SIR: Cryoablation for large tumours page 6

Interview: Palliative care in IO page 9



Profile: Jack Jennings page 14
First multi-society summit addresses the wants, needs and demands of IR on the global stage
Last month at the Society of Interventional Radiology (SIR) annual scientific meeting (23–28 March, Salt Lake City, USA), interventional radiology (IR) societies from nations worldwide sat around a table to consider the status of IR in their geographies. The Global Society Summit—the first meeting of its kind—heard international IR leaders discuss and define common challenges, to track a path for multinational collaboration and sustain a unified voice for IR in an increasingly competitive global healthcare environment.
Thirteen panellists in attendance, representing IR societies from every global continent, stood and updated the room on the status of IR in their country. “It’s heartening to hear that many of our challenges and thought processes are very similar worldwide,” said Alda Tam (MD Anderson Cancer Center, Houston, USA), SIR president and cocoordinator of the summit. Although at different stages down the path to subspecialty and specialty status, each society reported strikingly similar challenges, namely the recognition of the importance of clinical care in IR, difficulties with standardisation and training, practice economics and specialty distinction.
The IR clinical practice model was first to be dissected by the panel. SIR international division councillor and panel moderator Constantinos T Sofocleous (Weill Cornell Medical College Memorial Sloan-Kettering Cancer Center, New York, USA) began by discussing the value of routine outpatient IR clinical practice with longitudinal care for patients. Taking a poll, the majority of the panel agreed on the value of IR clinics and indicated that they offer this service.
“I think that in the USA,” said Parag Patel (Medical College of Wisconsin, Milwaukee, USA) following this poll, “one of the critical aspects for our recognition as a specialty and from other specialties was the recognition that we take care of patients with the diseases that we manage.” Until the American Board of Medical Specialties recognised the important role that interventional radiologists play in the “longitudinal management of disease going forward”, he said, there was “no path to specialty”. However, he added that a young trainee who wants to take care of patients and do procedures will likely pursue an IR-dedicated training pathway that “involves or invokes” clinical practice as “mandatory”, Patel noted. This, however, is a highly streamlined training modality that is not frequently offered worldwide.
Adding to this point, Robert Lookstein (Icahn School of Medicine at Mount Sinai, New York, USA) noted that these direct training pathways are “critical to the success of [IR] at a global level”. Yet, in an effort to “refocus”, he shared data from a survey his centre carried out which asked US IR chiefs or clinical leads whether or not they provide outpatient clinical services. They found that 76% said yes and 24% said no, and these figures were similar when the same question was asked for inpatient services. “I share these because there are clearly opportunities for improvement, to meet the goal that we’re all stiving for here. We all want IR to have a singular focus on longitudinal clinical care to achieve clinical excellence. Is the distribution of clinical services similar in other countries?” Lookstein asked.
“In Europe, I think that the numbers are much lower,” said Christoph Binkert (Kantonsspital, Winterthur, Switzerland), “but heterogeneity is much higher, not just across Europe but even within my country.” Although Binkert noted that Switzerland is not entirely representative of Europe, he explained that outpatient clinics have become the norm. “All of the big players do it—if you’re not offering outpatient clinical care, patients will not come to you.”
In the UK, Robert Morgan (St George’s Hospital NHS Foundation Trust, London, UK)—British Society of
An advantage of progressing from behind is that you learn from others’ mistakes.”
Continued on page 4
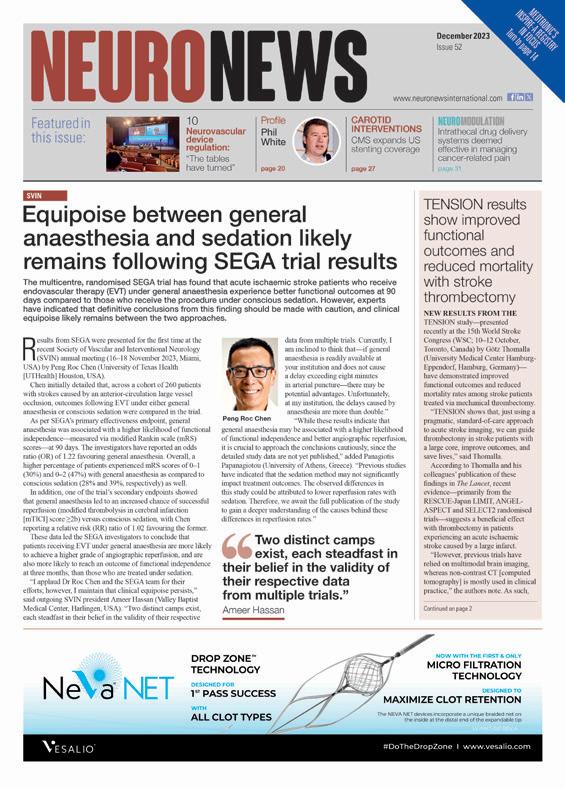
Largest liver venous deprivation registry set to release positive preliminary results at ECIO
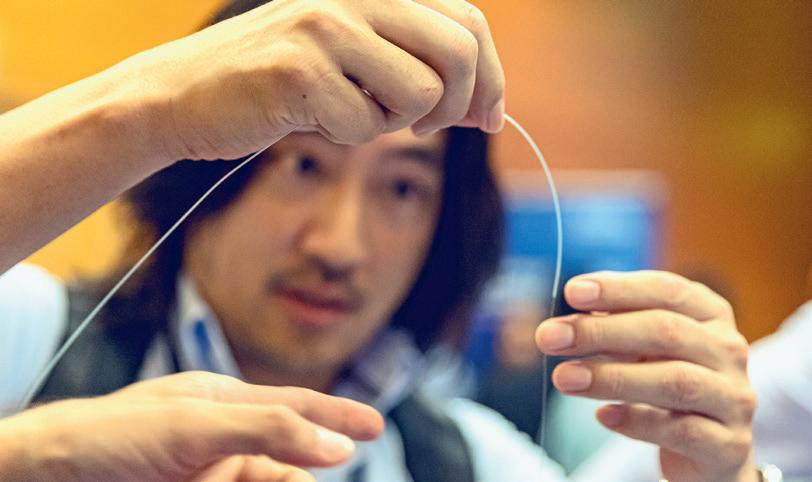
IN 2020, A SINGLE-CENTRE STUDY conducted by Kosuke Kobayashi (University of Lausanne, Lausanne, Switzerland) confirmed the superiority of liver venous deprivation (LVD) over portal vein embolization (PVE) alone, inducing faster hypotrophy of the future liver remnant. In April 2024, “exciting” preliminary results from the largest global LVD registry—EuroLVD—are set to be released at the European Conference of Interventional Oncology (ECIO) annual meeting (28 April–1 May 2024, Palma de Mallorca, Spain), setting sights on a soon-to-be reached consensus for this promising treatment modality.
Lead investigator Alban Denys (Centre Hospitalier Universitaire Vaudois [CHUV], Lausanne, Switzerland) and previous chairman of ECIO, spoke to Interventional News on sharing their initial results at the upcoming ECIO meeting.
“I think this could impact the clinical practice of centres that are still not convinced on LVD,” Denys said. “Our main messaging during this presentation will be to not be afraid to start. It’s a safe procedure, it’s not very complex and it enables better outcomes from your patient, so don’t be afraid to go for it—and even participate in the EuroLVD registry if you do implement the procedure.”
EuroLVD is an initiative that has been set up between interventional radiology and hepatobiliary surgery groups in Lausanne to collect information about LVD. “It’s almost copy and pasting what has been done for the associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) technique,” Denys explained. ALPPS is a surgical technique that combines transection of liver parenchyma and the ligation of the portal vein to the diseased liver. It allows higher, “more efficient” degrees of hypertrophy of the future liver remnant (FLR) in a short time, Denys explained. However, studies have shown a high rate of morbidity and mortality associated with
Continued on page 6 ECIO
www.interventionalnews.com April 2024 | Issue 94
PREVIEW
SIR GLOBAL
Interventional News Spring Edition
Greetings dear readers,
I have just returned from an excellent Society of Interventional Radiology (SIR) annual scientific meeting (23–28 March) in Salt Lake City, USA. This was the 49th meeting of the SIR, and next year, the society will celebrate its 50th congress since its inception. There were several sessions at SIR 49 on the status of interventional radiology (IR) worldwide—i.e. global IR—and this topic will be the focus of this brief editorial to open the April 2024 edition of Interventional News.
While IR is a mature discipline in many areas of the world (including North America, Europe, North East Asia and Australasia), in many other parts of the world, the field is in various stages of development. To a large extent this is due to local economic circumstances, the national status of healthcare, and the enthusiasm of device manufacturers to promote sales in these countries; although this latter issue could be regarded as a chicken and egg situation (i.e. industry may be reluctant to expend resource in less well-developed markets).
Many global IR leaders consider that there is an obligation by mature IR societies to assist in the development of countries with less IR resources. This baton has already been taken up by individuals in SIR, the Cardiovascular and Interventional Society of Europe (CIRSE) and the Asia Pacific Society of Cardiovascular and Interventional Radiology (APSCVIR) with several initiatives already underway.

spend on device costs.
To deliver local training to interventional radiologists in their countries, major societies and individuals have organised local outreach training. For example, the APSCVIR in collaboration with SIR and CIRSE has organised several outreach educational courses in Myanmar and this year will provide a course in Mongolia. Another example of outreach training is provided by Sang Joon Park (Seoul National University Hospital, Seoul, South Korea) and colleagues from Seoul, who regularly provide on-site training at hospitals in Ethiopia. There are many other similar enterprises by other individuals ongoing.
 Robert Morgan
Robert Morgan
For example, for many years CIRSE and SIR have sent representation to National Society congresses around the world. Most recently, the 2023 Society of African Interventional Radiology and Endovascular Therapy (SAFIRE) congress (3–5 November) in Cape Town, South Africa was attended by representatives of CIRSE and SIR. Connections made at these meetings are important to foster communication and to share local problems and devise potential solutions.
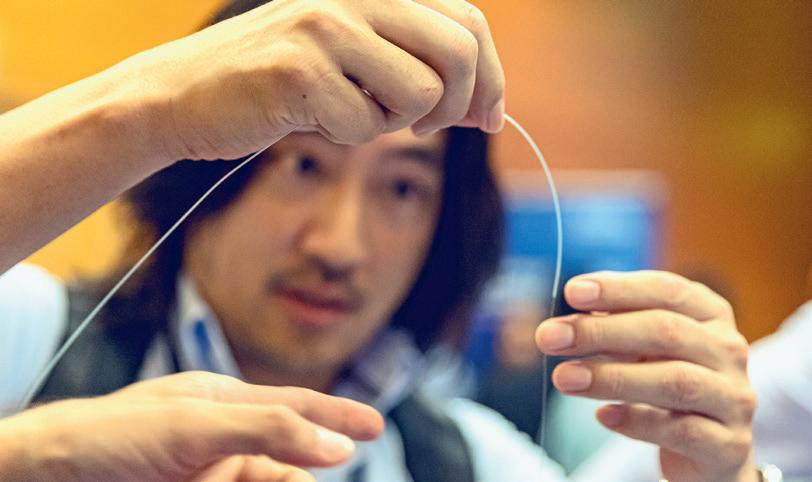
To address the issues of high costs of embolic agents for many interventional radiologists, Vincent Vidal (Marseille University Hospital Timone, Marseille, France), has developed the FAIR-Embo concept using surgical suture material to deliver an inexpensive embolic agent to interventionists with limited financial resources. This type of clever invention is ideal for those with little funding to
The SIR Global IR Society Summit, which is described in a feature piece in this edition of Interventional News deliberated many of the major issues facing interventional radiologists around the world. There was also a separate session that focussed on the specific needs of Africa. All of those present concurred that these types of session are a useful start. However, there is much to be done to enable IR to be delivered consistently to the global population irrespective of local circumstance.
All delegates agreed that these discussions must form just the start of a journey. I sincerely hope that similar sessions to build on these beginnings will be held at future international IR congresses. I believe that we have a responsibility to endeavour to ensure that the benefits of interventional radiology are made available to patients wherever they live in the world.
ROBERT MORGAN is professor of interventional radiology at St George’s University Hospitals NHS Foundation Trust (London, UK) and the president of the British Society of Interventional Radiology.
n SIR 2024 BEST OF ABSTRACTS:
This year’s Society of Interventional Radiology (SIR) annual scientific meeting (23–28 March, Salt Lake City, USA) gave recognition to select abstracts during the closing plenary session. Introduced by SIR 2024 programme chair Bulent Arslan (Rush University, Chicago, USA), who commended the “strong” and “compelling” presentations, speakers challenged preconceptions about disease states and treatment strategies.

For more on this story go to page 8.
n CX 2024 PERIPHERAL ARTERIAL PROGRAMME:

Andrew Holden (Auckland City Hospital; University of Auckland, Auckland, New Zealand)—one of the CX Symposium co-chairs—gives his predictions on debates and controversies ahead of this year’s meeting. Holden sets sights on the unmissable peripheral arterial programme, which will tackle global controversies and host heated debates. For more on this story go to page 11.
n THE HIDDEN INTERVENTIONAL RADIOLOGISTS:

A new study conducted by the Harvey L Neiman Health Policy Institute (HPI) has identified a large percentage of unidentified interventional radiologists ‘hidden’ within Medicare data. The research has uncovered a previously unforeseen trapdoor, in which self-designated specialty in Medicare claims data has proven to be an “inadequate selection method” resulting in the omittance of practising interventional radiologists from records.
For more on this story go to page 17.


2 interventionalnews linkedin.com/company/interventional-news/ Editors-in-chief: Professor Robert Morgan, Professor Andy Adam, Professor Brian Stainken Publisher: Stephen Greenhalgh | Content director: Urmila Kerslake Editor: Éva Malpass | Editorial contribution: Jocelyn Hudson, Will Date, Bryan Kay, Jamie Bell and Adam Pearce Design: Terry Hawes, Josh Lyon and David Reekie Advertising: Michael Broughton michael@bibamedical.com Subscriptions: subscriptions@bibamedical.com Published by: BIBA News, which is a subsidiary of BIBA Medical Ltd BIBA Medical, Europe, 526 Fulham Road, Fulham, London, SW6 5NR, United Kingdom Tel: +44 (0) 20 7736 8788 BIBA Medical, North America, 155 North Wacker Drive, Suite 4250, Chicago, IL 60606, United States Tel: +1 708-770-7323 Printed by: Buxton Press. Reprint requests and all correspondence regarding the newspaper should be addressed to the editor at the United Kingdom address. © BIBA Medical Ltd, 2024. All rights reserved.
NEWS IN
LATEST
BRIEF THE
STORIES FROM THE INTERVENTIONAL WORLD
EDITORIAL
Alda Tam, SIR President addresses congress
MASTERING EMBOLIZATION
ET2024
June 1 - 4 | Vienna, AT
Join us for the world’s premier conference on embolization !
ET 2024 will place a spotlight on the importance of embolization through a variety of innovative, engaging session formats, providing the most comprehensive platform for interventionalists to discuss all hot topics in the field, find out about the latest research, and grow their network.
Browse the programme
ET 2024 will cover the entire range of embolotherapy treatments, from basics and well-established therapies to the latest developments, over the course of nearly 100 lectures from expert faculty members.
Register
Register in advance of the congress to save and be ready to experience ET from the first session onwards!
All-Access Pass
For even more savings for onsite registration and to gain access to all of CIRSE’s online educational offerings year-round, including all congresses, the CIRSE Academy, and the CIRSE Library, get the 2024 All-Access Pass !
Flight discount
Attendees of ET 2024 can enjoy reduced rates when traveling with the Lufthansa Group. Scan the QR code to get the discount code !
See you in Vienna !
ET’s official travel partner, Kuoni Tumlare Congress, has secured a great number of hotel rooms at very competitive prices and offers an easy-to-use booking tool for congress participants.
www.etconference.org


EUROPEAN CONFERENCE ON EMBOLOTHERAPY
TODAY!
REGISTER
The SEO of IR: ChatGPT offers “exciting” data for patient perception and referral
Using Chat generative pre-trained transformer (GPT) to understand the public perception of interventional radiology (IR), Chloe Cross (Icahn School of Medicine at Mount Sinai, New York, USA) and colleagues presented new data which provide “exciting” insights into how and when IR is suggested for treatment for patients using artificial intelligence (AI).
CROSS ET AL DETAILED THEIR study titled ‘Settling turf wars: When does ChatGPT refer you to an interventional radiologist?’ at the Society of Interventional Radiology (SIR) annual scientific meeting (23–28 March, Salt Lake City, USA), in a session dedicated to emerging technologies within IR.
Developed by OpenAI, ChatGPT is a conversational AI-based chatbot which provides answers to questions or prompts. “Although it’s not specifically designed for medicine,” Cross explained, “many patients are using ChatGPT for medical decisionmaking—similar to how patients use WebMD. Our purpose was to understand public perception of IR and when IR
treatments are offered.”
Cross and colleagues developed a standardised prompt that reflected a realistic patient query, adhering to a ‘I have a disease process, what type of doctors can treat this?’ formula. The researchers created a list of disease processes in various systems treated by IR which were selected from a literature review. Each prompt was repeated three times and then the number of times IR was suggested and an average rank was recorded. Their results showed that ChatGPT mentioned IR in 51 (73.9%) of 69 prompts, with an average rank of
First multi-society summit addresses the wants, needs and demands of IR on the global stage
Continued from page 1
Interventional Radiology (BSIR) president and cocoordinator of the summit—shared that being given “permission” to provide outpatient clinics is not always given in UK hospitals for interventional radiologists. He believes that there is “much to be done” to increase recognition by UK Hospital Trusts of dedicated, protected time, within work hours to see patients before procedures and at follow up in outpatient clinics.
In Denis Szejnfeld’s (Certa Hospital, São Paulo, Brazil) view, issues arise as interventional radiologists often do not specialise early in training. Confirming this statement, Ethel Rivas Zuleta (Universidad Dr José Matías Delgado, La Libertad, El Salvador) commented that in Latin America, graduates must choose between two paths early in their training—private practice or institutional national practice, also referred to as academic hospitals, which leaves little room for deviation.
In other nations worldwide, training can be limited due to a lack of resources, as audience member Chidubem Ugwueze (Icahn School of Medicine at Mount Sinai, New York, USA) conveyed. Addressing the panel, he explained his involvement with a training programme in Nigeria which provides a well-rounded IR course preparing trainees for the European Board of Interventional Radiology (EBIR) examination. He referenced one of his trainees who he says has all of the clinical requirements he would need to pass the EBIR examination—this is not the issue in these
3.3. Of all the disease states, IR was consistently ranked first for stroke angiography and splenic artery aneurysm embolization. Cross offered that for the splenic artery, this result may be due to the level of literature published on this diagnosis in IR. “We are pretty much the only ones who are doing splenic artery aneurysms in the recent past, so you can see where this result is coming from. It speaks to the importance of having our name in new searches published in these realms.”
Their data, however, showed that IR was not suggested for the treatment of pulmonary embolism (PE) or image-guided bone biopsy, and was only suggested once for the treatment of benign prostatic hyperplasia. Interestingly, Cross added that IR was only mentioned once and ranked far behind other specialties for image-guided percutaneous ablation of renal carcinoma, a treatment frequently performed by interventional radiologists.

“It’s important to note that IR was cited for the treatment of many diseases, which is quite exciting. This may help to improve patient awareness of IR, especially for referrals,” said Cross. Yet, she stated that these data indicate a “need for more public outreach” concerning the disease
African nations, he said. “The biggest obstacle is that trainees can have all of the technical skills to do the procedures, but they don’t have reliable access to the devices needed to perform these,” Ugwueze said. “I see a lot of big names in this room who can move mountains and change these circumstances. I also see people who have already solved these problems elsewhere—how would you go about changing this?” he asked.
In response to Ugwueze, interventional radiologist Sangjoon Park (Seoul National University Hospital, Seoul, South Korea) shared his experience in Ethiopia and recounted difficulties in transporting enough lipiodol to the centre there. Park averred that trainee interventional radiologists there should not be trained in these procedures if they have no access to the devices/therapeutic agents. “Bottom line, there’s some things that you can do and some things that you can’t—so you have to decide on what procedures you can do to the best of your ability.”
“I did not want to touch on the lack of materials,” Rivas Zuleta commented. “Coming from Latin America, these disparities are ingrained, and what we must focus on is these materials come from companies who earn millions of dollars/euros in Europe and the USA. They aren’t going to give us free products, so we have to focus on what we can do.”
Referencing a previous session that day—Extreme IR—Rivas Zuleta noted that her first thoughts were “oh my god, what an expensive case”. In this session, one particular case reported the use of 12 coils for a single patient. “All I was thinking was, ‘I wouldn’t be able to use coils for the rest of the year’. Coming from relatively low-income countries means that we have to focus on what procedures are possible for us,” she said.
Another voice from the audience was past president of the Society of Interventional Radiology (SIR) Brian Stainken—interventional radiologist and current co-editor-in-chief of Interventional News—who stated he was “a little disappointed” more speakers
processes such as PE where IR was not indicated.
One limitation of their study was that they do not know the “inner workings” of ChatGPT, Cross relayed, so any conclusions drawn may be speculative. There is also little understanding of how patients are interacting with the technology as it is still relatively new.
“New versions of these large language models are coming out constantly. We may see changes in the generative answers that we obtain from this research, however for now, ChatGPT can help us understand public perception of IR and we are being suggested for many diseases we are able to treat, so that is very exciting,” Cross told attendees. She concluded that future research should explore ChatGPT’s role in medicine in order to better understand how the patient pathway to IR can be expedited through this new technology.
It’s important to note that IR was cited for the treatment of many diseases, which is quite exciting”
had not addressed a glaringly obvious issue. “I’m old enough now to know it’s all about the dollars. Practice economics is something that isn’t much talked about on the international stage but it’s very real. There are lots of reasons given to why these medical device companies aren’t selling in these countries, but the big one is there’s no market. There’s no market because the market hasn’t been made.”
Wael Saad (University of Utah, Salt Lake City, USA)—representing the Society of African Interventional Radiology and Endovascular Therapy (SAFIRE)—responded that each society can help to “push in the right direction” in terms of moving mountains for countries requiring resources. “It’s very impactful for physicians in Africa to be able to help patients in need with minimal equipment and there is a lot of need there. An advantage of progressing from behind is that you learn from others’ mistakes and misfortunes,” Saad added.
Closing the summit, Morgan asked the panel how they believe the forum should go forward, to which Patel added that, yes, although their needs are varied, how can they “identify and prioritise support needed in each region?” Patel continued that the forum is intended to be a “continued effort in partnership with SIR and the Cardiovascular and Interventional Radiological Society of Europe (CIRSE)”, holding global summits at each of their respective meetings to “continue conversations, identify society needs and maintain collaboration to elevate IR, so that it is recognised universally as a distinct specialty that can provide exquisite care”. Sofocleous indicated that on behalf of SIR alongside Patel and Morgan, the summit will prioritise the described international IR needs for the next agenda to be discussed at CIRSE 2024 (14–18 September, Lisbon, Portugal). The coordinators stated that this inaugural summit is the “first of many” that will help to empower local interventional radiologists. In doing so, they hope to join international forces to increase IR outreach in each corner of the globe.
4 April 2024 | Issue94 ChatGPT
Chloe Cross
COVER STORY continued
The double-edged sword of private practice in the MENA region
Interventional radiologists Mohammed Almoaiqel (King Abdulaziz Medical City, Riyadh, Saudi Arabia), Karim Abd El Tawab (Ain Shams University Hospitals, Cairo, Egypt) and Mohammad Al-Twalah (Dawali Clinic, Riyadh, Saudi Arabia) speak to Interventional News about the pros and cons of private practice in the Middle East and North Africa (MENA) region, surveying the spectrum of opportunities and challenges faced by interventionists today.
THE SIGNIFICANT TRACTION OF interventional radiology (IR) as a specialised field has been marked on a global scale in recent years. For interventionists in the MENA region, demand for IR’s minimally invasive procedures has steadily increased year on year with growing awareness of its benefits for a range of indications. Although public healthcare systems in the MENA region have traditionally been the primary providers of interventional treatments, a tangible uptick in private healthcare institutions—or office-based labs (OBLs)—has been observed.
In Almoaiqel’s view, private practice runs alongside his role at the government hospital in Riyadh, which means that from 8am–5pm he can be found at the hospital, and from 5–9pm he covers a private IR clinic. In his OBL setting, he is able to perform “pure, elective IR procedures” such as embolization— including prostate artery embolization (PAE) and uterine artery embolization (UAE)—as well as vascular procedures via their diabetic foot service. He stated that around 30–40% of interventional radiologists in his region also work in both settings.
“It gives us freedom—freedom to see more patients and practice IR,” Almoaiqel said, commenting on the clinical autonomy that private practice has afforded him. In many countries worldwide, IR’s distinction from diagnostic radiology (DR) or radiology is still being forged, which equally applies to the MENA region. As Abd El Tawab added, most interventionists that open OBLs still perform DR procedures alongside IR, and the number of “true IR” clinics are still few.
The prevalence of these catch-all clinics, Abd El Tawab pointed out, may be in part due to the competitive nature of private practice IR in Egypt, where he practises. “No one will refer to us—no

urologist, gynaecologist, or surgeon will send patients to us. All patients are self-referred, so we have to recruit them,” he stated.
Due to the increasingly saturated market, establishing a reputable presence to recruit patients has equated to marketing initiatives, with OBLs differentiating their services via social media advertisements. In Egypt, medical advertising is legal, which means Abd El Tawab’s private practice runs Facebook ads to reach patients—“they see the ads, they come, and they are convinced”, he said.
No one will refer to us—no urologist, gynaecologist, or surgeon will send patients to us. All patients are selfreferred, so we have to recruit them”
Karim Abd El Tawab
To Al-Twalah, the age of social media advertising in private practice IR has been “very challenging”, particularly in Riyadh. “People have moved online, they’re watching videos on TikTok and Instagram and you have to be there to be seen—it’s not us, but we have a team for that. We have daily challenges with this.”
Viewing social media as a double-edged sword, Almoaiqel attested to the benefit of educational campaigns which have been furthering the reach

of IR, and what their procedures can do. Erecting a booth near their private clinic, his team have distributed brochures in the past, in order to spread awareness of IR treatments in their community.
“It’s a slow process,” Almoaiqel said, “but our community awareness must be improved—many women are not aware of fibroid embolization as a non-surgical alternative option, and our rate of amputation for diabetic foot is very high. We could save those feet and limbs by doing endovascular procedures.”
However, caseloads in public hospitals remain high, all three speakers asserted. Despite the lack of visibility of IR procedures, interventionists are experiencing long wait times and convoluted patient access. For this reason, Almoaiqel detailed his governments initiative to “relieve pressure” on public hospitals and insurance companies. He said that they have “facilitated investment” into private practice, “simplifying the opening of new facilities”. This support for OBLs also relieves pressure on the government to pay for the health sector, he continued.
Yet, as the government “injects support” into private practice, Almoaiqel said, challenges arise as “most patients are not insured, and they have to pay from their own pocket—this is a limitation”. He added that IR procedures are not cheap, some even working out to be more expensive than surgical procedures, via the specialist materials and technology that are required. “This limits us to patients who are able to pay,” he said. Abd El Tawab added that, in Egypt, patients’ insurance often “covers everything or nothing”, highlighting a discrepancy between funding and insurance coverage, which may be blocking patient access to private IR treatment.
Historically, private practice has provided interventional radiologists with a higher earning potential compared to that of public hospitals. Yet, in Al-Twalah’s experience, the value in switching to private practice came from being “able to do what you want to do”. “Life is short—your work has to be enjoyable for both you and the patient, and in a good setting with a focused team.” Often private practices have a condensed, multidisciplinary team working under “one umbrella”, which Almoaiqel believes is the key to “long-term success” in private practice.
“In our clinic we have phlebologists, interventional radiologists, vascular surgeons and a podiatrist. In supporting each other to forward this vision for IR, the continuity of care we can achieve for patients is limitless,” Almoaiqel said.

5 Issue94 | April 2024 Private Practice IR
PAIRS
Karim Abd El Tawab
Mohammad Al-Twalah Mohammed Almoaiqel
Cryoablation highly effective for breast cancer patients with large tumours
Cryoablation—a minimally-invasive technique that uses ice to freeze and destroy small, cancerous tumours—has now been proven effective for breast cancer patients with large tumours, providing a new treatment path for those who are not candidates for surgery, according to new research presented at the Society of Interventional Radiology (SIR) annual scientific meeting (23–28 March, Salt Lake City, USA).
“FOR PATIENTS WHO HAVE LARGER tumours but can’t undergo surgery, this approach could be more effective than the current standard of care for patients who are not surgical candidates,” said Yolanda Bryce (Sloan Kettering Cancer Center, New York, USA). “When treated with only radiation and hormonal therapy, tumours will eventually return. So, the fact that we saw only a 10% recurrence rate in our study is incredibly promising.”
Cryoablation uses imaging guidance such as ultrasound or computed tomography (CT) scan to locate tumours. An interventional radiologist will then insert small, needle-like probes into the breast to create an ice ball that surrounds the tumour, killing the cancer cells. When combined with hormonal therapy and radiation, patients can have nearly 100% of their tumours destroyed. If the tumours do grow, patients can be treated with cryoablation multiple times to
ECIO PREVIEW continued
Largest liver venous deprivation registry set to release positive preliminary results at ECIO
Continued from page 1
the procedure.
“The idea of LVD is to be more efficient than PVE but less morbid and with a lower mortality than ALPPS,” said Denys. In his team’s view, striking this balance may provide a “significant benefit” in terms of hypertrophy of the left lobe of the liver when resection of the right lobe is necessary, but the left lobe is “too small”, without additional morbidity/ mortality.
“The technique has only been invented a few years ago however, so there is not much depth in the literature,” he added. Aside from Kobayashi et al’s monocentric retrospective analysis, Denys noted that there are “almost no prospective data”, leading his team to build their comprehensive registry.
The registry has collected data from centres in Switzerland, France, the USA, and the UK, with centres continuing to join week by week. “We have more than 200 patients now included in this series, and it’s about to be the largest registry of its kind. We not only want to evaluate the functional effect of the technique, but the volumetric effect of the technique on liver function. So, it’s really to build evidence based on large numbers and, although it took time to start, it’s now very successful, and each week we
control growth. The treatment has been successfully used to treat tumours smaller than 1.5cm, but its effectiveness on larger tumours was not extensively demonstrated until now.

Yolanda Bryce
This retrospective study assessed outcomes for 60 patients who underwent cryoablation because they were not candidates for surgery or refused surgery after consultation with a breast surgeon due to age, cardiac issues, hypertension, or currently undergoing chemotherapy for another cancer. Their tumour sizes ranged from 0.3—9cm with an average size of 2.5cm. Patients with tumours larger than
have new cases that are registered by internationally renowned centres, such as the MD Anderson Cancer Center in Houston, Texas, USA.”
Denys explained that to date the Dragon 1 trial has been the largest collection of data in this arena. Dragon 1 assessed combined portal- and hepatic-vein embolization (PVE/HVE) to accelerate FLR hypertrophy in patients with borderline resectable colorectal cancer liver metastases, and was based in The Netherlands. “We are close to Dragon in numbers currently, but by summer we believe we will surpass this threshold,” Denys speculated.
Offering an impression of the results to be presented at the ECIO meeting, Denys stated that first data are confirming that LVD allows “faster kinetic growth rate” of the left lobe of the liver and higher hypotrophy that has previously been reported in the literature for PVE. Their data, however, are showing that morbidity and mortality for the procedure is “very low”, and his team has not seen complication associated with HVE used in addition to PVE.
“The results are quite positive,” Denys commented. He explained that his teams’ intention is to provide this initial detail and subsequently subdivide their cohort by disease groups based on liver function characteristics recorded before patients underwent LVD. In doing so, Denys and his team will seek answers to questions, such as—is the liver normal? Has the patient received chemotherapy?
Is it a cholestatic liver? Is it a cirrhotic liver? In asking these questions, they aim to define how LVD works in various groups.
Anticipating what responses their preliminary results will glean from
1.4cm were treated with multiple probes (one probe placement for each centimetre of disease). In a follow-up after 16 months, the recurrence rate was just 10%.
“Surgery is still the best option for tumour removal, but there are thousands of women who, for various reasons, cannot have surgery,” said Bryce. “We are optimistic that this can give more women hope on their treatment journeys.”
The procedures were performed with local anaesthesia or minimal sedation, depending on the eligibility and preference of the patient. The freezethaw cycle started with 5–10 minutes of freezing, followed by 5–8 minutes of passive thaw, and then 5–10 minutes freezing at 100% intensity. Patients were able to go home on the same day, following the treatment.
The researchers will continue to follow the patient cohort to collect data on long-term effectiveness and to better understand the impact that adjuvant (e.g. hormone therapy and radiation) therapies combined with cryoablation can have on this patient population.
We are optimistic that this can give more women hope on their treatment journeys.”
ECIO 2024 delegates, Denys believes their presentation will prove to be “interesting”. Considering that previous studies of LVD have offered single-centre data, he hopes theirs will “get rid” of any inclusion bias that can occur in such settings. “Ultimately, we want to confirm these monocentric studies, which have provided optimistic data that have informed our present registry,” Denys said. “There is already a very positive signal supporting LVD and its superiority
There is already a very positive signal supporting LVD and its superiority over PVE for every single patient.”
over PVE for every single patient.”
Denys noted that observing marginal indications for liver preparation techniques, such as LVD and PVE, will be “very interesting” when they are able to analyse the final data of their registry.
“When your left liver lobe volume is at its limit, what preparation technique should you decide to go with, if at all? What do you get in terms of results?
If you are able to shorten hospital stay and reduce morbidity, that’s very interesting information. There’s also room for expanding the indication for liver preparation techniques to broader
indication criteria, as the technique has very low morbidity and this is what we want to confirm—the more liver you leave in place after surgery, the better the patient outcome in the postoperative period.” This, he stated, may be due to faster recovery time and less complications—all endpoints that he anticipates can be achieved with LVD, or at least this is what his team are seeing “at the moment”.
Finally, Denys added that interventionists should not be “afraid” to use LVD and hopes that any centre which begins to deploy the technique may consider becoming involved in the registry. His presentation of their preliminary data at ECIO is aimed to

6 April 2024 | Issue94 SIR Coverage
SIR
EMBOLIZE trial launched to rectify unmet need in treatment of chronic pelvic pain
The EMBOLIZE trial, a prospective, randomised controlled trial—the first of its kind—was recently launched at the Society of Interventional Radiology (SIR) annual scientific meeting (23–28 March, Salt Lake City, USA), and seeks to investigate the effects of ovarian vein embolization (OVE) and pelvic vein embolization in reducing symptoms in women experiencing chronic pelvic pain due to pelvic venous disease (PeVD).
THIS TRIAL IS A MULTISOCIETY collaboration between SIR Foundation and The VIVA Foundation, in partnership with Penumbra, and will be led by Ronald S Winokur (Weill Cornell Medicine, New York, USA) and Gloria Salazar (The University of North Carolina, Chapel Hill, USA).
PeVD occurs when enlarged veins develop in the pelvis surrounding the uterus or ovaries, which can lead to severe chronic pelvic pain. Speaking to Interventional News, SIR Foundation chair and member of The VIVA Foundation board of directors Maureen P Kohi (The University of North Carolina, Chapel Hill, USA) referenced a call to action from the World Health Organization (WHO), which looked at global data citing pelvic pain as a central manifestation of the disease in women.
“The main treatment that we’ve been offering is OVE, and we know that the
data show a substantial improvement in chronic pain, but we’ve not been able to produce high-quality evidence to support that treatment option. Not only for the scientific community but also to our payers. Many women do not have insurance coverage for this procedure,” said Kohi. In women, these veins can be difficult to see and feel, Neil Mansho Khilnani (Weill Cornell Medicine, New York, USA)—a member of the EMBOLIZE steering committee—explained, which has driven “scepticism” over diagnosing and treating the pain. “The payers also hear this scepticism and jump on that as an opportunity to reduce expenses to their budget.”
The study investigators are seeking women over the age of 18 who have dilated uterine, ovarian or pelvic veins that are causing chronic pain. To determine efficacy, the study will compare changes in the patients’ pain
More hysterectomies can be averted with earlier uterine artery embolization for postpartum haemorrhages
New research presented at the Society of Interventional Radiology (SIR) annual scientific meeting (23–28 March, Salt Lake City, USA) has found early intervention with uterine artery embolization (UAE) can help women avoid hysterectomy due to severe bleeding after childbirth.
“THESE FINDINGS ARE IMPORTANT AND may help more women avoid hysterectomy and other very serious complications of uncontrolled haemorrhage,” said lead author Younes Jahangiri (Michigan State University, East Lansing, USA), a resident interventional/diagnostic radiologist. “As the medical community looks for ways to provide better care for women to address maternal health and peripartum care, this is one more option on the table that could help many women.”
scores on a visual analogue scale from four weeks before treatment through six months post-treatment to evaluate the outcome of vein-directed intervention for venous-origin chronic pelvic pain. Investigators will also evaluate other quality-of-life improvements, improvements in the pelvic vein varices, and changes in pain medication usage.

“Pain is a tricky thing to quantify as there are many variables,” commented Khilnani. “The impact of pain is more important because pain doesn’t just cause pain, it interferes with your life, how many days you’re with your spouse, missing work or how much you are able to do things in your life that are important to you.” To ensure the quality of patientreported outcomes, the investigators will conduct cognitive interviews to get an accurate “picture” of how pain is affecting the patient.
Salazar is confident that due to the large size of the centres from which the investigators will draw participants, enrolment should begin quickly. “Referral will not be a problem. A problem will be selecting appropriate patients for this study. We have evidence for the role of venous compression in this patient population

The study was a retrospective review of 66 patients with a median age of 31 who underwent UAE for uncontrolled postpartum haemorrhage at a single, high-volume medical centre between 2014–2022. UAE successfully controlled postpartum haemorrhaging in 62 of the 66 patients (94%). Four patients required hysterectomies to stop the bleeding, all of whom lost at least 2,400ml blood prior to presentation for UAE and showed symptoms of diffuse intravascular coagulopathy, a clotting abnormality that can happen after large-volume haemorrhage due to rapid consumption of clotting factors.
Postpartum haemorrhage is a rare, but potentially deadly complication of childbirth. To stop it, obstetricians will initially use conservative approaches to replace the lost blood or to promote clotting. If these measures are insufficient, hysterectomy is usually performed. Alternatively, interventional radiologists can be brought in to perform UAE, injecting tiny particles into the arteries that supply blood to the uterus using fluoroscopic imaging guidance. Once placed in the arteries, the particles temporarily block blood flow to stem uterine bleeding.
“Based on these findings, we would encourage obstetricians to involve interventional radiologists early, to be ready to perform UAE if more conservative approaches are not managing
and so we have specific criteria in terms of evaluating the ovarian minimalisation outcomes,” she said. The investigators added that, in the setting of challenges in gaining reimbursement for this procedure, the EMBOLIZE trial is actively encouraging providers to refer potential participants who they cannot treat. “It’s in our best interest to broaden the conversation to touch patients who might be looking for treatment as both arms of the study are fully funded,” Khilnani stated, explaining that participants in the untreated arm will eventually receive treatment after six months.
The multi-society partnership with Penumbra is hoped to expand the reach of the trial to give many women in pain the opportunity to participate. “Patients with pelvic venous disease have few treatment options available to them,” said James F Benenati, chief medical officer at Penumbra. “Dedicated to advancing innovative therapies that address a significant unmet need, Penumbra’s support of this study will help provide clear evidence of the benefits of OVE and pelvic vein embolization to help patients worldwide.”
postpartum haemorrhage,” said senior author James Morrison (Michigan State University, East Lansing, USA).
Researchers in this study found a 36% incidence of post-embolization syndrome, which presents with abdominal pain and flu-like symptoms. The study found that it was more likely to occur in patients who experienced greater blood loss before embolization.
Jahangiri, Morrison and their colleagues plan to expand their research to include multiple institutions and ultimately to conduct a prospective study that examines longer-term outcomes of UAE.
UAE successfully controlled postpartum haemorrhaging in 62 of the 66 patients (94%)
7 Issue94 | April 2024 SIR Coverage
Younes Jahangiri
Gloria Salazar
SIR 2024: Best of abstracts
This year’s Society of Interventional Radiology (SIR) annual scientific meeting (23–28 March, Salt Lake City, USA) gave recognition to select abstracts during the closing plenary session. Introduced by SIR 2024 programme chair Bulent Arslan (Rush University, Chicago, USA), who commended the “strong” and “compelling” presentations, speakers offered data which challenge preconceptions about disease states and treatment strategies.
Abin Sajan (Columbia Irving Medical Center, New York, USA), presenting first, relayed the team’s evaluation of the long-term efficacy of haemorrhoid artery embolization (HAE) in patients with symptomatic haemorrhoids.
Providing initial background, Sajan noted that haemorrhoid disease affects between 5–10% of the general population and is the third most common outpatient gastrointestinal diagnosis. Current treatment options, he outlined, range from least to most invasive, including lifestyle modifications, office-based procedures such as rubber-band ligation, and lastly surgical haemorrhoidectomy. Sajan explained however that office-based procedures currently have recurrence rates as high as 40-50%.
With intent to confirm the effectiveness of HAE, Sajan then described his team’s retrospective, singlecentre study of 221 patients—“the largest sample size to date”, the speaker noted. All patients had symptomatic internal haemorrhoids and were observed over the course of two years between August 2021 and April 2023. Their cohort, comprised of 115 males and 106 females, had an average age of 57.1 years and an average haemorrhoid grade (HG) of 2.1. Patient symptoms ranged from less than 5 years to more than 20 years, which truly “shows the disease burden of this population”, Sajan said.
After undergoing embolization of the abnormal vascular blush at the haemorrhoidal cushion, patients were evaluated at baseline, 1-, 3-, and 6-12 months for haemorrhoid-related pain (HRP), haemorrhoidal symptoms score (HSS), quality of life (QoL), French bleeding score (FBS), and HG.
Here, Sajan detailed their results, stating that for “every single outcome measure was significant across every single timepoint”. Technical success was achieved in 100% of cases and a 90% clinical success was also reported, with 21 patients requiring repeat embolization. 19 out of the 21 patients had a middlerectal artery supply which was embolized.
“Haemorrhoidal artery embolization is an effective and durable treatment option for haemorrhagic disease with a very low risk profile,” he summarised. “Next steps will include a comparison to standard treatments such as rubber-band ligation.” Finally, Sajan asserted that the current evidence is sufficient to place HAE within the treatment algorithm for symptomatic haemorrhoid treatment.
Novel ex vivo human liver for microwave ablation research
Following Sajan, Carlos B Ortiz (University of Texas Health Centre at San Antonio, San Antonio, USA) discussed the novel creation of dual-perfused ex-vivo human liver models for the investigation of microwave ablation (MWA).
In collaboration with local transplant surgeons and the Texas Organ Sharing Alliance (TOSA), Ortiz and his team gained research consent and received human research livers from deceased organ donors using standard surgical and transplant preservation techniques. He described that a fluoroscopic compatible ex vivo dual arterial and portal perfusion system was used to perfuse and oxygenate the organ. MWA was performed using a 2.45GHz system
(Angiodynamics) at 140 Watts for six minutes followed by placement of a spinal needle to mark the trajectory of the probe. MWA zones were segmented along the MWA trajectory to obtain maximal short axis diameter (SAD) and long axis diameter (LAD) measurements. Ellipsoid volume and sphericity were then calculated.
Receiving a total of 12 livers, seven underwent “successful” perfusion and MWA procedures, with an average cold ischaemic time of 76.8 hours. Continuous bile production was observed in five perfused livers, including the two cirrhotic livers, while average oxygen consumption was 11.4 + 8.3mL/ min. No bile production was noted in livers with >60 hours cold ischaemic time. Comparing perfused and non-perfused MWA, Ortiz expanded that perfused

Jolie Jean
Our study demonstrates that cryoablation can be performed effectively in patients with large tumours”
resulted in significantly smaller MWA dimensions than nonperfused ablations, with a difference of approximately 28%. Additionally, in a sub-analysis, the speaker described a “statistically significant increase” in perfused MWA zones in livers with steatosis compared to those with cirrhosis.
“We report the successful creation of a dualperfused human liver model,” Ortiz continued, “this model can produce the heat-sink effect and enable the study of different tissue types.”
Breast cancer recurrence after cryoablation
Jolie Jean (Weill Cornell Department of Radiology, New York, USA) was next to present, addressing breast cancer recurrence after cryoablation. Giving brief context, Jean outlined that the National Comprehensive Cancer Network (NCCN) in the USA set guidelines in which surgery is the “cornerstone for locoregional control” of breast cancer. “Presenting a unique challenge,” she said, “are women who are poor surgical candidates or who refuse surgery.”
Breast cryoablation has been studied in recent clinical trials which have demonstrated its effectiveness in low-risk cancers less than 1.5cm, Jean said. Due to a “paucity” in literature, Jean’s team set out to evaluate breast cancer recurrence after cryoablation in a broader range of cancer subtypes a and sizes, who were poor surgical candidates or refused surgery.
Their single institution retrospective study included 60 patients with an average age of 75. Of these patients, 48 had invasive ductal carcinoma (IDC), five with invasive lobular carcinoma, and seven who had other histology. Tumour size ranged from (0.3-9cm), with average size of 2.5cm±1.8cm. Jean stated that a multi-probe approach was taken for tumours greater than 1.4cm with a series of freeze-thaw cycles to achieve a 1cm margin.
“All procedures were well tolerated,” Jean described for attendees, noting that “minimal or no” sedation was used based on patient preference. Following the procedure, patients were imaged using mammography and ultrasound, which at a median follow-up of 16 months, showed a recurrence rate of 10% (six patients).
Patients with poorly differentiated disease had higher risk of recurrence, while invasive lobular carcinoma status, oestrogen/progesterone receptor status and triple-negative breast cancer (TNBC) status did not contribute to the risk. Jean added that tumour size did not differ between recurrence and nonrecurrence groups.
“To date, this is the largest single-institution retrospective experience describing recurrence rates after cryoablation of primary breast cancer. Our study demonstrates that cryoablation can be performed effectively in patients with large tumours using a multi-probe approach,” Jean summarised, adding that they hope this research and prior studies will “pave the way” for US Food and Drug Administration approval and insurance reimbursement.
Radiofrequency ablation for intrahepatic cholangiocarcinoma Qian Yu (University of Chicago, Chicago, USA) was next to the podium, describing a 20-year analysis of radiofrequency ablation for intrahepatic cholangiocarcinoma (iCCA). In this “rare but very aggressive” indication, Yu began, the majority of tumours are not resectable at the time of diagnosis, and following resection, recurrence can be high.
Data on this topic are “sparse”, thereby, through using the Surveillance, Epidemiology, and End Results (SEER) database from 2000–2020, the researchers extracted data from approximately 27% of the US population diagnosed with cancer, evaluating trends in survival among iCCA patients undergoing thermal ablation. For a total of 192 patients, the median overall survival (OS) in these data was 28 months, with one, three, and five-year OS of 79.3%, 35.8%, and 19.8%, respectively. Looking closely at the data, Yu noted that patient survival increased after 2010, and that “as expected”, tumour burden correlated with survival.
“The survival curve of local disease appears better than extrahepatic disease,” Yu said, with tumours of less than 3cm demonstrating better survival than larger tumours. For patients with tumours of less than 3cm, survival was reported as an “impressive” 49 months, Yu detailed. “This tells us that ablation can be effective in carefully selected patients.” Yet, there is still a need for high-level evidence, Yu stated, drawing attention to the size of their cohort despite the 20-year time range. “It is beyond a single-centre’s ability to gather a homogenous, yet large enough sample size—future institutional collaboration is key for this research to move forward,” Yu finalised.
8 April 2024 | Issue94 SIR Coverage
SIR
Peeling the “onion”: Pain palliation’s developing role in cancer care
At this year’s Society of Interventional Oncology (SIO) annual conference (25–29 January, Long Beach, USA), Dimitrios Filippiadis (Athens, Greece) moderated and presented in a session focused on palliative interventions, an area of rising interest within interventional oncology (IO). Filippiadis is an associate professor of diagnostic and interventional radiology (IR) at the National and Kapodistrian University of Athens, whose practice centres on musculoskeletal (MSK) and oncologic interventions, and cancer pain management. Catching up with Interventional News, he gives an update on palliative care as it stands today, the treatments that work, and the broader significance of palliation in light of a global opioid crisis.
What were the key takeaways from your presentation and the overall session at SIO?
My talk in this palliative session focused on injections for cancer patients, so the main focus was pain reduction, mobility improvement, and improvement of life-quality in cancer patients. The fact is that, currently, there is a very high percentage of cancer patients that experience pain. Almost 80% of patients will experience pain during the course of their disease, and the vast majority of these patients are not adequately treated for their pain today. Therefore, this is a very large patient pool that we need to help.
Specifically for nerves, we can inject a wide variety of different agents, ranging from corticosteroids, local anaesthetics, alcohol of phenol, and rarely, hyaluronate acid derivatives for intra-articular injections. For example, you have a patient who is suffering either from degenerative disease in the spine or from metastases in the spine, and the result is neuralgia going all the way down to the lower extremities. To help these patients, you can inject corticosteroids with local anaesthetic. If you want something more permanent, you can perform neurolysis. An alternative to that is temperature mediated neurolysis—which will use radiofrequency or cryoneurolysis—in order to destroy the nerves. When you are performing any type of neurolysis, you interrupt the pain signals from the periphery to the brain, providing the patient with immediate pain relief, which complements life quality improvement.
Let’s take, for example, pancreatic cancer—in the guidelines, neurolysis of coeliac plexus or splanchnic nerves is included for the management of pancreatic cancer-related pain. In the National Comprehensive Cancer Network (NCCN) guidelines from 2021, and in the revised version of 2023, IO techniques including injections, neurolysis, augmentation techniques and ablation, are included for the management of adult cancer pain. For too many years, myself and
Additionally, one of the greatest advantages of our percutaneous or transarterial approaches is that they can be combined in a single session. A patient can visit the hospital once and receive ablation, plus structural augmentation, and maybe transarterial embolization—whenever it’s necessary. This is not only beneficial for the patient, but for the hospital and its finances as well.
What influences your judgement when deciding on a pain management pathway?

my colleagues believed that pain palliation is an extra fourth step in the well-known analgesic ladder from the World Health Organisation (WHO). But right now, everybody’s convinced that our techniques—IO percutaneous, minimally invasive techniques—are not an extra fourth step, but actually an intermediate step which should be performed before switching from weak to strong opioids. Thus, the earlier we perform this kind of therapeutic approach, the better the result we are seeing. By doing so, we can significantly reduce strong opioid administration and we can positively impact the global opioid overdose crisis.
How significant is palliative care to your oncology practice?
Palliative care is a major part of our everyday clinical practice. In my hospital, we have weekly multidisciplinary board meetings to discuss pain management, which are held separately from the multidisciplinary team (MDT) tumour board meetings.
We have orthopaedic surgeons and neurosurgeons, medical and radiation oncologists, anaesthesiologists, interventional oncologists, and we speak about different cases with a clear focus on pain management. Therefore, for the last three years that we have been holding these meetings, running palliative procedures has become around 50% of our everyday clinical practice. There is also a wide variety of techniques that we can offer; as well as neurolysis, we offer ablation, vertebral augmentation, or bone augmentation techniques. For patients with lytic spinal or peripheral skeletal metastasis, which cause pain and mobility impairment, we can offer percutaneous ablation, which can result in both local tumour control, prolonged overall survival, and pain reduction followed during the same session by an augmentation technique for structural support.
Following our weekly MDT meetings to decide which therapy should be performed, we consult with the patient to clearly explain what their expectations should be. Expectations differ case by case—you can have a patient with less extensive disease and the goal could be a combination of local tumour control, plus symptomatology improvement. You can have patients who have extensive metastatic disease and the goal there is to first identify the source of pain and treat it. In these cases, you will offer improvement of the symptomatology in terms of pain reduction and mobility improvement. And last but not least, you also have cancer patients who have been treated, but they’re suffering from pain as an adverse event of the treatment. For example, you can have breast cancer patients who have undergone mastectomy, or patients with lung cancer, who have undergone thoracotomy and, respectively, these patients after surgical operation might suffer from post-mastectomy or postthoracotomy pain syndrome. We also help these patients with neurolysis by taking out specific nerves for each case.
Looking past pain, you can have patients suffering from other symptoms, such as breast cancer patients with hot flashes, or patients with abdominal malignancy that suffer from nausea or vomiting. Cryoneurolysis of specific nerve targets in specific cases can also help in improvement and resolution of these symptoms as well.
Is
every
interventional oncologist equipped to
provide pain palliation? What soft/hard skills are required to perform these techniques? This is the million dollar question. As interventional oncologists, we are clinicians, we are fully fledged clinicians. And we should start by explaining to everybody that we are treating the patient and not the images. There is a long list of
clinical skills that are required to first decide on the correct therapy and then perform this treatment. Interventional oncologists should be able to consult with the patient, analyse the medical and clinical record, see the list of drugs the patient is taking, identify the source of pain, the source of symptomatology in general—and this will happen if you combine clinical and physical examination with evaluation of the diagnostic imaging.
Once we have this ability—and trust me, interventional oncologists, we do have these abilities because we were trained for that—we can proceed for selection of an appropriate therapeutic technique. I strongly believe that interventional oncologists should be involved in the decisionmaking process, simply because we know better than anybody else, the advantages and disadvantages of our therapeutic approaches, and therefore we can offer an optimal utilisation of these therapies.
We should also be involved in the follow-up of the patient—in pain, I explain it to my patients through an example of an onion. There are lots of large layers on the outside which cover the smaller layers inside. When you remove these outer layers, you must check to see what effect this has had on the inner portion. Which is to say we should follow up with the patient to see whether additional treatments are necessary. In the era of personalised medicine, it’s not who owns the patient, but who is clinically responsible for a specific section of their disease.
Major interest in palliative treatments in IO has spiked in the last five to 10 years. This may perhaps be due to the opioid crisis, as previously mentioned, but also due to its inclusion in the 2019 NCCN guidelines. I have participated in a group of authors who published a paper in 2019 which has been referenced in The NCCN Adult Cancer Pain Guidelines. Pain has also had a major impact on cancer patients, and it can drive them away from systemic and local therapies. If you have a patient who is in pain, it’s
9 Issue94 | April 2024 Interventional Oncology
Dimitrios Filippiadis
Ultrafast contrast-enhanced ultrasound for PAD patients shows promise in early feasibility research
Majorie van Helvert (University of Twente, Enschede, The Netherlands) and Michel Reijnen (Rijnstate Hospital, Arnhem, The Netherlands) are currently conducting research on ultrafast contrast-enhanced ultrasound blood flow quantification in peripheral arterial disease (PAD) patients after endovascular treatment. Early findings show that the new technique could offer an innovative imaging alternative.
INTERVENTIONAL NEWS RECENTLY SPOKE
with both van Helvert and Reijnen, and they went into more detail about their findings. Traditionally, conventional ultrasound systems are used in the diagnostic work-flow of PAD. These systems have limited temporal resolution which is typically capped out at 10–100 frames per second. However, with the novel technique that Reijnen and van Helvert used, they were able to increase that framerate to thousands or even tens of thousands of frames per second. This may be necessary to adequately quantify very high velocities and short-lived flow disturbances, for instance, in and around stenoses.
“Within that technique we use a new type of ultrasound transmissions, which is called plane wave ultrasound,” Reijnen explained. “When you look at regular ultrasound, and its image reconstruction, it’s done line-by-line. So, they make the image in separate lines, and all these lines are combined into one image. With plane wave, all transducer elements are simultaneously active in transmit and receive, thus you construct the image in one go. That enables you to get much more frames per second.”
Besides the increased framerate, the team also used contrast microbubbles. For this purpose an IV [intravenous drip] needs to be inserted to allow for contrast administration prior to the ultrasound acquisitions. “Once we use the ultrasound, these contrast microbubbles make sure that the echogenicity of the blood is enhanced,” van Helvert said. “Next to that, they can be used as tracer particles; that is really the basis for this technique in deeper structures, like the iliac arteries. When we’re looking at more superficial arteries, we don’t really need the contrast as we can perform our analysis based on the bloodspeckle signal itself.”
Reijnen explained that, when you look at anatomy, you are going to mostly use computed tomography (CT) angiography or magnetic resonance
imaging (MRI). “Those are the two most important modalities,” Reijnen said. “When we look at functional imaging, there’s mostly duplex ultrasound. A duplex ultrasound is a regular ultrasound combined with doppler. It gives us flow velocities in one direction, generally in the middle of the vessel.”
He continued by saying that there are some drawbacks to duplex ultrasound, next to the aforementioned temporal resolution. “One of them is that it’s only in one directional. Also it requires a beam-to-flow angle correction which makes it highly operator dependent.”
While MRI technologies offer acceptable imaging, there are still some drawbacks to that as well. Namely, Reijnen explains, it’s time consuming, expensive, and the fact that multiple cardiac cycles are combined during image reconstruction may filter out important diagnostic information. “Another important drawback for example,” Reijnen said, “when there are stents, metal and MR is not a good combination. So, there may be disturbances because of the material of the stent.”
Once the images from the ultrafast contrastenhanced ultrasound have been compiled, the more technical aspect comes into play. In order to determine blood flow patterns, the recorded images from the contrast-enhanced ultrasound are divided into different sub-windows. An algorithm then registered how the microbubbles moved across the images.
“We calculate a cross correlation, and the peak in this cross correlation defines the most probable movement that these microbubbles made between two consecutive images that we captured,” van Helvert stated. “Combined with the time in between the frames, we can calculate a velocity vector per sub-window.”
After the images are captured, they must be filtered to see the microbubble contrast compared to the tissue clutter. The thousands of images that the team


captures through ultrasound and thereafter analyse, allows them to build a velocity vector field over time. However, one unfortunate downside of this is that the images and the velocity vector field are still twodimensional compared to the three-dimensional flow characteristics.
“But, the upside of this technique compared, for instance, to MRI-based flow imaging, is that we measure a couple of cardiac cycles and its proven feasible inside stents.. So, it does provide added information in that sense,” van Helvert explained. Reijnen went into more detail. “We can really track these bubbles during the cardiac cycle, and we can assess different patterns from that. So, we can see recirculations, we can see stasis of blood, we can see forward flow and backflow. We can also see that there is difference in blood flow at the anterior wall and the dorsal wall of the blood vessel where there a re bifurcations.”
“What we’re aiming for is, at least my view on things, that in an early disease stage you can do such measurements reliably and minimally invasive to assess if patients have favorable or unfavorable blood flow with respect to disease progression,” van Helvert said.
As for the next steps, Reijnen noted: “At this stage we’re looking at the technique itself, so we’re looking at which parameters can we reliably derive. How can we standardise them and how can we quantify them? And when we’ve done that, then we can do clinical studies in which we start to look at the predictive value of each of them.”
“There’s a lot of steps ahead of us,” van Helvert told us. “We’re in the very first stage.”
10 April 2024 | Issue94 Peripheral Interventions
PERIPHERAL
Michel Reijnen Majorie van Helvert
New data and heated debates set to spark controversy in CX 2024 peripheral arterial programme
“These will be important, salutary lessons. Should a controversy arise again involving a proven efficacious therapy, we now know that stopping access to that therapy may result in unwanted and unexpected negative effects on patient care.” These are the preluding thoughts of Andrew Holden (Auckland City Hospital; University of Auckland, Auckland, New Zealand)—one of the Charing Cross (CX) Symposium 2024 (23–25 April, Londo, UK) co-chairs—ahead of this year’s meeting, referencing the paclitaxel mortality controversy. Here, Holden sets sights on the unmissable peripheral arterial programme, which will tackle global controversies and host heated debates.
“The peripheral arterial programme is jam-packed with controversy this year— controversy being the theme for CX 2024,” says Holden, highlighting this fact by noting that the first session will address paclitaxel mortality. The paclitaxel mortality controversy in peripheral arterial disease (PAD) will be punctuated by a late-breaking presentation from Eric Secemsky (Beth Israel Deaconess Medical Center, Boston, USA), who plans to examine whether the meta-analysis and subsequent regulatory body restrictions on paclitaxel caused harm.
“Although the original paclitaxel mortality controversy did not make sense in terms of causation theories, it was appropriate to take this report very seriously. However, in many geographies this resulted in stopping a therapy that had been shown to be more effective and durable than our nondrug-coated strategies,” details Holden. “An important question that hasn’t been addressed to date is when depriving patients of a more effective treatment modality, were we causing patients harm? With the benefit of hindsight, can we learn important lessons regarding this?”
“Hopefully we will provide the final chapter of this controversy. We have key opinion leaders presenting new data, and some input from regulators such as the US Food and Drug Administration (FDA) and the UK Medicines and Healthcare products Regulatory Agency (MHRA),” Holden says. “I’m very grateful to Eric and his group for providing additional data to allow us, for the first time, to dive into this issue.”
Holden notes that during this session, speakers and audience members will have the opportunity to ask the regulators what their thoughts are with regard to the removal of access to paclitaxel-coated devices and the duration of time it has taken to have these therapies reinstated.
Paclitaxel-coated devices also feature

in later sessions, Holden contributes, commenting that the ‘Paclitaxel and sirolimus-coated balloons in the femoropopliteal arteries’ session will end with a debate, which asks if “following the FDA announcement, do paclitaxel-coated devices now beat limus-coated devices”. He adds that drug-coated technologies will be of “great interest” at this year’s CX Symposium and will provide delegates with the opportunity to share their thoughts and experiences.
“Promising” future for bioresorbable scaffolds in the tibial arteries
Later in the peripheral programme, speakers will turn to bioresorbable scaffolds in the tibial arteries. Brian DeRubertis (Weill Cornell Medicine, New York, USA) will present latebreaking data in the LIFE-BTK clinical trial evaluating the safety and efficacy of the everolimus-eluting Esprit belowthe-knee (BTK) system (Abbott) in chronic limb-threatening ischaemia (CLTI) patients with infrapopliteal artery disease.
“Bioresorbable scaffolds have been the holy grail for lower limb arterial interventions for many years,” Holden
When depriving patients of a more effective treatment modality, were we causing patients harm?”
details. He draws attention to the high percentage of cases that require a scaffold due to issues such as dissection and recoil after angioplasty, but also the long-term negative effects of metal stents when placed in the tibial arteries.
“We’ve looked for a bioresorbable
scaffold that works in the acute phase, but then dissolves with time and allows arterial structure and physiology to be restored. Many trials have failed both above and below the knee,” he says. However, following the LIFE-BTK trial results in 2023, which showed a statistically significant benefit for primary bioresorbable scaffolds, Holden believes this year’s CX is positioned well for a “timely deep dive” into the subject and “promising” emergent technologies.
Inaugural Roger M Greenhalgh late-breaking trials session
On both Tuesday 23 and Wednesday 24 April at CX 2024 the inaugural Roger M Greenhalgh late-breaking trials sessions will take place. “I believe Professor Greenhalgh would be very proud of the late-breaking trial sessions we are hosting in the peripheral arterial space at CX 2024,” says Holden.
At a glance, he highlights that deep venous arterialisation is a topic of “growing interest” that will feature in this session. He states the session will provide an opportunity for attendees to evaluate where this new technology may sit within physicians’ current armamentarium, particularly in patients with advanced CLTI. New data from the CLARITY trial will be presented by Anahita Dua (Massachusetts General Hospital, Boston, USA), evaluating transcatheter arterialisation of deep veins for no-option CLTI.
Holden also places focus on the sixmonth SHOCC study data, which will be presented by Athanasios Saratzis (University of Leicester, Leicester, UK). The trial analysed the Shockwave lithotripsy device (Shockwave Medical) for patients with PAD and will produce new data during Wednesday’s Roger M Greenhalgh late-breaking trials session. This data, Holden shares, will shed light on the device’s “effectiveness” at the trial’s UK centre.
CLTI and imaging modalities
Elsewhere in the peripheral programme, Holden highlights the comprehensive coverage of CLTI trials—including updates from BEST-CLI and the BASIL-3 podium first—and points toward the imaging modalities session.
“One of the big challenges with imaging and CLTI is trying to identify the patients who are going to respond to revascularisation. We know that CLTI patients often have a multifactorial cause for their disease in addition to their macrovascular arterial disease. In many cases, we can spend a lot of time revascularising patients who don’t benefit so we need to get a better idea of favourable responders,” says Holden.
Holden restates the importance of pre-procedural and intra-procedural imaging, which will be explored during this session, enabling physicians to get to grips with new technologies to assist in measuring when a therapeutic endpoint has been reached during a revascularisation procedure”.
“Imaging and CLTI is an expanding and very important topic that we’re going to certainly delve into on the Thursday [25 April] of CX 2024,” he adds.
Great debates in the peripheral arterial programme
The CX 2024 peripheral programme will also play host to a variety of controversial debates including paclitaxel versus limus-coated devices, and bypass versus endovascular surgery, affording CX delegates the opportunity to cast their votes. Aptly devised, the debates in the peripheral arterial programme are centred on controversial topics and are hoped to spark lively discussion. To this end, Holden believes that they will “drive consensus and effectively further the conversation” surrounding these complex treatment modalities.
11 Issue94 | April 2024 CX 2024
Andrew Holden
Fostering development: Using social media as an interventional radiologist

Evgenia Efthymiou
Point of View
As a member of the Cardiovascular and Interventional Radiological Society of Europe social media subcommittee, Evgenia Efthymiou (University of Athens, Athens, Greece) expands on the importance of visibility and the valuable interventional initiatives that can be achieved online.
The advent of social media has generally transformed the healthcare landscape, facilitating communication, collaboration, education, and patient-centered care. Interventional radiology (IR), a technologically driven specialty, inevitably experiences the impact of platforms like X, LinkedIn, Facebook and Instagram. Past research has shown a significant increase in the adoption of social media within the radiology community,1 while a recent Australian study showed that the majority of interventional radiologists use at least one social media account.2
Sharing educational content, such as intriguing cases and innovative approaches to complex clinical scenarios, is among the most prevalent
and efficient uses of social media within the IR community.3 Εvery post with a popular hashtag could be widely shared and may commence a vivid discussion regarding technical details, risk of complications and postoperative care etc.
Educational posts are shared not only among qualified interventional radiologists, but also between medical students and residents. It is essential to highlight the role of social media in early medical education, as nowadays, multiple accounts are available on X (@ETF_IRtrainees, @IR_Juniors) along with Instagram and Facebook accounts and groups, which provide a wealth of images and case-based discussions about IR. The importance of social media use in early medical
education and during residency could be easily addressed, by observing the constant increase of followers across various accounts as well as the increasing frequency of reposted content.
Social media serves as a crucial platform for mentoring and motivating medical students and young interventional radiologists. Presently, numerous accounts are accessible, providing students, prospective residents, and fellows with insights into the daily experiences of IR and the training programmes available. These accounts may belong to societies and training centres, but they can also be managed by current trainees and interventional radiologists, who—in a more direct and personal manner— share insights into their training journey and the challenges they face.
Besides educational purposes, social media facilitates communication and interaction, allowing active participation in online discussions. These interactions are instrumental in developing a professional network and can enhance one’s career by creating opportunities for collaboration. Platforms like LinkedIn or ResearchGate showcase individuals’ curriculum vitae (CV) and research interests, facilitating recruitment efforts and enabling participation in multicentre research projects. It has also been proven, that sharing research via social media is linked with higher citation rates.4 In addition to personal accounts, radiology departments, journals and radiology professional societies use social media platforms for research dissemination.
Social media can also raise awareness among other medical professionals and patients, advocating for the important role of IR in modern medicine. It highlights the availability of alternative
Is it time for IR to embrace AI?
“It’s time for all of us to embrace artificial intelligence [AI], because it’s my prediction that interventional radiologists who use AI will certainly have better patient outcomes,” were the words of Dania Daye (Massachusetts General Hospital, Boston, USA) presenting at the Pan Arab Interventional Radiology (PAIRS) annual congress (10–13 February, 2024, Dubai, United Arab Emirates). Her talk focused on AI in interventional radiology (IR) and how it can augment practice efficiency.
SPEAKING FROM HER CENTRE’S experience, she first noted the “rapid” development of US Food and Drug Administration-approved AI-based medical devices, with over 720 having been approved in the most recent report. However, while there are very few algorithms approved for use in IR today, she stated, the opportunities for “improving practice efficiency and patient care” are abundant. Daye’s presentation highlighted various opportunities for AI implementation across different aspects of IR practice. These included patient-facing care, pre-procedural planning, intra-procedural support, patient risk stratification, and non-clinical applications aimed at improving practice efficiency. In patient-facing care, AI offers tools for “patient selection, triage, and care coordination” she explained. Applications range from identifying suitable candidates for IR procedures to streamlining referrals
and coordinating care through communication aids and chatbots. The speaker continued that AI also plays a role in augmenting patient-facing care through chatbots, health risk prediction, and interpreting physician notes. Notably, large language models like ChatGPT have demonstrated significant potential in improving patient understanding of radiology reports, Daye added.
Pre-procedural planning benefits from AI-driven segmentation, dosimetry support for Y90 procedures,
AI will no doubt change the way we practice medicine in the next 10 years”
minimally invasive treatments and showcases the positive impact IR procedures can have on patients’ lives.
A primary concern regarding the use of social media in healthcare is the potential breach of patient confidentiality, which can occur easily. Discussing specific procedural details or complex and rare cases could compromise patient privacy. Additionally, social media platforms do not undergo the rigorous peer review process of scholarly articles, making them susceptible to misinformation. Therefore, each post should undergo further personal review before dissemination. Lastly, maintaining professionalism consistently in all interactions is crucial, as misunderstandings can easily occur.
To sum up, social media has become an indispensable aspect of the contemporary world, including within IR, providing a multitude of opportunities such as promoting medical education, fostering career development, facilitating networking, and disseminating research, among others. As we expand our presence on social media, the field of IR will have greater influence in the swiftly changing medical environment.
References:
1. Patel SS, Hawkins CM, et al. Professional social networking in radiology: Who is there and what are they doing?. Acad Radiol. 2017;24(5):574-579. doi:10.1016/j.acra.2016.09.026
2. Wang MT, Foo M, Maingard J, et al. Social media in interventional radiology. J Med Imaging Radiat Oncol 2021;65(2):182-187. doi:10.1111/1754-9485.13142
3. Kassin MT, Ukeh I, Bunch PM, Sabri SS. Social media considerations for the interventional radiologist. Radiographics. 2022;42(6):E165-E166. doi:10.1148/ rg.220157
4. Widmer RJ, Mandrekar J, Ward A, et al. Effect of promotion via social media on access of articles in an academic medical journal: A randomized controlled trial. Acad Med. 2019;94(10):1546-1553. doi:10.1097/ ACM.0000000000002811
Evgenia Efthymiou is an interventional radiologist at the Attikon University Hospital, Athens, Greece.

Dania Daye
device sizing, and electronic medical record (EMR) information extraction. Daye outlined that intra-procedural support includes AI applications for image fusion, surgical robotics, needle guidance, and patient risk stratification. The speaker went out to outline the nonclinical applications of AI in IR which can improve practice efficiency. Sharing AI applications within scheduling, clinical trial recruitment, coding for procedural billing, and insurance pre-authorisation, “which in the USA has really changed how we bill for these procedures”, she stated.
Daye’s presentation emphasized the potential of AI in IR practice, predicting that its integration will lead to better patient outcomes. “AI will no doubt change the way we practice medicine in the next 10 years,” she told delegates. While challenges remain, including the need for further research and development, “embracing AI” Daye sees is essential for the betterment of IR efficiency in the future.
12 April 2024 | Issue94 Technology
Five-year outcomes show transurethral ultrasound ablation successful in treatment of prostate cancer
A minimally invasive treatment using magnetic resonance imaging (MRI) and transurethral ultrasound instead of surgery or radiation is effective in treating prostate cancer, according to new research presented at the Society of Interventional Radiology (SIR) annual scientific meeting (23–28 March, Salt Lake City, USA).
The traditional treatment options of radiation or surgery often come with a risk of side effects, including urinary incontinence and erectile dysfunction that cause significant morbidity and adverse lifestyle effects. Researchers said that some patients now have a durable alternative for whole-gland treatment with MRI-guided transurethral ultrasound ablation (TULSA) that does not preclude future treatment with surgery or radiation.
“The success of TULSA represents a revolution in whole-gland treatment for prostate cancer,” said lead author Stephen S Raman (University of California, Los Angeles, USA).
“Prostate cancer is the most common form of cancer in men, affecting one in eight men in their lifetimes. We have more research to do, but if validated, TULSA has the potential to change the standard of care for thousands of men.”

In the TULSA procedure, a small catheter-like device is inserted through the urethra into the prostate. Once there, MRI is used to guide precise positioning of 10 therapeutic ultrasound elements into the prostate. MR thermometry is used to monitor the tissue while heating to more than 55 degrees within the prostate and limiting heat to the sensitive nerves surrounding the prostate as the device rotates around the entire gland. The procedure can be performed in an outpatient or inpatient facility under general or spinal anaesthesia in two to three hours.
According to Raman this image guided therapy: “maximises our ability to kill cancer cells while minimising collateral damage to the prostate to achieve the ultimate trifecta in prostate cancer treatment—full local cancer control while maintaining urinary continence and potency. The latter are the complications of most prostate
A new class of microcatheter can be created that overcomes manoeuvrability deficits which can cause unsuccessful catheterisation.”
Christopher Bailey
cancer therapies that patients hate and often result from a lack of precision in treatment monitoring.”
In the prospective observational study, participants showed improvement in the reduction of the presence of cancer, prostate size and prostate-specific antigen levels (PSA), which are markers for cancer. Cancer was undetectable on follow-up biopsy by 76% at one year after TULSA with a decrease in median prostate volume by 92% within one year and a decrease in PSA from 6.3ng/ml to 0.63ng/ml at five years.
because of residual or new tumours. Through this process, researchers learned the early predictors of TULSA failure related to calcifications between the urethra and prostate cancer and better monitoring of prostate swelling, targeting and misalignment, leading to improved detection and management of these preventable errors during the procedure.

Stephen S Raman
TULSA had a very favourable side-effect profile compared to alternative surgical, radiation and thermal therapy showing that, up to five years, 92% of patients recovered continence and 87% preserved erectile function. During the study, 115 men were enrolled across 13 sites in five countries. Of those treated, 25 men received follow-up conventional treatment with surgery or radiation
Raman noted that the study affirms that interventional radiologists now have a meaningful role in detection and management of prostate cancer care as they already had in other types of cancer, such as lung, kidney and liver cancers. He said interventional radiologists’ expertise in imaging and image-guided procedures and experience with ablation make them a critical part of the prostate cancer care team.
The research into TULSA’s effectiveness continues with the CAPTAIN trial, a randomised controlled trial comparing TULSA with radical prostatectomy.
Interventional radiologists’ expertise in imaging and image-guided procedures and experience with ablation make them a critical part of the prostate cancer care team”
13 SIR Coverage Issue94 | April 2024
JACK JENNINGS
Jack Jennings is a professor of radiology and chief of musculoskeletal radiology for Mallinckrodt Institute of Radiology (MIR) at Washington University School of Medicine in St Louis, USA. Best known for his innovation in musculoskeletal and spine interventions, Jennings is no stranger to blending niches, combining skills gained from his experiences in interventional radiology (IR), neuroradiology, and musculoskeletal radiology for a range of tumours in the bone, spine and soft tissue.
What attracted you to a career in IR?
Since I was young, I always wanted to be a doctor and do something with my hands in medicine. I spent a lot of time in the operating room with a neurosurgeon friend of my family, so I naturally had neurosurgery as my chosen pathway. This trajectory was modified late in medical school based on the wisdom and advice of my mentors Don Hilbelink, my doctorate advisor, and Reed Murtagh (both University of South Florida, Tampa, USA) a neuroradiologist. I was introduced to radiology and IR concurrently, though a quick lastminute pivot resulted in me matching to a radiology residency.
Who were your mentors?
At MIR, I was fortunate to work under internationally respected pioneer in musculoskeletal (MSK) radiology and interventions, Louis Gilula, who sadly passed away in 2014. Lou pushed me as a resident and fellow to meet and spend time with Afshin Gangi and Matt Callstrom who both blazed the trail for MSK interventional oncology (IO). I was fortunate and able to go to Strasbourg, France at the beginning of my career and spend time with Afshin and his team. This was my introduction to advanced bone and soft tissue ablations, including the treatment of spine metastases. Matt Callstrom was very instrumental in MIR developing a bone ablation practice over 15 years ago and guided me through the process. His direction was invaluable. He helped us navigate the reimbursement and third-party payer issues in an era before there were current procedural terminology (CPT) codes for the majority of the ablation procedures we were doing. I am forever grateful for all of their guidance, mentorship, and very close friendship. The ability to combine imaging with cancer-related treatments has been the perfect blend for my career satisfaction. IR is always developing new procedural techniques, ablation and procedural devices, imaging guidance, and ablation evaluation/ confirmation. This allows us to have a very close relationship with industry and work with research and development teams in the creation of therapeutic devices for the treatment of cancer. This relationship and the overlapping goals we share, has fostered many wonderful mentors and friends.
I have been blessed with incredible mentors at every step of this journey. Having one great mentor in your career is a blessing but to have as many as I’ve had is beyond words. Maybe it speaks of how much guidance I need i.e. too much. I have such gratitude for all of them and I would encourage early career
physicians to reach out and find a mentor or two. This is the beauty of societies such as the Society of Interventional Oncology (SIO), the American Society of Spine Radiology (ASSR), the Society of Interventional Radiology (SIR) and the Cardiovascular and Interventional Radiological Society of Europe (CIRSE), as they all have programmes and mechanisms for students to early IR/IO to meet with programme/society faculty and/ or be involved with the mentor programmes. These relationships that you will develop with mentors, colleagues and being involved in societies, will give a dimension and satisfaction to your career that goes beyond the everyday grind.
Could you describe a particularly memorable case of yours?
My most memorable case was my first cryoablation case. Lou had a case involving metastatic thyroid cancer to the bone with lesions increasing in size, and he convinced myself—a fellow at the time—and Daniel Wessell, first-year faculty, to do the first bone cryoablations at MIR. Talk about pressure! We did six lesions that day, which took us nearly 12 hours (obviously very novice and very slow) and let’s just say my scrubs were drenched; however, it was the nidus for us to begin to build what is now a very robust ablation practice.
You formed a multidisciplinary metastatic spine working group (MMSWG) in 2014 that led to published recommendations for the treatment of metastatic spine disease. What are the most important factors when devising recommendations?
The MMSWG came about by the efforts of radiation oncologist Cliff Robinson (Washington University in St Louis, St Louis, USA), Bob Poser, vice president of Global Spinal Therapies at Merit Medical, and myself. This group was made up of radiation, surgical and medical oncologists and interventional radiologists from institutions from the USA and Europe. We used level-one evidence and recommendations available at the time to develop a treatment algorithm for patients with spine metastatic disease. This included an in-person, day-long roundtable discussion, presentations of the evidence and formulation of the treatment pathways for various scenarios of spine metastatic disease. To this day, we follow this algorithm and even updated it a few years ago with a follow-up manuscript as we learned that, as an institution, we were more aggressive and had promising results when operating on patients with metastatic spinal cord compression.
What is the most exciting development in the musculoskeletal interventional arena in the last five years?
FACT FILE
CURRENT APPOINTMENTS
2020–present: Professor of radiology and orthopaedic surgery, MIR (St Louis, USA)
2018–present: Musculoskeletal radiology section chief, MIR (St Louis, USA)
2010–present: Treasurer, Society of Interventional Oncology (SIO) Executive Committee
PREVIOUS APPOINTMENTS (SELECTED)
2022–2023: President, American Society of Spine Radiology Executive Committee
2020–2023: Scientific programme committee member, SIO
SPONSORED CLINICAL TRIALS (SELECTED)
Co-investigator, STAND trial
Co-investigator, OSPREY diagnostic accuracy trial
Principal investigator, MOTION cryoablation trial
Site and national principal investigator, STARRT trial
MSK IR has gone from being a niche subset of IR 15 years ago with only a few people in the audience at scientific meetings—by few I mean the speakers mostly attending each other’s talks—to a rapidly advancing field with ever increasing adoption, hands-on courses all over the world, and positively affecting the lives of many cancer patients with osseous metastatic disease. Cancer patients are living much longer and many will have bone metastases. Our mission is to educate and train as many IR physicians as possible in these procedures so that they can offer them in their practice.
As previous president of the ASSR, what was your experience holding this post?
This society has been so kind to me and took me in as a young attending and really an outcast i.e. MSK radiologist in a neuroradiology society! The mentorship and career fostering by this society, including past presidents Josh Hirsch (Massachusetts General Hospital, Boston, USA), Allan Brook (Montefiore Medical Center, New York, USA), Bassem Georgey (University of California San Diego, La Jolla, USA), and Adam Flanders (Thomas Jefferson University Hospital, Philadelphia, USA) was incredible, and I am very appreciative of them. This society is unique in that it focuses on diagnostic and interventional spine treatment, and it has greatly impacted the advancement of spine procedures from adoption to reimbursement. The rebirth of its workshop has been an overthe-top success with attendees and with our industry partners. This synergy has led to its success and I am sure this will continue for many more years.
Currently, you are treasurer of the SIO. How did you become involved with the society and what does your current role entail?
SIO has really been one of the greatest highlights in my career as it has made great strides in solidifying IO as the fourth pillar of oncologic treatment of cancer patients. Very similar to ASSR, I am blessed that this group has allowed me to be involved in this journey for the advancement of IO patient care. Being on the board and executive committee has allowed me to work with the incredible team of interventional physicians including Muneeb Ahmed (Beth Israel Deaconess Medical Center, Boston, USA), Matt Callstrom (Mayo Clinic, Rochester, USA), Bill Rilling (Medical College of Wisconsin, Milwaukee, USA), Alexis Kelekis (National and Kapodistrian University of Athens, Athens, Greece), Sean Tutton (University of California San Diego, La Jolla, USA), and Michael Soulen (University of Pennsylvania Health System, Philadelphia, USA) who continue to mentor and educate me. As this society continues to grow and as more society-sponsored trials and educational efforts go forward, the immediate and future financial stability becomes more complex and requires much accountability.Working closely with SIO staff and the finance committee, we are focusing on developing a very solid
14 Interview April 2024 | Issue94
PROFILE

financial foundation. I have learned much throughout this process and it could not be done without the support of our SIO team led by Jena Stack.
Yours was recently the first US hospital to be accredited with the International Accreditation System for Interventional Oncology Services (IASIOS). How will this benefit your practice?
With the rapid growth, depth and breadth of IO, having a baseline accreditation such as IASIOS for quality and safety will ultimately result in greater uniformity and validity making us all better at caring for patients. I am very thankful to Andreas Adam (King’s College London, London, UK), Liz Kenny (Royal Brisbane and Women’s Hospital, Queensland, Australia) and CIRSE for all of their help with this process and their continued support. Our quality and safety office was very excited to be a part of IASIOS. The application process educated us on some deficiencies and we have already begun making modifications in our patient workflow.
What is the most exciting development in IO at present?
IO is rapidly growing in its scientific advancements and multidisciplinary adoption. The increased presence in the National Comprehensive Cancer Network (NCCN) guidelines and multidisciplinary tumour boards will allow for broader adoption and knowledge to the other oncology specialties who are not aware of what IR can offer. Likewise, the study and use of combined therapies including ablation and immunotherapy and radiation therapy will continue to advance the treatment of patients especially in those who have failed multiple lines of treatment. These collaborative efforts will surely lead to better patient care.
What is the greatest challenge facing interventional radiologists today?
The rapid growth of IO comes with a responsibility to be able to provide these services to as many individuals as possible across this world—we need growth beyond the walls of ‘ivory towers’. We will need
"We need growth beyond the walls of ‘ivory towers’. We need to train and educate more individuals.”
to continue to train and educate more individuals, both residents and those already in practice, to go out and provide these services and to emphasise the importance of a multidisciplinary approach to cancer care. This is a very exciting time for IR and IO, but we must continue the education, training, and scientific pursuits to make a solid pillar in cancer treatment. We also must continue to educate our insurance companies and thirdparty payers of the advances that have been made and their scientific legitimacy to mitigate this being a barrier for patient treatment.
What are your hobbies and interests outside of medicine?
I have nine children (seven biologic and two step), and we are very sports-driven family— sports such as basketball, hockey, football, volleyball, and soccer. Nearly every second of my free time is filled with my family. The only exception is that I run/workout every morning. We also like to travel. My wife French so we like to go to France every summer and we travel frequently throughout Europe.
15 Interview Issue94 | April 2024
alisonlang.com
First applied ethics discussion at PAIRS 2024


Tauqir Rana
Eric J Keller
Point of View
Tauqir Rana and Eric J Keller discuss a session at the Pan Arab Interventional Radiologists Society Pan Arab (PAIRS) annual congress (10–13 February, 2024, Dubai, United Arab Emirates) featured the first session on ethics in IR in the region, discussing issues such as futility, surrogate decision-making, and conflicts of interest.
The session stimulated a lively discussion and highlighted important cultural differences, which can shape these challenging issues faced in IR practice.
Futility was the first issue raised. Interventional radiologists often care for critically ill patients and can be faced with requests for procedures that offer little chance of benefit. Common examples include gastrostomy tubes in patients with severe dementia or numerous biliary drains for patients with advanced cancer and malignant biliary
obstruction. Advance care planning and partnerships with palliative care can be helpful in navigating these requests. Perceptions of value, risks, and preferences vary widely, so it is important when faced with these requests to understand the patient’s and family’s goals of care and values to differentiate palliative from futile care. The talk then transitioned to consent and surrogate decision-making. The audience raised questions about family requesting that elderly patients not be told about their terminal diagnosis and
how to facilitate informed consent when patients and family defer to whatever the doctor thinks is best in certain cultures.
The modern ideal of consent has moved away from paternalism (what the doctor orders) as well as deferring solely to patient autonomy (whatever the patient/ family wants). Rather, we are challenged to facilitate shared decision making where we respect patients’ preferences and encourage their involvement in the decision-making process but also offer recommendations and guidance as content experts. Patients have a right to know/make decisions about their care, but they also have the right to defer to others to make decisions on their behalf, and this preference should be respected.
The audience was then asked about requiring suspension of Do Not Resuscitate (DNR) and Do Not Intubate (DNI) orders to have an IR procedure. American surgical and anaesthesia guidelines have recommended against requiring suspension for procedures, advising that code status should instead be rediscussed. Yet, a study of IR practices in the USA found that about a third of practices require the patient to be full code for IR procedures. Most participants agreed with required suspension, noting that their anaesthesiologists (and selves) want the ability to resuscitate their patient if something happens intraoperatively.
The final questions raised involved conflicts of interest and relationships with industry. Conflicts of interest
(COIs) are a natural part of professional life and are not always financial. The issue is not necessarily to the existence of conflicting interests or relationships with industry, but the potential bias caused by these relationships. Interventional radiologists’ relationship with industry is viewed as invaluable, but the question becomes how can we effectively manage bias associated with these valuable relationships?
The PAIRS 2024 Applied Ethics in IR session was critical in initiating these key conversations across the world of IR. We hope to continue raising important issues facing our specialty to develop practical strategies and tools to help navigate them across cultures.
References:
1. H D Rockwell, et al. Utilisation of Goals of Care Discussions and Palliative Care Prior to Image-Guided Procedures Near The End of Life. Clinical Radiology. 2022 Feb 14; 10.1016/j.crad.2022.01.050.
1. Tia Forsman, et al. Consent in Interventional Radiology—How Can We Make It Better? Canadian Association of Radiologists Journal. 2022 May 25; 10.1177/08465371221101625
1. Eric D Cyphers, et al. Required Suspension of Do Not Resuscitate and/or Do Not Intubate Orders in Interventional Radiology: A Survey of Prevalence and Practices. Journal of Vascular and Interventional Radiology. 2022 Dec 20; 10.1016/j.jvir.2022.12.032.
1. Thomas Webb, et al. The Prevalence of Financial Conflict of Interest Disclosures by Endovascular Specialists on X (Twitter). Journal of Vascular and Interventional Radiology. 2024 March 19; 10.1016/j. jvir.2024.03.017
Tauqir Rana is a consultant interventional radiologist at King Faisal Specialist Hospital, Riyadh, Saudi Arabia and Eric J Keller is a senior IR resident at Stanford Health Care, Stanford, USA.
Preliminary programme is online!
LINC 2024, the Leipzig Interventional Course, will feature numerous live cases performed from leading interventional centers worldwide, news on the latest developments, KOL in-depth discussions on hot topics, company symposia, and poster sessions.
LINC 2024 will take place from Tuesday, 28 May through Friday, 31 May 2024 in Leipzig, Germany.
Event status assessed by Ethical Medtech CVS: overall compliant.
Don’t miss LINC 2024 – register today!


16 April 2024 | Issue94 Point of View LEIPZIG INTERVENTIONAL COURSE 28–31 May 2024 | Leipzig, Germany Visit our website and subscribe to our newsletter to stay informed: www.leipzig-interventional-course.com Provascular GmbH · Leipzig Interventional Course (LINC) · Markkleeberg, Germany
LI24 ad_225x153_linc_MAY.indd 1 22.03.24 09:44
The hidden interventional radiologists: New study uncovers those lost in data
A new study conducted by the Harvey L Neiman Health Policy Institute (HPI) has identified a large percentage of unidentified interventional radiologists ‘hidden’ within Medicare data. The research has uncovered a previously unforeseen trapdoor, in which self-designated specialty in Medicare claims data have proven to be an “inadequate selection method” resulting in the omittance of practicing interventional radiologists from records.
MIKKI D WAID (HARVEY L NEIMAN
Health Research Policy Institute, Reston, Virginia) and colleagues reference interventional radiology (IR) as arguably one of the most poorly understood fields of medicine in the introduction to their research. They assert that the overlap in services across radiology has created a “challenge” for identifying interventional radiologists.
The authors note that definitions of IR to date have been “insufficient” for identifying “replicable samples of interventional radiologists for research”. Additionally, they posit that the self-designated physician specialty found in Medicare data—which are typically derived from the Medicare Provider Enrolment, Chain, and Ownership System (PECOS)— have been shown to be “unreliable” and does not accurately represent the true level of self-described interventionists when compared with physicians’ own websites.
“This research does not attempt to make a judgement on which radiologists should be considered interventional radiologists,” Waid and colleagues underline. Rather, their research sought to identify if interventional radiologists are accurately represented in the available data.
The primary sources for their analysis were the 2015–2019 Centres for Medicare and Medicaid Services (CMS) Provider and Payment Utilization and Payment Data Physician and Other Supplier Public Use File (PUF), and 2015–2019 data from Optum’s de-identified Clinformatics Data Mart (CDM) database.
The PUF provides physician-level data including gender, self-designated specialty, state, zip code of practice, and counts and payments by service performed. The CDM database includes full patientlevel medical claims data from approximately 20 million members enrolled in commercial and Medicare Advantage plans.
To identify practicing interventional radiologists within PUF and CDM data, Waid et al looked at the number of procedures that were billed as IR-related treatment and rank-ordered radiologists IR-related work as a percent of total-billed work relative value units (wRVUs). Characteristics were analysed at various threshold percentages. The authors also note that external validation used Medicare records with the Society of Interventional Radiology (SIR) membership records.
Their results show that, of the 37,131 unique radiologists, in the Medicare data, 8,010 (21.6% of total unique self-designated diagnostic radiologists and interventional radiologists), 3,572 (9.6%), and 2,060 (5.5%) met the 10%, 50%, and 90% thresholds, respectively. Above a 10% IR-work threshold only 24% of selected practicing interventional radiologists were designated as such in the data; above 50% and 90% thresholds, percentages rose to 42% and 48%, respectively. The average IR-related work (surgical, invasive, and evaluation and management services) reported among practicing interventionists was 45, 84 and 96% of total wRVUs, for the 10, 50 and 90% thresholds. Pulling key takeaways
from their results, the authors highlight that in both datasets, most practicing interventional radiologists at all IR-work levels up to 95% were designated as diagnostic radiologists in the source data. They contend that, even at the highest levels of IR-related work effort, no more than 47.6% of interventional radiologists are “appropriately” self-designated in the Medicare sample.
Furthermore, Waid et al identified characteristics that were associated with “greater likelihood” of being a practising interventional radiologist. Among these characteristics were male sex, fewer years since training, practicing in a metropolitan area, and employment within a “smaller” practice. The authors opine that future research exploring the “relationships between workforce, practice, system, and community factors” to understand the fundamental IR workforce dynamics could illuminate “factors that predict patient access to IR services”.
The fluidity of IR in definition and the pervasive overlap of its services has created statistical invisibility for practicing interventional radiologists, the authors salient conclusions assert. “Physicians’ self-designation could vary over time—defined as diagnostic one year and interventional the next. They also do not necessarily always define themselves. Their institution or billing provider may take on this power, particularly in the PECOS system,” the authors state.
There is an absence of an available gold standard for assigning specialty that reflects both training and medical practice”

Mikki Waid
STRIDE subgroup analysis provide new data for Penumbra’s Indigo aspiration system
During the Society of Interventional Radiology (SIR) 2024 annual scientific meeting (23–28 March, Salt Lake City, USA), newly presented data from a subgroup analysis of the STRIDE study showed that Penumbra’s Indigo aspiration system used in a single session without the need for overnight tissue plasminogen activator (tPA) is safe and effective for patients with lower extremity acute limb ischaemia (ALI).
“ALTHOUGH THE USE OF TPA following aspiration thrombectomy with [the] Indigo system was not limited during the STRIDE study, the majority of patients did not receive it and still experienced excellent outcomes,” said STRIDE investigator Jayer Chung (Baylor College of Medicine, Houston, USA).
“These findings demonstrate that
the use of aspiration mechanical thrombectomy, without overnight tPA, yields high procedural success, low complication rates, and high target limb salvage rates in [lower extremity] ALI.”
A press release details that, although widely used, there are many complications associated with tPA and other clot-busting drugs. In the case of the overnight lytic group, tPA was also
“There is an absence of an available gold standard for assigning specialty that reflects both training and medical practice,” Waid and colleagues pose. “Identifying IR physicians in claims data poses a challenge that hinders the progress and comparability of research to broadly characterise and measure the value of this important independent medical specialty.” The authors conclusions demonstrate a need for better representation and definition of IR and call for improved selection method to avoid the omittance of “the majority” of practicing interventional radiologists.
associated with an increased need for intensive care unit (ICU) monitoring as shown by the higher median length of ICU stay among those patients.
“The high risk of associated major bleeding is a notable limitation of thrombolytics as an intervention across many disease states, and [lower extremity] ALI is no exception,” said Thomas Maldonado (New York University of Langone Health, New York, USA), national principal investigator of the STRIDE study. “The data show that aspiration mechanical thrombectomy is a safe and effective minimally invasive procedure, which may offer an option to eliminate thrombolytic use for some patients.”

STRIDE is an international, prospective, single-arm, multicentre, observational study of patients with lower extremity ALI and using the Indigo aspiration system as a frontline intervention. The latest findings include:
• No significant differences were detected between patients who received overnight tPA and those who did not for target limb salvage rate at 30 days, patency at 30 days and 30-day mortality.
• ICU resource utilisation was significantly lower in single-session Indigo patients.
Penumbra notes that ALI is associated with a high risk of amputation and death. Studies have shown that ALI patients treated with catheter-directed thrombolysis often risk further vascular complications, such as major bleeding.
17 Issue94 | April 2024 News
DATA
Indigo system
AASLD releases updated guidance for use of TIPS
The American Association for the Study of Liver Diseases (AASLD) has recently published updated practice guidance on the use of transjugular intrahepatic portosystemic shunt (TIPS) procedures. The guidance, featured in the journal Hepatology, sought to account for “technical refinements” that have occurred in recent years.
In the initial summary of the update, Edward Wolfgang Lee (University of California, Los Angeles, Los Angeles, USA) and colleagues set out that the AASLD guidance—which provides a data-supported approach for the use of endovascular therapies in this setting—is separate to the AASLD guidelines, which are supported by “systematic reviews of current literature, formally rated on the quality of evidence, and strength of the recommendations”. The recent guidance was developed by the AASLD Practice Guidelines Committee, who state that, in most instances, a “sufficient number of randomised controlled trials [RCTs] were not available to support meaningful systematic reviews and meta-analyses” on the topic.
TIPS creation is typically performed percutaneously to create a portosystemic shunt that is used to treat complications that arise from portal hypertension, particularly in cases of liver cirrhosis and other endstage liver diseases. By establishing a shunt between the portal and hepatic veins, TIPS effectively reduces portosystemic pressure gradient (PSPG), addressing issues like variceal bleeding and refractory ascites. The guidance assert that the procedure requires
careful patient selection and diligent postprocedural management to optimise outcomes and minimise risks.
In relation to TIPS, the guidance statement highlights that polytetrafluoroethylene (PTFE)–covered stent-grafts should be considered standard of care. Also, bland portal vein thrombosis (PVT) does not preclude creation of TIPS which used to be considered as a relative contra-indication of TIPS. Regarding the latter, the statement adds that referral to experienced centres should be considered. In agreement with other societal recommendations such as BAVENO 7 and ALTA, the AASLD guidance statement recommended a pre-emptive TIPS (known as early TIPS) in patients present with acute variceal bleeding within 72 hours.
In terms of patient selection, the guidance emphasises that “absolute” contraindications for TIPS include heart failure, severe pulmonary arterial hypertension, uncontrolled hepatic encephalopathy, and systemic infection or sepsis. Lee et al also warn that TIPS creation may be “difficult” in patients with polycystic liver disease, hepatic or portal vein occlusion, and intrahepatic tumours.
The authors add that complication occurrence during TIPS is “rare”—complications were reported in less than 5% of cases in a contemporary series conducted by Xiaochun Yin (Nanjing Drum Tower Hospital, Jiangsu, China) et al. Complications that have been identified in these cases include intraperitoneal bleeding, arterial injury, liver infarct, hepatic capsular puncture, haemobilia, immediate TIPS thrombosis and sepsis. The guidance states that preTIPS workup should ideally include cross-sectional imaging to achieve an “adequate anatomical map” of the portal vein and hepatic veins.
Study shows transradial and transfemoral access PAE produce similar technical results yet ischaemic attack “concern” remains
A recent study published in the Journal of Vascular and Interventional Radiology comparing the efficacy and safety of prostatic artery embolization (PAE) via transradial access (TRAPAE) versus transfemoral access (TFA-PAE) to assist access selection have demonstrated “similar” technical results, however complications relating to TRA-PAE remain “a concern”.
CONDUCTED AT A SINGLE centre between April 2014 to August 2022, the study evaluated procedural outcomes and adverse events of 998 patients who underwent PAE. Andrew Richardson (Jackson Memorial Hospital, Miami, USA) lead author of the study, and colleagues performed their analysis with institutional review board (IRB) approval.
The researchers detail that 821 (82%) patients underwent TRA-PAE (Group R) while 177 (18%) underwent TFA-PAE (Group F). Of their patient cohort, mean age and prostate size of Groups R and F were 69.2 years and
117.4g, and 75.2 years and 127.2g, respectively. Using the Barbeau test on patients who underwent TRA-PAE—a test which assesses the patency of the radiopalmar arch—116 patients were diagnosed with Barbeau A, 700 with Barbeau B and five with Barbeau C compression. Furthermore, procedural and patient-specific metrics were reviewed, and adverse events were recorded according to the Society of Interventional Radiology (SIR) adverse events classification.
Andrew Richardson and colleagues, report that technical success—defined as achieving bilateral PAE—was high
Most recently, the AASLD guidance also states that preprocedural correction of coagulopathy must be sought.
Post-procedural care and surveillance are also addressed in the guidance, which emphasises the importance of monitoring the post-TIPS portosystemic pressure gradient (PSPG) level. The authors convey that this level is predictive of rebleeding risk—“lower values are associated with lower bleeding recurrence and, inversely, predictive of post-TIPS complications such as hepatic encephalopathy and worsened liver function”.
Following the publication of the guidance, the AASLD commented: “The practice guidance aims to equip care providers with an in-depth understanding of the use of TIPS and/or variceal embolization/ obliteration such as retrograde transvenous obliteration (RTO) or antegrade transvenous obliteration (ATO) in the management of variceal haemorrhage.
The goal is to facilitate multidisciplinary discussions between hepatologists, gastroenterologists, interventional radiologists, and surgeons in the selection of endovascular treatments for patients with variceal haemorrhage.”
The recent guidance addresses a need for standardisation in approaches to TIPS use, crucially accounting for advancements in technology and therapeutic strategy. Moving forward, the guidance is hoped to inform clinical decision-making and stimulate further research in the field of interventional hepatology. Lee and colleagues conclude that further research should provide evidence on the best technical approaches to TIPS, “understanding the effects of TIPS in patients with non-alcoholic fatty liver disease—now the fastestincreasing aetiology of cirrhosis— and its therapeutic role as compared with emerging endovascular therapies”.

in both groups, with 97.2% of patients in Group R and 93.2% in Group F achieving this outcome. Indications for PAE included lower urinary tract symptoms, acute or chronic urinary retention, and haematuria. Mean procedural time, single- and continuous-rotation fluoroscopy time, dose area produce and air kerma, were “significantly” lower in Group R when compared to Group F.
Moreover, Richardson et al found that six patients in Group R and nine patients in Group F had access site ecchymoses, whereas five patients in Group R and six patients in Group F had access site haematomas. Of
concern, the researchers note that two patients experienced transient ischaemic attacks (TIAs) after TRAPAE. They comment that both of these patients were self-resolving and were discharged safely home within 48 hours of initial treatment. Additionally, two occult radial artery occlusion were reported, but no patient experience hand ischaemia.
Richardson and team went on to emphasise the importance of these findings for interventional radiologists when selecting the appropriate access route for PAE procedures. “Our study highlights the comparable technical success of TRA-PAE and TFA-PAE, with the added benefits of reduced access site complications and radiation exposure associated with transradial access,” said Richardson et al in their conclusion.
Technical success achieved in 97.2% in Group R and 93.2% in Group F 2
patients experienced transient ischaemic attacks (TIAs) after TRA-PAE
18 April 2024 | Issue94 Embolization
EMBOLIZATION
Analysis shows high renal function preservation following image-guided cryoablation
A recent study published in CardioVascular and Interventional Radiology has found that patients undergoing percutaneous image-guided cryoablation for small renal tumours have high preservation of renal function. Conclusions drawn from the study suggest that the treatment should be considered as “an opportunity” for patients with small renal tumours and solitary kidneys.
LEAD AUTHOR PIA I PIETERSEN
(University of Southern Denmark, Odense, Denmark) states that their aim was not to explore the differences between renal function reduction after image-guided cryoablation versus partial nephrectomy, but to “estimate” the reduction. In doing so, they hoped that their results may add information and evidence, allowing oncologist surgeons and interventional radiologists in the future to act as a “multidisciplinary team” by making decisions based on the “advantages and disadvantages” of cryoablation in this patient population.
Cryoablation, a minimally-invasive technique, involves the use of extreme cold to destroy cancerous tissue. It has emerged as a promising alternative for treating small renal tumours, offering potentially favourable outcomes while
preserving renal function.
Pietersen et al extracted data from the European Registry for Renal Cryoablation (EuRECA) database concerning patients with renal cell carcinoma (RCC) who had undergone image-guided percutaneous cryoablation from 2014 until 2024. Patients with multiple tumours, who had been previously treated, or have had more than one cryoablation procedure were excluded. Renal function parameters, including glomerular filtration rate (GFR) and serum creatinine levels, were evaluated before and after the procedure to assess any changes or adverse effects.
A total of 222 patients with solitary kidney and biopsy-confirmed renal cancer were entered into the database. Of these, 184 patients met Pietersen and colleague’s inclusion criteria and
Both microwave and cryoablation show “high” efficacy in treating solid enhanced renal masses
In a recent study published in the Journal of Vascular and Interventional Radiology, researchers have reported “high” technical success and local disease control for both microwave ablation (MWA) and cryoablation (CA) in treating solid enhancing renal masses ≤4cm in adult patients.
THE STUDY, CONDUCTED AT A SINGLE high-volume institution across a 12-year period between January 2008 and December 2020, aimed to determine the technical success, adverse events, local tumour recurrence, and survival rates associated with each treatment modality. The retrospective review included data from 279 small renal masses in 257 patients following an institutional review board (IRB) approval of Thomas Jefferson University. The patient cohort
70 patients had sufficient data from baseline to follow-up available via the database which were included in the authors’ analysis.
Of patient demographics, the authors add that the median age was 67.5 years old and the majority of the patients were men (67.1%). Additionally, RENAL nephrology score was available for all patients with a median of six.
Their findings show high preservation of renal function among patients with solitary kidney following cryoablation. Despite a statistical decrease in renal function of 11% after three months post-procedure, all patients avoided the need for acute dialysis, and none showed severe advancement in chronic kidney disease (CKD) stage.
The findings contribute valuable insights to the existing body of literature on renal tumour management, particularly in patients with solitary kidneys. They support the growing evidence base for the use of cryoablation as a viable alternative to traditional surgical approaches, offering potential benefits in terms of renal function preservation and overall patient outcomes. However, Pietersen et al do note that several variables should be included in the decisionmaking on management and treatment of these patients, such as the quality of life, adverse events, side effects of focal versus systemic therapy. They also add that, although literature for
had a median age of 71 years of age (range, 40–92 years) and were each deemed clinically suspicious by imaging for cT1a renal cell carcinoma (RCC). Of these masses, 191 were treated with CA, while 88 underwent MWA. The study evaluated adverse events, treatment effectiveness, and therapeutic outcomes for both procedures, as well as disease-free, metastaticfree, and cancer-specific survival rates. Additionally, the researchers examined changes in renal function using the estimated glomerular filtration rate.
active surveillance for patients with tumours in solitary kidneys is “limited”, it should be considered particularly in “elderly and fragile” patients.
Noting prevalent limitations of their study, Pietersen and colleagues state that follow-up regimes in the different countries and institutions did not allow them to collect the missing data retrospectively. Plus, due to the non-controlled, non-randomised nature of their analysis, “biased” selection of patients is “probable”.
Pietersen et al wrote of their results, explaining that image-guided cryoablation appears to be a promising
Whether an 11% reduction is clinically relevant with severe cancer diagnosis in mind is debateable”
treatment that maintains a “low” effect on renal function. “Whether an 11% reduction is clinically relevant with severe cancer diagnosis in mind is debateable and depends on each specific patient,” they conclude. “This treatment should be considered as an opportunity for patients with small renal tumours and solitary kidneys.”

Led by George Sun (Sidney Kimmel Medical College, Philadelphia, USA) et al, analysis revealed no significant differences in patient age or sex between the MWA and CA groups. However, cryoablated lesions were reported to be larger and more complex compared to those treated with MWA. Notably, the technical success rate for MWA was 100%, with only one of the 191 cryoablated lesions requiring retreatment for residual tumour.
Moreover, there was no significant impact on renal function following either CA or MWA. Subsequent analysis using propensity score matching demonstrated that there were no significant differences in local recurrence rates, adverse event rates, cancer-free survival, or overall survival between matched cohorts of patients who underwent MWA and CA.
In their discussion, Sun et al state that: “in the
early years of small renal mass ablation, CA was the only ablation modality used, and most patients were treated using moderate sedation. With the advent of MWA in 2013, a need to treat more complex lesions, and an increasing number of obese patients (>40%) in clinical practice, general anaesthesia became the standard of care for these procedures.”
“This retrospective review showed a tendency to treat smaller, less complex lesions with MWA,” the researchers conclude. Their study findings indicate that both microwave ablation and cryoablation achieve high technical success and local disease control in treating small renal masses. The observed higher adverse event rates following CA may be attributed to the treatment of larger and more complex lesions with this approach.
Cryoablated lesions were reported to be larger and more complex compared to those treated with MWA”
19 Issue94 | April 2024 Renal Interventions
RENAL
George Sun



*Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the neuro interventional arena Editorially independent Visit neuronewsinternational.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** Subscribe today Available in print and digital formats and through our social channels


MMA embolization trials represent “major shift” in subdural haematoma treatment
THREE RECENTLY PRESENTED clinical trials have demonstrated positive outcomes associated with middle meningeal artery (MMA) embolization in chronic subdural haematoma (SDH) patients, representing a “landmark moment” and “major shift” in the treatment of this condition.
Findings from the EMBOLISE, MAGIC-MT and STEM trials—all of which were disclosed for the first time at the 2024 International Stroke Conference (ISC; 7–9 February, Phoenix, USA)—evaluated the addition of minimally invasive MMA embolization to standard medical care, as compared to standard care alone, and found that the procedure was linked to reduced failure rates without an increased occurrence of serious complications.
“This is a landmark moment in the treatment of SDHs,” said ISC 2024 chair Tudor Jovin (Cooper University Health Care, Camden, USA). “This is a moment to which I draw parallels with the thrombectomy trials in 2015. It’s a similar situation—this technique has been in practice at certain centres, inconsistently—but, now, we have level-one evidence from not one but
three trials of unequivocal benefit, both in patients who require surgery and those receiving medical management only.”
The EMBOLISE randomised controlled trial (RCT) was the first of these studies to be delivered at ISC, with leading investigators Jason Davies (State University of New York, Buffalo, USA) and Jared Knopman (Weill Cornell Medical College, New York, USA) taking to the podium to outline first-time data. The trial enrolled 400 adults—all of whom were about to undergo surgery for a subacute or chronic SDH, and considered able to care for themselves and likely to survive for at least one year—across 39 US hospitals.
EMBOLISE’s primary endpoint was the rate of SDH recurrence requiring surgical drainage within 90 days, which was observed in 4.1% of patients who underwent surgery plus MMA embolization, compared to 11.3% with surgery alone—a “highly significant” difference.
“The EMBOLISE trial showed that there was a nearly three-fold reduction in reoperation for patients that were treated with surgery plus embolization,” said Davies. “Fewer trips to the
operating room mean less potential for pain, complications and expense, and better recovery, for the patient.”
The second MMA embolization RCT featured at ISC, assessed the Onyx (Medtronic) system, was presented by Ying Mao (Huashan Hospital/ Fudan University, Shanghai, China), who detailed 90-day outcomes from the prospective MAGIC-MT study. A total of 722 symptomatic, nonacute SDH patients from 31 centres across China—randomised to receive either standard care (surgical drainage and/or non-surgical management) plus embolization, or standard care alone—were included in the trial’s analysis. As per MAGIC-MT’s primary endpoint, 7.2% of patients in the MMA embolization group died, or experienced symptomatic SDH recurrence or progression, within 90 days post-randomisation, comparing favourably to 12.2% in the control group.
This is a moment to which I draw parallels with the thrombectomy trials in 2015.”
Tudor Jovin
The third and final RCT presented at ISC, the STEM study, evaluated the Squid liquid embolic system (Balt), and was delivered by co-principal investigator Adam Arthur (University of Tennessee Health Science Center, Memphis, USA). As per STEM’s
ASTER2 analysis links combined thrombectomy approach to improved reperfusion in proximal occlusions
A subgroup analysis of the ASTER2 clinical trial has found that a first-line combined thrombectomy approach, which involves using contact aspiration and a stent retriever in tandem, may produce better reperfusion outcomes compared to use of a stent retriever alone in patients whose ischaemic stroke is caused by an internal carotid artery (ICA) terminus occlusion with or without an M1-middle cerebral artery (MCA) occlusion.
Writing in the journal Stroke, Arturo Consoli (Foch Hospital, Suresnes, France) and colleagues do note, however, that the same superiority was not observed in stroke patients with isolated M1-MCA occlusions.
For this analysis, researchers included patients enrolled in ASTER2—a randomised trial comparing the effects of combined versus stent retriever-only thrombectomy in large vessel occlusion (LVO) stroke patients. These were patients with an ICA terminus occlusion with or without an M1-MCA occlusion, as well as those with an isolated M1-MCA occlusion.
Consoli et al evaluated the effects of combination therapy against stent retriever-only thrombectomy as first-line approaches via angiographic and clinicoradiological outcomes. The former meant looking
at the rate of first-pass effect, expanded treatment in cerebral infarction (eTICI) score ≥2b50, and eTICI ≥2c, at the end of the first-line strategy and at the end of the procedure. The latter consisted of 24-hour National Institutes of Health stroke scale (NIHSS) scores, European cooperative acute stroke study (ECASS-III) grades, and three-month modified Rankin scale (mRS) scores.
primary effectiveness endpoint, there were three distinct modes of failure in the trial: residual or reaccumulated SDH (≥10 mm) at 180 days postintervention; reoperation after index procedure or surgical rescue within 180 days of randomisation; and a new, major disabling stroke, myocardial infarction or death from any neurological cause within 180 days of randomisation. Preliminary results outlined by Arthur indicated a failure rate of 15.2% with MMA embolization compared to 39.2% without—data ultimately associated with an odds ratio of 3.6 favouring the intervention.
“Chronic SDH is an exceedingly common problem, and these findings will be relevant to a large population of patients,” said David Fiorella (Stony Brook Cerebrovascular Center, Stony Brook, USA), co-principal investigator for STEM alongside Arthur. “The presented data indicate that this novel, adjunctive procedure represents an important advance.”
In an official statement following these three presentations, the Society of Neurolnterventional Surgery (SNIS) acknowledged MMA embolization as a beneficial adjunctive treatment for chronic SDH, describing the procedure as a “major shift” in the management of this disease.
“In many ways, these data are really just the beginning—there will be a tremendous amount of additional insight coming very soon,” Fiorella added, alluding to the recently completed MEMBRANE RCT evaluating the Trufill n-BCA liquid embolic system (Cerenovus/J&J), as well as a planned, combined analysis of all four of these major MMA embolization studies.
Rates of eTICI ≥2b50 after the first-line technique were significantly higher with the combined approach (100%) compared to the stent retrieveronly approach (75.8%) in patients with ICA terminus±M1-MCA occlusions (odds ratio [OR], 11.83; 95% confidence interval [CI], 2.32–60.12), Consoli and colleagues report. They add that the rate of eTICI ≥2c in the combined group (66.7%) was roughly double that of the stent-retriever group (33.3%; OR, 4.09; 95% CI, 1.39–11.94). However, the same trend was not present in patients with isolated M1-MCA occlusions.

Arturo Consoli
A total of 362 patients were included in the post-subgroup analysis—299 had an isolated M1-MCA occlusion, 150 of whom were treated with a first-line combined approach, and 63 had an ICA terminus±M1-MCA occlusion, with 30 undergoing a first-line combined approach.
Across the 63 patients with ICA terminus±M1MCA occlusions included in the analysis, the authors also relay that they found a modified first-pass effect rate of 33% with the combined thrombectomy approach, compared to 21.2% with use of a stent retriever only. The need for rescue treatments was distinctly higher in the stent retriever-only group (42.4%) versus the combined-thrombectomy group (20%). However, positive clinical outcomes were more even between the two—as per three-month rates of mRS scores of 0–2, which were 37.9% in the stent-retriever group and 40.6% in the combined group. Decreases in NIHSS scores at 24 hours were also similar across groups, at −0.2 points (95% CI, −3.5–3.2) in the former and –0.7 points (95% CI, –4.2–2.9) in the latter.
21 Issue94 | April 2024 Neurointervention
NEUROINTERVENTION





Education, News, Insights
Join the CX Vascular platform today to connect and engage with the global vascular community, share expertise and experiences, and stay up-to-date with the latest education and news in the vascular world. Members will also have access to exclusive content including live discussions on the latest advances in the vascular field and interviews with key thought leaders in the space.
Register now
the community at https://cxvascular.com
Join
CX programme to feature latebreaking data across peripheral, aortic and venous domains
This year’s Charing Cross (CX) Symposium 2024 (23–25 April, London, UK) will once again play host to a plethora of Podium-First presentations. Data from across the peripheral, aortic, venous, renal and acute stroke domains of vascular surgery are set to be delivered throughout all three days of the meeting.
The Peripheral Arterial Controversies programme and discussions around the paclitaxel-mortality controversy in peripheral arterial disease (PAD) will be punctuated by a late-breaking presentation from Eric Secemsky (Beth Israel Deaconess Medical Centre, Boston, USA), who plans to examine whether the meta-analysis and subsequent regulatory body restrictions on paclitaxel-coated devices caused harm.
Later in the morning, Brian DeRubertis (New York, USA) will also disclose the newest data from the LIFE-BTK clinical trial evaluating the safety and efficacy of the everolimus-eluting Esprit below-the-knee (BTK) system (Abbott) in chronic limb-threatening ischaemia (CLTI) patients with infrapopliteal artery disease. Elsewhere on the peripheral section of the programme, new data from the CLARITY trial and final results from the PROMISE UK trial will be presented by Anahita Dua (Massachusetts General Hospital, Boston, USA) and Hany Zayed (Guy’s and St Thomas’ NHS Foundation Trust, London, UK), respectively.
Within the Vascular Access Masterclass, Andrew Holden (Auckland City Hospital; Auckland University Hospital, Auckland, New Zealand) is set to present IN.PACT AV Access outcomes and outline the role of the IN.PACT AV drug-coated balloon (DCB; Medtronic) in end-stage renal disease patients with a dysfunctional arteriovenous fistula for haemodialysis.
The programme for day one will close with a session dedicated to the podium-first presentation of BASIL-3—a multicentre randomised controlled trial (RCT) assessing the clinical outcomes and cost-effectiveness relating to drug-coated angioplasty balloons and drug-eluting stents in the management of severe limb ischaemia caused by femoropopliteal disease. Presentation of the study’s background, methodology, results, and take-home messages, will be led by principal investigator Andrew Bradbury (University of Birmingham, Birmingham, UK).
Day two
Wednesday’s Thoracic Aortic Controversies programme will also feature several podium-first presentations, with the first of these coming from Fiona Rohlffs (University Hospital HamburgEppendorf, Regensburg, Germany), who is set to discuss findings on the outcomes of fenestrated versus branched thoracic endovascular aortic repair (TEVAR) for aortic arch pathologies.
Later in the day, outcomes relating to acute aortic dissection in the UK will be disclosed by Arun Pherwani (University Hospitals of North Midlands NHS Trust, Stoke-on-Trent, UK), followed immediately by Frank Arko (Charlotte, USA) detailing experiences based on more than 500 patients and posing the question: does sex or ethnicity matter in type B aortic dissections? Additional podium firsts in this session include Konstantinos Spanos’ (Larissa General University Hospital, Larissa, Greece) presentation of a meta-analysis on endovascular techniques in adult coarctation and Vincent Riambau’s (Universitat Autònoma de Barcelona,
Barcelona, Spain) delivery of data on low-profile TEVAR durability in a real-world registry.
Elsewhere, Stephen Black (Guy’s and St Thomas’ NHS Foundation Trust, London, UK) will attempt to define the need for a dedicated inferior vena cava (IVC) stent as part of the Venous and Lymphatic Controversies section of the programme. Later on in the same session, efficacy results from the SAVVE trial—pertaining to long-term use of a bioprosthetic valve for patients with chronic deep venous reflux— will be presented by David Dexter (The Vein Center of Virginia, Virginia Beach, USA).
Three more podium-first presentations are set to

take place in the afternoon under the umbrella of Superficial Venous Controversies, with the first of these seeing Tobias Hirsch (Halle, Germany) deliver the results of the prospective SYNCHRONOUS trial evaluating the role of simultaneous, prophylactic anterior accessory saphenous vein (AASV) ablation in patients also undergoing endovenous laser ablation (EVLA) of an insufficient great saphenous vein (GSV). Following this will be Manj Gohel (Cambridge University Hospitals, Cambridge, UK) and Kathleen Gibson (Lake Washington Vascular, Bellevue, USA), both of whom are scheduled to present on randomised clinical trials comparing cyanoacrylate glue closure with thermal ablation and surgical stripping using the VenaSeal (Medtronic) SPECTRUM dataset.
This year’s Acute Stroke and Carotid Controversies programme will include the first European release of data from PERFORMANCE II—a single-arm study evaluating carotid artery stenosis treatment using the Neuroguard integrated embolic protection (IEP) system. Ralf Langhoff (Sankt GertraudenKrankenhaus GmbH, Berlin, Germany) is set to present these results on Wednesday morning.
Day two’s inaugural Roger M Greenhalgh late-
breaking trials session will also take place on the Wednesday, with six-month SHOCC study data presented by Athanasios Saratzis (University of Leicester, Leicester, UK) and a ‘first look’ at findings from the PREVISION first-in-human (FIH) study presented by Holden featuring among several above-the-knee (ATK) trials. A further podiumfirst presentation from Peter Schneider (University of California San Francisco, San Francisco, USA) will examine the safety and efficacy metrics of a transvenous arterial bypass system based on pooled analyses, and comprehensive evaluation of objective performance goals.
The focus of the session will then shift to BTK trials, as first-time data from the randomised SAMBA study comparing a paclitaxel DCB to plain-balloon angioplasty are delivered by Gunnar Tepe (Klinikum Rosenheim, Rosenheim, Germany); an interim analysis of the DEEPER REVEAL trial is disclosed by Mahmood Razavi (Providence St. Joseph Hospital, Stockton, USA); and final results from DEEPER LIMUS are presented by Leyla Schweiger (Medical University of Graz, Graz, Austria).
Day three
On Thursday in the aortic programme, the CX Juxtarenal Controversies programme will kick off with a podium-first from Hence Verhagen (Erasmus University Medical Center, Rotterdam, The Netherlands) relating to aneurysm-sac dynamics and its prognostic significance following fenestrated/ branched endovascular aneurysm repair (EVAR). Following this, one-year outcomes with fenestrated ringstent-based endografts from the global FACT registry will be presented by Michel Reijnen (University of Twente, Arnhem, The Netherlands), before Holden returns to the podium to discuss a new endo-anchor system for enhanced endograft fixation and seal.
The morning’s session on advanced imaging and reducing radiation will see Rohlffs appear once again to present on a phantom study indicating the influence of operator positioning on radiation dosage.
Later that afternoon—within the Abdominal Aortic Aneurysm (AAA) Controversies section of the programme—Sean Lyden (Cleveland Clinic, Cleveland, USA) will be delivering an update on the JAGUAR trial, including post-market experiences with the Alto abdominal stent graft system (Endologix). This will precede another podium-first from Reijnen, who intends to outline long-term outcomes from the ICEBERG study, and from Verhagen, who is set to discuss long-term, health-related quality of life after acute type B aortic dissection within a cross-sectional survey study.
In addition, as part of the CLTI Controversies programme, Patrick Coughlin (Nuffield Health, Cambridge, UK) is scheduled to present two-year data in an effort to elucidate whether CLTI clinics can reduce amputation rates. Subsequently, Bradbury will return to the podium alongside Matthew Menard (Boston, USA) for a late-breaking session entitled: “BEST-CLI versus BASIL-2—outcomes when comparing apples with apples”.
The Innovation Showcase on day three is also set to play host to multiple podium-firsts, with Firas Mussa (Texas Medical Center, Houston, USA) outlining ‘how we plan to merge data’ in a presentation based around the large, superiority IMPROVE-AD trial comparing a strategy of medical therapy plus upfront TEVAR versus medical therapy plus surveillance for deterioration in uncomplicated type B aortic dissection patients. Later on in this session, firsttime findings from the BeYond venous post-market clinical follow-up study will be presented by Michael Lichtenberg (Klinikum Arnsberg, Arnsberg, Germany) as well.
23 Issue94 | April 2024 CX 2024
CX PROGRAMME
Charing Cross Symposium 2023
FastWave Medical announces third utility patent for intravascular lithotripsy technology
FastWave Medical, a clinical-stage medical device company developing intravascular lithotripsy (IVL) technology, has announced the issuance of its third utility patent by the United States Patent and Trademark Office (USPTO).
The newly granted patent supports the differentiated design of FastWave’s next-generation IVL system, which aims to address challenges associated with treating calcified arteries in patients with occlusive vascular disease, a condition affecting millions of people worldwide. By developing advanced lithotripsy platforms, FastWave aims to solve the gaps with existing IVL technology while improving ease of use and patient safety by reducing procedural complications.
Society of Interventional Oncology announces third European site approved in ACCLAIM trial
The Society of Interventional Oncology (SIO) announces the European Institute of Oncology (IEO) in Milan, Italy, as the next European site approved for enrolment and activated for the society’s primary clinical trial, Ablation with Confirmation of Colorectal Liver Metastases (ACCLAIM) prospective trial for microwave ablation as a local cure.

In this multicentre, international trial, SIO proposes to establish microwave ablation (MWA) as the preferred treatment option for selected colorectal liver metastases that can be ablated with sufficient margins. The study is the first global, prospective trial to use an objective and reproducible technical outcome in its study design, which SIO believes will drive important changes to future treatment guidelines. The study will incorporate software to assess the ablation zone and margins and determine if achieving complete margins during an ablation equates to procedural success, where the primary outcome is local disease progression at two-years post-ablation. Participants of the ACCLAIM trial will be patients
with a diagnosis of colorectal cancer liver metastases.
Endologix initiates postmarket study of the Detour system Endologix has announced the initiation of the Percutaneous transmural arterial bypass (PTAB)1 postmarket study. This study marks the beginning of a comprehensive postmarket study aimed at evaluating the real-world performance of the Detour system in patients undergoing treatment for long complex superficial femoral artery (SFA) disease.
AngioDynamics receives 510(k) clearance for AlphaVac system in treatment of PE
AngioDynamics, a leading medical technology company focused on restoring healthy blood flow in the body’s vascular system, has announced that the US Food and Drug Administration (FDA) has cleared the AlphaVac F1885 system for the treatment of pulmonary embolism (PE), enhancing its utility in critical medical scenarios such as PE.
patient recovery experience than open surgery, according to Silk Road.
Avicenna.AI receives FDA 510k approval for PE and stroke severity technology
Detour system

The study will leverage the Vascular Quality Initiative (VQI) registry infrastructure developed and supported by the Society for Vascular Surgery Patient Safety Organization (SVS PSO), a company press release notes.
The PTAB1 postmarket study evaluates the Detour system’s performance in patients with very long (TASC D) SFA lesions. The study plans to enrol up to 450 patients, with a focus on including at least 200 women and also features an imaging substudy. Recruitment will involve up to 200 sites, with five-year follow-up.
TriSalus releases real-world data showing success for pressureenabled drug delivery
TriSalus Life Sciences, an oncology company integrating delivery technology with immunotherapy in the treatment of patients with liver and pancreatic tumours, has announced the publication in Current Medical Research and Opinion—a manuscript detailing a real-world study of the use of the pressure-enabled drug delivery (PEDD) method with the TriNav device for transarterial chemoembolization (TACE) and transarterial radioembolization (TARE) in patients with hepatocellular carcinoma (HCC) and liver metastases.
The study revealed that, in TACE procedures, interventional radiologists could deliver more of the chemotherapeutic agent to the tumour when using TriNav vs. the amount delivered using standard catheters, a critical treatment goal. TriNav patients had fewer 30-day inpatient visits postprocedure, than non-TriNav patients.
The expanded FDA indication allows for the utilisation of the AlphaVac F1885 system for the treatment of PE, which broadens the applicability of the AlphaVac F1885 system in the nonsurgical removal of thrombi or emboli from the venous vasculature. The indication expands treatment options for patients with PE, reducing thrombus burden and improving right ventricular function.
“FDA clearance marks a significant advancement in patient care and safety. This milestone underscores our commitment to merging physiciancentric design with patient outcomedriven solutions,” said Juan Carlos Serna, AngioDynamics senior vice president of scientific and clinical affairs. “In addition to meeting our primary endpoints, the trial also showed a meaningful, favourable reduction in clot burden, ultimately improving patient outcomes.”

Silk Road adds Enroute NPS Plus device to TCAR portfolio
Silk Road Medical has announced the launch of its Enroute transcarotid neuroprotection system Plus (NPS Plus), which the company describes as a key component of its transcarotid artery revascularisation (TCAR) portfolio.
As per a Silk Road press release, this next-generation device builds upon the prior Enroute transcarotid neuroprotection system to deliver smoother arterial sheath insertion, greater flow precision, and a further streamlined prep experience for surgical teams—all while maintaining “unparalleled” neuroprotection during the TCAR procedure.
“With the launch of the NPS Plus, we’re thrilled to empower our TCARtrained physicians with a solution that addresses their insights and feedback to streamline the TCAR procedure,” said Chas McKhann, chief executive officer of Silk Road. “Our focus on new product innovation reflects our ongoing commitment to leadership in the treatment of carotid disease.” TCAR delivers periprocedural stroke rates of less than 1% and a better
Medical imaging artificial intelligence (AI) company Avicenna.AI have today announced that it has received 510(k) clearance from the US Food and Drug Administration (FDA) for its CINAiPE and CINA-ASPECTS products. Using a combination of deep learning and machine learning technologies, the company develops AI solutions that automatically detect and prioritise lifethreatening conditions, assess them for severity, and then notify clinicians.
Addressing the serious issue of delayed and missed findings in diagnostic imaging, CINA-iPE is an AI-powered tool that detects incidental pulmonary embolism (PE) during routine computed-tomography scans. Unsuspected PE is a common finding in routine CT scans of the chest, but as little as 25% of emboli are reported during the initial interpretation, the press release explains. This is particularly relevant in the cancer patient population, where PE is a significant cause of mortality.
Getinge and Cook Medical enter US commercial distribution agreement for iCast covered stent Getinge and Cook Medical have announced an exclusive sales and distribution agreement for the iCast covered stent system, which received US Food and Drug Administration premarket approval for the treatment of symptomatic iliac arterial occlusive disease.

Cook Medical will assume sales, marketing and distribution rights for the product in the USA over the coming months. The iCast covered stent system will continue to be manufactured by Atrium Medical Corporation (Merrimack, USA), which is part of Getinge. “This agreement with Cook Medical ensures that the iCast covered stent system will reach the optimum number of patients who will benefit from it in the USA,” said Patricia Fitch, president of Getinge in North America. Mark Breedlove, senior vice president of Cook Medical’s vascular division stated: “This product fills the need of a covered stent in our vascular portfolio with a proven technology. iCast has five-year data aligned with our commitment to long-term clinical evidence and predictable results for [peripheral arterial disease] therapies.”
24 Market Watch Product News April 2024 | Issue94
Principal investigator at the study site, Franco Orsi and co-investigator Paolo Della Vigna were recently approved as the eighth site overall, and third European site, activated in the ACCLAIM trial.
Product News
iCast covered stent
Clinical News





*Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the vascular arena Editorially independent Visit vascularnews.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** Subscribe today Available in print and digital formats and through our social channels
THIS ADVERTORIAL IS SPONSORED BY VARIAN
A new era for advanced microwave ablation therapy and imaging
In the realm of interventional radiology (IR), technological advancements and innovation are continuously reshaping the landscape of patient care. This has become more evident in recent years in the field of ablation, which has long been a staple for a range of oncologic and interventional treatments. As technology continues to evolve, however, so too does the need to refresh the ablation space to keep pace with innovation and patient-specific needs.
MICROWAVE ABLATION (MWA) HAS emerged as an effective treatment modality for hepatocellular carcinoma (HCC) and metastatic liver cancer (mCRC), and as a promising alternative to surgery for in selected patients. However, as MWA assumes a more prominent role in treating primary and metastatic liver cancers, there is a concurrent need for an update in technologies that reflect the advancements that have been made in improving procedural predictability and outcomes.
Imaging and theraputic advancement
One of the key areas driving the need for advancements is the significant progress in therapeutic and imaging technologies. These advancements have enabled medical professionals to target and treat abnormal tissue with improved accuracy, minimising damage to surrounding healthy tissue and improving patient outcomes.
With the current technologies, physicians can face challenges ablating large tumours that require the use of more than one probe. This can result in overlapping ablation zones, creating procedural complexity, as well as necessitating extensive planning to ensure the best positioning of probes to treat the patient with confidence. The ability to consistently predict and plan what is needed for individual patients is essential. When planning, parameters that need to be considered can include temperature, power, or number of probes, which are all necessary factors to gain a real-time, accurate understanding of the ablation zone.
To meet expectations of interventionalists today, ablative technologies should incorporate continuous registration capabilities throughout the procedure to ensure precise localisation of the patient’s anatomy. As physicians ablate, the initial target may become obscured, making accurate targeting difficult. With current tools that cannot always guarantee repeatability, interventionalists must have extensive experience to achieve consistent accuracy.
The ongoing Ablation with Confirmation of Colorectal Liver Metastases (ACCLAIM) prospective trial for MWA as definitive local tumour control (local cure), seeks to confirm the importance of ablative technologies, and the potential of MWA to treat metastases that can be ablated with sufficient margins. Led by Constantinos T Sofocleous (Memorial Sloan Kettering Cancer Center, New York, USA) et al., the researchers hypothesise that MWA of colorectal liver metastases (CLMs) of ≤2.5cm with confirmation of an ablation margin over 5mm, will achieve definitive local tumour control (local cure) with minimal morbidity. Currently, this international study is enrolling subjects with one to three CLMs using any United States Food and Drug Administration (FDA)-cleared or

CE-marked MWA device. The procedure will be performed with the intent to create a minimum margin of ablation of 5mm, ideally ≥10mm from the edge of the target tumor to the ablation periphery. Minimum margin size will then be assessed immediately after MWA using an FDA cleared image-processing software to provide a three-dimensional (3D) assessment of the ablation zone and margin.
“If someone is doing liver tumour ablation, they should be doing margin confirmation in some way, shape or form, 100% of the time, to ensure good clinical outcomes. Newer technologies will make it better for physicians not doing it every day to achieve this,” said William Rilling (Medical College of Wisconsin, Milwaukee, USA) and ACCLAIM investigator during a recent interview featured on VISion—Varian’s blog about breakthroughs, resources, and expert insights for IR professionals.
The ACCLAIM trial seeks to affirm the importance of margin confirmation and pre and postprocedural imaging, driving a much-needed update in technologies that are utilised for MWA. Co-sponsored by Varian, the trial reflects Varian’s commitment to advancing procedural efficiency to support interventional radiologists in the future.
New groundbreaking technology
At the recent Society of Interventional Radiology (SIR) annual meeting (23–28 March, Salt Lake City, USA), Varian announced its newest ablation technology. The IntelliBlate MWA system* by Varian, a Siemens Healthineers company, combines microwave technology with advanced imaging capabilities.
Aiming to meet elevated levels of performance required to achieve optimal patient outcomes, IntelliBlate MWA system allows clinicians to tailor
treatment plans to each patient’s unique anatomy and pathology. With its real-time monitoring and feedback capabilities, the system provides visual and audible cues to streamline setup and interaction for the clinician.
“This is a tangible result of our synergy and collaboration with Siemens Healthineers— IntelliBlate [is] the cornerstone of a futurefocused integrated imaging and treatment ecosystem from a single provider,” said Frank Facchini, president of Varian Interventional Solutions during the unveiling of the system.
The system also includes the Ximitry* probe, which is comprised of a laser alignment disc, LED status indicator, fixed burn center with symmetrical ablation zone growth pattern, and intuitive temperature sensors. Varian believes that a single Ximitry probe can be used for large ablation zones, sparing healthy tissue and providing consistent control across diverse tissue types, leading to optimal treatment outcomes while minimising the risk of complications.
The IntelliBlate system also integrates with the myAblation Guide* software and is further complemented by the myNeedle Companion workflow, which is available on select Siemens Healthineers imaging systems. This enables healthcare providers who use a range of systems to seamlessly transition their ablation practice to align with the most recent innovations.
Next-generation microwave ablation
The need to advance the ablation space is apparent. Due to the rapid advancements in both therapy and imaging technologies, interventionalists and innovators alike strive to provide patients with the best possible care. The IntelliBlate MWA system has the potential to reshape the landscape of ablation therapy and to provide better procedural control for physicians.
“Our dedication to understanding the performance of our new microwave ablation system goes beyond conventional preclinical research. We have invested significantly in gathering comprehensive data across various tissue types, including perfused tissues. This extensive preclinical testing has provided robust insights that we believe truly distinguish our next-generation microwave system,” says Theresa Caridi, director of medical affairs at Varian Interventional Solutions.
In summary, with the latest addition to Varian’s arsenal of tools soon to be available, innovative solutions aimed at improving predictability and planning when providing ablative therapies are on the horizon. Among the evolving technologies, the IntelliBlate MWA system is noteworthy for its potential to influence the direction of ablation therapy, with the goal of pursuing improved outcomes in this patient population.
References:
1. Han Y, Zhao W, Wu M, Qian Y. Efficacy and safety of single- and multiple-antenna microwave ablation for the treatment of hepatocellular carcinoma and liver metastases: A systematic review and network metaanalysis. Medicine (Baltimore). 2022 Dec 23;101(51):e32304. doi: 10.1097/ MD.0000000000032304. PMID: 36595779; PMCID: PMC9794220.
2. Dou Z, Lu F, Ren L, Song X, Li B, Li X. Efficacy and safety of microwave ablation and radiofrequency ablation in the treatment of hepatocellular carcinoma: A systematic review and meta-analysis. Medicine (Baltimore) 2022 Jul 29;101(30):e29321. doi: 10.1097/MD.0000000000029321. PMID: 35905207; PMCID: PMC9333547.
3. Tang Y, Zhong H, Wang Y, Wu J, Zheng J. Efficacy of microwave ablation versus radiofrequency ablation in the treatment of colorectal liver metastases: A systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2023 Aug;47(7):102182. doi: 10.1016/j.clinre.2023.102182. Epub 2023 Jul 20. PMID: 37479137.
4. Benson AB, D’Angelica MI, Abbott DE, et al. Hepatobiliary Cancers, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2021;19(5):541-565. Published 2021 May 1. doi:10.6004/ jnccn.2021.0022
*The IntelliBlate microwave ablation system and the myAblation Guide software are pending 510(k) clearance and are not yet commercially available in the USA or any other markets.
©2024 Varian Medical Systems, Inc. VARIAN, XIMITRY and INTELLIBLATE are trademarks of Varian Medical Systems, Inc., pending or registered U.S. Pat. & Tm. Off. The following trademarks of Siemens Healthineers are registered or pending with U.S. Patent and Trademark Office: SIEMENS HEALTHINEERS, MYNEEDLE COMPANION, and MYABLATION GUIDE.
26 Advertorial April 2024 | Issue94
Industry News
Johnson & Johnson to acquire Shockwave Medical
Recently announced, Johnson & Johnson is to acquire Shockwave Medical. Under the terms of the transaction, Johnson & Johnson will acquire all outstanding shares of Shockwave for US$335.00 per share in cash, corresponding to an enterprise value of approximately $13.1 billion including cash acquired. The transaction was approved by both companies’ boards of directors.
The acquisition of Shockwave further extends Johnson & Johnson MedTech’s position in cardiovascular intervention and accelerates its shift into higher-growth markets, Johnson & Johnson said in a press release. The acquisition will expand Johnson & Johnson’s medtech cardiovascular portfolio into coronary artery disease (CAD) and peripheral artery disease (PAD).
Joaquin Duato, chairman and chief executive Officer of Johnson & Johnson, said: “With our focus on innovative medicine and medtech, Johnson & Johnson has a long history of tackling cardiovascular disease— the leading cause of death globally. The acquisition of Shockwave and its
Conference calendar
23–25 April
Charing Cross Symposium
London, UK
www.cxsymposium.com
28 April
5th Annual Endovascular Interventions Symposium
Palm Springs, USA
https://na.eventscloud.com/ website/53519/
leading IVL technology provides a unique opportunity to accelerate our impact in cardiovascular intervention and drive greater value for patients, shareholders and health systems.”
Sirtex Medical appoints
Matt Schmidt as new chief executive officer
Sirtex Medical, a manufacturer of interventional treatment solutions, has announced the appointment of Matt Schmidt as chief executive officer and board of directors member, effective March 25, 2024.
Since joining Sirtex in 2023, Schmidt has been an integral part of the company’s executive leadership team, collaborating with senior leaders and shareholders to set corporate strategy, accelerate organisational performance, deliver strong results and build a winning culture, a press release states.
globe,” said Weikun Tang, chairman of Grand Pharmaceutical Group. “Matt’s performance-driven leadership capabilities, as well as his commitment to partner with physicians to provide patients with innovative solutions, positions him as the right person to lead Sirtex into its next phase of growth. We are excited to work closely with Matt as Sirtex continues to create value for patients, physicians, employees and shareholders.”

“I am optimistic about the future and honoured to lead the Sirtex team during this exciting time in company history, especially given some of the transformative solutions we have brought to market over the last year,” said Schmidt. “We are a patientcentred organisation with talented employees who are dedicated to improving lives. I am very much looking forward to what we will achieve together.”
Shape Memory Medical advances endovascular embolisation by completing $38 million in financing

with participation from both new and existing investors.
Shape Memory stated in a press release that its proprietary shape memory polymer is a low-density, porous embolic material that is crimped for catheter delivery. According to this press release, it is also self-expanding upon contact with blood for rapid conversion to organised thrombus. It is the company’s hope that this new technology will offer unique properties, including vascular space-filling, radiolucency, low radial force, and stimulation of the immune response and healing system.
“I am confident Matt will advance Sirtex’s vision of providing minimally invasive cancer and embolization therapies to more patients around the
28 April–01 May
European Conference on Interventional Oncology (ECIO)
Palma de Mallorca, Spain
https://www.ecio.org/
16–19 May
Global Embolization and Oncology Symposium Technologies (GEST)
New York, USA www.thegestgroup.com
28–31 May
Shape Memory Medical has announced that it has completed US$38 million in Series C financing, which has been led by Earlybird Venture Capital, along
Leipzig Interventional Course (LINC)
Leipzig, Germany
www.leipzig-interventional-course. com
01–04 June
ET
Vienna, Austria
https://www.etconference.org/
Shape Memory also recently announced that the US Food and Drug Administration (FDA) granted the company an investigational device exemption (IDE), which will allow it to begin a prospective, multicentre, randomised, open-label trial to determine the safety and effectiveness of the Impede-FX RapidFill device in improving abdominal aortic aneurysm (AAA) sac behaviour, when used with elective endovascular aneurysm repair (EVAR).






14–15 June
Endo Vascular Access (EVA)
Patras, Greece
https://www.evameeting.org/
05–07 August
The Interventional Radiology Society of Australasia (IRSA)
Christchurch, New Zealand https://irsa.com.au/annualscientific-meeting-asm-2024-savethe-date/
14–18 September
The Cardiovascular and Interventional Radiological Society of Europe (CIRSE)
Lisbon, Portugal
https://cirsecongress.cirse.org/
26–27 September
Vascular Access Society of Britain & Ireland (VASBI)
Cardiff, UK
https://www.vasbi.org.uk/annualscientific-meeting-2024/
Interventional News is a trusted, independent source of news and opinion in the interventional world.
Sign up for a free print subscription* and e-newsletter subscription**
www.interventionalnews.com
*Available for US and EU readers only
** Available worldwide
27 Market Watch Issue94 | April 2024
Matt Schmidt








*Available for US and EU readers only **Available worldwide Visit renalinterventions.net and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** Subscribe today Available in print and digital formats and through our social channels A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the field of renal disease management Editorially independent






 Robert Morgan
Robert Morgan