

THE RURAL & REMOTE ISSUE


FASA
&
Outen
Hamlyn – Darling Downs,

A message from the CEO
This special Rural and Remote Issue of Soundeffects News shines a light on the sonographers who deliver essential imaging care far beyond our major centres, from Emerald to Invercargill, Nhulunbuy to Ashburton.
Across Australia and New Zealand, rural sonographers are often the first, and sometimes the only, point of access to diagnostic imaging.
Their adaptability, resilience, and dedication ensure patients in even the most remote locations receive timely, high quality care. Through this edition, we celebrate their stories and their impact: the ingenuity required to manage limited resources, the close community connections they build, and the commitment they bring to improving health outcomes.
The ASA’s advocacy focus this year has been firmly on rural and remote health through addressing workforce shortages, student placement challenges, and the need for equitable access to ultrasound services. Our work continues to ensure that no matter where patients live, they can access expert sonography close to home.
To every sonographer working beyond the city limits, thank you. Your expertise, compassion, and perseverance strengthen healthcare across our region.
Regards
Tony Coles CEO, Australasian Sonographers Association


SPECIALISE WITH A MASTER OF MEDICAL ULTRASOUND.

Enhance your clinical practice with CQU’s specialist postgraduate master’s for practicing sonographers. Study entirely online via our hyperflexible mode and tailor your degree to your interests across advanced unit options in fetal echocardiography; musculoskeletal sonography; vascular sonography; obstetric and paediatric sonography; and clinical education. CONTEMPORARY
Rural Healthcare
The
challenges and opportunities for patients and sonographers from
a policy and advocacy perspective
This article uses the word ‘rural’ broadly, to encompass those living in regional, rural and remote communities.
The needs of the rural population
A significant proportion of Australians and New Zealanders live outside metropolitan areas, where the majority of health services are located. In Australia, 28%1 of the population lives in rural areas, and in New Zealand, it is 19%.2
Every rural community is different, with its own unique circumstances. Yet on average, compared to those living in metropolitan areas, rural communities face poorer access to healthcare and lower utilisation of services. Rural communities typically have a higher proportion of elderly and low-income households, and many are impacted by wider socioeconomic factors such as poor access to employment and education opportunities, and poorer housing conditions.
From an overall health perspective, people living in rural areas are more likely to live with conditions that make them more prone to poor health outcomes, such as high blood pressure, being regular smokers, or being overweight. People living in these communities are also more likely to suffer from preventable conditions and death from avoidable causes.1,2
Without equitable and timely access to healthcare, rural communities are at risk.

The challenges for rural patients in accessing healthcare
GEOGRAPHIC ISOLATION
Geographic isolation and the need to travel to larger centres to access healthcare are significant barriers for many people living in rural areas. This impacts access to timely diagnosis, treatment, and ongoing care, and can result in more complex presentations and poorer health outcomes.
Travelling what can be large distances costs patients time and money. This includes transport costs, the need to take time off work, and making childcare arrangements if relevant. Depending on the number and timing of appointments and the capacity of the individual, some rural patients also face the cost of an overnight stay. While some patients have access to public transport, health service shuttles, or financial assistance for travel, many do not. In addition, it is more difficult for rural patients to utilise short-notice appointments that arise from cancellations, which further impacts their access to care.
The provision of telehealth and virtual reporting has progressed significantly post-COVID, and while this has helped across many areas of healthcare, it is not always the answer, as households living in rural areas are also less likely to have access to mobile technology or reliable internet connections. For example, in New Zealand, only 65% of people in remote locations have a cellphone, and 75% have internet access.2 Even where internet access is available, digital literacy and affordability can be barriers. Importantly, many patients also require, or prefer, in-person services.

Several initiatives go some way to assist patients, such as mobile clinics operated by imaging or multidisciplinary teams using tailored equipment, scheduled specialist days when practitioners travel to rural areas to deliver services, together with financial and practical assistance to support patients in travelling to receive care. However, further funding and work are needed to ensure the needs of all rural patients are met.
WORKFORCE SHORTAGE
Despite their needs, the maldistribution of healthcare professionals across Australia and New Zealand means patients living in rural areas face poorer access to healthcare compared to those living in metropolitan areas. This includes general and allied healthcare as well as access to emergency, pregnancy, and specialist care. The number of healthcare professionals per capita can be significantly lower in rural areas than in metropolitan areas. When it comes to ultrasound exams, this includes not only sonographers, but also radiologists, general practitioners, nurses, other allied health professionals, and support staff. As sonographers are often the first point of contact, shortages can have flow-on effects. Combined, this can result in longer wait times and delayed care across maternity care, cancer pathways, MSK injuries, and more.
In the ASA’s 2024 Employment and Salary Survey Report3, only 4% of sonographers report working in rural or remote areas, and a further 29% in regional towns.
There has been a shortage of sonographers on both sides of the Tasman for well over a decade, with the profession listed on the Australian occupation shortage list4 and on the New Zealand Green List.5
The shortage in New Zealand is acute, with sonography classified as a tier 1 profession, meaning eligible visa applicants can access

immediate residence status. The situation is impacted by the fact that there is currently only one accredited education provider, resulting in a heavy reliance on overseas qualified sonographers. Each year, more than half of all new sonography registrants to the regulatory body (the Medical Radiation Technologist Board) are overseas qualified.6
Reducing red tape for suitably qualified internationally trained sonographers, and the use of incentives to take up rural positions, can go some way to easing the workforce shortage when supported by cultural competency training and assistance to help new staff become familiar with local and cultural norms. Use of locum and FIFO workers can also help address access issues, although some patients may feel more comfortable accessing care from someone they are more familiar with.
WIDER SOCIOECONOMIC FACTORS
While governments and employers alike use financial and other incentives to attract and retain sonographers in rural areas, it can be hard to keep
staff longterm. As well as isolation, other influencing factors include a lack of available or affordable housing, higher living costs, and a lack of education, recreation and employment opportunities for family members.
The challenges for sonographers working in rural areas
Working in rural areas can be incredibly rewarding. Here, sonographers are often exposed to a wide range of presentations and have opportunities to extend themselves professionally. Sonographers working in rural areas often get to know patients well and can make a meaningful impact on and connection with local communities.
However, it is not without its challenges. Sonographers working in rural areas can be faced with inadequate infrastructure and limited resources – such as outdated equipment, limited workspace, unreliable technology, and fewer supporting services. For sole practitioners or sonographer-owned clinics, the economics of operating in rural areas can be particularly difficult due to higher costs and lower patient volumes.
PROFESSIONAL ISOLATION AND BURNOUT
Rural sonographers are at risk of professional stress or burnout, as they are often working in small and isolated teams, if not alone. It can be difficult to take leave due to the acute shortage of replacement cover or the pressure of knowing their workload will have grown during their absence.
Social and professional isolation is also a major issue with fewer opportunities for professional collaboration and support than those working in larger centres, including fewer opportunities to debrief or discuss complex or challenging cases. And while online learning systems have expanded exponentially in recent years, offering flexible CPD and virtual networking, making meaningful connections can be challenging in a virtual format.
less likely to have a medical practitioner onsite to provide support to patients, and more likely to have feelings of isolation and being ineffective at work than those working in metropolitan areas.
SONOGRAPHY STUDENTS
Sonography students from rural areas face a very real challenge, with many needing to move away from their usual location to access education and clinical placements, meaning they need to find affordable alternative accommodation and establish financial and social support.
Preliminary findings from ASA’s research into student placement poverty8 highlight the challenges for sonography students, with a third rating the financial and other stress of undertaking

Conversely, it can be very difficult for employers and supervising sonographers in rural locations, already struggling with a workforce shortage, to have the time or resources to support a student on placement despite the value of doing so.
Advocating for sonographers living and working in rural areas
The ASA recognises the vital role sonographers play in rural communities and knows they are often working under challenging conditions with limited resources and support. We thank rural sonographers for supporting patients across the full spectrum of healthcare needs, from pregnancy care to endometriosis and cancer diagnosis, to providing musculoskeletal interventional procedures where permitted.
ASA ADVOCACY, PROJECTS, AND STAKEHOLDER ENGAGEMENT
The ASA continues to advocate on behalf of sonographers living and working in rural Australia and New Zealand by ensuring their needs are understood and heard. This includes advocating for accessible pregnancy care for patients and ensuring government funding reflects that rural patients may require multiple or extended exams in one day. Our professional development and events teams continue to work hard developing extensive clinical guidelines and supporting resources, and ongoing professional development and networking opportunities, including online modules and flexible delivery options to support members who work in rural areas.
The ASA has a variety of exciting projects planned for the coming year that aim to support sonographers working in both rural and metropolitan areas, including a project to investigate the models and feasibility of sonographer reporting, a project to investigate models of training, and another to assess sonographer-performed musculoskeletal


interventions. This is in addition to professionwide projects to develop a sonographer career progression framework and an entry-level scope of practice for Australian sonographers.
The ASA advocates for sonographers and patients in rural areas through regular meetings with the chief allied health officer on both sides of the Tasman, and through our membership of organisations such as the Australian National Rural Health Alliance, Allied Health Professions Australia, and Allied Health Aotearoa New Zealand.
For our members in New Zealand, we are thrilled to now have a dedicated New Zealand-based executive officer, together with a passionate and engaged 10-member New Zealand Sonographer Advisory Group, and a current New Zealand-based Board member. Over the next 6–12 months, we will continue advocating for improved access to obstetric ultrasound services and contribute to the work being undertaken by the Medical Radiation Technologists Board, including the scope of practice review and the position statement on remote care.
In Australia, we thank the Sonographer Policy and Advisory Committee, supported by the Special Interest Groups, for their ongoing work in developing position statements and supporting submissions – including 2 new position statements on AI and clinical training placements, and the recent Medicare reviews where committee members highlighted the importance of ensuring the needs of rural patients can be met in a single visit if needed. Over the coming year, we will continue working on priority issues such as advocating for statutory regulation for Australian sonographers, supporting recommendations to help ease the workforce shortage, and raising awareness of the role and skills of sonographers.
FEEDBACK WELCOME
We warmly invite feedback from our members and partners. If you have a question or thoughts to share about rural healthcare, or initiatives to better support sonographers living and working in rural communities, please email the ASA Policy and Advocacy team at policy@sonographers.org
REFERENCES
1. National Rural Health Alliance. Rural Health in Australia Snapshot 2025. Available at: https://www.ruralhealth.org.au/wp-content/uploads/2025/02/ NRHA-Rural-Health-in-Australia-Snapshot-2025.pdf
2. Hauora Taiwhenua | Rural Health Network. Rural Health New Zealand Snapshot 2024. Available at: https://htrhn.org.nz/wp-content/ uploads/2024/10/Rural-Snapshot-2024-HT-FINAL-Spread-Updated.pdf
3. Australasian Sonographers Association. ASA Employment and Salary Survey 2024. Available at: https://www.sonographers.org/publicassets/f9272863-bf9bef11-9135-0050568796d8/2024-ASA-Employment---Salary-Industry-Report. pdf
4. Jobs and skills Australia. Occupation Shortage List. Available at: https:// www.jobsandskills.gov.au/data/occupation-shortages-analysis/occupationshortage-list
5. New Zealand Immigration. Green List Roles. Available at: https://www. immigration.govt.nz/work/requirements-for-work-visas/green-listoccupations-qualifications-and-skills/green-list-roles-jobs-we-need-peoplefor-in-new-zealand/
6. New Zealand Medical Radiation Technologists Board. Annual Reports. Available at: Annual Reports | Medical Radiation Technologists Board
7. Australasian Sonographers Association. ASA Workplace Health and Safety Report 2023. Available at: https://www.sonographers.org/ secureassets/5db2455b-d71b-ef11-912f-0050568796d8/2023-ASA-WHSSurvey-Report.pdf
8. Australasian Sonographers Association. ASA survey of sonography students on placement in Australia. Undertaken September – October 2025. Full analysis and results yet to be finalised and released. For more information, please contact policy@sonographers.org
OTHER USEFUL RESOURCES
Australian Institute of Health and Welfare. Rural and remote health [Internet]. Updated 30 April 2024. Available at: https://www.aihw.gov.au/reports/ruralremote-australians/rural-and-remote-health
Australian Government – Department of Health, Disability and Ageing. Rural health workforce [Internet]. Available at: https://www.health.gov.au/topics/ rural-health-workforce
New Zealand Ministry of Health. New Zealand Rural Health Strategy. Available at: Rural Health Strategy | Ministry of Health NZ
TIM OVENS
Emerald, Queensland
From city practice management to regional small business ownership, sonographer Tim Ovens has built a career defined by adaptability, community connection, and a passion for delivering quality healthcare where it’s needed most. Now based at Emerald Radiology in Central Queensland, Tim shares how he transitioned from therapeutic radiography to ultrasound, what makes rural practice uniquely rewarding, and the opportunities and challenges of providing essential imaging services in regional Australia.

My journey to Emerald Radiology is a culmination of a career working in hospitals, suburban practices, tutoring, and the unexpected death of my mother. When my mother passed suddenly, I was helping manage a private practice in Brisbane but looking to invest in a small clinic. It was a daunting prospect that had been put on hold until my family circumstances had changed, when my mother’s death sparked me into taking some action. An opportunity arose to purchase a single machine practice in Emerald, Queensland, and after a rapid tour of the community, my wife and I decided to take the plunge into small practice ownership.
What makes working as a sonographer in Emerald different from practising in metropolitan areas?
Regardless of where we work, we all make a significant impact on people’s lives and their health outcomes. After years of improving my scanning, including upskilling in MSK and vascular studies, I was fortunate to take these skills to a regional community.
Can you share what first drew you to sonography, and how you came to be working at Emerald Radiology in Queensland?
I started my career as a therapeutic radiographer working closely with medical imaging facilities, utilising CT scanners for radiotherapy planning purposes. Over time, I built a rapport with the medical imaging teams, including the sonographers who encouraged me to pursue a career in ultrasound. At the same time, radiation oncologists were discouraging me from pursuing a medical career due to the time required to qualify, the commitment, the duration of study, and the massive hours required as a junior doctor. Sonography appeared to offer a better lifestyle, good remuneration, job security, the opportunity to upskill, challenge the intellect, and become a vital part of the diagnostic team with significant input.
Encouraging sonographers to work remotely is challenging due to the numerous opportunities available on the coast or in the city.
I’ve found the work to be similar in both settings, although when working regionally, it helps to be a good all-rounder with experience. Sonographers working in regional settings are often by themselves and without a radiologist on site. Although the work is similar in both locations, the connection to the community and other health professionals is vastly different; a good comparison would be working within radiology in a small hospital. When there are findings that require immediate action, we can’t simply send them to a large emergency centre as we would in the city. We are often called

What a place to work
upon and encouraged by our radiologists to ‘make the call’ and liaise with the requesting practitioners and emergency centres so our patients get the appropriate help and best health outcomes. Many of our patients travel up to four hours (one way) to be seen at our practice, so they need to be directed immediately to the appropriate medical professionals to seek help. Our referrers and our surrounding hospitals want to be contacted directly; therefore, our sonographers have corresponding phone numbers to expedite the process. Referrers in regional communities seem eager and accommodating to speak with technicians and will often step out of a consult to take a call. We are a small community, and there is certainly a strong sense of camaraderie among the healthcare workers.
What are some of the biggest opportunities you’ve experienced, as well as the challenges, in delivering ultrasound services in a rural community?
The biggest opportunities I’ve experienced are practice management/ownership, community connection, and the opportunity to improve radiology access for our region. Owning a practice
has plenty of challenges, with the majority being financial, staffing, and finding time to do all the administration required to keep a practice running effectively. There are no human resources, marketing, accounts payable, IT, payroll teams, etc., for a single regional practice! Our small team of 10 does all we can to make these things happen, and over the last 5 years, I’ve learnt plenty in this space.
Sonographers are hard to come by, so much like our metropolitan colleagues, running at capacity can be challenging. Encouraging sonographers to work remotely is challenging due to the numerous opportunities available on the coast or in the city.
To ensure our growth, I’ve been fortunate to help train a few sonography students who have continued with the practice upon graduation. Emerald Radiology is also blessed to have a few experienced part-time sonographers who have worked in the practice for years, offering flexibility and experienced hands to lean on.
We currently fly in radiologists to perform steroid injections for the region, being the only local clinic to do so. It’s a fantastic community service, saving


Where all the hard work gets done, Ultrasound Room 1
thousands of hours of driving, financial savings, and reducing inconvenience for our patients. Due to the lack of cytotechnologists in the region, we do not offer FNA services. We will endeavour to offer this service in the future, but we need to overcome a few hurdles to do so.
How does providing ultrasound in a rural setting allow you to make a direct impact on your patients and the wider community?
Being able to provide a regional ultrasound service in Emerald reduces the need for the community to travel to Rockhampton or Mackay. It’s extremely inconvenient to travel 6–8 hours for an examination that takes 30 minutes. With the help of the other private imaging provider in town, the 2 radiology clinics can accommodate most ultrasound services for a 700 km radius. Patients can take less time away from their family and work commitments, with the additional benefit of reduced accommodation and travel costs.
What role does collaboration between health professionals play in delivering ultrasound services in your area?
Strong collaboration between health professionals in a rural community is vital to the best health outcomes for our patients. This is particularly important in urgent situations. Like most regional settings, high-end medical services are not available, and patient transportation time can be the difference between life and death. In urgent situations, it’s imperative that imaging is provided with haste and that all healthcare professionals involved work closely together to give referrers/ specialists access to imaging and reports so the appropriate medical advice can be given, and if required, patients are airlifted to the appropriate healthcare facility rapidly. We work very closely with the main and satellite hospitals in the region to make this happen.

Maraboon Dam – at full capacity can hold three Sydney Harbours. Provides water for irrigation of cotton, grapes and citrus in the region
What changes or support would make the biggest difference for sonographers working in regional, rural or remote areas in Australia?
I think we are rather lucky to work in this profession at this moment in time. In the last 5 years, our professional bodies have offered some amazing professional development online, reducing the need for any of us to travel. We often watch these clever individuals present after hours from the comfort of our own homes! This is particularly important for remote sonographers, as the time it takes to travel and the ability to take time away from the practice are very difficult. As previously mentioned, many remote sonographers are the only source of ultrasound services for a community or hospital, so without them on site, this service is no longer available. More online professional development would not only help our remote sonographers but everybody in the profession.
Financial limitations to enhance professional development for remote sonographers can be a significant hurdle to improving their scanning. Various professional organisations offer financial help to support sonographers located outside of metropolitan centres to attend conferences, etc., The ASA has offered scholarships and support for remote sonographers for many years, and you will often find funding for conferences and professional development in places you never thought to look! In my very first week in Emerald, a local doctor asked how I could make a difference in the region, so I asked where he felt medical imaging was currently lacking. He was quick to respond with MRI (oh yeah), but paediatric and vascular ultrasound were also flagged as major hurdles for the community. With the aid of this medical professional and Health Workforce Queensland, my master’s in paediatric and vascular ultrasound was funded, and in time, we could offer those services to the community. Eventually, we got there with MRI!
Interview with Tim Ovens – Emerald, Queensland

Working remotely can be isolating, so perhaps more collaboration between remote sonographers would benefit not only the individuals but the practices they work in. Remote sonographers face unique challenges, and it would be great to liaise with others in a similar situation about the issues faced and how they’ve gone about improving their work environment. From personal experience, I’ve found locum work to perform a similar role, as at times you get to work in clinics with other sonographers who tackle issues differently from yourself. A sonographer exchange would be great to broaden our horizons (for all parties) and understand that there are often different or better ways to tackle a scanning technique or other issue. The exchange would give an opportunity for metropolitan sonographers to experience a welcoming rural community and open their eyes to another world.
Can I finish with a cheeky idea? To encourage not only sonographers but all healthcare workers and those seeking employment in any field, a reduction in income tax for those working outside of metropolitan centres would improve staffing shortages in rural communities and provide a great opportunity for those willing to work in those regions. We all know there is a national shortage of sonographers, but there are shortages across most industries in rural communities.
Emerald Radiology front entrance
PIP JEFFREY
Ashburton, New Zealand
As team lead at Ashburton’s rural imaging branch, Pip Jeffrey plays a vital role in delivering ultrasound services to her Canterbury community. A general sonographer, her varied case load spans obstetrics, vascular and small parts. Pip shares her insights into the rewards and realities of practising in a regional centre, from the strong sense of community connection to the challenges of working with limited resources and providing essential imaging access for patients across rural New Zealand.



How does providing ultrasound in a regional centre like Ashburton differ from working in larger New Zealand cities?
What does your role as a sonographer in Ashburton involve day to day?
As a general sonographer, my day consists of scanning a varied worklist, including abdomens/ pelvis, obstetrics, vascular and small parts ultrasound. I love the variety of patients I see, from paediatrics to the elderly and everything in between – no 2 days are the same. I am also the team lead for our branch, so I oversee the effective running of our little rural branch, which provides ultrasound and X-ray services.

Working in a regional centre like Ashburton involves working with a more close-knit team and smaller community, providing a strong sense of direct patient care and community connection. It also requires more autonomy and an adaptive approach to patient care, with fewer resources available compared to our city counterparts. We do not have a radiologist onsite nor an emergency department locally, so prompt patient care, open referrer communication and direct transfer of patients to tertiary centres when required, is paramount.
What are the main types of patients or cases you typically see in your community?
We image a range of outpatients for a variety of reasons, from acute to chronic conditions; for example, possible DVTs or ectopic pregnancy cases, abdominal pain, period complaints, routine obstetrics, to lumps and bumps, plus a lot of musculoskeletal injuries.
How important is access to local imaging for people living in rural Canterbury?
Ashburton is a large rural town that services a wide patient catchment from surrounding districts, with some patients travelling up to 100 km to our branch. Consequently, access to local imaging is critically important for our community to ensure prompt patient care, which in turn
Avon River Christchurch
Sharplin Falls Washpen Falls track

aids our local primary health providers in making quicker diagnoses and treatment. As a result, this reduces delayed diagnoses and associated costs, while minimising the necessity of travel for sick and vulnerable patients.
What opportunities or challenges do you encounter working in a regional health setting?
The benefit of working in a regional health setting is that it helps to build strong community relationships between us and referrers, as well as with patients. I enjoy the autonomy that goes with working regionally and the challenges of having to be more resourceful and versatile in my diagnostic approach.
Being able to provide an essential service like ultrasound in regional New Zealand is rewarding
Being a small team can sometimes prove challenging when it comes to staff sickness and staff shortages. Working regionally can sometimes feel isolating when working solo, with a lack of peer support and onsite radiologist input. Limited resources and equipment can also prove challenging from time to time.
From your perspective, what makes sonography rewarding in a place like Ashburton?
I love the work-life balance working locally provides. I can do the school run in the mornings and be home at a reasonable hour at night to spend quality time with the family. Ashburton is a beautiful place to live, surrounded by scenic landscapes to explore, with a range of outdoor activities on offer such as hiking, biking, skiing and water sports.
Being able to provide an essential service like ultrasound in regional New Zealand is rewarding; knowing we are helping to address disparities in access to healthcare is a great feeling. Patients are very appreciative of having scans offered locally, as it means less disruption to their personal and professional lives by reducing the need for longdistance travel. This is especially true for our elderly community, who may not have the means to travel or are too sick to travel.

Corsair Bay Christchurch
Mt Hutt Ski Field
NATALIE CLEMENTS, FASA Bunbury, Western Australia

With a career that spans more than 25 years and a passion for mentoring the next generation, Natalie Clements has become a cornerstone of sonography in Western Australia’s southwest. From her early days helping shape the state’s first medical imaging program, to leading busy regional departments, Natalie shares how regional practice has shaped her career and why investing in local training is key to the future of sonography in regional Australia.
Can you tell us about your journey in sonography and how it led you to working in Bunbury?
I was one of the first medical imaging students at Curtin University in Western Australia, and a student at SJOG Subiaco, then employed there full-time. I was enrolled in MRI Honours back when there was only one machine in the entire state. However, I saw the dark side of a dimmed ultrasound room and got that gel on my fingers, and I was permanently on the ultrasound roster. I worked closely with my 2 incredible sonographer friends, who guided me through my Diploma in Medical Ultrasound, alongside 4 very special radiologists.
My career took me to Geraldton Regional Hospital, where I did FIFO (fly in fly out) half a week and the rest of the week at SJOG Subiaco. Four months in, and I moved permanently to Geraldton, where I was the only sonographer and on call 24/7. Back then the teleradiology was pretty basic, especially on weekends, and I’d spend more time processing films in the dark room and uploading them than I did actually scanning the patient!

The move down south to Bunbury came thanks to my then-boyfriend, who was soon upgraded to husband. I worked at a new SKG Radiology, built a house on the beach and started a family with two gorgeous boys who have kept me busy ever since. Almost 25 years later, I am still here and loving every moment of this journey.
From your experience, what are the biggest health needs or imaging demands in your region?
From my experience, the biggest health needs and imaging demands in my region are quite pressing. Throughout my entire scanning career, I’ve never seen a time when we have had enough sonographers and enough appointment slots –there is simply never enough capacity.
Like many places, we are facing a significant shortage, but regionally, it’s reached a crisis point with waitlists stretching from 6 to 8 months as the norm.
Research
shows that country allied health practitioners or GPs are more than 7 times more likely to return to their hometown after their studies.
SKG Radiology Bunbury
However, I think it is a broader health issue and not just sonographer-related. Patients struggle to get timely appointments with GPs, often lack continuity of care with the same doctor, and end up relying on emergency clinics when they really need help. Wait times to see surgeons are long, which means more up-to-date imaging is required, and the cycle goes on.
As someone who grew up in the country and works with many rural sonographers, I’m aware of how important it is to encourage local students into this profession. Research shows that country allied health practitioners or GPs are more than 7 times more likely to return to their hometown after their studies.
That’s why I am passionate about connecting with the next generation of potential sonographers at local schools. We host dedicated health career evenings where students can even try scanning on a machine. I’ve given school career talks explaining what and how far ultrasound careers can go. I talk about ultrasound careers to any school-aged student I have as a patient. This year alone, we’ve hosted 13 students on work experience at our department, and I know of at least 4 local students that have continued to university to pursue ultrasound careers.
How does working in a regional hub influence the professional opportunities available to sonographers?
Working in a regional hub opens up a wide range of professional opportunities that you might not get in a metropolitan setting. Early in my career, I realised that regional and remote sonographers often become generalists by necessity – and become local educators to the broader healthcare team. I still remember the surgeon who had never seen intussusception on ultrasound, let alone 3 in one week! Or the groundbreaking news that I can see a stenosis in the common iliac artery – true story, I kid you not! These kinds of experiences show how much value we can add, especially when our work means patients don’t have to travel long distances for specialist imaging.
There is also a great sense of professional autonomy. You need to trust your skills, knowledge and judgement to deliver the best outcomes for the patients. You learnt to back yourself, as there was no one else to scan; you just had to get on with it back then, with a dog-eared anatomy book. Nowadays, there is an app for that, or google to answer any

Interview with Natalie Clements – Bunbury, Western Australia
Three Waters of Bunbury – ocean, bay and inlet
question. Mind you, you need a working internet or decent phone coverage. Even with modern tools, that self-reliance and confidence in your own ability is something that regional practice really builds.
The variety of pathology I encountered was incredible – often more complex or rare than I expected. One case that has stayed with me was a twin pregnancy where one baby had anencephaly. I followed that journey through all the growth scans, and eventually, the mother made it far enough along to go to Perth for delivery and organ donation. It was a powerful reminder of the role we play in people’s lives. Of course, the workload can be intense, especially with on-call and barely a day away from the ultrasound machine. The sense of community in the hospital made all the difference. Everyone supported each other, and I always felt part of the team. Looking back, those experiences pushed me out of my comfort zone in the best way –and gave me far more than I ever expected.
What role does professional development and mentorship play for sonographers outside metropolitan centres?
Professional development and mentorship are incredibly important for sonographers working in regional areas. One of the few positives to come out of COVID has been the growth in online learning and virtual meetings. While telehealth meetings existed before, the pandemic really opened the door for us to connect more easily. Now there’s nothing stopping regional sonographers from joining meetings, conferences or presentations from anywhere in the world – on just about any topic. There are entire websites dedicated to on-demand learning, and I can watch sessions from the ASA Annual International Conference when it suits my schedule. It’s amazing how hard it used to be to find enough educational activities, and now they’re everywhere!
I’ve also been able to be involved with the ASA and ASAR committees, which wouldn’t have


been possible without tools like Zoom and Teams. Giving back to the profession in this way has been incredibly rewarding.
Mentorship has always played a big role in my development as a sonographer. I was lucky enough to have the support of numerous sonographers as a support network. These days, I can send images for review in real time, even before the patient leaves the department – making clinical decisions easier. It’s exciting that this is being developed into a resource and will be more accessible to everyone.Locally, we’ve also taken the initiative to support each other by forming the ASA group South West WA.
It came about purely from the need for more professional development and mentorship. We hold regular case study nights, which are informal and engaging, and it’s been great to see quieter members grow in confidence with each meeting. The discussions are always lively, and the group includes sonographers from across the region, including those who work in FIFO or DIDO roles.
What do you think makes practising sonography in regional Western Australia unique compared with other parts of the country?
Ultrasound in regional Western Australia is unique because of the vast distances we cover to provide services. Sonographers often travel long hours to reach communities, which means patients don’t have to make the journeys themselves to Perth.
Newest ASA Gnome – Sono Gnome at Gnomesville
Interview with Natalie Clements – Bunbury, Western Australia
Some of my patients travel hundreds of kilometres to have scans, and then, if required, we try to fit in any other needle biopsies or injections on the same day. It is a big commitment, and it shows how dedicated we are to delivering high quality care no matter where we are.
Despite working in regional or remote areas, we maintain the same standards of scanning and service that you would expect in Perth. There is a real sense of purpose in knowing we are providing essential healthcare to communities that might otherwise have limited access.
Even with modern tools, that self-reliance and confidence in your own ability is something that regional practice really builds.
On a personal level, the daily commute for me is driving through a Tuart forest, then along the beach, currently checking for whales or the resident dolphin pods. I live 20 minutes from the wineries of the Geographe region and 40 minutes from the wineries or beaches of the Margaret River region.

Work is 5 minutes from the best shoe shop in Australia, the local beach and the IKEA of food – the Bunbury Farmers Market!
Looking ahead, what innovations or system changes could strengthen ultrasound services in regional areas?
To start this wish list – first and foremost, we still need reliable mobile phone coverage and faster internet services throughout rural, regional and remote WA. Since so much of our reporting happens electronically, improving connectivity is essential and long overdue.
Artificial intelligence will definitely play an important role in the future. Beyond assisting with diagnosis, I can see AI helping to streamline patient management; for example, automatically generating the appropriate follow-up requests and even booking the next available appointments when a certain pathology is detected on the scan. This would make the health system more efficient and help patients receive more timely care, especially in areas where access to specialists is limited.
To support regional sonographers and encourage junior sonographers, we need to look at regional placements and HECS debt write-off, like medical officers have available to them from the government. To enable this, those junior sonographers would need support in training, professional development and for workforce retention. Remote supervision and mentoring have to play a critical role by enabling real-time scan sharing and audiovisual communication to enable a remote but instant connection to experienced mentors. It will provide clinical guidance and enhance diagnostic accuracy and learning, but will also help to reduce professional isolation. This support would build confidence, improve job satisfaction and contribute to retaining skilled sonographers in areas where they are most needed.
Koombana Bay Bunbury
Each year, the ASA supports sonographers living and working beyond metropolitan centres through the Rural and Remote Conference Support Grant, offered in partnership with Marsh Insurance. The program provides full conference registration, flights and accommodation, helping to bridge the distance for those who might otherwise be unable to attend.
At ASA2025 Melbourne, rural and remote sonographers joined colleagues from across the profession for 3 days of education, collaboration and connection. Below, recipients reflect on what the experience meant to them – from new clinical insights to practical changes they’ve already put into practice back home.
The conference was amazing and I am just so grateful that I was able to attend in person. As a solo sonographer, being given the opportunity to attend in person has been extremely beneficial. I was able to learn new scanning techniques from the workshops and the masterclass I attended, and I’ve already been able to use them since returning!
I loved the location of the motel and conference. Melbourne was new to me, so I had no idea where things were, but it was very easy to navigate.
The Friday morning coffee meet and greet was perfect to meet the other sonos and ease my social anxiety.
Alaina George – Ayr, Queensland


Thank you very much for the opportunity to attend this year’s ASA Conference. It was a very well-organised and informative event, with high quality speakers. I attended on all days, throughout the whole day.
The program had a lot of diverse topics, with multiple fantastic speakers. It was difficult to choose which lecture to attend! Thankfully, this is still available online, although I wish it could be online forever so that I can rewatch it in what little spare time I have.
I really enjoyed the lectures from Dr Daren Gibson and Dr Simon Meagher (who was sponsored by GE) at lunchtime; the headphones worked well for the crowd! I was
so engrossed in learning that I didn’t have enough time to eat or look around all the exhibitors during lunchtime.
Overall, I was very impressed with the quality of speakers and the large range of topics at the ASA Conference in 2025. Talks given by fellow sonographers, particularly sonographers who work at Monash Health, and esteemed doctors from different specialities, to give their side of healthcare. A lot of the lectures were given at an intermediate/expert level, which I found very relevant to me, to understand and bring these new or updated concepts to my everyday practice in rural WA.
Sharon Chan – Karratha, Western Australia
The conference was absolutely fabulous. It far exceeded my expectations. The range of speakers was very broad, with many real ‘gems’, plus locals with years and years of experience and passion to share.
I am still pinching myself that I was granted the R&R scholarship. It certainly made a big difference to me – to be able to attend from so far away.
I consider myself so fortunate. I am immensely grateful that ASA runs such a generous scheme. I have come back to my site all fired up, applying new knowledge and digging out resources. I’ve also already arranged further apps training for myself and preset tweaks on my machine so that I feel I am keeping up with (in particular) first-trimester fetal heart advances.
The only problem was that there were so many great talks, I couldn’t attend all! But I can watch them in review.
Alison Stock – Manjimup, Western Australia

HAYLEY LINDSAY
Invercargill, New Zealand
At the southern tip of Aotearoa, Hayley Lindsay delivers vital ultrasound services to the Southland community, from Invercargill to Te Anau, Gore, and even Stewart Island. Born and raised in the region, Hayley combines local insight with specialist expertise in obstetrics and gynaecology, playing a crucial role in early detection and patient care for those far from tertiary hospitals. She reflects on the privilege of caring for familiar faces, and the deep satisfaction that comes from ensuring her community has access to high quality imaging close to home.

to have a broad clinical exposure. This has allowed me to step out and not only develop my skills in obstetrics and gynaecology, but to find new passions within other avenues of sonography, such as MSK imaging. Learning MSK ultrasound was imperative to save patients having to go elsewhere to get MSK scans.
We have closer professional relationships with referrers and specialists, which builds up a good continuity of care.
Are there particular health conditions or patient needs in Southland that shape the kind of work you do most often?
Invercargill is New Zealand’s southernmost city. What is it like delivering ultrasound services in such a unique location?
I feel incredibly lucky that I get to provide ultrasound services to Invercargill and the wider Southland community. No day is ever the same. I can start the day with antenatal or general ultrasound, knowing an acute scan can come in at any time. As Invercargill is so far away geographically from a tertiary centre, ultrasound imaging is relied on heavily by both our local referrers and out-of-town specialists.
Being a sonographer in Southland really broadened my skills due to the wide range of cases.
I feel privileged that there is a huge variety of work. As a general sonographer, who trained in a large city with tertiary centres, I have always had a strong interest and subspecialised in obstetrics and gynaecology. I am fortunate since working rurally
High level obstetric ultrasound is critical, given the large distance to higher level maternal care. Our closest maternal fetal medicine is roughly a 7-hour drive from Invercargill. Early detection of fetal abnormalities or pregnancy complications allows early referral to Dunedin or Christchurch. Some fetal abnormalities require the mothers to give birth in Auckland (a 2-hour flight away). Picking up these fetal abnormalities antenatally can be lifesaving.
Acute/emergency work is also important in Southland, since definitive surgical or specialist interventions may require patient transfer out of the region.

Twilight with Ralph at Oreti Beach, Invercargill (Riverton in the distance)
Interview with Hayley Lindsay – Invercargill, New Zealand

How do you think geography influences access to imaging for people living in your region?
Invercargill has a very large and wide catchment area. We service not only the Invercargill population, from Te Anau, Gore, the bottom of the South Island and Stewart Island. On any one day, it is not uncommon to have a few patients drive 150 km+ to arrive for their ultrasound examination. Patients from farming communities and remote areas rely heavily on accessible imaging. This means that while we have the patients in the department, we adjust our bookings so that most anatomy scans are completed on the day, rather than having to get the patients back for completion.
If the patient has to travel to Invercargill for a specialist appointment, we facilitate same-day appointments to lessen the burden of travel on our patients. We also try to extend examinations if needed to limit out-of-town travel.
The nearest tertiary hospital is Dunedin Hospital; this is over 2.5 hours away by road. This means imaging services in Invercargill play a crucial role in providing timely diagnostics without patients having to travel long distances.
In Southland, the climate is often cold, wet, windy or snowy. This heavily affects patients’ travel from out of town or flights in from Stewart Island.
What do you enjoy most about working in Invercargill and serving this community?
I am originally from Invercargill, so it is nice to be back in my hometown serving the community, as Invercargill is a smaller, close-knit community.
I get to build a rapport with patients. I am privileged to scan patients throughout their multiple pregnancies, so you end up getting to know the patients personally, making care more connected and tailored.
We have closer professional relationships with referrers and specialists, which builds up a good continuity of care. I also love that we have monthly multidisciplinary meetings discussing abnormalities with our specialists; the discussions are great as we get some feedback on scans and answers to clinical questions.
Have there been any moments in your work that really highlight the importance of having sonographers based locally?
There are so many, but honestly, on the days when an abnormality or pathology is identified, this can avoid dangerous delays, sparing patients stressful and costly travel for an examination that we can do locally. This is rewarding as it allows clinicians to act immediately.
Looking ahead, what changes or improvements would make the biggest difference for sonographers working in Invercargill or in the Southland region?
Honestly, just having more sonographers down here would be the dream. Maybe having one or two sonographers Te Anau or Gore-based, would make a huge difference in the amount of travel our patients would have to do. I would also love to be involved in multiregional CPD so that I am always learning and my skills are always developing.
Invercargill’s Queens Park with the historic Feldwick Gates at the park main entrance
DAVID OUTEN Nhulunbuy, Northern Territory
After more than 2 decades in East Arnhem Land, David Outen has become a familiar and trusted face in remote imaging across the Northern Territory. From establishing ultrasound services in Nhulunbuy to delivering outreach clinics across East Arnhem communities, David has witnessed firsthand the evolution of healthcare in one of Australia’s most remote regions.

Over that time, what changes have you seen in sonography and healthcare delivery in the Territory?
The position in Nhulunbuy many years ago was pure radiography, but I brought ultrasound into the mix and worked as a sole practitioner until 2018.

Service expansion saw us employ another rad/ sono, and we began on outreach service – flying to East Arnhem communities to deliver ultrasound locally. This has been a great success, resulting in an expansion of healthcare to very remote communities.
You’ve been working in the Northern Territory for over 20 years. What first brought you here? What has kept you in the NT?
I moved here from Darwin when my kids were young and fell in love with the place. Gove is perfect for young families – the streets are safe; there are beautiful local beaches and camping spots. If you are into fishing, it is a paradise!
As my children have grown and moved away, I have stayed, overseeing a growing medical imaging department and building a small empire.

In 2021, Gove District Hospital installed a CT scanner, and we slowly expanded by employing another radiographer.
The
outreach ultrasound is
challenging but fun. Flying to work in a small plane beats a traffic jam any day!
We have recently gained another sonography position and plan to increase ultrasound services remotely so that we visit each community twice per month. The technological developments in high quality, truly portable ultrasound over the years have made this possible.
What are the most common types of cases or imaging needs you see in Nhulunbuy?
Our population base in town is very young, so there is a lot of obstetric scanning.
A high rate of rheumatic heart disease, diabetes, renal disease and Hep B keeps us busy with abdominal and renal work.
Macassan Beach (Garanhan)

Apart from that, there is the usual mix of small parts, MSK and vascular that you would find anywhere.
How do you approach working with Aboriginal and Torres Strait Islander communities, and what have you learned from that experience?
I have found East Arnhem Land to be one of the last places in Australia where Indigenous culture still survives – even thrives. If you get the chance to visit the Garma Festival, I recommend it, where local culture is on display.
There are cultural differences which everyone learns about when first employed, and I have studied the local language – Yolngu Matha, at CDU in Darwin, and can speak a little to clients, which makes them feel more at home in a modern hospital setting.
What are some of the practical challenges of delivering imaging services in such a remote part of Australia?
A lot of our clients live very remotely, requiring a long drive across dirt tracks or a light plane to access hospital services.
We don’t have a local radiologist on-site, so we mostly run the show ourselves, but we can call Darwin for advice when needed. The outreach
ultrasound is challenging but fun. Flying to work in a small plane beats a traffic jam any day!
After two decades in the NT, what do you find most rewarding about your work, and what advice would you give to others considering remote practice?
I enjoy working with a small team of radiographers and sonographers. There is more responsibility, and we feel more appreciated in the hospital.
Being in a small hospital (33 beds) means I know every staff member – conversations are friendly and positive, and less combative than at larger workplaces.
I am on call for CT, X-ray and ultrasound – and my day involves moving between all 3 modalities – so there is a lot of variety, which I enjoy greatly.
If work in the city is getting you down, whether that is the long commutes or unfriendly work environments – I would definitely recommend a change, and a remote hospital ultrasound might be just what you need!
Give it a go at least once in your career!

Gove District Hospital
Gove Boat Club at sunset
TINA HAMLYN
Darling Downs, Queensland

From the Torres Strait Islands to outback Queensland, Tina Hamlyn has built a career defined by adaptability, service, and a commitment to care. As a state reliever with Queensland Health, she travels wherever she’s needed most, often to communities with limited access to imaging. Tina reflects on the resourcefulness required in rural healthcare and the powerful connections formed through delivering essential imaging to patients who might otherwise go without.
What does your role as a state reliever with Queensland Health involve?
I provide general radiography and ultrasound services wherever Queensland Health requires relief. Assignments usually run for about three weeks and can be anywhere, from the Torres Strait Islands to outback towns like Charleville. Some placements also include outreach work, where I travel to smaller communities that don’t have ready access to imaging services. Over the years, many rural facilities have secured permanent radiographers, so not every posting requires me to use both skill sets – but having that flexibility can make a real difference in rural areas.
How do you balance both ultrasound and X-ray when working in smaller facilities?
It’s all about teamwork and understanding priorities. The medical and nursing staff are incredibly supportive – they know that urgent cases come first. Administration staff also build breathing space into the ultrasound schedule to allow for the X-ray side of

Thursday Island Hospital with the world’s greatest located hospital chopper pad
things. Patients, too, show remarkable patience. Many travel long distances and often have other errands to run while they’re in town, so they’re quite adaptable. There’s a shared sense of ‘we’re all in this together’, which makes juggling both roles manageable.
What are the main challenges of moving between different sites and teams?
The trickiest part is always those first few hours –figuring out local processes and navigating the different IT systems. Luckily, hospital staff are consistently welcoming and quick to lend a hand. After more than 5 years as a reliever, you often cross paths with the same people at different sites, adding familiarity to the constant change. The work can feel isolating at times, so I make a point of staying connected with a network of sonographers I can call for advice or to exchange ideas. I also deliberately pick up contracts in regional and metropolitan hospitals now and then. It keeps my skills sharp, exposes me to new techniques, and reminds me of the variety that first drew me to this career.
Rural work is unique; the challenges are real, but the rewards are unmatched.
How important is access to imaging in the rural communities you support?
Access to imaging is absolutely vital in rural and remote communities. Without it, diagnoses are
Interview with Tina Hamlyn – Darling Downs, Queensland
delayed, treatments are pushed back, and patients face poorer outcomes. On top of the health risks, there’s the personal toll – many people have to travel hours, sometimes days, away from their homes, families, and work. The costs of travel and accommodation add another heavy layer of stress. I’ve met patients who’ve postponed essential tests simply because they couldn’t afford the time or expense of travelling to a larger centre.
That’s where our work makes a real difference. And the gratitude is immense – you see it in the patients, and you feel it from the medical teams.
By providing imaging locally, we can also reduce unnecessary transfers for the purpose of imaging. This allows services such as the Royal Flying Doctor Service and Life Flight, which are heavily relied on, to keep their critical services available for genuine emergencies.
What kinds of cases or patient needs do you see most often in country towns like Charleville?
Everything walks through the door, like a mix between private practice and an emergency department. You’ll do the standard outpatient work, but trauma is a big part of the load: motor vehicle accidents, farm injuries, and the occasional horse mishap. Obstetrics also makes up a large share. We often manage high risk pregnancies in partnership with tertiary centres, doing scans locally to save women from constant travel to metropolitan hospitals.

The work is anything but routine. Patients are tough – many won’t seek care until their symptoms seriously disrupt daily life – so you encounter conditions you’ve never even read about, let alone imaged. It keeps you on your toes, and it keeps the work fascinating.
Looking back on your experiences travelling across Queensland, what have been the most rewarding aspects of your job, and what advice would you give to other sonographers considering rural or relief work?
The greatest reward is simple: knowing you’re making an immediate difference. In places where medical resources are thin, every scan matters. Nearly every patient will remind you of that, often with a heartfelt ‘thank you’ that stays with you long after the day is done.
For anyone thinking about taking the leap into rural or relief work, do it. You’ll meet some of the toughest, most grateful people you’ll ever know, and you’ll collect stories that stay with you for life.
It will push you outside your comfort zone, but in the best way – it sharpens your skills and deepens your perspective. Rural work is unique; the challenges are real, but the rewards are unmatched.
My advice? Don’t go it alone. Build a support team of fellow sonographers you can call for advice, share ideas with, or simply debrief.
You’ll discover that the determination and heart of rural medical teams create a kind of healthcare that’s as special as it is inspiring. Medical resources might be limited, but the teamwork and the big-hearted spirit make it an incredibly special environment to work in.
Afternoon visitors at Charleville Hospital
On
the road with the Deadly Heart Trek: Dr Lucy Law on cardiac care in remote Australia

Combining clinical expertise with a passion for equity in healthcare, Dr Lucy Law is a cardiac sonographer whose work spans some of the most remote communities in Australia. Based in Canberra and travelling regularly to the Northern Territory, she supports projects such as the NEARER SCAN initiative and the Deadly Heart Trek, providing lifesaving cardiac screening and education in Indigenous communities. Lucy shares how collaboration, cultural connection and innovation are helping to close the gap in access to cardiac ultrasound for Aboriginal and Torres Strait Islander peoples across rural and remote Australia.
Can you tell us a little about your current role as a cardiac sonographer and where you are based? After completing my PhD and returning to Australia, I aimed to work in Indigenous health, particularly rheumatic heart disease (RHD). In 2023, I volunteered as an echocardiographer for the NEARER SCAN (Non-Expert Acquisition and Remote Expert Review of Screening Echocardiography images from Child and AnteNatal clinics) project (Jones et al., 2024) run by the Menzies School of Health Research.
This led to roles as a research officer on this and related projects and as an echocardiographer with a private company serving remote communities in the Top End and Central Australia. I’m based in Canberra and regularly travel to the NT.

What does your work usually involve, particularly in rural and remote communities?
Before a trip, I pack personal items, the portable machine, and other equipment. The next morning often starts early for a flight or a long drive. On arrival, I meet the clinic manager, set up my space, and discuss the day’s workflow with the clinic staff.
Workflow often relies on word of mouth, patient availability and transport options, as well as community business. For screening, if appropriate, we may visit homes and schools with hand-held ultrasound gear, always guided by cultural liaisons and local health staff. Trips last 1–5 days. All scans are reviewed remotely, with cardiology support available by phone.
How did you first become involved in the Deadly Heart Trek, and what drew you to participate? Deadly Heart Trek (DHT) was conceived and is currently led by a group of inspirational clinical and academic individuals with extensive experience in First Nations health provision and advocacy, with whom I have had the privilege of working during my time in the NT. My firsthand experience seeing the lack of resources, meeting the people this affects, as well as witnessing the wide range of avoidable consequences this has for First Nations health outcomes, motivates me to want to use my skill set, passion and privilege to be part of a
Early morning commute Mparntwe (Alice Springs) to Kaltukatjara (Docker River)
sustainable, accessible and culturally safe solution to this problem. The DHT strives to make genuine connections with the communities they visit, not only offering essential services that are otherwise not accessible, but to providing education and support to these communities in person, on country.
The most outstanding thing about the experience was the teamwork.
What was your role during the Trek, and what stood out to you most from the experience? Teams are small, so you have multiple roles. My expert role was as an echocardiographer performing RHD screening echoes, and when required, full studies.
My additional roles included driver, car packing expert and interior designer. Interior design was the hardest role as you were in a different community space (classrooms or such) every day, so reorganising the room to create functional clinical

and education spaces was a daily challenge. The most outstanding thing about the experience was the teamwork.
Each person worked hard to fulfil their multiple roles while keeping a happy and positive attitude, ensuring an efficient and high standard of workflow, as well as engaging with the community and all the chaos kids bring! Most of us had never worked together either!
Just shows how amazing teamwork can be if you all have a common goal.
From your perspective, what difference does the Deadly Heart Trek make for Aboriginal and Torres Strait Islander peoples in the communities you visited?
Most remote communities may never see a sonographer, cardiologist, paediatrician, or paediatric cardiologist. Having a specialist team on site to assess, consult, and develop a treatment plan with the clinic and family saves critical time and resources.

Working with colleagues in Dili (Timor Leste) and Milikapiti (Melville Island) on the NEARER SCAN/ LENO BESIK project. *LENO BESIK is the title of the project in Timor Leste
Community education – through engagement, face-to-face interaction, and conversations on country – is vital to improving health outcomes. Working alongside local health professionals,
Advancements in AI for ultrasound may also enhance future screening and diagnostic capabilities, further supporting timely and accessible care.
community members, and families builds trust and mutual understanding. It also ensures care is delivered in a culturally safe and respectful way. Aboriginal Liaison Officers (ALOs) and senior community members, who speak the language and understand community dynamics, are essential to meaningful service delivery. Their role is irreplaceable. Data collected from these visits is shared with local health services, helping to refine
care and build a clearer picture of disease burden. This collaborative, community-centred model supports sustainable improvements in healthcare access and outcomes for First Nations and Torres Strait Islander peoples in remote regions.
Looking more broadly, what do you see as the biggest challenges and opportunities in improving access to cardiac ultrasound in rural and remote Australia?
There are significant challenges in rural and remote healthcare, especially around funding, resources, and support.
Remote work requires diverse skills and strong cultural awareness. Increasing sonographer exposure and education in this space would help improve access. The NEARER SCAN project addresses this by training First Nations community members – such as Aboriginal Health Practitioners (AHPs), nurses, and some remote doctors – to use simplified echo protocols with handheld devices to screen for RHD. This collaborative, communityled approach builds local capacity and creates a

Some of the 2025 DHT team (Lucy bottom right)
sustainable care model. Studies are uploaded to a cloud server, reviewed by experts, and followed by a management plan.
The goal is to embed this process into routine care, enabling early detection and treatment for children and young people in remote areas. Advancements in AI for ultrasound may also enhance future screening and diagnostic capabilities, further supporting timely and accessible care.
What protocols are in place for urgent or abnormal findings when working in remote or rural clinics?
Each health service will have its own protocols. On arrival, it is very important to review these and speak with clinic management. Communication with the clinic staff is essential as they know their patients’ history and condition as well as the clinic’s capacity. Often, you will not be with a cardiologist, so it is important to have a good line of communication with them. Due to distance and limited resources, triaging of the situation is very important, and if deemed acute or in need of more advanced management, transport to another health facility can be arranged.
Taking time to find the best set-up that is both private for the patient and optimal for scanning is essential.
Do you always still scan a full TTE protocol on each patient, or are they more focused?
No. When screening for RHD, we use a highly abbreviated protocol (Remenyi et al., 2020), which allows for gross assessment of the left heart structure and function, which is primarily affected in RHD. If disease is detected, a full TTE protocol will be completed. If the patient is being followed by the cardiology team, a full protocol will be completed. The same goes if we have not seen the patient
before or in a long time. In some cases, limited studies are all that can be acquired, but we do our best to get as much information as we can, as we know there is a high chance that the patient will not be able to have an echo again for some time.
Are ergonomic set-ups similar to metro areas (what are the facilities like)?
No. As we will take a portable ultrasound machine on these trips, we must get a little bit creative with how we set up the space we have access to. I have frequently worked on basketball courts, in classrooms and in mobile trailer clinics.
Taking time to find the best set-up that is both private for the patient and optimal for scanning is essential. I always try and arrive early (if possible) and ask for equipment or environment modifications if I can. Resources are limited, so being understanding and patient is key.
Are there strategies to help avoid burnout, especially if there are overbookings?
The workflow and patient load in a day can vary greatly. A lot of flexibility is required, so taking breaks when there is downtime is encouraged. Communication, support and understanding with your colleagues is crucial. We also strive to share the load with rural and remote trips where possible. Taking some creature comforts with you (noise-cancelling headphones, a book), eating well, stretching, fresh air, engaging with the communities you visit (speaking to elders, going to arts centres) and sleeping well also help me avoid burnout.
Remenyi B, Davis K, Draper A, Bayley N, Paratz E, Reeves B, Appelbe A, Wheaton G, da Silva Almeida IT, Dos Santos J, Carapetis J, & Francis JR (2020). Single parasternal-long-axis-view-sweep screening echocardiographic protocol to detect rheumatic heart disease: A prospective study of diagnostic accuracy. Heart Lung Circ, 29(6),859–866. https://doi. org/10.1016/j.hlc.2019.02.196
Pioneering remote care: ASA Rural and Remote Sonographer of the Year, Sadie Atkins

When Sadie Atkins boards a small charter plane bound for a remote Northern Territory community, she knows she’s not just carrying her ultrasound machine, she’s carrying vital healthcare to people who might otherwise go without. The first-ever recipient of the ASA’s Rural and Remote Sonographer of the Year award this year, Sadie has built her career on resilience, adaptability, and a passion for connection. In this interview, she shares what drives her, the misconceptions she hopes to challenge, and the memorable moments that have shaped her journey in remote sonography.
What first inspired you to take your sonography career into rural and remote practice?
Coming from a small community allows people to build strong, collaborative working relationships with other healthcare professionals – whether it’s doctors, midwives, nurses, or allied health staff.
In a rural setting, we’re not just colleagues; we’re part of a close-knit team working towards a shared goal where we trust and support each other. That connection enhances communication, trust, and ultimately, patient care. Working remotely also enables professionals to develop broader skills –independence, adaptability, problem-solving, and leadership.
I love living remotely. Rural life allows for a slower, more grounded pace, where you’re not constantly rushing. You can focus on what matters most –family, work you care about and time outdoors.
What are some of the biggest misconceptions people have about healthcare in rural and remote areas?
Being in a remote setting can sometimes lead to the misconception that we are behind the times or not in touch with the latest advances in our field. However, that couldn’t be further from the truth. Despite the challenges of distance and limited access, we are deeply committed to staying current through continued education – whether that’s through online learning platforms, professional development, or participating in yearly ultrasound workshops. We understand that providing high quality care means staying informed, and we make it a priority to bring the latest knowledge and best practices to the communities we serve.
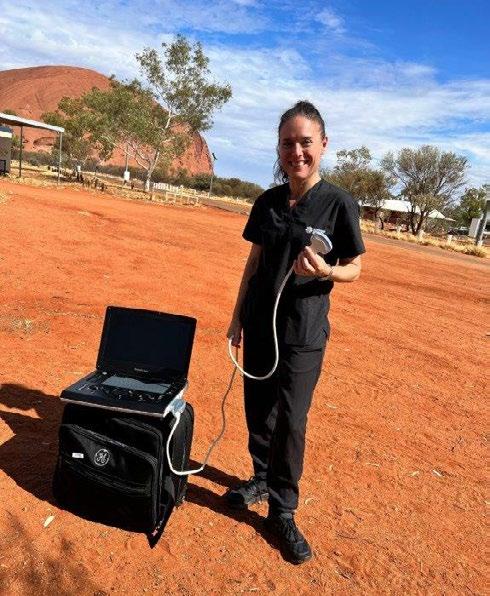
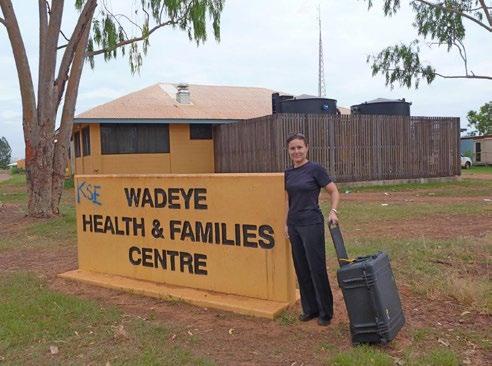
The remote ultrasound service involves travelling in small, chartered aircraft, often accompanied only by the pilot.
Scanning ultrasound at Uluru
There is also the misconception that being in a remote area means limited medical services. However, using a portable ultrasound machine ensures that no location is out of reach. We operate across vast distances, travelling by small, chartered aircraft to remote Indigenous communities throughout the Northern Territory and Arnhem Land. Our team provides diagnostic imaging in a range of settings – scanning patients in local renal units during dialysis, attending to individuals during GP visits, and delivering essential ultrasound services within the correctional system. This model demonstrates that high quality, patient-centred care can be effectively delivered even in resource-limited and geographically isolated environments.
What has been one of the most surprising or unexpected experiences you’ve had while working in a remote community?
Working in remote communities has provided me with many memorable experiences over the years. The remote ultrasound service involves travelling in small, chartered aircraft, often accompanied only by the pilot. Even just reaching these communities can be unpredictable, particularly during our tropical wet season. On one occasion, after flying all the way to Maningrida in the North Central coast of Arnhem Land, we were unable to land due to a buffalo refusing to move off the runway. There have


been times when landings were aborted because of severe electrical storms or unexpected encounters with flocks of birds.
One time, I shared a return charter flight with a patient and her midwife after detecting abnormal obstetric Dopplers during a scan. Upon arrival in Darwin, I was able to personally drop them directly at the hospital, highlighting the integrated nature of our remote service delivery.
Remote sonographers play a crucial role in bridging the healthcare gap, especially in rural or underserved communities.
Maningrida community charter flight
Scanning ultrasound at Uluru
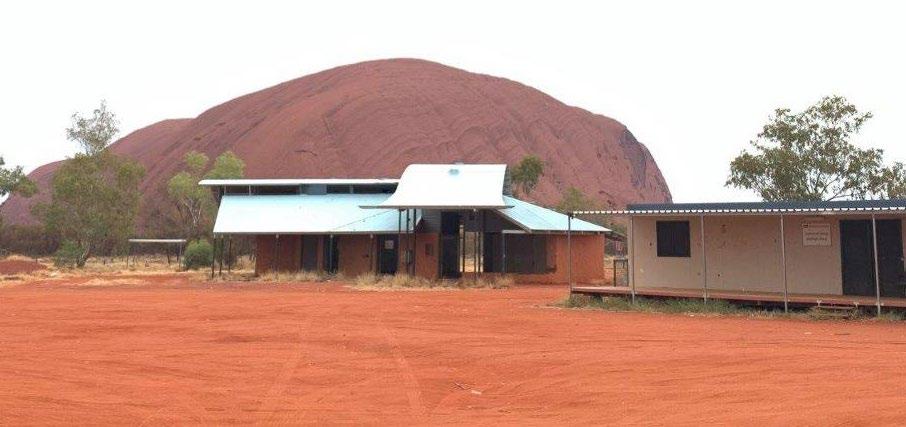
One particularly special moment was my first visit to the Mutitjulu community at the base of Uluru. The flight over Uluru and Kata Tjuta was breathtaking. On another trip, with some spare time, the pilot kindly offered a scenic flight over Kakadu National Park – an unforgettable experience.
Although I no longer participate as often in remote trips due to my current role as ultrasound educator, I take great pride in our dedicated team of sonographers who consistently demonstrate outstanding adaptability and commitment, delivering vital healthcare services to some of the most remote and isolated regions of Australia.
You are the first recipient of the ASA’s Rural and Remote Sonographer of the Year award. What does this recognition mean to you personally and professionally?
No achievement is ever accomplished in isolation – it is the result of the unwavering support and dedication of a loyal team. I do not view this award as a personal accolade, but rather as a tribute to all

the sonographers of the Northern Territory, whose tireless efforts and passion ensure the delivery of high quality care, even in the most remote regions of our Territory. Professionally, I hope this recognition serves as an inspiration to our students, demonstrating the rewarding and diverse career that lies ahead of them. Their enthusiasm and commitment to learning continue to inspire and motivate us all.
Wadeye community
Mutitjulu Community
How do you hope this award will inspire or influence others working in rural and remote healthcare?
To realise that sonography can be flexible, impactful, and a deeply rewarding profession.
Remote sonographers play a crucial role in bridging the healthcare gap, especially in rural or underserved communities.
Their work reinforces the principle that patient outcomes are improved when dedicated professionals are behind the scenes. I also hope this award encourages more sonographers to consider joining our team and embracing the unique and meaningful experiences that come with delivering care in remote settings.
Looking ahead, what’s one change or innovation you’d love to see that could make your work easier or improve patient care in remote settings? Air-conditioning, a patient bed that can move up and down, a chair to sit on while scanning, and a flushing toilet, ha ha! The simple things in life!

Wadeye community
soundeffects news is the biannual magazine of the Australasian Sonographers Association (ASA) Ltd.
The information in this publication is current when published and is general in nature; it does not constitute professional advice. Any views expressed are those of the author and may not reflect ASA’s views. ASA does not endorse any product or service identified in this publication. You use this information at your sole risk and ASA is not responsible for any errors or for any consequences arising from that use.
Please visit www.sonographers.org for the full version of the ASA’s publication disclaimer.
