospt.2020.0606
5. Requejo-Salinas N, Lewis J, Michener LA, et al. International physical therapists consensus on clinical descriptors for diagnosing rotator cuff related shoulder pain: A Delphi study Braz J Phys Ther 2022;26(2):100395. doi:10.1016/j.bjpt.2022.100395
6. van Kampen DA, van den Berg T, van der Woude HJ, et al. The diagnostic value of the combination of patient characteristics, history, and clinical shoulder tests for the diagnosis of rotator cuff tear. J Orthop Surg Res 2014;9(1):70-74. doi:10.1186/s13018-014-0
070-y
7. Gismervik SØ, Drogset JO, Granviken F, Rø M, Leivseth G. Physical examination tests of the shoulder: a systematic review and meta-analysis of diagnostic test performance. BMC Musculoskelet Disord 2017;18(1):41. doi:10.1186/s12891-017-140 0-0
8. Hegedus EJ, Goode AP, Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med 2012;46(14):964-978. doi:10.11 36/bjsports-2012-091066
9. Cadogan A, McNair P, Laslett M, Hing W, Taylor S. Diagnostic accuracy of clinical examination features for identifying large rotator cuff tears in primary health care. J Man Manip Ther. 2013;21(3):148-159. d oi:10.1179/2042618612y.0000000020
10. Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination. Part I: the rotator cuff tests. Am J Sports Med 2003;31(1):154-160. doi:10.1177/036354650303 10011101
11. Yuen CK, Mok KL, Kan PG. The validity of 9 physical tests for full-thickness rotator cuff tears after primary anterior shoulder dislocation in ED patients. Am J Emerg Med. 2012;30(8):1522-1529. do i:10.1016/j.ajem.2011.12.022
12. Zou AP, An FM, Xin YQ Diagnostic value of physical examination tests for supraspinatus tendon tears. Zhongguo Gu Shang 2022;35:220-224. doi:10.1 2200/j.issn.1003-0034.2022.03.005
13. Liu YL, Ao YF, Yan H, Cui GQ. The hug-up test: a new, sensitive diagnostic test for supraspinatus tears. Chin Med J (Engl) 2016;129(2):147-153. doi:10.4103/0 366-6999.173461
14. Bak K, Sørensen AKB, Jørgensen U, et al. The value of clinical tests in acute full-thickness tears of the supraspinatus tendon: does a subacromial lidocaine injection help in the clinical diagnosis? A prospective study Arthroscopy 2010;26(6):734-742. d oi:10.1016/j.arthro.2009.11.005
15. Sgroi M, Loitsch T, Reichel H, Kappe T. Diagnostic value of clinical tests for infraspinatus tendon tears. Arthroscopy. 2019;35(5):1339-1347. doi:10.1016/j.arth ro.2018.12.003
16. Yazigi Junior JA, Anauate Nicolao F, Matsunaga FT, Archetti Netto N, Belloti JC, Sugawara Tamaoki MJ. Supraspinatus tears: predictability of magnetic resonance imaging findings based on clinical examination. J Shoulder Elbow Surg. 2021;30(8):1834-1843. doi:10.1016/j.jse.2021.02.013
17 Dinnes J, Loveman E, McIntyre L, Waugh N. The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review Health Technol Assess 2003;7(29):1-166. doi:10.3310/hta7290
18. Hippensteel KJ, Brophy R, Smith MV, Wright RW. A comprehensive review of physical examination tests of the cervical spine, scapula, and rotator cuff J Am Acad Orthop Surg. 2019;27(11):385-394. doi:10.54 35/jaaos-d-17-00090
19. Tokish JM, Decker MJ, Ellis HB, Torry MR, Hawkins RJ. The belly-press test for the physical examination of the subscapularis muscle: electromyographic validation and comparison to the lift-off test. J Should Elbow Surg 2003;12(5):427-430. doi:10.1016/s1058-2746(03)00047-8
20. Collin P, Treseder T, Denard PJ, Neyton L, Walch G, Lädermann A. What is the best clinical test for assessment of the teres minor in massive rotator cuff tears? Clin Orthop Relat Res. 2015;473(9):2959-2966. doi:10.1007/s11999-015-4392-9
21. Chalmers PN, Cvetanovich GL, Kupfer N, et al. The champagne toast position isolates the supraspinatus better than the Jobe test: an electromyographic study of shoulder physical examination tests. J Shoulder Elbow Surg. 2016;25(2):322-329. doi:10.1016/j.jse.2015.07.031
22. Ackmann T, Schneider KN, Schorn D, et al. Comparison of efficacy of supraspinatus tendon tears diagnostic tests: a prospective study on the “fullcan,” the “empty-can,” and the “Whipple” test. Musculoskelet Surg. 2019;10:12306-12319.
23. Greis PE, Kuhn JE, Schultheis J, Hintermeister R, Hawkins R. Validation of the lift-off test and analysis of subscapularis activity during maximal internal rotation. Am J Sports Med. 1996;24(5):589-593. doi:1 0.1177/036354659602400505
24. Hertel R, Ballmer FT, Lambert SM, Gerber CH. Lag signs in the diagnosis of rotator cuff rupture. J Should Elbow Surg 1996;5(4):307-313. doi:10.1016/s1058-27 46(96)80058-9
25. Forbush SW, White DM, Smith W. The comparison of the empty can and full can techniques and a new diagonal horizontal adduction test for supraspinatus muscle testing using cross-sectional analysis through ultrasonography Int J Sports Phys Ther 2013;8:237-247.
26. Barth JR, Burkhart SS, De Beer JF. The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear Arthroscopy 2006;22(10):1076-1084. doi:10.1016/j.arthro.2006.0 5.005
27 Portney LG. Foundations of Clinical Research -Applications to Evidenced Based Practice. 4th ed. FA Davis; 2020.
28. Nicholson GP, Naylor AJ, Rao AJ, Cvetanovich GL, O’Brien MC, Charles MD. Do champagne toast and champagne pour clinical tests correlate with location and size of rotator cuff tears? Arthroscopy 2019;35(12):e26. doi:10.1016/j.arthro.2019.11.067
29. Sciascia AD, Spigelman T, Kibler WB, Uhl TL. Frequency of use of clinical shoulder examination tests by experienced shoulder surgeons. J Athl Train. 2012;47(4):457-466. doi:10.4085/1062-6050-47.4.09
Download: https://ijspt.scholasticahq.com/article/67934-survey-on-knowledge-use-and-diagnostic-applicability-ofspecial-tests-for-rotator-cuff-involvement-in-clinical-practice/attachment/ 134874.docx?auth_token=G1cQBv6LdWXj6sQy2Eu7
Takumi Fukunaga a , Connor Fedge, Timothy Tyler, Michael Mullaney, Brandon Schmitt, Karl Orishimo, Malachy McHugh, Stephen Nicholas
Keywords: elbow, forearm, emg, overhead athlete, rehabilitation https://doi.org/10.26603/001c.68073
The flexor-pronator mass of the forearm contributes dynamic stability to the medial elbow Training this muscle group is essential for overhead athletes, however, there is lack of evidence supporting use of training exercises. The purpose of this study was to measure the extent of EMG activity of the flexor pronator musculature during two distinct forearm strengthening exercises using resistance bands. It was hypothesized that two exercises would elicit at least moderate level of muscle activity, but the activation would be different in the pronator versus the flexor muscles.
10 healthy subjects (all males, age 36±12 years) were included. Surface EMG activity was measured on three muscles of the dominant-side forearm: flexor carpi ulnaris (FCP), flexor digitorum superficialis (FDS), and pronator teres (PT). After measurement of maximal voluntary contraction (MVC) for each muscle, subjects performed wrist ulnar deviation and forearm pronation exercises using elastic band resistance. Resistance was set to elicit moderate exertion (5/10 on the Borg CR10 scale). Order of exercise was randomized and three repetitions of each exercise were performed. Mean peak EMG activity in each muscle across repetitions during the eccentric phase of each exercise was calculated and expressed as a percentage of MVC. Moderate level of activity was defined as 21% of MVC or higher Peak normalized EMG activity in each muscle was compared using two-way (exercise x muscle) repeated-measures ANOVA with post-hoc pairwise comparisons if a significant interaction was found.
There was an exercise by muscle interaction effect (p<0.001). The ulnar deviation exercise selectively activated FCU (40.3%) versus FDS (19.5%, p=0.009) and PT (21.5%, p=0.022). Conversely, the pronation exercise selectively activated FDS (63.8%, p=0.002) and PT (73.0%, p=0.001) versus FDS (27.4%).

The ulnar deviation and pronation exercises using elastic band resistance studied targeted and activated the flexor-pronator mass musculature. The ulnar deviation and pronation exercises using elastic band resistance are practical and effective means of training the flexor-pronator mass. These exercises can be readily prescribed to athletes and patients as part of their arm care program.
Corresponding author:
Takumi Fukunaga, DPT, SCS, ATC, CSCS
Mailing address: Nicholas Institute of Sports Medicine and Athletic Trauma, Manhattan Eye Ear & Throat Hospital, 210 East 64th Street, 5th Floor, New York, NY 10065 USA
E-mail address: tak@nismat.org
Overhead throwing places an extreme amount of valgus stress on the medial elbow 1,2 This valgus stress is predominantly experienced during the late cocking and acceleration phases of throwing and is primarily resisted by the anterior bundle of the ulnar collateral ligament (UCL).2,3 This repetitive stress placed upon the UCL is considered a contributing factor to the increasing rate of UCL tears.4
The maximum force that the UCL is able to resist is about 54% of the valgus force experienced during pitching.2 Therefore, it has been postulated that dynamic elbow stability is provided by the flexor-pronator musculature of the medial elbow 5–11 Specifically, the flexor carpi ulnaris (FCU), flexor digitorum superficialis (FDS), and the pronator teres (PT) have been suggested as active stabilizers of the elbow during valgus stress.5,6,8,10,11 This suggestion is based on the anatomical location of the flexor-pronator mass being in close proximity to the UCL.5,10 It has also been shown that isometric contraction of the medial forearm musculature decreases humeral-ulnar joint space during a valgus stress11 and medial elbow stability decreases with fatigue of the forearm musculature,12 further suggesting their dynamic contributions to stability
The medial forearm musculature also demonstrates high electromyographic (EMG) activity during the throwing motion, specifically during the late cocking and early acceleration phases of pitching.13–16 These pitching phases have previously been demonstrated to involve the highest valgus stress on the medial elbow,2 leading researchers to suggest that the flexor-pronator mass provides dynamic stabilization of the medial elbow.13–15 Additionally, the forearm musculature is considered a key component to pitching accuracy and ball movement further establishing the importance of the flexor-pronator musculature to the throwing athlete.17,18
Based on the flexor-pronator musculature’s role during the throwing motion, strengthening these muscles have been deemed an important component of a rehabilitation program for overhead athletes and have a potential beneficial role of mitigating UCL injuries.5,6,8,16,19 To date, there is a paucity of evidence to suggest specific interventions that target the flexor-pronator forearm musculature. Elastic band resistance provides for a portable and convenient means of performing flexor-pronator muscle strengthening. However, the extent of EMG activity of the flexorpronator musculature when using elastic resistance has not been reported. Therefore, the purpose of this study was to measure the extent of EMG activity of the flexor pronator musculature during two distinct forearm strengthening exercises using resistance bands. It was hypothesized that two exercises would elicit at least moderate level of muscle activity but the activation would be different between the pronator versus the flexor muscles
Number of subjects
10 (all male)
Age 36 ± 12 years
Height
1.77 ± 0.04 m
Weight 79 ± 5 kg
Values are mean ± SD
Ten male subjects were recruited as a sample of convenience from the local community. All subjects were healthy at the time of testing, did not have a history of elbow or wrist pathology, and were confirmed to have normal, functional range of motion in their dominant wrist and forearm and were able to perform the tasks involved in this research study Eight out of the ten subjects participated in regular strength training at least three times weekly; however, none of the subjects reported doing strengthening exercises specifically targeting the forearm musculature. Four out of the ten subjects had history of participation in throwing or overhead sports. Before participation in this research study, each subject provided written informed consent in accordance with institutional review board regulations (Northwell Health IRB # 19-0586)
A 16-channel BTS FREEEMG 300 system, CMRR: >110 dB at 50–60 Hz; input impedance: >10 GΩ (BTS Bioengineering, Milan, Italy) was utilized for the EMG collection during this study
Previously described anatomical landmarks for surface EMG placement were identified for FCU, FDS, and PT muscles.20,21 The subject’s exposed skin was prepared by shaving, cleaning, and lightly abrading. Disposable Ag/AgCl passive dual surface EMG electrodes (2.0 cm interelectrode distance; Noraxon, Scottsdale, AZ) were placed on the identified landmarks on the right proximal forearm of each subject (Figure 1). Muscle activity was sampled at 1000 Hz.
Once the surface electrodes were attached to the subject, a maximum voluntary contraction (MVC) was performed, in the previously described manual muscle testing (MMT) position for each muscle.22 A single tester, a physical therapist with over 20 years of clinical experience, performed the MMT for all subjects.
Subjects then determined the level of resistance they would use for their trial by performing wrist ulnar deviation for five repetitions while holding a resistance band (Nonlatex TheraBand, Hygenic Corporation, Akron, OH). The resistance band was cut to the length of each subject’s leg length, to provide extra length for wrapping around the hand. To standardize the level of resistance across the two exercises, subjects determined which resistance level elicited exertion of 5 out of 10 on the Borg CR10 Scale.23 This process was repeated for forearm pronation. Instructions were provided to each subject to ensure that there was
no tension or slack in the resistance band at the start of the exercise, as elongation of the resistance band influences perceived resistance and associated muscle activity 24
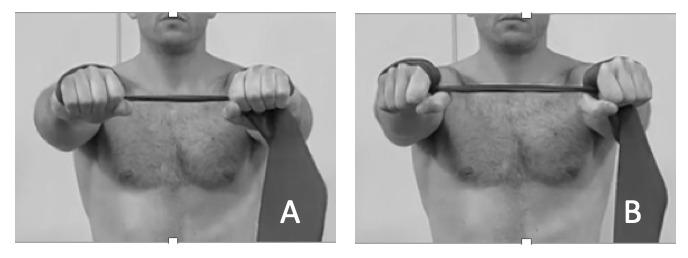
Two exercises, wrist ulnar deviation and forearm pronation were performed in random order These exercises were included in the Evidence Based Arm Care program previously published with links to exercise videos.25 Randomization was done by pulling a card out of an opaque envelope with the exercise written on the chosen card to be done first. Wrist ulnar deviation was performed by the subject holding the resistance band with elbows extended, palms facing down, and arms held at shoulder height. The resistance band was wrapped twice around the subject’s hands, with the band resting without slack or tension when arms were kept shoulder-width apart (Figure 2A). The subject then moved his wrist into ulnar deviation (Figure 2B), performing this movement for three repetitions. The subject was asked to match movement speed to a metronome set to 20 beats/min, guiding the subject to move through a 3-second concentric phase and a 3-second eccentric phase, to enable controlled movement in both phases of the exercise.
Forearm pronation was performed with the subject in seated position. The resistance band was looped twice around the hand. The subject then tensioned the resistance band reaching halfway down their lower leg and stepping on the band with their right foot. Their forearm was placed on their right thigh, in supinated position, with their right wrist crease at the edge of their patella. (Figure 3A). The subject was instructed to move through the entire available range of forearm pronation motion for three repetitions (Figure 3B). Movement speed was matched to a metronome set to 20 beats/min, leading to a 3-second concentric phase and a 3-second eccentric phase.
All EMG data were processed according to previously described methods.26 Briefly, raw EMG signals were high-pass filtered at 10 Hz, full-wave rectified and smoothed using an RMS filter with a 100-ms window. For each muscle, the peak EMG activation level was identified during each exercise. The mean activation level of each muscle from 250 milliseconds before the peak to 250 milliseconds after the
 Figure 1. EMG Electrode Placement: (A) Pronator Teres, (B) Flexor Digitorum Superficialis, (C) Flexor Carpi Ulnaris
Figure 2. Wrist ulnar deviation (A) starting position (B) end position.
Figure 1. EMG Electrode Placement: (A) Pronator Teres, (B) Flexor Digitorum Superficialis, (C) Flexor Carpi Ulnaris
Figure 2. Wrist ulnar deviation (A) starting position (B) end position.
peak was then calculated. This was then averaged over the three repetitions for each exercise and each muscle. After processing, the EMG data were normalized to the maximum EMG activities recorded during maximal voluntary contractions (MVC) and expressed as a percent. Muscle activity level was classified according to the system of DiGiovine et al. as 0% to 20% MVC low activity, 21% to 40% MVC moderate activity, 41% to 60% MVC high activity, and greater than 60% MVC very high activity.14
Descriptive statistics were calculated for mean normalized peak muscle activity for each muscle during each exercise. Effect of exercise and muscle on mean normalized peak EMG activity was compared using two-way (exercise x muscle) repeated-measures ANOVA. If an interaction effect was found, Bonferroni-adjusted post-hoc simple main effects were calculated. Significance level was set a priori at p = 0.05. All statistical analyses were performed using IBM SPSS Statistics 25 (IBM Corp, Armonk, NY).
Mean normalized muscle activity for each muscle during each exercise studied is shown in Table 2 There was an exercise by muscle interaction effect (p < 0.001). The ulnar deviation exercise selectively activated FCU (normalized peak EMG of 40.3%) versus FDS (19.5%, p = 0.009) and PT (21.5%, p = 0.022). Following the classification system of DiGiovine et al., the ulnar deviation exercise elicited moderate muscle activity in FCU, low activity in FDS, and moderate activity in PT Conversely, the pronation exercise selectively activated FDS (63.9%, p = 0.002) and PT (73.0%, p = 0.001) versus FCU (27.4%). The pronation exercise elicited very high muscle activity in FDS and PT, and moderate muscle activity in FCU.
The results of the current study demonstrate that exercises using elastic band resistance selectively targeted and elicited moderate to very high activity in the flexor-pronator musculature. The normalized peak EMG was significantly higher in the FCU compared to the FDS and PT during the ulnar deviation exercise, while the normalized peak EMG was significantly higher in the FDS and PT during the pronation exercise. Therefore, the FCU was predominantly activated during the ulnar deviation exercise, while FDS and PT were more active during the pronation exercise.

The flexor-pronator mass is an important muscle group in overhead athletes, as it provides dynamic stability to the elbow to resist valgus forces.5–11 This dynamic stabilization is critical, as pitching places high degrees of stress on the UCL,1,2 and UCL tear rates are rising.4 Additionally, the flexor-pronator muscles have high levels of activity during overhead throwing13–16 and are important toward control and velocity of pitches.17,18 Despite their role in overhead throwing, minimal evidence exists in how to effectively train these muscles and if these muscles can be targeted with strengthening exercises.
The knowledge that these exercises selectively activate the flexor-pronator muscles is important for overhead athletes, as well as strength and conditioning and rehabilitation personnel, due to the potential for increasing dynamic stability of the elbow and potentially decreasing the stress on the UCL.5,6,8,16,19 These results can influence clinical decision making as more than one exercise is required to strengthen all muscles of the flexor pronator mass and to best strengthen the dynamic stabilizers of the medial elbow
This research study had several limitations. The study sample included only healthy male participants and this limits generalizability of its findings, particularly to injured patient populations as patients with a history of UCL injury demonstrate alterations of musculature activity 19 The
Figure 3. Forearm pronation (A) starting position (B) end position.Table 2. Average muscle activity for the muscles and exercises studied.
All values are mean % MVC ± SD
* FCU significantly higher activity than FDS (p = 0.009) and PT (p = 0.022)
** FDS (p 0.002) and PT (p 0.001) significantly higher activity than FCU
cross-sectional nature of this research study precludes study of training effects of these exercises. Future studies are needed to elucidate their training effects on muscle strength, muscle activation during overhead throwing, and medial elbow stability
The findings of the current study suggest that ulnar deviation and pronation exercise using resistance bands can target and activate the flexor-pronator mass. This information is useful for clinicians and strength and conditioning specialists who work with overhead athletes, as these exercises
may be prescribed as an effective component of an arm care exercise program.
The authors declare that there is no conflict of interest.
Submitted: August 19, 2021 CST, Accepted: December 23, 2022
CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Werner SL, Fleisig GS, Dillman CJ, Andrews JR. Biomechanics of the elbow during baseball pitching. J Orthop Sports Phys Ther. 1993;17(6):274-278. doi:10.2 519/jospt.1993.17.6.274
2. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med 1995;23(2):233-239. doi:10.1177/03635465950230021 8
3. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11(5):315-319. doi:10.1177/0363546 58301100506
4. Leland DP, Conte S, Flynn N, et al. Prevalence of medial ulnar collateral ligament surgery in 6135 urrent professional baseball players: A 2018 Update. Orthop J Sports Med 2019;7(9):2325967119871442.
5. Davidson PA, Pink M, Perry J, Jobe FW Functional anatomy of the flexor pronator muscle group in relation to the medial collateral ligament of the elbow. Am J Sports Med. 1995;23(2):245-250. doi:10.1 177/036354659502300220
6. Park MC, Ahmad CS. Dynamic contributions of the flexor-pronator mass to elbow valgus stability J Bone Joint Surg Am. 2004;86(10):2268-2274. doi:10.2106/00 004623-200410000-00020
7 Lin F, Kohli N, Perlmutter S, Lim D, Nuber GW, Makhsous M. Muscle contribution to elbow joint valgus stability J Shoulder Elbow Surg 2007;16(6):795-802. doi:10.1016/j.jse.2007.03.024
8. Udall JH, Fitzpatrick MJ, McGarry MH, Leba TB, Lee TQ Effects of flexor-pronator muscle loading on valgus stability of the elbow with an intact, stretched, and resected medial ulnar collateral ligament. J Shoulder Elbow Surg 2009;18(5):773-778. doi:10.101 6/j.jse.2009.03.008
9. Gregory B, Nyland J. Medial elbow injury in young throwing athletes. Muscles Ligaments Tendons J 2013;3(2):91-100. doi:10.32098/mltj.02.2013.06
10. Otoshi K, Kikuchi S, Shishido H, Konno S. The proximal origins of the flexor–pronator muscles and their role in the dynamic stabilization of the elbow joint: an anatomical study. Surg Radiol Anat. 2014;36(3):289-294. doi:10.1007/s00276-013-1168-3
11. Tajika T, Oya N, Ichinose T, et al. Flexor pronator muscles’ contribution to elbow joint valgus stability: ultrasonographic analysis in high school pitchers with and without symptoms. JSES Int 2020;4(1):9-14. doi:10.1016/j.jses.2019.10.003
12. Millard N, DeMoss A, McIlvain G, Beckett JA, Jasko JJ, Timmons MK. Wrist flexion exercise increases the width of the medial elbow joint space during a valgus stress test. J Ultrasound Med. 2019;38(4):959-966. doi:10.1002/jum.14779
13. Sisto DJ, Jobe FW, Moynes DR, Antonelli DJ. An electromyographic analysis of the elbow in pitching. Am J Sports Med 1987;15(3):260-263. doi:10.1177/03 6354658701500314
14. Digiovine NM, Jobe FW, Pink M, Perry J. An electromyographic analysis of the upper extremity in pitching. J Shoulder Elbow Surg 1992;1(1):15-25. do i:10.1016/s1058-2746(09)80011-6
15. Hamilton CD, Glousman RE, Jobe FW, Brault J, Pink M, Perry J. Dynamic stability of the elbow: electromyographic analysis of the flexor pronator group and the extensor group in pitchers with valgus instability J Shoulder Elbow Surg 1996;5(5):347-354. doi:10.1016/s1058-2746(96)80065-6
16. Lipinski CL, Donovan L, McLoughlin TJ, Armstrong CW, Norte GE. Surface electromyography of the forearm musculature during an overhead throwing rehabilitation progression program. Phys Ther Sport 2018;33:109-116. doi:10.1016/j.ptsp.201
8.07.006
17. Hirashima M, Kadota H, Sakurai S, Kudo K, Ohtsuki T Sequential muscle activity and its functional role in the upper extremity and trunk during overarm throwing. J Sports Sci. 2002;20(4):301-310. doi:10.1080/02640410275357607
18. Keeley DW, Wicke J, Alford K, Oliver GD. Biomechanical analysis of forearm pronation and its relationship to ball movement for the two-seam and four-seam fastball pitches. J Strength Cond Res. 2010;24(9):2366-2371. doi:10.1519/jsc.0b013e3181b2 2aea
19. Glousman RE, Barron J, Jobe FW, Perry J, Pink M. An electromyographic analysis of the elbow in normal and injured pitchers with medial collateral ligament insufficiency. Am J Sports Med. 1992;20(3):311-317 doi:10.1177/03635465920200031
20. Zipp P Recommendations for the standardization of lead positions in surface electromyography. Europ J Appl Physiol 1982;50(1):41-54. doi:10.1007/bf009522
21. Remaley DT, Fincham B, McCullough B, et al. Surface electromyography of the forearm musculature during the windmill softball pitch. Orthop J Sports Med. 2015;3(1):232596711456679. do i:10.1177/2325967114566796
22. Kendall FP, Kendall McCreary E, Provance PG, Rodgers M, Romani W. Muscles: Testing and Function, with Posture and Pain Wolters Kluwer Health; 2014.
23. Andersen LL, Andersen CH, Mortensen OS, Poulsen OM, Bjørnlund IB, Zebis MK. Muscle activation and perceived loading during rehabilitation exercises: comparison of dumbbells and elastic resistance. Phys Ther. 2010;90(4):538-549. doi:10.2522/ptj.20090167
24. Mullaney MJ, Perkinson C, Kremenic I, Tyler TF, Orishimo K, Johnson C. EMG of shoulder muscles during reactive isometric elastic resistance exercises. Int J Sports Phys Ther. 2017;12(3):417-424.
25. Mullaney M, Nicholas S, Tyler T, Fukunaga T, McHugh M. Evidence based arm care: the throwers 10 revisited. Int J Sports Phys Ther 2021;16(6):1379-1386. doi:10.26603/001c.29900
26. Orishimo KF, McHugh MP Effect of an eccentrically biased hamstring strengthening home program on knee flexor strength and the lengthtension relationship. J Strength Cond Res 2015;29(3):772-778. doi:10.1519/jsc.00000000000006
Robert Manske 1 a , Katherine Podoll 2 , Alycia Markowski 3 , Maureen Watkins 3 , Lorna Hayward 3 , Murray Maitland 4 1 Physical Therapy, Wichita State University, 2 University of Washington, 3 Physical Therapy, Northeastern University, 4 Department of Rehabilitation Medicine, University of Washington
Keywords: Musculoskeletal Ultrasound, Differential Diagnosis, Diagnostic Imaging https://doi.org/10.26603/001c.68137
Ultrasound diagnostic imaging (USI) is widely utilized in sports medicine, orthopaedics, and rehabilitation. Its use in physical therapy clinical practice is increasing. This review summarizes published patient case reports describing USI in physical therapist practice.
Comprehensive literature review.
Literature Search
PubMed was searched using the keywords “physical therapy” AND “ultrasound” AND “ case report” AND “imaging” In addition, citation indexes and specific journals were searched.
Study Selection Criteria

Papers were included if the patient was attending physical therapy, USI was necessary for patient management, the full text was retrievable, and the paper was written in English. Papers were excluded if USI was only used for interventions, such as biofeedback, or if the USI was incidental to physical therapy patient/client management.
Categories of data extracted included: 1) Patient presentation; 2) Setting; 3) Clinical indications; 4) Who performed USI; 5) Anatomical region; 6) Methods of USI; 7) Additional imaging; 8) Final diagnosis; and 9) Case outcome.
Of the 172 papers reviewed for inclusion, 42 were evaluated. Most common anatomical regions scanned were the foot and lower leg (23%), thigh and knee (19%), shoulder and shoulder girdle (16%), lumbopelvic region (14%), and elbow/wrist and hand (12%).
Fifty-eight percent of the cases were deemed static, while 14% reported using dynamic imaging. The most common indication for USI was a differential diagnosis list that included serious pathologies. Case studies often had more than one indication. Thirty-three cases (77%) resulted in confirmation of a diagnosis, while 29 case reports (67%) documented significant changes in physical therapy intervention strategies due to the USI, and 25 case reports (63%) resulted in referral.
This review of cases provides details on unique ways USI can be used during physical therapy patient care, including aspects that reflect the unique professional framework.
Cooresponding Author: Robert.Manske@wichita.edu
Ultrasound diagnostic imaging (USI) is becoming more widely utilized in sport medicine, orthopaedics, and rehabilitation to extend the physical examination and avoid delays in diagnosis. Indications for USI continue to increase because of its advantages compared to other diagnostic imaging modalities. Benefits include no radiation, cost-effectiveness, portability, and it is non-invasive. Clinical providers can gain immediate imaging information for a broad spectrum of patient presentations. USI results in real-time, high-resolution visualization of anatomical structures across physiological systems. The unique properties of USI can be used to assess vasculature, lungs, joints, bones, tendons, and muscles.1–3 Additionally, ultrasound allows the clinician to interact with the patient to guide the examination of specific patient complaints.4 Musculoskeletal USI has become a valuable tool to objectively assess musculoskeletal structures, as well as functionally, during range of motion and muscle activation both statically and dynamically 5,6
Physical therapists (PTs) have a unique practice framework and scope of practice compared to other healthcare providers.7 Their practice framework emphasizes anatomy, pathoanatomy, and biomechanics of movement. Consequently, published literature on the use of musculoskeletal USI in physical therapist practice may provide unique information about the benefits of this imaging modality A survey of PTs in the United States found that of 646 respondents, 241 had recommended or referred patients for USI.8 However, the respondents reported having a more substantial knowledge base and skills for recommending or ordering radiography (x-ray) and magnetic resonance imaging (MRI) over USI. Thus, increased awareness of USI in clinical practice may improve its appropriate utilization by PTs.
Boissonnault and Ross9 examined the use of diagnostic imaging by PTs by synthesizing 78 case reports. They found that PTs recognized indications for diagnostic imaging such as worsening of symptoms without cause, inconsistent findings compared to the referral diagnosis, associated symptoms such as fatigue, and lack of progress despite treatment. Boissonnault and Ross9 reported that PTs’ referrals for diagnostic imaging resulted in subsequent diagnoses across a spectrum of categories, including fracture, cancer, visceral disease, cardiovascular, and urogenital. However, these authors did not identify the imaging modalities. At present, clinical implications for USI have not been established for the physical therapy community Linking USI case reports to the unique practice framework of PTs could improve the incorporation of USI into physical therapy clinical practice.
To our knowledge, no publications synthesize published case reports of USI in physical therapy practice. Patient case reports provide insights for PTs and other providers regarding patient presentations, red flag recognition, diagnosis, and how therapists used USI to identify and manage these various conditions. Published case reports provide documentation of clinical reasoning in complex circumstances, which can inform clinicians by providing details
regarding patient-specific examination information. Since the incorporation of USI into physical therapy practice is relatively new, case reports are a large proportion of the available evidence. These case reports are proposed to have significant educational value because they advance medical knowledge and constitute preliminary evidence for evidence-based medicine. Synthesis of case reports can also provide the foundation for other research methods.
The purpose of this review is to summarize published patient case reports that describe the use of USI in PT’s practice to diagnose and manage patient conditions.
One of the authors of this paper (MEM) conducted a computerized database search of PubMed using the keywords “physical therapy” AND “ultrasound” AND “ case report” AND “imaging”. In addition, Physical Therapy, the Journal of Orthopedic and Sports Physical Therapy (JOSPT) (standard and Case Reports versions), and the International Journal of Sports Physical Therapy (IJSPT) were searched specifically. Once a paper was identified, the PubMed citation index similar papers listings were reviewed, along with the paper’s reference list, for any additional papers matching the inclusion criteria. Literature searches were conducted from July 2021 to August 2022.
Papers were included if the patient was attending physical therapy, USI was necessary for the patient management process, the full text was retrievable, and the report was written in English. It was not required that a PT conduct the USI. Papers were excluded if USI was only used for interventions, such as biofeedback, or if the USI was incidental to PT patient/client management. For example, papers were excluded if the PT did not have an explicit role in recommending, referring, or conducting USI. Case series were included if each case met the inclusion/exclusion criteria.
The authors developed a data extraction form based on the work of Boissonnault and Ross,9 the authors’ collective knowledge of diagnostic USI, and knowledge regarding differential diagnosis and medical screening. The categories of data included: 1) Patient presentation, including primary complaint and demographics; 2) Setting; 3) Clinical reasoning that led to USI; 4) Who performed USI; 5) Anatomical region assessed; 6) Whether USI was static, dynamic, or Doppler; 7) Other imaging; 8) Final diagnosis; 9) Outcome of the case.
Clinical reasoning categories indicating the appropriate use of USI were derived from Boissonnault and Ross.9 Papers were categorized as to whether 1) the differential diagnoses included serious pathology that could not be ruled out without diagnostic imaging (hereafter described as “ serious differentials”, 2) red flag symptoms were present (“red flags”), 3) there was no clinical progress despite treatment (“no progress”), or 4) if the PT’s examination findings did not concur with the referral diagnosis (“disagreement”). Other clinical reasoning categories were generated if a case report did not fit any of these categories. A single case report may have more than one indication for USI. Clinical reasoning categories were required to be explicitly stated.
The researchers collected the anatomical regions assessed with USI to understand more common presentations and suggest necessary USI skills. When one or more regions were explicitly stated, all regions were recorded. Where the regions were not explicitly stated, USI images were used to determine the region. The reports may not have always reported all anatomical areas that were imaged. Similarly, when case reports did not specify whether tests were static or dynamic, the nature of the test was inferred by the published images.
Outcome categories were limited to patient referral, arriving at a diagnosis, or a change in physical therapy intervention strategies. The imaging case reports focused on diagnostic strategies and often did not include patient-specific clinical outcomes.
Following the acquisition of full-text case reports that met the inclusion/exclusion criteria, entire papers were reviewed independently by two researchers (RCM and KRP). Each case report’s data was hand entered into the data extraction form in Microsoft Excel. A third researcher (MEM) then reviewed all data to verify accurate data logging and resolve discrepancies. The authors met to discuss all the collected cases, compare findings, and generate summaries. The authors reached a consensus for all case-report data.
The initial search strategy resulted in 172 papers being reviewed by title and abstract for inclusion/exclusion criteria. Most of the excluded papers at this stage used USI for the medical diagnosis and the patient was referred for physical therapy Since the initial search strategy was not specific, these papers were identified but did not meet the inclusion criteria. Forty-five complete published case reports were obtained for reading and data tabulation. One paper included two cases. Following a complete review, two cases were ultimately excluded because USI was used solely for ultrasound-guided percutaneous electrical nerve stimulation. One paper was excluded because USI was used for drug delivery. One paper was excluded because the relationship of USI to physical therapy practice was indeterminable. Thus, 42 cases were assessed by the researchers.
The Journal of Orthopaedic and Sports Physical Therapy had 24 case reports. The more recent journal version, JOSPT Cases, had 8 case reports. The earliest JOSPT case report was from 1994. More recently, JOSPT had a special feature titled “Musculoskeletal Imaging,” which started in 2008 and was the primary source of case reports. JOSPT launched the Cases version in 2021 and continues the same format for imaging cases. The International Journal of Sports Physical Therapy and its predisesor, the North American Journal of Sports Physical Therapy had nine reports. Physiotherapy Theory and Practice had three cases. Physical Therapy Journal had one case report. Thirty-five cases were from within the United States, and eight were from other countries.
Patient primary complaints, anatomical regions, and final diagnoses are listed in Table 1 The average patient age was 37 years (range 15-73). Case reports included 25 males,
18 females, and the sex of one patient was not reported. Diagnostic ultrasound was performed by PTs 22 times, by another health care professional in 15 cases, and a sonographer was unidentified in six cases. Settings varied little, with most patients from outpatient orthopaedic (27) and sports (14) clinical environments. One patient was seen in a pelvic health clinic, and only one case report was from an inpatient physical therapy setting.
Anatomical regions with the largest proportion (n, %) of physical therapy USI case reports are the foot and lower leg (10, 23%), thigh and knee (8, 19%), shoulder and shoulder girdle (7,16%), lumbopelvic region (6, 14%), and elbow/ wrist/hand (5, 12%). There were very few case reports for the spine (3, 7%), head and neck (3, 7%), and hip/groin region (1, 2%). One case report focused on the lungs.
Case reports either documented a single type of USI (static, dynamic, or Doppler) or more than one type. Eighteen case reports did not specify whether the patient was static or dynamic during USI. These cases were inferred to be static tests from the published images and were added to the seven case reports that specified the patient was static, resulting in a total of 25 cases (58%). The authors assumed that dynamic and Doppler tests would be preceeded by static imaging. Six case reports reported dynamic testing (14%). Eight case reports specified that Doppler imaging was used (19%). See the listing of all case reports, presenting complaints, anatomical regions assessed, and final patient diagnosis in Table 1
Case reports often had more than one indication for USI (32, 74%). The most common reason for USI during examinations was when the differential diagnosis list included serious pathologies (26, 60%). For example, Hoglund, Silbernagel, and Taweel31 reported that moderately severe lower leg pain with full weight-bearing that originated from running includes stress fracture as a differential. Rosenthal, Hawkes, and Garbrecht45 reported that unilateral calf pain and cramping, with negative spine examination and negative compartment syndrome tests, could include popliteal artery entrapment as a differential.
Eleven cases (26%) reported specific red flags. Red flags are important to discern as it is an indication of possible serious pathology including inflammatory, neurological conditions, structural musculoskeletal damage or disorders, circuilatory problems, suspectived infections, tumors or even systemic disease processes.
No change from previous treatment was reported in twelve cases (28%). The average duration before the PT recognized a lack of progress was 3 months, with a range of 0.5 to 12 months. The most commonly reported duration before the PT initiated imaging was 2 months, indicating a high degree of suspicion early on in the treatment process. For example, Stanley and Berkoff49 reported that a patient had 8 physical therapy sessions over 1 month before the patient was referred for imaging because of failure to progress.
A disagreement occurred between initial diagnosis and final outcome in 16 cases (37%). At times this occurred when a referral for a given pathology was determined to be a different pathology In some instances this happened af-
Table 1. Included case reports, presenting complaints, anatomical regions assessed with USI, and final patient diagnoses.
Author(s)
Angelopoulou and McReynolds10
Beneck, Gard and Fodran11
Patient presenting complaint
Left lateral knee pain
Low back pain
Anatomical Region Assessed
Final diagnosis
Knee/leg Fibular collateral ligament tear
Lumbopelvic Spondylolisthesis
Boggs and Nitz12 Left lateral foot pain
Low back pain and left posterior thigh pain
Lumbopelvic Hypomobility, decreased activation of multifidus
Foot/ankle Oblique fracture of the 5th metatarsal Brenner, Gill, Buscema, and Kiesel13
Brindisino, Mourad, and Maselli14
Buchanan and Rawat15
Buchanan and Rawat16
Left subscapular and shoulder pain
Medial ankle pain
Medial elbow pain
Burzynski et al.17 Chronic perineum pain
Crane, Young, and Koppenhaver18
Davis, Brooks, and Bryceson19
DeLisa, Hensley, and Jackson20
Faltus, Boggess, and Bruzga21
Fink and Stoneman22
Fisher, Lento, and Mabry23
Flatt and Rawat24
Garbrecht, Reynolds, and Rosenthal25
Left unilateral abdominal pain
Right anterior ankle pain and swelling
Left upper extremity swelling
Right anterior thigh pain
Left knee pain
Left ankle pain
Bilateral hip pain, burning and popping in right hip
Right anterior shoulder pain
Ghaly, Boggs, and Ross26 R hand pain, some paresthesia, and diminished sensation
Hassett, Kulig, and Colletti27
Hellem, Jelsing, and Hurd28
Ho, Gross, Gaal, and Nguyen29
Ho, Ho and Colletti30
Hoglund, Silbernagel, and Taweel31
Kardouni32
Kirkham and Rawat33
Krause and Smith34
Bilateral anterior knee pain
Left medial elbow pain
Left anterior hip pain
Difficulty opening mouth; right temporomandibular pain
Right lateral leg pain
Right lateral ankle pain
Right shoulder pain
Right anterior arm pain
Shoulder/upper arm Elastofibroma
Foot/ankle Schwannoma of posterior tibialis nerve
Elbow/wrist Elbow apophysitis
Lumbopelvic USI test for bladder retention was negative
Lumbopelvic Hypoechoic band, symptomatic trigger point
Foot/ankle Pseudo-aneurysm of anterior tibial artery
Shoulder/upper arm Paget-Schroetter syndrome and primary effort thrombosis
Hip/thigh Rectus femoris muscle tear
Knee/leg
Foot/leg
Superficial femoral vein thrombosis and popliteal deep vein thrombosis, bilateral pulmonary emboli
Transsyndesmotic fibular fracture
Hip Bilateral metallosis
Shoulder/upper arm Thrombosis in middle subclavian and axillary veins
Elbow/wrist/hand Cystic mass compressing the ulnar nerve
Knee/leg Xanthomatous tendinosis
Elbow/forearm Ulnar neuritis with medial apophysitis
Hip/thigh
Temporomandibular joint
Knee/leg
Nondisplaced fracture of the anterior superior iliac spine
USI lateral capsule-condyle distance test was positive; temporomandibular hypomobility
Fibular stress fracture
Foot/ankle Oblique fracture of the distal fibula
Shoulder/shoulder girdle
Shoulder/arm
Fracture of humerus, multiple partial muscle tears
2nd-degree strain of biceps brachii
Author(s)
Leech, Bissett, Kot, and Ntoumenopoulos35
Mechelli, Preboski, and Boissonnault36
Monteleone, Gismant, Stevanato, and Tiloca37 Case 1
Monteleone, Gismant, Stevanato, and Tiloca37 Case 2
Murphy, Stockden, and Breidahl38
Neville, Meyers, and Hojnowski39
Painter, Ogle, and Teyhen40
Pape, Pape, De Martino, and Christensen41
Pujol-Marzo and Balius42
Rainey, Taysom, and Rosenthal43
Rainey, Taysom, and Rosenthal44
Rosenthal, Hawkes, and Garbrecht45
Said and Bevelaqua46
Sillevis, Shamus, and Mouttet47
Sillevis and Swanick48
Stanley and Berkoff49
Torstensen, Meen, and Stiris50
van Duijn and Felton51
Wood, Konin, and Nofsinger52
Zosel et al.53
Patient presenting complaint
Respiratory deterioration, secretion retention, and widespread crackles to lung auscultation
Low back pain
Atrophy of the right deltoid
Anatomical Region Assessed
Final diagnosis
Lung Pleural effusion
Lumbopelvic Abdominal aortic aneurysm
Shoulder/arm Quadrilateral space syndrome
“Hollow” in the right shoulder
Shoulder/arm Quadrilateral space syndrome
Acute right-sided abdominal pain
Left medial foot and ankle pain
Left buttock pain and urinary incontinence
L lower leg swelling (after skiing injury, feeling snap, on-site diagnosis of soleus tear)
Chest pain
Left posteromedial knee pain, snapping
Right shoulder pain, paraesthesia digits, swelling
Low back pain, left leg pain, paraesthesia
Left proximal posterior thigh pain
Right-sided foot pain
Headache
Left lateral calf pain
Right shoulder pain
Right medial elbow pain
Left medial elbow pain
Left-sided neck pain
ter referral from a physician, while other times it occurred following an initial diagnosis after direct access examination.
Another common reason for including USI in the diagnosis was to expand the clinical examination to include more specificity (5, 12%). This is important for PT’s for many reasons. During the examination process, the medical his-
Lumbopelvic 2nd-degree strain of the abdominal oblique muscle
Foot/ankle Advanced focal degeneration or partial tear of tibialis posterior tendon
Lumbopelvic Dysfunctional motor control of the transversus abdominis and pelvic floor muscles
Foot/leg
Shoulder/shoulder girdle
Knee/leg
Shoulder/arm
Knee/leg
Hip/thigh
Foot/ankle
Head/neck
Deep vein thrombosis in the calf
Stress fracture in the sternum
Benign mass in the posteromedial knee
Upper extremity deep venous thrombosis subclavian and axillary veins
Popliteal artery entrapment
Benign vascular malformation
Plantar fasciitis with thickening
Cervicogenic headache due to spine immobility
Knee/leg Schwannoma
Shoulder/arm
Supraspinatus muscle degeneration
Elbow/forearm Complete tear of the ulnar collateral ligament
Elbow/forearm Ulnar collateral ligament sprain
Head/neck/ Shoulder/arm Upper Extremity superficial venous thrombosis
tory may not seem to exactly line up with the physical examination. This could be something as simple as the patient has been in therapy for some time and not improving, and has recently experienced unexplained weight loss. In this instance, the PT used USI to expand the diagnsosis to other areas, or for assessing for other potential confuounding conditions.
Six cases included both pre- and post-testing USI. As a part of foundational PT treatments, demonstrating progress or regression of conditions is required for medicolegal purposes and insurance requirements. Improvement can be used to obtain approval for further continued care, while lack of progress is helpful for seeking different treatment options or referral back to physician or another health care provider
Other imaging modalities used in conjunction with USI depended on the case’s patient-specific nature. Depending on the case, USI was followed up with another imaging modality to clarify the nature of the pathology Follow-up imaging was seen in 23 patients. These follow-up tests included an x-ray, MRI, and magnetic resonance angiography In some cases, another specialist repeated USI. On the other hand, previous negative imaging tests, including MRI, radiograph, or other USI negative results, may have preceded positive USI results. In retrospect, this finding is expected because of the complex nature of appropriateness criteria54 and imaging clinical reasoning rules. One case had concurrent imaging performed. Fourteen of the cases did not require further follow-up imaging; in one case, follow-up imaging was unable to be determined.
Outcomes of case reports focused on diagnosis. Thirtythree cases (77%) resulted in a confirmed diagnosis from the USI. Because of the confirmation of a diagnosis, twentynine case reports (67%) documented significant changes in physical therapy intervention strategies due to the USI. Twenty-five case reports (63%) stated that the USI resulted in referral. Only two case reports used USI to monitor improvements in patient status over time.
The purpose of this review was to summarize published case reports that describe the use of USI in PTs practice for the diagnosis and management of patient conditions. Case reports can be used to examine how PTs utilize USI for diagnostic purposes and develop clinical skills.55 This review of case reports corroborates the previous work of Boissonnault and Ross.9 Physical therapists in orthopaedic and sports medicine environments recognized indications for imaging, resulting in improved diagnostic validity for the patient. This diagnostic validity is essential for appropriate care and reduces the potential delay of diagnosis, which causes unnecessary patient hardship. This seems critical as PTs primarily rely on their clinical suspicion when screening for serious pathology, while at the same time are uncertain about their differential diagnostic abilities.56 USI was used as an extension of the physical examination and added valuable data in justifying referrals or monitoring patient change over time. In many instances, PTs were the provider performing the USI examination or were the person referring patients to have USI conducted.
Physical therapists are uniquely positioned to optimize USI as a powerful examination and treatment tool. Ultrasound allows a clinician to view not only static but dynamic anatomical images. Of all healthcare professionals, PTs are movement experts. Due to PTs knowledge and education in
anatomy, kinesiology and biomechanics, and physical examination, they are equipped to acquire and interpret static and dynamic images and can relate these images to pathology. A physical therapist can move back and forth between physical examination, history taking, and imaging without losing sight of the primary objectives of the clinical examination. Physical therapists are trained to examine the entire kinetic chain and thus can quickly identify how a region distant to the actual site of symptoms may contribute or be the cause of dysfunction. This ability to perform a more complete assessment of a given condition, including medical screening, may flag a different or more serious differential diagnosis not even suspected by another provider. The ability of physical therapists to discern more serious pathology was seen in the present study which found that 11 cases (26%) reported red flag conditions associated with the patient presentation. For example, Mechelli et al.36 described a case in which a 38-year-old male was initially referred to therapy for chronic lower back pain. The patient also had red flag symptoms of insidious onset unrelenting, deep, boring pain that was constant, irrespective of movements of posture changes or time of day. The resulting USI demonstrated an abdominal aortic aneurysm. Garbrecht et al.25 reported that a patient had exercise-induced unilateral upper extremity arm swelling with negative cervical and shoulder musculoskeletal examinations. Doppler ultrasound discovered a thrombosis of the subclavian and axillary veins. Both of these cases demonstrate the physical therapists ability to differentiate between appropriate and inappropriate conditions ameanable for physical therapy treatment.
Disagreements between the initial diagnosis and what was ultimately determined to be the cause of pathology was not uncommon occurring in 16 (37%) of the reviewed cases. Depending on the seriousness of the condition examined with musculoskeletal-US, a disagreement that is not resolved can be a matter of life or death. For example, Flatt and Rawat,24 initially treated a patient following total hip replacement, that ended up having metallosis which is a rare build-up of debris within tissue resulting in osteolysis and loosening of a prosthetic. Additionally, despite receiving a Well’s screening score of 0, Pape et al.41 report on a patient with a medical diagnosis of partial soleus tear, who ultimately was found to have a deep vein thrombosis.
In review of these case studies another common reason for including USI in the diagnosis was to expand the clinical examination to include more specificity (5, 12%). For example, Beneck et al.11 reported the case of a 57-year-old woman. A longitudinal view of the lumbar facet joints demonstrated marked anterior displacement of the L3-4 and L4-5 facet joints, indicating possible spondylolisthesis. A grade II spondylolisthesis was confirmed by follow-up radiography In another case report, Brenner et al.13 used USI to confirm decreased multifidus activation in a person with chronic low back pain.
Six cases included both pre- and post-testing USI. For example, Ho et al30 measured temporomandibular motion during active mouth opening to identify a movement im-
pairment and followed up with additional measurements after 10 physical therapy sessions.
Prior to making a patient/client management decision, PTs utilize the diagnostic process in order to establish a diagnosis for a specific condition in need of the PTs attention. When indicated, a physical therapist can order appropriate tests, including but not limited to imaging and other studies, that are performed and interpreted by other professionals. Additionally, when a patient is referred with a previously established diagnosis, the physical therapist should determine that the clinical findings are consisten with that diagnosis. If the diagnostic process reveals findings that are outside of the scope of PTs knowledge, experience, or expertise, the physical therapist should refer the patient/ client to an appropriate practitioner In the reviewed case studies, typical of the physical examination process, case presentations often started with a patient complaint of pain in a general anatomical area. When the results of history and physical examination were inconclusive or suggestive of an alternate diagnosis, USI performed by the PTs or a referral for USI resulted in a final diagnosis that was more specific.
USI offers several unique strengths for the evaluation of soft tissues. There were cases where USI discerned information that was not gleaned from either MRI or x-ray 4 USI has a higher special resolution than MRI, which is extremely helpful when viewing superficial soft tissue structures. Studies have shown that USI performs comparably to MRI in the detection of pathologies such as full-thickness and partial-thickness rotator cuff tears, with a sensitivity and specificity of up to 95%.57–60
Physical therapy focuses on movement-related health. Physical therapists may provide a unique perspective on USI for assessing the dynamic function of soft tissues. An example includes observing muscles contract and relax. Due to improvements in hardware and software, including portable hand-held units, the clinician can quickly and efficiently compare the patient’s involved and non-involved sides while continuing to interact with the patient directly The ability to interview the patient while examining various structures helps determine the actual injury from the differentials. Reports such as these support that USI is a valuable point-of-care imaging modality tool to extend the physical examination in the physical therapy clinic.61–63
There were several case reports where the resulting diagnosis was vascular pathology 22,25,36,45 These vascular-related case reports suggest that PTs should maintain a high degree of suspicion for these differentials, and Doppler might be an appropriate imaging modality for some physical therapy patients. For example, Garbrecht et al.25 used same day Doppler USI which ruled in a occlusive throbus in the middle subclavian and axillary vein of a 23-year-old male active-duty Marine with complaing or anterior shoulder pain after multiple episodes of transient shoulder pain. In another military case, Fink and Stoneman22 report on a case of a 21-year-old healthy athletic male cadet who had leg pain following a long car ride. Ultimately he was found to have a lower extremity DVT despite displaying minimal DVT risk factors.
In the orthopaedic clinic, it is challenging to discern precise anatomical structural anomalies without imaging. For example, a review of physical examination tests of the shoulder found that the clinical performance (sensitivity and specificity) of single tests is limited.64,65 Combinations of shoulder physical tests provide better accuracy, but marginally 64 Individual pathoanatomical structures that cause shoulder pain, such as impingement syndrome, cannot be isolated by motions or external stresses. Also, shoulder physical assessment has been found to lack acceptable levels of reliability.66 Because of these limitations, when the clinical examination is ambiguous, shoulder radiography, MRI, and ultrasound are recommended depending on each modality’s indications and clinical efficiency 67
Based on this review of case studies, PTs often perform diagnostic USI during examination of the extremities. This predominance of USI for these regions may reflect a larger number of patient presentations of these areas in standard outpatient orthopedic clinics. Learning USI skills and understanding pathology may be easier when analyzing these areas. More cases are needed that describe USI use by PTs in other regions such as the spine, hand and wrist, the elbow, and the hip.
Most of the cases described in this paper were patients from an orthopaedic outpatient or sports medicine setting. Since PTs work with patients across diagnostic categories and USI images anatomical structures across physiological systems, more case studies should address other practice areas. Only one case described use in an inpatient physical therapy setting. Indeed, the total number of case reports should increase to provide additional clinical reasoning and diagnostic guidance.
A published case report may stimulate other clinicians to report similar cases, which may, in turn, prompt further investigations to more systematically evaluate a new hypothesis related to diagnosing via USI. The authors encourage standardized data reporting and detailed clinical decision-making descriptions in future imaging case reports. Although the CARE68 case report checklist covers general items, imaging case reports should provide readers with additional information on clinical reasoning. Useful information for standardized reporting of USI cases may include:
1) How the patient accessed physical therapy services (e.g., referral or direct access); 2) The clinical setting in which services were provided (including whether this was a specialty service); 3) If and when a patient was referred for ultrasound by another professional; 4) The professional designation of the person who performed the USI; 5) other diagnostic testing methods and the results; 6) The PT’s specific role in patient triaging and referral; 7) A chronological list of patient care from the onset of symptoms to the date of the examination; and 8) Specific outcomes. Table 2 is a checklist of information the authors feel would be beneficial when publishing USI case studies. The highlighted areas are those not included in the CARE68 case report checklist.
The limitations of this case report synthesis are primarily due to publication bias. Authors of case reports must be motivated and possess the time and skills to submit a
Title 1 The diagnosis or intervention of primary focus followed by the words “US” and “case report”
Key Words 2 2 to 5 key words that identify US, the diagnosis, or interventions in the case report
Abstract 3a Introduction: What is unique about this case and what did US imaging add to the case
3b Main symptoms, complaints, or important clinical findings
3c The main diagnosis, US diagnosis, reasons for use of US imaging and ultimate outcomes
3d Conclusion: What is the main “take away” lesson from this US case?
Introduction 4 1 or 2 paragraphs summarizing why this US case is unique
Patient information
5a De-identified patient specific information
5b Primary concerns and symptoms of the patient (medical history)
5c Chronological list of patient care from date of onset of symptoms to date of care
5d Medical, family, and psychosocial history including relevant genetic information
5e What was the clinical setting (Out-patient, inpatient)?
5f How did patient access PT (referral from who, direct access)? Clinical
6 Describe significant PE and important clinical findings Timeline 7 Historical and current information from this episode of care organized on a timeline
adherence and tolerability (How was it assessed?)
10d Adverse and unanticipated events
Discussion 11a A scientific discussion of the strengths AND limitations associate with this case report 11b Discussion of the relevant medical literature with references
11c The scientific rational for any conclusions (including assessment of possible causes)
11d The primary “take-away” lesson of this US case report (without references) in one paragraph
Patient Perspective 12 The patient should share their perspective in 1 to 2 paragraphs on the treatment they received
Informed Consent
13 Did the patient give informed consent? Please provide copy
PE= Physical examination; US= Ultrasound manuscript. Journals require case reports to be focused on a novel aspect of clinical practice. The actual frequency of USI for patients utilizing physical therapy and their outcomes is unknown. It is likely that the case reports vastly underrepresent the actual numbers of patients that undergo USI. Also, it is unknown whether patients present with signs and symptoms that are indicators for imaging,
but these patients are not referred. The literature search used to gather these case reports may not have captured all studies, especially because the researchers only included papers in the English language. Future research should be more systematic in observations, and methods to standardize USI in clinical practice may provide more accurate information on the impact on patient care. Lastly, future studies
are needed to determine if the clinical reasoning associated with USI in physical therapy differs from other professional environments.
Ultrasound imaging provided information for physical therapy patient care beyond a traditional physical exam, including aspects that reflect the unique professional framework.
PTs are utilizing USI for clinical reasoning associated with various patient presentations that can result in the diagnosis of muscle and ligament strains and sprains, fractures, and vascular problems.
Submitted: November 20, 2022 CST, Accepted: December 26, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Hodges PW, Pengel LH, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003;27(6):682-692. doi:10.10 02/mus.10375
2. Zheng Y, Wang L, Han X, et al. Combining contrast-enhanced ultrasound and blood cell analysis to improve diagnostic accuracy of plasma cell mastitis. Exp Biol Med (Maywood) 2021;247(2):97-105. doi:10.1177/15353702211049361
3. Zhou J, Liew D, Duffy SJ, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: a health economic analysis. Circ Cardiovasc Qual Outcomes 2021;14(5):e006789. doi:1 0.1161/circoutcomes.120.006789
4. Alves TI, Girish G, Kalume Brigido M, Jacobson JA. US of the knee: scanning techniques, pitfalls, and pathologic conditions. Radiographics 2016;36(6):1759-1775. doi:10.1148/rg.2016160019
5. Pillen S, van Alfen N. Skeletal muscle ultrasound. Neurol Res 2011;33(10):1016-1024. doi:10.1179/1743 132811y.0000000010
6. Whittaker JL, Teyhen DS, Elliott JM, et al. Rehabilitative ultrasound imaging: understanding the technology and its applications. J Orthop Sports Phys Ther. 2007;37(8):434-449. doi:10.2519/jospt.2007.235 0
7 American Physical Therapy Association. Physical Therapist’s Scope of Practice. Published September 13, 2017 Accessed February 1, 2022. https://www.apt a.org/apta-and-you/leadership-and-governance/polic ies/position-scope-of-practice
8. Rundell SD, Maitland ME, Manske RC, Beneck GJ. Survey of physical therapists’ attitudes, knowledge, and behaviors regarding diagnostic imaging. Phys Ther 2021;101(1). doi:10.1093/ptj/pzaa187
9. Boissonnault WG, Ross MD Physical therapists referring patients to physicians: a review of case reports and series. J Orthop Sports Phys Ther 2012;42(5):446-454. doi:10.2519/jospt.2012.3890
10. Angelopoulou K, McReynolds K. Use of dynamic ultrasound imaging for assessment of the fibular collateral ligament of the knee. J Orthop Sports Phys Ther. 2019;49(3):210. doi:10.2519/jospt.2019.8460
11. Beneck GJ, Gard AN, Fodran KA. Spondylolisthesis identified using ultrasound imaging. J Orthop Sports Phys Ther 2017;47(12):970. doi:10.2519/jospt.2017.7363
12. Boggs RG, Nitz AJ. Musculoskeletal ultrasonography to detect a displaced fracture of the fifth metatarsal. J Orthop Sports Phys Ther. 2018;48(11):903. doi:10.2519/jospt.2018.7884
13. Brenner AK, Gill NW, Buscema CJ, Kiesel K. Improved activation of lumbar multifidus following spinal manipulation: a case report applying rehabilitative ultrasound imaging. J Orthop Sports Phys Ther. 2007;37(10):613-619. doi:10.2519/jospt.20 07.2470
14. Brindisino F, Mourad F, Maselli F. Elastofibroma presented as shoulder pain in an amateur swimmer: screening for referral in physiotherapy A case report. Physiother Theory Pract 2021;38(12):2257-2267 doi:1 0.1080/09593985.2021.1920077
15. Buchanan V, Rawat M. Schwannoma of the posterior tibial nerve. J Orthop Sports Phys Ther 2020;50(2):111. doi:10.2519/jospt.2020.9103
16. Buchanan V, Rawat M. Elbow apophysitis in an adolescent tennis player J Orthop Sports Phys Ther Cases. 2021;1(3):159-160. doi:10.2519/josptcases.202 1.9842
17 Burzynski B, Jurys T, Burzynski K, Cempa K, Paradysz A. Physiotherapeutic assessment and management of chronic pelvic pain syndrome: A case report. Medicine 2021;100(15):e25525. doi:10.1097/m d.0000000000025525
18. Crane J, Young B, Koppenhaver SL. Imaging and quantification of an abdominal muscle trigger point using shear-wave elastography J Orthop Sports Phys Ther Cases. 2021;1(3):183-184. doi:10.2519/josptcase s.2021.10081
19. Davis M, Brooks D, Bryceson W Pseudoaneurysm: a rare complication of ankle arthroscopy. J Orthop Sports Phys Ther 2017;47(1):42. doi:10.2519/j ospt.2017.5544
20. DeLisa LC, Hensley CP, Jackson S. Diagnosis of Paget-Schroetter Syndrome/primary effort thrombosis in a recreational weight lifter Phys Ther 2017;97(1):13-19. doi:10.2522/ptj.20150692
21. Faltus J, Boggess B, Bruzga R. The use of diagnostic musculoskeletal ultrasound to document soft tissue treatment mobilization of a quadriceps femoris muscle tear: a case report. Int J Sports Phys Ther 2012;7:342-349.
22. Fink ML, Stoneman PD Deep vein thrombosis in an athletic military cadet. J Orthop Sports Phys Ther. 2006;36(9):686-697 doi:10.2519/jospt.2006.2251
23. Fisher TB, Lento P, Mabry LM. Unstable transsyndesmotic fibular fracture. J Orthop Sports Phys Ther Cases 2021;1(2):112-113. doi:10.2519/jospt cases.2021.10329
24. Flatt S, Rawat M. Metallosis after total hip arthroplasty J Orthop Sports Phys Ther Cases 2021;1(3):197-198. doi:10.2519/josptcases.2021.1033
25. Garbrecht JD, Reynolds W, Rosenthal MD Upper extremity effort thrombosis. J Orthop Sports Phys Ther. 2020;50(9):532. doi:10.2519/jospt.2020.9585
26. Ghaly B, Boggs RG, Ross M. Ulnar neuropathy at the wrist. J Orthop Sports Phys Ther Cases 2021;1(3):148-149. doi:10.2519/josptcases.2021.9793
27. Hassett EK, Kulig K, Colletti PM. Xanthomatous tendinosis. J Orthop Sports Phys Ther 2012;42(4):379. doi:10.2519/jospt.2012.0406
28. Hellem AR, Jelsing EJ, Hurd WJ. Refractory ulnar nerve symptoms in an adolescent pitcher with medial apophysitis. J Orthop Sports Phys Ther 2018;48(5):419. doi:10.2519/jospt.2018.7359
29. Ho KY, Gross R, Gaal W, Nguyen A. Incomplete fracture of the anterior superior iliac spine. J Orthop Sports Phys Ther. 2019;49(5):355. doi:10.2519/jospt.2 019.8504
30. Ho KY, Ho S, Colletti PM. Use of ultrasonography for assessing treatment efficacy in a case with ankylosis of the temporomandibular joint. J Orthop Sports Phys Ther 2016;46(3):225. doi:10.2519/jospt.2 016.0404
31. Hoglund LT, Silbernagel KG, Taweel NR. Distal fibular stress fracture in a female recreational runner: a case report with musculoskeletal ultrasound imaging findings. Int J Sports Phys Ther 2015;10(7):1050-1058.
32. Kardouni JR. Distal fibula fracture diagnosed with ultrasound imaging. J Orthop Sports Phys Ther. 2012;42(10):887 doi:10.2519/jospt.2012.0418
33. Kirkham CA, Rawat M. Isolated fracture of the greater tuberosity. J Orthop Sports Phys Ther Cases. 2022;2(1):32-33. doi:10.2519/josptcases.2022.10349
34. Krause DA, Smith J. Ultrasound assessment of an acute biceps brachii injury. J Orthop Sports Phys Ther. 2012;42(6):569. doi:10.2519/jospt.2012.0411
35. Leech M, Bissett B, Kot M, Ntoumenopoulos G. Physiotherapist-initiated lung ultrasound to improve intensive care management of a deteriorating patient and prevent intubation: a case report. Physiother Theory Pract 2015;31(5):372-376. doi:10.3109/09593 985.2014.1003629
36. Mechelli F, Preboski Z, Boissonnault WG. Differential diagnosis of a patient referred to physical therapy with low back pain: abdominal aortic aneurysm. J Orthop Sports Phys Ther. 2008;38(9):551-557 doi:10.2519/jospt.2008.2719
37 Monteleone G, Gismant M, Stevanato G, Tiloca A. Silent deltoid atrophy in beach volleyball players: a report of two cases and literature review. Int J Sports Phys Ther 2015;10:347-353.
38. Murphy M, Stockden M, Breidahl B. Acute tearing of the oblique abdominal wall insertion onto the iliac crest in an Australian football player: a case report. Int J Sports Phys Ther 2016;11:1125-1134.
39. Neville C, Meyers K, Hojnowski L. Ultrasound assessment of the tibialis posterior tendon. J Orthop Sports Phys Ther 2010;40(10):667 doi:10.2519/jospt.2 010.0417
40. Painter EE, Ogle MD, Teyhen DS. Lumbopelvic dysfunction and stress urinary incontinence: a case report applying rehabilitative ultrasound imaging. J Orthop Sports Phys Ther 2007;37(8):499-504. doi:10.2 519/jospt.2007.2538
41. Pape MH, Pape SH, De Martino E, Christensen SWM. Deep vein thrombosis in a young, physically active man. J Orthop Sports Phys Ther Cases 2021;1(3):166-167. doi:10.2519/josptcases.2021.1018 0
42. Pujol-Marzo M, Balius R. Stress fracture of the sternum. J Orthop Sports Phys Ther Cases. 2021;1(4):240-241. doi:10.2519/josptcases.2021.1032 3
43. Rainey CE, Taysom DA, Rosenthal MD Snapping pes anserine syndrome. J Orthop Sports Phys Ther. 2014;44(1):41. doi:10.2519/jospt.2014.0402
44. Rainey CE, Taysom DA, Rosenthal MD Upper extremity deep venous thrombosis. J Orthop Sports Phys Ther 2014;44(4):313. doi:10.2519/jospt.2014.04 05
45. Rosenthal MD, Hawkes N, Garbrecht JD. Popliteal artery entrapment syndrome. J Orthop Sports Phys Ther 2020;50(9):531. doi:10.2519/jospt.2020.9568
46. Said R, Bevelaqua AC. Benign vascular malformation at the ischial tuberosity. J Orthop Sports Phys Ther 2016;46(7):607 doi:10.2519/jospt.20
16.0410
47. Sillevis R, Shamus E, Mouttet B. The management of plantar fasciitis with a musculoskeletal ultrasound imaging guided approach for instrument assisted soft tissue mobilization in a runner: a case report. Intl J Sports Phys Ther 2020;15(2):274-286. doi:10.26603/ij spt20200274
48. Sillevis R, Swanick K. Musculoskeletal ultrasound imaging and clinical reasoning in the management of a patient with cervicogenic headache: a case report. Physiother Theory Pract. 2019;37(11):1252-1262. doi:1 0.1080/09593985.2019.1686793
49. Stanley LE, Berkoff DJ. Benign peripheral nerve sheath tumor in a distance runner. J Orthop Sports Phys Ther 2017;47(2):125. doi:10.2519/jospt.2017.678
50. Torstensen TA, Meen HD, Stiris M. The effect of medical exercise therapy on a patient with chronic supraspinatus tendinitis. Diagnostic ultrasound-tissue regeneration: a case study. J Orthop Sports Phys Ther 1994;20(6):319-327 doi:10.2519/jospt.1994.2
0.6.319
51. van Duijn AJ, Felton SD. Ultrasound imaging of ulnar collateral ligament injury J Orthop Sports Phys Ther 2016;46(12):1086. doi:10.2519/jospt.2016.0420
52. Wood N, Konin JG, Nofsinger C. Diagnosis of an ulnar collateral ligament tear using musculoskeletal ultrasound in a collegiate baseball pitcher: a case report. N Am J Sports Phys Ther. 2010;5:227-233.
53. Zosel KL, Dummar MK, Adams BG, Henderson NC, Westrick RB. Upper extremity superficial vein thromboses presenting as acute neck pain in a young and healthy male: a case report. Int J Sports Phys Ther 2021;16(3):854-861. doi:10.26603/001c.23429
54. American College Of Radiology ACR Appropriateness Criteria. American College of Radiology Accessed February 1, 2022. https://www.ac r.org/Clinical-Resources/ACR-Appropriateness-Criter ia
55. Sayre JW, Toklu HZ, Ye F, Mazza J, Yale S. Case reports, case series - from clinical practice to evidence-based medicine in graduate medical education. Cureus 2017;9(8):e1546. doi:10.7759/cure us.1546
56. Budtz CR, Rønn-Smidt H, Thomsen JNL, Hansen RP, Christiansen DH. Primary care physical therapists’ experiences when screening for serious pathologies among their patients: a qualitative study. Phys Ther 2022;102(5). doi:10.1093/ptj/pzac026
57 Al-Shawi A, Badge R, Bunker T The detection of full thickness rotator cuff tears using ultrasound. J Bone Joint Surg Br. 2008;90(7):889-892. doi:10.1302/0 301-620x.90b7.20481
58. Iannotti JP, Ciccone J, Buss DD, et al. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am 2005;87(6):1305-1311. doi:10.2106/jbjs.d.02100
59. Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am 2004;86(4):708-716. doi:1 0.2106/00004623-200404000-00007
60. van Holsbeeck MT, Kolowich PA, Eyler WR, et al. US depiction of partial-thickness tear of the rotator cuff. Radiology. 1995;197(2):443-446. doi:10.1148/rad iology.197.2.7480690
61. Ahmadi O, Motififard M, Heydari F, Golshani K, Azimi Meibody A, Hatami S. Role of point-of-care ultrasonography (POCUS) in the diagnosing of acute medial meniscus injury of knee joint. Ultrasound J 2022;14(1):7. doi:10.1186/s13089-021-00256-0
62. Franks N, Gress J, Joseph R. Point-of-care ultrasound for suspected pectoralis major rupture: a case report. Clin Pract and Cases Emerg Med. 2021;5(1):93-96. doi:10.5811/cpcem.2020.10.50802
63. Richman M, Kieffer A, Moss R, Dexeus D Patella fracture identified using point-of-care ultrasound. Prague Med Rep 2021;122(4):308-312. doi:10.14712/2 3362936.2021.29
64. Hegedus EJ, Goode AP, Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med 2012;46(14):964-978. doi:10.11 36/bjsports-2012-091066
65. Gismervik S, Drogset JO, Granviken F, Rø M, Leivseth G. Physical examination tests of the shoulder: a systematic review and meta-analysis of diagnostic test performance. BMC Musculoskelet Disord 2017;18(1):41. doi:10.1186/s12891-017-140
0-0
66. May S, Chance-Larsen K, Littlewood C, Lomas D, Saad M. Reliability of physical examination tests used in the assessment of patients with shoulder problems: a systematic review. Physiotherapy. 2010;96(3):179-190. doi:10.1016/j.physio.2009.12.002
67 Pierce J, Anderson M. Update on diagnostic imaging of the rotator cuff. Clin Sports Med. 2023;42(1):25-52. doi:10.1016/j.csm.2022.08.009
68. CARE Case Report Guidelines. What are the CARE guidelines? https://www.care-statement.org
Alexandra Diggles a
Keywords: cesarean section, female athlete, pelvic floor dysfunction, post-partum, return to sport
https://doi.org/10.26603/001c.65894
Increasing numbers of elite female athletes are competing in professional sport, and many wish to become pregnant and return to competitive sport after childbirth. Athletes have a higher risk of pelvic floor dysfunction (PFD) than non-athletes (54% versus 7%) and there is also an increased prevalence in post-partum women compared to nulliparous women (35% versus 2.8-7.9%). Additionally, PFD has been shown to influence athletic performance. High quality evidence for elite athletes is lacking, and there are no exercise guidelines specifically for these women to prepare or effectively guide their safe return to sport (RTS). The purpose of this case report is to detail the management of an elite athlete who presented following cesarean section (CS) with the goal of RTS within 16 weeks.
A 27-year-old primiparous Caucasian professional netballer presented at four weeks postcaesarean section (CS) for RTS screening and assessment of pelvic floor muscle (PFM) function. Assessment included readiness and fear of movement screening, dynamic pelvic floor muscle function, structural integrity of the CS wound, levator hiatal dimensions, bladder neck descent, and early global neuromuscular screening. Measures were collected at four weeks, eight weeks, and six months post-partum. The post-partum athlete demonstrated alterations in pelvic floor muscle function, reduced lower limb power and psychological readiness. A functionally staged dynamic and sport specific pelvic floor muscle training program was implemented and adapted to the patient for her early post-partum timeline.
Rehabilitation strategies were effective in achieving the primary outcome of RTS at 16 weeks post-partum with no adverse events reported at 6 months follow-up.
This case highlights the need for a holistic and individualised RTS management approach that includes women’s and pelvic health risk factors in a professional athlete.
Level of Evidence 5
Female participation in elite sport has increased significantly in the last 10 years.1,2 Athletes returning to sport
Corresponding author:

Alexandra Diggles. BPhty (Hons.), MPHealth Pelviology Physiotherapy.
Address: Brisbane 4169, Australia.
Email: info@alexandradiggles.com
post-partum is also more common. Limited evidencedbased protocols, established time frames or injury risk data exist to guide the post-partum athlete’s return to sport (RTS).2,3 Athletes have a higher risk of pelvic floor dysfunc-
tion (PFD) than non-athletes (54% versus 7%)4–6 and there is also an increased prevalence in post-partum women compared to nulliparous women (35% versus 2.8-7.9%).5,7,8 It is suspected that there is an increased risk of PFD for postpartum athletes and therefore there is a need to identify best-practice for RTS in this population.
There are mixed reports of the optimal timeline for returning to sport post-partum. A recent editorial advocates for a multidisciplinary, biopsychosocial injury rehabilitation model for postpartum return to high impact activities yet such a model has not been investigated.9 Evidence suggests that 71% of athletes return to training within six weeks post-partum.10 Similarly, survey data indicates that 40% of post-partum recreational runners return to running at four weeks11 and 78% at 12 weeks.12 Contrary to this, guidelines based on expert opinion for return to running identify potential risk factors in returning to running in the first three months post-partum.8 The prevalence of urinary incontinence (UI) or vaginal heaviness was reported by more than 30% and musculoskeletal pain by 84% in early post-partum runners.12 Urinary incontinence increases the risk of having musculoskeletal pain with running (RR 1.97 95% CI (1.37, 2.84)12 and negatively influences performance and participation.13 Additionally, authors have shown reduced abdominal wall strength post-partum irrespective of delivery mode which may contribute to poor trunk control, PFD and suboptimal RTS.14 Given the high rates of PFD and pain in post-partum women returning to exercise and the influence on performance, there is a clear need to evaluate PFD within a global neuromuscular assessment prior to RTS.
The purpose of this case report is to detail the management of an elite athlete who presented following cesarean section (CS) with the goal of RTS within 16 weeks. It draws on the current sports literature of physical and psychosocial factors that influence successful RTS15,16 and factors specific to post-partum RTS, referred to herein as the “mother load”.17
GT, a 27-year-old primiparous caucasian professional netballer presented at four weeks post-CS for RTS screening and assessment of pelvic floor muscle (PFM) function. Her healthcare team included a sports physiotherapist, performance manager, coach, dietician, psychologist, obstetrician, sports physician, and pelvic health physiotherapist (author). GT consented to this case being published.
GT had been playing elite netball for 10-years and had no time off training or playing due to injury. Prior to childbirth, she had no prior urinary or anal incontinence, obstructive emptying or sexual health concerns during sport or daily life.
GT reported coping well throughout pregnancy and in the acute post-partum phase. Her weight gain during pregnancy was within normal range (11.5-16Kg) based on her
pre-pregnancy body mass index.18 She experienced minimal medical, musculoskeletal, or pelvic health issues during pregnancy and continued to train non-contested with the netball team until 30 weeks gestation, remaining physically active until birth in line with current guidelines.19,20 She did not complete pelvic floor muscle training during pregnancy There was no other relevant medical history
GT underwent an elective low segment CS with standard wound closure due to breech presentation.17,21 There were no peri-operative or post-operative complications for mother or infant. Lochia stopped at three weeks post-partum. Breastfeeding was established on day four with no latching concerns, nipple, or breast discomfort. GT and infant were discharged on day five, a standard length of stay in an Australian private hospital. GT reported having a small pre-pregnancy breast size and an insignificant size increase.22 GT reported being well supported personally and by her team and team support staff. She reported her post-partum weight at her four-week initial review was 5Kg greater than pre-pregnancy.
At four weeks post-CS, she was walking 30 minutes daily at a casual pace and performing two sessions per week of three sets of light intensity unweighted squats and lunges (rate of perceived exertion 2-3/10).20 There was no itching, discolouration, or discomfort around the scar 21 She did not report any symptoms, nor bother related to her pelvic floor function.23 She had not returned to sexual activity. She reported general fatigue and an average of six to eight hours accumulated sleep per night. When asked, GT identified some concerns with RTS: “birth can cause pelvic floor muscle injury and prolapse and that it can get worse if you do the wrong thing”
• Play in round one of the national competition at 16 weeks post-partum
• Assess her individual PFD risk
• Commence pre-season training at 12 weeks post-partum
• Continue to exclusively breastfeed for the first six months post-partum
GT’s history suggested a low predictive risk of PFD16,24 confirmed by the validated Australian pelvic floor questionnaire (APFQ) (Appendix A).23 Psychosocial screening evaluated factors known to influence RTS and post-partum wellbeing including post-partum depression and anxiety, sleep quality, readiness to return to sport, and fear of movement scales (Table 1).9,15,17
Early post-partum physical performance tests were compared to pre-partum data (Appendix B) provided by GT’s sports physiotherapist, and which were relevant to early intervention (Table 2). Evidenced-informed screening for high level neuromuscular performance in netball8,15,29,30 was planned to be completed by the sports physiotherapist at eight weeks post-partum. A summary of key examination findings is found in Tables 1 and 2
Table 1. Outcome measures and examination findings at 4 weeks, 8 weeks and 6-month follow-up
higher the EPDS score, the higher the likelihood of a depressive illness of varying severity
the severity of emotional symptoms from within normal limits (low score) to extremely severe (highest score)
APFQ23 (domain score _/10)
The additive score for each domain is the divided by the number of questions to give an evenly weighted score for each domain. Higher scores relate to worse function.
Patient reported co-ordination with IAP (DL jump) to volitional failure to control
EPDS Edinburgh post-partum depression scale | DASS-21 Depression anxiety stress scale | APFQ Australian Pelvic Floor Questionnaire | POP Pelvic organ prolapse | IAP Intra-abdominal pressure | ^ using International continence society grading of Pelvic floor muscle (PFM) strength and tone | MVC maximal voluntary contraction | GH genital hiatus is measured from the posterior fourchette to the middle of the urethral meatus and PB perineal body is measured from the posterior fourchette to the middle of the anus. | IRD inter-rectus distance with a normal value of <25mm | POSAS 2.0 The patient and observer scar assessment scale version 2.0 The lowest score is ‘1’ for each category which corresponds to the situation of normal skin. Score 10 equals the largest difference from normal skin (i.e. the worst imaginable scar or sensation). | SL single leg |DL double leg | NA not assessed as achieved normative range |WNL within normal limits |* significant reduction compared to pre-partum
GT did not meet diagnostic criteria for PFD such as urological or anorectal disorders, prolapse or pain syndromes31 or diastasis rectus abdominis (DRA).14,27 Given that the definition of PFM dysfunction requires patient concern and alteration in normal pelvic floor muscle function,31 GT’s examination identified sub-clinical alterations in PFM:
• Neuromotor deficits
◦ delayed recruitment (voluntary and functional)
◦ delayed relaxation
• Reduced endurance with sustained and rapid contractions
• Reduced power during a rise in intra-abdominal pressure (IAP)
Musculoskeletal screening identified reduced rectus abdominis strength (as per previously published testing guidelines),14,28 reduced lower limb strength compared to her pre-partum data (Appendix B) and reduced stationary balance testing of < 30seconds.
Biopsychosocial screening identified changes commensurate to four weeks postpartum9,17 including:
• Moderate fear of movement
• Belief that all women are at risk of PFD post-partum impacting her ability to RTS.
Stage one of GT’s pelvic health physiotherapy management started in the immediate post-partum phase2 as part of a collaborative and criteria based RTS model (Figure 1).8,15,29,30,32 During this stage, the pelvic health physiotherapist directed case management.
Management was informed by time-based wound healing principles17,21 and criterion-based assessments such as asymptomatic response to exercise testing.15,20,30,32 Dur-
ing all stages, the patient was asked to keep a diary to record training, breastfeeding, sleep, and symptoms. Exploratory interviews with post-partum athletes suggest that social support, childcare, and training specificity are all enablers of successful return.9,17 The shared-decision and development of GT’s netball-specific exercise program considered child minding, caring needs, lactation, and GT’s availability while targeting optimal training dosage.29,32
)
The focus of pelvic health physiotherapy intervention in Stage 1 was:
• multidisciplinary engagement
• education to reduce fear of movement and address PFD beliefs
• sleep optimization
• wound healing
• PFM rehabilitation
Obstetrician clearance to return to a graded training schedule was given at six weeks post-partum. Nutritional and psychology reviews were initiated given their link to UI2,16,17 and RTS readiness, performance, and sleep.11,15,17 DEXA scans were undertaken as per the team’s medical protocol for all athletes. For GT, this enabled monitoring of unattenuated axial bone loss associated with lactation and the consequent increased risk of bone stress injury 10,17
Individualized education sessions provided clear, simple and evidence-informed knowledge that a CS is unlikely to result in pelvic floor muscle injury.12,24 This was facilitated by a lecture-style and teach-back approach that outlined the neuromuscular changes that occur in pregnancy and compare and contrasting modes of delivery During the teach-back discussion and when asked GT reported reduced fear of PFM injury with RTS. Other major themes of generalized education were sleep optimization,8,17 feeding pos-
tures, bra considerations,9,17,22 and timing of physical activity around expressing.2,17
Relative contraindications to early post-partum exercise were increasing longitudinal wound tension and wound pain (> 4/10).11,21 In the immediate post-partum phase, there is minimal scar integrity (< 30% tensile strength).21 Scar dressing with silicone tape and daily massage to reduce hypertrophic scarring21 were taught and patient selfefficacy confirmed. Abdominal wall compression wear during activity was recommended8,21,33 given it may be more effective than core-based exercise in the immediate postpartum phase for pain intensity and perceived function.33 Abdominal wall exercises were not specifically given, and wound pain was used to guide her response to general exercise. To minimize longitudinal scar tension, verbal and visual instructions were given to avoid trunk rotation and limit cross-body exercises.
There is insufficient evidence in pelvic floor rehabilitation guidelines regarding pain rating and training load early post-partum.8,11 In early post-partum studies, women reported no pain from commencing PFM exercises immediately post-birth, therefore early PFM training was commenced.34
GT’s PFM training program (Table 3) was developed in line with exercise prescription15,29,32 and PFM training guidelines8,20,26,30,35,36 to target GT’s impairments and train specifically for the characteristics of netball.15,29,37 Netball requires endurance and repeated explosive effort (power). Athletes involved in impact sports have been shown to have, and require above, normal PFM strength38 to withstand the increased IAP that occurs with running and jumping.2,4,6,12,36,38 The aim of this PFM training program was to achieve hypertrophy,26,35 speed of muscle recruitment during explosive tasks36 and endurance.2,26,35 Verbal feedback, digital palpation and patient verbal con-
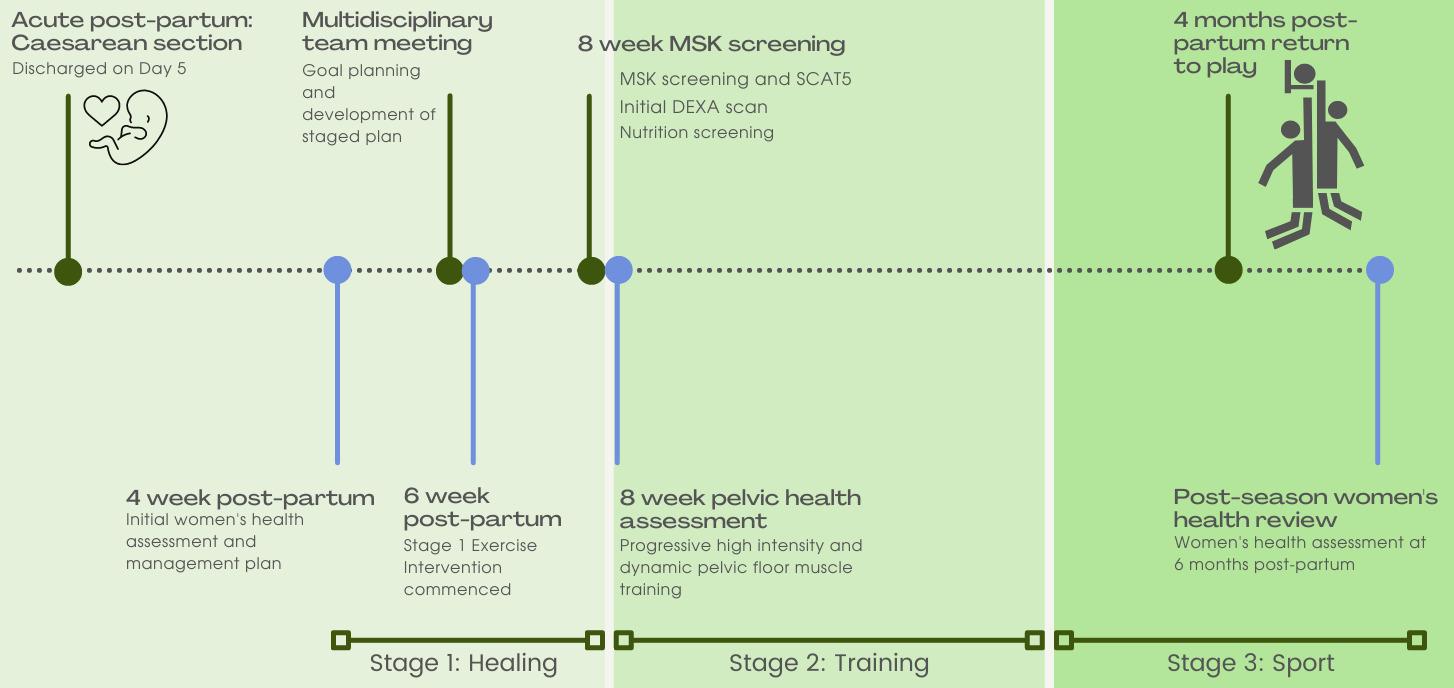
firmation of awareness were used in all prescribed postures to facilitate a correct technique.35,36 Early training (week 4) focused on repeated daily exposure to achieve neural adaptation with normalisation of motor recruitment and relaxation. Initial intra-vaginal pressure biofeedback (Peritron®, discontinued, Cardio-Design, Victoria) was conducted to guide correct sub-maximal voluntary contraction and relaxation at her first session. Progressive daily PFM training has been shown to be effective in addressing PFM dysfunction26,35 with greater benefit from a combined strength and neuromotor program (Table 2, week 6).39 GT was shown how to self-progress her repetitions and postural load if the quality of PFM contraction was maintained. Progressive overload was achieved by increasing repetitions or increasing load by modifying task to challenge IAP demands.30,32,40 Recommendations were given to perform the strength-based exercise earlier in the day and the endurance-based exercise later in the day to allow for sufficient recovery 15 However, a shared-decision making approach was taken to optimise the likely times of exercise completion around breastfeeding and other childcare needs. Other strategies included metronome pacing and an activity diary to facilitate adherence.39
At her week eight assessment, GT had reduced abdominal strength compared to pre-partum. With wound and abdominal fascial strength continuing to increase to 80% at 12 weeks,2,8,17,21 graded abdominal strengthening and trunk rotation activities were permitted, with continued scar taping21 and symptom monitoring. Insufficient evidence currently exists for best-practice abdominal wall strengthening post-partum.14,41 All women post-partum, with and without a diagnosis of DRA, have reduced abdominal wall
Figure 1. Patient management timeline. Blue time points represent individual evaluation with the pelvic health physiotherapist. Green time points represent key rehabilitation milestones.strength compared to nulliparous controls, however the importance of this remains unknown.14,41,42 Expert opinion supports a focus on integrated abdominal wall control compared to isolated muscle strength variables.43 In consideration of an integrated approach to rehabilitation, initial abdominal wall exercise was prescribed as isometric lower abdominal wall activation in supine and quadruped postures as outlined in Berg-Poppe et al41 and progression principles were applied as outlined by Christopher et al.30 Given the lack of specificity identified in the literature for post-partum abdominal wall rehabilitation,41,42 exercises were progressed when able to achieve five sets of 10, with 15-second recovery periods as based on abdominal wall training guidelines for sporting injuries.32 Quadruped exercise was progressed to add in upper limb movement once perceived as easy by GT and confirmed by the physiotherapist that there was minimal trunk deviation, no compensation, doming or breath-holding during the task. Static exercise such as plank and side plank were progressed from knee based to full versions using the same criteria of observed quality and once achieving one minute endurance, five repetitions. The abdominal wall program was completed three non-consecutive days per week.
The PFM training program was progressed to focus on power training and netball-specific dynamic exercises to induce pre-active and supra-maximal PFM contraction (Table 3).35–37 This included PFM pre-activation with a cough, a five-meter chest pass at rapid speed, lunge to knee drive, and progression from double to single leg jumping to volitional failure.36 Throwing distance, weight, IAP demand and hop distance were progressed based on symptom monitoring and perceived levels of exertion.29,30,32,40
Having attained normal PFM function and being asymptomatic during Stage 1 functional testing, GT commenced a return to run program at 10 weeks post-partum.29
Ongoing PFM training was integrated into GT’s conditioning sessions to maintain function following the 12-week training program. Her program included PFM control during multi-directional stepping/hopping to volitional failure and PFM endurance.36 GT was prescribed PFM training three times per week to align with exercise prescription guidelines for rest and recovery given her high intensity training load at this stage.9,15,32,37 Abdominal wall exercise included cross-body control with load and progressive balance demands, and ongoing plank and quadruped exercise. Scar taping was ceased. Throwing and catching drills with reaching outside base of support provided ongoing challenge for abdominal function.
The primary outcome was successful return to full match play at 16 weeks post-partum. Reassessment at six months post-partum identified improved PFM function. There was no injury reported during the season. GT continued successfully breastfeeding. As little is known about early postpartum recovery and the influence of high-impact activ-
ity,2,8,17,44 a six-month review identified no de novo PFD A critical component of GT’s successful RTS was communication between all stakeholders and consideration of all biopsychosocial factors.9,17 GT provided her perspective on RTS: "It has really helped having Netball (state) and the state team, they’ve been amazing." Her satisfaction with intervention: "It was really well planned out for me; it was very doable"
Current post-partum guidelines do not provide clear criteria to evaluate a post-partum athlete prior to RTS, however several criteria have been suggested when returning to sport following injury: pain/symptom free clinical evaluation, minimal range of motion/strength deficits, sport specific functional field testing, and no apprehension during full effort.10,15,29 These criteria can be applied in pelvic health to evaluate a holistic post-partum RTS management plan.
Clinical evaluation for post-partum RTS should include screening for PFD risk factors. Pre-existing PFD risk factors include: pre-pregnancy symptoms, prior vigorous exercise, depression and recurrent urinary tract infection (rUTI).7,24,25 Most significantly, pre-pregnancy symptoms (and severity) are associated with a 15-17 times increased risk of persistent UI or urgency24 and these are the most prevalent symptoms in athletes.6,24 In a multivariate analysis, vigorous exercise (> 4 times per week), depression and rUTI were all associated with a 40-200% increased risk of post-partum PFD.16 While exercise status correlates with greater risk of developing symptoms, recent studies identify a two- to three-fold increased chance of earlier return to running with higher weekly running volumes and running during pregnancy 11,12,44 Therefore, both volume of exercise and the presence of PFD need to be evaluated. The author suggests that ante-natal screening for PFD, knowledge of an athlete’s exercise habits, and the use of a validated PFD screening questionnaire23 may identify risk factors as well as identify athletes antenatally that would benefit from assessment and intervention. In GT’s case, an asymptomatic history was an enabling factor for RTS.
Fascial support and pelvic floor resting position have a direct influence on urethral closing pressure and the development of PFD.26,38 Tissue distensibility increases during pregnancy irrespective of delivery mode.45 Many studies identify increased rates of UI, POP and anal incontinence (AI) with longitudinal studies reporting birthing mode as an independent risk factor 24 While CS has been shown to be protective for the incidence of urinary symptoms and prolapse (POP),7 pregnancy may change the risk profile during the immediate post-partum phase for an asymptomatic athlete, sub-optimal function should also be addressed to achieve RTS. In relation to CS birth, there is no significant difference of pelvic floor morphology and bladder neck mobility during pregnancy and post-birth with a return to prepregnancy values observed.45 Women experiencing vaginal heaviness were 50% less likely to return to running and this correlated with pre-pregnancy urinary symptoms,
rUTI and vigorous exercise.11,12,24 Wound healing,21 selfselected timing of RTS,17 higher levels of fatigue,17 nutritional demands17 and post-operative pain2,12,17 may be a reason for a CS not being an enabling factor for return to running11 despite being a lower PFD risk.16,24 An additional factor can be the influence on abdominopelvic control. Current research suggests that abdominal wall strength and control remains reduced at 26 weeks post-partum irrespective of activity levels or type of birth.14 Unfortunately, the mixed quality and heterogeneity of the re-
search has provided low certainty as to the type and benefit on improving function of the abdominal wall with post-partum rehabilitation.14,33,41,42
Athletes have been shown to have UI despite strong PFM, whereas increased bladder neck descent (BND) was a risk factor for UI.4,25,26,38 Similarly, excessive lengthening of the urogenital hiatus over time is an independent risk factor for UI and POP and may be related to altered perineal muscle function, repetitive high IAP as well as vaginal birth.7,25,45 Early return to heavy work post-partum has
been associated with a three-times increased risk of POP symptoms.44 However, women who return to high-impact exercise early post-partum have no difference in PFM strength, reported UI or POP symptoms compared to nonexercisers at six weeks or 12 months.44 Interestingly, intensity and long training hours of athletes correlate with the onset of PFD16 suggesting chronic overload may be a risk factor versus exercise itself This may place an athlete with a full-time training load at greater risk of developing PFD on RTS. This case study evaluated urogenital hiatus and bladder neck descent using 2D transperineal ultrasound at rest and under load, performed longitudinally to monitor structural change.25,26 A consideration for future studies would be pre- and post-training assessments of tissue distensibility and whether this correlates to the development of symptoms and influences RTS. On reflection regarding this case, earlier engagement of a pelvic health physiotherapist prior to pregnancy would have allowed better planning in the post-partum phase.9 In future practice, the acute post-partum phase (up to six weeks) would be advocated as a time for tissue restoration and building psychosocial resilience. Further multidisciplinary planning would be beneficial to include technical skills/drills in early stages of rehabilitation in a low intensity and controlled environments.
Optimizing neuromuscular pelvic floor function can improve urethral closing pressures and the levator plate position.26,31,35,39 PFM strength, timing, and coordination are highly correlated with UI,26,35,36 and vital to support IAP loads during running and landing in netball.2,4,16,26,40 Impaired reaction times are associated with a three-fold risk of UI.36 There is grade 1 evidence for PFM training in the general population,35 and sport and training specificity should be considered when prescribing PFM training.4,15,46 The authors acknowledge the limitation of the sport specific training protocols provided in this case and support future work to provide multi-disciplinary RTS protocols. The author suggests promotion and engagement with stakeholders and sporting decision-makers to create greater opportunities for primary pelvic health screening in female athletes.
The lack of PFM functional measures that offer predictive validity of pelvic health risk and RTS was a clinical challenge in this case and the research is underdeveloped compared to other rehabilitation protocols.4,15,30 While not validated, the author considered symptom responses during jumping to identify any issues prior to the introduction
of sport-specific training. There is currently limited evidence for the prevention of PFD with PFM training. Specific ante-natal PFM training has been shown to reduce the risk of developing UI by 62%,47 however, research in general sporting populations would suggest targeted training does not prevent injury.15,29,32 Further research into the prognostic value of PFM functional field testing may assist safe RTS.
A postpartum athlete experiences the “mother load” of perinatal musculoskeletal and physiological changes as well as experiencing the demands of early high intensity training. Current evidence suggests PFD has a significant influence on returning to exercise and that athletes are at greater risk of PFD The RTS timeline in GT’s case is limited to an asymptomatic woman following CS returning to netball. This case study proposes a battery of tests to detect PFD and integrates pelvic health into a RTS program. Multidisciplinary planning should begin during early pregnancy and include a pelvic health physiotherapist. A range of factors should be considered, PFD, delivery, wound healing, sleep, breastfeeding, and breast changes. Future areas of research include developing post-partum RTS protocols, diagnosis, prevention, and management of PFD in athletes and the longitudinal effects of PFD and RTS.
The author does not have any financial or personal relationship with people or organizations that may inappropriately bias the work.
The author wishes to thank Dr Kerrie Evans PhD, MHealthSc(ManipPhty), BAppSc(Phty), FACP, GAICD and Dr Margaret Sherburn PhD, MWmnsHlth, BAppSci (Phty).
The author of this paper has nothing to disclose.
Submitted: March 20, 2022 CST, Accepted: October 10, 2022 CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Girl Power: Measuring the Rise of Women’s Sport in Australia. Nielsen.com. Published March 6, 2019. h ttps://www.nielsen.com/au/en/insights/article/2019/g irl-power-measuring-the-rise-of-women-s-sport-in-a ustralia/
2. Bø K, Artal R, Barakat R, et al. Exercise and pregnancy in recreational and elite athletes: 2016/17 evidence summary from the IOC Expert Group Meeting, Lausanne. Part 3—exercise in the postpartum period. Br J Sports Med 2017;51(21):1516-1525. doi:10.1136/bjsports-2017-09 7964
3. Schilaty ND, Bates NA, Hewett TE. Relative dearth of ‘ sex differences’ research in sports medicine. J Sci Med Sport. 2018;21(5):440-441. doi:10.1016/j.jsams.2 017.10.028
4. Pires T, Pires P, Moreira H, Viana R. Prevalence of Urinary Incontinence in High-Impact Sport Athletes: A systematic review and meta-analysis. J Hum Kinet 2020;73(1):279-288. doi:10.2478/hukin-2020-0008
5. Bø K, Sundgot-Borgen J. Are former female elite athletes more likely to experience urinary incontinence later in life than non-athletes? Scand J Med Sci Sports. 2010;20(1):100-104. doi:10.1111/j.160 0-0838.2008.00871.x
6. Gram MCD, Bø K. High level rhythmic gymnasts and urinary incontinence: Prevalence, risk factors, and influence on performance. Scand J Med Sci Sports. 2020;30(1):159-165. doi:10.1111/sms.13548
7 Blomquist JL, Muñoz A, Carroll M, Handa VL. Association of Delivery Mode With Pelvic Floor Disorders After Childbirth. JAMA 2018;320(23):2438-2447. doi:10.1001/jama.2018.1831 5
8. Donnelly G, Brockwell E, Goom T Return to running postnatal - guideline for medical, health and fitness professionals managing this population. Physiotherapy 2020;107:e188-e189. doi:10.1016/j.phy sio.2020.03.276
9. Donnelly GM, Moore IS, Brockwell E, Rankin A, Cooke R. Reframing return-to-sport postpartum: the 6 Rs framework. Br J Sports Med 2022;56(5):244-245. doi:10.1136/bjsports-2021-104877
10. Sundgot-Borgen J, Sundgot-Borgen C, Myklebust G, Sølvberg N, Torstveit MK. Elite athletes get pregnant, have healthy babies and return to sport early postpartum. BMJ Open Sport Exerc Med 2019;5(1):e000652. doi:10.1136/bmjsem-2019-00065 2
11. Christopher SM, Cook CE, Snodgrass SJ. What are the biopsychosocial risk factors associated with pain in postpartum runners? Development of a clinical decision tool. PLoS One 2021;16(8):e0255383. doi:1 0.1371/journal.pone.0255383
12. Moore IS, James ML, Brockwell E, Perkins J, Jones AL, Donnelly GM. Multidisciplinary, biopsychosocial factors contributing to return to running and running related stress urinary incontinence in postpartum women. Br J Sports Med 2021;55(22):1286-1292. do i:10.1136/bjsports-2021-104168
13. Dakic JG, Hay-Smith J, Cook J, Lin KY, Calo M, Frawley H. Effect of pelvic floor symptoms on women’s participation in exercise: a mixed-methods systematic review with meta-analysis. J Orthop Sports Phys Ther 2021;51(7):345-361. doi:10.2519/jospt.202 1.10200
14. Deering RE, Cruz M, Senefeld JW, Pashibin T, Eickmeyer S, Hunter SK. Impaired trunk flexor strength, fatigability, and steadiness in postpartum women. Med Sci Sports Exerc. 2018;50(8):1558-1569. doi:10.1249/mss.0000000000001609
15. van Melick N, van Cingel REH, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506-1515. doi:10.1136/bjsports-2015-0 95898
16. Simeone C, Moroni A, Pettenò A, et al. Occurrence rates and predictors of lower urinary tract symptoms and incontinence in female athletes. Urologia. 2010;77(2):139-146. doi:10.1177/039156031 007700210
17 Mottola MF. Exercise in the postpartum period: practical applications. Curr Sports Med Rep. 2002;1(6):362-368. doi:10.1249/00149619-20021200 0-00010
18. Rasmussen KM, Yaktine AL, Committee to reexamine IOM pregnancy weight guidelines, Food and nutrition board, board on children, youth and families, Institute of Medicine, National Research Council. Weight Gain during Pregnancy: Re-Examining the Guidelines National Academies Press; 2009.
19. Artal R, O’Toole M. Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period. Br J Sports Med. 2003;37(1):6-12; discussion 12. doi:10.1136/bjsm.37.1.6
20. Brown WJ, Hayman M, Haakstad LAH, et al. Australian guidelines for physical activity in pregnancy and postpartum. J Sci Med Sport. 2022;25(6):511-519. doi:10.1016/j.jsams.2022.03.008
21. Atkinson JAM, McKenna KT, Barnett AG, McGrath DJ, Rudd M. A randomized, controlled trial to determine the efficacy of paper tape in preventing hypertrophic scar formation in surgical incisions that traverse Langer’s skin tension lines. Plast Reconstr Surg 2005;116(6):1648-1656; discussion 1657-8. do i:10.1097/01.prs.0000187147.73963.a5
22. Brisbine BR, Steele JR, Phillips EJ, McGhee DE. Can physical characteristics and sports bra use predict exercise-induced breast pain in elite female athletes? Clin J Sport Med. 2021;31(6):e380-e384. do i:10.1097/jsm.0000000000000831
23. Baessler K, Mowat A, Maher CF. The minimal important difference of the Australian Pelvic Floor Questionnaire. Int Urogynecol J 2019;30(1):115-122. doi:10.1007/s00192-018-3724-1
24. Durnea CM, Khashan AS, Kenny LC, et al. What is to blame for postnatal pelvic floor dysfunction in primiparous women—pre-pregnancy or intrapartum risk factors? Eur J Obstet Gynecol Reprod Biol. 2017;214:36-43. doi:10.1016/j.ejogrb.2017.04.036
25. Dietz HP, Lekskulchai O Ultrasound assessment of pelvic organ prolapse: the relationship between prolapse severity and symptoms. Ultrasound Obstet Gynecol 2007;29(6):688-691. doi:10.1002/uog.4024
26. McLean L, Varette K, Gentilcore-Saulnier E, Harvey MA, Baker K, Sauerbrei E. Pelvic floor muscle training in women with stress urinary incontinence causes hypertrophy of the urethral sphincters and reduces bladder neck mobility during coughing. Neurourol Urodynam 2013;32(8):1096-1102. doi:10.1 002/nau.22343
27 Vesting S, Olsen MF, Gutke A, Rembeck G, Larsson MEH. Clinical assessment of pelvic floor and abdominal muscles 3 months post partum: an interrater reliability study BMJ Open 2021;11(9):e049082. doi:10.1136/bmjopen-2021-049082
28. van de Water ATM, Benjamin DR. Measurement methods to assess diastasis of the rectus abdominis muscle (DRAM): A systematic review of their measurement properties and meta-analytic reliability generalisation. Man Ther 2016;21:41-53. doi:10.101 6/j.math.2015.09.013
29. Hickey JT, Timmins RG, Maniar N, et al. Pain-free versus pain-threshold rehabilitation following acute hamstring strain injury: A randomized controlled trial. J Orthop Sports Phys Ther. 2020;50(2):91-103. do i:10.2519/jospt.2020.8895
30. Christopher SM, Gallagher S, Olson A, Cichowski S, Deering RE. Rehabilitation of the postpartum runner: A 4-phase approach. J Womens Health Phys Therap 2022;46(2):73-86. doi:10.1097/jwh.00000000 00000230
31. Frawley H, Shelly B, Morin M, et al. An International Continence Society (ICS) report on the terminology for pelvic floor muscle assessment. Neurourol Urodyn. 2021;40(5):1217-1260. doi:10.100 2/nau.24658
32. Thorborg K, Reiman MP, Weir A, et al. Clinical examination, diagnostic imaging, and testing of athletes with groin pain: An evidence-based approach to effective management. J Orthop Sports Phys Ther. 2018;48(4):239-249. doi:10.2519/jospt.201 8.7850
33. El-Mekawy H, Eldeeb A, El- Lythy M, et al. Effect of abdominal exercises versus abdominal supporting belt on post-partum abdominal efficiency and rectus separation. Int J Medical Med Health Sci 2013;7:44-48.
34. Neels H, De Wachter S, Wyndaele JJ, Wyndaele M, Vermandel A. Does pelvic floor muscle contraction early after delivery cause perineal pain in postpartum women? European Journal of Obstetrics & Gynecology and Reproductive Biology 2017;208:1-5. do i:10.1016/j.ejogrb.2016.11.009
35. Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 2018;10(10):CD005654. doi:10.1002/14651858.cd0056 54.pub4
36. Moser H, Leitner M, Eichelberger P, Kuhn A, Baeyens JP, Radlinger L. Pelvic floor muscle displacement during jumps in continent and incontinent women: An exploratory study Neurourol Urodynam 2019;38(8):2374-2382. doi:10.1002/nau.24 161
37 Birdsey LP, Weston M, Russell M, Johnston M, Cook CJ, Kilduff LP. Acute physiological and perceptual responses to a netball specific training session in professional female netball players. PLoS One 2022;17(2):e0263772. doi:10.1371/journal.pon e.0263772
38. Kruger JA, Dietz HP, Murphy BA. Pelvic floor function in elite nulliparous athletes. Ultrasound Obstet Gynecol 2007;30(1):81-85. doi:10.1002/uog.40 27
39. Hay-Smith EJC, Herderschee R, Dumoulin C, Herbison GP Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev. 2011;12:CD009508. doi:10.1002/14651858.cd009508
40. Egger MJ, Hamad NM, Hitchcock RW, et al. Reproducibility of intra-abdominal pressure measured during physical activities via a wireless vaginal transducer Female Pelvic Med Reconstr Surg 2015;21(3):164-169. doi:10.1097/spv.00000000000001 67
41. Berg-Poppe P, Hauer M, Jones C, Munger M, Wethor C. Use of exercise in the management of postpartum diastasis recti: A systematic review J Womens Health Phys Therap 2022;46(1):35-47 doi:1 0.1097/jwh.0000000000000231
42. Gluppe S, Ellström Engh M, Kari B. Women with diastasis recti abdominis might have weaker abdominal muscles and more abdominal pain, but no higher prevalence of pelvic floor disorders, low back and pelvic girdle pain than women without diastasis recti abdominis. Physiotherapy. 2021;111:57-65. doi:1 0.1016/j.physio.2021.01.008
43. Dufour S, Bernard S, Murray-Davis B, Graham N. Establishing expert-based recommendations for the conservative management of pregnancy-related diastasis rectus abdominis: A delphi consensus study. J Womens Health Phys Therap 2019;43(2):73-81. doi:1 0.1097/jwh.0000000000000130
44. Tennfjord MK, Engh ME, Bø K. The influence of early exercise postpartum on pelvic floor muscle function and prevalence of pelvic floor dysfunction 12 Months postpartum. Phys Ther. 2020;100(9):1681-1689. doi:10.1093/ptj/pzaa084
45. Stær-Jensen J, Siafarikas F, Hilde G, Benth JŠ, Bø K, Engh ME. Postpartum recovery of levator hiatus and bladder neck mobility in relation to pregnancy. Obstet Gynecol 2015;125(3):531-539. doi:10.1097/ao g.0000000000000645
46. Vieira GF, Saltiel F, Miranda-Gazzola APG, Kirkwood RN, Figueiredo EM. Pelvic floor muscle function in women with and without urinary incontinence: are strength and endurance the only relevant functions? a cross-sectional study Physiotherapy. 2020;109:85-93. doi:10.1016/j.physio.2 019.12.006
47 Woodley SJ, Boyle R, Cody JD, Mørkved S, HaySmith EJC. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2017;12(12):CD007471. doi:10.1002/146518 58.cd007471.pub3
Download: https://ijspt.scholasticahq.com/article/65894-the-mother-load-and-return-to-sport-a-case-report-ofreturning-to-professional-netball-following-cesarean-section/attachment/ 132091.pdf?auth_token=18U0rk4AOSemZSz2Dd6P
Download: https://ijspt.scholasticahq.com/article/65894-the-mother-load-and-return-to-sport-a-case-report-ofreturning-to-professional-netball-following-cesarean-section/attachment/ 132092.pdf?auth_token=18U0rk4AOSemZSz2Dd6P
Case Reports
1
American Academy of Manipulative Therapy, 2 Wellward Regenerative Medicine, 3 Tybee Wellness & Osteopractic regenerative medicine, shoulder pain, rehabilitation, platelet rich plasma, prolotherapy, blood flow restriction exercise, dry needling https://doi.org/10.26603/001c.68143Keywords:

Platelet-rich plasma (PRP) and prolotherapy have resulted in promising outcomes in patients with various types of shoulder injuries. However, there is a lack of preliminary evidence supporting preparation of PRP production, timely application of these therapies and regenerative rehabilitation protocols. The purpose of this case report is to describe the distinct method including orthobiologic preparation, tissue-specific treatment and regenerative rehabilitation of an athlete with a complex shoulder injury
A 15y/o competitive female wrestler with a complex shoulder injury presented to the clinic after unsuccessful conservative rehabilitation. Unique methods were incorporated to optimize PRP production, specific tissue healing and regenerative rehabilitation. Multiple injuries required different orthobiologic interventions at different time frames, in order to promote optimal healing and stability of the shoulder
The described interventions resulted in successful outcomes including pain, disability, full return to sport, and regenerative tissue healing confirmed with diagnostic imaging.
5
Acromioclavicular joint (ACJ) separation injuries are commonly seen in athletics. Although there is a paucity of recent evidence on the epidemiology of ACJ separation, the most recent data suggests that these injuries account for up to 53% of athletic related shoulder injuries.1 Interestingly, concomitant intra-articular joint pathologies (e.g., labral tears, supraspinatus tears, inferior glenohumeral ligament tears) have been reported, ranging from 14-77%.2–5 Because multiple sites and tissues can be affected, such injuries can be regarded as complex shoulder injuries. Labral tears and supraspinatus tears have been identified as two of the more common intra-articular pathologies associated with ACJ separation.2–6 Interestingly, the incidence of con-
comitant labral tears associated with ACJ separation seems to be linear, and ranges from 60% in grade 1 ACJ injuries to 100% in grade 4 ACJ injuries.4 Research investigating conservative non-surgical treatment (physical therapy/corticosteroid injections) of these types of complex shoulder injuries is scant, with most quality trials on shoulder pain addressing the more encompassing diagnosis of subacromial impingement syndrome.7–10 This seemingly may be an important barrier to effective comprehensive management of a complex shoulder injury, as each injured tissue likely needs to be addressed independently at specific time frames for optimal outcomes.
Intuitively, there seems to be a need for novel point-ofcare strategies to identify and promote specific tissue healing at each pathoanatomical site of a complex shoulder in-
Corresponding author:
James Escalonijury, while improving functional outcomes in a safe/timely manner. Orthobiologic medicine complimented with appropriate regenerative rehabilitation may be an attractive option. Platelet-rich plasma (PRP), and prolotherapy are two common therapies used within the spectrum of orthobiologics/regenerative medicine.11,12
PRP is a preparation of autologous plasma enriched with a platelet concentration above that normally contained in whole blood.13 Following exsanguination, it is generally prepared in a centrifuge to separate its contents for a greater concentration of platelets within the blood. It is within this concentration that the platelets are extracted and re-injected into specific areas of musculoskeletal injury Once injected, the PRP exerts a strong bioactive effect, releasing a plethora of key growth factors that promote healing.14 The overall goal of using PRP is to have supratherapeutic platelet concentration in a small volume of plasma, in order to promote healing of tissues (joints, cartilage, tendons and ligaments) that have intrinsically poor healing capacity.13 Further, preparation of blood-based orthobiologic compounds such as PRP may be enhanced with specific exercise prior to exsanguination.15,16 Unfortunately, the use of PRP for the management of shoulder conditions is not without controversy 17,18 However, recent evidence has suggested that PRP results in short and long term improvements in pain and function in patients with partial rotator cuff tears.19–21 Only one case series has suggested improved outcomes treating the glenoid labrum with PRP.17,22 To date, there seems to be minimal evidence supporting the use of PRP in conservative orthopaedics, with a strong recommendation for standardization of PRP production, treatment and post-treatment rehabilitation protocols.6,12,23–25
Prolotherapy is an additional therapy that introduces a small amount of a natural irritant solution to the site of painful and degenerated tendon insertions, joints, ligaments, and adjacent joint spaces.26 Commonly, prolotherapy consists of a concentrated dextrose solution that creates an environment to reintroduce a local inflammatory cascade, triggering the release of growth factors that aid with collagen deposition around areas of injury or laxity 12,26,27 Hence, a major goal of prolotherapy is to treat ligamentous laxity and related musculoskeletal and arthritic conditions by improving the tensile strength of specific intra-articular and extra-articular tissues.12,26,28 Overall, the evidence supports the use of dextrose prolotherapy for tendinopathy, specific joint osteoarthritis, and spinal/pelvic ligament dysfunction.26 A recent trial29 reported short-term (2-week) improvements in pain, disability and shoulder AROM following prolotherapy to patients with supraspinatus tendinopathy Smaller studies have given some plausible insight for the use of prolotherapy for the ACJ and complex shoulder injuries, however, there are no larger trials to reinforce these findings.30,31
Rehabilitation following orthobiologic therapy is described by the American Physical Therapy Association as the integration of interventional orthobiologic techniques coupled with appropriate rehabilitation strategies that harness the healing mechanisms through movements to aug-
ment the orthobiologic therapies.12 The goal of rehabilitation after orthobiologic therapy is to return a patient to optimal function by combining the science and research behind both rehabilitation and regenerative medicine. Further preliminary data with progressive tissue healing protocols are needed to support its use following orthobiologic therapy
In this case, four unique methods were incorporated to optimize this patient’s healing and functional recovery. These included blood flow restriction therapy (BFR)32–35 prior to the blood draw (pre-exsanguination) and during specific rehabilitation, dry needling with electrostimulation,36–38 and a specific protein supplement regimen designed to amplify the effects of tissue loading.39,40 Each of these unique elements were combined in a manner not before described in the literature. The purpose of this case report is to describe the distinct method including orthobiologic preparation, tissue-specific treatment and regenerative rehabilitation of an athlete with a complex shoulder injury.
A 15-year-old competitive female wrestler with persistent shoulder pain presented after unsuccessful management of her shoulder pain with conventional physical therapy The injury occurred during a wrestling practice when another wrestler fell (full bodyweight) on the anterior shoulder in a position of end range abduction/external rotation. No immediate diagnosis was made on the field. The athlete was able to continue with wrestling but with significant limitations in her performance, persistent resting pain and disturbed sleep. Following the wrestling season, she underwent three months of physical therapy including glenohumeral joint mobilizations, range of motion and traditional rotator cuff exercises. This rehabilitation approach resulted in minimal improvement in symptoms or sport specific function. The athlete had no prior injuries to the shoulder, cervical, or thoracic spines.
The subject subsequently presented to the physical therapist and physician for a co-evaluation, The physician was a dual-board certified anesthesiologist and pain management physician with a specialty in regenerative medicine. The physical therapist was board certified, and fellowship trained in orthopaedics. Informed consent was obtained from the subject/parents prior to the history and physical examination. The subject’s pain on the numeric pain rating scale (NPRS)41,42 was 5/10 at rest and 8/10 during athletic activity (Figure 1). She described the pain as widespread with poor localization, and her initial Quick-DASH43,44 score was 18% (Figure 2). The subject was unable to perform wrestling off-season practice or run due to a feeling of instability and pain in the shoulder Pull-up motions and bench press motions were notably limited due to pain and feelings of instability during supervised team weight training. Further. skills position of a wrestling “under-hook” position could not be performed due to instability Importantly, prior to injury, her spring sport participation was unrestricted and included four days per week of wrestling
practice with three days per week of strength training. Preinjury, one-repetition maximum testing was reported to be 65lb bench press, 50lb pound dumbbell row, and 145lb deadlift.
Visual observation revealed normal position of the glenohumeral joint (GHJ) with a minor misalignment/swelling around the ACJ. Initial screening for the cervical spine involvement was negative and included a negative Spurling’s test for reproduction of symptoms, a positive Shoulder Abduction Sign for exacerbation of shoulder symptoms, and no symptoms below the elbow.45 The initial shoulder exam revealed full active range of motion in flexion, abduction, external rotation at 90 degrees abduction and internal rotation at 90 degrees abduction. Pain was reproduced from 90 degrees of shoulder elevation through end range, with more severe pain at end range. Impingement testing was negative.10,46 Special testing for the labrum revealed a positive compression rotation test, with pain reported deep in shoulder 47,48
Special testing for the acromioclavicular joint included painful palpation, cross-body adduction, resisted acromioclavicular extension, and a positive active compression test.49,50 Laxity was in the ACJ joint in anterior to posterior direction. Superior glide mobility testing of the ACJ was painful, with a firm ligamentous end-feel when compared to the contralateral side. Laxity of the GHJ was also noted ipsilaterally during the anterior load and shift test.51
Strength of the rotator cuff (internal and external rotators) was 5/5 in neutral position but was limited by pain (4/5) in 90 degrees of flexion and abduction. Strength testing of the scapular musculature (middle trapezius, lower trapezius, rhomboids) in prone was similar in that testing at greater than 90 degrees of shoulder flexion or abduction was limited by pain. The tentative diagnosis from the physical examination included an ACJ sprain and suspected labral tear with anterior laxity of the glenohumeral joint.
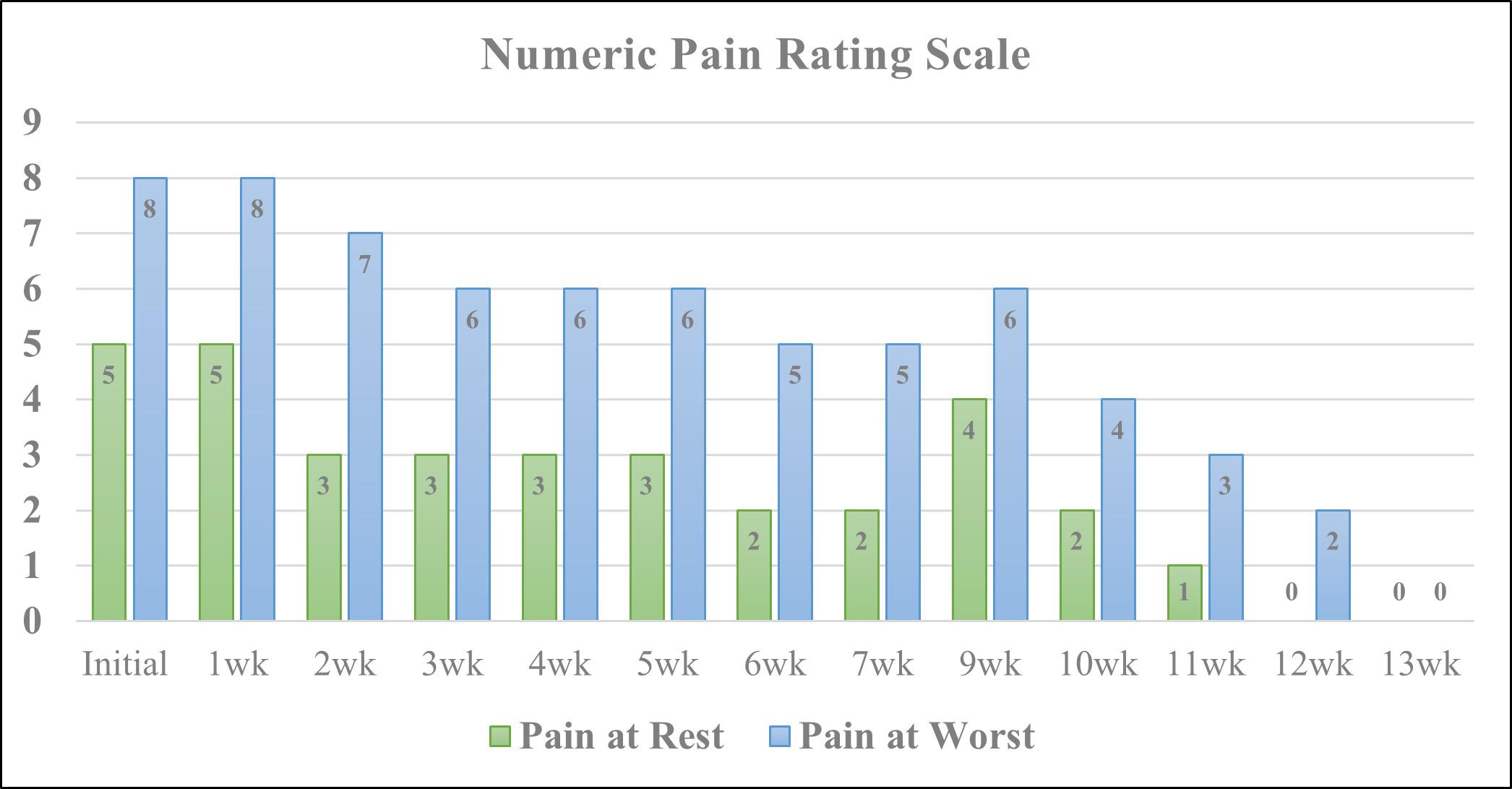
Diagnostic ultrasound imaging (GE Logiq E9; 2010) of the biceps tendons, tendons of the rotator cuff, rotator interval, labrum and anterior/posterior ACJ was performed immediately following the physical examination. Ultrasound confirmed misalignment of ACJ (clavicular portion elevated) with distinct hypoechoic patterns noted on both the clavicular and acromial attachments of the capsule, with associated bony abnormalities (Figure 3A, 4A). Further, a small supraspinatus myotendinous partial thickness tear was also identified. The labrum was not adequately visualized with the ultrasound study.
Based on the physical examination/ultrasound findings and a lack of progress with conservative treatment, magnetic resonance imaging (MRI) was ordered to guide further treatment considerations. An MRI with contrast was performed using a 3-tesla magnet and revealed a small focal tear in the superior labrum at the biceps labrum attachment (Figure 5A), with an intact biceps tendon. Further, arthritic/ cystic changes were noted in the acromion, though the ACJ ligaments were still intact. Importantly, the supraspinatus tear found during the diagnostic ultrasound was not ad-
Figure 1. Numeric pain rating scale; 0-10, Initial (initial PRP injection to labrum),1wk-7wk (outcomes post PRP injection), 9wk (2 days-post first prolotherapy injection to ACJ), 10wk-11wk (1-2wk post first prolotherapy injection), 12wk (prolotherapy injection to posterior ACJ), 13wk (final outcome measures taken).Figure 2. Quick-Disabilities of the arm shoulder and hand; 0-100%, Initial (initial PRP injection to labrum),1wk-7wk (outcomes post PRP injection), 9wk (2 days-post first prolotherapy injection to ACJ), 10wk-11wk (1-2wk post first prolotherapy injection), 12wk (prolotherapy injection to posterior ACJ), 13wk (final outcome measures taken).
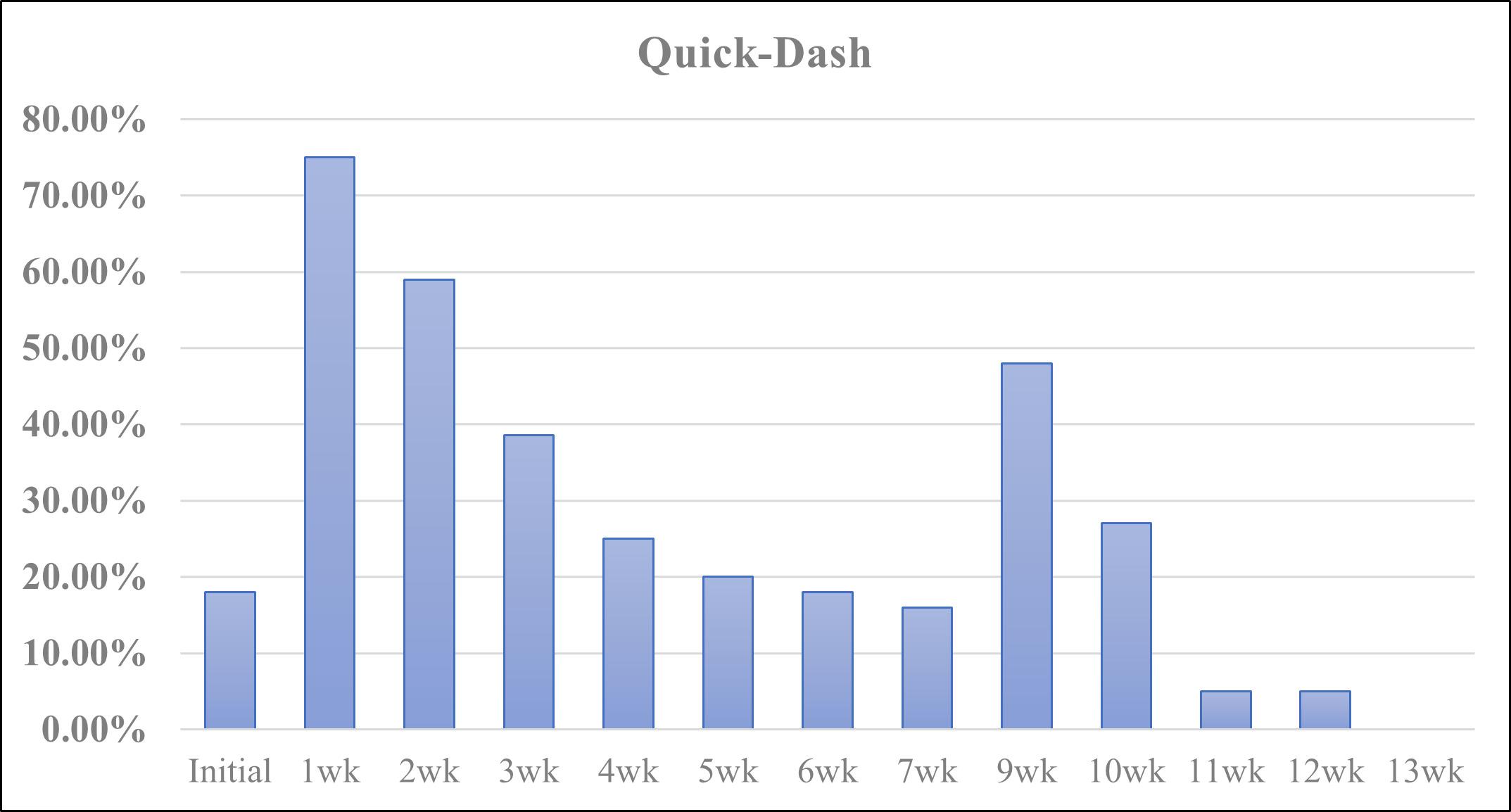
Figure 3. Diagnostic Ultrasound: Anterior View of Acromioclavicular Joint: Initial and 1-Year Follow-up
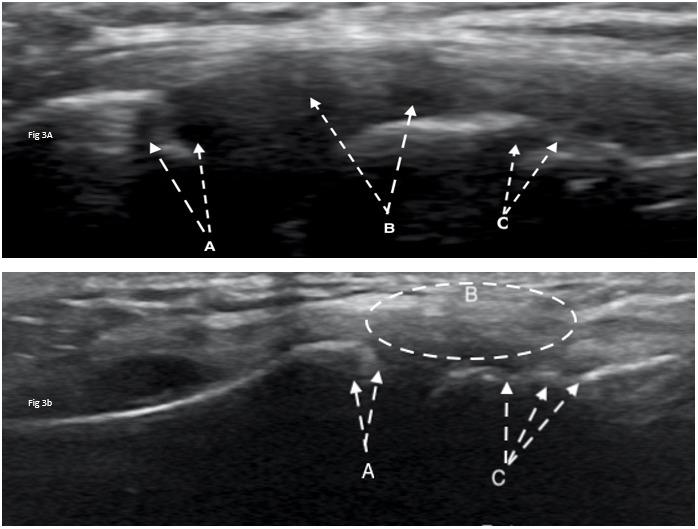
A: Hypoechoic patterns showing denudement of the distal clavicle and separation of the capsule from the clavicle (A-arrows); tears in the mid and acromial regions of the capsule (Barrows); and bony abnormalities at the acromion (C-arrows) at initial evaluation.
B: Reduction of denudement on distal clavicle (Arrow-A); tissue growth (hyperechoic filling) throughout joint capsule (B-circle); and filling in of bony abnormality (C-arrows), at 1-year follow-up.
Figure 4. Diagnostic Ultrasound: Posterior View of Acromioclavicular Joint: Initial and 1-Year Follow-up
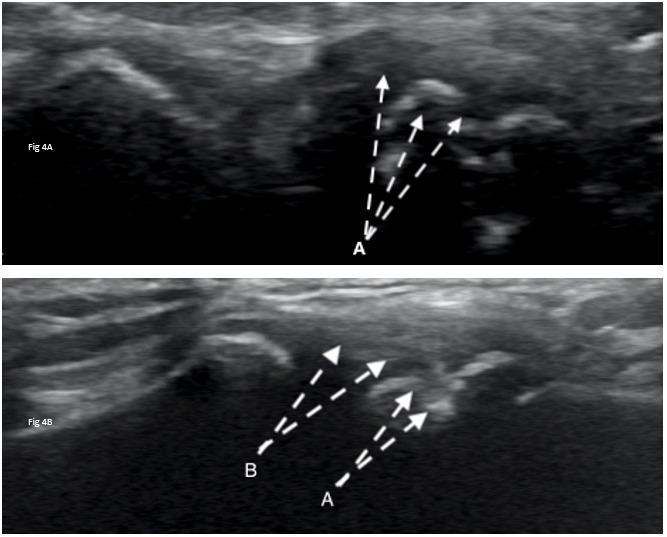
A: Hyper-calcific regions at the capsule anastomosis of acromion signifying a failing joint capsule or avulsions (A-arrows) at initial evaluation.
B: Remodeling of the calcific lesions, tissue growth (hyperechoic filling) and adherence of the capsule to the acromion (B-arrows) at -1year follow-up.
equately visualized on the MRI scan and the labral tear found on the MRI was not adequately visualized on the ultrasound. Hence, both imaging techniques were indicated.
Due to the complex nature of the shoulder injury (ACJ, labrum, rotator cuff) and the athlete having an impending soccer season, the labrum was prioritized, and addressed first with a PRP injection. The PRP procedure was the initial focus, because of the inflammatory cycle52 and the longer period of recovery needed with this type of regenerative procedure.18,20,21
Prior to exsanguination, a novel technique of blood flow restriction (BFR) exercise53 was performed (Appendix) to amplify important circulatory components of healing in in the subject’s whole blood.16,32,33,35,54–56
The platelet-rich plasma was prepared using 160mL whole blood exsanguinated using a 20-gauge antecubital access. This was drawn into 10mL vials containing citrate as an anti-coagulant. The first spin was performed at 1500 RPM for 10 minutes to segregate the plasma, platelets, and leukocytes from red blood cells. The serum layer was extracted manually down to buffy coat and transferred to two new vials. The second spin was performed at 2500 RPM for eight minutes. The serum was removed from each vial un-
til 6mL of serum with a platelet plug remained from each vial. This was then mixed to reconstitute a total of 12mL of leukocyte rich platelet-rich plasma (LR-PRP), which is approximately 13x the concentration of platelets.
The injection area was identified with Logiq E9 ultrasound using a linear probe in virtual curvilinear mode. To target the biceps tendon insertion on the labrum and the labral tear, the probe was positioned in the anterior shoulder in an axial plane to visualize the pectoralis major and short head of the biceps tendon overlying the anterior labrum. The needle was inserted in short axis and advanced to the labrum, confirming needle placement with hydro-dissection of tissue using LR-PRP. The needle was progressively walked cephalad noting the needle palpatory feedback and ultrasound visualized hydro-dissection to confirm placement. Upon overlap with the coracoid process and loss of visualization of the labrum, the needle was directed cephalad by palpation alone. Approximately 4mL of LR-PRP was injected into the labrum and intra-articular space. Despite its absence on MRI, a small myotendinous junction supraspinatus tear was appreciated on ultrasound, and the remaining 2mL of LR-PRP was injected into the supraspinatus myotendinous junction and sub-acromial bursa.
The subject was followed regularly with a specific physical therapy protocol based on time frames of recovery to aid with tissue loading and healing.52 This protocol was developed in order to better stimulate growth factors15,16,53 and encourage stress relaxation of the collagen associated with the injured tissue.39 Prior to each exercise session the sub-
ject was instructed to consume 15 grams gelatin in the form of hydrolyzed collagen combined with 225 mg vitamin C to help stimulate collagen synthesis, which in turn has the potential to improve the function and integrity of an impaired tendon.39,40,57 In order to further enhance the healing response, the subject received electrical dry needling38 to the shoulder according to a protocol developed by Dunning et al.10 All components of the post-procedural rehabilitation program are detailed in the Appendix.
Following successful completion of her eight-week plan of care after the PRP injection, the subject noted a distinct difference in the level and location of pain. Prior to the PRP intervention, she was unable to localize pain in her shoulder and described it as wide-spread pain at rest (NPRS=5/ 10) and with movement (NPRS=8/10). After the PRP and regenerative rehabilitation, she noted the lower/inferior 50% of her shoulder pain had resolved but an upper, more anterior pain remained at rest (NPRS=2/10) and with movement (NPRS=5/10). This was correlated clinically with negative special testing of the labrum/rotator cuff and no changes in the provocative ACJ exam. These findings from the follow-up examination and self-report outcomes (Figure 1, 2) helped confirm the labrum tissue as a potential independent source of pain, allowing a more confident transition into phase II of her orthobiologic intervention.
The second phase began with an ultrasound guided prolotherapy injection (20% dextrose + 0.2% lidocaine) into the anterior acromioclavicular joint. A second prolotherapy injection was determined to be necessary at a follow-up visit due to posterior ACJ pain during heavier weightlifting and
plyometric activities. The second ultrasound guided prolotherapy injection (with identical concentration) was directed to the posterior ACJ based on local tenderness and symptom provocation. A less rigid rehabilitation protocol was followed in this phase due to the nature of healing with prolotherapy.58 (Appendix).
At the three-month (13 week) follow-up after the initial treatment, disability dropped to a 0%, and the subject was able to perform soccer, heavy weightlifting, and intense wrestling practice without limitation or pain (Figure 1, 2). Reevaluation of provocative special testing of the shoulder at three months was negative. Intense wrestling practice at the three-month time frame included plyometric activities through the shoulder, ability to perform under-hook positions dynamically and against resistance, and full painless participation in supervised team weight training. Weight training returned to pre-injury strength testing levels and subject returned to running without feelings of instability or pain, allowing unrestricted participation in soccer and wrestling concurrently
At the one-year follow-up, the subject reported no pain (NPRS=0/10) and full return to athletics (QDASH =0% disability). A follow-up MRI at one year revealed no discrete labral tears, minimal supraspinatus tendinopathy, and normal visualization of the ACJ (Figure 5B). Similarly, a oneyear follow-up diagnostic ultrasound revealed normal appearance of the supraspinatus tendon, its myotendinous junction and ACJ (Figure 3B, 4B).
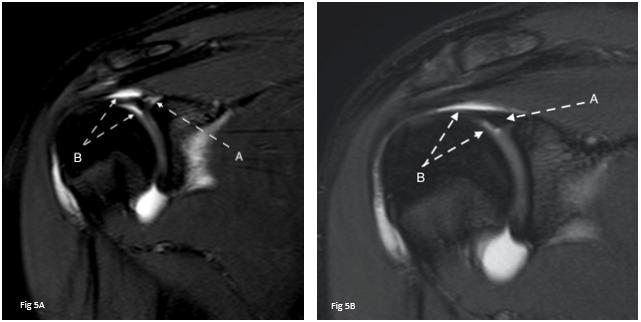
This case report describes the successful short and longterm outcome of a competitive female wrestler with a com-
Figure 5. MRA of Shoulder: Initial and 1-Year Follow-up A: Initial MRA. Tear in the superior labrum at the biceps labral attachment (A-arrows) and surrounding inflammation (B-arrow) at initial evaluation B: MRA. Healing of glenoid labrum (Arrow A) and reduction in surrounding inflammation (Arrow B) at 1yr follow-up.plex shoulder injury who failed conservative treatment and returned to sport without pain or the need for surgery. The novel methods of PRP preparation, tissue specific orthobiologic therapy, and regenerative rehabilitation protocols may have contributed to the overall outcomes and timely return to full function.
The use of PRP for tissue healing is based on the underlying capacity of platelets to supply and release supraphysiologic amounts of essential growth factors and cytokines from their alpha granules. This process provides a regenerative stimulus that augments healing and promotes repair in tissues with low healing potential.13 Growth factors that are commonly described for their utilization include but are not-limited to: platelet-derived growth factor (PDGF), transforming growth factor-b (TGF-b), vascular endothelial growth factor (VEGF) epidermal growth factor (EGF), basic fibroblast growth factor (bFGF), and insulin-like growth factor (IGF-1).13,59
Blood flow restriction (BFR) exercise has been described as a training method which partially restricts arterial inflow and fully restricts venous outflow in the working musculature during exercise.34 It exerts physiologic effects under low loads that would normally occur under heavier loads but cannot be performed due to injury, healing or surgery This has been shown to produce improved strength and muscle hypertrophy changes in a more expedient manner than with traditional high-load strength training.60,61 It additionally improves a variety of measures correlated with improvements in strength and the positive effects of exercise.35,62,63 It has been suggested that BFR exercise results in increased mobilization of hematopoietic stem progenitor cells, proliferation of myogenic stem cells, increased cytokine responses, increases in the number of circulating CD34+/KDR+ endothelial progenitor cells, and increased VEGF.32,33,35,54–56 Thus, in this case report, BFR was used during exercise to “amplify” the yield / healing capacity of PRP by utilization pre-exsanguination and during rehabilitation, respectively. A recent study suggested that BFR can be considered a way to manipulate point-of-care blood products such as PRP to increase product yield.16 To date, no prior studies have used BFR as an adjunct to orthobiologic therapy or as a part of the regenerative rehabilitation process.
Dry needling with electrical stimulation was incorporated after exercise to continue to facilitate the healing process after orthobiologic injection. Dry needling is described as an intervention whereby thin, monofilament needles are used to penetrate the skin and stimulate underlying neural, muscular and/or connective tissues for the management of pain and disability associated with neuromusculoskeletal conditions.64 Dry needling with electrical stimulation has been found to aid with improved analgesia in many painful conditions, including subacromial pain syndrome, and has been shown to aid with wound and tissue healing in experimentally induced trauma.37,38,65–69
To further attempt to augment the healing process, the subject was required to take 15 grams of hydrolyzed collagen with 225 mg of vitamin C one hour prior to rehabilitation exercise. This was consistent with prior research
supporting collagen synthesis and tendon healing.39,40 Although Baar39 described the successful rehabilitation of patellar tendinopathy, it appears that tendons and the shoulder labrum both contain a similar collagen matrix,70 and may result in similar changes when supplementing the effects of the regenerative rehabilitation protocol.39,40,57,71,72 Further research is needed in this area.
Following, the first phase of the orthobiologic/rehabilitation process, prolotherapy was directed at the ACJ to reduce laxity and address remaining pain in the shoulder Interestingly, there were greater reductions in disability after the prolotherapy injections (16% to 0%) than the PRP injections (18% to 16%). Similarly, activity related pain (pain at worst) followed a similar trend after the PRP (8/10 to 5/10) and prolotherapy (5/10 to 0/10). Clinically and pathoanatomically there may be several plausible theories behind these changes. First, with multiple areas of tissue injury, it is very difficult a patient or the clinician to decipher individual components of injury and related pain/ disability. Second, the reduction in the initial higher pain thresholds after the PRP/rehabilitation may have been related to the selected tissue healing and initial return to function. However, the laxity and remaining pain in the ACJ tissues during the provocative exam may have been the key pathoanatomical component associated with the stagnant disability From an orthobiologic/regenerative medicine perspective, addressing the correct tissue based on its healing time frame, surrounding structural integrity, and results of imaging and physical examination seems to be of paramount importance.
Finally, it should be noted that because this is a case report, the results or theoretical constructs do not indicate a cause-and-effect relationship. Results such as those experienced by this subject may not be seen in all subjects. Additionally, a six-month follow-up with diagnostic ultrasound and or MRI would have been ideal to correlate with specific tissue healing. Further investigation comparing outcomes after conservative versus typical surgical management is needed. Additionally, future studies/trials need to consider standardizing blood-based orthobiologic preparation and specific regenerative rehabilitation protocols to better determine the effect of these novel techniques.
This case report demonstrates the successful outcome of a competitive female athlete with a complex shoulder injury who failed prior conservative rehabilitation. Detailed imaging and evaluation procedures indicated tissue pathology at multiple joint sites. Tissue specific orthobiologic interventions with novel preparation, in conjunction with a comprehensive regenerative rehabilitation protocol, resulted in a full return sport without restrictions at the three-month follow-up. At the one-year follow-up, MRI and diagnostic ultrasound imaging confirmed notable tissue healing in all original injury sites.
The authors report no conflicts of interest.
Submitted: June 14, 2022 CST, Accepted: December 23, 2022
CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0
International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Skjaker SA, Enger M, Engebretsen L, Brox JI, Bøe B. Young men in sports are at highest risk of acromioclavicular joint injuries: a prospective cohort study Knee Surg Sports Traumatol Arthrosc 2021;29(7):2039-2045. doi:10.1007/s00167-020-0595 8-x
2. Ruiz Ibán MA, Moreno Romero MS, Diaz Heredia J, Ruiz Díaz R, Muriel A, López-Alcalde J. The prevalence of intraarticular associated lesions after acute acromioclavicular joint injuries is 20%. A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2021;29(7):2024-2038. do i:10.1007/s00167-020-05917-6
3. Jensen G, Millett PJ, Tahal DS, Al Ibadi M, Lill H, Katthagen JC. Concomitant glenohumeral pathologies associated with acute and chronic grade III and grade V acromioclavicular joint injuries. Int Orthop. 2017;41(8):1633-1640. doi:10.1007/s00264-0 17-3469-3
4. Shah SS, Ferkel E, Mithoefer K. High prevalence of superior labral anterior-posterior tears associated with acute acromioclavicular joint separation of all injury grades. Orthop J Sports Med 2020;8(8):2325967120941850. doi:10.1177/232596712 0941850
5. Markel J, Schwarting T, Malcherczyk D, Peterlein CD, Ruchholtz S, El-Zayat BF. Concomitant glenohumeral pathologies in high-grade acromioclavicular separation (type III – V). BMC Musculoskelet Disord. 2017;18(1):439. doi:10.1186/s12 891-017-1803-y
6. Chahla J, Cinque ME, Piuzzi NS, et al. A call for standardization in platelet-rich plasma preparation protocols and composition reporting: a systematic review of the clinical orthopaedic literature. J Bone Joint Surg Am. 2017;99(20):1769-1779. doi:10.2106/jbj s.16.01374
7 Rhon DI, Boyles RB, Cleland JA. One-year outcome of subacromial corticosteroid injection compared with manual physical therapy for the management of the unilateral shoulder impingement syndrome: a pragmatic randomized trial. Ann Intern Med. 2014;161(3):161-169. doi:10.7326/m13-2199
8. Burger M, Africa C, Droomer K, et al. Effect of corticosteroid injections versus physiotherapy on pain, shoulder range of motion and shoulder function in patients with subacromial impingement syndrome: A systematic review and meta-analysis. S Afr J Physiother 2016;72(1):318. doi:10.4102/sajp.v72i1.31
9. Pieters L, Lewis J, Kuppens K, et al. An update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain. J Orthop Sports Phys Ther 2020;50(3):131-141. doi:10.2519/jospt.2020.8498
10. Dunning J, Butts R, Fernández-de-las-Peñas C, et al. Spinal manipulation and electrical dry needling in patients with subacromial pain syndrome: a multicenter randomized clinical trial. J Orthop Sports Phys Ther 2021;51(2):72-81. doi:10.2519/jospt.2021.9 785
11. Dhillon MS, Behera P, Patel S, Shetty V. Orthobiologics and platelet rich plasma. Indian J Orthop 2014;48(1):1-9. doi:10.4103/0019-5413.12547
12. Centeno CJ, Pastoriza SM. Past, current and future interventional orthobiologics techniques and how they relate to regenerative rehabilitation: a clinical commentary Intl J Sports Phys Ther 2020;15(2):301-325. doi:10.26603/ijspt20200301
13. Wu PI, Diaz R, Borg-Stein J. Platelet-rich plasma. Phys Med Rehabil Clin N Am 2016;27(4):825-853. do i:10.1016/j.pmr.2016.06.002
14. Filardo G, Di Matteo B, Kon E, Merli G, Marcacci M. Platelet-rich plasma in tendon-related disorders: results and indications. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):1984-1999. doi:10.1007/s0016 7-016-4261-4
15. Joshi S, Mahoney S, Jahan J, Pitts L, Hackney KJ, Jarajapu YP Blood flow restriction exercise stimulates mobilization of hematopoietic stem/progenitor cells and increases the circulating ACE2 levels in healthy adults. J Appl Physiol (1985). 2020;128(5):1423-1431. doi:10.1152/japplphysiol.00109.2020
16. Callanan MC, Plummer HA, Chapman GL, Opitz TJ, Rendos NK, Anz AW Blood flow restriction training using the delfi system is associated with a cellular systemic response. Arthrosc Sports Med Rehabil. 2021;3(1):e189-e198. doi:10.1016/j.asmr.202 0.09.009
17 Schneider A, Burr R, Garbis N, Salazar D Plateletrich plasma and the shoulder: clinical indications and outcomes. Curr Rev Musculoskelet Med. 2018;11(4):593-597 doi:10.1007/s12178-018-9517-9
18. Lui M, Shih W, Yim N, Brandstater M, Ashfaq M, Tran D. Systematic Review and Meta-Analysis of nonoperative platelet-rich plasma shoulder injections for rotator cuff pathology. PM R. 2020;13(10):1157-1168. doi:10.1002/pmrj.12516
19. Kwong CA, Woodmass JM, Gusnowski EM, et al. Platelet-rich plasma in patients with partialthickness rotator cuff tears or tendinopathy seads to significantly improved short-term pain relief and function compared with corticosteroid injection: a double-blind randomized controlled trial. Arthroscopy 2021;37(2):510-517 doi:10.1016/j.arthr o.2020.10.037
20. Sari A, Eroglu A. Comparison of ultrasoundguided platelet-rich plasma, prolotherapy, and corticosteroid injections in rotator cuff lesions. J Back Musculoskelet Rehabil 2020;33(3):387-396. doi:10.323 3/bmr-191519
21. Giovannetti de Sanctis E, Franceschetti E, De Dona F, Palumbo A, Paciotti M, Franceschi F. The efficacy of injections for partial rotator cuff tears: a systematic review. J Clin Med. 2020;10(1):51. doi:10.3 390/jcm10010051
22. Vander Kraats R, Doss A. Glenoid labral tear: follow up case series on ultrasound guided autologous platelet rich plasma in conjunction with a progressive rehabilitation program. F1000Res 2012;1:68. doi:10.12688/f1000research.1-68.v1
23. de Andrade ALL, Sardeli AV, Garcia TA, Livani B, Belangero WD PRP does not improve the objective outcomes of anterior cruciate ligament reconstruction: a systematic review and metaanalysis. Knee Surg Sports Traumatol Arthrosc 2020;29(9):3049-3058. doi:10.1007/s00167-020-0634
8-z
24. Hussain N, Johal H, Bhandari M. An evidencebased evaluation on the use of platelet rich plasma in orthopedics – a review of the literature. SICOT J. 2017;3:57 doi:10.1051/sicotj/2017036
25. Fadadu PP, Mazzola AJ, Hunter CW, Davis TT Review of concentration yields in commercially available platelet-rich plasma (PRP) systems: a call for PRP standardization. Reg Anesth Pain Med 2019;44(6):652-659. doi:10.1136/rapm-2018-100356
26. Hauser RA, Lackner JB, Steilen-Matias D, Harris DK. A systematic review of dextrose prolotherapy for chronic musculoskeletal pain. Clin Med Insights Arthritis Musculoskelet Disord 2016;9:139-159. doi:1 0.4137/cmamd.s39160
27 Reeves KD, Sit RW, Rabago DP Dextrose Prolotherapy: A narrative review of basic science, clinical research, and best treatment recommendations. Phys Med Rehabil Clin N Am. 2016;27(4):783-823. doi:10.1016/j.pmr.2016.06.001
28. DeChellis DM, Cortazzo MH. Regenerative medicine in the field of pain medicine: Prolotherapy, platelet-rich plasma therapy, and stem cell therapy Theory and evidence. Techniques in Regional Anesthesia and Pain Management. 2011;15(2):74-80. d oi:10.1053/j.trap.2011.05.002
29. Lin MT, Chiang CF, Wu CH, Huang YT, Tu YK, Wang TG. Comparative effectiveness of injection therapies in rotator cuff tendinopathy: a systematic review, pairwise and network meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2019;100(2):336-349.e15. doi:10.1016/j.apmr.2018.0 6.028
30. Hsieh PC, Chiou HJ, Wang HK, Lai YC, Lin YH. Ultrasound‐guided prolotherapy for acromial enthesopathy and acromioclavicular joint arthropathy: a single‐arm prospective study. J Ultrasound Med 2019;38(3):605-612. doi:10.1002/ju m.14727
31. Seenauth C, Inouye V, Langland JO Dextrose prolotherapy for chronic shoulder pain: a case report. Alternative Therapies in Health & Medicine 2017;23(7).
32. Joshi S, Mahoney S, Jahan J, Pitts L, Hackney KJ, Jarajapu YP Blood flow restriction exercise stimulates mobilization of hematopoietic stem/progenitor cells and increases the circulating ACE2 levels in healthy adults. Journal of Applied Physiology 2020;128(5):1423-1431. doi:10.1152/japplphysiol.001 09.2020
33. Nielsen JL, Aagaard P, Bech RD, et al. Proliferation of myogenic stem cells in human skeletal muscle in response to low-load resistance training with blood flow restriction. J Physiol 2012;590(17):4351-4361. doi:10.1113/jphysiol.2012.2 37008
34. Patterson SD, Hughes L, Warmington S, et al. Blood flow restriction exercise: considerations of methodology, application, and safety. Front Physiol. 2019;10:533. doi:10.3389/fphys.2019.00533
35. Patterson SD, Leggate M, Nimmo MA, Ferguson RA. Circulating hormone and cytokine response to low-load resistance training with blood flow restriction in older men. Eur J Appl Physiol 2013;113(3):713-719. doi:10.1007/s00421-012-2479-5
36. Dunning J, Butts R, Mourad F, Young I, Flannagan S, Perreault T. Dry needling: a literature review with implications for clinical practice guidelines. Phys Ther Rev. 2014;19(4):252-265. doi:10.1179/108331913 x13844245102034
37 Butts R, Dunning J, Perreault T, Mourad F, Grubb M. Peripheral and spinal mechanisms of pain and dry needling mediated analgesia: a clinical resource guide for health care professionals. Int J Phys Med Rehabil. 2016;4(2):2-18. doi:10.4172/2329-9096.1000 327
38. Wang R, Luo D, Xiao C, et al. The time course effects of electroacupuncture on promoting skeletal muscle regeneration and inhibiting excessive fibrosis after contusion in rabbits. Evid Based Complement Alternat Med. 2013;2013(869398):1-16. doi:10.1155/2 013/869398
39. Baar K. Stress relaxation and targeted nutrition to treat patellar tendinopathy Int J Sport Nutr Exerc Metab. 2019;29(4):453-457. doi:10.1123/ijsnem.201 8-0231
40. Shaw G, Lee-Barthel A, Ross ML, Wang B, Baar K. Vitamin C–enriched gelatin supplementation before intermittent activity augments collagen synthesis. Am J Clin Nutr 2017;105(1):136-143. doi:10.3945/ajc n.116.138594
41. Castarlenas E, Jensen MP, von Baeyer CL, Miró J. Psychometric properties of the numerical rating scale to assess self-reported pain intensity in children and adolescents: a systematic review Clin J Pain 2017;33(4):376-383. doi:10.1097/ajp.00000000000004 06
42. Kahl C, Cleland JA. Visual analogue scale, numeric pain rating scale and the McGill pain Questionnaire: an overview of psychometric properties. Physical Therapy Reviews 2005;10(2):123-128. doi:10.1179/108331905x55776
43. Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (Quick DASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 2006;7(1):44. doi:10.1186/ 1471-2474-7-44
44. Mintken PE, Glynn P, Cleland JA. Psychometric properties of the shortened disabilities of the arm, shoulder, and hand questionnaire (quick dash) and numeric pain rating scale in patients with shoulder pain. J Shoulder Elbow Surg 2009;18(6):920-926. doi:1 0.1016/j.jse.2008.12.015
45. Katsuura Y, Bruce J, Taylor S, Gullota L, Kim HJ. Overlapping, masquerading, and causative cervical spine and shoulder pathology: a systematic review Global Spine J. 2020;10(2):195-208. doi:10.1177/21925 68218822536
46. Tate AR, McClure PW, Young IA, Salvatori R, Michener LA. Comprehensive impairment-based exercise and manual therapy intervention for patients with subacromial impingement syndrome: a case series. J Orthop Sports Phys Ther. 2010;40(8):474-493. doi:10.2519/jospt.2010.3223
47 Somerville LE, Willits K, Johnson AM, et al. Clinical assessment of physical examination maneuvers for superior labral pnterior to posterior lesions. Surg J (N Y) 2017;3(4):e154-e162. doi:10.105 5/s-0037-1606829
48. Gismervik SØ, Drogset JO, Granviken F, Rø M, Leivseth G. Physical examination tests of the shoulder: a systematic review and meta-analysis of diagnostic test performance. BMC Musculoskelet Disord 2017;18(1):41. doi:10.1186/s12891-017-140 0-0
49. Chronopoulos E, Kim TK, Park HB, Ashenbrenner D, McFarland EG. Diagnostic value of physical tests for isolated chronic acromioclavicular lesions. Am J Sports Med. 2004;32(3):655-661. doi:10.1177/0363546 503261723
50. Powell JW, Huijbregts PA. Concurrent criterionrelated validity of acromioclavicular joint physical examination tests: a systematic review Journal of Manual & Manipulative Therapy 2013;14(2):19E-29E. doi:10.1179/jmt.2006.14.2.19e
51. Eshoj H, Ingwersen KG, Larsen CM, Kjaer BH, Juul-Kristensen B. Intertester reliability of clinical shoulder instability and laxity tests in subjects with and without self-reported shoulder problems. BMJ Open 2018;8(3):e018472. doi:10.1136/bmjopen-201 7-018472
52. Duchesne E, Dufresne SS, Dumont NA. Impact of inflammation and anti-inflammatory modalities on skeletal muscle healing: from fundamental research to the clinic. Physical therapy 2017;97(8):807-817 do i:10.1093/ptj/pzx056
53. Patterson SD, Hughes L, Warmington S, et al. Blood flow restriction exercise: considerations of methodology, application, and safety Front Physiol 2019;10:533. doi:10.3389/fphys.2019.00533
54. Drummond MJ, Fujita S, Takashi A, Dreyer HC, Volpi E, Rasmussen BB. Human muscle gene expression following resistance exercise and blood flow restriction. Med Sci Sports Exerc 2008;40(4):691-698. doi:10.1249/mss.0b013e318160ff
55. Van Craenenbroeck EM, Vrints CJ, Haine SE, et al. A maximal exercise bout increases the number of circulating CD34+/KDR+ endothelial progenitor cells in healthy subjects. Relation with lipid profile. J Appl Physiol (1985) 2008;104(4):1006-1013. doi:10.1152/ja pplphysiol.01210.2007
56. Beamer B, Hettrich C, Lane J. Vascular endothelial growth factor: an essential component of angiogenesis and fracture healing. HSS J 2010;6(1):85-94. doi:10.1007/s11420-009-9129-4
57. Baar K. Training and nutrition to prevent soft tissue injuries and accelerate return to play Sports Science Exchange 2015;28(142):1-6.
58. Centeno CJ, Pastoriza SM. Past, Current and future interventional orthobiologics techniques and how they relate to regenerative rehabilitation: A Clinical Commentary. Int J Sports Phys Ther. 2020;15(2):301-325. doi:10.26603/ijspt20200301
59. Wasterlain AS, Braun HJ, Dragoo JL. Contents and formulations of platelet-rich plasma. Operative Techniques in Orthopaedics 2012;22(1):33-42. doi:1 0.1053/j.oto.2011.11.001
60. Takarada Y, Takazawa H, Sato Y, Takebayashi S, Tanaka Y, Ishii N. Effects of resistance exercise combined with moderate vascular occlusion on muscular function in humans. Journal of Applied Physiology 2000;88(6):2097-2106. doi:10.1152/jappl.2 000.88.6.2097
61. Lixandrão ME, Ugrinowitsch C, Berton R, et al. Magnitude of muscle strength and mass adaptations between high-load resistance training versus lowload resistance training associated with blood-flow restriction: a systematic review and meta-analysis. Sports Med 2018;48(2):361-378. doi:10.1007/s4027 9-017-0795-y
62. Ozaki H, Loenneke JP, Buckner SL, Abe T Muscle growth across a variety of exercise modalities and intensities: Contributions of mechanical and metabolic stimuli. Med Hypotheses 2016;88:22-26. do i:10.1016/j.mehy.2015.12.026
63. Fahs CA, Loenneke JP, Thiebaud RS, et al. Muscular adaptations to fatiguing exercise with and without blood flow restriction. Clin Physiol Funct Imaging. 2015;35(3):167-176. doi:10.1111/cpf.12141
64. Escaloni J, Butts R, Dunning J. The use of dry needling as a diagnostic tool and clinical treatment for cervicogenic dizziness: a narrative review & case series. Journal of Bodywork and Movement Therapies. 2018;22(4):947-955. doi:10.1016/j.jbmt.2018.02.015
65. Langevin HM, Schnyer R, MacPherson H, et al. Manual and electrical needle stimulation in acupuncture research: pitfalls and challenges of heterogeneity J Altern Complement Med 2015;21(3):113-128. doi:10.1089/acm.2014.0186
66. Langevin HM, Bouffard NA, Badger GJ, Churchill DL, Howe AK. Subcutaneous tissue fibroblast cytoskeletal remodeling induced by acupuncture: Evidence for a mechanotransduction-based mechanism. J Cell Physiol 2006;207(3):767-774. doi:1 0.1002/jcp.20623
67. Dunning J, Butts R, Fernández-de-Las-Peñas C, et al. Spinal manipulation and electrical dry needling in patients with subacromial pain syndrome: a multicenter randomized clinical trial. J Orthop Sports Phys Ther 2020;(0):1-46.
68. Parmen V, Taulescu M, Ober C, Pestean C, Oana L. Influence of electroacupuncture on the soft tissue healing process. J Acupunct Meridian Stud 2014;7(5):243-249. doi:10.1016/j.jams.2014.03.003
69. de Almeida M dos S, de Aro AA, Guerra F da R, Vieira CP, de Campos Vidal B, Rosa Pimentel E. Electroacupuncture increases the concentration and organization of collagen in a tendon healing model in rats. Connect Tissue Res 2012;53(6):542-547 doi:10.3 109/03008207.2012.710671
70. Alashkham A, Alraddadi A, Felts P, Soames R. Histology, vascularity and innervation of the glenoid labrum. J Orthop Surg (Hong Kong) 2018;26(2):2309499018770900. doi:10.1177/23094990 18770900
71. Baar K. Minimizing injury and maximizing return to play: lessons from engineered ligaments. Sports Med 2017;47(Suppl 1):5-11. doi:10.1007/s40279-01 7-0719-x
72. West DW, Lee-Barthel A, McIntyre T, Shamim B, Lee CA, Baar K. The exercise-induced biochemical milieu enhances collagen content and tensile strength of engineered ligaments. J Physiol. 2015;593(20):4665-4675. doi:10.1113/jp270737
Download: https://ijspt.scholasticahq.com/article/68143-novel-orthobiologic-preparation-and-regenerativerehabilitation-of-a-complex-shoulder-injury-in-a-competitive-adolescent-female-athlete/attachment/ 135721.docx?auth_token=BwoF44jiquxJmcai6ioM
Bullock G, Collins G, Adams R, Thigpen C, Shanley E. Personalized Injury Reduction Strategies in Sports Medicine: Lessons Learned from Advances in Breast Cancer Treatment: A Clinical Commentary. IJSPT. Published online February 1, 2023:253-261.
7
Garrett Bullock 1,2,3 a , Gary Collins 4,5 , Rober Adams 6 , Charles
Thigpen7 , Ellen
Shanley1 Department of Orthopaedic Surgery, Wake Forest School of Medicine, 2 Department of Biostatistics and Data Science, Wake Forest School of Medicine, 3 Centre for Sport, Exercise and Osteoarthritis Research Versus Arthritis, University of Oxford, 4 Centre for Statistics in Medicine, Nuffield Department of Orthopaedics, Rheumatology, and Musculoskeletal Sciences, University of Oxford, 5 Oxford University Hospitals NHS Foundation Trust, 6 Department of Radiation Oncology, University of North Carolina School of Medicine, 7 ATI Physical Therapy
Keywords: Risk, Risk Management, Prediction, Confounding
https://doi.org/10.26603/001c.57680
Injury rates across sport have risen over the past twenty years, despite increased efforts in training and injury prevention. The rise in injury rates suggest that current approaches to estimating injury risk and risk management are not effective. One factor limiting progress is the inconsistency in screening, risk assessment, and risk management strategies to guide injury mitigation approaches.
How can sports physical therapists identify and apply lessons learned from other healthcare fields to improve athlete injury risk and risk management strategies?
Breast cancer mortality has consistently decreased over the last 30 years, largely attributed to advances in personalizing the prevention and treatment strategies which include modifiable and non-modifiable factors when assessing risk, the transition to personalized medicine, and the systematic approach used to investigate individual risk factors. Three critical phases have facilitated the identification and importance of individual risk factors and developing targeted, personalized strategies for breast cancer risk including:
1) Establishing the potential relationship between factors and outcomes;
2) Prospectively investigate the strength and direction of the relationship;
3) Investigating if intervening on identified factors alters prognosis.
Applying lessons learned from other healthcare fields could improve shared decision making between the clinician and athlete concerning risk assessment and management. Examples include calculating only non-modifiable risk, creating individualized screening schedules based on risk assessment, or calculating the influence of each intervention on the athlete’s injury risk. A systematic approach to identify and intervene on risk is needed to improve athlete outcomes.
Corresponding author:
 Garrett S. Bullock, PT, DPT, DPhil
Garrett S. Bullock, PT, DPT, DPhil
Department of Orthoaedic Surgery & Rehabilitation
Wake Forest School of Medicine
475 Vine St. Winston-Salem, North Carolina, 27101
Email: garrettbullock@gmail.com
The World Health Organization Physical Activity Action Plan identifies that sport is an underutilized, yet important, physical activity contributor 1 However, sport participation has inherent injury risk,2,3 with 30% of all emergency department visits due to sport injury.4 Injury rates continue to rise, with a 35% increase in female soccer anterior cruciate ligament tears over 25 years.3 The rise in injury rates suggest that current approaches to estimating injury risk and risk management are not effective.5 One factor limiting progress is the inconsistency in screening, risk assessment, and risk management strategies to guide injury mitigation approaches. For example, individual potential risk factors are often times preemptively deemed important in all sport sub populations, when in reality, additional larger and repeated studies are needed to understand the generalizability of a specific risk factor.5 This spuriously concludes a ‘catch all’ risk factor at all competition levels, when this specific risk factor may only be influential in a sub-population, or worse, demonstrate no actual risk due to influence from another confounding variable, providing biased injury risk results.5,6
In order to improve our understanding of injury risk, and move towards effective injury mitigation in sport physical therapists and clinical researchers must apply lessons from other healthcare professions. One medical disease that has steadily demonstrated improved patient outcomes is breast cancer.7–9 The inclusion of both modifiable and non-modifiable factors when assessing risk,10,11 the transition to personalized medicine,10,12,13 and the systematic approach used to investigate individual risk factors14 have created a system that can be replicated in other fields of medicine. Therefore, the purpose of this commentary is to describe breast cancer risk research and risk management strategies and how these strategies can be implemented in sport, using baseball as a practical example, to improve athlete outcomes.
One sport that is highly researched for injury risk is baseball.15–18 A 2019 scoping review reported that 678 studies focused on baseball research.19 Baseball is played throughout the world, with 160 countries associated with the World Baseball and Softball Federation.20 Over 16 million people participate in baseball within the United States alone, with professional leagues throughout Australasia, Latin America, and North America.20,21 Baseball is considered a relatively safe sport but injury rates have more than doubled over the last two decades.15,17,22,23 Injury incidence ranges from 0.8 to 4.0 injuries per 1,000 athlete exposures.24–31 with the greatest incidence attributed to the shoulder,15,23 elbow,17,23,32 and trunk,23 with throwing overuse injuries being the most common.25,33 The number of injuries is greater compared to other throwing sports.28,29,31 Baseball players have a greater risk of injury (1.7 times greater odds) compared to softball players, and pitchers with a 4.57
greater odds compared to position players.29 Injury burden is high, with time loss, replacement, and health care costs continuing to rise at all baseball levels.34 The escalation in frequency,2,3,7,21,23,33–35 severity,28,29,36 and cost34 of injuries in baseball suggests that the approaches to understanding and preventing baseball injuries are not effective.
The available empirical evidence has identified only a fraction of the complex interactions of risk factors in baseball.19,37 A primary limitation of current baseball research is that there are no prospective studies examining multiple intrinsic and extrinsic risk factors to inform injury prevention programs. Previous studies do not control for nonmodifiable confounders that can act as effect modifiers changing the impact of the study variables on the ultimate outcome 15,35,38,39 Further, the focus of previous research has often been on one specific physical factor in isolation,15–18 without attempting to control for or understand its relation to other modifiable and non-modifiable confounders. Therefore, the complex interaction of multiple risk factors and injury mechanisms are unclear and inhibit clinical examination, prevention strategies, and clinical decision making.
Breast cancer mortality has consistently decreased over the last 30 years,7,8 largely attributed to advances in personalizing the prevention and treatment strategies which include modifiable and non-modifiable factors when assessing risk,10,11,40 the transition to personalized medicine,10,12,13 and the systematic approach used to investigate individual risk factors (Figure 1).14 These key steps have seen decreased breast cancer mortality rates by 6.9% from 2002 to 2006 alone, with an average of a 2% decrease per year in Europe.41 Within the United States, breast cancer mortality has decreased by 38% from 1990-2003.9 These reductions in mortality trends have been observed across all age groups,9,41 and particularly in younger women.9
Besides advances in surgical42 and chemotherapy treatments,43 the improvements in breast cancer survival have been attributed to innovations in breast cancer screening, risk assessment, and risk management.10,12,13 Risk assessment is defined as a, “systematic approach to characterizing adverse exposures.”44,45 While risk management is defined as selecting strategies to reduce risk of the outcome.44 In order to improve attributable risk identification and management, the United States Preventive Services Task Force in 2009 changed their breast cancer mammography screening guidelines, stating, “screening should be an individual one and take into account patient context, including the patient’s values regarding specific benefits and harms (pg. 294).”46 These alterations were implemented due to specific changes in understanding of breast cancer risk, particularly in the advent of personalized medicine.
Personalized medicine is defined as when medical treatment is customized for an individual patient.47 Within
breast cancer, personalized medicine has been implemented due to the understanding and inclusion of both modifiable and non-modifiable risk factors when assessing outcome risk. For example, the advent of genetic research, specifically investigations of the BRCA1 & BRCA2 genes and single nucleotide polymorphisms (SNPS),12,13 and their relationships to breast cancer have created a better understanding of non-modifiable risk.10,11 The inclusion of nonmodifiable risk factors helps guide shared decision making between the clinician and patient on screening strategies and potential primary and secondary risk management approaches for modifiable factors.10 For example, if the 10-year breast cancer risk is higher for a specific 40-yearold, compared to the average 50-year-old, it may be advantageous to begin mammogram breast cancer screening 10 years prior to the nationally recommended screening age.10 The understanding of non-modifiable risk may also inform how intervening on modifiable risk factors will change breast cancer risk. Modifiable breast cancer risk factors include changes in weight after the individual reaches 18 years old to present age, physical activity habits, nutrition, and alcohol consumption.11,48 A clinician can calculate if intervening on these modifiable risk factors (through educational, lifestyle, and medical interventions), changes a particular patient’s breast cancer risk. This information helps apprise the clinician on the cost benefit of different screening measures (such as MRI versus traditional mammogram), the potential intensity and adherence needed to focus on modifiable risk factor interventions, and potential educational counselling on false positive tests (in case increased screening is required) to create a more individualized tailored medical approach.10,48
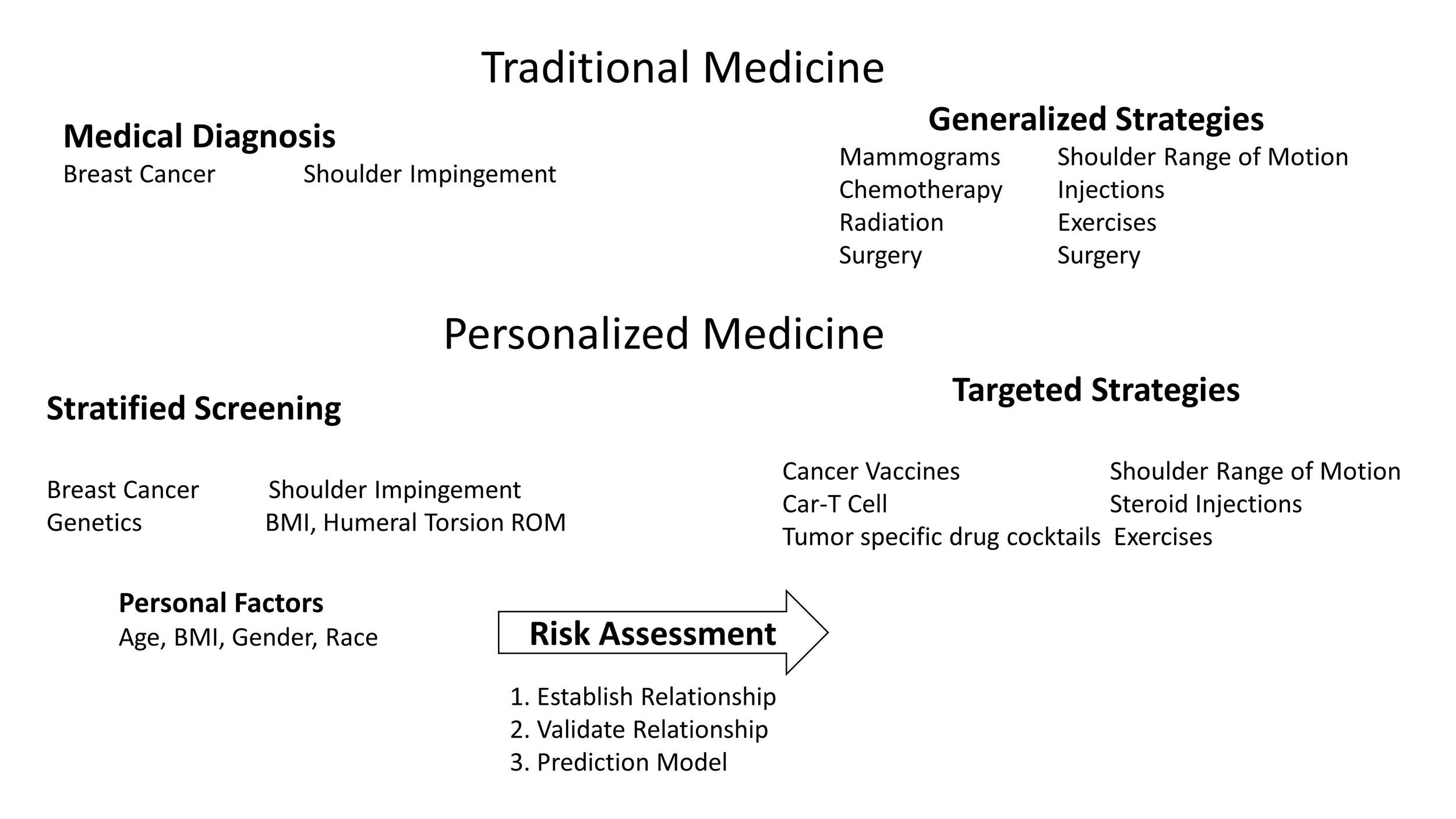
So far, we have briefly highlighted screening, risk assessment, and management strategies in breast cancer The question of how this applies to sport, which does not deal with life and death, but at worst, career ending injuries needs to be answered? Currently, baseball injury risk and risk management does not account for non-modifiable risk factors, and assumes equal risk between all populations and subgroups. Within breast cancer, a systematic approach has been proposed to investigate potential risk factors and incorporate these risk factors into one comprehensive risk assessment.14 This systematic approach can be used as a template for improving baseball outcomes and more generally in sport.
Three critical phases have facilitated the identification and importance of individual risk factors and developing targeted, personalized strategies for breast cancer risk.14 First, level one studies establish the potential relationship(s) between factors and outcomes of interest, which generates future, testable hypotheses. These studies identify statistical relationships between a potential risk factor and the outcome, without controlling for confounders. Baseball research remains at this level. Level two studies prospectively investigate the strength and direction of the relationship between the risk factor and outcome, while controlling for confounding. These studies can also investigate potential sub group relationship differences between the risk factor and outcome. Within baseball, this is the next logical step in risk factor research and can be easily implemented through replicating past study designs and cohorts, while controlling for confounders. Level three
Figure 1. Three Steps to Assess and Intervene on Outcome Risk Using a Disease and a Musculoskeletal Examplestudies can entail prediction model development and validation studies seeking to understand if intervening on a factor alters prognosis.14 Within baseball, randomized control trials on modifiable risk factors and the development and validation of prediction models is warranted to better calculate injury risk and improve risk management.
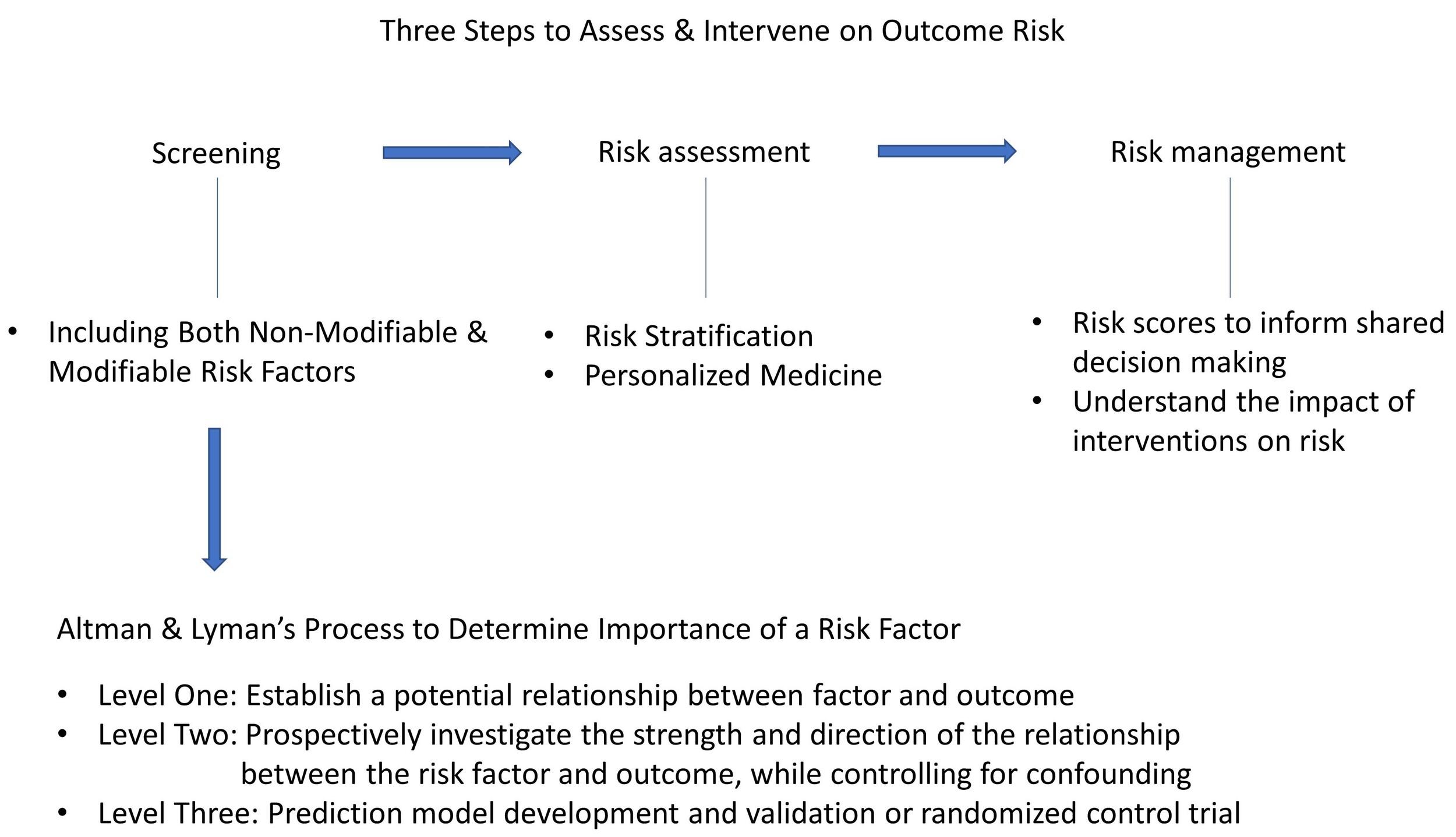
To use a hypothetical example for context, a clinician scientist wants to understand if shoulder range of motion is a risk factor for arm injuries in baseball pitchers. To initially investigate this issue, this clinician scientist performed a level one retrospective cohort study, in which shoulder range of motion was compared between injured and non-injured baseball pitchers. The clinician scientist could perform an analysis of variance (ANOVA) or a logistic regression to ascertain if there are differences in shoulder range of motion between injured and non-injured baseball players. In this hypothetical example, a 20º difference in total shoulder rotation (external plus internal shoulder rotation) was observed between injured and non-injured pitchers, which is beyond the standard error of measure and minimum clinically importance difference.49 From these findings, the clinician scientist surmises that shoulder range of motion might be an injury risk factor in baseball pitchers. However, the clinician scientist knows there are specific biases that need to be controlled for in order to help understand if this is truly a risk factor
Following the level one study results, the researcher decided to perform a level two prospective study on shoulder range of motion. Shoulder range of motion was measured in spring training, along with potential confounders, including hand dominance, body mass index,50 injury history,51 shoulder strength,52 lower extremity range of motion,53 balance,32,35 and pitch velocity 54 Each pitcher was followed for the entire season with injuries and total athlete
exposures (in the form of pitching appearances and number of pitches) collected. The clinician scientist then performs a Cox survival analysis or a relative risk regression to compare injured versus non-injured pitchers. The clinician scientist also performs sub group analyses for left and right handers, as these sub populations have demonstrated different clinical phenotypes, including demonstrating different height,55 mass,50 humeral torsion,56,57 and pitch velocity.58 The clinician scientist observed that there is still a difference in total shoulder rotation between injured and non-injured pitchers, which after controlling for all confounders, is 12º. Further when analyzing left and right handers separately, left handers demonstrated a 9º difference and right handers demonstrated a 15º difference. These differences between left and right handers were beyond the standard error of measure and thus suggests there may be clinical differences in shoulder rotation injury risk between hand dominance. The clinician scientist hypothesizes that shoulder range of motion can be used to help ascertain injury risk and should be intervened upon. However, before interventions can be recommended, these risk factor needs to be assessed for efficacy in relation to modifiable and non-modifiable risk factors, and if there is a causal relationship between shoulder range of motion and injury. Examples of a non-modifiable risk factors include age, humeral torsion,56,57 and previous arm surgical history
To answer these level three questions, the clinician scientist performs a multiyear prospective study, including both modifiable and non-modifiable risk factors, to develop a prediction model. The developed prediction model demonstrated good prediction performance following best practice guidelines and improved with the inclusion of shoulder range of motion as a predictor.59 The clinician sci-
Figure 2. Three Phases to Defining a Risk Factorentist then performs a clustered randomized control trial performing manual therapy to the shoulder in the treatment arm and standard care (not including manual therapy) performed in the control arm for an entire season. The research determines that there is a 30% reduction in arm injuries in the treatment arm compared to the control arm. When assessing the intervention effectiveness in left and right handers, it is observed that left handers demonstrated a 20% reduction in injury rates and right handers a 40% reduction in injury rates. The clinician scientist concludes that intervening on this modifiable risk factor, using the prediction model to identify pitchers at risk for injury, can help decrease arm injury risk in pitchers. Further, modifying shoulder range of motion has different injury risk management effectiveness (20% difference) between left and right handers.
The proposed approach is not reflected in the current state and progression and sport injury risk screening, assessment and intervention strategies. To use a baseball clinical example, current best evidence-based practice suggests that baseball pitchers are at a higher risk for injury when a pitcher’s dominant (throwing) shoulder total range of motion is 10º less than the non-dominant (non-throwing) shoulder 17,60 Current clinical decisions would recommend that this at-risk pitcher would receive specific shoulder range of motion interventions (such as stretching and manual therapy), until the pitcher’s dominant shoulder total range of motion was below 10º different than their nondominant shoulder 61 The current best practice recommendation implies that this will effectively mitigate this particular pitcher’s injury risk through this specific intervention. A current limitation with this approach includes assuming that all populations and subgroups demonstrate a similar risk relationship between the proposed risk factor and injury Further, it is ambiguous if this particular injury risk would be managed through this intervention, due to lack of specific understanding as to how this particular risk factor relates to other modifiable and nonmodifiable risk factors and if there is a causal relationship between shoulder range of motion deficits and arm injuries in baseball pitchers.
The sports medicine and research community could gain insight from the lessons learned and implemented in breast cancer. These experiences could help improve a particular pitcher’s current injury risk assessment and allow for personalized interventions. Improved injury risk assessment would be ascertained by accounting for non-modifiable risk
factors such as the pitcher’s injury history,51 previous pitching exposure,62 pitching mechanics,37 and osseous adaptation.63 Understanding how these non-modifiable risk factors interplay with the modifiable shoulder range of motion risk factor,17,60 along with other modifiable risk factors such as shoulder strength52 and balance,32,35 could be enhanced though controlling for confounders in prospective injury risk studies from previous level one studies. Development of an injury prediction model would be a logical progression within the tiered level three study paradigm. This information could then be used in shared decision making between the clinician and athlete concerning risk management. Specifically, calculating current injury risk could determine if individualized screening schedules throughout the season are warranted, beyond the traditional preseason screening. One could also calculate only non-modifiable injury risk, which would illuminate how intervening on all modifiable risk factors would potentially impact risk mitigation strategies. Another option would be to calculate the influence of each intervention on the athlete’s injury risk, providing a better plan for creating a personalized approach to their risk management.
These are only a few of the potential next steps that could improve sport injury research and inform clinical practice across body regions, specific injuries, and athlete groups. It should be noted that current practice suggests taking detailed patient histories should be followed by performing a thorough and comprehensive physical exam. However, each of these pieces are not amalgamated into one comprehensive injury risk assessment nor risk management strategies (such as understanding casual factors or a comprehensive prediction model), and considered in isolation from a risk assessment and management perspective. Learning and implementing lessons from medical research and services for diseases such as breast cancer, would only improve patient care in the sports medicine setting.
Current research, athlete screening, risk assessment, and risk management are ineffective in sport, demonstrated by the continued rise in injury rates and severity over the last twenty years.15,17,22,23 As demonstrated through breast cancer screening strategies,10,11,48 an improved understanding of risk is not ascertained without the inclusion of both modifiable and non-modifiable risk factors. Until the sport community applies the lessons learned from other health care professions, sport injury outcomes will be suboptimal, continuing to provide a disservice to athletes.
Submitted: April 11, 2022 CST, Accepted: November 30, 2022
CST This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. World Health Organization. Global Action Plan on Physical Activity 2018-2030: More Active People for a Healthier World. World Health Organization; 2019.
2. Emery CA, Meeuwisse WH, McAllister JR. Survey of sport participation and sport injury in Calgary and area high schools. Clin J Sport Med. 2006;16(1):20-26. doi:10.1097/01.jsm.0000184638.72075.b7
3. Agel J, Rockwood T, Klossner D Collegiate ACL injury rates across 15 sports: national collegiate athletic association injury surveillance system data update (2004-2005 through 2012-2013). Clin J Sport Med. 2016;26(6):518-523. doi:10.1097/jsm.000000000 0000290
4. Kang J, Hagel B, Emery CA, Senger T, Meeuwisse W. Assessing the representativeness of Canadian Hospitals Injury Reporting and Prevention Programme (CHIRPP) sport and recreational injury data in Calgary, Canada. Int J Inj Control Safe Promot. 2013;20(1):19-26. doi:10.1080/17457300.2012.656315
5. Bahr R. Why screening tests to predict injury do not work—and probably never will…: a critical review. Br J Sports Med 2016;50(13):776-780. doi:10.1136/bjs ports-2016-096256
6. Meeuwisse WH. Assessing causation in sport injury: a multifactorial model. Clin J Sport Med. 1994;4(3):166-170. doi:10.1097/00042752-19940700 0-00004
7. La Vecchia C, Bosetti C, Lucchini F, et al. Cancer mortality in Europe, 2000–2004, and an overview of trends since 1975. Ann Oncol 2010;21(6):1323-1360. doi:10.1093/annonc/mdp530
8. Levi F, Bosetti C, Lucchini F, Negri E, La Vecchia C. Monitoring the decrease in breast cancer mortality in Europe. Eur J Cancer Prevent. 2005;14(6):497-502. do i:10.1097/00008469-200512000-00002
9. Jatoi I, Chen BE, Anderson WF, Rosenberg PS. Breast cancer mortality trends in the United States according to estrogen receptor status and age at diagnosis. J Clin Oncol 2007;25(13):1683-1690. doi:1 0.1200/jco.2006.09.2106
10. Maas P, Barrdahl M, Joshi AD, et al. Breast cancer risk from modifiable and nonmodifiable risk factors among white women in the United States. JAMA Oncol 2016;2(10):1295-1302. doi:10.1001/jamaonco l.2016.1025
11. Sprague BL, Trentham-Dietz A, Egan KM, TitusErnstoff L, Hampton JM, Newcomb PA. Proportion of invasive breast cancer attributable to risk factors modifiable after menopause. Am J Epidemiol 2008;168(4):404-411. doi:10.1093/aje/kwn143
12. Olopade OI, Grushko TA, Nanda R, Huo D. Advances in breast cancer: pathways to personalized medicine. Clin Cancer Res 2008;14(24):7988-7999. do i:10.1158/1078-0432.ccr-08-1211
13. Mavaddat N, Michailidou K, Dennis J, et al. Polygenic risk scores for prediction of breast cancer and breast cancer subtypes. Am J Human Genetics. 2019;104(1):21-34. doi:10.1016/j.ajhg.2018.11.002
14. Altman DG, Lyman GH. Methodological challenges in the evaluation of prognostic factors in breast cancer Breast Cancer Res Treat 1998:379-393.
15. Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med 2011;39(2):329-335. doi:10.1177/0363546510384223
16. Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in Glenohumeral Passive Range of Motion Increase Risk of Shoulder Injury in Professional Baseball Pitchers: A Prospective Study. Am J Sports Med. 2015;43(10):2379-2385. doi:10.1177/03635465155943 80
17. Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: a prospective study. Am J Sports Med. 2014;42(9):2075-2081. doi:10.1177/036354651453839
18. Wilk KE, Macrina L, Fleisig GS, et al. Glenohumeral passive range of motion and the correlation to elbow injuries in professional baseball pitchers. Orthop J Sports Med. 2013;1(4 Supplement 1):2325967113S0001. doi:10.1177/2325967113s00017
19. Bullock GS, Uhan J, Harriss EK, Arden NK, Filbay SR. The Relationship Between Baseball Participation and Health: A Systematic Scoping Review J Orthop Sports Phys Ther 2020;50(2):55-66. doi:10.2519/josp t.2020.9281
20. Kelly WW Is baseball a global sport? America’s ‘national pastime’ as global field and international sport. Global Networks. 2007;7(2):187-201. doi:10.111 1/j.1471-0374.2007.00164.x
21. Kelly M. Participation in baseball on the rise. Published 2019. https://www.mlb.com/news/basebal l-participation-increases
22. Conte S, Camp CL, Dines JS. Injury trends in Major League Baseball over 18 Seasons: 1998-2015. Am J Orthop (Belle Mead NJ) 2016;45(3):116-123.
23. Posner M, Cameron KL, Wolf JM, Belmont PJ Jr, Owens BD. Epidemiology of Major League Baseball injuries. Am J Sports Med 2011;39(8):1675-1691. do i:10.1177/0363546511411700
24. Bonza JE, Fields SK, Yard EE, Dawn Comstock R. Shoulder injuries among United States high school athletes during the 2005-2006 and 2006-2007 school years. J Athl Train. 2009;44(1):76-83. doi:10.4085/106 2-6050-44.1.76
25. Collins CL, Comstock RD Epidemiological features of high school baseball njuries in the United States, 2005-2007 Pediatrics 2008;121(6):1181-1187 doi:10.1542/peds.2007-2572
26. Kerr ZY, Roos KG, Djoko A, Dompier TP, Marshall SW. Rankings of high school sports injury rates differ based on time loss assessments. Clin J Sport Med 2016;27(6):548-551. doi:10.1097/jsm.0000000000000 405
27 Krajnik S, Fogarty KJ, Yard EE, Comstock RD Shoulder injuries in US high school baseball and softball athletes, 2005-2008. Pediatrics. 2010;125(3):497-501. doi:10.1542/peds.2009-0961
28. Powell JW, Barber-Foss KD Injury patterns in selected high school sports: a review of the 1995-1997 seasons. J Athl Train 1999;34(3):277-284.
29. Pytiak AV, Kraeutler MJ, Currie DW, McCarty EC, Comstock RD. An Epidemiological comparison of elbow injuries among United States high school baseball and softball Players, 2005-2006 Through 2014-2015. Sports Health. 2018;10(2):119-124. doi:1 0.1177/1941738117736493
30. Saper MG, Pierpoint LA, Liu W, Comstock RD, Polousky JD, Andrews JR. Epidemiology of shoulder and slbow injuries among United States high school baseball players: school years 2005-2006 through 2014-2015. Am J Sports Med. 2018;46(1):37-43. doi:1 0.1177/0363546517734172
31. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS. Incidence of injuries in high school softball and baseball players. J Athl Train 2011;46(6):648-654. do i:10.4085/1062-6050-46.6.648
32. Garrison JC, Johnston C, Conway JE. Baseball players with ulnar collateral ligament tear demonstrate decreased rotator cuff strength compared to healthy controls. Int J Sports Phys Ther. 2015;10(4):476-481.
33. Petty DH, Andrews JR, Fleisig GS, Cain EL. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med 2004;32(5):1158-1164. doi:1 0.1177/0363546503262166
34. Knowles SB, Marshall SW, Miller T, et al. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj Prev 2007;13(6):416-421. doi:10.1136/ip.2006.014720
35. Garrison JC, Arnold A, Macko MJ, Conway JE. Baseball players diagnosed with ulnar collateral ligament tears demonstrate decreased balance compared to healthy controls. J Orthop Sports Phys Ther 2013;43(10):752-758. doi:10.2519/jospt.2013.46 80
36. Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of medial ulnar collateral ligament reconstruction. Am J Sports Med. 2016;44(3):729-734. doi:10.1177/0363546515622407
37 Bullock GS, Menon G, Nicholson K, Butler RJ, Arden NK, Filbay SR. Baseball pitching biomechanics in relation to pain, injury, and surgery: A systematic review J Sci med Sport 2021;24(1):13-20.
38. Hannon J, Garrison JC, Conway J. Lower extremity balance is improved at time of return to throwing in baseball players after an ulnar collateral ligament reconstruction when compared to pre-operative measurements. Int J Sport Phys Ther 2014;9(3):356-364.
39. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sports Med 2011;39(9):1997-2006. doi:10.1177/ 0363546511408876
40. Krzyszczyk P, Acevedo A, Davidoff EJ, et al. The growing role of precision and personalized medicine for cancer treatment. Technology 2018;6(03n04):79-100. doi:10.1142/s23395478183000 20
41. Bosetti C, Bertuccio P, Levi F, Chatenoud L, Negri E, La Vecchia C. The decline in breast cancer mortality in Europe: an update (to 2009). The Breast 2012;21(1):77-82. doi:10.1016/j.breast.2011.08.001
42. Ruiterkamp J, Ernst MF, van de Poll-Franse LV, Bosscha K, Tjan-Heijnen VCG, Voogd AC. Surgical resection of the primary tumour is associated with improved survival in patients with distant metastatic breast cancer at diagnosis. Eur J Surg Onc 2009;35(11):1146-1151. doi:10.1016/j.ejso.2009.03.01
43. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;365(9472):1687-1717 doi:10.1016/s014 0-6736(05)66544-0
44. Samet JM, Schnatter R, Gibb H. Invited commentary: epidemiology and risk assessment. Am J Epidemiol. 1998;148(10):929-936. doi:10.1093/oxfordj ournals.aje.a009569
45. Council NR. Risk Assessment in the Federal Government: Managing the Process.; 1983.
46. United States Preventative Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009;151(10):716-726. doi:10.7326/0003-4819-151-1 0-200911170-00008
47 Hamburg MA, Collins FS. The path to personalized medicine. N Engl J Med. 2010;363(4):301-304. doi:10.1056/nejmp1006304
48. Tamimi RM, Spiegelman D, Smith-Warner SA, et al. Population attributable risk of modifiable and nonmodifiable breast cancer risk factors in postmenopausal breast cancer Am J Epidemiol 2016;184(12):884-893. doi:10.1093/aje/kww145
49. Hayes K, Walton JR, Szomor ZL, Murrell GA. Reliability of five methods for assessing shoulder range of motion. Aus J Physiother. 2001;47(4):289-294. doi:10.1016/s0004-9514(14)6027
4-9
50. Forsythe CM, Crotin RL, Greenwood M, Bhan S, Karakolis T. Examining the influence of physical size among major league pitchers. J Sport Med Phys Fit 2016;57(5):572-579.
51. Kucera KL, Marshall SW, Kirkendall DT, Marchak P, Garrett WE. Injury history as a risk factor for incident injury in youth soccer Br J Sports Med 2005;39(7):462-462. doi:10.1136/bjsm.2004.013672
52. Byram IR, Bushnell BD, Dugger K, Charron K, Harrell FE Jr, Noonan TJ. Preseason shoulder strength measurements in professional baseball pitchers: identifying players at risk for injury Am J Sports Med 2010;38(7):1375-1382. doi:10.1177/036354650936040
53. Li X, Ma R, Zhou H, et al. Evaluation of hip internal and external rotation range of motion as an injury risk factor for hip, abdominal and groin injuries in professional baseball players. Orthop Rev. 2015;7(4). doi:10.4081/or.2015.6142
54. Bushnell BD, Anz AW, Noonan TJ, Torry MR, Hawkins RJ. Association of maximum pitch velocity and elbow injury in professional baseball pitchers. Am J Sports Med 2010;38(4):728-732. doi:10.1177/03 63546509350067
55. Loffing F, Hagemann N. Performance differences between left-and right-sided athletes in one-on-one interactive sports. In: Laterality in Sports Elsevier; 2016:249-277.
56. Takeuchi S, Yoshida M, Sugimoto K, Tsuchiya A, Takenaga T, Goto H. The differences of humeral torsion angle and the glenohumeral rotation angles between young right-handed and left-handed pitchers. J Shoulder Elbow Surg 2019;28(4):678-684. d oi:10.1016/j.jse.2018.09.002
57 Takenaga T, Goto H, Sugimoto K, et al. Lefthanded skeletally mature baseball players have smaller humeral retroversion in the throwing arm than right-handed players. J Shoulder Elbow Surg 2017;26(12):2187-2192. doi:10.1016/j.jse.2017.07.014
58. Solomito MJ, Ferreira JV, Nissen CW. Biomechanical differences between left- and righthanded baseball pitchers. Sports Biomech 2017;16(2):143-151. doi:10.1080/14763141.2016.1186 725
59. Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD) the TRIPOD statement. Circulation 2015;131(2):211-219. doi:10.1161/circulationaha.11 4.014508
60. Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in glenohumeral passive range of motion increase risk of shoulder injury in professional baseball pitchers: a prospective study Am J Sports Med 2015;43(10):2379-2385. doi:10.1177/03635465155943 80
61. Bailey LB, Thigpen CA, Hawkins RJ, Beattie PF, Shanley E. Effectiveness of manual therapy and stretching for baseball players with shoulder range of motion deficits. Sports Health 2017;9(3):230-237 do i:10.1177/1941738117702835
62. Erickson BJ, Chalmers PN, Axe MJ, Romeo AA. Exceeding pitch count recommendations in Little League baseball increases the chance of requiring Tommy John surgery as a professional baseball pitcher Orthop J Sport Med 2017;5(3):232596711769508. doi:10.1177/2325967117
695085
63. Noonan TJ, Thigpen CA, Bailey LB, et al. Humeral torsion as a risk factor for shoulder and elbow injury in professional baseball pitchers. Am J Sports Med 2016;44(9):2214-2219. doi:10.1177/036354651664843 8
1 Denver Nuggets Basketball Club, 2 New York Red Bulls, 3 School of Physical Therapy, Regis University
Keywords: Manual Therapy, Sports Physical Therapy, Symptom-Modification, Pain https://doi.org/10.26603/001c.67936
Symptom modification techniques have been recently dichotomously labeled as either passive or active therapies. Active therapy such as exercise has been rightfully advocated for while “passive” therapies, mainly manual therapy have been regarded as low value within the physical therapy treatment spectrum. In sporting environments where physical activity and exercise are inherent to the athletic experience, the utilization of exercise-only strategies to manage pain and injury can be challenging when considering the demands and qualities of a sporting career which include chronically high internal and external workloads. Participation may be impacted by pain and its influence on related factors such as training and competition performance, career length, financial earning potential, educational opportunity, social pressures, influence of family, friends, and other key stakeholders of their athletic activity. Though highly polarizing viewpoints regarding different therapies create black and white “sides,” a pragmatic gray area regarding manual therapy exists in which proper clinical reasoning can serve to improve athlete pain and injury management. This gray area includes both historic positive reported short-term outcomes and negative historical biomechanical underpinnings that have created unfounded dogma and inappropriate overutilization. Applying symptom modification strategies to safely allow the continuation of sport and exercise requires critical thinking utilizing not only the evidence-base, but also the multi-factorial nature of sports participation and pain management. Given the risks associated with pharmacological pain management, the cost of passive modalities like biophysical agents (electrical stimulation, photobiomodulation, ultrasound, etc), and the indications from the evidence-base when combined with active therapies, manual therapy can be a safe and effective treatment strategy to keep athletes active.
Level of Evidence 5
Physical therapy is at the forefront of promoting movement, maximizing health care, and minimizing the medical burden placed on society It has been identified as a costeffective means to reduce the medical burden on individuals and society, especially when access to physical therapy is provided early in the course of care.1–3 In particular, sports physical therapy and rehabilitation is crucial to limiting the burden of injuries and pain on athletes.4–6 Despite the focus on active movement-based strategies, restoration
Corresponding author:
 Steven M Short Denver Nuggets Basketball Club 1000 Chopper Circle Denver, CO,
Steven M Short Denver Nuggets Basketball Club 1000 Chopper Circle Denver, CO,
USA
steveshortdpt@gmail.com
of prior activities and overall clinical outcomes is often limited by pain and related deficits such as motor inhibition, altered movement patterns, and activity impairments within sport (i.e inability to perform tasks such as running, jumping etc).
Pain and our society’s understanding of pain have led to growing medicalization of numerous conditions such as non-specific low back pain, various tendinopathies, and an array of arthropathies. Additionally, conditions such as non-specific low back pain are driving factors towards the management of pain over the prioritization of function and
movement. Often the front line to managing pain in orthopedic and sports medicine conditions is one of pharmacological nature, including non-steroidal anti-inflammatory drugs (NSAIDs) and opioids, despite numerous documented adverse reactions (gastrointestinal, renal, delayed bony and soft tissue healing, addiction, etc).7,8 Pain is not necessarily indicative of tissue injury, and in sporting environments, it is important to differentiate injury, the impact of pain on the perceived safety of sporting participation, and related pain management.9 The demands of training and competition on athletes and the associated biopsychosocial responses can elicit varying pain responses.10 For the sports medicine professional, safe, low cost symptom modifying tools may have a place in reducing medicalization and unnecessary imaging, pharmacological use, and overall medical utilization while increasing patient autonomy
Orthopedic manual physical therapy is a specialty area of practice that is based on manual examination and a myriad of treatment techniques applied through clinical reasoning. These techniques include integrating exercise, patient education, and other physical therapy modalities to address pain, loss of function, and wellness.11 It is important to note that the definition and application of manual therapy practice is evolving and requires consistency to improve its usefulness in patient care.12 Current definitions and utilization of manual therapy are not passive, and labeling as such discredits its application.13 While the overall strength of evidence supporting manual therapy is limited,14 Level 1 and 2 randomized controlled trials have offered indications for utilization to improve short-term outcomes.15 Manual therapy has been identified as a cost-effective and low risk means to assist in the management of pain and modify symptoms to promote movement.2,14,16 Further, early manual therapy was also associated with a lower likelihood of receiving magnetic resonance imaging (MRI),17 pain management injections, and opioids, as compared with late manual therapy.18 When applied appropriately, there is the potential to reduce overmedicalization of orthopedic conditions often seen in athletics.15,19
A combination of the scientific process and modern methods of information distribution such as social media, have identified the value and importance of exercise not just within the physical therapy profession, but in health care as a whole.20,21 While “active” exercise therapies such as heavy-slow resistance and sprint training hold a primary function in the management of athletes, exercise may not always provide the desired analgesic and therapeutic effect when the athlete is already in pain, be it either acute or chronic.22 Further, in those with chronic pain, exercise induced hypoalgesia is reduced,23 potentially limiting its effectiveness. Thus, persistent pain with various therapeutic exercise or sporting exercise that does not achieve hypoalgesia for an athlete may facilitate chronic pain habits, ongoing medicalization, and likely requires intervention strategies beyond just “active” exercise therapies. Often,
athletes are already hitting a prescribed level of exercise load, resulting in an era of load management and that focuses on a sweet spot of comprehensive exercise load. Pain itself is often a barrier to the numerous benefits of exercises and additional strategies and interventions may be needed to maximize the benefits of exercise and enhance sport participation.24 Thus, there is a place in clinical practice for symptom management and addressing pain with manual therapy while maintaining adequate sporting qualities through training.
When appropriately applied in an athletic setting, manual therapy may elicit short-term effects that enable a more enjoyable, manageable and sustained exercise experience.10,25 Reductions in pain, increased perceptual recovery and reducing athlete injury anxiety may lead to reduced injury risk and improved confidence in performance.26 In doing so, physical therapists are maximizing their practice by assisting in long-term, comprehensive musculoskeletal management and can facilitate physical activity longevity and favorable health care outcomes beyond an athlete’s playing career 3,10,27,28
Physical therapy and manual therapy is not without risk.29 As with all health interventions, providers must weigh the risk against potential benefits of various treatments available to the patient and clinician. The risk of major adverse events in manual therapy is very low, including manipulation to the cervical spine, and has been shown to be lower than the risk of taking various medications and similar to that of exercise and control/passive/sham interventions.30 Furthermore, even with a significant body of research surrounding manual therapy, papers generally provide minimal detail regarding volume, intensity and descriptions of techniques. In general research has indicated limited value to manual therapy because of the common issues of small effect sizes and absence of documented long-term positive effects on outcomes.12
A significant and frequent danger when providing manual therapy is the utilization of nociceptive language.31–33 Language that is dated, focusing on inaccurate pathoanatomic nature in examination34 and injury mechanism,35 specificity of technique,36 and unreasonable expectations of outcomes related to techniques37 are common pitfalls. An overreliance on unsupported biomechanical mechanisms of manual therapy within clinical reasoning and patient education have consistently contributed to pitfalls related to the intervention. This includes outdated manual therapy concepts such as “functional leg length discrepancies,” “sacral torsions” and labeling patients as having joints “out of place/alignment” Other common unsupported labels include “adhesions” “trigger points” and “subluxations” amongst many others. These concepts have been consistently shown to be unreliable in examination and theory, and can create unnecessary fears, pathoanatomical anxiety, and fear avoidance patterns following examination and treatment.32
These problems have the potential to drive dependency on manual therapy and ultimately limit patient independence and function.20,21 This overmedicalization of manual therapy has led to its perception as a low-value health care option, particularly in the context of long-term outcomes. In sports physical therapy, this can lead to negative feelings and emotions prior to competition and potentially hamper performance capabilities. Creating anxiety in athletes is a known risk factor for future injury38 and a therapist must ensure that modern and informed language match their interventions. Further, delaying safe and efficacious physical training and exercise therapy while waiting to resolve these perceived impairments often leads to deconditioning of athletes and inadequate sporting load.
Therapists must understand the current concepts of mechanical input and associated neurophysiologic effects of manual therapy. When a therapist provides a manual intervention, a mechanical stimulus is applied upon an athlete and produces input into the dorsal horn of the spinal cord. This initiating a multi-factorial cascade of neurophysiologic effects stemming from the nervous system. Both the peripheral and central nervous system provide signal pathways that induce responses throughout the body These include neuromuscular (i.e muscle activity), autonomic (i.e heart rate, cortisol), endocrine (opioid) pain modulatory, and non-specific (context, beliefs fear, expectations, etc) responses (Figure 1).16,35,39,40
With multiple body systems responding to the therapist’s treatment strategy, manual therapy requires patient
education pre-, during and post- intervention. Patient education regarding manual therapy techniques needs to include honest discussion of its benefits and limitations. Despite the previously discussed limitations and pitfalls, providers can highlight the importance of understanding of and leveraging of the positive short-term outcomes (interand intra-session and between session) for long term improvement in outcomes41,42 With the patient and therapist properly informed and aligned as well as honest expectations discussed, manual therapy can then be reasonably applied.43
The prescription, dosage and progression are a crucial component of manual therapy intervention but are extremely challenging to define. To improve internal validity and stay true to the medical model of research, a prescriptive application of manual therapy within randomized controlled trials has been trialed to varying degrees of success and application.44–47 This has been challenged12,48–50 due to the pragmatic nature of clinical practice, and is a likely contributor to inconsistent manual therapy findings and small effect sizes found in the literature. For physical therapists imbedded in a team setting, reimbursement considerations (i.e number of visits and services billable to insurance) may not be a restriction to provide care. In these instances, diligence must be provided to ensure to not overprescribe therapeutic intervention (exercise or manual therapies). Conversely, the increased frequency of athlete visits combined with their daily internal and external workload demands and the absence of pressure of reimbursement furthers the short-term efficacy of manual therapy utilization.
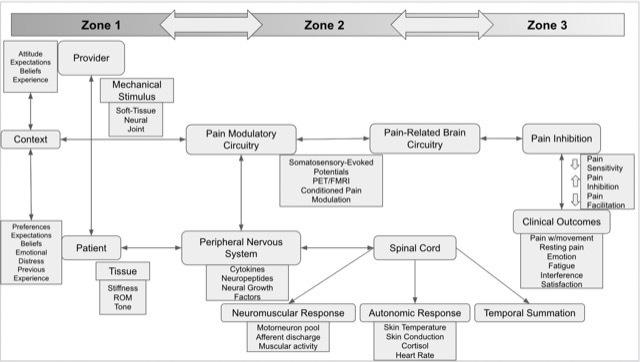 Figure 1. Multi-factorial neurophysiologic mechanisms of manual therapy (modified from Bialosky et al)35
Figure 1. Multi-factorial neurophysiologic mechanisms of manual therapy (modified from Bialosky et al)35
When practicing in an athletic training room or sports physical therapy clinic, the time-cost benefit of a technique must also be considered. The clinician’s clinical reasoning and ongoing evaluation of patient response is essential in appropriate and effective dosage of manual therapy. A clinicians preference and confidence with a specific intervention or technique has been shown to impact outcomes,35,41 which may be important when considering that multiple variations of manual techniques and interventions can result in similar outcomes.
12,41,51 If an athlete is a responder to manual therapy, the dosage of should be based on achieving a clinically meaningful improvement to focally addressed symptoms (i.e 7/10 knee pain) and be related to a functional chief complaint (sport impairment i.e impaired jumping performance). Changes to the type, time, frequency, intensity, and volume of manual related to athlete improvement demonstrates the pragmatic nature of application.48–50
Consistent re-evaluation of functional movements and athlete limitations (i.e running, jumping, cutting, etc) should be performed within session to assess the shortterm effectiveness of applied manual therapy techniques. This may also allow the therapist to identify if different techniques may need to be applied or if the individual is not responding to the specific intervention (Figure 2).
41,51,52
To improve athlete autonomy and independence, longterm application of manual therapy should be appropriately titrated so as not to foster dependence on any one provider or manual therapy technique.13,53 A transition to symptom-modifying mobility exercises that mimic or reinforce previously applied manual therapy interventions may replace the therapist as symptoms are reduced and function is restored. Ultimately this accomplishes the goal of creating athlete independence and transitioning to techniques
that focus on active exercise variations.13 This progression is necessary for the athlete in order to promote long-term autonomy in their musculoskeletal management, physical attribute development and overall performance enhancement.

There is an inherent time-cost benefit to all intervention forms available to physical therapists which makes intervention selection quite important. When providing athlete care, the provider must consider the demands placed on the athlete, both within and outside the sporting realm. When comparing outcomes against other “passive” therapies within the physical therapy evidence-base, manual therapy consistently is identified as more efficacious when compared to other interventions (electrophysiologic agents, taping, etc) outside of education and exercise. Recently a comparison of the effects of manual therapy has been likened to that of biophysical agents and other traditional modalities.54 As athletes seek to manage pain and continue competing and training, it is not a question of if the athlete will receive “passive” therapies, rather it is a question of which “passive” therapy will provide the most effective and efficient results within their comprehensive care model that includes ample exercise activity via the sport and its associated training.
While a full comparative review is beyond the scope of this commentary, the practicing sports clinician must consider how to compare and weight the cost-benefit of the numerous and easily applied manual therapy techniques with other pain and symptom modification modalities that are available. Manual therapy may have a challenged evidence base, varying non-specific mechanisms of action, and vari-
Figure 2. Applied clinical reasoning feedback loop for manual-therapy (Modified from Rhon)13ance in application, but clinicians must acknowledge that not all symptom modification techniques are equal when comparing against other forms of intervention within physical therapy practice.15,19,44,55,56 In fact, the field of manual therapy likely acknowledges these deficiencies more than the those who use theory-based, non-outcome informed application of modalities such as electrical stimulation, ultrasound, and lasers. Practically speaking, the cost of machinery and technology and time required for utilization is often not worth the minimal potential benefits, which has led to changes in ethics statements, physical therapy education, reimbursement and overall trends of use.57–60 Meanwhile, manual therapy, which is an entrylevel skill, may provide a cost-effective, mobile, and efficacious intervention that is consistently supported by clinical practice guidelines15,19,56,61,62 which provide related intervention comparisons and recommendations.
A multi-factorial, multi-disciplinary approach is necessary to improve outcomes within sports medicine settings. Within that construct, the benefits of manual therapy which includes building therapeutic alliance via touch, improving function via safe, cost-effective short-term pain modulation and facilitating education and exercise to be more impactful when they are limited less by pain and anxiety
The following are examples of how clinically-reasoned manual therapy within a multi-modal musculoskeletal care model facilitates conservative management in an athletic setting:
The athlete reports to physical therapy 72 hours following an acute ankle inversion and resultant lateral ligament sprain. The Ottawa Ankle Rules are negative and the athlete desires to return to play within two days. Visual examination reveals moderate swelling and ecchymosis of the ankle region. The objective examination reveals limited ankle dorsiflexion in supine and weightbearing, the ability to resist manual strength assessment in all-planes, impaired balance during performance of a single leg squat test and antalgic pattern with running gait. The patient notes that their confidence in running is limited by pain that is 7/10 on the Numeric Pain Rating Scale.
The athlete reports applying ice and compression therapy independently The therapist elects to provide anterior to posterior graded mobilization to the talus on the tibiofibular joint. Ankle dorsiflexion range of motion is improved in supine but not in weightbearing. The therapist then performs an ankle dorsiflexion mobilization with movement
technique until near symmetry is restored in a weightbearing ankle dorsiflexion test. A single leg squat test is again performed to compare pain and movement quality, both of which are improved. Following this improvement, running is attempted, with a noted decrease in the NPRS to 4/10. Local eccentric inversion and plantar flexion strengthening, single leg balance and lower compound lower extremity strengthening exercise were prescribed following this bout of manual therapy. The athlete is educated on continuing their compression and ice therapy independently Education is provided on the natural history of ankle sprains, the encouragement of early weightbearing and returning to sport when able to meet the Pain, Ankle impairments, Athlete perception, Sensorimotor control, Sport functional performance (PAASS) criteria.19,63
The athlete follows up with the physical therapist prior to competition. Manual therapy is provided again, with the prior two techniques performed prior to assessment of the PAASS constructs with further reduction in pain on all assessment. Due to lingering ankle dorsiflexion limitations during single leg squat and 3/10 pain with activity, the therapist decides to utilize a talocrural and rearfoot distraction manipulation.45 The athlete is able to pass PAASS criteria and is provided a semi-rigid brace to compete in.
On future visits, the therapist provides a home exercise program consisting of banded self-mobilization with movement into dorsiflexion that mimics previous manual therapy techniques that the athlete can perform independently prior to sporting activity. Manual therapy is tapered off during future visits and is performed as needed according to pain presentation and when indicated post-exercise for recovery Education and exercise programming is provided to the athlete on continuing a lower extremity single leg balance and strengthening program and to continue in order to reduce the risk of future lateral ankle sprain and chronic instability.
A basketball athlete is boxing out an opponent. The opponent then outjumps the athlete who is in a flexed, athletic position. The opponent lands on the athletes back, forcing the athlete into loaded flexion and rotation before both fall onto the floor. The athlete attempts to continue participation but reports being unable to continue due to worsening perceived lumbar spine tightness. Evaluation by the physical therapist reveals no radicular symptoms and sensory and motor function is normal in all extremities. There is notable increase in tone of the paraspinal musculature on palpation assessment. Range of motion is limited in flexion (forward bending) and extension (backward bending), to a lesser extent. There is no glaring strength loss but a Gower’s sign is noted on the return from forward bending assessment. Slump assessment is negative for radicular symptoms.
The athlete states that moist heat and laying prone relieves their symptoms. They are fearful to try and touch their toes. The treating therapist elects to perform soft tissue mobilization to address the increased tone about the paraspinals before re-addressing the fear of movement. Re-assessment of forward and backward bending reveals normalizing extension range of motion but apprehension persists with lumbar flexion. Graded lumbar central posterior to anterior mobilization was provided to identified painful segments.
Traditional mobilization grades 1 and 2 are described as oscillations before the end range of motion to theoretically assist in pain control. Grade 3 and 4 mobilizations are various oscillations at end range tissue resistance to theoretically increase range of motion. Although the validity of the grades are up for debate, the actual application of grades 1-4 likely operate mechanistically within the neurophysiologic effect spectrum of manual therapy mechanisms.35 In this case, the grade of mobilization started as low grade, and was progressed per their reported pain response with posterior to anterior assessement and associated carry over to functional movement. Upon re-evaluation, pain was decreased with forward bending and the patient states that they had decreased apprehension to move. The athlete was then provided quadruped lumbopelvic range of motion exercises and cardiovascular exercise for 20 minutes that did not exacerbate their symptoms. Education was provided on the natural history of low back pain and the positive expectations as the individual was absent of radicular pain. The athlete remains apprehensive of sporting activity and their next competition is in 48 hours. The athlete’s home exercise program consists of continued low intensity cardiovascular activity and the same lumbopelvic range of motion exercises, and they are set for follow up assessment in the athletic training room three hours prior to the upcoming competition. As they noted symptom reduction with heat and extension, they were educated on continuing those therapies as indicated.
Upon evaluation prior to competition, the athlete has nearly restored their range of motion in all planes. However, Gower’s sign persists, with residual pain that is 3/ 10, and they note some apprehension in absorbing contact similar to the mechanism of injury during skill training. The athlete is educated on the purported neurophysiologic mechanisms of spinal manipulation and agrees to the treatment. The athlete is provided a side lying lumbar manipulation with immediate reassessment of forward bending. Pain and movement quality are improved, and the therapist
introduces quadruped and closed chain motor control/ strengthening exercises to reinforce the reduction in symptoms and improved movement tolerance. The athlete notes improved confidence and in consultation with team physicians and key stakeholders, the athlete returns to competition.
The following day, the athlete is instructed on mobility exercises that simulate the manual therapy techniques. Further proximal trunk and lower extremity strengthening drills are installed into their resistance training program in communication with the acting strength and conditioning coach. Manual therapy is provided as indicated only if the symptoms worsen or required further medical evaluation.
Education and exercise are the foundation of physical therapy intervention. When considering the barriers to these pillars, which include pain, anxiety, fear of movement and further injury, it is reasonable to consider the utilization of manual therapy as an adjunct to improve patient comfort, confidence, and to leverage short-term outcomes in a sporting environment where participation of exercise is already necessary The primary goals of manual therapy are to reduce pain and promote safe and efficient movement. This is paramount in a sports setting, as short-term symptom modification is a significant driver in improving athlete comfort, confidence, and safety and thus potentially influencing athlete availability to rehabilitation, training, and competitive participation. Manual therapy is generally safe and cost-effective within a sports-medicine environment compared to, or performed in combination with alternative forms of care (pharmacologic, electrophysical, etc).17,18
A balanced and updated approach must be taken, as overdiagnosis and overmedicalization via manual therapy may result in more harm than good. A modern and clinicallyreasoned approach can make these treatment interventions efficacious and move beyond the “passive” label by facilitating continued activity
The authors state no conflict of interest in the creation of this manuscript.
Submitted: May 31, 2022 CST, Accepted: November 03, 2022
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Hon S, Ritter R, Allen DD Cost-effectiveness and outcomes of direct access to physical therapy for musculoskeletal disorders compared to physicianfirst access in the united states: systematic review and meta-analysis. Phys Ther 2020;101(1). doi:10.109 3/ptj/pzaa201
2. Demont A, Bourmaud A, Kechichian A, Desmeules F. The impact of direct access physiotherapy compared to primary care physician led usual care for patients with musculoskeletal disorders: a systematic review of the literature. Disabil Rehabil 2021;43(12):1637-1648. doi:10.1080/09638288.2019.1
674388
3. Rhon DI, Fraser JJ, Sorensen J, Greenlee TA, Jain T, Cook CE. Delayed rehabilitation is associated with recurrence and higher medical care use after ankle sprain injuries in the united states military health system. J Orthop Sports Phys Ther. 2021;51(12):619-627 doi:10.2519/jospt.2021.10730
4. Strack DS, MacDonald CW, Valencia EB, Davison M. Case for the specialised sports physical therapist to be an essential part of professional athlete care: letter from America no. 1. Br J Sports Med 2019;53(10):587-588. doi:10.1136/bjsports-2017-0975 75
5. Lifshitz L. A sport physiotherapist as medical director: taking a leadership role. J Orthop Sports Phys Ther 2012;42(9):748-749. doi:10.2519/jospt.201
2.0110
6. Bayer ML, Magnusson SP, Kjaer M. Early versus delayed rehabilitation after acute muscle injury N Engl J Med 2017;377(13):1300-1301. doi:10.1056/nej mc1708134
7. Malve HO. Sports pharmacology: a medical pharmacologist’s perspective. J Pharm Bioall Sci 2018;10(3):126-136. doi:10.4103/jpbs.jpbs_229_17
8. Ziltener JL, Leal S, Fournier PE. Non-steroidal anti-inflammatory drugs for athletes: an update. Ann Phys Rehabil Med. 2010;53(4):278-288. doi:10.1016/j.r ehab.2010.03.001
9. Hoegh M, Stanton T, George S, Lyng KD, Vistrup S, Rathleff MS. Infographic. pain or injury? Why differentiation matters in exercise and sports medicine. Br J Sports Med 2021;56(5):299-300. doi:1 0.1136/bjsports-2021-104633
10. Hainline B, Derman W, Vernec A, et al. International Olympic Committee consensus statement on pain management in elite athletes. Br J Sports Med 2017;51(17):1245-1258. doi:10.1136/bjsp orts-2017-097884
11. Orthopaedic Manual Physical Therapy: Description of Advanced Specialty Practice 2018 American Academy of Orthopaedic Manual Physical Therapists; 2018.
12. Cook CE, Donaldson M, Lonnemann E. ‘Next steps’ for researching orthopedic manual therapy J Man Manip Ther. 2021;29(6):333-336. doi:10.1080/10 669817.2021.2008010
13. Rhon DI, Deyle GD Manual therapy: always a passive treatment? J Orthop Sports Phys Ther. 2021;51(10):474-477 doi:10.2519/jospt.2021.10330
14. Babatunde OO, Legha A, Littlewood C, et al. Comparative effectiveness of treatment options for plantar heel pain: a systematic review with network meta-analysis. Br J Sports Med 2019;53(3):182-194. d oi:10.1136/bjsports-2017-098998
15. George SZ, Fritz JM, Silfies SP, et al. Interventions for the management of acute and chronic low back pain: revision 2021. J Orthop Sports Phys Ther 2021;51(11):CPG1-CPG60. doi:10.2519/jospt.2021.03 04
16. Bishop MD, Torres-Cueco R, Gay CW, LluchGirbés E, Beneciuk JM, Bialosky JE. What effect can manual therapy have on a patient’s pain experience? Pain Management 2015;5(6):455-464. doi:10.2217/pm t.15.39
17 Fritz JM, Brennan GP, Hunter SJ. Physical therapy or advanced imaging as first management strategy following a new consultation for low back pain in primary care: associations with future health care utilization and charges. Health Serv Res 2015;50(6):1927-1940. doi:10.1111/1475-6773.12301
18. Wang D, Mueller K, Lea R. Outcomes associated with manual therapy for workers with non-chronic low back pain. Workers Compensation. Published online 2021.
19. Martin RL, Davenport TE, Fraser JJ, et al. Ankle stability and movement coordination impairments: lateral ankle ligament sprains revision. J Orthop Sports Phys Ther 2021;51(4):CPG1-CPG80. doi:10.251 9/jospt.2021.0302
20. Zadro JR, Décary S, O’Keeffe M, Michaleff ZA, Traeger AC. Overcoming overuse: improving musculoskeletal health care. J Orthop Sports Phys Ther. 2020;50(3):113-115. doi:10.2519/jospt.2020.010
21. Nicholls DA. The active future for the passive therapist. J Orthop Sports Phys Ther 2021;51(7):318-321. doi:10.2519/jospt.2021.10536
22. Gajsar H, Nahrwold K, Titze C, Hasenbring MI, Vaegter HB. Exercise does not produce hypoalgesia when performed immediately after a painful stimulus. Scand J Pain 2018;18(2):311-320. doi:10.15 15/sjpain-2018-0024
23. Vaegter HB, Handberg G, Graven-Nielsen T. Hypoalgesia after exercise and the cold pressor test is reduced in chronic musculoskeletal pain patients with high pain sensitivity. Clin J Pain. 2016;32(1):58-69. doi:10.1097/ajp.0000000000000223
24. Rice D, Nijs J, Kosek E, et al. Exercise-induced hypoalgesia in pain-free and chronic pain populations: state of the art and future directions. J Pain 2019;20(11):1249-1266. doi:10.1016/j.jpain.201
9.03.005
25. Brukner P, Khan K. Brukner & Khan’s Clinical Sports Medicine Vol 1: Injuries. 5th ed. McGraw-Hill Education (Australia); 2016.
26. Cook CJ, Beaven CM. Individual perception of recovery is related to subsequent sprint performance. Br J Sports Med. 2013;47(11):705-709. doi:10.1136/bjs ports-2012-091647
27 Palmer D, Cooper DJ, Emery C, et al. Self-reported sports injuries and later-life health status in 3357 retired Olympians from 131 countries: a crosssectional survey among those competing in the games between London 1948 and PyeongChang 2018. Br J Sports Med 2021;55(1):46-53. doi:10.1136/bjspor ts-2019-101772
28. Cockerill IM. They think it’s all over, but it may not be! Br J Sports Med. 2005;39(12):880-883. doi:10.1 136/bjsm.2004.016642
29. Hagley GW, Mills PD, Shiner B, Hemphill RR. An analysis of adverse events in the rehabilitation department: using the veterans affairs root cause analysis system. Phys Ther 2018;98(4):223-230. doi:1 0.1093/ptj/pzy003
30. Carnes D, Mars TS, Mullinger B, Froud R, Underwood M. Adverse events and manual therapy: a systematic review. Man Ther. 2010;15(4):355-363. do i:10.1016/j.math.2009.12.006
31. Mintken PE, Derosa C, Little T, Smith B. A model for standardizing manipulation terminology in physical therapy practice. J Man Manip Ther 2008;16(1):50-56. doi:10.1179/106698108790818567
32. Flynn TW, Childs JD, bell S, Magel JS, Rowe RH, Plock H. Manual physical therapy: we speak gibberish. J Orthop Sports Phys Ther 2008;38(3):97-98. doi:10.2519/jospt.2008.0103
33. Stewart M, Loftus S. Sticks and stones: The impact of language in musculoskeletal rehabilitation. J Orthop Sports Phys Ther. 2018;48(7):519-522. doi:1 0.2519/jospt.2018.0610
34. Fryer G, McPherson HC, O’Keefe P The effect of training on the inter-examiner and intra-examiner reliability of the seated flexion test and assessment of pelvic anatomical landmarks with palpation. Int J Osteopath Med. 2005;8(4):131-138. doi:10.1016/j.ijos m.2005.08.004
35. Bialosky JE, Beneciuk JM, Bishop MD, et al. Unraveling the mechanisms of manual therapy: modeling an approach. J Orthop Sports Phys Ther 2018;48(1):8-18. doi:10.2519/jospt.2018.7476
36. Slaven EJ, Goode AP, Coronado RA, Poole C, Hegedus EJ. The relative effectiveness of segment specific level and non-specific level spinal joint mobilization on pain and range of motion: results of a systematic review and meta-analysis. J Man Manip Ther 2013;21(1):7-17 doi:10.1179/2042618612y.0000 000016
37 Kamper SJ. Engaging with research: linking evidence with practice. J Orthop Sports Phys Ther 2018;48(6):512-513. doi:10.2519/jospt.2018.0701
38. Timpka T, Jacobsson J, Bargoria V, et al. Preparticipation predictors for championship injury and illness: cohort study at the Beijing 2015 International Association of Athletics Federations World Championships. Br J Sports Med 2017;51(4):271-276. doi:10.1136/bjsports-2016-0965 80
39. Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther 2009;14(5):531-538. doi:10.1016/ j.math.2008.09.001
40. Bialosky JE, George SZ, Bishop MD. How spinal manipulative therapy works: why ask why? J Orthop Sports Phys Ther. 2008;38(6):293-295. doi:10.2519/jos pt.2008.0118
41. Cook C, Learman K, Showalter C, Kabbaz V, O’Halloran B. Early use of thrust manipulation versus non-thrust manipulation: a randomized clinical trial. Man Ther. 2013;18(3):191-198. doi:10.1016/j.math.20 12.08.005
42. Cook CE, Showalter C, Kabbaz V, O’Halloran B. Can a within/between-session change in pain during reassessment predict outcome using a manual therapy intervention in patients with mechanical low back pain? Man Ther. 2012;17(4):325-329. doi:10.101 6/j.math.2012.02.020
43. Décary S, Zadro JR, O’Keeffe M, Michaleff ZA, Traeger AC, Légaré F. Overcoming overuse part 5: is shared decision making our excalibur? J Orthop Sports Phys Ther 2021;51(2):53-56. doi:10.2519/jospt.2021.0 103
44. Cleland JA, Abbott JH, Kidd MO, et al. Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther 2009;39(8):573-585. doi:10.2 519/jospt.2009.3036
45. Cleland JA, Mintken PE, McDevitt A, et al. Manual physical therapy and exercise versus supervised home exercise in the management of patients with inversion ankle sprain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther 2013;43(7):443-455. doi:10.2519/jospt.2013.4792
46. Dunning JR, Cleland JA, Waldrop MA, et al. Upper cervical and upper thoracic thrust manipulation versus nonthrust mobilization in patients with mechanical neck pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther 2012;42(1):5-18. doi:10.2519/jospt.2012.3894
47. Dunning J, Butts R, Fernández-de-Las-Peñas C, et al. Spinal manipulation and electrical dry needling in patients with subacromial pain syndrome: a multicenter randomized clinical trial. J Orthop Sports Phys Ther 2021;51(2):72-81. doi:10.2519/jospt.2021.9 785
48. Hohenschurz-Schmidt D, Kleykamp BA, DraperRodi J, et al. Pragmatic trials of pain therapies: a systematic review of methods. Pain 2022;163(1):21-46. doi:10.1097/j.pain.0000000000002 317
49. Lerner-Lentz A, O’Halloran B, Donaldson M, Cleland JA. Pragmatic application of manipulation versus mobilization to the upper segments of the cervical spine plus exercise for treatment of cervicogenic headache: a randomized clinical trial. J Man Manip Ther 2021;29(5):267-275. doi:10.1080/10 669817.2020.1834322
50. Roenz D, Broccolo J, Brust S, et al. The impact of pragmatic vs. prescriptive study designs on the outcomes of low back and neck pain when using mobilization or manipulation techniques: a systematic review and meta-analysis. J Man Manip Ther 2018;26(3):123-135. doi:10.1080/10669817.201
7.1398923
51. Cook CE, George SZ, Keefe F. Different interventions, same outcomes? here are four good reasons. Br J Sports Med. 2018;52(15):951-952. doi:1 0.1136/bjsports-2017-098978
52. Kent P, Marks D, Pearson W, Keating J. Does clinician treatment choice improve the outcomes of manual therapy for nonspecific low back pain? a metaanalysis. J Manipulative Physiol Ther 2005;28(5):312-322. doi:10.1016/j.jmpt.2005.04.009
53. Short S, Short G, Strack D, Anloague P, Brewster B. A combined treatment approach emphasizing impairment-based manual therapy and exercise for hip-related compensatory injury in elite athletes: a case series. Intl J Sports Phys Ther 2017;12(6):994-1010. doi:10.26603/ijspt20170994
54. Page P. Making the case for modalities: the need for critical thinking in practice. Int J Sports Phys Ther 2021;16(5):28326. doi:10.26603/001c.28326
55. Willy RW. Innovations and pitfalls in the use of wearable devices in the prevention and rehabilitation of running related injuries. Phys Ther Sport 2018;29:26-33. doi:10.1016/j.ptsp.2017.10.003
56. Cibulka MT, Bloom NJ, Enseki KR, Macdonald CW, Woehrle J, McDonough CM. Hip pain and mobility deficits-hip osteoarthritis: revision 2017. J Orthop Sports Phys Ther 2017;47(6):A1-A37 doi:10.2519/jos pt.2017.0301
57. Robertson VJ, Baker KG. A review of therapeutic ultrasound: effectiveness studies. Phys Ther 2001;81(7):1339-1350. doi:10.1093/ptj/81.7.1339
58. Kharel P, Zadro JR, Maher CG. Physiotherapists can reduce overuse by choosing wisely. J Physiother. 2021;67(3):151-155. doi:10.1016/j.jphys.2021.06.006
59. American Physical Therapy A. Exclusive use or use of multiple biophysical agents HOD P06-18-17-27 Published online 2018.
60. Greco JL, Lamberg EM. Biophysical agent curriculum in entry-level physical therapist education programs across the united states: a survey J Phys Ther Educ 2020;34(2):138-149. doi:10.1 097/jte.0000000000000128
61. Blanpied PR, Gross AR, Elliott JM, et al. Neck pain: revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1-A83. doi:10.2519/jospt.2017.0302
62. Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges J. Knee pain and mobility impairments: meniscal and articular cartilage lesions. J Orthop Sports Phys Ther 2010;40(6):A1-A35. doi:10.2519/jos pt.2010.0304
63. Smith MD, Vicenzino B, Bahr R, et al. Return to sport decisions after an acute lateral ankle sprain injury: introducing the PAASS framework—an international multidisciplinary consensus. Br J Sports Med 2021;55(22):1270-1276. doi:10.1136/bjsports-20 21-104087
Kevin Wilk, PT, DPT, FAPTA 1,2 a , Zachary M Thomas, PT, DPT, OCS, CSCS 3 , Christopher A Arrigo, MS, PT, ATC 4 , George J Davies, PT, DPT, ATC, CSCS 5,6,7
1 Vice President National Director Clinical Education & Research, Champion Sports Medicine, Select Medical, 2 Director of Rehabilitative Research, American Sports Medicine Institute, 3 Sports Physical Therapy Fellow, Champion Sports Medicine, 4 Advanced Rehabilitation, 5 Physical Therapy, Georgia Southern University, 6 Coastal Therapy & Sports Rehab, 7 Gundersen Health System
Keywords: ACL injury, neurocognitive training, reactive testing, return to play https://doi.org/10.26603/001c.67988

The incidence of knee injuries in sport, particularly involving the ACL, appears to be increasing yearly, especially in younger age athletes. Even more concerning is the frequency of ACL reinjury also appears to be increasing year after year Improving the objective criteria and testing methods used to determine return to play (RTP) readiness following ACL surgery is one aspect of the rehabilitation process that can significantly help in reducing reinjury rates. Currently, the majority of clinicians are still using post operative time frames as their number one criterion for clearance to RTP. This flawed method demonstrates an inadequate reflection of the true unpredictable, dynamic environment athletes are returning to participate in. In our clinical experience, objective testing to allow for clearance to sport participation following an ACL injury should incorporate neurocognitive and reactive testing due to the nature of the injury typically occurs because of failed control of unanticipated reactive movements. The purpose of this manuscript is to share a neurocognitive testing sequence we currently employ consisting of 8 tests in 3 categories: Blazepod tests, reactive shuttle run tests, and reactive hop tests. The use of a more dynamic reactive testing battery may decrease the reinjury rates when an athlete is cleared for participation by measuring readiness in chaotic circumstances that are more truly reflective of the sporting environment the athlete is working to return to and in the process give them a greater sense of confidence.
It is estimated there are between 200,000 to 250,000 anterior cruciate ligament (ACL) knee injuries sustained annually in the United States, resulting in approximately 150,000 to 165,000 ACL surgeries each year 1,2 The incidence of these serious knee injuries appears to be increasing yearly, especially in high school aged athletes. More troublesome than the frequency of ACL injuries, is the rate of reinjury also appears to be increasing year after year. Investigators have reported reinjury rates following ACL surgery to range as high as 30-39%.3,4 This rate of reinjury results in as many as 4 in every 10 surgeries being attributed to reinjury. This level of reinjury following ACL surgery is unacceptable. In these instances, the athlete has already suffered one significant knee injury, undergone surgery, and worked through the rehabilitation process afterwards only to suffer another ACL injury to either the opposite or the previously reconstructed knee. As health care providers we need to critically examine every available
way to reduce ACL reinjury rates. One area that can significantly help in reducing these reinjury rates is improving the methodology used in return to play (RTP) testing following ACL surgery
The cause of these unacceptably high reinjury rates has been attributed to a number of factors. First, there is a surprising overall lack of RTP testing generally utilized in making RTP decisions. Barber-Westin and Noyes3 reported in a large meta-analysis and systematic review of 716 articles that only 13% utilized objective criteria in determining readiness to return an athlete back to participation following ACL surgery. This lack of testing is extremely disappointing when you consider that a reduction in reinjury rates has been demonstrated by utilizing objective RTP testing in the decision-making process.5–7 Second, athletes are returning to participate in sport without completing the entire rehabilitation process, often due to insurance plan limitations, an inability to afford rehabilitation following the exhaustion of benefits, or self-discharge. Each of these factors results in incomplete rehabilitation, placing the athlete at risk of reinjury. Third, is the frequent lack
of high-level activities and functional sport-specific challenges during the rehabilitation process. When an athlete is not challenged in a similar environment, with replicating demands matching those of the sport, they are often returning to the result inadequately prepared and therefore a higher risk of reinjury. Next, is the fact that most of the RTP tests currently in use are single task drills with anticipated movements. Sports are seldom single task activities and often involve unanticipated movements. Brophy et al8,9 and others10,11 have reported the majority of soccer injuries sustained to the female player occurred during defending and/or with unanticipated reactive movements. For example, a soccer player may be performing soccer drills with other players to create an environment of distraction, controlled chaos, and dual tasking. This combination of variables and the hierarchy of tasks inherent to sport makes single task drills insufficient to assess RTP readiness. Lastly, the athlete often goes back to their sport or activities unprepared and at risk of reinjury for a combination of the reasons listed above.
The present RTP testing methodology is underutilized and when employed not satisfactorily effective to appropriately determine RTP readiness of the athlete following ACL surgery Most decisions are made in the Physician’s office, based solely on physical examination and subjective reporting. Typically, when RTP testing is performed, it is not done in the same environment or with sport specificity. Testing needs to be conducted with an emphasis on the performance of multiple tasks, neurocognitive challenges, and motor control. RTP decisions should be made by a team of health care providers looking at the athlete’s readiness from a variety of viewpoints to make an informed decision based on subjective, objective and functional data. RTP criteria should not be a single event to determine readiness to return athletes to all levels of sport.
RTP testing for the lower extremity following ACL surgery has been discussed extensively in the literature since the mid 1980’s. There are over 500 articles that present various testing procedures and protocols. These testing procedures include single leg hop testing, shuttle running, balance testing and functional movement screening, isokinetic testing, and limb symmetry index assessment to list just a few.12–19 While these tests are all good measures of what they are designed to assess, they all test a single task, and none involve reactive assessment. Even the tests used that replicate drills employed in sport training, are simply drills and not truly specific sport related activities. These tests are good, serve a vital purpose and we recommend them as tests to assist in determining rehabilitation progression.
Historically all these tests have been referred to as RTP tests. They are more appropriately tests suited to determine athlete readiness to begin progression through rehabilitation, running, jumping, agility drills, or other transitional programs. They are not true measures to assess readiness to return to competitive play. These tests are predictable, in that the athlete is asked to perform a specific movement or task and is evaluated based on their resultant performance of this movement. In sports, there are numerous
unpredictable movements that the athlete must perform, most of these are reactive in nature and have multiple stimuli occurring simultaneously Therefore, to effectively assess return to play readiness during the recovery after ACL surgery, the RTP tests must measure those types of sport activities, movements, and reactions. The problem is these tests do not assess reaction time, dynamic stabilization, dynamic reaction movements and do not tell us if the athlete is ready to initiate competitive practice or return to competitive play
Although there are limitations in the previous metrics for clinical decision making for RTP, it is important to recognize some of the research of the tests which provide the criteria to progress to the neurocognitive testing. Refer to the list below for an example checklist or functional testing algorithm for a criterion-based approach for progression through rehabilitation and in preparation for using the advanced testing methods.20
• VAS/NPRS
• PROs
• Kinesiophobia
• Anthropometric measurement for effusion
• Static balance/Dynamic balance
• AROM/PROM – Knee/PF
• Strength Testing – TLS: LSI, Unilateral ratios, Allometric scaling to BW
• Special Tests for ligament stability: Lachman’s, Pivot Shift, KT1000/2000
• Walking/running gait analysis
• Functional movement patterns
• Jump Test
• Hop Tests
• T-drill hop test
• Change of Direction Test
• LEFT (adds acceleration/deceleration [anterior/retro] and acute fatigue factor
Even though the “missing link” is the neurocognitive reactive testing, there must be preparatory testing that leads to criterion-based metrics that prepares the patients to perform the neurocognitive reactive testing. Therefore, criteria that can be used to determine the patient’s readiness for performing these advanced neuro-cognitive reactive tests are described in Table 1.
The purpose of this manuscript is to present a proposed testing and RTP model we currently use clinically This RTP testing includes neurocognitive testing, reactive motor control testing, dual tasking, and psychological readiness with the main focus on reactive unanticipated test movements.
Appropriate testing of RTP readiness following ACL surgery, should not only assess if the athlete appears ready to resume play but also be directed toward minimizing the risk of reinjury To accomplish this, testing must be more dynamic, sport oriented, and even unpredictable in nature. A neurocognitive testing battery must include measures
of reactive response and incorporate
sport-type reactions and movements. Testing must also be safe, easy to perform and measure, and require minimal equipment to complete. Neurocognitive testing is a way to measure various aspects of cognitive function non-invasively These cognitive functions include things like reaction time, multi-tasking, attention, memory, and perception. Short tests designed to assess these functions produce objective measures that can be compared to standard scores or to an individual’s baseline scores when available. Readiness to return to sport involves more than just the readiness of the musculoskeletal system. The neurocognitive system is a vital aspect of sport due to the constant use of cognitive functions such as reaction time and multi-tasking. Reaction time testing has been shown to be highly reliable and can be used to assess an athlete’s cognitive and athletic ability.36 Musculoskeletal injuries affect the neurocognitive system as well, so assessing and training this system can lead to better outcomes when determining readiness to return to play Simon et al37 demonstrated that the addition of a neurocognitive and anticipatory component to the traditional hop test series resulted in a statistical difference in performance and may improve functional return to sport testing. When comparing reactive versus preplanned agility testing, Ser-
pell et al38 demonstrated a difference in mean reaction time between elite and subelite groups in the way in which they contributed to perceptual skills and/or reaction ability All of these factors combine to make the incorporation of neurocognitive training and testing elements crucial to advancing the effectiveness of RTP testing following ACL surgery and help to minimize the risk of reinjury as the athlete returns to competition.
The neurocognitive testing sequence we currently employ consists of a total of 8 tests in 3 categories: Blazepod tests, reactive shuttle run tests, and reactive hop tests. Testing is performed sequentially using 3 Blazepod tests, 2 reactive shuttle runs and finally 3 reactive hop tests. Adequate rest and recovery are allowed between tests. Based on the duration of the tests, the patients are permitted a 1-3 minute rest between tests. The testing measures are:
Each target light is 60 inches apart.
The lateral slide test begins with four Blazepods positioned in a straight line five feet apart (60 inches). (Figure 1) The pods are configured in a randomized pattern using a single target color (blue) and five distracting colors (purple, green, orange, red, and yellow). One pod will light up the target color (blue) and the remaining three will be lit in distracting colors. Lights are set to transition on a hit and with zerotime delay between each transition. The athlete is instructed to begin in the center of the pods and will shuffle laterally targeting the blue light. Athletes are required to maintain a mini squat in an athletic position throughout the test and must avoid hopping or running between lights. Another individual will be tossing a soccer ball towards the target light. The athlete is instructed to catch the ball, tap the target light then toss the ball back while locating the next light and shuffling to it in a good athletic ready position. Once the test begins the goal is to tap as many lights as possible in 30 seconds. The total number of taps as well as average reaction time is calculated and scored following completion of the test.
The 4 corners reactive test begins with four Blazepods positioned in a square 21 feet (252 inches) apart. (Figure 2) As in the first test the pods are configured in a randomized pattern where one pod will light up the target color (blue) and the remaining three will be a distracting color (purple, green, orange, red, and yellow). Lights are set to transition on a hit and with zero-time delay between each transition. The athlete is instructed to begin in the center of the pods and locate the blue light. Another individual will be tossing a soccer ball towards the target light. The athlete is instructed to catch the ball, tap the light then toss the ball back while locating the next light. Once the test begins the goal is to tap as many lights as possible in 30 seconds. Total number of taps as well as average reaction time is calculated following completion of the test.
The standing right versus left reactive test begins with four Blazepods positioned in a rectangle 36 inches in length and 12 inches wide. (Figure 3) The pods are configured in a randomized pattern so that any of the four can illuminate with only one at a single point in time. Lights are set to transition on a hit, with zero-time delay between each. In this test both blue and red are set as the target colors which represents the color in which the single pod will illuminate. The athlete begins in double limb stance with their feet shoulder width apart between the four pods performing fast feet. If the pod illuminates blue they are instructed to hit it with their left foot and if red, then hit it with their right foot. After each hit the pods will change color and the athlete must react to contact the next target color. Once the test begins the goal is to tap as many target lights as possible in 15 seconds. Total number of taps, number of errors, as well as average reaction time is calculated following completion of the test.


The reactive 10-yard T shuttle run test begins with 4 cones positioned in a “T”. (Figure 4) The individual cone is positioned 10 yards from the other three which are each 5 yards apart forming a “T” The athlete begins at the individual cone and is instructed to sprint towards the cone directly in front of them. Once two thirds to the first cone, the tester will call out right or left, signifying the direction the athlete will begin to shuffle laterally towards. They are instructed to slide laterally 5 yards to the furthest cone, tap it, then reverse and slide laterally 10 yards to the furthest cone in the opposite direction and tap it. Once they tap the second cone, they reverse slide 5 yards back to the middle cone. Finally, after taping the middle cone the athlete will pivot and run 10 yards back to the starting position. The goal is
Figure 1. Lateral slide test with light targets (Blazepods Inc.) Figure 2. Four corner target light test (Blazepods Inc.) Each light target is 21 feet apart.to complete the test as quickly as possible. The time begins when they start their run and stops when they pass the final cone.
The reactive 10-yard L run test begins with 4 cones positioned in a “T” (Figure 5) The individual cone is positioned 10 yards from the other three which are each 5 yards apart. The athlete is instructed to begin at the individual cone and sprint towards the cone directly in front of them. Once two thirds to the first cone, the tester will call out which direction the athlete will go. Once the direction is called, the athlete will turn in the direction named and sprint around the far cone. To finish the test the athlete will sprint back to
the middle cone, pivot and then sprint back to the starting position, completing the “L” The goal is to complete the test as quickly as possible. The time begins when they start their run and stops when they pass the finally cone.
REACTIVE SINGLE LIMB HOP FOR DISTANCE
The reactive single limb hop for distance test begins with the athlete standing on one limb. The athlete is instructed to hop forward from the starting position as far as possible. (Figure 6) While in the air the tester will call out right or left designating the foot in which the athlete is required to land on. The goal of the test is to hop as far as possible and land solidly on the designated leg. Athletes must stick the landing for 2-3 seconds for the test to count. Three consecutive repetitions are performed, and the distance is averaged. The distance is measure from the starting line to the back of the landing leg heel.
REACTIVE SINGLE LIMB CROSS OVER HOP FOR DISTANCE
The reactive single limb cross over hop for distance test begins with the athlete standing on one limb. The test begins with the athlete hopping as far as possible off the single limb. While in the air the tester will call out the foot in which the athlete is required to land on, either left or right, crossing the center line of the testing field. (Figure 7) They will then complete the sequence by completing two more cross over hops on the same limb. The athlete is instructed to hop as far as possible with each hop and stick the final landing for 2-3 seconds. They will complete three consecutive repetitions and take the average distance between each test as the final score. The distance is measure from the starting line to the back of the athlete’s heel at the final hop.
The reactive single limb alternating cross over hop for distance test begins with the athlete standing on one limb (Figure 8). The athlete is instructed to hop forward as far


 Figure 3. Standing Right versus Left Reactive target light test.
Targets are placed 3 feet apart and the participant is instructed to tap the right foot to the red target & the left foot to the blue target.
Figure 4. Reactive 10-yard T Shuttle Run Test.
This test involves a 10-yard run then a side shuffle to one direction for 5 yards & then in opposite direction for 5 yards and then turn and run back to start line.
Figure 5. Reactive 10 Yard L Run Test.
This test is performed with a 10 yard straight run then a turn to instructed direction for 5 yards and then a turn back to start position.
Figure 3. Standing Right versus Left Reactive target light test.
Targets are placed 3 feet apart and the participant is instructed to tap the right foot to the red target & the left foot to the blue target.
Figure 4. Reactive 10-yard T Shuttle Run Test.
This test involves a 10-yard run then a side shuffle to one direction for 5 yards & then in opposite direction for 5 yards and then turn and run back to start line.
Figure 5. Reactive 10 Yard L Run Test.
This test is performed with a 10 yard straight run then a turn to instructed direction for 5 yards and then a turn back to start position.
as possible. While in the air the tester will call out a foot on which the athlete is required to land, either left or right. The athlete will then complete the sequence by performing two more cross over hops successively on alternating limbs. The athlete is instructed to hop as far as possible with each hop and stick the final landing holding for 2-3 seconds. They will complete three consecutive repetitions and take the average distance between each test. As with the other tests the distance is measure from the starting line to the back of the athlete’s heel.
Videos of the drills and tests in this manuscript can be found here: VIDEO FOLDER
Although these are examples of some of the tests that are currently being used clinically because of ecological validity, nevertheless, we have to acknowledge the limitations of
these tests. The tests have not been tested for reliability, validity or predicative validity regarding follow-up effectiveness for athletes to return to play, return to performance or prevention of reinjury
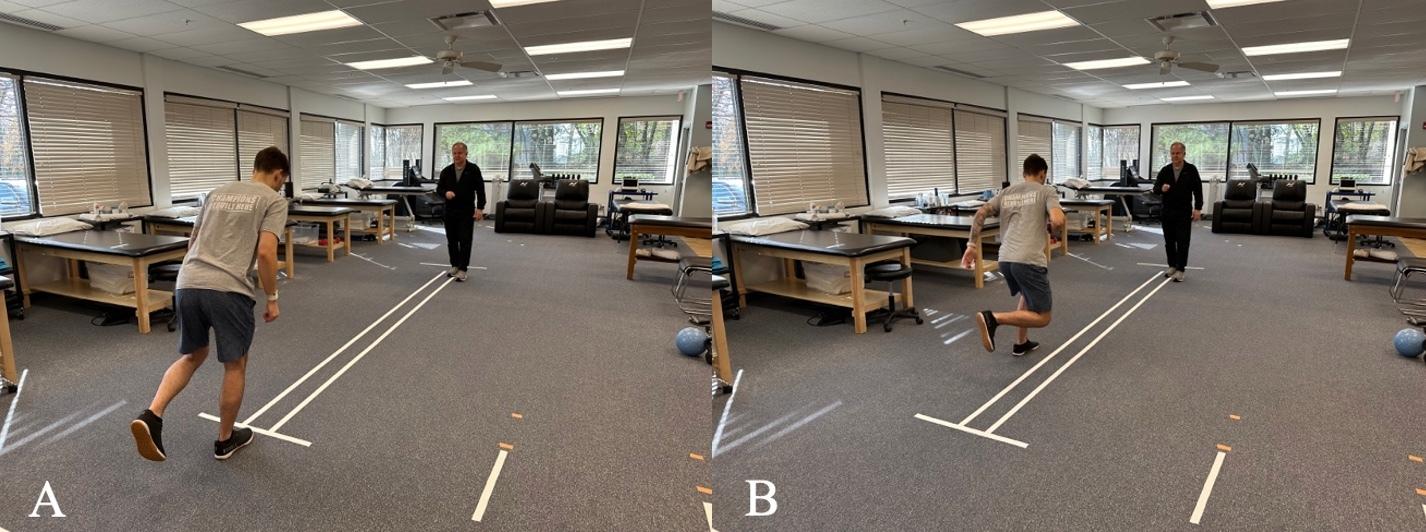
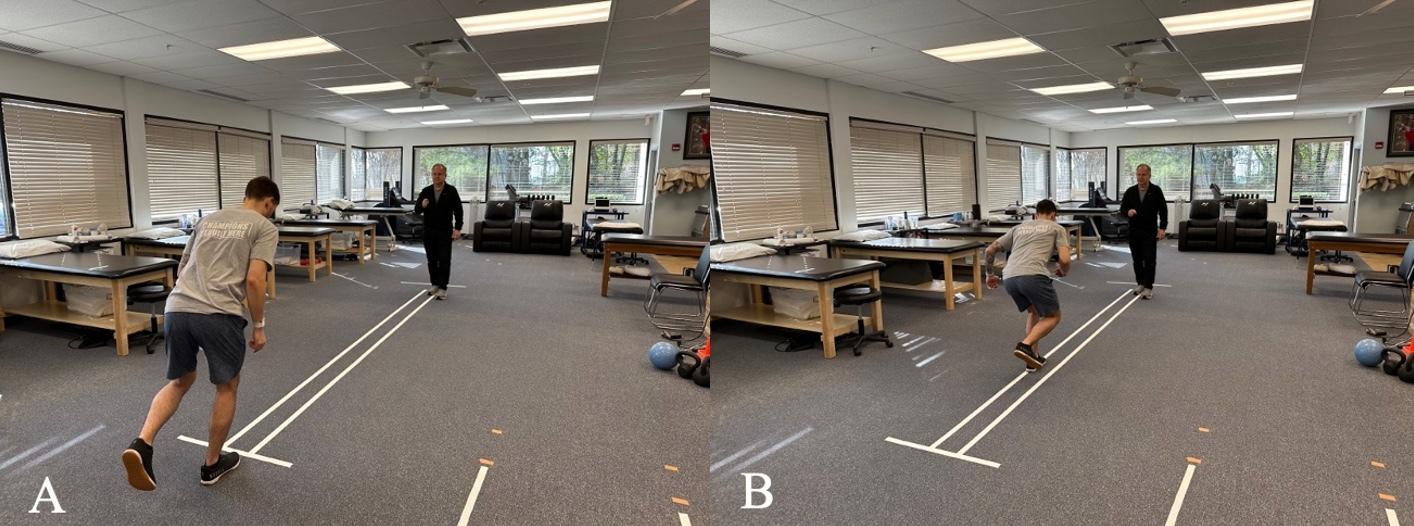
The current state of RTP testing following ACL surgery is inadequate and does not reflect the true unpredictable, dynamic environment athletes are returning to. Not only is there a need for better utilization of RTP testing for predicting readiness, the significant incidence of reinjury must also be drastically reduced. These needs require both an improvement in the type of tests utilized and the overall use of subjective, objective and functional RTP testing in determining readiness to resume unrestricted activity. It is our hope that presenting this theoretical model for the use of neurocognitive testing in assessing athletic readiness that
Figure 6. Reactive Single Leg Hop for Distance Test. The participant stands on one foot and hops outward – as the participant hops, they are instructed which foot to land on. Figure 7 Reactive Single Limb Cross Over Hop for Distance Test. The participant stands on one foot and hops outward – as the participant hops, they are instructed which foot to land on and they must cross over the center tape. They will then complete the sequence by completing two more cross over hops on the same limb.more critical thought will be placed on the type of testing needed to help determine when an athlete is capable of returning to sport. Also, the use of a more dynamic testing battery may decrease the reinjury rates when an athlete is cleared for participation.
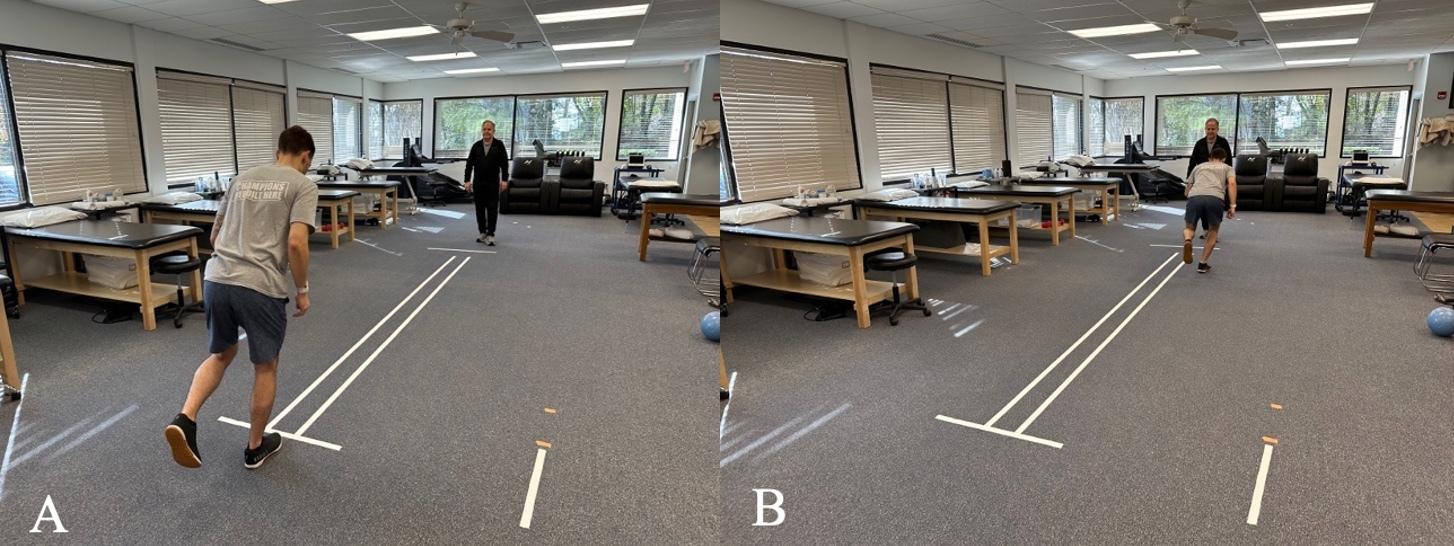
Submitted: December 21, 2022 CST, Accepted: January 16, 2023
CST
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
Figure 8. Reactive Single Limb Alternate Cross Over Hop for Distance Test. The participant stands on one foot and hops outward – as the participant hops, they are instructed which foot to land on and they must cross over the center tape. The athlete will then complete the sequence by performing two more cross over hops successively on alternating limbs.1. Fu FH, Bennett CH, Lattermann C, Ma CB. Current trends in anterior cruciate ligament reconstruction. Part 1: Biology and biomechanics of reconstruction. Am J Sports Med 1999;27(6):821-830. doi:10.1177/03 635465990270062501
2. Wilk KE. Anterior Cruciate Ligament Injury Prevention and Rehabilitation: Let’s Get it Right. J Orthop Sports Phys Ther 2015;45(10):729-730. doi:1 0.2519/jospt.2015.0109
3. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy 2011;27(12):1697-1705. doi:10.1016/j.art hro.2011.09.009
4. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport. Am J Sports Med. 2014;42(7):1567-1573. doi:10.1177/0363 546514530088
5. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study Br J Sports Med 2016;50(13):804-808. doi:10.1136/bjsports-2016-096 031
6. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946-951. doi:10.1136/bjs ports-2015-095908
7 Hurley ET, Mojica ES, Haskel JD, et al. Return to play testing following anterior cruciate reconstruction – a systematic review & metaanalysis. Knee 2022;34:134-140. doi:10.1016/j.knee.2 021.11.010
8. Brophy RH, Stepan JG, Silvers HJ, Mandelbaum BR. Defending Puts the Anterior Cruciate Ligament at Risk During Soccer: A Gender-Based Analysis. Sports Health. 2015;7(3):244-249. doi:10.1177/19417381145 35184
9. Brophy R, Silvers HJ, Gonzales T, Mandelbaum BR. Gender influences: the role of leg dominance in ACL injury among soccer players. Br J Sports Med 2010;44(10):694-697. doi:10.1136/bjsm.2008.051243
10. Walden M, Krosshaug T, Bjorneboe J, Andersen TE, Faul O, Hagglund M. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases. Br J Sports Med. 2015;49(22):1452-1460. doi:10.1136/bjsp orts-2014-094573
11. Stuelcken MC, Mellifont DB, Gorman AD, Sayers MGL. Mechanisms of anterior cruciate ligament injuries in elite women’s netball: a systematic video analysis. J Sports Sci 2016;34(16):1516-1522. doi:10.1 080/02640414.2015.1121285
12. Gokeler A, Dingenen B, Hewett TE. Rehabilitation and return to sport testing after Anterior Cruciate Ligament Reconstruction: Where are we in 2022? Rehabilitation and Return to Sport in Athletics 2022;4(1):E77-E82.
13. Logerstedt D, Grindem H, Lynch A, et al. Singlelegged Hop Tests as Predictors of Self-reported Knee Function After Anterior Cruciate Ligament Reconstruction: The Delaware-Oslo ACL Cohort Study Am J Sports Med 2012;40(10):2348-2356. doi:1 0.1177/0363546512457551
14. Barber SD, Noyes FR, Mangine RE, McCloskey JW, Hartman W Quantitative assessment of functional limitations in normal and anterior cruciate ligamentdeficient knees. Clin Orthop Relat Res. 1990;255:204-214. doi:10.1097/00003086-19900600 0-00028
15. Noyes FR, Barber SD, Mangine RE. Abnormal Lower Limb Symmetry Determined by Function Hop Tests after Anterior Cruciate Ligament Rupture. Am J Sports Med. 1991;19(5):513-518. doi:10.1177/0363546 59101900518
16. Bolgla LA, Keskula DR. Reliability of lower extremity functional performance tests. J Orthop Sports Phys Ther 1997;26(3):138-142. doi:10.2519/jos pt.1997.26.3.138
17. Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41(6):377-387. doi:10.2 519/jospt.2011.3547
18. Anderson MA, Gieck JH, Perrin D, Weltman A, Rutt R, Denegar C. The relationships among isometric, isotonic, and isokinetic concentric and eccentric quadriceps and hamstrings force and three components of athletic performance. J Orthop Sports Phys Ther 1991;14(3):114-120. doi:10.2519/jospt.199 1.14.3.114
19. Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther 1994;20(2):60-73. doi:10.2519/jospt.1994.20.2.6 0
20. Davies GJ, Zillmer DA. Functional Progression of a Patient Through a Rehabilitation Program. Orthopaedic Physical Therapy Clinics of North America. 2000;9:103-118.
21. Savalli L, Hernandez-Sendin MI, Puig PL, Trouvé P Douleurs après ligamentoplastie du ligament croise antérieur: démembrement et prise en charge. Ann Readapt Med Phys 2004;47(6):299-308. doi:10.1016/ j.annrmp.2004.05.005
22. Hill GN, O’Leary ST. Anterior cruciate ligament reconstruction: the short-term recovery using the Knee Injury and Osteoarthritis Outcome Score (KOOS). Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1889-1894. doi:10.1007/s00167-012-222 5-x
23. Turk R, Shah S, Chilton M, et al. Critical Criteria Recommendations: Return to Sport After ACL reconstruction requires evaluation of time after surgery of 8 months, >2 functional tests, psychological readiness, and quadriceps/hamstring strength. Arthroscopy. Published online October 7, 2022. doi:10.1016/j.arthro.2022.08.038
24. Huang H, Nagao M, Arita H, et al. Reproducibility, responsiveness and validation of the Tampa Scale for Kinesiophobia in patients with ACL injuries. Health Qual Life Outcomes 2019;17(1). doi:10.1186/s12955-0 19-1217-7
25. Relph N, Herrington L. Knee joint position sense ability in elite athletes who have returned to international level play following ACL reconstruction: A cross-sectional study. Knee. 2016;23(6):1029-1034. doi:10.1016/j.knee.2016.09.005
26. Shelbourne KD, Benner R, Gray T, Bauman S. Range of Motion, Strength, and Function After ACL Reconstruction Using a Contralateral Patellar Tendon Graft. Orthop J Sports Med 2022;10(11):232596712211381. doi:10.1177/23259671 221138103
27 Shelbourne KD, Freeman H, Gray T Osteoarthritis after anterior cruciate ligament reconstruction: the importance of regaining and maintaining full range of motion. Sports Health. 2012;4(1):79-85. doi:10.117 7/1941738111430201
28. Zumstein F, Centner C, Ritzmann R. How limb dominance influences limb symmetry in ACL patients: effects on functional performance. BMC Sports Sci Med Rehabil 2022;14(1):206. doi:10.1186/s 13102-022-00579-y
29. Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength Asymmetry and Landing Mechanics at Return to Sport after Anterior Cruciate Ligament Reconstruction. Med Sci Sports Exerc. 2015;47(7):1426-1434. doi:10.1249/mss.00000000000 00560
30. Setuain I, González-Izal M, Alfaro J, Gorostiaga E, Izquierdo M. Acceleration and Orientation Jumping Performance Differences Among Elite Professional Male Handball Players With or Without Previous ACL Reconstruction: An Inertial Sensor Unit-Based Study PM R. 2015;7(12):1243-1253. doi:10.1016/j.pmrj.201 5.05.011
31. Ebert JR, Edwards P, Preez LD, Furzer B, Joss B. Knee extensor strength, hop performance, patientreported outcome and inter-test correlation in patients 9–12 months after anterior cruciate ligament reconstruction. Knee. 2021;30:176-184. do i:10.1016/j.knee.2021.04.012
32. White AK, Klemetson CJ, Farmer B, Katsavelis D, Bagwell JJ, Grindstaff TL. COMPARISON OF CLINICAL FATIGUE PROTOCOLS TO DECREASE SINGLE-LEG FORWARD HOP PERFORMANCE IN HEALTHY INDIVIDUALS. Intl J Sports Phys Ther. 2018;13(2):143-151. doi:10.26603/ijspt20180143
33. Negrete R, Simms S, Gross J, et al. The Test ReTest Reliability of A Novel Single Leg Hop Test (TDrill Hop Test). IJSPT. 2021;16(3):724-731,. doi:10.26 603/001c.23677
34. Worst H, Henderson N, DeCarreau R, Davies GJ. A Novel Test to Assess Change of Direction: Development, Reliability, and Rehabilitation Considerations. IJSPT 2019;14(2):228-236.
35. Tabor MA, Davies GJ, Kernozek TW, Negrete RJ, Hudson V A multi-center study of the test-retest reliability of the lower extremity functional test. J Sport Rehab. 2002;11(3):190-201. doi:10.1123/jsr.1 1.3.190
36. Spiteri T, Cochrane JL, Nimphius S, et al. The evaluation of a new lower-body reaction time test. J Strength Cond Res 2013;27(1):174-180. doi:10.1519/js c.0b013e318250381f
37 Simon JE, Millikan N, Yom J, Grooms DR. Neurocognitive challenged hops reduced functional performance relative to traditional hop testing. Phys Ther Sport. 2020;41:97-102. doi:10.1016/j.ptsp.2019.1
2.002
38. Serpell BG, Ford M, Young WB, et al. The development of a new test of agility for rugby league. J Strength Cond Res 2010;24(12):3270-3277


Robert C. Manske, PT, DPT, Med, SCS, ATC, CSCS
Michael Voight, PT, DHSC, SCS, OCS, ATC, CSCS, FAPTA
Chris Wolfe, PT, DPT, OCS, Cert Dip PT
Phil Page, PT, PhD, ATC, CSCS, FACSM
Quadriceps muscle injury is a common occurrence, especially among athletes. While a careful history and a thorough physical examination are important steps in the assessment of quadriceps muscle pathology, it is still difficult to differentiate the type and severity of the pathology. Because of this difficulty, musculoskeletal ultrasound (MSK-US) is an invaluable tool in the diagnosis of quadriceps muscle or tendon injury. Utilizing this noninvasive imaging technique, medical professionals can easily diagnose and monitor muscle and tendon disorders to quickly determine the correct treatment plan for each individual case. The ability to view these structures in real-time allows identification of any present pathologies. MSK-US has become a useful component in diagnosing quadriceps muscle and tendon injuries due to its ability to clearly display the affected structures without exposing the patient to radiation or utilizing ionized contrast media. MSK-US provides valuable insight into fluid dynamics around joints and can even detect myotendinous tears that might otherwise be overlooked with the clinical examination or symptoms usually reported by patients. MSK-US can provide precise visualization of edema and can easily distinguish between benign and potentially pathological findings
which make it an integral part of any holistic evaluation of quadriceps muscle and tendon injury. Additionally, it can be used to track the progress of physical therapy treatments and monitor tissue healing. This information is invaluable in ensuring an optimal outcome for any quadriceps muscle and tendon injury. Therefore, when used in combination with clinical tests, MSK-US can drastically increase the accuracy of the clinical examination. By utilizing this technology, healthcare practitioners have reliable access to more comprehensive diagnostics for musculoskeletal injuries and diseases than ever before. Clinicians are then able to tailor rehabilitation plans more effectively and ensure their patients receive proper treatment. As a result, recovery times may be shortened, and patients are able to return to their normal activities more quickly.
Traditionally, quadricep complex soft tissue injury has been difficult to quantify with the clinical evaluation. Clinical success is always predicated upon an accurate diagnosis and understanding of the pathological process. MSK-US imaging has revolutionized the diagnosis of quadriceps muscle and tendon injuries. While a careful history and a thorough physical examination are important
Patient is supine with a bolster placed under the knee for 30 degrees of flexion, reducing the patella “locking” on the femur as in full extension.
Transducer Placement: Short Axis (SAX) Probe is placed one probe width proximal to the patella.
Patient is supine with a bolster placed under the knee for 30 degrees of flexion, reducing the patella “locking” on the femur as in full extension.
Transducer Placement: Long Axis View (LAX). Probe is placed on the proximal portion of the patella.
Figure 1a. (Left) Figure 1b. (Right)Figure 2a and 2b: SAX view showing the cortex of the femur as the linear reflection deep on the image. Mixed echoes of fat and muscle are superficial to the bony margin. The quadriceps tendon is normally seen as a hyperechoic fibrous texture. Tissue texture should be uniform and light grey in appearance. There should be no darkened areas which may be indicative of injury.
Figure 3a and 3b: LAX view of normal tendon showing the patellar cortex superficial and to the right on the image. Hyperechoic fibrous echotexture of the quadriceps tendon is superficial and tapers to its attachment on the patella.


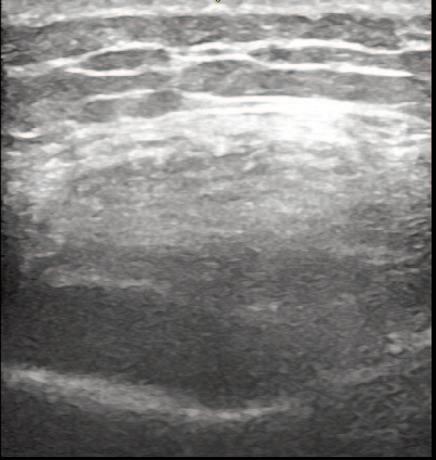
steps in the assessment of quadriceps pathology, MSK-US provides high-resolution static of dynamic images that enable successful visualization and separation of soft tissues from adjoining bones and ligaments. MSK-US has become an invaluable component in diagnosing quadriceps muscle and tendon injuries due to its ability to clearly display the affected structures without exposing the patient to radiation or utilizing ionized contrast media. MSK-US can provide precise visualization of edema and can easily distinguish between benign and potentially pathological findings which make it an integral part of any holistic evaluation of quadriceps muscle tendon injury. The speed and accuracy of ultrasound imaging make it a useful tool in differentiating muscle contusion from tendinopathy or strain. In addition to the diagnostic benefits, MSK-US is also beneficial for monitoring progression and recovery of quadriceps muscle and tendon injuries. The accuracy of images helps clinicians evaluate patient progress during physical therapy sessions and make necessary adjustments to treatment plans if needed. This allows for more precise track-
ing of muscle healing, enabling clinicians to identify any setbacks early on and provide timely intervention if required.
In conclusion, MSK-US is an effective diagnostic tool for assessing quadriceps muscle and tendon injuries. MSK-US has minimal risk with no radiation involved and it can provide valuable information about the extent and progression of injury. By understanding MSK-US and its benefits, medical professionals can better diagnose and treat patients with quadriceps muscle and tendon injuries, leading to more successful outcomes. This makes it an invaluable tool for healthcare professionals when treating musculoskeletal disorders. MSK-US should always be used alongside other techniques such as physical examinations, laboratory tests and patient history to accurately diagnose quadriceps muscle and tendon injuries. MSK-US is essential for providing insight into the structures affected by injury and helps clinicians create tailored physical
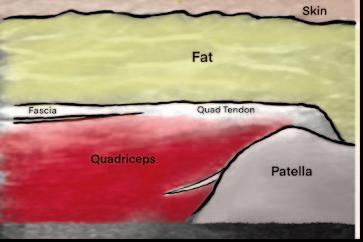 Figure 2a.
Figure 2b.
Figure 3a.
Figure 3b.
Figure 2a.
Figure 2b.
Figure 3a.
Figure 3b.
therapy plans that lead to optimal outcomes. With its accuracy, precision, and non-invasive nature, MSK-US has become an integral part of diagnosing and treating quadriceps muscle injuries. The goal of this article is to provide a few tips and tricks to assist in using MSK-US as a diagnostic tool for the assessment of quadriceps pathology.
LAX view showing quadriceps tendinopathy associated with symptoms has a higher rate of tendon hypoechogenicities, hyperechogenicities and neo-vascularization, with the tendon appearing thicker and with a greater diameter.
LAX view showing quadriceps tendon rupture with 3.4 cm retraction of the tendon (curved red arrow).
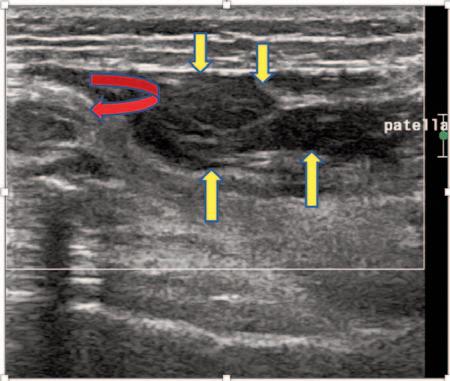
A large heterogeneous 3.5 x 1.2 x 6 cm suprapatellar bursal hematoma (yellow arrows).
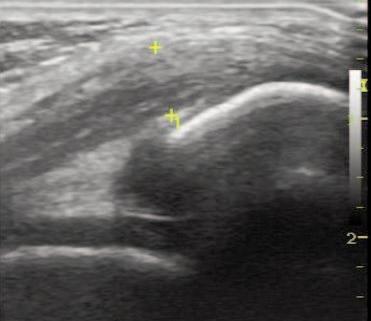 Figure 4a. LAX View of Quadriceps Tendon. Case courtesy of Maulik S Patel, Radiopaedia.org, rID: 25215
Figure 4b. LAX View of Quadriceps Tendon. Case courtesy of Craig Hacking, Radiopaedia.org, rID: 56032
Figure 4a. LAX View of Quadriceps Tendon. Case courtesy of Maulik S Patel, Radiopaedia.org, rID: 25215
Figure 4b. LAX View of Quadriceps Tendon. Case courtesy of Craig Hacking, Radiopaedia.org, rID: 56032
u Patients and athletes who walk in a HydroWorx pool are better equipped to transfer what they learn to land than their counterparts who engage in self-directed shallow water walking.

u Aquatic therapy is bene昀cial to achieve threshold-intensity training while lowering the stress on the joints that is caused by land running.
u The bene昀ts of water therapy on the underwater treadmill included reduced soreness, body fat and in昀ammation while also improving muscle mass and strength performance.
u Clinical results show that athletes who participate in water rehabilitation and land-based post rehabilitation have better scores on postural sway, indicating better balance and fewer episodes of re-injury.
u Bene昀ts of hydrotherapy exercises included a lean body mass increase with underwater treadmill training, with gain seen mainly in the legs.





Stimulates the body’s natural repair mechanisms with our non-invasive current. The unique combination of Winback energy & manual treatments offers great rehabilitation results and a faster recovery of muscle and joint functions.









