








As I am not the most sociable of individuals, it will not surprise you that I have yet to engage in merry banter with any of the new Chatbot functions being rolled out by the software industry. Someone who insists on selecting his own music rather than asking Alexa to do it is scarcely going to rush to talk to Bard or ChatGPT. But that’s me as a private individual. Professionally, I am excited to see what new technology can bring to our organisation and our sector. As an organisation, we are already using chatbot functions to improve our service to members. How far can we use artificial intelligence (AI) functionality to provide advice to members, enabling our in-house experts to concentrate on nuanced and specialist cases? And will AI reduce clinical risk and defray the number of potential insurance claims?
For the sector, the possibilities are even more enticing. Improved technology should allow for a reduction in the administrative burden of practice. More profoundly, the ability of new technology increasingly to perform some of the basic repetitive optometric tasks and, over time, to move slowly into diagnosis, will transform optometrists’ day-to-day activities. For patients, the ability for new technology to allow images to be reviewed remotely allows them to potentially access services in areas where there is a shortage of optometrists or, in time, even from the comfort of their own homes. Yet there is no question that technology carries with it risk. Not only is there the threat to jobs represented by increasing automation, but there is an ongoing danger that AI models developed in response to data gathered about eye conditions among predominantly white, western patients may fail to deliver to the needs of a diverse population. Equally profound is the risk arising from our regulatory models that are ill-equipped to control AI-enabled offerings based outside the UK. Our positioning should not be to seek to stop the rise of technology but to influence its use. There are questions we need to ask: What are the areas where it will be useful? Where are we most worried? How can we ensure that control remains in the hands of people who know optics? What are the risks and how can we mitigate them? And how can we ensure that optometrists continue to survive and thrive?


Adam Sampson, AOP chief executive

“Professionally, I am excited to see what new technology can bring to our organisation and our sector”


07-23
The news in digest
Picture this
Cameron Optometry marks the end of mask-wearing in its practice
OT reports
The workforce needs of the profession are discussed in Parliament
The edit
Optics in 16 stories
100% Optical
OTreviews show highlights from 2023
Supplier insight
Myopia management and axial length explored
Industry profile
SpaMedica’s Christine Purslow on AI’s potential in cataract care
AOP Council
A report on the March Council meeting
AOP round-up
#SightWontWaitcampaign success, Council appointments, the HSOC, and vision and driving

“We’re committed to raising awareness of the importance of regular vision checks for driving”
Henry Leonard, AOP head of clinical and regulatory PAGE 23
25-31
The trends, launches and looks
OT focuses on...
Children’s vision
Me and my glasses
Floral Street founder, Michelle Feeney
Get the look // Anatomy of a frame
With Lizzy Yeowart
The shortlist
The June/July selection Behind the brand LOOK

33-36
Voices from optics and beyond Perspectives
Professor Julie-Anne Little; Doug Perkins; Imran Rahman
My vision
Michael Bayley
“Healthcare has all the ingredients to flourish”
Imran Rahman, CEO of CHEC PAGE 35





Business insight and career development
The roundtable
OThosted a roundtable exploring the patient contact lens experience
How I got here
Optometrist, Alvaro Borges
Pre-reg focus
Isha Saghir and Rochelle Anderson
Life as a locum
Aneesa Saleem
Becoming a business owner
Simon Hyde
IP and me
IP optometrists discuss contact lens and corneal infiltrates
How do I...
Engage with AI as an optometrist?
Key milestones
Altris on harnessing AI technology
Eyes on wellbeing
Bullying in the workplace









and environmental standards. The
Professional development for optometrists, DOs and CLOs
CPD welcome



From putting data in the hands of patients to predicting which children will develop high myopia, OT explores the potential of AI for eye care. Inside we speak to optometrists Dr Stephanie Campbell and Kishan Devraj, and Professor Daniel Ting
Establishing the impact of sight loss and the need for vision rehabilitation 73 Deaf awareness: it’s all about access
78 The leadership ‘A’ list
83 Your wellbeing matters for you and your patients
88 Cases in clinic
Career
Cubitts’ head of optometry, Dipa Patel, on why working autonomously is key for employees I could not live without...
”My digital video slit lamp,” says optometrist, Katie Burrows Last word Dr Ceecee Britten-Jones’ secret life

OTvideo highlights OT’s roundtable with VivaQuity explores floaters
Watch the video on www.optometry.co.uk
Listen to The OT Podcast today
Our first four episodes, featuring Professor Nicola Logan, Ian Cameron, Keith Valentine and Dr Peter Frampton are available to listen to on all main podcast platforms
Contact OT with your experiences and observations from practice: newsdesk@optometry.co.uk








8 OTREPORTS
Key insights from the APPG on Eye Health and Visual Impairment
12 CLINICAL ROUND-UP
Links between deprivation and glaucoma severity, and more of the latest research
14 100% OPTICAL OT'svideo production editor picks out five unmissable interviews from the 2023 show

“Our smiles are back“
After more than three years, the team at Cameron Optometry has removed their masks, marking the end of mask-wearing at the independent practice in Edinburgh. Posting the news on its Instagram page, the practice shared its delight with followers, commenting: “No more muffled conversations and no more hiding our smiles when we see you try on your new glasses.” The practice said that while non-mask wearing would be the norm, patients could request staff wear a mask at any point.
June/July 2023

Volume 63:03 Issn 0268-5485
ABC certificate of circulation 1 January 2022–31 December 2022
Editor: Emily McCormick emilymccormick@optometry.co.uk
Deputy editor: Lucy Miller lucymiller@optometry.co.uk
Features editor: Selina Powell selinapowell@optometry.co.uk
Senior reporter: Kimberley Young kimberleyyoung@optometry.co.uk
Web content and social media manager: Leah Boyle leahboyle@optometry.co.uk
Clinical editor: Dr Ian Beasley ianbeasley@optometry.co.uk
Clinical editor for multimedia: Ceri Smith-Jaynes cerismithjaynes@optometry.co.uk
Video production editor: Laurence Derbyshire laurencederbyshire@optometry.co.uk
CPD enquiries: 020 7549 2076 CPDhelp@optometry.co.uk
AOP membership and OT subscription team: subscriptions@aop.org.uk
Advertising:
Sonal Mistry 020 3771 7247 sonal.mistry@thinkpublishing.co.uk
Advertising production: aop@ccmediagroup.co.uk
Art director: Grant Pearce
Senior designer: Juanita Adu
Associate director: Anna Vassallo
Executive director: Jackie Scully
Published bimonthly for the Association of Optometrists by Think Media Group
20 Mortimer Street, London, W1T 3JW
Printed by Acorn Web, Normanton Ind Estate, Loscoe Close, Normanton, West Yorkshire, WF6 1TW
All rights in and relating to this publication are expressly reserved. No part of this publication may be reproduced in any form or by any process without written permission from the AOP or the publisher.

“VITAL AND ESSENTIAL” NEEDS OF EYE CARE WORKFORCE DISCUSSED
The AOP’s Adam Sampson and Dr Peter Hampson spoke at the April meeting of the APPG on Eye Health and Visual Impairment, which addressed the eye care workforce
The eye care workforce was discussed at the meeting of the All Party Parliamentary Group (APPG) on Eye Health and Visual Impairment on Wednesday 26 April.
APPG co-chair, Marsha de Cordova MP, began the session by speaking about the Government’s soon to be published workforce plan, emphasising that “it is really important that it takes in the vital and essential needs of our sector, particularly when it comes to optometry and ophthalmology.”
1“AI IS A BUZZWORD AT THE MOMENT, BUT IN REALITY, IT’S ANOTHER WAY OF SAYING: HOW DO WE INCREASE PRODUCTIVITY WITHIN THE EXISTING WORKFORCE?”
The AOP’s clinical and professional director, Dr Peter Hampson, spoke about the Association’s research into the UK eye care workforce, collated from corporate and NHS England data, the Office for National Statistics, and the General Optical Council (GOC) register.
Pairing this data with existing information that the AOP has on the 82% of UK optometrists who are members offers up “a fairly robust data set,” Hampson said.
“We can model the rate at which the number of optometrists will increase based on current trends of GOC data, on trends of how we think the number of optometry schools are able to change over the next two, five or 10 years, and how population will change in the demographic areas,” he said.
Modelling in order to see changes in productivity has also been possible, Hampson said, adding:
“AI is a buzzword at the moment, but in reality, it’s another way of saying: how do we increase productivity within the existing workforce? If we increase that burden on practitioners, do they have the capacity to cope?”
AOP data suggests there is the right number of optometrists, Hampson said, but the spread across the country is unbalanced.
“There are enough optometrists to deliver this care,” Hampson said, adding that time to build capacity needs to be factored in. In five years, he believes the optometry workforce will be in a position to take on a “significant amount” of work that was previously being performed in hospitals.
2“OPTOMETRY SHOULD BE AT THE HEART OF PATIENT-CENTRED EYE CARE IN THE UK”
Professor Leon Davies, president of the College of Optometrists, outlined his desire for optometrists to be positioned at the heart of a patientcentred eye care workforce.
“Patients in all four nations of the UK should be able to access all eye care services via their primary eye care optometrists in the first instance, with optometrists established as the first contact practitioners,” Davies said.
The pandemic allowed optometrists to prove their skills, he said, and “we all now have a unique opportunity to build on these achievements to address the backlog and build cost-effective, clinically safe, sustainable eye care services for the benefit of our patients.”
Services, including higher qualifications, must be


commissioned and collaboration with universities should be facilitated, he said. Data should inform workforce planning in order to meet patient need and improve outcomes.
“In order to improve eye care services and patient outcomes, it is clear the way forward is to help services to better utilise multidisciplinary eye care teams, including making the most of the full core skills and competencies of optometrists,” Davies added.
3
“THERE IS A STRONG DESIRE FROM THE WORKFORCE TO HAVE FLEXIBLE WORKING”
AOP chief executive, Adam Sampson, spoke about future workforce challenges that the profession should be aware of.
Sampson emphasised the changing demographic of optometry. “We now have a strongly female entry into the profession, which is a distinct change and in the long-term will provide us with some interesting challenges about retention and career progression,” Sampson said.
A “huge appetite” for flexible working was evident in the most recent AOP member survey, he shared, adding: “There is a strong desire from the workforce to have flexible working.”
AOP members have clearly expressed a desire to carry out an increased amount of clinical work, Sampson shared.
There is a strong desire for more enhanced skills, and this is a key part of how the existing optometry workforce can be retained.
A market-led approach needs to be taken when commissioning services, Sampson added, and IT connectivity needs to be embraced in order to reach hard to access areas.
4
“WE LOVE HAVING OPTOMETRISTS IN OUR CLINICS”
Liz Tomlin, head orthoptist at Guy’s and St Thomas’ Hospital, explained that Minor Eye Conditions Service optometrists regularly attend specialist clinics, where they have been able to develop relationships with consulting ophthalmologists –allowing them to take their extended knowledge into their communities.
“We love having optometrists in our clinics,” she said, “but it’s a rare beast that comes to work for the NHS five days a week.”
One day a week contracts for optometrists to work in the hospital while remaining in community practice for the other four days are helpful, she explained.
5
“WE ARE PASSIONATE ABOUT THE NHS AND THE DRIVERS FOR CHANGE”
Seema Verma, consultant ophthalmologist at St Thomas’ Hospital, spoke about the hospital’s ophthalmology department both before and during the pandemic, citing issues including an increasing workload, limited medical workforce, increased waiting times, and irreversible sight loss. “The workforce has always been the challenge,” she said.
Fragmentation of referral patterns and pathways, optometrists not always being where they are needed, competing interests and funding challenges within the NHS, and issues with IT connectivity between primary and secondary care are all identifiable issues “which we have known about for a long time,” Verma added.
A “massive collaborative effort” has seen solutions including community optometry clinics, teaching and upskilling by consultants, and optometrists being trained so they can manage more in the community, Verma shared. “We’re all here because we want to make a change,” she said, noting that there are multiple opportunities available to work in different ways – for example, with the potential of remote consultations.










“We are now at a critical stage in the effort to curb myopia, where we have the tools to create meaningful change”
Yvette Waddell, CEO of Brien Holden Vision Institute, highlighted the importance of engaging with myopia management as the organisation hosted Myopia Awareness Week 2023 from 22–26 May. The month was full of myopia-related news and education, including the AOP’s MAYopia Day event. If you missed it, why not watch the recordings back at: www.aop.org.uk/events-and-education

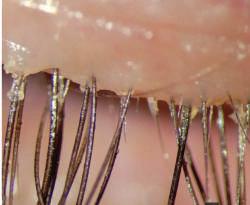
Haag-Streit UK has launched its 2023 Slit Lamp Imaging Competition. Open until 11 August, this marks the fifth competition held by the manufacturer, offering eye care professionals an opportunity to showcase their slit lamp imaging skills. Uptal Sarkar from Disha Eye Hospitals Barrackpore in Kolkata, India, was named winner of the 2022 competition. Read more information online at: bit.ly/412E9dV
4.76% Nearly one million
EssilorLuxottica has formed an exclusive licensing agreement for the design, manufacture and worldwide distribution of eyewear between the Roger Federer (RF) and Oliver Peoples brand. The inaugural collection will launch in spring 2024. Roger Federer said he was “thrilled” to collaborate with Oliver Peoples, adding: “We both found great commonality in how we approach our work, and they are a perfect partner for the debut of my RF eyewear collection in 2024.”






Data recorded by Specsavers suggests that the multiple performed nearly one million clinical eye health appointments through enhanced optical services (EOS) between March 2022 and February 2023, up from 453,000 appointments for the same period in 2018–2019. The largest group of patients were seen for a Minor Eye Condition Service style consultation, the multiple found.





01438 740823
www.bibonline.co.uk

Domiciliary eye care company, OutsideClinic, has introduced a new lightweight kit bag. Designed by OutsideClinic Southwest regional manager, Dan Young, and senior designer, Jon Richards, the new bag features pre-cut slots for each piece of equipment and weighs 6.4kg compared to the previous 10kg.

Data released by EuromContact on the market for soft contact lenses in 2022 revealed growing numbers of contact lens wearers in Europe. Total wearers were up 4.76% in 2022 over 2021. Of the 11 European countries covered in the report, 6.6% of the population between 15 and 64 years old wear soft contact lenses, the association said.
Ocushield is among 148 companies to be recognised in the first King’s Awards for Enterprise. The accolade was previously known as The Queen’s Award for Enterprise, and has been renamed to demonstrate King Charles’ desire to continue recognising outstanding UK businesses. Ocushuield, founded by Dhruvin Patel (pictured), can now use the King’s Award emblem for the next five years.


60 DAYS IN 16 STORIES
Scientists from Trinity College Dublin have shown that gene therapy is capable of lowering intraocular pressure in mouse and monkey models of glaucoma. Describing their findings in ScienceAdvances, researchers highlighted that a single injection of a viral vector can increase the flow of aqueous fluid from the front of the eye – resulting in a decrease in pressure. Find the full story on OTat: bit.ly/41k4TXt

Toku Inc, co-founded by Dr Ehsan Vaghefi (pictured), closed an $8 million Series A Preferred financing round, co-led by Topcon and National Vision. It aims to accelerate the development of technologies using AI to analyse retinal images for biometric markers linked to health and risk of cardiovascular events, stroke or diabetes.

52%
A study published in Journal of the American Heart Association found that people who experienced high levels of workplace discrimination were 52% more likely to report high blood pressure during an eight-year followup than those with low discrimination. The study by University of California involved 1246 adults.
70,000
Moorfields Eye Hospital has opened a new hub at Stratford Broadway, its second largest standalone site, that is expected to provide around 70,000 appointments per year.
“We’re thrilled to be able to help Eye Docs to offer community-based services to patients and help to reduce the burden on the NHS”
Professor Shehzad Naroo, from Aston University, discussed the launch of a Knowledge Transfer Partnership (KTP) between the university’s optometry and business schools, and Eye Docs. The KTP will work to develop a new shared care model, identifying which patients need to be seen by Eye Docs surgeons and which can be seen in primary care optometry practices.
“It was like magic”
Mahnoor Khan, final year student at the University of Huddersfield, described how her experience of wearing spectacles as a child sparked a curiosity for optometry in OT’s A to Optometry series: bit.ly/45Bow0p

Optometrist, outgoing AOP chairman and lecturer, Julie-Anne Little, was appointed professor at the University of Ulster in April. Professor Little leads the centre for optometry and vision science. She spoke to OT about the future of optometric education, her advice to her younger self and the rewards of research. Read the findings at: bit.ly/3MWu6mB

A consultation on changes to primary care ophthalmic services in Wales will close on 19 June. The Welsh Government hopes the consultation will help guide an increased scope for eye care services in Wales. The AOP has strongly encouraged members to respond to the consultation, and will also be responding to the proposals with, and on behalf of, members in Wales.
Read more at: bit.ly/44tBAnR
“Patients, if you listen carefully, are always teaching you something new”
Paul Adler, senior optometrist and director at Paul Adler Opticians, a Hakim Group independent practice, shared how he followed his father’s footsteps into optometry, how he learns from his patients, and why you should follow your dreams. See more at: bit.ly/3nx6bjZ


Scientists from the University of Edinburgh and Princess Alexandra Eye Pavilion have examined the relationship between deprivation and the severity of glaucoma at diagnosis.
The research, which was published in Eye, found that 14.3% of patients living in the most deprived areas had a standard automated perimetry mean deviation (MD) equal to or worse than −6 dB in the better eye at diagnosis, compared to only 6.8% of patients living in the least deprived areas. Only 0.8% of patients living in the least deprived areas had a MD equal to or worse than −12 dB in the better eye at diagnosis, compared with 4.8% of patients in the most deprived areas. The researchers highlighted that people in lower socio-economic groups are more likely to have long term health conditions and develop multiple illnesses at a younger age.
“Those from lower socio-economic backgrounds may experience barriers to accessing health care, for example due to direct costs such as transport or medication costs, or due to indirect costs

“Those from lower socioeconomic backgrounds may experience barriers to accessing health care”
such as loss of earnings due to time away from work,” the researchers shared.
They added that uptake of eye care services is still uneven across different socio-economic groups, even though the Scottish Government introduced free eye examinations for all people living in Scotland in 2006.
“Costs may still be a barrier due to the potential costs of spectacles or ancillary tests,” the authors noted.
“As late diagnosis is a major risk factor for glaucoma blindness, it is important that measures are taken to reduce inequalities in glaucoma diagnosis due to deprivation,” they concluded.
New research has revealed disparities in the proportion of children with autism spectrum disorder (ASD) who receive vision screening in the US.
The study, which was published in Pediatrics, involved analysis of 63,829 ‘well-child visits.’ The children were aged between three and five, with the visits carried out between January 2016 and December 2019 in Delaware, Pennsylvania and Florida. Researchers found that 37% of children with ASD received vision screening as part of the visit, compared to 60% of children without ASD.
The scientists also found that the disparities were highest among black children with ASD. Among this cohort, only 28% received vision screening. Senior study author, Dr Brittany Perry,
of Nemours Swank Autism Center, shared that she undertook the research after observing that many patients attending appointments had never received vision screening.
“I wanted to study whether this might be a broader disparity,” she said. The study authors highlighted that photoscreening – where a specialised camera or video system is used to capture images of a child’s eyes – can be helpful for children with ASD as they cannot always understand or respond to instructions in a conventional visual acuity test.
“Increased use of photoscreening may prove to be a great tool for reducing disparities and increasing vision screening in more vulnerable populations with autism,” Perry said.
NEUROSCIENCE
Spiders lose vision when hungry
Scientists believe that a new study describing the effect of starvation on jumping spiders could hold insight for the development of age-related macular degeneration.
The research, which was published in Vision Research, involved studying two groups of captive spiders. One group was fed an unrestricted diet while the other group was given half portions.
They found that photoreceptor degeneration was exacerbated in the underfed group of spiders.
Rathore et al.
DOI: 10.1016/j.visres.2023.108185
CHILDREN
Low-concentration atropine lowers incidence of myopia New research has explored the effect of low-concentration atropine eye drops on myopia incidence.
The study, which was published in JAMA, involved the recruitment of 474 nonmyopic children between the ages of four and nine. The researchers concluded that nightly use of 0.05% atropine eye drops resulted in a significantly lower incidence of myopia compared with placebo, as well as a lower percentage of participants with fast myopic shift after two years.
Yam et al.
DOI: 10.1001/jama.2022.24162
NEUROSCIENCE
COVID-19 and face blindness
Scientists have described a case of face blindness in a 28-year-old woman after contracting COVID-19.
Writing in Cortex, researchers highlighted that the patient had normal face recognition before she became infected with COVID-19 in March 2020.
She noticed that when her COVID-19 symptoms relapsed, she would have difficulties recognising faces – including members of her own family.
A survey of 54 respondents with long COVID found that the majority reported reductions in visual recognition and navigation abilities.
Kieseler et al.
DOI: 10.1016/j.cortex.2023.01.012



CPD courses available, with more courses added regularly

Choose from a wide range of topics from dry eye to electromagnetic radiation
Access our Essential Contact Lens Practice book, a comprehensive resource on Contact Lens practice, from understanding the market through to practical fitting advice
Choose a learning style that works for you Supporting Excellence in Patient Care VISION




OT reviews the stats for 100% Optical 2023 and picks out unmissable video interviews from the show
OT’S HIGHLIGHT REEL



With summer here, 100% Optical 2023 already feels like a fond memory.
The optical trade show gained its highest attendance yet, with more than 10,600 delegates meeting in London at the ExCeL Centre in late February.
A post-show delegate survey by the organisers of 100% Optical has found that 96% of respondents were either very satisfied, fairly satisfied or somewhat satisfied with the show.
The show has achieved a Net Promoter Score (NPS) of 45.95, a rise on 2022’s 42.30. The industry average NPS is 14.58, the organisers said.
Nathan Garnett, show director for 100% Optical, explained: “Most organisers use NPS as a benchmark as to how they are performing. We focus on improving that score every year.”
Show spending power was up 60%, reaching £4.3 billion.
Garnett suggested that the pandemic may have had an effect on spend in 2022, whereas this year: “We’ve seen it bounce back. I think that is reflected in the increase.”
“I think it is also to do with the fact that the show is more rounded,” he

said, noting that the show covers a variety of sectors. Key reasons cited by survey respondents for attending the show included to see new products, understand market trends, attend education and gain CPD points.
What comes next?
Plans have already begun to be laid for 2024, which will mark the 10th anniversary of the show.
Garnett said: “The show we’ve just done was our biggest yet, and this upcoming one looks like it is going to be even bigger.”
Dr Ian Beasley, AOP head of education and OT clinical editor, commented: “The 2024 event offers delegates the opportunity to top up interactive CPD points, meet their peer review requirement and tick off all domains early on in the final year of the cycle.”
100% Optical 2024 will take place from 24–26 February at ExCeL London. To find out more visit the show’s website: www.100percentoptical.com
As media partner for 100% Optical, OT’s coverage continues online. Join in at: www.aop.org.uk/ot/optical2023
Show spend reached £4.3 billion in 2023. This was seen in:
£866m CONTACT LENSES
Laurence Derbyshire, video production editor for OT, picked out five unmissable interviews from 100% Optical 2023.

1
100% Optical 2023
Show review
With the dust still in the air, I looked back at the show that just-was: all the looks, hardware and education fresh in mind.
youtu.be/QVCiGVw8wt8
2
Hyperparallel OCT from Cylite

This fascinating piece of tech coming out of Australia seems to be coming at OCT from a different direction, bringing new ways of visualising both the anterior and posterior eye.
youtu.be/UYMJgv9hPdQ

3
Prue Eyewear from MAC Eyewear
Dame Prue Leith shares her opinions on colour, which is that we aren’t showing enough of it. A sentiment I can always get behind. youtu.be/dvlZz8yLQ0w
4 Myah taking axial length measurements with Topcon Myopia management is becoming more and more prevalent, making anything that can help you take better care of your young patients that little bit more important.
youtu.be/yS7oX6FfGnQ

5 Bird Eyewear on low carbon projects
Ed Bird is the kind of person who really wants to do what is right for the environment. He discusses the improvements the brand has made to their processes as well as some of his project outside of eyewear.
youtu.be/tEJ5wfjbj0Y









OT heard from manufacturers designing instruments to support the measurement of axial length, and sought out additional free tools
Guidance from professional optical bodies suggests that axial length is a key outcome measure in myopia management, and equipment manufacturers have created platforms to help capture these measurements, in a way that can also be easily communicated to patients and their parents or guardians.
Danielle Lee, Topcon Healthcare’s clinical affairs manager for the UK and Ireland, explained that there has been an increase in demand for devices that can measure axial length since the release of new myopia management guidance from the College of Optometrists in 2022.
“While it’s not a requirement for practices to be able to measure axial length, there are more and more practices taking the view that, if it’s the gold standard, then maybe we should be incorporating that into clinics,” she explained.
Considering the growing levels of awareness of myopia management, Darren Taylor, optometrist and product training manager at Essilor Instruments UK, said: “I can see similarities to what happened with OCT in the market a few years ago: the more patients and parents enquire about myopia management, and the more practitioners talk about it, the more it will become the norm.”
Taylor suggested practices are keen to gather more data to enhance eye examinations and offer more to patients.
Essilor’s Myopia Expert 700 features corneal topography with integrated
optical biometer, for axial length measurement. It can offer pupillometry and fluorescein assessment. Data capture can also be delegated if required.
The Myopia Care software supports practitioners with communication, allowing for axial length data from the Myopia Expert 700 and refraction data to be combined with patient questionnaires and myopia risk factors. Data is presented in graphs and percentile growth charts and can be turned into a PDF report for patients and guardians to take home.
Discussing the importance of communicating this data, Taylor noted the length of time a patient may be on the treatment pathway, sharing: “It is very important to have a way to keep them engaged throughout that time.”
For parents and guardians in particular, Taylor said: “For most people, it's fairly easy to understand where we are now, but parents always want to know: where are we likely to be heading in the future?”
Haag-Streit’s Lenstar Myopia report displaying axial length with treatments and Tideman myopia risks
The Myah device offers corneal topography, keratoconus screening and pupillometry, along with capturing axial length measurements, and the measurement process can be delegated. The device also incorporates a suite of dry eye assessment tools.
The device can be used to assess risk and start myopia conversations, monitor axial length and compare measurements with growth curves, drawing on the Erasmus University dataset.
Lee explained that this “huge” European-specific dataset has been gathered over a number of years, assessing patient populations. Incorporating this data into normative growth curves provides an indication of where the patient is in comparison to what is expected, similar to height and weight charts.
“From a clinician’s point of view, it enables those conversations to be had earlier, as we can see how the prescription and axial length are changing over time, what to then expect in later life, and the risk of the patient becoming myopic or a high myope,” Lee said, adding that once an intervention has been started, “we can utilise that data to monitor treatment efficacy and compliance.”
This provides a multifactorial approach, as the data can be utilised in different ways, depending on where the patients are in their myopia management journey, and can be exported into a variety of reports, including a report for the patient.

AOP guidance recognises that while measuring axial length change is optimal for myopia management, “these measurements are not widely used in mainstream clinical practice at present.”
Resources are available that can provide a place for practices to get started in myopia management without a biometer, and the AOP website offers guidance on consistent methods of measurements that can be taken. The guidance is available on the AOP website here: bit.ly/449ie7E.
The Brien Holden Vision Institute (BHVI) offers a free Myopia Calculator which shows the range of myopia management options and demonstrates the possible benefits over time of starting to treat myopia progression.
The BHVI shared with OT that, in the 12 months between the end of March 2022 and start of April 2023, the calculator received more than 100,000 page views – an increase of 9% on the previous year, and a 17% increase in unique page views.
The International Myopia Institute also provides free online resources for myopia management, such as the IMI Facts and Findings Infographic, as well as white papers and clinical summaries, while Ulster University has produced the PreMO Risk Indicator and Axial Length Growth Charts.
Lenstar Myopia
Haag-Streit has seen demand for its optical biometer, the Lenstar Myopia, “increase dramatically” in the last year, Grahame Wood, national sales manager at Haag-Streit UK, said.
The Lenstar Myopia system is made up of the Lenstar 900 optical biometer with corresponding EyeSuite Myopia software. The biometer enables axial length measurement, pupillometry, vitreous chamber depth, central corneal thickness and keratometry, and the software allows for previously collected data from refraction and measurement devices to be imported, and environmental factors to be defined.
Designed to help facilitate the consultation and education of patients and parents, the software also utilises axial length growth curves from the Erasmus University Medical Center, and produces easy-to-read reports.
“This will aid practitioners on when to intervene, for example, if growth is too fast. In addition, it shows the effectiveness of treatments over time on slowing the rate of growth,” he added.
The right time to invest in a device for measuring and monitoring axial length will be individual to each practice and manufacturers emphasised the importance of education and keeping up to date with research for practices new to myopia management, or who may not feel ready to invest in a biometer.
Lee shared: “We’re seeing practitioners that have never done myopia control before that are getting on board with it and using a device like this as their introduction to it, to help them along the way with that learning.”
Read your 2023 Myopia Guide which arrives with this edition of OT
Features include displays for tracking treatment interventions, showing refraction curves, axial length measurement and environmental factors, such as outside time versus screen time and parental history of myopia.
Haag-Streit plans to launch an additional smart software add-on to the Lenstar Myopia. Wood explained: “The AMMC (Age Matched Myopia Control) module developed by Dr Kaymak looks at speed of axial length growth of the patient over time and categorises the speed of growth using a simple traffic light system that is easy for patients and parents to understand.”
Taylor recommended considering how many children are on the practice database, and how many the practice would like to see in the future, where the device will be located, who will operate it, and the value it could add to the practice. He pointed out that there can be multiple pathways for purchasing equipment.
Lee also recommended considering the clinic workflow, and additional functionality a device might offer.
For those looking into this kind of instrument, Wood said: “If you are already conducting myopia management, or wishing to introduce this, then investment in this type of technology will certainly add value to your practice, both from a clinical and patient loyalty perspective.”


















Christine Purslow, director of optometry at SpaMedica, on the potential applications for artificial intelligence and keeping the patient journey in focus


There are so many potential applications for artificial intelligence (AI) in eye health but two areas with immediate impact and appeal for eye care in the UK are already with us and growing. One is the use of AI in patient support – the simplest version is the AI chatbot that can provide an ‘always on’ solution to patient queries; and the other is the application of AI based on deep learning to medical imaging, including retinal imaging.
Detecting abnormal features in retinal vasculature, lesions, optic nerve head images and optical coherence tomography (OCT) images will standardise and improve care, whilst facilitating different models of care. Ocular imaging is key to audit, telemedicine and virtual support, all of which allow us to plan safe and effective care for patients without the most senior clinician personally examining every individual.
AI is already with us. Chatbots are in use across several medical areas, including ophthalmology, and several options already exist in glaucoma and diabetic eye care to help identify high probability of abnormality, but not all of them utilise deep learning. The most useful role, so far, appears to be screening and detection in pathology with characteristic changes in fundus appearance.
“The number one question will always be: what does it do for the care of our patients?”
In cataract care, co-morbidities in an elderly cohort are fairly common. Hypertension and cardiovascular disease, to name just two, plus other eye pathology, so there will always be a screening element to the pre-assessment visit. The clinician has to establish suitability for surgery
and if any co-pathology needs prior management. Any tool that helps us to identify retinal disease – particularly through hazy media – is most welcome. At pre-op assessment we also grade lens opacities, but this is subject to clinician interpretation – if this could be automated to flag up posterior polar cataract, for example, this could be beneficial. Patients with posterior polar cataract are at higher risk of intra-operative complications so sure knowledge of this condition directly impacts surgical planning.
We are always looking for intelligent solutions that improve the care and outcomes for our patients. Having access to technology that can easily identify abnormal retinal images and raise suspicion for clinicians before they examine the patient has the potential to increase the effectiveness of the consultation.
Digital imaging systems already facilitate shared care and virtual review, via the exchange of accurate information. If we can also rely on AI to remove false positives or false negatives from a screening or monitoring service, this is likely to improve collaborative working further, and reduce the frustrating number of unnecessary or inaccurate referrals into secondary care.
The number one question will always be: what does it do for the care of our patients? Every other consideration stems from that – disease detection rates, how does it compare with the clinician alone, do we detect disease earlier, does it reduce the need for visits to the clinic? Referral refinement, screening, monitoring stable eye conditions, and identifying progression are all resource-heavy areas for ophthalmology and optometry – AI technology can be part of the solution. I’m eager to see where it takes us.




Togetherwe providegreat outcomes; ultimatelyimprovingour patients'qualityof life
UK's largest provider of NHS cataract surgery, with 48 hospitals across England
NHS appointments available four weeks from referral -surgery within four weeks Free transport for patients
Patients return to community optometrists for post-op assessment
SCAN THE QR CODETO FIND OUT MORE:
Regular communication from SpaMedica at every stage of the patient journey
Specialist advice to community optometrists to support you with your patients/ referra Is 24-hour emergency hotline for your patients


“An important symbolic moment” and the pressure created by test times were discussed at the March AOP Council meeting
Resources on managing risk in practice and a growing awareness of eye health in parliament were discussed at an AOP Council meeting on 15 March (AOP offices, London).
AOP chairman, Professor Julie-Anne Little, shared with Councillors that work on the AOP’s Whole Life Course project is progressing.
The initiative aims to collect patient and practitioner stories to demonstrate the contribution of optometry over a lifetime. “This project is now well underway and we will continue to engage with Council members across this work,” Little said.
AOP chief executive, Adam Sampson, shared with Council that the MP for Battersea, Marsha de Cordova, is expected to have a second reading of her National Eye Health Strategy Bill on 24 November.
Sampson described how de Cordova asked Prime Minister Rishi Sunak if he would back the bill during parliamentary questions.
He added that the way Sunak answered the question made it clear that he was expecting it and that eye care was included within his briefing.
“That was an important symbolic moment,” Sampson emphasised.
“If we think about where we were a couple of years ago, to where we are now – with Number 10 thinking about eye health – that is progress,” he said.
AOP policy director, Carolyn Ruston, gave Councillors an update on public affairs and policy work. Ruston highlighted that the AOP was
invited to give evidence to the All Party Parliamentary Group on Eye Health and Vision in April about workforce capacity issues in eye health (read more on page 8). She shared that the AOP is making an average of one or more submissions to consultations and calls for evidence each month – and being actively encouraged to participate in consultations by other organisations.
“I think that is important from an influencing point of view,” Ruston observed.
“If
we think about where we were a couple of years ago, to where we are now – with Number 10 thinking about eye health – that is progress”
AOP chief executive Adam Sampson
AOP policy adviser, Kathy Jones, delivered a presentation to Council about managing risk in practice in light of discussions within the profession about test times. She noted that the AOP employment team deal with queries from optometrists who are concerned about the risks created for patient safety from short sight test times.
Jones added that locum optometrists can feel vulnerable when it comes to test times as they may be concerned about the implications if they ask for longer appointments. “They may not be asked to come back to a practice,” she said.
Jones shared that the AOP has traditionally been reluctant to set a minimum test time because each eye examination is tailored to the patient in the chair.
Councillors provided feedback on whether the AOP policy position could be improved, and if further resources are needed for AOP members on managing risk in practice.
Opening the discussion, Little observed that the appointment length only serves an administrative purpose.
“You only know how much time you need once you’ve started to see the patient,” she said.
Councillor Karan Vyas shared that some companies can be inflexible about limits on test times – and will force out managers and staff who disagree with this approach.
“They will find a locum who will work to those time pressures,” he said.
Councillor Kevin Wallace said that if a minimum testing time is set, then there is the risk that some companies will try to apply this time for every patient.
He highlighted the importance of test times that adapt to the needs of different patients. “Any proper diary management system should have that flexibility built in,” he said.
Councillor Will Holmes observed that developments in technology may also influence test time requirements.
“I think it is going to be a moving target over the next decade. That is another reason not to go with a minimum time because it is going to change relatively quickly,” he said.
Councillor Fatima Nawaz shared that test times are an issue that affects resident optometrists as well as locums, and those working in independents as well as multiples. She said that unrealistic test times set optometrists up to fail. “I do hope that our work with employers going forward will result in progress on this issue,” she added.
The AOP hosted its AGM on 7 June, which was followed directly after by its Council meeting where newly-appointed Councillors in designated positions were welcomed. Read more on page 22.
OT breaks down the highlights from the response to the AOP’s campaign

The AOP’s Sight won’t wait campaign received a “phenomenal” response, with coverage across national, regional, online and sector press, the association has shared.
The campaign launched on 21 March, following a Freedom of Information request by Optometry Today which revealed that patients have lost their sight due to NHS backlogs.
An AOP survey found that 43% of members had serious concerns over the number of patients they had seen who could lose sight unnecessarily as a result of long NHS waiting lists and cancelled appointments, while a poll of 498 Macular Society members also shed light on the experience of patients.
The AOP called for the Government to commit to a national eye health strategy, enabling more people to access care quickly and locally.
The campaign reached TV and radio, with interviews featuring AOP chief executive, Adam Sampson, optometrist and AOP clinical adviser, Farah Topia, and chief executive of the Macular Society, Cathy Yelf. Patients also shared their own experiences.
This included a primetime slot on BBC 1 Breakfast, and coverage on Sky News and BBC Look North, as well as a lead slot on Radio 4 In Touch.
online media, including 12 national print pieces, in the The Guardian, The Daily Telegraph, The Independent, I News, Daily Mail, Scottish Mail, Daily Express, The Sun, The Scottish Sun, The Scotsman, Daily Star, and Evening Standard, as well as 67 regional publications.

Sight won’t wait was discussed in 70 radio interviews, including BBC Radio Ulster and Global Wales
The campaign also received almost 200 hits across national, regional and
3
70
The 14 Councillors join the AOP Council to represent the diverse membership of the AOP
The AOP has welcomed 14 Councillors to its Council in designated positions.
The new Councillors were confirmed following an appointment process that ran between February and March 2023.
Appointed Councillors are:
Mehul Patel, director of a multiple practice
Kevin Thompson, director of an independent practice
Josie Evans, employee of an independent practice
Karan Vyas, employee of a multiple practice
Meera Sodha, locum optometrist
Paul Chapman-Hatchett, domiciliary care optometrist
Alisha Mann, hospital optometrist
Ankur Trivedi, independent prescriber
More than 170 online pieces were written on the campaign, including the 12 national papers, and major online media such as Sky News, ITV, AOL, MSN, Yahoo! and MyLondon
The campaign, #SightWontWait, can be found on the AOP website at: www.aop.org.uk/ sightwontwait, along with a template letter for members to contact their MP about the campaign.
Read OT’s investigation into the numbers of patients losing sight as a result of delays to treatment since 2019 at: bit.ly/3KZYJpo
170
12
Priya Tanda, pre-registration optometrist
67 REGIONAL PUBLICATIONS
Habeeb Rahman, undergraduate student optometrist
Ali Yasen, newly-qualified and early-career optometrist
Brian McKeown, optometrist for Northern Ireland
Erica Campbell-Walker, optometrist for Scotland
Kamal Kalsi, optometrist for Wales.
The AOP Councillors began their terms of office on 7 June 2023. The undergraduate student and pre-registration optometrist positions have a term of office of one year. All other designated positions have a three-year term. The full list of Councillors is available at: www.aop.org.uk/councillors
The Council is made up of 34 members, with 14 elected to represent geographical areas across the UK, and 20 Councillors with designated positions, representing the different modes of practice and career stages seen across the AOP membership.
AOP members are able to contact Councillors through the online community forums at: https://community.aop.org.uk
The in-person event will take place in November
The AOP will host a refreshed conference designed for hospital and specialty optometrists working in primary and secondary care settings this November.
Developed by the AOP alongside the Hospital Optometrists Committee, the Hospital and Specialty Optometrists Annual Conference will take place from 4 November to 5 November at Warwick University in Coventry.
The event, previously known as the Hospital Optometrists Annual Conference, was held virtually for three years following the pandemic but has now been
reimagined for 2023 to welcome specialty optometrists alongside hospital optometrists.
Organisers suggested this move recognises “the importance of bringing together primary and secondary care and offering opportunities to share learnings and best practice for the benefit of patients.”
More details about the event, including the conference programme, will be released later this year.
Members can register interest in the event to receive updates at: www.aop.org.uk/HSOC

la Your Viaion Roadworthq?
fail to meet the most basic eyesight standard for driving.
A third of those who failed the number plate test had been prescribed corrective lenses but were not wearing them at the time they were stopped.
Of the drivers who failed the Is Your Vision Roadworthy? roadside screening, 85% had their licence revoked on the spot under legislation known as Cassie’s Law
The campaign also found that 42% of drivers undertaking the roadside vision screening had not had an eye test in the last two years.
The Is Your Vision Roadworthy? campaign launched over the first May bank holiday
The AOP is supporting a new public campaign to educate motorists on standards of vision for driving. Optical bodies partnered with motoring organisations to launch the Is Your Vision Roadworthy? campaign, which encourages motorists to maintain routine eye tests to prevent their vision becoming a safety hazard. The campaign was launched to coincide with the early May bank holiday from 28 April–1 May. Ahead of the launch, 23 out of 45 police forces in England, Scotland
Read more about the campaign on OT: bit.ly/41LxgyR
and Wales carried out roadside vision screening between 27 February and 12 March, submitting data for 898 motorists, which was collated and analysed by Dr Carol Hawley, from the University of Warwick and CARGY Research.
The study suggested that 2.2% of number plate tests resulted in failure. Extrapolating the data across the number of active driving licence holders in the UK, campaign organisers said this suggests more than 900,000 British drivers would
Responding to the “deeply concerning” findings, Henry Leonard, AOP head of clinical and regulatory, suggested the figures “shine a spotlight on just how many people are taking to UK roads without meeting the legal vision standards for driving.”
“We’re committed to raising awareness of the importance of regular vision checks for driving which is why we’re delighted to be working with partners on this campaign to reinforce the message to the public,” he added.
The campaign, which was made possible by a grant from the Central Optical Fund, saw national roadside posters, media relation activity, a podcast and social media activity.
You can read and download AOP resources on driving and vision standards at: www.aop.org.uk/dontswerve










Sun-ready myopia management
Hoya has launched a sun range with Miyosmart sun spectacle lenses that combine DIMS Technology with protection from UV rays and intense sunlight, for effective and non-invasive myopia management outdoors. Miyosmart Chameleon is a photochromic spectacle lens that offers a two-in-one solution for myopia management both indoors and outdoors. Coming soon, the Miyosmart Sunbird polarised spectacle lenses slow myopia progression and provide visual comfort from sun glare in intense sunlight, Hoya explained. Both Miyosmart sun lenses are available at the same price as clear. www.hoyavision.com/uk

Dibble Optical has increased its range of children’s eyewear with a new exclusive collection, Flex Frames. The frames are designed with no metal parts and manufactured from a soft, malleable material. The frames are free from rubber and latex, BPA-free and phthalate-free, and can hold prescriptions up to +/-28. The collection includes 13 models in a range of sizes and colours. www.dibbleoptical.co.uk
Mix and match
Tomato Glasses UK is highlighting its new Mix and Match service which enables children to swap elements of frame designs to suit their own preferences. Within each of the ranges, children can select a frame front, sides, ear tip colour and headband. Parts can only be mixed within the same range. The service is offered without charge, with the company sharing: “Children love to choose.” www.tomatoglassesuk.com






Caledonian Optical, part of Duncan and Todd Group, has launched its myopia management lens solution, Imperium. The lens features two zones of positive power to induce myopic defocus in the lateral areas of the lens. The company suggested that these zones “coincide with areas of increased retinal cell distribution, thereby reducing the stimulation for the eye to elongate.” A vertically orientated zone on the lens provides the prescribed power. www.caledonianoptical.com
Want to v,ork in a store you could end up ov,ning?




Optometrist and lifestyle blogger, Lizzy Yeowart, selects striking styles inspired by iconic figures
Three sun styles worn by female style icons.

Founder of eco-friendly fragrance brand, Floral Street, on expressing her style
1
I own about 30 pairs of glasses in total. When I moved into my home, I had three drawers built into my bedroom just to house them all. My glasses of the moment are quite bold, hexagonal and fern green. I get so many compliments when I wear them. Wherever I go in the world, they certainly get me noticed.
2
I’ve worn glasses for about the last 18 years, since my early forties when my sight definitely started to change. Since then, I get a yearly check-up which is also a chance to choose new styles. I spend more on glasses than I do on jewellery. I wear contact lenses when I’m doing TV appearances, or when I’m going out for an evening.
3
You can really express your individual style and character through the frames you choose. They can enhance an outfit, boost your confidence, and make you stand out from the crowd. I think Prue Leith has put glasses on the map: she’s made it cool for mature women to have fun with their choices.
4
Glasses have become a key accessory in my life, so I have multiple. I like bold statement varifocals for the day to go with my outfits, and then for computer work and reading I have lighter weight frames with magnifying lenses. Also, I often put prescription lenses into my sunglasses so I can read when I’m on my sunny vacations.

A classic icon
The ‘Manhattan’ is an exact replica of the iconic sunglasses worn by Holly Golightly in Breakfast at Tiffany’s Originally designed by Oliver Goldsmith, this frame has gone on to inspire countless interpretations. www.olivergoldsmith.com

Royal inspiration
Referring to our late majesty, Queen Elizabeth II, this eyewear proudly recalls the frame worn by the Queen in the 70s and 80s. https://francoispinton.com

Catwalk vintage
This cool take on a vintage cat’s eye style is reminiscent of one Grace Kelly wore in the famous beach scene in To Catch a Thief www.eyespace-eyewear.co.uk
Frames
Eyewear jewellery
As part of its 50th anniversary celebrations, Prodesign Denmark has reissued the ‘Iris’ frame, first launched almost 20 years ago, in a new version for 2023. The model is available in three shapes, one based on the original ‘5104,’ a deeper square, and a big cat’s eye (pictured). The curved front has been refined to make the frame more comfortable to wear, and a new defined angle in the sides provides more adjustability.
designeyeweargroup.com
Frames
Clash of colours
J.F. Rey has released a new optical line, Whisper, a minimalist style available in a round shape with refined metal. Taking inspiration from eyeshadow make-up styles that bring a flattering ‘pop’ of colour to a look, the frames, including ‘JF3016’ (pictured), feature vivid shades with bold colour schemes contrasted against vibrant graphics on the sides. www.jfrey.fr


Frames
A spring in your step
Charmant has revealed the new Spring/Summer 2023 collection from Esprit Optical, with ‘joy’ at the heart. Styles in the collection include modern retro, thin geometric models and bold frames. Featured in the collection, the men’s contemporary rectangular ‘ET33475’ (pictured) frame is vintage-inspired and features thin sides, with 3D volume design details on the front and end pieces and an accentuated brow line with matte finish. www.charmant.com
Instrument
Precision colour
Cerium Visual Technologies has launched the latest version of the Intuitive Colorimeter, the Wave. The instrument has a re-designed and space-saving footprint, with new cloud storage capability and aesthetically refreshed and improved software. The enhanced features of the Wave allow for a high level of precision in a “robust and efficient assessment,” and also aligns with the Practical diagnostic guidelines for visual stress protocol. https://ceriumvistech.com



To feature in OT’s Hit list, contact kimberleyyoung@ optometry.co.uk



Eyewear as icons
Mondottica has introduced the Vivienne Westwood 2023 Sun Collection which draws from the timeless styles immortalised by the Hollywood starlets of the 50s and 60s. The collection includes statement frames like the ‘Ada’ (pictured), which takes inspiration from Georgian jewellery lockets, featuring intricate metal pearl-inspired detailing as a focal point.
https://mondottica.com
AI-powered design
EssilorLuxottica has launched its new progressive lens, the Varilux XR series, designed using artificial intelligence. Researchers from EssilorLuxottica gathered more than one million data points to develop a behavioural modelling system to predict how individuals with presbyopia look at objects around them. Norbert Gorny, co-chief operating officer at EssilorLuxottica, explained that with the technology, “we can now establish a visual behaviour profile for every single prescription and provide the first eyeresponsive lens that respects the natural behaviour of the eye.” https://ecp.essilor-pro.com/gb
The Body Doctor, the company behind The Eye Doctor range, has introduced an in-practice deep cleansing kit for dry eye. The Zocular Eyelid System Treatment (ZEST) pack uses patented Zokrex technology and activated natural Okra polysaccharide complexes to gently exfoliate the eyelids. ZocuSwab foam applicators are used to lift debris from the eyelid margin. www.the-body-doctor.com





































































































































Vittore and Cristiana Tormen, CEOs
Our production is 100% Italian and always will be
With our products, we cover all age groups starting from newborn babies with their first pair of glasses
We make frames that perfectly combine aesthetics and functionality. 1 2 3

Unpicking a standout frame, by OT columnist Lizzy Yeowart


Can you tell us about LOOK’s approach to, and history of, manufacturing in Italy?
LOOK was born 45 years ago in the cradle of eyewear, in the Dolomites. We still make our frames entirely here. We are siblings, the second generation of the Tormen family to lead the company founded by our father Gino. We are happy to have picked up his baton and feel the responsibility to carry it forward with commitment and passion. In our work we are driven first and foremost by a strong family bond that accompanies every phase of our life in the company and outside.
What makes LOOK’s eyewear unique?
From the very beginning at LOOK, we have tried to distinguish ourselves by an evolved vision, in which style and technique are the prerogative of a product designed to meet the user’s needs. Glasses are a product for everyday use. Comfort and lightness therefore become two essential factors. We have always stood out for the quality and authenticity of ethical, truly Italian production, that is consistent with what we claim.
Are there any new collections or projects in development that you can tell us about?
At LOOK we never stand still. We recently released our Spring/Summer 2023 collection with sunglasses in addition to prescription frames. In the past, we had sunglasses in the sample collection, and now we have a complete offer that is consistent with LOOK’s style.
Available in a wide choice of colours
3D printed frame from Götti’s Dimension collection

Eyewear is created on demand so requires fewer raw materials and means less wastage


























I“Where the responsibility lies is a key question that needs to be answered”
Professor Julie-Anne Little
joined the GOC as a qualified optometrist in 2003. Back then, while fundus photography was available, it wasn’t embedded in practice in the way that it is now. At the same time, the likes of the IOLmaster was relatively new for ocular biometry. That was the type of tech available, and everything was absolutely still on paper. Over the past two decades, we have seen a massive shift in electronic care records affecting how we work and what we can do in terms of our ability to bring everything together digitally on a patient record. Yet with developments to these electronic systems, even decades later we’re still not connected well between primary and secondary care – it’s very much a patchwork across the postcodes of how well we can connect with NHS colleagues when we refer.
The arrival of AI
Artificial intelligence (AI) is here. Machine learning assisted information is happening – it’s already what we are using in many applications on our smartphones. In terms of healthcare, research trials and outcomes continue to be shared at pace – there’s a lot of research into wearable digital tech, as well home monitoring, for example, but clinicians still play a key role in how that data is interpreted to direct patient care. There are a lot of positives that we, as a profession, could harness with AI. There is a lot of data that AI can efficiently sift out, while flagging the stuff of interest. However, for me, the uncertainty isn’t exactly in where it might go, but in the regulation that is needed around it: the ethical, regulatory and legal frameworks. It feels like this is really overdue now.

I think there is a lot of fear in the profession in relation to AI, and a sense of ‘Is this going to replace us? And is everything going to become automated?’ This is natural, and while I think part of the clinical processes will become automated, I also feel there will always be a need for the interpretation and understanding of that information. We need to be fully engaged in the quality of the information going into the algorithms to make sure they are answering our questions adequately. Where the responsibility lies is a key question that needs to be answered through these developments. Is it the company who built the machine that will be responsible for the decision-making, or is it the clinician who is deploying it and using that decisionmaking process? That is a real concern in terms of medical malpractice and clinical negligence.
The patient in focus
In terms of AI and patients, I’m certain in the future there will be developments in home monitoring. Patients could benefit greatly from tools that, for example, in the future might be able to flag when somebody is showing a sign of an issue and sending this forward to be seen. Overall, it strikes me that whilst there’s a rise in technology and its ability, there’s also a rise in the public valuing contact. People place a real value on contact and human expertise. I am confident that the profession will continue to be well-placed to provide that in the future.
Professor Julie-Anne Little is an optometrist, outgoing chairman of the AOP Board, and a senior lecturer at Ulster University.
What is your view?
Email OT with your comments newsdesk@ optometry.co.uk

AOP chair
Professor Julie-Anne Little formally handed AOP chairmanship to Emma Spofforth during the Association’s AGM on 7 June.

I“Change is coming and we must be ready for it”
Doug Perkins



have always been a keen advocate for a continuous rise in the standard of optometry. As the technology revolution unfolds, our clinical journey needs to be easier and more accessible than ever. We are living in a decade of change – I am convinced our industry is going to see more change in the next decade than in the previous 30 years, and that high quality clinicians will continue to be absolutely fundamental.
Technology is driving other options for access to refractions and product. Online fulfilment in various iterations, sight testing in pop-up booths and artificial intelligence (AI)-assisted clinical decision making already exists. They will become more prominent and accessible. Some people think this will be the end of community optometrists but in my view community optometry has a great future.
“I am convinced our industry is going to see more change in the next decade than in the previous 30 years, and that high quality clinicians will continue to be absolutely fundamental”
OTwebsite For news and insight updated daily, visit our website: www. optometry.co.uk
Language and technology
I use the term ‘AI-assisted clinical decision making’ quite deliberately because tools that make use of AI help optometrists detect disease. It’s the optometrist who must ask the right questions during the eye examination and make the decision about the management plan.
We need to support clinicians to adapt and thrive in this brave new world, and this will safeguard patient outcomes. As long as we manage change and demonstrate our value to the patients we are caring for now, they will be less likely to consider other providers or care options that may lower the standard of their overall care. We want to look after everyone we can in our communities and do more to help the health service, so there has never been a more critical time to invest in training and technology to enable clinicians to be the best they can be. We must remember that many of the refraction and screening
processes will become fully automated in this decade. Technological adoption now will allow optometrists to provide high quality eye care more readily. This includes using the power of clinical data to improve outcomes and to provide people with choice on how they interact with us. My vision is to improve both the patient and practitioner experience and allow more time for quality interactions with patients to better understand their needs and also to help them appreciate that they are in expert hands. Alternative sight testing will only become more accessible and prevalent in coming years. The only way to safeguard the public and their eye health is to raise awareness of the benefits of the expert services delivered by community optometrists.
Educating and informing patients
Optometrists need to educate each and every patient about the importance of regular eye care in their clinics, explaining the long-term benefits of good eye health care, including patients in the decision making, and demonstrating their expertise so they keep coming back. Through innovation and a proactive approach, we can keep our patients coming into optometry practices, providing them with the full scope care and experience they are seeking.
Practitioners need to embrace change. My call is for optometrists to upskill using higher qualifications and to assist in the development of those around them. A perfect example of where optometrists can make a huge difference right now is by helping to upskill and mentor their teams. As our industry transforms, we need to recognise that people are the single most critical element in delivering this change – clinicians and the teams that support them. We must develop career pathways that attract and retain strong clinical teams and leadership that brings our clinicians on this journey with us. Change is coming and we must be ready for it. Failing to adapt is not an option. We must safeguard our expertise and the eye health of our nation.
Doug Perkins is joint group CEO and co-founder of Specsavers.

R“British healthcare has all the ingredients to flourish in a technologicallydriven future”
Imran Rahman
ecent years have seen the narrative around UK healthcare dominated by discussion of high demand and slow movement, with NHS waiting lists at an all-time peak of 7.22 million. Despite these problems, Britain possesses a resource, key to rapidly advancing its healthcare offering: its dominance in the development of innovative healthtech. Through the increased use of technology, British healthcare has the potential to improve its quality while streamlining services and cutting down on waiting lists. With investment in UK healthcare technology soaring over the past decade, Britain has developed into a leading nation in the global healthtech revolution, a prominence which will be crucial in supporting the country’s healthcare services over the coming years.
Lending a robotic hand, or four…
Over the past century, medicine has witnessed an exponential progression in breadth and its sophistication; yet healthcare is far from immune to the risks of human error. The next step for medicine is to develop technology which can significantly reduce the impact of human error and knock-on delays or pressures. Through ever-improving robotic technologies, medical professionals protect their patients from human fallibility. The Da Vinci System is one such example. The four-armed robot, specifically designed for medical use, has been employed by the NHS for over two decades; yet the past few years have witnessed an explosion in Da Vinci’s usage across a vast array of medical procedures and innovative surgeries. With the increased precision they offer, these “robotic surgeons” play a significant part in reducing human error while streamlining procedures to render them less invasive, minimising healing time and further potential costs to the NHS. Beyond putting a barrier between patient care and human error, healthcare technologies can help surgeons hone
their own skills, thereby improving their own accuracy. With investment in healthtech soaring over recent years, the growing application of technologies such as Da Vinci and augmented reality will be the major factor in advancing the quality of UK healthcare into the future.
To have a tangible impact on reducing waiting lists, it is vital that British healthcare continues to advance and embrace cutting-edge technology. Alongside reducing human error, surgical robots have the capacity to minimise the risks of medical procedures – reducing the chance of complications and recovery time, and consequently freeing up hospital beds. Through technological progress, quality of care can go hand in hand with efficiency of service.
Moreover, technology can help to streamline processes across all aspects of healthcare. Indeed, since the COVID-19 pandemic, day-to-day healthcare has taken a clear step towards the digital, with over 54,500 healthcare and medical apps available on the Google Play Store by the end of 2022. With such a broad range of possibilities, these healthcare apps have the dual impact of reducing patient stress and increasing the efficiency of GPs, hospitals, pharmacies, and medical centres.
A digital future
British healthcare has all the ingredients to flourish in a technologically-driven future. By facilitating new research, improving standards of medical practice, and expediting the patient experience, technology offers an answer to growing waiting lists experienced across the UK. What is key now is that providers embrace this opportunity, exploring the myriad ways that technology can be advanced in support of medicine, ensuring a brighter future for healthcare in Britain.
Imran Rahman is a consultant ophthalmologist and CEO of CHEC.
“The next step for medicine is to develop technology which can significantly reduce the impact of human error”

“I want to help other people and increase awareness”
Michael Bayley
In 1982, I broke a pair of glasses and I went to get them repaired. They did the sight test and checked my pressures. The optometrist said I needed a referral to hospital. Over the years I was started on eye drops and then I had surgery. I received regular checks but five years ago things started to deteriorate. It was two years ago that I was registered as sight impaired. I had to stop driving and stop working.
I joined a local group, the East Cheshire Eye Society –they have social groups and walking groups. You are not on your own. You meet people with different eye conditions and you can find out how they cope with things. I have become more social than before I was registered sight impaired. It is good to have something local to me because if you have to travel a long way that is more of a challenge. When you are first diagnosed, it is a lot to take in. The East Cheshire Eye Society gave me advice on what resources were available. They were able to guide me in the right direction.
I can’t see out of my right eye at all and in my left eye I can see a small amount from the centre. The field of vision has come right in. In the early stages you can have vision loss, but you don’t notice it because your brain is adjusting. When you have massive chunks of sight loss, you notice it because one day you wake up and your vision has changed. When my vision deteriorated two years ago, it was quite a shock. Over the years I was told what could possibly happen, but even with all the surgeries and treatments, you can only slow down the sight loss for so long.
I walk into things – my vision changes in the bright light or in dull light. In my own house, I can get about because I am familiar with it. If I am reading anything it has to be magnified.
It is important that you go for your sight tests so that it can be picked up early. Make sure everyone in your family is getting their sight checked. Continue to go for your sight tests – don’t just do it once and then think you are alright. Once your vision goes, there is no cure to bring it back. It will never return to what it was.

“I feel for people who are referred to hospital and then have to wait for a long time for their appointment”
During COVID-19, the time between appointments increased. You can have a lot of damage to your sight in that time that can’t be reversed. The doctors and the surgeons were trying their best but they couldn’t get people in. I feel for people who are referred to hospital and then have to wait for a long time for their appointment. Different areas have different waiting times. I feel like eye care has been one of the things that was forgotten, to an extent, during the pandemic. If nothing is done to address the waiting list, the NHS will come under a massive strain when they are dealing with the sight loss as a result. Doing something now would save money in the long run. This is not a problem that is going to go away. If you lose your vision, it’s harder to work. There is an economic cost to the country. This should be a serious priority. I want to help other people and increase awareness about taking care of your eyes.
0
Patient leaflets
The AOP has produced a series of downloadable eye condition leaflets www.aop.org.uk/patients





43 How I got here
Optometrist and Gloucestershire LOC chair, Alvaro Borges, on his passion for health equality
45 Pre-reg focus
Isha Saghir on how technology is helping her uncover pathology in her pre-reg year

51 How do I... Engage with AI as an optometrist? With the AOP’s Dr Peter Hampson

In a roundtable discussion, hosted in partnership with CooperVision, OT investigates how practitioners can optimise the soft contact lens fitting journey both inside and outside the consulting room
How can optometrists ensure a smooth journey when it comes to contact lenses – both for their patients, and for the running of the practice?
In association with CooperVision, OT held a roundtable with four eye care practitioners to answer this multi-layered question.
Preparing for the patient
The first question for our roundtable participants is: what are the most important
things for practitioners to consider ahead of a contact lens fitting appointment?
Independent prescribing optometrist, Eleanor Hickman, makes sure she has potentially appropriate lenses for every patient before they arrive: a full trial bank with a range of lenses, which is regularly renewed.
“You can’t have something for absolutely everyone, particularly patients that have got special requirements – but you can
certainly have a good range of lenses in the practice,” Hickman said.
To aid this she has a discussion with every patient, whether existing or new to the practice, about their requirements and expectations ahead of their visit. Questions cover full or part-time wear, and what they are hoping to improve on. Hickman has a patient currently who only wants lenses for when she’s running, for example.
55 Eyes on wellbeing As calls to the AOP’s Peer Support Line grow, OTexplores bullying in the workplace
Craig McArthur, optometrist and practice owner at Peter Ivins
Eyecare, Bearsden
Jen Martin, contact lens optician at Boots
Opticians, Glasgow
Rebecca Troughton, optometrist and practice owner at Specsavers
Northallerton
Eleanor Hickman, IP optometrist at Duncan and Todd, Aberdeen.
She emphasised the importance of having a contact lens for the patient to try so they can get a feel for it, even if it is not the final one they will leave with.
“It might not be the final lens, but it means we have something to try, and that’s a good starting point for the patient’s experience, as well as for the practice, so they don’t have too many trips back and forth,” she explained.
In Northallerton, Rebecca Troughton’s practice utilises teamwork when it comes to contact lens appointments. A contact lens optician, a contact lens manager and Troughton herself take ownership of the contact lens section of the practice diary, ascertaining
whether the patient has worn contact lenses before, if there is any history, or if it is a new fit, ahead of the appointment.
A pre-visit questionnaire to identify why the contact lenses might be required allows the practice to order lenses in preparation, Troughton said.
All retail and front of house staff have been trained in the questionnaire, and it is then reviewed by a clinician who decides which lenses should be ordered.
The majority of the time, this means the correct products are in stock when the patient visits – with the exception of those with more bespoke requirements, Troughton notes.
She said: “For the 10% that need amending, it is better to experience something rather than come in and have nothing there and have to have another journey.”

Troughton also has a protocol for replenishing stock, so the lens bank does not become diminished.
“Putting a process in place for the core team who have ownership of it has made a big difference in having everything that we need there ahead of the appointment,” Troughton said, adding that this cuts the amount of time wasted and makes the best use of people’s skills.
She added: “I think patient experience has been significantly improved by having one cohesive experience in one trip.”
Craig McArthur was keen to emphasise how early preparing a contact lens patient for their appointment should start.
“The journey doesn’t start when the patient enters your practice, and it certainly doesn’t end when the patient leaves the practice,” he said. “We’ve got some really clever tools at our disposal to try and offer a more complete patient journey. You can begin communicating and educating patients before they set foot in your practice.”
He continued: “Once the patient makes the appointment, you’ve got another trigger point to communicate with them, educate them, gather
“The
journey doesn’t start when the patient enters your practice”
Craig McArthur
information about them. We do this electronically, with a lifestyle questionnaire to get a feel for what they’re going to be using the contact lens for: is it going to be daily, etc. That allows us to tailor the visit before they make the journey to the practice.”
He added: “In terms of contact lens patients, you’re trying to educate them a little bit and remove some of the fear of the unknown.”
OT asked Jen Martin about
whether she finds preparing patients ahead of the visit beneficial, and what tools her practice uses to support this.
“I think it’s very beneficial to the patient, for them to know what they’re expecting, but also for us in terms of our time expectations once the patient makes it into the practice,” Martin said.
She phones new patients to gather information on their contact lens history ahead of the appointment. The practice’s front of house team also audits the clinic to ensure stock lenses are available.
For the practice’s existing patients, she discusses contact lenses in practice and provides a leaflet that includes QR codes for training videos.
Troughton also uses QR codes to engage patients. The majority book online, she explained, so having something digital to send out is helpful.
At Duncan and Todd, Hickman uses a buddy system: patients have the phone number of a member of the practice team, and are encouraged to call whenever they have a question. If they are on a contact lens trial, they also receive a phone call after the fitting to ensure they are on track.
Hickman emphasised the importance of getting the information to the patient, either digitally or in a more analogue way, so whatever situation might arise can be prepared for.
“It’s about communication. If the person has booked online, you need to make sure you have everything you need. The last thing you

“Patient experience has been significantly improved by having one cohesive experience in one trip”
Rebecca Troughton
want is a patient turning up on the day, and you end up turning them away [without trying contact lenses]. So communication, communication, communication.”
In response to how a patient might feel if turned away without trialling contact lenses on the day of their fitting appointment Hickman added: “We know what we’re talking about. We know what a multifocal is, we know what a daily is, we know what a monthly is. But the patient just wants to be able to see. They don’t necessarily understand the complexities of what might make that difficult.”
Non-chair time: optimising the journey OT is interested in how practices can optimise the patient journey to improve their experience, and particularly in how the number of practice visits can be reduced.
Hickman has convenience at the forefront of her mind due to her practice’s rural location.
Troughton, also in a rural location, is equally as happy to have remote consultations so her patients can avoid making 30 or 40-mile round trips to visit in person. It is convenience that takes priority when decisions over
appointments are being made, she shared.
Working in Glasgow city centre, Martin also believes changes in patient behaviour come from a need to maximise time.
“It’s almost a time poverty thing,” she said. “There are a lot more people interested in whether they can have remote consultations, and if we can send things out.”
Troughton added: “Having that flexibility is the most crucial thing. It has to be patient-centred, because that’s the whole point.”
The staff in Troughton’s practice are almost all trained to teach contact lens fitting, she explained, meaning that concerns about extra practice visits [for application and removal] are almost non-existent –patients go away with all the information they need after their initial visit.
“It’s doing the teach there and then, and having all the samples ready,” she said. “That replenishment of the stock bank means that, at the very least, somebody is going to get enough lenses to try out.”
Troughton continued: “If they try them and they like them, they can sign up to have a delivery straightaway. They don’t need to come back in. In an ideal world, somebody will see us once and that should be the ball rolling
“There
from there.” She makes an exception for nervous patients who might benefit from a second teach, or for more complex cases – such as a recent RGP wearer with nystagmus.
Martin’s practice ensures that at least two people with application and removal training are on the shop floor every day, and that everyone knows who is going to be responsible for each patient as they come in.
“We’re trying to keep it out of the clinic and make sure it’s a very streamlined process for the shop floor staff,” she said.
McArthur advised having a diary for contact lens teaches alongside the regular practice diary, and using a morning meeting to ensure that enough appropriately trained staff members are available.
In terms of utilising front of house staff to support the handling and experience of contact lenses for new wearers once they have left the practice, McArthur also uses a buddy system. Avoiding drop-out is something the practice focuses heavily on, he said.
“The contact lens buddies are the patients’ point of contact,” McArthur explained. “Our front of house support staff are key to making that work.”
He continued: “The entire team is involved – it could
are a lot more people interested in whether they can have remote consultations, and if we can send things out”
Jen Martin

“The patient just wants to be able to see. They don’t necessarily understand the complexities of what might make that difficult”
Eleanor Hickman
be a dispensing optician or a clinical assistant. The contact lens buddy conducts the teaching session with some technology alongside, for example the Captiv8 platform – so they’ll have [application and removal] videos to aid the teaching session. They’ll then send those videos on to back things up. They will also call the patient the next day, to try and iron out any problems in the first 24 hours.”
A follow-up is scheduled within two weeks, McArthur said, adding: “We try to baby them through that delicate initial period of contact lens wear, because we know dropout is really high in the first couple of months.”
He noted that: “Sometimes an unhappy patient views you negatively. You might lose them as a patient if you fail to fit them with the contact lens.”
McArthur added: “These patients are really valuable, once you get them through that initial period. A longterm contact lens patient, to us, is more than twice as valuable as a spectacle wearer.”
In the chair
Troughton believes that the choice to fit on day one depends as much on the type of lens as it does on the patient themselves –Troughton would consider

the chance of infection with daily disposables, for example, or whether it is a low-risk lens.
Patient choice is the main thing, she said, although her confidence in fitting on the day will be improved “if they’re competent in their teach and they ask all the right questions, we’ve given them written information to support, they know we’re there seven days a week to get in touch, and we’ve got that rapport with them.”
Hickman will also consider whether the patient has a history of contact lens wear.
“With an existing wearer, I am quite comfortable with signing them off in a single appointment, because they know when things aren’t right,” she explained. “They tend to get back in touch quite readily if they’re not happy about something. I’m a bit more anxious about a new fit. They get a lot of information all at once.”
Follow-up calls are essential to consolidate what these patients know, she said.
Troughton agreed: “Whether you’re having that conversation face-to -face or whether you’re having it remotely, it’s important the conversation is had. Having that personal care is the reason patients stay with you. It’s an invaluable follow-up.”








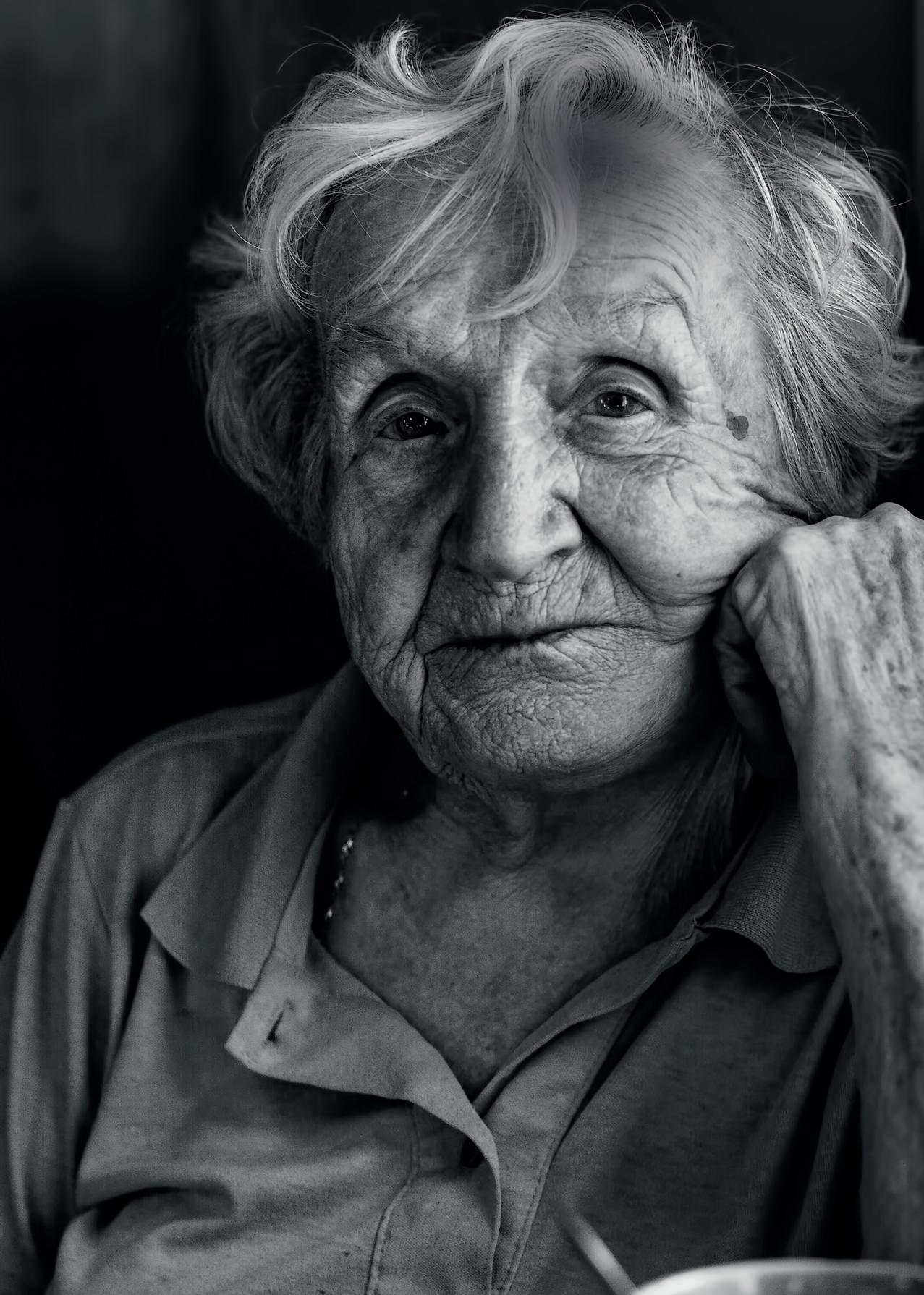
HOW I GOT HERE

“The best way to grow is to face my fears”
Optometrist and Gloucestershire LOC chair, Alvaro Borges, on his beginnings in Portugal and uncovering a passion for challenging health inequality
In Portugal, my dad started his optical career as a sales representative. When I was 16, the two of us designed and put his first practice together. Being part of that journey was exciting. There were very few graduate optometrists in Portugal at the time, and ophthalmologists dominated optics. This, together with becoming myopic, made me want to pursue a career in optometry. I wanted to examine people’s eyes and make their lives better.
In 2005, I wanted to study abroad. The rumour was that the ERASMUS programme was available to all undergraduate degrees, except optometry. I enquired with the student exchange office. There was a printing error on the guide and, in fact, there were options available. I did the first semester of my fourth year in Barcelona. I learned two languages, had lots of fun, and met my partner. I had to return to Portugal for my last semester, but I liked Catalonia so much that I secured access to the EU Leonardo da Vinci programme to do my pre-reg.
In 2009, I opened my own practice. It was the beginning of the financial crisis and it hit Portugal hard. I couldn’t have
chosen a worse year. After all the hard work and savings put into it, it was heartbreaking to endure days with few patients and dispenses. The following three years were painful. Regardless of how much effort I put into building the practice, nothing worked.
In 2012, the UK was still part of the European Union and the expertise and level of practice in UK optometry was miles from any other European country. I had a sister-in-law in the Midlands, so I thought, ‘I’ll try my luck. I’ll go to the UK.’
I came to the UK without any prospects. The General Optical Council (GOC) was thorough in understanding my level of expertise. That reassured me that they had a strict process in place, but my anxiety was through the roof. I was living in the UK, with no guarantee that I would be able to practise here.
The GOC asked me to do a hospital placement. For two months, I called all hospital eye departments within 100 miles, every single day. Eventually, I found an orthoptist who helped me. I attended clinics in all sorts of ophthalmology specialties, orthoptics, and advanced
contact lenses. That was an interesting time and a steep learning curve.
At the same time, Specsavers in Cheltenham had a vacancy for an optical assistant. The workplace atmosphere was excellent. Soon after, my qualification was recognised and I started working as an optometrist. I’m grateful to the practice: they were willing to take me in as an optical assistant and later as an optometrist while I was still doing my optometry title conversion.
My interest in reducing health inequality came because of a particular incident. I was working in practice when, during my lunch break, I approached a rough sleeper. I kneeled to talk to him, and noticed a right hypopyon with severe hyperaemia. I arranged for him to be treated the same day. This experience made me think about inequalities in eye health. I realised that people who suffer from health inequalities are less likely to seek care. We need to reach out to them and make sure they have easy access to the care they deserve.
In May 2022, Gloucestershire Integrated Care System (ICS) was the first in England to fund a homeless eye care clinic. The project was initiated by the Local Optical Committee, with support from Vision Care for Homeless People. It provides help to people experiencing vision issues, or who haven’t
“People who suffer from health inequalities are less likely to seek care”
“My Plan B?” I could have easily gone into economics or international relations.
been able to access eye tests. The project demonstrates how early intervention can help homeless people. Since then, I’ve been advocating with the ICS for further efforts to tackle inequalities in eye care.
I am involved with IT solutions for image sharing between primary and secondary care. NHS Gloucestershire has launched a project called Community Ophthalmic Link, allowing optometrists in primary care to access patients’ hospital eye service imaging, GP discharge letters, and diabetic eye screening records in real time. This is having a positive impact, for example by leading to a reduction in referrals to secondary care.
I currently work in an independent practice two days a week, for the Local Optical Committee Support Unit as an optical lead two days a week, and have chaired the Gloucestershire LOC since 2019. In my free time I volunteer at the Gloucester homeless eye clinic. I am also a father of three and I value spending time with my family.
So far, my career has been marked by pushing the boundaries. I’ve learned that the best way to grow is to face my fears, push outside of my comfort zone, and keep moving forward. This is true for both my personal and professional life.

Our latest breakthrough in managing myopia progression
Myopia is becoming more common every passing year, with clear trends showing higher prevalence in the younger population. 1 As we are sure you know, the healthy development of a child's eyes is crucial - it shapes their future.
As industry leaders, our latest innovation to help address this growing issue is ZEISSMyoCare - our first age-specific myopia management portfolio with lenses designed to help slow down the progression of myopia.
The ZEISSMyoCare range consists of two lenses:
MyoCare - for children younger than 10 years of age. Shows an average emmetropic progression ratio for axial length of 63% 2 for children aged 7-9 years.
MyoCare S - for children aged 10 years and above.
ZEISSMyoCare S shows an average emmetropic progression ratio for axial length of 86% 2 for children.
Both lenses come with full UV protection, and feature aesthetically appealing ring-like microstructures as a functional zone.
100% of children wearing this range of lenses confirmed that they adapted to them within 1 day.3
ZEISS MyoCare average absolute reduction of progression: Reduced spherical equivalent refractive error by -0.22D. Reduced axial length progression by 0.14mm
ZEISS MyoCare S average absolute reduction of progression: Reduced spherical equivalent refractive error by-0.33D. Reduced axial length progression by 0.13mm
The innovation within

C.A.R.E.® technology
Patented Cylindrical Annular Refractive Elements (C.A.R.E.®)induce alternate defocus and correction zones expanding towards the periphery of the lens. These microstructures mean additional power is added to the base lens power and induces the intended relative myopic defocus.

A unique point-by-point, free-form optimised back surface aimed to minimise the hyperopic defocus to maintain the patient's refractive correction as well as the intended myopic defocus for all gaze directions.
The ZEISSMyoCare lens portfolio is built on more than a decade of ZEISSinnovation and experience in myopia management, in collaboration with optical experts, eye care practitioners and academics. These lenses incorporate scientific concepts from proven scientific research, evidencebased learnings and effective treatments.
If you believe in offering the best to your patients, offer ZEISS MyoCare.
Get in touch with one of our specialist team on 0121 332 4400 or email us at customercare.vision@zeiss.com
1 HoldenBA,et al. GlobalPrevalenceof Myopiaand HighMyopiaand TemporalTrendsfrom 2000 through2050. Ophthalmology.2016 May;1Z3(5):1036-42. 1 Age-weightedabsoluteeffects.1 Theefficacyof the MyoCarerange hasbeen scientificallyestablishedviaa two-year prospective,double-blind,randomizedcontrolledclinicaltrial lead by WenzhouMedicalUniversityEyeHospital,China,2021, on 78 myopicchildrenwearingZEISSMyoCareRxlenses, 72 myopicchildrenwearingZEISSMyoCareS Rxlensesand 76 myopicchildrenwearingZEISSSingleVisionlenses for 12 months.(Unpublishedresults.)
PRE-REG FOCUS
Pre-reg optometrist, Isha Saghir, explains how she has adapted to the use of technology in the practice setting
The use of technology in practice improves the efficiency of eye care services and provides significant benefits for patients and the multi-disciplinary team involved in their care.
Technology aids with early detection, prompting early intervention, documentation of disease progression, accurate referrals, and patient education, as they can visualise and process the information they’re given about their ocular health.
In my practice, we have an Optomap and optical coherence tomography (OCT). The Optomap allows for a widefield view of the retina without the need to dilate, which has proven useful if a patient is unwilling to be dilated or where dilation is contraindicated.
The OCT provides deeper scans, showcasing the layers of the retina, aiding accurate diagnosis and efficient referrals. They both provide a method of documentation and are non-invasive, quick, and easy to perform.


The skill of accurately interpreting scans requires practice and experience, which was challenging as these are both things that come with time. Due to the detailed nature of the information provided, I found it best to start off familiarising myself with simpler scans showing healthy eyes, so when I was presented with an abnormal result, I would be able to spot the anomalies more easily.
“The
skill

to familiarise myself with the limitations of practice equipment, to allow for realistic expectations.
Aiding diagnosis
I saw a patient a few months ago who had attended for a routine eye examination with no presenting symptoms, so when it came to performing Volk, I was not expecting to see anything abnormal.
However, the patient had two retinal holes in
of accurately interpreting scans requires practice and experience, which was challenging as these are both things that come with time”
I also found it beneficial to be able to interpret images for more common ocular complications, for example, dry versus wet age-related macular degeneration, cystoid macular oedema, and vitreomacular traction, before expanding my knowledge to more complex cases. As good as technology is, it has its limitations. It was useful
I was able to adapt to my practice’s clinical technology by... being open minded about learning a new system in a new environment. I hadn’t worked at Vision Express beforehand, so it was a great learning curve, but thankfully welcome sessions were available. My level of learning has become more enhanced with use of the OCT machine, providing me with a more in-depth understanding.
the extreme temporal periphery, one superior and one inferior, with vitreous traction between the two. This was the case in both of her eyes, and was completely unexpected for both the patient and myself.
When I was explaining my findings and management to the patient, I was able to show her exactly what I was
I am currently working towards... completing my Stage 1 journey. Later, I will be studying for Stage 2 and focusing more on what clinically interests and challenges me for further learning. I would love to widen my knowledge as much as I can whilst on placement.
I am most looking forward to... covering my competencies, and having more clinical
Education Library
OT’s Education Library contains CPD and Skills guides on 31 topics www.optometry.co.uk/ education-library
talking about. The Optomap proved extremely useful, as it fully documented my concerns and helped me show them to the patient. It also helped me to perform a swift referral.
I referred the patient urgently due to the size of the retinal holes and the accompanying vitreous traction. She returned a few weeks later to update me on the laser the hospital eye service had performed, and was extremely grateful for the services provided.
My practice does not use artificial intelligence currently, however it has been discussed. I think it is something that will be a great tool to improve diagnostics and potentially initiate earlier intervention, as algorithms can be used to aid with early detection of common ocular pathology.
At the time of writing, I am preparing for my Stage 2 assessments, which are both only a few days away. I am aiming to sit the July OSCEs, which does seem like an achievable goal.
0
discussions and interactive sessions at the training days in Nottingham. Moving into Stage 2, and continuing to deepen my understanding of the various coding languages I’m learning, such as Python and JavaScript, to help me potentially move into the IT optometry sector in the future.
RochelleAndersonisa pre-registrationoptometrist atVisionExpressChiswick



UI Tn A® contact L I rv----\ lenses with >MoistureSeal®TECHNOLOGY


really nervous. You think, ‘Oh, what have they got?’ But once you get used to it, after the first day, you’re fine.
“I don’t think I’d ever go back into full-time work”
Locum optometrist, Aneesa Saleem, tells OT about the learning curve she has experienced working for herself
Before I became a locum... I was working as a resident optometrist locally, in an independent practice. It was a quiet practice, and they didn’t need an optometrist as much as I wanted to work at that point. I wanted to see, with locum work, if I could find work close by, and if I could pick when I wanted to work.
When I started as a locum, I wish I had known… That local optical committee (LOC) websites tell you how to do referrals. If you look on an LOC website and type in whatever area it is, the local committee will have information about referrals.
I didn’t know this existed initially. I’d rely on people to tell me, and not everyone knew. It would be very difficult. You panic. You think ‘oh, how
do I do a referral? No one knows.’ I’d try and get in contact with optometrists who had worked in the practice previously, to get guidance on what to do. When I realised the LOC websites existed, I started finding the local pathway for the area that way, and then it was so much easier.
The person who has helped me most in locuming is…
My husband. He started locuming before I did, so he would give me tips.
My biggest locum challenge is…
When you’re new to a practice and there’s lots of new equipment, especially optical coherence tomography. You need to figure out how to use each different programme. Equipment is the biggest thing. Walking up to the practice, sometimes I get
“With my little boy, I try and work on the days he’s at nursery, so I’m not missing out on him too much since he’s there for a chunk of the day”
Practices can make life easier for locums by… Not starting them with the patient right away. Give them half an hour after the opening time.
While I arrive early, practices don’t always open early, so you don’t get in until 9am anyway. If your first patient is booked in for 9am, you’ve got to just get on with it. So maybe start a little bit later, or let the locum start a bit earlier, just so they can get used to everything – especially if it is a new practice for them.
My favourite thing about being a locum is… Convenience. With my little boy, I try and work on the days he’s at nursery, so I’m not missing out on him too much since he’s there for a chunk of the day.
I don’t think I’d ever go back into full-time work. Maybe when he’s at school, if I can get a school hours job. It’s okay while he’s in nursery, but when he gets to school it might be a bit more difficult. I don’t want to be working weekends then, because he’ll be at home. At the moment, I can work when I want to.
As a locum, I’ve adapted my days by… Getting up earlier. Because I was working locally when I was a resident optometrist, I could wake up later. Now I’m slightly further out, often locuming in Stoke-
About Aneesa 0 0 0
Name: Aneesa Saleem
Location: Birmingham
Locum since: 2016.
on-Trent and travelling from Birmingham, so it involves waking up early.
The biggest difference between being a resident optometrist and a locum is… When I was a resident optometrist, I could follow up on patients whenever I wanted. As a locum you’re not guaranteed to come back, so you can’t book them in for a different day. All your referrals have to be done. It’s difficult leaving them for someone else, because then they’ve got to figure out why you’re dilating them, or why you’re doing certain things. If you’ve got it all done in one day, it’s easier in the long-term – but it is hard, because everything has got to be done right then that day.
The one thing I would change about locum work is...
Because I’ve completed postgraduate certificates in medical retina and glaucoma, if there were specific clinics I could be involved in, I would be. If they existed, that would be nice for locums. But I don’t see many opportunities. I think they are more for resident optometrists in hospitals.
AOP support
If you are thinking about becoming a locum, and want to talk this through in more detail, contact regulation@aop.org.uk























Taking on two practices, starting a conversion course in optometry, handling a pre-Christmas break-in, preparing for summer exams, planning a move 260 miles north: it’s all in a year’s work for Simon Hyde, new owner of West Sussex’s Direct Optical.
In May 2022, Hyde took on Direct Optical’s two practices, in Worthing and Littlehampton. He had previously worked with the practices as a locum dispensing optician, which helped when the question of taking over arose.
The previous owner “wanted to find a person with the right attitude toward his patients,” Hyde said. He explained: “I had worked with him for a couple of years. He was happy with the way I was treating his patients. He could see that his legacy could continue.”
Practice ownership is the latest in a string of roles that Hyde has held in optics. His career started three decades ago, when he began as a trainee technician at Salisbury Specsavers in January 1990.
Alongside practice ownership, in early 2023 he enrolled on a distance learning conversion course in optometry – something that he felt was essential if he was to succeed as a practice owner.
“I’ve been in optics for 32 years,” Hyde explained. “I’ve done every level, aside from optometry. I could have
“I’m quite a procrastinator, and if
I can leave it, I will. I’ve had to learn, in business, to do it straightaway”

thought. I thought I knew everything about optics, but I knew nothing about the accounting side of it.”
Looking ahead
BECOMING A BUSINESS OWNER
“If you’re not pushing yourself, you’re going backwards”
Simon Hyde, new owner of Direct Optical in Worthing and Littlehampton, on how he is balancing business ownership with an optometry conversion course
stayed as a locum dispensing optician until I was 70 years old, or [I could] take the plunge. It had always been an ambition.”
Taking on the optometry course at the same time as the practices was, he said, “potentially ill-advised –but if you’re not pushing yourself, you’re going backwards.”
He added: “I had wanted to do the optometry conversion course for a long time. It’s the last brick in that wall of experience, from being a trainee technician 32 years ago, all the way through to technician to optical assistant to dispensing optician to manager to director. The last thing to do is optometrist.”
In Hyde’s own words he has, in recent months, had “literally as much going on as possible.”
An early annoyance was a break-in at Direct Optical’s Worthing practice, which happened three weeks before Christmas and saw entire frame collections from Oakley and Ray-Ban being taken. Diplomatically,
Hyde describes the burglary as “badly timed.”
Moving on, does he feel that having already been self-employed as a locum helped him in the early days of practice ownership?
“Being a locum assisted me in understanding staff and locum needs,” Hyde said. “Because I’ve been in their position, as a dispensing optician, I understand their frustrations a lot more. I know you need to have consistency to know where you are.”
But his new venture is entirely different to being a sole trader locum, he shared.
“It’s been a massive learning curve. From the accounting side, it’s been much more than I
As he marks the one-year anniversary of owning Direct Optical, Hyde’s next few months are unlikely to be any less busy: he is currently preparing for his summer exams, after which he will move from Brighton to Bradford to begin his fulltime optometry course.
He plans to travel back to the south coast at weekends for the 10 months that he will be based in Yorkshire.
A cautious rebrand is also planned for the summer, and Optix software has recently been installed at the practices.
Aside from everything else, a new location is also planned for the Worthing practice – from its current home in east Worthing to a more central location, which will allow for a second consulting room to be opened – which Hyde will also be able to use during his pre-reg.
“That is going to be another challenge,” Hyde said – although, like everything else, it doesn’t appear to be one that has any prospect of phasing him.
0
Three tips on new business ownership
1 Prepare for admin: “You have to start from scratch, and cross the t’s and dot the i’s on everything. That has been the biggest learning curve.”
2 Avoid procrastination: “If you leave things for later, it becomes overwhelming. You’ve got to chip away at it. Try not to let things mount up – deal with them at the time.”
3 Don’t worry about not having a business partner: “Decision making is much easier because I’m not having to run it past anyone else.”

OT presents a clinical scenario to three of its resident IP optometrists. Here, we consider a contact lens wearer with a photophobic and painful eye and corneal infiltrate
Farah Topia, AOP clinical adviser, IP-qualified: 2016. 0 0 0
Kevin Wallace, AOP clinical adviser, IP-qualified: 2012
Ceri Smith-Jaynes, OT clinical multimedia editor, IP-qualified: 2018
The question:
A daily contact lens wearer presents with a photophobic and painful right eye. She last wore her contact lenses yesterday morning and removed them due to discomfort. Slit lamp examination reveals a 1-2mm round corneal infiltrate with indistinct edges, which does not stain with fluorescein. The anterior chamber is quiet and the visual acuity remains good. How would you manage this patient?
OT’s panel says... Kevin Wallace (KW): The most important thing in a case of a contact lens wearer presenting with a sore eye is to rule out
microbial keratitis. If the lesion is small, not central and there is no anterior chamber reaction, then it is likely that it is a sterile infiltrate, but in the early stages the signs and symptoms can be similar.
It is very important to monitor the patient closely, particularly over the next few days, and you should have a low threshold for seeking advice if the condition worsens.
This patient has already done the most important thing, which is removing the contact lens. She should be instructed not to wear them again until the eye has fully healed. It can be useful to keep the contact lens (and case if they are reusable) in case they need to be cultured.
Ceri Smith-Jaynes (CSJ): I agree. My management on this would depend on how bad the symptoms are and whether I’m around for the next 48 hours to keep in touch with the patient. Contact lens associated infiltrates tend to cause a foreign body sensation rather than pain, so I’m already a bit twitchy about this one.
I would always keep Acanthamoeba, bacterial keratitis and fungal keratitis in mind in these cases. Size matters too: this one is a bit big for an infiltrate, but then it doesn’t stain and there is no anterior chamber activity, which is a good thing. If there was any lid swelling or discharge, that would tip me over into immediate referral. I would have to see it and talk to the patient myself, but I think this one is just an infiltrate, which is inflammatory rather than infective. Lubricant drops can help with comfort and, if I am right in the diagnosis, it should be getting better over the next 24 hours, not worse.
I would leave the chat about contact lens hygiene and blepharitis management for the follow up appointment. We would need to consider the fit of the lens too – is it too tight?
“Contact
lens associated infiltrates tend to cause a foreign body sensation rather than pain”
Ceri Smith-Jaynes, OT clinical multimedia editor
Farah Topia (FT): I am in agreement too. In all likelihood, this is a sterile ulcer, but as the differential diagnosis is microbial keratitis, we would need to watch very closely.
I would ideally review the patient at 24 hours and then again at 48 hours to ensure that there is no further pain, redness, discharge or anterior chamber activity. If it is a sterile ulcer, most signs and symptoms would have resolved by 48 hours. It is also more likely to be a sterile infiltrate if this has happened before, so an awareness of the history is useful.
This could also be marginal keratitis, and I would have a good look for any signs of blepharitis as a potential underlying cause. I might also suggest a lubricant to help with the symptom of discomfort in the short term. The key message is to keep a close watch with this one.
For more information
If you are unsure about managing a scenario in practice, email: regulation@aop.org.uk
If there is a scenario that you would like to hear our IP optometrists’ views on, email: lucymiller@optometry.co.uk
Clinical director at the AOP, Dr Peter Hampson, provides an introduction to the often complicated subject of artificial intelligence HOW DO I...
John McCarthy, a computer scientist from Stanford University, defined artificial intelligence (AI) as: “The science and engineering of making intelligent machines, especially intelligent computer programs. It is related to the similar task of using computers to understand human intelligence, but AI does not have to confine itself to methods that are biologically observable.”
As a healthcare professional, you might be wondering where you can go to learn about AI in this area specifically. As you might imagine, there are plenty of online resources.
Those provided by IBM are a good place to start. They cover basic definitions and offer some free courses and training materials, including how AI can work in healthcare and why healthcare organisations are choosing to utilise it.
AI in optometry practice
The short answer to whether any optometrists are already using AI software in practice is yes, but this might be so simple as to be slightly

misleading. There is a natural instinct to think AI is new, but it isn’t – in fact, many optometrists will have been using basic versions of AI for many years. Take, for example, visual fields testing and the commonly used algorithms built in to speed up the testing process. This is an example of AI.
We are starting to see the first commercially available products that can help to analyse optical coherence tomography (OCT) data and spot defects. You might have this or similar software in your practice already.
Ethical concerns
The ability to do anything about ethical concerns in AI is not in the control of AOP members. The ethical questions involve much wider issues that society is grappling with.
Some of the risks in this area include:
Bias in the AI software, based upon the training data used: Is your patient accurately represented within the training data the AI has used to ensure that the answer given is correct? This may not always be the case
“The short answer to whether any optometrists are already using AI software in practice is yes, but this might be so simple as to be slightly misleading”
Further reading
Read more articles from our extensive How do I... series on our website www.optometry.co.uk/ how-do-i
The Government’s AI regulation: a pro-innovation approach white paper: bit.ly/435emE6
From the AOP: What lies ahead: The promise of technology: bit.ly/3KcjbCW
From IBM:
What is artificial intelligence (AI)? https://ibm.co/3KxF3do
How AI is impacting healthcare: https://ibm.co/3U9JSg2
What is artificial intelligence in healthcare? https://ibm.co/3Gi1DnE
Access for all parts of society, regardless of ability to pay: A number of emerging AI applications involve the assessment of OCT scans, but what if the patient can’t afford the scan? This might mean they cannot benefit from the earlier diagnosis that OCT, in combination with AI, may bring The risk of not understanding the technology, or its limitations: Specsavers refers to AI internally as ‘supported decision making.’ But when do you pay attention to its advice, and when do you ignore it? What does ‘being a professional’ mean if you start to defer decision making to technology? This is another question that does not have a straightforward answer Regulation: The Government has recently
launched an AI regulation white paper which appears to favour a light touch approach. This is linked to the previous point: if you do not understand what the AI technology is doing and it ultimately gets it wrong, who should be responsible? The technology provider, or the professional utilising it?
These are the questions that as a profession and as a society we must address if we are to make use of AI and not simply find ourselves being used by it. Of course, this means a longer and more in-depth conversation than one that is likely to take place between optometrists at a practice level.
Get in touch
For further information, contact the AOP’s regulation team on: regulation@aop.org.uk













“Our goal is to help, because AI cannot ask all the questions”
Chief medical officer at Altris, Maria Znamenska, explains how software that uses AI to speed up interpretation of OCT scans came into being
01 Altris was founded in 2017. We had two years of development, and in 2019 received the CE mark as a medical software in the European Union. Customers felt more secure once we had this confirmed. For a conservative field such as medicine, and for optometrists and ophthalmologists, it’s sometimes hard to accept new technologies. When they see the certificates, and that it is developed by a team of retinal experts on a data basis, they feel safer and are more comfortable trying it. Sales grew after that. We now have users from more than 140 countries.
02 During COVID-19 we were still working, but maybe not as fast as we had planned. The development of Altris AI never stopped, it was just a bit slower in those years. When I look back on all that we went through, we did a great job.
We have lots of people working for Altris from Ukraine. We had a pause in our work when the war started, for the first couple of months. Some people left, and some people relocated inside Ukraine to safer cities and regions. Some of our team members are now in different countries.
Post-COVID-19 and despite the war, we have made huge improvements during the last year. We are not going to stop. We will continue building this product. It’s like a train; we are just moving forward.
03
We then give this data to our artificial intelligence (AI) specialists. When they build new features they show us, and we make an evaluation. If we see results that we are not satisfied with, we recollect data.
Our team is not small, but it’s not a huge corporation where it takes years to approve anything new. We are doing things quickly. We are continuously improving the numbers, accuracy, and usability.
It’s our everyday work to improve. We are continuously listening to our customers. They give us ideas, and we consider if we can do them.
04
Altris AI accounts currently active in the UK
100% Optical 2023 was our first time at such an exhibition in the UK. We were met with a great interest from the industry. Not only eye care specialists, but also from optical coherence tomography (OCT) manufacturers and other people. We were pleased to see that what we are doing is interesting to people, and that it could be useful.
05
We are continuously improving our software. We update our tools every two weeks. No product can be perfect, and we understand that.
The main goal of our ophthalmology clinic in Kyiv is data collection and annotation by retinal experts.
“My wish for all eye care specialists is not to be afraid of using new technology in their everyday practice”
Our next step is to improve the product we have today: improve the accuracy of detection of more pathologies. For the commonly observed diseases we are pretty good, but there are some diseases that are not seen so often, so we are always working on improvement. We have an idea around glaucoma risk analysis, and this is what we are working on.
AI can detect minor pathology in the very early stages. Also, it can provide
risk analysis. We can recommend that the patient follows up more frequently. Our goal and our dream is to make more of those early diagnoses, where we can prevent or treat diseases in the early stages, while they still can be treated. In the late stages, unfortunately, sometimes things cannot be treated. We don’t want to see patients with irreversible blindness.
06
We are currently in the FDA approval process, where Altris AI is being considered as medical software for the US market. My wish for all eye care specialists is not to be afraid of using new technology in their everyday practice. I understand this is something new, and new things sometimes look scary. But we need to understand, whether we want it or not, that new technology is around us today. We need to use it to improve our practice. Using these new technologies is a win-win situation for everybody: for the patient, who is diagnosed in time, for the eye care specialist, who has a second opinion, and for the whole eye and healthcare system, because of correct referrals and triage of patients.
The main question that everyone asks is whether AI will replace doctors and optometrists. No, it will not, and this is not our goal.
Our goal is to help, because AI cannot ask all the questions. It doesn’t have all the other information that can be gathered by a clinician. There is no reason to be afraid of such things. We need to use it and take the benefits from it.












In 2022, bullying entered the top five issues discussed on the AOP’s Peer Support Line (PSL) for the first time. Worryingly, bullying now makes up 10% of all calls received by PSL volunteers.
Here, OT outlines how you can identify when bullying is taking place at work, how to take proactive steps to deal with it, and when bullying might cross the line into discrimination.
The Advisory, Conciliation and Arbitration Service (Acas) defines bullying as “unwanted behaviour from a person or group that is either offensive, intimidating, malicious or insulting,” or “an abuse or misuse of power that undermines, humiliates, or causes physical or emotional harm to someone.”
The bullying could be regular or one-off, happen face-to-face or on channels such as social media or on the phone, and happen either at work or in nonwork related situations, Acas goes on to say. The organisation adds that incidents do not have to be noticed by other people to be classed as bullying.
The NHS says that: “Bullying is not always a case of someone picking on the weak. Sometimes a person’s strengths in the workplace can make the bully feel threatened, and that triggers their behaviour,” adding: “Bullying can make working life miserable. You can lose all faith in yourself, you can feel ill and depressed, and find it hard to motivate yourself to work.”

As the number of calls to the AOP’s Peer Support Line related to bullying increases, OT looks into how to handle the issue in the workplace
Examples could include a colleague putting you down, undermining your authority, or spreading rumours about you, or a manager giving you a heavier workload than other people, Acas says.
SupportLine adds that constant criticism, shouting, intimidation and harassment, withholding of essential information, using offensive or threatening language, removal of responsibilities, wrongly placing blame and setting unrealistic standards are other potential examples of bullying in the workplace.
Mind advises looking into your workplace’s bullying policy initially, before trying to resolve the issue informally, possibly utilising a colleague who you trust to discuss the issue with the person you believe is bullying you. You should retain evidence of the bullying to support your accusations, as these will be required if you take
the issue to HR or your manager. If you do not feel comfortable speaking to someone at work about the issue, Mind suggests seeking independent advice – possibly from visiting the Acas website, or calling the service’s helpline.
Likewise, the NHS advises staying calm, attempting to speak to the bully in case their behaviour is not deliberate, and keeping a diary to record incidents before progressing to a formal complaint. If the situation does continue and you decide
to raise a formal complaint about the individual or individuals you believe are bullying you, your workplace should have a policy that can guide you in how to do this.
The Acas website also has a large number of resources for those who might be experiencing bullying at work.
When bullying becomes discrimination
As seen in OT’s Time to Speak series, optometrists are often at risk from discrimination in the workplace – both from members of the public and from colleagues. Acas identifies when bullying might cross the line into discrimination. Via the organisation’s website, you can find answers on discrimination at work in general, as well as around disability, age and religion, and equal pay. The site also outlines how discrimination at work is covered by the Equality Act 2010. The Acas site also has guidance for employers on what they should do if a bullying, discrimination or harassment complaint is received by an employee, including their duty of care responsibilities.
The AOP provides members with access to a range of wellbeing resources and expertise
Call the Peer Support Line on 0800 870 8401
Read the AOP’s resources on managing stress at work: www.aop.org.uk/stress
Read OT’s article on tackling bullying in the workplace: bit.ly/44dfiqi
If you believe you have or are being discriminated against at work, contact the AOP’s employment team for advice on employment@aop.org.uk


'


20 Individually Wrapped Pre-Moistened Towelettes


From putting data in the hands of patients to predicting which children will develop high myopia, OT explores the potential of artificial intelligence technology for eye care





On 11 May, 1997, world chess champion, Garry Kasparov, caught the elevator to the 35th floor of a skyscraper in Manhattan. He took his place at a table with two small flags, a chess board and his opponent: IBM supercomputer Deep Blue.
“I had many emotions sitting down,” he later told the podcast, In Machines We Trust.
“It was hard to explain my experience because I was really the first worker to have my job threatened by a machine,” he said.
Kasparov explained that he was accustomed to reading the body language of his opponent. He would prepare for each match by studying the previous games and tendencies of the rival player.
But Deep Blue was a blank slate, coming up with moves that the computer engineer who built it did not understand.
“It’s easy for a chess machine, after all. They don’t care if they win or lose. They don’t even know they’re playing chess,” Kasparov said.
Deep Blue beat Kasparov in six games, becoming the first computer to beat a human in a traditional chess tournament.
More than two decades later, artificial intelligence (AI) has become integrated into the fabric of daily life. It is there at the supermarket checkout, on the phone in your pocket, a disembodied voice on the kitchen benchtop telling you might need a jacket as well as a jumper as you walk out the door.
Within eye care specifically, the first AI-based medical device to receive US Food and Drug Administration approval was a tool for automatically grading retinal
images named IDx. Deep learning has been applied to fundus photography and optical coherence tomography (OCT) scans to detect diabetic retinopathy, glaucoma, age-related macular degeneration and retinopathy of prematurity.
With advances in AI, some clinicians will empathise with Kasparov’s concerns when he sat across the table from Deep Blue –would this computer replace him?
An article published in the Journal of Optometry in 2022 described the views of 400 US optometrists on AI.
While the majority (72%) agreed that AI will improve the practice of optometry, one in four expressed concern that AI would replace providers.
You would forgive Kasparov, who walked away from his 1997 defeat without talking to reporters, for holding a grudge. But decades later Kasparov is a strong advocate for the potential of AI.
“Technology doing our work is the whole history of human progress,” he told the In Machines We Trust podcast, hosted by Jennifer Strong. “It’s a tool and makes us smarter. The way a
telescope augments our vision –what matters is how we focus it,” Kasparov said.
For optometrist Dr Stephanie Campbell, a formative experience that illustrated the potential of technology occurred when she was testing the vision of a young boy with Down’s Syndrome while completing her PhD at Cardiff University.
Campbell was struggling to test the vision of her patient without glasses, when he reached for her iPad and started searching for videos. “He could find the YouTube icon but when he got into YouTube, he couldn’t really see much detail,” she said.
Campbell began to wonder if she could develop a video game where patients would tap on the objects that they can see. Technology that could be used from the comfort of a patient’s home would also lessen the stress that some patients feel when attending a sight test.
“If we could gamify the measurement of vision, it makes someone less nervous, and you actually get better data when the patient is relaxed,” Campbell explained.
After discussing the idea with software engineers at an NHS Hack





Day in Cardiff, a prototype was developed and eventually patented in 2015.
A decade after the sight test that first inspired her, Campbell leads Okko Health – a company with 20 staff based in London and Bristol that develops home-monitoring apps for measuring vision. During the development of the technology, Campbell has become aware of the variety of measurements of visual function that can be assessed using an app – including colour vision, distortion, motion perception and contrast sensitivity alongside visual acuity.
“I think the penny drop moment was when we realised that this is a visual sciences lab in everybody’s pocket,” she said.
“If we can do this really well and get it calibrated, then the discoveries that clever people in universities have made over decades can be translated for patients who would never usually have access to those diagnostics,” Campbell explained.
Home monitoring for AMD
Campbell presented results from an initial pilot of 50 AMD patients using an Okko Health app to monitor their vision at the Association for Research in Vision and Ophthalmology annual
conference in 2022. The pilot found that the Okko Health app was a feasible method for monitoring visual function at home, and there was good adherence among the Nottingham Hospital patients who downloaded and registered with the app.
A new study will see 500 AMD patients across Oxford Eye Hospital and Nottingham Hospital testing their vision at home three times a week with an Okko Health app.
Society provided feedback on everything from colours and fonts to the images used within the app.
“It was a delight and it continues to be – that we built this technology with the people who are going to be using it,” Campbell told OT.
The average age within the volunteer group was 77. As the user experience testing was conducted during lockdown, it occurred over video calls – many volunteers had learned to use Zoom in order to communicate with their grandchildren.
Campbell highlighted that the aim is for the Okko Health app to flag deterioration of disease so the patients who need care are seen in hospital sooner.
The app also provides reassurance to those who are at low risk and can self-test at home.
“The whole point of the AI we are developing is to keep people out of hospital who don’t need to be there,” Campbell shared.
“This approach is really about driving better outcomes and preventing sight loss at scale,”
“I think the penny drop moment was when we realised that this is a visual sciences lab in everybody’s pocket” Dr Stephanie Campbell
An AI algorithm will be trained using information collected through the app, alongside OCT scans and clinical information gathered in secondary care.
“Essentially this study, from a vision science perspective, is looking at whether structure and function correlate and to what extent,” Campbell explained.
Campbell describes the technology that is being developed by Okko Health as “patientdriven” AI. When the app was first being tested in 2020, a group of 100 volunteers from the Macular
she said. Campbell believes that alongside improving clinical care, Okko Health has potential to improve the patient experience. If people are able to monitor their vision at home, it gives them greater control over their lives.
“Once they know that they don’t need that anti-VEGF treatment for four months, they can plan for that holiday,” she said.
“From a patient perspective, I think we underestimate how much of a burden that eye disease is to their daily lives,” Campbell shared.
During lockdown, many people developed new hobbies – perhaps they baked banana bread or began to learn a language. Optometrist, Kishan Devraj, developed a chatbot to answer the questions of patients with genetic eye disease.
Devraj, who has been building websites in his spare time for the past decade, collaborated with Professor Mariya Moosajee in order to make the information on her new Gene Vision website more accessible.
“If you have a genetic eye condition, or you have someone in the family who has a genetic eye condition, you can have a conversation with this chatbot,” Devraj explained.
Since the launch of the chatbot, Devraj has embarked on a new project led by Moosajee called Oversight. They aim to create technology that harnesses digital activity to analyse the daily impact of an eye condition. The background data collection that occurs on smartphones – for example, step count, mobility and walking speed
– would be analysed to see if it correlates with clinical information and scans connected in the clinic.
“I thought we could take a lot of this data and compare it against fundus images and visual acuity. If eye disease is getting worse, how are these metrics from the phone changing? Perhaps we could use that as a way to assess eye disease,” Devraj explained.
Devraj shared that Moosajee initially approached him to see if an app could help to measure the impact of new treatments for genetic eye disease.
“She wanted to assess their visual function better. There were many treatments out there and there was no good way of assessing how someone’s eye disease was changing or improving,” he said.
the technology. He aims to recruit 200 patients over the course of his doctorate. Alongside readily accessible smartphone information, Devraj has received agreement from Apple to have access to more specific data such as measurement of light levels and assessing how someone uses the keyboard.



Devraj is now completing a pilot at Moorfields Eye Hospital as part of a PhD that will focus on developing
“I think optometrists should be aware that the profession is changing for the better”
Kishan Devraj
“How fast do they type? How many mistakes are they making?” Devraj said.
“With people with inherited eye disease, in certain light conditions, their mobility is less. If we could assess the amount of light on their phone and compare it with how they move around, we could tell how their eye disease is changing,” he shared. The impact of eye conditions on mental health is also explored through analysis of sleep data and the types of words that patients use in messages.
“We wouldn’t be able to extract exactly what they are saying on their messages – but we can get sentiment analysis where we can see if the words being used are positive or negative,” Devraj shared.

Although currently the project is at an early stage, in the future there is potential for AI to extract insights on disease progression.
“It will be able to compare clinical changes from results in the test room to changes in the data collected in the app,” he said.
Devraj believes that clinicians have a vital role to play in shaping AI going forward. He highlighted that many people who build technology do not have an experience of working with patients.
“I think optometrists should be aware that the profession is changing for the better and there are a lot of opportunities out there. They can get involved outside the test room. Healthcare needs you because you are at the frontline,” he said.
Professor Daniel Ting is head of artificial intelligence and digital
innovation at the Singapore Eye Research Institute.
His team developed the Singapore Eye Lesion Analzyer Plus (SELENA+) –a CE-marked deep learning system that screens for diabetic retinopathy.
Ting and colleagues have also developed two AI algorithms with applications for myopia.
The first algorithm helps to screen for myopic macular degeneration and myopic choroidal neovascularisations among adult myopes – as well as identifying those who are at risk of developing the conditions.
The second algorithm, published earlier this year in Nature Digital Medicine, uses baseline fundus imaging alongside clinical data (age, gender, race, parental myopia, and baseline spherical equivalent) to predict the five-year risk of a patient developing high myopia.
Crystal ball gazing
Ting told OT that once patients are identified as being at risk, preventative action can be taken – for example, through lifestyle, medical or optical interventions. “We have AI that has the ability to look into the future. I think this is one of the powerful things that these algorithms are able to offer,” he shared.
When it comes to mitigating the risks of relying on AI, Ting outlines three

approaches to deployment. AI can either be fully automated – where AI makes the call – or assistive, where the human stays in the loop and makes the final call.
However, in Ting’s view, a third hybrid model holds the most promise. Under this approach to deployment, AI would hold full responsibility for simple decisions, but would require oversight for more challenging or borderline cases.
Ting highlighted that as well as making the most economic sense, this approach makes use of the innate strengths within human and artificial intelligence. Human clinicians are good at recognising normal eyes – because this is what they see all day in clinic – while AI excels at identifying the abnormal.
“If you combine the strengths
“We have AI that has the ability to look into the future”
Professor
Daniel Ting
between what AI can do and humans can do that is a win-win situation,” Ting emphasised.
Ting shared that eye care is a field that has access to advanced technology and a plethora of images – which serve as a valuable database for AI.
“To me, it is like diamonds because I use this data for AI all the time,” he shared.
Ting highlighted that for AI to be effective, it is important to have comprehensive and seamless digital records within optometry
April:
JAMA Ophthalmology researchers report on an AI chatbot that scored 46% across 125 multiple-choice questions for board certification in ophthalmology
A deep learning AI model is found to be capable of identifying retinopathy of prematurity from retinal images in Lancet Digital Health
March:
Writing in eLife, scientists describe a deep learning model capable of predicting an individual’s chronological age from retinal scans with a margin of error of 3.3 years
A British Journal of Ophthalmology study of 4795 participants in China demonstrates the dependability of the Airdoc retinal AI system for detecting multiple retinal diseases in a primary healthcare setting.
January:
Authors describe a deep learning system for predicting the five-year risk of children developing high myopia in Nature Digital Medicine
Researchers outline a deep learning model for predicting the treatment effect of orthokeratology in Frontiers in Pediatrics.


practices. “We want the patients to have a one-stop service where you can access the entire eye care history that this patient has,” he told OT.
“AI itself is great, but it has to work within a digital ecosystem,” Ting shared.
As AI has developed, some clinicians have expressed concern about whether all groups will benefit from the technology equally.
Writing in the Community Eye Health Journal in 2022, Professor Andrew Bastourous and Dr Charles Cleland highlighted that the accuracy of an AI system depends on the quality and the suitability of the data it is trained on.
The authors observed that algorithms for diabetic retinopathy screening have typically been trained in well-resourced health systems that have access to large databases of retinal images.
“This further leaves behind those living in low-resourced health settings, an issue which has recently become known as health data poverty.”
optometrists surveyed for the Journal of Optometry around half (53%) expressed concern around the diagnostic accuracy of AI.
Responding to concerns around bias within AI, Ting highlighted that regulatory approval processes involve establishing whether the algorithm is generalisable. “If a company has already got approval from your local regulatory body, then I think that is safe to use,” he said.
Ting shared that a crucial part of the research and development process is establishing who the intended user of an algorithm is. If insufficient data exists for a certain group, there are AI techniques that can be harnessed to make up for this shortfall, such as federated machine learning. One of the research streams being undertaken by Ting’s lab is looking into the creation of synthetic AI – where data could be artificially generated.
Ultimately, Ting sees AI as a tool for addressing the fact that half of the 2.2 billion people worldwide with visual impairment lost vision because their condition was not detected early enough.



you could reduce that avoidable sight loss,” Ting shared with OT.
Dr Carlos Ciller is chief executive of RetinAI, a Swiss company that provides a range of software solutions to improve patient outcomes. Alongside data management – enabling the harmonisation of data from disparate sources – RetinAI has AI algorithms for the classification and segmentation of retinal disease, as well as predicting patient outcomes.

“We have progression prediction algorithms in retinal diseases, including geographic atrophy, that
“We see a major opportunity to democratise access to Dr Carlos Ciller
enable us to understand how the disease is going to evolve with and without treatment, and with different treatment regimes,” Ciller shared.
Using RetinAI’s software, clinicians can drag and drop patient data and receive a report with AI analysis. The software is certified as a medical device in the US and European markets, with AI models certified in Europe. Although RetinAI’s initial focus is ophthalmology, Ciller also sees the potential of the software for optometrists working in primary eye care. “We see a major opportunity to democratise access to expertise to evaluate complex diseases,” he said. “I think it will improve efficiencies within the healthcare system and close the gap of long wait times for treatment,” Ciller observed.
He shared his view that AI has the potential to enable clinicians to spend more time on important tasks – such as spending more time with patients. “The human touch is what matters. That is the thing that cannot be replaced by a machine,” he said.
“I think consistently what we have seen with the advent of any new technology is that jobs are a collection of tasks. Some of these
tasks evolve over time. We see technology helping optometrists and ophthalmologists to do things more efficiently,” Ciller emphasised.
Ciller sees the potential of AI for enabling screening in countries where the eye care workforce would previously not have supported this at scale.
He shared that clinicians should not be overly reliant on the decisions made by AI until they are confident that it is performing a task properly.
“At the same time, if you have certainty that it has gone through a process of validation, testing and regulatory approval, I think it is a staggered approach. You start as a co-pilot, then you move to delegating menial tasks,” he said.
Ciller encouraged optometrists to have an open mind when it comes to incorporating AI in practice. “I think AI, with the appropriate regulations, an open mindset and the right clinical environment, can do a lot of good things,” he said.
From code to clinic Moorfields Eye Hospital consultant ophthalmologist, Pearse Keane, is a professor of artificial medical intelligence at University College London. Keane shared with OT that AI will save sight by
allowing earlier detection of sightthreatening disease.
He added that the technology will also reduce the burden of chronic eye disease on patients by reducing the number of times they have to attend hospital.
“I think the main benefit of AI in eye care will be its ability to bring highly specialised expertise out of the hospital eye services and into the community and homes of patients,” he said.
While there is enormous potential for the application of AI to eye care, Keane highlighted that there can be challenges in “going from code to clinic.”
AI must be proven to be safe and effective in large clinical trials and receive regulatory approval as a medical device.“This is a very expensive and time-consuming process and – as yet – only a small number of AI systems have achieved it. There are also challenges in how these systems can be integrated and deployed in healthcare systems and questions about the business models – how much will they cost and who will pay for them?” he said.
Keane believes that the development of foundation models in AI hold potential for eye care.
He explained that ChatGPT is an example of a foundation model that

“By far the biggest advance in AI in the last few months has been the advent of large language models such as ChatGPT and GPT-4 from Open-AI, and Bard from Google
“These are effectively chatbots but their key feature is that, because they have been trained on huge amounts of data, and because they have billions of parameters, their scale gives them potential for a wide range of applications.
“These models are already being incorporated into search engines and other commonly used pieces of software. Some of these models have proven powerful enough that they can pass medical licensing or university entrance examinations. They haven’t yet been employed in eye care, but this is likely to happen very soon.”
In April, US researchers reported that ChatGPT had scored 46% answering a practice test for board certification in ophthalmology (bit.ly/3VEdaUL).

Software developed by Advanced Ophthalmic Systems


uses language, but these models can also be trained on large amounts of images and other data.
“These are exciting because they are likely to prove useful in diagnosis of less common and rare eye diseases, and because they are also likely to work better across a wide range of ethnicities and other demographic groups,” he said.
Karl Jeebaun is the chief executive of Sparca, a software development company that includes Advanced Ophthalmic Systems (AOS) within its portfolio. Jeebaun is also the chairman of the Optical Suppliers Association’s e-health focus group.
AOS provides clinicians with software that can objectively grade the anterior segment through image analysis. The software mimics the way a human brain would interpret a result if it had all the information stored in an image not visible to the naked eye. “AOS utilises a branch of AI called computer vision to enable highly accurate and repeatable, objective outcomes,” Jeebaun said. AI is also used by the company within AOS VA to monitor a patient’s distance from the screen during a remote visual acuity test.
Reflecting on how AOS technology is incorporated into practice, Jeebaun shared that many practitioners consider how technology can improve the way they work.
“For the vast majority it has really boiled down to the use case. How can technology improve, streamline or retain the current client services or processes they do manually today?” he said.
Jeebaun observed that while an increasing number of AI systems are receiving regulatory approval, wide scale adoption within optometry practices is another matter.
“Until there is clear guidance for use of this type of technology from industry then as much as professionals get excited, their default position is ‘Am I allowed to use this technology?’,” he shared.
“Getting to a point where AI is truly embraced is still a way off, in my opinion,” Jeebaun added.
He highlighted that opportunities presented by AI include reducing waiting lists and limiting avoidable
“AI in its current form is designed to assist and streamline processes not replace the practitioner”
Karl Jeebaun
sight loss, while also conserving the resources of the NHS.
Unaccredited systems that have not been clinically validated are one of the key risks that Jeebaun is wary of. “It really only takes one of these rogue systems to have a bad patient outcome and set the whole industry back years,” he said.
Through Jeebaun’s role on the OSA, he is developing a digital checklist for suppliers to understand the standards they need to meet to enter the UK market, alongside a database that buyers can use to check if a product has the appropriate accreditation.
As part of the NHS working group for eye care transformation, Jeebaun is contributing to a project to standardise digital imaging formats in order to improve interoperability between the NHS and community optometry. Jeebaun believes that the objective analysis provided by AI will lead to better outcomes for patients. “In the majority of cases, AI in its current form is designed to assist and streamline processes not replace the practitioner. The practitioner today will always have the final say on pathology, treatment and diagnosis,” he said.















C-105155
LEARNING OUTCOME
REMEMBER TO UPLOAD YOUR CPD POINTS TO YOUR MYGOC
Practitioners will understand the characteristics of good leadership to facilitate effective collaborative working.
C-105081
LEARNING OUTCOMES
Practitioners will understand how and when to explore whether a patient needs functional or emotional support following sight loss
Practitioners will understand the roles of health and social care colleagues in the sight loss sector and pathways available to patients for functional support.
DEAF AWARENESS: IT’S ALL ABOUT ACCESS
C-105090
LEARNING OUTCOME
Practitioners will be aware of the changes that can be made in practice to accommodate the needs of Deaf patients.
C-104759
LEARNING OUTCOME
Practitioners will understand how to maintain their wellbeing to help reduce stress and avoid potential negative impact on patient care. YOUR WELLBEING MATTERS FOR YOU AND YOUR PATIENTS
CASES IN CLINIC
C-104859
LEARNING OUTCOME
Practitioners will be able to assess a range of clinical cases and determine management within their scope of practice.
EXAM QUESTIONS, REFERENCES & DECLARING CPD POINTS
MCQs for OT’s CPD appear online at www.optometry.co.uk/CPD. Exams in this issue will be live from 10 June to 1 September, 2023. When taking an exam, the MCQs may require practitioners to apply knowledge that
has not been covered in the article. Visit www.optometry.co.uk/CPD, and click on ‘Related CPD article’ to view the article and references in full. In the new CPD cycle, registrants are responsible for declaring their CPD
points viatheir MyGOC account. If you pass an exam with OT,you will receive a certificate to use as evidence when declaring your CPD points. Certificates will be available to download in your MyAOP.
ONLINE FROM 10 JUNE
Jane Macnaughton PhD, FCOptom, Prof Cert LV and Professor Keziah Latham PhD, FCOptom, Prof Cert LV
IN BRIEF This article highlights the roles and responsibilities of health and social care colleagues working in the sight loss sector.
The need for assistance with daily living tasks, mobility, or assistance specifically within the school or workplace is central to any discussions that practitioners may have with their patients who have experienced irreversible sight loss. However, this may not be an area of clinical practice that is familiar to all those who work primarily within primary care. The purpose of this article is to raise awareness of health and social care colleagues within the sight loss sector, to highlight their roles and responsibilities, and to inform practitioners of the pathways of communication, so they are able to appropriately advise and signpost patients who have demonstrated a need for further intervention.
Eye care practitioners spend significant chair time focusing on the clinical needs of patients to allow them to make a timely diagnosis, and thus, an appropriate referral for onward management. However, clinical measures, such as the measurement of distance visual acuity or contrast sensitivity, do not capture an individual’s response to their vision impairment and the impact that impairment may have upon daily living. The impact of permanent sight loss varies between individual personality traits, across generations and across cultures. For example, the difficulty in reading cooking instructions or the inability to set the cooker to the correct temperature may be of high importance to one person but may have less relevance to another if they have no need to cook for themselves. Similarly, the disabling effect resulting from the inability to drive following the withdrawal of a driving licence may be devastating to one person but of little consequence to another who has little need to drive.
Unsurprisingly, alongside the functional decline in activities of daily living, sight loss is also associated with an overall reduction in quality of life, increased levels of depression, an increase in the likelihood of falls, a higher prevalence of loneliness and a loss of self-esteem.1-6 It follows that to reduce the long-term burden on health
and social care, timely support for those in need should be made available. Eye care practitioners are rarely equipped with the skill set or appropriate funding to be able to deal with such functional and emotional needs. However, it is a duty of care to be able to discuss the impact of sight loss with patients, and thus, be able to make appropriate and timely referrals to those who can. Therefore, practitioners need to know what questions to ask to be able to determine if a referral for interventions is indicated, who to refer patients to for assistance and the pathways open to be able to do so.
WHO IS ENTITLED TO
Anyone with a disability who demonstrates a need for functional or emotional support is entitled to assistance from the health and social care sector. In the case of sight loss, the majority of service providers will be vision rehabilitation specialists. There are several routes to access these services, and these will vary between the four nations and between different health boards, local authorities, or local social services departments.
One of the primary pathways to access rehabilitation services is following formal certification of sight loss from within hospital eye service (HES) departments.
Certification of sight loss as either sight impaired (SI) or severely sight impaired (SSI), refers to the level of sight loss that the individual has demonstrated, whereas registration refers to the process of that patient being added to the local register of individuals with sight impairment. The registrar may be the local authority, council, health board or appointed charity. The process varies slightly across the four nations, but the Certificate of Vision Impairment (CVI) used to initiate that process has clear guidelines on the level of distance acuity and visual field measured. The identified levels for SI and SSI certification are presented in Table 1 7
Age-related macular degeneration (AMD) continues to be the leading cause of certifiable vision impairment in the UK.8,9 Glaucoma is currently the second most common cause, with hereditary retinal disorders (for example, retinitis pigmentosa), cerebrovascular disease,
and diabetic retinopathy or maculopathy, making up the remainder of the five most common causes.10
In addition to collecting epidemiological data on common causes, or those affected by sight loss, the CVI is the most reliable route for the individual to be brought to the attention of vision rehabilitation services. However, people with a CVI may choose whether to be included in their local register of vision impairment and inclusion is not automatic. It follows, therefore, that published data of people registered as SI or SSI is not definitive and is only a guide to the true number of adults living with acquired sight loss.
While registration is necessary to apply for financial support or concessions such as tax and welfare benefits, registration is not mandatory to access vision rehabilitation services. All individuals are eligible for an assessment of needs and for care to be provided if that need is established. Therefore, those who are struggling with early sight loss who may not meet the identified criteria for registration outlined in Table 1, may also be eligible for assistance.
Eye care practitioners may refer or simply signpost their patients directly to locally based vision rehabilitation services. When the CVI was first introduced in 2005, the Low Vision Leaflet (LVL) was also established for primary care practitioners to assist in signposting their patients for an assessment of needs.11 These leaflets can be obtained from the local health board, council or vision rehabilitation teams for distribution to our patients within primary care. Similarly, within HES clinics, the Referral of Vision Impairment (RVI) can be used for a similar purpose. This form may be filled in by the clinic staff or a sight loss advisor, such as an eye clinic liaison officer (ECLO),
to bring the patient to the attention of the local service provider. Regional variations do exist, so it is worthwhile understanding what mechanisms are in place in the local area.
As previously mentioned, although SI and SSI certification has clear guidelines on the level of sight loss measured, it is not a clear cut off between those who may be struggling with sight loss and those who are not. Eye care practitioners should, therefore, discuss the functional impact of sight loss following a reduction in any of the measures of visual function taken during an eye examination; even a small degree of loss may have a significant impact upon the ability to complete tasks independently. While the reduction in visual function may not be at a level that is certifiable, the patient should still be signposted for assistance, especially where their level of independence has been compromised.
Table 2 (see page 70) gives an example list of common questions for the eye care practitioner to consider when examining a patient with sight loss to determine whether signposting to local vision rehabilitation services is indicated. The emphasis of the discussion should ideally be centred around the impact the sight loss has had on the patient’s level of independence. Where the need for signposting has been identified, primary care practitioners can use local pathways in place (which may include use of the LVL) to bring their patients to the attention of rehabilitation services.
The aim of the last two questions in Table 2 is to identify symptoms of depression in patients with chronic physical health problems. These questions are underpinned by guidance from the National Institute for Health and Care Excellence (NICE).12 If a patient
Table 1 Current criteria of visual acuity and visual field status for certification as sight impaired or severely sight impaired7
Severely sight impaired (SSI)
Visual acuity of less than 3/60 (1.30 logMAR) with a full visual field
Visual acuity between 3/60 and 6/60 (1.30–1.00 logMAR) with a severe contraction of the visual field
Visual acuity of 6/60 (1.00 logMAR) or better with a clinically significant contracted field of vision which is functionally impairing the person, for example, significant reduction of inferior field or bitemporal hemianopia
Sight impaired (SI)
Visual acuity of 3/60 to 6/60 (1.30–1.00 logMAR) with a full field of vision
Visual acuity between 6/60 and 6/24 (1.00–0.60 logMAR) with moderate contraction of the visual field, for example, superior or patchy loss, media opacities or aphakia
Visual acuity of 6/18 (0.50 logMAR) or better if they have a marked field defect, for example, homonymous hemianopia
Table 2 List of common questions for the eye care practitioner to consider when examining a patient with sight loss
Example functional, mobility, self-care and social questions
• What are you most struggling with?
• Do you live alone? - house/flat/bungalow
• Any difficulty using stairs?
• Do you go out on your own? – any mobility problems/glare in sunlight/recent falls?
• Do you do your own shopping? Can you see prices/labels in shops?
• Can you see your coins to pay? Are you able to use a debit card?
• Can you see the TV – how close do you sit to the TV/how big is the TV screen?
• Can you see to cook for yourself? Can you see food on the plate?
• Can you pour liquids with ease? Do you ever scald yourself or spill the drink?
• Can you see appliance dials/buttons? – microwave/hob/oven/washing machine/telephone?
• Do you use a mobile phone/tablet/laptop/computer/Kindle?
• Any hobbies where your vision is affecting your ability to perform the task? – for example, sewing/reading/crafts/playing cards/piano/singing?
• Charles Bonnet syndrome – have you been having any unusual hallucinations in your vision since your sight loss?
Example questions relating to previous assistance or vision rehabilitation
• Have you previously been registered as sight impaired/severely sight impaired? How long ago?
• Have you received any assistance from social care services or vision rehabilitation services? How long ago?
• What sort of assistance did you receive?
• Has anything changed since that visit (consider loss of spouse, support or moving to a new home)?
• Do you feel you might benefit from a review by a vision rehabilitation specialist?
Emotional wellbeing: identification of depression in patients with chronic physical health problems12
• During the last month, have you often been bothered by feeling down, depressed, or hopeless?
• During the last month, have you often been bothered by having little interest or pleasure in doing things?
responds positively to either of those questions, the practitioner should notify the patient’s general practitioner (GP). In addition, the locally placed ECLO or sight loss advisor would be able to advise on locally placed counselling services to assist those with sight loss.
Sight loss advisors
In the early 1990s, feedback from patients attending hospital eye clinics highlighted the need for more emotional support and information on services following sight loss; this led to the development of several sight loss advisor roles across the four nations. For example, the Royal National Institute of Blind People (RNIB) developed a role known as the eye
clinic liaison officer (ECLO) and now employs over 100 ECLOs across the UK. In some areas, ECLOs may be employed by local sight loss charities. In Scotland, a similar role, known as a patient support worker, was also developed; at the current time, a large number are employed by Visibility Scotland. Comparable roles may exist in many other HES departments, and although qualifications or titles may vary, their roles and responsibilities remain similar.
The majority of sight loss advisor roles are based within hospital eye clinics and are actively involved in the process of certification. Their aim is to bridge the gap between the hospital clinical processes and local health and social care provision by signposting new service users for appropriate support. Following an
initial person-centred assessment of needs, the sight loss advisor may also provide emotional support, information, signposting and onward referral as necessary. The views of various health and social care professionals across the UK were analysed in a qualitative study which found that sight loss advisors are well placed within the HES to provide emotional support and information, and contribute significantly to the smooth running of eye clinics.13 Another study found that most clinical staff admit to not having the time or expertise to provide emotional support or practical advice to patients about living with sight loss.14 Having sight loss advisors available to refer patients who require extra support allows clinical staff to focus on their clinical obligations.
It is worthwhile understanding the communication pathways in place for contacting locally placed sight loss advisors as these may vary according to area. In one area an advisor may only be able to access records relating to current patients; in other areas the advisor may have access to previously discharged patient records. Thus, if a patient presents in primary care who would benefit from, for example, a review of their certification status, that sight loss advisor might be able to initiate this process without the need for the eye care practitioner to refer the patient back into the system through their GP.
The RNIB’s Sightline Directory provides a comprehensive list of ECLOs across the UK.15 In Scotland, a similar directory of locally based patient support workers can be accessed through VisibilityScotland 16
Vision rehabilitation and habilitation specialists
Once a new service user is brought to the attention of the health and social care teams, an assessment will take place in the person’s home to determine their support needs. Functional assessments may be conducted by one of a growing number of vision rehabilitation and habilitation specialists, where the term rehabilitation refers to specialists working with adult groups and habilitation refers to working with children and young people (0 to 25 years). In some areas, the name rehabilitation officer (RO) or rehabilitation officer of the visually impaired (ROVI) may still exist. In recent years, newly qualified vision rehabilitation specialists are trained through graduate-level teaching courses, and in April 2022 a professional register was accredited by the Professional Standards Authority with the Rehabilitation Worker’s Professional Network (RWPN) maintaining a register of both vision rehabilitation
“THE IMPACT OF PERMANENT SIGHT LOSS VARIES BETWEEN INDIVIDUAL PERSONALITY TRAITS”
and vision habilitation specialists.17 At the point of publication, the RWPN registers includes approximately 500 vision rehabilitation specialists and 120 vision habilitation specialists within the UK.
During the initial home visit, the vision rehabilitation specialist will assess the adult service user’s needs and discuss with them how their sight loss has impacted upon various aspects of daily living such as the ability to cook for themselves, personal care and mobility needs. In the main, the focus of service delivery is to address the functional impact of sight loss with an emphasis on maintaining both independence and safety. An example of the latter may be to provide adaptations within the home to reduce the possibility of falls or accidents in the kitchen while cooking.
The impact of other disabilities is also assessed such as hearing impairment, dementia, or other physical disabilities. After a full assessment of needs, possible solutions are outlined, goals agreed and an action plan created to achieve those goals. Where services are not available, or where the vision rehabilitation specialist has identified needs beyond their professional remit, there is a duty of care for the rehabilitation team to refer the service user on for additional support.18 It follows therefore, that more than one professional may be involved in the management of an individual with sight loss.
While a multidisciplinary approach to vision rehabilitation and low vision service provision is encouraged,19 there is still a lack of evidence to confirm the most effective, accessible and cost-efficient model of service delivery across the UK.20-22 Ideally, referral to and between rehabilitation services should be seamless for the service user, but this may be difficult to achieve when individuals have different needs which may require input of multiple service providers.
A survey commissioned by the Thomas Pocklington Trust found that 60% of support services were delivered by the local authority with the rest provided primarily by the voluntary sector.12 Services were also found to be less likely to assess or deliver emotional support, with the report suggesting that this was a result of financial pressures or lack of training for providers. An absence of emotional support may also lower social participation, further impacting upon emotional wellbeing.23
Ideally, all local health authorities should provide both practical and emotional support at an early stage in
the sight loss journey, to reduce long-term demands on health and social care systems.24
Delayed referrals for appropriate support and intervention can result in care needs intensifying, or the individual losing the motivation to retain independence.
A lack of awareness of rehabilitation interventions has been cited as one of the main reasons why professionals do not make timely referrals.14,25,26 For example, a qualitative study found that ophthalmologists did not consider referring their patients for social care needs until all possible clinical interventions had been exhausted, despite participants reporting that they would have liked to have been offered support sooner.14
A lack of awareness and understanding of service availability by patients themselves may also be a key reason why some people with a vision impairment do not seek help sooner, with those who are not registered as either SI or SSI less likely to be aware of available services or how to access them.25,27
Geographical location and the distance or time taken to access services has also been shown to be a significant barrier.28,29 Other factors such as depressed mood, or the patient’s level of family support, may also constrain an individual’s motivation to engage in rehabilitation strategies.30-32
The majority of those with acquired vision loss have a progressive condition and thus the level of sight loss may change over time. Furthermore, a service user’s personal circumstances may also change, such as moving to a new house or job or losing a supportive family member; therefore, there is a need for a process of review.22,33-35 However, just as there is no standard model of vision rehabilitation service across the UK, there appears to be no standard of follow-up or review


process for those vision rehabilitation services already in place. Guidance underpinning current service delivery across the UK is broad, with only a brief suggestion that the need for review is made locally, where teams are advised to offer follow-up appointments ‘as appropriate’ to the service user.36,37 In a recent study, the authors investigated the change in rehabilitation needs over time and established that there remained a need for continued support and intervention at 12 months following the initial vision rehabilitation assessment.38 The study also suggested that early identification and support for activities highlighted as being of high importance to the service user such as hobbies, crafts or DIY, could prevent such goals being relinquished, the result of which may have an impact upon emotional wellbeing. Finally, without a formal review process, any measures to determine the impact of assistance or intervention are either difficult to achieve or simply not possible.
To identify and signpost patients into existing health and social care systems in a timely manner has longterm benefits. It is not unusual for practitioners to come across patients with irreversible sight loss who have been discharged from the local eye department following the end of observation or treatment. Where relevant, it is important to be able to establish whether the patient has been seen by the local health and social care teams, and if so, how long ago. Any significant change in personal or functional circumstances may indicate signposting the patient back for review, especially where there is a concern over personal safety or emotional wellbeing. Where there has been a significant drop in clinical visual function, a referral back into the HES to acquire a change in certification from SI to SSI may also be indicated for the patient to access the change in entitlements that may bring. 0
Dr Jane Macnaughton is an experienced educator, author and hospital optometrist. She is currently a specialist optometrist at University Hospitals of Leicester NHS Trust and a senior lecturer at Anglia Ruskin University. Macnaughton has worked within the sight loss sector for over 30 years and authored two textbooks. She is currently the low vision service lead for Leicestershire and Rutland, hosted in association with Vista
Professor Keziah Latham is professor of optometry at Anglia Ruskin University, where she leads the Vision & Hearing Sciences Research Centre. Latham’s principal teaching, research and clinical interests are in low vision. She runs the low vision clinic within the university eye clinic and is a trustee of local voluntary organisation Cam Sight
Maryna Hura MEd, PGCE, BSc (Hons), FBDO, FHEA
IN BRIEF This article provides useful tips on how to improve the patient experience for Deaf people attending an optical practice.
The term ‘deaf,’ with a lower case ‘d,’ is generally used to describe people with all degrees of hearing loss, including Deaf, deafened and hard of hearing, while the term ‘Deaf,’ with an upper case ‘D,’ is often used to refer to members of the Deaf community who consider deafness as being a part of their cultural identity. These individuals are likely to be profoundly deaf since birth and will probably use British Sign Language (BSL) as their first language.1 This article will consider the existing barriers that the Deaf community regularly face when accessing healthcare and explore the potential means of overcoming such barriers within an optical practice setting.
According to the Office for National Statistics (ONS), the 2021 census figures show an increase of over 6000 BSL signers in England and Wales since 2011. A careful analysis of the data across England, Wales and Scotland leads to the conclusion that a figure of some 70,000 Deaf BSL users across the UK (including 6500 in Scotland) could be considered a credible estimate. A figure at least twice as large, in the region of 150,000, can be estimated if all BSL users are included, with the annual survey consistently measuring BSL users as 0.3%-0.5% of the adult patient population.2
BSL is a language with a unique vocabulary, construction and grammar, which is not based on the grammatical rules of English language. BSL is not a visual interpretation of English; it is a complete language of space and movement which utilises the hands, body, face and head. For many Deaf BSL users, English is their second, or even third language, which is why their written English may appear ‘foreign’ and grammatically inaccurate.3
Fingerspelling is used to represent specific English words for which there are no signs, for example, names or places. In BSL, facial expressions, body and hands are all equally important; Deaf people watch
the face when signing, not the hands. BSL is different from other sign languages, for example, American Sign Language (ASL), Irish Sign Language (ISL) and French Sign Language (FSL). BSL was recognised as an official British language by the UK Government on 18 March 2003.1
The story of Hazel, a Deaf BSL user, was reported in a recent study of the health of Deaf sign language users in the UK.4,5 Hazel felt unwell at work and went to a walk-in clinic, where there was no interpreter available at short notice, so she communicated with the nurse using written notes. The nurse advised Hazel to see the general practitioner (GP) who, in turn, referred her to the hospital. Having waited for hours to be seen, followed by more written notes, the patient was kept overnight in an emergency department, where the doctor told her (again, using written communication) that she had probably suffered a mild stroke. Hazel can read, but like many Deaf people, only at a basic level. Since Hazel felt better, she was sent home, but her condition worsened over the next couple of days, which resulted in hospitalisation. A week later, Hazel was discharged from the hospital and had another consultation with her GP, this time with an interpreter present. It transpired that the patient suffered from hypertension but did not realise that it was a lifelong condition and had stopped taking her tablets because she did not like them. Lack of accessible information on medication and not having interpreters during consultations resulted in two weeks of worry and frustration, multiple visits to the GP and hospital, spending one week on the ward and a preventable stroke.
According to research,5 ‘the reasons behind the increased prevalence of risk factors for chronic health conditions demonstrated in the Deaf population
are complex’ and include social, environmental and lifestyle factors, as well as difficulties in communicating with health professionals. A number of Deaf participants who took part in the study, stated that ‘poor communication in consultations with their doctor is a barrier and that this affects their trust in their GP’ which, in turn, leads to a compromised ‘understanding of chronic conditions, adoption of changes in lifestyle, and adherence to treatment.’5
Written communication using pen and paper may be useful for basic short exchanges of information; however, it is not always appropriate when conducting an eye examination, delivering important information relating to eye health or dealing with ocular emergencies. As with users of other languages, the simple solution to this would be to communicate through a BSL interpreter.3
Over 5% of the world’s population require rehabilitation to address their ‘disabling’ hearing loss, which represents 432 million adults and 34 million children).6 It is estimated that by 2050 over 700 million people – or one in every 10 – will have disabling hearing loss.6 In 2019, there were approximately 390,000 deafblind people in the UK, with this figure set to increase to over 600,000 by 2035.7
Given the barriers which the Deaf community experience when accessing primary healthcare in general, optical professionals should consider how this picture translates within the eye care sector. For instance, how many Deaf patients lack awareness of the critical signs/symptoms of eye disease and systemic conditions with ocular implications, simply because the educational material is not easily available in their preferred language?

Imagine being the only hearing person applying for a job within a Deaf-led organisation and joining a team of Deaf colleagues. Think about how you would go about communicating in your new working environment, in the absence of an interpreter. Imagine having no idea what is being said yet giving the opposite impression by nodding your head in approval during staff meetings or not being able to join in conversations during social events.8 Now, imagine trying to access healthcare services and having to explain what is wrong in a country where you do not speak their language. How confident would you feel to consent to a surgical procedure or take prescribed medication?
3 This is a great way to put
yourself in the shoes of a Deaf or hard of hearing person. Consider the barriers that Deaf people face on a daily basis; these include difficulty communicating with hearing people, educational barriers, difficulty in securing a job, along with the safety implications associated with hearing impairment. Having to face such barriers can leave a person with a feeling of isolation, depression, lack of confidence and being excluded from society.1 Furthermore, cultural differences can lead to confusion and misunderstanding in certain situations. For instance, to gain attention in the hearing world, one would either call out, whistle or shout. However, in the Deaf world, gaining attention of another person relies on different methods, for example, tapping, waving, flashing a light or stamping feet. Among other key aspects of effective communication within the Deaf community are pointing and eye contact, which may be considered rude by hearing people who have been brought up to learn that staring and touching is rude behaviour; nevertheless, these are very natural behaviours for Deaf people.1 There is a common belief that hearing aids or cochlear implants can replace normal hearing. Research with Deaf users demonstrates that these technologies can distort noises and adults may have an especially hard time relearning how to interpret sounds. It also depends on the level of spoken language that the Deaf person has managed to acquire as a child. Another misconception is that lipreading is sufficient to communicate effectively; however, it has been
shown that ‘reading’ lips without sound provides approximately 30% of information in English, since most sounds are formed within the mouth, with the rest being educated guessing. Even those words that are visible can be confusing – ‘it is like guessing ongoing crosswords without pen and paper every day.’8
Perhaps hearing people take for granted their daily verbal interactions in a workplace, restaurants, pubs, shops, banks, train stations, yet the dependence on verbal communication and sound in these environments has a significant impact on Deaf people, who regularly struggle to access information. More work has to be done by hearing and nondisabled people to remove these barriers, so that Deaf people do not feel embarrassed about asking for something to be repeated or having to ask for conversations to move towards accessible formats such as written communication. There is a need to shift the expectation that Deaf people alone are responsible for accessibility.9
Meaningful communication does not have to be verbal. While disability, including deafness, is one of the nine protected characteristics under the Equality Act 2010,10 the notion of being disabled is often rejected by the members of the Deaf community, as it may be interpreted as ‘less than’ or lacking something. For most Deaf people, deafness is a key aspect of their cultural identity, a natural characteristic, rather than a label which carries any associated stigma.
Eileen O’Banio, a Deaf advocate, believes that ‘It’s all about the perspective. If you are Deaf you see the world differently. Your way of communication is different. You seek out other Deaf people as they understand you. You don’t want to be fixed – as you don’t believe you have any disability.’11
Under the Equality Act 2010, service providers, including optical practices, have a duty to provide ‘reasonable adjustments to improve service for customers with disabilities who would otherwise be at a substantial disadvantage compared with people with no disabilities;’ therefore, optical professionals should be aware of the legal aspects and local protocols and recognise what reasonable adjustments must be made for their Deaf patients.5 The most apparent solution to overcome the language barrier is to communicate through a registered BSL interpreter. While the interpreting services are generally available, either in person or virtually, there may be
an issue of cost, staff may not be aware of how to access them or not enough notice is given to arrange the service in time for the appointment.12
All patients have the right to be fully involved in the decisions about their care, be able to access information in a form they can understand, be listened to and have their dignity and privacy respected. Furthermore, practitioners must recognise the limits of their professional competence. However, it is difficult to appreciate how the above can be achieved when a healthcare professional and their patient do not use the same language. The reality is that access to health services is almost always in another language for Deaf people whose preferred language is BSL, whether it is in the form of a leaflet or online video with subtitles.3
From August 2016, all organisations providing NHS care or publicly funded adult social care must follow the Accessible Information Standard (AIS). The purpose of the AIS is ‘to establish a clear, consistent approach to the information and communication support needs of patients, service users, caregivers, and parents with a disability, impairment, or sensory loss.’13 The five steps of AIS are:
1 Ask people if they have any information or communication needs and find out how to meet their needs
2 Record those needs clearly and in a consistent way
3 Flag or highlight in the person’s file or notes so it is clear they have information and/or communication needs and how to meet those needs
4 Share information about people’s information and communication needs with other providers of NHS and adult social care, when consented or have permission to do so
5 Take steps to ensure people receive information they can access and understand and receive communication support if needed.13
There are some steps that optical practices can take to make the experience more patient-friendly for those with hearing impairment, from the first interaction, such as booking an appointment, through to performing delegated tasks, conducting an eye examination and dispensing.
If the practice team is aware that a Deaf patient has arranged a sight test appointment and requested a BSL interpreter, every attempt should be made to accommodate their request as a ‘reasonable adjustment,’ at least two weeks before
“IT IS IMPORTANT FOR HEALTHCARE PROVIDERS TO PROMOTE ENGAGEMENT WITHIN THE COMMUNITY BY MAKING JOBS IN HEALTHCARE, HEALTH POLICY, RESEARCH AND EDUCATION MORE ACCESSIBLE”
the appointment. If booking an interpreter in person is not possible, consider using a video link interpreting service. Whether it is reasonable for the practice to pay for something like BSL interpreters will depend on the circumstances, and the practice should consider the factors listed in the Quality and Human Rights Commission (EHRC) code.14 If a practice has restricted resources, it would be expensive to arrange the interpreter. If there is no financial assistance available from the NHS towards the costs of the interpreter, it would not be reasonable to expect the practice to pay for this service. If it is not possible for the practice to fund an interpreter, other reasonable adjustments that could be offered to the patient include:
• Accommodating a BSL interpreter arranged by the patient
• Providing information in an accessible written format
• Providing a longer sight test appointment.
It should be noted that not all Deaf people use BSL; some prefer to lipread and speak, so it is important to establish their preferred communication method prior to the appointment. Upon arrival, a Deaf patient is likely to inform a member of staff that they are deaf either by saying it or signing it, but it is worth remembering that deafness is a hidden disability.1
Be aware that, unless the patient has an interpreter with them, they will not hear when their name is called in the waiting area, unless there is some form of a visual alert. The practitioner will need to approach them, establish eye contact and use gestures or written notes to communicate with them. It is only polite to ask for permission to use written communication. Explain clearly what is required and expected of the patient before conducting any diagnostic tests. Remember that they will not be able to see to lipread or watch the interpreter when they are undertaking visual field assessment or having their intraocular pressures measured.1
During the sight test, it is important for the practitioner to explain what is required before starting and using hands to point and gesture where they want the patient to look. When using terminology, explanations should be given in a
simple way, using visual aids, such as pictures or diagrams to describe what is meant; this is helpful even if an interpreter is present. When the sight test is completed, and if the patient requires a dispense, it is important to notify the next member of staff that the patient is Deaf.1
Further practical steps to ensure a better experience for Deaf patients could be to organise a Deaf awareness training session for all staff and promoting online booking of appointments. Every time a new Deaf patient is seen in practice, staff can ask how they prefer to communicate and make a note on their clinical record. Ensure there is a system in place for booking interpreters and all staff are aware of it, remembering that it can take two to three weeks to find an available interpreter. Note that using lipreading or asking a family member or friend to interpret are not examples of a ‘reasonable adjustment’ under the Equality Act, unless requested by the patient.5
While hard of hearing people, who are usually older and are able to speak and read English, are happy to receive written information and leaflets, Deaf sign language users may need more thorough and careful explanation of eye conditions, procedures and treatment plans, using visual aids, such as props, images, drawings and gestures.5 The practitioner must remember to maintain eye contact while they are talking and look at the Deaf person when they are talking or signing, ensure their face is well lit, and show first, then talk. Above all, be patient and allow time for effective communication.
Over the last year, there have been reports of an increased interest in BSL among the hearing population.14 One of the reasons for this is the presence of Deaf contestants in popular TV shows, for example, Rose Ayling-Ellis in Strictly Come Dancing, Tasha Ghouri in Love Island, and more recently, ITV’s Life After Deaf, featuring John Bishop and his son Joe. In 2021, BSL Courses reported that they had received 711 free trial enrolments on 31 October, compared to the usual 20 to 30 per day. The Learn BSL webpage had 675 views in August, rising to 1155 views in September and 1468 in October, as Rose progressed through the competition.15 However impressive the impact of celebrities has been on the popularity
of BSL, it was an important political event that changed Deaf history forever. A Bill to recognise BSL as a language of England, Scotland and Wales passed unopposed by peers in the House of Lords on 27 April 2022. The passing of this historic Bill was a cause for celebration within the Deaf community, which came after many years of campaigning for the recognition of their language and the right to access public services, such as health and education in BSL.16
If learning BSL is something that is of interest to a practitioner or colleagues within practice, what are the next steps? A number of providers offer face-to-face classroom-style learning, with many more providing a wide range of online courses. Completing a Deaf awareness course, together with a free trial or a taster BSL session, can be an excellent starting point. It is worth finding out from the local Deaf centre, or a Deaf charity operating in the region, if they are able to tailor the sessions to satisfy CPD requirements for optical professionals.
For those wanting to take their learning experience further, BSL level 1 is a starting point for anyone wishing to attain a formally recognised qualification and can be taken without any previous experience. Level 2 training is suitable for those who wish to learn BSL at an intermediate level, whereas level 3 enables the learners to communicate confidently with Deaf people in a variety of work and social settings and level 4 meets the learning needs of those who already have competence in BSL level 3 and are interested in developing their skills and knowledge further.17 Finally, level 6 is for those who wish to learn sign language at a fluent level involving highly advanced skills and language in complex situations.18
There are some excellent educational tools available, which can help learners to make progress through any of the above courses. An online BSL sign dictionary19 provides an extensive range of signs; it is easily accessible through a web browser or an app and can be used as a reference point when communicating with Deaf patients in practice. For those who prefer textbooks, there are many to choose from. While there are plenty of online

resources, accessing free taught lessons can be challenging not only for healthcare professionals, but also for Deaf people, their families and friends. Courses can be expensive, and while some are funded for parents of Deaf children, there is no funding for Deaf adults to learn BSL.8
Optometrists and dispensing opticians have an opportunity to enquire about bespoke Deaf awareness and BSL courses via their local optical committees (LOC) or optical membership organisations. CPD events have already been delivered by the Leeds LOC and ABDO, in partnership with a Leicester-based charity, Action Deafness.20,21
Deaf people tend to experience poorer physical and mental health compared to the hearing population and face significant inequalities in terms of access to healthcare services, including eye care. Fulfilling patient-centred outcomes for Deaf sign language users is distinctly different from the rest of the population due to the unique cultural and linguistic aspects. Fundamental principles for the better promotion of patient-centred care for Deaf people includes facilitating greater opportunities for them to engage in influencing their healthcare and investing in preventative and supportive programmes to build knowledge concerning their health in ways that are linguistically accessible and culturally appropriate. In addition, investing in appropriate means to elicit Deaf people’s healthcare experiences, so that these can be incorporated into more sensitive structures for measuring healthcare impact, would provide valuable insight.22
It is important for healthcare providers to promote engagement within the community by making jobs in healthcare, health policy, research and education more accessible, thus maximising positive outcomes for Deaf patients. By doing so, society may see improvements in the socioeconomic status of those who have hearing loss and a greater representation of the Deaf community in clinical practice and health education, which will benefit not only Deaf people, but their hearing colleagues.12
Maryna Hura has worked in optics since 2003, qualifying as a dispensing optician in 2008, and divides her time between lecturing at Bradford College and working in practice. Hura is currently working towards her BSL level 3 qualification, is a member of Leeds Local Optical Committee and Huddersfield Deaf Centre committee, as well as a General Optical Council Education Visitor Panel Member.
Peter Greedy BSc (Hons), MCOptom, MAC
IN BRIEF This article examines the attributes of great leadership and how these contrast with toxic behaviours that can be present in the work environment.
What makes a great leader? Does it come naturally, or is it a learned behaviour? Whether people are born with an innate ability or have to be trained as managers, team leaders and supervisors, being a great leader requires ongoing learning and openness to change and growth.
Nobody enjoys working in a toxic environment and research shows that it is the number one reason people leave their jobs.1 It is, therefore, essential to be fully aware of what both good and bad leadership practice looks like. This type of article can never be exhaustive as each individual will bring their own personality, skills and knowledge to their role. Here, the author shares his ‘A’ list, which outlines 10 attributes of great leadership and considers how their toxic antitheses can manifest in the workplace.
Authenticity is fundamentally about being a true representation of someone’s core values and beliefs and expressing these in the way they speak and behave. The root of the word authentic is 'genuine’. Not being authentic implies failing to represent a genuine version of oneself. How often do people consider that they would behave differently if no one was watching or listening to them? That’s not to say that the accepted norms of appropriate behaviour for various situations, for example, being professional in the practice environment, should be ignored. But consider those times when a person says they agree with someone when they don’t; or say what they think people want to hear rather than what they actually believe. These actions can result in the individual being a people pleaser because of employer or peer pressure, without thinking that this is compromising who they authentically are. To be authentic, it is important to have an awareness of core values and beliefs and how these can manifest in the work environment.
Many people are likely to see work as a ‘doing’ thing rather than a ‘being’ thing and do not take enough time to reflect upon who they truly are. Doing a review of
individual values and beliefs is a useful exercise. But what are values and beliefs? A simple definition to consider is that values are ideas, whereas beliefs are concepts that are held to be true.
Some examples of values are justice, equality, honesty, integrity, fairness and loyalty. Beliefs may be world or religious views such as opinions on global warming, racial equality, abortion, or immigration. Both values and beliefs can change over time and beliefs tend to change more frequently than values. For example, the author’s spiritual beliefs have changed many times over the years and are continually evolving, whereas his value of equality is unflinching.
Being authentic requires courage to hold steadfast to values and beliefs in the face of challenge; the courage to raise a hand when asked if anyone else has something to add; the courage to speak up when witnessing someone being singled out and picked on unfairly, instead of choosing to remain silent or even joining in.
Antithesis to authenticity: fake There is a common expression thrown around these days ‘Fake it ‘til you make it’, a notion that encourages people to pretend to be something or someone they are not until they are successful. Those adopting this approach will tend to be loud and brash, and sadly in some work cultures, those who shout the loudest can get the attention, rewards and promotion.
Tolerating and rewarding this kind of behaviour is very toxic and thoroughly demotivating. It adversely affects the performance of the rest of the team who are more likely to underperform and engage in what is known as ‘quiet quitting’ or working to rule, as a form of protest against the employer who they feel is either tacitly or actively supporting such behaviour.
Managers and leaders can be fearful of addressing this issue because they don’t want to lose a ‘star player’ and the great results produced by this type of character; this is a misguided approach and dealing with such a person, either through directing behaviour change or accepting they are likely to leave, will increase
the performance of the rest of the team. With good leadership, the sum of the incremental performance improvements will outweigh the loss of the one ‘star player’ in the longer term.
This attribute of leadership be described as holding to the values and mission of the team or wider organisation. There is often a large overlap between personal values (authenticity) and corporate values. If this isn’t the case, then the individual is probably in the wrong job. In an optical setting, there are different types of practice such as volume retail; bespoke service value proposition; hospital; domiciliary or academia. As a locum optometrist, the author has worked in various settings over the years and has become very clear on the type of practice he prefers to work in and be aligned with. It is important for an individual to identify which setting best aligns to their preferences.
Antithesis to alignment: self-serving
This is where our actions and behaviours are aligned to personal outcomes, rather than the good of the team or the organisation. The self-serving person, while being understandably and acceptably ambitious, may use underhand measures to further their career, such as taking credit for someone else’s ideas or work, undercutting prices to make a sale, or giving a false impression of their achievements to make them look better. As a leader, giving credit to the originator of ideas and work demonstrates alignment to the collective contribution of the team.
Awareness is an attribute that involves all our senses including those from our sensory organs as well as emotional intelligence and intuition. All this data travels inward to be processed by the individual. When working in teams, there are three types of awareness to consider:
• Intra-team awareness is tuning in to everything going on within the team. This could be the front-of-house team, dispensing colleagues, or the clinical team
• Inter-team awareness is the dynamic between the team and other teams working in the organisation towards the same goals. For example, all teams ensuring that the patient journey from arrival to departure is smooth and efficient
• Extra-team awareness is looking beyond the organisation to factors in the environment that can influence the goals of the team and may be outside of internal control, things like weather, economic factors, competing companies, or a global pandemic.
Antithesis to awareness: obliviousness Obliviousness can be conscious, the so-called ‘head in the sand approach,’ or unconscious. An oblivious leader or team member may exhibit limited emotional intelligence, sympathy or empathy, and they may be unaware of, or simply ignore, everything that does not directly affect them.
If the direction of information transfer in awareness is from outside to in, the information, signals, data, emotional intelligence and intuition of attention are inside to out. We ‘pay’ attention because there is a cost, such as time, focus, listening, emotional and cognitive labour to those in our sphere of responsibility. However, there is also great value to this ‘paid’ attention to the recipient. How a person responds to everything they are aware of and experience in any given moment is an expression of attention. The goal is to be able to respond in a healthy way, rather than in a toxic way.
Where do people place their attention at any given time? Is their attention where it should be? Is their mind wandering? It is natural for the mind to be drawn away by competing demands, often for safety, and should not be seen as a negative. Rather, it’s our mind switching from one thing to another, for instance, looking up from a phone to cross the road can be lifesaving.
Mindfulness, a process of learning to tune in to oneself and the current situation can increase attention on the present. The relationship between physical exercise and physical health is familiar to all, but do most people actively work to keep their minds fit and healthy? Mindfulness can be taught, learned and improved with dedicated books on the topic such as Peak Mind by Amishi Jha.2
Antithesis to attention: neglect
It is easy to recall a situation when chatting to a colleague, friend or relative where they are constantly responding to message notifications on their phone, or when we say something in a meeting and are interrupted and spoken over as if our contribution is of no value? In that moment how do we feel?
Neglected perhaps?
At a more serious level, neglect is a form of abuse. As with many things there is a spectrum, and in this case, from not giving full attention to full neglect and we all sit somewhere on this spectrum at any one time. Most of us will recognise that we can work to be better at giving our attention rather than being neglectful. During back-to-back patient consultations,
it could be all too easy to let the routine be an excuse to drift into autopilot. Practising mindfulness and being observational and attentive to the patient’s responses can help them to open up, which it turns allows the practitioner to optimise their care.
Attention and neglect framing
This is a simple thought exercise to conduct for any relationship, which is taken from the Unlocking Us podcast with John Gottman and Julie Schwartz Gottman, hosted by Brené Brown.3,4 Here, they discuss the concept of turning toward, turning away and turning against. Consider a real-life scenario where you are working at the dining table looking out into the garden. Your partner enters the room and spots a robin in the garden and says, ‘Oh darling, look at the beautiful robin.’ In the moment, you have three possible responses:
• Turn towards – take a moment to observe the robin and acknowledge how pretty it is and then carry on with your work. This approach pays attention to your partner, both parties appreciate a point of connection, and it all took about 10 seconds
• Turn away – ignore your partner’s comment and continue working, saying nothing. A failure to pay attention can result in both parties having private negative thoughts
• Turn against – with frustration you say to your partner, ‘Can’t you see I’m working?’ A hostile conflict ensues, costing time and emotional labour to chat through and resolve. Probably a good half an hour wasted.
How we frame the story here is so critical:
Option 1: your partner is simply seeking a brief point of connection to share a thing of beauty to enjoy, allowing for a positive moment together before resuming the task at hand after minimal disruption Option 2: you tell yourself that your partner is being selfish and doesn’t care that you are working and should know that it is important to not interrupt and if she really loved me, she would know this and not do it. Which approach is likely to deliver the best outcome?
5 AUTONOMY
Autonomy in leadership can be described as granting those who work for, or alongside, the freedom to do their thing – the thing they were hired to do – and, assuming a good recruitment process, the thing they are great at. Granting autonomy to those in the team or business means letting go while also striving to provide the best environment for them to succeed. Regularly checking in with the team regarding their roles and
“ACCOUNTABILITY ALLOWS LEADERS TO RECOGNISE THAT THEY ARE FALLIBLE... WE ALL FAIL AND HOW LEADERS HANDLE THEMSELVES WHEN THIS HAPPENS SPEAKS TO THEIR INTEGRITY ”
offering support where required is essential. Great leaders will optimise the work environment for their team, accommodate personal needs where possible, give encouragement and have people’s backs if needed.
Antithesis to autonomy: micromanaging
Micromanaging is perhaps one of the easiest things to slide into subconsciously. It often can come from a place of wanting to help deliver the best outcome, but for those on the receiving end, it can be negative and invalidating. Very competent people will often feel they know the best way to do something, and they probably do – for themselves. But that does not mean their way is the best way for other people who have different skills and thought processes.
Micromanaging can be expressed in various ways: overly frequent, dictatorial communications; unnecessary supervision; excessive criticism; a need to know every detail; too frequent updates; lack of delegation and redoing other people’s work. All of this is a clear expression of a lack of trust and can lead to apathy and disrespect from the team, not to mention the burnout of the micromanager.
Micromanaging can also be a form of perfectionism. The author believes that perfect is the enemy of good ‘Good enough’ is exactly what it says and seeking perfection is subject to the law of diminishing returns and can be extremely time consuming and inefficient. In optics, this is one reason for tolerances – because within tolerance is good enough.
Accountability allows leaders to recognise that they are fallible. They own their mistakes, apologise and make amends. We all fail and how leaders handle themselves when this happens speaks to their integrity, honesty, and ultimately, the level of trust the team has in them. Accountability can be at different levels: upwards to a boss; laterally to peers; and downwards to those in the team. Each of these are important contracts to engage in and as a leader something to role model well. A helpful question to ask ourselves is, ‘Who am I accountable to in my current situation?’ It is always good to review this standpoint.
Antithesis to accountability: blame and shame
Typical behaviour of those who feel no need to be accountable and take responsibility for their actions when things go wrong is to hide behind a wall of blame and shame. There may be deflection of responsibility for things on to other people, for instance, claims that others made mistakes or were late with their contribution, that someone didn’t explain the brief properly and a hundred other excuses. Similarly, shaming tactics may also be used as well as gaslighting to make others question themselves. A common phrase used to gaslight people is ‘You’re overreacting;’ this is almost always more about the person saying it than the one receiving it. Learning from failure and facing inadequacies is a strength, requiring vulnerability in the workplace and is a means to effective learning.
Agency is where the leader grants themselves and those in the team the ‘power to’ act in the best interests of the business. As a leader, it provides the feeling of control over both actions and consequences. For those in the team, it grants them the same agency to do the job, so that they have the feeling of control, and are free to make mistakes – the most powerful way of learning, yet for some, the hardest thing to let go of. In the early stages of the working relationship, ‘power with’ is appropriate, where the leader works alongside those in the team to ensure they know all they need to and have the right tools at their disposal to do the job. Demonstrating and supervising is good initially, although this needs to be reduced over time as agency is transferred to colleagues. It is that letting go of the saddle of the child learning to ride a bike without stabilisers for the first time so they can ride free. Holding on too long results in a power struggle, which invariably results in a crash.
Antithesis to agency: power over ‘Power over’ is not good leadership but control, domination and coercion, such as methods used by cult leaders to control their followers. It takes away critical thinking and generates a group of followers rather than a team of individually empowered, talented players. Toxic, and especially narcissistic leaders will always feel their way is the best and only way. They end up creating clones of themselves from those who allow themselves to be manipulated; this generates a non-diverse, one-dimensional team with limited capabilities. For those subject to this kind of leadership, there is no scope for personal growth.
Agility is the ability to adapt quickly and easily in response to changing circumstances, for example, when a team member is ill or gets another job, the computer system crashes, a supplier fails to deliver, or new legislation is introduced. How do we adapt to these changes that are outside of our control? Can we think creatively and be flexible and find new solutions for the new situation? Do we see changes as obstacles or opportunities? Do we carry the weight of this responsibility on our own or do we get the team involved?
Agility is synonymous with a growth mindset, a belief in the ability to learn and adapt; this does not mean abandoning values and vision. Learning and experimentation are key, with a willingness to change as needed. Times are often volatile, uncertain, complex and ambiguous; this means change is inevitable and being agile is not optional, it is essential.
Antithesis to agility: fragile and fixed Inflexible things are either so solid they are fixed and immovable or fragile and snap under pressure. Fixed thinking applies to many areas, for example, it sees intelligence and talent as innate and, therefore, unable to be developed. Neuroscience shows us that the brain is changing all the time, for instance, by just reading this article, neurons in the brain will have rewired and made new connections. Change happens whether we like it or not, so why not engage in this change and ensure we are feeding our minds with the good stuff?
A fixed mindset reduces self-knowledge and is more focused on external rewards and validations. It inhibits taking risks through fear of failure and can cause unhealthy competition and foster the ‘win at all costs’ mentality.5
Acceptance without judgement and with the assumption of positive intent is one of the toughest challenges in leadership. The assumption of positive intent is about relating to people from a place that assumes they are doing their best and that we do not always know their story, that is to say, what is going on in their lives at that particular moment. It is so easy to assume when someone makes a mistake that it is because they weren’t trying hard enough or paying enough attention. It is helpful to reframe the situation by asking the question – did the person do it on purpose? Giving people room to fail and make mistakes is so important for growth and yet it is all too easy to jump to negative thoughts and words in those moments. Maybe the team member had received some
“GREAT LEADERS BUILD A HEALTHY CULTURE IN ORGANISATIONS. THEY ARE AUTHENTIC WITH A FINELY TUNED AWARENESS AND BEHAVE IN FULL ALIGNMENT WITH THE GROUPʼS VALUES AND MISSION”
bad news that day and their mind was distracted with concerns, so their focus was not on the task. Leaders need to be compassionate and supportive and help in any way they can.
Antithesis to acceptance: judgement (rejection)
People are programmed to judge everything and are very good at it. Negative experiences can have a more profound impact and stay in the memory longer and more prominently than positive ones.
How can a leader avoid negative judgement? In Brené Brown’s book Dare to Lead, non-judgement is number six in her acronym BRAVING, a process for transforming relationships in the workplace. BRAVING stands for boundaries, reliability, accountability, vault (speaks to not gossiping), integrity, non-judgement and generosity.6 A good approach for a leader to avoid judgement is to always consider, ‘What’s their story?’
Appreciation is a crucial practice to be developed by all leaders and should be expressed regularly, sincerely and generously. A regular ‘thank you’ and ‘great job’ from the boss goes a long way and should not be restricted to moments of success. To take it to the next level, a good leader will say ‘thank you for the work you are doing, and do you have what you need here?’ This expresses so much more in terms of care for the person. At other times, a more significant gesture of appreciation is important: a handwritten card, a bunch of flowers, or a celebratory event. Many other ways of showing appreciation are available too, such as providing the team member with additional responsibility, benefits, perks, learning and development opportunities, promotion, and of course, a salary increase.
The author suggests the following as an excellent mantra for bosses: ‘Stop catching people doing things

wrong and start catching people doing things right’. Those that have been on the receiving end of someone always pointing out things they think should be done differently or better, that is to say, done their way, will know how frustrating and demoralising this can be. Choosing to look for and appreciate the good that people do is a mindset that should be embraced, and with practice, can become the norm.
Antithesis to appreciation: contempt
In a mild form, contempt is expressed as being taken for granted, which can be defined as a failure to properly appreciate (someone or something), especially as a result of overfamiliarity. Nobody likes to be taken for granted.
At its worst, contempt is a very toxic form of disrespect and is cited as the largest negative impact on employees’ ratings of their company’s culture.7 It is usually directed as part of a belief that not only has a person done something wrong, but that they have some deep, fundamental flaw. Contempt goes beyond saying ‘What you did was bad,’ and says, ‘You are bad.’ Constantly being ignored is hard to take and demotivating, especially for the conscientious employee striving to do their best. Enduring the disrespect of contemptuous comments and behaviours is likely to drive good people away from the business, resulting in lost time and the expense of finding, hiring and training a replacement. Carrot or stick? Carrot every time.
Great leaders build a healthy culture in organisations. They are authentic with a finely tuned awareness and behave in full alignment with the group’s values and mission. They foster individual autonomy and agency in those they lead, accepting and appreciating the value each one contributes to the whole. Above all, they work in service of those they are privileged to lead.
Peter Greedy is an optometrist with extensive experience of professional and management roles, with proven leadership skills from over 30 years in healthcare. He thrives on innovating unique and effective solutions to situations. Greedy is an accredited coach and passionate about personal, professional and leadership development, addressing toxic cultures and bringing trust and belonging into the heart of organisations. Outside of optometry, he is also the inventor and owner of an award-winning, patented shoelace system.
Sheena Tanna-Shah BSc (Hons)
IN BRIEF This article will explore how small steps can lead to big improvements in mental and physical wellbeing, bringing benefits for the practitioner and their patients.
We all lead busy lives navigating our way through work, family life, social commitments, continuous learning, daily chores and everything in between. As a result, it can be difficult to find time to check in with ourselves, to question how we are feeling and how our life is impacting us. It is easy to ignore stresses, little niggles, blame lack of time, or simply feel that looking after our wellbeing is unnecessary because there is so much else to do and so many other people to focus on. Maybe the only time we really do reflect on this is when we hit mental exhaustion, burnout, or are physically ill and almost forced into re-evaluating our lifestyle. Rather than wait for these crisis moments, it is far better to take a proactive approach as a failure to effectively manage your wellbeing could impact on both your personal and professional life.
A World Health Organization (WHO) report showed that an estimated 15% of working age adults have a mental health disorder at any one point in time. As of 2019, 301m people globally were living with anxiety.1 In the UK, one in four adults have a diagnosable mental health condition, with 75% diagnosed by the age of 25.2 If your wellbeing is poor, it can reflect in everything you do and who you interact with, no matter how much you try to ‘just get on with it.’
This article will explore four key categories of wellbeing3 and use illustrative case studies to outline steps that can be taken to make improvements to many aspects of daily life.
How are your emotions and feelings in your daily life and towards certain situations and circumstances? Do you have high levels of
confidence, self-worth and self-esteem? Do you feel positive and have a growth mindset in moving forward with goals? Is your mood always up and down? Do you become easily frustrated or irritated and blame other people and situations for it?
If you think your wellbeing is suffering, what steps do you need to take to start feeling good? Talking to someone is always a good place to start, whether that’s a friend or family member, or if that feels too close to home, then speaking to a health care professional or accessing the wide range of support that is available online. If you are registered with a general practitioner (GP) you can even self-refer for support via the NHS talking therapies service.4
It’s not always easy talking about how we feel and often might not know where to begin or how to describe our thoughts. A first step could be to write down your thoughts as when these are continuously going around in our mind it can escalate and feel overwhelming. Putting your thoughts down on paper can help to start making sense of things.
Just 10 minutes of doing something each day that makes you feel good can really make a difference, whether that’s enjoying a cup of tea, reading a book, doing a short workout, going for a walk or listening to music.
Using stress relieving techniques such as breath work, meditation, journaling, yoga or taking a warm bath can all help to make you feel calmer and more relaxed.
Consider how you feel in your physical self. Do you feel energised, healthy, nourished and sufficiently hydrated? Or do you feel lethargic, tired, sluggish and have health issues?
Take time to review your sleep patterns. We often underestimate the power of sleep, but it is vital for the body to rest and heal. Do you get sufficient quality sleep or when you have promised yourself an early night it ends up being midnight before you go to bed and then you wake up hitting the snooze button multiple times in the morning?
How much exercise do you do weekly? Exercising is vital to keep the body fit, strong, mobile and healthy. Whether you go to the gym, go for a walk or run, or simply making a conscious decision to always take the stairs rather than the lift, doing something is better than doing nothing. Is there something that prevents you from scheduling in some movement, and if so, can you adapt your routine to build in short periods of regular physical activity?
How well are you nourishing your body? Are you skipping meals, eating in a rush or defaulting to convenience foods? Planning and preparing your meals and being mindful of what you are eating can make a huge contribution to your physical wellbeing.
How much water are you drinking? Is it enough and if so, how are you tracking it? Our body weight is made up of 55% to 75% water and is required for many vital bodily functions, including flushing toxins out.5
What can you do to support and improve your physical health? Understanding the benefits of looking after your health and staying accountable either using a tracker, chart, journal, or buddying up with another person can help you to stay consistent.
Consider how you are in a social setting? Whether it’s with friends, family, or at a club, do you feel good, supported, and enjoy the connections, or do you feel anxious, don’t feel like you fit in or feel like
you don’t belong? Have you outgrown the people you surround yourself with? Could you make new connections with other interests you may have?
It’s important to spend time alone and have that self-care time but as humans we like to connect and feel a sense of belonging, but is your tribe making you feel good?
Consider the following questions:
• Do you feel content in your current role?
• Are you happy with your work environment, colleagues and line manager?
• Do you feel supported with the work you are doing?
• Do you feel that you have opportunities to progress your career ambitions if you so wish?
• Do you have the right resources and tools to help you work?
Try giving yourself a score in each of those areas from one to 10 (one being very poor – 10 being perfect) to gauge where your workplace wellbeing is? What small steps and actions can you take to increase the score? When can you take these steps? How will you know when you have achieved them? How will you feel when you begin to increase the score in these areas?
Think about a time when you’ve had some worries in your personal life, or had a health concern to deal with, how has your day at work been on these occasions? When your wellbeing isn’t where it should be in any of these areas it can impact your daily thoughts, feelings, actions and ultimately your reality.
Another way to approach your wellbeing is to look at the ‘five ways to wellbeing’ from MIND (see Figure 1).6
Connect
Speak to and meet up with friends and family, share your thoughts and ask them about their day. Do an activity together, go for a walk or meet for a coffee. Connecting in person can really support wellbeing by giving us a sense of comfort and belonging.
Be active
Keep exercise simple, achievable and fun. A fiveminute stretch in the morning, a walk during your lunch break, through to organising a sporting event with your work colleagues or friends can all help support you being active, fitter and healthier.
Take notice
Be mindful of the present moment and enjoy it. In your practice, maybe you can get a small plant to enjoy, relax with a coffee without thinking of chores, enjoy the nature when you are outside, notice people around you and what they may be feeling and saying.
Keep learning
Learning new skills can really help to boost your confidence and self-esteem; this could be at work through continuing professional development, taking on a new hobby, doing puzzles or reading books, all of which can really help you feel good.
Give
Research has shown that doing an act of kindness once a week for six weeks can increase wellbeing.7 Buying a cup of coffee for someone, opening a door, smiling, checking in with your neighbour, through to sharing your favourite book with a friend, can all help in the art of giving.
Kylie returned to work at the practice three weeks ago on a part-time basis after finishing her maternity leave. She is feeling overwhelmed by having to juggle her home life, looking after her family, lack of sleep and returning to work after being off for a year. When she comes to work, she is feeling emotional, tired and lonely, and just about makes it through the day.
Managing expectations and communication is vital here for Kylie. She needs to understand that she doesn’t have to be a super parent or a super worker and try to deal with everything on her own. Speaking to her manager should be the first step. Sharing feelings isn’t always easy but taking a few minutes to talk about ways of easing back into work can make a huge difference. Support could mean
increasing testing times for a short period or having an appointment slot set aside so she can refresh her knowledge on products or system changes. Often lunch breaks can mean catching up on jobs or doing a bit of shopping, but Kylie should try and take time out to enjoy her lunch, have a coffee, read a book, take a short walk or listen to a podcast.
Getting support is important, and if the line manager isn’t providing this for Kylie, then she should reach out to someone above them for advice.
Kylie should also recognise the importance of making small adjustments at home such as meal prepping, getting an early night if sleep is broken and scheduling in self-care time, even if it’s just 10 minutes with a cup of tea.
If the struggle persists then seeking professional help is also advisable, speaking with a healthcare professional and/or looking at the online support that is available from websites such as the NHS.4
John has been having to look after his elderly mum who struggles with health issues, which has meant he’s had less time for his own self-care. When he comes to work, he’s feeling a little irritated and is known to be a bit short with people.
John needs to work on managing his commitments and incorporating time for self-care, including socialising and ensuring he is staying hydrated and nourished. He needs to recognise that although he wants to be there for his mum, if it begins to impact upon his own health and wellbeing then how will he be able to support others effectively? John should reflect on his last two to three weeks and look at the meals he ate, his sleep pattern and how much time he had to do something for himself. If he hasn’t eaten properly, slept well or had time to switch off,

he is more likely to be irritable. Creating a timetable of when he will be helping his mum and when he will have time for his own needs is key. Looking at further assistance and help to support his mum may also be something that needs to be considered. Communicating with a peer or line manager about his personal circumstances is important, so that the right support is provided at work too. When others at work are aware of the struggles a person is going through, they can make adjustments, for instance, allowing a five-minute breather if things are getting too much, or making time to go for a walk with them during the lunch break to check in on their wellbeing.
Amandeep has been having problems in her relationship. She hasn’t spoken to many people about it as she feels uncomfortable and embarrassed; however, it’s causing her stress and her emotions are unstable. When she comes to work, colleagues are often wondering what mood she will be in, whether to talk to her or leave her alone. While Amandeep cannot fully control the circumstances in her personal life, she can dictate how she responds and manages them, and the priority is to deal with stress. Considering things such as practising mindfulness, meditation, breathwork, yoga and journaling are all simple strategies to reduce stress.
Often during stressful periods, it’s easy to neglect doing things like exercising or meeting friends. Exercise can really support stress reduction by releasing hormones that elevate mood. It’s also important that Amandeep connects with her friends and family to talk through her worries and help her to feel safe, secure and supported as she moves forward. Reaching out to professional support networks could be a helpful alternative for Amandeep if she is not quite ready to speak to her friends and family.
Whatever you are going through, no matter how big or small, it is all valid when it impacts your day-today life. When your wellbeing is not being managed,

it can impact upon professional relationships with your team and patients. It’s noteworthy that only 7% of communication is received verbally and 93% nonverbally through body language and tone (Figure 2).8
When you are not feeling happy or good within yourself, clarity, focus and presence will be impacted. During a consultation, engagement with the patient may be reduced, body language and tone will be impacted, and you may simply not be the best version of the eye care professional that you would like to be.
Looking after your wellbeing also means that ultimately, you are looking after your patient to the very best of your abilities. You may be the best clinician, giving the best examination and recommendation but if the patient doesn’t feel their experience was good then they will leave feeling dissatisfied. Patients want to feel heard and understood, with a good explanation of the results, time to ask questions and feel at ease during the consultation.9
When we are not feeling good at work our productivity, motivation and purpose in the role starts to diminish; this turns into a vicious cycle of further emotional stress. We may start to turn up late to work, have moments of daydreaming, poor focus and concentration, which can put a strain on our relationships within the team.
Mental health really does matter and it’s up to us to make changes to improve our wellbeing. We have a duty of care to ourselves and our patients to be the very best version of ourselves. There is always one positive step you can take to improve your mindset and make changes for a happier positive future.
If you feel you need support, there is a range or organisations that can help.4,6 The AOP peer support line is a confidential, free-phone helpline for individuals (members and non-members) at any stage of their optical career to call and discuss their problems with a trained, empathetic peer who recognises the pressures of optical practice.10
Sheena Tanna-Shah is an optometrist and also runs her own wellbeing company which offers rapid transformation therapy, mindfulness and mediation, mindset coaching and neurolinguistic programming. Tanna-Shah is the author of PerfectlyImperfectMumand her work has featured on BBC News, ITV’s ThisMorning, BBC Radio and a wide range of national publications.








0
Alan Hawrami MSc, BSc (Hons), MCOptom, Prof Cert Med Ret, Dip Glauc, DipTP (IP), OPwSI
IN BRIEF This article features a series of clinical cases. Readers are invited to review the images and access additional resources where necessary to answer the questions.

A patient presents with symptoms of gradual blurred vision in one eye over the last year. They mention that they had eye surgery in both eyes approximately 10 years ago.
01 What is the most likely diagnosis based on the image above?
a) Corneal scarring
b) Posterior capsular opacification
c) Subluxated lens
d) Vitreous floaters
02 What is the most likely treatment for this presentation?
a) Corneal transplant
b) Intraocular lens exchange
c) YAG laser capsulotomy
d) YAG laser vitreolysis
03 The patient has declined the option of referral. What is the most appropriate next step?
a) Refer the patient anyway
b) Discharge from the practice
c) Advise on the non-urgent nature of the condition and monitor within the practice
d) Rebook them to see a different clinician to persuade them to be referred on

A 12-year-old girl presents with left eye pain, blurred vision and light sensitivity. She reports play-fighting with her younger sister that morning.
04 She finds it very difficult to open her eye during examination. What would be the most appropriate next step to aid assessment?
a) Instil a topical anaesthetic
b) Instruct the patient’s mother to force her eye open
c) Wait until she can open her eyes naturally
d) Accept she cannot open her eyes and make an educated diagnosis
05 What is the most likely diagnosis based on the above image?
a) Corneal ulcer
b) Decompensated cornea
c) Corneal abrasion
d) Filamentary keratitis
06 What next step could be considered as an appropriate course of action?
a) Cycloplegic drops
b) Topical antibiotics
c) Topical lubricants
d) All of these options

A patient attended due to intermittent pain and photophobia in one eye over the past three days. They have been feeling unwell and stressed recently due to a death in the family.
07 What sign or symptom is leastlikely to be expected in this case?
a) Redness
b) Watery discharge
c) Floaters
d) Blurred vision
08 Based on the image above and taking into account the history, what is the most likely diagnosis?
a) Herpes simplex keratitis
b) Marginal keratitis
c) Peripheral ulcerative keratitis
d) Corneal desiccation
09 The patient informs you that they wear contact lenses. How does that change your management of the patient?
a) No change
b) Treat as acanthamoeba keratitis until proven otherwise
c) Prescribe a topical antibiotic eye drop
d) Prescribe a topical steroid eye drop

A patient attended with finding shown in the image.
10 Which of the following signs is most apparent?
a) Trantas dots
b) Corneal guttata
c) Punctate epithelial erosions
d) Mutton-fat keratic precipitates
11 Which of the following is leastlikely to be associated with this case?
a) Anterior chamber cells
b) Posterior synechiae
c) Iris neovascularisation
d) Hypopyon
12 The patient also has high intraocular pressures. Which hypotensive eye drop class would you most likely want to avoid in this patient?
a) Prostaglandin analogue
b) Carbonic anhydrase inhibitor
c) Alpha-agonist
d) Beta-blocker

Alan Hawrami qualified as an optometrist in 2012 and has extensive experience working within community ophthalmology and the hospital eye service, mainly in a casualty setting. He is a director of a practice in Tonbridge, Kent which provides community ophthalmology and enhanced eye examinations. Hawrami has also completed a master’s degree in advanced clinical optometry and ophthalmology at University College London and the professional diploma in glaucoma.

MY CAREER ADVICE
“EMPLOYEE
Dipa Patel, head of optometry at Cubitts, on why ability to work autonomously is key for employees at the practice group
What advice would you give someone who wants to work for Cubitts?
Look at our core company values: Pioneering, Proud, and For All. We look for friendly, enthusiastic, hard-working, honest people, who uphold these principles.
What do you look for when shortlisting candidates?
Variety in different types of practices is good, but experience in independents is preferable. An empathetic nature and a genuine passion for their work is paramount. We are very patientfocused and the eye exam experience is important to us. Our eye exams are 40 minutes long and one hour for optical coherence tomography (OCT) eye exams, to allow our optometrists time to provide the best clinical, yet friendly and approachable service to our patients. We want everyone to leave feeling as if they’ve been listened to.
How important is experience?
As we’re introducing OCTs to more of our practices, experience in this is preferred but not necessary as we can provide training if required.
All our practices are single testing, so optometrists have to be comfortable working autonomously and making the majority of their clinical decisions alone. We do have internal peer communication groups for those times when a colleague’s advice is
needed. Because of this, we look for a minimum of five years experience post pre-reg.
How important is the cover letter? Applications can be made directly through our website, so a cover letter isn’t always required. However, attaching a cover letter does give applicants the opportunity to differentiate themselves – this allows us to have a better understanding of the person applying for the role.
What is the biggest mistake made in interviews?
Applicants not being themselves. My advice is to show us who you are –that’s why we want to interview you.
What are the most important values at Cubitts?
The Cubitts Code of Conduct reflects our company values. Pioneering: we improve things, by doing things better or more simply, celebrating both innovation and failure. Taking the lead: we don’t wait to be told what to do, and we stay positive in the face of challenges and change. Proud: we take pride in doing things properly, even when we are exhausted. We are deeply committed to the highest standards, with a relentless drive for consistency in quality and detail. For All: we treat
How do you go about ensuring fairness and equality in your hiring process?
We have recently been certified as a B Corp, and as part of this we demonstrate our ongoing commitment to diversity, equity and inclusion within all aspects of the business, including our workers. We have transparent salary grades for optometrists and every other position in the company.
everyone with the same warmth and respect, and without ego. We listen and communicate openly and honestly, respecting all opinions.
What tip would you give a new employee for their first week?
Enjoy it. Immerse yourself in your new team and practice, and don’t be afraid to ask for help – we’ve all been the new person in something. Our team will always be happy to help you if you are ever unsure on anything.
How important is employee wellbeing?
Employee wellbeing is vital to Cubitts. We all have access to financial health support on Bippit and mental health support through Thrive, ensuring that we all know where to turn to when we need support in the workplace.
“Variety in different types of practices worked in is good, but experience in independents is preferable”




It couldbe, if you're lookingfor a role that'sfocusedon clinicalcare and providinga high-quality serviceto NHS patients.Due to our recent expansion, we have vacancies in multiple locations, where you'll have the opportunity to work with some of the UK's leading ophthalmologists, nurses and HCTs. You'll benefit from fantastic training and professional development opportunities too.
We're patient-focused, providing clinical expertise and support for all our patients throughout every step of their patient journey.
We're busy-as the UK's largest provider of NHS cataract surgery, we have thousands of patients choosing our services and are proud to be able to support them in improving their sight and, ultimately, their quality of life.
Our patients really value the service we deliver-we've received 5-star reviews from more than 8,600 NHS patients across our 48 hospitals -you can read these on NHS UK.
You'll be GOC registered, with at least 12 months' post-registration experience -we provide full training so previous hospital experience isn't required.
You'll be someone that enjoys variety, is calm under pressure, great at problem solving and is willing to go the extra mile to provide the best service and advice for our patients.






























































Computerised test charts have revolutionised distance vision assessment -now it is time to do the same for near vision testing.
The ThomsonNear Chart allows you to link your PCto any mobile device (Apple, Android or Windows) and display a huge range of calibrated near vision tests directly on the device -no wires attached!
Simply select the required test on your PCand it instantly appears on the device. "Thissystemwill











With retinal imaging and optical coherence tomography (OCT) widely available in practice, our patients have become accustomed to seeing the back of their eyes in great detail on screen.
As practitioners, we have come to rely on this technology for detection, monitoring and education of posterior pole conditions. But are patients being disadvantaged if we don’t give their anterior eye complaints the same attention?
I COULD NOT LIVE WITHOUT...
I started using a digital video slit lamp in 2020, and am still finding new ways to utilise its full range of capabilities. The system can capture still images and record video clips, which are easily reviewed and manipulated within its software. With some practice, it has become quick and simple to integrate into my usual slit lamp routine. I’m predominantly using the digital slit lamp to document and monitor anterior eye conditions and for troubleshooting contact lens issues, but it can also take really good retinal images through a Volk lens.
Patient engagement and progress
For me, the biggest advantage of using a digital slit lamp has been patient engagement. Nothing beats showing a patient an image of their own eye to explain their condition and why we are recommending a treatment. The images and videos are impressive. Having a recognisable, personal image to reference makes explaining what is normal or potentially abnormal easier for them to understand.

“The patient gets to see first-hand the difference any management plan is making”
Having a digital slit lamp also gives me the ability to record an accurate baseline and to monitor progress pictures at subsequent visits. This can be particularly useful with conditions like blepharitis. Here the patient gets to see first-hand the difference any management plan is making, which has been great at keeping patients motivated to continue with their treatment. It can also highlight to them a lack of improvement with poor compliance, or when a different management strategy may be needed. In a similar way, taking a few moments to record a video of a toric soft contact lens swinging off axis can very simply demonstrate to a patient why they’re experiencing intermittent blur. Having this available allows them to appreciate why we may recommend a new fit or upgrade and why this could alleviate their symptoms.
They say a picture is worth a thousand words, and this is certainly the case with digital slit lamp images. The captures are clear and detailed, and are stored for comparison at future visits. This level of documentation feels much more accurate and watertight than written notes and drawings. This can be particularly useful if the patient is seen by another practitioner for follow up appointments.
Within the software, areas of interest on the images can be magnified, measured and analysed, meaning small, subtle changes are more easily identified and acted upon. We have confidence in monitoring these patients and can provide better quality, more timely referrals hen necessary. The images taken also create a great educational resource for patients and for in-house training.
In truth, a digital slit lamp doesn’t show me anything through the eyepiece that an ordinary slit lamp couldn’t. However, for the patient it opens up a whole new understanding of their eye health and creates a real ‘wow’ moment in a consultation.
Discussing the images with patients has helped to better educate and inform them of their conditions, keep them on track with treatments, and retain them for ongoing care and product purchases. I’ve come to rely on the digital slit lamp in the same way as retinal imaging and OCT, and my patients have come to expect it as part of a comprehensive, advanced examination.
June/July 2023 www.optometry.co.uk



Dr Ceecee Britten-Jones on the sense of community she has found within disc golf
Disc golf seemed to be a pretty natural transition when I stopped playing ultimate frisbee competitively in 2019. I was able to transfer some of the skills that I used in ultimate frisbee and learn new techniques at the same time. Disc golf is very chilled and fun. You can train as much or as little as you want. Considering the myopia epidemic, it is also a really good way of getting your outdoor time.
It is like golf, but instead of hitting balls into holes, you are throwing discs into baskets. We generally play 18 holes. You play with different discs that have different aerodynamic properties – there are drivers for long distances, putters for short distances and mid-range discs. My husband plays disc golf as well. We have at least 100 in our house, they are everywhere.
“I remember being about to throw a disc and there were these sheep and cows casually walking through the middle of the course”
My secret life
Do you have a personal passion to share with readers? Get in touch with selinapowell@ optometry.co.uk
I remember being about to throw a disc and there were these sheep and cows casually walking through the middle of the course. That was perfectly normal for that course.
Every time I play with my husband, we have to go and retrieve a disc from somewhere bizarre. I am not a risky thrower – I tend to stay within my repertoire – and my throws are pretty predictable, whereas my husband is a very creative thrower and he can throw at some amazing angles. We have spent hours climbing in bushes and he has waded into lakes to retrieve discs.
On every disc, people will write their name and phone number.

One of my favourite courses is in Adelaide – it is an amazing course right in the centre of the city in the parklands. My husband’s family is from Adelaide so we have gone back for Christmas every year. Every time we go, we will play disc golf four or five nights a week.
There is a disc golf course in Auckland, New Zealand where the baskets are quite hidden.
We have had discs discovered by strangers and returned six months after they were lost. We have also found discs in unusual places and returned them to their owners. It is like a treasure hunt, if you think about it.
Disc golf is a very welcoming sport. We have taken my parents to disc golf and we have friends who take their children. It is a game for all ages and demographics. Everyone should try it if they come across a course.
SupplementaryCodes
2.0 Cycloplegicrefractionfollowingroutineprimaryeyeexaminationonachild 2.1 Paediatricreview(withoutdilation)
ProducedfortheopticalprofessionintheUKbyFODOsupportedbyABDOandAOP
Peter Pham CEO and Founder of ZEST
“The ZEST Kit offers practitioners a convenient and low-cost treatment which shows a dramatic improvement in patients with dry eye and ocular discomfort. It is simple to perform but yields unrivalled clinical results.”

Gentle microexfoliation powered by Okra for immediate and durable clinical improvements

ZEST® is an in-practice deep cleansing system, utilising patented Zokrex™ technology and activated natural Okra polysaccharide complexes for a gentle, highly effective treatment. The Zocuswab foam applicators are used to gently exfoliate the eyelid margin, binding and lifting debris to remove biofilm that may be blocking the Meibomian Glands’ orifices, contributing to inflammation, redness and dry, flaky skin.