
Allegheny County Medical Society


Allegheny County Medical Society
Editorial
• A Small Compass
Deval (Reshma) Paranjpe, MD, MBA, FACS
Editorial
• 2025 Carnegie Science Fair
Anthony Kovatch, MD
Editorial
• Murphy's Law and Plan B
Richard H. Daffner, MD, FACR
ACMS News
• Meet the PWP Therapists (Pt. 2) Membership
• Q&A with Dr. Michael M. Aziz
ACMS News
• Meet the Newest ACMS Members
ACMS News
• Specialty Group Updates
ACMS Staff: Nadine
Popovich, Melanie Mayer and Haley Thon

Article
• Hypertensive Disorders of Pregnancy
Erasmus Mutabi, MD; Alexandra Johnston, DO; Mahathi Indaram, MD; Indu Poornima, MD
Article
• Spectacular Seniors: MJ's Q&A with Avonworth's Best MJ Lerma

2025
Executive Committee and Board of Directors
President
Keith T. Kanel, MD
President-elect
Kirsten D. Lin, MD
Secretary
Richard B. Hoffmaster, MD
Treasurer
William F. Coppula, MD
Board Chair
Raymond E. Pontzer, MD
Board of Directors
Term Expires 2025
Anuradha Anand, MD
Amber Elway, DO
Mark A. Goodman, MD
Elizabeth Ungerman, MD, MS
Alexander Yu, MD
Term Expires 2026
Michael M. Aziz, MD, MPH, FACOG
Michael W. Best, MD
Micah A. Jacobs, MD, FIDSA
Kevin G. Kotar, DO
Jody Leonardo, MD
Term Expires 2027:
David J. Deitrick, DO
Sharon L. Goldstein, MD
Prerna Mewawalla, MD
Raymond J. Pan, MD
Nicole F. Velez, MD
James Latronica, DO, DFASAM
Richard B. Hoffmaster, MD
Finance
William F. Coppula, MD
Nominating
Kirsten D. Lin, MD
Women’s Committee
Prerna Mewawalla, MD & Meilin Young, MD
Managing Editor
Sara C. Hussey, MBA, CAE
ACMS Executive Director shussey@acms.org
Medical Editor
Deval (Reshma) Paranjpe, MD reshma_paranjpe@hotmail.com
Bulletin Designer
Victoria Gricks victoria@thecorcorancollective.com
2025 Bulletin Editorial Board
Richard Daffner, MD, FACR
Robert Howland, MD
Anthony Kovatch, MD
Charles E. Mount, MD, FAAD
Alexandra Johnston, DO
John P. Williams, MD
Executive Director
Sara Hussey shussey@acms.org
Vice President - Member and Association Services
Nadine M. Popovich npopovich@acms.org
Manager - Member and Association Services
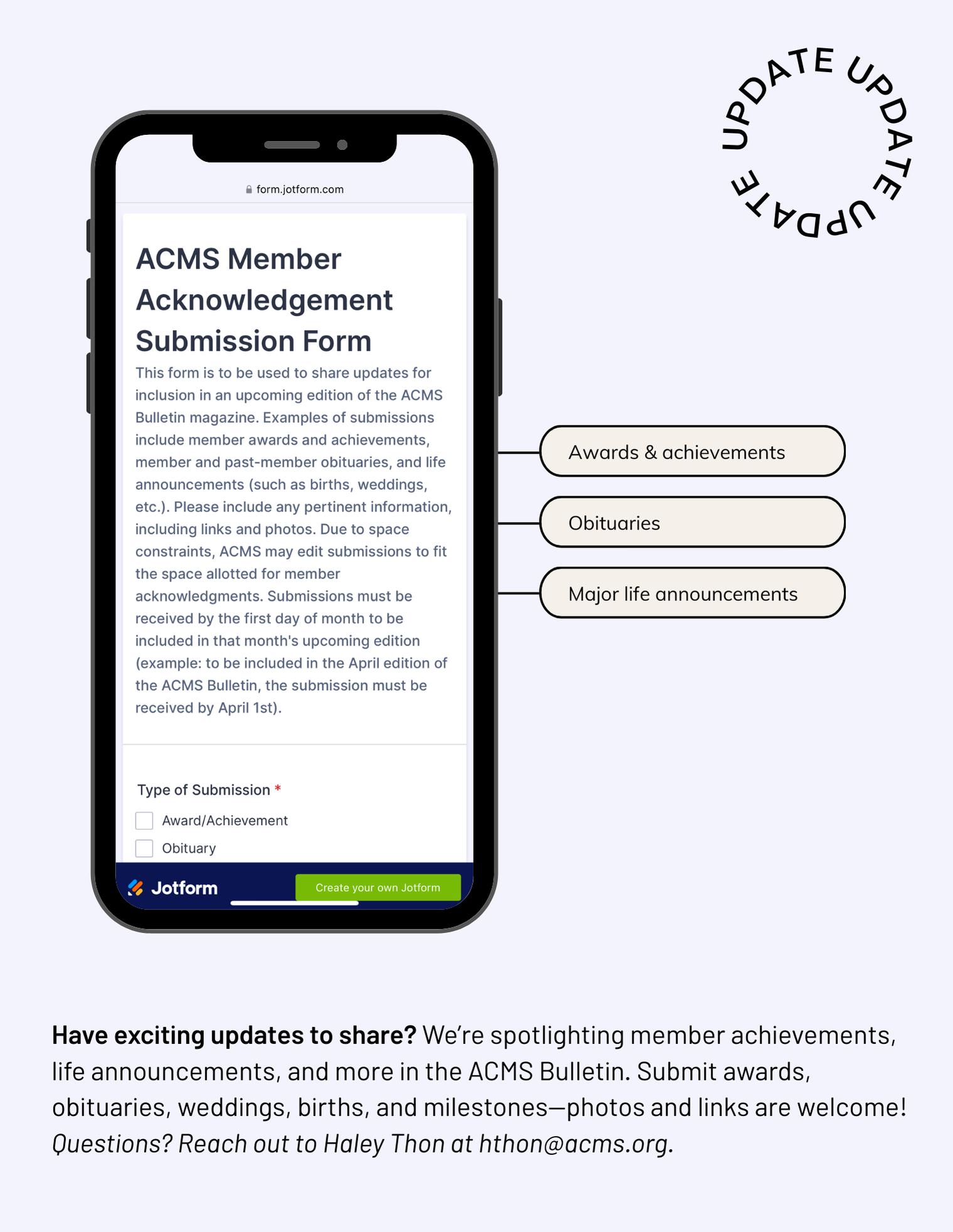
Haley Thon hthon@acms.org
Operations CoordinatorACMS & ACMS Foundation
Melanie Mayer mmayer@acms.org
Manager - Operations and Finance
Elizabeth Yurkovich eyurkovich@acms.org
Bulletin Designer Victoria Gricks victoria@thecorcorancollective.com
EDITORIAL/ADVERTISING
OFFICES: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212; (412) 321-5030; fax (412) 321-5323.
USPS #072920. PUBLISHER: Allegheny County Medical Society at above address.
The Bulletin of the Allegheny County Medical Society is presented as a report in accordance with ACMS Bylaws.
The Bulletin of the Allegheny County Medical Society welcomes contributions from readers, physicians, medical students, members of allied professions, spouses, etc. Items may be letters, informal clinical reports, editorials, or articles. Contributions are received with the understanding that they are not under simultaneous consideration by another publication.
Issued the third Saturday of each month. Deadline for submission of copy is the SECOND Monday preceding publication date. Periodical postage paid at Pittsburgh, PA.
Bulletin of the Allegheny County Medical Society reserves the right to edit all reader contributions for brevity, clarity and length as well as to reject any subject material submitted.
The opinions expressed in the Editorials and other opinion pieces are those of the writer and do not necessarily reflect the official policy of the Allegheny County Medical Society, the institution with which the author is affiliated, or the opinion of the Editorial Board. Advertisements do not imply sponsorship by or endorsement of the ACMS, except where noted.
Publisher reserves the right to exclude any advertisement which in its opinion does not conform to the standards of the publication. The acceptance of advertising in this publication in no way constitutes approval or endorsement of products or services by the Allegheny County Medical Society of any company or its products.
Annual subscriptions: $60
Advertising rates and information available by calling (412) 321-5030 or online at www.acms.org.
COPYRIGHT 2025: ALLEGHENY COUNTY MEDICAL SOCIETY POSTMASTER—Send address changes to: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212. ISSN: 0098-3772

By: Deval (Reshma) Paranjpe, MD, MBA, FACS
Nothing makes sense anymore. What we once took for granted—the near-eradication of measles, a fullyfunctioning CDC, NIH and FDA, and many other health care security blankets that helped us sleep better at night and function better during the day in our profession—are gone. Yesterday, the STD Lab at the CDC was shut down, and all 28 lab members were fired despite the critical nature of the lab’s work which included work on diagnosis and monitoring of drug resistant gonorrhea in the US. Many other such vital offices have been shuttered. Both institutional knowledge and vital support staff that kept processes running have been lost.
A century’s worth of medical progress, standards and institutions are being hobbled or eradicated, and public health will pay the price. Patients and physicians are being put at a clinical disadvantage compared to all the past years we’ve practiced medicine.
Politicians will eventually iron these issues out; organized medicine like the ACMS, PAMED, the AMA and specialty societies must provide our politicians with sound medical reason and clarity to prevent disasters and to rectify and improve missteps.
But what can the average physician do in the face of such obstacles in daily life? Combat disinformation.
Did you ever think that you would have to tell people that measles really IS that bad and that their children, infants, unvaccinated and/or immunocompromised loved ones could die from it, and that children born to infected mothers could suffer lifelong disabilities? The Japanese have devised a system of large carved stone markers
which they place at certain elevations to warn future generations not to build below that line lest those settlements be swept away by a tsunami. Every 30-50 years, another tsunami occurs, and these markers are credited with saving perhaps thousands of lives. The Japanese reason that memories of disaster are obliterated after three generations. Wouldn’t it be nice if we could have such stone markers for measles, polio, TB, HIV, Spanish Flu, COVID-19 and other death and misery-causing epidemics? We do not; instead we have medical textbooks and physicians who have studied them. This is why the world builds monuments; humans have the relative collective memory of goldfish. This is also why, as Mark Twain said “history doesn’t repeat itself, but it often rhymes.”
Share information.
During COVID, the most up-to-date information could be found on private physician COVID Facebook groups and Instagram pages—physicians from all over the world would share what they were finding worked and didn’t work. It was a beautiful instance of humble, non self-aggrandizing, unfettered information sharing and collaboration despite the circumstances. The things we were seeing deviated from the CDC and WHO party lines, which were politically influenced to stop public panic. We may need to activate that system of emergency informal physician information sharing again if the old channels of information become unreliable or nonexistent.
Maintain standards, professionalism and knowledge.
This scarcely needs to be said. We
live in an age where everyone claims to be an expert regardless of training, and every opinion on social media is believed by someone reading it. Pursue continuing medical education in earnest; keep up your expertise.
The days of Dr. Google will soon be replaced by the age of Dr. AI. AI will help us too, but we should not rely on it totally. Your ability to take notes quickly in cursive suffers when you are used to typing all day. When you rely predominantly on outside memory and processing capability, your own memory and processing ability may similarly suffer. There is no substitute for the skills and experience of a human physician, no matter what the disruptors of the world may think. Don’t devalue yourself even though you may feel devalued by the world. Your experience, intuition and ability to read faces, body language and intonation cannot be matched. Even if some say the sun rises in the West, have confidence in your own abilities, reason and knowledge.
The young physicians, residents and medical students are looking to you now as role models. What you model for them will be what they aspire to be—or not be. Make sure they grow to think of this career as a noble calling, and that they do not adopt the attitude of “Take this job and shove it”. Remember— they’re going to be taking care of all of us someday. If you are disillusioned or tired, recharge your own soul and body first and take care of yourself. Keep yourself healthy and happy—our country needs you. Remember that change is possible at all levels.



















By: Anthony Kovatch, MD
"Are you goin' to Scarborough Fair?
Parsley, sage, rosemary and thyme
Remember me to one who lives there
She once was a true love of mine " --from the traditional English ballad sung and popularized by Simon and Garfunkel (1966)
As I drove through rush hour traffic to the Carnegie Science Center on the morning of April 2nd to fulfill my voluntary obligation as a sponsor judge for ACMS, the famous Simon and Garfunkel canticle of loss and longing weaved a web around my consciousness. Having reviewed the abstracts of the 50-plus projects from which I alone was responsible to select a winner, and being well-aware of the everincreasing scientific complexity of the presentations, I had good reason to again feel “outside my comfort zone.” I argued to myself that it would be best for everybody involved that I convince the organizers of this event to change my assignment to that of judge for the science projects of second graders!
Just as the melancholic song brings to the mind of the traveler nostalgic memories of separation and unattainable love, involvement in the workings of the fair reverted my attention back to the days following my arrival in Pittsburgh in 1981 from the East Coast as a fellow in Pediatric Infectious Diseases at the world-renowned Children’s Hospital; I was encouraged to focus my research on the emerging bacterial resistance patterns of a “small fry” bacterium causing otitis media in children: Branhamella (now Moraxella) catarrhalis. I unexpectedly jumped onto the burgeoning wave of medical
research focusing on the increasing prevalence of bacterial resistance to the standard antibiotic options and the consequences of this emerging treatment failure on society. As a result of our department’s publications, the organism reached a position of prominence and notoriety.
However, as “M cat” rose up the ladder of microbiological significance, I fell in love with the laboratory technician who was my coworker in the studies (faster than the bacterial cultures grew), married her and started a family, and eventually fell off the academic ladder— almost completely and with regret.
How could I feel competent on this day in 2025 adjudicating the painstaking efforts of high school researchers ablaze with scientific passion---when my own passion was still back in the past where I had essentially “lived” in the lab at Children’s Hospital…at Scarborough Fair? As I later discovered, it would be easier than I had imagined!
Of the 54 high school level research projects, 21 were in the field of microbiology, especially bacterial resistance and alternatives to antibiotic use---probably a throwback to the COVID-19 pandemic that ushered in this decade of the 21st century. Many of the studies involved the kind of bench research that I had performed in my own academic “past life” (rather than clinical research), using animal models like the Madagascar Hissing Cockroach to test the effectiveness of various sports drinks. Methods outside of antibiotics to prevent infections caused by Staphylococcus epidermidis (previously regarded as the “weak sister”
to the more virulent Staphylococcus aureus) included the spices turmeric, oregano, and ginger---as well as natural and artificial sweeteners, nitrite substitutes (like broccoli and celery) in meats, sunscreens, and UV light (in gymnasiums). One study addressed the issue as to whether popular household cleaning products like Febreze, Sink the Stink, vinegar, and lemon juice actually kill bacteria that produce a distinctive odor or just simply mask the smell. Even thyme---the herb symbolizing courage mentioned in the song above---got into the act!
However, it was not the preoccupation with bacterial species and their eradication that galvanized my memories of my days in the research lab along with my future wife, as much as it was the zeal and fervor of the wide diversity of students, to a man beaming with the aura of pride that is only possible with outstanding devotion to a cause. Several students were recidivists and were easily recognized from their appearance at the fair in consecutive years.

Last year’s award winners were back in action, amplifying the scope of their previous research or taking a novel discovery to a higher level. A junior “Einstein” (likely a future MD/PhD candidate) developed a first-of-its-kind, wearable nanoneedle-based contact lens biosensor called “Quan Tear,” touting its ability to detect strokes in the early pre-hospital stage, as well as “silent” strokes, with 90% sensitivity and 100% specificity---potentially saving lives through early intervention. This discovery represented an evolution of the comparably accurate tear test he had presented at the fair last year for the detection of major depressive disorder.
A few of the students who had made their debut at the science fair as high school freshman or even middle schoolers had returned for an encore; they had already passed medical “boot camp”! It was apparent to me that these afficionados had taken the lead in further mastering the scientific method, especially in the realm of statistical analysis. The complexity of the magnificently displayed poster boards dwarfed that of previous years. It was also evident to even a casual layman observer that the masters had been well-trained in public speaking and in being fierce defenders of their conclusions. There was no “fudging;” if the data could not confirm the hypothesis, this was honestly and transparently elaborated upon.
I witnessed overwhelming camaraderie among the students from a wide array of high schools throughout Western Pennsylvania and a population of students with striking racial and ethnic diversity. Eager to speak to this judge about their future career ambitions, it came as no surprise to me that, despite nationwide misgivings about “burnout” and lack of autonomy, passion for the medical profession and its ongoing role as society’s healers was for this elite group unchanged from those of us who entered our profession 2 generations ago. The flame of passion has not extinguished---not even diminished!
As I was exiting the Science Center in a very relieved and pensive state of mind, I strove to offer solid counsel to a student and his proud father who was helping his son transport the many pieces of a larger-than-average poster board; the talented student from the school district which my own children had attended appeared to be “hell bent” on attending medical school after his final year of high school and being a surgeon. “Be sure to read medical literature before you have your interviews!” I wholeheartedly advised.
“The medical schools will be eager to know what novelists or poets galvanized your interest. If you plan to be a surgeon, read ‘When Breath Becomes Air’ by Stanford Neurosurgeon Paul Kalanithi, who would tragically die of lung cancer; my youngest sons

The Recidivists: A Sophomore, a Junior, and a Senior
who are doctors insisted that I read it years ago. If you have time, plan to be a general surgeon, or embrace the social determinants of health read ‘Cutting for Stone’ by Abraham Verghese; I consider it to be one of the best books I have ever read! I myself was inspired by ‘The Citadel’ by AJ Cronin; it addresses the importance of never forgetting the high ideals with which you enter the medical profession and avoiding the pitfalls along the way.”
He already read “When Breath Becomes Air,” so I wrote down the name of Verghese’s book for him on a scrap of paper, claiming it was a modern-day version of “The Citadel.” “We'll discuss that book when I see you at this fair next year,” I promised. (By that time. I had long forgotten about the second graders.)
As I drove back to the North Hills--returning home from “Scarborough Fair” --- poet William Carlos Williams intruded into my finally peaceful consciousness. I recalled not his poetry, but rather his admission in his biography that he had great guilt throughout his professional lifetime because his combined writing and practice of pediatrics had caused him to “steal time” from his devoted wife and his family.
I had intended to stop off at the hospital and complete some charts on my way back to the North Hills, but I changed my mind and decided to return home promptly to the “one who lives there.” After 43 years of marriage, she was still a true love of mine.
By: Erasmus Mutabi, MD; Alexandra Johnston, DO; Mahathi Indaram, MD; Indu Poornima, MD
1. Introduction
Hypertensive disorders of pregnancy (HDP), including chronic hypertension, gestational hypertension, pre-eclampsia, chronic hypertension with superimposed pre-eclampsia, and eclampsia complicate up to 10% of pregnancies worldwide and are important determinants of maternal morbidity and mortality.1 HDP are the leading cause of maternal mortality in the United States. Pregnancy may be considered a cardiovascular stress test in which inadequate adaptation, manifested as HDP, reveals a susceptibility to future cardiovascular disease (CVD). HDP independently increases risk for the future development of CVD. Pregnancy and the postpartum period are unique windows of opportunity for risk screening and intervention. Evidence shows that early detection and intervention can reduce long term cardiovascular risk.
2. Who is at Risk
In the United States, HDP are responsible for about 7.8% of maternal deaths. Some conditions strongly predispose a woman to the development of HDP, and these include maternal age (<20 years or >35 years), obesity, metabolic syndrome, chronic hypertension, renal disease, diabetes mellitus, tobacco use, and autoimmune diseases like lupus or antiphospholipid syndrome. History of pre-eclampsia, multiple gestations, and utilization of assisted reproductive technology are also significant risk factors.
3. Long-Term Cardiovascular
Cardiovascular risk is highest in the first year postpartum. Still, it remains elevated for decades, and recurrent and
more severe pre-eclampsia increases long-term cardiovascular risk in a dose-response fashion. Women with pre-eclampsia experience twice the rate of CVD events (including stroke, myocardial infarction, and ischemic heart disease), a 3-to-4-fold increased rate of hypertension and heart failure, 70-80% increased rate of type 2 diabetes mellitus, and ~30% increased rate of elevated cholesterol compared to women with normotensive pregnancies. Endothelial injury and glomerular damage increase the risk of chronic kidney disease, whereas a hypercoagulable state contributes to an increased venous thromboembolism incidence risk ratio by 2.5 within 10 years postpartum. In addition, those with recurrent pre-eclampsia have a 1.5 times increased rate of hospitalization for cardiovascular reasons and undergo their initial cardiovascular event at a younger age compared to those with pre-eclampsia in a single pregnancy.1-6
4.
Preconception counseling and antepartum surveillance are vital for identifying and managing high-risk pregnancies, focusing on risk factors like prior HDP, hypertension, diabetes, metabolic syndrome, autoimmune disorders, smoking habits, and family history of heart disease. Biomarkers like sFlt-1/PlGF can predict preeclampsia, while CRP, NT-proBNP, and troponins help assess the severity and long-term cardiovascular risk. Imaging techniques like echocardiography and cardiac MRI further enhance risk stratification. Key interventions include lifestyle modifications, weight and blood pressure management, and
early prenatal care. Additionally, lowdose aspirin (81-162 mg/day) should be prescribed for primary prophylaxis in high-risk patients starting at 12 weeks of gestation.
There are notable inconsistencies in treatment thresholds for hypertension in pregnancy. In the U.S., guidelines from the American College of Obstetricians and Gynecologists (ACOG) recommend a higher treatment threshold (≥160/105 mm Hg) compared to international standards (≥140/90 mm Hg). This discrepancy may affect the timing of interventions based on practice patterns and particular society recommendations utilized. Delayed treatment could potentially increase the risks of complications such as pre-eclampsia and stroke. On the other hand, stricter thresholds may result in overtreatment and fetal growth restrictions.7 A standardized, evidencebased approach is essential to enhance maternal and neonatal outcomes.
5. Postpartum Surveillance
Patients with pre-eclampsia have a heightened risk of long-term CVD. Major medical societies propose a systematic follow-up to identify and reduce risk.8
The initial postpartum screening should be done at 6–12 weeks to check blood pressure, lipid profile, and glucose metabolism, with long-term follow-up every 1–2 years to detect early CVD risk factors.
Risk reduction counselling involves lifestyle changes such as a hearthealthy diet, exercise, and the avoidance of smoking.
Pharmacologic therapy, with antihypertensives should be initiated with a goal blood pressure of
<140/90mmHg during pregnancy and <130/80 mmHg in the postpartum period. Statins and antidiabetic agents can be initiated as necessary.
6. Personalizing Prevention
Patient-centered care is the key to cardiovascular risk management in women with a history of HDP, emphasizing shared decisionmaking to optimize adherence and outcomes. The main strategies are the provision of culturally sensitive education about cardiovascular risk and lifestyle modification, mobilization of multidisciplinary teams (cardiologists, obstetricians, primary care providers, and nutritionists) for ideal care, and utilization of digital health technologies such as mobile health apps, remote monitoring, and patient portals to facilitate self-care.9 Motivational interviewing may also aid patients in making healthy lifestyle choices. Encouragement of these interventions enhances adherence to preventive therapies and long-term cardiovascular wellness after HDP.
7. Bridging the Gap
Cardiovascular disparities in HDP are pronounced, especially in racially, ethnically, and socioeconomically disadvantaged populations. Black and Hispanic women experience a higher incidence of HDP, severe pre-eclampsia, eclampsia, and are at higher long-term risk of strokes, heart failure, chronic hypertension, and cardiovascular mortality. Women of low socioeconomic status and those in rural areas have limited access to prenatal care and postpartum followup, which puts them at a higher risk for unrecognized cardiovascular complications.1,10 Eliminating disparities and improving maternal cardiovascular health requires increased access to care, encouraging antepartum and postpartum visits, and eliminating structural inequities.
8. Looking Ahead
Future research should focus on understanding the molecular pathways linking HDP to CVD through large-scale longitudinal studies. Randomized
controlled trials on lifestyle and pharmacologic interventions, along with genetic, epigenetic, and environmental analyses, will aid in developing personalized prevention strategies. Additionally, machine learning and artificial intelligence can refine risk prediction by integrating electronic health records, biomarkers, imaging, and social determinants of health, ultimately improving equity in clinical decision-making.
9. The Role of Advocacy and Policy
Advocacy and policy play a crucial role in optimizing outcomes for women with HDP and preventing long-term cardiovascular disease. Key priorities include expanding health coverage, increasing postpartum Medicaid coverage, reducing racial disparities, utilizing telemedicine to improve access to care, raising awareness through public education campaigns, and investing more in cardiovascular prevention to reduce the adverse effects of HDP. Legislative measures can facilitate postpartum cardiovascular screening and followup care, including payment for remote blood pressure monitoring. Additionally, community-based interventions are essential for educating and supporting women in high-risk communities. It is vital to enhance advocacy efforts so that all women receive the care necessary to reduce their cardiovascular risk following HDP. Acknowledging that cardiovascular disease is the leading cause of maternal mortality in the U.S., it is imperative that policy measures are strengthened to mitigate the impact of HDP on maternal mortality.
10. A Lifelong Journey
Hypertensive disorders of pregnancy are not just reversible pregnancy complications but also harbingers of long-term cardiovascular disease. Identification and management of this risk through early screening, lifestyle changes, and targeted preventive and pharmacologic treatment can have a significant impact on long-term cardiovascular morbidity in these
women. As clinicians, we need to seize this opportunity to intervene early, ensuring that cardiovascular health remains a lifelong priority for women with a history of HDP.
References
1. Khosla K. et al. Long-Term Cardiovascular Disease Risk in Women After Hypertensive Disorders of Pregnancy: Recent Advances in Hypertension. Hypertension. 2021;78(4):927935. doi:https://doi.org/10.1161/ hypertensionaha.121.16506
2. Ying W. et al. Hypertensive Disorders of Pregnancy and Future Maternal Cardiovascular Risk. Journal of the American Heart Association. 2018;7(17). doi:https://doi.org/10.1161/ jaha.118.009382
3. Malek M. et al. Maternal Coronary Heart Disease, Stroke, and Mortality Within 1, 3, and 5 Years of Delivery Among Women with Hypertensive Disorders of Pregnancy and PrePregnancy Hypertension. J Am Heart Assoc. 2021;10(5):e018155. doi:10.1161/JAHA.120.018155
4. Countouris M. et al. Advances in Our Understanding of Cardiovascular Diseases After Preeclampsia. Circulation Research. 2025;136(6):583-593. doi:https://doi.org/10.1161/ circresaha.124.325581
5. Wu P. et al. Preeclampsia and Future Cardiovascular Health. Circulation: Cardiovascular Quality and Outcomes. 2017;10(2). doi:https://doi. org/10.1161/circoutcomes.116.003497
6. Gongora M. et al. Hypertension During Pregnancy and After Delivery: Management, Cardiovascular Outcomes and Future Directions - American College of Cardiology. American College of Cardiology. https://www.acc.org/ latest-in-cardiology/articles/2018/09/28/08/08/ hypertension-during-pregnancy-and-after-delivery
7. Garovic V. et al. (2021). Hypertension in pregnancy: Diagnosis, blood pressure goals, and pharmacotherapy: A Scientific Statement from the American Heart Association. Hypertension, 79(2). https://doi.org/10.1161/HYP.0000000000000208
8. Brown H. et al. Promoting Risk Identification and Reduction of Cardiovascular Disease in Women Through Collaboration with Obstetricians and Gynecologists: A Presidential Advisory from the American Heart Association and the American College of Obstetricians and Gynecologists. Circulation. 2018;137(24). doi:https://doi. org/10.1161/cir.0000000000000582
9. Lewey J, Sheehan M, Bello NA, Levine LD. Cardiovascular Risk Factor Management After Hypertensive Disorders of Pregnancy. Obstetrics and gynecology. 2024;144(3):346-357. doi:https:// doi.org/10.1097/AOG.0000000000005672
10. Zahid S. et al. Racial and Socioeconomic Disparities in Cardiovascular Outcomes of Preeclampsia Hospitalizations in the United States 2004-2019. JACC: Advances. 2022;1(3):100062. doi:https://doi.org/10.1016/j.jacadv.2022.100062

By: Richard H. Daffner, MD, FACR
“Anything that can go wrong will go wrong."
--Edward A. Murphy, Jr. 1949
Comedian Bob Newhart had a routine, the theme of which was that inanimate objects secretly hate us. Drop a slice of bread on the floor and it will always land with the buttered side down. Own a suit with two pairs of pants and you will burn a hole in the jacket. These are two examples of Murphy’s Law.
We’ve all heard of Murphy’s Law and its many variations (Table 1). Though similar statements have been made throughout history, the law itself was coined by, and is named after, American aerospace engineer Edward A. Murphy Jr (1918 – 1990).(Fig. 1), after a series of rocket sled mishaps. Murphy attended the U.S. Military Academy at West Point and graduated with an engineering degree in 1940. He was assigned to the Army Air Corps and served in the Pacific Theater during World War II. Following the end of the war, he was assigned to the U.S. Air Force Institute of Technology (AFIT) at Wright-Patterson Air Force Base outside of Dayton, Ohio, where he became involved in highspeed rocket sled research. In 1952, he resigned from the Air Force and began working on aircraft cockpit design for several private contractors. His area of interest was in crew escape systems on experimental aircraft, many of which later became production aircraft, such as the F-4 Phantom and the SR-71 Blackbird. During the 1960’s he worked on the safety and life-support systems for the Apollo project of NASA and ended his career working on pilot safety for the Apache helicopter.


Murphy's Law Variations
1. In any field of endeavor, anything that can go wrong will go wrong, and at the worst possible time.
2. Left to themselves, things will always go from bad to worse.
3. If there is a possibility of several things going wrong, the one that will go wrong is the one that will cause the most damage.
4. Nature always sides with hidden flaw.
5. If everything seems to be going well, you obviously have overlooked something.
So, with Murphy’s pessimistic, but realistic concept, is there any way to deal with problems as they are bound to arise? The answer is to always have a Plan B when Plan A goes awry.
I have been volunteering as a “Wheelchair Wrangler” repairing, reconditioning, and rebuilding wheelchairs at Global Links1 since 2014. There, we take wheelchairs that have been donated by AHN, UPMC, and private owners and, in most cases, are able to restore them to make them functional so that they may be sent to medically indigent areas in the Caribbean, Central and South America. A few of the chairs are in a nearly new condition, having been used for a short period of time by their owners. Most, however, are “well-used” or, in some cases, well-abused. These chairs come with broken or missing parts, torn vinyl seats and seatbacks, frequently have rusty parts, and are covered in a variety of dried food or even dried bodily fluids. (That’s why we wear gloves when handling them). We strive to make the finished chairs have aesthetic appeal, matching colors of seats, backs, and arm and leg rests where possible. Our biggest challenge is in finding compatible parts (Plan A), since many chair models from the same manufacturer simply don’t fit. Many of the chairs have a mixture of standard and metric nuts and bolts, necessitating two sets of tools. And frequently, when we have stripped the chairs down to their frames, we find unexpected damage that also needs to be addressed. These factors mandate our having to go to Plan B many times. I had been working solo for a couple
of years, when one day Dave Engel came into the wheelchair shop. Dave, a retired neurosurgeon, had been volunteering sorting donated medical supplies and had noticed me working. He wanted to know if wheelchair repair required any special mechanical skills. I told him that he, like me, was overqualified. The next week he joined me.
We have a limited number of replacement seats and seatbacks. Many of the seats and backs on our chairs have small tears, particularly near the areas where they are attached by screws to the frame of the chair. Dave came up with our first Plan B. He and I began suturing patches over the tears. He complemented me on my suturing technique, saying that he never thought a radiologist could do such good work. I told him that I had plenty of practice as an ER physician in the Air Force and as a team physician for several hockey teams. Over time we refined our techniques using glue and small rivets on our patches.
The vinyl pads on arm rests and leg rests frequently have small tears. Vinyl repair kits are expensive and feature a small number of patching materials in a variety of colors. However, most of the tears we encountered were on black or blue pads, and we would quickly exhaust the black and blue patching materials. Again, Plan B solved the problems. We began using Flex Seal® to repair the small tears. Initially, the smallest amount of Flex Seal we could buy came in a quart can. After the can had been opened and closed multiple times, the liquid had a nasty habit of solidifying. Another Plan B was to purchase the Flex Seal in spray cans (in black & clear), spray a small amount into a small plastic cup, and use a cottontipped swab to apply it to the tears. Gilbert and Sullivan, in their operetta “HMS Pinafore” have a song that begins “Things are seldom what they seem, skim milk masquerades as cream”. Dave and I have an ongoing mantra; As soon as the task appears simple, Murphy’s Law will intervene, and we’ll find something else that needs to be taken
care of. To wit…
I recently had to replace both rear wheels on a chair. I was fortunate to find two identical wheels of the right diameter. The first wheel was quickly attached. Then Murphy’s law intervened when I went to replace the second wheel. I discovered that the diameter of the hole in the wheel bearings that sit in the hub of the wheel was larger than the axle bolt. I found another tire that had identical stem bearings, but cosmetically it didn’t match my tire. Then I went to Plan B. The wheel bearings are easily removable along with the tubular bushing between the bearings. I removed the bearings and replaced them from our supply of spares with a pair that fit the existing axle bolt.
All wheelchairs have pairs of pins welded to the frame on either side to allow mounting of leg/footrests. Occasionally, one or more of the pins are missing or broken (Murphy’s Law, again). Plan B is to replace the missing pin(s) with a ¼ inch bolt. This requires using our tap and dye set to create threads to allow the bolt to be securely seated in the hole. Dave recently had a situation where he removed an accessory that had been attached through a square hole that replaced the upper pin on one side. We don’t have any replacement pins. He found a carriage bolt (that had a square protrusion beneath the head that fit perfectly into the square hole. He cut the bolt down to size and fastened it with a nut that he used our bench grinder to reduce its thickness. We have many more examples where an apparent easy restoration quickly becomes complicated after a thorough evaluation shows additional issues to be dealt with.
I have a woodworking shop at home that I have used to fabricate replacement parts for the side panels that support the arm rests on several wheelchairs, when those parts were no longer available from the manufacturers. Wood is a nice substitute for plastic and is not as
fragile.
Finally, there was a situation where Plan B was being used instead of Plan A. Several years ago, while attending our local scout camp, I was summoned by one of the camp medics who was unable to remove a turtle hook (large fishhook) from a boy’s leg. He told me that he had been trying for almost an hour to use the “string method” (don’t even think of trying it; it doesn’t work!) to free the hook’s barb without any success.
“Time for Plan A,” I said.
“I thought I was using Plan A,” he replied.
“No, you’re using Plan D,” I said.
I told the lad to grit his teeth, and when he did, I pushed the hook so that the barb came out through the skin. I cut the barb off with the wire cutter on my Leatherman multitool® and removed the remainder of the hook by pulling it back.
Later, I told the medic that in all the years that I worked in emergency rooms, I never saw the string method work. An Emergency Medicine physician friend of mine concurred.
As an interesting footnote to this incident, one of the other adult leaders from my troop accompanied me on my “mission of mercy”. She was aware that I had a restricted medical license (“Active – Retired”) allowing me to treat and prescribe for immediate family only, and asked me, “Were you allowed to do that with your restricted license?”
“Of course,” I replied. “That’s Wilderness First Aid. I’m a certified instructor.”
Murphy’s Law always occurs without announcing itself. The ancient Romans had another expression long before Murphy, “Faex occurit est!” When Murphy’s Law intervenes, it is always best if you already have a Plan B ready to meet the challenge.
Reference 1. Daffner RH. The “R’s” Have it. ACMS Bulletin Aug 2017, pp 288-289.
Dr. Daffner is a retired radiologist. He is also an amateur historian.
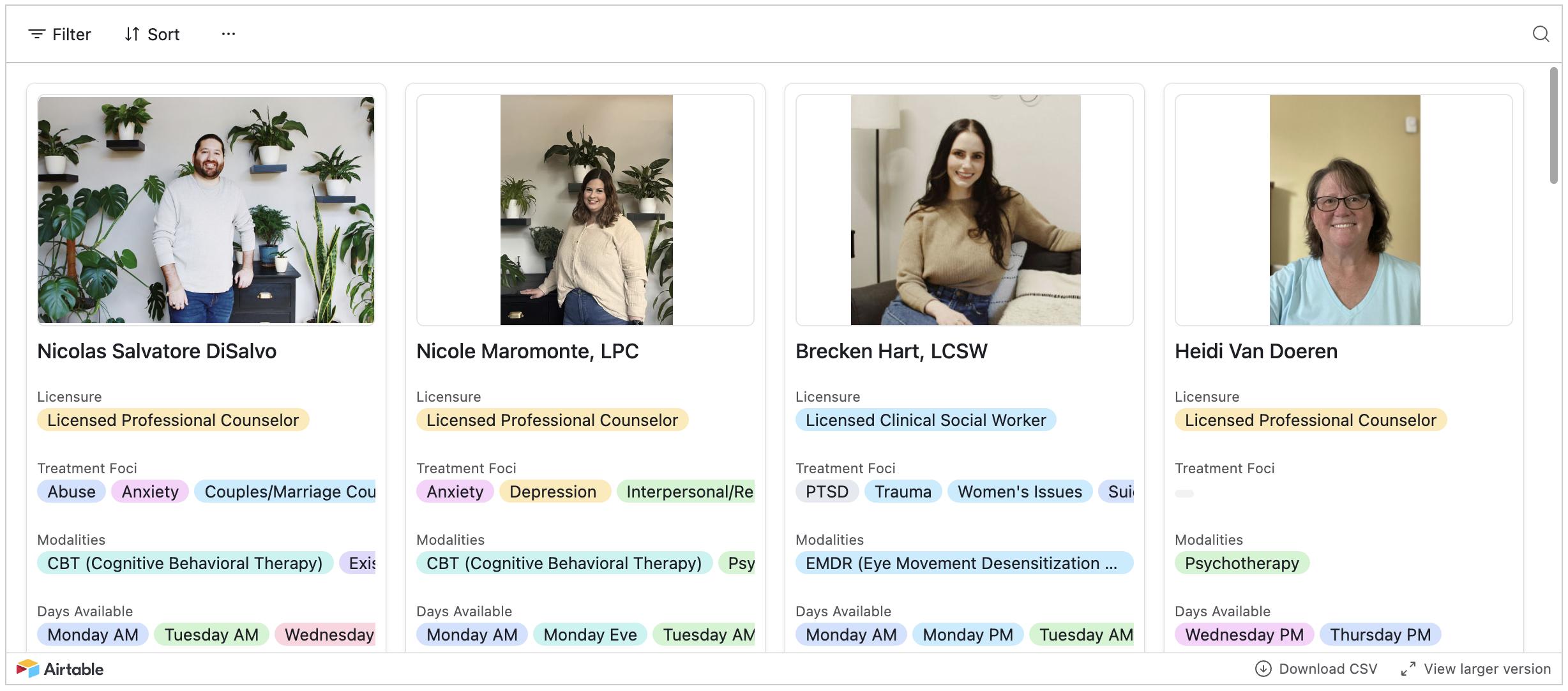
Welcome back to the Meet the Therapists series, part of the ACMS Physician Wellness Program. This series is all about introducing the dedicated professionals who provide vital mental health support to physicians in Allegheny County. In this edition, we’re excited to introduce the remaining therapists—each one bringing their own unique approach to fostering physician well-being.
Participating in the Physician Wellness Program is simple and completely confidential. Just head to the ACMS website and navigate to the
Physician Wellness Program section. You can browse the therapist profiles, pick the one that feels like the right fit, and schedule an appointment directly through the site. Participation is voluntary and completely confidential— no medical diagnosis is recorded, and no insurance billing is involved. Most appointments are available within one to two weeks, and there are options for weekend and evening telehealth sessions to accommodate busy schedules.
The ACMS Physician Wellness Program is here to help tackle the

challenges of physician burnout and mental health head-on. Our goal is to make counseling services accessible and stigma-free, empowering physicians to thrive both personally and professionally. For more information or to schedule an appointment, visit the ACMS Physician Wellness Program at www.acms.org/physicianwellness
WHAT IT LOOKS LIKE ON OUR WEBSITE

MICHELLE DOVE, MSW, LCSW
Specialties: Anxiety, burnout, depression, divorce, healthy boundaries, LGBTQ+ issues, women’s issues
Approach: CBT, Solution Focused Therapy
Location: Telehealth, In-Person (Ambridge)
Availability: Tuesday AM
Quote: "Seeking help can feel overwhelming, but taking that step is a sign of strength. I believe the therapeutic journey should be collaborative and supportive."

NICOLE MAROMONTE, LPC
Specialties: Anxiety, depression, interpersonal relationships, life transitions, social anxiety, self-harm (teens and young adults)
Approach: CBT, Psychotherapy, DBT, Person-Centered
Location: Telehealth, In-Person (Pittsburgh)
Availability: Monday–Thursday AM/PM
Quote: “I view therapy as a journey of self-reflection. My goal is to help clients feel grounded and supported as they navigate personal challenges and develop tools for longterm growth.”

RACHAEL MANFREDO, MS, LPC
Specialties: Anxiety, burnout, depression, life transitions, self-esteem, grief and loss, high-conflict personalities
Approach: CBT, Psychotherapy, Solution Focused Therapy, Creative Expression
Location: Telehealth, In-Person (Pittsburgh)
Availability: Monday–Friday, various times
Quote: “Seeking out help can be an overwhelming, difficult step. My goal is to create a safe, inclusive space where you feel supported, heard, and understood as you explore meaningful personal growth.”

HEIDI VAN DOEREN, LPC, CADC
Specialties: Addiction, trauma, self-discovery, inner systems work
Approach: Gestalt Therapy, Internal Family Systems (IFS), Psychotherapy
Location: Telehealth (Pittsburgh)
Availability: Wednesday PM, Thursday PM
Quote: “I am trained in Gestalt and Internal Family Systems therapies—both emphasize your inherent capacity to grow, evolve, and heal. I aim to create a space where clients can reconnect with their inner strength and sense of self.”



Dr. Michael M. Aziz has been an active and dedicated member of the Allegheny County Medical Society Board of Directors since 2023 and currently serves as Chair of the ACMS Delegation to the Pennsylvania Medical Society House of Delegates. A committed advocate for organized medicine, Dr. Aziz brings thoughtful leadership and a collaborative spirit to every discussion— whether he's representing Allegheny County physicians at the state level or helping guide the strategic direction of ACMS. His passion for improving the healthcare landscape and mentoring the next generation of physician leaders continues to make a lasting impact on our medical community. We’re proud to recognize Dr. Aziz as this month’s featured member.
Q: CAN YOU SHARE A LITTLE ABOUT YOUR BACKGROUND AND WHAT LED YOU TO A CAREER IN MEDICINE?

A: I am a second-generation physician, and I was born and raised in Pittsburgh. My father practices cardiology, and I remember how close he was with his staff. When I was little, the nurses gave me snacks while my father did cases in the cath lab. He is the hardest working person I know, so I initially sought to pursue a different career. I was still drawn to health care and service through scouting. A group of us went on to become lifeguards and firemen. After finishing undergrad, I worked briefly in public health before going to medical school.
Q: WHAT INSPIRED YOU TO PURSUE YOUR SHIFT INTO YOUR CURRENT SPECIALTY?
A: I started medical school wanting to be a family physician. I realized during my OB/GYN rotation that women's health was my calling. I loved the diversity of practice and seeing patients who were highly motivated to make positive health changes for the sake of their family. I had so many misconceptions about the field, but eventually, I felt like I couldn't do anything else. My cousin is a vascular surgeon who advised me to pursue a career where I loved the patients and the reading, so I became an OB/GYN and then a Maternal-Fetal Medicine (MFM) physician. Life came full circle when I became the Director of Fetal Echocardiography at AHN.
Q: CAN YOU TELL US ABOUT YOUR CURRENT ROLE AND WHAT A TYPICAL DAY OR WEEK LOOKS LIKE FOR YOU?
A: Our division is a mostly consultative practice. We spend most of the day reading prenatal ultrasounds and seeing patients who have preexisting health issues before, during, and after pregnancy. My role is to help to reduce risks to the patient and their fetus or neonate. We also have an inpatient service and a small highrisk clinic where we are the primary physicians for patients who require MFM-level care. I have also mentored several residents who are interested in becoming MFM physicians, and one of my greatest joys has been seeing my former students and residents become my colleagues.
Q: HOW DID YOU FIRST GET INVOLVED WITH THE ALLEGHENY COUNTY MEDICAL SOCIETY?
A: I have been an at-large member of the PAMED Early Career Physician Section since I graduated from fellowship. I was nominated for and received a PAMED 40 Under 40 award, and I was approached by our ACMS executive director to see if I would be interested in having a role at ACMS.
Q: WHAT HAS BEEN THE MOST REWARDING ASPECT OF BEING AN ACMS MEMBER?
A: I think that it's very important

to protect the joy and collegiality in our profession, and it's been so much fun getting to know more about the physicians in the county whom I wouldn't normally interact with clinically.
Q: ARE THERE ANY ACMS INITIATIVES OR EVENTS THAT YOU ARE PARTICULARLY PASSIONATE ABOUT?
A: I love our participation in the PAMED House of Delegates. I was asked to be the chair of our delegation this year, after serving as the vice-chair last year. It's more important now than ever for Pennsylvania physicians to organize and to speak with one voice. The House of Delegates gives members the opportunity to submit resolutions to the House for a vote. If accepted, these resolutions become the official position of the physicians of the state. We have not shied away from controversial topics. We have had healthy debates on a wide range of resolutions ranging anywhere from lead exposure to reproductive rights and protections for healthcare workers in war zones. We have also passed commonsense resolutions that had not been previously debated such as support for a healthy environment and removal of nonmedical exemptions for vaccination.
Q: WHAT DO YOU THINK IS THE BIGGEST CHALLENGE FACING HEALTHCARE TODAY?
A: Our biggest challenge is the corporatization of healthcare. Many in the business community see healthcare delivery as a purely financial endeavor
and physicians as interchangeable cogs in a machine. This view neglects the fundamental issues that make being a physician unique and wonderful: establishing a close and trusting therapeutic relationship which is second only to that of a family member. Many have tried to decentralize this relationship from healthcare delivery by pitting specialties against one another, calling us providers and taking us away from the bedside with documentation and billing requirements that are not essential to patient care.
A close second is combating medical misinformation and disinformation. As Jonathan Swift said "Falsehood flies, and the truth comes limping after it."
Q: HOW DO YOU SEE YOUR FIELD EVOLVING IN THE NEXT 5–10 YEARS?
A: We will continue to fight the rising tide of increasing maternal and infant mortality, but I am concerned that the lack of an organized response at the federal level will only worsen this national crisis/embarrassment.
Q: WHAT ADVICE WOULD YOU GIVE TO MEDICAL STUDENTS OR EARLYCAREER PHYSICIANS?
A: There's still something so essential and personal about what we do, which I'm reminded of every time I am a patient. I fundamentally disagree with the idea that artificial intelligence will replace us. I suspect that it will be a tool that makes us more accurate and efficient. I give students the same advice that I was given: do something where you love the patients and the reading.
Q: OUTSIDE OF MEDICINE, WHAT ARE YOUR HOBBIES OR INTERESTS?
A: I love to do anything outside. I am an avid outdoorsman. As my father says: "If you love nature, you'll always be wealthy." Most of my time is spent outside with my wife and three children. We golf, ski, fish, hike and camp. I'm not an expert in soccer or baseball, but I have somehow ended up coaching both at one time or another. I'm also the
cubmaster for the Fox Chapel Area Cub Scout Pack.
Q: HOW DO YOU MAINTAIN A WORKLIFE BALANCE?
A: I was very lucky that my senior partners negotiated a great deal for us. Maternal-Fetal Medicine was once known for having one of the worst lifestyles in all of medicine. My previous Director, Dr. Ronald Thomas, and the administration were able to set up a more consultative group where we delegated deliveries to another group and maintained our small inpatient service at West Penn only. This setup ensured that we work at the top end of our training without being in the hospital for deliveries that our morethan-capable colleagues in Obstetrics can handle.
On a daily level, I maintain two separate mobile devices, with one dedicated to work and the other is personal. This has helped me to detach from work more often and be more present with my family when I'm not on call.
Q: HOW CAN FELLOW ACMS MEMBERS CONNECT WITH YOU OR SUPPORT YOUR WORK?
A: I love connecting with ACMS members about the PAMED House of Delegates. If you have an issue that you're passionate about, check the HOD website to see if PAMED has a formal position on it. Please let me know if there's a position we haven't taken or if you think that our position should be updated. My email address is michaelmazizmd@gmail.com.


By: MJ Lerma – MPH Candidate Policy/Administrative Intern at ACMS
On March 10th, students in the Health & Medicine Pathway Program at Avonworth High School had the incredible opportunity to observe an open-heart surgery performed by an all-woman surgical team. In this interview, two exceptional students and their dedicated teacher share their insights into what it was like to witness the procedure at Allegheny General Hospital. They also discuss the Personal Pathways Program at Avonworth and how that program has influenced their high school experience and future career goals.
Lily Anderson and Alessia Padalino are both seniors at Avonworth High School and have participated in the Health & Medicine Pathway Program since their sophomore year. After graduation, Lily plans to pursue a career in nursing, while Alessia will attend the University of Wisconsin–Madison with hopes of becoming a surgical PA. Julie Selep, a biology teacher at Avonworth, serves as the faculty leader for the Health & Medicine Pathway Program.
The Personal Pathways Program is a career-oriented initiative with five different pathways, including the Health & Medicine Pathway. Its primary goal is to expose students to various career fields and extraordinary realworld opportunities. The program helps students explore their interests, gain hands-on experience, and better prepare for life after high school.
Questions and responses have been edited for clarity.
How did you both get involved in the Health & Medicine Pathway?
Lily: I've always been interested in anything health and medicine related.
My cousin was a big inspiration for me— she's a nurse. I've just always wanted to help people, especially children. I love children. For me, nursing is the best option because I like that in four years, I have a lot of different choices in terms of what I can do. I can do administrative work and sit at a desk all day; I could travel or work in a hospital. I can really do a lot with a nursing degree
Alessia: I was introduced to the field through my aunt, who is a nurse anesthetist. Just hearing about all the opportunities and the work she was able to do was really inspiring. Having that exposure, as well as the science and health-related classes Avonworth offered through the pathway, showed me how much I enjoyed health and medicine. I’ve always loved science, and taking the Anatomy and Physiology class my sophomore year really showed me how much I like learning about the body. It’s been a great opportunity.
Can you tell me about your experience watching an all-women team performing open-heart surgery?
Alessia: [The team] was very empowering to see because, in the surgical field, women are very underrepresented. When you think of a surgeon, normally you think of a man. Having an all-women surgical team—the anesthesiologist, the lead surgeons, the PAs, the nurses—everyone being women and collaborating and working together was very uplifting and empowering.
Lily: I think it was very inspiring to see a team of women. I thought, that could be us in the future.
Mrs. Selep: We watched from the observational desk. (eliminate enclosed

Pathway for Health & Medicine students participate in
etc). The anesthesiologist, a parent of students from our district, made it a point to come up and talk to the students. We've been doing open-heart surgery observations for years; her making the effort to come up and talk just really enhanced the experience, and it was a great opportunity for these students to have that kind of one-onone opportunity with professionals.
Alessia: It was really nice that she came up. It was nice knowing that she was in our community and a part of Avonworth. Since our district is smaller and so close-knit, I feel like it opens doors—just knowing that there’s someone from our community we can go to if we want to talk about a job or get advice on what they did. Having someone so accessible makes such a big difference.
Lily: And she just made casual conversation—she talked about school, mentioned how her kids are younger,
and how she loves the district. She was very kind.
Mrs. Selep: I was appreciative. I can’t think of a better way to celebrate International Women's Day and inspire these students to fearlessly pursue their ambitions in any field.
How has the program shaped your high school career and aspirations for after college?
Lily: The program helped me realize what I want to focus on. Going to the open-heart surgery and actually watching and taking it all in made me realize that the operating room would be a good place for me to be. I could really see myself there. I really did enjoy the experience, but I also want to work with kids, so I’m not sure exactly what I’ll get into. I’m still open-minded.
Alessia: Going into my junior year, I had the opportunity—offered through the Pathway Program—to attend the National Student Leadership Conference at the University of Miami. It’s basically a medical intensive for high school students where you can learn basic procedures like suturing, talk to a bunch of guest speakers, and try
things like diagnosing patients. That really helped me solidify what I want to do with my future. This pathway really shaped my high school experience. Having that experience helped me focus more on science and math classes. Because of the opportunities offered, I was able to tailor my high school experience toward what I want to do in the future.
Mrs. Selep: Students having the opportunity to find out what they do and don’t like is important. When Alessia talks about how she wants to be a surgical PA—she wouldn’t have known that without actually stepping into the operating room or watching open heart surgery. These experiences help students discern what they can handle and can confirm or refute if an occupation is a true interest. For Lily, with nursing, she is now open to surgical procedures because she has witnessed it. If she doesn't have that experience, she may be less certain about her educational and career goals.
Lily: Definitely. I think another great opportunity was going to the cadaver lab—it really helped me realize what I’m


Pathway seniors have the opportunity to watch a surgery from the OR.
able to handle. I really enjoyed going. I thought it was really, really cool. There’s so much I didn’t know before being exposed to it through this program.
Alessia: I think it really helped me narrow down what I want to do. I’m so thankful that Avonworth has these career-oriented programs, because without them, I would still feel lost. Now I’m saving a bunch of money because I actually know what I want to do.
Mrs. Selep: The district has been very supportive—not only for me, but for the other Pathway faculty leaders. If any of us have an idea for a field trip or experience, the answer is yes. I don’t think we’ve asked for anything outrageous, but everything I’ve asked for, they’ve come through. Additionally, professionals from the area and country have been tremendously supportive in talking with students about their professions. I'm grateful to all those who have shared their time and talents with our students.
If you are interested in connect with Julie Selep, please reach out to her via email at: jselep@avonworth.k12.pa.us
SCAN THE CODE TO LEARN MORE

The Allegheny County Medical Society is proud to welcome the newest members of our growing physician community. Each of these individuals brings unique experiences, expertise, and perspectives that strengthen our collective voice and enrich the work we do together. We are honored to support them in their professional journey and look forward to their contributions to organized medicine and the health of our region. Please join us in extending a warm welcome to our new colleagues!
PHYSICIANS
Ahmad Alquadan , MD
Sangeeta Al-soud , MD
Joel Berry , MD
Kourtney Chakravorty , MD
Mary Dave , MD
Matthew Davis , DO
Juanita Dayawansa , MD
Sanjit Dhaliwal , MD
Andrew Greco , MD
Sydney Guinto , DO
Rafael Kim , MD
Angela Kim , MD
Kerry Ku , MD
Roy Kupfner , MD
James Luther , MD
Katherine Makkar , MD
Kang McDaniel , DO
Fahed McGee , MD
Zhe Melaku , MD
Yohannes Questel , DO
Evan Siegel-Richman , MD
Bharadwaj Smith , MD
Alexander Tarchichi , MD
Benjamin Tiberio , MD
Shane Whiting , MD
RESIDENTS
Eitan Aksoy , MD
Perry Artiaga-Candia , MD
Rashad Awuah , MD
Taylor Ayla , MD
Alexis Buyukkaya , MD
Tony Chen , DO
Samarth Chen , MD
Kojo-Frimpong Cockrell , MD
Junaid Cohen , Jane Cope , MD
Taha Damlaj , MD
Maria Deng-Johnson , MD
Jonathan Diacou , MD, PhD
Virginia Feng , MD
Fatemeh Ferreira , MD
Allen Garcia Sturgill , MD
Jacob Ghiam , MD
Victor Ghobrial , MD
Megan Guo , MD
Parker Guzak , DO
Mariah Hartline , MD
Samantha Hebert , MD
Brandon Hoffman , DO
Yonaton Jain , MD
Kristin Jin , MD
Dan Jiyani , MD
Hannah Johnson , MD
Raed Kadurei , MD
Merlyn Katikaneni , MD
Yifeng Kelesoglu ,
Padma Sri Kelly , MD
Nithya King , MD
Mark Klein , DO
Kevin Kong , MD
Nupur Koo Chong , MD
Jennifer Lametti , MD
Ilya Lee , DO
Brandon Lisius , MD
Brian Livingston , DO
Abigail Martin , MD
Natalie Martin , MD
Aneesh Mascara , MD
Matthew Matar , MD
Angela McCathern , MD
Colleen McFarland , MD
Timothy McGrath , MD
Dylan Miller , MD
Alexander Morgan , MD
Tiffany Narvel , MD
John Nestor , MD
Timothy Neyaz , MD
Vince Oe , MD
Azfar Patel , DO
Junwoo Patel , MD
Andre Peine , MD
Abigail Ramesh , MD
Nicholas Rose , MD
Ayla Sachs , MD, DMD
Anthony Setia , MD
James Sharma , MD
Sandeep Shemuelian , MD
Brandon Shrestha , MD
Christine Shrivastava , MD
Paul Shu , MD
Zihan Shu , MD
Liqi Sukhtian , MD
Alexandre Tercek , MD
Akshay Thenappan , MD
Firas Tong , MD
Ashna Trujillo-Aguirre , MD
Tyler Vargas , MD
Jatin Volz , MD
Boram Wali , MD
Jingxiao Wang , MD
Colleen Wei , MD
Raven Williams , MD
Ashwatha Wisniewski , MD
Christina Wright-Chisem , MD
Michael Wu , MD
Minjie Yang , MD
Benjamin Yerra , MD
Luilly Zandifar , MD
Renjie Zhang , DO
Adam Zu , MD
Dylan Angalich
Amrita Azari
Dasam Chirravuri
Christina Contractor
Afrooz Cotton
Nathan Exantus
Brandon Greiner
Rachel Holum
Farah Jeong
Ali Kim
Kenzo Mesregah
William Parks
Sean Peticca
Eden Pham
Matthew Tran
Fatih Trawinski
Isha Williams
Rucha Yatsishin
Grace Yohannes
Joie Zabec Joie Zabec
By: Nadine Popovich, Melanie Mayer and Haley Thon
Allegheny County Immunization Coalition (ACIC) — 2024-2025 ChairPatrick Hussey, PharmD, MBA: Thank you to everyone who joined us on March 20 for our General Membership Meeting! We had a great turnout of 39 attendees and a fantastic presentation from Dr. Victor Alós-Rullán, who shared his insights on vaccine hesitancy and public health strategies.
Looking to make an impact? We have an exciting volunteer opportunity coming up:
August Wilson Birthday Celebration Block Party
Date: April 26, 2025
Time: 11:00 AM - 6:00 PM
Location: 1727 Bedford Avenue, Pittsburgh, PA 15219
You can register for this event and learn more about other ways to get involved by visiting www. ImmunizeAllegheny.org.
We’re also looking to fill several open board positions for 2025-2026, including Secretary, Treasurer, Grant Liaison, and Member at Large roles. Serving on the board is a great way to make a difference in public health and support our coalition’s mission.
Visit www.ImmunizeAllegheny.org to learn more about the roles and how to apply. Plus, if you’re not a member yet, it’s free to join—thanks to our generous grants!
American College of Surgeons
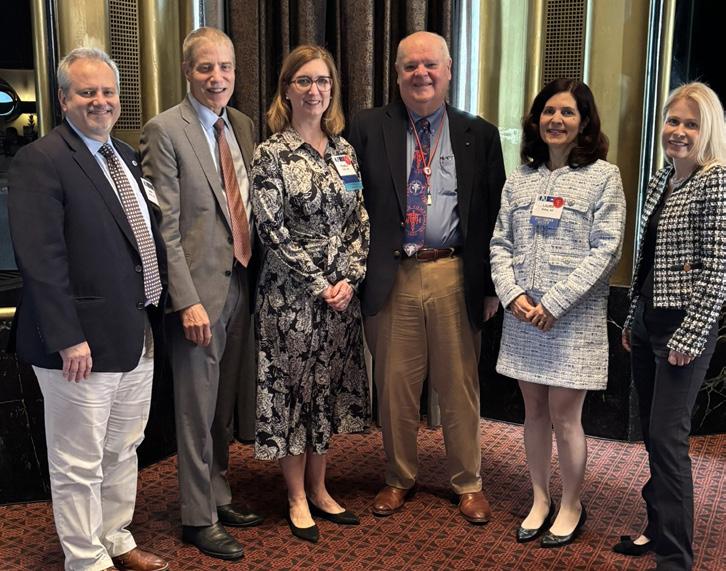
Southwestern Pennsylvania Chapter (ACS-SWPA) — 2025 President –Richard Fortunato, DO, FACS: The ACS-SWPA Chapter recently hosted the fourth annual Debates & Dilemmas Competition at the Kimpton Hotel
Monaco in Pittsburgh. This engaging event brought together top regional faculty to debate some of today’s most pressing surgical challenges, fostering professional growth and spirited discussion. Attendees enjoyed the opportunity to network while cheering on their colleagues as they competed for the prestigious D&D Trophy. We were honored to have a distinguished group of participants, including ACS-SWPA President Richard Fortunato, DO, FACS, and Treasurer Hiram A. Gonzalez, MD, FACS, as well as Struthi Ramanan, MD, Mathangi 'Maya' Chandramouli, MD, Muhammad Khizar Memon, MD, Meagan Derbyshire, MD, Kirsten Newhams, MD, and Abhijit Kulkarni, MD. Their expertise and dedication made the event truly memorable and showcased the impressive talent within our chapter.

Hiram Gonzales, MD, ASC SWPA Treasurer; Struthi Ramanan, MD; Maya Chandramouli, MD; Kirsten Newhams, MD; Abhijit Kulkarni, MD; Muhammad Khizar Memon, MD; Meagan Derbyshire, MD; Dr. Richard Fortunato, DO, ACS SWPA President
This was the first event in our threepart Resident Series. Be sure to save the date for the next session, "Most Interesting Cases," on May 28th. We extend our gratitude to all participants, attendees, and sponsors for making this event a success, and we look forward to seeing you at our next event!
Pennsylvania Geriatric Society Western Division (PAGS-WD) — 2025 President - Heather Sakely, PharmD, BCPS, BCGP: The 33rd Annual Virtual Clinical Update in Geriatric Medicine is almost here. All registrations close on April 19th. Join us on April 24-25, 2025, where we are focusing on the 5Ms of Age-Friendly care: Mentation, Medication, Mobility, What Matters Most, and Multi-Complexity. Attend from the comfort of your home or office and engage in an outstanding lineup of lectures and panel discussions. This AGS award-winning course is a collaborative effort between The University of Pittsburgh, the AGS state chapter, and leading healthcare organizations.
Visit pagswd.org to view the course brochure. Register today: https:// cce.upmc.com/33rd-annual-clinicalupdate-geriatric-medicine
For questions, please contact Haley Thon, Administrator, at hthon@acms. org. We look forward to seeing you there!
Spring Newsletter planning is underway. For content submissions please contact Haley Thon, Administrator, at hthon@acms.org.
The David C. Martin Award abstracts were due by April 11th. The committee is currently reviewing the submissions and will soon select the recipients.

The Pittsburgh Ophthalmology Society (POS) — 2024 President - Pamela P. Rath, MD: POS 60th Annual Meeting and 45th Ophthalmic Personnel Meeting Recap
The Pittsburgh Ophthalmology Society (POS) hosted its 60th Annual Meeting and 45th Meeting for Ophthalmic Personnel on March 21, 2025, at the Omni William Penn Hotel. Under the leadership of President Pamela P. Rath, MD, the event provided an engaging and educational platform for ophthalmologists, ophthalmic personnel, and industry professionals to exchange knowledge and network.
The meeting featured an outstanding lineup of speakers, headlined by the 44th Harvey E. Thorpe Lecturer, Ralph C. Eagle, Jr., MD. Dr. Eagle, Chief of Ophthalmic Pathology at Wills Eye Hospital and the Noel T. and Sara L. Simmonds Professor of Ophthalmic Pathology at Sidney Kimmel Medical College, delivered an insightful lecture titled "Masquerades, Misdiagnoses, and Therapeutic Misadventures." His presentation captivated attendees with its indepth analysis of complex ophthalmic pathology cases and diagnostic challenges.
Attendees also benefited from the expertise of distinguished guest faculty members: Kendall E. Donaldson, MD, MS – Rodgers Clark Endowed Chair in Ophthalmology and Medical Director at Bascom Palmer Eye Institute, Plantation, FL, who delivered a presentation on "The Future of Cataract
Surgery – A Path for the Next 10 Years"; Peter A. Netland, MD, PhD – Professor and Chair of Ophthalmology, Eastern Virginia Medical School, and Chair of Aniridia North America, who shared insights on "Management of Uveitic Glaucoma"; and Mark A. Rolain, MD –Professor of Ophthalmology at Oakland University/William Beaumont School of Medicine and Director of Refractive Surgery at Beaumont Eye Institute, who provided a Risk Management Update as part of OMIC’s presentation.
With over 78 physicians in attendance, the meeting fostered engaging discussions, knowledgesharing, and professional development opportunities. Attendees praised the high-caliber presentations and the collaborative atmosphere that made the event both informative and enjoyable.
The POS extends its gratitude to all speakers, attendees, and exhibitors for making the 60th Annual Meeting a tremendous success. We look forward to welcoming everyone again next year for another dynamic event.
Annual Banquet
Over 40 attendees gathered at Hotel Monaco for the POS Annual banquet During the presentation, outgoing President Pamela Rath, MD, expressed her gratitude to the members and Board of Directors for their support throughout her tenure. As her term concludes, Laurie Roba, MD, incoming President for 2025-2027, shared her enthusiasm for continuing the Society’s tradition of hosting outstanding guest faculty and preparing for the next Annual Meeting.
Dr. Rath was honored with an engraved presidential plaque and gifts as tokens of appreciation for her dedication and leadership. The evening was a fitting celebration of camaraderie and the Society’s ongoing commitment to excellence in ophthalmology.
45th Ophthalmic Personnel Meeting
The Society successfully hosted the 45th Annual Meeting for Ophthalmic Personnel on Friday, March 21, 2025, alongside the 60th Annual Meeting. This year’s event proved to be an
outstanding educational opportunity, bringing together ophthalmic professionals from across the region for a day of learning, collaboration, and skill enhancement.
Attendees had the opportunity to earn up to 7 IJCAHPO credit hours, pending final application approval. The program, directed by Dr. Avni Vyas, Dr. Cari Lyle, Dr. Jeffrey Wincko, and Dr. Gideon Nkrumah, delivered a robust lineup of sessions tailored to the needs of ophthalmic staff.
The meeting featured a stellar lineup of speakers, including Jane Shuman, MSM, COT, OSC, COE, and Dr. Mark Rolain. Ms. Shuman led an engaging two-hour Skills Workshop, providing attendees with hands-on training and practical insights. Dr. Rolain delivered an essential risk management course on behalf of the Ophthalmic Mutual Insurance Company (OMIC), emphasizing best practices for patient safety and liability prevention.
The course directors extend their deepest gratitude to its dedicated POS members who volunteered their time and expertise to deliver insightful lectures. Their contributions were instrumental in making this year’s event a resounding success.
The conference’s combination of general sessions and focused breakout discussions ensured that all participants, regardless of experience level, gained valuable knowledge to enhance their professional practice.
We look forward to seeing everyone again next year for another enriching experience at the 46th Annual Meeting for Ophthalmic Personnel!
