Evolving new consensus should help guide diagnosis and management.

The Power of Four Innovative procedures look at ways to use corneal lenticules. ALSO IN THIS ISSUE

Evolving new consensus should help guide diagnosis and management.

The Power of Four Innovative procedures look at ways to use corneal lenticules. ALSO IN THIS ISSUE
Refractive Femtosecond Laser Comparison Compare available refractive platforms at a glance.
Towards a More Inclusive Ophthalmology Working together to address the challenges of inclusivity and equity.
De veloped using a patented algorithm
Cr eated for maximum light utilization
Designed to redefine clarity and precision
Benefit from proven technology that minimizes disturbances while maximizing performance, ensuring unparalleled visual outcomes for every patient.
Available as:
• PRELOADED
• T ORIC
• 4 LOOP
• C LOOP







Finding a Keratoconus Consensus Evolving new consensus should help guide diagnosis and management.

04 Editorial: Beyond EURETINA: A loss for all of ophthalmology
06 Inside ESCRS: Survey is Informing New Leadership and Business Programmes in 2024
07 ESCRS Update: Inclusive Programming; IOL Calculator Update; Heritage Interview
08 ESCRS Analysis: Towards a More Inclusive Ophthalmology
16 Treating the Nonhealing Corneal Ulcer
Amy Lin MD
17 Alternatives to Penetrating Keratoplasty
Jennifer Rose-Nussbaumer MD
18 Ray of a New Dawn in Corneal Infection Research
Detlev Holland MD
20 New Approach to Keratoconus
Ceren Ece Semiz MD
21 A Promising New Option for Keratoconus
Bojan Pajic MD, PhD, FEBO
22 Knowing Iris Repair: Aniridia
Soosan Jacob MS, FRCS, DNB
&
24 Refractive Femtosecond Laser
26 Femtosecond Laser Table
28 Overcoming Obstacles to Presbyopia-Correcting IOLs
Joaquin Fernández MD, PhD
30 Flexing Four-Flanged Scleral Fixation
Markus Schranz MD
31 Hyperopic Lenticule Extraction
Pavel Stodůlka MD, PhD, FEBOS-CR
32 The Power of Four Suphi Taneri MD
33 Rethinking the Femtosecond Laser
Kevin L Waltz MD
34 Can Glaucoma Patients Gain Long-Term IOP Control?
Norbert Koerber MD, PhD and Simon Ondrejka MD
36 Combining Canaloplasty and Trabeculotomy
Melissa Chin MBBS, FRCS(Ophth) (Glasg)
37 Preserving the Ocular Surface
Matteo Mario Carlà MD





Publisher
Filomena Ribeiro
Executive Editor
Stuart Hales
Editor-In-Chief
Sean Henahan
Senior Content Editor
Kelsey Ingram
Creative Director
Kelsy McCarthy
Graphic Designer
Jennifer Lacey
Circulation Manager
Lucy Matthews
Contributing Editors
Cheryl Guttman Krader
Howard Larkin
Dermot McGrath
Roibeárd O’hÉineacháin
Contributors
Laura Gaspari
Soosan Jacob
Timothy Norris
Colour and Print
W&G Baird Printers
Advertising Sales
Roo Khan
MCI UK
Tel: +44 203 530 0100 | roo.khan@wearemci.com
EuroTimes® is registered with the European Union Intellectual Property Office and the US Patent and Trademark Office.
Published by the European Society of Cataract and Refractive Surgeons, Suite 7–9 The Hop Exchange, 24 Southwark Street, London, SE1 1TY, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983

We are deeply saddened by the sudden and unexpected passing of EURETINA President Ramin Tadayoni. European ophthalmology and the ESCRS have lost a true leader and inspiration, and many of us have lost a dear friend.
Death leaves a heartache no one can heal, but love leaves a memory no one can steal. The death of Professor Ramin Tadayoni weighs heavily on many hearts—not only in EURETINA, the society he served as the current president. A world-renowned retina specialist, Ramin has touched many hearts with his dedication, his noble character, his kindness. To know him was to like him—and to respect all his achievements. He was a man of great productivity, innovation, and, above all, integrity. His life was cut short at just 54 years old. Abraham Lincoln’s famous remark that it is not the years in our life that count but the life in our years is so true. And yet, it offers little comfort when faced with such a tremendous loss.
Professor Tadayoni was the Head of the Ophthalmology Department at the Fondation Adolphe de Rothschild and the Lariboisière and Saint-Louis University Hospitals in Paris; a Professor of Ophthalmology at the University of Paris; and former Head of the Retina Department at Cochin Hospital in Paris. He was also the Director of the new French Institute of Myopia. Ramin Tadayoni was known worldwide for his research on retinal disease, vitreoretinal surgery, and imaging. He was the author of nearly 200 medical and scientific articles and numerous contributions to ophthalmology textbooks.
In a heartfelt statement, the EURETINA board paid tribute to their beloved leader: “Ramin was a world-renowned visionary and a true force for good in the field of retina. He was a mentor to all who had the privilege of working
EDITORIAL BOARD
Noel Alpins (Australia)
Bekir Aslan (Turkey)
Roberto Bellucci (Italy)
Hiroko Bissen-Miyajima (Japan)
John Chang (China)
Béatrice Cochener-Lamard (France)
 Thomas Kohnen Chief Medical Editor
Thomas Kohnen Chief Medical Editor
Oliver Findl (Austria)
Nino Hirnschall (Austria)
Soosan Jacob (India)
Vikentia Katsanevaki (Greece)
Daniel Kook (Germany)
Boris Malyugin (Russia)

with him and learning from him. Perhaps most notably, he was a treasured friend whose loss feels immeasurable in this moment.” If you ever had the pleasure of meeting Ramin or, like almost all of us on our Society’s Board, had the privilege of collaborating with him, you’ll totally agree. ESCRS and EURETINA are partners in the best sense, and some of our annual congresses have been held within days of one another at the same venue. These congresses ran in perfect harmony, and the collaboration with Ramin was always uncomplicated and enjoyable for everyone involved. If you knew him, you liked him.
We at ESCRS are all feeling the pain of our friends and colleagues at EURETINA. Our hearts go out to Ramin’s family at this difficult time. We also want to say a big thank you to a wonderful ophthalmologist and inspiring leader: Ramin, you will be missed, but your memory will live on in our hearts forever. Rest in peace.
H Burkhard Dick MD, PhD
 José Güell Medical Editor
José Güell Medical Editor
 Paul Rosen Medical Editor
Paul Rosen Medical Editor
Marguerite McDonald (US)
Cyres Mehta (India)
Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands)
Filomena Ribeiro (Portugal)
Leigh Spielberg (The Netherlands)
Sathish Srinivasan (UK)
Robert Stegmann (South Africa)
Ulf Stenevi (Sweden)
Marie-José Tassignon (Belgium)
Manfred Tetz (Germany)
Carlo Enrico Traverso (Italy)
Burnout is a chronic issue in ophthalmology, leading a growing number to abandon the field early in their careers. What should be done to reduce unnecessary stress in training and practice, allowing for a successful long-term career?
Young ophthalmologists are invited to submit their answer to that question in an 800-word essay for the John Henahan Writing Prize. The author of the winning essay will receive a €500 bursary and a specially commissioned trophy, awarded during the 2024 ESCRS Congress in Barcelona, Spain. The winning essay will be published in EuroTimes.
The competition is open to ESCRS members (including the free membership available to trainees) age 40 or younger on 1 January 2024.
DEADLINE APPROACHING! Essays must be received by 14 June.
For details, please see the dedicated page on our website https://www.escrs.org/eurotimes/john-henahan-writing-prize
A
year-round programme will complement Leadership and Business Innovation Day at the 2024 Annual Congress.
BY STUART HALES, EXECUTIVE EDITORSpecialist training and qualification in ophthalmology might seem to be a ticket to financial security, but judging from responses to a current survey, many eye surgeons need more knowledge on how to effectively establish and manage a business— whether it be their private practice (should they choose to enter one) or a public/academic hospital.
The survey, conducted by the ESCRS Leadership Development and Business Innovation Committee, is designed to reveal the challenges facing ophthalmologists today and identify topics for future education programmes. The survey questions include:
• What is the one leadership skill you would like to improve?
• What is the one business management skill you would like to improve?
• If you were to attend a Leadership and Business Innovation programme this year, what topics would be of interest to you?
• Which topics would be of interest to you for a weekend workshop in 2024?
Financial literacy was the leadership skill that rated the highest (37.5%), while strategic planning (35%) and financial skills (29%) ranked highest and second highest among business management skills. More than half of respondents said they would attend a weekend workshop about business planning (53.8%) and financials for ophthalmologists (52.6%), and almost as many would attend a programme about financing a private practice in 2024.
“It’s clear we need to deliver a programme about business in healthcare, which will apply to those in private practice as well as those in government-funded practice,” says Paul Rosen, chair of the ESCRS Leadership Development and Business Innovation Committee. “We want to raise business standards in the public sector, but we also want to provide the necessary tools for people who want to develop their own private practice.”
The committee is planning an ambitious agenda for 2024 to address not only business and financial issues but also topics such as value-based healthcare and factors that influence patients’ care decisions. Two intensive weekend workshops and four podcasts are being lined up to support these learning objectives. The first podcast, which features David Lockington and Julien Buratto and focuses on achieving work-life balance and mentorship, will aim to provide prac -


tical advice and strategies to maintain personal well-being while managing professional responsibilities.
Additionally, on Sunday at the ESCRS Annual Congress in Barcelona, the LDBI Committee will (1) host a day-long programme geared towards practice administrators and clinic teams and (2) co-sponsor a lunchtime workshop with ESONT (European Society of Ophthalmic Nurses and Technicians) on successfully implementing innovative technology in your practice. (Space will be limited, and registration will be available through the Annual Congress registration website. Lunch will be provided.)
“With the help of the workshops, webinars, podcasts, and videos that will be conducted throughout the year— and the comprehensive programme at the Annual Congress—we believe we will be building a cohesive story,” says Basak Bostanci, another committee member. “We will also use social media
Whether you’re looking to refine your skills in a private practice, lead more effectively in academic or public health settings, or simply improve the operational aspects of your clinical practice, our 2024 offerings are tailored to help you succeed.

to actively improve awareness in the LDBI programme.”
The survey has also revealed a high degree of interest in mentoring and in a “mini-MBA” programme. Although the latter is especially challenging—“We’ve looked at that over the years, and it’s expensive to offer,” Rosen says—the committee is considering a streamlined certificate focused on leadership, which would offer essential business management skills at a fraction of the cost. To further reduce financial barriers for participants, the committee is investigating potential funding opportunities.
Together, the offerings in store for 2024 are intended to equip doctors at any stage of their career with essential business and leadership skills relevant to public, private, and academic practices. These skills are crucial for those aiming to establish or manage a private practice, lead in university settings, or enhance operational efficiency in public healthcare environments.
“Ophthalmologists should approach their public-sector practices with the same business acumen required in private practices,” says Artemis Matsou, another committee member. “The principles of efficient management are universal, whether in the public or private sector. Our aim is to provide the necessary leadership and management skills for both.”
ESCRS is conducting a survey to collect demographic data about the Society’s members and the ophthalmology industry at large and to identify the challenges ophthalmologists face daily in overcoming barriers to inclusion.
The survey is part of a larger initiative led by ESCRS President Filomena Ribeiro to create a culture of inclusivity for Society members, partner societies, industry, and ophthalmologists around the world.
“Our starting point is to enhance the collection and analysis of data and evidence about our membership, thus enabling us to better understand and acknowledge the needs and impact of our work,” Prof Ribeiro said.
The survey takes less than five minutes to complete and will enhance ESCRS programmes this year and beyond. The results will be presented at the Annual Congress in Barcelona in September.
The ESCRS online IOL calculator is becoming more powerful and useful with the addition of calculations for toric IOLS and ongoing efforts to include calculations for keratoconus and cases after refractive surgery.
Launched in 2022, the calculator has quickly proved its value, receiving more than 450 uses per day. The calculator employs web scraping to enable results from several current calculators, including Barrett, Cooke, Evo, Hoffer, and Kane, thereby allowing ophthalmologists to obtain multiple calculations with only one data entry session.
“The IOL calculator stands as a testament to innovation and collaboration within the ophthalmology community, bringing together experts with the shared goal of enhancing patient outcomes,” says ESCRS President Filomena Ribeiro.
Developed by Dante Luis Buonsanti and Miguel Raimundo, the calculator is gradually broadening its reach and attracting interest from other formula creators wanting to collaborate with ESCRS. In addition to the keratoconus and post-refractive calculations under development, possible longer-term enhancements include:

Scan the QR code to access the survey.
• Incorporating artificial intelligence more deeply into the calculator so surgeons can better understand the variables between different eye/lens structures; and
• Collating more specific data points around patients who have already gone through laser eye surgery and have cataracts.
A “Visionaries Past and Present” interview that recounts the evolution of IOL surgery from perilous to commonplace is now available for viewing.
The interview, conducted at the ESCRS 2024 Winter Meeting in Frankfurt, is moderated by EuroTimes Editor-in-Chief Sean Henahan and features Dr Richard Packard (Packard Medical Practice), Prof Thomas Neuhann (EuroEyes Clinic Group), and Prof Hans-Reinhard Koch (University of Bonn).
The professors describe early phaco surgery uncertainties, industry struggles, and the genius of IOL visionaries like Dr Charles Kelman and Dr Richard P Kratz.
The video is available at https://www. youtube.com/ watch?v=OpSBVDDCAsU&t=41s.

The only way to face challenges to inclusivity and equity is to work together without barriers.
LAURA GASPARI REPORTSAs 2024 marks an important year for ESCRS in raising awareness of diversity, equity, and inclusivity (DEI) issues in ophthalmology, many challenges need to be acknowledged and faced, according to ESCRS President Filomena Ribeiro MD, PhD, FEBO and ESCRS consultant Kris Morrill.
Professor Ribeiro stated clearly that social responsibility, equity, and inclusivity are the priorities ESCRS will embrace during her tenure as president.
“Diversity and inclusion are about making sure everyone feels welcomed and respected for who they are,” she said. “It is about understanding and appreciating that people are different in many ways.”
Most know uniqueness is strength, not weakness: in ophthalmology, it can bring different perspectives and experiences, enhancing innovation to achieve better results. Many challenges currently serve as obstacles to more inclusive, equal, and diverse ophthalmol-
ogy, such as the under-representation of minorities (especially in leadership positions), unequal career, mentorship, and surgical training opportunities. Additional discrimination factors include gender identity, sexual orientation, age, religion, and political views.
The more visible example is the representation of women in ophthalmology, especially as surgeons. A recent survey published by the Journal of Cataract & Refractive Surgery on surgical training in Europe revealed female specialists reported a mean 18% fewer entire cataract surgical procedures than their male counterparts. Women also felt less confident about their surgical skills, and female residents in ophthalmology reported continued gender bias.
“In 2024, we should not see barriers if people want to become surgeons in ophthalmology. There should be pathways to do that,” Kris Morrill stated. “It is very difficult to become a
We should not see barriers if people want to become surgeons in ophthalmology.
surgeon in certain countries—especially for women, because of family issues, motherhood, et cetera. This should not be happening, and we need to stop it.”
One of the greatest barriers to overcome is unconscious bias, or judging someone based on stereotypes and cultural backgrounds without even realising it. “The first step is to understand nobody is immune to
unconscious bias and all decisionmaking processes we make are influenced by it,” Prof Ribeiro said. In this regard, ESCRS collaborated with Project Implicit, a think tank led by scientists from Harvard University and the University of Virginia, in refining an online tool to measure unconscious biases.
“The immediate reaction I saw from most people was saying they had no biases; they were very open-minded and made no judgements,” explained Ms Morrill. “Then, you start to dig in a little deeper and realise every single decision we make is based on some preconceptions in our minds. So, you start to scratch the surface and start to think twice about decisions and how you react to people. It is a very interesting process.”
ESCRS is tackling this issue by introducing new activities addressing it, such as the workshop last Winter Meeting in Frankfurt. “Leaders need
to face this challenge to start a process of change that should be transversal to all members,” Prof Ribeiro affirmed. The next step, she said, is involving membership and industries. Frankfurt’s escape room experience took a step towards that, providing an opportunity for people to work together.
The ESCRS annual meeting in Barcelona will have a DEI symposium, workshops, and instructional courses. Most importantly, ESCRS is preparing a survey for its members to assess the real obstacles to DEI issues they face, using their input to develop a more effective DEI strategy. The survey is based on the one proposed by the British Hip Society and published in the British Medical Journal.
“As their demographics reflect ours, we asked their permission to use their survey with adaptations to ophthalmologists and to benchmark against another surgical society,” Ms Morrill
explained. The hope is this survey will establish a baseline as there is no existing data on the topic, according to both Prof Ribeiro and Ms Morrill. A good starting point is reflecting on the issue and working towards a common goal, even if the change will not be fast and smooth.
“I think people should plan to attend activities in Barcelona to learn and understand where we stand today as a Society, as well as where we want to go,” Ms Morrill concluded.
Even if surgeons think they know the way forward, Prof Ribeiro encourages attending the sessions willing to learn.
“It is important to be open-minded and willing to learn from others who are different from us,” she concluded. “By taking these steps, we can help break some barriers and create a more inclusive environment for everyone.”

Evolving new consensus should help guide diagnosis and management.BY DERMOT MCGRATH

One of the primary hurdles in managing keratoconus lies in defining progression reliably. Unlike many other progressive conditions, keratoconus lacks a universally accepted definition of ectasia progression, leading to inconsistencies in treatment approaches and clinical trials. Factors such as changes in corneal shape, visual acuity, and corneal thickness are usually considered, yet reaching a consensus remains challenging despite advances in imaging technologies.
“With better instruments, we have tighter measurements, but the current definition is still somewhat vague and less specific than most of us would like,” conceded José Güell MD, PhD. “Generally speaking, we are still following the guidelines that came from the first Delphi Panel, which was published in 2015.1 The guidelines need updating, and this is what we are just starting to work on.”
The progression of keratoconus is usually determined by comparing the results of corneal tomographic measurements
at different time points. Kmax (maximum anterior sagittal curvature) is the most commonly used parameter to detect or document ectatic progression and is also regularly used as an indicator for cross-linking’s efficacy. The Delphi Panel advised combining parameters from both the anterior and posterior cornea and corneal thickness, where the magnitude of the change is above the normal noise of the testing system. The panel acknowledged, however, that specific quantitative data to define progression is lacking.
In the absence of clear parameters, the discernment and experience of the treating clinician take on greater importance, Professor Güell noted.
“From my perspective, any increases in mean corneal power higher than 1.0 D or corneal astigmatism higher than 1.0 D are usually strong clues for deciding that keratoconus is progressing,” he said. “While there might be different opinions and nuances worldwide, these two main measurements are still broadly used to determine if a patient is progressing.”
Establishing a consensus on what constitutes progression is paramount, as it not only guides treatment decisions but also facilitates the development of uniform protocols for monitoring and managing the disease, Ingemar Gustafsson MD, PhD pointed out.
“The Global Consensus from 2015 is still valid, in that it tells us which anatomical changes we must consider. It also specifies that we need to consider what it calls the ‘noise’ or measurement error of the measurement system. However, we consistently fail at that aspect, which makes it so troublesome,” he said. “We have become fixated on detecting an increase of Kmax at 1.0 D, which is not so helpful in scientific and clinical practice. Many adhere to the classic increase of Kmax of 1.0 D—in part by tradition, in part because that is what many other clinicians use. I would be glad to review more articles justifying the use of the selected parameters for the diagnosis of progressive keratoconus and the evaluation of the treatment efficacy.”
With better technology available to clinicians, the critical question now is less about diagnosing a patient than determining the optimal intervention time to perform cross-linking, Dr Gustafsson believes.
“The diagnostic aspect is generally not difficult with modern Scheimpflug-based equipment and optical coherence tomography (OCT). For patients aged 18 or [younger], we proceed with cross-linking (CXL) upon diagnosis as we know these patients can progress rapidly. Otherwise, for patients 18 or [older], we make four initial measurements at one visit, and then we follow up after 4 to 6 months to see if there is any progression,” he said. “We include Kmax and the A (anterior), B (posterior), and C (minimal corneal thickness) parameters based on inter-day repeatability and stratified according to the disease severity. If there is no progression, we follow them for another 4 to 6 months [before making] another set of measurements after another year. If nothing happens, then we tell them to come back if they have any visual disturbances.”
Close follow-up of younger patients is advised given the risk of progression is much higher in this cohort, advised Prof Güell.
“For our young patients, a significant number of them will probably have progression in the 10 years following diagnosis. For those older than 18, if the proper treatment was performed and there is no subsequent trauma—basically no eye rubbing—then the number of cases with progression is extremely low,” he explained. “In cases of progression, we first need to check if the cross-linking treatment performed was the correct one. With the new modalities of epi-on, shorter treatments, new devices, et cetera, many patients have not received a standard protocol for treatment. The rate of retreatments in this particular population may be moderately high.”
Prof Güell noted the threshold to administer cross-linking has evolved since the Delphi Panel consensus, with surgeons now less concerned about possible complications associated with cross-linking.
“There is definitely less fear to indicate cross-linking despite not having objective information on the progression. Cross-linking has some potential complications, but the rates are quite low, and it is not always possible or practical to ask patients to undergo new examinations every few months,” he said. “For certain cases, we may decide to do cross-linking as a prophylactic treatment and not as a direct treatment for confirmed progression.”
He added a decision to treat may also be motivated by low patient compliance in the case of confirmed keratoconus.
“This is crucial because even with the best tools and technologies available, if the patient continues rubbing their eyes and does not respect the visit intervals for follow-up, then you have a major problem,” he said. “Although it is not my standard, if you think the compliance of your patient is going to be low, perhaps you will be more inclined to decide to perform cross-linking.”
Dr Gustafsson said the policy in his clinic is to perform cross-linking only if deemed necessary.
“We need to reflect on what is best for the patient and make the best use of our resources. We cross-link fewer patients in our clinic than before, even though we have many more new referrals. This is due to our more precise detection limits, which have reduced the number of unnecessary cross-linking procedures,” he said. “The CXL resources have thus been directed to those having the most to gain from cross-linking, providing a timely treatment which is essential in terms of preserving vision. Although cross-linking is safe in general, we prefer not to expose patients to a painful treatment and possible side effects unless we are sure it is appropriate.”
While advances in corneal imaging devices and artificial intelligence-driven algorithms should facilitate more accurate
and objective assessments, the effectiveness of these tools ultimately hinges on the availability of high-quality data for training algorithms, noted Olivia Li MD, a cornea consultant based in London.
“I believe we should be collecting quality data through routine practice in a way that can be used to inform and train algorithms and contribute to our knowledge of keratoconus in the future,” she said. “There needs to be leadership and engagement from all parties really to work towards that goal.”
Dr Li points to the medical retina domain, and diabetic retinopathy in particular, as an example of what can be achieved using the right approach.
“What we have seen is how diabetic retinopathy databases across the world have been the foundation of clinically useful algorithms that are now functioning quicker, better, and more efficiently than humans in terms of diagnosing classified diabetic retinopathy,” she said. “It is no coincidence that the first FDA-approved AI algorithm in health was for diabetic retinopathy screening.”
The key reason for that, Dr Li explained, is the longitudinal data set for diabetic retinopathy uses a standardized method to collect quality data from fundus images which are accessible, usable, and transferable.
“All of these factors currently limit many aspects of what we do in the field of cornea. Most corneal databases, even
internally within hospitals, are gathered across a number of imaging devices. And not all of them adopt the DICOM format—the usual means of storing and transferring medical images in a hospital’s database,” she explained. “That limits what you can do with the data. If you can’t get the raw image, you get derived parameters and human-generated numbers as a surrogate.”
Despite these drawbacks, Dr Li and colleagues at Moorfields Eye Hospital have drawn on more than a decade’s worth of longitudinal data of keratoconus patients to build a risk calculator capable of predicting progression and time to cross-linking.2
“It’s not perfect but it is certainly helpful in discussing various options with the patient and planning their treatment,” she said. “It’s particularly helpful for young people who have been otherwise completely healthy to understand the disease and its implications more because often these patients haven’t had to deal with a significant and life-changing diagnosis.”
Dr Li and co-workers have also focused on the variability of same-day measurements using the Pentacam HR (Oculus).3
“For the key markers commonly used to define keratoconus progression, we generated limits of agreement, so the clinician knows exactly what has been defined. The definition for progression is when the change is greater than the 95% limit of agreement,” she said. “Essentially this means

ESCRS iLearn is an online learning platform, free for ESCRS members.
Visit elearning.escrs.org to access over 30 hours of interactive, assessed, and accredited e-learning content, including surgical videos, diagrams, animations, quizzes, and forums.
there’s a 95% chance any change won’t be just from measurement variability.”
Moreover, the limit of agreement will change depending on the severity of disease present.
“Measurements are usually more repeatable for early disease and less repeatable for advanced disease,” Dr Li explained. “What we have done is to put numbers to the different levels of Kmax, K2, and pachymetry, and we have done that for every dioptre to refine the definition of progression based on severity.”
Although progress is being made to avoid both under- and overdiagnosis using such adaptive thresholds, there is still room for further improvement.
I would encourage colleagues to publish data in open-access repositories, collaborate, and create dedicated registries, as big data permits greater leaps in scientific progress.
“The problem is we still don’t really know what constitutes true progression. We have to draw the bar somewhere. A 1.0 D change in Kmax has worked relatively well for the last couple of decades as a decision for crosslinking—but we don’t know what the ground truth is as we
move towards a more holistic assessment of progression instead of relying on single parameters,” she said. “As we start to use raw images, we will probably get closer to a tighter definition of progression because the richness of the data offers a much greater dimension of studying the disease, enabling us to get tighter progression thresholds.”
With the latest Delphi Panel expected to start work later this year, the hope for everyone in keratoconus research is that a new consensus will finally bring clarity to existing grey areas. As Dr Gustafsson sees it, the key to making progress on all these issues lies in collective endeavour.
“I would encourage colleagues to publish data in open-access repositories, collaborate, and create dedicated registries, as big data permits greater leaps in scientific progress,” he concluded. “And don’t be afraid of using more recent detection limits while we await the outcomes of the next global consensus.”
For citation notes, see page 40.
José Güell MD, PhD is Director of the Cornea and Refractive Surgery Department at IMO Grupo Miranza and Associate Professor of Ophthalmology at Autònoma University, Barcelona, Spain. guell@imo.es
Ingemar Gustafsson MD, PhD is senior consultant of the cornea service at Skåne University Hospital, Lund, Sweden. gustafsson.ingemar@gmail.com
Olivia Li MD is a cornea consultant based at Chelsea and Westminster Hospital, London, UK. olivialieyes@gmail.com

Need a quick introduction or refresher about a surgical procedure? Have a tip to share about a technique or approach you use that makes surgery easier?
The ESCRS 100 is the place to go. It’s a library of short (roughly 100 seconds), high-quality instructional videos about all fields of cataract and refractive surgery.
More than a dozen videos have already been created, and additional videos are being uploaded each month. Current videos include the following topics:
• Phaco rolling
• LASIK: Lifting the flap
• Descemet membrane stripping
—PUT THE ESCRS 100 VIDEO SERIES ON YOUR LIST OF MUST-WATCH EDUCATIONAL RESOURCES !

Multipronged approach encompasses accurate diagnosis, recognising confounding factors, ocular surface support, and careful introduction of adjuvant treatments.
CHERYL GUTTMAN KRADER REPORTSRose Bengal-mediated photodynamic therapy (PDT) demonstrated potent antimicrobial activity against fungi and methicillin-resistant Staphylococcus aureus in vitro as well as encouraging results in a pilot clinical study investigating it to treat severe, progressive infectious keratitis.
Now, Rose Bengal Electromagnetic Activation with Green light is being evaluated as a treatment for fungal and Acanthamoeba keratitis in a randomised phase 3 study and will be tested for treating bacterial corneal ulcers in a second phase 3 trial, said Amy Lin MD.
While waiting to see if the PDT approach offers hope for providing better treatment for nonhealing corneal ulcers, Dr Lin described a practical approach for managing these challenging cases cornea specialists might consider the bane of their practice.
“Do everything you can to secure an objective diagnosis by taking a step back, getting a complete history, and keeping an open mind,” she said. “Then do everything you can to encourage healing, and proceed with caution using certain adjuvant therapies that can have benefits as well as risks.”
Gathering a complete history of past and current medications is important because one or more clinicians have seen some of these patients with nonhealing corneal ulcers. Steroid and topical anaesthetic use, in particular—often given out by emergency room doctors—should be elicited, Dr Lin said.
In keeping an open mind, she cautioned about avoiding the “anchoring” bias that occurs when paying too much attention to a single sign or diagnostic test.
“Keep in mind cultures are only positive about 50% of the time,” Dr Lin said. “So, consider reculturing, especially after stopping all medications for 24 to 48 hours, and using other testing, including confocal microscopy and, as a last resort, corneal biopsy.”
The presence of confounding factors that can interfere with therapeutic response should also be investigated. In
addition to topical anaesthetic use, these factors include topical medication-related toxicity, poor patient compliance, concurrent ocular surface disease or exposure, autoimmune disease, neurotrophic keratitis, illicit drug use, and severe nutritional deficiency.
In addition to antimicrobial therapy, supportive care to encourage healing is important for achieving a successful resolution. The approach should include aggressive lubrication with preservative-free artificial tears and ointments, punctal plugs, and autologous serum tears. Oral agents that inhibit matrix metalloproteinase-9 activity can also be prescribed, including vitamin C ≥1000 mg daily and doxycycline or minocycline ≥100 mg twice daily.
Although topical steroids, bandage contact lenses, amniotic membrane, conjunctival flaps, and topical cenegermin (recombinant human nerve growth factor) can be helpful adjuvants in certain situations, Dr Lin noted the need to use them cautiously considering their potential to be a double-edged sword.
“Steroids can interfere with epithelial healing and must be used carefully in fungal, Nocardia, and Acanthamoeba infections. Bandage contact lens application, amniotic membrane transplantation, and conjunctival flaps should only be done when there is good infection control,” she explained. “And while cenegermin can be helpful in cases of concurrent neurotrophic keratitis, it can exacerbate infection and inflammation.”
Dr Lin spoke during ASCRS 2024 Cornea Day in Boston, US.
Amy Lin MD is an Associate Professor (Clinical), Moran Eye Center, University of Utah, Salt Lake City, US. amy.lin@hsc.utah.edu
Cornea findings and comorbidities considered in surgical decisions for endothelial dysfunction.
CHERYL GUTTMAN KRADER REPORTSEndothelial keratoplasty (EK) has become the standard of care for the surgical management of endothelial dysfunction. And when it comes to choosing an EK procedure, Jennifer Rose-Nussbaumer MD relies on Descemet membrane endothelial keratoplasty (DMEK) as the workhorse for the majority of her patients.
However, Ultrathin Descemet stripping automated endothelial keratoplasty (UT-DSAEK) has an important role for select eyes with endothelial dysfunction, and some patients may even be candidates for Descemet stripping without EK (aka, Descemet stripping only [DSO]), Dr Rose-Nussbaumer said.
Descemet stripping only can be considered an option for patients with Fuchs’ corneal endothelial dystrophy having only central guttata (<4.5 mm) and a good peripheral endothelial cell count (≥1000 cells/mm2). Dr Rose-Nussbaumer observed the availability of imaging technology (CellChek 20 PLUS, Konan Medical) affording visualisation of the endothelium in the peripheral cornea enables her selection of patients for DSO.
Although technically a straightforward procedure, there are two keys to achieving success. To enable cell migration and proliferation, surgeons must incorporate as many guttata as possible and be careful to avoid disrupting the stroma.
Adjuvant use of a rho kinase inhibitor appears to improve DSO outcomes, although ripasudil, which is commercially available only in Japan, seems more effective than Europe and US-approved netarsudil. Further studies of netarsudil are underway. In the meantime, Dr Rose-Nussbaumer said ripasudil can be readily acquired through online sources.
DMEK vs UT-DSAEK
Although technically more difficult than UT-DSAEK, DMEK has an advantage of allowing faster and better visual recovery. As a tip for surgeons performing DMEK, Dr Rose-Nussbaumer noted controlling anterior chamber depth is important for enabling graft unfurling.
“Surgeons should modulate anterior chamber depth by allowing egress of fluid so that there is enough room for the graft to unfurl but not so much room for the graft to curl right back up,” she said.
Concern about greater endothelial cell loss over time after DMEK versus UT-DSAEK was raised in a randomised controlled trial conducted by Dr Rose-Nussbaumer and colleagues.1 The difference between procedures was not statistically significant in prespecified models but was in a repeated measures analysis. An ongoing National Institutes
of Health-funded trial is investigating if DMEK is still good for complex eyes and whether cell loss is higher in DMEK in general, which is important as it may reduce the longevity of the graft.
Dr Rose-Nussbaumer said she chooses UT-DSAEK in complex cases where difficulty with DMEK graft positioning is anticipated, such as in eyes with severe corneal scarring, aphakia, aniridia, or a scleral fixated IOL. She illustrated her point by presenting a patient who had sustained a traumatic injury leading to lens loss, implantation of a scleral-fixated artificial iris implant, and corneal oedema. The completed UT-DSAEK procedure used a pull-through technique with sutures to pull the graft into place. At six months postoperatively, the patient had 20/25 visual acuity.
If assistance is needed with visualisation during DMEK or DSAEK, Dr Rose-Nussbaumer said she has implemented anterior segment OCT or chandelier lighting.
“Inserting the chandelier is very straightforward, even for us as anterior segment surgeons, and has been a game-changer for me because it completely lights up the intraocular world,” she said.
Dr Rose-Nussbaumer spoke at ASCRS 2024 Cornea Day in Boston, US.
For citation notes, see page 40.
Jennifer Rose-Nussbaumer MD is Associate Professor of Ophthalmology, Stanford Byers Eye Institute, Palo Alto, California, US. rosej@stanford.edu


Will UVC light the way as a potential treatment for microbial keratitis?
DERMOT MCGRATH REPORTSAnovel treatment using ultraviolet-C (UVC) light developed by Photon Therapeutics Ltd shows promise as a potentially safe and effective alternative to existing treatments for microbial keratitis, according to Detlev Holland MD.
“It is still early days, but preclinical studies of low-dose UVC in vitro, ex vivo, and in vivo have shown promising results regarding safety and efficacy. It is fast and non-invasive and can be performed at the slit lamp,” he said. “If we have a treatment that can be used directly, which is quick and without complications, it could be really helpful in patients with corneal infections.”
Corneal infections are one of the leading causes of blindness worldwide, with patients suffering from a wide range of complications, Dr Holland noted.
“There is also the issue of increasing resistance worldwide to antibiotics, which is driving the search for new therapies,” he said. “UVC is directly targeted on the microbial DNA, so there is no resistance to this treatment.”
It is still early days, but preclinical studies of low-dose UVC in vitro, ex vivo, and in vivo have shown promising results regarding safety and efficacy.
Ultraviolet light has different wavelengths from 100 to 400 nm and is commonly divided into three bands: UVA (400 to 315 nm), UVB (315 to 280 nm), and UVC (280 to 100 nm).
“UVC is of particular interest as it is ‘germicidal’ and known to have efficacy against a range of microorganisms, including bacteria, viruses, fungi, and protozoa,” Dr Holland explained.
For the in-vitro tests, a range of bacteria—staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa, and streptococcus pyogenes—were exposed to a 4.5 mm diameter 265 nm


beam at a fixed intensity and distance of 8.0 mm for 1, 2, and 4 seconds.
“It was shown that as little as one second of UVC exposure had an anti-microbial effect. The density of growth inhibition increased with exposure time—and the highest efficacy in this test demonstrated for Pseudomonas aeruginosa and the least efficacy for E coli,” he said.
To evaluate the safety of UVC exposure at bactericidal doses, the team exposed confluent monolayers of primary culture of human corneal cells to UVC for 1, 2, 4, 5, 10, or 30 seconds. A live/dead cytotoxicity assay was then performed to measure cell death and compared it with a non-treated control group.
“The dead/live ratio was the same for the treated group as in the control group,” he said. “Moreover, the exposure time did not change the cell death ratio. So, it seems relatively safe with no adverse effects on the human corneal epithelial cells.”
Dr Holland also presented results from in vivo tests on mice, showing that UVC light is comparable to antibiotic treatment in reducing infection.
“The UVC light was comparable to the treatment eyes, which were treated with antibiotics,” he said. “A two-time application of 15-second UVC treatment was highly effective in managing P aeruginosa keratitis, with only 25% of mice requiring a second dose.”
Although further studies are needed to assess the safety and efficacy of UVC in human eyes, Dr Holland noted the
treatment may help to answer an unmet need in treating corneal infections.
“New treatment options could be very helpful,” he concluded. “Sometimes, when we have a patient with keratitis—and we don’t know exactly which bacteria we are dealing with— corneal scraping and lab tests can take 24 to 72 hours to yield results, prolonging the patient’s journey to treatment. UVC light therapy gives a potential empiric rapid and safe way to address these infections as it is effective against all microbes.”
Dr Holland presented at the 2024 ESCRS Winter Meeting in Frankfurt.
Detlev Holland MD is a cataract and refractive surgeon at Augenzentrum.ONE, Kiel, Germany. He is a shareholder in Photon Therapeutics Ltd. holland@augenzentrum.one
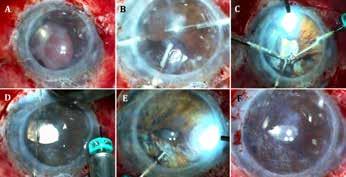
Corneal regeneration with lenticule implantation.
DERMOT MCGRATH REPORTSPatients with keratoconus and other progressive corneal diseases may soon benefit from a novel treatment involving implantation of intrastromal lenticules capable of stimulating corneal stromal regeneration, according to a study presented at the ESCRS Winter Meeting in Frankfurt.
“Fresh myopic intrastromal lenticular (FML) implantation seems to offer a safe, economical, and reliable technique that leads to increased corneal thickness, improved visual acuity, and the regeneration of healthy keratocytes, extracellular matrix, telocyte cells, and stem cells that are involved in stromal regeneration,” reported Ceren Ece Semiz MD.
FML may offer a number of advantages over current techniques to treat advanced keratoconus, which typically involve invasive surgery such as penetrating keratoplasty—carrying a high risk of complications such as infectious keratitis, tissue rejection, or even endophthalmitis.
Dr Semiz’s study included 60 eyes of 40 patients with advanced keratoconus indicated for corneal transplantation (stage 2 or 3 advanced keratoconus according to the Amsler–Krumeich classification) at the Eye Hospital Pristina, Kosovo. A lenticular implant was removed from donor patients who underwent SMILE (VisuMax; Carl Zeiss Meditec AG) surgery for refractive error correction. The lenticules extracted from the donor eyes were implanted in the 60 keratoconic eyes on the same day and followed for up to five years.
Dr Semiz highlighted key aspects of the surgery using the VisuMax femtosecond laser.
“The surgeon (Faruk Semiz MD) created a stromal pocket with a diameter of 8.00 mm, which is larger than the optical zone of the donor lenticule, and a cap thickness set to 130 µm from the corneal surface and a 2.09-mm incision according to high keratometric value,” she said.
Although intrastromal lenticule implantation has already been reported as a safe and effective surgical option for advanced keratoconus, previous studies have used lenticules preserved in eye banks or decellularised by cross-linking (CXL). The rationale behind Dr Semiz’s approach is the fresh lenticules contain extracellular matrix, keratocytes, telocytes, and stem cells—all of which play an integral role in stromal regeneration and damage repair. “Extracellular matrix provides a suitable environment for the implanted lenticule to survive, while telocytes are responsible for homeostasis, intracellular communication, and stem cell activation,” she said.
Another key consideration is the shape of the lenticule because the central part of the myopic lenticule is thick, whereas its periphery is thin.
“In the keratoplasty indicated advanced keratoconic eyes— even though the fundus examinations are normal—these eyes have high myopia due to irregular astigmatism and increased cornea elasticity,” she said. “Therefore, based on the topog-

raphy, the central thick part of the donor lenticule should be placed on the thinnest part of the recipient cornea to transform the conic cornea shape into an ellipsoid form.”
For histopathological, immunohistological, and electron microscope examinations, lenticular samples were randomly extracted from treated keratoconus patients several times in the one to five years after surgery. SMILE was not applied again. The extracted volume was then replaced with a new lenticule.
Electron microscope images showed disorganised and thinned collagen fibres as well as apoptotic cells in the cornea with keratoconus. In contrast, the control eyes implanted with the fresh lenticules demonstrated well-organised parallel lamellar structures.
Postoperative immunofluorescence images displayed both telocytes and stem cell-like cells. Additionally, five years after surgery, corneal biopsy samples were stained immunohistochemically with a CD34 marker to highlight progenitory cells and telocytes. An increase in progenitory and telocyte cell activity was observed, indicating stromal reorganisation and regeneration.
Dr Semiz presented at the 2024 ESCRS Winter Meeting in Frankfurt.
Ceren Ece Semiz MD is an assistant in the Department of Ophthalmology at Eye Hospital Pristina, Kosovo. cerensemiz99@gmail.com
Bowman’s layer transplantation shows promise in early trial.
TIMOTHY NORRIS REPORTSBowman’s layer transplantation (BLT) could soon become an effective and safe treatment option for patients with advanced keratoconus, offering a viable alternative when cross-linking and intracorneal ring segments are not valuable options due to corneal thinning or steepening, according to Bojan Pajic MD, PhD.
Cautioning this technique is still in the experimental stage—lacking a prospective study—he conducted a preliminary study aiming to investigate BLT as a potentially valuable technique for corneal ectasia stabilisation through the strength of the graft and wound healing reaction. The study sought to evaluate the hypothesis the acellular nature of Bowman’s layer graft could reduce the risk of graft rejection.
Before making the lenticule, Dr Pajic said it is necessary to mount the tissue in an artificial chamber. A lenticule with diameter of 8 to 9 millimetres and a 100-micron thickness, including the Bowman’s layer on one side, is then cut out from the graft with a femtosecond laser. After the preparation phase, the procedure can start with the femtolaser-induced dissection of the recipient cornea central stromal pocket over 360 degrees to the limbus (with a diameter of around 9 to 9.5 millimetres) to allow a safe insertion of the lenticule. The Bowman’s layer is then inserted into the recipient’s corneal pocket and stretched to the corneal periphery. As a sutureless procedure, BLT can decrease further corneal surface irregularities.
While this procedure could be done with a mechanical cut, Dr Pajic said a femtosecond laser is undisputedly a better choice for especially low tolerance, such as thin corneas. Femto-
second laser use, compared to mechanical cuts during corneal surgery, reduced higher order aberrations in the first postoperative phase while also significantly decreasing postoperative corneal oedema, which could be the cause of refractive errors.
“One month after BLT, patients with keratoconus showed a significant decrease in measured simulated keratometry of approximately 4.5 D and maximum keratometry of 7.5 D,” he said. “The flattening was particularly pronounced in advanced keratoconus cases with a central cone and remained significant one year postoperatively, but after that period we achieved good and long-lasting results in terms of visual acuity.”
The procedure showed low rates of complications. Of the 103 eyes in the study, only 3% required a consecutive penetrating keratoplasty. Six per cent of eyes developed acute hydrops, and 2% had mild keratitis. One case of Pseudomonas corneal ulcer caused by contact lens use was observed.
Despite these encouraging results, Dr Pajic stressed the need for larger prospective, multicentred studies to eventually confirm these preliminary findings. Moreover, with the addition of an intraoperative OCT, the safety and precision will also increase, he said.
Dr Pajic presented his research at the 2024 ESCRS Winter Meeting in Frankfurt.
Bojan Pajic MD, PhD, FEBO is Consultant in the Division of Ophthalmology, Department of Clinical Neurosciences, University Hospitals of Geneva, Switzerland.
Contact: YO@ESCRS.org YO.ESCRS.org

This next part in our series helps surgeons feel more prepared for aniridia cases.
DR SOOSAN JACOB MS, FRCS, DNBAniridia refers to the absence of iris tissue. It can be congenital or acquired and can be partial or total. Acquired causes include post-traumatic and iatrogenic (post-surgery).
Congenital aniridia is associated with a mutation in the PAX6 gene on chromosome 11p13. It is inherited most commonly as an autosomal dominant disease (85%), but also sometimes as autosomal recessive or as a de novo mutation (sporadic -13%).
Sporadic aniridia may be associated with Wilms tumour, genitourinary abnormalities, and growth retardation (WAGR syndrome). Wilms tumour is seen in one-third of sporadic cases since the deletion of the short arm of chromosome 11 may involve both the PAX6 gene and the adjacent Wilms tumour gene. Autosomal recessive aniridia is called Gillespie syndrome and has aniridia, cerebellar ataxia, and mental retardation as associations.
Congenital cases are not truly aniridic in the strict sense, as a small hypoplastic iris is often visible on gonioscopy. This peripheral stump can result in peripheral anterior synechiae and angle closure glaucoma by the second decade. Other associated ocular abnormalities include myopia, limbal stem cell deficiency, corneal pannus, microcornea, microspherophakia, cataract, ectopia lentis, foveal and optic disc hypoplasia, coloboma, nystagmus, strabismus, and amblyopia. Evaluation of family members and regular ultrasound for ruling out Wilms tumour is required in sporadic cases. Genetic evaluation may also be useful.
Traumatic and iatrogenic aniridia
Traumatic aniridia may occur following a blunt or penetrating injury where a part of or the entire iris is lost or has to be excised during reconstruction.
Iatrogenic aniridia refers to partial or complete loss of the iris during a surgical procedure. This may be intentional—e.g., a large sector iridectomy during a previous surgery—or accidental, such as inadvertent iris avulsion during phacoemulsification/cortex aspiration or nucleus extraction in manual small incision cataract surgery.
Congenital aniridia management
Patients with congenital aniridia should receive amblyopia therapy and treatment for strabismus. Coloured contact lenses or tinted glasses can help decrease photophobia and improve vision. Prophylactic goniotomy may be of benefit in preventing glaucoma. The onset of glaucoma should routinely be looked for, and surgery is often required for intraocular pressure control, with maximal success rates given by glaucoma drainage devices. Co-existing cataract and/or ectopia lentis may necessitate surgery if visually significant.
Aniridia IOLs and iris prostheses are available and will be discussed in the next episode of this series. Depending
on the severity, aniridia-associated keratopathy may need treatment ranging from just preservative-free artificial tears to simple limbal epithelial transplantation with or without keratoplasty. Graft failures are common, however. Prognosis for congenital aniridia is poor due to the frequently associated ocular comorbidities.
Large sector iridectomies may seem daunting to correct but can be tackled efficiently in many cases. Microforceps are introduced through a paracentesis, and the residual stump of the iris drawn in to see the actual available tissue, which is often more than what is initially visible because of the tendency for the cut ends of the iris to retract. In addition, the cut ends may fibrose and incarcerate into peripheral anterior synechiae (PAS)—often possible to release by careful blunt dissection from the overlying stroma, taking care not to tear the iris.
The risk of creating a Descemet’s detachment during synechiolysis decreases by pushing the iris away from the cornea rather than pulling it towards the anterior chamber (AC). A microscissor can be useful to cut the corneal attachment of the PAS. Some bleeding may occur during these manoeuvres, and continuous infusion through an AC maintainer serves to tamponade and arrest bleeding. This can be aided by withdrawing instruments temporarily and increasing infusion pressure. Alternately, all manoeuvres may also be done with viscoelastic filling the AC.
Once the iris stumps on either side are released, the microforceps gently stretch the two ends towards the centre to see how much mobility can be obtained towards the opposite stump and the intended final position of the pupil. If impossible to repair, iris prosthetic devices may be used.
If apposition is possible, a combination of several techniques continues iris repair. Care should be taken to use
gentle, controlled manoeuvres to prevent iris tearing, iridodialysis, haemorrhage, and other complications.
An SFT technique brings the two edges of the iris stroma together. Decreased tension on the iris leaflets can be attempted, released by gentle and careful tugging on the iris roots to release any small synechiae in the angles. Multiple SFT passes taken adjacent to each other approximate the iris leaflets as much as possible without causing cheese-wiring or iris stromal holes.
This initial part of the repair results in the two iris leaflets coming together in an iridodialysis-type configuration.
The next part of the repair therefore addresses the gap present between the distal arc of the repaired iris and the scleral wall. The motility of the repaired iris towards the scleral wall and the displacement of the pupil on attempted apposition of the iris to the scleral wall are assessed both visually and by using microforceps to gently manipulate the iris.
In case the iris is mobile—but the pupil gets displaced on the apposing iris base to sclera—a trocar-assisted hang-back technique may be performed using a double-armed 10-0 or 9-0 polypropylene suture with long, thin needles on both ends. The iris is ‘hung back’ in a non-appositional manner from the scleral wall using the prolene suture, allowing the pupil to
remain in the desired location. For a detailed description of this technique, see part three of this series on iris repair.
Classical iridodialysis repair
In case the iris is mobile enough to appose against the scleral wall without displacing the pupil being displaced, any one of the various iridodialysis repair techniques is acceptable.
Pupillary relocation
If the pupil is pulled to the side of scleral fixation, it can be recentred using the vitrector or microscissors to enlarge the pupil in the desired direction. If this enlarges the pupil too much, an additional SFT on the iridodialysis side (provided iris tissue allows) makes it small again. Mid-stromal iridodiathermy on the side to which the iris needs to be moved using the endodiathermy probe with just sufficient power to cause mild iris stromal contraction can also help relocate the pupil.
An alternate repair method is to first sclerally fixate the stumps of the iris, align them towards each other, close the gap using an SFT suture, then centre the pupil (see Figure).
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.

There are many different femtosecond laser surgical platforms to choose from, and it can be hard to keep them all straight. We have prepared a table allowing you to compare these at a glance, along with some comments from some of our members who use these lasers regularly.
Béatrice Cochener-Lamard MD, PhD on the ELITA Femtosecond Laser by Johnson & Johnson Vision (J&J).
“After many years of using lenticule extraction surgery, we are now seeking new strategies in refractive surgery, aiming to transform the procedure from a product to a true concept. As one of the biggest fans of lenticule extraction surgery with SMILE, I was contacted by J&J—a pioneer in femtosecond laser—and asked to become one of the European investigators for their new platform called ELITA.”
One of the main features of ELITA Femtosecond Laser is the new proprietary procedure of lenticule extraction, smooth incision lenticule keratomileusis (SILK). According to Prof Cochener-Lamard, ELITA is providing the same outcome in terms of safety and efficacy compared to the VisuMax 800 (SMILE) platform, with a visual recovery of two to four days and a short learning curve. The specificities are based on the biconvex profile of the lenticule, which receives half of the correction on each side, extended by a thin layer addition “flat-add” at the periphery that facilitates the removal of the lenticule.
“We have no intraoperative complications to report after more than 150 cases performed in our centre. The treatment nomogram integrates corrections of spherical aberrations, compensation of the applanation effect, and transition zones. Like all the other recent KLEx devices, the machine offers adjustable centration and compensation of cyclotorsion thanks to an interactive screen.”
The ELITA platform is on an ongoing trial in 50 centres. It was approved by the US FDA and recently validated with the CE mark.
Francesco Carones MD on Alcon WaveLight® FS200 Femtosecond Laser.
A valid and easy-to-use device, the FS200 by Alcon WaveLight® allows the
surgeon to perform LASIK procedures, corneal inlays, and intrastromal channels for segments.
“This device always keeps paying off. After 10 years of continuous use, I never encountered a single major issue. Never a poorly cut flap, nor the need to stop mid-procedure.”
The FS200 stands out for the twostage suction system: while the first part applies a vacuum between the suction ring and the patient’s limbus, the second stage connects the suction ring and the applanation cone. With this, the eye remains very still, creating a wonderful stabilisation both for the alignment phase and the procedure. It might not be very easy to perform at first and may require a little practice, he observed.
Another important feature of the FS200 is the ability to customise, adapt, and modify data, even after the suction phase. Dr Carones noted it is not necessary to centre before this phase. If a decentration is detected, the only way to fix the issue is to repeat the alignment. On the contrary, the FS200 makes it possible to adjust via software by calibrating the X and Y axes and the cyclotorsion right on the spot.
The FS200 is fast, creating an 8.5/9.0 mm flap in 9 to 12 seconds, which Dr Carones said could be further improved with a quicker scan time. It would also benefit from the implementation of a remote assistance service, he noted.
Antonio Leccisotti MD, PhD, MSc, FWCRS on FEMTO LDV Z8, Ziemer. “I have operated around 100,000 eyes performing LASIK and femto-LASIK in my career—of which I conducted at least 90,000 with the FEMTO LDV Z8 by Ziemer. This is a device that always provided optimal flaps, very few losses of suction, almost no cases of DLK, but especially smooth cut surfaces every single time. It is the most advanced instrument in our armamentarium.”
The LDV Z8 features a moveable and articulated arm that can be placed over the patient, bringing the machine close to the eye and not vice versa. This provides better handling of the device, allowing a swift switch from a femto to the excimer laser, like in the case of a LASIK procedure, he suggested. Moreover, LDV Z8 also comes with an integrated
intraoperative OCT scan acting as guidance and providing information during surgery and an automatic centration/ alignment option, very useful in KLEx.
What makes this device special is also the laser, Dr Leccisotti explained. Set at low energy and with small, narrow impulses, it can create a very smooth surface, sensibly improving precision and refractive outcomes. Along with LASIK, cataract, intrastromal lens, and corneal transplants, the LDV Z8 provides the surgeon with the means to perform CLEAR, an application enabling a safe and fast KLEx. It is also “a wonderful machine for lenticule extraction,” he observed.
He commented the laser velocity is a little slow when it needs to perform the cut. But the device overall is safe and effective and so simple to use—it could be used in training.
Roberto Bellucci MD on Bausch + Lomb VICTUS®
“I have a long experience with the VICTUS device by Bausch + Lomb. I started using it in 2012 for cataract and LASIK surgery, and I am still using it today.”
A great fan of VICTUS, Dr Bellucci considers it an incredibly versatile device for LASIK, capable of “making even a cup of coffee if the surgeon re-
Laser Type: Pulsed femtosecond solid state laser, Laser class 4 (IEC 60825-1)
Wavelength: 1030 +/- 5 nm
Pulse Duration: 350 (+50/-150) fs
Pulse Frequency: 200 kHz
Patient Contact Interface: Applanation cone supported with automatic Beam Control Check (BCC), Suction ring, Vacuum tubing
System Components: Main laser unit; Swivelling patient bed; Operator interface, including keyboard, control panel, moveable joysticks, and high-resolution monitor; Highly advanced microscope; Applanation cone; Control panel patient bed; Laser and centre pedal; WaveLight® FS200
Femtosecond Laser Patient Interface
Laser Type: Diode-pumped, solid-state laser (DPSSL)
Wavelength: 1040 +/- 25 nm
Pulse Frequency: 80 or 160 kHz, depending on procedure
Pulse Duration: 290–550 fs
Patient Contact Interface: Suction ring type
System Components: Main laser unit; Patient bed included; Sterile Patient Interface kit; Visualisation; Real-time, high-contrast and high-speed Swept-source OCT; High-resolution video camera; Optional external microscope; Patient interface intelligent pressure sensors, Curved patient interface with separate suction cup
Laser Type: Mode locked, diode-pumped, Ytterbium-doped fibre laser
Spot Size: < 2 µm
Pulse Frequency: 10 MHz
Wavelength: 1040 nm
Pulse Duration: 100–200 fs
Patient Contact Interface: Suction ring type
Patient Interface: Single use
Laser Type: Class 3b
Repetition Rate: Up to 4 MHz
Max Laser Output Power: 500 mW
Wavelength: 1030 +/− 50 nm
Pulse Duration: < 295 fs
Operating Conditions: Room temperature 18–24°C
Relative Humidity: 30–70%
Interface: One-size patient interface for single use
Other: Eye tracking semi-automated centring of patient eye, including static cyclotorsion compensation
quires it, so to speak,” he complimented with a bit of humour.
As a pre-KLEx generation femtosecond laser, it is an extremely adaptable instrument, capable of doing almost everything, from LASIK to cataract, astigmatic cuts, intrastromal rings, and corneal transplants in a very reliable and safe manner, Dr Bellucci observed. It is very fast by today’s standards, able to cut a flap in less than 20 seconds.
VICTUS features an intraoperative camera and OCT that gives the surgeon the possibility to observe corneal flap formation from different perspectives.
“You can observe the thin line of bubbles forming in real time and [the
Applications: LASIK, lamellar and penetrating keratoplasties, intracorneal ring segments
Features: WaveNet™ Computer Network, PerfectPulse Technology™, Smart Calibration and Beam Control Check (BCC), Advanced Suction Technology for patient interface
Applications: cataract, LASIK, intrastromal rings, keratoplasty
Features: Intraoperative camera OCT, Suction ring separated from the device
2010
Applications: SILK, LASIK
Features: Cyclotorsion, Biconvex lenticule shape, Fast tight pulse delivery scanning, Sub-micron precision optics, Ultra-precise laser pulse, Interactive screen
Applications: KLEx, LASIK
Features: Cyclotorsion compensation, Single-size patient interface, Semi-automated eye tracking-guided centration and docking
November 2011
March 2023
July 2020
depth of] the cut, a beautiful feature that can have maybe less use in LASIK than in cataract, but it is a fascinating spectacle on its own.”
One of the strongest points of VICTUS, Dr Bellucci noted, is the suction ring. Although separated from the device, it can be applied with a little help from intraoperative microscopy. The ring is placed on the perilimbal conjunctiva and has a two-phase suction, adjustable to maximise precision. Surgeons can centre their procedure on the clip, but with VICTUS, they can also move the clip if the centration is insufficient.
Ivan Gabrić MD on SCHWIND ATOS femtosecond laser.
“We always thought KLEx would never be a match for LASIK, as the early visual recovery was measured on days, not hours. Also, with the lack of cyclotorsion control with previous generation devices, it was not great for high astigmatic corrections. We thought lenticule procedures will always take longer to recover. However, with the SCHWIND ATOS femtosecond laser, each challenge fell apart quickly. KLEx is not a difficult surgery anymore, and with properly optimised laser settings and surgical techniques, more than 95% of patients have monocular vision of 20/20 or better on day one.”
One of the best features of ATOS is customisation, Dr Gabrić said.
“Everything can be surgeon-tailored, making every little desired change in settings, including optical zones of up to 8.0 mm. It can be a little
challenging and overwhelming for inexperienced users at first, but after a dozen cases, it’s easy. Docking is semi-automated and amazingly easy and fast to achieve, and the device allows a KLEx with zero lenticule thickness edge for safer removal.”
Moreover, he reported integration of other external diagnostic hardware and software is possible and simple. It can be a little slow in the warmup and the energy check, but once the laser fires, it is quick.
Simonetta Morselli MD
on ZEISS VisuMax 500 and 800. “VisuMax by Zeiss is the first femtosecond laser of this new generation. It is a trailblazer and the first device allowing the surgeon to perform lenticular surgery, the original ReLex SMILE. I have been using this device since its release in 2012.”
VisuMax has all the features required for a highly customisable refractive surgery, with a very versatile laser that provides all the options for a personalised LASIK and KLEx—by selecting flap thickness, depth of residual posterior stroma, and myopia correction from -0.50 D to -10.0 D with -5.0 D of astigmatism, she noted.
The laser is still a bit slow on the SMILE side, with 32 seconds of suction time, Dr Morselli observed, but that improved in the VisuMax 800. Despite some issues related to cyclotorsion and posterior centration, she said it is a versatile device that reliably offers access to every desired procedure.

(VisuMax 500)
Wavelength: 1043 nm
Laser Pulse Rate: 500 kHz
Pulse Duration: 220–580 fs
Operating Conditions: Room temperature 18–25°C
Atmospheric humidity 30–70%
Accessories: Single-use contact glasses, Treatment pack (sizes S/M/L and type KP), Keratoplasty adapter for patient supporting system
System Components: Patient supporting system, including platform-integrated uninterruptible power supply (UPS), Surgical microscope with additional slit illumination, Video camera with integrated digital recording
(VisuMax 800)
Laser Type: femtosecond laser
Available Treatment Options: Flap, SMILE® pro, CIRCLE®, ICR, Keratoplasty
Digital Assistant Systems: Centration aid, CentraLign®, Cyclotorsion adjustment, OcuLign®, Nomogram tool VISULYZE®5
Max Laser Frequency: 2 MHz Wavelength: 1043 nm
Pulse Duration: 220–580 fs
Surgical Microscope Magnification: 0.7x
Factors for Magnification Change: 0.4 / 0.6 / 1.0 / 1.6 / 2.5
Eyepiece Magnification: 12.5x (10.0x)
Filters: Blue, Barrier filter (yellow)
Slit Illumination: Slit width ≤ 0.3 mm / 0.7 mm, Slit height 11.0 mm
Ambient Conditions for Operation: Temperature: +18–25°C
Humidity: 30–70%
Device Mass: 520 kg Minimum Floor Load: 2.5 kN/m2
Footprint Standalone: L x W: 1710 mm x 925 mm
Laser Type: Solid state mode locked, diode-pumped
Wavelength: 1020–1060 nm
Max Pulse Frequency: < 10 MHz with ±10% tolerance
Pulse Duration: 200–500 fs Max Pulse Energy: < 6 µJ
Spot Size: < 2 µm
Dimensions: Base footprint 1.0 m x 0.6 m; Height (floor to screen) 1.4–1.7 m
Patient Contact Interface: Applanating patient interface, Liquid patient interface
System Components: Base station integrating the laser cavity, fixed mirror articulated arm (FMAA), power supply, computer, touchscreen monitor, suction unit, OCT box, and safety system; Handpiece integrating the cutting lens and topview camera; Disposable accessories, including procedure pack with liquid patient interface (LPI) for cataract surgery and with applanating patient interface (API) for corneal surgery
Applications: SMILE, LASIK, keratoplasty
Features: Centration aid, Cyclotorsion adjustment nomogram tool (500) 2011 (800) January 2024
Applications: refractive (CLEAR, LASIK, Intrastromal pockets), cataract (Z-Cataract), keratoplasty, tunnels for intracorneal rings
Features: Multipurpose laser, Intraoperative OCT imaging, Seamless workflow integration, Low energy concept, Multiple applications
May 2014


New technology can smooth the path to premium IOL acceptance.
Many of the principal barriers to the adoption of presbyopia-correcting intraocular lenses can be overcome with a combination of rigorous preoperative screening procedures, personalised IOL selection, and patient counselling, according to Joaquin Fernández MD, PhD.
“The most recent ESCRS Clinical Trends Survey showed the cost to the patient and concerns about the night-time quality of vision and loss of contrast sensitivity are the major concerns of surgeons in implanting presbyopia-correcting
IOLs,” he said. “We think the postoperative complaints can be prevented or minimised with screening procedures in the preoperative period and appropriate technology selection in the postoperative period. Concerns about the costs can be managed with cost-effectiveness research studies from the patient’s perspective.”
Although results from the ESCRS Clinical Trends surveys show that presbyopia-correcting IOL use has been increasing in recent years, premium IOLs are still implanted in a
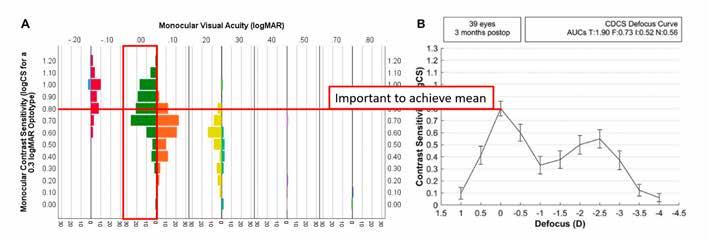
During the past 7 days, how bothersome did you find when you experienced visual artifacts around the lights at night, such as streetlights, car front lights, or car brake lights?
If answer is equal to or about moderately, and any of the following indexes is accomplished, it could be a psychological reason, not optical
minority of cases. In 2023, just 11% of respondents were implanting presbyopia-correcting IOLs, the same percentage as the previous year.
“Surgeons with more than 10 years of experience and in private practice present slightly higher ratios of concern,”
Dr Fernández noted. “Surgeons in eastern Europe were also slightly more concerned about patient cost than their counterparts in western Europe.”
Looking at the key issues involved, Dr Fernández said the policy in his clinic is never to dismiss or diminish potential concerns about a potential loss of contrast sensitivity.
Surgeons with more than 10 years of experience and in private practice present slightly higher ratios of concern.
or estimate it with these indices, whose cut-offs for contrast sensitivity ≤0.8 logCS have been calculated as >1.25, <7.67 and >1.0, for OSI, DLI, and PNS, respectively.
A similar approach may also prove effective in anticipating issues with night-time quality of vision, Dr Fernández said.
His team carried out a study to assess the photic phenomena (PP) and positive dysphotopsia in patients using light distortion index (LDI) and parameters obtained from a simulator, both of which were combined with subjective disturbances related to PP.2 This enabled them to obtain cut-off values for LDI that better predicted patients passing from “slightly” to “moderately” bothersome in terms of photic phenomena. The team also assessed the relationships between LDI and objective cataract grading methods, including OSI, DLI, and PNS.
“Patients reporting moderately or higher bothersome levels in the preoperative period and with LDI less than 15.20%, less than 2.8 for OSI, greater than 7.6 for DLI, and less than 2 for PNS might deserve special attention in the multifocal intraocular lens selection,” he advised. (Figure 2)
“It is very important in the preoperative examination to determine the contrast sensitivity of those patients with visual acuity of 20/20 or better,” he said. “We use direct screening measures with a preoperative measurement of the contrast sensitivity defocus curve in the range of +0.50 D to -0.50 D with best distance correction using the Multifocal Lens Analyser application, which can be downloaded on an iPad (https://apple.co/3TSGlDd). It enables us to determine the cut-off point at which the patient will start to experience a negative impact on their contrast sensitivity from an implanted multifocal IOL.” (Figure 1)
Dr Fernández and co-workers validated this approach in a recent study in which they measured distance-corrected contrast sensitivity defocus curve (CSDC) and visual acuity and graded crystalline lens sclerosis with three objective metrics: Ocular Scatter Index (OSI), Dysfunctional Lens Index (DLI), and Pentacam Nucleus Staging (PNS).1 The surgeons can therefore decide to directly measure the contrast sensitivity
Finally, in terms of the additional costs associated with presbyopic IOLs, Dr Fernández said it was important to explain the cost-effectiveness of such procedures from a patient’s perspective, since the patient is usually responsible for these additional costs, drawing on effectiveness published studies in the scientific literature. Dr Fernández’s team has developed a tool named IOLEvidence ( https://apple.co/498YGC5 ), which provides updated information on IOL effectiveness as provided by studies of intraocular lenses organised by the new evidence-based functional classification. 3
Dr Fernández presented at the ESCRS Winter Meeting in Frankfurt.
For citation notes, see page 40.
Joaquin Fernández MD, PhD is CEO and Medical Director of the Ophthalmology Department at Qvisión in Vithas Virgen del Mar Hospital, Almería, Spain. JoaquinFernandezoft@Qvision.es
Study results reveal 80% of patients end up with good refractive outcomes.
TIMOTHY NORRIS REPORTSUsing a four-flanged intrascleral intraocular fixation approach can produce good refractive outcomes, but there is room for improvement, a new prospective, longitudinal single-site study suggests.
The study of 28 eyes of 28 patients aimed to evaluate the four-flanged technique, first described by Sergio Canabrava1 , using a 6.0 Prolene suture and the PhysIOL Micropure IOL with an A-constant of 119.4. Led by Markus Schranz MD, the study included patients requiring a scleral fixation IOL, with strict selection criteria. Patients with corneal ectasia or dystrophy, surgery, scleral buckling, and macular diseases were excluded.
One of the most important steps of the surgery is marking the spots where to externalise the sutures, placing two spots 3.5 millimetres apart from each other and 2.5 millimetres posterior to the limbus. Dr Schranz stressed the importance of symmetry and its great influence on tilt decentration.
Axial length, TK mean, and white-to-white (WTW) distance were all in normal range. Absolute surgically induced astigmatism was 1.0 D at three months. Considering the mean refractive prediction error, the majority of patients ended up more hyperopic than intended. However, the prediction error appears to correlate with several factors, he said.

Considering the absolute error, 80% of patients ended up within the 1.0 D range of intended, which is quite good for scleral IOL fixation.
Axial length was associated with prediction error. The surgery was associated with more hyperopic outcomes in short eyes and more myopic outcomes in longer eyes, probably due to effective lens position (ELP) instability.
“Considering the absolute error, 80% of patients ended up within the 1.0 D range of intended, which is quite good for scleral IOL fixation,” Dr Schranz observed.
The researchers evaluated correlations between the prediction error and biometry parameters to find a reason for that outcome, revealing how the axial length played an important role. With increasing axial length, the refractive prediction error becomes more negative.
“So, shorter eyes are more hyperopic, and longer eyes tend to be more myopic than intended. No significant correlation was found considering True K or WTW,” Dr Schranz said. “On the other hand, aqueous anterior chamber depth (ELP minus CCT) did show a positive correlation with the prediction error, which is not surprising.”
Improving the refractive outcomes is important for patients’ quality of vision. As Dr Schranz suggested, a possible step could be the search for landmarks visible in the anterior segment optical coherence tomography (AS-OCT) as well as under the microscope in the OR to improve ELP consistency. He cited the scleral spur as one of these landmarks, as it is visible in AS-OCT and as a blue line during surgery. Finding correlations between the ELP and this landmark could create a more precise lens calculation.
“Patients are nowadays getting more and more demanding, asking for the same and previous refraction outcomes,” Dr Schranz noted. “A better understanding of the correlation between AS-OCT and anatomical landmarks should be key to improving IOL calculations in the future.”
Dr Schranz presented at the 2024 ESCRS Winter Meeting in Frankfurt.
For citation notes, see page 40.
Markus Schranz MD is a researcher at the Department of Ophthalmology and Optometry, Medical University of Vienna, Austria. markus.schranz@meduniwien.ac.at
Early study results suggest stable outcomes with little astigmatism.
TIMOTHY NORRIS REPORTSThe approval of a lenticule extraction procedure for hyperopic patients in Europe could be imminent. This safe and effective procedure will soon take its place amongst the most interesting innovations in refractive surgery, according to Pavel Stodůlka MD, PhD.
Lenticule extraction is an increasingly popular procedure now evolving into different variations, with companies selecting their own names for the same procedure. Starting with ReLex by Zeiss in 2011 and eventually copyrighted as SMILE, this procedure now is called SILK in Johnson & Johnson devices, CLEAR by Ziemer, SmartSight by Schwind, and renamed KLEx by the editors of the Journal of Cataract & Refractive Surgery and Journal of Refractive Surgery.
According to Dr Stodůlka, this can be further simplified to lenticule extraction—a suitable and simple name to avoid confusion and misleading terminologies. In recent years, lenticule extraction has become more advanced, rivalling or even outperforming LASIK in speed, recovery, and lesser complications. As the lasers become faster and more precise, innovative technologies and techniques enter the pipeline.
It is now possible to perform a lenticule extraction in less than 10 seconds, which is quite fast, Dr Stodůlka said. Cyclotorsion compensation is already available, and in the future, it could be possible to have even automated offset compensation for lasers. Robotic femtomatrix laser treatment, which could theoretically achieve a lenticule extraction procedure in less than 5 seconds, is another possibility.
Results warranting anticipation
Hyperopic lenticule extraction is now one of the most anticipated procedures by keratorefractive surgeons, as it cuts the lenticule differently. It is typically an 8-mm-wide lenticule with a thinner centre and thicker periphery than the standard myopic procedure and a 120-micron-cap thickness.
We performed the world’s first surgery at our clinic and are now waiting for one-year results.
Dr Stodůlka presented the results of an international study by Zeiss. In a one-year follow up, patients showed very nice results, with postoperative UDVA the same or better than preoperative CDVA in 78% of cases, without a single eye with a two or more line loss. Refractive outcomes were within 0.5 D in 53% of eyes and 1.0 D in 76%. Regarding cylinder, 95% had 0.5 D and below with 99% up to 1.0 D. A presbyopia-correcting lenticule extraction study on more than 100 patients involving six international centres will soon reach the oneyear follow-up mark, he noted.
“We performed the world’s first surgery at our clinic and are now waiting for one-year results,” Dr Stodůlka said. “This procedure already shows very nice results for something usually much more challenging to correct than myopia. The laser also induces spherical aberration that, in combination with mini-monovision, can enhance depth of vision.
“This should just bring spectacle independence to most of our patients, and I am very enthusiastic about it,” he concluded.
Dr Stodůlka presented his findings at the 2024 ESCRS Winter Meeting in Frankfurt.
Pavel Stodůlka MD, PhD, FEBOS-CR is founder, chief surgeon, and CEO of Gemini Eye Clinics, Czech Republic and Vienna. stodulka@lasik.cz

Finding uses for corneal lenticules, once considered a waste product.
TIMOTHY NORRIS REPORTSSince implementing keratorefractive lenticule extraction (KLEx) in refractive surgery, corneal lenticules are often considered nothing more than waste products, usually disposed of after the procedure. However, according to Suphi Taneri MD, this could be a trend set to change in the near future.
Four novel and different procedures considering corneal lenticule use are under investigation as possible treatment options for specific conditions.
Small-incision corneal intrastromal lenticule implantation for hyperopia correction (FILI) was the first mentioned, an effective technique where a lenticule extracted from a donor myopic eye after a KLEx procedure is subsequently implanted into a hyperopic eye.
This field of intrastromal lenticule implantation was founded by Drs Sri Ganesh and Sheetal Brar, who dedicated an entire decade to the development. It is a surgical technique in evolution, an elegant method that has shown interesting and positive results in the outcomes of a five-year study. This technique uses untreated human tissue, unlike the second procedure, Dr Taneri explained.
While some patients around the globe may not approve of porcine lenticule implantation, he added, small-incision lenticular intrastromal keratoplasty (LIKE) uses a denatured lenticule from a porcine eye graft, which is first cross-linked and then inserted in the cornea of a patient with keratoconus. This lenticule is much stiffer than the keratoconic stroma and can be inserted in a corneal pocket to stabilise and flatten an ectatic cornea.
The third technique, pioneered by Dr Aylin Kılıç, comes with the three-year study results on allogenic inlays made

from corneal donor tissue, designed to increase depth of focus of presbyopic patients. The allogenic inlay inserted is so small and biocompatible it is almost invisible—even to a slit lamp analysis, allowing the eye to gain a broad defocus curve of -4.0 D reading distance.
Lenticule rotation was the last technique Dr Taneri mentioned, a principle developed by Dr Jesper Hjortdal and reported on a clinical level for the first time by Dr Pavel Stodůlka for treating extreme astigmatism. The technique aims to create a lenticule with half of the manifest refractive cylinder and rotate it 90 degrees—without removing any corneal tissue from the patient.
Clinical cases presented showed no sign of opacification after eight months, along with a myopic shift, probably due to the dissection of the corneal lamellae. The myopic shift is acceptable and, in some cases, beneficial for the hyperopic patient.
Lenticule implantation—either human, allogenic, or crosslinked—or the rotation of the patient’s lenticule inside the corneal pocket are at the base of four promising approaches for four special indications, such as presbyopia correction, ectasia, hyperopia, and extreme corneal astigmatism.
Dr Taneri presented during the 2024 ESCRS Winter Meeting in Frankfurt.
Suphi Taneri MD is the Director of the Center for Refractive Surgery Muenster, Germany. taneri@refraktives-zentrum.de

Device finds new applications in refractive and glaucoma surgery.
TIMOTHY NORRIS REPORTSFemtosecond laser is still showing remarkable potential for the future of cataract, refractive, and glaucoma surgery, with novel techniques and applications already showing promising results. According to Kevin L Waltz MD, femto will continue to be a pivotal part of ophthalmology, as surgeons can do things with it they could not do otherwise, suggesting it should be recognised today as a digital scalpel more than just a laser.
Dr Waltz observed the technology had a rough start. After the first attempts in glaucoma surgery in the 1990s that did not work for technical reasons, femto shifted to refractive surgery with encouraging results. Now, with almost 30 years of successful use in refractive surgery, femtosecond laser is being employed again in glaucoma surgery.
Performing a trabeculotomy with a femtosecond laser allows a non-invasive procedure with no risk of intraocular infection. It is possible to do 500 microns wide, 200 microns high, and 400 microns deep internal openings, depending on the target structure, with precision and consistency impossible for the human hand. The cohort of patients operated in this way showed a significant decrease in IOP from baseline at 18 months, which, according to Dr Waltz, was sustained over the more than two years of follow up.
Rethinking the femtosecond laser as a digital scalpel could potentially further innovate or even revolutionise refractive surgery. Enter LIRIC (laser-induced refractive index change), a new procedure aiming to change the refractive index of corneal tissue instead of reshaping corneal tissues.
“We are not cutting anything—we are actually changing the refractive index, one atom at a time,” he said, pointing out

a different way of using the femtosecond laser. “Nine million pulses change the collagen structure and refractive index, creating diffractive patterns, and using an incredibly small amount of energy.”
Dr Waltz added that LIRIC is already showing promising results with remarkably good quality of vision and excellent visual acuity with the first attempts performed in 2015 and the possibility to treat presbyopic eyes with high-quality outcomes, fast recovery, and low risk of postoperative complications. No inflammation, scatter, and scarring of the cornea were observed at a slit lamp examination in all 27 treated patients. Furthermore, the procedure showed no damage to the corneal nerves due to the extremely low energy involved. There is no change in the corneal curvature, only a change in the refractive power.
Improving the efficiency of today’s femtosecond lasers was key for innovation, Dr Waltz emphasised. What investigators are working on could be available to treat glaucoma in Europe this year, and, in a few years, the US.
“A new way to think and treat glaucoma, to change our patient’s refractive outcome, even change IOL power inside the eye,” he observed. “We will be able to do things we have only dreamed of.”
Dr Waltz delivered his presentation at the 2024 ESCRS Winter Meeting in Frankfurt.
Kevin L Waltz MD is Partner, Central American Ophthalmic Research Consultants, Indianapolis, Indiana, US. kwaltz56@gmail.com

New study shows promising long-term results for novel procedure.
TIMOTHY NORRIS REPORTSAb interno canaloplasty effectively maintains longterm IOP control in glaucomatous patients, reducing the need for topical medications, a long-term follow-up study suggests. A six-year, single-centre study recently published in the Journal of Glaucoma looked at ab interno canaloplasty with the iTrack microcatheter (Nova Eye) performed as a standalone procedure or combined with cataract surgery in patients with mild to moderate primary open-angle glaucoma (POAG).1
Ab interno canaloplasty is a novel MIGS procedure. Contrary to a common misconception, it is not necessary for a MIGS procedure to involve implant use, explained Simon Ondrejka MD, one of the study authors.
Circumnavigating the canal
This procedure starts with inserting the iTrack catheter into Schlemm’s canal through the anterior chamber and the trabecular meshwork. The device then circumnavigates the canal, separating the herniations of the meshwork into the collector channels, breaking inner lumen adhesions, and opening stenotic segments present. After navigating 360 degrees, the device is slowly withdrawn while releasing viscoelastic, thus completing the process of dilation of Schlemm’s canal. The trabecular meshwork and the collector channels remain dilated, directly addressing the aqueous outflow resistance and enhancing the physiological drainage of the aqueous humour.
Dr Ondrejka said this is a sutureless, safe, and effective procedure that can significantly reduce IOP in patients with POAG in the long term.
Of the 27 treated eyes, 4 underwent canaloplasty as a standalone procedure, and 23 received the combined treatment. Reduction of IOP was more than 20% in 61% of eyes, with a steady decrease up to 27% after six years—the longest ab interno canaloplasty follow-up available in the literature, he noted.
The study showed almost all patients were able to gradually reduce glaucoma medications. The mean reduction was 52% from 1.9 medications at baseline to 0.9 at six years, with no significant difference between combined and standalone procedures. Of note, 39% of the patients were completely medication free after six years.
These patients are just grateful to be able to reduce their medications significantly or even entirely, observed co-author Norbert Koerber MD, PhD. Many of them suffered the burden of side effects before the procedure.
39%
39% of the patients were completely medication free after six years.
To investigate medication reduction, patients in the study were divided into groups according to the baseline number of medications. When conducted, this was the first time for an ab interno canaloplasty in Europe, so there was no precedent data to rely upon, Dr Koerber said.


Of the 18 patients already under IOP-lowering drugs, 4 were receiving three medications at baseline, 7 were receiving two medications, and 7 a single medication. Of these, 3 underwent the standalone procedure and 15 treated in combination with phacoemulsification.
Most striking is how significantly medication use was reduced in the long run, Dr Koerber noted. After three years, 1 eye was treated with three medications, 4 with two medications, and 6 with one medication only. Seven were medication free. Compared to preoperative measures, 16% of eyes took more medications at three years postoperatively than baseline, 22% took fewer medications, and 61% partially or completely reduced the overall quantity. The mean number of medications was lowered from 1.8 at baseline to 0.4 after one year, and this value remained substantially stable, with only a slight increase, over the study period.
This was a remarkable improvement for both the physicians and the patients, Dr Koerber said. Canaloplasty made it possible to obtain these results without implanting a foreign body in the eye, but only through the dilation of Schlemm’s canal, with long-lasting effects.
We are very happy to have a procedure that does not use any metal device in our patient’s eye while still achieving a significant reduction.
“We are very happy to have a procedure that does not use any metal device in our patient’s eye while still achieving a significant reduction, both in IOP and the number of medications,” he said. “All of this with no serious complications observed.”
Drs Ondrejka and Koerber presented at the 2024 ESCRS Winter Meeting in Frankfurt.
For citation notes, see page 40.
Ophthalmic YAG and SLT Laser System / Ophthalmic YAG Laser System
"Precision treatments with the YAG/SLT laser"
Optics that enhance clarity and contrast
Sharp aiming beam
Precise
Refined YAG laser delivery with lower plasma threshold
Unique SLT assist function "SLT-NAVI"
Coaxial illumination for better visualization (optional) NEW
Norbert Koerber MD, PhD currently works at Augencentrum Köln, Germany, and the Clinica Oculistica, University-Hospital of Padova, Italy. He is one of the pioneers of the canaloplasty procedure. N.koerber@gmx.de
Simon Ondrejka MD is a cataract and glaucoma specialist at Augencentrum Köln, Germany.
www.nidek.com
Novel glaucoma procedure performs effectively in real-life study.
Anovel surgical device capable of combining two ab interno treatments in a single procedure delivers consistent reductions in intraocular pressure (IOP) and topical glaucoma medications in patients with moderate to advanced glaucoma.
“We found the OMNI Surgical System (Sight Sciences) resulted in a statistically significant reduction in intraocular pressure and reduction in topical glaucoma treatment at six months in our cohort of patients with moderate to advanced glaucoma compared to what has been mentioned in the literature,” said Melissa Chin. “We didn’t find any difference in outcomes between the type of glaucoma treated, whether or not it was combined with cataract surgery and whether or not patients had previous trabeculectomy.”
The OMNI Surgical System enables surgeons to treat glaucoma using viscocanaloplasty and trabeculotomy sequentially in the same surgical session using a single corneal incision with a single device.
Dr Chin’s retrospective study reviewed the real-world outcomes of all OMNI glaucoma surgeries performed between October 2022 and August 2023 at a regional National Health Service ophthalmic centre in the United Kingdom. Baseline data was compared with six-month outcomes, including IOP, number of medications, complications, and further glaucoma surgery.
A total of 94 eyes of 86 patients were identified, 42 of which had six-month data. Most eyes (60%) had primary open-angle glaucoma (POAG), 21% had primary angle closure glaucoma (PACG), 14% had normal tension glaucoma, and 5% had pseudoexfoliation glaucoma. Just under half of the eyes (48%) had standalone OMNI procedures, while 52% underwent OMNI combined with cataract surgery.
The results showed a mean 23.2% reduction of IOP and an average reduction in medications of 1.43 topical glaucoma agents.

“A subgroup analysis showed the patients with a lower baseline intraocular pressure (below 18 mmHg) did not actually have any reduction in IOP, but they had a greater mean reduction in medications of 2.00,” Dr Chin said. “The patients with an IOP of 18 mmHg or more had a greater reduction in IOP of 33.9% and a reduction in topical medications of 1.15 agents.”
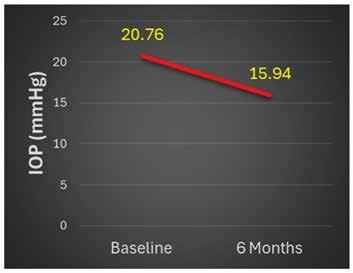
Mean intraocular pressure at baseline and at 6 months. Chin, M Nasir, T Jordan, V Shaikh, A. Six-month, real-world outcomes of the OMNI® Surgical Systm at a regional NHS Ophthalmic Centre in the UK. Poster presented at the 2024 ESCRS Winter Meeting in Frankfurt, Germany.
The study found no statistically significant difference in mean IOP reduction or reduction in number of topical medications between eyes with standalone surgery and those combined with cataract surgery, those with a history of trabeculectomy, and those with no prior glaucoma surgery—or between eyes with POAG and PACG, Dr Chin added.
Complications included hyphaema in 10%, early raised IOP (over 21 mmHg) in 26%, late raised IOP (more than 30 days postoperatively) in 10%, and iridodialysis in 2%. Further surgeries included repeat OMNI in 7% and Preserflo in 1%.
Summing up, Dr Chin said that while further studies are needed, the OMNI Surgical System seems to offer a safe and effective treatment for moderate to advanced glaucoma. Furthermore, the technique is relatively straightforward to master for experienced glaucoma surgeons.
“In this study, the surgeons performing OMNI all had prior experience doing angle surgeries, so I think once you get past that hurdle, the learning curve is not too steep,” she said.
Dr Chin presented her study at the 2024 ESCRS Winter Meeting in Frankfurt.
Melissa Chin MBBS, FRCS(Ophth)(Glasg) is a Locum Consultant Ophthalmic Surgeon at Buckinghamshire Healthcare NHS Trust, Aylesbury, United Kingdom. mcchin88@hotmail.com or melissa.chin2@nhs.net

MIGS can help reduce problems associated with drops.
The treatment and management of glaucoma with drops, while often effective, also come with potential adverse effects that can trouble patients. Given that these drops, particularly those containing benzalkonium chloride, can cause corneal toxicity and dry eye symptoms, preservation of the ocular surface may be one of the less appreciated benefits of minimally invasive glaucoma surgery (MIGS), notes Matteo Mario Carlà MD.
While the surgical approach could resolve these issues, Dr Carlà said it can also be the cause of different postoperative adverse effects. It is now recognised that reducing the number of treatments improves overall outcomes. However, even after a successful trabeculectomy, other potential adverse problems can present, such as filamentary keratitis, Dellen keratitis, and corneal epithelial abnormalities.
MIGS is strongly indicated for patients with mild to moderate glaucoma who are especially intolerant to medical therapy. This approach has the advantages of both reducing medications and having fewer adverse effects than surgery, Dr Carlà said.
MIGS has the advantage of minimising surgical trauma and conjunctival manipulation while keeping a good safety profile. For example, a study on XEN Gel Stent showed preservation of goblet cells and limited ocular surface inflammation compared to standard trabeculectomy. Patients undergoing combined surgery with cataract had higher levels of inflammatory cells in both the conjunctiva and the limbus.
Dr Carlà presented the results of a prospective study of another MIGS device, PreserFlo MicroShunt. The study examined 48 eyes undergoing PreserFlo implantation alone or in combination with phacoemulsification. One-year follow-up data looked at subjective and objective parameters of the ocular surface balance.
“The results showed that PreserFlo really keeps the eye on steady lowered intraocular pressure,” he said. “Some 56% of
patients achieved a complete surgical success, with an IOP below 18 mmHg and complete medication independence after one year.”
The success rate was around 80%, with an average improvement of the patients’ ocular surface. Subjective parameters were already increased 1 month after surgery, while tear breakup time and Schirmer results improved in 6 to 12 months. Similarly, the Oxford scale showed a significant positive impact—with a lot of patients showing no signs of epitheliopathy on fluorescein staining. Focusing on the objective parameters, tear osmolarity and minimal epithelial thickness improved during the first year after surgery.
Ocular surface parameters were transiently worse in the phaco-PreserFlo surgery group—with OSDI and tear osmolarity scores showing significantly higher rates than the standalone group 1 month after surgery. These findings clearly underline how cataract surgery may impact the reconstitution of the ocular surface, Dr Carlà said. However, all parameters stabilised and were comparable among the two groups at the 6 and 12-month follow-ups.
Dr Carlà observed the results showed PreserFlo MicroShunt use may interrupt the vicious cycle of ocular surface inflammation caused by medication, with significant improvements in tear breakup time, Schirmer testing, and the Oxford grading scale. Some 95% of eyes had a tear osmolarity below 302 mmOsm/L, which is the average of a healthy individual, a clear sign of improvement in quality of life, he concluded.
Dr Carlà spoke at the 2024 ESCRS Winter Meeting in Frankfurt.
Matteo Mario Carlà MD is a researcher at the Catholic University of the Sacred Heart, Rome, Italy. mm.carla94@gmail.com
During his Charles D Kelman Innovator Lecture at the 2024 ASCRS Annual Meeting, Dr David F Chang presented a video of his experience using ForSight Robotics’ ORYOM™ Surgical Robotics Platform to perform a complete, remote robotic cataract procedure on an animal eye while sitting at a workstation located 20 feet away. The ORYOM (“daylight” in Hebrew), the world’s first robotic surgery platform for cataracts, utilises AI-based algorithms, advanced computer vision, and miniaturised mechanics to enhance surgical precision and safety.
www.forsightrobotics.com
AEYE Health has received the first US FDA clearance for Optomed Aurora, a fully autonomous and portable device equipped with artificial intelligence to diagnose referable diabetic retinopathy from retinal images obtained with a handheld camera. The device uses AEYE Diagnostic Screening technology (AEYE-DS), which is already FDA-cleared and commercially available with a tabletop imaging device. Clearance of the new handheld device is based on two large-scale prospective phase 3 studies, where it demonstrated a sensitivity of 92%–93% and a specificity of 89%–94%. In both studies, more than 99% of patients received a diagnostic result using a single image from each eye, most often without pupil dilation.
www.aeyehealth.com
Rayner—a global manufacturer of products for cataract surgery—proudly announced the delivery of its 5 millionth RayOne lens (and 11 millionth lens made from RayAcryl, its proprietary hydrophilic acrylic material). RayOne is Rayner’s fully preloaded IOL injection system. The milestone comes during the year that marks the 75th anniversary of the first IOL implantation in 1949. The PMMA IOL was designed by Sir Harold Ridley and manufactured by Rayner. The company also recently announced its acquisition of the Swiss-based Sophi phacoemulsification machine.
https://rayner.com
NIDEK has announced the winners of the 4th Annual IMAGE OF THE YEAR Award. Marlon Rafael García Roa MD, Mexico, was awarded first prize for “20/25 how long,” a 163-degree ultrawidefield colour image of a right eye with diabetic retinopathy taken from the temporal position with the Mirante Scanning Laser Ophthalmoscope. The contest theme was “invisible to visible,” featuring diabetic retinopathy cases often requiring examination of the fovea to the extreme periphery. Eye care professionals worldwide voted online and onsite at AAO 2023 to choose the winning image. In response to submissions and votes, NIDEK made a donation to the International Agency for the Prevention of Blindness.
www.nidek.com


The central-hole design of the V4c Visian Implantable Collamer Lens (ICL; STAAR Surgical AG) appears to eliminate the risks associated with a low vault reported with earlier models, according to the findings of a 10-year follow-up study. The retrospective and comparative case series involved 90 eyes with 10 years of follow-up after implantation with the V4c ICL. The eyes included 37 with a low vault (less than 250 µm) and 90 with a high vault (between 250 µm and 800 µm). Throughout follow-up, no eyes developed ICL-induced anterior subcapsular opacity, and the IOP remained stable. The loss of endothelial cell density from preoperative values at follow-up was 3.8% and 4.5% in the low and normal vault groups, respectively. Two (5.4%) and eight (8.9%) eyes in the low and normal vault groups needed ICL exchange. One (2.8%) and two (2.2%) eyes in the low and normal vault groups required excimer laser treatment to correct residual refractive error.
B Alfonso-Bartolozzi, et al. “Ten-year follow-up of posterior chamber phakic intraocular lens with central port design in patients with low and normal vault,” 50(5): 441–447.
IMAGE-BASED ALGORITHM ACCURATELY PREDICTS ICL VAULT HEIGHT
A new image-based AI model can predict the postoperative vault of the implantable collamer lens (ICL) with a high level of accuracy, according to the findings of a retrospective machine learning study. To develop their deep learning model, the study’s authors trained a neural network on demographic data and 3,059 preoperative and postoperative high-frequency digital ultrasound images of 437 eyes of 221 patients who underwent ICL implantation. The algorithm achieved a mean absolute error of 66.3 µm for the 12.1 mm lens, 103 µm for the 12.6 mm lens, and 91.8 µm for the 13.2 mm lens. All predictions were within 500 µm for the 12.1 mm lens, as were 99.0% and 96.6% of predictions for the 12.6 mm and 13.2 mm lenses.
T Nasser, et al. “VAULT: vault accuracy using deep learning technology: new image-based artificial intelligence model for predicting implantable collamer lens postoperative vault,” 50(5): 448–452.
High-quality, US-registered cataract trials have enrolled acceptable proportions of women, but race and ethnicity remain underreported, according to the findings of a cross-sectional database study. The authors identified 100 clinical cataract-related randomised controlled trials (RCTs) that used double (or greater) masking with results published through a registry or scholarly journal. Of those studies, 97—which included 67,697 patients—reported sex demographics. Using the Global Burden of Disease database of sex-based cataract disease burdens for prevalence values, the authors determined the patients’ pooled participation-to-prevalence ratios (PPRs) for female sex to be 0.89, with values between 0.8 and 1.2 constituting sufficient study enrolment. Ethnicity and race were reported in 9 and 26 trials, respectively. Among trials that reported race, 84.44% of patients were white.
B K Tao, et al. “Diversity in enrolment to clinical trials for cataract medicine and surgery: meta-analysis,” 50(5): 460–467.
Explore IOL solutions and demystify common misunderstandings with insights into a refractive future that offers more improved postoperative outcomes—exclusively on the ESCRS website.
escrs.org/eurotimes/ supplements/
Finding a Keratoconus Consensus
Page 10
1. Gomes JA, et al. “Global consensus on keratoconus and ectatic diseases,” Cornea, 2015 Apr; 34(4): 359–69.
2. Maile Howard P, Li Ji-Peng Olivia, et al. “Personalized Model to Predict Keratoconus Progression from Demographic, Topographic, and Genetic Data,” of Ophthalmol, ajo.2022.04.004
3. Li Ji-Peng Olivia, Maile Howard P, Bunce Catey, et al. “A Comparison of Keratoconus Progression Following Colla gen Cross-Linkage Using Standard or Personalised Ker atometry Thresholds,” s41433-024-02994-6
Alternatives to Penetrating Keratoplasty
Page 17
1. Chamberlain W, Lin CC, Austin A, et al. “Descemet Endothelial Thickness Comparison Trial: A Randomized Trial Comparing Ultrathin Descemet Stripping Automat ed Endothelial Keratoplasty with Descemet Membrane Endothelial Keratoplasty,” 19–26.
Overcoming Obstacles to Presbyopia-Correcting IOLs
Page 28
1. Fernández J, Burguera N, Rocha-de-Lossada C, Rachwani-Anil R, Rodríguez-Vallejo M. “Objective cataract grading methods and expected contrast sensitivity reestablishment with multifocal intraocular lenses,” Int Ophthalmol, 2023;
Committee representatives of ESCRS organise and present sessions at meetings organised by our national and sister societies. These sessions are typically delivered by a group of speakers on a current topic selected by ESCRS in person or virtually.
These sessions provide useful education as well as collaboration between societies promoting and sharing benefits across both memberships.
escrs.org/education/academies/
June 1–4
2024 European Glaucoma Society Congress
Dublin, Ireland
June 5–8
2024 Retina International World Congress
Dublin, Ireland
September 6–10
2024 ESCRS Congress
Barcelona, Spain
November 28–29
UKISCRS
75th Anniversary of the IOL
London, United Kingdom


1 Jun
6 Sep 5 Jun

28 Nov

Minimally Invasive Glaucoma Surgery (MIGS) has emerged as a pivotal advancement in the management of glaucoma, offering a new option between medical treatment and more invasive surgical treatments.
There is a growing recognition of the need to shift towards earlier procedural interventions to mitigate the problems associated with topical treatment, such as compliance and tolerability issues. Taking compliance out of the patient’s hands may result in more consistent IOP control, thus reducing the risk of disease progression and vision loss. However, the question arises as to whether the risk-benefit ratio justifies the earlier surgical intervention.
The safety and efficacy of the iStent technologies have been proven in many studies, being documented in more than 300 peer-reviewed publications.
EFFICACY OF MIGS WITH ISTENT INJECT® W IMPLANTATION
The reported IOP reduction after iStent technologies implantation ranges from 15.2% to 42.3% depending on the study population and surgical goals1,2
The functional progression rate of glaucoma, measured as change in visual field, after iStent technologies implantation has been analysed in a recent meta-analysis3.
The review of 2794 articles revealed 15 peer-reviewed publications (1115 eyes), which fulfilled the selection criteria and had a sufficient follow-up period.
During the mean follow-up duration of 37.9 months, IOP reduction was 26,6%. Mean visual field defect progression was −0.01±0.42 dB/year after combined procedures and −0.07±0.62 dB/year after iStent stand-alone procedures. The reported progression rates did not differ significantly between the original iStent and the iStent inject®3
To my best knowledge, this is the first analysis on the impact of a MIGS device on the glaucoma progression rate. It is impressing – as the authors of the meta-analysis state – it would take a healthy eye more than 1000 years to become blind at this rate of progression.
PERIOPERATIVE SAFETY OF MIGS WITH ISTENT INJECT® W
MIGS procedures, characterized by their minimal tissue
 BY FRITZ HENGERER, MD, PHD
BY FRITZ HENGERER, MD, PHD
• Chief Medical Officer and Senior Head Physician, Buergerhospital Eye Clinic, Frankfurt, Germany
• International Vision Correction Research Centre, Heidelberg, Germany
• David J. Apple International Laboratory of Ophthalmic Pathology, Department of Ophthalmology, University of Heidelberg, Germany
trauma and shorter recovery times, demonstrate excellent safety profiles in the perioperative period.
Pivotal studies with the iStent inject® have shown low rates and risks of intraoperative complications and adverse events4. For instance, iStent inject® implantation, has been shown to have a low risk of transient hyphema and intraocular inflammation and in a randomized study with 505 patients, none of the patients showed signs of choroidal effusions, myopic shift, flat anterior chamber, cyclodialysis and significant hyphema4
LONG-TERM SAFETY OF MIGS WITH ISTENT INJECT® W
Long-term safety outcomes following MIGS are crucial in assessing the durability of intraocular pressure (IOP) reduction and the occurrence of late complications. In general, MIGS procedures are associated with fewer sight-threatening complications such as hypotony, bleb-related infections, or corneal decompensation, compared to more invasive surgical treatments, such as trabeculectomy. This confirms the place of MIGS in the new treatment algorithm as an early surgical treatment option, which helps to delay more invasive surgical treatments.
Preservation of ocular anatomy and function is another hallmark of MIGS, as these procedures spare the conjunctiva and maintain the potential for future interventions if needed.
Endothelial cell loss (ECL) and peripheral anterior synechia (PAS) have been associated with various types of glaucoma surgery. However, the endothelial cell safety with iStent inject® has been demonstrated to be similar to cataract surgery alone over 5 years5.
Published results on the efficacy and safety of the iStent inject®, as well as my personal clinical experience, encouraged me to start earlier with minimally invasive surgical interventions in my glaucoma patients.
The recent meta-analysis of the very low progression rate of the visual field defect after iStent technologies implantation foster my treatment strategy.
References: 1. Shalaby WS, Jia J, Katz LJ, et al.. iStent inject: comprehensive review. J Cataract Refract Surg 2021;47:385–99. 2. Healey PR, Clement CI, Kerr NM, et al.. Standalone iStent trabecular micro-bypass glaucoma surgery: a systematic review and meta-analysis. J Glaucoma 2021;30:606– 20. 3. Gillmann K, Hornbeak DM. Rates of visual field change and functional progression in glaucoma following trabecular microbypass implantation of iStent technologies: a meta-analysis. BMJ Open Ophthalmol. 2024;9(1):e001575. 4. Samuelson TW, Sarkisian SR Jr, Lubeck DM, et al. Prospective, Randomized, Controlled Pivotal Trial of an Ab Interno Implanted Trabecular Micro-Bypass in Primary Open-Angle Glaucoma and Cataract: Two-Year Results. Ophthalmology. 2019;126(6):811-821. 5. Voskanyan L, García-Feijoó J, Belda JI, Fea A, Jünemann A, Baudouin C; Synergy Study Group. Prospective, unmasked evaluation of the iStent inject system for open- angle glaucoma: Synergy trial. Adv Ther. 2014 Aug;31(8):189-201. doi: 10.1007/s12325-014-0131-2. Epub 2014 Aug 9. PMID: 25108116;
PMCID: PMC4140028.
iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATION FOR USE: The iStent inject® W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject® W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject® W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS: • For prescription use only. • This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject® W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject® W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.” • There are no known compatibility issues with