Trends in the treatment of paraophthalmic aneurysms in the era of flow diversion Morgan 1Donald
1 Krush ,
Timothy G White
2 MD ,
and Amir R Dehdashti
2 MD
and Barbara Zucker School of Medicine at Hofstra/Northwell, 2Department of Neurosurgery, North Shore University Hospital, Northwell Health, Manhasset, NY, USA
Background Paraophthalmic aneurysms present a unique challenge to surgeons and ideal management of these aneurysms remains up for debate. The three main treatments for these aneurysms are: surgical clipping, endovascular coiling, and flow diversion. Each of these techniques comes with their own advantages and disadvantages. The use of endovascular coiling versus surgical clipping of ruptured intracranial aneurysms was compared in the International Subarachnoid Aneurysm Trial (ISAT).1 Since then, use of coiling has been steadily increasing. The newest of these technologies are flow diverting stents (FDS) such as the Pipeline and Flow Re-Direction Endoluminal Device (FRED) systems. No randomized trials have been conducted to compare the treatments of aneurysms in this specific location.
Objectives To review the use, benefits, and drawbacks of surgical clipping and endovascular coiling of paraophthalmic aneurysms in the time of flow diversion.
Methods A retrospective chart review of 109 patients who received treatment for a paraophthalmic aneurysm at North Shore University Hospital over the past 6 years was performed. Demographic data, aneurysm and patient characteristics at baseline, intervention data, imaging findings, and clinical and radiological follow up was recorded for each patient. Complications were recorded in three categories: ischemic events, intracranial hemorrhage, and visual field deterioration and defects. Data was collected in a REDCap database.
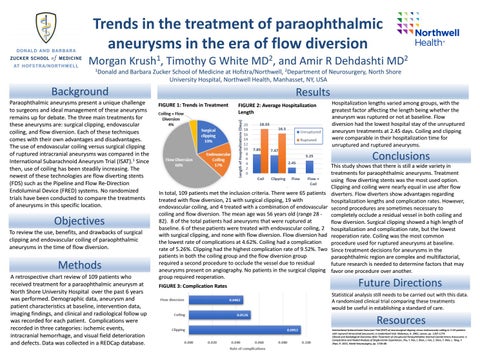
Results FIGURE 1: Trends in Treatment
FIGURE 2: Average Hospitalization Length
Hospitalization lengths varied among groups, with the greatest factor affecting the length being whether the aneurysm was ruptured or not at baseline. Flow diversion had the lowest hospital stay of the unruptured aneurysm treatments at 2.45 days. Coiling and clipping were comparable in their hospitalization time for unruptured and ruptured aneurysms.
Conclusions In total, 109 patients met the inclusion criteria. There were 65 patients treated with flow diversion, 21 with surgical clipping, 19 with endovascular coiling, and 4 treated with a combination of endovascular coiling and flow diversion. The mean age was 56 years old (range 28 82). 8 of the total patients had aneurysms that were ruptured at baseline. 6 of these patients were treated with endovascular coiling, 2 with surgical clipping, and none with flow diversion. Flow diversion had the lowest rate of complications at 4.62%. Coiling had a complication rate of 5.26%. Clipping had the highest complication rate of 9.52%. Two patients in both the coiling group and the flow diversion group required a second procedure to occlude the vessel due to residual aneurysms present on angiography. No patients in the surgical clipping group required reoperation. FIGURE 3: Complication Rates
This study shows that there is still a wide variety in treatments for paraophthalmic aneurysms. Treatment using flow diverting stents was the most used option. Clipping and coiling were nearly equal in use after flow diverters. Flow diverters show advantages regarding hospitalization lengths and complication rates. However, second procedures are sometimes necessary to completely occlude a residual vessel in both coiling and flow diversion. Surgical clipping showed a high length of hospitalization and complication rate, but the lowest reoperation rate. Coiling was the most common procedure used for ruptured aneurysms at baseline. Since treatment decisions for aneurysms in the paraophthalmic region are complex and multifactorial, future research is needed to determine factors that may favor one procedure over another.
Future Directions Statistical analysis still needs to be carried out with this data. A randomized clinical trial comparing these treatments would be useful in establishing a standard of care.
Resources International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Molyneux, A. 2002, Lancet, pp. 1267-1274. Clinical and Radiological Outcomes After Treatment of Unruptured Paraophthalmic Internal Carotid Artery Aneurysms: a Comparative and Pooled Analysis of Single-Center Experiences. Zhu, Y. Pan, J. Shen, J. Fan, Z. Shen, Y. Wen, L. Tong, Y. Zhan, R. 2015, World Neurosurgery, pp. 1726-38.