






Thank you for joining us to celebrate University Hospitals Department of Surgery’s 7th Annual Research Day. This event showcases innovative research endeavors across the Department of Surgery at University Hospitals in conjunction with Case Western Reserve University School of Medicine as well as other affiliated institutions including Northeast Ohio Medical University. It highlights the Department’s commitment to advancing surgical science and improving patient care In addition, promotes a culture of research and academic excellence within the Department and offers a unique opportunity for researchers to network, collaborate, and learn from each other, fostering a community of scholars and future leaders in surgery.
Today’s presentations from medical students, residents, fellows, and research associates associates reflect the diverse spectrum of our Department’s research, including basic and translational science, clinical, health services and outcomes, and surgical education research It covers a variety of surgical specialties and topics, demonstrating the Department’s breadth and depth of research knowledge and expertise
We are pleased to welcome Julie A Freischlag, MD, FACS, FRCSEd(Hon), DFSVS, MAMSE as this year’s honored guest for the Oliver H Payne Lectureship Dr Freischlag will be presenting her lecture “Clinical and Personal Comparative Effectiveness” during Grand Rounds.
This year’s presentation format will consist of 29 quick shot presentations Each medical student presenter will have 3 minutes for an oral presentation followed by a 2 minute Q&A session. Each trainee presenter will have 4 minutes for an oral presentation followed by a 2 minute Q&A session Prizes will be awarded for the top medical student and trainee presentations at resident graduation
Presentation Evaluation Form
https://redcap.link/researchday2024evaluations

Please use the link/QR code above to access the evaluation form. For each presentation, select the applicable presenter/abstract title from the drop-down list and use the slide bar to cast your vote in the evaluation categories.

UH RISES (Research in Surgical Outcomes and Effectiveness) is a collaborative surgical outcomes research center at University Hospitals Cleveland Medical Center It brings together attending physicians, residents, fellows, and students to build on UH’s academic mission and support advances in health care The mission of UH RISES is to leverage the understanding of surgical disease, technology, and patient experience to continuously improve outcomes
Established in 2018, the UH RISES Center serves to centralize health science research within the Department of Surgery through research support services, research meetings, and structured mentorship within areas of research interest and professional development Research support provided through UH RISES includes study and protocol design, data management, access to an inventory of secondary data sources, statistical analysis, and regulatory affairs
UH RISES holds bi-monthly research meetings on the 2nd and 4th Thursdays of each month from 2-4pm. All UH faculty, residents, staff, and students are welcome to attend to share research ideas, receive feedback on proposals or grant applications, troubleshoot current research activities, or practice for upcoming conference presentations
To Heal:
Leveraging our knowlege of surgical disease, we strive to continuously improve outcomes and future care for ou patients through the study of patient experience

To Teach:
We aim to advance health sciences within the UH Department of Surgery through developing faculty, residents, and medical students as researchers
To Discover:
We seek to improve all patient outcomes and advance the reputation of University Hospitals as a clinical and quality leader
University Hospitals, a community hospital network that serves patients across Northeast Ohio, is one of the nation’s leading academic medical centers Its mission – To Heal To Teach To Discover – is fulfilled through its prestigious clinical and research programs
The Department of Surgery at University Hospitals is known for its excellence in education, research, and clinical care It includes a wide range of surgical disciplines:
Bariatric Surgery
Cardiac Surgery
Colorectal Surgery
General Surgery
Pediatric Surgery
Plastic and Reconstructive Surgery
Surgical Oncology
Thoracic and Esophageal Surgery
Transplant and Hepatobiliary Surgery
Trauma, Critical Care, and Acute Care Surgery
Vascular and Endovascular Surgery
The Department of Surgery has a long tradition of training leaders in surgery and offers a variety of residency and fellowship programs. These programs benefit from a broad network of teaching hospitals and a diverse faculty, preparing residents and medical students for leadership in the surgical field We offer advanced training opportunities across various surgical specialties, emphasizing our commitment to academic and clinical excellence
The Department of Surgery is invested in advancing surgical practices through cutting-edge research and innovation With a focus on collaborative, multidisciplinary studies, the Department has been successful in integrating clinical care with scientific discovery, which has significantly enhanced patient outcomes and surgical techniques This commitment is further exemplified by its leadership in developing novel surgical materials and methodologies, ensuring that both the medical community and patients benefit from the latest advancements in surgical care


Chief Executive Officer of Atrium Health Wake Forest Baptist
Chief Academic Officer and Executive Vice President of Advocate Health
Executive Vice President for Health Affairs at Wake Forest University
Dean of Wake Forest School of Medicine
Grand Rounds Presentation: “Clinical and Personal Comparative Effectiveness”
Julie A Freischlag, MD, FACS, FRCSEd(Hon), DFSVS, MAMSE, is chief executive officer of Atrium Health Wake Forest Baptist, chief academic officer of Advocate Health and executive vice president for health affairs of Wake Forest University As a member of the executive leadership team, she is responsible for the academic core of Advocate Health, the third largest nonprofit integrated health system in the United States In this role, she oversees research and discovery for the entire Advocate Health system, including all educational and research programs at Wake Forest University School of Medicine, Atrium Health Cabarrus College of Health Sciences and Atrium Health Carolinas College of Health Sciences. As CEO of Wake Forest Baptist, Freischlag has overall responsibility for the health system’s clinical, academic and innovation enterprises and its annual operating budget of more than $4 billion
With more than 15 years of leadership experience, Freischlag – who has been CEO of Wake Forest Baptist since 2017 – joined Atrium Health in October 2020, when Atrium Health underwent a strategic combination with Wake Forest Baptist Health and Wake Forest University School of Medicine A practicing vascular surgeon specializing in the treatment of thoracic outlet syndrome, Freischlag has led education and training programs at top medical schools in her role as professor and chair of surgery and vascular surgery departments. Freischlag also has more than 30 years of experience leading patient-care services as chief of surgery or vascular surgery at nationally ranked hospitals. Previously, she served as professor, chair of the surgery department and surgeon-in-chief at Johns Hopkins Medical Institutions Additional leadership positions held throughout her career include vice chancellor for Human Health Sciences and dean of the School of Medicine at UC Davis
Her national leadership includes serving as the 2021-2022 president of the American College of Surgeons, a former governor and secretary of the Board of Governors and a regent and past chair of the Board of Regents of the American College of Surgeons She is the past president of the Society for Vascular Surgery and the Society for Vascular Surgery Foundation, and past president of the Association of VA Surgeons and the Society of Surgical Chairs. Freischlag was the editor of JAMA Surgery for 10 years (20052014) and is currently a member of the JAMA Oversight Committee and the editorial boards of the Annals of Vascular Surgery, Journal of the American College of Surgeons, British Journal of Surgery and the Journal of the American Medical Association Currently, Freischlag serves on the Board of Directors of the Association for American Medical Colleges, National Institute of Health Clinical Center Research Hospital Board and Aga Khan University Board of Trustees She is also chair of the Health Services Committee, University of Pittsburgh School of Medicine Board of Visitors and the University of Illinois Health Advisory Council Most recently, the Association of American Medical Colleges named Freischlag as chair-elect of its board of directors, with her term to begin in November 2024
Freischlag has received numerous teaching and achievement awards, including an achievement award from the Department of Veterans Affairs She was elected to the National Academy of Medicine in 2015 Freischlag holds a bachelor of science degree from the University of Illinois and a medical degree from Rush University She completed her general surgery residency and fellowship training in vascular surgery at UCLA Medical Center She also holds a Fellow of the American College of Surgeons credential, a Distinguished Fellow of the Society for Vascular Surgery designation and a Fellowship of the Royal Colleges of Surgeons

7:00 AM – 8:00 AM
Grand Rounds – Keynote Speaker, Dr. Julie A. Freischlag “Clinical and Personal Comparative Effectiveness”
8:15 AM – 9:15 AM Resident Case Conference
9:15 AM – 9:45 AM Resident Career Development
Kulas Auditorium
UH Lakeside 5th Floor
9:45 AM – 12:45 PM BREAK
12:45 PM – 1:00 PM Welcome and Introduction
1:00 PM – 2:11 PM Medical Student Research Presentations
2:12 PM – 2:30 PM BREAK
2:30 PM – 4:28 PM Trainee Research Presentations
Kulas Auditorium
UH Lakeside 5th Floor
Kulas Auditorium
UH Lakeside 5th Floor
4:30 PM – 4:40 PM Closing Remarks

Wolstein Auditorium
Wolstein Research Building
Wolstein Auditorium
Wolstein Research Building
Wolstein Lobby
Wolstein Research Building
Wolstein Auditorium
Wolstein Research Building
Wolstein Auditorium
Wolstein Research Building
12:45 PM – 1:00 PM WELCOME / INTRODUCTION
Christopher Towe, MD
1:00 PM – 1:05 PM 1) Matthew Chen, BA (Faculty Advisor: Richard Hoehn, MD)
The Role of Patient Navigation in Cancer Treatment: A Systematic Review
1:06 PM – 1:11 PM 2) Claire Drigotas, BA (Faculty Advisor: Richard Hoehn, MD)
Dosing Strategies for Cytoreductive Surgery with Heated Intraperitoneal Chemotherapy in Treating Malignant Peritoneal Mesothelioma: A Review
1:12 PM – 1:17 PM 3) Andrew Fiorentino, MS (Faculty Advisor: Chloe Williams, MD)
Camryn Hawkins, PhD, MS (Faculty Advisor: Chloe Williams, MD)
Does Timing Matter? The Impact of Interhospital Surgical Transfer on Patient Outcomes in Necrotizing Soft Tissue Infections
1:18 PM – 1:23 PM 4) Meaghan MacRae, BS (Faculty Advisor: Eiichi A. Miyasaka, MD)
Characteristics of the Patient and Appendix that Increase Visualization of the Appendix by Ultrasound
1:24 PM – 1:29 PM 5) Allison Gasnick, BS (Faculty Advisor: Christopher Towe, MD)
Physician Research Productivity: A Bibliometric Analysis
1:30 PM – 1:35 PM 6) Isabel Ho, BA (Faculty Advisor: Howard Wang, MD)
Evaluation and Management of Head and Neck Hemangiomas in Infancy
1:36 PM – 1:41 PM 7) William Julian, MS (Faculty Advisor: Lee Ocuin, MD)
Comparison of Hospital Volume and Risk-Standardized Mortality Rate as a Proxy for Hospital Quality in Complex Oncologic Hepatopancreatobiliary Surgery
1:42 PM – 1:47 PM 8) Gillian Michaelson, BS (Faculty Advisor: Eiichi Miyasaka, MD)
Simplifying Universal Pediatric Pre-Operative Anesthesia Screening Using the NARCO Score for Pediatric Anesthesia Risk Stratification
1:48 PM – 1:53 PM 9) Kathleen Mulligan, BA (Faculty Advisor: Richard Hoehn, MD)
Disparities in Receipt of Adjuvant Immunotherapy Among Stage III Melanoma Patients
1:54 PM – 1:59 PM 10) Alice Qian, BS (Faculty Advisor: Cristian Baeza, MD)
Presenting: Gabriel Tensol Rodrigues Pereira, MD (Faculty Advisor: Cristian Baeza, MD)
Percutaneous Decannulation Of Extracorporeal Membrane Oxygenation Using MANTA Device: A Real- world Single-center Experience
2:00 PM – 2:05 PM 11) Hailey Seibert, BA (Faculty Advisor: Luke Rothermel, MD, MPH)
Social Determinants of Health Predict Lower Receipt of Systemic Treatment, Influencing Survival in Patients with Metastatic Melanoma
2:06 PM – 2:11 PM 12) Henry Stitzel, BS (Faculty Advisor: Lee Ocuin, MD)
Initiation of a Single-Institution Hepatic Artery Infusion Pump Program for Colorectal Liver Metastases and Intrahepatic Cholangiocarcinoma: Safety, Feasibility, and Circulating Tumor DNA Tracking

2:12 – 2:30 PM BREAK
2:30 PM – 2:36 PM 13) Aria Bassiri, MD (Faculty Advisor: Christopher Towe, MD)
Revisiting N3 Non-Small Cell Lung Cancer: Assessing Survival Parallels to N2 Disease and the Impact of Neoadjuvant Therapy with Surgery
2:37 PM – 2:43 PM 14) Christina S. Boutros, DO (Faculty Advisor: Richard Hoehn, MD) A Comprehensive Analysis of Metastatic Disease following Surgery for Clinically Localized Cutaneous Melanoma
2:44 PM – 2:50 PM 15) Hamza Nasir Chatha, MD (Faculty Advisor: Jeffrey Marks, MD)
Elevated Preoperative Lower Esophageal Sphincter Pressure Predicts Improved Clinical Outcomes after Per Oral Esophageal Myotomy (POEM)
2:51 PM – 2:57 PM 16) Susan J. Doh, MD (Faculty Advisor: Megan Miller, MD)
Adjuvant Chemotherapy is Underused in Women Aged < 50 with HR+ HER2- Breast Cancer in the National Cancer Database
2:58 PM – 3:04 PM 17) Weichuan Dong, PhD (Faculty Advisor: Richard Hoehn, MD) Socioeconomic Status and Dermatologist Accessibility, and Early vs. Late-Stage Melanoma Risk
3:05 PM – 3:11 PM 18) Mohamedraed Elshami, MD, MMSc (Faculty Advisor: Lee Ocuin, MD) To Revise Or Not to Revise? Isolated Margin Positivity in Localized Pancreatic Ductal Adenocarcinoma
3:12 PM – 3:18 PM 19) Jessica Hungate, MD (Faculty Advisor: Gregory Rushing, MD; Pablo Ruda Vega, MD) Left Atrial Appendage Exclusion During MIDCAB
3:19 PM – 3:25 PM 20) Hanna Kakish, MD (Faculty Advisor: Luke Rothermel, MD, MPH) Immunotherapy Use in AJCC8 Stage IIIA Melanoma: A Single Institution Experience.
3:26 PM – 3:32 PM 21) Mamadi Papus Keita, MD (Faculty Advisor: Yakov Elgudin, MD, PhD) Building a Ross Procedure Program, Keys to Success
3:33 PM – 3:39 PM 22) Saher-Zahra Khan, MD (Faculty Advisor: Jeffrey Marks, MD) Predictors of Recurrence After Paresophageal Hernia Repair
3:40 PM – 3:46 PM 23) Alexander Loftus, MD (Faculty Advisor: Lee Ocuin, MD) Cost and Resource Use Analysis of Extended-Spectrum Penicillin Antibiotic Therapy after Pancreatoduodenectomy in Intermediate- and High-Risk Patients
3:47 PM – 3:53 PM 24) Daniel Praise Mowoh, MD (Faculty Advisor: Leena Khaitan, MD) Does race play a role in the failure of primary bariatric surgery?

3:54 PM – 4:00 PM 25) Kimberly R. Rebello, MD, MSc (Faculty Advisor: Gregory Rushing, MD; Pablo Ruda Vega, MD) Avoiding Atriotomy; University Hospitals GP Maze: Operative Technique and Early Outcomes
4:01 PM – 4:07 PM 26) Erik L. Risa, MD (Faculty Advisor: Andrew Loudon, MD) Don't Break the Bank: Transfusion of Survival Outliers in Hemorrhagic Shock
4:08 PM – 4:14 PM 27) Ananya Tawde, MD (Faculty Advisor: Zoe Stewart Lewis, MD, PhD) Case Report: Failed SVR12 in Two HCV Naïve Recipients of HCV Viremic Deceased Donor Kidneys Requiring Additional DAA Treatment
4:15 PM – 4:21 PM 28) Heming Hannah Zhao, MD (Faculty Advisor: Scott Wilhelm, MD) Management Strategies and Timing of Parathyroidectomy In Tertiary Hyperparathyroidism Post-Kidney Transplant: A Comparative Analysis
4:22 PM – 4:28 PM 29) Mina A. Ibrahim, MD (Faculty Advisor: Leena Khaitan, MD) Long-Term Outcomes of Magnetic Sphincter Augmentation in Sleeve Gastrectomy and RGBP Patients: A Comprehensive Analysis
4:30 PM – 4:40 PM CLOSING STATEMENTS

Background: Patient navigation programs have been shown to improve the quality of cancer care for certain populations The impact of patient navigation has been well-established in improving screening rates and diagnostic resolution This systematic review aimed to characterize the multifaceted role of patient navigators within the realm of cancer treatment.
Materials and Methods: A comprehensive electronic literature review of PubMed and Embase databases was conducted to identify relevant studies investigating the role of patient navigators in cancer treatment from August 1, 2009 to March 27, 2023 Results from both databases were aggregated and duplicates were removed
Results: A total of 59 unique articles were included in this review article. These studies investigated the roles of patient navigators in treatment initiation, treatment adherence, patient satisfaction, quality of care indicators, and palliative care Amongst studies focused on cancer treatment initiation, 71% found a significant increase in treatment initiation amongst patients who were enrolled in patient navigation programs while 65% of studies focused on treatment adherence demonstrated significant improvements in treatment adherence 80% of studies investigating patient satisfaction showed significant benefits, and 81% of studies reported a positive impact of patient navigators on quality care indicators. All three palliative care studies found beneficial effects of patient navigation
Conclusion: This systematic review provides compelling evidence supporting the value of patient navigation programs in cancer treatment. The findings suggest that patient navigation interventions play a crucial role in improving access to care and optimizing treatment outcomes, especially for disadvantaged cancer patients. Incorporating patient navigation into standard oncology practice can reduce disparities in cancer treatment and improve the overall quality of cancer care

Strategies for Cytoreductive
Claire Drigotas, BA, Alexander Loftus, MD, John Ammori, MD, Luke Rothermel, MD, MPH, and Richard Hoehn, MD.
Significance: Malignant Peritoneal Mesothelioma (MPM) carries a poor prognosis representing 10-30% of mesothelioma diagnoses Cytoreductive surgery (CRS) with heated intraoperative intraperitoneal chemotherapy (HIPEC) improves survival in MPM There is no standardized HIPEC protocol with respect to chemotherapeutic agent, dose, administration temperature, or duration. In this study, we analyze common practices and outcomes of published HIPEC regimens to gain insight into current practice to inform future directions of study.
Methods: PubMed literature search for investigational studies of CRS and HIPEC for treatment of MPM in adults Studies representing the same patient cohort were included in origin analysis and excluded from subsequent analyses
Results: 35 studies were analyzed for geographic origin and 29 were analyzed for regimens and outcomes. 91% of studies were single-institution and 83% were from European or North American Institutions Median publication year was 2017 The most common drug regimens were mitomycin C, cisplatin/doxorubicin, and cisplatin/mitomycin C. Studies used a variety of dosing strategies. Perfusion temperatures ranged from 40-45°C. 90 min was the most common perfusion time. Study outcomes were heterogeneous and included median survival (40.9 +/- 19.1 mos), grade III/IV complications (29 +/- 13.2%), and perioperative mortality (3 +/- 3.4%).
Conclusions: While CRS with HIPEC is an established treatment for patients with MPM, available evidence suggests wide variability in the type of HIPEC regimen used for these patients Future projects standardizing protocols across multi-institutional collaborations would better assess the role of agent, dose, and perfusion time in achieving survival benefits for MPM.

Chloe Williams, MD, Andrew Fiorentino, MS, Camryn Hawkins, PhD, MS, Omkar Pawar, MSCE, BDS, Matthew Moorman, MD, MBA, Amy Page Rushing, MD, FACS, and Brandon Radow, MD, FACS.
Introduction: Necrotizing soft tissue infections (NSTIs) are life-threatening and require prompt diagnosis, early surgical intervention, and complex perioperative care. Transfer to tertiary care hospitals (TCH) is often requested. We hypothesized that interhospital transfer of NSTI patients may preclude timely surgical debridement, thereby worsening outcomes
Methods: We conducted a retrospective review of adult patients treated for surgically-confirmed NSTIs from 2016-2021 at a tertiary care hospital. Patients were grouped by first presentation at either TCH or OSH; the OSH patients were further divided into those who underwent index operation prior to transfer vs after. We compared patient and presentation characteristics between groups. Outcomes included time to first surgery, total surgeries, hospital and ICU length of stay, fecal diversion, mortality, consultants, and disposition
Results: 145 patients with NSTI were included: 23 TCH (15 8%), 108 (74 4%) OSH/TCH first surgery, and 16 (11.0%) OSH first surgery. Demographics and comorbidities were similar between groups. There was no difference in minutes to first surgery between TCH (731371) and OSH patients (867498); p=0 22 There was no difference in ICU days for patients who presented at TCH (M= 4 52, SD= 5 10) and those transferred from OSH (M= 3 74, SD= 5 68); p=0 56 Those who started at TCH had on average more surgeries than OSH patients (4 vs 2 8, p=0 02) There was no difference in our other pre-defined outcomes
Conclusions: These findings suggest that transfer status does not independently predict the outcomes for NSTI patients. Transfer to TCHs for NSTI management before or after first surgery can be safely done within regional hospital networks

Meaghan MacRae, BS, Megan Callaghan, BS, Omkar Pawar, MSCE, BDS, and Eiichi Miyasaka, MD.
Introduction: Ultrasound (US) is a commonly employed method to aid in the diagnosis of acute appendicitis. However, US accuracy is dependent on the operator and location of the appendix, contributing to a high nonvisualization rate This study aims to describe patient characteristics that predict the visualization of the appendix by US We also aim to describe patient features that warrant further investigation for non-visualized appendices (NVA)
Methods: We performed a retrospective chart review of 795 pediatric patients who underwent 743 US for suspected appendicitis at a pediatric emergency department from November 2017 through December 2021 Imaging findings were characterized as positive, negative, equivocal, or NVA Appendix location was classified as central, pelvic, retrocecal, anterior, or not visualized Patient age, sex, body mass index (BMI), pediatric appendicitis score (PAS), c-reactive protein (CRP) and diagnosis by surgical pathology were recorded. Descriptive statistics were obtained and comparisons between groups were done using chi-squared tests.
Results: Of the 743 ultrasounds in our study, 186 visualized the appendix while 557 were NVA The appendix was more likely to be visualized in males (30 7% vs 20 4%), with the highest visualization rate between ages 8-11 years in males (42 1%) and 10-12 years in females (35 5%) Visualization rate was lower after age 13 (18 3%), declining in both sexes. Visualization was inversely related to patient BMI, with 32.4% visualization for BMIs < 17.9, 26.9% for BMIs 18 – 22.9, and 7.3% for BMIs > 23. There were 139 patients who underwent CT after NVA by US and 51 patients who underwent primary CT Distribution of appendiceal location is shown in Figure 1
Of the NVA, 51 patients (9 2%) had acute appendicitis These patients had higher average PAS (6 2 vs 4 4, p< 001), WBC count (15.5 vs 9.7, p<.001), neutrophil count (12.1 vs 6.0, p<.001), and CRP (7.6 vs 3.5, p<.001) compared to those without appendicitis. There was no correlation with sex, age, BMI for NVA and the eventual diagnosis of acute appendicitis
Conclusions: Ultrasound has highest visualization rate between the ages of 8 and 12, with better rates in patients with lower BMIs Other diagnostic modalities including CT and observation should be more strongly considered in patients outside this category. Central and retrocecal locations of appendixes were less likely to be visualized on US, suggesting that a targeted re-scanning of this area may help improve US visualization rates.

Characteristics of the Patient and Appendix that Increase Visualization of the Appendix by Ultrasound

Figure 1. Distribution of appendiceal location by CT imaging was significantly different between those who underwent CT after initial NVA by US versus those who underwent primary CT scan (p=.015). 60% of appendices that were originally not visualized by US were either in the central or retrocecal positions

Allison Gasnick, BS, Avanti Badrinathan, MD, Christina Boutros, DO, Aria Bassiri, MD, Jillian Sinopoli, DO, and Christopher W. Towe, MD.
Introduction: Research is crucial in academic medicine, contributing to career advancement, institutional reputation, and patient care However, factors like temporal constraints, which can vary across specialties, and demographics can affect research productivity This study aims to understand factors that can enhance research productivity by investigating correlations between surgeon research productivity and specialty, medical school attended, year of graduation, and gender.
Methods: This study is a bibliometric analysis of publishing trends among providers who are actively practicing medicine in the United States A list of physicians was obtained using data from the Centers for Medicare & Medicaid Services (CMS), as well as their specialty of practice, medical school graduation and year, and gender Physicians were excluded if their primary specialty was non-surgical or they had missing specialty information. The outcome of interest was the number of citations listed in MEDLINE database. The database was accessed using the Entrez programming utilities for Python 3 as provided by the National Center for Biotechnology Information A Python 3 environment was utilized to develop a “scraping” method to derive publication information for a given author’s name using the Entrez utility and MEDLINE parsing utility This information was then imported into a pandas dataframe for further analysis. Providers were categorized by primary specialty as listed in the CMS database and duplicates were removed. The relationships of provider characteristics and citations were analyzed with linear regression
Results: Providers in the field of surgical oncology demonstrated an association with higher citation numbers than all other specialties considered (coeff 12 46,CI 4 77 – 20 15, p=0 002) Providers who attended medical schools that resulted in a MD degree, as opposed to DO, also demonstrated an association with higher citation numbers (coeff 16.16, CI 0.39 – 31.64, p=0.045). The number of years from medical school graduation to the timing of this study demonstrated a negative association, suggesting that younger providers are associated with higher citation numbers than their older counterparts (coeff -0 74, CI (-1 25, -0 22), p=0 005) Citation counts were similar among males and females
Conclusion: We show that surgical oncologists and younger physicians demonstrate higher research productivity. The competitive landscape of residency and fellowships and the increasingly competitive field of surgical oncology may contribute to these associations Medical schools with robust research resources, particularly MD schools, may play a vital role in preparing providers for successful academic careers

Physician Research Productivity: A Bibliometric Analysis .
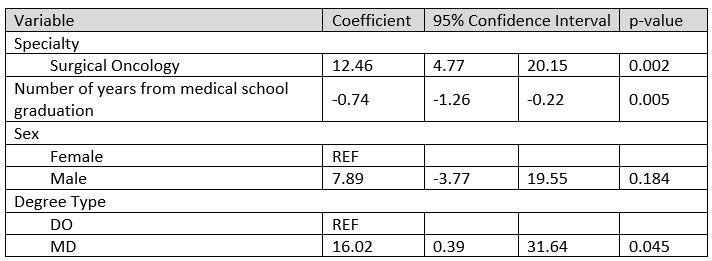
Table 1. Linear regression of factors associated with increased physician research productivity, as measured by citation count in the MEDLINE database. DO – Doctor of Osteopathic Medicine; MD – Doctor of Medicine.

Background: Hemangiomas are one of the most common head and neck masses encountered in the pediatric population and can be broadly classified into infantile and congenital hemangiomas. Accurate diagnosis and classification are essential for selecting the appropriate treatment approach, including observation, medical therapy, or surgery The aim of this study is to review our clinical experience and early outcomes with evaluation and management of infants less than one year of age with hemangiomas in the head and neck region
Methods: A retrospective review of all infants with hemangiomas in the head and neck region managed by our team over a 3-year period were included. Clinical characteristics, such as location, depth, symptoms, imaging, biopsy, and treatment modality, were tabulated. Hemangiomas were classified into infantile hemangioma (IH), rapidly involuting congenital hemangioma (RICH), and non-involuting congenital hemangioma (NICH) Physician assessment at around one year of age of whether of patients needed further treatment was obtained from review of patient chart and clinical photographs
Results: A total of 164 patients with 262 hemangiomas met inclusion criteria. Of the vascular lesions identified, 160 patients had IH, 2 had RICH, and 2 had NICH. The most common locations were the scalp (n=55, 21.0%), eyelid/periorbital region (n=28, 10 3%), and the neck (n=25, 9 5%) The average number of hemangiomas per patient was 1 6 ± 0 1 The average age of initial evaluation was 6 6 ± 1 7 months 18 (11 1%) patients reported symptoms related to the hemangioma including ulceration, bleeding, and visual obstruction Most did not require imaging for diagnosis (n=134, 81.2%), although some underwent ultrasound (n=18, 10.9%), MRI (n=7, 4.2%), or both (n=5, 3.0%), to aid in diagnosis or to exclude visceral involvement if suspected (e.g. liver ultrasound). One patient met diagnostic criteria for PHACE Only one patient underwent biopsy of their hemangioma Most patients underwent medical treatment for their hemangiomas (n=139, 84 2%), with only one (0 6%) undergoing surgical excision, and 22 (13 3%) opting for observation alone Two patients (1 2%) underwent both medical and surgical treatment in the first year of life. Systemic propranolol was the most common initial medical therapy (n=107, 77.5%), followed by topical timolol (n=29, 21.0%) and oral atenolol (n=2, 1.5%). The average length of follow-up was 11 1 ± 1 8 months Of the patients treated with propranolol, only 14 (13 1%) experienced complications, mostly minor complications such as cold hands and feet (n=9, 8 4%) and sleep disturbances (n=4, 3 7%) No patients were required to stop treatment due to complications At the most recent follow-up, a majority of the patient were deemed to unlikely need any additional treatment (74 55%)
Conclusion: Most head and neck hemangiomas can be diagnosed based on history and physical exam alone. Beta blocker therapy is the mainstay of treatment in infancy for head and neck IH that require treatment, with an excellent safety profile Surgical management may be indicated for select cases of IH for diagnostic or treatment indications Congenital hemangiomas present with unique features and require a different treatment approach, with surgical resection usually indicated in cases of NICH

Comparison of Hospital Volume and Risk-Standardized Mortality Rate as a Proxy for Hospital Quality in Complex Oncologic Hepatopancreatobiliary Surgery
William T. Julian, MS, Mohamedraed Elshami, MD, MMSc, John B. Ammori, MD, Jeffrey M. Hardacre, MD, Jordan M. Winter, MD, and Lee M. Ocuin, MD.
Background: Oncologic hepatopancreatobiliary operations are complex, and centralization to more experienced centers has been recommended but remains controversial Hospital volume and risk-stratified mortality rates (RSMR) are metrics for interhospital comparison. We aim to compare facility operative volume to facility RSMR as a proxy for hospital quality.
Methods: Patients who underwent surgery for liver (LC), biliary tract (BTC), and pancreatic (PDAC) cancer were identified in the National Cancer Database (2004-2018) Hierarchical logistic regression was used to create facilityspecific models for RSMR. High-volume centers (HVC) were in the top quintile, and low-volume centers (LVC) were in the lowest. High-performance centers (HPC) were in the lowest RSMR tercile, whereas those in the highest were low-performance centers (LPC). Primary outcomes included median facility RSMR and RSMR distributions Volume and RSMR-based redistribution was simulated and compared for reductions in 90-day postoperative mortality Case mixes and procedure-specific mortality was also compared for both volume and RSMR-stratifications
Results: 106,217 patients treated at 1282 facilities were included, of whom 17,695 had LC, 23,075 had BTC, and 65,447 had PDAC Analysis of case mix and patient demographics were similar overall, however 90-day mortality rates at low-volume centers compared to high-volume centers were ~2-fold higher for liver cancer (11 0% vs 5 8%, p<0 001), ~2-fold higher for BTC (6 7% vs 13 3%, p<0 001), and ~1 6-fold higher for pancreatic cancer (7 8% vs 4.8%, p<0.001). For RSMR-based stratification, 90-day mortality rates at low-performance centers compared to high-performance centers were ~2.5-fold higher for liver cancer (13.7% vs 5.5%, p<0.001), ~2.5-fold higher for BTC cancer (16.3% vs 6.2%, p<0.001) and ~3-fold higher for pancreatic cancer (12.0% vs 4.0%, p<0.001). HVC had lower RSMR compared to medium-volume and LVC for LC, BTC, and PDAC (all p<0 001) HPC had lower RSMR compared to MPC and LPC for LC, BTC, and PDAC (all p<0 001) Volume-based redistribution required 16 0 patients for LC, 11 2 for BTC, and 14 9 for PDAC reassigned to 15, 22, and 20 centers per life saved within each US census region. RSMR-based redistribution required 4.7 patients for LC, 4.2 for BTC, and 4.9 for PDAC reassigned to 316, 403, and 418 centers per life saved within each US census region.

Conclusion: Our findings indicate that RSMR may outperform volume as a proxy for hospital quality with oncologic hepatobiliary surgery RSMR-based redistribution was more efficient in reducing patient mortality per patient moved, requiring 2-3 fold fewer patients to be moved compared to volume-based redistribution while achieving the same reduction in mortality. RSMR-based redistribution placed patients in more recipient centers, suggesting that RSMR-based redistribution could limit the logistic difficulties associated with redistribution. Additionally, this study finds that differences in postoperative mortality are driven primarily by facility-specific factors rather than patient-specific or case-specific factors, a finding that we believe is novel These findings have important implications given the context of centralization and patient redistribution, particularly given the high morbidity and mortality rates associated with such oncologic surgical procedures

Gillian Michaelson, BS, BA, Lucille Hu, MPH, Shelley Ohliger, MD, Anuja Sarode, MPH, and Anne K Mackow, MD, MPH.
Purpose: Universal pre-operative anesthesia screening is resource-prohibitive in certain hospital settings. Risk stratification could decrease the overall intensity of universal screening by limiting inperson screening to those patients with the highest anesthesia risk. We investigated whether a modified version of the NARCO (Neurologic, Airway, Respiratory, Cardiac, Other) pre-surgical pediatric risk score could effectively stratify pediatric surgical patients into high- and lowanesthetic-risk groups and whether this stratification would be predictive of postanesthetic/post-surgical complications
Method: A retrospective analysis was conducted using 132,881 records from the American College of Surgeons National Surgical Quality Improvement Program-Pediatric (2019 ACS NSQIP-P®) Comorbidities were sorted into NARCO categories and assigned presumptive scores using two methodologies one considered uncertain comorbidities as high-risk (overestimating the highrisk group) and another that considered these low-risk (overestimating the low-risk group). These groups were evaluated by demographic and adverse outcome data using chi-square or Wilcoxon-Mann-Whitney analyses (p<0.05).
Results: In both methodologies, the occurrence of 23 of 24 adverse events were significantly (p<0 05) associated with the high-risk group; premature infants and neonates were significantly more likely to be sorted into this group Additionally, a strong correlation was found between anesthetic risk as determined by both NARCO and ASA scores.
Conclusion: We conclude that a modified version of the NARCO pre-surgical risk assessment for pediatric patients can accurately stratify patients into high- and low-risk groups based on non-granular patient data Regardless of methodology, this risk stratification identified patients at highest risk for post-anesthetic and postsurgical complications, which can identify those who require intensive pre-surgical screening.

Kathleen M. Mulligan, BA, Hanna Kakish, MD, Omkar Pawar, BDS, MSCE, Fasih Ali Ahmed, MD, Mohamedraed Elshami, MD, MMSc, Luke D. Rothermel, MD, MPH, Jeremy S. Bordeaux, MD, MPH, Iris Y Sheng, MD, Ankit Mangla, MD, and Richard S. Hoehn MD.
Background: Melanoma survival has greatly improved with the advent of immunotherapy, but unequal access to these medications may exist due to non-medical patient factors such as insurance status, educational background, and geographic proximity to treatment.
Methods: We used the National Cancer Database to assess patients with non-metastatic cutaneous melanoma who underwent surgical resection and sentinel lymph node biopsy (SLNB) with tumor involvement from 2015-2020 We evaluated rates of adjuvant immunotherapy among this patient population based on patient, tumor, and facility variables including insurance status, socioeconomic status, pathological stage (IIIA-IIID), and treatment facility type and volume.
Results: Adjuvant immunotherapy was associated with improved survival for stage III melanoma, with slight increase in 5-year OS for stage IIIA (87 9% vs 85 9%, p=0 044) and higher increase in stages IIIB-D disease (70.3% vs. 59.6%, p<0.001). Receipt of adjuvant immunotherapy was less likely for patients who were older, low socioeconomic status, or uninsured. Low volume and community cancer centers had higher rates of adjuvant immunotherapy overall for all stage III patients, whereas high volume and academic centers used adjuvant immunotherapy much less often for stage IIIA patients compared with those in stages IIIB-D
Discussion: Our results demonstrate inconsistent use of adjuvant immunotherapy among patients with stage III melanoma, despite a significant association with improved survival. Notably, there was a lower use of adjuvant immunotherapy in patients of lower SES and those treated at high volume centers. Equity in access to novel standards of care represents an opportunity to improve outcomes for patients with melanoma

Presenting: Gabriel Tensol Rodrigues Pereira, MD
Clinical Resident, Internal Medicine
Percutaneous Decannulation of Extracorporeal Membrane Oxygenation Using MANTA Device: A Realworld Single-center Experience.
Ioannis Milioglou, Alice Qian, Pedro Rafael Vieira de Oliveira Salerno, Gabriel Tensol Rodriguez Pereira1, Luis Augusto Palma Dallan, Kelsey Gray, Michael Morrison, Yasir Abu-Omar, and Cristian R. Baeza
Introduction: The MANTA Vascular Closure Device (VCD) represents a novel approach to achieving hemostasis after large-bore femoral access procedures Numerous clinical studies have evaluated the efficacy of the MANTA device across a range of patient populations undergoing different procedures. However, there is still a paucity of data available concerning the use of MANTA devices in aiding the decannulation of VAECMO. Therefore, our study aims to present our single-center experience of utilizing the MANTA VCD in patients undergoing this procedure
Methods: This single-center study included all patients undergoing percutaneous decannulation of femoral VA ECMO using the MANTA plug-based VCD between January 2021 and October 2023 at University Hospitals Cleveland Medical Center Inclusion criteria were adult patients who required prolonged (>24 hours) hemodynamic support with VA-ECMO Outcomes included all-cause mortality, hemostasis, bleeding, limb ischemia and site infection Vessel closure technique: Once the ECMO circuit was disconnected, the arterial cannula was clamped and cut leaving about 5 centimeters length distal to the clamp. Using 3 medium size tegaderms at the distal end of the cannula, a water-sealed membrane was created. The clamp was removed and then an 18G needle was used to perforate the tegaderm membrane to push the guide wire inside the artery. Once the wire was secured inside the artery, the cannula was removed holding manual compression while the Manta sheath was pushed over the wire Subsequently, the insert piece was removed from the sheath and the closure unit was inserted The toggle was then released, the assembly component withdrawn, and the collagen pad secured onto the anterior arterial wall using the stainless-steel lock.

Clinical Resident, Internal Medicine
Percutaneous Decannulation
MANTA
Results: This is a retrospective cohort study of 19 patients. Baseline characteristics and pre-decannulation labs are shown in Table 1. The most common ECMO indication was acute coronary syndrome (ACS) complicated by cardiogenic shock at 36 8% The mean length of ICU stay for these patients was 18 8 days (± 8 42) Seventeen out of 19 patients survived to discharge The MANTA device was successfully deployed in 19 patients, with 10 procedures conducted at the bedside and 9 in an operating room setting Complete hemostasis was achieved within 5 minutes of MANTA deployment in 17 out of 19 patients. In 2 patients manual compression after Manta deployment was required to achieve adequate hemostasis. Additionally, acute lower extremity ischemia was noted in two patients, necessitating endovascular interventions. No infections were reported at the site of MANTA deployment
Conclusion: Overall, based on our experience and that of other centers, the MANTA VCD has proven to be a simple, safe and effective percutaneous technique for facilitating in the OR, but most of all it opens the opportunity for bedside VA-ECMO decannulation. Post decannulation ischemic complication are higher in this series of sick patients when compared with elective procedures like TAVR and EVAR Additionally, operators should be mindful of the incidence of ischemic complications Distal Doppler pulse signals should always be checked, in order to indicate bailout options when this occurs

Hailey Seibert, BA, Hanna Kakish, MD, Maira Bhatty, MS, Adam Wade, BA, Henry Herrera, BA, Richard S Hoehn, MD, and Luke D Rothermel, MD, MPH.
Introduction: Melanoma is more common in high socioeconomic status (SES) population, yet low SES populations present with more advanced disease We set out to understand the effect of social determinants of health and other factors on the receipt of systemic treatment for stage 4 melanoma patients within our regional health system
Methods: We reviewed patients with metastatic melanoma at our institution (2010-2021) We collected information on baseline demographics, SES (based on the Area Deprivation Index [ADI], highest quartile considered ‘low SES’), tumor characteristics, and treatment details. We stratified our cohort into two groups based on the receipt of any type of systemic treatment. Intergroup comparisons were computed using Pearson Chisquare test, Fisher’s exact test, and Mann-Whitney U-test as appropriate Multivariable regression analysis was performed to identify predictors of no systemic treatment receipt We reported granular information on reasons for not receiving systemic treatment Finally, multivariable Cox hazard models were fit for OS
Results: We included 179 patients in our analysis, of whom 60 (33.5%) did not receive any type of systemic treatment. Non-receipt of systemic treatment was higher in patients who were older (≥66 years= 40.4% vs. <66 years= 25 9%), of low SES (46 6% vs 23 7%), of race other than Non-Hispanic White (62 5% vs 30 7%), without any history of previous melanoma (43 6% vs 22 4%), symptomatic at presentation (39 3% vs 20 0%), and diagnosis between 2010-2017 (42 7%) vs 2018-2021 (16 1%) (all p<0 05) On multivariable analysis, Low SES, higher ECOG score, and diagnosis between 2010-2017 were associated with no systemic treatment receipt. Reasons for nonreceipt of systemic treatment included: advanced disease that precluded treatment initiation and recommended for hospice care (48 3%), receipt of other treatment (metastasectomy +/- radiation) (23 3%), poor medical conditions (16 7%), refusal despite medical advice (6 7%), and death due to other cause/missing (5%) We reported those reasons based on the SES status in Figure 1 Multivariable Cox analysis demonstrated worse survival for patients who did not receive systemic treatment (HR= 2.31, 95% confidence interval [CI]= 1.40-3.81), no spouse/significant other (HR= 1.83, 95% CI= 1.14-2.94), and higher ECOG score (HR= 1.33 per one value increase, 95% CI= 1.04-1.69).
Conclusion: The results of this study showed that in our regional hospital system, we can predict less receipt of systemic treatment by identifying patients coming from regions having higher rates of medical deprivation, as determined by ADI. Notably, those reasons more often included advanced disease and poor medical condition, which are not modifiable at the time of diagnosis. The best option to improve the receipt of systemic therapy for patients with lower SES may be to invest in primary care efforts to improve baseline health, allowing for all treatment options in the face of metastatic melanoma

Social Determinants of Health Predict Lower Receipt of Systemic Treatment, Influencing Survival in Patients with Metastatic Melanoma
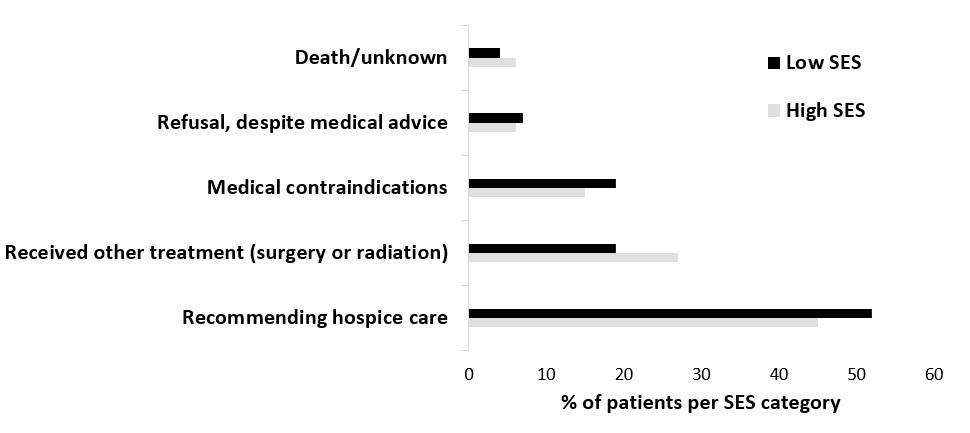
Figure 1: Granular reasons for not undergoing systemic treatment for patients at our institution diagnosed with stage IV melanoma 2010-2021, separated by SES

Initiation of a Single-Institution Hepatic Artery Infusion Pump Program for Colorectal Liver Metastases and Intrahepatic Cholangiocarcinoma: Safety, Feasibility,andCirculatingTumorDNATracking
Lee M. Ocuin, MD, Henry Stitzel, BS, Michelle Chung, MD, Sree Harsha Tirumani, MD, Maria Tomaro, MSN, CNP, OCN, David Bajor, MD, Sakti Chakrabarti, MD, Melissa Lumish, MD, Madison Conces, MD, Amit Mahipal, MD, Jennifer Miller-Ocuin, MD, Emily Steinhagen, MD, Ronald Charles, MD, Michael Liu, MD, David Dietz, MD, Meagan Costedio, MD, John B. Ammori, MD, and J. Eva Selfridge, MD, PhD.
Introduction: Hepatic artery infusion (HAI) with floxuridine (FUDR) is a treatment option for patients with colorectal liver metastases (CRLM) or intrahepatic cholangiocarcinoma (ICC). Outcomes from newer HAI centers are understudied ctDNA tracking has not been described in patients receiving HAI Herein, we describe safety, feasibility, oncologic outcomes, and results of dynamic circulating tumor DNA (ctDNA) in patients treated with HAI at a new HAI program
Methods: All patients who underwent HAI pump placement from April 2022 through March 2024 were included. Data were collected by retrospective chart review Outcomes included safety, technical success rate (post-operative nuclear medicine study showing no extrahepatic perfusion and bilobar hepatic perfusion), feasibility (receiving >1 cycle of FUDR), relative dose intensity (RDI) of FUDR received, radiographic response (RECIST 1 1), and quantitative ctDNA response.
Results: A total of 29 patients underwent HAI pump placement by one surgeon (LMO), co-managed by two medical oncologists (JES, ML) Twenty-five (86%) had CRLM and four (14%) had ICC Most (97%; 28/29) received systemic chemotherapy (median: 6 cycles) prior to pump placement
One operation was performed robotically, and the remainder were done with an open approach. 32 concomitant procedures were performed in 19 (76%, n=19/25) patients with CRLM (colectomy [n=13], proctectomy [n=3], partial hepatectomy [n=10], microwave ablation [n=6]) There were no 30 day mortalities and 1 patient experienced rapid tumor progression and died within 90 days Of the patients that have reached 90 days postoperatively, five patients (20%, n=5/25) experienced Clavien-Dindo Grade >3 complications Three patients (10%) experienced a total of 5 HAI pump-specific complications (pump pocket [n=3], hemorrhage [n=1], biliary sclerosis [n=1]).

Initiation of a Single-Institution Hepatic Artery Infusion Pump Program for Colorectal Liver Metastases and Intrahepatic Cholangiocarcinoma: Safety, Feasibility,andCirculatingTumorDNATracking
Technical success was 100%. Feasibility was 97% (n=28/29). Median time from surgery to initiation of HAI was 14 days Median number of FUDR cycles received was 5 13 patients (46%, n=13/28) experienced a dose reduction and 20 (71%, n=20/28) experienced a dose hold Median RDI was 74 0% (CRLM: 74 0%; ICC 72 5%) 19 patients (68%, n=19/28) had measurable disease on pre- and post-HAI pump implantation At the time of data analysis, disease control rate was 95%; 12 patients had demonstrated partial response and 7 had stable disease. Five patients (20%, n=5/25) with CRLM underwent complete metastasectomy within 12 months of pump implantation. Quantitative ctDNA was obtained on 11 patients (38%). Nearly all patients (n=9, 82%) had initial decrease in ctDNA level upon initiation of HAI Rising ctDNA level appeared to occur with extrahepatic disease progression
Conclusions: Implementation of a new HAI program is safe and feasible with promising early oncologic outcomes ctDNA tracking is achievable in this patient population and dynamic changes in ctDNA may correlate with radiographic response to treatment.

Initiation of a Single-Institution Hepatic Artery Infusion Pump Program for Colorectal Liver Metastases and Intrahepatic Cholangiocarcinoma: Safety, Feasibility,andCirculatingTumorDNATracking
Figure 1. Quantitative ctDNA tracking data for all patients with ctDNA values drawn on the first day of FUDR treatment. The x axis highlights time from FUDR initiation in days, the y axis represents the percent change in quantitative ctDNA from baseline, and the arrows indicate a hold or reduction in FUDR dosing Figure 4A is represents patients with ICC, whereas Figure 4B-E represents patients with CRLM


Aria Bassiri, MD, Christina Boutros, DO, Grigory A. Manyak, BA, Boxiang Jiang, MD, Jillian Sinopoli, DO, Leonidas Tapias Vargas, MD, Philip A. Linden, MD, and Christopher W. Towe, MD.
Background: Patients with clinical N3 non-small cell lung (NSCLC) cancer are traditionally treated with definitive chemoradiation followed by immunotherapy. We hypothesize that survival outcomes between cN2 and cN3 disease after lobectomy are similar and that neoadjuvant therapy followed by surgery may be appropriate for select patients with cN3 disease
Methods: This is a retrospective analysis of the 2020 National Cancer Database (NCDB). Adult Patients with clinical N2 or N3 non-metastatic NSCLC were identified. Patients were further categorized into two groups based on treatment: Definitive chemoradiation with immunotherapy versus neoadjuvant therapy followed by surgery (lung lobectomy) The outcome of interest was overall survival Demographic, clinical, and institutional characteristics were compared between the groups utilizing bivariate analysis Multivariable logics regression, adjusted for pertinent variables, was performed to assess association with treatments Adjusted multivariable Cox regression with interaction analysis, Kaplan Meier (KM) survival analysis, and log-rank test were performed to determine the association with clinical N stage, treatment choice, and overall survival amongst patients with clinical N2 and N3 A further survival analysis utilizing the same statistical method was performed to evaluate survival amongst patients with cN3 disease comparing overall survival between different treatments Data is shown as odds ratio (OR) or hazard ration (HR) and 95% confidence interval Statistical significance was defined as p value ≤0.05.
Results: In total, 345,813 patients were identified with clinical N2 (73.8%, n=255,137) or N3 (26.2%, n=90,676) non-metastatic lung cancer Among patients with cN2 and cN3 disease, 24,824 (cN2:16,986, cN3:7,838) underwent definitive chemoradiation with immunotherapy and 12,301 (cN2:12,301, cN3:646) underwent neoadjuvant chemoradiation followed by surgery In multivariate logistic regression adjusted for clinical and demographic characteristics, patients with cN3 were more likely to undergo definitive chemoradiation with immunotherapy compared to patients with cN2 disease (OR 0.11, CI 0.10-0.12). In Multivariate Cox regression and KM analysis, compared to patients with cN2 disease that underwent neoadjuvant therapy followed by surgery, patients with cN3 disease demonstrated similar overall survival (HR 0 97, CI 0 88-1 08; log rank test: p=0 708 Figure) Lastly, among patients with cN3 disease, those who were treated with neoadjuvant therapy followed by surgery had a survival advantage compared to patients that underwent definitive chemoradiation with immunotherapy (HR 1.03, CI 1.02-1.04, log rank test: p<0.001. Figure) and patients with pathologic N2 and N3 demonstrated inferior survival compared to patients with pathologic N0.

Conclusions: N3 non-metastatic NSCLC patients have survival outcomes similar to N2 disease after neoadjuvant therapy followed by surgery Among patients with N3 disease, neoadjuvant therapy with surgery demonstrated improved overall survival compared to definitive chemoradiation followed by immunotherapy These findings challenge the dogma that patients with clinical N3 NSCLC should be non-surgical.
Figure – Kaplan Meier survival estimate among patients with clinical N2 and N3 non-metastatic non-small cell lung cancer stratified by treatment (neoadjuvant therapy followed by surgery and definitive chemoradiation with immunotherapy) from 2004-2019 in the National Cancer Database

Christina S. Boutros, DO, Hanna Kakish, MD, Alexander W. Loftus, MD, John B. Ammori, MD, Jeremy Bordeaux, MD, MPH, Ankit Mangla, MD, Iris Sheng, MD, Gary Schwartz, MD, Luke D. Rothermel, MD, MPH, and Richard S. Hoehn, MD.
Introduction: The NCCN considers “baseline staging” (whole body PET scan +/- brain MRI) for all asymptomatic melanoma patients with a positive sentinel lymph node biopsy (SLNB) Metastatic workups are increasingly used for node-negative patients with high-risk tumors that may benefit from adjuvant systemic therapies The true yield of these workups is unknown
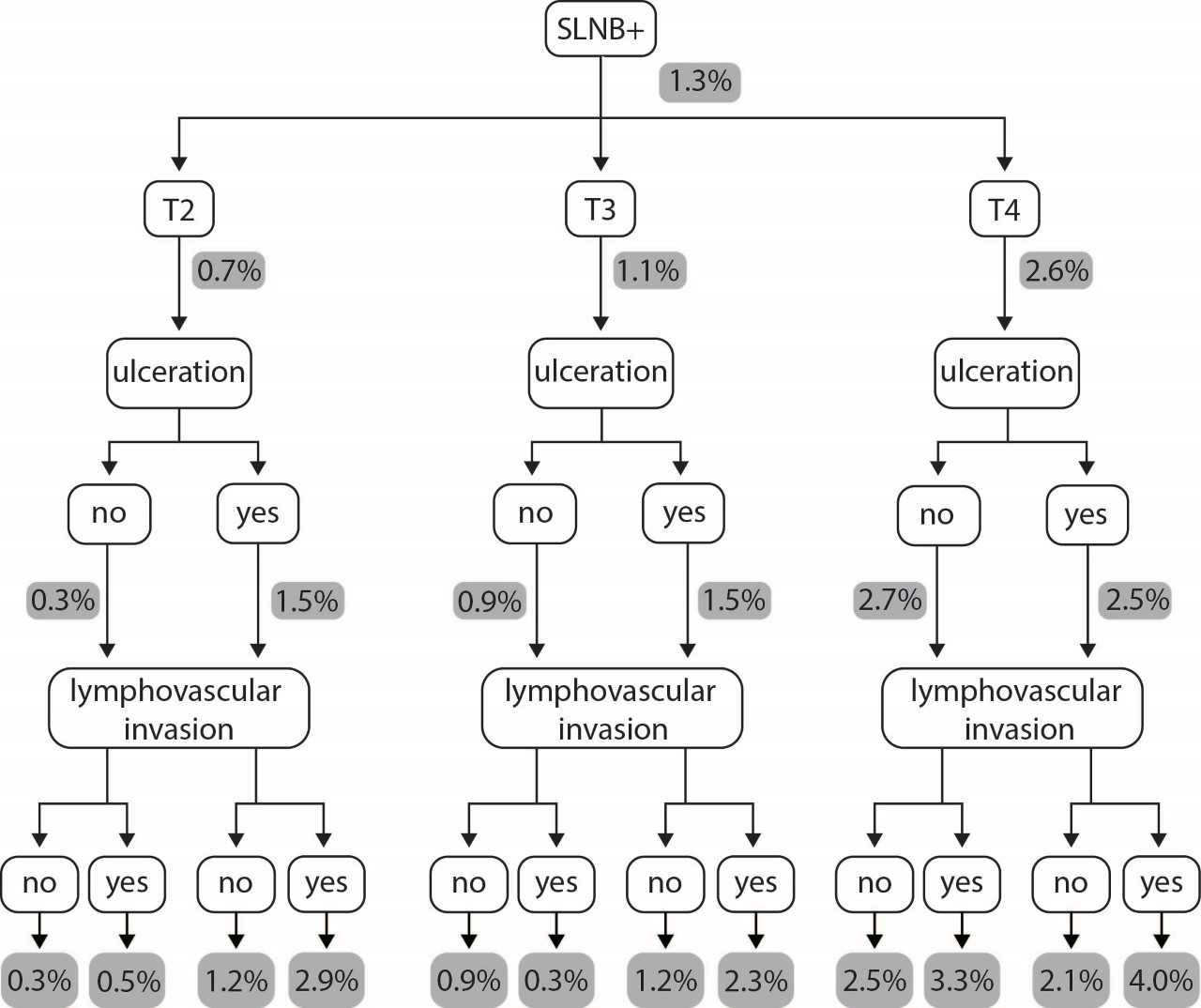
Methods: We created cohorts of adult malignant melanoma patients, T2-4, using the National Cancer Database (NCDB, 2012-2020) to mimic three common clinical scenarios: (1) clinically node negative, with positive sentinel lymph node(s) (SLNB[+]); (2) clinically node negative, with negative sentinel lymph node(s) (SLNB[-]); (3) clinically node positive who underwent lymph node dissection or other form of biopsy and had proven pathologic nodes (cN[+]) Demographic and clinical characteristics were compared by univariable analysis Multivariable regression identified independent predictors of metastasis in each cohort. Supervised decision trees classified the rates of metastasis based on key clinical variables.
Results: 12,083 patients were SLNB[+], 65,939 were SLNB[-], and 10,771 were cN[+] Rates of any metastatic disease and brain-only metastases across cohorts were as follows: (1) 169 (1 4%) / 37 (0 3%); (2) 203 (0 3%) / 26 (<0.1%); (3) 325 (10.5%) / 49 (1.6%) (p < 0.001). There was a significant increase in rates of metastases with increased T stage for cohorts 1 and 2 (p <0.001). T4 tumors (OR 2.55, p < 0.01, CI 1.50-4.49), ulceration (OR 1.48, p = 0 026, CI 1 04 - 2 09), and LVI (OR 1 7, p = 0 008, CI 1 14 – 2 42) associated with greater risk of metastatic disease for both SLNB[+] and SLNB[-] patients on multivariable regression For cN[+] patients, only lesions found on the lower limb as well as nodular and lentigo maligna subtype associated with greater risk of metastases on multivariable regression. A supervised decision tree to classify the rates of any metastasis for SLNB[+] and SLNB [-] patients was completed. The only groups with >2% risk of metastatic disease were T4 tumors or T2/T3 tumors with ulceration and LVI. Most groups had a negligible risk (<0.1%) of brain-only metastases.
Conclusion: This is the first analysis to guide pragmatic use of metastatic imaging for patients following melanoma excision and SLNB Among cN0 patients, metastatic disease is uncommon and brain-only metastases are exceedingly rare. Further investigation could promote a tailored and value-based approach to metastatic workups guided by individual risk factors.

Figure 1. Supervised decision tree which describes the rates of metastatic disease given different clinical and tumor characteristics. Grey boxes indicate the rate of any metastatic disease for each branch of the tree.

Hamza Nasir Chatha, MD, Joshua Lyons, MD, Christina Boutros, DO, Saher-Zahra Khan, MD, Patrick Wieland, MD, Iris Levine, BS, Jamie Benson, MD, Christine Alvarado, MD, Guy Katz, MD, and Jeffrey M. Marks, MD.
Background: Although per oral endoscopic myotomy (POEM) has shown to be beneficial for the treatment of achalasia, it can be difficult to predict who will have a robust and long lasting response. Historically, it has been shown that higher lower esophageal sphincter pressures have been associated with poorer responses to alternative endoscopic therapies such as Botox therapy and pneumatic dilation This study was designed to evaluate if modern preoperative manometric data could similarly predict a response to therapy after POEM
Methods: This was a retrospective study of 237 patients who underwent POEM at a single institution over a period of 13 years (2011-2023) and who had a high-resolution manometry performed preoperatively and an Eckardt symptom score performed both preoperative and postoperatively. The achalasia type and integrated relaxation pressures (IRP) were tested for potential correlation with need for any further achalasia interventions postoperatively as well as the degree of Eckardt score reduction using linear regression model
Results: The Achalasia type on preoperative manometry was not predictive for further interventions or degree of Eckardt score reduction (p= 0.76 and 0.43, respectively). A higher IRP was not predictive of need for further interventions, however it was predictive of a greater reduction in postoperative Eckardt scores (p=0 03) as shown by the nonzero regression slope
Conclusion: In this study, achalasia type was not a predictive factor in need for further interventions or the degree of symptom relief. Although IRP was not predictive of the need for further interventions, a higher IRP did predict better symptomatic relief postoperatively. This result is opposite that of other endoscopic treatment modalities (Botox and pneumatic dilation) Therefore, patients with higher IRP on preoperative high-resolution manometry would likely benefit from POEM which provides significant symptomatic relief postoperatively
Keywords: Integrated Relaxation Pressure (IRP); Achalasia; Manometry; Eckardt score; per oral endoscopic myotomy (POEM)

Elevated Preoperative Lower Esophageal Sphincter Pressure Predicts Improved Clinical Outcomes after Per Oral Esophageal Myotomy (POEM)
Figure 1. Eckardt score reduction vs Preoperative IRP showing a positive correlation


Adjuvant Chemotherapy is Underused in Women Aged < 50 with HR+ HER2Breast Cancer in the National Cancer Database
Susan J. Doh, MD, Amanda L. Amin, MD, MS, FACS, FSSO, Ashley B. Simpson, DO, FACOS, FACS, Lisa Rock, MD, FACS, Robert Shenk, MD, FACS, and Megan Miller, MD, FACS.
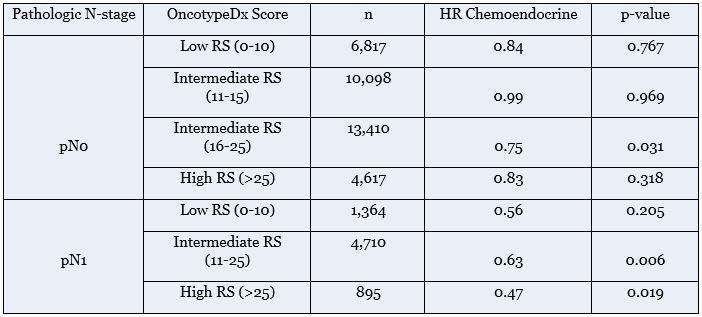
Introduction: For HR+ HER2- breast cancer, the TAILORx and RxPONDER studies established the benefit of adjuvant chemoendocrine therapy over endocrine therapy alone in women aged ≤50 with N0 disease and OncotypeDx recurrence score (RS) 16-25, and N1 disease and RS < 25, respectively Our aim was to determine factors associated with chemotherapy receipt in women < 50 with stage I-III HR+ HER2- breast cancer in clinical practice and assess overall survival (OS) for comparison with clinical trials data
Methods: We queried the NCDB 2004-2020 for women aged 18-49 with stage I-III HR+ HER2- breast cancer who underwent surgery. Patients with inflammatory breast cancer, bilateral disease, unknown RS, and neoadjuvant systemic therapy receipt were excluded Univariable logistic regression and multivariable Cox proportional hazards assessed factors associated with chemotherapy receipt and OS
Results: Of 69,542 patients, 82.5% were pN0, 17.3% were pN1, and 0.1% were pN2+. RS was similar in pN0 and pN1 patients: low RS (0-10) 19.7% and 19.4%, intermediate RS (11-25) 66.8% and 67.3%, and high RS ( >25) 13 6% and 13 3% Chemotherapy receipt increased with greater burden of nodal disease (24 1% pN0, 46 8% pN1, and 88 1% pN2+, p< 0 001) and with RS (4 9% low, 56% intermediate, 39% high, p< 0 001) The vast majority of pN0 patients who received chemotherapy had RS 16-25 (46 7%) or >25 (44 9%) However, in the N0 group, 68 6% of RS 16-25 and 15.1% of RS >25 patients did not receive chemotherapy. Of pN 1 patients, 70.5% of low RS and 52.6% of intermediate RS patients did not receive chemotherapy. Factors positively associated with chemotherapy receipt were intermediate and high RS (OR 4.04 and OR 57.17, both p < 0.001), grade 3 histology (OR 3.66, p < 0 001), larger tumors (pT2-4 OR 1 48-3 07, p < 0 001), and nodal positivity (pN1 OR 3 17 and pN2+ OR 12 29, both p < 0 001) For patients who received endocrine therapy (n = 65,238, 93 8%), there was an OS benefit with chemoendocrine therapy in pN0 patients with RS 16-25 (HR 0 75, p=0 031) A similar OS advantage was observed for pN1 patients with intermediate (HR 0.65, p=0.006) and high RS (HR 0.4, p=0.02).
Conclusions: Acknowledging the exclusion of neoadjuvant treatment, less than half of women with HR+ HER2breast cancer aged < 50 and pN0 RS 16-25 or pN1 RS < 25 in the NCDB received adjuvant chemoendocrine therapy despite the OS benefit established in clinical trials and largely confirmed in this study Our results likely reflect complex decision-making, including the potential replacement of chemotherapy with ovarian suppression, and highlight opportunities to refine application of the recent TAILORx and RxPONDER findings to oncologic practice.

Adjuvant Chemotherapy is Underused in Women Aged < 50 with HR+ HER2Breast Cancer in the National Cancer Database
Multivariable Cox Proportional Hazard Ratios for Chemoendocrine vs Endocrine Therapy alone in women aged <50 with HR+ HER2- breast cancer

Socioeconomic Status and Dermatologist Accessibility, and Early vs. Late-Stage Melanoma Risk
Weichuan Dong, PhD, Brock Montgomery, Uriel Kim, PhD, MBA, Hanna Kakish, MD, Johnie Rose, MD, PhD, Siran M. Koroukian, PhD, Jeremy S. Bordeaux, MD, MPH, Luke D. Rothermel, MD, MPH, and Richard S. Hoehn, MD.
Background: Socioeconomic status (SES) and dermatologist accessibility can influence the detection and diagnosis of melanoma The objective of this study is to understand the association between early and late-stage melanoma incidence rates with neighborhood-level SES and dermatologist accessibility
Methods: This cross-sectional study included individuals diagnosed with melanoma in Ohio from 2011 to 2020 from the Ohio Cancer Incidence Surveillance System. Incidence rates of early-stage (defined as local stage) and late-stage (defined as regional or distant stage) melanoma were calculated at the neighborhood-level using the Max-P regionalization method to ensure statistical stability and safeguard patient confidentiality SES was measured using the area deprivation index, while dermatologist accessibility was captured using the 2-Step Floating Catchment Area method that accounted for dermatologist density, population, and travel time We identified and characterized neighborhoods with suboptimal melanoma detection (low rates of early-stage and high rates of late-stage disease). We then examined how suboptimal melanoma detection is associated with SES and dermatologist accessibility using geospatial analysis pairwise t-tests
Results: The study included 20,138 individuals, with 99% of patients who were White living in 259 neighborhoods. The median (interquartile range) of early-stage and late-stage incidence rates were 16.5 (14.020.1) and 4.1 (3.5-4.7) per 100,000 persons, respectively, across the neighborhoods. We found that neighborhoods with low early-stage, high late-stage incidence rates were more likely to be socioeconomically disadvantaged and have lower dermatologist accessibility They were additionally characterized by higher degrees of rurality, chronic disease burden, poorer health behaviors, and a higher proportion of African American residents Our analyses also suggest that SES and dermatologist accessibility was associated with early-stage incidence rates, but neither was associated with late-stage incidence rates (Figure).
Conclusions: Early-stage incidence rates in high-SES neighborhoods may have been driven by diagnoses of lowrisk melanoma that may not progress to late stage The risk of late-stage melanoma may not change by improved screening uptake in low-SES areas, data from high-SES areas indicate similar late-stage incidence rates Efforts should be prioritized on developing meaningful risk-stratified melanoma screening and highly effective treatments to target rapidly progressing melanoma.

Socioeconomic Status and Dermatologist Accessibility, and Early vs. Late-Stage Melanoma Risk
Figure 4. Bivariate maps of socioeconomic status and dermatologist accessibility and their association with early and late-stage incidence of melanoma.

Note: NS: not significant, ** p < 0.01, *** p < 0.001

To Revise Or Not to Revise? Isolated Margin Positivity in Localized Pancreatic Ductal Adenocarcinoma
Mohamedraed Elshami, MD, MMSc, Victoria S. Wu, BA, Henry J. Stitzel, BS, Jonathan J. Hue, MD, Alexander W. Loftus, MD, Ravi K. Kyasaram, MS, John Shanahan, BS, John B. Ammori, MD, Jeffrey M. Hardacre, MD, and Lee M. Ocuin, MD.
Background: Revision of positive margins during pancreatectomy for pancreatic adenocarcinoma (PDAC) is of unclear benefit We determined the proportion of patients who had margin-positive disease and no other adverse pathological findings (APF) using institutional and administrative datasets and estimated the fraction of patients who would derive potential benefit (FDPB) from margin revision.
Methods: Patients with clinical stage I-II PDAC who underwent pancreatectomy within our institution (20102021) and the National Cancer Database (NCDB; 2010-2020) were identified Isolated margin positivity (IMP) was defined as margin+ and absence of other APF (node+, PNI+, LVI+; institutional data) or margin+ and node/LVI- (NCDB) IMP* in the NCDB was estimated by multiplying IMP by the average rate PNI- calculated based on the current study and previous studies (83.8%). FDPB from neck margin revision was estimated by FDPB=IMP%×NMP%×NAPF% where NMP is the fraction of patients with a positive neck margin and NAPF is the fraction of patients with no APF. FDPB# in the institutional cohort and FDPB* in the NCDB cohort (location of positive margins is not captured) were calculated utilizing overall margin-positive rate
Results: We included 225 patients from our institution and 23,598 patients within the NCDB. The overall rate of margin positivity was 21 8% (institution) and 20 3% (NCDB) The rate of IMP was 0 4% (institution) and the rate of IMP* was 0.5% (NCDB). In the institutional cohort, 154 patients (68.4%) had recurrence. Of these, 34.4% were local and 65 6% were distant The rate of distant recurrence ranged from 61 1% (n=11/25) in patients with all pathological findings positive to 83.3% (n=5/6) in patients with no APF. Nine patients (4.0%) had a positive neck margin; six neck margins were analyzed by intraoperative frozen section, and three of these margins were positive None of the three margins were revised intraoperatively.
Within the institutional cohort, the FDPB was calculated using the following values: IMP, 0 4%; NMP, 4 0%; and NAPF, 6.2%. Therefore, 1 in 100,000 patients might derive a potential survival benefit from revision of a positive pancreatic neck margin (Table 1A) The FDPB# estimates approximately 1 in 18,500 patients might benefit from revision of any positive margin. For the NCDB analysis, FDPB* was calculated using the following values: IMP*, 0 5%; MP, 20 3%; and NAPF*, 3 9% Thus, approximately 1 in 25,000 patients might benefit from revision of a positive margin to negative (Table 1B).

To Revise Or Not to Revise? Isolated Margin Positivity in Localized Pancreatic Ductal Adenocarcinoma
In the institutional cohort, the median RFS was not reached for IMP, 63.3 months for NAPF, 14.8 months for negative margins+ 1 APF, 20 3 months for positive margins and 2+ APF, and 12 9 months for all APF positive Within the NCDB, patients with IMP had lower median survival than patients with no APF (20.5 vs. 39.0 months) but higher median survival than margin positivity+1 APF (20 5 vs 18 0 months) or all APF positive (20.5 vs. 15.4 months).
Conclusions: IMP in resected PDAC is rare and most patients recur distantly. Intraoperative revision of a positive margin after resection of PDAC is unlikely to confer benefit to most patients and should not be routinely performed


Jessica R. Hungate, MD, Gregory D. Rushing, MD, and Pablo F. Ruda Vega, MD.
Background: Recent trials support more aggressive management of the left atrial appendage during cardiac surgical operations In our division, minimally invasive coronary bypass, MIDCAB (LIMA to LAD), has become the therapy of choice to treat proximal LAD lesions not suitable for stenting. Elderly patients who are considered for MIDCAB often have a higher risk of bleeding and stroke. We present our initial experience excluding the left atrial appendage during MIDCAB.
Methods: In 2022 sixty-three patients underwent MIDCAB Of these seven underwent concomitant left atrial appendage exclusion Mini left anterior thoracotomy was used in all patients, one patient underwent multi-vessel grafting. Left atrial appendage exclusion was performed thoracoscopically (1), and via direct mini left anterior thoracotomy (6).
Results: The average age was 79 years; there were 4 men and 3 women The average CHADS2VASC2 score was 5 14, the average HASBLED score was 3 71 Four patients had an established diagnosis of atrial fibrillation Average follow up was four months; there were no myocardial infarctions, no strokes, and no deaths. All patients had TEE verified complete exclusion of the left atrial appendage.
Conclusions: Surgical left atrial appendage exclusion is feasible in minimally invasive coronary revascularization Concomitant left atrial appendage exclusion should be used to expand the indications for hybrid revascularization, especially in the elderly population


Immunotherapy Use in AJCC8 Stage IIIA Melanoma: A Single Institution Experience.
Hanna Kakish, MD, Kevin Xu, BA, Iris Sheng, MD, Ankit Mangla, MD, Richard S Hoehn, MD, and Luke D Rothermel, MD, MPH.
Introduction: Adjuvant immunotherapy for stage III melanoma demonstrated significant recurrence-free survival (RFS) benefits overall outweighing the risk of adverse events. However, literature on the benefits of adjuvant therapy on AJCC-8 stage IIIA-specific survival benefits is less robust, and it *is concerning that the risks of treatment-related adverse events (TRAEs) outweigh the benefits of adjuvant therapy in this subgroup of patients We set out to study adverse events in patients with AJCC-8 stage IIIA melanoma
Methods: We conducted a single-center retrospective study of adult patients with AJCC-8 stage IIIA melanoma who received either immunotherapy or surveillance between January 2015 and March 2022. We collected data on demographics, tumor details, and follow-up by searching through the electronic medical record We compared patients receiving immunotherapy vs clinical surveillance, and recorded clinically significant TRAEs experienced by the patients on immunotherapy We defined clinically significant TRAEs as any toxicity requiring additional treatment, referral to another specialty, or disruption of adjuvant treatment and reported the rate of each TRAE of the total patients receiving adjuvant immunotherapy Kaplan Meier survival curves were generated to compare RFS, overall survival (OS), and melanoma-specific survival (MSS) between patients who received adjuvant immunotherapy vs clinical surveillance Finally, we identified the characteristics of patients who had significant higher rates of recurrence
Results: We included 72 patients, of whom 36 patients (50%) received adjuvant immunotherapy and 36 patients (50%) received surveillance. The vast majority of patients (86.1%) had maximal nodal deposits <1 mm. 25 patients (69 4%) experienced at least one irAE The most common irAEs were dermatologic reactions (rash and/or pruritus) in 9 patients (25 0%) and hypothyroidism in 7 patients (19 4%) Other notable irAEs included transaminitis (11 1%), colitis (8 3%), arthralgia (5 6%), myositis (5 6%), and adrenal insufficiency (5 6%) (Table 1) Of patients who received treatment, 12 (33.3%) permanently discontinued treatment due to an adverse event, none of whom were started on a second-line therapy. No deaths were attributable to adverse events in our cohort. After a median follow-up period was 2 7 years, 17 patients (23 6%) experienced a recurrence Kaplan-Meier estimates for RFS, OS, and MSS at 2 years were not significantly different between the two groups based on immunotherapy receipt There were also no differences in time to any recurrence between patients who received systemic treatment versus those on surveillance (833 days vs 603 days, p=0.700). Finally, higher rates of recurrence were seen with larger nodal deposits (median of 0.06 [Interquartile range [IQR]= 0.02-0.2 mm] vs. 0.45 [IQR= 0.041.2 mm]).

Immunotherapy Use in AJCC-8 Stage IIIA Melanoma: A Single Institution Experience.
Conclusion: Our analysis reported relatively high rates of irAEs and discontinuations in immunotherapy-treated IIIA patients without any clear survival benefits The majority of patients in our cohort had <1mm nodal deposit, for whom recurrence rates are low at baseline Therefore, while prospective studies are needed to confirm these findings, clinicians should consider the relatively high adverse events with immunotherapy especially for patients with low risk stage IIIA melanoma.
Table 1: Treatment related adverse events for patients at our institution diagnosed with AJCC-8 stage IIIA melanoma 2010-2021, receiving adjuvant immunotherapy


Mamadi Papus Keita, MD, Mohammad El Diasty, MD, PhD, Travis Wilder, MD, Yasir Abu-Omar, MD, PhD, Rakesh Arora, MD, PhD, Cristian Baeza, MD, Kelsey Gray, MD, Igo Ribeiro, MD, Pablo Ruda Vega, MD, Gregory Rushing, MD, Marc Pelletier, MD, Joseph Sabik, MD, Yakov Elgudin, MD, PhD.
Objectives: This abstract provides a roadmap for launching a successful Ross procedure surgical program with focus on the logistics of team building and streamlining patient management to mitigate the impact of a steep learning curve on surgical outcomes
Methods: This is a narrative description of a division's experience with the initiation of a surgical program dedicated to performing Ross procedure. We describe the process and provide tips that we believe have contributed to the success of the program.
Results: Surgical Training: The program was initiated by two experienced surgeons with experience in aortic root surgery and with defined goals for a successful program A list of potential patients was developed The surgeons attended a formal training course at a center of excellence in Ross procedures. This course was comprised of dedicated lectures, wet lab sessions, and live surgery observation. Surgeons participated in other wet labs, including one on the morning before performing their first case, aided by a proctoring surgeon with Ross procedure expertise Two attending surgeons worked together in all cases and three other surgeons were added as the program grew to form a core group
Patient Selection: A patient selection pathway with specific eligibility criteria was established and distributed among all cardiac surgeons and referring cardiologists to ensure the capture of potential Ross procedure candidates
Standardized Procedure: Efforts were made to standardize all aspects of the surgery On the day of surgery, team members (including surgeons, anesthesiologists, scrub nurses, and perfusionist) participated in a comprehensive team huddle to discuss the technical details of the planned procedure and any potential variations.
Postoperative Care: An internal standardized order set was used to ensure that all members of the intensive care team managed these patients in a cohesive manner This included specific instructions on fluid management, inotropic/vasopressor support, and target blood pressure in the immediate postoperative period.

Follow-up: All Ross patients are captured in an institutional database, including clinical and radiological parameters for all patients. A dedicated nurse practitioner was designated to provide regular contact with patients after discharge to ensure full adherence to strict blood pressure targets for the first 6 months after surgery.
Monitoring Outcomes: A standardized quality process was utilized to continually review surgical outcomes and detailed multidisciplinary team discussions were held to review any serious complications
Program Growth Timeline: The program was launched in July 2022. During the planning phase (0-2 months), surgeons attended preparatory courses and wet labs. The following phase lasted for the next 6-8 months, during which, surgeons performed their first cases where they double scrubbed with each other for support and to gain more exposure to the procedure After that, three more experienced surgeons from the team started performing the procedure under the proctorship of the two lead surgeons The detailed program structure is presented in Figure 1.
Conclusions: Building a successful program for Ross procedure requires meticulous planning, team building, and a standardized perioperative care pathway These factors contribute to the program development and the achievement of excellent surgical results

Mamadi Papus Keita, MD
Surgical Fellow, Cardiac Surgery
Building a Ross Procedure Program, Keys to Success


Saher-Zahra Khan, MD, Christine Alvarado, MD, Jamie Benson, MD, Christina Boutros, DO, Patrick Wieland, MD, Hamza Nasir Chatha, MBBS, Guy Katz, MD, Joshua Lyons, MD, and Jeffrey M Marks, MD.
Introduction: Recurrence rates after laparoscopic paraesophageal hernia (PEH) repair have been reported anywhere up to 60%. Several technical maneuvers have been thought to reduce risk of recurrence including measures such as fundoplication, hiatal mesh placement, and gastropexy. We sought to identify patient and operative factors that are predictive in PEH recurrence
Methods: This was a retrospective review of patients that underwent PEH repair at a single tertiary academic institution between 2010 and 2023. Recurrence was identified radiographically or endoscopically. Patients were excluded from analysis if they were missing data on recurrence or if they had a previous PEH repair. Univariate comparison of patient and operative factors between patients that did and did not have recurrence was completed using Wilcoxon rank sum test for continuous variables and Chi-squared test for categorical variables Univariate logistic regression to predict recurrence was completed using these factors; factors with a p-value less than 0 05 were included in multivariate logistic regression
Results: A total of 1,171 were included in the final analysis of which 178 had recurrence (15.2%).
497 (42.4%) of patients were aged over 65 years and 706 (60 3%) had a BMI greater than 30 Of the patients that recurred, 67 (37 6%) underwent surgical revision, 14 (7 9%) within 90 days There were no demographic differences between patients that recurred and patients who did not Patients that recurred more frequently had short gastric vessels divided (77.8% vs 66.7%, p = 0.007), fundoplication performed (56.3% vs 46.1%, p = 0.013), and had gastropexy performed (33.3% vs 23.1%, p = 0.004). Patients that recurred were less likely to have hiatal mesh used (6.3% vs 12.0%, p = 0.026). On univariate analysis, number of symptoms present (OR 1.15, 95% CI 1.03 to 1.28), divided short gastric vessels (OR 1 75, 95% CI 1 16 to 2 62), fundoplication (OR 1 51, 95% CI 1 09 to 2 09), and gastropexy (OR 1 66, 95% CI 1 17 to 2 36) were associated with recurrence Use of hiatal mesh was not associated with recurrence (OR 0 49, 95% CI 0 26 to 0 93) On multivariate analysis, use of mesh (OR 0 47, 95% CI 0 23 to 0 96) was not associated with recurrence while gastropexy (OR 1.60, 95% CI 1.09 to 2.35) was.
Conclusions: Patients that recurred were more likely to have fundoplication or Gastropexy performed, short gastric vessels divided, or have more symptoms and less likely to have hiatal mesh on univariate analysis On multivariate analysis, gastropexy was still associated with a 60% increased likelihood of recurrence while mesh was half as likely to be associated with recurrence. Our results suggest that gastropexy should be rarely used and only in select patients where data supports use. Although our data supports mesh use, a low proportion of patients had mesh place likely reflecting its use in selective patients as well.

Allen Scholar, General Surgery
Predictors of Recurrence After Paraesophageal Hernia Repair
Table. Univariate and Multivariate Regression to Predict Paraesophageal Hernia Recurrence
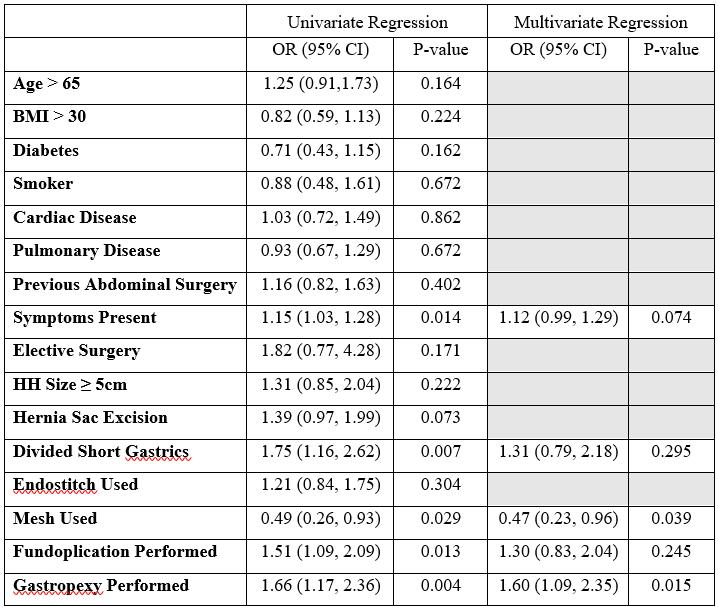

Cost and Resource Use Analysis of Extended-Spectrum Penicillin Antibiotic Therapy after Pancreatoduodenectomy in Intermediate- and High-Risk
Alexander Loftus, MD, Victoria S. Wu, BA, Richard Hoehn, MD, Mohamedraed Elshami, MD, MSc, Jonathan J. Hue, MD, Samuel L. Douglas, MD, John B. Ammori, MD, Jordan M. Winter, MD, Jeffrey M. Hardacre, MD, and Lee M. Ocuin, MD.
Background: Clinically relevant postoperative pancreatic fistula (CR-POPF) remains a challenge following pancreatoduodenectomy We previously reported that extended antibiotic therapy following pancreatoduodenectomy with soft gland texture and fistula risk score (FRS) >3 is associated with 83% lower odds of CR-POPF We hypothesize that extended antibiotic therapy after pancreatoduodenectomy in higher-risk scenarios is associated improvements in resource utilization and overall costs.
Methods: We performed a retrospective cohort study of patients who underwent elective pancreatoduodenectomy (2018-2022) with soft gland and FRS >3 who received standard antibiotics (continued for <24 hours) or ten days of piperacillin-tazobactam, converted to amoxicillin-clavulanic acid on discharge Cost data were obtained for the 90-day postoperative window and groups were compared based on development of CR-POPF (yes/no), stratified by receipt of extended or standard antibiotics. We calculated and compared aggregate costs based upon treatment group and development of CR-POPF, which included costs for hospital length of stay (LOS), repeat surgery, interventional procedures, antibiotics, and emergency department visits In addition, we compared number of percutaneous drainage procedures, total drain days, number of CT scans, and days of antibiotic therapy within 90days of surgery between treatment groups and stratified by development of CR-POPF
Results: A total of 87 patients were included in the analysis, of whom 34 received extended antibiotics and 53 received standard antibiotics There were no differences in baseline clinicodemographic characteristics between the extended or standard antibiotics groups As published, extended antibiotics were associated with a decreased rate of CR-POPF (11 8% vs 37 7%; OR=0 17, 95% CI: 0 04-0 68)
In patients who developed CR-POPF, those who received extended antibiotics were older (74 vs. 60 years, p=0.03) and underwent fewer image-guided drains placements as compared to patients who received standard antibiotics (75% vs 100%, p=0 022) There were no differences in index LOS, 90-day composite LOS, 90-day readmission rate, 90-day mortality rate, total antibiotic days, total drain days, or number of CT scans Overall, the cost associated with CR-POPF was higher than no CR-POPF ($60527 vs $25631, p=0 028) Costs were lower in patients who received extended antibiotics ($50,005 vs. $71,995, p=0.165), but this did not reach statistical significance.
In patients who did not develop CR-POPF, those who received extended antibiotics had more antibiotic days (10, IQR: 10-14 vs 4, IQR: 0-11; p=0 003) Costs were similar between patients who received extended antibiotics or standard antibiotics ($31,462 vs $35,417 p=0 685)

and Resource Use Analysis of Extended-Spectrum Penicillin Antibiotic Therapy after Pancreatoduodenectomy in Intermediate-
For the overall treatment cohorts, costs were lower in patients who received extended antibiotics ($31,708 vs $49,096, p=0.058). Our risk-based model, implemented to decrease heterogeneity in cost data, predicted an average cost savings of $15,795 per patient who received extended antibiotics.
Conclusion: Extended antibiotic therapy following pancreatoduodenectomy in patients with soft gland texture and FRS >3 is associated with cost savings, and in patients who develop CR-POPF, there is an associated decrease in number of percutaneous image-guided drain placements These cost savings likely are driven by decrease in rate of CR-POPF, which are associated with higher cost. These outcomes will be formally tested in a randomized controlled trial (NCT05753735).
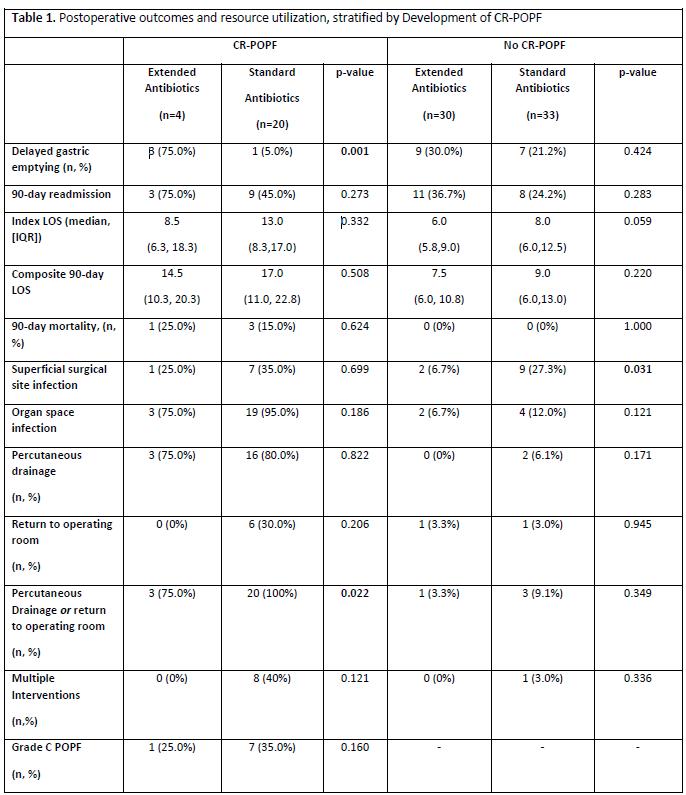

Does race play a role in the failure of primary bariatric surgery?
Daniel Praise Mowoh, MD, Mina Ibrahim, MD, Mai Al Khadem, MD, Omkar Pawar, MSCE, BDS, Mujjahid Abbas, MD, and Leena Khaitan MD-MPH.
Introduction: Studies have shown that revisional bariatric surgery comprises a significant proportion of currently performed bariatric procedures Racial disparities have been implicated in primary and revisional bariatric surgery however, its impact on revisional bariatric procedures for indications of weight regain and inadequate weight loss has not been described Hence, our study aims to demonstrate the role of race in revisional bariatric surgery for weight regain/inadequate weight loss (IWL/WR).
Methods: The MBSAQIP PUFs for 2020 were queried for revisional bariatric surgeries Other procedures were excluded The study population was then categorized by indications Our study group underwent these surgeries for IWL/WR and the comparison group underwent revisional surgery for all other indications Univariate analysis was used to compare categorical variables between groups and multivariate logistic regression was used to evaluate the likelihood of revision or conversion for IWL/WR.
Results: 20387 patients underwent revision and conversion for all indications 10715 had indications of IWL/WR 85 4% were female and 14 6% were male 63 3% of the population were Caucasian, 24 4% were black/African American, 12.3% Hispanic, 0.5% Asian. The most notable index surgeries in our study population were sleeve gastrectomy (38.1%), gastric bypass (4.9%), and gastric band (52.4%). Multivariate logistic regression showed that Black or African American race had higher odds of being revised or converted for weight regain or inadequate weight loss compared to white race (OR 1 24, 95%CI 1 14–1 34, p = 0 000) after adjusting for age, sex, BMI class, and comorbidities and so did Hispanic ethnicity (OR 1 36, 95%CI 1 22–1 5, p = 0 000)
Conclusion: Our study showed that minority patients are more likely to undergo revision or conversion bariatric surgery for the indication of weight gain or inadequate weight loss. This indicates racial disparities that could lead to the failure of primary bariatric surgery
Keywords: revision, conversion, bariatric surgery, weight loss surgery, weight regain, inadequate weight loss, racial disparities.

Kimberly R. Rebello, MD, MSc, Pablo Ruda-Vega, MD, and Gregory D. Rushing, MD.
Background: Atrial fibrillation (Afib) is the most prevalent arrhythmia both in the United States and globally, with an estimated national prevalence of over 5.6 million, and global prevalence of 50 million. It is associated with increased adverse outcomes including 2.4-fold stroke risk, 1.5 myocardial infarction risk, and 1.6-fold risk of chronic kidney disease The presence of Afib at the time of cardiac surgical intervention has been shown to worsen 30-day outcomes and overall survival Re-establishing normal sinus rhythm would reduce these above risks, however, we still do not see rising rates of ablative intervention in all applicable procedures The Cox-Maze procedure for surgical treatment of atrial fibrillation (Afib), requires formal atriotomies–even in minimally invasive approaches. Our method uses ablation technologies to create the Cox-Maze IV lesion set, through the left atrial appendage (LAA), and purse string access used for retrograde cardioplegia cannulation
Methods: This prospective study included 21 patients (median age 66 years [quartile 1 (Q1), quartile 3 (Q3): 63, 73]), without need for atriotomy, who received a Cox-IV Maze lesion set We employed a midline sternotomy, cardiopulmonary bypass (CPB), and retrograde cardioplegia. Box pulmonary vein isolation was performed using bipolar radiofrequency energy. Through the LAA tip, the mitral valve annular and LAA circuit lines were ablated with cryothermy The tricuspid annular circuit line was ablated with cryothermy via the retrograde coronary sinus at the purse-string access site All other lesions were completed epicardially with cryothermy Patients were followed with electrocardiogram and 7-day Holter monitoring at 3-, 6-, and 12-months, with the primary outcome being freedom from Afib with or without anti-arrhythmics and anticoagulants.
Results: Within our cohort, 9 (42.9%) had paroxysmal Afib, 5 (23.8%) had persistent Afib, and 7 (33.3%) had longstanding persistent Afib The median CHA2DS2VASc score was 3 (Q1, Q3: 3, 5) and HASBLED score was 2 (Q1, Q3: 2, 3) There was no operative mortality and need for only one pacemaker placement in the setting of complete heart block The median CPB and aortic cross-clamp times were 146 and 98 min, respectively The most common concomitant procedure with the GP Maze was coronary artery bypass (n=18, 85.7%), followed by aortic valve repair or replacement (n=5, 23.8%), and then ascending aortic replacement (n=2, 9.5%). At each of the 3 follow-up intervals, all patients were free from atrial dysrhythmias with many not requiring further anticoagulation or antiarrhythmics within 3-months (Table) Of those that have reached the 1-year interval, only 1 patient still remains on antiarrhythmic therapy The average length of stay in-house was 6 days, with 90 5% of patients going home. No patients required an intra-aortic balloon pump, or had complications related to mesenteric ischemia, renal failure (with or without dialysis), mediastinitis, or perioperative myocardial infarction.
Conclusion: The GP maze is an effective procedure with respect to maintaining normal sinus rhythm, with reduced need for anticoagulation and antiarrhythmics This is a new operative technique that maintains equivalent durability of the Cox-IV Maze lesion set, without formal atriotomy

Avoiding Atriotomy; University Hospitals GP Maze: Operative Technique and Early Outcomes
Table: Early outcomes of the 21 patients enrolled in the study. Values are n(%) or median (Q1, Q3). *Defined as death during the hospital stay, or within 30 days of their index operation †Only accounts for those patients who have reached that timepoint since surgery
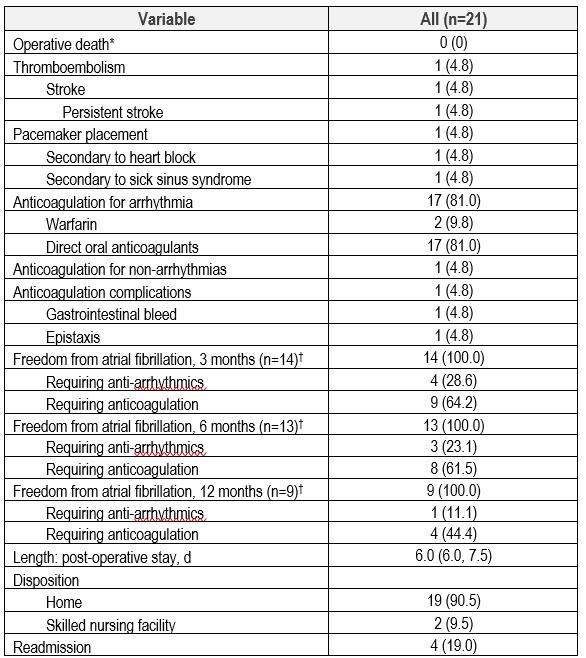

Don't Break the Bank: Transfusion of Survival
Andrew M. Loudon, MD, Erik L. Risa, MD, Avanti Badrinathan, MD, Amy P. Rushing, MD, and Matthew L. Moorman, MD.
Background: A massive transfusion resuscitation must consider available resources and patient response Survival is 50% after 11 units (U) PRBC. In high-volume transfusions, chance of survival is low, but not futile. No mechanism accurately predicts those few survivors. We describe characteristics predictive of survival after highvolume resuscitation of hemorrhagic shock.
Methods: Retrospective analysis of 2019 American College of Surgeons Trauma Quality Improvement Program (ACS-TQIP) data was performed Trauma patients ≥16 years old who received transfusion within 4 hours of arrival were included. Patients were excluded if they died in the Emergency Department, were dead on arrival, received <2 units (U) PRBC, did not receive FFP, or were missing data. Survivor outliers (SO)were defined as survivors receiving more blood than 95% of the surviving population Characteristics associated with SO were identified by multivariable logistic regression
Results: 17,407 patients received transfusion, 12,585 (72%) survived. 5.3% (663/12,585) of survivors were SO receiving ³17U PRBC. At ³17U PRBC, SO were more likely than high-volume mortalities (HVM) to have lower age (AOR 0 97, 95% CI 0 97-0 98), lower ISS (AOR 0 97, 95% CI 0 97-0 98), balanced transfusion (AOR 1 66, 95% CI 1 18-2 32), high shock index (AOR 1 57, 95% CI 1 12-2 20), and maintained GCS (AOR 1 12, 95% CI 1 10-1 15) SO were more likely to require hemorrhage control on an extremity (AOR 2 87, 95% CI 1 11-7 45) HVM arrived more often without vital signs (AOR 0 58, 95% CI 0 35-0 96) and require hemorrhage control by thoracotomy (AOR 0.35, 95% CI 0.16-0.74).
Conclusions: Blood stewardship requires the assessment of survival profile Standardized assessment protocols should be created around patient factors associated with survival in high-volume resuscitation to identify patients with a favorable survival profile The decision to continue resuscitation should be made on a case-by-case basis to improve utility of blood in massive transfusion. Resuscitation of survivor outliers yields few survivors and strains the blood supply.

Don't Break the Bank: Transfusion of Survival Outliers in Hemorrhagic Shock


Report: Failed SVR12
Ananya Tawde, MD and Zoe Stewart Lewis, MD, PhD.
Background: There has been an increasing incidence of transplantation of hepatitis C viremic (HCV+) deceased donor kidney transplants (DDKT) into hepatitis C naïve (HCV-) recipients Current literature shows earlier initiation of direct-acting antiviral (DAA) therapy results in shorter duration of recipient viremia and reduced risk of potential viral exposure for patient caregivers There have been rare reports in transplant recipients of HCVviremic donor organs of failure to achieve a sustained virologic response when screened 12 weeks after completion of standard DAA therapy (SVR12). Treatment failures usually occur from disruption in the treatment course due to adverse clinical events or medication noncompliance and very rarely from viral strains with mutations conferring DAA resistance
Case Summaries: Presented here are two cases of DDKT patients receiving a kidney from the same HCV viremic genotype 3 organ donor. The donor was a 38-year-old HCV viremic brain dead donor, with a cause of death secondary to drug overdose. The Kidney Donor Profile Index was 59%, with an admit creatinine of 1.3 mg/dL, and terminal creatinine 7 0 mg/dL Both kidney recipients had delayed graft function (DGF) and required hemodialysis in the immediate post-operative period, as expected with the high terminal donor creatinine
Patient 1 was a 67-year-old female with end stage renal disease (ESRD) secondary to Type II Diabetes Mellitus who was pre-dialysis. She was initiated on a 12-week DAA course with Sofosbuvir/Velpatasvir (Epclusa®) on post-operative day 30 Patient 2 was a 61-year-old female with ESRD secondary to type 1 Diabetes Mellitus on chronic hemodialysis She was initiated on a 12-week DAA course with Glecaprevir/Pibrentasvir (Mavyret®) on post-operative day 39 However, both patients failed to achieve SVR12 despite becoming aviremic after 4 weeks of DAA therapy. Neither patient had a disruption in medication administration. Both were subsequently treated with an additional course of Sofosbuvir/Velpatasvir/Voxilaprevir (Vosevi®) and have become aviremic, with pending SVR12 follow-up and genetic resistance testing.
Discussion: With the advent of DAA therapy, HCV viremic donor organs are now routinely transplanted into HCV naïve recipients with informed consent This case report highlights the critical need for protocolized followup to ensure all transplant recipients achieve SVR12. DAA treatment failures occur in 3%-5% of HCV positive patients, most commonly from patient medication non-compliance. In addition, it is incumbent upon transplant centers utilizing HCV-positive donor organs to have robust patient informed consent and caregiver education to avoid unintended viral transmissions until each patient achieves SVR12

Case Report: Failed SVR12 in Two HCV Naïve Recipients of HCV Viremic Deceased Donor Kidneys Requiring Additional DAA Treatment
Abbreviations: DGF: delayed-graft function DAA: direct-acting antivirals; HCV: hepatitis C virus; NAT: nucleic acid testing, SVR: sustained virologic response; DSA: donor-specific antibodies, AASLD: American Association for the Study of Liver Disease; CKD: chronic kidney disease; ESRD: end-stage renal disease
Keywords: Renal transplant, Hepatitis C, antiviral drugs, organ donors

Heming Hannah Zhao, MD and Scott M. Wilhelm, MD.
Introduction: Tertiary hyperparathyroidism (THPT) is defined as persistent elevation of parathyroid hormone (PTH) six months post-transplant (TXP). Management strategies for THPT include medical therapy (cinacalcet) and parathyroidectomy (PTX) Prior studies have demonstrated the superiority of PTX over cinacalcet in managing hypercalcemia and preserving renal allograft function in THPT patients Despite available evidence, an underutilization of PTX in the management of THPT has been observed in several single-institutional studies We aimed to evaluate THPT patients after kidney transplant based on management strategy (cinacalcet or PTX) utilizing a national database.
Methods: Data was collected from the TriNetX Dataworks, utilizing de-identified records from approximately 100 million patients from 83 healthcare organizations. We included kidney transplant patients diagnosed with THPT between 1998 and 2021, aged 18 years and older We compared patients who underwent PTX with those who received medical treatment Additionally, we examined subgroups of THPT patients who underwent PTX within different time frames post-transplant (within 6 months, 6 months to 1 year, and between 1-3 years)
Descriptive statistics and relative risks were calculated. All analyses were performed in TriNetX Live.
Results: Patients who received cinacalcet without undergoing PTX (n=161) were 1 8 times more likely to have persistent hypercalcemia (RR 1.77, CI:1.27-2.47, p<0.05) and a 1.7 times more likely to have elevated PTH levels (RR 1.73, CI:1.33-2.24, p<0.05) compared to those who underwent PTX (n=344) within three to ten years after the index event (start of cinacalcet or surgery). There were no significant differences in the risk kidney stones, GFR < 60 ml/min, hyperphosphatemia, elevated creatinine, or blood urea nitrogen (BUN) levels between the two groups
For operative timing, patients who underwent PTX within 6 months of kidney transplant (n=55) were 62% less likely to have persistent hypercalcemia (RR 0 38, CI:0 19-0 78, p=0 01), hyperphosphatemia (RR 0 38, CI:0 190 78, p=0 01), and kidney stone formation (RR 0 38, CI:0 19-0 78, p=0 01) between the third and tenth-year postsurgery compared to those who underwent PTX between 6 months and 1-year post-transplant (n=21). In contrast, when comparing PTX performed 1 to 3 years after transplant (n=57), patients who underwent PTX within the first year (n=132) were 57% less likely to form kidney stones (RR 0 43, CI: 0 19-0 98, p<0 05), and were two times more likely to maintain normal GFR (RR 2 03, CI:1 10-3 73, p<0 05)
Conclusion: Our findings confirm that PTX is more effective than cinacalcet in managing THPT post-kidney transplant Additionally, our results suggest that early PTX, performed within 6 months after transplant, may provide better control of hypercalcemia, hyperphosphatemia, kidney stone formation, and GFR compared to delaying surgery.

Mina A Ibrahim, MD, Daniel P Mowoh, MD, Mai Al Khadem, MD, Mujjahid Abbas, MD, and Leena Khaitan, MD, MPH.
Introduction: Management of gastroesophageal reflux disease after bariatric procedures can be challenging. There are very few long term studies in this arena. This study aims to evaluate the long-term outcomes of the Magnetic Sphincter Augmentation (MSA) Reflux Management System in a cohort of bariatric patients who had previously undergone sleeve gastrectomy and RGBP (Roux enY Gastric Bypass), with a focus on assessing gastroesophageal reflux disease (GERD) scores, medication use and patient-reported symptoms
Methods: We conducted a retrospective chart review of 16 consecutive bariatric patients who received MSA implants following sleeve gastrectomy (n=14) or gastric bypass (n=2) surgeries. Data was collected regarding BMI, Gerd quality of life assessments (Gerd-HRQL), reflux symptoms, and use of PPIs in the sleeve/RGB patients through an extended period with a mean follow-up of 48 months
Results: Patients were followed up for a range of .5-84 months. Preoperative assessments included upper gastrointestinal imaging (UGI), high resolution manometry, Bravo pH studies, and esophagogastroduodenoscopy (EGD) Three patients exhibited reflux on UGI, and 13/13 patients had positive Bravo studies preoperatively Sixteen patients had a lower esophageal sphincter (LES) pressure under 18 mmHg, and eight patients had biopsy proven esophagitis Long term outcomes are as follows Daily PPI use fell from 88% to 25% at greater than three years GERD quality of life assessment scores fell from 50 6 at baseline (range 27 to 70) and normalized at long term follow up. GERD symptom of regurgitation completely resolved. At long term two patients had dysphagia and two patients had ongoing reflux. No adverse events were noted.
Conclusion: This is the first long-term outcomes study of Magnetic Sphincter Augmentation placement after bariatric surgery Our study showed the majority of patients had long-term improvement in GERD-HRQL scores and resolution/ relief of their reflux symptoms, with decreased use of PPIs. MSA is a safe, effective and durable management tool for reflux after bariatric surgery in carefully selected patients.


Aria Bassiri, MD
PGY2 / Allen Scholar
Hometown: Tehran, Iran
Undergraduate: B.Sc., University of Toronto
Graduate: M.Sc., Boston University
School of Medicine; MD, Wayne State University School of Medicine
Faculty Advisor: Christopher Towe, MD

Christina Boutros, DO
PGY2 / Allen Scholar
Hometown: Oyster Bay, NY
Undergraduate: New York Institute of Technology
Graduate: DO, New York Institute of Technology College of Osteopathic Medicine
Faculty Advisor: Richard Hoehn, MD
Matthew Chen, BA
Medical Student, CWRU School of Medicine
Hometown: Philadelphia, PA
Undergraduate: BA, Case Western Reserve University
Graduate: In-Progress, Case Western Reserve University School of Medicine
Faculty Advisor: Richard Hoehn, MD

Susan J. Doh, MD
PGY2 / Allen Scholar
Hometown: Glenview, IL
Undergraduate: University of Chicago
Graduate: University of Illinois at Chicago
Faculty Advisor: Megan Miller, MD

Research Fellow
Hometown: Lahore, Pakistan
Graduate: Shifa College of Medicine, Pakistan
Faculty Advisor: Jeffrey Marks, MD

Health Services Researcher, CWRU School of Medicine
Hometown: Shanxi, China
Undergraduate: Heilongjiang University of Science and Technology
Graduate: Kent State University
Faculty Advisor: Richard Hoehn, MD

Claire Drigotas, BA
Medical Student, CWRU School of Medicine
Hometown: Baltimore, MD
Undergraduate: BA, The University of Chicago
Graduate: In-Progress, Case Western Reserve University School of Medicine
Faculty Advisor: Richard Hoehn, MD

Mohamedraed Elshami, MD, MMSc
Research Fellow, Surgical Oncology
Hometown: Gaza, Palestine
Graduate: MD, Islamic University of Gaza, Gaza, Palestine; MMSc; Harvard Medical School, Boston, MA.
Research Mentor: Lee Ocuin, MD

Allison Gasnick, BS
Medical Student, CWRU School of Medicine
Hometown: Wayne, NJ
Undergraduate: BS, Emory University
Graduate: In-Progress, Case Western Reserve University School of Medicine
Faculty Advisor: Christopher Towe, MD

Camryn Hawkins, PhD
Medical Student, Northeast Ohio Medical University
Hometown: Youngstown, OH
Undergraduate: The Ohio State University
Graduate: In-Progress, Northeast Ohio Medical University
Faculty Advisor: Chloe Williams, MD

Andrew Fiorentino, MS
Medical Student, Northeast Ohio Medical University
Hometown: Tampa, FL
Undergraduate: MS, University of Florida
Graduate: In-Progress, Northeast Ohio Medical University Faculty Advisor: Chloe Williams, MD

Isabel Ho, BA
Medical Student, CWRU School of Medicine
Hometown: Great Falls, VA
Undergraduate: BA, University of Virginia
Graduate: In-Progress, Case Western Reserve University School of Medicine
Faculty Advisor: Howard D. Wang, MD


Jessica Hungate, MD
PGY2 / Allen Scholar
Hometown: Sugar Land, TX
Undergraduate: University of Texas at Austin
Graduate: Texas Tech University (El Paso) School of Medicine
Faculty Advisor: Gregory Rushing, MD; Pablo Ruda Vega, MD
Mina Aziz Ibrahim, MD
Clinical Instructor Fellow
Hometown: Hauppauge, NY
Undergraduate: SUNY Stony Brook University
Graduate: Lewis Katz School of Medicine at Temple University
Residency: General Surgery at Rutgers Health
Faculty Advisor: Leena Khaitan, MD

William Julian, MS
Medical Student, CWRU School of Medicine
Hometown: Cleveland, OH
Undergraduate: MS, University of Vermont
Graduate: In-Progress, Case
Western Reserve University School of Medicine
Research Mentor: Lee Ocuin, MD


Hanna Kakish, MD
Research Fellow, Surgical Oncology
Hometown: Amman, Jordan
Graduate: Jordan University of Science and Technology
Research Mentor: Luke Rothermel, MD, MPH

Mamadi Papus Keita, MD
PGY6 / Surgical Fellow
Hometown: Guinea, West Africa
Undergraduate: The Citadel, The Military College of South Carolina
Graduate: The University of Medicine and Health Sciences, St Kitts
Residency: General Surgery at Carle Illinois College of Medicine, Urbana, IL
Faculty Advisor: Yakov Elgudin, MD, PhD

Saher-Zahra Khan, MD
PGY2 / Allen Scholar
Hometown: Wayne, PA
Undergraduate: BS, Villanova University
Graduate: MD, The Ohio State University College of Medicine
Faculty Advisor: Jeffrey Marks, MD

Alexander Loftus, MD
PGY2 / Allen Scholar
Hometown: Buffalo, NY
Undergraduate: BS, Cornell University
Graduate: MD, Jacobs School of Medicine and Biomedical Sciences, State University of New York, University at Buffalo
Faculty Advisor: Lee Ocuin, MD
Meaghan MacRae, BS
Medical Student, CWRU School of Medicine
Hometown: Medford, MA
Undergraduate: BS, Georgetown University
Graduate: In-Progress, Case Western Reserve University School of Medicine
Faculty Advisor: Eiichi Miyasaka, MD

Gillian Michaelson, BS, BA
Medical Student, CWRU School of Medicine
Hometown: Westport, CT
Undergraduate: BS,- BA, Brown University
Graduate: In-Progress, Case Western Reserve University School of Medicine
Research Mentor: Eiichi Miyasaka, MD

Kathleen Mulligan, BA
Medical Student, CWRU School of Medicine
Hometown: Phoenix, AZ
Undergraduate: AB, Princeton University
Graduate: In-Progress, Case Western Reserve University School of Medicine; Incoming Resident in Otolaryngology – Head and Neck
Surgery at UCLA
Faculty Advisor: Richard Hoehn, MD

Daniel Praise M. Mowoh. MD
PGY2 / Allen Scholar
Hometown: Ndop, North West Region, Cameroon
Undergraduate: BS, University of Maryland
Graduate: MD, Howard University College of Medicine
Faculty Advisor: Leena Khaitan, MD

Alice Qian, BS
Medical Student, CWRU School of Medicine
Hometown: Pittsburgh, PA
Undergraduate: BS, Case Western Reserve University
Graduate: In-Progress, Case Western Reserve University School of Medicine
Faculty Advisor: Cristian Baeza, MD


Kimberly R. Rebello, MD, MSc
PGY3 / Clinical Resident
Hometown: Farmington, CT
Undergraduate: University of Connecticut
Graduate: University of Connecticut
Faculty Advisor: Gregory Rushing, MD; Pablo Ruda Vega, MD

Erik Risa, MD
PGY2 / Clinical Resident
Hometown: Bellevue, WA
Undergraduate: BS, Santa Clara University
Graduate: MD, University of Washington School of Medicine
Faculty Advisor: Andrew Loudon, MD
Hailey Seibert, BA
Medical Student, CWRU School of Medicine
Hometown: Massillon, OH
Undergraduate: BA, Case Western Reserve University
Graduate: In-Progress, Case
Western Reserve University School of Medicine
Research Mentor: Luke Rothermel, MD, MPH


Henry Stitzel, BS
Medical Student, CWRU School of Medicine
Hometown: Akron, OH
Undergraduate: BS, St. John's University, Queens, NY
Graduate: In-Progress, Case Western Reserve University School of Medicine
Research Mentor: Lee Ocuin, MD

Ananya Tawde, MD
PGY1 / Clinical Resident
Hometown: Cincinnati, OH
Undergraduate: BS, University of Akron
Graduate: MD, Northeast Ohio
Medical University
Faculty Advisor: Zoe Stewart Lewis, MD

Gabriel Tensol Rodrigues Pereira, MD
PGY3 / Clinical Resident
Hometown: Belo Horizonte, Brazil
Undergraduate: Colégio Bernoulli
Graduate: Universidade Federal de Minas Gerais (Federal University of Minas Gerais)
Faculty Advisor: Cristian Baeza, MD
 Heming Hannah Zhao, MD
Heming Hannah Zhao, MD
PGY2 / Allen
ScholarHometown: Blacksburg, VA
Undergraduate: BS, Cornell
University
Graduate: MD, Rutgers Robert Wood Johnson Medical School
Faculty Advisor: Scott Wilhelm, MD


On behalf of the Department of Surgery, we would like to thank our staff and faculty for organizing this event
Erica Coleman
Heather Cigoi, JD, MBA-HCA
Lisa DiNardo, PhD
Omkar Pawar, MSCE, BDS
Reagan Stevens, CMI
Christopher W. Towe, MD
