HIGH STREET HEROES










Welcome
My walk to the office is a traditional one, following the route taken by generations of medieval herdsmen driving their livestock from the countryside to be sold at Smithfield Market. Over time, it has come to look very different: people skirt Pret wrappers rather than cow pats, pass horse troughs planted out with flowers, and drink in former printworks now repurposed as cocktail bars.
Over the past year or two, that picture has changed once more. When I started at the AOP last June, we were still deep in lockdown and all the shops were shuttered. Over the months, those at the top end of my route, in Islington itself, have gradually reopened. Yet many of those in the heart of the City remain closed, and the accumulated post indicates that they will never reopen. This is not just a London phenomenon: across large swathes of the UK, the pace of recovery in villages and towns has far outstripped that in city centres. A combination of the pandemic and online purchasing is transforming the way we consume. The High Streets of the future may look very different from the High Streets pre-pandemic, let alone those of medieval past. This trend seems to affect optometry too. On my walk, I pass nine optometry practices, ranging from multiples and high-end boutique chains, to sole traders. All are back up and running; all, at a glance at least, are doing a decent trade. Unlike so many traders around here, few optometry businesses appear to have succumbed to the pandemic.
As this edition of OT discusses, some practice owners are beginning to ask themselves serious questions about whether the traditional optometry business model needs to change. Given the rise in online purchasing, do they seek to increase their clinical income stream? Conversely, given the financial limitations on NHS spending on optometric services (signalled by a totally inadequate increase in the level of the GOS fee), is it time to eschew NHS work? Or should smaller providers seek the shelter and economies of scale of a bigger group to reduce their level of personal risk? The future of the profession is likely to be diverse and it will be for practice owners to make their own decision about what sort of business they want to be. But one thing is certain: in 50 years’ time, the business of optometry will have changed as fundamentally as the look of my walk from Highbury Corner to Smithfield Market.


Adam Sampson, AOP chief executive

“It will be for practice owners to make their own decision about what sort of business they want to be”
Smithfield Market


07-21
SPOTLIGHT
The news in digest
Picture this
Haag-Streit’s in development simulator to support trainning in retinal examinations on premature babies
OT reports
100% Optical insight: what to know before the show
The edit
Optics in 16 stories
Clinical round-up
Heart attack risk predicted by AI
Supplier insight
The synergies of audiology and optometry
Industry profile
Federation of Small Businesses on High Street challenges, with Martin McTague
AOP affinity partner
Complete Background Screening
AOP roundup
100%Respectcampaign, a membership survey, and Mayopia event launched
Spotlight 100%Respectcampaign
“We’re committed to safe working environments in which all employees are protected from discrimination and treated equally”
Serena Box, AOP PR manager
PAGE 20
25-31
HIT LIST
The trends, launches and looks
OT focuses on...
Myopia management
Me and my glasses
Saxophonist, presenter and MBE recipient, Jess Gillam
Get the look // Anatomy of a frame
With Lizzy Yeowart
The shortlist
The April/May launches selection
Behind the brand
Eyeplan



33-37
COVID-GENERATION
SPECIAL REPORT
“‘Hopeful,’ ‘optimistic,’ ‘apprehensive’ and ‘uncertain’”
Huda Hathaf, AOP student representative

PRACTICE TEAM GUIDE THE PERFECT FIT


39-52 IN PRACTICE
Business insight and career development
The discussion Neighbouring practices discuss working in harmony since 1991
How I got here
Black & Lizars optometrist, Eilidh Thomson
The workshop
Lloyd & Whyte’s William King advises on insurance policies
IP and me
IP optometrist, Susan Bowers
Eyes on wellbeing
Nadia von Scotti; Kaupo Kikkas; Getty
Practical workplace wellbeing tips from Mental Health at Work’s Alison Pay Pre-reg focus
Thaksha Sritharan and Holly Leitch
Key milestones
Setting up a menopause support group
Becoming a business owner
Sofia Fazal
From learning sign language to promoting healthy lifestyles, OT profiles the diverse ways practitioners are giving back to their communities. Plus: private eye care – three practice owners share insight into their business models
Professional development for the eye care practitioner
65 CPD welcome
66 Low vision first aid
71 An introduction to intelligent systems in ophthalmology
75 Does my face look big in this?
80 Ocular allergic disorders
86 Corneal topography
88 A day in the hospital clinic
90-98 END NOTES
Jobs
Looking beyond the CV by Leightons Opticians & Hearing Care recruitment manager, Stuart Jackson
I could not live without...
”OCT,” says locum optometrist, Aman Sandhu
Secret life
Dr Greg Hammond on becoming a COVID-19 vaccinator
ONLINE

An interactive CPD video on childhood eye disease
Watch the video on www.optometry.co.uk/cpd
Contact the OT team with your experiences, observations and lessons from practice today: newsdesk@optometry.co.uk
















08 OT REPORTS
Spotlight
100% Optical show organisers share the five things to know ahead of the event
12 CLINICAL ROUND-UP
A bionic eye, and using artificial intelligence to predict heart attack risk
20 AOP SUPPORT
The AOP’s campaign against discrimination, a new myopia event, and a member survey
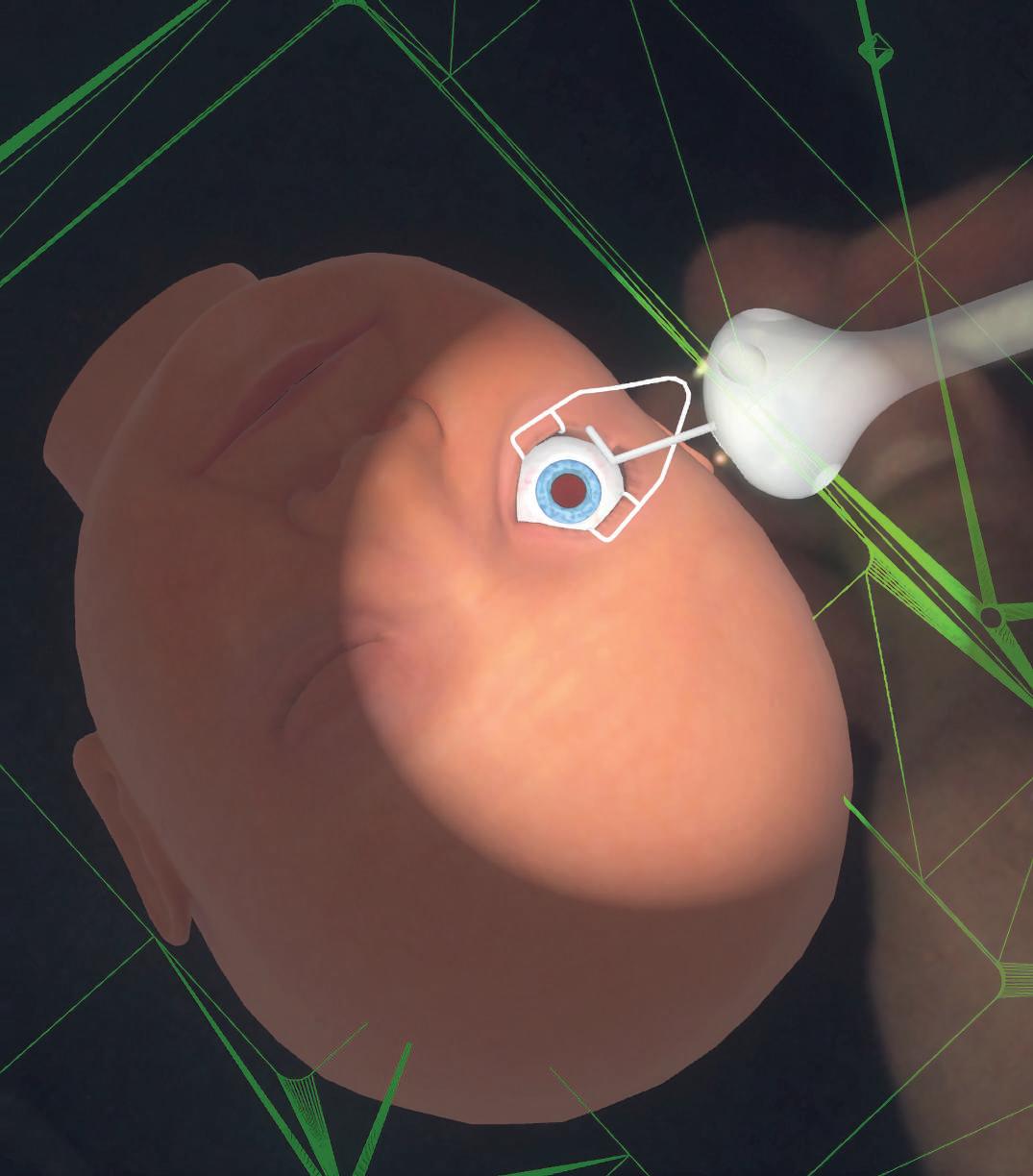
Developing tech
Haag-Streit Simulation is designing a simulator to support training in retinal examinations of premature babies. The ROP-Simulator would enable trainees to practise on virtual patients by simulating the physiology and pathology of an infant and mimicking the ophthalmoscope hardware, as well as reproducing the haptics of indenting the eye.

KNOW BEFORE YOU GO: FIVE 100% OPTICAL INSIGHTS
April/May 2022

Volume 62:02 Issn 0268-5485
ABC certificate of circulation 1 January 2020–31 December 2020
Editor: Emily McCormick emilymccormick@optometry.co.uk
Deputy editor: Lucy Miller lucymiller@optometry.co.uk
Assistant editor: Selina Powell selinapowell@optometry.co.uk
Senior reporter: Kimberley Young kimberleyyoung@optometry.co.uk
Web content and social media executive: Leah Boyle leahboyle@optometry.co.uk
Clinical editor: Dr Ian Beasley ianbeasley@optometry.co.uk
Clinical editor for multimedia: Ceri Smith-Jaynes cerismithjaynes@optometry.co.uk
Video production editor: Laurence Derbyshire laurencederbyshire@optometry.co.uk
CPD enquiries: 020 7549 2076 CPDhelp@optometry.co.uk
AOP membership and OT subscription team: subscriptions@aop.org.uk
Advertising: Matt Hall 020 3771 7257 matt.hall@thinkpublishing.co.uk
Advertising production: aop@ccmediagroup.co.uk
Senior designers: Grant Pearce, Juanita Adu
Client engagement director: Anna Vassallo
Executive director: Jackie Scully
Published bimonthly for the Association of Optometrists by Think Media Group 20 Mortimer Street, London, W1T 3JW
Printed by Acorn Web, Normanton Ind Estate, Loscoe Close, Normanton, West Yorkshire, WF6 1TW
All rights in and relating to this publication are expressly reserved. No part of this publication may be reproduced in any form or by any process without written permission from the AOP or the publisher.


After a gap of two years following pandemic restrictions, 100% Optical 2022 is just around the corner, bringing CPD, new products, and the opportunity for in-person networking.
Nathan Garnett, show director for 100% Optical, told OT: “We are feeling really positive about the show.”
KEY TRENDS ON THE SHOW FLOOR
Over 200 exhibitors will be at the show, explains Celsa Vazquez, event sales manager: “More than we’ve ever had.” Giving insight into the innovations set to be on display, she explained that the event organisers are seeing “really innovative handheld diagnostic equipment” from equipment manufacturers. In eyewear, new materials will be the biggest talking point, as well as the opportunity to meet new brands entering the UK. Virtual ‘try-on’ solutions, supported by augmentedreality, are set to be a key feature. Meanwhile, the presence of
audiology providers and suppliers is increasing in 2022. With many practices looking at introducing audiology, Vazquez said: “It’s definitely an area that we want to grow moving forwards.”
Delegates will see creative approaches from shop fitting providers, Vazquez added: “What they are going to be showcasing, and what they can do, is going to be quite eye opening for practices.”
Over 200 exhibitors
500 brands
More than 130 education sessions
Four poster trails.
Keeping up to date
As the official event partner and education provider for the show, the AOP has produced a programme of more than 130 education sessions, including workshops, lectures and peer reviews. The programme has been designed around the General Optical Council’s new CPD scheme, with sessions covering all of the new domains and interactivity requirements.
Dr Ian Beasley, OT clinical editor and head of education for the AOP, shared: “100% Optical is a valuable opportunity for delegates to keep up to date on key topics such as myopia management, optical coherence tomography, and many more. The education programme has been tailored to support delegates in meeting their CPD requirements, offering plenty of choice in topics covered and the style of delivery.” Beasley noted that education at the show is incredibly popular and encouraged delegates to review the sessions they have booked, and cancel any they no longer wish to attend.
THE POSTER TRAILS
Education provision at the show will include four poster trails, with one non-interactive CPD point available for completing each trail.
“There is something for every practitioner,” Beasley explained. “The poster trails are a beneficial way to use any downtime delegates might have during the show, between CPD sessions or meetings with exhibitors, and a chance to take even more value away from the show experience.”
“New for 2022, AOP members and OT subscribers will be able to scan a QR code on the posters to take the exam live, and receive an instant result and certificate,” Beasley said.
Maps showing the six different locations of the posters will be available for delegates to collect at the AOP Lounge.
Under the GOC's new CPD scheme, registrants are required to upload their own evidence of CPD completion. More information and guidance on how this can be done is available on the AOP website: www.aop.org.uk/events-and-education
“Plan ahead. Delegates should think about what exhibitors they want to visit and any queries they might have for the AOP while they have the opportunity to meet face-to-face with the team.”
Safe and efficient
Using the 100% Optical show app, now available to download, attendees can look through exhibitors, book appointments, network with other delegates, or post to social media.
Garnett explained the app is useful for creating a personal schedule of meetings and CPD.
Though COVID-19 restrictions have been lifted in England, hand sanitiser and masks will be available for those wishing to use them.
With visitor safety and wellbeing a top priority, James Champion, head of exhibition sales at ExCeL London, shared with OT that, “we’re continuing measures, such as our enhanced cleaning regimes, hand sanitisers located throughout the venue and increased ventilation in line with the latest guidance – all aimed at reassuring attendees and exhibitors alike.”
Say hello at the AOP Lounge
The AOP has been working with the exhibition organisers to ensure the show will be an informative and engaging event. The AOP Lounge (L03) will provide a dedicated area hosting a programme of education,
RECOGNISING RAMADAN
This year, 100% Optical will coincide with Ramadan (approximately 2 April until 1 May), and event organisers, along with the AOP, are collaborating to ensure adjustments will be available for delegates who will be observing the holy month. Champion highlighted: “There is a prayer
with sessions including peer reviews and content delivered in partnership with Johnson & Johnson Vision.
room on site – located beside Hall S9 – available for anyone to use as they wish.”
Exhibitors will be asked to be considerate of delegates observing Ramadan, and many are making plans to ensure accessibility for show visitors who will be fasting, Garnett said, adding: “The key thing is ensuring exhibitors are aware, acknowledge it, and make people feel welcome.”
Individuals from the AOP will be on the stand for members and non-members alike to meet.
Read more insight ahead of the show online: www.aop.org.uk/ ot/100-percentoptical
Members can request meetings on specific issues through the 100% Optical website.
IAN’S TOP TIP
Medical Air Sanitisers
Clean air has never been so important
Is your practice a Safe Air Space?



Stop the spread of viruses
Reduce allergy symptoms all-year-long
Comply with highest hygiene standards
Keep staff safe, healthy and at work
Reassure your patients
Promote health and raise productivity
Reduce sick-leave
6 STAGE FILTRATION TECHNOLOGY



AIR8 280 Nano
Ideal for the consulting room
Effective area up to 24m2
AIR8 720i Edge
Ideal for staff area or small front of shop area
Effective area up to 64m2
AIR8 1200i Pro
Ideal for large front of shop
Effective area up to 110m2

01438 740823
sales@bibonline.co.uk
bibonline.co.uk
“Renewable and sustainable ways of doing things are going to be here to stay. Every year awareness grows and people’s viewpoints come along on that journey too”

Tom Wolfenden, managing director at Wolf Eyewear, introduced OT to the brand’s new 'Inspirit philosophy.' The philosophy incorporates sustainability into all decision-making processes and the way the business operates. Read more online: https://bit.ly/373LovN
28%
The Childhood Eye Cancer Trust found parents’ concerns for their children’s eye health have dropped to the lowest point in eight years. The survey of more than 1000 parents with children up to six years old found 28% had taken their child to an optometrist for an eye test, compared to 37% in 2019. The charity, which supports families affected by retinoblastoma, emphasised the importance of resuming routine eye checks.

Lenstec Optical Group has proposed closing its Leeds facility, with 21 positions at risk. The optical supplier, part of the Essilor Group, cited a reduction in household names on the High Street, and a decline in independent practice market share as part of the decision.
Orbis International has revealed that female garment workers in Bangladesh suffer from high rates of near vision impairment, which is associated with earning a lower monthly salary, even after adjusting for factors such as years in employment and working hours. The charity suggested addressing this could help to reduce poverty and gender inequality in the country.
Alcon has launched its new Total30 monthly reusable contact lens in the UK, with features designed to mimic ocular biology. The lenses are aimed at wearers seeking a premium performance, and who likely have prior experience of reusable lenses, so the company launched “an aftercare programme with a difference,” including mindfulness podcasts, playlists, and reminders around contact lens care.
In the Spring Statement, Chancellor Rishi Sunak announced plans to increase Employment Allowance, which cuts National Insurance for small businesses, from £4000 to £5000 this month (April). A temporary business rates discount of 50% (up to £110k) was announced for retail, hospitality and leisure businesses for the 2022–2023 tax year.
1600
Residents across Wiltshire donated more than 1600 pairs of glasses to help people experiencing homelessness through a campaign led by Haine & Smith and regional charity, Alabaré. Anna Lewin, clinical lead optometrist, said: “When we launched our campaign, we didn’t imagine we would get such a good response.”


SCIENCE & VISION

THE EDIT
60 DAYS IN 16 STORIES
A study in Experimental Eye Research indicated the potential benefits of exercise in improving tear breakup time (TBUT) and tear secretion. A study involving 52 students aged 18 to 25 and divided into ‘athletes’ and ‘nonathletes’ found that while both groups saw improvements in TBUT, tear secretion and visual acuity following exercise, athletes displayed more marked improvements.
“We are… finding out what the needs of people with sensory conditions are and looking at potential solutions to the challenges they are faced with on a daily basis”
Dr Wasim Ahmad, of the Communication, Sensing and Imaging (CSI) Research Group, discussed how accessibility has not always kept pace with the progression of technology at an event displaying assistive technology.
PROFESSIONAL SUPPORT


The GOC has met 17 of the 18 Professional Standards of Good Regulation in the Professional Standards Authority’s (PSA’s) annual performance review for 2020–2021. It did not satisfy Standard 15 (Fitness to Practise) due to the length of time taken to conclude cases. The PSA noted that the GOC had made “significant progress” in implementing its improvement plan, and was the only healthcare regulator to have reduced its open caseload of older cases since the start of the pandemic.
“The announcement of a 2% increase will be a blow to primary eye care providers”
The Optometric Fees Negotiating Committee (OFNC) expressed disappointment following an announcement from the Department of Health and Social Care that the General Ophthalmic Services fee for sight tests will increase 2% from this month (April). The OFNC highlighted that the change in fee represents “in real terms a cut to funding” due to rising inflation.
IN PRACTICE

No7 Contact Lenses has launched a website dedicated to providing optical students in the UK with information and education on gas permeable lenses. The free-to-access site aims to support students through their professional development and spark an interest in specialist contact lenses. Professional services manager, Ian Sexton, said: “The primary aim of this site is to help students gain the critical skills needed to become fully rounded eye care practitioners.”
%
Research has found that hospital admission rates across England and Wales for diseases of the eye and adnexa increased by 73% between 1999 and 2019. Sharing the findings in International Journal of General Medicine, the scientists noted that the ageing population and increased life expectancy contributed to the rise over two decades. The most common reason for hospitalisation was disorders of the lens.
Optometry, regulatory and government bodies have signed a joint letter to the profession, highlighting the importance of vaccinations against COVID-19. The letter illustrates a “strong recommendation” that those in patient-facing roles should be vaccinated, and provides advice where someone is not fully vaccinated: https://bit.ly/3Ih4Emz

“I had no idea that a brain tumour could cause you to lose your eyesight”
Patient, Carla Hempe, shared her experience of a sight test that led to an urgent referral, later uncovering a meningioma compressing her optic nerve, and how her awareness of the importance of sight tests has changed: https://bit. ly/3tLdF1Z

Pexels/Gustavo Fring
A new eye clinic will open at the University of Huddersfield, supported by the independent optical group, Valli Opticians. University Valli Opticians will support clinical and commercial experiences of working in an optometry practice, as well as provide placement and employment experiences.

Clinical round-up
OT’s Selina Powell reviews the latest clinical news and research papers
AI PREDICTS HEART ATTACK RISK
Artificial intelligence (AI) developed by an international team of researchers has estimated the risk of someone having a heart attack over the next year on the basis of retinal scans.
A study describing the research, which was published in Nature machine intelligence, highlighted that the AI system had an accuracy of between 70% and 80%.
Professor Alex Frangi, from the University of Leeds and the Alan Turing Institute, shared that the technology opens up the possibility of “revolutionising” the screening of cardiac disease.
“Retinal scans are comparatively cheap and routinely used in many optician practices. As a result of automated screening, patients who are at high risk of becoming ill could be referred to specialist cardiac services,” he said.
To train the AI system, the technology analysed the retinal and cardiac scans of 5000 people.
The system identified associations between pathology in the retina and changes in the patient’s heart. Sven Plein, from the University of Leeds,

“Patients
who are at high risk of becoming ill could be referred to specialist cardiac services”
shared that the AI system can be used to unravel complex patterns that exist in nature.
“That is what we have found here – the intricate pattern of changes in the retina linked to changes in the heart," he said.
The authors concluded: “Our results indicate that one could identify patients at high risk of future myocardial infarction from retinal imaging available in every optician and eye clinic.”
MOORFIELDS EYE HOSPITAL PATIENT RECEIVES BIONIC EYE
An octogenarian who was previously blind in her left eye has been able to detect signals following the insertion of a bionic chip at Moorfields Eye Hospital.
The patient, from Dagenham, is the first in the UK to receive a bionic eye as part of a Europe-wide clinical trial.
Surgeons implanted the 2mm chip, which receives signals from specialised glasses containing a video camera under her retina. The chip captures the visual scene projected by the glasses and transmits this to a small computer attached to the patient’s waistband.
Artificial intelligence algorithms within the computer direct the glasses to focus on what is deemed to be the main object in the image.
The image of this object is projected as an infra-red beam on to the chip, which is then converted into an electrical signal
that passes through to the brain as if it were natural vision. Four to six weeks following the operation to insert the chip, the system is tested by switching the chip on to see if the patient detects a signal.
The patient then undergoes a rehabilitation programme to adjust to this new form of vision. The 88-year-old patient shared: “I am thrilled to be the first to have this implant, excited at the prospect of enjoying my hobbies again, and I truly hope that many others will benefit from this too,” she shared.
Consultant vitreoretinal surgeon at Moorfields Eye Hospital, Mahi Muqit, highlighted: “The success of this operation, and the evidence gathered through this clinical study, will provide the evidence to determine the true potential of this treatment.”
DIABETES
Link between eating disorders and eye disease
A new study published in Journal of Diabetes and Metabolic Disorders has highlighted that people with diabetes who develop eating disorders are at an increased risk of eye disease.
Scientists from Anglia Ruskin University looked at data from 1100 participants across several studies. This research revealed that those with an eating disorder were 2.94 times more likely to develop diabetic retinopathy than those without pathological eating behaviours.
Trott et al.
DOI: 10.1007/s40200-022-00980-x
CHILDREN
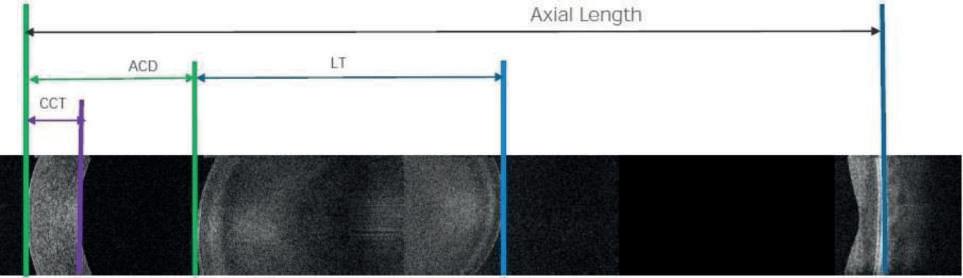
Using contact lenses to accelerate axial growth in hyperopes
New research has found that axial growth can be accelerated in hyperopes using centre-near multifocal soft contact lenses.
The study, which was published in Ophthalmic and Physiological Optics, involved 22 hyperopic children between the ages of eight and 14 years.
Axial growth during the two-year intervention period was close to three times greater in the test group than the control group (0.17mm versus 0.06mm).
The Aston University researchers concluded that rate of eye growth can be accelerated in children with hyperopia by imposing relative peripheral hyperopic defocus using multifocal contact lenses.
Beasley et al.
DOI: 10.1073/pnas.2102975118
RETINA
Clues to mortality risk found in the eye
Scientists have developed a deep learning model that predicts an individual’s age on the basis of fundus images.
The research, which is published in British Journal of Ophthalmology, describes a deep learning model that predicted an individual’s age to within 3.55 years.
By analysing mortality data, the scientists found that each oneyear increase in the gap between actual chronological age and age predicted on the basis of fundus scans was associated with a 2% increase in all-cause mortality.
Zhu et al.
DOI: 10.1136/bjophthalmol-2021-319807



The synergies of audiology and optometry
With demand for audiology services growing, OT looks at how partnerships between audiology providers and
independent optical practices are on top of this shift
Providers agree that audiology is growing. Paul Surridge, chairman of the British Irish Hearing Instrument Manufacturers Association (BIHIMA), has experienced both sectors, having previously led SightCare as chief executive for 19 years.
“The trend of opticians and audiologists working together has been underway for a number of years now and is a growth opportunity,” he said, adding: “As experts in the senses, there is a natural affinity between eye and ear specialists.”
Hearing care has not always had the footprint in optical practices that it does now. Dave Murphy, managing director of Amplify Hearing, a business focused on bringing audiology and optometry together in practices, explained: “Then some of the big retailers realised the synergy between the eyes and the ears, and how they could leverage their optical business and include audiology.”
“I think it was always really difficult for independent optical practices to get involved in audiology,” he continued, adding, “but I know for a fact that it is growing,” with the company onboarding an extra 100 practices this year.
Ryan Leighton, founder of The Hearing Care Partnership, and CEO of Leightons Opticians and Hearing Care, agreed: “We’ve seen more people over the years starting to think about audiology and optometry running alongside each other.”
The Hearing Care Partnership has grown to 170 practices since 2017. “In the independent sector, it seems like a lot more people are looking to introduce audiology alongside optometry because it’s clearly a very significant, natural fit for businesses,” Leighton said, “to the point where, if opticians are not part of audiology, it almost becomes a lack of a competitive advantage for them.”
Rebecca Wagstaff, hearing aid audiologist at Amplifon, also sees the advantage: “The smaller independents are now dipping their hands in because – competition wise – if you can provide hearing care and eye care in the same place, that is going to stop you losing your patient base to the bigger chains.”
The hearing care retailer operates day centres in 20 optical practices, making up two thirds of its locations.
Practices have long-standing relationships with their patient bases that they want to nurture, Wagstaff added, so providing an extra service “makes sense.”
“Audiology is here, and is here to stay inside the optical space”
Dave Murphy, managing director, Amplify Hearing
Drivers of demand
Audiology has experienced a reduction in the availability of services in the NHS in England, leading more patients to turn to private practices, the experts said.
“That has driven the independent audiology market across the UK, not just in optometry settings, but across the whole sector,” Murphy suggested.
If services are less available in the NHS, the High Street can act as an access point, he said: “We’re creating a route where people can be seen on the High Street, and creating an audiology journey, without involving the GP and NHS.”
The pandemic has only increased pressures on NHS audiology. Leighton noted, with lengthening waiting lists, “that means there are more people in the population, and in communities, who are looking for direction for hearing loss, and might be looking outside the NHS.”
Many GP practices have also not been providing wax removal services in recent years, adding that as a result, “there has been quite a big movement from the private sector to provide services to help people with earwax removal.”
Reflecting on the increasing need for audiology services, Leighton summarised: “There’s clearly a lot of demand from the ageing population. On top of that, we’ve got a previously very efficient NHS audiology provision across the UK, which has been struggling because of COVID-19. People are looking for a solution, so will look to providers of audiology services in the local community.
“I think certainly in the next couple of years we’re going to see increased demand. There is the potential, if done well, for a lot more patient footfall in optical practices,” he continued.
Pressure and propulsion
Face-to-face activity in audiology halted when the country went into lockdown in 2020, though audiology remained operational as an essential service in the latter lockdowns. Since then, hearing aid sales returned to pre-pandemic levels, Surridge said, and the sector is now “in growth once again.”
“The industry worked together to establish remote provision, in a safe and accessible way using clever technology solutions, which has really advanced the sector,” he added. “Not only has it
allowed people to access their audiologist on a more frequent basis for check-ups and tuning, all from the comfort of their home, but it has also allowed audiologists to understand their patients’ needs in a real-world setting.”
Murphy told OT: “What we saw with the pandemic was suppliers and manufacturers delivering technology in three months, that they would otherwise have rolled out over 24 months.”
Technology enabling remote access to hearing instruments, and therefore creating the space for remote appointments and clinics, has been “fantastic” Murphy emphasised, “because it gives the patient choice.”
Leightons moved to host phone or Zoom calls with patients who were experiencing hearing loss or had an issue that needed resolving which meant, when patients could be seen in practice again, audiologists could provide an abbreviated assessment.
“That’s enabled us to do things in a more effective way. For patients who maybe can’t get into the practice and want to be seen about their hearing and whether it has changed, the audiologist can remotely reprogramme their hearing aids,” Leighton highlighted.
A holistic service
The providers agreed that patients benefit most from the convenience of having both services in one place.
When future-proofing practices it’s important to consider factors that provide a “great patient service experience and value,” Leighton said, adding: “From our point of view, optometry and audiology are a great fit in that regard.”
This could also support patient loyalty and advocacy, Leighton suggested: “What you will hopefully see is a stronger foundation of patients within your database in the local community, and more awareness, and therefore you should be able to build a stronger and more sustainable business.”
Wagstaff explained that she, and the optical practice she works in, both have access to her diary to make appointments: “I’m only there one day a week, but it is full every week.”
The partnership approach means practices retain their patient base, and also don’t have the initial outlay to buy the audiology equipment, or to employ and train a member of staff, she shared.
Considering the reasons practices might engage with the audiology sector, Murphy told OT: “On a more holistic level, it is about the clinical relationship between eyes and ears and making sure the health and wellbeing of patients is first and foremost.”
“It’s clear that audiology is here, and is here to stay inside the optical space,” he continued, recommending a collaborative approach: “Let’s create an environment where it works for everybody.”
WHAT INNOVATION ARE YOU MOST EXCITED TO SEE IN AUDIOLOGY?
Murphy: I think remote care is a huge part of how we can deliver the best patient care in the future. We don’t want to turn into a remote care business; it is about being able to triage and possibly fix patient instruments remotely.
Leighton: Hearing aids are communicating with your iPhone or TV. It’s exciting to think about how that technology becomes more accessible to people. There is really amazing work going on around the world with regards to hearing aid implants, which could be the next stage on from where we are today.
Wagstaff: There is a rechargeable custom hearing aid that has just been made available. A rechargeable option is going to benefit those patients on the older side who don’t want anything fancy, they just want something they can use.
Surridge: I think health monitoring will be a major development for the sector. Extending hearing devices beyond just hearing ‘aid’ or ‘sound delivery’ device, and into the world of healthables; monitoring heart health, tracking weight or exercise, medication routines, and fall detection.

























sales@bibonline.co.uk
www.bibonline.co.uk

Challenges facing the High Street
Martin
McTague, national chair of the Federation of Small Businesses, on the pressures facing small businesses on
the High Street


Small businesses on the High Street definitely have a lot on their plates at the moment, following two years of uncertainty, restrictions, and change. The rises in National Insurance contributions (NICs) and business rates will increase small businesses’ costs before they have earned a penny of income, while spiralling inflation is causing input prices and utility bills to soar. It’s no surprise that retail businesses registered the lowest confidence level in the Federation of Small Businesses’ (FSB) Small Business Index research in the final quarter of last year, at -40 (against -8.5 for all businesses).
The Spring Statement did contain one big win for small employers. An increase in the Employment Allowance from £4000 to £5000 will allow small businesses to offset some of the impact of the rise in NICs.
for rent arrears which are due to the pandemic. Landlords are aware that the commercial property landscape has shifted, with premises in formerly red-hot locations such as central London now seeing lower levels of footfall. Meanwhile, commuter town locations are enjoying higher numbers of shoppers as people who are working from home tend to stay local.
to keep on top of their stock levels, and are necessitating changes to stock management processes. In a fashiondriven area such as eyewear, knowing what customers will be looking for in three months’ time is becoming more important than ever, while retailers cannot afford sales of items such as contact lenses and supplies to be interrupted due to a lack of stock, for fear that customers will turn elsewhere.
Challenges and cost pressures abound, but many small businesses are bullish about the future, now that COVID-19 restrictions have been lifted, and the pent-up demand for products and services (such as eye examinations and new glasses purchases) begins to make itself known. We are still some way from the pre-pandemic norm in many ways, but people are starting to think about purchases and check-ups, which they put off during the height of previous waves of the pandemic.
The FSB’s Small Business Index found retail businesses registered the “lowest confidence level” for the final quarter of 2021.
Business rates relief schemes in the various nations of the UK across the pandemic have rightly focused on the most at-risk sectors, including High Street-based retail businesses. But the relief schemes won’t last forever; we want to see thousands of small firms in England lifted out of paying rates, by increasing the ceiling for small business rates relief to a rateable value of £25,000. The 50% business rates relief for eligible retail, hospitality, and leisure properties from April, announced in the Spring Statement, is welcome however.
The Government’s levelling up agenda is yet to be fleshed out, but if it brings more life to local communities and High Streets, it is to be welcomed. We will push the Government to consider the needs of small businesses as it looks to advance the agenda, as well as pointing out that the many areas which would not normally be thought of as needing to be ‘levelled up’ will still have small firms which have had a tough time.
The restrictions on commercial evictions brought in as a response to the COVID-19 pandemic expired towards the end of March. Although there are still protections in place
Many businesses have been affected by supply chain issues, and shipping costs remain higher than a year ago. Delayed delivery times are having an impact on retailers’ ability
The arguments for staying local to shop are strong and are being heard by consumers. Now is the time for small firms to band together and work with local government, development agencies, and community groups to explore how to make their High Street a great destination for residents and visitors. As our research shows, small firms have the appetite to grow – it is up to the Government to ensure they have the opportunity and the right environment to do so.
EBBING CONFIDENCE













































“We listen and learn, and make sure the journey is as pleasant, easy, and quick as it can be”
Rachel Bedgood, lead signatory at Complete Background Screening, on the updates members can expect to see in background checking services
Complete Background Screening (CBS) has partnered with the AOP for many years. Through this partnership, we have been able to offer members a standardised and streamlined background checking process, and the feedback we receive from members is always super positive.
There have been a lot of updates in regards to the Disclosure and Barring Service (DBS) in recent months, particularly in light of the pandemic. Like everything, COVID-19 had an impact on DBS and background checks in recruitment. Completion times were slightly longer as there weren’t the staff or the resources to complete the checks and processes. In addition, there where delays within the DBS and its partners, such as the local police forces.
However, the DBS introduced a fasttracking service allowing applications to be processed free of charge if they were contributing to the pandemic support efforts and offered a check against the child and adult barred lists within 24 hours. This was hugely beneficial in helping the healthcare sector rapidly screen individuals to place into frontline roles that were required at the time.
Changes in checking
As life has begun to settle, the DBS has had time to introduce some new ideas and changes. Firstly, with government approval, the DBS reduced the costs of checks from 6 April. Previously, basic and standard DBS checks were charged at £23, and enhanced DBS checks were charged at £40. Now it will reduce to £18 for basic or standard checks, and £38 for enhanced. It is only a couple of pounds less for the enhanced level disclosures – the check required to be on the NHS Performers List – but a cost saving is a cost saving.
The DBS intends to introduce digital ID checking as early as this month (April), which is going to be a mini revolution.

For many businesses, ID checking can feel like a labour-intensive and lengthy process for employer and employee. With the digital ID offering in place, employees will see a much quicker and smarter way to verify their ID. They will not need to meet with anyone faceto-face, meaning DBS applications can be submitted much faster. Quicker submissions mean quicker turnaround times. From an employer’s point of view, this can save them time and money. It also takes away the pressures of the process and the potential margins of error when checking a person’s ID manually.
Checks increasing
Most AOP members we see opt for the enhanced level disclosures with barred list checks. Some employers might decide to run additional checks. CBS is a background screening house with a global reach. As such, we can undertake international criminal checks, Right to Work checks and employment screening. Very often employing candidates can be quite a long and drawn out process, but when the wrong decisions are made it can become very expensive to resolve this later.
Within optometry, we see a large volume of individuals opt to subscribe to the Update Service, which means they potentially have a portable DBS check and won’t need to undertake multiple additional checks.
For more information on the services available from CBS through its affinity partnership with the AOP, visit: www.aop.org.uk /benefits
Employment was on the rise throughout 2021, particularly in the healthcare sector, and the volume of DBS checks processed continues to increase year-on-year. The DBS currently processes nearly six million enhanced checks alone.
This service was born from a Home Office enquiry revealing that individuals who might work in the same type of role in different settings, were still subjected to multiple criminal checks. The Home Office decided to create portability, so a person working in similar environments has the ability to move that DBS between organisations. This also allows us and employers to determine if a person’s criminal record has changed. A perceived flaw within the DBS system previously was that, in theory, the criminal certificate was only valid on the day it was issued, but those signed up to the Update Service can give their employer or organisation continued peace of mind.
MAKING THE PROCESS EASIER
Rachel says: “We are very aware that nobody thinks: “I can’t wait to have a DBS check.” There is a level of apprehension around background screening, and understandably so as they can be invasive. However, the checks are very necessary. We listen and learn, and make sure the journey is as pleasant, easy, and quick as it can be for the applicant.”
L-R Sarah Nicholls, finance manager; Rachel Bedgood; Sarah Lloyd, operations manager


A pledge against discrimination
The AOP has launched a new campaign which asks individuals and businesses to take steps to promote inclusivity in optometry
This April the AOP will launch its 100% Respect campaign, asking individuals and businesses to pledge to create inclusive environments.
The digital campaign has been launched ahead of 100% Optical, to encourage attendees to sign up to the pledge, and coincides with Ramadan.
Corporate businesses, independent practice owners, employees, locums, and students, are all encouraged to sign up to the pledge.
The campaign encourages anyone who sees or experiences discrimination to report it, and the AOP is working with senior industry leaders and business owners to create inclusive environments by following the association’s guidance for employers.
Serena Box, PR and media manager for the AOP, explained: “We’re committed to safe working environments in which all employees are protected from discrimination and treated equally.”
Mastering myopia
Focus areas were identified using data from the AOP’s Voice of Optometry survey, which found that racial discrimination was more prevalent than any other form – cited by 60% of survey participants – though sexism, religious and agerelated discrimination were also reported widely.
Experiences shared by members in the survey also indicated that in 80% of cases, it was patients who were “the perpetrators of discrimination.”
As a result, the campaign highlights resources, such as practice posters, to help to foster a healthy environment and illustrate a zero tolerance approach to discrimination, as well as social media and digital assets.
“We all have a duty to call out discrimination and tackle inequality,” Box said, adding that the AOP seeks to be “an advocate of change and support the enforcement of zero tolerance policies to ensure our members feel safe and protected in their workplace.”
More information about the #100Respect campaign can be found on the AOP website: www.aop.org.uk/Respect
The MayopiaDayvirtual event will deliver a programme of education to update practitioners on myopia management
OT, in partnership with the AOP, will host a series of virtual education sessions focused on myopia management in May, bringing the profession together to hear from experts and share learnings.
Mayopia Day, which is headline sponsored by CooperVision, will be held online on 22 May, featuring key topics in myopia management and offering interactive CPD points. Education will be delivered by CooperVision, Johnson & Johnson Vision, Hoya and Essilor. Members can attend for the full programme, or specific sessions of interest.
OT clinical editor and AOP head of education, Dr Ian Beasley, said: “The programme is designed to appeal to all, from those who are new to myopia management, to experienced practitioners wishing to consolidate and update their knowledge in the subject area.”

AOP PREPARES NEW MEMBERSHIP SURVEY
John White, AOP communications director, shares why it is important to get involved
WHAT IS THE AIM OF THE SURVEY?
Membership surveys are a vital listening exercise for the AOP. They enable us to ask members about their evolving attitudes to their profession and career, and this insight helps us to review and enhance what we offer members based on their individual needs.
WHY IS THIS RESEARCH IMPORTANT?
We recognise that the profession is changing – and the speed and scale of these changes has accelerated during the pandemic. Our survey will explore the experiences of optometry professionals and the expectations members hold about the profession in the future. For example, what services do members believe optometry will offer in the community – and how will the optometrist’s role and practice team’s role adapt? We also plan to ask about members’ individual career ambitions and development needs.
HOW CAN MEMBERS TAKE PART?
The research company will invite members to take part in focus group work, followed by the survey which will take around 15 minutes to complete. Questions will vary based on mode of practice and career stage. For the results to be statistically meaningful, we would like to see as many members as possible take part. Members need to check their ‘MyAOP Communications’ setting to make sure they are receiving information about AOP surveys.
“With a rapidly changing evidence base and an evergrowing portfolio of clinical solutions available, it is important that practitioners are updated on the latest developments in the field and incorporate myopia management tools within their skillset,” Beasley added.

More information about MayopiaDay,including education sessions and bookings, can be found on the AOP website, www.aop.org.uk/events, from 18 April.

AOP EXPERT AOP EXPERT
Commercial Policy
Sarah Melzack, AOP membership benefits officer
How has the AOP’s mentoring programme been received?
We’ve had a huge number of mentors sign up, and over two thirds of mentees who are on the platform have matched themselves with someone for support and are in active relationships. For mentees, it is a fantastic opportunity to cherry pick someone who has experience in the area they are looking to develop in.
How many mentors are currently in the scheme?
We have almost 100 mentors. Over half of our mentors have 20 years of experience in practice or above, and over two thirds of mentors have more than 11 years of experience. We have a great balance between mentors working in the corporate and independent space. Of our mentors, 20% are locum optometrists, and 15% are optometrists working in hospitals or academia.
What led to the expansion of the programme to locum members?
While locums may return to some practices, there are a lot of locums who are oneperson bands. They don’t have that stable sense of team or supervision. Mentoring can give the locum the space for those conversations outside of day-to-day relationships, and still have someone in their corner on a regular basis.

Carolyn Ruston, AOP director of policy
How would you describe your career journey so far?
I have worked in the NHS for over 15 years. However, my career originally began in information science. I love working in healthcare and the opportunity to be part of something that impacts positively on people’s lives.
AOP members can sign up for a mentor through the AOP website: www.aop.org.uk/adviceand-support/health-andwellbeing
What have you learnt from your previous experiences that you intend to carry across into your policy work at the AOP?
where possible. I am looking forward to working with sector partners and our members to grow and sustain the future of optometry, especially in the context of imminent health reforms that will have impact on the commissioning and delivery of primary care.
What are you most excited about for the year ahead in your new role?
When everything else in a locum’s day-to-day can be segmented, a mentor can sew it all together – understanding where the locum has been and what they are going on to. If an optometrist is new to locuming, it can also be nice to speak to someone who has been doing it for a while.
For me, it is important to think about the outcome or impact you want to have by developing a particular piece of policy and managing a specific programme. Having the patient at the forefront of our thinking should always be the priority. I am a strong advocate for coproduction and collaboration
A COMPLETE
treatment plan for ChiLDhOod mYopiA
Health reform and the formation of Integrated Care Systems present some exciting but challenging opportunities in optometry. I am looking forward to working with members and the sector to shape the future of optometry, and how we work with colleagues to alleviate backlogs in secondary care and improve health outcomes for our local communities.
The full interview with Carolyn can be found online: https://bit.ly/3tq6Hzh















Menicon Bloom™ in your store enquiries@menicon.co.uk 01604 646216 www.menicon.co.uk



























































FOCUSES ON... MYOPIA MANAGEMENT
A blossoming system
Menicon has launched its Menicon Bloom Myopia Management system to offer “a complete treatment plan that extends beyond vision correction.” This includes CE-approved contact lenses and care products, while a Menicon Bloom app and Menicon Bloom Easyfit software help practitioners monitor wearer compliance to reduce the progression of myopia. The company has also launched training and e-learning modules for practitioners to become certified Menicon Bloom specialists. www.menicon.co.uk/professional

Hit list
The trends, launches and looks

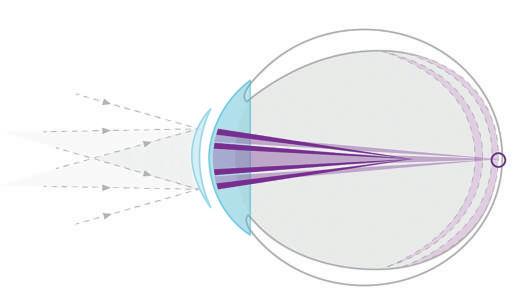
Combined approach
Lenslet tech
Essilor’s Stellest lenses have arrived in the UK. The lenses feature a design that aims to control and slow down myopia progression, using Highly Aspherical Lenslet Target (HALT) technology, a constellation of invisible aspherical contiguous lenslets over 11 rings on the surface of the lens. The lenses aim to create a volume of unfocused light in front, and following the shape of, the retina, which helps to slow down eye elongation. ecp.essilor.co.uk
Haag-Streit UK has partnered with Hoya Lens UK to provide the Lenstar Myopia by Hoya, based on the Lenstar 900 optical biometer and EyeSuite myopia management software. The combination of the lens and device “creates a strong one-two approach to diagnose and manage myopia and provides eye care professionals with an end-to-end comprehensive package that equips them to combat the progression of myopia,” the companies said. hsuk.co/HOYALenstarMyopia

Entering the market





EssilorLuxottica and CooperCompanies have finalised a joint venture operating agreement for SightGlass Vision to accelerate commercialisation of its lens technology. SightGlass Vision’s Diffusion Optics Technology incorporates thousands of microdots in the lens to scatter light, which reduces contrast on the retina and aims to reduce myopia progression. Commercialisation of the technology is progressing with the first European launch in the Netherlands. www.linkedin.com/company/ sightglassvision



















Jess Gillam

GET THE LOOK
Optometrist and lifestyle blogger, Lizzy Yeowart, on statement pieces from the most recognisable design houses
During the pandemic, retailers reported steep rises in accessory sales, especially investment pieces from heritage and designer brands. Here are three pieces of eyewear from long-established fashion houses.

Undeniably Dior
This bold butterfly sun style makes a statement, and the gold-finish CD monogram leaves no doubt that this is unmistakeably Dior. www.dior.com
The award-winning saxophonist and BBC Radio 3 presenter on her bold eyewear
1
I started wearing glasses when I was about seven. The first pair I had were those awful NHS octagonal frames and I look back now and question: ‘what was I thinking?’ I come from a line of glasses wearers so my mum had probably thought she should take me for an eye test.
2
I really love that my current pair have seethrough acetate with black patterns on. I wear quite bold clothes on stage so the fact that they’re see through and black means they pair with any colour. Because I’ve always worn glasses, they’re part of my everyday outfits so it's important they sit well on my face and they’re comfortable. Because I've worn glasses for so long, I don’t recognise myself without them on.
3
I have one pair of glasses that I fall in love with and then hold on to for as long as humanly possible. I’ve got one pair of glasses and a spare next to the bed so I know that I’ve got one pair that I can wear to find my glasses with, and one pair of sunglasses.
4
Glasses are an important part of my identity and look, especially on stage. It’s important for my confidence levels. I can’t see without my glasses for one point, but even with contacts, I feel slightly bare. I’m so grateful to opticians and people who have made it possible to be able to see the world properly because it makes such a difference. I am grateful for being given good vision through my glasses.

Bio beauty
A modern silhouette made from biodegradable bio-acetate and highlighted with a gold-plated ‘B’ and detachable chain with Burberry lettering. uk.burberry.com

Pearlescent treasures
Chanel’s iconic strap is reimagined in this stunning optical style with chain-link detail on the top and sides. It comes with a detachable strap fashioned from calfskin and imitation pearls. www.chanel.com/gb
Spectacles
Street style
International Eyewear has introduced 10 new frames in the Humphrey’s 2022 collection, which is inspired by street style and aimed at a young generation “with a zest for life.” Highlights include a bold oversized frame “for the more adventurous” wearers, while the ’582354’ (pictured) presents new shapes in trending metal materials. www.internationaleyewear.co.uk
Sunglasses
A new dawn
Neubau Eyewear has launched a special collection featuring two sunglasses to represent “the spirit of new beginnings” and capture the sense of night turning to day. The ‘Transition’ frames, ‘Xenon’ and ‘Neon,’ host a colourful beta titanium feature along the brow line and mirrored lenses. The frames are both made from the brand’s natural3D sustainable material, a bio-based polymer made from castor oil beans, then processed in a 3D printing “no-waste” method. www.neubau-eyewear.com


Spectacles
At the core
Eco Eyewear, a Modo Eyewear brand, has launched its spring/ summer 2022 collection with four ‘families’ centred around different sustainable materials: 95% recycled metals, bio-based plastics, ocean plastic and bio acetate. In the recycled metals collection, the new ‘Osier’ sunglasses (pictured) are available in a rounded square style with polarised lenses in colours ranging from yellow to denim. www.eco-eyewear.com
Equipment
Assessment technology
Grafton Optical has launched a new module from SBM Sistemi to enable practices to turn their slit lamps into a digital dry eye assessment tool. The DSLC200 Slit Lamp Imaging Module features a 3.1 megapixel camera with 1/1.8” sensor and optical image splitter. Used with the DSLC200 module, the DEM100 Dry Eye Module includes examinations for interferometry, tear meniscus, bulbar redness, meibography, blepharitis, NIBUT and anterior segment imaging. www.graftonoptical.com

Nadia
von Scotti

To feature in OT’s Hit list, contact kimberleyyoung@ optometry.co.uk

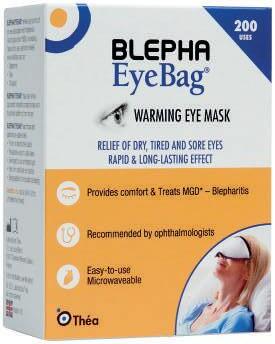
Dry eye
Bags of potential
Théa Pharmaceuticals has added the Blepha EyeBag to its range of eyelid care products. The Blepha EyeBag is designed to treat eye conditions including meibomian gland dysfunction, blepharitis, stye, chalazion, and dry eye disease. The compress is made from silk and cotton, with flax (linseed) filling, and can be reheated up to 200 times. www.thea-pharmaceuticals.co.uk



Spectacles
Pastel perfection
William Morris London has highlighted three new “stand-out and eccentric” styles from its spring/summer 2022 collection, suggesting that “playful designs and bright colour splashes” are ideal for the season ahead. Included in the collection, the ‘LN50238’ (pictured) acetate frames feature splashes of pastel colours in unique designs, with the blossom-inspired hues including blues, greens, and pinks. www.williammorris.co.uk
Sunglasses
A lasting statement
Retrosuperfuture has introduced its spring/summer 2022 collection, which features an approach designed to “last beyond the season.” The collection includes four new sunglass silhouettes, while the optical range features seven new styles. In sunglasses, the brand highlighted ‘Zenya’ (pictured) an oversized cat’s eye frame with thick rims, wide rectangular lenses, and a V-shaped brow line. The design is available in three shades: all-black, spotted Havana, and a purple and black checked acetate. www.retrosuperfuture.com



















EYEPLAN
Commercial director, Chris Clemence, on the increased uptake of the Eyeplan model
EYEPLAN //
1 2 3
Eyeplan was founded 23 years ago, and the founders, Simon Mills and Fraser Robertson, are still leading the business
Mills and Robertson were involved in taking HMRC (then HM Customs and Excise) to court in 1995 in a VAT case for optometrists
Eyeplan’s sister company is the Eyetech group of practices.

ANATOMY OF A FRAME
Unpicking a standout frame, by OT columnist Lizzy Yeowart

What is Eyeplan? What was your most recent launch?

We design eye care schemes for practices, help them with their pricing, marketing and staff training, and provide a core service of direct debit management. We’ve been doing this for about 23 years. The main thing we have brought to the market over the last few years is the new management platform, Opti. The platform allows users to create tailor-made eye care packages for patients.
Are there any new solutions in development that customers should be aware of?
Uptake has increased dramatically since COVID-19. Practices were grateful for the investment they made in creating the contracted income. It was probably one of our busiest periods of patient communications and talking to practices about how to survive and maintain their patient base, but it worked. I think people are rapidly moving away from GOS, and it is probably the most common topic I discuss. Another thing that is driving practices towards the Eyeplan model is the extension of services that optometrists are able to offer.
What do you see as key trends for practice management in the year ahead?
Our focus is to have Opti as standard practice across our family of associates. The roll-out is about 50% to 60% complete. We want to keep adding associates to the Eyeplan family. This is happening currently at a rate of about two or three a week, which is quite high.

Clockwise from left: Tailoring packages; Chris Clemence; marketing support.



SPECIAL REPORT:
COVID19 GENERA TION THE OUTLOOK

“’Hopeful,’ ‘optimistic,’ ‘apprehensive’ and ‘uncertain’ are words used by students to describe their future,” suggested Huda Hathaf, AOP student representative and third-year optometry student, when asked how students might be feeling about the pre-reg application process and their readiness for joining the profession.
Students graduating from universities in recent years may be entering the profession knowing only the form of optometry that emerged through the pandemic – one of personal protective equipment (PPE), communicating behind a mask, and with a stronger emphasis on history, symptoms and triaging than ever.
The availability of pre-reg placements has varied throughout the pandemic, and though there is a recovery, some students are still feeling the effects.
Providing a view into the experience of students, Dr Leanne Smewing, clinical lead optometrist for the School of Health professions at the University of Plymouth, told OT: “Students have certainly found applying for pre-reg a little more difficult this academic year.”
The university has been supporting second and third year students with CV writing, and Smewing added: “It has been important to emphasise what year they are studying, as we know employers are receiving applications for students aiming to start pre-reg in both 2022 and 2023.”
Anil Kirit Rach, student representative for Optometry Scotland and fourth year optometry student, told OT: “Some of my fellow students have had concerns about securing their pre-reg placement due to changes in the number of pre-reg places available.”
Some practices have had to reduce the number of pre-regs they take on, while in some cases, students have encountered delays caused by an overlap with the previous pre-reg.
Although, Rach noted, “most students are still able to join the practice and gain experience front-
of-house until there is testing room space for them.”
The majority of students feel there has been a lot of support in securing a placement, Rach found.
Third-year optometry student in Wales, Martha Glain, has also seen a level of anxiety from fellow thirdyear students about selecting a pre-reg placement.
Part of the reason for the concerns, she suggested, has been that some practices have not been able to offer work experience opportunities due to capacity issues resulting from COVID-19 restrictions.
“Some students have not been able to visit their chosen store to meet staff, or even get a feel for the area where the practice is located, before signing their contracts,” she said.
Increasing opportunities
Employers have been seeking to support pre-reg optometrists and provide new opportunities.
Among those expanding availability, Specsavers told OT that places have risen from 450 in 2019, to over 500 in 2020.
For the 2021–22 period the company has made more than 550 offers and continues to support
“’Hopeful,’ ‘optimistic,’ ‘apprehensive’ and ‘uncertain’ are words used by students to describe their future”
Huda Hathaf, AOP student representative
students “who have been unable to secure a position elsewhere.”
“There is an enormous amount of competition for places, particularly in the popular city centre and more central locations,” Victoria Taylor, head of graduate recruitment at Specsavers, said. “Many of our vacancies in those areas will typically receive more than 100 applicants per role.”
The company has adopted a more flexible approach to its pre-reg programme to “withstand the challenges” of recent years. For example, the onboarding process has evolved from a focus on the autumn months to extend beyond this.
David Clulow also intends to broaden placement availability in its practices, offering 10 places for the 2022–23 cohort.
This follows on from the positive experiences of three pre-reg optometrists within the company, explained Natasha Luthra, resident optometrist at David Clulow’s Wigmore Street flagship site, as well as “the growth in interest from our optometrists to supervise, and the capacity to add additional testing rooms to several practices.”
“We’ve already had a mammoth surge in CVs to head office through word-of-mouth, as London placements are so highly sought after,” she continued.
THE SCHEME FOR REGISTRATION

Providing insight into the pre-reg process, Lizzy Ostler, director of education at the College of Optometrists, confirmed the Scheme for Registration is still provided around the GOC’s temporary Handbook and amendments: “This currently includes a reduced daily capacity for OSCE examinations, to allow for cleaning time between stations, an online experience that replaces the Hospital Eye Service for those who need it, and a blend of remote and face-to-face work-based assessments.”
Numbers indicate that over 95% of both the 2020–21 graduating cohort, and the previous cohort, have found a placement and enrolled on the Scheme. Despite the impact of the pandemic, 2021 saw the largest number of new optometrists the College has qualified to date.
The temporary handbook changes for pre-reg, made in response to the challenges of the pandemic, were extended for the 2022–23 academic year, and the College will be undertaking a review in September.
“We are learning from the experiences offered by changes introduced in 2020, and will be seeking to retain those that offer a more effective or efficient assessment experience,” Ostler said. “For example, we are now working towards recognising a blended approach to the Hospital Eye Service experience – taking the best elements of online provision and, where appropriate, combining these with in-clinic observation sessions.”
Advertising of the pre-reg programme will also be rolled out.
Boots Opticians currently has 11 pre-regs on its programme, with the intention of welcoming around 85 new members to its team in the summer, the company shared.
Jayne Johnson, learning and development manager at Boots Opticians, told OT that plans to integrate virtual elements into its programme were accelerated as a result of the pandemic.
Elements of the application process moved online, with virtual interviews and sessions
with optometry schools. Running the programme online for the year helped Boots to scope out its programme further for the future, Johnson said.
In independent practice, Claire Slade, head of professional advancement and governance at the Hakim Group, told OT: “We have crafted our pre-reg experience to ensure it’s not based around volume, but really creating well rounded optometrists of the future who could work anywhere, and achieve all their aspirations with multiple pathways for career progression.’’
“Previously there hasn’t been one port of call for pre-regs interested in working in independent practice,” she shared. The business has created a central resourcing team to act as a key point of contact for students interested in pursuing a pre-reg in independent practice.
This work is beginning with engaging universities and talking to second years about independent practice. Meanwhile, the team is keen to support the current cohort of graduates and pre-regs, to try and place more people.
“We’ve got so much to offer in independent practices, and I think it can really be the best place to train,” Slade said.
Challenges to confidence
Discussing the challenges students have faced over recent years, Hathaf told OT: “One of the concerns students face following the pandemic is transitioning from a student to a confident clinician.”
For some, a difficulty in developing that clinical confidence has come about as a result of struggles to secure work experience during the pandemic.
Work experience is valuable for supporting the understanding of students. University of Plymouth’s Smewing shared: “Particularly in dispensing clinics, those who have worked in optical practice and have dispensed before show real confidence and achieve the necessary episodes and competencies at a faster rate.”
To support students who do not feel as confident, the university runs sign-up sessions to gain that additional experience.
Third-year optometry student, Amy Cooper, recognised that “understandably, practices aren’t too keen on bringing in additional unnecessary people,” and that often it has not been possible to have a student in the testing room with the optometrist, while maintaining a reasonable distance.
Explaining why this is worrying to students, she shared: “I think that some people are concerned that they should have more to show on an application, or think that it’s absolutely crucial to have lots of work experience.”
Concerns about confidence and ‘having more to show’ on applications have been common issues identified amongst broader populations of young people.
Research by the Institute for Employment Studies (IES), an independent centre for research in employment and human resources, considered experiences amongst young people.
Cristiana Orlando, health foundation research fellow, explained: “Young people are concerned that, increasingly, we are moving into a more competitive labour market, where employers have more stringent requirements for recent graduates.
“There is a generalised anxiety of ‘I have to show something,’ and that the lack of experience of the practical side would be a deterrent that would play against them when looking for a job,” she added.
Careers consultant, Estanis Bouza, at The Careers Group in City, University of London, also noted this nervousness from students: “I think we will always look back on the last couple of years as a period of time when lots of students missed valuable opportunities. Many have struggled in different ways over this time. I have spoken to many students about the anxiety that missing out on opportunities has caused them.”
While the group recognised that organisations “made great efforts” to provide virtual experiences during lockdowns, there was an overall reduction in availability, and “it is difficult to replicate some of the benefits of an in-person experience.”
Some students have been particularly hard hit by the shrinking of opportunities experienced during the pandemic.
Research in 2021 by the Sutton Trust, an organisation championing social mobility, indicated a
“I think that some people are concerned that they should have more to show on an application, or think that it’s absolutely crucial to have lots of work experience”
Optometry student, Amy Cooper

94%
of employers believe skills like confidence, motivation and resilience are as, or more important, than academic qualities, research by the Sutton Trust has found
drop in students from low-income backgrounds participating in extracurricular activities.
Dr Rebecca Montacute, senior research and policy manager at the Sutton Trust, explained that, as focus shifted to core learning, “extra-curricular activities and work experience placements have fallen down the priority list, and this has affected disadvantaged students most keenly.”
This could have knock-on effects to accessing the workplace, she said.
“Our previous research, in 2017, highlighted how important ‘essential life skills’ – things like confidence, motivation, and resilience – are for the workplace, with 94% of employers saying these skills are as, or more, important than academic qualities,” Montacute added, sharing that it is “vital” all young people have access to these opportunities.
The
market and perceptions
The fluctuating levels of confidence seen amongst students have been reflected in the labour market. As job and work experience places began reappearing, IES noted a discrepancy between this recovery and young people’s perceptions of the market.
“That speaks about the lasting impact on confidence and motivation,” Orlando identified. “Young people who have had to transition from one stage of education to the next, or into the labour market, during the height of COVID-19, have had to face something humongous. It is stressful to bounce back from that.”
Looking forwards, the careers market seems positive, she told OT, and Bouza agreed: “According to the Institute of Student Employers’ Vacancy Survey 2022, graduate vacancies have surpassed prepandemic levels, and are set to increase by 20% compared to prepandemic levels in 2019.”
“Students are not putting themselves forward for opportunities as much as employers would like to see,” he observed, acknowledging the potential impact of the pandemic on student confidence but emphasising that employers are looking for good quality applications.
In Scotland, Rach told OT that some students are worried about their experience levels and “meeting the expectations of practices,” however, he identified: “Practices have been very supportive.”
Having observed the impact of the pandemic on previous year groups, Indy Ghuman, final year optometry student and chair of the AOP student committee, said: “I had somewhat discounted that those experiences would be viable for us and I was grateful I had an optical job that was providing experience.”
However, many of his peers have also been able to secure optical jobs
alongside studies, suggesting: “Despite the pandemic coming in between, especially in 2020, towards the middle and end of 2021, it seemed there were opportunities for students.”

Reflecting on his experience, Ghuman shared that while there have been difficulties, particularly in accessing hospital experience, “I had quite a diverse, enriched experience compared to what could be described as a very challenging environment.”
Employer requirements
To address student concerns around work experience, OT reached out to a number of pre-reg employers, who concurred that while valuable, similar skills could be demonstrated outside of optical placements.
Asked the extent to which having work experience or prior part-time work within a practice is considered in applications, Luthra, from David Clulow, said it is “hugely desirable and can help those looking for a placement secure one early if they’re already known candidates to us.”
However, “leadership, good organisational skills, and the ability to self-motivate as well as work in a team, are important transferrable skills,” she suggested.
RECOGNISING THE IMPACT OF THE PANDEMIC
As part of its research, IES put together recommendations for employers. Speaking to OT, Orlando said: “The first element is to listen to what young people are saying.
“What do they talk about when discussing positive experiences? From being provided with a diverse learning experience, to being given guided opportunities to actively develop new skills, feeling that the employer is involved in their development but also their wellbeing –mental health in the workplace is becoming increasingly important.”
She noted: “One of the things that young people themselves suggested was: ‘give us more opportunities from an earlier stage to start developing skills, don’t wait for us to graduate’.”
Montacute at the Sutton Trust highlighted: “It’s important for organisations to keep in mind when looking at applications that young people will likely not have been able to gain as much work experience over the last couple of years.”
“Workplaces should assess candidates based on their future potential, and not necessarily the experiences they have undertaken,” she added.
The Institute of Student Employers’ Vacancy Survey 2022 indicates the graduate jobs market is recovering, with vacancies 20% higher than in 2019
These can be demonstrated through extra-curricular interests in a CV or cover letter, Luthra said.
Specsavers’ Taylor said: “It is fair to say that having some exposure to a busy practice environment is an advantage. However experience working in any customer-facing role is also valuable and is of benefit to the individual themselves as well as a prospective employer.”
Taylor added that the business understands that not everyone can take on part-time employment to build their CV, so suggested: “I’d encourage you to consider bringing to light other examples in areas of your life where you might have been part of a team – sports clubs; charity and volunteer work.”

At interview stage, Boots looks for skills such as leadership, teamwork, customer care, and problem solving, Johnson said. Outlining that “optical experience is not a must-have,” she explained: “These examples can come from optical experience, but also any work experience, college or university experience, or from any other life situation.”
Acknowledging that “optical experience is fantastic,” the Hakim Group’s Slade highlighted that they are looking for ambitious individuals “who will go the extra mile.”
“Sometimes the people who are best suited, are the ones who have perhaps done something different,” she said. “If that means that they’ve had an experience, like running charity events or being a Guide leader, but they haven’t had that weekend or holiday job in a practice, that’s fine by us.”
“We want to know about every experience like that – where you’ve pushed yourself above and beyond. We want people who engage with the environment around us,” she said, and pointed out that applicants need to put a lot of thought into the experiences they might have had in their journey so far.
A new generation
Ghuman reflected that while their experiences have been different, such as with the addition of PPE, they have brought their own benefits. “Developing those communication and interpersonal skills would have been more difficult,” he illustrated. “But doing so would be very beneficial, because you’ve got that extra skillset of being able to build a rapport with a patient while wearing a mask, and being able to show that you are listening, and engaging with them, with these extra obstacles in your way.”
“We are going to see a lovely generation of optometrists come through who have a unique skill set that they have had to take on board”
Claire Slade, head of professional advancement and governance at Hakim Group
Ghuman added: “I think something that employers and other optometrists in the profession will maybe notice about the graduates coming up through the pandemic, is that they are a lot more adaptable to change.”
Similarly, Bouza said students have showcased flexibility, “perseverance and stamina to keep going.”
“They all count,” he continued, adding: “Employers love candidates who can reflect on what they have learned and can explain clearly the value of this.”
Speaking to OT, the employers all recognised that students and graduates will have a different set of skills following the pandemic.
Considering this, Slade observed: “When I look at the students who have come up in the last 18 months, I think they must have bravery and tenacity in bucketloads to adapt through COVID-19.”
“I do think we are going to see a lovely generation of optometrists come through who have a unique skill set that they have had to take on board, and it will arm them very well,” she added.

THE STUDENTS:
WHAT ONE THING WOULD YOU WANT EMPLOYERS AND THE PROFESSION TO KNOW?
Glain: The massive impact COVID-19 has had on our studies. Once, in-person clinics would have been a hub of activity. Now, with the limited characteristics of patients in university clinics, there are fewer opportunities to understand why you are doing certain tests.
Cooper: We are, and have been, trying our best to make the most of a challenging situation. We are acutely aware that we may have missed out in some aspects, and we’ve done as much as we could and developed other skills, such as adaptability and independence.
Hathaf: Employers and professionals are going through the same struggles. Unfortunately, COVID-19 is something we’ll have to live with for a long time. However, it has highlighted the importance of working together and adapting to new situations.
Rach: Interviews have been via video calls, rather than in-person, which means students haven’t always had the chance to see the practice and meet the team, so providing an opportunity to come into practices would be welcomed.
Ghuman: I think we have been trained to work in this environment now. While optometrists in the field faced a landslide change in PPE and adapting their tests, university students have been equipped to the new way of working, which I think is a good thing.

Five resources from the AOP
Students and pre-reg members can use the AOP’s Pre-reg register to list their availability: www.aop.org.uk/ advice-and-support/business/pre-reg-register
OT’s Education library hosts skills guides along with archived CET and CPD articles, covering a range of topic areas: www.optometry.co.uk/cpd/education-library
The AOP Peer Support Line offers a free and confidential helpline for members and non-members at any stage of their career. The line can be accessed at 0800 870 8401 or found at: www.aop.org.uk/peersupportline
The AOP’s employment team is available to support and advise AOP members on pre-registration contracts and employment law, and can be contacted at employment@aop.org.uk
The AOP’s new mentoring programme is available online at: www.aop.org.uk/mentoring
In practice
43 How I got here
Black & Lizars’ Eilidh Thomson explains how a chance meeting changed the course of her career
THE DISCUSSION
45 The workshop
How to ensure you have the right insurance policy for your independent practice
49 Pre-reg focus
Business insight and career development
Pre-reg at Manchester Royal Eye Hospital, Thaksha Sritharan, on managing complex patients
High Street harmony
51 Key milestones Setting up a menopause support group for colleagues across Specsavers

In Brighton, a local independent and a branch of Specsavers have worked side-by-side since 1991. OT found out what they have learnt from each other
Existing on the same Brighton street for over three decades, Specsavers North Street and independent practice, Eyesite Opticians, provide a blueprint for how to work collaboratively as local businesses operating within the same sector. Here, they tell OT how it is done.
The working relationship
Jim Green joined Eyesite in 2005 after qualifying as a dispensing optician, before becoming practice manager in 2012 and then managing director in 2017.
“Specsavers,” he explained, “has been next door to us all that time. I think they signed
their lease within the same six months as we did, here on North Street in 1991.”
Lateef Iqbal is newer to his practice, having taken over as ophthalmic director for Brighton’s two Specsavers stores 18 months ago.
Green believes the business direction and goals of the two practices allow them to work well alongside each other. “Being an independent allows us to differentiate ourselves,” he said. “We don’t chase the price-sensitive market and we position ourselves differently in terms of the products and services we offer. It seems to work well for both of us. It’s been a
good relationship, which has continued even as directors and practice management has changed in each business.”
He also notes that “even when times are challenging, you still end up having a chat with the guys next door. In Brighton city centre, there are six or seven opticians in about four square miles, so it’s not just Specsavers as the competition. We know a lot of the optometrists who work there, and we naturally see them at industry events in the community.”
Transparency has been key, he said: “There’s always been a lot of honesty along the way, and we’ve always
OT’s panel
Lateef Iqbal, ophthalmic director of Specsavers Brighton
Jim Green, managing director of Eyesite Opticians, a Hakim Group practice.
managed to avoid an acrimonious relationship. It seems to work well for us.”
Avoiding rivalry
Iqbal emphasised the importance of customer service in avoiding
rivalries appearing between the practices: “There’s certainly been no rivalry in my time here, and I don’t believe there ever has been,” he said. “Customer choice is really important, and I think there’s enough of a difference in what we offer to be able to happily co-exist.
“While having an independent as close as Eyesite is unusual, having more than one practice on the High Street is a good thing. It offers choice and convenience, and encourages people to visit and support the local economy.”
Green agrees: “Because we’re operating in the same sector, but in different demographics, I don’t find there is a rivalry. When you have an ambition to provide eye care to your community, not just for the current generation, but for generations to come, that changes your mentality. That attitude means we are always keeping our patients at the centre of what we do. We’ve found that adopting a patient-centred approach makes our decision making a lot more straightforward. While we are competitors, we want to make sure we’re doing right by our patients every step of the way.”
He added: “Healthy competition is necessary; it keeps us on our toes. We relish being able to demonstrate our difference.”
Fostering relationships
Green believes local competition can attract attention to eye care.
“Key for us is making sure you’re clear about your vision, your ambitions, and the direction of your
business,” he said. “If that means evolving your model, moving into a more premium sector, for example, then don’t be afraid to do so. Being an independent means you can make decisions and adapt quickly. You can be in charge of your own destiny.”
Speaking about Specsavers specifically, he added: “I would definitely avoid going for the same market. We don’t have that buying capacity. Generally, the multiples are good at what they do, so build your strategy and vision based on your strengths and how you want to drive the business.”
Iqbal sees communication, mutual respect, and a patientcentric ethos as the most important factors: “Never criticise your colleagues, because all you’re doing is criticising your own profession,” he said. “If an issue arises, discuss it. We’re all in it together, and the customer has the choice to walk away from both of us. We need to give them a reason to see an optician rather than order frames online. It’s important that people seek professional advice, and we all need to work together to make sure people value what High Street opticians offer.”
Green agrees: “It’s important to ensure a personal relationship with all your neighbours,” he said.
“I’d advocate going for a
“Having more than one practice on the High Street is a good thing. It offers choice and convenience”
Lateef Iqbal
coffee with the directors, to have a chat about how you see the optical market. If we are all in the same mindset, which is to provide eye care for our communities, we should have the same principles. If that’s where the emphasis is, there’s no reason why that relationship can’t become stronger. If each party knows which demographic they’re catering for, we can stick to our business model and stay true to our values.”
What would Green and Iqbal say to those who are sceptical that multiples and independents can work together cohesively?
Green is unequivocal: “We’ve proved since 1991 that it can work. I understand that if you transpose this into a village it might be different. But I still think patients will make their buying decisions and be loyal to a practice where they’ve been all their lives, whether that be because of personal relationships or rapport over the years.
“At the same time, it would be naive to assume that they couldn’t look elsewhere. That makes it even more

important to provide clarity about your offering and to make sure you look after them. Patients only tend to leave an opticians if they are unhappy with something. By looking after them you can minimise the chance of this.”
Iqbal is on the same page: “We need each other. As a large business we are able to raise awareness about the importance of eye health, encouraging people to get an eye test wherever they choose. We can learn from each other and improve how we work. The more the merrier, as long as they are delivering clinical excellence and value to their patients.”
What is the most important thing they have learnt from each other?
Green is quick to identify the lessons independents can take from having a multiple on their doorstep: “We’ve learned the power of marketing. But I also think they have remained true to their business model, and how they operate clinically is in line with this. We’ve had to learn how to be different from that.”
“It’s important ensure a personal relationship with all your neighbours”
Jim Green

Iqbal also finds inspiration from having Eyesite so close: “I enjoy looking in their window as they have a different approach to us,” he said. “The important thing is that we are different enough to happily co-exist. There is definitely room for both of us on the High Street.”




































































“Optometry
just
popped into my head”
Black & Lizars optometrist, Eilidh Thomson, on a chance meeting that changed the course of her career
Throughout school, I wanted to study law. It’s strange looking back, because I was better at sciences.
After leaving school, my doubts began. I didn’t want to do medicine, but I hadn’t considered other medical professions. Then, the idea of optometry just popped into my head.
My parents thought I shouldn’t write law off, so I decided to go. I was a month into the course, on the train with a friend, telling her that I should have done optometry, and next to her was a gentleman. He was a director of Black & Lizars. He said, “It’s fate that you’re talking about this. I want to help.”
It was because of that meeting that I’m here. I went to a Black & Lizars practice for work experience and met staff, including the practice manager, an optometrist, and a pre-reg, who was talking about how he’d found a really exciting career.
Afterwards, the director said, “If you’re serious, we’ll help you.” I dropped out of university, and he created a reception position for me at a practice close to home.
I worked for Black & Lizars for a year and then applied to Glasgow Caledonian University, starting the following year. They kept me on as a Saturday girl throughout university. I’m still in touch with that director today.
Completing my prereg with Black & Lizars wasn’t guaranteed. There were six of us working Saturdays, and three places. I was lucky to get one, in the Milngavie practice. Everyone was invested in my success. Reception had my competencies, so if a patient phoned with criteria I needed, they’d book them with me.
My newly-qualified position was working between two single testing practices. That was a challenge: I was working alone, without another optometrist. But
“There’s satisfaction in treating a problem rather than just diagnosing it”
it made me confident in my decision making. A supervisor was always a phone call away, but I quickly learned to trust my own judgement. I was challenged, but I didn’t feel unsupported.
I became an independent prescriber in 2017. When I was newly-qualified, my practice was quite far from the eye hospital, so I knew being able to prescribe would be helpful. There’s satisfaction in treating a problem rather than just diagnosing it. You see patients come back; you’ve managed their condition; they’re better. It’s a very satisfying aspect of the job.
I joined the Optometry Scotland executive committee in 2019. It’s interesting to focus on community optometry, being a part of a solution to make things better. Recently, we’ve had a 3% rise in our General Ophthalmic Services (GOS) fee, a success that Optometry Scotland was influential in. More important was the recognition of an annual review of the GOS budget. We hope future reviews consider the work the sector does in Scotland and at least keeps pace with inflation.
At the start of the pandemic, almost everyone was furloughed. I covered remote triage for four Edinburgh practices. When you’re thrown into that situation, you have to get comfortable making decisions based on limited information.
I’m now in a professional services role with Black & Lizars. I’m testing four and a half days a week, with half a day for professional
“My Plan B?” My plan B would have been to continue with law – who knows where I’d have ended up.
services work. That involves recruitment, handling clinical claims, training – anything that comes under the clinical umbrella. It gives us more ownership of the company. Your ideas can change how things progress.
I was part of the pilot for NHS Education Scotland Glaucoma Award Training (NESGAT). The idea is that patients are discharged from eye hospital to NESGAT optometrists in the community, who manage their care. We had our first face-to-face meeting in February 2020, then moved online. We did our hospital placements towards the end of 2020 and into 2021. The next step will be putting it into practice and managing glaucoma patients myself.
I’m also part of an Optometry Scotland working group, working with Education Strategic Review stakeholders to secure the best version of the new education system. Hopefully, we’ll get something in place that works for everyone.
A highlight was seeing my first pre-reg qualify. It’s a proud moment, when you’ve helped mould someone’s career. Being able to impart wisdom to someone else is very fulfilling.
Share your career journey with OT.Email lucymiller@ optometry.co.uk






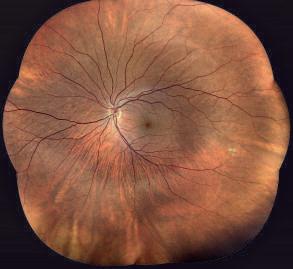



for these incidents to be insured, and therefore were left without cover.
THE WORKSHOP
Finding the right insurance policy
William King, commercial development manager at Lloyd & Whyte, explains the importance of securing a bespoke insurance policy for your independent practice
The scenario
Laura, practice owner
“I’m a new business owner, currently getting my paperwork in place before I open the doors to my first High Street practice. I’m a little confused about what type of insurance I need. Some people have said I need specialist insurance designed specifically for the healthcare sector, whilst others have suggested retail. Could you advise on a solution?”
The advice

William King, commercial development manager at AOP affinity partner, Lloyd & Whyte
Setting up your own High Street practice is exciting, but it can also be fraught with concerns over ensuring the most appropriate cover is in place for you, your staff, and your patients. Whilst it may seem simpler just to go online and get an ‘off-the-shelf’ retail policy, you could be leaving yourself vulnerable to gaps in cover or being underinsured. Sometimes the quick and easy solution is not always the right one. That is why speaking to healthcare sector insurance experts, like Lloyd & Whyte, will pay dividends and ensure that you have the
optimum cover to meet your needs.
How do you know what type of insurance you need?
Online providers will ask you which elements of cover you wish to include, for example public liability, employers’ liability, contents, and so on. You may not realise the importance of each aspect of cover and omitting one could leave you exposed. A bespoke, tailor-made policy for healthcare professionals approved by the AOP can help ensure you make an informed decision.
For example, I had a client that didn’t have legal expenses cover, as they thought employers’ liability would cover them for any potential employee disputes or unfair dismissal claims. It was only when making a claim they realised they needed legal expenses cover
Advice on sums insured and risk management
Underinsurance is a key aspect to avoid. Often there is confusion around the market value for items rather than the new value, as well as not knowing how much a ‘normal’ optometry practice cover would be. Whilst we can’t specifically tell you what the sums insured will be, we can have conversations to help establish this.
Retail vs healthcare policies
Sometimes a ‘shop’ policy has been designed for retail units rather than specifically for an optical practice. Whilst there are 100s of variations of insurance policies, it is impossible to compare them all. Examples of key differences to look out for can be:
Limits to glass cover –some policies will not be sufficient to cover the shop front of an optometrist
Equipment breakdown –opticians and optometrists rely on certain specialist equipment, so if one key piece of equipment fails and causes the practice to close or operate at a reduced capacity, this may not be covered.
With tonometers costing £3000–£10,000 and keratometers priced at a minimum of £2000, for example, protecting such valuable assets makes sense. Mobile pieces like ophthalmoscopes can set you back anywhere from £500 to £1000 and need to be covered if taken away from the premises.
“Sometimes the quick and easy solution is not always the right one”
Dedicated experienced claims team
Not only do you get specific, helpful advice when setting up the policy through a specialist, but at the point of claiming our in-house claims team has brilliant experience when helping to calculate potential loss of earnings following a fire at the practice, for example. Our aim is to make the whole claims process as hassle free as possible.
Advice on additional applicable policies
Only relying on a traditional ‘business’ policy may leave you exposed in areas you may not consider, such as cyber insurance, directors and officer insurance, and entity insurance. A qualified, specialist insurance adviser like Lloyd & Whyte can help explain these policies and how they would apply to your situation. We offer complimentary commercial insurance reviews to AOP members. We review your policies, identify any gaps, and make practical recommendations to better protect your business. Contact us to benefit from specialist financial advice including pension advice and retirement planning plus exclusive rates on essential home, travel, and practice insurance.
Member support
Read about the benefits available through AOP affinity partners: www.aop.org.uk/membership

“Our local GPs have not seen eyes for many years”
Susan Bowers, one of the first UK optometrists to become an independent prescriber, tells OT about her most memorable cases
I became an IP optometrist because… Doing so much contact lens work meant I did lots of anterior eye and dry eye work, so it was a natural progression.
My first prescription was… So long ago, in 2009 – but was probably dry eye, as this is the most common problem I encounter.
My latest case was… A very naughty 75-yearold female, who was referred with suspected glaucoma after a domiciliary visit by Specsavers two or three years ago and did not take the referral letter to her GP. She presented for a Minor Eye Conditions Service (MECS)
After I told her that I suspected she had glaucoma she sheepishly admitted not progressing her previous referral, hoping the glaucoma would go away.
The case that kept me up at night was… I have photography, so I can record exactly what each case looks like and review the following day. I tend to be confident whist treating patients.
My most memorable case was… I enjoyed treating a Thygeson’s case, and saving patients trips to hospital and long waits in A&E. I would be reluctant to treat conditions where there is no one in clinic the next day to monitor, but we have three IPs at our practice so that is rarely the case.
We take referrals from pharmacists, GPs, and local non-IP colleagues, and patients also walk in, especially if they have been before.
The benefits IP brings to the business are… Our kit is comprehensive, enabling us to get accurate diagnoses. We have Zeiss Forum software to do structural and functional loss in glaucoma. This means we see private patients, as well as MECS and those from outside our catchment area.
appointment with eye pain and discomfort. Her pressure was 27mmHg, with extensive visual field loss and optic nerve damage on optical coherence tomography scans. After checking with a consultant colleague and because of the backlog, I put her on Latanoprost (as I have the professional diploma in glaucoma) and I will be referring her to the glaucoma clinic, where I also work, for a formal diagnosis of primary open angle glaucoma by the ophthalmologist.
DID YOU KNOW?
Starting in October 2022, Coventry & Warwickshire Local Optical Committee is part-funding optometrists to do the basic certificate in glaucoma
My ambitions for the future are… I got my diploma in glaucoma in late 2019 and wanted to learn Selective Laser Trabeculoplasty and PIs in the hospital setting, but COVID-19 got in the way. I also reduced my hospital hours to help cover a colleague’s maternity leave. Now at 68, I am looking forward to retirement.
Being IP-qualified has helped the reputation of my practice by… All three of us have FP10 pads, and our local GPs have not seen eyes for many years.
“After I told her that I suspected she had glaucoma she sheepishly admitted not progressing her previous referral, hoping the glaucoma would go away”
Patient response to my IP skills has been… My speciality is digging out embedded metal, and I have had a lot of practice. Patients are often not quite as grateful when the anaesthetic wears off.
The implications of IP on other areas of optometry are… If low dose atropine becomes available for myopia control in this country, you will need IP – but I am not keen to supply high doses due to the side effects. You can also get contact lenses with hay fever drugs (from Johnson & Johnson Vision).
IP AND ME
With Stress Awareness Month in April, OT spoke to Alison Pay, managing director of Mental Health at Work, about the value of early conversations, and how employees can prepare for them.
When should someone seek help for their stress?
Stress is not a diagnosable mental health issue. At Mental Health at Work, we encourage early conversations in the workplace about our mental health: with colleagues, with managers, with Mental Health Allies and sometimes with human resources or occupational health, along with early access to the right signposting. If this is not enough to support a movement back to health and we move towards issues or illness, you should then seek professional help.
The role of the workplace is not to diagnose or advise, but if it can provide an environment which supports our psychological health and safety, then early action may be all that is needed to keep us well.
What practical solutions should people incorporate into their working day to relieve stress?
Practical solutions for managing stress at work will be an individual decision.
EYES ON WELLBEING
“Our wellbeing at work is critical”
Alison Pay, managing director of Mental Health at Work, gives OT some practical tips for workplace wellbeing during April’s Stress Awareness Month
Our mental health is unique, and one size does not fit all.
Having conversations, particularly with our line managers, can help support us to manage our mental health and wellbeing at work.
A structured conversation, built around a wellness action plan, which asks open questions around how you stay well at work, can help both manager and employee to agree what works for an individual and how this can be accommodated within each role and workplace.
How would you recommend preparing to discuss stress with a manager?
Part of the success of the outcome is how prepared your manager is to receive
Other ways the AOP is supporting your health and wellbeing
The AOP’s Peer Support Line is turning five years old next month. It is a free, confidential helpline for members and non-members at any stage of their career, and can be accessed 24 hours a day. Volunteers are on duty to return calls between 8am and 8pm, and an external answering service is available outside these hours.
Contact the Peer Support Line on 0800 870 8401.
the conversation. That is important, because you need them to to be able to listen to you. Part of the answer is not expecting your manager to solve it for you, because that’s not their job, and they’re not qualified to do it. You would ideally like them to listen, and ask how they can support you to be able to manage your work.
“Your mental health is your mental health. No one else is an expert in it”
It is important that, ahead of the conversation, you have considered some suggestions about what is right for you. What’s right for one person is not going to be right for another. There is a myriad of complexities. So, do the thinking beforehand, about what could make the difference for you. Having more than one suggestion is important, because this is going to be a conversation. Think as broadly as possible about how the workplace can
Building the happiness habit: join the AOP’s new wellbeing webinar series
The AOP’s happiness webinar series aims to equip members with practical skills that will help them reconnect with their happiness.
The first hour-long webinar took place on 22 March and focused on aiming for happiness. The recording can be watched via the AOP’s events and webinars page: www.aop. org.uk/events. The next three webinars focus on achieving happiness (29 June), stabilising your happiness (27 September), and protecting your happiness (24 November.) Book your place via the link above.
support you. Your mental health is your mental health. No one else is an expert in it.
What is the one message you would like members to take away?
Our wellbeing at work is critical. It is important that we recognise in ourselves and in others when we might be moving away from it. The earlier you can act, the more likely that you’re going to find preventative or protective actions to enable you to move back to health. The earlier you have the conversation, the better.
More information
Mental Health at Work is a notfor-profit, Community Interest Company. To work with them to build capability around workplace mental health in your organisation, contact team@mentalhealthatwork.com


PRE-REG FOCUS
“I now fully understand my role as a trainee”
Pre-reg optometrist at Manchester Royal Eye Hospital, Thaksha Sritharan, on organising her competencies six months in
I
t is six months since I started my pre-reg position at Manchester Royal Eye Hospital. Compared to the beginning of my pre-reg, I feel more settled in and I now fully understand my role as a trainee. I also see how the Scheme for Registration is training me to become a better practitioner. For instance, a competency that you need to look out for will act as a reminder to ask questions in history and symptoms.
A varied schedule
My day-to-day schedule at the hospital changes between different clinics in the morning and afternoon, which is nice because I have variety in my week. I have a three-week rotating timetable. Throughout the week I see patients in the core, dispensing and paediatric clinics. Most of my time is spent in the core clinic, where I build up my refraction, contact lens and low vision skills. I also have clinics that I can shadow during the week, such as


the macular treatment centre, glaucoma clinics, optometric lead glaucoma assessment, cataract clinics, paediatric low vision clinics, and the emergency eye department. Due to having a timetable, my pre-reg schedule hasn’t changed much, however my confidence in taking on more complex patients has grown. I know I will be fully supported by my supervisors no matter how complicated the case, so I am

I was looking forward to, because I wanted to see more of the UK. In addition, getting a placement at a hospital really confirmed my choice in terms of location because I knew I would have a unique pre-reg experience in an excellent environment for learning and training. Moving to a new city did bring up more things to become familiar with, however I was well
“Reviewing a competency as soon as you have found a suitable record is a great way to keep on top of studying”
always up for a challenge in order to learn more from the experience.
A new city for pre-reg I am confident in my decision in terms of location. I went from studying optometry in London as an international student to moving to Manchester to complete my pre-registration. The change in location was something
My favourite part of the pre-reg is… being able to apply the skills and knowledge I have learned at university in the real world. I love interacting with different patients every day, and helping them in any way that I can.
My least favourite part of the pre-reg is… the effect that the COVID-19 pandemic has had
supported by my colleagues and they really helped me with the transition. If I didn’t get the hospital placement I wouldn’t have shied away from leaving London – I would have chosen the location where I felt the most supported. I would recommend this way of thinking for anyone deciding between pre-reg placements, as it is a very
on the work environment: the restrictions between patients and optometrist due to personal protective equipment and social distancing, as well as additional difficulty when assessments are carried out virtually.
Before I started my pre-reg I wish I had known… how important my logbook was
Education Library
OT’s Education Library contains CPD and Skills guides in 31 topics www.optometry.co.uk/ cpd/education-library
‘full on’ period during your early career and it will be the time where you are most susceptible to picking up habits, good and bad.
Managing competencies
Working full time and studying can be overwhelming. I find that taking it on little by little is the best way to approach it. For example, any time I see interesting pathology or I am unsure of something I note it down, and I look into it at the earliest opportunity. I find this to be advantageous as it strengthens the theory behind findings.
I also think reviewing a competency as soon as you have found a suitable record is a great way to keep on top of studying.
I often write a to-do list in my agenda. This way I can keep track of what I have reviewed and I can plan ahead. I also think it is important to destress if you are feeling particularly burnt out, with activities or hobbies you enjoy.
going to be for keeping track of the different patient types and test characteristics that I have come across, and how important it is to use as evidence at different stages throughout the registration scheme.
HollyLeitchisapre-reg optometristatUrquhart Opticians,Kilmarnock



KEY MILESTONES
“We want to support one another to help women through this”
Louise Furby, senior events, planning and communications manager at Specsavers, on using her personal experience to launch a menopause community for staff
01
I started my own menopause journey in 2015, and two years later found myself experiencing some tough personal challenges that were beginning to impact my work. The biggest issue was brain fog, which, coupled with migraines, often left me exhausted at the start of the working day. I also experienced joint pain, weight gain, and heart palpitations, which were incredibly worrying. Feeling anxious and despondent, I did a Google search and discovered the likely cause of all these symptoms: menopause. I realised managers and team members were uninformed and ill-equipped to support anyone experiencing menopause. As I trawled through the quagmire of information, I had to find a way to inform and educate my (male) line manager. Communication and honesty was key, but the experience left me questioning how well the business was set up to support women going through this stage of life.
members to record short videos and endorsements. A lot of people still feel awkward about menopause. Historically, it’s been all about mood changes and hot flushes, so we wanted to keep the conversation light to help those less familiar with the topic to appreciate that it’s not embarrassing.
AOP menopause support
The AOP has a suite of resources to support members affected by the menopause: www.aop.org.uk/ menopause
02 I started being more open about my journey, and this led to honest conversations with colleagues. We agreed we needed an outlet: somewhere we could be open about our menopause experiences, and able to support one another. That’s when MenoTalk was born.
03

Once the group was established, we realised word-of-mouth was our best approach to get members. Whilst we worked up a timeline for a wider launch, we began reaching out to specialists via social media and recommendations. Our board sponsor, along with our director of reward and policy, both supported whilst we navigated myriad training options.
04
We began with a soft launch to store colleagues and support office personnel. We used our intranet to introduce the group, engaging our existing
05 We use Microsoft Teams for all our MenoTalk activity. We asked members whether they wanted to be an advocate, identifying and driving actions to support the agenda through in-function representation; a champion, building awareness of the group and providing feedback to contribute to the agenda and help land key messages across the wider business; or an affiliate, an ally, group member, and supporter of the agenda. We are conscious that everyone’s journey differs and some just want advice. Three tiers of membership allowed us to meet all needs, particularly early on.
06 We are working towards World Menopause Day 2022 (1 October), and our intention is to have a suite of training materials for our support office, store colleagues, mental health first aiders and MenoTalk members to access. We are keen to introduce “MenoMondays,” where we’ll
feature webinars and Q&A panels to give our members advice and support. We want to broaden our membership appeal to members who are not directly impacted by menopause, but who want to feel equipped to support team members, family members or friends.
07 Our MenoTalk motto is to be United Through Menopause. We want to support one another to help women through this period, and retain the workforce at a time when many women are at the peak of their career. My ultimate ambition is to have a menopause network with at least one representative member in every Specsavers store, and for our menopause training to be mandatory for all new starters. We need to educate colleagues early about menopause, to help remove the stigma and provide a safe and confidential environment for everyone to talk and share experiences. If our MenoTalk group can help prepare and comfort just one woman who is feeling isolated during her menopause journey, we have already succeeded.
“My ultimate ambition is to have a menopause network with at least one representative member in every Specsavers store”
The owner of Wolverhampton’s Bushbury Eyecare, Sofia Fazal, had a long journey into practice ownership, working in multiples and the corporate world before finally setting out to fulfil her long-held ambition in autumn 2021.
“I started off in optics, working across the sector,” she explained, “and had various opportunities to take on franchise opportunities. But, having small children, I decided to wait until they were old enough for me to focus my energy into having my own practice.”
She added: “When I got into my late 30s, I was in a position to start thinking about it.”
Building ambition
This ambition, Fazal said, came from experiences in multiples, where she was unable to spend as much time with her patients as she would have liked.
“I was missing out on stretching my skills and making sure the patient’s best interest was kept in mind,” she said. “I really wanted to be able to deliver best practice, and I felt that I was unable to do that when I was working for other people.”
Then, a curveball came about: Fazal became the professional services manager at Zeiss, a company that she describes as “the Bentley of optics.”
She remained at Zeiss for two and a half years, working across UK and global marketing, and in training and development, implementing business models for independents and larger corporations, “to increase the bottom line and really make a difference,
BECOMING A BUSINESS OWNER

“My background is different to a regular optician buying an independent”
Sofia Fazal, former professional services manager at Zeiss, on moving from the corporate world into independent practice ownership
whether they were small or had lots of stores.”
During the pandemic though, Fazal did a lot of reflecting. “I thought, ‘Where is my North Star? Where am I going with this?’”
Fazal made the difficult decision to leave Zeiss, “with nothing planned,” posting on LinkedIn that she wanted to venture into practice ownership. Within a few days, she had had six people reach out to see if she would be interested in buying their practice. She immediately saw potential in what is now Bushbury Eyecare, made the decision to go ahead, and received the keys on Saturday 18 September, 2021. Testing began the following Tuesday.
Practice priorities
Fazal’s immediate priority was restocking and rebranding, and changing the shopfront and interior, whilst being careful not to alienate existing customers: “I want them to feel comfortable and that they have enjoyed the experience,” she explained. Despite early changes, Fazal was realistic: she expected to build the practice for a year. “But,” she said, “it
happened more quickly than I expected, I think because I had vision and commitment. I was so sure I wanted to do this. I think you’ve got to have that mindset. You can’t sit on the fence. Once you’ve made that decision, you’ve got to be ready to go.”
Project management skills learnt at Zeiss, as well as her optical experience, helped her stay organised. Within a couple of weeks,
Becoming embedded within the community was also a priority: “We should be seen as an integral part of the society we live in.”
Importance of community
For new practice owners, Fazal emphasises the importance of “syncing up with other independents who have been there and done that,” and not being afraid to lean on peers for advice.
She said: “We’ve all been there. I’m only six months in, but there are practices who’ve been there for years. Learning from their experience is important.”
She also advises reaching out to the AOP for any clinical queries.
Future focus
When it comes to buying a second practice, it’s a case of when, not if – but Fazal has learnt not to rush. “I’m ambitious,” she said. “I love what I do. But I have to make sure this practice is running smoothly. I’m very happy
“I love being my own boss. It feels so rewarding when you see the
you make”
she had her marketing plan for the year, and on day one had organised new frame supplier visits.
Fazal says understanding local demographics is key, and that project plans and timelines are vital in keeping achievements on schedule. She also takes Wednesdays and Fridays as strategy and marketing days, because “if you’re not disciplined, you’ll end up inundated.” Fazal’s first three months were about footfall, reputation building, and making sure her team worked well together.
difference
with what we’ve achieved in the first six months. We’ll definitely be looking for another practice in the next year, though.”
She added: “I love being my own boss. It feels so rewarding when you see the difference you make.”
She wants those embarking on practice ownership to “reach out to people like myself, who have practices. The door’s always open. I’m happy to help anyone who needs it. We’re all in it together.”
NOTICEOFTHEAOPANNUAL GENERALMEETING
To all members of the Association of Optometrists (AOP). The AGM of the AOP will be held at the Crowne Plaza London Kings Cross Hotel, 1 King’s Cross Road, London WC1X 9HX on Wednesday 8 June 2022. The AGM will commence at 9am.
Agenda for the Association of Optometrists’ Annual General Meeting 2022
1. Introduction by the chairman
2. To receive and approve the minutes of the last Annual General Meeting held on 9 June 2021
3. Roll of deceased members
4. To receive the chairman’s report
5. To receive the chairman of Finance Committee’s report
6. To approve the Annual Financial Report and Accounts for the year ended 31 December 2021
7. To consider and, if thought correct, approve the proposal of the Board that BDO LLP be re-appointed as the Association’s auditors
8. Any other business.

By Order of the Directors. Adam Sampson, chief executive, 2 Woodbridge Street, London EC1R ODG
1. Please note that a full set of the 2021 accounts will be available at www.aop.org.uk in advance of the AGM
2. A member entitled to attend and vote at the meeting convened by the notice set out above is entitled to appoint a proxy to exercise all or any of his or her rights to attend and speak and vote in his or her place. A proxy need not be a member of the Association


PEER
SUPPORT LINE FROM THE AOP
Supporting members at all career stages
The AOP launched its confidential, free-phone Peer Support Line in May 2017. Since then, it has received 1172 calls from practitioners looking for a safe space to discuss any problems they may be experiencing.
In 2021, volunteers took 293 calls, averaging 24 calls per month. The three main reasons given for calling for support
were: employment (17%), stress (17%), and mental health (16%). The service aims to provide members and non-members at any stage of their optical career with the opportunity to talk with a trained, empathetic peer who recognises the pressures of optical practice.
What is the Peer Support Line?
Speaking to one of the AOP’s 29 Peer Support Line volunteers enables practitioners to talk through their problems in a dedicated, non-judgemental space. Volunteers are trained AOP members who will not give advice, but will offer other possible sources of support and, where relevant, help callers to reach a resolution or take action. Importantly, the volunteers understand the benefits
“The volunteer was very kind and understanding”
3. A form of proxy is available on the AOP website at www.aop.org. uk. To be effective, the instrument for appointing a proxy must be deposited with the Association’s chief executive at the Association’s office (Janicephillips@aop.org.uk) no later than 3.45pm on Friday 3 June 2022. Completion of the proxy does not preclude a member from subsequently attending and voting at the meeting in person if he or she so wishes.
The AOP’s Annual Report will be available at www.aop.org.uk
of having someone listen who is impartial and has no personal agenda. Calls can be on a range of issues, including workplace pressure, bullying, ill health, financial worries, bereavement, or anxiety about exams. No issue is too small or too trivial.
Calls are completely anonymous and only a first name or alias will be requested.
Practitioners who have used the service have told us
“The man I spoke to was very encouraging, patient and positive – thank you for your help.”
“The volunteer was very kind and understanding.”
The number Call 0800 870 8401. Calls are answered 24 hours a day by an external answering service, with volunteers on duty to return calls between 8am and 8pm.
The Peer Support Line IN NUMBERS
CALLS RECEIVED IN 2021
CALLS RECEIVED SINCE ITS LAUNCH IN MAY 2017
NUMBER OF CALLS RELATED TO MENTAL HEALTH HAS DOUBLED SINCE 2019
100% OF CALLERS RATED THE CONVERSATION AS SUPPORTIVE OR VERY SUPPORTIVE*
*Of those who left feedback.
100% OF CALLERS WERE EITHER SATISFIED OR VERY SATISFIED*




















Aa week after the first lockdown, a herd of wild goats roamed past shuttered shops in Llandudno.
It was a moment that illustrated the great emptying of British High Streets – the only window shopper in the previously bustling Welsh seaside town a Kashmiri mountain goat grazing on spring flowers.
Dwindling footfall as a result of the pandemic, after years of desertion by customers in favour of online shopping, caused some business owners to question the future of bricks-and-mortar High Streets. When restrictions eased, and the goats returned to the hills, would the shoppers come back?
Fast-forward two years and the pandemic has created opportunities

HIGH STREET HEROES
From learning sign language to promoting healthy lifestyles, OT profiles the diverse ways optical professionals are giving back to their communities
for High Streets, as well as challenges. AXA’s Small Businesses: the Big Picture report provided a snapshot of UK small and medium businesses in 2021.
The analysis outlines how consumer loyalty to neighbourhood businesses rose during the pandemic, while revenue from local customers also increased.
Of those surveyed, 43% of small and medium businesses reported a newfound appreciation for their local community and other surrounding local businesses.
These reciprocal forces – of local loyalty and businesses serving their neighbourhoods – underline the idea that High Streets are not solely about transactions but the relationships that form around them. OT explores the unique ways that optometrists are contributing to their local High Street.




THE OPTOMETRIST WHO STARTED A SHORT STORY COMPETITION Durham optometrist, Simon Berry, started a short story competition for young people in celebration of World Book Day 2018. Memorable submissions have included a story written in Makaton – basic sign language – and a non-fiction
account by a refugee whose house had been bombed in Syria.
“It was written in the child’s language – so it was very matter of fact. Only as an adult reading it do you go ‘Oh my word’,” Berry shared. Young authors wrote stories on the topic of random acts of kindness during the pandemic – from making ornaments out of old tyres to emptying the dishwasher when it was not their turn.
“When you think of random acts of kindness, you might picture grand gestures, but during the pandemic in lockdown it was often the small things that made the difference,” Berry shared.
The latest competition, in 2021, received 75 entries. A compilation of the stories was launched with an official book signing at Waterstones.
Berry recently learned that alongside a local priest and war hero, the local school had named a classroom after him following a vote
by pupils and staff. “I was really surprised – it proves that you are part of the community and that what we are doing in practice is having an impact on people,” he observed.
THE OPTOMETRIST WHO LEARNED SIGN LANGUAGE
Optometrist Clare Pearce started learning sign language 15 years ago as a way of improving the experience of deaf patients who visited the practice where she worked.
She completed an entry level sign language qualification at a local college, where she learned the alphabet and basic conversational skills. “I love the language; it is really expressive. There is a beautiful depth to it,” she shared.
Pearce observed that even being able to sign the first letter of a word is useful during a sight test. “It is amazing how just a little bit of sign language can really facilitate your eye examination. The patients reacted really positively.”
there is a massive push to keep people in primary care. The role of the High Street optometrist is really important. I don’t think we will see that waning,” she said.
THE PRACTICE MANAGER
PUTTING A SPRING IN SANTA’S STEP
Visitors to the Somerset village of Saltford in early December may chance upon on an unusual sight –a sea of Santas running through the streets. However, there will be no double-takes among the residents of Saltford and Keynsham, with the annual event holding a cherished place in the local festive calendar since it started in 2013.
“The race is well known now and people have Santa dash parties at their house – families will get together and cheer the Santas on when they run past,” Norville Opticians Keynsham practice manager, Beth Bracey, shared with OT.






“Everybody deserves the best care and I will do what I can to make sure there aren't barriers”
Clare Pearce
A passion for accessible healthcare has also seen Pearce certify her two Cardiff practices as dementia-friendly. Pearce emphasised her belief that optometry services should be available to everybody.
“Everybody deserves the best care and I will do what I can to make sure there aren’t barriers in place,” she said.
Pearce believes that now is an important time for the High Street in the UK. “Within Wales
For young children within the area, it is as though all their Christmases have – quite literally – come at once.
“The kids’ eyes nearly pop out of their heads when they walk around the corner and they see all of these people dressed as Santa.”
Norville Opticians Keynsham, which joined Hakim Group in 2020, sponsors race numbers in the annual Santa run, while runners also collect their costumes from the practice in the lead up to the race.





The race has raised £103,500 for different charities since it was started. The oldest runners are in their 80s, while a mini dash is held for those aged under 12. A best dressed dog competition is also sponsored by a local grooming business.
Bracey, who volunteers wearing a high-vis vest with ‘Santa’s little helper’ on the back, shares that there is a strong sense of community spirit within Keynsham.
“The High Street is really important as a social hub where people meet,” she said. “We are not
just here to make money – we are here to help,” Bracey added.
THE OPHTHALMOLOGIST IMPROVING EYE CARE ACCESS




During the pandemic patients were hesitant about visiting the hospital –particularly those involved in clinical trials who did not require treatment.
Professor Francesca Cordeiro, from Imperial College London, shared that this hesitance underlined a general trend of some groups within the population not volunteering for clinical trials.
“There are certain postcodes that we never see patients come from,” she shared.
Cordeiro came up with the idea of bringing a mobile unit to underserved populations, rather than asking them to come to the hospital. A donated van was refurbished and equipped with all the technology necessary to provide a full eye examination using funding from the Imperial Health Charity.
While currently in a proof-ofconcept phase, if successful, the model has potential not just for clinical trials but for screening – which could result in earlier detection of disease.
Working as an ophthalmologist, Cordeiro observes patients presenting with avoidable sight loss.
“It is quite often that you see profound vision loss in someone presenting for the first time,” she shared. Cordeiro outlined her belief in “doing something different to make a difference.”
“You need to do disruptive things to make progress in any field… I think innovation in ophthalmology should try to eliminate sight loss ever occurring.”



THE OPTOMETRY PRACTICE BRINGING THE NEIGHBOURHOOD TOGETHER
When Sohail Hakim started working at Alan Miller Optometrists a decade ago, patients would come to him whose great-grandparents had had their eyes tested in the same practice.
“So many patients come in and tell us, ‘I remember sitting in that chair when I was five years old’,” he shared with OT
The practice is located in Irlam and Cadishead – an industrial area of Manchester, with the 20,000 strong population separated from the city centre by a canal.
“It is a very close-knit community,” Hakim said. “People choose to stick to businesses that are local and reliable. There is that continuity in terms of who they are seeing and where they are going,” he added. Alan Miller Optometrists, also part










“We are not just here to make money – we are here to help”
Beth Bracey



of Hakim Group, has served its community for more than 90 years. The practice provides sight tests to members of the Greater Manchester police force and supplies safety eyewear to local manufacturers. In pre-pandemic times, it was normal for patients to be offered a cup of tea and a biscuit.
“When I am travelling to work, it is like going from one home to another,” Hakim shared.
“The practice has been moulded by the community. It has always been there like the butcher, grocer, restaurant or newspaper store. This is the local practice that serves everyone’s eye care needs.”
THE OPTOMETRIST PROMOTING HEALTHY LIFESTYLES
A passion for prevention has seen optometrist Shamina Asif spearhead an initiative that involves optometry practices offering smoking cessation, alcohol screening and weight management services as well as NHS Health




“We hope to improve health outcomes across the whole community”
Tom Mackley
violence – the optical practice in effect becomes a hub to support their own communities,” she shared.
THE OPTOMETRIST GIVING CHILDREN A BETTER START
THE PRACTICE DIRECTOR
DONATING PART OF HER SALARY TO LOCAL CHARITIES
When optometrist Sue Haine was growing up in a small farming village, she observed how everyone in the community helped each other.




Checks. The Healthy Living Optical Practices (HLOPs) scheme has been introduced across Nottingham, Derbyshire and Greater Manchester, with Worcestershire recently commencing the service.
“As optometrists, we are already picking up signs of cardiovascular disease and other systemic conditions, so it only makes sense to have public health commissioned services in optical practices too,” she shared with OT.
Alongside public health specialist, Michelle Dyoss, Asif has set up a consultancy to help other local optical committees secure funding and establish HLOPs.
Asif emphasised that optical practice staff are in a good position to talk about healthy living and the prevention of disease.
“A lot of the patients develop good relationships with optical staff and with the introduction of other possible services – like mental health and signposting for domestic


A pioneering initiative in Blackpool aims to address healthcare inequalities by connecting vulnerable families with optical practices.
Optometrist Tom Mackley shared that the Better Start project aims to link families with with pharmacy, dental, and optical practices using community connectors – a person from their neighbourhood who the family trusts.
“We are trying to focus attention on where we can make a difference. Some families don’t readily access primary care services. We must understand the barriers and overcome them,” Mackley said.
Mackley is chair of the Lancashire & South Cumbria Local Eye Health Network for NHS England.
Three practices have initially enrolled in the project within central Blackpool. Once the pilot is completed, there is potential to extend it to areas within Lancashire and South Cumbria with similar demographics.
“I’d be naïve to think that we are going to end health inequalities, but if we can demonstrate that families we have seen continue to engage in healthcare in the long-term, then I think we will have succeeded,” Mackley shared.
“Ultimately, we hope to improve health outcomes across the whole community. Better Start delivers that by focusing on the children.”
“There was never any question of exchanging money for a service – I grew up with the idea that one good turn deserves another,” she shared with OT.
Haine is now a director of Haine & Smith Opticians, which has 20 independent practices in Wiltshire, Gloucestershire and Oxfordshire.
Since 1995, Haine and her fellow director have donated a portion of their salaries to a charitable trust that supports local endeavours.
More than £150,000 has been donated to 600 community organisations in that time.
Haine emphasised that it is the local people who keep Haine & Smith in business.
“We have a duty to look after them,” she shared.
Haine highlighted that High Streets are more than just shops – but places to meet and socialise.
She believes this quality will draw people back to the High Streets as the UK recovers from the pandemic.
“It can mean a great deal to people to be able to wave through a shop window to a familiar face.”






SIGHT TEST BY SUBSCRIPTION
Meal kit, gym, Netflix… eye plan? OT talks with practices about switching to private care and asks whether the future of eye care will be by monthly payment

For Keval Sejpar, principal optometrist at McAusland Optometrists, the pandemic was the straw that broke the camel’s back.
Switching to private care was a conversation that had rumbled in the practice tearoom for years before the Exmouth independent made the change in July 2020.
Following the outbreak of COVID-19, falling patient numbers as a result of social distancing restrictions and the added cost of personal protective equipment reignited conversations about changing the practice business model.
Underlining these considerations were frustrations with the administrative burden and scant reimbursement from General Ophthalmic Services (GOS).
“It was an opportunity to take ownership of our business model
rather than continue putting up with something that wasn’t sustainable,” Sejpar said.
The practice now offers two options for patients – a pay as you go model and a payment plan, where a monthly fee covers all of a patient’s clinical care. Sejpar shared that the vast majority of patients have signed up for the payment plan, with less than 10% opting for pay as you go.
“Nowadays, there is familiarity with subscription models almost across the board,” he shared.
In the year leading up to February 2020, around 81% of examinations performed at McAusland
“There is familiarity with subscription models almost across the board”
Keval Sejpar
Optometrists had a GOS component. However, Sejpar calculated that he could afford to lose 40% of patients receiving solely GOS services and still break even. In the first year, he estimates that he lost fewer than 10% of patients following the switch.
He described the change to a private model as liberating –enabling all members of the practice team to focus on what is best for the patient.
“It has empowered everyone in the team, from the receptionists to the optometrists and the dispensing opticians, to say, ‘you don’t need to worry about the money element of this, just do what is best for the patient’,” Sejpar said.
PAPERWORK OVERLOAD
I-Care Optometry in East Grinstead chose to end its GOS contract on 1 January 2021.
Practice owner, James McAlinden, explained to OT that while GOS fees had previously accounted for around 7% of practice turnover, this type of sight test was responsible for roughly half the practice’s paperwork.
The initial response to the practice’s subscription model has been positive, McAlinden shared.
“It is early days, but it is building in a healthy way,” he added. In the 35 years that McAlinden has been working in optics, he
highlighted that the GOS fee has changed relatively little – despite advancements in technology and the quality of eye examinations over that time.
“The NHS fees didn’t reflect the level of expertise, the level of equipment and the amount of time and care that we provided,” he said.
He believes that optometry should have a fee structure that reflects the expertise and clinical standing of all the eye care professionals involved in a patient’s care.
“I feel that in my own little way I would like to contribute to that idea. I am 52 this year, so it is not necessarily my future, but I think it is the correct way for optometric practice to go,” McAlinden said.
Changing to a private model has also provided benefits to staff. Optometrists take their time with patients, with between six and eight appointments a day.
“I have worked for many different companies over the years in optics. In the clinics where you are seeing 20 patients a day, people are stressed and there is more capacity to miss something because you are running at full tilt. This is to my mind a better environment,” he shared.
THE AOP PERSPECTIVE

AOP CLINICAL AND REGULATORY HEAD, HENRY LEONARD
It’s important to think carefully about the implications of reducing or ceasing GOS work because a formula which works well for a particular type of practice, in a particular area, may not be successful elsewhere. Think about the demographics of your patient base. It’s also important to consider what type of practice you are running; a well-established boutique-style practice will probably find it easier to transition than retailers towards the budget end of the market. It may be possible to pivot from one type of practice to another before making the switch, but if you’re thinking of doing so, you should consider whether there is a market for this. It’s also worth remembering that you don’t need a GOS contract in order to claim optical vouchers, so even after you’ve terminated your GOS contract, you can still accept and claim vouchers. Members can contact regulation@aop.org.uk
described the switch to the subscription model as a matter of “professional pride.”
“The Government has no desire to increase the GOS amount when they see practices giving away free eye tests and we will never get beyond that situation until something really radical happens,” Bennett emphasised to OT.
“The NHS fees didn’t reflect the level of expertise, the level of equipment and the amount of time and care that we provided”
James McAlinden
For David Bennett, of Brooks and Wardman Optometrists in Nottingham, the decision to switch to a private model of care was a straightforward one.
“During the first lockdown in 2020 we realised that the underfunded GOS amount was never going to cover the practice needs, and more importantly the patient needs, as we emerged slowly from lockdown,” he shared.
Patients pay a monthly fee for unlimited clinical care. Bennett
GOS AND PUBLIC HEALTH
While many practices have experienced challenges around the administrative burden of GOS and inadequate levels of reimbursement, Professor Darren Shickle has examined the public health implications of the way sight test funding currently operates.
A trained medical doctor, the University of Leeds academic does not have a background in eye care. He became interested in the public health issues surrounding GOS after
he received a knock on his university office door from an ophthalmologist over 15 years ago.
“At that time there was concern within the primary care trusts in Leeds around the relative number of GOS sight tests that were being provided relative to the rest of the region and the rest of the country,” Shickle shared.
He has since worked on a portfolio of research including work that examines the true cost of a sight test and analyses disparities in eye care access linked to areas of deprivation.
The work was at times painstaking – combing through boxes of paper GOS forms to extract relevant information – and revealed stark differences in eye care access.
For example, in 2011, people aged 60 and older living in the least deprived areas of Leeds were 71% more likely to access an NHS sight test than those in the highest areas of deprivation.
For the under 16s, young people were 23% more likely to attend an NHS sight test if they lived in the least deprived neighbourhoods.
Shickle and colleagues also found inequalities in uptake of NHS funded sight tests in Essex within an analysis of 2013–2015 GOS data.
Shickle emphasised that visual impairment is an important public health problem.
“You wouldn’t want people from deprived backgrounds to be at increased risk from heart disease, for example, so why would you allow them to be at an increased risk of sight loss? Both sight loss and heart disease are preventable,” he said.
A shortfall between those who are eligible for a free sight test and those who take up the offer exists at a national scale.
Shickle calculated that if all those aged under 16 had a sight test at the recommended minimum frequency, there would have been 10.1 million GOS claims over a year in 2012. However, GOS statistics revealed an uptake that was less than a quarter of this figure.
For those aged 60 and over, the estimated need was 9.2 million – with uptake higher at 60%.
THE IMPORTANCE OF PROXIMITY
Research has supported the idea that how close someone lives to an optometry practice can predict their likelihood of accessing a GOS sight test. Work carried out by a Public Health Action Support Team in 2009 within London’s Tower Hamlets found that 13% of people living within 0.1km of an optometry practice had received a sight test in any one year.
This figure dropped to 4% among those living 1km or further away from a practice.
The traditional business model within optometry of compensating for poorly reimbursed clinical services through the sale of spectacles means there is no incentive to set up practices in economically disadvantaged neighbourhoods.
“Sight tests have always been a loss leader. That is partly one of the issues that I have
with the system – the business model is not really conducive to public health benefits,” Shickle said.
“If you were to plot out the locations of practices in relation to deprived areas, you are much less likely to find a practice right in the middle of a deprived area of Leeds. At best you might have one right on the edge,” he said.
Research led by Shickle in 2014 estimated the cost of offering a sight test. While the exact cost varied depending on assumptions made within the model, every option resulted in insufficient income.
The researchers concluded that it was reasonable to assume that the GOS sight test fee only compensated for half the ‘true cost’ of the test.
Shickle is quick to point out that he prefers to remain neutral over the perennial conflict between optical bodies and the NHS regarding the GOS sight test fee.
“What I’ve always been cautious about is being a critical friend of the sector,” he said.
“The optical bodies would love for me to say ‘The GOS fee should go up,’ but actually what I would want is a change in the business model rather than maintenance of the current model,” Shickle emphasised.
HIGH STREET VERSUS HEALTH
During qualitative interviews with people living in deprived areas, Shickle delved into some of the reasons that people in these communities were hesitant to access eye care.
The words of a young participant stuck with Shickle – that having your eyes tested is a High Street experience rather than a health experience.
“The things that would attract the target audience into an opticians in a shopping centre – where they are brightly lit, with high-end furnishings – might give a sense of reassurance and the quality of the experience if you are middle class. Whereas if you are from a socially deprived background, you might think, ‘that is just extra cost, that is why frames
cost so much’,” Shickle highlighted. In an ideal world, Shickle would like to see the clinical services offered by optometry practices separated from dispensing services.
“I would be happy for the sale of glasses to be entirely in the private sector, although you would still want to have vouchers because there would be some people who can’t afford any spectacles,” he said.
“The important thing in terms of clinical services is for it to become a health experience. That would mean looking at the model of general practice and general dental practice. You don’t tend to find dentists or
“The business model is not really conducive to public health benefits”
Professor Darren Shickle
GPs in the centre of cities or towns in shopping malls, you will find them in small buildings within communities.”
An initial exploratory trial of this idea in 2016 involved employing an optometrist to work part-time within a GP practice.
Patients were made aware of the service through a written reminder in a similar way to how GPs raise awareness of other screening services.
Shickle noted that in order for this model to be rolled out, the NHS would have to cover the full cost of eye examinations.
“That would be offset by patients being picked up with glaucoma and AMD at an earlier stage – there would be costs averted down the line.”
Shickle reflected on his research over the preceding 15 years.
“An ageing population means that the public health importance of eye health continues to increase. While my research pointed to changes that might address this public health need, very little has changed because of the political, economic, and professional barriers that remain.”







CPD
IN THIS ISSUE
C-100803
LEARNING OUTCOMES
Practitioners will be able to provide appropriate collaborative care for patients with low vision
Practitioners will be able to communicate effectively to identify the specific needs of patients with low vision.
C-100804
LEARNING OUTCOME
Practitioners will be updated on the implications of artificial intelligence for clinical practice.
OCULAR
C-101001
LEARNING OUTCOMES
Practitioners will be able to elicit symptoms and explain the management of ocular allergy to patients Practitioners will be able to manage patients presenting with ocular allergy within their scope of practice.
C-100368
LEARNING OUTCOME
Practitioners will be able to interpret corneal topography plots. CORNEAL
C-100955
LEARNING OUTCOMES
Practitioners will be able to communicate with patients to guide appropriate frame selection
Practitioners will be aware of how the characteristics of the frame can be tailored to meet patient needs. DOES MY FACE LOOK GOOD IN THIS?
C-100361
LEARNING OUTCOME
Practitioners will be able to assess common hospital clinic cases and determine management within their scope of practice.
If you pass an exam with OT, you will receive a certificate to use as evidence when declaring your CPD. Certificates will be available to download in your MyAOP. EXAM QUESTIONS, REFERENCES & DECLARING CPD POINTS
MCQs for OT’s CPD exams appear online at www.optometry.co.uk/CPD. Exams in this issue will be live from 9 April to 1 July, 2022. When taking an exam, the MCQs may require practitioners to apply knowledge that has not been covered in the related
CPD article. Visit www.optometry.co.uk/CPD, and click on ‘Related CPD article’ to view the article and accompanying references in full. In the new CPD cycle, registrants are responsible for declaring their CPD points viatheir MyGOC account (www.optical.org).
LOW VISION FIRST AID
IN BRIEF This article outlines how practitioners can support patients with low vision, while also taking into account the impact of the COVID-19 pandemic.
INTRODUCTION
For many practitioners, their recollection of low vision at university is often one of ray diagrams and working distances. Most would believe that this is something that cannot be done effectively in primary care the funding structure of low vision services.
One of the casualties of the coronavirus pandemic has been low vision services. This vital service was considered non-essential and was suspended in March 2020. In many areas it was one of the last services to resume and there are continuing waits for many patients. This is due to the space in clinic being required for more acute service provision.
Some low vision services were able to continue with teleconsultations and limited face-to-face appointments throughout the last 18 months. However, the demographics of a low vision service is skewed towards those most at risk of COVID-19 complications. This means many patients are still reluctant to come for face-to-face consultations, and infection control reduces the number of appointments available. This increases the waiting list further.
The waiting list for cataract surgery and laser treatment for posterior capsule opacification (PCO) is rising too and, as a result, there are people living with sight loss temporarily. Practitioners may not consider a person waiting for these interventions as living with sight loss, knowing that when they have treatment their vision will be restored, but until that day arrives, they are having to deal with the same issues as anyone else with a sight loss condition. This means that they may be at increased risk of falls,1 burns and depression,2 and a poorer quality of life. Optometrists and dispensing opticians are in an ideal position to help provide low vision first aid. Early intervention can make a big difference to the safety, independence and quality of life of a person with sight loss.
WHERE DO YOU START?
Often in a busy clinic, especially with personal protective equipment (PPE) and infection control
issues to deal with, practitioners often want to help someone with sight loss but do not know where to start and how to manage this in a time sensitive way. As with any aspect of eye care, a systematic approach is required. Start with what practitioners do best –assess the functional vision. What is the type of sight loss? Then, think about what that means to the patient – what activities is it likely to affect? Finally, move on to what can easily be done to help them now by having a toolbox of strategies, resources and ideas to choose from. Using this approach is efficient and less overwhelming.
WHAT MATTERS TO THE PATIENT?
No two people with sight loss will have the same experience, issues or difficulties. As discussed earlier, practitioners can have an educated guess based on the functional vision results as to what the impact of the sight loss is on the individual. However, the only real way to find out is to ask:
● How are you coping at the moment?
● What do you find difficult or frustrating?
● Have you had any falls or near misses this last year?
● How are you in yourself?

Dr Louise Gow BSc (Hons), MSc, OD, MCOptom
Observation is also helpful in assessing the needs of the patient. Are they in clean clothes? Do they look as well presented as they used to? Knowing a little about their situation helps too.3 Have they got anyone at home that helps them? Are they working? What are their hobbies? Are they suffering from comorbidities, managing lots of medications?
Based on these questions and observations it is possible to assess risks and difficulties very quickly. Start with the issue that is the greatest risk. For example, are they able to see well enough to selfmedicate? Have they suffered multiple falls in the last year? Are they depressed?4
LOW VISION FIRST AID TOOLKIT
There are some very straightforward strategies that can be discussed with patients to help them cope with their situation. Some of these are conversations that, to an extent, probably already happen during a consultation. For most patients it will be several different strategies that will cover the issues they are facing. A combination of practical suggestions, information and signposting to help might seem basic but can be transformative. The range of practical suggestions follow the bigger, brighter, bolder5 and sensory substitution approach to adaptations.
Lighting
Lighting is something that is often discussed with patients, especially if they are presbyopic. For people with low vision, it is essential as it can mean the difference between achieving a task and giving up.
The golden rule of lighting is to ensure a balance by not having too much light nor too little.6 Having even lighting throughout the house without glare sources, such as unshaded lamps, reduces discomfort, disability glare and the risk of falls. Many people with sight loss have difficulty with light adaptation so keeping the light even throughout is extremely important. Task lighting specific to the activity, such as a reading lamp, under-cupboard lights on work surfaces, or LED lights on magnifiers, can be used to increase contrast without creating glare. A torch is a valuable tool for spotting curbs in the evening when out and about, and for tasks such as looking in kitchen cupboards. Most people have a torch in their pocket in the form of a mobile phone, but for better light quality, directing people to LED, rechargeable lights such as a foldable design is a good idea (see Figure 1)
Sunlight can be a wonderful bonus or a source of discomfort and disability. Any advice about lighting should also include the control of sunlight into the house or workplace. When out and about, the use of a hat with a brim or wraparound sunglasses can improve vision and comfort significantly. It is

possible to get glare shields that fit over prescription spectacles in a wide range of colours and depths of tint. Blue blockers can help people with poor contrast sensitivity but generally there are no rules around the colour of the tint; this is a matter of personal preference. It is a good idea to keep a small stock of fit-over glare shields and encourage the patient to try different colours and depths of tint in the environments that cause the symptoms. For some people that might mean a different glare shield for specific activities.
Simple adaptations at home
Serious injuries can occur from trips, falls and burns that could easily have been avoided with advice and support about adapting the environment. Some recommendations would be:
● Check around the home and workplace for potential hazards. This could include rugs, low level trip hazards such as uneven surfaces, and ornaments and plants in the general walkways in the home
● Advise friends, family and work colleagues not to move furniture or objects from their usual locations; this means that they are easier to locate and less likely to become trip hazards
● Lighting around steps or other hazards
● High contrast tape along cupboard doors or along steps inside and outside the house, bold black felt tip pens for writing, contrasting plates and placemats
● For cooking, suggesting simple changes like one cup kettles which reduces the risk of over filling cups with boiling water, or ready chopped vegetables to reduce the chances of cuts can be helpful.
Figure 2 PenFriend
Table 1 Recommended resources
Type of support
Practical support with activities of daily living
Wellbeing: emotional and physical safeguarding
Resources to store
Local sensory needs team at social services
Local sight loss society
RNIB sight loss advice line
Local ECLO
Counselling services through RNIB/ Macular Society/ local sight loss society through GP
GP and local safeguarding contacts
Mental health charities MIND/ Rethink/ Anxiety UK
Local ECLO
Employment and welfare rights
Technology: starting out or learning new skills
Education: learning support for all students
Information to take away in preferred format
Useful links
Access to work details
Employment and legal support services through RNIB/other sight loss charities
Local sight loss society support RNIB Tech for Life support service
DSA information
Local QTVI (qualified teacher for visually impaired)
Children and young people’s teams at local sight loss society or RNIB Book share scheme RNIB
RNIB starting out, confident living and eye conditions booklets
Eye condition specific organisations
Systemic condition specific support organisations
https://www.diabetes.org.uk/ https://glaucoma.uk/ https://www.macularsociety.org/ https://www.sightlinedirectory.org.uk/ https://www.rnib.org.uk/ https://britishblindsport.org.uk/
Sensory substitution
Sensory substitution is the term used to refer to the use of an alternative sense to achieve a task that sight loss has made difficult. You may think that these options are reserved for people with severe sight loss, but many day-to-day tasks can be made easier with the inclusion of audio or tactile aids. For example, someone who could read with a magnifier may choose to listen to an audio book instead because it is more enjoyable.
Audio
The most well-known of the audio options is Talking Books, which are available free through the RNIB. There is also a wide range of audio book providers through app stores and local library services. Many kitchen appliances have audio options too, such as microwaves,
scales and thermometers. These devices make cooking more enjoyable and safer.
If the person is struggling to enjoy TV programmes, then they could try enabling audio description. Audio description explains what is happening on screen so that the person has an understanding of the visual detail alongside the dialogue.
The Penfriend is a device that enables the patient to record and read aloud information on labels (see Figure 2)
Tactile
There are simple tactile aids such as Bumpons, which are small rubber spots that can be stuck onto the TV remote, appliance settings or draw handles (see Figure 3). Using a tactile marker reduces the need

to come up close to kitchen appliances with a magnifier to check the setting.
Selfcare
Tasks such as shaving, applying make-up, picking out clothes and managing medications or health conditions can all be overwhelming. There are some simple tips that can be shared by the practitioner to help with these tasks.
Managing medication
Medication mistakes can be very serious, so it is vital that the patient is advised to flag concerns with their general practitioner (GP) and also the pharmacist. There are various options available, but perhaps the most popular is the use of dosette boxes where the pharmacist dispenses the tablets into blisters that contain the tablets and dosage for each day and, if necessary, which part of the day.
For people who need to monitor their blood pressure or blood sugar levels, there are talking monitors. Sometimes these are difficult to use so the GP can arrange community nurses to help out. Nowadays, there is a raft of technology for managing diabetes7 and the patient can discuss appropriate options with their diabetes nurse.
Instilling drops can also be very difficult for those with sight loss, so it is really important to check with patients who need drops that they are managing this adequately. Using a drops dispenser is a quick and inexpensive way to solve the problem for most people but learning techniques to put drops in can help.8
Make-up and getting dressed
This can be difficult and upsetting for people to cope with, and while might seem unimportant, these problems can have a significant effect on someone’s emotional wellbeing. Magnifying mirrors and task lighting might be the only adaptation that is required to help someone manage. There are some really useful blogs and YouTube videos that help people learn other techniques such as those by Holly Tuke9 and Elin Williams.10
Choosing clothes can also be difficult, but this can be solved in various ways such as:
● Tactile markers sewn into clothes with a different shape for each colour
● Arranging the wardrobe in colour order with the assistance of someone else initially
● Colour apps on mobile devices that can detect the colour such as Seeing AI.
Emotional support and wellbeing
Sight loss has a significant impact on emotional wellbeing and is a grieving process where many people need counselling and support before they can take on ideas and practical support. Identifying when someone is struggling can be difficult but asking if they need any support is always important. Helping them to reconnect with leisure activities through local societies and national organisations, such as British Blind Sport UK, is also important.
Magnification
Simply making things bigger can certainly be of help to some people. For example, sitting at 2m from the TV rather than 4m doubles the size. This may require some encouragement as the patient may be worried about sitting too close.
Large print books and large print versions of everyday items, such as calculators, calendars, timers and remote controls are very effective for those who just need a little bit of help up to 2x.
It is possible to purchase magnifiers online up to around 15x, which can be a tempting option for patients to consider while waiting for a low vision assessment. However, it is advisable for the practitioner to steer them away from these purchases unless it is a replacement for a previously prescribed magnifier or a low level of magnification. The use of magnifiers is not intuitive and it is difficult to predict the best power without trying it first. If the patient wants to buy through the practice or online, make sure there is a returns policy that is clear for the patient. The rule of thumb that is a good starting point is: Magnification estimate = current visual acuity/ required visual acuity. However, there should be 1.3:1 acuity reserve for spot reading or a 3:1 acuity reserve for fluent reading.5 Always demonstrate either with a magnifier or in a trial frame the short working distance of the lens and the need to hold the magnifier close to the eye to get the required effect. Most patients find an illuminated magnifier better than a simple magnifier. As this is not always the case, it is helpful to demonstrate this in the consulting room.
TECHNOLOGY
Most people carry around a smartphone and often have a tablet or laptop at home. These devices can offer all of the strategies in one:
Figure 3 Bumpons
Functional vision assessment – what can they see and how usable is their vision?
Needs assessment – what is the impact of the sight loss?
First aid toolkit:
Adaptations – bigger, brighter, bolder, audio tactile
Take away information
Referral and signposting
● Bigger: built in magnifiers and accessibility options. The options for the level of magnification at normal working distances are immense and only dependent on the quality of the screen
● Brighter: built in torchlights
● Bolder: high contrast, adjustable screens
● Audio: voice over, audio messaging, screen reading apps, apps for people with visual impairment, such as Seeing AI or audio books
● Tactile: some specialist devices include refreshable braille screens.
All that is required is a suggestion that they might explore the functions of the device they already have. There are accessibility features built in and apps that can be downloaded. Age should be no limit; those who have not grown up with technology may be a little reluctant, but the practitioner can demonstrate the options using their own phone or tablet in the consulting room so that the fear can be outweighed by the possibilities. It is important to avoid stereotyping as nobody should be considered too old, too cognitively impaired or too visually impaired to try technology. There is support to help someone get started through RNIB’s Tech for Life team or through similar services at local sight loss organisations.
ESSENTIAL CHECKLIST
As with medical first aid there should be an essentials checklist (see Figure 4):

● Have you dealt with any risk factors such as medication, falls, selfcare and safeguarding?
● Have you asked how they are in themselves?
● Have you considered the impact on the things that they want to do, or on their work and hobbies?
● Have you given them enough information in their preferred format that empowers them to access the support that is available while they wait for their low vision assessment?
This might seem like a long list which equals a lot of time in a busy clinic, but in most cases it will simply be a case of signposting, or better still, referring to other services. All that is needed is a set of resources either in a desktop file or paper file in the consulting room; Table 1 will help to organise this. It can be seen there is overlap in much of the table so a referral to one organisation can open multiple doors. If in doubt as to what is available in the local area a good starting point is the sightline directory database.
CONCLUSION
If the pandemic has taught us anything it is that a little bit of help goes a very long way. Taking a bit of time to go through this checklist could save someone’s job and livelihood, improve their quality of life or even save their life without even touching a ray diagram.
Dr Louise Gow is the specialist lead for eye health at the RNIB. She is an optometrist with 30 years’ experience in primary care and specialist settings. She specialises in low vision and eye care for people with learning disabilities. She also works for SeeAbility in the Special School Eye Care service and low vision clinics at St Thomas’ Hospital, London. Her doctoral thesis explored how it is possible to adapt primary eye care for children with an ASD.
Figure 4 Low vision first aid process
AN INTRODUCTION TO INTELLIGENT SYSTEMS IN OPHTHALMOLOGY
Dr Helen Kuht PhD, BMedSci, AFHEA and Dr Mervyn Thomas MBChB, PhD, AFHEA, FRCOphth
IN BRIEF This article provides a brief overview of artificial intelligence and the application of this technology to ophthalmology.
INTRODUCTION
Artificial intelligence (AI) is rapidly becoming part of our everyday living, perhaps without many of us even being aware we are using it. AI is frequently used commercially but has also demonstrated promising advances in healthcare, within specialities of radiology, pathology and, more recently, ophthalmology. This article provides an overview of the history of AI and explains how it is being applied to ophthalmology, including key considerations for new guidelines and potential risks associated with implementation.
WHAT IS AI?
AI describes the ability for a computer or machine to mimic human intelligence. Early work by mathematician and computer scientist Alan Turing, leading to his theory of computation, was a key milestone in AI history.1 Simultaneous discoveries in the fields of neurobiology and information theory raised the possibility of creating an ‘electronic brain.’2,3 This subsequently led to Turing’s question of whether machines could demonstrate intelligent behaviour. His seminal paper in 1950 which considered the question ‘Can machines think?’ was a catalyst for AI research.4 In 1956, AI was first described as a machine capable of independent thinking and mimicking human behaviour, following training.5 Since then, AI has become increasingly more prevalent in business and healthcare. Today, AI is used for many different tasks but can broadly be identified as demonstrating the following behaviours: planning, learning, problem solving, perception, motion, and manipulation.
Machine learning (ML) is a type of AI (see Figure 1, page 72) which describes the ability of a computer to perform tasks without being explicitly programmed. There are three main types of ML algorithms:
1. Supervised ML – in the training stage of the model, the algorithm requires both the data (for example, images) and annotations (for example, classification) that have been allocated by the human interpreter. The system is then validated on just the data without annotations
2. Unsupervised ML – in the training stage the algorithm only receives the data with no annotations. The intelligent system independently determines the inherent structure of the data and classifies accordingly
3. Reinforcement ML – the algorithm receives and interprets the data independently, but through a dynamic process with evaluative feedback, to maximise reward function.
WHAT IS DEEP LEARNING?
Deep learning (DL) is a classification of ML which can handle large amounts of data and has the ability to interpret features and classify, without the requirement for expert input to first extract the features of an image before submitting to the model.6 The DL system is modelled on the structure of the human brain and neural networks. Often these neural networks have many layers and are given the term ‘convolutional neural network’ (CNN) (see Figure 2, page 73). This structure of a DL model facilitates the analysis of images, videos and unstructured data. The development of DL systems for image classification, among other tasks, is largely possible due to our access and ability to handle ‘big data.’ Computing power has exponentially increased over the last few decades while dramatically reducing in cost. DL models have largely contributed to the success of AI in medicine.7 DL in medicine provides a panoramic view of an individual’s case, subsequently allowing for more precise diagnoses and unique management plans. Furthermore, AI in healthcare allows efficient processing and interpretation of big data, such as whole genome sequencing, electronic health records and medical imaging, a task notoriously challenging to manage and execute.8-10 DL is particularly effective in image recognition as currently demonstrated in radiology, pathology and, more recently, ophthalmology.11-13
AI IN OPHTHALMOLOGY
Ophthalmology has arguably been at the forefront of AI development in healthcare, with promising
proof-of-concept work in diagnostic and analytical clinical scenarios.7 DL models are commonly used for ophthalmology research and have been developed for data analysis, segmentation, diagnostic and predictive systems.14 Intelligent systems are predominantly developed in ophthalmology for image analysis, such as with fundus photographs or optical coherence tomography (OCT) interpretation. Screening tools for diabetic retinopathy and glaucoma have been developed, offering the potential for an earlier diagnosis.15-21 Furthermore, proof-of-concept for the use of AI to predict disease and disease progression has been demonstrated in age-related macular degeneration (AMD) and diabetic retinopathy.17,22-25 More recently, DL has demonstrated high levels of accuracy for differentiating between sightthreatening papilloedema and pseudopapilloedema.26 Many of these developed intelligent systems demonstrated impressive performance, often surpassing human capabilities. For example, the diagnostic performance of detecting diabetic retinopathy has excelled following the introduction of DL, achieving 96.8% and 87.0% sensitivity and specificity, respectively.15
With both ageing and growing populations, the burden on healthcare systems worldwide is increasing.27,28 Additionally, imaging technologies, such as OCT, are becoming increasingly available and far exceeding the availability of expert clinicians to interpret results.29 Therefore, we are at a critical time to introduce intelligent systems to aid the clinical pathway and reduce the pressure on clinicians.
To date there have only been limited applications of AI in paediatric eye disorders.30-34 This is likely due to the lack of sufficiently large annotated paediatric datasets to allow for training and validation. As a result, the paediatric
demographic is commonly overlooked, and hence, paediatric populations are often deprived of novel technologies.
Currently, retinopathy of prematurity and congenital cataracts are the two main areas of research for AI in paediatric ophthalmology.33,34 Additionally, the use of ML with strabismus detection, reading disability and refractive error are slowly developing.30-32 Identifying, quantifying and classifying childhood ophthalmological disease with the use of AI has the potential to augment the clinical pathway.
GUIDELINES FOR AI STUDIES: LEGAL CONSIDERATIONS AND CONSENT
The majority of studies associated with AI in healthcare are performed on a retrospective basis, with clean, annotated datasets.35 However, this is not representative of real clinical data, where often data is unstructured and messy.36 Outcomes from these retrospective studies, therefore, should be considered proof-of-concept and hypothesis generating, rather than concrete evidence of a successful algorithm.35 To assess the actual performance of an intelligent system, prospective clinical trials must take place in real-time clinical scenarios, to represent patient care.
To perform a clinical trial, specific guidelines must be adhered to. Consolidated Standards of Reporting Trials (CONSORT) were first introduced in 1996,37 and were recently extended in 2020 to include guidelines for any clinical trial which involves an AI component.38-40 Parallel with CONSORT-AI, a statement was issued for clinical trial protocols; SPIRIT-AI (Standard Protocol Items: Recommendations for Interventional Trials – AI).41-43
The first autonomous AI diagnostic system to be authorised by the US Food and Drug Administration (FDA) was an intelligent system designed to detect diabetic retinopathy.15 Proof-of-concept studies for the use of DL in medicine are increasing rapidly; however, to date, prospective clinical trials are scarce. As of September 2020, publicly available data is only accessible for 11 clinical trials in healthcare related AI-systems,15,44-52 four of which were in the field of ophthalmology.15,35,44-46
The term ‘big data’ is often associated with AI and describes the large datasets required to train and validate intelligent systems to ensure sufficient data is available to reduce the risk of underfitting of the model. Underfitting describes the poor performance of the model on the training dataset because the model is unable to draw conclusions on the relationship between the input variables and the output variables. In healthcare, these large datasets are often obtained from patients over time, from multiple different sites, for example, hospitals. Data privacy is a key consideration and one reason why robust guidelines have been developed to ensure the most appropriate approach to studies involving AI.
The General Data Protection Regulation (GDPR) was first implemented in 2018 to regulate the protection of
Figure 1 Relationship between artificial intelligence, machine learning and deep learning
Artificial intelligence
Machine learning
Deep learning
Figure 2 A simplified overview of a supervised DL model. (A) the training stage of the algorithm using both data and annotations inputted into the model through a convolutional neural network. The algorithm then progressively learns from the data and annotations inputted. (B) the validation stage of the algorithm which involves just data inputted into the system, and predictions being generated
personal data in Europe.53 As part of this regulation, all health data is considered to be personal data; however, if the health data is being used for research purposes, then this may be exempt.54 GDPR therefore introduced a new version of de-identification named ‘pseudoanonymisation’ to allow the use of exempt personal data in research provided there is a legal basis;55 this describes only the removal of data which is directly identifying.55 Studies developing AI systems for healthcare often involve multi-centre collaborations to ensure the collection of a sufficiently large and diverse dataset. Multi-centre efforts are particularly important when developing systems for rare diseases. Such studies naturally involve some form of data sharing, which inherently increases the risk for data breaches.56 One new approach which can be implemented to protect data privacy is called ‘federated learning,’56 which was first proposed in 2017 by Google AI and describes the decentralisation of algorithms. This decentralisation allows the algorithm to be trained on data within the protected environment, for instance, a hospital or university,57 which enables multiple centres to access the algorithm, without having to distribute their protected data across multiple sites.7 A similar approach to minimise the risk of re-identification would be the local training of generative adversarial networks (GANs) and the subsequent sharing of the GANs rather than sharing of the data. GANs are a recent advance and require the use of generated synthetic data, meaning that the performance of the model may be subject to bias and risks safety and efficacy.56
ADVANTAGES OF AI IMPLEMENTATION TO HEALTHCARE
DL in healthcare has the potential to empower clinicians and enhance the clinical pathway by supporting clinical decision making.58 However, it is important to consider that AI is not here to replace the clinician. When a patient attends a clinic and, for example, an abnormality of the optic nerve on OCT assessment is identified, this is not looked at in isolation, but the larger clinical picture is considered including medical history, clinical assessments, patient reported symptoms and other aspects of the clinical work up. The same principle goes for AI in healthcare, that is to say, while AI may allow for a more efficient process of classifying an abnormality, the clinical work-through and clinician input remain a crucial element of the pathway.35 With this in mind, the implementation of AI in healthcare requires a ‘human-inthe-loop’ approach, which is particularly important when navigating through complex cases.35 Introducing AI to healthcare can facilitate a more efficient clinical pathway enabling clinicians to spend more time with the patient. Due to the inevitable introduction of AI tools into routine practice, it is important that clinicians are educated accordingly.59 Clinicians are likely to be involved in developing, validating and implementing these systems and, therefore, require some instruction or knowledge to perform these tasks.
The development of automated DL systems has the potential to play a central role in the democratisation of AI in healthcare. Automated DL describes an accessible
user interface that allows users with minimal or no prior coding knowledge to navigate and develop DL models.60 Clinical applications with automated DL have already been demonstrated in proof-of-concept studies. One such example is the feasibility study for classification of medical images (images of skin lesions, chest x-rays and retinal photographs) using an automated DL design with clinicians with no prior coding experience.60
Supervised ML models are often implemented for intelligent healthcare systems, due to the ability to train the algorithm with pre-existing classification systems or grading systems in place. However, sometimes subtle features may easily be missed by the human interpreter and may not have been considered when classifications were developed. Training algorithms on pre-defined groups may prevent the algorithm from looking past the limitations and bias from human clinicians.61 One benefit of using an unsupervised ML approach for classification is the ability for the intelligent system to cluster images based on similar features. Although the algorithm will not be able to state, for example, ‘diagnosis of diabetic retinopathy,’ it will be able to group together similar images. In this capacity, AI may enable new discoveries associated with conditions or uncover previously missed subtle changes.
LIMITATIONS AND RISKS ASSOCIATED WITH IMPLEMENTING AI IN HEALTHCARE
Although promising studies have demonstrated the high performance of AI systems, there are many barriers to implementing AI in healthcare.62 Technologies incorporating AI introduce concerns and associated risks.63 One common concern around the use of DL is the ‘black box’ nature of the systems.64 This term describes the opaque nature of the algorithm and the subsequent inability to uncover how the intelligent system reaches a conclusion on the image classification. However, recent advancements in explainable AI (for example, GradCAM) may help to demystify the systems by providing an explanation output of the patterns the system is looking at in the image to conclude a prediction.65
An important consideration with using supervised ML models is that all of the annotations provided for the


data (ground truths) have been assigned by the clinician or researcher. There will always be an inherent human error with classification and assignment.61 Validation accuracy of developed intelligent systems therefore will never reach 100% due to this inherent error. However, introducing a team of expert clinicians to all classify the images may reduce this error and improve efficiency and diagnostic accuracy. A further challenge associated with translating these intelligent systems into clinical practice is the inconsistency of analysing data from different OCT devices and the lack of standardisation of imaging protocols.66
Despite the efforts to de-identify patient data, technological advances may enable re-identification of data in the future.56,67 Already the ability to identify gender, age and cardiovascular risk factors from fundus photographs has been demonstrated.68
Often DL systems are developed using heterogenous populations. This has the potential to develop biased models which may perform poorly when introduced to different populations. This highlights the importance of including diverse datasets to develop and validate DL models prior to implementing into healthcare to ensure all populations are widely represented. Without including diverse datasets, diagnostic and predictive inaccuracies are inevitable. This also highlights the importance of performing clinical trials to validate a system using AI, to prevent causing any harm to patients and potential misdiagnosis.
35
CONCLUSION
Developing AI-enabled screening tools in conjunction with telemedicine could contribute to the democratisation of the healthcare system in ophthalmology to screen and monitor patients from a primary eye care setting.69 This has the potential to reduce NHS cost burden, increase accessibility to healthcare and improve the clinical pathway. However, most of the aforementioned DL systems in ophthalmology remain at the proof-ofconcept stage, with very few having been translated into clinical practice. A rise in clinical trials for AI-enabled screening and diagnostic tools and the eventual clinical implementation in years to come is anticipated.
Helen Kuht is a research orthoptist and completed her PhD at the University of Leicester. She was recently granted a Wellcome Trust Early Career Fellowship Award and undertakes clinical orthoptic work in the Midlands. Kuht graduated from the University of Sheffield in 2016 with first-class honours in orthoptics. Her current role is focused on introducing the application of AI into paediatric ophthalmology with the use of OCT. Kuht has presented this work at conferences, subsequently being awarded presentation prizes and the ARVO international travel grant.
Dr Mervyn Thomas is a clinical lecturer in ophthalmology and genomic medicine at the University of Leicester and clinical commitments at the Leicester Royal Infirmary. He has been the recipient of prestigious awards for his achievements, and his research has been supported by grants from Medical Research Council, Wellcome Trust, Academy of Medical Sciences, Health Education England and Fight for Sight. Thomas was elected to the ARVO program committee, is a scientific advisor for Nystagmus Network and on the Global Albinism Alliance Scientific Committee.
DOES MY FACE LOOK GOOD IN THIS?
Amy Rose BSc (Hons), FBDO, FHEA
IN BRIEF This article considers how to undertake appropriate frame selection taking into account the material and the facial characteristics of the patient.
INTRODUCTION
The General Optical Council (GOC) requires that all registered practitioners are able to dispense suitable optical appliances, considering the patient’s comfort, age and lifestyle, along with the durability and cosmetic appearance of the appliance.1 Some of these aspects are easier to meet than others. For instance, patients who have nickel allergies will not be dispensed with frame materials that are likely to elicit a reaction; those with high prescriptions will warrant a smaller lens aperture to minimise weight and improve the cosmetics. It is when there are fewer specific requirements or necessities to be met when the practitioner’s knowledge of stock and skills can be demonstrated.
MATERIAL
The properties of frame materials have been discussed extensively elsewhere so will not be explored in depth here. The material affects the cosmetics of the frame, and the nature of the front will generally dictate the bridge fitting, although alterations can be made to modify the fitting, for instance, by adding pads on arms to a plastic front to accommodate certain bridge projections. The selection of the frame material can be for both practical and aesthetic purposes. A heavyhanded patient, persistently presenting with damaged frames, may benefit from a titanium frame, selected for its durability; similarly, a patient very sensitive to weight on their nose may be dispensed with a titanium frame due to its lower specific gravity compared to other materials. The frame material can also help to improve the cosmetics of the finished spectacles or complement the personality of the patient. Cellulose acetate, propionate or acrylic frames (see Figure 1) offer a thicker rim and sides, which can meet a patient’s

requirement for a retro or vintage style. In contrast, metal materials tend to result in thinner, less obtrusive rims and sides; stainless steel or titanium frames may reflect a patient’s minimalistic style. Combination frames can draw advantages from both plastics and metals. For example, lightweight fronts to increase comfort and thicker sides to disguise lens thickness.
Patients who prefer a unique style can consider frames produced from natural materials, such as horn or wood, or less common materials like acrylic. It is the responsibility of the practitioner to communicate with the patient, not only to determine their requirements for the dispensing, but also to advise the patient on the options available to them; this includes sharing details on the frame, including advantages and disadvantages of the material properties and construction.
COLOUR
Frames are available in every colour imaginable. As with frame shapes, colours can either complement or contrast with a patient’s natural tones. Complexions can be classified by observing hair
Figure 1 Acrylic frame. Image courtesy of Kirk & Kirk
and eye colour in relation to skin tone2 and the terms ‘warm’ and ‘cool’ give a general description. Warm complexions typically have a darker or yellow undertone, with darker hair: browns, reds, dark or strawberry-blonde, and darker eyes such as hazel or brown. Those with cool complexions are fairer skinned, with light blonde, grey and white hair, and blue, grey and light green eyes. These broad terms can then be narrowed down into ‘springs,’ ‘summers,’ ‘autumns’ and ‘winters’ (see Figure 2). Spring complexions consist of fair skin tones, with strawberry-blonde to varying shades of dark to golden-blonde hair. The frame colours that complement these complexions include orangey-reds, tans, golden-browns and gold, and lighter neutral colours such as ivory, cream and beige. Patients with light hair and eye colour and fair skin tones can be classed as ‘summers’ and tend to suit desaturated colours such as blues, greys, pink, dull silver, light gold, ash-browns, rosebrowns and rose-beiges. Patients with an autumn complexion have red-brown or red tones, auburn or golden-brown hair, and dark colouring and golden skin undertones. Like those with summer complexions, frames with softer, desaturated colours typically suit these patients, including
olives, ambers, orangey-reds, rust, copper, moss green, teal, golden-browns and gold. Those with a winter complexion have a darker colouring, or strong contrast between their skin, eyes and hair colours. Frame colours that suit these patients are stark cool colours, including cool blues, emerald greens, burgundy, black, dark brown and silver. Plastic frames can also be produced with patterns and fabric inserts (see Figure 3, page 78) and with other materials, all of which will need to complement the patient’s colouring and preferences.
Determining a patient’s complexion can sometimes be difficult; however, asking what colour clothing the patient tends to wear or avoid, can help the practitioner to select colours or patterns that will complement their complexion as well as style. Of course, the best method to determine whether a frame colour suits a patient is to try the frame on.
In addition to the frame colour suiting the patient’s colouring, it should also complement their facial features. Darker colours will suit heavier facial features, such as darker, thicker eyebrows. In contrast, lighter frame colours will suit more delicate facial features. If a thick, dark frame is placed on a face with delicate, light features, it can appear ‘heavy’ and overpower the features. A light frame on a face with darker features can sometimes appear almost invisible, while others, out of place.
Factors external to the patient’s appearance can influence the choices made, such as the patient’s occupation, hobbies, lifestyle and the season. For instance, members of the police force are advised to wear discreet colours3 and other professionals may wish to avoid certain colours or vibrancy as part of their profession. In contrast, some may wish to be more outgoing in their frame colour or pattern choices, to accentuate their personality.
The season can affect the colours of frames available and what the patient desires with frames produced for autumn/winter collections being typically darker than those of spring/summer.
SHAPE
A common question from patients during frame selection is: What shape(s) suit my face? To produce the most cosmetically appealing results, the frame should help to create a balanced facial shape. Selecting a frame that has opposing features to the shape of the patient’s face helps to create an optical
Figure 2 Colour palette wheel for different complexions
Face shape
Characteristics
Oval Considered to be the ‘ideal’ face shape
Balanced proportions in facial features and positions
Oblong
Face appears longer than it is wide
Frame selection
Most frame styles suit this face
Avoid oval shapes
Ensure the frame front size is proportionate to that of the face
Deeper frames reduce the appearance of the face length
Frames with stronger horizonal features increase the apparent width of the face
Round
Square
Desire to make face appear longer, to mimic oval shape
Wide face shape, with almost parallel ‘sides’
Diamond Central portion of the face is widest
Narrows towards top and lower portions
Heart/base up triangle
Wider at the top
Narrows towards chin
Base down triangle Jawline appears widest part of the face
illusion of a balanced face shape. For example, a rectangular frame will widen a thin face as the apparent greater width than depth of the front creates the illusion that the face is wider than is actually is. To be able to advise on a frame shape that best suits the patient, the practitioner first needs to be able to identify common face shapes. These shapes are drawn from the proportions of the face at different points: oval, oblong, round, square, diamond, base-up triangle and base-down triangle (see Table 1)
Oval faces are generally considered to be the most desirable face shape. The proportions reflect those of the ‘ideal’ face, with the forehead, eyes
Round frames emphasise roundness of face
Shallow frames lengthen face shape
Avoid definite vertical sides
Lengthen facial appearance
Rounded shapes, such as round and oval to soften squareness
Rounder frames, or quadras with rounded corners
Upswept frames suit some
Avoid sharp angles on frames
Square and pilot shapes to draw the appearance of the face out in the lower portion
Upswept or oval frame shapes to balance face shape, widening it nearer the top portion
and nose, and the mouth and chin, each occupying around a third of the face height, and the eyes, nose and temples each occupying a fifth of the face width.2 This face shape is able to wear most frame shapes; however, oval frames should be avoided. To enhance the cosmesis of the spectacles, ensure the size of the frame front is proportionate to the face. Oblong faces appear longer than they are wide. A deep frame helps to reduce the apparent length of the face, as will fronts with a consistent, as opposed to two-tone, colouring. To increase the apparent width of the face, a frame with more emphasis on the horizontal sides, such as a quadra or oval shape, should be selected.
Table 1 Characteristics of face shapes and frame advice
“THE ABILITY TO PERFORM A FRAME SELECTION USING MORE THAN A PRESCRIPTION AS THE GUIDE IS COMPLEX AND NOT EASILY TAUGHT. IT COMES WITH EXPERIENCE”
Round and diamond faces are wide. Diamond faces are widest in the central horizontal portion, narrowing towards the forehead and chin. Diamond faces can appear quite angular, which is emphasised with sharp corners and angles on frames. Rounded frames help to soften the angles, as do quadra shapes with more rounded corners. Quadras, more square than rectangular, will also help round faces appear thinner and longer. Rounder shapes on these faces will emphasise the roundness so should be avoided. Upswept frames can be beneficial for these facial shapes as a slight upsweep will help a round face appear thinner and longer, while on a diamond shape it can help to widen the top portion of the face. However, it is important that the front width does not extend further than the widest part of the face and the peak of the upsweep is not too sharp.
A face that appears short and wide, with parallel ‘sides,’ can be described as square. As with round faces, the aim is to lengthen the facial appearance. Frames with definite, almost parallel sides, such as quadras, will emphasise the squareness of the face; however, this can be softened with rounder shapes, such as oval and round frames. Shallower frames will help to lengthen the face.
The widest part of the face is used to describe the base direction in triangular faces. Base-down triangle faces are widest in the lower portion, narrowing towards the top. The presence of a spectacle frame can help to balance the face

shape and this can be further enhanced using an upswept or oval frame to draw the eye upwards and outwards. Base-up triangle faces can also be referred to as heart-shaped where the face is widest in the upper portion and narrows towards the chin. In these patients, using pilot or quadra shapes can help to balance the lower portion of the face. A pilot shape does the same to a base-up face shape as the upswept does for base-down, drawing the eye down and out, broadening the appearance of the lower portion. In both cases, choosing the frame shape that follows the same direction as the face, will emphasise its widest point.
Our eyebrows are heavily involved in non-verbal communication4 used in combination with the eyes to convey non-verbal cues as to intentions, understanding and meaning. As a general rule, the spectacle rim should never cover the eyebrows in ophthalmic spectacles, nor should they be visible within the lens aperture. For optimum cosmesis, and to facilitate non-verbal communication, the frame brow line should follow the line of the eyebrows, which should remain visible.
As well as balancing the overall face shape, the frame can be used to change the appearance of the nose. The apparent length of the nose is dependent on how much is visible beneath the bridge.5 In the same manner that a shallow frame lengthens the appearance of the face, exposing more of the nose makes it appear longer. Other methods to lengthen the appearance of the nose includes selecting frames with high-positioned, keyhole or thin bridges, all of which help to expose more of the nose. In the case of keyhole bridges, it is recommended to use darker colours to emphasise this feature the most.
Shortening the appearance of the nose can be achieved by dispensing frames with thicker bridges, mid- or low-positioned bridges, or saddle bridges. Thicker and mid- or low-positioned bridges conceal more of the nose, making it appear shorter. Saddle bridges sit on the crest of the nose, lower compared to other bridge types, which shortens the appearance of the nose.5 It is of course, imperative that the bridge fitting is suitable for the patient in all instances, as this is the weight bearing point of the spectacles and cannot always be adjusted at a later date. Balancing the effect that the shape of the frame will have on the appearance of the finished lenses, while still being cosmetically pleasing on the patient can be challenging, particularly in cases where a higher prescription needs to be considered.
Figure 3 Tartan fabric insert. Image courtesy of FACEAFACE

This requires the practitioner to explain the effect of the frame shape on the finished lenses to the patient, who should be given the necessary information to make an informed decision on the finished spectacles, including appearance and weight. In some instances, it will be more challenging to strike the balance between dispensing for the prescription and the cosmetics.
MANUFACTURING PROCESS
Innovations in technology and an increased awareness of the need to reduce carbon footprints have led to breakthrough methods of spectacle frame production, such as 3D printing and recycled materials. For patients who are conscious of the environmental impact of their spectacles, these frames offer an alternative to those produced through traditional, less sustainable methods. It is important that practitioners are aware of not only common materials and their properties, but also new and emerging materials and manufacturing innovations, which slowly trickle down into high street practice. Greater awareness of, and the need to improve sustainability, will undoubtedly ensure that this area will grow in the coming years. Patients will actively seek out suppliers of frames that they are drawn to and will expect practitioners to have a thorough knowledge of the product.
COMMUNICATION
The success of any dispense is reliant upon effective communication between the practitioner
and the patient. Practitioners are experienced and trained to ask questions relating to aspects such as visual task analysis, occupation and hobbies; however, to dispense a frame that truly suits a patient, it is important to spend time ascertaining information about their personality, style and preferences using a mixture of open and closed questions such as:
● What colours do you tend to wear?
● Are you planning to dramatically change your hair style or colouring?
● Would you like a frame that is very ‘on trend’ or something more conservative?
This line of questioning should never be accomplished through an interrogation, but through an open conversation. Some elements can be determined non-verbally by observing what the patient is wearing, their hair style and colouring and the frames they are drawn to. Equally, observe the frames they avoid and ask why. The practitioner may wish to encourage them to try a style they may not otherwise have considered but could suit them.
CONCLUSION
Frame selection is an equally important part of a dispensing as lens recommendations. While the lenses enable patients to see clearly, the frame is responsible for the comfort, durability and functional operation of the spectacles. A poor frame selection can lead to negative reviews, or the patient not returning at all whereas frame selection which meets the patient’s requirements and desires is hugely rewarding for the practitioner and beneficial for the wider reputation of the practice.
The ability to perform a frame selection using more than a prescription as the guide is complex and not easily taught. It comes with experience, a good knowledge of frame availability and the materials and production methods used. The cosmesis and optics of the finished spectacles needs to be considered throughout the dispense and during any recommendations made by the prescribing practitioner, as this is where the foundations of a dispensing begin.
Figure 4 Frame constructed from stainless steel and 3D printed insert around the rim. Image courtesy of Mykita
Amy Rose is a dispensing optician with over 10 years’ experience working in independent practice and is currently a lecturer in optometry at the University of Hertfordshire.
OCULAR ALLERGIC DISORDERS
Dr Sandeep Dhallu PhD, BSc (Hons), MCOptom
IN BRIEF Allergic eye disease affects a large proportion of patients and appropriate diagnosis and treatment is necessary in order to relieve symptoms. This article provides an overview of allergic eye disease.
INTRODUCTION
We are exposed to a vast array of toxic and allergenic substances on a daily basis. Allergic eye disease is a common condition that affects a large proportion of the world’s population, with 15% of eye related consultations in the UK primary care setting reported to occur as a result of allergic conjunctivitis.1 It is often linked with other atopic conditions such as asthma, eczema and food allergies. Allergic disease as a whole represents a substantial burden on the NHS2 and can significantly impact on a person’s quality of life.3 It has also been linked with poorer exam performance in UK teenagers.4
Sufferers of ocular allergy tend to self-medicate or do not seek help for their ocular symptoms and this can lead to poor symptom control. Appropriate diagnosis and treatment are necessary in order to relieve symptoms and prevent complications from arising.
HYPERSENSITIVITY REACTIONS
The immune system provides protection by differentiating between self and non-self in order to eliminate foreign substances using either innate or adaptive immunity. The innate system, which is present from birth, is the initial defence response and utilises an antigen non-specific mechanism. If the innate system cannot overcome the foreign substance, the adaptive system takes over, using an antigen-specific defence mechanism.5-7
Hypersensitivity reactions are immunologically based adverse reactions and have traditionally been classified into four categories. Allergies and hayfever are examples of type I reactions and involve immunoglobulin E (IgE) antibodies as well as two types of white blood cells (mast cells and basophils). Initial exposure to the allergen results in allergen specific IgE antibodies binding to the cell membranes of mast cells and basophils so that when re-exposure occurs, the allergen is recognised and there is a rapid immune response, which results in the symptoms of allergy.5 Type II reactions occur mainly as a result of immunoglobulin G (IgG) and
immunoglobulin M (IgM) antibodies interacting with body cells and tissues, and these can sometimes cause damage to tissues. Type III reactions, like lupus and rheumatoid arthritis, occur due to immune complexes which can trigger an inflammatory response and may cause tissues to become damaged in the process of these complexes getting broken down by enzymes. Type IV reactions, like chronic asthma, do not involve antibodies but T cell lymphocytes. When there is an initial exposure to an allergen, memory T cells are produced and any subsequent exposure initiates a faster and stronger immune response, which can also cause tissue damage. Allergic eye disease is an immune response to allergens on the ocular surface and encompasses all four types of hypersensitivity reaction.8
OCULAR ALLERGIC CONJUNCTIVITIS
In 2012, a new classification for ocular allergic disorders was proposed in which there was a distinction between allergic and non-allergic hypersensitivity reactions, and a further subdivision of allergic reactions into IgE and non-IgE mediated hypersensitivities, as shown in Figure 1 9
Seasonal allergic conjunctivitis and perennial allergic conjunctivitis
Allergic conjunctivitis is the commonest but also mildest form of ocular allergic disease and involves a solely type I hypersensitivity reaction which usually begins within seconds to minutes of exposure to the allergen.10 It can be categorised as seasonal (SAC) or perennial (PAC), with the main difference between the two being the chronicity of symptoms. Seasonal triggers include temporary allergens like pollen, whereas perennial triggers include longer lasting allergens such as house dust mites and animal dander. Smaller allergens like animal dander have a higher chance of causing symptoms compared with larger allergens such as house dust mites, which cannot remain airborne for as long after disturbance. SAC is an IgE mediated allergic reaction that tends to be more prevalent in particular seasons; typically,
mediated
mediated
SAC, PAC, VKC, AKC CBC, VKC, AKC
hypersensitivity
Figure 1 Classification for ocular allergic disorders.9 SAC (seasonal allergic conjunctivitis), PAC (perennial allergic conjunctivitis), VKC (vernal keratoconjunctivitis), AKC (atopic keratoconjunctivitis), CBC (contact blepharoconjunctivitis), GPC (giant papillary conjunctivitis)
spring/early summer when pollen levels are high. Symptoms include itchiness, epiphora, bulbar hyperaemia and eyelid swelling, with the severity of symptoms varying according to the patient’s exposure to the allergen.
PAC is also an IgE mediated reaction to allergens that are present all year round such as dust mites, animal dander and mould. It is characterised by the same symptoms as SAC, with the differentiating factor being that PAC is chronic, and thus, the often-mild symptoms persist for longer. As a result of the COVID-19 pandemic and the consequent increase in people both working and studying from home, a larger proportion of the population have stayed indoors for longer than they might otherwise have done, thereby prolonging any contact and exposure to perennial triggers.
With both SAC and PAC there is no corneal involvement; however, there can still be a substantial impact on a sufferer’s quality of life.3,9 SAC and PAC is generally underdiagnosed and when the symptoms of SAC and PAC arise, sufferers generally tend to selfmedicate using over-the-counter medications as the first course of action;11 these may be of limited value and can also produce undesirable side effects, especially with those that contain preservatives. Most sufferers of allergic conjunctivitis also tend to suffer from other atopic conditions such as asthma and eczema, thus a targeted ocular history will help to better diagnose SAC and PAC, and differentiate it from other ocular conditions with overlapping symptoms (see Figure 2, page 82) 12
ATOPIC KERATOCONJUNCTIVITIS, VERNAL KERATOCONJUNCTIVITIS, GIANT PAPILLARY CONJUNCTIVITIS AND CONTACT
BLEPHAROCONJUNCTIVITIS
Other forms of ocular allergic disease include atopic keratoconjunctivtis (AKC) and vernal keratoconjunctivitis (VKC), which can produce more severe adverse reactions including epithelium remodelling and even vision loss. Giant papillary conjunctivitis (GPC), which is also known as contact lens papillary conjunctivitis (CLPC), is traditionally included in this group of ocular allergic diseases, although it is caused by repeated microtrauma from contact lens wear. VKC is a persistent form of severe ocular allergy that typically affects boys between the ages of four and 12 years, who often present with intense itching, tearing and photophobia. It can be both IgE and nonIgE mediated. VKC is rare in western countries, with an estimated prevalence in Europe of 3.2/10,000, but is much more prevalent in subtropical countries.13 There are two forms: the tarsal form, which is more prevalent in western countries; and the limbal form, which is more prevalent in sub-tropical countries. Those with the tarsal form may present with irregularly sized hypertrophic papillae of the upper tarsal plate, while those with the limbal form can have transient conjunctival gelatinous infiltrates with white points at the limbus known as Horner-Trantas dots. Unlike SAC and PAC, the cornea can be affected with VKC; punctate keratitis, epithelial micro-erosions and ulcers are all signs of corneal involvement with VKC.
AKC is a fairly rare disease and can be considered as an ocular manifestation of atopic dermatitis which may affect the eyelids, conjunctiva and cornea. Like VKC, it is mediated by both IgE and non-IgE mechanisms. AKC generally occurs in young adulthood and may persist for many decades. It is often associated with complications such as keratoconus, conjunctival fibrosis, retinal detachment and cataract, all of which can affect vision.
GPC is an example of a non-allergic hypersensitivity reaction, usually to contact lenses (see Figure 3), hence the alternative name, CLPC. However, it may also occur in response to ocular prosthetics, scleral buckles and post-operative sutures. It is characterised by symptoms such as foreign body sensation, itchiness, blurred vision and an increase in mucus production. It can be resolved by discontinuing use of the triggering agent.
Contact blepharoconjunctivitis (CBC) is an allergic reaction to a substance that is applied to the eyelid skin and is characterised by itching, burning, swelling and redness of the eyelids. There may also be bulbar hyperaemia but if this absent then this would indicate that the allergen only came into contact with the eyelid.9
POTENTIAL SOURCES OF OCULAR ALLERGY
Well known triggers for ocular allergy include pollen, mould, animal dander and dust mites. In addition, there are also other more atypical sources found in commonly used products, such as cosmetics and toiletries, which might also give rise to an allergic response.
Cosmetics
Modern cosmetic products undergo rigorous testing and are safe for most users; however, adverse reactions
may still occur. Sensitivity to preservatives, perfumes and dyes used in these products are common reasons for allergic reactions.14 Metals such as nickel, cobalt, chromium and lead, which are used in make-up products like eyeshadow and eyeliner, can also be a source of ocular allergy.15 Allergic responses to mascara can manifest as an asymptomatic follicular response of the tarsal conjunctiva, as well as contact dermatitis of the eyelid as a result of ingredients such as black iron oxide, nickel and shellac, among others.16 Hypersensitivity to dyes used to tint the eyelashes and eyebrows can also lead to symptoms of lid oedema and chemosis, as well as keratoconjunctivitis and blepharitis.17
Perfumes are quite often added to cosmetics and toiletries and, therefore, can be difficult to avoid. An allergic reaction to perfumes in products may result in dermatitis of the skin in the affected area, including the eyelids. Interestingly, perfumes have been found to cause a degradation of laser optics and thus it has been suggested that laser centres should advise staff and patients to avoid wearing perfume inside laser suites 18 Products that are applied topically to the skin such as moisturisers and cleansers can also cause ocular irritation, even when they are applied some distance away from the eyes; this can occur as a result of the spreading behaviour of such products over the skin and towards the eyes.19 Ocular cosmetics and ointments applied to the periocular skin can migrate from the site of application to the ocular surface, with greater and quicker migration found to occur when cosmetic products are applied closer to the ocular surface such as along the inner eyelid versus 2mm away from the lid margin.20 This is in agreement with the findings of a study exploring the migration of a cosmetic eye pencil that was applied either behind the lash line along the inner lid margin or along the periocular skin next to the lash line, which found that migration occurred more readily when the product was applied behind the lash line.21 It was postulated that this occurs due to small vertical movements of the muscles of Riolan, which are located just next to the lid margin, helping to move products that are applied around the eyes towards the tear film. In addition, the warmth of the eyelid was thought to further aid the mobility of lipid products.21,22 Thus creams and cosmetic products that are applied to the face, even if some distance away from the eyes, may be the source of an allergic response in the eye.
Allergic contact dermatitis from cosmetics is common and the reason why consumers are generally encouraged to patch test a product if using it for the first time. The face is exposed to a large number of different cosmetics and therefore, dermatitis around the eyes and eyelids
Figure 2 Differential diagnosis of ocular allergy
is more likely to occur. Use of shampoo, cleansers and moisturisers, as well as make-up products like foundation, mascara, eyeliners and make-up removers, are all potential sources of adverse ocular reactions.
Pollutants
While there is an established association between levels of air pollution and certain systemic diseases such as stroke, heart disease and respiratory diseases, ocular associations are less well known. In large cities, vehicles are the primary source of pollutants, which produce particulate matter (PM), for example PM2.5, PM10, diesel exhaust particles, as well as gaseous emissions like nitrogen oxides (NOx). A recent study investigating the link between pollutants and ocular allergic diseases in Japan found that VKC was significantly associated with the larger PM10 and gaseous NOx, while AKC was found to be associated with nitrogen dioxide (NO 2); thus, nitrogen oxides were found to be linked with both refractory forms of allergic conjunctivitis.23
THE EYE’S DEFENCE AGAINST ALLERGENS
The surfaces of the body (skin, mucous membranes) provide a physical barrier against foreign substance and infections, which is reinforced by secretions. The eyelids act as a barrier, not only to ocular injury, but also to allergens. The tear film provides protection, as well as lubrication24 and inflammatory conditions such as allergic conjunctivitis can change both the composition and volume of tear production.25,26 Exposed surfaces like the conjunctiva and cornea, which form the outermost layer of the eye, come into direct contact with allergens and pollutants, and are therefore, common sites for allergic reactions.
CLINICAL FEATURES OF OCULAR ALLERGY
Ocular allergy is commonly associated with symptoms of watery, itchy, red, sore, swollen and stinging eyes.27 Those with chronic symptoms may develop an eye rubbing habit which over time can lead to complications such as keratoconus, spikes in intraocular pressure (IOP), as well as other rare complications such as acute hydrops and iris prolapse.28 The clinical features of each of the main ocular allergies are given in Table 1 (see page 84)
DIFFERENTIAL DIAGNOSIS
Due to a similarity in the ocular manifestations of hypersensitivity reactions with some ocular diseases, ocular allergy can be misdiagnosed. Comprehensive history and symptom taking is important in both aiding the correct diagnosis as well as identifying potential triggers. A detailed slit lamp examination of the eye and
adnexa will also help to confirm diagnosis of ocular allergy and to differentiate it from other ocular diseases. Tear film dysfunction can lead to similar symptoms like irritation, grittiness, burning, and itching, and is usually more common in adults and those with auto-immune disorders. Infections like bacterial and viral conjunctivitis tend to produce discharge, while inflammatory conditions such as blepharitis are characterised by crusting of the lashes as well as lid margin hyperaemia.
ANTI-ALLERGY MEDICATION
Mild ocular allergic reactions such as SAC and PAC usually resolve without the need for medical intervention. Sufferers with ocular symptoms should be advised to avoid the allergen, use cold compresses for symptomatic relief as well as ocular lubricants to improve the barrier function of the tears.
For delayed or more severe hypersensitivity reactions, anti-allergy medication may be considered. Current treatment for allergy includes antihistamines, mast cell stabilisers, combined dual action mast cell stabiliser with antihistamine, vasoconstrictors, non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroids. It is preferable to use preservative-free eye drops where possible.
Oral antihistamines can be effective in relieving nasal and conjunctival symptoms of allergy; topical antihistamines are preferable and faster acting when the symptoms of allergy are primarily ocular.29 Mast cell stabilisers, such as sodium cromoglicate, prevent degranulation and may be used prophylactically to stop the release of inflammatory mediators in order to reduce the signs and symptoms of allergy. Dual action options, such as olopatadine, provide the benefit of both a rapid
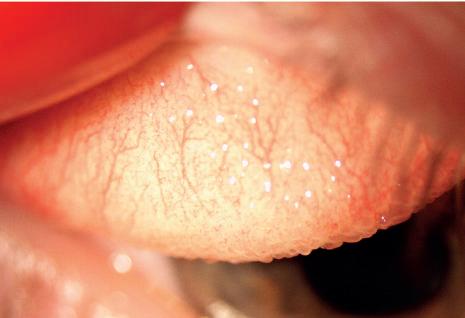
Figure 3 Ocular signs of giant papillary conjunctivitis. ImagecourtesyofJohnson&Johnson
Table 1 Summary of the clinical features of the main ocular allergies. Adapted from Leonardi etal20129
Eyelids
Oedema
Conjunctiva Follicles/ papillae
OedemaOedema
Follicles/ papillae Giant papillae, large cobblestone papillae (tarsal)
Cornea - - Superficial punctate keratitis (SPK), ulcer, vernal plaque
Limbus - - Thickened, Horner-Trantas dots (limbal)
“IT IS IMPORTANT TO BOTH CORRECTLY DIAGNOSE OCULAR ALLERGY AND ALSO TO IDENTIFY POSSIBLE TRIGGERS”
relief in symptoms combined with the longer-term benefits associated with mast cell stabiliser use.
Vasoconstrictors are designed to ease conjunctival redness but do not have any action on the underlying cause of the ocular allergic response. Thus, they are not usually recommended, but if used should be done so with caution. Antihistamine eye drops, which have vasoconstricting properties, are available over the counter as a treatment for ocular allergy. Although such eye drops are intended to relieve symptoms of allergy such as itchiness and ocular discomfort, they may be used inappropriately to make the eyes look wider and whiter. Their usage can lead to adverse effects such as rebound conjunctival hyperaemia and follicular conjunctivitis, blurred vision, a change in IOP, acute

Dr Sandeep Dhallu works as a lecturer in the optometry department at the University of Hertfordshire having previously worked as a research fellow in optometry at Aston University. She has also worked within clinical research at Moorfield’s Eye Hospital following the completion of her PhD, where she evaluated ways of improving assessment of premium intraocular lenses. Her current research interests include ocular nutrition, dry eye and contact lenses. SAC
Oedema, meibomitis, blepharitis - Erythema, eczema
Papillae, fibrosis Giant papillae
SPK, ulcer, plaque, opacities, neovascularisation
Thickened, Horner-Trantas dots (limbal)
Hyperaemia, follicles
Rarely involved -
Hyperaemia-
angle closure, iritis and corneal epithelial pigment deposition, among others.30
NSAIDs like ketorolactrometamol 0.5% and diclofenac can provide relief from ocular itching. Use of topical corticosteroids should generally be avoided in SAC and PAC but may be used for VKC 31 and AKC 32 if the cornea is involved. They should not be recommended for longterm use due to associated risks such as raised IOP and cataract formation.33
CONCLUSION
Allergic eye disease affects a large proportion of the population and can have a considerable impact on a sufferer’s quality of life. It is important to both correctly diagnose ocular allergy and also to identify possible triggers so that they can be avoided in order to help relieve symptoms and prevent longer term complications from developing. Triggers such as pollen, mould and animal dander are well known; however, less common sources such as those found in everyday items should also be considered as these can also contribute to an ocular allergic response.











CORNEAL TOPOGRAPHY
Wee Heong Chu BSc, MCOptom, DipTp (IP)
IN
BRIEF
This feature presents a series of corneal topography images. Practitioners are invited to interpret the images and answer the accompanying questions using additional resources where required.
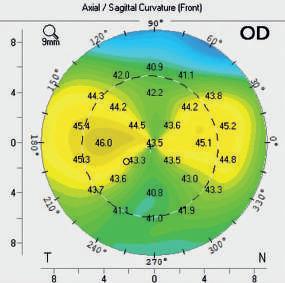
01 Which of the following bestdescribes the topography in the image?
a) Keratoconus
b) With-the-rule astigmatism
c) Against-the-rule astigmatism
d) Corneal scarring evident
02 Which is the steeper meridian?
a) Horizontal
b) Along 60°
c) Vertical
d) None of these options
03 Which of the following procedures would benefit from this information?
a) Contact lens fitting
b) Cataract surgery
c) Refractive surgery
d) All of these options
CPD POINT
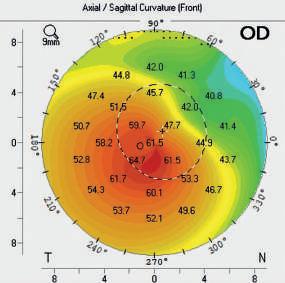
04 Based upon the topography shown, what other signs would you expect to see on slit lamp examination?
a) Corneal guttae
b) Corneal oedema
c) Corneal thinning
d) Corneal abrasion
05 Which of the following statements regarding the condition indicated by the topography is false?
a) Often associated with a history of atopy
b) Typically leads to progressive non-inflammatory corneal ectasia
c) Frequently leads to blindness
d) Less common in Caucasians
06 Which of the following management options is contraindicated in this condition?
a) Contact lens fitting
b) Spectacles
c) Refractive surgery
d) Corneal cross-linking
IMAGE A
IMAGE B
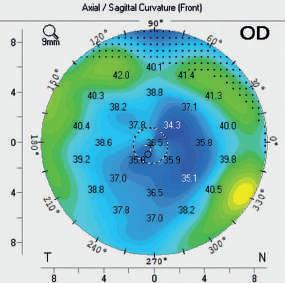
07 Which of the following bestdescribes the corneal curvature shown in the image?
a) Steep centrally
b) Normal
c) Asymmetrical
d) Flat centrally
08 What is the mostlikely explanation for the above topography?
a) Deep anterior lamellar keratoplasty
b) Full-thickness corneal graft
c) Corneal cross-linking
d) Refractive surgery
09 What type of refractive error was mostlikely to be present prior to this procedure?
a) Astigmatism
b) Myopia
c) Hyperopia
d) Presbyopia
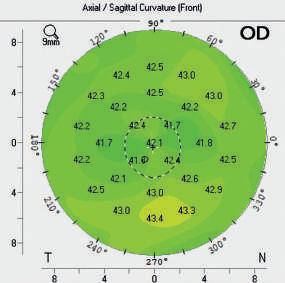
10 Which of the following bestdescribes the central corneal curvature in the image?
a) Oblate
b) Steep
c) Astigmatic
d) None of these options
11 Assuming an axial length of 23.50mm and the topography given, what is the mostlikely refractive error in this case?
a) -1.00 / -5.50 x 90
b) +7.50
c) +0.25
d) -12.50 / -0.50 x 45
12 Which of the following is trueof normal corneal curvature?
a) It is uniform across the cornea
b) There is progressive flattening from the centre to the periphery
c) It is always flattest temporally
d) None of these options

Wee Heong Chu qualified as an optometrist in 1997 and currently works full time at Raigmore Hospital, Inverness. In the hospital setting she covers a variety of core optometry and extended role clinics, and has a special interest in corneal and medical corneal contact lenses.
M A G E I N T E R P R E T A T I O N
IMAGE C
IMAGE D
A DAY IN THE HOSPITAL EYE CLINIC
Dr Deborah Armstrong PhD, MCOptom, DipTp (IP)
IN BRIEF This feature outlines a selection of cases commonly seen in the hospital eye clinic. Readers are invited to review the images and use additional resources where necessary to answer the questions.
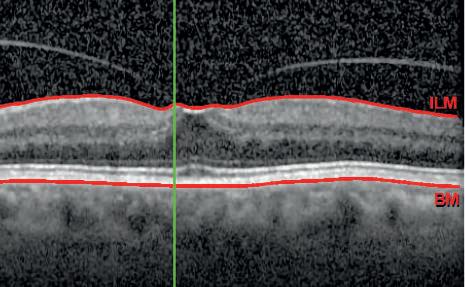
A 77-year-old male patient with visual acuities of R 6/6
L 6/9+1 complains of occasional photopsia in the left eye with no floaters noted. Amsler chart testing reveals mild distortion centrally in the left eye
01 What is your diagnosis?
a) Vitreomacular traction
b) Cystoid macular oedema
c) Central serous chorioretinopathy
d) Subretinal choroidal neovascularisation
02 Which of the following is the leastlikely risk factor for the condition shown?
a) Wet age-related macular degeneration
b) Stickler’s syndrome
c) Retinal vein occlusion
d) High myopia
03 Which of the following management options would an ophthalmologist be mostlikely to use in this case?
a) Anti-VEGF injections
b) Pars plana vitrectomy
c) Ocriplasmin injections
d) Watchful waiting with regular OCT and Amsler chart self-monitoring

A 63-year-old female patient complains of glare when driving at night and gradual onset slightly reduced vision in the right eye. Visual acuities are R 6/9 L 6/6+2
04 What is your diagnosis?
a) Posterior subcapsular cataract
b) Posterior capsular opacification
c) Subluxed intraocular lens
d) Cortical cataract
05 Which of the following is the mostlikely risk factor for this condition?
a) Glaucoma
b) Corneal dystrophy
c) Older age
d) Diabetes
06 What is the treatment for this condition?
a) Phacoemulsification with intraocular lens implant
b) Nd:YAG laser peripheral iridotomy
c) Nd:YAG laser capsulotomy
d) Selective laser trabeculoplasty
IMAGE A
IMAGE B
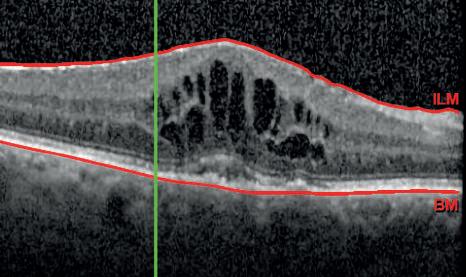
A 67-year-old male patient presents for a post-operative assessment following cataract surgery in the right eye six weeks ago. He reports the vision in his right eye to have gradually deteriorated over the past week. His visual acuities are R 6/24 L 6/5. There is no pain or red eye and the intraocular lens is clear and well-placed
07 What is your diagnosis?
a) Central serous chorioretinopathy
b) Subretinal choroidal neovascularisation
c) Cystoid macular oedema
d) Pigment epithelial detachment
08 Which of the following is the leastlikely risk factor for developing this condition after cataract surgery?
a) Diabetes mellitus
b) Age-related macular degeneration
c) Epiretinal membrane
d) Thyroid eye disease
09 Following cataract surgery, patients are routinely prescribed corticosteroid drops. Which of the following is mostlikely to occur as a result of using these drops?
a) Elevated intraocular pressure
b) Uveitis
c) Corneal decompensation
d) Posterior capsular opacification
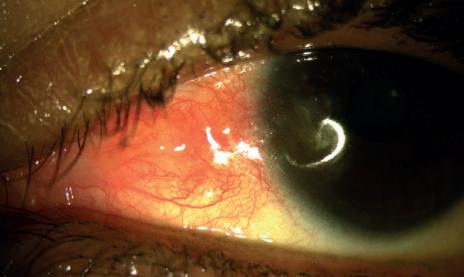
A 47-year-old female patient complains of acute onset watery, red, mildly irritated right eye for approximately one week. Vision is unaffected and there is no corneal involvement or anterior chamber activity
10 What is your diagnosis?
a) Episcleritis
b) Bacterial conjunctivitis
c) Anterior uveitis
d) Pingueculitis
11 Which of the following is the leastlikely predisposing factor for this condition?
a) Rheumatoid arthritis
b) Diabetes
c) Herpes zoster ophthalmicus
d) Systemic lupus erythematosus
12 Which of the following would be the most appropriate treatment in this case?
a) Cold compresses and fluorometholone drops for one to two weeks
b) Cold compresses and Maxitrol drops for one to two weeks
c) Cold compresses and artificial tears for one to two weeks
Acknowledgement
Images courtesy of ELHT ophthalmology department
d) Cold compresses and systemic naproxen 500mg for seven to 10 days I M A G E I N T E R P R E T A T I O N

Dr Deborah Armstrong graduated from Aston University. She worked as an optometrist in both a primary care setting and the hospital eye service before completing the investigative ophthalmology and vision science glaucoma course at the University of Manchester and a PhD at the University of Bradford. Armstrong now combines work as a specialist optometrist in glaucoma for East Lancashire Teaching Hospitals NHS Trust with teaching at the University of Bradford.

MY CAREER ADVICE
“SHORTLISTING GOES BEYOND LOOKING AT A CV”
Stuart Jackson, recruitment manager at Leightons
Opticians & Hearing Care, explains why understanding the company’s DNA is so important for candidates
What is the one piece of advice that you would give to someone who wanted to work for Leightons Opticians & Hearing Care?
When you look at Leightons – our history, our quality of service and stellar reputation within a clinical setting – you will find that the bedrock of all this is great people.
Listen, Empathise, Educate and Delight (LEED) is our DNA, running through everything we do, and how we treat our patients and each other. As a business, of course we want the best talent, so it is important that you tell us about your achievements and skills, but we’ll also look beyond that to understand relatable experiences that encapsulate our DNA, which makes us a special place to work.
So, our advice is: be proud, and highlight what you can bring from a skills and experience point of view, but also how you’ll bring our DNA to life.
When you are shortlisting candidates, what is the first thing you look for?
First and foremost, we look for the right skills and experience for the role. However, shortlisting goes beyond looking at a CV. We try to make it a personal experience and
one that benefits both Leightons and the applicant. It is important for us that the people we hire will create great experiences for our customers and colleagues. However, what runs alongside that is “how can Leightons work for you?” What can Leightons provide the applicant to enhance their own career?
How important is the cover letter in applications that you receive?
Very. You can only get so much from a traditional CV; a cover letter is a chance for the applicant to tell a greater story. It tells us that the applicant has taken the time to think about why a career with Leightons is something they truly want.
What is the biggest mistake that someone can make in an interview for Leightons?
We actively listen to our candidates and want to understand what they can bring to the role they are applying for, and why they want to work for us. It is vital that candidates are able to talk to us about this in their interview.
How do you ensure fairness and equality in your hiring process? We have a robust recruitment process that not only allows us to view an
“It is important for us that the people we hire will create great experiences for our customers and colleagues”
How important is employee wellbeing at Leightons?
We can’t stress enough how important this is to us. We are a people business with a genuine focus on the wellbeing of all our employees, and want everyone who works with us to thrive. As well as day-to-day support from within the business, we offer additional support such as a 24/7 confidential Employee Assistance Programme that is completely independent and offers information and advice.
applicant on their merits, but also a system that allows us to capture candidate equality information anonymously.
We ensure everyone has the opportunity to request reasonable adjustments as part of the process, so we can make accommodations as required. We also ensure an equitable interview process for all candidates.
A new employee is preparing for their first week at Leightons. What tip would you give them to be successful?
Enjoy it. This is a great time for us, as we get to welcome amazing new people into the business. There will be lots of support and development on offer. Meet new colleagues, ask lots of questions, and enjoy your new role with us.




























































Marketplace
Services and products for the practitioner
AN OCT DEVICE
Locum optometrist, Aman Sandhu, on how working with optical coherence tomography has revolutionised his practice
I have been using optical coherence tomography (OCT) since October 2018. Working as a locum, in that time I have seen the popularity of it grow among most High Street opticians, where it is now often offered as standard in contrast to once only being accessible in hospital settings.
The most common OCT machine I have used in practice is the Nidek RS 330 model, but there are other brands, such as those made by Zeiss, Heidelberg and Topcon. OCT can also be used for the anterior segment.
Benefit for patients
The implementation of OCT has resulted in more detail being obtained from the back of the eye. Historically, the use of the digital retinal camera has been a great tool to help diagnose pathology. However, the downside to this has always been that only a 2D image can be obtained. OCT gives 3D images of the different layers of the back of the eye. This is a great advantage as many eye diseases begin beneath the surface. Thus, being able to give patients information and/or refer accordingly before symptoms develop is a huge step forward.

I COULD NOT LIVE WITHOUT...
traction (VMT) may occur if the vitreous pulls on the macula, this can then lead to macula complications. An OCT scan will show if there is VMT and if intervention, for example pars plana surgery, is required, or whether patients just need to be told of symptoms to watch out for.
I’ve found OCT particularly helpful in the management and diagnosis of retinal detachments and tears, retinoschisis, agerelated macular degeneration, glaucoma, papilloedema, and epiretinal membrane.
An improved view
Patients are very impressed when they are shown an OCT image and realise the importance of having it conducted at regular sight tests. I find it helpful to describe the image as layers of cake, explaining that the fundus photo is like looking at the top of the cake whilst the OCT scan is like slicing through
“Being able to give patients information and/or refer accordingly before symptoms develop is a huge step forward”
the cake and being able to see all the different layers. This helps patients to better understand the scan.
A common condition we see in practice is posterior vitreous detachment (PVD). OCT has helped improve how we mange PVD by giving us more information. A complication of the condition can be macula involvement, and an OCT scan shows if a PVD has had any of this. A vitreomacular
OCT, along with other diagnostic tools, helps build a far better picture of the health of the eyes. However, it is important to note that it does need to be used with other tests and not just as a standalone measure in order to be able to get the true picture of the ocular health, thus enabling correct management.
Having more information has helped detect early pathology, and knowledge and experience of OCT has helped improve referrals by giving more information to secondary care and also by managing more cases in primary care. This monitoring is far more accurate from being able to compare OCT scans from sight test to sight test. It has also provided more opportunity for interaction with patients, allowing practitioners to be able to discuss and inform them of changes and give the necessary advice.
MY SECRET LIFEAS...
WOptometrist Dr Greg Hammond tells OT about his experience as a COVID-19 vaccinator
hen the opportunity to become a vaccinator came up, I was entering the last few months of my PhD at Cardiff University so I was beginning to think about looking for a job. It was at that time that Cardiff and Vale Health Board said that they wanted optometrists, dentists and others to help out with the vaccination programme. I thought it would be a chance to get involved and learn something new.
“In20years’timewhen someoneasksme,‘What didyoudoduringthe pandemic?’Icansay, ‘Well,actually,Ihelped endit’”
There was some e-learning, an online webinar and at least one practical training session. You went to the vaccination centre and sat in with people who would tell you how to use the computer system, the questions to ask people coming in, and the process of giving vaccines. There were no dummy arms. The first time I was given a needle, it went straight into a real person. It was a bit scary. I thought ‘I’ve never done this before. Am I going to hurt them?’, ’How much force do I need to use?’ It is very strange that first time, but you quickly get a feel for it and realise that the needles are made for this purpose.
My secret life Do you have a personal passion to share with readers? Get in touch with selinapowell@ optometry.co.uk
bring someone else in. On a busy day I might vaccinate between 50 and 100 people.
The youngest person I vaccinated was 16 and the oldest was in their 80s. Seeing the range of emotions and the gratitude was amazing – we saw many elderly people who were terrified just to leave their home. But when they left the vaccination centre they felt like they could be more confident. For young people, they didn’t have to worry about putting their family at risk.
I remember one person skipping into the cubicle because they were so excited to have their vaccine.

I remember just before the lockdown came in, going for a walk with my partner and saying to him, ‘I wonder if this is our ‘Your country needs you’ moment?’ I wondered if all healthcare professionals would be drafted in and I would be asked to help in the hospital.
I worked at Bayside Vaccination Centre in Cardiff full-time between April and September. In a day it is difficult to say how many people you would vaccinate. Generally we would be so busy that we couldn’t keep a tally. I would vaccinate one person, clean everything and then
That didn’t happen on the scale that we thought it might but I knew that I wanted to help when I got the opportunity. My family and friends were so proud when I told them I was becoming a vaccinator. It is a really great feeling to think that in 20 years’ time when someone asks me, ‘What did you do during the pandemic?’ I can say, ‘Well, actually, I helped end it.’


Sustainability Matters
A 2021 report by the Intergovernmental Panel on Climate Change says that without action, the world will reach or exceed 1.5 degrees of warming by 2040. This will lead to extreme heatwaves, oceans rising, and the destruction of 70% to 90% of the coral reefs.3
CooperVision and sustainability.
In 2019, CooperVision teamed up with organisations worldwide to align with the United Nations Sustainable Development Goals aimed at building a better, more sustainable future over the next decade. We decided to prioritise environmentally responsible practices across four key areas: water, energy, recycling, and people.
During the production process, we recycle 95% of the materials used and 99% of plastics.*
We are also the first contact lens manufacturer to make all of our one-day contact lenses plastic neutral in the UK and Ireland.1,2





What’s plastic neutrality?
Plastic neutrality is achieved when a company recovers or recycles the same amount of plastic it puts into the marketplace.
We’ve made our one-day contact lenses plastic neutral through our partnership with Plastic Bank.®3,4
We've partnered with Plastic Bank® to stop oceanbound plastic by offsetting our plastic consumption through their Certified Plastic Neutral programme. We purchase credits equal to the weight of the plastic we use in our one-day contact lenses,3 the blister and outer carton packaging here in the UK and Ireland – and an equal amount of plastic is collected by Plastic Bank.®4















































“Like many companies, we’re on a sustainability journey. We identified that plastic neutrality is a meaningful action we can take today while we work on longer-term innovation.”







Why use plastic at all?
1. Sterility.
2. Enhanced safety.
3. Increased comfort.
4. Innovative application.






Heathcliffe Clash, Head of Marketing Communications – EMEA, CooperVision.











“The latest climate science reports make it clear that we have to take action in this decade to help manage climate change... we can all play our part by making changes to our lifestyle as individuals, but also in how we run our company in the UK, Ireland and globally.”





Currently, plastic is necessary in healthcare for a number of important reasons:
As CooperVision’s Doug Bairner states,

Even though the total waste generated by the average contact lens wearer is a tiny fraction of household waste, there is room to be more sustainable.5



























Scan the QR code and get involved.





















Doug Bairner, Country Manager, UK & Ireland, CooperVision.
“Plastic is really important in keeping the manufacture of our contact lenses hygienic and safe. But we have to balance that with sustainability.”
















It's easy to make a difference.
Our journey towards a more responsible, sustainable way of living and doing business is just beginning. We've used innovation to shape the way forward. But how easy is it for our customers?
Being a part of CooperVision’s Plastic Neutral initiative is effortless.
If you recommend or wear our one-day contact lenses in the UK and Ireland, you’re reducing plastic in the ocean, and supporting coastal communities.
It’s a simple and powerful way for everyone to be more sustainable.























We’ve made our one-day contact lenses plastic neutral through our partnership with Plastic Bank® . 1,2

Get involved.