TEC
ADDRESSING TRAUMA ACHIEVING EQUITY ENGAGING COMMUNITY
COMPREHENSIVE PLAN 2023
 Jill Bowen, Ph.D. Commissioner
Jill Bowen, Ph.D. Commissioner



45 Acknowledgments
48 Appendix
A. P.A.C.E. TEC Crosswalk
B. Significant Incident Response Model
C. Prolonged Strategy Report
D. Focus Group Transcript: People Who Have Perpetrated Crimes
E. Childrens Behavioral Health and Prevention in Schools
F. ReCast Overview
G. Network of Neighbors Overview and Expansion
H. Philadelphia Alliance for Child Trauma Services Overview and Expansion
I. Philadelphia System of Care Overview
J. Community Mobile Crisis Team Overview and Expansion
K. Crisis Intervention Response Team Overview
L. BHTEN Trauma Trainings
M. Communications Strategy
N. Trauma Card Series
a. General
b. School-age Children
c. Gun Violence
d. Early Pre-K
O. Social Determinants of Health Equity Unit Logic Model
P. Systems Integration One Stop Shop Flyer
Q. Community Services and Resources Guide
R. Neurobiology of Trauma
S. Substance Use Early Intervention Services
TEC COMPREHENSIVE PLAN 2023 5 CONTENTS 7 Message from the Commissioner 9 Introduction 10 Population Health Approach 11 Behavioral Health Treatment Continuum 12 TEC and P.A.C.E. 12 TEC Vision 13 TEC Strategies 14 TEC Initiatives 16 ADDRESSING TRAUMA 16 Trauma Overview 17 Trauma in Philadelphia 17 Vision and Approach to Addressing Trauma 18 Trauma Challenges 18 Current Trauma Programming 21 Impacts of Trauma on Children 22 Services for Children and Families 23 Continuum of Child & Adolescent Services 24 Gap Analysis 26 Trauma Metrics 28 2022 Data Driven Efforts Shootings and Network of Neighbors responses 28 Significant Incident Response Model 32 External Stakeholder Learning Collaborative and Subcommittees 34 Proposed New and Innovative Programming 36 Achieving Equity 38 Engaging Community 40 TEC Workplan

MESSAGE FROM THE COMMISSIONER
In December 2020, I was honored to be selected as Commissioner of the Department of Behavioral Health and Intellectual disAbility Services for the City of Philadelphia. At that time, the world was still in the uncertainty of a global pandemic, there was national civil and political unrest, and locally we were grappling with how to provide behavioral health services to the city’s most vulnerable citizens where health disparities were that much more apparent.
In addition, Philadelphia is the sixth largest city in the nation, has one of the highest poverty rates, and experiences violence that devastates families and communities. Philadelphia is challenged with a substance use crisis that results in those with substance use disorder as well as people living in highly impacted communities witnessing the ravages of the opioid epidemic every day.
Considering these tremendous challenges, I wanted to make meaningful, systemic, and lasting changes during my tenure as Commissioner and beyond. I wanted to focus the Department on what I saw as challenges nationally and locally, and I wanted to do so in a way that addressed root causes of issues that the behavioral health system could seek to address. Most importantly, I wanted to include the voices and perspectives of those who often go unheard and who often struggle through systems to find the supports and services they need.
Committed to these tenets, I have created and guided DBHIDS through our priority lens TEC, which stands for Trauma, Equity and Community. Through this lens, we are committed to transforming our system to reduce trauma, ensure equity in our service delivery, and engage communities to inform all aspects of our work.
This plan outlines the incredible work that has been in place before I took the helm and exciting, impactful, new work that has been developed and/or expanded during my tenure thus far. This plan shows how our work fits together as we seek to be a system that is nimble, flexible, and responsive to the needs of individuals and communities, as those needs emerge. Most importantly, this plan is about improving the quality of life and wellness for individuals and communities across Philadelphia. I invite you to read this plan and affirm your organization’s or community’s role in advancing this work. It is because of the engagement and commitment of you and so many others, that Philadelphia is a leader in behavioral health services nationally.
We know the challenges we face were not created overnight. We know we need immediate and long-term strategies that help those struggling today, and strategies to transform systems to perform better tomorrow. Today, I am asking for your commitment in continuing forward with DBHIDS for the entire journey: to address Trauma, achieve Equity, and engage Communities so all Philadelphians can thrive.
Best,
Commissioner, City of Philadelphia Department of Behavioral Health and Intellectual disAbility Services

TEC COMPREHENSIVE PLAN 2023 7

INTRODUCTION
The City of Philadelphia Department of Behavioral Health and Intellectual disAbility Services (DBHIDS) is proud to offer behavioral health care, intellectual disability supports, and early intervention services in one comprehensive integrated system.
The mission of DBHIDS is to educate, strengthen, and serve individuals and communities so that all Philadelphians can thrive.
We envision a Philadelphia where every individual can achieve health, well-being, and self-determination.
Our services are offered through a network of provider agencies. We also collaborate with the Philadelphia School District, the child welfare and judicial systems, and other stakeholders. It is through our many partnerships that we can serve Philadelphians who need our help and support.
DBHIDS serves all Philadelphians as evidenced by our longstanding commitment to recovery, resilience, and self-determination. Traditionally, we have prioritized services to individuals who are experiencing a mental health or substance use-related condition or intellectual disability to improve their outcomes.
While that focus remains, today, we are also intensively aware of the needs facing all in the community –those in need of behavioral health treatment and those who strive for behavioral wellness. We take an active role in promoting the health and wellness of all Philadelphians through our population health approach and through our priority lens TEC by addressing Trauma, achieving Equity, and engaging Community.
This report provides an overview of DBHIDS’ TEC programs and strategies that are operating and those we plan to implement over the next one to three years. Our strategies include immediate actions that will address pressing issues as well as longer-term strategies to address trauma, achieve equity, and engage community as we seek to transform our system.
TEC COMPREHENSIVE PLAN 2023 9
POPULATION HEALTH APPROACH
Philadelphia has a population of 1.57 million people, of which 750,000 are Medicaid eligible. By applying a population health approach, DBHIDS is seeking to improve the health of all Philadelphians, including the approximately183,000 individuals we serve annually.
Our approach includes
1. Working upstream (earlier intervention)
2. Broad set of strategies
3. Working with at-risk and healthy populations
4. Delivering health promotion interventions
5. Working in non-treatment settings
6. Health activation approaches empowering others
7. Working at the community level
8. Wellness for all
9. Addressing the Social Determinants of Health (SDOH)
10. Developing innovative community partnerships
Through Medicaid and County dollars, we can provide support to low income, under-insured and uninsured residents. People are able to access DBHIDS services in a variety of ways, which is reflects our outreach and engagement efforts as well as lessons learned from communities and stakeholders. The “front-doors” of our system include:
1. 988/ Philadelphia Crisis Line
2. WarmLine (Operated by people with lived experience and clergy)
3. Community Behavioral Health Member Services
4. Network of Neighbors
5. Crisis Response Centers
6. EPIC – Ask for it by name
7. Community Outreach Events
8. In-Community Behavioral Health Screening Events
9. Boost Your Mood
10. Provider Network
11. Health Minds Philly
12. Outreach and Engagement Teams
13. Schools
14. Mental Health First Aid
15. Targeted Engagement (Engaging Males Of Color and Immigrant Refugee Wellness Academy)
16. Intellectual disAbility Services
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 10
TEC COMPREHENSIVE PLAN 2023 11 BEHAVIORAL HEALTH TREATMENT CONTINUUM Harm Reduction (Outreach & Engagement) 1 Community Settings (Treatment, Prevention, & Neighborhoods) 2 Inpatient Treatment 3 CBH MEMBER SERVICES 24/7 365 DAYS/YEAR HOTLINE: 1-888-545-2600 INDIVIDUALS CAN CONTACT OR GO TO ANY LICENSED TREATMENT PROVIDER TO GAIN SYSTEM ENTRY. FQHCS - Federally Qualified Health Center STEP - Suppot Team for Education partnerships
TEC AND P.A.C.E.
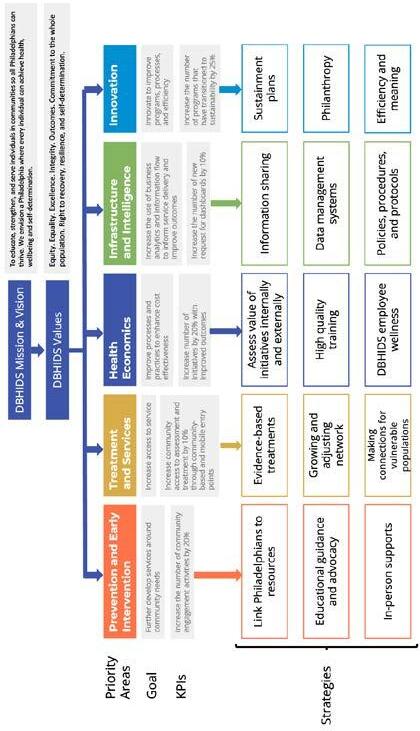
The TEC lens layers on top of the DBHIDS Strategic Plan P.A.C.E. (Prioritizing to Address a Changing Environment). The P.A.C.E Framework has five priority areas along with corresponding goals and key performance indicators that include (see appendix 1):
1. Prevention and Early Intervention – further develop services around community needs.
2. Treatment and Services – increase access to services
3. Health Economics – improve processes and practices to enhance cost effectiveness
4. Infrastructure and Intelligence – increase the use of business analytics and information flow to inform service delivery and improve outcomes
5. Innovation – innovate to improve programs, processes, and efficiency.
TEC VISION
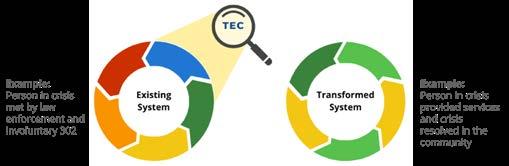
Below outlines the TEC lens. DBHIDS seeks to transform existing systems by shifting processes and practices based on the following lens:
1. Addressing Trauma means creating a system that is trauma-responsive, trauma-informed, and trauma-mitigating. DBHIDS recognizes institutional trauma as a type of systemic trauma that can result from institutional action and inaction. With TEC, DBHIDS is addressing various types of traumas, including institutional harm, by creating programs that aim to ameliorate the risk of institutional wrongdoing.
Charge:
a. Reduce traumatic experiences in the system
b. Change processes to be trauma responsive and trauma mitigating
c. Shift systems to be trauma reducing
2. Achieving Equity requires DBHIDS to intentionally identify and address institutional and structural racism, transform systems to reduce behavioral health disparities, and promote racial equity for Black, Indigenous, and People of Color (BIPOC). The DBHIDS Diversity, Equity, and Inclusion (DEI) unit is constantly working to inform programs and processes to promote equity within the Department and externally.
Charge:
a. Identify and change processes that create disparities
b. Review/evolve hiring, contracting, and community engagement processes and practices to reduce disparities.
3. Engaging Community encourages DBHIDS to connect individuals to community-based services and integrate community wisdom into program development and operations. DBHIDS recognizes the importance and effectiveness of fully integrating programs into the community and is working actively to shift its programs in this direction as much as possible. DBHIDS also wants communities to have a voice in program development as a way of ensuring successful implementation of communitybased programs.
Charge:
1. Shift Services from institutions to community settings
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 12
System Transformation
Using a TEC lens to shift system responses that add a layer of trauma to those that mitigate against trauma by shifting processes and practices
TEC STRATEGIES
Our TEC vision is implemented through a range of strategies, supporting the vision. The strategies have evolved over time, to be responsive to needs as they have emerged. The strategies include:
1. Addressing Trauma – Blanketing the city Trauma Supports
a. Individual Interventions
b. Community-based Interventions
c. Website Resources
d. Trainings
e. Communications strategies (hard copy materials, radio, TV, film, social media, podcasts)
f. Hospital-based Programs
g. Stakeholder Committees to develop and support trauma strategies
h. Implementation of the trauma stakeholder committee workplan
i. Trained Community Responders to respond to traumatic incidents in their communities
2. Achieving Equity – Reduce Disparities and Promote Racial Equity
a. Conscientious Contracting
b. Data Driven programming
c. Scaling/expansion of programs to ensure services are available to every community
d. Monitoring tools that track data points that identify and address disparities
e. *Include language below on DEI
3. Engaging Communities – Increase Community-based Programming and Input
a. TEC Talks and Community Conversations
b. DBHIDS Conferences - TEC Conference, Faith and Spiritual Affairs Conference
TEC COMPREHENSIVE PLAN 2023 13
c. TEC Tour
d. Providing resources at community events
e. Public facing websites – DBHIDS.org, CBHPhilly.org and Healthy Minds Philly
f. Committees that include community-based organizations and community members

g. Developing more community-based programs
The Big Picture
TEC INITIATIVES
Below are a few of the programs that illustrate the types of initiatives under each category for context. A listing of all the programs across the department organized by TEC category can be found in the PACE/TEC Crosswalk.
1. Addressing Trauma – Blanketing the city with Trauma supports (more than 40 programs). The programs highlighted in “Blanketing the City with Trauma Supports” are built on the importance of community connectedness and shifts access to services and resources to meet people where they are - in their communities. These programs help to connect individuals and communities to the vast array of services provided by DBHIDS, as well as connecting people further to the providers within the behavioral health and intellectual disability networks.
a. Network of Neighbors (expanded in 2022)
b. Engaging Males of Color – Trigger Film (2022)
c. Community Wellness and Engagement Unit
d. ReCAST (launched in 2022)
e. Faith and Spiritual Affairs
f. Healing Hurt People
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 14
g. Behavioral Health Crisis System transformation and launch 988 (2022)
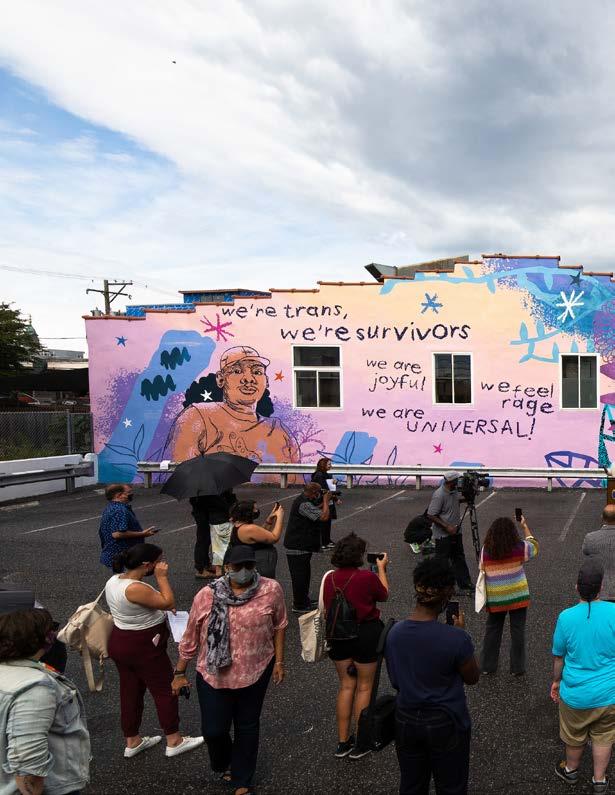
h. Porch Light Initiative/Mural Arts
i. Trauma External Stakeholder Learning Collaborative (launched in 2022)
2. Achieving Equity – Reduce disparities and promote racial equity (more than 30 programs)
a. Social Determinants of Health Equity Unit (launched in 2022)
b. Forensic Equity Unit (launched in 2023)
c. Mobile Outreach and Response Services expansion
d. Mobile Methadone Maintenance Treatment (2023)
e. Peer Institute
f. Alternatives to Detention
g. Stepping Up Initiative
h. Forensic Support Team
i. Immigrant and Refugee Wellness Academy (launched 2022)
j. START (launched in 2022)
3. Engaging Community (more than 20+ programs)
a. TEC Talks (launched in 2021)
b. TEC Talk Community Conversations (launched in 2022)
c. TEC Conference (held in 2023)
d. TEC Tour (scheduled for 2023)
e. TEC Podcasts (scheduled for 2023)
f. Faith and Spiritual Affairs Conference (held in 2023)
g. NAMI Faith WarmLine
h. Community Affairs Unit – Community Wellness and Engagement
i. Peer Culture Transformation Advisory Board
j. Philadelphia Systems of Care communities
k. Healthy Minds Philly
l. Family Member Committee
m. Youth Move Philadelphia
n. Suicide Prevention Task Force
TEC COMPREHENSIVE PLAN 2023 15
Healing Occurs in the Community: Blanketing the City with Trauma Supports
DBHIDS is committed to bringing services to individuals and communities across the City. The services listed below show the shift in service delivery from provider and clinical settings to include community spaces that meet people where they are. These models demonstrate the need for a variety of engagement approaches to make services available to all Philadelphians.
Network of Neighbors Expansion
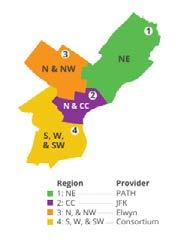
Regional Team Model Expansion of the Network of Neighbors staff will include four teams working across four regions of the city, along with administrative staff to support the overall operations of the program
Engaging Males of Color Initiative
2021 EMOC focused on the traumatic of impact social justice issues on males of Color
Community Wellness Engagement Unit
Designed to provide greater access to Behavioral Health support, guidance, and linkages to care on a community level
• Peer Culture and Community Inclusion – those with lived experiences engaging the peer community and the integration of those with lived experience across the continuum
Mural Arts
Themed Murals: Trauma and Healing
External Stakeholder Group
To leverage services, resources, expertise, and wisdom from key community-based organizations, providers, people with lived experience, academicians, stakeholders from all corners of the community
Faith and Spiritual Affairs
Trauma and healing from a faith-based perspective
ADDRESSING TRAUMA
TRAUMA OVERVIEW
Trauma is an emotional experience to a terrible event or series of events that could have occurred once or multiple times over an extended period. Trauma poses a significant threat to the overall health and wellbeing of individuals, families, and communities. First responders, health care workers, and counselors are also at risk and may experience vicarious trauma in their efforts to provide supports.
We know that people who experience traumatic events have an increased risk of developing a range of chronic physical and behavioral health concerns, and children are particularly vulnerable. Trauma can impact anyone, regardless of socio-economic status. However, many people in poverty routinely witness violence in their communities and experience various forms of discrimination that exert a toll on their health.
To address trauma, DBHIDS administers programming, maintains and develops partnerships, and implements evidence-based practices and innovative approaches to address the effects of trauma in the City of Philadelphia.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 16
TRAUMA IN PHILADELPHIA
Philadelphia has the third highest poverty rate in the U.S. at 23 percent. This is down from 25 percent in recent years, but unfortunately has continued to sustain at 37.3 percent poverty rate for children. Poverty in and of itself is traumatic. We know that food insecurity, housing insecurity, and lack of basic needs, also referred to as the Social Determinants of Health, impacts one’s health and life expectancy (Healthy People 2030).
Adverse childhood experiences (ACEs) are potentially traumatic events that occur in childhood. ACEs can include violence, abuse, and growing up in a family with mental health or substance use problems. ACEs are linked to chronic health problems, mental illness, and substance misuse in adulthood. Previous studies on ACE’s in Philadelphia have shown that half of Philadelphia’s zip codes have more than 30 percent of children experiencing 4+ ACE scores.
The prevalence of gun violence has been devastating for individuals, families, and communities across Philadelphia, particularly for Black men. As of April 2023, there have been 134 homicides in Philadelphia due to gun violence. While that number is down 14 percent from 2022, it is still 134 lives, families, and communities impacted. Of those killings, 94 percent were Black men. Chronic exposure to gun violence is traumatic, and there is a relationship between trauma exposure and negative mental health experiences. Higher rates of community violence are concentrated in areas impacted by long-term systemic racism and disinvestment, which disproportionately impacts low-income communities of color. Strategies addressing the confluence of chronic exposure to gun violence, community violence, poverty, and trauma are needed. We believe that by increasing community and trauma supports for “at-risk” individuals through prevention, intervention, and postvention in support of a wholistic, citywide effort, we can disrupt the cycle of gun violence. Below shows the total shooting victims and shooting fatalities from 2015-2022.
With these grim statistics, we have engaged stakeholders and examined our existing programming to discuss how DBHIDS can increase and target trauma resources and supports for prevention, intervention, and postvention programming to reduce the negative outcomes of trauma in highly impacted communities.
VISION AND APPROACH TO ADDRESSING TRAUMA
Our vision is to ensure that there is an accessible continuum of services that addresses the various types and stages of trauma for all Philadelphians. DBHIDS will accomplish this through a diverse and effective network of supports programs that address the variety of challenges communities face regarding social economic status, race, or gender.
The framework for this approach features the following steps:
1. Understand existing and needed resources, utilize best practices, and make data-driven decisions.
2. Deepen our work with stakeholders to ensure equitable access to resources and to bring solutions from and sustain solutions in communities.
3. Recognize the impact of traumas associated with many factors including isolation, violence, racism, substance use, the pandemic, etc.
4. Recognize the resources – in-school prevention, supports and treatment, evidence-based models in the continuum, community outreach, support, and engagement.
TEC COMPREHENSIVE PLAN 2023 17
Year 2015 2016 2017 2018 2019 2020 2021 2022 Total Shooting Victims 1,294 1,340 1,263 1,449 1,473 2,259 2,337 2,263 Shooting Fatalities 233 262 259 301 311 448 506 474
5. Enact a comprehensive strategy to support people and communities across the city experiencing a variety of traumatic events or circumstances. Within this, the Department has created a landscape review, gaps analysis, communications plan, and stakeholder committees to address specific areas of trauma.
TRAUMA CHALLENGES
To approach addressing the varying traumas people experience, we created categories to frame our thinking and to begin to identify what services already exist in our system and services that need to be developed. Below includes some of the main categories of trauma identified by our workgroups. Many are related to the COVID-19 pandemic and others are persistent over time. They include:
1. Disruption to behavioral health and physical health services due to the pandemic
2. Pandemic relate illness, death, and isolation
3. Pandemic related emotional and physical disturbance
4. Prolonged and complex trauma
5. Systemic, generational, and direct experiences of racism
6. Political and social unrest
7. Personal and community experiences of violence
8. Poverty: housing, economic, and food insecurity
CURRENT TRAUMA PROGRAMMING
DBHIDS funds programs serving adults and youth across five main categories: individuals, communities, website/media, trainings and hospital-based programs. Highlighted below are some of our most visible programs. A full listing of all of the trauma programs can be found in the P.A.C.E. and TEC crosswalk and on public facing web page dbhids.org/trauma which list all of the department’s resources available to the general public.
1. Individual-level Interventions
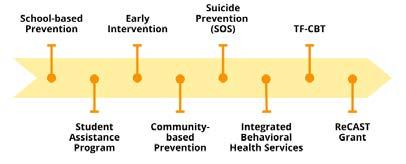
a. Trauma-focused Cognitive Behavioral Therapy (serves youth) - designed to help children, adolescents and their parents to overcome the negative effects of traumatic life events.
b. Prolonged Exposure Therapy (serves adults) - aims to reduce post-traumatic stress (PTSD) symptoms by helping individuals approach traumatic related thoughts feelings and situations that had previously been avoided.
c. Intensive Behavioral Health Services (serves youth) - wrap around services for children in their homes, schools and communities
d. Philadelphia Crisis Line – 988 (serves all) - 24/7 crisis line to assist people and their families with behavioral health crisis.
e. Crisis Intervention Response Teams (serves adults) - Co-responder model with the Philadelphia Police Department to respond to behavioral health crisis related calls
f. Community Mobile Crisis Response Team (serves all) - 24/7 regional response teams that engage, screen, assess, and provide resolution focused crisis interventions.
g. Mobile Outreach and Recovery Services (serves adults) - serves individuals seeking treatment for behavioral health services in communities deemed high risk for substance misuse and overdose.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 18
h. Student Assistance Program (serves youth) - behavioral health assessment available in all public, parochial and charter schools to ensure students behavioral health needs that may impact their school performance are addressed
i. Signs of Suicide Intervention and Prevention (serves youth) - educates youth on signs related to suicide.
j. COPE2Thrive offers three Cognitive Behavioral Therapy-based (CBT) programs designed to help children, teens, young adults, and adults dealing with anxiety, stress and depression by teaching them how to develop the skills needed to stop negative thoughts and start thinking and behaving in more positive ways. COPE2Thrive offers nonclinical approaches to help shift the youth’s mindset to reduce or minimize the probability of them using drugs or alcohol to cope with trauma or violence they encounter daily.
k. Behavioral Health and Intellectual disAbility Trauma Screener (serves all)– screens disable individuals for trauma
l. Crisis Response Centers (serves all) - operates 24/7 on emergency basis for screenings and placement/linkage to appropriate levels of care and services
m. Urgent Care – PATH UCC for children (serves children) - serves youth experiencing behavioral health challenges
n. Social Drivers of Health Programming (serves all) – mitigates the trauma of poverty by providing food, transportation, technology, employment, housing
2. Community-level Interventions
a. Network of Neighbors (serves youth 9+ adults) - provides trauma supports to any community across the city that has experienced a traumatic event. Communities can be defined by, but not limited to geography, schools, churches, places of work, etc.
b. Porch Light/Mural Arts (serves all) initiative that creates public murals that seek to transform neighborhoods and promote the health of neighborhood residents and individuals who help create the mural.
c. Engaging Males of Color (serves all) - organizes events to engage men and boys of color in dialogs designed to address the impact of trauma, health, economic, and educational disparities.
d. Diversity Equity and Inclusion Healing Spaces (serves all) - safe, supportive spaces for discussions to help people process traumatic events with others.
e. Peer Culture and Community Inclusion (serves adults) - supports efforts to engage people with lived experience of mental health challenges and/or substance use disorder.
f. Community Wellness Engagement Unit (serves adults) - regionalized teams that provide services across the city to community members by linking them with community resources and supports addressing behavioral health wellness and trauma.
g. Behavioral Health and Intellectual disAbility Planning Initiative (serves adults) - an integrated system of care for individuals with co-occurring mental health disorders and intellectual disabilities which includes implementation of the START model (START Model is a communitybased crisis intervention for individuals with intellectual and developmental disabilities and mental health needs. The model is evidence informed, person-centered, solutions-focused approach that employs positive psychology and other evidence-based practices. START Stands for Systemic, Therapeutic, Assessment, Resources, and Treatment)
TEC COMPREHENSIVE PLAN 2023 19
h. Philadelphia System of Care (serves youth) - resource network for youth and their families to access behavioral health support and trauma related services to support youth experiencing significant emotional and behavioral health challenges impacting them in their school, home and communities.
i. Resilience in Communities after Street Trauma Grant- ReCAST (serves youth and young adults)addresses the impact of stress and trauma on youth/young adults and their families caused by community violence, particularly gun violence, by linking them to trauma-informed services and supports, and to reduce violence by and against youth/young adults by implementing evidencebased prevention programs and supporting positive youth and family programming in six specific neighborhoods using a collaborative community and city participatory process
3. Systems Connectors
a. Website/Media
i. Film- Invisible Opioids (serves adults) - film educating the community on what opioids are and dispelling misconceptions in the black community.
ii. Film – TRIGGER (serves adults) - film about gun violence in Philadelphia from multiple perspectives including the shooters, victims, and their families, and more broadly, about healing from trauma.
iii. MindPHLtogether.com (serves all) - collaboration between the City and Blue Cross Blue shield to improve mental health.
iv. Boost Your Mood (serves all) - campaign to acknowledge stress caused by the pandemic, violence and racism that all cause trauma.
v. Health Minds Philly (serves all) - offers wellness tools designed to support mental health and well-being for all Philadelphians regardless of insurance or income.
vi. Behavioral Health Screenings (serves all) - Online and in-person screenings to learn whether a person may be experiencing symptoms of a mental health disorder.
b. Trainings and Conferences
i. Trauma Awareness Trainings (serves adults) - training for providers that discuss various types of traumas and supports providers with implementing trauma informed practices
ii. BHTEN Trauma Training Series (serves adults) - trainings for providers, addressing trauma that include the trauma resilience series ranging from interventions, to secondary traumatic stress, psychological first aid and understanding racial, social, and intergenerational trauma.
iii. ReCast Provider Trainings (serves youth and adult) - expands culturally competent, trauma informed behavioral health practices in schools and community youth programs through training in evidence-based practices designed, such as PLAAY (Preventing Long Term Anger and Aggression in Youth)
iv. Mental Health First Aid (serves youth 16+, adults) - eight-hour course that teaches skills needed to identify, understand, and respond to signs of behavioral health challenges or crisis.
v. Crisis Intervention Trainings (serves all) - coordinated effort between the Philadelphia Police Department and DBHIDS to promote empathy and understanding while increasing effective communication with community members when they are in very vulnerable situations.
vi. Faith-based and Spiritual Affairs Conference (serves all) –is hosted annually and on April 28, the theme was “Healing from the Hurt with Trauma Informed Care.” Attended by faith leaders,
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 20
providers, community-based organizations, and members from across the city to learn about resources and tools available to address trauma.
vii. Addressing Trauma, Achieving Equity, Engaging Community Conference (serves all) - held on March 24, the theme was “Trauma, Equity and Community in the City of Brotherly Love and Sisterly Affection.” Attended in-person and virtually by 400-plus people including providers, community-based organizations, and member to learn about the city’s trauma supports that “blanket the city,” the importance of BIPOC therapists and culturally competent care, addressing trauma experienced by people with intellectual disabilities, secondary traumatic stress, and additional topics.
c. Hospital-based Programs
i. Cure Violence Philadelphia (serves all) - violence intervention program utilizing a Chicago-based public health model focusing efforts to stop shootings and murders in North Philadelphia.
ii. Healing Hurt People (serves all) - trauma-informed, hospital-based violence intervention program that offers case management and linkages to referrals for people who have been victims of violence.
iii. Warm Hand Off Program - program operating in area hospitals and emergency department, utilizing peers to connect people to treatment services upon discharge.
IMPACTS OF TRAUMA ON CHILDREN
We know people who experience traumatic events have an increased risk of developing a range of behavioral health concerns, and children are particularly vulnerable. Child traumatic stress occurs when children and adolescents are exposed to traumatic events or situations (school or neighborhood violence; domestic violence; physical abuse; sexual abuse; neglect; serious accidents; sudden or violent death of a loved one, natural disasters, terrorists’ attacks, and war).
Traumatic experiences suffered in childhood can alter the production of neurotransmitters and hormones, which can lead to mood disorders, inability to regulate stress, and an overactive sympathetic nervous system. Symptoms of trauma in children include nightmares and trouble sleeping; avoidance of thoughts, feelings, reminders of the trauma; bed-wetting; attention problems; anger, irritability, temper tantrums, and aggressive behavior; flashbacks and intrusive thoughts of the traumatic event; withdrawal, dissociation (feeling of detachment), and numbness; sadness; loss of trust in others; increased risk-taking behaviors; and poor school performance.
We have also seen more acute presentations of mental illness in children due to the social isolation from the pandemic causing limited access to services. Our goal is to continue and increase resources that children need through our continuum of care.
The diagram below lists services for children and families including individual and community-based interventions.
TEC COMPREHENSIVE PLAN 2023 21
SERVICES FOR CHILDREN AND FAMILIES
Below are services for children ages K-12, beginning with prevention services, through individual and community-based interventions
Included in the below diagram is a mapping of the Continuum of Child and Adolescent services for children from infancy, through young adulthood and ranging from prevention to acute services.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 22
CONTINUUM OF CHILD & ADOLESCENT SERVICES
Adolescence
Young Adult (18-21st birthday)
Prevention
Community Treatment Supports
Natural and Community Based Supports, Prevention programs via DHS/DBH/OVR/OAS/IDS/Courts/School District
Case Management (BCM, COC)
HiFi Wrap Assessment
Crisis Assessment
Outpatient Assessment Access Centers
Provider Based Assessments (Psychiatric, Psychological, Master’s Level, FBA/skills)
Children’s Mobile Crisis Teams (CMCT)
Crisis Intervention
Community Based Child and Family Treatment Services
Alcohol and Other Drug Treatment
Residential Services
Acute Services
Crisis Mobile Intervention Service (CMIS)
Crisis Stabilization Units
Outpatient Treatment (Individual, Family, Group)
Intensive Behavioral Health Services (IBHS)- Individual and Group Services (BC, MT, BHT, Group MT, CTSS)
IBHS Applied Behavior Analysis (ABA)
Early Childhood Treatment Program
Long Term Partial Family Services (FBS, FFT, MST-PSB, PHIICAPS)
Outpatient
Intensive Outpatient Treatment
Short and Long Term Residential
Community Residential Rehabilitation- Host Home Psychiatric Residential Treatment Facility
Adult Residential Treatment Facility
Acute Partial Hospital
Acute Inpatient Hospital
TEC COMPREHENSIVE PLAN 2023 23
Early
Infancy Early Childhood Childhood
Adolescence
GAP ANALYSIS
DBHIDS conducted a gaps analysis and received feedback from DBHIDS staff and the Prolonged Trauma and Children and Families Trauma subcommittees to identify some of the areas of opportunity to increase services and/or resources in our current system. Some of the topic areas that guided our discussion included:
1. Geographic distribution of services
2. Equitable access to services based on population, including: age, race, gender, immigrant and refugee status, intellectual disability, etc.
3. Community-level engagement and inclusion program input and feedback
4. Quality and quantity of services along the continuum: prevention, early intervention, treatment, postvention, policy
5. Diversity of community partners engaged in our work
6. Zip codes not served vs. not served proportionate to needs
Below are some of the gaps identified and recommendations that were proposed:
General Recommendations
1. Trauma-informed approaches need to be developed to serve the intellectual and/or developmental disabilities (IDD) population more effectively. The system needs training and education for staff to ensure staff are able to communicate and serve people with ID and, in particular, non-verbal individuals
2. There should be a due diligence checklist to ensure all special populations are considered when creating new programs/services. Ensure all programs are accessible and available, as applicable to:
a. LGBTQIA+
b. Veterans
c. Seniors
d. People with physical disabilities
e. Reentering
f. Immigrant populations
g. Incarcerated individuals
h. Children in child welfare or out-of-home placement.
3. City partnerships could be further enhanced to promote health equity and justice related to trauma. Partner with PDPH on campaigns to educate the public about trauma and the impacts on health. Leverage health systems through collaboratives such as COACH reach deeper into communities to promote available services to address trauma.
4. There are not enough BIPOC and/or culturally competent providers, providing trauma services to BIPOC communities. Connect with BIPOC providers to better serve BIPOC communities. Connect with community-based organizations such as HIAS Pennsylvania and the Nationalities Services Center to better serve immigrant and refugee communities.
5. There is a significant shortage of trauma specialists, trained clinicians, and general behavioral workforce staff. This is causing tremendous strain on the existing systems, decreasing capacity of
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 24
programs and increasing burnout of existing staff. Need to address behavioral health workforce staffing challenges.
6. DBHIDS should consider using Philly ACEs scores as one of the metrics to locate programming.
a. Ensure all zip codes with children who have an average of 4+ ACES, have access to all our main resources.
b. Create a community resource asset map to assist in locating services in areas with high needs.
c. Build protective factors and resiliency resources in zip codes with high ACE
7. Secondary trauma support is needed for supervisors who are working with and supporting front line clinicians. Create programming that is regularly made available to support staff
8. Some effective trauma programs and intervention are not considered treatment – and therefore are not billable – but should be funded as a part of the trauma services continuum. Set aside funding for trauma interventions that are not Medicaid billable.
9. There is no chat feature or interactive feature on the DBHIDS website. A chat feature or chatbot would be helpful in navigating the site’s services.
10. The public as well as providers are not clear on all the trauma resources available through DBHIDS. Host annual conferences for providers to understand how to access all DBHIDS services including how to refer to trauma resources.
11. Include a link to DBHIDS trauma resource and 988 on all phila.gov pages
Program-specific Gaps and Recommendations
1. Trauma Focused Cognitive Behavioral Therapy - expand to unserved areas, i.e. West Philadelphia. Explore use in addressing racial trauma and cultural competence.
2. Youth Mental Health First Aid – expand training in schools and Out of School Time programs
3. Boost Your Mood- help with navigation. Find additional ways to distribute this resource for people that do not have internet access
4. Behavioral Health screenings - not accessible at all literacy levels. Adapt the screening to be more accessible.
5. Need trauma resources for early childhood care providers for children ages five and younger. Need for immediate response to daycare and pre-k programs in events where young child or class is exposed to or experiences a traumatic event.
6. Need trauma training for children’s mobile crisis teams.
7. Expand language access to include all refugee populations
8. Need early intervention screening: bridging the gaps between non-early intervention substance abuse programs or PACTS providers and OAS services
9. Early Intervention or Substance Abuse Services-providers need access to trauma training
10. Need to work with The Philadelphia Department of Human Services to better address trauma experienced when a child is removed from their home.
TEC COMPREHENSIVE PLAN 2023 25
Additional Feedback from the Gaps Analysis Discussions
1. The system needs to clearly define the word “equity” so a shared understanding is used to evaluate how services are distributed, managed, awarded, and accessed.
2. There needs to be a real conversation about those that have privilege/power and making room for people that do not have privilege/power to have a voice in creating and implementing services.
3. Include community members and community driven data in program design/development
4. Understand why some programs do well “on paper,” but are not programs that are “trusted” by the people that they serve. Understand if this is only an issue of cultural competency or other factors. Need additional or alternate evaluations to identify this challenge.
5. Larger and well-resourced organizations are better positioned to obtain additional funding. Smaller organizations that may be very effective may not have funding for evaluation and research and this decreases their potential to increase their capacity. Technical assistance and support should be provided to increase equity in awarding contracts to smaller organizations.
6. Ensure programs have trauma-reducing policies. Ensure that programs don’t “exit” people from programming with harsh disciplinary policies but instead are designed to keep people included and set up for success.
7. Fund programs that seek to “interrupt” the cycles of violence and serve the whole family, such as interrupting the school-to-prison pipeline. Serve the whole family and teach the family how to advocate for their family members and themselves.
8. Peer voices should always be included at the development level of any program.
9. Address survivorship bias. We can’t just look at people who’ve been successful in programs. We need to also look at people who weren’t successful and what about those programs/policies that did not work.
10. Understand how different systems work with each other to see the intersections that can or currently cause trauma. Overly stressed and siloed systems hide issues and practices that may cause trauma. Need to focus more on institutional coordination.
11. There is a bridge between academia and practice of about 10-14 years. We need to figure out how to more quickly apply research to practice.
12. Institute modular approaches to therapy interventions for faster results, i.e., MATCH-ADTC – Modular Approach to Therapy for Children with Anxiety, Depression, Trauma or Conduct problems.
TRAUMA METRICS
Metrics are tracked on every trauma initiative. These metrics vary based on the program with regard to number of people served, number of community events, program type, etc. In addition to tracking outputs, DBHIDS seeks to track outcomes, demonstrating the effectiveness of each of the programs administered, as well as track trends over time and overlay public data sources to increase our ability to make data driven decisions.
The current data we collect on each program as applicable includes:
1. Number of people served
2. Number of events/sessions/trainings/responses
3. Number of events per zip code
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 26
4. Number of participants served per zip code
5. Number of website visits
6. Annual program cost/costs per participant and trends month over month/year over year
7. Utilization rates
8. Recidivism rates
9. Zip codes NOT served
10. Where people live that are receiving a particular service/where people are receiving services
We are currently able to overlay our program data with following public data sources:
1. Police data – shooting, homicides, arrests
2. Percent of people living in poverty in each zip code
3. Percent of Medicaid eligible individuals per zip code
4. Percent of suicides
5. Hunger rate per zip code
6. Literacy rate per zip code
7. Overdose deaths
8. Hospital sites
9. Health centers
10. Crisis Response Centers
11. Schools
TEC COMPREHENSIVE PLAN 2023 27
2022 DATA DRIVEN EFFORTS SHOOTINGS AND NETWORK OF NEIGHBORS RESPONSES
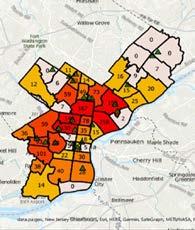
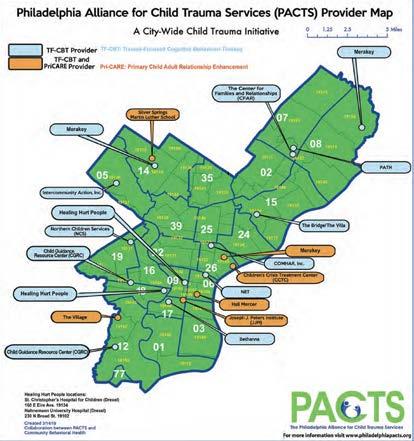
Below is an example of a data overlay that we are using to understand how our presence corresponds with activities in communities. Below shows Network of Neighbors responses in green triangles, per zip code, overlaid with the number of shootings per zip code, which are color coded and numbered. This type of data will help to inform our strategies around resources needed and deployed.
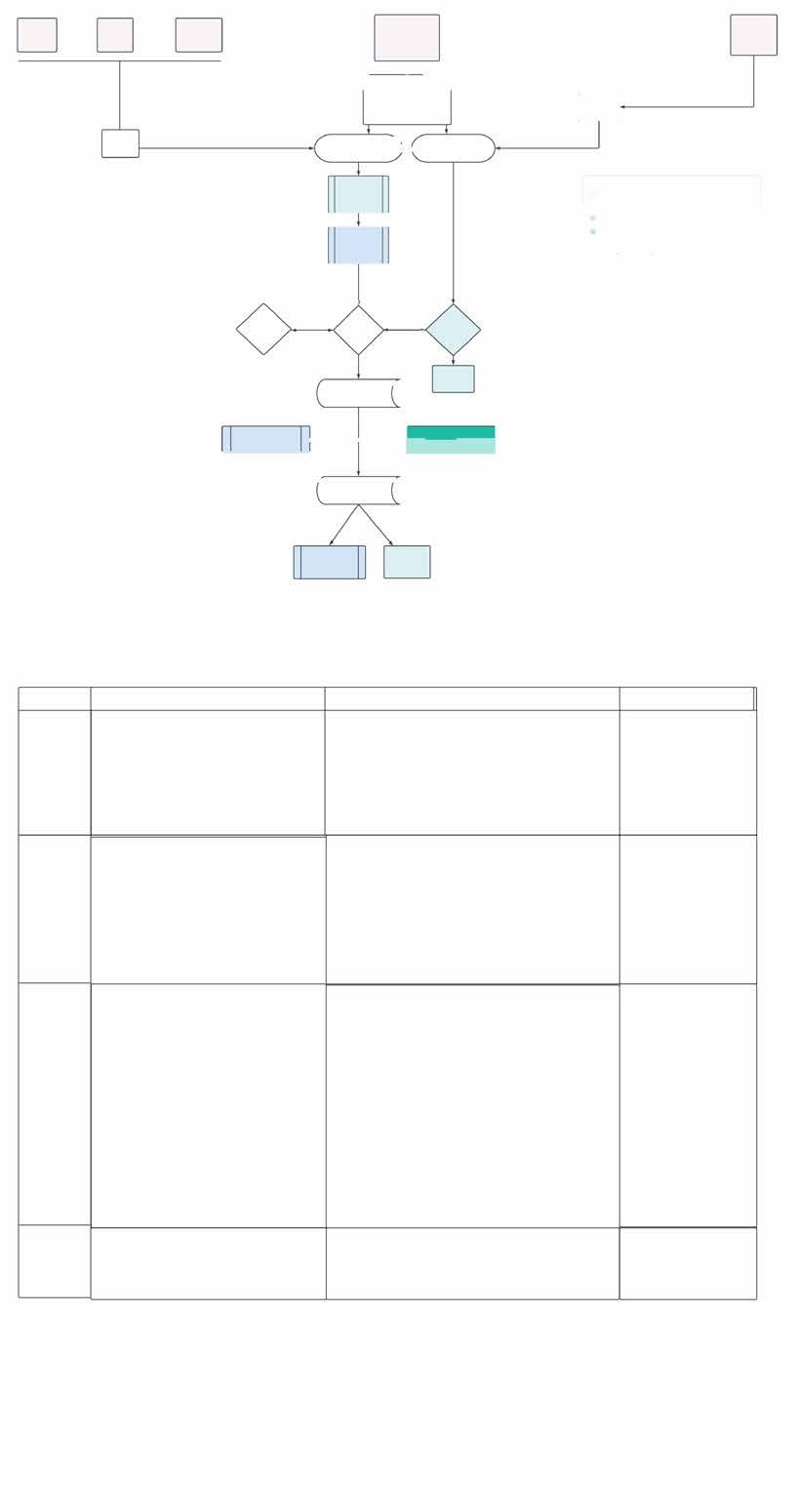
SIGNIFICANT INCIDENT RESPONSE MODEL
DBHIDS is often engaged by external stakeholders and the community to provide mental health support after a traumatic event. Events such as the Fairmount fire in 2022 and the Roxborough High School shooting later that year are examples of incidents that posed significant trauma to those directly involved. To respond to external requests from the community at large for various supports and resources in the instance of serious incidences, DBHIDS has created an Incident Response Flow Chart of how requests are triaged to ensure a timely and effective response to community needs.
The purpose of the protocol is to create a clear outline to access department wide resources by external stakeholders. Below are the Stages of the Incident Response Flow. (Appendix B)
Stage 1 - Post Trauma Impact and Needs Assessment
a. Description
Post-Trauma Impact and Needs Assessment is the first phase of the Post-Traumatic Stress Management (PTSM) continuum of trauma and evidence-informed, population, and public health community interventions, and thus communities an intervention on its own. The Post-Trauma Impact and Needs Assessment is coordinated by Network of Neighbors staff and implemented by the impacted community’s natural leadership (Community Connectors) and continues throughout the duration of the response. Since the Impact and Needs Assessment is a joint effort between Network of Neighbors staff, systems partners, and the impacted community’s leadership, at least one community point-of-contact (Community Connector) must be identified prior to beginning the process. It should be noted that the Network of Neighbors’ incident response process occurs separately for each impacted community that makes contact with the Network of Neighbors. Community here is defined as any group of people with a common affiliations or experience (e.g., witnesses, first responders, neighbors, friends, classmates, etc). This means that this process may
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 28
be in effect for multiple communities at the same time who were impacted by the same incident (in different ways)
b. Components
i. Virtual and in-person meetings with the impacted community’s natural leadership (Community Connectors) who can serve as trusted credible messengers, advocates, and gatekeepers for the impacted community. These community members are in the best position to re-establish a sense of emotional or psychological safety after the traumatic incident, which is the first step in assisting a community after a traumatic incident. During these meetings, Network of Neighbors Staff provide technical assistance, guidance, information and referrals to Community Connectors, who in turn provide the Network of Neighbors with the specifics in reference to 1) how their community has been impacted, 2) what the needs are, and 3) norms, boundaries, culture and local context. Skipping this step risks further harm to the impacted community, as well as increased distrust between the impacted community and supports and services available to it.
ii. Identification of impacted subgroups within the community based on experience, relationship, as well as gender, age and development level (e.g. eye witnesses, neighbors, parents and caregivers, classmates, friends, colleagues, etc.)
iii. Technical assistance, making use of existing resources, supports, and services – including the community’s own natural strengths and healing practices – service and support referrals (for individuals and families), and overall guidance around the implementation of a traumainformed community response.
c. Goals:
i. To establish a non-intrusive, compassionate presence to help the impacted community to marshal their own resources as well as existing supports and services in order to manage the short and long-term impact of the trauma in a way that taps into and strengthens the community’s natural resiliency and connections.
ii. Assessment of community’s capacity to handle short-term (acute) issues (and identification of needed resources)
iii. Assessment of community’s capacity to handle long-term psychosocial disruptions (and identification of needed resources)
iv. Identification of leadership structure (to assist with responsive planning)
Stage 2 – Response Coordination
a. Description
Response Coordination involves the planning of community and group-level interventions, recruitment of impacted community members, as well as the alignment of stated community needs with the available supports and services. This phase includes ongoing coordination with Community Connectors, as well as Responding Partners, which includes stakeholders and entities involved in the response process, either at the local or system level.
b. Components
i. Response Planning with Community Connectors – Identification of a date/time for the response (or multiple), location, recruitment of impacted community members, messaging, etc.
ii. Coordination with Responding Partners (system alignment)- information sharing and
TEC COMPREHENSIVE PLAN 2023 29
coordination of supports and services around the community’s stated needs and preferences. For Philadelphia public schools, the Philadelphia School District Office of Prevention and Intervention is always a Responding Partner, as well as Uplift Center for Grieving Children (when a student or staff member has died). Responding Partners vary depending on the impacted community’s existing relationships and connections as well as their stated needs.
iii. Outreach to CTR’s (Community Trauma Responders) and internal DBHIDS supports/ programs. Depending on the incident, its impact on the community in question and their stated needs and preferences, the Network of Neighbors reaches out to their network of trained Community Trauma Responders to support the community response, as well as trained DBHIDS staff and DBHIDS programs that are appropriate for the specific response. The Network of Neighbors may consider specific needs and preference when reaching out to Community Trauma Responders and internal DBHIDS staff and programs: including language, experience, professional qualifications, affiliation with the impacted community, etc. The Network of Neighbors always completes a “Response Briefing” regardless of whether the community response is supported by Community Trauma Responders or internal DBHIDS staff. However, if they are invited to support their response, their participation in the Response Briefing is mandatory to ensure consistent communication and mitigate the risk of harm.
c. Goals
i. Alignment of community’s stated needs, boundaries, norms, preferences, and cultural considerations with available supports and services.
ii. Planning of a community response that includes the community’s voice and ensures that the response takes place as a date, time, and location that is safe, accessible, and convenient for community members.
Stage 3 - Community Response
a. Description
Community response involves community and group-level interventions that take place wherever the impacted community regularly meets or feels comfortable at a date and time that they have chosen. These interventions vary in their purpose and goals (according to the phase of the community’s healing process, or the time elapsed since the traumatic incident).
The goal section outlines the goals (and purpose) unique to the different kinds of interventions (PTSM, PIES and PGA). Overall, the goal of these interventions is to:
i. Protect the space for the impacted community to come together for comfort, healing and connection.
ii. Reduce and mitigate the impact of the trauma (stress)
iii. Provide accurate information, either about the incident or about common reactions to overwhelming stress and practical strategies for coping.
iv. Foster peer connection and healthy coping
v. Identify community members who may benefit from additional support and services or higher levels of behavioral/mental healthcare.
vi. Provide support within the context of the community so that the information and the resources are sustained with the community past the duration of the response.
b. Components
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 30
i. PTSM Orientation Sessions – 0-72 hours, or up to one week post traumatic incident open to the entire impacted community
ii. PTSM Stabilization Group/s - Up to two weeks post traumatic incident – small group discussions for the groups with homogeneous exposure
iii. PTSM Coping Group/s and PTSM Follow-Up Coping Groups – Two to three weeks – three month/one year post traumatic incident – small group discussions for groups with homogeneous exposure. Include suicide specific protocols.
iv. PTSM Compassion Care Discussions – can occur anytime (preventative) or after a traumatic incident, depending on the nature of the impact and the experience of the community members. These discussions focus on the how the “work” you do impact you, which can include the work of being a part of a certain community of performing a certain job/role.
v. PTSM Pre-Intervention Overviews – Structured information sessions/meet and greets, designed to build trust and safety with impacted community members before a PTSM small group discussion.
vi. P.I.E.S. Discussion – P.I.E.S discussions are not part of the formal PTSM evidence and trauma informed curriculum but are used to build safety and trust with impacted community members before a group intervention. P.I.E.S discussions are also used within classroom setting and whenever the experience, relationship, and degree of impact of community members is unknown.
vii. PFA Response – Psychological First Aid (PFA) is a one-to-one intervention (also appropriate for working with families), that is used by the Network of Neighbors during the Post Trauma Impact and Needs Assessment process, as well as during the P.I.E.S and PTSM intervention on an as-needed basis. However, PFA Responses involve dispatching Network of Neighbors (or PFA trained DBHIDS staff) to community events organized outside of the department to provide PFA support as needed.
c. Goals
i. PTSM Orientation Sessions – Dissemination of accurate information from stakeholders that can provide needed information (e.g. Philadelphia Police Department, Parks and Rec, Risk Management, Licenses and Inspection, etc.) to calm rumors and reduce orienting the community to additional supports, and identifying “Community Connectors” or potential subgroups of impacted community members.
ii. PTSM Stabilization – Emphasis on grounding and mindfulness techniques to reduce stress and arousal and safety plan for the short-term aftermath, including preparation for the funeral (if applicable)
iii. PTSM Coping – Opportunity for similarly impacted community members to tell their story, discuss thoughts and reactions (normalize reactions), reduce stigma, received accurate information and support, discuss coping strategies and begin the healing process.
iv. Compassion Care discussion – Address stress associated with the “work,” as well as challenges and rewards of the “work.” Compassion care discussions are preventative but sometimes utilized in the aftermath of an incident depending on the community’s unique situation and experience.
v. P.I.E.S Discussion – Opportunity for community members to share thoughts ad reactions, support each other and assess/identify the impact as well as community members who cannot identify safety or support.
TEC COMPREHENSIVE PLAN 2023 31
vi. PFA Responses – PFA responses occur in community settings, designated events or in the immediate aftermath of a traumatic incident. The goal of PFA is to assess immediate needs of survivors and connect them to safety and support.
Stage 4 – Post Response
a. Description
Post response is also an ongoing process, as multiple “responses” may take place over the course of several months or years. The process involves ongoing communication and checking in with the Community Connector/s who can monitor “the pulse” of the community and assess interest in additional interventions or supports.
b. Goals
i. Connection to long-term supports (e.g., internal DBHIDS programming, Uplift Center for Children and ongoing grief groups, or any supports or services that can fill gaps identified during the response process)
ii. Ongoing technical assistance and Post-Trauma Impact and Needs Assessment
iii. Trainings (in topic identified by the community to include Psychological First Aid and/or Post Traumatic Stress Management training)
iv. Surveying of the Community Connectors for outcome and evaluation.
c. Goals
i. Provision and connection to long-term supports in a manner that respects the impacted community’s timeline, boundaries and stated needs and preferences.
ii. Increased trust between the impacted community and existing support and services.
EXTERNAL STAKEHOLDER LEARNING COLLABORATIVE AND SUBCOMMITTEES
The External Stakeholders Learning Collaborative (ESLC) serves as an external engagement mechanism to discuss and receive feedback on the vast array of trauma activities funded and/or planned by the department, as well as an opportunity to discuss best practices, leverage opportunities to work with partners and increase knowledge across all stakeholders in addressing trauma. This group meets bi-monthly with the intent to exchange information and stay abreast of current programming and issues related to trauma, in the city.
The collaborative is comprised of 100-plus members: including community members, advocates, staff from community-based organizations and hospital systems, academicians, local subject matter experts and DBHIDS staff.
Subcommittees were developed to focus on specific priorities identified by the ESLC and subcommittee members. Subcommittees meet monthly and have thus far provided recommendations that DBHIDS has developed into multi-year work plans – what we refer to as “recommendations to action” to address the following areas:
1. Prolonged trauma
2. Trauma impacting children and families
3. Secondary trauma
4. Trauma related to violence
5. Defragging the system
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 32
Prolonged Trauma
The charge for this committee is to identify policies and practices to address prolonged trauma in Philadelphia. Below are the main recommendations. See appendices for the full Prolonged Strategy report.
1. Develop External Stakeholders Trauma workgroup. Include academicians, practitioners and community members.
2. Start with clear definitions of equity, power, privilege, diversity, and inclusion.
3. Identify various stakeholder groups for which trauma awareness training/trauma 101 and implicit bias training should be prioritized.
4. Develop trauma informed resources/trainings for pre-schools and daycares (ECE)
5. Identify specific, standardized metrics that are asset-based.
6. Standardize metrics that are collected related to trauma related from DBHIDS provider network.
7. Identify and provide specific resources to address STS and vicarious trauma among the peer provider workforce.
8. Develop trauma certification for CPS, CRS.
9. Revise polices that expel individuals for non-compliance with programmatic restrictions (not trauma informed) i.e., review policies with providers to ensure opportunities for further engagement versus expelling people from programs.
Children and Family Trauma
The charge for this committee is to identify areas to improve and/or expand DBHIDS services for children and families.
1. Young children 0-5. Need for immediate response to daycare and pre-k programs in events where young children are exposed to traumatic events.
2. Build capacity for trauma training of child and family serving organization and family members.
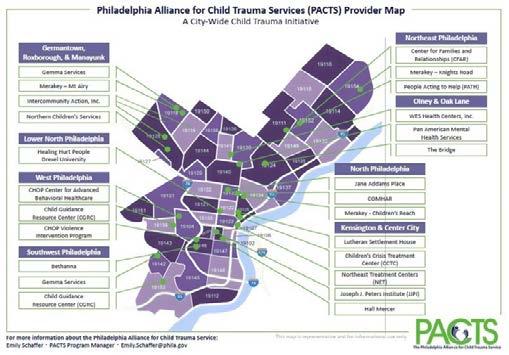
3. Expand TF-CBT into underserved areas, i.e. Southwest Phila – PACTS now has providers to serve these communities. PACTS will update maps.
4. Address workforce trauma training
5. Disseminate educational materials more broadly and widely, including community level.
6. Need for additional in class clinical support for ECE level providers.
7. Modify PACTS trainings to incorporate focus on racial trauma.
8. Children’s Mobile Crisis team- identify possible need for trauma specific training.
Secondary Traumatic Stress
This charge for this committee is to recommend best practices and provide resources for social service professionals.
1. Speaker’s series in the External Stakeholder Learning Collaborative.
2. Directory of supports for staff – Behavioral Health Community Supports Directory (Will be made publicly available on dbhids.org this year)
3. Partner with NAMI and NASW around messaging for the behavioral health workforce related to secondary trauma.
4. Social media messaging and infographic to access supports.
TEC COMPREHENSIVE PLAN 2023 33
Defragging the System
The charge of this subcommittee is to recommend activities to reduce traumatic experiences and barriers people may face while trying to access services, through multiple systems.
1. Systems Mapping – DBHIDS plus other city health and human services agencies (Will be made publicly available at dbhids.org this year)
2. Identify systems to defrag (i.e., hospitals, schools, universities, city agencies, etc.).
Trauma Related to Violence
The charge for this committee is to understand how to serve and provide services and resources to individuals, families, and communities impacted by the trauma of violence.
1. Focus group with people who have perpetrated crimes to understand their perspectives and how they could have been helped.
2. Focus group with people who have been victims of crimes to understand their experiences of pre and post their trauma, including survivorship guilt.
3. Focus group with youth to understand their experiences with trauma in their neighborhoods and school environments, what supports they need and what they want adults to know about how to support them.
4. Public Service Announcements of DBHIDS resources.
5. Gun shootings mapping and responsive actions.
6. Annual TEC conference
7. Social media and infographic to access supports.
PROPOSED NEW AND INNOVATIVE PROGRAMMING
DBHIDS is also seeking funding for opportunities to create new programming to address youth experiencing trauma. Below are two new proposed programs and one program expansion that we see as urgent in implementing now to alleviate trauma for youth living in neighborhoods highly impacted by trauma.
1. Program - Trauma to Triumph
This program will disrupt the pervasive presence of trauma for low-income BIPOC people highly impacted by trauma by acknowledging their traumatic experiences, celebrating their strengths, and encouraging their hope and belief in themselves for a positive and productive future. The resources will be delivered with behavioral health supports.
The program will be designed to work in partnership with local nonprofit organizations and behavioral health providers that have demonstrated excellence in youth-focused, trauma-driven programming throughout the City of Philadelphia.
The program will serve 100 people between the ages of 10-24 over the course of 12 months. Selection of applicants will be prioritized for youth living areas that have high poverty and crime rates.
The program will consist of the following modules:
a. Post Secondary Transition Supports
b. Trauma Support Groups
c. Turning Pain into Art
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 34
d. Black Boy & Girl Joy
The anticipated outcomes include:
a. Positive engagement of youth that promotes healing and well-being
b. Increased hope for a positive and productive future as reported by youth
c. Increased overall engagement in positive and productive activities as reported by youth
2. Trauma-responsive and Trauma-mitigating Programming with Community-based Organizations
This activity will address the pervasive trauma experienced by individuals and communities and must also include the work and efforts of existing community-based organizations engaged in gun violence prevention work. This recommendation comes from both the ESLC and Councilman Kenyatta Johnson’s panel. We see operationalizing this recommendation by:
a. Soliciting 501(c)(3) organizations addressing trauma through:
i. Innovative, non-conventional activities for at-risk youth in high crime areas.
ii. Group supports for grieving families.
iii. Piloting new ideas developed by people with lived experience to prevent and end gun violence.
3. Community Wellness Engagement Unit Youth Focused Support Team
This team will provide wellness supports in a variety of settings where children live, learn, and play. This work will complement available behavioral health supports and will focus on wellness and prevention. The CWEU Youth Focused Team will create a schedule and rotation each academic year ensuring there is capacity for all schools to be provided in person supports. A branding strategy will also be implemented to ensure all schools and families are aware of all of DBHIDS’ resources and availability to respond to school-wide and individual (parent, child, teacher) level concerns.
a. The team will engage children in settings such as:
i. Schools (prioritizing community schools)
ii. Out-of-school time programs
iii. Recreation centers
iv. Playgrounds and other public places
b. Youth will be offered coping and life skills, referrals to services, and supports for the challenges children face including:
i. Stress
ii. Trauma
iii. Social media-related issues including bullying, drill music, and damaging self-esteem messages.
iv. Basic needs related to the social determinants of health and
v. Behavioral health referrals included but are not limited to Tier 2 and T3 supports in and out of schools.
c. The team will consist of a clinical-level supervisor, behavioral health workers, and community wellness specialists that will deliver in person programming. A family navigator will provide supports that will include the interest of the child and extend to the needs of their families as needed. And a program evaluator will ensure the goals and outcomes of the program are tracked,
TEC COMPREHENSIVE PLAN 2023 35
enabling the team to ensure that the programs’ strategies are effective and impactful.
d. We anticipate this specialized team will bridge the gap in connecting behavioral health and related resources needed for children and families supporting children to have better academic and health outcomes.
e. This work will help to reduce racial disparities by providing resources in communities that have experienced disinvestment due to structural and systemic racism. Addressing the social determinants of health and will support low income and BIPOC children who experience disproportionately higher levels of poverty access basic needs that can support their health and well-being.
ACHIEVING EQUITY
DBHIDS seeks to shift our systems to reduce behavioral health disparities through a variety of approaches and by intentionally addressing structural racism and advancing health equity and justice. We aim to make services more available and accessible to individuals and communities that have been historically underserved, close service gaps and improve service delivery.
In our charge to identify and change processes that create disparities, we:
1. Created the Social Determinants of Health Equity Unit in 2022 – this unit promotes health equity by connecting individuals with behavioral health needs to resources that address the social determinants of health.
2. Created the Forensic Equity Unit in 2023 – this unit will address the deep racial inequality within the justice system for people with serious mental illness by preventing incarceration for those at risk of justice involvement, reducing the length of stay for incarcerated individuals, reducing reincarceration for the justice-involved, increasing connections to treatment and support for those returning to the community from institutional settings, and targeting social determinants of health (SDOH). The unit’s focus on social determinants of health directly aligns with the Commonwealth’s Health Care Reform Recommendations by addressing food insecurity, health care, housing, transportation, childcare, employment, utilities, clothing, and financial strain within the justice-involved population with behavioral health challenges. These initiatives will ensure the success achieved in resolving the NSH waitlist is sustained while addressing the deep racial disparities within the justice-involved Philadelphia SMI population.
3. Transformed our crisis systems by:
a. Expanded our Community Mobile Crisis teams to serve the entire city
b. Implemented and promoted 988 and have seen a considerable increase in call volume with positive success stories and outcomes
4. Seek to engage BIPOC Providers (DEI and Racial Equity Change Team)
a. Expanding our behavioral health provider network to include more BIPOC-owned and operated community-based behavioral health organizations that focus on a culturally and linguistically centered continuum of quality care to increase utilization of non-acuity behavioral health services and change the behavioral health service experience of Philadelphia’s BIPOC adults.
b. Increased intentionality on BIPOC community collaboration and partnership. We are seeking to explore and develop new and innovative diverse community outreach and engagement strategies that advance knowledge and enhance awareness of our department and the vast array of resources, services, and treatment modalities we provide while recognizing the unique
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 36
perspectives and needs of BIPOC communities in the way we serve their cultural differences. We are also committed to enhancing mechanisms to monitor the BIPOC Treatment experience to eliminate bias, racist, and discriminatory practices.
5. Included information on how to connect with BIPOC providers on Healthy Minds Philly
6. Use data to understand where there may be service desserts and/or where we may need to right size resources
7. Operate a Housing Unit – addresses the social determinant of health – housing, for street homeless individuals who are largely BIPOC.
8. Operate a DEI unit that houses Immigrant and Refugee Affairs and Language Access ServicesAssesses the needs of immigrant and refugee communities as well as service providers, to identify gaps and determine how DBHIDS can deliver culturally and linguistically appropriate services to the communities
9. Expanded Network of Neighbors in 2022 which allows the team to meet the needs of every community across the city through a regionalized approach.
10. Fully operationalized the Community Wellness Engagement Unit – regionalized throughout the city providing coverage to every council district to meet the needs of every community across the city.
11. Created the Racial Equity Opioid Overdose Committee in 2022 to address the rise in overdose deaths in BIPOC communities and equity in services and delivery.
In our charge to review and evolve hiring, contracting and community engagement processes and practices to reduce disparities, we are committed to what we call “conscious contracting” that aims to remove barriers and promote equity.
Additionally, we work internally to ensure that staff across all divisions and levels of leadership are representative of the communities of we serve.
2023 Minority, Women, Disabled/Disadvantaged Business Enterprises Statistics for our provider network and DBHIDS.
1. Over 90 percent of DBHIDS funds support non-profit agencies
2. 79 percent of DBHIDS staff are minority
3. DBHIDS Executive Leadership – 75 percent minority, 50 percent women
4. D DBHIDS Contracted Agencies –
a. Workforce – 52 percent minority, 65 percent women
b. Executive – 33 percent minority, 59 percent women
c. Board of Directors – 40 percent minority, 44 percent women
Moving forward in 2023, we plan to:
1. Continue DEI efforts to increase diversity in the provider network.
2. Host focus groups with BIPOC providers to understand challenges and barrier with becoming part of the network with the goal of increasing the number of providers.
3. Conscious contracting - work to increase diversity in the provider network by valuing cultural competence, community presence and other factors that are consistently valued.
4. Develop monitoring tools that track data points that can ensure services are equitable delivers in every community.
TEC COMPREHENSIVE PLAN 2023 37
5. Continue data-driven responses to racial and geographic disparities.
6. Continue our diversity, equity, and inclusion efforts to address racial equity in the overdose epidemic.
7. Publish the Behavioral Health Supports Directory which lists providers by categories including: LGBTQ, BIPOC, Seniors, Immigrants and Refugees, Intellectual Disabilities, Secondary Traumatic Stress, Deaf/ Sign Language Needs, Children’s Supports, Sight Impaired, and Domestic Violence.
8. Host TEC tours in neighborhoods across the city to understand the unique needs of the people and the identities of those communities in addressing trauma and delivering services.
9. Seek sustainable funding sources to continue to address the social determinants of health for the people we serve.
ENGAGING COMMUNITY
We work across the city every day through numerous teams and in a variety of formats. We seek solutions from and sustain solutions in communities. We also actively seek to embed sustainable funding and operational activities within our providers and community-based organizations where possible.
Below are some of our programs that actively engage and work in partnership with communities. A listing of all the programs across the Department organized by TEC category can be found in the P.A.C.E. /TEC Crosswalk. (Some programs that engage communities are also noted and already defined in the trauma section of this report)
1. Engaging Males of Color
2. Community Affairs – provides behavioral health resources and information at community events across the city.
3. Community Wellness Engagement Unit
4. Faith and Spiritual Affairs (FSA) - Engages the faith-based community, organizes the FSA Advisory Board, hosts an annual conference, and is dedicated to:
a. Enhancing understanding of behavioral health conditions
b. Reducing the stigma associated with behavioral health challenges.
c. Promoting inclusion and connectedness in one’s community,
d. Aiding in the integration of spirituality into behavioral health care and treatment
5. Porchlight program with Philadelphia Mural Arts
6. Immigrant Refugee Wellness Academy- In 2022, DBHIDS launched the Immigrant/Refugee Wellness Academy (IRWA) pilot program. IRWA is a free training program designed to empower and prepare Philadelphia’s multilingual/multicultural immigrants and refugees with knowledge, resources, and tools necessary to engage in activities that address behavioral health and intellectual disability challenges, trauma, and inequity experienced within the immigrant and refugee community. The benefits of this certificate program include behavioral health and intellectual disability knowledge and understanding,
7. Peer Culture and Community Inclusion - PCCI is a community partnership promoting pathways to wellness. Our goal is healthy individuals, families, and communities, free of stigma, with equal access to health resources sharing their lived experiences for continued holistic wellness. In order to realize this mission, the PCCI Unit actively engages, supports, and models the promotion of hope, wellness and empowerment throughout the Behavioral Health system of Philadelphia and beyond
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 38
8. Mobile Outreach and Recovery Services
9. Homeless Outreach and Huddles - Street outreach engages homeless individuals living on the streets of Philadelphia. Staff offers emergency housing and treatment options as well as water and assistance meeting their immediate survival needs. More important for persons experiencing chronic street homelessness, street outreach represents building reliable relationship that assist individuals in addressing barriers to coming inside. Outreach assists persons in identifying their needs, wants and desires as they recover their lives. Outreach acts as a bridge to a life beyond street homelessness. Outreach Special Initiatives Unit along with AR2 and the Managing Director’s Office
10. Philadelphia Systems of Care/Councils - (PSOC) - Community-driven councils that are representative of local neighborhood families, youth, and partners, who are committed to community empowerment and to addressing the social determinants connected to youth behavioral health, resiliency, and wellness
11. Youth M.O.V.E. Philadelphia - is a local chapter of Youth M.O.V.E. National (Motivating Others through Voices of Experience). YMP is devoted to improving services and systems that support positive growth and development by uniting the voices of individuals who have lived experience in various systems including mental health, juvenile justice, education, and child welfare.
12. Suicide Prevention Task Force - The Philadelphia Suicide Prevention Task Force (P-SPTF)’s mission is to work toward zero suicides in Philadelphia. This mission will be achieved through a collaboration of all stakeholders and by engaging in a coordinated and integrated approach across the city.
13. TEC Talks and Community Conversations hosted by Dr. Jill Bowen - engages community members, staff and our provider network in addressing TEC
14. Family Committee - Family Member Committee is comprised of family members of children with a variety of behavioral health needs. These meetings provide an opportunity for family members to network with each other, receive support and to also provide input into policies and programs of DBHIDS affecting children and families. It is a safe forum where family voice is heard and can move our system in directions that better serve children and families.
15. Community Autism Peer Support (CAPS) - program pairs an individual with autism who has completed a peer support training program, with other individuals with autism to achieve personal wellness and community participation goals
Moving Forward in 2023, we plan to:
1. TEC Talks and Community Conversation - conversion and expansion to podcasts
2. Distribution of materials in new spaces this year- i.e. 52 public schools, more playstreets.
3. Create an external facing web page for the community to learn about and have the opportunity to join our community groups.
4. Ensure ongoing representation, post TEC tours, at community led events, as requested by communities.
TEC COMPREHENSIVE PLAN 2023 39
TEC WORKPLAN
Short-term 1 to 12 months (green); Mid-term 13 to 24 months (blue); Long-term 24+ month (dark blue) Implementation Schedule
TRAUMA
Prolonged Trauma
1. Develop External Stakeholders Trauma workgroup. Includes academicians, practitioners, and community members
2. Start with clear definitions of equity, power, privilege, diversity and inclusion
3. Identify various stakeholders and groups for which trauma awareness and training 101 and implicit bias training should be prioritized.
4. Develop trauma informed resources/trainings for pre-schools and daycares (ECE)
5. Identify specific, standardized metrics that are asset based.
6. Standardize metrics that are collected related to trauma from the DBHIDS provider network
7. Identify and provide specific resources to address STS and vicarious trauma among the peer provider workforce.
8. Develop trauma certification for CPS, CRS.
Children and Family Trauma
1. Young children 0-5. Need for immediate response to daycare and pre-k programs in events where young children are exposed to traumatic events.
2. Build capacity for trauma training of child and family serving organizations and family members.
3. Expand TF-CBT into underserved areas, i.e. southwest Phila.
4. Address workforce trauma training.
5. Disseminate educational materials more broadly and widely, including community level.
6. Need for additional in class clinical supports for ECE level providers
7. Modify PACTS trainings to incorporate a focus on trauma.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 40
or
Recommendations or Activities Term
Committees
other
Committees or other Recommendations or Activities Term
8. Children’s Mobile Crisis team - identify possible need for trauma specific training
Trauma Related to Violence
1. Focus group with people who have perpetrated crimes to understand their perspectives and how they could have been helped
2. Focus group with survivors of crimes to understand their perspectives and how they could have been helped
3. Focus group with youth to understand their experiences with trauma in their neighborhoods and school environments, what supports they need and what they want adults to know about how to support them.
4. Public Service Announcement of DBHIDS resources
5. Gun shootings mapping and responsive actions
6. Annual TEC conference
7. Social media and infographic development on supports
Defragging the System
1. Systems Mapping of DBHIDS and other city health and human services agencies. Make DBHIDS mapping tool publicly available on DBHIDS.org
2. Identify systems to defrag (i.e. hospitals, schools, universities, city agencies, etc.)
Secondary Traumatic Stress
1. Speakers Series in the External Stakeholder Learning Collaborative
2. Directory of supports for staff - Behavioral Community Supports Directory. Make publicly available on dbhids.org
3. Partner with NAMI and NASW around messaging for the behavioral health workforce related to secondary trauma.
TEC COMPREHENSIVE PLAN 2023 41
Committees or other Recommendations or Activities Term
Gaps and Recommendations
New and Innovative Programming
EQUITY
1. Develop a plan to prioritize and implement feasible recommendations
1. Seeking program funding and support. If awarded will implement within 6-12 months, post award.
1. Continue DEI efforts to increase diversity in provider network.
2. Host focus groups with BIPOC providers to understand the challenges and barriers with entering the network – with the goal of increasing the number of providers
3. Conscious Contracting- work to increase diversity in the provider network by valuing cultural competence, community presence and other factors that are consistently valued.
4. Develop monitoring tools that track data points that can ensure services are equitable delivers in every community.
5. Continue data driven responses to racial and geographic disparities
6. Continue Diversity, Equity and inclusion efforts to address racial equity in the overdose epidemic.
7. Publish the Behavioral Health Supports Directory which lists providers by categories including: LGBTQ, BIPOC, Seniors, Immigrants and Refugees, Intellectual Disabilities, Secondary Traumatic Stress, Deaf/Sign Language needs, Children’s Supports, Sight Impaired and Domestic Violence
8. Host TEC tours in neighborhood across the city to understand the unique needs of the people and the identities of those communities, in addressing trauma and delivering services.
9. Seek sustainable funding sources to continue to address the social determinants of health for the people we serve.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 42
Committees or other Recommendations or Activities Term
COMMUNITY
1. TEC Talks and Community Conversationsconversion and expansion to podcasts
2. Distribution of Materials in new spaces this year, i.e., 52 public schools, more Playstreets.
3. Create an external facing web page for the community to learn about and have the opportunity to join our community groups.
4. Ensure ongoing representation, post TEC tours at community led events as requested by communities.
TEC COMPREHENSIVE PLAN 2023 43
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 44
ACKNOWLEDGMENTS
We thank you for your contributions.
DBHIDS Staff
Emily Auerbach
David Ayers
Catherine Bracaliello
Andrea Brooks
Gina Booker
Gabriel Bryant
Raekwon Burton
Kyle Carter
Tapiwa Chadambura
Kleckner Charles
Christina Crews
Eduardo Collazo
Lisa Colton
Natalie Dallard
Laura Derrigi
Elana Dicocco
Dominique Dillworth
Racquel Fetzer
Kathleen Fox
Stacey Galonka
Tamika Harvey
Yolanda Hughes
Monava Jones
H. Jean Wright
Jessica Smith
External Stakeholders
Jonathan Arrieta, Impact Services
Burke Bodo, Philly Spark
Meagan Corrado, West Chester University
Dorothea Davis, Vision for Equality
Nicholas DeMarco, PMHCC
Jeanne Felter, Jefferson University
Charles Horton, Septa
Reginald Howard, Drexel university
Sara Jaffee, University of Pennsylvania
Leslie Leiberman, Health Federation of Philadelphia
Samantha Joseph Rivera, Office of Children and Families
Kamela Johnson
Jon Korczykowski
Laura York
Iris Lozada
Joe Lowry
Shintele Malloy
Sam Margolius
Paola Maysonet
Adelaide Mooney
Sharon Musser
Andrea October
Valarie Oulds
Kevin Pack
David Poyser
Katrina Pratt-Roebuck
Richard Rosario
Tierra Pritchett
Sosunmolu Shoyinka
Pamela Sigman
Richard Tull
Amber Lee Venti
Faith Washington
Kristen Williams
Nikita Weaver
Marquita Williams
Kelly Moore, Rutgers University
Michael O’Bryan, Drexel, Lindy Institute
Casey Odonnel, Impact Services
Joe Pyle, Scattergood Foundation
Grace Ryder, Childrens Crisis Treatment Center
Antonio Valdes, Chidrens Crisis Treatment Center
Laura Vega, Children’s Hospital of Philadelphia
Roy Wade, University of Penn
Roberta Waite, Drexel University
Rex Yin, Philly Spark
TEC COMPREHENSIVE PLAN 2023 45


APPENDIX A
P.A.C.E. TEC CROSSWALK
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 48
City of Philadelphia
Services
Department of Behavioral Health and Intellectual disAbility
 Jill Bowen, Ph.D. , Commissioner November 2022
Jill Bowen, Ph.D. , Commissioner November 2022
P.A.C.E. TEC
CROSSWALK
Introduction
The Philadelphia Department of Behavioral Health and Intellectual disAbility Services (DBHIDS) P.A.C.E. (Prioritizing to Address our Changing Environment) strategic plan outlines the department’s priorities, goals for each of these priorities, and the path way to achieve these goals. Each of the five priority areas features a key performance indicator (KPI) that helps DBHIDS measure its progress toward the goal, and three strategies that are used to help move the needle. This document serves as a map to hel p DBHIDS employees understand how their work fits within P.A.C.E. priority areas as well as the TEC (Addressing Trauma, Achieving Equity, and Engaging Community) framework. The work of DBHIDS is multifaceted and holistic; one project or program can often a ddress several priority areas and aspects of TEC at the same time. Divisional leadership helped to identify key projects within each division, which have been mapped to each P.A.C.E. priority area and TEC component.
DBHIDS Systems Integration Unit pg. 1
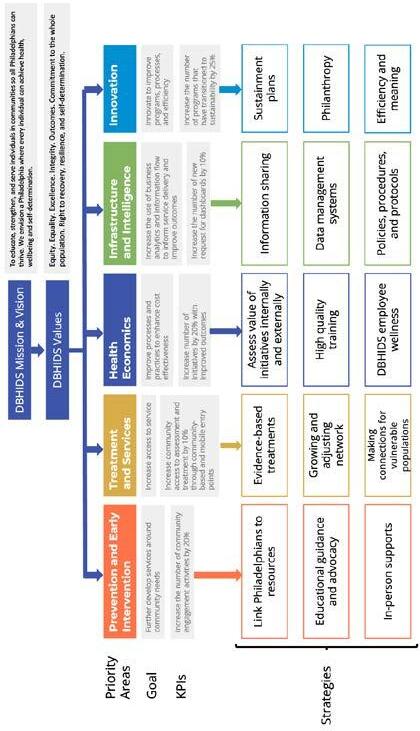
DBHIDS Systems Integration Unit pg. 2 P.A.C.E.
Framework
ddressing Trauma means creating a system that is traumaresponsive, traumainformed, and traumamitigating.
DBHIDS recognizes institutional trauma as a type of systemic trauma that can result from institutional action and inaction. With TEC, DBHIDS is addressing various t ypes of traumas , including institutional harm, by creating programs that aim to ameliorate the risk of institutional wrongdoing. Achieving Equity requires DBHIDS to intentionally identify and address institutional and structural racism, transform systems t o reduce behavioral health disparities, and promote racial equity for Black, Indigenous, and People of Color (BIPOC). The DBHIDS Diversity, Equity, and Inclusion (DEI) unit is constantly working to inform programs and processes to promote equity within the department and externally to the public. Engaging Community encourages DBHIDS to connect individuals to communitybased services and integrate community wisdom into program development and operations. DBHIDS recognizes the importance and effectiveness of fully integrating programs into the community and is working actively to shift its programs in this direction as much as possible. DBHIDS also wants communities to have a voice in program development as a way of ensuring successful implementation of commun itybased programs.
DBHIDS Systems Integration Unit pg. 3 TEC Lens A
ENGAGING COMMUNITY
• GoalsShift services to be increasingly communitybased and sustain through integrating initiatives more fully into communities.
• Charge Shift Services from institutions to community settings.
• P.A.C.E. overlayEnsure communities are heard and contribute to longterm sustainment strategies.
ACHIEVING EQUITY
• GoalTransform systems to reduce behavioral health disparities and promote racial equity amongst Black, Indigenous, and People of Color (BIPOC).
• Charge
Identify and change processes that create disparities. Review/evolve hiring, contracting and community engagement processes and practices to reduce disparities.
• P.A.C.E. overlayUse an equity focused lens.
ADDRESSING TRAUMA
• GoalTransform operations to be traumamitigating.
• Charge
Reduce traumatic experiences in the system.
Change processes to be traumaresponsive and traumamitigating.
Shift systems to be traumareducing.
• P.A.C.E. overlayEnsure KPIs use a traumainformed lens.
DBHIDS Systems Integration Unit pg. 4
ENGAGING
ACHIEVING EQUITY COMMUNITY
• DBHIDS SDOH (Social Drivers of Health) Workgroup
• DBHIDS Prevention
• DBHIDS SDOH (Social Drivers of Health) Workgroup
• DBHIDS Prevention
• DBHIDS SDOH (Social Drivers of Health) Workgroup
• DBHIDS SDOH (Social Drivers of Health) Workgroup
• DBHIDS Prevention
• DBHIDS TEA (Technology Equipment Access)
• DBHIDS FEEDS (Food Engagement through Efficient Delivery)
• DBHIDS MASS (Mobility Access through Supplemental Services)
• DBHIDS SDOH (Soci al Drivers of Health) Workgroup
• DBHIDS Prevention
• DBHIDS TEA (Technology Equipment Access)
• DBHIDS FEEDS (Food Engagement through Efficient Delivery)
• DBHIDS MASS (Mobility Access through Supplemental Services)
• DBHIDS SDOH (Social Drivers of Health) Workgroup
• Employment
• DBHIDS Quickscreen
• DBHIDS Organizational Mapping
• DBHIDS TEA (Technology Equipment Access)
• DBHIDS FEEDS (Food Engagement through Efficient Delivery)
Prevention and Early Intervention
• DBHIDS SDOH (Social Drivers of Health) Workgroup
• DBHIDS Prevention
• DBHIDS Trauma Workgroup
• DBHIDS FEEDS (Food Engagement through Efficient Delivery)
• DBHIDS Quickscreen
Treatment and Service
Health Economics
Infrastructure and Intelligence
• DBHIDS Organizational Mapping Innovation
• DBHIDS FEEDS (Food Engagement through Efficient Delivery)
• DBHIDS MASS (Mobility Acce ss through Supplemental Services)
• DBHIDS SDOH (Social Drivers of Health) Workgroup
• DBHIDS Quickscreen
• DBHIDS Prevention
• DBHIDS FEEDS (Food Engagement through Efficient Delivery)
• Supplemental Services)
• DBHIDS SDOH (Social Drivers of Health) Workgroup
• DBHIDS Prevention
• DBHIDS Quickscreen
DBHIDS Systems Integration Unit
pg. 5
Commissioner’s Office ADDRESSING TRAUMA
ENGAGING COMMUNITY
• Engaging Males of Color (EMOC) (Diversity, E quity, and Inclusion (DEI))
• Faith and Spiritual Affairs (CBSD)
• Porch Light: CommunityBased Services Development Unit (CBSD)
• Increase youth advocacy and engagement with alcohol, tobacco, and drugs (CEU)
• Community Districts Behavioral Health Outreach (CWEU)
• Storytelling Training (PCCI)
• Recovery Walk (PCCI)
• Peer Institute (PCCI)
• Peer Force (PCCI)
• Same Day Work and Pay Peer Support (PCCI)
• Community Support Program (PCCI)
• Certified Peer Specialist (CPS) Training (PCCI)
• CPS and Certified Recovery Specialist (CRS) Professional Development
• Community Coalition Wellness Initiative (CCWI) (CEU)
• Community Support Program (PCCI)
• Community Districts Behavioral Health Outreach (CWEU)
• Storytelling Training (PCCI)
• Peer Institute (PCCI)
Planning Innovation
ACHIEVING EQUITY
• Faith and Spiritual Affairs (CBSD)
• Porch Light: CommunityBased Servi ces Development Unit (CBSD)
• Increase and enhance community linkage relationships and increase community access points defined as touch down sites and hubs (Community Wellness Engagement Unit (CWEU))
• Storytelling Training (PCCI)
• Recovery Advocates (PCCI)
• Pe er Institute (PCCI)
• Same Day Work and Pay Peer Support (PCCI)
• Community Support Program (PCCI)
• Certified Peer Specialist (CPS) Training (PCCI)
• CPS and Certified Recovery Specialist (CRS) Professional Development
• Storytelling Training (PCCI)
• Recovery Advocates (PCCI)
• Peer Support Toolkit (PCCI)
• Peer Institute (PCCI)
• Community Support Program (PCCI)
• Peer Force (PCCI)
• Community Support Program (PCCI)
• Certified Peer Specialist Training (PCCI)
• Engaging Males of Color (DEI)
• Faith and Spiritual Affairs (CBSD)
• Porch Light (CBSD)
• Same Day Work and Pay Peer Support (PCCI)
• LGBTQ Initiative (CBSD)
ADDRESSING TRAUMA
• Porch Light: CommunityBased Services Development Unit (CBSD)
• Engaging Males of Color (EMOC) (Diversity, Equity, and Inclusion (DEI))
Prevention and Early Intervention
• Faith and Spiritual Affairs (CBSD)
• Community Districts Behavioral Health Outreach (CWEU)
• Wellness Recovery Action Plans (Peer Culture and Community Inclusion (PCCI))
• Storytelling Training (PCCI)
• Peer Institute (PCCI)
• Same Day Work and Pay Peer Support (PCCI)
• Community Support Program (PCCI)
• Certified Peer Specialist (CPS) Training (PCCI)
• CPS and Certified Recovery Specialist (CRS)
Professional Development
• Educational FilmsIndividual Opioids
• MindPHL
• Boost Your Mood
• PI Sponsorship events
• Network of Neighbors (NoN)
• Community Districts Behavioral Health Outreach (CWEU)
• Wellness Recovery Action Plans (PCCI)
• Certified Peer Specialist Training (PCCI)
• CPS Employment and Technical Assistance Program (PCCI)
• Faith and Spiritual Affairs (CBSD)
• Porch Light (CBSD)
• LGBTQ Initiative (CBSD)
• Peer Support Toolkit (PCCI)
• Same Day Work and Pay Peer Support (PCCI)
Treatment and Service
• Storytelling Training (PCCI)
• Peer Institute (PCCI)
• Community Support Program (PCCI)
• Certified Peer Specialist Training (PCCI)
• Cure Violence
• Healing Hurt People
• DBHIDS Diversity Gaps Analysis and Employee Survey (DEI)
Health Economics
• Healing Spaces (DEI)
• Wellness plans across all PI units (PCCI)
• Engaging Males of Color (DEI)
• Faith and Spiritual Affairs (CBSD)
• Porch Light (CBSD)
• Same Day Work and Pay Peer Support (PCCI)
DBHIDS Systems Integration Unit
Innovation
pg. 6
ENGAGING COMMUNITY
• Regional Collaborative
Biobehavioral Catchup Program
• Attachment
• Philadelphia That All May Worship
• Project Impact
• Behavioral Health/Intellectual disabilities Community Treatment Team (BHID CTT) Initiative
• Coaching Across Settings
• IDS Quality Management Initiative
Services
ACHIEVING EQUITY
• LifeSharingEverybody deserves a family
• Social Emotional Support for PHL PreK
• Project Impact
ADDRESSING TRAUMA
• Connect Philadelphia's infants and toddlers, who are at risk for social/emotional concerns, to Infant Toddler Early Intervention (ITEI)
Prevention and Early Intervention
• Social Emotional Support for PHL PreK
• LifeSharingEverybody deserves a Family
• Behavioral Health/Intellectual disabilities Community Treatment Team (BHID CTT) Initiative
• Coaching Across Settings
• Behavioral Health/Intellectual disabilities Community Treatment Team (BHID CTT) Initiative
Treatment and Service
• Trauma Screener
• Coaching Across Settings
Health Economics
DBHIDS Systems Integration Unit pg. 7
Intellectual disAbility
ENGAGING COMMUNITY
• Crisis Intervention Training (CIT)
• Civil Mental Health Court
• 911 Triage
• MacArthur Safety and Justice Challenge
• Veteran Initiative Unit
• CoResponder Pilot Program
• Expanded Community Residential Treatment Beds
• First Judicial District Mental Health Court
• MacArthur Safet y and Justice Challenge
• Expanded Community Residential Treatment Beds
• First Judicial District Mental Health Court
Behavioral Health and Justice Division
ACHIEVING EQUITY
• Crisis Intervention Training (CIT)
• Philadelphia Municipal Accelerated Misdemeanor Program (AMP) Expansion
• Department of Corrections Re entry
• Forensic Certified Peer Specialist Team
• MacArthur Safety and Justice Challenge
• Forensic Support Team
• HiFive Supportive Housing Initiative
• COVID19 Master Lease Program
• Reentry Initiatives
• Alternatives to Detention Philadelphia Department of Prisons (PDP) Reentry
• Pretrial Services
• 911 Triage Desk
• CoResponder Pilot Program
• Expanded Community Residential Treatment Beds
• Adult Probation and Parole Department ATD
• CHIPPS and Norristown State Hospital (NSH) Downsizing
• Department of Corrections Reentry
• Forensic Certified Peer Specialist Team
• HiFive Supportive Stepping Up Initiative
• COVID19 Master Lease Program
• Reentry Initiatives
• Alternatives to Detention PDP Reentry
• MacArthur Safety and Justice Challenge
• Philadelphia Municipal AMP Expansion
• HiFive Supportive Housing Initiative
• Stepping Up Initiative
• Crisis Intervention Training (CIT)
• MacArthur Safety and Justice Challenge
• 911 Triage Desk
• Step ping Up Initiative
• CoResponder Pilot Program
• Expanded Community Residential Treatment Beds
ADDRESSING TRAUMA
• Crisis Intervention Training (CIT)
• Philadelphia Municipal Accelerated Misdemeanor Program (AMP) Expansion
Prevention and Early Intervention
• Suicide Prevention Task Force
• Increase the number of individuals released from jail who are connected to BH Services within 7 to 30 days
Treatment and Service
• Adult Probation and Parole Department Alternatives to Detention (ATD)
• Department of Corrections Reentry
• Forensic Certified Peer Specialist Team
• MacArthur Safety and Justice Challenge
• Forensic Support Team
• HiFive Supportive Housing Initiative
• COVID19 Master Lease Program
• Reentry Initiatives
• Alternatives to Detention Philadelphia Department of Prisons (PDP) Reentry
• Pretrial Services
• 911 Triage Desk
• Veteran Initiative Unit
• CoResponder Pilot Program
• Expanded Community Residential Treatment Beds
• Adult Probation and Parole Department ATD
• CHIPPS and Norristown State Hospital (NSH) Downsizing
• Department of Corrections Reentry
• Forensic Certified Peer Specialist Team
• HiFive Supportive Stepping Up Initiative
• COVID19 Master Lease Program
• Reentry Initiatives
• Alternatives to Detention PDP Reentry
• MacArthur Safety and Justice Challenge
• Philadelphia Municipal AMP Expansion
• Pretrial Services
• Expanded Community Residential Treatment Beds
• HiFive Supportive Housing Initiative
• Stepping Up Initiative
• Improve linkages and data sharing to extend community tenure
• CHIPPS and NSH Downsizing
• Crisis Intervention Training (CIT)
• MacArthur Safety and Justice Challenge
• Philadelphia Municipal AMP Expansion
• 911 Triage Desk
• Stepping Up Initiative
• CoResponder Pilot Program
• Expanded Community Residential Treatment Beds
Health Economics
• Pretrial Services
• Expanded Community Residential Treatment Beds
• HiFive Supportive Housing Initiative
• Stepping Up Initiative
Infrastructure and Intelligence
• CHIPPS and NSH Downsizing
• Crisis Intervention Training (CIT)
• MacArthur Safety and Justice Challenge
• Philadelphia Municipal AMP Expansion
• 911 Triage Desk
• Stepping Up Initiative
• CoResponder Pilot Program
• Expanded Community Residential Treatment Beds
Innovation
pg. 8
DBHIDS Systems Integration Unit
ENGAGING
• Mobile Outreach and Recovery Services (MORS)
• BHSI (covers uninsured and underinsured individuals)
• Mobile Methadone Maintenance Treatment (MMT)
• Warm Handoff
• Homeless Outreach
• Targeted Case Management ( MH and SUD)
• Electronic Pre and Post Surveys for Prevention Programs
• Mobile Outreach and Recovery Services (MORS)
• Mobile MMT
• Electronic Pre and Post Surveys for Prevention Programs
ACHIEVING EQUITY
• Prevention Services
• Student Assistance Program (SAP)
• Early Intervention Programs
• Core Substance Use Treatment Services
• Mobile Outreach and Recovery Services (MORS)
• BHSI (covers uninsured and underinsured individuals)
• Mobile Methadone Maintenance Treatment (MMT)
• Pregnant and Parenting Services
• JOH Peer Pilot
• JOH Couples Program
• Recovery Houses
• Returning Citizens Housing Program
• Residential Housing Services
• Warm Handoff
• Homeless Outreach
• Targeted Case Management (MH and SUD)
• Electronic Pre and Post Surveys for Prevention Programs
• Update to Mainstay
• Qlik Reporting
• Prevention Services
• Mobile MMT
• JOH Peer Pilot
• JOH Couples Program
• Returning Citizens Housing Program
• Electronic Pre and Post Surveys for Prevention Programs
ADDRESSING TRAUMA
• Prevention Services
• Student Assistance Program (SAP)
• Problem Gambling Prevention
Prevention and Early Intervention
• Early Intervention Programs
• Core Substance Use Treatment Services
• Mobile Outreach and Recovery Services (MORS)
Treatment and Service
• BHSI (covers uninsured and underinsured individuals)
• Mobile Methadone Maintenance Treatment (MMT)
• Wound Care
• Pregnant and Parenting Services
• JOH Peer Pilot
• JOH Couples Program
• TIP
• Safe Havens
• Recovery Houses
• Returning Citizens Housing Program
• Residential Housing Services
• Warm Handoff
• Homeless Outreach
• Targeted Case Management (MH and SUD)
• Mental Health Treatment and Services
• Returning Citizens Housing Program
• Mobile MMT
• Wound Care
• Housing Subsidies
• Shared Housing Project
• MORS
Infrastructure and Intelligence
• Journey of Hope (JOH) Peer Pilot
• (JOH) Couples Program
DBHIDS Systems Integration Unit
Innovation
pg. 9 Behavioral Health Division
COMMUNITY
TRAUMA
• Trauma Training • Training for Providers and Community
• Trauma Aware Community
• Grant Writing
• Grant Writing • Reinvestment Plans
• Training for providers and community
• Trauma training for staff and community
• Trauma Training
• Training for Providers and Community
• Trauma Aware Community
• Health Choices Contract Oversight
• Compliance training
• Workforce Planning
• Health Insurance Portability and Accounta bility Act (HIPAA) Compliance
• Fiscal Staff Cross -Training
• Post Review Process
• Hybrid Work Planning
• Fiscal Policies and Procedures Manual
• Performance Improvement Plan (PIP) process
• Help Desk Support
• Business Intelligence
• Data Management
• Disposition of paper files and records
• Reinvestment Plans
• Sustainment Plans
and Service
• Training for providers and community
• Trauma training for staff and community
• Employee Wellness
• Process for Sanctions and Exclusions
• Background checks for providers, vendors, consultants
• MSD Manual
• Onboarding and Offboarding
• Project Management
• Project Repository
• Hybrid Work Planning
• Grant Writing
• Quality Management Dashboard
and Intelligence
• Quality Oversight
• Complaints Process
• Complaints and Grievances Oversight
DBHIDS Systems Integration Unit pg. 10 Administration, Finance, and
ADDRESSING
ACHIEVING
ENGAGING COMMUNITY Prevention
Quality
EQUITY
and Early Intervention
Treatment
Health Economics
Infrastructure
Innovation
Engaging Community
• Suicide Prevention Task Force
• Behavioral Health Screenings
• Healthy Minds Philly
• Philadelphia System of Care
• Philadelphia Systems of Care (PSoC) Communities of Care
• Youth Move Philadelphia
• Healthy Minds Philly
• Philadelphia System of Care
• PSoC Communities of Care
• Ad ult Mobile Crisis Response Teams
• Alternative Response (AR2)
• Healthy Minds Philly
• PSoC Communities of Care
Achieving Equity
Office of the Chief Medical Officer Addressing Trauma
• Behavioral Health Screenings
• Healthy Minds Philly
• Philadelphia System of Care
• Philadelphia Systems of Care (PSoC) Communities of Care
• Family Member Committee
• Behavioral Health/Intellectual disAbilities (BHID) Clinical Consultations
• Healthy Minds Philly
• Philadelphia System of Care
• PSoC Communities of Care
• Healthy Minds Philly
• PSoC Communities of Care
• Clinical Fieldwork Pipeline
• Suicide Prevention Task Force
• Philadelphia System of Care
• Philadelphia Systems of Care (PSoC) Communities of Care
Prevention and Early Intervention
• Youth Move Philadelphia
• Behavioral Health/Intellectual disAbilities (BHID) Clinical Consultations
• Continuity of Care
• Alternative Response (AR2)
Treatment and Service
• Philadelphia System of Care
• PSoC Communities of Care
• Philadelphia Crisis Line (PCL)
• Adult Mobile Crisis Response Teams
• Crisis Response Center (CRC) Expansion
• Behavioral Health Urgent Care
• Admissions, Discharges and Planning Team (ADAPT)
• BHID Clinical Consultation
• Philadelphia Crisis Line (PCL)
• Reducing Coercive Care Strategies: 302 Strategies
• Care Traffic Control
• PSoC Communities of Care
• Clinical Fieldwork Pipeline
Health Economics
Infrastructure and Intelligence
Innovation
DBHIDS Systems Integration Unit
pg. 11
Community Behavioral Health
ENGAGING COMMUNITY
• Cognitive Behavioral Therapy (CBT)
• Parent Child Interaction Therapy (PCIT)
• Ecosystemic Structural Family Therapy (ESFT)
• Philadelphia Alliance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Intensive Behavioral Health Services (IBHS)
• Cognitive Behavioral Therapy (CBT)
• Parent Child Interaction Therapy (PCIT)
• Ecosystemic Structural Family Therapy (ESFT)
• Philadelphia Alliance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Intensive Behavioral Health Services (IBHS)
• High Fidelit y Wraparound
• Evidence Based Practices Program Designation
• Recovery Oriented Cognitive Therapy
• Residential Taskforce Recommendations
• Value Based Purchasing
• Cognitive B ehavioral Therapy (CBT)
• Parent Child Interaction Therapy (PCIT)
• Ecosystemic Structural Family Therapy (ESFT)
• Philadelphia Alliance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Intensive Behavioral Health Services (IBHS)
• Value Based Purchasing
• Value Based Purchasing
• Philadelphia Alli ance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Intensive Behavioral Health Services (IBHS)
• High Fidelity Wraparound
• Community Autism Peer Specialist (CAPS)
ACHIEVING EQUITY
• Cognitive Behavioral Therapy (CBT)
• Parent Child Interaction Therapy (PCIT)
• Ecosystemic Structural Family Therapy (ESFT)
• Philadelphia Alliance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy ( TFCBT)
• Intensive Behavioral Health Services (IBHS)
• Cognitive Behavioral Therapy (CBT)
• Parent Child Interaction Therapy (PCIT)
• Ecosystemic Structural Family Therapy (ESFT)
• Philadelphia Alliance for Child Trauma Services
• High Fidelity Wraparound
• Evidence Based Practices Program Designation
• Recovery Oriented Cognitive Therapy
• Value Based Purchasing
• Intensive Behavioral Health Services (IBHS)
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Cognitive Behavioral Therapy (CBT)
• Parent C hild Interaction Therapy (PCIT)
• Ecosystemic Structural Family Therapy (ESFT)
• Philadelphia Alliance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Intensive Behavioral Health Services (IBHS)
• Value Based Purchasing
• Value Based Purchasing
• Philadelphia Alliance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Intensive Behavioral Health Services (IBHS)
• High Fidelity Wraparound
ADDRESSING TRAUMA
• Cognitive Behavioral Therapy (CBT)
• Parent Child Interaction Therapy (PCIT)
• Ecosystemic Structural Family Therapy (ESFT)
Prevention and Early Intervention
• Philadelphia Alliance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• I ntensive Behavioral Health Services (IBHS)
• Cognitive Behavioral Therapy (CBT)
• Parent Child Interaction Therapy (PCIT)
Treatment and Service
• Ecosystemic Structural Family Therapy (ESFT)
• Philadelphia Alliance for Child Trauma Services
• High Fidelity Wraparound
• Evidence Based Practices Program Designation
• Recovery Oriented Cognitive Therapy
• Dialectical Behavior Therapy (DBT)
• Prolonged Exposure (PE)
• Residential Taskforce Recommendations
• Value Based Purchasing
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Intensive Behavioral Health Services (IBHS)
• Cognitive Behavioral Therapy (CBT)
• Parent Child Interaction Therapy (PCIT)
• Ecosystemic Structural Family Therapy (ESFT)
• Philadelphia Alliance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Intensive Behavioral Health Services (IBHS)
• Value Based Purchasing
• Value Based Purchasing
• Philadelphia Alliance for Child Trauma Services
• TraumaFocused Cognitive Behavioral Therapy (TFCBT)
• Intensive Behavioral Health Services (IBHS)
• High Fidelity Wraparound
Health Economics
Infrastructure and Intelligence
Innovation
DBHIDS Systems Integration Unit pg. 12
APPENDIX B
SIGNIFICANT INCIDENT RESPONSE MODEL
Stage Description
1 Post-Trauma Impact & Needs Assessment
Post-Trauma Impact & Needs Assessment is the first phase of the Post-Traumatic Stress Management {PTSM) continuum of trauma and evidence-informed, population and public health community interventions, and thus constitutes an intervention on its own. The Post-Trauma Impact & Needs Assessment is coordinated by Network of Neighbors staff and implemented by the impacted community’s natural leadership (Community Connectors) and continues throughout the duration of the response. Since the Impact & Needs Assessment is a joint effort between Network of Neighbors staff, system partners, and the impacted community’s leadership, at least one community point-of-contact (Community Connector) must be identified prior to beginning the process, It should be noted that the Network of Neighbors incident response process occurs separately for each impacted community that makes contact with the Network of Neighbors. Community here is defined as any group of people with a common affiliation or experience (e.g., witnesses, first responders, neighbors, friends, classmates, etc.). This means that this process may be in effect for multiple communities at the same time who were impacted by the same incident (in different ways).
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 62
Components Goals
1. Virtual and in-person meetings with the impacted community’s natural leadership (Community Connectors) who can serve as trusted credible messengers, advocates, and gatekeepers for the impacted community. These community members are in the best position to re-establish a sense of emotional or psychological safety after the traumatic incident (Macy et. al., 2004), which is the first step in assisting a community after a traumatic incident (Hobfall et.al., 2007). During these meetings, Network of Neighbors staff provide technical assistance, guidance, information and referrals to Community Connectors, who in turn provide the Network of Neighbors with specifics in reference to 1) how their community has been impacted 2) what the needs are and 3) norms, boundaries, culture, and local context. Skipping this step risks further harm to the impacted community, as well as increased distrust between the impacted community and supports and services available to it.
2. Identification of impacted subgroups within the community, based on experience, relationship, as well as gender, age, and developmental level (e.g. eye-witnesses, neighbors, parents and caregivers, classmates, friends, colleagues, etc.)
3. Technical assistance, making use of existing resources, supports, and services-including the community’s own natural strengths and healing practices-service and support referrals (for individuals and families), and overall guidance around the implementation of a trauma-informed community response.
1. To establish a non-intrusive, compassionate presence to help the impacted community marshal their own resources as well as existing supports and services in order to manage the short and long-term impact of the trauma in a way that taps into and strengthens the community’s natural resiliency and connections.
2. Assessment of community’s capacity to handle short-term (acute) issues (and identification of needed resources)
3. Assessment of community’s capacity to handle long-term psychosocial disruptions (and identification of needed resources)
4. Identification of leadership structure (to assist with response planning)
APPENDIX 63
Stage Description
2 Response Coordination Response Coordination involves the planning of community and group-level interventions, recruitment of impacted community members, as well as the alignment of stated community needs with available supports and services, This phase includes ongoing coordination with Community Connectors, as well as Responding Partners, which includes stakeholders and entities involved in the response process, either at the local or system level.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 64
Components Goals
1. Response Planning with Community ConnectorsIdentification of a date/time for the response (or multiple), location, recruitment of impacted community members, messaging, etc.
2. Coordination with Responding Partners (system alignment)-information sharing and coordination of supports and services around the community’s stated needs and preferences. For Philadelphia public schools, the Philadelphia School District Office of Prevention & Intervention is always a Responding Partner, as well as Uplift Center for Grieving Children (when a student or staff member has died). Responding Partners vary depending on the impacted community’s existing relationships and connections, as well as their stated needs.
3. Outreach to CTRs (Community Trauma Responders) and internal DBHIDS supports/programs-Depending on the incident, its impact on the community in question and their stated needs and preferences, the Network of Neighbors reaches out to their network of trained Community Trauma Responders to support the community response, as well as trained DBHIDS staff and DBHIDS programs that are appropriate for the specific response. The Network of Neighbors may take into account specific needs and preferences when reaching out to Community Trauma Responders and internal DBHIDS staff and programs: including language, experience, professional qualifications, affiliation with the impacted community, etc. “The Network of Neighbors always completes a “Response Briefing” regardless of whether or not the community response is supported by Community Trauma Responders or internal DBHIDS staff. However, if they are invited to support their response, their participation in the Response Briefing is mandatory to ensure consistent communication and mitigate the risk of harm.
1. Alignment of community’s stated needs, boundaries, norms, preferences and cultural considerations with available supports and services.
2. Planning of a Community Response that includes the community’s voice and ensures that the response takes place at a date, time, and location that is safe, accessible, and convenient for community members.
APPENDIX 65
Stage Description
3 Community Response Community Response involves community and group-level interventions that take place wherever the impacted community regularly meets or feels comfortable, and at a date and time that they have chosen, These interventions vary in their purpose and goals (according to the phase of the community’s healing process, or the time elapsed since the traumatic incident).
The goal section outlines the goals (and purpose) unique to the different kinds of interventions {PTSM, PIES, and PFA). Overall, the goal of these interventions is to:
1. Protect the space for the impacted community to come together for comfort, healing.
2. Reduce and mitigate the impact of the trauma (stress)
3. Provide accurate information, either about the incident or about common reactions to overwhelming stress and practical strategies for coping
4. Foster peer connection and healthy coping
5. Identify community members who may benefit from additional supports and services, or higher levels of behavioral/mental healthcare.
6. Provide support within the context of the community, so that the information and resources are sustained within the community past the duration of the response.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 66
Components Goals
PTSM Orientation Sessions---0-72 hours, or up to 1 week post traumatic incident-open to the entire impacted community
PTSM Stabilization Group/s-0 -2 weeks post traumatic incident-small group discussions for groups with homogeneous exposure
PTSM Coping Groups/s and PTSM Follow-Up Coping Groups-2 Weeks-3 months/1 year post traumatic indentsmall group discussions for groups with homogeneous exposure. **Includes suicide specific protocols
PTSM Compassion Care Discussions-can occur anytime (preventative) or after a traumatic incident, depending on the nature of the impact and the experience of the community members. These Compassion Care discussions focus on how the ‘’work” you do impacts you, which can include the work of being a part of a certain community or performing a certain job/role.
PTSM Pre-Intervention Overviews-Structured information sessions/meet-and-greets designed to build trust and safety with impacted community members before a PTSM small group discussion.
P.I.E.S. Discussions-P.I.E.S. discussions are not part of the formal PTSM evidence and trauma-informed curriculum but are used to build safety and trust with impacted community members before a group intervention. P.I.E.S. discussions are also used within classroom settings and whenever the experience, relationship, and degree of impact of community members is unknown.
PFA Response-Psychological First Aid (PFA) is a oneto-one intervention (also appropriate for working with families) that is used by the Network of Neighbors during the Post-Trauma Impact & Needs Assessment process, as well as during the P.I.E.S. and PTSM interventions on an as-needed basis.
However, PFA Responses involve dispatching Network of Neighbors staff (or PFA trained DBHIDS staff) to community events organized outside of the department to provide PFA support as needed.
PTSM Orientation Sessions: Dissemination of accurate information from stakeholders that can provide needed information (e.g. Philadelphia Police Department, Parks and Rec, Risk Management, L&I, etc.) to calm rumors and reduce heightened stress and arousal. Additional goals include orienting the community to additional supports, and identifying “Community Connectors” or potential subgroups of impacted community members.
PTSM Stabilization: Emphasis on grounding and mindfulness techniques to reduce stress and arousal and safety plan for the short-term aftermath, including preparation for the funeral (if applicable)
PTSM Coping: Opportunity for similarly impacted community members to tell their story, discuss thoughts and reactions (normalize reactions), reduce stigma, receive accurate information and support, discuss coping strategies and begin the healing process.
Compassion Care discussion: Address stress associated with the ‘’work”, as well as challenges and rewards of the ‘’work.” Compassion Care discussions are preventative but sometimes utilized in the aftermath of an incident depending on the community’s unique situation and experience.
P.I.E.S. Discussion--Opportunity for community members to share thoughts and reactions, support each other, and assess/identify the impact as well as community members who cannot identify safety or support.
PFA Responses: PFA responses occur in community settings or designated events or in the immediate aftermath of a traumatic incident. The goal of PFA is to assess immediate needs of survivors and connect them to safety and support.
APPENDIX 67
Stage Description
4 Post-Response
Post-Response is also an ongoing process, as multiple “responses” (see above) may take place over the course of several months or years. The process involves ongoing communication and checking in with the Community Connector/s, who can monitor “the pulse” of the community and assess interest in additional interventions or supports.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 68
Components Goals
1. Connection to long-term supports (e.g. internal DBHIDS programming, Uplift Center for Grieving Children ongoing grief groups, or any supports or services that can fill gaps identified during the response process).
2. Ongoing Technical Assistance and Post-Trauma Impact and Needs Assessment
3. Trainings (in topics identified by the community, to include potentially Psychological First Aid and/or PostTraumatic Stress Management training)
4. Surveying of the Community Connector/s for outcome evaluation
1. Provision and connection to long-term supports in a manner that respects the impacted community’s timeline, boundaries, and stated needs and preferences.
2. Increased trust between the impacted community and existing supports and services
APPENDIX 69
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY
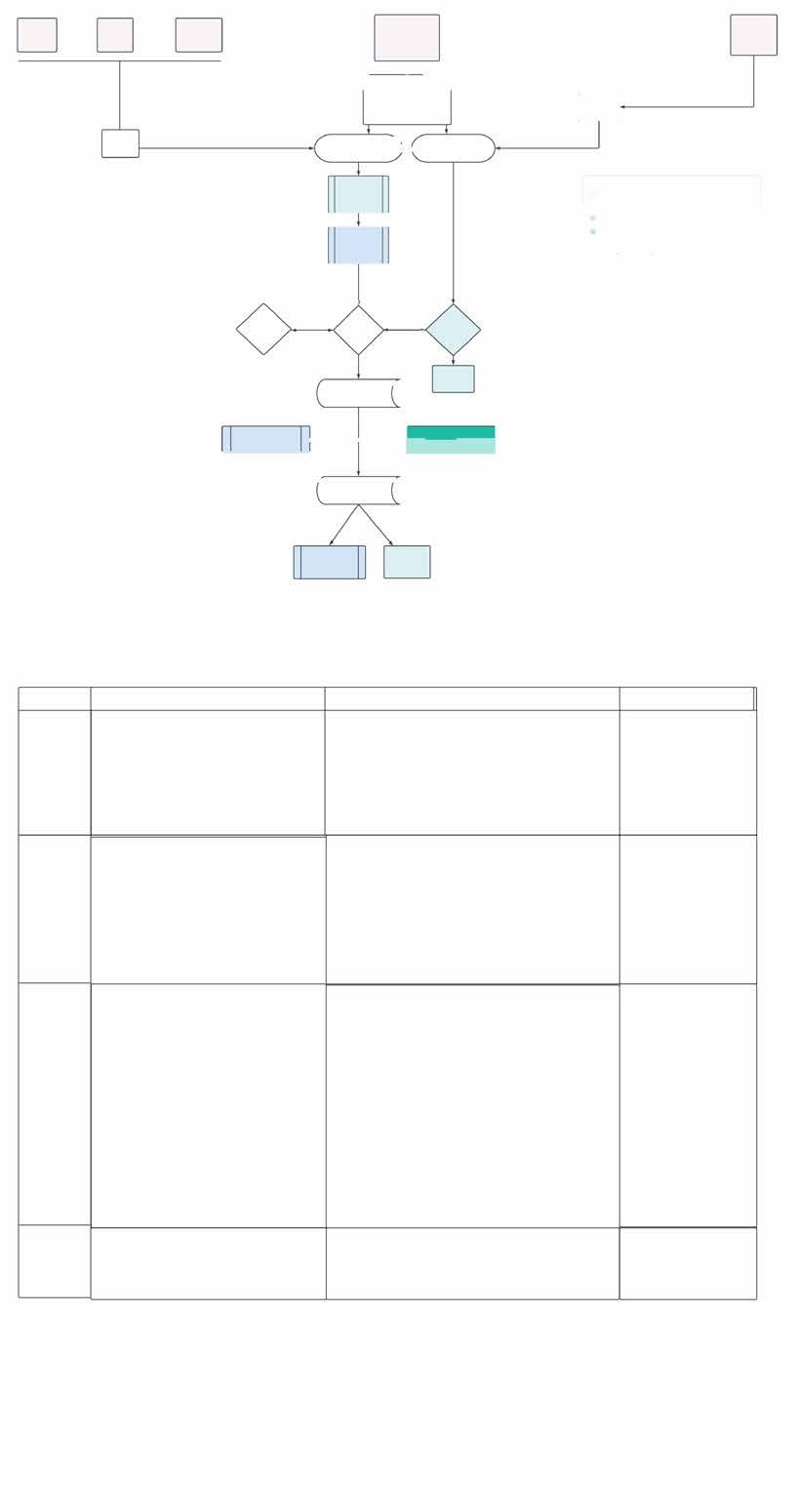
' Elected Officials Stage 1 Stage 2 Stage 3 Stage 4 ""Schools ..PSD requests
through PSD Prevention &Intervention (P&I) Impacted Community (Direct) DBHIDS/Other City Dept. ' Internal/External Stakeholders I "C••�-� non-crisis + + 0-24 hrs/evening/weekend ,.....__________ Trauma Response &
Preparedness Unit ' Network of Neighbors: Trauma \-------. Response Network ,._, Emergency Preparedness
Coordination
' Response Planning w/ Community Connectors Community Response, Outreach to ""CTRs/lnternal DBHIDS Supports Pre-Response Briefing Management
P&,diUlughoal
-Group/Community i.-------t-------<►I (PF'A)
lnl8nlendon *CTRs=Community
11 11 �� �� , Post-Response
, Post-Response Debriefing
go
Emergency
Identification of Community Connector/s (Point/s-of-contact) Post-Trauma Impact & Needs Assessment
w/ Responding Partners (system alignment)
(PTSM)
Fi nllAld
· 1-ly lnteiventions
Trauma Responders (Community Members, School Staff, & agency/city dept. personnel trained in PFA/PTSM) Post-Traumatic Stress
PTSM Follow-Up TrainingfTechnical Assistance Connection to long-term supports
hrs/evening/weekend
Mass Care Coordination
External Stakeholders
*CTRs=Community Trauma Responders (Community Members, School Staff, & agency/city dept. personnel trained in PFA/PTSM)
Diagram Key
Q Entry Point
Q Post-TraumaUc Stress Management (PTSM) Continuum of Trauma & Evidence-Informed, Resiliency-Focused Commuojty Interventions
Q Process Steps inclusive of internal DBHIDS programs (CWEU, PACTS, EMOCS, DEi, etc.)
• Psychological First Aid (PFA) Trauma & Evidence-Informed, Resiliency Focused Individual & Family Intervention-Can be utilized across department/system: including PCL line, Mobile Crisis Teams, CWEU, etc.
APPENDIX 71
Fi
11 �-
APPENDIX C
PROLONGED STRATEGY REPORT
The mission of the City of Philadelphia Department of Behavioral Health and Intellectual disAbility Services (DBHIDS) is to educate, strengthen, and serve individuals and communities so that all Philadelphians can thrive.
We envision a Philadelphia where every individual can achieve health, wellbeing, and self- determination. The principles on which this Prolonged Trauma Research and Best Practices Strategic Framework is built, in alignment with the core values of DBHIDS, include:
• Strength-based approaches that promote hope.
• Community inclusion, partnership, and collaboration
• Person- and family-directed approaches.
• Family inclusion and leadership.
• Peer culture, support, and leadership.
• Person-first (culturally competent) approaches.
• Trauma-informed and trauma-responsive approaches.
• Holistic approaches toward care.
• Care for the needs and safety of children and adolescents.
• Partnership and transparency.
*Read more about the Practice Guidelines for Resilience and Recovery Oriented Treatment at dbhids.org/practice-guidelines.
Overview
DBHIDS is engaged and positioned to address the behavioral health challenges experienced by Philadelphians across a variety of traumatic experiences. Our strategy includes administering existing programming, increased stakeholder engagement at the community-based organization and community level, inclusion of best practices identified across the country, and developing new programming to ensure populations most impacted by immediate and prolonged trauma are given the resources, tools, and supports to heal and ultimately thrive.
Our vision is to ensure there is an accessible continuum of services to address the various types and stages of trauma for all Philadelphians. We do this by:
• Enacting a comprehensive strategy to support people and communities across the city experiencing a variety of traumatic events or circumstances.
• Understanding existing and needed resources, using best practices, and making data-informed decisions.
• Deepening our work with stakeholders to ensure equitable access to resources.
• Bringing solutions from and sustaining solutions in communities.
From October 2021 through March 2022, DBHIDS convened the Prolonged Trauma Research and Best Practices group, a think tank of area experts from academic institutions and community-based organizations.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 72
The goals of the work group were two-fold:
• To develop a roadmap for policies and practices to address prolonged/complex trauma in Philadelphia that will be included in DBHIDS’ comprehensive trauma plan for internal use.
• To create a repository of toolkits, effective interventions, and evidence-based practices to guide the city’s strategic response to prolonged/complex trauma.
The group met monthly for six months. Each month’s meeting was focused on one of the five P.A.C.E. priority areas to garner knowledge and expertise from the experts around Prevention and Early Intervention, Treatment and Services, Health Economics, Infrastructure and Intelligence, and Innovation related to prolonged trauma. This strategic framework is a result of this work.
Defining Trauma
“Trauma” refers to a single event, multiple events, or a set of circumstances that is experienced by an individual or community as physically and emotionally harmful or threatening and that has lasting adverse effects on the individual’s physical, social, emotional, or spiritual well-being. Common traumatic events include domestic and intimate partner violence, physical abuse, community and school violence, medical trauma, natural disasters, terrorism, neglect, and refugee and war zone trauma.
Prolonged trauma, also known as complex trauma, describes the exposure to prolonged, repeated, multiple traumatic events and the effects of this exposure. These events are severe and pervasive, such as abuse, violence, or neglect (Adapted from National Child Traumatic Stress Network definition).
A community can experience prolonged trauma in addition to its individual members. By taking a population health approach, DBHIDS recognizes a need for initiatives that shift from event-based trauma to complex trauma experienced by a larger population, such as racism or poverty, and their effects that can last for generations.
Social Determinants of Health Related to Trauma
The Philadelphia Health of the City 2020 report found that one in five Philadelphians live in a household with an income below the federal poverty line. Although poverty rates declined in recent years, Hispanics and non-Hispanic Blacks are still twice as likely to live in poverty compared to non-Hispanic Whites. Poverty contributes to health disparities within communities. Accessibility to health care and safety from community violence are inhibited by increased poverty. Poverty rates are highest in North and West Philadelphia neighborhoods.
Likewise, these areas have the highest instance of gun violence. City-wide gun violence in 2021 was up 20 percent from 2020. Black men and children make up the majority of gun-related deaths amongst adults and adolescents. Increased prevalence of gun violence contributes to the cyclical effects of traumatic events that influence behavior and health.
Adverse Childhood Experiences in Philadelphia
Adverse childhood experiences (ACEs) are events during childhood, such as abuse, neglect, or exposure to violence, that contribute to trauma. Children of parents with behavioral disorders or who have experienced ACEs themselves or parents who are not present, experience higher instance of ACEs throughout their lives. Prolonged traumatic exposure is linked to increase risk of chronic disease and younger mortality, as well as increased engagement in risky behavioral activities into adulthood.
More than 70 percent of Philadelphia’s adults have experienced one or more ACEs, and members of higher poverty neighborhoods are more likely to experience ACEs and prolonged traumatic exposure. Half
APPENDIX 73
of Philadelphia’s neighborhoods have over 30 percent of resident children experiencing 4+ ACEs. NonHispanic Blacks and Hispanics possess disproportionate rates of ACEs compared to non-Hispanic Whites. Consequently, trauma-related illness and behavioral outcomes in combination with poverty and other social determinants of health increase disparities across Philadelphia’s regions. Disproportionate rates amongst race and neighborhoods suggest a need for services targeted toward stressors unique to each group. Goals of the strategic framework Include:
• To ensure that trauma services are delivered in a racially and socially conscious way
• To reduce individuals’ unnecessary exposure to traumatic events
• To avoid re-harming or re-traumatizing people served
• To create a cohesive repository of trauma resources in Philadelphia
• To align trauma-informed care across mental health and substance use treatment modalities
• To include peers and individuals with lived experience in meaningful roles throughout the traumainformed continuum
• To strengthen connections within the behavioral health system and its partners
• To assess internal organization culture to ensure provider wellness
• To incentivize quality trauma-informed care within community partners
Addressing Special Populations in Prolonged Trauma Behavioral Health Care
The Prolonged Trauma Research and Best Practices framework aims to be accessible to all Philadelphians regardless of unique or specialized needs. Services must be adequately trained and resourced to meet the needs of specialized populations, including, but not limited to, the LGBTQ+ population; individuals with co-occurring behavioral health diagnoses and intellectual disabilities (BHID); immigrants and refugees; and transition-aged youth. When needed, language accommodations, interpreter services, or communication assistance for those using text-based communications devices will be provided. Additionally, all facilities and transports will be compliant with the Americans with Disabilities Act and emotional support and other service animals will be accommodated in facilities. A focus on equity and cultural appropriateness will be applied as trauma research and best practices are developed and expanded. DBHIDS initiatives will provide trauma training and resources that will be modified for occupation-specific needs, including law enforcement, child services and education staff, and health service workers, to ensure wellness amongst care providers in order to adequately address the unique needs of the communities they serve.
Alignment with DBHIDS P.A.C.E. Strategic Plan
In 2018, DBHIDS introduced the P.A.C.E. Strategic Plan. P.A.C.E. stands for Prioritizing to Address Our Changing Environment and is the blueprint for how DBHIDS divisions work together to align, coordinate, and integrate initiatives across the organization has been aligned with the P.A.C.E. Strategic Plan to demonstrate continuity and congruency within and across city agencies and the provider network’s delivery of services within the crisis continuum.
P.A.C.E. is comprised of five key priority areas that include:
• Prevention and Early Intervention
• Treatment and Services
• Health Economics
• Infrastructure and Intelligence
• Innovation
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 74
Each of these priority areas is accompanied by Department-wide strategic goals and key performance indicators that will help us assess our progress towards meeting our goals. Every component of the proposed strategic framework will be guided by the P.A.C.E. Strategy. Learn more about the DBHIDS PACE Strategic Framework at dbhids.org/about/PACE.
DBHIDS TEC Framework: Trauma. Equity. Community.
The City of Philadelphia Department of Behavioral Health and Intellectual disAbility Services works to educate, strengthen, and serve individuals and communities so that all Philadelphians can thrive. In order to focus our efforts, DBHIDS works through a lens we call TEC by asking ourselves every day whether our work addresses Trauma, achieves Equity, and engages Community.
To address Goal By
Trauma Transform operations to be trauma informed Reduce traumatic experiences within systems; shift systems to be traumareducing
Equity Transform systems to reduce behavioral health disparities and promote racial equity amongst Black, Indigenous, and people of color (BIPOC)
Community Shift services to be increasingly communitybased; sustainment through integrating initiatives more fully into communities and neighborhoods
Intentionally address structural and institutional racism; shift systems to achieve equity
Shift services from institutions into community settings
Addressing Prolonged Trauma with P.A.C.E.
Prevention and Early Intervention
Prevention and early intervention services are the foundation of our population health approach, aiming to help individuals protect their health and sustain their wellness. At the community level, activities that support prevention and early intervention include those specifically focused on substance use prevention, as well as those focused on addressing trauma, social isolation, unemployment, homelessness, and other social determinants of health (SDOH) early on, which could otherwise threaten health and wellbeing and contribute to health disparities. Community-level activities also involve infusing communities with a range of advocational, educational, and other supports that increase the number of allies beyond the formal system. DBHIDS follows a three-tiered approach to prevention, developing prevention programming that is universal (for the general public), selective (for individuals or subgroups of the population at risk due to biological, psychological, and/or social factors), and targeted (high-risk individuals with detectable symptoms of mental health disorders). Key components of prevention and early intervention services should be peer-led, using community engagement teams.
Treatment and Services
Comprehensive trauma and mental health services are crucial elements of behavioral health systems. Appropriate trauma-informed services can improve outcomes for individuals, reduce cyclical trauma and violence in communities, reduce over-reliance on law enforcement interventions, and facilitate access to other necessary behavioral health services and supports.
Availability and access to behavioral health services continue to be a complex gap in Philadelphia’s behavioral
APPENDIX 75
health system. Evaluating the efficacy of programs is often victim to survivorship bias—efficacy based on those who “survived” or finished treatment. Special consideration toward those in which treatment and services were not successful could highlight areas in which trauma care can be improved for more diverse populations. By increasing the array of trauma-responsive services available within the communities, the goal is to ensure timely access to the most appropriate treatment resources. With improved and expanded trauma services, we can ultimately create a seamless integrated behavioral health care system, where more Philadelphians can receive appropriate, timely, and quality care.
Health Economics
Thoughtful investments within health systems for effective delivery of trauma care improve health outcomes by focusing on upstream interventions that prevent higher-cost treatments, trauma-influenced behaviors within the community, and potentially retraumatizing treatments. Effective upstream strategies include leveraging the skills and experience of peers within community and clinical settings to improve complexity and competency of care and focusing on the sustainability of participants within programs to ensure wellness before exiting. To succeed in these strategies, a value-based foundation within services can incentivize providers to shift greater focus toward the early identification of trauma and trauma-related health outcomes.
Infrastructure and Intelligence
Each division must have ready access to the specific information it needs to make evidence-based decisions, determine whether our services have the desired impact, and continually improve our system. Infrastructure and intelligence will facilitate transparency and accountability in the operation of a more prolonged traumainformed system. Up-to-date, relevant business intelligence will facilitate a transition from paying for volume to paying for value while improving health outcomes for our city’s most vulnerable residents. Organizational collaboration across all seven DBHIDS divisions and into the community ensures conscious and relevant decision-making for the health of all Philadelphians.
Innovation
As a community, we face unprecedented, complex challenges, exacerbated by the COVID-19 pandemic. The need for innovative approaches that satisfy the goals of the framework, but are adaptable to our changing world is paramount. The Prolonged Trauma Research and Best Practices Strategic Framework sets forth innovative solutions to prolonged trauma at the systemic, community, and individual levels. Innovative use of technology and the arts allows self and population expression that can serve to heal and thrive through creation and community bond while revealing hidden themes in the community that could lead to better-targeted programming. The proposed framework will utilize innovative public health approaches to prolonged trauma treatment to transform the city’s behavioral health system.
Framework Strategies
Through conversations with the Prolonged Trauma Research and Best Practices work group, recommendations were given under overarching themes reflected below. The following table visualizes how each recommendation contains targeted strategies that align with PACE and TEC.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 76
Recommendations
Develop and Improve Asset-based Programming
Asset-based approaches to program formation accounts an individual’s well-being and strengths instead of using numbers like ACEs to determine efficacy within the program. An effective and underutilized community tool to improve trauma-based services is using the skills of the people to leverage their own abilities for sustainable future change. Innovative ways the department can move toward asset-based, skills-focused programming to prevent trauma and treat trauma-impacted individuals include:
• Mentoring and Big Brother/Big Sister programs
• Arts/athletics/other recreational activities
• Re-entry employment programs and entrepreneurial skills workshops
• Summer employment and recreational programs for adolescents at risk of juvenile justice involvement
• Co-designing spaces for place-based projects (parks, housing, art, etc.) within communities
DBHIDS’ Network of Neighbors Trauma Response Network recognizes the power of community members to address trauma within their communities. The program is designed to strengthen local efforts first, and recede into the background as neighborhood networks emerge and strengthen. The Network of Neighbors program falls under the Trauma Response and Emergency Preparedness (TREP) unit and serves as a postvention program, but the department can use these tools and existing connections to further train community members to be trauma-informed even when no immediate response is needed within a community. Educating and supporting trusted leaders within the community, like faith leaders, to understand trauma and its impact on their neighbors can provide upstream, community-based interventions that alleviate the need for clinical treatment or postvention responses along the continuum of services and supports.
There are several programs operating in Philadelphia that address trauma from an asset-based, upstream approach. Please see Appendix A for a listing of programs recommended by the work group.
APPENDIX 77
Prevention and Early Intervention Treatment and Service Health Economics Infrastructure and Intelligence Innovation Trauma Equality Community Asset-based Programs x x x x x x x Capacity Building x x x x x x x x Inclusion x x x x x x x Strengthen Collaboration Between Systems x x x x x x x x
Asset-based approaches must also be applied from an infrastructure and intelligence lens. Current literature rejects catastrophizing approaches to adverse childhood experiences and other prolonged trauma exposures. For example, using data to state that someone with four or more ACEs has a shorter life expectancy than someone with one or fewer ACEs removes power from individuals and communities. DBHIDS must promote the use of asset-based measurement tools as opposed to negative.
Targeted Approaches to develop and improve asset-based programming
• Implement metrics and measures that are asset-based (e.g. measuring social capital, mentorship, belonging, etc. As opposed to trauma exposures, ACEs scores, etc.)
• Develop community-based training programs (similar to Network of Neighbors) to enhance community capacity to prevent and respond to trauma.
• Invest in upstream approaches to trauma prevention and treatment, such as healing therapies through the arts, music, green spaces, etc.
Expand Upon Individual, Organizational, and Systemic Capacity Building
Philadelphia’s past approaches to moving interventions and services toward being trauma Informed have been disproportionately focused on staff-client relationships. A more sustainable approach will include more institutional approaches toward organizational culture, within the department itself, and within community organizations. Although community wellness is DBHIDS’ mission, ensuring the wellness of providers and the organization overall should be a priority to deliver the best interventions to the community. Mitigating secondary, or vicarious, traumatic stress can improve the behavioral health workforce to protect those that serve our most vulnerable populations. Organizational stress can severely impact the ability to provide for our community, from how we combat overarching collective disturbances throughout the behavioral health system, down to avoiding workplace violence and keeping providers safe. To improve the trauma-informed organizational culture, programs can start with a self-assessment:
• Professional quality of life measure proqol.org
• Trauma-informed organization assessment (includes STS) bit.ly/Trauma-informed-STS
• STACI (University of Kentucky) uky.edu/ctac/stsscale
• VTORG: Vicarious Trauma Organizational Assessment bit.ly/VTORG
DBHIDS can further assess capacity by integrating more interdisciplinary perspectives to trauma interventions throughout the whole department. By training our staff across different divisions and throughout our provider network to be more trauma-informed and how to effectively deliver EBPs, we can move siloed trauma practices toward a more multifaceted approach.
Targeted approaches to expand upon individual, organizational, and systemic capacity building
1. Address implicit biases among DBHIDS provider network staff. We will not be able to effectively build trauma-informed practices and policy without first addressing personal bias.
2. Conduct an organizational self-assessment of DBHIDS to address secondary traumatic stress internally.
a. Can repeat this process externally across the DBHIDS provider network.
3. Review existing data from CBH, EPIC, NIAC, and DBHIDS to assess DBHIDS provider network capacity (licensure, skills, trainings, etc.) and identify gaps
a. Develop a summary report of readiness within the DBHIDS provider network
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 78
b. Develop a needs assessment for education and training of the provider network
4. Develop an inventory of trauma-informed and healing-centered programming in Philadelphia (see Appendix A).
5. Institute modular approaches to therapy interventions for faster results. Explore Modular Approach to Therapy for Children with Anxiety, Depression, Trauma, or Conduct Problems (MATCH-ADTC). EBPs, when available, can be cumbersome for families to maintain/follow through the full course of treatment. Modular approaches introduce EBPs in segments (modules) and potentially allow individuals to gain skills and make progress in fewer sessions.
6. Build network ability to serve the whole family. Examine billing policies and practices that only allow providers to bill for the primary recipient of services when the trauma is a systemic/family concern.
7. Create educational programming that teaches individuals and families how to navigate complex systems and advocate for themselves.
Institute Multifaceted and Meaningful Inclusion Practices
To address trauma within the city, acknowledging where strategies fall short is important to amend programs and avoid re-harming or re-traumatizing the people served. A pillar of this framework is a theme of inclusion—including lived experience and community voice in the program development and decisionand policy-making processes. Through this, the department can recognize what existing trauma-informed programs are not working. Inclusion of the community voice through the implementation of services shares power within the transparency of decision-making between the community and the department and ensures that programs have trauma-reducing policies targeted to the direct needs of the people served. Transferring power outside of city government into the hands and voices of community members is a proven method of ensuring needs are met through an on-the-ground perspective. Promoting policies that were designed through a participatory process ensures that programs have traumareducing policies. By sharing peer experiences through the power of storytelling, the department can learn how people navigate through the behavioral health system and find solutions where wellness and safety fall short. Community listening sessions hosted by DBHIDS can provide a new point of view for the department to work from while offering the community an outlet to discuss matters around trauma within the city. Through these sessions, different perspectives from different communities, especially those who have been underrepresented within programs, can speak to how different SDOH influence trauma and healing. Using these sessions as qualitative information gathering can be a form of departmental self-reflection on how current programs are meeting the specific needs of some communities but leave out others and can orchestrate how researchers collect quantitative data to find better evidence-based trauma interventions for community wellness.
Targeted approaches to institutes multifaceted and meaningful inclusion practices:
1. Focus on diversity, equity, and inclusion efforts across the DBHIDS provider network.
a. Start with clear definitions of equity, power, privilege, diversity, and inclusion.
b. Acknowledge the privilege and power that DBHIDS maintains, and begin to work towards providing tangible opportunities to redistribute the system’s power to the people without power and privilege.
c. Ensure that shared definitions of power, equity, and inclusion are used when evaluating programs or services, who is awarded funding, and who is accessing services.
2. Examine programs’ inclusion/exclusion policies. Revise policies that expel individuals for noncompliance/non-adherence to programmatic restrictions.
APPENDIX 79
a. Address survivorship bias – consider people for whom programs were not effective, and examine what it was about those programs or policies that did not work for them.
3. Develop future DBHIDS programming and policy through a participatory process (DBHIDS advisory board, community meetings, etc.)
4. Collect qualitative data and emphasize the value of storytelling and qualitative data collection. Qualitative data must inform quantitative evaluation approaches
Strengthen Collaboration Between Systems
Collaboration with other Philadelphia public systems—the Department of Public Health, the Department of Human Services, the School District of Philadelphia, the Philadelphia Police Department—can ensure delivery of trauma-informed care at all levels while being aware of what sectors cross at the wrong paths. Integrating services where they should not be can be retraumatizing. Non-traditional approaches to treatment and services like meeting people and families within the communities they live, work, and play in to deliver behavioral health care, instead of a clinical setting, allows interventions to be delivered where people feel safest. Additionally, conducting a gap analysis within the DBHIDS network can improve collaboration between systems. Coordination of shared data between systems can connect divisions within community conversations to bring trauma programs they are needed most in the city.
DBHIDS can explore innovative funding streams to support providers in care coordination and their ability to work with families and caregivers to incentivize family models of care and address SDOH. The department can play a role in leading organizations in advocacy for increased and enhanced funding opportunities at the state and federal level.
It is critical to incentivize EBPs by offering enhanced reimbursement rates for designated providers and increase capacity of EBPS throughout the behavioral health system. Providers that receive the EBP Program Designation rates are expected to develop strategies to direct financial incentives to the clinicians delivering the EBP. Enhancing staff compensation and retention of EBP-skilled staff is a crucial strategy for EBP sustainability.
Targeted approaches to strengthen collaboration between systems
1. Conduct an assessment based in “user experience” at the intersection of multiple systems: where are the pain points? Where could someone be traumatized or re-traumatized? Focus on institutional coordination to approach an individual holistically.
2. Cross-system review of traumatic events in schools (modeled from OD-STAT)
3. Standardize metrics that are collected from DBHIDS provider network
4. Standardize screening practices across DBHIDS provider network
5. Develop the External Stakeholders Trauma Workgroup to translate research into practice
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 80
What’s Next?
The Department of Behavioral Health and Intellectual disAbility Services is seeking to expand and improve the continuum of prolonged trauma services in Philadelphia. Through discussions with stakeholders, as well as Request for Information (RFI) and Request for Proposal (RFP) processes, DBHIDS is soliciting information and ideas from behavioral health providers, law enforcement, community-based organizations, family members, people with lived experience, and other stakeholders to expand and re-imagine the adult behavioral health crisis continuum, and procure provider partners.
DBHIDS serves the city’s most vulnerable individuals, families and communities as evidenced by our longstanding commitment to recovery, resilience, and self-determination. As the leader of Philadelphia’s behavioral health system, DBHIDS has developed the Prolonged Trauma Research and Best Practices Strategic Framework to envision an expanded and improved trauma continuum in Philadelphia. The Strategic Framework responds to DBHIDS’s mission by providing an evidence-based, real-world vision to advance Philadelphia’s adult crisis system.
Acknowledgments
Jonathan Arrieta (Impact Services)
Meagan Corrado, DSW, LCSW (West Chester)
Jeanne Felter, Ph.D., LPC (Jefferson)
Racquel Fetzer, CPS, CFPS (DBHIDS)
Reginald Howard, CPS, CHW (Drexel)
Sara Jaffee, Ph.D. (Penn)
Leslie Liberman (Health Federation of Philadelphia)
Kelly Moore, Psy.D. (Rutgers)
Michael O’Bryan (Drexel, Lindy Institute)
Casey O’Donnell (Impact Services)
Joe Pyle (Scattergood Foundation)
Mary Grace Ryder (CCTC)
Antonio Valdes (CCTC)
Laura Vega, DSW, LCSW (CHOP)
Roy Wade, Jr., M.D., Ph.D., MPH, MSHP (Penn)
Roberta Waite, Ed.D. (Drexel)
APPENDIX 81
APPENDIX D FOCUS GROUP – PEOPLE WHO HAVE PERPETRATED CRIMES
Focus Group Draft Report
RE: Focus Group with those who perpetrated violence to learn about ideas to curb future violence in Philadelphia County
DATE: Feb. 8, 2023
FROM: Systems Integration Unit
Overview
This project came out of the DBHIDS “Trauma Related to Violence” subcommittee discussions. This subcommittee works on supporting the Philadelphia community who have trauma related to violence. Dr. Megan Corrado suggested that this subcommittee gather qualitative research through conversations with individuals who committed violent crimes in Philadelphia to understand the root causes of violent crime and to propose solutions. Following up on this idea, we gathered five individuals who committed violent crimes in their past and listened to their life experiences and what led them to violence. We listened to their insight, from their lived experience, about what actions could have changed the trajectory of their life and have proposed solutions to prevent violent crime in Philadelphia.
Conversation 1: Adults who committed violent crime in Philadelphia
We spoke to five adults who currently work for Philadelphia Anti-Drug Anti-Violence Network (PAAN) who self-identified as growing up in Philadelphia and who committed violent crimes. George Mosee from PAAN connected these individuals to Kyle Carter, Assistant Director of Systems Integration, and Rebecca Curry, Master of Public Health Intern, to participate in this focus group. The interviewees all accepted the invitation and actively participated in this discussion. The focus group was administered over Zoom on Dec. 19, 2022, at 6 p.m.
Below are the notes from this conversation. Included are the questions asked of the participants and their answers.
1. How has violence impacted your life personally?
a. Participant A – affected life since a kid. Grandfather used to abuse grandma, he shot her in the head, but she didn’t die. 1992 his friend was murdered. Been around violence whole life. Whole life and raised – if someone slighted you, violence was response. Learned violence.
b. Participant B – grew up around violence. Grew up in 70s and gangs then in Nicetown. Watched as a kid, six years old riding a big wheel, gang members hitting each other over head with wine bottles, saw guy stabbed in the arm, and mom grabbed him and took him inside. Seen people get shot in the street. Working at PAAN he was shot in the right arm, by a kid (16/17 years old). He has coped with it all because he was immune to it. Violence been around whole life – streets, father abused mother when he was young, seen people being shot.
c. Participant C – Violence comes from family – father overly aggressive with mother and he took out his aggression he saw at home and took it out with those in the streets since he couldn’t fight his father. Saw people in the crowd was fighting and that was his surroundings.
d. Participant F – grew up around it. Closest cousin was shot and killed when he was 16 and participant was 12. Uncle doing life, he saw intimate partner violence with his mom. Seen a lot.
e. Participant D– violence was around her whole life. Saw her mom beaten by a man, two brothers
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 82
facing life, cousin was shot at the corner of her block (started to tear up when talking).
2. Do you feel like the presence of gangs or cliques is leading to the uptick of violence?
a. Participant E – yes, gangs. Sees on a daily basis on social media for cliques. Five or six guys with no structure and violence comes from there.
b. Participant A – Gangs since the 70s. Cliques are not new. Different neighborhoods have fist fight every now and then. Now seeing a lot of guns. Uptick in stabbings – couple months quadruple. Stabbed with knives. Triggered over drill music, rap music, Reddit. Younger people – shooters and victims are getting younger.
c. Participant B – For A lot of these kids drill music was explained to him recently music has a tendency to influence young people and can get folks to want to participate in what is in the music. Desensitized to violence, even to guns. Ghost gun – order different parts to get shipped and assemble the guns themselves. Kids that are as young as 13/14 years old. Shaped by surroundings and the older kids and think it’s “cool” to kill someone. Kids think it is some kind of game until they see the outcome – jail. Kids don’t think they are going to get shot. Same day that a kid was shot, someone died. Shooter didn’t see who he wanted to shoot so decided to shoot up the corner –one died. Two kids were shot when that happened shot, and other person was shot as well.
d. Participant E – Kids don’t understand the consequences of the violence. Kids are getting younger doing the crimes. “Wave of death” carries on way after the act itself. Goes to the Juvenile Justice Center to talk to youth. When a crime is committed, it affects the whole community. Kids don’t understand this.
e. Participant C – used to ask the old heads but don’t have old heads. Who you socialize with everyday are all the same age. No one to look up to anymore because old heads are on drugs, dead, or in jail. Young people have no one to respect/look up to.
3. Do you feel that underlying issues of respect or distrust with police are fueling inner city violence?
a. Participant C - Lack of respect. Kids don’t have any guidance. There is no respect for the police today. Threatening police today and someone is teaching young kids that they will not be held accountable as an adult will be. Kids do not respect authority. No one cares.
b. Participant E – only care about the white people
c. Participant D – Racism is a big part. On TV, white people get away with stuff. Black people won’t shoot a white person and will shoot their own
d. Participant A – All the isms play a big role/part. How the cops treat those in our community plays a part. Modern policing theory is that it was based off of slavery. Deep conversation and deep roots.
e. Participant B – agrees with participant. Cops are out there to do a job. Politics play a role. Participant was incarcerated but he was blamed for something that he didn’t do (threatening someone when he wasn’t there) and the news media were involved. This led the to distrust the police/media/investigative reporting. Politics is involved, selling of newspapers was important to them. Participant was given a life sentence. He was sentenced under the crack law. Participant learned the crack law (disparity between crack and cocaine sentences). Some cops might care but for a lot of them it was just business. Spent around 17 years in prison. Race did play a role in the sentencing he was sentenced under. A lot of components. Act like they care but don’t really and we get the bad end of it. We are self-destructing out here. Adding insult to injury. Need to change the mindset of the people/kids and convince them that this is not the way to go. Late ’80s – carrying a firearm without a license and disorderly conduct before selling crack. Said the cops were shocked that he didn’t have a criminal record at 18 – graduated high school and started community college.
APPENDIX 83
Racism – wants to look at you like always associated as criminals and violence. Crack law came about when the basketball player snorted crack and died. He has been home 2.5 years.
f. Participant D – Kids not having anyone to look up to. Older people are taken away due to crooked laws and left with no one to look up to so they only have each other to look up to and are now killing each other. One big vicious cycle. They are not interested in WHY things happened and just wanted to lock people up.
g. Participants C & E – no one to look up to – only the radio, videos they are making, social media.
4. If anyone has been in the probation process, what resources that might have not been offered that maybe should have been that can potentially prevent someone from reoffending?
a. Participant A – he is on life time parole as a juvenile lifer. His group is different – folks like him got a lot of resources and support. Digital literacy, housing support, how to use an iPhone, he was prepared to go home. He was in prison. Didn’t ask what our needs were, they just told us what our needs were. He has been home for a couple of years. He has not had issues with his probation officer. People he has talked to have not had problems with their probation officer. Maybe because he is older. He got what he needed and he thought it was that way across the state. Support groups who met twice a month for support.
b. Participants – C & E – when he came home, not set up? One little misstep, they will get locked up.
c. Participant D – few years ago got off of probation in a surrounding county. Popping up during her probation. They never reached out to ask how she was doing or asked about her kids.
5. What do you think would be helpful to keep people from committing violence?
a. Participants C, D, & E - Guidance – didn’t get the help they needed. If he had someone to say hey, it would have changed his life.
b. Participant B – if you have a positive person in your life who is a positive influence. Needs schooling. Mentee’s mother passed away, his father isn’t around, kid called Participant “old head.” Participant has adopted him as his old head and can reach out to the participant. Participant is telling him from experience. Telling the kids from experience is helpful he thinks. Participant started his time in Kansas. POSITIVE INFLUENCE. If the kids still want to take that route, the kids cannot say they didn’t know what to expect. Show the younger generation what to do and word spreads that way. Doesn’t have to be an old head who has lived experience but someone to show them the way/another way.
c. Participants C & E – someone who was there consistently would have helped to change the direction of his life. Male figure consistent. Didn’t think he had to listen to no one, he’s fly, and he doesn’t have to listen to anyone. Start from home. He is a product from everyone.
d. Participant D – mom of four sons. Keeps her sons in positive things and keep positive people around them. She doesn’t have a male relationship because she doesn’t want people in and out of her kid’s life.
6. What programs needed?
a. Participant D – need trauma counseling, no mothers, no fathers, they need love. Mental health, background checks for people that work at these places.
b. Participant A – focus on awareness, more rec centers that are operational, spaces for kids.
c. Kyle - Mental health awareness and as African Americans – mental health challenges that are unique to this situation. ELSC mentioned that we have resources but not everyone knows about them.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 84
d. Participant B – influence of money situation. Financial education. Budget money. Simple things like care for themselves. Need all programs – how to cook and take care of oneself- life skills. Nutrition information. Kids focus on money – rob someone for little or nothing. Kids might not have responsible a adult. Learn how to get a job and be responsible themselves. Teach a brother how to fish. Mindset needs to change to learn how to make a legitimate living – may prevent robberies. Teach how to earn money legitimately. Change mindset.
e. Participants C & D – financial literacy.
Takeaways
Many of the interviewees had similar experiences in their youth including domestic violence, feelings of not belonging, lacking in life skills, unmet social determinants of health, and lacking in supportive adult figures for stability. In addition, highlighted below are some take aways from this conversation:
• Drill music trivializes the seriousness of situations and makes the issues mentioned in the music seem “cool,” reinforcing this mentioned behavior.
• Youth are resourceful in obtaining weapons, even purchasing pieces and assembling weapons themselves.
• Social media boundaries are only helpful when there is an adult in the household to monitor social media use.
• The loss of adult mentors or “old heads” hierarchy in neighborhoods and cultures of communities.
• Acknowledgment of racism in the police infrastructure and criminal legal policies. Communities of Color and Black communities do not trust and experience violence at the hands of police.
Ideas for Next Steps
Reflecting on insights gleaned from this conversation, we offer a few suggestions.
• Work alongside domestic violence agencies to support youth who live in households where there is or has been domestic violence.
• Connect youth and the Parks and Recreation Department for safe environments to play and for food access.
• Connect youth to life skills training through the school district of Philadelphia.
• Implement and monitor universal behavioral health screening and social determinants of health screening for youth.
• Connect “opportunity youth” to mentoring programs such as Big Brothers, Big Sisters, and MENTOR to provide adult support to this population.
• Expand the Police Athletic League to build trust between youth, the community, and police.
• Create and manage a network of support groups for individuals and families who have been affected by gun violence. There should be differentiation between support groups for survivors of gun violence, families of survivors of gun violence, and families of victims of gun violence. These groups have different needs, and each need could be best addressed separately.
Conclusion
This focus group was a powerful and unique lens to look at the gun violence issues in this city. This conversation centered the humanity of individuals responsible for gun violence and created a space to learn more about the reasons choices were made to proactively prevent future violent crime. We believe that everyone should have an opportunity to choose a different path for themselves besides a violent one. We look forward to supporting policy changes and programs for Philadelphia’s youth to give them a chance at a healthy and successful life without violence.
APPENDIX 85
APPENDIX E
CHILDREN’S HEALTH AND PREVENTION IN SCHOOLS
City of Philadelphia
Department of Behavioral Health and Intellectual disAbility Services
Substance Use Services Provided in Schools
Below highlights the prevention services available to students and that is coordinated through DBHIDS and the School District’s Office of Prevention and Trauma. All schools have some prevention programming (i.e. SAP Student Assistance Program). The list below includes additional programs that may be selected through conversation between the providers and the SDP’s Office of Prevention Intervention and Trauma to determine additional programs that are a best fit for their school. High needs schools, such as in Kensington, have received program expansion from the prevention providers. Programs funded by Pennsylvania Department of Drug and Alcohol Programs unless otherwise noted.
Program Populations Purpose
1 Student Assistance Program
Elementary, Middle, and High School Students
2 Incredible Years Preschool and Elementary School Students
To assist school personnel in identifying issues including Alcohol, Tobacco and Other Drugs (ATOD) and mental health issues which pose a barrier to students’ success. Services include screening/assessment, consultation, referral and/or small group education for SAP identified youth.
To promote emotional and social competence and to prevent, reduce, and treat behavioral and emotional problems in young children (2 to 12 years old) through three comprehensive, multi-faceted, and developmentally based curricula for parents, teachers, and children.
3 Life Skills Training (LST) Elementary, Middle, and High School Students
To provide elementary students, middle school/junior high students, and high school students with the necessary skills to resist social pressure to smoke, drink, and use drugs; helps them develop greater self-esteem, self-mastery, and self-confidence; enables children to effectively cope with social anxiety; increases their knowledge of the immediate consequences of substance misuse; and enhances cognitive and behavioral competency to reduce and prevent a variety of health risk behaviors.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 86
Program Populations Purpose
4 Nurturing Parenting Programs
The Nurturing Parenting Programs are a family-centered trauma-informed initiative designed to build nurturing parenting skills as an alternative to abusive and neglecting parenting and child-rearing practices. The long-term goals are to prevent recidivism in families receiving social services, lower the rate of multi-parent teenage pregnancies, reduce the rate of juvenile delinquency and alcohol misuse, and stop the intergenerational cycle of child abuse by teaching positive parenting behaviors.
5 Positive Action (PA) Preschool, Elementary, Middle, and High School Students
Positive Action is an integrated and comprehensive curriculumbased program that is designed to improve academic achievement; school attendance; and problem behaviors such as substance use, violence, suspensions, disruptive behaviors, dropping out, and sexual behavior. It is also designed to improve parent–child bonding, family cohesion, and family conflict. All materials are based on the same unifying broad concept (one feels good about oneself when taking positive actions) with six explanatory sub-concepts (self-concept, positive actions for your body and mind, managing yourself responsibly, treating others the way you like to be treated, telling yourself the truth, improving yourself continually).
6
To help students understand the consequences of drug use, recognize the benefits of nonuse, build norms against use, and identify and resist pro-drug pressures. Project ALERT is a school-based prevention program for middle or junior high school students that focus on alcohol, tobacco, and marijuana use through small-group activities, question-andanswer sessions, role-playing, and the rehearsal of new skills to stimulate students’ interest and participation. It seeks to prevent adolescent nonusers from experimenting with these drugs, and to prevent youths who are already experimenting from becoming more regular users. Based on the social influence model of prevention, the program is designed to help motivate young people to avoid using drugs and to teach them the skills they need to understand and resist pro-drug social influences.
APPENDIX 87
Project ALERT Middle School Students
Program Populations Purpose
7 Project Towards No Drug Abuse (TND)
High School Students Project Towards No Drug Abuse (Project TND) is a drug use prevention program for high school youth. The current version of the curriculum is designed to help students develop selfcontrol and communication skills, acquire resources that help them resist drug use, improve decision making strategies and develop the motivation to not use drugs. It is packaged in 12 40-minute interactive sessions to be taught by teachers or health educators. The TND curriculum was developed for highrisk students in continuation or alternative high schools. It has also been tested among traditional high school students.
8 Too Good for Drugs (TGFD) Elementary, Middle, and High School Students
Too Good for Drugs (TGFD) is a school-based prevention program for kindergarten through 12thgrade that builds on students’ resiliency by teaching them how to be socially competent and autonomous problem solvers. The program introduces and develops social and emotional skills for making healthy choices, building positive friendships, communicating effectively, and resisting peer pressure. TGFD teaches five essential social and emotional learning skills:
1. Goal Setting
2. Decision Making
3. Bonding with pro-social others
4. Identifying and managing emotions
5. Communicating effectively
9 CATCH My Breath Middle and High School Students CATCH My Breath is a youth E-cigarette and JUUL prevention program developed by. The University of Texas Health Science Center at Houston School of Public Health. The program provides up-to-date information to equip students with the knowledge and skills they need to make informed decisions about the use of E-cigarettes, including JUUL devices. CATCH My Breath includes active student-centered learning facilitated by peer leaders. The program offers in-class activities, teacher education, online resources, and take-home materials for parents. The program’s key learning objectives include knowledge of-cigarettes and potential harms, understanding and analyzing deceptive advertising techniques, developing, and practicing socially acceptable refusal skills and practicing peer modeling techniques in small groups.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 88
Program Populations Purpose
10 The Council for Boys and Young Men
The Council is a strengths-based approach to promote boys’ safe, strong, and healthy passage through preteen and adolescent years. Using the Council program model, professional mentoring/counseling services, and trained volunteers, the program introduces healthy role models and promotes prosocial behaviors. The Council follows a structured, group curriculum and uses incentives for participation. Each week, for 10weeks, a group of boys of similar age and development meet with two facilitators for two hours. Boys are encouraged to attend for ten weeks or more to get the full benefit of the Council model.
11 Alcohol and Other Drugs (AOD)
Elementary and Middle School Students
Includes alcohol and other drug environmental activities such as policy change, social norms marketing and town hall meetings. EXCLUDES Tobacco-related environmental activities, which are recorded under Tobacco Prevention Activities.
12
Elementary and Middle School Students
Includes alternative activities such as ATOD-free recreational and/or social opportunities, recognition events and leadership/ mentoring activities. 13
Elementary and Middle
Includes community-based process activities such as multiagency collaboration, marketing and developing programs, assessing community needs, and strategic planning.
14 ATOD Education
Youth and Adults Includes alcohol, tobacco, and other drugs prevention education activities. This includes educational programs intended to develop life skills such as refusal skills, decision making and stress management.
Youth and Adults Includes information dissemination activities such as health fairs, speaking engagements, and distribution of brochures, flyers, newsletters, PSAs, etc.
Funded by Pennsylvania Department of Drug and Alcohol Programs
APPENDIX 89
Environmental Activities
Alternative Activities
Alcohol Tobacco and Other Drugs (ATOD)
ATOD Community Based Process Activities
Students
School
Activities
Dissemination Activities
15 ATOD Information
Program Populations
16 ATOD Materials Development
Youth and Adults
Purpose
The creation of original documents and other educational pieces for use in information dissemination activities related to substance misuse and its effects on individuals, schools, families, and communities. Services under this category include audiovisual materials, printed materials, newsletters, public service announcements, and resource directories.
Funded by Pennsylvania Department of Drug and Alcohol Programs
17 ATOD Non-SAP Problem ID and Referral Activities
Elementary, Middle and High School
Includes problem identification and referral activities such as risk screening, referral to services and follow-up. EXCLUDES screening, referral and follow-up done as part of the Student Assistance Program.
Funded by Pennsylvania Department of Drug and Alcohol Programs
18 Beginning Alcohol and Addictions Basic Education Studies (BABES)
Elementary, Middle and High School
Beginning Awareness Basic Education Studies (BABES) is a primary prevention program designed to give children a lifetime of protection from substance misuse. BABES accomplishes this by assisting young people to develop positive living skills and by providing them with accurate, nonjudgmental information about the use and misuse of alcohol and other drugs.
19 PA STOP Campaign Youth and Adults
20 Tobacco Prevention Activities
21 Narcan Training and Distribution
Youth and Adults
Youth and Adults
This strategy is used to capture activities associated with the dissemination and marketing of the Commonwealth Prevention Alliance’s PA STOP campaign which includes education around issues such as opiate misuse.
Types of services included under this program include tobacco education, training, compliance checks, etc.
Since 2016, DBHIDS has offered the opioid overdose prevention and Narcan rescue training in support of bringing awareness to the opioid epidemic in Philadelphia. The training explains the Good Samaritan Act 139 & Pennsylvania’s Standing Order for Naloxone (Narcan) identifies how to recognize signs and symptoms along with risk factors that occur during an overdose. Individuals learn how to administer the life-saving medication and receive Narcan kits once they have completed the training.
Funded by Pennsylvania Department of Drug and Alcohol Programs and Pennsylvania Commission on Crime and Delinquency (PCCD)
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 90
Program Populations Purpose
22 STEP Elementary, Middle and High school Students
The STEP initiative provides mental health, behavioral health and social service support to students and families in select District schools. Each STEP team has a combination of STEP positions that can include a STEP Clinical Coordinator, a STEP School Behavioral Consultant, a STEP Case Manager and a STEP Family Peer. This team of mental health professionals can provide therapy, case management, behavior planning and peer support as well as consult on school wide initiatives with a trauma informed lens. Students and families are wrapped in thoughtful, consistent, and culturally responsive services that can and should lead to better outcomes for students in the classroom and in the community.
Funded through HealthChoices
23 Intensive Behavioral Health Services (IBHS)
Elementary, Middle and High School Students
Intensive Behavioral Health Services (IBHS) support children, youth, and young adults with mental, emotional, and behavioral health needs.
OBHS offers a wide array of services that meet the needs of these individuals in their homes, schools, and communities. IBHS has three categories of services:
1) Individual services which provide services to on child:
2) Applied Behavior Analysis (ABA) which is a specific behavioral approach to services; and
3) Group services which are most often provided to multiple children at a specific place. Evidence- based treatment can be delivered through individual services, ABA services and group services.
Funded through HealthChoices
APPENDIX 91
APPENDIX F
RECAST OVERVIEW
Resiliency in Communities After Stress and Trauma (ReCAST)

ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 92
APPENDIX G
NETWORK OF NEIGHBORS OVERVIEW AND EXPANSION
Network of Neighbors: A Trauma Response Network
The Network of Neighbors is a community-driven trauma response network that works to reduce violence and trauma by responding more effectively to it by working alongside the community to address their experience, define needs and boundaries, and puts community safety and choice first.
The Network utilizes Psychological First Aid (PFA) and Post-Traumatic Stress Management (PTSM), two trauma-informed interventions, for supporting communities impacted by trauma.
DBHIDS Network Response Planners and community members trained as Community Trauma Responders to support — and lead — responses to stress, trauma, loss, and violence within their own communities and aligns with local and citywide supports to protect the safety, dignity, and voice of the impacted community.
Regional Team Model
Network of Neighbors Expansion
Regional Team Model Expansion of the Network of Neighbors staff will include four teams working across four regions of the city , along with administrative staff to support the overall operations of the program



Community Trauma Responders
Members of the community
Trained in trauma-informed approaches , including Psychological First Aid and PostTraumatic Stress Management
Responding to invitations from the community in collaboration with DBHIDS Response Planners

Share skills and enhance the community ' s natural support and strength
Response Planners and Engagement Specialists
Organize community responses

Facilitate interventions and trainings
Conduct community presentations
Recruit Community Trauma Responders
Identify needs and establish ongoing relationships with communities
54
APPENDIX 93
* Response Planners and Engagement Specialists will serve their regions and serve as city -wide responders based on their specialties and skills
APPENDIX H
PHILADELPHIA ALLIANCE FOR CHILD TRAUMA SERVICES OVERVIEW AND EXPANSION


ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 94
2021 PACTS Provider Network
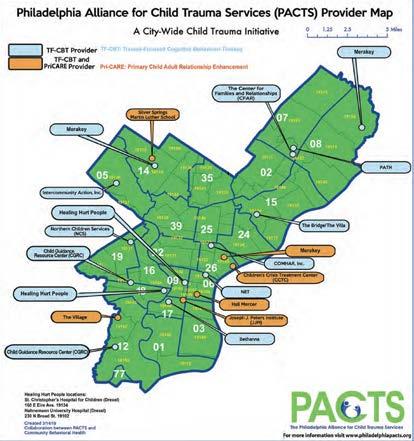
APPENDIX 95
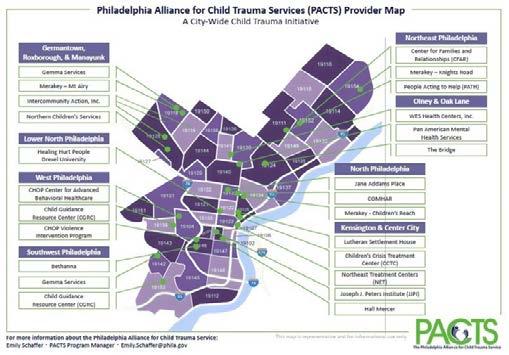
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 96 2023 PACTS
APPENDIX I
PHILADELPHIA SYSTEM OF CARE OVERVIEW

APPENDIX 97
APPENDIX J
COMMUNITY MOBILE CRISIS TEAM OVERVIEW AND EXPANSION
Community Mobile Response Expansion – CMCRT
Creating 24/7 regionalized, city-wide coverage through four providers managing 15to 20 teams that cover shifts throughout the day,evening, bridge, overnight and weekends. Each provider has one program director, two supervisors, six clinicians, six peer specialists, and four medical professionals.
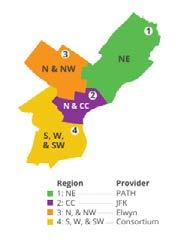
1. Two New Providers: Elwyn & PATH
2. Two Existing providers: JFK & Consortium Team Configuration
1. Behavioral Health Crisis Intervention Specialist
2. Certified Peer Specialist or Family Advocate
3. Medical Professional Activities
Engage, screen, assess, provide resolution-focused crisis intervention, de-escalate, develop safety plans, and link/transport to appropriate treatment and/or community services as indicated. Work with community when not resolving crises to provide education,support and to develop relationships.
Mobile Teams Regionalization
The four regions identified through historical data reviews of crisis service use. This clarity of the boundaries can allow for consistent data tracking and analysis.
Regionalization can promote community awareness of the service, improve efficiency of services and promote greater care coordination.
A committed presence in a defined area builds stronger relationships.
Providers described in RFP responses, established relationships and service offices in the assigned regions. Additionally, when not responding to crises, the providers will be tasked with ongoing engagement activities within assigned communities.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 98
APPENDIX K
CRISIS INTERVENTION RESPONSE TEAM OVERVIEW
CIRT Co-responder Expansion
1. CIRT pairs mental health professionals with CIRT-trained police officers from the Philadelphia Police Department (PPD). The program has expanded with the formation of the PPD Behavioral Health Unit and is available city-wide during the weekday shift. Further expansion is planned in 2023.
2. CIRT teams respond to behavioral health related police involved incidents with the goal of:
a. De-escalating crisis;
b. Reducing the use of force, arrest, and incarceration of individuals with behavioral challenges;
c. Increasing access to treatment and other services in the community.
3. The program includes CIRT Outreach Teams consisting of Outreach Specialists and Certified Peer Specialist or Recovery Specialists to provide brief solution-focused care coordination and on-site assistance with community linkages and supports after the crisis event has been resolved.
APPENDIX 99
APPENDIX L
BEHAVIORAL HEALTH TRAINING AND EDUCATION NETWORK TRAUMA TRAININGS
Trauma Training Initiative
Trauma Theory 101: What Everyone Needs to Know about the Impact of Trauma, Adversity and Toxic Stress
Three one-day sessions per year
Upcoming Sessions:
6/26/23
10/23/23
2/26/24
CEUs Cost Available Modalities
SW, APA, PCB, CPRP, IACET
$30 Live virtual webinar
The purpose of this training is to provide foundational information about what neuropsychological trauma is and its impact on individuals across the life span. The prevalence of these issues is discussed. The course reviews the developmental, physiological, cognitive, and emotional results of experiencing trauma, particularly early childhood trauma. Up-to-date Information is provided on how individuals who have experienced trauma can remain affected, and how they present in behavioral health settings.
Community Resilience Model TBD by DBHIDS SW, APA, PCB, CPRP, IACET
TBD TBD
The Community Resiliency Model© (CRM©) is designed to support the creation of trauma responsive and resiliency- focused communities (adults and children) by offering a common understanding of the impact of trauma and chronic stress on the nervous system. This easy to learn, user-friendly, skills-based model focuses on how individuals can restore or increase resilience even during challenges in order to be able to bring their nervous systems back into balance. Once individuals learn the model they can teach it to other staff, peers, family members, neighbors. This training focuses on defining the Resilience or “OK” Zone and participants being able to Identify their own Resilience Zone and how to use CRM© skills to widen that zone. This introductory session focuses on teaching participants three of the five basic CRM skills and offering them the opportunity to practice them.
Trauma Informed Recovery, Resilience Tools and Supports Quarterly Upcoming Session: 5/3/23
APA, PCB, CPRP, IACET
$30 Live virtual webinar
This training provides information and practice strategies as well as specific tools for behavioral health and other human services staff working to support persons needing to recover from trauma, with a focus on how to interact with persons receiving services using trauma-informed approaches. The prevalence and neurophysiological impact of traumatic and toxic stress, particularly in early childhood is discussed. This training provides opportunities to practice and use at least 2 trauma-informed activities/tools.
Understanding Trauma: The Impact and the Intervention Quarterly TBD None
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 100
$0 Live virtual webinar
Trauma Training Initiative
CEUs Cost Available Modalities
Trauma is a significant public health concern and the need to address it is viewed as an important component of effective behavioral health service delivery (SAMHSA, 2014). This training will explore the foundational principles of trauma by defining, illustrating different types of trauma and explain the neurological process of trauma. The training will also offer solutions for a trauma informed approach which will include the 6 Guiding principles to a trauma informed approach and how to support trauma informed workplace.
Responding to Vicarious Trauma Quarterly TBD
None $0 Live virtual webinar
This training is designed to define vicarious trauma and understand its impact on the helper professional. It will explore signs and symptoms while identifying preventative strategies to intervene and decrease its impact
Supervision to Support Staff Wellbeing: Addressing Trauma Exposure Response
Quarterly Upcoming Session: 5/10/23
APA, PCB, CPRP, IACET $0 Live virtual webinar
Trauma Exposure Response can reduce direct service and clinical staff’s capacity to be effective, caring, engaging, hopeful and enthusiastic in the delivery of services. It is essential for staff, with support and information from their supervisors to understand and attend to the possible impact of serving individuals and families with histories of childhood abuse and adversity. This training will present strategies and tools that supervisors can use in their program settings to help prevent and address the impact of vicarious traumatization and secondary trauma. Trauma Exposure Response, Vicarious Traumatization, and Secondary Trauma will be defined and discussed.
Trauma Informed Supervision: Addressing the Realities Annually Upcoming Session: 9/27/23
SW, APA. PCB, CPRP, IACET
TBD Live virtual webinar
Discussion and activities in this course build on BHTEN’s training Supervision to Support Staff Wellbeing: Addressing Trauma Exposure Response. This session will delve into the role of organizational culture, and other institutional issues that affect service efficacy such as staff’s ability to do meaningful traumainformed work. Focus will include presenting and discussing strategies for supervisors to address any existing barriers. Opportunities will be provided to examine best practice concepts and collective experience from the perspective of supervision in order to envision what an effective trauma- informed organizational culture at participants’ agencies/programs can look like.
DIY Storiez: Trauma Narratives and Urban Youth Annually Upcoming Session: 4/19/23
SW, APA. PCB, CPRP, IACET
$30 Live virtual webinar
This training begins with an introduction to trauma (defining trauma, exploring trauma exposure and urban youth, and considering the consequences of trauma exposure). It then explores trauma treatment for youth (best practices, treatment modalities, common factors, and trauma narratives). Finally, the DIY Storiez intervention is presented using didactic material, video content, and participatory activities. Storiez is a 9-step framework to assist urban youth as they create, voice, and honor their life narratives. The DIY Storiez intervention is an adapted version of the full trauma narrative process. It supports trauma survivors in creating abbreviated trauma narratives with the support of teachers, program leaders, coaches, and other community support.
APPENDIX 101
Trauma Training Initiative CEUs Cost Available Modalities
Storiez-Trauma Narratives for Urban Youth-Clinician Training Annually Upcoming Session: 6/14-15/23
SW, APA. PCB, CPRP, IACET
$60 Live virtual webinar
This training guides clinicians through the process of helping trauma survivors create, voice, and honor their narratives. It begins with an introduction to trauma (defining trauma, exploring trauma exposure and urban youth, and considering the consequences of trauma exposure). It explores trauma treatment for youth (best practices, treatment modalities, common factors, and trauma narratives). Finally, the Storiez intervention is presented using didactic material, video content, and participatory activities. Storiez is a 9-step framework to assist urban youth as they create, voice, and honor their life narratives using a variety of artistic formats and mediums.
Trauma Basics Annually Upcoming Session6/6/23
SW, APA. PCB, CPRP, IACET $30 In-Person Workshop
Whether or not it is fully recognized, human services workers are working with survivors of trauma. Given the prevalence and impact of violence amongst this population, the need for integrated services that are informed of trauma theory and include interventions designed to address the impact of trauma is evident. This introductory training aims to increase awareness and understanding on the part of services providers at all levels of the prevalence of trauma in consumers, the impact of that trauma on consumers, their behaviors and beliefs, and finally, how a more trauma-informed approach will enhance work with survivors of all ages.
Men’s Trauma Empowerment Model
TREM Versions
Women’s, LGBTQIA+, Adolescent
2-Day Training
Upcoming Session –
6/7-8/23
TBD
SW, APA. PCB, CPRP, IACET
$75 In-Person Workshop
This is a 2-day course. The TREM model is an evidenced-based 24-session, manualized group intervention that addresses the impact of interpersonal violence and trauma on persons with serious, persistent mental illness and/or substance use disorders. Documentation of three to five hours of prerequisite training in basic trauma theory is required for TREM training participants to receive certificates of completion for this two-day workshop. At the end of the workshop participants should be able to co-facilitate this group model. Participants in this training have completed the required application process and review.
Psycho-education: Helping
Adults Heal and Grow after Trauma
Annually
Upcoming Session:
4/27/23
SW, APA. PCB, CPRP, IACET $30 Live virtual webinar
Psycho-educational interventions for people who have experienced trauma, complex trauma, vicarious traumatization and/or traumatic loss are increasingly used to promote resilience, recovery, and posttraumatic growth. This webinar will help participants learn content and methods for enhancing psychoeducation and family education interventions, as well as what to avoid, based on available research. Participants will have an opportunity to select an adult target population within their area of interest and expertise, then begin developing a psycho-educational intervention for that population.
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 102
APPENDIX M
COMMUNICATIONS STRATEGY
Commissioner’s Message
This plan supports DBHIDS’s efforts to address Trauma, achieve Equity and engage Community (TEC) to help all Philadelphians thrive. Included in this plan are the materials and distribution strategies that will be employed to provide individuals with information and resources to connect trauma-addressing, -mitigating, and -reducing services. This plan will evolve to be responsive to needs as they emerge. Our intent is to ensure a diverse and robust strategy that reaches all demographics as DBHIDS is here to serve all Philadelphians.
Organization of the Plan
This plan is organized with new and existing materials produced by the Department over many years of programming and addressing a variety of behavioral health needs. This plan reflects the varied and innovative programming with community-based organizations and stakeholders that spans beyond traditional behavioral health interventions and includes efforts utilizing a population health approach. The materials are meant to be informative and engaging to provide access to trauma resources. Included in this plan is our distribution strategy for multiple outlets, social media, radio, TV, billboards, and partnership with other City agencies, behavioral health providers, and community-based organizations. Our intention is to blanket the city with trauma resources and supports.
Materials and Platforms
DBHIDS has developed materials in multiple formats to educate Philadelphia residents about various resources addressing trauma. Below include some of those resources and/or strategies to deploy messaging.
1. Palm cards
Palm cards were created to educate and inform Philadelphians about trauma resources. We worked with committees and with individuals with lived experience to help us to answer the questions: What is trauma? What is specific trauma (violence, pandemic, racism, etc.)? What types of events are traumatic? How does trauma feel? Who can I call for help? What can I expect when connecting to these resources?
These cards address the questions and provide an avenue to educate the public on impacts of trauma with easy –to understand access points to services. Through this process, we identified and prioritized four palm cards. The cards are a general trauma card, a gun violence trauma card, early childhood trauma card, and a school-aged trauma card. Future cards recommended were domestic violence, child abuse, physical or emotional neglect, racism or discrimination, grief and loss, pandemic-related isolation, vicarious trauma, secondary traumatic stress, practical skills for coping with trauma, and resilience. The four cards that were created have been distributed in several settings including schools, libraries, play streets, health centers, community-based organizations, and more.
2. Public service announcements (PSAs) and podcasts
DBHIDS is in the process of creating PSAs and podcasts. We hope these will reach individuals across AM/FM radio stations and via streaming services at different times of day across a multitude of platforms.
APPENDIX 103
3. Social media
We coordinated with Snap 2 Marketing/PR which recommended the following strategy: General:
a. Position DBHIDS as THE go-to resource for trauma-related mental health care in Philadelphia.
b. Show residents how to access services, especially those that are community-based.
c. Educate the public about trauma – the sources, symptoms, disparities, and solutions.
d. Engage the DBHIDS network of providers in spreading awareness about trauma and the Department.
e. Humanize the Department and TEC as it is important for the public to see the humanity inherent in the work.
4. Content Strategy
a. Follow the 80/20 rule for social media – for every four posts that provide useful/helpful information, one post can be about DBHIDS (e.g. a quote from Commissioner Bowen)
b. Linking: Link content to easily accessible information on the DBHIDS website or on HealthyMindsPhilly.org. The primary content here will be a series of blogs about trauma (one to two per month).
c. Content mining: Enlist trauma subcommittees and various units to write the blogs as well as to furnish factoids, research, and events.
d. Produce videos to highlight DBHIDS’ approaches to trauma, success stories, and how to access services.
e. Produce a social media toolkit with content on trauma that others can share.
f. Highlight the work of providers. (Note: This type of reciprocity will encourage them to share trauma toolkit posts.)
5. Timing, Type and Frequency
a. For the next six months, 80 percent of the content on DBHIDS’ social channels will be focused on TEC work and messaging. This includes access to services and education.
b. Another 15 percent will be related to IDS.
c. The remaining 5 percent will consist of other City agency initiatives in the Health and Human Services cabinet, i.e. Office of Public Health and the Office of Children and Families.
d. Frequency:
i. Facebook – DBHIDS averages 36/posts month. About 28 will be TEC-related.
ii. Twitter – DBHIDS averages 120 posts/month. About 90 will be TEC-related (some of these can be repeated or use slightly different graphics/copy).
iii. Instagram – DBHIDS averages a few posts/month. Frequency TBD.
iv. LinkedIn—While a LinkedIn page exists, it is underutilized. If one of the goals is to communicate with professionals, a separate LinkedIn strategy should be developed.
6. Type
i. The content will be a combination of news-related, event driven, and evergreen (trauma facts for example).
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 104
ii. TEC events should be promoted three times each – say two weeks and two days beforehand and once after (with a photo from the event). Larger events (e.g. Faith and Spiritual Affairs Conference) could be promoted more.
iii. A six-month social media calendar will be created and shared with the TEC team to provide ample time for planning and execution.
7. Creative Strategy
a. Engage the community with very simple, relatable content: one fact at a time.
b. Develop the creative with an outside-in mindset, always cognizant that it’s about needs and solutions.
i. As an example, a video on Porch Light would tell the story about art as a healing mechanism to trauma, the people involved and the WHY, not just the WHAT of Porch Light.
c. Use photography as much as possible to humanize the work and, where it makes sense, accompany the photos with posts that use a storytelling approach.
d. As resources allow, utilize videos to capture the attention of followers.
8. Sample Content Ideas
Trauma awareness and education
A campaign of multiple posts (10 or more) featuring simple facts about the sources, the symptoms, and the disparities around trauma. Each post will have a call to action (Such as “Call 988”). A campaign like this is evergreen.
These posts can form the basis of the social media toolkit which can be shared with providers in the network and other City departments.
9. Position DBHIDS executives as trauma thought leaders
Commissioner Bowen’s statement during the tragic house fire in February is a great example of this type of content. Key messages from presentations made and attributed information from reports are other examples of this type of content.
10. Events
Media coverage from the previous year can be a powerful way to engage on social media. There are numerous creative ways to promote events—a photo collage from previous years, quotes from people who attended in the past, media coverage, photos of presenters, etc.
11. Blogs
There is existing trauma-related content on the HealthyMindsPhilly.org website that can be repackaged and shared on social channels.
12. Humanize DBHIDS
While photos of staff at work should be used judiciously it is good to pull back the curtain from time to time – for example to tease a big announcement by showing the team planning it a few days ahead, or to promote the culture while encouraging job applicants.
13. Website
In 2022, DBHIDS created a trauma page on the DBHIDS.org website dbhids.org/trauma as a one-stop landing page for all 37 programing resources including individual, community, website/trainings, and hospital-based programs. This web-page details each program, allowing the user to connect to each resource. This page also includes state and federal trauma resources. Another website was designed
APPENDIX 105
as an online resource and tool to support and improve Philadelphians mental health and well-being called HealthyMindsPhilly.org. This website is linked to the DBHIDS trauma website and vice versa to provide connection to all the resources that DBHIDS has to help residents connect to supportive resources.
14. Distribution Plan
DBHIDS intends to have a reliable cadence to distribute educational trauma resources. Our intention is to have permanent placement of trauma materials and to distribute physical materials in a variety of settings. Below is our distribution plan for each platform.
a. Palm cards and hard copy materials- we plan to distribute paper copies of the palm cards on a biannual basis to the following:
i. DBHIDS providers
ii. PDPH health centers
iii. Free libraries
iv. Parks and Rec centers
v. Barber shops + beauty shops
vi. Corner stores
vii. Schools/community schools
viii. State legislative offices
ix. City Council offices
x. Police stations
xi. Municipal service buildings
xii. Community Crisis Intervention Program (CCIP)
xiii. Events (concerts, etc.)
xiv. Resources kits, tabling etc.
xv. Halfway houses
xvi. Places of worship
xvii. Faith-based organizations
xviii. Philadelphia Housing Authority
xix. Community resource centers
xx. County Assistance Office
xxi. Hospitals
xxii. SEPTA bus wrappers/signage in subways
Key distributors will include:
xxiii. Planning and innovation teams
xxiv. Philadelphia System of Care
xxv. ReCAST - community conversations
xxvi. Healthy Minds Philly and DBHIDS.org
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 106
xxvii. Behavioral health providers
xxviii. Mayor’s Office of Civic Engagement and volunteer services
xxix. Door-to-door palm card distribution
xxx. Trauma captains/block captains
xxxi. Community-based organizations
The four palm cards have been translated into the top ten languages spoken in Philadelphia: Spanish, Chinese (simplified), Russian, Vietnamese, Portuguese, Haitian Creole, Arabic, Dari, French, and Bengali. The palm cards will be shared these languages and language assistance is available at all trauma resources mentioned in the palm cards.
b. Social Media - twice a week, our communications team will post information about the DBHIDS trauma resources for the purpose of informing the public of all the resources and how to access the resources. These posts will be across all DBHIDS platforms to include Instagram, Facebook, and Twitter.
The DBHIDS communications team drafted the TEC social media campaign below:
i. Professional audiences two to three times weekly, i.e. LinkedIn from 8 to 11 a.m.
ii. Community partners, provider organizations and general audience 3x weekly Facebook/6-9 p.m. and noon to 3 p.m.
iii. Community partners, provider organizations and general audience 3x weekly Twitter/9 a.m. to noon
iv. Community influencers two to three times weekly; Intagram from 6 to 9 p.m. and noon to 3 p.m.
v. Film screenings three times a month
vi. Conferences every other month
vii. Trainings three times a month
viii. Monthly events two to three times a week
ix. Support groups three times a month, scattered throughout the month
x. Community events two times a month (BBQs)
xi. City events two times a month (such as school district events)
xii. Week prior reminders to register for upcoming events
xiii. Placeholders for general info and generic info for TEC
APPENDIX 107
c. Radio/podcasts - we plan to run radio advertisements on both WURD and WHYY radio stations drawing Philadelphians to our DBHIDS.org/trauma web-page and social media channels for information on DBHIDS trauma resources and how to access these resources. Podcast outlets TBD.
ADDRESSING
108 Month Facebook Twitter LinkedIn Instagram 1 Conference STD Conference STD Conference STD Conference STD 2 3 Training Training Training 4 5 Film screening Senior Expo & Wellness Senior Expo & Wellness Film screening 6 7 Promote Resource Fair Promote Resource Fair Promote Resource Fair Promote Resource Fair 8 9 Conference register Conference register Conference register Conference register 10 11 Film screening promo Film screening promo Film screening promo Film screening promo 12 13 Training Training Training Training 14 15 Services/upcoming events Services/upcoming events Services/upcoming events 16 17 Support groups Support groups Support groups Support groups 18 19 Training Training Training Training 20 21 Film screening promo Film screening promo Film screening promo 22 23 Promoting free food popup Promoting free food popup Promoting free food popup 24 25 Post conference photo Post conference photo Post conference photo Post conference photo 26 27 Workshops Workshops Workshops Workshops 28 29 Community events Community events Community events Community events
TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY
Have You Experienced Traumatic Stress?
Have You Experienced Traumatic Stress?
Trauma is an emotional response to a terrible event or series of events.
Trauma can occur from a single experience or prolonged experiences.
Trauma is a frightening or violent event that can pose a threat to how you feel physically and/or how you feel emotionally inside.
Traumatic events might include:
Violence
Racism
Neglect
Physical or emotional abuse
Pandemic related isolation
Grief and Loss
Trauma can feel like:
Heart racing or skipping
Body aches
Emotional swings
Outburst of anger or rage
Support is available:
For help with the impact of trauma, please contact:
Member Services 888-545-2600
(For mental health and substance use services)
Philadelphia Crisis Line 988 or 215-685-6440 Network of Neighbors 267-233-4837
(respond to trauma in communities)

Fear Depression Anxiety No energy
You can expect: Compassionate professionals to listen and connect you to services. Insurance and paperwork assistance to get the help you need. Ongoing support as needed, including contacting professionals.
For more tips and resources visit D B H I D S . O R G / T R A U M A
Sources: traumaresourceinstitute com and unicefusa org
APPENDIX 109
1. 2. 3.
your boost mood boost boost
Trauma is an emotional response to a terrible event or series of events.
Numbers to Know 24/7
988 Suicide and Crisis Lifeline
Member Services
Trauma can occur from a single experience or prolonged experiences. Trauma is a frightening or violent event that can pose a threat to how you feel physically and/or how you feel emotionally inside. or 215-686-6440
Care Connect Warmline
888-545-2600
mental health crisis mental health and substance use
Places to Go
Friends Hospital 4641 Roosevelt Blvd. 215-831-2600
Einstein Medical Center 5501 Old York Road 215-951-8300
484-278-1679
substance use navigation
for behavioral health emergencies
Hall Mercer 234 S. Eighth St. 215-829-5433
Episcopal Hospital 100 E. Lehigh Ave. 215-707-2577
Websites to Visit
For 24/7 online behavioral health screenings, Mental Health First Aid trainings, events, and resources, visit
H e a l t h y M i n d s P h i l l y . o r g
Children’s Crisis Response Center 3300 Henry Ave., Falls Center 2, Suite 3N 215-878-2600
NET Access Point (Substance Use Treatment) 1007 W. Lehigh Ave. 215-408-4987
To find mental health and substance use services and providers for Medicaid recipients online, visit C B H P h i l l y . o r g

For more resources, use your cell phone camera to scan the QR code or visit D B H I D S . O R G / B O O S T wellness • behavioral health • intellectual disability early intervention • community supports

We take an active role in promoting the health and wellness of all Philadelphians through our population health approach. By empowering the entire community to take charge of their health, DBHIDS helps to create a Philadelphia in which every resident can thrive.

110
Photo: Steve Weinik
School-aged Children Trauma Card
Children's Trauma Supports
Children's Trauma Supports
School-age
Trauma is an emotional response to a terrible event.
Trauma can occur from a single experience or prolonged experiences. Trauma is a frightening or violent event that can pose a threat to how you feel physically and/or how you feel emotionally inside.
Traumatic events might include:
Violence
Racism
Neglect Grief and Loss
Trauma can feel like:
Stomach Aches Headaches
Easily Frightened
Physical or emotional abuse
Pandemic related isolation
Clinging to Adults
Feeling aggressive No Energy
For Help, Contact: Member Services 888-545-2600
Difficult to console Outbursts of Anger
(ask about Intensive Behavioral Health Services, Phila. Alliance for Child Trauma Services, and Trauma-Focused Cognitive Behavioral Therapy)
Children's Crisis Treatment Center 215-496-0707
Network of Neighbors 267-233-4837
(responds to trauma in communities)
How to get help:
Talk to a supportive friend or relative
Talk to your school counselor and staff you can trust Talk to a trusted friend or relative
For more tips and resources visit D
Sources: City of Philadelphia Office of Children and Families

APPENDIX 111
H
B
I D S . O R G / T R A U M A
Numbers to Know 24/7
Suicide and Crisis Lifeline
Children's Resources
DHS Helpline
267-519-5326
988 or 215-686-6440
Court Appointed Advocates 215-590-4923
Center for Child Protection
267-519-5326
Places to Go for behavioral health emergencies

Children’s Crisis Response Center 3300 Henry Ave., Falls Center 2, Suite 3N 215-878-2600
Children’s Crisis Treatment Center 1080 N Delaware Ave., 6th Fl. 215-496-0707
Websites to Visit H e a l t h y M i n d s P h i l l y . o r g
For 24/7 online behavioral health screenings, Mental Health First Aid trainings, events, and resources, visit
To find mental health and substance use services and providers for Medicaid recipients online, visit C B H P h i l l y . o r g
For more resources, use your cell phone camera to scan the QR code or visit D B H I D S . O R G / B O O S T wellness • behavioral health • intellectual disability early intervention • community supports

We take an active role in promoting the health and wellness of all Philadelphians through our population health approach. By empowering the entire community to take charge of their health, DBHIDS helps to create a Philadelphia in which every resident can thrive.
Created in collaboration with Leah Mundy-Maher, LSW, Behavioral Health Training and Education Network

ADDRESSING 112
Photo: Steve Weinik
your boost mood boost boost
The Trauma of Gun Violence The Trauma of Gun Violence
Trauma is an emotional response to a terrible event or series of events. Trauma can occur from a single experience or prolonged experiences. Trauma is a frightening or violent event that can pose a threat to how you feel physically and/or how you feel emotionally inside.
Traumatic events might include:
Being a victim of a shooting
Witnessing a shooting
Losing a loved one to a shooting
Trauma can feel like:
Feeling unsafe
Loss of appetite
Trouble sleeping
Difficulty concentrating
Support is available:
Heart racing
Body aches
Emotional swings
Outburst of anger
For help with the impact of trauma call:
Member Services 888-545-2600
(For mental health and substance use services)
Philadelphia Crisis Line 988 or 215-685-5440
Network of Neighbors 267-233-4837
(respond to trauma in communities)

You can expect:
1 2 3
Fear Depression Anxiety
No energy
Supports include:
Community Crisis Supports
Trauma Focused
Therapy
Peer Supports
Compassionate professionals to listen and connect you to services.
Insurance and paperwork assistance to get the help you need.
Ongoing support as needed, including contacting professionals.
For more tips and resources visit D B H I D S . O R G / T R A U M A
Sources: City of Philadelphia Office of the Victim Advocate
APPENDIX 113
For

boost mood boost boost

114
24/7
Mental Health
Aid trainings,
and
to Know 24/7
online behavioral health screenings,
First
events,
resources, visit your
Numbers
D B H I D S
O R G / B O O S T wellness • behavioral health • intellectual disability early intervention • community supports
take an active role in promoting the health and wellness of all Philadelphians through our population health approach. By empowering the entire community to take charge of their health, DBHIDS helps to create a Philadelphia in which every resident can thrive. Websites to Visit H e a l t h y M i n d s P h i l l y . o r g
find mental health and substance use services and providers for Medicaid recipients online, visit C B H P h i l l y . o r g 888-545-2600 Member Services mental health and substance use services 215-232-1984 Homeless Outreach
For more resources, use your cell phone camera to scan the QR code or visit
.
We
To
Created in collaboration with Adara Combs, Esq., Office of the Victim Advocate 215-567-6776 215-940-0550 215-228-1718 Victim Advocate Phila. Anti-Drug Anti-Violence Network Mothers in Charge 988 or 215-686-6440 Suicide and Crisis Lifeline
Photo: Steve Weinik
Pre-K Children Trauma Card
Children's Trauma Supports
Trauma is an emotional response to a terrible event. Trauma can occur from a single experience or prolonged experiences. Trauma is a frightening or violent event that can pose a threat to how you feel physically and/or how you feel emotionally inside.
Traumatic events might include:
Violence
Racism
Neglect Grief and Loss
Trauma can feel like:
Stomach Aches Headaches
Easily Frightened
For Help, Contact:
Physical or emotional abuse
Pandemic related isolation
Clinging to Adults
Feeling aggressive No Energy
Member Services 888-545-2600
Difficult to console Outbursts of Anger
(ask about Intensive Behavioral Health Services, Phila. Alliance for Child Trauma Services, and Trauma-Focused Cognitive Behavioral Therapy)
Children's Crisis Treatment Center 215-496-0707
Network of Neighbors 267-233-4837
(responds to trauma in communities)
You can expect: Resources and the connections for needed services and supports Children and families receive the help they need Ongoing support as needed
For more tips and resources visit D B H I D S . O R G / T R A U M A
Sources: City of Philadelphia Office of Children and Families

APPENDIX 115
Children's Trauma Supports Pre-K to Five
your boost mood boost boost
Numbers to Know 24/7
Suicide and Crisis Lifeline
Children's Resources
DHS Helpline
267-519-5326
988 or 215-686-6440
267-519-5326 Court Appointed Advocates
Places to Go for behavioral health emergencies

Children’s Crisis Response Center 3300 Henry Ave., Falls Center 2, Suite 3N 215-878-2600
Websites to Visit
Center for Child Protection
215-590-4923
Children’s Crisis Treatment Center 1080 N Delaware Ave., 6th Fl. 215-496-0707
For 24/7 online behavioral health screenings, Mental Health First Aid trainings, events, and resources, visit
H e a l t h y M i n d s P h i l l y . o r g
To find mental health and substance use services and providers for Medicaid recipients online, visit C B H P h i l l y . o r g
PACTS serves youth in Philadelphia who have experienced potentially traumatic events and are living with traumatic stress. P h i l a d e l p h i
For more resources, use your cell phone camera to scan the QR code or visit D B H I D S . O R G / B O O S T wellness • behavioral health • intellectual disability early intervention • community supports

We take an active role in promoting the health and wellness of all Philadelphians through our population health approach. By empowering the entire community to take charge of their health, DBHIDS helps to create a Philadelphia in which every resident can thrive.
Created in collaboration with Kate Eisenpress, Director of Early Childhood Strategic Initiatives

ADDRESSING 116
Photo: Steve Weinik
P A C T S
a
. o r g
APPENDIX O
SOCIAL DETERMINANTS OF HEALTH EQUITY UNIT LOGIC MODEL
Goal of Unit: To increase and promote health equity across Philadelphia’s Behavioral Health System by addressing social determinants of health such as economic mobility, access to food, increasing mobility and increasing access to technology as well as developing sustainable funding sources to enhance current SDOH Programs and implementing additional programs to meet the needs of residents to increase their quality of life and life expectancy.
SDOH System Recommendations: Facilitating Internal SDOH Core Group and Larger SDOH Group Across all Systems
Employment: Promoting Economic Mobility
DBHIDS Role Supporting SDOH Program: Employment Systems Program Specialist
• Management of DBHIDS Employment Clearinghouse, including four DBHIDS funded Employment Services Programs and other community partners:
a. COMHAR
b. Consortium
c. First Step Staffing
d. Horizon House
e. Pathways-WorkForce
f. Philly WINs
• Facilitating active Outreach and Engagement
• Hosting First Step Staffing monthly hiring events and expanding events to other partners such as:
a. BDT CEO Mobile Unit
b. Assurance Wireless
c. ID Philly
d. 1199C
e. Providing the following documents:
- Health literacy
- Employment Myths
- How to obtain ID Documents
Food DBHIDS Role Supporting SDOH Program: Social Drivers and Clinical Collaboration Specialist
• Develop and retain collaborative partnership with Philabundance.
a. Bi weekly food delivery for one year to 100 households
b. Nutrition Counseling
c. Incentive Cards for completion of program surveys
• Coordinate with OHS Committee
• Connecting participants receiving food resource with additional benefits and resources with support of Benefits Data Trust (BDT)
Transporation DBHIDS Role Supporting SDOH Program: Social Drivers and Clinical Collaboration Specialist
• Linkage to monthly SEPTA Transportation Passes which provides the following:
a. Increases choice regarding location for healthcare needs and employment options
APPENDIX 117
Technology DBHIDS Role Supporting SDOH Program: Social Drivers and Clinical Collaboration Specialist
• Providing a free of cost Chromebook to DBHIDS participants which will increase access to the following:
a. Telehealth-Healthcare options
b. Remote access
c. Transportation location and assistance
d. Building social connections
Future SDOH Implementation: Collecting qualitative data by completing surveys, collecting quantitative data by SocialScape Platform, developing a Commodity Fund as SDOH Program, expand economic mobility by establishing a Benefits Specialist role, increasing affordable housing and develop a Community Health Worker role within the unit to support with promoting health literacy, tracking SDOH needs, and linkage to community resources.
Philanthropy: Develop Philanthropy Affinity Network and explore grant funding opportunities to expand SDOH programs.
Building Partnerships: Local retail stores
118
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY
APPENDIX P
SYSTEMS INTEGRATION ONE STOP SHOP FLYER
DBHIDS Employment Initiative
One Stop Shop
I f y o u a r e r e c e i v i n g D B H I D S s e r v i c e s a n d n e e d h e l p f i n d i n g a j o b o r l e a r n i n g v o c a t i o n a l s k i l l s , w e c a n h e l p y o u f i n d e m p l o y m e n t a n d c o m m u n i t y r e s o u r c e s t o s u p p o r t y o u r e c o n o m i c m o b i l i t y .
O p e n a t 1 2 : 3 0 p . m . f o r r e s o u r c e s a n d a t 1 p . m . t o d i s c u s s e m p l o y m e n t o p p o r t u n i t i e s w i t h F i r s t S t e p S t a f f i n g . S i g n - u p i s m a n d a t o r y t h e F r i d a y b e f o r e .
B r i n g t w o f o r m s o f I D A s t a t e I D i s r e q u i r e d t o e n t e r t h e b u i l d i n g , a p i c t u r e o f t h e
I D i s a c c e p t a b l e .
F i r s t T u e s d a y s
8 0 1 M a r k e t S t . , P h i l a . , 1 9 1 0 7
E n t e r t h e b u i l d i n g o n 8 t h S t r e e t .
P a r t i c i p a t i n g P r o v i d e r s
P h i l l y I D • B e n e P h i l l y • G e n M o b i l e • F i r s t S t e p S t a f f i n g • L i b e r t y R e s o u r c e s
T o s i g n u p o r f o r m o r e i n f o r m a t i o n e m a i l K a d i s h a . A l b e r g a @ p h i l a . g o v o r c a l l 2 6 7 - 9 9 0 - 4 7 6 4 o r 2 6 7 - 8 5 8 - 9 4 0 5
Brought to you by the DBHIDS SDOH Equity Unit Our goal is to support people receiving services seeking employment while linking with additional community resources which may be supportive of them obtaining and retaining employment, supporting with economic mobility

APPENDIX 119
APPENDIX Q
COMMUNITY SERVICES AND RESOURCES GUIDE
COMMUNITY SERVICES AND RESOURCE GUIDE Healthcare
Housing
Office of Homeless Services
215-686-7175
24/7 Emergency Shelter Assistance
Home Repairs 215-448-2160
Phila. Division of Housing and Community Development helps homeowners with basic repairs
Utility Shut-off Assistance
215-972-5170
See if you are eligible for money from the Utility Emergency Services Fund.
Gas Heating Bill 866-857-7095
Call LIHEAP for help with your gas bill.
Low-income Housing Online bit.ly/PHLhousing
Search for apartments in Philadelphia
Affordable Housing bit.ly/AffordPHL
Search affordable apartments in Philadelphia

Rental Assistance Programs rentassistance.us
Employment
First Step Staffing
215-333-3349
$12 to $18/per hour same-day jobs, interviews, and rides to job sites No experience is needed
Job Coaching and Services
215-560-1900
Call the Phila. Office of Vocational Rehabilitation for help with interviews, finding work, and keeping jobs, or visit 801 Market St., Suite 6034, Phila., PA 19107. Including people with intellectual disabilities
Job Search 833-750-JOBS (5627)
Call to schedule an appointment with CareerLink
Philadelphia Crisis Line 988 or 215-685-6440
24/7 Mental Health Crisis and Suicide Prevention
Community Behavioral Health
888-545-2600
Mental health and substance use treatment services for Philadelphians with Medicaid.
Behavioral Health Services 215-599-2150
Learn if you qualify for mental health and addiction services with the Targeted Case Management Unit
BHSI Substance Use Treatment 215-546-1200
Call Behavioral Health Special Initiative for addiction treatment options if you have limited or no insurance
Free Grief and Loss Support
Domestic Violence Hotline
215-685-7408/7411
866-723-3014
To apply for Medical Assistance and Insurance call Medicaid at 215-560-7226, CBH Member Services at 888-545-2600, or online at compass state pa City Health Center phila gov/services/mentalphysical-health/city-health-centers
PHMC Dental 215-309-6223
Call the Public Health Management Corp for virtual telehealth and emergency dental services
Medical and Dental Services 215-320-6187
Call the Stephen Klein Wellness Center to schedule an appointment.
Children's Resources
215-836-0958
Call or visit Cradles to Crayons at 4700 Wissahickon Ave , Suite 142, Phila , PA 19144
Updated: Jan 2023
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 120
C I T Y O F P H I L A D E L P H I A
DEPARTMENT OF BEHAVIORAL HEALTH AND INTELLECTUAL disABILITY SERVICES
COMMUNITY SERVICES AND RESOURCE GUIDE
Food Assistance
Food Distribution Sites phila gov/food/# Find free groceries and meals near you No ID is required
Food pantries 311 or 800-5HUNGRY
Call the Coalition Against Hunger for hot meals and food assistance in your area City Health Centers phila gov/services/mental-physicalhealth/city-health-centers
Older Adult Meal Sites
215-765-9040
Call the Phila Corporation for Aging to reserve 5 to 7 free meals per week
SNAP Hotline
215-430-0556
Call to apply for food stamps and other benefits. Free Grocery Delivery amazon.com/snap-ebt
Sign up with your EBT card
Internet Access
High-Speed Internet Subsidy
833-511-0311
Transportation
Medical Assistance Transportation - Modivcare
877-835-7436
Transportation to appointments for people with Medicaid
Medical Appointment Transportation 215-580-7145
Get rides to medical appointments or help with costs
Paratransit Services 888-545-2600
Call SEPTA for the Share-Ride program and Paratransit services information
Transportation Access Programs lyft com/lyftup
Get rides to the things you need like groceries, jobs, voting, and vaccines.
Additional Resources
Find Help findhelp org

Search for food, utilities, transportation, and more. Where to Turn Guide projecthome org/where-to-turn
Regularly updated list of resources related to health & safety, benefits, and legal assistance, and more
Call to apply for a monthly internet subsidy, mail-in applications, or visit GetEmergencyBroadband org
Computer Training
215-867-9732
Call, email, or visit the Phila. Office of Innovation and Technology online to learn computer skills. Digital Navigator Helpline

215-426-7049
Internet and Computer Access for Philadelphia Residents
Online QR Codes






For more online resources, use a cell phone camera to scan the QR code. Employment Housing Food Assistance
Same-day Food Housing Delivery Hot Meals Coaching Search Shelters Utilities

APPENDIX 121
@DBHIDS
Photo: Steve Weinik
APPENDIX R NEUROBIOLOGY OF TRAUMA
In the last 20-plus years, neuroscientists’ research findings have contributed to groundbreaking discoveries made possible by significant technological progress for studying the brain. Opportunities have been created to focus on the impact childhood trauma/toxic stress can have on the nervous system across the lifespan. Included is the discovery that due to neuroplasticity our brains are highly malleable, even into adulthood.
Neurobiology of trauma helps to explain many of the common experiences and behaviors that can affect survivors of childhood trauma and toxic stress. When someone experiences a traumatic event or experiences extreme fear, brain chemistry is altered and the brain begins to function differently – this is called the “Fear Circuity,” a protective mechanism which all of us have. The neurobiology of trauma – essentially the effects of trauma on the brain – is important to understand because it helps break down commonly occurring misconceptions about childhood trauma leading to victim-blaming and survivor self-blame throughout their lifespans. When neurobiological information and interventions relating to trauma are available it can help survivors understand their traumatic experiences and manage the aftermath in new ways.
During and after a childhood traumatic experience, survivors experience a cascade of physical, emotional, cognitive, behavioral, relational, and spiritual responses that can make them feel unbalanced and threatened. Evidence-based neuroscience interventions have been developed for managing such responses. Of particular importance is the role some of these findings play as part of trauma-informed care. The research has contributed to opportunities for behavioral health staff, helpers in the natural support system and survivors of trauma themselves to promote healing and recovery from trauma. Specific skills can be learned to manage the often lifelong neurological aftermath of these traumatic experiences.
A good number of neurobiological interventions have been developed (Miller-Karas, Levine, Siegel, Sebring, Ogden, Fisher, Porges among others) to address these responses. An example of one approach focuses on acquiring substantial relevant skills to help manage especially intense responses to childhood trauma/toxic stress. The Community Resilience Model (CRM) one of two related models is available through the Trauma Resource Institute. BHTEN has sponsored the introduction of this model to provider staff and DBH expressed interest in expanding the training’s availability to additional behavioral healthcare staff and community members.
The CRM explains common responses to trauma from a biological perspective, reframing the human experience from one of shame and pathology to one of hope and biology. Studies cited by one of the models’ creators have demonstrated significant reductions in depression and anxiety and increases in well-being using the Community Resilience and Trauma Resilience models described available through the Trauma Resource Institute. (Miller-Karas, E. 2023).
ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 122
References
Fisher, S. F. (2014). Neurofeedback in the treatment of developmental trauma: Calming the fear-driven brain. W W Norton & Co.
Herman, J. L. (2023). Truth and repair: how trauma survivors envision justice (First edition.). Basic Books.
Herman, J. (2015). Trauma and recovery. Basic Books.
Levine, P. A. (2010). In an unspoken voice: how the body releases trauma and restores goodness. North Atlantic Books.
Levine, P. A. (1997). Waking the tiger: healing trauma : the innate capacity to transform overwhelming experiences. Berkeley, Calif., North Atlantic Books.
Miller-Karas, E. (2023). Building Resilience to Trauma: The Trauma and Community Resiliency Models (2nd ed.). Routledge. doi.org/10.4324/9781003140887
Ogden, P., Minton, K., & Pain, C. (2006). Trauma and the body: A sensorimotor approach to psychotherapy. W. W. Norton & Company.
Porges, S. W. (2011). Norton Series on Interpersonal Neurobiology. The Polyvagal Theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. New York, NY: Norton.
Siegel, D. J., & Bryson, P. H. D. T. P. (2012). The whole-brain child. Random House. van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Viking.
Prepared by
Kalma Kartell White, Trauma Training Specialist, Behavioral Health Training & Education Network
APPENDIX 123
APPENDIX S SUBSTANCE USE EARLY
INTERVENTION SERVICES
The City of Philadelphia Department of Behavioral Health and Intellectual disAbility Services

Substance Use Early Intervention Services
Single County Authority
DBHIDS Early Intervention Services supports individuals who are at risk of addiction and builds their resiliency and positive decision-making skills.
Who we serve Goal
Services are for Philadelphia residents ages 10 and up with pre-diagnostic levels of addictive substance use and for those exposed to substance-use living in the home or in their surroundings.
The aim is to help young people and their families recognize the harmful consequences of substance use and addiction. Parents/caregivers and siblings of enrolled youth are welcome to participate.
Accessing services
Anyone can make a self or peer referral for service by contacting a provider directly.


ADDRESSING TRAUMA , ACHIEVING EQUITY ENGAGING COMMUNITY 124
us
Harvey
Contact
Tamika
Tamika.Harvey@phila.gov 215-599-4972
Early Intervention Services
Virtual or in-person sessions are offered for a three- to six-month period and include:
• Cognitive Behavioral Therapy

• Community Engagement
• Life Skills
• Expressive Writing
• Evidence-Based Practices
• Motivational Interviewing
• Leadership Skills
• Parent Workshops
• Conflict Resolution
• Work Ready Programs
Provider agencies and contacts
Cora Services 8540 Verree Road Philadelphia, PA 19111 215-342-7660
Northern Children Services 5301 Ridge Ave. Philadelphia, PA 19128 215-482-1423
Youth Advocate Program 900 W. Jefferson St. Philadelphia, PA 19122 215-599-2174 ext.1505, 1506, 1515
ODAAT 2532 N. Broad St. Philadelphia, PA 19132 215-226-7860
Jewish Family and Children Service 2100 Arch St. Philadelphia, PA 19103 215-356-1851
The Wedge Recovery Centers 6711 Old York Road Philadelphia, PA 19126 215-276-3922
Pro-Act 1701 W. Lehigh Ave. Philadelphia, PA 19132 215-223-7700
Gaudenzia 2751 N. Fifth St. Philadelphia, PA 19133 215-423-5766
APPENDIX 125
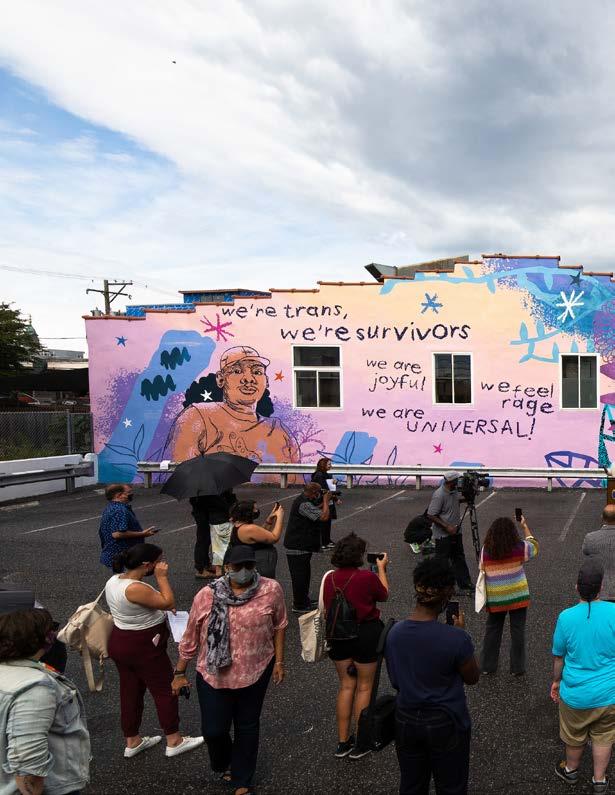



Addressing trauma, achieving equity, and engaging community. Jefferson Tower 1101 Market St. Philadelphia, PA 19107 215-685-5400 DBHIDS.org @DBHIDS
Photo credit: Steve Weinik
 Jill Bowen, Ph.D. Commissioner
Jill Bowen, Ph.D. Commissioner







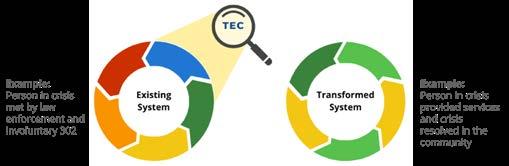

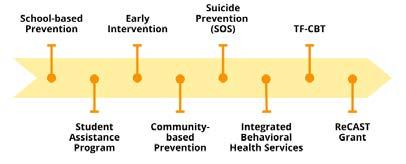
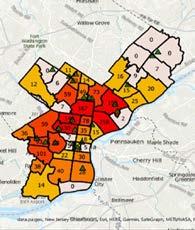


 Jill Bowen, Ph.D. , Commissioner November 2022
Jill Bowen, Ph.D. , Commissioner November 2022