Evaluating Upper Extremity Lymphedema following Hand Surgery in Patients with Previous Ipsilateral Lymph Node Surgery 1,2,
1,2 BS ,
Michael J. Fitzgerald MD Jesse Galina Peter Olivares Emily Kolodka Ariel Henig 1,2 1,3 1,2 1,2 Cesar Iturriaga BS , Susan Maltser MD , Lewis B. Lane MD , and Kate W. Nellans MD, MPH 1Donald
Background • Lymphedema is a feared complication following breast cancer surgery with axillary lymph node (LN) dissection or sentinel lymph node biopsy. • Medical professionals often advise against all upper extremity interventions on ipsilateral side following axillary lymph node surgery (ALNS), however: • mechanism regulating the onset of lymphedema is theoretical & poorly understood • limited scientific literature supporting avoidance recommendations
1,2 BS ,
and Barbara Zucker School of Medicine at Hofstra/Northwell 2Northwell Health Orthopedics 3Northwell Health PM&R
Results
Nevertheless, patients develop significant anxiety about developing lymphedema, and are hesitant to undergo ipsilateral hand procedures despite paucity of evidence linked to poor outcomes following small hand procedures. Goals: • better understand the risk associated with the development or exacerbation of upper extremity lymphedema following hand surgery or steroid injection in patients with a history of axillary lymph node surgery • decrease patient anxiety and avoidance of interventions on the ipsilateral upper extremity
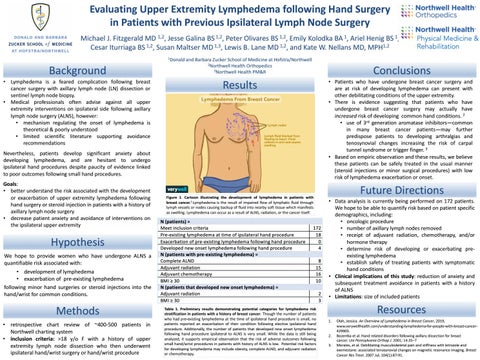
Figure 1. Cartoon illustrating the development of lymphedema in patients with breast cancer.1 Lymphedema is the result of impaired flow of lymphatic fluid through lymph vessels or nodes causing backup of fluid into nearby soft tissue which manifests as swelling. Lymphedema can occur as a result of ALNS, radiation, or the cancer itself.
Hypothesis We hope to provide women who have undergone ALNS a quantifiable risk associated with: • development of lymphedema • exacerbation of pre-existing lymphedema following minor hand surgeries or steroid injections into the hand/wrist for common conditions.
Methods • retrospective chart review of ~400-500 patients in Northwell charting system • inclusion criteria: >18 y/o F with a history of upper extremity lymph node dissection who then underwent ipsilateral hand/wrist surgery or hand/wrist procedure
1 BA ,
Table 1. Preliminary results demonstrating potential categories for lymphedema risk stratification in patients with a history of breast cancer. Though the number of patients who had pre-existing lymphedema at the time of ipsilateral hand procedure is small, no patients reported an exacerbation of their condition following elective ipsilateral hand procedure. Additionally, the number of patients that developed new onset lymphedema following hand procedure ipsilateral to ALNS is very small. While the data is still being analyzed, it supports empirical observation that the risk of adverse outcomes following small hand/wrist procedures in patients with history of ALNS is low. Potential risk factors for developing lymphedema may include obesity, complete ALND, and adjuvant radiation or chemotherapy.
1 BS ,
Physical Medicine & Rehabilitation
Conclusions • Patients who have undergone breast cancer surgery and are at risk of developing lymphedema can present with other debilitating conditions of the upper extremity. • There is evidence suggesting that patients who have undergone breast cancer surgery may actually have increased risk of developing common hand conditions. 2 • use of 3rd generation aromatase inhibitors—common in many breast cancer patients—may further predispose patients to developing arthralgias and tenosynovial changes increasing the risk of carpal tunnel syndrome or trigger finger. 3 • Based on empiric observation and these results, we believe these patients can be safely treated in the usual manner (steroid injections or minor surgical procedures) with low risk of lymphedema exacerbation or onset.
Future Directions • Data analysis is currently being performed on 172 patients. We hope to be able to quantify risk based on patient specific demographics, including: • oncologic procedure • number of axillary lymph nodes removed • receipt of adjuvant radiation, chemotherapy, and/or hormone therapy • determine risk of developing or exacerbating preexisting lymphedema • establish safety of treating patients with symptomatic hand conditions • Clinical implications of this study: reduction of anxiety and subsequent treatment avoidance in patients with a history of ALNS • Limitations: size of included patients
Resources 1. 2. 3.
Olah, Jessica. An Overview of Lymphedema in Breast Cancer, 2019, www.verywellhealth.com/understanding-lymphedema-for-people-with-breast-cancer429903. Bozentka et al. Hand related disorders following axillary dissection for breast cancer. Uni Pennsylvania Orthop J. 2001; 14:35–7 Morales, et al. Debilitating musculoskeletal pain and stiffness with letrozole and exemestane: associated tenosynovial changes on magnetic resonance imaging. Breast Cancer Res Treat. 2007 Jul; 104(1):87-91.