NEWS AND NOTES

The Michigan Institute for Imaging Technology & Translation (MIITT) is on a mission to improve standard MRI methodologies utilizing cutting-edge research. Working within the radiology department gives MIITT researchers a first-hand look at the challenges radiologists are facing when reading MRI scans.
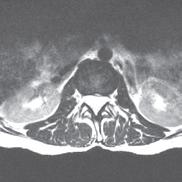
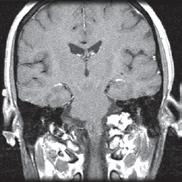
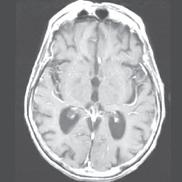
“When using standard MRI approaches, we are limited to brighter and darker shades of gray,” says MIITT co-director, Nicole Seiberlich, PhD, Research Professor of Cardiovascular Imaging and Associate Professor of Radiology. While radiologists are both skilled and experienced at reading and interpreting these images, introduction of a numerical measurement technique eliminates subjectivity, providing readers with specific data. “With our proprietary method, Magnetic Resonance Fingerprinting (MRF), radiologists can acquire quantitative data on multiple important properties simultaneously, which improves the accuracy of the diagnostic information. These quantitative tissue property maps include actual numbers that give experts reproducible and actionable results. It has been evaluated in brain, prostate, liver, cardiac, and musculoskeletal imaging.”
“Our goal is not only to solve immediate problems but also to develop long-term solutions for radiologists by converting technically feasible research methods into clinically useful tools,” adds Dr. Seiberlich, who co-founded MIITT in July 2019. In 2023, MIITT received the Dean’s Award for Technology and Innovation, recognizing their unique approach to technology development and translation.
It is truly my pleasure to update you on some of the many exciting things happening in our department. We continue to engage in robust clinical expansion, adding hours, sites of service, and new service lines. (Learn more about the scale and scope of our operation in the article and infographic in this edition.) Radiologic imaging and intervention are the daily work of the majority of our 1700+ member team, and we are proud of our outstanding service to patients and the medical community. Our clinical work also provides a firm foundation for growth and innovation in research and education. While we are actively engaged in present day clinical work, we are also making the discoveries that will enable future excellence in the field, and training the technologists, clinicians, and scientists who will lead us in the future.
This edition of our newsletter highlights several of our research and clinical collaborations, and introduces readers to a new educational outreach project: The Radiology Vault. Read on to learn more about how we are expanding the reach of Michigan Radiology, and stay engaged with us throughout the year. We welcome feedback and updates from our alumni, and would love to profile more of you in our future newsletters.
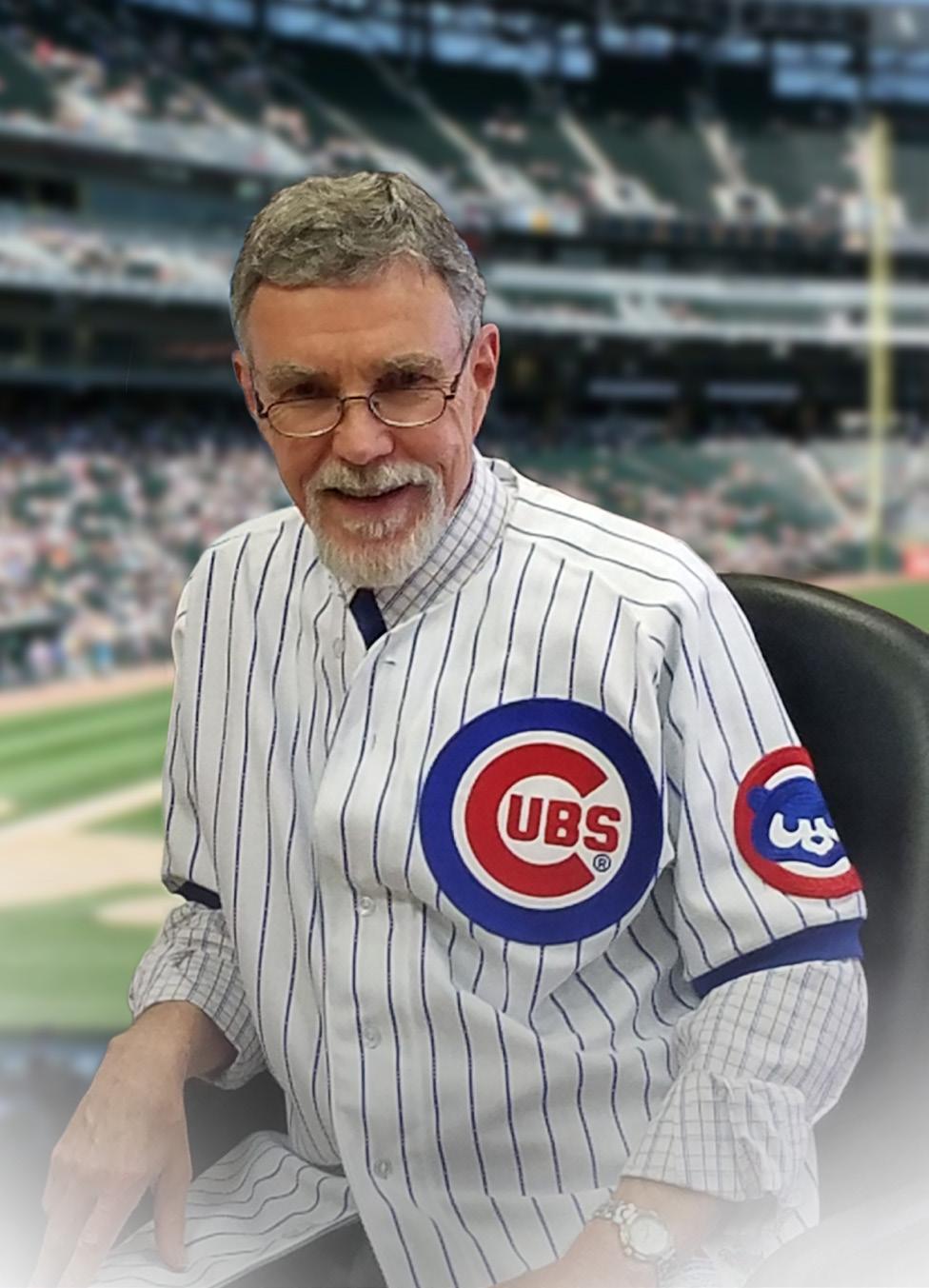
It has been an honor to succeed N. Reed Dunnick, MD as the Fred Jenner Hodges Professor and Chair of this department. Dr. Dunnick has remained deeply engaged with our department and has been a generous advisor to me and other leaders since stepping down as chair in 2019. After an energetic second career as Editor-in-Chief of Academic Radiology, Dr. Dunnick has elected to retire in earnest, and we had the opportunity to celebrate him as a department this summer. His impact on the field of radiology cannot be overstated, and his accomplishments are outnumbered only by his grateful mentees.
We look forward to continuing to see him at departmental gatherings. He is also working with Dr. Jim Ellis on writing the history of our department, and I look forward to learning more from his efforts!
Sincerely, Vikas


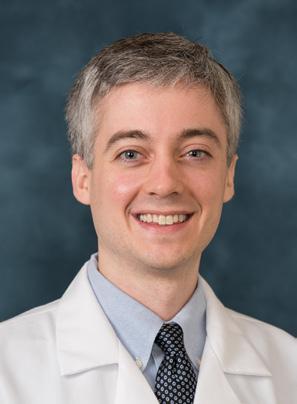
Nathan Amann, MD
Medical School
Case Western Reserve University
Favorite Thing
Bass fishing and exploring new restaurants
Devon Clark, MD
Medical School
University of Rochester
Favorite Thing
Catching up with family, I have a standing call with my grandparents every Thursday night!
Rylee Friel, MD
Medical School
Indiana University
Favorite Thing
Reading and baking
Emily Fuller-Lechton, MD
Medical School
University of Iowa
Favorite Thing
Running, hiking, reading
Sanja Ghanshani, MPH, MD
Medical School
Wayne State University
Favorite Thing
Enjoying the outdoors with my husband and our dog
Chance Hebert, MD
Medical School
Louisana State University
Favorite Thing
Going outside to touch grass or find a body of water to stare at
Andrew Holmes, MD
Medical School
University of South Dakota
Favorite Thing
Enjoying the outdoors (such as hiking, running, cycling) with my wife, McKayla, and our two dogs, Nora and Theo
Alex Landschulz, MD, MS
Medical School
University of Michigan
Favorite Thing
Enjoying the outdoors and spending time with friends
Samantha Scott, MD
Medical School
Albany Medical College
Favorite Thing
Being outside on a long walk or hike
Amir Mostafavi Sterabadi, MD
Medical School
Texas Christian University
Favorite Thing
Trying new restaurants, spending time with friends and family, fishing
Hanna Thompson, MD
Medical School
University of Louisville
Favorite Thing Baking
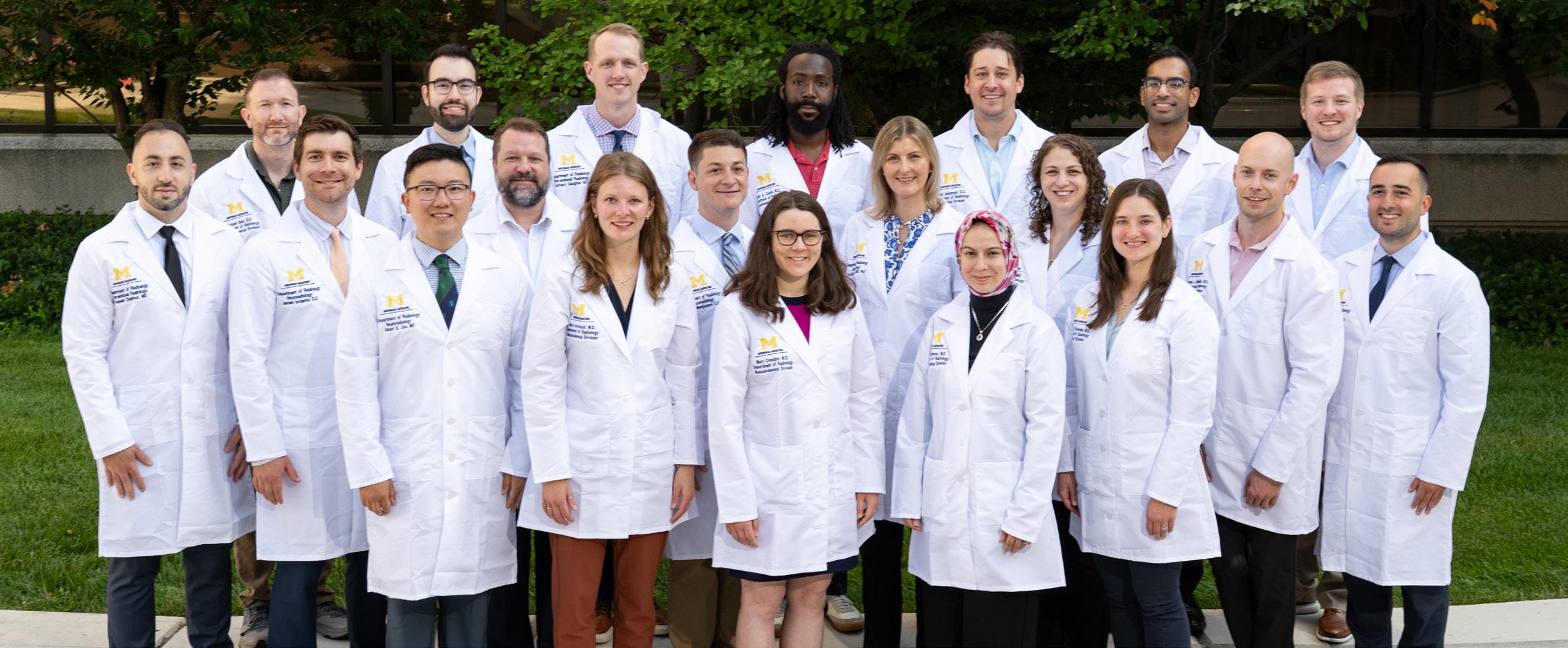
Third row: Michael Bair, DO (Musculoskeletal); Orlin Sergev, MD (Neuroradiology); Zachary Gaughan, MD (Interventional Radiology Independent); Mark Cooks, MD (Abdominal); Alex Jessmore, DO (Abdominal); Kevin John, MD (Neurointerventional); Michael Ramalia, DO (Abdominal)
Second row: Hussein Chahrour, MD (Interventional Radiology Independent); James Iordanou, DO (Neuroradiology); Nicholas Rasmussen, MD (Musculoskeletal); Mark Manganaro, DO (Neuroradiology); Jennifer Hayes, MD, PhD (Neuroradiology); Antigone (Annie) Mitchell, MD (Abdominal); Steven Machusko, MD (Abdominal); Luke Odisho, MD (Neuroradiology)
First row: Albert Jiao, MD (Neuroradiology); Alexa Arvidson, MD (Musculoskeletal); Mary Creedon, MD (Musculoskeletal); Mariam Salman, MD (Breast Imaging); Raelynne Shanker, MD (Abdominal)
Not pictured: Anjelica Abate, MD (Breast Imaging); L. Jordan Breyfogle, MD (Interventional Radiology Integrated); Nathan Loudon, MD (Interventional Radiology Integrated); Laura O’Donohue, MD (Pediatric); Lisa Philips, MD (Cardiothoracic); Madhusudan Reddy, MD (Nuclear Medicine)

Effie Adjei, MD
Assistant Professor
Abdominal Radiology/Nuclear Medicine from University Hospitals
Cleveland Medical Center
Cleveland, OH
Reve Chahine, MD
Assistant Professor
Abdominal Radiology from Michigan Medicine (Fellow)
Ann Arbor, MI


James Frencher, MD, PhD
Assistant Professor
Vascular & Interventional Radiology from UMass Chan Medical School
Worcester, MA
Xhorlina Marko, MD
Assistant Professor
Vascular & Interventional Radiology from Henry Ford Health
Detroit, MI
Marisa Martin, MD
Assistant Professor
Abdominal Radiology
from University of California San Francisco San Francisco, CA

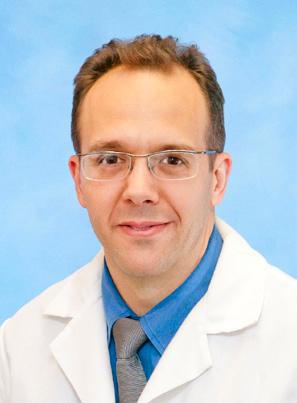
Jon Jacobson, MD
Professor
Musculoskeletal Radiology from Lenox Hill Radiology/RADNET
New York, NY
Sean Miller, MD
Assistant Professor
Nuclear Medicine
from Michigan Medicine (Fellow in Radiation Oncology) Ann Arbor, MI

Tayson Lin, MD
Assistant Professor
Emergency Radiology from Michigan Medicine (Fellow)
Ann Arbor, MI
Rajashree Vyas, MBBS
Instructor
Community Radiology from Desert Radiology Las Vegas, NV

Matthias Wilms, PhD
Assistant Professor
Computer Aided Detection and Artificial Intelligence
from University of Calgary Calgary, Alberta, Canada






Yuni Dewaraja, PhD
Honored with the Hal Anger Lectureship Award by the Society of Nuclear Medicine and Molecular Imaging (SNMMI)

Ansel Hillmer, PhD
Named Vice President-Elect for the SNMMI Brain Imaging Council, and a 2025 Distinguished Investigator by the Academy for Radiology & Biomedical Imaging Research
Prabesh Kanel, MS, PhD
Received grant funding from the Michael J. Fox Foundation


Oliver Kripfgans, PhD
Named a 2025 Distinguished Investigator by the Academy for Radiology & Biomedical Imaging Research
Gary Luker, MD
Installed as N. Reed Dunnick Research Professor, U-M Radiology

Gunjan Malhotra, MD
Named Radiology Faculty Lead for M2 Education in Surgery and Applied Sciences
Katherine Maturen, MD, MS
Appointed as Associate Chair for Communication and Development, U-M Radiology
Mishal Mendiratta-Lala, MD
Named to the Society of Advanced Body Imaging (SABI) Board of Directors
Douglas Miller, PhD
Received Fry Award for lifetime achievement from the International Society of Therapeutic Ultrasound (ISTU)
Shruti Mishra, MD, PhD
Received grant funding from New Investigators Award Program (NIAP), a collaboration between the Alzheimer’s Association and the National Alzheimer’s Coordinating Center (NACC)
Venkatesh Murthy, MD, PhD
Received Masters of ASNC (MASNC) designation from the American Society of Nuclear Cadiology (ASNC)

Brian Ross, PhD
Appointed as Associate Chair for Innovation, U-M Radiology





Peter Scott, PhD
Named Fellow of the World Molecular Imaging Society and appointed as Associate Chair for Basic Science Research, U-M Radiology
Judy Sebolt-Leopold, PhD
Named a 2025 Distinguished Investigator by the Academy for Radiology & Biomedical Imaging Research
March 2 – 6, 2026
Arizona Biltmore, A Waldorf Astoria Resort Phoenix, AZ
Kimberly Shampain, MD
Appointed as Division Director of Abdominal Radiology, U-M Radiology
William Sherk, MD
Appointed as Division Director of Vascular & Interventional Radiology, U-M Radiology
Benjamin Viglianti, MD, PhD
Appointed as Division Director of Nuclear Medicine, U-M Radiology
Ashish Wasnik, MD
Appointed as Associate Chair for Faculty Affairs, U-M Radiology
Michael Zintsmaster, MD
Named Clinical Content Director at the American Educational Institute (aeiseminars.com), expanding CME offerings in Radiology and other medical specialties
This five-day course will provide a broad overview of selected radiology/imaging subjects of particular importance to diagnostic radiologists in clinical practice. A broad range of lecture topics, with emphasis on practical applications, will be presented. Topics will include, but are not limited to: breast imaging, musculoskeletal, thoracic, abdomen, MRI, CT, nuclear medicine imaging, ultrasound, and neuroradiology.
Janet Bailey, MD Breast Imaging
Remy Lobo, MD Neuroradiology
Mishal Mendiratta-Lala, MD Abdominal Radiology
Smita Patel, MD Cardiothoracic Radiology
Joel Platt, MD Abdominal Radiology
Samer Soussahn, MD Musculoskeletal Radiology
Benjamin Viglianti, MD, PhD Nuclear Medicine
The University of Michigan Department of Radiology gathered with pride and gratitude this summer to celebrate the career and retirement of our chair emeritus, N. Reed Dunnick, MD. We have had the honor of working with a true luminary in our field, who wrote seminal manuscripts and textbooks and led most of our major national organizations, impacting thousands of radiologists and ultimately their patients.
Despite his fame and well-deserved accolades, Dr. Dunnick remains unchanged -- modest, steady in his habits, and motivated by the success of others. He knows the value of being present and has shown up for his department in every possible venue: walking through radiographer work areas, attending morning conference, making time to see a resident’s first scientific abstract presentation, and traveling to witness a faculty’s gold medal award or honorary professorship. He has demonstrated and promoted the value of volunteerism in radiology, encouraging and sponsoring us to participate and lead in local and national organizations, enhancing both the reputation of the department and the careers of its members.
Dr. Dunnick’s legacy in our department lives in its infrastructure, finance, culture, and most importantly its people. In retirement he plans to continue to support our mission by assisting with fundraising and development, as well as writing a book on the history of the department. We wish him every happiness in the next chapter!





Expanding acc E ss and pati E nt-c E nt E r E d car E across s outh E ast Michigan
The demand for clinical imaging services has never been higher, and our department continues to grow, both in the size of our team and the number of sites of service. This includes new facilities “on the hill” and in our communities, and extended hours for advanced imaging at existing sites. The continued expansion illustrates the department’s commitment to equitable, high-quality, and patient-centered care.
t roy cE nt E r for s p E cialty c ar E: c oM pr E h E nsiv E outpati E nt r adiology

Michigan Medicine broke ground on the Frances and Kenneth Eisenberg Troy Center for Specialty Care in June 2025, and what will be the largest outpatient medical facility in our system is set to open in spring 2027. Thanks to a transformational gift from Sidney and Madeline Forbes of Bloomfield Hills, MI, the radiology department has announced plans for the Sidney and Madeline Forbes Advanced Imaging Center, a separate state of the art facility to be constructed on the same campus. This location will offer a comprehensive lineup of all eight imaging modalities and service lines, ensuring that patients in the metro-Detroit area have access to a full range of diagnostic and interventional radiology services.
y psilanti hE alth cE nt E r: Expanding a cc E ss
In June 2025, Ypsilanti Health Center moved into a new larger location, offering multiple services including primary care in a federally designated shortage area, numerous medical specialty clinics, and a broad range of diagnostic imaging services - CT, ultrasound, x-ray, bone density, and breast imaging.
Behind the scenes, a dedicated team of radiology staff and faculty made this launch possible, navigating complex operational and logistical hurdles. Their expertise and hard work turned vision into reality, and has brought exceptional care closer to home for more patients. The community is already benefitting from this expansion. In the first two months of operation, more than 1,800 imaging exams have been performed.

t h E pavilion: a nE w Era for i npati E nt c ar E
Opening in Fall 2025, the D. Dan and Betty Kahn Health Care Pavilion at the main hospital complex will provide 264 private inpatient rooms and advanced specialty services in a new 12 story tower. This multi-year project has relied on collaboration among faculty, technologists, nursing staff, the capital projects team, radiology IT, and leaders across Michigan Medicine. Radiology will be centrally located on the 3rd floor, offering MRI, CT, general imaging, ultrasound, and interventional radiology services, with a dedicated nursing team for patient prep and recovery.
The Pavilion will also include advanced neurointerventional radiology capabilities with two procedure suites in the sixthfloor operating rooms and a state-of-the-art

MR/OR suite staffed by MRI technologists. Thanks to the integration of surgical and imaging resources and dedicated staff, precise care for complex cases will be made possible at this location.

In early 2025, outpatient wait time for adult MR imaging at U-M climbed to >50 days. Patients seeking clarity on uncertain diagnoses or treatment plans experienced added anxiety and frustrating delays. With state Certificate of Need regulations limiting installation of new MRI scanners, extending operational hours became the next best solution to increase capacity and reduce wait times.
On March 17, 2025, the Northville Health Center became the first Ambulatory Care Unit within Michigan Medicine to offer 24-hour MRI services, marking a significant step in patient access. The results have been impressive. In the five months after implementing round-the-clock service, average wait time decreased by 40%, allowing patients timely access to essential diagnostics. The community response has been overwhelmingly positive, with appointments quickly filling the expanded schedule, no matter the time of day, or night.
From Ypsilanti to Troy, and Northville to the Pavilion, these expansions are about more than just growth. They focus on strengthening our connection to the communities we serve. With every opening, the department commits to a standard of excellence unrelated to geography. We maintain consistent service, image acquisition, and exam interpretation across all of our sites so that the highest quality imaging and procedures are available wherever our patients live, work, and care for their families.
by Shelby Beard
985,657
875,597 PATIENTS SERVED
Positioning MIITT within radiology rather than the biomedical or electrical engineering departments kept the scientists both mentally and physically close to the end users.
“Our field of research takes place at the intersection of medicine and engineering,” says Principal Investigator, Gastao Lima da Cruz, PhD. One of the many benefits of the MIITT translational research group is in open collaboration between clinicians and engineers. Six medical doctors with MIITT primary affiliations are in active collaboration with the research scientists, postdoctoral fellows and graduate students. Working side by side in the Medical Science I building, investigators gain an understanding of real world clinical problems, then work together to solve them utilizing technology.
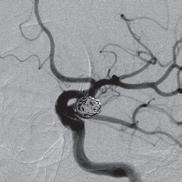
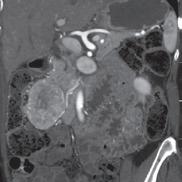
“This is a good example of a problem I’m having clinically that’s being solved by our research group,” says radiologist and scientist, Shane Wells, MD, Associate Professor of Radiology and Urology whose research focuses on improving diagnostic information to help urologists make more informed decisions. “I currently use ultrasound or CT to put needles into the liver to treat tumors. The needles get hot at the end and burn the tumor. It’s a minimally invasive procedure that can actually cure liver cancer and patients can go home the same day. However, one of the shortcomings of the current technology is that we can’t target tumors very well, which negatively affects patient outcomes. Now, the platform that we’ve developed at MIITT combines ultrasound and MRI to improve that tumor targeting.”
“One solution that we found is to use our Siemens MAGNETOM Free.Max 0.55T MRI Scanner,” says Dr. Seiberlich. As one of the few locations nationwide that owns and operates this “low field” machine, the MIITT team and UM Radiology have identified niche utilities, including the ability to conduct “in bore” biopsies--meaning the patient stays in the MRI scanner throughout the procedure. Now radiologists can clearly see the area that they want to biopsy, and accurately direct metallic needles without risk of damaging surrounding tissue. In addition to a wider bore, initially intended for larger patients or those with claustrophobia, the image quality of the scans is less affected by metal implants at low field strength. This is also advantageous when scanning patients with prior joint replacement surgery. “We can also capture MRI scans of parts of the body that are in motion, such as the heartbeat or blood flow,” she says. “Instead of a one second scan to make an image of a stationary body part, we can create a usable image in 20 milliseconds. We continue to discover special use cases that make this machine an exciting tool for us to have in radiology.”
Two of the Graduate Student Research Assistants in the Seiberlich Lab have made significant progress in their individual areas of interest with the aid of the MIITT scanners.

One of the many benefits of utilizing the MRF method as opposed to traditional MRI techniques is that it can be applied across vendors and machines to enable quantitative comparisons. “Before MRF, the shades of gray you received depended on all sorts of factors,” says Tom Griesler, MS, third year BME PhD candidate, whose research interests include MRF sequence design and optimization for brain and abdominal imaging. Results varied based on the series, settings, and manufacturer. Using MR Fingerprinting, numerical physical parameters enable comparison across time and space.
“We’re also developing something called quantitative T1rho mapping, an MRI-based measurement technique for contrast-free myocardial fibrosis detection,” says Sydney Kaplan, MS, 4th year BME PhD candidate. “This is part of my research where we’re trying to avoid administering gadolinium based contrast agents to patients who may have kidney disease. With standard scanning technology, we can’t see fibrosis on an MRI image. However, by using T1rho or an alternative method, Magnetization Transfer (MT), both of which are sensitive to macromolecules like collagen or proteins, we can see subtle changes in heart tissue.”
Going forward, MIITT may be venturing into deep learning to improve the resolution of multiple parameter maps and decrease scanning time. Its goals will continue to revolve around solving the challenges that radiologists have on a daily basis using MRI to diagnose disease. “We will continue to look for collaborators who have questions that we can seek to answer with MRI technology,” says Dr. Seiberlich.
by Nikolas Charles
Patients who have been diagnosed with localized prostate cancer have an opportunity to seek treatment in a health care environment where every aspect of their care will be addressed. At the U-M Weiser Center for Prostate Cancer, “our focus is entirely on patient-centered care,” says co-director and prostate MRI specialist, Matthew Davenport, MD, MBA, Professor of Radiology and Urology and Vice Chair of Radiology. The center, which opened in January 2022, is the direct result of a $30 million philanthropic gift from U-M regent and prostate cancer survivor, Ron Weiser. In addition to ensuring that all patients receive world-class medical care, “we want them to feel like they’re entering a sanctuary where they’re empowered not only to survive — but to thrive. We do this by utilizing a multidisciplinary structure,” which means newly referred patients can consult with an integrated team of urologists, radiation oncologists, and radiologists, often during the same visit. This allows the Weiser team to offer different perspectives when assessing each patient’s condition, to plan the most effective treatment options.
Located in the University Hospital, the Weiser Center’s 360-degree approach is guided by two additional co-directors, Todd Morgan, MD, Professor of Urology, specializing in Urologic Oncology and Bob Dess, MD, Associate Professor of Radiation Oncology and coordinated by Program Manager, Martina Jerant, MPH. “The whole idea behind the donation was to find ways to provide high-quality comprehensive care by a team of experts,” says Dr. Dess. Through expertise, collaboration and innovation, the patient is at the center of every decision. “The amazing thing about our team is the
intense focus on elevating the patient experience. There’s constant attention given to their voice,” says Dr. Morgan.
An important aspect of treating the whole person---beyond their cancer--includes both physical and psychological rehabilitation from potential side effects of treatment. “Patients who are treated with hormonal therapy, radiation or surgery may experience feelings of loss about sexual changes, urinary issues and other physical impacts,” says Associate Director, Daniela Wittmann, PhD, Clinical Associate Professor Emerita in the Department of Urology and certified sex therapist.
“As the psychosocial clinician and researcher in the center, my focus has been sexual health. And because of my training as a mental health worker, I’m very aware of the psychological impacts this disease and the side-effects of treatment can have on both the patient and their partner.” Rather than silently suffering with the possible negative effects of the treatment, Dr. Wittmann wants people to know that there are interventions available to mitigate these issues, such as sex therapy, physical therapy, and mental health support.
From the moment patients arrive throughout the completion of their care, every detail has been pre-planned to make their health care as efficient as possible. A roadmap has been created for them to follow that includes education, navigation and peer mentoring. Patient Education provides access to relevant information during each phase of care. By selecting the resources tab on the website, an informative, video-enriched educational platform features such topics

as: Navigating your diagnosis, Planning your first visit, and Post-treatment care. An AI tool is also being developed that will allow patients to search and locate curated content such as documents and guidelines specific to their needs.
Patient Navigation is a system of compassionate, personalized one-on-one logistical, operational and emotional support. Social worker and public health specialist, Jan Gamboa, MPH, LBSW, meets newly diagnosed patients provide answers to common questions. More importantly, she’s a support person to help alleviate the stress and anxiety that may come with a prostate cancer diagnosis. “It’s a new role and the first of its kind within the Michigan Medicine Health System,” says Ms. Gamboa. “Every patient and partner interaction that I have is very genuine.” While much of her time is spent preparing newly diagnosed patients for their first appointment, she’s also available to speak with them throughout their cancer treatment journey.
Peer Mentoring provides an invaluable service by connecting current patients in all stages of their care with previous patients. Advocate volunteers are available to answer questions from the perspective of someone who has first-hand experience. Some of these same advocates are an integral part of the decision-making process in the ongoing development of the center. One of those highly regarded peer
mentors is Rick Haas, 67, from Toledo, Ohio, who was diagnosed with advanced prostate cancer during the pandemic of 2020. He had a prostatectomy (surgical removal of all or part of the prostate gland) at Michigan Medicine. “The surgery was successful, but there was still some cancer left in the prostate bed (the space between the bladder and bowel), says Mr. Haas. “I did 39 treatments of radiation and hormone therapy, during which I would try to cheer up other people going through the same process. That’s when I decided to become a mentor.”
Another appreciated advocate is U-M alumnus, Tom Prew, 74, from Rochester Hills, who was diagnosed with prostate cancer in September 2021. Dr. Morgan performed a prostatectomy a few months later. “I had one of the best surgeons I could possibly have at one of the best hospitals in the nation. The entire Weiser team provided exceptional care, from the doctors, surgeons and anesthesiologists to the RNs and lab techs.” After his successful treatment, he enthusiastically volunteered to work as a peer mentor. “I’m fortunate that I found a way to give back and provide a valuable service to newly diagnosed patients at the Weiser Center for Prostate Cancer.”
by Nikolas Charles
After two years in action, Michigan Medicine’s Mobile Mammography program has succeeded in improving access to care for underserved patients and promoting community engagement. Now the goal is shifting to bring that same high quality health care directly to women in need in additional areas of the state, making it more convenient and accessible.
“Where people live and play and pray is important to us as we think about where to deploy the unit,” said Tony Denton, senior vice president and chief environmental, social and governance officer of U-M Health and Michigan Medicine. “From a patient satisfaction perspective, it’s been very successful. From a health care access perspective, it’s been very successful. We have a dedicated team committed to trying something new. Our vision is evolving as we continue to learn and continue to grow this model of care. But the overall vision is to improve access.”
A collaborative effort between Michigan Medicine and the Department of Radiology, the mobile mammography unit
provides screenings to women who face significant barriers to care, including lack of insurance or transportation.
According to Breast Imaging Manager Laura Braid, some sites that the mobile unit serves are also backlogged due to a lack of sufficient equipment. “Women are having to wait months in some areas just to get in for a screening, which in a matter of months could be a completely different result than what they could get now,” she said. “And there are often a lot of healthcare staffing issues in these communities, too.”
Feedback from patient surveys shows that the Mobile Mammography program has had a definite impact on health outcomes. For example, one woman was going to skip her mammogram because of transportation issues, but she decided to have it at the mobile unit since it was close to her home. Breast cancer was identified and diagnosed early, then she opted for surgery.
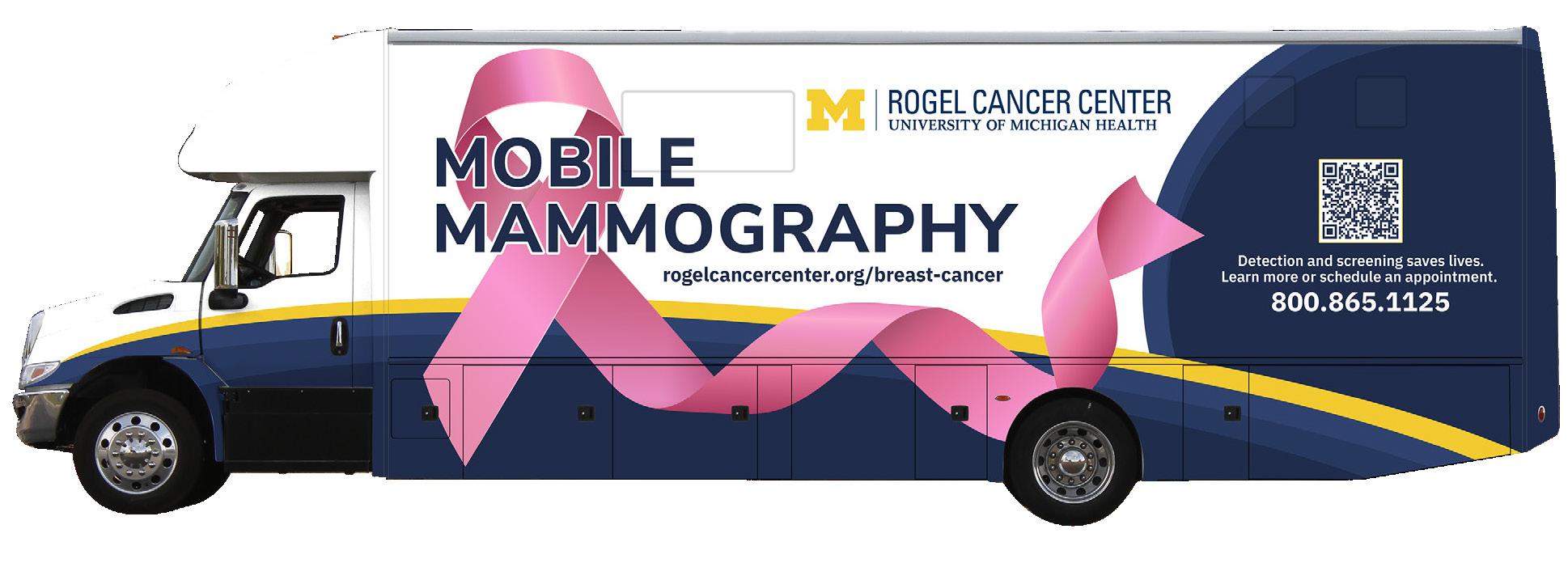
“I think it saved my life,” she wrote.
Other patients have indicated that they simply feel more comfortable in the mobile unit.
“Some patients don’t feel completely safe going to a hospital, just with past trauma that they’ve had in their life experiences,” said Emily Ferroni, Mobile Mammography Program Manager. “After building a relationship with communities, a lot of patients have given us feedback that they’ve always felt very safe and comfortable and had a good experience getting a screening in our mobile unit, compared to going to a larger facility, which is maybe more commercialized and not as personal.”
The mobile mammography unit started out in Ypsilanti, providing services three days a week, until the new U-M Ypsilanti Health Center opened in June. Mobile Mammography continues to provide screenings in Ypsilanti, servicing the Packard Health site and at various community events. Following the initial rollout in Ypsilanti, the mobile unit extended its road trips to Flint, Detroit and various southeast Michigan communities, Battle Creek and Kalamazoo, with plans to venture into the northern part of the state.
“We are slowly working to branch out from the local surrounding areas to eventually provide screening services across the Lower and Upper Peninsula of Michigan,” said Ferroni. “There are a lot of logistics to figure out involving staffing and the necessary travel, but our goal is to get up into the Alpena area, Cheboygan area, and, hopefully, to Michigan’s Upper Peninsula as well. There is a high need in the Upper Peninsula, especially in tribal communities.”
c
Taking a mobile unit on the road is, both literally and figuratively, a journey.
While the equipment itself -- including a state-of-the-art GE Pristina Mammography scanner – is the same high-quality technology that is used at U-M’s fixed breast imaging locations, the mobile unit has its own unique drawbacks. Like a large RV, the unit’s greatest challenge is just making sure that it is always fully operational, which requires thoughtful care and regular preventive maintenance.
Winters may require navigating the unit through icy weather or snowstorms. And while the unit runs on gas to drive, it can’t function without running water once it’s parked and open for business. Making sure the pipes don’t freeze is another concern, and the mobile unit stays plugged in at night so that its generator can provide electricity during the day.
The health care clinics that Mobile Mammography serves have challenges as well, including high no-show rates.
“If a community finds that they’re having high no-show rates, we encourage them to overbook our schedule by x-number of appointments, and we encourage walk-ins as well,” Ferroni said. “For example, one of the communities that we went to only completed nine appointments the very first time. Since then, we’ve serviced them quarterly and they’re now completing 19 appointments, which is typically a full schedule.”
The Mobile Mammography program has mostly been working with healthcare facilities to schedule and promote breast screenings, but Ferroni said the staff is also building more community partnerships to promote the unit’s services at various events.
For example, sometimes a community may want to offer multiple mobile services at once, such as a flu clinic, a primary care clinic and mammogram screening. Providing tours of the mobile unit at local community events is another way of establishing community relationships that subsequently lead to more bookings.
“When we’re in an underserved community, they like what they know, and what they know is their community,” Radiology Operations Director Lauren Esch said. “So, we never try to just drive our unit with the big block M anywhere to make people feel uncomfortable, making them wonder, ‘Oh, what’s U of M doing here? I like where I go.’ People don’t like change. So, we rely on the community a lot to promote the events.
“Mammogram screenings are not everybody’s favorite,” she continued. “It’s like going to the dentist. You don’t really want to do it, but you should. The clinics we partner with reach out to their patients themselves to get the patients on the schedule. They do all the coordinating, so that way it keeps patients feeling comfortable that they’re still being cared for by their facilities.”
Mammograms are not free, but breast cancer screenings are covered by insurance, including Medicaid. Most health centers that partner with Mobile Mammography are Federally Qualified Health Centers (FQHCs), which accept and provide services to patients with Medicaid.
Michigan Medicine also partners with the Breast and Cervical Cancer Control Navigation Program (BC3NP), a federal program which provides low-income women access to breast and cervical cancer screening services and follow-up care if needed. The BC3NP is funded by the Centers for Disease Control and Prevention (CDC) and administered by the Michigan Department of Health and Human Services.
“Prior to any patient being screened on our unit, we ensure that they have some sort of insurance, or we can enroll them in the BC3NP program,” Esch said. “That way, they are not receiving the bill. We ensure that every patient has access to a PCP (Primary Care Physician) and access to some sort of financial payment for their screening, so at the end of the day we know they’re being taken care of.”
by Lynn Waldsmith
The goal of Michigan Medicine’s Mobile Mammography program is to reach areas of need within underserved communities across the state of Michigan . Michigan Medicine and the Department of Radiology began offering this service in February 2023 in Ypsilanti . As of July of 2025, the unit has completed 2,220 mammograms in various southeast Michigan communities, with plans to expand services across the Lower and Upper Peninsulas of Michigan .
“We want communities to thrive,” said Tony Denton, senior vice president and chief environmental, social and governance officer of U-M Health and Michigan Medicine . “In addition to improving access, we think mobile mammography improves earlier diagnosis and provides a better health care experience overall . As we look at areas that are underserved, we’re also trying to improve a sense of belonging by having U-M Health and Michigan Medicine being perceived as a partner in care . And that means being where people live . ”
The mobile mammography unit is currently servicing or is scheduled to serve clinics in the following cities:
• Ann Arbor (FQHC*)
• Battle Creek (FQHC & Tribal)
• Dearborn (FQHC)
• Detroit (FQHC)
• Dowagiac (Tribal)
• Flint (FQHC/Community Partners)
• Fulton (Tribal)
• Inkster (FQHC)
• Kalamazoo (FQHC)
• Rochester (Community Partner)
• Taylor (FQHC)
• Ypsilanti (FQHC)
*An FQHC, or Federally Qualified Health Center, is a communitybased healthcare organization that provides primary care and preventive services to underserved patients, regardless of their ability to pay or insurance status .
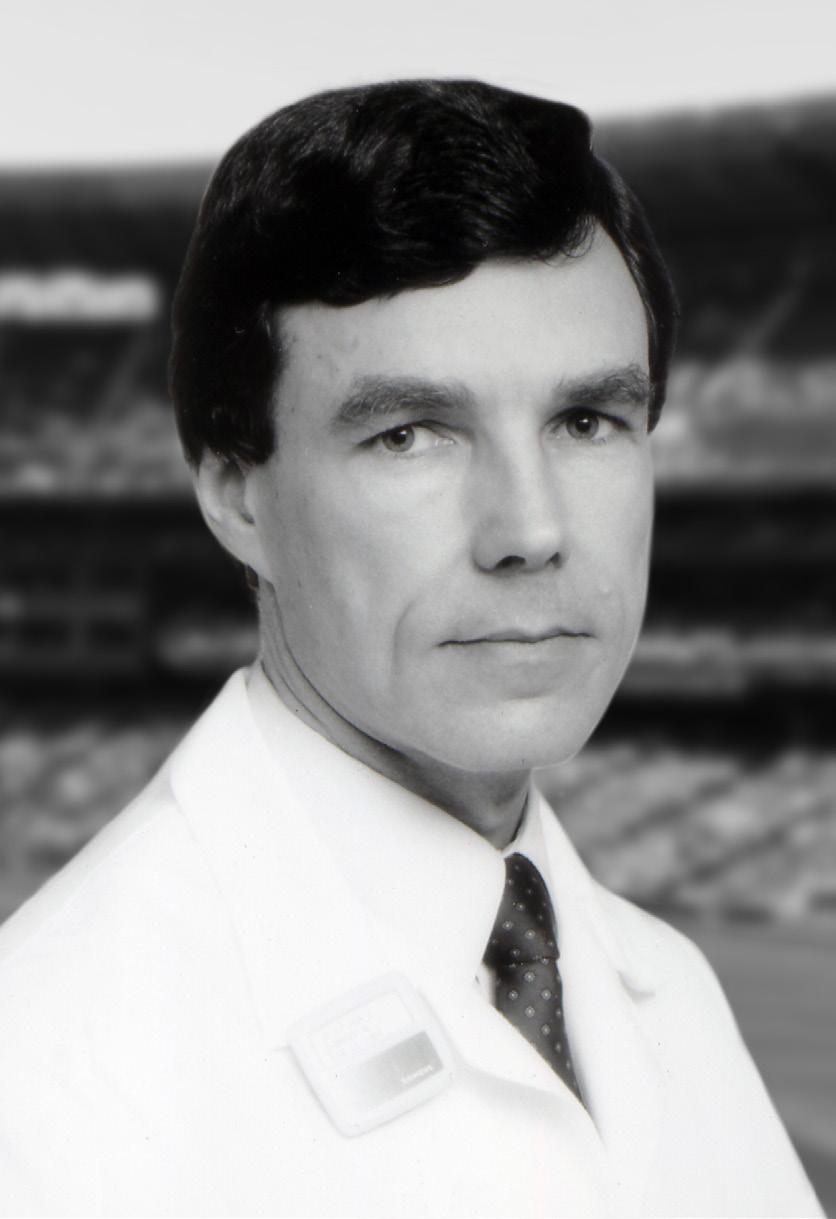
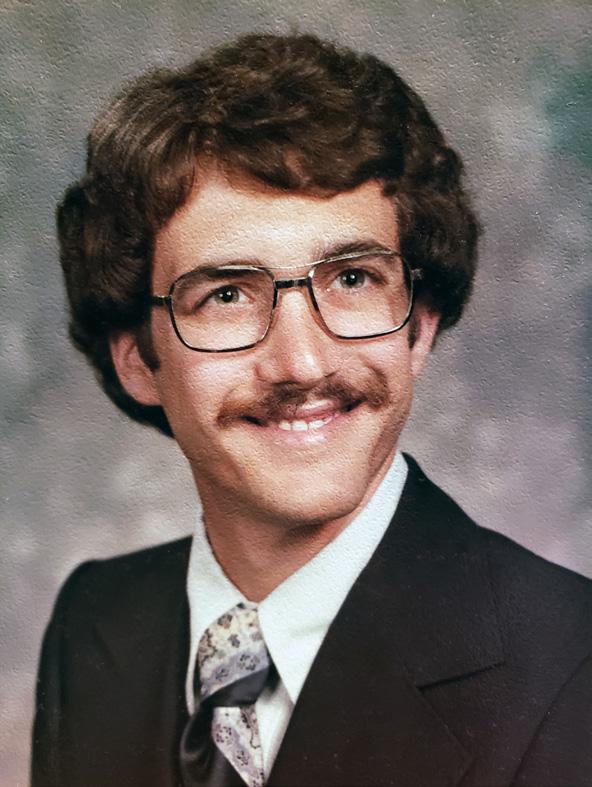
Born in Manhattan, New York in 1944 to Berdie and Ralph Silver, Terry M. Silver, MD, FACR, FAIUM, FSRU, FSUR, Professor Emeritus of Radiology, died on September 6, 2025. He was a devoted father to Jill (Dr. Craig) Levine, David (Angela Aquino-Silver) Silver and Michelle (Stephen) Levine, and loving grandfather of Josh, Samantha & Rylie Levine, Jonah Silver and Ari & Eli Levine and the late Robbie Levine, and is survived by Kathy Richard, his loving companion for over 10 years.

An avid New York Yankees fan, Terry knew in high school that he wanted to be a physician. Attracted to the University of Michigan by the strong academic programs and sports tradition, he first ventured to Ann Arbor in 1962 to begin his undergraduate studies, graduating with a B.S. with distinction in 1966…and became a passionate Wolverine! He returned to New York for medical school, receiving his MD degree with Cum Laude honors from the State University of New York (SUNY), Downstate Medical Center, College of Medicine. During his internship in internal medicine at Downstate Medical Center-Kings County Hospitals in Brooklyn, New York he was mentored by Jack Rabinowitz, MD, the Chair of Radiology, setting him on his journey into radiology. Thereafter, the lure of Ann Arbor and Wolverines was strong, and Terry spent his entire professional career in the Department of Radiology at the University of Michigan Medical School. He was thrilled to return to Ann Arbor in 1971 for his Diagnostic Radiology Residency, after which he joined the faculty in 1974. He rapidly ascended the academic ladder, rising to the rank of full professor with tenure in 1981 at the age of 37, younger than any prior faculty member in the illustrious history of the Department at that time.
Dr. Silver served as Director (1976-1987) and Co-Director (1987-1992) of the Division of Diagnostic Ultrasound, the
director of postgraduate medical education programs in radiology (1994-2002), and as the first Associate Chairman of Radiology in the Department (19841992) during a time of rapid growth of the Department, and was instrumental in the recruitment of many top notch faculty, including Drs. Gary Glazer, Paul Carson, Melvyn Korobkin and Robert Bree.
A pioneer in the development of diagnostic ultrasound, he was described by the dean of the medical school as “an outstanding leader in the field of ultrasound”. While Dr. Silver’s research interests encompassed all areas of diagnostic ultrasound, they were primarily focused on problems and applications related to pediatric, genitourinary, and gynecologic diseases, as well as intraoperative sonography. In the late 1970’s, he was very active in developing the newly emerging ultrasound technique known as neonatal neurosonography (cranial ultrasound), which became the gold standard for detecting intracranial hemorrhage in premature infants. As a clinical investigator, he was externally funded on 7 grants, many of which were from the National Institutes of Health and focused on ultrasonic technology development and applications, published 81 scientific articles in peer reviewed journals, 4 book chapters, and 50 medical abstracts and contributed 16 scientific exhibits to various national medical meetings.
A committed educator, Terry was an engaging teacher “at the alternator” who loved to share his passion for radiology with medical students, residents, fellows and colleagues. He was in his element when surrounded by learners when reading cases. You could tell as they physically leaned in that they were transfixed by his explanations of anatomy and disease as seen through diagnostic imaging. He charmed them through his knowledge, charisma and passion for “seeing the light bulb go off over their heads!” In addition
“Dr. Silver’s dedication to education was evident not only in his daily teaching on the clinical service, but also the courses he organized in ultrasound. He was the leading force in establishing the successful model for the University of Michigan Radiology CME course in Phoenix. This course has become the model for all of our off site courses.”
- Dr. N. Reed Dunnick
to giving 125 presentations and lectures at national meetings and radiology postgraduate courses, and being a visiting professor at 27 different medical centers and universities both in the U.S., and abroad, his passion for teaching led him to initiate and serve as Director of two of the most successful University of Michigan radiology postgraduate medical education courses, “A Seminar in Diagnostic Ultrasound” in Ann Arbor held annually for 24 years (1977-2000), and “Radiology in the Desert” in Scottsdale, AZ for 9 years (1994-2002). Terry was the consummate master of ceremonies with a “hands on” approach, warmly greeting and getting to know each of the registrants and their families, learning about where they practiced and helping guide them to make sure they enjoyed not only their time at the meeting in the sunny, warm desert southwest as respite from the colder northern winter climate. It was no surprise that many people came back year after year. Terry passed the torch to Dr. Joel Platt, who whole-heartedly embraced Terry’s approach and has carried that through each year ever since with his own personal touch.
Dr. Silver was active in professional societies and served in many leadership positions in diagnostic radiology and the subspecialty of diagnostic ultrasound. He was honored with fellowship status in four radiologic organizations, the American Institute of Ultrasound in Medicine (AIUM), the American College of Radiology (ACR), the Society of Uroradiology (SUR) and the Society of Radiologists in Ultrasound (SRU). He was honored by the Alumni Society of SUNY-Downstate College of Medicine with the Alumni Achievement Award, the Harry Z. Mellins MD Master Teacher Award in Radiology, and the Frank L. Babbott MD Memorial Award for distinguished service to the medical profession and the community. One of the professional society activities Terry most enjoyed was his service to the American Board of Radiology, from which he would receive the Distinguished Service Award in recognition of his many years of devoted service, including serving as an oral examiner in the Ultrasound category 14 times over 10 years.
Among his many activities, Dr. Silver was one of the original founding 20 members of the Society of Radiologists in Ultrasound (SRU) and served on the executive and fellowship committees. He was also a member of the Board of Governors of the AIUM where he served on numerous committees, served on the Board of Directors of the Society of Uroradiology, and on the executive Boards of the Michigan Sonographers Society (MSS), and the Society of Diagnostic Medical Sonographers (SDMS). In addition, he was very active in the American College of Radiology (ACR), serving on two commissions and numerous committees
on federal relations, education and training, quality assurance and residency training, and served on the scientific program committee of the Radiological Society of North America (RSNA). He was a reviewer for 5 medical journals, on the editorial board of 3 journals, and served as co-editor of the Yearbook of Diagnostic Radiology.
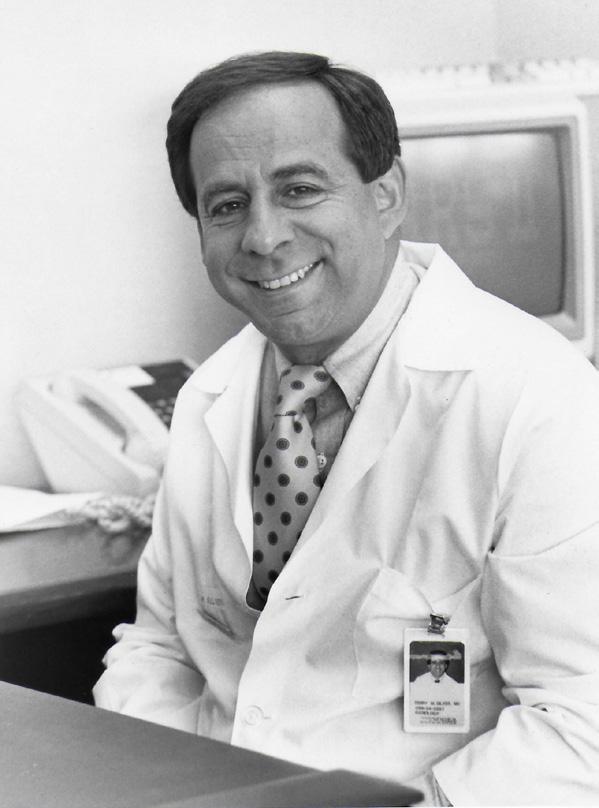
After a 38-year career, Dr. Silver retired in 2009 as an honored professor emeritus, and remained an active member of the University community, including the Medical Center Alumni Society, and the Victors and Presidents Club. The Terry M. Silver Professorship was created in honor of his dedication and commitment to radiology education and the generations that would follow. It was truly an honor for me to be named the first Terry M. Silver Collegiate Professor in Radiology. Terry had taken an interest in my career as a junior faculty, and along the many years would check in on me, offer pearls of advice and was a great listener. After his retirement, I have fond memories of meeting with Terry for breakfast at Angelo’s or the Northside Grill or catching up over dinner when he wintered in Arizona during the Michigan Radiology course. He shared many stories about his adult children and grandchildren, always beaming with pride and eager for his next visit with them. He was eager to hear how I was doing, both personally and professionally. We always sat at the same table. If you knew Terry, you understand and are smiling as you read this.
True to how Terry did things, he prepared me over 15 years ago for the moment I would write this memoriam, passing to me a sealed manila envelope stamped “confidential” all over the front and back one day at breakfast, and repeating his clear instructions to open it upon news of his passing. Now open, within it was a brief biosketch … an extended biosketch … and his last academic CV… again, so very, very, Terry … smile on.
May his memory be a blessing and an inspiration.
by Ella A. Kazerooni, MD, MS
“I first met Terry after arriving in Ann Arbor to pursue a residency in Internal Medicine. I frequently took the bus to work at 7 am. One January day when the bus was late, a car pulled up and this guy asked me if I wanted a ride. Turned out, the driver was Terry doing a good deed. We talked a lot about new developments in Radiology which sparked my interest in the field. I will always remember that day when a generous stranger offered me a ride.”
- Dr. Mark Helvie
Today’s medical trainees have fundamentally changed how they learn, turning to the internet rather than traditional textbooks for their education. This shift means that our medical students, residents, and fellows are increasingly learning from sources outside the University of Michigan, despite our world-class faculty who are among the brightest minds in radiology. The Michigan Radiology Vault addresses this challenge and ensures that our trainees and learners worldwide benefit from the knowledge and innovation that defines our training programs.
Understanding that modern learners prefer concise, engaging content over lengthy lectures, the Radiology Vault delivers on-demand education through expertly crafted short-form videos. Hosted on YouTube, this free collection of concise (<10 minute) high yield topics showcases our faculty’s clinical and research expertise in an accessible format. We currently offer more than 70 videos and anticipate doubling that number by June 2026. Some videos have already been viewed thousands of times.
At Michigan Radiology, we have an ambitious goal of becoming the nation’s premier radiology residency program. Every video shared through the Radiology Vault communicates our commitment to education, extending Michigan Radiology’s influence and ability to attract top-tier candidates. We welcome your suggestions and input on this new publicly available resource for radiology education.





















The department has raised about 75% of the $1M needed to endow the James H. Ellis, M.D. and Jean A. Lawton, M.D. Early Career Professorship in Radiology, and we seek support from our alumni for the final push. In addition to honoring a cherished member of the department, endowments are an important mechanism to ensure long term financial stability and prosperity for our department and, by extension, academic radiology and the field we love. Drs. Ellis and Lawton, and Department chairs Drs. Dunnick and Gulani, have all made generous gifts to this fund, and we invite you to learn more and potentially contribute.
early-career professorship will continue those efforts for young faculty for the future; in doing so, it will honor something very important to me: encouraging others to succeed. The greatest pleasure of being an academic radiologist for me has been watching our trainees and young faculty become great radiologists who help patients every day. Some have additionally created new knowledge through their research, or taken on leadership roles. Many are teaching their craft to the next generation of radiologists. It has truly been an honor to have participated in this process.

I think it is more difficult for beginning faculty to carve out time for academic pursuits than it was when I was starting in Radiology. There is more clinical work required, more required mandatory learning modules, more administrative paperwork now. That’s part of the appeal of an early-career professorship. It will be a way to help junior faculty have protected time to devote to academic pursuits early in their careers, when that time is really needed.”
“The Department of Radiology has been my professional home for over 40 years. Over those years, I have been very well supported by the Department of Radiology. That encourages my wife and me to give back to the department, and help the Department attract and keep outstanding new faculty in the future. An early-career professorship can do just that: it can be a recruitment tool to secure new faculty or it can be a retention tool to keep promising young faculty.”
Most endowed professorships are awarded to senior faculty, to acknowledge their professional stature and contributions to the field. By contrast, Jim has a unique vision for this professorship: it is designed to help a young faculty member create a spectacular career. Here is what he has in mind:
“I’ve always been interested in mentoring faculty, fellows, and residents in the department, and helping them start their careers, in whatever venue they choose. An
Will you join us in building this legacy of excellence? If you are ready to make a donation to this effort, you can do so using the button below.
Support our mission! Your gift, pledge, or bequest can make a lasting impact on our education, research, and clinical efforts. To discuss giving options, please contact:

Ryann Eff Senior Associate Director of Development effr@med.umich.edu
| 419.392.3040
We would love to hear what you are up to and potentially feature you in a future newsletter. Residency and fellowship graduates please fill out the Alumni Update Form to send us your news and update your contact information.
Go to the Alumni Update Form

FOLLOW US @UMICHRADIOLOGY
Editor
Katherine Maturen, MD, MS
Media Services
Sarah Abate
Danielle Dobbs
Feature Articles
Shelby Beard
Nikolas Charles
Ella Kazerooni, MD, MS
Lynn Waldsmith
Communications Specialist
Vanessa Allen
Thank you to Aaron Amin, Chris Benyi, Lauren Esch, Carol Kruise, Michele Mangner, Angie Shultis, and Rebecca Torres for content support and Tejaswi Worlikar PhD for editorial assistance
Executive Officers of Michigan Medicine: Marschall S. Runge, MD, PhD (Dean, U-M Medical School; Executive Vice President, Medical Affairs, University of Michigan; Chief Executive Officer, Michigan Medicine); David C. Miller, MD, MPH (President, U-M Health; Executive Vice Dean for Clinical Affairs; U-M Medical School Professor of Urology); Steven L. Kunkel, PhD (Executive Vice Dean for Research, U-M Medical School; Chief Scientific Officer, Michigan Medicine; Peter A. Ward Distinguished University Professor; Endowed Professor of Pathology Research); George A. Mashour, MD, PhD (Interim Executive Vice Dean for Academic Affairs, U-M Medical School; Interim Chief Academic Officer, Michigan Medicine; Senior Associate Dean for Faculty and Faculty Development; Professor of Anesthesiology and Pharmacology) Regents of the University of Michigan: Jordan B. Acker; Michael J. Behm; Mark J. Bernstein; Paul W. Brown; Sarah Hubbard; Denise Ilitch; Carl J. Meyers; Katherine E. White; Santa J. Ono (ex officio) A Non-discriminatory Employer. © 2025 Regents of the University of Michigan