E3 Advocacy
empower, engage, and educate
When Care Is ‘Accessible’ But Not Reachable

empower, engage, and educate
When Care Is ‘Accessible’ But Not Reachable
The purposes they serve and how to get involved.
Navigating the Canadian Healthcare System and Understanding Health Insurance
Hidden Reasons Behind Self-Sabotage


CACHEducation is evolving to better serve the needs of patient advocates and healthcare professionals with its rebrand to CACHEducation Academy. This transformation reflects an expanded commitment to delivering high-quality, structured learning experiences tailored to the ever-changing landscape of patient advocacy and healthcare education. As part of this rebrand, CACHEducation Academy will introduce Advanced Curriculum offerings starting in April 2025, providing deeper insights, specialized training, and enhanced skill development for those looking to elevate their expertise. This next phase marks a significant step forward in strengthening the capacity and impact of patient advocates through comprehensive and innovative education.
“Enrolling in CACHEducation was a game-changer for me as a patient advocate. The program provided invaluable knowledge, practical skills, and a supportive community that empowered me to make a real impact in healthcare advocacy.”

A Heal Canada Digital Magazine
OCTOBER 2025 | Issue 10
Founders Note
PRINCIPAL TOPIC
Navigating the Canadian Healthcare System and Understanding Health Insurance
Value-Based Healthcare
Social Determinants of Health in Canada
Emerging Treatments in the Canadian Healthcare Environment
Health Insurance in Canada: A Cornerstone of Equity, Diversity, and Inclusion
MENTAL HEALTH
Reading for Well Being
Doomscrolling In A Time Of Tariffs
From First Step to First Session: Accessing Mental Health Care in Canada
Understanding Why We Self-Sabotage
Finding Friendship in Retirement Living
Radio Taiso 3 Minute Japanense Routine
Diabetes and Seniors - 5 Facts
PEDIATRIC HEALTH
Digital and Social Media Impact on Children
ADVOCACY SPOTLIGHT
When Care Is ‘Accessible’ But Not Reachable
Grassroots engagement for change
The Disorder Channel What Is HT?
Staywell
Health Advisory Network
From the Oil Sands to Mental Health
Advocacy
Talk About the Yew Tree
Elianna’s Journey
Unware of Thier Might (Poem)
Goal Setting Made Simple
How Cholesterol Denialism went from Reasonable Skepticism to Pseudoscience
5 Tips for Eating Healthy in a Time Crunch (plus recipes!)
The Smile File
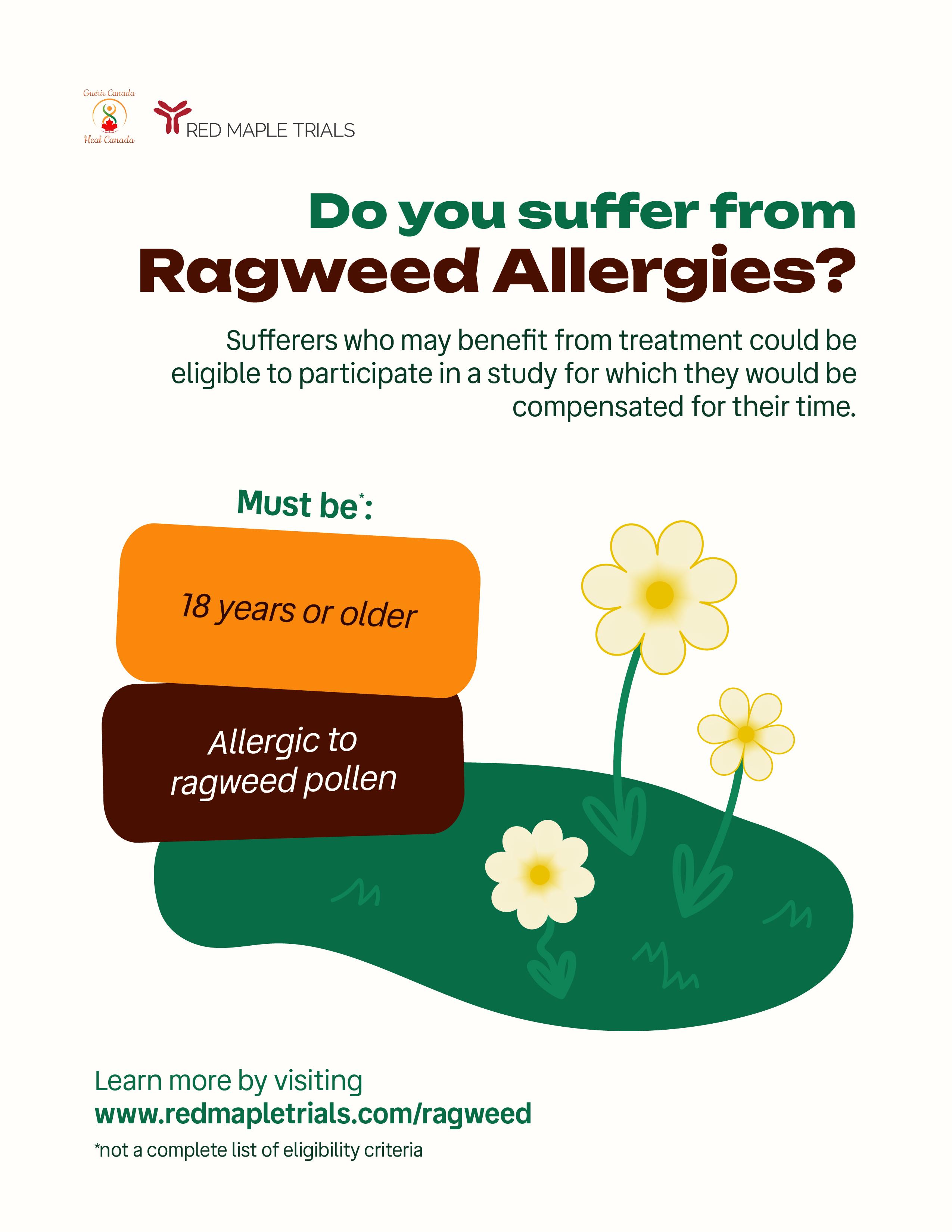
The Importance of Clinical Trials
Heal Canada Resources
Clinical Trials and Registries
Alliances Supporters
Heal Canada Team
Team Members: Cheryl Petruk, Wendy Reichental, and Anna Trubaieva
Designer: Richie Evans
E3 Advocacy is a bimonthly patient advocacy magazine distrubted by Heal Canada. It has been running for 10 issues over 1 year and is seen globally, serving a variety of patient communities.
Heal Canada is a registered Non Profit Organization in Canada
Visit healcanada.org to download this current issue and subscribe for future issues admin@healcanada.org
Disclaimer: The Patient Advocacy Digital Magazine provides general information and resources to promote patient empowerment and awareness. The content is not a substitute for professional medical advice or treatment. Always consult with qualified healthcare professionals for personalized guidance regarding your specific medical condition or situation.

ISSN 2819-2265
© 2025 E3 Advocacy Digital Magazine. All rights reserved.
No part of this publication may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the publisher, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law. For permission requests, please contact: admin@healcanada.org
E3 Advocacy is a publication of Heal Canada, supporting education, empowerment, and engagement in patient advocacy.
By Cheryl Petruk, Founder, Heal Canada
As we unveil the October issue of E3 Advocacy Digital Magazine, I am filled with excitement and gratitude. This issue marks a new chapter — not only in design, with a refreshed, dynamic look, but also in purpose. The transformation reflects our ongoing commitment to deliver meaningful, relevant, and empowering content for Patients, Advocates, and Healthcare Professionals around the world.
Within these pages, you’ll find incredible articles that inform, inspire, and ignite conversations. Each contribution — from thought-provoking editorials to lived patient experiences and expert insights — embodies what E3 Advocacy stands for: Educate, Empower, Engage. Together, these stories strengthen our shared mission to elevate the patient voice and build bridges between advocacy, healthcare, and innovation.
It is with great humility that I share an extraordinary milestone: E3 Advocacy now reaches over 54,000 readers worldwide. This achievement is a testament to the passion of our writers, the trust of our readers, and the collective belief that education and collaboration can drive meaningful change in healthcare.
Today, E3 Advocacy has become one of Heal Canada’s signature programs — a vibrant platform that fuels our team’s passion every single day. Through every article, conversation, and connection, we are reminded that advocacy is not just our work; it’s our purpose.
Thank you for being part of this journey, for reading, sharing, and championing the patient voice. Together, we continue to make advocacy matter.

With appreciation and inspiration,
Cheryl Petruk Founder, Heal Canada & E3 Advocacy Digital Magazine


By Cheryl Petruk
Canada’s healthcare system is one of the defining features of its national identity— publicly funded, universally accessible, and guided by the principle that healthcare should be based on need rather than ability to pay. Yet, for many Canadians and newcomers alike, understanding how the system functions—who pays for what, which level of government is responsible, and how private or supplementary insurance fits in—can be confusing.
This article provides an overview of how the Canadian healthcare system works, highlighting the roles of federal and provincial governments, how public health insurance operates, and how private insurance fills coverage gaps.
Canada’s healthcare system—commonly referred to as Medicare—is not a single national plan but a collection of provincial and territorial health insurance plans operating under shared
national principles established by the Canada Health Act (CHA) of 1984.
The Canada Health Act outlines five key principles that every province and territory must meet to receive full federal funding:
1. Public Administration: Health insurance plans must be administered on a non-profit basis by a public authority accountable to the provincial government.
2. Comprehensiveness: All medically necessary hospital and physician services must be covered.
3. Universality: All residents are entitled to the same level of care.
4. Portability: Coverage must follow residents across provinces and territories and provide limited coverage when travelling abroad.
5. Accessibility: Services must be provided on uniform terms and conditions without financial or other barriers.
These principles ensure that healthcare remains equitable, publicly administered, and accessible to every Canadian citizen and permanent resident.
The federal government and provincial/territorial governments share responsibility for healthcare delivery and financing, but their roles differ.
The Government of Canada, through Health Canada and related agencies, plays several key roles:
• Setting national standards through the Canada Health Act
• Providing financial support to provinces and territories via the Canada Health Transfer (CHT)—the largest federal transfer to provinces, amounting to over $50 billion annually
• Supporting public health and health research, including disease prevention and emergency preparedness through agencies like the Public Health Agency of Canada and the Canadian Institutes of Health Research (CIHR)
• Delivering healthcare directly to specific populations (Indigenous peoples living on reserves, Canadian Armed Forces members and veterans, Federal inmates, and Refugee claimants under the Interim Federal Health Program)
The federal government also regulates pharmaceutical safety, medical devices, and food and drug standards through Health Canada.
Each province and territory administers its own health insurance plan and is primarily responsible for:
• Managing and delivering healthcare services
• Determining which services are insured
• Negotiating physician fee schedules
• Funding hospitals and health authorities
• Regulating healthcare professionals
Because of this provincial autonomy, healthcare systems differ across Canada. What’s covered in one province may not be covered in another, leading to variations in wait times, prescription drug programs, and access to specialized services.
All provinces and territories provide public health insurance that covers medically necessary hospital and physician services. Residents must register with their provincial health authority to obtain a health card that allows access to publicly funded care.

Under the Canada Health Act, the core publicly funded services include:
• Hospital care (inpatient and outpatient)
• Physician services (general practitioners and specialists)
• Diagnostic services (such as lab tests and imaging when medically necessary)
• Some surgical dental procedures are performed in hospitals
Many essential health-related services fall outside the scope of the CHA and are not universally covered:
• Prescription drugs (outside hospitals)
• Dental care
• Vision care
• Physiotherapy, chiropractic, and other allied health services
• Long-term care, home care, and mental health services (beyond basic levels)
Because these services are excluded from the Canada Health Act, provinces determine the extent of their coverage individually, leading to significant regional variation.
Each province and territory has its own public health insurance plan, with specific names and administrative processes. Examples include:
• Ontario Health Insurance Plan (OHIP)
• Alberta Health Care Insurance Plan (AHCIP)
• Régie de l’assurance maladie du Québec (RAMQ)
• Manitoba Health, Seniors and Active Living
• British Columbia’s Medical Services Plan (MSP)
While all cover hospital and physician services, they differ in supplementary coverage. For instance:
• Quebec mandates participation in a public or private prescription drug plan.
• Ontario covers prescription drugs for youth under 25 and seniors over 65 through the Ontario Drug Benefit Program.
• British Columbia operates a Fair Pharmacare program based on household income.
These programs offer residents some level of protection, but out-of-pocket costs can still occur for those without private insurance.
Approximately two-thirds of Canadians have private health insurance, most often provided through employers or professional associations. Private insurance plays a complementary role to the public system—it does not replace it.
Private insurance typically covers:
• Prescription medications not covered by provincial plans,
• Dental and vision care,
• Paramedical services (e.g., physiotherapy, massage therapy),
• Semi-private hospital rooms,
• Out-of-country medical care, and
• Medical equipment or prosthetics.
Canadians who are self-employed, retired, or unemployed often purchase individual or family health plans from providers such as Manulife, Sun Life, Green Shield Canada, or Blue Cross. Private coverage helps reduce financial strain and ensures broader access to services that contribute to quality of life, particularly for those with chronic conditions or specialized needs.
The interaction between federal and provincial governments in healthcare financing is crucial to maintaining the system’s stability. The Canada Health Transfer (CHT) is the primary mechanism through which the federal government supports provincial health expenditures.
Provinces must comply with the Canada Health Act to receive the full CHT allocation. If a province allows user fees or extra billing by physicians for insured services, the federal government can withhold equivalent amounts from its transfer payments—ensuring compliance and equity across Canada.
Beyond financial support, Ottawa collaborates with provinces on national health priorities, such as:
• Mental health and addictions,
• Reducing surgical wait times,
• Expanding long-term and home care, and
• Addressing Indigenous health disparities.
Understanding how to access healthcare can make a significant difference in navigating Canada’s complex system. The process typically involves several steps:
1. Primary Care Access:
Most Canadians access healthcare through a family physician or nurse practitioner, who acts as the first point of contact and coordinates referrals to specialists.
2. Walk-in Clinics and Telemedicine:
For those without a family doctor, walk-in clinics and virtual health platforms provide nonemergency care. Many provinces now support telehealth services, allowing patients to consult healthcare professionals remotely.
3. Emergency and Hospital Services:
Emergency departments are accessible to all residents, though wait times vary. Patients are not billed for insured hospital services.
4. Specialist Referrals:
Most specialists require a referral from a primary care provider to ensure continuity and cost control.
5. Pharmacy and Prescription Coverage: Prescription drugs must be paid out-ofpocket unless the patient is covered under a public drug plan (e.g., seniors, low-income households) or private insurance.
6. Cross-Provincial and International Care:
Under the portability principle, residents temporarily in another province remain covered for necessary services. However, international travel usually requires private travel health insurance.
While the Canadian healthcare system is admired globally, it faces persistent challenges that require coordinated action:
• Wait Times: Long wait times for elective surgeries, diagnostics, and specialist appointments remain a concern.
• Access to Primary Care: Millions of Canadians lack a regular family physician, leading to fragmented care.
• Aging Population: Growing demand for long-term care, home care, and chronic disease management is straining provincial budgets.
• Pharmacare and Mental Health: The absence of universal drug coverage and uneven access to mental health services create inequities.
• Health Human Resources: Staffing shortages, especially in rural areas, affect timely access to care.

Efforts are underway to modernize the system. In 2023, the federal government announced a 10-year, $198-billion healthcare funding agreement to support provinces in addressing these issues, including data sharing, workforce retention, and improved mental health services.
One of the most significant policy discussions in Canada today is the creation of a national pharmacare program—a public plan that would ensure universal access to prescription drugs.
Currently, drug coverage is a patchwork of provincial programs and private plans. As a result, one in five Canadians reports difficulty affording medications.
The Advisory Council on the Implementation of National Pharmacare (2019) recommended a universal, single-payer public pharmacare program phased in over time. Discussions continue between federal and provincial governments, with cost-sharing models and administrative logistics still under negotiation.
Indigenous peoples in Canada face substantial disparities in health outcomes due to historical, social, and structural inequities.
The First Nations and Inuit Health Branch (FNIHB) under Health Canada delivers or funds health services in collaboration with Indigenous communities, while provinces provide hospital and physician services. Efforts to advance Indigenous self-determination in health governance—such as British Columbia’s First Nations Health Authority (FNHA)—are reshaping how care is delivered and accessed in Indigenous communities.
For patients and families managing complex or chronic conditions, understanding insurance coordination is essential.
• Patients with multiple coverages (e.g., employer plan plus provincial drug program) must coordinate benefits—usually the employer plan pays first.
• Reimbursement systems vary by province; for example, Ontario’s Trillium Drug Program requires patients to meet an income-based deductible before coverage begins.
• Appeals and exceptions processes exist for high-cost drugs not listed on provincial formularies, though these can be lengthy and complex.
Patient advocacy groups play an important role in helping individuals navigate these reimbursement systems, ensuring equitable access to treatments and bridging communication between patients, providers, and policymakers.
Canada’s healthcare system is at a crossroads. Future sustainability will depend on modernization and collaboration across all levels of government and sectors.
Key reforms underway include:
• Integration of digital health records for continuity of care.
• Expansion of team-based primary care models.
• Greater emphasis on value-based healthcare, where outcomes are measured relative to cost.
• National coordination on data, pharmaceuticals, and innovation.
The vision is a more patient-centered, outcomedriven system that aligns public funding with measurable improvements in population health.
Navigating Canada’s healthcare system requires understanding its federal-provincial structure, the scope of public insurance, and the role of private coverage in filling gaps. While Canadians benefit from universal access to essential hospital and physician care, disparities remain in areas such as drug coverage, dental care, and mental health services.
As Canada continues to evolve its healthcare model—balancing universality with sustainability—the collaboration between governments, healthcare professionals, and patient advocacy organizations will be crucial in shaping a system that truly reflects the values of accessibility, equity, and compassion at the heart of Canadian society.


Cheryl A. Petruk is a multifaceted professional whose career spans patient advocacy, business, and post-secondary education, showcasing her dedication to significantly impacting these areas.


By Cheryl Petruk
Value-based health care (VBHC) shifts the system’s focus from “how much care was delivered” to “what outcomes mattered to patients and at what cost across the full care journey.” In Canada’s publicly funded ecosystem—where budgets are finite, needs differ by region, and health equity is a core principle—VBHC offers a practical, measurable way to improve results while stewarding resources responsibly. Healthcare Excellence Canada (HEC) frames VBHC as linking resources over a patient’s journey to the outcomes that matter most to patients and communities—emphasizing experience, health outcomes, equity, and sustainability alongside cost. This orientation fits Canada’s policy goals and patient-centred ethos.
The canonical definition of VBHC pairs patientimportant outcomes with the total costs of delivering care across a cycle (e.g., from diagnosis to rehabilitation). Organizations such as ICHOM have operationalized this idea by publishing global standard sets of patient-centred outcome measures that enable apples-to-apples
comparisons and learning. For Canadian teams, these sets help anchor clinical pathways, quality improvement, and procurement to the metrics patients actually care about (function, symptom relief, participation in life), not just process counts.
HEC has built practical tools—like a VBHC toolkit and organizational self-assessments— to help systems translate the concept into implementation. These resources walk through governance, measurement, costing, and change management—key building blocks for moving from pilots to durability.
1. Measuring outcomes that matter to patients When clinical teams routinely measure standardized outcomes (including PROMs and PREMs), they can spot variation, iterate pathways, and share what works. This is the engine of VBHC: transparent, comparable outcomes tied to clinical practice. Internationally, the spread of ICHOM sets illustrates how outcome measurement becomes a common language across providers and payers, and Canadian programs can plug into that network to accelerate learning.
2. Paying for results across a full episode
Episode-based or “bundled” funding motivates integrated, coordinated care (e.g., surgery through rehab) and discourages fragmentation. Ontario’s bundled care for hip and knee replacements is a prominent Canadian example: hospitals, home care, and outpatient rehab align around a defined episode, with one payment covering the full cycle. Evaluations and expansion work through the Health System Performance Network (HSPN) and CIHI documentation show how bundles standardize best practices, clarify accountability, and create incentives to reduce preventable complications and readmissions. At the clinic level, programs have translated
“VBHC offers a practical, measurable way to improve results while stewarding resources responsibly.”
the policy model into operational rules of the road—such as clear reimbursement ceilings for community physiotherapy within the bundle— so frontline partners understand scope, roles, and the value levers (functional recovery, safe discharge, supported self-management).
3. Reducing low-value care to free up capacity Canada’s Choosing Wisely movement illustrates a complementary VBHC lever: systematically de-implementing tests and treatments that do not help patients. Implementation research associated with Choosing Wisely highlights both the opportunity (a meaningful share of spend and patient burden is tied to low-value care) and pragmatic strategies to reduce it (clinician feedback, order set redesign, shared decisionmaking). Reducing low-value care improves patient experience and safety while creating “headroom” for investments that matter—an essential ingredient of value.
4) Using health technology assessment (HTA) to buy value, not volume CADTH/CDA (Canada’s pan-Canadian HTA body) supports VBHC by informing coverage and procurement decisions with rigorous evidence on clinical effectiveness, cost-effectiveness, and system impact. Increasingly, HTA in Canada also incorporates equity considerations to
avoid widening gaps when new technologies are introduced. This ensures that investments generate meaningful patient and population outcomes per dollar spent and align with Canadian commitments to fairness.
Canadian policy leaders have been building VBHC-enabling infrastructure for years: standardized outcome frameworks, costing methods, learning collaboratives, and data platforms. HEC’s national work on value, along with provincial payment and pathway innovations (e.g., Ontario bundled care), shows both proof-of-concept and momentum. Moreover, VBHC aligns with the system’s social contract: publicly financed care delivered equitably, with accountability for results that patients feel. Scholarly and policy commentary in Canada points to VBHC as more than a buzzword: it is a structured path to modernize care—prioritizing prevention, early diagnosis, and integrated management to achieve better outcomes at the same or lower total cost.

1. Start with one pathway and publish the outcomes.
Pick a high-volume, high-impact pathway (e.g., total joint arthroplasty, heart failure, diabetes). Implement a recognized outcomes set (or adapt from ICHOM), collect PROMs routinely, and report results transparently to clinicians and patients. Tie QI to what you learn.
2. Bundle across the full episode.
Define the episode’s start/stop, accountable team, and shared budget. Use Ontario’s experience as a template—clear roles for surgical centres, home care, and community rehab; standard discharge criteria; and pragmatic reimbursement rules for partners.
3. Systematically de-implement low-value care. Adopt Choosing Wisely recommendations locally with real workflow changes: revise order sets, embed clinical decision support, auditand-feedback, and patient-facing materials. Reinforce with leadership goals and clinician champions. Measure utilization and patientimportant outcomes pre/post.
4. Procure for value using HTA and equity lenses.
Use CADTH evidence and methods to shape formularies and device procurement, and to structure outcomes-based agreements with suppliers where appropriate. Make equity impact an explicit criterion during topic selection and decision-making.
5. Invest in data and costing.
VBHC requires linking clinical outcomes, PROMs/PREMs, and patient-level costing across settings. Provincial data assets (and CIHI reporting standards) can support this—teams should design data collection to be lightweight for clinicians and meaningful for patients. (See CIHI’s bundled care reporting specs for an example of episode-level data elements.)
6. Build capability and culture. Use HEC’s VBHC toolkit and organizational assessments to align leadership, governance, and frontline teams. Train clinicians in interpreting PROMs, engaging in shared decision-making, and running small tests of change. Celebrate outcome improvements that matter to patients.
Better patient outcomes and experience. When teams aim at the outcomes patients value, unnecessary steps fall away and recovery improves (e.g., improved function after joint replacement, fewer complications, faster return to life). Bundled care models support smoother transitions and reduce the “handoff harms” patients often experience. Health System Performance Network
Improved equity. By measuring outcomes by population group and incorporating equity into HTA, organizations can identify gaps, target supports, and avoid widening disparities when new technologies arrive.
VBHC is not a single program—it’s a way to run the health system. Canada already has many of the ingredients: a patient-centred ethos, national HTA capacity, provincial payment innovation, and pan-Canadian quality resources. Health organizations that start with one pathway, measure outcomes, bundle funding around the episode, de-implement low-value care, and procure using HTA and equity can deliver better results for patients and the system alike.
“When teams aim at the outcomes patients value, unnecessary steps fall away and recovery improves.”
System sustainability. Reducing low-value care and buying based on value redirect scarce resources to interventions with proven benefit— essential in a publicly funded system under pressure.
Professional satisfaction. Clinicians see the impact of their work when results are tracked and shared, and they gain tools to change practice (order sets, patient materials, bundles) in ways that help patients most.
By Cheryl Petruk

When we think of health care in Canada, the universal Medicare system often dominates the conversation: doctor visits, hospital care, basic diagnostics. But health isn’t simply the absence of disease or the services we receive — it is deeply shaped by the “social determinants of health” (SDOH): the social, economic, and environmental conditions in which people live, work, grow, and age. For advocacy organizations and insurers alike, bridging the divide between these upstream factors and downstream treatments is essential to achieving equity and sustainability.
The Government of Canada defines social and economic factors — such as income, social status, education, employment conditions, early childhood development, housing, food security, social supports, and access to health services — as core determinants of health. In the public health and health equity literature, these are distinguished from the “health care” system itself; they constitute the context in which health is either supported or undermined.
Canada is far from immune to health inequities rooted in these determinants. People with lower incomes, marginalized racial or Indigenous backgrounds, or precarious employment face higher rates of chronic disease, mental health challenges, and unmet health needs — not necessarily because of individual choices, but because of systemic barriers in housing, food access, employment conditions, and social inclusion.
While Medicare ensures that most medically necessary physician services and hospital stays are
covered, large gaps remain in coverage for many treatments, interventions, and supports (e.g. medications, dental care, physiotherapy, mental health care, home care). In Canada, approximately 30% of total health spending comes from private out-of-pocket or private insurance sources.
These gaps mean that social disadvantage often translates directly into poorer health outcomes — and worse, into financial hardship, as people forgo needed care or accumulate debt.
1. Access to “non-core” treatments is mediated by socioeconomic status
Because public coverage in Canada excludes or limits many services that people often need — such as prescription drugs (outside hospital), dental and oral health, many mental health therapies, physiotherapy and rehabilitation — individuals rely on private insurance or pay out-of-pocket. Those with stable employment, good benefits, or higher income are more likely to hold such coverage; those in precarious work, part-time jobs, or marginalized communities are less likely to benefit.

Thus, social determinants (employment, job security, income) become gatekeepers to access. A person with chronic back pain in a low-wage job may not be able to afford physiotherapy or pain management services, exacerbating disability and downstream medical costs.
2. Claim denials and administrative barriers disproportionately burden disadvantaged groups
Emerging research from health systems outside Canada underscores how social determinants can shape interactions with insurers. In one U.S.-based study, patients in lower income brackets and with lower educational attainment faced significantly higher odds of insurance claim denials for preventive services — even when coverage should exist. Although contexts differ, the mechanisms — administrative complexity, coding errors, knowledge barriers — can similarly disadvantage marginalized populations in Canada when dealing with private insurers.
In effect, even when coverage theoretically exists, complexity and bureaucratic barriers can act as “soft rationing,” disproportionately affecting those with fewer resources or literacy to navigate claims/ resistance.
3. Untreated social needs drive downstream cost burdens
When social determinants are neglected — for instance, poor housing that worsens asthma, food
insecurity that compounds diabetes, or social isolation that deepens mental illness — the health system pays a higher price later through emergency visits, hospitalizations, and advanced disease.
From an insurance economics perspective, covering upstream interventions (or more holistic care) could reduce downstream expensive claims. For example, ensuring access to mental health counselling or physiotherapy early can prevent relapse or complications that spiral into costly acute care.
From an advocacy standpoint, if our health policy solely focuses on “coverage for more services,” we may miss the deeper problem: inequitable distribution of risk and access. A better model is one that internalizes social risk, offering sliding scale premiums, cross-subsidization, or embedding social care supports into health benefit plans.
Canada has begun to experiment with reforms and programs that address these intersecting gaps:
• The Canadian Dental Care Plan, rolled out in phases beginning in 2023–2025, offers dental coverage to Canadians without other dental insurance and below a certain income threshold. This is a direct policy move to cover a historically uninsured health service, partially mitigating an SDOH-mediated gap.
• Provinces are increasingly adopting social-determinant-aware frameworks. In Ontario, for instance, the Social Determinants of Health Framework seeks to embed non-medical social supports (housing, food, transportation) into care planning and resource allocation.
• Advocacy groups and health equity networks are pushing for universal pharmacare, expanded mental health coverage, and more generous home- and community-care models — all of which would reduce the reliance on private insurance and out-of-pocket payments.

These are important steps, but they remain partial and fragmented. The systemic inequity between those who have access to extended benefits and those who do not still looms large, especially for working-age adults outside public benefit programs.
For E 3 Advocacy readers, bridging the divide between social determinants and insurance coverage offers opportunities for leverage. Below are some strategic directions:
1. Promote “social risk adjustment” in benefit design
Insurance plans (public or private) might incorporate risk-adjustment formulas that weigh social disadvantage, such that groups bearing higher social risk receive proportionately lower out-of-pocket costs or higher covered benefit levels.
2. Embed social supports within health coverage
Health plans could fund or refer to allied social services (housing assistance, nutrition programs, transportation subsidies) for medically vulnerable individuals. This integration ensures that coverage is not only clinical but holistic.
3. Advocate for universal coverage policies for historically excluded services
Dental, vision, mental health, physiotherapy, rehabilitation, and pharmacare are core areas to target. The more these become part of a universal standard, the less access depends on either job benefits or individual wealth.
4. Make claims systems equitable and accessible
Simplify administrative processes, provide support for claimants who may struggle with paperwork or appeals, and audit for bias in denials. If claim denials disproportionately affect marginalized groups (as in international evidence), mitigation must be a priority.
5. Strengthen data collection and equity evaluation
To determine the effectiveness of reforms, insurers and public agencies must collect and analyze data along axes of income, race, disability status, geography, and other social axes. This allows for monitoring of whether coverage expansion is reducing disparities.
6. Incentivize preventive and upstream investment
Rather than focusing solely on acute costly interventions, insurers and governments should support programs (e.g. community wellness, healthy housing, nutrition) that reduce the incidence or severity of disease, thus lowering claims in the long run.
In Canada, the promise of Medicare is incomplete. The social determinants of health continue to shape who becomes ill, who recovers, and who avoids care entirely. Insurance coverage — whether through public plans, private benefit systems, or hybrid models — cannot fix social inequities, but it can either perpetuate them or ameliorate them. For a healthier, more equitable Canada, advocacy must push not only for more covered treatments, but for insurance systems structured with social justice in mind: equitable access, social supports, simplified administration, and a holistic focus rooted in prevention.

New treatments offer hope to patients and their loved ones. Here, we present new therapies that are available to Canadians.
This section also addresses challenges around access to new medication. Our readers will find important information to help them understand Canada’s drug review processes.
An informed and engaged patient is an empowered one. We aim to equip our readers with the tools and knowledge to navigate the complex healthcare landscape because, more than ever, patients need to raise their voices to get access to services. Accessing innovative medicines can save patients’ lives.
By Cheryl Petruk

Canada’s therapy landscape is shifting fast. Below are five areas where Health Canada approvals or active reviews signal meaningful change for patients and clinicians—plus what to know about access and implementation.
What’s new (Canada): Two anti-amyloid monoclonal antibodies—lecanemab (Leqembi) and donanemab (Kisunla)—are in the Canadian pipeline. Health Canada accepted donanemab for review in February 2024; lecanemab has also been filed in Canada. In the U.S., both have regulatory milestones, with ongoing long-term data emerging internationally.
Why it matters: These agents target amyloid and are intended for early Alzheimer’s (MCI due to AD or mild dementia), aiming to slow decline rather than just treating symptoms.
What to watch in Canada:
• Regulatory decisions (Health Canada).
• Health technology assessment (CDA/INESSS) recommendations and provincial drug plan listings that determine real-world access and infusion infrastructure needs (infusion capacity, MRI monitoring, APOE4-related risk counselling).
What’s new (Canada): Health Canada granted marketing authorization to exagamglogene autotemcel (exa-cel; CASGEVY) in September 2024 for patients ≥12 years with sickle cell disease (recurrent vaso-occlusive crises) or transfusion-dependent beta-thalassemia—Canada’s first approved CRISPR-edited cell therapy in hematology. CADTH subsequently issued a recommendation (context for coverage decisions).
Why it matters: Following one-time autologous therapy and conditioning, many patients experience significant reductions in VOCs or transfusion burden, leading to a transformation in their quality of life.
What to watch in Canada:
• Centre readiness & equity: The treatment is complex (conditioning, apheresis, transplant-like workflows). Ensuring geographically equitable access and culturally competent supports is crucial.
• Funding models: Given high upfront costs, expect outcomes-based or managed-access arrangements to be part of provincial negotiations, as seen internationally.
What’s new (Canada):
• Semaglutide 2.4 mg (Wegovy) received Health Canada authorization in 2021 for chronic weight management and, in November 2024, a label expansion to reduce the risk of non-fatal myocardial infarction in adults with established cardiovascular disease—aligning treatment with hard CV outcomes, not just weight.
• Tirzepatide (Zepbound)—the first dual GIP/GLP-1 receptor agonist—was approved and available in Canada in July 2025 for obesity/overweight with comorbidities. Updated Canadian guidance (2025) now incorporates tirzepatide and other agents.
Why it matters: These medications deliver substantial, sustained weight loss and—critically— cardiovascular risk reduction (for semaglutide). They also reshape approaches to NAFLD/MASH, sleep apnea, and diabetes prevention.
What to watch in Canada:
• Coverage variability: Public and private formularies differ significantly; prior authorization and supply constraints can limit access. Pricing dynamics may shift further as generics/biosimilars arrive in the coming years.
What’s new (Canada): Health Canada expanded the Arexvy (GSK) RSV vaccine indication in November 2024 to adults aged 50–59, making Canada an early adopter for this younger risk group. (Previously, approval was for ≥60, similar to Pfizer’s Abrysvo.)
Why it matters: Adults with chronic conditions begin to see a higher RSV hospitalization risk in their 50s. Earlier vaccination windows may blunt seasonal surges and protect multimorbid patients.
What to watch in Canada:
• Provincial program decisions (publicly funded vs. private purchase), and targeted roll-outs in long-term care, Indigenous communities, and among those with cardiopulmonary disease
TROP2-targeting ADCs, notably datopotamab deruxtecan, are moving globally; the FDA approved Dato-DxD for specific indications in January 2025. In Canada, datopotamab deruxtecan is under review at Health Canada, signalling potential near-term access if positive assessments follow. Expect substantial practice change in metastatic disease sequencing and combinations.
Access pathway in Canada: what determines “real” availability?
1. Health Canada authorization (Notice of Compliance) establishes safety/efficacy and marketing.
2. CDA/INESSS health-technology assessments recommend whether public plans should fund a drug, often with criteria.
3. pCPA and provincial formularies negotiate/list (timelines vary by province/territory).
4. Clinical infrastructure (e.g., infusion/monitoring for Alzheimer’s antibodies; transplant-like programs for gene therapy) and workforce capacity ultimately shape equitable access.
Practical takeaways for patients, advocates, and clinicians
• Ask about eligibility now. Even pre-listing, specialists can advise on trial options, compassionate programs, and future criteria.
• Document outcomes. For high-cost therapies (gene therapy, ADCs, obesity medications), robust patient-reported outcomes and real-world data can support sustainable funding and equitable access.
• Capacity plan. Introducing infusion or cell/gene therapies demands coordinated pathways across centres—advocates can champion resourcing and travel supports to avoid two-tier access.

Remember to look out for new episodes of our podcast, Empowering Voices, dedicated to amplifying the stories and insights of patients, healthcare professionals, and advocates in the blood disorder and rare disease communities.
Each episode will feature meaningful conversations on patient experiences, emerging research, and the evolving landscape of healthcare advocacy. Through Empowering Voices, we aim to educate, inspire, and drive change by bringing realworld perspectives to the forefront. Stay tuned for our first episode, coming soon— because every voice matters!
Listen now at https://www.healcanada.org/empowering-voice-podcast




In this section, we provide information on ensuring that ABC/DEI is part of the patient conversation in our Health ecosystem. Our focus is to illuminate the pathways through which individuals grappling with health challenges can not only find their voice but also harness it to drive their own journey.
Healthcare and the patient’s experiences should not be determined by social determinants of health.
We believe that an informed and engaged patient is an empowered one. Through enlightening articles, expert insights, and inspiring stories, we aim to equip our readers with the tools and knowledge necessary to navigate the complex healthcare landscape.

By Cheryl Petruk
Access to equitable healthcare is often cited as a fundamental Canadian value. Yet, for many citizens and residents, gaps remain in what our publicly funded healthcare system actually covers. From prescription drugs and dental care to mental health services, vision, and home care, millions of Canadians still face barriers to accessing essential care. For marginalized groups — including Indigenous peoples, racialized communities, newcomers, people with disabilities, and low-income earners — these gaps can deepen inequities and undermine inclusion.
In the framework of diversity, equity, and inclusion (DEI), comprehensive and accessible healthcare insurance is more than an administrative policy; it is a moral and structural necessity for achieving health justice in Canada.
Canada’s healthcare system, grounded in the
Canada Health Act (1984), promises universality, accessibility, comprehensiveness, portability, and public administration. These five principles shape our publicly funded “Medicare” model, which covers medically necessary hospital and physician services. However, the system does not automatically ensure equal access to all health services.
Services such as prescription drugs outside hospitals, dental care, mental health counselling, physiotherapy, and vision care — often deemed essential for well-being — are not universally covered. Instead, they depend on employer benefits, private insurance, or limited provincial programs. For equity-seeking groups, particularly those in precarious employment or without stable income, this patchwork of coverage results in fragmented care and health inequities (Canadian Institute for Health Information [CIHI], 2023).

While most Canadians have access to basic physician and hospital care, insurance inequities persist across socioeconomic and demographic lines.
• Indigenous Peoples: Many Indigenous communities experience poorer health outcomes due to historical trauma, systemic racism, and jurisdictional disputes in healthcare delivery. Coverage gaps under programs like the Non-Insured Health Benefits (NIHB) plan have left some individuals without consistent access to necessary medications and specialized care (Allan & Smylie, 2015).
• Racialized and Immigrant Populations: Newcomers and racialized Canadians are more likely to hold part-time or temporary employment, where benefits such as private health insurance are rare. This leads to lower access to prescription drugs and mental health services, contributing to worse outcomes for preventable and chronic diseases (Statistics Canada, 2022).
• Low-Income and Uninsured Populations: An estimated one in five Canadians lacks adequate prescription drug coverage (Hoskins, 2019). Without coverage, individuals may skip medications, delay treatment, or face catastrophic out-of-pocket expenses.
• People with Disabilities: Despite higher health needs, individuals with disabilities often face exclusion from private plans due to income limits, part-time employment, or high premiums (Canadian Human Rights Commission, 2021).
These realities contradict the DEI promise of fairness and inclusion and reveal how health insurance access functions as both a determinant of health and a measure of social equity.
1. Health Equity and Financial Protection
Universal healthcare coverage without universal insurance is incomplete. Prescription medications and dental or mental health care can consume significant portions of household budgets. Expanding public or hybrid insurance models — such as a national pharmacare program — can protect vulnerable populations from financial hardship, aligning healthcare policy with DEI principles.
2. Trust and Cultural Safety
Insurance gaps often reinforce distrust among marginalized groups who already experience discrimination within healthcare settings. Expanding coverage through culturally competent and equitable insurance programs can foster inclusion, strengthen trust, and encourage engagement with the healthcare system.
3. Economic Participation and Productivity
Access to comprehensive insurance improves workforce participation, especially for women, racialized individuals, and persons with disabilities. Employees with coverage are healthier, more productive, and experience
Canada is at a pivotal moment in redefining what “universal healthcare” truly means.
National Pharmacare Initiative: In 2024, the federal government introduced the Pharmacare Act — the first step toward a national program to provide essential medicines to all Canadians, beginning with diabetes medications and contraceptives. This initiative addresses long-standing inequities in prescription drug coverage (Government of Canada, 2024).
Dental Care Expansion: The Canadian Dental Care Plan (CDCP) launched in 2023 provides coverage for uninsured Canadians with annual household incomes below $90,000. This is a landmark step toward reducing oral health inequities, particularly among seniors, children, and low-income families (Health Canada, 2024).
Mental Health and Home Care Investments: Provincial and federal negotiations continue to expand funding for community-based mental health and home care services — critical needs for marginalized Canadians, especially those in

DEI advocacy in healthcare must go beyond workforce diversity and cultural competence. It must tackle structural inequities in who can access care and who can afford it. Patient advocates, community organizations, and policymakers play a key role in:
Championing National Pharmacare – Support equitable, universal drug coverage as a DEI priority.
Expanding the Definition of “Medically Necessary” – Advocate for mental health, dental, and vision care as integral to health, not optional extras.
Ensuring Culturally Safe Coverage Policies – Design programs that consider the linguistic, cultural, and geographic realities of diverse populations.
Measuring Equity Outcomes – Collect disaggregated data to monitor gaps and ensure that insurance programs close — not widen — health disparities.
Canada’s health system has long been a point of pride, yet the persistence of inequitable access to insurance for essential health services undermines the very values of universality and inclusion. In the context of diversity, equity, and inclusion, access to comprehensive healthcare insurance is not a luxury — it is a right and a measure of justice.
Expanding and equalizing healthcare insurance will not only improve health outcomes but also strengthen Canada’s social fabric. For DEI advocates, ensuring equitable access to health insurance is an indispensable part of building a Canada where every individual — regardless of race, gender, income, or ability — has the opportunity to live a healthy and dignified life.


A dedicated space where we embrace the journey towards mental wellness with open arms and open hearts.
We believe that an informed and engaged patient is an empowered one. Through enlightening articles, expert insights, and inspiring stories, we aim to equip our readers with the tools and knowledge necessary to navigate the complex mental health care landscape.
Join us as we explore how patient advocacy, active engagement and comprehensive education can transform the experience of mental health care, turning obstacles into opportunities for growth and healing.
By Joanna Pozzulo, Ph.D.
Whether it is a change in season or a change in circumstance, transitions can be anxietyfilled. Dealing with “everyday anxiety” (or stress or nervousness) can be challenging to handle for many of us (I fall into this category!). I was curious to read Good Anxiety: Harnessing the Power of the Most Misunderstood Emotion (2021) by Dr. Wendy Suzuki. How could anxiety be “good”?
Neuroscience professor Suzuki takes you on a science-filled journey of how anxiety works in our brains and how you can change those pathways for a more positive experience. It should be noted that Suzuki makes a distinction between clinicallevel anxiety and everyday anxiety. Although the mechanisms may be similar, the book is oriented toward helping us cope with and change our perceptions and reactions to everyday anxiety.
Not only is there a lot of science in this book, but there are also several case examples that help illustrate the information. Suzuki chronicles her journey after the unexpected passing of her younger brother. She takes stock of where she is in her life and how she wants to live it moving forward.
The notion of good anxiety is about coping and changing our perceptions and reactions to anxiety so that it becomes a strength and motivator; “our superpower,” as Suzuki notes. Three themes that emerge centre around making time for meditation, exercise, and sleep. These elements may help you move from bad to good anxiety. It’s not easy to make the shift when you’re feeling depleted.
The book contains several questionnaires to give you a sense of where your anxiety level is now and what some of your anxiety triggers may be. Becoming conscious of your reactions to anxiety is the first step. Suzuki offers numerous guided strategies to help individuals make the shift to managing anxiety effectively.
https://carleton.ca/mental-health/reading-forwell-being-podcast/
Happy reading (and listening)!
“The book is oriented toward helping us cope with and change our perceptions and reactions to everyday anxiety.”
Shifting from bad to good anxiety will require some effort, but it is well worth the try for improved well-being.
For more evidence-based picks for well-being, sign up for the Reading for Well-Being Community Book Club, https://carleton.ca/mental-health/ book-club-sign-up/
Check out the Reading for Well-Being Podcast for interviews with authors of my book picks,

Joanna Pozzulo, Ph.D. Chancellor’s Professor Department of Psychology Director, Mental Health and Well-Being Research and Training Hub (MeWeRTH) carleton.ca/mental-health Carleton University
By Andrea Lawson and featured Researcher Marisa Young
If the news makes you feel more powerless rather than more informed, it might be time to rethink how you’re engaging with it. Constant access to news keeps us informed in a fast-moving world, but it’s important to find ways to navigate the news cycle to protect our mental health, a McMaster sociologist says.
“With 24/7 updates, social media algorithms that prioritize extreme content, and an endless stream of crisis-driven headlines, it’s no surprise that many people feel more anxious and overwhelmed than ever,” says Sociology associate professor Marisa Young, the director of the Centre for Advanced Research on Mental Health and Society.
“At the end of the day, staying informed should help us understand the world — not make it feel unbearable,” she explains. Young shares insights on the impact of the news cycle, as well as tips on how to safeguard mental health.
WHAT IMPACT DOES THE SEEMINGLY ENDLESS WAVE OF CONSEQUENTIAL (AND NEGATIVE) NEWS STORIES HAVE ON OUR MENTAL HEALTH?
Constant exposure to negative news can take a real toll on our mental well-being. It’s not just about feeling sad or frustrated in the moment — it can create a sense of ongoing stress, almost like background noise or what we refer to as an “ambient stressor” that never really goes away.
Sociologists think about stress in different ways, and one important distinction is between short-term
stressors, like a single upsetting news story, and chronic stressors, which build up over time. The news cycle today often makes bad news feel relentless, and that can contribute to chronic stress, where people feel like they’re always bracing for the next crisis.
In addition to the content of the news that matters, but also the way we consume it. When we’re bombarded with distressing stories — whether it’s about political turmoil, climate disasters or economic uncertainty — it can create a sense of powerlessness, which is especially harmful to mental health.
People may start to feel like no matter what they do, things won’t change, and that can lead to feelings of anxiety, hopelessness, or even emotional exhaustion. This is something sociologists call “stress proliferation,” where one type of stress spills over into other areas of life.
For example, worrying about a financial crisis after reading the news can make someone more anxious about their job security, which then affects how they interact with their family, how they sleep, and so on.
Yes, and that’s a really important part of the conversation. Not everyone experiences stress from the news in the same way.

People who are already dealing with uncertainty in their lives — whether it’s students worried about their future, parents juggling responsibilities, or workers in precarious jobs — are likely to feel the weight of bad news more heavily. If someone is already struggling to pay rent, then reading about rising interest rates or job layoffs isn’t just distressing — it’s personal.
Students, in particular, can be vulnerable because they’re in a life stage where so much is uncertain. They’re making decisions about their future while constantly hearing that the economy is unstable, the climate is in crisis, and political divisions are deepening. It’s a lot to process.
Parents also uniquely experience this stress, especially when the news relates to safety, education, or financial security. Many parents already feel stretched thin, and hearing about school violence, climate disasters, or rising living costs can intensify feelings of anxiety.
And then there’s the bigger picture of inequality. People in lower-income households, racialized communities, or those facing discrimination tend to experience more structural stressors in daily life. For them, the news doesn’t just report on crises—it often reflects ongoing realities they already live with.
So, while negative news can affect everyone, it doesn’t land the same way for all of us.
It’s tricky because we all want to stay informed, but there’s a fine line between being engaged and feeling emotionally drained.
One sign that news consumption might be becoming harmful is if it starts affecting your mood in a lasting way — if you feel anxious, hopeless, or even exhausted after scrolling through headlines. Some people find themselves compulsively refreshing their news feeds, almost like they’re looking for the next piece of bad news. That’s sometimes called “doomscrolling,” and it can create a cycle where the more we consume, the worse we feel, but we keep going back for more.
Another red flag is if news starts interfering with daily life — like if you find yourself checking updates the moment you wake up, staying up late reading negative stories about distressing events, or feeling overwhelmed to the point where you’re withdrawing from conversations with friends or family. If the news makes you feel more powerless rather than more informed, it might be time to rethink how you’re engaging with it.
Definitely. The goal isn’t to avoid the news altogether, but to be more intentional about how we engage with it. One of the most effective things people can do is set boundaries around when and how they consume news. Instead of checking updates constantly throughout the day, setting aside specific times — maybe in the morning and then again in the evening — can help prevent the feeling of being constantly bombarded.
It’s also helpful to be mindful of where you’re getting your news. Sensationalized headlines and 24/7 breaking news coverage tend to focus on the most extreme, emotionally charged stories, which can make the world seem even more chaotic than it is. Balancing that with sources that provide context, analysis, or even solution-focused reporting can help shift the focus from feeling overwhelmed to feeling informed.

And finally, it’s important to recognize when it’s okay to step back. Just because something is happening in the world doesn’t mean you have to absorb every detail in real time. Sometimes taking a break — whether it’s for a day or even just an evening — can help reset your perspective and allow you to engage with the news in a way that feels less draining.
If the news is making you feel overwhelmed, the first thing to remember is that you’re not alone. A lot of people are feeling this way, and part of that is because we’re not just dealing with bad news — we’re dealing with bad news that’s constant and often feels out of our control.
One of the best ways to counteract that is to focus on the things that are within your control. One approach is to shift from passive consumption to active engagement. Instead of just absorbing negative stories about distressing social situations, finding small ways to take action — whether that’s volunteering, donating or even just having conversations about issues that matter — can help restore a sense of agency. Research shows that when people feel like they’re contributing to solutions, even in small ways, it can reduce feelings of helplessness and anxiety.
Social connection is also a key buffer against stress. Talking with friends, family or community groups about how you’re feeling can help put things in perspective and remind you that you’re not facing the world’s problems alone. Sometimes, just voicing anxieties out loud can make them feel more manageable.
Finally, grounding yourself in activities that are separate from digital spaces — things like going for a walk, exercising, reading a book, or engaging in hobbies — can help counterbalance the mental overload that comes with constant news exposure.
The goal isn’t to ignore what’s happening in the world, but to make sure that staying informed doesn’t come at the expense of your well-being.
Published here with the kind permission of the author, Andrea Lawson and researcher Prof. Marisa Young. Our thanks for sharing their insights with Heal Canada readers. This article was first published on Brighter World. Read the original article.

Marisa Young is an Associate Professor in the Department of Sociology at McMaster University, a former Early Career Fellow at the Work-Family Research Network (formally the Sloan Foundation), a Canadian Research Chair in Mental Health and Work-Life Transitions, Director for McMaster University’s Centre for Advanced Research on Mental Health Society (ARMS), and Past-Chair of the Canadian Sociological Association Mental Health Research Cluster. Her research investigates the intersection between work, family, and residential contexts to bring a greater understanding of social inequalities in mental health for parents and children.

By Vanessa Sales and Danielle Rice
Over the past several decades, Canada has made important progress in reducing the stigma associated with mental health challenges. Mental health and well-being involve considering the way someone thinks, feels, and acts. How someone deals with stress, understands their strengths and weaknesses, builds relationships, and takes part in their community all influence well-being.1 Mental health can look different for everyone and is an important part of overall wellness.2 In Canada, mental health problems are one of the main reasons people have trouble with day-today tasks (e.g. doing chores, socializing).
In fact, 1 in 5 Canadians experience a mental health problem or illness each year (e.g. anxiety, depression).3 Poor mental health can impact life at home, work, school or in relationships.4 With this in mind, it can be helpful to consider how to work on your well-being by improving lifestyle factors, connecting with others, or reaching out to a mental health professional. Often, once someone has decided to pursue professional
help, it can feel overwhelming and unclear how to easily access these services. Given this, we provide an overview of accessing mental healthcare within Canada, including:
• The types of mental health services that are available
• Where and how to find help
• How to get the most out of therapy
There are many types of mental health supports in Canada offered by different professionals and in different formats (e.g., virtual or online). For example, counselling and therapy services can be provided by psychiatrists, psychologists, psychotherapists, counsellors, psychological associates, and social workers.5 Figure 1 below highlights how these health professionals can provide help. These titles may change or look different between provinces, but this list can help as a starting point, especially when speaking with a family doctor.
Regardless of the professional that you reach out to for support, it is important that you feel comfortable with them. As noted above, these professionals provide psychotherapy to help people work on their mental health goals or speak about challenges they have experienced. For many people, psychotherapy can improve the quality of life, reduce mental health problems, and make everyday tasks easier. When considering the type of professional you will connect with, it can be relevant to think about what you hope to get out of therapy.
Many different types of psychotherapy can be offered, such as one-on-one (individual), in a group, or with your family or partner (i.e., couples therapy). Individual therapy involves you and a therapist, while group therapy involves a therapist and a group of people typically experiencing similar mental health or substance use challenges.6 Individual sessions often last 20-50 minutes, while group sessions can last longer.6 The type of therapy you choose may depend on what is available in your region, the challenge you’re seeking help with, and your preferences. Figure 2 highlights common types of
A family doctor or nurse practioner are often the first people you speak to for a discussion about mental health, assessment, or referral.
A medical doctor with expertise in mental health and substance use conditions who can diagnose and treat mental health problems; they often prescribe medication and sometimes provide counselling.
A health professional that has completed graduate school training to assess, diagnose, and treat mental health problems through talk-therapy. Psychologists are often experienced in conducting research.
Similar to a psychologist in Ontario, but usually had completed fewer years of graduate school training.
A health professional who helps with mental health, wellness, and relationships through talktherapy.
A health professional that helps people, families and communities through providing talktherapy and connecting people with resources in their communities.
Figure 2. Common Types of Psychotherapy and Descriptions
Provides people with information about their mental health with understanding, problem solving, and communication.
Involves learning new info and applying these learnings.
Can range from 5-24 sessions.
A therapy that helps people deal with their mood and current relationships and life events.
Helps people identify and address challenges with grief, role transitions, role disputes, and interpersonal challenges.
Usually takes place over 12-16 weeks.
A flexible therapy that is based on the relationship between the person and the therapist.
Therapy is focused on speaking about what you are struggling with and recieving emotional support and validation.
Number of sessions depends on what is needed.
A short-term therapy focused on thoughts, emotions, and behaviours that teaches skills and strategies to improve mental health.
Future oriented and change focused.
Commonly 6-20 sessions.
Focused on goals. Typically involves homework.
psychotherapy: cognitive behavioural therapy (CBT), supportive counselling, interpersonal therapy (IPT), and psychoeducation.7 Mental health professionals often use skills from many types of therapies, and while it is not necessary to select the exact type of therapy you would, it can help to understand a few types of therapies that exist and consider what you may or may not want (e.g., out-of-session homework).
In Canada, some mental health services need a referral from a doctor, while others can be found online and accessed on your own.8 Mental health services can be publicly available (paid for by the government) or private (paid for through work benefits or purchased directly).8 Examples of services offered publicly in Canada are visits with family doctors, nurses, walk-in clinics (for people without family doctors), community mental health services, and some culturally specific services. Private
services do not require a referral and can be accessed through extended health benefits where sessions are covered by your insurance or can be paid directly be the client and in these examples, you can typically choose your own mental health provider (e.g., psychologist, psychotherapist). Employee assistance programs can also offer psychotherapy sessions and crisis support for workers and their families. Universities or colleges also typically offer short-term psychotherapy. Freely available services like support groups, hotlines, crisis text lines are also ways that individuals receive support for mental health or substance use challenges.
• Online Mental Health Courses: support better understanding, care and prevention
• BounceBack: a program that is designed to help adults and youth develop skills to deal with a range of mental health problems
• Ontario Structured Psychotherapy Program: free mental health and skillbuilding support for individuals dealing with low mood or anxiety
• 9-8-8: Suicide Crisis Helpline: available to anyone in Canada (bilingual, culturally appropriate, informed)
• Kids Help Phone: 24/7 support for kids and teens
• Hope for Wellness Helpline: 24/7 support for Indigenous people across Canada
Culturally specific supports are also available to help people from different backgrounds with mental health problems.
• Across Canada, Integrated Youth Service centres give young people a space to receive mental health and sibstance use support.
• ACCESS Open Minds (AOM) is a national youth mental health network that aims to improve access to services, lead research and knowledge sharing, and collaborate with youth and families. AOM also provides specific mental health care to First nation, Inuit and Métis youth and families through centering a space where community members can learn and work together.
Now, imagine you decided you would like to make a first therapy appointment. Maybe you have asked your family doctor for a referral or found recommendations for a therapist online. Before your first appointment with a mental health professional, it can be helpful to set yourself up for success. Figure 3 highlights some considerations for therapy before starting:
1.
Before you start, think about your patterns of sleep, physical activity, substance use, how you handle stress, your friendships and relationships, and what you eat.
Could you start working to improve one or more of these lifestyle factors?
Why do you want to do therapy? What are your broad goals or hopes for feeling better?
For example, you may feel uninterested in activities you used to enjoy, and you
are wanting to increase your motivation and take part in these activities again.
Or maybe you want to decrease feelings of anxiety or learn how to cope better when stressed - these are all great goals and things you can speak about during your final appointment.
Understand what you want to get from therapy, how much time you can spend on it, and the format that works best for you.
For example, you can think about your schedule and how often you want to meet with a mental health professional and whether that be online or in-person.
Take time to note down what is working well or has worked well in the past.
For example, if previously you have found speaking to friends helps you feel better, or going for a run, these are helpful pieces of information you can share during your first appointment. 4.
Think about if you are okay with your mental health clinician working together with other care providers.
After each season, take some time to think, reflect, and relax.
6. GOALS
Mental health challenges can be difficult to work through, and knowing where to reach out is not always clear. It can be worthwhile to think about how best you can prioritize your mental health and if therapy is something you may be open to trying. If you are still not sure what is right for you, a good first step is talking to your family doctor or visiting the Canadian Mental Health Association (CMHA). Everyone deserves access to mental health support, and we hope this article can provide a starting point, open the conversation about mental health with a loved one, or maybe even be used as a reminder to speak with a medical provider you work with about your well-being.
1. Mental Health 101: Mental health: Definitions, diagnoses and use of language. Accessed June 23, 2025.
https://moodle8.camhx.ca/moodle/mod/book/ view.php?id=48&chapterid=5
2. Mental health. Accessed June 23, 2025.
https://www.who.int/news-room/fact-sheets/ detail/mental-health-strengthening-ourresponse
3. Mental Illness and Addiction: Facts and Statistics. CAMH. Accessed June 23, 2025.
https://www.camh.ca/en/driving-change/thecrisis-is-real/mental-health-statistics
4. Kirkbride JB, Anglin DM, Colman I, et al. The social determinants of mental health and disorder: evidence, prevention and recommendations. World Psychiatry. 2024;23(1):58-90. doi:10.1002/wps.21160
5. How to get mental health help. CMHA National. Accessed June 24, 2025.
https://cmha.ca/find-help/how-to-get-help/
6. Malhotra A, Mars JA, Baker J. Group Therapy. In: StatPearls. StatPearls Publishing; 2025. Accessed June 24, 2025.
http://www.ncbi.nlm.nih.gov/books/ NBK549812/
7. Psychotherapy talk therapy. CAMH. Accessed June 24, 2025.
https://www.camh.ca/en/health-info/mentalillness-and-addiction-index/psychotherapy
8. Where to Get Care – A Guide to Navigating Public and Private Mental Health Services in Canada. Mental Health Commission of Canada. July 25, 2025. Accessed July 29, 2025. https://mentalhealthcommission.ca/resource/ where-to-get-care-a-guide-to-navigatingpublic-and-private-mental-health-services-incanada/


Vanessa Sales, BScH, recently obtained a Bachelor of Science (Honours) in Psychology at Queen’s University. She holds several research assistant positions at St. Joseph’s Healthcare Hamilton, University of the Fraser Valley, and Queen’s University. She plans to pursue a career as a clinician-scientist. vvanessasales55@gmail.com
Dr. Danielle Rice is a Clinical and Health Psychologist and Clinical Lead at the Mood Disorders Treatment and Research Clinic at St. Joseph’s Healthcare Hamilton, and an Assistant Professor at McMaster University in the Department of Psychiatry and Behavioural Neurosciences. experts.mcmaster.ca/display/riced


By Dr. Robyne Hanley-Dafoe
Why do we sometimes lose sight of our goals, hold ourselves back, play small, or limit our own success?
It can look like holding onto the dream of writing your own book, but constantly telling yourself it’s not the right time. It can look like staying in a familiar work environment or a toxic relationship, even though you imagine something better. It can appear as downplaying or not sharing your achievements out of fear of standing out. It can even look like small daily choices, such as staying up late the night before a morning workout and then blaming fatigue for skipping it.
We’ve all been there. Despite having the best of intentions, we find ourselves getting in our own way and being derailed by our own actions.
Self-sabotage happens when we engage in a behaviour that undermines our goals, progress, success, or well-being. Sometimes we consciously engage in these behaviours, while other times it is unconscious. The reality is that
every behaviour serves a purpose, even if it is working against us.
There are both internal and external forces behind this pattern of self-sabotage and the tendency to play small.
A strong force behind some of our selfsabotaging behaviour and why we play small is external pressure. The reality is that we receive so many messages about what is acceptable when it comes to ambition and success. We want to be successful, but not too successful. We’re told to dream big, but not too big. Celebrate your wins, but not too loudly.
There’s a tendency in our culture to criticize or cut down those who stand out, achieve too much, or rise too high. This phenomenon is known as Tall Poppy Syndrome.
As social beings, we instinctively want to feel accepted within a group. What happens is that we begin to hold ourselves back and dim our light for fear of standing out. We worry that if we step out too boldly, someone might have an opinion. We fear being criticized, judged, or excluded, so we choose to play small.
Self-sabotage is often a protective response to fear, judgment, and uncertainty. Self-sabotaging behaviours are often rooted in our need to feel safe or in control, even if it means undermining our goals and chances of success.
Some common internal reasons behind selfsabotage:
• The need for control
• Comfort in the familiar
• Low self-esteem or self-worth
• Fear of failure
• Fear of judgment
• Fear of success or greatness
When we step into uncertainty, whether it’s a new role, a creative project, or putting ourselves out there in some way, the outcome
“In protecting ourselves, we miss out on our own greatness and limit what’s possible in our lives.”
feels unpredictable. To manage that risk, we sometimes choose not to try fully, we procrastinate, or we even give up. This way, if things don’t work out, it feels less like an unpredictable failure and more like a chosen outcome, even if it’s not optimal.
Here are some starting points for overcoming some of the internal and external drivers behind self-sabotage:
Surround yourself with the right supporters
Find those who believe in your potential, lift you up, cheer you on, and genuinely celebrate your growth, rather than those who limit your dreams.
Notice your go-to excuses
We all have familiar stories we tell ourselves: “It’s not the right time,” “It probably wouldn’t work,” or “I’m not ready.” Get curious about these internal narratives and the stories you tell yourself. Are they true, or are they protective stories you’ve rehearsed into beliefs? Naming them is the first step to letting them go.
Reclaim your belief in your capability
Self-sabotage thrives when we overestimate the challenges ahead and underestimate our ability to figure things out. If you think about your gifts, skills, and talents, you were given them to be able to serve and be useful to others. Lean into the truth that you can do great things.
Practice micro-bravery
You only need a spark of courage to step boldly into opportunity and toward what matters to you. There’s never that imagined “perfect” time. The right time to go for your goals is when you decide it is.
Allow hope
Don’t be afraid to get your hopes up. Rather

than protecting yourself by setting low expectations, allow yourself to hope and to believe in your potential. You are worthy of your big, bold, audacious goals and well-equipped to handle whatever comes with pursuing them.
Self-sabotaging behaviours tend to prioritize short-term comfort and safety over our longterm goals. Yet in protecting ourselves, we miss out on our own greatness and limit what’s possible in our lives. Over time, these choices can leave us feeling frustrated, dissatisfied, and unfulfilled.
So, what big, bold thing are you holding back on? Where in your life are you playing it safe? Where are you getting in your own way?
Taking the leap of going back to school, starting a business, leaving an unfulfilling situation, or allowing yourself to dream again will always require courage. Anything that is really worth doing will require you to choose to be brave.
My final gentle invitation to you is to notice when you’re holding yourself back, and ask
yourself: What would happen if I took that brave, bold step and everything worked out?
This article originally appeared on Psychology Today on August 22, 2025, and is reprinted here with permission.

Dr. Robyne Hanley-Dafoe is an educational behaviourist and globally recognized speaker and scholar.
She is the award-winning author of Calm Within the Storm and Stress Wisely, and she will release her next book, I Hope So, on February 10, 2026, furthering her work on hope, resilience, and navigating life’s challenges.
drrobyne.ca

In today’s society, the health of senior citizens stands as a paramount concern, particularly within the framework of the Canadian healthcare system. This heightened focus is more than just a response to the growing number of seniors. Still, it is deeply rooted in recognizing their invaluable contribution to society and their unique challenges in their twilight years.
As people transition into their senior years, they bring unique health and social needs. This shift presents challenges and opportunities for the Canadian healthcare system and society.
In our Seniors Health section, we will provide information to help you in your journey, navigate daily life as a Senior, and provide resources to help you have the best quality of life.

By Peg Bocci A Transition That Opens the Door to Connection
Moving is never easy, and for many older adults, downsizing or transitioning to a retirement living residence comes with an extra layer of emotion. It’s not just about packing up a lifetime of memories; it’s about leaving behind a home, familiar routines, and sometimes longtime neighbours. But what I’ve seen time and time again is that, on the other side of that change, there’s often something wonderful waiting: new friendships and a sense of connection that can truly brighten life.
I have had the privilege of helping older adults through this transition, and one of the most rewarding parts of my work is watching new friendships take shape. For many, moving into a new residence can feel intimidating at first. The unfamiliar surroundings and routines can create anxiety, and the thought of starting over socially may be daunting. But retirement living is uniquely designed to foster connection. From shared meals and activity programs to casual coffee chats and hobby clubs, these environments are structured to encourage interaction and engagement.
One of the most important things I remind my clients is that friendships don’t have to happen
overnight. Just like any new relationship, they take time to develop. Attending events or joining a class can feel uncomfortable at first, but often, that small step leads to unexpected companionship. I’ve seen residents meet over an exercise class. Card games, or even volunteering within the residence. They discover shared interests, exchange stories, and gradually build bonds that are just as deep, if not deeper, than the friendships they left behind.
The benefits of friendship in retirement living extend far beyond social enjoyment. Studies consistently show that meaningful social connections can improve mental and physical health, reduce stress, and even enhance longevity. For someone navigating the emotional aspects of downsizing or moving, having friends nearby provides a sense of belonging and security. It turns a new environment from a temporary stop into a vibrant home.
One story that I always think about is a client I will call Mary. She was very hesitant to leave her home, which she’d lived in for 40+ years, worried she wouldn’t fit in, and worried that she’d lose her independence. But a few months after moving, she joined a weekly book club and met a few women who shared her love of reading, laughter, and afternoon tea.
Those simple connections grew into deep friendships that gave her a new sense of confidence, laughter and a renewed sense of purpose. Mary often tells me that some of her closest friends today are people she met after her move.
Finding a connection often comes down to mindset. When older adults stay curious, kind, and open to community life, friendships seem to appear naturally. A smile in the hallway, a chat over coffee, or lending a hand at an event can spark relationships that make each day brighter. Families can help by encouraging loved ones to get involved, offering gentle support rather than pressure.
“For someone navigating the emotional aspects of downsizing or moving, having friends nearby provides a sense of belonging and security.”
At its heart, transitioning into retirement living is a journey of growth. Yes, it’s about adjusting to a new space and routine, but it’s also about opening the door to friendship and rediscovering joy in everyday moments. This stage of life can be filled with laughter, shared memories, and a renewed sense of belonging.
If there’s one thing I’ve learned, it’s that moving into a retirement living residence doesn’t mark the end of connection; it often marks the beginning. Friendship can blossom at any stage of life.
It just takes openness, a little courage, and that first simple “hello”.

Peg Bocci
is
Founder & CEO of Silver Lining Senior Advisors.
She has worked in the senior living industry for over 20 years and has acquired a wealth of knowledge of this dynamic industry and the people living and working in it. www.silverliningsenioradvisors.com peg@silverliningsenioradvisors.com 647-771-8276


There’s much to learn from how the world’s longestliving people stay active. In Ikigai: The Japanese Secret to a Long and Happy Life, authors Héctor García and Francesc Miralles interviewed more than 100 centenarians in Okinawa, Japan—a Blue Zone renowned for longevity. Their takeaway: lasting vitality doesn’t require a gym or marathon training, just movement naturally woven into everyday life.
Say hello to Radio Taiso (also known as radio callisthenics), Japan’s beloved morning exercise tradition.
By April Hattori
Radio Taiso (also known as radio calisthenics) is a short, gentle exercise routine broadcast across Japan every morning—yes, on the radio! Schools, workplaces, parks, and neighborhoods often gather together to do the routine in unison. It’s such a part of daily life in Japan that many people know it by heart from childhood.
The routine takes only 3 minutes to complete and includes a series of rhythmic, flowing movements designed to:
• Increase joint mobility
• Improve posture and flexibility
• Wake up your muscles and circulation
• Help people of all ages stay active
The best part? You can do it standing or seated, making it accessible for seniors, beginner exercisers, and anyone looking for a daily dose of movement.
Here’s a breakdown of the moves with repetitions and seated modifications so you can follow along at your own pace. The goal isn’t perfection—it’s daily movement and joyful consistency!
Standing: Raise arms overhead and stretch tall, then circle them to your sides.
Seated: Sit tall, lift arms overhead, and lower them gently. Repetitions: 2 times
Standing: Bend knees, while lifting both arms out to the side, shoulder height
Seated: Lift both arms out to the side, shoulder height. Repetitions: 8 times
Lateral overhead arm circles
Alternate circles inward and outward. Repetitions: 4 times

Open Arms
Arms out to the side
Open arms to stretch chest muscles.
Repetitions: 4 times
Overhead Side Stretch Arms
Standing: Right arm overhead, leaning left: 2 times; Left arm overhead, leaning right: 2 times. Repeat sequence.
Seated: Right arm overhead, leaning left once for a count of 2; Left arm overhead, leaning right for a count of 2. Repeat sequence.
Bend at the waist 3 times. Place your hands on your lower back and lean back for a count of 3. Repeat sequence
Arms swing laterally left, right, left, right and then diagonal up left 2x
Arms swing laterally right, left, right, left and then diagonally up right 2x
Heels and Arms Up
Step out left while fingers of both hands go to the shoulders
Lift heels, arms up
Step center, arms down to sides
Step out right while fingers of both hands to your shoulders
Lift heels, arms up
Step center, arms down to sides
Reach and Open
Reach for left toes: 2 times
Stand up and open chest for 2 counts
Reach for right toes: 2 times
Stand up and open chest for 2 counts
Around the World
Bend at the hips and circle to the left
Bend at the hips and circle right
Bend at the hips and circle to the left
Bend at the hips and circle right Bend at the hips and circle to the left
Standing: Do 4 hops and then 2 jumping jacks, arms out shoulder level (Modification: Do single step outs right and left instead of jumping jacks.)
Seated: No jumps. Shake arms down 4 times and lift arms shoulder level 2 times.
Standing: Bend knees, while lifting both arms out to the side, shoulder height
Seated: Lift both arms out to the side, shoulder height. Repetitions: 8 times
Full-Body Stretch and Opening Arms
Standing: Raise arms overhead and stretch tall, then circle them to your sides.
Seated: Sit tall, lift arms overhead, and lower them gently.
Repetitions: 4 times
In Japan, this routine is more than just movement—it’s a shared experience that connects people to their community and helps them age with strength and independence. Whether you’re 7 or 87, Radio Taiso is a joyful and effective way to move your body every day.
Even better? It only takes 3 minutes, so there’s no excuse not to try!
Reprinted with the kind permission and support of April Hattori of yes2next.
To watch the tutorial video with step-by-step standing and seated options please visit the yes2next website: Try out Radio Taiso!

April Hattori is the founder of yes2next, who is passionate about helping people of all ages say yes 2 their next steps of fitness and joy. She is a certified personal trainer with additional certifications in Senior Fitness and Fitness Nutrition from the American Council on Exercise.

By Verve Senior Living
When we age, our bodies undergo various changes, and one of the most significant health concerns for seniors is diabetes. Often referred to as a “silent condition,” diabetes is a chronic disease that causes our body’s blood sugar (glucose) levels to fluctuate at unhealthy levels.
As our body turns the food we eat into sugar, called glucose, it also needs insulin to help said glucose get into our cells for energy. If you have diabetes, your body either isn’t producing enough insulin on its own or is unable to facilitate it, or both. What makes diabetes especially concerning for adults over 65 is how quietly it can progress and how serious its complications can become if not managed properly.
According to the Centers for Disease Control and Prevention (CDC), more than 33% of adults aged 65 and older live with diabetes. Yes, that’s a pretty big number. But here’s the good news: with the right information and some smart lifestyle tweaks, you can keep it in check and keep living your best life.
You may be a senior yourself or caring for a loved one; whichever it is, understanding the facts about diabetes in seniors can be life-changing.
In this article, we’ll explore five essential facts every senior should know, along with practical advice for managing diabetes and promoting a healthy lifestyle in your golden years.
First and foremost, understanding the difference between type 1 diabetes and type 2 diabetes is key to effective care and management.
“More than 33% of adults aged 65 and older live with diabetes.”

Type 1 diabetes occurs when the immune system mistakenly attacks insulin-producing cells in the pancreas, resulting in your body not producing enough insulin. This eventually causes glucose to build up in the bloodstream. While type 1 diabetes usually develops early in life, it can manifest in older adults, as well. And the unfortunate truth is, there are no known risk factors and therefore surefire ways to prevent it.
Type 2 diabetes, on the other hand, may be more common and is also more lifestyle-based. Factors such as poor diet, inactivity, and being overweight contribute significantly to its onset. The good news is that this can be reduced by losing excess weight through proper diet and exercise, which improves the body’s ability to use insulin and process glucose. Moving your body just 30 minutes a day can have a huge, healthy impact. Coupled with healthy eating habits that focus on fresh veg and fruit, whole grains, and lean protein, while simultaneously cutting back on red meat.
While type 1 diabetes requires insulin therapy for life, type 2 diabetes can often be managed or even reversed with diet changes, regular activity, and weight control.
Your Next Steps:
• Know your diagnosis. Ask your doctor which type you have. Treatment plans can be quite different.
• Track blood sugar regularly, as seniors may experience fluctuating glucose levels.
• Consider joining a diabetes education class through your local senior center or health provider.
Managing diabetes isn’t just about controlling blood sugar. It’s about protecting your whole body. If left unchecked, you can have too much blood sugar (glucose), it can damage your blood vessels and nerves throughout your entire body.
Here are five serious conditions linked to diabetes in seniors:
1. Heart Disease and Stroke: Diabetes doubles the risk of heart attacks and strokes in seniors. It can accelerate the buildup of plaque in arteries, leading to cardiovascular events.
2. Kidney Disease (Nephropathy): Over time, diabetes can damage the small blood vessels in the kidneys, leading to kidney failure. Seniors may need dialysis if not addressed early.
3. Vision Issues and Blindness: Diabetes is a leading cause of diabetic retinopathy, cataracts, and even complete vision loss. In this case, regular eye exams become necessary.
4. Nerve Damage (Neuropathy): Tingling, numbness, or pain in the hands and feet are signs of nerve damage, which can eventually lead to mobility issues or even amputation.
5. Foot Problems and Infections: Seniors with diabetes often experience slow-healing wounds. Left untreated, small cuts or sores can become serious infections.
• Schedule annual eye exams and kidney screenings.
• Inspect your feet daily for cuts, swelling, or redness.
• Don’t ignore symptoms like numbness or pain. These could be signs of diabetes-related complications.
One of the most challenging things of diagnosing diabetes in seniors is that its symptoms often resemble other age-related issues. It manifests in the body with symptoms that range from mild to severe.
Fatigue, vision changes, and frequent urination might seem normal with age. But they could be signs of something more serious. So, if you have any doubt at all that a symptom might be pointing towards a larger issue, do not hesitate to contact your trusted healthcare provider right away.
Common diabetes symptoms include excessive thirst and hunger, frequent urination, especially at night, blurred vision, fatigue or dizziness, unexplained weight loss, tingling or numbness in hands and feet, and slow-healing cuts or sores.
What Can You Do As A Senior?
• Keep a symptom journal to observe the changes.
• Share even minor concerns with your doctor. The earlier you detect, the better.
• Get routine blood glucose screenings during wellness checkups.
Prediabetes means your blood sugar levels are higher than normal but not high enough for a diabetes diagnosis. It’s a wake-up call, not a life sentence. According to StatsCAN Plus, from 2016 to 2019, 4% of Canadians aged 20 to 79 were living with prediabetes. Among them, Canadian seniors aged 60 to 79 (8%) were twice as likely to be living with prediabetes as those aged 40 to 59 (4%).
Prediabetes is when the body has higher-than-normal levels of glucose, putting it at greater risk for type 2 diabetes, heart attack, and stroke. A healthy lifestyle is often all it takes to get back on track, but it’s still important to get your glucose levels checked regularly and speak with your trusted healthcare provider if further testing or medication is required.
Key risk factors for prediabetes include being over 45, overweight or obese, having a family history of diabetes, lack of physical inactivity, and high blood pressure or cholesterol.
For the next step, ask your doctor about your A1C level, which reflects your average blood sugar over 3 months. Aim for 30 minutes of gentle activity (like walking or swimming) most days, and choose meals rich in fiber, whole grains, and vegetables.
It may sound simple, but adopting a healthy lifestyle is one of the most powerful tools seniors have for preventing and managing diabetes. Even if you’re already diagnosed, prediabetic, or at risk, maintaining a healthy lifestyle is one of the most effective ways for seniors to manage diabetes and support overall well-being.
Even light physical activities like chair yoga, gardening, or a daily walk can significantly improve insulin sensitivity. A balanced diet that includes lean protein, whole grains, and plenty of fresh fruits and vegetables is essential, while limiting processed foods and sugary drinks helps keep blood sugar levels in check.
Furthermore, chronic stress can also impact glucose levels, so incorporating calming activities such as deep breathing exercises, listening to music, or spending time in nature can be super beneficial. Aim for 7 to 9 hours of quality sleep each night, and stay proactive with regular doctor visits and routine health screenings to catch potential issues early.
Additionally, small steps, such as swapping white bread for whole grain or adding a 15-minute walk after dinner, can also make a big difference over time.

Let’s Keep It Simple, Shall We?
Truth be told, living with or preventing diabetes in seniors doesn’t have to be overwhelming. By understanding the type of diabetes, recognizing the symptoms, and addressing related health issues early on, seniors can stay in control of their well-being.
Remind yourself that you are not alone, and diabetes is manageable with the right knowledge, support, and habits.
Take proactive steps today. Don’t wait for tomorrow. Book a check-up, tweak your diet, and add more movement to your day. This new chapter you’ll start today can lead to better health outcomes for tomorrow.
Need some more inspiration to get started? Read about ways to promote healthy aging in our Inspiring Stories, and check out just how Verve’s resident-centric support promotes health and wellbeing in our residents.
Your journey toward better health starts today!
This article originally appeared on the Verve Senior Living website and is reprinted here with permission.

Staying physically active is crucial for seniors to maintain their overall health and quality of life. Engaging in regular fitness activities helps improve strength, flexibility, balance, and cardiovascular health, reducing the risk of injury and chronic diseases. Fortunately, many free workout resources are available, particularly online. One such valuable resource to try is the
It is a mother-and-daughter dynamic duo showcasing a variety of exercises specifically tailored for those 50 and beyond and for individuals with limited mobility. Their YouTube channel offers you more than 200 free fitness videos.
Whether it’s gentle stretches, chair exercises, or low-impact cardio routines, yes2next provides a convenient and effective way for seniors and everyone to stay active and maintain their well-being.


We believe that an informed and engaged parent is an empowered one. Through enlightening articles, expert insights, and inspiring stories, we aim to equip our readers with the tools and knowledge necessary to navigate the complex pediatric health care landscape.
Join us as we explore how patient advocacy, active engagement and comprehensive education can transform the pediatric health care experience, turning obstacles into opportunities for growth and healing.
By Cheryl Petruk

In today’s connected world, children are growing up with a digital savviness, having been surrounded by technology that has shaped how they learn, communicate, and play. From early childhood through adolescence, screens—smartphones, tablets, gaming systems, and social media—have become woven into the fabric of their daily life. Society generally recognizes that digital and social media can provide educational and social benefits. However, growing evidence suggests that excessive or unmonitored use of social media can also harm children’s mental health, cognitive development, and overall well-being. As parents, educators, and healthcare professionals, we need to understand these impacts as a society, as they are essential to guiding healthy digital habits.
Digital technology has had a transformational effect on how children interact with the world. While educational platforms, interactive apps, and virtual classrooms have opened new learning opportunities where children can explore science through simulations, practice reading and math in gamified formats, and connect with peers across cultures, this can be seen as a massive transformation in our societal environment. During the COVID-19 pandemic, technology bridged gaps in education and socialization that might otherwise have isolated children completely. This was an unprecedented time in our history. While technology has assisted us in our daily lives, we can reflect on how we have become dependent on it.
However, much research that has been conducted in recent years has been able to show us that constant access to screens can blur the line between beneficial and harmful use. Research from the Canadian Pediatric Society (CPS) notes that while technology can enhance learning, excessive exposure—especially to entertainment or social media—has been linked to attention difficulties, disrupted sleep patterns, social consequences, and reduced physical activity. The challenge we face lies in moderation: harnessing digital benefits without letting them dominate a child’s day-to-day life.

Social media platforms such as TikTok, Instagram, Snapchat, and YouTube have become integral to how preteens and teens express identity and seek connection. However, these platforms are not designed with the developing brain in mind. Children and adolescents are particularly vulnerable to the dopamine-driven reward systems embedded in social media algorithms. Likes, comments, and views trigger cycles of validation and comparison, which can lead to anxiety, low self-esteem, and even symptoms of depression or narcissistic behaviours.
Recent studies, including one published in JAMA Pediatrics, have found correlations between high social media use and mental health concerns in youth, particularly among girls. Constant exposure to curated, idealized content often fosters unrealistic expectations about body image, lifestyle, and success: cyberbullying, peer pressure, and fear of missing out (FOMO) further compound emotional stress. For many young users, the digital world becomes a mirror reflecting insecurity rather than confidence.
Early and excessive screen exposure has measurable effects on attention span, language development, and executive functioning. The American Academy of Pediatrics (AAP) cautions that children under two years of age should avoid digital media (except video chatting), as their brains develop best through human interaction. For older children, prolonged screen use— especially multitasking across devices—has been associated with decreased focus, reduced empathy, and difficulties in emotional regulation.
Sleep disruption is another critical concern. The blue light emitted from screens suppresses melatonin, delaying sleep onset and reducing overall rest quality. Inadequate sleep for children has been linked to impaired learning, mood disorders, and weaker immune responses. Establishing “screen-free” zones—such as bedrooms and family mealtimes—can help counter these effects.

Digital engagement often replaces outdoor play and physical activity. The World Health Organization (WHO) recommends at least 60 minutes of moderate to vigorous physical activity daily for children aged 5 to 17. Yet, according to Statistics Canada, many children fall short of this goal, partly due to increased screen time. Extended sedentary behaviour contributes to rising rates of childhood obesity, poor posture, and vision strain.
Excessive gaming or media use can lead to “tech-neck” and repetitive strain injuries, conditions once seen primarily in adults. Encouraging balance—such as regular movement breaks, outdoor time, and non-digital hobbies—helps safeguard both physical and mental health.
Parents, caregivers, and educators have a pivotal role in modelling and monitoring healthy technology use. The Canadian Pediatric Society encourages co-viewing and active discussion around online content. When parents engage with children about what they see and do online, it helps them develop critical thinking and digital literacy. These skills need to be developed in children and are essential so that when children encounter misinformation, online predators, or inappropriate content, they can critically think about the situation and the decisions that may need to be made in response.
Community organizations, schools, and healthcare providers can also contribute by promoting digital wellness education. Through programs offered in our communities and school systems that focus on media literacy, emotional resilience, and safe online communication, we can empower children to navigate the internet responsibly and teach them to distinguish between reality and fiction. Pediatricians can screen for problematic media use as part of regular health visits, offering early interventions when necessary. School counsellors can also monitor behavioural issues that may be demonstrated by children in the classroom setting, from overuse of digital tools.
Creating a healthy relationship with technology requires intentional effort from families, educators, and society at large. Here are several evidence-based strategies to support balanced use: Set Clear Boundaries: Establish consistent screen-time limits that reflect age-appropriate guidelines (for example, less than 2 hours of recreational screen time per day for children over 5).
1. Encourage Screen-Free Zones: Keep devices out of bedrooms and mealtimes to promote better sleep and family connection.
2. Promote Active Media Use: Replace passive scrolling with creative activities such as coding, photography, or educational games.
3. Model Healthy Behaviour: Children emulate adult habits—when parents put their phones away during family time, children are more likely to follow suit.
4. Foster Open Dialogue: Talk about social media pressures, online safety, and the difference between real and filtered lives.
5. Encourage Offline Play: Engaging in outdoor exploration, sports, and social activities is vital for development and stress reduction.
The digital landscape is evolving faster than ever, and so are the pressures faced by children growing up within it. While banning technology isn’t realistic—or necessarily beneficial—empowering children to use it wisely is both possible and essential. Through awareness, education, and thoughtful boundaries, families and communities can ensure that digital and social media enhance, rather than hinder, a child’s growth.
In the end, balance remains the key. Technology should be a tool for creativity, learning, and connection—not a substitute for the laughter, movement, and face-to-face interactions that nurture healthy, happy childhoods. Some words of wisdom: keep a box of crayons, colouring books, blank paper, a deck of cards, board games, handy. Take the opportunity to use time away from digital media to have a conversation with your children and stimulate their creativity.

G
Genu varum
Hand and upper extrem
Limb deformities
Limb length discrepan
Metabolic and heritabl
Neuromuscular condit
Painful conditions of th
Plastic reconstruction
Scoliosis and spine def
Skeletal dysplasia
Sports medicine





The My Blood My Health program is dedicated to empowering individuals affected by Hematological issues by providing trusted education, advocacy, and support. Through patient- centered resources and expert collaborations, we strive to enhance awareness and improve access to critical information for those navigating their blood health journey. Stay tuned for the next edition of the My Blood My Health digital magazine, coming in March, featuring insightful articles, patient stories, and the latest updates in hematology.




Heal Canada and Pat ADV Hub in the USA have embarked on a collaborative journey, aiming to revolutionize the realm of patient advocacy across North America. This pioneering partnership brings together two influential organizations from neighbouring countries, combining their extensive expertise and resources.
The objective is to expand and enhance the access to critical information for patient advocates, ensuring that individuals across the continent receive the best possible support and guidance in their healthcare journeys.
By bridging the gap between Canadian and American healthcare advocacy, this alliance promises to foster a more informed, empowered, and connected community of patient advocates, significantly contributing to the improvement of healthcare experiences for countless individuals.
patadvhub@gmail.com
www.patadvhub.org

Heal Canada and Pat ADV Hub are colloborating on a project!
Do you have a recipe or two that helps you live a better Quality of Life with your disease or diagnosis? Send your recipe to: recipes@healcanada.org
In your email, tell us about yourself, your diagnosis, and how your recipe helps you live a better quality of life.


This unique feature aims to introduce these vital organizations to a broader audience, highlighting their missions, achievements, and the critical support they offer patients and their families.
Each edition of this segment meticulously selects a different group, delving into their specific focus areas, ranging from rare diseases to everyday health challenges. Heal Canada amplifies these groups’ voices and fosters a deeper understanding and connection within the broader healthcare community by showcasing their stories, initiatives, and community resources.
This section is more than just an informational piece; it celebrates these advocacy groups’ tireless efforts and significant impact and empowers readers by connecting them with valuable resources and support networks.

By Angelina Wiggins
The Canada Health Act establishes a fundamental promise of universal access to medically necessary services for all Canadians. However, this commitment often manifests as a paradox for a significant portion of the population, as theoretical eligibility for care does not reliably translate into actual, timely access. For many Canadians, complex navigational barriers transform the healthcare system from a safety net into an obstacle course.
This analysis examines three critical barriers that contribute to the pervasive accessibility paradox: debilitating waitlists, fragmented referral silos, and daunting geographic and literacy disparities. It then outlines concrete, clinician-level actions necessary to help bridge this systemic gap for patients.
Timely access to specialist care is crucial for effective medicine, serving as the juncture where complex conditions are managed, diagnoses
are refined, and suffering is mitigated. When access is delayed, the consequences are far more severe than mere inconvenience; the wait becomes a clinical burden that imposes a heavy cost on patient well-being and the healthcare system.
The impact of specialist wait times on Canadians is substantial and extensively documented. According to Statistics Canada, 36% of Canadians waited three months or longer for an initial consultation with a medical specialist, a delay identified as a primary reason for unmet healthcare needs. More than half of older adults who reported unmet care needs attributed the difficulty to still waiting for an appointment. In fact, “waiting for a visit” was the most frequently cited barrier to accessing specialist care in several provinces, including Alberta (76.71%), British Columbia (55.13%), and Ontario (59.53%).
This prolonged uncertainty carries a human cost, affecting nearly two-thirds (64%) of Canadians who consulted a specialist within the 12 months preceding the survey. Of those affected by wait times, the consequences were severe, with 66% experiencing worry, anxiety, and stress, placing a psychological toll on top of their physical ailment. Furthermore, 36% endured
ongoing pain, and 22% reported that their health condition had deteriorated while waiting, turning manageable issues into more urgent problems. Unsurprisingly, satisfaction levels are directly linked to wait time, with fewer than one in five Canadians (17%) who waited for longer than three months reporting that they were very satisfied or satisfied with the wait time.
In Canada’s two-tiered healthcare system, a referral from a primary care provider acts as the essential gateway to specialized care. However, the referral process itself is frequently described as “complex, time-consuming, and fragmented.” This state leads to critical failures where referrals may be refused, lost, or simply overlooked, leaving patients and providers frustrated long before they reach a waitlist. Alarmingly, a recent study indicated that 36% of referrals were not acknowledged within seven weeks of being sent, forcing primary care providers and their patients to wait without confirmation that their request for care was received.
Family physicians serve as the system’s primary “gatekeepers”, but this burden is intensified for


the growing number of Canadians who lack a regular provider. Those without a regular healthcare provider reported that their lives were significantly affected by wait times more often (71%) compared to those who have one (63%). The dysfunction is bidirectional as primary care providers express dissatisfaction with the opaque process and the lack of timely specialist responses, while specialists voice dissatisfaction with the quality of referral letters, which often lack a clear clinical question and sufficient information needed for appropriate and timely triage.
Overcoming procedural hurdles is only part of the accessibility challenge; effective healthcare navigation also requires patients to surmount physical distance to services and possess the necessary literacy to engage with the inherently complex system. For many, the confluence of geography and health literacy creates nearly insurmountable obstacles.
A stark disparity exists between urban and rural physician distribution. While approximately 20% of Canadians reside in rural or remote communities, only 8% of the nation’s physicians practice in these areas. This imbalance forces rural patients to carry a heavy travel burden. On average, rural Canadians must travel over 35 km to see their doctor -more than double the travel time for those in larger centers. Furthermore, specialized services, such as surgeries and cancer treatments, are typically concentrated in larger urban centers.
A national deficit in health literacy exacerbates the challenge of navigating this complex and distributed system. According to the Public Health Agency of Canada, 60% of Canadian adults and 88% of seniors are not health literate. Health literacy is defined as the ability of an individual to obtain, understand, and apply basic health information and services necessary to make informed health decisions. For example, some seniors lack the literacy skills to follow instructions on a medicine bottle, making self-advocacy within the complex healthcare structure impossible. For a patient who must travel 35 km for care, low health literacy further diminishes their navigational capacity to coordinate travel, confirm appointments, or understand complicated previsit instructions, resulting in a damaging cycle of missed opportunities.
While these systemic issues demand largescale policy reforms, frontline clinicians have a professional responsibility to act within their sphere of influence to shield patients from the very failures - waitlist ambiguity, referral
black holes, and navigational challenges - that undermine universal access.
Given specialist frustration regarding incomplete or unclear referrals, a high-quality referral letter serves as a crucial instrument of patient advocacy. It streamlines the process, enables better triaging, and reduces the risk of rejection or delay. Clinicians should draft referrals that clearly articulate the clinical question, outline the specific expectation (such as advice only versus shared care), and provide sufficient clinical information for the specialist to triage the case appropriately.
With the staggeringly high rate of low health literacy, clinicians cannot assume patients understand the next steps in their care journey. Clinicians must proactively guide and advocate for vulnerable patients, especially those facing complex social or administrative barriers, such as newcomers who lack provincial coverage. In cases where a patient is medically uninsured, providers should consult with local hospitals to determine their policies regarding what constitutes an emergency. If referring a patient you fear may be dismissed, such as an uninsured refugee child who was turned away from an ER despite a medical need, do not rely on verbal instructions. Provide a specific, written referral letter for ER staff detailing the clinical findings and explicitly stating why the condition constitutes a medical emergency. This crucial act of documentation can prevent the patient from being turned away.
The practice of “send and forget” poses risks to patient safety in a system where many referrals often go unacknowledged after seven weeks. To prevent care from stalling indefinitely in administrative silence, clinicians should
implement a simple, practice-level system to track referrals. If acknowledgement is not received from the specialist’s office within a reasonable timeframe, the practice must proactively follow up to confirm receipt and inquire about the status.
Canada’s universal healthcare mandate, enshrined in the Canada Health Act, is persistently undermined by the accessibility paradox, resulting in significant unmet needs among vulnerable populations. Systemic barriers, including prolonged wait times, fragmented referral systems, and social determinants such as geography, income, and low health literacy, contribute to inequitable access to care. These barriers fall most heavily on people who are younger, live in rural areas, have lower household incomes, or lack a regular family physician, making it more difficult for them to access needed specialist services. While addressing these broad structural failings requires largescale policy solutions, frontline clinicians play a vital role in patient advocacy. By mastering the referral handoff, acting as system navigators, and proactively tracking patient progress, providers can implement targeted interventions to protect their patients from being lost in the system’s administrative voids.

Angela Wiggins is a secondyear Master of Physical Therapy student at Western University. She previously completed an Honours Bachelor of Psychology at the University of Windsor and is passionate about patientcentered care and improving access to health services.
1. Canadian Pediatric Society (CPS). Caring for kids new to Canada: Navigating the Health System. Last updated March 2014.
2. George Szasz, CM, MD. Basic health literacy: Canada is doing poorly. BCMJ (British Columbia Medical Journal). January 12, 2023.
3. Heal Canada. Submission Guidelines for Heal Canada’s E3 Advocacy Digital Magazine. (Date not specified).
4. Healthcare For Real (Canadian Medical Association). Does where I live affect my health care? (Date not specified).
5. Keely, E., & Liddy, C. Transforming the specialist referral and consultation process in Canada. CMAJ: Canadian Medical Association Journal, 191(15):E408–E409. 2019 Apr 15. doi: 10.1503/cmaj.181550.
6. Lan, M., Alemu, F. W., & Ali, S. The doctor will not see you now: investigating the social determinants of specialist care using the Canadian Longitudinal Study on Aging (CLSA). Frontiers in Public Health, 12. 2024 Sep 27. doi: 10.3389/fpubh.2024.1384604.
7. Pandey, M., Kamrul, R., Rocha Michaels, C., & McCarron, M. Identifying Barriers to Healthcare Access for New Immigrants: A Qualitative Study in Regina, Saskatchewan, Canada. Journal of Immigrant and Minority Health, 24, 188–198. February 2022. doi: 10.1007/s10903021-01262-z.
8. Statistics Canada. Wait times to see a medical specialist in Canada, 2024. Released: 202507-29.
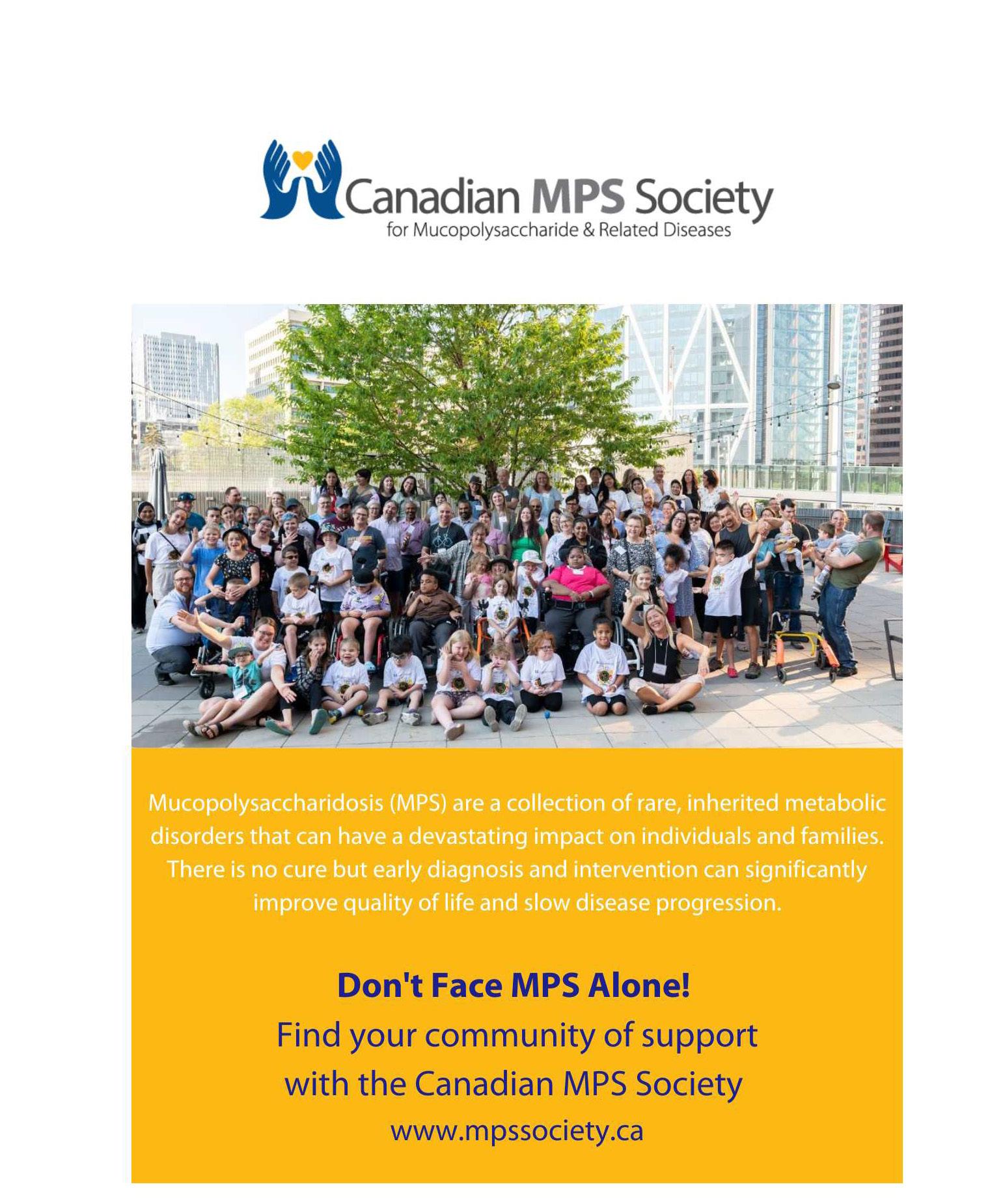



For Canadians living with lethal diseases such as aggressive cancers or rare genetic conditions, time is often the most critical — and limited — resource. But while science continues to advance, Canada’s healthcare and regulatory systems are lagging behind. The time it takes for new treatments to move from discovery to the hands of patients can stretch into years — time many do not have.
The Life Saving Therapies Network (LSTN), a Canadian non-profit organization, has launched a petition on Change.org titled “Urgent Call to Reform Approval and Access to Treatments of Lethal Diseases.” The petition is a direct appeal to the Government of Canada to create a dedicated framework for faster and more equitable access to promising therapies for patients facing lifethreatening illnesses.
According to the petition, the current approval and reimbursement systems treat all diseases with a similar process, regardless of how aggressive or terminal the illness may be. This “one-size-fits-all” approach can result in patients with rapidly progressing or incurable diseases being forced to wait years for access to a drug, even when strong early evidence suggests it could help.
The petition outlines a proposed Lethal Disease Framework (LDF) — a system that would adapt the approval and access process specifically for lethal diseases. The core of this proposed framework involves several key reforms.
First, the petition calls for accelerated and adaptive regulatory oversight. Specifically, it proposes that patients with lethal diseases should be granted conditional access to new therapies following Phase 2a trials — the point where preliminary efficacy and safety are typically demonstrated. This would allow patients to access potentially life-saving drugs earlier, while further data is gathered in realworld conditions.
Second, the petition highlights the importance of an integrated, pan-Canadian approach to healthcare access. Under the current system, drug availability, diagnostic services, and funding decisions can vary dramatically between provinces. The proposed framework seeks to ensure consistent access across all regions of the country, so that a patient’s location does not determine their chance of survival.
Third, the petition calls for greater use of real-world evidence and decentralized clinical trials, allowing data to be collected from patients receiving treatment outside of traditional trial settings. This could help bring promising treatments to market faster while continuing to evaluate their performance
in real-time.
Another major concern raised is the lack of timely access to diagnostics, such as MRIs, CT scans, and PET imaging — tools that are essential for early and accurate disease detection, monitoring, and treatment planning. The framework urges investment in both technology and personnel to improve diagnostic turnaround times nationwide.
The petition also targets the bureaucratic delays built into the current system. Even after a treatment receives Health Canada approval, there are multiple additional layers of review — including costeffectiveness assessments and provincial drug plan negotiations — that can add years of delay. The LDF proposes that these processes should run in parallel, not sequentially, and should be bound to specific timelines, such as 60 days for reimbursement decisions.
Finally, the petition supports wider use of Drug Access Navigators — professionals who assist patients in accessing treatments through compassionate use programs, private insurance, or manufacturer programs, while public access is still being negotiated.
LSTN’s petition is part of a broader conversation already happening in other parts of the world. In the United States, the Food and Drug Administration (FDA) has long offered programs such as Accelerated Approval and Breakthrough Therapy Designation, which allow earlier access to drugs for serious or life-threatening conditions. Similarly, the European Medicines Agency (EMA) provides Conditional Marketing Authorizations for treatments that meet unmet medical needs.
While Canada does have mechanisms for early access — such as the Special Access Program — these are often limited, underutilized, and inconsistent across jurisdictions. LSTN argues that a formalized national framework would ensure better coordination, accountability, and fairness.
This is not just a matter of policy — it’s a matter of survival. The petition argues that Canada’s health system must evolve to match the speed of science and the urgency of patient need.
Canadians can read and sign the petition online at Change.org, and are encouraged to share it with their networks and elected officials. The Life Saving Therapies Network believes that with the right framework, Canada can lead in providing faster, smarter access to treatments for those who need them most.
In the face of lethal disease, time is everything. For patients across the country, that time should not be wasted in the waiting room.
To sign the petition, please visit https://www.change.org/supportLSTN or scan the QR code below:

Anris
Kica, Co-CEO of Life Saving Therapies Network
https://www.lifesavingtherapies.com/

The most rare stories on earth streaming free to your TV.

HOPE comes streaming in.
The Disorder Channel is a first-of-its-kind streaming platform dedicated exclusively to showcasing stories from the rare disease community. Available on Roku and Amazon Fire TV, it offers a curated collection of short films, documentaries, talk shows, and animated shorts that illuminate the lived experiences of individuals and families affected by rare conditions. With content ranging from feature films to shorts, from deeply personal narratives to educational programming, The Disorder Channel serves as both a storytelling hub and a powerful advocacy tool.
Founded in 2020 by Daniel DeFabio and Bo Bigelow, two fathers of children with ultra-rare diseases, The Disorder Channel emerged from a shared frustration and a bold vision. Both dads had created short films about their children—Daniel’s son Lucas, who had Menkes disease, and Bo’s daughter Tess, who lives with USP7-related disorder (Hao-Fountain Syndrome). While their films found some success at traditional film festivals and medical conferences, they quickly realized the limitations of these venues. Film festivals offered broad appeal but lacked targeted interest in medical stories, while medical conferences had the right audience but were often expensive and inaccessible to families.
As so often happens for rare disease families, upon discovering that the solution they needed did not exist, they decided to create it. Since no platform existed to consistently showcase films of rare disease stories, they would build one. Their first step was launching DISORDER: The Rare Disease Film Festival in 2017, which brought together filmmakers, patients, clinicians, and industry leaders to share and witness rare disease narratives. The festival was a success, but its reach was still limited by geography and logistics. Then came the COVID-19 pandemic, which forced the cancellation of the 2020 edition of the festival. Rather than pause their mission, Daniel and Bo pivoted—and The Disorder Channel was born.
The Disorder Channel is more than just a digital extension of the film festival; it’s a media outlet with a singular focus: rare disease storytelling. It features films that were screened at past festivals, as well as new content that might never have found a platform elsewhere. Viewers can explore a wide range of topics, from genetic diagnostics and caregiving to mental health and advocacy. Shows like Once Upon a Gene TV, Pain Points, Unfixed, Stronger Every Day, and Taking Care with Rose Reif offer episodic content that blends education with empathy. There’s even room for creative formats—some films use puppets, animation, or fantasy elements to convey complex emotional truths.
What sets The Disorder Channel apart is its commitment to making the rarest stories in the world accessible and visible. With over 10,000 known rare diseases affecting more than 300 million people worldwide, these conditions are often overlooked in mainstream media. The Disorder Channel fills that gap by giving patients and families a voice, and by educating viewers about the realities of living with rare disease.
“We know families facing a rare disease diagnosis will search the internet, and so much of what they learn there is dire news and a disheartening or devastating prognosis. But if, in addition to the medical papers, they can also find films like those we offer, films of how rare disease families go on to live their lives and build the best futures possible, we can offer not only comfort and community, but a possible path to hope,” says Daniel DeFabio. “Our film and talk shows don’t change the medical facts, but they put them into the context of how you might live this different life.”
The Disorder Channel is a way to watch these intimate stories on the largest screen in your home. It is free to add and easy to access, making it a low-barrier entry point for anyone interested in rare disease awareness. It’s a testament to what happens when personal experience meets creative action. Daniel and Bo didn’t just wish for better representation—they built it. Their work has helped shift the narrative around rare disease from isolation to connection, from silence to storytelling. As part of their mission to make these stories of the rare disease lived experience more seen and better understood, The Disorder Channel will often license films to conferences and events. Selections from their collection of more than 250 films and videos have screened at health and rare disease conferences, including BIO, World Orphan Drug Conference, The National Institutes of Health, Pharma Forum, Global Genes Summit, Sanford CORDS Great Plains Rare Disease Summit, Takeda’s Executive Leadership Summit and Access USA, among others.
The founders have also led storytelling training workshops to prepare rare disease advocates to tell their own stories with more impact, whether in videos, podcasts, blogs or face-to-face. These inperson and virtual workshops often feature faculty recruited from the rare disease filmmakers and podcasters featured on The Disorder Channel.
In a media landscape dominated by mass-market entertainment, The Disorder Channel stands out as a niche platform with a global purpose. It’s not just about watching films—it’s about witnessing lives that are too little understood, learning from them, and joining a movement that believes every story, no matter how rare, deserves to be heard.

Daniel DeFabio,
Co-Founder
Disorder: The Rare Disease Film Festival
The Disorder Channel
https://www.rarediseasefilmfestival.com

By Cheryl Petruk
Health Technology Assessment, often abbreviated as HTA, is a structured, multidisciplinary process that evaluates health “technologies” — including medicines, medical devices, tests, surgical procedures, digital health tools, programs or health services — across multiple dimensions (clinical, economic, social, ethical, organizational). The goal is not merely to produce academic knowledge, but to inform realworld decisions by health authorities, payers, and policy makers about whether a new (or existing) technology should be adopted, covered, funded, or used, and under what conditions (O’Rourke, Oortwijn, & Schuller, 2020)
In simpler terms: HTA helps decision makers answer “Is this health technology good value for patients and for the health system?” It examines benefits, risks, costs, and wider impacts—so that scarce health resources can be used as wisely and fairly as possible.
HTA is increasingly common around the world. Many countries require HTA for new medicines or technologies before they are reimbursed or introduced into public health systems. The European Union has moved toward a joint HTA framework, beginning joint assessments from January 2025 onwards.
While every HTA agency uses its own precise methods, key phases are broadly shared. Below is a simplified “lifecycle” of an HTA, and where patients and advocates can engage.
Topic identification / Scoping / Priority setting
Health systems and HTA agencies must first decide which technologies or interventions are worth evaluating. This involves setting priorities (e.g. high-burden diseases, novel therapies, unmet needs). Patients or advocacy groups can sometimes propose topics or signal which innovations matter most.
The HTA team frames the question in terms of Population, Intervention, Comparator, and Outcomes (PICO). Here, patients can help decide which outcomes truly matter (e.g. quality-of-life, symptom relief, side-effects) rather than only some surrogate biomarkers.
The HTA team gathers available scientific and real-world evidence: clinical trials, observational data, registry data, and sometimes qualitative evidence (patient experiences). Patients can submit “patient-based evidence”—surveys, stories, experience data—to fill gaps not captured in clinical trials.
This is where costs (e.g. drug price, monitoring, side effects, hospitalizations) are weighed against benefits (life extension, symptom relief, avoided complications). Sometimes qualityadjusted life years (QALYs) or other valuation metrics are used. Patients can assist by validating assumptions about use patterns, adherence, or resource use in real life.
“HTA helps decision makers answer
‘Is this health technology good value for patients and for the health system?’”
At this stage, panels (which may include clinicians, economists, ethicists, and sometimes patient representatives) review the evidence and make recommendations (e.g. yes/no funding, use under certain restrictions, or “coverage with conditions”). Patient voices here can challenge assumptions, highlight lived-experience tradeoffs, and ensure the decision reflects what patients prioritize.
Implementation/monitoring/re-evaluation
Once a decision is made, the technology is (or isn’t) adopted. Post-launch monitoring may collect real-world outcomes, safety data, utilization, and cost impacts. HTA may be revisited or updated over time. Patients may help in monitoring, reporting outcomes, or revising assumptions over time.
Over time, HTA agencies are increasingly assessing how meaningful patient engagement has influenced decisions, processes, or outcomes. Frameworks like the “Three-Domain Impact Framework” classify impact in (a) changes in HTA results or recommendations, (b) effects on the HTA organization and culture, and (c) benefits or burdens to patients themselves.
Throughout this process, transparency, clear communication, and well-defined roles are critical to effective and respectful patient engagement.
Clinical trials often focus on measurable endpoints (e.g. tumor size reduction, biomarker change) that may or may not reflect what patients care about most (daily functioning, fatigue, sideeffect burden, psychological impact). Involving patients ensures that HTA considers real-world impacts that matter.
HTA is ultimately about allocating limited healthcare resources. Decisions about which treatments to fund or restrict have ethical consequences. Patient involvement helps to ensure fairness: that marginalized voices are heard, that benefit-risk tradeoffs reflect lived realities, and that decisions have legitimacy and public trust.
Often, clinical trial data are incomplete, or populations studied differ from the “real-world” patients. Patients can help identify what evidence is missing (e.g. long-term side-effects, impact on daily life) and help shape research priorities or conditional access agreements.
If reimbursement decisions don’t reflect patient realities (e.g. complexity of use, monitoring burden, comorbidities), uptake and adherence may suffer. By injecting patient insight into HTA, recommendations may be more feasible and patient-friendly, improving ultimate benefits.
When HTA processes invite patient roles openly, decision-making becomes more transparent and accountable. Patients can witness how evidence is weighed, question assumptions, and see why certain decisions were made — which strengthens trust in the system.
Meaningful participation fosters patient empowerment. Patients can gain a greater understanding of health systems, advocate more effectively, and build capacity in their communities. Over time, this can enhance policy change from the ground up.
While many HTA agencies now include patient voices, the path is not straightforward. Some common challenges:
• Lack of awareness or knowledge among patients about HTA and how to engage effectively.
• Limited or unclear guidance on how and when to involve patients, or insufficient procedural support.
• Tokenistic engagement — involving patients superficially rather than in decision-making roles.
• Representativeness — ensuring that patient contributors reflect the diversity of the full patient population (age, severity, socioeconomic status).
• Time, resource, and training constraints — patient contributors may lack time, compensation, or training to engage fully.
• Conflicts of interest — e.g. patient organizations sometimes receive industry funding, which must be managed.
• Evaluation gap — many HTA bodies do not systematically evaluate how patient involvement influenced outcomes, and reporting is inconsistent.
Nevertheless, initiatives and tools are emerging to surmount these barriers. For example, the Guidelines International Network (GIN) has published tools to support patient involvement in HTA (e.g. guidelines, templates, training). Some HTA bodies are piloting consensus methods (e.g. Delphi panels) to integrate patient input in scoping or prioritization stages.
If you are a patient advocate or working with a patient community and want to engage in HTA, here are some guiding principles:
• Start early — being involved from the scoping or topic selection stage is more powerful than joining late.
• Be clear about roles — understand how your input will be used, timelines, decision stages, and expectations.
• Seek capacity building and training — many HTA agencies or stakeholders now offer training modules for patients.
• Use evidence and stories together — blending quantified experience data (e.g. surveys) with narratives adds powerful context.
• Be transparent — disclose conflicts of interest or funding sources to preserve trust.
• Advocate for feedback cycles — ask HTA bodies to report how patient input changed decisions or was (or was not) used.
• Collect evaluation data — gather reflections on your involvement: what worked, what didn’t, so future advocacy improves.
• Work in networks — collaborate with other patients, advocacy networks, or HTA interest groups (e.g. HTAi Patient & Citizen Involvement) to share insights and increase impact.

Health Technology Assessment is a cornerstone of modern health policy. It helps bring rigor, transparency, and accountability to decisions about which health innovations should be adopted, funded, or restricted. But it is not purely a technical exercise — the “human” dimension matters deeply. Without the voice of patients and advocates, HTA risks missing what really matters in people’s daily lives, and decisions may lack legitimacy or feasibility.
For patients and advocates, engaging proactively in HTA is an opportunity to shape decisions that affect access to therapies, fairness of health systems, and the relevance of medical innovation. The road to meaningful involvement has challenges—but with capacity building, clear frameworks, and mutual respect between HTA bodies and patient groups, it is possible to make HTA not only scientifically robust, but truly patient-centered.

Imagine being forced to choose between life-saving medical care and the financial burden of relocating to Toronto to access it. This is the reality for many patients, alongside their caregivers and family who must travel far from home to receive critical treatment. The added challenge of securing safe, affordable housing in an unfamiliar city often makes an already difficult journey even harder. This financial burden may force patients to either delay or forgo necessary medical care.
This is where StayWell Suites Charity steps in.
StayWell provides affordable accommodations to Canadians who must relocate for medical treatment. Through partnerships with major hotel chains and professional furnished apartment providers, we offer subsidized patient rates, alleviating the financial burden and ensuring patients can stay close to hospitals, alongside their caregivers and family, while receiving treatment.
The inspiration for StayWell Suites Charity came from the personal experience of Tina Proulx, a patient from Ottawa, who faced a similar challenge in 2015. Diagnosed with a rare, life- threatening disease, Tina needed a double lung transplant at Toronto General Hospital, over 400 kilometres from her home in Ottawa. In Toronto, the areas surrounding the hospitals are amongst the most expensive in the city. Tina and her husband Joel decided to make the move and had to take leaves of absence
from work – they found themselves living in one of the most expensive cities in the country without any income.
Matt Regush, a partner at Sky View Suites, learned of Tina’s relocation challenges in the fall of 2015, when her family inquired about furnished accommodations and instantly provided them with a fully furnished unit at a reduced cost. This encounter led to the creation of StayWell Suites Charity. “If you cannot afford to live in Toronto and you’re making the choice not to accept treatment, then you are basically making the choice to die” says Tina, reflecting on her experience. In December 2015, Tina received her transplant and made a full recovery, inspiring StayWell’s mission to help other patients facing the same challenges.
From our start in 2018, providing three patients of the Princess Margaret Cancer Centre, including their families and caregivers, with 135 nights, we have grown significantly. By the end of 2024, we will have supported over 5,500 patients with over 90,000 room nights across all major hospitals in Toronto. Patient stays range from a few days to over a year. Earlier this year, we concluded an agreement with the SickKids Foundation to provide $250,000 in accommodation support over the next five years.
Looking ahead, StayWell will expand to other cities across Canada in 2025, continuing to rely on the support of dono s and partners to fill the gap between accommodation costs and what patients can afford. StayWell Suites Charity is committed to providing safe, affordable accommodations to patients, along with their caregivers and family, during their medical journey. Your support can make a life-changing difference for families like Tina’s, ensuring that no patient has to choose between their health and affordable accommodations.
Patients/caregivers can go to our website staywell.ca and select the Book Now link.

By Kim Hanson

Living with diabetes has taught me the importance of sharing my story—whether it’s with researchers developing studies, companies improving medications and devices, or government agencies striving to deliver better services. But over the years, I’ve often wondered: How do my experiences compare to those of someone facing cancer or cardiovascular disease? Could we uncover valuable solutions by looking at what connects us, alongside what makes our challenges unique?
At HealthPartners, these questions inspired something big. For over 35 years, we’ve brought together workplaces, health charities, and communities they serve to improve the lives of people affected by illness. Now, we’re taking the next step.
We’re proud to introduce the Health Advisory Network (HAN)—a national platform where people like you can share your experiences, highlight challenges, and collaborate on solutions to improve healthcare across Canada.
Share Your Voice: Participate in quick online surveys and consultations about your experiences as a patient or caregiver.
Get Paid: Your time and insights are valuable, and we make sure they’re compensated.
Drive Change: Help tackle challenges in workplaces, healthcare systems, and communities.
Why now? Because the numbers speak for themselves:
• 45% of Canadians live with at least one major chronic condition.
• 2.5 million Canadians report unmet healthcare needs.
• 1 in 2 Canadians will act as caregivers during their lifetime.
The Health Advisory Network creates a unified space for people affected by health conditions to connect, share, and make a meaningful impact. It’s not here to replace the incredible work of health charities or patient-oriented research groups—it’s here to amplify it. Together, we can uncover shared challenges and opportunities to build a stronger, more inclusive healthcare system.
Join the Health Advisory Network today and help shape the future of healthcare in Canada.
Sign up today and start making an impact.
healthpartners.ca


For over 35 years, HealthPartners has brought together workplaces, health charities, and people with lived healthcare experience to improve lives across Canada.
The Health Advisory Network is a national platform that invites individuals affected by illness to share their stories through paid surveys and consultations. Your lived experience can help shape research, policies, and programs that make healthcare better for everyone.
Improving healthcare through lived experience. healthpartners.ca/network


The “Patient’s Journey” section of E3 Advocacy Digital Magazine is close to our hearts. This magazine is dedicated to patients and caregivers. We are proud to offer a platform to our community so that we can share, learn, and grow together.
Here, patients can share their experiences and empower readers by connecting them with our Heal Canada community. By doing so, we can understand that whatever the situation we face, we are not alone! United, we stand in Advocacy!

How Cognitive Behaviour Therapy Changed My Life — and Can Change Yours
By Landon Gregory Barrowman
When I look back on the year that changed everything, I see it in chapters, each one heavier than the last. First came the separation from my partner. Then my father passed away. A cancer scare followed, and finally, the loss of my job in the Alberta oil sands.
Those events weren’t just setbacks; they were seismic shifts in my life. They left me questioning my future, my stability, and even my identity. Like many men in the trades, I had been taught to “push through” and keep working, no matter what was happening inside. But the truth was, I was struggling.
That’s when I found Cognitive Behaviour Therapy (CBT).
CBT is a form of psychological therapy built on a simple but powerful idea: our thoughts, feelings, and behaviours are interconnected. By identifying and challenging unhelpful thinking patterns, behaviours, and emotions, we can change the way we feel and act. It’s practical, structured, and focused on problem-solving, a style that resonated deeply with me. Plus, you can do it yourself every day!
For men in the trades, CBT’s appeal is that it’s hands-on and results-oriented. There’s no vague jargon or endless analysis of the past. Instead, it gives you tools, real tools, for dealing with stress, anxiety, anger, and depression. It’s like having a mental “toolkit” you can carry with you, whether you’re on the job site or at home.
In the wake of my personal losses, CBT helped me separate what I could control from what I couldn’t. It taught me to spot the mental “shortcuts”, like assuming the worst ( catastrophizing), blaming myself for everything (personalization), or thinking nothing would ever change (fortune telling), that were making things harder.
By challenging those thoughts and replacing them with balanced, evidencebased thinking, I started to see real changes. My mood lifted. I began making better decisions. I found the energy to move forward. This wasn’t just about “thinking positive.” It was about rewiring the way I approached life.
At first, I wrote The Working Man’s Guide to Mental Health for my coaching clients as a way for them to review the techniques we’d talked about in our sessions. But as I wrote, I realized it could help anyone who works with their hands, lives in a high-stress environment, or has been told to “tough it out” instead of addressing their mental well-being.
I published the book on Amazon and soon got a call from the Edmonton Construction Association, inviting me to speak about mental health in the trades. That led to another realization: not everyone is a reader.
“In the wake of my personal losses, CBT helped me separate what I could control from what I couldn’t.”
Then I worked on behavioural observation and emotional regulation. All are very important parts of CBT.
What started as personal recovery grew into a new career. I enrolled in university to study psychology. I began coaching others in CBT techniques, especially men in the trades and oil sands, where mental health struggles often go unspoken.
I noticed something powerful: when you explain CBT in plain language, without clinical jargon, people use it. They see results. And that’s when I realized I needed to put these tools into a format that anyone could access.
So I recorded a series of free video lectures covering the same concepts as the book. They’re available on YouTube for anyone who prefers to learn by watching and listening.
CBT didn’t just help me survive my hardest year; it opened doors I never imagined. I’ve connected with workers, employers, and community groups across Alberta who are hungry for real, practical conversations about mental health. I’ve been invited to speak, teach, and share my story.
Most importantly, I’ve seen men who once brushed off the idea of “mental health” start using CBT tools in their daily lives, handling stress better, improving their relationships, and taking back control.
The oil sands and construction industries are built on resilience, problem-solving, and teamwork. Those same qualities are at the heart of CBT. When we treat mental health like any other skill, something you can learn, practice, and get better at, we start breaking down the stigma that keeps
so many men silent. Shame.
I’m proud to call St. Albert home, proud of my years in the trades, and proud to now be part of a movement that says mental health isn’t a weakness, it’s a skill worth mastering.
If my story can inspire even one more person to pick up these tools, then the journey has been worth it.

Landon Barrowman is a University of Athabasca student of Psychology who has worked in the Alberta Oilsands for over a decade and now works as a peer perspective Cognitive Behaviour Coach. He is a loving father, musician, talk show host of the Midnight Tonight Show and Author of the Working Man’s Guide to Mental Health
By Ingrid Karmark

I consider myself to be active and relatively healthy. I am middle-aged and busy myself with tutoring online students who need lessons in Math and English. During my leisure time, I pride myself on being able to swim the breaststroke non-stop in a warm pool for an hour a week – perhaps two per cent of people can do this at my age, and it would also be a challenge for many younger people. I exercise by walking around the neighbourhood block with my husband every day. We eat a balanced diet, alternating our animal, fish and poultry types. I only drink a glass or two of sparkling wine on the weekend as a treat. I don’t smoke or vape.
I also attend screenings at my medical practice assiduously. Every three years, the British National Health Service invites women to attend mammograms to be screened for signs of breast cancer. I have never missed a screening. A couple of years ago, I received a letter informing me of the result of a negative test for abnormalities after my last due screening.
However, this Spring, I noticed a dimple in the lower part of my right breast. My first thought was that this was simply a natural part of the ageing process. After all, I was a postmenopausal woman. Initially, I told myself that changes in my breast shape could simply be a sign of ageing, couldn’t they? But then it occurred to me: why was the dimpling affecting only the right breast? I had seen a poster on a job centre toilet wall back in 2019 (where I had worked as a welfare advisor), which had a myriad of mini diagrams showing abnormalities of the breast as possible signs of cancer.
I decided that it was time to make an appointment with my doctor. I got a prompt date with her. At the surgery, on inspection, she could see the dimple for herself. Further, there was now tenderness in the affected area that had not been there before. She was sufficiently concerned to book an urgent cancer pathway appointment at the local Kent and Canterbury General Hospital. Within less than a fortnight, I was seen by a consultant who examined me thoroughly and told me that he suspected breast cancer. Secretly, I had been hoping that the lump that was now at the site of the dimpling was just a case of necrosis: a benign condition that can be caused by an injury. As someone who swims so vigorously, I tried to convince myself that it was likely caused by my numerous breast strokes. However, he booked another urgent appointment with a mammographer. Just over a week later, I was back at the same hospital. I had two scans – mammography and ultrasound. I spent a long time in the scanning rooms. The senior doctor asked me if she could insert titanium markers into me. I gave her my permission. At this point, I understood that these markers would guide a surgeon to identify and potentially help a surgeon remove the masses, which I had now seen for myself on her computer screen. The doctor had told me she suspected cancer from the mammograms, but the biopsy of some samples she had taken would prove conclusively. I asked her why I appeared to have cancer. She told me bluntly: “It’s because you are a woman.”
A fortnight later, I was seen by a breast surgeon, who confirmed the worst news of breast cancer. Within a few weeks, the same surgeon removed two masses from my right breast in a full mastectomy at Queen Elizabeth the Queen Mother Hospital in Margate, Kent. I was massively relieved to have had them removed so rapidly. In the weeks prior to the operation, the growth of the tumours had begun to feel painful, and I now needed painkillers to get through the days. I was given a private room at QEQM to recover overnight, which was unexpected and made the operation recovery more comfortable. Just a month later, I had to be given axillary lymphatic node clearance of the right armpit because the sentinel node biopsy done during the first operation had revealed a cancerous node. The highly experienced surgeon was right to carry out the axillary node clearance because metastatic cancer had been found near some of the eighteen lymph nodes he had removed.

I now await further treatment. I am currently being treated with radiotherapy in the right chest area. Given the high estrogen and progesterone receptivity of my cancer cells, I have also been given hormone blocker pills for ten years.
A gene-based Oncotype DX cancer genetics test has guided me and the medics on the benefit or not of chemotherapy prior to radiotherapy. In my case, it turned out that hormone blocking treatments (plus radiotherapy) alone are just as effective as chemotherapy in controlling and killing residual cancer cells.
During my recovery time, I have been doing some research on breast cancer and treatments. I found it most surprising that one type of breast cancer chemotherapy treatment – taxane - comes from the Pacific Yew tree bark. This tree grows in the forest of British Columbia. The properties of the bark enable it to kill cancer cells. If ingested, the untreated bark, needles and berries are toxic, yet when pharmaceutically formulated, they give hope and life to patients.
One in seven women will be like me in their lifetime: they will be diagnosed with breast cancer. It is one of the most common cancers. Men can get breast cancer too, but around one per cent will get this news. Bronwen Wallace, the Canadian poet and novelist, was also diagnosed with breast cancer and passed on in her forties in 1989.
My takeaway from the experience of my own cancer diagnosis is that we need annual mammograms for certain high-risk patients or for those who request them. It is possible that had I been due for an annual check at the beginning of this year or even last year, my cancer would have been less extensive and required fewer interventions. It seems to me that cancer detection runs up against the cost/benefit constraint of our healthcare service. Yet surely, it is also cost-effective to treat cancer patients at the earliest opportunity and improve survival rates with more frequent breast scans? I would urge everyone to check their breasts regularly; to not be afraid of contacting their doctor when they suspect there is something different going on with their body. Breast cancer is more easily treatable in its earliest stage. Vigilance can save lives.

Ingrid Karmark was born in Saskatchewan and now lives in England. She is a Modern Languages and Law graduate and is currently working as an online tutor while writing fiction and non-fiction articles in her spare time. She has had four pieces published in Folklore (Sask) magazine in the last two years. During the Covid pandemic, she worked as a welfare rights advisor (2019-22) for the public organization Citizens Advice and also had her articles published in its in-house magazine CAVE. She currently lives in the picturesque medieval town of Faversham with her husband and six parrots.

By Trinidy Kuchuk
Life in its smallest form has so many miracles, from the moment of conception to the pure joy of hearing the first cries of a brand-new baby being born. Elianna was born a beautiful baby girl weighing at 6 lbs 13oz in November 2019, everything that came with her birth was perfect, the doctors and staff smiling and marveling at her ten fingers, ten toes, and even the way she immediately put her hand to her cheek as she fell asleep, but life for her would soon become one of many specialist appointments, medical tests, and constant watch and wait results, tears, and questions.
On a camping trip when she was six months old, we noticed light brown spots developing on her body. Through the reference of a friend, it was time to have her assessed by her family doctor. The result is questionable NF1 or, in medical terms, Neurofibromatosis Type 1, a genetic disorder which causes tumours to grow on the nerves in the body. Finding a specialist to confirm became a task, from being called a Google mom, to being told to leave my worries at the door, there was nothing wrong with my daughter, I felt helpless. I returned to my family doctor, who looked around for a specialist who was willing to hear us out.
At a year old, we found a pediatric specialist willing to sit down with us. It was explained a diagnosis for NF1 would have to have a requirement of two

criteria out of six to be met: Café-au-lait spotting (The brown spots that were already present on her), freckling in the armpit or groin area, plexiform or fibroma neurofibromas (which are lumps that present on the skin), lisch nodules, and a immediate family history of it. Elianna presented three of the criteria: café-au-lait spots, freckling in her armpit, and lisch nodules. It was enough to send her for genetic testing to get a more positive result, but not enough to be confirmed until the results came back.
It was a long, gruelling wait, but the results had come in; Elianna was positive for NF1! A follow-up appointment would now be booked to explain the next steps. The next steps were explained to be many more appointments and specialist teams that would be all working together, Brain MRIs to check for tumours, Ophthalmology appointments to watch for sight issues and tumours that can grow on the optic nerve, Neurosurgeon appointments to watch for any changes that may take place, and genetic counselling to go over the what-ifs.
First was the genetics counselling, Elianna was a hit with all the specialists in the office, running around and baby-gabbing all her stories to any of the staff that would listen to her, she was definitely having the time of her life, as a mother about to hear the news of what to expect, I was not. We were sitting down in a desked office as a tall, younger man came in with his student
and sat down. Here comes the truth: Elianna was classified as a rarer form of NF1; her condition was not passed down by me or her father, but rather mutated on her own in the embryonic stages of my pregnancy. Her condition was listed as spontaneous Neurofibromatosis Type 1, not affecting every nerve, rather only some, but which nerves it could affect, only time could tell us, as the genetic testing could not. I sat and listened, almost numbing out the information he was giving to me, until he asked if I had any questions. What do you ask? What do you say? I had nothing. It was then that he recommended research, do as much as I could, because for the next 18 years, I would be learning more and more about what she would be going through, and sadly, the references from the medical teams were limited, as there was not a lot of knowledge regarding this disorder, which I learned quickly over time.
Everything seemed to be pretty calm and repetitive, jumping from one specialist to another, introducing Elianna and me, all the while Elianna catching the attention of all the doctors and nurses with her fun-loving spunk and affection. Until it felt like the world crashed down, the results of her first MRI were in. I will never forget the day I received the call. I was standing at my son’s school, waiting for him to get out, Elianna sleeping soundly in her car seat in the car. The call came from her pediatric specialist, “Elianna’s MRI results are in. Are you in a place where you can talk?” I wasn’t really, but I had hope there was nothing truly wrong, so of course I said “Yes”. They had found a mass, near her third ventricle, a brain tumour, and a team of doctors would be meeting to discuss what the next steps would be. In the meantime, an in-office appointment would be needed, she said. The feelings that went through me, I can’t even explain; the worst was that this was all during COVID. What more could the world throw?
It was later advised that the best option for her was a watch-and-wait approach, which allowed


them to continue monitoring her through blood work and yearly MRIs. I spent the next few weeks researching as much as I possibly could on NF1, malignant and benign tumours, about NF1 in itself, and about all the other tumours that could come from it. reaching a roadblock with nothing else to learn, I found myself needing to know more, I had become obsessed with learning about it, I reached out to a clinic, a non for profit foundation in the United States, who sent me more information and options to have Elianna come to their clinics, which I decided on against for the time being, I reached out to Facebook groups and other moms who were in the same situation, they became my teaching and my support, I even attended conference after conference online to gain information from doctors and from people suffering with NF1. Research and learning became my mission, so that when my daughter gets older, she will have answers.
Elianna is now five years old, her specialist appointments have moved from one year, to six months, to now three months. Her MRIs continued to show a growing mass that we watched and waited on, only recently learning it has resolved itself. She has begun to develop fibromas on her body and countless more café au lait spots and freckling. She has been continuously watched for her bone structure, ensuring that any bowing that is seen is immediately treated, and that her eyes continue to show no optic nerve gliomas. From head to toe, she is monitored by the countless specialists who, every day, are faced with the unknowns of NF1.

As Elianna’s mom, I frequently get told, “Looking at her, you cant even tell she is sick”, no, you cant, because she is not sick, she has a progressive disease that lies inside of her, waiting to decide what it will do, she is normal in every other way, she plays, she laughs, she is like every five year old rambunctious little girl, she even has the best of the best temper tantrums, but she has NF1.
She is a warrior and for her entire life will have people surrounding her, walking her on this path she will take, will it be easy for her, no! but she has a fight in her that is unstoppable. The worst part of this disease, is at anytime, it can sneak up on its victim, and change the whole form of its system, it can progress mildly, or it can change to severe, NF1 is unpredictable, and as of today, does not have a cure, but the foundations, the teams of doctors, the families who are faced with this everyday, like we are, fight, we fight for the hope of a cure, that one day, the tumors, both benign and malignant, will be managed, or cured, that those faced with this disease will be able to smile, knowing someone is “just that much closer to finding a cure”, and that the feeling of not being beautiful enough because of this disease, will finally diminish. This is Elianna’s Journey, and although it is just beginning, she will never be alone in it, because no matter what, we all fight together.

Trinidy Kuchuk is Elianna’s mom and lives in Edmonton, Alberta.
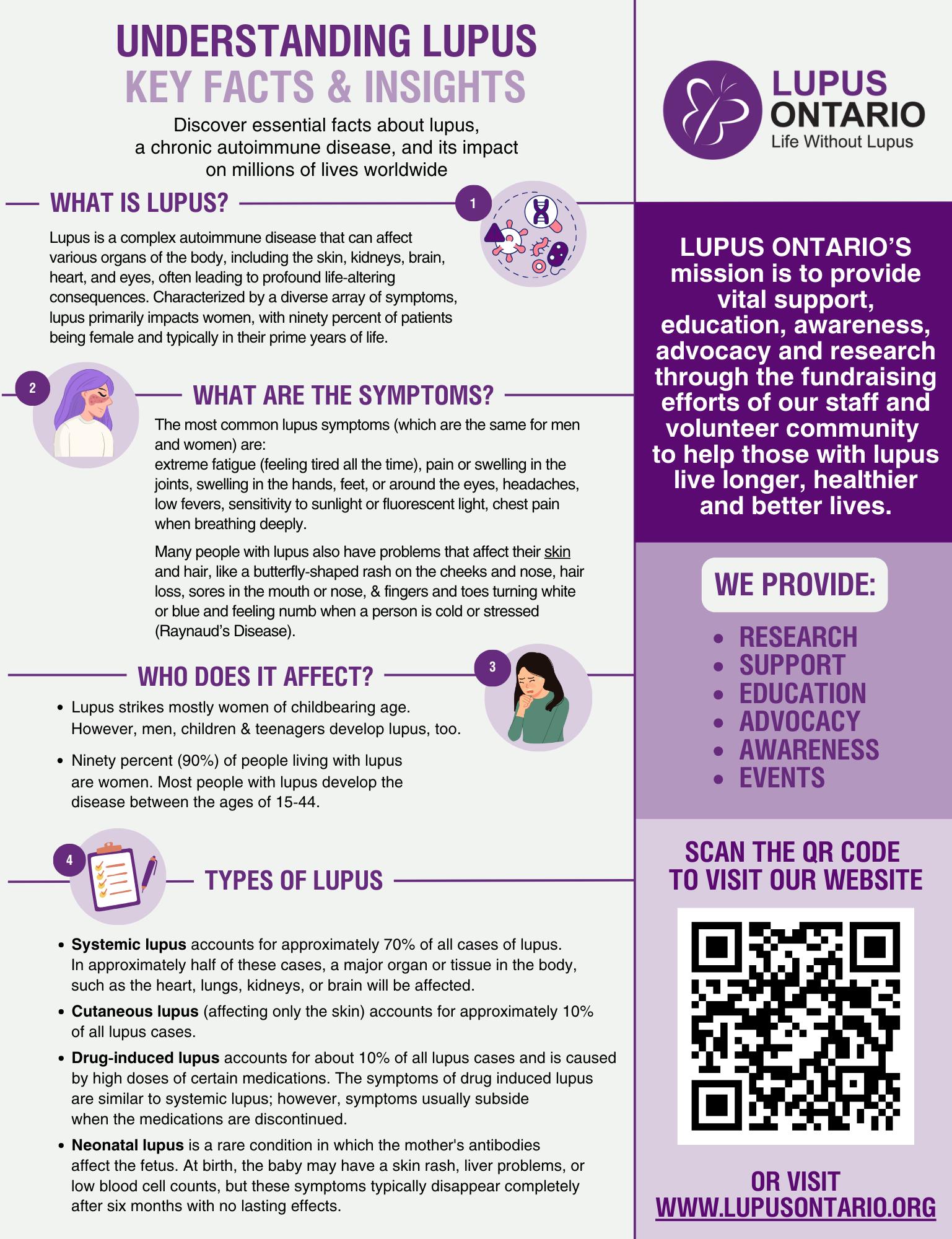

If you would like to share your story about your journey, as a patient, caregiver, or advocate, send us a short (150 words) description of your journey, for consideration in an upcoming issue!
Email your submission to: digitalmagazine@healcanada.org

By Alvina Nadeem
I have been distracted lately, finding it hard to focus. This happens to me every 3 months. It’s not some biological or seasonal phenomenon, but it has become that over the last 2 years. And today, just like I did 3 months ago, I will get the clarity I am seeking when I meet my oncologist for my last 3-month checkup. After today, it will be every 6 months for the next 3 years.
And honestly, it can be such an anxiety-producing thing, not the actual appointment, but the wait and anticipation that starts 2 weeks before the event.
When every little tick or tock inside my body feels like the “ticking” of a potential recurrence.
Where lower back pain turns into, “Is there a mass pressing on my insides again?”
It is a powerless feeling, and I could keep spiralling, but instead I decided to sit down last night and remind myself of my might.
And then, I was thinking about all the wonderful people I have met over the last few years: advocates, researchers, nurses, doctors, and ot working in different parts of the healthcare ecosystem. Some behind the scenes, some more vocally, and so I decided to remind us all of our might.
Enjoy the read! ❤️
Have you ever met a being so quiet and so powerful, And somehow unaware of what they carry?
They walk through the world looking for strength in stars, in stones, in anyone but themselves.
And yet…
They can command the air to move in ripples and waves, to send patterns of meaning across space, to shift another mind with nothing but breath …and call that power, speaking!
They can ignite storms in the silence of their minds, tiny flashes, one after another, turning questions into understanding, and ideas into change …and call that power, thinking!
They can take light that has travelled for millions of years, bend it through the lens of their eyes, and turn it into vision, story, beauty, truth …and call that power, seeing!
They can move matter, convince wood, stone, and steel to hold the shape of a spark, an idea, to make imagination solid …and call that power, building!
And still, somehow…they forget.
They forget how mighty they truly are.
So this is your reminder, Dear mighty being, reading this poem: What you call speech, is air rearranging itself to carry your intent. What you call thought, is electricity carving pathways through your mind. What you call sight, is light surrendering itself to be understood. What you call creating, is atoms moving where you asked them to go.
This may sound like metaphor, but really,
it’s just physics disguised as poetry.
You are already moving the world every time you think, see, build, or speak!
Own these powers. Use them with care.
Because you were never small, You just got used to your might. And forgot how powerful you really are.

Alvina Nadeem is a mechanical engineer, certified coach, and change management expert. With over 15 years of experience, she specializes in project and change management, delivering sustainable, inclusive solutions that address complex challenges across organizations, communities, and industries.
Certified in EQ-i 2.0/EQ 360 and ProSci Change Management, Alvina combines technical expertise, emotional intelligence, and coaching to guide organizations through transformation. She integrates a systems-focused engineering background with a deep understanding of human dynamics, ensuring that solutions are both technically sound and people-centered.
Following her ovarian cancer diagnosis in 2023, Alvina shifted her focus toward healthcare transformation, patient engagement, and system efficiencies.
Your Voice, Your Power: Help Shape the Future of Patient Care
Take 10 minutes to complete the Heal Canada & My Blood My Health Patient Surveys—because your experience matters in driving real change.
Visit our website at: https://www.healcanada.org/survey
Check often as more surveys are being added!
The following Quality of Life Survey’s are currently open and eagerly seeking respondents.
Take some time to complete them if you’re eligible!



Here, we explore the many facets of well-being, from nourishing your body with wholesome nutrition to rejuvenating your mind through meditation and mindfulness. You’ll find practical advice on exercise, mental health, and preventive care, all tailored to fit into your busy lifestyle.
But “Living Well” is more than just a guide; it’s a community. We encourage you to engage with us, share your journeys, and learn from others who are on similar paths. Whether you’re taking the first steps towards a healthier you or are further along your journey, we’re here to support and inspire you at every turn.
“Living Well” will provide topics that matter the most to your health and happiness. Let’s celebrate the joy of living well together!
By Alice Funk

Let’s be real: the words “goal setting” can sound a little… stiff or corporate. Like something a boss talks about at a Monday meeting while clicking through too many PowerPoint slides. But goals aren’t just for corporate types or hyper-productive morning people with colorcoded planners.
Goals are for you. Yes, you — even if you’re juggling work, family, brain fog, and a body that sometimes feels like it has a mind of its own.
In fact, if you live with chronic pain/illness, setting good goals might be one of the most powerful tools you can use to feel a little more in control, a little less overwhelmed, and a lot more proud of yourself.
This article is all about why goals matter, how to make them SMART (and not stressful), and some practical tips for getting started without burning yourself out.
Let’s face it, life has enough chaos without adding more to your plate. But that’s exactly why goal setting works — it brings some order to the chaos.
Goals
(a.k.a. “Where am I going again?”)
Without goals, life can feel like driving without GPS: you end up somewhere, but not necessarily where you wanted to go. Goals act like a friendly voice saying, “Turn left here!” (But unlike GPS, they don’t yell at you if you miss the turn — you just re-route.)
Ever cross something off a to-do list and immediately feel like a rockstar? That’s dopamine at work — your brain’s way of throwing a mini-party. When you hit small goals, you get that same boost, which makes you want to keep going. Just remember – actions become motivation!
When you have chronic pain/illness, it’s easy to feel like life is one big “to be determined” or “I don’t know.” Goals give you proof that you can follow through — even if it’s something as simple as “Do gentle stretches today” or “practice breathing techniques.”
Let’s be honest: some days, just taking a shower or even getting dressed feels like an Olympic event! Goals help you notice those victories instead of brushing them off. And yes, you deserve gold medals for everyday stuff too.
Ever make a goal like “I’ll get healthier this year” and then, months later, you have no idea what that even meant or how you were going to achieve it? Yeah, so do 90% of other people who made New Year’s resolutions. That’s where SMART goals come in.
SMART is just a fancy acronym that stands for:
• Specific – Get clear. What exactly are you trying to do?
• Measurable – How will you know you did it?
• Achievable – Can you actually do it without needing superpowers?
• Relevant – Does it actually matter to you right now?
• Time-bound – When will you get it done?
Here’s a quick example:
• Vague goal: “I want to be more active.”
• SMART goal: “I will walk (or dance in my kitchen) for 10 minutes, three times a week, for the next two weeks.”
See the difference? One is wishful thinking. The other is a plan you can actually check off — and maybe even have a little fun with. TIP: Actually having something to physically “check off,” like a weekly calendar, is helpful as it’s a visual of what you are doing and have done.
Here’s the good news: you don’t need a fancy planner or all the answers to start setting goals. Here’s a super simple process:
Step 1: Pause and Check In
Before you write anything down, take a minute to ask:
• How am I feeling physically?
• What matters to me this week?
• Do I have the energy for something big, or do I need to keep it tiny?
Step 2: Brain Dump
Write down all the things you want to do. Big things, small things, fun things, boring things. Don’t edit — just get them out of your head and onto paper. Also, doesn’t matter how outrageous they are either. Skydiving? Write it down. Clip your toenails? Write it down.
Step 3: Pick One to Three Goals
Resist the urge to go wild here. Too many goals = overwhelm. Ask yourself: “If I only got ONE thing done this week, what would make me feel proud and/or accomplished?”
Step 4: Make Them SMART
Run each goal through the SMART test. If it feels too big, shrink it down. Instead of “clean the house,” try “tidy one drawer.” Instead of “run a marathon,” try “walk to the mailbox.” (Unless you actually want to run a marathon — then, by all means, go get it!).
Goals are the end game, the actions you do, and practice consistently are what help you reach those goals. You can’t eat a Big Mac in one mouthful; you have to take smaller bites in order to finish it.
Step
This step is key for people with chronic pain/illness: plan for flare-ups.
• Plan A: The original goal.
• Plan B: The “bad pain day” version.
• Plan C: The “I just can’t today, but I still want to feel accomplished” option. Example:
• Plan A: Walk 10 minutes outside.
• Plan B: Do gentle chair stretches for 5 minutes.
• Plan C: Take three deep breaths and wiggle toes. (Yes, that counts!)
Step 6: Track and Celebrate
Put your goals somewhere visible — fridge, journal, phone app. And when you complete one, celebrate! Text a friend, dance it out, or give yourself a dramatic slow clap. You can even assign a reward to accomplishing a goal – a piece of your favorite dessert, a new book, etc.
Chronic pain/illness can make life feel like you’re constantly playing catch-up. Plans get cancelled, energy disappears, and you might even start to feel like you’ve lost a piece of yourself. Goals help change that narrative. You define YOU, not your illness!
Even if pain controls some parts of your life, goals remind you that you still get to decide what you focus on. You get to steer the wheels where you want to go!
Think of your energy as a limited phone battery. Goals help you spend that battery on what actually matters instead of letting notifications (and other people’s demands) drain you. Boundaries can also play a big role in this, as well as learning to say “No” when needed. If you say “No” to something, that means you get to say “Yes” to something else, and the reverse is true as well. All about priorities and not spreading yourself out thin!
Instead of staring at a messy room and feeling defeated, you can break it down: “Today I’ll just clear the nightstand.” Little goals are like those tiny scrubbing bubbles on the cleaning commercial — they save the day one small area at a time.
Chronic pain/illness can make you feel stuck. Goals give you something to look forward to and celebrate, which is a big deal when every day feels the same. Mark your calendar with a variety of celebrations – birthdays, holidays, upcoming sales at your favorite store, even your cat/dog’s grooming day – anything counts!
Each one is clear, realistic, and gives you a little dopamine hit when you check it off.
• Be Kind to Yourself: Goals aren’t a pass/fail test. Adjust them if needed. Change them up – they are not written in stone. These are YOUR goals, not someone else’s.
• Stack Goals: Tie new goals to existing habits — e.g., stretch after brushing teeth.
• Use Reminders: Phone alarms, sticky notes, or even a friend who texts “Did you do your thing yet?”
• Reward Yourself: Celebrate effort, not just results. Even a halfway-done goal is progress.
• Reflect Often: Each week, ask what worked and what didn’t. Tweak for next time.
Once you get comfortable with small goals, you can zoom out and start setting bigger ones — like going back to work, trying a new hobby, or planning a trip. SMART goals give you stepping stones instead of asking you to cross the whole river at one time.
Goal setting doesn’t have to be scary, boring, or reserved for overachievers. It’s really about designing a life that feels doable — and even joyful — one small step at a time.
So, grab a pen, write down one small goal, and start there. Whether it’s stretching, drinking water, or finally watching that show everyone’s been talking about, celebrate it when you do it.
Because life with chronic pain/illness can be tough — but with a few well-placed goals, you can make room for more wins, more laughter, and more days where you get to say, “Yep, I did that.”
I have included an easy “Plan A, B, C” Pain-Day Planner sheet for you to download to use. Have fun with it and remember to CELEBRATE all the wins, no matter how small or big they are!

Alice Funk is a Mental Fitness Mindset Coach from Sturgeon County, Alberta, who loves to encourage and guide others to be their true selves and reach their goals. Her own journey and experiences have taught her that learning to know yourself and what you need is the mightiest step to take (and sometimes the scariest one as well).
The first step on your new path is finding you! If you would like to chat with Alice, please contact her at info@newpathsolution.com or book a FREE Connection Session!
Because some days are “crush it” days, some are “crawl through it” days — and you deserve a plan for both.
STEP 1: PICK YOUR FOCUS
What do you want to work on this week? (Choose one area: movement, self-care, connection, home project, etc.)
My focus area:
STEP 2: CREATE YOUR PLANS
Plan A: “Feeling Pretty Good”
Your ideal plan for when you have a good energy day. What I’ll do:
When:
How long:
Example: Go for a 10-minute walk outside after breakfast.
Plan B: “Meh, But Manageable”
Your modified plan for a medium day - make it shorter, easier, or lighter. What I’ll do:
When:
How long:
Example: Do 5 minutes of chair stretches instead.
Plan C: “Today is Rough”
Your bare-minimum plan for when pain or fatigue is at its worst — but you still want to do something. What I’ll do:
When:
How long:
Example: Take 3 slow breaths and wiggle my toes in bed.
CELEBRATE!
After you do ANY of these (A, B, or C), check it off and do a tiny happy dance. (Even if it’s in your head.)
Notes / Wins
“Something is always better than nothing.”

By Dr. Christopher Labos
You wouldn’t normally think there was much overlap between cholesterol denialism and antivaccination rhetoric. But there is. Statin skeptics frequently claim Covid-19 vaccines killed thousands, a view unsupported by science. But the interesting thing is, cholesterol denialism wasn’t always a pseudoscience.
Cholesterol holds a special place in the popular imagination that sets it apart from the many other cardiac risk factors we talk about. Nobody thinks diabetes is good for you, and nobody dismisses the dangers of high blood pressure. Nobody today is under the delusion that smoking is harmless or that our increasingly sedentary lifestyle is serving us well. But cholesterol remains a source of doubt for many in the media, the general public and, sadly, amongst physicians too.
While it is easy to pour scorn on this position, not that long ago, it was actually somewhat justifiable. In September 1989, The Atlantic’s cover proclaimed: “The Cholesterol Myth: lowering your cholesterol is next to impossible with diet, and often dangerous with drugs – and
it won’t make you live longer.” And they weren’t actually wrong.
The cholesterol controversy can be summarized in broad strokes. It began in 1913, when Nikolai Anitschkow fed rabbits purified cholesterol and demonstrated that they developed atherosclerosis. Although seemingly definitive, his findings drew criticism because they couldn’t be replicated in other animals like rats and dogs. We now know species handle cholesterol differently, but at the time, it was dismissed as a rabbit-specific quirk, irrelevant to human health. What’s true in animals is not necessarily true in humans.
In retrospect, the dietary studies weren’t outright failures. Many did lower cholesterol, and some did reduce cardiovascular events. But their modest, inconsistent benefits fueled skepticism. Hopes then shifted to the new cholesterol medications. The 1970s and 1980s saw the publication of studies on clofibrate and cholestyramine. The biggest of these, the Coronary Primary Prevention Trial, was in some ways definitive. There was a significant
reduction in cholesterol, which translated into a significant reduction in cardiovascular events.
The story could have ended there, but caveats remained. Cholestyramine caused many side effects and, while it reduced events, it didn’t lower mortality. Some argued there was little point in treatment if it didn’t help people live longer, a view many shared at the time.
We reach the 1989 Atlantic cover declaring: “Lowering your cholesterol is next to impossible with diet, and often dangerous with drugs – and it won’t make you live longer.” Technically true, it marked a turning point. Early drugs were ineffective by today’s standards, but history shows cholesterol clearly played a role in atherosclerosis: whenever it dropped significantly, heart attacks declined. The problem was simply a lack of the tools to make a major dent in people’s serum lipid profiles.
As long as statins were the only useful cholesterol medications available, you could maybe convince yourself the benefits were unique to that drug class. But they aren’t the only medication out there anymore. The development of ezetimibe (which blocks cholesterol absorption in the intestine) and PCSK9 inhibitors (which act on the cholesterol receptor in cells) has made that argument unsustainable.
The striking thing about cholesterol medications is their linear benefit: If you plot out all the studies of cholesterol medications (both statin and non-statin treatments), they fall along a very straight line. The more they lower cholesterol, the greater the cardiovascular protection. Diet helps a little, while newer PCSK9 injectables cut risk dramatically. Statins aren’t special; it’s the degree of cholesterol reduction that matters.
“The ‘lipid hypothesis’ is no longer a hypothesis; cholesterol’s role in heart disease is clear. ”
In the 1990s, everything changed with statins. The 4S study showed simvastatin lowered cholesterol, cut heart attacks, and reduced both cardiovascular and all-cause mortality. Twenty-six randomized studies later, it became clear that statins did what they promised. They reduced cholesterol and prevented cardiovascular disease. But the deniers still had one last redoubt. Maybe it wasn’t about cholesterol. After all, previous cholesterol trials had been disappointing. Maybe there was something special about statins, and they prevented heart disease via a mechanism independent of cholesterol. Had you been alive at the time, you might have said the same. I was, and I did.
You will hear people argue that statins are too expensive, that the benefits are too marginal in a generally low-risk population, or that they don’t want to endure the side effects. It’s worth pointing out that statins are now off-patent, and no pharmaceutical company is lobbying for their use. The benefits of statins are inherently higher in high-risk populations and lower in low-risk ones. All medications work this way. But even in patients without cardiovascular disease, there is a cardiovascular benefit. It just isn’t as marked as what you see in patients who have a history of heart attack or stroke.
As for the side effects, they are overrepresented in the media, and many of the subjective symptoms people suffer are due to

the nocebo response. What’s more, anyone who doesn’t want to use statins to lower cholesterol is free to use any of the newer (albeit more expensive) cholesterol medications on the market now. Just don’t think you can get away with natural therapies like fish oil, cinnamon, garlic, turmeric, or red yeast. These have been tested head-to-head against rosuvastatin, and the statin came out on top.
You can argue that there are better ways to measure cholesterol beyond the simple characterization of good (HDL) cholesterol versus bad (LDL) cholesterol. You can argue that, in low-risk populations, the cost of therapy outweighs the benefit. You can argue that we should be doing more to encourage lifestyle change and healthy eating habits, especially among children. All of these are interesting arguments, but they are questions of policy, not science.
A lot of the anti-cholesterol talking points were valid arguments decades ago. It was once valid to argue that Betamax was better than VHS. Had you been alive at the time, you might have said the same. But if you bring that up now, you would no longer be relevant.
The “lipid hypothesis” is no longer a hypothesis;
cholesterol’s role in heart disease is clear. To deny it is to ignore evidence and repeat outdated arguments, which is how cholesterol denialism slid into pseudoscience.
This article is reprinted with the kind permission of Dr. Christopher Labos and the publication The Skeptic. To view the original article in its entirety, please visit https://www.skeptic.org.uk/2024/02/ how-cholesterol-denialism-went-from-reasonable-skepticism-to-pseudoscience/
Dr. Christopher Labos is a cardiologist with a master’s degree in Epidemiology. He is a columnist with The Montreal Gazette and Medscape, featured on the Sunday Morning House Call on CJAD radio, and has a regular TV segment on CTV Montreal and CBC’s Morning Live
He is an associate with the McGill Office of Science and Society and co-hosts the award-winning podcast The Body of Evidence. He is the author of Does Coffee Cause Cancer? published by ECW Press, a book about food epidemiology and why food headlines are often misleading.

By Sue Lemoine Plus Recipes!
One of the most common reasons people give me for skipping healthy meals or exercise is: “I just don’t have the time.”
And I get it. Life is busy. Between work, family, and everything else on your plate, it can feel almost impossible to prioritize your health. But here’s the truth: the people you see glowing with energy, the ones who seem to “have it all together” with their nutrition and lifestyle? They don’t have extra hours in the day that you don’t. They’ve simply learned how to make health a priority—and you can too.
The good news is that eating well doesn’t have to be complicated or time-consuming. With a few simple tweaks and some planning, you can nourish your body and feel amazing, even on your busiest days.
Here are 5 simple, doable tips for eating smart when life is moving fast.
When life gets busy, preparation is your secret weapon. Think of it as setting your future self up for success.
It takes the same amount of time to peel a banana or grab a hard-boiled egg as it does to unwrap a pastry from the vending machine. The only difference? The vending machine is always ready and waiting. That’s why your job is to make sure healthy options are just as convenient.
A quick weekend grocery shop can make all the difference. Stock up on easy staples—rotisserie chicken, pre-washed veggies, eggs, fruit, nuts . . . and you’ll always have the makings of a simple, nourishing meal on hand. A little prep time now saves stress (and regret) later.
Most of us rotate through the same handful of meals anyway. Why not make yours healthy and effortless?
Think of your “go-to meals” as your personal toolbox for busy days. Maybe it’s overnight oats with fruit, a smoothie, or a quinoa and veggie scramble. Once you have a few favorites that you can make quickly (even when you’re tired), eating well feels automatic.
Spending a little time on Sunday to plan these out sets you up for an entire week of healthier choices—and saves time, money, and energy in the process.
Eating on the go doesn’t have to mean drive-thru food. Pack your own healthy lunch or snacks, and suddenly you’re in control of what fuels your body.
Invest in a cooler bag, a stylish lunch tote, or even a car-friendly hot pot. Old-school Thermoses are lifesavers too. Having your own prepared food means you’ll cruise right past the fast-food temptation at 3:00 pm and head into the afternoon with steady energy instead of a sugar crash.


Even with the best planning, sometimes you end up eating out. The key? Learn how to navigate menus with confidence.
Most restaurants now offer lighter options, and if they don’t, don’t hesitate to ask for what you need. Remember: you’re the customer. You can absolutely request grilled protein, extra veggies, or dressing on the side.
Don’t be afraid to Google the restaurant’s menu ahead of time so you can walk in already knowing your healthiest picks.
Here’s the most important tip: release the idea of perfection. Healthy living isn’t about never having dessert or always packing the perfect lunch. It’s about consistency, balance, and selfkindness.
If you miss a day of planning or end up grabbing something less than ideal, it’s not failure—it’s just life. Simply refocus at your next meal. Over time, these small, consistent choices add up to lasting change.
Your health is one of your greatest treasures. With a little preparation and a few go-to strategies, you can absolutely eat well—even in the busiest seasons of life.
I like to keep a bag of nuts in my bag at all times because when I get hungry, eating a few nuts will keep the hunger at bay until I can eat my next meal. This means I stay prepared, and that one small tweak keeps me balanced, fueled, and feeling like my best self.
And you deserve to feel like your best self too.
Want more support in building healthy habits that fit your busy life? I’d love to help! Email me at sue@flourish-nutrition.ca, and let’s make clean eating effortless for you.

Sue Lemoine, RNHP
Holistic Nutrition & Lifestyle Coach Menopause Coaching Specialist Certification
A Holistic Health and Wellness Practitioner based in Edmonton, supporting women around the globe through the transitions of perimenopause and menopause. With a deep belief that this stage of life can be one of power, clarity, and joy, Sue helps her clients naturally balance their hormones through personalized nutrition and lifestyle strategies. Her programs gently guide women back to vitality, reducing symptoms, restoring confidence, and reigniting their spark.
If you’re navigating the challenges of perimenopause or menopause and are ready to feel like yourself again, reach out for a complimentary consultation: sue@flourish-nutrition.ca | flourish-nutrition.ca
Grab a copy of my complimentary Perimenopause Weightloss Blueprint


MAKES 5 SERVINGS
INGREDIENTS:

1 cup raw almonds
1 cup walnuts or cashews
½ cup pumpkin seeds (pepitas)
½ cup unsweetened dried cranberries or cherries
½ cup dark chocolate chips (70% or higher)
Mix everything together in a large bowl.
Divide into five small reusable snack bags or containers. Keep one in your purse, car, or desk for a quick grab when hunger strikes.
Healthy fats and protein from nuts keep blood sugar stable, pumpkin seeds add magnesium for stress support, and a little dark chocolate satisfies the sweet craving while providing antioxidants.
MAKES 4 SERVINGS
INGREDIENTS:
• 4 whole-grain tortillas or wraps
• 1 cup hummus (store-bought or homemade)
• 1 cucumber, cut into thin sticks
• 1 red bell pepper, sliced into strips
• 1 carrot, julienned
INSTRUCTIONS:
1. Spread ¼ cup hummus on each tortilla.
2. Lay cucumber, pepper, and carrot sticks across the middle.
3. Roll up tightly, then slice into 4–5 bite-sized rounds.
4. Store in a sealed container for up to 2 days.
WHY IT WORKS: Fiber-rich veggies + protein-packed hummus = a satisfying snack that travels well and helps curb cravings. The colour alone makes it feel like you’re treating yourself, not depriving yourself.

INGREDIENTS:
• 2 cups rolled oats
• 1 cup unsweetened applesauce
• 1 scoop vanilla protein powder
• 1 tsp cinnamon
• ¼ cup raisins or chopped dates
INSTRUCTIONS:
1. Preheat oven to 350°F (175°C).


2. Mix oats, applesauce, protein powder, cinnamon, and raisins in a bowl until combined
3. Drop spoonfuls onto a lined baking sheet and flatten slightly.
4. Bake for 12–15 minutes, until firm.
5. Cool completely, then store in an airtight container.
WHY IT WORKS: These soft cookies feel like comfort food but are packed with protein and fiber.Perfect for tossing in a bag before work or school pickup.
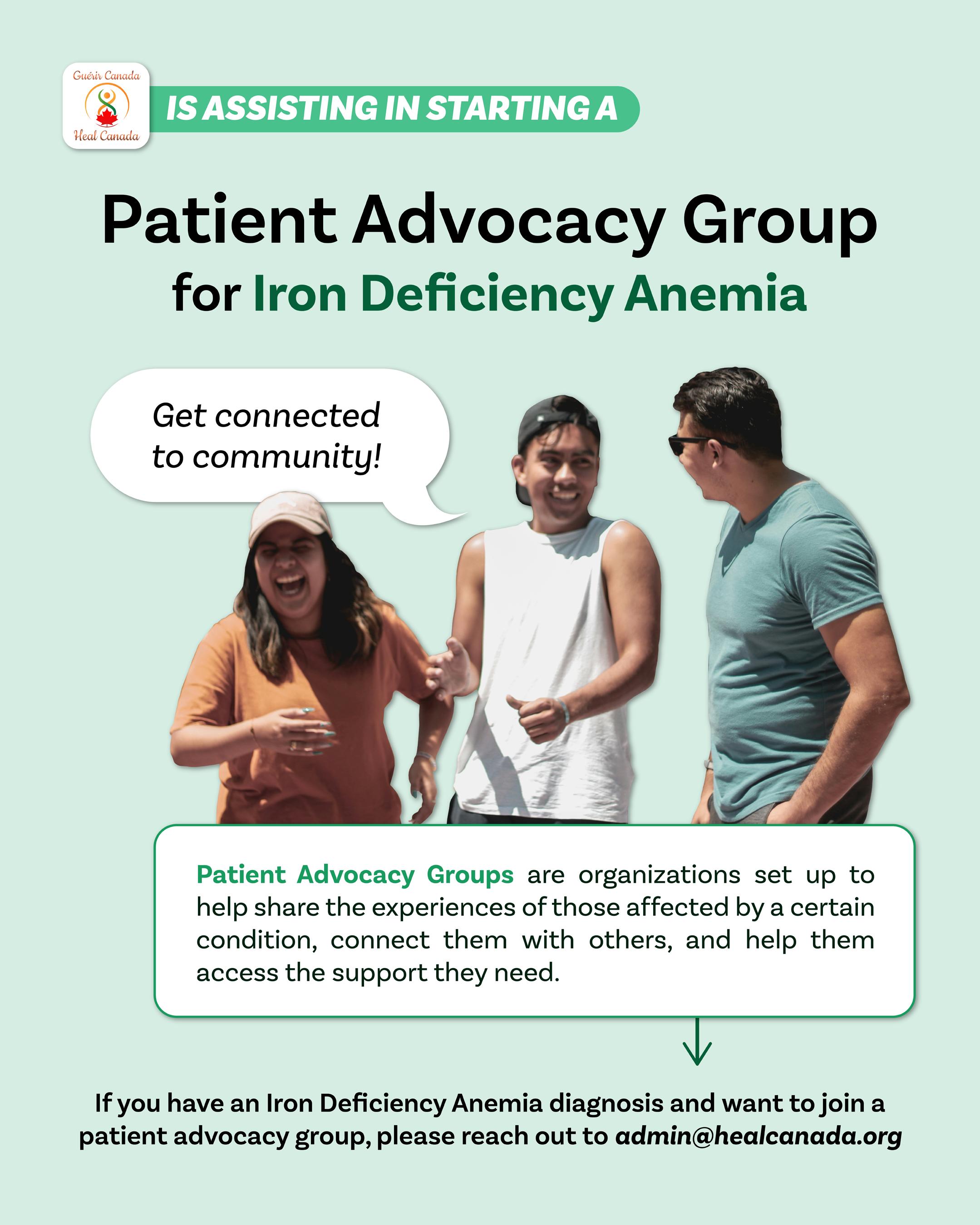

In our pursuit to empower patients and their advocates with knowledge, this section bridges the gap between medical professionals and our readers, offering clear, accurate, and practical answers to your most pressing questions. Whether you’re navigating the complexities of clinical trials, seeking advice on managing chronic conditions, or exploring the latest in wellness trends, our experts are here to provide you with insights grounded in the latest research and clinical experience.
Let’s embark on this journey of understanding together, fostering a community where informed decisions lead to better health outcomes.
By Maureen Carpenter
The purpose of clinical trials is to gather data to support or debunk the intervention being studied. Improved health outcomes through clinical trials can include drugs, vaccines, surgical or radiological procedures, devices, preventive care and psychotherapies, to name a few. Clinical trials are crucial, ultimately, in enhancing patient outcomes. Some trials are used to help in the early diagnosis of a disease before symptoms occur.
The history of clinical trials goes back further than expected. Evidence of the world’s first clinical trial can be found in the Bible in the ‘Book of Daniel’. King Nebuchadnezzar was a military leader who had ordered his people to only eat meat and drink water to improve their health. A group of young royals didn’t follow orders and consumed a diet of beans and water. After ten days, the young royals reported feeling better and stronger than the meat and water diet group.
In 1747, a Scottish doctor with the Navy tested diet supplements to help combat scurvy. Sailors would be at sea for prolonged periods of time, and many would become stricken with rotting gums and open sores in the skin, causing them to become bedridden. This often would lead to death.
The doctor’s idea was to prevent the disease with acids. A group of twelve sailors was broken up into pairs. All six pairs were given
different dietary supplements in addition to the core diet. Some were given cider, or vinegar, or seawater. One duo received two oranges and a lemon as their diet supplement. This pair showed sudden and visible improvements in the symptoms they were exhibiting that indicated scurvy. The study was well documented and resulted in the discovery of the cause of scurvy and a treatment/prevention. Sailors were then managed with lime juice as a dietary aid in scurvy prevention.
With clinical trials comes the importance of informed consent. The result of the War Crimes trial, after the Second World War, was the Nuremberg Code. The significance of this was in direct reflection of the reported and documented experiments carried out by doctors on concentration camp prisoners. The Geneva Conventions of 1949 included this code explicitly. Countries throughout the world have their own Federal laws and codes that protect patients during clinical trials, with the baseline thread being the informed consent and ethical treatment of the human patient. Throughout the years since the initial writing of the code, there have been adaptations for technology and changes in federal laws regarding research on human beings. Those unable to provide informed consent, like children and other populations, are now part of the ethical research considerations.
Positive outcomes have occurred due to clinical trials. Immunotherapy drug trials have helped those with lung cancer live longer. This therapy targets the immune system in creating a means for the body’s own defences to attack the cancer cells. Kidney transplant medicine has shown the benefits of receiving an organ from a live donor, regardless of being a perfect match. Clinical trials have helped advance the technology of vaccines. While immunization agents help to reduce or eliminate diseases, people need to be open to receiving a vaccine or series to help prevent outbreaks, as in measles or polio. The development through clinical trials of a myeloma therapy that prolongs a patient’s life in a cancer that currently cannot be cured is another example of positive outcomes.
Artificial Intelligence (AI) and other technologies have been enlisted to aid in the design of clinical trials. Digital technology can help reduce the cost and complexity of current clinical trials. The traditional approach to clinical trials required the patient to be in direct or closer proximity to the research group or facility. Now with virtual capabilities, trials can be successful in recruitment and retention of participants via email, texting, and social media. Data collection is being investigated in the use of smartphones or other mobile devices.
AI has been successful in acquiring data and interpreting it to lead to diagnosis and treatment in certain fields. Some success has been found in the decision-making aspect in pediatric cataract cases. The antibiotic dosing for septic patients and management of hypotension in intraoperative patients has also been a win for AI system applications.
Worldwide, the top three clinical trial areas are Cancer Research, Mental Health and Behaviours, and Nervos System diseases. The largest clinical trial to date was in 1954, the field application of the Polio vaccine. Many countries have online lists of their current clinical trials
that can be accessed online via clinicaltrials. gov.
Where would we be without clinical trials and research? At one time, the treatment for mental health issues was to drill holes in the skull to release the ‘evil spirits.’ Milk was thought to be a cure for cholera via transfusion. Cholera had other horrific treatments, one being the use of boiling tobacco-infused enemas. Smallpox would still be a deadly disease without vaccine clinical trials. Many of the most effective treatments today would not be possible without clinical trials. Chemotherapy, cholesterolreducing medications, vaccines, and cognitive behavioural therapy have advanced and saved or improved lives as a direct result of clinical trials.
1. www.nih.gov
2. www.hopkinsmedicine.org/research/ understanding-clinical-trial
3. www.nia.nih.gov/health/clinical-trials-andstudies
4. www.definitivehc.com
5. clinicaltrials.gov
6. Rosa C, Marsch LA, Winstanley EL, Brunner M, Campbell ANC. Using digital technologies in clinical trials: Current and future applications. Contemp Clin Trials. 2021 Jan

Maureen Carpenter is a a BSC RN in Alberta. She has worked as an ICU/Emerg. Nurse in Edmonton, Medivac/Flight Nurse, in the NWT and currently works for the Dept. of National Defense in a Nursing Role. Maureen previously served our country in the Canadian Air Force and NATO operations.

The International Consortium for Health Outcomes Measurement (ICHOM) is a global organization dedicated to transforming healthcare systems by defining, measuring, and reporting outcomes that truly matter to patients. By creating standardized sets of outcome measures across medical conditions, ICHOM empowers healthcare providers, policymakers, and researchers to improve care quality, efficiency, and transparency. At its core, ICHOM’s mission is to ensure that patients are not just recipients of care, but active partners in shaping what highvalue healthcare looks like.
Engaging patients and patient advocates as active members of the ICHOM Patient Partner Alliance is essential to ensuring that healthcare outcomes truly reflect what matters most to those receiving care. Their lived experiences and perspectives help define meaningful measures, such as quality of life, functional recovery, and emotional well-being, that go beyond traditional clinical indicators. By joining the Alliance, patients and advocates contribute their voices to a global movement for more transparent, equitable, and person-centered healthcare, helping to shape a future where every health system measures success through the eyes of the patient.
Find out more at ICHOM Patient Partner Alliance




Patients, caregivers, patients organizations, healthcare professionals and other stakeholders, we want to help you.
Reach out to share your story, connect with our allied organizations, and explore ongoing clinical trials.
NEED INFORMATION AND SUPPORT?
Visit our website for resources that can assist you as a care partner for patients with their diagnoses, treatments and a better quality of life. www.healcanada.org
WANT TO SHARE YOUR STORY?
If you would like to share your story about your journey, send us a short description of your journey for consideration. | digitalmagazine@healcanada.org
Send your coordinates to Heal Canada and be part of our registry, so patients and their care partners can find you!
HEAL CANADA CAN ASSIST YOUR PATIENT ORGANIZATION:
• Increase awareness
• Fundraising
• Improve your understanding of the Canadian Healthcare system Supporting your submission to CDA (CADTH) and INESSS admin@healcanada.org | www.healcanada.org
If you would like to share your expertise with our reader. Send us a short description of your proposal for consideration. | digitalmagazine@healcanada.org
NEED INFORMATION AND SUPPORT?
Visit our website for resources needed to help you work with advocacy groups. | www.healcanada.org












































is a multifaceted professional whose career spans patient advocacy, business, and post-secondary education, showcasing her dedication to significantly impacting these areas.
Family circumstances drove her transition into patient advocacy During the last 15 years, she has worked tirelessly to bridge the gap between the healthcare system, patients, and pharma stakeholders. Her empathetic approach and dedication to advocacy have made her a respected figure in this field. She lobbies for a healthcare system based on patient- centricity. She supports other patient organizations in becoming better advocates by leading Heal Canada and CACHEducation. Cheryl has recently achieved her greenbelt in VBHC, and is in pursuit of her DBA.
is the Program Manager at Heal Canada. Wendy holds a B.A. and a Diploma in Human Relations and Family Life Education from McGill University. She is certified in foot reflexology.
Throughout her career, she has showcased her insightful perspectives through her writings, which have appeared in publications such as The Montreal Gazette and Ottawa’s Globe and Mail. She has also contributed to specialized platforms like Booming Encore and Refresh Reflexology Magazine, demonstrating her versatility in addressing diverse audiences. Her unique observation on the initial days of the pandemic lockdown is captured in the anthology Chronicling the Days: Dispatches from the Pandemic, published by Guernica Editions in the spring of 2021.
is the Administrative Coordinator at Heal Canada. Anna holds a B.A. in Management of Organizations and Business Administration.
Throughout her career, Anna has brought clarity to complex business challenges by leveraging data. With over six years of experience in data analysis and operations, she has held key analyst roles at different companies. Her expertise spans reporting, process optimization, and strategic insight generation, supporting decision-making across departments and international teams. Now, she continues to apply her skills to improve performance and efficiency of Heal Canada.

OCTOBER 2025 | Issue 10
Navigating Insurance and Coverage
Remember to check out our issue of our other magazine, My Blood, My Health, coming out in a few month!