ENHANCING MENTAL HEALTH SUPPORT FOR
WORKERS
STRIVING FOR PERSONCENTRED CARE
THE ROLE OF GAMIFIED EXERCISE IN FALLS PREVENTION
THE QUEST FOR NEW OSTEOPOROSIS TREATMENTS




WORKERS
STRIVING FOR PERSONCENTRED CARE
THE ROLE OF GAMIFIED EXERCISE IN FALLS PREVENTION
THE QUEST FOR NEW OSTEOPOROSIS TREATMENTS


Welcome to the first issue of Aged Health for 2024. As I step into the role of editor, the aged care sector is in a state of evolution towards the concept of person-centred care.
In this issue we take a look at the feasibility of the proposed new Aged Care Act, with insights from aged care consultant Professor Rodney Jilek. According to Jilek, provisions in new Act that place the safety, health and wellbeing of aged care users at the heart of its requirements are a welcome move. However, he believes some care facilities may struggle to achieve compliance. Turn to page six to read more about the feasibility of the new Act.
Recent research conducted by the Violet Initiative found that nearly half of aged care workers exposed to death and dying are impacted professionally and mentally — but despite this, only 16% seek help, information or support. Kate Carnell AO, Chair of the Violet Initiative, takes a look at the importance of supporting workers as they care for residents reaching the end of their lives.
Other topics explored in this issue include gamified exercise and its role in falls prevention, high-quality dementia care and the quest for new osteoporosis treatments.
I welcome article submissions from our readers — so if you would like to offer any insights or expertise for future issues of the magazine, please do get in touch on the email address below.
Hope you enjoy this issue!
 Amy Steed Editor ah@wfmedia.com.au
Amy Steed Editor ah@wfmedia.com.au





Expand your comfort zone with this innovative and powerful design:
• Compact and Lightweight Lasts all day
• Ergonomically Designed
• Quiet

Caire provides everything you need for your oxygen therapy, from oxygen concentrators to accessories, we are dedicated to helping you breathe easy.

Combining portability with clinical efficiencygiving you the freedom to travel and enjoy life on the go:
• Compact and transportable Extended Battery Life
• Quiet
• 24/7 Use

Stationary oxygen concentrator that’s durable with a high continuous flow:
• Higher flow options for patients in hospitals or long-term care facilities
Dual flow option allowing two patients to use simultaneously Easy to service and maintain

A power efficient stationary oxygen concentrator is the must have for your home oxygen delivery needs:
Lightweight and easily transportable
• Low failure rate with no preventative maintenance schedule
Lockable flow meter caireaustralia.com.au



The Royal Commission into Aged Care Quality and Safety exposed a litany of complaints from aged care users in Australia, and was a wake-up call for policymakers and service providers throughout the sector, writes
AMY SARCEVIC.One key revelation was that the current Aged Care Act 1997 is no longer fit for purpose, given its lack of emphasis on the quality of life of service users.
“It is structured around providers and how to fund them — not about the people accessing services and what they need,” said a spokesperson for the Aged Care Quality and Standards Commission (ACQSC).
This has prompted the design of a new Aged Care Act, focused on the safety, health and wellbeing of older people.
This year, subject to it being passed by the parliament, Australian aged care providers, workers and subcontractors will have to abide by this new Act, which carries larger penalties and added consumer safeguards.
So, what does the new Act entail and how feasible will it be for aged care providers to meet its obligations?
The Royal Commission heard countless stories of aged care consumers having their dignity undermined through transactional rather than person-centred care.
Alongside allegations of abuse, people in residential aged care facilities were allegedly given nutrient-poor diets and inadequate dental care, and were subjected to demeaning practices around incontinence management.
In response, the new Act places the safety, health and wellbeing of aged care users at the heart of its requirements. These extend from peoples’ initial contact with aged care providers, right through to routine elements of daily care.
Aged Care Consultant Professor Rodney Jilek said these provisions are a welcome move, but is concerned about the sector’s capacity to meet person-centred interventions. >>
“Provisions of the Act around personcenteredness and individual rights are in conflict with the building blocks of the aged care sector, which is about providing basic care for the masses, at the lowest cost,” he said.
“In one way, this Act is trying to move aged care closer towards the NDIS, but without the resources and funding to do it. That will be a big struggle for providers, even those with the very best of intentions to be compliant.”
In fact, Jilek is concerned some of the provisions may do more harm than good, by robbing resources from direct care.
“The new Act looks great on paper. The reality is, the administrative burden on providers is getting larger and, without any increase in resources, I’m worried it will take attention away from where it is needed most: with the people who use the services.”
At best, the provisions are unlikely to create meaningful improvements, he said.
“We have seen this already with the 2023 mandate for sufficient nurse staff ratios. This sounded great, but the reform should have come in 15 years ago with an adequate buildup. Instead, we tried to go from zero to 100 in six months and wondered why we couldn’t meet the obligation — there was no workforce to pull from.”
That said, Jilek is pleased to hear that those who expose misconduct might be better protected under the new Act, given the legal repercussions whistleblowers sometimes face.
“If added whistleblower protections do come into effect, they will be very welcomed. It’s difficult for people to highlight problems or take action now, as everything is protected information. All reports from the Royal Commission are heavily redacted and bear little resemblance to the original SITE audit reports. So hopefully they do fix that,” he said.
Health Economist and Board Director Dr Stephen Duckett is more optimistic, claiming a small shift in management priorities could help providers meet their obligations.
IN ONE WAY, THIS ACT IS TRYING TO MOVE AGED CARE CLOSER TOWARDS THE NDIS, BUT WITHOUT THE RESOURCES AND FUNDING TO DO IT. THAT WILL BE A BIG STRUGGLE FOR PROVIDERS, EVEN THOSE WITH THE VERY BEST OF INTENTIONS TO BE COMPLIANT.

“It will require change — but not impossible change,” he said. “For example, at the moment, a lot of providers prefer the flexibility of having lots of part-time staff. But I think a person-centred approach will require permanent, full-time workers who can develop an ongoing relationship with consumers. And with wages on the increase this finally looks like a more reasonable prospect.
“The same applies for improving meals,” he continued. “We have all seen terrible pictures of food in aged care facilities. It doesn’t cost a lot to make more appetising food, especially now we have the funding mechanisms to support that. It just requires management to stop and think about who they are hiring for catering and how they might do things differently.”
The ACQSC acknowledges the challenges of meeting the new obligations, but said it is prepared to support the sector.
“We understand that the new Act represents a significant amount of change across the aged care system, and that providers and workers will need support to understand what this means for them. The department will continue to work closely with the aged care sector on this significant reform […].”










The Australian population is aging at an increasing pace, with over 65s expected to double and over 85s to triple in mere decades. To support and care for our aging population successfully, our precious aged care workers need to feel similarly supported and comfortable reaching out for help and support, writes
KATE CARNELL AO, Chair of the Violet Initiative.Recent research conducted by the Violet Initiative uncovered nearly half (41%) of aged care professionals exposed to death and dying are impacted professionally and mentally, but only 16% seek help, information or support — and nearly a third (29%) have considered leaving their occupation. Research respondents admitted that while caring for ill, old and frail patients was a rewarding experience, it also took a mental toll.
The number of deaths each year is predicted to double by 2040. It is no secret that aged care workers are overworked, overstretched and overstressed, which is resulting in significant workforce issues for providers nationally. Creating an environment where our aged care workforce is supported and protected will be key to caring effectively for Australians through the last stage of life.
Below are some considerations for aged care leaders to support staff effectively and, in turn, better care for the aging community.
Empowering staff to talk about death and dying, as well as the challenges they face when caring for their residents, is critical. It is equally important to establish policies that support workers outside of a professional environment, such as encouraging them to take leave regularly to rest, reset and reduce instances of burnout.
Aged care leaders could create an environment where open discussions around the mental health impacts of their roles are normalised and encouraged by establishing a peer-to-peer support group. This could create an environment where experiences and knowledge are shared to help aged care workers support each other and feel a sense of community.

Establishing a ‘buddy system’ whereby workers are paired together can also be beneficial and enable them to regularly check in and support each other.
Ongoing education can also help leaders support and protect their staff. Providing training and mental health education for workers to learn strategies to navigate grief, mental health challenges, improve their wellbeing and better communicate and care for their residents is invaluable.
Work delivered by the Violet Initiative over recent years has confirmed that many staff want to increase their capability, confidence and willingness to open and manage sensitive conversations about the last stage of life, to better support residents, family members, caregivers and other staff.

Spotting signs of stress and burnout in staff is vital to providing support promptly and effectively. Some warnings signs to be aware of can include: low productivity and lack of concentration, a noticeable lack of energy or exhaustion, or increased absenteeism. Leaders may also spot noticeable shifts in a staff member’s interactions with them, such as a change in their mood.
Implementing a ‘check-in policy’ whereby leaders meet regularly with staff to gauge their thoughts, experiences and be on the lookout for warning signs are important. From those conversations, strategies can be created to address burnout, fatigue and distress, such as offering reduced hours or leave, or access to internal or external initiatives to support them further.
It can be common for aged care workers to overlook their own grief when supporting a resident’s loved ones in the event of their death. Allowing staff to access existing, external initiatives to process grief and navigate

mental health challenges is just as vital as internal programs. Leaders can implement debriefing, counselling or confidential support services, provided by a third party.
Ultimately, government funding and support for initiatives designed to assist aged care workers is critical. Digital support, tools and resources, and the provision of dedicated hotlines (already established in countries such as the UK) are specifically designed to support healthcare workers, offering a listening ear and an opportunity to discuss challenges openly and without judgement.
Initiatives that use technology to offer roundthe-clock support are also emerging and can be utilised by aged care professionals. For instance, at the Violet Initiative, technology has been greatly beneficial to those who access the organisation’s services. The organisation has started implementing AI tools, including a ‘conversation with Violet’ which is always on, and always free, delivering information and advice 24/7, helping people access strategies and guidance to navigate challenges while caring for someone through the last stage of life.
A lack of preparation, discussion and funding for the last stage of life can result in dire consequences, including decreased workplace productivity due to unresolved grief, aged care workforce burnout and unplanned hospital admissions, increasing pressure on our already overstretched hospitals. Encouraging regular, open discussions about death and dying, implementing policies and initiatives, and accessing external programs are vital to keeping aged care staff healthy, happy and equipped to care for the aging community effectively.
IMPLEMENTING A ‘CHECK-IN POLICY’ WHEREBY LEADERS MEET REGULARLY WITH STAFF TO GAUGE THEIR THOUGHTS, EXPERIENCES AND BE ON THE LOOKOUT FOR WARNING SIGNS ARE IMPORTANT. FROM THOSE CONVERSATIONS, STRATEGIES CAN BE CREATED TO ADDRESS BURNOUT, FATIGUE AND DISTRESS.

Kate Carnell is Chair of the Violet Initiative, a national not-for-profit organisation that provides information, resources and support to help people navigate the last stage of life and grief. Previously, Kate has held positions as ACT Chief Minister, inaugural Australian Small Business and Family Enterprise Ombudsman (ASBFEO), CEO of the Australian Chamber of Commerce and Industry, CEO of beyondblue, CEO of the Australian Food and Grocery Council, CEO of the Australian General Practice Network (AGPN) and CEO of the National Association of Forest Industries (NAFI). Kate was appointed an Officer of the Order of Australia in 2006 for her services to the community through contributions to economic development and support for the business sector, knowledge industries, the medical sector and medical technology advances.







The introduction of the Improved Payment Arrangements added a substantial administrative burden to the already overstretched aged care workforce.
With every service event needing to be claimed individually, care managers are battling piles of untracked, and sometimes handwritten, invoices that need to be individually entered into their ERP, reconciled to the appropriate visit in AlayaCare, and claimed via Services Australia. A recent AlayaCare and Redmap survey found that 50% of aged care providers have three or more hands managing their invoices from receipt to entry into your home and community care software system and the ERP.
The consequences?
• Untracked invoices mean zero transparency for the care provider
• Stressed and over-worked care managers spending time on data entry instead of client care
• High risk of missing a Services Australia claim and being left out of pocket
• Difficulty locating specific invoices for any vendor enquiries
• Poor cashflow if not pre-booking care events
• Potential to forfeit the claim if the recipient has departed (under the 70-day rule) The changes have already seen providers large and small question the sustainability of continuing to service this market. It is imperative that the aged care sector adapt in order to continue to provide a high level of care to older Australians.
In 2022, RMIT-Cisco Health Transformation Lab released a report in response to the Royal Commission into Aged Care Quality and Safety. This report highlighted the critical role that technology and digitalisation have to play in transforming the aged care sector, emphasising the need to automate and streamline non-care duties.
In response to this clear need, AlayaCare and Redmap teamed up to develop an integrated accounts payable solution, specifically designed to support home care providers by automating reconciliation of vendor invoices to visits. Redmap Accounts Payable Automation can scan vendor invoices to extract the information (even if hand-written) and reconcile it to the booking event in AlayaCare. Plus, Redmap will check whether the vendor is registered for GST, ensure the invoice isn’t a duplicate, and verify the bank details against the system to minimise the risk of fraud.
This automated solution alleviates the administrative burden on care managers and your accounts department by reducing the process from invoice receipt to filing from seven steps down to one.
The governance and compliance benefits
Automating your accounts payable process has additional governance and compliance benefits. How long does it take your team to check the vendor’s bank details against the system, verify the dollar value against the
event booking, confi rm whether the vendor is registered for GST, confirm the invoice isn’t a duplicate, and manually enter the invoice into the system?
When you automate the process, not only are these steps completed instantly and automatically, but the team has visibility into committed spend against funding claims every step of the way. Eliminating the untracked invoices on people’s desks and within individual email accounts gives unprecedented insight into business cashflow. Redmap’s AP Automation also enables easy PTRS reporting with a feature that checks and tracks the invoice email receipt date, payment date and customer terms.
Supporting your team
A 2023 Aged Care Workforce Report from CompliSpace recently highlighted that “Almost a third of workers plan to quit within the next three years. Around half plan to quit within the next five. The top reasons for leaving are stress, excessive overtime/expectations and too much paperwork.”
It is imperative that the sector take steps to reduce this burden, and Accounts Payable Automation is one step organisations can take towards signifi cant effi ciency gains, leaving more time and resources to focus on providing better care to older Australians.




There is absolutely no doubt that aged care funding needs urgent reform. Starting to tackle the true issues around funding — including user contributions, sustainability and equitable funding for regional and remote providers — is a necessary and positive move. However, factors such as the right model of care, organisational culture, empowered people and correct workforce design, also play an important role in ensuring that providers can deliver the level of care we rightfully expect for older Australians, writes
CHRIS MAMARELIS, CEO of Whiddon.
In 2019, when called as a witness at the Aged Care Royal Commission, l spoke to the core premise of what we do at Whiddon — providing relationship-based care. We know the forming of these deeper and richer relationships between care recipients and caregivers is integral to the delivery of quality care.
It is an unfortunate reality that the current focus on mandated care minutes and 24x7 registered nurse requirements is directing the focus onto compliance, rather than driving quality care and truly meeting the needs of residents.
As a sector on the verge of significant reform, this marks an important inflection point. We must ask ourselves, is this driving the right behaviour — and the right incentives for providers — to create the best possible, person-centred care for our older Australians?
The most current aged care data released in the UARC Aged Care Sector Report draws attention to some serious risks to quality care.
More than 78% of providers are not currently meeting their mandated care minutes. In addition, they are struggling to comply with the 24x7 registered nursing requirements, particularly on overnight shifts. This has coincided with a dramatic 400% increase in the proportion of direct care time provided by casual third-party contractors.
As providers are required to direct more funding to care roles, which are becoming increasingly more cost-intensive, some providers may be forced to choose between meeting their care minutes through expensive agency staff and delivering other core supports such as wellbeing programs, hospitality and maintenance services.
l believe that what is of even greater importance than the conversation on the cost of casual third-party contractors is the impact on the delivery of quality care in a system that is becoming increasingly reliant on agency staff (quality over quantity).
Back in 2022, the Productivity Commission reviewed the quality effects of agency staffing in residential aged care. At the time, agency or contractor staff represented a small percentage of our total aged care workforce.
Whilst the report stopped short of any directions around caps on the use of agency staff by aged care providers, it did identify that providers with a greater reliance on agency care staff have “poorer quality, as perceived by residents”. It recommended that future research should assess the risks of using temporary workers versus having staffing shortfalls in terms of how it impacts quality care outcomes.
Given the drive to meet care minutes targets and a huge spike in the use of agency staff across the sector, it seems high time that this assessment is now a priority.
There is no disputing agency and contractor staff have an important role to play in aged care. ​ However, the difficulties created through intermittent work schedules, increased workload for permanent staff and the impact on resident relationships suggest contractors should be used as a short-term measure for staffing gaps — not part of our core aged care workforce. >>

This is even more relevant for our critical regional and remote homes, identified in the recent UARC report as already experiencing the highest rates of sustainability concerns. The reason these matter is because quality, continuous care means providing a pathway for older Australians to stay connected to their beautiful local communities, families and history.
It is well documented that these homes face far more challenges and costs in areas such as employment, transporting and sourcing food and supplies, maintenance and general support. If we are serious about quality care, we need to ensure we are throwing our support behind our regional and remote providers, to ensure local high-quality care is always an option.
So, what is required? How can we ensure that eagerly awaited reform and recommendations from the Aged Care Taskforce deliver on the primary goal of the original Royal Commission — quality care?
We need to work towards workforce design that supports and incentivises quality care. This may include exploring improved commercial arrangements with nursing agencies and contractors, at a global or industry level. Royal Commission Recommendation 87 speaks to safeguards to ensure that providers are prioritising permanent, direct employees. Given
this emerging issue, is it time for the Commonwealth to consider regulating the labour hire sector attached to aged care?
What is clear is that continued investment in our workforce is critical to ensure that our direct and indirect care employees are fully empowered, remunerated and rostered in a way that supports relationship-based care.
Rather than directing funds towards a mandated compliance model, let us invest directly in the people caring for our elders with improved clinical training, dementia education, digital literacy, leadership and wellbeing programs. Further, and given the influx of overseas workers, directing funding to support those transitioning to working life in Australia is another key area that will enhance our services. The priority for regulators and providers alike needs to be holistic, person-centred care rather than perpetuating the battle between providers to simply fill rosters. Are older Australians genuinely benefiting from this?
It’s also about regulating agencies further to stop price gouging and working collaboratively across health, NDIS and aged care to address our shared challenges, such as increased competition, compliance burden and workforce retention.
And finally, reviewing our supports for regional and remote care of older Australians needs our unwavering commitment and attention. With over 34% of Australians living in rural or remote areas of Australia, it is incumbent on current providers and the government to work together to improve the sustainability of our care offerings in these communities.

Chris Mamarelis is the Chief Executive Officer at Whiddon, a not-for-profit aged care organisation caring for close to 3000 people through residential aged care, community care and retirement living. He leads a team of over 2500 employees.

The telemedicine trend is exploding, with virtual consult & services being the most well-known and popular among patients. Telehealth consults occur in Care Facilities, Hospitals and at Home in all locations from Major cities to the remotest locations across Australia and the Pacific Region.
What is telemedicine (or telehealth)? There are several definitions, but they all point to the same general idea: Telemedicine is the transfer of medical information from one site to another via electronic communications to improve patients’ health outcome.
Patients and Care Givers have embraced telemedicine enthusiastically and here’s why:
1. They can access care easily from a tablet, smartphone or computer, meeting through a safe, secure, and confidential video connection. Surveys show that patients are just as satisfied with a virtual face-to-face visit as a live one.
2. Patients can connect with a qualified health care provider right away, and get a diagnosis
and treatment as needed. Some tests can even be conducted during a virtual visit and prescriptions can be ordered afterwards.
3. Patients get convenient care, when and where they need it, without the hassle of driving or waiting to be seen. Virtual consults can be available seven days a week, for extended hours if required.
4. In addition to being fast, easy, and flexible, virtual consults are more affordable. Ergotron combine the power to support onboard diagnostics and videoconferencing with Ergotron’s Mobile Carts and Wall Mount Solutions. Healthcare organizations can rely on Ergotron’s more than 30 years of expertise and service to build a solution that matches their needs and budget. Visit our website https://www.ergotron.com/ en-au/markets/healthcare
Alternatively reach out to your local Ergotron representative for an independent consultation. Email: robin.burgess@ergotron.com Mobile +61421080303


Not-for-profit aged care provider mecwacare's $40 million Simon Price Centre in Mont Albert North in Melbourne, with a capacity for 100 residents, is officially open.
The non-denominational provider has been caring for vulnerable Victorians since 1959 and now cares for more than 20,000 people each week through its network of aged care and disability services.
The Simon Price Centre is mecwacare’s 18th facility and is its most advanced residential care centre to date, connecting residents to round-the-clock high-quality care and services delivered by specialist staff.
As part of the carefully planned design, car parking and hospitality services are located on the lower ground level to minimise the impact on the surrounding green environment. The facade nestles into the street at the north-west end — an effect enhanced by two glorious eucalypts standing majestically on the corner. The presence of native trees at both the front and rear setbacks showcases the thoughtful landscape design of the property.
The centre, with an ‘aging-in-place’ approach, differs from other facilities in that it offers a number of suites where resident couples can live together in a studio-style apartment. Residents also have access to an onsite cinema, hair and beauty salon, private dining space, library, wine bar and cafe.
An extensive lifestyle program is complemented by the scientific benefits of pet therapy. Courtesy of visits from local volunteers and their pets, residents may experience improved cognitive function; reduced levels of depression, anxiety and loneliness; lower levels of agitation and confusion; and improved mood and lucidity. >>
Chipo Nyemba, mecwacare’s Regional Manager for Melbourne, believes people’s deep trust in the care and services provided to their loved ones at the Simon Price Centre sets the organisation apart.
“I started working in aged care 16 years ago, after my dad started needing aged care. My motivation was that I wanted things done right, and I’ve stuck to that every day of my career since,” Nyemba said.
“My role with mecwacare enables me to keep that promise I made myself — I’m proud to now be delivering it the residents who call our facilities home.”
The facility’s first resident, Elaine, believes that the standard of care and facilities provided at the Simon Price Centre is unparalleled.
“The care I get here has helped put me and my family at ease, and is the best thing about this place,” Elaine said.
“I receive attentive care and we know I am in good hands — it makes me feel special.
“Previously, my condition meant that I was struggling to maintain weight with a healthy diet… since moving in here with mecwacare, my recovery has improved. The food here is really helping with that and I’m looking forward to enjoying the full menu.”
The new facility is named after the late Simon Price OAM, a long-serving Board Member and Life Governor of mecwacare. Price and his late wife Jane were significant contributors to the mecwacare community for many years, and the centre has been named in honour of his selfless commitment to serving vulnerable Victorians..



“THE CARE I GET HERE HAS HELPED PUT ME AND MY FAMILY AT EASE, AND IS THE BEST THING ABOUT THIS PLACE,” ELAINE SAID.
The Smileyscope virtual reality technology solutions are aimed at reducing a patient’s pain, stress and anxiety when having common medical procedures, such as blood tests, vaccinations and medical imaging.
The company’s digital headsets change potentially stressful environments, such as hospitals and clinics, to relaxing virtual locations, like underwater worlds full of colourful fish.
By using virtual reality technology to make needle procedures less scary for children, procedures could be completed faster and without the need for sedation or rescheduling appointments. This could help children get access to the treatment they need without delay.
Smileyscope’s headsets are medical grade and fully wipeable, which means they can be used in acute care settings from an infection control point of view. They are lightweight and can be used by children as young as four years old.
Smileyscope
www.smileyscope.com.au

Galvin’s simple and smart bathroom solutions for safety and water and temperature monitoring have been developed with comfort, care and convenience in mind. They are designed to help increase autonomy and dignity for older people without compromising safety and functionality.
The tapware features touch-free sensors, thermal disinfection, hygiene flush feature and smooth tubular spout for easy cleaning and to minimise bacteria growth both internally and externally. The grab rails and accessories are architecturally inspired.
Galvin Engineering Pty Ltd
www.galvinengineering.com.au

Lenexa Medical’s LenexaCARE is a fabric-based sensor technology paired with AI software that monitors patient position and pressures in real time to enable personalised pressure injury prevention.
The solution is designed to continuously monitor the patient’s position and presence, as well as their high-pressure areas, ultimately providing real-time, patient-specific, non-subjective data to guide clinicians and carers to deliver quality care.
LenexaCARE is designed to minimise patient suffering and also assist clinicians and reduce the burden on the wider healthcare system.
Lenexa Medical
www.lenexamedical.com


Falls in older people can be reduced by gamified step exercises, a large randomised control trial has found.
With a steadily aging population, the researchers say scalable and effective fall prevention strategies are needed to address the growing impact of falls in the community.
A trial conducted by a team of Neuroscience Research Australia (NeuRA) and UNSW researchers made use of smart±step, an exercise gaming console that anyone can use without requiring assistance from a therapist. smart±step is connected to a television screen, and once a game of choice is selected, it requires the person to step on target panels on a step mat, just like one would with a game controller.
During the trial, it was found that those over the age of 65 who participated in these at-home gamified step exercises were less likely to suffer a fall. In fact, the number of falls was reduced by 26% when compared to a control group. The results of the trial were published in Nature Medicine
“Regular balance-challenging exercise is effective at preventing falls, so we tried to make exercise fun and easy to do,” said Dr Daina Sturnieks, lead author of the study and Senior Research Scientist at NeuRA and UNSW Sydney.
769 people over 65 — all living in the community — participated in Sturnieks’ study. They were asked to do smart±step exercise games for 120 minutes per week over the course of 12 months. Participants reported their falls over this period and this data was compared to a control group, who only received a public health pamphlet about preventing falls.
Over the 12 month-study period, participants who received the exercise intervention showed significantly fewer falls compared to the control group: 36% of the exercise group had a fall in the study period, whereas 48.2% of the pamphlet group had a fall.
While these results are encouraging, the researchers said one limitation of the research was that the sample primarily consisted of well-educated and high-functioning older people.
“The findings cannot be generalised to frailer older people,” the researchers said.
“Furthermore, participants were not blinded to their intervention, therefore the level of expectancy for preventing falls may have differed between the groups, which may contribute to a placebo effect that might impact the findings.”
One in three people over the age of 65 living independently will experience a fall every year. Falls are a significant public health issue, contributing to mobility-related disability and loss of independence, and they are also the second leading cause of unintentional injury deaths worldwide.
The best evidence for fall prevention in the community is balance-challenging exercise, according to Sturnieks.
“We’ve known for a long time that, if done correctly and consistently, balance-challenging exercises can prevent falls. But the problem is that often people don’t keep up with their exercises because they can get boring very quickly,” she said.
This led Sturnieks and the team at the Falls, Balance and Injury Research Centre at NeuRA to explore the idea of gamifying the balance exercises.
“People get addicted to games because they are fun and they become motivated to beat their high score and just get lost in the game,” she said.
WE’VE KNOWN FOR A LONG TIME THAT, IF DONE CORRECTLY AND CONSISTENTLY, BALANCECHALLENGING EXERCISES CAN PREVENT FALLS. BUT THE PROBLEM IS THAT OFTEN PEOPLE DON’T KEEP UP WITH THEIR EXERCISES BECAUSE THEY CAN GET BORING VERY QUICKLY.
The advantages of smart±step exercise games — or exergames — go beyond physical exercise benefits: people are also undertaking cognitive training, which is easily incorporated into these games.
“These exergames require people to think quickly, unlike traditional exercise programs where you often just go through the movements,” Sturnieks said. The smart±step exergames involve stepping on a mat, which acts as a controller.
The exergames vary in content and range, from collecting treasures to stomping on moving cockroaches or avoiding obstacles. Overall, the games require timely movements and quick thinking to keep up.
“Exergames are like a two-in-one: you get physical benefits but also you are keeping yourself cognitively challenged, which is good for the brain and healthy aging. Plus, it’s fun!”





Sandra Osborne’s long-time passion to become a nurse started right from the time she was in high school.
Now Director of Care Services at Whiddon Grafton, Sandra’s enthusiasm for nursing was realised during Year 10 at school. She applied for work experience at the local hospital, spent two weeks working there and already knew by that stage that she wanted to be a nurse. After finishing Year 12, she then moved from her hometown of Grafton to Brisbane to study as a pupil enrolled nurse at the Royal Brisbane Hospital.
“This time away from home gave me life skills as well as a varied knowledge of nursing care for all situations including emergency, surgery and public relations,” said Sandra said.
“After completing my course and becoming registered with Ahpra, I moved back to my hometown in the hope of getting work at our local base hospital.
“I decided to widen my options and I was encouraged by family to apply at a local aged care home — known then as Livingstone House (Frank Whiddon Masonic Homes).”
Sandra personally canvassed the home, dropping her resume in on a Thursday. By Friday, she had already received a call.
“They were impressed with my resume and qualifications, and I was asked to start work on the Saturday afternoon,” Sandra said.
This was 35 years ago — but, to this day, Sandra is still working with Whiddon. The company has supported her career into management roles, from Deputy Director to Director of Care Services.
“I can clearly remember my very first shift as though it was yesterday,” Sandra said.
“I was met at the front door by one of the female residents who showed me to the staff area. She then took me to the registered nurse on duty, stating as she left to ‘Make sure you are at my room promptly at 7 pm to put me in my night attire and tuck me into bed’. This comment was the first of many during my nursing years. After 35 years with Whiddon, there are so many stories to tell!”
Sandra has also seen a considerable number of changes in the aged care sector during these years. However, the one thing that hasn’t changed — and the main reason she has remained working in aged care — is the residents.
“Being involved with the residents and being an aged care nurse means that I can make a difference in someone’s life,” Sandra said.
“Being able to become a part of their family and they, ours. To listen to their stories and share in their life stories. This interaction is so heartwarming — even just having the ability to put a smile on somebody’s face.”
Sandra starts her day with a catch-up with her clinical staff. This involves a focus on the wellbeing of all residents, and making sure the roster has the correct skills mix with care staff for each of the facility wings.
“I stop and chat with any resident who is up and about. By 10 am, our residents have made their way to our activity room and this is where I have the time to interact with most of our residents,” Sandra said.
“There is usually a bit of singing and lots of laughter. I always have an open door for staff, residents and their families.
“It is a privilege for me to be a part of a resident’s journey during their stay with us. In particular, providing comfort and being with them at the end of their journey is both emotional and special. To give support to their family in their difficult time to say goodbye. It has had a huge impact on my own life and values — and it has made me the person I am today.”


Dementia prevalence in the community and residential aged care is significant. We know 68.1% of aged care residents have moderate to severe cognitive impairment and two in three of the 421,000 Australians with dementia live in the community, writes
With this high prevalence, everyone working across the healthcare industry, including health, aged care and disability, ought to be receiving compulsory education about dementia to increase their understanding, knowledge and skills in dementia care.
When people living with dementia receive care from professionals that have completed dementia education, there are fewer incidents of changed behaviour and people living with dementia have a more consistent experience of quality care.
We know dementia education leads to a reduction in high-risk incidents, lower rates of inappropriate medication use and more positive staff attitudes and morale, which ultimately results in better service delivery and quality of life for people living with dementia.
MAREE McCABE, CEO at Dementia Australia.
Dementia Australia is focusing on implementing change in the following areas:
• Dementia support pathways: People living with dementia, their families and carers must have optimal access to the integrated services and supports they need to live the life they choose.
• Building workforce capability: The workforce, leadership and culture must understand and support dementia and have the skills and knowledge to sustainably embed quality dementia care.
• Dementia-friendly design: Physical environments must support people living with dementia to be as independent as possible.
All of these things are underpinned by people living with dementia placed firmly at the centre.
With a longer-term focus and vision that includes dementia specialisation in all pathways to nursing and aged care qualifications, we can ensure aged care and dementia will become a more appealing career to pursue for healthcare professionals and will attract the qualified staffing numbers needed for the future.
In the short term, upskilling the current workforce using existing education tools from the Centre for Dementia Learning at Dementia
Australia will begin to alleviate some of the pressures and challenges of caring for someone living with dementia.
Educating the workforce has been the focus of the Centre for Dementia Learning for a number of years and four Leadership and Practice Change education programs for care workers have recently been launched.
These programs will deliver engaging education to build the dementia capability of future leaders in the sector, as well as creating lasting change through leadership and culture change that in turn promotes improved behaviours, attitudes and care practices for all care workers.
Strong leadership in aged care is fundamental to the delivery of high-quality dementia care. It
was recognised as a critical element of sustained practice improvements by the Royal Commission into Aged Care Quality and Safety, and in response, also by the federal government.
At the heart of these programs, the Centre for Dementia Learning works to engage, enable and empower participants to develop real insights into what it is like to live with dementia, and in so doing, change their attitudes and behaviours — which in turn transforms their practice.
The sooner the aged care workforce is accessing appropriate dementia care education and training the sooner we will begin to see the changes needed to improve the health, lifestyle and care outcomes for people of all ages living with all forms of dementia, their families and carers. We know from our work and broad consultation with people living with dementia, their families and carers that if we get quality care right for people living with dementia then there will be quality care for all. Maree McCabe is the CEO of


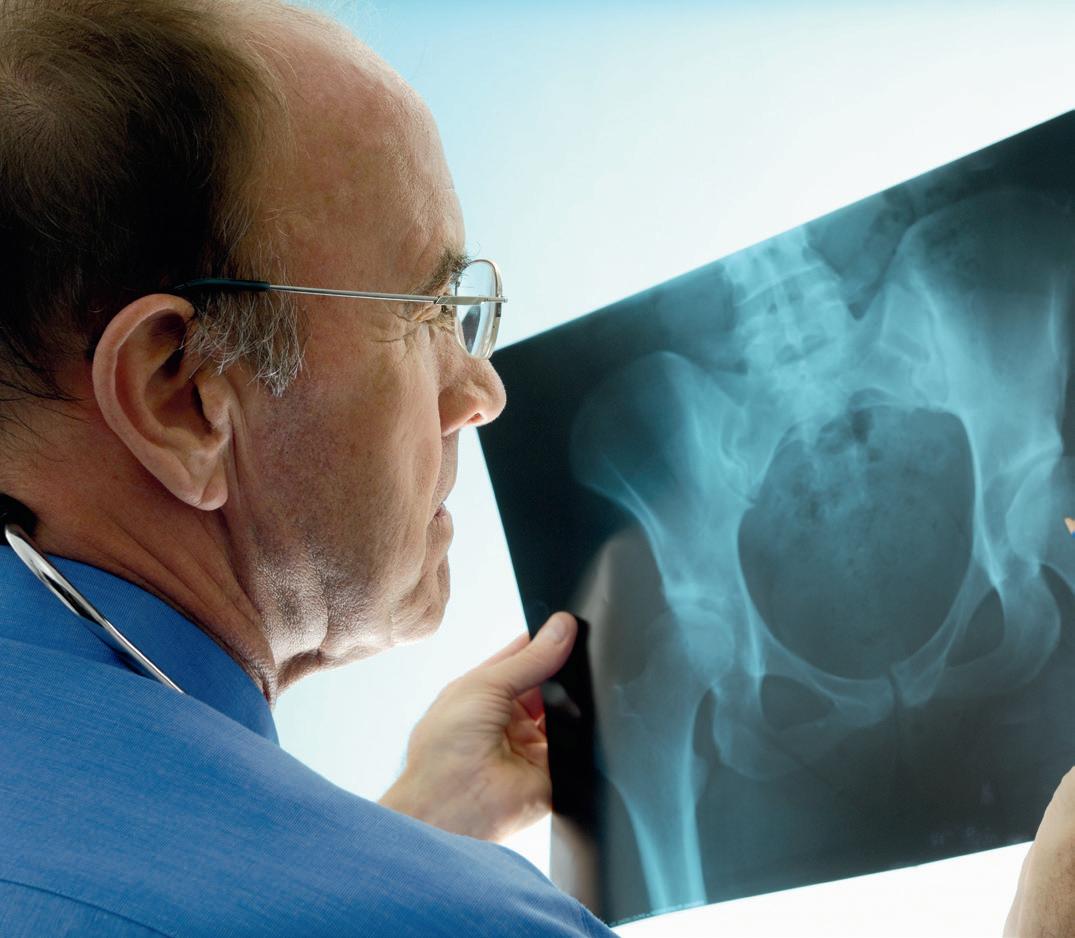
Astudy to be undertaken by Mater researchers may yield some new ways to treat osteoporosis.
Osteoporosis — a disease in which the skeleton becomes fragile and prone to fracture — is one of Australia’s most common chronic diseases, affecting more than 1.2 million people.
Half of all women over 50 will suffer an osteoporosis-related bone fracture, and a quarter of those who suffer a hip fracture are likely to die within six months.
The National Health and Medical Research Council announced that it will award more than $1.58m to Mater Research to conduct the largest genetic association study of bone mineral density on hundreds of thousands of individuals.
Dr John Kemp, Mater Research’s Musculoskeletal Genomics Group Leader, said medicines used to treat osteoporosis can slow bone loss, and in some cases partially restore lost bone. However, a cure for osteoporosis has not yet been found.
“Osteoporosis remains a major health burden for society and considerable scope exists to identify and develop new therapeutics that can restore lost bone,” Kemp said.
“Development of new therapeutics for osteoporosis has been hampered by a limited understanding of the genes that control bone, as well as the different cell types in which they function.
“Our study is likely to identify cellular and genetic mechanisms that control bone and prioritise those that can be targeted by new therapeutics to restore the structural integrity of bone.”
Kemp’s team will also develop a web-based platform that will allow the international research community to explore their data.
“Knowledge sharing is key to accelerating the development of new therapeutics for osteoporosis,” he said.
Acting
Art
Art/Production:
Copy
Advertising
PUBLISHED
22 152 305 336
www.wfmedia.com.au
Head Office
Unit 5, 6-8 Byfield Street, North Ryde Locked Bag 2226 North Ryde BC NSW 1670
AUSTRALIA ph: +61 2 9168 2500
If you have any queries regarding our privacy policy please email privacy@wfmedia.com.au
Subscriptions for unregistered readersprice on application
The magazine you are reading is just one of 11 published by Westwick-Farrow Media. To receive your free subscription (magazine and eNewsletter), visit the link below.