








































































There's exciting times ahead for the MyDay® daily disposable contact lenses. Turn over to meet the family.




When I became chairman of the AOP in the summer of 2017, I recall people asking me: ‘what are your aims, Mike?’ It is an understandable question. I was clear then, and am now, that the role is not about presidential missions and manifestos, but to act as a figurehead, to facilitate the Board and Council, and to support the chief executive to achieve the best results possible for members.
No one could have predicted the impact of COVID-19, and it has shaped the final year of my chairmanship. Many of the issues the AOP faced in 2017 remain – crucially among them being the changing role of optometrists and what they are paid. How the pandemic has affected the profession has served to heighten these questions. It has also placed new demands on the AOP staff to support members in practice – and to do so seamlessly, while working from home.
Looking back, the AOP’s decision to reduce membership fees by 20% in response to the COVID-19 pandemic was a big moment – and one I am proud we made. The Board knew many within the profession were worried about their job security, health, family and finances. The fee reduction meant we used a large portion of the AOP’s reserves, but it was important the Board was able to take a big and ambitious step that would affect members meaningfully, alleviating the financial strain many were facing.
Throughout my chairmanship, our chief executive, Henrietta Alderman, has been by my side. Henrietta’s work to develop and re-shape the association over her eight-year tenure means, as she retires in June, she leaves the AOP stronger and more resilient than ever.
For Julie-Anne Little and Adam Sampson, our incoming chair and chief executive respectively, much work remains. The vast scale of NHS England and the Department of Health will always be a challenge – and we can draw lessons from the devolved nations. In a world shaped by COVID-19, the NHS needs to be reminded of optometry’s role as a key healthcare service. At times during the pandemic, professional bodies struggled to align their positions – and the AOP will need to continue to make sure leadership is provided to our members.
Now, more than ever, we need to be openminded about what the future might look like. The pandemic’s impact on hygiene and infection control is just one example of this. The AOP must continue to ask members for their ideas and views, and to listen carefully – but we also should remember that members expect us to work out the answers and fight for change.
For the AOP to remain relevant, we need multigenerational representation, reflecting different fields within the profession. We need to find out and understand

our members’ aspirations. One way we have improved this is by changing the structure of the Council, with more appointed positions bringing in people with skills and background for different areas (see pages 8–10).
What makes the AOP so valuable to our members is that its staff provide constant support to them as and when they need it, while also looking at what is coming down the road and considering what the future of optometry, healthcare, technology, litigation and so on will be.
As our members’ scope of practice changes (and it inevitably will), we need to help them on this journey –be it what they do in the consulting room, what they do virtually, and what the demands are for optometry to take on work from other parts of the health service.
For the AOP to shape the future of the profession, it is crucial that members engage and contribute to the conversation. I wanted to influence my future so I got involved – and I urge members to do the same. As an optom once told me: “If you are not at the table, you might be on the menu.”
Mike George AOP chairman, 2017–2021

07-25
SPOTLIGHT
The news in digest
Picture this
Nasa’s Expedition 65 mission
OT reports
AOP Councillors on the biggest challenges facing the profession
The edit
Optics in 16 stories
100% Optical
The May online event reviewed
Industry profile
CooperVision’s president, Dan McBride
Clinical roundup
The “ice cube tray” that could restore sight
Supplier insight
Ophthalmic lens solutions
AOP roundup
A new chief executive, the launch of the Strategy for Optometry, and a guide to support practice teams
Spotlight AOP SUPPORT
“The additions to the education programme are designed to enable the whole optical practice team to flourish and grow their skill set”
Ian Beasley, head of education
PAGE 24
27-33
HIT LIST
The trends, launches and looks
OT focuses on...
Contact lenses
Me and my glasses
British ultrarunner, Alice Hector
Get the look // Anatomy of a frame
With Lizzy Yeowart
The shortlist
The June/July selection
Behind the brand
Akoni Group


35-39
PERSPECTIVES
Voices from optics and beyond
Perspectives
Simon Raw, Marcus Dye, Melanie Hingorani
Letters
PPE and the environment
My vision
Lora Fachie
“We now have a huge backlog of patients – how many, we simply don’t know”
Melanie Hingorani, ophthalmologist and clinical lead for the National Eye Care Recovery and Transformation programme







Business insight and career development
The roundtable
OT and SpaMedica ask ECPs about the impact of virtual consultations
Pre-reg focus
Emily Mather and Peter Grant
How do I...
Build an online retail presence?
What I have learned
Launching an augmented reality project
Becoming a busines owner
Roshni Dalia
The workshop
Cyber protection, with Lloyd & Whyte
Key milestones
The story behind Moorfields’
Department of Digital Medicine
story The big questions
What are the most pressing challenges facing the profession – and how do we respond? From mega-mergers to sight test funding, and from big data to PPE, OT asks the experts for their views on what the future might hold PAGE 57-64
90-98 ENDNOTES
Jobs
The Specsavers’ take on recruitment I could not live without...
Tearstim and Idra, says Claire and Rebecca Gough
Last word
Tanjit Dosanjh’s secret life
65 CET welcome
66 Persistent epithelial defects: covering the gaps
70 Macula, magnifiers and more
74 Can contact lenses still be an option for patients with dry eye disease?
79 The causes and impact of amblyopia
84 Cases of gradual vision loss
86 Anterior eye cases in practice
88 CET author Q+A: Dr Nery Garcia-Porta
In this edition of OT, practitioners can test a range of competencies: Education and training for the eye care practitioner
OT video highlights A roundtable on virtual consultations in practice Watch the video on www.optometry.co.uk
Contact the OT team with your experiences, observations and lessons from practice today: newsdesk@optometry.co.uk






















































08 OT REPORTS
New AOP Councillors offer their views on the issues that matter within optometry
Watch this space
21 CLINICAL ROUND-UP
A vision-saving 'ice cube tray,' and how an octopus vision test could detect AMD risk
24 AOP SUPPORT
Launch of the AOP's Strategy for Optometry and Adam Sampson takes on CEO role

NASA astronaut, Mark Vande Hei, uses Heidelberg Engineering's Spectralis optical coherence tomography device on board the International Space Station. Astronauts undergo regular vision checks while in space to monitor for signs of Space-Associated Neuro-Ocular Syndrome. Hei is a flight engineer for Expedition 65 – a mission that began on 21 April 2021. www.nasa.gov
June/July 2021

Volume 61:03 Issn 0268-5485
ABC certificate of circulation 1 January 2020 – 31 December 2020
Editor: John White johnwhite@optometry.co.uk
Deputy editor: Emily McCormick emilymccormick@optometry.co.uk
Senior content editor: Lucy Miller lucymiller@optometry.co.uk
Assistant editor: Selina Powell selinapowell@optometry.co.uk
Senior reporter: Kimberley Young kimberleyyoung@optometry.co.uk
Web content and social media executive: Leah Boyle leahboyle@optometry.co.uk
Clinical editor: Dr Ian Beasley ianbeasley@optometry.co.uk
Clinical editor for multimedia: Ceri Smith-Jaynes cerismithjaynes@optometry.co.uk
Video production editor: Laurence Derbyshire laurencederbyshire@optometry.co.uk
CET enquiries: 020 7549 2076 CEThelp@optometry.co.uk
AOP membership and OT subscription team: subscriptions@aop.org.uk
What does 2021 have in store? And how will the profession respond? OT asked some of the AOP’s new Council intake for their reflections, goals and concerns
Advertising: Richard Ellacott 020 3771 7242 richard.ellacott@thinkpublishing.co.uk
Advertising production: aop@ccmediagroup.co.uk
Senior designers: Grant Pearce, Juanita Adu
Client Engagement Director: Anna Vassallo
Executive director: Jackie Scully
Published bimonthly for the Association of Optometrists by Think Media Group
20 Mortimer Street, London, W1T 3JW
Printed by Acorn Web, Normanton Ind Estate, Loscoe Close, Normanton, West Yorkshire, WF6 1TW
All rights in and relating to this publication are expressly reserved. No part of this publication may be reproduced in any form or by any process without written permission from the AOP or the publisher.


“One of the biggest issues within optometry currently is the changing professional landscape, with an ageing population, an overstretched hospital eye service and underfunding for primary eye care services,” Rachel Hiscox told OT. She explained that expanding the role of the optometrist through standardised shared care schemes across the UK would “not only offer improved patient care, but also increase the scope of the optometrist.”
Paul ChapmanHatchett also recognised the significance of the ageing population, explaining that “we need to raise the awareness of the role domiciliary optometrists can have in providing General Ophthalmic Services (GOS) and also ophthalmology services in a community setting.”
Stephanie Kearney felt that there are “many issues” facing optometry currently, ranging from an increased workload, to commercialism and greater investment in the specialities within
optometry. She added that, “with the rising prevalence of myopia in children in the UK, the management of progressive myopia is an issue we will all be facing at some point during our professional career.”
Jasmin Matharu identified that many hospital optometrists self-fund extra courses with no additional financial support,
highly skilled clinicians. It is my concern that any significant overhaul, or change to the way in which optometrists are educated and trained, could harm the profession, and our patients,” he asserted. Indy Ghuman also noted the importance of the ESR. “With new optometry programmes under the new requirements to start from 2023–2024, the incoming 2021 cohort of optometry students will be present to see the tangible overlap
“We need to build on the gains the professions have made. Every practitioner deserves to be given the opportunities to maximise their skill-set”
Kris Cottier
explaining that “networking with each other would give an insight to how we can get funds for our development.”
For James Brawn, the most important issue in the profession is the General Optical Council’s ongoing Educational Strategic Review (ESR). “The current educational system is well established, and consistently produces
with their studies and consequences of this gigantic development in optometric education,” he said. Looking to the short-term, Ghuman commented that the focus must be on the phased return of university learning on campus as a key issue for student optometrists. “There is a hope of ‘ordinary’ student life returning for the 2021–2022 year,” he said.
AS A NEWLY ELECTED COUNCILLOR, WHAT CHANGES WOULD YOU LIKE TO SEE TO HELP THE PROFESSION MOVE FORWARD?
Kearney told OT there is a need for a more balanced workload.
“Optometrists are increasing becoming involved in shared care schemes as well as the utilisation of more advanced techniques such as OCT. However, the additional time required to analyse such scans or to see such patients is not always accounted for in the commercial environment many of us work in.” She also mentioned increased investment in GOS to reflect the increasing specialism of optometry and its role in supporting the hospital eye service, and greater public awareness and appreciation of the key services optometry practices provide.
Hiscox agreed, highlighting the importance of seeing an appropriately funded NHS eye examination fee, which “takes into account inflation, the scope of the eye examination and the expertise of optometrists.”
She also called on the introduction of nationwide shared care schemes, enhancing the role of the optometrist and “enabling improved patient care within the community, without an unfair patient postcode lottery.”
Matharu noted that there is a lack of standardisation between hospitals. “It is important that we all deliver the same level of care to our patients. This will allow for transparency between different trusts,” she said. Matharu highlighted the need to represent the interests of hospital optometry within the AOP, and planned to help hospital
optometrists communicate with peers to raise their concerns, and create a bridge between High Street and hospital optometry.
Karan Vyas explained that he would like to see reform of education where students are able to “better gain clinical experience and are exposed to more pathology before leaving university.” Vyas also called for changes in daily practice to make sure that practitioners are not exposed to discrimination in the workplace.
Ghuman told OT that, with the GOS sight test fee increase in April 2021 for the first time since 2015, he hoped to see “greater appreciation for an optometrist’s value and the skilled work they do. Changing the sight-testing funding infrastructure will be pivotal to help sustainably fuel and elevate the profession to meet the changing eye health needs of the UK population.” He also noted that further embracing myopia-control treatment options was important, empowering patients to “make decisions on their health that will in turn boost the profile of optometrists.”
“I am passionate about pushing the boundaries for hospital optometrists. As optics continues to diversify it is important to adapt to the changes”
Jasmin Matharu
Clean air has never been so important
your practice a Safe Air Space?

Stop the spread of viruses
Reduce allergy symptoms all-year-long
Comply with highest hygiene standards
Keep staff safe, healthy and at work
Reassure your patients
Promote health and raise productivity
Reduce sick-leave 6 STAGE FILTRATION



AIR8 280 Nano Ideal for the consulting room Effective area up to 24m2
AIR8 720i Edge Ideal for staff area or small front of shop area Effective area up to 64m2
AIR8 1200i Pro Ideal for large front of shop Effective area up to 110m2

New AOP Council members will begin in post from 9 June 2021, following the results of elections that took place between 12 March and 26 March 2021. AOP members were invited to vote in the seven constituencies where there were more candidates than vacancies: Scotland, North West England, East Midlands, West Midlands, London, South East England, and Yorkshire and the Humber. The AOP Board appointed additional Councillors to represent different sectors of the membership. In 2021, for the first time, this included Councillors representing directors of independent practices, directors of multiple practices, domiciliary care optometrists, employees of independent practices, employees of multiple practices, independent prescribing optometrists and locum optometrists. Incoming chair of AOP Council, Dr Julie-Anne Little said: “It’s great to see such enthusiasm in the profession to share experiences and tackle issues together. The new structure also offers a different dynamic with an increased number of posts that reflect the diverse roles of our members.”
Emma Spofforth East of England
Tushar Majithia East Midlands
Jagdeep Kaur Gill London
Angela Henderson North East England
Dharmesh Patel North West England
Rachel Hiscox South East England
Ed Bickerstaffe South West England
Francesca Marchetti West Midlands
Stewart Mitchell Yorkshire and the Humber
Nizz Sabir Yorkshire and the Humber
Julie-Anne Little Northern Ireland
Brian McKeown Northern Ireland
Stephanie Kearney Scotland
Eilidh Martin Scotland
Kevin Wallace Scotland
James Brawn Wales
Kamaljit Kalsi Wales
Inderpal Ghuman Undergraduate student optometrists
Luke McRoy-Jones Pre-registration optometrists
Sana Asif Newly-qualified & early career optometrists
Ali Yasen Newly-qualified & early career optometrists
Vijay Anand Hospital optometrists – chair of hospital optometrists committee
Jasmine Kaur Matharu Hospital optometrists
Fatima Nawaz Independent prescribing optometrists
Paul Chapman-Hatchett Domiciliary care optometrists
Kris Cottier Locum optometrists
Mehul Patel Directors of multiple practices
Kevin Thompson Directors of independent practices
Karan Vyas Employees of multiple practices
Josephine Evans Employees of independent practices
Jonathan Bennett Franchisee/joint venture optometrists
James Dawson Dispensing opticians
Will Holmes University lecturers
Phillip Buckhurst University lecturers – nominated by the Optometric Schools Council
“Optometrists have a huge opportunity to take a more holistic primary role in eye care with the support of our ophthalmology colleagues; one that delivers on our patients’ needs and remunerates fairly”
Mehul Patel
Chapman-Hatchett noted that housebound individuals “have the same right to access high quality eye care as the wider population and we can help highlight where obstacles currently exist which impede this.” Explaining that domiciliary care continues to grow, he said the profession needs to help support and shape professional standards and development of optometrists.
Mehul Patel concluded that the pandemic has “forced the industry to adopt a different mode of working within a short space of time,” but added: “Optometrists have a huge opportunity to take a more holistic primary role in eye care with the support of our ophthalmology colleagues; one that delivers on our patients’ needs and remunerates fairly. With more and more practices embracing technology and investing in OCT, core training needs to encompass these advancements and produce skilled professionals who can competently manage patients under supervision of the hospital eye service.”
Cottier told OT: “We need to build on the gains the professions have made. Every practitioner deserves to be given the opportunities to maximise their skill-set and work to the full extent of their capability. We need to continue to highlight the advantages of eye care in the primary eye care setting rather than in secondary care. We need to continue to be seen as the go-to practitioner for all things eyes.”





















CooperVision has acquired No7 Contact Lenses. The business will operate as part of the CooperVision Specialty EyeCare group, but will retain the No7 name. The acquisition is set to enable CooperVision to establish direct-to-practitioner operations for specialty lenses in the UK, and is also expected to expand access to contact lens designs, and support the development of myopia management solutions.

“The delays in diagnosis we have seen in 2020 have the potential to seriously impact the prognosis for babies and children with eye cancer”
Patrick Tonks, chief executive of the Childhood Eye Cancer Trust, highlighted the pressures on the health service over the past year but stressed the effects for diagnosis of retinoblastoma. The charity reported that it took over six months for a diagnosis to be given for 24% of children who were diagnosed with retinoblastoma in 2020.

























“Opticians have really shown how important we are to the general health system and I think we’ve really proved our worth this year”
Shamir Optical Industry has become the optical performance partner for the Alpine F1 Team, establishing what the partners have called “the first vision performance lab in Formula 1.” The partnership will provide ophthalmic assessments and Shamir safety equipment and lenses to the Alpine F1 team and base personnel.

Lisa Kassell, practice manager at Conlons of Barrow Opticians and Hearing Care, a Hakim Group practice, celebrated receiving a Cumbria Business Innovation Special Performance Certificate by High Sheriff Julie Barton.









“I would recommend that anyone considering a new OCT scanner in 2021 seriously look at the Optopol range. I have been very impressed with the scan quality, ease of use and comprehensive functionality of the software”
Sundeep Kheterpal MA MRCOphth FRCSEd


of respondents in a Théa survey of 2000 people did not know any of the symptoms of dry eye disease. The No Eyedea survey, conducted by YouGov, found a “lack of awareness” around dry eye disease. Despite this, the company suggested many had experienced the symptoms but almost a third of respondents admitted waiting to see if the symptoms would go away by themselves.
Johnson & Johnson Vision has received US Food and Drug Administration approval for its Acuvue Abiliti Overnight Therapeutic Lenses, with the company suggesting this is the “first and only” FDA-approved orthokeratology contact lens for myopia management. The news follows a collaboration announced between Johnson & Johnson Vision and Menicon earlier this year, designed to bring forward therapeutic contact lenses for myopia management.
Following an appearance on Dragon’s Den, glasses chain and necklace designer, CotiVision, secured an investment of £50,000 from investor Deborah Meaden. Co-founders Nancy Gries and Julie Hawkins said of the experience: “We are loving every moment and can’t wait to see where we can go from here.”

Researchers from Cardiff University are investigating whether bone marrow stem cells could help to prevent sight loss in glaucoma patients. Scientists have already demonstrated that transplanting bone marrow stem cells into a model of glaucoma can prevent the death of retinal ganglion cells. Now scientists aim to separate exosomes from the bone marrow stem cells to replicate the same benefits without the need for a transplant.
60 DAYS IN 16 STORIES

University College London scientists will investigate if inherited retinal faults could be treated using gene editing technology. Funded by Fight for Sight, the research uses CRISPR-CAS9 base editing technology to directly repair faulty genes. Research lead, Dr Jacqui van de Spuy, said the study will advance the application of direct base editing as a therapeutic approach for inherited retinal diseases and accelerate base editing technologies towards a clinical treatment.

The World Council of Optometry has passed a resolution advising optometrists to incorporate a standard of care for myopia management into practice. The resolution defines evidencebased standard of care as comprising the mitigation, measurement and management of myopia. The resolution also included an encouragement for public education, and early, frequent discussions with parents around myopia.
NHS England has published Eye Care Planning & Implementation guidance for commissioners, highlighting that primary care pathways should be commissioned across England, including urgent eye care, referral filtering, monitoring and cataract post-operative care. The AOP suggested this is a positive step with the potential to fulfil the AOP’s call for the NHS to deliver more eye care through optical practices in England. More on the timelines can be read online: https://bit.ly/2QNgFLN
OThas heard from a panel of 16 eye care professionals about the key changes they expect to see in optometry in the year ahead, with themes ranging from further collaboration between primary and secondary care, to an increased demand for domiciliary services, a growing need for dry eye treatments, and a continued use of teleoptometry.
For further insights from our panel of optometrists, read OT's feature online: https://bit. ly/3wgefnX
dry eye patients report being unable to work because of the condition, according to a survey of 500 dry eye patients commissioned by Santen across five countries. The survey found that, within the UK, approximately one in five (22%) dry eye patients felt that their symptoms had become worse during the pandemic.
Moorfields Eye Hospital and Kings College Hospital have collaborated to allow surgeons from the latter to operate on 15 patients using Moorfield’s facilities at Duke Elder Eye Unit in St George’s Hospital, London. The agreement during the latest wave of the pandemic, enabled glaucoma and emergency vitreoretinal operations to take place that would have been deferred.

“I have gained so much knowledge and developed new skills by working within a rapid access Minor Eye Condition Clinic. I have seen cases that I would only see in Kanski’sClinical Ophthalmology”
Speaking to OT for the online My inspiration series, optometrist Pretty Basra, described the impact her A-level chemistry tutor had on her journey into optometry and also shared how her practice has been affected by the pandemic.

Over 390 optometrists qualified in the spring round of Objective Structured Clinical Examinations. The assessment marked the largest in the history of the Scheme for Registration with 499 candidates taking part. Commenting on the pre-reg experience during COVID-19, recently-qualified optometrist, Toritse Eferakorho pictured above), shared: “I believe the lessons I learned throughout my pre-reg experience will make me a better optometrist.”

100% Optical Online offers a new platform for the industry show
that will continue to be built upon in the future
The end of May saw eye care professionals log on to join 100% Optical Online – the first time that 100% Optical has run as a virtual show, with the May 23–24 event seeing more than 1800 delegates join the platform, hosted via SwapCard.
Nathan Garnett, event director, said of the virtual event: “We all missed meeting and catching up at the show, but this was a very effective way for people to learn and chat, connect with suppliers and see what is happening in optics.” The show gave delegates an opportunity to attend lectures, view the latest in eyewear and meet with suppliers, he added.
Bringing together all modes of practice
The show featured an AOP-led programme of education with seven CET sessions, each offering an interactive
100% OPTICAL IN NUMBERS
More than 1800 active delegates
6800 messages exchanged
More than 50 exhibitors
Over 500 products, frames and services on display
CET point. The programme included a session from the AOP’s clinical negligence team on spotting the red flag signs and symptoms of intracranial tumours, along with sessions on myopia, the role of the tear film in relation to the health of the ocular surface, and dry eye.
Lectures also explored retinal imaging modalities and contemporary approaches to subjective refraction.
Dr Ian Beasley, AOP head of education and OT’s clinical editor, said: “The AOPled education stream delivered a platform to bring together practitioners from all modes of practice to learn, engage with expert speakers and earn valuable interactive CET points in the final year of the cycle.”
Recordings of the sessions will remain on the platform for optometrists to revisit. No CET points are available for viewing the presentations on demand.
Beasley added: “The AOP’s attention will now focus on building its extensive programme of education for the faceto-face 100% Optical event in January 2022 which will gently ease practitioners into the transition to the General Optical Council’s new CPD scheme.”
Creating a community
The event platform will remain available for delegates to rewatch content on demand and arrange meetings, and will also be built on in the future, with Garnett explaining: “The move towards digital learning and interaction is here to stay. I see this as a great supplement to the exhibition in January, when people will be able to come back together after two very hard years.”
SPEAKER INSIGHT
Why is your topic so important for optometrists to engage in?
SESSION RED FLAGS
SPELL DANGER
Speaker: Dr Peter Hampson, clinical director of the AOP, and Efa Schmidt, AOP head of clinical negligence
“Thankfully most patient presentations in optometric practice aren’t life or death. However, this is one area where they could be, or at least the outcomes could be life-changing for the patient. We would like to reduce the risk of harm to patients without overburdening already busy practitioners.”
SESSION BARRIERS TO MYOPIA MANAGEMENT – AN UPDATE
Speaker: Dr Manbir Nagra, optometrist, educator and researcher in myopia, contact lenses and health technologies
“Clinical care is rarely limited to clinical tasks such as refraction or fundus examination etc.
Communication plays a central role. By appreciating the influences on our decision making and the views of parents, patients, and practitioners, we can make better informed decisions.”
SESSION gO C THE PERIPHERY
Speaker: Simon Browning, optometrist and lecturer
“We live in an age where patients expect higher standards of care. With the new technologies available, there is no excuse for us not to access that level of care that our patients want. It's not just this area in the middle of the eye that is available to us. We're all getting older – populations are generally ageing – and so pathology is only going to increase. Myopia is on the rise, diabetes is on the increase. This is why we need to be looking at the whole retina.”
Find the platform at: www.100percent optical.com/whats-on/100-optical-online
As planning shifts to the 2022 event, Garnett suggested that there is more to come from 100% Optical, telling OT: “We are delighted to continue working with the AOP to deliver world leading content to our followers. We've got exciting talks and education planned for the remainder of the year, so watch this space."
100% Optical 2022 will take place on 22–24 January at ExCel London
















President of CooperVision, Daniel McBride, talks to OT about the key trends in the contact lens market, the impact of COVID-19, and the need for practices to innovate
The recovery of the contact lens market has been impressive, from what was a complete pit that all markets fell into. What we found is that when the markets opened up, there was a strong recovery.
In North America much of the market is nearing a full recovery, but there is still a lot of opportunity in places like California and New York, where business is still down. Looking at the Asia-Pacific market, which was highly sensitive to the pandemic, we are starting to see a pretty strong recovery there now too. Probably the weakest region is Europe, and that appears to be based on the slow vaccine rollout.
We’re seeing a strong recovery when markets open, but when a country goes back into lockdown, we immediately see a pullback. Consumers are relatively healthy. There is certainly a segment that was extremely negatively affected in losing their jobs because of the pandemic, but by and large consumers are ready to buy once the markets open.
A big worry in the middle of the pandemic was for practices that were damaged quite severely and just watched their business dry up. Supporting that recovery has been a large part of CooperVision's focus.
One of the trends we observed over the course of the year was a big spike in online purchases. Consumers were looking at where they could get their product, and they couldn’t always get it from their normal eye care practice, so they were finding online vendors.
I think practices do need to stay aware of this, though what we did find is that consumers like to go back to their normal shopping habits so there was a good rebound for practices. But when I think about it globally, online was around 18–20% of the market pre-pandemic and it has shifted up to maybe 20–22% of the market. This shift definitely has a longterm impact on practices. Practices are still the place to go, however, and the eye care practitioner (ECP) still has the

“It has been a tough year for everyone, but contact lenses is a great industry to be in”
primary relationship with the customer. If they leverage that relationship, then our observation is that many consumers like to buy from their practitioners.
One of the biggest trends, still, is daily disposable silicone hydrogel (SiHy) contact lenses. We have a massive trend of people moving into daily disposable contact lenses and that becoming the lens of choice from the very beginning. In the industry, over half of daily disposable lenses are still in older products and standard hydrogel products, so the amount of people shifting into a healthier and higher oxygen modality is exciting.
From a small base to a standard of care, adoption of myopia management has been growing
A major focus for the profession currently is myopia management, McBride told OT, describing it as “the most exciting area of optometry right now,” and a “sea-change in terms of what we do for people’s vision.”
Recently, the company has made a series of moves focused around myopia management, including a partnership with EssilorLuxottica to accelerate commercialisation of technologies from SightGlass Vision, a company
developing spectacle lenses to reduce the progression of myopia.
The company also partnered with the World Council of Optometry (WCO) to encourage practices to incorporate a standard of care for myopia management into practice.
McBride explained that the focus around myopia management has moved from a question of whether the clinical science would support a WCO resolution, towards engaging parents
and encouraging the adoption of myopia management in practice.
He noted that practitioners will need to determine how to incorporate myopia management into practice, and highlighted that the company expects to see an increase in myopia diagnosis following the pandemic, adding: “Eye care practitioners have to be ready.”
Read more from McBride on the journey to the adoption of myopia management on the OTwebsite.
Daily disposables were previously for a select few people who could fit them, because they were more expensive and more difficult to make. It was for sphere patients, a limited range of toric patients, and even fewer multifocal patients –nobody else could really go into the lens. I think that is a big change now. We’re expanding our toric ranges on all of our daily disposable products. We intend to offer a toric range that is the same as your standard FRP range so that anybody can make a choice in products.
The other exciting piece of this is understanding that the category can be so much bigger and recognising that there is no real reason to limit people on what products they can have. There are a host of people at a certain age, who will say: “I can’t wear contact lenses, they don’t make them for me.” That is not true anymore. We will make contact lenses for anybody and any eye.
The industry has talked about telehealth for a long period of time, but has been really slow to adopt. I think the pandemic has accelerated the trend towards that. When we think about things like myopia management, for example, we know that it requires multiple parent conversations. Telehealth allows ECPs to do that in a safe space – parents can be at home and can research what you are telling them.
We are seeing models being tested out globally where whole segments of practice are going into telehealth – at least on a screening or repeat consumer basis.
I think it is a big benefit for contact lenses. The one complaint that we get about contact lenses is that they take longer to fit, and so take longer in the chair. If you can take some of that burden off the practice, it allows you to get more people through.
Fitting glasses is quicker and more profitable in the shortterm. But there is a lot of data to suggest that contact lens wearers are more profitable consumers. They spend more in the store at the end of the day. Having stores recognise that contact lens wearers are their strongest consumers will be important. Telehealth helps to eliminate some of the perceived downside that they can take longer to service.
We are going to be innovating, bringing expanded parameter ranges, doing new things within the science and bringing in new clinical information, so ECPs are better able to explain to consumers what they are getting.
But it is going to require a little bit of investment on the ECP side too. That is going to involve making sure you are up to date on the latest in the clinical information. But you are also going to have to innovate within your practice too. Telehealth is a great example of that: you need to be able to reach consumers in their homes and in different ways to provide them with greater pieces of information.
Practices are probably going to have to embrace some e-commerce. Consumers want to buy products when they want to buy them. So, at midnight when they are online, can they buy their product from you? Because they want to buy from you if you have made it convenient for them.
The benefit of this is that we have an industry that is phenomenal. It is growing and there are new products available to engage with customers. It has been a tough year for everyone, but it is a great industry to be in.
THE NUMBERS:
A survey by the General Optical Council (GOC) of more than 2000 people exploring the public perceptions of the profession has found that confidence and satisfaction in eye care professionals remains high. Marcus Dye, GOC acting director of strategy, said: “We’re extremely pleased to see that confidence in the professions remains high, especially during the COVID-19 pandemic.”
96% of respondents were satisfied with their last visit
97% were satisfied with the coronavirus measures put in place
9IN10 (94%) were either fairly or very confident in the standard of care provided by optometrists. In line with, and slightly higher, than that for doctors, dentists and pharmacists
The report revealed a continued shift in public perception, with more patients agreeing they would attend an optometrist first with an eye issue – a figure which has been on an upwards trajectory since 2015 –and more seeing optometrists as a healthcare service
30%
of respondents said they would attend an optometrist first if they woke up with an eye problemThis represents an 11-percentage point increase since 2015
OVER 1/3 of respondents perceive optometrists to be solely a healthcare serviceThis is an increase of fourpercentage points since 20191/2 of respondents perceived optometrists to be a mix of retailer and healthcare service
Data source: General Optical Council, Public perceptions research 2021, carried out by M·E·L Research


















University of Wisconsin-Madison

OT’s Selina Powell reviews the latest clinical news and research papers
Researchers at the University of Wisconsin-Madison have tackled the challenge of delivering photoreceptors to the retina with a tiny scaffold that resembles an ice cube tray.
The study, which is published in Science Advances, describes a micro-moulded patch designed to be implanted under a damaged or diseased retina.
be used to create many other types of soft scaffolds for various biomedical applications,” he highlighted.
The research team is preparing the scaffold patch for surgical testing in large animals. If successful, then the technology will be tested in humans.

Microscopy revealed that the completed scaffold was capable of holding more than 300,000 photoreceptors in approximately the area of the human macula.
Professor of electrical and computer engineering at the University of Wisconsin-Madison, Zhenqiang Ma, described the results as “exciting and significant.”
“Once we figured out the recipe, mass production became immediately possible, and commercialisation will be very easy. The fabrication methods can
OCTOPUS VISION TEST COULD HELP PINPOINT PATIENTS AT RISK OF AMD
UK scientists are developing technology that could be used by optometrists to screen for patients with low macular pigment levels.
A new study, which was published in Journal of Experimental Biology, describes using technology to test how well a colour blind octopus can detect polarised light.
The research team found that octopuses have the most sensitive polarisation vision system of any animal tested to date.
David Gamm, director of the McPherson Eye Research Institute, shared his hope that early generation retinal patches will be safe and will restore some vision. “Then we’ll be able to innovate and improve upon the technology and the outcomes over time,” he highlighted.
“The fabrication methods can be used to create many other types of scaffolds for various biomedical applications”
position at the University of Bristol and the University of Aston, highlighted that humans can perceive polarisation because of macular pigments in the eyes.
“By inventing a method to measure polarisation vision in octopuses, we were able to use the core technology to develop a novel ophthalmic device that can quickly and easily screen people for low macular pigments, a strong risk factor for increased susceptibility to macular degeneration,” he said.
“I hope this serendipitous invention will help empower people to do more to look after our eyes”
Temple is developing the technology through his start-up company Azul Optics.
Study confirms safety of virtual care
New research published in eClinicalMedicine has found that a virtual accident and emergency eye care service has a similar safety level to an in-person eye casualty service.
The research examined the case notes from 404 patients treated through Moorfields Eye Hospital’s video consultation service, which was introduced in response to the social distancing requirements of the pandemic.
These patient episodes were compared to the case notes of 451 patients who attended eye casualty in person. Researchers found comparable safety levels between the two services, while 97% of patients seen through the video platform were satisfied with their care.
Li et al.
DOI: 10.1016/j.eclinm.2021.100818
Treatment not always needed in patients with high IOP
New US research has highlighted that patients with elevated eye pressure do not always need treatment to prevent vision loss from glaucoma.
The research, which was published in JAMA Ophthalmology, described results from the Ocular Hypertension Treatment Study.
A total of 1636 patients with high intraocular pressure were regularly monitored between February 1994 and December 2008. Observations were also taken after 20 years of follow up.
Researchers found that around one in four participants went on to develop vision loss in at least one eye from glaucoma – which was lower than expected.
Kass et al.
DOI: 10.1001/jamaophthalmol.2021.0341
Drinking red wine may reduce cataract risk
Researchers have found that low to moderate alcohol consumption is associated with a lower chance of requiring cataract surgery.
Subsequent research led to a method of testing macular pigment levels –which can be linked to an individual’s risk of developing age-related macular degeneration later in life. Professor Shelby Temple, who holds an honorary
“We are all living longer and expecting to do more in our older age, so I hope this serendipitous invention will help empower people to do more to look after our eyes, so they don't suffer from this devastating disease,” he said.
The research, which was published in Ophthalmology, showed that adults who consumed alcohol within the maximum UK weekly limit of 14 units per week were less likely to undergo cataract surgery.
The most significant reduction in the risk of requiring cataract surgery was among wine drinkers.
Chua et al.
DOI: 10.1016/j.ophtha.2021.02.007

As changing patient lifestyles drive suppliers to source new solutions, OT takes a look at the technology behind three lens solutions meeting the needs of growing patient groups
Patient requirements are at the heart of innovations across optics, and key patient groups are emerging as important areas of focus for manufacturers.
Recent months have seen Hoya introduce its Miyosmart lens for myopia management, and Essilor its Varilux Comfort Max for the presbyopic market – solutions for patient groups that are set to continue growing with the anticipated rise in myopia and an ageing population. Modern lifestyles are also having an impact – something that has only built during the pandemic – and that Zeiss has explored in its SmartLife portfolio.
With these patient needs unlikely to abate any time soon, OT asked the three suppliers about these key areas and the technology behind their innovations.
A key shift in patient behaviour has been the increased use of digital devices. Paul Hopkins, optometrist and professional services manager at Zeiss Vision UK and Ireland, told OT: “Connectivity is increasing regardless of age. More than 50% of the world’s population now carries a portable digital device.”
“This connectivity means that we rarely switch off,” Hopkins said, suggesting: “Over time, the constant need to multitask and change our viewing distances between devices, screens, another person or task means the way our eyes behave has also changed.”
The use of devices has evolved over the pandemic, with Zeiss finding in a survey with OnePoll that 61% of
respondents use a laptop and another digital device simultaneously, whilst 57% use a smartphone and another device simultaneously.
“Considering the recent changes in working habits due to the global pandemic, of those we surveyed, 60% agree that they multitask more when they’re working from home,” Hopkins noted. The survey found that 42% think their eyes are having to multitask by looking at screens, while 34% think their eyes have to multitask by switching between different distances.
The survey also found that 26% of people experienced problems with clarity of vision when switching between different distances.
The company argued that this constant connection can lead to eye strain and has also led to new patterns of posture and eye movement. Illustrating this, a 2019 study by the Zeiss Vision Science Lab found that regular use of smartphones has led people to look down more than we used to, using more of the lens –particularly the lower part of the lens.
These changes occur on top of the shifting visual needs that patients already experience through ageing, particularly the decrease in the amplitude of accommodation, and a decrease in pupil diameter.
Hopkins suggested the Zeiss SmartLife lens portfolio is designed to widen
a patient’s clear field of view and cater for the changes in accommodation and pupil diameter that occur through ageing. In order to address the varying needs of the different age groups, the portfolio is made up of three different lens types.
The lenses have been developed with Zeiss SmartView Technology, which includes the use of object-space-models and “design fingerprints” (distribution of vision zones) adapted to the visual behaviours of wearers.
The object-space-model is used to account for the dynamic visual behaviour of wearers, flattening the distribution of dioptric power in the lens periphery in order to create smoother vision –something the company found was needed for the frequent changes in head and eye posture that is observed in the way people interact with their devices.
Presbyopia is a key area of focus for the industry, suggests Dr Andy Hepworth, professional relations manager for Essilor, highlighting: “Within the UK, we have an ageing population and figures highlight that in about 2025, a third of the population will be over 55.”
Hepworth suggests this shift could mean that multifocal spectacles –varifocals in particular – could become ever more dispensed to the wearer.
Last autumn, Essilor launched its Varilux Comfort Max, a new addition to its varifocal lenses, designed to offer wearers greater flexibility in the postures they can adopt whilst still being able to see sharply, created specifically for wearers with busy lifestyles who take part in activities that result in static postures or cause prolonged strain on the eyes.
The lens was designed using Essilor’s Flex Optim technology to increase the ‘useful vision zone’ of the lens by up to 46%, enabling wearers to adopt a broader range of head movements. In particular, this expansion also enables the wearer to adopt up to 495 different body postures when looking at a computer or desktop screen.

Explaining the reason behind this, Hepworth highlighted that with people now needing to multitask more within the
arm’s length area: “It has become quite clear to our research and development (R&D) team and market researchers that members of the public – presbyopic and pre-presbyopes – need correction that satisfies the use of digital devices.”
To model how wearers behave and move in their spectacles, Essilor’s R&D teams developed a new simulation process. The LiveOptics process utilises avatar simulations to mathematically model the conditions of an “infinite number” of real-life vision tasks.
While first touched on in the development of the Varilux X series in 2018, the process was robustly used within the framework of the Varilux Comfort Max, Hepworth said. Describing how the avatars are used to form a prototype ahead of live testing, he shared: “What these avatars do is tell us what needs to be built into a Varilux design. The R&D teams look at that information, add the features in and then can keep tweaking.”
Meanwhile, the technology can also help to inform future innovation. Hepworth told OT: “The R&D teams can continue using these avatars to try and work out what is going to be happening in the future, and what the Varilux lens needs to have the ability to do.”
Innovating in myopia
Hoya has also been addressing the needs of a key group with a focus on myopia.
Andy Sanders, professional services director at Hoya Lens UK, said: “Myopia is a significant global public health and socioeconomic problem and has been steadily increasing in recent decades.”
To address the issue of myopia progression Hoya launched its
MiyoSmart lens, featuring a patented technology called Defocus Incorporated Multiple Segments (DIMS), which the company suggests helps to slow myopia progression and axial elongation.
The concept began, Hoya told OT, when Dr Chi-ho To, head of the school of optometry at the Hong Kong Polytechnic University and chair professor of experimental optometry, had been exploring resources detailing myopia control methods. When on a bus, he noticed the dark tinted windows had contra-vision film which allowed those inside the bus to see out but not vice versa. Sanders said: “Being a myopic patient himself, he removed his glasses to see through the little holes that the window film had, and to his surprise, he could see clearly with a very acceptable visual acuity.”
The professor reviewed optical alternatives that slow down the progression of myopia, finding nothing about optical defocus, Sanders shared. “From his experience with the window film on the bus, and the findings from his recent literature review, he concluded that a way to control myopia could be in combining two stimuli, one with minus power and another one with plus power.”
Having reviewed data from a contact lens trial that involved simultaneous defocus, the professor worked on a model that would use a defocus incorporated multi-segment spectacle lens design to manage myopia progression. Sanders added: “This would override the eye movement that we experience while we wear glasses (versus contact lenses), with a stable vision of near and distant vision with myopic defocus.”
WHAT DOES INNOVATION MEAN FOR LENS SUPPLIERS?
The Optical Suppliers Association’s lens focus group highlights the key innovations within lens manufacturing
"Arguably, the biggest innovation within the lens industry was the democratic revolution of freeform. The arrival of ‘digital surfacing’ as a new production method for generating lenses was more significant than many realised. Around the turn of the 21st century, we suddenly had a new way of producing progressive addition lenses from single vision (SV) blanks. With the right software, any SV lens could now be produced as a progressive lens design. New lens designs were quicker to the market. This offered more choice to the profession who could offer a wider choice of lifestyle and personalised lenses to an increasingly demanding public.

The MiyoSmart lens hosts a clear central hexagonal area of 9.4mm diameter which provides the patient with the full myopia correction. This area is then surrounded by a treatment zone of 33m which consists of micro-lenslets, each with a +3.50D power and measuring 1.03mm in diameter, distributed exactly 1.5mm centre to centre.
Describing how this approach addresses myopia, Sanders explained: “Unlike standard spectacle lenses, which produce peripheral hypermetropic defocus on the retina, which is hypothesised to drive myopia progression, the MiyoSmart lens creates peripheral myopic defocus reducing the progression trigger.”
Likened to a honeycomb, the defocus zone provides an average ratio of myopia correction to defocus of 50:50. Sanders added: “When the patient looks directly through the defocus zone, visual acuity remains almost unchanged.”
Hoya plans to build on the technology, Sanders confirmed and is "investigating potential improvements and additional lens options to enhance its myopia management offering.”
Lifestyle is built into almost everything we buy, and ophthalmic lenses are no different. Only by asking the right questions will you find out what the consumer wants. We have seen that working from home has increased the demand for ‘computer specs.’ Specialist selective/absorbing coatings can deal with excessive exposure to UV, infrared, the challenges of night driving, and even offer anti-microbial protection. Meanwhile, sports vision, mobile devices and active leisure pursuits provide specialist dispensing opportunities. People are beginning to understand that we ask a lot of our eyes today and they expect lenses to be able to cope with the demands of our day-to-day lives. The best eye care and the best possible vision should go hand-in-hand, whatever the lifestyle, whatever the demands."
Read more from OSA's lens focus group in OT online
The AOP's Strategy for Optometry aims to highlight the key role optometry plays as part of the NHS and where the profession can further relieve pressure on the health service
The AOP has launched its Strategy for Optometry, a plan setting out a vision for the future of the profession.
Aimed at MPs, NHS Commissioners and other key decision makers, the publication is designed to highlight the key role optometry does, and could, play as part of the NHS.
The AOP noted that eye care in the UK has already gone through “fundamental change” as a result of the coronavirus pandemic, with optical practices providing patient eye care where hospitals and GPs could not.
“It prompted commissioners and clinicians to innovate. But NHS primary eye care beyond the sight test remains patchy in England, creating a postcode lottery that is confusing and unfair for patients,” the association continued.
The AOP’s Strategy for Optometry outlines where optometrists are qualified and equipped to deliver on more NHS work, addressing how this could relieve
Supporting the practice team


pressure on overstretched hospital eye and emergency departments.
Incoming chair of AOP Council, Dr Julie-Anne Little, said: “Our strategy has been developed with the AOP Council and sets out a vision for key decision makers – showing how optometry can work better and smarter for the NHS and ensuring the skills of eye care professionals are used to their full potential. But it also highlights the reforms needed in eye care funding to make sure patients in every community retain access to the care they need.”
A summary of the strategy has been included in this edition of OT for all practising, student and career break AOP members.
The AOP’s Strategy for Optometry can be read in full on the website at: www.aop.org.uk/optometrystrategy
From successful triage to contact lens retention, OT and the AOP have produced new resources focused on supporting and upskilling the practice team
Alongside the June/July edition of the journal, Optometry Today (OT) has launched a new guide covering key issues affecting the whole practice team.
The guide tackles some of the biggest issues facing practice teams including developing a successful triage process, dealing with complaints and ensuring an inclusive environment.
Features also explore the balance between selling and recommendation, insight on how to make contact lenses an integral part of practice, and tips for eyewear selection.
The guide, released in partnership with Johnson & Johnson Vision, will be distributed to members working in an independent practice setting; features from the guide will also be made available on the OT website throughout June and July.
To further support practices, the AOP has launched a new webinar series, also in partnership with Johnson & Johnson Vision, aimed at upskilling the practice team in key areas. The four webinars will be available from the end of June, through to mid-July and will be free to access for the whole practice team.
Adam Sampson joins on 14 June
The Board of the AOP has appointed Adam Sampson as the new chief executive. He takes up the role on 14 June, succeeding Henrietta Alderman who held the post since 2013.
Sampson recently held the position of chief executive of St Elizabeth’s Hospice and has previously held roles as chief executive of Shelter, and was the inaugural CEO of the Legal Ombudsman. He has also previously been an interim CEO of the General Optical Council (GOC).
Mike George, AOP chairman, said: “The fact that this role demands an external focus and the ability to navigate across a complex stakeholder landscape in a changing sector really appeals to him, and we believe his experience in this area is ideal for the role of chief executive at the AOP.”
George thanked Alderman for her “outstanding contribution” to the AOP, adding: “We wish her the very best for her retirement.”
On his appointment, Sampson said: “As I know from my time at the GOC, optometrists play a critical role in maintaining the nation’s eye health. The AOP is the leading representative membership organisation for optometrists and I look forward to leading the association in its vitally important mission of helping to shape the future of the optical profession.”
The sessions will explore some of the key issues and challenges faced by dispensing opticians, optical assistants and frontline workers in practice teams.
Dr Ian Beasley, AOP head of education, said of the series: “These new additions to the AOP education programme are designed to enable the whole optical practice team to flourish and grow their skill set, which is why we’ve made them open to AOP members and non-members.”
The first webinar in the series will explore common clinical and non-clinical dilemmas that may be faced by frontline practice staff on a typical day in practice and how to manage them. This will be followed by a session on what to consider when dispensing progressive powered lenses. A third webinar will advise on visual fields and optical coherence tomography for the optical assistant. The final webinar will provide guidance on recruitment and retention in contact lenses.
More information about the webinar series can be found at www.aop.org.uk/events

AOP EXPERT
Sarah Melzack, project manager of the Peer Support Line
How has the Peer Support Line (PSL) been supporting members in the past year?
In the last 12 months our amazing volunteers have assisted with almost 100 hours of support conversations; listening to problems, providing understanding, and helping callers to work through their worries to gain some perspective or a plan of action. While 2020 saw a 65% rise in calls, fuelled by stresses and work/life changes caused by the pandemic, 2021 seems to be plateauing but with an increase in mental health issues, an unfortunate repercussion following such an unstable and strained year. Thankfully, a lot of callers report a sense of relief and clarity after speaking to us.
What are your plans for the PSL in the year ahead?
With the rise in mental health issues, we will be concentrating
on upskilling our volunteers in this area. We’re also conducting an (delayed due to the pandemic) 'onboarding' of recruits so it will be great to have some new perspectives brought to the wonderful volunteer community that we have.
What would you like members to know about the PSL in 2021?
The PSL volunteers are optometry professionals who can understand the context and implications of caller’s problems, be them large or small, professional or personal, and they operate in a completely anonymised and confidential space. Previous callers have often referenced wishing they’d called sooner, so to members struggling I would say, please don’t delay.
ThePSLcanbeaccessedvia www.aop.org.uk/peersupportline orbycalling08008708401

AOP EXPERT
Leah
Boyle, web content and social media executive
What is the OTtalkssocial mediaseries?
This is an online video series that aims to offer the latest advice and insight into how to get the best out of using social media – from simple tips and tricks to ethical responsibilities surrounding professionalism and confidentiality. OT interviews industry experts, as well as optometrists and students with an established social media presence, who each offer a different perspective.
What led to the concept?
Over the past year we’ve all witnessed the growth of online activity. Some practitioners may have used this time to think about what they offer online and the social media platforms they invest time into, so we thought this was the perfect opportunity to release a
video series that could help them. There is a plethora of information and guidance online about social media best practice, but we wanted to create something bespoke and relevant for optometrists.
How do you hope this will benefit optometrists?
I hope this helps optometrists to feel more informed, confident and better-equipped when using social media in their practice or as students, and perhaps try new things. The OT team would like to continue with this series so we would welcome any budding optometry influencers to contact us.
TheOTtalkssocialmedia seriescanbefoundon InstagramandFacebook: @optometry_today























Blending technologies
Johnson & Johnson Vision’s Acuvue Oasys Multifocal lens with Pupil Optimised Design has received CE Mark approval in Europe. The product for patients with presbyopia is set to launch in the UK this summer, from July. Expanding the Acuvue Oasys portfolio, the two-week reusable lens features the Pupil Optimised Design technology that is currently available in the 1-Day Acuvue Moist Multifocal and also follows the same fit process. www.jnjvisioncare.co.uk
Sealing in comfort



Bausch + Lomb has launched its ULTRA Multifocal for Astigmatism, expanding its monthly reusable range. The contact lens features Moisture Seal Technology, incorporated through a proprietary twophase manufacturing process that helps lenses to retain moisture and wettability. It also combines Bausch + Lomb’s 3-Zone Progressive Design, for clear vision across near, far and intermediate distances, and OpticAlign Design, which the company suggests provides <5 degrees of rotation on 95% of patients for stable vision.
www.bausch.co.uk
Extending availability
Menicon has extended its Miru 1day Flat Pack range to include plus powers of up to +2.00D (in -0.25D steps). The contact lenses use Smart Fit technology to allow it to orient correctly, no matter how it is applied. The lens features a bi-aspheric, thinner toric design, in order to match natural eyelid contours and also bonds with tears to lock in moisture. Menicon has updated its online toric calculator to include the new plus powers. www.menicon.co.uk


Immersive engagement
Alcon has launched Precision1 daily disposable contact lenses in both spherical and toric designs. The product features Alcon’s proprietary Smartsurface technology; a permanent, micro-thin layer of moisture at the lens surface, which the company suggests helps support a stable tear film. The lens is designed to meet the needs of ‘high performance seeking’ wearers, while addressing the key drivers of new wearer dropout. Alongside the product release, the company launched an augmented reality patient support programme. Read moreabouttheprojectonpage50. www.uk.alcon.com































































































The professional ultrarunner, former Team GB triathlete and Bollé ambassador, on what she looks for from her eyewear
1
I have around 12 pairs of sunglasses, all of which are Bollé, who I am an ambassador for. The vast majority of frames I have are sports sunglasses for running and cycling but my lifestyle collection is growing. Outside of sport, I live in my ‘Merit’ sunglasses that have a very flattering design.
2
The most important things about my eyewear are sun and fly protection. It’s amazing how many bugs hit the lenses, and how much grit and wind the lenses also protect me from. The right frames can give you a ‘game face’ too. My competitors can’t see my eyes and when you are suffering in a race that poker face is an advantage.

Optometrist and lifestyle blogger, Lizzy Yeowart, on summer glamour
It is time for glasses wearers to emerge butterfly-like from the cocoon of lockdown confinement and embrace every social opportunity with gusto and celebratory eyewear.

Etnia
David Bowie exemplified an unapologetic individuality and fearless self-expression. Etnia Barcelona pays tribute to the icon with its eponymous collection.
Etnia’s ‘Ziggy Stardust’ www.etniabarcelona.com

Jimmy Choo
3
I prefer bright and colourful frames, which match my occasional desire to stand out from the crowd. I find wearing the right colours elevates my mood, especially when having a tough patch in a race. It’s the little touches, such as my sunglasses, that can add to that.
4
A great fit where I barely feel I am wearing glasses is important. For cycling and running there can be a fair amount of head movement, so a strong but comfortable fit is key to ensure they don’t slip. The lens has to be right for the conditions. The light-reactive Phantom works well for me as I can be out for very long hours in really mixed weather.
This black ruthenium oval sun style is characterised by a clip-on chain, complete with Swarovski crystals and signature ‘JC’ logo. The chain can be detached and worn as a necklace. Jimmy Choo’s ‘Shine’ in black ruthenium with grey lenses www.safilogroup.com/en/2-jimmy-choo

Eyewear from Pier Martino is made using top-quality materials and set with Swarovski crystals. Its styles are for those that dare to be different and who wish to express their personality.
Pier Martino’s ‘6627’ www.piermartino.it
Style icons
Porsche Design Eyewear has launched a limited edition sunglass model inspired by its 2021 brand ambassador, the Hollywood actor, director and race car driver, Patrick Dempsey. Based on the ‘P’8928’ frame, a modernised take on brand’s first sunglasses with an interchangeable lens mechanism, the ‘P’8928 P Collector’s Edition’ features a squared aviator shape and a titanium frame available in a dark grey and black colourway. The frame is available with four additional pairs of coloured interchangeable lenses in a traveller box.
www.rodenstock.com


JF Rey has introduced its spring 2021 collection focusing on minimalism and geometric effects, with features including graphic cutouts and architectural structures. The collection includes nylor frames, semi-rimmed or full-metal styles. Within the collection, the ‘JF2932’ (pictured), ‘JF2933’ and ‘JF2934’ designs feature two-toned frames with thin metal lines. The company explained the appearance “comes from the folding and meticulous hand colouring of a piece of metal assembled on the frame to give the optical illusion of fine interwoven lines on the top.” www.jfrey.fr/en

Sunglasses
Movie magic
Barton Perreira and EON Productions Limited has released Series 2 of the BP x 007 collaboration, ahead of the September launch of NoTimeToDie. The release introduces four new colours for the ‘Joe’ frame, inspired by locations in the film. The ‘Matera/Green Smoke’ design draws on the colours of the Matera village in Italy, while ‘Hakadal/Noir’ is inspired by the landscapes of Norway. ‘Port Antonio/Safari Polarised’ evokes the beaches surrounded by jungle in Port Antonia, Jamaica, and the ‘El Nido/Old English Polarised’ (pictured) is inspired by a scene set at Havana’s El Nido Bar. www.bartonperreira.com
Zeiss Vision Care has launched Zeiss DuraVision AntiVirus Platinum UV, the company’s first lens coating with antiviral and antibacterial properties. The coating uses nano silver technology to actively kill 99.9% of potentially harmful viruses and bacteria on the lens surface. The coating has been tested and has shown compliance with ISO standards for antiviral or antibacterial testing by external laboratories and institutes in China, Germany and Canada. More information on the testing can be found on the Zeiss website.
www.zeiss.co.uk



Simple refractions
BiB Ophthalmic Instruments has introduced the HandyRefract binocular trial lens holder. The tool features an arm positioned to enable the optometrist or patient to hold in their hand for a “quick and handy refraction.” The HandyRefract includes two sprung front cells, fully-rotational with axis markings for lens insertion. Both sprung cells can be removed for cleaning. www.bibonline.co.uk
Imaging
Next-gen captures
To feature in OT’s Hit list, contact kimberleyyoung@ optometry.co.uk

Mainline Instruments has revealed the DRSplus from iCare, described as “the next generation in confocal fundus imaging.” The device uses a white LED illumination, combined with confocal scanning, to produce TrueColour and detail-rich images, the company shared, suggesting it provides greater image sharpness, optical resolution and contrast compared to traditional fundus cameras. Due to the confocal technology, the DRSplus can also scan through cataracts to aid clinicians in the diagnosis of ocular disease. www.main-line.co.uk


Crystalline glamour
De Rigo has presented the limitededition Chopard Red Carpet 2021 style, inspired by a bracelet in the high jewellery collection of the same name. The 23K gold-plated metal frame features a square-shaped front piece, with 214 hand-set crystals, colour coordinated to match the hues of the lenses. The frame is available in traditional gold and palladium-hued crystal with gold flash mirrored lenses, or blue and purple-coloured crystals with blue gradient lenses. www.derigo.com









































CEO, Rosario Toscano, on adapting as a young brand

AKONI GROUP//
Founded in 2019, the team is headquartered in Lugano, Switzerland
Collections are designed in California by Jeff Solorio and John Juniper, the founders and former designers of DITA
Made in Japan, the frames are created through a combination of traditional and cutting-edge production techniques.
OT columnist, Lizzy Yeowart

What makes Akoni’s eyewear unique?

Our eponymous Akoni collection was created for people who appreciate timeless design, exceptional materials, and uncompromising craftsmanship. We avoided the stereotypical categorisation by gender and age, and instead organised the collection into five unique categories based on inspiration, design, and materials. We use planet-friendly materials and processes whenever possible.
What is the latest collection you have released, and why does it stand out?
We just launched the Balmain and Akoni spring/summer 2021 collections to enthusiastic receptions. The Balmain collection was featured in the house’s amazing fashion show held in the Air France hangar at Paris’ Charles de Gaulle airport. Highlights of this season’s collection include an evolution of the iconic ‘Wonder Boy’ colourway in Silver and Blu, and new additional elements in acetate and titanium grill.
How has COVID-19 affected Akoni, and how has it had to adapt?
COVID-19 has presented the world with enormous challenges, and our hearts go out to everyone who has lost a loved one to this terrible pandemic. I’m an eternal optimist, so with respect to COVID-19’s business impact, I would say that the flipside of challenge is opportunity. Although Akoni Group launched in one of the most challenging business climates in recent memory, the fact that we’re a small, experienced, dedicated team allowed us to quickly pivot and adapt to the new and constantly changing landscape.


Voices from optics and beyond

A“I love my job as a domiciliary optometrist so much more now than I did working in practice”
Simon Raw
t the age of 15, when I was exploring careers and work experience, I had no idea which path I wanted my life to take. My mum was heading out to the opticians, who happened to be one of her old school friends, when she commented that it was a possible career I could explore. I completed work experience including at an independent and in a hospital clinic. I loved the gadgets and the job’s caring nature, which offered more social hours than other medical roles.
At 18, I left home to go to complete three happy years at the University of Manchester Institute of Science and Technology (UMIST) – making lifelong friends and receiving my degree. A Boots pre-reg followed in the city centre store in Newcastle where I worked in a fabulous team and developed the skills learned at uni. I took a career break to travel the world and worked for six months in Christchurch, New Zealand, for OPSM Opticians. On returning to the UK, I became a store manager and pre-reg supervisor with Boots.
Inspiring suitable candidates
After three years at university and seven years in practice, I still had no idea what domiciliary optometry involved and only had stereotypes and myths in my mind. I imagined that all patients would have dementia, poor communication skills, poor personal hygiene and would not be suitable for a proper, complete eye examination. How wrong could I have been?
Thirteen years of full-time domiciliary work later, I have to say it was the best career
move I ever made. As an optometry student, I would have liked to have known all the possible career options earlier. Some fabulous optometrists out there would be perfect for this role, but they haven’t given domiciliary a second thought.
To assist the universities in their career development, OutsideClinic asked me to deliver an online lecture to university students on the rewards and challenges of domiciliary work. Working closely with former OutsideClinic colleague, optometrist, Dr Rakhee Shah, a domiciliary lecture has already been built into the course at two institutions, with the rest keen to follow suit. With this, and my newly developed lecture for all optometry students, I hope we will now be able to dispel the myths and inspire suitable candidates on this fantastic career path.
The lesson consists of the legal and NHS requirements for domiciliary. We discuss the need for enhanced communication skills and flexibility in each patient’s specific requirements. There includes a display of the different equipment that can be used and an explanation of the need for excellent record keeping. We highlight case records to show examples of what a domiciliary optometrist may encounter.
COVID-19 has changed all our lives, and domiciliary care is no different. At OutsideClinic, we have adapted and are often complemented by patients about how safe they feel with the changes we have made to our routine.
What is your view?
Email OT with your comments newsdesk@ optometry.co.uk

“With an everageing population and increasing life expectancy, we will need many more domiciliary optometrists to see everyone”
With an ever-ageing population and increasing life expectancy, we will need many more domiciliary optometrists to see everyone. Hopefully, I can inspire some students to take up the role and enjoy it as much as I do.
Simon Raw is an optometrist for OutsideClinic



A“At the GOC, we are committed to finding ways to be more agile and responsive in the face of adversity”
Marcus Dye
s we begin to move towards a ‘new normal,’ we have been reflecting at the General Optical Council (GOC) about how we’ve responded to the COVID-19 pandemic, and what changes might be here to stay going forward.
Early on in the pandemic, we received many queries from registrants looking to us for advice and guidance. As an independent regulator, we were able to support registrants by removing any unnecessary regulatory barriers to the provision of clinical care, in line with government guidance, and to clarify any ambiguity in our legislation or rules.
“It would have also been beneficial to have a ‘go-to’ list of partners for an emergency like this and this is something we will implement for future emergencies”
To do this, we issued a series of statements that clarified changes to our regulatory processes, and clarified current practice – for example on the supply of spectacles and contact lenses and infection prevention and control. Alongside this, we sought emergency legislation from the Government, and worked with professional bodies, the NHS and the Department of Health and Social Care to clarify the Government’s guidance.
Internally, there were adjustments we had to make quickly, including closing the GOC office and delivering our work remotely. We also moved our fitness to practise hearings online, which was a first.
We had to do our best to be quick on our feet and there were some things we had to learn along the way. One of these things was that it is possible to achieve rapid consultation with key stakeholders during emergency situations, including professional and representative bodies, NHS,
employers and national commissioners, and that change can be developed and implemented in much shorter timescales than previously thought. We also learned that we needed to work extremely closely with sector partners from the very beginning. Although we did this early on, we acknowledge that it could have been sooner. It would have also been beneficial to have a ‘goto’ list of partners for an emergency like this and this is something we will implement for future emergencies.
Much is still unknown
The pandemic highlighted to us that we need to do more to better inform registrants about our role and what we do. Some of the questions we received were outside of our remit and due to this lack of understanding, a couple of petitions were started calling for us to stop routine eye tests. This is not something that is within our role or powers and we will continue to work to educate our registrants and the public about what we do.
Because we had to provide guidance so quickly, we weren’t able to consult with the wider sector on our COVID-19 statements. To ensure everyone had the chance to share their views, we held a consultation which sought feedback on the proposal to align our statements to the College of Optometrists’ traffic light system so that we can make it clearer when they will apply going forward.
We also asked for views on whether any of our statements should be policy positions or become part of our Standards of Practice beyond the pandemic. We commissioned Enventure Research to analyse the responses and produce a consultation report and we are currently considering our response, which we will share in due course. From the consultation responses, most registrants are supportive of the content in our statements and how we propose they will apply going forward in line with the College’s traffic light system. We will be using this insight going forward to inform our decisions as we move towards a ‘new normal.’
With the Government proceeding with its route out of lockdown, there is a feeling of optimism –although much is still unknown about how the pandemic will continue to progress. One thing we do know is that we can be more agile and responsive in the face of adversity, and will be much better prepared for any future pandemic.
Marcus Dye is acting director of strategy at the General Optical Council

E“If we recognise that we want to change eye care, what we really need is data to be collected as business-as-usual”
Melanie Hingorani
ven before COVID-19, in the world of optometry and ophthalmology we knew there was a big problem brewing. We had escalating demand from older and more diabetic patients, and we had big delays despite having far more treatments to offer patients. We just weren’t coping and patients were being harmed.
And then COVID-19 came along – and it either shut down services or dramatically slowed them. We now have a huge backlog of patients – how many, we simply don’t know. People with glaucoma and retinal problems need to be seen on time and the truth is they have not been.
However, COVID-19 has opened peoples’ minds to what is possible – and created opportunities for us to do things differently and get things done more rapidly than NHS bureaucracy would have allowed before.
A new process has emerged where the patient only needs to come into hospital for the diagnostics; at a separate point the clinician then reviews the test results, and if the patient is fine, they are sent a letter, and if they are not, they have a video consult follow-up.
The assumption that we can’t see patients virtually because they won’t like it, or they will be inept digitally, has been proved wrong. Actually, patients find they like the luxury of sitting in their own home for their consultation.
There is much evidence to support the role of optometry to tackle the backlog. My experience through the shared care work I have done bears this out. Patients were really happy to see their optometrist; they already knew them, and it was so much more convenient to arrange a visit locally.
When shared care pathways work less well, the reason is a lack of an effective partnership between ophthalmology and optometry. We have to work together; both sides have to be prepared to learn and feed back on what’s gone well and what’s gone badly. If we put that effort in from the beginning, it can work

brilliantly. Issues occur when commissioners do not talk to the hospital and decide to run a repeat measures scheme in optometry that is completely divorced from everything else. We are let down by a lack of routine national data collection at any level of detail. In hospitals, we don’t diagnostically code: our backlog of ophthalmology cases can only be divided into ‘new,’ ‘follow-up,’ ‘child,’ and ‘adult.’ This means we do not know who has got what disease; we don’t capture how many people are seen via optometry referral nor where the variation in referrals is coming from. With optometrists performing enhanced roles, how many patients are going through this route, and at what scale was hospital visits avoided?
Health economics modelling
“The assumption that we can’t see patients virtually because they won’t like it, or they will be inept digitally, has been proved wrong”
The question of renumeration is sensitive, but we need to be grown up and achieve consistency of payments. Some clinical commissioning groups are paying one thing, some are paying another; where is the evidence to support that is the right approach, underpinned by logic and evidence related to the risk and complexity of the work? There is a huge difference in terms of the time and knowledge you need to manage simple post-cataract eye surgery, versus a glaucoma assessment where the patient could go blind if you get it wrong.
Nobody wants a system like GOS, where optical practices in the community feel they are
Read more Insight into the National Eye Care Recovery and Transformation Programme www.locsu.co.uk/ recovery-reform
using their business to prop up the NHS. But asking the NHS to pay optometrists the same fee that it would for a patient going into the hospital is not going to fly. It has to be more affordable.
While we can talk about adopting a GOS+ approach in England that replicates the model in Scotland and Wales, the direction of travel from NHS England is to decentralise commissioning.
The first thing I would do is collect data on what’s being paid for schemes nationally. We need to see the variation and understand what is reasonable using health economics modelling.
Share your views. Send letters and tributes to OT via email to johnwhite@optometry.co.uk
Am I alone?
Am I alone in being concerned about the amount of plastic waste being generated in the current circumstances? Am I alone in questioning the indiscriminate use of single-use, disposable, plastic aprons and gloves? Am I alone when my heart sinks every time I rip off my plastic apron, and peel off my plastic gloves?
COVID-19 is not the only crisis in our world. The environmental, plastic waste and climate crisis was with us long before it hit, and will be here long after COVID-19 is no longer in the headlines.
The issue is not about the use of appropriate PPE for staff dealing with COVID-19 patients. Neither is the issue about the correct disposal of plastic waste. It is not even about the financial cost of all this additional plastic, although that can’t be inconsequential. And I hope that plastic isn’t being used just to make the public ‘feel safer.’
In hospitals, our tariffs and pricing have a methodology behind it that takes into account the overheads and what we did for the patient, divided by how many patients we see. Without the same overheads in High Street practice, let’s explore what the economics are that justify the difference in what a hospital is paid versus community optometry.
Melanie Hingorani is clinical lead for the National Eye Care Recovery and Transformation programme. She is also a consultant ophthalmologist at Moorfields Eye Hospital, and chair of professional standards at the Royal College of Ophthalmologists

The issue is about the amount of plastic waste currently being generated, and how plastic should only be used if it really needs to be. It is about not leaving a legacy of plastic waste that is used for a matter of minutes, but takes decades to degrade. It is about balancing out the competing demands of the current pandemic with the environmental, plastic waste and climate crisis, which will affect all of us… and our children…and our children’s children…
I have written about this issue to Public Health England, NHS England, the NHS Sustainable Development Unit and my hospital
bosses. I have not made any inroads, so far.
If I am not alone, if there is even a modicum of common sense in what I am saying, will ‘somebody’ take up this issue with the ‘powers that be’? Will the ‘optometry bodies’ raise their heads above the parapet, and question the rationale for what has become the ‘new normal’?
Peter Pawson, optometrist
OTreserves the right to edit letters and points out that the views expressed may not be those of the journal or the AOP
“It is like sunshine in a bowl”
Lora Fachie
When I was born, I had a hereditary sight loss condition that also affects my mum and two brothers. My mum had some useable vision until she was about 16. My eldest brother could read large print until the age of eight. My middle brother can see light and dark.
Up until the age of five I had some vision – I could read large print. My two eldest brothers would use me to find the football in the back garden. Now I have light perception.
As a member of the British cycling team, I have access to what is called a performance lifestyle adviser who helps athletes with any issues that are not cycling related – it could be anything from buying a house to education.
A couple of years ago I was really struggling with cycling mentally. My adviser suggested coming up with something extra on the side of cycling that I could focus on. We got chatting and he said, ‘Well why don’t you write a blog?’
He encouraged me to start writing about my cooking and eventually I decided to take the plunge. That was two years ago.
I find cooking really relaxing. With my cycling training programme, everything I do is very regimented. I have specific numbers that I try to hit.
I love to cook with every different type of spice because of the sensory experience. And not just when you eat it but when you are cooking it too – how the spices change as they are cooked. My meals may not always look as good as a meal that someone who is sighted could plate up, but they are always tasty.

“You get very good at problem solving when you can’t see. The world isn’t designed for people with sight loss so, to get by in life, you have to find your own way”
I am very scientific and analytical. But when it comes to cooking, i find that I just cannot follow a recipe and do what I’m told. I am chalk and cheese with training and cooking.
Patient leaflets
The AOP has produced a series of downloadable eye condition leaflets www.aop.org.uk/patients
I would love to learn more cooking technique. At the moment I won’t attempt any filleting of fish or anything where you have to handle a lot of hot liquid – such as work with sugar. I have an ongoing argument with my husband because he doesn’t want me to use a blow torch. You get very good at problem solving when you can’t see. The world isn’t designed for people with sight loss so, to get by in life, you have to find your own way. Growing up, we were taught never to accept no for an answer.
There are a couple of things that I use for cooking that are adapted. I have a talking kitchen scale and tactile markers.
I try to keep things as simple as possible. If you keep your hot pans to a minimum you are less likely to burn yourself or accidentally knock something over. Tasty food doesn’t need to be complicated. I love being able to cook for people and providing something for someone else. My husband’s favourite meal that I make is chicken creole. It is a curry with banana and pineapple served with coconut rice. It is like sunshine in a bowl.
Altrincham-based para-cyclist, Lora Fachie, won gold in the tandem pursuit at the Rio 2016 Paralympic Games. She posts recipes and nutrition tips on her blog, Blindingly Good Food



47 Pre-reg focus Time to take on more complicated clinical challenges, Emily Mather tells OT
Over the past 12 months, the patterns of optometric practice have evolved in radical and unexpected ways in order to deliver eye care during a pandemic. OT and SpaMedica brought two experienced optometrists together to reflect on a year unlike any other. We asked them to unpick what role virtual consultations have played in their practice, how they have captured and used patient feedback to inform their work, and what artificial intelligence (AI) could mean for the profession in 2021 and beyond.
The only experience of telemedicine most optometrists are likely to have had pre-2020 was when seeing diabetic screening patients, Joanne Tutt, a senior optometrist and clinical lead of Birminghambased The Eye Collective, said – but observed that this changed with the pandemic.
“Over the last 12 months, we have been taking part in the COVID-19 Urgent Eyecare Service (CUES), and this has meant we have been triaging and offering remote consultations for patients,” Tutt explained.
“It has been quite challenging. One early learning was that it was easier to do a telephone consultation with the patient rather than a video call.”
50 What I have learned How Alcon and EyeKandy teamed up in order to reach a new contact lens audience
52 The workshop Let’s talk cyber protection. Lloyd & Whyte’s Will King reviews the core principles for practices
55 Key milestones Setting up Moorfields’ Department of Digital Medicine with Peter Thomas
ROUNDTABLE
How virtual consultations have won the support of patients and allied healthcare professionals – and why the change in approach and extended scope of practice for optometry should stay post-pandemic
Using the example of a patient with red eye, Tutt said she would ask them to send a photo, and then would arrange a follow-up call.
“This gives me, as a clinician, time to assess the data and information that the patient is sending. I would then call back having reviewed the data. This approach worked better than using a video platform
such as Zoom – we found that patients would get a distracted by the phone, plus they would expect an immediate answer.”
Tutt added that she was “seeing a lot of patients” who were not existing customers with the group of practices, which meant that she had no access to their information.
“You are doing a history and symptoms check as well.”
“We found some patients would say that they had not used their phone to take photographs before”
David Brett Williams
David Brett Williams, optometrist, clinical lead and JVP of Specsavers Luton, agreed with the limitations of video for triage. “Photos tend to be far more effective, and far more diagnostically significant, than using video, which is low resolution.”
Williams told OT that his practice sticks to a script with the patient, and requests a photo beforehand, which includes instructions on how to take selfies. “We found some patients would say that they had not used their phone to take photographs before – so we realised that patient education was required.”
The appreciation of patients
Asked about the response of patients to virtual consultations, both panellists agreed the reception had been extremely positive.
“Patients like the fact you are there at the end of the telephone, that they can send photographs, and you can message them back with different questions,” Tutt said.
Using practice staff to triage patients as the practices opened back up to routine care has also played an important role, Tutt said. “Receptionists field initial calls, and if a clinical issue is flagged, an optometrist can carry out a follow-up to find out the specifics of the issue – that way we then have a better idea of what we are dealing with if that patient needs to come into practice.”
And for Tutt, the whole practice team can get involved in the triage process.
Joanne Tutt
“Ensure that the patient has a copy of their referral letter if they are going to be referred into the hospital. Arm them with the important info and point them to NHS website advice. The ophthalmology consultation might be remote too, and the advantage of remote care is that patients often feel more comfortable in their own homes and are more likely to ask questions. As an optometrist, give them the support and info so that they feel they can ask the important questions of the consultant.”
“As a company we decided remote consultations are really here to stay. We created a training video for all staff on how to communicate better with patients over the telephone, including a crib sheet of what to ask. The CUES pathway we use is also really good – it has dropdown menus and boxes where you can capture data.”
The scale and speed of the profession’s shift to telemedicine has been startling, Tutt said. “You think back to a year ago, and it feels like we have been doing virtual clinics for so much longer.”
This observation was echoed by Williams, who explained with a smile that he had “underestimated” the level of interest from patients and allied health professionals for the virtual consultation 0800-number service he offers via a contract with four clinical commissioning groups.
“We had to get the service up and running at speed. When outpatient appointments were stopped and GPs stopped seeing patients in person, demand rose. In particular, we saw that patients from A&E were being discharged if they were coming in with eye injuries including foreign bodies. They simply were not seen – and were told to call our 0800-number,” he explained.
The appreciation of patients for virtual consultations was palpable, Tutt and Williams explained.
“With the optimism of the vaccines on offer today, it is hard to recall how gloomy it was back at the start of the pandemic in March 2020,” Williams said. “When we
David Brett Williams
“I remember in the summer a patient phoned in, who had been discharged with a cinder that had entered his eye from a fire. I facetimed with him, got him to buy contact lens solution, and taught his girlfriend how to irrigate his eye to remove the cinder. It worked and he was fine.”
spoke to patients, who felt at times like they were being bounced between services, we found that they were so relieved to actually get hold of someone to speak to. As an optometrist, it makes the long hours and the difficulty all worthwhile.”
Both panellists also pointed to an experience in the last year that has been “massively professionally rewarding,” observing that during the pandemic the clinical skills of the profession has been tested in new ways.
For Tutt, it is “through necessity” that ophthalmologists have had to give optometry more leeway in how the profession interacts and treats patients. “Optometrists are more confident, and in turn this has given ophthalmologists more belief in our ability. And patients are simply pleased that there is help out there.”
Williams noted that optometrists involved in virtual consultations see a far wider range of cases than pre-COVID-19, including minor eye conditions service (MECS) schemes, primarily because hospital services are so limited.
“Our optometrists love it. The practice does have to shift up the gears – and our reception team who were taking calls that were once about the costs of lenses are now getting calls
about symptoms – and are prioritising which patients might need to come into the practice. Success for us was being systematic and processdriven with these patients,” Williams explained.
New optimism, new pressures
During the pandemic, the use of smartphone adapters and apps for assessments has evolved at pace.
Williams said he had looked at a range of video conferencing apps but concluded that they did not offer the clarity needed.
Both Tutt and Williams highlighted that the simplicity of email offered tangible benefits.
“We may have had email for decades, but it helps immensely,” Williams said.
“We use email to share instructional materials, including the Amsler grid for patients that have been diagnosed with AMD. Plus, we can send a copy of any information we have sent to the GP to the patient via email as well.”
Tutt agreed, using the example of how the practice group now proactively emails links to eye condition leaflets, including dry eye syndrome, provided by the AOP to patients.
Tutt said the group also use email to send a questionnaire to patients to capture their
To watch the roundtable, hosted by OT and SpaMedica, visit www.youtube.coc/c/ Optometry-Today_ AOP/videos

feedback on the service, as well as the performance of the optometry staff.
The experiences shared by Tutt and Williams spoke of a need to marry clinical care and support to patients alongside pastoral and emotional care. How did the practice team find time to manage these dual pressures?
Tutt explained that The Eye Collective “always worked to deliver satisfaction not volume. We offer a 30-minute testing time, and we are seeing fewer patients in the day. We have found that virtual consultations can save time; it means we can use the time more valuably, offering a holistic service, rather than one that is simply all about refractions and specs.”
For Williams, the NHS faced a “tipping point” that he and his colleagues had to respond to – and are continuing to do so.
Williams highlighted that capturing patient data plays an important role in cementing the value that optometry is playing, particularly through the triaging of patients, adding that the practice software shows 97% of calls from patients are answered in eight seconds.
While noting her practice group was not on the scale of Williams’, Tutt explained they had found that the data they collected was useful. “We have been looking at who has accessed virtual clinics, how receptive they were to the experience, and how we as a group can look at using remote care more. We are also looking at why some practices have done more CUES than others.”
Faced with the opportunities and challenges of COVID-19,
Professor Christine Purslow, director of optometry at SpaMedica “During the roundtable, I particularly liked the insight about patients’ adoption of the virtual consultation technology, and how willing they were to adopt it, as well as how flexible and creative optometry has been to find solutions in different environments. The experience has meant that optometry has turned a corner. We at SpaMedica recognise community optometry as the go-to place for eye care. SpaMedica naturally partners with optometrists: we rely on the expertise of community optometrists to diagnose and refer NHS cataract surgery patients to us and conduct patient post-op assessments through our accreditation scheme. We champion the community optometrist, and if there are ways that we can work together differently then that’s great for everyone: the patients, optometrists and hospital ophthalmology teams.”
Clockwise from top left: John White; Professor Christine Purslow; David Brett Williams; Joanne Tutt
the panel was asked about the role of AI – both for improved patient care and for practice management.
Williams concludes: “We are on the cusp in practice. This has been pushed by necessity. But having made this ground I do not think we will go backwards.”
He added that evolution is needed in AI, pointing to dry eye and AMD as the most readily applied avenues in practice, and adding the caveat: “We have to justify the number of patients that benefit versus the investment needed.”
For Tutt, the ‘new normal’ is a balance that “uses virtual consults to enable more patient touchpoints. Plus, we don’t need to only think local – we have patients nationally now.”
Williams shared that his dream AI innovation is a tool that “analyses the data we have to create a risk profile for the patient and guide how we manage their care. We have fundus photography for patients going back 10 years, OCT scans going back four years – and I’d love to have a software platform that takes these images and comes up with a prompt for the clinician to say, ‘consider this scenario, watch out for this sign, capture this data, ask this question.”
David Brett Williams
“There should be a huge push for stable glaucoma to be monitored in the community. Every hospital eye service is struggling to keep up with stable glaucoma and as a profession we are qualified to manage these patients –and can refer them back in if anything is amiss. There are a lot of stable glaucoma patients in the hospital service who have had their 12-month review delayed and are facing even longer waits.”
Tutt agreed, stating: “We have the data, and we have responsibility to do something with it. I want to be able to make clinical decisions more confidently.”
Looking to future, Tutt concludes that “COVID-19 has pushed us out of our comfort zone as clinicians, and we have stepped up and shown what we can do. There is a need for us to offer more face-to-face appointments, but remote consults are really useful. We must not lose the momentum and get complacent. We have shown ophthalmology what we can do. We need to look for the opportunities, preempt them and adapt.”
For Williams the profession has “progressed a lot,” adding: “I always wanted to have a greater role than as a refractionist. COVID-19 will be with us to stay, and we know we will have other issues to face. The impetus is on CCGs and national bodies to commission the services.”


PRE-REG FOCUS
“I’m enjoying it more every single day”
Pre-registration optometrist at Moorfields Eye Hospital, Emily Mather, on finding a supportive community in her first four months
The first four months of my pre-reg have flown by. I’m enjoying it more every single day and feel like I’m becoming more confident in my ability. I’m enjoying the hospital setting and the variety of clinics is great. Pre-reg is hard –there’s no denying that – and things in the hospital are sometimes very challenging, but I feel like I’m learning a lot every day. We’re busier in clinics than we were at the start and we are working a lot more independently than we were initially. We’ve started taking low vision patients – which is exciting, as I can implement a lot of what I learned at university.
A hospital is an unusual place to be during COVID-19. A lot of the patients are very happy to see us, and many of them haven’t seen or spoken to anyone else for a long time – so they’re just happy to interact with other people. We’re in scrubs during

Peter says…

clinics too, which I love, as I don’t have to spend ages picking out what to wear in a morning (or do any ironing).
A culture of support
Everyone is really looking out for one another as COVID-19 has been a challenging time for everyone, which is lovely. The team of optometrists at Moorfields is huge and everyone is always making sure pre-regs are supported – not only just with pre-reg

everyone is always willing to help. I have some amazing supervisors, who sit down with me before I take a patient and talk through their existing history and any challenges I might potentially face, and how to overcome them. The supervisors also let us get really stuck in as pre-regs and now we’ve been here a little longer they’re helping us take on more complicated challenges.
“The supervisors let us get really stuck in as pre-regs and now we’ve been here a little longer they’re helping us take on more complicated challenges”
work, but emotionally and with anything else that we might be struggling with.
I have been supported by so many people at Moorfields. The great thing about the hospital is there are lots of people you can ask about so many different things, and
A great thing about doing a pre-reg at Moorfields is there is a little group of four of us. We can all help each other with competencies, patient records and other pre-reg queries. It’s nice to be able to talk to each other
I would tell my early pre-reg self to… Make the most of the extra testing time you have to nail down practical techniques and iron out any areas you have trouble with. You will have some difficult days, but one bad day does not make you a bad optometrist. You’ve just got to dust yourself off and remember that you are still learning and will get better with experience.
The next thing I hope to achieve is… Completing Stage 1 of the Scheme for Registration over the next couple of months by getting outstanding competencies signed off at my remaining visits. Having recently reached the required number of refractions, I hope to do the same with contact lens patient encounters as soon as I can.
Education Library
OT's Education Library contains CET, Skills guides and CPD www.optometry.co.uk/ cet/education-library
about anything we’re finding challenging.
We’re all in the same boat and going through the same thing, so being able to share experiences and gain help and advice from people in the same position is invaluable.
It’s been a challenging four months of settling in, managing working full time and going home to revise in the evening. Now things are opening up a little more, London is a great place to explore. I’m desperately trying to manage my time effectively in order to make the most of the city. I have a community placement coming up too, which will be great to gain experience in another optometric setting. I’m excited as it will allow me to build a new set of skills and work in a new team. I’m looking forward to the next couple of months of pre-reg and learning even more.
My best experience of the pre-reg period so far is… It is hard to pick one, but I've really enjoyed developing my own way with patients and the sense of achievement I feel when they leave happy having been under my care.
PeterGrantisapre-reg optometristatJulianDavies Opticians,StMellons,Wales
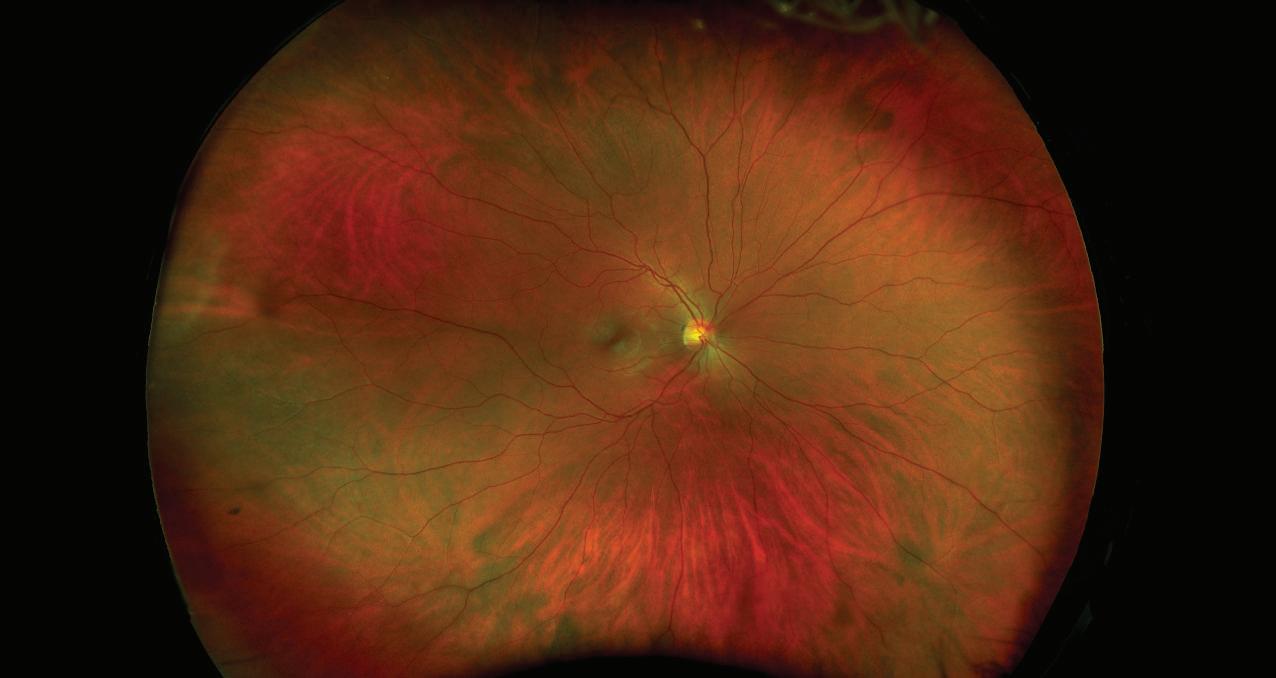









Optometrist and practice owner of Valarie Jerome Optometrists, Dr Valarie Jerome, discusses how building her business during the pandemic led her to establish an online offering
Creating an online shop for my practice was a necessity. Having only been open four months at the time of the first lockdown, I didn’t have any recalls or email lists to market to and therefore needed to find a way of making money.
Initially, I worked on building the practice’s social media presence, and getting more engagement on social media. In doing that, I realised that there was no point in getting people engaged online if I couldn’t offer them anything online. As a result, I set up my own web shop and filled it with eye care products and sunglasses, with free home delivery in the local area.
Shortly afterwards I began to stock an eye care product called We Love Eyes, and, as one of the only suppliers in the UK, people across the country began to discover it and order it through my online shop.
I would love to expand the shop and will be adding an area where people can view, but not purchase, the optical frames that are available in practice. This will work as an online shop window. It will allow potential patients to see what is on offer, and feel more comfortable and confident when they come in.
e-commerce platforms
Creating the shop really was quite simple and has paid
dividends for the business during the pandemic. I would encourage other independent practices to explore it as an option.
I began by simply doing some research on what the best e-commerce site to use was. While I initially opted to use a site that had a free offer, I have since switched to a platform that allows my credit card terminal to run through it – this is something that I would recommend practice owners consider when selecting a platform.
Most e-commerce sites will offer users a pin plate that enables you to build the template for your web shop. I found using these templates was similar to programmes like Canva and PowerPoint, so it was very easy to use.
“Creating the shop really was quite simple and has paid dividends during the pandemic”
I picked it up as I went along and believe most practitioners would be able to do so as well. It took me around four days, working between three and four hours a day on it, to set the web shop up.
The part of the process that took the longest was adding the descriptions for each product. While this

isn’t mandatory, I think it is beneficial for the customer.
I then shared the designs with friends and family to get their opinions on the look and feel, and to test it out, and made some adjustments following their feedback.
Prior to setting up the web shop, I did a lot of local research, including on social platforms such as Instagram.
I also spoke to retailers locally and in doing so built up an idea of what would work for the local area, what people like and what they want. This research helped inform and support my decisions on what products I would offer on the web shop. It was an important phase as it allowed me to get to know more about the wants and needs of potential customers. The web shop would only work if it catered for the right audience.
I also had to be sure that my online store married with the in-store experience and ethos that I was offering. For example, I considered investing in virtual try-on software to support potential customers in making their purchasing decisions. However, in the practice we provide a bespoke and boutique experience, during which we curate and guide our patients when selecting frames and a virtual try-on service online didn’t fit with this.
To read more on businessrelated news, insight and experiences, visit our website www.aop.org.uk/ot/ in-practice
1. Be patient
2. Do your e-commerce research to see what works best for you and the products you stock
3. Ask around and talk to local retailers for advice: there is a wealth of knowledge out there.
Business benefits
Having an online shop has brought my practice more exposure. It hasn’t just been about selling the products. The increased visits that it has brought to the website means that the practice now ranks higher on Google and is a lot easier to find via a web search than it was previously. I’ve not paid for Google Ads; I’ve built the practice’s online presence organically. When I first started, if you typed in ‘opticians Newbury’ into the search engine, my practice wouldn’t come up. But now it is listed with the big guys.
Having a web shop has made my website more popular, in turn making it more popular with Google and, as a result, has made the practice easier to find for potential patients. However, the web shop didn’t bring in business or boost our online presence overnight. I had to give it time. It certainly has paid off now.

the heart of the programme. We really focused on how they think, the questions they have around contact lenses, even their word choice and intonation. These choices were pulled through – even in the ECP section – so that they would use the same language with their patients.
“We needed to be disruptive to reach our target audience”
Alcon UK & Ireland’s Eddie Pigott, and Eyekandy’s Garrett Albanese, on taking patient support to an augmented reality platform
What led to the launch of the augmented reality platform alongside Precision1?
Eddie Pigott, brand manager, Alcon UK & Ireland (EP): Research shows that contact lens drop out is still an issue, especially in the first three months. We found that patients could have difficulties, but they may not contact their eye care professional (ECP). However, practitioners often reach out to us for support tools to share with their patients.
Using the Precision1 patient support programme powered by augmented reality (AR) was an opportunity to provide support to both ECPs and patients. We wanted to provide support that was
“AR
available 24–7 and easily accessible by scanning a QR code. We saw in other markets that apps or simple websites were not the ideal way to engage patients. So, we needed to be more disruptive to reach our target audience who are young and active and use mobile phones for everything – this is why AR was the ideal technology to deliver a great support programme to both patients and ECPs.
What were your key considerations when creating the platform?
EP: We defined two clear sections: one for wearers (or potential wearers) and one for ECPs. New, young contact lens wearers were at
has moved beyond the novelty factor of PokemonGo and now has very real life practical applications in patient care”
Garrett
Albanese, Eyekandy chief marketing officer
What have you learned about the applications for AR in the contact lens sector?
EP: Although the evolution of technology is hard to predict as it is moving incredibly fast, and our new contact lens wearers are younger and tech savvy; we need to anticipate what our consumers expect. We are seeing more applications of augmented reality in daily life, all designed to engage consumers around an experience, so though disruptive today in eye care, there are still many avenues to explore in optometry.
What do you think AR offers in engaging patients?
Garrett Albanese, Eyekandy chief marketing officer (GA): In an AR experience, patient communication moves from what is often a linear and static education series to a fully immersive journey that allows for the discovery of information in an interactive format. This allows a healthcare company to centralise a suite of disparate, yet relevant assets into an experience that is a new way to engage the patient. AR has moved beyond the novelty factor of PokemonGo and now has very real life practical applications in patient care. Companies like Alcon can leverage multiple triggers to assist anyone, ranging from ECPs to patients.
What do consumers enjoy about engaging with companies through AR?
GA: Eyekandy has run proprietary research to understand consumer engagement with AR and discovered that: 67.6% of people would engage with interactive AR product packaging if provided to them; and 70.33% of people are more likely to buy a product if offered a relevant AR experience.
Unlike ‘traditional digital’ forms of content, AR offers a fully immersive and non-linear experience that allows users to go deeper into educational materials from brands. The attention of each individual user is also amplified, with attention levels 45% higher than with traditional media channels like video and print. This multimedia/multi-sensory format meets the new behaviour of users, who have become accustomed to being surrounded by content in their daily media consumption. AR modernises a brand’s omnichannel strategy in one centralised experience.
What have you taken away from this project?
GA: Technology has advanced in such a way over the past 18 months that patients no longer need to download an app to activate AR. This was a significant barrier that has been eliminated in patient education – allowing healthcare companies to scale activations quickly.
Share your story
Get in touch if you would like to share your experience with OT kimberleyyoung@optometry.co.uk
Roshni Dalia ventured into practice ownership at the age of 27 when she purchased Notting Hill Gate Opticians.“It was always my ambition to become a practice owner,” she told OT.
Qualifying in 2012, Dalia initially worked as a resident optometrist at an independent opticians, before venturing into locuming.
Crediting her early experience in independent practice for giving her the confidence to realise her ambition, Dalia shared: “I learned a lot about running a business when I worked for an independent practice. I was able to observe how my boss ran the business, his relationships with staff and how he adapted the practices to change with trends.”
Surreal and scary
In order to prepare herself to become a practice owner, Dalia later began locuming in independent and multiple settings in order to develop her “optical and commercial experience in businesses with different strategic objectives.”
“This killed two birds with one stone,” the optometrist explained.
“It helped me earn as much as I could, which I could later invest in the practice, and it gave me insight into how people run practices differently, which enabled me to better gauge what type of systems I wanted to incorporate into my practice and what type of service I wanted to offer.”
Realising her goal in 2018, Dalia described receiving the keys to her practice as “surreal, scary and exciting all at the same time. I remember feeling a weight fall on my shoulders as I felt the keys fall into my hand.”

What do you most like about being a practice owner?
BECOMING A BUSINESS OWNER
“In the end, I had to give a six-month rent deposit”
Roshni Dalia on finding the right practice and adapting to changing business requirements
Opportunity to grow Dalia would keep an eye out for practices up for sale via business management consultancy website, Myers la Roche. When she came across an advertisement for Notting Hill Gate Opticians 2018, she knew the time was right. A key reason she opted to purchase in the area was its “unique demographic, which included elderly patients, school children and families,” she told OT. Although Dalia’s desire to become a business owner was driven by the freedom of operating your own practice, she was also attracted to Notting Hill Gate Opticians as it afforded her the opportunity to grow an existing business. It also allowed her to “put my own stamp on the practice.”
By her own admission, Dalia had no business experience before becoming a practice owner. However, she had worked hard to prepare herself. But Dalia admits that there were many surprises
along the way. When purchasing the practice, Dalia was assigned an existing lease for the building that the practice is based in, which came with difficulties as her landlord expressed concerns about her age and lack of experience.
“In the end I had to give a six-month rent deposit instead of three months, which was money that I could have been spent on new equipment and stock.”
While she found NHS bureaucracy “quite smooth,” she admits that the “lengthy process” involved in applying for an NHS contract meant that, as completion neared, she grew concerned about being unable to offer NHS eye tests and the impact it would have on the continuity of care for her patients.
On taking over the practice, Dalia meticulously planned a new brand identity, which included a new logo and ethos. She also introduced online booking functionality to enable customers to book
I enjoy the freedom of operating the practice; I am in a position where I can analyse my demographic clearly and make key decisions based on my patients’ needs to ensure they feel valued.
What has been the biggest surprise as a business owner?
The overwhelming sense of togetherness and the community spirit with not just our patients but also local businesses.
What are your tips for purchasing a practice?
1. Spend time in the area so you can judge footfall
2. Ask if you can locum before taking over so people can get used to you and you get used to the patients and procedures
3. Make sure you keep a good relationship with the previous owner as having their support is of paramount importance.
an eye test out of hours. She then designed price lists, business cards and appointment cards featuring the new branding.
Offering advice to others considering practice ownership, she advised:
“There’s no black and white way of running a practice; it depends on a number of different things. Something that might work well in one practice, often doesn’t work at all in other practices.”






OTposesamonthlyscenariofromapractitioner. Thismonth,welookatcybersecuritywith Lloyd&Whyte’sWill King
The scenario
Anna, independent practice owner
“I’ve seen lots of press coverage about cyber-attacks and scams increasing since COVID-19 hit. As an independent, I’m worried about the impact this might have on my business. After the year we’ve had, the last thing we need is more disruption. Can you advise on how I can minimise the practice’s risk?”
The advice

Will King, commercial development manager at Lloyd & Whyte
Over the last year, over a third of small businesses suffered an average cost of £3650 from lost data or assets and that it costs the UK healthcare sector £5.2 million – almost double that of the global average. As cyber-crime becomes more prevalent it is also becoming more sophisticated.
What are the risks to your business?
Since the pandemic, we have radically changed how we work, with nearly half (48%) of the UK workforce now doing some work from home. This may include your support staff, such as practice managers. The ability to work from
Actual invoices have details changed so that funds are diverted into the criminal’s bank accounts. In an industry that has a wide supply chain, security issues like this are a growing concern.
How to mitigate risk
Start with a risk assessment to identify areas and people most at risk. We have a cyber risk self-assessment form available on our website.
access
any device has made access and mobility easier. Unfortunately, the use of personal devices also gives hackers more doorways into networks. Leading insurer Beazley reports that the two most common forms of attack to deploy ransomware are phishing emails and breaching poorly secured remote desktop protocol (RDP). RDP enables employees to access their work computer desktops or company’s primary server from home with the press of a button, but the convenience also comes with added risks. Additionally, social engineering is being deployed, whereby cyber criminals impersonate employees, creating seemingly legitimate communications.
Issues raised by remote working can be mitigated by implementing strong security protocols, including encryption. Use a multifactor authentication-enabled virtual private network and have a limited number of password attempts. Given that 80% of hacking breaches involve stolen passwords or credentials, correct passwords protocol is vital.
Passwords should contain at least eight characters and comprise a combination of numbers, symbols and upper and lowercase letters. They should not be shared or used across different platforms –and need changing regularly.
Educate users
Beware of phishing emails and keep up to date with the latest scams that exploit current trends. The overwhelming majority of breaches start with malicious emails or other social engineering where victims are tricked into revealing confidential information. Risks can be reduced if employees are able to recognise scams, via ongoing security awareness training.
“No matter how secure you believe your system to be... breaches can and will still occur”
Back-ups and firewalls
Ensure regular back-ups that are verified and stored safely offline are completed. Allowing automatic updates on your firewall, anti-virus software and cloud storage system will greatly reduce the vulnerability in your system and subsequently the chance of you suffering a breach.
Up to 80% of cyberattacks can be prevented by undertaking Cyber Essentials – the Government-backed cyber security certification scheme. The Government’s guidelines on managing your security can be found online.
No matter how secure you believe your system to be, or how well trained your employees are, breaches can and will still occur. Such incidences are unlikely to be covered by traditional insurance policies, therefore, it is important to have the correct cyber cover in place. Things to consider when deciding on a policy include: Access to a 24/7 incident response
Cover for any data protection breaches and reimbursement of any costs of notifying your clients
Forensic experts to identify how the breach occurred and implement fixes
Overtime costs paid
Includes human error. Technical expertise and real-world claims handling experience can make the difference between suffering a catastrophic loss or getting back online quickly.
For more information from Lloyd & Whyte, visit www.llyoydwhyte.com/aopcyber




















“Everything is pushing in the direction of digital transformation”
Peter
Colleagues and I had been thinking about learning from the digital work we’d been doing, and looking forward to see how we could scale and embed it. How could we go from monitoring 500 patients with macular degeneration at home, using a smartphone app, to doing that for 10,000 patients? It requires a huge amount of work, not just in terms of deploying new technologies within the hospital and maintaining them – there’s also an entire piece of work around getting your workforce ready.
A major part of the thinking behind the Department of Digital Medicine is to create a central entity that can help staff to develop skills to make sure that, when we identify a need to deliver care digitally, we
can make services as scalable and as safe as possible for our patients.
02 We formally created the Department of Digital Medicine in February 2021.
We’re now in the process of making sure we’ve got the right senior leadership, governance structure and project management in place.
It’s an ongoing process, but it is happening rapidly.
I think when COVID-19 struck, even those of us who were optimistic about this were surprised by how quickly it was possible to adapt. I think it’s the same story across a lot of NHS trusts; people are saying they’ve achieved more in
the last six months than they have in the previous six years because suddenly everything was pushing in the direction of digital transformation.
03 There was a growing realisation that this wasn’t going to be something that traditional hospital structures were going to be able to cope with. If we have a quarter of a million decisions being made a year by different artificial intelligence (AI) systems, we need a new entity. People have started to talk about departments of clinical artificial intelligence, for example, to oversee these processes. That was another part of the logic: to make sure we’re not taken by surprise when we do get these capabilities.
This is a clinical department, and the idea is to get clinicians really centrally involved in this kind of work. They’re the ones who can be leading this, bringing the perspective that clinicians bring to these situations. They are the experts.
04
We’re now bringing through other senior leaders, and getting all the aspects of the department coordinated and then, hopefully, rapidly working over the rest of this year. We’re doing a lot of work with NHS X, NHS England and NHS Digital around the national transformation of ophthalmology with digital technology, and this has really been the first
“It is very different to things we’ve done in hospital in the past”
big project where all these entities within Moorfields are now working closely together. We’re already underway with the first big projects.
05
We’ve tried to get the initial set-up future-proofed. I hope we’re setting up a structure that’s going to be robust to future development, so that when AI comes along, for example, we’ve got that appropriate clinical safety work stream that can handle, implement and monitor it and make sure we're getting all the benefits without any risks. We’ve tried to think ahead. For us, the major goal is to make everything that happens in the hospital as slick as possible using technology.
06
Part of the drive is to make sure that we’re able to make our expertise available digitally. There are moves towards better connectivity between primary care and hospitals. If there is a community optometrist or an ophthalmologist in another centre that needs a sub-specialist opinion for something, the Department of Digital Medicine will be able to support us in receiving those requests and giving clinical advice to support care outside the hospital. Reducing the amount of care that we centralise in hospital is in most people's roadmaps. I think we can use digital means to support that. By linking people together, you support the entire system to improve.






From sight test funding to mega-mergers and the environmental impact of PPE, OT explores five issues facing the profession
Canadian optometrists threaten a withdrawal of services while UK optometrists consider the future of GOS
Optometrists working in Ontario, Canada came together in March this year for a virtual town hall meeting to address a question that has hung over each consulting room, each day, for decades.
How can the profession achieve equitable funding of sight tests?
With close to nine in 10 Ontario optometrists in attendance, 96% voted in favour of a withdrawal of services from 1 September unless the Government agrees to make changes enabling a sustainable funding model.
Optometrist Dr Derek MacDonald told OT that since he first started working 29 years ago, provincial funding for sight tests has increased by less than $6 CAD (£3.50).
Despite the slow pace of advancement, this is the first time the optometrists of Ontario have proposed a withdrawal of services.
“For years, we’ve had times where a spark flares up and there is some hope of change and then it gets doused,” MacDonald said.
“Across the province within the profession there is a palpable sense that we are now at a point now where something is going to give,” he added. Within Canada, decisions about the distribution of healthcare funding are made by the provincial Government.
Unlike other healthcare professions, such as nursing and medicine, optometrists do not have a formal negotiation process regarding how much they are reimbursed for performing Ontario Health Insurance Plan (OHIP) sight tests.
The fee for an OHIP sight test when MacDonald first started working was
$39.15 and is now around $45 (£26.50). MacDonald estimates that in Ontario, between 70% and 75% of patients seen by practices are funded through OHIP. Optometrists are unable to opt out of provincially-insured sight tests and patients are not permitted to pay out-ofpocket, or use private insurance to pay for provincially-insured services.
He described the level of provincial funding as a “losing proposition” where the care that professionals train for many years to deliver is the loss-leader.
“It is inarguable that it is inequitable. How can you expect a private practice, which is in essence a small business, to survive when they are losing money on every service they provide?” MacDonald emphasised.
The pandemic limited the number of patients that practices could see creating a challenging time for the optometry profession. MacDonald noted that during the 11 weeks optometry practices were closed in Ontario, some optometrists began to wonder if they would ever be able to open their doors again.
“It pushed a lot of people to breaking point,” he said.
While funding is the tangible issue that the profession has focused on, MacDonald believes it is indicative of a lack of respect for the profession.
He added that successive governments from a variety of political persuasions have refused to engage with optometrists.
“We have always resisted the urge to withdraw services but there comes a point where you have no other cards to play,” MacDonald noted.


The Ontario Association of Optometrists is now calling for two measures to avoid a withdrawal of OHIP services in September.

Firstly, an agreement that requires regular formal discussions between the association and the Ministry of Health, and secondly, the funding of OHIP sight tests on at least a cost-recovery basis.
“Our hope is that something changes long before 1 September and we can continue providing the services that we are trained to offer,” MacDonald told OT.
MacDonald practises alongside his wife, who he met while studying to be an optometrist, at his practice in Waterloo, Canada.
He continues to work in the building where he started his first job – driving to the same address each working day for the past 29 years.
“It sounds cliché, but it really is the best job in the world. If I reach up into the cabinet above my desk, I still have the day sheet from my first day in practice. I still see some of the patients whose names are on that sheet.”
Although funding has been an everpresent bugbear, MacDonald would not change his career choice.

“What trumps that 100 times over is that the patients we see value the care they get,” he emphasised.
The GOS gap
When Dr Martin Smith took over the helm of his Lincoln optometry practice 17 years ago, there was no computer to be seen in the consulting room and the most expensive piece of equipment was a fundus camera.
Now he takes a call from OT in a room containing £150,000 worth of




Dr


“IT IS INARGUABLE THAT IT IS INEQUITABLE”
Dr Derek MacDonald
equipment to explain why his practice is parting with one constant in a world of evolving demands and technology –the General Ophthalmic Services (GOS) sight test.
“When I took over there was no thought of the possibility of not offering GOS tests, it was just what you did,” he shared. “Everything we do has changed so much since then. The GOS fee has gone down in real terms over time, the IT demands have gone up, you have got to jump through so many more hoops. There comes a point where you stand back from it and think: ‘This is ridiculous. What am I doing?’”
Smith will stop offering GOS sight tests at his practice from 1 August. His practice began offering an optional subscription model for receiving eye care six months ago, which has been positively received by patients.
Smith shared that two other independent optical practices within his local area have also opted to stop offering GOS following the pandemic.
Rather than being a decision based in finances, Smith said the outbreak
of COVID-19 gave him the time to consider the big picture around how his practice was operating.
“It was more an ethical decision,” he emphasised. “It feels honest, as a healthcare professional, to be working for a realistic fee,” Smith shared.
Fewer than one in 10 patients who come through the doors of Smith’s practice currently receive purely GOS services.
He noted that, over time, the gap between what his practice offers through GOS and the service provided through a private sight test has evolved to the point where there are few common elements – and where the optical regulator expects more from professionals than they are reimbursed for by the NHS.
When Smith started offering independent prescribing clinics, it highlighted the distortion that a low GOS fee creates in the market.
“You are charging a normal clinical fee for prescribing because there are no spectacle sales to make up the loss – suddenly your fees look massively disproportionate,” he observed.
Despite the long legacy of GOS at Smith’s practice, he does not feel anxious about his decision. “I was massively, massively relieved. Once I made the decision to make that leap, it was like the scales falling from my eyes.
I was thinking: ‘Why didn’t I do this sooner?’”
Optometrist and chairman of BBR Optometry, Nicholas Rumney, shared that his practice continues to offer GOS even though he finds the level of reimbursement to be inadequate.
“We choose to work within the NHS because our area has nine enhanced care schemes enabled after years of persuasion and negotiation, and they won’t work with us if we leave the GOS,” he said.
Rumney emphasised that whether practices choose to remain with GOS or leave is dependant on a variety of factors.
“But it is not the responsibility of our profession to make up for deficiencies in government support,” he added.
Myers La Roche director, Dominic Watson, first helped a practice to go private seven years ago – a move which was considered unusual at the time.
The practice saw a short-term dropoff in patient numbers and profit, before rebounding to normal levels within two years.
Watson shared that the practice owner had a better quality of life as a result of the switch.
”
Dr Derek MacDonald
“People throw around the term ‘life-changing’ in a pretty cavalier fashion, but I believe optometry is. A year after referring an elderly patient with bilateral swelling of the optic nerve, I went to call him for his regular appointment in a waiting room full of people. He stood up and literally shouted ‘This is the man who saved my life.’ Those are the moments that I can remember like it was yesterday. Optometrists do that kind of thing across the province each and every day.”

He believes that this year’s GOS increase signals a shift in approach from government towards the profession.



“IT FEELS HONEST, AS A HEALTHCARE PROFESSIONAL, TO BE WORKING FOR A REALISTIC FEE“
Dr Martin Smith
“He had patients telling him: ‘You look about 10 years younger’,” he told OT.
He observed that while there has been an increase in practices moving away from GOS, owners should give the move careful consideration. “I can see some people potentially getting burned. I think it is going to be brilliant for many, but it is not for everybody. It is understanding your patient base and your model.”
Gordon Ilett took over the role of chair on the Optometric Fees Negotiating Committee (OFNC) in April. The national eye care body is responsible for negotiating the GOS fee with government.
When asked why he took on a role that involves tackling government inertia while also, at times, facing criticism from within the profession, Ilett said that he felt a sense of duty.
“What we must ensure is that those who are most vulnerable in society don’t lose out,” he said.
“I have yet to meet a critic who can come up with a good argument to say – ‘If you do this, you will get more money.’”
This year the OFNC confirmed that the Government would increase the GOS sight test for the first time since 2015 – from £21.31 to £21.71.
“NHS England is waking up to the good that we do. They have recognised that they have fallen behind on the sight test fee as paid on inflation-adjusted ground alone, without taking into account the service improvements and developments in the scope of practice,” Ilett shared.
However, Ilett highlighted that the OFNC is aware that the increase is “nowhere near enough” to compensate practitioners for the time and resources they put into providing a service for the NHS.
In terms of his focus for the coming year, Ilett is planning to build on the work of his predecessor, Paul Carroll, who strengthened engagement with NHS England and the Department of Health during the course of the pandemic.
“We seem to have built relations to the point where we can have a dialogue about the symbiotic development of the eye care sector,” he said.
With the NHS is facing burgeoning waitlists and an ageing population, optometrists are ideally placed to take some of the strain off secondary care by managing conditions within the community.
“As a nation, I think the time is ripe to have a discussion about our funding for social care and for health care,” Ilett noted.
Ilett would like to see more research undertaken that assesses the difference between the cost of offering a sight test in the UK and the level of reimbursement.
Understanding the impact of practices choosing not to offer GOS sight tests is also key, he observed.
“Will that disadvantage certain groups of the population? Will we end up with excellent services concentrated in affluent areas where people can afford to pay privately and will people in less affluent areas fail to be able to obtain even a basic examination?”



How can independent practices remain resilient in the wake of COVID-19?


Will PPE outlast the pandemic? How can clinicians reduce its environmental impact?
Masks and other forms of personal protective equipment (PPE) have quickly become an essential part of practising as an optometrist during the pandemic.
As case numbers fall, will the use of PPE also decline? And if it remains, how can the environmental impact of PPE be minimised?
COVID-19 has prompted a period of significant change on British High Streets.
Waves of shop closures prompted many independent practices to wonder what shape their local business hub would take as the UK emerges from the pandemic.
In 2020, an average of 48 shops, restaurants and other leisure outlets closed each day across Great Britain. How can optometry practices thrive amid an altered retail landscape?
Dominic Watson, of Myers La Roche, has recently published a report detailing his predictions for ‘megatrends’ that will shape the future of independent optics.
Turning to the steps that independent practices can take to remain resilient, Watson noted that
tenants are in a good position to renegotiate their lease following the pandemic.
“There are massive opportunities to reduce fixed overheads on property,” he said.
A trend that Watson terms ‘islandification’ – where High Street businesses are marooned amid closed premises and shops that convert into residential units – means that footfall may not be the same as it was pre-pandemic.
“It is really important to either become a destination or look at moving,” Watson shared.
He noted that landlords are eager for new tenants, even in prime locations, which may help to sway practices considering a move.
“If you get it right, you can quickly claw back the cost of the refit and move,” he said.
Shifting working patterns present opportunities for independent practices to attract new customers into their practice who may have previously worked in an urban centre but are now seeking eye care closer to home.
Watson recommends that practices understand their catchment population, understand what their practice is offering and make sure the two elements are aligned.
“There is an opportunity to get new patients through the door by very much playing on the local.”

AOP head of clinical and regulatory, Henry Leonard, shared his view that PPE will continue in some form as we emerge from the pandemic.
“Despite the challenges inherent in examining patients while wearing PPE, and the extra time needed to follow more stringent infection prevention and control measures, many practitioners believe at least some of these measures are likely to remain in place for the foreseeable future,” he highlighted.
Leonard said that while the use of direct ophthalmoscopy has declined as a result of the pandemic, some procedures still involve getting close to the patient.
Examinations often take place in poorly ventilated consulting rooms and may last for a prolonged period of time – increasing the risk of transmission, not just of COVID-19, but other diseases such as flu.
“As healthcare professionals, we are mindful that these pathogens can still result in serious complications for older, more clinically vulnerable patients, who may have a range of underlying health issues,” he said.
Leonard noted that many practitioners are keen to wear at least a face mask going forward to provide themselves and their patients with greater protection.
“This should also result in fewer staff absences due to illness and help reduce the spread of diseases within the wider community,” he shared.
UK researchers from Royal Sussex County Hospital assessed the environmental impact of personal protective equipment in a paper published in the Journal of the Royal Society of Medicine in March this year.
“THE IDEAL SITUATION WOULD BE THAT ALL FUTURE DESIGN, MANUFACTURE AND USE OF PPE CONSIDERS SUSTAINABILITY AS ONE OF ITS PRIORITIES”
Dr Annie Pinder

Chantelle Rizan, Malcolm Reed and Mahmood F Bhutta estimated the environmental impact of PPE distributed by NHS England in the first six months of the COVID-19 pandemic using a life cycle assessment.
They calculated that the carbon footprint of the PPE distributed over the period was 106,478 tonnes of carbon dioxide emissions.
The authors note that, per day, this carbon footprint is equal to 244 return flights from London to New York.
Li Fang and Annie Pinder are both anaesthetists in the final stages of specialty training in the North West Deanery and became sustainability fellows in 2021. With colleagues, they published a letter in the British Medical Journal in March discussing the need to mitigate the environmental impact of plastic PPE.
In response to questions from OT, Fang noted that single-use PPE during the COVID-19 pandemic has added to the already significant impact that healthcare had on the environment pre-pandemic. She shared that healthcare-related


“THERE ARE MORE SUSTAINABLE ALTERNATIVES TO OUR CURRENT PPE REPERTOIRE”
Dr Li Fang
activities are responsible for around 5% of the UK’s total carbon emissions, as well as contributing to air pollution, water pollution and other ecological damage.
“Climate change and air pollution affect human health through multiple factors and worsen existing inequalities, so as clinicians we should seek to prevent further damage if we are to work towards a healthier population,” Fang emphasised.
“While we acknowledge the many circumstances where PPE is required, we believe there are more sustainable alternatives to our current PPE repertoire,” she added.
Fang would like to see a reduction in single-use PPE, such as gloves,
BY
THE NUMBERS
5%
the proportion of UK carbon emissions that healthcare is responsible for
244
the number of return trips from London to New York that is equivalent to NHS England's daily PPE carbon footprint
20 KILOMETRES
the distance a petrol car would travel to equal the carbon footprint of 100 plastic gloves
plastic aprons, face masks and plastic visors.
She noted that many instances of glove-wearing are unnecessary, with research showing that proper hand washing is equally effective in preventing transmission.
“Increased recycling and proper disposal of PPE would help to reduce the impact of plastics in landfill and incineration, and on our wildlife. We would also like to see more research focussed on production of sustainable and reuseable PPE,” Fang shared.
When asked what steps clinicians can take, co-author, Annie Pinder, noted the importance of avoiding unnecessary PPE use.
She shared that every box of 100 gloves used has the equivalent carbon footprint of driving 20 kilometers in a standard petrol car.
“We think there is a role within all our professions to influence the procurement of equipment, opting for re-usable items, and ideally aiming to have supplies that are made domestically instead of abroad to eliminate the substantial emissions from international travel, especially by air freight,” Pinder highlighted.
She shared that the pair are currently working on a project to calculate the carbon footprint of new PPE that has been designed for healthcare settings.
Pinder and Fang will highlight areas of carbon cost and work with designers and developers to mitigate the impact where possible.
“The ideal situation would be that all future design, manufacture and use of PPE considers sustainability as one of its priorities.”
How can information improve eye care?
When thinking about resources in primary care optometry, it is tempting to focus on the latest pieces of equipment.
But perhaps one of the most valuable resources is less tangible: the data that accrues every single time a sight test is performed in practice.
How can this be harnessed to lend insight on the progression of disease and enhance future treatment options?
Research optometrist, Fiona Buckmaster, is working on a project to collect, classify and curate a retinal image repository from optical practices across Scotland.
While similar databases have been developed internationally using retinal images from secondary care, this is the first time that an image repository of this scale has been developed drawing from data held in primary care.
“As an optometrist, I am really excited by this. I think it has potential to really impact the way that primary care optometry is delivered,” Buckmaster emphasised.
In Scotland, 1700 optometrists perform two million sight tests each year from around 900 optical practices. Since 2006, routine sight tests using high-resolution retinal cameras have been funded by the NHS in Scotland.
“It means that there is now over a decade of rich longitudinal resources that are currently being stored in High Street practices,” Buckmaster said.
She shared that the data stored in optical practices has potential to lend insight not just into ocular

Optometrist and AOP clinical director, Dr Peter Hampson, on how advancements in the use of data will affect optometry
Data in optometry has historically existed in discreet unconnected systems that makes comparison and follow up difficult. This can mean that optometrists are often unaware of what the patient’s status was at their last appointment. This can make it difficult to detect change and can lead to assumptions over the patient’s status and also unnecessary re-referral to secondary care. Advancements in the use of data should help to tackle this challenge in a couple of ways. The first is to be able to more easily detect any change in a patient and the ability to quantitively monitor the progression of disease across a wider scope of environments. Data sharing across modes of care will reduce gaps in care, improve access and ultimately improve health outcomes for patients. This should in turn allow quicker and more timely interventions as data trends become easier to spot and the inter-observer variability becomes less important.
disease, but systemic disease – with research suggesting that there can be retinal manifestations of conditions such as Parkinson’s, Alzheimer’s and cardiovascular disease. “We want to know whether a routine eye examination could tell us more about patients’ health,” Buckmaster said.
The Scottish Collaborative Optometry-Ophthalmology Network eResearch (SCONe) project are currently undertaking a two-year feasibility study.
Optometrists in Scotland can register interest in joining the SCONe network as pilot practices by email (scone@ed.ac.uk). Those in Scotland
The second, but linked point is that by increasing the volume of accessible data and the use of deep learning, our understanding and recognition of disease will also advance. One of the criticisms raised against current optical coherence technology (OCT) databases is that certain patients are underrepresented, leading to patients without disease being incorrectly flagged as outside of normal limits.
However, if we imagine a world where all of the data captured from OCTs was pooled and categorised, we could have a far greater understanding of what the “normal” patient actually looks like. This in turn should enable us to detect disease at an earlier stage and instigate treatment quicker, improving outcomes for patients and enhancing the role of primary care.
This is advantageous for patients, but also improves the role of clinicians and helps them to more fully utilise the extent of their training. For many this may also allow them to practise optometry in the way they envisaged when they embarked on their career.
and other areas of the UK are invited to complete an online survey to help researchers understand what images optometrists are capturing and the data management infrastructure they are using.
What does the acquisition of GrandVision by EssilorLuxottica mean for independent practices?
The European Commission approved the acquisition of GrandVision by EssilorLuxottica in March this year – with approval conditional on the divestment of some optical retail stores in Belgium, Italy and the Netherlands. Three years after a merger between two global companies dominating the sale of lenses and frames respectively, what will the expansion into supplying directly to the consumer mean for independent optical practices in the UK?
UK optometrist Dr Cindy Tromans is president of the European Council of Optometry and Optics (ECOO), which represents optometrists and opticians working throughout Europe. The sector the organisation represents is largely comprised of independent optical practices in the majority of ECOO's member states.


Tromans noted that vertical integration is expected to have a direct impact on these smaller players in the field.
“The effects of the Essilor and Luxottica merger in 2018 have been felt in the optical market already, so this new development gave rise to even greater concerns. For instance, it has the potential of limiting competitor access upstream and to provide restricted or delayed access to products downstream.”
Tromans noted ECOO members have highlighted concerns that, as a result of the acquisition, the company will be competing directly with independent practices and obtain a “significant competitive advantage.”
“This progressive market consolidation is a real risk for smaller players in their ability to compete and is expected to lead to higher prices for the customer in the medium to longterm,” she said.
The European Commission conditions in Belgium, Italy and the Netherlands involve divesting around 350 stores across the three countries.

While the restrictions are “a step in the right direction,” Tromans does not believe the conditions go far enough.
She also contends that the European Commission should have extended the conditions imposed within these nations to countries with similar market environments. Tromans noted that a delay in access to innovative products is a risk for smaller market stakeholders. “The concentration process that started at the industrial manufacturer level has now extended into the retail field. We think the next logical step will be an acquisition of a contact lens manufacturer and that
“THE CONCENTRATION PROCESS THAT STARTED AT THE INDUSTRIAL MANUFACTURER LEVEL HAS NOW EXTENDED INTO THE RETAIL FIELD”
Dr Cindy Tromans


the US market is a blue print for their strategy.”
The AOP is calling for members who experience a change in their relationship with EssilorLuxottica to share their experiences with the policy team (policy@aop.org.uk). Insight on closures, price changes and other information that provides a picture of the UK market is also welcome.


66Persistent epithelial defects: covering the gaps
LEARNING OBJECTIVES
LEARNING OBJECTIVES
• Communicate effectively with the patient to investigate the potential cause of corneal epithelial pathology
• Be aware of the implications of corneal epithelial pathology with regard to the indications and contraindications of CL wear
• Manage patients presenting with corneal epithelial defects
LEARNING OBJECTIVES
• Understand the natural progress and determine the severity of corneal epithelial pathology
• Recognise when it is appropriate to refer cases of corneal epithelial pathology for specialist opinion
LEARNING OBJECTIVES
• Be aware of different treatment approaches for managing corneal epithelial defects
LEARNING OBJECTIVES
• Communicate effectively with the patient to investigate the potential cause of corneal epithelial pathology
• Be aware of the implications of corneal epithelial pathology with regard to the indications and contraindications of CL wear
• Communicate effectively with patients with sight and hearing impairment
• Provide advice on interventions to support the needs of patients with sight impairment
LEARNING OBJECTIVES
• Communicate effectively with patients with sight and hearing impairment
• Provide advice on interventions to support the needs of patients with sight impairment
74Can contact lenses still be an option for patients with dry eye disease?
LEARNING OBJECTIVES
• Be aware of the evidence relating to the therapeutic use of CL to manage ocular surface disease
LEARNING OBJECTIVES
• Obtain relevant history and symptoms from CL patients presenting with discomfort
• Manage patients presenting with CL discomfort
LEARNING OBJECTIVES
• Explain to patients about the significance of amblyopia
• Assess visual function in children with amblyopia
• Identify different causes of amblyopia
LEARNING OBJECTIVES
• Explain to patients about the significance of amblyopia
• Be aware of the different causes of amblyopia
loss
LEARNING OBJECTIVES
• Interpret the presenting signs and symptoms for a range of sudden vision loss cases
86 Anterior eye cases in practice
LEARNING OBJECTIVES
• Obtain relevant history and symptoms from CL patients presenting with discomfort
• Manage patients presenting with CL discomfort
LEARNING OBJECTIVES
• Be aware of the different approaches for managing patients presenting with CL discomfort
EXAM QUESTIONS & REFERENCES
LEARNING OBJECTIVES
• Manage patients presenting with anterior segment pathology
LEARNING OBJECTIVES
• Assess cases of anterior segment pathology and manage the patient accordingly
MCQs for OT’s CET exams appear online at www. optometry.co.uk. Exams cannot be submitted after this date. Please note that when taking an exam, the MCQs may require practitioners to apply additional knowledge that has not been covered in the related CET article. CET points will be uploaded to the GOC within 10 working days. AOP members and subscribers will then need to log into the CET portfolio by clicking on ‘MyGOC’ on the GOC website (www.optical. org) to confirm points. Visit www.optometry.co.uk, and click on the ‘Related CET article’ title to view the article and accompanying ‘references’ in full.
THE CET EXAMS WILL EXPIRE ON: 3 SEPTEMBER 2021
Dr Scott Cutting MBBCh, BSc and Tahmina Pearsall MBCHB, FRCOphth, FRCSEd, MRCOphth, MSc
This article will provide an overview of persistent corneal epithelial defects. It will cover the aetiology, assessment, current management and potential future therapies.
Introduction
Given that the cornea is responsible for the majority of the refractive power of the eye, maintaining its integrity is crucial in order to provide good vision.1 The corneal epithelium is important in this regard; it acts as a barrier to infection and, along with the tear film, provides a smooth refractive surface. Under normal circumstances, the epithelial surface is constantly renewed by limbal stem cells.1,2 Corneal epithelial defects can result in significant issues for patients, including severe pain, reduced visual acuity (VA), infections and perforation. In an otherwise healthy cornea, defects usually take two to three days to heal. A persistent corneal epithelial defect (PCED) is a term arbitrarily reserved for epithelial defects that are still present after two weeks, by which time it should have healed in an otherwise healthy cornea.3 The precise incidence of PCEDs is unknown but is estimated to be less than 100,000 in a US population of around 315 million, making it a relatively rare disease.4
Aetiology
In order to discuss how the cornea can become compromised and lead to PCEDs, it is useful to consider the normal healing process. The corneal epithelium is thought to be renewed from stem cells located in the limbus. Limbal epithelial cells produce basal epithelial cells which then migrate towards the central cornea and replenish the more superficial layers of the epithelium. Epithelial cells are normally adherent to surrounding cells and also to the underlying basement membrane. These connections prevent disruption of the corneal epithelium, for example, during blinking.2
When the corneal epithelium is damaged, cells next to the defect break their attachments to the cells surrounding them and move centripetally as a single layered sheet to cover the wound.5 They then proliferate to reform the normal layers of the epithelium and also re-establish their adhesions to surrounding cells.2,5
The cornea is supplied by nerves from the ophthalmic division of the trigeminal nerve. These nerves are important for corneal sensation and the blink and tearing reflexes which protect the cornea. They also release nutrients and trophic factors which are crucial
for maintaining a healthy cornea.6 Factors released by these nerves, such as substance P (SP) and calcitonin generelated peptide (CGRP), are important for the corneal wound healing;6 therefore, it follows that abnormalities in epithelial adhesion, limbal stem cells and corneal innervation can affect the ability of the cornea to heal (see Table 1).
Neurotrophic keratopathy
Neurotrophic keratopathy is caused by impairment of corneal innervation; this leads to a loss of the normal interactions between the corneal epithelial cells and corneal nerves resulting in a reduction in the release of nutrients and trophic factors which otherwise maintain a healthy cornea and promote wound healing. Reduced corneal innervation also impairs corneal sensation and, therefore, the protective blink reflex and tearing reflex will become less effective; thus, injury to the cornea will be more likely.1,2 In addition, defects in the cornea may not cause severe pain in these patients due to aberrant sensation and they may only seek medical attention when complications arise. Many conditions can result in damage to the corneal nerve supply. One of the most common causes is herpetic keratitis, but other causes include strokes and diabetes.1,7
Impaired epithelial adhesion
Problems with epithelial cell connections to the underlying basement membrane or with the basement membrane itself can increase the risk of PCEDs. Basal epithelial cells are connected to the underlying basement membrane by hemidesmosomes and fibril connections. Abnormalities in these connections can lead to recurrent erosions which in turn can result in overproduction of matrix metalloproteinases (MMPs). These MMPs can disrupt the basement membrane and its connections.2 Most commonly, recurrent corneal erosions are found after an initial corneal abrasion, which can result in inflammation and cause disruption of the epithelial basement membrane.1,8 Hemidesmosomes can be abnormal or absent in epithelial basement membrane dystrophy (EBMD, otherwise known as map-dot-fingerprint dystrophy), which can, therefore, also lead to recurrent corneal erosions.2
Aetiologies of PCED
Neurotrophic keratopathy
Impaired epithelial adhesion
Toxicity
Eyelid malposition
Limbal stem cell deficiency
Toxicity
Examples of responsible conditions
Herpetic keratitis
Diabetes
Topical medication
Surgical trauma
Stroke
Tumours
Prior trauma
EBMD
Topical anaesthetics
Topical glaucoma medications
Preservatives
Lagophthalmos
Entropion
Ectropion
Direct injury (chemical, thermal, surgical)
Stevens-Johnson syndrome
Ocular cicatricial pemphigoid
Contact lens-induced keratopathy
Aniridia
Many topical eye drops can affect the integrity of the cornea. For example, topical anaesthetics affect the adhesion between epithelial cells and the basement membrane by affecting the hemidesmosomes. They can also affect migration of epithelial cells which can impair corneal renewal and wound healing.2 Topical glaucoma medications can have adverse effects on the ocular surface as well by increasing inflammation and affecting the quality of the tear film.9 Preservatives are another common cause of ocular surface toxicity, the most frequent offender being benzalkonium chloride (BAK). BAK disrupts the tear film but is also directly cytotoxic to corneal epithelial cells.10
Eyelid malposition
Abnormalities in eyelid position can have significant effects on the health of the cornea by disrupting the tear film. In lagophthalmos, the lids do not close completely; this can lead to exposure keratopathy where the eye dries out, meaning the protective benefits from the tear film are lost. The eyelids also protect the eye from trauma and this function is compromised in lagophthalmos.11 On the other hand, entropion and trichiasis cause direct damage through rubbing on the surface of the cornea, which can result in recurrent abrasions and disrupt healing of epithelial defects.2
Limbal stem cell deficiency
As mentioned previously, limbal stem cells are responsible for repopulating the cornea with epithelial cells after trauma. Thus, deficiency of these stem cells leads to an inability to regenerate the epithelium.2 There
are multiple causes of limbal stem cell deficiency (LSCD); these can be direct chemical, thermal or surgical injury to the stem cell population. Likewise, inflammatory conditions such as Stevens-Johnson syndrome or ocular cicatricial pemphigoid can deplete the limbal stem cells as can contact lens-induced keratopathy. LSCD can also be hereditary in the case of aniridia.2,12
Initial assessment of PCEDs should be tailored to try and determine the underlying cause. A careful history should be able to identify prior trauma or infection, use of topical medications or contact lenses, prior surgery and relevant past medical history. During the examination, special attention should be paid to eyelid position and closure, evidence of anterior segment inflammation, corneal sensation, signs of infective keratitis and evidence of pathology in the fellow eye. If the underlying cause or causes can be identified, then therapy can be tailored appropriately.
A good history and examination are critical in managing PCEDs as management should initially be to treat the underlying cause if possible (see Table 2, page 68).3 As well as assessing and treating any underlying conditions, other therapies can be attempted to help the defect heal; these will be discussed in a stepwise manner, starting with medical therapies before going onto surgical therapies.
Lubrication
Lubricating eye drops and eye ointments are an easy option to start with in order to prevent the ocular surface from drying out and are usually first line. These can be used very frequently, initially every one to two hours, and should ideally be preservativefree.2,3 Improving the quality of the tear film is also
Table 2
Underlying pathology
Dry eyes
Toxicity of topical medications
Exposure keratopathy/eyelid malposition
Herpetic keratopathy
Limbal stem cell deficiency
Examples of specific treatment
Lubricating drops/gels
Punctal occlusion
Identifying and stopping/ replacing drops causing toxicity
Lid surgery
Decompression
Antivirals (to clear ongoing viral infection)
Steroids (to reduce inflammation)
Limbal stem cell transplant
beneficial, for instance, by identifying whether the patient has blepharitis and giving them advice on hot compresses and lid hygiene. If lubrication of the ocular surface isn’t adequate despite these measures, then punctal occlusion can be considered to reduce the drainage of tears.3 The puncta can be permanently closed using cautery, but it is often useful to trial punctal plugs as a temporary solution beforehand; this can identify patients who may not tolerate long-term punctal occlusion due to the development of significant epiphora.
Review of topical medications
Many eye drops can cause toxicity of the ocular surface, which may be due to the medication itself or the preservatives present in the drops, for example, BAK. This toxicity can be an important factor, adversely affecting the healing of the cornea and can be exacerbated in patients with a poor tear film who are unable to effectively clear the medication from the ocular surface.3 If ongoing treatment is necessary, for example, in glaucoma patients, preservative-free or less toxic alternatives should be tried. Alternatively, other treatments could be considered to reduce the drop burden for the patient, such as laser procedures.3
Bandage contact lenses and pressure patching
Soft bandage contact lenses are sometimes used to protect the epithelium from significant trauma during blinking. This can be useful in promoting healing of the underlying defect in certain cases within a secondary care setting and also provide symptomatic relief for the patient in what can be a very uncomfortable condition. Preservative-free lubricating eye drops should be used concurrently to prevent the contact lens adhering to the ocular surface.3 With a contact lens and an epithelial defect, infection is a risk. Therefore, an antibiotic drop should also be prescribed, and steroid eye drops are usually avoided. Close follow-up is also recommended in this situation.2,3 Pressure patching involves taping pads over the eye while the eyelids are closed to prevent opening of the eye. This provides similar benefits to a bandage contact lens
although it may be more difficult to tolerate for the patient. Prolonged patching may impair healing of the defect and, therefore, patients need to be reviewed regularly. Similarly, to the bandage contact lenses, it can also increase the risk of infection.3 It is important to note that optometrists should avoid the routine use of therapeutic contact lenses and pressure patching in cases of corneal abrasion.13
Gas permeable scleral contact lenses can also be used in cases which are refractory to conventional treatment. They provide an environment that promotes healing in three main ways. Firstly, they have a high oxygen permeability which is important for growth and repair of the epithelium. As they do not come into contact with the cornea, they also create a reservoir of fluid between the lens and the corneal surface which provides continuous lubrication.14 Finally, they reduce friction on the cornea. As with soft contact lenses, there is an increased risk of infection and, therefore, prophylactic antibiotic drops are needed and the patient requires close follow-up.3
If other treatments fail, then another option is to use autologous serum. The patient’s own blood is centrifuged and the serum is then taken and used in drop form. Unlike lubricating eye drops, the serum contains high concentrations of growth factors necessary for healing of the cornea. This treatment can be very effective, with studies consistently showing substantial improvement in the size of non-healing epithelial defects which were previously unresponsive to conventional therapies.3,15 However, regulatory restrictions involved in processing blood prevent widespread use of autologous serum drops. The main health concern with using autologous serum drops is their propensity to grow bacteria if contaminated, which could lead to infection. Therefore, sterile preparation of the drops is essential, as is hygienic use and proper storage of the drops by patients.3,15 In patients unable to use their own blood for the production of autologous serum due to illness, donor blood or umbilical cord blood can be used.2,3
Epithelial debridement
Thickened edges of the corneal epithelium surrounding the PCED can impede more peripheral epithelial cells from migrating across to cover the defect. Gentle debridement of these edges can, therefore, promote healing.2,3
n Dr Scott Cutting is an ophthalmology specialty trainee working in Surrey. He graduated in medicine with honours from Cardiff University where he also received a first-class bachelor’s degree in pharmacology.
n Tahmina Pearsall is a consultant ophthalmic surgeon practising at Whipps Cross University
Tarsorrhaphy
Tarsorrhaphy involves fusing the upper and lower eyelid margins, partially or completely. This reduces the exposure of the cornea and prevents both desiccation of the ocular surface and friction from blinking. This can be undertaken using temporary sutures or Botulinum toxin
A injections or can be permanent.1–3
Conjunctival flap
A flap of conjunctiva can be created to cover a PCED and promote healing. However, it will impair the vision of the patient, and the ability of the clinician to assess the underlying structures. The procedure can be reversed but often there will be significant underlying scarring, and to restore vision, a corneal transplant may be required. Conjunctival flaps also tend to damage limbal stem cells and, therefore, can have long-term disadvantages.1,3
Amniotic membrane grafting
As well as protecting the cornea from frictional forces during blinking, amniotic membranes provide growth factors for epithelial healing and can act as a scaffold for growth. They also have anti-angiogenic, antiinflammatory, anti-fibrotic and possibly anti-microbial properties.2,16 Amniotic membranes can be very useful for PCEDs, with success rates reported from 64% to 91%.16 They can be sutured or glued onto the ocular surface.
Limbal stem cell transplantation and keratoprostheses
In cases of LSCD, transplants of healthy limbal stem cells have been shown to be an effective way of achieving corneal re-epithelialisation. There are multiple methods described for limbal stem cell transplantation (LSCT). In cases where there is unilateral limbal stem cell deficiency, the patient’s other eye can be used to harvest limbal stem cells for transplantation.2,17
Graft rejection is the most common cause of failure of LSCT and, therefore, allografts require systemic immunosuppression which comes with its own complications.3,17 Synthetic keratoprostheses have also been used in patients with LSCD.2,3
Thymosin beta-4
Thymosin beta-4 is a peptide involved in promoting epithelial proliferation and re-epithelialisation of the cornea. It is thought to do this by preventing production of pro-inflammatory cytokines such as nuclear factor
Hospital – part of the Bartshealth Trust. She is UK trained at Moorfields Eye Hospital, St Thomas’ and Addenbrooke, which enables her to provide medical and surgical care across all aspects of ophthalmology. Her research and surgical achievements have won many prizes both nationally and internationally and most recently she has been nominated for the Hospital Heroes award.
kappa light chain enhancer of activated B cells (NFkB) and tumour necrosis factor alpha (TNF-alpha). There have been some promising results in human trials.2
Nexagon
Nexagon is an antisense oligodeoxynucleotide used to reduce expression of connexin43, which is a protein found in gap junctions that allows cell-tocell communication and is thought to be involved in apoptotic spread. Nexagon has had some encouraging results in human trials with reduced inflammation and re-epithelialisation in patients with PCEDs.2,3
Mesenchymal stem cells
The use of mesenchymal stem cells (MSCs) is being investigated for tissue regeneration in multiple aspects of medicine. With regards to the cornea, they have been shown to reduce inflammation and promote wound healing;18 this may be via the production of cytokines and trophic growth factors to stimulate healing responses. It is unclear whether they can differentiate directly into corneal epithelial cells.19
Blood-derived products
Platelet-rich plasma has been investigated as an alternative to autologous serum. Platelets release granules containing growth factors such as EGF (epidermal growth factor) and IGF-1 (insulin-like growth factor-1) and, therefore, platelet-rich plasma may be better at stimulating corneal healing.2,3,20 Also research is being done into purifying individual components of serum, for example, EGF and IGF-1.21
Nerve growth factor restores corneal sensation, promotes corneal healing and nerve regeneration and can also increase tear production.22 Oxervate, which contains cenergermin, a recombinant human nerve growth factor, has been recently approved for treatment of neurotrophic keratitis in Europe and the US.2,22
Conclusion
PCEDs can be difficult to treat but there are many medical and surgical therapies which can be of benefit and newer options may soon be available. Appropriate treatment relies on accurate assessment of the underlying aetiology.
This article describes the impact of visual impairment on patients with age-related macular degeneration and how this can be managed
Age-related macular degeneration (AMD) is recognised as the leading cause of sight loss in the older population in the UK.1,2 On the one hand, blindness attributable to wet AMD has reduced since the introduction of novel treatments,3 with sight loss slowed down using intravitreal (IVT) vascular endothelial growth inhibitors (anti-VEGF).4,5 On the other hand, up to a quarter of wet AMD patients are anti-VEGF non-responders,6 which can lead to profound sight loss and affect independence and quality of life (QoL). Patients benefit from a network of friends and family, both practically as well as psychosocially.
7 However, consideration should be given to the impact on the carer’s QoL, especially if caring responsibility has been imposed upon them. The input from the carer can be reduced by helping the patient become more independent and by providing care from third parties. Each individual person has different priorities when it comes to their desired and achievable level of independence. The low vision practitioner needs to be equipped to offer assistive devices and interventions in alignment with the specific needs of each patient.
This case scenario serves as an example of a patient who is undergoing treatment for AMD.
The increase in patients receiving treatment for AMD has led to the introduction of virtual clinics, whereby optical coherence tomography (OCT)8 and LogMAR vision are being used for grading. The time patients spend with optometrists and ophthalmologists is minimal, although counselling at strategic points during the process has been shown to improve alignment of expectations and adherence to treatment.9 Treatment and sight loss can have a significant emotional and psychosocial impact on the patient.10 During a low vision assessment, these issues, as well as the more practical needs for magnification and support can be addressed.
This case is about a patient who has been treated
with IVT anti-VEGF in both eyes for many years until the injections no longer made any difference and treatment had to be ceased as her vision dropped below 6/96.11 Her visual loss has caused her to have low moods and to feel frustrated and less motivated as she has to depend on others for her daily needs. Like many patients presenting with low vision, she hoped that stronger glasses would help; this is not a realistic expectation in this case and, in fact, she is eligible for registration of severe sight impairment (SSI).12 Expectations need to be managed in a positive way, offering alternatives to compensate for visual impairment and dealing with the emotional issues related to visual loss. Table 1 summarises the relevant clinical details.
At this level of vision, optical magnifiers may be a solution for spot reading tasks such as reading correspondence, checking cooking times, reading dials and looking up phone numbers. One can work out the approximate required magnification for reading mail as follows: in order to read N10, this patient needs 4x (N40:N10) magnification; however, for fluent reading an acuity reserve of 2:1 is usually needed,13 which means that 8x magnification is required. Magnifiers of this strength are small in diameter and, therefore, slow down reading speed significantly. These limitations need to be explained and demonstrated and alternative options discussed. The use of technology, such as apps, as well as CCTV systems and electronic magnifiers can be very good alternatives, providing that the patient is motivated to learn new skills. Practitioners can provide information about local technology resources for visually impaired people, such as library sessions, Royal National Institute of Blind People (RNIB) sessions and online support. Strategies can also include non-optical aids. For example, bills can be requested in large print, tactile stickers can be used for dials and frequently used phone numbers can be printed in bold large print for the patient to use (see Figure 1). Other items can be considered, such as large-dial phones, keyboard stickers, tactile games and kitchen utensils and the use of contrast and lighting. Audio books, magazines and newspapers can be considered as well as audio description for theatre and cinema.
This patient felt that she had to depend on others for many things as her sight deteriorated. The fear of losing her eyesight further contributed to her low mood. There are various questionnaires that can be used to assess if a patient would benefit from emotional support. The Geriatric Depression Scale questionnaire (GDS-15) is fairly detailed, but practitioners can also simply ask two questions as follows:14 ‘During the last month have you often been bothered by:
‘Feeling down, depressed or hopeless?
‘Having little interest or pleasure in doing things?’
If both questions are answered in a confirmatory manner, various steps can be taken. The patient can be referred to their general practitioner (GP), the eye clinic liaison officer (ECLO) or to the RNIB for counselling. Practitioners can also provide information about peer support groups, such as the Macular Society as this also has a positive impact on QoL in patients with AMD.15 Having to depend on others can also impact QoL and some of these issues can be addressed by the RNIB. For example, a blue badge can make it easier to access places. RNIB and Guide Dogs mobility training can improve independence and the ‘My Guide’ service can allow patients to go out without the need to ask friends or relatives. The RNIB can give advice on benefits and entitlements. It is important to ask the patient about visual hallucinations, also known as Charles Bonnet Syndrome as this is a relatively common experience, affecting around 25% of patients with visual loss16 and people don’t always find it easy to initiate a conversation about this topic for fear of being seen as someone with dementia or psychosis. It can be very reassuring when a low vision practitioner explains that this is a relatively common phenomenon with sight loss.
Hearing loss is a common comorbidity in the elderly population with SI. This scenario describes some of the ways in which practitioners can support a patient with dual sensory loss in a low vision practice.
Isolated SI and hearing impairment (HI) each lead to many challenges in terms of accessing information, mobility, independent living and social interaction. Both conditions are becoming increasingly prevalent as the population gets older.17,18 It has been estimated that around 71% of people over the age of 70 have HI,19 with rates for SI18 and HI20 set to rise in the next two decades. In this case report, the focus is on hearing loss which is acquired later in life.
Communication can be a challenge for an elderly person with dual sensory loss, who relies on hearing aids and lip-reading. This case report addresses aspects of communication during the consultation and also the available support for patients with acquired deafblindness later in life (see Table 2).
A patient in her late 80s attends the low vision clinic for the first time with a history of AMD in both eyes. Her better right eye is stable with a vision of 6/15. She has not been offered (and is not eligible for) SI registration.12
Her visual loss affects her in terms of managing correspondence, functioning in the kitchen and mobility. She has not tried the use of magnifiers
Greet the patient with a smile
Face the patient when you address them
Avoid talking to the carer, friend or relative instead of the patient
Avoid glare/ light scatter from a window or other light source
Avoid clutter around the face such as hair, hands or a scarf
Avoid looking down or writing while speaking
Avoid walking around while speaking
Explain procedures before switching lights off
Find out what ear is preferred and position yourself optimally
Find out if patient prefers low or high pitch
Speak slowly, but not too slowly as facial expressions and mouth patterns need to remain natural
Speak clearly, but don’t shout (negative facial expressions)
Get closer to the patient if this helps
before. Due to her severe HI, she finds it hard to follow conversations, even with one hearing aid in. This is complicated further due to the difficulty in recognising faces and facial expressions and she has never mastered the art of lip-reading. Her HI makes it difficult for her to make phone calls. It is common for people with dual sensory loss to experience difficulty with communication.21 People with SI or HI tend to use the other sense to compensate.22–26 For those with SI and HI, this strategy cannot be applied. Despite barriers in communication, she does not feel isolated and has
a strong social network. Her friends take her out to places, but she would like to be more independent. A significant number of patients attending a low vision service experience HI as well as SI. It is important to be aware of HI at the beginning of the assessment. The practitioner can make adjustments according to preferred ear and preferred pitch, tone and volume. In any case, it is helpful to face the patient when talking and to make sure the lighting conditions are optimal, for instance avoiding light scatter, to facilitate lip-reading and recognition of
n Cirta Tooth is an optometrist with a special interest in visual impairment. After several years working in community optometry, she is now primarily based in a hospital setting where she works in paediatric, macular and low vision clinics. She has developed strong relationships with healthcare professionals, local support
facial expressions. It may be necessary to sit quite close to the patient. It is important to avoid talking and walking or talking and writing simultaneously so that the practitioner is always facing the patient. These small adaptations can make a big difference in terms of effective communication. Table 3 summarises the relevant findings for Case 2.
As the acuity is N16 in this case, for reading correspondence fluently (acuity reserve 2:1), a magnification of around 3 to 3.5x should be sufficient, whereas 1.6x should be adequate for spot reading. Illuminated magnifiers or electronic magnifiers could be tried to enhance contrast. A typoscope can be helpful when contrast sensitivity is low. This lady was encouraged to print essential phone numbers in bold N24 print and she already manages her bills successfully online. The ECLO can recommend a phone with pre-set numbers and/or large dials and display.
Transportation and assistance with errands are common needs in people with dual sensory loss.27 My Guide and the RNIB offer mobility training and My Guide also offers sessions for family and friends of people with visual impairment with information about common eye conditions as well as advice about safe and effective guiding. My Guide has trained volunteers who help patients improve confidence on familiar routes.
Kitchen safety is an important issue to consider when dealing with patients with sight loss. For some patients, cooking can provide enjoyment while maintaining a healthy lifestyle. It can be difficult to see dials, chop vegetables and pour drinks. Kitchen safety assessments can be carried out by the RNIB with a view to providing tactile stickers, liquid level indicators, contrasting chopping boards, kitchen gadgets and improving task lighting. Simple strategies such as pouring drinks over the sink can also be discussed.
groups and voluntary organisations. She recently completed postgraduate education in low vision and paediatric optometry as well as clinical teaching, clinical audit and research skills. She is involved in teaching optometrists, orthoptists, ophthalmologists, paediatricians, QTVIs, RNIB staff and postgraduate ophthalmology students.
Table 1
Combined HI and SI can lead to profound difficulties in communication and a holistic approach is indicated. It is worth discussing strategies, such as optimal positioning in a room, lighting to enhance contrast on people’s faces, reducing clutter in the room and also around the face to allow for better lip-reading and distinguishing facial expressions. The effect of sitting closer to people during conversations can also be helpful. One can imagine that the COVID-19 pandemic has affected people with dual sensory loss significantly due to the use of face masks and social distancing. Face shields and transparent face masks can alleviate this problem to some extent. Deaf Action can assist with the use of a flashing phone with loop system, a flashing doorbell and gadgets for voice enhancement. Hearing aids can be reviewed and lipreading courses can be offered. Patients often really appreciate it if an optometrist liaises with services for HI people. Support groups for the hearing impaired as well as for the visually impaired can make a difference to many patients. As can be seen from this case, the low vision practitioner can make adaptations to improve communication in the clinical environment to suit individual needs.28 Deaf awareness training for health professionals has been shown to have a positive impact on effective communication and patient satisfaction.29 Good links with relevant professionals and organisations can have a greater impact than if SI is addressed in isolation.
As shown in the cases in this article, addressing an elderly patient’s needs around SI can be much more than simply handing out a magnifier. The impact of sight loss is much more profound than not being able to read. Mobility, independence and social interaction as well as emotional wellbeing need to be addressed as well. It is important to take into account that ageing is often associated with other health issues. Hearing loss, systemic disease and dementia are just some examples that create additional issues that the practitioner needs to be prepared to deal with. It is incredibly rewarding to support patients in this way and make a significant difference to their QoL.
an option
Dr Nery Garcia-Porta MSc, PhD, PG Cert (HE), FHEA and Thom Finney BSc (Hons), MCOptom, PG Cert (HE), FHEA
This article will review the association between dry eye disease and contact lens wear, highlighting the use of contact lenses in the management of the condition.
Introduction
From the silicone hydrogel revolution at the turn of the century, to the recent introduction of lenses for myopia control, the past two decades have seen a number of breakthroughs in the field of contact lenses.1 The current range of soft and rigid gas permeable (RGP) lens designs means that most patients are now able to be fitted with a lens type that may benefit their lifestyle in some way. There are numerous studies which even suggest that making the switch to contact lenses can have a positive impact on quality of life. In general, lenses tend to offer fewer restrictions for those with active lifestyles, such as when exercising or performing outdoor activities, for adults but children alike.2–6
Unfortunately, it hasn’t all been plain sailing for contact lens wearers, with lens wear being a well-known risk factor for those who are susceptible to dry eye disease (DED).7 While often overlooked, DED has been found to have a significant impact on both productivity and quality of life, with a concerning association also seen in patients presenting with depression.8,9 Alongside variable vision, ocular discomfort is a common presenting symptom for lens wearers who suffer with DED. The TFOS International Workshop on Contact Lens Discomfort report highlighted the significance of this, suggesting that as many as 51% of contact lens dropouts are as a result of ocular discomfort.10 Some studies have even stated that contact lens dropout is precipitated by the majority of typical signs and symptoms of dry eye, with the exception of changes to the structure and function of meibomian glands.11,12 Research shows that when lens wearers initially experience ocular discomfort, it is common for patients to reduce their wearing times, often leading to a temporary or permanent discontinuation of lenses altogether.10 Hence, in order to minimise dropouts and to ensure our patients are successful contact lens wearers, it is vital to investigate any reports of ocular discomfort and to correlate their symptoms with the assessment of the ocular surface. While similar, it is important to note that not all wearers who present with contact lens discomfort (CLD), suffer with clinical DED. The first aim of this article is to differentiate between the definitions of these two conditions.
According to the TFOS DEWS II report, DED is described as a multifactorial disease of the ocular surface, characterised by a loss of homeostasis within the tear film. It states that DED is ‘accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play aetiological roles.’11 While the use of contact lenses might exacerbate a pre-existing case of DED, it is also common for non-lens wearers to present with similar symptoms. These patients would, therefore, pose a higher risk of lens intolerance should they choose to try them in the future. Given this, when fitting new wearers, it is worth considering treating any symptoms of DED first, prior to fitting the initial lens choice. This early treatment of underlying conditions should reduce the possibility of ocular symptoms later down the line, particularly those which may otherwise have led to contact lens intolerance or discontinuation.12
When classifying symptomatic patients, the term ‘CLD’ tends to be used for those whose issues are directly as a result of lens wear. A common presentation would be where the symptoms increase towards the end of the day, after wearing lenses for several hours. CLD is defined as a condition ‘characterised by episodic or persistent adverse ocular sensations related to lens wear, either with or without visual disturbance, resulting from reduced compatibility between the contact lens and the ocular environment, which can lead to decreased wearing time and discontinuation of contact lens wear.’10 A common defining feature of CLD is the patient reporting an improvement in ocular symptoms upon removing their lenses. Typically, DED symptoms tend to persist despite contact lenses no longer being on the eye, therefore, terms such as ‘contact lens related/associated dry eye’ are usually reserved for patients who have pre-existing DED, which may have been exacerbated by lens wear.10 It is also worth differentiating CLD from the initial irritation that some new wearers might experience during their adaptation period. CLD often appears later in habitual contact lens wearers, long after the adaptation period has ceased. In summary, while the symptoms reported in CLD











































and DED are practically identical (for example, ocular discomfort, dryness, irritation), and often exacerbate one another, the early diagnosis of DED patients is an important factor in predicting and preventing future cases of CLD.
The TFOS DEWS II report suggests that the best way to diagnose DED involves starting the assessment with a thorough history and symptoms, prior to evaluating the ocular surface (see Figure 1). Validated questionnaires can be a useful tool here, both initially to grade the severity of the symptoms, but also to monitor any changes by re-evaluating during subsequent aftercare visits. There are many validated questionnaires currently available (for example, the Ocular Surface Disease Index (OSDI),







and the Dry Eye Questionnaire (DEQ-5)) with some designed to be used specifically with lens wearers (such as the Contact Lens Dry Eye Questionnaire (CLDEQ-8)). This process can allow for a more tailored slit lamp assessment to be performed, looking for signs such as corneal staining, meibomian gland dysfunction, ocular inflammation or any alteration to the characteristics of the tear film (stability, volume, osmolarity). Assessing the symptoms can also ascertain the optimum time of day for follow-up appointments, aiming to examine the patient when they are most symptomatic. This approach should aid in providing an accurate diagnosis and classification of DED, be it evaporative, aqueous deficient or a mixture of the two.9 While DED and CLD can frequently co-exist, many symptomatic wearers will present without clinical
fit and wearing modality
signs. So, what factors may have an impact on lens comfort and what can we try for those wearers who present with ocular dryness or discomfort but show no clinical signs?
There are a number of factors of lens design which can influence whether a patient may experience CLD. These can include water content, dehydration, base curve, edge design, lens thickness and modulus to name but a few. Additionally, the lens fit and care regime also play significant roles. For example, despite the benefits of silicone hydrogel lenses, a common side effect can be the build-up of lipid deposits on the lens surface, particularly when in reusable form.13,14 Solving this problem can often mean experimenting with a change in modality or lens material. Reusable lenses also require the consideration of lens solutions, with the care regime and patient compliance being key factors in avoiding CLD. Away from the lenses themselves, there is a myriad of patient characteristics to consider, all of which may affect the lens comfort. These include age, gender, ocular and/or systemic diseases, medications, tear production and/or stability and ocular surface health. Similarly, the patient environment such as humidity, air quality or the visual tasks being performed can also impact on lens comfort. Given these considerations, a 2013 TFOS workshop categorised CLD into two main classifications: discomfort that is directly related to the lenses; and discomfort that is as a result of the surrounding environment (see Figure 2).15
History and symptoms
A common presenting complaint for contact lens wearers is the inability to comfortably achieve their desired
wearing times. While this may be as a result of DED, be it pre-existing or exacerbated by lens wear, it may also be due to one of the many causes of CLD outlined in Figure 2. As previously mentioned, alongside validated questionnaires, performing an extensive history and symptoms can be an excellent way to help to differentially diagnose the cause of the problem. Having a systematic approach to questioning can prevent missing important information and help to rule out certain characteristics such as environment (aircon), side effects of medication or preservatives (topical or systemic), co-existing ocular or systemic disease (pingueculae, or rheumatism) or allergies. Remembering not to ignore other unmodifiable factors such as age and gender is also important, albeit simplistic.
When and where?
It could be argued that knowing when a patient is most symptomatic is one of the vital pieces of knowledge needed to successfully manage CLD. Some lenses may produce minimal symptoms under normal conditions, yet increase significantly under prolonged exposure to adverse environments, such as low humidity or rooms with dusty or smoky air.16 Aiming to see patients ‘at their worst’ is a great way to tease out any clinical signs that have otherwise appeared absent. Similarly, informing and advising lens wearers to avoid any known problematic environments where possible, can also help to minimise levels of discomfort. Should these environments be unavoidable, protective eyewear could also be considered with varying degrees of success.17 Due to the close relationship between DED and CLD, known modifiable factors in DED such as a heathy diet and good hydration could also be suggested to patients affected by discomfort. A suggested summary of the strategies to manage CLD can be seen in Figure 3.
Lens fit and design
Upon ruling out external factors, there are several things to consider in cases where the ocular discomfort is thought to be exclusively related to the contact lenses. As previously touched upon, the lens fit, the care regime and the lens itself need to be reassessed before making any changes to the lens parameters. For example, it is not uncommon for a mishandling of the lenses, such as aggressive cleaning, to be responsible for damaging the edge of soft lenses or causing problematic surface
scratches to RGPs. Defective lenses such as these can be a clear source of discomfort and, if found, can prevent making unnecessary changes to the lens fit.17 As a general rule, lenses which prove too flat will be symptomatic immediately, often exacerbated by the reflex tears upon insertion. Conversely, steep lenses tend to be initially asymptomatic, becoming uncomfortable over time due to factors such as lens deposits, dryness or compression of the bulbar conjunctiva.18 Studies suggest that examples of thin designs with a knifepoint edge profile provide superior end of day comfort, when compared with lenses of a thicker and more rounded edge design.19 Similarly, lenses with a higher modulus of elasticity, that is to say, those with less flexibility, may also increase patient awareness of the lens; however, there is currently little literary evidence of silicone hydrogel lenses being any more (or less) comfortable than their hydrogel counterparts.20 The CLDEQ-8 is a useful validated questionnaire which is able to detect changes in the scores for lens discomfort, when patients are refitted with new lenses.21 Hence, using tools such as these to assess and monitor the efficacy of clinical interventions can be a great way to clarify which management methods have been successful.
Wettability and care
Poor lens wettability is another factor that can adversely affect ocular comfort, with some designs incorporating components to aid and maintain surface wettability.22 The use of solutions that contain wetting agents can also be highly beneficial; however, their effects are often limited after several hours of lens wear.17 Similarly, applying preservative-free wetting drops to the ocular surface
can be a successful method in reducing symptoms, particularly towards the end of the day. Contact lens deposits are another common cause of discomfort, with proteins being the most common form found with hydrogel lenses and lipids seen more with silicone hydrogel materials.17 However, we can find any type of lens deposit in any lens material because this also depends on the patient characteristics. Good patient compliance is vital in minimising the accumulation of deposits on the lens surface, specifically with reference to adequate cleaning and lens replacement. This is a key step in avoiding the formation of deposits and one that patients can often need reminding of. An alternative action for minimising deposits would be to increase the frequency of lens replacement or, where possible, switching to daily disposables; this would also eliminate any sources of discomfort caused by the preservatives found in some lens care solutions, which in some cases can produce a hypersensitive or toxic response. On the other hand, if reusable lenses are the optimum modality for a patient, then devising a care system using products designed to target specific deposits would be another option.23 In any case, good practice would be to pay attention to the ingredients (and concentrations) of any lens solution and to try to avoid the pitfall of choosing a solution based entirely on cost or ease of supply.
Despite being a well-known risk factor for those susceptible to developing DED, contact lenses have been valuable tools in the management of DED patients for a number of years now.24
About the authors
n Dr Nery Garcia-Porta is an optometrist with a master’s degree in clinical optometry, who got her PhD in Vision Sciences at the University of Santiago (Spain) in 2015. Her PhD research in the field of contact lenses involved several internships at research centres including Aston University and the University of Minho in Portugal. In 2017, she moved to Anglia Ruskin University (ARU) to develop a project focused on the evaluation of the ocular surface in glaucoma patients, thanks to a Marie SklodowskaCurie Individual Fellowship. She is currently working as a lecturer in optometry at ARU. Garcia-Porta completed a clinical internship in the Illinois College of Optometry in Chicago (US) and she has worked as optometrist in Spain’s Quironsalud Hospital.
Similarly, in patients with corneal pathology, lenses can also act to reduce corneal desiccation by providing mechanical protection against the lids and surrounding environment.
Scleral contact lenses
Scleral contact lenses can be used to protect the ocular surface by maintaining corneal hydration. The fluid reservoir created between the corneal epithelium and the posterior lens surface acts to keep the ocular surface moist.25 Studies have shown that the use of scleral lenses in severe dry eye patients can improve best corrected visual acuity, reduce subjective discomfort and even have a notable improvement in quality of life.26,27 As these lenses are composed of RGP materials they often have a high Dk; however, due to the lens thickness and induced tear layer, scleral lenses should not be considered for overnight use.25
Bandage contact lenses
Therapeutic soft contact lenses (or bandage contact lenses) are used with the aim of improving comfort and protecting the ocular surface, by reducing the effects of an adverse environment. While they can be replaced daily, in general, they are used on an extended wear basis, often being exchanged at monthly intervals.28,29 This level of wear time is possible thanks to the development of high Dk soft lens materials such as silicone hydrogel. These lenses can be used with many ocular surface conditions, such as recurrent corneal erosions, post-corneal surgeries or filamentary keratitis, in addition to many dry eye related situations such as Sjögren’s syndrome.24,28 Other applications of therapeutic soft lenses include improving the stability of the tear film, relieving patient discomfort and reducing ocular
n Thom Finney is an optometrist who splits his time between the hospital eye service and higher education, where he is the course leader for the contact lens optician pathway at Anglia Ruskin University (ARU). Entering the profession in 2004, he completed his initial BSc in ophthalmic dispensing at ARU, before studying optometry at Cardiff University. Following his pre-registration year at Leicester Royal Infirmary, he spent several years in community eyecare before returning to the hospital setting. Alongside his role at ARU, Finney specialises in medical retina and emergency eye care at the Royal Stoke University Hospital and is deputy glaucoma module lead at Moorfields Eye Hospital. He has recently completed the therapeutic prescribing course at Glasgow Caledonian University.
staining, particularly in patients where lid or lash interaction with the cornea has been troublesome.28,29 Unfortunately, as with other forms of extended wear lenses, managing the increased risk of ocular infection can often result in extra chair time, therefore, clinicians should consider the pros and cons on a case-by-case basis.30
In recent years, researchers have been exploring the use of contact lenses as a drug delivery system for patients suffering with DED.31 The aim is to achieve a continuous delivery of pharmaceutical agents onto the ocular surface, something which has not been possible with the current topical options such as ointments or drops. While this option is not available yet in clinical practice, studies have suggested that a delivery method such as this should provide a healthy increase in drug efficacy. By having the agent in contact with the cornea for a longer period, this is thought to provide an improvement in the drug bioavailability of up to 50%, in addition to reducing the possibility of systemic side effects.32–34
Contact lenses are well-known by the general population to be an excellent way in which to correct refractive error, while escaping the use of spectacles. What is lesser known are the interesting ways in which they can be used therapeutically in ocular conditions such as DED. With current research on how lenses can be used as drug delivery systems, in conjunction with the steady rise in independent prescribing optometrists, it will be exciting to see how the role of the optometrist will evolve in this field over the coming decade
Fabrizio
This article considers the different causes of amblyopia and the impact it can have on patients throughout life.
Introduction
Amblyopia is a binocular vision dysfunction defined as a unilateral or bilateral reduction of visual acuity (VA) not improvable solely by optical correction nor caused by ocular abnormalities.1,2 So, amblyopia is a neurophysiological disorder in which the visual pathway from the eye to the visual cortex does not develop properly due to some type of interference during the critical or sensitive period. Reduced VA in amblyopia is accompanied by one or more amblyogenic factors such as strabismus, anisometropia, high refractive error, or more rarely, by an obstruction in the optical pathway that reduces retinal image quality, such as congenital cataract.3,4 Naturally, if these factors are left untreated, they interfere with normal development of the visual pathway during the critical period of maturation resulting in permanent visual impairment.3 Addressing amblyopia or amblyogenic factors early is essential to provide the best outcome. Idiopathic amblyopia can occur with no apparent history of strabismus or visual deprivation but may be a result of an amblyogenic factor early in life, such as anisometropia, which resolved prior to presentation.
Amblyopia is second only to uncorrected refractive error as the most common reason for VA impairment in a young population.5 Amblyopia in the UK is the most common binocular vision disorder in children, affecting 2–5% of children, and the second most common cause of visual impairment in children in low-income countries.6,7,8 Williams et al reported an amblyopia prevalence of 1.1% in children that had received preschool screening, versus 2% in those not screened.9 From a clinical point of view, unilateral amblyopia, which is more frequent than binocular amblyopia, is defined as a difference in best-corrected visual acuity (BCVA) between the two eyes of 0.20 LogMAR units, that is to say, two lines on the acuity chart. A difference of 0.10 LogMAR units between the two eyes is usually considered to be normal. Unilateral amblyopia arises after selective disruption of visual input to one eye during critical periods of development.10 A study using OCT images found subtle modifications in amblyopic eyes which might affect
the outer nuclear layer at the fovea suggesting the possible involvement of the photoreceptors.11 Others have found significantly thicker retinal nerve fibre layers (RNFL) in amblyopic eyes than those in the fellow, non-amblyopic eye.12 Bilateral amblyopia is defined as a reduction of 0.20 LogMAR units or more compared with the developmental norms for BCVA at a given age. However, refractive and strabismic amblyopia are the most common types. Anisometropic and strabismic amblyopia account for 90% of all amblyopia. Isoametropic amblyopia is rare, accounting for only 1–2% of all refractive cases of the condition.13Additional risks of developing amblyopia include: neurodevelopmental syndromes;14,15 prematurity or low birth weight;16,17 retinopathy of prematurity;18 family history of strabismus, anisometropia, isoametropia or amblyopia; and congenital cataract.19,20
It is well known that there are windows in early life when neural connections can be robustly restructured in response to experience. The existence of these time-limited critical periods has been demonstrated for many brain areas and functions, including those involved in visual processing.21 The critical period term in the context of the developing mammalian visual system was described by Hubel and Wiesel in their experiments, where one eyelid in cats and monkeys was sutured in order to evaluate the effects on the visual circuitry.22–24 The authors found that monocular deprivation during very early life caused functional blindness in the involved eye, but the retina of this eye was surprisingly fully functional after the suture was removed. They also found a physiological shift in responsiveness of neuronal activity in the visual cortex to light stimulation when one eye was deprived of vision early in life. The change in the eye best-able to excite neurons in the visual cortex was defined as having ocular dominance plasticity and was most robust during a specific age period and diminished once the cat became older. Hubel and Wiesel suggested
that there was a period of development when changes in the external visual environment can alter existing neuronal connections.
More recent studies in animals have suggested that brain plasticity can be dramatically enhanced in enriched environments, increased by constant physical exercise, stimulation, and substantially reduced by stress.25,26 Hooks and Chen defined three phases of plasticity during the critical time period.27 The pre-critical period is the initial formation of neuronal circuits and is not dependent on visual experience. Before the critical period, there is also a period of ocular dominance column formation during which there is robust spontaneous activity and visual experience. One developmental event that marks the passage from the pre-critical period to the critical period is the activation of a GABAergic circuit. The second phase is termed the critical period: a distinct onset of robust plasticity in response to the visual experience when the initially formed circuit can be modified by experience. It seems that the critical period starts very shortly after the relevant sensory information first becomes available. In this period, there are changes not only at the level of synaptic transmission, but increasingly accompanied by structural changes, which result in closure of the critical period. The final phase, closure of the critical period, marks the end of the critical period, where visual experience no longer elicits the same degree of plasticity.
A common misconception in managing patients with amblyopia is that it cannot be treated successfully beyond eight years of age. However, the Pediatric Eye Disease Investigator Group found that in seven-to-12-year-old participants, 53% of those receiving two to six hours of occlusion therapy (and atropine) demonstrated an improvement in VA of at least 10 letters versus just 25% in those receiving optical correction only. In participants aged 13 to 17 years, 25% receiving occlusion therapy (without atropine) responded to treatment versus 23% given optical correction alone. Importantly, for participants in the older group without a previous history of occlusion therapy, the treatment response rate was 47% for those who were patched during the study, versus just 20% in those receiving optical correction only.
If not treated effectively at early age, children with amblyopia can develop visual deficits that may result in less efficient visual performance and lead to occupational exclusions in adulthood. In addition, patients with amblyopia may also have strabismus and a greater risk
of losing vision in the better eye (three times that of a normal adult; 17 times that of a normal child).29,30 Adults with a VA of 6/18 or worse in their amblyopic eye are also more likely to have a road accident.31 They can be also excluded from a wide range of jobs, which increases with the severity of VA impairment.
32
Furthermore, reduction in stereopsis is associated with reduced fine and gross motor and reading skills.33,34 The amblyopic eye may have lower grating acuity and vernier acuity, lower contrast, along with spatial perception disturbances such as misperception of orientation, positional uncertainty and localisation difficulties.
35 Binocular vision perception is usually impaired in patients affected by amblyopia due to suppression or abnormal retinal correspondence leading to degraded sensory fusion and decreased or even absent stereopsis.
36 Fayi et al reported a prevalence of amblyopia of 2.5% in a group of medical students. The effect of amblyopia on these students was moderate, but it did not affect their academic performance.
37 Others found that in a group of students aged nine to 15 years, amblyopia affected participation in sport and social activities as well as performance in school.
38 Further work has demonstrated that reading ability is impaired in children with strabismic amblyopia; this occurs during monocular viewing with the amblyopic eye as well as with the nonamblyopic eye, but also under binocular conditions.
39
Unilateral or bilateral uncorrected refractive errors are the most common cause of amblyopia.40 Refractive errors can result in permanent vision loss and can prevent a child from developing the appropriate visual and perceptual abilities, and eye-hand coordination skills, which are prerequisites to learning.
Anisometropic and isometropic amblyopia are the two main types of refractive ambyopia.40Anisometropic amblyopia occurs only in one eye and is caused by a distinct difference in refractive error between each eye. In this form, the difference in refractive error causes the image on one retina to be more blurred than in the fellow eye and is often associated with strabismus. A greater amount of anisometropia or astigmatism significantly increases the risk and severity of amblyopia.41,42 In isoametropic amblyopia, the amount of refractive error in both eyes is similar, but the VA reduction is bilateral, although it is less common and typically less severe than anisometropic amblyopia.40 In isometropic amblyopia due to high hyperopia, usually greater than +4.50D, accommodation may also lead to strabismic amblyopia. Conversely, children with symmetric myopia rarely
1

develop amblyopia as they simply reduce their working distance to obtain a clear image. The refractive error range that can lead to isoametropic amblyopia has been defined as a minimum of around 6D to 8D in myopic patients, 4D to 5D in hyperopes and 2D to 2.5D in astigmats.45,46 For anisometropes, 3D or more of myopic anisometropia, 1.5 to 2D of astigmatic anisometropia and 1D of anisohyperopia can result in amblyopia.45,46 Recent research suggests that anisometropic patients also have asymmetric accommodative responses between eyes, which adversely affects VA potential. In addition, the image degradation associated with amblyopia results in profound changes in accommodative accuracy and facility, fixation stability, along with saccade and pursuit function. Amblyopic eyes with a lead of accommodation in the distance and a lag at near seem to have a poorer prognosis following occlusion therapy.47
In strabismic amblyopia, VA is impaired due to unilateral and constant strabismus that onsets during early childhood. Eccentric fixation, in which the child has difficulty directing the fovea at the object, is a significant
motor anomaly associated with strabismic amblyopia, especially in those with constant esotropia. Amblyopia due to strabismic disorders seems to result from competitive or inhibitory interaction between neurons processing the nonfusible inputs from the two eyes, which leads to domination of cortical vision centres by the healthy eye and chronically reduced responsiveness to input by the non-fixating eye. Children with strabismic amblyopia can present with a wide range of VA impairment, from slightly worse than 6/6 to poorer than 6/60. The average BCVA is around 6/24.48 When both anisometropia and strabismus are present, the average reported VA is around 6/30.48 Children with intermittent or alternating strabismus rarely develop amblyopia, or only to a minimal degree, since each eye is able to receive visual stimulation at one time or another and VA in these cases is usually 6/19 or better. The most common cause for strabismic amblyopia is infantile esotropia.49 In these children, the ocular deviation is usually constant and the prognosis for normal sensory motor fusion is poor (see Figure 1) 49 Children with exotropia tend to have an intermittent ocular deviation, so amblyopia is less likely (see Figure 2) 49
In deprivation amblyopia, light to the eye is obstructed, for instance by ptosis, haemangioma or optical media opacities. It is a type of amblyopia secondary to occlusion of the visual axis early in life, resulting in a lack of foveal stimulation.50 Congenital cataracts are a common cause of deprivation amblyopia, especially when dense. Peripheral lens opacities or punctate opacities, and

opacities less than 3mm in diameter can be observed closely and successfully managed by treating the associated amblyopia with patching and spectacles.51 VA impairment due to deprivation tends to be more severe with a poorer prognosis than in strabismic and refractive amblyopia. Successful treatment of amblyopia greatly depends on early detection and treatment of predisposing disorders such as congenital cataract. Understanding the genetic reasons for congenital cataract leads to more effective screening tests, early detection and treatment of children who have high risk for hereditary congenital cataract.52 Organic amblyopia occurs in association with structural anomalies such as macular coloboma and optic nerve hypoplasia. It is very important to make a prompt diagnosis as these patients may have some component of amblyopia which can improve with optometric management.53
Functional amblyopia is a visual disorder caused by emotional factors rather than physical or physiological changes.54 A child with functional amblyopia will present with poor vision and the practitioner is unable to find the cause during optometric examination. This form of amblyopia is often seen in children with conversion disorder, a condition in which the child presents with neurological symptoms without an apparent neurological cause. It is thought that this disturbance arises in response to psychological conflict in the child’s life and is considered to be a psychiatric disorder.55,56 Children might experience motor deficits such as poor coordination and paralysis and may develop sensory problems that include visual disturbances, deafness, or loss of the sense of touch. Langman et al assessed 26 patients who complained of sudden reduction in vision. The visual change was bilateral in 50% of the patients and causes included family problems (30%), school problems (25%), mild head trauma (4%), and unknown (41%).57 The treatment of these patients consisted of discussion and psychological therapy, optical correction and pharmacological therapy. In a period of one to three months, the VA was re-evaluated, and 90% of patients recovered to normal levels, while only 10% needed to continue with psychotherapy.
This article highlights the common causes of amblyopia and demonstrates the key role that practitioners play in the early detection and appropriate management of these patients. Timely intervention and effective communication with parents is required to deliver the best prognosis for these patients.
About the author
n Fabrizio Bonci is the clinical optometry lead and vision therapist at Ocular-Optikus Clinic in Kecskemét, Hungary. He has worked mostly in eye clinics in Italy and was also a clinical research fellow at the Department of Clinical Neuroscience and Mental Health, Imperial College London, Charing Cross Hospital.
The Benevolent Fund is here to help during those difficult circumstances
For you — let us know if we can help you
Needs you — please help us identify those in need
From you — please support us financially
Situations can arise that prevent us from pursuing our career, supporting ourselves and our families, and planning for the future in the usual way
Prashant Shah MCOptom, PGDipOphth, DipClinOptom and Yashita Shah MCOptom, PGDipOphth
This feature presents four cases of sudden vision loss. Readers are invited to review the images and access additional resources where necessary to answer the questions.

A 70-year-old patient presents with left eye sudden
1m.
01 Which of the following is the most likely diagnosis of the condition shown in the image?
a) Cilioretinal artery occlusion
b) Branch retinal artery occlusion
c) Central retinal artery occlusion
d) Ophthalmic artery occlusion
02 Which of the following statements is false?
a) The central macula is described as cherry red colour because its vascular supply is from the choroid and not from the inner retinal vessels
b) Vasospasm is a more common cause of the condition shown than carotid plaque emboli
c) The condition shown is a medical emergency
d) Acetazolamide can reduce intraocular pressure to help dislodge an embolus
03 Which of the following is not a risk factor for this condition?
a) Hypercholesterolaemia
b) Diabetes
c) Hypotension
d) Carotid atherosclerosis

A 69-year-old patient presents for examination after hitting a parked car while driving. He has been a smoker for over 50 years.
04 Based on the history and the image shown, what visual field defect would be expected in the right eye?
a) Temporal hemianopia
b) Nasal hemianopia
c) Temporal quadrantanopia
d) Nasal step
05 Where is the most likely location for the lesion in the visual pathway?
a) Left optic nerve
b) Optic chiasm
c) Right optic radiation
d) Left lateral geniculate nucleus
06 What is the most likely cause?
a) Stroke
b) Whiplash injury from road traffic accident
c) Pituitary gland tumour
d) Retinitis pigmentosa

A 57-year-old patient presents with reduced visual acuity of 6/12 in the left eye. Visual acuity in the right eye is 6/6.
07 Which of the following is the least likely symptom for the condition shown?
a) Photopsia
b) Floaters
c) Superior visual field loss
d) Ocular pain
08 Which of the following signs is least likely to be found on clinical examination?
a) Raised intraocular pressure
b) Tobacco dust
c) Red blood cells in the vitreous
d) Vitreous haemorrhage
09 Which of the following is the least likely risk factor for this condition?
a) Hyperopia
b) Previous cataract surgery
c) Recent eye trauma
d) Positive family history
About the authors
n Prashant Shah is an experienced optometrist and CET author with postgraduate diplomas in ophthalmology and in clinical optometry.

10 Based on the image, what condition is the patient likely to have had?
a) Primary open angle glaucoma
b) Pseudoexfoliation syndrome
c) Closed angle glaucoma
d) Pigment dispersion syndrome
11 Which of the following symptoms is the patient likely to have presented with initially?
a) Haloes around lights
b) Ocular pain
c) Nausea
d) All of these options
12 Which of the following is not a predisposing risk factor for the condition?
a) East Asian ethnicity
b) Positive family history
c) Systemic medications such as topiramate
d) Myopia
n Yashita Shah is an experienced optometrist working in independent practice. She holds a postgraduate diploma in ophthalmology.
Stanley Keys FCOptom, Dip Glauc, Dip Tp (IP)
This visual recognition feature presents a series of anterior eye cases that may present in routine practice. Review the images and use additional resources where necessary to complete the questions.
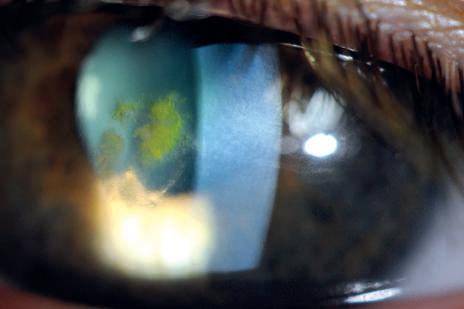
01 Which of the following is the most likely diagnosis of the condition shown?
a) Herpes simplex keratitis
b) Acanthamoeba keratitis
c) Microbial corneal ulcer
d) Corneal abrasion
02 Which of the following is the least relevant check in this case?
a) Staining with fluorescein
b) Checking under both upper and lower eyelids for foreign body
c) A clear history and symptoms
d) Corneal swabs
03 Which of the following statements in relation to the management of this condition is false?
a) A cotton pad should be applied over the eye with medical tape
b) Topical ocular lubricants and ointments are beneficial
c) Topical antibiotics can be used as prophylaxis
d) Cyclopentolate may be used if the eye is very sore

04 What feature is shown in this image?
a) Anterior chamber cells
b) Keratic precipitates
c) Vogt’s striae
d) Superficial punctate keratopathy
05 Which of the following conditions is most likely to result in this finding?
a) Anterior uveitis
b) Acanthamoeba keratitis
c) Dry eye
d) Herpes simplex keratitis
06 Where do the changes shown occur?
a) At a corneal epithelial level
b) Within the stroma
c) On the corneal endothelium
d) Within the tear film

07 What is the most likely cause of the signs shown in the image?
a) Chemical injury
b) Penetrating ocular injury
c) Blunt ocular trauma
d) Viral conjunctivitis
08 Which of the following is least relevant to check in this case?
a) Corneal pachymetry
b) Comparison of the intraocular pressure reading with respect to the fellow eye
c) Visual acuity
d) Checking that the anterior chamber is properly formed
09 Which of the following examinations is least helpful in cases of this type?
a) Checking for full ocular movements
b) Undertaking a dilated fundus examination
c) Checking the anterior chamber for a hyphema
d) Colour vision testing
n Stanley Keys is an experienced hospital optometrist based in Raigmore Hospital Inverness. He has gained independent prescribing status and in 2012 became a fellow of the College of Optometrists. His main clinical interest is in

10 What is shown in the image?
a) Corneal chemical injury
b) Band keratopathy
c) Granular dystrophy
d) Keratic precipitates
11 Which of the following statements in relation to this condition is false?
a) The lesions lie primarily in the corneal endothelium
b) Recurrent erosion syndrome can develop due to these lesions
c) It is a bilateral condition
d) Vision can eventually become affected
12 Which of the following is not a form of treatment for this condition?
a) Corneal graft in severe cases
b) Ablation with excimer laser
c) Lubricant and bandage contact lens to manage erosions
d) Corneal crosslinking
glaucoma. He is also involved in optometric education as a CET contributor to Optometry Today, giving lectures at a range of events and conferences and is the developer of the optometry-evolution website.
Dr Nery Garcia-Porta

Dr Nery Garcia-Porta is an optometrist with a master’s degree in clinical optometry, who got her PhD in Vision Sciences at the University of Santiago (Spain) in 2015. Her PhD research in the field of contact lenses involved several internships at research centres including Aston University and the University of Minho in Portugal. In 2017, she moved to Anglia Ruskin University (ARU) to develop a project focused on the evaluation of the ocular surface in glaucoma patients, thanks to a Marie Sklodowska-Curie Individual Fellowship.
Tell us about your role…
I split my time between teaching and research at ARU. I am lucky because teaching about contact lenses is my professional passion. I have been module leader in different contact lens modules for three courses (BOptom, PGCert CLO, FdSc ophthalmic dispensing). I am also collaborating with researchers from different institutions on several projects.
What are you most proud of?
Despite having studied optometry in Spain and completed my PhD, I managed to get a Marie Skłodowska-Curie Individual Fellowship – a very competitive European grant with a success rate of around 10%. Also, I achieved my dream of becoming a lecturer in optometry in the UK, which is considered the point of reference for optometrists in Europe.
What do you like most and least about your working day?
I enjoy sharing my knowledge with students and seeing how they learn and improve their clinical skills. It is also rewarding that students appreciate the hard work behind each lecture and lab session. We have a very supportive team at ARU, and having a good working environment is very important to me. What I like least is how hard it can be to find time and resources to run research projects and also the stress we are exposed to in academia, which is a very competitive world.
How do you manage a work/life balance?
My husband works in Spain, so this year was a challenge due to the travel restrictions. Under normal circumstances, we travelled a lot. We are both in academia so we understand the particularities of this work and support each other. In addition, we ensure we have everyday time for us (even at a distance).
Kindle or hardback? Kindle
Cheese or chocolate? Chocolate
Apple or Android? Android
Takeaway or fine dining? Finedining
Trainers or heels/brogues? Heels/brogues
Beach bum or culture vulture? Beachbum
Strictly or X Factor? IwouldsayTheITcrowd
n 21st century low vision care: virtual reality, augmented reality and new devices
Michael Crossland
n Management of cataract surgery complications
Jo Mackenzie
n Treatment of children with amblyopia
Fabrizio Bonci
n Omega 3 and ocular health – what’s the deal?
Iain Johnson
n Cases in casualty Alan Hawrami
n Ancillary tests in practice Prashant Shah
LIVE CET OT has a range of CET videos and articles available online, including:
n Infection control and prevention – 2021 update
n Ocular trauma and assessment
n Primary care assessment and management of macular holes
n Communication essentials: health literacy in practice
n Management of the anisometropic child
n Dispensing children in a special needs school environment
The CET articles are available at www.optometry.co.uk/cet

Dr Ian Beasley
is the clinical editor for OT and head of education for the AOP, with responsibility for delivering education in the journal and at face-to-face events. He began his career as an optical technician and later went on to train as a dispensing optician ahead of qualifying as an optometrist in 1997. In 2013, Dr Beasley became the first person in the UK to graduate with a doctorate in optometry from Aston University and received a research excellence award from the College of Optometrists in the same year for his published work on susceptibility to pattern glare following stroke. He maintains strong links with academia as a visiting lecturer at Aston, and is continuing his research by exploring the effect of peripheral defocus on axial growth and modulation of refractive error in hyperopes.
Do you have an idea or request for a CET article? Email the clinical editor ianbeasley@optometry.co.uk



MY CAREER ADVICE
“WE’RE ALWAYS LOOKING FOR PEOPLE WHO LOVE TO ENGAGE WITH CUSTOMERS”
Alan Gregg, head of recruitment services at Specsavers, shares his advice on joining the multiple
What is the one piece of advice that you’d give to someone who wanted to work for the company?
We’re a people business, so we’re always looking for people who love to engage with customers and their colleagues, and really have that customer-first mindset.
What’s the very first thing that you look for?
Past experience, and what they’re passionate about. We’re able to tailor people towards the type of store that would suit them best. Also, anyone who takes an active part in their own learning. Anyone who is looking to further themselves professionally, and who want to go the extra mile to deliver the highest customer service. It all comes back to the customer for us.
How important is the cover letter?
We don’t require cover letters from optometrists. We have a specialist team that speaks to optometrists, all day, every day, so we make it as easy as possible to express interest. We’ll unearth everything that you might put in a cover letter – we’ll make sure we’re getting all the information out so we can pass it on to the store partners to find the best possible fit. Putting pen to paper is not necessary.
“We’re
How do you go about ensuring fairness and equality in your hiring process? Do you have specific programmes in place to ensure that?
The recruitment team speaks to everybody. Because of the 1000 plus businesses that we have across the UK and Ireland, this allows us to help tailor the right role for the right person.
Every store is run by its own directors, and so everyone will get to see every candidate, and every candidate will get to see the store that might suit them best. It might be that you want to work in a big city centre store, or you may want to work in a smaller store, in an outpost somewhere. Or it could be that you want part time, or full time – all of those things can be taken into account to make sure you see every possible role.
The flexibility that the partners have in terms of what they can add and put into contracts makes things flexible and supportive for each individual.
So, whether that’s supporting future development courses, if it’s working around particular hours or days – that can all be completely accommodated.
able to tailor people towards
the type of store that would suit them best”
WHAT STEPS DOES HAKIM GROUP TAKE TO ENSURE THAT THE HIRING PROCESS IS FAIR?
Probably placing emphasis on things that aren’t always the most important. That’s probably talking mainly about things like remuneration above other parts of the role. If a candidate is making it all about money, then it’s probably not going to be the right role for them. I think people should be taking into account other things: progression, opportunities to become a senior clinician or a partner, and the flexibility on offer, rather than concentrating purely on salary. That would be probably the biggest thing.
A new employee is preparing for their first week at Specsavers: what tip would you give them to be successful?
We’ve got a first-class induction programme for new colleagues. The advice would be to absorb all of the different ways that our business model operates, because it is unique. And even if you’ve worked in the industry before, our systems and processes could be different from what you used in the past. Because our businesses are operated locally by joint venture partners, it is important to understand the family of the store you join, and what part they play in the community.

















































































Practice owner of CG Optical, Claire Gough, and assistant manager, Rebecca Gough, on how Tearstim has enabled the business to better diagnose and treat dry eye patients

Adry eye service is an emerging growth area for eye care professionals that helps broaden their offering, addresses the day-to-day challenges that the condition brings to patients, and can increase revenue.
At CG Optical, we look after the eye care needs of many elderly patients and are all too familiar with their daily struggles to dispense drops or use eye bags to relieve sore eyes.
meibomian gland dysfunction (MGD) an alternative to drops. As the only practice in the surrounding area offering a dry eye service, we saw a huge demand for treatment and the feedback we get from patients has been positive.
The procedure is performed within a few minutes and involves covering the patient’s eyes with protector shells. We recommend a course of four treatments and an annual top up.
For patients who required additional help following treatment, such as a drop or a gel to correct a PH imbalance
to inform patients about how well the Tearstim procedure is likely to work for them, and whether they will need the back up of a supplement, gel or drop, before they commit to any investment.
We genuinely believe it is best to provide the most accurate diagnosis from the onset, so we don’t build hopes up and later disappoint.
Idra has become a show piece for us in-store and patients have commented about how impressive it looks. They also like to get involved with the analysis by looking at the pictures and asking questions about their glands. This all helps them understand the dry eye diagnosis and why we are recommending specific treatments.
Reading an article about Tearstim, which uses regulated pulsed light technology (IRPL) to get the meibomian gland functioning properly again, gave us fresh hope and we took a leap of faith and established a dry eye service for our patients.
After sourcing further information on Tearstim and the procedure it uses from our sales manager at Essilor Ltd, we quickly made the decision to invest in the equipment. In November 2019, we became the first practice in the UK to exclusively offer Tearstim to patients and were able to provide those with Sara
“As the only practice in the surrounding area offering a dry eye service, we saw a huge demand for treatment”
in their tears, and to improve patient satisfaction, we also invested in Idra dry eye analysis from Essilor Ltd to enhance our service further.
Idra performs a full assessment of the ocular surface via a series of quick tear film tests to classify the type of dry eye disease. When used alongside Tearstim, it can provide eye care practitioners with a complete diagnosis and treatment service for patients living with the most common cause of dry eye, MGD. Using Idra allows us
On establishing our dry eye service, we designed a marketing campaign to promote it to patients and advertised in the local newspaper, in addition to using leaflets and an A-board. Word of mouth has also proved powerful. One patient recently travelled from the High Peaks, about three hours away, and another customer brought her mum to visit from Wales for treatment after being happy with the results herself. A steady stream of patients are also referred following a routine eye exam.
Offering a dry eye service has been healthy for business and provided a timely additional income stream as part of our business model. It gives us a unique edge that other independents locally do not have and helped increase footfall when routine eye exams dropped during the pandemic. Although we didn't perform as many eye exams during the pandemic, we ran a lot of dry eye consultations because patients didn't want to sit at home and suffer in silence, especially when it can be exacerbated by extra screen time from working from home and keeping in touch with family via Zoom.

Optometrist and founder of the Prison Opticians Trust, Tanjit Dosanjh, OBE, on how his dad’s experience in prison inspired him to give former inmates a second chance
“Formerprisoners areextremelyloyal employees.Itisbuilt intotheirpsyche thatno-oneis evergoingto givethem achance again”

y dad was in prison while I was completing my optometry degree and immediately afterwards. Eventually, when you go visit a family member in prison you end up talking about the same sort of things – ‘what are you doing with your time?’ Through my visits to my dad, I had a good understanding of the types of training programmes that exist in prison. All of the training courses are very basic and didn’t seem like they were setting inmates up for a meaningful career.
When I graduated, I wanted to set up a business with a social purpose behind it. The Prison Opticians charity was founded in 2015. Since then, we have trained 65 prisoners, with 45 entering into jobs as optical advisers or lab technicians. Looking ahead, we want to be not just a small training organisation – we want to train 50 or 60 prisoners every single year. We want to set our own labs up in prisons and start glazing for the independent market, supplying the wider optical sector with our products and services.
After someone has been through our training programme, they will have had a minimum of 10 weeks of
My secret life Do you have a personal passion to share with readers? Get in touch with selinapowell@ optometry.co.uk
training in optics. If you are hiring someone off the street, you are not going to get that.
Above and beyond the idea that it makes good business sense, these people are part of our community. They have shown me that they want to change, and they want a second chance. If this can help someone to live a crime-free life, it is good for the community. Employment is one of the key ways that you can stop people from reoffending.
Former prisoners are extremely loyal employees. For prisoners, it is built into their psyche that no-one is ever going to give them a chance again. That is part of their DNA. The first person who gives them a decent job and gives them an opportunity – they stay with them.
I have been in contact with my dad throughout the process of setting up Prison Opticians. At first, while he was a serving prisoner, he was sceptical. Like many prisoners, he believed that anything that is good for prisoners would be shut down. He was unsure whether it was the best way to spend my time. Now he has seen the project succeed, he is pleased that we are giving people who were facing the same circumstances opportunities to progress. He is proud that he has a son who is helping the sort of people who he was locked up with.



…the contact lens patient retention programme from CooperVision, designed to help reduce drop out and support remote patient care.
















Step 1














Step 2





































3



















If we can give step-by-step support to new contact lens wearers, we can help reduce contact lens drop out - allowing new wearers to enjoy the freedom provided by contact lenses and live their lens life to the full.
My Lens Life is a category programme that provides patient communication tools at every step of the contact lens journey, for all your contact lens patients, regardless of the lenses they are wearing.
To find out more please contact your CooperVision Business Development Manager. coopervision.co.uk/mylenslife






