



A conference sponsored by the Center for Theology and Ethics in Catholic Health and the Institute for the Liberal Arts at Boston College
MARCH 20-21, 2026, AT BOSTON COLLEGE
Keynote Speaker

The “Artificial Intelligence, Authentic Mercy: Navigating AI Ethics in Catholic Health” conference will bring together physicians, nurses, health care administrators, biomedical engineers, technologists, theologians and ethicists to explore the opportunities and challenges presented by AI in Catholic health care settings. The goal is to ethically analyze AI in health care through the lens of Catholic moral teaching and theological ethics.
Illustrations by J.S. Dykes
4 ACCESSIBLE, AFFORDABLE, BENEFICIAL: HOW CAN U.S. HEALTH CARE BE RESHAPED TO BETTER SERVE PATIENTS?
Elizabeth Garone
9 TREATING FEAR: STEPS TO HELP YOUR IMMIGRANT PATIENTS
Monica Maalouf, MD, Amy Blair, MD, and Mark Kuczewski, PhD
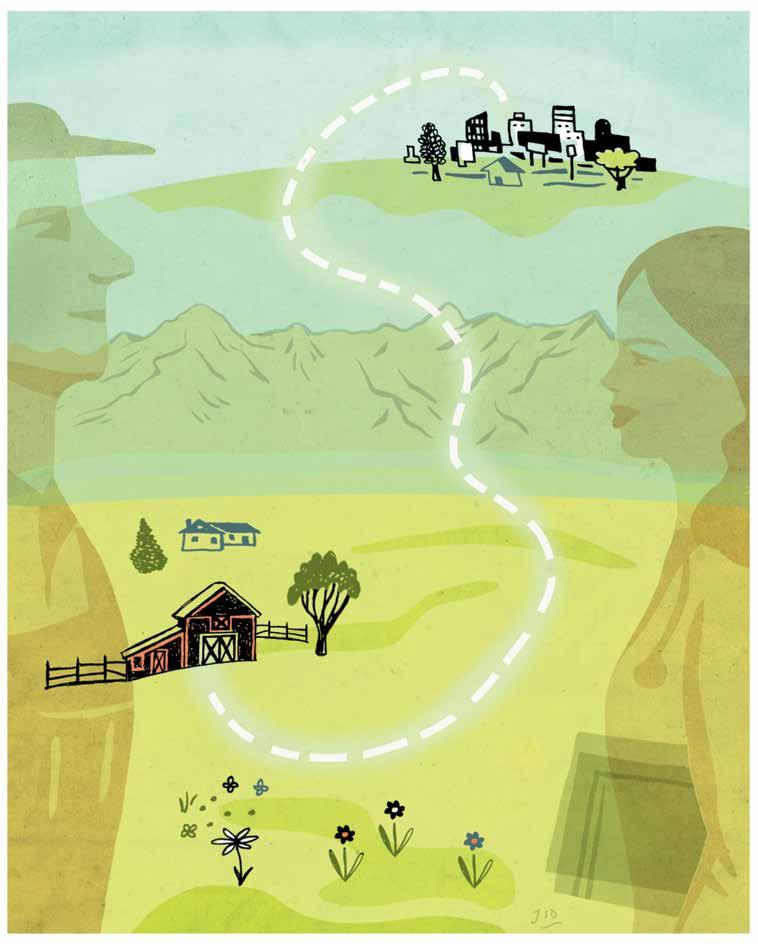
15 RALLYING AROUND RURAL CARE: HOSPITALS STRIVE TO DELIVER ACCESSIBLE SERVICES
Robin Roenker
22 ARTIFICIAL INTELLIGENCE WITH A PURPOSE AT PROVIDENCE
Sara Vaezy, MHA, MPH
26 ACCOUNTABLE CARE ORGANIZATIONS SAVE BILLIONS, BUT STRUGGLES REMAIN IN THE SHIFT TO VALUE-BASED CARE
Kelly Bilodeau
32 MARYLAND’S TOTAL COST OF CARE MODEL ALIGNS HEALTH INNOVATION WITH MISSION-DRIVEN CARE
Mitch Lomax, MBA, Trevor Bonat, MA, MS, and Olivia D. Farrow, Esq.
36 PLACE HUMAN DIGNITY AT THE CENTER OF HEALTH CARE REFORMS
Sarah Reddin, D.HCML, and Richard Fogel, MD, FACC, FHRS
40 FINDINGS FROM CHA SURVEY: FORMATION REACHES DEEPER INTO MINISTRIES, INCREASES DEMAND FOR NEW RESOURCES
Darren M. Henson, PhD, STL
2 EDITOR’S NOTE BETSY TAYLOR
47 COMMUNITY BENEFIT
What’s the Point of Doing a Needs Assessment and Improvement Plan if They Don’t Lead To Real Change?
STEPHANIE MOXLEY, CAROLINE GAGNE and MADISON THOMPSON
50 ETHICS
50 Years Later: The Enduring Legacy of Karen Ann Quinlan Continues to Influence End-of-Life Decisions
BRIAN M. KANE, PhD
54 MISSION Weaving Foundational Mission-Related Competencies Into Workplace Expectations
DENNIS GONZALES, PhD, BART RODRIGUES, MDiv, MA, MBA, JOYCE MARKIEWICZ, RN, BSN, MBA, and LAURA CIANFLONE, MA
58 FORMATION
A Sign of Hope, 30 Years Later
DARREN M. HENSON, PhD, STL
61 THINKING GLOBALLY
Why We Need Serenity, Courage and Wisdom Now to Protect Our Most Vulnerable BRUCE COMPTON and NEERAJ MISTRY, MD
31 POPE LEO XIV — FINDING GOD IN DAILY LIFE
64 PRAYER SERVICE

IN YOUR NEXT ISSUE AGING & LONGEVITY
When it comes to thinking about this issue of Health Progress exploring Health Care Across America, it’s helpful to consider: What are our values, and how are those reflected in our health care system?1

In a Catholic care environment, articulation of values is clearer than in many other settings, and consideration of that question is woven throughout this issue. And I think this question leads to other ones, including: Who do we value? In Catholic social teaching, the Church “proclaims that human life is sacred and that the dignity of the human person is the foundation of a moral vision for society.” As the U.S. bishops summarize in a reflection on these teachings, “We believe that every person is precious, that people are more important than things, and that the measure of every institution is whether it threatens or enhances the life and dignity of the human person.”2
We don’t just value someone if they’ve got the correct papers and pay their bills. Those matters are important, but they’re not the litmus test by which a Catholic health care ministry provides care. Are our institutions threatening or enhancing the life and dignity of all people? And if, in Catholic institutions, we feel we do better at this than some other organizations — or at least aspects of it better — is there a way to raise our voices together to tend to a national health care system in need of reimagination?
Across our nation, people are confused by a splintered health care system. They may swim in medical debt, have trouble understanding a doctor’s guidance, or be in pain, afraid or even just bone-tired. I could cite a study, but every one of us has seen this with our own eyes at one point or another.
And it is not enough to shrug off a broken system, because we — Catholic health care collectively — are in the system-fixing business. And we are in the system-fixing business because the nation’s patients deserve nothing less than that.
1. This video, by The Washington Post, features a lot of food for thought about other nations’ health care systems, and what they may reveal about our own system, including a few speakers who discuss the role that a society’s values play related to its health care system: “What Experts Say About Who Has the World’s Best Health Care System-Opinion,” The Washington Post, June 17, 2021, YouTube video, 9:14, https://www.youtube.com/ watch?v=wfsJXo1h1G0.
2. “Seven Themes of Catholic Social Teaching,” United States Conference of Catholic Bishops, https://www.usccb.org/beliefs-and-teachings/ what-we-believe/catholic-social-teaching/ seven-themes-of-catholic-social-teaching.
VICE PRESIDENT, COMMUNICATIONS AND MARKETING
BRIAN P. REARDON
EDITOR
BETSY TAYLOR btaylor@chausa.org
MANAGING EDITOR
CHARLOTTE KELLEY ckelley@chausa.org
GRAPHIC DESIGNER
NORMA KLINGSICK
ADVERTISING 4455 Woodson Rd., St. Louis, MO 63134-3797, 314-253-3447; fax 314-427-0029; email ads@chausa.org.
SUBSCRIPTIONS/CIRCULATION Address all subscription orders, inquiries, address changes, etc., to Service Center, 4455 Woodson Rd., St. Louis, MO 63134-3797; phone 800-230-7823; email servicecenter@chausa.org. Annual subscription rates are: complimentary for those who work for CHA members in the United States; $29 for nonmembers (domestic and foreign).
ARTICLES AND BACK ISSUES Health Progress articles are available in their entirety in PDF format on the internet at www.chausa.org. Photocopies may be ordered through Copyright Clearance Center, Inc., 222 Rosewood Dr., Danvers, MA 01923. For back issues of the magazine, please contact the CHA Service Center at servicecenter@chausa.org or 800-230-7823.
REPRODUCTION No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage and retrieval system, without permission from CHA. For information, please contact copyright@chausa.org.
OPINIONS expressed by authors published in Health Progress do not necessarily reflect those of CHA. CHA assumes no responsibility for opinions or statements expressed by contributors to Health Progress.
2025 AWARDS FOR 2024 COVERAGE
Catholic Media Awards: Magazine of the Year — Professional and Special-Interest Magazines, Second Place; Best Cover — Small, First Place; Best Special Section, Second Place; Best Special Issue, First Place; Best Regular Column — Spiritual Life, Honorable Mention; Best Coverage — Disaster or Crises, Third Place; Best Feature Article — Professional and Special-Interest, Third Place; Best Reporting of Social Justice Issues — Dignity and Rights of the Workers, Second Place; Hot Topic — Eucharistic Revival, Third Place; Hot Topic — 2024 Election, Third Place; Best Writing — Analysis, First Place; Best Writing — In-Depth, Second Place.
American Society of Business Publication Editors Awards: Print — Special Section, National Bronze Award and Regional Gold Award; All Content — How-To Article, Regional Silver Award.
Produced in USA. Health Progress ISSN 0882-1577. Fall 2025 (Vol. 106, No. 4).
Copyright © by The Catholic Health Association of the United States. Published quarterly by The Catholic Health Association of the United States, 4455 Woodson Road, St. Louis, MO 63134-3797. Periodicals postage paid at St. Louis, MO, and additional mailing offices. Subscription prices per year: CHA members, free; nonmembers, $29 (domestic and foreign); single copies, $10.
POSTMASTER: Send address changes to Health Progress, The Catholic Health Association of the United States, 4455 Woodson Road, St. Louis, MO 63134-3797.

Follow CHA: chausa.org/social


Trevor Bonat, MA, MS, chief mission integration officer, Ascension Saint Agnes, Baltimore
Sr. Rosemary Donley, SC, PhD, APRN-BC, professor of nursing, Duquesne University, Pittsburgh
Fr. Joseph J. Driscoll, DMin, director of ministry formation and organizational spirituality, Redeemer Health, Meadowbrook, Pennsylvania
Jennifer Stanley, MD, physician formation leader and regional medical director, Ascension St. Vincent, North Vernon, Indiana
Rachelle Reyes Wenger, MPA, system vice president, public policy and advocacy engagement, CommonSpirit Health, Los Angeles
Nathan Ziegler, PhD, system vice president, diversity, leadership and performance excellence, CommonSpirit Health, Chicago
ADVOCACY AND PUBLIC POLICY: Lisa Smith, MPA; Kathy Curran, JD, MA; Clay O’Dell, PhD; Paulo G. Pontemayor, MPH; Lucas Swanepoel, JD
COMMUNITY BENEFIT: Nancy Zuech Lim, RN, MPH
CONTINUUM OF CARE AND AGING SERVICES: Indu Spugnardi
ETHICS: Nathaniel Blanton Hibner, PhD; Brian M. Kane, PhD
FINANCE: Loren Chandler, CPA, MBA, FACHE
GLOBAL HEALTH: Bruce Compton
LEADERSHIP AND MINISTRY DEVELOPMENT: Diarmuid Rooney, MSPsych, MTS, DSocAdmin
LEGAL, GOVERNANCE AND COMPLIANCE: Catherine A. Hurley, JD
MINISTRY FORMATION: Darren Henson, PhD, STL
MISSION INTEGRATION: Dennis Gonzales, PhD; Jill Fisk, MATM
PRAYERS: Karla Keppel, MA; Lori Ashmore-Ruppel
THEOLOGY AND SPONSORSHIP: Sr. Teresa Maya, PhD, CCVI

HEALTH CARE ACROSS AMERICA

ELIZABETH GARONE
Contributor to Health Progress
As a cardiologist in the Philadelphia area, Dr. Peter Kowey treated countless patients over the decades for different heart ailments. So, he wasn’t surprised when he received a call from one of them. What was surprising was that the patient was asking him about her hip replacement surgery. She was in extraordinary pain and had gone in to see her surgeon for a follow-up appointment.
“The surgeon came in and said, ‘This device is broken. We’re going to have to replace it,’ and then he walked out, leaving her with a gazillion questions,” said Kowey. Totally frustrated and unable to get her questions answered, she called Kowey, knowing he would take the time to explain everything to her.
As anyone enmeshed in the world of health care will share, doctors are under increasing pressure to see more patients but for shorter amounts of time, often to bolster the bottom line. Compounding this and other pressures is the uncertainty around the future of the health care landscape with the July 4, 2025, passage of the One Big Beautiful Bill Act (OBBBA). One aspect remains certain: The health care system has a lot of work to do to make care more accessible, affordable and beneficial to everyone, especially given the constraints of the new law, with many pieces of the legislation going into effect in 2026. The Congressional Budget Office is projecting OBBBA to cause around a $1 trillion reduction in federal health care spending through 2034 and increase the number of uninsured people by 10 million.1
As health care continues along this uncer -
tain path, there are many issues that need to be addressed.
For doctors to do their jobs well and for patients to get the answers they need, something has to give, according to Kowey, a professor of medicine and clinical pharmacology at Thomas Jefferson University in Philadelphia who recently authored the book Failure To Treat: How a Broken Healthcare System Puts Patients and Practitioners at Risk. Otherwise, very few doctors can give the attention and care necessary to fully address patients’ concerns and symptoms.
“We’re stacking the patient schedule every 15 to 20 minutes per patient, and the patients suffer, of course, because they don’t think that they have enough time,” said Kowey. “By the time the technician puts the patient in the room and gets a cardiogram and vital signs, we’re halfway through the visit. So, part of the problem is that even when you get in, you don’t necessarily have a satisfactory visit, or that you don’t walk out feeling like you got what you needed.”
It isn’t just patients feeling unsatisfied. Due to
myriad pressures, physicians are walking away or retiring earlier than planned. In a recent MedCentral survey, more than one-third (35%) of physicians said they have considered leaving the medical practice since the start of 2025. Top reasons cited include personal burnout, early retirement and clinical demands. 2 If the current situation continues, the U.S. can expect a physician shortage of up to 86,000 physicians by 2036, according to the Association of American Medical Colleges.3
One area that needs to be addressed is the haphazard approach to health care in the U.S., according to Dr. Jeff Salvon-Harman, CPE, CPPS, vice president of safety for the Institute for Healthcare Improvement (IHI). “In the U.S., we have not done a great job at keeping people from becoming patients,” he said. “As a result, what we’re seeing that is affecting hospitals is patients with four or five chronic, comorbid conditions that impact each other, such that when any one of them causes an acute complication, the multiple others that are in the background are also being impacted. We have to do a better job in communities, in ambulatory care, in primary care, not only delivering care, but creating safer environments for people, so that people don’t have to become patients.”
In 2023, approximately 76% of U.S. adults reported one or more chronic conditions, and about 51% reported multiple chronic conditions. That number jumped to nearly 79% for older adults, according to the Centers for Disease Control and Prevention.4
A more strategic approach needs to be taken, according to Salvon-Harman. “Part of what we have to acknowledge is that the health care system that we have today did not come to be through intentional design. Nobody convened a committee or a working group or a task force to say, ‘Let’s design perioperative care for the whole country. Let’s design primary care for the whole country. Let’s design specialty care, inpatient and outpatient for the whole country.’ Every health system has pulled together, starting out with individual hospitals becoming multiple hospitals, and then becoming a large organization. They’ve adapted and adopted and added as they needed to for their business models or as care paradigms changed.”
At New Jersey’s Saint Peter’s Healthcare System,
President and CEO Leslie Hirsch is seeing the shift from inpatient to outpatient visits that many hospitals across the country are experiencing. Medical procedures that, in the past, would have required multiple days in the hospital, such as hip surgery, can now be done as a one-day appointment for otherwise healthy patients.
While the advancements in technology that make this possible are, as Hirsch describes, “incredible,” it has also meant that insurers want to pay less wherever they can. “The role that insurers play in pre-authorization and denials for consumers and then for providers has resulted in an extremely complex and frustrating system for both consumers and providers,” said Hirsch. Even if a patient stays in the hospital for multiple nights, but insurance classifies them as “observation status,” they are still considered an outpatient. That means insurance pays a fraction of what it would have paid had it been an inpatient visit, yet the patient is receiving the same level of care and services, and the hospital is using just as many resources and staff. “What’s going to happen is the payer, the insurance company, is going to deny us payment on that, and then we’re going to have to appeal,” he said. Hospitals end up having to leave millions of dollars on the table because of this. “It’s just this is the game that insurers play,” said Hirsch.
Technological advances have saved many lives and a lot of time, but they must be carefully implemented, according to Salvon-Harman. Many manual surgeries and open surgeries have become laparoscopic and are now becoming robotic. “Those kinds of changes happen over time. None of that was intentional. Nobody said, ‘We need to have a robot to do surgeries, because it’ll be better than laparoscopes and open surgeries.’ The technology evolved and emerged, and we said, ‘Yes, we could use that because that looks like it’s better, that might be more effective, that might be more consistent [for some surgeries].’”
As a result of the way our health system has evolved, there are a lot of inconsistencies. “When you move across one organization to another, sometimes even within the same parent organization, different sites of care may be doing things differently. And so, we’re always trying to balance the structures, the processes and the culture of the large parent organization, but also each and
every one of the individual sites of care, whether a hospital or an outpatient practice,” said SalvonHarman. “So, there’s still a lot to do around achieving those higher levels of consistency and, in some cases, being in sync with other parts of the system. Technology holds some promise in closing some of those gaps, moving us in that direction, but it hasn’t yet done it completely successfully.”
Many of the new technologies are intended to help us “work smarter, rather than harder, and are supposed to increase the efficiency or the effectiveness of what we do,” said Salvon-Harman. But we need to be cognizant of the ways they introduce additional complexity. “They have a learning curve for how to use them optimally. They have various influences, like what we call human factors: how the human interfaces with that piece of equipment or that technology that may introduce risk at the same time that it is eliminating other risks.”
At the same time, we are at a point when new technologies must be embraced, as they can keep health care moving forward and are what many patients have come to expect, according to Yunan Ji, an assistant professor of strategy with a focus on the design and regulation of health care markets at the Georgetown University McDonough School of Business. With more transparent pricing than in the past, health care organizations also need to find effective ways to communicate “nonprice attributes,” such as clinical outcomes and patient experience, in ways that resonate with consumers who are making choices about where to receive care.
platforms — ranging from online scheduling and virtual visits to personalized cost estimators and mobile engagement tools — will be better positioned to attract and retain patients. In a competitive environment where convenience, transparency and digital experience matter more than ever, digital maturity is becoming a key differentiator for providers.”
At Bon Secours Mercy Health, one of the goals is to make health care easier for patients and for consumers. In 2024, Bon Secours Mercy Health launched a conversational, artificial intelligence (AI)-powered digital guide called “Catherine,” (named in honor of Catherine McAuley, the founder of the Sisters of Mercy) aimed at transforming how patients access information and resources when they have knee, hip and shoulder pain.5
“Conversational AI represents the modern era of patient engagement,” said David Cannady, Bon Secours Mercy Health’s chief strategy officer. “It’s time to offer a solution that goes beyond what patients can currently access in Google searches or on social media platforms.” In addition, the health system is working toward same-day access
“In a competitive environment where convenience, transparency and digital experience matter more than ever, digital maturity is becoming a key differentiator for providers.”
— YUNAN JI
“This shift also reflects a broader transformation toward a more digital, consumer-oriented health care ecosystem — accelerated by the rise of telemedicine, on-demand care and virtual-first models. Just as consumers have come to expect seamless, intuitive digital experiences in sectors like retail and banking, they now bring those same expectations to health care, particularly for elective services, outpatient care and administrative interactions,” Ji said. “Hospitals and health systems that invest in modern, user-friendly digital
for patients, which Cannady believes will be driven by AI and automation. “We utilize AI to help patients access the right care at the right time by simplifying the process, from appointments and scheduling to finding the appropriate provider for their health needs, whether preventive or acute.”
Leaders at Bon Secours Mercy Health are watching several legislative and regulatory discussions that could have a potential impact on patient care and the providers of that care, said Cannady. “Key topics include Medicaid and Affordable Care Act

Exchange enrollment eligibility and other proposed reductions,” he said. “Should enrollment and public program reimbursement decline, health systems might face decisions such as the rationing of services to sustain a viable community-based model of care. In some cases, unfortunately, there may be closures of service lines or even hospitals in rural and other communities.”
For IHI’s Salvon-Harman, it means thinking about new delivery paradigms, new ways to identify what is meaningful. “Is it better for a patient to have a 15-minute appointment monthly, three months in a row? Or is it better for that patient to have 45 minutes with their health care provider one time in three months but get a much more substantive dose of health care in that 45-minute appointment?” he asked. “Do we need to think about how we acquire information in the health care setting, and how we process information? Do the standard tools for a history and physical examination that have been taught for over 100 years and used for over 100 years still serve the purpose?”
He suggests we look at adapting those models and collecting information differently so we can analyze that information, and we can apply the thinking from that analysis to each patient. “I feel like that’s really where we’re at now in ambulatory care: needing to really question the models we’ve been using and their effectiveness, and identifying and testing new models to see if they enhance our ability to diagnose more accurately, more timely,” said Salvon-Harman. “And to better coordinate across different specialties more efficiently and effectively, creating venues for more cross talk in real time, across specialties and across providers, leveraging AI and leveraging virtual technology to support better information sharing closer to real time. I think those are a lot of the opportunities that are emerging but haven’t yet been successfully harnessed.”
There are also error and human factors, according to Thomas Jefferson’s Kowey. While AI and technology can help, they can’t replace human judgment. “We’re not dealing with widgets here. We’re dealing with biological organisms with feelings, with emotions, with expectations, with
fear and anxiety,” he said.
Everything comes down to making systemic changes, according to Kowey, who was motivated to write his book by the “tremendous number of problems” in the U.S. health care system. “As the title says, it’s broken. It’s impacting both the quality of patient care and the well-being of providers. Burnout is real. But I truly believe it doesn’t have to be this way,” he said. “It’s a call to action for patients, legislators, administrators and providers. We still have options, but not a whole lot of time. If things keep going the way they are, we may lose the quality of care we’ve come to expect, possibly for good.”
ELIZABETH GARONE is a freelance writer who has covered health, business and human-interest topics. Her writing has appeared in The Wall Street Journal, The Washington Post, BusinessWeek and The Mercury News, among other publications.
1. “Health Provisions in the 2025 Federal Budget Reconciliation Law,” KFF, August 22, 2025, https://www.kff. org/medicaid/health-provisions-in-the-2025-federalbudget-reconciliation-law.
2. Marcia Frellick, “Survey Shows One-Third of Physicians Considering Leaving Medicine,” MedCentral, June 17, 2025, https://www.medcentral.com/biz-policy/ survey-shows-one-third-of-physicians-consideringleaving-medicine.
3. “The Complexities of Physician Supply and Demand: Projections From 2021 to 2036,” Association of American Medical Colleges, March 2024, https://www. aans.org/wp-content/uploads/2024/05/aamc-2023workforce-projections-report.pdf.
4. Kathleen B. Watson et al., “Trends in Multiple Chronic Conditions Among U.S. Adults, by Life Stage, Behavioral Risk Factor Surveillance System, 2013–2023,” Preventing Chronic Disease 22 (2025): http://dx.doi.org/ 10.5888/pcd22.240539.
5. “Mercy Health Cincinnati First to Launch AI Powered Digital Assistant,” Mercy, December 20, 2024, https://www.mercy.com/news-events/news/ cincinnati/2024/mercy-health-cincinnati-first-tolaunch-ai-powered-digital-assistant.

MONICA MAALOUF, MD, AMY BLAIR, MD, and MARK KUCZEWSKI, PhD
Stritch School of Medicine, Loyola University Chicago
First, remember your vocation. Caring for patients is the main thing that doctors, nurses and health care professionals do. Navigating the nuances of immigration policy? Not so much. Unfortunately, immigration enforcement has become highly politicized, impeding the ability of healers to effectively treat their patients and to promote their health. Health care professionals need tools to address the social influencers of health related to immigration enforcement.
Discussing immigration often arouses suspicion of a hidden political agenda. However, the duty to care for patients is at the heart of the healer-patient relationship.1 Health care professionals are trained to set aside personal opinions and reactions to social circumstances in the service of optimizing patient care. Policies and opinions of recognized professional bodies, such as the American Medical Association, support addressing immigration-related barriers to care.2 We propose actions for clinicians that follow from the values that comprise the identity of the healing professions.
Because Catholic health care institutions espouse a commitment to carry out the healing ministry of Jesus Christ, marginalized and stigmatized patients are a focus of attention. Migrants and refugees are often among the named groups for which Catholics and Catholic institutions must exercise special care because they are politically underrepresented and lack opportunities to make their voices and concerns heard. As Pope John Paul II stated, “The Church in America must be a vigilant advocate, defending against any unjust
restriction the natural right of individual persons to move freely within their own nation and from one nation to another. Attention must be called to the rights of migrants and their families and to respect for their human dignity, even in cases of nonlegal immigration.”3
This recognition of migrants’ dignity or worth as rooted in their humanity has a long history that cuts across differences between so-called “liberal” or “conservative” Catholics and is encoded in key documents such as the Catechism of the Catholic Church. Pope Francis articulated that the situation of migrants should be seen as on par with “grave” bioethical questions.4 Of course, these foundational teachings are distilled into Catholic health care’s touchstone, the Ethical and Religious Directives for Catholic Health Care Services (ERDs).
The ERDs articulate the social mission of Catholic health care to those “whose social condition puts them at the margins of our society ... immigrants and refugees.”5 And they remind us that our respect for the worth or dignity of the human person “extends to all persons who are served by Catholic health care.”6 Undermining
that mission by violating patient privacy or in any way violating the trust of vulnerable patients cannot be tolerated.
Employees of a Catholic health care institution must respect and uphold the religious mission of the institution and adhere to these Directives. They should maintain professional standards and promote the institution’s commitment to human dignity and the common good.7
Second, create a culture of safety in the providerpatient relationship. The Trump administration has rescinded guidance that designated hospitals as protected sites, locations where routine immigration enforcement should not take place.8 For many who are undocumented, the act of seeking care and providing personal information is now an act of courage. Recent reports show that since the beginning of the year, 20% of lawfully present immigrants in the U.S. say they or a family member have limited their participation in activities outside the home due to concerns about drawing attention to immigration status.9
patients of varying immigration status. The key tenets of this approach include open-ended communication, collaborative care approaches, active listening and empathy.
Open-ended communication is essential to ensure patients can guide the visit, express their goals and health concerns, and not feel pressured by the provider’s priorities for the visit. Openended questions also help frame patients as active agents in sharing their health care story, provide them with a sense of control, and increase the collaborative nature of the visit.11
As patients feel a baseline sense of safety, providers can enhance a deeper sense of trust through active listening. This skill can help the provider elicit clues, either verbal or nonverbal, that may signal the larger social and structural factors influencing the patient’s health. For example, patients may report a general sense of worry about current events or exhaustion over elements outside of their control. Patients may express worry about a family member or the ability to safely travel to appointments.
A provider who demonstrates empathy and communicates nonjudgmentally is more likely to assuage some of the fear brought by immigration status, allowing patients to access the care they need.
One way many people with immigrationrelated fears respond to increased immigration enforcement is to avoid health care altogether. In one study, Hispanic patients were less likely to report having a regular care provider or attending preventive visits.10 These patients were also less likely to present for diabetes care. The implications of this care avoidance can be devastating for individuals, resulting in social and financial losses due to illness going untreated, as well as the loss of early cancer detection and modifiable disease prevention.
For the physicians and providers who see and treat patients, fostering trust and a sense of safety is crucial to ensure patients do not fear accessing the care they need. The principles of trauma-informed care and patient-centered care are useful frameworks for addressing fear among
Providers may open additional avenues for conversation by normalizing fearful circumstances. For example, a provider might say, “Some of my patients find that current events are causing fear that affects their health. Is that something you have experienced?”
Another helpful strategy is summarizing what has been said to encourage specificity. For example, “You said that the chest pain is worse when you are feeling stressed. Can you tell me anything else about the situations that are particularly stressful for you right now?” These foundational patientcentered techniques can facilitate communication, validate patient concerns and foster safety for patients sharing their stories.
However, providers should also be cautious to avoid retraumatization or probing for details that a patient might be unwilling to share. Active listening can again be used to notice signs of discomfort or pauses in the patient’s story, demonstrating hesitancy. These situations warrant a slow and deliberate approach that focuses on the patient’s needs. Like all discussions of difficult topics in the health care setting, patients should feel in control and be able to slow or stop conversations at their

discretion.
A provider who demonstrates empathy and communicates nonjudgmentally is more likely to assuage some of the fear brought by immigration status, allowing patients to access the care they need. Patients who do feel comfortable discussing immigration status may disclose varying levels of details of past events or future fears. Providers in primary care relationships may choose to assure patients that they can talk about it again in the future, when the patients are ready.
Third, recognize and address the manifestations of fear. Accessing affordable health insurance is a complex task for most Americans, but even more so for immigrant patients. Undocumented patients face significant barriers because they are not eligible for federally funded programs such as Medicare or coverage through the Affordable Care Act marketplaces. Most private insurance plans require a Social Security number or proof of lawful residency, which undocumented individuals typically cannot provide.
While federal Medicaid is largely off-limits to undocumented individuals, some states — including New York, California and Illinois — have created programs using state funds to fill in gaps, especially for children, those who are pregnant and those with urgent medical needs. However, financial challenges in public insurance have caused programs such as the Illinois Health Benefits for Immigrant Adults to be implemented, paused and then canceled, all in four years.12
manifest in the medical encounter. Some patients may ask for expedited or expansive testing that is outside of what is indicated by accepted standards of care. For example, women may ask for early mammograms or scans to “make sure” no serious complications are present. Some patients may also request additional refills of medications needed for diabetes, high blood pressure or other chronic diseases.
These requests stem from the uncertainty of both future insurance coverage and future ability to safely present for care. Patients who request additional services may be mistakenly written off by health care teams as unreasonable, overly anxious or experiencing somatization.
To optimize the health of all patients, providers should seek to understand the patient perspective and provide flexibility. Acknowledging the fear patients are experiencing and calling out the uncertainty of the system can also empower the patient-provider relationship. Helpful statements may include, “We cannot predict whether the policy (access) will change in the future, but I am an advocate for your health and will ensure we make the best decisions for you today.”
optimize the health of all patients, providers should seek to understand the patient perspective and provide flexibility. Acknowledging the fear patients are experiencing and calling out the uncertainty of the system can also empower the patient-provider relationship.
This rapidly changing landscape of eligibility and the prospect of financial catastrophe that people without health insurance face is at the forefront of patients’ decision-making. Turbulent times perpetuate fear and discomfort in seeking care. Beyond fears related to the cost of treatment, many who are undocumented avoid interfacing with public benefit systems simply to avoid disclosing private information that may compromise their safety.
For those patients who do seek health care, it is important for providers to recognize how fear can
Physicians can offer patients flexibility by offering virtual or telephone visits, after-hours health care options, and by providing extra refills of chronic medications between visits if it is safe to do so.
During these periods of legal and political uncertainty, it may be difficult for members of the health care team to project reassurance or calm, particularly when health care providers may have personal concerns about their rights or legal status. Relying on communities of practice focused on justice within a health care team is essential for maintaining strength amid uncertainty.
Fourth, make your clinic a safe and resourcerich environment. Earlier, we provided some ideas on interacting with patients to create a culture of safety in the provider-patient relationship. It is also important that health care professionals draw upon developed resources to make their clinic a safer place for these patients.
One easy-to-use resource to analyze your clinical environment’s preparedness for this era of ubiquitous immigration enforcement is the Model Policy developed by the Illinois Alliance for Welcoming Health Care. 13 This outstanding resource can walk you through the needed protocols of a “front door policy” to guide preparation for a potential entry into your facility by U.S. Immigration and Customs Enforcement or other law enforcement officials seeking to perform immigration enforcement. It will also guide you through specific practices regarding the allimportant designation of private spaces. If you desire further context on how these practices fit with what other health care facilities have done, we recommend consulting the Doctors for Immigrants’ tool kit.14 Furthermore, patients need usable information to take control of their situation, including resources and emergency planning materials. The number of outstanding online resources that can help with these tasks is rapidly growing, and it is tempting to provide a long list of links. However, most patients are better served by referral to a small number of useful and reliable resources that will enable them to begin taking action.
easy access to reliable information is an important way that you can parlay your credibility into patient empowerment.
Above all else, become the healer your patients need. We have focused on basic ways to support immigrant patients. Becoming a maximally effective health care provider for these patients requires some skill development and refinement that can be tailored to your patient population. This requires engagement.
Engage with your relevant professional organizations. For instance, the American Academy of Pediatrics has a Council on Immigrant Child and Family Health, the Society of General Internal Medicine boasts an Immigrant and Refugee Health Interest Group, and the American Society for Bioethics and Humanities has an active Immigration Affinity Group. The American Medical Association regularly issues policy statements regarding the humane care of immigrant patients.
Engage with relevant community organizations. Such networks can enhance your ability to support your patients significantly.
Such communities foster values formation and provide information regarding current developments and patient needs. Similarly, keeping abreast of advocacy information that is posted by CHA can secure and build your foundational knowledge.16

The Sanctuary Doctor tool kit was created to provide this information in a succinct, one-stopshopping kind of way. The website is available in English and Spanish.15 Convenient two-sided wallet cards with the QR codes to the English and Spanish web pages are available upon request from sanctuarydoctor@luc.edu. This is an easy and unobtrusive way to provide patient access to needed information on finding an immigration lawyer and developing an emergency plan.
While pointing patients toward such resources may seem insignificant, immigrant communities are often preyed upon by opportunists who misrepresent themselves as attorneys and defraud this already vulnerable population. Providing
Engage with relevant community organizations. Such networks can enhance your ability to support your patients significantly. For instance, while the legal resources section of the Sanctuary Doctor tool kit can assist your patients in finding qualified representation in your area, networking with local immigration advocacy organizations often results in knowledge of nearby legal services available to low-income clients on a pro bono or sliding scale basis. Similarly, such organizations can provide services and workshops that empower your patients. Contact with such groups can also enhance your understanding of the concerns your patients are facing.
In closing, we hope that you will find this information useful and helpful in supporting your
patients. Do not be overwhelmed by concerns about being inadequate for the task or not yet having the knowledge and skills you believe are optimal. As with most aspects of clinical practice, assistance is all around you, and you will quickly come to see how valuable your efforts are. Most importantly, your patients will respond to your care and reward you with trust. And, of course, in a trusting relationship, your patients will also become your teachers.
At Loyola University Chicago Stritch School of Medicine, DR. MONICA MAALOUF is an associate professor of medicine and the assistant dean of diversity, equity & inclusion. DR. AMY R. BLAIR is a professor of family medicine and is the assistant dean of medical education. MARK KUCZEWSKI is the Fr. Michael I. English, SJ, professor of medical ethics and the director of the Neiswanger Institute for Bioethics.
1. Sabrina Derrington et al., “Plan, Safeguard, Care: An Ethical Framework for Health Care Institutions Responding to Immigrant Enforcement Actions,” Hastings Bioethics Forum, April 1, 2025, https://www. thehastingscenter.org/plan-safeguard-care-an-ethicalframework-for-health-care-institutions-responding-toimmigrant-enforcement-actions/.
2. Rachel F. Harbut, “AMA Policies and Code of Medical Ethics’ Opinions Related to Health Care for Patients Who Are Immigrants, Refugees, or Asylees,” AMA Journal of Ethics 21, no. 1, (2019): https://journalofethics. ama-assn.org/article/ama-policies-and-codemedical-ethics-opinions-related-health-care-patientswho-are-immigrants/2019-01.
3. Pope John Paul II, “Ecclesia in America,” The Holy See, January 22, 1999, section 65, https://www.vatican.va/content/john-paul-ii/en/apost_ exhortations/documents/hf_jp-ii_exh_22011999_ ecclesia-in-america.html.
4. Pope Francis, “Gaudete et Exsultate,” The Holy See, March 19, 2018, section 102, https://www.vatican.va/ content/francesco/en/apost_exhortations/documents/
papa-francesco_esortazione-ap_20180319_gaudeteet-exsultate.html.
5. Ethical and Religious Directives for Catholic Health Care Services: Sixth Edition (Washington, DC: United States Conference of Catholic Bishops, 2018), 9.
6. Ethical and Religious Directives, 13.
7. Ethical and Religious Directives, 9.
8. Lynn Damiano Pearson, “Factsheet: Trump’s Recission of Protected Areas Policies Undermines Safety for All,” National Immigration Law Center, February 26, 2025, https://www.nilc.org/resources/factsheet-trumpsrescission-of-protected-areas-policies-underminessafety-for-all.
9. Shannon Schumacher et al., “KFF Survey of Immigrants: Views and Experiences in the Early Days of President Trump’s Second Term,” KFF, May 8, 2025, https://www.kff.org/racial-equity-and-health-policy/ poll-finding/kff-survey-of-immigrants-views-andexperiences-in-the-early-days-of-president-trumpssecond-term/.
10. Abigail S. Friedman and Atheendar S. Venkataramani, “Chilling Effects: U.S. Immigration Enforcement and Health Care Seeking Among Hispanic Adults,” Health Affairs 40, no. 7 (2021): https://doi.org/10.1377/ hlthaff.2020.02356.
11. Jeffrey D. Robinson and John Heritage, “Physicians’ Opening Questions and Patients’ Satisfaction,” Patient Education and Counseling 60, no. 3 (2006): 279-285, https://doi.org/10.1016/j.pec.2005.11.009.
12. Peter Hancock, “Illinois on Track to End Health Coverage Program for Immigrant Adults,” WTTW News, May 14, 2025, https://news.wttw.com/2025/05/14/illinoistrack-end-health-coverage-program-immigrant-adults.
13. “The Model Policy,” Illinois Alliance for Welcoming Health Care, https://www.ilalliancehealth.org/policies.
14. “Our Toolkit,” Doctors for Immigrants, https:// doctorsforimmigrants.com/ourwork/#ourtoolkit.
15. “Treating Fear: Sanctuary Doctoring,” Loyola University Chicago Stritch School of Medicine, https://www.luc.edu/stritch/bioethics/ medicaleducation/sanctuarydoctor/.
16. “Advocacy: Immigration,” Catholic Health Association of the United States, https://www. chausa.org/advocacy/issues/immigration.
HEALTH CARE ACROSS AMERICA

ROBIN ROENKER Contributor to Health Progress
Roughly 1 in 5 Americans — more than 60 million in all — live in rural areas across the country. For these residents of rural ZIP codes, locating accessible health care can feel like an uphill battle.1
The striking provider disparity between urban and rural areas in America is one key reason why. While urban areas currently average 31 providers per 10,000 people, rural areas have just 13 per 10,000 residents. And while urban areas boast 263 specialists for every 100,000 individuals, rural areas have only 30 specialists available per 100,000 people, according to the National Rural Health Association.2
Across the country, Catholic hospital systems are working diligently to bridge this divide and provide greater health care access to residents of small towns and farm communities.
When it comes to maximizing rural health care delivery, “It’s really a theme of each patient getting the right care at the right place at the right time,” said Kevin Post, DO, chief medical officer for Avera Health. To pursue that mission, Avera has prioritized “keeping the patient at the center of focus, while leveraging innovative tools” to support rural health care providers, Post said.
Other systems, including SSM Health and Intermountain Health, are doing the same. Drawing on innovative telehealth applications, creative
staff recruitment initiatives and organizational models that optimize the reach of available staff and facilities, Catholic health systems strive to provide all patients with top-notch care, unhindered by community size.
Historically, rural residents have poorer health outcomes, on the whole, than those who live in urban areas. 3 Death rates from heart disease, cancer, stroke and respiratory disease tend to be higher in rural areas,4 leading to a life expectancy for rural residents that’s roughly 2.5 years lower than their urban counterparts — a gap that continues to widen.5 These outcomes are tied to a myriad of health determinants, from smoking rates and obesity rates to residents’ access to nutritious food, health insurance and accessible health care, among other factors.
Hospital administrators said tackling this rural-urban disparity will require a multipronged approach, with telehealth programming serving as a powerful tool to help level the health care playing field.
Beginning with telehealth programming for critical care in 2014, Intermountain Health has grown its telehealth services footprint to include 105 programs, including telestroke, telehospitalist, teleoncology, telechaplaincy and telecrisis (behavioral health) services. The telehealth programs serve Intermountain Health’s entire 33-hospital footprint, including five Catholic hospitals across Montana and Colorado, as well as 43 hospitals outside of the Intermountain Health system that receive services on a contract basis.
“Through telehealth, we can bring specialty care to the patients, instead of bringing the patient to specialty care,” said John Williams, Intermountain Health’s assistant vice president of telehealth services. Having access to specialists via telemedicine reduces travel time for patients, allowing them to receive expert care in smaller, local, critical access hospitals, which frequently do not have specialists, like neurologists, on staff.6
“If we have a patient who walks into the emergency room who is suspected of having a stroke, staff will call our command center to be immediately connected with our telestroke team,” Williams said. “Typically, in under three minutes, [the remote specialists] are able to see that patient, and they’re able to run through their assessments, using video technology, to work with the local physician or local APP [advanced practice provider], depending on how that hospital is staffed, to help develop a care plan for that patient.”
“Our patients [in rural hospital settings] will see local, advanced practice providers, while getting remote access to specialists — perhaps back in Sioux Falls — so they really feel like they’re getting cared for by a team,” Post said.
Operating 23 hospitals across Illinois, Missouri, Oklahoma and Wisconsin, SSM Health, too, is “leaning heavily into telehealth to see how we can better open up care access for our patients,” said Stephanie Duggan, MD, the system’s chief clinical officer. She notes that SSM Health’s adoption of specialty services using telehealth — including stroke services — is well integrated across their network. Their next goal: integrating primary care using telehealth just as effectively, drawing on a regional service model.
“We need to lean into [telehealth] resources in a different way,” she said. “Telehealth can feel a bit impersonal, but if we can develop a regional telehealth center [where patients see the same, regionally based primary care providers] … we can help patients gain greater trust and confidence in the person on the other end of that camera.”
Like many systems, SSM Health, Intermountain Health and Avera Health also use telehealth services paired with remote monitoring technology as a prevention tool. These programs provide real-time biofeedback for patients at risk of cardiovascular disease, diabetes or even prepartum7 or postpartum complications. This allows providers to identify and address possible red flags before symptoms progress to critical levels.
“Through telehealth, we can bring specialty care to the patients, instead of bringing the patient to specialty care.”
— JOHN WILLIAMS
Systems generally transfer patients to tertiary sites if a higher acuity of care or an ancillary service is needed to maintain quality and safety of care.
At Avera — where 37 hospitals serve a footprint of 72,000 square miles across South Dakota, North Dakota, Nebraska, Iowa and Minnesota — a similar approach uses telehealth to deliver specialty services, like cardiac or oncology care, to rural facilities without those specialists on staff. “Telehealth services allow us to leverage our care team to the top of license,” said Post, noting that 90% of Avera’s hospitals are critical access facilities with 25 or fewer beds.
From a health care provider’s perspective, having the support of telehealth services can, in some cases, lessen the challenges of accepting a post in a rural area, where staffing can be stretched thin. Avera is among the systems that have found success, for example, in implementing an artificial intelligence-supported virtual nursing program that lets remote, central hub teams use in-room cameras to monitor patient fall or bed sore risk, reconcile medications and do other routine tasks.8 This addition of “virtual eyes on beds” helps free on-site nurses to focus their expertise on other, high-level responsibilities, Post said.
Additionally, Intermountain Health found that hospitals using its nighttime telehospitalist services discovered it’s now easier to retain staff, Williams said. “Because this service allows us to


handle admit orders overnight virtually, on-site physicians no longer have to be on call 24/7. It allows the on-site teams to refresh and have some time with their families. As a result, these communities are able to recruit and retain physicians much more successfully.”
Recruiting and retaining staff is a critical concern at rural hospitals and clinics, as it is everywhere in health care.
Administrators at SSM Health, Intermountain Health and Avera Health agreed that building a pipeline of rural care providers remains a key focus. Each system is developing specific outreach programming to address ongoing staffing needs.
“We have to have people see rural medicine in a different light,” Duggan said, pointing to the power of offering on-site, rural shadowing opportunities for young physicians. “It’s about showing [them] how vital and what an important role and a difference one can make by being a part of
a smaller community,” she said. “Often that is enough for them to say, ‘Hey, maybe I could see myself living in a more rural community, even though I didn’t grow up there.’”
For some providers, the rural setting is a real draw. SSM Health’s two southern Illinois hospitals, St. Mary’s Hospital in Centralia and Good Samaritan Hospital in Mount Vernon, for instance, have found notable success recruiting locally. Partnering with area community colleges, the hospitals offer a nursing extern program that allows current nursing students to gain hands-on training while still in school. To date, roughly 85% of program participants have gone on to accept full-time SSM Health nursing positions in either Centralia or Mount Vernon. The hospital system hopes to expand the program soon to include other modalities, including respiratory therapy.
SSM Health also actively works to build partnerships with area high schools, sending representatives to career days and health class presentations, all with the hope of attracting local stu-
dents to the diverse array of health careers at an earlier age.
“We’re having to get more creative to build our own [workforce] pipelines,” said Damon Harbison, president at both SSM Health St. Mary’s Hospital — Centralia and Good Samaritan Hospital. “While we of course welcome outsiders, what we have found is that when you’re able to attract locals who already have staked their claim to the area, so to speak, you’re going to have more success in retention.”
For its part, Avera has found traction in attracting and retaining nurses through internships and an innovative internal travel nurse recruitment program. This program offers high-paid travel placements limited to 13 Avera sites across three states.
“It’s a win-win,” Post said. “Participating nurses get the benefit of a higher compensation rate, but with the security of having employment by a health system. Meanwhile, from a system perspective, we’re getting the benefit of placing our own team members who can move seamlessly between sites because they’re comfortable with our care protocols.”
Since 2005, 112 hospitals serving rural counties across the country have closed completely. During the same period, another 84 rural-serving hospitals converted to non-acute or non-inpatient care, according to the University of North Carolina at Chapel Hill’s Cecil G. Sheps Center for Health Services Research.9
In the last five years, more than 100 rural labor and delivery units have closed across the U.S. Today, fewer than half of America’s rural hospitals offer maternity services.10
These closures offer glimpses of what could become a growing trend. Already, roughly 44% of rural hospitals in America are operating with negative margins, according to KFF (formerly the Kaiser Family Foundation).11
As hospital system margins become further squeezed by health cost escalations and dwindling reimbursements, rural systems, especially, will need to continue making careful decisions regarding where and how best to deliver care to maximize efficiencies, leaders said.
Service delivery challenges may become even more difficult after the passage in July of HR-1, better known as the One Big Beautiful Bill Act. Those who opposed this legislation fear that reductions

in Medicaid and Medicare funding could lead to the shuttering of many rural care facilities.
Just after the bill’s passage, Ascension posted a statement from its president, Eduardo Conrado, noting that the impending cuts “risk destabilizing the health care system, especially in rural and underserved areas.”12
While the newly signed legislation does include $50 billion in federal funding for a new “rural health transformation program,” that figure represents only slightly more than one-third of the estimated loss of federal Medicaid funding in rural areas, according to KFF.13
While some details of the fund’s allocation remain unclear, it’s expected that half will be distributed equally across all 50 states, with CMS retaining discretion regarding allocation of the remaining $25 billion.14
In times when there’s a challenging operational climate, rural systems will be forced to rethink their delivery approach, Harbison said.
“Twenty-five or 30 years ago, every community hospital was trying to offer every service they possibly could. Those times are over,” he said. “With the impending reimbursement cuts, there will be a lot of boardroom discussions about the need to potentially close services or consolidate or close hospitals.”
In navigating those decisions, SSM Health will focus on how best to deliver the precise, tailored services each community needs, Harbison said. To identify those services, the system already leverages a multistep approach, including patient surveys, dialogues with providers, and formal community needs assessments.
SSM Health also plans to continue building partnerships with community agencies and even competing health systems to ensure health services remain available in small market areas.
“If we can help patients by doing something together, then that’s the right thing to do,” Harbison said.
At Avera, care delivery optimization plans include ramping up core care services at its regional hospitals, so patients in very remote areas can still access critical care within, say, a two-hour drive rather than needing to travel four or more hours to an urban, tertiary site, Post said.
Avera also plans to remain laser-focused on meeting community service needs and developing local partnerships to address rural citizens’ food, housing and transportation insecurities.
Additionally, across the country, many small
hospitals have found success working with larger regional hospitals — as either managed or affiliate partners — to leverage efficiencies in supply chain management, regulatory protocols and other top-level administrative demands.
These partnerships have led to substantial cost savings and operational advantages for participants in Illinois, said Harbison, who serves as president of SSM Health’s Southern Illinois rural health network.
“Over the last several years, we have worked with smaller hospitals in the area to … build relationships to ensure that everyone is working at the top of their scope to help their communities,” Harbison said.
“I think we are going to see this more and more, that [community] hospitals are going to partner up with bigger systems” to operate successfully, Harbison added. “There’s a sense that we don’t need to be operating in silos. People are realizing there’s power in working as a system to create a [best practice] playbook for rural health.”
Finally, health care providers must continue assessing the quality of their care delivery through the lens of patient experience. At every turn, health care leaders said, their goal is to provide streamlined, accessible, top-notch care, regardless of an area’s population size.
“I think one of the most important things we can do,” SSM Health’s Duggan said, “is to lean into available technology, standardizing where it makes sense, so our patients have a consistent, quality care experience.”
ROBIN ROENKER is a freelance writer based in Lexington, Kentucky. She has more than 15 years of experience reporting on health and wellness, higher education and business trends.
1. “How We Define Rural,” Health Resources & Services Administration, February 2025, https://www.hrsa.gov/ rural-health/about-us/what-is-rural.
2. “About Rural Health Care,” NRHA, https://www. ruralhealth.us/about-us/about-rural-health-care.
3. Kendal Orgera, Siena Senn, and Atul Grover, “Rethinking Rural Health,” AAMC, September 27, 2023, https:// www.aamc.org/advocacy-policy/rethinking-rural-health.
4. Sally C. Curtin and Merianne Rose Spencer, “Trends in Death Rates in Urban and Rural Areas: United States, 1999-2019,” NCHS Data Brief, no. 417 (2021): https://dx.doi.org/10.15620/cdc:109049; Macarena C.
Garcia et al., “Preventable Premature Deaths from the Five Leading Causes of Death in Nonmetropolitan and Metropolitan Counties, United States, 2010-2022,” Morbidity and Mortality Weekly Report: Surveillance Summaries 73, no. 2 (May 2, 2024): http://dx.doi.org/ 10.15585/mmwr.ss7302a1.
5. Jaime Aron, “What’s Health Care Like in Rural America? We’re Taking a Close-Up Look,” American Heart Association News, April 30, 2024, https://www.heart. org/en/news/2024/04/30/whats-health-care-like-inrural-america-were-taking-a-close-up-look; Jack M. Chapel, Elizabeth Currid-Halkett, and Bryan Tysinger, “The Urban-Rural Gap in Older Americans’ Healthy Life Expectancy,” The Journal of Rural Health 41 (2025), https://doi.org/10.1111/jrh.12875.
6. “Critical Access Hospitals,” Rural Health Information Hub, https://www.ruralhealthinfo.org/topics/ critical-access-hospitals.
7. Julie Minda, “Avera Health Uses Remote Monitoring to Improve Health Outcomes for New Moms in Eastern South Dakota,” Catholic Health World, June 2025, https://www.chausa.org/news-and-publications/ publications/catholic-health-world/archives/june-2025/ avera-health-uses-remote-monitoring-to-improvehealth-outcomes-for-new-moms-in-eastern-southdakota.
8. “Avera Expands Telemedicine Efforts to Virtual Nursing,” Avera, Balance (blog), December 12, 2023, https://www.avera.org/balance/family-medicine/ avera-expands-telemedicine-efforts-to-virtual-nursing/.
9. “Rural Hospital Closures,” Cecil G. Sheps Center for Health Services Research, https://www. shepscenter.unc.edu/programs-projects/rural-health/ rural-hospital-closures/.
10. “Stopping the Loss of Rural Maternity Care,” Center for Healthcare Quality & Payment Reform, June 2025, https://chqpr.org/downloads/Rural_Maternity_Care_ Crisis.pdf.
11. Zachary Levinson and Tricia Neuman, “A Closer Look at the $50 Billion Rural Health Fund in the New Reconciliation Law,” KFF, July 24, 2025, https://www.kff.org/ medicaid/issue-brief/a-closer-look-at-the-50-billionrural-health-fund-in-the-new-reconciliation-law/.
12. Eduardo Conrado, “Statement on Medicaid and ACA Cuts in Newly Passed Legislation,” Ascension, July 3, 2025, https://about.ascension.org/news/2025/07/ statement-on-medicaid-and-aca-cuts-in-newly-passedlegislation.
13. Levinson and Neuman, “A Closer Look at the $50 Billion Rural Health Fund.”
14. Levinson and Neuman, “A Closer Look at the $50 Billion Rural Health Fund.”






SARA VAEZY, MHA, MPH Chief Transformation Officer, Providence St. Joseph Health
At Providence, our commitment to delivering high-quality, mission-driven care guides us in everything we do, including leveraging technology solutions. To help give time back for what matters most — patient care and human connection — we’re investing in artificial intelligence (AI)-enabled tools designed to streamline workflows and simplify day-to-day processes.
In our 2030 strategic plan, we are focused on making Providence the best place to give and receive care, as we create a delivery model for the future supported by innovation and positive change. Our five-year road map is anchored in three strategic pillars: be the best place to give and receive care, create the delivery model of the future, and drive focused innovation for positive change.
Using technology as a tool to transform and improve the patient and caregiver experience enables all three strategic pillars. At Providence, all our employees are called caregivers, recognizing that each of us plays a part in caring for patients and each other.
Pertaining to patient care, Providence is focused on patient experience and has established three focus areas to help our patients navigate their care: making it frictionless, personalized and navigable. Frictionless means making it easier for people to find and use our services. For example, we aim to ensure that all schedulable appoint -
ments have the option of being booked online. While that option is currently not exercised at each location, we know that, as a system, we seek to have everyone operating from the same data. Whether an appointment is made by phone or online, we help patients get the most information about where to get care.
We’re also focused on the personalization of care. We serve 5 million patients annually in our seven-state footprint. Each patient is different, with different needs, motivations and expectations of the services they are using. We connect with patients in a way that keeps them engaged.
Finally, when it comes to navigation, patients want to be able to navigate getting and receiving health care the way they are used to doing things in real life, just as they do with online shopping and banking. We focus on web, mobile and call center experiences to make it easy for our patients to get care. Navigation means being able to easily get into the right care at the right time, find the information you need, and get the job done (for example, booking an appointment) as a patient with minimal effort.
Providence Considers Health Care Trends as It Determines How Best To Use AI
Ongoing uncertainty and volatility in government
Changing supply and demand/ economic trends
Distribution, decentralization and emergence of ecosystems
Ongoing workforce challenges and competition for workforce
Digital enablement of consumer experience
Consolidating ambulatory environments
The rise of the “payvider”
A new flavor of health system mergers and acquisitions
Growing focus on diversification
Artificial intelligence adoption and data emerging as differentiators
Providence leaders gather data and forecasts as they plan for the future. They begin with a foundational understanding of the provision of health care as a public good, and examine the impact of the overall geopolitical landscape, the nature of supply and demand, workforce concerns, anticipated changes in reimbursement, and shifting market dynamics, such as the rise of the payvider, which is an entity that provides both insurance and care delivery services.

On the clinical side, we are focused on using AI technology to give our providers more quality time with our patients through what we call “sacred encounters.” For instance, an overwhelming number of messages that patients submit through their patient portal take a lot of clinician time away from direct patient interaction because care teams must respond to messages. Providence clinicians receive about 7 million patient-generated messages annually, and responding to these messages is a source of clinician burnout and fatigue.
We are taking a multipronged approach to this problem: by reducing the number of patientgenerated messages by providing direct patient access to the information they need or the task they’re trying to complete; by triaging messages to the right member of the care team; and by helping clinicians efficiently respond to messages.
All this said, AI within the health care realm is complicated and requires oversight, governance and guardrails. We’ve put in place key initiatives to ensure that we keep patients and caregivers safe and set ourselves up for success.
There are two key bodies of work happening at Providence, each composed of multiple initiatives. The first is our internal AI work groups. The Clinical AI Work Group is a dedicated multidisciplinary team led by clinicians who provide oversight, feedback and guidance around priority work areas for clinically oriented AI. The second work group is our Enterprise AI Guardrails Work Group. With so many AI-based solution implementations in flight, Providence leaders need visibility into these projects to provide guidance. This group evaluates AI solutions for safety, equity, risk, legal, compliance,
ethics and privacy guardrails. The team implements a governance structure to prioritize, safeguard patient data, prevent bias and ensure access to innovations for all, including underserved populations.
The other body of work is the Office of Transformation. The office aims to create a multidisciplinary and cross-functional approach that brings together technology, operations, clinical and financial aspects to drive large-scale changes throughout our system. There are two workstreams built into the Office of Transformation: current initiatives and future initiatives.
Current efforts this year are focused on reducing clinical administrative burden through clinician-facing documentation and charting support with ambient solutions, and supporting the
reduction and response to in-basket messages. These tools can save clinicians time during and after care. The tools also allow providers to spend more meaningful time with patients and still wrap up their day at a reasonable hour.
One guiding principle is that we are not going to automate what isn’t working — it is not substitutive. We will do things better and think about these issues more materially. Our future initiatives include workflow automation and new models of care delivery through virtual and asynchronous care. All will incorporate AI solutions as part of the process. When done right, AI is going to help our patients and caregivers.
SARA VAEZY is chief transformation officer for Providence St. Joseph Health in Seattle.
1. As you think about how Providence St. Joseph is working to ensure patient experiences that are frictionless, personalized and navigable, what struck you about the way the system is involving technology and artificial intelligence (AI) in their processes? What interested you most about the approach?
2. Does your organization have internal work groups similar to those this system is using? What aspects of creating groups like a Clinical AI Work Group and an Enterprise AI Guardrails Work Group appealed to you?
3. In Catholic health care, keeping humanity at the center of care is foundational to the work. What can you contribute to your organization’s understanding of the use of AI, whether it’s a perspective on mission, ethics, clinical, all of these, or your own distinct perspective? What are some ways to discuss these evolving issues and how they are implemented where you provide care?
4. How might Catholic social teaching, organizational ethics and bioethics inform the appropriate design, implementation and use of AI in health care?

KELLY BILODEAU Contributor to Health Progress
Accountable care organizations (ACOs) are reshaping American health care, cutting billions in costs and improving patient outcomes through a patient-centered, preventive approach. Despite these successes, ACOs are facing growing challenges, prompting calls for reform to help these models achieve their full potential.
The money saved by ACOs often comes from seemingly small changes in clinical practice that can yield outsized benefits. An example comes from Hospital Sisters Health System (HSHS), which launched its ACO in 2015 in central and southern Illinois. At the time, doctors rarely screened for depression during visits, even though the condition puts a substantial clinical and financial burden on both the patient and the health care system.
Experience and research show that patients with untreated depression have high use of acute care services, and that is costly, especially when the underlying condition isn’t addressed, explained Dr. Leanne M. Yanni, president and CEO of Illinois Physician Enterprise for HSHS.
The organization wanted to do more for patients to respond to this “common mental health condition that needs both screening and timely treatment,” she said.
As part of the Medicare Shared Savings Program (MSSP), a value-based ACO model established by the Affordable Care Act and implemented by the Centers for Medicare and Medicaid Services (CMS) in 2012, the organization made depression screening a priority. As a result,
screening rates increased from 2 in every 10 patients to near universal levels, leading to more prompt treatments and better patient outcomes, Yanni said.
ACOs, like this one, have shifted away from a fee-for-service model toward a coordinated, preventive care approach that targets chronic conditions and social and behavioral determinants. The approach is producing tangible benefits. In 2023, the MSSP ACOs generated more than $3 billion in total earned shared savings, according to CMS.1
“The story of ACOs has been a very positive story, about growth, savings, improved clinical outcomes, better care, better health, lower cost,” said Emily Brower, president and CEO of the National Association of ACOs (NAACOS), which advocates for health care members of these organizations. “They’ve been incredibly successful.”
While they’ve shown broad improvements overall, ACOs are not equal, said Rob Saunders, PhD, senior research director for health care transformation at the Duke-Margolis Institute for Health Policy. “There are ACOs out there that have done amazing things and have really bought in, and their leadership is on board,” he said. Other ACOs have struggled. They may have conflicting
incentives, limited capital for making upfront investments, or their leadership is managing multiple priorities, he explained. “Not surprisingly, their results are often underwhelming.”
Spotty commitment isn’t the only issue affecting ACO performance. NAACOS and other advocates say that more than a decade into the ACO era, structural challenges with models, including the MSSP, are hindering progress. NAACOS is now advocating for revised reimbursement structures that better reward high performers and reduce administrative burdens. They also seek to create incentives to encourage organizations that are still sitting on the sidelines to engage in these value-based initiatives. Nearly 90% of 168 health care professionals in a recent NAACOS survey cited financial risk as a primary barrier to valuebased care.2
“We’ve produced enough evidence that these models are good for patients and providers. Let’s keep going and keep making it better,” Brower said. “Nobody wants to revert to fee-for-service because there’s not enough opportunity, or for organizations to drop out of ACOs because of the heavy administrative or regulatory burden.”
ACO models come in many different forms. Medicare’s MSSP was the first major driver for ACO adoption, although there were some earlier predecessors, Saunders said. Today, it’s one of several federal ACO models, including CMS Innovation Center models such as ACO Reach, ACO Primary Care Flex Model and the Enhancing Oncology
which now cover more than half of Medicare beneficiaries, are also driving value-based care, but do it by using capitated payments for each patient, rather than the ACO shared savings approach. 5 (Capitated payments are fixed, prearranged payments per patient.)
There are also commercial ACOs, coordinated by insurers such as Aetna, UnitedHealthcare and Cigna, which were once smaller than federal programs, but have grown rapidly and now rival or exceed Medicare ACOs in size, Saunders said. In 2022, approximately 45% of doctors participated in commercial ACOs, compared to about 38% in Medicare ACOs, according to the American Medical Association.6
Shared savings models vary in the amount of financial risk they place on ACOs. Some offer upside-only arrangements, where organizations only get a share of savings and no penalty for losses. Others, such as the MSSP Enhanced track, offer the opportunity to earn more from shared savings, but the program can also cost them more in losses.
Since they began, ACOs have achieved a 2% to 3% improvement in overall cost trends. While these percentages may sound slight, the reductions are in relation to trillions in expenditures, Duke’s Saunders said.
St. Louis-based Mercy has seen successes through its participation in the Enhanced track of CMS’s MSSP, the higher-risk and reward model. “Over the last five years, we’ve managed the total cost of care at 6% to 8% [it varies by year] lower than our peers in our given markets and our given communities,” said Dave Thompson, senior vice president, chief growth officer and president of population health at Mercy.
Organizations often need to invest in changes for three to five years before their efforts pay off, Saunders said. “You can’t just start an accountable care organization tomorrow and suddenly be able to improve quality and reduce costs,”
he said. “It
takes time.”
Model, among others.3 More than half of Medicare beneficiaries are now aligned in an accountable care relationship with a provider, according to CMS.4 In addition, Medicare Advantage plans,
In contrast to high-performing organizations like Mercy, many struggle to achieve results. Nearly 40% of Medicare ACOs made no savings or incurred losses, according to a report from Arcadia CareJourney.7
Organizations often need to invest in changes for three to five years before their efforts pay off, Saunders said. “You can’t just start an accountable care organization tomorrow and suddenly be able to improve quality and

reduce costs,” he said. “It takes time.”
Comparing results from federal and commercial programs is difficult because commercial programs rarely release public data and because of program variability. This variability also presents a challenge for organizations trying to participate across multiple programs, Saunders said.
While data isn’t available on all ACOs, a Congressional Budget Office report identified performance trends across Medicare programs. Those that do the best are those run by physician groups or have a larger proportion of primary care providers, and those who initially invested more in the programs than the regional average.8
It’s not surprising that physician-led ACOs tend to outperform hospital-led models because it’s often an apples-to-oranges comparison, Saunders said. Hospitals, which tend to be larger organizations with a lot of infrastructure, may face difficulties if they try to quickly change things like their workflows, processes and structures, he explained.
In addition, hospitals often face built-in disincentives under ACO models for hospitals. An ACO program typically allows an ACO to share in savings if health care quality remains constant or improves. However, a hospital may lose direct revenue if it cuts down on inpatient admissions or the number of emergency room visits. This means a hospital-based ACO might not be in a better place financially if it makes improvements. “However, an ACO led by a physician group would not have the same conflict if they reduce hospitalizations or emergency room visits,” he said.
high-quality care.’ Despite that intention, most providers still struggle to provide recommended care that is known to produce the best outcomes,” said Dr. Christopher Funes, president of the Louisiana-based Health Leaders Network (HLN) and the Franciscan Missionaries of Our Lady Health System (FMOLHS) medical director for ambulatory quality. “The difference under the ACO is intentionality. We don’t just recommend that our patients get colon cancer screening. We ensure that our providers can easily order it, follow up to make sure the patient has done it, and work continuously to close those care gaps using a ‘whole team’ approach.”
Today, more than 80% of HLN patients get the recommended colon cancer screening, compared to 30% at the program’s outset. “We’re catching more colon cancer earlier, when it’s more easily treated, and preventing colon cancer deaths,” Funes said.
“The difference under the ACO is intentionality. We don’t just recommend that our patients get colon cancer screening. We ensure that our providers can easily order it, follow up to make sure the patient has done it, and work continuously to close those care gaps using a ‘whole team’ approach.”
— DR. CHRISTOPHER FUNES
While there are financial risks associated with ACO participation, many think the long-term benefits outweigh the challenges. Michelle Wieczorek, former HSHS system director of accountable care, said their organization joined the MSSP to better align with its Franciscan mission of delivering compassionate, high-quality care to Medicare beneficiaries.
An ACO can help turn intent into reality. “Every provider wants to give their patient ‘good,
ACOs also help health care organizations take a broader view of care. “There’s a holistic approach to patient care with an ACO approach that really reinforces the importance of being proactive in a patient’s care and also providing high-quality preventative health screenings and behavioral changes, addressing the whole patient, and certainly the social drivers of health as well as behavioral health,” said Dr. Gavin Helton, president of primary care at Mercy.
Despite their successes, several factors hinder ACO performance. Administrative complexity is one. Tracking ACO requirements, measures and charting progress takes a lot of effort and
money. And recent program changes have added to the burden. CMS recently rolled out updated quality reporting requirements, Thompson said. “They’re well-intended, but they’re more focused on administrative tasks versus actual outcomes. So, it’s crucial that we keep that outcome orientation.”
Financial benchmarks also present barriers. Program targets are often based on past performance, so as organizations improve, it becomes harder to generate savings.
“On the Medicare side, we’re now seeing some groups that were the rock star ACOs start to drop out because the cost benchmarks that they’re being held accountable to were ratcheted down. At some point, that’s not sustainable for them,” Saunders said. “The ACO program design is going to need to be tweaked in order for them to be effective going forward.”
Yanni said that fluctuations in reimbursement, like annual fee schedule changes, also make it difficult for organizations committed to an annual budgeting process to participate in ACOs, because it’s difficult to plan and stay on track financially.
There are other factors as well. “One of the biggest challenges to success in ACOs is the amount of investment required to be effective in valuebased care,” Funes said. Certain types of facilities, including rural hospitals and community-based practices, however, face even steeper hurdles getting into the ACO model. Brower said NAACOS also hopes that future reforms will include new incentives to help more organizations clear those barriers.
Funes agrees that support could encourage participation. “More resources are needed in human capital, data and analytics, and in processes and support systems for providers,” he said. “It’s hard to make that kind of investment when you can’t be sure of the return. If we’re doing well in a particular ACO model, but CMS suddenly cancels that model, or pushes our group out of that model, it makes it really difficult to make future investments.”
However, some of the drag on performance comes from operational issues within the ACO. Many groups aren’t involving doctors in the improvement process. “It’s really important for hospitals to work with primary care well. It’s important for our specialists to work with their primary care
referral points in the hospitals,” Wieczorek said.
But many organizations don’t take this step. “ACOs have used different strategies for improving care. Some ACOs have tried involving care coordinators to smooth transitions from hospital to home or to manage referrals and data between different clinicians. These ACOs have not really engaged their front-line clinicians,” Saunders said. “And there’s a reason for that, but it makes it hard to get buy-in from clinicians for broader care delivery improvements.”
Changing clinical practices requires commitment from the doctors providing care. It also requires feedback. Providers need to see and understand what strategies are working and which are not, Wieczorek said.
A 2024 NAACOS report outlined some additional characteristics of the highest-performing ACOs.9 Many of the most successful organizations establish value-based care agreements with multiple payers and have tools in place that allow them to track and manage the different policies and programs. They also have engaged leaders who are committed to accountable care and lead the culture shift. Additionally, they use data and tools to identify areas for improvement, track progress and build trust with patients by involving them in the care decisions.
Experts are now pressing for changes to help ACOs thrive and to encourage more organizations to join in outcome-focused initiatives. These efforts come amidst new uncertainties about the road ahead.
“A year ago, I would have said there’s predictability in the evolution of ACOs, we don’t think it’s going to go away, but we think it’s going to continue to evolve in a positive way with increasing risk and hopefully more nationally directed support for what hospitals need to be successful,” Yanni said. That picture has shifted. If carried out in their present form, Medicaid cuts enacted through the recent federal budget reconciliation bill could affect ACO participation by increasing financial pressure on health systems and hospitals, Yanni said. “That will likely have a significant negative impact on health system finances, creating less willingness and ability to invest in valuebased care,” she said.
With Medicaid cuts and benchmarks potentially squeezing ACOs, the question is: Will

policymakers tweak ACO models quickly enough to keep providers on board?10 NAACOS’s Brower remains confident that there is bipartisan support for value-based models. “I think what we’re seeing today is still lots of support for accountable care from the new administration and continuing support from members of Congress,” she said.
Even so, organizations are preparing for change. Wieczorek said there’s work to be done to prioritize investments to keep the program on track. “We have been successful because we’ve developed the rigor and the discipline and the teamwork that it takes to do work in these riskbearing structures. It’ll just be harder as fiscal realities are challenging us,” she said.
Experts hope that ACO programs will continue to make progress. As the U.S. health care system continues to evolve, ACOs remain a central pillar of patient-centric reforms. But policy adjustments will be critical if they are going to realize their full potential.
KELLY BILODEAU is a freelance writer who specializes in health care and the pharmaceutical industry. She is the former executive editor of Harvard Women’s Health Watch. Her work has also appeared in The Washington Post, Boston magazine and numerous health care publications.
1. “Shared Savings Program Fast Facts,” Centers for Medicare and Medicaid Services, January 1, 2025, https://www.cms.gov/files/document/2025-sharedsavings-program-fast-facts.pdf.
2. “The State and Science of Value-Based Care 2025,” National Association of ACOs, https://www.naacos. com/wp-content/uploads/2025/05/State-and-Science-
of-VBC-2025.pdf.
3. Shveta Mehrotra and Katie Everts, “8 Trends Among Top-Performing MSSP ACOs in 2022,” Arcadia CareJourney, January 8, 2024, https://carejourney.com/ trends-top-performing-mssp-acos-2022/; “Innovation Models,” Centers for Medicare & Medicaid Services, https://www.cms.gov/priorities/innovation/models?cat =Accountable+Care+Models.
4. “CMS Moves Closer to Accountable Care Goals with 2025 ACO Initiatives,” Centers for Medicare and Medicaid Services, January 15, 2025, https://www.cms.gov/ newsroom/fact-sheets/cms-moves-closer-accountablecare-goals-2025-aco-initiatives.
5. Meredith Freed et al., “Medicare Advantage in 2024: Enrollment Update and Key Trends,” KFF, August 8, 2024, https://www.kff.org/medicare/issue-brief/ medicare-advantage-in-2024-enrollment-update-andkey-trends/.
6. Andis Robeznieks, “Nearly 60% of Doctors Work in a Practice That’s Part of an ACO,” American Medical Association, October 30, 2023, https://www.ama-assn. org/practice-management/payment-delivery-models/ nearly-60-doctors-work-practice-s-part-aco.
7. Mehrotra and Everts, “8 Trends Among Top-Performing MSSP ACOs in 2022.”
8. “Medicare Accountable Care Organizations: Past Performance and Future Directions,” Congressional Budget Office, April 16, 2024, https://www.cbo.gov/ publication/59879.
9. “ACO Drivers for Success,” National Association of ACOs, September 2024, https://www.naacos.com/ aco-drivers-for-success/.
10. “President Trump-Signed Reconciliation Bill: Budget, Economic, and Distributional Effects,” Penn Wharton, University of Pennsylvania, July 8, 2025, https://budgetmodel.wharton.upenn.edu/issues/2025/7/8/presidenttrump-signed-reconciliation-bill-budget-economic-anddistributional-effects.

“Society’s well-being depends upon their being given the ability to develop their God-given gifts and capabilities, and to respond to the demands of the times and the needs of others with a free and generous spirit.”
— Pope Leo XIV’s message to the Second Annual Rome Conference on Artificial Intelligence on June 20, 2025
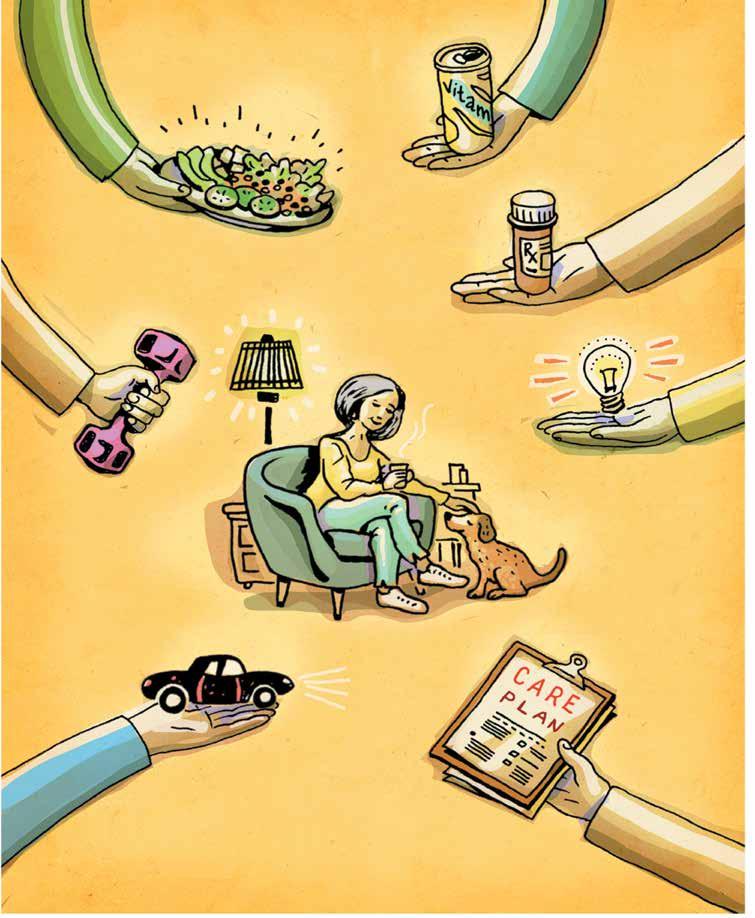
HEALTH CARE ACROSS AMERICA

MITCH LOMAX, MBA, TREVOR BONAT, MA, MS, and OLIVIA D. FARROW, Esq.
Ascension Saint Agnes Hospital
A60-year-old woman living with chronic conditions such as asthma, polymyositis, rheumatoid arthritis and depression sought emergency care due to worsening shortness of breath. Following her discharge from the emergency department, she continued to struggle with her symptoms while also navigating significant barriers to recovery, including food insecurity, lack of transportation and the need for home-based medical support.
However, through Maryland’s Total Cost of Care (TCOC) Model,1 the woman changed the course of her condition, leading her on a road to health and recovery through whole-person care that bridged her clinical and social needs. She is not being identified by name to respect her privacy.
The TCOC Model operates under a unique Medicare waiver that began in 2019, in which Maryland assumes the full financial responsibility for the total cost of care for Medicare beneficiaries. The Total Cost of Care Model establishes global budgets for hospitals, providing predictable revenue streams while simultaneously creating accountability for managing the total cost of care for their populations.2 For Catholic hospitals, with their long-standing commitment to serving the poor and vulnerable, the model’s support of integrated care allows the opportunity to align financial incentives with their core values of compassion, justice and community service.
The Health Services Cost Review Commission serves as the central regulatory body of the model, setting hospital budgets and monitoring performance against cost and quality targets. Each hospital receives an annual global budget that covers all inpatient and outpatient services, fundamentally changing the financial dynamics of health care delivery.
Unlike traditional reimbursement models that pay for each service provided, global budgets create incentives for efficiency and population health management. Hospitals that successfully manage their attributed populations within budget while meeting quality standards can retain savings, while those that exceed their budgets face financial penalties.3
Unlike traditional fee-for-service models that reward volume, this waiver allows Maryland to assume complete financial risk for Medicare
beneficiaries’ total health care costs across all settings and providers.4 In the model’s first years, from 2019-2021, Maryland generated more than $689 million in excess Medicare TCOC savings.5
A unique and innovative initiative of the TCOC Model is the development of the Maryland Primary Care Program (MDPCP). 6 This program serves Medicare patients and places an emphasis on the utilization of their primary care services. Through voluntary participation by primary care providers, funding is awarded to support the delivery of advanced primary care to a vulnerable population. The MDPCP provides hospitals with flexible funding that allows for the creation of resources and support that give primary care providers the ability to have a deeper role in the prevention and management of chronic diseases, and thus yields a reduction in hospitalizations.7
physical and occupational therapy.
For Catholic health care organizations, the TCOC Model offers a unique opportunity to align financial incentives with their fundamental mission of serving those most in need. Catholic hospitals have historically struggled with the tension between their commitment to providing charity care and the financial pressures of operating in a fee-for-service environment. The TCOC Model resolves this tension by creating financial incentives that support rather than penalize missiondriven activities.
The TCOC Model’s success suggests that the future of health care lies not in choosing between mission and margin, but in creating systems where serving the common good and achieving financial sustainability are mutually reinforcing goals.
The model includes specific requirements for care coordination services, including nutrition counseling, pharmacy services, behavioral health integration and health education. These requirements recognize that effective health care delivery requires addressing patients’ comprehensive needs, not just their immediate medical conditions. Hospitals must demonstrate meaningful engagement with community partners and show measurable improvements in care transitions and patient outcomes.8
Through Maryland’s comprehensive care coordination model, the patient with multiple chronic conditions was promptly connected with services, including home health care, the Moveable Feast meal program for Marylanders, and durable medical equipment like an oximeter and rollator. Care managers accelerated her primary care follow-up, provided emotional support, assisted with Maryland Transit Administration Mobility services, and ensured she had access to
Perhaps most significantly for mission-driven organizations, the TCOC Model includes explicit incentives for reducing health care disparities and improving access for vulnerable populations. The model measures and rewards reductions in disparities between different racial and ethnic groups and improvements in outcomes for patients living in high-poverty areas. Early results have shown promising reductions in disparities. Gaps in unplanned readmissions, preventable admissions and timely followup care narrowed by a range of 26% to 40% between Black and white beneficiaries.9
Maryland’s experience with the TCOC Model has important implications for health care transformation efforts nationwide. Last year, the Centers for Medicare & Medicaid Services announced plans to expand similar models to other states through the AHEAD (States Advancing All-Payer Health Equity Approaches and Development) Model,10 suggesting that Maryland’s innovations would become more widely adopted.
The TCOC Model’s success suggests that the future of health care lies not in choosing between mission and margin, but in creating systems where serving the common good and achieving financial sustainability are mutually reinforcing goals. For Catholic health care organizations and other mission-driven providers, this represents not just an opportunity for financial success but a pathway to more fully realize their fundamental calling to heal and serve.
For the 60-year-old Ascension St. Agnes patient, this approach meant she received medication reconciliation and proper inhalers, and she adhered to her care plan, remaining safely at home without any hospital readmissions. Her successful recovery illustrates how Maryland’s all-payer, value-based health care model supports patients far beyond episodic treatment. Unlike fee-forservice systems that often end care at discharge, Maryland’s model integrates medical, social and behavioral support services to address root causes and reduce readmissions.
The proactive, wraparound care received — ranging from timely follow-up to transportation and nutritional support — demonstrates how coordinated care under the Maryland model leads to better outcomes, enhanced independence and more efficient use of health care resources.
For Ascension Saint Agnes Hospital in Baltimore, MITCH LOMAX is chief financial officer.
TREVOR BONAT is chief mission integration officer. OLIVIA D. FARROW is vice president of external affairs. LAURETTA OSOMIHA, a nurse and case manager, contributed information for this article.
NOTES
1. “Maryland Total Cost of Care Model,” Centers for

Medicare & Medicaid Services, https://www.cms.gov/ priorities/innovation/innovation-models/md-tccm.
2. “Maryland Total Cost of Care Model.”
3. “Hospital Rate Setting: Successful in Maryland but Challenging to Replicate,” Healthcare Value Hub, June 1, 2020, https://www.healthcarevaluehub.org/ advocate-resources/publications/hospital-ratesetting-promising-challenging-replicate.
4. “The Maryland Model,” Maryland Hospital Association, https://mhaonline.org/wp-content/ uploads/2024/06/mha-maryland-model-valuegraphicdb8ede355f24402c9499fb957022b01c.pdf.
5. “Maryland Total Cost of Care Model: Evaluation of the First Four Years (2019–2022),” Centers for Medicare & Medicaid Services, https://www.cms.gov/ priorities/innovation/data-and-reports/2024/ md-tcoc-1st-progress-rpt-aag.
6. “Maryland Primary Care Program,” Maryland Department of Health, June 2021, https://health.maryland.gov/ mdpcp/pages/home.aspx.
7. “Maryland Primary Care Program.”
8. “Maryland Total Cost of Care Model: Evaluation of the First Four Years (2019–2022).”
9. “Maryland Total Cost of Care Model: Evaluation of the First Four Years (2019–2022).”
10. “States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model,” Centers for Medicare & Medicaid Services, https://www.cms. gov/priorities/innovation/innovation-models/ahead.
Ascension Saint Agnes Hospital authors Mitch Lomax, Trevor Bonat and Olivia D. Farrow describe ways in which the Total Cost of Care Model offers a unique opportunity to align financial incentives with the fundamental mission of serving those most in need. They describe ways it allows for care coordination.
1. This program operates through a unique Medicare waiver. What lessons can be learned from this approach, including for those who live in other states?
2. Do you work with anyone or glean helpful information from an author or thinker who advocates for health care transformation in a way that makes considerable sense to you? Who?
3. What significant changes might be needed to create “systems where serving the common good and achieving financial sustainability are mutually reinforcing goals,” as the authors write of the Maryland model?
4. Reflecting on the mission, vision and values of your organization, how do you see the Maryland program as a creative way to reimagine health care and services to the most vulnerable in your community?
HEALTH CARE ACROSS AMERICA

SARAH REDDIN, D.HCML Vice President, Ministry Formation-Mission Integration, Ascension
RICHARD FOGEL, MD, FACC, FHRS
Former Executive Vice President and Chief Clinical Officer, Ascension
Health care in America is in need of a transformation. Average costs of care are consistently double those of other developed countries, 1 while outcomes in the U.S. — like life expectancy, infant mortality and chronic disease management — fall short.2 Access remains a consistent issue with almost 8% of Americans, or 26 million people, without health insurance.3 Millions more are underinsured, causing them to delay or avoid care altogether.
How we, as health care providers, understand our patients and communities will become even more essential to serving in nuanced and personalized ways. In turning to the workforce itself, burnout, moral injury and administrative burdens cause distress, health concerns and professional disconnect, with many choosing to leave the profession altogether.
With so many cracks in the foundation, it can be hard to know where to turn for solutions. One source of strength comes from the very principle that gave birth to Catholic health care in the first place: human dignity. This commitment is drawn from Genesis 1:26-27 and the firmament of the imago Dei, which powers our ministries to know we are made in God’s image and that we grow in God’s likeness through each act of loving service we make. Wherever human suffering is occurring — including throughout health care in this country and our own ministries — we can detect an affront on human dignity.
The roots of our 2,000-year-old Catholic
Christian tradition grow from the Judaic tradition that is more than 2,000 years its elder. And within that tradition lies the principle of tikkun olam, meaning “repairing the world.” While it has evolved to take on different applications in different contexts, from a Judaic social justice perspective, tikkun olam compels persons to engage in works of social justice, in charitable endeavors, in activism, in acts of kindness to make the world a better, more equitable place. At its core is the understanding that each person has a personal moral responsibility to alleviate human suffering and contribute to the well-being of others.
Most people seeking health care do so not because they want to, but because they have to. In these realities, medicine and health systems across the country have designed sites of care, access models, scheduling tools and more from the perspective of the provider. These models communicate that the patient must be seen on the timeline and terms of the provider to maximize his or her efficiency and experience. They
also convey that associates must accomplish their work in standard patterns, sometimes at odds with their own basic needs.
If we focus on pulling the most fundamental commitment from our Catholic heritage to the forefront, we can flip this script. What is required here is a heart shift from “they are fortunate to see us” to “it is our privilege to encounter and serve them.” And from “this is the way the work is” to “let’s design new ways of working, together.” This, in turn, generates a mindset shift in clinicians, associates and administrators alike that causes us to move mountains in service to the individuals and communities we care for and are a part of. It generates clarity. It focuses our attention. And it drives results in a human-centric way that differentiates the experience for all.
Our tradition is replete with examples of reverent service. In fact, the very term we use for our primary sites of care, hospital, indicates as much. Drawing its roots from the Latin word hospes, meaning “guest” or “stranger,” hospital is derived from the Old French word ospital, meaning hostel, lodging or shelter for the needy.
Going deeper into our tradition, however, the verb “to hospitalize” is based on the AramaicHebrew word ashpez, meaning to host or invite a guest into your home and look after them hospitably. Phonetically and in its meaning, ashpez is similar to hospice/hospital, both in its historical use and in modern Hebrew. It is therefore possible that the word hospital is derived from Aramaic.4 This was the language of Jesus, which offers insight into the threads of the vocabulary of our ministry identity even today.
The emphasis on “all” is incomplete without emphasizing the capacity within the imago Dei for “un-othering.” When we see our own humanity reflected in those leading lives quite different from our own, the motivation toward justice in the form of true right relationship is activated in powerful ways. Knowing that the immigrant’s humanity is our humanity — just as much as the humanity of our own child, spouse or an unhoused person is our humanity — ensures we are ever-challenging ourselves to see the real face of God in those we are so blessed to serve and serve beside.
When we see our humanity reflected in those leading lives quite different from our own, the motivation toward justice in the form of true right
relationship is activated in powerful ways. Making this commitment to honor and make a guest of each person means taking practical action. Being dedicated to the concept takes us only so far. As Pope Francis was known to say through his actions and words, “realities are more important than ideas.”5
At Ascension, we have been taking this humancentric commitment to those we serve into new horizons, testing how we can decrease cost, improve access, and raise the bar on consumer, clinician and associate experience.
Innovation in access: In our focus on caring for all people, understanding the distinct needs of the unique populations we serve by various demographic sets, and then investing in their specific needs, we see this approach reaping positive outcomes at Ascension. By working with our patients and understanding their access patterns, we have opened up primary care visits elsewhere in our ecosystem and have achieved a 5% drop in preventable emergency department visits.6 This is reverence in action.
‘Real-time listening’: Every health system has some way of collecting patient feedback, with those participating in Medicare using the Hospital Consumer Assessment of Healthcare Providers and Systems survey as a standard mechanism. Striving to truly listen to the heart of our patients’ and their families’ care journey — from scheduling through care delivery and bill payment — is the rigor that the Ascension Consumer Experience team has brought to those we serve. This is demonstrated through an enhanced behavioral science method married to our mission in a realtime listening strategy.
Through interdisciplinary efforts led by consumer experience, technology and mission integration teams, our human-centered design has made the process of surveying, from point to point, more relevant to the patient, the clinician and the leader. And, when something goes awry and a patient or family member communicates that through a survey, we can act quickly. This real-time recovery cultivates right relationship and trust.
We are also challenging ourselves to meet not just health care industry standards but those set by the broader consumer experience sector. By democratizing data, making it viewable and
accessible via easy-to-navigate digital platforms, the responsibility has grown, and our patient satisfaction scores have improved right along with it. Using data sets that span understandings of human behavior outside of just health care — such as the net promoter score to indicate patients’ overall levels of satisfaction with their entire care journey — has amplified our care teams’ ability to see the holistic views of the patient experience.
Further, there is much to be said on the term “consumer” in and across health care, including our own ministries. Conversations with colleagues across the field have led our teams at Ascension to consider how the health care ministry ought to ensure the term is anchored in the dignity of the human person. How we have done so previously with other terms, such as “the patient” and “the poor,” has led to new understandings of the people we serve and serve beside. In this sense, considering what the person is “consuming” might be a right starting point to flip the script on where we focus our attention: Is all that they take in — the care, the communication — in “right relationship” with their humanity?
‘Always on listening’: Inspired by feedback from our front-line care providers, Ascension’s Associate Experience team, in collaboration with mission integration, nursing leaders, physicians and partners in technology, launched a new strategy, focused on better listening to and solving problems with our associates, with initial focus on our hospital-based nursing teams. Through a quick, mobile-friendly survey designed to easily share feedback, nurses can describe unresolved challenges in the physical environment, for example, or moments deserving recognition, like a great moment of teamwork. Cases are routed to the appropriate response team, communicated and/or celebrated at huddles, and tracked by leadership to ensure prompt action.
Feedback on this tool has been positive, as it cuts through the complexities of prior processes and is designed in a user-friendly format. Ensuring that the application of our core values also includes those we serve beside is essential to living out our commitment to the dignity of all human persons.
Fixing health care in America will require a return to foundational principles, particularly a focus on
the inherent dignity of every human person. Centering the people we serve in our processes in real and recognizable ways and designing solutions with them generates the path.
Through the daily recommitment and reconnection to our tradition, we make new that which is eternal: the love that God has for each of us and the capacity we hold to heal society through acts of moral service. By more transparently sharing our practices across ministries, we draw upon our combined strength to heal a broken health care system not by force or by will, but by love.
SARAH REDDIN serves as vice president of ministry formation–mission integration at Ascension. She was also a member of CHA’s 2022 class of Tomorrow’s Leaders. DR. RICHARD FOGEL retired from Ascension earlier this year from his role as executive vice president and chief clinical officer.
1. “How Does the U.S. Healthcare System Compare to Other Countries?,” Peter G. Peterson Foundation, August 16, 2024, https://www.pgpf.org/article/how-does-theus-healthcare-system-compare-to-other-countries/.
2. David Blumenthal et al., “Mirror, Mirror 2024–A Portrait of the Failing U.S. Health System: Comparing Performance in 10 Nations,” The Commonwealth Fund, September 2024, https://www. commonwealthfund.org/sites/default/files/2024-10/ Blumenthal_mirror_mirror_2024_final_v4.pdf.
3. Sara R. Collins and Avni Gupta, “The State of Health Insurance Coverage in the U.S.,” The Commonwealth Fund, November 21, 2024, https://www.commonwealthfund.org/publications/surveys/2024/nov/state-healthinsurance-coverage-us-2024-biennial-survey.
4. Simon Wein, “The Origins of the Word ‘Hospital,’” Hektoen International, 2023, https://hekint.org/ 2023/03/23/the-origins-of-the-word-hospital/.
5. Pope Francis, “Evangelii Gaudium,” The Holy See, November 24, 2013, https://www.vatican.va/ content/francesco/en/apost_exhortations/documents/ papa-francesco_esortazione-ap_20131124_evangeliigaudium.html.
6. Erica Carbajal, “Ascension’s Path to a 5% Drop in Preventable ED Visits,” Becker’s Hospital Review, May 16, 2025, https://www.beckershospitalreview.com/ uncategorized/ascensions-path-to-a-5-drop-inpreventable-ed-visits/. Note that since the time of publication, the 5% threshold has been achieved.

DARREN M. HENSON, PhD, STL Senior Director of Ministry Formation, Catholic Health Association
“Formation is widely recognized as a crucial tool for embedding Catholic identity and essential for aligning personal values with Catholic health care’s mission,” writes Shaikat Sen, executive vice president of HSM Group and lead researcher for CHA’s nationwide study of ministry formation across its membership. Launched in the fall of 2024 to build on findings from CHA’s 2022 Mission Leader Survey, the survey’s goal was to discover members’ activities and needs related to ministry formation.
The three-part study reveals points of maturation in formation across the Catholic health ministry. Sen observes that mission and formation leaders “in this study appear to be completely personally invested in ministry formation.”
When we read those words from an outside consultant without prior knowledge and experience of formation in Catholic health care, we realize that formation has reached a milestone in this ministry of healing. This is not to say that formation is at a point of maturity, but rather that outside perspective affirmed the ministry’s years of dedication to growth in this area.
The study points to evidence of growth in formation compared to 10 and 20 years prior. It reveals the depth and breadth of formation activities across Catholic health care ministries beyond senior leadership formation programs, including mid-level leader programs and formation touchstone experiences for hourly workers ranging from bedside to business offices and beyond.
This report shows four things. First, it reveals the variety of activities and breadth of sources
used in formative experiences. Second, the study’s responses detail formation needs for the organization, and third, it reveals the needs of individual leaders to grow in their competency in creating and facilitating formation experiences. Lastly, this report outlines discoveries about future formation plans across the ministry, demographic information about the nearly 200 respondents from CHA member organizations, opportunities and challenges, and finally, conclusions and analysis of the study’s findings.
CHA’s ministry formation electronic survey was sent to all mission and formation leaders known to CHA and was open for several weeks in October and November 2024.
CHA’s survey plan entailed three parts: qualitative one-on-one interviews, a quantitative survey administered digitally, and a data collection process on systems’ senior leadership formation programs.
Sen first conducted 10 in-depth virtual inter-
SPENT CREATING/LEADING
views with individuals recruited by CHA. All shared a commonality in that they were mission or formation leaders engaged in leading, creating or facilitating formation experiences. They differed in terms of the scope of responsibility, professional titles, system or facility size, geography and years in Catholic health care, spanning from as little as three years to more than 40 years. These interviews provided rich background information that helped HSM and CHA craft the quantitative survey.
The quantitative survey included approximately 35 questions across four main categories: time and involvement in formation activities, personal and organizational formation needs, participation and effectiveness, and demographic and other administrative data. The survey was designed to take less than 20 minutes to complete. All responses were anonymous, with individual information secured by HSM. CHA received only aggregate and de-identified data.
Altogether, the survey was sent to nearly 500 mission or formation leaders, with 196 responses. Among those who took the survey, approximately 20% had formation in their professional title. CHA was pleased with the response rate from members, as it was within reach of industry standards
of +/-5% margin of error, suggesting that the findings accurately reflect the ministry as a whole.
The first question on the electronic survey tool asked the leader, “What does formation mean to you?” followed by an open box to receive written responses. HSM manually analyzed the responses. There, they found reliable congruency for the definition of formation articulated in CHA’s 2020 Ministry Formation Framework. The top three themes include: personal reflection, exploration or calling; integration of Catholic identity with daily work or personal values; and lifelong growth and learning.
Additionally, respondents noted that formation reinforces organizational values, creates connections that build community and enables transformative experiences. These responses reverberate the language of CHA’s member-driven formation definition that says it enables “connections between personal meaning and organizational purpose,” so participants can articulate, integrate and implement “the foundational elements of Catholic health ministry” so that it “flourishes now and into the future.”1
When asked about an individual’s involvement
in formation, nearly all mission and formation leaders confirmed some activity, and 1 in 5 dedicate half or more of their time to formation. The survey asked respondents to specify formation activities they have led at least once during the past 12 months. The results reflect a broad scope and depth of formation, and the following percentages reflect the proportion of respondents confirming their involvement.
Formation activities by mission and formation leaders range from leading reflections at leadership meetings (97%) or department meetings (89%), creating or leading a ritual celebration/ blessing (84%), facilitating an onboarding or orientation (82%), leading didactic programmatic experiences (71%) and creating formation curriculum (63%). Among those experiences, leaders are more likely to facilitate these experiences with mid-level leaders, followed by senior leaders, and then hourly workers. Just over half of the
respondents report leading reflections for boards of directors (55%) and facilitating discernment processes (57%).
Among the data, a new discovery emerged: the prominence of time dedicated to mid-level leader formation activities. On average, nearly one-third of all mission or formation leaders’ time is given to this area of the organization, with 28% of their time dedicated to executive leadership, and 22% spent with front-line workers (see chart on page 41).
The survey asked leaders to identify top formation-related needs for the organization, summarized in the graph shown below. Respondents were given a list of 18 options (including “other”) and asked to select up to five and rank them in order. The top three needs were clinician and physician formation (53%), demonstrating for-
Clinician and physician formation
Demonstrating formation’s impact
Ongoing formation
Gaining leadership buy-in for protected time for formation
Establishing formation programs and expectations
Content resources and sample modules
Formation programs strategy and design
Mentoring
Short huddle reflections
Financial resources
Board formation
Presenters and subject matter experts
Practice and feedback on integrating theology and spirituality
Source: The HSM Group, 2024 CHAUSA Ministry Formation Survey Report
mation’s impact on the organization (47%), and ongoing formation opportunities and content (42%). The next most frequent responses relate to system and leadership support, such as gaining leadership buy-in for protected time for formation (34%), establishing formation expectations for all leaders (31%) and financial resources (21%).
Mentoring newer or less experienced formation leaders and partners gained favorability by more than a quarter (27%) and was ranked first by nearly 10% of all respondents. Leaders also cited the need for content resources and sample modules (30%) and formation strategy and design support (28%).
Similarly, the survey presented 18 options to identify source content that mission and formation leaders typically use when facilitating a formative experience. Top sources include a ministry’s mission statement and core values, followed by heritage stories, including those of Jesus and the founding congregations. Rounding out the top five was the Catholic social tradition. When presented with the same list yet asked where the need is for new materials, Catholic social tradition emerged as the fourth most frequent option, along with spirituality and inspirational authors or wisdom figures (43% each) and theological tradition and sources (40%). This means that mission and formation leaders frequently resource the Catholic social tradition, and they also desire fresh resources related to it.
When posed with the idea that CHA could potentially create fresh materials in 10 different identified areas, respondents chose justice and disparities as well as individual spirituality (47% each), leadership (46%) and discernment (36%). While not in the top tier, the following areas resonate with up to 25% of leaders: care for creation and environmental sustainability, synodality and lay leadership in the Church, accompanying seniors and the chronically ill, and ethics.
We asked leaders about their plans over the next two to three years. In open-ended responses sorted by the consultants, the most frequent response was developing and improving leadership programs (27%). The next three top areas cited by 1 in 5 leaders included formation for all workers; integrating the Catholic social tradition, mission and values; and honing delivery methods and evaluating program length. These were followed by clinician formation and the integration
of spirituality. One in 10 noted plans related to board formation.
We wanted greater understanding of the aspects of formation where individual leaders desired to grow. CHA has long articulated formation as a core competency of excellence in mission leadership. CHA’s 2022 Mission Leader Survey found that overall, mission leaders ranked formation as their top area for growth. In this current survey, the tool offered more than a dozen skills or areas for potential individual growth related to formation (see graph on page 44). Respondents were asked to rank three. Three quarters (75%) cite connecting with and applying the theological tradition (including the Catholic social tradition) in accessible and relevant ways as the overwhelming areas where leaders would like to grow. As many as 3 in 4 respondents picked this as one of their top three needs.
The next grouping of areas for growth includes evaluating and assessing formation experiences, the art of storytelling, and connecting personal values to the overall organizational purpose or mission. Up to 33% of all respondents identified these areas. In the next notable tier (20%-24%), respondents cited crafting useful prompts, sourcing content and curriculum development.
When asked about the likelihood of signing up for a program, participants favored a facilitation skills workshop, in addition to individual mentoring and communal spiritual practices.
The survey concluded with a series of questions related to demographics. The questions repeated the majority from the 2022 Mission Leader Survey and other past surveys to build longitudinal analytics. This study validated the integrity of data reported from the 2022 survey, particularly in terms of race and ethnicity.2 The current study reflects a statistically equal split between women and men mission leaders, closing a gap reflected in the 2013 survey, where women held a clear majority (70%), perhaps due to the historical prevalence of women religious in these roles.3
The current study also inquired deeper than past surveys into leaders’ educational backgrounds. While past CHA surveys of mission leaders also inquired about education and degrees, this study had a keen interest in understanding any distinctiveness in the theological training
Connecting and applying theological tradition (and Catholic social teaching) in accessible ways
Formation evaluation and assessment
The art of storytelling and connecting with mission, values, vision and individual purpose
Connecting personal values and experiences to overall purpose and mission
Sourcing content for reflections and presentations
Creating useful prompts
Curriculum development
Integrating content to the group’s needs
Group facilitation
Planning for formation experience
among those leading formation experiences.
The data affirm that today’s mission and formation leaders are steeped in the theological and spiritual tradition, as 84% have a university education in theology, religious studies and/or spirituality. Furthermore, responses revealed that nearly 7 in 10 have a master’s degree and 17% have a doctoral degree, whether a PhD, DMin or other applied doctorate. These data indicate consistency with the 2013 Mission Leader Survey.4
The current study broke new ground by specifically inquiring about a Master of Divinity (MDiv). The significance is that the MDiv is typically a minimum of 81 graduate credit hours, whereas other master’s programs are typically 36 graduate credits, less than half the credit hours of an MDiv. Moreover, the latter is the basic academic credential for ecclesial partners in ordained ministry. This formation survey shows more than a quarter of respondents have an MDiv (27%), an impressive accomplishment.
Lastly, this study inquired about previous work experience, believing that past participation in other aspects of church forms an individual for ministry. Most respondents had prior work expe-
Source: The HSM Group, 2024 CHAUSA Ministry Formation Survey Report
rience in a Catholic ministry. Fewer than a quarter had no experience in other Catholic ministries. Forty percent had worked in either a Catholic parish or an educational setting, ranging from grade school through higher education.
Religious Life and Seminary Formation
Perhaps more fascinating is the finding that well more than half of respondents have experienced formation as a part of a religious community, seminary and/or ordained ministry. This is significant as one hypothesis is that the community of mission leaders has long benefited from former religious or former priests and seminarians, yet it will one day have diminishingly few from these ranks and be comprised of individuals with little to no experience with other facets of church life.
These data suggest that current mission and formation leaders are well-represented by those settings. What is more, of the 95 individuals indicating previous experience in religious life or seminary, 80% of them spent at least five years in that setting, and 57% spent 10 years or more.
In addition to intellectual preparedness, this survey also forged toward a fresh frontier by inquiring about ongoing spiritual growth. Interestingly, nearly half of all respondents engage
Formation flows from the head to the heart and the whole. In an age of information and data saturation, formation forges a path for the whole person to flourish, particularly as it offers opportunity and nourishment for the spiritual dimension of being human.
with a spiritual companion or director on a consistent basis. This is important because decades ago, when women religious led the ministry, there could be a very solid assumption that each sister had a spiritual director. Spiritual direction is part and parcel of a religious community. Yet this cannot be assumed for lay leaders in a ministry. There is no structure for communal support, never mind accountability, for lay spiritual growth and development. This study, however, offers indicators that a sizable portion of mission and formation leaders demonstrate an objective commitment to spiritual life as a key aspect of their own ongoing formation.
Robust and Evolving
This study validated years-long developments in ministry formation that once focused nearly exclusively on senior leaders and now extends deep and wide in the ministry. The data show how mission and formation leaders have responded to the call to extend formation beyond executive positions, all the way to hourly workers. This is evidenced by mission leaders’ time commitments to orientations for all workers and new leaders. Further evidence appears in plans to fortify formation for all workers. Formation is truly integrated throughout the entire continuum of care in highly complex organizations.
Spirituality as a Formative Experience
There is a need and desire for spiritual resources. This underscores a critical distinguishing feature of formation — that it is more than an intellectual exercise. Formation flows from the head to the heart and the whole. In an age of information and data saturation, formation forges a path for the whole person to flourish, particularly as it offers opportunity and nourishment for the spiritual dimension of being human.
Spiritual development is a key path for ongoing formation. Unlike degree programs or professional certifications, formation is not primarily about undergoing one program only to then embark upon another. Rather, tending to the spiritual life of being human is a primary means and an indispensable method of ongoing formation. Programs serve a critical function, akin to an initiatory process. They help leaders gain a deep understanding and experience of being immersed in a ministry and connecting and integrating their professional expertise into the needs and vision of the organization, which also happens to conduct the work of the Church. In other words, they become more fully aware of what it means to be part of a ministry. From there, leaders in ministry are called to commit to fostering contemplative practices that attune their awareness to the transcendent in the ordinary, and to make these connections for the teams they lead.
Clear direction for more support and resources for formation emerged as a notable need from CEOs and executive leaders in this recent study. Leaders cited a need for financial resources, and other indicators of executive support emerged, such as protected time for leaders to fully participate in formation programs. Do leaders and sponsors know which members of the executive team have completed a formation program, and do they unequivocally promote their participation in those programs?
Another perennial need in the field of formation is tools and processes to translate the individual formative experiences, outcomes and value of formation to the overall organization into a dialect understood and appreciated by operational leaders. It has been said that the sisters who founded
our ministries often eschewed the spotlight, in the most positive sense. They were committed to their calling and ministry of care for others in need and did not invest much in telling their own story.
Today is different, and with near-exclusive lay leadership across the ministry, there is a greater need to tell the good news of our own work. Formation is no different, and formation has very good stories (and data) to tell. Such work underway by CHA and many member organizations relates to how to do that, for whom and by what methods.
Three points summarize a heap of information. First, we must celebrate and offer high praise for the work, dedication and development of ministry formation. A quarter of a century ago, when sisters insisted on embedding formation in the operations of the healing ministry, they may have only dreamed of the breadth and depth of activities cited in this study.
Second, our ministries must grow their investments in formation programs and activities. This includes people, time, organizational culture and financial resources. Continual improvements and innovation in established programs emerged as a top organizational need. A follow-up article on current practices in senior leadership formation programs will be forthcoming in the next issue of Health Progress.
And third, there remains a hunger for integrat-
ing elements of Catholic identity, particularly the social tradition, and then demonstrating the impact that formation has on individuals and the organization. CHA has materials in development that will support members’ excellence in both of these areas, and updates will be shared in the near future.
DARREN M. HENSON is senior director of ministry formation at the Catholic Health Association, St. Louis.
1. Framework for Ministry Formation (St. Louis: Catholic Health Association, 2020), https://www.chausa.org/ store/products/product?id=4363.
2. Dennis Gonzales and Jill Fisk, “Survey Reveals Encouraging Trends—and Concerns—for Future Mission Leaders,” Health Progress 104, no. 1 (Winter 2023): https://www.chausa.org/news-and-publications/ publications/health-progress/archives/winter-2023/ mission---survey-reveals-encouraging-trends-andconcerns-for-future-of-mission-leaders.
3. Brian P. Smith and Sr. Patricia Talone, RSM, “New Survey: Mission Leaders Respond,” Health Progress 94, no. 6 (November-December 2013): https://www.chausa.org/news-and-publications/ publications/health-progress/archives/novemberdecember-2013/new-survey-mission-leaders-respond.
4. Smith and Talone, “New Survey.”

Community health needs assessments (CHNAs) and community health improvement plans (often known as CHIPs or implementation strategies — same thing!) represent major investments, not just in time and resources, but in the potential for meaningful change. While the names vary, these plans follow the CHNA and are required as part of a process to collect data from and about the community’s health and then make a plan with partners to improve the health of area residents.
Communities spend months collecting survey data, conducting interviews and focus groups, building consensus and selecting health priorities. Hospitals and health departments dedicate staff and other resources to not only meet Internal Revenue Service and Public Health Accreditation Board requirements (requiring that this process happens every three years), but also to connect with community partners and create community health improvement.
But here’s the hard truth: Too often, these plans end up shelved, with goals unmet and momentum lost. If this sounds familiar, you’re not alone. Across the country, health leaders are wrestling with the same frustrating question: What’s the point of all this planning if it doesn’t lead to real impact?
The gap between planning and implementation is common. Leadership changes can derail momentum. New directors may shift focus, while staff turnover creates knowledge gaps that stall coordination.
Then there’s the resource reality check. Many plans look great on paper but crumble under realworld constraints. Without dedicated staff and accountability, even the best intentions get sidelined by daily demands.
Perhaps most critically, stalled implementa-
tion erodes trust. Community members who contribute to CHNAs invest their time in the hope of change. When they see no change, rebuilding that trust becomes an uphill battle.
Unrealized CHIPs don’t just jeopardize compliance; they represent missed opportunities to prevent disease, reduce disparities and improve lives. When plans sit idle, improvement work doesn’t get done well or doesn’t happen at all. Resources scatter, partnerships weaken and faith in collaborative efforts fades.
To explore how communities can move from planning to impact, we, at Moxley Public Health, hosted a national networking call with CHA titled “What’s the Point of Doing a Community Health Needs Assessment and Improvement Plan if It Doesn’t Lead to Real Change?” That conversation, which followed another session we conducted this past summer at National Association of County and City Health Officials’ NACCHO360 annual conference, highlighted strategies communities across the nation are using to make CHIPs successful.
The most successful implementations have one thing in common: someone whose job it is to make the CHIP happen! Whether it’s a project manager,
public health planner or team lead, this coordinator keeps the process on track. It’s important to remember that this person is not doing all the work; rather, they ensure the plan stays on track. These leaders facilitate communication, maintain accountability and help partners stay aligned. Partners collaborating on a CHIP serve residents in various ways; they may be local governments, area schools or other organizations working toward community health improvement. Some communities pair internal staff with external “champions” for specific strategies. Others boost engagement by allowing staff to lead work that aligns with their passions. When people care deeply about the issues they’re addressing, implementation energy sustains itself more naturally.
Many CHIPs falter when the hospital or health department is expected to do all the work itself instead of building genuine community ownership. Aside from aligning community resources, successful implementation also involves sharing leadership with community partners.
Successful communities prioritize what’s realistic while staying ambitious. They set realistic goals while still pushing for meaningful change, finding that sweet spot between ambition and achievability.
Gone are the days of large, unfocused meetings where little gets done. Effective communities rely on smaller, goal-oriented work groups that meet regularly and report to a larger steering committee or the dedicated leadership of the CHIP. These groups function best with clear roles, consistent schedules and concrete deliverables. We have seen success when these groups meet regularly with clear agendas and then report quarterly to the broader collaborative. Pilot testing work group configurations helps identify the right mix of people willing to roll up their sleeves, not just attend meetings.
Too often, CHIPs aim to create new programs rather than optimize existing ones. Effective implementation starts with comprehensive resource mapping — understanding not just what’s available but also how it connects and where gaps exist.
Some communities hold “Did You Know?” webinars to increase partner awareness of available resources, leading to better collaboration and less duplication. In many communities where the CHIP is most successful, health partners create integrated approaches in which all plans reinforce the same priorities instead of having initiatives pulling in different directions.
This means involving community partners not just during implementation but also in the assessment and planning process. It means creating opportunities for residents to participate meaningfully. Some communities even have pathways for community members who want to join work groups.
Most importantly, community partnership means listening to subject matter experts in the community rather than having just a few leaders dictate community health priorities. One NACCHO360 conference participant offered wise advice: “Listen to your local organizations. Don’t let leaders alone dictate CHIP priorities.”
Technology and Transparency
Simple tools can have a big impact. Communities using shared documents for work plan updates report better engagement between meetings. Live dashboards track goal progress and create visibility, creating both accountability and celebration opportunities.
Some communities use program management systems to help track CHIP activities, but the technology isn’t what matters. Instead, it’s consistent documentation and regular progress monitoring embedded into organizational routines that can make a difference.
Acknowledging ‘Less Is More,’ and Sustaining Commitment
Perhaps one of the most important lessons from communities is to resist the urge to fix everything at once. As one leader put it, “Less is more. It’s a hard lesson to learn because we want to fix it all.”
Successful communities prioritize what’s realistic while staying ambitious. They set realistic goals while still pushing for meaningful change, finding that sweet spot between ambition and achievability.
Aside from setting realistic expectations, the communities sustaining their CHIP work over multiple years share certain practices. They celebrate progress through annual reports that highlight accomplishments while maintaining accountability for ongoing work. They adapt their approaches based on what they learn, viewing implementation as an ongoing process rather than a one-time event.
Most importantly, they’ve embraced the collective impact model: recognizing that lasting change requires sustained commitment from multiple community organizations working toward shared goals with coordinated effort and support.
CHIPs can drive real change and improve the health of communities, but only with intentional, ongoing implementation. This means investing in coordination, aligning resources, building authentic partnerships and staying focused.
The question isn’t whether your CHIP can transform community health. It’s whether you’re ready to move from planning to action, from good intentions to measurable results. For communities ready to make that commitment, the tools are there — and so is the opportunity to create lasting impact.
At Moxley Public Health, STEPHANIE MOXLEY is CEO and lead consultant. CAROLINE GAGNE and MADISON THOMPSON are public health consultants.
(Required by 39 U.S.C. 3685)
1. Title of publication: Health Progress
2. Publication number: 0882-1577
3. Date of filing: September 3, 2025
4. Issue frequency: Quarterly
5. No. of issues published annually: 4
6. Annual subscription price: free to members, $29 for nonmembers
7. Location of known office of publication: 4455 Woodson Rd., St. Louis, MO 63134-3797
8. Location of headquarters of general business offices of the publisher: 4455 Woodson Rd., St. Louis, MO 63134-3797
9. Names and complete addresses of publisher, editor and managing editor: Catholic Health Association, Publisher; Betsy Taylor, Editor; Charlotte Kelley, Managing Editor; 4455 Woodson Rd., St. Louis, MO 63134-3797
10. Owner: Catholic Health Association of the United States, 4455 Woodson Rd., St. Louis, MO 63134-3797
11. Known bondholders, mortgagees and other security holders: None
12. The purpose, function and nonprofit status of this organization and the exempt status for federal income tax purposes has not changed during the preceding 12 months.
13. Publication name: Health Progress
14. Issue date for circulation data below: Summer 2025 Average No. Copies Actual No. Copies of Each Issue During Single Issue Published Preceding 12 Months Nearest to Filing Date
15. Extent and nature of circulation:
a. Total no. copies (net press run)
b. Paid and/or requested circulation (1) Paid/requested outside-county
mail subscriptions stated on Form 3541
(2) Paid in-county subscriptions
(3) Sales through dealers and carriers,
street vendors, counter sales and other USPS paid distribution (4) Other classes mailed through the
USPS
c. Total paid and/or requested circulation
[sum of 15b (1), (2), (3) and (4)]
d. Free distribution by mail (samples, complimentary and other free)
(1) Outside-county as stated on Form
3541
(2) In-county as stated on Form 3541
(3) Other classes mailed through the
USPS (4) Free distribution outside the mail
(Carriers or other means)
e. Total free distribution [sum of 15d (1), 879
(2), (3), (4)]
f. Total distribution (sum of 15c and 15e)
g. Copies not distributed
h. Total (sum of 15f and g)
i. Percent paid and/or requested circulation
(15c divided by 15f times 100)
16. This statement of ownership will be printed in the Fall 2025 issue of this publication.
I certify that the statements made by me above are correct and complete. Betsy Taylor, Editor
The case of Karen Ann Quinlan remains a watershed moment in both Catholic bioethics and secular ethical and legal thought. On its 50th anniversary, its impact resonates in evolving understandings of dignity, autonomy and the role of modern medical technology.

On April 15, 1975, 21-year-old Quinlan collapsed at a party in New Jersey after ingesting alcohol and tranquilizers, resulting in two 15-minute periods of anoxia and irreversible brain injury. Her friends initially put her in bed to recover; then, when she stopped breathing, one of them performed mouth-to-mouth resuscitation. They then called emergency services when she continued to be unresponsive.
She was transported to Newton Memorial Hospital in Newton, New Jersey. Upon clinical examination, she had a temperature of 100 degrees, her pupils were unreactive and she was unresponsive even to deep pain. The attending physician, Dr. Paul McGee, requested a consultation from neurologist Dr. Robert Morse.
Morse found that Quinlan was comatose with evidence of decortication, a condition relating to derangement of the cortex of the brain. The condition causes a physical posture in which the upper extremities are flexed and the lower extremities are extended. She required a respirator to assist her breathing. Subsequently, she was transferred to St. Clare’s Hospital, which was Catholic, under the care of Morse. He and other physicians diagnosed Quinlan as being in a persistent vegetative state.1
To distinguish between a persistent vegetative state and the determination of death by neurological criteria (brain death), persistent vegetative state is a diagnosis of severe damage to the “thinking” parts of the brain; however, those parts of the brain that control autonomic nervous system responses (for example, breathing and tem-
perature regulation) are still intact. So, there is a lack of consciousness, but the body will still maintain some regulatory functions. The determination of death by neurological criteria has as its standard the irreversible cessation of all functions of the entire brain. It is established through clinical tests, such as apnea testing, when a patient is removed from a respirator to determine if they breathe on their own.2
So, according to her physicians, Quinlan was not dead. She was in a persistent vegetative state and required a ventilator and feeding tube for survival.
Her devout Catholic parents were conflicted about how to proceed with her care. According to one author, Quinlan’s mother, Julia, and her siblings, Mary Ellen and John, believed that the ventilator should be discontinued. Quinlan’s father, Joseph, was not initially convinced.3 The family consulted with their parish priest, who said that discontinuing treatment was not sinful. Quinlan’s father then agreed that her ventilator should be discontinued. The family had evidence that Quinlan did not wish to be kept alive by extraordinary measures.
Central to Catholic moral thought is the distinction between ordinary (proportionate) and extraordinary (disproportionate) means of preserving life.4 This doctrine, based on St. Thomas Aquinas and many centuries of theological reflection, maintains that individuals must use ordinary means to preserve their life, but may forgo extraordinary treatments. So, for example, one is morally obligated to have regular medical appointments to assess one’s health, but does not have to undergo chemotherapy if the burden ex-
ceeds the benefit. Quinlan’s ventilator aptly illustrated a potentially extraordinary intervention.
Generally, every person should make their own decisions regarding medical treatment. In situations where the patient is no longer competent to decide, like Quinlan, a person should be appointed to act in their name, making choices the person would have made for themself. This is important. If a surrogate decision-maker acts for the incompetent patient, they are not making decisions for them. Instead, they are making decisions as them. Usually, today, the person who is incapacitated will have made the decision of who will act on their behalf when they are competent. Otherwise, the selection of that person is made under legal requirements. But it is also essential to note that during Quinlan’s time, this was not yet a usual practice.
So, having made the judgment that the ventilator was extraordinary care, the family asked Morse and St. Clare’s Hospital to remove Quinlan from the ventilator. They both refused, arguing that since Quinlan was diagnosed as being in a persistent vegetative state, it would be contrary to medical ethics to remove her from the respirator. Since she was not dead, their position was that life-sustaining technologies should be used to preserve her life.5
The Quinlan family made their request to discontinue the ventilator based on their Catholic beliefs and theology. They were supported by their local parish priest, Msgr. Thomas Trapasso, and Bishop Lawrence Casey of the Diocese of Paterson, New Jersey. But those beliefs and theology were not sufficient in changing the decisions of the physician and the hospital. With their request denied, the Quinlans filed a civil lawsuit in 1975 against Morse and St. Clare’s Hospital.
In their suit, the Quinlans made three arguments. First, it was argued that denying the choice to remove the ventilator based upon their Catholic beliefs was a violation of religious rights under the First Amendment to the U.S. Constitution. Second, keeping Quinlan on a ventilator was a form of “cruel and unusual punishment,” which violated the Eighth Amendment to the U.S. Constitution. Lastly, they argued that Quinlan had a right to privacy, to make her own medical decisions, and that her father should be empowered to
make them for her as a surrogate decision-maker.
The New Jersey Superior Court ruled in favor of Morse and the hospital. It argued that the decision to discontinue care was a medical one, not a personal one. Further, it said that even if Quinlan had said that she would not want extraordinary treatment, she said this as a young person while discussing a theoretical situation, not the one she was in now. The Quinlans appealed to the highest state court.
The New Jersey Supreme Court rejected the first two arguments of the suit. For the first argument, that of religious freedom, the court wrote that “Simply stated, the right to religious beliefs is absolute but conduct in pursuance thereof is not wholly immune from governmental restraint.”6 With regard to the argument that keeping Quinlan on a ventilator was “cruel and unusual punishment,” the court stated that the context for the Eighth Amendment was related to penal punishment, not medicine. However, the court agreed with the third argument, that Quinlan had a right to privacy, overturning the ruling by the New Jersey Superior Court.
The recognition of a right to privacy was first proposed in a Harvard Law Review article in 1890.7 However, it did not become formally recognized as a legal principle in a judicial decision until 1965, in the U.S. Supreme Court case of Griswold v. Connecticut. That case involved a suit by Estelle Griswold, the executive director of the Planned Parenthood League of Connecticut, who was arrested and charged with violating a Connecticut law passed in 1879 that banned the use of any drug, medical device or other instrument in furthering contraception. Griswold argued that the law violated the right to privacy of married couples. They had a right to be left alone with their choices regarding sexual relations. The U.S. Supreme Court agreed and ruled in favor of Griswold.
From 1965 until the New Jersey Supreme Court reached its decision on Quinlan, the right to privacy was invoked in several cases.8 The Quinlan decision stated that the right to privacy also extended to medical interventions. Although Quinlan never met the legal criteria for brain death, the court concluded that the withdrawal of ventilatory support, once deemed medically futile, did not constitute homicide. In the words of the court:
We have no hesitancy in deciding … that no
More advanced technologies, from artificial intelligenceguided interventions to gene editing, heighten these ethical stakes, but the core of the Quinlan teachings — dignity, consent and reasoned restraint — remain vital.
external compelling interest of the state could compel Karen to endure the unendurable, only to vegetate a few measurable months with no realistic possibility of returning to any semblance of cognitive or sapient life. We perceive no thread of logic distinguishing between such a choice on Karen’s part and a similar choice which, under the evidence in this case, could be made by a competent patient terminally ill, riddled by cancer and suffering great pain … .9
Further, the court appointed Quinlan’s father, Joseph, to be her surrogate decision-maker.
Quinlan’s physicians gradually weaned her from the respirator during May of 1976. She continued to breathe on her own. The family did not want artificial nutrition and hydration stopped, because they thought that these interventions were ordinary, proportionate care, although the State Supreme Court gave permission for all life support to be withdrawn. Quinlan lived another 10 years, dying on June 11, 1985.
The Quinlan case created a national template for later decisions like Cruzan v. Director, Missouri Department of Health (1990). In Cruzan, the Supreme Court upheld states’ ability to require “clear and convincing” evidence before allowing surrogates to refuse treatment for incompetent patients. 10 It also underscored the importance of advance directives. Public awareness following Quinlan’s case led to widespread adoption of advance directives and living wills. The federal Patient Self-Determination Act (1990) required health care institutions to inform patients of these legal tools — a direct outgrowth of the Quinlan precedent.
Quinlan continues to inform discussions on assisted suicide, artificial hydration, brain death and definitions of personhood. More advanced technologies, from artificial intelligence-guided interventions to gene editing, heighten these ethical stakes, but the core of the Quinlan teachings —
dignity, consent and reasoned restraint — remain vital.
The shift championed by Quinlan’s case — from paternalism toward collaborative, patientcentered care — continues as clinicians integrate medical insight with value-sensitive choices, mediated by ethics committees and ethics consultants. As can be seen in the New Jersey Superior Court’s decision, prior to Quinlan, the tendency was to empower physicians to have the final choice in decision-making. After this case, the emphasis has been on informing patients about their choices so that they can choose to accept or reject medical treatments. This shift, however, does not mean that they can compel physicians to provide any care that they want.
On its 50th anniversary, the Quinlan case stands as an ethical landmark. For the Catholic Church, it validated theological distinctions between ordinary and extraordinary care and gave momentum to formal guidance grounded in compassion. For secular bioethics, it laid the groundwork for the autonomy movement, institutional ethics, legal precedents and public policies that empower individuals facing end-of-life dilemmas.
Centuries from now, as new medical capabilities emerge, the Quinlan principles — balancing respect for life with a humane acceptance of death — will continue to guide society in difficult moments. In honoring Quinlan’s journey, we honor a legacy that transcends technology and ideology, affirming our shared humanity.
BRIAN M. KANE, PhD, is senior director, ethics, for the Catholic Health Association, St. Louis.
NOTES
1. “In Re Quinlan,” Justia, https://law.justia.com/cases/ new-jersey/supreme-court/1976/70-n-j-10-0.html.
2. In 1968, Harvard Medical School released a report titled “A Definition of Irreversible Coma,” which proposed brain death as a new legal standard for determining death based on the irreversible loss of neurological function. See: “A Definition of Irreversible Coma:
Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death,” JAMA 205, no. 6 (1968): 337–340, https://doi.org/10.1001/ jama.1968.03140320031009 (requires paid access). This report, often referred to as the “Harvard definition,” significantly impacted the understanding and legal acceptance of brain death as a criterion for death in the United States. In 1975, at the time of Karen Quinlan’s condition, the Harvard definition was not yet fully enacted as law in all states. It was not until 1980 that the Uniform Law Commission adopted the Uniform Determination of Death Act, which would become the model for states enacting legislation that would establish neurological criteria for the determination of death. It would take many years after that for states to adopt the language. At the present time, most, but not all, states recognize neurological criteria for the determination of death. It is important to note that there are other tests beyond apnea testing.
3. Matthew Stonecipher, “The Evolution of Surrogates’ Right to Terminate Life-Sustaining Treatment,” Virtual Mentor 8, no. 9 (2006): 593-598, https://doi.org/10.1001/ virtualmentor.2006.8.9.hlaw1-0609.
4. Rev. Donald Henke, “A History of Ordinary and Extraordinary Means,” National Catholic Bioethics Quarterly 5, no. 3 (2005): 555-575, https://doi.org/10.5840/ncbq20055333.
5. This 1975 article from The New York Times gives context to Dr. Morse’s decisions: Joseph F. Sullivan, “Doctor Tells Court He’d Refuse to Let Woman in Coma Die,” The New York Times, October 21, 1975, https://www.nytimes.com/1975/10/21/ archives/doctor-tells-court-hed-refuse-tolet-woman-in-coma-die-her-doctor.html.
6. “In Re Quinlan,” Justia.
7. Samuel Warren and Louis Brandeis, “The Right to Privacy,” Harvard Law Review 4, no. 5 (1890): 193-220, https://doi. org/10.2307/1321160. Louis Brandeis was a future U.S. Supreme Court Justice and Samuel Warren was his law partner. The article came about in part because of intrusions by reporters and newspaper photographers into the life of the Warren family. Together, he and Brandeis argued in their article that there was an implied right of privacy, to be left alone in their own lives to make decisions, in the U.S. Constitution.
8. See, for example, the following cases: “Eisenstadt v. Baird, 405 U.S. 438 (1972),” Justia, https://supreme.justia.com/cases/ federal/us/405/438/; “Roe v. Wade, 410 U.S. 113 (1973),” Justia, https://supreme.justia. com/cases/federal/us/410/113/.
9. “In Re Quinlan,” Justia.
10. “Cruzan v. Director, Missouri Department of Health 497 U.S. 261 (1990),” Justia, https://supreme.justia.com/cases/federal/ us/497/261/.
When I joined the Mission team at CHA in January 2020, one of my first major projects was to lead a comprehensive revision of the Mission Leader Competency Model. The model had remained unchanged for nearly a decade and no longer reflected the evolving responsibilities of mission leaders in Catholic health care. Recognizing the importance of this work, we convened a diverse work group that included mission leaders, human resource professionals, leadership development experts and others. To ensure the model was grounded in real-world insights, we also conducted focus groups with CEOs, senior mission leaders, sponsors and additional partners across the ministry.

DENNIS GONZALES
The result was an enhanced model that elevated three critical competencies — operations, strategy and advocacy — underscoring the increasingly strategic and integrative role of mission leaders. We also reinforced that general leadership competencies are essential for mission leaders, as they are for their peers, and
these are now woven throughout all seven core mission competencies. A notable example of this integration comes from Catholic Health based in Buffalo, New York, which developed the MissionDifferentiated Leadership Competency Model. Their approach illustrates the reciprocal value of embedding mission into leadership expectations at every level, reinforcing mission as a central, unifying force throughout the organization.
ANNUAL
BART
RODRIGUES, MDiv, MA, MBA, JOYCE MARKIEWICZ, RN, BSN, MBA, and LAURA CIANFLONE, MA
At Catholic Health, we stand at a pivotal moment, charged with leading with clinical excellence and a sacred purpose rooted in the healing ministry of Jesus Christ. As the presence of vowed religious diminishes and lay leaders take on more significant roles, the question arises: How can we uphold our mission while meeting the operational demands of modern health care? Our answer lies in the Mission-Differentiated Leadership Competency Model. This innovative model equips a mission-differentiated leader in Catholic health care to embrace
and manage the paradoxes and complexities of business and mission, as well as the balance between margin and mission. It tailors specific competencies and behavioral expectations to career ladders or leadership stages. It is designed to drive the organization’s sacred purpose, vision, mission and values, and we believe it has the potential to shape the future of Catholic health care.
ACROSS DISCIPLINES AND CAREER STAGES
Our leadership development consultancy part-



Spiritually Grounded
Mission and Values Integration
Values-Based Decision-Making/ Decision Quality
Care for the Poor and Vulnerable Persons
Displays self-awareness of personal values and spiritual purpose
• Seeks guidance from mentors
• Participates in spiritual formation opportunities
• Aligns professional goals with organizational mission
Demonstrates commitment to core values
• Participates in mission-driven projects
• Makes informed decisions based on available data
• Seeks input from peers
• Evaluates short-term impacts
Participates in community service activities
• Raises awareness about poverty issues
• Supports charitable initiatives
Servant Leadership
• Supports team members' growth and development Listens actively to team concerns
• Provides constructive feedback

Mission-Differentiated Leadership Competency Model Examples of Workplace Behaviors
Encourages the team to find balance and purpose
• Integrates mindfulness practices in meetings
• Supports team members' spiritual needs and growth
Ensures team activities reflect core values
• Communicates the importance of mission alignment
Recognizes team members who uphold values
• Balances team input with organizational goals
• Uses data-driven decisionmaking Considers long-term consequences
• Organizes team efforts to support the needy Encourages volunteerism Partners with local charities
• Fosters a supportive and inclusive team environment Encourages collaboration and teamwork
• Recognizes and rewards team contributions
Integrates spiritual principles in decision-making
• Promotes ethical behavior, mentors and develops others
• Facilitates regular reflections on mission, vision and values
• Develops strategies that uphold mission and values Aligns departmental goals with organizational mission
• Evaluates team performance based on value integration
• Evaluates the long-term impacts of decisions
• Incorporates risk management Aligns decisions with strategic objectives
• Develops programs to aid underserved communities
• Allocates resources for social initiatives
• Measures the impact of community programs
• Mentors emerging leaders and promotes collaboration Builds a culture of trust and respect
• Empowers team members to take initiative
• Promotes a culture of spirituality and ethical standards
Champions Catholic social teachings
• Serves as a visible role model of Catholic faith
• Advocates for mission-driven initiatives
Ensures strategic plans reflect mission and values
• Promotes mission alignment across departments
• Makes strategic decisions with high impact
• Balances innovation with risk
• Ensures decisions support organizational growth
• Champions initiatives for social responsibility
• Advocates for policies supporting the poor
• Collaborates with NGOs and government agencies
• Advocates for servant leadership principles
• Develops leadership programs
Models humility and empathy

Embodies spiritual values in leadership style
• Leads with integrity and compassion
• Champions a spiritually grounded organizational culture
• Leads by example, reinforcing mission and values
• Makes mission-centric decisions
• Cultivates a culture of mission and values
• Ensures decisions align with the overall vision
• Leads with strategic foresight
• Makes high-stakes decisions confidently
• Leads large-scale efforts to address social drivers of health
• Integrates social responsibility into business strategy
• Influences public policy for poverty alleviation
• Models servant leadership in all interactions Prioritizes the well-being of caregivers
• Creates a legacy of servant leadership
observable behaviors (see Figure 1 above, with more details about the model available with the online version of this column). These competencies are now embedded in our annual leadership performance reviews.
This tailored, scalable model reflects Catholic health care’s dual nature — as both a sacred mission and a complex business — reinforcing Catholic Health’s shared commitment to its future. By engaging in a strategic collaboration to develop
er, they provide a holistic approach to personal and professional growth, ensuring that mission integration is not only understood but actively embodied in daily operations and leadership practices.
The Leadership Enhancement and Development program was launched a couple of years ago to support the professional development of leaders across our system. Through this yearlong program, participants learn to build highly effective
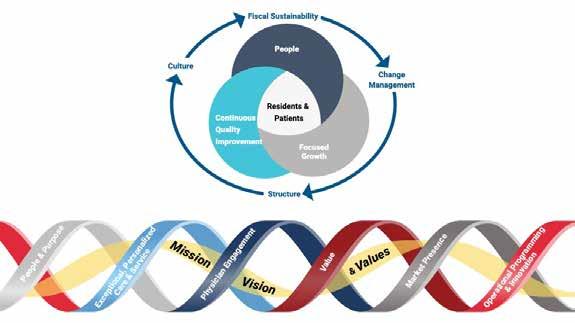
teams, navigate change and deliver exceptional results, thereby developing their leadership skills and advancing their careers.
Ministry formation programs offered through CHA and internally within our system at Catholic Health create experiences that invite those who serve in Catholic health care to discover connections in the purpose between the “personal why” (personal purpose) and “organizational why” (organizational purpose). They serve as a wellspring for personal renewal and professional resilience, ensuring that our leadership practices remain faithful to the Church’s healing ministry.
Our Ministry Formation program has adopted CHA’s Framework for Ministry Formation. We are building on this framework by incorporating our model’s five core competencies: spiritually grounded; mission and values integration; decision quality and values-based decision-making; care for the poor and vulnerable persons; and servant leadership. Each competency includes a behavioral framework that articulates observable behaviors at various proficiency levels, fostering both accountability and growth, as embedded in annual performance evaluations for
leadership.
Embedding mission competencies and observable behaviors into annual performance strengthens the case for the importance of ministry formation amid ongoing economic challenges. By leveraging our model’s competency and behavior framework, ministry formation proposes a set of integrated elements and a shared language that supports the organization’s mission and Catholic identity, driving cultural transformation.
Annual performance evaluations, competencies and behaviors: Competencies define the necessary knowledge and skills, while behaviors describe how leaders apply those competencies in practice. By evaluating both competencies and behaviors, organizations gain a holistic view of a leader’s contribution, ensuring they not only possess technical expertise but also demonstrate the interpersonal and professional qualities needed to deliver high-quality patient care.
Performance reviews that affirm and reward desired behaviors can significantly contribute to employee satisfaction and retention. Leaders are evaluated not just on outcomes, but on how they
achieve those outcomes in alignment with Catholic identity and values.
Annual planning, integration and balanced scorecard: Rather than treating mission as an add-on or as a parallel track to operations and business, both mission and business aspects are embedded like a ribbon, woven together and integrated, serving as the core of our six strategic pillars (see Figure 2 on page 56): people and purpose, exceptional personalized care and service, physician engagement, value, market presence, and operational programming and innovation. Our priorities — people, continuous quality improvement and focused growth — are centered on patients and long-term residents. At the same time, we are mindful of critical success factors, such as structure, culture, fiscal sustainability and effective change management in our annual planning and balanced scorecard efforts. What distinguishes this Mission-Differentiated Leadership Competency Model is its integration not only into our annual performance evaluations for leadership but also into our annual balanced scorecard priorities. (Such scorecards allow for strategic planning and management at organizations.)
Health care is evidence-based — the need for data, measurement and influence: In today’s evidence-based health care environment, Catholic Health continues the shift from paper to digital, which enables us to more effectively support our mission by aligning leadership development with both our spiritual values and strategic goals.
By capturing insights from annual self-assessments and manager evaluations, we can now track competency growth across both mission-driven and operational areas, identify emerging leaders, and design coaching, mentoring and formation programs grounded in real performance data. This approach enhances accountability and transparency, ensuring that individual goals are meaningfully aligned with our organizational priorities. Most important, this transformation fosters a culture of continuous learning and im-
provement, essential to our promise of delivering high-quality, person-centered care rooted in the healing ministry of Jesus.
We have much work ahead of us to fully embed the vision established here, which requires partnership and collaboration among mission, human resources, leadership and other stakeholders. It is a multiyear initiative that is worthy of the effort. We aim to establish clear expectations, create a nurturing environment, foster well-being and career growth, promote increased engagement and retention, improve performance and facilitate professional development that enables our workforce to flourish.
Commitment, accountability and sustaining a sacred legacy: As lay leaders assume roles traditionally held by religious members, shared accountability becomes essential. The competency and behavior model supports online 360-degree evaluations and reinforces the legacy of Catholic health care sponsors. As the Church entrusts more leadership to the laity, this framework becomes essential. It is not only a response to an internal need, but also a proactive measure and a strategic foresight, aimed at securing the future of Catholic health care.
This proactive approach should reassure the skeptics about the future of Catholic health care. This work is also a testimony to hope. By equipping leaders who can carry forward the ministry with integrity, compassion and competence, Catholic Health demonstrates a commitment to both its legacy and its future.
DENNIS GONZALES, PhD, is senior director, mission innovation and integration, for the Catholic Health Association, St. Louis. At Catholic Health, based in Buffalo, New York, BART RODRIGUES is executive vice president and chief mission and ethics officer. JOYCE MARKIEWICZ is president and chief executive officer. LAURA CIANFLONE is senior vice president of human resources.
Imagine writing a letter, or rather an explanatory email today, to colleagues and that email remaining relevant and incisive more than a generation later. That’s exactly what happened when I recently reread “A Sign of Hope,” by the late Archbishop of Chicago Cardinal Joseph Bernardin. This was a pastoral letter on health care, released nearly 30 years ago on October 18 (the feast of St. Luke, the physician). Pastoral letters typically pertain to the people within a bishop’s diocese, yet the content, message and timing of this one reached from shore to shore.

Last year, when Pope Francis designated 2025 the Jubilee Year of Hope, I pondered connections to health care, and my mind jumped to Bernardin’s pastoral letter. As I dusted off the booklet from my shelf, I rediscovered key themes and passages that remain compel ling and fuel hope today.
First, Bernardin made a bold statement “that health care is a ministry of the entire community of faith, the Church. Indeed, it is an essential ministry. Therefore, each health care … system should see itself as part of the whole Church… .”
Continuing to enact the heal ing ministry of Jesus in the 21st century is an essential ministry and activity of the community of faith and not merely a nicety.

Second, there are obstacles inherent to this work and ministry, and Bernardin names both internal and external challenges. These parallel his observations on the tensions between ministry and the business of doing health care. These tensions remain perennial weeds among our work.
Third, Bernardin appeals to social issues. He was masterful at weaving points from the Catholic social tradition into his remarks and homilies.
The pastoral letter notes the need for human solidarity and community. In addition, he called for compassion and to promote the common good. Fourth, the social issues are not abstract ideas for him. Rather, these are integral to the Catholic imagination, which can only be fed and formed by attending to the spiritual and theological formation of a vision that health care is more than the delivery of a service. “Economic, technological, systemic and medical realities are not enemies. Rather, it is also to them that we bring our ministry of Christian hope.” 2 In other words, our very presence and contributions to the wider field of health care, medicine, nursing, counseling, wellness and more help form and inform them. Our ministries bring an added dimension of the Reign of God to the business and contractual relations, which, in turn, sparks reflection for our partners on what matters most and how they may contribute more justly to the needs of society and those served.
When I realized this would be the pastoral letter’s 30th anniversary, I contacted Fr. Michael Place. Not only is he CHA’s past CEO and president who served from 1998 to 2005, but he was Bernardin’s theologian prior to that, contributing research and drafts for speeches and major works, includ-
ing “A Sign of Hope.” I was curious if my reading of the pastoral letter resonated with the author’s intention. We sat down together to reflect on the pastoral letter in light of the current environment.
Fr. Place, what remains relevant in Bernardin’s pastoral letter for us today, 30 years later?
Well, Part One does. As I reflected back to the time, I wondered, were we just talking to ourselves, or did the pastoral message have more value than the five years or so around the time of the letter? But I think it still works, at least for me.
Yes! It works for me as well. Rereading the letter, I noticed a lens that Bernardin offers in the opening pages. He says the Genesis story “does not describe a cosmic battle in which order triumphs over chaos once and for all. … But chaos continues to exist. It is a part of life. At times, it can seem to get the upper hand and overcome the order, purpose and sense of meaning in our lives. But God’s creative work is ongoing. God continues to order the chaos we encounter, making it possible for us to live our lives under his protection.”3
Hope is all over the place in Bernardin’s writing. I was looking for a quote recently and did a word search of several speeches, and it’s everywhere. I had no idea how pervasive it is.
For the health care pastoral, I wanted to find a leitmotif that had a scriptural grounding to it, rather than a dogmatic warrant. The experience of illness predates dogma, our receipt of it. Jesus, as healer, was in continuity with the experience of the Hebrew people, who knew God as healer. We should begin in that space, not in the space of ecclesial ministry, which tends to get structural. We land there, but the beginning of the letter starts with experience, which was Bernardin’s style.
Part One, on the promise of life in the midst of chaos and hope in the Christian life, still works for me. Now, you have to stand inside a faith heritage to appreciate it. If you’re just appropriating a business, I don’t think it would be a convincing argument for someone with no faith background. Whether they might find affinity or resonance, that’s another thing. Chaos is chaos. The hope comes not from the chaos, but from outside of it.
Cardinal Joseph Bernardin’s main point in Part One of “A Sign of Hope” is that “God’s creative activity includes the promise that we are able to live our lives, even in the face of the chaos of illness and death. God’s promise of life is the basis for Christian hope.”4
Bernardin then states what he means by “hope.” He writes, “The hope of which I speak is an attitude about life and living in God’s loving care. Hope, rooted in our trust of God’s love for us in Christ, gives us strength and confidence; It comforts us with the knowledge that, whatever is happening to us, we are loved by God through Christ.”5
— DARREN HENSON
What needs do you see for spiritual formation among health care leaders in the ministry today, so they can be grounded in and offer the kind of Christian hope illuminated in this letter?
We have to orient people to God. We have to begin with where their human yearnings are. I’ve seen success when people have an experience of personal transformation. The feedback on ministry formation has been that it’s been life-changing. They’re better people and leaders, and they know there is more out there for them to encounter.
‘NO PATH FORWARD WITHOUT PRAYER’
Fr. Place’s comments on spirituality echoed those he gave in a talk to a gathering of Catholic health ministries in Illinois, where he revisited “A Sign of Hope.” His insights are worth reprinting and an apt closing to this homage to Bernardin’s “A Sign of Hope”:
I am convinced that there is no path forward without prayer. What we are about is a powerful vision of the best of being human, but we are about more than a vision. What we are about can enlighten and inspire, but we are about more than inspiration. What we are about requires the hard labor and creativity of many, but we are about more than human thought and labor.
Our “more” is nothing less than being the individuals who are personally called and sent by Christ to proclaim “the Gospel to the poor” and “to heal the brokenhearted” (Luke 4:18, KJV), and in so doing to be the individuals who proclaim that the Reign of God is at hand. Our “more” is something that is deeply personal. It is about you and I, and our Saving God. It is about being in relationship, a deeply personal relationship with the one who died and rose to save us and sent His Spirit to be with us until He comes again in triumph at the end of time.
For this personal relationship to flourish, it needs to be nourished like all relationships. Thus, the importance is that as individuals and as organizations, we be intentional about nurturing the spirit and reality of prayer. Which is to say, we nurture the possibility that individually and collectively, the presence of God can be encountered. We are not about an ideology.
We are about a living person, Jesus Christ.6
For this, we are signs of hope, as we continue to commit ourselves as leaders of this essential ministry that is part of the whole Church.
DARREN M. HENSON, PhD, STL, is senior director of ministry formation at the Catholic Health Association, St. Louis.
1. Joseph Cardinal Bernardin, A Sign of Hope: A Pastoral Letter on Healthcare (Archdiocese of Chicago, 1995), 9. 2. Bernardin, A Sign of Hope, 16. 3. Bernardin, A Sign of Hope, 2. 4. Bernardin, A Sign of Hope, 3. 5. Bernardin, A Sign of Hope, 3. 6. Rev. Michael D. Place, STD, “‘A Sign of Hope’ Revisited: A Work of Justice” and “‘A Sign of Hope’: Will They Be Our Future?” (presented at the Illinois Catholic Health Association Annual Meeting, Chicago, IL, October 6, 2023).


To better navigate the complexity of today’s global health relationships, we must ground our work in Catholic social teaching and embrace the wisdom of the Serenity Prayer, which begins: “God grant me the serenity to accept the things I cannot change; courage to change the things I can; and wisdom to know the difference.”
This posture will help strengthen our global relationships and deepen our witness to justice, compassion and the common good by engaging in a culture of encounter in our fractured world.
To help us reimagine global health partner-
Iships, Dr. Neeraj Mistry, a global health consultant, shares how we can embark on this initiative through humility, shared responsibility and deep listening. His call is a timely invitation for Catholic health care in the U.S. to align more fully with the global Church as we live out our faith in service.
NEERAJ MISTRY, MD
t is interesting how context and environment shape our actions and the path we follow through our lives. For me, growing up as a person of color in apartheid South Africa grounded my commitment to social justice. I chose to apply myself to the study and practice of health and medicine to address the inequalities that the system of apartheid had created. When I started as a doctor in clinical practice, I served one patient at a time within a health and social system that, at times, worked against the well-being of my patients and community.
While I found the immediacy of clinical practice fulfilling, I soon realized that to achieve systemwide change, I needed a wider scope of action and impact. Consequently, I dedicated my efforts to global health on HIV/AIDS, tuberculosis, ma-
laria and neglected tropical diseases. My decision to focus on these diseases — broadly described in the Bible as pestilence and famine — emerged from the desire to “change the things I can” in terms of the health of the poorest and most vulnerable in our societies. These vulnerabilities arise from system failures and structural imbalances that leave us with a world of “haves” and “have-nots” that correlate broadly to north-south, urban-rural, educated-uneducated and whitepeople of color.
And I am far from alone in this work. The past century has witnessed dramatic improvements in global health and development, indicators that are a collective success borne from decades of hard work by the global health and development community. Here, I must acknowledge that further
scrutiny reveals that despite aggregate improvements (for example, in education, maternal and child health, and life expectancy indicators), lowresourced and vulnerable populations have seen a much slower rate of improvement.
This bifurcated pace of progress has created an ever-widening gap between poorer and betterresourced sectors of society. Our limited success shows where there is still work to be done. The task of “loving more,” as Pope Leo XIV reminded us in his first homily, is clearly set before us.
We are now living in a time of volatile political and economic uncertainty that undermines and threatens the hard-won gains in health and development,1 potentially setting the health and development status of vulnerable populations back by decades.2 The global health and development community has suffered setbacks resulting from changes in bilateral and multilateral aid, shifts in economic and trade policy, and a widespread retrenchment of health and development personnel that have left government programs in endemic countries reassessing their national plans. Through this transition, the poorest have become even more marginalized.
This global predicament has led me to reflect on a time in my life when my South African community was working to dismantle a deeply entrenched system: the anti-apartheid struggle. Apartheid’s deeply discriminatory policies were pervasive across all sectors and disciplines of society, and opposing this system required an equally broad range of resistance actions employed by citizens at every level of society.
Philosopher Friedrich Nietzsche’s truism that “he who has a why to live for can bear almost any how” is helpful when withstanding periods of discord, division and degradation, but is perhaps less useful when charting a collective path out of the desolation of prejudice and the weaponized fear of our differences. I have found both solace and inspiration in the Serenity Prayer, which was introduced to me by one of my country’s faithbased anti-apartheid comrades. The Serenity Prayer beautifully holds us as we acknowledge and grieve what is loved and lost, and then take our individual and collective actions to love more.
I share this reflection in a world that is becoming increasingly unjust, unstable, unpredictable and polarized. It is ultimately the poorest and
most vulnerable among us who bear the brunt of this rise in instability. Indeed, the role of the Church and faith-based communities to champion the poor and vulnerable has never been more relevant. As Pope Francis said, “Today, as in the past, liberating the poor, the oppressed and the persecuted is an integral part of the mission entrusted by God to the Church.”3
The withdrawal of the U.S. from the foundational role it played in global health and international development has disrupted the global health and development ecosystem. Not only was the U.S. the major financial supporter of health and development, albeit at a lower proportion of its GDP when compared to other industrialized countries,4 but it had also set up the institutions and the human capital critical to sustaining the effort. Furthermore, it enabled other sectors to complement the foundational role, where we saw private foundations and philanthropists having the bandwidth for nimble innovation and experimentation, nongovernmental organizations and faith-based groups focusing on community and last-mile related work, universities providing academic robustness, and businesses bringing about economic growth and development. These respective efforts were enabled by steadfast, reliable and sincere leadership from the U.S.
The world still needs that committed partner for development. Mis- and disinformation on social media, misaligned corporate incentives, partisanship and political infighting, and rising inflation and cost of living are just some of the factors leading to discord and distrust in society. The Church, together with the broader faith-based community, can provide that solid foundation of hope. As Pope Leo XIV has said, “a leaven for a reconciled world,” has never been more urgent.5
What would it take for the Church to organize itself as we strive to “love more” for global health? What would it take to better mobilize ourselves to serve as the leaven of unity, communion and fraternity within the development community? These questions can be challenging, especially given that under the broad umbrella of Catholicism, Christianity and the even more expansive faith-based sector, there is much division of parallel work.
Resources beyond financial ones abound in the sector, and the starting point that unites all
faiths is the ethic of service. Could the Church better be that reliable and consistent partner for the poorest and most vulnerable? How can we work collectively to provide ourselves with the courage to change what we can and provide each other with the wisdom to know where best to place our talents and efforts?
It is through discernment that Catholic health care, as a ministry of the Church, can move from working within the status quo (or the past’s paradigm) to a new role of partnership and fraternity with and for the poorest and most vulnerable. It is through fraternal and courageous action that the faith-based sector mobilizes as a force through its instrumental role in effecting change. And we must have the wisdom to appreciate the dynamic state of acceptance and change in an ever-changing global landscape in this moment, as Pope Leo XIV describes as an “hour for love.”6
BRUCE COMPTON is senior director, global health, for the Catholic Health Association, St. Louis. DR. NEERAJ MISTRY is an independent global health consultant based in Washington, D.C. He served as managing director of Global Network for Neglected Tropical Diseases and medical director of the Global Business Coalition on HIV/AIDS, TB and Malaria.
1. Shereen Hussein and Jonathan Samet, “Measuring Population Health Impact of the Trump Administration’s Withdrawal from WHO and Cuts to USAID: Time to Start Counting,” Population Health Metrics 23, no. 13 (2025): https://doi.org/10.1186/ s12963-025-00376-y.
2. Sharon Basaraba, “Life Expectancy Then and Now: 1800 vs. Today,” Verywell Health, August 8, 2025, https://www. verywellhealth.com/longevity-throughouthistory-2224054#; John Stover et al., “The Effects of Reductions in United States Foreign Assistance on Global Health,” SSRN, April 8, 2025, http://dx.doi.org/10.2139/ ssrn.5199076.
3. Pope Francis, “Address of His Holiness Pope Francis to the Members of the Plenary Council of the International Catholic Migration Commission,” The Holy See, March 8, 2018, https://press.vatican.va/content/ francesco/en/speeches/2018/march/ documents/papa-francesco_20180308_ icmc.pdf.
4. “Official Development Assistance (ODA),” OECD, https://www.oecd.org/en/ topics/official-development-assistanceoda.html.
5. Pope Leo XIV, “Homily of the Holy Father Leo XIV,” The Holy See, May 18, 2025, https://www.vatican.va/content/leo-xiv/ en/homilies/2025/documents/20250518inizio-pontificato.html.
6. Pope Leo XIV, “Homily of the Holy Father Leo XIV.”



FOR MORE INFORMATION: Contact Bruce Compton Senior Director, Global Health bcompton@chausa.org

JILL FISK, MATM, DIRECTOR, and KARLA KEPPEL, MA, ASSOCIATE DIRECTOR, MISSION SERVICES, CHA
Ancient cultural and religious practices of hospitality are deeply embedded in the Judeo-Christian tradition. The nomadic lifestyle and barren wilderness meant that when you encountered fellow humans, it would have been necessary to stop, rest and restock supplies.
In the harsh desert of the Middle East, providing hospitality could mean the difference between life and death. The host was expected to share food, shelter and protection. By accepting this hospitality, the traveler was expected to honor their gift and refrain from hostility, even if their host was a known enemy.
Throughout the Old Testament, we see this play out. When Abraham and Sarah welcome three strangers (Genesis 18:1-15), Abraham’s extravagant welcome is a stark contrast to how Lot receives visitors in Genesis 19. Whereas Lot only offers the minimum, Abraham goes above and beyond, and unknowingly welcomes special guests of God. Later, Rahab, a Canaanite woman, welcomes Israelite spies (Joshua 2) and ultimately becomes one of only five women named in the genealogy of Jesus (Matthew 1:1-17).
Finally, in the Gospel of Luke in the New Testament, Martha and Mary welcome Jesus into their home. While Martha works to offer physical sustenance to Jesus, we see that sometimes a ministry of presence, like Mary’s, is the higher calling. As Pope Francis reminds, “A guest is not merely to be served, fed, looked after
in every way. Most importantly he ought to be listened to.”1
Then and now, hospitality is seen as a reflection of God’s own generosity and the limitless love that is offered to all people.
At any given moment, no matter the geographic location or the specialty, a warm welcome is ministry practice as patients arrive for appointments, testing, procedures and everything in between. Regardless of your role, first touches are critical in experiencing a culture of healing.
More than mere behavior and deeper than customer service, living out the values of the Catholic health ministry relies on an inner disposition of hospitality, empowered by God’s gracious welcome and expansive love, which we embody.
Prayer can help us cultivate an inner disposition of love. With intentional practice, we more deeply reflect God’s generous love as we greet those who come to us for care.
As you pray with the following prompts, consider how you might prepare yourself to be fully present to the healing needs of patients, families and associates. How might you prepare your heart for hospitality? How might you serve as a conduit of God’s generous and loving hospitality for all those you encounter?
As one who offers welcome, try this practice as a prompt to start each day:
Begin by taking a few slow, deep
breaths. Let your breath permeate from your belly, radiate up through your heart, and reach toward the crown of your head. Practice this a few times until you can allow yourself to settle into the loving hospitality of God, present with and within you, at this very moment and in the day ahead. Invite the Divine to lead and guide you as you pray. Slowly recall the events of yesterday, recalling what you did and who you were with. Linger over each event; ask yourself, “Where was God present in what I saw, smelled, tasted, touched and heard?” Can you notice how the loving, attentive presence of God cared for your needs? As you reflect on yesterday, what about God’s hospitality seems most significant?
Consider the day ahead: What is on your calendar? Are there interactions you anticipate or dread? Considering your whole self, what do you need from God to be a loving and attentive presence with others today? How will God’s hospitality toward you change the way you will greet others — the way you look upon them, listen to them, speak to them, love them and help meet their healing needs? Finally, with what you have received and what you desire in this time of prayer, seek the expansive and limitless love of God in your call to serve. Let love be your guide.
NOTE
1. Pope Francis, “Angelus,” The Holy See, July 17, 2016, https://www.vatican.va/content/ francesco/en/angelus/2016/documents/ papa-francesco_angelus_20160717.html
Duquesne University offers an exciting graduate program in Healthcare Ethics to engage today’s complex issues.

Courses are taught face-to-face on campus or through online learning for busy professionals.
The curriculum provides expertise in clinical ethics, organizational ethics, public health ethics and research ethics, with clinical rotations in ethics consultation.
Doctoral students research pivotal topics in healthcare ethics and are mentored toward academic publishing and conference presentation.
MA in Healthcare Ethics (Tuition award of 25%)
This program requires 30 credits (10 courses). These credits may roll over into the Doctoral Degree that requires another 18 credits (6 courses) plus the dissertation.
Doctor of Philosophy (PhD) and Doctor of Healthcare Ethics (DHCE)
These research (PhD) and professional (DHCE) degrees prepare students for leadership roles in academia and clinical ethics.
MA Entrance – 12 courses
BA Entrance – 16 courses
Graduate Certificate in Healthcare Ethics
This flexible program requires 15 credits (5 courses). All courses may be taken from a distance. The credits may roll over into the MA or Doctoral Degree (PhD or DHCE).
OCTOBER 21–23, 2025
Each day from 2 to 5 p.m. ET
Learn the basics of community benefit through CHA’s highly regarded program. Taught by experienced community benefit leaders, the virtual event provides ample opportunities for participant questions and engagement.
Attendees will receive a copy of CHA’s A Guide for Planning and Reporting Community Benefit and 24/7 access to recorded sessions, tools and resources. To learn more and register, visit chausa.org/events or scan the QR code.
