SPECIAL FOCUS GLAUCOMA CATARACT & REFRACTIVE | CORNEA | RETINA PAEDIATRIC OPHTHALMOLOGY June 2020 | Vol 25 Issue 6
NAVIGATING THE MIGS MAZE

Belong to something inspiring. Join us. See into the future of eye surgery and patient care. Visit www.escrs.org for information about membership & benefits
Publisher Carol Fitzpatrick
Executive Editor
Colin Kerr
Editors
Sean Henahan
Paul McGinn
Managing Editor Caroline Brick
Content Editor
Aidan Hanratty
Senior Designer
Lara Fitzgibbon
Designer
Ria Pollock
Circulation Manager
Angela Morrissey
Contributing Editors
Howard Larkin
Dermot McGrath
Roibeard Ó hÉineacháin
Contributors
Maryalicia Post
Leigh Spielberg
Gearóid Tuohy
Priscilla Lynch
Soosan Jacob
Colour and Print
W&G Baird Printers
Advertising Sales
Amy Bartlett
ESCRS


Tel: 353 1 209 1100
email: amy.bartlett@escrs.org
Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the managing editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983

As certified by ABC, the EuroTimes average net circulation for the 10 issues distributed between February and December 2019 was 47,863 P.16 CONTENTS A EUROPEAN OUTLOOK ON THE WORLD OF OPHTHALMOLOGY www.eurotimes.org REGULARS 35 Industry news 37 Practice management 39 Calendar SPECIAL FOCUS GLAUCOMA 4 Navigating the MIGS Maze – is it best alone or in combination with cataract surgery? 6 The future of glaucoma surgery 8 Dealing with high myopia in glaucoma patients 9 Micro-bypass stent shows good results 10 Triple approach proves safe and effective 11 Attentive evaluation of the optic disc is invaluable CATARACT & REFRACTIVE 12 Adapting to the new normal – returning to work after COVID-19 14 Dealing with complications of surgery 16 Stress is a major issue among younger surgeons 17 Mono-EDOF lens provides intermediate vision without sacrifice of distance vision 18 JCRS highlights 19 Femto shows no clear benefit over phaco
CORNEA 20 New surgical techniques aid treatment of hydrops in keratoconus 21 Methodical approach brings speed without haste in dry eye assessment
keratitis
cases of endothelial pathology RETINA 26 What’s next for OCT-angiography? 27 Genome sequencing and inherited retinal disease 28 Can regenerative medicine help diabetic retinopathy? 30 Biomarker classifier outperforms human experts with OCT scans 31 Ophthalmologica highlights PAEDIATRIC OPHTHALMOLOGY 32 New formulations of cyclosporine showing good results in paediatric OSD 33 Multifocal IOLs achieve good results in paediatric cataract P.15 Included with this issue... ESCRS Survey on COVID-19 Practice Patterns Ophthalmologists ESCRS Survey COVID-19 PRACTICE PATTERNS PATTERNS EUROTIMES | JUNE 2020
22 DWEK and ROCK inhibitors combine to treat Fuchs’ dystrophy 23 Sixteen-year review of bacterial keratitis 24 Study shows corneal cross-linking is as effective as antibiotics in healing infectious
25 Cataract surgery in
MEDICAL EDITORS
2020 ESCRS Virtual Congress offers a personal touch




Dear Colleagues,
Amid ongoing disease, death and uncertainty around the world, one regrettable casualty of the COVID-19 crisis is the 2020 live ESCRS Congress. It was to be held in Amsterdam in October. Instead, we will host our first ESCRS Virtual Congress on Friday 2 October through Sunday 4 October.
This decision was taken in part because current Netherlands meeting safety protocols make a live conference of some 9,000 delegates and 6,000 industry representatives unfeasible in the available space, if at all. In addition, it remains unclear whether travel and quarantine restrictions will allow widespread attendance.
Most of all, protecting our delegates and other stakeholders from potential infection in a crowded meeting space is our overriding concern. We hope this early notice gives you the time you need to arrange your participation for the virtual meeting.
Note that “virtual” does not mean “impersonal.” Building on the success of our innovative moderated poster sessions and dispersed free paper format, this year’s meeting will feature cutting-edge research in a highly interactive setting
Note that “virtual” does not mean “impersonal.” Building on the success of our innovative moderated poster sessions and dispersed free paper format in Paris and Vienna, this year’s meeting will feature cutting-edge research in a highly interactive setting, with online messaging available from your home or office.
To further encourage
interaction, we plan to bring named lecture presenters and major symposia panels to Amsterdam where possible for the in-depth analysis and vivid discussions that ESCRS is known for.
As with live events, CME credits are being arranged for select digital programmes. Meeting contents will also be available afterward via ESCRS On Demand, allowing you access to the latest science and education on your schedule.
INTERNATIONAL EDITORIAL BOARD
Noel Alpins (Australia), Bekir Aslan (Turkey), Roberto Bellucci (Italy), Hiroko Bissen-Miyajima (Japan), John Chang (China), Béatrice Cochener-Lamard (France), Oliver Findl (Austria), Nino Hirnschall (Austria), Soosan Jacob (India), Vikentia Katsanevaki (Greece), Daniel Kook (Germany), Boris Malyugin (Russia), Marguerite McDonald (USA), Cyres Mehta (India), Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands), Leigh Spielberg (The Netherlands), Sathish Srinivasan (UK), Robert Stegmann (South Africa), Ulf Stenevi (Sweden), Marie-José Tassignon (Belgium), Manfred Tetz (Germany), Carlo Enrico Traverso (Italy)
Our industry partners are also lending their full support. In addition to helping out with the enormous technical challenges this congress presents, they will be hosting a virtual exhibit hall as well as lunchtime educational events. We will take care to also include some entertaining moments that are going to be quite memorable!
Finally, recognise that this event is a work in progress. Much will depend on how circumstances develop. Watch for details here and at ESCRS.org. We look forward to seeing you in October.

EDITORIAL 2
A WORD FROM
GUEST EDITORIAL
Prof. dr Rudy MMA Nuijts, ESCRS President
RUDY MMA NUIJTS MD, PhD
Emanuel Rosen Chief Medical Editor
José Güell
Rudy MMA Nuijts
Thomas Kohnen
EUROTIMES | JUNE 2020
Paul Rosen
78 % of readers trust its content
Reach
47,863 *
* Average net circulation for the 10 issues circulated between 1 February 2019 to 31 December 2019. See www.abc.org.uk Results from the EuroTimes Readership Study 2017
NUMBER 1!
NAVIGATING THE MIGS MAZE

RCTs and the FDA say ‘no’ to standalone MIGS; experience may say ‘yes’. Howard Larkin reports
Minimally invasive glaucoma surgery techniques (MIGS), including trabecular bypass procedures as well as suprachoroidal and, potentially, subconjunctival shunts, offer surgeons a wide range of options for treating mild to moderate glaucoma and ocular hypertension. But should they be used alone or only in combination with cataract surgery?
The answer is simple, said Keith Barton MD, FRCP, FRCS, in a debate at ESCRS Glaucoma Day 2019 in Paris, France. “MIGS are only fit for combined surgery. Why? Because the only randomised clinical trial evidence is in combined surgery.”

It’s a matter of risk vs benefit, explained Dr Barton, of Moorfields Eye Hospital, London, UK. So far, the proven efficacy of
MIGS procedures of all types is modest, he noted. For patients already undergoing cataract surgery the risk is reasonable. “For a standalone procedure, you have a much higher bar … [and] there is no real standalone evidence,” he argued. Dr Barton cited several studies in support of his argument. For example, a prospective randomised study involving 240 patients with primary open-angle glaucoma and cataract implanted with the iStent (Glaukos,
Laguna Hills, California, USA) trabecular bypass device with cataract surgery found 72% of iStent eyes reached a target IOP of 21mmHg or less compared with 50% for cataract surgery only eyes one year after surgery, and 66% and 48% respectively saw IOP reduction of 20% or more. The results are statistically significant, but the gains over cataract surgery alone are not huge. (Samuelson TW et al. Ophthalmology 2011;118:459-467.)
EUROTIMES | JUNE 2020 SPECIAL FOCUS: GLAUCOMA 4
MIGS are only fit for combined surgery. Why? Because the only randomised clinical trial evidence is in combined surgery
Keith Barton MD, FRCP, FRCS
Similarly, before it was removed from the market, a two-year study of the CyPass (Transcend Medical, Menlo Park, California, USA) supraciliary microstent involving 505 patients found mean unmedicated IOP 2.0mmHg lower in the CyPass group than the cataract surgery group, with medication use 67% lower in the Cypass group – once again significant, but modest, gains. (Vold S et al. Ophthalmology 2016;123:2103-2112.).
The US FDA agrees that MIGS should be limited to use with cataract surgery, Dr Barton said. “The FDA obviously does not apply in Europe, but it is noteworthy that the US FDA believes [MIGS] are only fit for combined surgery. … it’s because the only evidence is with combined surgery.”
ARE SUBCONJUNCTIVAL DEVICES MIGS?
One exception is the Xen Gel Stent subconjunctival drainage device, which the FDA has cleared for implantation as a standalone procedure or in conjunction with cataract surgery, Dr Barton said. However, the manufacturer does not refer to it as a MIGS device, he added.
While there has been much debate about what qualifies as MIGS, “it’s interesting that the device that has been out there the longest that is most appropriate for standalone surgery doesn’t call itself ‘MIGS’”, Dr Barton noted.
Similarly, Santen steers away from describing its Preserflo MS as a MIGS device “because the term MIGS seems to be associated with only modest efficacy”, Dr Barton said.
In summary, the only randomised clinical trial evidence for MIGS efficacy is in combined surgery; one major licensing agency has only licensed MIGS for combined surgery; and the devices with the strongest arguments for standalone usage shy away from calling themselves “MIGS”, Dr Barton said.
STANDALONE MIGS
Arguing for MIGS use in both standalone and combined procedures, Julian Garcia Feijoo MD, PhD, of San Carlos Hospital, Complutense University, Madrid, Spain, first sought to clarify MIGS as a concept. He subdivided it into true MIGS, including Schlemm’s canal stents and suprachoroidal shunts, and MIGS involving blebs and use of mitomycin C shunting to the subconjunctival space.
These differing devices clearly involve varying levels of risk, have different suitable patient profiles, and differing efficacy, Dr Garcia Feijoo said. “We have many surgical procedures. That way we can find the patients who can benefit from the different glaucoma devices and MIGS.”
Therefore, Dr Garcia Feijoo believes that the decision to use MIGS or MIGS involving blebs should be taken in the context of other medical and surgical options based on the

patient’s condition and circumstances.
Factors to consider include diagnosis, stage and rate of progression, ocular characteristics and pathologies, age and life expectancy and other factors, such as topical medication tolerance and adherence. “When making the decision consider the patient needs and preferences and tailor the treatment accordingly,” Dr Garcia Feijoo said.
The real question, though, is whether MIGS can be effective as standalone treatments, or do they need cataract surgery to be effective, Dr Garcia Feijoo said. Many papers suggest they can be.
Dr Garcia Feijoo agreed with Dr Barton that bleb-forming devices such as the Xen Gel Stent (Allergan, Curr Clin Opthalmol 2018. Stalmans. ICGS 2016) and Preserflow (SANTEN, Batlle JF et al J Glaucoma 2016. Garcia Feijoo. AAO 2018) have proven standalone efficacy (Curr Clin Opthalmol 2018. Stalmans. ICGS 2016) and may be considered as an alternative to trabeculectomy for moderate to severe cases.
For trabecular bypass and Schlemm’s stenting MIGS approaches, Dr Garcia Feijoo believes these may be appropriate for patients needing high to mid-teens intraocular pressure control. Studies suggest complication rates are similar to or lower than cataract procedures, and the chances of controlling IOP for two-to-five years without medication is 60-to-75% in suitable patients with early disease, which can be very helpful for patients with low medication tolerance, he said.
Several prospective studies have demonstrated efficacy of trabecular bypass stents for open-angle glaucoma patients. These include a prospective study showing 36-month efficacy (Hengerer FH et al. Adv Ther 2019
Jul;36(7):1606-1617.) and a second series out to 42 months (Katz J et al. Clin Ophthalmol in press.), Dr Garcia Feijoo said. “Do they work? Yes. For how long, we don’t know.”
Suprachoriodal devices may be useful for more advanced cases, slowing progression and the need for topical medications for more than four years in a pseudophakic patient (Garcia Feijoo et al. J Ocul Pharmacol Ther 2018;34(7):538-542.).
In summary, standalone MIGS provide efficacy – though not to the level of trabeculectomy – as well as improved quality of life and reduced medication burden for many patients. “These things are true for both standalone and combined surgery,” Dr Garcia Feijoo said.
REBUTTAL
Still, FDA clinical trial guidelines and AAO technology assessments question the use of standalone MIGS procedures, Dr Barton countered. These patients typically need more than the moderate IOP lowering MIGS provides, he added.
He noted that a 2011 AAO technology assessment found “it is not possible to conclude whether these novel procedures are superior, equal to, or inferior to surgery such as trabeculectomy or to one another. The studies provide the basis for future comparative or randomized trials of existing glaucoma surgical techniques”.
“In other words, we really don’t know where we are. Are we really going to do these procedures on people who need a standalone procedure?” Dr Barton asked.
In addition, FDA trial guidelines for MIGS studies explicitly rule out patients with advanced glaucoma, ocular hypertension or vision-threatening visual field defects – “basically anyone you’d want to do standalone surgery on”, Dr Barton said. He contended that both the financial and opportunity costs of standalone MIGS are not worth the benefit.
While conceding long-term studies are needed to better understand the effects of MIGS procedures, Dr Garcia Feijoo believes surgeons should use their judgment, and use MIGS in standalone surgery when it will benefit specific patients, specially pseudophakic patients with early glaucoma. Trabecular bypass surgery can be useful early on and suprachoroidal approaches may be useful for intermediate glaucoma. “There are opportunities for every device and we have to decide wisely which patients can benefit from each,” he said
EUROTIMES | JUNE 2020 SPECIAL FOCUS: GLAUCOMA 5
There are opportunities for every device and we have to decide wisely which patients can benefit from each
Julian Garcia Feijoo MD, PhD
When making the decision consider the patient needs and preferences and tailor the treatment accordingly
Julian Garcia Feijoo MD, PhD
THE FUTURE OF glaucoma surgery
Will minimally invasive glaucoma surgery (MIGS) replace trabeculectomy?

The answer may be a partial “yes” –although increasingly severe and rapidly progressing disease in ageing populations may increase absolute trabeculectomy numbers, debaters argued at the ESCRS Glaucoma Day 2019 in Paris, France.

While trabeculectomy will likely remain the go-to procedure for the minority of patients with severe and/ or rapidly progressing glaucoma, MIGS devices already have displaced filtration surgery in many milder cases, said Leon Au BSc, MBBS, FRCOphth, consultant ophthalmologist at Manchester Royal Hospital, UK.
MIGS procedures are more than adequate for the vast majority of glaucoma patients, and future, more effective MIGS will likely capture even more patients, Dr Au added. Where 20 years ago there
were almost no treatment choices between maximum medication and invasive filtration surgery, today’s options range from SLT and other laser procedures to MIGS trabecular, supraciliary and subconjunctival stents, to canaloplasty and viscocanalostomy.
These less-invasive options fulfil patients’ desire to keep disease asymptomatic while minimising eye drops and invasive, uncomfortable, surgical interventions – not to mention reducing time off work and in hospital, Dr Au said.
In addition, few glaucoma patients actually need the sub-12mmHg intraocular pressure trabeculectomy can provide, and this largely
comes down to disease severity and age, Dr Au said. “I’d hope to intervene earlier with less invasive procedures to avoid patients progressing to end-stage disease treated with one too many eye-drops”, said Dr Au.
Glaucoma is generally diagnosed late in life and progresses slowly or not at all, so moderate IOP reduction is enough to prevent visual disability in most patients.
For example, a large longitudinal study of open-angle glaucoma patients in the UK found mean age at diagnosis was more than 71 years, with 30% dead in 10 years, 44% in 15 years and 63% in 20 years. Average time from presentation to death was just over 7.5 years – not surprising
Advancing technology and ageing populations will likely mean more of both trabeculectomy and MIGS.
Howard Larkin reports
EUROTIMES | JUNE 2020
I’d hope to intervene earlier with less invasive procedures to avoid patients progressing to end-stage disease...
SPECIAL FOCUS: GLAUCOMA 6
Leon Au BSc, MBBS, FRCOphth
given an overall UK life expectancy of 81 years, Dr Au pointed out (Sharma T, Salmon JF, Br J Ophthalmol. 2007 Oct; 91(10): 1282–1284. Shahid H, Salmon JF. Br J Ophthalmol. 2013 Feb;97(2):2356. King C et al. Br J Ophthalmol. 2018 Dec;102(12):1663-1666).
As a result, “some of the new devices have managed to displace trabeculectomy”, Dr Au said. He cited a study at Manchester in which the iStent (Glaukos) implant proved sufficient for three-quarters of 16 trabeculectomy candidates, which included those on acetazolamide (Diamox) pre-op, or who had cup-to-disc ratios greater than 0.7, required more than two IOP drops, had IOP over 21.0mmHg and visual field mean deviation of -4.0dB or more. During seven years’ follow-up, only four required trabeculectomy, sparing 12 patients the more invasive and riskier procedure (Ziael H, Au L. 8th World Glaucoma Conference, 2019, Melbourne, Australia).
“I think that displacement may be called replacement, and for me, the future of MIGS is very bright,” Dr Au said.
AGE DRIVING UP TRAB NEED
Arguing for the continuing need for trabeculectomy, Kuldev Singh MD, MPH, of Stanford University, California, USA, allowed that most glaucoma patients do not need the dramatic IOP reduction trabeculectomy affords and may need no surgery at all. He refers to these lowseverity patients as having “glaucoma light”. Most of “glaucoma light” is treated pharmaceutically and only a small subset of patients with glaucoma currently undergo any surgery at all whether it be MIGS, trabeculectomy or something else.
While most glaucoma patients are slow progressors, the 3-to-5% who are fast or very fast progressors may need IOP levels that cannot be achieved with MIGS procedures and thus may benefit from trabeculectomy.
However, while rapid progressors are not
frequent, they do sometimes require very low IOP and even slow progressors may need trabeculectomy if they live long lives after developing glaucoma. Most of the MIGS procedures have only been studied for oneto-three years and there exists decades-long follow-up with trabeculectomy to know that there is the potential for long-term success.
“There is that 5% where you need a really low pressure and there’s nothing that does it like a trab,” he said. So while MIGS will undoubtedly grow in numbers, and that is a good thing, it will not completely replace the need for trabeculectomy. The two classes of surgery can and should co-exist, he believes.
Large prospective trials, including the landmark Tube v Trab study, demonstrate that trabeculectomy can reliably reduce IOP to the low single digits for five years or more (Gedde SJ et al. AJO 2012;153(5):789803). Other studies suggest a correlation between big drops in IOP and actual improvement in visual fields, Dr Singh added (Caprioli et al. Ophthalmology 2016;123:117-128).
“Six [mmHg] may be the new 12 for the very severely affected patients and/or those who continue to show progression with low double-digit IOPs. An IOP of 12mmHg is by no means a guarantee of visual preservation, especially when the optic nerve is severely damaged and there is very little reserve.
And while the average lifespan after glaucoma diagnosis was historically short, it is getting longer, Dr Singh noted. As more people age into their late 80s, 90s and even 100s, the incidence of rapidly progressing glaucoma is jumping, with

many previously slow progressors speeding up later in life. He believes this will mean a rise in the absolute number of patients requiring trabeculectomy, even though the proportion relative to MIGS may fall.
Trabeculectomy is not only the most reliable procedure for long-term IOP reduction, it is also titratable and, when performed by an experienced surgeon with careful attention to follow-up, does not have to be associated with a high risk of complications, Dr Singh said. However, achieving good long-term results requires technical skill, knowledge of how to modulate wound healing and, most of all, time with patients during the perioperative period, Dr Singh said.
Already, Dr Singh is noticing that patients are travelling long distances to see him for trabeculectomy as the number of more recently trained surgeons have either not learned the procedure or have stopped doing it, and these are not mutually exclusive scenarios. In his opinion, those who were not adequately trained to perform trabeculectomy before beginning practice are ultimately more likely to abandon the procedure due to frustration with results.
“We will absolutely still need trabeculectomy in the future. If you want to call yourself a glaucoma specialist, learn trabeculectomy and how to follow those patients. This does not mean you cannot and should not also embrace MIGS – the choice of procedure should obviously be individualised based upon what each patient needs,” said Dr Singh.
Leon Au: Leon.au@mft.nhs.uk
Kuldev Singh: Kuldev.Singh@stanford.edu
EUROTIMES | JUNE 2020
SPECIAL FOCUS: GLAUCOMA 7
There is that 5% where you need a really low pressure and there’s nothing that does it like a trab
VISIT OUR WEBSITE FOR INDIAN DOCTORS www.eurotimesindia.org INDIA
Kuldev Singh MD, MPH
High myopia glaucoma surgery


New options may address scleral thinning, other long-term complications. Howard
Larkin reports
High myopia presents special challenges for advanced glaucoma treatment. And while surgical approaches ranging from trabeculectomy to minimally invasive procedures (MIGS) have pluses and minuses, their wide variety means it’s often possible to find an option that meets individual patient needs, said Antonio M Fea MD, PhD, at the ESCRS Glaucoma Day 2019 in Paris, France.
“Are we afraid of glaucoma surgery? I would say in general, yes. In the case of myopic patients, it is even more difficult,” said Dr Fea, of the University of Turin, Italy.
High myopia glaucoma patients often present a treatment conundrum. On one hand, they are typically young, phakic and likely to progress with intraocular pressures (IOP) in the high teens – factors favouring trabeculectomy to sustain a target IOP low enough for long-term vision preservation.
On the other hand, highly myopic patients are at higher risk for hypotony maculopathy following filtration surgery – gravitating against trabeculectomy (Costa VP, Arceiri ES. Acta Ophthalmol 2007;586-597. Fannin LA et al. Ophthalmology. Jun 2003;110(6):1185-91). Male patients are at even higher risk as are those who underwent trabeculectomy with antifibrotics, Dr Fea said. (Stamper RL et al. Am J Ophthalmol 1992; 114(5):544-53).
The risk is long-lived. In a recently published case, a 34-year-old man developed hypotony maculopathy 14 years after trabeculectomy, apparently due to progressive scleral thinning and morphologic change leading to collapse of the scleral wall during hypotony (Kao ST et al. J Glaucoma 2017;26:e137-e141). Therefore, trabeculectomy, when used in myopic patients, should be done with minimal or no antimetabolites, sutured tightly and checked to ensure complete conjunctival sealing, and followed closely, Dr Fea said.
Similarly, hypotony may be a significant risk for high myopia patients in other glaucoma surgeries. About onethird experience it after deep sclerectomy (Hamel M et al. J Cataract Refract Surg. 2001 Sep;27(9):1410-7.), while myopiarelated morphological responses in drainage channels may limit the effectiveness of trabecular MIGS (Chen Z et al. Ophthalmic Physiol Opt 2018;38:266-272).
WEIGHING OPTIONS
Dr Fea recently treated a 53-year-old male with -6.25 dioptres myopia with -2.75 dioptres cylinder and glaucoma that progressed about -10.0dB in 10 years in his right eye, with IOP of 18-24mmHg on four medications. To avoid hypotony, Dr Fea ruled out trabeculectomy, while ab interno MIGS didn’t offer enough potential IOP reduction. To avoid possible clogs requiring needling and complications with the patient’s contact lenses, he decided against a XEN (Allergan), opting for a PreserFlo (Santen) shunt implanted through a scleral incision.
Nine months after a surgical revision, the patient’s IOP is around 10-14mmHg. Whether that is enough remains to be seen, Dr Fea said, though the possibility of additional surgeries was preserved.
Antonio Fea: antoniomfea@gmail.com
Practice Management & Development ESCRS
further details email: innovation@escrs.org Submission Deadline Friday 24 July 2020 Grow Your Practice Through Innovation Win a €1,500 Bursary ESCRS Practice Management and Development Innovation Award EUROTIMES | JUNE 2020 SPECIAL FOCUS: GLAUCOMA 8
For
iStent plus cataract surgery

Favourable glaucoma outcomes with micro-bypass stent and cataract surgery. Dermot McGrath reports

Implantation of the iStent inject (Glaukos) in combination with cataract surgery significantly and safely reduced intraocular pressure (IOP) and the medication burden in eyes with various types and severities of glaucoma, according to a study presented at the 37th Congress of the ESCRS in Paris.
“This real-world experience from a number of different Australian surgeons augments the existing evidence for iStent inject as a promising and safe treatment option for glaucoma and is the largest multicentre cohort of patients treated with iStent inject to date from the Asia-Pacific region,” said Colin I Clement PhD, FRANZCO, of Sydney Eye Hospital, Australia.
Describing the properties of the iStent inject, Dr Clement said it was a trabecular micro-bypass system made up of two titanium stents for ab interno implantation. The stents, which are just 230 microns in diameter and 360 microns in height, are designed to increase access to collector channels with multiple lateral lumens facilitating aqueous outflow from the anterior chamber.
“The minimal tissue disruption of the stent leaves the natural anatomy intact and preserves the potential for future treatment options,” he said.
Dr Clement presented data from a retrospective case series of 165 eyes of iStent inject procedures combined with phacoemulsification carried out by five different Australian surgeons. The vast majority of patients were primary open angle glaucoma (70%), but other indications included appositional angleclosure, pseudoexfoliative glaucoma and ocular hypertension. Key outcome parameters were IOP reduction, medication use, visual acuity and adverse events.
The mean patient age at baseline was 71.4 years, mean IOP was 18.3mmHg (± 5.4) and mean medications were 1.7. The severity of the glaucoma was recorded as mild in 70%, moderate in 18% and severe in 12%.
The results showed a statistically significant reduction of 23.2% in mean IOP and a 71.5% reduction in mean medication use from 1.7 to 0.47 after 12 months.
“Overall around 85% of patients had an improvement in their IOP control and a similar majority had a reduction in medications required to reduce their IOP,” said Dr Clement. There were very few complications overall, with two of 165 eyes with incorrectly positioned stents, two with corneal oedema, two with prolonged anterior chamber inflammation, one stent that came in contact with the iris and one case of hyphema, which resolved without treatment.
Overall, the visual acuity was 20/40 or better in 97% of patients after surgery at 12 months compared to 93% before surgery. Three eyes went on to have additional glaucoma procedures to reduce their IOP down to target levels.
“The real-world evidence demonstrated significant IOP and medication reduction achieved in various types of glaucoma and the safety profile of the stent was favourable with a low complication rate similar to that following cataract surgery alone,” he concluded.
Be everywhere. See everything Catch up on what you’ve missed
ESCRS On Demand, members can view the presentations from any conference. Catch up on all the sessions at a time and place that suits you.
www.escrsondemand.org With
SPECIAL FOCUS: GLAUCOMA 9
Colin I Clement PhD, FRANZCO
Triple procedure FOR CATARACT & GLAUCOMA

Goniotomy-viscodilation-cataract surgery lowers IOP and medication use at one year. Howard Larkin reports

Combining dual-blade goniotomy and viscodilation of the outflow channels with cataract surgery is a safe and effective way to reduce intraocular pressure (IOP) and reliance on IOP-lowering medications for cataract patients with moderate-to-advanced glaucoma, Linda L Burk MD told the 37th Congress of the ESCRS in Paris, France. The triple procedure also reduces the financial burden of, and improves patient compliance with, glaucoma treatment, said Dr Burk, of UT Southwestern Medical School, Dallas, Texas, USA.
In a study involving 120 patients, Dr Burk removed 180 degrees of the trabecular meshwork with a Kahook Dual Blade and then directly flushed the collector channels with viscoelastic in a procedure she refers to as “clean the gutters and powerwash the down spouts”. The patients, half of whom had moderate-to-severe glaucoma and one-third of whom had previous glaucoma surgery, also underwent cataract surgery and implantation of an intraocular lens. Because so many patients had active disease, no medication washout was attempted before surgery.
One year after surgery, mean IOP fell 2.3mmHg, from 18.8 ± 5.4 to 16.5±5.4mmHg; mean topical glaucoma
medication use fell by 1.5, from 1.7± 0.9 to 0.2 ± 0.5; and the percentage of patients using no drops to control IOP increased from 0% to 90%, Dr Burk reported. This improves patient therapy compliance and greatly reduces medication costs. At $50 per bottle, the saving would be $84,000 annually for the group, she pointed out. Overall, 94% of patients were at or under 21mmHg and 42% at or under 15mmHg. Among patients with moderate-toadvanced glaucoma, 45% reached an IOP of 15mmHg or less with no medications, Dr Burk said.
REJUVENATION
The combined goniotomy-viscodilationcataract procedure results from a fouryear search for a combined glaucoma
procedure that is effective in lowering IOP, economical and compatible with implantation of premium lenses, Dr Burk said. Among its advantages are ease of combining the glaucoma procedures with cataract surgery, no expensive hardware needed, no foreign bodies left behind, a low complication rate and fast recovery.
Perhaps more importantly, the procedure removes diseased trabecular meshwork and creates direct access to multiple collector channels. This allows direct viscodilation with nothing more than a Healon cannula, restoring aqueous outflow, Dr Burk said.
“Many glaucoma experts think the collection channels are damaged beyond repair. I beg to differ. I think they can be rejuvenated by this technique,” Dr Burk concluded.

Linda Burk: LindaLBurk@gmail.com

EUROTIMES | JUNE 2020
SPECIAL FOCUS: GLAUCOMA 10
Kahook Dual Blade removes trabecular meshwork
Viscoelastic cannula fits snug into Schlemms Canal and allows viscoelastic to directly dilate the collector channels
Courtesy of Linda
L Burk MD
EuroTimes is your magazine! Contact EuroTimes Executive Editor Colin Kerr at colin@eurotimes.org Do you have ideas for any stories that might be of interest to our readers?
Linda L Burk MD
Early detection
Diagnostic suspicion of optic disc hinges on presence of corroborating findings. Cheryl Guttman Krader reports
Attentive evaluation of the optic disc in clinical practice provides invaluable information for identifying glaucoma, but no single feature provides diagnostic certainty, said Francisco Goñi MD at the ESCRS/EGS Glaucoma Day meeting in Paris, France.
“When a sign of glaucoma is detected, search carefully for other signs and place the information in the context of the complete examination,” advised Dr Goñi, a glaucoma specialist practising in Barcelona, Spain.
In his talk, Dr Goñi discussed the approach to optic disc examination and signs that raise suspicion of glaucoma. Through a series of clinical examples, he showed that individual signs can lack specificity for glaucoma and thus the need to look for corroborating evidence.
To assess the optic disc, Dr Goñi recommended performing the examination


through a dilated pupil and prior to knowing information about IOP or the findings from OCT imaging, which could bias the subjective judgment of the optic disc. He also emphasised the importance of comparing the optic disc appearance between eyes by moving the slit-lamp from one eye to the other.
Systematic evaluation of the optic disc focuses on size, cupping and the neuroretinal rim. Dr Goñi said that when considering the cup-to-disc ratio (CDR), however, clinicians must remember that disc size matters.

“We cannot classify patients in terms of glaucoma based only on the CDR. It must be put into the context of cup size because a large disc usually has large cupping and a small disc usually has small cupping,” he explained.
IS OR ISNT?
Care is also needed in evaluating neuroretinal rim thickness, recognising that the “ISNT”
Making your wishes come true: OCULUS Introduces its Shooting Stars

rule, stating that normal disc rim thickness of inferior the region is ≥ superior ≥ nasal ≥ temporal is not obeyed in 50% of normal eyes and also does not apply to non-standard optic discs. In eyes with a CDR >0.57, clinicians may consider the IS rule (inferior≥superior) that is more specific than the ISNT rule.
Dr Goñi observed that positional changes of vessels at the optic disc that occur due to narrowing of the neuroretinal tissue are important to observe when looking for glaucoma progression but they are not typical as an early sign. Retinal nerve fiber layer defects and disc haemorrhages may also be signs of glaucoma but they are not specific and so need to be considered in the context of whether there are additional glaucoma signs. Beta zone paripapillary atrophy can also be a clue to glaucoma, but is not a definite sign.
Francisco Goñi: francisgoni@yahoo.com
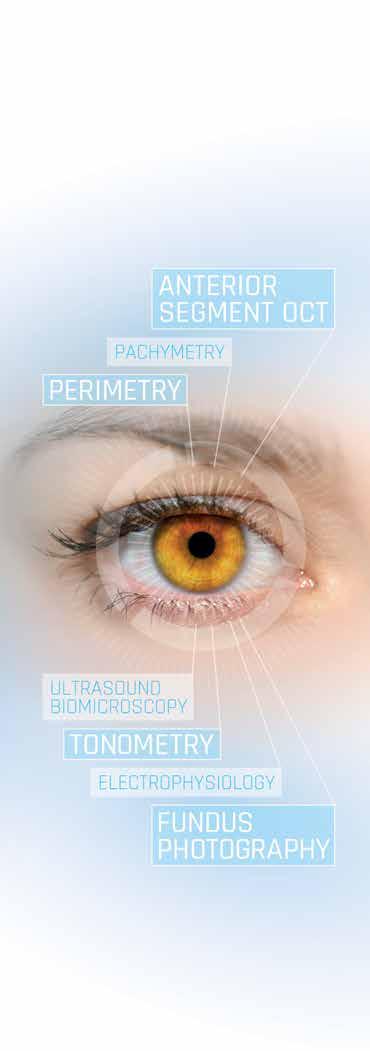
OCULUS perimeters – fast, small, EMR ready
OCULUS perimeters are purposefully optimized for monitoring functional impairment in glaucoma. Marked by shortened examination time, a more intuitive analysis of findings as well as increased patient comfort they each provide a modern all-in-one clinical solution for visual field testing. And all of this despite their small footprint! Learn more about the Easyfield ®, Centerfield ® 2 and Smartfield at www.oculus.de

EUROTIMES | JUNE 2020 SPECIAL FOCUS: GLAUCOMA 11
Follow us! www.oculus.de Eurotimes Centerfield Easyfield Smartfield - Störer Sternschnuppe 178x130 e 04.20.indd 1 21.04.2020 18:58:13
The New Normal
EUROCOVCAT is a group of cataract and refractive surgeons that has met on Zoom several times to discuss how to get back to practising ophthalmology in the most safe, efficient manner in the months and years ahead. This article, written exclusively for EuroTimes, provides an insight on how to rethink cataract care, not only for the current COVID-19 situation, but for the "new normal" following a global pandemic.
Brézin A.P., Université de Paris, Hôpital Cochin, Paris, France; Burdon M., Queen Elizabeth Hospital, Birmingham, UK; Cummings A.B., Wellington Eye Clinic, Dublin, Ireland; Evren Kemer O., University of Health Sciences, Ankara City Hospital, Turkey; Malyugin, B.S., Fyodorov Eye Microsurgery Federal State Institution, Moscow, Russian Federation; Prieto I., Prof. Dr. Fernando Fonseca Hospital, Portugal; Rejdak R., Department of General Ophthalmology, Medical University of Lublin, Poland; Teus M.A., University of Alcalá, Madrid, Spain; Tognetto D., University Eye Clinic, Trieste, Italy; Törnblom R., TYKS Hospital, Turku, Finland; Sallet G., ASZ Hospital, Aalst, Belgium.
INTRODUCTION
Countries are at different starting points with regard to COVID-19 epidemiology and response, availability of personal protective equipment, testing requirements, current cataract patient pathways (some have overnight stay), economic situations and patient demographics.
Clinic settings for cataract surgery also vary from standalone private practices, ambulatory surgical centres to large specialised clinics and departments located within the general hospitals.
Financing of cataract surgery differ too, quite significantly: though standard cataract is publicly reimbursed throughout Europe, some interventions, such as Advanced Technology IOLs, are covered by private insurance or co-payment.
Therefore, guidance on cataract surgery recovery needs to be quintessentially local and adapted to the specific clinical setting.
However, there are important overarching considerations that span across all practices:
COVID-19 patient and medical staff safety protocols will be here to stay, at least well into 2021.
Risk/benefit assessments will be crucial in determining when and how to restart cataract procedures.
This also provides an opportunity to critically reframe the patient pathway to future-proof cataract care.
Why we need to put a spotlight on Cataract in the next phase of COVID-19 recovery? The development of cataract is an inevitable fact of ageing. Cataract surgery is therefore among the top three most commonly performed surgical interventions across Europe. In many countries, waiting lists are already long; and suspension of all interventions due to the outbreak of COVID-19 has further affected patients’ access to care.
While the evidence suggests that the impact of cataract surgery on a patient’s quality of life is overwhelmingly and compellingly positive, in some countries, health authorities are tempted to deprioritise
cataract surgery in recovery planning as it is considered as a less urgent elective surgery.1,2,3
Patients on prolonged waiting lists for cataract surgery may experience negative outcomes during the waiting period, including vision loss and ultimately, poorer health-related quality of life (HRQoL).4
Untreated cataract also increases the risk of falls and with it the incidence of hip and knee fracture and head injuries. Conversely, cataract surgery decreases the risk: in a cohort of US Medicare beneficiaries aged 65 years and older with a diagnosis of cataract, patients who had cataract surgery had lower odds of hip fracture within one year after surgery compared with patients who had not undergone cataract surgery.5
At the same time, cataract surgery is a safe procedure typically performed in an outpatient setting and with local or topical anaesthesia. Compared to most other elective surgeries, it can be performed efficiently even with COVID-19 safety protocols.
What needs to be considered when re-starting Cataract Surgery? Due to the high volume of patients now on cataract waiting lists, there are pressing questions if and how to prioritise patients.
There is agreement in this group that a pragmatic stance should be taken to patient triaging to facilitate the restart. We propose a number of considerations:
1. Consider patients in chronological order of those already scheduled prior to the COVID-19 surgical suspension and assess their willingness for surgery.
2. Quality of life: Strong consensus that priority should not be based on visual acuity alone, but on Quality of Life vs. Risk. Therefore, simple questions on quality of life, daily function and personal preferences should be asked to ascertain readiness.
3. Age: Must consider age when triaging patients and speaking of Quality of Life, as any delay of surgery is significant for a septuagenarian and octogenarian relative to life expectancy.
4. Patient condition (comorbidities): We should also consider the conditions that place patients in the group of higher risk for COVID-19 outcomes: Older people and people of all ages with pre-existing medical conditions (such as diabetes, high blood pressure, heart disease, lung disease, or cancer) appear to develop serious illness more often than others.6 If chronic health issues and comorbidities can meaningfully be improved, there is a rationale to wait.
5. Ocular priorities (other concomitant ocular disease): Poor vision, narrow angles or other risk factors, anisometropia or high refractive errors should be considered. Operating on the second eye may be lower on the list if the anisometropia is not reducing the quality of life and increasing the risk of falls for example.
Consequently, we should aim for quality rather than quantity, and accept the fact that the number of cataract surgery procedures per day prior to COVID-19 may not be reached in the near future.
How will the cataract surgical pathway need to change to best protect patients and staff? We agree that the clinic is actually in most cases the highest risk area, not the operating arena itself, so there is a strong need to completely rethink the consultation protocol.7
No setup can guarantee complete COVID-19 safety, but control measures need to become standard.
We have highlighted some overarching considerations:
• The new reality calls for a one-stop clinic setup.
• Consistently reduce human contact to a minimum – this applies to number of staff in clinic as well as accompanying family members.
• Specific pathway for COVID-19 positive patients. There is no need for a specific diagnostic pathway, but rather the “red room” where the patient can be consulted about the deferred surgery.
• New waiting room configuration and methods (i.e. in-car waiting and patient distancing).
12 EUROTIMES | JUNE 2020 CATARACT & REFRACTIVE
• Facility disinfection on a regular basis – after each patient as well in time intervals.
• Mask distribution to all those who enter – either provided by each individual or the clinic.
• Air system evaluation to possibly cut central air in clinics and hospitals to avoid spread.
• Patient and team’s anxiety and safety management is crucial: clearly communicating all the procedures and protocols ahead of time to reassure them that we are taking COVID-19 seriously and will do our best to make sure that our centres are the safest place that they can be outside of their homes.
Each critical phase of the cataract care pathway needs to be evaluated in greater detail:
Pre-surgical assessment:
• First assessment can be done by phone one-to-three days prior to surgery:
- If have symptoms currently or had symptoms previously.
- If and how much patient is bothered by their vision.
- Understand readiness to come in for surgery.
- Explain that risk cannot be quantified.
• Possible use of interactive history forms that can be completed on patients’ phones, iPads or PCs that can include all the questions that we would normally ask in the clinic, such as reason for visit as well as visual expectations, or willingness to pay for Premium IOLs.
• Do only the mandatory in-clinic assessments (e.g. biometry, OCT, topography, tomography and specular microscopy).
• Pre-op COVID-19 testing should be integrated into one-stop pre-surgical assessment where required and possible. Testing is a subject of debate with many unresolved questions on types of tests, availability and reliability. As cataract surgery is done under local anaesthesia and integrated in a fast-track approach, many centres will not require PCR testing and all patients are to be managed as potential COVID-19 carriers.
We agree that the following is suggested whether or not any testing is performed:
• Pre-triage by phone the day before surgery:
Questionnaire to assess if symptoms, risk – if yes to one question, postpone surgery if possible.
• Triage at the check-in the day of the operation:
- Questionnaire to assess if symptoms, risk – if yes to one question, postpone surgery if possible.
- Consent process – needs to clearly articulate that COVID-19 infection risk cannot be quantified.
Surgical process:
• Dilation – possible to be done by patient before coming to clinic or by intracameral injection in OR during the surgery.
• Limit communications with the patient during the surgery to strict minimum.
• Reduce number of people present in OR (i.e. one surgeon and two nurses) and consider the needs for others including anaesthetist, assistants and residents in training.
• Bilateral same-day sequential surgery now being recommended in more countries and should be considered in alignment with country legislation. However, one must be aware of the risks this can entail and inform patients about these risks. The choice to perform bilateral contemporary surgery remains the surgeon’s choice.
• Staff protection: the staff should wear surgical mask8, gloves, should be trained about wearing and taking out of personal protection equipment.
• Phacoemulsification instruments should be covered properly and single use; protecting shields for operating microscopes, ‘like slit-lamp separators’, should be attached to oculars.9
Post-op:
• Only phone call and video assessment one day post-surgery as this is already in place in some markets.10
• Limit post-op visits to only four weeks postoperative visit unless there are any issues.
• Possibility to do visits through teleconsultation if patient and caregivers agree.
• Need to evaluate current mobile apps that could be used. We recognise that the list of recommendations is clearly not exhaustive and should be adapted and augmented locally to be fit for purpose.
CONCLUSION
We need to get back to doing cataract surgery. Vision is a vital part of general health and cataract waiting lists have only become longer in the past few months. There is a need for cataract surgery to start again as a priority. The primary factor that needs to be considered is how the cataract is impacting the patient’s quality of life. If the impact is minimal, of course surgery can wait. If the current quality of vision, however, is so that it is reducing the patient’s quality of life, then the cataract surgery should be performed sooner rather than later. The surgery itself will be different to what we are used to. There will be limited access to cataract surgery slots due to social distancing guidelines and some older patients may be reluctant to come to hospital settings for cataract surgery while COVID-19 is still in the news. More intense preoperative screening, swabs prior to surgery if possible,
increased use of PPE, fewer people in the operating room including in some instances working without an anaesthetist and using topical anaesthesia only, are all possible and even likely scenarios. Postoperative exams can be done virtually, either with a video call or even just a phone call, calling patients back for in-person consultations only when there are potential problems.
This text is not intended to replace local guidelines or any legislative recommendations. We had the opportunity to meet a few times using videoconferencing to discuss our main challenges and share ideas on how to face and overcome these challenges. When the discussion ended (for the moment anyhow), the final document was found to be especially useful by all of us, and hence we agreed that it may be found useful by our colleagues in the wider ophthalmological community. The decision to share the text more widely was unanimous. It is noticeably clear to us that we are all facing similar challenges in the face of this unprecedented event and we are unearthing and thinking of new ways of doing things every day. The situation is very dynamic, both from a health and an economic standpoint and we are certain that within weeks, there will be a lot to add to our collective thinking. At this point in time, there is no golden rule for exactly how cataract surgery should be restarted in Europe. However, it needs to be restarted. Each surgeon will have to consider a number of issues and then based on their experience, their local conditions and sentiment, and their patients’ willingness to proceed with surgery, take the first careful steps to the new normal for cataract surgery. We hope that you find the thoughts expressed here useful and we welcome further discussion.
1. Sammartino, Maria, et al. Cataract 29. Perioperative Care of the Elderly: Clinical and Organizational Aspects (2017): 190.
2. Lamoureux, Ecosse L., et al. The impact of cataract surgery on quality of life. Current opinion in ophthalmology 22.1 (2011): 19-27.
3. Busbee, Brandon G., et al. Cost-utility analysis of cataract surgery in the second eye. Ophthalmology 110.12 (2003): 2310-2317.
4. Hodge, William, et al. The consequences of waiting for cataract surgery: a systematic review. Cmaj 176.9 (2007): 1285-1290.
5. Tseng VL1, Yu F, Lum F, Coleman AL Risk of fractures following cataract surgery in Medicare beneficiaries. JAMA. 2012 Aug 1;308(5):493-501
6 https://www.who.int/emergencies/diseases/novelcoronavirus-2019/question-and-answers-hub/q-adetail/q-a-on-on-covid-19-for-older-people
7. Curr Eye Res. 2020 Apr 23:1-6. doi: 10.1080/02713683.2020.1752737. [Epub ahead of print] Facing COVID-19 in Ophthalmology Department. Romano MR, Montericcio A, Montalbano C, Raimondi R, Allegrini D, Ricciardelli G, Angi M, Pagano L, Romano V
8. https://www.nap.edu/read/11637/chapter/4#38
9. Wong DHT, Mak ST, Yip NKF, Li KKW. Protective shields for ophthalmic equipment to minimise droplet transmission of COVID-19 [published online ahead of print, 2020 Apr 22]. Graefes Arch Clin Exp Ophthalmol. 2020;1‐3. doi:10.1007/s00417-020-04683-y
10.Tinley CG, Frost A, Hakin KN, McDermott W, Ewings P Is visual outcome compromised when next day review is omitted after phacoemulsification surgery? A randomised control trial. Br J Ophthalmol. 2003 Nov;87(11):1350-5
13 EUROTIMES | JUNE 2020 CATARACT & REFRACTIVE
-
COMPLICATIONS of surgery
As precision surgeons aiming for excellent unaided distance and near visual acuity, we feel uncomfortable hearing the word “complications”. However, the best way to manage complications is to be prepared. I like to think of complications as those that I am terrified of, those that worry me a lot and others.
TERRIFIED OF
Endophthalmitis and infections: This terrifies each of us because of the potential of even best planned surgeries going wrong. Key in these situations is early identification and referral to the vitreoretinal surgeon.
It is important to communicate with the patient, to not lose trust and to help them navigate this unexpected territory. It becomes imperative to educate lay population, media as well as governmental agencies about the multi-factorial causation for endophthalmitis, especially in cluster outbreaks.
Supra-choroidal and expulsive haemorrhage: This is rare but has the potential to turn ugly, rapidly. Shallowing of the anterior chamber (AC), a firm eye, loss of red reflex and bulging of the posterior capsule should be recognised immediately. Your first aim should be to withdraw instruments and suture all incisions closed. The AC may be deepened with viscoelastic if possible. Prolapsed iris may need to be excised and any further surgery should be deferred. Surgical drainage via sclerotomy is not advisable, as it results in loss of tamponading effect and further bleeding.
WORRIES ME A LOT
Posterior capsular rent (PCR): Most important here is not to pull out the phaco or I/A probe abruptly, as this can result in extension of the tear and vitreous prolapse. Viscodispersive viscoelastic is injected under the remaining pieces and over the PCR and the probe is gently removed. Key here for me, is the stage at which PCR occurs.
If entire/ large part of a hard nucleus is present, I prefer to convert to manual small-incision cataract extraction, which is self-sealing while allowing safe removal of nucleus.
If it is only a soft cataract or a small fragment left behind, I bring it over the iris and then perform an IOL scaffold technique by preplacing a three-piece IOL into the sulcus with optic capture and then emulsifying the nucleus. The cortex, however, should be removed before implanting the IOL. I do this with a vitrector probe via a pars plana approach, alternating between cut and aspirate modes to avoid vitreous traction while allowing easy cortex aspiration.
Persistent corneal oedema: Preoperative specular count helps identify early Fuchs’ dystrophy. Viscodispersive viscoelastic, in-the-bag chop, low energy usage, torsional ultrasound all help decrease corneal damage. In advanced cases, phaco may be combined with endothelial keratoplasty (EK).
If corneal oedema is seen postoperatively in a patient with normal preoperative endothelial count, I do an ASOCT to rule out Descemet’s detachment (DD), which if present can be easily bubbled. Bullous DD may occur during stromal hydration of side port. This may not respond to air/ long-acting gas alone and I do Relaxing Descemetotomy to drain trapped fluid.
In recalcitrant oedema, I prefer doing pre-Descemet’s EK using three techniques also described by me – endoilluminator and air pump-assisted techniques as well as host Descemetic scaffolding, which make surgery easier, repeatable and decrease chances of graft detachment.
Retinal complications: Chances increase in high myopes and complicated surgeries.

A retinal surgeon should be consulted immediately. Postoperative cystoid macular oedema may also occur and prophylactic topical NSAIDs are helpful to prevent it. This should be treated aggressively if present.
Malpositioned IOL: An IOL that is not

properly placed or that gets dislocated worries me since it requires a second intervention. Eyes with deficient anterior/ posterior capsular support need stable IOL fixation during primary surgery in the form of iris or scleral fixation or an ACIOL. A single-piece acrylic IOL placed with haptic in sulcus can cause uveitisglaucoma-hyphema syndrome and needs to be repositioned. Late postoperative dislocations can occur because of suture degradation and progressive zonulopathies.
OTHER COMPLICATIONS
Refractive error: In patients who opt for premium IOL to decrease spectacle dependence, I generally find that having done a proper preoperative counselling sets expectations straight for small postoperative refractive errors. However, large refractive surprises can be upsetting and may entail either cornea-based refractive surgery, piggyback IOL, IOL exchange or sometimes an IOL rotation. Dysphotopsias: Positive dysphotopsias such as glare, haloes etc occur secondary to poor optics of the eye (increased higherorder aberrations, large-angle kappa) or the IOL (diffractive IOLs, truncated edges, high refractive index IOLs) and can be treated by pharmacological pupillary constriction. Unresponsive and persistent cases may need an IOL exchange. Negative dysphtopsias are managed by special glasses that block light entering from the side. Just waiting for capsular opacification to cause light scatter on to the dark area of the retina may also work. Surgical options include removing nasal overlapping capsule, reverse optic capture, orienting optic haptic junction to horizontal meridian or exchanging with a three-piece silicone IOL. Pupillary constriction can, however, worsen it.
Other complications such as postoperative glaucoma, inflammation, posterior capsular opacities etc may occur and can generally be handled well with appropriate and timely treatment. Complications in special situations such as IOL opacification following
14 EUROTIMES | JUNE 2020 CATARACT & REFRACTIVE
Any number of complications can occur in or after surgery, and it's important to keep things in perspective.
Soosan Jacob, MS, FRCS, DNB reports
intracameral air in hydrophilic IOLs, corneal melts in patients with rheumatoid arthritis, severe postoperative inflammation in uveitic patients etc need special evaluation and planning pre- and postoperatively.

Other forms of refractive surgery can also have complications, though the rate is generally low.
PHAKIC IOLS (PIOLS)
PIOLs have distinct complications depending on whether they are AC or posterior chamber (PC) PIOLs. The vaulting of a PCPIOL is important and a low vault can cause cataract while an excessive vault can cause shallow AC, angle closure and increased IOP. ACPIOLs can cause endothelial decompensation, glaucoma and pupillary abnormalities/ distortion.
My personal preference is to place a PCPIOL as it is easier for me and for the patient if I have to treat a potential cataract formation than a potential endothelial decompensation. Since these are all intraocular surgeries, they do carry the risk of complications such as uveitis, retinal detachment, endophthalmitis etc. I give prime importance to performing a thorough dilated retinal examination preoperatively to avoid potential retinal detachments and avoid operating on very high-risk patients.
CORNEA-BASED REFRACTIVE SURGERY COMPLICATIONS TERRIFIES ME
Infections: Luckily, the rate of infections post-refractive surgery is very low and proper precautions continue to maintain this so. Post-PRK infections may occur secondary to epithelial defect and use of contact lenses. Post-LASIK infections are unlike usual corneal infections and proper management is a must. Interface involvement, delayed presentation, steroid usage, atypical and resistant organisms, inadequate drug penetration, indolent course and slow response to therapy are seen.
WORRIES ME A LOT
Flap complications: Buttonholes, free caps, perforations, decentred flap, amputated flap, partial flap all occur more often with microkeratome but also do occur with femtosecond laser. Buttonholes are managed by deferred surface ablation, whereas free caps can undergo excimer ablation with careful flap replacement. Partial flap with microkeratome is deferred for later treatment whereas if with femtosecond, the cut can be resumed. Small-incision lenticule extraction (SMILE®) can have complications with lenticule creation, dissection and extraction.
Ectasia: Preoperative evaluation and risk scoring is important. Sometimes a patient who has no risk factor on tomography may still present with ectasia. Preoperative biomechanical screening may be useful in the form of Corvis Biomechanical index and Tomographic Biomechanical index. Ectasia should be treated early with cross-linking
to minimise damage to vision as well as avoiding more invasive surgeries such as deep anterior lamellar keratoplasty.
In advanced cases, intra-stromal corneal ring segments such as Intacs and CAIRS (Corneal Allogenic Intrastromal Ring Segments) can be used simultaneous with CXL to improve uncorrected visual acuity. Aberrated optics: This may occur secondary to central island, decentred ablation, irregular astigmatism and even early post-LASIK ectasia. Patients have glare, haloes and decreased uncorrected and best-corrected visual acuity, often worse at night. Tomographic evaluation is needed to rule out ectasia. I then generally give some time for epithelial remodelling and also use brimonidine eye drops for pupillary constriction to try and relieve symptoms non-surgically.
Unresponsive and persistent cases may respond to rigid gas permeable contact lenses or topography-guided therapeutic refractive surgery. In SMILE, partially retained lenticule can cause irregular astigmatism and symptoms. Fourier domain OCT and diluted IVTA can be used to delineate the retained fragment and remove it. In Epi-LASIK, stromal injury from blade can cause irregular astigmatism and in case of an uneven bed, ablation should be postponed.
Dysphotoptic symptoms: These are more common with larger corrections, smaller optic zone, aberrated optics (see above) and larger pupil size (more important with older laser technology). Transient light sensitivity occurs in some patients but generally responds to treatment.
Epithelial ingrowth, Striae, Diffuse Lamellar keratitis (DLK), Interface debris: These complications can generally be addressed with good resolution. I leave subtle peripheral striae and inactive, peripheral epithelial ingrowth alone but symptomatic ones need intervention. DLK always needs to be treated aggressively with steroids and in more advanced cases with flap lift and wash.
OTHER COMPLICATIONS
I always make sure that refractive expectations are set right by proper counselling. I take care to explain that though refractive surgery in its current form gives excellent results, both efficacy and safety-wise, it cannot guarantee spectacle independency for all activities for every single patient
Consent and patient counselling should include complications such as dry eye and the possibility of some residual refractive error. Over-corrections and undercorrections may occur and are generally treatable after refractive stabilisation. Aggressive topical steroids can be used for under-corrections. Deep surface ablations can be prone to haze/regression and Mitomycin-C is used intraoperatively.
To conclude, complications are an inevitable part of every surgeon’s life and these should be dealt with properly either by the surgeon or through specialist referral.
Dr Soosan Jacob is Director and Chief of Dr Agarwal's Refractive and Cornea Foundation at Dr Agarwal's Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
EUROTIMES | JUNE 2020 CATARACT & REFRACTIVE 15
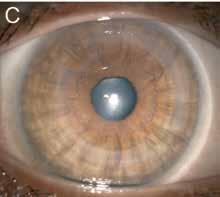
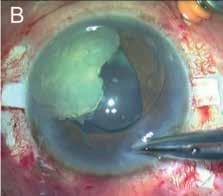
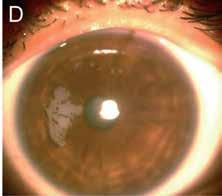
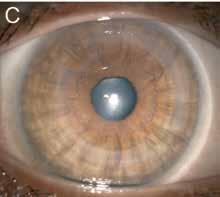
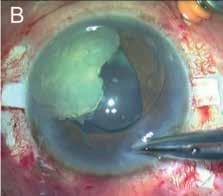
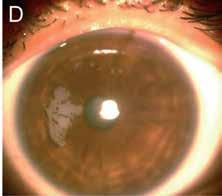
A: Capsular tension ring implantation in subluxated cataract; B: IOL scaffold for PCR; C: CAIRS (Corneal Allogenic Intrastromal ring Segment) for corneal ectasia; D: Post-SMILE epithelial ingrowth
Stress kills
Stress leading to burnout is an under-recognised problem among surgeons. Roibeard Ó hÉineacháin reports

Around two-thirds of surgeons endure prolonged unrelieved stress, potentially undermining their physical and psychological health, leading to obesity, cardiovascular problems, depression and early death, said Prof Michaela BayerleEder MD, PhD, Department of Clinical Pharmacology and Department of Endocrinology and Metabolism, Medical University of Vienna, Vienna, Austria.
“Stress perception and stress management are under-acknowledged in the surgical community and you need to be aware that you may be among those who are over-stressed,” she told the 37th Congress of the ESCRS in Paris, France.
Prolonged stress leads to increased cortisol and catecholamine levels, she said. A potential consequence of that is metabolic syndrome. She noted that about one-third of young male surgeons suffer from obesity, one-third have impaired glucose tolerance leading to diabetes and more than 40% have lipid disorders.
In addition, some estimates suggest that up to 68% of surgeons suffer from burnout and this is accompanied by depression that is mild-to-severe in up to 20%. In addition, around 15% of all surgeons are addicted to drugs. The stressors appear to have lifeshortening effect. For, example a study of Brazilian neurosurgeons showed they had an average lifespan of only 68 years, Prof Bayerle-Eder pointed out.
Another important aspect of stress is its effect on an individual’s relationships, she said. Stress reduces levels of testosterone and oestrogen resulting in reduced libido and fertility. Furthermore, research shows that stress can impair the amygdala, making one less cognizant of other’s emotions, as expressed in facial expressions and other non-verbal cues.
In the classical model of stress, when confronted with a challenge, the stress levels rise, but as the challenge is overcome, the stress levels subside. However, a prolonged period of stress will result in burnout, when
the stress reaction is replaced by a nonreactive apathy and resignation to stress.
In the general adaptation stimulus model, a stressful stimulus leads to an alarm reaction, arising mainly from the brain stem and then there is a stress adapt reaction. This activates the hypothalamus pituitary adrenal (HPA) axis, increasing levels of cortisol and testosterone, adrenaline and dopamine, all of which can be beneficial when presented with a challenge. But again, when the stress adaptation reaction is prolonged it leads to burnout, Prof Bayerle-Eder explained.
The fight-or-flight response tends to be more pronounced in males because it is mediated not only by norepinephrine and adrenaline but also by testosterone. Females generally have a more “tend and befriend” approach to problems and manage stress through socialising. That encourages the secretion of oxytocin, which is a relaxing and antidepressant
hormone and is mediated by oestrogen. Under stressful conditions the hypothalamus causes the pituitary to release adrenocorticotropin hormone (ACTH) causing the adrenal cortex to release cortisol. There is also an activation of the sympathetic branch of the nervous system inducing fightor-flight response through the release of epinephrine and norepinephrine.
When a surgeon focuses on a procedure, they will have the classical release of norepinephrine and adrenaline as well as dopamine, which is the "endogenous cocaine" that provides the feeling of satisfaction that comes with meeting a challenge and accomplishing a task. Increased levels of acetylcholine further enhance their attention.
“It is only the over-activation of this system that leads to the bad consequences,” she said. However, surgeons and others who have reached the burnout stage can recover a healthy and happy existence and, in the process, become a more able practitioner. Steps that might be taken to alleviate and prevent burnout include changes in diet and exercise to improve cardiovascular health and enhance sexual function. Maintaining a good social and sexual life is also important, to maintain good oxytocin levels. Good sleep hygiene is also necessary for optimal function, she added.
Michaela Bayerle-Eder:
michaela.bayerle-eder@meduniwien.ac.at
CATARACT & REFRACTIVE 16 EUROTIMES | JUNE 2020
Stress perception and stress management are under-acknowledged in the surgical community...
Prof Michaela Bayerle-Eder MD, PhD
Mono-EDOF lens improves vision
New lens provides intermediate vision without sacrifice of distance vision. Roibeard Ó hÉineacháin reports
The new Tecnis® Eyhance (Johnson & Johnson) refractive aspheric monofocal extended depth of focus (EDOF) IOL appears to provide very good distance vision and slightly improved intermediate distances vision compared to a standard aspheric monofocal IOL, reports Ewa MrukwaKominek MD, PhD, University Clinical Centre Katowice, Poland.
In a pilotage study involving 10 patients who underwent implantation of the new Eyhance IOL, uncorrected distance visual acuity (UCDVA) and uncorrected intermediate visual acuity (UCIVA) was significantly better postoperatively (p<0.05) than it was preoperatively. Patients also reported significant improvement in the performance of daily activities connected to vision, she told the 24th Winter Meeting of the ESCRS in Marrakech, Morocco.
Prof Mrukwa-Kominek and her associates performed the cataract procedures with standard ultrasound phacoemulsification. They measured the preoperative and postoperative refractive error using the maximum plus technique. They calculated the power of implanted lenses for emmetropia using the Barret TK Universal II formula. These ranged from 19.0D to 25.5D (mean 21.3D).
One month after the procedure, both the mean uncorrected distance visual acuity (UCDVA) and the mean uncorrected intermediate visual acuity (UCIVA) were significantly better than they were preoperatively (p<0.05). Postoperatively the mean UCDVA was Snellen 0.9, compared to 0.2 preoperatively, and the mean UCIVA, using the Jaeger standard at 66cm J10 preoperatively and J6 postoperatively. In addition, the average refractive error improved from -1.50D to -0.25D. No adverse effects or decentration of the IOL were observed, Prof Mrukwa-Kominek said.
The patients’ responses to the Catquest-9SF questionnaire showed significant improvement of performance of daily activities after implantation of the Tecnis Eyhance lens. Prior to the procedure, seven patients said they were very dissatisfied or fairly dissatisfied with their vision. One month postoperatively, nine patients said they were very satisfied or fairly satisfied with their vision, Prof Mrukwa-Kominek said.
The new Tecnis one-piece IOL (ZCB00) has the same base geometry as all other Tecnis one-piece lenses but has a continuous aspheric surface. The dioptric power of the lens changes from the periphery to the centre, without diffractive rings or refractive zones, in a manner designed to provide better intermediate distance vision compared to a monofocal aspherical lens. In addition, the lens material provides simultaneous correction of chromatic aberration.
“It seems that the innovative Tecnis Eyhance intraocular monofocal lenses with ‘extended depth of focus’ provide very good distant vision and slightly improved vision at intermediate distances. Implantation of Tecnis Eyhance IOLS can be considered in all patients who have opted for a monofocal lens implant,” Prof Mrukwa-Kominek concluded.
Ewa Mrukwa-Kominek: emrowka@poczta.onet.pl

17
EUROTIMES | JUNE 2020 CATARACT & REFRACTIVE
Ewa Mrukwa-Kominek MD, PhD
THOMAS KOHNEN European Editor of JCRS


JCRS HIGHLIGHTS

VOL: 46 ISSUE: 4 MONTH: APRIL 2020
ACCELERATED CXL IN PAEDIATRIC KERATOCONUS
A five-year follow-up study supports the use of corneal collagen cross-linking (CXL) in paediatric keratoconus and suggests advantages for using an approach with increased irradiance over a shorter application time. The retrospective case-controlled study compared two different accelerated CXL protocols in 143 eyes of 86 patients with a mean age of 15 years. One group received four minutes of illumination at 30mW/cm2, and the second group received five minutes of illumination at 18mW/cm2. Both treatments halted progression of keratoconus. Patients in the second group showed a statistically significant reduction in total higher order aberrations and coma during the five-year visit when compared with the preoperative visit. This was not seen in the first group. A Agca et al., “Accelerated corneal crosslinking in children with keratoconus”, Volume 46, Issue 4, pp517-523.


TORIC IOLS AFTER CORNEAL REFRACTIVE SURGERY
Patients who have had LASIK or PRK in the past show significant decreases in astigmatism when implanted with toric IOLs according to a retrospective study.







The study included 56 eyes with previous myopic LASIK/PRK and 19 eyes with previous hyperopic LASIK/PRK. Vector analysis was used to assess the preoperative corneal and postoperative refractive astigmatism. Mean corneal astigmatism in myopic cases declined from 1.34D preoperatively to 0.36 after IOL implantation. Hyperopic cases showed similar improvement, from a mean 1.66D before surgery to 0.34D after toric IOL surgery. A majority of eyes, 80% of myopic cases and 84% of hyperopic cases, had refractive astigmatism of 0.50D or less at postoperative follow-up. D Cao et al., “Outcome of toric intraocular lenses implanted in eyes with previous corneal refractive surgery”, Volume 46, Issue 4, pp534-539.
ROCK INHIBITORS AND EYE BANKS
Rho-associated protein kinase (ROCK) inhibitors, better known as a glaucoma treatment, may have a role to play in preserving corneal tissue in eye banks. Apoptosis of corneal endothelial cells is a known problem in grafts stored in storage medium and is related to graft suitability for transplantation. Corneal endothelial cell survival in donor corneal tissue is essential for the transparency of the graft. Selective ROCK inhibitors have been shown to decrease apoptosis of cultured human corneal epithelial cells. A study conducted in human donor corneolimbal rings stored in commercial storage medium demonstrated a reduced rate of early apoptosis and late cell death at one week when a ROCK inhibitor (Y-27632). This could have important implications for corneal tissue storage in eye banks. Moreover, ROCK inhibition could prove to be useful in promoting future graft survival, the investigators note. Future studies are planned. A Achiron et al., “Effect of Rho-associated kinase inhibitor on human corneal endothelial cell apoptosis”, Volume 46, Issue 4, pp612-616.
CATARACT & REFRACTIVE 18 JCRS is the official journal of ESCRS
ASCRS
and
EUROTIMES | JUNE 2020
Femto vs Phaco: The latest
Femtosecond laser-assisted cataract surgery (FLACS) is neither safer nor more effective than standard ultrasound phacoemulsification and is considerably less cost-effective, according to the findings of the largest prospective randomised controlled trial conducted to date comparing the two procedures, published in the January 2020 issue of The Lancet
















“The main point to take home from this study is that FLACS is a very safe procedure because we didn’t observe any significant adverse event related to the laser procedure by itself, but on the other hand, the advantages proposed for this advanced technology does not translate into any clinical benefit for patients compared to standard phacoemulsification whatever the cataract severity grade,” the study’s lead investigator Cédric Schweitzer MD, Bordeaux University Hospital, France, told EuroTimes in an interview.
The Femtosecond laser-assisted versus phacoemulsification







Cataract surgery (FEMCAT) trial involved 1,476 eyes of 907 patients who were randomly assigned to undergo bilateral cataract surgery either with FLACS with the Catalys® system (Johnson & Johnson) or standard phacoemulsification between Oct 9, 2013, and Oct 30, 2015. Participants were masked to the surgical treatment allocation until the last follow-up visit at 12 months after surgery. Those in the phacoemulsification group underwent a sham laser procedure.



The primary clinical endpoint was the success rate of surgery, defined as a composite of four outcome criteria at a threemonth postoperative visit: absence of severe perioperative complication, a best-corrected visual acuity (BCVA) of 0.0 LogMAR or better, an absolute refractive error of 0.75 D or less and 0.5 D or less change in corneal astigmatism and 20°or less change in cylinder axis.
On that basis the study’s investigators found no significant difference in the success rate of surgery between the FLACS group (41.1%) and the standard phacoemulsification (43.6%). The incremental cost-effectiveness ratio was €10,703 saved per additional patient who had treatment success with PCS compared with FLACS. At the same time there were no significant differences between the two groups in terms of complications. Most of the complications in the FLACS group occurred during the phacoemulsification phase of the procedure or post-operatively.
“The cost-effective ratio of phacoemulsification surgery is one of the best in medicine, whatever the specialty. Surgeons can choose to use the femtosecond laser, but it is too costly. If the costs were similar or there were improvements in the technology that could provide a greater clinical benefit to patients, perhaps related to new intraocular lenses, as was the case with foldable IOLs and phacoemulsification, we could change the paradigm,” Dr Schweitzer said.
19 forum.escrs.org A library of symposia, interviews, video discussions, supplements, articles and presentations Spotlight on: Toric IOLs and Presbyopia
Glaucoma
Ocular Surface Disease
Corneal Therapeutics
FEMCAT trial fails to show clinical benefit of FLACS over standard phaco. Roibeard Ó hÉineacháin reports
EUROTIMES | JUNE 2020 CATARACT & REFRACTIVE
[FLACS] does not translate into any clinical benefit for patients compared to standard phaco
Cédric Schweitzer MD
Treating hydrops
New surgical techniques make acute hydrops in keratoconus a treatable disease. Roibeard Ó hÉineacháin reports
Conservative treatments for hydrops in keratoconus patients are becoming obsolete with the advent of new surgical approaches such as compression sutures and miniDescemet’s patch grafting, which can greatly reduce the duration of the condition, reports Prof Bjӧrn Bachman MD, PhD, FEBO, University Hospital Cologne, Germany.
“Compression sutures and mini-DMEK contribute to a paradigm shift from conservative to surgical treatment of acute hydrops in keratoconus,” Dr Bachman told the 24th ESCRS Winter Meeting in Marrakech, Morocco.
He noted that acute hydrops occurs in 2.5-to-3% of eyes with keratoconus and is unilateral in most cases. The condition usually occurs in the second and third decade and predominantly in male patients, as is the case with keratoconus. Spontaneous resolution of corneal oedema generally occurs between one and nine months.
Conservative treatments have long been the mainstay of treatment for corneal hydrops. However, they are mostly palliative in nature and generally do not shorten the duration of the condition. Furthermore, the conservative approach has a limited effect on the potential for complications, such as corneal scarring, which occurs in nearly all cases and will be extensive in some cases. In addition, hydrops occurring close to the limbal area can provoke severe corneal neovascularisation. Other potential complications include microbial keratitis and corneal perforation.
BRINGING DESCEMET’S MEMBRANE AND STROMA
Hydrops in keratoconus results from a failure of the less flexible Descemet’s membrane to align with the inner surface of the ectatic stroma. The rupture and detachment of Descemet’s membrane allows the influx of aqueous humour into clefts within the stroma. Surgical treatments introduced in recent years are designed to bring the Descemet’s membrane and stroma back into alignment with each other or to patch the rupture with a small Descemet’s endothelial graft.
The first surgical approach to be introduced was intracameral injections octafluoropropane (CF38) gas at non-
expanding concentration 14%. Research suggests that it can at best bring about a slow improvement in the condition. In a retrospective study, the mean time for resolution of the oedema was 78.7 days in 62 eyes that underwent intracameral C3F8 injection and 117.9 days 90 eyes that received conservative treatment (p<0.0001) (Basu et al. Ophthalmology 2011;118:934-9).
“The problem is if there is too much distance between the detached Descemet’s membrane and the corneal stroma. If you have a large tear in the membrane, the gas can just pass through the hole and fill up the space between Descemet’s and the corneal stroma and then you will have the opposite effect from what was intended,” Dr Bachman said.
A real step forward was compression sutures and intracameral gas tamponade technique, he noted. It involves drawing two-to-five full-thickness sutures with 10-0 nylon across the Descemet’s membrane tear to draw the ectatic stroma and the DM into conformation with each other. That is followed by the intracameral injection of C3F8 or SF6 gas in non-expanding concentrations. Patients undergo suture removal two to six weeks after surgery. In a study involving 15 acute hydrops keratoconus patients, average time for resolution of corneal oedema following the procedure was 8.87 days (Rajaram an et al, Cornea. 2009 Apr;28(3):317-20).
Marc Muraine MD later introduced a variation of the technique where the suture only extends though the stroma (Br J Ophthalmol 2015;99:773-7). The technique has also been combined with OCT guided drainage of acute hydrops, which helps clear the cornea even faster (Siebelmann et al, Cornea 2019).
MINI-DMEK
A new approach in acute hydrops is the use of mini-DMEK grafts, sized 5.0mm or less, to patch the disrupted Descemet’s membrane. In a study he and his associates performed, four mini-DMEK procedures in three eyes of three patients, UCVA logMAR improved from 1.6 before to 1.2 after six-to-eight weeks. They had to repeat the procedure in one patient because the Descemet’s membrane of patient had so much tension the patch did not attach. They removed a piece of Descemet’s membrane from that patient. There was a partial detachment of graft without relapse of hydrops in two eyes.
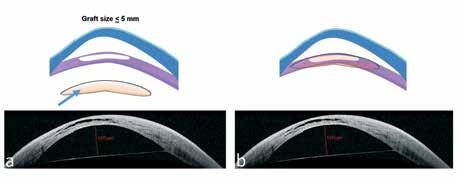
Comparing Mini-DMEK vs compression sutures, Dr Bachman noted that miniDMEK has the advantage of eliminating any risk of suture loosening and leakage from the stitch canal. In addition. unlike compression sutures, mini-DMEK can treat massive oedema. Its main disadvantages are that it requires general anaesthesia and is a complex technique best performed with intraoperative optical coherence tomography (OCT). The main advantages of compression sutures are that it is an easy technique requiring no special equipment and can be performed with local anaesthesia. The main disadvantages with the technique are the risk of leakage and the risk of relapse in eyes with large amounts of oedema.
“Acute hydrops has become a treatable disease. In most patients surgical approaches rather than a purely conservative treatment is advisable. The new surgical treatments provide a rapid improvement in visual acuity and presumably results in less scar formation or vascularisation of the corneal stroma and reduce the risk of requiring a penetrating keratoplasty,” Dr Bachman concluded.
Björn Bachmann: bjoern.bachmann@uk-koeln.de
EUROTIMES | JUNE 2020 CORNEA 20
(a) The graft for mini-DMEK (blue arrow) is adapted in shape and size to defects in the recepient’s Descemet's membrane (DM). Those grafts can be used to patch ruptures in DM occuring in acute hydrops in keratoconus patients (b)
Courtesy of Prof Bj
ӧ rn Bachman MD, PhD, FEBO
Ophthalmologists
ESCRS Survey on COVID-19 of PRACTICE PATTERNS PRACTICE PATTERNS
A Message From Professor Rudy MMA Nuijts, ESCRS President




The ESCRS COVID-19 survey on the practice patterns of ophthalmologists conducted from April 5 to April 24, 2020 offers us some valuable insights into the issues that have been addressed by ophthalmologists since the outbreak of the pandemic. I would like to thank all of my colleagues who took the time to answer our survey during this very stressful time.
In the following pages, you can see the results of the survey, which will help the ESCRS and the wider ophthalmological community plan a way forward for our community as we do our best to return to the level of services we were able to provide to our patients before the outbreak of the pandemic. There will surely be successes and failures along the way, but I am confident that the courage we have shown in fighting this terrible virus will help us to create a new dawn for ophthalmology.
President
Executive Summary
This survey demonstrates an interesting cross-section on the views of ophthalmologists on the COVID-19 pandemic.
While approximately 75% of the respondents were continuing to do less than 15% physical visits for consultations, there was variation in practice amongst countries, with ophthalmologists in Germany scaling down their in-person visits least compared with colleagues in other European nations. For infection prevention during physical visits, physical distancing and requesting patients to use hand disinfection and wear a surgical mask were the measures being used most often.
Variation in lockdown restrictions between countries was also seen in the responses to the questions about type of care being provided, percentage of physical consultations and percentage of surgeries being performed that showed patterns differing among ophthalmologists in different countries.
As an alternative to physical visits, telephone was the most common tool being used to communicate with patients; only about 15% of respondents were using video consultation.
Almost all of the respondents, around 90%, reported doing less than 15% of their usual surgical volume, including almost 60% who reported doing no surgeries. Approximately 10% of the respondents had been transferred to a COVID ward to provide patient care.

Overall, those ophthalmologists who responded to the survey appeared satisfied with the measures taken by their governments to control the COVID-19 pandemic. Here too, however, there were notable differences by country. Whereas in many countries more than 50% of respondents were satisfied with their government’s actions, looking at the two most heavily affected countries, only about 10% of respondents in Spain were satisfied compared with approximately 40% of those in Italy.
Responses to the survey’s questions about personal protection equipment (PPE) provide testimony to the dedication and initiative of the medical community. The limited availability




of basic resources such as masks, hydroalcoholic solutions and gowns at the peak of the epidemic show that the virus took us by surprise and did not allow us to anticipate needs. Even if the reorganisation capacities of the health authorities varied from one country to another, however, the survey results indicate that the mobilisation of the medical profession was a common denominator across nations and had an undeniable role as the main actor in managing the crisis.
Less than 30% of the respondents were satisfied with access to COVID-19 testing for their employees, and this lack of satisfaction was consistent among ophthalmologists across countries. In addition, less than 50% of the respondents said they were satisfied with the personal protective equipment (PPE) provided by their clinic or hospital.
FFP2 masks were being used more heavily in Spain and Italy compared with other countries and satisfaction with PPE was less than 30% in both Spain and Italy.
Most members participating in the survey believed they would restart performing elective surgery in May or June. Their responses also indicated they would be changing their practice logistics in the future.
Asked about how the pandemic would change their future practice behaviour, nearly
half of responding ophthalmologists indicated they would incorporate phone and/or video consulting on a routine basis. Out of necessity, technology has been increasingly adopted for professional communications, but perhaps without due consideration to the downsides.
We are maintaining links through conference calls and a growing number of webinars, but these modern communication options may set aside data protection and bioethics.
We know, however, that in-person physicianpatient communication is very important in all of medicine and that physical examination, including the use of multiple diagnostic devices, is critical for appropriate decisionmaking in ophthalmology. Furthermore, many of our patients may not have access to the technology that is needed for participating in a remote consultation. Time will tell whether ophthalmologists who turned to phone and video consulting during the pandemic because there was no other option will continue to use these methods when the pandemic is over.
Finally, and maybe surprisingly, there are a large number of ophthalmologists who say they do not plan any changes to their practice.
We cannot predict the future, but we would suggest that our future behaviour may change more substantially than our survey results suggest.

COVID-19 Practice Patterns of Ophthalmologists I
Prof. dr Rudy MMA Nuijts ESCRS
Prof. dr Rudy MMA Nuijts
Prof. Thomas Kohnen
Prof. Oliver Findl
Prof. Béatrice Cochener-Lamard
How many years have you been in practice post training?
COVID-19 Practice Patterns of Ophthalmologists II 70% EUROPE 30% REST OF THE WORLD 30% REST OF THE WORLD Location of respondents total respondents 1,376 60% male female 40% 0% 10% 20% Surgeon-owned practice
Corporate-owned practice Hospital-owned practice Private Hospital Public Hospital Academic Institution 30% 40% 50% 60% Currently in training (e.g. resident/fellow) 0-10 year 11-20 years > 20 years 0% 10% 20% 30% 40% 50% 60%
What type of practice do you work in? (more than one possible answer)
What type of
are you currently providing ? (multiple an
possible)
Q.1 What type of care are you currently providing? (multiple answers possible)
Q.2 What percentage
COVID-19 Practice Patterns of Ophthalmologists III 0% 10% 20%
percenta ge of consultations do you still see physically? Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=891) Re st of the World (n=385) Austria (n=27) Belgium (n=38) Fra nce (n=23) Germany (n=25) Gre ece (n=59) Ital y (n=76) Netherlands (n=125) Por tugal (n=40) Ro m ania (n=32) Spain (n=236) UK (n=81) Non e 1-15% 15-25 % 25-50% >50%
What
of consultations
see
do you still
physically?
swe rs
Europe Vs Rest of the World Selected European Countries Eu ro pe (n=886) Re st of the Wo rld (n=387) Emergency care only Intrav it re al injections Laser procedures Some electi ve su rg er y (e.g. second eyes after 1st phaco) Follow-up visits af ter previous electi ve surgery 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Austria (n=27) Belgium (n=37) Fra nce (n=23) Germany (n=25) Gre ece (n=59) Ital y (n=70) Netherlands (n=123) Por tugal (n=38) Ro m ania (n=28) Spain (n=228) UK (n=78)
care
Q.3 How do you contact non-physical patients? (multiple answers possible)
Q.4 What percentage of surgeries do you still perform?
COVID-19 Practice Patterns of Ophthalmologists IV 0% 10% 20% Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=889) Re st of the World (n=383) Austria (n=27) Belgium (n=38) Fra nce (n=23) Germany (n=24) Gre ece (n=59) Ital y (n=75) Netherlands (n=125) Por tugal (n=40) Ro m ania (n=32) Spain (n=236) UK (n=81) Phone By emai l By video consulting By app Do not prov ide non-emergency care
0% 10% 20% Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=887) Re st of the World (n=385) Austria (n=27) Belgium (n=37) Fra nce (n=23) Germany (n=25) Gre ece (n=59) Ital y (n=76) Netherlands (n=123) Por tugal (n=40) Ro m ania (n=32) Spain (n=235) UK (n=81) Non e 1-15% 15-25 % 25-50% >50%
Q.5 When do you expect to restart elective surgery again?
Q.6
COVID-19 Practice Patterns of Ophthalmologists V
to control the COVID-19 pandemic? 0% 10% 20% Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=891) Re st of the World (n=386) Austria (n=27) Belgium (n=38) Fra nce (n=23) Germany (n=26) Gre ece (n=59) Ital y (n=75) Netherlands (n=124) Por tugal (n=40) Ro m ania (n=32) Spain (n=236) UK (n=81) Ve ry satisfie d Satisfie d Neutral Dissatisfied Very dissatisfie d
How satisfied are you with the measures taken by your government
0% 10% 20% Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=843) Re st of the World (n=389) Austria (n=23) Belgium (n=34) Fra nce (n=23) Germany (n=23) Gre ece (n=54) Ital y (n=72) Netherlands (n=102) Por tugal (n=37) Ro m ania (n=30) Spain (n=219) UK (n=68) April May June July August September October November December January 2021
Q.7
Yes, wa s assigned to COV ID wa rd Ye s, wa s assigned to ICU depar tment
Self-isolation
Alternative ophthalmic ta sks (research, protocol pre para tion, educationa l activities)
Non
COVID-19 Practice Patterns of Ophthalmologists VI
measures have you taken to protect your staff? (multiple answers possible) 0% 10% 20% Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=885) Re st of the World (n=385) Austria (n=27) Belgium (n=37) Fra nce (n=23) Germany (n=26) Gre ece (n=57) Ital y (n=75) Netherlands (n=124) Por tugal (n=40) Ro m ania (n=32) Spain (n=234) UK (n=81)
fo r some
Q.8 What
Dismissal
Work in separated teams
hou
Re d uction of wo r king
rs
e Tra nsfer to medical wa rd s
child
Social leave (eg. because of
ca re)
0% 10% 20% Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=888) Re st of the World (n=384) Austria (n=27) Belgium (n=38) Fra nce (n=23) Germany (n=26) Gre ece (n=58) Ital y (n=75) Netherlands (n=124) Por tugal (n=40) Ro m ania (n=32) Spain (n=234) UK (n=81)
Have you been assigned to provide general medicine or critical care?
No
Ye s, wa s assigned to none-COVID re la te d duties
Q.9 Which prevention measures are your patients requested to use? (multiple answers possible)
Europe vs R est of the World
Physical distancing (including distance between seats)
Hand glove s
Su rg i cal mouthnose mask
Hand disinfection
COVID-19 Practice Patterns of Ophthalmologists VII
0% 10% 20%
Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Austri a (n=27) Belgiu m (n=38) France (n=23) Germany (n=25) Greece (n=59) Italy (n=74) Netherlands (n=124) Po rt ugal (n=39) Romania (n=30) Spain (n=236) UK (n=80) Europe (n=888) Re st of World (n=386)
Q.10
What personal protection equipment ( PPE ) are you using besides routine measures such as hand desinfection etc.? (multiple answers possible)
Non e
Access to te stin g if re queste d
FFP2 mas k
FFP1 mask
Face shield
Eye prote ction visor or gog gles
Slit lamp barrier or breath shiel d
Hand glove s
Su rg i cal mouthnose mask
COVID-19 Practice Patterns of Ophthalmologists VIII
0% 10% 20% Europe vs R est of the
Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Austria (n=27) Belgium
Fra nce
Germany (n=25) Gre ece (n=59) Ital y (n=75) Netherlands (n=123) Por tugal (n=38) Ro m ania (n=30) Spain
UK (n=81) Europe (n=889) Re st of World (n=386)
World
(n=38)
(n=23)
(n=236)
Q.11 How satisfied are you with the availability of PPE as provided by your clinic or hospital?
Q.12 How satisfied are you with the access to testing for your employees?
COVID-19 Practice Patterns of Ophthalmologists IX
0% 10% 20% Europe vs R est of the
Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=875) Re st of the World (n=381) Austria (n=25) Belgium (n=37) Fra nce (n=23) Germany (n=24) Gre ece (n=58) Ital y (n=75) Netherlands (n=122) Por tugal (n=40) Ro m ania (n=29) Spain (n=232) UK (n=81) Ve ry satisfie d Satisfie d Neutral Dissatisfied Very dissatisfied 0% 10% 20% Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=875) Re st of the World (n=381) Austria (n=27) Belgium (n=38) Fra nce (n=23) Germany (n=25) Gre ece (n=55) Ital y (n=73) Netherlands (n=122) Por tugal (n=39) Ro m ania (n=31) Spain (n=230) UK (n=81) Ve ry satisfie d Satisfie d Neutral Dissatisfied Very dissatisfied
World
Q.13 Will the COVID
pandemic change your future practice behaviour? (multiple answers possible)
-19
Europe vs R est of the World
Ye s, will adopt bilateral cataract surgery
Ye s, will decrease frequency of physical postoperati ve exa mination after surgery
Yes, will incorporate phone/ video consulting on a ro u tine basis
COVID-19 Practice Patterns of Ophthalmologists X
0%
Selected European Countries 0% 10% 20% 30% 40% 50% 60% 70% 10% 20% 30% 40% 50% 60% 70% Austri a (n=27) Belgiu m (n=37) France (n=22) Germany (n=25) Greece (n=57) Italy (n=72) Netherlands (n=123) Po rt ugal (n=39) Romania (n=32) Spain (n=231) UK (n=81) Europe (n=875) Re st of World (n=379) No
Q.14
Q.15 Have you encountered ocular abnormalities in patients with COVID-19?
XI
healthcare authorities/insurance companies in regard to teleconsultations? 0% 10% 20% Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=873) Re st of the World (n=378) Austria (n=27) Belgium (n=38) Fra nce (n=23) Germany (n=25) Gre ece (n=55) Ital y (n=73) Netherlands (n=122) Por tugal (n=39) Ro m ania (n=31) Spain (n=230) UK (n=81) Ve ry satisfie d Satisfie d Neutral Dissatisfied Very dissatisfied
How satisfied are you with the reimbursement strategy of your
0% 10% 20% Europe vs R est of the World Selected European Countries 30% 40% 50% 60% 70% 80% 90% 100% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Europe (n=888) Re st of the World (n=387) Austria (n=27) Belgium (n=37) Fra nce (n=23) Germany (n=25) Gre ece (n=59) Ital y (n=75) Netherlands (n=125) Por tugal (n=40) Ro m ania (n=30) Spain (n=235) UK (n=81) Yes, conjunctivitis No Does not apply –Have not dealt with COV ID-19 cases ye t Yes, other COVID-19 Practice Patterns of Ophthalmologists
Dry Eye Diagnostics
Dry eye disease (DED) assessment has many pitfalls, but most usual situations can be overcome with a 10-minute examination, said Prof Marc Labetoulle, South Paris University, France, during a keynote address at Cornea Day during the 24th ESCRS Winter Meeting in Marrakech, Morocco.
The Tear Film & Ocular Surface Society’s DEWS II guidelines have provided precise yet complex flow charts for the diagnosis procedures and treatment of dry eye disease. However, time constraints mean that, unfortunately, it is not always possible to use them comprehensively in a clinical setting, he noted.
In a busy clinic there might be a tendency to rush through the consultation. But there really is no need to do so since a fairly definitive diagnosis of the underlying cause of the patient’s condition and arriving at an appropriate prescription is possible with a five-to-10minute examination in 90% of dry eye patients, he said.
LISTEN TO THE PATIENT
The first step in the consultation is to listen to the patient’s description of their dry eye symptoms. That involves having the patient complete an Ocular Surface Disease Index (OSDI) questionnaire (or equivalent) while still in the waiting room and then hearing the patient’s spontaneous complaints as well as information about risk factors including age, ethnicity, contact lens wear and previous refractive surgery.
The patient’s description of the symptoms can provide important diagnostic information. For example, if a patient says their discomfort is the same every day, but if the maximum
discomfort is in the morning, then Meibomian gland dysfunction (MGD) is likely a contributor to the condition. However, if the symptoms are most intense during the evening, an aqueous deficiency likely contributes more to the condition.
In patients who report having symptoms only at certain times, a complaint of pain that awakens them in the morning is strongly indicative of finger dot dystrophy. If the condition tends to occur only during certain times of year or during certain activities, allergy is a likely aetiological (or associated) suspect, Prof Labetoulle said.
SLIT-LAMP EXAM PEARLS
Slit-lamp examination can provide further clues to the main mechanism of DED. For example, eyes with mild aqueous deficiency will tend to be very bloodshot with a reduced sheen of the cornea and debris in the tears. In the more severe cases of aqueous deficiency there will be conjunctival folds with confluent staining and/or filaments.
In eyes with MGD, the redness and staining will be greatest in the inferior part of the ocular surface and there may be neovascularisation at the limbus. Examination of the eyelid will show inflammation at the edge and plugging and drop-out of Meibomian glands.
One should also be careful not to miss signs of other ocular surface diseases, such as superior limbal keratitis, a common cause of recalcitrant dry eye disease that is characterised by conjunctival folds and increased staining in the superior limbus, he advised.
He noted that when testing tear breakup time (TBUT) it is important not to instil too much fluorescein, which will overestimate TBUT, or too little fluorescein, which will underestimate it.
Prof Labetoulle’s own protocol for reproducible TBUT is to instil a low concentration of fluorescein and wait 20-to-30 seconds, allowing spontaneous blinking, until the green staining is translucent (not too much fluorescein, and not too little). He assesses the TBUT test three times in a row and estimates the mean value.
It is also essential to get an idea about the level of tear secretion at least once in the check-up of a new patient, he noted. Schirmer test and phenol red thread tests are reliable, and assistants can be trained to perform them effectively prior to the consultation. Tear meniscus measurement, using optical coherence tomography or corneal topography, can be a practical alternative although there are no precisely validated normal values for the parameter.
INCLUDE THE PATIENT IN THE TREATMENT STRATEGY
Once these tests and examinations are complete, a prescription may be formulated that specifically addresses both the patient’s symptoms and the underlying disease in the majority of cases, Prof Labetoulle said.
“The biggest mistakes people make are providing prescriptions without explanation, with successive attempts of a new eye drop after the previous one has failed,” Prof Labetoulle said.
Treatment options include liquid solutions such as saline solution and glycol derivatives for hydrating the ocular surface, and vinyl- and cellulosebased gel solutions with mucomimetic properties. There are also drops with both hydrating and mucomimetic properties such as the hyaluronates, he noted.
Drops are also available that address osmolarity, or the oxydative stress, to reduce inflammation and some that act as lipid substitutes, which are useful in MGD. Lid hygiene measures are also useful in MGD. For cases where autoimmune disease is a factor, cyclosporine is available. In recalcitrant cases the options include physical treatments to improve lid hygiene, punctal plugs, scleral lenses and autologous serum, he added.
Marc Labetoulle: marc.labetoulle@aphp.fr

EUROTIMES | JUNE 2020 CORNEA
A methodical approach brings speed without haste in dry eye assessment. Roibeard Ó hÉineacháin reports
21
The biggest mistakes people make are providing prescriptions without explanation, with successive attempts of a new eye drop after the previous one has failed
Prof Marc Labetoulle
From DMEK to DWEK
Atechnique combining Descemetorhexis without endothelial keratoplasty (DWEK) and a postoperative topical regimen of the rho-kinase (ROCK) inhibitor ripasudil (Glanatec, KOWA), is showing promise in the treatment of Fuchs’ dystrophy, said Professor Friderich E Kruse MD at the 10th EuCornea Congress in Paris France.
“The primary advantage of this technique is that you do not need a graft. A graft as we know is foreign tissue and has certain immunological disadvantages. There are also significant cost-savings with this technique,” said Prof Kruse, University of Erlangen-Nürnberg, Erlangen, Germany.
STANDARD TREATMENT
He noted that since the 1990s there has been a trend in the treatment of endothelial disease towards less invasive procedures that leave as much of the host cornea intact as possible. Procedures like Descemet’s stripping automated endothelial keratoplasty (DSAEK) ultrathin DSAEK and Descemet’s membrane endothelial keratoplasty (DMEK) have therefore become standard treatments for bullous keratopathy and Fuchs’ dystrophy.
Continuing in that same evolutionary path, research now suggests, and clinical evidence supports, the feasibility of treating Fuchs’ endothelial dystrophy simply by performing a 4.0mm Descemetorhexis and allowing the corneal endothelium’s own natural healing ability to restore the missing tissue and provide a clear cornea . Moreover, the studies also show that the rho-kinase inhibitor, ripasudil, can enhance and speed up the corneal endothelium’s regeneration.
“We were all taught that corneal endothelial cells would not migrate or proliferate. But this not completely true. For example, if you look at DMEK grafts that are decentred or there is a gap between the graft and host endothelium, endothelial cells often migrate into the gap after a few months,” Prof Kruse said.
He added that several anecdotal reports have described cases of spontaneous corneal endothelium regeneration following accidental Descemetorhexes occurring during cataract surgery. Furthermore, research published by Gerrit Melles MD has demonstrated that endothelial cells
from the host and/or the graft would similarly migrate to fill the gap in eyes that have undergone quarter-DMEK grafts, although some eyes required rescue DMEK procedures.
Reports on several small series of Fuchs’ dystrophy patients undergoing primary DWEK have also shown varied results, with success rates ranging from no success in three eyes to 14 successes in 17 eyes. The early trials showed that the technique appeared to be successful in most eyes in studies where a 4.0mm Descemetorhexes was used.
The studies also suggest that the success of DWEK procedures is limited to the subtype of Fuchs’ dystrophy where the guttae is at the centre and there is good endothelium in the periphery. It is not effective for bullous keratopathy, where most of the endothelium is affected.
RECENT DEVELOPMENT
A more recent development in the DWEK technique has been the use of ripasudil eyedrops following surgery. Ripasudil is a rho-kinase inhibitor approved in Japan in 2016 in for the treatment of ocular hypertension and glaucoma. The Rho-associated protein kinase (ROCK) enzyme has two isoforms, ROCK-1 and Rock-2. They are activated in response to wounding or integrin stimuli and they play
a critical role in cell adhesion, migration, proliferation, differentiation and apoptosis via modulation of the cytoskeleton.
In the laboratory, ripasudil, a ROCK1 inhibitor, has been shown to promote corneal endothelial cell proliferation in cultured human cells and wound healing and corneal endothelium regeneration in an in vivo rabbit eye model.
Recent clinical trials are now appearing to bear out the laboratory findings regarding the potential value of the ROCK-inhibitor in eyes undergoing DWEK. For example, in a study involving 12 patients who underwent 4.0mm Descemetorhexes, a regimen of topical ripasudil treatment resulted in clear corneas in eyes where DWEK was not initially successful (Moloney et al, Cornea 2017;36:642-648).
A subsequent double-blind study involving 18 patients undergoing 4.0mm DWEK procedures showed that those receiving a two-week regimen of ripasudil eyedrops four times daily recovered vision significantly more quickly (4.6 weeks vs. 6.5 weeks, p<0.01) and had a statistically significantly higher average endothelial cell density than those who did not receive the eyedrops (Macsai et al, Cornea 2019; 38 :529-534).
PLANNING STAGES
Prof Kruse and his associates are now conducting a similar double-blind trial comparing outcomes of DWEK with and without ripasudil. He noted that the agent is not yet approved in Europe, although a phase II multi-centre randomised controlled trial involving 60 patients undergoing DWEK is now in the planning stages.

He commented that a disadvantage of DWEK is its long recovery period of up to four months, during which time vision is very poor. In contrast, a patient undergoing DMEK will generally recover the vision they had before surgery by one week after surgery.
“After Descemet’s stripping, visual acuity goes down tremendously the patient only has hand movements and that is certainly something for both the doctors and the patients to consider when deciding whether to adopt this technique,” Prof Kruse said.
CORNEA 22 EUROTIMES | JUNE 2020
New technique requiring no donor tissue showing promise in the treatment of Fuchs’ dystrophy. Roibeard Ó hÉineacháin reports
The primary advantage of this technique is that you do not need a graft.
A graft as we know is foreign tissue and has certain immunological disadvantages
Friderich E Kruse MD
Friderich E Kruse MD
Infectious Keratitis
Fluoroquinolone-resistant
A16-year review of bacterial keratitis isolates tends to support the use of fortified vancomycin and tobramycin drops for ulcerative keratitis, reported Allan Slomovic MSc, MD, FRCS(C), at the 24th Winter Meeting of the ESCRS in Marrakech, Morocco.
The Canadian research showed that Gram-negative bacteria remain more susceptible to standard antibiotics than do Gram-positive bacteria. Significantly, susceptibility of all Gram-positive isolates to vancomycin was 100% for all 16 years of the study.
“High susceptibility to vancomycin reinforces the empirical use of fortified tobramycin and vancomycin in the initial management of severe bacterial keratitis and in cases unresponsive to fourthgeneration fluoroquinolones,” said Dr Slomovic, Professor of Ophthalmology, Department of Ophthalmology and Visual Sciences, University of Toronto, Toronto.
The study involved a total of 2,330 corneal scrapings taken from January 1, 2000, through December 31, 2015.
Pathogens were recovered in 1,335 samples (57.3%), with bacterial keratitis accounting for 1,189 (86.0%) of the positive cultures. Other pathogens recovered included fungi in 9%, a third of which were yeasts, and Acanthamoeba in 2%. In addition, 9% had viral infections.
Gram-positive bacteria accounted for 75% of bacterial growths, with coagulasenegative staphylococcus being the most common, accounting for 59% of Grampositive bacteria isolates and 37% of all bacterial isolates. Gram-negative bacteria accounted for 25% of bacterial isolates with pseudomonas aeruginosa being the most common, accounting for 47% of Gram-negative and 11% of all isolates.
Dr Slomovic noted that they obtained multiple isolates in 11% of cases, which were bacterial in 92%, fungal in 5%, viral in 2% and Acanthamoeba in 1%.
Risk factors for polymicrobial infections included trauma, decreased systemic immunity, and ocular surface disease.
“Multiple isolates accounted for approximately One-in-10 cases of infectious keratitis, so it is important to think about polymicrobial infection when the patient is not responding as expected,” he added.

Ó hÉineacháin reports
GRAM-NEGATIVE MORE RESPONSIVE THAN GRAM-POSITIVE BACTERIA
The Gram-negative isolates were very susceptible to the five most commonly used antibiotics for the pathogens, with mean sensitivity rates of 96% for ciprofloxacin sensitive, 95% for gentamicin, 94% for tobramycin, 91% for ceftazidime and 95% for piperacillin/ tazobactam. Pseudomonas was sensitive in every case to ceftazidime, tobramycin and piperacillin/tazobactam. Serratia marcescens was sensitive in every case to ciprofloxacin, gentamicin and piperacillin/tazobactam.
However, the Gram-positive bacteria were less susceptible to standard antibiotics with mean sensitivities of 56% to erythromycin, 66% to cefazolin, 87%, trimethoprim/ sulfamethoxazole, but 100% for vancomycin. Staph aureus, the most common Gram-positive pathogen detected in the study had sensitivities of 75% to erythromycin, 96% to cefazolin and 100% to vancomycin. Methicillin resistant staph aureus (MRSA) accounted for 1% of isolates, and methicillin-resistant coagulase-negative Staphylococcus accounted for 39% of isolates.
“Similar to other reports we found that the susceptibility to tested antibiotics for Gram-negative bacteria to be excellent, above the 90% range. By contrast, and again similar to other reports, we found that the susceptibility to tested antibiotics for Gram-positive bacteria to be far less sensitive between 56% to 87%, except for vancomycin to which all tested isolates have been 100% sensitive for all 16 years of the study,” Dr Slomovic said.
Among the trends observed since 2010 were that corneal cultures rates have been decreasing significantly and there has also been a significant decrease in percentage of Gram-positive isolates, including streptococcus (p<0.0001) and staphylococcus (p<0.005).
“This is largely due to the introduction and effectiveness of fourth-generation fluoroquinolones. Many community ophthalmologists are treating these ulcers without obtaining cultures. At the University where the cultures are being performed, we are only seeing the more serious ulcers or the ones not responding to treatment of with fourth-generation fluoroquinolones,” Dr Slomovic said.
LOOMING CRISIS
There was also a significant increasing trend towards resistance to erythromycin. The other antibiotics evaluated did not show any significant trend in resistance patterns. However, Dr Slomovic noted that both Gram-positive and Gram-negative bacteria have become increasingly resistant to fluoroquinolones.
He emphasised that a crisis appears to be looming with regard to antibiotic-resistant bacteria, which currently account for 35,000 deaths a year and increased morbidity in 2.8 million. According to the United Nations, if current trends continue, the global death toll from antibiotic resistance will reach 10 million in 2050.
“It has been 15 years since the fourthgeneration fluoroquinolones entered the market. Since that time there really have been no new ophthalmic antibiotics,” Dr Slomovic added.
Meanwhile the use of topical steroids in conjunction with topical fortified antibiotics is showing promise in the treatment of infectious keratitis. In the Steroids for Corneal Ulcers trial (SCUT), among patients with positive bacterial ulcers who received topical steroids 48 hours after commencing antibiotic therapy, all those treated with topical steroids, other than those with nocardia ulcers, had better visual acuity at 12 months (Srinivasan et al, Arch Ophthalmol 2012, 130(2):143-50.). It is recommended that topical steroids are added only after the offending organism has been identified, antibiotic sensitivities have been determined and there is evidence of improvement. Corneal cross-linking (CXL) is also showing promise in the treatment of infectious keratitis. Several investigators have reported on the efficacy of CXL in infectious keratitis and a new trial, SCUT II, investigating the use of topical steroids combined with CXL, is now under way, Dr Slomovic said.
EUROTIMES | JUNE 2020 CORNEA 23
bacteria a growing problem in the treatment of infectious keratitis. Roibeard
A characteristic slit-lamp photo of a corneal ulcer Courtesy of Allan Slomovic MSc, MD, FRCS(C)
C XL for Keratitis
Corneal cross-linking alone as effective as antibiotics in healing infectious keratitis in phase III RCT. Roibeard Ó hÉineacháin reports
PACK-CXL (photo-activated chromophore for infectious keratitis-corneal crosslinking) appears to be an effective alternative to standalone treatment for infectious corneal infiltrates and early corneal ulcers, according to the preliminary results of a phase-III RCT (randomised controlled trial) presented by Emilio Torres-Netto MD, at the 24th ESCRS Winter Meeting in Marrakech, Morocco.
“Even with a tendency for a longer healing, 85% of eyes treated with PACK-CXL healed without the use of antimicrobial therapy,” said Dr TorresNetto, ELZA Institute and University of Zurich, Zurich, Switzerland.
The prospective multi-centre, randomised controlled trial involved 30 patients with infectious keratitis. All had infiltrates and early ulcers up to 4mm in diameter and 350μm in depth. Grampositive cocci were the most commonly identified pathogens. there were also five case of filamentous fungal keratitis (Aspergillus sp), he noted.

The study randomised patients to two treatment groups, namely PACKCXL or the current standard of care, antimicrobial therapy. Patients already receiving antibiotic or antifungal therapy stopped their treatment at least one day before undergoing their assigned treatment. Prior to treatment, the mean infiltrate size was 1.8mm for the medication group and 2.4 mm for the PACK-CXL group (p=0.113).
“Our objective was to analyse the time to corneal epithelialisation with PACKCXL as a first-line treatment in early infectious corneal ulcers and compare it to the current standard of care, antimicrobial therapy,” Dr Torres-Netto said.
In the PACK-CXL group, removal of the epithelium around the borders of the ulcerations was followed by application of a riboflavin and irradiation with UV-A (total energy 5.4 or 7.2J/cm2), Dr Torres-Netto explained.
He noted that there was no significant difference between the groups in terms of corneal re-epithelisation time, which was 12.3 days in the PACK-CXL group and 6.8 days for standard treatment. One patient in the medication group developed a corneal perforation on the eleventh day after initiation of antibiotic therapy and one patient in the PACK-CXL group developed
fungal keratitis and received antifungals from day four of the study. Both patients were excluded from the analysis.
However, he noted that even on an intent-to-treat basis the PACK-CXL was effective in 85% of patients.
THE NEED FOR NEW TREATMENTS
Dr Torres-Netto noted that infectious keratitis due to corneal infection is a major cause of global blindness and severe visual impairment. The socioeconomic costs related to corneal ulcers and their treatment are immense. In addition, antibiotic resistance has become a global problem and the development of new antibiotics has been at a virtual standstill for decades.
“One of the most recent antibiotics that we have today are the fluoroquinolones and in some series we have already 50% resistance in patients with chronic use of fourth-generation fluoroquinolones, so it’s a great concern at this time,” he added.
He pointed out that PACK-CXL – a new term to distinguish the use of CXL for infectious keratitis treatment from its use for corneal ectatic disorders – does not require expensive medication, but only Vitamin B2 solution and a UV light source. In addition, previous data show that PACK-CXL may also be efficient in antibiotic-resistant and mixed infections.
In addition, a soon-to-be published meta-analysis of studies involving PACKCXL appears to support the present study’s findings. The meta-analysis included only studies involving the use of the therapy for infectious keratitis with robust reporting of epithelial healing times and comprised four
studies and 12 case reports and case series. In those studies, the re-epithelialisation times following PACK-CXL were similar to those in the current study, except one study where CXL was combined with antibiotics but in which 70% of the infections were of fungal origin.
A further meta-analysis including the present study looking at 72 eyes in all showed no significant difference between PACK-CXL with antibiotics and PACKCXL without antibiotics in terms of the likelihood of successful re-epithelialisation. The only significant factor found to affect the success of treatment was the diameter of the lesion, which had inverse correlation with re-epithelialisation time. Therefore, treatment should commence as early as possible, he said.
“Our results suggest that PACK-CXL may become an alternative standalone treatment for infectious corneal infiltrates and early corneal ulcers. While the preliminary results of this multi-centre randomised trial are promising, a larger sample is needed to further investigate the efficacy and safety of this treatment modality,” Dr Torres-Netto said.
This preliminary phase of the study was led by the ELZA Institute in Zurich, Switzerland and conducted jointly with the Centre for Applied Biotechnology and Molecular Medicine at the University of Zurich (Zurich, Switzerland), the Narayana Nethralaya Eye Hospital (Bangalore, India), the BenGurion University of the Negev Sheva (Beer-Sheva, Israel) and the Wenzhou Medical University (Wenzhou, China).
Emilio Torres-Netto: emilioatorres@me.com
EUROTIMES | JUNE 2020
CORNEA 24
Infectious keratitis (Streptococcus Viridans) prior to (left) and (right) 21 days after accelerated high fluence PACK-CXL (7.2 J/cm2). The eye showed complete re-ation at 21 days postoperatively
Courtesy of Dr Boris Knyazer, Ben-Gurion
Phaco & corneal disease
Low endothelial cell density a challenge in cataract cases.
Dermot McGrath reports
Cataract surgery in cases of low endothelial cell density remains a challenging proposition even for more experienced surgeons, according to Vincenzo Scorcia MD.
“Performing cataract surgery alone in patients with a low endothelial cell count is very challenging, mainly because of the high risk of endothelial damage from the phacoemulsification. It makes it a difficult decision for the surgeon to decide whether to proceed with cataract surgery alone or to combine it with keratoplasty,” he told delegates attending the joint ESCRS/EuCornea Symposium at the 37th ESCRS Congress.
Dr Scorcia said that there are several issues to be addressed before embarking on cataract removal in patients with pathologies such as Fuchs’ endothelial corneal dystrophy (FECD), which is the most common indication, or those who have previously undergone penetrating keratoplasty or experienced complications from anterior chamber phakic IOL implantation.
“We need to ask if the patient could improve their vision from cataract surgery alone, so we need to determine if the main problem is the cataract or the corneal disease,” he said.
Cataract-related symptoms include blurred vision and glare as well as change in refraction, which is often a myopic shift induced by cataract.
Corneal symptoms are typically represented by glare, said Dr Scorcia,
University of Magna Graecia, Catanzaro, Italy. In the early stages this is characterised by an increasing number of guttata in the centre of the cornea even if the light transmission is normal, he said.
“The debilitating symptoms can occur even when there is little to no stromal or epithelial oedema and the pachymetry is relatively normal,” he said.
Light scattering starts to occur at more advanced stages of guttata, explained Dr Scorcia, and is related to increased corneal thickness and subsequent light scattering caused by separation of the collagen fibrils of the cornea.
“At this point the patients usually complain of a degradation of visual acuity and this problem is more prevalent in the morning,” he said.
Once the surgeon decides to proceed with phacoemulsification, the next key issues are to assess the risk of corneal decompensation after cataract surgery and then to determine which preoperative parameters should be considered as risk factors for corneal failure, said Dr Scorcia.
He pointed out that the threshold number of endothelial cells necessary to main corneal deturgescence, which is the state of dehydration necessary to maintain the transparency of the cornea, is currently unknown. Furthermore, non-uniform endothelial cell loss often results in sampling errors.
“We know that peripheral endothelial cells have a higher density than in the central part of the cornea, yet the cells
are usually counted only in the central zone so we are lacking a lot of valuable information about the reservoir of cells in the periphery,” he said.
Dr Scorcia added that it is also difficult to obtain an accurate count of endothelial cells in the presence of corneal oedema, which leads to poor specular microscopy images.
Another key parameter is preoperative central corneal thickness (CCT), which above a threshold of 640 microns is usually considered predictive of corneal decompensation in FECD patients.
“We should perhaps treat this as a guide rather than a strict rule, since we still do not know what the normal thickness value should be and there is poor reliability of ultrasound pachymetry readings. There is also a very high diurnal variation of CCT in patients with FECD, which hinders identification of true corneal thickening,” he said.
Previous studies have shown up to 90% of Fuchs’ patients who underwent cataract surgery did not need corneal transplants and achieved a postoperative best-corrected visual acuity of 20/35, said Dr Scorcia.
“In a large number of cases, opting for cataract extraction alone despite endothelial pathology may be a good option because the patients are often satisfied with less than perfect visual outcomes and it avoids the potential complications associated with endothelial keratoplasty,” he said.
Vincenzo Scorcia: vscorcia@libero.it
European Union Web-Based Registry
The aim of the project is to build a common assessment methodology and establish an EU web-based registry and network for academics, health professionals and authorities to assess and verify the safety quality and efficacy of corneal transplantation.
www.ecctr.org
EUROTIMES | JUNE 2020 CORNEA 25
ECCTR is a project funded by the ESCRS with initial support from the EU
What lies ahead with OCT-A?
OCT-angiography offers huge potential, but questions remain.
Leigh Spielberg MD reports
Software updates have significantly improved the quality of OCT-angiography (OCT-A) imaging systems since they were first developed, but not all instruments are created equal. There are also significant differences regarding what can be seen in each segmented layer of the retina, according to Giovanni Staurenghi MD, Milan University Eye Clinic, Italy.
Dr Staurenghi gave a talk on the future of OCT-A at the 19th Annual EURETINA Congress in Paris, France. As a member of the International Nomenclature for Optical Coherence Tomography Panel, which was assembled to define a consensus for OCT imaging technology, he has a particular expertise in the capabilities and limitations of both OCT and OCT-A.
“Although the software driving OCT-A image creation tends to improve approximately every three months, distinctions remain between the many instruments available on the market,” he said. This is because they are fundamentally different.
OCT-A refers to a group of OCT imaging methods that facilitate visualisation of blood flow in the retina and choroid. Like Doppler OCT techniques, OCT-A detects motion in the imaged sample. In contrast to Doppler OCT, however, OCT-A ignores the quantitative measurement of blood flow, and instead uses blood flow motion as a contrast medium to visualise the blood vessels. To detect this vascular flow information, the OCT-A algorithms generate images based on the motion signal between repeated OCT B-scans at the same position.
Instruments vary based on which scan technique is employed. Some OCT-A machines use spectral domain imaging in (SD), while others use swept source (SS). The differences can be significant.
Advantages of SS-OCT imaging over SD-OCT include the faster scanning speed and its use of a longer wavelength and its reduced sensitivity roll-off. These result in enhanced light penetration through the RPE, as well as better detection of signals from the deeper layers. However the signal-to-noise ratio is higher with SD, particularly for the inner retina, allowing much more contrast and visualisation for this layers.
Several factors differentiate OCT-A from traditional fluorescein angiography. Paramount among these differences are OCT-A’s image segmentation possibilities. This allows for the separate visualisation of individual layers of the retina and choroid. Segmentation can be based on structural OCT or flow signal.
“When segmentation is based on structural OCT, we have a division of the retina into the superficial capillary plexus and the deep capillary plexus,” he explained. “In this case, the inner plexiform layer seems to belong to the superficial capillary plexus. Alternately, when the segmentation is based on flow signal, the inner plexiform layer gets divided between the superficial vascular plexus and the intermediate capillary plexus.” This influences the final image, rendering a particular blood vessel visible in some machines’ scans and invisible on others, potentially creating misinterpretation if different instruments are compared.
Crucial to most users, whether researchers or clinicians, is resolution. This concerns the distance between B-scans, which determines the spatial resolution. This can vary from 5.7μm to 12.9μm depending on different instruments, said Dr Staurenghi.
Each of these variables can have an impact on the quality and usefulness of the resulting images.
“This leads to image disparities that can have significant impacts on measuremnents. Crucial values such as mean vessel density, fractal dimension and foveal avascular zone size can vary widely between the different instruments,” said Dr Staurenghi.
He cited a paper from the American Journal of Ophthalmology (Corvi F. et al. Am J Ophthalmol 2018;186:25–31) in which these values were measured side-by-side, and large differences emerged.

Dr Staurenghi, who refers to himself as a “multi-imaging supporter”, concluded that “although we still have some difficulties to work out, OCT-A is a fantastic tool, and it could be added to our armamentarium for the diagnosis and management of retinal disease”.
Some within the retina community believe that given the shorter time and lower cost of image acquisition, greater convenience, greater comfort and greater safety of imaging with OCT-A, it is just a matter of time before OCT-A becomes the gold standard for imaging such pathologies as choroidal neovascularisation.
Giovanni Staurenghi: giovanni.staurenghi@unimi.it
EUROTIMES | JUNE 2020 RETINA 26
Giovanni Staurenghi MD
This leads to image disparities that can have significant impacts on measuremnents
Giovanni Staurenghi MD
Inherited retinal disease diagnosis
Whole genome sequencing can help determine the cause of unexplained disease. Roibeard Ó hÉineacháin reports
Whole genome sequence can reveal hidden variants of genes associated with inherited retinal disease that will not be detected by conventional exonbased gene (exome) sequencing, said Susanne Roosing PhD, Radboud University Medical Center, Nijmegen, The Netherlands.
“The ultimate goal is to use this knowledge for gene therapy, often gene variant specific gene therapy,” said Dr Roosing at Retina 19, a meeting held in Dublin, Ireland, by Fighting Blindness, a patient-led charity.
She noted that inherited retinal diseases (IRDs) have a high degree of heterogeneity. An estimated 60% of retinitis pigmentosa cases have a genetic cause of disease that can be found using exome sequencing, which is currently the most widely applied method for disease gene variant identification. Among those cases solved by exome sequencing, about 15% are caused by canonical splice site variants that are always conserved so always linked to exon skipping or noncanonical splice site variants that may also have an effect on splicing.
However, exome sequencing – the sequencing of those parts of the gene that are included in the final RNA product – has the inherent limitation that it will not detect the non-coding intronic variants of the genes. Whole genome sequencing, on the other hand, enables identification of causative deep intronic variants and can also detect variants in genes not previously associated with inheritable retinal disease.
Dr Roosing and her associates performed whole genome sequencing on 40 Irish cases and 60 Dutch or Israeli cases of unexplained IRD. In this way they were thus far able to determine the genetic cause in 12 cases, and candidate variants in 41 cases. In 26 cases they found no variants and in 21 their analysis is ongoing.
UNDETECTED VARIANTS
Among those cases where they found a genetic cause were 13 previously undetected variants in coding regions of known IRD genes. They included homozygous variants in known IRD genes (which were not included in the Target5000 panel) and a very large deletion in gene PDE6B.
The candidate variants in non-coding variants included deep intronic variants in the Bietti and Oguchi retinitis pigmentosa phenotypes associated with known IRD genes. They also found a very large inversion spanning numerous exons in a gene called EYS.
“Our next steps are to perform segregation analysis for candidate genes and variants where applicable, perform midigene assays for selected candidate variants based on different criteria to provide proof-of-pathogenecity and continue analysis of remaining cases.
Unsolved cases will be further investigated for causative intronic variants (which aren’t yet identified as such), splice enhancers, splice silencers. Much knowledge remains to be gained,” Dr Roosing concluded.
Susanne Roosing: Susanne.Roosing@radboudumc.nl
Convenient Web-Based Registry Cataract, Refractive and Patient Reported Outcomes in One Platform
The patient-reported outcome is linked to clinical data in EUREQUO. This enables better knowledge of indications for surgery and o ers a tool for clinical improvement work based on the patients’ outcome.
EUROTIMES | JUNE 2020 RETINA
Join Track the EUREQUO Platform your Surgical Results EUREQUO is free of charge for all ESCRS members www.eurequo.org 27
Regenerative medicine
Endothelial progenitor cells may aid therapy in diabetic retinopathy. Roibeard Ó hÉineacháin reports
Regeneration of the damaged vasculature in retina from patients with diabetic retinopathy may be possible through the use of progenitor cells to restore blood flow and prevent progression to the late, sight-threatening stages of the disease, said Prof Alan Stitt PhD, Queen’s University Belfast, Northern Ireland, UK, at a meeting held in Dublin by Fighting Blindness, an Irish patient-led charity.
Watch the latest video content from ESCRS and EuroTimes, FREE on the ESCRS Player
Advanced Instructional Courses
Eye Contact Interviews
Video of the Month
Video Journal of Cataract, Refractive & Glaucoma Surgery
Young Ophthalmologists
Videos: “Early cases with expert discussion”
Online Museum
player.escrs.org
Prof Stitt noted that there is growing evidence that dysfunction of resident progenitor cells in vascular beds can lead to blood vessel damage and non-perfusion of diseased tissues. The normal reparative capacity of the retinal vascular endothelium is compromised in diabetes and this may, at least in part, underlie the vessel degeneration and progressive ischaemia that we see in proliferative diabetic retinopathy (PDR) and diabetic macular oedema (DME).
He added that detailed pre-clinical studies have shown that introducing a type of vascular progenitor cell, called endothelial colony-forming cells (ECFCS), into the ischaemic retina can regenerate blood vessels and restore perfusion thus preventing sight-threatening pathology such as proliferative retinopathy or oedema. These ECFCs can be isolated from umbilical cord blood but also from the peripheral blood of adults. The cells have many progenitor features that allow them to target areas of tissue hypoxia and participate in de novo vessel formation and integration with the existing retinal vessels, Prof Stitt said.
“These cells integrate into the resident retinal vascular endothelium and promote perfusion. They have great therapeutic potential since they can be readily isolated, expanded in the laboratory setting and, potentially, delivered to patients after appropriate tissue-typing. We have been able to achieve a significant treatment effect with as few as a thousand cells so they have quite a high level of potency,” he added.
These cells integrate into the resident retinal vascular endothelium and promote perfusion
Alan Stitt PhD
It has been noted that the introduction of new treatments for DME, including intravitreal vascular endothelial growth factor inhibitors (anti-VEGFs) and new forms of steroid delivery has lowered the ranking of diabetic retinopathy as a leading cause of blindness across Europe, but it still remains a very significant disease that causes vision loss. Moreover, around 40-to-50% of DME patients do not respond optimally to the currently available therapies.
Although the evidence is only building at this point, There are also some concerns that long-term anti-VEGF therapy could impact on the endogenous, homeostatic and reparative capacity of the retina and the choroid.
“It would be beneficial to develop a therapy that can promote blood vessel repair in the retina at the early and intermediate stages, Prof Stitt added.
Alan Stitt: a.stitt@qub.ac.uk
EUROTIMES | JUNE 2020 RETINA
28
2–4
October 2020
The 20th EURETINA Congress, scheduled to take place in Amsterdam, will instead take place as a virtual congress experience in October 2020. For all information and updates please visit the website
www.euretina.org

th
Euretina Congress
Learn online in your own time, with self-paced and assessed ESCRS iLearn courses on:

∙ Cataract Surgery
∙ Cornea
Biomarkers in retinal disease
Automated system outperforms human experts for biomarker
identification. Dermot McGrath reports
Initial trials of an automatic biomarker classifier show that it is capable of outperforming human experts in the task of biomarker detection in optical coherence tomography (OCT) scans, paving the way for more efficient and economical ocular disease screening and detection, according to a study presented at the 19th EURETINA Congress in Paris.
“The reality is that humans have a hard time with biomarker detection – at least, compared to a machine that has been specifically trained for the task,” said Thomas Kurmann, a PhD student at the ARTORG Center for Biomedical Engineering Research at the University of Bern.
OCT is the gold standard in the diagnosis of retinal diseases such as age-related macular degeneration (AMD) or diabetic macular oedema (DME), with trained experts diagnosing patient scans by searching for biological markers, said Mr Kurmann.
“It is a very difficult task for human experts. It is time consuming, tedious, error prone and expensive when one considers that it takes about five minutes per scan for an expert grader,” he said.
The team from the ARTORG Center jointly with the Department of Ophthalmology at the Bern University Hospital set out to test its hypothesis that an automatic biomarker classifier could perform as well as or better than human grading experts in the task of biomarker detection in OCT B-scans.
In total, 470 volume scans of 327 patients were included, making a total of 23,030 OCT B-scans, with an additional test set of 1,000 Scans from 21 AMD patients using the same device type and scanning protocol.
Morphological biomarkers included subretinal fluid, intraretinal fluid, intraretinal cysts, hyperreflective foci, drusen, reticular pseudodrusen, epiretinal membrane (ERM), geographic atrophy, outer retinal atrophy and fibrovascular pigment epithelial detachment. A healthy biomarker was also included to denote the lack of any previously mentioned biomarker.
∙ Refractive Surgery
∙ Visual Optics
Trainers: use the task list to assign courses for trainees and monitor their progress.
The automatic classifier achieved higher Kappa values for eight biomarkers compared to the median human grader, with highest values recorded for ERM and the lowest for reticular pseudodrusen.
“The biomarker detector is accurate and 100 times faster than a human grader. With a single server at our lab we can compute every single volumetric scan that is taken worldwide in real-time. Automated analysis of scans using machine learning algorithms provide a cost-effective and reliable alternative to assist ophthalmologists in clinical routine and research,” he concluded. For more information about the study, please see https://bit.ly/ ET-Kurmann
Thomas Kurmann: Thomas.kurmann@artorg.unibe.ch
RETINA 30 EUROTIMES | JUNE 2020
more at https://elearning.escrs.org
Keep learning. Whenever, wherever.
Learn
It is a very difficult task for human experts. It is time consuming, tedious, error prone and expensive Thomas Kurmann
SEBASTIAN WOLF Editor of Ophthalmologica

OPHTHALMOLOGICA
VOL: 243 ISSUE: 3
RISK FACTORS IDENTIFIED FOR RETINAL PATHOLOGIES IN FELLOW-EYE PCV PATIENTS
Unilateral polypoidal choroidal vasculopathy (PCV) contralateral eyes with BVN requires careful monitoring for future development of PCV or neovascular AMD (nAMD) choroidal neovascularisation, a retrospective study suggests. The study included 48 patients with unilateral PCV. At five years’ follow-up, 17% developed PCV or CNV in their fellow eye.Baseline characteristics in the fellow eye that correlated significantly with the development of PCV included subfoveal choroidal thickness (p=0.001), irregular retinal pigment epithelium elevation (p<0.001), choroidal vascular dilation (p<0.001), choroidal vascular hyperpermeability (p<0.001) and the presence of branching vascular network (BVN )(p<0.001). The only significant risk factor for the development of nAMD was BVN (p=0.045, odds ratio = 24.66).K Kim et al, “Five-Year FollowUp of Unaffected Fellow Eyes in Patients with Polypoidal Choroidal Vasculopathy”, Ophthalmologica 2020, Volume 243, Issue 3.
AUTOFLUORESCENT LIFETIMES LONGER IN GEOGRAPHIC ATROPHY THAN STARGARDT’S DISEASE
A new study indicates that atrophic regions of the retinal pigment epithelium (RPE) have longer autofluorescence lifetimes in patients with age-related macular degeneration (AMD) than they do in eyes with Stargardt’s disease (STGD). In 30 geographic atrophy patients with a mean age of 78 years, mean retinal autofluorescence lifetimes were significantly longer than in 13 STGD patients with a mean age of 43.7 years, in both the short 498-560nm spectral channel (997ps vs 363ps) and the long 560-720nm spectral channel (880ps vs 39 ps). The findings may provide additional clues into the pathogenetic mechanisms underlying the conditions, the authors note. Y Solberg et al, “Fluorescence Lifetime Patterns of Retinal Pigment Epithelium Atrophy in Patients with Stargardt Disease and Age-Related Macular Degeneration”, Ophthalmologica 2020, Volume 243, Issue 3.
TPA AND SF6 GAS EFFECTIVE IN LIFTING SUBMACULAR HAEMORRHAGES

Intravitreal injection recombinant tissue plasminogen activator (rtPA) and sulphur hexafluoride gas (SF6) can displace large submacular haemorrhages (SMH), allowing postoperative diagnostic testing to guide further treatments, a new study indicates. The authors analysed medical records of 96 consecutive SMH patients who underwent intravitreal injection of rTPA and SF6 followed by facedown positioning. They found that the SMH was displaced from the fovea in 76% of eyes. There were statistically significant correlations between the macular findings revealed after blood displacement and the additional treatments selected for the underlying disease.
E Maggio et al,“Intravitreal Recombinant Tissue Plasminogen Activator and Sulphur Hexafluoride Gas for Submacular Haemorrhage Displacement in Age-Related Macular Degeneration: Looking behind the Blood”, Ophthalmologica 2019, Volume 243, Issue 3.

NUMBER 1!
79 %
of readers say EuroTimes contains up-to-date information
47,863 * Reach
*Average net circulation for the 10 issues circulated between 1 February 2019 to 31 December 2019. See www.abc.org.uk
Results from the EuroTimes Readership Study 2017
Ophthalmologica is the peer-reviewed journal of EURETINA EUROTIMES | JUNE 2020
RETINA 31
Cyclosporine A Update
New
Newer formulations of cyclosporine A (CsA) are transforming the treatment of severe paediatric allergic ocular surface diseases, with proven efficacy and safety data now available, the 10th EuCornea Congress in Paris, France, heard.
Paediatric Ophthalmologist Dominique Brémond-Gignac MD, Paris, France, prepared an expert update on the use of cyclosporine in allergic conjunctivitis which was delivered by her colleague Dr Frederic Chiambaretta, during the dedicated session on ocular surface diseases in paediatric patients.
Severe allergic conjunctivitis alone is estimated to effect 6-to-30% of the population, in up to 30% of children alone or in association with allergic rhinitis. It is a diagnostic and therapeutic challenge in children; it has multiple clinical forms and ranges from mild to severe, causing loss of quality of life and visual impairment.
Vernal keratoconjunctivitis (VKC) and atopic keratoconjunctivitis (AKC) are rare and potentially debilitating forms, which are characterised by allergic inflammation of the ocular surface, with clinical manifestations involving the tarsal (palpebral) and/or bulbar conjunctiva that can have a seasonal course, but also may be chronic with acute exacerbations, Dr Brémond-Gignac wrote.
Key signs and symptoms of VKC include photophobia, tearing, conjunctival hyperaemia, itching, stringy mucous discharge, giant papillae on the upper tarsal conjunctiva, papillae and gelatinous infiltrates on the limbus with white-yellow nodules (Horner-Trantasdots), superficial
punctate keratitis and corneal shield ulcers. VKC is a disease that affects primarily boys and children from age three to 16 years old and usually disappears at adolescence, Dr Brémond-Gignac’s presentation outlined.
Prompt, correct diagnosis and treatment of VKC is key due to the risk of blindness, cataract, glaucoma, epithelium defects and herpes or fungus, and consequently steroid-sparing treatment is important. The immunosuppressant drug CsA is thus an effective treatment, Dr Brémond-Gignac outlined in her ESCRS presentation.
There are a number of different concentrations of CsA (0.05-2mg/ml) available in different countries with different indications. The minimum effective concentration for the treatment of VKC remains unknown, with no studies having compared the efficacy of different concentrations according to Dr Brémond-Gignac’s presentation.
NEW DATA
However, newer CsA formulations (0.1%, specific clinical indication for VKA) have shown good efficacy in severe VKA in four key studies to date. Specifically, Prof Brémond-Gignac’s presentation outlined the results of research she was involved with – the VErnal KeratoconjunctiviTIs Study (VEKTIS), a phase III, multi-centre, double-masked, vehicle-controlled trial that evaluated the efficacy and safety of an investigational therapy for severe VKC, CsA cationic emulsion (CE), an oil-in-water emulsion with increased bioavailability versus conventional CsA formulations.
Paediatric patients (4-18 years) with

active severe VKC (grade of 3 or 4 on the Bonini severity scale) and severe keratitis (corneal fluorescein staining [CFS] score of 4 or 5 on the modified Oxford scale) were recruited for the study.
One-hundred-and-sixty-nine patients were randomised to CsA CE 0.1% (1mg/ ml) eye drops four times daily (high dose), CsA CE twice daily (low dose) plus vehicle twice daily, or vehicle four times daily for four months.
Differences in least-squares means versus vehicle for the primary endpoint were statistically significant for both the high-dose (0.76; p=0.007) and the low-dose (0.67; p=0.010) groups, with treatment effect mainly driven by CFS score.
Significant differences were found between both the active treatment groups and vehicle for use of rescue medication. VKC symptoms and patient quality of life (assessed by visual analogue scale and the Quality of Life in Children with Vernal Keratoconjunctivitis questionnaire) improved in all three groups, with significant improvements for high-dose (four-times daily) CsA CE versus vehicle.
The study concluded that the efficacy of high-dose CsA CE in improving keratitis, symptoms, and quality of life for those with severe VKC was demonstrated in the recruited patients. In addition, in this study cohort, CsA CE was well tolerated, and the results were maintained during 12 months; “So this is an effective and safe treatment option for these patients.”
Dr Bremond-Gignac’s presentation also emphasised the importance of washing and hygiene for the diseased eyes to optimise results.
EUROTIMES | JUNE 2020
formulations of cyclosporine showing good results in paediatric ocular surface diseases. Priscilla Lynch reports
PAEDIATRIC OPHTHALMOLOGY 32 Free Membership Membership to WSPOS is available for FREE on www.wspos.org World
Ophthalmology
Society of Paediatric
and Strabismus
Multifocals in children
Multifocal IOLs achieve good results in treatment of paediatric cataracts.
Roibeard Ó hÉineacháin reports
Multifocal intraocular lenses are a good option for children with cataracts, provided that the patients are selected appropriately, said Laurence Lesueur MD, Toulouse, France.
“In 2019, multifocality in children with the latest generation of premium hydrophobic acrylic IOLs should be proposed and discussed, especially for unilateral and bilateral cataracts after the age of five years,” Dr Lesueur told the WSPOS Subspecialty Day in Paris, France.
She cited the French SAFIR study, in which 41 eyes of 33 children underwent multifocal IOL implantation and had a minimum follow-up of one year and a mean followup of 25 months. The mean distance best-corrected visual acuity (BCVA) improved from a preoperative value of 0.66 logMAR to 0.24 logMAR and the mean postoperative distance uncorrected visual acuity (UCVA) was 0.42 logMAR. In addition, the mean near postoperative UCVA was 0.44 logMAR and the mean near BCVA was 0.28 logMAR. Moreover, 43.5% of patients were spectacle-independent postoperatively.
The children in the retrospective multicentre study were aged nine months to 15 years, with a mean age of seven years. This included 30 unilateral and 11 bilateral cataract cases with congenital, traumatic or iatrogenic cataracts.
Children under five years of age also underwent posterior capsulorhexis and anterior vitrectomy. The study’s exclusion criteria were corneal disease, glaucoma, microphthalmos, pupil deformation, retinopathy, neuro-ophthalmic disease and ocular inflammation.
The lenses used in the study included the ReSTOR SN 60 AD3-AD1 (Alcon), the Tecnis ZMA00, the AMO NXG1, and the Acri.LISA Toric (ZEISS). There were no significant differences between the different types of multifocal IOL in terms of visual outcome or the incidence of posterior capsular opacification requiring YAG laser capsulotomy, which occurred in 43.5% of cases overall.
She noted that several other notable studies have investigated the use of multifocal IOLs for paediatric cataracts. They suggest that the myopic shift is greater in the eye without the implant in unilateral cases and that bilateral cases tend to achieve the greatest degree of stereopsis. Studies also show promising results in some of the newer trifocal IOLs.
Dr Lesueur noted that while questions remain about the sometimes-unpredictable myopic shift that can occur in patients even in the second decade of life, where necessary, laser refractive surgery performed in adulthood can achieve good refractive and anatomical results.
WCPOS V | 2020
is now WSPOS
World Wide Connect 2020
In light of the concerns and uncertainties presented by the Covid-19 pandemic, it has been confirmed that WCPOS V, scheduled to take place in Amsterdam, will instead be presented in virtual format, WSPOS World Wide Connect 2020.
We at WSPOS believe that with every challenge comes opportunity and this challenge now presents us the opportunity to deliver all the conference sessions to a global audience via a virtual platform.
In the words of Ralph Waldo Emerson “Do not go where the path may lead, go instead where there is no path and leave a trail” Please join us in the coming weeks and together we will create a trail seldom seen.
EUROTIMES | JUNE 2020 PAEDIATRIC OPHTHALMOLOGY
www.wspos.org 33
...multifocality in children with the latest generation of premium hydrophobic acrylic IOLs should be proposed and discussed
Laurence Lesueur MD

ASCRS is your trusted source for innovative education and philanthropy, for every stage of your career. Join today: ASCRS.org
INDUSTRY NEWS
NIDEK launches CP-9 Chart Projector
The CP-9 is a user-friendly chart projector that provides a brighter and clearer chart display with a white LED, according to NIDEK. The long-life light source achieves high cost-efficiency for daily examination. Additionally, an optical zoom enables a variable installation distance. Easy focus adjustment by rotational LED aperture is also available. “Combining a sophisticated design with these innovative features, the CP-9 is easy to put into practice in various facilities, and it particularly works well with other NIDEK refraction products,” says Motoki Ozawa, President and CEO of NIDEK CO., LTD. “We will continue to enrich the optometry product line-up and further strengthen proposals to meet a wide range of customers’ needs.”
www.nidek.com
CE CLEARANCE
ZIEMER has received CE clearance for its new Lenticule Application

“CLEAR” for the treatment of myopia and astigmatism.
“CLEAR” stands for “Corneal Lenticule Extraction for Advanced Refractive Correction.” “CLEAR” can be purchased and upgraded with a new software package. The CE clearance also authorises surgeons to use the FEMTO LDV Z8 Laser Platform for children’s cataract surgery.
“‘With our new developments, we are keen to offer doctors and patients the benefit of a large variety of treatments. So, we are delighted to be reaching a new milestone in this regard with our solution-oriented innovations,” said Frank Ziemer, CEO and President of Ziemer Ophthalmic Systems. www.ziemergroup.com
INNOVATION AWARD
Rayner has been recognised for its excellence in innovation by winning the esteemed and internationally recognised Queen’s Award for Enterprise (QAE) for its RayOne fully preloaded IOL injection system, designed to create the smallest fully preloaded IOL incision during cataract surgery.
Now in its 54th year, the Queen’s Awards for Enterprise are the most prestigious business awards in the United Kingdom and Rayner (a previous winner of the award in 2009) is one of only 220 organisations nationally to be honoured with the achievement.
Rayner CEO, Tim Clover, said: Were able to meet their needs. I’m incredibly proud to see that Rayner is once again recognised as a leading innovative British technology company.”
www.rayner.com
FREE 5 year membership for trainees
ESCRS Membership
• Reduced Registration Fees for ESCRS Congresses

• Subscription to Journal of Cataract & Refractive Surgery
• Access to ESCRS Grants, Bursaries and Research Awards
Access to:
• ESCRS iLearn
Online CME accredited interactive courses
• ESCRS On Demand
Online library of presentations from ESCRS Congresses
• EUREQUO
European Registry of Quality Outcomes for Cataract and Refractive Surgery
• ECCTR
European Cornea and Cell Transplantation Registry
today. EUROTIMES | JUNE 2020 INDUSTRY NEWS
www.escrs.org Join
35
Exceptional clinical education is 0ne
click away!
Visit ASCRS.org today!
ASCRS.org is a dynamic web portal featuring a new design and enhanced features, and delivering an exceptional user experience.
The new web portal features one-touch video playback, seamless navigation across all ASCRS online platforms, and more!
Visit ASCRS.org today!
Explore hundreds of surgical videos, presentations, webinars, and more by type, topic, or meeting date Find the latest and most relevant anterior segment surgery techniques and trends by keyword, type, topic
Track your current CME credit status through real-time access to your CME transcript and certificates
ASCRS.org is your 24/7, one-stop resource for anterior segment surgical online education.

COVID-19
& ophthalmic practice
Ido not believe that there is any practice of medicine, including all of ophthalmology, that has not been impacted by the Covid-19 pandemic in some way or another. Practices have been impacted in multiple ways, with clinics being concerned for the health of their staff and patients and then having an equally great concern about the economic challenges that lie ahead.
Clinics that have based their revenues on mainly elective procedures have seen their income drop by 99%. Patients are also nervous and are highly unlikely to be queueing up to spend time in densely populated waiting rooms. When the all clear is given to start practising elective medicine again, it’s not going to be like a light switch that is switched on but it is going to take time for people to venture out again and seek medical help. The recovery is going to be slow.
When people do venture out, however, they are going to be far more inclined to visit a clinic where space is a feature and where high people density is absent. I also predict that patients are going to be more inclined to want their surgeries performed in a day-care centre or even better, an ambulatory surgery centre or clinic, rather than a hospital. Bear in mind that most ophthalmology patients are not unwell and prefer to remain that way.
I have been following what is happening in Asia and have been somewhat surprised that refractive surgery has returned at a greater pace than cataract surgery. Once I understood the reasoning, namely that refractive surgery patients are younger and therefore less frightened by the virus, it did make sense.
I already see some clinics spending money advertising on how clean, sterile and virus-free their facilities are and believing that this would be a differentiator. In my view, this will not be a differentiator but rather what is called a

“hygiene factor”. It goes without saying that you have to offer these infection-control protocols in order to practice safely. This is a time to continue focusing on what really makes you different. If everyone is practising the same level of infection control, then this is clearly not a differentiator.
Some of the lessons that I have learned is that the investment that we have made over the years in our team is paying off enormously with the team pulling together, coming up with ideas and plans on how things may look in the “new normal” and generally seeing this significant challenge as an opportunity to do things better after COVID-19 has been beaten, whenever that may be. We certainly foresee a future where telemedicine or digital communication forms a greater part of the routine eye examination experience at the clinic.
The history taking and determining of the motivations for surgery would be established remotely with telemedicine, the patient would then be seen at the clinic only to have their scans and the eye examination by the medical team and would then return home again and be followed up with a telemedicine call again to discuss the options and review the exam. This way you are protecting both patient and practitioner with less exposure to one another than before. You are also allowing the clinic to generate the same level of throughput as before, as now patients are physically spending less time in the clinic than before.
I imagine that if I were to write about this very topic again in just a few days from now, I will have a different view on certain aspects. That is how fast the impact of this pandemic is impacting clinical practice. Being mentally agile, adaptable, and having a positive attitude and stamina is going to be required to come out the other side looking remotely as healthy as we did just a few months ago, before the pandemic broke.
Returning to work after the pandemic will be a challenge for everyone.
EUROTIMES | JUNE 2020 PRACTICE MANAGEMENT 37
Arthur Cummings FRCSEd reports
Five Phases of the Crisis
Taking a look at the immediate and long-term effects of the COVID-19 pandemic on ophthalmic practices. Rod Solar reports
Shortly following the WHO announced a global pandemic, we locked ourselves in a room for two full days to map out the future for our cataract and refractive surgery clients. We resolved to make informed predictions of how the COVID-19 Crisis would impact the elective surgery market in the short and medium-term and what this could mean for you and your practice, clinic or hospital.
We developed a solid framework to help practice owners strategically plan for the expected (and predictable) changes that are coming. With this information, we hope that you can take strong and specific actions to help you maintain and protect your practice (which in this economy would be an achievement), and could even enable you to achieve modest growth.
Don’t react. Respond
We all have a lizard brain, a monkey brain, and a visionary brain. Be diligent not to stimulate your lizard brain – the one that makes you fight, flight or freeze. Resist the comfortable denial of the monkey brain – this is not the time to blindly do what others do.
Instead, it’s time to stay in your visionary brain as much as you can. It will be hard. The choices you’ve made and will need to make will tax your resolve. Your visionary brain that likely led you to start your practice in the first place. That’s the calm, deliberative, creative, and optimistic brain that asks –“what do I want to see in the world, and how do I want to engineer it?”
PHASE 1: Denial (one-to-two weeks before your shutdown)
In the denial phase, your market is conducting “business as usual”. People are distracted, but they’re carrying on. This group is in full-on monkey-brain mode and is carrying on as they always have done. These folks will keep their appointments because, for them, nothing has materially changed. That is the minority, and they’re typically younger Millennials – your LASIK market. If your country is in Phase 1, you have an immediate opportunity to help some patients but you need to act now.
PHASE 2: Panic (two-to-three weeks of shock)
During this phase, there is an immediate and sudden contraction of supply and demand for elective healthcare services as physiological, and safety needs supersede everything else. Your inquiries will likely slow to ZERO in this phase. Don’t market to anyone in the panic phase. The key at this time is to prepare appropriately for the next three phases.
PHASE 3: Boredom (six-to-12 weeks after your shutdown)
In the boredom phase, people will be hungry for information and entertainment that distracts them from current events and the sheer monotony of life inside four walls. This is your chance to create and disseminate content that is either informative, educational or entertaining while maintaining a sensitive tone to current affairs – less aspirational, more grounded in utility. Most importantly, make this content interactive.
PHASE 4: Hope (one-to-16 weeks from your shutdown)
After 12-to-16 weeks from your shutdown, we will be through the worst of it, and people will begin planning for their future. There will likely be steep economic decline followed by a period of bumping along the bottom, like an aeroplane, struggling to take off. Hear me now and quote me later –this recession will likely mark the end of elective surgery as a commodity. Position it as a luxury and adjust your servicelevel accordingly.
PHASE 5: The ‘new’ normal (four months from your shutdown up to two years)
In February, I’d only read the phrase “social distancing” once. Now, it’s everywhere. And unless experts’ most optimistic models come to pass, we should expect to be subject to social distancing. Consider a typical reception/waiting room that’s about 7×7 metres (23×23 feet) with 32 chairs all neatly placed together – set mere inches apart. Now take those chairs and distance them by 6 feet/2 metres each – in every direction. Now, in a space you could fit 32 people, you can only fit nine chairs. Your reception room capacity has just reduced by 72%.
Another point worth mentioning is, no matter how safe you feel your environment is, people who’ve avoided restaurants for two months aren’t about to go out for dinner twice a week. If you decide to do anything this week, add video appointments to your service offering. Before the coronavirus, they were already becoming a standard feature in today’s society – particularly the health sector. Today, they are a must if you want to protect your patient pipeline during the coronavirus crisis shutdowns, and beyond.
Now is the time to help, to share, and to support each other through this challenge.
Rod Solar is Director of Practice

Development Consulting of LiveseySolar
https://www.liveseysolar.com/
38 EUROTIMES | JUNE 2020 PRACTICE MANAGEMENT
Rod Solar, speaking at the the 36th Congress of the ESCRS in Vienna, Austria
Due to the COVID-19 virus, a number of meetings have been cancelled or rescheduled. The information in this calendar is correct at the time of going to print; please check the meeting website or email the conference organisers to confirm all meeting dates.
JUNE
WOC2020 Virtual ® 26 – 29 June http://icowoc.org/
JULY
1st Virtual HSIOIRS Congress
34th HSIOIRS Congress
7 – 10 July www.hsioirs.org/
JULY
2020 ASRS
Annual Meeting
24 – 26 July www.asrs.org
SEPTEMBER
5th International Glaucoma Symposium
4 – 5 September
Mainz, Germany
https://glaucoma-mainz.de/
SFO 2020 Congress
5 – 6 September
https://www.sfo.asso.fr/
OAS 34th Annual Scientific Meeting
11 – 13 September
Chicago, USA

www.eyeanesthesia.org/
49th ECLSO Conference
18 – 19 September
Paris, France
https://www.eclso.eu/
EUROTIMES | JUNE 2020 CALENDAR 39
The OAS 34th Annual Scientific Meeting will take place in Chicago, USA
49th ECLSO Conference will take place in Paris, France
OCTOBER
38th Congress of the ESCRS
Virtual Meeting
2 – 4 October
www.escrs.org
20th Euretina Congress
Virtual Meeting
2 – 4 October
www.euretina.org
11th EuCornea Congress
Virtual Meeting
Date to be confirmed www.eucornea.org
WSPOS World Wide Connect 2020 Virtual Meeting
www.wspos.org
NOVEMBER
BEAVRS 2020
November
https://beavrs.org/
AAO 2020
14 – 16 November
Las Vegas, USA
https://www.aao.org /annual-meeting
100th SOI National Congress
25 – 28 November
Rome, Italy
https://www.congressisoi.com
XXI International Congress of the Brazilian Society of Ophthalmology
26–28 November
Rio de Janeiro, Brazil
https://sistemacenacon.com.br/site/ sbo2020/mensagem
DECEMBER
14th EGS Congress
14 – 16 December
Brussels, Belgium www.egs2020.org/
2021
MARCH
6th San Raffaele OCT & Retina Forum
5 – 6 March
Milan, Italy
https://www.octforum2021.eu/
JUNE
AECOS 2021 European Symposium
3 – 6 June
Florence, Italy https://aecosurgery.org/ 2021-european-symposium/
46th Meeting of the European Paediatric Ophthalmological Society (EPOS)
17 –19 June
Copenhagen, Denmark https://epos2021.dk/
JULY
AECOS 2021 Summer Symposium
15 – 18 July
Utah, USA

https://aecosurgery.org/ 2020-summer-symposium/
33rd APACRS–SNEC
30th Anniversary
Joint Meeting
29 – 31 July
Suntec City, Singapore
https://apacrs-snec2020.org/
CALENDAR 40 Continue your education online all year with our new range of online resources Ready when you are. Visit education.escrs.org EUROTIMES | JUNE 2020
The AECOS 2021 Summer Symposium will take place in Utah, USA
Announcement of Virtual Meeting
38th Congress of the ESCRS
2- 4 October 2020
As the Annual Congress can not take place in Amsterdam as planned, ESCRS is excited to offer an online digital experience instead.
Please visit the website for updates & further information
www.escrs.org
Research Education Innovation
ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.