Reimagining the Interprofessional Care Team in the Virtual Space during the COVID-19 Pandemic Joy Achuonjei MS, Lauren Block MD MPH, Daniel J. Coletti PhD Division of General Internal Medicine, Hofstra Northwell School of Medicine examine timing, content, and methods of communication between members of the interprofessional care team in addition to their communications with patients over a period of 5 weeks starting in May of 2020 where all team members were working remotely. Would add to methods
Results
Introduction
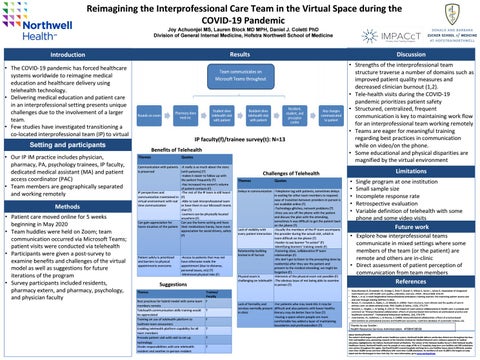
• The COVID-19 pandemic has forced healthcare systems worldwide to reimagine medical education and healthcare delivery using telehealth technology. • Delivering medical education and patient care in an interprofessional setting presents unique challenges due to the involvement of a larger team. • Few studies have investigated transitioning a co-located interprofessional team (IP) to virtual
IP faculty(f)/trainee survey(t): N=13
Setting and participants • Our IP IM practice includes physician, pharmacy, PA, psychology trainees, IP faculty, dedicated medical assistant (MA) and patient access coordinator (PAC) • Team members are geographically separated and working remotely
Methods • Patient care moved online for 5 weeks beginning in May 2020 • Team huddles were held on Zoom; team communication occurred via Microsoft Teams; patient visits were conducted via telehealth • Participants were given a post-survey to examine benefits and challenges of the virtual model as well as suggestions for future iterations of the program • Survey participants included residents, pharmacy extern, and pharmacy, psychology, and physician faculty
Discussion
Benefits of Telehealth Themes
Quotes
Communication with patients -It really is so much about the story is preserved [with patients] (T) -makes it easier to follow up with the patient frequently (T) -Has increased my extern’s volume of patient contacts (F) IP perspectives and -The rest of the IP team is still heard communication maintained in (F) virtual environment with real -Able to task interprofessional team time communication or have them in our Microsoft teams chat (T) -Learners can be physically located anywhere (F) Can gain appreciation for Can see the home setting and have home situation of the patient their medications handy, have more appreciation for social drivers, safety (F)
Patient safety is prioritized and barriers to physical appointments overcome
-Access to patients that may not have otherwise made the appointment (due to distance, personal issues, etc) (T) -Minimized physical risks (F)
Suggestions Themes Best practices for hybrid model with some team members remote Telehealth communication skills training would be appreciated Training on use of telehealth platform to facilitate team encounters Enabling telehealth platform capability for all team members Precede patient visit with visit to set up technology Divide responsibilities with one telehealth resident and another in-person resident
Trainee/ Faculty F T F T T T
• Strengths of the interprofessional team structure traverse a number of domains such as improved patient quality measures and decreased clinician burnout (1,2). • Tele-health visits during the COVID-19 pandemic prioritizes patient safety • Structured, centralized, frequent communication is key to maintaining work flow for an interprofessional team working remotely • Teams are eager for meaningful training regarding best practices in communication while on video/on the phone. • Some educational and physical disparities are magnified by the virtual environment
Limitations
Challenges of Telehealth Themes
Quotes
Delays in communication -Telephone tag with patients, sometimes delays in waiting for other team members to respond; ease of transition between providers in person is not available online (T) -Technology-glitches, network problems (T) -Once you are off the phone with the patient and discuss the plan with the attending, sometimes it was difficult to get the patient back on the phone (T) Lack of visibility with -Usually the members of the IP team accompany every patient interaction the provider during the actual visit, which is more difficult on the phone (T) -Harder to see learner “in action” (F) -Identifying learners’ training needs (F) Relationship building -Fostering close, collaborative IP team limited in IP format relationships (F) -We don’t get to listen to the precepting done by resident(s) after they see the patient and present to the medical attending; we might be forgotten (F) Physical exam is -Elements of the physical exam not possible (F) challenging on telehealth -The obvious issue of not being able to examine in person (T)
Lack of formality and -For patients who may need ASL it may be services normally present difficult and also patients with lower healthy in clinic literacy may do better face to face (T) -Having a space where people are more comfortable has added a layer of maintaining boundaries and professionalism (T)
• • • • •
Single program at one institution Small sample size Incomplete response rate Retrospective evaluation Variable definition of telehealth with some phone and some video visits
Future work • Explore how interprofessional teams communicate in mixed settings where some members of the team (or the patient) are remote and others are in-clinic • Direct assessment of patient perception of communication from team members
References • Reiss-Brennan B, Brunisholz KD, Dredge C, Briot P, Grazier K, Wilcox A, Savitz L, James B. Association of integrated team-based care with health care quality, utilization, and cost. JAMA. 2016;316(8): 826-34. • Block, L. et al. A novel longitudinal interprofessional ambulatory training practice: the improving patient access care and cost through training (IMPACcT) clinic. • Bower, P., Campbell, S., Bojke, C., & Sibbald, B. (2003). Team structure, team climate and the quality of care in primary care: an observational study. BMJ Quality & Safety, 12(4), 273-279. • Buscemi, J., Steglitz, J., & Spring, B. (2012). The impact of team science collaborations in health care: a synopsis and comment on “Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes”. Translational behavioral medicine, 2(4), 378-379. • Zwarenstein, M., Goldman, J., & Reeves, S. (2009). Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane database of systematic reviews, (3).
Thanks to our funder: Health Resources Services Administration. #T0BHP28558 About Northwell Health The nation’s third-largest non-profit secular healthcare system, Northwell Health delivers world-class clinical care throughout the New York metropolitan area, pioneering research at the Feinstein Institute for Medical Research and a visionary approach to medical education, highlighted by the Hofstra Northwell School of Medicine. The winner of the National Quality Forum’s 2010 National Quality Healthcare Award, Northwell Health cares for people at every stage of life at 21 hospitals, long-term care facilities and 450 ambulatory care centers throughout the region. Northwell Health’s owned hospitals and long-term care facilities house about 6,400 beds, employ more than 10,000 nurses and have affiliations with more than 12,000 physicians. Its workforce of over 61,000 is the largest on Long Island and the third-largest in New York City. For more information, go to www.northwell.edu