The Use of Ultrasound in The Face of Diagnostic Uncertainty For Necrotizing Enterocolitis in Neonates Saira Khan, Michelle Kallis, MD, Alpna Aggarwal, MD, Aaron Lipskar, MD, Chethan Sathya, MD RESULTS
BACKGROUND
➢ Twenty-nine patients (53.7%) had a positive diagnosis for Necrotizing Enterocolitis.
➢ Necrotizing enterocolitis (NEC) is a devastating intestinal disease in newborns with high associated morbidity and mortality. NEC is characterized by severe inflammation of the intestines, leading to necrosis or perforation. It is most commonly seen in premature neonates, likely due to immaturity of intestinal epithelial cells and immune system. ➢ Once there is clinical suspicion, abdominal radiograph is used to look for characteristic findings like pneumatosis intestinalis (air in the intestinal wall), abnormal persistent distended bowel loops, bowel wall thickening, pneumoperitoneum and portal vein gas.
➢ Of the positive patients, pneumatosis was identified by abdominal ultrasound in 22 patients (75.9%) and by abdominal radiograph in 6 patients (20.7%), (p<0.01). ➢ Of the negative patients, absence of pneumatosis was confirmed in 100% of patients by abdominal ultrasound and in 48% of patients by abdominal radiograph (p<0.01).
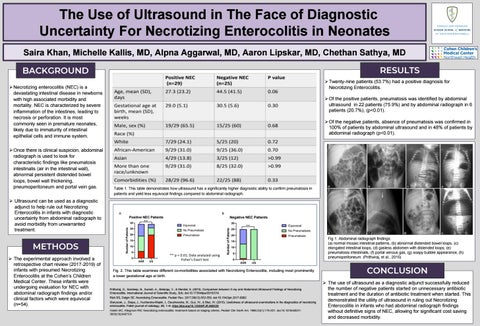
Table 1. This table demonstrates how ultrasound has a significantly higher diagnostic ability to confirm pneumatosis in patients and yield less equivocal findings compared to abdominal radiograph.
➢ Ultrasound can be used as a diagnostic adjunct to help rule out Necrotizing Enterocolitis in infants with diagnostic uncertainty from abdominal radiograph to avoid morbidity from unwarranted treatment. Fig 1. Abdominal radiograph findings: (a) normal mosaic intestinal patterns, (b) abnormal distended bowel loops, (c) elongated intestinal loops, (d) gasless abdomen with distended loops, (e) pneumatosis intestinalis, (f) portal venous gas, (g) soapy bubble appearance, (h) pneumoperitoneum. (Prithviraj, et al., 2015)
METHODS ➢ The experimental approach involved a retrospective chart review (2017-2019) of infants with presumed Necrotizing Enterocolitis at the Cohen’s Children Medical Center. These infants were undergoing evaluation for NEC with abdominal radiograph findings and/or clinical factors which were equivocal (n=54).
Fig. 2. This table examines different co-morbidities associated with Necrotizing Enterocolitis, including most prominently a lower gestational age at birth.
Prithviraj, D., Sandeep, B., Suresh, A., Balaraju, V., & Mondal, S. (2015). Comparison between X-ray and Abdominal Ultrasound Findings of Necrotizing Enterocolitis. International Journal of Scientific Study, 3(4). doi:10.17354/ijss/2015/319 Rich BS, Dolgin SE. Necrotizing Enterocolitis. Pediatr Rev. 2017;38(12):552-559. doi:10.1542/pir.2017-0002 Staryszak, J., Stopa, J., Kucharska-Miąsik, I., Osuchowska, M., Guz, W., & Błaż, W. (2015). Usefulness of ultrasound examinations in the diagnostics of necrotizing enterocolitis. Polish journal of radiology, 80, 1–9. https://doi.org/10.12659/PJR.890539 Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33(1):179-201. doi:10.1016/s00313955(16)34975-6
CONCLUSION ➢ The use of ultrasound as a diagnostic adjunct successfully reduced the number of negative patients started on unnecessary antibiotic treatment and the duration of antibiotic treatment when started. This demonstrated the utility of ultrasound in ruling out Necrotizing Enterocolitis in infants who had abdominal radiograph findings without definitive signs of NEC, allowing for significant cost saving and decreased morbidity.