09 APSCVIR: Reflections from the Mongolia Outreach Programme
14 Profile: Alexis Kelekis

18 Arterial access: Challenges and solutions in paediatric patients



09 APSCVIR: Reflections from the Mongolia Outreach Programme
14 Profile: Alexis Kelekis

18 Arterial access: Challenges and solutions in paediatric patients

Burnout in interventional radiology (IR) has advanced from anecdotal or subspecialty-specific to a prominent and increasingly researched global concern. Since the publication of Jacon J Bundy (University of Michigan Health System, Ann Arbor, USA) et al’s 2020 survey, which demonstrated the disproportionate severity of the condition among interventional radiologists, several papers have warned of burnout as not only a qualityof-life issue but a structural threat to the IR workforce capacity and patient care.
At this year’s Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual congress (14-18 September, Barcelona, Spain) a new session titled ‘Managing your life as an IR’ is throwing burnout and other factors associated with maintaining a healthy work-life balance as an interventional radiologist into sharp relief.
“Most of the doctors who attend the [CIRSE] congress are diligent clinicians—we all know how to treat patients, but we are not prepared to take care of ourselves,” says interventional radiologist Anna Alguersuari Cabiscol (Juaneda Hospitales, Balearic Islands, Spain) speaking to Interventional News. Set
to present during the session, Alguersuari’s goal is to expose the “taboo” she believes burnout is still considered. Sharing a personal account, Alguersuari describes that four years ago she experienced “complete burnout” and subsequently quit her job as an interventional radiologist.
“I didn’t care. I didn’t care if I was treating a patient with cancer. I only wanted to finish my work without being questioned by anyone. She also refers to sometimes feeling disregarded by superiors who, in hindsight she believes, were likely unhappy with her performance. “I was so detached from my colleagues’ needs regarding their patients that I wouldn’t try to collaborate. I was known as Dr No,” Alguersuari retells. During this time, she cites total disconnection from peers and colleagues, while losing all motivation for interventions she once found exciting. In retrospect, she thinks a long lasting feeling of chronic demotivation and lack of puropose favored behaviours that were not always civil or respectful. Respect, she explains, encourages a team to “collaborate more productively; if we can’t trust our colleagues enough to
Continued on page 5

IR notably reduces morbidity in post-surgical complication management compared with second surgical attempt, study finds
radiology (IR) has been found to “significantly” reduce recovery time and prevent morbidity associated with re-exploration following major pancreatic surgery, which even in high-volume centres has a morbidity and mortality rate of between 30–50% in the literature.
Published in the Journal of Clinical Interventional Radiology, the authors state that IR’s synergistic and less invasive role is “crucial” in managing postpancreatectomy complications.
“Interventional radiologists play a critical role in the management of patients with pancreatic and periampullary disease, seldom preoperatively and often postoperatively for the management of complications associated with pancreatic surgery,” states lead author Suyash Kulkarni on behalf of his team at Tata Memorial Centre in Maharashtra, India.
In recent years, Kulkarni et al continue, IR has been increasingly integrated into the treatment of postoperative pancreatic complications. Commonly performed procedures for the early successful management of complications are percutaneous image-guided drainage for intra-abdominal collections, postoperative pancreatic fistula placement, percutaneous transhepatic biliary drainage for patients with biliary leak or stricture, and angioembolization for patients with postpancreatectomy haemorrhage (PPH), the authors state. They emphasise that early identification of these complications and appropriate management is “vital” to successful outcomes in this patient population.
Continued on page 4

Do you remember the days when medical publications focused almost exclusively on medicine? They seem to have gone with the wind, and I am not sure why.
MEDICAL JOURNALS HAVE AN IMPORTANT role in the dissemination of knowledge and the promotion of new ideas. At their best, they are an important building block in the construction of a solid base for the practice of medicine.
Of course, it is entirely appropriate for medical journals, particularly ones that belong to national medical societies, to include articles that concern broader issues that influence health, such as environmental factors and social determinants of disease. And it is acceptable for such articles to discuss matters that may not yet be supported by solid scientific data; indeed, at their best, they may point out possibilities that have not been explored yet and encourage their investigation.
Medical newspapers and magazines, such as Interventional News, usually include commentaries on the significance of scientific advances by the authors of scientific articles, and by other experts in the field. They combine such articles with reports of political and institutional issues relevant to medicine.
The editors of medical publications have to tread carefully. Medical politics are relevant and interesting to many readers. But there are significant challenges related to issues that are only tenuously related to medicine. Handling them appropriately requires objective, unbiased reporting and editing, as well as avoiding being obsessed with these issues and highlighting them repeatedly. Editors can have passionate views about certain subjects, but they must set them aside when they are preparing the next issue of their journal.
Let’s take the example of climate change: depending on your views, this is an acute emergency that necessitates immediate action or a natural cyclical event that should be mitigated, as it always has been. Judging whether an article on this topical subject in a medical publication is a sensible analysis of legitimate concerns, or a venting of one’s frustrations, depends on the balance between true medical issues and matters that are outside the expertise of most doctors. If most of the text focuses on subjects such
as the impact of climate on medication supply chains, or on temperature fluctuations affecting the demand for treatment related to climate-induced illnesses like heatstroke and respiratory issues, it is likely to be a sensible analysis of genuine climate-related problems. But an article that briefly mentions such matters and then discusses at great length how governments should change their energy policies to achieve net zero, and lectures readers on the obligation of citizens to protest the mining of fossil fuels, does not belong in a medical publication.
I am not suggesting that physicians are not entitled to hold strong opinions about controversies related to gender, race, politics, wars, or climate change. But if they want to express their views in public they should do so in the mainstream media. Using medical publications to try to influence their colleagues about issues on which they have no special expertise is an abuse of their position. It is regrettable that several previously respectable medical journals have allowed themselves to be used in this way, week in and week out, and even worse that some editors are playing this game and demeaning themselves and their publications.
My next editorial will analyse in detail how Greenland could annex the USA.
It is regrettable that several previously respectable medical journals have allowed themselves to be used in this way, week in and week out”
n IO CRYOABLATION:
Is cryoablation the pinnacle of interventional oncology (IO)’s deescalation philosophy? In Frano Orsi’s (Milan, Italy) view, cryoablation embodies this philosophy, enabling patients seeking treatment for breast cancer with a minimally invasive alternative to surgery. Here, he discusses why he believes this to be true and what needs to happen to secure cryoablation as ‘standard’ for breast cancer intervention.

For more on this story go to page 6.
n NEW HORIZONS:
Welcome to this new section of Interventional News focused on the life, ambitions, and opinions of young interventional radiologists in training and early practice. We want to hear from those of you in training and early practice. Tell us about your everyday and your dreams— what is good, what needs to change? What holds you back? How do you view your future career as an interventionist? Have your say via New Horizons. For more on this story go to page 17.
n VASCULAR ACCESS:


Percutaneous cholecystostomy is a valuable intervention for managing acute cholecystitis in high-risk surgical patients. Yet, the choice between transhepatic and transperitoneal access routes remains a topic of ongoing debate. In this article, Nikolaos-Achilleas Arkoudis and Stavros Spiliopoulos (both Athens, Greece) analyse viewpoints to provide concensus on the best treatment pathway.


For more on this story go to page 19.
Editors-in-chief: Professor Robert Morgan, Professor Andy Adam, Professor Brian Stainken
Publisher: Stephen Greenhalgh
Editor: Éva Malpass | Editorial contribution: Jocelyn Hudson, Will Date, Bryan Kay, Jamie Bell
Design: Terry Hawes, Josh Lyon and David Reekie
Advertising: Abbie Richardson abbie@bibamedical.com
Subscriptions: subscriptions@bibamedical.com
Published by: BIBA News, which is a subsidiary of BIBA Medical Ltd
BIBA Medical, Europe, 526 Fulham Road, Fulham, London, SW6 5NR, United Kingdom Tel: +44 (0) 20 7736 8788 BIBA Medical, North America, 155 North Wacker Drive, Suite 4250, Chicago, IL 60606, United States Tel: +1 708-770-7323
Printed by: Buxton Press. Reprint requests and all correspondence regarding the newspaper should be addressed to the editor at the United Kingdom address. © BIBA Medical Ltd, 2025. All rights reserved.
interventionalnews linkedin.com/company/interventional-news/ @in_publishing
Subscribe here
If you have comments on this issue or suggestions for upcoming editions write to eva@bibamedical.com




IR notably reduces morbidity in post-surgical complication management compared with second surgical attempt, study finds
Continued from page 1
The focus of their study was to establish the role of IR in the management of potentially lifethreatening postpancreatectomy complications such as PPH, thus preventing re-exploration. To do so, Kulkarni and colleagues enrolled 758 patients who underwent pancreatic surgery between January 2014 and December 2019. All patients who developed post-surgical complications within 90 days of primary hospitalisation were included. Complications were classified according to the International Study Group of Pancreatic Surgery (ISGPS).
The types of surgery included in the study were pancreatectomy (4%), pancreaticoduodenectomy (73.8%), enucleation (1%), pancreatectomy and vein resection (4.85%), and multivisceral pancreatic surgery (16.5%). Of the 758 patients included, 206 (27.2%) developed post-surgical complications. Of these, 46 patients (6%) experienced PPH, with 30 patients (3.96%) requiring intervention; 13 patients (43.3%) underwent angioembolization, of whom five (38.46%) died due to causes unrelated to PPH, while 17 patients (56.7%) underwent surgical reexploration.
The authors note that the 90-day mortality rate in patients with PPH was 17.39%, which is comparable
with other studies in the literature. For patients who underwent primary angioembolization for PPH, the mortality rate was 38.46%—which is not statistically significant, they detail. The causes of death for these five patients included biliary sepsis with multiorgan dysfunction, myocardial infarction, hepatic decompensation, and major hepaticojejunostomy and pancreatojejunostomy leaks. Kulkarni and colleagues state that “although PPH may have been a contributing factor, the causes of death were not directly related to the condition”.
“These five patients who underwent re-exploration were beyond the scope of management by IR,” state Kulkarni and colleagues, who explain that mortality rates in patients with PPH “remain high despite aggressive intervention”. They do note, however, that these patients also tend to have associated complications and comorbidities which contribute to increased mortality and morbidity rates. They describe that common comorbidities among this patient population are diabetes, hypertension, hypothyroidism and coronary artery disease; 45 patients in their study cohort presented with one comorbidity and 47 with multiple.
Elsewhere in their results, the researchers observed intra-abdominal fluid collections in 173 (22.8%) patients, with 147 (85%) undergoing image-guided interventions and 23 (13.3%) undergoing surgical re-exploration. The 90-day mortality rate after percutaneous image-guided intervention was 6.12% and after primary surgical re-exploration was 21.7%.
Among other results, the authors identified that biliary complications occurred in 31 patients (4%), of which 18 (58%) underwent image-guided intervention and 11 (35.5%) underwent surgical re-exploration. The 90-day mortality rates were 27.78% and 35.5% in the IR and surgical groups, respectively. Further,
As artificial intelligence (AI) continues to gain traction in interventional radiology (IR), a new checklist developed by researchers at the National Institutes of Health (NIH) aims to address mounting concern around the overuse of AI models in clinical study. The Checklist for Artificial Intelligence Research Evaluation (iCARE) seeks to support the development of safe, generalisable technologies, providing a “code-to-clinic” pipeline for AI model deployment in research.
PUBLISHED IN THE JOURNAL
Cardio Vascular and Interventional Radiology (CVIR), lead author James T Anibal (National Institutes of Health, Bethesda, USA; University of Oxford, Oxford, UK) and colleagues write that common issues such as limited data availability, poor model generalisability, and algorithmic bias have hindered the clinical translation of many AI solutions, with some systems offering “little practical improvement” over human expertise.
Despite these challenges, AI has the potential to “enhance the performance and efficiency of the healthcare system, improving patient outcomes”, state the authors. However, researchers must navigate risks including hallucination, bias, and model confabulation, which are issues that are often amplified by insufficient transparency and a lack of
robust evaluation processes, Anibal et al continue.
Several reporting mechanisms have emerged to promote rigour and reproducibility in AI research, yet Anibal et al note that existing guidelines “do not capture modern, specialtyspecific details”. The authors write that current standards typically focus on classical statistical tests, without sufficient consideration of topics such as pre-trained models or the design of learning objectives or annotation strategies.
the incidence of pancreatic fistula was observed in 20% of patients, 91.8% of whom were prevented from undergoing surgical re-exploration by use of IR management. The 90-day mortality rate in patients who underwent percutaneous drainage was 2.7% and 30.3% in those who underwent primary surgical re-exploration.
“Image-guided interventions successfully prevented re-exploration in 61.5% of PPH cases, 88.9% of biliary complications, and 99.3% of intra-abdominal fluid collections,” state Kulkarni et al, emphasising the “pivotal role” IR plays in managing post-surgical complications.
“IR provides a minimally invasive alternative to surgical re-exploration, reducing recovery time and preventing morbidity associated with re-exploration,” say the authors. They highlight that “early recognition and prompt intervention” are key in patients with PPH, biliary leak and portal vein thrombosis, as these are conditions associated with high mortality and morbidity rates. However, in cases where surgical re-exploration is required, this is “often due to complications which are beyond the scope of percutaneous management”, Kulkarni et al point out.
“Despite the success of IR procedures, some patients may still require reoperation in situations such as anastomotic dehiscence, or peritonitis. Moreover, increased frequency of complications is associated with a higher risk of mortality,” the authors state.
Finalising thoughts on the present findings, Kulkarni and colleagues conclude that IR procedures are safe and effective, and represent a cooperative, minimally invasive approach to managing postpancreatectomy complications, to “reduce recovery time and prevent morbidity associated with re-exploration”.
or anticipated need for AI within their specific area of research”, say Anibal et al. They state that this step encourages critical evaluation of the use of AI and its relevance to IR research.

James T Anibal
The checklist guides researchers through a detailed reporting process which begins with pre-training data that can be used as a foundation for large language models (LLMs), for example. The authors describe that AI models often benefit from initial exposure to large datasets to enhance performance across tasks; however, pre-training is not always feasible especially in data-scarce or resource-limited settings. iCARE provides a structure for authors to justify their approach, including the application of pre-trained models. This, according to Anibal et al, helps to determine how novel generative AI models like GPT are being leveraged in IR contexts.
the framework incorporates structured reporting on bias, ethics, patient consent and data privacy. Sixteen categories of potential bias are included, offering a full pathway for authors to disclose the limitations of their models.
In addition, iCARE addresses reproducibility, prompting researchers to report on the accessibility of their models, while assessing whether these resources are usable by other researchers. Anibal and colleagues describe that often AI projects are “technically available but in a disorganised state— lacking standardisation, completeness, documentation, clear data usage guidelines, and overall ‘AI-readiness’”.
To address this, the newly proposed iCARE framework is designed to help ensure that interventional radiologists using AI models “comprehensively report all AI methods described in their manuscript and clearly justify the current
Interpretability is another critical component highlighted by the authors, who state that “black box” AI systems may offer limited clinical utility if their decision-making processes cannot be adequately explained. Thus, the iCARE checklist encourages authors to describe any efforts made to interpret model outputs, while also acknowledging that full explainability may not always be achievable.
Beyond technical considerations,
Finally, the checklist explores clinical deployment and asks authors to consider how their AI tools could be integrated into existing IR workflows. Historically, the authors note, many AI models developed in research settings have failed to reach clinical practice, underscoring the importance of early consideration of “potential challenges to deployment”.
“The incorporation of AI in IR is inevitable, and organised processes are necessary to ensure the practical, ethical use of data-driven methods within this cutting-edge discipline,” Anibal et al summarise. They conclude that the present framework offers a comprehensive, IR-specific evaluation framework, which hopes to support the safe and meaningful incorporation of AI into IR practice.
question and we don’t treat each other with respect, it’s a complete failure and you will never treat the patient as well as you should”.
Burnout can affect physicians to varying degrees across specialties, causing mental fatigue and even physical illness. In the aforementioned Bundy et al survey, data distinguished specialties in which level of burnout is more severe. The survey was shared via the Society of Interventional Radiology (SIR) Connect Open Forum website, which on the day of posting (7 January 2019) had 7,402 members. From the total membership, there were 339 complete responses. The prevalence of burnout was 71.9% (244 respondents).
This abundance of burnout places interventional radiologists in the upper range of that reported amongst all medical specialties. The prevalence of this condition in medicine as described in the literature varies from 30–75%. In fact, the authors of the survey write: “Interventional radiologists report manifestations of burnout at a rate higher than not only the general public (28%) but also diagnostic radiologists (54–61%) and surgeons (40%).”
Statistics on burnout in IR are increasing, however on review of data available today Alguersuari believes the prevalence of the phenomenon is still underestimated, making it impossible to “give a clear idea of how big the problem is”. In her view, and particularly in Spain where she practises, clinicians are reluctant to divulge their struggles to peers or senior staff members for fear of being seen “as a loser—as a failure, yet it affects so many people who are afraid to share it”, she says.
impostor syndrome. Key characteristics of impostor syndrome are self-doubt, fear of failure and attributing success to external factors—a mindset that Alguersuari has dealt with “all her life”, she says.
“Unfortunately, this is more prevalent in women— it’s how we have been raised,” avers Alguersuari, explaining that, generally speaking, women in IR’s distorted view of their professional contribution may be why they feel the need to overwork.
“It’s a careful balance between confidence and competence. In IR, our competence is very high— we wouldn’t be where we are if it wasn’t. But my confidence, for example, is usually very low, because we don’t train for confidence, only competence,” Alguersuari describes. “They make sure we know how to treat the patient, but not how to look after ourselves with all the pressure we experience. When confidence is too low, burnout appears, as you feel insecure about your abilities,” she says.
“I’m still angry to this day”
Although the session set to take place on Saturday at CIRSE 2025 is directed toward all interventional radiologists,



“As there is no direct IR residency in Israel, I was a diagnostic radiology resident, and my team—even the women on my team—did not support me. I was not entitled to designated time for breastfeeding for example, something that is mandated by law nowadays. The attitude was ‘if it’s been tough for me, it will be tough for you’ and I’m still angry to this day,” Mauda-Havakuk retells. “In my department at the time, a male colleague had broken his little finger and had been given sick leave for six months. That was longer than my maternity leave,” she shares.
Pregnancy is a small portion of a woman’s career, Mauda-Havakuk states, highlighting that “we’re talking about two to three years within a 30-year career” in which women should be provided additional support. She states that institutions and individuals must do more to raise awareness, but that “more men must talk about these issues”. “It’s empowering to talk about amongst women, but if we want a true push, we need male voices to join us,” she says. To this call Alguersuari abides, stating that “if nothing is done and societies neglect to talk about this, there will be fewer interventional radiologists and this will become a chronic problem”.

“Confidence and competence”
IR demands that practitioners hone technical skills, aptitude for time-management and the ability to make good decisions in high-pressure situations. Coupled with irregular hours and on-call duties, managing work-life balance can be challenging, arguably none more so than for those in training, Ana Marija Alduk (University Hospital Centre Zagreb, Zagreb, Croatia) believes.
During the CIRSE session, Alduk is set to speak on the needs of young interventional radiologists. She shares that, although she is no longer a junior, she did experience the line blurring between personal and work life when she was training. To her, the “transition to working independently can be extremely stressful, as you are required to perform high-stakes procedures where patient outcomes can be life-changing”.
“Performing procedures without direct supervision and making clinical decisions alone requires a high level of responsibility, confidence and competence, all while young interventional radiologists are still establishing their professional identities and are working longer hours to prove themselves, which can be difficult to manage,” Alduk shares.
Echoed by Alguersuari, finding harmony between confidence and competence can be difficult for interventional radiologists of any age, but she believes women more frequently experience an imbalance—or
I didn’t care if I was treating a patient with cancer. I only wanted to finish my work without being questioned”
Anna Alguersuari Cabiscol
challenges vary across genders when considering family responsibilities. Research conducted by Najafi et al in 2024 found that women bear a disproportionate share of caregiving duties. When paired with an unpredictable work schedule, this can be a significant threat to a sustainable work-life balance.
To Michal Mauda-Havakuk (Tel-aviv Sourasky Medical Center, Tel-aviv, Israel)—also due to speak during the upcoming session—all interventional radiologists struggle to maintain work-life balance in relation to family responsibilities, not just women. In her view, this is most acutely felt during new parenthood. Mauda-Havakuk highlights that men in heterosexual relationships today “want to exercise parenthood” just as much as women, placing importance on equal maternity/paternity leave.
Mauda-Havakuk does however emphasise the importance of providing support for interventionalists who are pregnant or breastfeeding—support which was not provided to her as a resident diagnostic radiologist.
“The culture is shifting” In her return to IR, Alguersuari credits a shift in focus as the key to her renewed enthusiasm to practise IR. “I decided that patients were the focus and nothing else mattered—not my ego, nor my need to show that I knew things,” Alguersuari shares. In retiring the concept that independence and selfsufficiency equate to an effective interventionist, Alguersuari sought to collaborate more with her team, while showing “vulnerability, even to the patient”.
Alduk agrees that creating a “supportive environment that encourages asking questions and learning, not only from successes, but from failure, is crucial for building confidence”, which can be easily achieved through mentorship, she says. To Alguersuari, this is the “only solution” to the issue, and that “mentorship is vital to teach trainees how to look after themselves”.
“We have a very stressful specialty. This is a fact we cannot escape,” says Alguersuari. “If you see stress as a bad thing, it could kill you. However, if you see stress as a challenge, as something that makes you find better resources to solve the problem, this will transform your mental strength,” she advises.
Alduk states that setting clear boundaries and delegating tasks can help in reducing stress, a skill that she feels the younger generation are better at doing. In her experience, the older generation often “accepted longer hours and personal sacrifice”.
“But the culture is shifting,” Alduk details, “there is more emphasis on balance and wellbeing now.” She sees the increased awareness of stress among younger interventionists to be “positive”, however does believe that this may make them more “susceptible” to stress as they “place greater emphasis on achieving worklife balance and so may feel the effects of stress more acutely when this balance is disrupted”.
Above all, the speakers emphasise the benefit of mentorship programmes that can support residents and trainees, to increase job satisfaction and reduce rates of burnout. Although there are few well-established mentorship schemes in place globally and data are “lacking” on how best to implement them, Alguersuari believes this is a goal to work toward collaboratively.
“What everyone must take away is that we are all at risk. I love my job. I really love my job, but I thought that I had chosen the wrong one. I believed that I had studied enough, and I did everything I was supposed to do, and I still experienced this,” Alguersuari concludes.
De-escalation is a principle applied in many fields throughout medicine to reduce the duration, dose and number of therapies a patient receives to preserve quality of life. The concept is rooted in ensuring the financial sustainability and accessibility of interventional treatments worldwide—a critical action amid the rising cost of global healthcare. In Frano Orsi’s (Istituto Europeo di Oncologia, Milan, Italy) view, cryoablation encapsulates this philosophy, providing patients seeking treatment for breast cancer with a minimally invasive alternative to surgery. Here, he discusses why he believes this to be true and what needs to happen to secure cryoablation as ‘standard’ for breast cancer intervention.
Why is cryoablation the ‘ultimate expression’ of IO’s de-escalation philosophy?
The philosophy of de-escalation is based on a principle of minimising treatment toxicity, preserving the patient’s quality of life without compromising the oncologic effectiveness.
Generally speaking, interventional radiology (IR) has applied this concept in many other areas, but when we apply this to breast cancer treatment, it amplifies the philosophy, enabling physicians to replace invasive surgical approaches and aggressive adjuvant therapies.
In the last few decades, the treatment of breast cancer has undergone a significant reduction in invasiveness, considering how we have scaled down from highly destructive procedures such as radical mastectomy, to more conservative approaches via lumpectomy, to very minimally invasive techniques like cryoablation.
Nowadays, more patients are being diagnosed with small, early breast cancer thanks to screening protocols available in many countries. When these small lesions are identified we aim to take advantage of this early diagnosis by descaling and reducing our invasiveness, which is a concept intrinsic to IO.
In the literature, de-escalation has become more prominent. Particularly since the publication of the COLLISION trial results, we have seen that thermal ablation for colorectal liver metastases has been demonstrated as an equal to resection in terms of efficacy, and we know that the percutaneous approach will dramatically reduce the invasiveness of the treatment, benefitting the patient.
You are principal investigator of the Percutaneous Cryoablation of Lowrisk Early Breast Cancer (PRECISE) study. How is this progressing?
The trial which is currently enrolling at the European Institute of Oncology in Milan, Italy, where I am based, is the first European protocol aimed to demonstrate cryoablation as a viable alternative to surgical resection in women 50 years of age and older with unifocal, small—up to 15mm in diameter—clinically node-negative, luminal A and B breast cancer.
A similar trial—ICE3—was conducted in the USA which had very good results in support of cryoablation as a comparable alternative to surgical lumpectomy. In our study, we have sought to finetune our protocol to show that we can successfully replace surgical resection entirely with cryoablation for these patients.
Surgery has been around for at least 4,000 years, so the general population has grown up thinking that surgery is the best option, particularly in oncology”
PRECICE is a multidisciplinary trial involving surgeons, pathologists, radiologists and interventional radiologists, and to date, we have enrolled 52 patients out of our intended 244. Our enrolment rate is lower than we would like; we have experienced friction, not only from surgeons, but even from patients—this is a
‘Be smart with your dose’: Radiation protection to glean focus at CIRSE 2025
NO MATTER THE AREA OF focus, radiation protection is a topic that concerns all interventionists.
At this year’s Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual congress (13–17 September, Barcelona, Spain) the Radiation Protection Pavillion has been designated the motto ‘Be smart with your dose’, seeking to expand the awareness campaign for radiation safety. The four-day programme will cover topics such as dose monitoring systems, hands-on tips for optimising dose as well as working as an interventional radiologist during pregnancy, and will deconstruct specific procedures, such as prostate artery embolization (PAE), to describe
very strange situation. It may be due to the common thinking that surgical approaches can cure all kinds of disease as this concept is embedded in our DNA. Surgery has been around for at least 4,000 years, so the general population has grown up thinking that surgery is the best option, particularly in oncology.
Often, the patient is not familiar with minimally invasive approaches as this pathway is far from the traditional one, and so they are afraid to expose themselves to something unknown. I have witnessed this process occur with ablation for liver disease for instance, which today, is very well established and patients often self-refer for this treatment.
This is not true of breast cancer just yet. We are absolutely a new player in the field, and it won’t be easy to be included in the standard treatment pathway for breast cancer. But, in order to do that in the best way, we need to produce and consolidate data.
Will the PRECISE data only apply to comparable healthcare systems? Is cryoablation accessible/applicable to low- and middle-income countries?
This is one of our main aims in conducting the PRECICE trial; by replacing surgical resection with cryoablation for select patients, the minimally invasive approach should have less of an impact on the healthcare system.
We don’t need general anaesthesia to carry out cryoablation and the patient is able to walk in and walk out in no more than 40 minutes. If we can show that this treatment may really replace surgical resection, we can hope to export this concept to developing countries where surgical approaches may cost significantly more or are hindered by infection which can often be a problem following resection. There is a cost for the device, of course, but the cost of the device and the procedure is much lower than the cost of surgery or anaesthesiologists. Plus, the impact on the patients’ social or working lives is less significant, enabling a return to normal activities that day or the day after. I believe that in most countries, especially developing regions where surgical activities are less established, cryoablation could offer a more affordable and straightforward

Orsi is set to present his Andreas Gruentzig Honorary Lecture on Monday 15 September at the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual congress (13–17 September, Barcelona, Spain).
Franco Orsi
radiation potential and protection measures.
A short talk by Peter Reimer (Klinikum Karlsruhe, Karlsruhe, Germany)—chairperson of the CIRSE Radiation Protection Subcommittee— will address updates to the CIRSE and Society of Interventional Radiology (SIR) Standards of Practice document, explaining the action points which every interventional radiologist should be implementing within their practice.
Speaking to Interventional News ahead of the annual congress in Barcelona, Reimer underlines the programme’s motto, sharing that their
focus centres on practical tips and tricks for radiation safety. “The programme will host a safety conference session held over the weekend,” he states, adding that another important area of discussion is women in IR. “This session will feature the personal experiences of our female colleagues working throughout pregnancy,” Reimer details.
Finally, he directs attendees to the ‘game-show style’ session which hopes to “engage participants in a fun and interactive way, testing their knowledge of radiation safety under the title: Radiation Safety Pursuit,” Reimer states.
A new randomised controlled trial has found that listening to music during computed tomography (CT)-guided interventions “significantly decreases” patient-reported anxiety levels. The research team state that, beyond interventional radiology (IR), their findings highlight the important connection between anxiety levels and pain felt by the patient during a procedure, and how music can be used to “potentially reduce complications, length of hospital stay, and the overuse of pain medication”.
THE TRIAL WAS LED BY
Florian Nima Fleckenstein (Charité Universitätsmedizin Berlin, Berlin, Germany), who will present the team’s findings at the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual congress (13–17 September, Barcelona, Spain).
Speakin to Interventional News, Fleckenstein explains that biopsy
procedures for unknown tumour masses—typically performed without general anaesthesia—were common procedures included in the trial.
“Patients who undergo biopsies are made aware that ‘something is wrong with your body, and we need to check it’, so they’re usually very afraid when they come in. We hypothesised that music could alleviate some of
“We aim to help interventional radiologists become masters of the live image,” says Tom Boeken (Hôpital Européen Georges Pompidou, Paris, France) describing the purpose of his team’s—six mathematical researchers— artificial intelligence (AI) lab specifically geared toward solving interventional radiology (IR) “problems”.
BOEKEN AND COLLEAGUES HAVE BEEN working on using geometry to develop AI systems for procedural assistance. “One of our key areas is geometry and how it can aid interventional radiologists in their day-to-day procedures,” Boeken shares with Interventional News
In the specialties adjacent to IR, AI has been successfully implemented, Boeken explains. Diagnostic radiology, for example, has “robust AI tools for pre- and post-procedural phases of treatment, as well as for prediction models in patient selection, like identifying features on an MRI [magnetic resonance imaging] or early follow-up imaging,” he says. “While all of this is interesting to interventional radiologists, it’s not unique to our field. These models can apply to surgery, chemotherapy and radiation therapy.”
“What is truly unique to IR, is our use of real-time imaging during interventions,” Boeken pinpoints. “Our focus on this, we hope, will empower our community in differentiation to other specialties that use imaging.”
Boeken and his research team are mainly working on two subtopics: 3D imaging and 2D and angiographic imaging and are set to discuss
their anxiety by creating a familiar and comfortable atmosphere,” says Fleckenstein. Patients were asked to complete the Numeric Rating Scale (NRS) pain assessment and the six-item short form of the State-Trait Anxiety Inventory (STAI-6) post-procedure.
“We saw a highly significant difference in reduction of anxiety levels between the two groups,” says Fleckenstein. He details that, typically, anxiety levels rapidly fall following a procedure for all patients; however, the researchers witnessed a “higher drop” in the group that had listened to music during their intervention.
“This study is important beyond the framework of IR; the bigger picture is that anxiety increases pain, and there are good publications showing quantitative markers, such as hormones and heart rate for example, which correlate anxiety with pain. This is then connected to higher complication rates, longer hospital stays and—in the USA—the overuse of pain medication such as fentanyl,” says Fleckstein.
their progress during the ‘AI in IR: Pre, post and intraprocedural prediction models’ session hosted by SPHAIRE (Spotlight on AI and emerging technologies in IR)—a dedicated area for emerging technologies at this year’s Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual congress (13–17 September, Barcelona, Spain).

Their work on 3D imaging looks at procedures such as thermal ablation, exploring how to guide a needle into a tumour, optimise margins, avoid damaging surrounding organs and eventually incorporate robotics. In 2D angiography, Boeken describes that his team are developing automation tools to better understand flow in vascular interventions—“like predicting which catheter will reach the target most effectively and supporting device deployment decisions”.
Prediction models using advanced statistics for IR procedures have become increasingly commonplace and have been successfully used in large studies such as the COLLISION trial. To Boeken, however, this doesn’t necessarily spell progress yet, as “globally, we’re still working to prove that our treatments are worth doing”, he says.
“Take liver ablation. Despite being performed for decades, we still must justify treating a 2cm tumour without surgery, so trials like COLLISION are crucial for our field and show that prediction models can help by improving outcomes through better patient selection. This way we can increase acceptance of our treatments. That’s the value of preprocedural AI,” Boeken details.
On the other hand, there are “drawbacks” to using AI for patient selection, he describes, one being the risk of becoming too selective, treating only the patients these models predict will respond well. “In the past, companies have sought perfect trial results and therefore only treated patients most likely to respond,” Boeken opines. He states that this has left many treatable patients excluded from trials in which they may have benefitted.
In Boeken’s view, it’s vital that interventionists continue to treat patients who might not have a high predicted success rate but who also have no other
Not only does music offer potential analgesic properties, but, Fleckenstein notes, it can also act as an “icebreaker” to make patients feel more at ease. “We had some very interesting encounters with patients around their choice of music. For example, some would recall seeing the artist in 1980-something with their wife and how it was a nice experience—and this is all while the procedure is taking place, so it’s a great way to divert the patient’s attention and reduce anxiety,” he notes. “Because of this study, I’ve had a lot of music from the 60s and 70s slip onto my Spotify playlist.”
The research team hopes their findings will encourage broader adoption of music as a low-cost, non-pharmacological adjunct during image-guided procedures. “There is no downside,” says Fleckenstein. “If something as simple as music can improve patient experience, reduce anxiety, and possibly enhance outcomes, then it should become part of our routine practice in IR.”
options: “If an AI model suggests a low probability of response, but the alternative is decline, we should still consider intervention,” says Boeken. He explains that, in the recruitment of trials, AI solutions have been used in debatable ways to improve efficiency and lower costs. Using pharmaceutical trials as an example, Boeken details how AI models can identify centres that are likely to underperform in recruitment and exclude them, even if there are patients who could be referred.
For some companies, Boeken shares that it is favourable to recruit fewer patients for financial reasons while ensuring that those who are enrolled meet stringent inclusion parameters which may indicate better treatment outcomes. Alternatively, he describes a branch of AI that can help to generate “fake” or synthetic data to bulk out clinical trial findings by enlarging a dataset for statistical purposes even if a small number of patients are recruited.
“As much as I’d like to have warnings concerning AI use in clinical trials, AI can also help interventional radiologists run clinical trials today,” Boeken says. “For instance, if five expert centres can only recruit 30–40 patients, synthetic data can help grow these data artificially and still be viable from a scientific perspective.”
“Our datasets are very small, and they will always be small. We’re not cardiologists that have 10,000-patient datasets or oncologists with 20,000 patients in a breast cancer screening programme. AI can really help our community be more scientifically credible and visible,” Boeken avers. “So, we must think differently about AI. Instead of relying on massive datasets, we’re building tailored models based on geometry and other mathematically structured methods.”
Thinking differently, Boeken and his team recently published the Checklist for Artificial Intelligence Research Evaluation (iCARE) to map a clearer pathway for AI’s use in IR research.
“We’ve gone pro,” Boeken states. “We were lacking a common direction. [Using iCARE], we’ve moved from a mindset of ‘AI is interesting’ to being able to conduct structured scientific research harnessing it—it’s very cool,” he says.

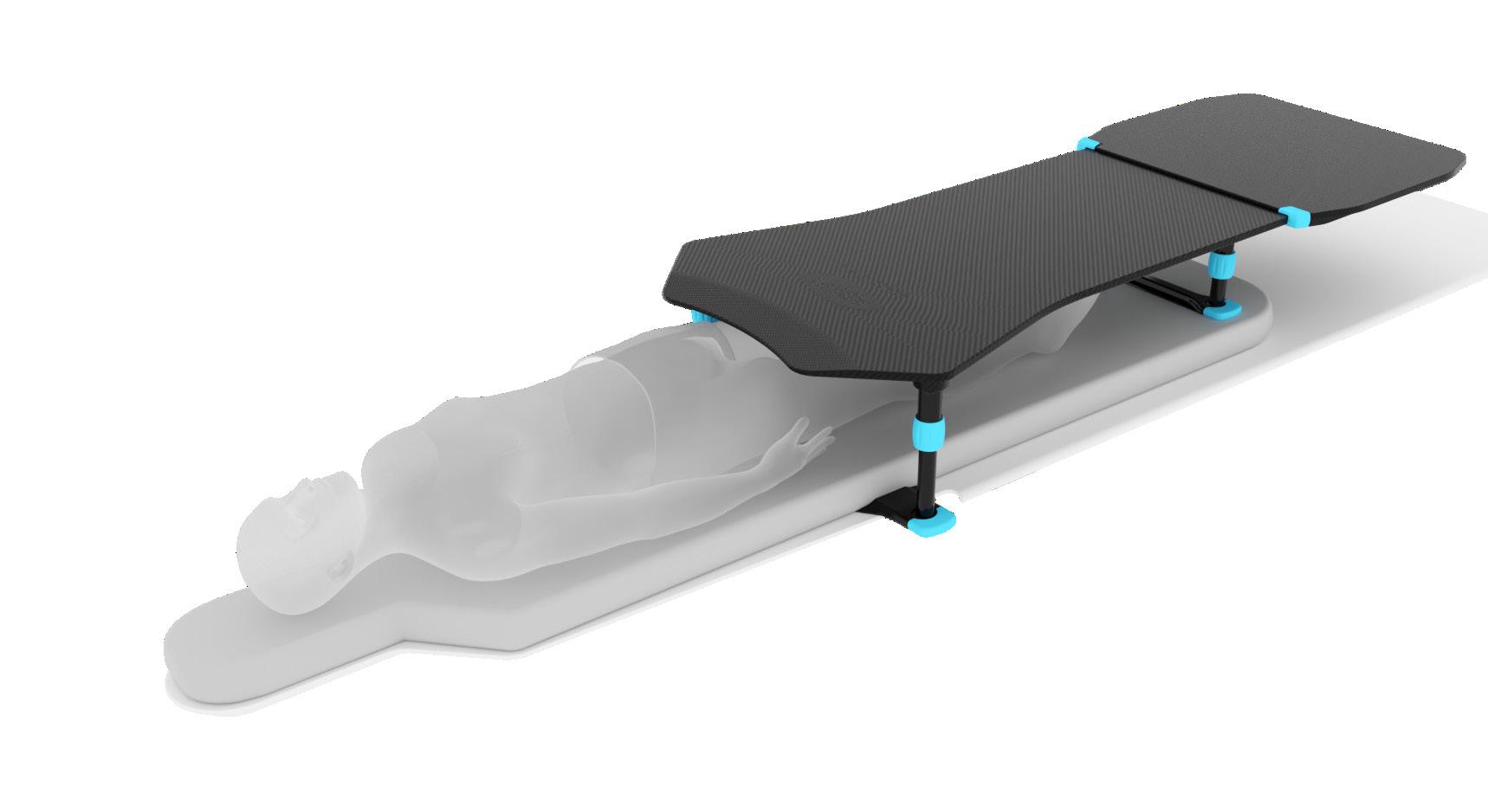
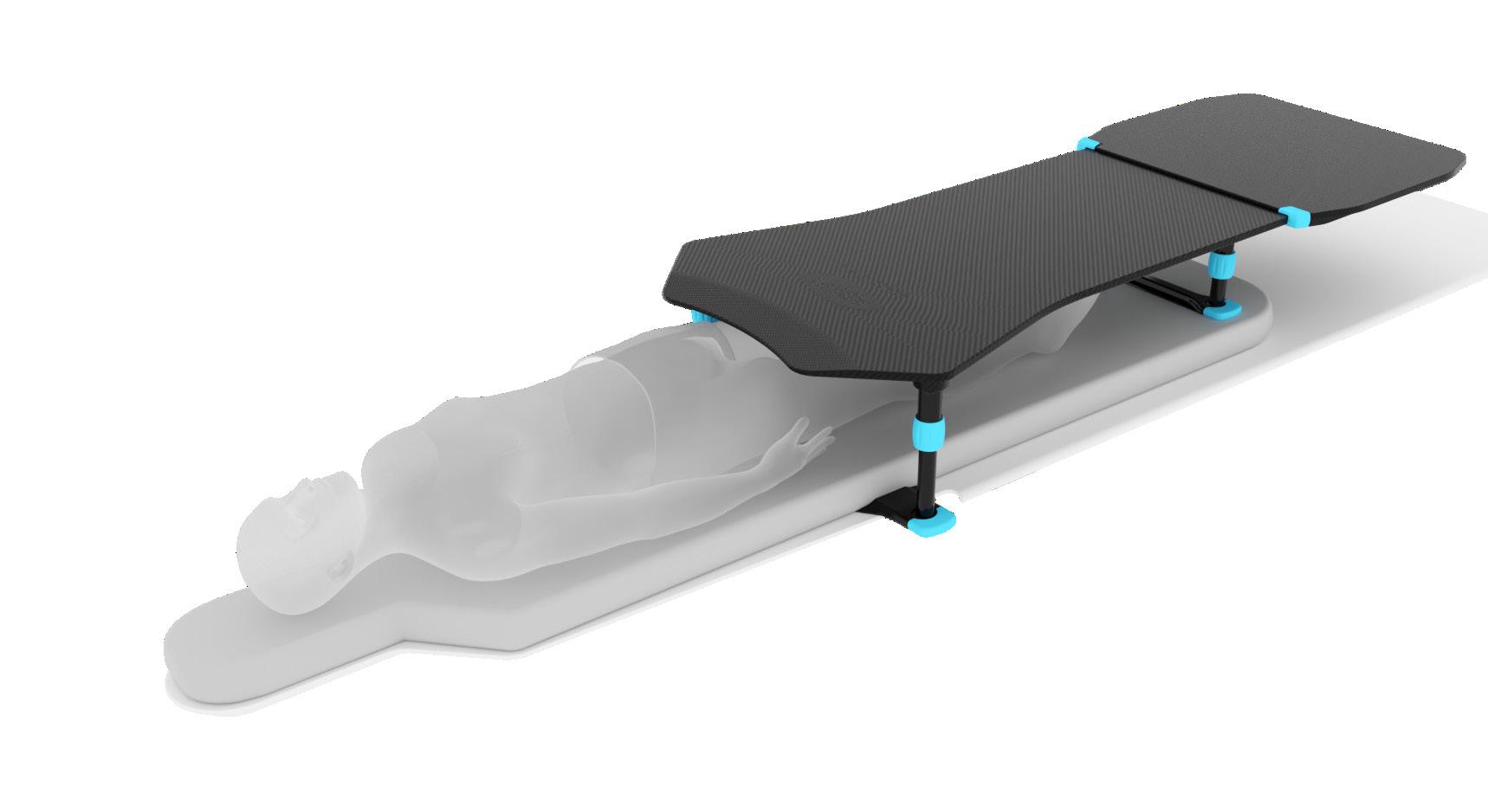
Now available in smaller sizes to support a wider range of patients and procedures.
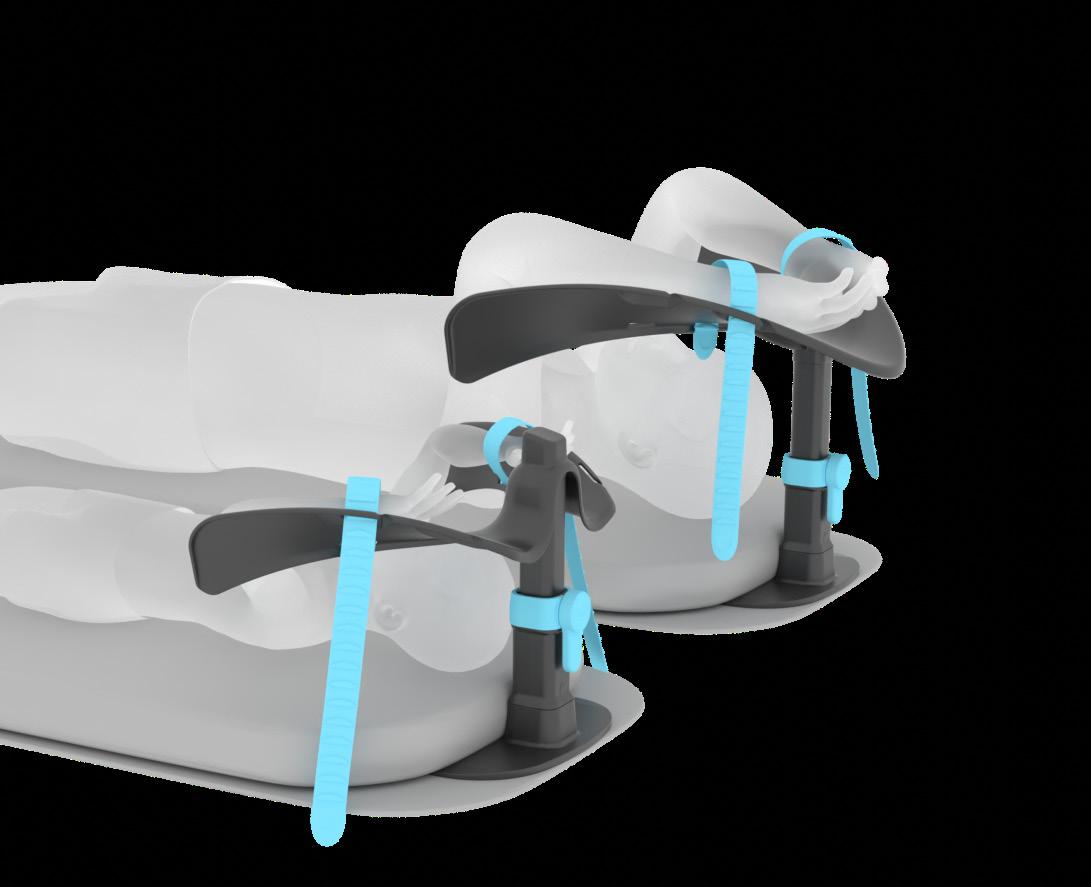
Compact platform designed to bring the clinician closer to the patient for retrograde access. Provides a stable surface for guidewire handling and supports varied procedural workflows.
Supports overhead positioning for small adults and paediatrics. Helps reduce shoulder flexion, improves stability, and can help minimise artefact during abdominal imaging. Suitable for use with C-arm, CT, and MR.

A growing commitment to elevate interventional radiology (IR) in underserved countries such as Mongolia came into focus with the latest instalment of the Asia-Pacific Society of Cardiovascular and Interventional Radiology (APSCVIR) Outreach Programme, delivered in collaboration with the Mongolian Society of Interventional Radiology (MSIR). Now in its third and final year, the programme aims to upskill local practitioners for long-term growth of IR across the region.
“THE IDEA IS TO EXCHANGE best practices, learn from one another and kickstart IR development in places where it’s still gaining traction,” said Shuvro Roy-Choudhury (Narayana Health, Kolkata, India), who was part of this year’s teaching faculty. “It’s not about a one-off visit, it’s about building a foundation,” he shared with Interventional News
The Outreach Programme, first launched under the leadership of APSCVIR past president Tan Bien Soo (Singapore General Hospital, Singapore), has travelled to countries including Bangladesh, the Philippines, and Myanmar over the past decade. Mongolia’s three-year cycle of training has brought together visiting faculty including Yasuaki Arai (National Cancer Center Hospital, Tokyo, Japan), Yozo Sato (Aichi Cancer Center Hospital, Nagoya, Japan), Je Hwan Won (Ajou

University Hospital, Suwon, South Korea), Joseph Kim (Presbyterian Medical Center, Jeonju, South Korea), and Robert Morgan (St George’s University Hospitals NHS Foundation Trust, London, UK) to deliver in-person teaching tailored to local needs and facilities. The visitors were welcomed by the local host faculty, including Onhod Batnasa president of MSIR and Erdenebulgan Batmunkh (Second State Central Hospital, Ulan Bator, Mongolia).
This year’s programme focused on aortic and venous disease, alongside hepatocellular carcinoma (HCC). Over the course of several days, participants
took part in lectures and hands-on device workshops. “We spent the first day performing video-recorded cases,” said Roy-Choudhury. “My colleagues did cases involving liver tumours and dialysis arteriovenous access, and I presented a prerecorded thoracic endovascular aortic repair case. These were shown during the following days to help anchor the lecture content,” he added.
Gerard Goh (Alfred Health, Melbourne, Australia), representing the APSCVIR board, also joined the teaching faculty and shared that the aim of the initiative is to remove barriers to entry, making IR training accessible in the Asia-Pacific region. “Rather than having trainees travel abroad, the idea is to bring the teachers to them,” he explained. “It’s about access, and it makes a real difference. The established interventional radiologists in Mongolia are great teachers in their own right and the momentum for advancing IR here is strong,” said Goh.
Over 100 attendees from across the country took park in this year’s programme, Ricky Cheng (Princess Margaret Hospital, Hong Kong, China)—APSCVIR executive board—recounting that many were young radiologists with a concerted interest in IR. “I think many will go on

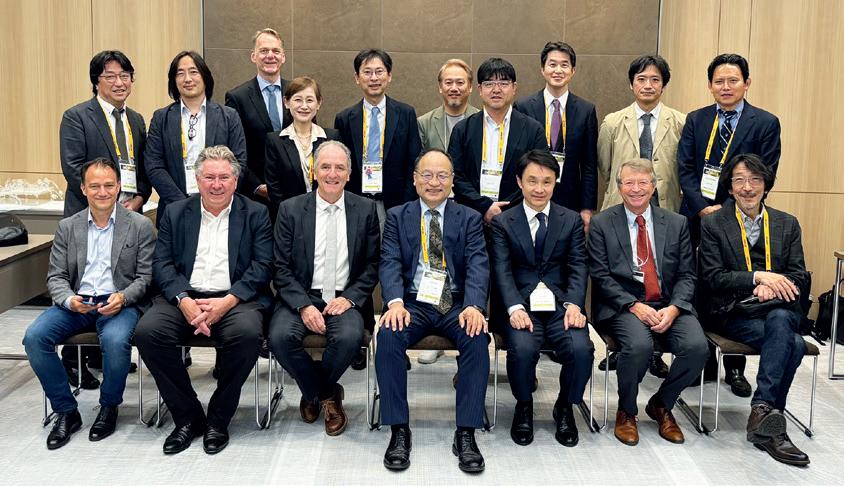
“They do not know the name of IR”: Key updates from JSIR and ISIR 2025 annual meeting
Popularising interventional radiology (IR) was the designated theme of this year’s 54th Japanese Society of Interventional Radiology (JSIR) and 15th International Symposium of Interventional Radiology (ISIR) held earlier this year (29–31 May, Tokyo, Japan). Facilitating a cross section of education, IR standardisation and debate, JSIR and AsiaPacific Society of Cardiovascular and Interventional Radiology (APSCVIR) president Koichiro Yamakado (Hyogo Medical University, Hyogo, Japan) shared key takeaways from this year’s meeting.
YAMAKADO—HAVING SERVED AS president of the JSIR since 2020 and the APSCVIR since 2022—set two goals which have characterised his term at the helm of both societies: first, to obtain accreditation for IR as a sub-specialty by the Japanese Medical Specialty Board; and second, to establish IR as a standard treatment in Japan. The former was granted in 2022. Still working to achieve the latter, Yamakado reflected on how the JSIR/ISIR 2025 programme was shaped to aid this objective.
“The content of our meeting has matured year on year and has already contributed greatly to the development of IR in Japan,” details Yamakado. “Communication with other non-IR societies in Japan and international IR societies has been very beneficial too. We also have good communication with government officials in Japan, which creates better opportunities for the future of IR. Promoting IR to the public has always been our goal each year and JSIR/ ISIR has been an invaluable vehicle to do so.”
Over 2,000 attendees took part in this year’s meeting, with involvement from the Cardiovascular and Interventional Radiological Society of Europe
(CIRSE), Society of Interventional Radiology (SIR) and other internationally recognised societies. Yamakado highlighted key sessions which focused on IR for obstetric and gynaecological malignancies and IR for palliative care.
The programme played host to a first-hand account of uterine artery embolization (UAE) delivered by actress Rie Shibata and a session detailing insurance coverage for IR procedures featuring talks from officials from the Ministry of Health, Labour and
The content of our meeting has matured year on year and has already contributed greatly to the development of IR in Japan”
to become interventional radiologists themselves,” Cheng commented. Despite enthusiasm around the programme, faculty noted that several challenges facing the growth of IR in Mongolia persist. Speakers shared that, while the capital Ulaanbaatar has numerous well-trained interventional radiologists, many of whom studied in Korea or Japan, access to IR treatments remains severely limited in rural areas. “There’s a need for IR to spread beyond the capital,” said Roy-Choudhury.
Roy-Choudhury also flagged deice availability as a barrier for IR in Mongolia and explained that the region particularly lacks devices for aortic disease or venous thrombectomy. He stated that “private sector device companies will need to think about how to support safer, more uniform access to IR procedures”.
The speakers each underlined the clear impact of the programme. “The hospitality from our hosts is always amazing and I felt privileged to be able to share knowledge and skills with fellow interventional radiologists and residents from other countries”, shared Goh.
Looking ahead, Cheng emphasised the drive to sustain momentum among Mongolian interventional radiologists. He stated that “further progress will come from things like research and publication in journals, attending international IR conferences, and access to overseas fellowships for Mongolian trainees”.
Welfare division, Pharmaceuticals and Medical Devices Agency (PMDA) and a key figure in the Japanese insurance system.
The programme served a wide variety of interests within IR, which Yamakado stated reflects rapidly developing areas of IR in Japan. Currently, “indications for radiofrequency ablation and cryoablation have been extended”, Yamakado says, describing the uptick of interest in this area. “Furthermore, we are planning to introduce Y90 radioembolization to Japan—interventional oncology is still popular. On the other hand, many IR procedures which feature pain control and palliative medicine such as genicular artery embolization, nerve block and musculoskeletal tumour embolization have become very popular,”
Yamakado stated.
This year’s JSIR/ISIR theme also alluded to “what should be done” to expand awareness of IR’s minimally invasive treatments, said Yamakado. He noted that the prevalent “problem” is that Japanese citizens “do not know the name of IR” and greater publicity must be sought to remedy this. Yamakado stated that the JSIR/IRIS congress will continue in efforts to achieve this goal, while they also hope to leverage social media in the near future to reach more patients.
CIRSE’s annual congress has been at the spearhead of minimally invasive imageguided treatments since its inception in 1985. This year, join us for the 40-year anniversary edition of the seminal meeting offering more than 460 presentations and 70+ hands-on training sessions!
Covering everything there is to know in IR
CIRSE 2025 will feature eight topic tracks ranging from arterial to venous, aortic, embolization, interventional oncology, neurointerventions, and more. In addition, MSK treatments and paediatric interventions will receive special attention.



Catch a sneak peek
Find out about some of this year’s hottest topics from the lecturers themselves!
Hands down the best hands-on!
CIRSE 2025 will offer participants the chance to gain practical experience with the latest tools and devices through a wide range of hands-on workshops on the following topics:
• Arterial atherectomy
• Arterial thrombectomy
• Closure devices
• Central lines and ports
• CBCT and image-guided fusion
cirsecongress.cirse.org
• Embolization: materials and tools
• Percutaneous arteriovenous fistulas
• Stroke thrombectomy
• Tumour ablation
• Varicose veins
• Venous stenting practice
• Venous thrombectomy/DVT-PE
• Vertebral augmentation
“Significant”
The use of degradable microspheres for uterine fibroid embolization (UFE) have demonstrated “excellent” infarction rates and fibroid volume reduction according to a recent study.
PRESENTED AT THE EUROPEAN Conference on Embolotherapy (ET; 11–14 June, Porto, Portugal), speaker Paul Lohle (ElisabethTweesteden Ziekenhuis, Tilburg, Netherlands) said the shift from permanent to temporary embolic material is of growing interest amidst increasing concern and questions—not only among patients— over “foreign materials and plastics” remaining in the body post-UFE. Lohle states that worry stems from the potential immune reaction to materials left behind. Driving their area of research, Lohle shared that studies have suggested a correlation between lower pregnancy rates and premature menopause following UFE with permanent particles.
“The disappearance of degradable microspheres after UFE offers the possibility of vessel restoration and uterine function, protecting the endometrium and allowing for vessel dilation during pregnancy for foetal growth, as well as lowering the risk of permanent ovarian damage or premature menopause,” detailed Lohle. He added that the degradation of the microspheres could also be beneficial in the event of fibroid recurrence requiring repeat UFE.
Lohle and colleagues’ study collected prospectively data from 51 patients between September 2023 and January 2025 with symptomatic uterine fibroids treated with 500–700µm followed by 700–900µm Nexsphere (Nextbiomedical) degradable microspheres. Patients underwent intentional unilateral or bilateral UFE based on contrast-enhanced magnetic resonance imaging (MRI) characteristics or angiographic features. Baseline and follow-up clinical results were collected by measuring health-related quality of life (HRQoL) metrics using the validated uterine fibroid symptom health-related quality of life (UFS-QOL) questionnaire. Fibroid and uterine volume, and fibroid infarction rate were assessed using T1-, T2and contrast MRI.
Patients had an average age of 48 years, with an average fibroid volume of 390cc and uterine volume of 821cc, while
Genicular artery embolization (GAE) with EmboCept S 50μm (Sirtex) resorbable microspheres provides “statistically significant improvements” to pain scores in patients with mild to moderate knee osteoarthritis, and preliminary oneyear results did not show inferiority compared to other resorbable or permanent embolics.
ALEKSEJS ZOLOVKINS (UNIVERSITY HOSPITAL SANT ANDREA, Rome, Italy) shared his team’s one-year experience with this technique highlighting baseline Kellgren-Lawrence (K-L) grade as the “most important indicator” of treatment success.
Zolovkins and colleagues treated 28 patients and 31 knees: 71% classified as K-L grade 1–3 (group one) and 29% as K-L grade 4 (group 2). Among patients treated, 15 were female and 13 were male, with a median age of 65.5±19.4 years.
Regarding clinical success, defined as ≥50% symptom reduction, the speaker reported a 90.3% success rate in 28 of 31 knees at 48 hours, 88% in 22 of 25 knees at six months, and 66.6% in 12 of 16 knees at 12 months.
Across both groups, Visual Analogue Scale (VAS) pain score showed “peak efficacy” with a 65.3% reduction at one month following GAE, which translated to 53.4% at six months and 54.6% at 12 months, a “relatively stable” trend, Zolovkins pointed out.
Using the Western Ontario and McMaster Universities Arthritis Index (WOMAC), Zolovkins reported a “rapid decrease” in scores at 48 hours for patients in group one, with a “sustained improvement” in WOMAC scores up to 12 months post-procedure.
“WOMAC scores [in group two] improved initially, but gradually returned to baseline values in the longer term,” he said.
Zolovkins stated that “the Kellgren-Lawrence grade is the most important predictor of treatment success”. He added that, the higher the WOMAC score at baseline, “the greater the improvement in symptoms” following treatment, which suggests that patients who are highly symptomatic may derive more benefit. Further, he and his team did not observe any correlation between outcomes and age or gender.

two patients had fibroids accompanied by adenomyosis. Of the 51 patients treated, Lohle and colleagues collected three-month follow-up data from 43 patients. Three-month follow-up MRI demonstrated high fibroid infarction rates (95%), as well as “significant” fibroid- and uterine-volume reduction: -158cm3 or 44% and -324cm3 or 37%, respectively.
Lohle stated that their results show “a significant improvement in the quality of life” of the patients included in the study. Key improvements in HRQoL metrics were reported across symptom severity, reported energy and the ability to engage in day-to-day activities.
Fibroid volume reduction
Lohle compared their data to those collected in Kichang Han et al’s randomised controlled trial in South Korea, which compared permanent agents with Nexsphere degradable microspheres. Han and colleagues found no significant difference between pain score or complete fibroid infarction; however, they found a significantly higher rate of recanalisation with Nexsphere microspheres compared with the permanent agents post-UFE (70% vs. 17%, respectively).
“Our preliminary results for UFE using a new degradable microsphere confirms its safety and efficacy with excellent fibroid infarction rates,” stated Lohle highlighting clinical improvement in the “vast majority”of patients.
Transcatheter arterial microembolization for Achilles tendinopathy yields better outcomes in recreational athletes,
A recent study has shown sustained pain relief and improved tendon function following transcatheter arterial microembolization (TAME) in patients with Achilles tendinopathy; however, superior success rates were observed in patients who engage in recreational exercise compared to competitive athletes.
analysis evaluated the short- and mid-term clinical outcomes in 82 patients diagnosed with Achilles tendinopathy who underwent TAME with imipenem cilastatin. Lead investigator Jia Cheng Yuan (University Hospital of Cattinara, Trieste, Italy) defined the research team’s focus as pain reduction and functional improvement.
TAME was performed via an ipsilateral antegrade femoral approach and patients were evaluated for all target branches of the posterior tibial artery and peroneal artery.
Using the Numerical Rating Scale (NRS) to assess pain, Yuan shared that 67 out of 82 patients achieved a ≥50% improvement om symptoms at 12 months post procedure. The mean baseline Victorian Institute of Sports Assessment Achilles (VISA-A) score was 48.4±19.1, which improved to
76.9±17.4 and 82.2±17 at six and 24 months, respectively.
In subgroup analyses carried out by Yuan et al, superior success rates were noted among recreational athletes (87.5%) following TAME compared to competitive athletes (61%). When stratified by technique, Yuan et al found that super-selective embolization had a success rate of 84.5%, compared to 63.6% for embolization from the main trunk. Regarding the superior success rates in recreational athletes, Yuan explained that: “Those that compete at a high level seek to go back to training as soon as possible, while the recreational athletes have the privilege of rest after their treatment. These findings support TAME as a viable option that offers these patients a potential pathway to recovery and restored activity levels,” said Yuan.

Minimally invasive and image-guided immunomodulation may transform local into systemic treatment through the multidisciplinary combination of drug plus device plus imaging guidance says Bradford J Wood (Bethesda, USA), speaking on immunotherapy in interventional oncology or ‘IO in IO’.
WHAT A COOL TIME TO BE IN interventional radiology (IR) and IO! An avalanche of immunomodulation locally delivered by interventional radiologists may soon dwarf all other indications for IO therapies combined. Combining IR devices with immunotherapy drugs like checkpoint inhibitors or injectables is a highly studied approach becoming more of a mainstream method of image-guided immunomodulation in specific scenarios. Instead of killing targeted cancer cells of local small tumours alone via ‘freeze, fry, shake, shock, irradiate, starve, or inject’, IO in IO uses these IR tools to stimulate a systemic immune response via a variety
of cellular processes, like upregulation of antigens (antigen presentation and damage-associated molecular patterns), recruitment of antigen-presenting cells (APCs), T-cell proliferation and trafficking, and downregulation of the pro-tumour “brakes” on the immune system (T-regs or myeloid-derived suppressor cells). Mini-nodes may even develop at the tumour ablation junction, called tertiary lymphoid structures, with a variety of immunocytes including T and B cells. Exactly how and where to apply which IO in IO tool in an optimised fashion to the right patients at the right time remains somewhat of a mystery, however.
We move fast as a discipline, embracing new devices and approaches at lightning pace by looking into the future to address unmet clinical needs with novel weapons and tools to better position image-guided minimally invasive therapies to help cancer patients live longer and live stronger. IR-stimulated immunomodulation promises to augment immunotherapies and has the potential to explode into a whole new paradigm where drugplus-device succeeds where standard drugs alone might fail by harnessing the immune response to cancer. Augmentation of immunotherapy was once a dream, but the evidence is beginning to roll in, as hundreds of clinical trials begin to fine tune specific ways to combine drugs with IR devices.
The Cardiovascular and Interventional Radiological Society of Europe (CIRSE) has partnered with academics/industry to fertilise this space via injectable immunotherapies combined with imageguided ablation.1 A similarly structured recent trial on ablation plus injected drugs for example reported stunning 87% overall response rates in patients with metastatic prostate cancer who failed prior therapies and were treated with IO in IO: cryoablation followed by an injectable multi-target drug cocktail (anti-CTL4 monoclonal antibody, anti-PD-1 monoclonal antibody, CD40 agonist monoclonal antibody, and TLR9 agonist).2 IO in IO primes the patient’s own immune system against the tumour. Typically, the immune system can recognise tumour as “foreign”, but the response is usually not robust enough to result in meaningful effects.
Initially unablatable patients with synchronous colorectal liver metastases (sCRLM) who successfully converted to ablatable status and underwent curative-intent microwave ablation (c-MWA) achieve comparable intrahepatic progression-free survival (ihPFS) and overall survival (OS) to initially ablatable cases undergoing radical MWA (r-MWA).
THESE WERE THE CONCLUSIONS DRAWN from a recent study published in the journal Clinical Radiology led by Liemei Chen and colleagues from the Sun Yat-sen University in Guangdong, China. They write that, due to the increased utilisation of preoperative chemotherapy and the emergence of new targeted therapies, there has been a “notable increase in tumour response rates”. Thus, providing an opportunity for an initially unablatable or inoperable subset of patients to potentially receive curative treatment.
The authors detail that 102 patients with initially unablatable sCRLM who underwent chemotherapy followed by MWA between 2013 and 2021 were enrolled in the study. According to ‘ablatability criteria’ defined by the authors as five or fewer tumours and tumours 3cm or smaller, patients meeting these criteria received c-MWA, while those exceeding
these markers received palliative-intent MWA (p-MWA).
In their findings, Chen et al state that the ihPFS of the p-MWA group was significantly shorter than that of the c-MWA and r-MWA groups (5.1 vs. 15 and 24.8 months). The OS did not significantly differ between the three groups (53, 66.3, and 78.5 months); however, after demographic matching, the c-MWA and r-MWA groups demonstrated similar ihPFS (15 vs. 18.9 months) and OS (66.3 vs. 64.7 months), with
Combination therapy is one answer. IO in IO may be the tip of an IO-altering iceberg and might soon change the foundation of how we practice IO on a daily basis.
The best outcomes and care often require a combined approach with years of multidisciplinary science to define high-level evidence for practice. Which is the best IR tool for immunomodulation? Intravascular catheter or intertumoral needle or conventional systemic? Cryoablation, histotripsy, thermal ablation, embolization, pulsed electrical fields, irreversible electroporation? When to give what drugs? How do IR tools biomodulate, interact with the compartments and tumour microenvironment? The window of opportunity to answer these questions remains open, but it won’t be forever. As soon as one approach makes a major impact, there will be fewer opportunities to perfect and optimise any approach. The time is now. Let’s do IO in IO!
References
1. CIRSE. (2024). Immunophotonics, CIRSE, and Next Research announce innovative phase 2/3 clinical trial: INJECTABL-3. [online] Available: www.cirse.org/ publications/cirse-insider/immunophotonics-cirse-andnext-research-announce-innovative-phase-2-3-clinicaltrial-injectabl-3/
2. Link, C.J., Kee, S., Prendergast, G.C., et al. (2025). Clinical responses to SYNC-T therapy: In situ personalized cancer vaccination with intratumoral immunotherapy in patients with metastatic castrationresistant prostate cancer (mCRPC). J Clin Onco 43(16_suppl), pp.2504–2504. doi: doi.org/10.1200/ jco.2025.43.16_suppl.2504.
Bradford J Wood is chief of interventional radiology and founding director of the National Institutes of Health Center for Interventional Oncology in Bethesda, USA.
no statistical difference in local tumour progression per lesion (6.4% vs. 7.6%).
Further, the authors identified that the p-MWA group had the highest complication rate (48.5% vs. 32.9% and 15.2%) and local tumour progression perpatient rate (44.8% vs. 20.5% and 9.9%, respectively) compared to the c-MWA and r-MWA groups.
In their discussion of the results, Chen et al suggest that tumour number and size are “not absolute contraindications for MWA with curative intent” and the ablatability of CRLM should be “continuously reassessed during conversion chemotherapy”.
They note that all initially unablatable patients who underwent MWA following chemotherapy, irrespective of their varying ablatability and even in patients who failed conversation therapy, resulted in a “notably satisfactory” median OS of 53 months.
“These findings suggest that such patients may derive survival advantages from MWA interventions, aligning with prior research indicating that local treatment by ablation with or without resection can improve long-term OS and PFS in patients with unresectable CRLM following chemotherapy compared to those who received chemotherapy alone,” Chen and colleagues write.
The authors draw attention to several limitations of their study, noting discrepancies across carcinoembryonic antigen (CEA) levels, tumour distribution and tumour size between groups. However, Chen and colleagues do not believe that these variations in overall patient demographics significantly impacted the comparison of survival outcomes across groups.
undermine and compromise PAE?”
“In the same way that a study is not needed to show that jumping out of a plane with a parachute yields better outcomes than without, there is no need to prove that glue has technical advantages over particles.”
THIS WAS A STATEMENT MADE BY Romaric Loffroy (University of Dijon School of Medicine, Dijon, France) during an animated debate with Clare Bent (University Hospitals Dorset, Bournemouth, UK) on liquid embolics for prostate artery embolization (PAE) at the recent Global Embolization Symposium and Technologies (GEST; 15–18 May, New York, USA). Countering Loffroy’s eagerness for glue to be assumed into the healthcare algorithm, Bent’s tack called for better data and dispelled ‘hypotheses’ which assume glue’s beneficial effect.
Loffroy’s first argument addressed the question that, if particles work, why change? In his view, “the main issue with particles—the Achilles heel and the reason we have recanalisation in most cases—is the lack of durability”, which has necessitated a “more aggressive and more robust initial optimisation”, namely PAE with glue, he stated. Illustrating this, he referenced Tiago Bilhim et al’s 2022 finding which showed a 58.1% reintervention rate at 10 years in patients who underwent PAE with polyvinyl alcohol particles.
“Would we keep the TV in black and white? No, because the standard is something to be changed all the time,” said Loffroy. Although data concerning glue are limited, Loffroy admitted, he contended that glue has ample technical benefits over particles, including real-time visibility, which reduces the risk of nontarget embolization, and provides a clearer endpoint.
While glue has a “learning curve” and its use should not be first attempted during PAE, Loffroy averred, comparative studies have found no significant difference in complication rates between glue and particles. Better yet, as newer glues emerge, he added that delayed polymerisation capabilities support better control thus reducing complication rates.
Lastly, set to disprove those who say glue is ‘too
expensive’, Loffroy asked: “What is your time worth? What about radiation exposure? What about recanalisation and recurrence?”
He stated that the cost of glue in Asia and Europe is less than that of particles, totalling €350 for 1ml of Glubran 2 (GEM) and 10ml of Lipiodol (Guerbet) in France where he practises. “How can you get any cheaper than that?” said Loffroy.

Loffroy

Summarising, the presenter stated that there is “no need to wait for a randomised controlled trial or 10-year follow-up data showing that glue has advantages over particles. It’s faster, cheaper, more visible, has a lower radiation dose and lower rate of recanalisation—with even better long-term clinical outcomes in my experience,” he rounded off.
Loffroy’s opponent, Bent began by describing the
Are we going to undermine and compromise PAE?”
Clare Bent
Clare Bent
Bent first highlighted the heterogeneity of glue, warning against using the “blanket term” ‘glue PAE’ as results seen in the literature to date show variable outcomes depending on material type. Divergent outcomes in trials have most commonly been due to the differing polymerisation kinetics, observed Bent. As some brands of glue polymerise quickly, Bent described that risks could range from proximal embolization, trapping of the catheter, or an exothermic reaction that can cause “significant inflammation and pelvic pain”. In terms of clinical benefit, she acknowledged that, between glue and particles, the limited data available have shown early outcomes are comparable but clarified that glue appears to offer a more conservative reduction in prostate size in the shorter term. Bent highlighted that reports have observed a 16–21% prostate size reduction with glue at three-month follow-up versus 30–40% with microspheres, which may influence embolic choice when performing PAE for other indications including neoadjuvant PAE prior to brachytherapy.
risk of promoting a technique with little evidence to prove its efficacy: “My first anxiety around liquids for PAE is that we have 20 years’ worth of data, five randomised controlled trials, 10 years of follow-up, all focused on the role of PAE to treat enlarged prostates using particles and microspheres; yet, our urology colleagues remain sceptical, and their respective societies still recommend that PAE continue under investigational use. If we introduce a modification to the technique, such as liquids, are we really using robust evidence to promote that? Are we going to
UK survey finds “huge resistance” to use of animal derivatives in devices even in emergency setting
“At the publication of this public census, we’ve opened Pandora’s box and we’re going to have to make a change,”
Pavan Najran (The Christie Hospital NHS Foundation Trust, Manchester, UK) said recently, referencing a UK-wide survey looking at the use of devices containing animal derivatives. Touted as the first and largest of its kind, Najran underlined the poignancy of the survey set against increasing patient autonomy, religious diversity in the UK and consent.
DURING HIS GLOBAL Embolization Symposium and Technologies (GEST; 15–18 May, New York, USA) presentation Najran shared that, via an electronic survey, he and his team collected responses from 407 patients who were given examples of emergency and nonemergency scenarios in which devices with animal derivatives may be used. The majority of responders
were white British/Welsh/Scottish/ Northern Irish, followed by Asian/ Asian British-Indian and Asian/Asian British-Pakistani. Most respondents had received higher education to undergraduate or postgraduate degree level. Those with no religion and meateaters made up a large proportion of respondents.
Religion as an influencing factor was a central focus for Najran and his team.
Drawing on her own practice with Glubran 2, Bent specified that glue does reduce radiation dose as the embolic injection is “quick”, but, that this does not mean the procedure itself is fast, particularly if using a plug and push technique for a more aggressive endpoint. “You don’t get immediate occlusion—that is not correct,” said Bent, displaying a case which illustrates extensive re-distribution of a glue embolic at four minutes post embolization. She stated that, yes, visibility is good; however it is only “hypothesised” that glue’s improved visibility equates to less nontarget embolization. In fact, a study by Etienne Salet et al found that both glue and particles caused glans necrosis in an equal number of patients, Bent shared.
“So, at what point are we saying that glue is better than particles?”asked Bent rhetorically. Her argument, erring on the side of adherence to evidence and caution against employing techniques without a solid basis for efficacy, concluded that PAE should only be used in the context of a trial. “It’s an exciting concept, but glue PAE isn’t quite ready for prime time just yet,” stated Bent.
Among respondents, 12 identified as Buddhist, 96 Christian (including all Christian denominations), 19 Hindu, six Jewish, 76 Muslim, two Sikh, nine preferred not to say and 16 marked ‘other’. Ranging from completely unacceptable to completely acceptable, Najran shared that across groups “there is huge resistance to the use of both bovine and porcine products in either emergency or non-emergency settings”.
“Looking at the Christian population, there is a move toward slightly more acceptable in all groups, but there is a significant proportion of those rejecting the use of such products,” said Najran. “In the Muslim population, as expected, there is a greater rejection in the porcine group, but actually in the bovine group as well.” Among responders who identified as having no religion (171) unacceptability was high, with 73.7% and 80.7% of responders stating no acceptability in an emergency and
elective setting, respectively. In the meat-eating group—which accounted for 149 respondents—33.5% specified no acceptability for the use of devices with animal derivatives in an emergency setting, and 40.9% responded no acceptability for their use in an elective setting. Vegetarians and vegans indicated greater rejection of these devices in any setting, a resistance Najran et al had anticipated.
Given the UK’s increasing diversity, Najran raised that “there is an increasing possibility of a mismatch between what is medically possible and what is personally acceptable”. He continued: “Right now, we can use such products in our patients without having to consent them or even discuss it with them before the procedure, which really needs to change. We need to approach our patients far more holistically and we need to consider the patient’s personal requirements and what is acceptable to them prior to performing a procedure.”
Expanding the limits of interventional radiology (IR), Alexis Kelekis (Athens, Greece) has had many firsts; as the first to perform vertebroplasty cases in Greece and the first international president of the Society of Interventional Oncology (SIO), Kelekis’ career has sought to drive the specialty forward both on the table and through society leadership. In his current roles as professor of diagnostic and interventional radiology and director of the third radiology department at the National and Kapodistrian Univeristy of Athens, Greece, he channels his enthusiasm and expertise to achieving excellence in patient care across interventional oncology (IO), IR, and musculoskeletal intervention. Here, Kelekis discusses his career from its earliest beginnings to present day while pinpointing the landmark developments in IR he has seen along the way.
What was it that drew you to medicine and to IR in particular?
I consider myself both fortunate and humbled to have been born into a medical family, with my grandfather, my uncles and my father practising as radiologists. At one point, my immediate family included no fewer than seven radiologists, each in a different subspecialty of radiology.
From a young age, I was immersed in this world. As a teenager, I would spend school vacations in the radiology department, helping in the lab, carrying, exposing, and printing films by hand, as was standard practice at the time—or archiving cases. Later, when the first digital angiography systems arrived, I began working with image post processing and enhancing. This was an exciting introduction to technology, and I still remember the fascination of working on some of the first computers I had ever seen.
My father, one of the pioneers of IR in Greece, made the radiology department and the interventional suite feel like a second home. Growing up in this environment, choosing radiology—and particularly IR—felt not just natural, but inevitable.
I will never forget the sense of awe and responsibility I felt as a young trainee, feeling the warmth of a patient’s blood on my gloves during my first groin puncture using the Seldinger technique. The meticulous process of cleaning, holding, and manoeuvring catheters and wires during those early cases left an indelible impression on me. Even now, that formative experience continues to shape my respect for the craft and my commitment to patient care.
Who have been your mentors throughout your career and what is the best advice they have given you?
I have been privileged throughout my career to have mentors and colleagues who supported me and taught me invaluable lessons, both professional and personal. In the moment, you rarely grasp the full significance of each encounter or experience, but looking back, you begin to appreciate the sequence of events and relationships that shaped you into the person you are.
My training in Switzerland at the University Hospital of Geneva under the guidance of François Terrier, was pivotal in developing my skills in IR, spine, musculoskeletal imaging, and pain management. One morning, as a young resident sipping coffee in front of a vending machine, I met Jean Baptiste Martin. From that day on, he took me under his wing
and taught me generously and without reserve.
In the same group, Daniel Ruefenacht and Christoph Becker trusted me to work in the first interventional magnetic resonance imaging (MRI) suite in the early 2000s, where I had the opportunity to practise some of the very first cryoablations and radiofrequency ablations in an MRI environment.
I feel fortunate to have been able to ride the crest of scientific innovation during the early days of bone augmentation procedures, working alongside true pioneers such as Harve Deramond in vertebroplasty and Jacques Theron in disc treatments. Those formative years instilled in me a love for creativity and innovation, and a sense of joy in the work itself.
One of the most enduring lessons came from Kieran Murphy, who taught me always to carry a piece of paper to sketch out ideas— to experiment, to improve procedures and treatments, and above all, to enjoy the process. My mentors and friends led by example and taught me to listen (thank you Sean). I learned from them that the greater the legend, the more humble the person.
Over 25 years, Jean Baptiste and I have worked side by side, always striving to improve procedures—talking, thinking, designing, and performing together—and having an incredible time every step of the way.
Could you outline one of your most memorable cases?
One of my most memorable cases was among the very first vertebroplasties I performed for bone augmentation, on a bedridden patient in Greece. The fracture and treatment were fairly standard. That evening, when I visited the ward, the patient was pain-free and, after six months confined to bed, was able to stand and walk.
I vividly remember the other patients in the ward rising to their feet, applauding and cheering. To them, it seemed nothing short of a miracle. They had witnessed this man arrive in agony, suffering intensely, carried in on a stretcher. And now, just hours later, he was walking out of the hospital. It wasn’t the most technically challenging or complex case I ever handled, but it was undeniably the most impactful moment in someone’s life. This is the memory I return to whenever I feel disappointed or discouraged—a reminder of how truly blessed I am to have the ability to change people’s lives.
You have recently taken on the role of
president of the SIO. How do you hope to make your mark in this position? What do you hope to achieve?
Being selected by one’s peers from across the globe to serve as their chair is both a tremendous privilege and a profound responsibility. My experience with the society has been an extraordinary journey of learning, guided by a board of exceptional colleagues who have generously shared their wisdom, experience, and patience.
CURRENT APPOINTMENTS
2024–present: Director, third radiology department, National and Kapodistrian Univeristy of Athens, Greece
2024–present: President, Society of Interventional Oncology (SIO)
2024–present: Board of directors (adjunct), Greek Society of Interventional Radiology (GSIR)
2020–present: Professor of diagnostic and interventional radiology, National and Kapodistrian University of Athens, Greece
PREVIOUS APPOINTMENTS (SELECTED)
2004–2024: Faculty, second radiology department, Medical School of the National and Kapodistrian University of Athens, Greece
CLINICAL RESEARCH (SELECTED)
Principal investigator, Percutaneous augmented peripheral osteoplasty in long bones of oncologic patients for pain reduction and prevention of impeding pathologic fracture: The Rebar Concept
Within SIO, I have rediscovered the creativity and inspiration that fuelled my earliest years in the field. Surrounded by likeminded individuals committed to advancing patient care, we focus on advocating for the benefits of minimally invasive oncology procedures. IO stands today as the fourth pillar of cancer care, and it is our mission to champion it loudly and proudly—for all the patients in the world that deserve the very best. It is a profound honour to serve as the first international president of SIO, and I am deeply committed to supporting and strengthening the society’s global character. We must foster an environment that promotes standardisation and verification of procedures, ensuring that percutaneous treatments are delivered with the highest quality and reproducibility. My hope is that SIO will continue to provide worldwide leadership and support for IO, advancing care and improving outcomes for patients everywhere.
Looking ahead, my vision is for SIO to be a beacon of innovation, education, and collaboration, uniting clinicians, researchers, and industry partners across all continents to transform cancer care through minimally invasive techniques. Together, we will set new standards, empower practitioners, and most importantly, improve the lives of millions of patients worldwide.
What do you anticipate will be the next big advancement in IO?
I believe that interventional percutaneous procedures for oncology will continue to gain wider acceptance, as we increasingly recognise their synergies with other treatments, together with medical therapy, surgery and radiotherapy. Emerging evidence suggests immunologic reactions associated with the release of molecules following percutaneous treatments, could potentially be harnessed by immunotherapy to create powerful synergistic outcomes and innovative therapies.
Both patients and physicians are becoming more aware of IO solutions and their ability to complement standard therapies, paving the way for more integrated and effective cancer care.
You performed the first academic vertebroplasty cases in Greece. Can you describe your experience?
Introducing a new technique and creating a paradigm shift is always extremely challenging and complex. Peers are, quite understandably, cautious about adopting new procedures—but in my experience, once these techniques are validated, they are quickly and enthusiastically embraced. The journey has been nothing short of a rollercoaster, with multiple layers to navigate—physicians, administrators, insurers, and of course, patients. And yet, I can say without hesitation that it has been worth every effort, and I would do it all over again. We faced significant scepticism along the way, but
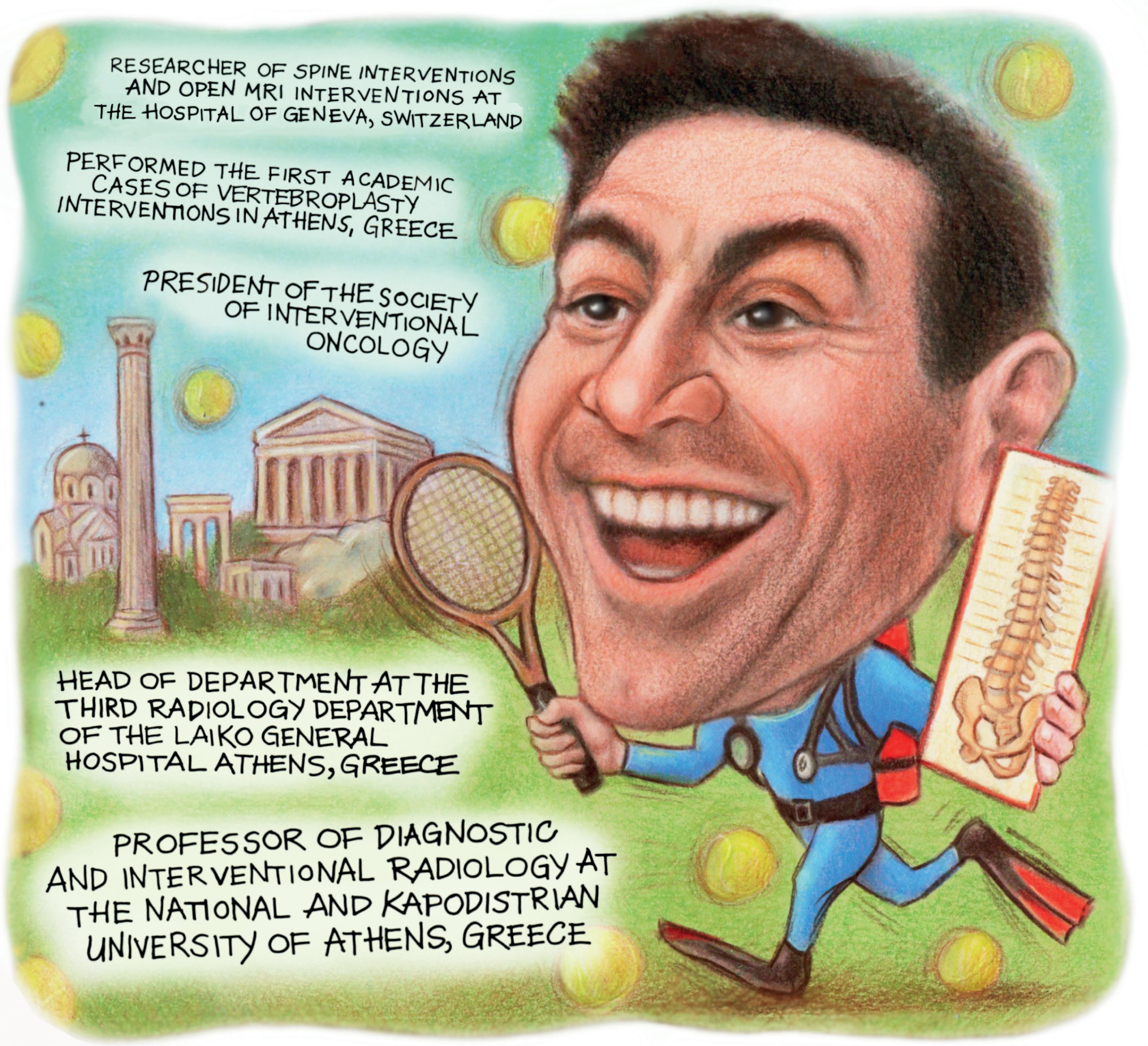
seeing a once incapacitated patient walking again is truly priceless.
Having played a role in numerous research papers regarding ablation, what do you believe will be the next significant development in ablative therapies?
In recent years, we have been fortunate to witness the ongoing evolution of ablation systems and devices—improving accuracy, reproducibility, and precision. The most recent advances are already transforming our practice, as enhanced planning, guidance, and confirmation tools are increasing our success rates. Integrating these technologies directly into imaging equipment enables better targeting and more effective tumour destruction. Our tools are evolving to provide optimised treatment solutions supported by real-time imaging, and interventional radiologists are now rigorously planning the technique and volumetrically verifying results. This three fold paradigm—planning, executing, and verifying, increasingly
supported by artificial intelligence (AI)-driven software—will truly transform the future of ablative therapies.
What have been some of the most important developments in IR over the course of your career so far?
As a child, I grew up in the era of cassette tapes, black and white televisions without remotes, and parents smoking in cars—so you can imagine that I’ve witnessed my share of changes over the years. IR has evolved right alongside this technological revolution, transforming itself completely over the decades. Some of the most monumental changes have come from the introduction of computerised imaging devices, such as angiographic equipment with subtraction imaging, as well as the development of catheters and wires with memory shapes, and new materials that made microcatheters and guidewires possible.
But the evolution of IR has not been purely technological. At its core, the specialty itself has grown and matured, building robust
"We faced significant scepticism along the way, but seeing a once incapacitated patient walking again is truly priceless”
clinical services and transforming from a niche subspecialty into one of the most sought after specialties in medicine, attracting some of the brightest and most creative minds.
What does your life look like outside of medicine?
What life outside medicine? No, I’m joking. There absolutely must be a life outside medicine, because one needs to regenerate one’s thoughts and replenish one’s soul. To be able to step outside the confines of one’s professional micro world and see things differently.
For me, life outside medicine is about my wife, my family, friends and pets; it’s about those, who remind me of the world beyond my profession and help me appreciate all that I have and all that I share. It’s about leisurely summer afternoons, lounging on a small boat in a quiet cove of a Greek island, listening to music with loved ones, enjoying the sunset with a great book at hand—praising nature and feeling grateful for living a full and meaningful life.
The Society for Cardiovascular Angiography & Interventions (SCAI) has released new, evidence-based clinical practice guidelines to support the treatment of chronic venous disease (CVD).
PUBLISHED IN THE JOURNAL OF THE Society for Cardiovascular Angiography and Interventions (JSCAI) with an accompanying technical review, the document offers recommendations on a range of therapeutic options.
“These are the first SCAI guidelines focused on chronic venous disease, and they come at a time of increasing recognition of the burden it places on patients and healthcare systems,” said Robert Attaran (Yale School of Medicine, New Haven, USA), chair of the guideline writing committee and member of the SCAI Vascular Disease Council.
The recommendations were categorised as either ‘strong’ or ‘conditional,’ depending on the certainty of the evidence. Among the recommendations, ablation
therapy is advised in combination with conservative management, is suggested for patients with symptomatic reflux in the great or small saphenous veins and ulcer-associated perforator vein reflux (conditional).
“These guidelines reflect SCAI’s commitment to bringing evidence-based standards to areas where our members are increasingly practising,” said SCAI president Srihari S Naidu (New York Medical College, New York, USA).
“As interventional cardiologists take a larger role in managing chronic venous disease, a common problem affecting millions of people, these recommendations will help ensure that patient care remains both consistent and personalised.”
Answering the questions of appropriate outcome measures after intervention for deep reflux as promising venous valve technology emerges

There is an old saying that goes, “As surgeons, we change the anatomy to improve physiology”. Correction of physiological abnormality should, then, result in clinical improvement. The assumptions behind such a three-step logic (anatomy-functionclinical outcome) are frequently challenged, modified and, sometimes, refuted when subjected to scientific examination. Recent developments in the field of chronic venous disease (CVD) make clear the need for such scientific examination of several basic assumptions, one of which is the role of reflux.
EPIDEMIOLOGICAL STUDIES
and clinical observations consistently demonstrate that patients with primary CVD have either deep or superficial venous reflux, or both. Superficial reflux is relatively easy to treat. Multiple clinical trials have shown that ablation leads to clinical improvement. Deep reflux data are less convincing. The introduction of surgical repair for deep venous valves generated several observational studies showing excellent long-term functional and good clinical outcomes.1,2 However, this operation requires the presence of a correctible valve, while most patients with deep reflux have valves damaged by the thrombotic process. Since valvuloplasty was universally performed in patients with terminal venous disease, consensus statements and guidelines restricted recommendations for deep vein reconstruction to patients with venous ulcers.3,4 More than 50 years of clinical experience performing deep reflux correction still did not answer the question of its role in the progression of CVD and the degree to which such correction changes the natural history of this disease process.
There is a definite need for a practical solution for deep reflux correction. Correction in patients with both primary and secondary CVD—preferably in non-terminal stages of the disease—should answer this question and define the place for such a procedure in clinical practice. Fortunately, several devices are currently in pre-clinical and clinical stages of testing, and the hope is that some solutions will be available soon. However, the path from initial trials to meaningful clinical data will not be easy.
The first challenge is patient selection. Haemodynamics plays an important role in the early stages of venous disease, but has minimal influence in advanced stages.5 The terminal stage is much more a chronic wound process, and correction of haemodynamic abnormalities, although beneficial, has a less clear benefit compared to earlier stages. Limiting the use of deep reflux correction to patients with venous ulcers will not answer the question of whether such a procedure can prevent disease progression. An additional challenge is choosing outcome measures that
are related more to haemodynamic correction than to other aspects of ulcer management. The only prospective randomised trial of deep venous valvuloplasty showed that patients with stable disease, or those that remained in the same clinical class for five years before surgery, do not benefit from deep valve repair, while those who progress to more severe disease have a significant clinical improvement.6 This suggests that it is reasonable to use reflux correction procedures in patients in early CVD stages who experience relatively fast progression. Another challenge is to demonstrate the relationship between improvement in haemodynamics and clinical outcomes. Existing measures of venous haemodynamics and the severity of venous disease are far from perfect and likely to be inadequate for addressing this challenge. The current definition of reflux, although clinically useful, has no meaning in terms of physiological or fluid dynamics. Reverse flow in venous segments is frequently a normal event, even when all valves
The path from initial trials to meaningful clinical data will not be easy”
are competent.7 The time of reversed flow depends on many factors outwith the presence or absence of valvular incompetence. The variability of reflux time measurements is so large that the same patient can be classified as having reflux if tested at different times by the same sonographer using the same procedures and equipment.8 Which parameters of reversed flow are physiologically relevant remain unknown. Suggested candidates range from the volume of blood refluxing back, the flow rate, velocity, vein wall sheer stress and near-wall sheer rate, to a combination of all these measures. Even if the specific factor is defined, ultrasound-based measurements provide information
only on one venous segment at a time. The impact of a single segmental reflux correction on the global haemodynamics of extremities is more likely to be clinically relevant and important to assess. Unfortunately, the only existing test for assessing global haemodynamics is plethysmography, which is even less reliable than ultrasound.
The instruments that are used to assess CVD severity were developed by expert consensus (the Venous Clinical Severity Score, or VCSS) or even by a single person (the Villalta score). They reflect more on current perceptions of what constitutes more-or-less severe disease, rather than on scientifically based indicators of disease severity. The exception would be some of the patient-reported outcomes—such as VEINES-QOL— that were psychometrically constructed and tested for several aspects of validity.
Like the physiological questions about deep venous valves, the question of appropriate outcome measures of reflux correction is likely to be answered by future clinical experience with valve correction devices. As practitioners managing patients with venous disease, we are at an exciting juncture—when many questions can be answered and the health of our patients can be improved. All we need is a solution that is practical and efficient at correcting deep venous reflux.
References
1. Kistner RL. Surgical repair of the incompetent femoral vein valve. Arch Surg. 1975 Nov;110(11):1336-42
2. Masuda EM, Kistner RL. Long-term results of venous valve reconstruction: A four- to twenty-oneyear follow-up. J Vasc Surg. 1994 Mar;19(3):391-403
3. Lurie F et al. Invasive treatment of deep venous disease. A UIP consensus. Int Angiol. 2010 Jun;29(3):199-204.
4. O’Donnell TF Jr et al. Management of venous leg ulcers: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2014 Aug;60(2 Suppl):3S-59S
5. Welkie JF et al. Hemodynamic deterioration in chronic venous disease. J Vasc Surg. 1992 Nov;16(5):733-40
6. Makarova NP, Lurie F, Hmelniker SM. Does surgical correction of the superficial femoral vein valve change the course of varicose disease? J Vasc Surg 2001 Feb;33(2):361-8
7. Lurie F. Anatomical Extent of Venous Reflux. Cardiol Ther. 2020 Dec;9(2):215-218
8. Lurie F et al. Multicenter assessment of venous reflux by duplex ultrasound. J Vasc Surg. 2012 Feb;55(2):437-45
Fedor Lurie is a associate director of the JOBST Vascular Institute in Toldeo, USA.

“It takes a long time to become young”
PABLO PICASSO

Welcome to this new section of Interventional News focused on the life, ambitions and opinions of young interventional radiologists in training and early practice.
FOREWORD BY EDITOR-IN-CHIEF BRIAN STAINKEN

LET’S TAKE A MINUTE AND THINK ABOUT the words that define the core culture in interventional radiology (IR). I’ll bet that words like groundbreaking, bold, disruptive, energetic and novel made it onto your list. Curiously, if you were to do the same thing and find words that describe youth, many would cross over.
That makes sense because, as medical specialties go, we are young; indeed in the USA we are the newest recognised primary medical specialty. Our closest sibling is 35 years older!
But, as anyone who was raised in a big family can attest, youth is relative. The elder siblings yield all too quickly to the kids busy climbing the tall walls, challenging authority and changing things.
This new section of Interventional News is all about those pesky kids.
We want to hear from those of you in training and early practice. Tell us about your everyday and your dreams—what is good, what needs to change? What holds you back? How do you view your future career as an interventionist?
While there is great variability across the world in the challenges you face, there is even greater opportunity.
What’s important and what’s not to an upper-level IR trainee
In this article, upper-level interventional radiology (IR) trainee, Monica Matsumoto (University of Pennsylvania, Philadelphia, USA) discusses the data that she and her collaborators collected on the quality and content of their training, distilling what is and isn’t important to her peers.
THE CURRENT IR TRAINING pathway with both integrated and independent residencies has been in place since 2017, with the most recent Match in March 2025 being the largest to-date.1 While several studies have focused on viewpoints regarding IR among medical students and incoming residents, insights from upper-level IR trainees are lacking and could provide valuable information, not only for junior residents and future IR trainees, but also for IR educators and residency leadership.2,3
We surveyed senior IR residents (PGY 5–7, n=48) in the USA, including integrated and independent pathways. Here are our top five takeaways:
1. Overall, residents are satisfied with their training
We found that upper-level residents were overwhelmingly happy, regardless of their IR training route. While there was a slight, nonstatistically significant preference of the integrated over the independent pathway, we could not make more definitive conclusions on the optimal pathway due to the limited number of responses.
2. Interpersonaland proceduralrelated programme components
Trainee happiness, faculty friendliness, ‘fit’
Once identified, solutions readily transfer across time zones and borders. Your world may seem unique to you, but most likely the same experiences are lived by some of your peers far, far away. We see it routinely when a touchstone article is published and cited globally. If it happens in the science of IR, what about the practice of IR, the economics, training, advocacy, device and patient access?
We hope that encouraging this sort of communication will help elevate practice standards and strengthen our global community.
Our first article in this series, authored by Monica Matsumoto, speaks to the experience of US IR trainees currently enrolled in dedicated IR training programmes. Their experience is an early indicator for how the future IR, trained primarily as a proceduralist, perceives the field as a primary specialty. Relevant outside the USA? Absolutely. The success story of this new training construct should help to inspire others climbing their tall walls toward a future where excellence is the first word you think of when you think of IR.
■ Have something to say? Get in touch with eva@bibamedical.com
with programme culture, procedure diversity and quantity, as well as development of procedural autonomy were selected as the most important components when selecting a programme.
3. A diagnostic foundation is key, with opportunities to develop ancillary IR training components
IR residents should be proficient in core diagnostic radiology components, with particular attention given to mastering body imaging, emergency radiology and ultrasound. Beyond the core components, programmes should offer varied elective opportunities based on resident preferences, such as a diagnostic procedural rotation and vascular surgery. Future areas for training innovation include ancillary opportunities, such as in practice development, business/financial literacy training and subspecialty (mini-)fellowships.

4. Intern year should be chosen based on personal priorities
Residents favoured intern year flexibility, with essentially a tie between preliminary surgery, categorical IR and no preference at all. However, residents noted that preliminary surgery and categorical intern years have more patient care emphasis than a transitional year.
5. There is no “one-size-fits all” training model
We found that residents’ reflections about programme components were predominantly heterogeneous. While this makes blanket conclusions more difficult, we believe the diversity is a strength of the current training model that accommodates and promotes different backgrounds and interests.
References
1. Kaufman JA, Mauro MA. The Path to Primary Specialty Recognition of Interventional Radiology and the IR/DR Certificate. JVIR. 2023;34(12):2052–2057.
2. Matsumoto MM, Shamimi-Noori S, Gade TP, et al A 5-Year Update on the IR Residency Match: 2022 National Survey Results of Program Directors and Matched Applicants Compared with 2017. JVIR 2023;34(9):1584–1598.e1549.
3. Oladini LK, Rezaee M, Thukral S, et al. Opportunities for Excellence in Interventional Radiology Training: A Qualitative Study. JACR. 2022;19(4):576-585.
Monica Matsumoto is an upper-level interventional radiology trainee at the University of Pennsylvania in Philadelphia, USA.

Lead paediatric interventional radiologist at Hong Kong Children’s Hospital, Kevin Fung specialises in vascular access, oncologic interventions and lymphatic imaging and interventions. In this article, Fung highlights the distinct clinical obstacles that arise when gaining arterial access in paediatric patients while sharing his best practices.
OBTAINING ARTERIAL ACCESS remains one of the most technically demanding aspects of paediatric angiography and endovascular intervention. Unlike adults, children present unique hurdles: smaller, spasmprone arteries, higher risk of dissection, and limited availability of paediatricspecific equipment (Figure 1). Notably, the mismatch between small-calibre arteries and adult-sized vascular sheaths
can result in arterial occlusion and thrombotic complications—reported in up to 16% of children weighing under 15kg.
Meticulous pre-procedural planning—including careful site selection, periprocedural optimisation, ultrasound-guided puncture, and attentive post-access care—can improve success rates and minimise adverse outcomes.
While transfemoral access remains the standard approach, alternative access routes can be useful in certain clinical scenarios. In neonates, umbilical vessels are often preferred to avoid access-related extremity complications. The umbilical artery provides direct systemic access via the internal iliac system, while the umbilical vein can be utilised if a patent ductus arteriosus or foramen ovale is present (Figure 2).
In cases of steno-occlusive aortoiliac disease or interventions involving steep visceral artery anatomy, upperextremity access—radial, brachial or axillary—can facilitate cannulation and device delivery. Brachial and axillary access can be considered in younger children when the radial artery calibre remains small. However, the interventionist must bear in mind the potential risk of upper limb ischaemia and compressive neuropathy in case of haemorrhagic complications. Although radial arteries <2mm were traditionally considered a relative contraindication
for radial access, new slender sheath technologies and the low incidence of clinically significant radial artery occlusion (RAO) have prompted reevaluation of these thresholds. Distal radial access at anatomical snuffbox may further reduce RAO risk.
Intraprocedural unfractionated heparin and vasodilators are essential to mitigate vasospasm and thrombosis. When arterial thrombosis occurs, systemic anticoagulation is first-line therapy for children, while catheterdirected thrombolysis or thrombectomy is reserved for chronic limb-threatening ischemia unresponsive to medical management. Fortunately, long-term sequelae are uncommon in children due to rich collaterisation. However, early surgical revascularisation should be considered in symptomatic children with claudication or limb length discrepancy.
Kevin Fung is an interventional radiologist at Hong Kong Children’s Hospital in Hong Kong.
Unlike adults, children present unique hurdles: smaller, spasmprone arteries, higher risk of dissection, and limited availability of paediatricspecific equipment”
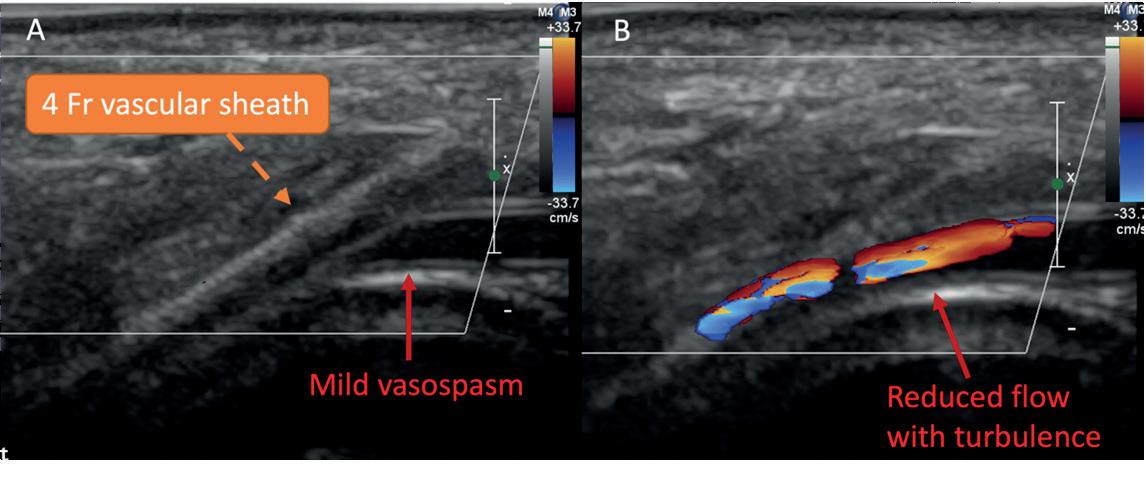


2 a-f: Given the small femoral arteries, a transumbilical venous approach was used to avoid accessrelated ischaemic complications in the lower limbs. Unique physiological connections between the systemic venous and arterial circulations exist in the perinatal period, making this technique possible

Results from the CLN-PRO-V007 pivotal phase 3 clinical trial of the acellular tissue engineered vessel (ATEV; Humacyte) in arteriovenous access for patients at high risk of autologous arteriovenous fistula (AVF) maturation failure with end-stage kidney disease (ESKD) were presented at the Society for Vascular Surgery (SVS) Vascular Annual Meeting (VAM 2025; 4–7 June, New Orleans, USA).
THE TRIAL’S RESULTS, PRESENTED BY Mohamad A Hussain (Brigham and Women’s Hospital and Harvard Medical School, Boston, USA), demonstrated the superiority of ATEV over autologous AVF in high-risk patients with ESKD.
CLN-PRO-V007 was a prospective, multicentre,
two-arm, randomised controlled trial comparing the efficacy and safety of ATEV and AVF in ESKD patients on haemodialysis undergoing singlestage surgical vascular access creation. ATEVs are bioengineered blood vessels grown from human vascular cells, designed to restore, replace or enhance
Controversies in transhepatic versus transperitoneal access for percutaneous cholecystostomy


Percutaneous cholecystostomy is a valuable intervention for managing acute cholecystitis in high-risk surgical patients.1 Yet, the choice between transhepatic and transperitoneal access routes remains a topic of ongoing debate. Here, NikolaosAchilleas Arkoudis and Stavros Spiliopoulos (both Athens, Greece) analyse contemporary viewpoints to provide concensus on the best treatment pathway.
THE TRANSPERITONEAL approach accesses the gallbladder directly without liver transgression, making it preferable for patients with liver disease or bleeding disorders. Still, because it lacks the protective effect of liver tamponade, it is considered to carry a higher risk of bile leakage, which can cause peritonitis.2 In contrast, the transhepatic approach has been traditionally reflected as a most popular route due to a lower chance of bile leakage, improved safety in cases where interposed tissues or fluid (ascites) are present, better catheter stability, and faster tract formation. However, due to the necessity of passing through the liver to reach the gallbladder, it is considered a higher risk of bleeding.2 Notably, recent studies show that the transperitoneal approach performs just as well as, if not better than the transhepatic approach. Particularly, studies by Michael D Beland et al and Joseph R Kallini et al demonstrated no statistically significant differences in the complication rates among the transperitoneal and transhepatic routes, while the Multicentre Audit
of Cholecystostomy and Further Interventions (MACAFI) retrospective evaluation of 913 patients found that the transperitoneal route had a lower haemorrhagic complication incidence, fewer episodes of acute cholecystitis recurrences and fewer hospital readmissions.3,4,5
Nonetheless, neither route should be considered inherently superior in all scenarios, as no single option is the best option for all cases. It is critical to understand that procedural nuance matters, and that individualised decision-making based on technique (trocar or Seldinger), anatomy, and operator experience should be considered. Every patient’s status and clinical scenario is different; therefore, it would make sense that every procedure should be tailored to the specific circumstances. We should integrate anatomy, urgency, co-morbidities and operator tools, and prioritise according to what makes the procedure easier for the physician and safer for the patient. For example, a transperitoneal trocar approach may be optimal when the gallbladder is
the function of damaged or diseased vascular tissue.
The trial enrolled a total of 242 ESKD patients, of which 110 were specified as high-risk of fistula nonmaturation (defined as all females and males with a body mass index [BMI] ≥ than 30kg/m2 and having diabetes).
ATEV was observed to have better functional patency, usability and a comparable access-related complication profile compared to AVFs in this highrisk subgroup of patients. The safety profile of the ATEV was reported to be comparable to AVF, with similarly low rates of infection.
The cohort of patients treated with ATEV had more thrombosis and stenosis events compared to AVF; however, the majority were successfully treated. Patients treated with ATEV had a lower need for maturation and surgical revision procedures compared to AVF.
well-distended with a clear direct path, minimising risks of bile spillage.6 Conversely, a transhepatic Seldinger approach may offer greater safety if the gallbladder is not adequately distended. Similarly, the transperitoneal Seldinger approach should be avoided due to the potential of bile spills, and the transhepatic trocar approach should be avoided due to the large bore of the catheter transgressing the liver.6
After all, despite earlier assumptions, recent trials have shown that the trocar and Seldinger techniques are equally safe and effective; therefore, as equally acceptable techniques, they may also subsequently affect route choice.7,8 Additional variables, such as expected catheter dwell time and plans for interval cholecystectomy, may all enter the equation.
Building on this controversy, recent consensus studies have reached differing conclusions, underscoring the complexity of the issue. One Delphi study recommended transhepatic access (83.4% agreement), while another
The lack of a one-sizefits-all solution highlights the need for interventional radiologists to lead this conversation”
suggested that both transhepatic and transperitoneal approaches are equally valid (80% agreement).9,10 These studies evaluated several statements regarding the management of high-risk patients with acute cholecystitis and were mostly represented by noninterventional radiology physicians.
The lack of a one-size-fits-all solution highlights the need for interventional radiologists to lead this conversation and provide guidelines for the different scenarios. As they are the specialists most familiar with the technical intricacies of percutaneous cholecystostomy, they are best
positioned to guide evidence-based decisions regarding the technical aspects of the procedure, while the rest of the issues regarding patient management can encompass the necessary multidisciplinary input. Until such consensus studies are led by the interventional radiology community, flexibility and clinical judgment must prevail, and percutaneous cholecystostomy access route selection should remain tailored to each patient’s anatomy, clinical condition and the operator’s preferred technique.
References
1. M. Yokoe et al., “Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos),” J Hepatobiliary Pancreat Sci, vol. 25, no. 1, pp. 41–54, Jan. 2018, doi: 10.1002/jhbp.515.
2. N.-A. Arkoudis et al., “Percutaneous cholecystostomy: techniques and applications,” Abd Rad, Jun. 2023, doi: 10.1007/s00261-023-03982-2.
3. M. D. Beland, L. Patel, S. H. Ahn et al., “ImageGuided Cholecystostomy Tube Placement: Shortand Long-Term Outcomes of Transhepatic Versus Transperitoneal Placement.,” AJR Am J Roentgenol, vol. 212, no. 1, pp. 201–204, Jan. 2019, doi: 10.2214/ AJR.18.19669.
4. J. R. Kallini, D. C. Patel, N. Linaval, et al., “Comparing clinical outcomes of image-guided percutaneous transperitoneal and transhepatic cholecystostomy for acute cholecystitis,” Acta radiol, vol. 62, no. 9, pp. 1142–1147, Sep. 2021, doi: 10.1177/0284185120959829.
5. P. E. Jenkins, A. MacCormick, J. Zhong et al “Transhepatic or transperitoneal technique for cholecystostomy: results of the multicentre retrospective audit of cholecystostomy and further interventions (MACAFI),” Br J Radiol, Jan. 2023, doi: 10.1259/bjr.20220279.
6. N.-A. Arkoudis, O. Moschovaki-Zeiger, and S. Spiliopoulos et al., “Transhepatic versus Transperitoneal Access for Percutaneous Cholecystostomy Remains Controversial: Interventional Radiologists Must Lead the Discussion,” Cardiovasc Intervent Radiol, May 2025, doi: 10.1007/s00270-025-04046-2.
7. L. Reppas et al., “Two-Center Prospective Comparison of the Trocar and Seldinger Techniques for Percutaneous Cholecystostomy,” AJR Am J Roentgenol, vol. 214, no. 1, pp. 206–212, Jan. 2020, doi: 10.2214/AJR.19.21685.
8. N.-A. Arkoudis et al., “US-guided trocar versus Seldinger technique for percutaneous cholecystostomy (TROSELC II trial).,” Abdom Radiol (NY), Apr. 2023, doi: 10.1007/s00261-023-03916-y.
9. J. M. Ramia et al., “International Delphi consensus on the management of percutaneous choleystostomy in acute cholecystitis (E-AHPBA, ANS, WSES societies),” Wor J of Emer Surg, vol. 19, no. 1, p. 32, Oct. 2024, doi: 10.1186/s13017-024-00561-8.
10. A. Pesce et al., “Management of high-surgical risk patients with acute cholecystitis following percutaneous cholecystostomy. results of an international Delphi consensus study,” Int J of Surg Mar. 2025, doi: 10.1097/JS9.0000000000002325.
Nikolaos-Achilleas Arkoudis is a consultant radiologist and Stavros Spiliopoulos is a professor of interventional radiology at the Attikon University General Hospital, National and Kapodistrian University of Athens, Athens, Greece.
BROWSE FULL PROGRAMME HERE
Safety – at the heart of everything we do Every procedure, every decision we make in IR, hinges on our ability to safeguard those in our care. Join us at the BSIR Annual Scientific Meeting 2025 to explore the latest innovations and protocols in IR designed to mitigate risks and ensure the highest standards of care.



To compliment the focus on safety, BSIR 2025 will include a series of sessions on emergency IR treatment. This series will include the treatment of vascular, gastrointestinal, and genitourinary emergencies, trauma, and iatrogenic complications.
Highlight topics
• treatment of chronic limb-threatening ischaemia
• vascular interventions
• iatrogenic complications
• paediatric IR
• emerging technologies
The Active Learning Zone returns in force this year, with over 15 stations enabling delegates to get hands-on with devices and phantoms across a range of IR procedures. This will be complimented by an array of in-depth workshops for small groups to deep dive in to topics such as radiation protection, liquid embolics, thrombectomy, and more.
Register by September 11 to access early bird fees!
FastWave Medical announces successful 30-day first-in-human data on Sola IVL technology
FastWave Medical announced the successful completion of initial firstin-human (FIH) procedures in its feasibility study of Sola, the coronary laser intravascular lithotripsy (IVL) device.
The multicentre study will assess Sola’s safety and performance in patients with calcified coronary artery disease. Sola is a rupture-resistant balloon catheter designed to help physicians treat hardened calcium in blood vessels with precision and control. Its laser energy delivers 360-degree pressure with each pulse, making therapy consistent and effective, even in challenging lesions.
“There’s a moment in every FIH study where you see if the technology lives up to its promise,” said Arthur Lee, director of Peripheral Vascular Services at The Cardiac and Vascular Institute (TCAVI) in Gainesville, USA. “With Sola, we saw that moment early on. It demonstrated exceptional crossability through complex anatomy where existing IVL technology might struggle, and its 5Hz pulse rate allowed us to deliver therapy efficiently— reducing ischaemic time in patients with compromised cardiac output.”
In a recent press release, the company highlighted that this milestone follows FastWave’s FIH study of Artero, its peripheral electric IVL (E-IVL) system, which demonstrated 100% procedural success and no adverse events at 30-day follow-up.
HistoSonics’s #HOPE4KIDNEY trial completes patient enrolment HistoSonics recently reported that it has completed enrolment in a pivotal trial to evaluate its histotripsy platform in treating kidney tumours.
The US company’s prospective, multicentre, single-arm pivotal #HOPE4KIDNEY trial is designed to evaluate the effectiveness and safety of the Edison system for the destruction of kidney tissue by treating primary solid renal tumours.
A total of 67 patients have been enrolled with a single, non-metastatic solid kidney mass ≤3cm. Patients will be treated with the Edison system and followed for five years post procedure,

with data at the 90-day evaluation point to be submitted in support of regulatory approval with the US Food and Drug Administration (FDA).
Penumbra’s STORM-PE randomised trial reaches enrolment completion Penumbra has shared that it has reached enrolment completion in the STORM-PE clinical trial. The pivotal, prospective, multicentre randomised controlled trial enrolled 100 patients to evaluate computerassisted vacuum thrombectomy (CAVT) using Penumbra’s Lightning Flash plus anticoagulation versus anticoagulation alone for the treatment of acute intermediate-high risk pulmonary embolism (PE).
“This is an important milestone that underscores Penumbra’s commitment to transforming care for patients with pulmonary embolism,” said James F Benenati, chief medical officer at Penumbra. “The trial successfully randomised patients well ahead of schedule thanks to the dedication of our clinical partners and the tireless efforts of our internal teams.”
The study follows the US Food and Drug Administration (FDA) 510(k) clearance of the AlphaVac F1885 system for the treatment of PE in the USA in April 2024 and its CE mark approval in Europe in May 2024. The RECOVER-AV trial is designed to evaluate the safety and efficacy of the AlphaVac F1885 system in support of its adoption in the global market, as well as to assess long-term functional outcomes for patients following
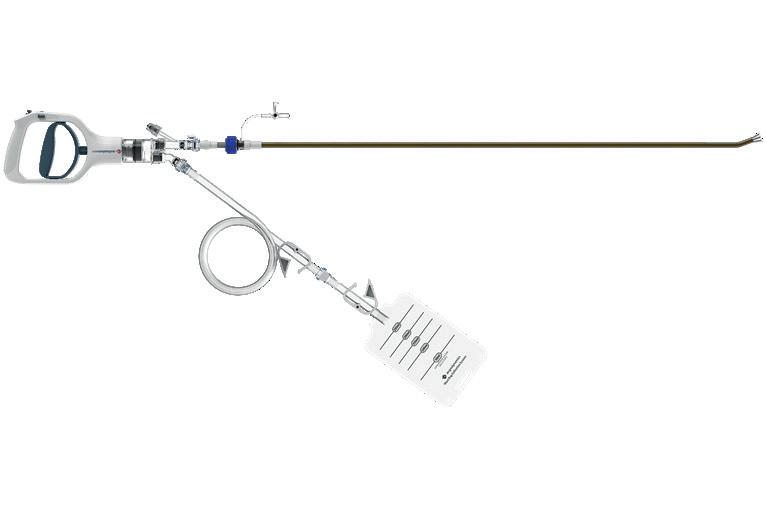
thrombectomy system.
The investigational device exemption study was carried out at 19 interventional cardiology, radiology and vascular surgery centres in the USA. E2’s system features a patented dual-action mechanism that combines aspiration with clot disruption.
In a recent press release, the company describes that the flow mitigation technology integrated into the system aids physicians in clot removal while reducing the loss of blood, a critical aspect of PE treatment.
Andrew Klein, ENGULF national principal investigator at Piedmont Atlanta Hospital in Atlanta, USA said: “The ENGULF trial represents an impressive journey of innovation during which E2 and investigators were able to introduce and evaluate several new technologies within the trial. “It is an exciting and dynamic period of evolution.”
OncoSil Medical announces completion of patient enrolment in PANCOSIL study
OncoSil Medical recently revealed the successful completion of patient recruitment for the PANCOSIL study.
The study is an open-label, singlearm phase 1–2 feasibility trial initiated by Amsterdam University Medical Center (Amsterdam UMC) in The Netherlands. The study is evaluating the safety and feasibility of computed tomography (CT)-guided percutaneous radionuclide therapy using the OncoSil device in patients with non-progressive, locally advanced pancreatic cancer (LAPC).
OncoSil Medical announced ethics committee approval for the PANCOSIL study on 5 June 2023 and the first patient treatment on 29 November 2023. A total of 20 patients have now been enrolled in the study. Its primary objective is to assess a novel delivery method for the OncoSil device via a CT-guided percutaneous approach. The company stated in a recent press release that this approach has the potential to simplify administration and lower barriers to adoption, supporting wider market penetration and real-world clinical use.
First patient enrolled in RECOVERAV trial of AlphaVac F18 system for treatment of acute PE AngioDynamics announced the first patient has been enrolled in the RECOVER-AV clinical trial, a prospective, multicentre, international, single-arm study evaluating the AlphaVac multipurpose mechanical aspiration (MMA) F1885 system in the treatment of acute, intermediate-risk pulmonary embolism (PE).
AngioDynamics continues to grow its global clinical presence and commitment to evidence-based care,” said Laura Piccinini, senior vice president/general manager, cardiovascular and international. “With AlphaVac already 510(k)-cleared in the USA and CE-marked in Europe for PE, we’re investing in high-quality data focused on functional recovery and quality of life that will equip clinicians, payers and patients with even greater confidence in the system’s safe, effective performance, and help broaden access to life-saving PE treatment across Europe and the wider global market.”
StentIt launches first-in-human trial of bioresorbable stent to treat below-the-knee CLTI
StentIt has revealed the successful implantation of its resorbable fibrillated scaffold (RFS). As part of the VITALIT 1 study, patients with chronic limb-threatening ischaemia (CLTI) below the knee have successfully been treated using the RFS implant. In this clinical procedure, revascularisation was achieved using an endovascular approach to restore blood flow to the foot.
StentIt’s RFS device is a bioresorbable stent built from microfibers, providing structural support to instantly open, and facilitate the reconstruction of the artery. Due to the porous design of the implant, patient’s own cells infiltrate into the mesh, triggering the formation of new vascular tissue. While the artery is being reconstructed from the insideout, the synthetic implant gradually resorbs and ultimately disappears over time.
Endovascular Engineering’s ENGULF pivotal trial completes patient enrolment
Endovascular Engineering (E2) has completed patient enrolment in the pivotal cohort of its ENGULF |trial, involving the Hēlo PE
BD to initiate real-world patient registry for Rotarex atherectomy system
BD announced plans to initiate a patient data registry for the Rotarex atherectomy system to measure realworld outcomes for patients with peripheral arterial disease (PAD).
Known as XTRACT, this prospective, multicentre, single-arm, post-market registry study will assess the clinical performance of the Rotarex atherectomy system in the treatment

of US patients with PAD lesions.
The XTRACT Registry is being led in partnership with co-principal investigators, Prakash Krishnan (Mount Sinai, New York, USA), an interventional cardiologist, and Todd Berland (NYU Langone Health, New York, USA), a vascular surgeon. The registry will enrol up to 600 patients at approximately 100 clinical sites across the USA, with the first patient enrolment expected later this year. Clinical follow-up evaluations will occur after 30 days, six months and 12 months post procedure.
“This registry will provide valuable data to support clinical decision-making and enhance patient outcomes in the management of PAD,” said Krishnan. “The Rotarex system has been extensively studied internationally, and we are excited to further evaluate its adaptability in treating a wide range of PAD lesions within the US patient population.”
Spanning 20,000 sq ft, Argon Medical’s new Distribution and Education Centre (ADEC) not only positions the company closer to customers, but also into better alignment with their training and education ethos. Strategically located in Derby, UK, the state-ofthe-art facility’s uses are threefold, functioning as a distribution warehouse, corporate offices, and a dedicated hands-on training centre to demonstrate their newest technologies for physicians and distributors. In July, Interventional News attended the grand opening of ADEC and sat down with Argon president and chief executive officer George Leondis and senior vice president of Europe, Middle East and Africa (EMEA) and Asia-Pacific (APAC) regions Matt Edwards to discuss their plans for the facility and how it fits into the company’s ambitious global expansion strategy.
Education, Leondis shared, has been at the centre of this project from inception and has been a unique identifier of Argon “from the beginning”, running right to the core of the business. “Teaching physicians early in their careers about how to use these devices, or, for example, how to perform procedures such as biopsy or drainage, has been mutually beneficial for us, and has allowed us to gain a foothold as an educator in the space,” Leondis says. “Education is one of the key characteristics we have become known for and one that we’re going to continue to focus on.”
The facility’s brand-new Clinical Education Centre can host in-person training demos or virtual education sessions. “This takes our ability to train our staff, distribution partners and also our physician users to a whole new level,” shares Edwards. “It’s not only going to enable hands-on simulation training that can replicate the procedure before the physician performs it for the patient, but it also means we can build a network of key customer partners, enabling us to expand our training and education offering.”
Having already welcomed distribution and physician partners to training sessions prior to the opening day, Edwards emphasises that the facility is already stretching its legs as a virtual and brick-andmortar education hub, helping them “achieve the level of clinical excellence that we demand for the new technologies we are bringing to market”, he states. During the grand opening, Argon’s senior clinical manager Anne-Marie Spence provided an introductory session for those present at ADEC and Argon’s clinical team who dialled-in virtually. Using a variety of Argon devices on realistic anatomical models, Spence illustrated the capabilities of the equipment, and the calibre of training offered at the facility. She pinpointed that individuals that have attended training to date have benefitted most from “real-time feedback” when using Argon devices in this environment, so that ultimately, “in real-life cases, they are supported and able to anticipate any issues that they could experience”.
Through education and training at ADEC, Argon is striving for clinical excellence when it comes to its products and their use in practice. Leondis reflected that historically “physicians, sales representatives or distribution partners would have to be taken to a
functioning operating room [OR] or the cath lab”, which could often be complex to arrange and carry out.
“We don’t have to do that anymore with this type of technology,” Leondis says, “this allows us to scale what we do.” In his view, the Clinical Education Centre’s ability to facilitate international training from the UK to physicians internationally was previously unachievable. “Now, we can simulate training in an OR or radiology lab with a physician and from there we can show them how a device works. I think it gives us a great opportunity to do this all over the world,” shares Leondis.
From a business growth perspective, Edwards highlights that the education focus of the facility builds into the broader framework of Argon’s future. “This facility ensures that we’re not only fit for purpose, but that we’re fit for future,” he shares, underlining the importance of this mentality considering Argon’s “rich research and development pipeline which is moving quickly”.
“As we gain approval within Europe, the technologies and products we’re offering are becoming more technical,” says Edwards. “With that comes a much greater need for training, both internally and externally. We want to make sure that we support the best technique, the best procedure but most importantly, the best patient outcomes,” he continues.
Leondis then speaks on Argon Medical’s key pillars— people, product and expansion. Having touched on ADEC’s capabilities, which he stated are a testament to the “world-class talent” at Argon who led the project, he emphasises the “large” pipeline of products and supply-chain expansion which will be facilitated by the centre.
“EMEA has been a big growth driver for us, and in APAC we’re growing well into the double digits in the region this year,” Leondis describes. “If you look back at Argon six years ago, 75% of our business was in the USA. Today, it’s a little bit over 50%. So, we are truly becoming a global business, and ADEC is giving us the opportunity to be close to our European customers and physicians,” Leondis says. Once fully operational, it is hoped ADEC will service approximately 80 countries worldwide.
Edwards details that a “big part” the company’s investment in the facility was to expand their support services. He shares that a key driver for this project was to strategically position customer service teams in
the same or similar time zones to customers, creating a “more local experience for direct and distributor business”.
“We’re also investing in warehouse staffing levels as well as our finance and back-office operations,” Edwards shares, “and that’s really where the majority of our investment is going to be placed—in people.”
Leondis adds that ironically “to be a global company you have to be close—you must be able to have people pick up the phone or be able to contact you in real time, and I think that’s one of the ways ADEC really fits into this strategy”.
Leondis—based in Argon’s global headquarters in Plano, USA—describes his first impression of the facility, of which he had previously only seen pictures. “I’ve been really excited about this. I was surprised by just how well this has been set up and how beautiful and functional it is. They did a fantastic job on the design, and it was great to see people’s positive reaction to it,” Leondis shares.
For Edwards, the experience on opening day was slightly different, having watched the facility be built from nothing. “I saw the evolution of it as the building was constructed and finished on the inside,” he describes.
Edwards continues: “I remember driving around the corner for the first time noticing that the position of the building is very prominent. This was confirmed yesterday when I brought George here for the first time and he asked me to stop the car to absorb the view,” Edwards retells.
“Every time I come here, I feel incredibly humbled and proud of what the team managed to achieve in a very short space of time and to such a high standard. I’ve also had the benefit of seeing some of our distribution partners come through here for training events, and again, the reaction was greater than I could have ever expected. So, I am very proud of what has been achieved here,” says Edwards.
Education is one of the key characteristics we have become known for and one that we’re going to continue to focus on”
George Leondis

This facility ensures that we’re not only fit for purpose, but that we’re fit for future”
Matt Edwards







Inari Medical, now part of Stryker, launches InThrill thrombectomy system
Inari Medical—now part of Stryker— has announced the launch of its next-generation InThrill thrombectomy system.
The company has stated in a recent press release that this is the first and only purpose-built small vessel and arteriovenous (AV) access thrombectomy system that can deliver fast, full luminal clot removal.
The second generation InThrill thrombectomy system is an 8Fr overthe-wire system comprising the InThrill thrombectomy catheter and the InThrill sheath. InThrill is built upon a familiar platform, optimised to become the standard for AV access and small vessel thrombectomy.
On May 19, 2025, Joshua Pinter and Anish Ghodadra of the University of Pittsburgh Medical Center (UPMC) in Pittsburgh, USA performed the first commercial case using the new InThrill thrombectomy system. “The next generation of InThrill has made our thrombectomies more effective and consistent than ever,” said Pinter. “Inari’s dedication to building a small vessel tool has changed our paradigm of treatment for AV access thrombectomy,” added Ghodadra.
“The launch of the next-generation InThrill thrombectomy system reflects our deep commitment to solving realworld challenges in vascular care,” said Tim Lanier, president, Inari Division. “This latest innovation delivers new tools and enriches our work with physicians in the vascular space.”
Philips receives FDA 510(k) clearance for image-guided navigation system for prostate cancer
Philips has announced the US Food and Drug Administration (FDA) 510(k) clearance of the latest Philips UroNav system.
In a recent press release made by the company, it states that the system includes a new advanced annotation workflow that supports clinicians during focal therapy procedures, helping deliver more precise, minimally invasive care.
“We’re entering a new era of precision prostate cancer care. Philips’ integrated focal therapy platform unifies imaging, biopsy pathology, treatment planning and 3D imaging guidance with magnetic resonance [MR] ultrasound fusion giving clinicians end-to-end efficiency and control,” said Ardeshir Rastinehad, vice chair of urology at Lenox Hill Hospital and system director of prostate cancer
at Northwell Health in New York, USA.
“With fused imaging and real-time ablation guidance in one place, we can personalise therapy with greater accuracy and spare patients the unnecessary side effects of traditional treatments.”
“We’re helping clinicians deliver more precise prostate cancer care by streamlining complex workflows and delivering the insights they need to support precise diagnosis and expand options for minimally invasive treatments,” said Martijn Hartjes, business leader, Clinical Informatics at Philips. “Our goal is to equip clinicians with the clinical tools required so they can deliver better care for more patients.”
In addition to clinical functionality, Philips UroNav delivers enhanced compatibility with ultrasound devices and needle guides and seamless integration with Philips DynaCAD systems for radiology and urology, says the company.
Varian lauches IntelliBlate mirowave ablation device in Europe
Siemens Healthineers’ Varian has introduced the next-generation microwave ablation solution— IntelliBlate—in Europe to treat soft tissue tumours.
Varian noted that this therapeutic device enhances Siemens Healthineers’ imaging and software solution suite, which includes myAblation Guide, myNeedle laser guidance system, and ultrasound for treatment management.
The addition of the device, which generates controlled spherical ablation zones for predictable treatment outcomes, facilitates clinicians in planning, placing, treating, monitoring, and confirming ablation therapy within a single environment.
In a recent press release, the company has stated that the Ximitry probe, a new feature of IntelliBlate, includes thermocouples for continuous temperature monitoring, providing clinicians with real-time data to inform treatment decisions. The system’s compact and portable design, with two generators in one system, features an intuitive interface for quick setup and preprogrammed settings, decreasing procedural hurdles.
Last year, the US Food and Drug Administration (FDA) granted 510(k) clearance for the IntelliBlate microwave ablation system. The company noted that following its FDA market clearance last year, IntelliBlate’s entry into the European market coincides with increasing clinical evidence supporting thermal ablation.
Varian interventional solutions president Franck Facchini said: “The results of the COLLISION trial mark a milestone in how we think about
ablation. We have reached the point where the clinical evidence irrefutably supports the use of thermal ablation as a first-line treatment option, and not just an option for patients who cannot undergo surgery.”
Medtronic to distribute FMD’s peripheral guidewires for transradial access in the USA Medtronic has announced it has entered into an exclusive US distribution agreement with Japan-based Future Medical Design Co (FMD) to sell specialty and workhorse peripheral guidewires. This agreement includes the first 400cm, 0.018″ peripheral guidewire available in the USA, expanding the Medtronic portfolio for transradial access for the treatment of peripheral arterial disease (PAD).
Medtronic shares that it is the sole distributor of 10 new F-14 and F-18 peripheral stainless-steel guidewires, available in 300cm and 400cm lengths. According to the company, the 0.018” 400cm wire, along with the 200cm working length IN.PACT 018 drug-coated balloon and Pacific Plus percutaneous transluminal angioplasty (PTA) catheter, provides physicians with a comprehensive suite of tools needed to reach lesions from a transradial approach.
“The F-14 and F-18 guidewires offer the tactile feedback, wire strength and control physicians need for lower extremity interventions, while also expanding radial access tools, a significant advancement,” said John Laird, chief medical officer for the Peripheral Vascular Health business, which is part of the Cardiovascular Portfolio at Medtronic.
Sirtex Medical granted FDA approval for SIR-Spheres
Sirtex Medical has revealed that is has received US Food and Drug Administration (FDA) approval for its SIR-Spheres Y90 resin microspheres for the treatment of unresectable hepatocellular carcinoma (HCC) in the USA.
With this approval, the company have stated in a recent press release, that SIR-Spheres are the only radioembolization therapy approved for the treatment of both metastatic colorectal cancer (mCRC) of the liver and HCC in the USA.
“This milestone reflects our ongoing commitment to delivering flexible, personalised therapies—with multiple dose options available daily—that empowers physicians to treat patients when and where it works best,” said Matt Schmidt, chief executive officer of Sirtex.
Cook Medical issues Class I recall for Beacon Tip angiographic catheters
Cook Medical has initiated a Class I recall of its Beacon Tip 5Fr angiographic catheter.
This follows reports of tip separation that could result in serious injury or death. The recall, identified as the most serious type by the US Food and Drug Administration (FDA), involves the removal of affected devices from clinical and commercial use.
In its notification to customers, Cook advised immediate examination of inventory to identify and quarantine any unused affected devices.
Distribution and use of the affected catheters must cease immediately. The manufacturer also stressed that the recall information should be communicated throughout relevant departments and to any third parties who may have received the devices.
Aventus thrombectomy system gains FDA clearance for PE treatment
Inquis Medical has recently shared that its Aventus thrombectomy system has received 510(k) clearance from the US Food and Drug Administration (FDA) for an expanded indication to treat pulmonary embolism (PE).The Aventus System is a next-generation mechanical thrombectomy platform.
“The FDA’s clearance of the Aventus system marks a major milestone for the company,” said Vahid Saadat, co-chief executive officer of Inquis Medical. “It validates the tireless efforts of our team and the deep partnerships we’ve built with our physicians, all focused on solving long-standing challenges in clot removal. Aventus is uniquely designed to meet the needs of physicians treating this life-threatening condition quickly, effectively, and safely.”
Penumbra receives US FDA clearance for Ruby XL system
Penumbra has announced the US Food and Drug Administration (FDA) clearance and launch =of the Ruby XL system.
The Ruby XL system is designed to help physicians achieve more efficient embolization, potentially reducing radiation exposure, and optimising outcomes—especially in large vessel and high-flow embolization, details a recent company press release.
“We’ve engineered Ruby XL to deliver more volume per coil than any other coil on the market, which may result in cost savings,” said Shruthi Narayan, president of Interventional Business at Penumbra. “Ruby XL embodies Penumbra’s commitment to innovation, delivering mechanical occlusion through more volume without sacrificing softness or deliverability.”
The Ruby XL System introduces three unique technologies—Ruby XL, POD XL, and Packing Coil XL—all of which can be delivered through a 0.035” diagnostic catheter.
Conventional pre-shaped microcatheter technology has evolved over the last decade, yet significant limitations still exist. In particular, the shape of a standard microcatheter cannot be changed or manipulated while inside a patient’s vasculature. As a user of this innovative technology, Jason C Hoffmann (NYU Langone Health, New York, USA) details his first-hand experience.
Selective cannulation of small arterial branch vessels for targeted/superselective angiography or embolization is commonly performed; however, conventional pre-shaped microcatheter use has limitations when in complex arterial vasculature, including tortuous or angulated vessels.
In these scenarios, the operator must often perform multiple microcatheter and wire exchanges to select the target vessel. This can take a considerable amount of time, require use of numerous devices, and may result in a substantial radiation dose to the patient and procedural staff. If the target vessel cannot be superselected, a less-targeted embolization must be performed, or the procedure is abandoned altogether. In either scenario, the case will take longer, with implications for increased cost and resource use, and has the potential for complications and untoward events.
The development of a steerable microcatheter (SwiftNINJA® steerable microcatheter; Merit Medical) is an innovation that offers an alternative approach to selective cannulation. This technology represents a new class of device, designed with a tip that articulates up to 180 degrees in opposing directions, providing real-time ability to change the angulation of the microcatheter tip while navigating through the vasculature.
The device can be used with or without a microwire which allows the injection of contrast while advancing or manipulating the steerable microcatheter. In my experience, this consistently leads to efficient selective cannulation of small vessels throughout the body, with a level of steerability that simply is not provided by any pre-shaped conventional microcatheter.
procedure time (75 vs. 112.5 minutes), and body-mass index (BMI) adjusted radiation exposure were found in the steerable microcatheter group.
Since publishing my early steerable microcatheter results, I have used the device in hundreds of prostate artery embolization (PAE) procedures, as well as superselective embolization of distal hepatic, renal, bladder, visceral and small pelvic arterial branches in a variety of scenarios. Cases have included treatment of traumatic injury, benign prostatic hyperplasia (BPH), hematuria, malignancy and non-traumatic causes of bleeding. Most of these procedures were performed with only the steerable microcatheter, and no microwire was needed. I continue to find that patients and my team benefit from steerable microcatheter use due to increased efficiency, high technical success rates, reliable target vessel selection and decreased radiation exposure.
Reducing vessel selection time in a prostate artery embolization case
An 85-year-old man with a long-standing history of BPH presented with severe lower urinary tract symptoms (LUTS) and intermittent gross hematuria. Despite multiple medical treatments, including three transurethral resection of the prostate (TURP) procedures over the past two years, the patient’s condition had not improved. His International Prostate Symptom Score (IPSS) was 29 (severe), and his Urinary Quality of Life Score was 5 (unhappy).

I can also inject contrast while advancing or manipulating the steerable microcatheter, allowing for precise control and improved vessel targeting. Decreased time to target vessel selection can have multiple benefits for the patient, primary operator, and procedural staff in the room. Advantages include decreased procedure times, increased procedural efficiency, fewer microcatheter and microwire exchanges, reduced fluoroscopy times, and lower radiation exposure.
SwiftNINJA steerable microcatheter use in moderate and high complexity angiography and/or embolization has routinely helped me to be successful and efficient. In 2019, I published my results, comparing steerable microcatheter to conventional microcatheter use in 40 procedures that involved moderate to highly difficult vessel selection.1
Statistically significant improvements in target vessel selection time—12 vs. 462.5 seconds (Figures 1a and b)—number of microwires used (0 vs. 2), total
Using a 2.4Fr SwiftNINJA through a 5Fr guide catheter, the left prostatic artery was selected in 12 seconds without a guidewire thanks to the steerability of the microcatheter tip. Proximal and then distal embolization of the left prostate artery with 300–500μ Embosphere microspheres (Merit Medical) was performed following the proximal embolization first, then embolize distal (PErFecTED) technique. The right prostate artery was then selected–again using the SwiftNINJA without a guidewire—in nine seconds and embolization was performed using the same technique.
Final angiography confirmed successful embolization of both left and right prostatic arteries. The patient was discharged the same day, with no hematuria or urinary retention reported since the procedure. At one month post-procedure, the patient’s IPSS decreased from 29 to 7 and Urinary Quality of Life score decreased from 5 to 1.
A 43-year-old female presented with chronic pelvic pain. Despite extensive diagnostic work-up, no definitive cause for the pain was found, except for
prominent left parauterine veins/varicosities and an enlarged left ovarian vein.
The patient was diagnosed with symptomatic pelvic venous reflux/pelvic congestion syndrome, and the plan was to proceed with venography and embolization. Due to extreme tortuosity of the gonadal venous vasculature preeminently, a 2.4Fr SwiftNINJA steerable microcatheter was used to efficiently navigate through the extremely tortuous vessels and into the inferior aspect of the left ovarian vein. Embolization was performed with sodium tetradecyl sulfate sandwiched in between packs of platinum microcoils.
Post-embolization digital subtraction venography demonstrated an appropriate angiographic result, with embolization of the left ovarian vein, but brisk antegrade blood flow in the left renal vein. The patient was discharged home in stable condition four hours post procedure, and experienced only mild flank discomfort for 24–36 hours post-procedure, relieved with ibuprofen. Her pelvic congestion syndrome symptoms markedly improved by the time she was seen for a post procedure office visit approximately six weeks later.
References 1. Hoffmann, JC, Minkin, J, Primiano, N et al., Use of a steerable microcatheter during superselective angiography: impact on radiation exposure and procedural efficiency. CVIR Endovasc 2, 35 (2019). https:// doi.org/10.1186/s42155-019-0078-9
Jason C Hoffmann is an interventional radiologist with NYU Langone Health in Mineola, New York, USA.
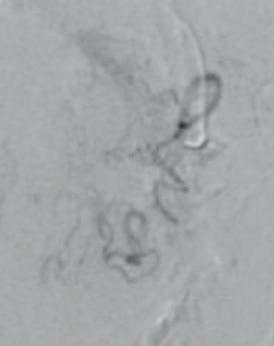

Figure 1. Left prostatic artery selected with SwiftNINJA steerable microcatheter. Initial internal iliac artery angiogram demonstrates Type 1 anatomy, with common origin of the left superior vesical artery and prostate artery (a). The microcatheter was moved from tip of 5Fr catheter to target vessel (distal aspect of main left prostate artery) in 12 seconds (b).
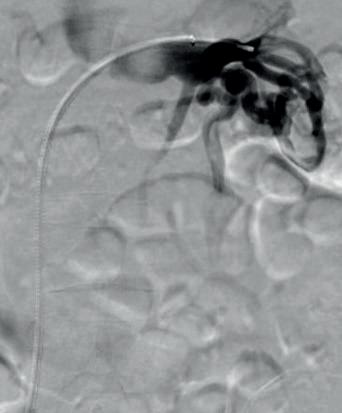

Figure 2. Left renal vein digital subtraction venography (DSV) via 5Fr catheter demonstrates patency of the left renal vein and inferior vena cava, with very prominent, tortuous and enlarged left gonadal vein (a). A 5Fr catheter was only able to select the most superior aspect of the left ovarian vein due to its extreme tortuosity. The SwiftNINJA steerable microcatheter was used to navigate through the multiple 180 and 360-degree turns to easily be passed inferiorly to the pelvis to perform embolization (b).





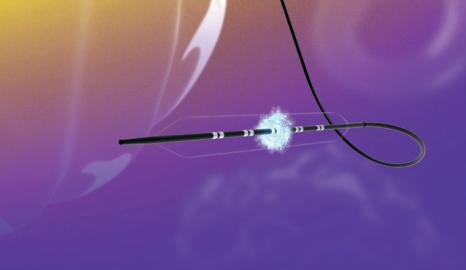
FastWave Medical secures eighth US patent for IVL portfolio FastWave Medical has secured its eighth US patent for its electric intravascular lithotripsy (E-IVL) platform, Artero, reflecting the company’s continued innovation in developing next-generation solutions for peripheral arterial disease (PAD) treatment, the company reports in a recent press release.
“IVL has become one of my frontline tools for treating peripheral arterial disease—it’s one of the most exciting breakthroughs we’ve seen in years,” said Constantino Pena (Miami, USA), a diagnostic and interventional radiologist at Baptist Health South Florida.
“Watching companies like FastWave push the envelope and bring fresh ideas to IVL technology makes this an incredible time to be in the field. The pace of innovation is truly inspiring, and it’s patients who stand to benefit most,” Pena stated.
The Artero system is designed to “streamline” PAD treatment with a simplified interface that delivers circumferential sonic pressure waves at 4Hz—twice the speed of existing IVL devices, according to the company.
“Too many medical devices are designed behind closed doors with limited user feedback. We wanted to flip that around and start with the daily frustrations physicians face and build from there,” said Scott Nelson, co-founder and chief executive officer (CEO) of FastWave Medical.

Merit Medical names Martha Aronson as new president and CEO Merit Medical recently announced the appointment of Martha Aronson as the company’s new president and chief executive officer (CEO), effective 3 October 2025. Fred P Lampropoulos
will remain as chairman of the board, president and CEO of Merit through 3 October. Upon Aronson’s appointment, Lampropoulos will continue to serve as chairman of the board.
“I am pleased to welcome Martha to Merit,” said Lampropoulos. “I believe the company has never been in a stronger position.
Martha is uniquely qualified to lead Merit into the future and drive its continued success.
Her keen intellect and proven track record of empowering global teams through collaborative excellence, consistent with ‘The Merit Way,’ makes her the ideal leader for Merit’s next stage of growth.
executive officer of Vivasure Medical.
“Achieving CE mark expansion for venous indications is an important step toward making our fully absorbable, sutureless solution more broadly accessible.”
MHRA announces UK medical device regulation amends
The Medicines and Healthcare products Regulatory Agency (MHRA) has launched important new steps to secure access for patients to the latest medical technologies available in Europe and other advanced countries.

Since our founding in 1987, we have achieved significant milestones, including strong returns delivered to shareholders since our IPO on 10 May 1990. I am incredibly proud of these achievements. With Martha’s experience and capability, I look forward to supporting her vision while she charts Merit’s course forward.”
Vivasure Medical submits premarket approval to FDA for PerQseal Elite closure system Vivasure Medical has submitted a premarket approval application to the US Food and Drug Administration (FDA) for its PerQseal Elite vascular closure system for arterial procedures.
In a recent press release the company has stated that the submission builds upon the successful results of the PATCH study as well as positive clinical use in Europe, reinforcing the system’s potential safety and performance profile. In addition, the company received European CE mark approval for an expanded indication for PerQseal Elite covering large-bore venous closure.
“We are proud to advance PerQseal Elite through these two key regulatory milestones as part of our commitment to delivering next-generation technologies for large-bore vascular closure,” said Andrew Glass, chief
As well as improving patient access to technologies, the proposals will boost MedTech industrial growth by reducing duplicative regulatory costs faced by manufacturers and instead focuses the domestic approvals route (UKCA) on first-in-market innovative technologies, including AI as a medical device.
The MHRA has now published the government’s response to its public consultation on future routes to market for medical devices in the UK, designed to modernise regulation and improve patient access to the latest innovative technologies.
In direct response to stakeholder feedback, the MHRA is also announcing its intention to consult later this year on the indefinite recognition of CE-marked medical devices.
In parallel, new international reliance routes will be introduced to allow swifter access to medical devices from trusted regulators in Australia, Canada, and the USA. This will allow eligible products to follow a streamlined pathway to market, helping bring the latest technologies to patients more quickly.
Minister of State for Science, Lord Patrick Vallance, said: “The MHRA’s new international reliance routes are excellent news for patients, who will now gain rapid access to new medical devices which have been approved as safe by our trusted regulatory partners. This is precisely the sort of streamlining of red tape that the Life Sciences Sector Plan calls for.
By making quick, informed, sensible decisions enabled by international
reliance, the MHRA will be able to better target its resources, focusing on regulatory activity and scientific advice that will advance the development of innovative new medical products— ultimately helping patients, and supporting med tech businesses to grow.”
Teleflex completes acquisition of Biotronik’s Vascular Intervention business
Teleflex has announced that is has completed the previously revealed acquisition of substantially all of the Vascular Intervention business of Biotronik.
The company notes in a press release that the acquisition adds a broad portfolio of therapeutic products to Teleflex’s portfolio of interventional access products.
On 27 February 2025, Teleflex announced its entry into a definitive agreement to acquire substantially all of Biotronik’s Vascular Intervention business. Under the terms of the agreement, Teleflex acquired the Vascular Intervention business for a cash payment of €760 million, less certain adjustments as provided in the purchase agreement, including certain working capital not transferring and other customary adjustments.
“We are pleased to announce the completion of the acquisition of substantially all of the Vascular Intervention business of Biotronik earlier than expected” said Liam Kelly, chairman, president and chief executive officer of Teleflex.
“The acquisition will significantly enhance our global presence in the Cath lab, expand our suite of innovative technologies, and improve patient care. We believe the acquisition will allow us to position this advanced coronary portfolio alongside our existing Interventional business and establish our global footprint in the fast-growing peripheral intervention market. The acquired business is rooted in robust research and development, clinical expertise, and global manufacturing capabilities, which we believe will further bolster Teleflex’s innovation pipeline, and position the company to participate in the emerging potential for resorbable scaffold technologies. We will provide additional details on our second quarter earnings conference call.”
13–17 September 2025
The Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Barcelona, Spain www cirsecongress.cirse.org
25–26 September 2025
Vascular Access Society of Britain & Ireland (VASBI) Bournemouth, UK www.vasbi.org.uk/asm-2025
9–11 October 2025
The Society of Interventional Radiology (SIR) EDGE San Diego, USA www.sirweb.org/learn/events/siredge-2025
17–19 October 2025
Symposium on Clinical Interventional Oncology (CIO) Miami, USA www.hmpglobalevents.com/cio/ agenda
7–8 November 2025
Vascular Embolotherapy and Nerve Interventions Targeting Inflammation and Pain (VENTI) Tokyo, Japan https://venti.or.jp
11–13 November 2025
British Society of Interventional Radiology (BSIR) Liverpool, UK www.bsir.org/events/bsir-asm
18–22 November 2025
VEITHsymposium New York, USA www.veithsymposium.org
27–30 January 2026
Leipzig Interventional Course (LINC) Leipzig, Germany www.leipzig-interventional-course. com/visitors/linc-2026
9–12 Februrary 2026
International Symposium on Endovascular Therapy (ISET) Miami, USA www.hmpglobalevents.com/iset
7–10 April 2026
The Pan Arab Interventional Radiology Society (PAIRS) Dubai, United Arab Emirates www.pairscongress.com