






The Department of Surgery is committed to providing expert, innovative and compassionate health care continuing our department’s proud 150-year tradition by training the next generation of surgeon leaders
OUR MISSION
The Department of Surgery will create a positive, substantive impact on human health, through collaboration among clinicians, scientists, medical and business professionals to achieve:
Highly effective, compassionate patient care
Innovative science and meaningful discovery
Superior, engaging education
OUR VISION
The Department of Surgery will be the best such academic group in the world, dedicated to: Improving patients’ chances of healthy survival while bettering the quality of their care
Discovering and developing insights, innovations and tools needed to better prevent and treat disease
Educating next generations of surgeons and researchers
OUR VALUES
The people of the Department of Surgery are committed to advancing medicine and serving humanity through living and teaching our core values of:
Respect and compassion
Collaboration
Innovation
Excellence

To say this year has brought new challenges would be an understatement We are learning to live our collective values and support inclusion in a changed organizational landscape, the level of uncertainty around federal research funding is at an all-time high, and we are living with ongoing threats of diminished healthcare funding such as Medicaid and Medicare cuts.
However, despite the substantial challenges placed before us, we continue to step up to deliver on our tripartite mission.
From a clinical perspective, this year brings the greatest opportunity we have had for growth Our biggest problem as a department is providing access to all the patients who want to come here to receive their care
The opening of the Pavillion this fall, and the related backfill of the University Hospital operating rooms, has allowed us to recruit new surgeons in colorectal, hepatobiliary, bariatric, plastic, thoracic and oral & maxillofacial surgery
From a research perspective, we remain at the top of NIH rankings, third in 2024 We have not been paralyzed by uncertainty we have continued to write and submit grants We have several faculty with excellent, fundable scores on K08 and R01 proposals, despite lower paylines. We have had major donations that will impact research for years to come, such as the 50-million-dollar gift our pancreatic cancer team, The Rogel & Blondy Center, under the leadership of Dr. Pasca Di Magliano and Dr. Frankel, received this past fall.
From an education perspective, we have been ranked by Doximity as the No 1 program in Surgery and No 3 program in Plastic Surgery for the fifth consecutive year This reputation ranking reflects how people around the country view our faculty, department and the quality of our graduating trainees
From a culture perspective, thanks to Dr Erika Newman’s prescient vision, and Dr Susan Pitt’s current leadership, the Michigan Promise programming around faculty, resident and staff development remains unchanged. The vision has always focused on supporting all members of the department to achieve excellence. Everyone has access to a launch team, a boost team, faculty exchange visits, leadership development and other offerings.
As tough as all this uncertainty and change is, I am confident we will continue to effectively navigate these challenges and show others the path to do the same We are privileged to have a tripartite mission that we all find great joy in pursuing that is still intact There are no doubt new barriers and challenges, but we have the right people, creativity and resolve to find our way through them together
Best,

Justin B. Dimick, MD, MPH
Frederick A Coller Distinguished Professor Chair, Department of Surgery Michigan Medicine







Christopher Sonnenday, MD, MHS Executive Vice Chair

Michael Englesbe, MD Resident Mentorship

Katherine Gallagher, MD Basic & Translational Science

Calista Harbaugh, MD, MSc Resident Professional Development

Tasha Hughes, MD, MPH Health & Well-Being

Andrew Ibrahim, MD, MSc Health Services Research

Grace Kim, MD Education
Jeffrey Kozlow, MD, MS Finance
Nabeel Obeid, MD Clinical Operations
David Odell, MD, MMSc Quality & Safety
Erin Perrone, MD Faculty Life
Robin Petroze, MD, MPH Global Surgery
Susan Pitt, MD, MPHS Faculty Development

Jenny Shao, MD Culture & Belonging








Andrew Benjamin, MD Division Chief, Acute Care Surgery

Craig Brown, MD Vascular Surgery

Alisha Lussiez, MD Colorectal Surgery
Kajal Mehta, MD, MPH Acute Care Surgery
Evan Glazer, MD, PhD Surgical Oncology

Nimesh Patel, MD Vascular Surgery
Ryan Howard, MD, MS Minimally Invasive Surgery/Veteran’s Administration

Alison Snyder-Warwick, MD Section Head, Plastic Surgery
Brittany L. Johnson, MD Pediatric Surgery








Christina Angeles, MD
Associate Professor of Surgery with tenure and Associate Professor of Dermatology

Robert Bealieu, MD, MSE Clinical Associate Professor

Andrew Chang, MD
Cameron Haight Collegiate Professor in Thoracic Surgery

Lesly Dossett, MD, MPH Professor of Surgery with tenure

Jonathan L. Eliason, MD Frankel Professor in Cardiovascular Surgery

Timothy Frankel, MD Professor of Surgery with tenure

Brian George, MD, MSE
Hugh Cabot Professor of Surgery

Jessica Hsu, MD, PhD Clinical Associate Professor

Kiran Lagisetty, MD Clinical Associate Professor
Paige Myers, MD, MPH Clinical Associate Professor
Andrea Obi, MD Wakefield Family Research Professor
Naveen Sangji, MD, MPH Clinical Associate Professor
Christopher Sonnenday, MD Professor of Surgery with tenure
Arul Thirumoorthi, MD Clinical Associate Professor
Weichao Wang, PhD Assistant Research Scientist
Yaqing Zhang, PhD, MS Research Associate Professor










DEPARTMENT OF SURGERY TAILGATE
SEPTEMBER 7, 2024

MICHIGAN WOMEN’S SURGICAL COLLABORATIVE SYMPOSIUM
NOVEMBER 14 & 15, 2024
FACULTY RETREAT
FEBRUARY 1, 2025
MEDICAL SCHOOL GRADUATION BRUNCH
MAY 16, 2025

MOSES GUNN RESEARCH CONFERENCE
MAY 30, 2025
NEW INTERN & FACULTY WELCOME RECEPTION
JUNE 24, 2025
We recognize that our success is due to the talent, commitment and vision of faculty and residents. We pledge that we will support each individual to achieve their full professional and academic potential. The Michigan Promise ensures that faculty and residents within our department, and our community as a whole, realize our goals as the leaders and best
We hosted the seventh ann delivered by Lola Fayanju, M Chief of Breast Surgery at P lecture was entitled “Towa Our (Surgical) Selves ”
Cultural Complications 2 0 academic year. Changes inc discussion, intentionality of of the healthcare inequity c invitation of healthcare equ conversation. The team loo feedback and additional ite
The Michigan Women’s Sur Collaborative (MWSC) host symposium The theme wa Inclusive Advantage: Stren Collective Mission.”
The Doctors of Tomorrow ( celebrates their 13 year se Technical High School stud School at Marygrove throug mentorship with M1 studen hosted their seventh annua Medicine Conference in per “Community Empowermen Health Equity Together” th
The Center for Surgical Inn innovation courses and reso across all departments, wit throughout Michigan Medic work at national medical ed with industry partners, furt


The department’s Junior Faculty Exchange program hosted 11 faculty over the course of the academic year, and 11 of our own faculty visited other institutions
Michigan visiting professors included: Rachel Hooper, MD (Stanford), Kyle Sheetz, MD (Duke), Meredith Barrett, MD (Massachusetts General Hospital), Molly Hunter, MD (The Ohio State University), Jenny Shao, MD (Northwestern), Hunter Underwood, MD (University of Wisconsin), Donnele Daley, MD (Vanderbilt), Lauren Krumeich, MD, MS (University of Alabama), Sean O’Neill, MD, PhD (Medical College of Wisconsin), Annie Ehlers, MD, MPH (University of Washington) and Calista Harbaugh, MD (MD Anderson Cancer Center)
Several Department of Surgery faculty participated in the Mini-Sabbatical Program this past year
The Leadership Development Program hosted its full program, this time inviting faculty from all over Michigan Medicine to participate
We partnered with the University of Colorado Department of Surgery to deliver the Mentorship Academy
Our 16-member department recruitment committee participated in 18 group interview sessions to assist the department in selecting the best candidates for open faculty positions in our general surgery, plastic surgery and thoracic surgery sections

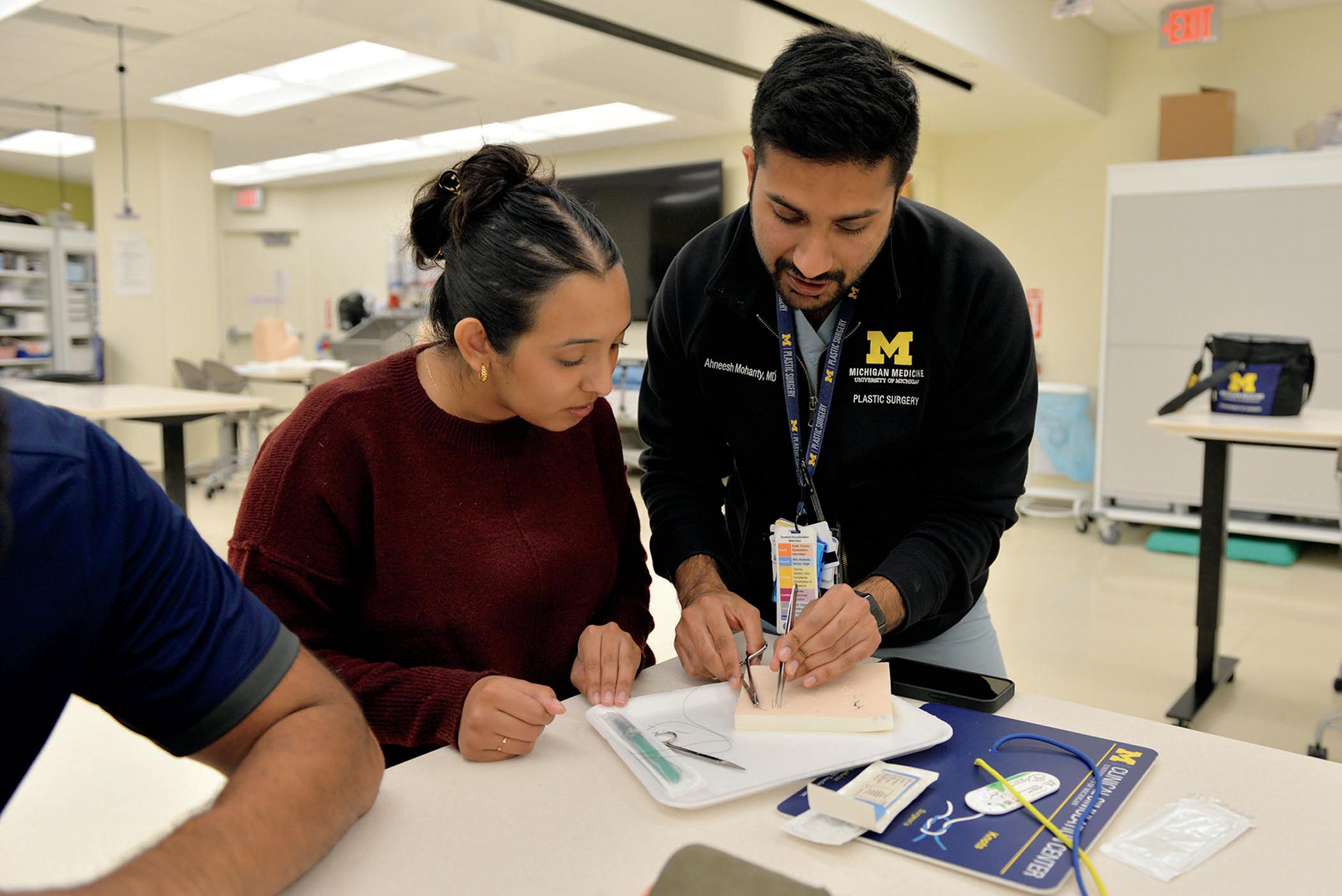
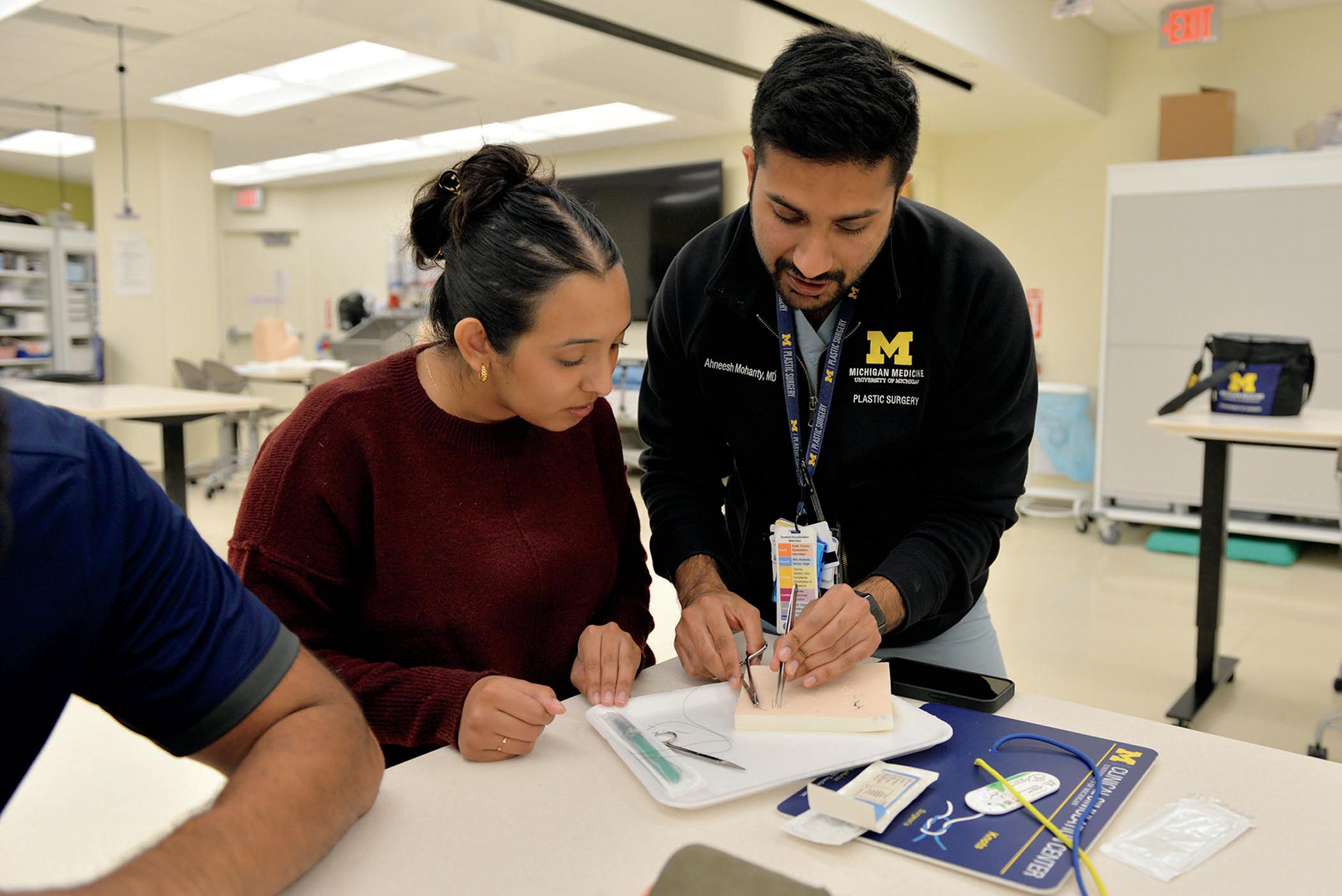
Home to the first teaching hospital in the U.S., the University of Michigan is a place where medical education has always been integral to our mission of improving human health in service of a life well-lived. Our team of more than 150 faculty are leaders not just in their clinical or research specialty, but also in surgery education.
We are committed to training surgeons who will be future leaders in the field of surgery. We offer numerous highly-ranked surgical residency and fellowship programs across a wide range of specialties. The Department of Surgery is nationally recognized for the excellence of its surgical training programs and consistently attracts outstanding candidates for trainee positions at the house officer and fellowship levels. With more than 100 residents and fellows across 10 specialties and sub-specialties, the learning experience at Michigan provides rich opportunities to learn with and from a diverse cohort.
Current programs include the M2 clerkship, the SCRUBS medical student surgery interest group, the Student Surgery Leadership Weekend, the Undergraduate Research Opportunity Program (UROP) and the Doctors of Tomorrow program.
RESIDENTS SUPPORTED BY T32 GRANTS
116 ACCREDITED HOUSE OFFICERS 100 RESIDENTS 16 FELLOWS 39 ADVANCED DEGREES HELD 11 WENT ON TO FELLOWSHIP 11
3 RESIDENTS SUPPORTED BY F32 GRANTS
43 UNDERREPRESENTED MINORITIES IN MEDICINE

RESIDENCY
General Surgery Residency
Hospital Dentistry General Practice Residency
Integrated Plastic Surgery Residency
Integrated Thoracic Surgery Residency
Integrated Vascular Surgery Residency
Oral & Maxillofacial Surgery Residency
Orofacial Pain Residency
FELLOWSHIP
Colon & Rectal Surgery Residency
Craniofacial Surgery Fellowship
CSTAR Fellowship
Endocrine Surgery Fellowship
Gender Confirmation Surgery Fellowship
Global Surgery Fellowship
Hand Surgery Fellowship
Head & Neck Oncology | Microvascular
Surgery Fellowship
Healthcare Administration Fellowship
Health & Design Fellowship
Microsurgery Fellowship
Minimally Invasive Surgery Fellowship
Pediatric Surgery Fellowship
Pediatric Surgery Fetal Medicine Fellowship
Pediatric Surgery Research Fellowship
Polly Suk-Yee Cheung Breast Surgical
Oncology Fellowship
Surgical Critical Care Fellowship
Surgical Innovation Fellowship
TMJ & Orthognathic Surgery Fellowship
Traditional Thoracic Surgery Fellowship
Transplant Surgery Fellowship
BY THE NUMBERS
Vascular Surgery Fellowship














Uchechukwu Amakiri, MD Integrated Plastic Surgery

Bradley Blitstein, DDS Oral & Maxillofacial Surgery

Luca Borah, MD, MPH General Surgery

Kyle Brown, DDS Orofacial Pain

Jessica Carducci, MD Integrated Thoracic Surgery

Juan "Sebastían" Cifuentes Muñoz, MD Integrated Vascular Surgery
Andrew Cheline, DDS Hospital Dentistry


Daniel Denson, MD General Surgery

Amelia Gavulic, MD General Surgery
Jeffrey Girardot, MD General Surgery - Prelim Interventional Radiology
Ekin Kayaalp, DDS Hospital Dentistry



Mihir Khunte, MD General Surgery - Prelim Interventional Radiology
Kayla Kolodychak, DDS Hospital Dentistry


Christine Lannon, MD Integrated Thoracic Surgery

Madison LeBlanc, DDS Oral & Maxillofacial Surgery

Jayna Lenders, MD Integrated Plastic Surgery

Maxwell Lohss, MD General Surgery - Prelim Interventional Radiology
Rachel Madar, DDS Hospital Dentistry


Gabriela Maica, MD, MBA General Surgery - Prelim
Estifanos Mehari, DDS Oral & Maxillofacial Surgery


Jeevan Murthy, MD General Surgery
Kenechukwu Odenigbo, MD General Surgery
Andrew Plumb, MD General Surgery - Prelim
Michael Saunders, MD, PhD Integrated Plastic Surgery
Vanessa Stitzlein, DDS Hospital Dentistry
Delaney Seger, DDS Hospital Dentistry
Reinie Thomas, MD General Surgery - Prelim
Olivia Waldron, MD Integrated Plastic Surgery
Baylee Wiechecki, MD General Surgery - Prelim
Alex Wu, MD General Surgery
Anna Noronha, MD General Surgery
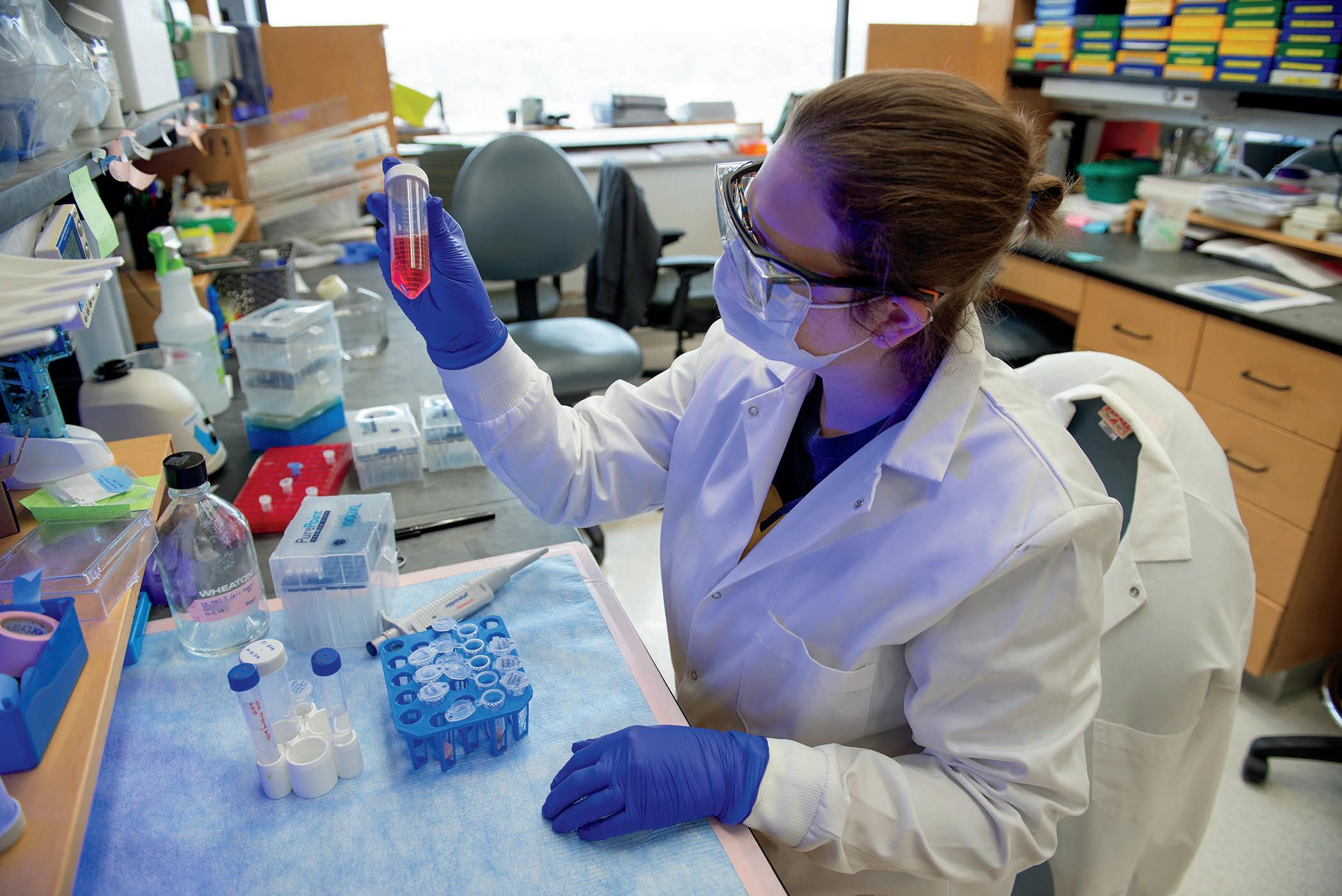
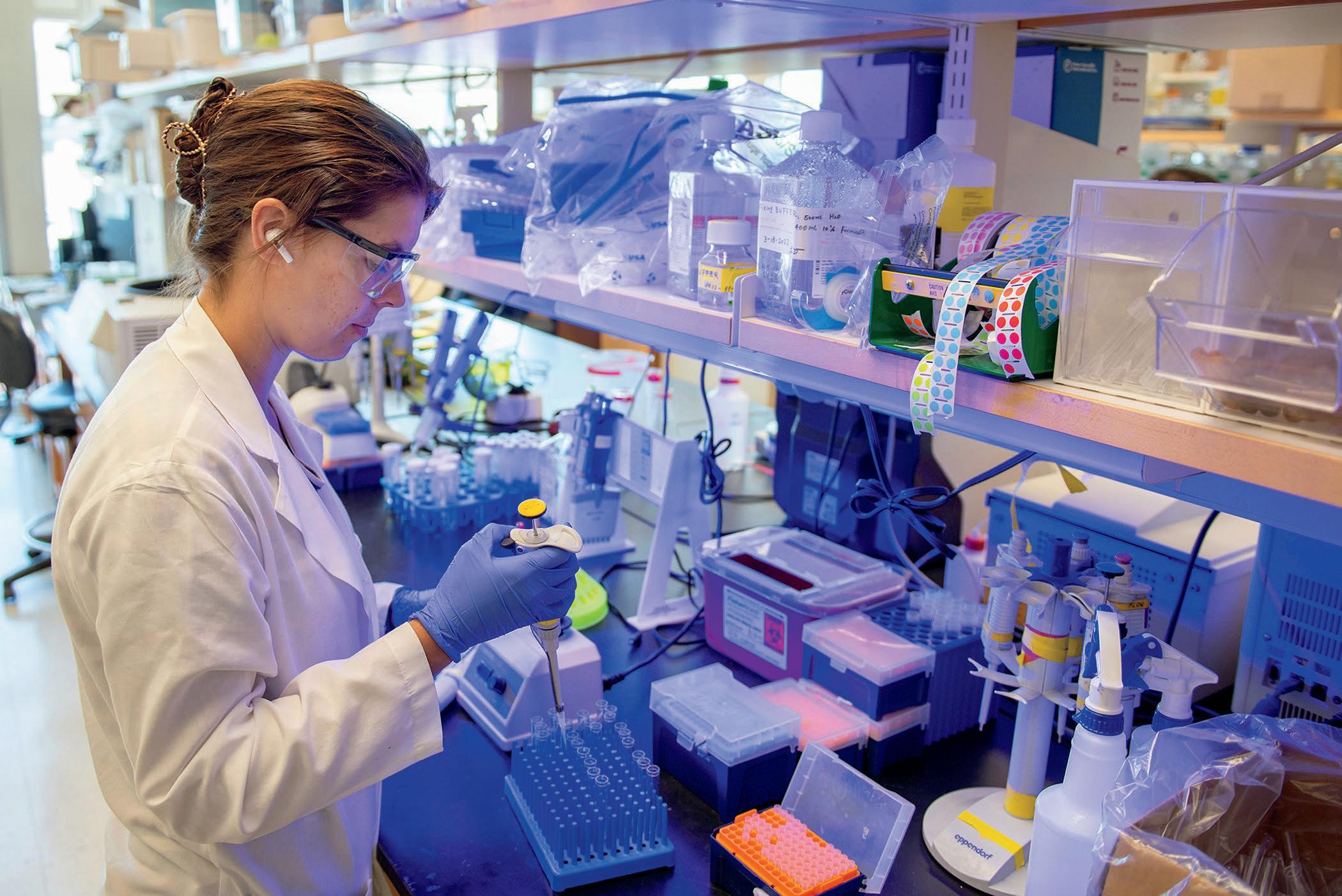
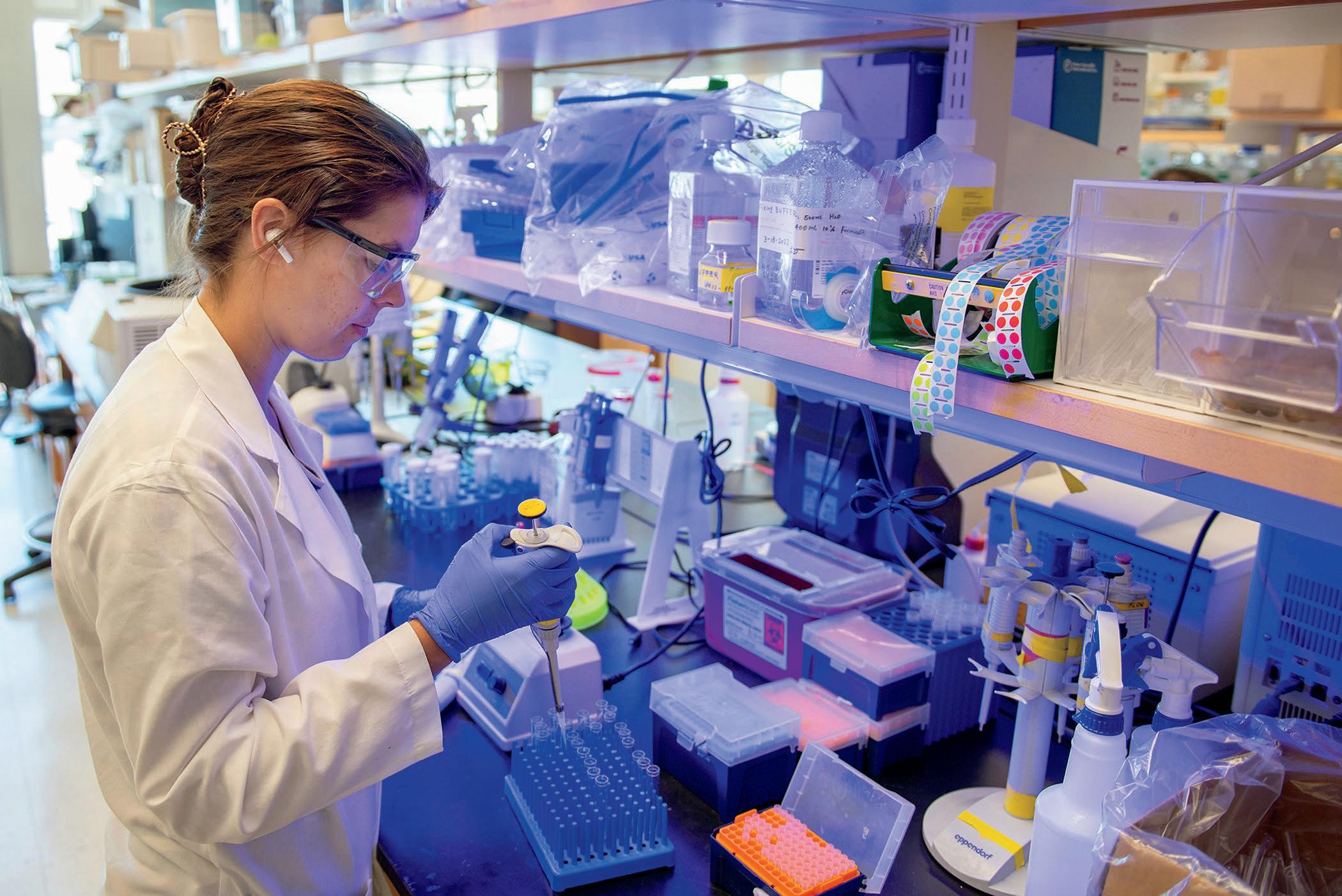
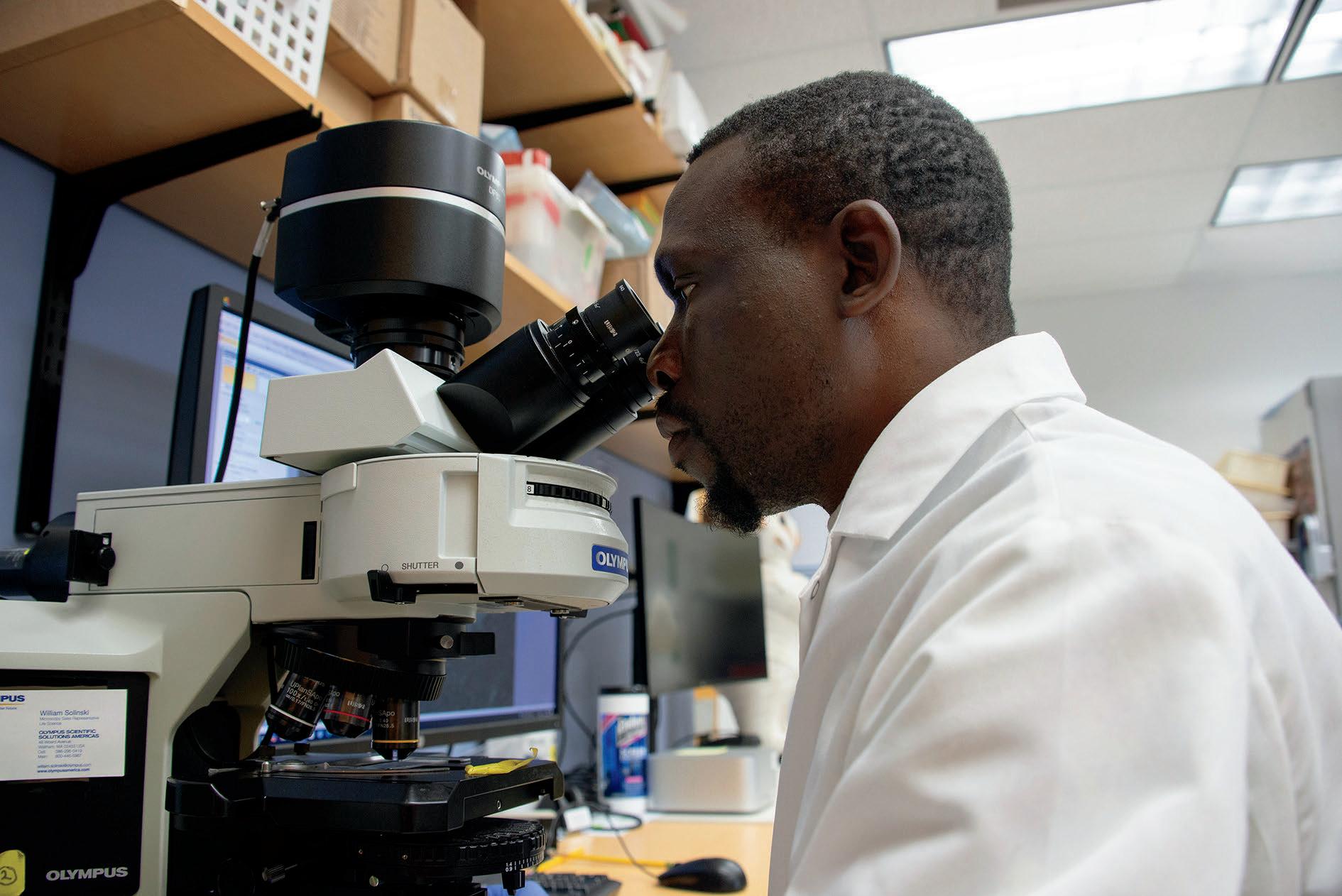
Scientific curiosity and a deeply human commitment to improving our patients’ quality of life guide our researchers at the Department of Surgery The Michigan Medicine Department of Surgery is dedicated to fostering a robust research environment that encourages our faculty, scientists and trainees to pursue discoveries that alter the future of surgery
We are always striving to provide high-quality, innovative patient care in addition to a cutting-edge training environment, and this depends on supporting the groundbreaking research conducted in the department. Our research spans basic science, translational, and health services investigation, and our impact speaks for itself: In 2023, our department ranked third for National Institutes of Health funding. We have more than 60,000 square feet of research space, and more than two dozen labs.
The department’s research centers and initiatives provide resources and a sense of community to not only those doing research in the department of surgery but across the institution. Researchers, ranging from undergraduate students to faculty members, come together to discuss work in core areas of focus, such as education research, basic science, health outcomes, or global surgery. Collaboration is key to the success of our research.
$25,857,902 TOTAL FUNDING
66 PRINCIPAL INVESTIGATORS
141 ACTIVE GRANTS
NIH AWARDS (R01, R03, K08, UM1, T32 & P30s)
49
5 AHRQ AWARDS
1 DEPARTMENT OF DEFENSE AWARD

3 MDHHS GRANTS
$8,715,392
TOTAL NIH FUNDING DEPARTMENT OF SURGERY RESEARCH FACULTY

BY THE NUMBERS

Mary Byrnes, PhD
Nadejda Bozadjieva Kramer, PhD
Ilona Kryczek, PhD
Peng Liao, PhD
Heng Lin, PhD
David Lubman, PhD
Andriy Myronovych, MD, PhD
Gurjit Sandhu, PhD
Randy Seeley, PhD
Weichao Wang, PhD
Jiali Yu, PhD
Jiajia Zhou, PhD
Weiping Zou, MD, PhD
CBATS provides a platform for basic and translational scientists across specialties to share resources and expertise to drive research advances.
CBATS hosted its first Grand Rounds, with Sayeed Ikramuddin, MD, MHA, Chair of the Department of Surgery at the University of Minnesota, speaking on the role of bariatric surgery in current practice CBATS also premiered an initiative to support faculty and trainee funding acquisition, featuring chalk talks where speakers workshopped developing proposals, and events that modeled the grants process, including an NIH mock study section and a guest presentation by a K99/R00 winner. Following her own chalk talk, Orsolya Lautner-Csorba, PhD, MSc, won the 2025 CBATS microgrant for her proposal, “Antibacterial hemodialysis catheter,” which will yield data for a future federal application CBATS member groups continued to have a strong impact on biomedical research, publishing in journals including Cancer Discovery, Cell and Nature
o global health education, international
The past year marked exciting growth for the Center for Global Surgery In Fall 2024, Robin Petroze, MD, MPH, became director, bringing renewed focus on surgical education A faculty workshop in November helped define the center’s evolving priorities. Phillip Hsu, MD, PhD, our second Global Surgery Fellow, received NIH Fogarty funding to develop a pediatric surgical training course. It was successfully piloted in five rural hospitals in Rwanda. Grace Kim, MD, earned the inaugural Global REACH Award for Outstanding International Engagement for her work on ALL-SAFE, a low-cost laparoscopic training system for resource-limited settings Jeffrey Punch, MD, continues to train teams in kidney transplantation in Rwanda, and 64 patients received transplants through this collaboration Dr Petroze performed Rwanda’s first pediatric liver cancer resection, expanding local capacity for complex pediatric care. The Center remains an active partner in the ACS/H.O.P.E. (Health Outreach Program for Equity in Global Surgery) initiative in Lusaka, Zambia
m throughout the department who conduct outcomes es.
In addition to Friday seminars, CHOP has increased its in-person programming to include two new offerings Data and Donuts takes place every other week, and focuses on covering quantitative analytical methods These sessions bring together our statisticians, faculty, fellows and staff to sharpen their statistical knowledge Additionally, CHOP is now hosting monthly Surgical Practice AI Research Community (SPARC) seminars SPARC is a multi-institutional community connecting stakeholders involved in the application of AI in healthcare. CHOP continues to publish at least 5 papers per week, and has 13 R01 funded investigators, as well as numerous K and society grant awardees This year CHOP welcomed Amy Suwanabol, MD, MS, to join the leadership team as Co-Director with Andrew M Ibrahim, MD, MSc
munity that aims to support innovative ideas and entrepreneurship in
The Center for Surgical Innovation is proud to mentor its sixth annual cohort of the Michigan Surgical Innovation Accelerator, supporting 10 funded projects with the help of seven innovation interns serving as project managers We also facilitated our third Surgical Innovation Discovery Course, where five surgical residents collaborated with engineers to explore novel ideas and develop functional prototypes In addition to strong partnerships with Biomedical Engineering faculty, we continue to collaborate across departments at Michigan Medicine to support interdisciplinary design projects and advance surgical innovation through sustained, cross-specialty engagement.
a community of educational scholars conducting research in teaching, learning, nt, curriculum, and the learning environment, with the shared goal of advancing the scholarship of evidence-based surgical education
CSTAR rebooted its fellowship program, welcoming Jamila Picart, MD, as the inaugural resident fellow and Alexandra Theall as medical student fellow, and we look forward to Marquise Singleterry, MD, joining as the next resident fellow Our robust curriculum engaged an average of 16 participants per session, spanning medical students, residents and faculty from the University of Michigan and nationally Notably, Andrew Krumm, PhD, secured $1 million in PCORI funding for a study on Personalized Patient Reported Outcome (PRO) Reports Using Machine Learning. Gurjit Sandhu, PhD continued to lead nationally as Director of the ASE Surgical Education Research Fellowship. Collectively, CSTAR faculty and trainees contributed over 30 scholarly publications this year, underscoring our commitment to advancing surgical education research
The Center for Surgical Trials aims to provide PI and recruitment support, liaise with institutional regulatory programs and create training opportunities in order to build a community of surgeon-trialists.
In its second year, the Center for Surgical Trials continues to support clinical research with hands-on assistance with regulatory, data and recruitment needs from a dedicated research team Within the department, there are currently 24 open clinical trial studies, 21 faculty Principal Investigators and 13 clinical trials are closed to accrual There are ongoing studies in nearly every section, with the most in the Sections of General Surgery and Vascular Surgery. WIth the help of comprehensive research support and educational programming, the center is strengthening trial capacity in the department and aiding the development of future generations of academic surgeon-scientists

The Department of Surgery at Michigan Medicine is one of the oldest departments of its kind in the country. Since 1849, our surgeons have been healing patients with a blend of Midwestern compassion and nationally renowned clinical expertise.
We treat more than 18,000 surgical cases a year, bringing together the combined knowledge and experience of more than 100 faculty physicians across more than 20 specialties We are highly ranked nationally for the quality of our clinical care, a fact that demonstrates the strengths we draw from our position within Michigan Medicine
We’re able to offer a caliber of care found only in a high-volume academic medical center because of the breadth of resources at Michigan Medicine, including its nearly 2,000 faculty members Our multidisciplinary programs bring together experts across specialties at the university to provide the best possible care for our patients
95,303 CLINIC VISITS
6,313 ADMISSIONS
579,493 RVUS
43,149 VIDEO VISITS

18,343 OR CASES
7,434 OR CASES (MAIN HOSPITAL)
3,493 OR CASES (AMBULATORY SURGERY CENTERS)
1,997 OR CASES (CVC)
3,754 OR CASES (MOTT)
1,665 OR CASES (NON-MM)


BY THE NUMBERS

Dana Telem, MD, MPH
Section Head, General Surgery

Lesly Dossett, MD, MPH Chief, Surgical Oncology
Paul Gauger, MD Chief, Endocrine Surgery
Andrew Benjamin, MD Chief, Acute Care Surgery
Michael McGee, MD Chief, Colorectal Surgery
Annie Ehlers, MD, MPH Chief, Minimally Invasive Surgery
Robert O’Rourke, MD Chief, Veterans Administration
Elizabeth Alore, MD, MPH
Christina Angeles, MD
Staci Aubry, MD
Filip Bednar, MD, PhD
John Byrn, MD
Kristen Carter, MD
J. Fintan Cooper, MD
Donnele Daley, MD
Justin Dimick, MD, MPH
Anne Ehlers, MD, MPH
Benjamin Ferguson, MD, PhD
Jonathan Finks, MD
Timothy Frankel, MD
Brian George, MD, MSE
Evan Glazer, MD, PhD
Calista Harbaugh, MD, MS
Mark Hemmila, MD
Ryan Howard, MD, MS
David Hughes, MD
Tasha Hughes, MD, MPH
Molly Hunter, MD, ScM, MA
Andrew Ibrahim, MD, MSc
Matthew Iyer, MD, PhD
Hope T Jackson, MD
Raymond Jean, MD, MHS
Jacqueline Jeruss, MD, PhD
Grace Kim, MD
Lauren Krumeich, MD, MS


Few specialties cover as much ground as General Surgery, as we advance life-changing treatments in areas like trauma, endocrine surgery, surgical oncology and veterans’ surgical care. Underlying our responsibility to clinical excellence is our commitment to training the next experts in academic surgery and developing knowledge and techniques that drive advancements for the future. Our approach to patient care is built on a model of coordination across multiple specialties, providing patients with a comprehensive experience that coalesces the best medical advice from a team of experts
35,198 CLINIC VISITS
7,532 ORCASES
$4.3 MILLION TOTAL FUNDING
5 RESIDENTS GRADUATED
9 FELLOWS GRADUATED
Our section received several large philanthropic gifts to support complex cancer care with new centers, including: $50 million to establish the Rogel and Blondy Center for Pancreatic Cancer and $25 million to create the Weiser Family Center for Breast Cancer.
Our general surgery residency program was ranked first in the nation by Doximity for the fifth year in a row
In research, we were awarded 22 new extramural grants
Dana Telem, MD, MPH, was appointed president of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Paul Gauger, MD, was elected president of the American Association for Endocrine Surgeons (AAES).
The Division of Acute Care Surgery provides care for major trauma and burn patients, as well as the management of emergency surgery and critical care services. Our Level 1 Trauma and Burn Verified Center is recognized by the American College of Surgeons and the American Burn Association as meeting or exceeding the highest standards of care for the most critically injured patients
The Division of Colorectal Surgery treats benign and malignant conditions of the small bowel, colon, rectum and anus, using both open and laparoscopic surgical techniques We provide multidisciplinary care through the U-M Comprehensive Cancer Center and the Michigan Bowel Control Program.
Established in 1979, we’ve grown to become one of the largest endocrine surgery divisions in the country. We provide medical and surgical care for patients with thyroid, parathyroid, adrenal, pancreatic and gastrointestinal endocrine disorders
Surgeons in the Division of Minimally Invasive Surgery focus on the diagnosis and treatment of diseases affecting the abdomen, the abdominal wall and the retroperitoneum including common conditions such as hernia, gallstones and heartburn. We also have a nationally recognized bariatric surgery program.
We provide operative care for cancers of the breast, skin, and gastrointestinal system We have special expertise in the management of patients with breast cancer, melanoma, pancreatic cancer, metastatic diseases of the liver and soft tissue sarcomas
Our VA Division is rare in that we focus exclusively on veterans’ care, building relationships and programs tailored to their needs. VA surgeons provide bariatric surgery, colorectal surgery, surgical oncology and general surgical services.
Gifty Kwakye, MD, MPH
Alisha Lussiez, MD
Kajal Mehta, MD, MPH
Lena Napolitano, MD
Hari Nathan, MD, PhD
Nabeel Obeid, MD
Sean O’Neill, MD, PhD
Pauline Park, MD
Lauren Perry, MD
Melissa Pilewskie, MD
Susan Pitt, MD, MPHS
Krishnan Raghavendran, MBBS
Scott Regenbogen, MD, MPH
Naveen Sangji, MD, MPH
Michael Sabel, MD
Jenny Shao, MD
Pasithorn Amy Suwanabol, MD
Hunter Underwood, MD
Gary Vercruysse, MD
Sven Holcombe, PhD, MS
Yuan Huang, PhD
Orsolya Lautner Csorba, PhD, MSc
Qiao Li, PhD
Yongqing Li, MD, PhD, MS
Marina Pasca di Magliano, PhD
Joseph Potkay, MS, PhD
Shuang Wei, PhD
Peng Zhang, PhD
Yaqing Zhang, MD, PhD
ACTIVE EMERITUS FACULTY
Robert Bartlett, MD
Richard Burney, MD
Alfred Chang, MD
Daniel Hinshaw, MD
James Knol, MD

Sean Edwards, MD, DDS
Section Head, Oral & Maxillofacial Surgery/Hospital Dentistry
CLINICAL FACULTY
Sharon Aronovich, DMD
Karen Carver, DDS, MD, MPH
Amy Chin, DDS, MD
Derek Holecek, DDS, MD
Hsiao Hsin Sung Hsieh, DDS, MS
John Nathan, DDS, MD
Paul Shivers, DMD, MD
Brent Ward, DDS, MD
Paulo Zupelari Goncalves, DDS, MSc, PhD
HOSPITAL DENTISTS
Stephanie Munz, DDS Chief, Hospital Dentistry
Ennis Bedair, BDS
Diane Chang, DDS
Lavika Mor, BDS
Kristine Phillips, DDS
COMBINED FACULTY
Jonathan McHugh, MD
Louise O’Brien, PhD, MS


The Section of Oral & Maxillofacial Surgery/Hospital Dentistry knows the importance of a holistic approach to health. That’s why our work combines excellence in patient care with the biomedical advances developed through our research to achieve outcomes that improve quality of life, from restoring a smile to easing chronic pain. We are a recognized center of excellence and one of the oldest units of its kind in the country Our strengths reflect the breadth of academic surgery, from diverse residency and fellowship experiences to skilled clinical care and impactful research
ORAL & MAXILLOFACIAL SURGERY AT A GLANCE
10,497 CLINIC VISITS
1,388 OR CASES
15 PUBLICATIONS $750,000 TOTAL FUNDING
3 RESIDENTS GRADUATED
3 FELLOWS GRADUATED
Our teams continue to research and develop treatments tailored to pediatric and adult patients. We successfully piloted a new interdisciplinary Sleep Fellowship program in partnership with ENT.
We continue to recruit and train exceptional individuals for our OMFS residency and TMJ fellowship programs Our Head and Neck Oncology fellowship remains strong, marked by the success of our latest graduate and our new, promising fellow Our anesthesia simulation project has gained national recognition and we are now a designation testing center for this training tool We also expanded our General Practice Residency program from five to seven residents
Our research mission remains centered on improving care quality, fostering education in evidence-based practice and inspiring a strong culture of curiosity. We also recently secured multiple grants to support clinical research
Karen Carver, DDS, MD, MPH, holds a leadership role with Women in OMFS, supporting efforts to advance gender equity in the specialty

The Section of Pediatric Surgery sets the standard for teamwork, compassion, education and innovation, as we achieve outstanding outcomes for patients, invent novel life-saving treatments and create a legacy of excellence in the field through advanced medical training. We’re proud of the well-rounded enterprise we’ve built with a high volume of operations annually in our fast-growing specialty practice, NIH-funded research and unique training experiences We’re motivated to provide the best care to our patients while improving the health of children everywhere, as we help create the future of pediatric surgery
PEDIATRIC SURGERY AT A GLANCE
4,197 CLINIC VISITS

Erika A. Newman, MD
Section Head, Pediatric Surgery
CLINICAL FACULTY
Meghan Arnold, MD
Joseph Church, MD
Peter Ehrlich, MD, MSc
Samir Gadepalli, MD, MBA
Ronald Hirschl, MD
Byron Hughes, Sr , MD, MPH
Brittany L Johnson, MD
George B. Mychaliska, MD
Erin Perrone, MD
Robin T Petroze, MD, MPH
66 PUBLICATIONS $200,000 TOTAL FUNDING
12 FELLOWS (ACGME & NON-ACGME)
4 FELLOWS GRADUATED 2,284 OR CASES
Our team remains fiercely committed to providing excellent care, continuing to expand our reach across the state for our Little Victors. We are further developing our interdisciplinary specialty programs, including our Solid Tumor Oncology, Fetal Diagnosis and Treatment center and Children’s Intestinal Rehabilitation program
We trained 12 future pediatric surgeons this year and are thrilled to welcome Brittany L Johnson, MD, our graduating senior fellow, as faculty Byron Hughes, MD, MPH, stepped into an associate program director role for the pediatric surgery fellowship.
Faculty and trainees are pursuing cutting-edge research on surgical care and social determinants of health, which is funded by R01 and T32 grants.
The section continues to thrive under the leadership of Erika A Newman, MD, who holds a strong national presence in the field Meghan Arnold, MD, is now Associate Chief Clinical Officer for C S Mott Children’s Hospital Erin Perrone, MD, was president of the Michigan chapter of the American College of Surgeons. Ronald Hirschl, MD, was elected president of the American Pediatric Surgical Association Foundation.
K Elizabeth Speck, MD
Arul Thirumoorthi, MD
ACTIVE EMERITUS FACULTY
Theodore Polley, Jr , MD

Alison Snyder-Warwick, MD
Section Head, Plastic Surgery

CLINICAL FACULTY
Steven Buchman, MD
Paul Cederna, MD
Kevin Chung, MD, MS
Robert Gilman, MD, DMD
Steven Haase, MD
Rachel Hooper, MD
Jessica Hsu, MD, PhD
Steven Kasten, MD, MHPE
Jeffrey Kozlow, MD, MS
Theodore Kung, MD
William Kuzon, Jr , MD, PhD
Lauren Marquette, MD
Adeyiza Momoh, MD
Paige Myers, MD
Hannes Prescher, MD
Noah Saad, MD
Erika Sears, MD, MS
Christian Vercler, MD, MA
Andrew Zwyghuizen, MD
RESEARCH FACULTY
Stephen Kemp, PhD
ACTIVE EMERITUS
Edwin Wilkins, MD


In the Section of Plastic Surgery, our biggest export is knowledge Our research and clinical breakthroughs improve how plastic surgeons practice everywhere and our training programs produce the next experts in the field. We are one of the largest divisions of its kind in the country. In our busy and rewarding practice, we have a singular focus on excellence in everything we do, constantly striving to provide the highest quality care possible for every single patient
30,348 CLINIC VISITS
3,813 OR CASES
166 PUBLICATIONS $2.3 MILLION
TOTAL FUNDING
3 RESIDENTS GRADUATED
4 FELLOWS GRADUATED
Our section performed over 3,800 major operations last year and saw over 30,000 patients in our outpatient clinics We provided comprehensive adult and pediatric plastic surgery care across the state at eight distinct locations. We also welcomed our new section head, Alison Snyder-Warwick, MD, and craniofacial surgeon, Hannes Prescher, MD, to the team.
Under the leadership of Paige Myers, MD, MPH, and Jessica Hsu, MD, PhD, the Integrated Plastic Surgery Residency program has been ranked third in the nation once again by Doximity
We have seven faculty members with extramural funding, demonstrating our commitment to all our academic missions
This year, Dr. Snyder-Warwick served as chair of the Plastic Surgery Research Council. Paul Cederna, MD, is currently serving as president of the American Association of Plastic Surgeons. Dr. Myers is the current chair of the Women in Plastic Surgery forum William Kuzon, MD, PhD, will be the president of the Society for Gender Surgeons this year


The Section of Thoracic Surgery draws on a legacy of impact and innovation in the treatment of surgical diseases of the chest as we continue to expand the field’s understanding of thoracic health, translating our discoveries to the clinic, and training the next generation of experts in thoracic surgery Pioneers of the transhiatal esophagectomy, we continue to lead in the treatment and research of surgical diseases of the trachea, lung, mediastinum, diaphragm and esophagus
3,242 CLINIC VISITS
15 PUBLICATIONS $1.8 MILLION TOTAL FUNDING 3 TRAINEES GRADUATED 10,497 OR CASES
The section continues to be the highest volume esophagectomy practice in the state of Michigan. We grew our lung cancer service line with the acquisition of intraoperative imaging tools to localize cancers and provide targeted surgical therapy.
This year, a 4+3 training program was approved in partnership with our general surgery residency program, providing an expedited pathway to thoracic surgical training Kiran Lagisetty, MD, will be program director for this new program and the thoracic surgery fellowship Dr Lagisetty and Chigozirim Ekeke, MD, were inducted into the Academy of Surgical Educators
Laura Kresty, PhD, MS, was awarded a UG3 award from the National Cancer Institute. David Odell, MD, MMSc, received R01 funding from the Agency for Healthcare Quality and Improvement and an investigator award from the American Association for Thoracic Surgery (AATS).
Faculty continue a tradition of national impact with Dr Odell leading the National Lung Cancer Quality Improvement Project for the American College of Surgeons and the Commission on Cancer Rishindra Reddy, MD, continues in his role as the Director of the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative.

David Odell, MD, MMSc Section Head, Thoracic Surgery
CLINICAL FACULTY
Andrew Chang, MD
Chigozirim Ekeke, MD
Kiran Lagisetty, MD
Jules Lin, MD
William Lynch, MD
Rishindra Reddy, MD, MBA
RESEARCH FACULTY
Laura Kresty, PhD, MS
ACTIVE EMERITUS FACULTY
Mark Orringer, MD

Michael Englesbe, MD


Section Head, Transplant Surgery
Meredith Barrett, MD
Ben Biesterveld, MD
Danielle Haakinson, MD
John Magee, MD
Jeffrey Punch, MD
Kyle Sheetz, MD, MS
Christopher Sonnenday, MD, MHS
Randell Sung, MD
Seth Waits, MD
Alvaro Rojas-Peña, MD

The Section of Transplant Surgery excels in research, education and clinical care, fostering a collaborative and compassionate approach to patient treatment and a dedication to advancing the field of transplant surgery. As one of the largest transplant centers in the country, we are ranked among the best for clinical outcomes.

$16.8 MILLION
TOTAL FUNDING
PUBLICATIONS
1 FELLOW GRADUATED 944 OR CASES
72
We take pride in treating patients who are not considered candidates for life-saving transplant or cancer care elsewhere Meredith Barrett, MD, has led our pediatric transplant programs, enabling earlier access to life-saving transplants through an expanded living donor liver transplant program.
Our liver transplant team was part of our institution’s first emergent living donor transplant, thanks to the extraordinary teamwork of over 200 clinicians. We had a very critical case with a young patient who didn’t have any viable transplant offers, so the team discussed using an emergent living donor transplant with one of the patient’s parents Together, they condensed a months-long testing process into a few hours, identified a parent donor and completed the transplant by the end of the day
Alvaro Rojas-Peña, MD, was named Director of the Robert H. Bartlett Extracorporeal Life Support (ECLS) lab. The lab has secured more than 20 years of continuous NIH research funding.
John Magee, MD, was elected as the President of the Organ Procurement and Transplantation Network Board of Directors (OPTN)

The Section of Vascular Surgery is pursuing advances in vascular surgical care that set the standard for our discipline: improving the lives of patients in our clinical practice, making discoveries in our labs and training future surgeon leaders. Our partnership with cardiovascular specialists across disciplines and our technologically advanced facilities make us uniquely equipped to treat difficult and complex cases and translate new treatments and approaches from the lab to the bedside
9,466 CLINIC VISITS
1,564 OR CASES
39 PUBLICATIONS $344,993 TOTAL FUNDING 1 RESIDENT GRADUATED 1 FELLOW GRADUATED
We grew our in-clinic procedures for the treatment of varicose veins with the Venous Health Program, saving OR time for more complex cases We partnered with Podiatry to expand our wound care, limb salvage and peripheral arterial disease programs and with Neurosurgery to provide an upper extremity clinic. Our patients have new treatment options for advanced peripheral arterial disease with DETOUR and LimFlow procedures and for abdominal aortic aneurysms with the GORE® EXCLUDER Thoracoabdominal Branch Endoprosthesis (TAMBE) implant
th
Our trainees remain well above the 90 percentile for open aortic and complex endovascular cases We created a new rotation with IR and Vascular Medicine exploring superficial and deep venous disease We’re hosting podiatry fellows with a new inpatient rotation for peripheral arterial disease.
The Conrad Jobst Research Lab developed two new animal models to advance the study of venous disease. The Computational Vascular Biomechanics lab made progress developing AI tools to extract information from angiography data to assess microvascular health and predict bypass graft patency
Frank Davis, MD, received a VA Career Development Award and Katherine Gallagher, MD, received a VA Merit Award. Dr. Gallagher also received the Joseph A. Vita Award from the American Heart Association. Andrea Obi, MD, received the Mid-Career Award and Lecture from the AHA’s Council on Peripheral Vascular Disease.

P , Section Head, Vascular Surgery
CLINICAL FACULTY
Robert Beaulieu, MD, MSE
Craig Brown, MD
Frank Davis, MD
Jonathan Eliason, MD
Katherine Gallagher, MD
Andrea Obi, MD
Nicholas Osborne, MD, MS
Nimesh Patel, MD
RESEARCH FACULTY
C Alberto Figueroa, PhD
Daniel Myers, DVM, MPH, DACLAM
ACTIVE EMERITUS FACULTY
Thomas Wakefield, MD
James Stanley, MD



Kathleen Alsup, PhD, MA Director, Anatomical Sciences

Glenn Fox, PhD, MS Director, Anatomical Donations Program
Andrew Barnosky, DO, MPH
David Brzezinski, MD, CGS
Amanda Kingston, PhD, MA
Mary Orczykowski, PhD
Cristina Prall, MS
Kelli Sullivan, PhD

The division is the educational center for human anatomy at the University of Michigan Medical School Our faculty design and facilitate curricula supporting the Medical School, School of Dentistry, and numerous undergraduate and graduate colleges Faculty are involved in anatomical research, pedagogical research and the development of premier tools for learning anatomy.
Our faculty taught more than 1,700 students throughout the University of Michigan this year, with a wider impact with the globally accessible Massive Open Online Course (MOOC).
We continue to pilot an adjunct extended reality portion of the curriculum for first-year medical students
Our leadership in open-access anatomy learning resources continues, with our website used worldwide at over 150 institutions promoting access and equity in educational resources for anatomy learners worldwide
We presented research on anatomical variation, curatorial techniques and teaching pedagogy at the American Association of Anatomists.

Boston and studied surgical research techniques at Harvard Medical School from 1966 to 1970 In 1970, he joined the faculty at the University of California, Irvine School of Medicine, before returning to U-M in 1980.
While at UC Irvine, Bartlett advanced work on ECMO, a technology that uses a circuit to oxygenate blood outside the body, allowing the heart and lungs to rest and recover. In 1975, his team first successfully used ECMO on a newborn, known as Baby Esperanza, who survived lung damage from meconium aspiration syndrome and went on to live a healthy life
professionals, but better people,” Rojas-Peña said

Bartlett’s leadership extended beyond Michigan He founded the Extracorporeal Life Support Organization (ELSO), which provides education, guidelines, and a global patient registry for ECMO programs.
“Dr Bartlett is best described as relentlessly curious and optimistic This is how he changed the world Our work will carry on in the spirit in which Dr. Bartlett founded the organization: welcoming and encouraging to all, fostering collaboration from everyone interested, using data to improve patient care and innovation, and bringing tenacity to our efforts to advance ECLS,” said Christine Stead, CEO of ELSO
Today, more than 261,000 patients worldwide have received ECMO support, with over 800 hospitals in 66 countries offering the technology ECMO gained wider public recognition and renewed importance during the COVID-19 pandemic Patients in intensive care units worldwide with acute respiratory distress caused by the novel coronavirus were placed on ECMO, with more than 17,000 recorded to date
At U-M, Bartlett served as chief of the Division of General Surgery, director of the Surgical Intensive Care Unit, director of graduate education in surgery, and chief of the Trauma/Critical Care Division. He also established the institution’s surgical critical care fellowship and helped expand mobile ECMO services through U-M’s Survival Flight program
Justin B. Dimick, M.D., M.P.H., chair of the U-M Department of Surgery, reflected on Bartlett’s legacy.
“There are two unique qualities Dr Bartlett possessed First, he never came across a subject he did not greet with great enthusiasm, whether medicine, science, music, or literature. Second, he never came across a student, or trainee, that he did not find worthy of inspiration Dr Bartlett’s legacy is not only pioneering ECMO, and all the years of life he gave generations, but also the future innovations of those he inspired through mentorship. We will miss Dr. Bartlett’s large scientific contributions to the department, and medicine broadly, but we will also miss the small magic moments of running into his energetic, animated self in the hallways,” said Dimick

of Medicine in 2003, and was named a fellow of the National Academy of Inventors in 2024. He translated life-support research to the marketplace, founding MC3 Cardiopulmonary acquired by Medtronic in 2024 and serving as medical director for CytoSorbents Corporation
Beyond medicine, Bartlett was a musician and supporter of the arts. As a medical student, he helped transform a raucous annual student roast into a musical parody tradition that continues today He was a founding member of the Life Sciences Orchestra and a longtime member of the Ann Arbor Civic Band. He also authored two novels and was an avid hockey fan.
Bartlett was preceded in death by his parents, Dr Robert M and Elizabeth Bartlett, and his sister, Jeannie Bonnell He is survived by his wife, Wanda Bartlett; his children Karl Bartlett, Keith Bartlett, and Karen (Joe) Fischer; siblings Bruce Bartlett (Genevieve Bartlett) and Beth Bartlett (Dave Winchester); grandchildren Sam, Helen, and Jason Bartlett and Samantha Fischer; and many nieces and nephews
Donations in his memory may be made to the Robert H. Bartlett Extracorporeal Life Support Laboratory, the University of Michigan Men’s Glee Club, or the University Musical Society
By Colleen Stone
Randy Seeley’s email inbox looks a lot different than it used to. A few years ago, it was a pretty typical academic researcher’s inbox: publication revisions, committee membership requests, communications with IACUC These days, the PhD basic science researcher in the Department of Surgery fields a barrage of inquiries from journalists and investment bankers looking for his perspective on GLP-1 drugs
Randy Seeley gets a lot of questions about GLP-1s. Here’s why.
The animal models he works with show that making a stomach very small has nothing to do with weight loss The change comes from how the brain communicates with the stomach via gut hormones, like GLP-1, which is thought to play a role in why a person stops eating.
GLP-1 is secreted after eating and is only active for about two minutes after eating, but modifications can be made to create analogs that last 24 hours, a week, and maybe even up to a month These analogs, like Ozempic, can effectively mimic surgery’s benefits without the need for invasive procedures.


Seeley has been studying communication between the gut and brain for over 30 years and how it translates into obesity and diabetes therapies. His research is well-known in the field – he’s published nearly 400 articles in several high-profile journals and his work has been cited more than 43,000 times (Though he’ll say some of those citations include times when you were wrong.)
Seeley is the director of the Michigan Nutrition Obesity Research Center, has served on numerous review panels for the NIH, and is the Senior Associate Editor for Diabetes He’s also worked closely with several companies seeking new therapies for obesity and diabetes. (See disclosure statement below.)
Seeley’s lab dissects bariatric surgery and how it affects communication between the gut and the brain. “When we first started working on bariatric surgery 20 years ago, the surgeons would tell you that it’s about physical restrictions by making your stomach super small That just made no sense to me,” Seeley said
“I’ve been studying this system for over 30 years, and no one really cared,” Seeley said. “And even when these were therapies for Type2 Diabetes, not that many people cared because it’s a smaller population and it animated fewer people to be concerned or think it was great.”
That was until the success of these drugs burst into the mainstream. Seeley started getting requests from journalists to comment on everything from the impact of the drugs on bariatric surgery to how they would affect the way users consume alcohol.
Seeley’s happy to answer the questions –especially if he can help educate people about how they work and combat some of the misinformation about the side effects and longevity of the drugs
The public shaming around the use of these drugs surprised Seeley, and it’s another angle he’s eager to discuss “I’ll admit to being naive I thought once people saw how effective these drugs were, thinking about obesity as a biological problem with a biological solution would seem obvious,” Seeley said.
Instead, individuals with obesity who have been shamed for the way their body is are shamed for using these drugs, as if they were using a cheat code to shed weight rather than pursuing an effective treatment. There’s a level of bias around obesity that undercuts the successes of the therapies.
Seeley talks to reporters to get a credible scientific perspective represented in the media It won’t stop the negative swell, but it can supply people with accurate information and maybe make more people feel like they deserve this kind of care
Seeley thinks of his lab’s work as reverse translational: They take a clinical phenomenon, bariatric surgery, back to the lab to understand how it actually works “It’s one of the most fun parts of my job – not just to be thinking about these problems from a pure curiosity about how the biology works, but how do you leverage that information into therapies that help patients?” Seeley said
That’s what pharmaceutical companies want answers to so that they can develop the next generation of therapies. Seeley and his lab have partnerships with companies like Novo Nordisk and Eli Lilly to help understand how these drugs work and solve problems that could lead to better versions
GLP-1 drugs won’t replace surgery or other treatments for obesity because they won’t work perfectly for every person What they do is give doctors more tools to help patients and build out care pathways to assess which options will be most helpful for any individual
Seeley sees this as an important evolution for obesity therapies in the future, which is a credit to the perspective he’s gained from his clinical collaborators
“I’ve spent nearly my entire career in a clinical department and it has helped my science enormously It’s made it more clear about what I should be trying to do and how I can apply my curiosity to the things that are going to matter the most,” Seeley said.
Disclosure: RJS has received research support from Novo Nordisk, Fractyl, Astra Zeneca, Congruence Therapeutics, Eli Lilly, Bullfrog AI, Glyscend Therapeutics and Amgen RJS has served as a paid consultant for Novo Nordisk, Eli Lilly, CinRx, Fractyl, Structure Therapeutics, Crinetics, Amgen and Congruence Therapeutics. RJS has equity in Bullfrog AI, Calibrate, and Rewind
By Gillian Golden

Everyone poops And colorectal surgeon Pasithorn Amy Suwanabol, MD, MS, believes everyone should be comfortable talking about it. Not just because it’s a very common bodily function, but being open about bowel habits can help you know if something’s wrong
If anyone’s happy to talk to you about your bowel movements, Suwanabol is It’s part of her job as a colorectal surgeon, and she feels it’s her duty (or her “doodie,” as she joked) to destigmatize conversations about it.
Suwanabol came to the Department of Surgery as faculty in 2015 when she was offered a job to practice out of the Ann Arbor Veterans Administration (VA). “Being at the VA is one of my happy places. It’s such a gift to be able to work at a VA and to provide care for veterans,” Suwanabol said Finding a fiercer advocate for the VA health system than Suwanabol would be a task – she loves the patient population and the supportive community there. And she’s always ready to champion the broad support the VA provides beyond physical care, including mental health and social support
In addition to her clinical duties at the VA, Suwanabol is the co-director of the Center for Healthcare Outcomes and Research (CHOP), where she supports health services research efforts within the department. This includes her own research, which largely focuses on qualityof-life care, especially for those with colorectal diseases
Is it difficult for Suwanabol to get her patients to open up about their bowel habits? Generally, no – they tend to be pretty open about what’s going on “When [my patients] come to see me, they already know I’m the poop doctor And they’re coming to see me because they’re having issues and I’m the ‘poop expert,’” Suwanabol said.
If her patients are uncomfortable talking about bowel habits, she tries to make the conversation feel very normal and gently remind them that being open will help her treat them and help improve their quality of life. Visual aids, like the Bristol Stool chart, also make it easier for patients to describe what they’re experiencing.
A sense of humor can also help lighten the mood and even be educational For example, Suwanabol has learned a lot of fun ways to describe an ideal bowel movement. “I call it a ghost poop – you wipe one or two times and you’re clean. Somebody else called it a phantom poop, and recently someone called it a spooky dookie,” Suwanabol said In another case, a friend of hers called it a “nirvana poop”
Helping patients understand what’s good and what’s concerning with their bowel habits is important to Suwanabol because it directly impacts quality of life, which is central to her clinical work and research.
Suwanabol treats a variety of colorectal diseases, but her specific patient population is those with colorectal cancer In recent decades, younger people are developing colorectal cancer at higher rates, and often, those diagnoses are happening in a more advanced stage of disease.
One reason is that younger people don’t fall in the screening guideline age range for colonoscopies, which could help catch the disease earlier “It’s a very curable cancer if you catch it early,” Suwanabol said.
What are some things to look out for to catch colorectal cancer early? Suwanabol has some advice:
Know your family history. If colorectal cancer or other hereditary cancers run in your family, make sure you get screened appropriately, which could mean getting a colonoscopy or doing stool testing
Look out for red flag symptoms Unintentional weight loss or persistent abdominal pain should be taken seriously. Also important is if you notice a change in your bowel movements not affected by your dietary habits, like a change in stool size, shape or consistency, or if you have blood in your stool
ASPIRATIONAL BOWEL MOVEMENTS: WHAT WILL AND WON’T GET YOU THERE
“I always tell people that a goal is having one to two soft-formed bowel movements a day that only require a couple wipes to get clean. Those are maybe aspirational poop goals, but those are good aspirational poop goals,” Suwanabol laughed
Getting to nirvana bowel movement status is achievable, and it starts with forming good habits. Here’s guidance Suwanabol gives her own patients:
Drink plenty of fluids
Make sure there’s enough fiber in your diet
Suwanabol says this should include insoluble fibers like fruits and vegetables as well as soluble fibers like oats, grains, and beans.
Consider probiotics Foods like yogurt are a great natural source
Use a bidet. It’s a gentle and effective way to clean up.
Get a Squatty Potty or toilet stool Squatting actually straightens out the ano-rectal angle and can help a bowel movement pass with ease.
What about habits and products that may get in the way of good colorectal health? Suwanabol has some guidance there too:
Avoid sitting on the toilet for a long time A bowel movement should happen fairly quickly, so you shouldn’t be there long enough to play a round of Candy Crush on your phone
Don’t strain to make a bowel movement happen
Aggressive wiping or cleaning isn’t necessary. The perianal skin is very sensitive, so be gentle and stick to water (and maybe a gentle soap)
Don’t use flushable wipes Environmental impact aside, they often have additives that can irritate or dry out the skin
Skip Preparation H. It can provide temporary relief, but tends to dry out the anus more and make symptoms worse.
Suwanabol happily dispenses this advice to her patients and anyone who may have questions or concerns. She and her fellow colorectal surgeons have seen and heard it all, so they don’t get squeamish talking about bowel habits with anyone, or even seeing pictures, because it’s a bodily function that affects everyone’s lives every day
“It’s our job and we know that a lot of people don’t have the same knowledge or experience, so we’re happy to see people and talk to them about it We want everyone to have good poops because it’s a quality of life thing,” Suwanabol said
By Gillian Golden
Acute care surgeons and automotive manufacturers have something in common: They want to minimize traumatic injuries after a car crash. With that in mind, collaborating is a natural choice.
The International Center for Automotive Medicine (ICAM) is a research center within Michigan Medicine where medical professionals and automotive engineers partner on work to improve automotive safety and preventing injuries. ICAM accomplishes its mission through three core avenues: cross-disciplinary education, computational biomechanics and policy-making
An example of the center’s education efforts is a fellowship that gives automotive safety engineers exposure to a medical perspective on automobile crash injuries ICAM’s assistant medical director, acute care surgeon Raymond Jean, MD, and engineering director, research scientist Sven Holcombe, PhD, took over as the co-directors of the fellowship this year, alongside medical director, Mark Hemmila, MD, continuing its roughly two-decade legacy
Prior to ICAM’s founding, Michigan Medicine was a medical center for the Crash Injury Research and Engineering Network (CIREN) CIREN is a federal program managed by the National Highway Traffic Safety Administration (NHTSA) that provides funds for research investigating car crashes to understand what factors contribute to injury outcomes.
Acute care surgeon Stewart Wang, MD, PhD, founded ICAM in 2010 to elevate and expand upon the research that he and his team had been previously providing as a CIREN center. ICAM’s projects investigate a broad spectrum of factors associated with automotive injuries, including data on vulnerable road users and vehicle occupants, injury severity prediction algorithms and the ICAM fellowship
ICAM’s research has helped improve vehicle safety systems, including validating how effective certain features are, according to Kristen Cunningham, MPA, ICAM’s director “One success story is that it was discovered that an airbag that the manufacturer was not sure was helpful actually did protect people from injury,” Cunningham said.
A success like that is a credit to ICAM’s network of collaborators, which also revealed an opportunity for education “One of the things that became very apparent is that the safety engineers wanted some experience in terms of what we see from the medical side of these trauma cases,” said Jean
So, Wang created the fellowship program and has partnered with General Motors, other manufacturers and tier-one suppliers for about 20 years, and has trained nearly 100 fellows.
The year-long program gives participating engineers basic instruction in trauma medicine and crash investigation.
The goal is to provide a medical perspective and help the engineers understand what they are trying to protect through regular crash case reviews and guest lectures from industry experts.
There are also hands-on exposures, such as the anatomy lab, where the fellows get an opportunity to see what a real body looks like, understand its physiology and how injuries can occur. “It’s been helpful for them to conceptualize a lot of the injuries we talk about that they’re trying to prevent,” Jean said.
Alongside this medical education, the fellows get to cut their teeth on the academic research process through a capstone project They conduct literature reviews, analyze data and try to answer a safety question, like how comorbidities factor into injury severity or how stature affects injury outcomes
It’s common for questions that pop up during fellowship case reviews to lead to research collaborations Jean noted a recent study that began as a question during a case review with the fellows: Do emergency automotive notification systems like OnStar help reduce transportation time to a hospital in the event of a crash?
Together, they conducted a retrospective study with data collected from case reviews and General Motors to validate that these systems do actually reduce time of transport. For Jean, these findings highlight an exciting future where artificial intelligence can be used to make safer cars, as well as the need for continued collaboration with the automotive industry
“Using AI to take the data that’s in your car and predict the severity of a car crash and how urgently an injury needs attention is where I see the future of automotive safety going, and industry partnerships are going to play a crucial role in this,” Jean said
The fellowship is designed to bridge the gap between different perspectives on what factors cause injury in a car crash Jean’s background in engineering puts him in a unique position where he can speak both languages.
But for the engineers and surgeons like Wang, this partnership is a valuable education
“As an occupant performance engineer, it’s easy to get immersed in data, but this program brought that data to life. Studying real-world crashes and human anatomy deepened my understanding and gave renewed purpose to my work,” said Leslie Sajovec, a current ICAM fellow and Vehicle Safety Performance Integration Engineer at General Motors.
Rashawndra Outlaw, a 2021-2022 ICAM fellow and Technical Expert at General Motors, feels similarly about the fellowship’s impact on her career and opportunities for innovation
“Through the program, I gained the ability to identify key body regions vulnerable to injury based on crash types and occupant factors. I also learned to assess injury severity using the Abbreviated Injury Scale (AIS) coding system,” said Outlaw
Helping engineers understand injury severity and causation illustrates why Wang felt it was important to create the fellowship. An added benefit? A more well-rounded perspective on the car crash injuries he saw as a surgeon
“The chance to marry the injuries I was seeing in the emergency department and link it to the crash through photos, road evidence and to reconstruct what happened demystified injury causation Once we better understood injury causation, I could partner directly with the engineers to improve the design of vehicle safety systems,” said Wang
Wang, Hemmila and Jean feel privileged to take part in this work with the fellows and help prevent more serious automotive injuries The feeling is mutual for the fellows – some of them have continued to work with ICAM after completing the fellowship. It’s a testament to the value of ICAM’s model of collaboration, which Jean thinks is made even richer because its home is in Michigan Medicine.
“Being close to Detroit – the automotive center of not only the United States, but also the world – you have the ability to bring together the best and brightest in terms of automotive safety. We’re fortunate enough to be considered the academic brain for that,” said Jean
By Gillian Golden


