Care Recommendations for EI

Helen Lill Cat Lancashire

What will we discuss?
● EI Skin care basics and example care routines


● Keratolytics and Retinoids
● Wounds, Blisters, and Allergies
● Infections - how to recognise trouble ●
●
Scalp care
Plantar-Palmar Keratosis (PPK)
● Temperature dysregulation ● Dealing with comments / Advocating for yourself
Life hacks
Travelling with EI
Current topics of interest
●
●
●
Skin care basics for EI
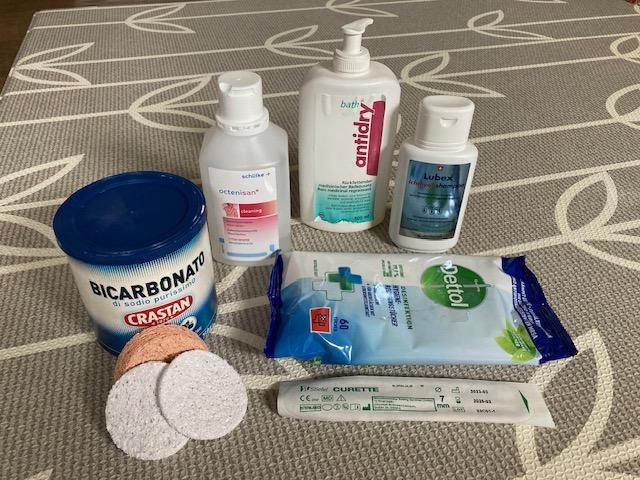
Bathing
- What to put in the bath and why?
- Bleach / Bicarbonate of soda / Salt / Oats
Exfoliation
- Wash cloth / Sponges / Exfoliators / Tools ● Moisturisers

-
Lotions / Creams / Ointments / Glycerin

●
●
Bathing
Suessmuth, K., et al (2020): Ichthyosis in Everyday Practice











Bathing https://www.firstskinfoundation.org/bathing-exfoliation FIRST (2023)
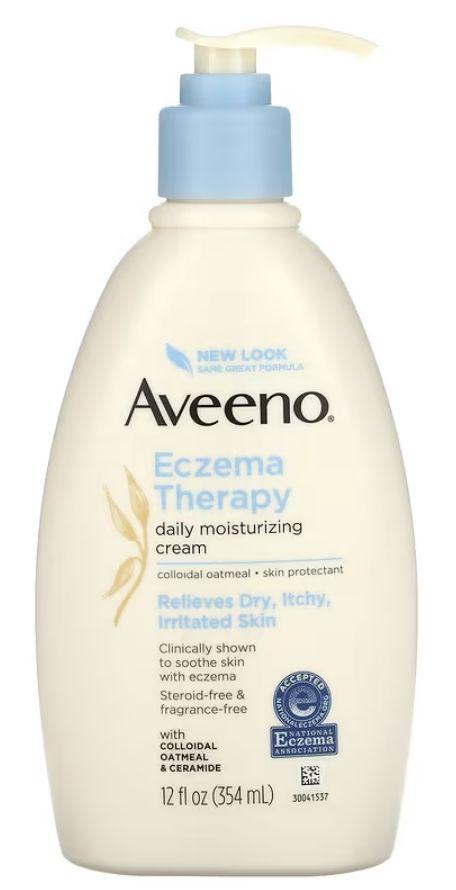
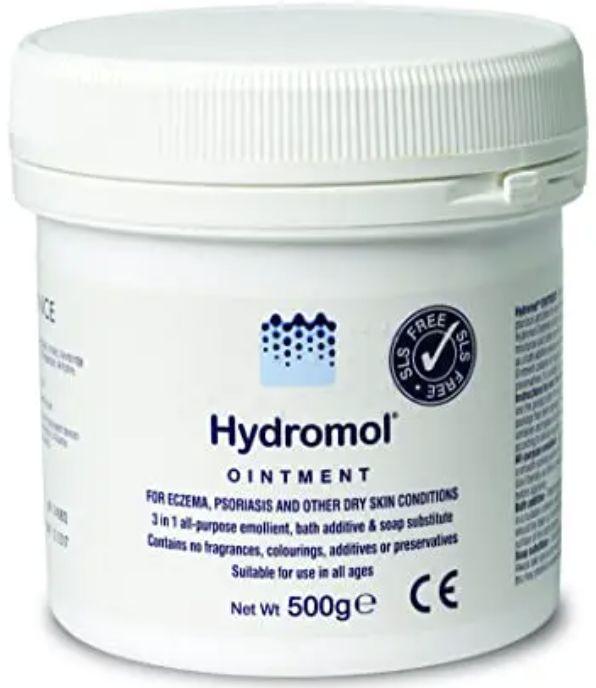
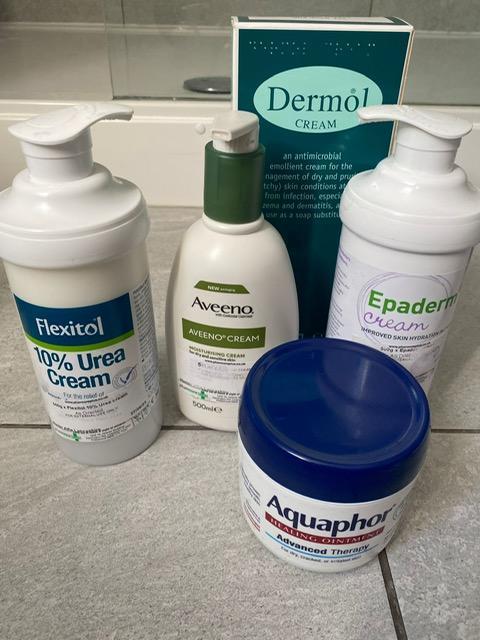
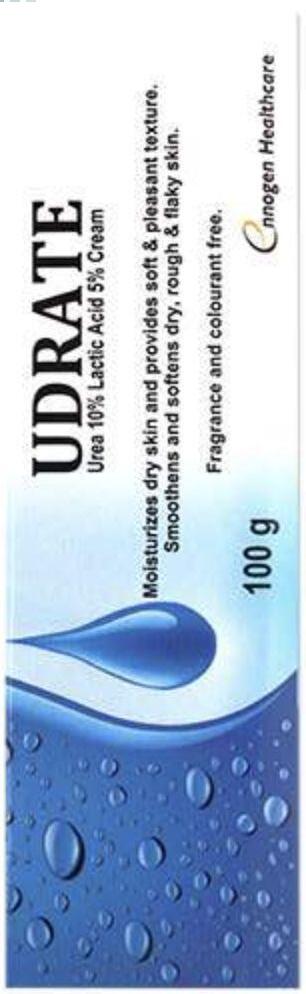
Moisturisers
Mazereeuw-Hautier, J., et al (2018); Chamlin, S., et al (2002); Rout, D., et al (2019); FIRST (2021)


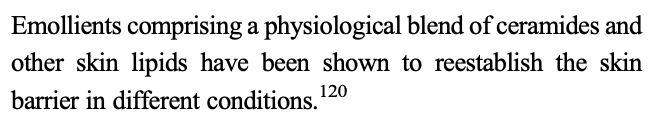
Ceramide lotion Vs Ointments

 Lill, H. (2022)
Lill, H. (2022)
Ceramide lotion Vs Ointments

 Lill, H. (2022)
Lill, H. (2022)
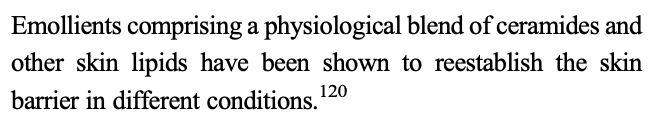
Ceramide lotions








Principles of skin care?




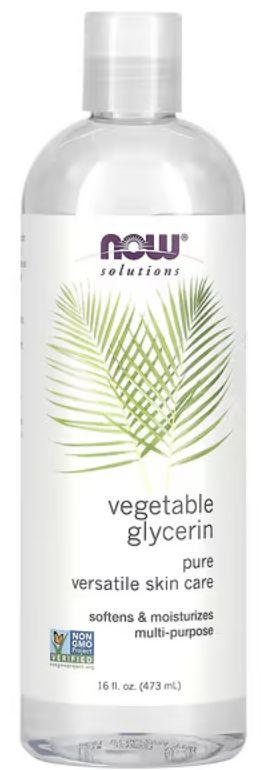
Humectant?


 Oberoi, J. (2022); Kraft, N. and Lynde, C (2005)
Oberoi, J. (2022); Kraft, N. and Lynde, C (2005)
Occlusive?

Kraft, N. and Lynde, C (2005);
Ghadially, R, Halkier-Sorensen, L, and Elias, P. (1992);


Oberoi, J. (2022)
Emollient?


 Sethi, A. et al (2016); Oberoi, J. (2022)
Sethi, A. et al (2016); Oberoi, J. (2022)
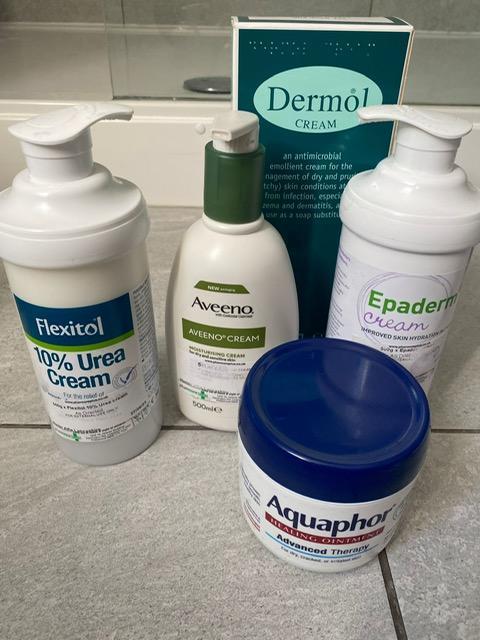
Find the right mix for you!
● Finding the right solution for EI skin is trial and error, but understanding the basic principles helps us find the right ingredients to work with


● Emollient = nourishes the skin biome and restores the skin barrier, but still allows the skin to breathe
● Humectant = makes the water from the bath last longer so that skin stays supple for longer.
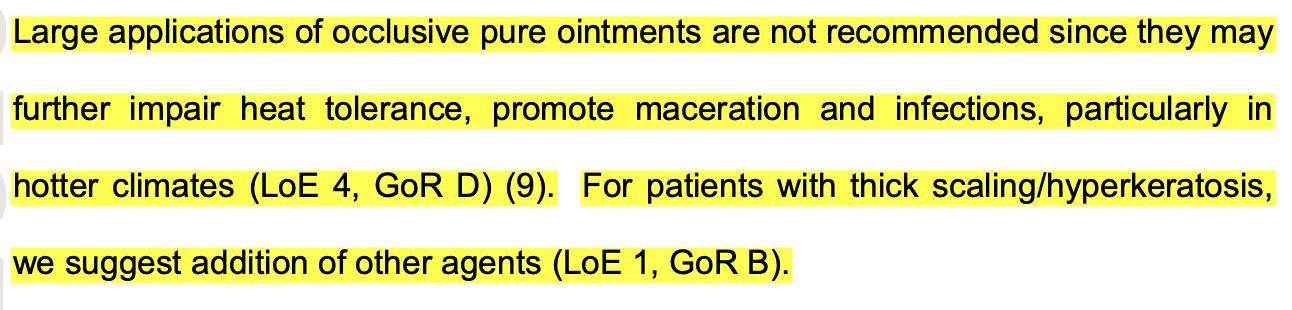
● Occlusives = Not ideal as a moisturiser for EI, but remain useful for wound care and sealing wounds
Care Routines



 Cat & Alfie
Helen & Arienne
Cat & Alfie
Helen & Arienne
Cat & Alfie
Bath & Exfoliation
Moisturisers & Keratolytics



Cat & Alfie
Infection care


Blister & Wound care


Helen & Arienne

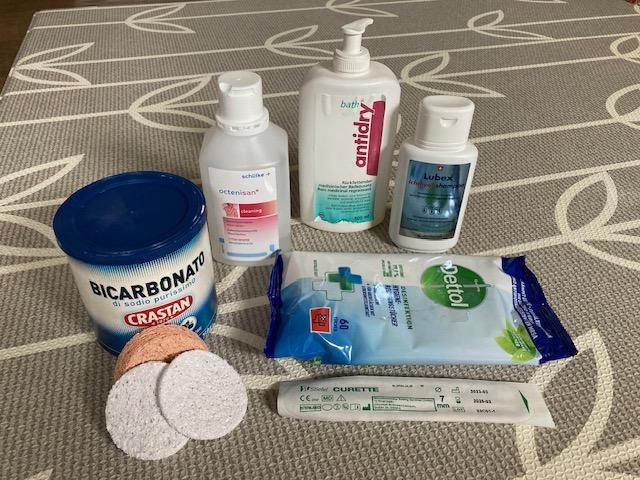


Bath & Exfoliation
Moisturisers & Keratolytics
Helen & Arienne
Skinnies WEB clothing

Exfoliation tools





Helen & Arienne
Odds & Sods!
Allergies & Fungal infections



Wound & Blister care


Keratolytics
● What are keratolytics?
- Examples include Urea, Salicylic Acid, Alpha-Hydroxy Acids
● How do they work?
- Soften the skin, and reduce the rate of hyperkeratosis
- Encourage completion of the shed skin cycle, or induce peeling
● When to use them
- Under 2 years: Only after discussion with HCPs (Urea 5-10%)
- Children and Adolescents: Urea 5% - 40% after discussion with HCPs, be wary of Salicylic Acid, and Alpha-Hydroxy Acids

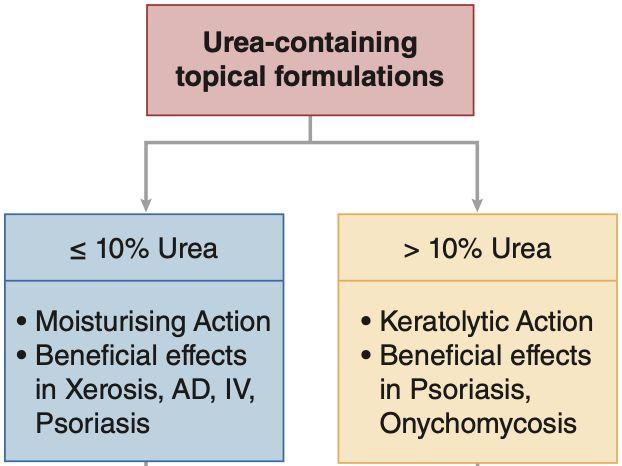
- Adults: Trial and error, consider 25-40% urea, or dual keratolytics

Keratolytics
Mazereeuw-Hautier, J, et al (2018): European guidelines; BJD



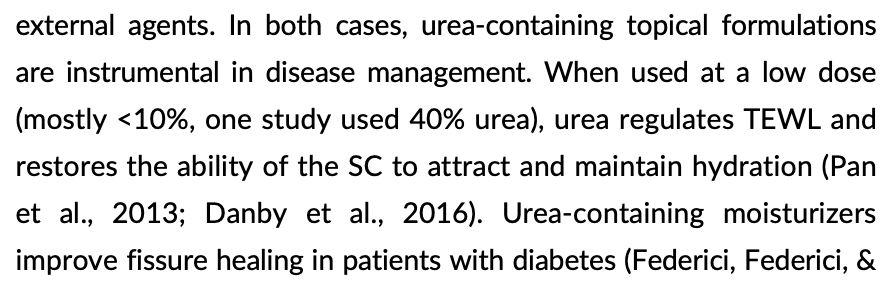
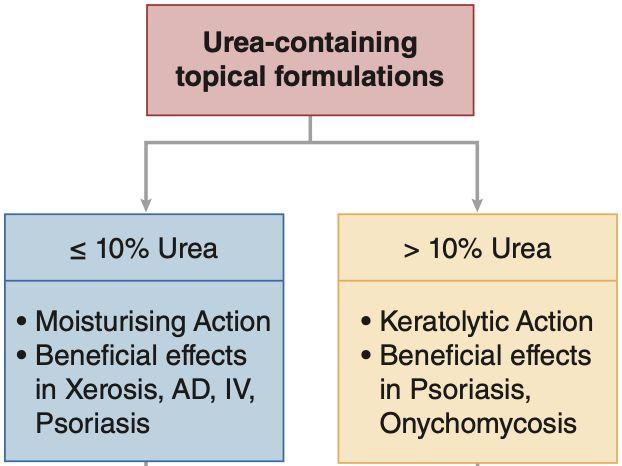
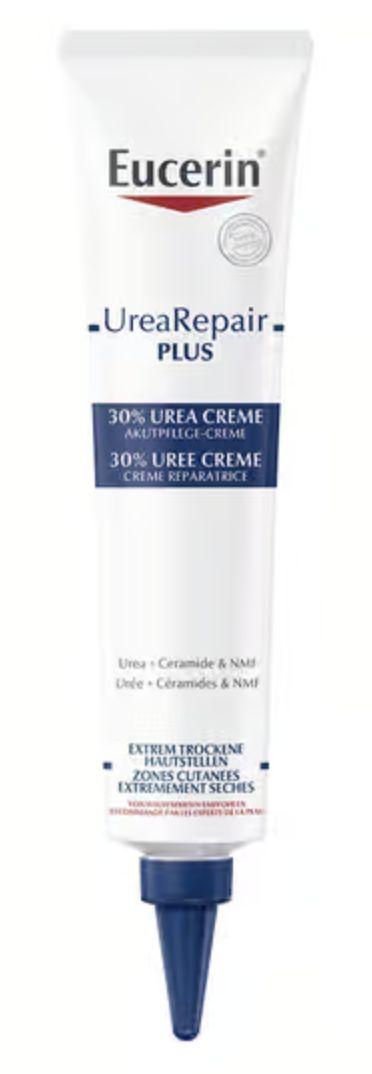
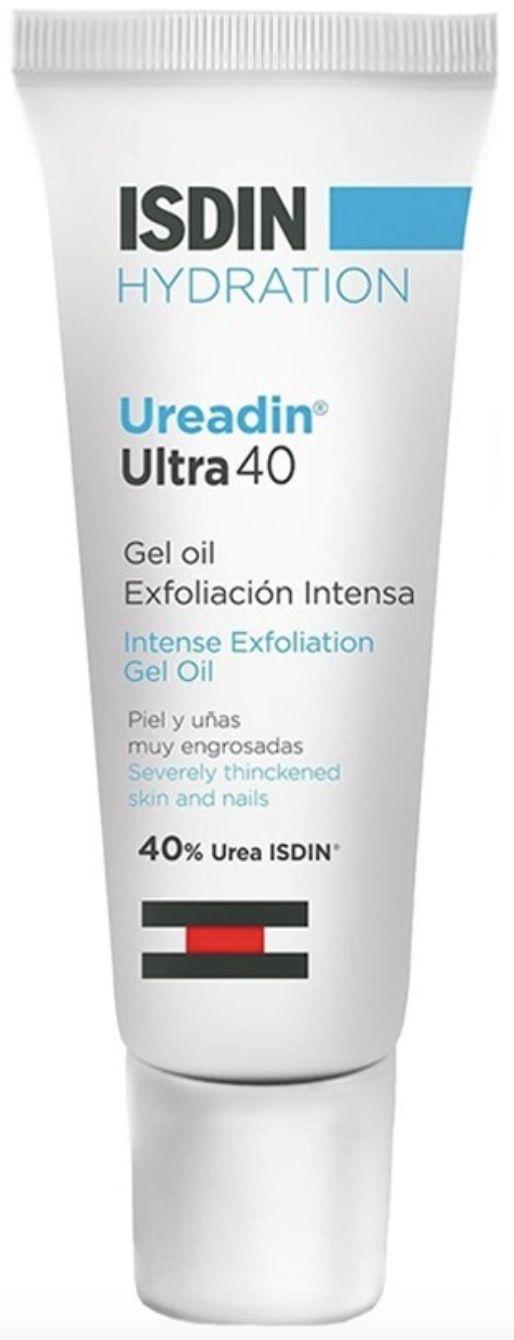
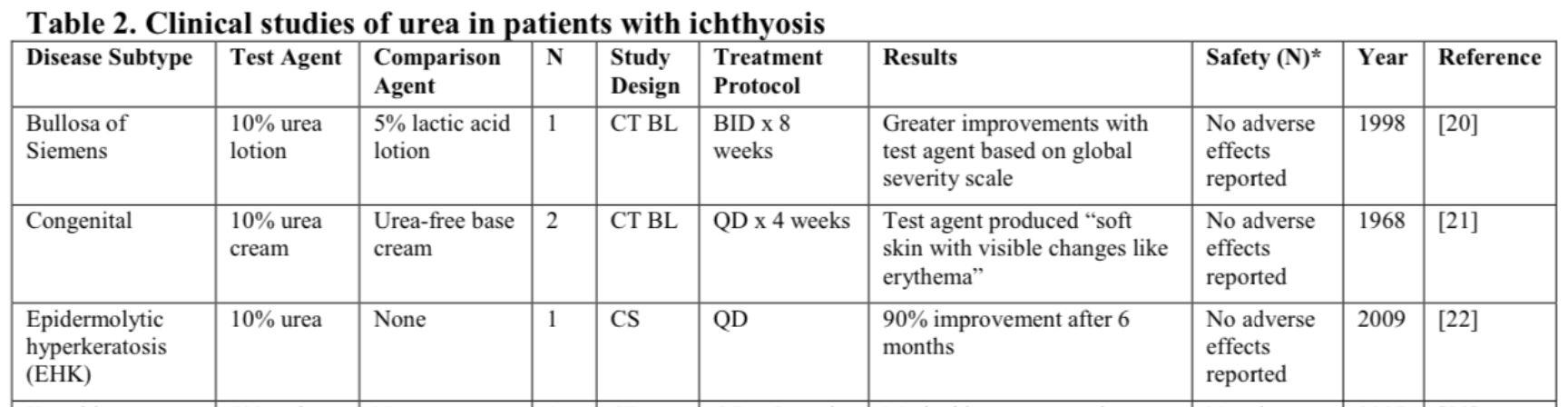
Keratolytics - Urea

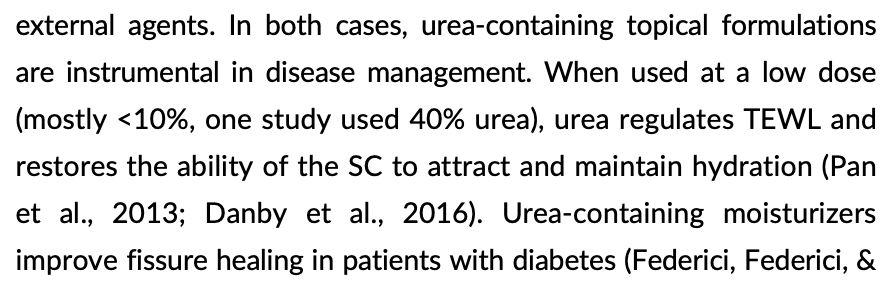

Cellano, L. (2018) Dermatologic Therapy; 31: e12690

Keratolytics - Urea
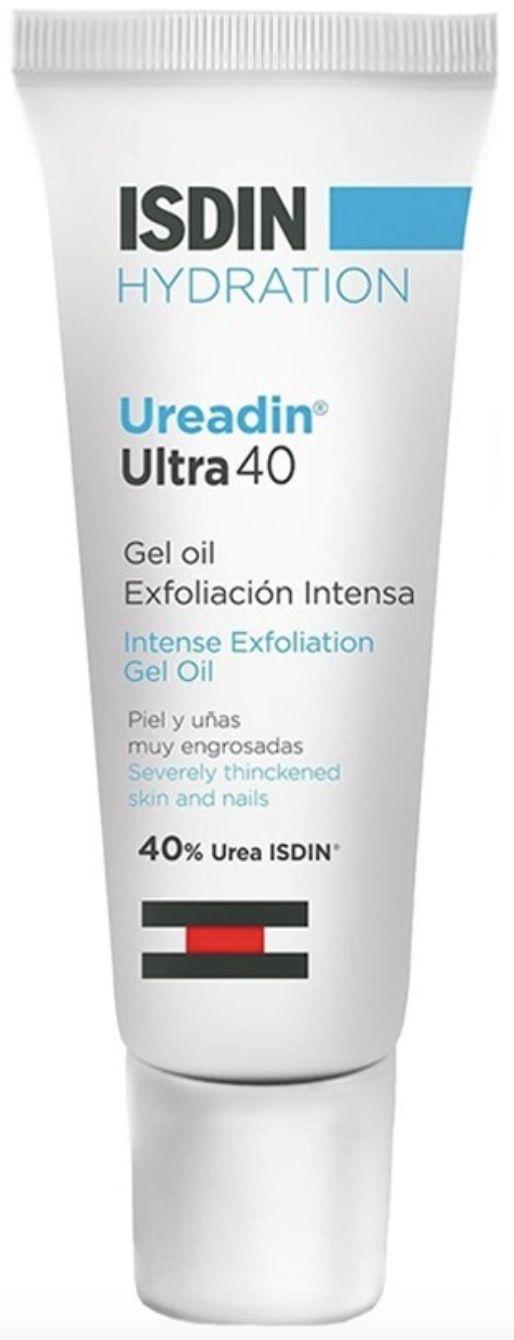





10% 12% 25% 30% 40%



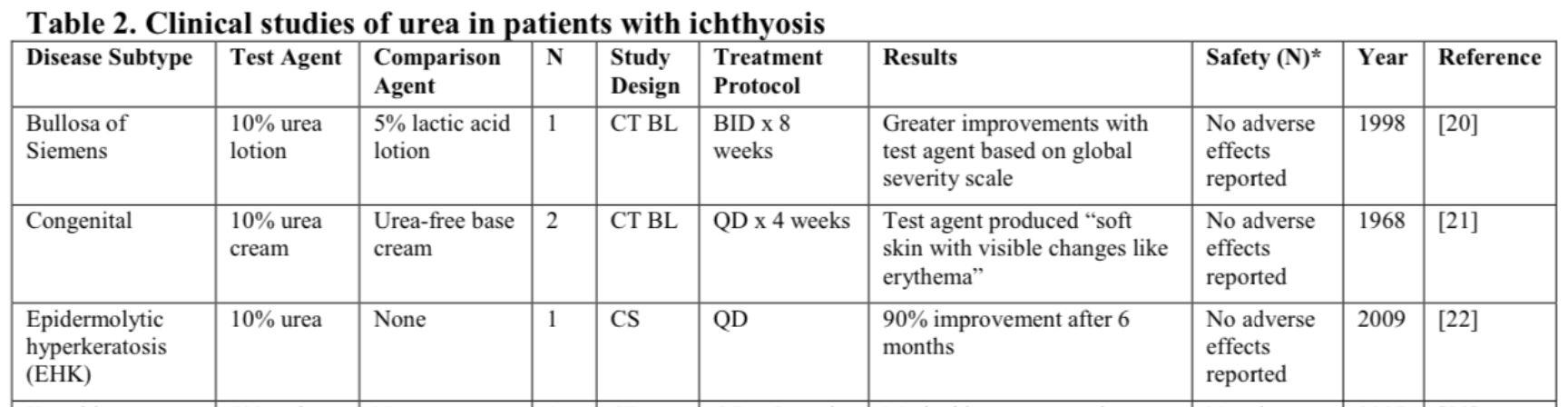
Keratolytics - Urea Pan,M et al (2013): Dermatology Online. Urea: A Review.
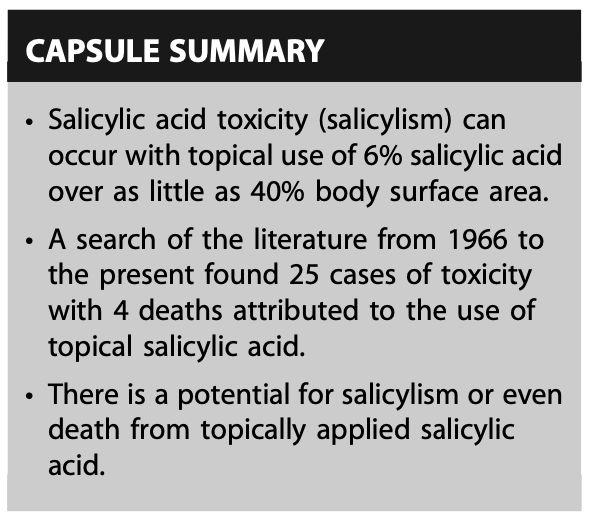
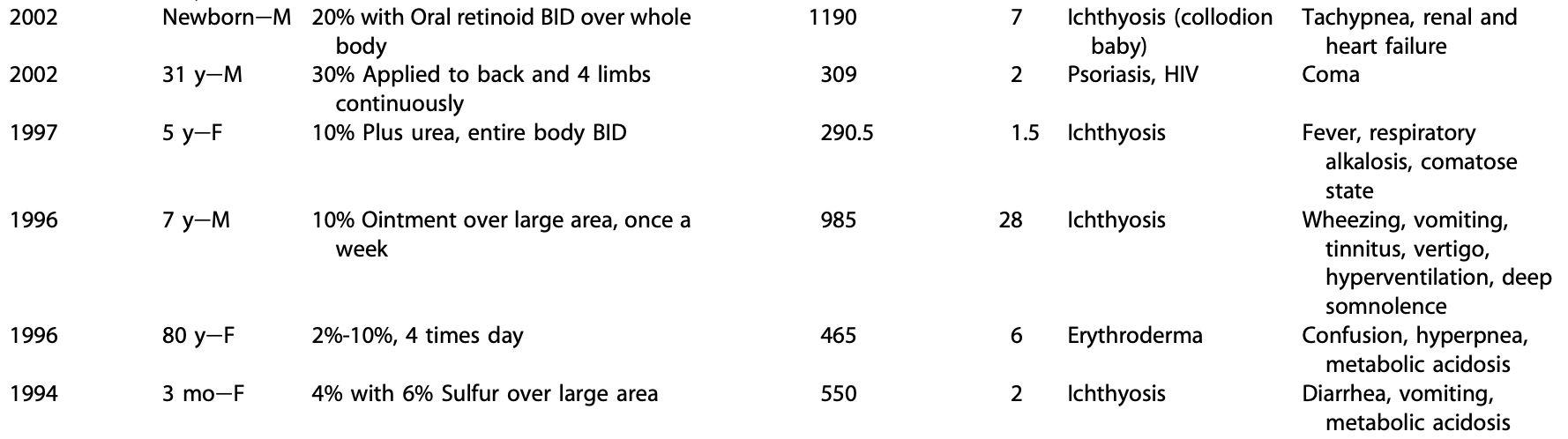
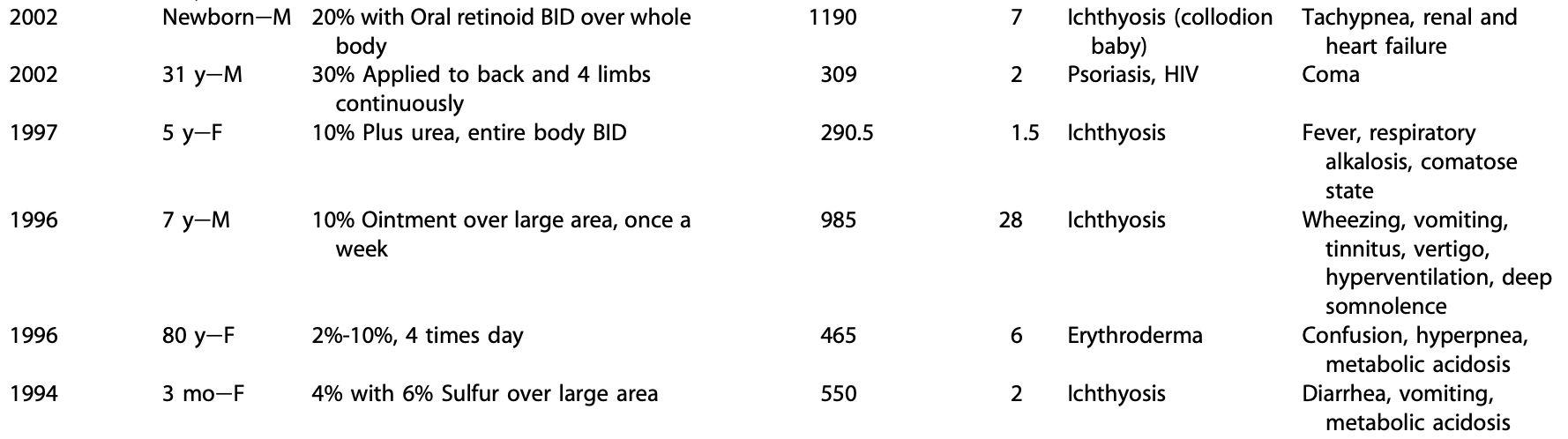
Keratolytics - Salicylic Acid

Madan, R. & Levitt, J. (2014) A review of toxicity from topical salicylic acid preparations. JAAD; Vol 70 (4)
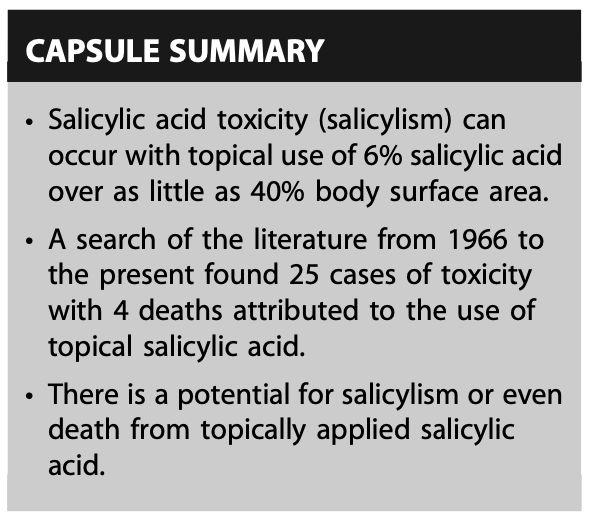


FIRST (2023) https://www.firstskinfoundation.org/creams-lotions-products

FIRST (2023) https://www.firstskinfoundation.org/bathing-exfoliation

US Food and Drug Administration (2022)

https://www.fda.gov/cosmetics/cosmetic-ingredients/alpha-hydroxy-acids#q4


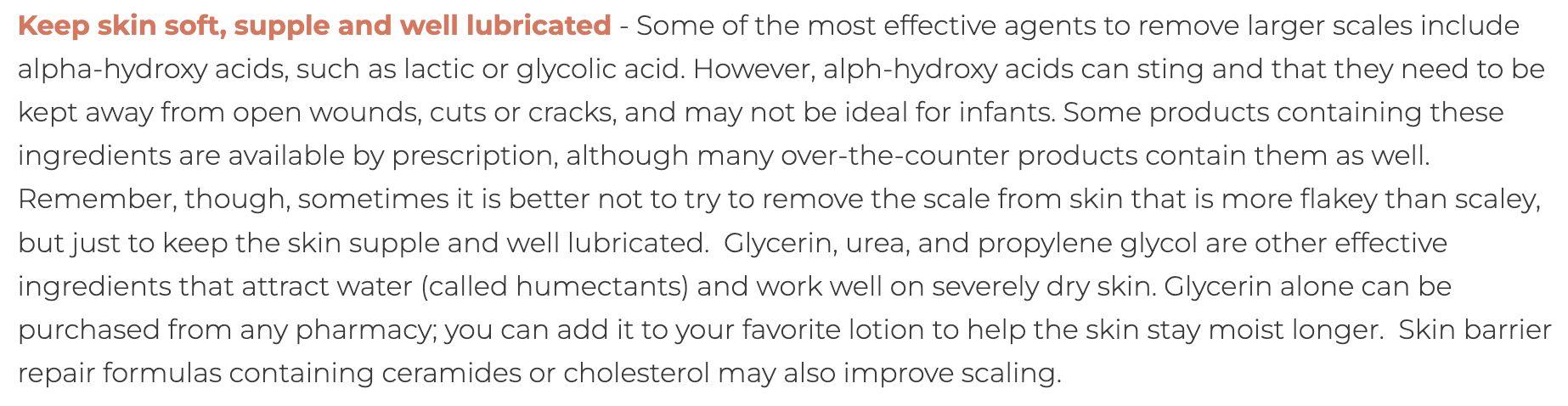
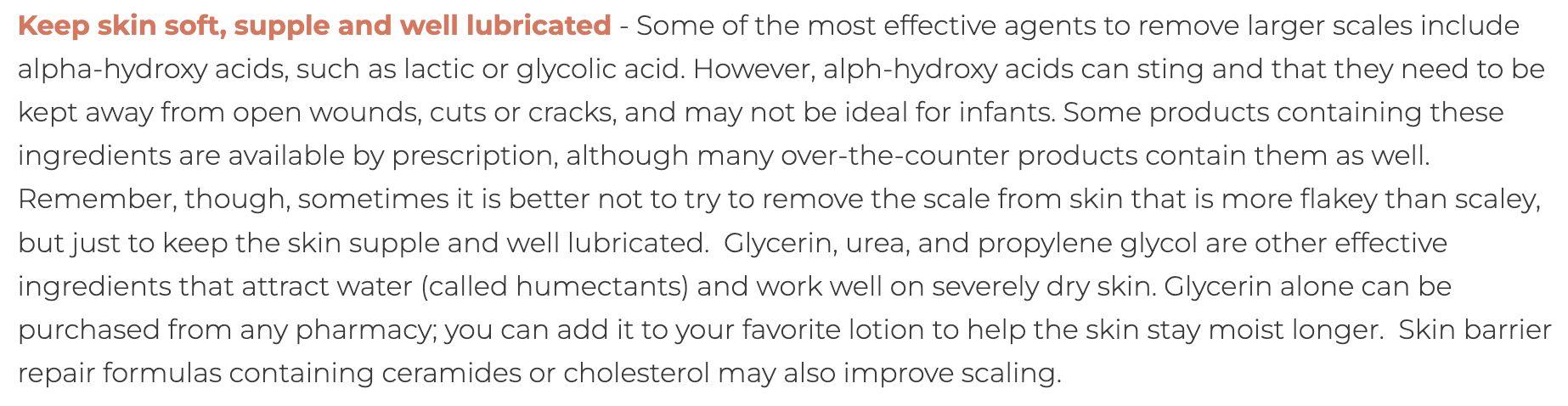
Keratolytics - AHAs
Keratolytics - AHAs
● AHAs are useful skin peelers
● They may cause burning, itching, and stinging due to their low pH
● They also increase the risk of sun damage to skin cell DNA

● The higher the strength, and the more frequent the use, the greater the risk of skin damage

ADULT USE ONLY
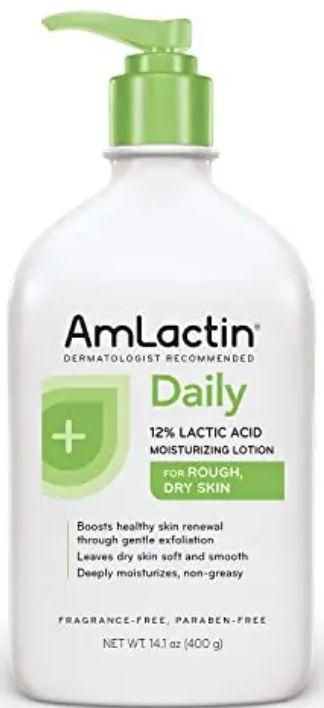
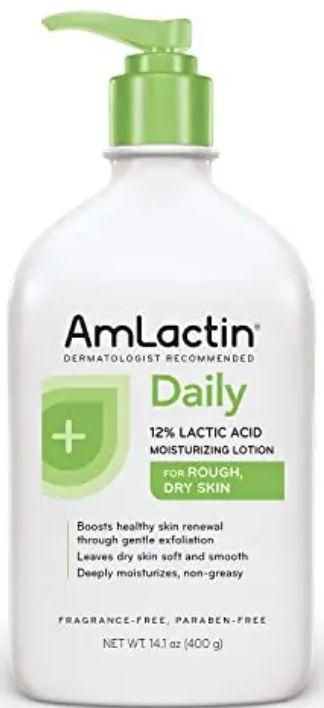
Dual Keratolytics
ADULT USE ONLY
10% Urea, 5% Lactic Acid
10% Urea, 5% Lactic Acid
10% Urea, 2% Salicylic Acid





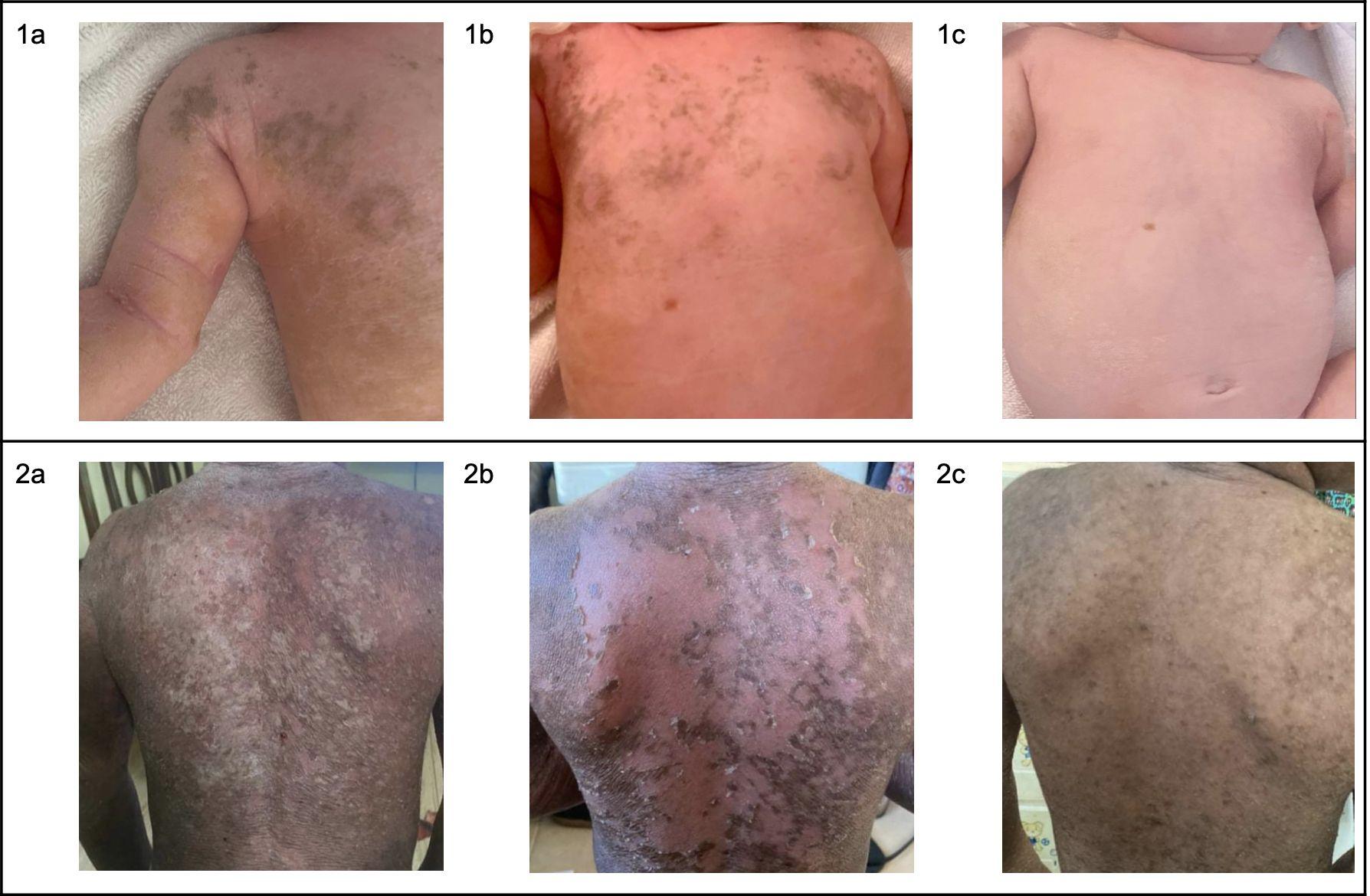
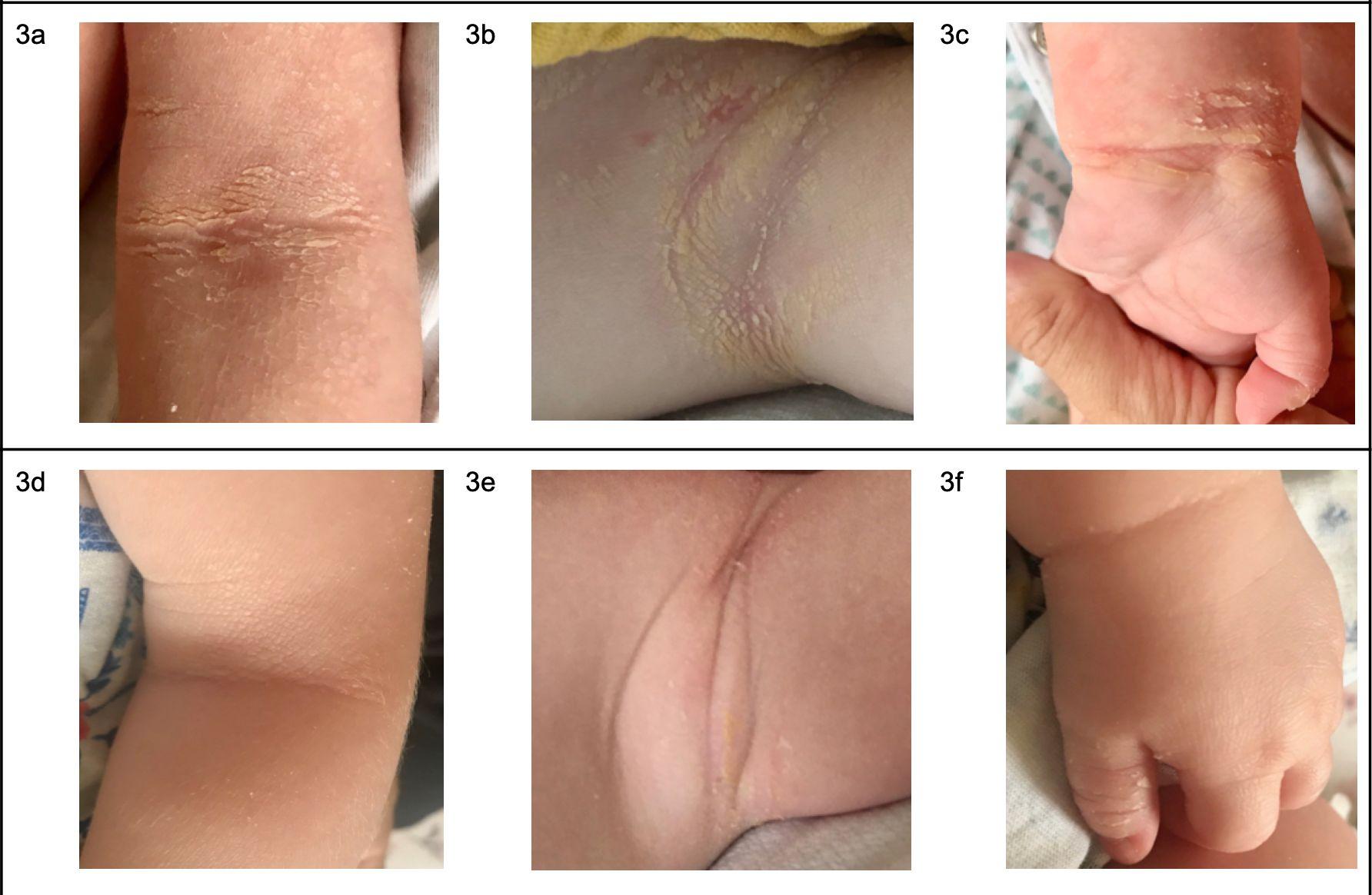
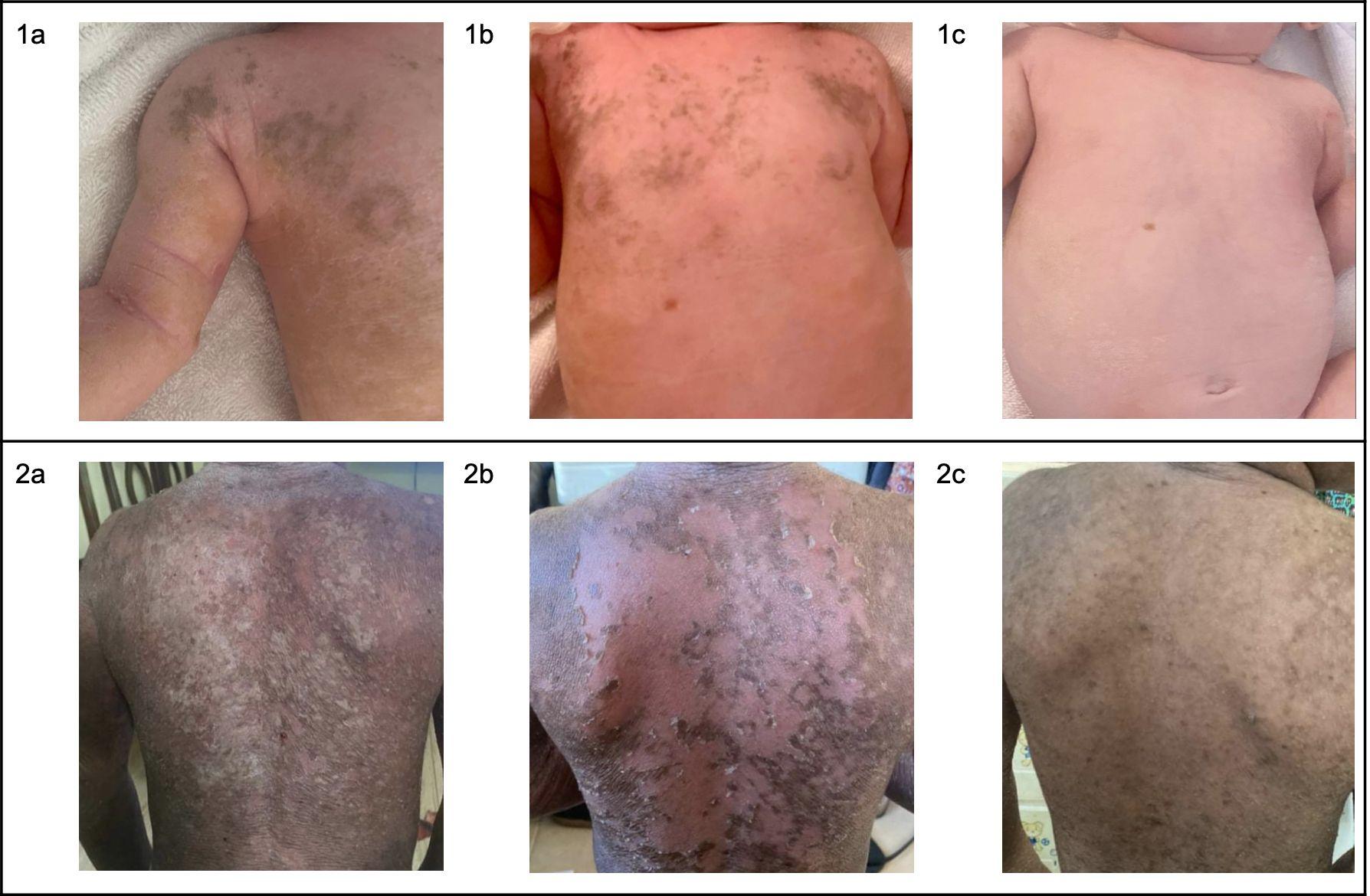
To do a care routine or not?

Right Arm
2 weeks
-No care
-No bath
-No exfoliation
-No creams
-No Keratolytics
= Thick, Itchy, Sore, & Uncomfortable
Left Arm
2 weeks
-Usual Care
-Daily bath
-Exfoliation
-Creams
-Keratolytic

= Controlled, Comfortable, & Confident

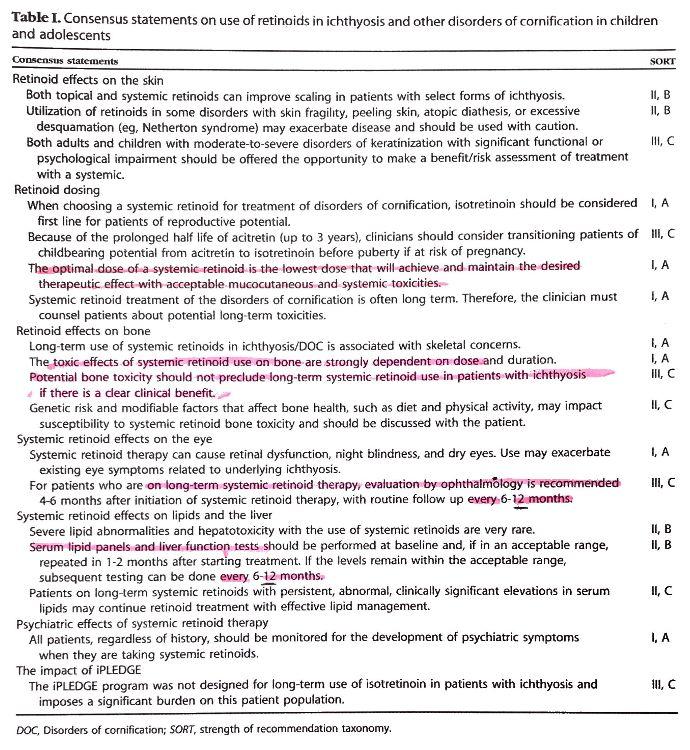
Retinoids
● What are retinoids?
- Topical or Oral medications which down-regulate keratinocyte / keratin production
● How do they work?
- No one is entirely sure, but they work best for KRT10
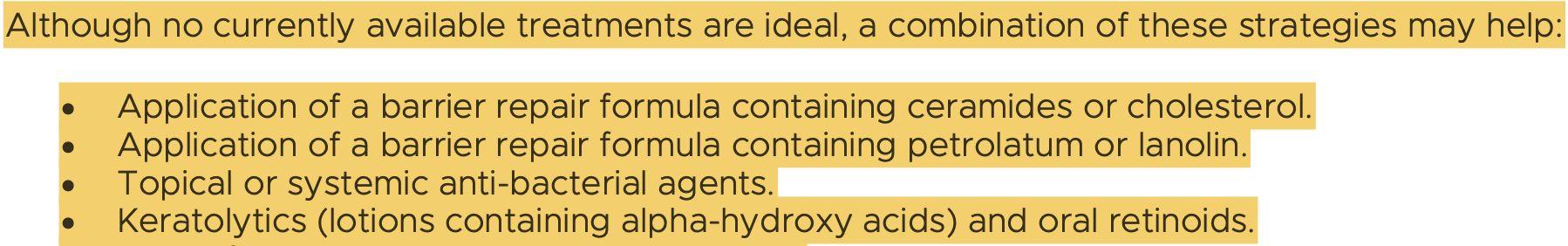
New Clinical Recommendations for Ichthyosis (2020)


- Indicate that low daily doses of oral retinoids are low-risk
● New products
- New trial for Topical Isotretinoin (Timber Pharmaceuticals)
●
Retinoids



Retinoids
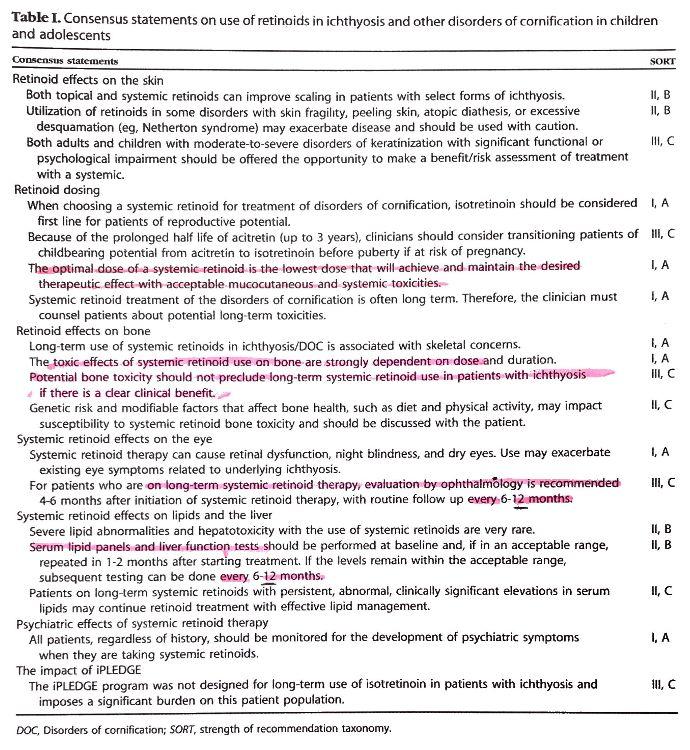
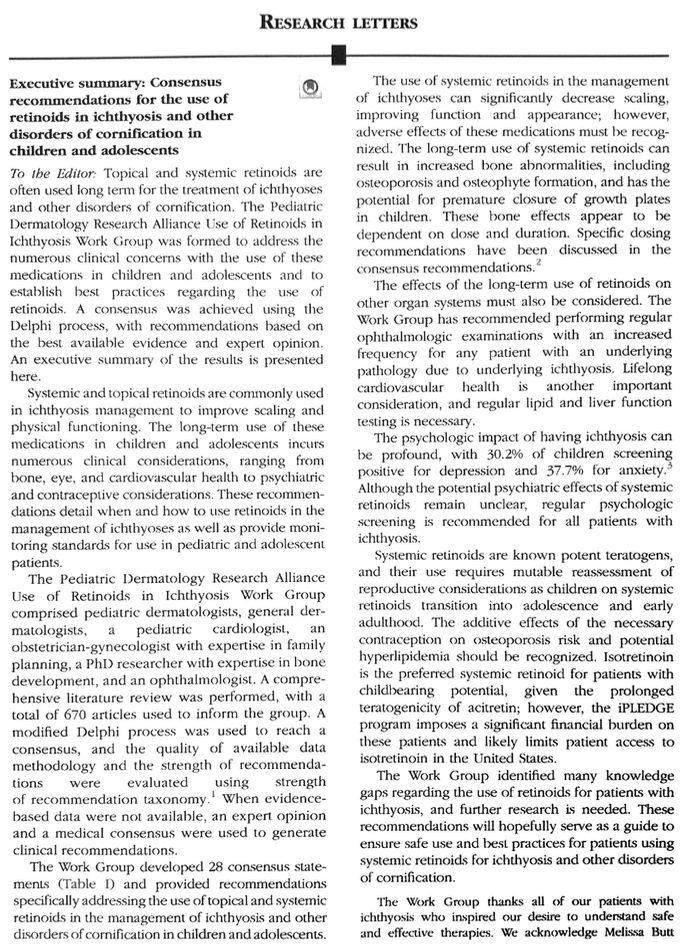


JMAD 86 (1)
Zaenglein, A, et al (2021):
Wounds and Blisters
● Wounds from trips and falls
- Remove loose skin / skin flaps
- Disinfect
- Cover with ointment / Consider zinc paste
- Use a dressing if this is what suits, or leave without and rest
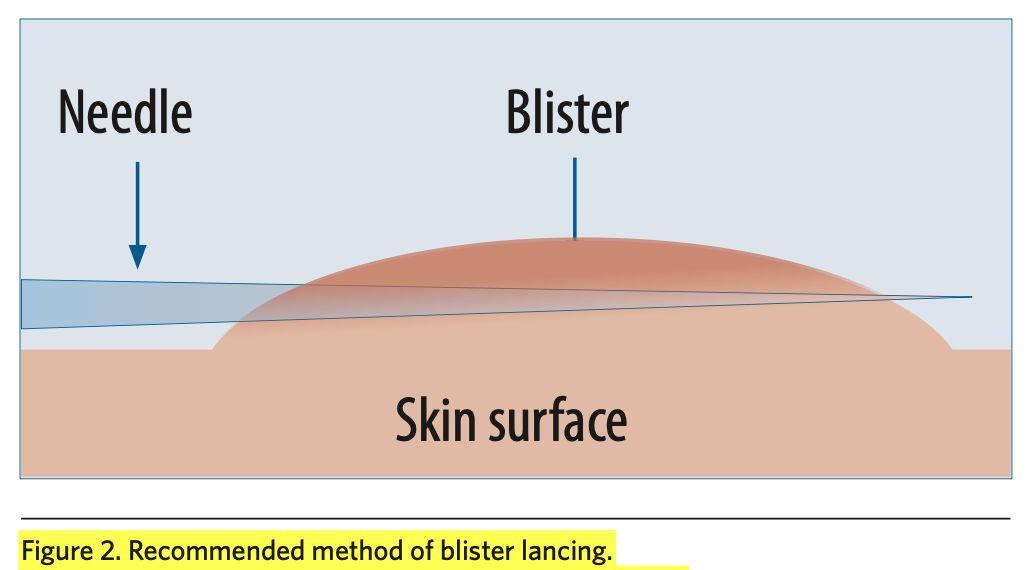
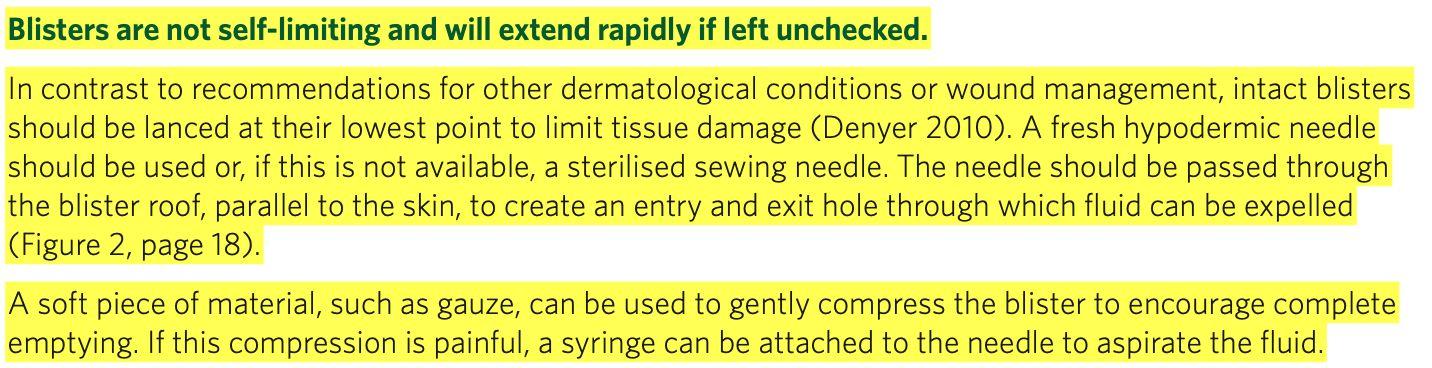
● Blisters
- Identify cause if possible, and remove source


- To pop or not to pop? De-roof or not?
- Secure the edge of the wound
- Manage as wound from now on
● Continue to bathe or not?
Wounds: Trips and Falls





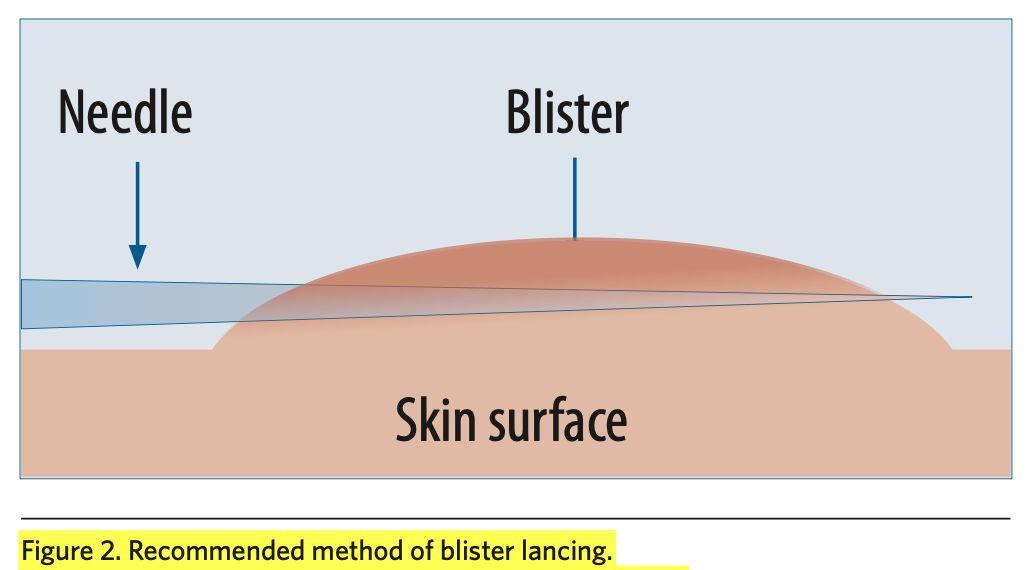
Blisters





Blisters
Denyer, J., et al. (2017) Best practice guidelines for skin and wound care in Epidermolysis bullosa: An International Consensus


Blisters and Heat Trauma





EI peculiarities





Bites and Allergies
● EI Skin tends to blister when experiencing: - A local allergic reaction to an insect bite; or - A systemic allergic reaction to food or medication.

● Blisters tend to be fluid-filled and in clusters and look different to the pus-filled ones you see with infections.
● Consider an allergic reaction if:
You see a cluster of small blisters in a specific location (After playing in the garden for example); or
-
You see a rash or extensive redness alongside extensive blistering (Within 1 -2 hours of eating or taking medication)
-

EI Skin and Allergies





EI Skin & Insect Bites





Allergy to Bites





Infections
● How to recognise a local infection
- Blisters with pus or yellow exudate that forms a crust
-
Local inflammation / redness / swelling / discomfort / itch
● How to recognise a systemic infection
- Starts from a local infection or sickness (Eg. Strep throat)

- Blisters appearing often and without obvious cause
- Blisters do not seem to heal / spreading quickly ● What to do
- Local: debride the wound, disinfect, treat infection topically
Systemic: Contact HCP, always try to swab first, treat infection, potential to change Antibiotics once swab results come back
-

Bacterial & Fungal Infection





Scalp care
● Recognising the problem
- Is it cradle cap or EI, or both?

● Different approaches to management
- Shampoos / oils / creams

- Leave to soak overnight, use a muslin cloth or cotton hat
● Products and tools to try
- P&S liquid / Dermaveen / Cocois / Treatments for psoriasis
- Silicon exfoliators / Lice comb / Rough towel rub
● Frequency of care and maintenance
- Period of consecutive days then weekly maintenance
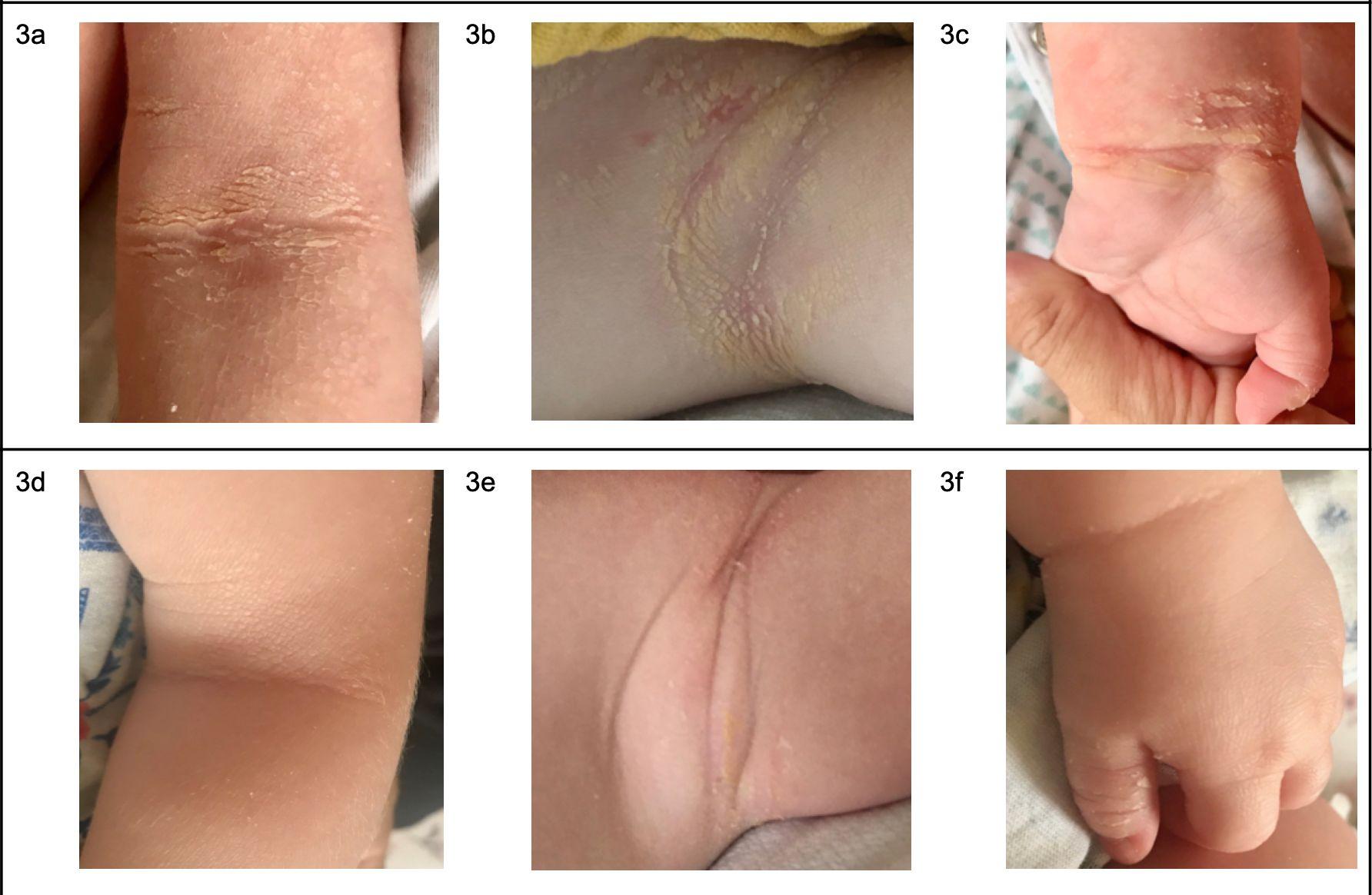
Plantar-Palmar Keratosis







Plantar-Palmar Keratosis
● Typically affects those with KRT1
- There are some with KRT10 who also have PPK
- Those with KRT9, only have PPK
● PPK has the potential to be very debilitating and affects development often
- Failure to meet usual developmental milestones (rolling over, crawling, walking)
- Difficulty with fine and gross motor control
- Pain and contractures can be problematic
● Often associated with additional care needs
-
Physiotherapy / Occupational therapy / Ergonomic support


Temperature Dysregulation
● Impaired skin barrier makes usual regulation of core temperature difficult

● Thick skin and barrier ointments block release of sweat
● Get too hot AND too cold much more quickly
● Signs of overheating - Patchy red face, scratching at neck and head, crying without obvious cause, sudden lethargy
● Signs of being too cold - Blue tinge to lips, shivering, crying without obvious cause

Temperature Dysregulation




Temperature Dysregulation








Dealing with comments
● Living with a visible difference typically invites many comments and stares from strangers
● Most people who make comments have good intentions but typically say things that can be upsetting
● Teach children to say something like: “Hello, my name is ____, do you want to learn about my skin?” to other children
● For adults who should know better than to stare, take the educational approach with something like: “My child has ichthyosis, it’s a skin condition they were born with. It’s not contagious. Do you have any questions?


Advocating for yourself
● EI is extremely rare (1 in 300,000), and this means you will often find that YOU become the expert

● Even very experienced dermatologists may have only seen 1 case of EI in their entire career, and misdiagnosis is still common
● This is even harder if you have to go to emergency care, where no one understands EI
● Use resources like this presentation to help show what is typical for EI and why you need help ●
If you are not getting the help you need, you have to be difficult and insist they reconsider, and/or seek out a second opinion
● The ISG can also help you to find an Ichthy-aware dermatologist

Travelling with EI
● It’s always best to plan ahead and be prepared
● Check luggage rules and rules for airport security such as restrictions on liquids (E.g. 100ml limit)
● Consider posting a box of supplies ahead of time

● Take a medical bag, which is a suitcase dedicated entirely to EI care supplies. Include: - Letter from dermatologist to confirm diagnosis, with description - Copy of prescription

● Explore options for bathing, including a portable bath/tub
● When camping, wild swimming is a fun bath solution!
Bathing while travelling




Life hacks
● Breakfast in the bath!
● Prepare/Cut dressings and bandages in bulk
● Use a kitchen degreaser in the bathroom
● Stand on something you can wash when applying moisturisers
● Keep a small EI first-aid kit with you on days out

● Coca-cola in the washing machine!
● Always take samples from pharma companies!
● Use bubble-wrap to teach about blister-care

Current topics of interest
● Recurrent infections
- Streptococcus particularly prevalent this year
- Seek help from specialist in infectious diseases
● Pain management
- Pain that is not directly caused by skin wounds
- Likely neuropathic pain, requires special care
- Seek help from specialist in pain management
● Autism and ADHD
- Many in our EI community are diagnosed

- Is there a genetic link, or is it induced by NICU trauma?
● Nutrition and the Gut / Skin biome

Academic References
- Suessmuth, K., Traupe, H., Metze, D., et al (2020) Ichthyosis in everyday practice: management of a rare group of diseases. J German Society of Dermatology: 225-243

- Mazereeuw-Hautier, J., Hernandez-Martin, A., O’Toole, E., (2018) Management of congenital ichthyosis: European guidelines of care - Part One. BJD
- Rout, D., Nair, A., Gupta, A., et al (2019) Epidermolytic hyperkeratosis: clinical update. Clinical, Cosmetic and Investigational Dermatology; 12: 333-344
- Foundation for Ichthyosis and Related Skin Types - FIRST (2022) Bathing and Exfoliation. Available at: https://www.firstskinfoundation.org/bathing-exfoliation

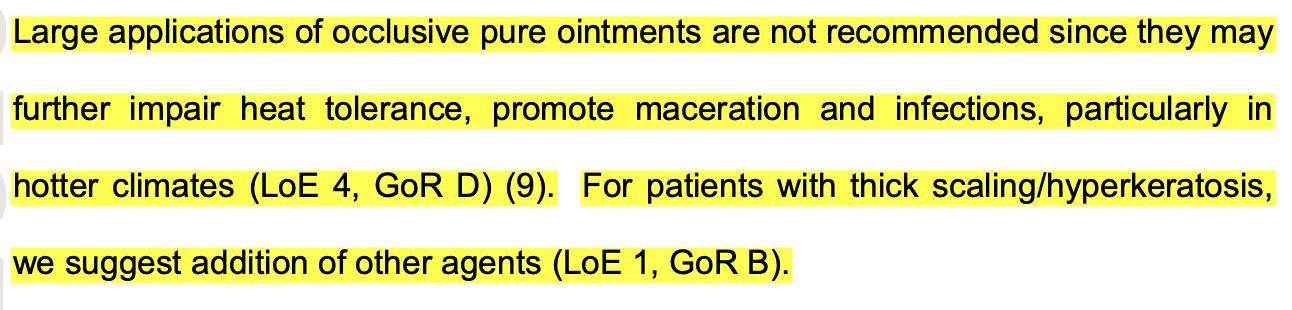
- Chamlin, S., Kao, J., Frieden, I., et al (2002) Ceramide-dominant barrier repair lipids alleviate childhood atopic dermatitis: changes in barrier function provide a sensitive indicator of disease activity. JAAD; 47 (2): 198-208
- Lill, H (2022) Ceramides Vs Ointments_Rationale for EI Skin. Available at: https://issuu.com/eicureproject/docs/ceramides_vs_ointments_in_epidermolytic_ichthyosis
- Sethi, A., Kaur, T., Malhotra, S., et al (2016) Moisturizers: The Slippery Road. Indian J Dermatol; 61 (3): 279-287
Academic References
- Kraft, N. and Lynde, C. (2005) Moisturizers: What they are and a practical approach to product selection. Skin Therapy Lett; 10: 1-8
- Ghadially, R., Halkier-Sorensen, L., and Elias, P. (1992) Effects of petrolatum on stratum corneum structure and function. J Am Acad Dermatol; 26 (3): 387-396
- Madan, R. and Levitt, J. (2014) A review of toxicity from topical salicylic acid preparations.
J Am Acad Dermatol; 70 (4):
- Oberoi, J. (2022) Types of Moisturisers: Humectants, Emollients, Occlusives. Available at:
https://lifepathdoc.com/moisturizer-a-complete-guide-from-types-to-layering/
- Pan, M., Heinecke, G., Bernardo, S., et al (2013) Urea: a comprehensive review of the clinical literature. Dermatology online journal; 19 (11)
- Cellano, L. (2018) Topical urea in skincare: A review. Dermatologic Therapy; 31: e12690
- Zaenglein, A., Levy, M., Stefanko, N., et al (2020) Consensus recommendations for the use of retinoids in ichthyosis and other disorders of cornification in children and adolescents.

Pediatric Dermatology; 00: 1-17




Thank you for coming! Contact Helen helenlill.eicureproject @gmail.com Contact Cat catlancashire.eicureproject @gmail.com