Risk Factors Associated with Development of Cerebral Edema Post-BAVM Embolization with Onyx Embolic Agent Madison Fraser1, Timothy White, MD2, Kevin Shah, MD2, Justin Turpin, MD2, Henry Woo, MD2
Background Brain arteriovenous malformations (BAVMs) are abnormal fistulous connections between the arterial system and the venous system made up of dysplastic plexiform vessels. Current treatment options include embolization, surgical resection, and radiotherapy. Treatment is often multimodal, involving a combination of the three options. Recently, surgeons have started treating BAVMs solely with embolization with a cure rate reported to be up to 24%.3 The management of BAVMs can be challenging as patients are often young, and each AVM can differ in its size, location, angioarchitecture, and imaging characteristics.
1Donald
and Barbara Zucker School of Medicine at Hofstra/Northwell 2Department of Neurosurgery at North Shore Hospital/LIJ
Results
Data was collected on 71 embolization procedures. Of those procedures, up to 50 of them (depending on the variable) were able to be analyzed for FLAIR signal. FLAIR MRI was unavailable or unable to be determined for the remaining procedures. The rate of severe cerebral edema development post-embolization when Onyx was used was 43% and the rate of mild or no cerebral edema was 56% (n = 41). The rate of severe cerebral edema development post-embolization when NBCA was used was 37% and the rate of mild or no edema was 62.5% (n = 8). The relationship between the rate of cerebral edema development and choice of agent was ultimately determined to be statistically insignificant (p = 1). Due to the limited availability of data on patients who have undergone embolization with NBCA agent as opposed to Onyx, the sampling size was significantly smaller for NBCA and may serve as a large source of error.
One injectable liquid embolic agent commonly used for the embolization of BAVM pedicles is Onyx™, which is a mix of ethylene vinyl-alcohol copolymer (EVOH), DMSO (dimethylsulfoxide), and micronized tantalum powder. Since its approval in 2005 for the endovascular treatment of AVMs, the risks and outcomes associated with Onyx usage has been mixed15,16. When accounting for the differing angioarchitecture/complexity of patients’ BAVMs, the periprocedural morbidity associated with Onyx usage when compared to the traditional embolic agent (NBCA) has shown no significant difference in mortality outcomes15.
Percent of the AVM embolized and the patency of the draining vein were also analyzed for a relationship to the development of cerebral edema post-embolization. These variables served to take into account the possibility of vasogenic edema from flow shunting (a result of the embolization procedure itself) as opposed to angiotoxicity edema resulting from the DMSO in the Onyx embolic agent. However, both the proportion of patients with occluded draining veins who developed cerebral edema and the proportion of patients with high percentage of AVM embolized who developed cerebral edema were determined to be statistically insignificant as well (p = 0.36 and p = 0.75, respectively).
Possible complications and adverse events of BAVM embolization include hemorrhage, infarct, neurological deficits, and development of cerebral edema.15-17 Limited literature suggests that the organic solvent component of the Onyx embolic liquid, DMSO, can be associated with angio- and neurotoxicity.18,19 The microvascular injury associated with DMSO infusion has lead to acute vasospasm and hemodynamic changes in animal models, however studies have yet to prove that this contributes to the adverse events seen after BAVM embolization with Onyx in human patients.18,19 The purpose of this study is to determine whether a possible association exists between the development of complications post-embolization with the use of Onyx embolic agent, with a specific focus on the development of cerebral edema.
Finally, there existed no correlation between the volume of Onyx embolic agent used during the embolization and the extent of cerebral edema post-procedure (⍴ = -0.127).
Hypothesis
These results signify that the choice and amount of Onyx used during BAVM embolization cannot be definitively linked to the development of cerebral edema.
The development of cerebral edema post-BAVM embolization is associated with the choice and amount of embolic agent.
Future Direction
Methods This study was a retrospective review of patients who underwent embolization treatment for cerebral AVMs at North Shore University Hospital and Southside Hospital between 1/1/2014 and 4/1/2020. In order to meet inclusion criteria for the study, patients had to have a confirmed BAVM diagnosed by MRI/MRA, CTA, and/or conventional angiogram. Patients were excluded from review if they had been diagnosed with dural arteriovenous fistula or spinal fistula or had a condition which complicated the nature of the BAVM (e.g. neurocutaneous syndromes such as cerebro-retinal angiomatosis (von Hippel-Lindau), encephalotrigeminal syndrome (Sturge-Weber), or Wyburn-Mason syndrome, or moya-moya-type changes of the BAVM). Data was ultimately collected on 46 patients. Clinical, radiographic, and procedural data was collected on all patients to determine the factors that predict outcomes in patients who undergo embolization treatment for their cerebral AVMs. The presence of cerebral edema post-embolization was determined by the intensity of T2-weighted (FLAIR) signal on 1-day post-op MRI. For purpose of analysis, the amount of FLAIR present on MRI was categorized as none/mild or severe. Each patient was denoted a score based on their FLAIR results: • 1 = none – mild FLAIR signal (none-mild cerebral edema) • 2 = high FLAIR signal (severe cerebral edema) The post-procedural FLAIR signals were then analyzed for relationship to the following procedural variables: • The amount of Onyx used in the procedure • The percent of BAVM embolized in the procedure (0-50% or 50-100%) • The usage of Onyx vs. NBCA embolic agent • The patency of the draining vein of the BAVM post-embolization (patent vs. occluded) Data was also collected on the features of each patients’ BAVMs, such as Spetzler-Martin score and the number of feeders, and on the clinical outcomes of the patient after embolization. This helped determine the rate of other complications in addition to cerebral edema, such as hemorrhage, seizures, and neurological deficits. Each patient’s 3-month follow-up MRI was also reviewed, if available, to determine whether any prior cerebral edema had resolved.
Conclusions
• Increasing the timeline of patient data retrospectively acquired may increase the sample size population of patients who received NBCA and improve data analysis when comparing embolic agents • Further analysis of other post-embolization complications, such as hemorrhage or infarct, and their possible link to Onyx usage
Resources Figure 7: Independent CRISPR knockout of CDK4 or CDK6 does not cause dropout in most breast cancer cell lines studied.
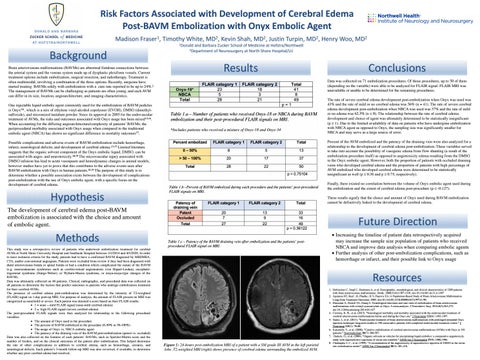
Figure 1: 24-hours post-embolization MRI of a patient with a SM grade III AVM in the left parietal lobe. T2-weighted MRI (right) shows presence of cerebral edema surrounding the embolized AVM.
1. Hofmeister C, Stapf C, Hartmann A, et al. Demographic, morphological, and clinical characteristics of 1289 patients with brain arteriovenous malformation. Stroke. 2000;31(6):1307-1310. doi:10.1161/01.str.31.6.1307 2. Apsimon HT, Reef ; H, Phadke ; R V, Popovic EA. A Population-Based Study of Brain Arteriovenous Malformation Long-Term Treatment Outcomes. 2002. doi:10.1161/01.STR.0000043674.99741.9B 3. Elsenousi A, Aletich VA, Alaraj A. Neurological outcomes and cure rates of embolization of brain arteriovenous malformations with n-butyl cyanoacrylate or Onyx: A meta-analysis. J Neurointerv Surg. 2016;8(3):265-272. doi:10.1136/neurintsurg-2014-011427 4. Crowley, R. W., et al. (2015). "Neurological morbidity and mortality associated with the endovascular treatment of cerebral arteriovenous malformations before and during the Onyx era." J Neurosurg 122(6): 1492-1497. 5. Saatci, I., et al. (2011). "Endovascular treatment of brain arteriovenous malformations with prolonged intranidal Onyx injection technique: long-term results in 350 consecutive patients with completed endovascular treatment course." J Neurosurg 115(1): 78-88. 6. Katsaridis, V., et al. (2008). "Curative embolization of cerebral arteriovenous malformations (AVMs) with Onyx in 101 patients." Neuroradiology 50(7): 589-597. 7. Dudeck, O., et al. (2006). "Organic solvents as vehicles for precipitating liquid embolics: a comparative angiotoxicity study with superselective injections of swine rete mirabile." AJNR Am J Neuroradiol 27(9): 1900-1906. 8. Chaloupka, J. C., et al. (1999). "A reexamination of the angiotoxicity of superselective injection of DMSO in the swine rete embolization model." AJNR Am J Neuroradiol 20(3): 401-410.