
Allegheny County Medical Society

Allegheny County Medical Society
Editorial
• Summer Nourishment
Deval (Reshma) Paranjpe, MD, MBA, FACS
Editorial
• Racing to Cure Sarcoma...With New Eyes
Anthony Kovatch, MD
Membership
• Q&A with Alexandra Johnston, DO
ACMS News
• Member Acknowledgements
ACMS News
• Meet the Newest ACMS Members
ACMS News
• Enhancing Member Value
Nadine Popovich
ACMS News
• Specialty Group Updates
ACMS Staff: Nadine
Popovich, Melanie Mayer and Haley Thon
Article
• Addressing Minority Mental Health Disparities
Erasmus Mutabi, MD and Alexandra Johnston, DO
Article
• 2025 Recap of the American Medical Association House of Delegates Annual Meeting
Donald S. Bourne, PhD, MPH
Article
• Private Practice Continues to Decline Among Physicians
Carol K. Kane, PhD

2025
Executive Committee and Board of Directors
President
Keith T. Kanel, MD
President-elect
Kirsten D. Lin, MD
Secretary
Richard B. Hoffmaster, MD
Treasurer
William F. Coppula, MD
Board Chair
Raymond E. Pontzer, MD
Board of Directors
Term Expires 2025
Anuradha Anand, MD
Amber Elway, DO
Mark A. Goodman, MD
Elizabeth Ungerman, MD, MS
Alexander Yu, MD
Term Expires 2026
Michael M. Aziz, MD, MPH, FACOG
Michael W. Best, MD
Micah A. Jacobs, MD, FIDSA
Kevin G. Kotar, DO
Jody Leonardo, MD
Term Expires 2027:
David J. Deitrick, DO
Sharon L. Goldstein, MD
Prerna Mewawalla, MD
Raymond J. Pan, MD
Nicole F. Velez, MD
James Latronica, DO, DFASAM
Richard B. Hoffmaster, MD
Finance
William F. Coppula, MD
Nominating
Kirsten D. Lin, MD
Women’s Committee
Prerna Mewawalla, MD & Meilin Young, MD
Managing Editor
Sara C. Hussey, MBA, CAE
ACMS Executive Director shussey@acms.org
Medical Editor
Deval (Reshma) Paranjpe, MD reshma_paranjpe@hotmail.com
Bulletin Designer
Victoria Gricks victoria@thecorcorancollective.com
2025 Bulletin Editorial Board
Richard Daffner, MD, FACR
Robert Howland, MD
Anthony Kovatch, MD
Charles E. Mount, MD, FAAD
Alexandra Johnston, DO
John P. Williams, MD
Executive Director
Sara Hussey shussey@acms.org
Vice President - Member and Association Services
Nadine M. Popovich npopovich@acms.org
Manager - Member and Association Services
Haley Thon hthon@acms.org
Operations CoordinatorACMS & ACMS Foundation
Melanie Mayer mmayer@acms.org
Manager - Operations and Finance
Elizabeth Yurkovich eyurkovich@acms.org
Bulletin Designer Victoria Gricks victoria@thecorcorancollective.com
EDITORIAL/ADVERTISING
OFFICES: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212; (412) 321-5030; fax (412) 321-5323.
USPS #072920. PUBLISHER: Allegheny County Medical Society at above address.
The Bulletin of the Allegheny County Medical Society is presented as a report in accordance with ACMS Bylaws.
The Bulletin of the Allegheny County Medical Society welcomes contributions from readers, physicians, medical students, members of allied professions, spouses, etc. Items may be letters, informal clinical reports, editorials, or articles. Contributions are received with the understanding that they are not under simultaneous consideration by another publication.
Issued the third Saturday of each month. Deadline for submission of copy is the SECOND Monday preceding publication date. Periodical postage paid at Pittsburgh, PA.
Bulletin of the Allegheny County Medical Society reserves the right to edit all reader contributions for brevity, clarity and length as well as to reject any subject material submitted.
The opinions expressed in the Editorials and other opinion pieces are those of the writer and do not necessarily reflect the official policy of the Allegheny County Medical Society, the institution with which the author is affiliated, or the opinion of the Editorial Board. Advertisements do not imply sponsorship by or endorsement of the ACMS, except where noted.
Publisher reserves the right to exclude any advertisement which in its opinion does not conform to the standards of the publication. The acceptance of advertising in this publication in no way constitutes approval or endorsement of products or services by the Allegheny County Medical Society of any company or its products.
Annual subscriptions: $60
Advertising rates and information available by calling (412) 321-5030 or online at www.acms.org.
COPYRIGHT 2025: ALLEGHENY COUNTY MEDICAL SOCIETY POSTMASTER—Send address changes to: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212. ISSN: 0098-3772

By: Deval (Reshma) Paranjpe, MD, MBA, FACS
It’s high summer, and great new restaurants are popping up like cheery dandelions everywhere.
Let’s start with the hottest hotspot that just opened on July 6th:
Palm Palm
5996 Centre Avenue — First Floor Pittsburgh, PA 15217
Dinner daily 3:30PM onwards; brunch Saturday and Sunday *Free parking in adjacent garage
Imagine Palm Springs with a dash of Palm Beach. Imagine stepping into a Slim Aarons photograph. When you step into Palm Palm, you are meant to feel light warm breezes and sundrenched glamor. Gilded high ceilings with custom murals, pastels and palm trees—they’re all waiting for you. Get ready to take a jet set vacation by going out to dinner without leaving Pittsburgh.
Partners Herky and Lisa Pollock and Chefs Ed and Amanda Smith from Ritual House bring you a Key West/ Palm Beach/Palm Springs inspired menu. A plethora of small plates ranging from truffled spaghetti-Os to deviled crab fritters to tuna sushi tots would take two weeks of daily dining to get through the menu. Mains are a small but solid selection of traditional steak and seafood plus Korean Fried Chicken. Desserts sound incredible— four mousse-based desserts (Coconut Mirage, Dark Desire, Orange, Yuzu/ Sesame) are must-haves along with Coconut Mango panna cotta and of course, Key Lime Pie. The cocktail list looks equally glamorous and
delicious. Housemade nonalc sodas include Lychee Coconut, Strawberry Passionfruit, Ginger Lemon and just to put a smile on the face of any New Yorker—a Chocolate Egg Cream. (A true egg cream contains neither egg nor cream. If you know, you know.)
Brunch promises to be spectacular. There’s something for every palate-ranging from standard two eggs and bacon to Wagyu steak and eggs, chicken and waffles, salads and Nashville hot chicken sliders. And then three types of avocado croissants including lobster and shrimp, Hawaiian French Toast, Tres Leches pancakes with mango, Fluffernutter waffles, and three types of Eggs Benedict. A broad range of enticing sides and both nonalc and regular cocktails round out the menu.
AVVA
235 Commercial Avenue Pittsburgh, PA 15215
Summer calls for outdoor dining. AVVA delivers. Picture a breezy seaside café in Istanbul on the Adriatic; forget you’re in Aspinwall on the Allegheny. Starters surpass the familiar hummus and babaganoush; try the tasty htipiti, ezme, haydari and trikafteri dips. Small plates include calamari and octopus; mains include a whole branzino, kebabs of every kind, and mixed grills from land and sea. Fresh and healthy salads offer a counterpoint, and baklava, kunefe, katmer and fresh fruit end the meal on a sweet note. You may recognize the pastry in kunefe as the crunch in the trendy and delicious Dubai Chocolates that are everywhere right now.
Ozone Bar and Grill
100 Fowler Road
Warrendale, PA 15086
Lunch and dinner daily starting at noon
Tucked just off Route 19 is a new concept from the owner of the great Kelly-O’s Diner next door. The great strength here is the chef, who insists on local sourcing wherever possible and the freshest and best ingredients. Picture classic American fare— appetizers, wings, flatbreads, salads, sandwiches and mains—but executed with exquisite attention to quality. I took my parents here and must say that I didn’t expect much when I looked at the menu—it looked like that of so many other restaurants. But when the food arrived--wow. Everything was fresh, high quality, delicious and made from scratch. My parents—notoriously picky eaters and seafood lovers—were impressed. They declared the seafood chowder the best they had ever had--and I agreed--the shrimp were incredibly fresh. This is a hidden gem— American cuisine done beautifully and with great pride and great service. Don’t miss this.
Bryant Street Tavern
5801 Bryant Street Pittsburgh, PA 15206
Wednesday & Thursday: 4-10PM
Friday: 2-11PM
Saturday: 11-11PM & Sunday: 11-9PM
*Closed Monday and Tuesday
Missing New England? Find all your favorites at this neighborhood pub where you can watch the game as well. A raw bar, lobster rolls, steamed
clams, crab cake sandwiches, fried calamari, sauteed mussels, clam chowder and fish and chips galore and peel-and-eat Gulf shrimp for good
measure. Landlubbers can have steak frites and burgers, and pasta and salad options as well. Brunch features crab beignets, shrimp and crab Louis salad,
and more. Fish tacos and Bang Bang Shrimp specials liven up Happy Hour. Reasonably priced cocktails ($11-14, not $20) are a nice touch.


By: Anthony Kovatch, MD
“Mariamma thinks about her own shattered illusions. Should she thank or curse the Condition and Lenin for bringing her here [to her mother]? The Condition takes away, but it also gives GIFTS that one might not have wanted.”
--from “The Covenant of Water” (2023) by Ethiopian-born author and physician, Abraham Verghese, who spent the early years of his career in America working with rural AIDS patients. The pathogenesis of the “condition” which is the focal point of the novel--a hereditary pattern of death by drowning because of an innate inability to swim—is ultimately uncovered by Mariamma in her medical training and comes to symbolize more generally the “human condition,” in particular our strivings to recognize, confront with courage, and heal the tragedies that inflict all families worldwide.

My participation in the 2025 Pittsburgh Cure Sarcoma (PCS) Annual Run/Walk on June 21st, starting at the storied North Park Lake boathouse, was a stark departure from my typical event running modus operandi. Instead of donning my race bib while emptying my bowel and bladder hidden inside a
port-a-potty at the starting line as the starting gun was going off, this solemn event saw me arrive over an hour before opening ceremonies in order to man the Allegheny County Medical Society booth; we were a Diamond Sponsor. I kept my glasses on at all times during the event so as to be able to read all the bibs until the starting gun went off.

Instead of pre-run warm-ups and last-minute chugs of water or electrolyte solutions, the crowd of over 1,400 silently prayed in unison as Dr. Mark Goodman, chairperson of the PCS Society and the Steel City’s most prominent orthopedic surgeon in the management and research of the tumors, took the podium and provided an inspirational update. However, I believe most of the crowd were eager to offer their personal gratitude for the cures and overwhelming comfort the “giant” had provided during over 40 years in practice. For us pediatricians, he was always the foremost advocate and our “go-to guy.” A member of ACMS since 1981, Dr. Goodman served as ACMS president in 2005 and has served as a delegate or alternate delegate to the Pennsylvania Medical Society since 1990.

Aside from the handful of elite runners who competed for winners’ medals, the vast majority of participants walked the 3.1 mile 5K course (and even some extra) at varying speeds; most were organized into groups representing a loved one--a survivor or a deceased family member or friend. At the 11th hour, perennial last place finisher “Slow Tony” decided to walk with the faithful; additionally, he feared succumbing to the heat and humidity. This time he would indeed run with his glasses on and had no intention of defending his last place finish in the Pittsburgh marathon.
I could recognize a sense of reminiscence or memorialization on all the walkers’ faces, imparting an aura of supreme hope and a spiritual reverence for the medical profession, and for healers in general. We walked in unison—united in a purpose well beyond our individual selves. Our group bonded so deeply that we almost forgot to cross the finish line and have our times recorded (I was thankful that I was not again designated “last to cross the finish line;” my “15 minutes of fame” had officially expired!) Instead of refueling with orange slices and bananas, yours truly digested a tutorial
by the dear mother of my old, nowthriving adult patients, Wendy Myers, LCSW, regarding Cancer Bridges--a free sarcoma support group which holds monthly virtual meetings on Zoom (www.cancerbridges.org) in partnership with PCS.

About 13,000 Americans are expected to be diagnosed this year with soft tissue sarcoma. More men (57%) typically develop sarcoma than do women (43%). Soft tissue sarcomas are more common in children, where they represent 15% of all childhood cancers. In adults, only about 1% of cancers are sarcomas. Life expectancy of soft tissue sarcomas depends on factors such as the tumor’s type, size, location, rapidity of tumor cell growth, and where it is located when first diagnosed. The National Cancer Institute (1) reports a 5-year survival rate of 65%.
Sarcomas that develop in bones are in a separate category from soft tissue sarcomas because they appear differently when examined under a microscope and have other clinical and treatment differences. Osteosarcomas are rarer than soft tissue sarcomas, with only about 1,000 new cases diagnosed in the United States annually (about half of which are in children and teens). The average 5-year survival rate for osteosarcoma is 60% but also differs depending on the location at diagnosis. The prognosis is better in children, teenagers, females, and having a tumor that can be completely removed surgically.
In 2019 the Pittsburgh Post-Gazette
published a bombshell series of articles entitled The Human Toll (2,3) linking fracking to the development of rare childhood cancers. From 20082018, in 4 heavily-fracked counties in southwestern PA (Washington, Greene, Westmoreland, Fayette), the reporters uncovered 27 cases of Ewing sarcoma--a very rare, but aggressive and frequently fatal, bone cancer of childhood--and 40 cases of other rare cancers, for a total of 67 rare cancers in children, teenagers, and young adults.
My retired pediatric colleague and former editor of the Pediablog, Edward C Ketyer, MD, FAAP, President of the Pennsylvania chapter of Physicians for Social Responsibility and a member of the AAP Council on Environmental Health and Climate Change, recently gave me a non-biased appraisal of the issue:
“Only about 200 cases of Ewing sarcoma are diagnosed in the United States each year. In Washington County, Pennsylvania’s most heavily fracked county where I’m from, 6 cases of Ewing sarcoma and 30 other rare childhood cancers were counted. These numbers are far more than would be expected to occur in a similarly populated, mostly rural area over a 10-year period. And new cases keep popping up in this region. Parents and physicians like me are very concerned that pollution and toxic waste from fracking operations may be to blame for this outbreak of rare childhood cancers.”

Until the final verdict is solidified, ongoing vigilance by the medical field and the press is warranted and crucial. As French writer Marcel Proust (“In
Search of Lost Time”) emphasized the importance of shifting and expanding our perspective:
“The real voyage of discovery consists, not in seeking new landscapes, but in having new eyes.”
Hence my glasses! Purely out of habit, I searched for the race time results for days after the event but was unable to find any link. Finally, I realized that the winners of this race had been determined long ago by their demonstration of fortitude and bravery and that, unknown to me, I had been little more than a spectator; the racecourse had already been consecrated long ago, as per the immortal words of a “giant” named Lincoln:
“But, in a larger sense, we can not dedicate—we can not consecrate—we can not hallow—this ground. The brave men, living and dead, who struggled here, have consecrated it, far above our poor power to add or detract.”

References
1. https://resources.healthgrades. com/right-care/cancer/sarcomaprognosis-and-life-expectancy
2. newsinteractive.post-gazette. com/childhood-cancer-pittsburghpennsylvania-canon-mcmillan-pollution/
3. newsinteractive.post-gazette.com/ fracking-and-health-2/

Introduction
By: Erasmus Mutabi, MD & Alexandra Johnston, DO
Each July, National Minority Mental Health Awareness Month draws attention to the persistent disparities in mental health care experienced by racial and ethnic minorities. Despite decades of research and reform efforts, Black, Hispanic/Latino, Asian American, Indigenous, and multiracial communities continue to face higher rates of psychological distress, reduced access to mental health care, and poorer outcomes compared to non-Hispanic White populations.1,2 In a 2023 national survey, 50% of White adults with poor mental health reported receiving services in the past three years, compared to 39% of Black and 36% of Hispanic adults.3 These disparities are deeply rooted in social determinants of health, systemic inequities, stigma, and limited access to culturally responsive care. Addressing them requires not only better clinical care but also policy changes, community engagement, and cultural reform within the health professions.
Mental illness affects all demographics, but minority populations often experience more severe, chronic symptoms and reduced access to care. Black and Hispanic/ Latino individuals, for example, are more likely to have prolonged depressive symptoms and less likely to receive accurate diagnosis or treatment, due in part to misdiagnosis, limited services, and lack of cultural awareness.4 Social determinants, such as poverty, housing instability,
unemployment, and discrimination, are more common in minority groups, increasing both vulnerability to mental illness and barriers to timely care.5
Intersectionality further compounds these challenges, as individuals with overlapping marginalized identities (e.g., LGBTQ+ people of color and undocumented immigrants) face added stigma, fewer protections, and greater exclusion.
Mental health care utilization among minorities remains low due to multiple interrelated barriers:
• Structural: Many face insurance gaps, limited provider availability, and transportation challenges. Clinics often operate during standard hours, making access difficult for those with rigid work schedules. These issues are worsened in underserved urban and rural areas where mental health providers are scarce.6
• Cultural: Stigma, fear of being judged, and cultural beliefs often discourage help-seeking. In some communities, mental illness is seen as a personal weakness or family disgrace. Mistrust of the healthcare system, shaped by historical malpractices such as the Tuskegee Syphilis Study and ongoing inequities, further limits engagement.7,8
• Systemic: Implicit bias and racial stereotyping can lead to misdiagnosis or inadequate care. Policies that limit coverage, restrict provider participation, or penalize those seeking mental health
support reinforce longstanding inequities in care delivery. Co-occurring substance use worsens mental illness; however, minority populations encounter greater barriers to care but higher rates of criminalization. In a large NYC jail study, Black and Hispanic individuals accessed mental health services half as often as Whites, yet twice as likely to face solitary confinement.9 After release, people of color with serious mental illness were nearly twice as likely to miss community care and over four times less likely to receive integrated treatment for both mental illness and substance use.10 Integrated models addressing both conditions are key to reducing these gaps. Among youth, minority adolescents face higher depression rates but lower treatment access. Only 29% of Latino, 32% of Black, and 21% of multiracial adolescents receive care, compared to 45% of Whites, often due to parental misconceptions, school-based challenges, and lack of youth-focused, culturally competent services.11,12
The COVID-19 pandemic exacerbated pre-existing mental health challenges in minority populations. These communities bore the brunt of COVIDrelated illness, mortality, job loss, and housing instability. Unsurprisingly, rates of anxiety, depression, substance use, and trauma surged, particularly among Black and Latino adults.13 While telehealth emerged as a key tool in expanding access, many minority individuals were left behind due to limited broadband access,
digital illiteracy, or language barriers, underscoring the digital divide as a new determinant of access.
Implementing culturally responsive care is a promising solution for improving mental health outcomes. Training clinicians in cultural competence, implicit bias mitigation, and trauma-informed care enhances patient trust and engagement. Integrated models, such as collaborative care, embed behavioral health professionals within primary care, improving mental illness diagnosis and treatment for minority populations. This approach reduces stigma by making mental health care a routine part of overall health services and patients are less likely to feel singled out or labeled.14 Additionally, culturally adapted psychotherapies that consider patients’ language, spirituality, and family structures demonstrate greater effectiveness and engagement, especially when community leaders or peers are involved in their delivery.15
Solutions should be communityinformed and policy-driven. Successful initiatives include peer-led programs, community health workers, and faithbased mental health efforts, which enhance access, reduce stigma, and improve cultural relevance. At the policy level, Medicaid expansion and mental health parity laws have improved access for minority populations, but potential funding cuts or changes in eligibility requirements could harm low-income and minority communities that rely on these services. Ongoing support is essential to maintain equitable access and prevent widening disparities. Policy support for workforce diversification, funding for minority-serving institutions, and culturally adapted mental health technologies is crucial. Policymakers must also tackle upstream factors like education, employment, housing, and environmental injustices, as these root
causes of psychological distress require system-level reform for community efforts to be truly effective.
A less-discussed but equally critical issue is the mental health of minority physicians and trainees. These individuals are more likely to experience discrimination, isolation, and impostor syndrome, leading to higher levels of burnout, depression, and career dissatisfaction.16 Medical culture often discourages vulnerability. Stigma, fear of licensure repercussions, and concerns about confidentiality prevent many minority trainees from seeking help. This is especially concerning as studies have shown that minority group physicians are underrepresented in leadership and wellness roles, which limits their influence on institutional mental health policies.17
Solutions could include:
• Confidential, low-barrier mental health services for medical trainees: These services should be easily accessible, stigma-free, and ensure privacy, allowing trainees to seek help without fear of judgment or career impact.
• Mentorship programs and affinity groups to promote a sense of belonging: Connecting trainees with mentors and peers from similar backgrounds can reduce isolation, build support networks, and foster professional growth.
• Removal of mental health disclosure questions on accreditation and licensure applications (both at the institutional and state level): Eliminating questions about past mental health treatment helps reduce stigma and encourages physicians to seek care without fear of professional repercussions.
• Institutional commitment to diversity, equity, and wellness: Medical institutions must invest in inclusive policies, leadership diversity, and wellness initiatives that prioritize the well-being of
underrepresented physicians and trainees.
When minority physicians feel supported, they are more likely to remain in the profession and continue serving underserved communities, thereby helping to address disparities within the system.
Conclusion: A Call to Action
Mental health disparities in minority populations are not merely a consequence of individual behaviors; they are a result of structural and systemic inequities. Addressing them requires more than cultural competence training or expanded clinic hours. It demands a fundamental rethinking of how we approach care, invest in communities, and prioritize equity at every level.
National Minority Mental Health Awareness Month reminds us that awareness must be followed by action. Whether through policy reform, clinical innovation, medical education, or community leadership, the path to mental health equity is one we must walk together, with urgency, humility, and commitment.

CHECK OUT THE REFERENCES

Dr. Johnston is an Internal Medicine physician as well as a medical educator. She is an Associate Program Director for the Internal Medicine Residency program at Allegheny Health Network, rounds on the inpatient teaching medicine service at West Penn Hospital and sees patients in her Internal Medicine clinic at West Penn Medical Associates. She has a passion for physician wellness and serves as the Wellness officer for the Medicine Institute at AHN as well as faculty for Drexel University College of Medicine and Clerkship Director for the Lake Erie College of Osteopathic Medicine.

Q: CAN YOU TELL US ABOUT YOUR CURRENT ROLE AND WHAT A TYPICAL WORKDAY OR WEEK LOOKS LIKE FOR YOU?
A: In my current role, I spend 50% of my time seeing patients, both precepting residents in clinic or in the hospital, and 50% of my time in my administrative role/teaching role. This time is spent preparing didactics, running our clinician educator track, advising and mentoring residents, working with the program and organization on wellness initiatives, and serving on committees for the residency program and affiliated medical schools. I run the inpatient and ambulatory clerkship at West Penn for internal medicine, so I frequently meet with students and spend time mentoring them.
Q: HOW DID YOU FIRST GET INVOLVED WITH THE ALLEGHENY COUNTY MEDICAL SOCIETY OR WHAT HAS YOUR OVERALL ENGAGEMENT BEEN WITH THE ACMS?
A: I joined ACMS/PAMED as a medical student and participated in some of the activities offered for students at that time. I became more involved a couple of years ago when I started as an alternate delegate to the HOD and then for the last couple of years as a delegate to PAMED HOD. I also recently joined the ACMS Wellness Advisory Committee. I love to participate in events that offer

the opportunity to mentor students and residents.
Q: WHAT HAS BEEN THE MOST REWARDING ASPECT OF BEING AN ACMS MEMBER?
A: The most rewarding aspect of being and ACMS member has been the opportunity to meet colleagues in different specialties and institutions and share experiences and network. It is always nice to be in a space with colleagues outside of work.
Q: ARE THERE ANY ACMS INITIATIVES (OR PAMED INITIATIVES) OR EVENTS THAT YOU ARE PARTICULARLY PASSIONATE ABOUT?
A: I'm very passionate about the Physician Wellness Program that ACMS has to offer. I think the services offered through the PWP that are free and

anonymous for physicians is a unique offering that the organization should be very proud of. I have provided this information to several colleagues and trainees, and it is an excellent resource to have available.
Q: WHAT DO YOU THINK IS THE BIGGEST CHALLENGE FACING HEALTHCARE TODAY?
A: I think one of the biggest challenges that healthcare is facing is going to be finding ways of providing equitable care to all patients as reimbursement is changing in the healthcare landscape. As reimbursement changes for specific populations there are likely to be hospital closures and decreased access to care, which will impact both patients and physicians. Of course, the integration of AI will also be a challenge in the way it compounds these impacts on physicians of different specialties.
Q: HOW DO YOU SEE THE HEALTHCARE FIELD EVOLVING IN THE NEXT 5-10 YEARS?
A: There will be many changes from the current state as healthcare continues to rapidly evolve, but what those changes are will depend much on
government and payor policy and the ways in which they are implemented. Physicians will need to advocate for policies that promote physician autonomy and the physician-patient relationship.
AI will likely have an impact on every specialty in some capacity as well as in the education of our medical trainees.
Q: WHAT ADVICE WOULD YOU GIVE TO MEDICAL STUDENTS OR EARLYCAREER PHYSICIANS?
A: Know your "why" and your mission and find a way to do something every day that will contribute to it in some way and set boundaries if too many other things are getting in the way. Although a lot has changed and will continue to change in healthcare and you may not always be able to implement things at the scale you had hoped, you can always impact the colleague or patient sitting next to you. Find a way to live your mission on a daily basis.
Q: OUTSIDE OF MEDICINE, WHAT ARE YOUR HOBBIES OR INTERESTS?
A: Running is something I love to do. Travel points has become my new thing over the past few months. Spending time with family/friends.
Q: DO YOU HAVE A FAVORITE BOOK, PODCAST, OR RESOURCE THAT YOU WANT TO SHARE WITH OUR MEMBERS (OR THAT HAS INFLUENCED YOUR CAREER!)?
A: Podcasts: White Coat Investor and Podcast Points for Normal People Book: Crucial Conversations and The Invisible String
Q: HOW CAN FELLOW ACMS MEMBERS CONNECT WITH YOU OR SUPPORT YOUR WORK?
A: X (AKA Twitter) @AlexJohnstonDO

By: Donald S. Bourne, PhD, MPH
The American Medical Association (AMA) convened its 2025 House of Delegates (HOD) Annual Meeting in Chicago from June 6–11th, bringing together over 700 delegates representing every corner of organized medicine. The meeting was marked by spirited debate on urgent national issues, with a central focus on defending science, protecting public health infrastructure, and preserving access to care for vulnerable populations.
As a delegate representing Pennsylvania, I want to highlight the business most relevant to our region’s physicians, especially the AMA’s decisive actions regarding the Advisory Committee on Immunization Practices (ACIP) and the protection of Medicaid in the face of pending federal legislation.
EMERGENCY RESPONSE TO ACIP OVERHAUL Background
On June 9, 2025, Secretary of Health and Human Services Robert F. Kennedy Jr. announced the removal of all sitting members of the ACIP, the CDC’s independent panel of vaccine experts. This move, justified by the administration as an effort to “restore public trust in vaccines,” was met with immediate and widespread condemnation from the medical and scientific community.1-3
AMA’s Emergency Resolution
The AMA responded with an emergency resolution, which:
• Condemns the removal of ACIP members: The AMA denounced the action as a direct threat to the integrity of national vaccine policy, emphasizing ACIP’s decades-long
role as a trusted, science-driven advisory body.2
• Calls for a Senate investigation: The resolution urges the Senate Health, Education, Labor, and Pensions (HELP) Committee to investigate Secretary Kennedy’s decision and the process by which ACIP members were removed.
• Demands immediate reinstatement: The AMA calls on Secretary Kennedy to reverse the decision and reinstate the original ACIP experts, citing the critical importance of their expertise.
• Commits to public advocacy: The AMA pledged ongoing advocacy to support the ACIP’s current structure and to explore alternative models for independent, evidence-based vaccine advisory if necessary.
• Reaffirms evidence-based guidance: The AMA reaffirmed its commitment to independent, science-based vaccine recommendations, recognizing that public trust and clinical integrity depend on such guidance.
PROTECTING MEDICAID: A TOP ADVOCACY PRIORITY
Advocacy Against Medicaid Cuts
A major focus of the HOD was the preservation of Medicaid and the Children’s Health Insurance Program (CHIP). The AMA adopted strong policy positions opposing proposed federal budget cuts exceeding $900 billion to Medicaid, arguing that such cuts would significantly harm the millions of Americans—including many Pennsylvanians—who rely on Medicaid for essential health coverage.
Key HOD Actions on Medicaid
• Preservation of Federal Funding and Eligibility: The AMA made the preservation of federal funding and eligibility for Medicaid and CHIP one of its top and most urgent legislative advocacy priorities.
• Opposition to Restrictions: The AMA strongly opposes any federal or state efforts to restrict eligibility, coverage, access, or funding for Medicaid and CHIP.
• Defending Access to Care: The HOD reaffirmed the AMA’s commitment to advocating for the protection and expansion of Medicaid, recognizing its vital role in supporting vulnerable populations, including children, seniors, and individuals with disabilities across Pennsylvania.
DEFENDING SCIENCE AND THE PATIENT-PHYSICIAN RELATIONSHIP
The 2025 HOD underscored that protecting science, clinical integrity, and the patient-physician relationship in the face of political interference is central to the AMA’s mission and a defining challenge of this moment in history. The AMA committed to:
• Sustained opposition to harmful policies: The organization will continue to oppose federal and state policies, proposals, and actions that undermine public health infrastructure, biomedical research, vaccine confidence, or evidence-based medicine and decision-making.
• Championing evidence-based practice: The AMA reaffirmed its dedication to ensuring that clinical decisions remain rooted
in scientific evidence, not political ideology, and that the patientphysician relationship is preserved as the foundation of quality care.
The ACIP’s recommendations and Medicaid funding directly impact clinical practice, patient access, and public health in Pennsylvania:
• Vaccine Policy: Disruption to the ACIP’s work could jeopardize insurance coverage for vaccines, increase administrative burdens, and heighten vaccine hesitancy in our communities.
• Medicaid and CHIP: Proposed cuts or restrictions would threaten coverage for hundreds of thousands of Pennsylvanians, including one in five Allegheny County residents4 , and strain the resources of practices and health systems serving vulnerable populations.
• Practice Integrity: Political interference in science-based decision-making undermines the trust that patients place in their physicians and the broader health care system.
The AMA’s actions this year reflect a renewed commitment to defending the pillars of science, access, and integrity in American health care. As a member of the Pennsylvania Medical Society and the incoming AMA Council on Science and Public Health, I urge my colleagues in Allegheny County to:
• Engage in advocacy: Stay informed and participate in efforts to protect Medicaid, vaccine policy, and evidence-based medicine. As physicians, we are uniquely positioned to speak on behalf of our patients, our communities, and the integrity of the healthcare system. Your story, your experience, and your expertise are powerful tools for change.
• Educate patients and policymakers: Provide clear and factual information to patients and
advocate for policies that support public health and clinical autonomy. A simple phone call, email, or meeting with your representative can help shape decisions that affect every aspect of our profession and our patients’ lives.
• Support organized medicine: Join or continue membership in the AMA, the Pennsylvania Medical Society, and the Allegheny County Medical Society to ensure our collective voice is heard. You can also donate to the Pennsylvania Medical Political Action Committee (PAMPAC) and the American Medica Association Political Action Committee (AMPAC), the nonpartisan political arm of organized medicine to support pro-medicine candidates.
The final actions of new AMA HOD policy positions will be available on the AMA website soon. Please reach out if you have questions or wish to get more involved. At this critical juncture, your participation in organized medicine is more important than ever.
Donald S. Bourne (dsb65@pitt.edu) is a 4th year medical student at the University of Pittsburgh. He is also an AMA Delegate, incoming AMA Council on Science and Public Health Member, and current Pennsylvania Medical Society Board of Trustees Member.
References:
1. National Foundation for Infectious Diseases. Experts sound alarm after ACIP members removed. Published June 10, 2025. Accessed June 30, 2025. https://www.nfid.org/expertssound-alarm-after-acip-membersremoved/
2. Muoi0, D. ‘All innuendo and conspiracy’: RFK Jr.’s vaccine advisory overhaul undermines vaccine confidence, experts say. Fierce Healthcare. Published June 10, 2025. Accessed June 30, 2025. https:// www.fiercehealthcare.com/providers/ all-innuendo-and-conspiracy-rfk-jrsvaccine-advisory-overhaul-underminesvaccine
3. US Department of Health and Human Services. HHS takes action to restore public trust in vaccines: ACIP announcement. Published June 9, 2025. Accessed June 30, 2025. https://www. hhs.gov/press-room/hhs-restore-publictrust-vaccines-acip.html
4. S iriwardane, V. Cut Medicaid? There’s no option that wouldn’t cause pain, says Pitt health researcher. PublicSource. Published March 24, 2025. Accessed June 30, 2025. https://www. publicsource.org/medicaid-cuts-trumpadministration-university-pittsburghhealth-researcher/


ACMS Welcomes AHN Residents and Fellows
The ACMS was pleased to participate in the Allegheny Health Network (AHN) Resident and Fellow Orientation, held June 26 and 27 at Allegheny General Hospital (AGH). Representing ACMS, Nadine Popovich, Vice President of Member and Association Services, engaged with incoming residents and fellows to highlight the importance of organized medicine and the many benefits of ACMS membership.
Attendees learned how ACMS supports physicians through professional advocacy, leadership development, networking
opportunities, continuing medical education (CME), and physician wellbeing resources, including the ACMS Physician Wellness Program (PWP).
The event proved to be a successful recruitment initiative, and it was especially rewarding to discover that many incoming residents and fellows were already ACMS members.
ACMS extends its sincere appreciation to AHN for the opportunity to connect with such a talented and promising group of future physician leaders.
ACMS is Seeking Physician Meet and Greet Opportunities
ACMS is actively seeking opportunities to engage with physicians across our region through staff meetings, orientations, and similar events. We welcome the chance to connect with medical professionals at all career stages to share how ACMS supports them through advocacy, leadership development, networking, CME, and wellness resources. If your institution or practice is planning an upcoming meeting or orientation, we’d be delighted to participate. Contact Nadine Popovich at npopovich@acms. org to discuss.

The Allegheny County Medical Society is proud to welcome the newest members of our growing physician community. Each of these individuals brings unique experiences, expertise, and perspectives that strengthen our collective voice and enrich the work we do together. We are honored to support them in their professional journey and look forward to their contributions to organized medicine and the health of our region. Please join us in extending a warm welcome to our new colleagues!
PHYSICIANS
Rim Abou Chakra, MD
Lindsay Bacik, MD
Lucas Haase, MD
Matthew Kocher, MD
Carl Makkar, MD
Arsalan Malik, MD
Mary ONeal, MD
SeHoon Park, MD
Tyler Pratte, DO
Bhawana Rathore, MD
Timothy Wong, MD
RESIDENTS
Eitan Aksoy , MD
PerrSalma Abousahle, MD
Diego Abreu Delgado, MD
Mahroo Aghababaei, DO
Kenneth Aguirre, MD
Hadiyah Ahmed, MD
Anjali Alangaden, MD
Amala Alenchery, MD
Aya Alfardous Alazm, MD
Richard Alfera, MD
Ahmad Ali, MD
Saif Al-Dien Al-Kailani, MD
Evan Ammerman, MD
Manan Arora, MD
Alvina Asif, MD
Muhammad Atif, MD
Armaghan Ayub, MD
Kathryn Bandi, MD
Joseph Bean, MD
Allison Beggin, MD
Navya Sai Bembavarapu, MD
Krish Bharat, MD
Lars Bjoernebo, MD
Helene Bloom, DO
Pooja Shivani Boddapati, MD
Robert Bortz, MD
Michael Bowling, MD
Patricia Bucci, MD
Emily Bucher, MD
Fatima Bukhari, MD
Theresa Bullen, MD
Alyson Burchell, DO
Anthony Casabianca, MD
Francheska Castro, MD
Andrea Caudill, DO
Rutvi Chahal, MD
Charlotte Chambers, MD
Diego Chamorro Ortiz, MD
John Chancellor, MD
Roshini Chandrasekhar
Marianne Chebli, MD
Smrithi Chidambaram, MD
Michelle Chisdak, MD
Ian Christie, MD
Chijioke Chukwudi, MD
Johnathan Clarke, MD
Rachel Contopoulos, DO
Dafne Cordero, MD
Tulio Loyola Correa, MD
Wenli Dai, MD
Marianna Daibes Rachid de Andrade, MD
Kyle Damen, DO
Adena David, MD
Luiz Paulo De Lima Guido
Morgan Decker, DO
Sahar Delavari, MD
Shraboni Dey, MD
Marielle Discipulo, MD
Alex Dobzanski, MD
Alejandro Dominguez, DO
Mahmoud El Baassiri, MD
Amira Elgogary, MD
Gitouf Elnema, MD
Andrey Ermak, MD
Hanna Ermesjo, MD
Mohamad Fares, MD
Aneeza Farooq, MD
Rogerio Ferreira, MD
Ethan Fitzgerald, MD
Sean Flannigan, MD
Elizabeth Ford, DO
Sarah Fribance, MD
Leah Furman, MD
Katelin Gardonis, MD
Adam Gargano, MD
Alexandria Gerber, MD
Bradley Gershkowitz, MD
Daniel Goetschius, MD, PhD
Harshini Gompa, MD
Lauren Green, DO
Jacob Gries, MD
Daniel Haddad, MD
Andrea Hall, MD
Sean Halloran, MD
Shaymaa Hegazy, MD
Omar Hejazi, MD
Andrew Henning, DO
Sandra Herrera, DO
Carlie Hoffman, DO
Darius Hossainian, MD
Jacob Hostetter, DO
Sarah Huyck, DO
Joanne Ike, MD
Paul Ilkka, MD
Abigail Jackovic, DO
Angela Jacob, MD
Emma Jacobs, MD
Olivia Jang, DO
Angelina Jessani, MD
Matthew Jester, MD
Vanessa Karlinski Vizentin, MD
Ramya Kaushik, MD
Roger Kayaleh, MD
Fatih Kelesoglu, MD
Katherine Kendall, MD
Megan Kerbag, DO
Himal Kharel
Grace Kim, MD, PhD
Mariyam Kim, MD
Valdemir Kim, MD
Kei Kobayashi, MD
Ayse Kolemen
Vijaya Rupa Konakanchi, MD
Kyle Kotleba, MD
Collin Kramer, MD
Kaylee Kriner, DO
Shruthi Kumar, MD
Nour Kurdi, MD
Steven Lam, MD
Julia Lauria, DO
Paul Lee, MD
Elizabeth Liao, MD
Emily Long, MD
Wanyan Ma, MD
Ebaad Malick, MD
Melika Marani, MD
Alexander Markes, MD
Katherine Marsh
Rachel Martin, MD
Muhammad Mazroua, MD
Sean Mcclaine, MD
Namratha Seetharam Meda, MD
Yilmarie Mercado-Vargas, MD
Onyi Mmagu, MD
Maxwell Modrak, MD
Swetha Movva, MD
Ahsan Nadeem, MD
James Nagel, DO
Saiyid Ahmad Ali Naqvi, MD
Anam Naseem, MD
Hasan Nassereldine, MD
Tsuyoshi Nemoto, MD
Ikemsinachi Nzenwa, MD
Jetina Okereke, MD
Elile Okoka, MD
Erika Ong, MD
Stanley Ozogbo, MD
Christie Pai, DO
Alexandre Paim Diaz, MD
Zoi Papalamprakopoulou, MD
Ashnee Patel, DO
Jamie Pattee, MD
Krishna Pichikala, MD
Bharat Pillai, MD
Danish Qureshi, MD
Nazar Rahmanov, MD
Daniel Ramos, MD
Timothy Ramseyer, MD
Khadeeja Riaz, MD
Hannah Rinehardt, MD
Troy Romero, DO
Spriha Rusmi, MD
Andy Sackey, MD
Dolores Sanchez Morey, MD
Joaquin Santos, MD
Saloni Savani
Mohammed Sayeem, MD
Nicole Schindler, MD
Alicia Schmidt, DO
Paula Sepulveda Beltran, MD
Dhruvil Shah, MD
Mehroash Shahid, MD
Dur E Shahwar, MD
Apurva Sharma, MD
Marina Shenouda
Matthew Sherman, DO
Ali Shields, MD
Sable Skewes, DO
Kristin Smoot, MD
Max Snider, DO
Yifang Song, MD, PhD
Zhixing Song, MD
Oyetunji Soriyan, MD
Brooke Stephens, MD
Meghan Sullivan, MD
Jon Suzich, MD
Muhammad Tahir, MD
Erica Talbot, MD
Sarah Tepe, DO
Megan Thompson, DO
Robin Tipps, MD, JD
Edward Tobin, MD
Matthew Topolski, DO
Douglas Tsahey, MD
Stephen Tse, MD
Anjitha Valiyil, MD
Rishi Vattikuti, MD
Jean-Marco Verdi Avila
Gina Vivino, MD
Lindsay Voltz, DO
Christine Wang, MD
Jasmine Wang, MD
Ronghua Wang, MD
Ezza Wasim, MD
Tyler Weigel, MD
Jonathan Weinhold, MD
David Willis, MD
Helena Winston, MD
Cherie Wong, MD
John Wroblewski, MD
Tuo Yang, MD
Adina Yerzhan, MD
Fatma Yilmaz, MD
Lauren Yoder Braff, MD
Amanda Zhou, MD
STUDENTS
Priya Aggarwal
Adham Ahmed
Farheen Ahmed
Matthew Ainsley
Margaret Atkinson
Beatrice Bacon
Mira Bagous
Anita Bargaje
Maria Basista
Logan Bass
Sarah Behr
Sarah Bell
Dustin Belliston-Fowkes
Story Bernstein
Abhinav Bhamidipati
Dionna Bidny
Lorenzo Bosque
Bergin Brown
Kristen Bucchin
Eleanor Burton
Caitlin Cahill
Matthew Cardillo
Maximilian Casey
Michael Cella
Alyssa Chafin
Lauren Charlton
Andres Chavez Barragan
Lingling Chen
Justin Cook
Blake Cooksey
Brian Costello
Ryan Cotter
Sierra Cowan
Natalie Curtis
Michael Daidone
Elizabeth Dakan
Emily Daum
Braden Denny
Gabriel DePinho
Mia DiFrancesco
Ashley Dillon
Jillian Dolan
Jennifer Duma
Emily Egbert
Aaron Etelamaki
Holly Everett
Trevor Fachko
Julianna Fairchild
Donald Falbo
Alyssa Famalette
Khushnood Faraz
Abigail Fish
Tiana Fleming-Hogan
Brandon Foster
Kelly Fox
Kierstin Frederick
Anthony Frost
Taylor Fusco
Megan Gaines
David Garyantes
Madeleine Glassner
Shawna Gloe
Daniela Gorski
Emily Grieco
Charles Hall
Gwyneth Hamilton
Marling Hardman
Alexis Haring
Emma Harvey
Jordan Head
Emma Hudson
Sarah Ingram
Zechariah Jung
Elizabeth Kairis
Karl Kamanousa
Ritesh Karsalia
Kiranjit Kaur
Taylor Kaye-Haley
Rachel Kim
Paige Kisling
Mikaela Koch
Serena Kothari
Emily Kuo
Fiona LaRoc
Adam Liu
Katherine Luca
Ryan Luca
Rachael Lutz
Samantha MacGavin
Angelina Makhoul
Andrea Makowski
Nickolas Malize
Alejandro Marrero Gonzalez
Daniel McLoughlin
Kayla McMillan
Sarah McNeilly
Cameron Mertz
Christopher Meyer
Angie Miller
Joy Mills
Lauren Nazzaro
Ana Negron Garcia
Brandon Nguyen
Kennedy Nicholson
Brian Niland
Emma Nowakowski
Elizabeth O'Neill
Andrew Ophus
Alyssa Osio
Christine Robert Pagotan
Joshua Palma
David Pan
Reema Patel
Nicole Pinzon
Jacob Popple
Robert Porter
Rohit Prem Kumar
Kathleen Price
Leah Prince
Sara Purchase
Anannya Pushkarna
Pooja Puttigampala
Amy Qin
Michelle Qiu
Mira Ramesh
Gabrielle Rauls
Spencer Regelson
Anthony Restaino
Philip Ripepi
Nicolas Ritcheson
Augusto Roca Fernandez
Paul Rodriguez
Joseph Rose
Alex Roth
Rebecca Roth
Molly Ruiz
Matthew Sanchez
Grace Scanlon
Clare Schmedes
Carl Schoephoerster
Cassandra Seifert
Julia Seraly
Ashani Shah
Gopiann Shah
Hannah Shanley
Amanda Shaw
Marie Shorokey
Zachary Shuckrow
Dina Silvestri
Alisha Sodhi
Madison Sofield
Daniel Soto
Charlotte Stahlfeld
Ananya Suram
Viswanath Swamy
Katherine Teixeira
Jacob Tepe
Hannah Tetreault
Vijay Viswanath
Alexander Wind
Emily Winterhalter
Klaudia Wojciechowska
Liam Wright
Madeleine Wright
Alexander Wu
Sharon Wu
Xinxin Wu
Vineetha Yadlapalli
Maxim Yaskolko
Hanxin Zhang
Junwei Zhang
Tyler James Znaczko

By: Nadine Popovich – VP of Membership & Association Services
As part of our continued commitment to enhancing the membership and ensuring the integrity of the benefits we provide, the Allegheny County Medical Society is introducing members-only access to certain resources, including:
• Member Benefits & Discounts
• The Digital Edition of The Bulletin These offerings will soon be housed behind a secure, members-only section of the ACMS website.
Why the Change
Over the years, ACMS has built a suite of valuable member benefits—ranging from exclusive discounts with local and national partners to physiciandriven content in The Bulletin. These resources represent real value in terms of cost savings. To preserve and protect that value, we believe it is essential to limit access to those who have made a commitment to the Society through their membership.
By securing these benefits, we ensure fair and exclusive access for our dues-paying members; enhance the credibility of our partnerships with benefit providers; reinforce the professional value of being part of a respected medical society and protect the integrity of our original content, created by and for local physicians.
• By August 1, all members will receive a unique username and password to access the secure members-only section. Members will have the option of changing their password after they establish their account.
• Easy-to-follow instructions will be included to guide you through the login process.
The August Bulletin will include instruction on how to access the members-only section, using your email, and will include screen shots as a guide.
Assistance with creating your account is a phone call or email away. Should you have questions or issues when you create your account, please contact Haley Thon at hthon@acms.org or to 412.321.5030 x105
By taking these steps, we are strengthening the value of membership while continuing to support the physicians of Allegheny County with the tools, community, and advocacy they deserve. In the coming months, we look to expand our benefits page with new benefits and discounts. Thank you for being a valued member of ACMS. We’re excited to continue providing you with high-quality, exclusive member resources and support.
Spotlight on MemberDeals: A New Exclusive Benefit for ACMS Members
We are excited to introduce MemberDeals, a new benefit provider offering access to exclusive savings on world-class entertainment and travel brands. MemberDeals gives ACMS members the opportunity to enjoy discounts on: Walt Disney World® Resort; Universal Orlando Resort™; Cirque du Soleil®; SeaWorld® Parks and Entertainment; hotels, car rentals, corporate gifts, and many more.
Whether you're planning a family vacation or looking to unwind with a weekend adventure, MemberDeals provides exceptional value to enrich your lifestyle—all just for being an ACMS member.
Look for MemberDeals on the Member Benefits & Discounts page beginning August 1st. ACMS will also feature upcoming deals in Snapshots.














53.2% in 2012.
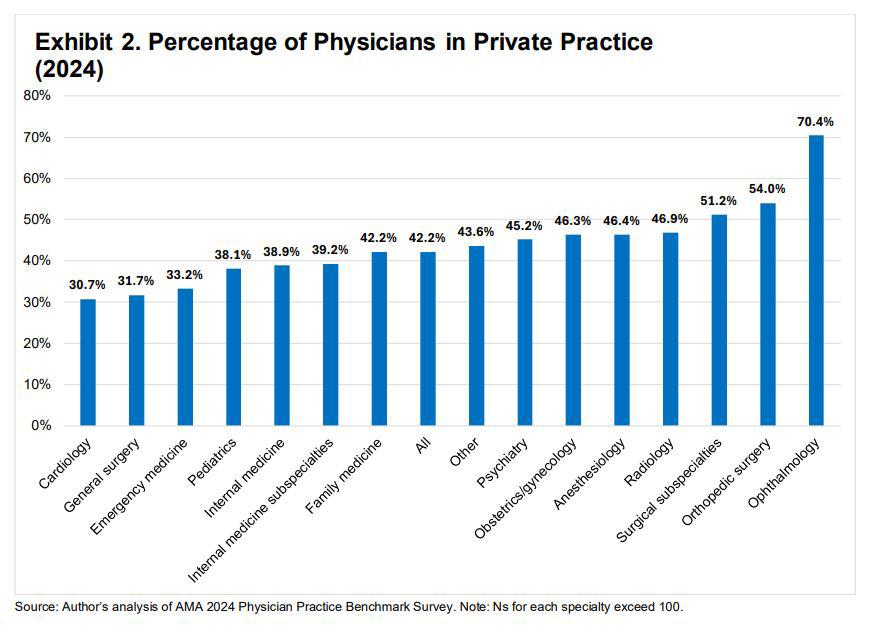
Over the past decade, the physician practice landscape has undergone a seismic transformation—shifting away from physician-owned private practice models and toward employment within larger health systems and corporate entities. The American Medical Association’s newly released report, Physician Practice Characteristics in 2024: Private Practices Account for Less Than Half of Physicians in Most Specialties, offers a clear-eyed assessment of this trend and its implications for the future of medicine. Drawing on data from the AMA’s biennial Physician Practice Benchmark Survey, this 2024 edition reflects the most comprehensive snapshot to date of how physicians work, who owns the practices they’re in, and what’s driving the decisions to stay independent—or to sell.
The AMA Policy Research Perspective, authored by Carol K. Kane, PhD, reveals that just 42.2% of physicians in the U.S. now work in physician-owned practices. That figure is down nearly 18 percentage points from 2012, when 60.1% of physicians reported practicing in privately owned settings. Ownership among physicians themselves is also on the decline, with only 35.4% holding an ownership stake in their practice today—down from
Perhaps most notably, these shifts are not occurring in isolation. They are accompanied by a broader trend toward larger, more consolidated practice models. For the first time since the AMA began tracking this data, fewer than half (47%) of physicians report practicing in groups of 10 or fewer. The small, independent practice that once defined American medicine is no longer the dominant structure.
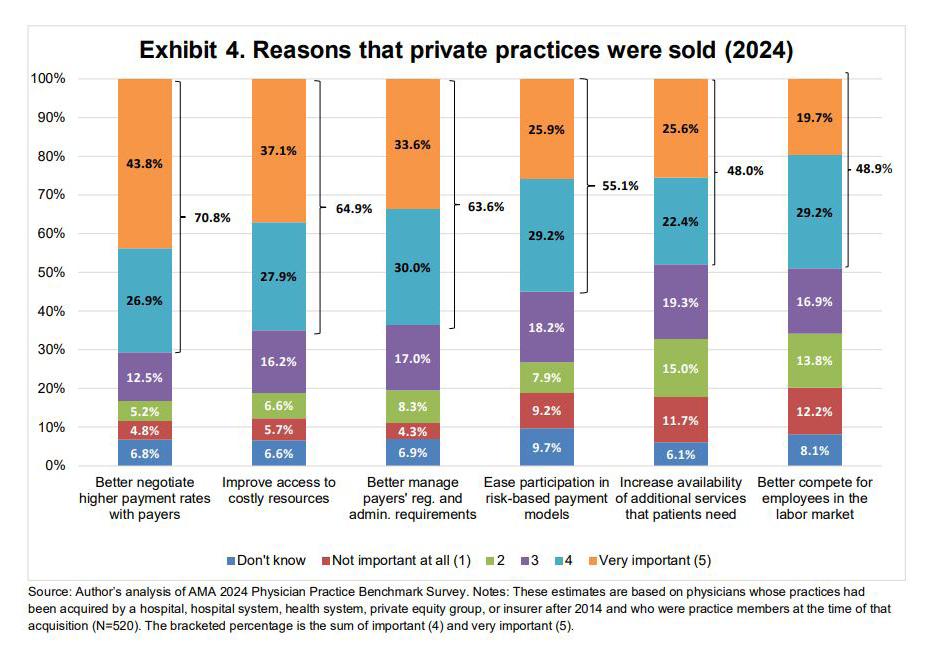
The report explores several underlying drivers behind these trends. Physicians cite a combination of economic and administrative challenges that are making private practice increasingly difficult to sustain:
• Inadequate payment rates,
• High costs for staffing, technology, and compliance,
• Burdensome regulatory and administrative requirements.
Together, these forces have made the overhead of private practice increasingly difficult to manage without the backing of a larger entity.
For many, employment by a hospital, health system, or private equity-backed group offers relief. Economies of scale, shared administrative services, improved payer negotiations, and more predictable income have led many physicians—especially younger ones— away from independent ownership.
What Types of Practices Are Growing?
According to the AMA data, hospital and health system ownership accounts for the majority of acquired practices. Among practices that changed ownership since 2015, 41.6% were purchased by hospitals or health systems. Private equity firms made up 15.3% of acquisitions—though nearly
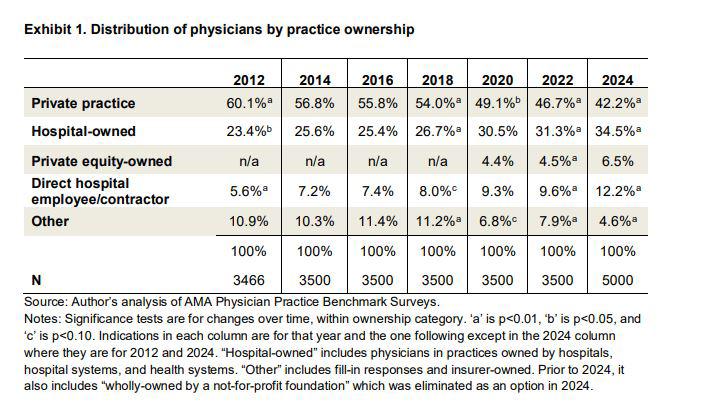
40% of those transactions have taken place since 2019, indicating increasing activity in that sector.
While the report highlights some uncertainty among physicians about who actually owns their practice—28% said they didn’t know who the purchasing entity was—the overall trajectory is clear: practice ownership is consolidating, and the players are increasingly institutional.
This trend is also reflected in practice structure. Single-specialty groups
still make up the largest share of physicians (37%), but multi-specialty practices (27.8%) are gaining ground. In 2012, the gap between the two was 23 percentage points; today it is less than 10. This reflects a larger trend toward integrated care delivery systems and team-based models.
One of the most interesting implications of the report is how generational preferences are
influencing the structure of medical practice. Newer physicians are more likely to seek employment than ownership. For them, the tradeoff between autonomy and stability often tilts toward the latter—particularly in a challenging post-pandemic economic environment.
For established physicians in private practice, this generational shift has real consequences. Recruiting and retaining new partners becomes more difficult. Succession planning becomes more complicated. And many physicianowners, facing growing administrative burdens and the rising costs of EHRs, staffing, and compliance, begin to see selling as their most viable option.
For organizations like the Allegheny County Medical Society, which serve a diverse, evolving physician workforce, these findings raise important questions about how to support physicians across practice models. Advocacy efforts must recognize the distinct pressures faced by private practices while also addressing challenges and needs of employed physicians—particularly around issues of autonomy, workplace culture, and physician voice in decision-making.
The full AMA report provides detailed charts, specialty breakdowns, and insights into the ownership structures shaping American medicine. We encourage ACMS members to read the complete document. This article was adapted as a summary of: Physician Practice Characteristics in 2024: Private Practices Account for Less Than Half of Physicians in Most Specialties by Carol K. Kane, PhD © 2025 American Medical Association. Reprinted with permission.

By: Nadine Popovich, Melanie Mayer, and Haley Thon
Allegheny County Immunization Coalition (ACIC) — 2024-2025 Chair - Patrick Hussey, PharmD, MBA: ACIC hosted its Quarterly Membership Meeting on Wednesday, June 19, 2025, from 9:00–11:00 AM, featuring guest speaker Biyanka Patel, MSL, of Bavarian Nordic. Her presentation, “Chikungunya – An Emerging Threat,” highlighted the rising clinical and public health concerns associated with the virus. Our next Quarterly Membership Meeting will take place on Wednesday, September 18, 2025, from 9:00–11:00 AM, and will feature Beth Hoffman, PhD, MPH, Assistant Professor in the Department of Behavioral and Community Health Sciences at the University of Pittsburgh School of Public Health. Dr. Hoffman will present “From TV to TikTok: Leveraging Media for Vaccine Communication.” Registration opens August 7th.
We also invite you to save the date for the 20th Annual Immunization Conference on Wednesday, November 5, 2025, at the Regional Learning Alliance in Cranberry Township. Conference details are available at www.immunizeallegheny.org, with registration opening in late summer. American College of Surgeons Southwestern Pennsylvania Chapter (ACS-SWPA) — 2025 President –Richard Fortunato, DO, FACS: The ACS Southwestern Pennsylvania Chapter is currently on summer hiatus and will resume programming in the fall with the third event in our resident series— Surgical Jeopardy. Details will be forthcoming.
In the meantime, we encourage members to consider attending the ACS
Clinical Congress 2025, taking place October 19–23 in Chicago. This annual meeting offers world-class education, unparalleled networking, and the latest updates across surgical disciplines. Learn more at facs.org.
We look forward to reconnecting this fall!
Pennsylvania Geriatric Society Western Division (PAGS-WD) — 2025 President - Heather Sakely, PharmD, BCPS, BCGP:
2025 Geriatrics Teacher of the Year Award – Nominations Needed
The Society is proud to announce that nominations are now being accepted for the 2025 Geriatrics Teacher of the Year Award. This prestigious annual honor recognizes two outstanding educators, one physician and one healthcare professional, who have shown exceptional commitment to advancing geriatrics education. Award recipients are individuals who have made a lasting impact on the training and development of future geriatric professionals and have significantly contributed to the growth of geriatrics education across the healthcare continuum. Full details, including eligibility requirements, selection criteria, and the nomination form, are available on the Society’s website at Pennsylvania Geriatrics Society - WD - Teacher of the Year.
Fall Program 2025
Planning is currently underway for the Fall 2025 Program. While the exact date is still to be determined, we’re excited to announce that the event will once again be held at the PNC Champions Club at Acrisure Stadium. The planning committee is actively reviewing potential topics to ensure a timely and
engaging agenda.
The Pittsburgh Ophthalmology Society (POS) — 2025 President - Laurie A. Roba, MD:
The Pittsburgh Ophthalmology Society announces 2025-2026 Monthly Meeting and Annual Meeting Dates
Laurie A. Roba, MD, President, along with the POS Board of Directors, is pleased to announce the schedule for the 2025-2026 POS Monthly Meeting Series and Annual Meeting dates. A total of six meetings are scheduled, starting in September and concluding with the Annual Meeting on March 20, 2026.
The Society will host these meetings as in-person events at the PNC Champions Club at Acrisure Stadium (100 Art Rooney Ave, Pittsburgh, PA 15212), centrally located on the North Side with nearby parking options. Additional details can be found on the POS website.
Each meeting will commence with registration at 4:00 pm, followed by the first lecture at 4:30 pm. The agenda includes a Resident Case Presentation featuring second-year residents from the University of Pittsburgh Department of Ophthalmology.
Members will receive registration information, including the registration link, one month prior to each meeting. Registration, managed exclusively online, is required (no walk-ins, please).
Please note our Cancellation and NoShow Policy. For more information, visit our website or contact Nadine Popovich if you are unable to attend a meeting.
The 2025-2026 monthly meetings are scheduled as follows: September 4, 2025, October 9, 2025, November 6,

2025, December 11, 2025 and January 22, 2026.
Please note that there will be no meeting in February due to planning the Annual and Ophthalmic Personnel meetings scheduled for March.
The Society is honored to host distinguished guest faculty:
• September 4: Asim Piracha, MD - Associate professor at
the University of Kentucky Department of Ophthalmology and University of Louisville’s Department of Ophthalmology and Visual Sciences. Board-certified ophthalmologist at Commonwealth Eye Surgery, Lexington, Kentucky.
• October 9: Jordan Deaner, MDUveitis and Vitreoretinal Surgery, Mid Atlantic Retina, Wills Eye
Hospital Assistant Professor of Ophthalmology Sidney Kimmel Medical College at Thomas Jefferson, University Philadelphia, PA
• November 6: Christopher Teng, MD, MBA - Professor and Chair of the Department of Ophthalmology and Visual Sciences, UMass Chan Medical School, Worcester, MA.
• December 11: Guest Speaker to be announced (visit www.pghoph.org periodically for updates).
• January 22: Raymond Cho, MD, FACS - Director of Ophthalmic Plastic and Reconstructive Surgery at The Ohio State University Wexner Medical Center, Columbus, Ohio Contact Nadine Popovich, administrator should you have questions about the monthly meeting series or annual meeting. She can be reached at npopovich@acms.org or to 412.321.5030 x110.

