Technology • Understanding the visual impact of the Stiles-Crawford effect • The importance of poroelasticity in soft contact lenses



Modern modalities require boundless imagination and limitless capabilities. Designed to support the requirements of scleral and ortho-k lens designs, Optimum Infinite’s unique properties offer you the opportunity to push the boundaries of speciality lens design.




32021 (88) ISSN:1386 0194
Fitting Background • Context in contacts Special Topic • New challenges in intra-ocular lens metrology Interview • Lynette Johns NOW AVAILABLE AT YOUR APP STORE Eyepress Fachmedien GmbH Saarner Str. 151, 45479 Mülheim a. d. Ruhr
Hyper Dk Tailored Modulus Inherently Wettable
optimum-infinite.com



Sustainability
The major issues of these times continue to be the corona crisis, the difficulties around global trade and production against a background of sustainability. The optical and contact lens industries are affected differently.
Let's focus on sustainability: Environmental protection is not always easy. Filtering contaminated water leaves a lot of waste that ends up being discharged more-or-less adequately, or at best recycled. Avoiding domestic air travel sometimes costs companies more in employee time and money than traveling by train. Electric cars may save CO2, but battery cell production requires a lot of energy and extraction of the raw materials required is associated with environmental and social problems. The list of such environmental dilemmas is endless.
Often it all comes down to choosing between the lesser of two evils: either in favor of the least harmful raw materials or the comparatively more environmentally friendly process. Does this all lead to nowhere and could we save ourselves the trouble? No! Experts believe that the next ten years will determine what the next 10,000 years will be like for our civilization. Thus there is no excuse for delay! All countermeasures, no matter how trivial they may seem, are important because they all add up in the end.
According to Statista, industry worldwide is responsible for 19% of all greenhouse gas emissions, and transportation for another 25%. The worldwide mass production of spectacle lenses, frames and contact lenses does its bit.
More and more companies that produce in our industry are realizing this. In a recent press release, CooperVision, for example, announced that it would produce its approx. 1 billion disposable lenses per day (!) in a plastic-neutral way in cooperation with Plastic Bank. This means that for every gram of contact lens and blister produced, the same amount of ocean-bound plastic waste is collected.Plastic Bank aims to reduce plastic waste in the world's oceans by building collection
and recycling infrastructures in countries where there is no functioning circular economy.
Bausch + Lomb has also continued to expand its sustainability efforts. The company currently reports to recycle more than 41 million contact lens, eye and lens care materials through collaboration with TerraCycle
Another example: Menicon has long developed a concept of sustainability. One environmentally friendly achievement is the development of their flat pack daily disposable lens. The plastics used in their manufacturing process are approximately 99% recycled. 100% recycled plastics are used for the outer packaging.
And the spectacle lens industry is also showing how this can be done in many areas. For example, the company Zeiss (Germany) claims to be CO 2 neutral by 2025. Essilor is committed to contributing to carbon neutrality, circular economy, worldview, integration and ethics. Emissions from direct operations are to be made CO2 neutral in Europe by 2023 and in other markets by 2025.
There are also more and more sustainable products that address this issue. Be it thinner semi-finished products that use less plastic, products made from sustainable materials, state-ofthe-art filtration systems, creative recycling options for production waste and much more.
But, even though the first step has been taken, most of the journey is still ahead of us.
How is your company doing in terms of sustainability? Write to me with your opinion. ■
SILKE SAGE Editor-In-Chief silke@global-cl.com

3
LETTER FROM THE EDITOR GlobalCONTACT 3-21
– not trivial but not impossible either!
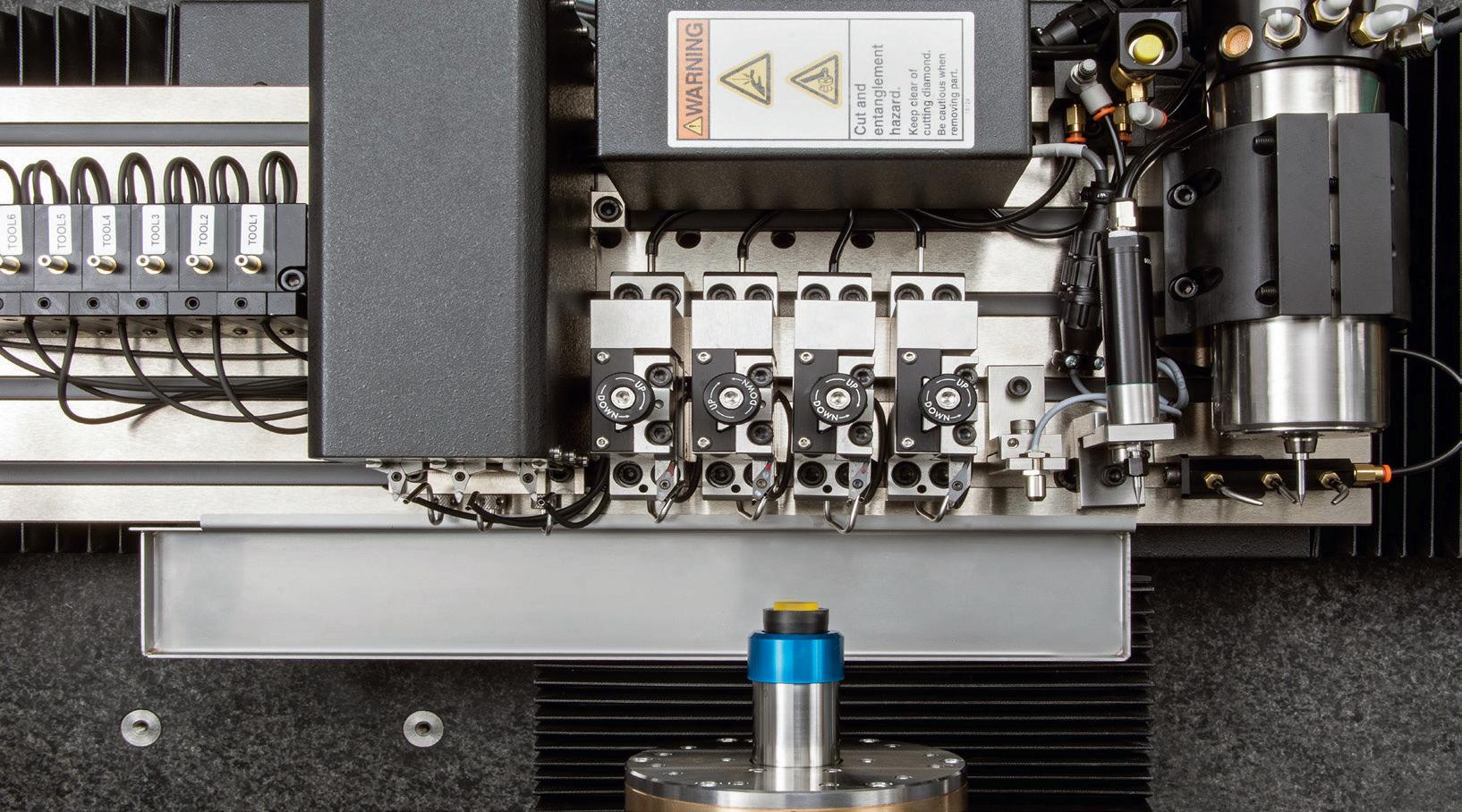
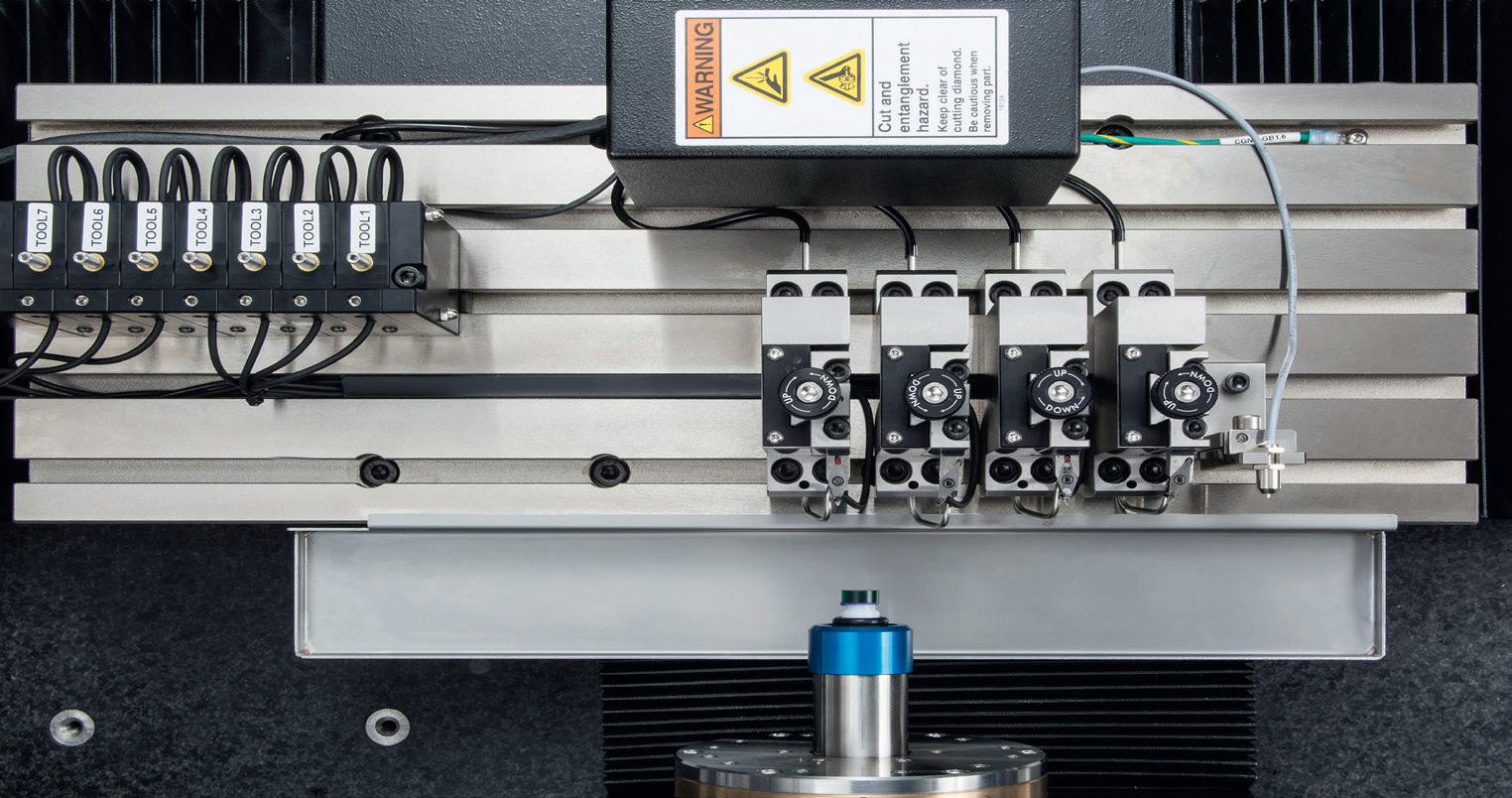
ULTRA-PRECISE AND ECONOMICAL MANUFACTURING OF CONTACT LENSES AND IOL

UPC 100 Vision // UPC nano
Highest surface accuracy and quality meet unprecedented productivity.

The compact and fully featured UPC 100 Vision is optimized for highly dynamic diamond turning of complex freeform surfaces like polish-free IOLs, mold inserts or complex contact lens designs.
The UPC nano is the most affordable and compact machine with on-board freeform capabilities and an optional laser for manufacturing high-quality contact lenses at maximum cost-efficiency.

Both machines can be easily integrated with an optional automation system.

www.schneider-om.com
INDEX TO ADVERTISERS
Title: Contamac, www.contamac.com
Inside front cover: Bausch + Lomb Inc., www.bausch.com
Page 4: Schneider GmbH & Co. KG, www.schneider-om.com


Page 7: REM Vision Tech, www.remvt.com
Page 9: OPTOCRAFT GmbH, www.optocraft.com
Page 13: K & Y Diamond Ltd, www.kydiamond.ca
Page 15: Optimec Systems Ltd., www.optimecsystems.com
Page 19: LAMBDA-X S.A., www.lambda-x.com



Page 21: Schneider GmbH & Co. KG, www.schneider-om.com
Page 25: Larsen Equipment Design Inc., www.larsenequipment.com
Page 35: AMETEK Precitech, Inc., www.precitech.com
Inside back cover: Efclin, www.efclin.com
Outside back cover: DAC International, Inc., www.dac-intl.com
NAMES TO NOTE
Joannes, Luc 36 Johns, Lynette 26 Kahlert, Marie 33 Kinder, Alina 16
Larsen, Erik 34 Roth, Hans-Walter 40 Vohnsen, Brian 22 van der Worp, Eef 30, 42
LETTER FROM THE EDITOR
3 Sustainability – not trivial but not impossible either!


Silke Sage
INTERNATIONAL NEWS
TECHNOLOGY
16 The importance of poroelasticity in soft contact lenses – pt. 2
Alina Kinder
Understanding the visual impact of the Stiles-Crawford effect
Brian Vohnsen
INTERVIEW
26 Interview with Lynette Johns – Drug delivery in scleral lens wear
Silke Sage
FITTING BACKGROUND
Context in contacts Eef van der Worp
Imaging techniques – case study Marie Kahlert
MANUFACTURING
TOPIC
HISTORY
Hans-Walter Roth
COLUMN
32021 (88) Technology • Understanding the visual impact of the Stiles-Crawford Effect • The importance of poroelasticity in soft contact lenses Fitting Background Context in contacts Special Topic New challenges in intra-ocular lens metrology Interview Lynette Johns NOW AVAILABLE AT YOUR APP STORE Eyepress Fachmedien GmbH Saarner Str. 151, 45479 Mülheim a. d. Ruhr optimum-infinite.com Modern modalities require boundless imagination and limitless capabilities. Designed to support the requirements of scleral and ortho-k lens designs, Optimum Infinite’s unique properties offer you the opportunity to push the boundaries of speciality lens design. Hyper Dk Tailored Modulus Inherently Wettable
10
14
6 All about you & event dates
All about research
All about products
22
33
30
34 Blocking scleral lenses Erik Larsen
SPECIAL
36 New challenges in intra-ocular lens metrology Luc Joannes
40 About the use of the “gel”-contact lens
CONTENT 5 GlobalCONTACT 3-21
42 Under pressure Eef van der Worp NEWS 44 Yellow Pages
All about you
Ten rules for the safe use of contact lenses endorsed by TFOS
The national campaign "Healthy Eyes Are in Your Hands", an awareness project dedicated to contact lenses and their safe use, promoted by the Tear Film & Ocular Surface Society TFOS and supported by ASSOTTICA (the Italian Contact Lens Association), promotes ten rules of correct hygiene and management of contact lenses.
The rules have also been summarized in the educational video "Healthy Eyes Are in Your Hands" in which children are the ones giving adults the indications of correct behavior. This video involves washing and drying your hands before handling contact lenses, never letting the lenses come into contact with water, not sleeping with contact lenses, and disinfecting lenses in a new solution after each use. If you wear disposable daily lenses, it is important to throw them away after taking them off and not reuse them, then follow the manufacturer's instructions and the specialist's instructions. The video campaign is available on the web: https://youtu.be/VdscomrqFsw and has already reached tens of thousands of views. "Contact lenses have a long history, and the materials with which they are made have evolved enormously over the years, thanks to intense scientific research. Today, new synthesis technologies have led to materials compatible with the ocular surface, reaching high standards of safety and comfort," emphasized Prof. Piera Versura, Head of the Ocular Surface Analysis and Translational Research Laboratory, Alma Mater Studiorum University of Bologna. “Unfortunately, we are distancing ourselves from this security mainly due to incorrect behavior. The Healthy Eyes Are in Your Hands Campaign can help you understand and remember that contact lenses are a medical device that we put in the eye, and they need care and maintenance."
CooperVision myopia control research receives Garland W. Clay Award
The American Academy of Optometry has awarded the 2021 Garland W. Clay Award to a team of researchers studying the effectiveness of CooperVision MiSight 1 day contact lenses in slowing the progression of myopia in children (aged 8-12 at the initiation of treatment). The prestigious award is given annually to the author(s) of the most important paper published in Optometry and Vision Science in the preceding five years. The authors of the winning paper, “A 3-Year Randomized Clinical Trial of MiSight Lenses for Myopia Control,” include:
• Paul Chamberlain, BSc (Hons.)
• Sofia C. Peixoto-De-Matos, MSc

• Nicola S. Logan, PhD
• Cheryl Ngo, MBBS, MMed
• Deborah Jones, BSc, FAAO
• and Graeme Young, PhD, FAAO
The Optometry and Vision Science editorial board bestows the annual Garland W. Clay Award based upon criteria including the number of citations in the world scientific literature, impact of vision science, value to the practice of optometry, and relevance to the mission of the American Academy of Optometry. After only two years since publication, the paper about MiSight 1 day contact lenses has been cited over 70 times according to Clarivate’s Web of Science and is the most cited paper in Optometry and Vision Science since 2016.
Optometry and Vision Science Editor in Chief Michael Twa, OD, PhD, FAAO stressed that his publication places a priority on quality evidence-
based publications noting that: “Clinical trial results provide strong evidence that it is possible to slow ocular growth that causes worsening myopia. Research into myopia control is rapidly evolving and effective treatments could do more than improve vision, they may also help lower lifelong risks for glaucoma, retinal detachments, and other degenerative eye conditions.”
CooperVision MiSight 1 day myopia control contact lenses are proven to slow the progression of myopia in children aged 8-12 at the initiation of treatment. Data gleaned from these three years of research laid the groundwork for FDA approval of CooperVision MiSight lenses in 2019. The study, a randomized double-masked clinical trial, demonstrated the effectiveness of MiSight lenses in reducing the rate of myopia progression in children (aged 8-12 at the initiation of treatment) by 59% on average over a three-year period.
CooperVision Director of Research Programs Paul Chamberlain, BSc (Hons.) said, “Our team is grateful to the Optometry and Vision Science Editorial Board and the American Academy of Optometry for recognizing our work. It is very satisfying to know that our research in myopia control is helping age-appropriate children and their parents around the world. And it is truly an honor to be associated with the other pioneering papers that have previously received this distinction.”
Chamberlain and team accepted the Garland W. Clay Award at the American Academy of Optometry’s Meeting in Boston on Thursday, Nov. 4.
6
GlobalCONTACT 3-21 INTERNATIONAL NEWS
Marcus Hughes elected to the BostonSight Board of Directors


BostonSight, a nonprofit eye healthcare organization and research center dedicated to saving sight and improving quality of life for patients, have elected Mr. Marcus Hughes to their Board of Directors. Mr. Hughes is Associate General Counsel at UMass Memorial Health Care in Worcester, MA. He serves as legal counsel to the UMass Memorial Health Care (UMMHC) System and its affiliates, with a primary focus on patient care matters. Prior to his role at UMass, Mr. Hughes was Attorney Fellow, Office of the General Counsel at Partners HealthCare in Boston, and Assistant Corporation Counsel for the City of Boston. Mr. Hughes began his legal career at Choate, Hall & Stewart in Boston. “Electing Mr. Hughes to the BostonSight Board is a tremendous benefit to the organization,” said Sara Yost, BostonSight President and CEO. “He is accomplished in legal healthcare
Johnson & Johnson Vision receives approval in Canada for Acuvue Abiliti 1-Day Soft Therapeutic Lenses for Myopia Management
Johnson & Johnson Vision received approval from Health Canada for Acuvue Abiliti 1-Day Soft Therapeutic Lenses for Myopia Management. Abiliti 1-Day lenses are a new option of daily wear, single-use, disposable lenses that have the potential to slow the progression of myopia and are specifically designed for children who are seven to twelve years old at the start of treatment. “The approval from Health Canada for Acuvue Abiliti 1-Day lenses marks another major step forward in our collaborative efforts with parents and eye care professionals to reshape the future of myopia,” said Xiao-Yu Song, MD, PhD, Global Head of Research & Development, Johnson & Johnson Vision. “Our researchers and scientists specifically designed
matters, including reporting and compliance, which will support BostonSight as we continue to lead in providing expert, compassionate patient care and scleral lens technology globally.” Mr. Hughes received his JD from Boston College Law School and his undergraduate degree from Middlebury College in Vermont where he was a Harry S. Truman Scholar Nominee and part of the New England Small College Athletic Conference All-Academic Team. He has spoken at events of the American and Boston Bar Associations on ethical behavior in the legal profession and operational challenges in responding to COVID-19, as well as written for the American Bar Association on COVID-19 and its impact on healthcare professional licensure and telehealth.
Abiliti 1-Day to be a novel soft therapeutic lens with the potential to slow the progression of myopia in children.”

The company also announced that each annual purchase of an Abiliti product would provide a free comprehensive eye health exam to a child in need through Sight For Kids – a joint program from Johnson & Johnson Vision and the not-for-profit Lions Clubs International Foundation (LCIF). Sight For Kids is one of the largest-known, school-based eye health programs that mobilizes Lions and eye care professionals to provide comprehensive eye health services in low-income schools around the world.

Abiliti 1-Day lenses are expected to be available in select areas of Canada starting as early as this year and expanding beyond in 2022. Parents and eye care professionals who want more information can visit www.seeyourabiliti.com.

Advertisement
Marcus Hughes. Source: BostonSight
Ultra precision CNC lathes for CL and IOL manufacturing Your smartest investment www.remvt.com INTERNATIONAL NEWS
EFCLLIN: PFAS-registry of ECHA: five EU member states have submitted the notification for restriction of PFAS

On 15th July, the five REACH competent authorities – from Denmark, Germany, the Netherland, Norway and Sweden – notified the European Chemicals Agency (ECHA) of their intention to restrict PFAS substances (Registry of Intentions). www.echa.europa.eu/registry-of-restriction-intentions/-/dislist/ details/0b0236e18663449b
Submitting a notification to ECHA’s Registry of Intentions (ROI) is step one of the restriction process – the five competent authorities flag a substance, allowing ECHA to get ready and industry to submit evidence. From this moment, the five competent authorities have twelve months to prepare a restriction proposal and collect all available evidence. All companies who are registered producers or users of the substance will also be notified so they can submit evidence to the
notifier. At the end of these twelve months, the five competent authorities will submit a restriction proposal after which ECHA will launch an open consultation via its website.
The proposal will then pass through several technical committees within ECHA who will give their expert opinion. The European Commission will have to decide whether to adopt or not the proposal using ECHA’s expert opinions as guidance. If they adopt it then it will be sent to the European Parliament and the Council of the European Union for their approval, after which it will be published and enter into force.
Over the next few months, ECHA will check whether the five competent authorities’ notification fulfils ECHA’s requirements. If it does, then they will publish the notification on the dedicated website page – the Registry of Restriction Intentions – allowing the public to follow the file’s progress.
CLMA remembers and honors Jo Svochak
Jo began her career in the contact lens industry alongside her husband, Frank Svochak, Sr., a true pioneer of contact lens machining in 1976 when they founded TruForm Optics. After Frank’s passing in 1982 Jo assumed the role as President of TruForm Optics, (1982-2019), and her passion to help people see their world better was made possible through TruForm’s countless contact lens design and machinery advancements throughout her 37 years of service to the industry.

Jo went on to be a pioneer in her own right, as she was the first female to hold the position of President with the Contact Lens Manufacturers Association (CLMA) from 1999 to 2000. In 2013 Jo received the Trailblazers Award, by the CLMA, for her outstanding achievement in product development to the enhancement of the contact lens industry. Since the inception of the Trailblazers Award in 1987 Jo remains the only female to receive the coveted award.
Among Jo’s notable work at TruForm Optics, she was proud of the contributions her late husband, Frank, and her son and current President of TruForm, Jan Svochak, made to advancing the industry forward, and she took great pride in the accolades she was able to see them receive: (1994) Jan Svochak received the Creative Design and Process
Award by the CLMA, for innovation in lens design and manufacturing process to the enhancement of the contact lens industry. (2006) Frank Svochak, Sr., received the Trailblazers Award for outstanding achievement in product development to the enhancement of the contact lens industry by the CLMA.
Jo attended her last CLMA meeting in 2018 and enjoyed the fellowship of her life-long friends and colleagues. Jo was also able to see her son, Jan Svochak, receive the Leonardo da Vinci Award for vision in establishing the focus of the CLMA and dedication to the achievement of its goals. This was a momentous event for the entire Svochak family.
Jo had a zest for life and a personal charm that drew people from all walks of life. Any conversation with Jo was a meaningful and memorable one. Above all of Jo’s career accomplishments and her unwavering dedication to the contact lens industry, her deepest love was being a mother, grandmother, and great grandmother. Jo had a special place in her heart for children, especially babies which always brought the brightest smile to her face.
Naomi “Jo” Svochak, was a compassionate and loving woman, and will be missed by all those who knew her.
8
GlobalCONTACT 3-21 INTERNATIONAL NEWS
Naomi “Jo” Svochak 1937-2021
GSLS 2022 https://na.eventscloud.com/website/22990/home
NCC 2022
https://contactlenscongress.com/?lang=en

EFCLIN 2022 www.efclin.com
ARVO 2022 www.arvo.org
EAOO & ECOO General Assembly www.visiondublin2022.com
ICSC 2022 www.icscmeeting.com
ECLSO Congress 2022 www.eclso.eu
Vision By Design www.orthokmeeting.com
AAO 2022 www.aao.org
IOFT 2022 International Optical Fair Tokyo www.ioft.jp/en-gb.html
Jan 19-22
Las Vegas, NV (USA)
Mar 13-14 Eindhoven (NL)
Apr 28-30 Barcelona/ Sitges (Spain)
May 1-4 Denver, CO (USA)
May 12-15 Dublin (Ireland)
July 29-30 Fort Lauderdale, FL (USA)
Sep 2-3 Paris (France)
Sep 28 - Oct 2 Bellevue, WA (USA)
Sep 30 - Oct 3 Chicago, IL (USA)
Oct 18-20 Tokyo (JPN)
the
please
whether the
takes
Know your quality: Contact and intra-ocular lens metrology made by Optocraft! Tel. +49 9131 69 15 00 email sales@optocraft.de
WEBINARS, CONFERENCES & TRADE FAIRS 2022
(due to
corona crisis,
check via the websites
event
place)
Advertisement
All about research
Studies on contact lens sensors, plastic pollution and the shape of light
A paper published by the journal Matter reports on the development of a new contact lens sensor system for smart contact lenses. The impact of contact lenses, specifically silicone hydrogels, as a source of plastic and microplastic pollution is the focus of a paper by a team of Arizona State University researchers. Further studies take a look at the influence of the shape of light on our vision and present a contact lens sensor for self-monitoring of intraocular pressure.
Ultra-thin sensor for smart contact lenses
In a paper published by the journal Matter, engineers from the University of Surrey together with partners from Harvard University, University of Science and Technology of China, UK National Physical Laboratory, George Washington University and Zhejiang University Ningbo Research Institute report on how they have developed a new contact lens sensor system for smart contact lenses.
The approach uses an ultrathin MoS2 transistors-based serpentine mesh sensor system. The integrated sensor systems contain a photodetector for receiving optical information, a glucose sensor for monitoring glucose level directly from tear fluid, and a temperature sensor for diagnosing potential corneal disease.
According to Dr Shiqi Guo, the first author of this study, the ultra-thin sensor layer is different from conventional smart contact lenses in that it could be mounted onto a contact lens and maintain direct contact with tears, thanks to its easy assembly, high detection sensitivity, good biocompatibility and mechanical robustness. He states that it also doesn't interfere with either blinking or vision.
Co-author Professor Sheng Zhang reports that the contact lens can provide diversified signals from eyes, which could be combined with advanced data analysis algorithms to provide personalized and accurate medical analysis for users.
Another potential that is mentioned in the abstract is that the integrated contact lens sensor system and fabrication strategy could allow for easy incorporation of other functional
10
GlobalCONTACT 3-21 INTERNATIONAL NEWS
components, such as an electrode array for electroretinography, antennas for wireless communication, and power modules for future in vivo exploration. The researchers believe that the system holds promise as next-generation soft electronics for healthcare and medical applications since the in vitro cytotoxicity tests revealed good biocompatibility.
Sources: Abstract of the paper [1], EurekAlert 2021-01-06 [2]
Plastic contact lenses in US wastewater

Arizona State University researchers Charles Rolsky, Varun Kelkar and Rolf Halden have studied the potential of disposable contact lenses as a high-volume pollution source. They conducted the first study to identify contact lenses, specifically silicone hydrogels, as a source of plastic and microplastic pollution. Using sales data and an online survey of lens users (n=416) alongside laboratory and field experiments at a conventional sewage treatment plant, the researchers determined the environmental fate and mass inventories of contact lenses in
the US. Their survey results revealed that around 21% of users flush their used lenses down the drain, a loading equivalent to 44.000±1700 kg y−1 of lens dry mass discharged into US wastewater. The researchers found that biological treatment of wastewater did not result in a measurable loss of plastic mass and caused only very limited changes in the polymer structure, as they determined by μ-Raman spectroscopy. They observed that the lenses accumulated as fragments in sewage sludge, resulting in an estimated accumulation of 24.000 ± 940 kg y−1 of microplastics destined for application on
11
GlobalCONTACT 3-21 INTERNATIONAL NEWS
agricultural soils contained in sewage sludge. Recycling of the contact lenses and their packaging amounted to only 0.04% of the total waste volume associated with contact lens use. In the discussion section of their paper, the researchers mention, that the study featured some limitations in that only 66% of the respondents answered a survey question regarding their age range, thereby reducing statistical power. Another factor is the unknown behavior of contact lens hydrogel polymers

during long-term, multiyear storage in septic tanks which is seen as interesting because an estimated 20% of households in the US use on-site septic systems for wastewater treatment. The team points out that hydrogel as an environmental pollutant through contact lenses could be almost completely avoided by properly disposing the lenses within solid waste. The paper states that at the time of the study, most products in the US contained no recommendations on how to properly dispose of the lenses and their packaging materials. The teams’ research suggests that although contact lenses are a small contributor to the plastic pollution epidemic, their unique chemistry presents a threat to the environment if they are improperly disposed of. They could act similarly to microbeads or microfibers, which are also flushed down the drain.
The shape of light changes our vision
Recent studies have shown that the first stage of vision, the perception of light itself, is extremely fast. But the analysis of this decisive step was carried out on molecules in solution in the laboratory. Scientists from the University of Geneva (UNIGE), in collaboration with Federal Polytechnic School of Lausanne (EPFL) and the University Hospitals of Geneva (HUG), Switzerland, reproduced the experiment on mice, in order to observe the processing of light by a living organism in all its complexity. This non-invasive study shows that light energy alone does not define the response of the retina. Its shape – short or long – also has an impact on the signal sent to the brain to form an image. This discovery, published in the journal Science Advances, opens up a new field of research into vision, diagnostics and possibly new curative possibilities. In the eye, the first stage of vision is based on a small molecule – the retinal – which, on contact with light, changes shape. When the retinal alters its geometric form, it triggers a complex mechanism that will result in a nerve impulse generated in the optic nerve. This process takes some time between the moment the eye perceives the light and the moment the brain decodes it. Physicists looked at the retinal to see how long it took to switch its shape. They isolated this molecule in a cuvette and subjected it to laser pulses to test its reaction speed. To their great surprise, the molecule reacted in about 50 femtoseconds.
To study this first stage of vision in detail, the scientists called on biologists, notably Ivan Rodriguez and Pedro Herrera, professors at the UNIGE Faculties of Science and Medicine, respectively, who placed a contact lens and performed an electroretinogram

on mice. When the light hit the retina, they were able to observe an electrical voltage at the cornea, thanks to an electronic amplifier. Their results showed that this stage took place with the same extreme speed as when the molecule is isolated.
The team continued the study by varying the shape of the pulses over time. Changing the shape should not induce any variation in the response of the retina because until now it was thought that only the number of photons captured by the eye played a role. But this was not the case. This result could be explained with the help of computer simulations performed in the group of Ursula Röthlisberger from EPFL.
The scientists observed that the eye did not react in the same way depending on the shape of the light, even though the light energy was identical. They also discovered that the eye’s reaction differed according to the order in which the colors were varied, for example as in a temporal rainbow, even though they follow each other extremely quickly. The retina believes that there is more or less light depending on the shape of the light, while the energy is similar, and therefore sends a stronger or weaker current to the brain depending on its response. This research is published in Science Advances, DOI: 10.1126/sciadv.abe1911.
Source: UNIGE [4]
12
Source: Nationwide Mass Inventory and Degradation Assessment of Plastic Contact Lenses in US Wastewater. [3]
GlobalCONTACT 3-21 INTERNATIONAL NEWS
Artist's view of femtosecond laser pulses arriving in an eye. Image: UNIGE Xavier Ravinet
Contact lens sensor for self-monitoring of intraocular pressure

A collaboration of researchers from different departments at Michigan State University, USA, has published a paper on a wireless, passive sensor that is capable of continuous monitoring of the change in the curvature of cornea caused by intraocular pressure fluctuations. It sits inside a customized, planar and circular doughnut-shaped contact lens. According to the abstract the sensor consists of a constant capacitor and a variable inductor in the form of a stretchable, closed-loop, serpentine wire that serves as both the sensor and the antenna.
Referenzen:

The abstract reports that the sensor shows a pressure responsivity of 523 kHz per 1% axial strain on a pressurized polydimethylsiloxane membrane and 35.1 kHz per 1 mmHg change in the intraocular pressure of a canine eye. Testing for stability showed unvaried characteristics after repeated cycles and parasitic movements. Predictable influences of temperature and humidity on the sensor response were verified experimentally and can be canceled out using real-time calibration with temperature and humidity sensors to integrate with a reader device. The researchers are convinced that the design has potential clinical applications.
Source: Abstract of the study [5]

[1] Guo S, Wu K, Li C, Wang H, Sun Z, Xi D, Zhang S, Ding W, Zaghloul ME, Wang C, Castro FA, Yang D, Zhao Y. Integrated contact lens sensor system based on multifunctional ultrathin MoS2 transistors. Matter. 2021 Mar 3;4(3):969-985. DOI: 10.1016/j.matt.2020.12.002. Epub 2020 Dec 30. PMID: 33398259; PMCID: PMC7773002.
[2] https://www.eurekalert.org/pub_releases/2021-01/uos-sub010621.php
[3] Charles Rolsky, Varun P. Kelkar, Rolf U. Halden. Nationwide Mass Inventory and Degradation Assessment of Plastic Contact Lenses in US Wastewater. Environmental Science & Technology 2020 54 (19), 12102-12108. DOI: 10.1021/acs.est.0c03121
[4] University of Geneva (UNIGE), 28.04.2021
[5] Hossein M., Kouhani M., Wu Jiajia, Tavakoli Arman, Weber Arthur J., Li Wen. Wireless, passive strain sensor in a doughnut-shaped contact lens for continuous non-invasive self-monitoring of intraocular pressure. Lab Chip, 2020,20, 332-342. DOI: 10.1039/C9LC00735K
Ultra Precision Diamond Tools DAC Optoform Moore Nanotech UPL Precitech Nanoform REM Vision CONTACT LENS AND IOL
Advertisement
www. ky diamond.ca
GlobalCONTACT 3-21 INTERNATIONAL NEWS
All about products

Contact Lens Metrology – upgrade your existing NIMO-TR1504 to the latest CLE-MENTOR software.


When it comes to contact lenses Metrology, CLE-MENTOR offers the most advanced software solution in terms of data integrity and integration. At the very core of the program, its user management options and its compatibility with the FDA CFR21 part 11 guidelines enable the protection of any data along with the traceability, warranties and full audit log.
Every NIMO-TR1504 currently in operation is compatible with CLE-MENTOR. Therefore, anyone can benefit from the new features of the program such as a powerful API offering unlimited possibilities of custom integration in your production workflow and a complete integration with FocalPoints, or the Secondary Aperture option dedicated to the control of segmented and decentered optics.
In addition to its optimised processing, new features and improved ergonomics, CLE-MENTOR offers a measurement time divided by two, reducing the cost while massively increasing the efficiency. For even faster measurements, NIMOevo associated to CLE-MENTOR reduces the measurement time of a lens to less than one second.

Depending on the use of the software, the R&D or the Production mode will meet the requirements and help achieve quality as well as improve the speed of the diagnosis.
Learn more about the software and its compatibility with your existing setup - visit our website: https://ophthalmics.lambda-x.com/cle-mentor/ - sales-ophthalmics@lambda-x.com
Gas Permeable Lens Virtual Education Series
Bausch & Lomb Boston Materials has introduced a virtual educational series on GP Materials. The program is a three-part webinar series that takes a deep dive into the importance of material selection in RGP Lens fitting.

Maria Walker, OD, MS, FAAO, FSLS, hosted Episode One: Selecting Gas Permeable Lens Materials, where she discussed the science that goes into GP material development. This episode provides an in-depth review of Boston materials, including their indications, quality, and manufacturing process.
In Episode 2; Susan Resnick, OD, FAAO, FSLS turned our attention to Gas Permeable Material
Selection for Scleral Lens Design. Here, she takes a closer look at Boston XO and Boston XO2 by highlighting her own case experience in her practice. Coming up in November 2021, the next episode will focus on Gas Permeable Material Selection for Overnight Orthokeratology. For more information on Boston Materials Webinar Series, to register for an upcoming program, or to receive on demand access to past recorded webinars, visit Fit-Boston.eu www.bausch.com
14
GlobalCONTACT 3-21 INDUSTRY NEWS
Optimum Infinite - Infinite Possibilities
Developed to meet the performance needs of modern modalities, Optimum Infinite offers hyper Dk (180 Dk), a tailored modulus and excellent wettability. These unique properties provide an ideal material for scleral and orthokeratology lens designs, offering laboratories an opportunity to push the boundaries of lens design and manufacturing. Optimum Infinite changes the paradigm so you don’t have to compromise when using hyper Dk materials. Contamac’s expert R&D chemists have rewritten the rules on hyper Dk materials, providing limitless capabilities for specialty lens designs. For more information on Optimum Infinite, contact your Contamac representative, or visit www.optimum-infinite.com. www.contamac.com, sales@contamac.co.uk

SortStation IOL: Inspection of intraocular lenses in production



OptiSpheric IOL PRO 2 offers fully automated IOL measurement. It is completed with WorkStation IOL and integrated SortStation IOL. This workplace is the best choice when it comes to carrying out all the steps upstream and downstream of the measurement in a simple, fast and safe process. It includes loading the sample holders with optimal illumination that makes it easy to ensure the ideal positioning of the lenses. Moreover, the lenses can safely be sorted after the measurement: Test results are automatically transferred to the display and made visible directly at the location of the samples. The fulfillment of the pass/fail criterion is displayed in a red/green color scheme and the reliable assignment of each lens is enabled. www.trioptics.com, info@trioptics.com

Advertisement
INDUSTRY NEWS
The importance of poroelasticity in soft contact lenses
Evidence of the pore space of a silicone hydrogel contact lens as transport path for pore diffusion and molecular diffusion – Part 2
Scleral lenses, hybrid lenses or Ortho-K: To ensure safe use of these types of contact lenses, the main focus is on the oxygen permeability of the plastic material of the lens. The metabolism of the cornea and the limbus should suffer as little irritation as possible. The aim of this article is to explain how this transport mechanism occurs and why it is so important. By Alina Kinder
Little is currently known about the pore space in silicone hydrogel contact lenses. The creation of artificial pores or pore space can occur in various ways. The contact lens material is a copolymer, produced by polymerization of a number of different monomers.
In the production of copolymer plastics, the type of structure and properties of the plastic are influenced by admixtures. The type of polymerization can also be used to control the size of the pore space. The cooling rates [19] of the individual manufacturing processes – whether they are produced by shape casting, centrifugal casting, or turning – are important for pore space design. Furthermore, changing pressure conditions during solidification of the plastic mass can lead
to pores and pore spaces. With the turning process, the plastic material is supplied in solid form, permitting the design of the pore space to be controlled to a certain extent. The polymer manufacturing process does not lie within the sphere of influence of the contact lens manufacturer but rather that of the material manufacturer.
In addition, it may be assumed that the first hydration, which transforms the contact lens material from a solid state into an amorphous or viscous structure, allows the actual pore space to develop or be formed. [20] During this process, soft contact lenses undergo a one-time increase in volume of approximately 30% which may correspond to the cavity volume.
Thus the cavity in soft material, resulting from pore diffusion
16
GlobalCONTACT 2-21 TECHNOLOGY
and molecular diffusion, seems to be shaped differently from that in porous solids. It needs to be considered whether the Dk or Dk/t value really is always the same in the different hydration states. [21] When addressing this issue, it should also be clarified whether the Dk/t value needs to take account of the particular state of the aggregate.
Fig. 3: SEM (Hitachi SU3800) photos of the surface of an Efrofilcon A (silicone hydrogel material).

Small Inset: Efrofilcon A before hydration; the surface shows surface damage from the blade.
Large Inset: Efrofilcon A after the first hydration; the surface appears to have a porous surface structure.
17
GlobalCONTACT 2-21 TECHNOLOGY
Fig. 4: Poly-HEMA; hydroxyethyl methacrylate polymer. A polymer that inhibits cell adhesion to growth surfaces in cultures. [22]

The type of polymerization and the composition of the individual components of the hydrogel or silicone-hydrogel plastic material are decisive for the material properties, and thus also for diffusion. The production and further development of the polymer material are key challenges for the material manufacturers. The composition of the material determines the wearing conditions of the contact lens on the eye, which are crucial for the health of the eyes. The manufacturing processes of the contact lenses are largely responsible for the geometry, comfort and vision. They are determined by the base curve (BC), the bevel, the size, the mobility and the surface lubricity. This calls for the expertise of the contact lens manufacturer.
Different cross-links of the polymers with different properties of elasticity and deformability can be created by the various polymerization processes. A preferred form of the long polymer chains is the random coil, which can change its shape dynamically. This dynamic gives rise to the elasticity known in natural rubber. Structural cross-linking occurs when at least four polymers are bonded together. Due to the regular arrangement and repetition of the individual monomers in a polymer it can be called a lattice structure, although the material exhibits amorphous properties. The definition of the Dk value should be adapted to the likely aggregate state. Furthermore, the term poroelasticity needs to be introduced into contact lens optics, because the structural crosslinking and the resulting elasticity cannot be adequately described by Young's modulus (modulus of elasticity) alone. [23,24]
The formation of this cross-linking during polymerization in the polymer material of a contact lens provides soft lenses with a pore space, leading to a corresponding effect on its elasticity. The elasticity of a contact lens is defined only by the modulus of elasticity (Young's modulus). However, in the context of wearing comfort and duration/rhythm, this one physical property is insufficient to fully describe the comfort and deformability during wearing. Thus, to improve wearing comfort, the industry is focusing on the design, surface roughness and coating of contact lenses. Another way to maximize wearing comfort is to modify the structure or composition of the contact lens. An integrated water gradient is designed to make the lens more
comfortable to wear. This allows better wetting of the contact lens and improves stability in the core.
Despite these efforts, no firm prediction can be made about the influence of the contact lens on the supply of oxygen to the cornea and wearing comfort. Not only the geometry of the cornea and the composition of the tear film but also the condition of the eyelids and the effects of the blink are important. During blinking, when pressure or frictional forces act on the surface of the contact lens, there is a momentary change in the cavity structure and oxygen may be released. The pore space of a contact lens is not a static space. On the one hand, particles/molecules that adhere and then detach again permanently change the volume of the pore space. On the other hand, the expansion and composition of the contact lens cavity depends very much on the surrounding conditions. Soft matter is an amorphous material that can be elastically deformed. During a normal blink, a pressure of 10.3 mmHg/ mm2 is exerted; during a conscious blink, pressures of about 51 mmHg/mm2 may be exerted [25] thus deforming the contact lens. Subsequently, wearing comfort appears to improve (as most contact lens wearers will confirm). This material property could well be defined by the magnitude of poroelasticity. It remains to be clarified whether this blinking effectively "squeezes out" oxygen from the pore space. Further, it also needs to be investigated which, or how many residual particles still in the pore space are detached from the pore walls. The blink of an eye can lead to speeds up to max. 20 cm/s. [26] The frictional force of the eyelid triggers shearing forces which act on the surface of the contact lens.
POROELASTICITY
Against this background, further research is required to determine whether the blink of an eyelid is capable of elastically altering the pore space of a silicone hydrogel contact lens to such an extent that adherent molecules can be dislodged. The term poroelasticity is scarcely used in contact lens optics, although poroelasticity well describes the elastic behavior of a porous plastic as well as defining the stiffness of the porous plastic. In fact, poroelasticity would be the material property that can realistically describe the dynamic behavior of a soft contact lens during wear. Current properties used can only define the contact lens in a static state (in the lab). The improvements in vascularization of the cornea observed since the introduction of the silicone hydrogel material have been attributed to the silicone content, and thus to the apparently improved circulation of oxygen. [27] It needs to be investigated whether the change in rigidity of more modern materials has not also improved the durability of the contact surface. Due to the extreme flexibility of the hydrogel material, very strong frictional forces may arise at the contact surfaces, which in turn may stimulate vascularity. [28]
In contact lens optics, the diffusion of oxygen into the tear film
18
GlobalCONTACT 2-21 TECHNOLOGY
is based on liquid diffusion. However, what has been discussed so far suggests that the transport of oxygen through a contact lens is more adequately described by pore or molecular diffusion than by simple diffusion processes.
Pore diffusion and molecular diffusion are processes widely used in physics and chemistry to describe the material property of amorphous bodies. For porous materials, the actual diffusion in liquids or solids does not apply while the diffusion within the pore space is more significant. Pore diffusion takes into account the tortuosity (turns) of the cavity as well as the transport path, which covers a much greater distance than just the material thickness of the contact lens.
Molecular diffusion does not leave out of consideration the interaction between the pore wall and the solute, so that the adsorption processes of the solute particles are included in the diffusion process.

ILLUSTRATION OF DIFFUSION THROUGH A PORE SPACE
The pore space itself now needs to be investigated. As a possible experimental approach, colored liquid can be diffused through the pore space as detached particles. This method of liquid staining can be used to demonstrate the effect of pore diffusion within a contact lens. The existence of cavities in a silicone hydrogel contact lens can be demonstrated by studying the diffusion over time (via video). On the basis of the known diffusion coefficient and the measured time, the Einstein-Smoluchowski equation (1) is used to determine the transport distance, which may be longer than the known center thickness of the contact lens.
D = <x>2/2t [m2/s] (1)

The path taken by the oxygen (dissolved in the tear film)
through the contact lens can be recorded and the time evaluated accordingly. Subsequently, the path length x can be determined via the diffusion constant D, which is known, and the measured time t using the Einstein-Smoluchowski equation.
As oxygen is difficult to dye, physiological saline solution stained with fluorescein can be used as a substitute. The diffusion of fluorescein is an obvious way of investigating diffusion. To measure fluorescein diffusion, the diffusion path of two contact lenses was examined and compared, in order to demonstrate the effect of pore diffusion.
Silicone hydrogel contact lens Efrofilcon A:
• Copolymer of silicone & fluorine and a lactam group N-vinyl pyrrilidone
• 74% water content
• Dk-value of 60*10 -11 ml(O2)*cm2/ml*mmHg*s or a Dk-value of 45*10 -11 ml(O 2)*cm 2/ml*hPa*s (center thickness = 0.266 mm, Ø = 16 mm).
Hydrogel contact lens Filcon II 3:
• Copolymer of MMA and a lactam group N-vinyl-pyrrilidone
• 75% water content
• Dk-value of 43*10 -11 ml(O2)*cm2/ml*mmHg*s or a Dk-value of 32*10 -11 ml(O 2)*cm 2/ml*hPa*s (center thickness = 0.225 mm, Ø = 16 mm).
These contact lenses were not coated and differ merely in their base material which in one case was a silicone material and in the other a MMA-VP material.
To prove that systematic errors can be excluded, a reference group consisting of two very similar hydrogel contact lenses was created.

Metrology solutions for CLE sales-ophthalmics@lambda-x.com - www.lambda-x.com Data integrity and traceability Measuring a contact lens in about one second Advertisement TECHNOLOGY
The reference group consisted of:
Hydrogel contact lens Hioxifilcon B:
• Terpolymer of glyceryl methacrylate
• 49% water content
• Dk-value of 15.8*10 -11 ml(O 2)*cm2/ml*mmHg*s or a Dkvalue of 11.9*10 -11 ml(O 2)*cm2/ml*hPa*s (center thickness = 0.235 mm, Ø = 16 mm).
Hydrogel Acofilcon B:
• Terpolymer of glyceryl methacrylate
• 49% water content
• Dk-value of 15.8*10 -11 ml(O 2)*cm2/ml*mmHg*s or a Dkvalue of 11.9*10 -11 ml(O 2)*cm2/ml*hPa*s (center thickness = 0.225 mm, Ø = 16 mm).
This table clearly shows that the resulting diffusion coefficient Derm – determined over time – appears to be of an order of magnitude less than the diffusion coefficient D of fluorescein dissolved in physiological saline would suggest.
Assuming fluorescein diffusion is conclusive, the pore diffusion in the contact lens made of the silicone hydrogel material is about six times higher than expected; in the reference lens it is about ten times higher. Due to its larger pore space, the silicone-hydrogel contact lens allows faster diffusion than the hydrogel material. In the reference group, the diffusion coefficients found were much smaller, so that the effect of pore diffusion was even up to 50-times greater than anticipated.
As far as is known, Fluorescein diffusion as discussed here has never been used to investigate the mode of diffusion through soft contact lens materials. Thus the aim here is to demonstrate the existence, effects and magnitude of pore spaces in contact lenses.
CONCLUSION
Diffusion path x erm = √(D*2t)[mm] Effect of the pore space x
These contact lenses, too, were uncoated and differed only in the base material. The Dk value and water content were the same. The effect of the pore space x PD can be determined based on the specified center thickness x and the actually measured diffusion path x erm Contact lens Center thickness of contact lens x [mm]
Efrofilcon A 0,266 0,67 2,52
Filcon II 3 0,225 0,73 3,24 Hioxifilcon B 0,235 1,61 6,85 Acofilcon B 0,225 1,65 7,33
Tab. 2: Influence of the pore space based on the increased diffusion path measured (for given diffusion coefficients).
Instead of the assumed diffusion paths corresponding to the center thickness of the contact lenses, 2.52- to 7.33-fold longer transport paths were measured. The Efrofilcon A lens had a shorter path than the Filcon II 3 reference lens, due to the composition of the copolymer material and the resulting different pore space. The control group with the same two hydrogel contact lenses also showed a transport path significantly longer than the actual center thickness of the two contact lenses. The diffusion paths determined for the two contact lenses Hioxifilcon B and Acofilcon B of 1.61 mm and 1.65 mm respectively were very similar due to their similar material composition. When the diffusion constants D and Derm are compared to each other, this results in the effect of pore diffusion EPD.
Contact lens Diffusion coefficient of fluorescein D [m²/s]
Diffusion coefficient determined from time D erm = x 2 /2t [m²/s]
Based on the results, when considering diffusion through a contact lens the concepts of porosity and tortuosity need to be taken into account in order to get closer to a more realistic understanding of diffusion. It is now evident that the concept of diffusion in a liquid on its own is not able to describe the complex process of particle transport.
Two different diffusion processes take place in the two different soft contact lens materials: In the hydrogel contact lens material, diffusion takes places through the aqueous phase, while in the silicone-hydrogel contact lens it is the interplay between pore diffusion and molecular diffusion that is the driving force behind oxygen diffusion.
With diffusion through the water phase in the hydrogel contact lens material, Brownian motion describes the diffusion process, allowing oxygen to diffuse through the contact lens. Random fluctuations of the water molecules are responsible for oxygen flow. The amount of diffusion is temperature dependent.
With the manufacturing process of hydration, the contact lens material undergoes expansion. During blinking, pressure or frictional forces are exerted on the surface of the contact lens.
This causes a brief change in the material structure, enabling oxygen to be pumped clear.
Effect of pore diffusion E PD = D/D erm
Efrofilcon A 0,42*10 -9 6,71*10 -11 6,26
Filcon II 3 0,42*10 -9 4,01*10 -11 10,48
Hioxifilcon B 0,42*10 -9 8,93*10 -12 47,01
Acofilcon B 0,42*10 -9 7,77*10 -12 54,04
Tab. 3: Effect of pore diffusion EPD, when the specified diffusion coefficient D is compared to the diffusion coefficient Derm measured (for a given center thickness).
Poroelasticity can adequately explain this "oxygen pumping" process and should thus be included in the description of the wearing comfort of a contact lens on the eye.
When considering diffusion in liquids, the viscosity of the solvent plays a role. The equation below refers to the viscosity η of the solvent and not the viscosity of the contact lens material. An increase in viscosity due to particles in the tear film leads to a slowdown of diffusion. The slowdown is not affected by the viscosity of the contact lens material itself.
20
PD = x erm /x
GlobalCONTACT 2-21 TECHNOLOGY
D = k BT / 6ηπR 0 (2)
k B = Boltzmann constant (1.380649 x 10-23 J/K)
T = Temperature
η = Viscosity
R 0 = Hydrodynamic radius
In the fluorescein diffusion above, the fluorescein dissolved in the reference group needed a much longer diffusion time than expected. Here diffusion occurs through the water content in the hydrogel material. The amount of oxygen diffusion via the pore spaces in the hydrogel material still requires further investigation.
Two diffusion processes play a major role in silicone hydrogel materials. One of these is pore diffusion, where the solvent diffuses through the pore space. The other is molecular diffusion, which takes account of the adsorption and capillary action of the solution in the pore space. The adsorption of solute particles in the phase or boundary layer of the pore walls changes the extent and nature of the pore space. This process is recurrent and thus does not represent a steady state. The capillary action within the pore space leads to different rates of diffusion which in turn affect the diffusion time. Pore diffusion can well represent the processes of diffusion in silicone hydrogel contact lenses. The interaction of pore diffusion through the cavity, and molecular diffusion which describes the diffusion rate through the shape of the cavity with the capillary action in the pore space, can be described by the material properties porosity and tortuosity. In addition, a more realistic insight into the amorphous nature of the polymeric contact lens material is achieved through consideration of the poroelasticity. The deformability of the material and the related development of forces such as suction and pumping forces in this connection should no longer be ignored. n
This is part 2 of this article. Read part 1 in GlobalCONTACT 2021_02 and in our app.
More information on using the GlobalCONTACT app on page 46
References are available on request from the editorial office or are listed in the GlobalCONTACT app.

Alina Kinder (EurOptom, Master of Science (Klin. Optometry)) is a lecturer at the Professional School for Optometry in Cologne (HFAK). She also works as an examiner on the examiner board of ECOO diploma and optometrist (ZVA/ HWK).

Living Innovation
www.schneider-om.com
Design the future with us!
The family-owned SCHNEIDER GmbH & Co. KG is one of world’s leading manufacturers of machines and system solutions in the fields of ophthalmics and (ultra-) precision optics. Known as the pioneer of freeform technology, we set new industry benchmarks by putting a heavy focus on R&D and new technologies.
As a full solutions provider, we offer our customers innovative solutions, ranging from the small individual machine to large and fully-automated Industry 4.0 lens production systems. Our company has more than 480 employees and is located in Germany, the USA, Brazil, Thailand and China.
Join our innovative team and apply for:
Specialist CL & IOL (f/m/nb)
Location: Fronhausen, Germany
Your responsibilities
Take full ownership for commissioning, installation, training, and servicing of our high-tech machines for custom contact lens (CL) and intraocular lens (IOL) production worldwide
Provide high-level customer support and expert training regarding all technical, quality and process aspects
Liaise with customers as well as internal departments to ensure satisfactory customer experience
Collaborate with our specialist departments to support machine optimization and product development

Enhance internal knowledge and transfer skills internally
Perform quality assurance and conformity testing of CL & IOL machinery, this includes the evaluation of lens geometries and surface inspection
Pilot test operation and presentation of machinery
Test and obtain machine acceptance of contact lens machines, including FAT & PDQ

Qualifications
Technical degree or relevant technical diploma/certificate Fundamental knowledge of contact lens or IOL manufacturing processes
Experience in customer support Knowledge of measurement and metrology devices for contact lenses or IOL inspection
Knowledge of analytical troubleshooting of CNC machinery’s hardware and software functionality
Benefits
Interesting and demanding tasks in a highly innovative environment
State-of-the-art workplaces
Flexible working hours Company pension scheme Workplace Health Promotion Numerous perks in a number of shops
High-quality and fresh food offers in the inhouse restaurant
Employee events Join our team to shape the future of the optical industry with us!
www.schneider-om.com/career/
SCHNEIDER GmbH & Co. KG
Biegenstrasse 8–12 D-35112 Fronhausen
Phone: +49 (64 26) 96 96-360 www.schneider-om.com
Advertisement GlobalCONTACT 2-21

22 GlobalCONTACT 3-21 TECHNOLOGY
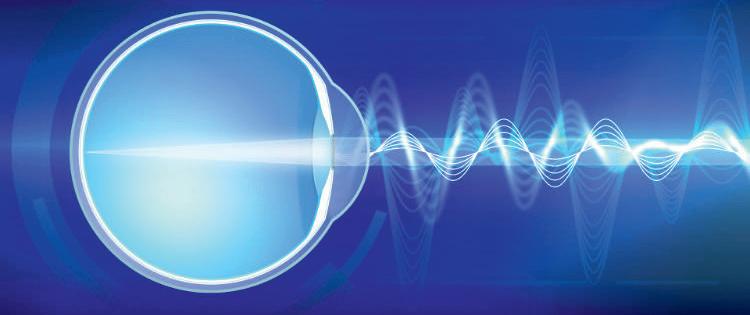
Understanding the visual impact of the Stiles-Crawford effect
The Stiles-Crawford effect (SCE) is a classic of visual optics that remains poorly understood. Discovered by Walter Stanley Stiles and Brian Hewson Crawford in 1932, it is a directional optical effect related to the very elongated shape of photoreceptors. The effect is only observed in photopic conditions and thus it is exclusively a cone photoreceptor effect. It is commonly analyzed for a single pupil point at a time in Maxwellian view corresponding to a single angle of incidence onto the retina. This differs markedly from normal vision through the entire eye pupil.
By Brian Vohnsen
The SCE is normally represented as a pupil apodization. Yet, as it originates in the optics of the retina itself, this approach is invalid, and the SCE provides a much stronger apodization than predicted with Maxwellian view. This has direct implications for vision and refractive optics of the anterior eye. In this contribution, the optics of the SCE is described with emphasis on the fact that photoreceptors themselves are active optical elements that impact vision on par with the optics of the anterior eye.

WHAT IS THE STILESCRAWFORD EFFECT?
Vision is highly sensitive to the angle of incidence onto the retina. This is due to the elongated structure of the photoreceptor cells where visual pigment is distributed in densely packed layers within the outer segments of each cell. The common assumption is that they act like optical fibers by guiding light from the inner to the outer segment of each cell. Yet, there are indications that lensing may also be in play in the high refractive index mitochondria that are densely packed in the ellipsoid between the inner and outer photoreceptor segments. The sensitivity to acceptance angle is described by a characteristic Stiles-Crawford function that resembles a Gaussian distribution in the pupil plane. The peak of the function is because photoreceptors point towards a common point near the pupil center whereas the width of the distribution describes the angular sensitivity of the photoreceptors. Thus, if a single ray of light is incident at a pupil eccentricity of 2.5 mm it will dampen the visual response by 50% and at 3.5 mm eccentricity by 75%.
WHAT CAUSES IT?
Although clearly of retinal origin, the mechanism causing the Stiles-Crawford effect remains elusive. Photoreceptors are believed to act as biological waveguides due to an elevated refractive index. Yet, vision is only triggered when light is absorbed in the outer segments where visual pigments are stacked and gradually renewed within an approximately two week cycle. Excess light is absorbed by the dark retinal pigment epithelium layer beyond the photoreceptors. That waveguiding is the principal cause of the Stiles-Crawford effect is challenged for a number of reasons: (1) foveal cones that are directional have a similar geometry to that of peripheral rods that lack directionality, (2) waveguiding does not describe what happens with the nonguided light, (3) the short length of outer segments allowing only a single or few reflections that may not build up modes effectively, (4) foveal cones are very densely packed very unlike those of individual optical fibers, and most importantly (5) waveguided oblique light would have a larger optical path
Left: The Stiles-Crawford function of the first kind (SCE-I) is usually expressed by a Gaussian pupil apodization with a characteristic directionality parameter of approximately rho = 0.05/mm2 at the fovea. It expressed the angular acceptance curve for the photoreceptors when measured with Maxwellian light at the pupil. Right: It is common practice to add the SCE-I function point-by-point across the pupil when analyzing its effect for the natural pupil size. Yet, this approach is flawed and severely underestimates its combined effect at the retinal plane. The effective truncation with a natural pupil is nearly an order of magnitude higher than with Maxwellian light.
23
GlobalCONTACT 3-21 TECHNOLOGY
Left: Light traverses stacked layers of visual pigments in the outer segments. The total absorption is proportional to the volumetric overlap between the light and the outer segments. For oblique light some light will leak into adjacent outer segments that will absorb the light according to the cone type.
Right: Cones are either isolated or grouped in small patches within the photoreceptor mosaic, whereas rods are grouped in larger patches with highly similar rods. The larger the patch of identical receptors, the smaller is the effective directionality. The plots show calculated SCE-I visibility curves for individual to larger and larger patches of identical outer segments in a hexagonal photoreceptor array. For rods the SCE-I directionality is practically absent.

The wavefront at the pupil has an accompanying wavefront slope at the retina only for even-order Zernike aberrations. For odd-order Zernike aberrations the point-spread function is similarly degraded, but the wavefront is incident along the axes of the photoreceptors and is therefore not attenuated in the same manner by the SCE-I.
trefoil) Zernike aberration orders as only the former has a wavefront slope in the retinal plane. Additionally, the plasticity of the retinal photoreceptors as being able to readjust to maximize light capture over a period of days suggest that they show a certain degree of phototropism like that of sunflowers. This may help understand visual adaptation as an optical mechanism to improve vision even in cases of blur and scattering of light, and ultimately help understand what optical mechanisms trigger and drive myopia in dim light such as indoors with larger pupil sizes.
HOW DO WE TAKE IT INTO ACCOUNT?
in the outer segments and therefore effective visibility should be larger, not smaller. Thus, I have recently argued that leakage of light rather than waveguiding may be the main reason for the Stiles-Crawford effect. This agrees with other reports of crosstalk between adjacent photoreceptors, but also explains why there is a small hue shift for oblique light (the Stiles-Crawford effect of the second kind) as light leaks into adjacent cones containing a different type of visual pigments (there are three cone types: long wavelength sensitive red cones, medium wavelength sensitive green cones, and a small fraction of short wavelength sensitive blue cones) whereas in the case of rods, any leakage into adjacent rods, will flatten the directionality response.
WHY DOES IT MATTER?
A careful understanding of the optics of the retina and photoreceptors is vital as it is the last optical element of the eye where images projected by the anterior eye trigger a visual sensation. The Stiles-Crawford effect shows that the angle of incident onto the retina is critical for vision. It also differentiates between even (defocus, spherical) and odd (coma, astigmatism,

Apodization of the pupil with a Stiles-Crawford effect is only valid on a ray-by-ray basis but not for the combined effect of vision through the natural pupil where its effect is nearly an order of magnitude larger with a drop-off in visibility with pupil size being closer to that of a power law and therefore there is a strong preference for small pupils. The time is due to consider the Stiles-Crawford effect rightfully in the retinal plane as only then can we evaluate its true role in vision. n
Brian Vohnsen, MSc, PhD, is a Fellow of Optica (Optical Society) and Associate Professor in optical physics at University College Dublin (UCD) in Ireland. He received his PhD in NanoOptics at Aalborg University in Denmark. His current research spans from advanced optical imaging techniques and adaptive optics to understanding vision with a special focus on the optics of the retina. He lectures both optics and physics, being twice a winner of the UCD College of Science teaching award and chairs postgraduate programs in physics and the physics committee on equality, diversion and inclusion. Contact: brian.vohnsen@ucd.ie

24
GlobalCONTACT 3-21 TECHNOLOGY
Larsen Equipment
In 2004, Keith Parker and I opened Advanced Vision Technologies (AVT). At that time, the economy was going through a very bad recession and as a result, it was impossible for a new business starting up to get a loan. We immediately reached out to Erik and Pam at Larsen Equipment to get refurbished equipment to use in our Laboratory. As AVT’s business grew, we invested in many different pieces of new equipment from Larsen Equipment and this helped us grow into one of the Premiere Labs in the United States. Our success is due in part to Erik and his Team with their state-of-the-art equipment and maintenance of their products. AVT is forever grateful for Larsen Equipment’s support of AVT. It is great to know AVT is working with Industry leaders with the Larsen Equipment and their Team!
Janine Bungo, VicePresident
QUALITY MANAGER: RANDY MINGOY
I have known Erik Larsen since 1992. Since then I have used just about every piece of equipment his company has built. My experience with Erik and the Larsen team has been one of great appreciation as they have always helped me in my needs of fully understanding equipment used to manufacture quality contact lenses. Erik has also been able to engineer any part needed for me even it was a custom part. Erik (Larsen Equipment) has been and still is a pioneer in the contact lens and optical industry, and I am thankful to him for his support over the years.
Randy Mingoy Quality Manager
PRESIDENT: KEITH PARKER
I have had the pleasure of working with Erik since the beginning of Larsen Equipment. The first piece of equipment, a 6 spindle horizontal arm polisher revolutionized our production of GP contact lenses. Through the years, I watched his business grow as he and his team listened to our Industry needs and developed now numerous products not only simplifying many tasks of manufacturing but improving the consistency of quality in our finished products. Innovation has been an ongoing experience of our Company only made possible through the innovation of necessary equipment developed and made available by the Larsen team.
Advanced
Vision Technologies
DIRECTOR OF OPERATIONS: JORDAN GOBEL
There can be a lot of moving parts when it comes to managing operations, so it is key to have reliable precision equipment that assists in overall efficiency. Larsen Equipment delivers just that! I have been utilizing Larsen manufacturing equipment for over 15+ years and have yet to run into an issue they could not resolve. I am a satisfied owner of bladder polishers, edge roller’s and auto-blockers etc. Each one of these units greatly assists in the reduction of rejects and manufacturing waste. Their ability to customize and retrofit specific tools certainly sets them apart from the competition. Larsen stands behind their equipment with a knowledgeable staff that provides exceptional service. Simply put, we are a better laboratory because of our relationship with the folks at Larsen.
Jordan Gobel
Director of Operations/Consultant
Advanced Vision Technologies

Larsen Equipment is a family owned business hosting a team of willing Staff all having the attitude of serving their Customer’s needs. As a Customer, we are made to feel like we have a friend in the business helping us develop a more efficient process allowing our Company to deliver better products for our Customers.
Our success of AVT simply could not have been possible without the help, assistance and dedication of Larsen Equipment. I will be forever grateful for my opportunity to work with Erik and his very capable Staff.
 Keith Parker President
Keith Parker President
969 S. Kipling Parkway, Lakewood, CO 80226 Phone: 303-384-1111 888-393-5374 Fax: 303-384-1124 www.AVTLENS.com
25
GlobalCONTACT 3-21 PR-Advert
Drug delivery in scleral lens wear
Interview with Dr Lynette Johns, Harvard Medical School Department of Ophthalmology
Drug delivery in scleral lens wear is still a bit uncharted territory, although talk about this and pioneering work in the field date back at least a few decades. The areas of potential application could be prevention against corneal infection in case of corneal defects, and particularly in case of persistent epithelial defect healing. These defects can be very difficult to re-epithelialize, and it is important to use prophylactic antibiotics, to prevent corneal infection in these vulnerable eyes. Another area of potential application could be the use of medication that prevents neovasculasation in the cornea. These drugs can prevent new blood vessel growth in the cornea. Other areas such as glaucoma medication application are still under investigation. Here, like in general scleral lens fitting, it is the balance between the benefits and the costs (including risks etc.) that need to be considered. Here is an overview of what we know so far.
By Silke Sage
GlobalCONTACT: Which drugs are generally suitable for the administration through scleral lenses?

Lynette Johns: If there is an epithelial defect on the cornea, it may be wise to have an antibiotic present to prophylactically prevent against a corneal infection. One of the antibiotics we use is Moxifloxacin – that provides dual protection against gram-negative and gram-positive microorganisms. Moxifloxacin is a preservative-free ocular therapeutic, which makes it ideal for applying in the reservoir of a scleral lens. Preservatives of topical medications are toxic to the cornea with extended exposure times or dosing in drop form. When preservatives are used in a scleral lens, they can cause dense superficial corneal staining.
GlobalCONTACT: When are they applied?
Lynette Johns: If there is a persistent epithelial defect, then this may be particularly useful. A persistent epithelial defect is a non-infectious focal loss of corneal epithelial cells. Often, they are caused by mechanical trauma, neurotrophic corneal disease, or post-surgically.
Depending on the underlying condition, they can be very difficult to re-epithelialize. Using aggressive lubrication and bandage soft contact lenses is typically needed. It is important to use prophylactic antibiotics as described above, to
26 GlobalCONTACT 3-21 FITTING BACKGROUND
prevent corneal infection in these vulnerable eyes. In extreme longstanding cases the eyelids are sewn partially closed (tarsorrhaphy) in order to heal and resurface the cornea. To prevent this, scleral lenses have been used to resurface corneal epithelial defects.
Drug delivery using scleral lenses was first suggested in a publication in 2000 by Dr. Perry Rosenthal and colleagues.[1] In this retrospective study, 14 eyes with persistent epithelial defects were treated with extended wear of scleral lenses and in some cases, there were prophylactic antibiotics placed in the reservoir of the lens with the saline. Unfortunately, there were four cases of microbial keratitis, but eight eyes completely resurfaced. Moxifloxacin was not used in this study. Later, this same group retrospectively reviewed 20 different cases with epithelial defects where
Moxifloxacin was used in all cases, and 17 eyes resurfaced. There were no cases of microbial keratitis in theses 20 cases using moxifloxacin in the reservoir. 2
I worked with Dr. Perry Rosenthal using extended wear of scleral lenses with prophylactic Moxifloxacin in the reservoir of the lens in many of these cases. It was remarkable to see how quickly and effectively this worked. The protocol for this treatment method was published by Ciralsky et al. in 2015.3

GlobalCONTACT: What is the requirement for these types of scleral lens fitting and how is the drug administered?
Lynette Johns: Basically, a scleral lens is fit as optimally as possible, with the plan to have no scleral lens compression or impingement on the conjunctiva. The lens is filled with preservative-free saline and one drop of moxifloxacin and applied on the eye using the typical method for scleral lens application (head parallel to the floor). The lens is worn on an extended-wear basis for 24 hours and the eye is examined carefully the next day. The lens is removed, photos are taken for comparison, the epithelial defect is measured, and all signs of microbial keratitis are ruled out. The lens is disinfected, and the same process is repeated daily until the defect has resurfaced. In some cases, the epithelium is very fragile and can break down the first night the lens is not worn. We would have patients wear the lens an extra night with the antibiotic to allow the epithelium to “tack down”. In my experience, the majority of corneas would resurface within two weeks. If
27 GlobalCONTACT 3-21 FITTING BACKGROUND
the healing was slow, we would manufacture two lenses for the patient and train him/her on careful application and removal of the lens. When proficient we dispensed both lenses. They would wear them on a “12/12” schedule. Basically, they would wear a fresh lens with the antibiotic in the morning while the nighttime lens is disinfecting during the day, and then remove that lens at bedtime and put a fresh lens in with the antibiotic and then disinfect the daytime lens overnight. When epithelial defects healed, the patients would wear the lenses daily and lubricate aggressively at night. If their lids open at night while sleeping, we would have them tape the eye closed while they slept.

GlobalCONTACT: Are there other potential fields of application?
Lynette Johns: Another medication used in the lens was topical 1% bevacizumab which is an anti-vascular endothelial growth factor (VEGF) medication. VEGF is a prominent factor that promotes neovascularization – new blood vessel growth in the cornea, and this drug can slow down the progression of that process. It has been injected into the eye to prevent retinal neovascularization and also injected into the conjunctiva against corneal blood vessel formation. It also had been used topically to prevent corneal neovascularization. I worked with Dr. Deborah Jacobs who was the first to use this medication in the lens for patients who demonstrated new blood vessel growth that was potentially sight-threatening. This use of 1% bevacizumab is off-label and carries potential risks of poor wound healing, corneal thinning, and ulceration of the cornea. To avoid systemic
absorption, the patients had punctal occlusion. The drug needed to be compounded made-to-order and preservative-free – which is expensive. The lens was worn daily only, and patients removed the lens and reapplied the drop midday for a total of two days dosing in the lens. This treatment continued for three months and was continued based on the discretion of the corneal specialist.4,5 Long-term results ranging from six months to eleven years of 13 patients who used a course of bevacizumab in the lens were reviewed and approximately 90% of eyes had a reduction in corneal neovascularization and approximately 75% had an improvement in best corrected visual acuity.6
GlobalCONTACT: How do you make sure, the dosage is correct?
Lynette Johns: In the previously described studies, one drop was placed in the reservoir with the saline solution. The problem with drug delivery in scleral lenses is dosing. The reservoir is different for each patient and the dilution would also be difficult to determine. It is unknown what percentage of the drug is ideal. Drug delivery with a scleral lens is a novel use of scleral lenses and is truly in its infancy. Practitioners should be cautious if delivering topical medications using this technique. In topical medications where drops are administered directly to the eye, most of the ocular medication is lost within 15-30 seconds after instillation.7 The tear turnover rate is approximately 16% per minute whereby all the drug disappears within ten minutes after dosing. Furthermore, the instilled drop is diluted by 1/3 of the original drop.8
28
GlobalCONTACT 3-21 FITTING BACKGROUND
GlobalCONTACT: When should scleral lenses vs eye drops be used?
Lynette Johns: I would be very cautious considering scleral lenses for drug delivery at this time unless further research is conducted. Risk and benefits should be clearly delineated before attempting drug delivery versus topical therapies such as eye drops. In the presence of an epithelial defect that does not respond to conventional therapy, I would use a scleral lens to resurface the defect with moxifloxacin since it has been shown to be effective. Close monitoring of the patient is required and may involve daily monitoring which can be difficult depending on practice scheduling. The expense of compounding drops for use in scleral lenses may be cost-prohibitive for some patients. But of course this needs to be performed in a highly controlled, hospital setting – and its use may be restricted depending on what part of the world and what profession you are in.
GlobalCONTACT: Does this cause any problems?
Lynette Johns: I think many people would like to consider using a scleral lens to deliver glaucoma medications; however, I think that’s premature at this time. I am concerned about the actual concentration of the drug in the reservoir of the lens. Would one drop of a conventional glaucoma medication be too strong for long-term exposure? Would it be ineffective and too diluted? We just don’t know those answers. Also, the volume of the actual reservoir of a vaulted scleral lens is unknown and changes with settling. I hope that this is researched to determine and titrate the appropriate concentration in the lens of all topical medications. Once it is carefully researched, this could be an effective pressure lowering treatment especially for noncompliant patients with glaucoma. To be clear, I am not advocating its use in this capacity at this time.
GlobalCONTACT: Is the application (over the surface of the cornea and limbus) evenly distributed by the scleral lenses? Or does it not matter?
Lynette Johns: This is a great question, and something that would need further study. But the same question applies to eye drops potentially too.
GlobalCONTACT: Is the medication of the eye drops generally different from the administration via scleral lenses – is only the quantity lower?
Or is a different concentration necessary?
Lynette Johns: Most probably it will be different, but we have no clue at this point on how much and why.
GlobalCONTACT: Is the application for non-professionals doable? Or does the optometrist or ophthalmologist have to apply it?
Lynette Johns: Patients have been able to apply the medications independently in the lens if they were proficient at application and removal. When using topical drugs in the lens, patients must be carefully watched by optometrists or ophthalmologists.

Again, it depends on the licensing and regulations of each country. Even in the United States, therapeutic licensing for optometrists varies from state to state.
GlobalCONTACT: Could atropine also be administered in this way? And if so, what would be the advantages?
Lynette Johns: Atropine is a very potent medication with significant side effects even with topical application. This most certainly requires further study before using in a lens on a patient.
GlobalCONTACT: Are there specifications for the lens material?
Lynette Johns: There are no specifications regarding lens materials in my experience with either of these medications. In the cases of anti-VEGF treatment, the highest Dk materials were used to enhance the oxygen permeability because of the presence of corneal neovascularization.
GlobalCONTACT: Thank you very much for this Interview!
References:
[1] Rosenthal P, Cotter JM, Baum J. Treatment of persistent corneal epithelial defect with extended wear of a fluid-ventilated gas-permeable scleral contact lens. Am J Ophthalmol. 2000 Jul;130(1):33-41. doi: 10.1016/s00029394(00)00379-2. PMID: 11004257.
[2] Lim P, Ridges R, Jacobs DS, Rosenthal P. Treatment of persistent corneal epithelial defect with overnight wear of a prosthetic device for the ocular surface. Am J Ophthalmol. 2013 Dec;156(6):1095-101. doi: 10.1016/j. ajo.2013.06.006. Epub 2013 Sep 25. PMID: 24075432.
[3] Ciralsky JB, Chapman KO, Rosenblatt MI, Sood P, Fernandez AG, Lee MN, Sippel KC. Treatment of Refractory Persistent Corneal Epithelial Defects: A Standardized Approach Using Continuous Wear PROSE Therapy. Ocul Immunol Inflamm. 2015 Jun;23(3):219-24. doi: 10.3109/09273948.2014.894084. Epub 2014 Mar 21. PMID: 24654929.
[4] Lim M, Jacobs DS, Rosenthal P, Carrasquillo KG. The Boston Ocular Surface Prosthesis as a novel drug delivery system for bevacizumab. Semin Ophthalmol. 2009 May-Jun;24(3):149-55. doi: 10.1080/08820530902802013. PMID: 19437350.
[5] Keating AM, Jacobs DS. Anti-VEGF Treatment of Corneal Neovascularization. Ocul Surf. 2011 Oct;9(4):227-37. doi: 10.1016/s1542-0124(11)70035-0. PMID: 22023817.
[6] Yin J, Jacobs DS. Long-term outcome of using Prosthetic Replacement of Ocular Surface Ecosystem (PROSE) as a drug delivery system for bevacizumab in the treatment of corneal neovascularization. Ocul Surf. 2019 Jan;17(1):134141. doi: 10.1016/j.jtos.2018.11.008. Epub 2018 Nov 20. PMID: 30468876; PMCID: PMC6340761.
[7] Shell JW. Pharmacokinetics of topically applied ophthalmic drugs. Surv Ophthalmol. 1982 Jan-Feb;26(4):207-18. doi: 10.1016/0039-6257(82)90081-
[8] Maurice D, Mishima S: Ocular pharmacokinetics. in SearsML (ed): Pharmacology of the Eye. New York, Springer-Verlag,1984, pp 19–116
[9] PMID: 7041308.
Many thanks to Eef van der Worp for his comments.
Dr. Lynette Johns is a research associate at Harvard medical school department of ophthalmology. She exclusively fits scleral lenses at Massachusetts Eye and Ear Infirmary. She is an author and co-editor with Melissa Barnett of the textbook: Contemporary Scleral Lenses: Theory and Application. She has published and speaks internationally on scleral and specialty contact lenses.
29
GlobalCONTACT 3-21 FITTING BACKGROUND
Let’s have a look at context within the contact lens industry. Context most commonly refers to the environment or setting in which something (whether words or events) exists. There may be a few context issues that are worthy of discussion, both here and at future meetings within our field. By Eef van derWorp

30 GlobalCONTACT 3-21 FITTING BACKGROUND
EPONYMS
The impressive British Contact Lens Association (BCLA) CLEAR papers – in which CLEAR stands for contact lens evidence-based report – shine an interesting light on terms used in our field. Laura Downie from the University of Melbourne in Australia is the lead author of part one of that series (eleven papers in all) that focuses on the anatomy and physiology of the anterior eye. She composed this paper with a team of experts from around the world including some European hotshots. Everybody who is active in the contact lens field should maybe have a look at this (the papers are open access from the Contact Lens & Anterior Eye website) to understand the landing tarmac of the lenses we so dearly love. The first thing the committee notes is that in general, the trend is to avoid eponyms where possible. An eponym is a person, place, or thing after whom or which someone or something is, or is believed to be, named. An example is Zeppelin (the first balloon with propellers that was directable), which is derived from the name of the German general and aeronautical pioneer Ferdinand von Zeppelin. In the cornea alone, we have several eponyms, the first being Bowman’s layer after the English physician, anatomist, and ophthalmologist William Bowman (1816–1892). This layer is thin but very strong. It separates the corneal epithelium anteriorly from the stroma. The new term for this, which would directly point to its location in the cornea and, to some degree, to its function, would be anterior limiting lamina. Don’t be surprised to see that term appear in future papers. The same is true with Descemet’s membrane (after the French physician Jean Descemet, 1732–1810). This would now become posterior limiting lamina, as it separates the posterior part of the cornea (the stroma) from the endothelial layer. There is discussion to do the same with Meibomian glands (after Heinrich Meibom, a German physician who lived from 1638–1700 and who first described these). There was no consensus within the CLEAR team at this point to change this to tarsal gland , but that may change in the future too.
“PINK EYE”
Laura Downie, in her BCLA presentation on her CLEAR paper, further explores the importance of the use of terms. She refers to a nice research article by Nickel et al: “Words do matter: a systematic review on how different terminology for the same condition influences management preferences”. In this systematic review, they look at several medical conditions and how they are described. One of them happens to be from the eyecare field; to describe the condition of conjunctivitis, you could use the term Pink Eye, or you could refer to it as Eye
Infection. One can imagine how this could have a huge impact on behaviour. And it does. Different terminology given for the same condition influenced management preferences and psychological outcomes in a consistent pattern, according to the study. Changing the terminology may be one strategy to reduce patient preferences for aggressive management responses to low-risk conditions. So, here is something to think about – from eye care practitioners toward their patients and also from manufacturer to client, and in everyday life on an almost constant basis, really – be careful what words or phrases you use in any given situation. It may change the outcome.
CONTACT LENS SAFETY
One ‘biggie’ in our field, of course, is contact lens safety. In many countries, there are unfortunately hefty discussions between ophthalmologists and contact lens specialists on the safety of orthokeratology. Is the ophthalmology world right? Depends on how you look at it, I suppose. If you see a number of MK (microbial keratitis) cases in a given week because of orthokeratology I can imagine that you may wonder whether this is the right modality (for children particularly). So, there is work to do: we need to make our contact lens practices as safe as possible, and there is room for improvement. Acanthamoeba infection, for instance, is almost exclusively contact lens-related and is also linked to tap water. Hence, it has been called a ‘preventable disease’. At the same time, all practitioners in large practices with whom I’ve spoken who do a lot with orthokeratology report hardly any cases of corneal infection with the modality in their database. It almost seems as though for the experts in the field who are on top of things, the infection rate is not all that high. But every infection is one too many. How to deal with this, in general, when you fit a pair of contact lenses? On one hand, you don’t want to scare newbie lens wearers. Contact lenses are a safe modality; pretty much everybody is on board with that. On the other hand, you don’t want to downplay things. You want to make sure that patients are compliant, that they follow the rules and regulation, and that they understand that there is a risk of infection. A little bit of good information about these risks seems warranted. So, it is about how you phrase things. This is a great profession to be in, but not necessarily a simple one per se.
LET’S MOVE ON – USE MICRON!
Another term that most likely will become more relevant going forward and will become the new standard in the contact lens field is ‘micron’. Microns of height are the new millimeters of radius in contact lens terminology. As we are moving away from central keratometry values to full corneal topography, we are also starting to think in elevation and height. The

31 GlobalCONTACT 3-21 FITTING BACKGROUND
appropriate term for that is micrometer (micron): which is, of course, 1/1000th of a millimeter.
The decision on when to fit a spherical corneal lens versus a toric corneal lens can now be made based on microns of height (typically in the 30-micron range is the cut-off point). This is true, too, for spherical versus toric orthokeratology. Also, the decision on when to go from a corneal lens to scleral lens is height dependent; studies at Pacific University have found that in 88% of cases, patients with less than 350 microns of corneal elevation difference along one meridian (the one with greatest variance) had good success with a corneal lens. But if there is more irregularity than that, then a scleral lens could be indicated. To top it off: when fitting scleral lenses, when is a toric scleral lens needed as an upgrade from a standard spherical scleral lens? We know from research by Greg DeNaeyer et al that if a 16 mm circle is drawn onto the scleral surface concentric to the limbus, less than 6% of eyes have a scleral asymmetry of more than 300 microns at 16 mm, which is considered ‘spherical’ by that definition. Anything more than that may be eligible for a toric or asymmetrical scleral lens design.
Scleral lenses have really opened our minds, and the road, toward using microns; everything from the elevation on the ocular surface, to clearance (fluid reservoir, vault) and trial sets for sclerals is in the micron nomenclature. And soft contact lenses are presented in overall sagittal height now too (in microns) – see my last contribution to GlobalCONTACT: ‘Mind the Gap’.
A THIN SKIN
To put things in perspective, and circling back to the anatomy and physiology of the anterior eye CLEAR paper, the thickness of the cornea is 540 microns and is considerably thinner in keratoconic eyes. The cornea is comprised of five principal layers, of which the most anterior layer (the epithelium) is approximately 50 microns thick. Extremely important tissue, of course, when it comes to orthokeratology. You may want to indent or massage that epithelium to some degree, but not the full thickness. The anterior limiting lamina (Bowman’s layer) is approximately 8 microns thick – as said, very thin but also very sturdy. The stroma is the bulk, with about 470 microns of tissue, which can swell (and thus increase) if oedema is present. Four percent swelling is considered physiological – e.g., this is the average amount of swelling that we see in the open eye upon awakening after a night of eyelid closure. The posterior limiting lamina (Descemet’s) is 3–20 microns thick; it increases in thickness with age. Finally, the endothelium is a very thin single cell layer (3–5 microns thick) that actually thins a bit with age. The normal human tear film is only 2-5 microns thick. In millimeters, the tear film would be 0.002 to 0.005 millimeters
thick. To get a good perspective of things, it would probably be better to switch to microns.
You see that in dealing with these layers and with our lenses, we are talking about very small numbers. People may be ‘thin-skinned’, as a figure of speech, when it comes to leaving curves behind and/or switching from millimeters to microns. But students in schools now start to think in microns first, with curves ‘second’. It may be time to move on.
AXL
Extending this to a new standard of care entering our field, myopia management: trying to not make this a lengthy article, myopia management is all about length. Myopia is an axial length disease. So, to keep it short, when you follow change in myopia development, it is all about axial length (AXL) of the entire eye. Managing myopia based on subjective or objective refraction is much too variant, and 0.25D steps are too coarse. At the recent ARVO meeting – the research congress in the ophthalmic field – the six-year data of a soft lens for myopia management (MiSight) was presented. This data showed that the maximum average change in six years that can be achieved is about half a millimeter: 0.529 mm, to be precise. Why not put this in microns? 529 microns sounds more exact and more applicable. In the MiSight study, 0.25D change in myopia was considered equal to 0.1 mm change…or shall we use 100 microns? Average growth of the eye between 10 and 13 years of age was 90 microns per year in the study, while for myopes not receiving treatment this was 160 microns annually. But the point is, shall we use microns here (instead of 0.09 mm and 0.16 mm, respectively, in this case)?
To follow change, this AXL measurement needs to be repeated on a regular interval (probably every six months). The changes are subtle; there is some discussion on what normal change is, and it may be dependent on the amount of myopia. But in any case, a parent would be more impressed if our treatment reached 110-micron reduction in myopia progression rather than 0.11 mm, presumably.
It is all about context. And what terms are used. n
Eef van der Worp, BOptom, PhD, FAAO, FIACLE, FBCLA, FSLS is an educator and researcher. He received his optometry degree from the Hogeschool van Utrecht in the Netherlands (NL) and has served as a head of the contact lens department at the school for over eight years. He received his PhD from the University of Maastricht (NL) in 2008. He is a fellow of the AAO, IACLE, BCLA and the SLS. He is currently adjunct Professor at the University of Montreal University College of Optometry (CA) and adjunct assistant Professor at Pacific University College of Optometry (Oregon, USA). He lectures extensively worldwide and is a guest lecturer at a number of Universities in the US and Europe.

32
GlobalCONTACT 3-21 FITTING BACKGROUND
Imaging techniques
Photograph
Kahlert (HFAK, Cologne, Germany)
What can be seen here?
During a routine procedure, a blood vessel was noticed in the temporal region of the iris during the examination of the marginal ring network of the right eye. This runs visibly from the outer edge of the iris (at approx. 8 o'clock) in a radial pattern to the centre of the iris and lies not in, but on the iris stroma.

Photo presentation: Students present their findings 1
Imaging technique:
Slit lamp (Haag-Streit BQ 900, Koeniz, Switzerland), diffuse illumination, image 1 with 25x magnification and image 2 with 40x magnification.
Finding:
Normally, the blood vessels contained in the iris stroma are not visible as they are hidden by the collagen fibres. The stroma contains the inner and the outer vascular ring, which are interconnected by small arteries. The blood vessels are responsible for supplying the iris with nutrients, transporting away metabolic products and foreign particles, and warming the aqueous humour in the anterior chamber of the eye so that it remains in motion.
The iris neovascularisation present here may possibly be the result of uveitis in the anterior segment of the eye (iritis), which can lead to rubeosis iridis.

Characteristics:
However, it is very likely that this is only a physiological anomaly, as the findings in relation to the medical history do not suggest a pathological change or possibly recurrent inflammation of the choroid in the iris area.
Further procedure:
No further therapy is necessary as progression of the neovascularisation is not expected due to the unchanged and persistent condition.
2
Marie
33 GlobalCONTACT 3-21 FITTING BACKGROUND
Blocking scleral lenses
Matching the tool to the back surface geometry
We at Larsen Equipment Design (LED) have been providing blocking solutions to the contact lens and IOL industries for decades. In the last few years, the concept of matching the convex blocking tool (arbor, chuck, etc.) to the back surface has re-emerged. This is especially true when making scleral lenses.


 By Erik Larsen
By Erik Larsen
In recent months we have attempted to provide matched blocking tools (arbors) to labs. We usually sell the blocking tools uncut so that the lab personnel can turn the tool to fit a range of back surface geometries. Thus, a set of five or six tools would suffice to span the range of the scleral designs. What has come to light is that some of the labs are making lenses under license to another lab. The licensed lens design is proprietary, and the licensed lab may not have access to the actual physical parameters of the back surface. The situation is problematic when they need to turn the blocking tool to approximate the back surface geometry of the lens. The basic idea of matching the blocking tool to the back surface geometry is to provide an approximate uniform
blocking compound (wax) thickness. The blocking tool would have a bi-curve (lenticulated) geometry that is close to the back surface geometry of the lens; only reversed. The benefit of this approach is to minimize the difference in wax shrinkage due to variation in wax thickness across the back surface.
We found (by graphics) that scleral lens designs in the 1416 mm diameter range may not benefit from the lenticulated blocking tool. The diameter of the base curve optic zone can be in the 11-12 mm range leaving a peripheral ring width of one to four millimeters. These lenses can have an edge lift of a fraction of a millimeter. The lens is about as thick as the edge lift, so deforming the edge due to wax shrinkage is
34
R8mm
A A B B 2 2 1 1 SV FINISH MATERIAL DIMENSIONS ARE IN INCHES TOLERANCES: FRACTIONAL: 1/32 ANGULAR: 1º FIRST PLACE DECIMAL: 0.030 TWO PLACE DECIMAL: 0.010 THREE PLACE DECIMAL: 0.005 FOURTH PLACE DECIMAL: 0.001 UNLESS OTHERWISE SPECIFIED: LARSEN EQUIPMENT DESIGN INC REVISION # REVISED DRAWN BY DATE SCALE: 5:1 APPROVED BY REQUIRED 1117 NW 52 ST SEATTLE,WA 98107 GlobalCONTACT 3-21 MANUFACTURING
R12mm 11mm 20mm 15mm
unlikely. For example (not a real lens design): A lens with a back surface radius (BCR) of 8 mm, optical zone diameter (OZD) of 11 mm, peripheral curve radius (PCR) of 11 mm, and a lens diameter of 15 mm. Here, a blocking tool with a single 8 mm radius would work fine because the increased thickness of wax at the edge is not enough to measurably pull the edge toward the arbor. The tendency of the wax shrinkage is to pull the edge of the lens toward the blocking tool resulting in a thicker edge than expected. In this example, the peripheral curve width is 2 mm with an approximate edge lift of around 0.7 mm. If the edge thickness is on the order of 0.5 mm, it is probably strong enough to resist deformation. So, when do you need a lenticulated blocking tool? Let’s look at a 20 mm diameter lens. Possible parameters could be: BCR of 8 mm, OZD of 12 mm, PCR 12 mm (again, not a real lens design). If we were to block this to an 8 mm single curve blocking tool, the edge lift at the 20 mm diameter would be about 2 mm. That is a volume of wax that will shrink significantly. If the effective wax shrinkage is 5%, that is a pull of 2 mm X .05 = 0.1 mm. The result is a thicker edge by about .1 mm. For an expected edge thickness of 0.5 mm, the actual edge thickness would be 0.6 mm. It is up to the fitter and patient to determine






if this is a significant deviation from the design of the lens. To be clear, the PC will return to the lathe turned radius, so the fit as indicated by fluorescein will not be steeper. However, the edge thickness may have increased which the patient may feel. Again, creating a blocking tool to approximate the back surface geometry is a good goal, but you need to temper that with the practicality of how many arbors you need to cover the range of scleral lens designs. Lenses in the 15-17 mm diameters are probably OK with the single radius arbors, but larger lenses may benefit with an arbor with a lenticulated geometry. n

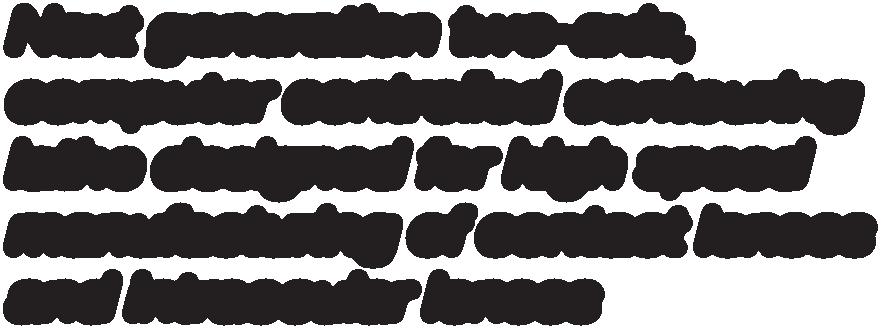
 Advertisement
Advertisement
MANUFACTURING
Erik Larsen graduated from the University of Washington with a Mechanical Engineering degree in 1981 and started Larsen Equipment Design later that year. Erik Larsen has industry awards from CLMA and EFCLIN.
New challenges in intra-ocular lens metrology

Recent functionalities and computation methods
As the complexity of IOL designs increases, metrology tools must become more and more powerful. Whether they are designed to generate multiple foci or an extended depth of focus, modern IOLs embed complex surface shapes and require ever more accurate metrology tools. By Luc Joannes
36 GlobalCONTACT 3-21 SPECIAL TOPIC
Besides the power and MTF benches described in the ISO-11979-2 standard, wavefront sensors are widely used in both R&D and production environments. Besides the instrument used for the raw measurement of the lens, a dedicated data processing and user interface is key for the IOL industry.

The Phase Shifting Schlieren, on which the Nimo technology is based, differs from other wavefront sensors methods by its high spatial resolution which makes the measurement of the most complex wavefronts possible and accurate.
The present paper introduces the most recent functionalities and computation methods implemented in the IOL-Mentor software application which push the limits of IOL metrology further.
A NEW SYNTHETIC MODEL EYE
The imaging performances of an IOL are evaluated in a lens system called ‘Model Eye’ (ISO-11979-2) accurately positioned in front of a wet cell containing the IOL (figure 1). The Model Eye simulates the power and spherical aberration of the cornea.
37 GlobalCONTACT 3-21 SPECIAL TOPIC
Fig. 1: An intraocular lens in the ISO-11979-2 Model Eye. Cornea model (left) and IOL in a wet well (right).
The imaging performance of the IOL is evaluated through the Modulation Transfer Function (MTF), at a specific aperture diameter (in the IOL plane) and for a given spatial frequency. The asphericity of the cornea model can be adjusted to match the manufacturer’s requirements.
To measure the MTF, a traditional lens bench takes both the cornea model and the IOL into consideration whereas wavefront sensors can measure the wavefront of the sole IOL. The contribution of the Model Eye can later be computed via numerical simulations. This capability has two major
advantages: in R&D, from a single IOL measurement, multiple Model Eye configurations can easily be simulated and compared; in production environments, the measurements are more consistent as they are not affected by the variability of the position of the IOL with reference to the cornea model. Ultimately, and this is non negligible, wavefront sensors and synthetic model eyes make it possible to measure IOLs in air and afterwards compute their performances in-situ and with the contribution of the Model Eye.


A straightforward method for the numerical simulation of the effect of the synthetic cornea on the MTF consists in summing the wavefront of the IOL and the wavefront the synthetic cornea generates in the IOL plane. This method, referred as ‘paraxial’, is valid for small apertures and when both the IOL and synthetic cornea have low aberrations, but it rapidly shows its limitations if these conditions are not met.
To overcome this problem, Lambda-X has developed a ‘nonparaxial’ ray-tracing method (patent pending) that is valid without restrictions on the amount of spherical aberration in the system. In contrast to the paraxial method, this non-paraxial approach accounts for the focusing effect of the Model Eye and therefore for the incident light entering the Model Eye not

Fig. 2: LB1157 simulated on Zemax
Fig 3: LB1157 processed on the Non-Paraxial Model Eye of IOL-MENTOR
Fig. 4: PMMA aspheric lens simulated on Zemax

Fig. 5: PMMA aspheric lens processed on the Non-Paraxial Model Eye of IOL-Mentor

38
GlobalCONTACT 3-21 SPECIAL TOPIC
Fig. 6: An EDoF IOL captured by IOLMentor and Nimo.
Fig. 7: Complex wavefront of the EDoF lens.
being collimated. In order to apply this method, the refractive index of the lens material and the overall lens geometry need to be taken into consideration as parameters for the measurement of the IOL (or its post processing).
The method has been validated against the lens design software Zemax for multiple IOL designs including toric lenses. A first demonstration is given in the simple case of a bi-convex glass lens (Thorlabs – LB1157) which has a power of 100D in air and a center thickness of 2.4 mm. The theoretical through frequency MTF in the best MTF (50 lp/mm) plane for an aperture diameter on 3 mm has been simulated in Zemax (figure 2). Figure 3 demonstrates the accuracy of the Non-Paraxial Model Eye available in IOL-Mentor. The MTF computed from the IOL wavefront measured first, in situ in a wet cell and then in air, perfectly matches the MTF simulated by Zemax. Note that the spherical aberration of the cornea model is chosen to be 0.1 µm but IOL-Mentor allows any value between 0.00 µm and 0.45 µm. IOL-Mentor can deal with any type of lens (biconvex, planoconvex) and any surface geometry (spherical, aspherical, toric, aspherical toric).
The method has also been validated for a 1.5 mm thick aspherical PMMA lens and for a large aperture (5 mm). Similar to the previous example, figure 4 is the MTF simulated by Zemax
Fig. 8: Measured through-focus MTF on the EDoF IOL. The aperture diameter is 3 mm and frequencies are 25 lp/mm (red), 50 lp/mm (Blue) and 100 lp/mm (Green). Power, cylinder and addition are calculated from the MTF peak positions at 50 lp/mm.
while figure 5 confirms the perfect match of the MTF computed by IOL-Mentor for the lens measured in air and in-situ.

EDOF CHARACTERIZATION
Nimo is also capable of measuring a large variety of extended depth of focus (EDoF) intraocular lenses (figure 6). Complex wavefronts can be captured as long as they do not include a diffractive step structure (figure 7). The through-focus MTF at a given frequency is generally used to extract the IOL power(s) and evaluate the imaging quality. Figure 8 shows the through-focus MTF curves of a commercial EDoF IOL measured with Nimo and computed with the Non-Paraxial Model Eye of IOL-Mentor. The cornea model has 0.15 µm of spherical aberration in this case.
CONCLUSION
The patent pending Non-Paraxial Model Eye implemented in IOL-Mentor opens way to a generalization of the use of wavefront sensors in IOL metrology for both R&D studies and production quality check.

Since the IOL can be measured in air and as a single lens, the operation is simpler, more consistent, and beneficial to IOL manufacturers and ultimately contributes to a better vision for the patient. n

39
GlobalCONTACT 3-21 SPECIAL TOPIC
THE PHASE SHIFTING SCHLIEREN, ON WHICH THE NIMO TECHNOLOGY IS BASED, DIFFERS FROM OTHER WAVEFRONT SENSORS METHODS BY ITS HIGH SPATIAL RESOLUTION WHICH MAKES THE MEASUREMENT OF THE MOST COMPLEX WAVEFRONTS POSSIBLE AND ACCURATE.
About the use of the “gel”-contact lens
Early guidebook for patients
The history of the soft contact lens spans just over half a century. The first publication on experiences with the soft plastic was published by the Prague researchers Wichterle and Lim in 1964. Their experiments with HEMA to produce contact lenses in a spinning process turned out to be almost adventurous. Due to the political situation, they were unable to complete the development. This was taken on by others, but it is to their credit that today the soft contact lens is used worldwide both as a refractive aid and as a therapeutic agent.
 By Hans-Walter Roth
By Hans-Walter Roth
There is little instructive literature from the early years of the hydrophilic contact lens. In 1971, the first Germanlanguage field report appeared in the clinical monthly bulletins, and in 1978 the first guidebook written by an ophthalmologist was published as a pocket book for patients. Until then, each lens manufacturer provided their own instructions for use for its product. Most of these writings are no longer preserved, now by chance a copy from the early years was found on Ebay. This document was published by the company Ergon from Prague, it was probably written around 1972. The company, which mainly supplied their products in East Germany in
40
EDUCATIONAL PUBLICATION
INSTRUCTIONS
COMPLICATION-FREE CONTACT
GlobalCONTACT 3-21 HISTORY
THIS HISTORICAL
CONTAINS THE MOST IMPORTANT
FOR
LENS WEAR, AND MOST OF THE RULES ARE STILL VALID TODAY.
those years, no longer exists. There is no information about its whereabouts. However, their instructions for use are still one of the standards for contact lens wear today. This historical educational publication contains the most important instructions for complication-free contact lens wear, and most of the rules are still valid today. For example, contact lens wearers were advised not to use cosmetics. Short fingernails ought to avoid conjunctival and corneal injuries. Eye drops or ointments should not be used together with lenses without medical advice.
Mercury-containing components such as thiomersal were intended to prevent fungal infestation, but led to toxic keratopathy in the sensitive eye. The alternative peroxide, originally recommended in a concentration of 10%, led to tearful epithelial damage of the cornea if neutralization was faulty.
Before sleeping, the contact lens should be removed from the eye. If the lens is stuck, it should be removed from the eye immediately. The same applies if rainbow-colored rings appear or the vision is fogged. After all, the symptoms of the tight lens syndrome or the overwear syndrome were already known, here you also have to remove the lens immediately. How to do that in an emergency is not explained in more detail.
NOTE ON POSSIBLE PROBLEMS
The trick to moisten the eye thoroughly beforehand is not yet known; many an erosio corneae after a failed attempt led the contact lens wearer to the outpatient eye clinic.
FIELD REPORT
IN 1971, THE FIRST GERMANLANGUAGE
APPEARED IN THE CLINICAL MONTHLY BULLETINS, AND IN 1978 THE FIRST GUIDEBOOK WRITTEN BY AN OPHTHALMOLOGIST WAS PUBLISHED AS A POCKET BOOK FOR PATIENTS.
The problems of dry eye are also mentioned. The room, in which one wears the lenses, is to be ventilated well, since the unsatisfactory air permeability of the lens can lead to oxygen deficit at the eye. The daily wearing time is thereby reduced.
Today, after 50 years, the soft disposable or disposable lens is one of the optics of choice, and complicated care procedures are eliminated with most replacement systems.
The biggest advance, however, is the price. Whereas the first soft hydrophilic lenses cost several hundred D-Mark each, today they cost only a few Euros. However, the risk of eye damage due to handling and hygiene errors or overlong wear remains. n
THERMAL DISINFECTION AND SAFETY INSTRUCTIONS
It is also advised to clean the hands carefully before each manipulation in order not to spread pathogenic germs to the eye. The lenses must be cleaned thoroughly after wearing and then sterilized. During the heat sterilization, which was common at that time, the container should be kept under supervision, because it could burst. After the heat treatment, the lenses may only be stored in a physiological solution, whatever was meant by that.
At that time, thermal disinfection was still a standard routine. The commercially available disinfectants of the time led to incompatibility reactions in many cases.
Dr. Hans-Walter Roth Institut für Wissenschaftliche Kontaktoptik Ulm E-mail: institut.roth.ulm@t-online.de

41
GlobalCONTACT 3-21 HISTORY
Under pressure
You may have heard about the impact that scleral lenses potentially may have on the intraocular pressure (IOP) of the eye. Is this true? And how harmful is it? Let’s see what the Contact Lens Evidence-based Academic Reports (CLEAR) papers by the BCLA (the British Contact Lens Association) have to say about this. These papers were published in the April issue of Contact Lens and Anterior Eye (open access) and consist of eleven different reports ranging from ocular anatomy and physiology to all types of lens modalities, including a special report on scleral lens fitting. The biggest hurdle for the team in writing the paper, and what generated the most discussion, was in fact IOP with regard to finding a well-balanced and evidence-based answer to the question raised above. By Eef van der Worp
GLAUCOMA
First things first: there is a beautiful but delicate balance between the amount of fluid that is produced by the ciliary body (which is located at the base of the crystalline lens) and the amount of drainage at the trabecular meshwork (located at the base of the iris anteriorly, in the corner that the iris forms with the cornea). The exact location of that trabecular meshwork and outflow is important, but we will get to that later. If the balance between the production and the drainage is ‘off’, then the pressure in the anterior chamber of the eye rises. This could lead to irreversible damage to the optic nerve head at the back of the eye – this condition is called glaucoma. The visual field of glaucoma patients can gradually decrease, which is usually symptomless until it is too late and only tunnel vision remains.
THE PRESSURE IS ON
So, the pressure is on eye care practitioners worldwide to monitor this on a routine basis, really. The IOP as such can be measured quite easily using an air-puff (non-contact IOP-

measurement) or by using a small probe that is placed on the cornea (after applying an anaesthetic) called Goldmann applanation tonometry. Basically, the amount of pressure needed to flatten the cornea to a plane state is converted to a number that is used in practice. The units used are millimeters of mercury (mm/Hg) pressure. Values under 21 mm/Hg are generally considered a safe level, although it can be a bit more complex than that in reality, but that is beside the point here.
ANCIENT SCLERALS
Ever since the very first introduction of (glass) scleral lenses, there has been talk about the potential effect that sclerals could have on IOP. One mechanism behind that could be that the scleral lenses exert force on the area where the trabecular meshwork is located and could prevent drainage. This indeed is the area where the scleral lens typically lands and rests. Another theory is that the ‘seal’ caused by sclerals may influence flow, and outflow particularly, of fluids in the anterior chamber. So why not just measure IOP during scleral lens wear and get on
42
GlobalCONTACT 3-21 COLUMN
with it? The problem is that it is hard to measure IOP during scleral lens wear because the scleral lens is literally in the way. The air forces or probe simply cannot be applied to the cornea during scleral lens wear. So, the first set of analyses of IOP in scleral lens wear always consisted of removing the lens and measuring IOP directly after lens removal. This has the obvious advantage that the lens is not in place at the time of measurement. Using this method, some found small but statistically significant increases in IOP.
THROUGH THE EYELID
To measure IOP with the lens in-vivo, it makes sense to measure the IOP not on the cornea but on the sclera just outside of the scleral lens borders. There are devices that indeed can measure IOP on the sclera or through the eyelid (no anaesthetic needed). The biggest pushback that studies with these instruments get is that the measurements are not the same as ‘corneal IOP’ and that the instruments are found to not be particularly reliable. Even so, using trans-palpebral IOP (measurement through the eyelid), two studies reported an average increase of 5.0 mm/ Hg after 1 or 4.5h of lens wear, while one study reported a 1 mm/Hg increase in IOP after 6h of lens wear.
THE HOLE STORY
A good new addition to the IOP-scleral story is a study in which investigators drilled a large hole in the center of the scleral lens and measured IOP through it. This does eliminate some of the other disadvantages. The lens is still in place, and we measure the corneal IOP values. They did report an average increase of 3.8 mm/Hg. An elevation in the measured IOP can occur quickly, as an increase was seen 1−2 min after lens application. A limitation of this method, though, is that the ‘seal’ that a scleral lens typically creates is broken. This model could be very viable though for fenestrated scleral lenses.
OPTIC NERVE HEAD OBSERVATION
The best thing to do, really, is to look at the optic nerve head directly and to measure the minimum rim width (MRW). Here, you can directly see and measure the effect of any potential IOP increase, if there is any. So far, two studies have looked at this. Maria Walker and colleagues in Houston (USA) have done some important groundwork in the field, and found a minimal effect on optic nerve head morphology in healthy adult eyes, using the non-scleral-lens-wearing eye as a control. Conversely, Samaha et al. from the University of Montreal (CA) observed a small but significant reduction in Bruch’s membrane opening minimum rim width after complete lens settling.
TAKE HOME MESSAGE
The take home message for clinical practice is that scleral lenses could alter IOP to some degree. But, the jury is still out, and definite conclusions cannot be drawn at this point based on the current evidence, the CLEAR paper states.
A couple of considerations for clinical practice: the values discussed are all averages, and relatively short-term effects were investigated. Potentially, the eye adapts to the new situation in the long run. Plus, there are huge inter-subject differences, and we cannot predict who will spike and who will remain stable, as Joseph Shovlin put it in a recent column in Review of Optometry. To add to the complexity, IOP measurement in keratoconus patients (a major indication for sclerals of course) is complex in itself, because the corneal parameters and rigidity are completely different from the normal cornea. Whether lens design, including non-symmetrical lens design options, is beneficial and could alleviate the problem is still to be seen. Avoiding scleral lenses in patients with progressive glaucoma seems to make sense but is not always easy. Sclerals are typically not worn ‘for fun’: there is usually a major indication to wear these lenses, and the benefits should be outweighed against the risks – while monitoring visual fields and optic nerve head changes. But in some other cases, alternatives, including corneal GPs, hybrids or soft custom lenses, can be considered potentially. n
Sources
- Barnett M, Courey C, Fadel D, Lee K, Michaud L, Montani G, van der Worp E, Vincent SJ, Walker M, Bilkhu P, Morgan PB. CLEAR - Scleral lenses. Cont Lens Anterior Eye. 2021 Apr;44(2):270-288
- Cheung SY, Collins MJ, Vincent SJ. The impact of short-term fenestrated scleral lens wear on intraocular pressure. Contact Lens Anterior Eye 2020;43(6):585–8.
- Fogt JS, Nau CB, Schornack M, Shorter E, Nau A, Harthan JS. Comparison of pneumatonometry and transpalpebral tonometry measurements of intraocular pressure during scleral Lens Wear. Optom Vis Sci 2020;97(9):711.
- Huggert A. Increase of the intraocular pressure when using contact glasses. Acta Ophthalmol (Copenh) 1951;29(4).
- Samaha D, Michaud L. Bruch membrane opening minimum rim width changes during scleral Lens Wear. Eye Contact Lens 2021 May 1;47(5):295-300
- Shovlin. Pressure Cooker. Review of Optometry. 2021 Aug 15th: p74.
- Walker MK, Pardon LP, Redfern R, Patel N. IOP and optic nerve head morphology during scleral Lens Wear. Optom Vis Sci 2020;97(9):661–8.
Eef van der Worp, BOptom, PhD, FAAO, FIACLE, FBCLA, FSLS is an educator and researcher. He received his optometry degree from the Hogeschool van Utrecht in the Netherlands (NL) and has served as a head of the contact lens department at the school for over eight years. He received his PhD from the University of Maastricht (NL) in 2008. He is a fellow of the AAO, IACLE, BCLA and the SLS. He is currently adjunct Professor at the University of Montreal University College of Optometry (CA) and adjunct assistant Professor at Pacific University College of Optometry (Oregon, USA). He lectures extensively worldwide and is a guest lecturer at a number of Universities in the US and Europe.

43
GlobalCONTACT 3-21 COLUMN
DAC International, Inc. Headquarters: 6390 Rose Lane Carpinteria, CA 93013 USA Phone: +1 805 684 8307 Fax: +1 805 566 2196 www.dac-intl.com info@dac-intl.com Europe: Phone: +44 (0) 7578 636 656 dgolden@dac-intl.com www.dac-intl.com

“Diamonds for all purposes”
APEX DIAMOND PRODUCTS LIMITED Unit 10, Bartleet Road, Washford Industrial Estate, Redditch,Worcestershire B98 0DQ
Unit 10, Bartleet Road, Washford Industrial Estate, Redditch, Worcestershire B98 0DQ
Tel: +44(0)1527 529011 Email: sales@apexdiamond.co.uk “Diamonds for all purposes”
United Kingdom
APEX DIAMOND PRODUCTS LIMITED www.apexdiamond.co.uk

Phone: +44(0)1527 529011 sales@apexdiamond.co.uk www.apexdiamond.co.uk
Diamond Tools
BRIO Ultrasonics
Calle Ciudad de Barcelona, 1J, Polígono Industrial Fuente del Jarro, 46988, Paterna, Valencia Spain
Phone: +34 96 134 11 09 info@brioultrasonics.com www.brioultrasonics.com
Machinery and Tools
Phone: +41 41 372 10 10 Fax: +41 41 372 06 83 www.efclin.com info@efclin.com
Boston Materials Group Bausch + Lomb Wintergasse 32 69469 Weinheim Germany
Boston Materials Group Bausch + Lomb Wintergasse 32 69469 Weinheim Germany
Phone: +49 6201 17869 tanja.malkus@bausch.com susanne.krostitz@bausch.com www.fit-boston.eu
Contact Lens Material
T +49 6201 17869 F +49 6201 62184 tanja.malkus@bausch.com www.fit-boston.com
Contamac LTD Carlton House, Shire Hill Saffron Walden Essex CB11 3AU United Kingdom
Phone: +44 1799 514800 sales@contamac.co.uk www.contamac.com Contact
K & Y Diamond Ltd. 1801 Boul Saint Regis Dollard-des-Ormeaux (Quebec) Canada H9B 2M9
Phone: +1 514 676 0640 Fax: +1 514 676 0645 sales@kydiamond.ca www.kydiamond.ca

44 46th EFCLIN CONGRESS EXHIBITION BUSINESS IN THE BEATING EUROPEAN FEDERATION OF THE CONTACT LENS AND IOL INDUSTRIES
Winkelbüel
Diamond Tools
EFCLIN
2 CH 6043 Adligenswil Switzerland
Association
Lens
Material
Machinery & Tools One Module per Year 510€ - 660€ please contact marie@global-cl.com
Contact Lens Handling Products For: Firm Lenses Scleral Lenses Hybrid Lenses Ortho K Lenses Available in Europe from: Prolens AG Josefstrasse 53 CH-8005 Zürich Switzerland +41 44 272 78 18 Zanesville, Ohio USA
® Contact Lens Handling Products For: Firm Lenses, Soft Lenses, Scleral Lenses, Hybrid Lenses, Ortho K Lenses Available in Europe from: Prolens AG Josefstrasse 53 CH-8005 Zürich Switzerland
+41 44 272 78 18 Manufactured by DMV Corporation Zanesville, Ohio USA www.dmvcorp.com Contact Lens Accessories
www.dmvcorp.com
Phone:
v1_58007_ADVERT_60MM_X_80MM_APEXDIAMOND.indd 1 12/11/2019 10:18
GlobalCONTACT 3-21 YELLOW PAGES
LAMBDA-X S.A. Avenue Robert Schuman 102 B-1400 Nivelles Belgium
Phone: +32 67 79 40 80 Fax: +32 67 55 27 91
info@lambda-x.com www.lambda-x.com
Instruments
Larsen Equipment Design 1117 N.W. 52nd Street Seattle, WA 98107 USA
Phone: +1 206 789 5121 Fax: +1 206 789 7756
erik@larsenequipment.com www.larsenequipment.com


Machinery and Tools
OPTOCRAFT GmbH Am Weichselgarten 7 D-91058 Erlangen Germany

Phone: +49 9131 691500 Fax: +49 9131 691511 sales@optocraft.de www.optocraft.de
MISUPCOTM
MisupcoTM Inc. 1378 Osceola Avenue Saint Paul, MN 55105 USA
MisupcoTM Inc. 1378 Osceola Avenue Saint Paul, MN 55105 USA
Phone: +1 651 353 8632 Fax: +1 651 698 0719 www.misupco.com mikef@misupco.com
Phone: +1 651 353 8632 Fax: +1 651 698 0719
mikef@misupco.com www.misupco.com
Blocking Wax
SCHNEIDER GmbH & Co. KG
Biegenstrasse 8 –12 35112 Fronhausen Germany
SCHNEIDER GmbH & Co. KG
Biegenstrasse 8 –12 35112 Fronhausen Germany
Phone: +49 (64 26) 96 96-0 Fax: +49 (64 26) 96 96-100 info@schneider-om.com www.schneider-om.com
Phone: +49 (64 26) 96 96-0 Fax: +49 (64 26) 96 96-100 info@schneider-om.com www.schneider-om.com
Instruments
RZ_Yellow_Pages_60x80_4C.indd 1
23.06.2020 12:37:08
Machinery and Tools S Y S T E M S Optimec Systems Limited Unit B3, The Haysfield Spring Lane North Malvern, WR14 1GF United Kingdom Phone: +44 1684 607006 www.optimecsystems.com info@optimecsystems.com Instruments TRIOPTICS GmbH Strandbaddamm 6 22880 Wedel Germany Phone: +49 4103 18006 0 www.trioptics.com sales@trioptics.com Instruments 45
Machinery & Tools Sterling Ultra Precision Division of AMETEK Precitech Inc. 8600 Somerset Drive, Largo Florida, 33773 USA Phone: +1 727 538 6110 fadi.achkouti@ametek.com Europe: +49 98 3797 8238 andreas.kuchler@ametek.com www.sterlingint.com Instruments V-Optics SAS 2, rue du travail 67400 Illkirch-Graffenstaden France
+33 (0) 3 67 10 28 60 info@v-optics.fr www.v-optics.fr GlobalCONTACT 3-21 YELLOW PAGES
Phone:
THE DIGITAL GLOBALCONTACT

The App on your tablet, smartphone or computer.
MASTHEAD GLOBAL

CONTACT
The Website and the Magazine: The complete communication system for the contact lens industry. The magazine, 2,500 copies, is distributed to contact lens laboratories, wholesalers and other organizations active in the contact lens and IOL industry. The website www.g lobal-cl.com is free for all industry related professionals
PUBLISHERS ADDRESS
Eyepress Fachmedien GmbH Saarner Str. 151, D-45479 Mülheim a. d. Ruhr Tel.: +49-208-306683-00 Fax: +49-208-306683-99 Website: www.g lobal-cl.com E-mail: info@ g lobal-cl.com
p.sioutis@eyepress.de
Silke Sage, Efstathios Efthimiadis, Petros Sioutis
EDITOR-IN-CHIEF Dipl.-Ing (FH) Silke Sage silke@global-cl.com britta@mafo-optics.com

John Saniter, Bopfingen, Germany
EDITORIAL BOARD
Wim Aalbers, Erik Larsen, Eef van der Worp
PRODUCTION & LAYOUT Efstathios Efthimiadis
PressUp GmbH, Postbox 70 13 11, D-22013 Hamburg Tel.: +49-40-386666-308, Fax: +49-40-386666-299
MEDIA CONSULTANT
Tel.: +49-208-306683-20 Fax: +49-208-306683-99 constanze@global-cl.com
ADVERTISING AGENT GREAT CHINA
Beijing FOCUS Optics Culture Commnication Co. Ltd. Room 319, Building 2, Nr. 1, Northbank 1292,
ocus@126.com Skype: jennywang611
FREE ACCESS
You do not have a subscription yet? Just go to our website and make sure you get all the benefits.

50
GlobalCONTACT 3-21
ADVERTISEMENT
Price list No. 10, valid from January 01, 2021 Publication Schedule 3 issues 2021: March, July, November SUBSCRIPTION COSTS PER YEAR European Union 80,00 € (plus VAT for German companies), Overseas Seamail 90,00 €, Overseas Airmail 110,00 €, United States Seamail 95,00 €, United States Airmail 125,00 €, Single issue 20,00 € (plus mailing costs) The Publisher requires three months written notice on cancellation. Subscribers please note that proof of notice may be required. BANK DETAILS Bank account: Sparkasse Aachen IBAN: DE21 3905 0000 1073 3925 06 SWIFT: AACS DE 33XXX PRODUCTION & PRINT Kollin Mediengesellschaft mbh, Neudrossenfeld The publisher takes no responsibility for unsolicited manuscripts. Please note also that photographs submitted for use in GlobalCONTACT cannot be returned. The publisher's written permission is required for any reproduction, translation or recording of material published in GlobalCONTACT, including extracts of such material. Permission will normally be given, subject to the usual acknowledgement. Copies made of published items must be limited in number and for personal use only. PHOTO CREDITS P.10: apinan, esthermm, P.12: Mulderphoto, P.16: Login, P.22: Lorant, P.30: New Africa, P.36: Axel Kock, P.42: witsawat /stock.adobe.com
of GlobalCONTACT App is now available
Nr. 15 Jianguo Eastroad, Beijing 100024 (Chaoyang), P.R. China Tel.: +86-10-8537-6529 g_f
RATES
Members
A WORLD OF OPPORTUNITIES 2022
Spanish culture combined with ancient and modern science has found Sitges/Barcelona to be the perfect location for business an d l e isur e ti me a s well. T h e 48t h EFCLI N Congres s & Exhibition takes place there f ro m 28t h – 30t h Apri l 2022. Fo r a n enga g in g lectur e p r o gram, manufacture r ’ s foru m an d th e best trade exhibition in the business, i t can’ t b e beaten . It’ s w here the Contact Lens & IOL Industry from Europe, the Far East, North Americ a an d beyon d com e together wil l yo u b e t he re?




48th EFCLIN CONGRESS EXHIBITION EUROPEAN FEDERATION OF THE CONTACT LENS AND IOL INDUSTRIES 28TH – 30TH APRIL 2022 BARCELONA/SITGES, SPAIN
REGISTER NOW WHILE THERE IS STILL TIME AT www.efclin.com/congress or e-mail us on
info@efclin.com
MORE INFORMATION
ADDRESS
WEB www.efclin.com MAIL info@efclin com PHONE +41 41 372 10 10 FACEBOOK search: EFCLIN TWITTER @EFCLIN#efclincongress
EFCLIN | Winkelbüel 2 | CH-6043 Adligenswil | Switzerland
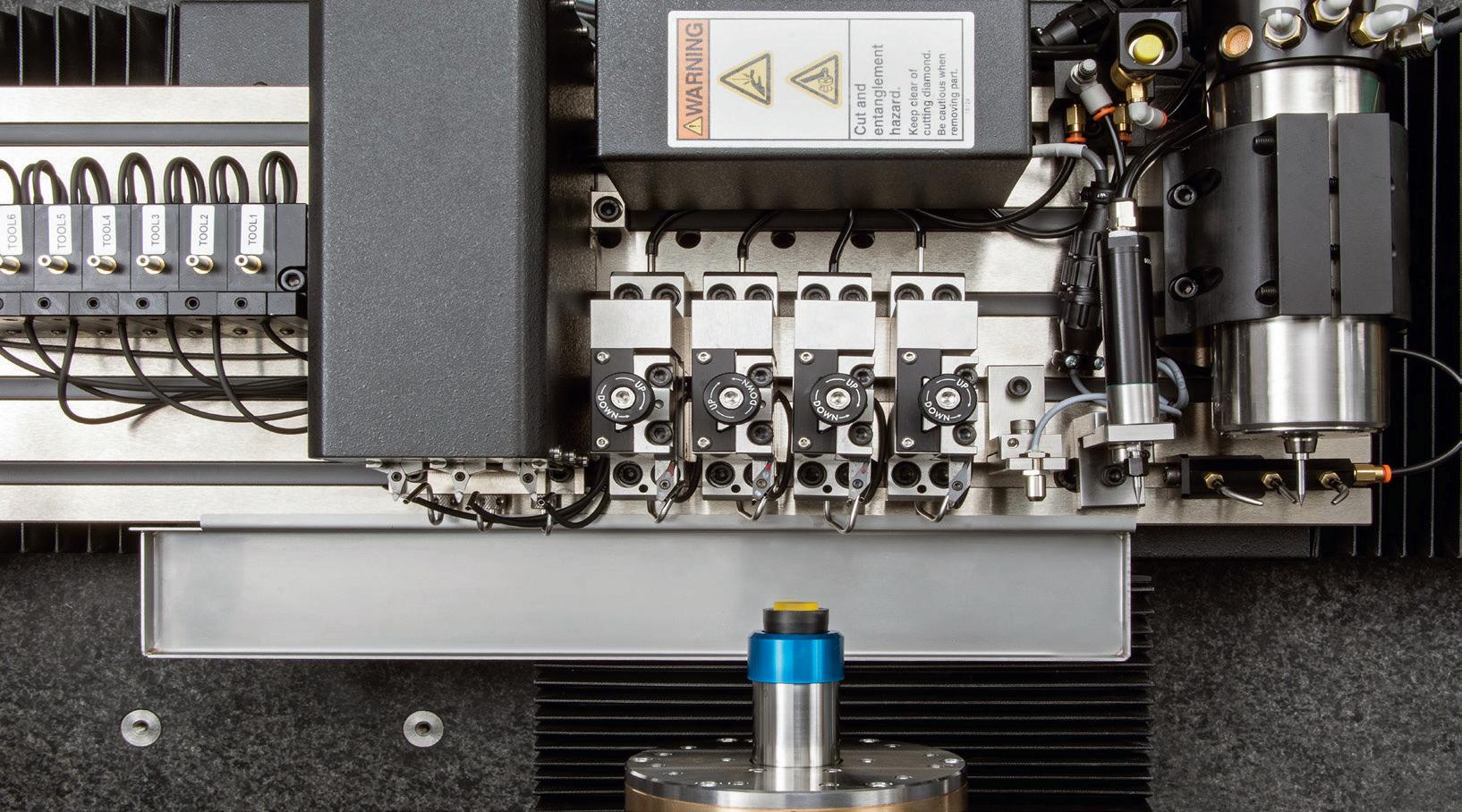
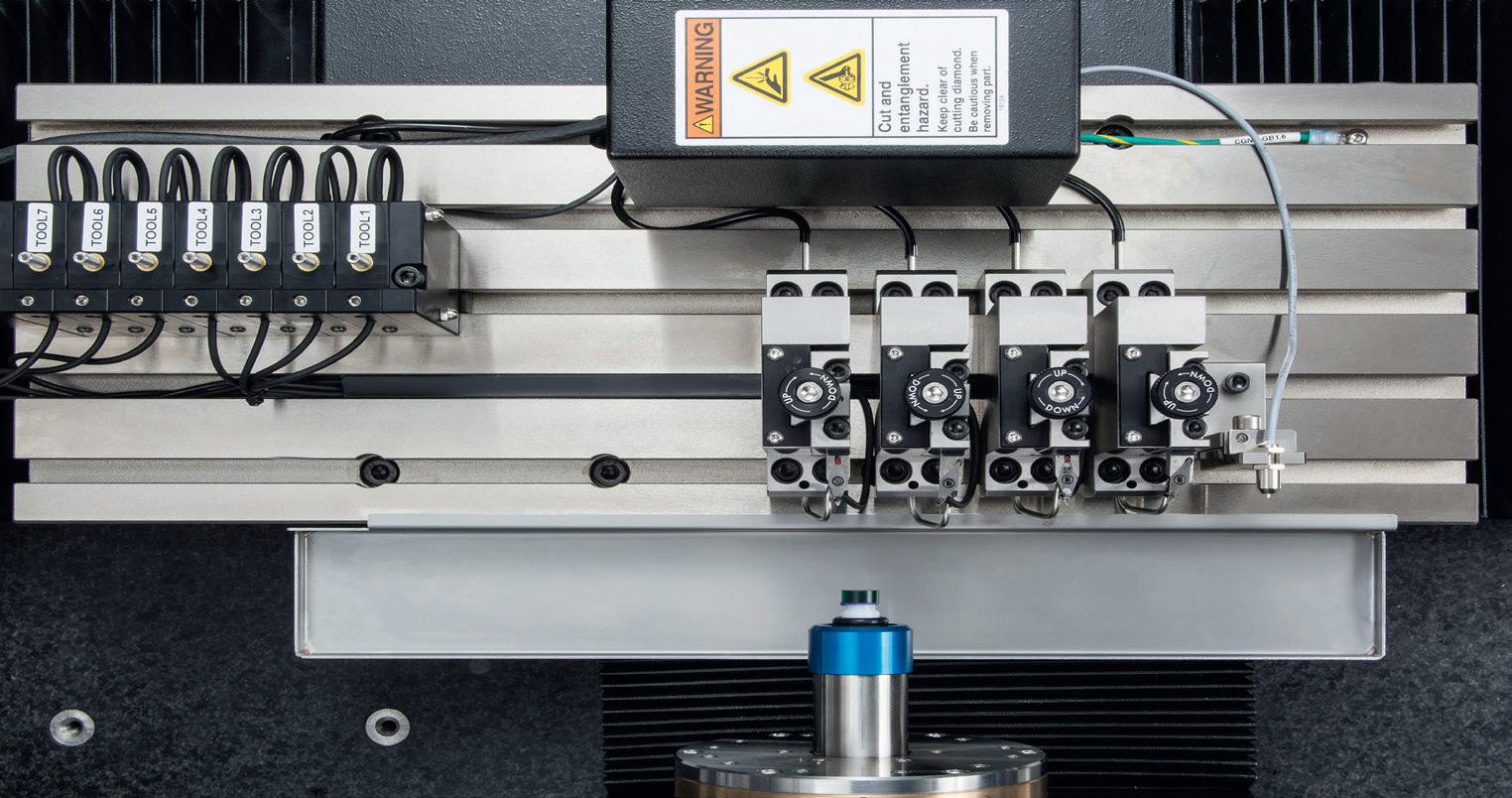
6390 Rose Lane, Carpinteria, CA 93013 USA Phone +1 805 684 8307 Fax +1 805 566 2196 dac-intl.com
Brown +1
745 1628
Chris Pantle +1 805 745 1610
DAC Offers Tooling Options That Grow With Your Business. THINK BIG START SMALL
Kurtis
805
kbrown@dac-intl.com
cpantle@dac-intl.com














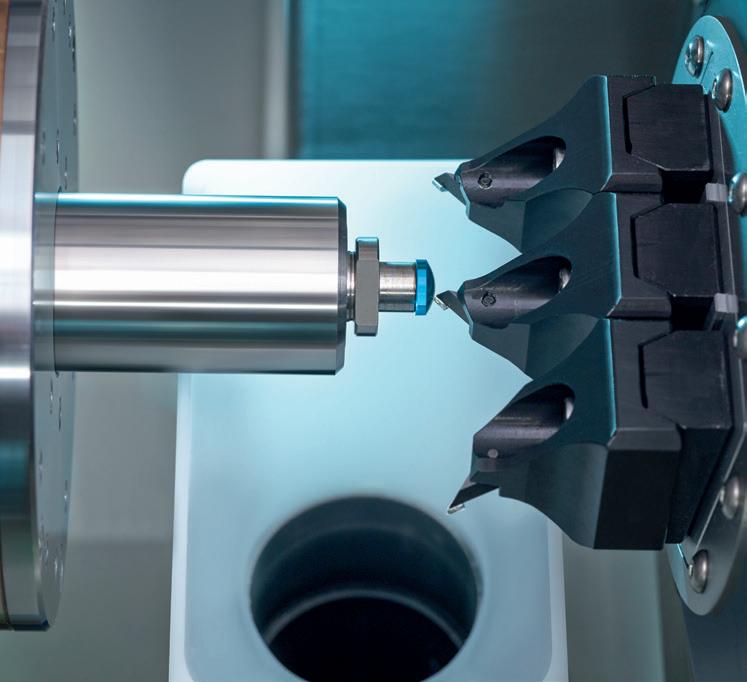












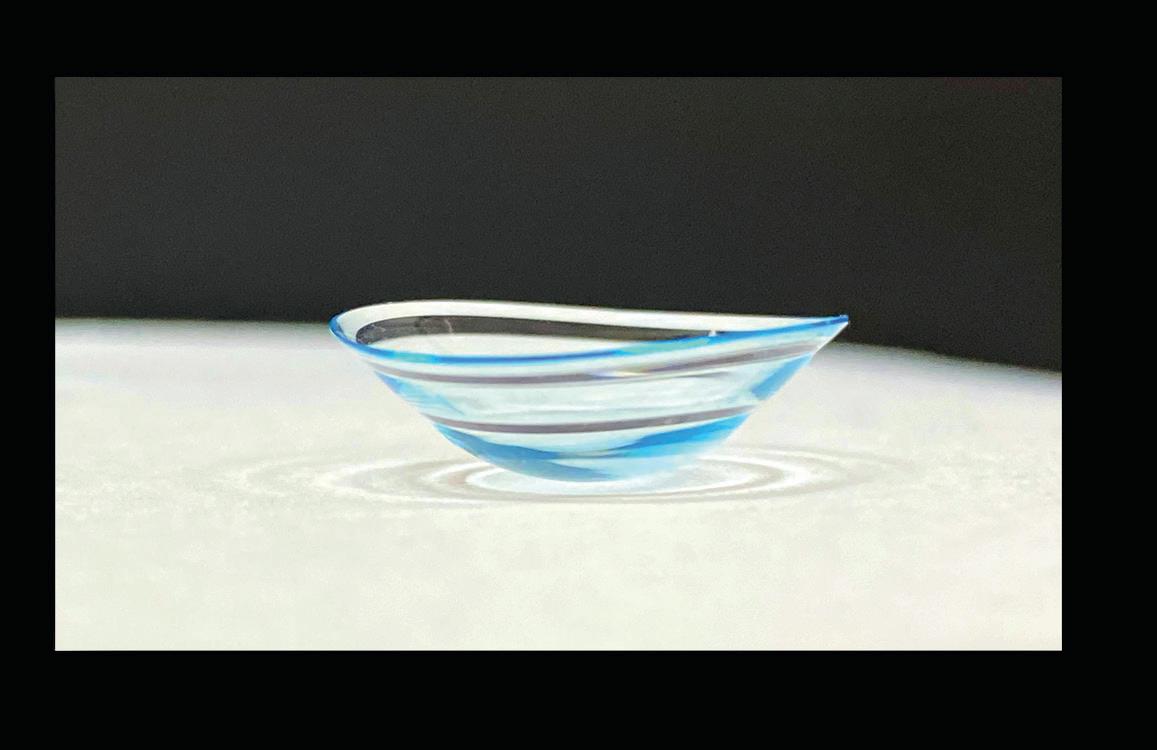






























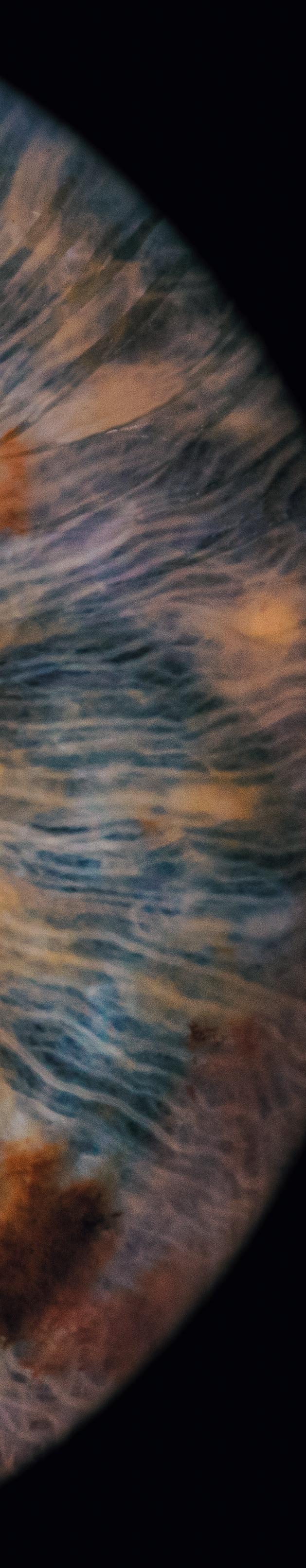





 Keith Parker President
Keith Parker President










 By Erik Larsen
By Erik Larsen

















 By Hans-Walter Roth
By Hans-Walter Roth