Volume 11 | Issue 01 | March 2023 | The Journal of the British Orthopaedic Association | boa.ac.uk Journal
Orthopaedics Dame Clare Marx
of Trauma and
OrthoFoam Knee Wedges




Nailing, nailed.
Simplify patient positioning for tibial or retrograde femoral nailing procedures with our range of trauma triangles. The knee remains in the correct position throughout the procedure with our durable foam providing the perfect balance of cushioning and stability.
Product Code:
OL.OF.KWS Ortholove Knee Wedge Small
OL.OF.KWM Ortholove Knee Wedge Medium



OL.OF.KWL Ortholove Knee Wedge Large
OrthoFoam Adult Ramp Elevator
Surgery, sorted.
Indicated for all surgical cases where elevation is necessary without offloading the heel. Frequently used in trauma cases to enable easy x-ray control. The ergonomic design, with slight concavity, ensures stable support of the limb without too much pressure on the calf.
Product Code: OL.OF.ARE
OrthoFoam SRE
Swelling no more.
Indicated following foot and ankle surgical cases for application in theatre or recovery or even preoperatively for trauma cases to ensure reduction of swelling. The ergonomic design ensures patient comfort, with stable elevation at heart level and without strain on the knee or hip. A home use version of the SRE allows patients’ seamless recovery after leaving hospital to the comfort of their home.
Product Code: OL.OF.SRE
Other shapes and sizes available. Call or email for more info
01480 457222 / info@ortholove.com / www.ortholove.com Distributed in the UK by LEDA Orthopaedics
In this issue...
32 Features: Supporting elective recovery through a short stay arthroplasty pathway
Jonathan Howell and Mary Stocker
38 Features:
20 Features: Dame Clare Lucy Marx Mark Bowditch and Deborah Eastwood
24 Features: Private Health Information Network (PHIN) and complying with the Competitions and Markets Authority Order: An update for BOA members Andrew Manktelow
28 Features:
‘Oops!’ Designing and implementing a novel peer-to-peer training session on learning from surgical mistakes Adam Stoneham, Simon Williams, John Hardie, Greg Neal-Smith and Fransiska Guerreiro
So you want to develop your own implant?
Paul Roberts
42 Features: Getting off the production line Bev Fitzsimons
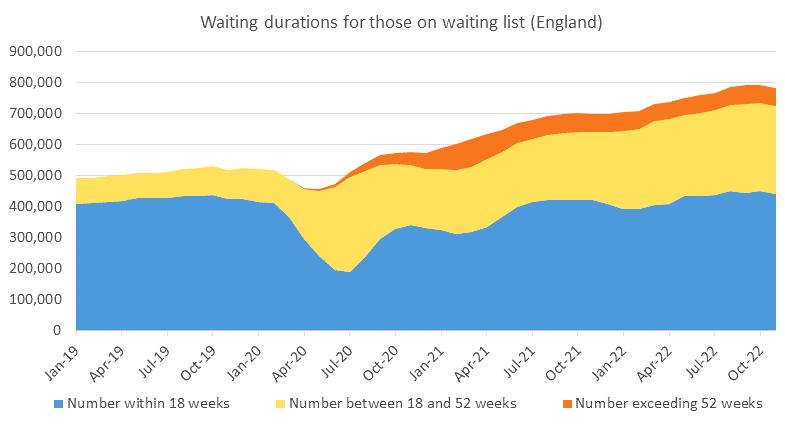
46 Medico-legal: The legal implications of treatment delays since the 2020 pandemic

Andrew Manktelow and Bertie Leigh
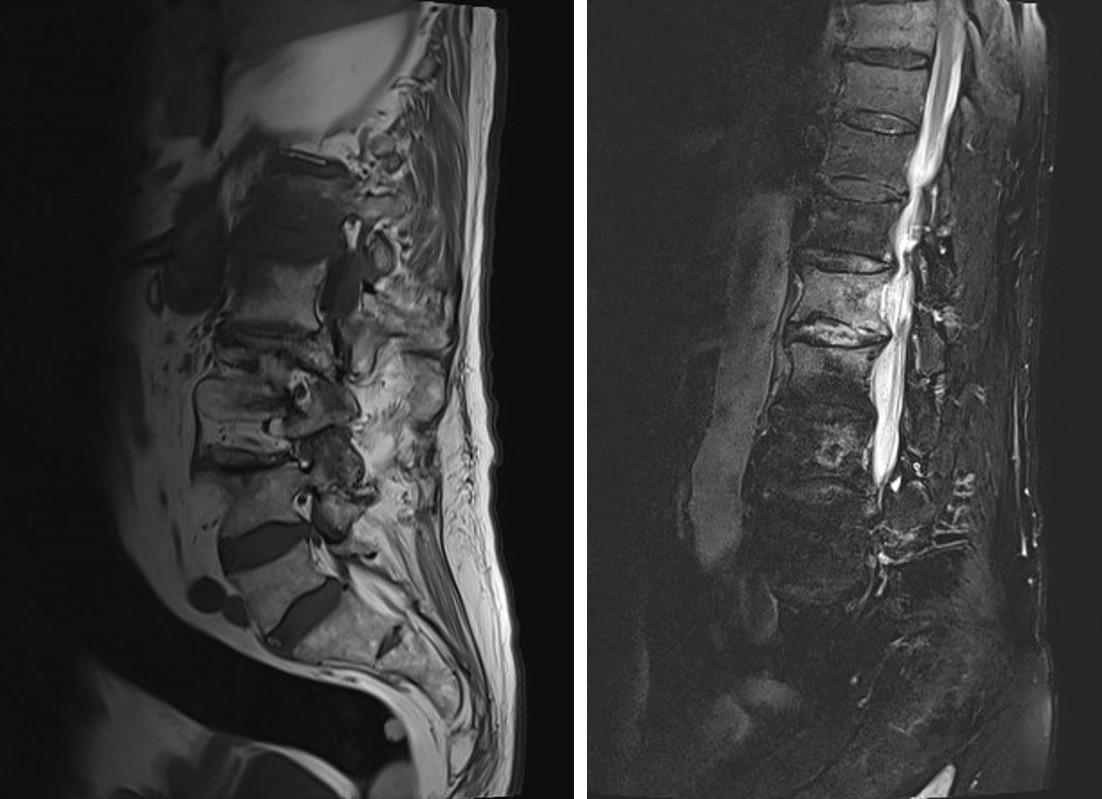
49 Subspecialty: Spinal surgery in the UK – an evolution


Niall Eames
50 Subspecialty:

Cauda equina syndrome - an overview
Sheweidin Aziz and Matthew Newton-Ede
Download the App



54 Subspecialty:
Spinal infection – an overview

Alex Goubran and James Tomlinson
58 Subspecialty:

Thoracolumbar fracture stability and the difficulties of classification systems
Alexander Durst and Sashin Ahuja
62 In Memoriam:
Dame Clare Lucy Marx

Eric Anderson
Bhaskar Bhowal
Alan William Frederick Lettin

The Journal of Trauma and Orthopaedics (JTO) is the official publication of the British Orthopaedic Association (BOA). It is the only publication that reaches T&O surgeons throughout the UK and every BOA member worldwide. The journal is also now available to everyone around the world via the JTO App. Read the latest issue and past issues on the go, with an advanced search function to enable easy access to all content. Available at the Apple App Store and GooglePlay – search for JTO @ BOA

Did you know that as well as advertising in our Journal publication, we can offer footer banner advertising on the JTO App! For more information please contact Wendy Parker Email: Wendy@ob-mc.co.uk | Telephone: +44 (0)121 200 7820




JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 01 3 From the Executive Editor
From the President
Simon Hodkinson 5
Deborah Eastwood
8-9 BOA Latest News
Contents Amputation the context T OrthopaedicsT Orthopaedics A Surgical Day Begins Volume 08 Issue 03Volume 08 Issue 02Volume 08 Issue 01 Volume 08 Issue 04 Journal of the British Orthopaedic Association The Journal of Trauma and Orthopaedics (JTO) has a dedicated news section, a features section containing interesting articles on various themes, a subspeciality section and a medico-legal section.
We are committed to sustainable forest management and this publication is printed by Buxton Press who are certified to ISO14001:2015 Standards (Environmental Management System). Buxton prints only with 100% vegetable based inks and uses alcohol free printing solutions, eliminating volatile organic compounds as well as ozone damaging emissions. Open Box Media & Communications are proud to be corporate sponsors of Heart Research UK (Midlands) 20 Cover
© portrait artist Alastair Adams
Journal of Trauma and Orthopaedics
image:
PPRP

www.heraeus-medical.com 11516 UK IMPROVE THE CHANCES Medical
patients
as reported in study results
57
TKA Read our article on RFI on page 65 of this edition. REDUCE RISK FOR INFECTION
Reduction of infection risk* using dual antibiotic-loaded bone cement in high risk
*
34 % in primary hip & knee arthroplasty 69 % in fractured neck of femur
% in aseptic revision
JTO Editorial Team
l Simon Hodkinson (Executive Editor)
l Hiro Tanaka (Editor)
l Simon Britten (Medico-legal Editor)
l Abhinav Singh (Trainee Editor)
l Niall Eames (Guest Editor)
BOA Executive
l Deborah Eastwood (President)
l John Skinner
(Immediate Past President)
l Simon Hodkinson (Vice President)
l Mark Bowditch (Vice President Elect)
l Fergal Monsell (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
l Bob Handley (Appointed Trustee)

BOA Elected Trustees
l Deborah Eastwood (President)
l John Skinner (Immediate Past President)
l Simon Hodkinson (Vice President)
l Mark Bowditch (Vice President Elect)
l Fergal Monsell (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
l Fares Haddad
l Amar Rangan
l Sarah Stapley
l Hiro Tanaka
l Cheryl Baldwick
l Deepa Bose
l Caroline Hing
l Andrew Price
l Andrew Manktelow
l Andrea Sott
l Paul Banaszkiewicz
l Stephen Eastaugh-Waring
Copyright
BOA Staff
Executive Office
Chief Operating Officer
- Justine Clarke
Personal Assistant to the Executive
- Celia Jones
Education Advisor
- Lisa Hadfield-Law
Policy and Programmes
Head of Policy and Public Affairs
- Gary Robjent
Head of Education and Programmes
- Alice Coburn
Programme and Committees Officer
- Eliza Heng
Educational Programmes Assistant
- Lina Mirghani
Communications and Operations
Director of Communications and Operations
- Annette Heninger
Marketing and Communications Officer
- Pujarini Nadaf
Membership and Governance Officer
- Natasha Wainwright
Interim Membership and Governance Officer
- Vicky McGuinness
Publications and Web Officer
- Nick Dunwell
Finance
Director of Finance - Liz Fry
Finance Assistant - Hayley Ly
Events and Specialist Societies
Head of Events - Charlie Silva
Events Coordinator - Venease Morgan
Exhibition and Events Coordinator
- Anna Prunty
UKSSB Executive Assistant - Henry Dodds
Credits
From the Executive Editor
Simon Hodkinson
Awarm welcome to this first edition of the JTO in 2023. It has been unseasonably warm, but all is not well in the NHS with previously unheard of strikes from our nursing colleagues and at the time of writing, our junior medical colleagues voting overwhelmingly for industrial action –very challenging times lie ahead!
I am sure you are all aware of the sad loss of Dame Clare Marx in November last year. Much has been written about her in the orthopaedic and national literature, however we wanted to include in this edition a piece in celebration of her life (page 20), a life well-lived to say the least. We hope we have done justice to a remarkable human being.
This edition covers a number of topical issues that many of us are currently facing. Andrew Manktelow’s update (page 24) for those of us engaging in private practice is timely. PHIN has had a difficult gestation, but it is gathering pace and he reminds us that the CMRs ruling are a matter of law and cannot be ignored.
He appears again in this edition in conjunction with Bertie Leigh, BOA Council lay member and senior solicitor, to discuss the medico-legal implications of the pandemic and the current waiting lists (page 46). A sobering article to say the least.
Copyright© 2023 by the BOA. Unless stated otherwise, copyright rests with the BOA. Published on behalf of the British Orthopaedic Association by: Open Box M&C
Advertising
All advertisements are subject to approval by the BOA Executive Board. If you’d like to advertise in future issues of the JTO, please contact the following for more information:
Wendy Parker - Media Manager
Email: Wendy@ob-mc.co.uk | Telephone: +44 (0)121 200 7820
Open Box M&C, Premier House, 13 St Paul’s Square, Birmingham B3 1RB
Disclaimer
The articles and advertisements in this publication are the responsibility of the contributor or advertiser concerned. The publishers and editor and their respective employees, officers and agents accept no liability whatsoever for the consequences of any inaccurate or misleading data, opinions or statement or of any action taken as a result of any article in this publication.
BOA contact details
The British Orthopaedic Association, 38-43 Lincoln’s Inn Fields, London WC2A 3PE Telephone: 020 7405 6507
Trainees from the Wessex rotation, lead by Adam Stoneham, present their experience in running a novel course in peer-to-peer learning from one’s mistakes (page 28). We all make them, but do we learn from them in a supportive environment? Frequently not, it would seem.
Jonathan Howell and Mary Stocker discuss the development of the Exeter short stay arthroplasty unit (page 32). Whilst we may not all have the luxury of the real estate required, the article presents their experience of setting up such a unit and the considerable success they have had in ‘day case’ arthroplasty, and the advances in patient care as a result.
Further on, Paul Roberts discusses his considerable experience in developing and bringing to market new implants (page 38) and Bev Fitzsimons invites us to get off the production line, (page 42). A thought provoking article that reminds us that whilst an element of standardisation can help our practice and our patients, surgery is not a production line!
Last but by no means least, is this month’s speciality series of articles, this month covering spinal surgery. Introduced by Niall Eames discussing the evolution of spinal surgery in the UK (page 49), and followed by articles covering topics we can all be exposed to on call –those of cauda equina syndrome (page 50), spinal infection (page 54) and thoracolumbar fracture stability and its classification (page 58).
I hope you enjoy reading this March edition of the JTO. n
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 03
Built by Clinicians, for Clinicians.
iMedDoc is a brand new practice management system designed to manage every aspect of your practice, securely. We simplify your daily tasks so you can focus on your patients.

The Consultants Mobile App
Our mobile application puts your practice in the palm of your hand giving you anytime, anywhere access to your business.
Dynamic Diaries
Our comprehensive diary system allows you to view your diary and the diaries of your colleagues side-by-side on the same screen.
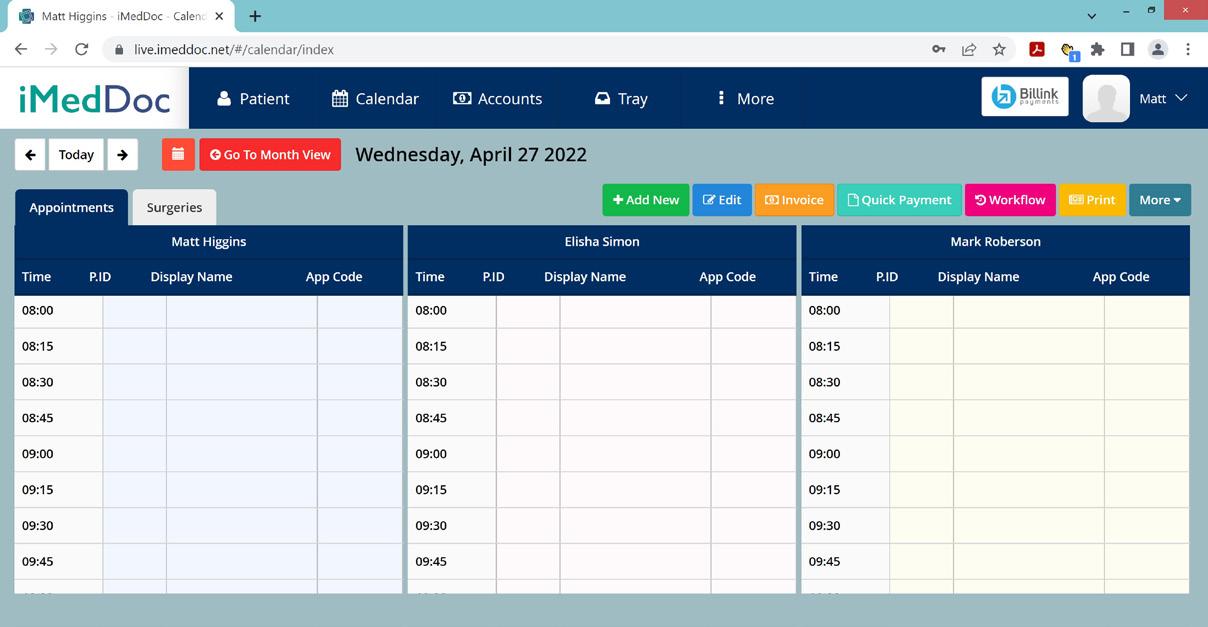
Electronic Medical Record
At the core of our system, is our cloud-based electronic medical record giving you everything you need to manage patient information.
Reporting and Analytics
Build a better business clinically and commercially. Track financial performance interpret medical records across your patient population. Book
www.imeddoc.com

+44 20 35141393
sales@imeddoc.co.uk

a demonstration with us today!
A kind word is like a spring day… it lifts your spirits (East
European Proverb)
Deborah Eastwood
As the snowdrops and daffodils flower and the sun brings warmth as well as light, we remember Clare’s joy in living and the strength she imparted with a warm smile and a kind word allowing those she met to thrive and grow.

Since Congress, our focus has been on growing and developing sustainable systems. At grass roots level all around the country, we have sown the seeds of projects on recruitment and retention, on new ways to educate, on recycling, on innovations to reduce our footprint and already, green shoots are appearing. Jointly with the NJR, we have appointed two Sustainable Surgery Fellows – Hammad Parwaiz and Rohan Prakash – and look forward to seeing their ideas flourish and bear fruit! We hope to be advertising fellowships for trauma surgery shortly.
We have finally made contact with the MHRA and been able to discuss the implications of the MDR and the UKCA marking. We have agreed to meet regularly and work more closely together to ensure a better understanding between regulators, industry and those who implant the devices for the benefit of our patients: perhaps common sense has won through?
Our BOA working party has produced guidance documents with respect to mitigating the risks of breast cancer in our female surgical colleagues by reducing exposure to ionising radiation and ensuring our PPE is fit for purpose. We are working with industry colleagues to devise suitable garments to improve protection to those at risk.
As part of a collaborative effort with BAPRAS and driven by Fergal Monsell and an able team of colleagues, the BOA has produced a series of webinars to support our colleagues in the Ukraine: these have now been edited to provide generic material for all those faced with disaster situations. We are working with WOC and colleagues at OrthoHub to develop further potential educational resources for those in low and middle income areas. Sustainable systems are important here too and may include the ability to service and repair existing equipment as much as sending ‘new’ materials.
I have had the opportunity to visit many colleagues around the UK and enjoyed celebrating Burns Night and ‘Stripping the Willow’ at the SCOT meeting: it was their first face-to-face meeting for some time and the joy and camaraderie was clear to see and the science was impressive. The STEP project reported that sadly, an unhappy and confrontational workplace culture was too common in departments across Scotland. At least we have now defined the problem and can set about putting it right.
But as spring arrives, we have to acknowledge that there are still many problems to face and a disenfranchised workforce is perhaps of most concern. The changes we have faced over recent years have been significant and challenging, and we must continue to support each other whilst challenging for further change. We hope that we are making some progress in presenting our case to those in government who might be able to change, for the better, the challenges we face. We were proud that the statement issued in support of our surgical teams was signed by all three Royal Colleges, all surgical specialty associations and all surgical trainee associations: all surgeons speaking with one voice and this is a position of some strength.
Growing up, one of my favourite novels was Anne of Green Gables, the author LM Montgomery was quoted as saying that ‘nothing ever seems impossible in spring’ so as we continue to face our local, regional and national challenges let us remember that and keep a smile on our face. n
From the President
President, British Orthopaedic Trainees Association (BOTA)
ST5 Specialty Registrar, North West Thames Rotation NIHR/RCS England Doctoral Research Fellow, University of Oxford Twitter: @OrthoSingh/@bota_uk
Ortho Update 2023
 Ronnie Davies
Ronnie Davies
After a COVID-19 induced move to an online format, the Ortho Update course returned to face-toface this year. This provided the opportunity to add some rather dramatic trauma simulation to the programme, enabling participants to get some major trauma resuscitation and spinal injury CEXs validated. A fantastic group of medical students added to the realism as simulated patients and gosh, what a performance they put on!
The focus was on trauma this year, and in a BOA first, we had a truly multidisciplinary bunch, including a general surgeon (and ATLS enthusiast) and a plastic surgeon who led case-based discussions about major burns. A personal favourite was the case-based discussion station of ‘the good, the bad and the ugly’, in which faculty aired their dirty washing to discuss the principles of fracture fixation. By the end of the course, candidates completed an average of six WBAs covering trauma topics that included compartment syndrome, neurovascular injuries and physiological response to trauma.
A highlight of the course was the thought-provoking plenary lecture by our very own Niall Eames entitled ‘The Second Victim’. This included a powerful video of a patient who was paralysed during a spinal operation. It was certainly the talking point at most tables over lunch.


We are already planning next year’s course, which is provisionally set to cover ‘Exams and Clinical Examination: how to pass the FRCS and examine like a pro’. Of course, there will be a few surprises to make it another excellent day of orthopaedic education. n

Abhinav Singh – Incoming BOTA President

Iam an Orthopaedic Registrar on the North West Thames rotation and a PhD Student at the University of Oxford. My research, funded by the NIHR/ RCS England Doctoral Research Fellowships, focuses on improving newborn screening for developmental dysplasia of the hip (DDH). I graduated from Peninsula College of Medicine and Dentistry in 2015 with a Merit in my medical degree and a first-class intercalated BSc in Biosciences from the University of Exeter. This was followed by foundation and core surgical training in London, during which I completed a Masters in Musculoskeletal Sciences with Distinction (University of Oxford) and a Postgraduate Certificate in Clinical Education (University College London). Outside of work, I remain a keen cricketer and runner.
My goals for the year
In the post-pandemic era, elective recovery continues to be slow, and trainees are facing immense challenges in achieving their required competencies. As President, I will champion effective engagement between regions and professional bodies to address trainee concerns and implement targeted improvements. Alongside this, I will ensure that BOTA continues to support trainees in undertaking impactful collaborative research and further develop its innovation/sustainability workstreams. Finally, I will facilitate a talented committee to work with industry partners, junior colleagues and BOA/BOTA Diversity Champions to ensure orthopaedics remains inclusive for all. n
06 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk News
“Genuinely one of the most useful courses I’ve attended. A real boost to my confidence.”
Fast,
Independent analysis of used medical devices



“Beyond Compliance and ODEP are delighted that the NHS Implant Analysis Service is going to facilitate this essential part of implant monitoring.”
- MR K TUCKER, CHAIR OF ODEP & BEYOND COMPLIANCE
-
08459 390018
efficient, cost effective analysis & reports for total hips, knees & other devices.
- nth-tr.implantanalysissupport@nhs.net
www.implantanalysis.nth.nhs.uk -
BOA-funded Nottingham University Clinical Trials Unit course
As part of BOA’s partnership with Nottingham University Clinical Trials Unit (NCTU), new opportunities are offered for BOA members to undertake courses about clinical trials, systematic reviews and developing your own trial ideas.
Developing your research ideas for trials in trauma and orthopaedics
A free, online, half-day course from Nottingham Clinical Trials Unit (NCTU), to help develop research ideas into fundable research applications is taking place between 9am and 1pm on 17th March 2023. To apply for a place on this course and for more information on other BOA- funded NCTU short courses, visit the NCTU website at: www.nctu.ac.uk/other-research/trauma-orthopaedics.aspx
BOA Educational Courses
Spinal cord injury BOAST published
We are pleased to announce the publication of a new Trauma BOAST (BOA Standard) on the Management of Traumatic Spinal Cord Injury. This BOAST was jointly developed by the BOA and the British Association of Spine Surgeons (BASS) and the British Association of Spinal Cord Injury Specialists (BASCIS). BOASTs are short standards documents that are produced by the BOA Trauma and Orthopaedic Committees. They are downloadable from our website and can be printed for display in hospitals. You can find a full list of BOASTs on the BOA website at www.boa.ac.uk/BOASTs.

Committee Appointments
Following a successful round of applications, the BOA would like to congratulate all those who have been appointed onto the BOA Committees:
Education and Careers Committee:
The BOA runs a wide range of courses under the Education Committee. These courses cater to the educational needs of a wide range of members (and nonmembers in some cases) at all stages of their careers. Upcoming Courses include:

Training Orthopaedic Education Supervisors (TOES)
The BOA Training Orthopaedic Educational Supervisors (TOES) course is now running entirely online. We have fully updated our training for educational supervisors to help you prepare for the new curriculum in 2023. Full details of the 2023 course dates can be found on the website at www.boa.ac.uk/toes
Training Orthopaedic Trainers (TOTs)
The underlying premise of TOTs is that if T&O trainers understand how people learn and how the T&O curriculum works, by translating that understanding into action, they should be able to improve their teaching. Much of the work can be done at a time, place and pace convenient to participants, with attendance at live virtual meetings to supplement personal learning. V-TOTs course will last for approximately six weeks. All of the 2023 course dates can be found at www.boa.ac.uk/tots
Julie Craig – SAS representative
Niel Kang – Lead for Medical Student Engagement
Rajesh Nanda – Lead for Fellowships and Courses
Medico-legal Committee:
Shyam Kumar (reappointed)
Orthopaedic Committee:
Alex Dodds
Research Committee:
Michael Whitehouse (reappointed)
Jeya Palan
Stephen McDonnell
Trauma Committee:
Aatif Mahmood – SAS representative
Alex Trompeter – BOAST Lead (reappointed)
Benjamin Ollivere
08 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Latest News
Clinical Impact Awards (ACCIA) 2023 process
The 2023 Clinical Impact Awards (successor of the Clinical Excellence Awards) will open for applications towards the end of March for an eight-week period.
For the 2023 process the ACCIA have decided to remove the role of National Nominating Organisations (NNO) such as the BOA and the RCS. The decision is based on a review of the 2022 scheme which concluded that the citation and ranking from NNOS made little difference to the overall decision making process and removing it would reduce bureaucracy, allow applicants more time to work on and submit their applications and hopefully increase the number and diversity of applications.
More information on the new process is available on the ACCIA web pages here: www.gov.uk/government/ organisations/advisory-committee-on-clinical-impact-awards
Battlefield trauma resources
The BOA and BAPRAS have created a series of videos on battlefield trauma to support surgeons who are working in military conflicts throughout the world. This project has brought together recognised experts with deployment experience, covering a wide range of topics relevant to the management of battlefield trauma. This content will be relevant to the provision of assistance in areas of conflict, independent of geo-political considerations.

You can view them on the BOA website here: www.boa.ac.uk/battlefield-trauma
UKITE 2022
2023 Council and Presidential Nominations
Attention Home Fellows – Council Trustee and Presidential nominations open on 15th March!
The BOA believes that Trauma and Orthopaedics should be an inclusive surgical profession that inspires, attracts and retains the best talent from a wide variety of backgrounds. One of the ways we believe we can best make that a reality is by ensuring we elect a Council that fully represents all our members and better reflects the broad and diverse population we serve.
You have the opportunity to bring your skills and expertise to help us grow and develop the BOA and Trauma and Orthopaedics as a whole. A more diverse BOA, and a broader range of voices, better serves our patients and best supports our colleagues and we welcome applications from across our membership.
Please be sure to submit your nominations for Council before the deadline of 15th April and for BOA President by 1st June.
More information and how to apply is available after 15th March on the BOA nominations website at www.mi-nomination.com/BOA
We had an excellent turnout of 796 trainees for UKITE in December 2022 from across the UK and Ireland joined by 179 candidates from Malta and South Africa. This year for the first time, candidates received question-level feedback on their responses to better support their learning, albeit after some technical delay.
Congratulations to West Midlands (Birmingham), who were the highest scoring training programme in 2022 with an average score of 58% for the 24 trainees who took part.
We couldn’t put UKITE together without our excellent team of editors and subspecialty leads who write and select the questions. Thank you all for your contributions. If you’re interested in getting involved for this year, you can find out more information at www.boa.ac.uk/ukite or email ukite@boa.ac.uk.
James Lind Alliance Priority Setting Partnership – First Time Soft Tissue Knee Injury
The BOA are pleased to announce that BASK & BOSTAA have recently identified the top 10 priorities for future research on the topic of First Time Soft Tissue Knee Injury for a James Lind Alliance Priority Setting Partnership.
You can read more about the project and the priorities here at www.jla.nihr.ac.uk/priority-settingpartnerships/first-time-soft-tissue-knee-injuries
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 09 Latest News
BOA sponsored Chatterjee travelling fellowship
In the summer of 2022 I completed my Chatterjee Fellowship at the Istituto Ortopedico Rizolli in Bologna, Italy. During my visit, I was able to spend time with Professor Davide Donati and the rest of the tumour team who graciously welcomed me into the department. They are a supra-tertiary referral centre for tumours and complex reconstruction, receiving referrals from all of Italy and surrounding European countries for both tumour work as well as complex revision arthroplasty, and has a specialist interest in the use of bulky allograft for reconstruction, which is something that we do not see used commonly in the UK.

I was able to observe the use of bulk allograft in both the reconstruction of complex revision arthroplasty surgery and tumour reconstruction. It was predominantly utilised for pelvic
 Omer Alanie
Omer Alanie
reconstructions, proximal tibia and foot and ankle reconstructions. I saw its use in a number of cases, but what I found most fascinating is the number of cases of patients who had ‘returns to theatre’ following the use of bulk allograft for infection or other complications. It highlighted that this is not a benign treatment, and that the risks of infection in this patient cohort with this treatment was not negligible, and can be of similar magnitude to the use of other reconstruction options.
It was very interesting discussing with the team there how they maintain their ability to provide such a service. This is because their ‘middle grades’ are on call for retrievals in a similar sense to a transplant retrieval team, and are on call for the entirety of Italy for this. This means that they can sometimes travel 5-6 hours to retrieve donor tissue which they can subsequently harvest and store for later use. This is something that perhaps is not feasible in the UK given the resource demands that such a service would require, but it was fascinating to see how they have established a network and retrieval team to allow provision of this service. Interestingly, the team felt the reason for lack of uptake of bulk allograft in the UK was predominantly due to concerns regarding prion transmission, rather than the logistical reasons. n
New BOA Trustee ( 2023 – 2025)
Stephen Eastaugh-Waring
Steve was appointed as a Consultant at North Bristol NHS Trust in 2003, initially with a broad practice of lower limb arthroplasty and trauma, but now focuses purely on hip surgery. Working during training as the lecturer in the University of Bristol responsible for undergraduate orthopaedic training, he took this interest forward into Consultant life. Shortly after appointment he became the postgraduate tutor for the Severn T&O rotation, subsequently moving up to the role of Training Programme Director for five-years. Head of School for Surgery followed this, eventually acting as the Chair for CoPSS (Confederation of the Postgraduate Schools of Surgery).
Throughout this period Steve enjoyed being a T&O examiner, and after his Deanery roles finished, he was appointed to be Chair of the ISB T&O examination for a three-year tenure. He still maintains close links, acting as an examiner assessor.
To complete a broad experience, Steve has also served a number of roles in clinical management, with five-years as Clinical Director for T&O (including a merger of two units into a large PFI hospital), then Divisional Director followed by Deputy Medical Director over the COVID-19 pandemic. A year’s ‘rest’ doing purely clinical work has now recharged the batteries and he is really looking forward to the challenges and opportunities offered by the BOA.
Steve is married to Tracey, a Consultant Anaesthetist (following ten years as an Intensivist) and has two daughters who are shortly embarking on their University undergraduate careers. An outdoor lifestyle offers a balance to a busy working life, and having represented Great Britain as an amateur in triathlon, an accumulation of injuries has now forced a transformation into a cyclist and motorbike enthusiast (don’t tell the trauma surgeons!!). n

10 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk News
Case of a patient with a previous bulk allograft of pelvis, now unfortunately infected
With co-visiting fellows in operating theatre
• Unique pivot joint enables freedom of movement

• 89% of users experienced improved quality of life1


• 94% of users would highly recommend2

SPORTS KNEE SURGERY Monday 6th and Tuesday 7th November 2023 Edgbaston Cricket Ground CPD points applied for Registration Open Convened by Tim Spalding, Pete Thompson and Andrew Metcalfe and an esteemed worldwide faculty, as we address the ‘How and Why’ for specific techniques in knee surgery. sportskneesurgery.com Supporting surgical education: From the atlas to the coccyx... The world’s most detailed and accurate 3D reconstruction of human anatomy Visit primalpictures.com to learn more about our catalogue of interactive learning tools, created from real body scans and imaging data – bringing the complexity of the musculoskeletal system to life. Spinomed® Core muscle group training device supporting management of osteoporotic vertebral fracturesnow with innovative pivot joint. medi. I
better www.mediuk.co.uk
feel
IP VOT JO TNI Intended purpose: Brace designed to actively relieve load and correct the lumbar spine / thoracic spine in the sagittal plane. 1. eurocom e. V. Published online at: https://www.eurocom-info.de/wp-content/uploads/2021/03/eurocom_Broschuere-Ruecken_Allensbach_web.pdf (Last access 23/08/2021). 2. medi GmbH & Co. KG, 2020 Scan for more information
BOTA update - 2022 Congress Review
Alexandra Haddon, James Chowdhury and Abhinav Singh
The BOTA 2022 Congress was held in the vibrant city of Liverpool, 22th – 25th November 2022, and focussed on sustainability with the theme ‘More green. More global. More diverse’. Delivered in collaboration with MedAll, this was the largest hybrid BOTA Congress to-date totalling an amazing 511 delegates. This included 61 Fair Medical Education Online Tickets for Low- and middle-income countries (LMIC) attendees, 30 online and 420 in-person tickets. The Congress’ huge success is a testament to the efforts put in by the outgoing BOTA 2022 Committee (led by Oliver Adebayo) and the Education Subcommittee (led by Adrian Andronic).

The pre-Congress face-toface courses included: the BOMSA Medical Student day, the ST3 Human Factors Bootcamp and the Postgraduate Orthopaedics FRCS Viva. The pre-Congress virtual courses were: Innovation in Orthopaedics and Equality, Diversity, Inclusion (EDI) Training. The Congress itself had some fantastic educational content thanks to BESS, AO, OTS, Let’s Talk Doctor and many of our industry partners. With increasing trainee interest in navigated and
robotics arthroplasty, there were interactive demonstrations of the MAKO (Stryker) and ROSA (Zimmer BioMet) systems. B. Braun also delivered an informative workshop on virtual surgery. Feedback demonstrated that all sessions were both well attended and received by junior and senior delegates

From a research perspective, a very healthy 174 free paper submissions demonstrated the industry of orthopaedic trainees over the past 12 months. Three podium presentation prizes were awarded to
negotiating culminated in a total of £4,000 being awarded to the following trainees: Chris Bretherton, Sarah Abbott, Zaid Hamoodi, Sohail Nisar and Ignatius Liew. The research funding was made possible through generous contributions from the BOA/RCS England Surgical Specialty Leads (SSLs) and AOUKI.

James Archer, Jamila Tukur Jido and Michael Pullinger. The Dragons’ Den session lived up to its name, with trainees pitching their work to Professors Siobhan Creanor, Caroline Hing, Xavier Griffin and Daniel Perry. Innovative presentations and some tough
The Congress hosted the first liveaudience recording of the Orthohub podcast, hosted by Kash Akhtar and Pete Bates. They were joined by a special guest, Sue Deakin, who provided a candid account of an adverse event as a consultant and how it has changed her career for the better. Thanks to a successful (and fiercely competitive) pub quiz and a brilliant gala dinner, over £2,000 was raised for Feet First Worldwide and Motec Life-UK charities. Congratulations also to Tim Petheram who was awarded the Trainer of the Year. Finally, for anyone who missed a session, recordings are available to watch on-demand on the MedAll website. The 2023 BOTA committee are already looking forward to welcoming everyone to the 2023 Congress in Edinburgh, 28th November – 1st December) n
12 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
News
“The Congress itself had some fantastic educational content thanks to BESS, AO, OTS, Let’s Talk Doctor and many of our industry partners.”
Dragons’ Den Research Session
Robotics session
Members of the 2023 BOTA Committee
by:

UCLH PRESENTS
3rd Annual
UCH Basic Shoulder Arthroscopy Course

Wednesday 08th May 2019
4th Annual Basic Shoulder Arthroscopy


Wednesday 13th May 2020
Course Convenor:
UCLH Education Centre, Euston London
Mr Abbas Rashid UCLH
Course Convenor:
Mr Abbas Rashid
8th Annual Basic Knee Arthroscopy Course

Thursday 14th May 2020
UCLH Education Centre, Euston London
Course Convenor:
Mr Sam Oussedik
Practical Skills for Orthopaedic ST3 Interviews

Wednesday 13th February 2019
- Experienced consultant faculty















Course Convenor:
- High ratio of faculty to participants
- Comprehensive programme
Mr Alistair Hunter
UCLH


staff
Suitable for CT1 to ST5 and Scrub staff

Accredited by:
For more information email: uclh.simulationcentre@nhs.net
For more information and to book email: uclh.simulationcentre@nhs.net

CPD POINTS APPLIED FOR POWER OF THE PAST FORCE OF THE FUTURE BOOKINGS OPEN THURSDAY 27TH & FRIDAY 28TH APRIL 2023 EDGBASTON PARK HOTEL BIRMINGHAM PatelloFemoral MASTERCLASS BIRMINGHAM oryon.co.uk/imaging/ 020 7042 1888 imaging@oryon.co.uk Contact us to become a referrer Refer to Oryon Imaging for affordable private diagnostic imaging in central London Same day MRI appointments Open 7 days a week Results in one working day IEP and Connect immediate access to results MRI £250 from Course Convenor: Mr Abbas Rashid UCLH 3rd Annual UCH Basic Shoulder Arthroscopy Course Wednesday 08th May 2019 Practical Skills for Orthopaedic ST3 Interviews Wednesday 13th February 2019 Course Convenor: Mr Alistair Hunter UCLH For more information email: uclh.simulationcentre@nhs.net Course Convenor: Mr Sam Oussedik 8th Annual Basic Knee Arthroscopy Course Thursday 14th May 2020 For more information and to book click here or email: uclh.simulationcentre@nhs.net UCLH PRESENTS UCLH Education Centre, Euston London Accredited by: Experienced consultant faculty High ratio of faculty to participants Comprehensive programme including meniscal repair Suitable for CT1 to ST5 and Scrub
British Orthopaedic Foot and Ankle Society (BOFAS) update
Paul Halliwell, BOFAS President
During the last 20 years, BOFAS has grown enormously in membership and activity. The BOFAS Principles of Foot and Ankle Surgery course has evolved to become required attendance by many Deaneries and has been delivered in countries including India and Africa. BOFAS was honoured to be Invited Society in 2022 by the European Foot & Ankle Society in Edinburgh and the American Foot & Ankle Society in Quebec. Educational resources offered through the BOFAS website are increasingly expansive and we have further developed the webinars necessitated by COVID-19 including a successful Master Techniques series.
BOFAS’ Scientific Committee has engaged with the National Societies Research Leads forum and is running the UK-Foot Ankle ThromboEmbolism project (UK-FATE) as well as continuing work with the NICE and the James Lind Alliance.
The BOFAS Registry continues to grow not only in size, but also in national significance. In June, NICE recommended input of any first MTPJ replacement onto the BOFAS Foot and Ankle Registry. Discussions with the BOA, GIRFT and NHS Digital regarding development of an implant registry continue. BOFAS meets with
Beyond Compliance / ODEP, and our Ankle Arthritis Networks Steering Group helps colleagues offer the most appropriate management to each ankle arthritis patient even if they themselves choose not to develop an ankle replacement practice. Networked care is increasingly important in other fields of care, especially that of the diabetic foot, so will figure highly during our March 2023 Congress in Liverpool.
These intense fields of work could be regarded as an impenetrable inner circle by the next generation, especially those who could be forgiven for believing there is a ‘typical’ Committee person. To understand this better and enhance accessibility we have created the role of BOFAS Equity, Diversity and Inclusion Lead.

BOFAS takes a pride in keeping patients’ interests at the centre of everything, whether directly by providing information through our website for example, or indirectly by training and mentoring the next generation, collecting clinical outcome data, raising the standards of research, or supporting colleagues to deliver their very best in a fulfilling and career-sustaining manner despite such challenging times. None of it is easy, but as you can see, BOFAS is up for it! n
Society for Back Pain Research (SBPR) update
Last summer the Society for Back Pain Research was finally able to meet and celebrate having reached 50 years, this had been delayed for two years by the pandemic, but we were thrilled to have the chance to see each other face-to-face and pick up discussions which had been on hold for a while.

There was an amazing session by some of our Honorary Members who reminded us of the task ahead of us and suggested ways that we may be able to make an impact on the problem we faced.
Our guest speakers were Frances Williams with her work with twin studies, Annina Schmid interrogating the concept of sciatica, Manuela Ferreira sharing her
experience of the Surgery for Spinal Stenosis (SUcceSS) Study.
The breadth of the society was demonstrated in the scientific content. The papers picking up awards were as follows:
President’s Award (2022): Adam WA Geraghty – Supporting self-management of low back pain with an internet intervention in primary care: Preliminary findings from the SupportBack 2 randomised controlled trial.
Secretaries Award (2022): Tamanna Rahman – Comparing three nuclectomy techniques: A high-resolution MRI study.
Honorary Members Award (2022): J Bell – X-ray scattering imaging of intervertebral discs under load.
New Investigator Award (2022): David Hohenschurz-Schmidt - Recommendations for the development, implementation, and reporting of (Sham) Control Interventions in efficacy trials of physical, psychological, and self-management therapies - The CoPPS statement.
Backcare Award (2022): B Saunders - Patients’ and general practitioners’ views and experiences of stratified primary care for patients with musculoskeletal pain: qualitative findings from the STarT MSK feasibility and pilot trial (paper presented to SBPR 2019 Sheffield, UK).
This year our SBPR meeting will be part of BritSpine 2023 – Glasgow SEC –18th – 20th April 2022. This will be a multi-disciplinary scientific conference and exhibition, which will bring together experts in spinal conditions, research, and treatment from across the world to expand knowledge and promote networking. Full details at: www.sbpr.info/meetings
SBPR welcomes new members, check out our website at www.sbpr.info n
14 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
News
Safe

Demonstrated to be as safe as autograft in a Level 1 human clinical study

E ective

Achieved a fusion rate of 97.3% at 24 months in a Level 1 human clinical study
Proven
A powerful cell attachment factor backed by Level 1 human clinical evidence







Spine

1 ACDF – 319 patients (IDE RCT)









“i-FACTOR subjects demonstrated higher overall success rate than control (autograft) subjects (68.75% and 56.95% respectively, p = 0.0382)”
2 PLF – 98 patients (RCT)

“This RCT indicates i-Factor being signi cantly superior to allografted bone in enhancing intertransverse fusion (p = 0.000)”

3 ALIF – 110 patients
“…high fusion rate and clinical improvements comparable to the published results for ALIF using autograft or BMP”
4 PLIF – 40 patients
“i-FACTOR is associated with faster formation of bridging bone when compared to autologous bone in patients undergoing PLIF”



Orthopedics
5 Long bone non-union and delayed union 22 patients –90% bone consolidation

“P-15 appears to o er a safe, economical, and clinically useful alternative to autograft in the repair of ununited fractures”































6 Foot and ankle – 170 patients
i-FACTOR yields 92% fusion at 12 months post-op across fore-, mid- and hindfoot joints











7 Foot and ankle – 16 patients
100% fusion at 12 months in hindfoot and ankle fusion revision procedures





8 Peri-acetabular osteotomy – 51 patients
Patients treated with i-FACTOR were 3x more likely to attain a partial or complete fusion at 6 months post-op compared to allograft
23 & 24 MARCH 2023 THE ASSEMBLY ROOMS BELFAST CPD POINTS APPLIED FOR REGISTER NOW
complete solution for opthalmology. Explore more: • Electrically powered functions • Dual articulating headrest • Exceptional surgical access aneticaid.com Book your demo today. sales@aneticaid.com +44 (0)1943 878647
to chance
Ophthalmic Stretcher The
Don’t leave fusion
Prioritise Bone Graft
Internal Unpublished Data Level 1 Prospective Study Published Case Series 1 2 5 5 6,7 5 8 3,4
107881 CER Journal Resize 190x130mm.indd 1 23/02/2023 15:33
British Orthopaedic Sports Trauma & Arthroscopy Association (BOSTAA) update
 Nick Nicolaou and Fazal Ali
Nick Nicolaou and Fazal Ali
This will be a busy year for the British Sports Trauma and Arthroscopy Association (www.bostaa.ac.uk) as we focus our efforts on advancing clinical practice and improving care for Orthopaedic sports injuries.
Our 2023 annual meeting will be held at the home of cricket, Lord’s, on 9th November. We look forward to presenting a high quality programme following on from our successful 2022 annual meeting focused on the Veteran Athlete.
Our involvement in the James Lind Alliance priority setting partnership for knee injuries reflects our aims in enhancing research and we look forward to the top 10 research priorities being decided this year.
The new BOSTAA Trainee committee has been active in organising the cadaveric lower limb surgical approaches course which will become a regular teaching event aimed at early stage surgeons by providing a subsidised course with experienced faculty. In addition, we look forward to producing regular podcasts to encourage engagement

with our younger members to complement the existing advanced arthroscopy course held every January.
Look out for the BOSTAA session at the BOA this autumn; in 2022 we were able to discuss sustainability in orthopaedics, a theme that will be key at the annual meeting this year. n
BOA Annual Congress 2023
19th – 22nd September, ACC, Liverpool
www.boa.ac.uk/Congress #BOAAC23
Registration
This year sees some changes to the BOA Annual Congress Registration. Registration will now open for all (both BOA Members and Non –Members) on Monday 3rd April 2023. BOA members can take advantage of their membership benefit and register at a discounted rate (100%) for an extended time period. This discount will run for 12 weeks from Monday 3rd of April to Sunday 25th June 2023.
BOA Abstract Submissions
Under the theme of ‘Sustainable Systems’ the 2023 Annual Congress will take place 19th – 22nd September, at the ACC, Liverpool. Once again we are closely working with the specialist societies to deliver revalidation and hot topic sessions. The programme will include keynote lectures, including the BOA’s Presidential Guest Lecture from Dr Kristy Webber and the Robert Jones Lecture being delivered by Professor Andrew Carr. The BOA President, Professor Deborah Eastwood, will also give an update on her presidential year.
BOA abstract submissions including Medical Students are now open and will close at 23:59 on Friday 5th May 2023. Categories include ATOCP/Physiotherapy, Basic Science, Developing World Orthopaedics, Education, Foot and Ankle, General Orthopaedics, Hands, Hip, Innovation in Simulation, Knee, Limb Reconstruction, Medical Students, Paediatrics, Quality Improvement, Shoulder and Elbow, Spines, Sports Trauma, Sustainable Systems, and Trauma and Tumours. Full details can be found on our website at www.boa.ac.uk/abstracts
This year’s abstracts are supported by Heraeus Medical.
Full details can be found on the Congress website at www.boa.ac.uk/registration
Please keep an eye on the BOA website over the upcoming months for updates on abstract submissions, programme, speakers, sponsors, accommodation and more – visit www.boa.ac.uk/annual-congress
Exhibition and sponsorship opportunities
Exhibit at the UK’s largest event for orthopaedic surgeons. Book your exhibition stand now and secure your space. To apply please contact exhibitions@boa.ac.uk
16 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
News





































BIOLOGICAL KNEE SOCIETY ANNUAL MEETING 2023 REDUCING REPLACEMENT BY
CPD
APPLIED FOR REGISTER NOW 24th & 25th April 2023 Southampton
REGENERATING
POINTS
Conference Listing 2023:
BHS (British Hip Society)
www.britishhipsociety.com
08-10 March 2023, Edinburgh
BOFAS (The British Orthopaedic Foot and Ankle Society)
www.bofas.org.uk
08-10 March 2023, Liverpool
BSCOS (British Society for Children’s Orthopaedic Surgery)
www.bscos.org.uk
09-10 March 2023, Southampton
BLRS (British Limb Reconstruction Society)
www.blrs.org.uk
23-24 March 2023, Belfast
BRITSPINE 2023
www.BritSpine.com
18-20 April 2023, Glasgow
BASK (British Association for Surgery of the Knee)
www.baskonline.com
16-17 May 2023, London
OTS (Orthopaedic Trauma Society)
www.orthopaedictrauma.org.uk
25-26 May 2023, Edinburgh
Joint Action update
2023 TCS London Marathon
On 23rd April, the London Marathon returns to its traditional spring schedule. Our amazing team of runners including, Jen Barwell, Alex Chipperfield, Paolo Consigliere, Larne JonesWhiting, Matt Owen, Satya Pydah, Hasan Rahij, Abhinav Singh, Amol Tambe and Dan Thurston will all be taking on the challenge. Please support our runners by donating at: https://2023tcslondonmarathon.enthuse.com/ britishorthopaedicassociation/profile

2023 RideLondon-Essex 100
Join us in 2023 by taking part in the Ford RideLondon-Essex 100 on Sunday 28th May 2023 and raise vital funds for Orthopaedic Research.
Ride for #TeamJointAction! We have a number of charity places currently available. If you are an experienced cyclist or someone who would just love the opportunity to take part in this iconic event, please email your interest to jointaction@boa.ac.uk
If you have been lucky enough to secure your own place through the ballot for either the
BOOS (British Orthopaedic Oncology Society)
www.boos.org.uk
09 June 2023, Burton-on-Trent
BESS (British Elbow and Shoulder Society)
www.bess.ac.uk
27-30 June 2023, Newport
UKPJI (UK Prosthetic Joint Infection)
www.ukpji.com
15-16 June 2023, Exeter
BIOS (British Indian Orthopaedic Society)
www.britishindianorthopaedicsociety.org.uk
07-08 July 2023, Windsor
BOA (British Orthopaedic Association)
www.boa.ac.uk
19-22 September 2023, Liverpool
BORS (British Orthopaedic Research Society)
www.borsoc.org.uk
25-26 September 2023, Cambridge
BOSTAA (British Orthopaedic Sports Trauma and Arthroscopy Association)
www.bostaa.ac.uk
09 November 2023, London
BSSH (The British Society for Surgery of the Hand)
www.bssh.ac.uk
22-24 November 2023, Glasgow
The BOA would like to thank everyone who generously donated to our Joint Action Christmas Appeal. With your generosity we have raised over £8,700 for Joint Action, the Orthopaedic Research Appeal of the BOA.

London Marathon or Ride London, we would still love for you to join us and run or ride for Joint Action. You will receive the same support as a charity place participant but there is no fundraising target, we simply ask that you raise as much as you can. All funds raised will support research into musculoskeletal disorders and any and all support is most welcome. Please contact the fundraising team at jointaction@boa.ac.uk to let them know.
North London Tough Mudder
The BOA have pulled together a team of staff members to raise funds for Joint Action and take part in the North London Tough Mudder on Saturday 15th April and are looking for a few more people to join the team. If you are interested, please contact the fundraising team as soon as possible at jointaction@boa.ac.uk
18 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk News
UCLH PRESENTS
Preparation for FRCS (Tr&Orth) Course
Wednesday 13th September 2023
UCLH Education Centre, Euston London
Course Convenor: Mr Alistair Hunter
The emphasis of this national course is on technique and aims to provide a framework early in a trainee’s preparation for understanding the nature of the FRCS (Tr&Orth) exam, develop strategies for optimising revision and for maximising scoring in the Viva and Clinical Examinations.

Accredited by:


For more information and to book http://training.ucheducationcentre.org/home/viewcourse/688/
COMBINED WITH COKS
16-17 MAY
CENTRAL HALL WESTMINSTER
LONDON

WWW.BASKMEETING.COM

REGISTER NOW
SUSTAINABLE SYSTEMS
THE BRITISH ORTHOPAEDIC ASSOCIATION ANNUAL CONGRESS 2023




19TH – 22ND SEPTEMBER, ACC LIVERPOOL




EXHIBIT AT THE UK’S LARGEST EVENT FOR ORTHOPAEDIC SURGEONS




Book your exhibition stand now and secure your space, to apply please contact exhibitions@boa.ac.uk

BASK 2 23
Dame Clare Lucy Marx
Clare was a true ‘one off’
Mark Bowditch and Deborah Eastwood
Clare was a remarkable woman and orthopaedic surgeon. An inspirational leader, good company with a mischievous sense of humour.
She was born in Coventry on 15th March 1954, her father an industrial chemist and her mother a schoolteacher and childcare specialist.
In her early years she spent time in Switzerland, where she had family. She learned French, became an accomplished skier and developed a love of Alpine walking that was to stay with her throughout her life.
Educated at Cheltenham Ladies College, she was introduced to medicine and surgery through an attachment to a local general surgeon in Coventry.
She subsequently studied medicine at UCH London. Thereafter, on the UCH/Westminster orthopaedic rotation, she developed a reputation as a hard worker who would never let you down – traits she continued to demonstrate throughout her career.
Following a fellowship in hip and knee arthroplasty at the Robert Brigham Hospital in Boston, she was appointed as a Consultant Orthopaedic Surgeon at St Charles Hospital Paddington, London, in 1990, moving into a new unit at St Mary’s hospital a year later.
With her passion for training already apparent, she promptly revised the medical student teaching, and took a keen interest in the Wednesday afternoon sessions. As well as developing her arthroplasty practice, she instigated daily trauma meetings, despite some resistance!
By this time, she had married her London neighbour, Andrew Fane, who had a family farm in Suffolk and decided a post nearer to ‘home’ was preferable.
When a post came up in Ipswich, she applied and became their first woman surgeon of any speciality, in 1993. Although potentially challenging, she experienced nothing but encouragement.

So, she joined seven rather large male consultants and naturally got given the nickname ‘Snow White’. After a few months, a colleague told her husband, as a compliment, that East Anglia hadn’t seen a woman wielding a knife like Clare, since Boudicca had been in business!
Things could be a bit different in rural Suffolk to central London. One registrar recalled being bleeped urgently by Clare to help in fracture
Features
20 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
clinic early one morning, only to arrive and then be asked to help catch a brood of ducklings that had hatched in the plaster room! They were given a new home in Clare’s pond. Her generosity and support for the T&O department was legendary. Many will fondly remember her lunchtime picnics in theatre with homebaked bread. She would host the annual department summer garden party for all staff, and would organise (and fund) the Christmas week staff buffet lunch in fracture clinic waiting room each year, visiting the wards over Christmas to thank the nursing teams.
She would welcome new colleagues joining Ipswich whenever possible with welcome dinners and indeed several current consultants stayed in the Fane farm selfcontained flat for a few months when first moving to Suffolk prior to finding a house.

She focused on high standards, patient safety, honest communication, and team engagement. Registrars treasured being on the ‘Marx firm’ for the ‘good surgeon’ apprenticeship, enhanced by her genuine personal interest, good humour, and generosity. For many, it established the core principles of their own professional practice.
Much of this was a daily demonstration of her ‘would you be happy for ourselves, or a family member, to be treated in that way’ approach to patient care.
Within a year of arriving in Ipswich, she was the clinical director for T&O, Rheumatology and A&E, quickly gaining the respect of
management and colleagues. Her door was always open, prepared to listen carefully first but never afraid to politely disagree with a characteristically unthreatening “may I suggest…” and a clear explanation of why. Always acting firmly in support of patient care.
She became the ultimate counsel for senior clinicians and executives alike. Referred to by some colleagues as the ‘headmistress’, somewhat cheekily and unbeknown to her, but always respectfully acknowledging a well-run team.

Her passion for high quality education ran through her entire career and led her to becoming Chair of the Joint Colleges Specialty Advisory Committee (SAC) in T&O, and as
Chair led a small group to produce the first T&O surgical curriculum in 2007. The T&O curriculum was a seminal piece of work and was the first of the surgical curricula and has been honoured worldwide.
In 2013/14 after 20 years at Ipswich, she was deeply honoured to be awarded the East of England Trainer of the year award, presented at Clare College, Cambridge.
She was elected British Orthopaedic Association President in 2008, a role she often described as the best and most enjoyable time of her career. She was the first woman President, breaking through a glass ceiling in a male dominated profession.

She brought diversity, fun, and strong but compassionate leadership to orthopaedics whilst Andrew similarly revolutionised the accompanying person’s programme. Together they were great company establishing friendships with orthopaedic leaders worldwide.

In 2009 she was elected to RCSEng Council with a role on the finance committee, and became Chair of the Invited Review Mechanism (IRM) in 2011. Her career long focus on >>

Features
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 21
“She was elected British Orthopaedic Association President in 2008, a role she often described as the best and most enjoyable time of her career. She was the first woman President, breaking through a glass ceiling in this male dominated profession.”
improving the quality of patient care was reflected in the RCSEng Good Surgical Practice document in 2014 and extended later into the GMC – the role of Good Medical Practice



















She became President of the RCSEngland in 2014, serving until 2017, and proved to be a true reformer as she drove through the redevelopment of the College buildings. This was not an easy time but her calm, measured approach and her ability to grapple with the difficulties she encountered meant that she was respected by all.

As at the BOA, she was the first female RCSEng President, but again this was never an issue for her. When someone commented that “at last the surgeons had appointed a woman President”, Sir Norman Williams, her predecessor as RCSEng President, retorted “My colleagues appointed Clare because she was best person for the job.”
Clare reluctantly stepped back from clinical work in 2014 after she had torn her rotator cuff whilst reducing a hip but did not slow down!
She became Associate Medical Director and was integral to the development of a major new elective orthopaedic centre for Ipswich and Colchester, appropriately now named the Dame Clare Marx Building.
In 2018, she became Chair of the Faculty of Medical Leadership and Management, and in 2019 the first woman Chair of the General Medical Council. At a time when its reputation amongst doctors was low, she brought a steadying sensible hand, enthused by the challenges.
She was honoured for her services to medicine, becoming a CBE in 2007 and a Dame in 2018.
Outside of medicine, in recognition of her contribution to the Suffolk community, she was appointed a Deputy Lieutenant in 2008, and in 2022 was one of five recipients to receive the Suffolk Medal.
She enjoyed life, particularly spending time with Andrew, enjoying the rural passions of the potting shed and countryside walks. She shared her love of music and opera with family and friends.
In 2021, she was diagnosed with pancreatic cancer and her GMC resignation letter highlighted Clare’s approach to medicine: “Since receiving this news, I’ve have been reminded once again of the importance and power of kindness in everything we do as doctors”.
Her husband recalled that this was brought home when as ‘Mrs Fane’ she was undergoing chemotherapy and a delightful elderly lady next to her regaled her with memories of a wonderful Miss Marx who had so kindly replaced her knee over 20 years ago – did Clare know her? – Clare admitted she did but nothing more.
She left us on the 27th November 2022.
The loss of Clare will be felt deeply across orthopaedic community and by those who knew and loved her, but her influence on the practice of surgery will be apparent for many years to come.
A senior surgeon in Norwich said, “it is a tribute to her that her fame and ennoblement never changed her – she remained the modest, charming, sharp witted and amusing young woman I remember from many years ago.”
Fittingly, the last words should go to her.
During an appearance on Radio 3 in April 2022 reflecting on her diagnosis she said:
“You only look back to learn, you must look forward for the future”
A truly remarkable woman. n
Features
22 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
“The loss of Clare will be felt deeply across orthopaedic community and by those who knew and loved her, but her influence on the practice of surgery will be apparent for many years to come.”









































































































Private Health Information Network (PHIN) and complying with the Competitions and Markets Authority Order: An update for BOA members
Andrew Manktelow
Andrew Manktelow
is a Consultant Orthopaedic Surgeon working within Nottingham University Hospitals NHS Trust, with a specialist interest in primary and revision hip surgery. A past President of the British Hip Society, Andrew has been on the BOA Council since 2019. Contributing to the Orthopaedic Committee Andrew reports to BOA Council on matters relevant to the Independent Sector.

With recent changes in process, a renewed impetus on delivery and with many having started their consultant life and work in private practice since the CMA Order of 2014, many BOA members will be unclear of what has been mandated by the CMA. In this article we aim to help colleagues understand their roles and obligations in this area explaining how recent developments will shape the process.
Background
Following a two-year investigation, the Competitions and Markets Authority (CMA) published a report in April 2014. This document identified a series of parameters surrounding consultant fee information, hospital and consultant performance, that the CMA required to be made available to inform patients as they sought to obtain the best available care in the Independent Sector (IS). This information was to be collated and published by the Private Health Information Network (PHIN). Private healthcare providers are required to collate and send data to PHIN and to fund PHIN’s processes. PHIN has always recognised that consultants need to be involved in producing data relating to their practice. Over the years PHIN has looked to engage with consultants in orthopaedics, and indeed all surgical specialities, to ensure that the data provided is accurate and validated prior to publication.
Alongside other representative bodies, the BOA has been in conversation with
PHIN over many years identifying concerns with data validity and data volume. The challenges that surround data interpretation, with minimal case mix adjustment and the complexity of providing meaningful Patient Reported Outcome Measures (PROMs) has been discussed. With the UK National Joint Registry (NJR), orthopaedic surgeons are already fully engaged and routinely involved in data collection. NJR Consultant Level Reports have become increasingly robust and helpful, allowing joint arthroplasty surgeons to review their practice within the appraisal process. Data collection and reporting outcome measures is also common away from arthroplasty practice, in foot and ankle, hand, shoulder and spine surgery. Orthopaedic surgeons are ahead of the game, demonstrated perhaps by a higher level of engagement than other surgical specialities with the PHIN process.
What data is required to be made available?
At the time of the original CMA Order it was identified that data on the following should be made available: surgeon volume, length of stay, infection rates, re-admission rates, revision surgery rates, mortality rates, unplanned transfers, patient feedback measures, links to registries and audits, improvements in health outcomes and frequency of adverse events.
PHIN has had variable success in collating and publishing data in these different areas, though remains clear in its objective to make progress in as many as are felt reasonable. With regard
Features
24 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
to performance, PHIN has been successful in publishing data relating to surgeons’ volume and length of stay. Recent progress has been made with PROMs, though other areas have proved more of a challenge.

In addition to clinical indicators, the CMA was keen that surgeons’ fees should be made available to ensure that patients are aware of any likely financial liability. There are significant challenges in this area. While out-patient fees are relatively easy to ascertain, Private Medical Insurers (PMIs) now increasingly influence and restrict consultants’ fees. Different PMIs have varying levels of remuneration for the same intervention. Additional complexity surrounds surgeons’ fees for ‘self-pay’ patients. Identifying the exact costs different hospital groups and different providers charge for the same procedures creates issues with open competition, making publishing this data a challenge. While this was not specifically required by the Order, it would seem more helpful if patients were able to compare the prices of a complete package of care transparently, including all consultant, anaesthetic and hospital fees.
Initially, it was hoped that much of the data would be relatively easy to collect. The true complexity has become more obvious over time. For example, PROMs collection could potentially seem straightforward. However different PROMs measures, collected at
different times and via different mechanisms makes direct comparison a challenge. Adequate numbers of different procedures by different surgeons are required. As such, PROMs data on hip and knee surgery is going to be published at site level rather than at consultant level.
More recently PHIN has identified areas of the Order that could be a challenge to deliver to the CMA. These included issues surrounding revision rate and mortality, which are both very difficult to assess without meaningful case mix adjustment.
Debate continues around what is best published at hospital and consultant levels. An example would be never events, something the CMA were keen to publish data on. Never events should be reported without blame and frequently indicate a system failure rather than issues with an individual consultant. Never events are probably best reported at hospital rather than at consultant level. There is a pre requisite that data published should be meaningful and helpful. Therefore data that has to be explained is unlikely to be useful and could confuse patients.
The BOA position
The BOA has identified challenges in large scale publication of private and NHS health information data, not least regarding data quality, interpretation and presentation. The BOA remains keen to see robust and accurate
data, presented in a manner that can be interpreted and understood, supporting the provision of a reliable, meaningful and useful resource for patients.
The BOA encourages surgeons to engage, to review and validate data submitted. The BOA has argued that the PHIN on-line portal should be user-friendly and easy to navigate, allowing consultants to flag and correct inaccuracies easily. For the reasons detailed above, it has always been the BOA’s position that certain data, such as revision rates, should not be published at an individual consultant level. The Royal College of Surgeons1 has also made clear the requirement for surgeons to engage and contribute to the PHIN process.
Data collection and validation
Processes by which data is collated and submitted varies. Surgeons are often not involved in validating data submitted to PHIN on their behalf by the private hospitals. Data is submitted to PHIN four times a year and is made available for publication around a month after submission. The BOA has been in conversation with various stakeholders aiming to improve this process. Surgeons must be in a position to access and review data, ensuring it is valid and accurate, possibly even before it is submitted. This should improve engagement and confidence in this process. >>
Features
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 25
At present, surgeons are required to review and to ‘sign off’ their data before data is published on the PHIN website. With confidence, engagement and verification of data variable, many surgeons who are active in the IS, do not have data published on the PHIN website. PHIN have made a decision that, in future, data will be published automatically unless a problem has been identified, though have reiterated that data published must be accurate and should not mislead patients or undermine consultants.
In moving ahead with this process, PHIN points out that surgeons should understand this data collection and provision was mandated by the CMA Order. This is designed to help our patients as they seek care within the IS. Pilots looking at how presumed publication is introduced are planned. These will review sequencing timelines detailing the risks, mitigations and issues involved as presumed publication becomes part of the PHIN strategy to implement the CMA Order.
The present situation
At the time of the current publication period (July 2021 – June 2022), 2,294 consultant orthopaedic surgeons appear in the data. 64% have created a profile about themselves. 37% have reviewed and verified their data for publication. 78% have submitted an approved fee structure information for publication. 37% have received a sufficient volume of feedback to allow a score to be published on PHIN’s website. It is reassuring to see that 98% of those consultants with sufficient feedback have achieved a patient satisfaction of 90% or higher and 84% have achieved a similarly good patient experience score. It would appear patients are happy with the care that they receive from orthopaedic consultants.

Recent changes and the future direction
During the time of the COVID pandemic, PHIN made a policy decision to take a backseat, feeling that consultants had enough to deal with. More recently, there has been a change in direction. The CMA has strengthened its expectation that the Order is to be delivered. PHIN has engaged with stakeholders to ensure that the process is made more urgent. Part of that process has been to review consultant engagement. The BOA have had an opportunity to contribute to that process.
Consultant engagement
PHIN has a stated aim to build confidence and trust in the data submitted, validated and published. Improving mechanisms by which data inaccuracy issues can be addressed. PHIN is keen for consultants to review the new portal, providing virtual sessions to help colleagues negotiate the process. PHIN plans to review whether other members of the surgical team and medical secretaries could input and verify profile data to the portal. It is understood that consultants are not a homogenous group and have different practices and levels of activity within the IS. More targeted communication is planned with additional improvements made to the PHIN consultant portal.
Recent changes in PHIN strategy
Under a changed PHIN leadership, there is a renewed impetus to ensure that the CMA Order is delivered. Healthcare providers who fund PHIN are also keen to see progress. In 2022, a delivery plan was submitted by PHIN to the CMA, with a stated aim to deliver the Order within the next four years. The CMA responded,
re-iterating the importance of the process, suggesting ongoing reviews with intermediate deadlines to ensure delivery. The CMA has already taken enforcement action for failure to comply and has described how a more robust approach will be taken with consultants who do not comply with their obligations. It is therefore important that consultants are aware of what is required and act accordingly.
The Federation of Independent Practitioner Organisations (FIPO) has provided a helpful briefing note detailing consultants’ responsibilities with regard to data submission and validation2. In the document it is identified that the only performance metrics to be made available to the public on the PHIN website are volumes of procedures and length of stay. Although it is important that colleagues check and validate their data, the document points out that PHIN cannot publish data it knows to be incorrect. Any inaccuracies should be identified. Correcting inaccurate data is not the consultant’s personal responsibility and should be undertaken by the provider. It has been noted that support for this correction can vary.
Summary
The requirement to provide meaningful and helpful data to patients as they seek care in the IS was mandated within the 2014 CMA Order. Consultants have an obligation to engage with the process and to facilitate the provision of meaningful information. Having taken a back seat through the COVID pandemic, PHIN has re-energised its processes to deliver the Order. Consultants should understand how data is collected and what data is submitted on their behalf. IS care providers should engage in that process, seeking to simplify how data is validated and specifically how any inaccuracies are rectified. While PHIN will move towards presumed publication, it recognises that no data will be published if it is known to be inaccurate. The CMA is taking a more robust approach and those that do not engage are likely to hear from the CMA directly. n
References
1. Royal College of Surgeons of England. Working in the Independent Sector. A guide to good practice. May 2022. Available at: www.rcseng.ac.uk/standards-and-research/ standards-and-guidance/good-practiceguides/working-in-independent-sector
2. Federation of Independent Practitioner Organisations (FIPO). PHIN and your responsibilities. Briefing note. September 2022.
Features
26 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
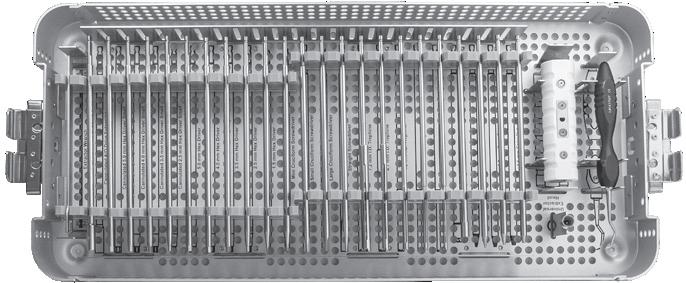
Star Bit Driver Set
Set consisting of four star bits — T10, T15, T20, & T25, a handle which accommodates any of the above bits, and a sterilization case


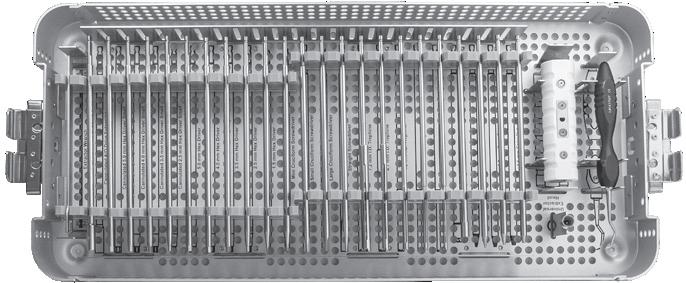
NO’S: 5194-00 [4 Star Bits w/Handle & Case] 5194-01 [4 Star Bits w/Case only]
Universal Screw Removal Instrument System
Designed to remove solid and cannulated screws
Flexible Osteotome System
Used for removal of stripped hex screws, buried screws, partial screws with broken screw heads





Wagner Osteotome Handle
Provides an assortment of osteotome blades for various orthopedic surgery procedures
Handle with Quick-Coupling End PRODUCT
[Set w/Quick-Coupling Handle and Case] S0012-00 [Set with Locking Nut Handle and Case]
Includes (also available indivually):
Optional Parts and Blades
Optional Strike Plate can be attached to the Handle for direct striking with a mallet


Optional Curved Chisel Blades are designed to help loosen the cement/prosthesis interval in TKA tibial tray and femoral component revisions. The curved design is useful in working around pegs & fins to get posterior cement access. Also helpful with removal of other implants, i.e shoulder, ankle, etc.




PRODUCT NO’S:
S1020-SP [Strike Plate for Handle]
Optional Osteotome Blades (Not Included In Complete Set):
S1123 [7.5" XL Osteotome Blade – 8 mm]
S1135 [6.75" Radial Osteo. Medial Curve – 11 mm]
S1136 [6.75" Radial Osteo. Lateral Curve – 11 mm]
S1137 [6.75" Radial Osteo. Medial Curve – 11 mm]
S1138 [6.75" Radial Osteo. Lateral Curve – 11 mm]


Optional Chisel Blades (Not Included In Complete Set):

S1233-L [2" Left Curved Chisel Bade – 8 mm]




S1233-R [2" Right Curved Chisel Blade – 8 mm]


S1222 [2.5" Chisel Blade – 8 mm]
S1223 [2.5" Chisel Blade – 10 mm]
S1224 [2.5" Chisel Blade – 12 mm]
S1225 [2.5" Chisel Blade – 20 mm]

S1229 [5" Chisel Blade – 8 mm]
S1228 [5" Chisel Blade – 10 mm]
S1231 [5" Chisel Blade – 12 mm]

S1230 [5" Chisel Blade – 20 mm]
S1227 [5.5" Long Chisel Blade]
S1232 [7.5" XL Chisel Blade]
S1234 [8.5" XL Chisel Blade]
S1235 [9.5" XL Chisel Blade]
S1236 [10.5" XL Chisel Blade]
S1237 [11.5" XL Chisel Blade]
S1238 [12.5" XL Chisel Blade]
Blade lengths reflect the actual working portion of the blade only. For overall length, add 1.5" (3,8 cm) to blade length listed above.


Medial and Lateral Curve Radial Blades designed by Henry Boucher, MD Curved Chisel Blades designed by William McMaster, MD

PRODUCT NO: S0010-00 [Complete System with Storage Case] Also sold individually Drive ends (A/O) designed for easy and quick engagement with universal handle Drive ends (A/O) designed for easy and
Cannulated Drive Extension Universal Instrument Handle Hex Drivers Screwdrivers Universal Extractor Trephines Screw Extractors
quick engagement with universal handle.
Also
PRODUCT
sold individually
Fracture Reduction Pick
5" Thin Blades Curved Thin Blades 3" Thin Blades Radial Blades Handle with Locking Nut
S1002
3" x 8 mm S1003 [Thin Osteotome Blade] 3" x 10 mm S1004 [Thin Osteotome Blade] 3" x 12 mm S1005 [Thin Osteotome Blade] 3" x 20 mm S1006 [Curved Thin Osteo. Blade] 3" x 12 mm S1007 [Curved Thin Osteo. Blade] 3" x 20 mm S1008 [Thin Osteotome Blade] 5" x 10 mm S1009 [Thin Osteotome Blade] 5" x 8 mm S1020 [Handle with Quick-Coupling End] 6" or S1021 [Handle with Locking Nut] 6" S1133 [Radial Osteotome] 5" x 10 mm S1120 [Radial Osteotome] 5" x 12 mm S1134 [Radial Osteotome] 5" x 14 mm S1121 [Radial Osteotome] 5" x 16 mm S1122 [Radial Osteotome] 5" x 20 mm S2007 [Slap Hammer] 12" 9018 [Case] Slap Hammer Case System Includes Choice of Handle Style
chisel design allows working around component pegs, fins, etc. Curved Radial Blades are helpful in the removal of total hip stems
NO’S: S0011-00
Set
[Thin Osteotome Blade]
Curved
Russell Wagner, MD
Designed by
is designed for easier gripping, rotational control, and use with a mallet with a standard 1/4” Lambotte osteotome Strike Plate for Handle 5" Chisel Blades 2.5" Chisel Blades Medial Curve Radial Blades Lateral Curve Radial Blades Long 5.5" Chisel Blade 2" Curved Chisel Blades 7.5” Extra Long Osteotome Blade 7.5", 8.5", 9.5", 10.5", 11.5", & 12.5" Extra Long Chisel Blades Designed for removal of well-fixed long bone intramedullary hardware FREE TRIAL ON MOST INSTRUMENTS 1.800.548.2362 103 Estus Drive, Savannah, GA 31404 info@innomed.net 912.236.0000 Phone 912.236.7766 Fax Innomed-Europe Tel. +41 41 740 67 74 info@innomed-europe.com © 2023 Innomed, Inc. ISO 13485:2016 www.innomed.net Innomed-Europe Alte Steinhauserstrasse 19 CH-6330 Cham Switzerland Tel: +41 (0) 41 740 67 74 www innomed-europe com UK Distributor: Hospital Innovations Ltd Concept House Talbot Green Business Park Pontyclun UK CF72 9FG Tel : +44 1443 719 555 www hospitalinnovations co uk
Handle
‘Oops!’ Designing and implementing a novel peer-to-peer training session on learning from surgical mistakes

Adam Stoneham is a post-CCT senior fellow in hand surgery at University Hospitals Southampton. His interests are in upper limb surgery and medical education. He is also the holder of a Guinness World Record. He developed the ‘Oops’ Programme after participating in a serious medical error as a junior trainee.
Mistakes in surgery are exceptionally common; they can harm surgeons as well as patients and are a major burden on healthcare systems in terms of wasted resources and the cost of litigation. Surgeons are not prone to seeking support for their mistakes and there are few forums available for them to discuss them with their peers. The aim of this article is to share our experience of developing and running a novel peer support training session and provide a blueprint for others to do the same. The session was entitled ‘Oops!’ (Optimising Outcomes through Peer Support) and was specifically targeted at Speciality Registrars. The objective was to provide a safe and confidential forum for participants to discuss their own mistakes and learn from each other’s.
Simon Williams is a Core Surgical Trainee working towards a career in orthopaedics. He has an interest in medical education and has a PGCert in Medical Education.


What are mistakes and why do they happen?
We defined a mistake as a decision or action which produced an unwanted result, either for the surgeon or the patient or both. The occurrence of errors in any human system is inevitable, but mis-management of these errors may lead to surgical incidents. Surgical incidents often result from complex interactions, decisions, and events rather than isolated, individual mistakes.
When workload exceeds the personal capacity of the surgeon, the likelihood of error increases1
This may be particularly applicable to surgical trainees who may not have performed the procedure recently (indeed sometimes at all). Other potential factors such as fatigue, distraction, or external pressures may further reduce capacity.
In surgery, a person’s experience (or lack of it) is critical. Whereas one would expect an individual’s competence to increase over their career, their perception of their own ability may in fact decrease. In 1999, Dunning and Kruger devised an experiment which showed that less skilled individuals consistently overestimated their ability whereas more highly skilled individuals were prone to underestimate it (see Figure 1 and 2)2. Appreciation of this effect both in ourselves – and just as importantly in those we supervise – may be strategic in predicting and avoiding mistakes 3
What is the scope of the problem in the NHS?
One in 20 hospital admissions results in avoidable patient harm 4. So-called ‘neverevents’ such as wrong site surgery and retained surgical instruments may happen as often as 1:100,000 and 1:10,000 respectively5
Threat of litigation is highly present in UK practice. Surgical mistakes contribute to the significant burden of NHS clinical negligence claims, with spending on pay-outs and settlements increasing rapidly in recent years, resulting in a bill of around £2.4 billion in
Features
“Only a fool learns from his own mistakes. The wise man learns from the mistakes of others.”
– Otto von Bismarck
Adam Stoneham, Simon Williams, John Hardie, Greg Neal-Smith and Fransiska Guerreiro
28 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
John Hardie regularly publishes, speaks, and directs courses in Human Factors in surgery. His early work was informed by his initial pilot training with the RAF, and subsequent General Aviation flying. He is a T&O registrar in the Wessex deanery.


Greg Neal-Smith is a T&O registrar in the Wessex Deanery. Outside of medicine he is an avid cook and has been trained by a Michelin starred chef in London. He is also a keen rugby player and is risking his surgical career once again when he captains his rugby sevens team in the Bournemouth Sevens this year!
2018-196. Surgical specialties are documented to have the greatest number of litigious claims, with 2,847 over a ten-year period to 2019, though obstetrics and gynaecology has the highest total value of pay-outs7
Fransiska Guerreiro is an ST5 in the Wessex Deanery. She won awards as a business manager, won the RCS Surgical Skills competition and Core Surgical Trainee of the year, and a prize at the European Society of Sports Knee Arthroscopy 2022 Congress. In her spare time she enjoys playing piano, guitar, and exploring the great outdoors with her husband and daughter.
Over 90% of surgeons report experiencing an intraoperative adverse event, most commonly within the last year. Whilst this can harm patients, the effect on the surgeon themselves can be significant and often overlooked. Amongst those surveyed they almost unanimously expressed strong feelings of anxiety, guilt, sadness, anger, shame, and/or embarrassment but few sought professional psychological counselling8

How can we avoid them?
It is estimated that there are over 500 million interactions between patients and the NHS a year 9. Although some mistakes are inevitable we believe this number could be reduced.
The study of Human Factors (HF) – or how systemic and individual characteristics influence behaviour – has been shown to improve safety and outcomes for those giving and receiving care. In recent years, healthcare has adopted proven HF concepts from the aviation, maritime and rail industries10. Examples include the WHO surgical checklist11,12, pre-operative planning techniques, standardised communication for safety-critical moments13 , structured team briefings, and dual surgeon operating14
Peer-to-peer teaching has proven benefits in medical education15. The aim of this session and the pre-course survey was to identify factors which had led to mistakes, as well as to share specific technical details which would enable other participants to anticipate and avoid the same thing happening in the future.
• Average claims for a new consultant: 1 in every 2.5 years
• A surgeon’s worst mistakes tend to occur in the first 3-5 years of autonomous practice
• 25% of consultants participate in wrong site surgery in their career

Peer-to-peer training session
An anonymous pre-course survey was circulated to all Orthopaedic Registrars in the Wessex Deanery. This collected basic information on level of training, sex, number of surgical errors encountered, and the factors which contributed to mistakes. Free text boxes were provided to cite examples of mistakes in which trainees had personally participated or directly observed.

Trainees were invited to prepare a brief 10-15 minute presentation of a particular error which they felt had relevant learning points for their peers. It was reinforced to colleagues that there was no requirement to submit a case, and any information provided would only be used with their consent. The day was hosted at a central but deliberately non-clinical venue. Only Speciality Registrars were invited in an attempt to create a safe atmosphere in which participants could be candid in their opinions. A single exception was made for a respected (recently retired) NHS Consultant with significant experience in medical education, surgery, and medical negligence. His role as mentor and mediator proved instrumental in the success of the day.
Well-known General Practitioner and comedian, Phil Hammond, was invited to present to the group on learning events throughout his career >>
Features
Figure 1: The original work of Dunning and Kruger2 showing actual vs. perceived ability. Low ability individuals consistently overestimated their performance whereas high ability individuals were prone to underestimate it.
Figure 2: How Dunning and Kruger’s work is more commonly represented to show how inexperienced individuals do not appreciate their lack of knowledge (‘you don’t know what you don’t know’).
Box 1: Mistakes in orthopaedic surgery. Experience from a leading UK indemnity provider.
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 29
and his collaboration with mainstream and social media to highlight wider failings in the National Health Service. This featured a degree of comedy to engage the group, ‘break the ice’ and provoke discussion.
The session adapted peer-to-peer teaching model – a format with proven benefits demonstrated in medical education research15. Psychological safety was established at the outset by agreeing to discuss all cases in confidence and adhere to Just Culture principles16 These principles include accountability for actions and an openness to learn from incidents but rejection of uncontextualised blame. Cases for discussion were anonymised by the presenters, and included incidents leading to adverse outcomes, and ‘near misses’ which did not lead to harm. As well as ‘technical mistakes’, presenters were encouraged to consider the wider context of the incidents and address learning points.
Pre-course survey results
Trainees reported a total of 76 ‘serious’ mistakes (e.g. missed diagnoses, wrong treatment, significant complications). The median number was three each over their career to date (range 1-10).

The nature of the mistakes varied greatly from misplaced hardwear, to wrong operation / wrong site surgery, to avoidable revision. A representative sample are displayed in Box 2.
The commonest reason cited for mistakes was lack of familiarity [n=8, 42%] followed by distractions [n=5, 26%]. Other reasons are shown in Figure 3.
In general, responders lamented their lack of preparation, failure to communicate effectively between junior and senior colleagues, and not ‘listening to their gut’ when they thought something was wrong.
• Lag screw passed behind IM femoral nail, unnoticed intra-operatively
• Reverse oblique proximal femoral fracture inappropriately treated with DHS with early failure
• Injury to superficial peroneal nerve during ankle ORIF
• Knee arthroplasty popliteal nerve injury, not subsequently recognised
• Hemiarthroplasty positioned too long
• Equipment not available due to holes in sterile sets
• DHS screw protruded medially into a calcified artery
• Too many passes of guidewire during DHS led to fracture of lateral wall whilst inserting lag screw
• Ankle Fixation in which the syndesmotic screws missed the tibia
• Inadvertent scaphoidectomy during routine trapeziectomy
What did we learn?
“Success is going from one failure to the next without losing enthusiasm” Unknown; sometimes attributed to Winston Churchill and cited by John Charnley
100% rated the course as ‘very beneficial to training’. The sessions delivered by Registrars, a recently retired Consultant, and Phil Hammond were the best received.
Features
Figure 3: Factors contributing to a serious error or near miss.
“When workload exceeds the personal capacity of the surgeon, the likelihood of error increases. This may be particularly applicable to surgical trainees who may not have performed the procedure recently (indeed sometimes at all). Other potential factors such as fatigue, distraction, or external pressures may further reduce capacity.”
30 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Box 2: Sample of errors which Registrars reported.
Certain specific cases were presented which highlighted particular equipment issues or ‘banana skins’ to avoid with individual operations. Some participants had never heard of some of the complications discussed and so left much better informed and able to avoid them themselves. It was refreshing to hear a balanced and realistic appraisal of our speciality including our less glamorous and less talked-about moments. There was a genuine feeling of comradery and whilst it is good to share our triumphs, participants took significant comfort in knowing they were not alone in their disasters.
Some themes came up repeatedly in the discussion. These included unfamiliarity with certain pieces of equipment and a lack of training and resources in some areas. The ‘quick Dynamic Hip Screw (DHS)’ was a particular cause of angst and it was suggested that this phrase be banned outright. Performing the procedure a few times on simulators (e.g. ‘Sawbones’) could be a minimum requirement for certain reproducible operations.
Consultant supervision was an important topic of conversation. Most of the cases presented had occurred when Registrars were operating unsupervised. It was the opinion of the senior Consultant present that on the whole this is no longer acceptable and indefensible in legal terms should a complication ensue. One of the more challenging errors had occurred because the consultant was inexperienced, and the trainee regretted that he had felt unable to speak out. Another serious mistake happened despite a very experienced surgeon being scrubbed in the room and the trainee felt their presence had in fact given them a false sense of reassurance.
The training of junior trainees by senior trainees was keenly debated. Many Registrars enjoy teaching and feel that it is necessary to facilitate to transition from trainee to Consultant trainer. Most agreed that it needs to be done in a safe environment and some expressed disappointment that they were not able to teach due to lack of senior support themselves. The extent to which trainees are ‘given enough rope by which to hang themselves’ is, of course, a matter of context and personal discretion, which develops with experience.
Learning from our practice (good and bad) is already a core curriculum outcome. Generic professional capabilities (GPC), established by the General Medical Council (GMC), which must be included in all post-graduate training curricula, include doctors learning from their “…own performance, that of others,
human factors and cognitive biases”17. This session was unanimously welcomed as a rare opportunity to put this into practice and we believe it would be a very welcome addition to any regions’ regular teaching programme as well as an incorporated or standalone annual national event.
• “See one, do one, teach one” is dead
• If you have never heard of it you can’t avoid it
• You don’t know what you don’t know
• Big mistakes happen through small holes
• Check twice cut once
• If it feels wrong it probably is
• Remember the seven P’s: proper prior planning prevents piss poor performance
Box 3: Some surgical truisms were aired.
Conclusion
“If you ain’t getting complications you ain’t operating” Anon
We were wary that this concept presents enormous scope with limited time. Therefore we had to be very selective regarding the content included. We tried to touch on legal aspects of medical errors and could easily have gone in many other directions including as human factors, psychology, non-technical skills etc. Other courses do exist in these areas.
Our peer-to-peer learning approach is not intended to replace departmental or national methods for clinical governance or incident investigation.
Wessex has traditionally had a very even split of the gender of trainees so it was surprising how few female Registrars participated in the survey or submitted cases to present on the day. Presuming men and women make equal numbers of mistakes (?) it would be worthwhile exploring whether this is a genuine trend and the factors underlying it.
We all make mistakes. Sometimes because we just lack technical ability but more often because of a litany of factors both within and beyond our control in any given context. Although we know we should – indeed we are professionally obliged to – reflect and learn from these events, there are currently very few forums in which to do so.
• Take a deep breath and step away from the table – obviously if safe to do so.
• Take another deep breath and tell someone senior and sensible in theatre there is a problem. Be cautious about just announcing in theatre, the patient may be awake, rumour control will have it out in the corridor before you can blink and by the time it comes back you will have removed the wrong hand and leg.
• Phone a friend or your boss. Preferably get them to come immediately to the theatre if on site, but if not, un-scrub and spend five minutes or longer talking to them about your options.
• Get them to join you if feasible and complete case with them there – you will be pretty unsettled and do not want any more issues.
• Write a full operation note.
• Have a cup of tea and large quantity of chocolate.
• Consider cancelling the rest of the list.
• Debrief team in theatre – don’t forget they will be upset and will be called on by investigation.
• Write a full account immediately and email to yourself and friend +/- Clinical Director/Lead clinician.
• Fill in Datix.
• Contact your defence union.
• Phone your friend/mentor/someone who knows the operation and talk about it. Most complications have been done before.
This all-new peer-to-peer training day was a great success; we would strongly encourage other regions getting in touch to replicate and share our experience. n
Acknowledgements
We are very grateful to Nigel Rossiter, Simon Hodkinson, Sophie Phillips, Alex Marshall-Lewis, Portia Ross, Alex Thomas, Sam Shamoon, and Jack Hurst.
References
References can be found online at www.boa.ac.uk/publications/JTO
Features JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 31
BOX 4: Words of advice from a senior surgeon upon making a serious mistake.
Supporting elective recovery through a short stay arthroplasty pathway
Waiting lists for elective orthopaedic surgery have been rising across the United Kingdom for several years, due to a combination of factors that include issues of demand, facilities and staffing. A lack of access to ring-fenced orthopaedic in-patient care in acute hospital sites has been one of the contributors to waiting list growth, and this pressure on facilities has become more acute since the COVID-19 pandemic, exacerbated by seasonal peaks in other infectious diseases.
at the Southwest Ambulatory Orthopaedic Centre. He is a Past President of the British Hip Society, and has published multiple scientific papers in the field of hip replacement and revision surgery.

One way in which elective care might be protected from the influence of acute pressures is to make more efficient use of the resources that are allocated to orthopaedic surgery. In 2021 we were given the opportunity to address the elective waiting list in Devon through the development of a new protected elective site, and to maximise the benefit gained by our system we undertook to transform the way in which elective arthroplasty surgery was delivered in our area.
Background
In March 2020, as the NHS faced an uncertain and potentially overwhelming need for acute care because of the
COVID-19 pandemic, the NHS in England responded with several secondary care initiatives that included establishing a number of new medical units, known collectively as the ‘Nightingale’ hospitals1 The Exeter Nightingale Hospital was the smallest and the last of these units to be opened; it was established on the site of a disused home improvements store (Figure 1), and during the COVID-19 pandemic it treated 247 patients from eight acute Trusts across three counties.
In May 2021, Devon Integrated Care System (ICS) was awarded funding from the National Accelerator Systems Programme, to support reduction in waiting times in key target areas. This funding was utilised to transform the site of the Exeter Nightingale Hospital for use by four specialities across the Devon system: elective orthopaedics, radiology, ophthalmology and rheumatology.
Building an elective orthopaedic centre New ways of working
At the inception of the project, we assembled a multi-disciplinary team (MDT) that included anaesthetic and orthopaedic clinical leads, as well as senior management, nursing and therapy leads, architects, estates, information technology and governance. The MDT set out to go beyond simple considerations of waiting lists numbers, and to use the Nightingale
Features
Jonathan Howell and Mary Stocker
32 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
“One way in which elective care might be protected from the influence of acute pressures is to make more efficient use of the resources that are allocated to orthopaedic surgery.”
Mary Stocker is joint clinical lead for SWAOC and is a Consultant Anaesthetist at Torbay and South Devon NHS Foundation Trust. She has a strong interest in day surgery and was the clinical lead for day surgery in South Devon for 14 years working, at the helm of their nationally recognised day surgery unit. She has been a member of the Council of the British Association of Day Surgery (BADS) since 2009 and served as their president for three years. She is currently their representative on the International Association of Ambulatory Surgery (IAAS), General Assembly.

transformation as a test of change for new ways of working. The ambition was to revisit every aspect of our existing patients’ journeys, to solve many of the challenges experienced at the base hospitals, and to implement new state-of the-art pathways for elective orthopaedic care. In particular, we were keen that improvements in our patient care would enable us to make drastic reductions in patients’ length of stay, an intention reflected in the name chosen for the new unit, The Southwest Ambulatory Orthopaedic Centre
(SWAOC). As a starting point the MDT gathered examples of best practice from within Devon and across the country, and we visited several other units to learn from their experience in short stay elective care. At a time when recruitment of clinical colleagues was very challenging, we undertook a campaign to attract candidates who had a stated interest for working in new ways, and across the clinical teams we built a culture of challenge and innovation. In line with Getting it Right First Time (GIRFT) recommendations, we have set a benchmark of a minimum four joints per all day list, and recognising that these primary surgeries at a protected elective site represent valuable training opportunities, we have worked with regional consultant colleagues to ensure that trainees have the opportunity to work at SWAOC.
New facilities



The Exeter Nightingale Hospital already had seven wards on site but planning laws and building regulations prevented us from placing theatres within the existing structure. We therefore commissioned modular units that included two theatres, each of which had separate anaesthetic and lay-up rooms, a recovery area and stores (Figure 2). The layout of the unit was optimised with patient flow and working efficiency at the heart of the design, as well as considerations necessary for establishing a green area within the theatre complex. The building and commissioning work was completed in January 2022, and despite the challenges of the winter of 2021/22, with the flexibility and willingness of clinical and management colleagues, SWAOC opened to patients in March 2022. >>

Features
Figure 1: Transformation from DIY store to hospital; Clockwise from top left: the building prior to transformation; a mural from one of the inside walls of the COVID-19 facility; one of the seven wards in the Exeter Nightingale Hospital.
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 33
Figure 2: Delivery and installation of the modular theatre complex.
The SWAOC Pathway
To reduce some of the challenges in redesigning all aspects of an elective orthopaedic pathway, and with the need to make an immediate significant impact on a substantial segment of the orthopaedic waiting list, the MDT decided that the project would initially focus on primary hip and knee replacement surgery. The success of the project has since allowed us to extend the scope of surgery to foot and ankle, with soft tissue knees, hip arthroscopy and spinal surgery also currently in advanced stages of planning for introduction at SWAOC. A summary overview of the primary knee and hip pathway is shown in Figure 3; every stage of the patient journey was redesigned, some selected aspects of which are discussed in more detail in this section.
Patient selection
SWAOC is a remote site, physically separated from the nearest acute hospital, and this created some potential difficulties with medical cover and the management of emergencies. As a result, the MDT designed a Red/ Amber/Green (RAG) rating system, based on a systemic review of patients’ comorbidities, and used this to select patients suitable for surgery at SWAOC. In the interests of safety, we limited our initial experience to patients deemed to be ‘Green’, with minimal co-morbidities, but in light of the safety and success of the unit we have been able to extend the facilities to those rated ‘Amber’ and even to some rated ‘Red’. The important thing to note is that every patient passing through SWAOC is placed on the same ambulatory pathway, so that everyone has the same chance of benefitting from day case arthroplasty.


Features
Figure 3 (part 1): Summary document showing an overview of the SWAOC pathway.
34 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Features
Preparation for surgery
Post op
Post op Care
o ALL Patients irrespective of complexity should follow these post op care goals and be optimized for short stay discharge
o IV fluids taken down in Primary Recovery, encourage oral intake
o Ensure Compact 125ml nutrition drink in Primary Recovery (all patients unless very brittle DM, OK for well controlled DM) – reduces first mobilisation dizziness, improves wound healing & immune function.

o Regular assessment of regression of spinal block and aim to mobilise within 1 hour of offset
o Patient able to demonstrate safe walking, transfers, stairs and exercises compatible with discharge utilising mobility aids as required/instructed.
o Encourage patient to eat and get dressed in ‘home clothes’ (as appropr iate to time of day/night)
o Avoid routine catheterisation, if symptomatic, bladder scan and in-out catheter with appropriate sterility precautions
o Aggressive management of any nausea symptoms
o Regular analgesia and supportive medications from post -op protocol to minimise side effects.
Discharge
Discharge Criteria
o Patient able to mobilise to standard compatible with discharge, safe transfers, stairs (if needed for discharge location) and exercises all confirmed as satisfactory by appropriately trained member of staff

o Wound checked (refer to nursing SOP)
o X-ray performed and reviewed as satisfactory by surgeon
o Able to drink & tolerate oral fluids.
o No urinary retention (refer to nursing SOP)
o Observations satisfactory (within acceptable limits for that patient)
o Haemocue® >100g/L. (BM appropriate if DM). Other bloods not routinely indicated post op.
o TTA medication available for discharge [pre-packed] with supportive instructions/ written patient information
o Safe place of discharge (doesn’t live alone, telephone access)
o Contact instructions for SOS provided to patient
summary.
Short stay arthroplasty demands that a patient’s medical condition is optimised for their operation, that their physiology is disturbed as little as possible during their stay, and that each patient receives consistent messaging and treatment along their pathway. We have created written and video patient information resources designed to promote day case or one night stay. Patients receive carbohydrate drinks the night before surgery and their food starvation period is limited to a maximum of six hours, with tea and coffee allowed up to two hours before and water to the point of their surgery. Premedication with a combination of Paracetamol, Celecoxib and Oxycodone helps to reduce post-operative pain and to promote early mobilisation.
Intra-operative care
5 post op doses* (ie stop day 2) 9 post op doses* (ie stop day 4)
5 post op doses (ie stop day 2) 10 post op doses (ie stop day 5) Oxycodone MR* 10mg po BD (5mg if age >70)
Oxycodone IR* 5 mg po PRN (for breakthrough pain – max 4 hrly) Not prescribed
Codeine 30-60mg po QDS (or tramadol if intolerant)






Ondansetron 4mg po TDS AND Macrogols 1 sachet po BD
o +appropriate VTE regimen with PPI cover Standard VTE prophylaxis THR TKR*
5 days. Commence on cessation of Oxycodone MR (ie start day 3)
7 post op doses (duration oxycodone)
+ 10 days supply laxative
10 doses supplied only*
4 days. Commence on cessation of Oxycodone MR (ie start day 5)
13 post op doses (duration oxycodone) + 10 days supply laxative
Day of Surgery (DO) ✓ ✓ All patients to receive Dalteparin⧫ 5000 units sc either predischarge home or 6-8 hours post op if remaining overnight at SWAOC
On discharge (TTAs) ✓ ✓ Aspirin to commence on discharge 150mg for 6 weeks
Notes:
With Lansoprazole 15mg for duration
• Please adjust Dalteparin⧫dose for high & low weight patients respectively
Please note: This is the units standard prophylaxis for low risk patients. Ensure you consult the full SWAOC Thromboprophylaxis protocol for any higher VTE risk patients or alternative regimens according to clinical need.
• If patient should remain in SWAOC or transferred to RDUH (E) longer than 1 night then Dalteparin to continue as inpatient
Notes
Pathway has been designed to reflect a fusion of best practice and best outcomes drawn from various high performing centres nationally and is supported by embedded data collection to track what is done matched to outcomes allowing further refinement
o □as defined by pre-assessment working group
Original Protocol Author: Dr Claire Blandford, Consultant Anaesthetist (v1 to v13)
Subsequent amendments: SWAOC team
Short stay arthroplasty care is promoted through highly protocolised anaesthetic techniques, augmented by surgical infiltration of local anaesthetic. General anaesthetics are avoided, and sedation minimised, to ensure patients recover rapidly; they spend just a few minutes in primary recovery before moving to the rehabilitation area. In consultation with anaesthetic colleagues, we developed two spinal protocols, based on either prilocaine or racemic bupivacaine, which wear off rapidly after surgery thus promoting early mobilisation.
Preoperative fluid balance is optimised and a maximum of 1,000 mls crystalloid is administered intraoperatively; we routinely perform cell salvage, with homologous transfusion in cases justified by collected volumes. >>
Figure 3 (part 2): Summary document showing an overview of the SWAOC pathway.
Pathway
THR/TKR/UKR*: [NB: manage UKRs as per TKR* each time mentioned in the flowchart] v 14 SWAOC THR.TKR. Original author Dr Claire Blandford© (v1 -v13) Nov 2022 Subsequent amendments SWAOC team Dec 2022. Please do not reproduce or alter without permission. (TTA) Discharge Medications o Use of pre-packed discharge medications. CD aspect will be pre-prescribed to allow for timely dispensing. o *Oxycodone prescribing must have written reinforced non-continuation of this via discharge
Drug
TKR
Paracetamol 1g
QDS 12 days 12 days Celecoxib 200mg po BD (Cautions: prev thrombosis, weight <50kg Contraindicated: eGFR <30, CCF stage II-IV, significant CVS history eg recent MI, UA)
SWAOC anaesthetic
THR and UKR
only
po
Page 2 of 2 = Post op Care & Discharge
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 35
Equiv carb to 2 slices toast
Theatre efficiency is promoted through agreed triggers for lay-up of the next case, communication with the admission area, and sending for patients. Anaesthesia is performed in a dedicated room, on the operating table, following which surgeons position patients before they are transferred tothe operating theatre.
Postoperative care and discharge
In the primary recovery area intravenous fluids are discontinued and patients are given a carbohydrate drink. After a brief period of monitoring, they are transferred to secondary recovery, where mobilisation starts as soon as the spinal has worn off. Pain scores and nausea are reviewed regularly with a low threshold for treatment, food is introduced early, post-operative X-rays are performed, and patients are encouraged to get dressed in their own clothes as soon as possible.
Discharge from the unit is protocolised and nurse led, and discharge paperwork is populated by different elements of the patient’s electronic pathway record. Patients receive a standardised pack of discharge medication that includes a strictly limited period of oxycodone use. Telephone calls are made to the patients on day one and day seven after discharge, and pain scores and patients’ opiate use are audited regularly.
SWAOC results
The first patients were treated in March 2022 and at the time of writing (January 2023), 740 primary hip and knee replacements have been carried out at the unit (Figure 4). The length of stay at SWAOC for all primary hip and knee replacements is shown in Figure 5, with the mean length of stay by procedure shown in Figure 6; 52% of primary arthroplasties performed at SWAOC have been day cases. Data from the author’s (JH) base trust shows that, in the year 2021/22, the median length of stay for both primary hip and knee replacements was three days. The data shown in figures 5 and 6 therefore represent a


significant downward shift in length of stay, which might be interpreted as resulting from patient selection. Indeed, the treatment of more complicated and frail patients has remained at the base trusts and SWAOC has treated more straightforward cases. However, learning from the pathways described has been incorporated into base trusts, and data from 2022/23 shows, that in the author’s (JH) Trust, the median length of stay for primary hip and knee replacement is now two days, even amongst this population of sicker, more complex patients.
Of course, length of stay is only one metric of interest, and we must ensure that patients’ care is not compromised by a relentless drive to reduce their time in hospital. Figure 7 shows the overall pain scores reported by SWAOC patients, demonstrating that only a very small proportion have severe pain, and the data in Figure 8 shows a high rate of patient satisfaction with the service they received at SWAOC.



Conclusion
SWAOC provided the Devon ICS, not only with an opportunity to reduce its waiting times for elective orthopaedic surgery, but also to develop new pathways for elective care that have allowed us to drastically improve our length of stay for high-volume low complexity procedures. This has been achieved through a multidisciplinary re-design of all aspects of our patients’ journey and through a greater protocolisation of the treatment that they receive. In this article the authors have discussed some aspects of these protocols, and we would like to thank all members of our MDT, and all those teams around the country, whose shared expertise helped us to achieve these results. The SWAOC MDT is in turn completely open to sharing our protocols with anyone interested in obtaining further information about them. n
References
1. Coronavirus: How NHS Nightingale was built in just nine days. Available at: www.bbc. co.uk/news/health-52125059
Figure 4: Numbers of primary hip and knee replacements performed at SWAOC (data last accessed 20th January 2023).
Figure 5: Length of stay for primary hip and knee arthroplasty at SWAOC.
Figure 6: Mean length of stay at SWAOC by procedure.
Figure 7: Overall pain experience of SWAOC patients.
Features 36 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk Miller’s
Figure 8: SWAOC patient satisfaction scores.
Miller’s Orthopaedic Review Course, Part I
Miller’s Orthopaedic Review Course, Part I
24–28 May 2023
24–28 May 2023
The Miller’s Orthopaedic Review Course, Part I, is a current, comprehensive review of orthopaedics unlike any other course. Taught by renowned surgeons across all subspecialties, the Miller's Orthopaedic Review Course, Part I, provides an in-depth analysis of key orthopaedic concepts to help you build knowledge and prepare for your future.
The Miller’s Orthopaedic Review Course, Part I, is a current, comprehensive review of orthopaedics unlike any other course. Taught by renowned surgeons across all subspecialties, the Miller's Orthopaedic Review Course, Part I, provides an in-depth analysis of key orthopaedic concepts to help you build knowledge and prepare for your future.
You can attend the 2023 course in person or virtually from the comfort of your preferred location. As a participant you will:
You can attend the 2023 course in person or virtually from the comfort of your preferred location. As a participant you will:
• Engage in five days of exciting live lectures from top faculty with on-demand versions available for 2 months of studying.
• Engage in five days of exciting live lectures from top faculty with on-demand versions available for 2 months of studying.
• Focus your learning through an intense and immersive comprehensive review of orthopaedics.
• Focus your learning through an intense and immersive comprehensive review of orthopaedics.
• Receive free one-year access to JBJS Clinical Classroom — an adaptive learning platform with over 4500 questions that builds knowledge by targeting areas that need strengthening.
And so much more!
• Receive free one-year access to JBJS Clinical Classroom — an adaptive learning platform with over 4500 questions that builds knowledge by targeting areas that need strengthening.
And so much more!
Learn more and register at millerreview.org
Learn more and register at millerreview.org
JBJS MRC International Ad 2023.indd 5 9/2/22 11:23 AM
So you want to develop your own implant?
Paul Roberts

Where do I start?
So, you have a concept of an orthopaedic implant you would like to develop. The essential questions to ask yourself are:
1. Is it novel? Implant companies are perfectly able to develop, produce and market ‘me to’ products without the involvement of surgeons.
Paul Roberts is a recently retired Consultant hip and knee arthroplasty surgeon. For most of his consultant career he was based at the Royal Gwent Hospital, Newport. He has a long-standing interest in the design and development of orthopaedic implants and instruments, and held numerous UK and foreign patents.
2. Is there likely to be continuing demand for it, taking into account the time it will take to bring it to market? Fashions change quickly in the orthopaedic implant world e.g. the rapid demise of metal-on metal hip replacements.
3. Will it be attractive to an implant company? Essentially, will they be able to make enough profit to justify the very high upfront costs of development, production, regulatory approval and marketing, and satisfy their shareholders?
If after answering these questions you wish to proceed, the issue that must be at the forefront of your mind is protection of your (embryonic) intellectual property (IP). Do not discuss your invention with anyone you cannot trust. Once an invention is in the public domain it cannot be patented, and any confidentiality agreement relating to it would be difficult to enforce. The public domain is wide, and would include for instance, a presentation at a local orthopaedic meeting. So be careful.
Do not use NHS facilities or time for any aspect of the development of your invention. This could leave you open to a claim by
the NHS on your IP in the future. Likewise, if you hold a University appointment, clarify with the relevant authorities what claim, if any, they may have on your IP.
Involving industry
To bring an orthopaedic implant to market you will inevitably have to involve the implant industry. The cost and expertise required for development, manufacture, regulatory approval and marketing are simply too great for an individual. For example, a PMA (pre-market approval) submission to the FDA in the USA is likely to cost upwards of $3 million and take at least five years to complete. So, the pertinent question is: when do you begin to interact with industry?
Clearly, your intellectual property is best protected with a patent. However, as discussed in the section on patents later, it is difficult and time consuming to patent an orthopaedic implant. Consequently, it is likely that you will need to approach an implant company relatively early in the pathway, as we did in our first project.
So, how do you choose which company to go to?
Firstly, you should choose a company which has a track record of interest in the type of implant you have invented, but also has a relevant gap in their portfolio. In my experience, small companies are most likely to be receptive to working with a single or small group of surgeons, and be interested in niche markets, but their resources may limit their development and marketing capabilities. The large multi-national implant companies have huge resources but can be
Features
38 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
“Clearly, your intellectual property is best protected with a patent. However, it is difficult and time consuming to patent an orthopaedic implant. Consequently, it is likely that you will need to approach an implant company relatively early in the pathway, as we did in our first project.”
difficult to work with if you are not on their ‘surgeons panel’. In particular, over the last 20 years it has become apparent that these companies, particularly the US based ones, are reluctant to work with individual surgeons in developing an implant, as they had done historically, but instead prefer to develop implants with a large ‘panel’ of surgeons, who can subsequently act as product champions and market influencers.
Whatever company you choose, do not discuss any details of your invention without them having signed a Confidentiality Agreement. These are easily and cheaply obtained on the internet, but may need some modification to meet your specific requirements. There are many anecdotes of surgeons having their invention rejected by an implant company, only for a very similar design to appear in the company’s portfolio some years later. A Confidentiality Agreement will provide a reasonable level of protection if well written, but obviously you must be prepared to take legal action if it is breached.
The more detail of the design features and applicability of your implant you are able to provide at the initial meetings, the greater is the chance that it will be taken up. At the
very least you should be able to provide a detailed summary of the design rationale and key design features, supported by good quality design drawings, all of which should be signed and dated by you. It may be worthwhile, as discussed earlier, to have some experimental data to support your claims at this stage, but this is not essential.
If the company decides to proceed with the project, the next phase is the preparation and signing of a contract that will define at least the company’s obligations to you, including financial compensation, your obligations to the company, and terms of termination. This contract will normally be drawn up by the company based on their own template, but there is no reason why you should not have a contract prepared independently. Whichever you choose, I would strongly recommend using a specialist life sciences attorney to prepare or check the contract and carry out further negotiations if necessary. Such lawyers do not come cheaply (£400-£500 per hour), but will be well versed in the tactics of the ‘David v Goliath’ situation you are effectively in. Money spent at this stage is likely to be money well spent. Contract disputes further down the line can be toxic, and difficult and costly to remedy. Only after the contract is agreed and signed should the development phase begin.
Patent applications

Patents are probably the most complex and least well understood aspect of intellectual property protection for the non-expert. If you are considering making a patent application, the following section will be relevant.
Background
The patent system exists to protect inventions and products; you cannot patent an idea per se. However, if you are able to develop your concept into an invention, you may be able to obtain patent protection.
To qualify as an invention in the patent process, three criteria must be met:
i) It must be novel. You cannot patent anything which is already in the public domain.
ii) It must demonstrate inventiveness. You cannot patent anything which would be obvious to a person well informed and experienced in the field. Likewise, it cannot be just a minor modification of an existing invention.
iii) It must have a practical, industrial application >>
Features
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 39
Assembly cross section.
Because of criteria (i) and (ii), in most cases it is unlikely that an orthopaedic implant will be patentable: it is unlikely to be novel, and it is likely to be considered a minor modification of an existing implant or previously patented, (although not necessarily marketed), design.
Whilst the whole implant may not be patentable, certain aspects of its design might be. For example, in 2012 we were able to obtain UK and European patents for a monobloc, chrome-cobalt acetabular component with transarticular screw fixation to be used in metal-on-metal hip resurfacing. Although the acetabular component itself was obviously not novel, the UK and European Examiners did consider that the design of the trans-articular screw fixation, with its ability to block transmission of fluid pressure waves and resist backing out, was novel and represented more than a minor modification of existing implants. Interestingly, although this implant was never brought to the orthopaedic market for a variety of reasons, following the publication of the patent we did receive numerous enquiries about the screw design from the marine engineering industry, with offers of collaboration.

The practicalities
It is possible to successfully apply for a patent without involving Intellectual Property lawyers. However, orthopaedic implants, and to a lesser extent instruments, are likely to be in the more complex range
Consequently, if you think your invention is going to be commercially viable, I would recommend using an Intellectual Property lawyer with a track record in life sciences from an early stage in the patent application. Details and advice can be obtained from the Chartered Institute of Patent Attorneys’ website. To minimise the costs, provide your chosen lawyer with the most detailed description and design drawings of your invention that you are able to produce. Likewise, if you have any experimental data to support your claims, a successful outcome is more likely.
The procedure
of the spectrum of patent applications. The work involved in the preliminary searches, and the drafting and filling of the application will be extensive and difficult if you do not have experience in the process. Likewise, responding to formal and detailed reports and questions from the patent examiners is a daunting challenge without expert guidance. It may not be possible to rectify errors made at this stage.
There is no such thing as a ‘worldwide patent’. Individual applications must be made to each country/jurisdiction in which you want patent protection (commonly UK, Europe and USA). There are two pathways you can follow: (i) individual country/ jurisdiction applications, or (ii) the Patent Cooperation Treaty (PCT) ‘international patent application’, covering most of the major industrialised countries of the world.
Features
“If you think your invention is going to be commercially viable, I would recommend using an Intellectual Property lawyer with a track record in life sciences from an early stage in the patent application.”
40 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Cup and screw assembly.
It is important to understand that the PCT system does not examine patent applications fully and it does not grant patents. However, once the PCT application is filed, it does provide immediate protection of your invention in the 142 member countries. It will also eventually provide you with information enabling you to judge the likely chance of success in subsequently obtaining patents from individual country/jurisdictions before potentially major costs are incurred.
For either pathway, the first stage is to file the patent application with your national patent office. In the UK this is the UK Intellectual Property Office. This establishes the priority date. This immediately gives you a 12-month period of protection and prevents anyone else in the UK obtaining a patent covering your invention, even if you do not subsequently complete the process.
If you decide to proceed down the individual country/jurisdiction patent route, it is important that the foreign applications are filed within one year of the priority date. In this situation they will be considered to have been filed on the priority date, effectively giving you retrospective protection.
If you choose the PCT route, the application should also be made within one year of the priority date for the same reason. You then enter the International phase, when the application is subject to both search (of relevant prior art) and examination of the design for inventiveness and industrial applicability. Within six months or so you will be provided with an International Search Report (ISR) and the Written Opinion of the International Search Authority (WOISA). If you do not challenge the WOISA, it is subsequently published without change as the International Preliminary Report on Patentability (IPRP), usually within 18 months of the priority date. This is essentially a non-binding opinion on the core patentability requirements: novelty, inventiveness and industrial applicability.
If you choose to continue the patent application process based on the result of the IPRP, you then enter the National phase, when individual applications are made to each country/
jurisdiction in which you want patent protection. Many countries will use the IPRP as the starting point for further examination. However, some countries, including the USA, ignore the IPRP and will conduct their own comprehensive search and examination.
In summary, the advantages of the PCT route compared to early filing of individual foreign patent applications include:
• Lower costs initially.
• The decision to pursue foreign patent protection, with the associated substantial costs, does not have to be made until the end of the International phase, when the IPRP will give you some indication of the likely probability of success.
The disadvantages include:
• Overall costs are higher.
• The process takes longer.
The costs when using an IP lawyer
It is difficult to provide an accurate estimate of the costs of even a UK patent application because of the many variables, including; the complexity of the application, the extent to which it is challenged by the examiner, and not least the fee structure of the IP firm you have chosen. An on-line search will produce wildly different results.
In May 2018, Hutchinson IP carried out a statistical analysis of the cost of their own successful direct UK patent applications (not UK National Phase). They concluded that the range was £3,300 - £10,200, with an average of £5,595.
Accepting that orthopaedic implant applications are likely to be at the expensive end of the range, and factoring in the increase in RPI since May 2018, the cost of a direct UK patent application now would be approximately £13,000, based on Hutchinson’s figures. Foreign applications are likely to be considerably more expensive. The cost of a PCT application currently is approximately £12,500.
For a ‘real world figure’, I have looked at the cost of the patent applications in 2012 mentioned above. We used a Partner in a well-known international IP firm. This turned out to be a complex and lengthy process, requiring multiple responses to questions and disputes with the various examiners. The total cost for applications in the UK (successful), Europe (successful,) and the USA (unsuccessful), taking in to account the increase in RPI, was approximately £40,000. On top of this are the not insubstantial annual renewal fees for each country/jurisdiction.
Key
reflections (many of which I did not follow)
1. If possible, work with a trusted friend/ colleague. You can share the costs (and benefits), but more importantly, you can support each other when times are tough, which they certainly will be. There were many times in the dealings with the implant companies that I would have given up if I had been acting alone.
2. Protect your intellectual property at all times. Keep detailed minutes of all meetings, and date, sign and keep any design drawings, however rough, you create at the meetings.
3. Employ the best life sciences attorney you can afford to prepare or check the definitive contract. We did not, and subsequently regretted it.
4. Don’t be overawed by the David v Goliath nature of the relationship with the implant companies. They are aware that you have ‘soft power’ with your influence in the wider orthopaedic community, and they will generally avoid overt confrontation with a surgeon-designer.
5. Learn to say no.
6. Don’t forget your family and friends, however busy or stressed you feel.
7. Enjoy the experience – easy to say in retrospect. Developing an implant is an immense intellectual challenge, which will take you outside your comfort zones on many occasions. In return, the satisfaction in seeing your idea come to fruition and benefit patients is huge. n
Read how Paul and his colleague Peter Grigoris developed two implants of their own, a new hip resurfacing system incorporating the Metasul bearing and a monobloc hip resurfacing acetabular component with trans-articular screw fixation, on Orthopaedics Online at www.boa.ac.uk/O2/implants
“If possible, work with a trusted friend/ colleague. You can share the costs (and benefits), but more importantly, you can support each other when times are tough, which they certainly will be. There were many times in the dealings with the implant companies that I would have given up if I had been acting alone.”
Features JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 41
Bev Fitzsimons is the Chief Executive of the Point of Care Foundation, a social enterprise with the mission to humanise healthcare. The Foundation runs Schwartz Rounds, a forum for reflective practice for staff in the NHS, which seek to help with the emotional and psychological impact of working in healthcare. The Foundation also runs patient experience programmes. A social scientist by background, Bev has worked in and around healthcare since the 1980s.
Getting of f the production line
Bev Fitzsimons
It is hard not to be despondent about the state of the NHS at the moment, with increased waiting times for ambulances and admission to hospital, a backlog of people waiting for treatment, reduced staffing levels, and a real difficulty hanging on to the clinical staff we have. But that is not the whole story. There is a genuine emotional burden in providing and receiving healthcare, and factors interfering with the process can cause moral injury1
The current working environment is brutal. Is it any wonder that we are losing our clinicians in droves? We attract high achieving, idealistic young people to our higher education institutions in ever greater numbers with the goal of becoming great doctors, nurses and therapists and making a difference to patients2 What is happening to make them want to leave, having worked so hard to get there?
As long ago as 2009, our Founder Jocelyn Cornwell wrote in the BMJ about the “difference between a hospital and a bottling factory”3. In it she describes both the benefits of standardisation (or indeed ‘industrialisation’) particularly in instances in which a patient’s journey might be reasonably predictable. Healthcare has many similarities with an industrial process: it involves many complex inter-connected processes, lots of hand-offs, it can be highly technical, and aspects can be standardised and delivered in the style of a production line.
Moreover, in some ways healthcare can resemble other industries. Like the law, healthcare can involve advocates – friends and family who speak on a vulnerable relative’s behalf. Like engineering or mechanics there is a diagnostic phase when the task (the treatment) may be unclear. Like education, the degree of specialisation means that the ‘inputs’ (the decisions about the processes of care) vary widely. In most cases there is a wide degree of discretion about the appropriate
treatment or care that will be informed by both patient, family, and professional preferences.
But healthcare is different in so many ways. Health and care bear witness to the greatest joys and the greatest losses in people’s lives. People in need of care are uniquely vulnerable. For this reason, over-reliance on industrial processes is problematic. And, even leaving aside the inherent humanity of health and care, the systems required to achieve production-line efficiency are not generally well implemented in our system, which has grown up piecemeal, with new elements, changed structures and bits added on over time. For example, we regularly hear about multiple IT systems that staff are required to use, each requiring a different login and password, and often requiring repetition of input. Patients also report inefficient administration of appointments and communications which add to the stresses and strains of their condition.
Even if the industrial approach was the ideal, with the best will in the world, we are not very good at it, either as professionals working in the system or as patients or family members seeking to navigate our way through it. Flawed processes cause enormous frustration to clinicians and patients alike.

Orthopaedic surgery, perhaps more than any other aspect of healthcare, has benefited greatly from ‘industrial’ approaches to process improvement, with increased standardisation4
Koenig et al.4 describe how standardisation of scheduling, preoperative testing, and perioperative coordination, was associated with improvements in cancellation rates, on-time operating room starts, and operating room utilisation. The same paper describes reductions in postoperative complications, shorter lengths of stay, and no difference in rates of discharge to home with standardised clinical pathways.
Features
42 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
A more recent paper, by Montori and Allwood, argues that over reliance on industrial approaches “turns patients into widgets and clinicians into production line workers, the work of caring reduced to processing people through the system”5. Transactional processes can only ever be part of the picture. As they say: “to care is human; policies, systems, institutions, or technologies cannot care.”
Since our launch as a charity ten years ago, the Point of Care Foundation has held to a vision of a more humanised healthcare system. But to move from industrial healthcare to humanised care requires a radical change in mindset.
What is to be done?

Too often, the interests of staff and patients are somehow pitted against one another. For the radical change in mindset that is needed to create a more human system, we must escape this false dichotomy. We are all on the same side.
First, as a society, we need to acknowledge the nature of the work, and the work environment, of the health and care system. This work makes huge emotional demands on those charged with delivering it. This needs to be recognised, and space created for those very normal human responses to be acknowledged and processed. It is important for people to be seen and heard.
As a system, we need to pay attention to wellbeing. And by this I don’t mean yoga classes! Thinking of Maslow’s hierarchy of needs6 it is astonishing that we hear repeated stories of the inadequate provision for even the most basic physiological needs for rest, food, hydration, and a place to sleep. We must pressure the system to be more human. For workers this means humane rotas and careful supervision, not treating junior doctors as cannon fodder, or denying people time off for their weddings or the funerals of loved ones. Neither clinical staff nor patients are widgets.
As leaders, it means prioritising the humanity of care. In the current context, systems leadership can’t quickly fix a systemic failure because it is built on shifting sands. However, the common denominator in healthcare is human and so isn’t relational leadership more important when the system fails? The Point of Care Foundation is responsible for implementing Schwartz Rounds, which is one manifestation of this. The underlying premise of Rounds is that healthcare staff are more able to work compassionately with patients and colleagues when they have greater insight into their emotional responses and when they themselves feel cared for. Having these practices embedded from early career / studenthood might just help us hang on to our staff a little better.
As co-workers, and sticking with Maslow for a moment, we can work to ensure one another’s psychological safety through respectful relationships at work. As Nick Schindler recently commented when discussing grief when a patient dies, people move miles to be with a great team (Figure 1).
Everyone makes a difference: I was reading today of the on-call room where the domestic staff have taken unbidden to making up the camp bed with clean sheets and towels every day. The member of staff commented “Honestly it’s made me feel more like a valued employee than anything else this week”, (Figure 2). >>
Features
Figure 1
“Too often, the interests of staff and patients are somehow pitted against one another. For the radical change in mindset that is needed to create a more human system, we must escape this false dichotomy. We are all on the same side.”
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 43
Keeping the focus on the patient
A concept which is familiar in the sphere of patient safety is that of the difference between the work ‘as imagined’ and the work ‘as done’. To do this well means keeping patients’ experiences at the front of our minds, understanding what it is like to be a patient or family member. One consultant we worked with described “… hearing about long and painful journeys to the hospital, getting lost, how taking blood can make the boys –and mothers – cry, and how clinic scheduling or delays can mean the families miss meals…”. These observations galvanised him to action in service of patients7
Let us not forget that patients, service users and families:
• Have expert knowledge, and understand the experience of receiving care.
• Have the right to be involved, as they are most affected by the care experience.
• Lend legitimacy and urgency to change – often changes that clinical staff have themselves been seeking.
• Can see waste and inefficiency.
• Understand personal and system obstacles to good care.
• Wish to share decision making and are realistic about what can be achieved.
• Are best placed to judge outcomes.
In short, patients can be clinicians’ greatest advocates and supporters.
As one colleague recently said, “I find that even if I can’t magically find a bed for a patient in a corridor, I can still get them a cup of tea. I’m not doing my job as a surgeon but at least I’m doing something as a human being. Healthcare in the NHS is really at that level these days”.

Conclusion
The imperfect, industrial nature of healthcare, which sacrifices the relationships inherent in care, has contributed to the exhaustion of care givers and patients.
Caring and being cared for is a symbiotic relationship in which both parties contribute to keeping the whole system going. As Montoni and Allwood say, “care requires a person to notice another’s human situation and to respond to it”. In a human system, no ‘big bang’ reorganisation or policy change is going to achieve the required changes to human behaviour. What will and does work however, is giving people – colleagues and patients – the space and tools to work together as a human system toward a common cause. n
References
1. Rosen A, Cahill JM, Dugdale LS. Moral Injury in Health Care: Identification and Repair in the COVID-19 Era. J Gen Intern Med 2022;37(14):3739-43.
2. 2022 – the hardest year in living memory to enter medical school. Available at: www.theguardian.com/education/2022/ jun/22/2022-hardest-year-in-living-memoryto-enter-uk-medical-school
3. Cornwell J. What’s the difference between a hospital and a bottling factory? BMJ 2009;339:b2727.
4. Koenig KM, Bozic KJ. Orthopaedic Healthcare Worldwide: The Role of Standardization in Improving Outcomes. Clin Orthop Relat Res 2015;473(11):3360-3.
5. Montori VM, Allwood D. Careful, kind care is our compass out of the pandemic fog. BMJ 2022;379:e073444.
6. Maslow AH. A theory of human motivation. Psychological Review. 1943;50(4):370-96.
7. The King’s Fund (2014). PFCC final report for the Health Foundation. Available at: www.health.org.uk/sites/default/files/PFCC_ finalreport.pdf
Features
Figure 2
44 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
“As a society, we need to acknowledge the nature of the work, and the work environment, of the health and care system. This work makes huge emotional demands on those charged with delivering it. This needs to be recognised, and space created for those very normal human responses to be acknowledged and processed. It is important for people to be seen and heard.”
Jig-guided hip revisions

For the first time, Gomina has developed an extraction set that allows a hip revision to be done with minimal bone loss. Thanks to innovative production technologies, it is possible to manufacture dimensionally rigid chisels with different radii. The precision ground, sharp cutting edges of the chisels are the result of Gomina’s many decades of expertise.

The bespoke crafted jigs manufactured by Gomina ensure the application of a precise separation of bone and prosthesis. This innovative pioneering extraction set from Gomina makes surgeon’s work far easier, leading to shorter operating times. Entirely for the patient’s benefit.

swiss quality Official Distributor for the UK Judd Medical Unity House, Buntsford Park Road, Bromsgrove, Worcestershire B60 3DX Tel. +44 (0)15 27 55 90 10, sales@judd-medical.co.uk, www. judd-medical.co.uk www.gomina.ch
Andrew Manktelow is a Consultant Orthopaedic Surgeon working within Nottingham University Hospitals NHS Trust, with a specialist interest in primary and revision hip surgery. A past President of the British Hip Society, Andrew has been on the BOA Council since 2019. Contributing to the Orthopaedic Committee Andrew reports to BOA Council on matters relevant to the Independent Sector.

The legal implications of treatment delays since the 2020 pandemic
Andrew Manktelow and Bertie Leigh
To say that the COVID-19 pandemic has created a challenge for orthopaedic care in the UK and beyond would be an understatement. Against a preexisting backdrop of progressively increasing waiting lists the COVID-19 pandemic had a sudden multifactorial effect on the ability to deliver effective orthopaedic care. This change has not been coterminous with the pandemic. The simple truth is that the NHS is not acutely ‘challenged’ or ‘under stress’: it has been failing to deliver an appropriate service within a reasonable timescale which has probably resulted in harm to some patients.
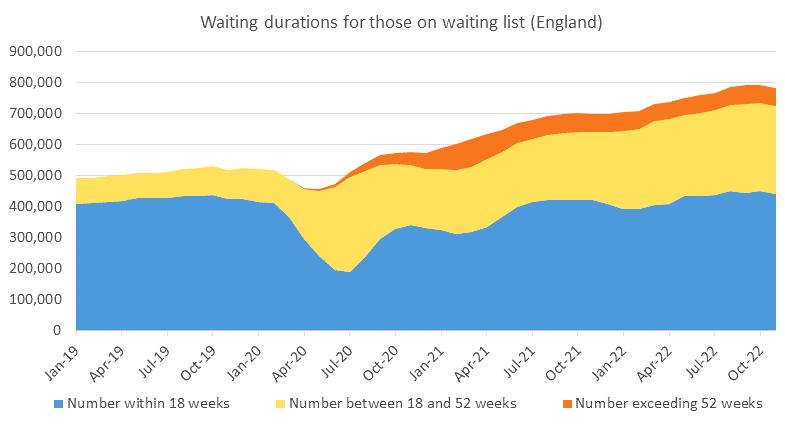
Bertie Leigh has been a consultant solicitor at Hempsons with extensive experience in medical negligence and in the law related to professional regulation. Bertie has had a close relationship with surgery and orthopaedics and was the chairman of NCEPOD for six years and was a non-executive director of the RNOH at Stanmore. He is particularly interested in issues related to consent and the effects of COVID-19 on what we need to discuss with our patients.

When the pandemic started, the planning to prepare for the unknown was disruptive. How the virus and its transmission would affect routine practices in the emergency department, in the
operating theatre and beyond was unknown and yet plans had to be made. Surgeons all remember meetings to discuss how services would need to be reconfigured, how doctors would need to be reassigned to support other services and how acute care could be delivered in the changed environment. All had to be reorganised at short notice and with little, if any, understanding of how things would progress. As doctors were alarmed by the reported experience from regions where the pandemic had progressed more rapidly, the anxiety created was disruptive in its own right.
Elective orthopaedic services were essentially shut down overnight. Many will remember being re-tasked to run minor injuries units. Many had the harrowing experience of working to support exhausted colleagues on medical wards and in the ITU. Re-learning old
Medico-legal
46 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Figure 1: Number of patients on waiting lists and duration of waiting times.
skills and working hard to apply ‘orthopaedic impetus’ to support other areas of medical practice. Preparations worked well in many situations, in other areas we might have been over prepared, however it would seem clear that in many, we were under prepared and illequipped for what transpired.
Circumstances were different in different areas of the country and at different times. The net effect was, and is, clear. Within elective orthopaedic surgery, NHS England data shows waiting times are now prolonged out of all recognition compared to those from prior to the pandemic and there is no evidence that things are improving. This is shown clearly in Figure 1, demonstrating how both the numbers of patients on waiting lists and the duration of their waiting time have increased since the start of the COVID-19 pandemic.
A huge amount of work is now being done with elective care centres and hubs designed to try and protect elective services from the unavoidable demands of emergency care within and away from orthopaedics. Behind the numbers are the practical consequences that are harder to encapsulate but are apparent to surgeons. Patients are now approaching elective surgery significantly deconditioned, poorly prehabilitated and with worsening comorbidity. Patients experienced worsened social support, isolation and anxiety during the COVID-19 pandemic that has further compromised their pre-operative situation. The lack of follow-up arrangements during the crisis, when face-to-face clinic appointments were stopped, led to patients re-presenting in very much more complicated situations. It has been difficult to review and identify bone loss or other factors of deterioration that have increased complexity. In the primary situation we are still dealing with cases with increased complexity where the bone has collapsed, where there has been progression of deformity. It is likely that surgical outcomes over time will be worse for many patients. Lengths of stay have increased with increased wound problems, infection and dislocation rates. It will take years for the full consequences of that situation to become truly understood and there is no evidence that things have reverted to normal.
Studies have demonstrated the impact of the COVID-19 pandemic on early clinical outcomes after total joint replacement. Anecdotally we are aware of cases, listed as routine that have now presented with very much more challenging bone loss and worse bone quality. Cases that were already complex are being admitted with 18 months of inactivity and deconditioning. These patients are likely to have worse outcomes. This additional technical complexity does not take
into account the dreadful experience that many of our patients have had, waiting for much longer than we would wish, in pain with restricted mobility and in isolation. A number of patients have been promised dates for surgery only to be deferred, allowing further progression of their pathological process, then requiring more complex reconstruction. Staged procedures have experienced prolonged intervals sometimes leading to acute complications such as infection, fracture and instability. Inactivity in elderly patients leads to muscle wasting that is likely to be permanent and the cause of additional morbidity and multi-system deterioration. All elective surgeons will know patients who have suffered harm as a consequence of delay. Much of this is directly COVID-19 related, but some is not: it is better seen as a consequence of an imploding system. Against that background in elective surgery, other orthopaedic patients have been managed differently. Early in the pandemic there was a situation in which some fractures that might previously have had surgery were being managed conservatively. All of this will have had negative consequences for our patient outcomes.
Green et al, detailed the experience of a highvolume elective centre (South West London Elective Orthopaedic Centre) comparing activity prior to COVID-19 with that after the first wave in 20201. They identified that patients waited longer, had an increased length of stay, more in hips than in knees, and higher in revision. They identified and described disease progression, patient deconditioning with increased pain and restricted function. There was less patient prehabilitation and education prior to surgery and patients experienced less family support and increased levels of anxiety. They also identified a surgical effect with decreased activity, all of which compromised outcomes of routine elective surgery1
In a widely-quoted work looking at the effect of joint replacement waiting lists, the Edinburgh Group reviewed their previous article detailing that patients described their experiences waiting for joint replacement as being a situation ‘worse than death’. They reported that the COVID-19 situation had compromised this yet further2
Unfortunately a number of our patients contracted COVID-19 while under our care. Many will have suffered consequences of varied significance and some tragically died with COVID-19 related conditions. Orthopaedic surgeons will be concerned by how all this and the way it has compromised our practice and our patients is likely to be viewed within a medico-legal context.
The likely response of the law
The gist of negligence is damage: whether anyone is liable is a secondary matter. The lawyers and their clinical advisors start with the damage and then see whether it can be shown to have been caused by a breach of a duty of care. In any individual case there will be arguments about whether the patient would have done better with appropriate care, but in many cases, subjected to the various concerns detailed above, sensible experienced expert witnesses are likely to agree that they probably would have done.
Here it will be clear that there has been a failure to deliver optimal care, by a country mile in many cases. However there had been a growing assumption in the decades up to 2020 that sub-optimal care was wrong. In many cases this has never been entirely realistic. Some hospitals have traditionally attracted the best surgeons and other staff, with better resources and equipment. But in a court of law that has rarely been an effective defence for the less well-equipped general hospital. Now all that has changed utterly: sub-optimal care has become more common and the law will need to revisit the problem, being more careful in defining the limits of what is acceptable. What is the duty of care owed to the patient in a system that cannot function as it should?
The NHS has often kept patients waiting too long and the courts met this in 1980. Mr Hincks and others had been waiting far too long for hip replacement surgery because the Good Hope Hospital in Birmingham needed rebuilding. The Court of Appeal ruled that the Secretary of State’s duty to provide throughout England and Wales hospital facilities “to such extent as he considers necessary” must be qualified.
“The funds are voted by Parliament, and the Health Service has to do its best with the total allocation of financial resources.”
In words prophetic of the present situation Lord Justice Bridge identified four deficiencies beyond his reach:
“…as we all know as a matter of common sense, the health service currently falls far short of what everyone would regard as the optimum desirable standard. That is very largely a situation which is brought about by lack of resources, lack of suitable equipment, lack of suitably qualified personnel and above all lack of adequate finance.
“I feel extremely sorry for the particular applicants in this case who have had to wait a long time, not being emergency patients, for necessary surgery. They share that misfortune with thousands up and down the country. I only hope they have not been encouraged to think that these proceedings >>
Medico-legal
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 47
offered any real prospects that this court could enhance the standards of the National Health Service, because any such encouragement would be based upon manifest illusion.”3
That judgement set the tone for all subsequent applications to the court for judicial review of treatment decisions. The court will not direct the Secretary of State to provide a better financed health service and individual applicants have tried to show that resources were distributed irrationally to their detriment. A failure to finance more gender reassignment surgery was held to be a reasonable prioritisation. A failure to provide more cancer therapy to a dying child was a reasonable treatment decision.
However that does not tell us how the court would have handled an application for compensation for the extra pain a patient has suffered as a consequence of unreasonable delay. The courts will always flinch from anything that looks like usurping the function of the executive and legislature in creating policy, as it would be in telling the Secretary of State how much to spend, but that does not mean that it will not order the NHS to compensate those individuals who have suffered damage as a result of unreasonable delay.
Since 2009, the NHS Constitution has set out rights for patients, public and staff. This looks very much like a contract between the taxpaying patient and the NHS. The terms of the Constitution take care to make it clear that it does not intend to create new legally enforceable rights, but it does create unmistakeable objective yardsticks by which potential breaches can be measured.
Legal rights infringed by a virus?
In 2020 it was assumed that the law would be much more forgiving: no-one could reasonably be blamed for failing to admit patients where the failure to admit was due to the system being swamped by a highly contagious and frequently fatal virus for which we had no effective treatment. No-one could reasonably be held liable for that delay or its consequences. The nation acknowledged the NHS’s heroic failure to deliver the previous service by applauding on their doorsteps.
However, several things have changed since the lock-down. First and foremost, as those events have drifted into the memory, the courts will become more analytical in picking out precisely which delays can be shown to be due to the virus.
Second, because the Service has failed to recover: during 2022 no hospital was closed
to admissions due to the virus. Delays due to that cause have elided with delays due to long term inadequacy of resource. Some is still directly attributable to the virus even after vaccinations and better treatment have made it less threatening to individuals, because there are still thousands of NHS beds diverted to the care of COVID-19 patients. Indirectly the virus still has an impact on the productivity of NHS facilities. Precautions against hospital acquired infections reduce throughput of patients. Staff have been depleted by the victims of the virus: a few have been killed or disabled, many more have been burned out or exhausted and we have increased sickness rates. Morale has been impacted by the realisation that the population who were prepared to come to their doorsteps to applaud NHS staff every Thursday evening were not led by a government that would ensure that their wages kept pace with inflation. We may be able to recruit new junior staff, but we cannot retain the experienced ones we need. All these contributions are much more softly focused.
How will a poor patient experience be viewed?
In time, long term PROMS and clinical outcomes will allow us to review things more objectively, but between now and then an increasing number of complaints will likely appear from patients who are rightly unhappy with their outcomes. It is not our purpose to debate these issues here, but the courts will have to decide which of them will provide a defence against a claim by a victim of delay. In theory, a sub-optimal service should make it harder for an individual to bring a claim: you cannot show that your damage is due to an unreasonable act or omission on the part of anyone. In reality such a proposition is a challenge to the ingenuity of the lawyers.
Can patients seek financial recompense if they felt forced to seek private care?
Many patients have sought care within the independent sector, funding expensive joint replacement surgery themselves. It is possible that such patients could seek financial compensation when they feel that they have had to seek self-funded independent care. Generally the NHS cannot be forced to reimburse patients for money they have spent elsewhere unless that service has been commissioned by an NHS provider.
How will a poor clinical outcome be viewed by the court?
In a claim that the NHS has failed to provide a safe or reasonable service, a patient could seek compensation for compromised fracture management, implant failures, inadequate remote reviews and increased complexity and complications of the surgery that they required. Certainly patients will
seek compensation when the fractures have resulted in malunions and deformity over time if they can show that it is the consequence of a failure to provide treatment within a reasonable period of time. This will make it more important to create contemporaneous documentation of any MDT and the rationale for any delay or specific management plan. If the Trust wishes to defend an apparently unreasonable delay it must create detailed records that will withstand scrutiny, demonstrating not only that there was a lot of delay about, but that the priorities of this individual patient were recognised and carefully considered.
How will contracting COVID-19 while under our care be viewed?
Much of what we are describing stems from the fallacy of the altered perspective. At the height of the pandemic no-one could complain if they contracted COVID-19 while under our care for emergency or more routine elective treatment. As time moves on and expectations change such claims will be feasible. The difficulty is that in preparing such a defence we had to create records of what happened at a time when we did not know we would need them, or the need to defend claims was a long way down the list of priorities.
Clearly this is an area that will concern clinicians and likely provoke increased legal interest in the future. Many of the issues, while similar to existing case law will not have been tested formally in the courtroom. Only time will tell how understanding the courts will be when reviewing activity delivered by an already compromised service then dealing with an additional, unexpected and debilitating challenge. n
References
1. Green G, Abbott S, Vyrides Y, Afzal I, Kader D, Radha S. The impact of the COVID-19 pandemic on the length of stay following total hip and knee arthroplasty in a high volume elective orthopaedic unit. Bone Jt Open. 2021;2(8):655-60.
2. Clement ND, Scott CEH, Murray JRD, Howie CR, Deehan DJ; IMPACT-Restart Collaboration. The number of patients “worse than death” while waiting for a hip or knee arthroplasty has nearly doubled during the COVID-19 pandemic. Bone Joint J. 2021;103-B(4):672-80.
3. R v The Secretary of State for Social Services ex parte Alan Hinks, Marie Flemming, Marjorie Lloyd and Leslie Smith [1980] BLM 1:93.
Medico-legal
48 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Spinal surgery in the UK –an evolution
Niall Eames
Niall Eames is an orthopaedic spine surgeon in Belfast. He has previously been Education Lead for the UKSSB and is past President of the Spinal Training Interface Group (STIG) Committee. Niall is Honorary Secretary of the British Scoliosis Society and Vice Chair of the BOA Education Committee.

Spinal surgery in the UK has undergone a very significant evolution over the last 50 years. From its early beginnings, it has now grown into a sub-specialty.
The establishment of Regional Spinal Networks across the country is part of the wider changes happening within the NHS, mirroring the setting up of trauma and cancer networks, all of which are aimed at improving patient care.
Both orthopaedic and neurosurgeons undertake spinal surgery, but in terms of training and experience, for trainees, there are significant differences between the two specialties. Spinal surgical procedures now compromise 14% of orthopaedic practice and 60% of neurosurgical practice. There are significantly more orthopaedic surgeons than neurosurgeons in the UK. The National Joint Registry lists over 400 hospitals providing hip replacement surgery across the United Kingdom at present compared with approximately 40 neurosurgical units across the United Kingdom and Ireland.
But, conversely, a greater percentage of neurosurgeons compared to orthopaedic surgeons undertake spinal surgery at varying levels of complexity. And the number of trainees differs dramatically with many more orthopaedic than neurosurgical trainees. However, a significantly higher proportion of neurosurgical trainees plan to undertake spinal surgery at the consultant level compared with orthopaedic trainees.
Training is central to any profession and to be successful, training must be of the best standard possible. In 2017, orthopaedics and neurosurgery came together to join the Interface Training Group, to establish a ‘network’ of cross specialty spinal fellowships across the
UK. This built upon the many high-quality fellowships in the UK in spinal surgery already existing. It provided a standardised curriculumbased fellowship programme jointly between neurosurgery and orthopaedics. Initially running as pre-CCT fellowships, these are now established and running as post-CCT fellowships.
Across the country, many non-spinal orthopaedic surgeons will see and take part in the initial management of patients with spinal pathology. For this short series of articles, the first Spinal Interface Training Group fellows in the UK, now consultants themselves, have come together with their mentors to look at three commonly occurring spinal conditions that all orthopaedic surgeons may encounter.
The first article looks at cauda equina syndrome and describes what to look for and some of the ongoing areas of confusion and research. This condition has the potential to cause devastating morbidity and needs rapid and appropriate care to achieve the optimum result for the patient.
The second article is an overview of spinal infection, looking at the differences between epidural abscesses and discitis and discussing how we manage infections in the spine. Finally, we have an article on thoracolumbar fractures and how we classify them. Stability has always been a major debate and this article looks at the various historical classifications and what is important when assessing these patients.
All three conditions have the potential to cause very significant patient harm and morbidity. All clinicians need to be aware of the management issues and ongoing debates involved in each, at the very least to allow appropriate initial treatment and referral. n
Subspecialty JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 49
“Both orthopaedic and neurosurgeons undertake spinal surgery, but in terms of training and experience, for trainees, there are significant differences between the two specialties.”
Cauda equina syndrome - an overview
Sheweidin Aziz and Matthew Newton-Ede
Sheweidin Aziz is a spinal consultant at the University Hospitals of Leicester and is a fellow of the RCSEng. She was one of the first Spinal Training Interface Group (TIG) Fellows in the UK. During her fellowship, she gained experience managing primary spinal tumours, metastatic spine disease, adult degenerative conditions, paediatric deformity, and trauma. She is a keen educator, previously awarded the ‘Outstanding Clinical Teacher’ of the year award by the University of Leicester Medical School.

Cauda equina syndrome (CES) is a clinically diagnosed syndrome resulting from the dysfunction of one or more of the lower sacral nerve roots. Back or leg pain or lower limb motor or sensory changes are often present but are not essential to the diagnosis. The presence of at least any of the following is required, bladder/bowel/sexual dysfunction and reduced sensation in the saddle area. CES cannot be excluded based on clinical signs alone. An emergency MRI scan must be performed even in the absence of CES signs. There are several stages of CES; the damage to nerve roots occurs continuously and progressively. Patients place more emphasis on pain, so clinicians must ask direct questions about red flags. The earlier the diagnosis and management, the better the outcome. There are no safe time thresholds, such as the 48-hour ‘safe’ time window. Both early and delayed surgery result in improved neurological outcomes.
Background
CES is a clinically diagnosed syndrome resulting from the dysfunction of one or more of the lower sacral nerve roots (S2 and caudal). One or more of the following symptoms or signs must be present:
• Bladder and/or bowel dysfunction
• Reduced sensation in the saddle area
• Sexual dysfunction
Matthew Newton-Ede is a spinal surgeon at The Royal Orthopaedic Hospital NHS Trust and Birmingham Children’s Hospital. He specialises in treating a wide range of spinal problems in adults and children including surgery of the neck and he has a particular interest in children’s spinal deformity surgery. He is a fellow of the RCSEng, and a member of the BOA, AO Spine, BASS and BSS.

Back or leg pain or lower limb motor or sensory changes are often present but are not essential to the diagnosis. Nerve root compression is almost always the cause, and MRI scanning is essential for confirmation1 CES occurs rarely in community populations and is only confirmed in 19% of those presenting with CES symptoms2
Duration of symptoms at presentation varies with a median of 48 hours. The commonest symptoms are sciatica, altered sensation in the saddle area, and micturition dysfunction. Sexual dysfunction is often omitted from the doctor’s enquiry, but when questioned, sexual dysfunction exceeds 90%3
Classification
The most useful modern descriptive classification (Lavy)1:
1. CES Suspected (CESS): Patients are at risk of developing CES. There is bilateral sciatica or motor/sensory changes in the lower limbs but no sphincteric or perineal sensory changes. Includes anyone at risk of developing CES, e.g. due to a large disc.
2. CES Early (CESE): In addition to CESS, there are perineal sensory changes or micturition symptoms. Bladder, bowel, and sexual functions are preserved.
3. CES Incomplete (CESI): Altered bladder function/sensation with/without perineal sensory changes, sexual or bowel dysfunction.
4. CES with retention (CESR): In addition to CESI, there is painless bladder retention and overflow.
5. CES Complete (CESC): Insensate bladder with overflow incontinence, no perineal, perianal or sexual sensation, and no anal tone.
The historical but useful classification (Tandon)1:
1. Type 1: Rapid onset of CES symptoms with no previous history of back problems (quite rare).
2. Type 2: Acute bladder/CES symptoms with back problems and sciatica history (commonest type). Patients are usually young (< 40 years) and have a high Body Mass Index (BMI).
3. Type 3: Longstanding back problems and gradually progressive CES (common in older patients with spinal stenosis – very rare), (Figure 1).
CESE and CESI are the most time-critical presentations with ‘more to lose’, and surgical decompression should be done as an emergency, especially in CESI. In CESR and CESC, although these are more likely to bear poor outcomes, surgical decompression remains beneficial; however, it appears less clear that it should be performed as an emergency (particularly overnight), although this is controversial with many spinal surgeons averring that all CES cases should be performed as an emergency.
Subspecialty
50 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Pathophysiology
CES is usually caused by the compression of nerve roots by lumbar disc herniation. The functional changes induced by compression can be caused by mechanical nerve fibre deformation compression and restriction of nerve root microcirculation, local ischaemia intraneural oedema and resultant Wallerian degeneration4
Diagnosis

The diagnosis consists of two critical points:

a) A history and examination consistent with suspicion CES (see above).
b) MRI (Figure 2) or CT5


Many patients ignore numbness, placing greater emphasis on pain. Doctors must ask about red flags. Nonetheless, red flag signs, including bilateral sciatica, altered perineal sensation, motor or sensory changes, and bladder/bowel/sexual dysfunction, have a low predictive value (a measure of the times that the value positive or negative is the true value). >>




Subspecialty
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 51 Introducing Arthrosamid®— a new class of injectable therapy to treat knee OA Safe and sustained pain relief with a single injection1 www. Arthrosamid .com @ConturaLtd Contura-Orthopaedics-Ltd Contura Orthopaedics Ltd OUS/ARTHRO/JAN2023/014 See our latest data and read about our patient experiences SCAN ME Reference: 1. Bliddal, H., et al. (2021). Polyacrylamide Hydrogel Injection for Knee Osteoarthritis: A 6 Months Prospective Study. J Orthop Res Ther. Vol 6(2). 1188. ISSN 2575-8241 For full details about warnings and precautions read the IFU. For more information and the IFU please visit https://www.Arthrosamid.com or contact us at enquiries@Arthrosamid.com
Figure 1: Sagittal and axial MRI T2 weighted images showing a central canal stenosis causing compression of the cauda equina, not requiring emergency decompression due to the absence of cauda equina symptoms and signs.
The usefulness of particular symptoms and signs:
a) Bilateral sciatica has a sensitivity of 32.4%, PPV 17.2%, and NPV 88.3%.
b) Post-void residual volume (PVR) of ≥ 200 ml has a sensitivity of 94.1%, specificity 66.8%, PPV 29.9% and NPV 98.7%6
Patients presenting with CES symptoms should have an emergency MRI scan even in the absence of clinical signs. Changes on PR examination are poorly correlated with findings of CES, and even though a post-micturition bladder scan is more useful, its ‘normality’ does not exclude CES (6% will be missed).
Emergency MRI is part of the triage of the suspected CES patient. It should always be performed locally7, as early diagnosis offers the best chance of a satisfactory outcome.
Timing of surgery
There is increasing understanding that damage to the cauda equina nerve roots occurs continuously and progressively, and thus, the earlier the surgical decompression, the better the outcome.
There are no safe time thresholds such as the 48-hour ‘safe’ time window described by Ahn8 because neurologic deterioration in CES can occur rapidly and unpredictably. There are commonly poor outcomes in CES patients leading to a lifetime of disabling, awful symptoms, loss of function and employment.
The British Association of Spine Surgeons (BASS) states that “Nothing is to be gained by
delaying surgery and potentially much to be lost”; surgery should be carried out as soon as is practically possible7
Removing a large central disc prolapse can be considerably more difficult than a routine discectomy and may require extensive exposure, and midline decompression and interlaminar decompression are the norm. The question of ‘whether to operate in the middle of the night’ with a ‘stable’ CES-I patient remains controversial; however, the authors of this article remind the reader that it is not possible to predict when a patient will progress from CES-I to CESR-R/C and consequently endure a far worse outcome. Emergency surgery is the expected norm9

Outcomes of surgical intervention of surgery
Neurological recovery is more likely with early surgical decompression. Patients who have a decompression whilst ‘in CESI’ have a better prognosis than those with CESR/C. Even when there is a delay in presentation with CESR/C, surgery offers improved outcomes. There is always ‘something potentially to be gained’ with decompression10
Approximately 75% of all CES cases will eventually have an acceptable urological function; however, often, there is the persistence of back pain and motor and sensory deficits. Of all CES patients, 1 in 5 will have a poor outcome, usually with the need for ongoing treatment, e.g. management of sexual dysfunction, self-catheterisation, colostomy, urological and gynaecological surgery, spinal injuries rehabilitation and psycho-social support. CESR/C patients are likely to have significantly worse long-term outcomes in bladder, bowel and sexual function compared to those with CESI11
Medico-legal aspects of cauda equina syndrome
The largest cause of claims is the delay in diagnosis and treatment. According to the National Health Service Resolution Report 2021/2022, orthopaedic surgery is in the top three specialities by volume of claims. From January 2008 to December 2018, NHS resolution received 827 claims for CES; the cost to the NHS was £186m.
Controversies and areas of further research
In patients with large or massive disc prolapses without clinical features of CES, i.e. CESS, these patients can be safetynetted, and emergency surgery is not warranted as they are likely to resolve spontaneously12
On the contrary, a small disc with clinical evidence of CES warrants surgical decompression, dependent on the stage.
There remains no agreed radiographic definition for CES. What defines a large disc? What is the crosssectional size? How much compression is needed? Does the presence of CSF exclude CES?
Take home messages
1. All patients with sciatica should be given surveillance advice concerning symptoms of CES (red flag ‘card’).
2. Doctors must enquire concerning red flags.
3. Neurological injury is time-critical.
4. Emergency scan, referral, and surgery.
5. There are no safe time thresholds. n
References
References
Subspecialty
can be found online at www.boa.ac.uk/publications/JTO
“Emergency MRI is part of the triage of the suspected CES patient. It should always be performed locally, as early diagnosis offers the best chance of a satisfactory outcome.”
52 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Figure 2: Sagittal and axial MRI T2 weighted images showing a large L5/S1 central disc prolapse causing compression of the cauda equina nerves.
Save The Date
SI Joint Dysfunction -

Hands-on International
Primary Surgeon Training
12-13 May 2023, Nice, France
Register here:
Don't miss: Don't miss:
Diagnosis algorithm for SIJ Dysfunction
Diagnosis algorithm for SIJ Dysfunction
Interactive Live Surgery Interactive Live Surgery
Professional discussions with specialties
Professional discussions with specialties
Save the date 12 -14 October 2023 · Basel · Switzerland

EBJIS
2023
41st Annual Meeting of the European Bone and Joint Infection Society
Theme From the beginnings of the AO foundation to modern treatment concepts in implant-related infections
Topics • Animal models in biofilm research
• Antimicrobials
• Biofilm and beyond - translation from in-vitro data to in-vivo strategies
• Diabetic Foot Infection and Diabetic Foot Osteomyelitis
Submit your abstract now!
Important dates
Abstract submission deadline: 12 April 2023
Early registration deadline: 3 July 2023
• Genetics in implant-related Infections
• Infection prevention
• Orthoplastic Surgery – from split skin to tailored tissue engineering? …and much more!

#EBJIS2023 www.ebjis2023.org

Alex Goubran is a Spinal Consultant at Musgrove Park Hospital, having completed his orthopaedic training in the South West Peninsula deanery. He was appointed as one of the inaugural Spinal Trainee Interface Group Fellows and completed this in Sheffield. He is keen on leadership, management and education.
Spinal infection –an overview
Alex Goubran and James Tomlinson
Spine infection covers a broad spectrum of disease from simple discitis that can usually be managed in a non-specialist centre, to complex infections with epidural collection, requiring emergency surgical management in a complex spine centre. Treating spinal infection is challenging and needs close collaboration between orthopaedics, radiology, microbiology and infectious diseases. It is a diagnosis that can be easy to miss in the early stages and a high index of suspicion is critical.
What is it?
James Tomlinson is a Consultant Spinal Surgeon at Sheffield Teaching Hospitals. He is Education TPD for T&O and has a significant interest in postgraduate training.


Osteomyelitis of the spine may result from haematogenous seeding of the adjacent disc space1 in a spondylodiscitis type picture; infection of the intervertebral disc and/or endplate. There may be delay in diagnosis and identification as it presents with common, often non-specific, symptoms of back and neck pain.
Though first described by Pott, specifically referencing Tuberculosis of the spine, the disease process can be caused by many pathogens. It may be isolated to the intervertebral disc space and termed spondylodiscitis2 but it is when the bony structures are involved, it would be termed vertebral osteomyelitis.
Who gets it?
Spinal infections have a bimodal distribution of incidence, with a peak below 20 years of age and another at 50-70 years of age. It is 2.5 times more common in females than males3. Certain risk factors are associated with discitis and are listed below. It is important to recognise that a large number of cases are seen in patients with no identifiable risk factors.
Common risk factors and association1 include age, immunocompromise, and active intravenous drug use. Diabetes mellitus, neoplastic disease and indwelling urinary catheters. Although post-operative infection is not common, it is still important to ask about recent spinal surgery in the context of relevant symptoms.
How common is it?
Spinal infection accounts for approximately 2-7% of all musculoskeletal infections. Its incidence is between 1:100,000 and 1:250,000 in developed countries. Its estimated mortality rate is 2-4%.
What are the causes?
In determining the cause or origin; pertinent history and evaluation of the patient should include history of antimicrobial use, prior surgical procedures as well as urinary tract infection, bloodstream infection, skin or soft tissue infection, and intravenous drug use2
The most common causative pathogen seen in Western societies are Staphylococcus aureus or E. coli1. Blood cultures are positive in approximately 50% of patients, and in these cases biopsy is therefore not needed. Patients with S. aureus bacteraemia must also undergo Echocardiographic assessment for evidence of infective endocarditis.
Discussion with microbiology and radiology colleagues is critical. Radiological guided biopsy is critical in the absence of either positive microbiology samples or positive blood cultures. Certain regions may have endemic Tuberculosis, and/or Brucella infection and Brucella. Tuberculosis remains a major cause of spinal infection worldwide and it is important to consider in certain areas of the UK, as well as in cases of recent foreign travel to high incidence countries. Those patients who are immunocompromised or who have human immunodeficiency virus may be at higher risk of infection with mycobacteria. High rates of Brucellosis are seen in the Mediterranean, Middle East, parts of Africa and Western Asia.
Fungal disease is extremely rare1. It is usually only seen in patients with significant risk factors.
In the paediatric population2, due to vascular anastomoses in the intervertebral disc, septic
Subspecialty
54 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
emboli do not usually cause bone infarction and bone infection in the same way as occurs in adults, but infection may be confined to the disc. In areas of endemic disease; pathogens such as Tuberculosis and Brucella should be considered.
How is it diagnosed?
The average time to diagnosis has been reported to be between 2-4 months2. Patients may initially present with very mild symptoms, and back or neck pain. It is critical to ask patients if their pain is different from any usual background pain –both in severity and distribution. New thoracic back pain, new radicular pain and/or weakness can be key findings.
Examination should elicit any signs of instability pain (pain on sitting on standing), and a thorough neurological examination is critical. Blood tests including inflammatory markers should be sent. Gold standard imaging is MRI whole-spine with axial and sagittal sequences. Wherever possible these scans should be done with Gadolinium to look for the presence of an epidural abscess. If an abscess is present ring enhancement will be seen. MRI scans may be normal in the early stages of discitis. In these cases a second scan should be done 14 days after the initial scan. Two normal scans 14 days apart makes spinal infection extremely unlikely.
If blood cultures are positive then radiologically guided biopsy is not usually needed, although only 50% of cases have positive blood cultures1 Radiologically guided needle biopsy is positive in up to 73% of cases if the infected site is radiologically accessible. Open surgical biopsy can be performed if needed and has a 92% positive culture rate.
Imaging
MRI of the spine has a sensitivity of 97%, specificity of 93% and an accuracy of 94% in diagnosis. Inability to distinguish margins between the disc space and adjacent vertebral marrow on the T1 weighted images associated with high signal intensity from disc and adjacent marrow on the T2 weighted images is considered the most salient radiological feature (Figure 1). If infection is centred on bone with spread under the anterior longitudinal ligament, TB must be suspected.
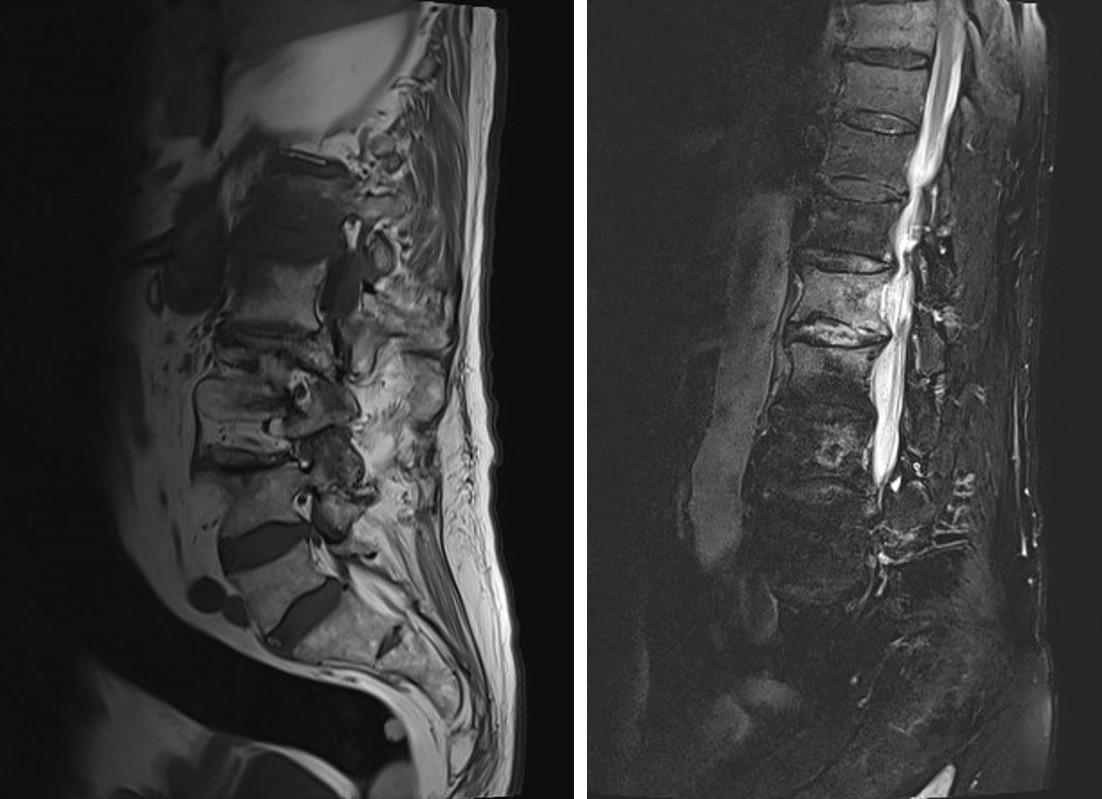
MRI can also distinguish between an infective process, degenerative disease, neoplasia or trauma. CT scanning is helpful in cases with significant bony destruction for surgical planning but is often less helpful when diagnosing early discitis with subtle changes.
Plain films should only be used to assess deformity and collapse as disease progresses
and is treated. They do not play any useful role in diagnosing discitis in the early stages of disease.
Medical and surgical management
Treatment should be targeted to an organism wherever possible. There are no universally agreed standards on the length of treatment. Uncomplicated discitis (not involving the epidural space) can usually be treated with two weeks of intravenous, then four weeks of oral, antibiotics. Infection with epidural involvement requires six weeks of intravenous antibiotics and a further six weeks of oral antibiotic therapy4
The Infectious Diseases Society of America guidance suggests withholding antimicrobial therapy until an organism has been cultured. Empirical antibiotics should however, be commenced in the face of sepsis, haemodynamic instability or neurological compromise. If treatment is commenced without cultures Flucloxacillin is often the first line treatment given that Staphylococcus aureus the most common causative organism.
Treatment response should be monitored with serial CRP measurements, ideally twice weekly. Repeat imaging is not routinely performed in simple discitis. Scan appearances may be abnormal for up to a year post infection, and thus repeat scans are not particularly helpful. In patients with
an epidural abscess an end of treatment scan should be performed before stopping antibiotics. This is to ensure the epidural collection has resolved5
Simple discitis without significant bony destruction can be managed in a nonspecialist centre. If significant bony destruction or epidural abscess is present patients should be managed in a specialist spine centre.
Surgical management
Absolute indications for surgery include epidural abscess with either neurological compromise, overwhelming sepsis or both. These patients may present in extremis and life threateningly unwell and need emergent decompression and drainage. Epidural abscess at cord level (above the conus) is also an absolute indication for emergency surgery (Figure 2). Such cases need urgent transfer to a specialist spine centre.
Relative indications for surgery are deformity and instability pain. Decision making in these cases is more nuanced and must include a detailed discussion with the patient and careful management of expectations.
When surgical stabilisation is needed it may be anterior, posterior or both and is usually bespoke to each case and the indications. The approach for decompression and >>
Subspecialty
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 55
Figure 1: MRI changes.
drainage of an epidural abscess is guided by the location of the abscess relative to the spinal cord - i.e. if whether an anterior or posterior approach is more suitable (Figure 3)6
Follow-up
It is almost impossible to give definitive guidance on which patients should or should not be followed up. Follow up may be with local orthopaedic teams, infectious diseases teams, spinal surgeons, or a combination of these.
Factors that shape follow up decisions include presence of epidural infection, treatment response (fall in CRP), causative organism (Gram negative infections may not fuse and develop chronic pain), and need for acute surgical
treatment. Patients with epidural space infection should all be followed up with an end of treatment MRI scan before stopping antibiotics. The other factors listed are all relative indications for follow up that should be considered.
Conclusion
Spinal infection is a complex spectrum of disease ranging from simple discitis in relatively well patients to complex epidural infection that may lead to life threatening illness or severe neurological compromise. A high index of suspicion is critical as this condition is often misdiagnosed or missed altogether. Once infection has been diagnosed on cross sectional imaging multispecialty input is needed to optimise treatment. n
References
1. Berbari EF, Kanj SS, Kowalski TJ, et al. Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adults. Clin Infect Dis. 2015;61(6):e26-46.
2. Duarte RM, Vaccaro AR. Spinal infection: state of the art and management algorithm. Eur Spine J. 2013;22(12):2787-99.
3. Baryeh K, Anazor F, Iyer S, Rajagopal T. Spondylodiscitis in adults: diagnosis and management. Br J Hosp Med (Lond) 2022;83(10):1-9.
4. Bernard L, Dinh A, Ghout I, et al. Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Lancet. 2015;385(9971):875-82.
5. Luzzati R, Giacomazzi D, Danzi MC, et al. Diagnosis, management and outcome of clinically- suspected spinal infection. J Infect. 2009;58(4):259-65.


6. Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ. Hematogenous pyogenic spinal infections and their surgical management. Spine Spine (Phila Pa 1976). 2000;25(13):1668-79.
Key learning points
• Spinal infection is often diagnosed late and it is critical to maintain a high index of suspicion.
• MRI imaging is the gold standard and should be performed early.
• Antibiotics should be withheld until an organism has been cultured unless a patient is systemically unwell.
• Input from spinal surgeons, microbiologists and infectious diseases is critical to optimise management.
• Simple discitis without significant bony destruction can be managed in a non-specialist centre. If significant bony destruction or epidural abscess is present patients should be managed in a specialist spine centre.
• Treatment response should be monitored with serial CRP measurements, ideally twice weekly. Repeat imaging is not routinely performed in simple discitis as scan appearances may be abnormal for up to a year post infection.
• Patients with epidural space infection should all be followed up with an end of treatment MRI scan before stopping antibiotics. Other factors may be relative indications for follow up that should be weighed individually.
Subspecialty
Figure 2: Epidural abscess.
Figure 3: Posterior stabilisation of cervical spine for bony infection.
56 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Ring enhancement on post contrast axial MRI
EDINBURGH INTERNATIONAL TRAUMA SYMPOSIUM AND TRAUMA INSTRUCTIONAL COURSE 15th-18th AUGUST 2023


TRAUMA SYMPOSIUM 16th-18th AUGUST 2023
Three day meeting suitable for established orthopaedic surgeons

Renowned international faculty


Focused on revalidation and update through short interactive lectures and CBDs

Break out sessions include cadaveric surgery focusing on surgical approaches and fixation techniques
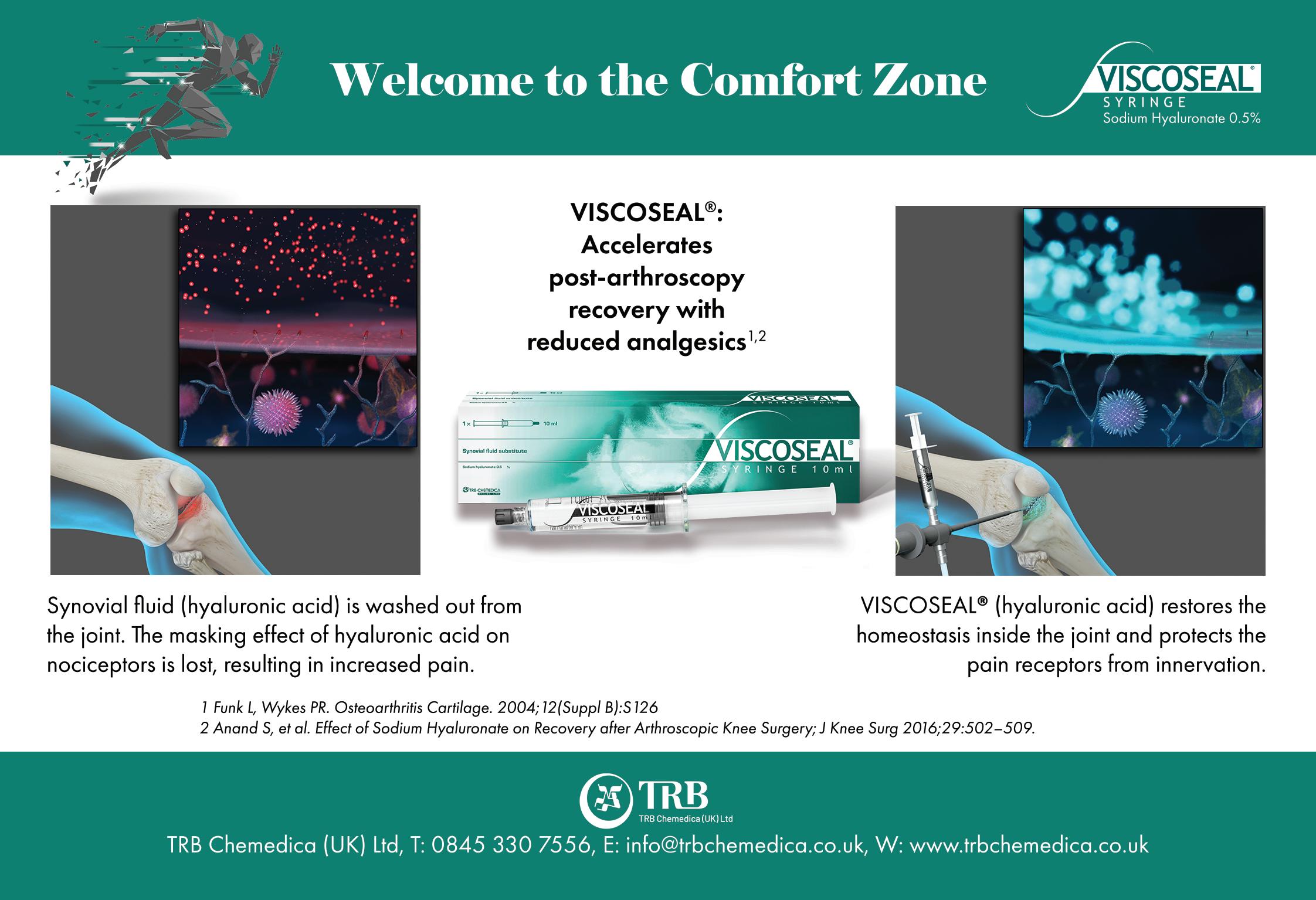
TRAUMA INSTRUCTIONAL COURSE 15th-18th AUGUST 2023
Four day orthopaedic trauma course suitable for established surgeons, trainees and AHP’s Comprehensive lectures and CBDs on the assessment and management of paediatric and adult fractures
Break out sessions including cadaveric anatomy teaching and FRCS viva practice
VENUE: SHERATON HOTEL AND EDINBURGH MEDICAL SCHOOL
For more information on booking and early bird discounts visit www.trauma.co.uk or email symposium@trauma.co.uk
Alexander Durst is currently a Senior Spinal Fellow at the Welsh Centre for Spinal Surgery and Trauma, in Cardiff. He was the first Spinal Trainee Interface Group Fellow for Health Education England. He subsequently completed a fellowship in Complex Spine Surgery at the University of Alberta, in Edmonton, Canada. His interests include spinal trauma and surgical education. He is an East of England T&O rotation alumnus.
Thoracolumbar fracture stability and the difficulties of classification systems
Sashin Ahuja is a Consultant

Orthopaedic Spinal Surgeon at Cardiff and Vale University Health Board since 2003. His practice covers the full spectrum of spinal disorders including paediatric deformity. He has worked on the executive boards of British Scoliosis Society (BSS), British Association of Spine Surgeons (BASS) and AO Spine. Sashin is the Chair of UKSSB (2021-2024), Co-Chair of the Spine ODEP & BC and has been Past President of BASS (20192021), AO Spine UK & I Council Chair (2017-2020). He is an expert advisor to NICE and MHRA.

Although the topic of fractures comprises a significant proportion of orthopaedic practice, and as such should be an area of common ground amongst us, in the spine it can produce apprehension. This can be partly attributed to controversies in the classification and management of spinal fractures, as well as the potentially devastating clinical implications associated with neurological injury. Even when discussing thoracolumbar fractures, a subject which is potentially less complicated than in the cervical spine, these disagreements can persist. As with most things in orthopaedics, reverting to basic principles and ‘keeping it simple’ can be a helpful method of understanding. We aim to highlight the important points from existing classification systems to help make them useful to clinical practice, future exam delegates and even our non-spinal colleagues examining them. We also hope to nix some unhelpful concepts in the process.
A historical perspective of thoracolumbar fractures
Until Wilhelm Röntgen discovered X-Rays in 1895, spinal fractures were classified clinically; based on whether or not they had neurological compromise. In a case series of 244 patients treated from 1864 through 1905 by Herbett Burrell (Boston City Hospital), an evolution in clinical assessment and
treatment was demonstrated. Initially, he did not consider injuries without paralysis to be spinal in nature, however he had re-evaluated this by 1900.
Burrell classified his patients into complete, incomplete or no paralysis groups, with mortality approaching 80% with paralysis. The majority were treated in a plaster jacket, with a few willing paralysed patients treated additionally with laminectomy, durotomy and removal of bone fragments. Neurological recovery was not consistent, and Burrell consequently advocated delayed surgery, since “an injury which has involved destruction of the cord is already done, and will get no worse in a few hours.”
In the period that followed, the development of spinal fracture management, as with much of modern orthopaedics, was strongly linked to early 20th century warfare. The first radiological series of spinal fractures was published by the Austrian (Nazi party member), Lorenz Böhler (Figure 1), of calcaneal angle fame. In his 1929 paper, “Technik der Knochenbruchbehandlung, vol. VIII” (English: Fracture Treatment, volume VIII) he suggested the importance of mechanism of injury, neurological status (paralysed or not) and fracture reduction. He described six types of fractures based on mechanism: compression, flexion, extension, lateral flexion, shear and torsion.
Subspecialty
“A stable spine is able, under physiological load, to maintain its normal movement so that there is no initial or additional neurological deficit, no major deformity, and no incapacitating pain.”
– White and Panjabi
Alexander Durst and Sashin Ahuja
58 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
In 1931, one of the fathers of British orthopaedics published his own series and classification. Reginald Watson Jones (Figure 2), who was later knighted due to his war efforts as a consultant to the Royal Air Force, believed thoracolumbar fractures were mostly pure flexion injuries. He treated them with hyperextension and plaster jacket immobilisation for four months. Anatomical reduction was allegedly almost always achievable and maintained, producing ‘excellent’ functional results.


These results were not found to be reproducible by EA Nicoll (Mansfield; Figure 3), who was commissioned by the Miners’ Welfare Commission, to tour North America in 1947 to research the treatment of traumatic paraplegia. In a series of 166 coal miners, Nicoll classified thoracolumbar fractures as stable or unstable, based on disruption of the interspinous ligament. As with Watson Jones, he believed most fractures had a flexion mechanism, likely due to the confined hunched positions miners worked in. However, his belief that most simple wedge fractures were stable challenged the zeitgeist so radically, that in public, good-humoured, back-and-forth lectures (including SICOT 1950, Paris) Watson-Jones and he comparatively criticised each other’s methods and results. Both presented a slide of one of their successes with a subsequent blank slide annotated saying, ’Nicoll’s method’ or ’Watson-Jones’ method’, respectively.
Nicoll’s work had enormous implications. At the time, a miner with a spinal injury was written off as a permanent cripple, unable to work again. However, 80% of Nicoll’s patients returned to hard manual labour in coal pits, and his report was accepted by Aneurin Bevan, the Minister of Health and founder of the NHS. Nicoll’s friend and colleague, Frank Holdsworth (Figure 4), who accompanied him on the North American tour, subsequently opened the Lodge Moore spinal injuries unit in Sheffield in 1954. Building on previous anatomical and biomechanical concepts, Holdsworth classified all spinal fractures according to four mechanisms of injury: flexion, flexion with rotation, extension and compression (Figure 5). Holdsworth also advocated a two-column model of the spine. His anterior column supported compressive loads, whilst the posterior column (consisting of everything dorsal to the posterior longitudinal ligament [PLL]) resisted tensile loads. He considered posterior column failure as the main determinant of instability in the spine. >>



Subspecialty
Figure 1: Lorenz Böhler: 1885 – 1973. Copyright 2005 Springer-Verlag London Limited.
Figure 2: Sir Reginald Watson Jones: 1902 – 1972. Watson Jones hyphenated his names in 1939, to differentiate himself from other Joneses, becoming Reginald Watson WatsonJones. Watson was his mother’s maiden name. Copyright 2005 Springer-Verlag London Limited.
Figure 3: E.A. Nicoll: 1903 – 1993. Copyright 2005 Springer-Verlag London Limited.
Figure 4: Sir Frank Wild Holdsworth: 1904 – 1969. Copyright 2005 Springer-Verlag London Limited.
JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 59
Figure 5: Drawings from Holdsworth’s posthumously published classic paper, demonstrating anatomy and mechanism of injury. Copyright 1970 by The Journal of Bone and Joint Surgery, Incorporated.
The three column concept (an examiner’s favourite)
Francis Denis’ (Minnesota; 1984) often misquoted (and mispronounced, as he was a Frenchman who moved to the USA!) review of 412 thoracolumbar fractures built on Holdsworth’s concept of posterior ligamentous rupture, however he did not believe that this alone was enough to produce instability. He recognised stability as a spectrum. His proposed middle column consisted of the posterior wall of the vertebral body, posterior annulus fibrosus and PLL. He did not mention halves or thirds of the vertebral body/disc. This may have been inferred from his drawings and quoted biomechanical work by Panjabi. He did not say that involvement of the middle column equalled spinal instability. Rather, his conceptual model aimed to explain mechanism of injury (as per Holdsworth) according to the modes of failure of the middle column. As this has seemingly brought confusion, subsequent classifications have ignored three-columns, and all in essence follow Holdsworth’s focus on mechanism and anatomy.
The Arbeitsgemeinschaft für Osteosynthesefragen (AO; English: Working group for bone fusion issues), or Magerl (1994), classification follows Holdsworth’s two-column model; with a compression resistant solid anterior column and tension resistant hollow posterior column of neural canal. It subdivides fractures by mechanism into compression (A-type), distraction (B-type) and rotation (C-type), in similar alphanumerical fashion to the AO long bone classification, with increasingly progressive instability. As with the other AO classifications, it can be complex to use for the non-initiated, but the principles remain clear: mechanism of trauma has a correlation to stability.
A new favourite classification amongst examiners
In 2005, a Delphi process of 40 ‘expert’ surgeons produced the Thoracolumbar Injury Classification and Severity Score (TLICS) based on 1) radiographic morphology, 2) posterior ligamentous integrity and 3) neurologic status, with no confusing mention of two- or threecolumn concepts. The three TLICS parameters essentially combine Holdsworth’s concepts with the pre-radiographic clinical classification of Burrell, producing a score to guide treatment. To truly classify according to TLICS, 1) plain radiographs/ computer tomography [CT], 2) magnetic resonance imaging [MRI] and 3) clinical assessment (by American Spinal Injury Association [ASIA] score) must be collated. A score < 3 is considered stable, not requiring surgery, whereas a score > 5 is considered unstable requiring surgery. Unfortunately, TLICS does not give an answer for injuries with a score of 4 (as stability is a spectrum). These are often the same injuries which produce debate when using other classification systems or treatment algorithms.
A more recent compromise between TLICS and Magerl is the 2013 updated AOSpine Thoracolumbar Injury Classification System, (Figure 6). As with
Holdsworth, Magerl and TLICS, a descriptive morphological classification based on mechanism is combined with posterior ligamentous integrity and a neurologic status modifier. Additional modifiers aim to aid surgeon decision making, however as with other classification systems they can confuse the uninitiated. As with other classification systems, we believe its best use is for communication between clinicians.
In our practice and teaching we believe that understanding a definition of stability (as per White and Panjabi), the importance of mechanism of injury, and how to aptly perform an ASIA neurological exam are keys to dealing with spinal fractures. Grasping these concepts should help surgeons, whether or not they are spinal by subspeciality. Then comes the next slew of controversial questions: what approach and technique by which to fix the fracture?! To brace or not?
Key learning points
1) Spinal stability is a spectrum.
2) Mechanism of injury correlates to stability.
3) Neurologic injury from trauma suggests spinal instability.
4) Neurologic damage occurs at the time of injury.
5) Classification systems should be reproducible communication tools. n
Selected references
• Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Joint Surg Br 1949;31B(3):376-94.
• Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am 1970;52(8):1534-51.
• Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8(8):817-31.
• White AA and Panjabi MM. Clinical biomechanics of the spine, Vol. xxiii. Philadelphia: Lippincott, 1990; p722.
• Vaccaro AR, Lehman Jr, RA, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005;30(20):2325-33.
• Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013;38(23):2028-37.

Subspecialty
Figure 6: The simplified ‘AOSpine Thoracolumbar Injury Classification System’ which 43 years on, bears similarities to Holdsworth’s drawings. Copyright by AOSpine International, Switzerland.
60 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
www.efort.org/vienna2023
24TH EFORT Congress
Vienna, Austria: 24-26 May 2023

Late registration deadline
02
MAY 2023
#EFORT2023
Congress Highlights | Main Theme: Building The Future Of Orthopaedics & Traumatology
Ageing Motion Analysis And Mobility
3D Printing For Patient Specific Implants



Robotics
Technological Advances In Diagnostic Equipment
Biological Implants
Key dates
Advanced Programme online: 01 April 2023
Virtual Learning Experience
Practical Applications Of Science & Techniques
Surgical Planning And Simulation
Patient reported outcome
Scientific & Clinical Networks
Late registration deadline: 02 May 2023
24
TH EFORT Congress 2023
Dame Clare Lucy Marx
15th March 1954 – 27th November 2022
Obituary by Mark Bowditch and Deborah Eastwood
Clare was born and brought up in the Midlands and attended Cheltenham Ladies College. She went on to study medicine at UCH London.
She subsequently joined the UCH orthopaedic rotation and following an arthroplasty fellowship in Boston USA, she was appointed as a Consultant at St Mary’s Hospital, London.
Having married, it soon became clear a post nearer to home was going be preferable.
A post arose in Ipswich and Clare became their first female surgeon in any surgical speciality in 1993. Although potentially challenging she experienced nothing but encouragement.
Her passion for high quality education led her to be Chair of the Joint Colleges Specialty Advisory Committee (SAC) and produce the first T&O surgical curriculum 2007.
She broke down barriers throughout her career and broke through the glass ceiling of male domination becoming BOA President in 2008, a time she described as the most enjoyable of her career. Although the first female president, this was never an issue for her.
She had an unfaltering sense of what was right for patients and colleagues which directed every decision and having got on to the RCSEngland Council, her focus was always improving patient care.
She rightly became the first woman President of the RCSEngland in 2014.
Having demitted as President of RCSEngland she did not stop and in 2018, she became chair of the Faculty of Medical Leadership and Management, and in 2019 the first woman chair of the General Medical Council. At a time when its reputation amongst doctors was low, she brought a steadying sensible hand, enthused by the challenges.

Honoured for services to medicine with CBE 2007 she was made a Dame in 2018.
In recognition of her contribution to the Suffolk community she was appointed a Deputy Lieutenant and in 2022 was one of five recipients to receive the Suffolk Medal.
In 2021, she was diagnosed with pancreatic cancer and her GMC resignation letter highlighted Clare’s approach to medicine: “Since receiving this news, I’ve have been reminded once again of the importance and power of kindness in everything we do as doctors”.
Clare passed away on the 27th November 2022. Her loss will be felt deeply across our orthopaedic community. n
Eric Anderson
22nd December 2022
It is with great sadness that we write to commemorate the life of our friend and colleague, Eric Anderson, who died shortly before Christmas 2022. Eric was one of the great leaders of the revolution in foot and ankle orthopaedic care over the last 50 years world-wide. He passed his FRCS in 1971 in London. He was appointed to his consultant post in the Western Infirmary, Glasgow in 1978, where he continued in his NHS practice until 2006.

As a trainer he inspired many that he taught to take up his beloved speciality. As a mentor his common sense and practical approach to problems meant that he was a go to for opinions on difficult cases.
His leadership was evident in the growth of the interest in foot and ankle surgery in the UK. He joined the British Orthopaedic Foot Surgery Society (as it was known in those days) in 1979 and became President in 1982. He was indeed President twice, also having that honour in 1995, at what might be described as the start of the modern era and the evolution to the British Orthopaedic Foot and Ankle Society in 2006. At a time of a little bit of an internal revolution, where the growing number of younger surgeons flexed their voting rights at an AGM, it was notable that Eric with his air of quiet common sense (particularly in matters of finance!) spanned the generations. Always an absolute gentleman in all senses of the phrase, you would however often see a little mischievous smile appear when these events unfolded.
In the early to mid-1990s he very much saw the importance of a united voice for foot and ankle surgery in Europe. He was heavily involved in bringing together the then two European societies (ESFAS and EFFAS) with the formation of EFAS in 1998 and was their first Treasurer.
He continued to contribute to the foot and ankle world in his later years not missing a BOFAS meeting for 40 years.
Sadly he lost his wife Liz only three months before he died, leaving his three children Colin, Heather and Fiona.
All who knew him will have a quiet smile at our fondest memory of him. n
In Memoriam 62 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
Obituary by Ian Winson and Don McBride
Bhaskar Bhowal
23rd October 1961 – 22nd December 2022
Obituary by Clare Wildin, Aamer Ullah and Joe Dias on behalf of Bhaskar’s Leicester colleagues
Bhaskar was naturally smart and a master of fine detail who never wrote with anything but a Mont Blanc pen. He qualified from Calcutta Medical College in 1984. At medical school he was the Culture Secretary, his love of music and fine food continued throughout his life. In 1991, he came to the UK to work at Morriston Hospital, Swansea, meeting Phil Matthews who sparked his interest in hand surgery. He was appointed as a Registrar in Leicester in 1993. Here he really developed his love of all things ‘British’, especially a good steak and going to ‘the pub’.
After his fellowship in Wrightington he was appointed as a Consultant Orthopaedic Surgeon at the University Hospitals of Leicester in 1999. Bhaskar never considered himself ‘the expert’ even though he was. He worked closely with his colleagues, shared opinions and co-operating on difficult cases. He evolved the paediatric hand surgery clinics with our plastic surgery colleagues and forged close working relationships with rheumatology and neurology. Bhaskar was a strong partner in all Leicester research activity, he was Principal Investigator for several National Institute for Health and Care Research studies on scaphoid fractures and Dupuytren’s disease and published numerous papers which have changed the treatment pathways for many hand and wrist conditions.

Alan William Frederick Lettin
06th January 1931 – 03rd January 2023
Obituary by Keith Tucker, John Getty and Jonathan Lettin
It is with sadness we report the death of Alan Lettin, BOA President 1994-95.

Alan was born in the East End of London and was proud of his humble heritage. He won a prestigious State Scholarship to UCH where he was awarded a BSc in physiology besides qualifying MB, BS, in 1956.
After National Service he entered orthopaedic training mainly at the Royal National Orthopaedic Hospital (RNOH) where his ideas as to how orthopaedic surgeons should be trained began to form. He collected his MS (1967) while at RNOH on fracture healing.
In 1967 he was appointed to Bart’s and Queen Elizabeth’s
Bhaskar’s true passion has always been with education. When aged 16 he was awarded the National Talent Search Scholarship by National Council for Educational Research and Training by the Indian Government, he delivered on his potential becoming East Midlands Deanery Training Program Director, Deputy Head of School of Surgery and Trauma and Orthopaedic SAC member. He was very proud of his trainees achieving an exemplary pass rate for the FRCS T&O exam. He co-authored the T&O curriculum for the General Medical Council, led on Technology Enhanced Learning and helped develop the BOA training course for supervisors. He helped run the Leicester Hand Fracture Course for over two decades and sadly only missed the last course because of ill health.
Bhaskar was much loved by all his colleagues in Leicester and was deeply involved with the Bengali community who regarded him as family. Bhaskar was supportive, obsessive, mischievous, kind and very often infuriating. His optimism was infectious. Despite his own health problems, he made us all smile.
He was a dear friend and colleague and we miss him greatly. n
Hospital Hackney and in 1969 he was also appointed to the RNOH whilst relinquishing his appointment at Queen’s.
During his long association with the RNOH he was involved with the development of the Stanmore knee, elbow and shoulder replacements and demonstrated them around the world. He was in fact a general orthopaedic surgeon but with a special interest in surgery for rheumatoid arthritis and back pain.
His name was on over 40 peer reviewed publications, 37 chapters in books and several books. He gave over 170 presentations to learned societies and served on over 100 committees, often as Chair. He was an examiner for several universities in the UK
He was a member of the Council of the Royal College of Surgeons before becoming a Vice President.
For many of us, what he will mostly be remembered for was his massive contribution to the formation (1969) of the Bart’s rotation, now known as the Pott rotation which he oversaw until he retired in 1995. The concept of progressive training, which was the hallmark of the Bart’s Rotation, was novel but was rapidly copied by numerous other orthopaedic departments. For Alan, training also involved teaching and he rarely missed his Wednesday teaching session with the Bart’s students.
After retirement, Alan moved to Suffolk where he had a small farm which he worked for a number of years.
Alan married Pat in 1954 and they had four children, three of whom survive him. Tragically they lost their daughter to a spinal tumour shortly after Alan’s appointment to Bart’s. They were an incredibly hospitable and generous couple and many of us remember the dinners at their house in Chigwell with fondness. Alan’s generosity will be forever remembered by the inscriptions in the Great Hall at Bart’s and the Alan Lettin room at the RCS.
Pat predeceased Alan in 2018 and age slowly took its toll before he died peacefully in his sleep three days before his 92nd birthday. n
In Memoriam JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk | 63
Products, Courses and Events
We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital equipment is fully protected in transit.

equipment is fully protected in transit. We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to




house implant samples, instruments and any other equipment.
MSK MRI Interpretation Courses
Step-by-step | Interactive | Case based
Web: https://uk.unitedorthopedic.com
Email: uk.service@unitedorthopedic.com
Telephone: +44 (0) 1827 214773
Trifibre Ltd
17 Boston Rpad Gorse Hill Industrial Estate
Leicester LE4 1AW
Telephone: 0116 232 3166
Email us: info@trifibre.co.uk
Web: www.trifibre.co.uk
We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to house implant samples, instruments and any other equipment.
Surviving trauma is just the start No
We provide national support and can help with:
• Legal advice
• Financial support
• Peer support
• 24hr counselling
• Benefits and welfare advice
Trifibre Ltd
17 Boston Rpad
Gorse Hill Industrial Estate
Leicester LE4 1AW
Telephone: 0116 232 3166
Email us: info@trifibre.co.uk

Web: www.trifibre.co.uk
We’re here for you and your patients:
Visit dayonetrauma.org/supporting-you

Call 0300 303 5648
Email dayone@dayonetrauma.org
Follow @dayonetrauma
Together, we will provide #MoreTraumaSupport
Charity number 1194227
The third National Orthopaedic Alliance (NOA) Annual Members’ Conference and second NOA Excellence in Orthopaedics Awards take place in Birmingham on 19 October 2023

The conference will be an impactful learning and networking opportunity for the orthopaedic community. It will address issues affecting orthopaedics and MSK, giving members an insight into national solutions and initiatives as well as opportunities to collaborate and share best practice. For the second year running, the award ceremony will shine a light on excellence in orthopaedics.
For further information including conference registration details and an overview of the awards, scan the QR code in this advert or email info.noa@nhs.net

Forthcoming courses via Zoom:
MSK MRI for Beginners Course

Covers: MRI of knee, shoulder and lumbar spine
Date: 22nd of April 2023
Further MSK MRI for Beginners Course
Covers: MRI of hip, elbow, ankle and cervical spine
Date: 25th March 2023
For details please visit: www.mskbeginner.com
For a registration form please email: admin@mskbeginner.com
For over 25 years, United Orthopedic has been a leading international designer, manufacturer, and distributor of versatile orthopaedic solutions that deliver world-class orthopaedic joint replacement implants which have made life better for hundreds of thousands of patients needing hip and knee replacements.

Find out more about our USTAR II Primary and & Revision Hinge Knee and Limb Salvage System which is part of the United Orthopedic portfolio of arthroplasty and limb salvage products.

• Platform-based approach - consistent design philosophy allows a platformbased approach to provide surgeons flexibility for a wide range of procedures
• Demand-matching - includes a wide range of product options for demandmatching to optimise solutions based on patient needs
• Advanced surgical technologies - builds on proven design philosophies with advanced surgical technologies to help deliver reproducible clinical outcomes and a streamlined procedure

64 | JTO | Volume 11 | Issue 01 | March 2023 | boa.ac.uk
one should be left to rebuild their life on their own
Arthroplasty and high-risk patients
How can results for patients at risk from infection be improved in a sustainable manner?
The main goal of arthroplasty is to relieve pain, improve and restore joint function and recover quality of life.
Periprosthetic joint infection (PJI) remains a complication that has to be taken seriously for those receiving arthroplasty surgery. The risk of infection for those receiving primary resection is up to 2%, rising to up to 5% for those undergoing revision.
There are many reasons why PJI can occur; it is sometimes down to the patient themselves. Patients each possess their own risk factors, which can increase the likelihood of developing an infection, both for those receiving primary and revision arthroplasty. For every ten patients over the age of 65, six will display at least two risk factors for infection. The latest studies suggest that individual risks or complications that can lead to PJI should be examined in relation to defined patient profiles. They provide initial findings that can be used, in the future, to develop promising arthroplasty treatment strategies that are geared towards different patients.
Approaches to arthroplasty surgery should be tailored to the patient
In clinical practice today, you can find different approaches aimed at avoiding complications and revisions in arthroplasty, such as PJI, periprosthetic fractures, dislocations and aseptic loosening, in an effective manner. What these all have in common is that the patient, with their individual risk profile, should be considered
in a situational manner to include the following in their treatment plan: the patient’s current comorbidities and the surgeryassociated risks.
Taking the patient-related risk factors into consideration

For example, patients that suffer from risk factors such as obesity, diabetes or cardiovascular diseases have a disproportionate risk of developing acute or chronic infections in the area surrounding the joint prosthesis following arthroplasty surgery. Many studies have shown there is a correlation between an increased Body-Mass-Index (BMI) and an increased risk of infection. Compared to non-obese patients, the rate of polymicrobial infection is higher in obese patients (60.3% compared to 33.3%, p<0.001). Uncontrolled diabetes is a known separate risk factor in the development of periprosthetic infection. For patients suffering from cardiovascular diseases, chronic blood vessel damage and medicines that influence clotting and thrombocyte function can all increase susceptibility to infection.
As many of these risk factors cannot be reduced in the short-term before surgery, targeted infection prophylaxis strategies are vital to help prevent infection. This also goes hand in hand with the decision to use antibioticloaded bone cement when fixing prostheses.
Indication-based treatment strategy: risk classification in primary arthroplasty
A patient’s individual comorbidities have a considerable influence on their risk of infection and should be considered when
selecting the optimal treatment algorithm. The first steps when deciding on the treatment and therapy to be deployed are to identify the patient’s comorbidities. When possible, this will go hand-in-hand with preoperative comorbidity optimisation.
Classifying patients at risk of infection, even for primary procedures
To prevent periprosthetic infection in patients at risk of infection in an effective manner, including during primary arthroplasty, a definition should be established to identify which patients can be classified as being at risk of infection. One approach from Spain takes the combination of a number of different risk factors into account, including comorbidities, the patient’s various pre-existing conditions and surgery-related risks. For example, in elective primary hip arthroplasty (TEP) and hip arthroplasty following trauma, a patient is classified as being at-risk if they have a combination of at least three risk factors, whereas for elective primary knee TEP, patients are classified as at-risk if they show at least two risk factors.
Infection reduction with dual antibiotic-loaded bone cement
It has been shown that for patients at risk of infection with a selected risk profile, the risk of developing PJI following primary hip or knee arthroplasty surgery can be additionally reduced through the application of dual antibiotic-loaded bone cement. A further report from Spain has shown a PJI reduction of 34% from 3.7% to 2.45% for primary hip and knee arthroplasty in high-risk patients through the use of a dual antibiotic-loaded bone cement, compared to the use of a single antibiotic-loaded bone cement. n
SPONSORED CONTENT www.heraeus-medical.com

What would you do if...? Did you know? The Medical Protection Society Limited (“MPS”) is a company limited by guarantee registered in England with company number 00036142 at Level 19, The Shard, 32 London Bridge Street, London, SE1 9SG. MPS is not an insurance company. All the benefits of membership of MPS are discretionary as set out in the Memorandum and Articles of Association. MPS® and Medical Protection® are registered trademarks. medicalprotection.org/nhs £549 Don’t be caught o guard - get protected from just * 2210214431:02/23 *Cost shown is the annual membership price for a UK Medical Consultant working exclusively in the NHS. Subject to protection requirements and underwriting approval. †Source: GMC Fitness to Practise Report, January 2023. Over 37,000 complaints were received by the GMC in the last 5 years.† If this happens to you, having the right support can make the experience a lot less daunting. You received a letter from the GMC Your personal conduct was called into question You received a complaint from a patient You were called upon as part of an inquest You needed to provide a formal report


























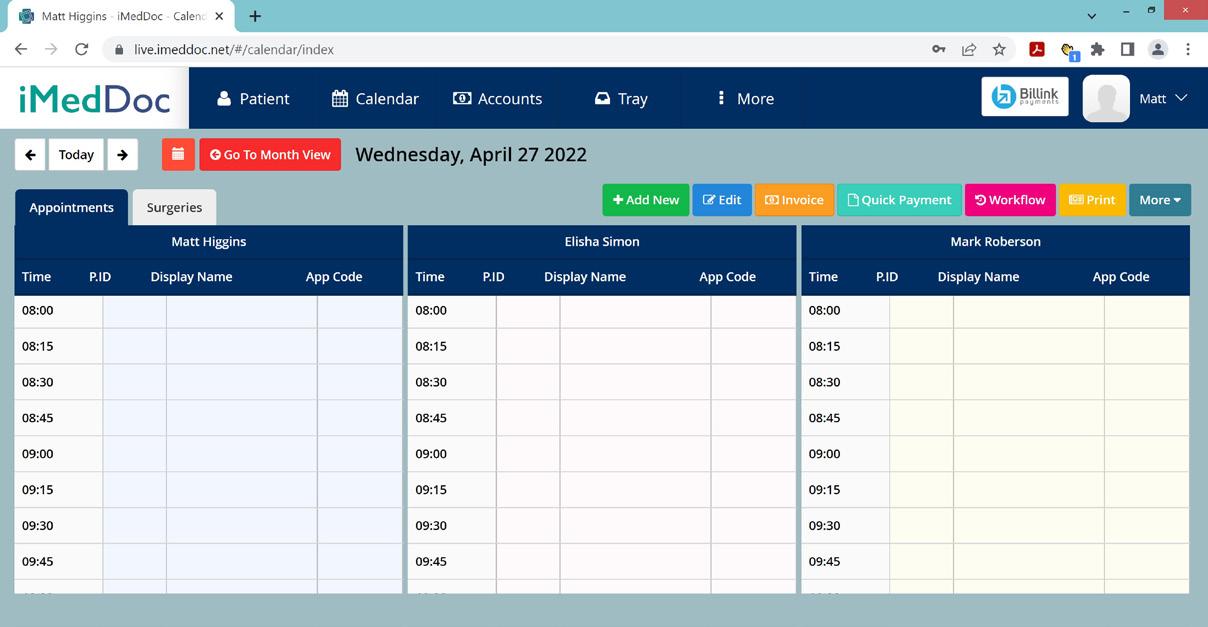



 Ronnie Davies
Ronnie Davies









 Omer Alanie
Omer Alanie


























































































 Nick Nicolaou and Fazal Ali
Nick Nicolaou and Fazal Ali