

Making waves
Contributors
Lara Anders

Lara is a passionate sonographer based in Cairns, Queensland. Lara has previously worked in hospital and outpatient settings and has recently embarked on a new chapter by starting her own sonography clinic, specialising in vascular, obstetrics and gynaecology. Lara is an enthusiastic volunteer, ASA Far North Queensland branch committee chair, and an active ASA Vascular SIG committee member. Lara thoroughly enjoys promoting ultrasound education by presenting at educational events and tutoring in clinics to assist in the development of other sonographers’ skills.
Madonna Burnett

Madonna obtained the DMU in Ultrasound in 1997 and has been a member of the ASA for almost 30 years. Madonna joined the ASA Qld branch in 1997/8 and has served on the committee in a number of roles, including chairperson, secretary and treasurer, until departing from the committee in 2022. She joined the Paediatric SIG committee several years ago and remains on the committee as of today.
Madonna worked as a radiographer/ sonographer for Mater Health Services from 1983–2018 (approximately). She began part-time work at the Queensland Children’s Hospital in 2014 and remains full-time as a radiographer/sonographer. Madonna has been married to her husband Rob for 37 years and they have 4 children and 1 little granddaughter.
Deanne Chester, AFASA

Deanne has been a clinical supervisor for more than 20 years and an academic lecturer for over 10 years and thus has a thorough understanding of the challenges in providing suitable clinical education to sonography students and trainees throughout Australia and New Zealand. She is passionate about maintaining standards in sonographer education, as well as engaging with innovative solutions to the chronic sonographer shortage.
Jessica Coffey

Jessica is an experienced clinical sonographer with a special interest in obstetric and gynaecological ultrasound. Over the past five years, she has worked in leading tertiary maternalfetal medicine units. She has a particular passion for training, education, and continuous professional development, and takes great pride in teaching, mentoring, and fostering learning within her field.
Kylie Elmore

Kylie has been a sonographer for 23 years. She commenced her vascular ultrasound training at the Townsville Hospital in 2008 and has worked for both public and private vascular surgeons since then. Kylie is currently a sonographer for Queensland X-ray in Mackay.
Peter Esselbach

Peter Esselbach works as an MSK specialist sonographer in Adelaide at Fowler Simmons Radiology and Radiology SA. He worked for 6 years in Queensland before moving to Adelaide to work as a sonographer. Peter also holds a physiotherapy degree and has worked for 20 years as a rehabilitation and musculoskeletal physiotherapist in Adelaide. He is a qualified Pilates instructor and enjoys combining his 2 professions to obtain the best management and diagnosis for his patients. Peter has a passion for seeing sonographers preventing and managing MSK injuries within their sonography careers.
Dr Michelle Fenech, FASA

Michelle is passionate about musculoskeletal ultrasound, teaching, and researching structural anatomy, and currently chairs ASA MSK SIG. She is a senior lecturer and head of course of postgraduate medical sonography studies at Central Queensland University, teaching advanced musculoskeletal ultrasound units in the Master of Medical Ultrasound course. She currently mentors sonographers in musculoskeletal ultrasound at the Royal Brisbane and Women’s Hospital and undertakes research with a musculoskeletal ultrasound, anatomical and teaching focus.
Contributors
Andrew Grant

Andrew is a regular presenter on MSK, vascular, paediatrics and general anatomy in Australia and internationally. Besides his skills in ultrasound imaging, Andrew also holds a commercial pilot’s licence, which he has used to fly in and out of remote communities, establishing a strong presence as a flying sonographer. Andrew has also worked for one of the top medical centres in the western USA, UCLA Medical Centre, where he assisted in setting up the musculoskeletal ultrasound program. Andrew recently completed his Master of Medical Sonography at UniSA and now practises at I-Med East Melbourne Radiology, where he is the ultrasound supervisor.
Gina Humphries

Gina Humphries is a senior sonographer with a keen interest in women’s ultrasound. After working as a zoologist, Gina studied radiography in 2007, before pursuing her passion for sonography in 2010. Gina is currently working in the private sector specialising in obstetric, gynaecological and breast imaging.
Emma Jardine

Emma is a sonographer working in Victoria. She has a passion for professional growth and believes that investing in ongoing education and training will benefit individual sonographers and contribute to better patient outcomes and overall healthcare experience.
Dr Lucy Law

Lucy is an Australian-trained echocardiographer with a PhD in the field of cardiorheumatology from Umeå University in Sweden and is certified by the ESCVI (European Society of Cardiovascular Imaging) as a congenital echocardiographer. Lucy is currently working on research projects, including a project aiming to teach basic echo skills to non-experts to increase the detection of rheumatic heart disease (RHD) in remote Australia and Timor Leste (Menzies School of Health Research), as well as a Swedish nation study reviewing the palliative pathways and outcomes of Fontan circulation for hypoplastic left heart syndrome (HLHS).
Cheelim Liew

Cheelim is a cardiac sonographer and a nurse practitioner with an interest in mechanical circulatory support systems. He completed his postgraduate degree in cardiac ultrasound (Distinction) at QUT in 2020. Reflecting his speciality, Cheelim is a member of the Australian Sonographer Association (ASA) cardiac ultrasound special interest group and a reviewer for the Sonography journal. He is also a representative in the Australian and New Zealand Intensive Care Society (ANZICS) Health Economics Committee and has co-authored economic costing guidelines for RCTs and ICU costing reviews. He is currently pursuing his PhD, which he expects to complete in 2028.
Lisa McGuire, AFASA

Lisa McGuire is a locum general sonographer with a Master of Medical Ultrasound. She has enjoyed volunteering in the mentorship program with Radiology Across Borders. Lisa is a member of the Emerging Technologies SIG.
Jenny Parkes, FASA

Jenny is a sonographer with extensive experience in sonographer clinical training. She has a master’s degree in medical ultrasound and a Grad Cert of Medical Education, both from Monash University. Jenny coordinates a unit of the Monash MMU and presents extensively on breast ultrasound – her main ultrasound passion. She is also keen to improve the clinical training experiences of students and encourage better-informed supervision. Professionally, Jenny was an ASA Board member for 8 years, including past president and secretary and is now in her 10th year as a director of the ASAR.
Assoc Prof Tristan Reddan, FASA

Tristan is the consultant radiographer/ sonographer at the Queensland Children’s Hospital in Brisbane, where he coordinates medical imaging research governance, provides state-wide paediatric ultrasound advice, and works clinically. He is also a clinical associate professor in the School of Clinical Sciences at the Queensland University of Technology (QUT), where he works as a sessional lecturer and collaborates on research projects and student supervision.
Contributors
Dr Jacqui Roots

Jacqui is a senior sonographer and PhD candidate at QUT. Her research investigates the use of ‘Shear Wave Elastography to Assess the Stiffness of Muscles in the Acute Stage Post Stroke’. Jacqui has worked in private and public, and in both Australia and the UK, and is a member of the ASA MSK SIG and Emerging Technologies SIG. She enjoys camping, hiking and the beach.
Jane Wardle

Jane Wardle is a dedicated educator and the head of course – medical sonography at CQUniversity, overseeing the course across multiple campuses in Australia. With a clinical background in radiography and sonography, she has extensive experience in healthcare and academic leadership. Jane is passionate about advancing sonographer education, emphasising patient-centred care, and fostering critical thinking in her students. A lifelong learner, Jane is currently exploring educational neuroscience, combining her interests in teaching and the science of learning to enhance student outcomes.
Alison White, AFASA

Alison is an accredited medical sonographer (cardiac) with over 25 years of experience in sonography. Alison has been a national clinical examiner for the ASUM DMU and is a past DMU Board member. Her clinical expertise has been recognised at both national (Australian Sonographer of the Year, ASUM, 2012; Associate Fellow of the ASA, 2023) and international levels (Fellow of the American Society of Echocardiography, 2017). She joined Griffith University in 2012 as a senior lecturer and program director, teaching cardiovascular and respiratory anatomy, physiology and pathophysiology and biomedical instrumentation. Alison is passionate about the professional development of sonographers and contributes to the ASA by reviewing articles for Sonography, presenting at the ASA National Conference and as a member of the Cardiac SIG.
Marilyn Zelesco

Marilyn Zelesco is a Western Australiantrained diagnostic radiographer who gained a postgraduate ultrasound qualification in 1991 and completed her master’s in ultrasound through RMIT in 2007. Marilyn has received professional awards from the Australian Institute of Radiography, the Australian Sonographers Association and the Australian Society for Ultrasound in Medicine.
Marilyn is the lead sonographer at the Fiona Stanley Hospital in Perth. Marilyn has an interest in hepatic, bowel and male reproductive tract ultrasound, elastography, CEUS, renal transplants, research, education and sonography in Indigenous healthcare.
VASCULAR
Diagnosing vasculitis with ultrasound: findings and pitfalls 6
VASCULAR
The diagnostic accuracy of temporal artery ultrasound and temporal artery biopsy in giant cell arteritis – A single centre Australian experience over 10 years 7

WOMEN’S HEALTH
Diagnostic performance of 3D automated breast ultrasound (3D-ABUS) in a clinical screening setting – a retrospective study 8

WOMEN’S HEALTH
Adverse pregnancy outcome in fetuses with early increased nuchal translucency: prospective cohort study 9
CARDIAC
Using artificial intelligence for rheumatic heart disease detection by echocardiography: focus on mitral regurgitation 10
CARDIAC
Noninvasive hemodynamic characterization of shock and preshock using echocardiography in cardiac intensive care unit patients 11
HEALTH & WELLBEING Incidence and cause of occupational burnout syndrome among sonographers 13
HEALTH & WELLBEING Sonographer wellbeing in Australia: Perceptions of job demands and resources in clinical working environments 14
HEALTH & WELLBEING
Building emotional resilience to foster well-being by utilising reflective practice in the sonography workplace 16
MUSCULOSKELETAL
Ultrasound had high accuracy in measuring hip joint capsule thickness 17
MUSCULOSKELETAL
High-resolution ultrasound approach to quadrangular joint in carpal boss: Everything musculoskeletal sonographer should know 18
GENERAL
The role of Doppler ultrasound in the evaluation of penile haemodynamics – A sonographer’s guide to the documentation of vasculogenic erectile dysfunction 20
GENERAL
Global trends in hepatocellular carcinoma epidemiology: implications for screening, prevention and therapy 21
CLINICAL SUPERVISORS
The ability for teaching self-efficacy by clinical preceptors in diagnostic medical sonography 23
CLINICAL SUPERVISORS
Common models and approaches for the clinical educator to plan effective feedback encounters 24
RESEARCH
Sonographers’ perspectives on research – A worldwide online questionnaire study 25
RESEARCH
Barriers to reporting guideline adherence in point-of-care ultrasound research: a cross-sectional survey of authors and journal editors 26
EMERGING TECHNOLOGIES
Artificial intelligence in breast ultrasound: application in clinical practice 27
EMERGING TECHNOLOGIES
The performance of ChatGPT-4.0o in medical imaging evaluation: a cross-sectional study 29
PAEDIATRIC
Ultrasonography of pediatric superficial soft tissue tumors and tumor-like lesions 30
Diagnosing vasculitis with ultrasound: findings and pitfalls
VASCULAR
Reviewer: Lara Anders
ASA SIG: Vascular
Authors: Schmidt W and Schäfer V
Journal: Therapeutic Advances in Musculoskeletal Disease. 2024; 16.
Open Access: Yes
Read the full article here
Why the study was performed
This study was conducted to address the increasing integration of vascular ultrasound into rheumatology for diagnosing and managing giant cell arteritis (GCA) and Takayasu arteritis (TAK). Ultrasound offers a noninvasive, rapid diagnostic tool that allows for direct visualisation of characteristic signs like the ‘halo sign’ and intima-media thickening (IMT). It supports timely treatment to prevent symptomatic complications, aligns with new European recommendations, and has been incorporated into rheumatology training. The study also emphasises its utility in detecting subclinical disease and guiding follow-ups in clinical practice.
How the study was performed
Schmidt and Schäfer performed a comprehensive review of current literature and guidelines to evaluate the role of ultrasound in diagnosing and managing large vessel vasculitis, particularly GCA and TAK. It explored the historical context, practical applications, and evolving recommendations emphasising ultrasound as a primary diagnostic tool. The review also analysed the integration of ultrasound into rheumatology training and its increasing use in clinical practice due to advancements in equipment and expertise supported by updated international guidelines.
What the study found
The study found that vascular ultrasound is highly effective for diagnosing GCA and TAK, demonstrating strong sensitivity and specificity when performed by qualified sonographers. Key ultrasound features, such as the ‘halo sign’ and IMT measurement, reliably identify vasculitis and support diagnosis. Ultrasound assessment of IMT measurement was found to be best used in monitoring disease progression and guide ongoing treatment decisions. Ultrasound proved valuable for early detection, intervention, and prevention, thus reducing hospitalisation rates, glucocorticoid doses and secondary complications. Additionally, its accessibility facilitates quicker diagnosis
of polymyalgia rheumatica and helps avoid common pitfalls, such as normal findings resulting from the rapid reduction in wall thickening following glucocorticoid treatment, which has been reported to occur as early as two days after commencement of treatment. The study also emphasised ultrasound’s role in updated classification criteria and its growing integration into current and future rheumatology practice and training.
Relevance to clinical practice
The study is highly relevant to clinical practice, as it emphasises the utility of vascular ultrasound for the timely diagnosis and management of GCA and TAK. Ultrasound enables noninvasive, real-time evaluation, reducing reliance on more invasive or resource-intensive tests. Its accessibility enables prompt intervention, preventing severe complications and improving disease management. Furthermore, the integration of ultrasound into rheumatology training and alignment with updated guidelines ensures that clinicians are well-equipped to utilise this technology to enhance patient care and streamline the diagnostic process in suspected vasculitis cases.
“rapid reduction in wall thickening following glucocorticoid treatment … has been reported to occur as early as two days after commencement of treatment”
The diagnostic accuracy of temporal artery ultrasound and temporal artery biopsy in giant cell arteritis –A single centre Australian experience over
10 years
Why the study was performed
Temporal artery biopsy (TAB) remains the gold standard in Australia for the diagnosis of giant cell arteritis (GCA). Obstacles to performing TAB include the increasing cost of healthcare, the need for hospital admission, potential perioperative complications and logistical issues for patients in areas that don’t have access to rheumatological services. This study aimed to assess the diagnostic accuracy of temporal artery ultrasound and therefore its potential use as a viable alternative.
How the study was performed
A single-centre retrospective study was performed over a 10-year period between 2011 and 2020. Patients with clinical symptoms of GCA and who had an ultrasound performed by a qualified sonographer were identified.
The ultrasound was considered positive for GCA based on the sonographic findings of:
• ‘halo sign’ or hypoechoic wall thickening of the temporal artery
• ‘compression sign’ or the inability to ablate the vessel lumen with probe pressure due to wall inflammation.
In addition to this, sonographers provided information on temporal artery patency, stenosis and flow velocity. Corresponding medical records were reviewed to retrieve biopsy findings.
What the study found
Ultrasound examinations were performed on 63 patients over the 10-year period and the data proposes that 20 per cent of ultrasounds performed were considered positive. Of those patients who had also undergone TAB, the study showed a moderately strong correlation between ultrasound and TAB results. Of the 32 negative temporal artery ultrasound examinations, only 4 patients had a positive TAB. Of the 12 patients who had a positive temporal artery ultrasound, only 2 were negative at TAB. This study found that temporal artery ultrasound had a sensitivity of 71.4% and a specificity of 93.3%. These findings were found to be comparable to international standards.
Relevance to clinical practice
In the hands of an experienced, qualified sonographer, the high specificity of a positive temporal artery ultrasound may reduce the need for TAB. This has the potential to reduce healthcare costs, patient morbidity, delay in diagnosis and logistical issues. Standardised protocols in reporting and performing ultrasounds for GCA as well as improved training for sonographers were identified strategies that could be utilised to further enhance patient outcomes.
VASCULAR
Reviewer: Kylie Elmore
ASA SIG: Vascular
Authors: He J, Williamson L, Ng B, Wang J, Manolios N, Angelides S, Farlow D and Wong P
Journal: International Journal of Rheumatic Disease
Open Access: Yes
Read the full article here
“If positive in the setting of a suggestive clinical presentation, a temporal artery ultrasound probably avoids the need for a temporal artery biopsy”
Diagnostic performance of 3D automated breast ultrasound (3D-ABUS) in a clinical screening setting – a retrospective study

WOMEN’S HEALTH
Reviewer: Jessica Coffey
ASA SIG: Women’s Health
Authors: Klein Wolterink F, Ab Mumin N, Appelman L, Derks-Rekers M, Imhof-Tas M, Lardenoije S, van der Leest M & Mann RM
Journal: European Radiology, 19 January 2024, Volume 34, pp. 5451–5460
Open Access: Yes
Read the full article here
Why the study was performed
Screening plays an important role in the early detection of breast cancer, with mammography used as the gold standard modality. Mammography is less sensitive in women with dense breast tissue due to the overlapping fibroglandular tissue. 3D automated breast ultrasound (3D-ABUS) has been proposed as a potential supplementary modality to improve cancer detection, specifically in this group of women. Several prospective studies of the performance of 3D-ABUS have reported additional cancer detection and increased sensitivity. However, they have also shown a decrease in specificity and an increase in the recall and biopsy rates. This study was conducted to evaluate the diagnostic performance of 3D-ABUS as a supplementary modality for breast cancer screening in a real clinical setting.
How the study was performed
This was a retrospective study of all patients who underwent 3D-ABUS for breast cancer screening at Radboud University Medical Centre in the Netherlands between January 2014 and January 2022. 3D-ABUS was offered in addition to mammography to all women undergoing clinical screening who had Volpara breast density C and D. 3D-ABUS alone was also offered to women who declined mammography or were younger than the mammography recommended age. Cases referred for diagnostic imaging were not included. 3D-ABUS and mammography were performed by trained radiographers using Seimens Acuson s2000 Automated Breast Volume Scanner Ultrasound System and Seimens Mammomat Revelation or Mammomat Inspiration machines. Studies were reviewed by one of six breast radiologists who had undergone training in the application and reading of 3D-ABUS before the installation of the machine. Statistical analyses were performed using IBM SPSS version 25 software.
What the study found
In total, 3616 3D-ABUS studies were performed in 1555 women over the 8-year trial. Of these, 152 examinations on 104 women were performed without mammography. The study found an additional cancer yield of 2.77 per 1000 screening tests. The overall recall rate was 5.2%, with a significant reduction over the time of the study (23.6% in the first year and 3.8% by year 8). The biopsy rate was 1.8%, with 52.8% of biopsies performed due to an abnormality detected on 3D-ABUS alone. The positive predictive value was 15.4%. These results are comparable in performance to previous prospective studies, with better recall and biopsy rates. The majority of cancers detected by 3D-ABUS alone were IDC, whereas the majority of cancers detected by mammography alone were DCIS.
Relevance to clinical practice
The findings of this study support the integration in clinical practice of 3D-ABUS as a supplemental screening tool for women with dense breast tissue. However, this would need to be balanced with the challenge of increased biopsy and recall rates, which are a source of anxiety for patients, as well as the additional costs of equipment, training and examination time.
“3D automated ultrasound screening performance in a clinical setting is comparable to previous prospective studies, with better recall and biopsy rates”
Adverse pregnancy outcome in fetuses with early increased nuchal translucency: prospective cohort study

WOMEN’S HEALTH
Reviewer: Gina Humphries
ASA SIG: Women’s Health
Authors: Bet B, Lugthart M, Linskens H, van Maarle M, van Leeuwen E, Pajkrt E
Journal: Ultrasound in Obstetrics & Gynecology
Open Access: Yes
Read the full article here
Why the study was performed
Increased nuchal translucency (NT) thickness > 3.5 mm is a known marker for congenital anomalies between 11 and 14 weeks gestation. There is limited understanding of its use as a screening tool before 11 weeks. This study aimed to investigate whether fetuses with an increased NT before 11 weeks are at risk of adverse pregnancy outcomes.
How the study was performed
This was a prospective cohort study that followed 109 women with a viable fetus, an NT measurement ≥ 2.5 mm and a CRL < 45 mm. An NT measurement of < 2.5 mm was considered normal at this scan. All women included in the study were referred to a fetal medicine unit and examined again when the CRL was > 45 mm. The NT was remeasured at this time. Patients were then allocated to one of two groups: those with a normalised NT < 3.5 mm and patients with a persistently increased NT > 3.5 mm. All patients were monitored until 4 weeks postpartum. The study then analysed the association between NT thickness before 11 weeks and adverse outcomes, and compared fetuses with a normalised NT to those with a persistently increased NT at the follow-up scan. Adverse outcomes were defined as aneuploidies and other genetic disorders, including chromosomal aberrations and (mono)genetic diseases.
What the study found
This study found an adverse pregnancy outcome in 35.8% of fetuses with an increased nuchal translucency (NT) thickness ≥ 2.5 mm before 11 weeks. The authors confirmed that fetuses with a persistently increased NT have an elevated risk of adverse outcomes when compared to fetuses with a normalised NT < 2.5 mm (65.2% vs 14.3%). The rate of adverse outcome was significantly reduced in fetuses with a normal NT measurement in the 11 to 14-week scan when compared to those with
a persistently increased NT at the followup scan (14.3% vs 65.2%). Importantly, for fetuses in which the NT normalised, the incidence of adverse outcomes was 8.5%, remaining higher than the baseline risk.
Relevance to clinical practice
This study draws attention to the benefit of evaluating the NT during a scan between 9- and 11-weeks gestation. Fetuses with an early increased NT before 11 weeks are at high risk of adverse pregnancy outcomes. In particular, the risk of chromosomal and structural anomalies remains higher than the baseline risk regardless of whether the NT remains increased or normalises after 11 weeks. Evaluation at this early stage may become routine for sonographers with an increased NT before 11 weeks, prompting a referral to a fetal medicine unit for detailed imaging and counselling about diagnostic and testing options.
“Fetuses with an early increased NT thickness are at considerable risk of an adverse pregnancy outcome, even if the NT normalises after 11 weeks”
Using artificial intelligence for rheumatic heart disease detection by echocardiography: Focus on mitral
regurgitation
Why the study was performed
Studies have shown that, by task-shifting screening echocardiography to non-expert operators, increased early detection of latent rheumatic heart disease (RHD) is possible. However, the issues regarding the lack of specialised personnel to diagnose RHD from these assessments remain. This study aimed to use deep and machine learning artificial intelligence (AI) methods to evaluate if the detection of RHD using mitral regurgitation (MR) criteria was comparatively accurate to expert cardiologists.
How the study was performed
Echocardiographic data used in this study was collected by experts using a specific imaging protocol and was part of a 2-year control trial study assessing the impact of secondary antibiotic prophylaxis in Ugandan adolescents and children with latent RHD. Using the 2012 World Heart Federation (WHF) criteria a panel of experts noted the presence or absence of RHD. Cases that were diagnosed using non-colour Doppler MR criteria, including spectral Doppler and morphological features, were excluded. In total, 511 (229 without RHD) were included in this study.
Multiple techniques were used to test and train AI algorithms. Localisation of the left atrium (LA) as well as identification of systolic frames was achieved by image harmonisation and convolutional neural networks. These processes were applied to address the inherent image differences that can occur such as spatial resolution and lack of electrocardiogram (ECG) trace. Subsequently, the machine learning approach was used to analyse MR jet length. Cross-validation and linear support vectors were used to identify 9 features that best describe and delineate the MR jet. The results of these methods were then compared to that of expert reviewers. The deep learning approach was also applied as an attempt to integrate intelligent image analysis which goes beyond factors identified by expert operators. This was achieved by
using two deep learning models specialised in processing multi-view (in this case parasternal long axis (PLAX) and apical 4 chamber (A4C) views) data; one dealing with special and temporal factors, and the other interframe temporal relationships.
What the study found
Image harmonisation for identification of the LA, from the PLAX and A4C views, had an accuracy of 0.99 and selected the correct systolic frame over 92% of the time. Localisation of the LA using the Dice coefficient exceeded 0.85 for both the PLAX and A4C views.
Machine learning techniques measuring MR jet length showed no statistically significant difference when compared to manual measurements performed by experts, with further analysis showing strong agreement between the methods. The combined deep learning methods performed best showing a precision of 0.78 and a diagnostic performance of 0.84 (De Long’s method).
Relevance to clinical practice
Using AI to analyse and interpret ultrasound images should not be done just because it is available but should add value to the process and help validate and define its place within sonography.
The authors have applied AI technologies to address a significant gap in service provision, namely the lack of the specialist’s capacity to review and diagnose RHD. The use of such technology in RHD endemic areas, which are under-resourced and low-middle income, could significantly aid in decreasing the global burden of RHD.
Reviewer: Dr Lucy Law
ASA SIG: Cardiac
Authors: Brown K, Roshanitabrizi P, Rwebembera J, Okello E, Beaton A, Linguraru M, Sable C
Journal: Journal of the American Heart Association (JAHA)
Open Access: Yes
Read the full article here CARDIAC
“Artificial intelligence (AI) could have important implications for scaling rheumatic heart disease (RHD) detection in endemic regions by nonexpert healthcare workers”
Noninvasive hemodynamic characterization of shock and preshock using
echocardiography in cardiac intensive care unit patients
Why the study was performed
Cardiogenic shock is a life-threatening condition associated with considerable morbidity and mortality among patients admitted to the ICU. Currently, it is difficult to distinguish the type of shock patients are enduring, with limited literature on the use of echocardiographic measurements in categorising the degree of shock. This review describes the transthoracic echocardiogram’s (TTE) characteristics for each shock classification for patients in the ICU. Clinical definitions of shock as classified in this article are summarised in the table below:
Term Definition
Hypotension
Presence of any of the following criteria:
• Admission systolic BP < 90 mmHg
• Minimum systolic BP < 90 mmHg during 1st hour
• Admission mean arterial pressure (MAP) < 60 mmHg
• Minimum MAP < 60 mmHg during first 1 hour
Hypoperfusion
Presence of the following criteria:
• Admission lactate > 2 mmol/L
• Urine output < 720 ml during first 24 hours
• Creatinine increased by ≥ 0.3 mg/dl during first 24 hours
How the study was performed
Classification Study Definition
Normal Neither hypotension nor hypoperfusion
Isolated Hypotension without hypoperfusion
Isolated Hypoperfusion without hypotension
Shock Both hypotension and hypoperfusion
This is a retrospective study using data from 2007 to 2015 from the Mayo Clinic Cardiac Intensive Care Unit (CICU), with 5375 patients included in the study. Data was collected and analysed on patients who had a TTE performed to assess LV ejection fraction (LVEF) within 1 day of admission to the CICU. Data collected included information on patient demographics, vital signs including blood pressure, blood and urine testing data and clinical observations correlating to the shock classification. Following shock classification, echocardiographic parameters were collected. Multiple statistical analyses were conducted to identify trends in the TTE parameters of patients in each shock classification.
What the study found (TTE features)
• Shock: decrease in biventricular systolic function, stroke volume (SV), increase in biventricular filling pressures
• Isolated hypoperfusion: reduction in ventricular forward flow
• Isolated hypotension: decrease in systematic vascular resistance
RV systolic function and hemodynamics
Reviewer: Cheelim Liew and Alison White, AFASA
ASA SIG: Cardiac
Authors: Jentzer J, Burstein B, Ternus B, Bennett C, Menon V, Oh J, Anavekar N
Journal: Journal of the American Heart Association
Open Access: Yes
Read the full article here
“TTE, including non-invasive Doppler hemodynamic assessment, can therefore be additive in the assessment of shock severity for prognostication and decisionmaking in CICU patients”
Noninvasive hemodynamic characterization of shock and preshock using echocardiography in cardiac intensive care unit patients (continued)
Relevance to clinical practice
• TTE can prognostically identify the different types of shock in ICU patients.
• Cardiac sonographers can utilise 2D and spectral Doppler measurements to categorise the type of shock.
• Early recognition of these patients through TTE performed by the cardiac sonographers could prompt timely and appropriate interventions that could make a difference in patients’ outcomes.
Figure 5, page 12

“Patients with isolated hypotension (normotensive shock) have lower forward flow and higher vascular tone than those with isolated hypotension (preshock), reflecting worse underlying cardiac compromise with preserved vascular compensatory mechanisms”
Incidence and cause of occupational burnout syndrome among sonographers
HEALTH & WELLBEING
Reviewer: Peter Esselbach
ASA SIG: Health and Wellbeing
Author: Tran M
Journal: Journal of Diagnostic
Medical Sonography
Open Access: Yes
Read the full article here
Why the study was performed
The study was performed to assess the level of occupational burnout in sonographers and to determine if there was an association between sex, number of hours worked per week and burnout.
How the study was performed
A survey and questionnaire were used to assess the prevalence of occupational burnout syndrome among sonographers who were members of the Society for Diagnostic Medical Sonography. The Maslach Burnout inventory survey was used, measuring emotional exhaustion, depersonalisation, and lack of personal accomplishment.
What the study found
A total of 1049 sonographers were surveyed of which 914 completed responses were analysed. The results indicated a moderate level of both disengagement and exhaustion overall. They concluded that a moderate degree of burnout syndrome was reported by the sonographer cohort. Between the two burnout dimensions, exhaustion appeared to be more prevalent than disengagement.
A significantly higher burnout score was seen in sonographers who worked more than 37 hours per week compared to those who worked fewer hours per week.
The survey found that 76% of respondents stated ‘they did not have enough energy for leisure activities after work.’ 81% responded that they were worn out and weary after work. Furthermore, 72% of sonographers said they felt emotionally drained during work.
The study found no significant differences when comparing the rate of burnout between men and women.
Relevance to clinical practice
The study suggested that sonographers who worked longer hours experienced higher levels of stress and developed a higher incidence of occupational burnout. This could indicate that a poor work-life balance often leads to higher levels of employee exhaustion and risk of burnout.
Workplace stress is a significant issue in sonography escalated by the increasing number of hours sonographers are working. Helping to manage workplace stress and the factors related to burnout would assist in improving the retention of sonographers within radiology.
“Assessing how burnout affects working sonographers could aid in managing workplace stress and improving employee retention”
Sonographer wellbeing in Australia: Perceptions of job demands and resources in clinical working environments
Why the study was performed
The study was performed to assess the workplace demands Australian sonographers are experiencing and to identify what resources are available for sonographers. The aim was to highlight which resources sonographers perceive to be the most effective in improving wellbeing in the workplace.
How the study was performed
A cross-sectional online survey of 69 Australian medical sonographers who were registered with the ASAR and worked a minimum of two clinical shifts per week were recruited for the study. The survey contained quantitative (demographic) and open-text questions related to workplace wellbeing.
SPSS Statistics Software was used to investigate any statistically significant data trends between the level of job satisfaction and independent variables (clinical environment, years of experience, subspeciality in ultrasound, age gender, role title, state in Australia, number of shifts per week and hours per week).
What the study found
• The largest number of participants were from the private sector (n = 39, 56.5%), 23 were from public hospitals and the remaining 7 participants were from private hospitals, specialists’ clinics and academic environments.
• The majority of participants were female (73.9%) and were clinical sonographers (78.3%).
• Fifty-eight per cent of participants had over 16 years of experience and the results suggested that with increased years of clinical experience, there were increased levels of job satisfaction. Overall, 39.1% of participants were moderately satisfied, 24.6% were very satisfied and 11.6% were moderately dissatisfied in their current role.
• Unrealistic workloads, time pressures and inadequate scheduled breaks were
universally reported by both private and public participants.
• The second most demanding factor for public hospital participants was unnecessary scans and scan extensions. This compares to private practices that reported incentivised workloads as the second most demanding factor.
• Participants reported inadequate remuneration and lack of role progression and professional development as factors that influenced their workplace demands.
• It was noted that patient-related factors that increased workplace demands included delivering unexpected findings, patients’ expectations of receiving immediate scan results and dealing with patient stress.
• Participants, in both private and public, noted workplace resources such as psychological support (employee assistance programs, employer support), injury prevention (workplace health and safety, physical therapy), workload reduction (scheduled breaks, workload reduction) and individual support (self-driven strategies) were resources available to them.
• Thirty per cent of private practice participants and 36% of public hospital participants identified psychological support as a workplace resource. Employer support strategies such as acknowledging hard work, financial rewards and regular team meetings were perceived to be effective resources.
• Forty-seven per cent of public hospital participants suggested that injury prevention, such as physical therapy and workplace health and safety, was an effective workplace resource. Physical resources to improve workplace wellbeing were less available to private practice participants, where 22.5% mentioned injury prevention and 15% mentioned workload reduction strategies.
• It was concerning to note that 42.5% of private practice sonographers reported no wellbeing resources were offered in their workplace.
• Reducing the repetitive nature of certain examinations and producing stretching videos were identified as beneficial resources to reduce injury rates and improve wellbeing.
HEALTH & WELLBEING
Reviewer: Emma Jardine
ASA SIG: Health and Wellbeing
Authors: Hall C, Pignata S, Tie M, Bezak E, Childs J
Journal: Sonography
Open Access: Yes
Read the full article here
Sonographer wellbeing in Australia: Perceptions of job demands and resources in clinical working environments (continued)
HEALTH & WELLBEING
Relevance to clinical practice
Workplace demands such as unrealistic workloads, time pressures, and the inadequate number of scheduled breaks were identified as the most frequent workplace stress by participants. When sonographers work under these pressures, patient care can be affected.
In 2023, Commonwealth health and safety laws came into effect in Australia stating, ‘employers must identify and manage hazards and risks to workers’ psychological health and safety’. Reduction in workload is perceived to be the most effective resource by participants to improve workplace wellbeing. Employers can ensure sonographer workplace wellness by implementing reasonable time frames per scan, capping the number of scans performed and ensuring a set number of breaks are taken per shift.
“New Commonwealth health and safety laws (2023) state ‘employers must identify and manage hazards and risks to workers’ psychological health and safety’. This study found that employers can ensure sonographer workplace wellness by implementing reasonable time frames per scan, capping the number of scans performed and ensuring a set number of breaks are taken per shift”
Building emotional resilience to foster well-being by utilising reflective practise in the sonography workplace
HEALTH & WELLBEING
Reviewer: Jane Wardle
ASA SIG: Health and Wellbeing
Authors: White A, Humphreys L, Oomens D
Journal: Sonography
Open Access: Yes
Read the full article here
Why the article was written
This article was written to explore the value of reflection, particularly affective reflection and reflective writing, as resilience-building tools for sonographers. Sonography professionals often face emotionally challenging and traumatic scenarios due to the nature of their work, including delivering difficult news or witnessing distressing situations. Such continual exposure can lead to compassion fatigue and burnout, impacting mental health and the quality of patient care. While reflection is widely practised in other healthcare fields for self-awareness and resilience, little research addresses its application within the sonography profession. The authors aim to demonstrate how reflective practices can support sonographers’ emotional resilience, helping to safeguard their wellbeing and sustain high standards in clinical practice.
How the review was performed
This article primarily reviews existing literature on reflective practice, affective reflection, and resilience within healthcare. It examines how sonographers could benefit from adopting reflective strategies, drawing from established methods and models in the literature, including the works of Donald Schön, Gibbs, and others on experiential learning. By incorporating theoretical frameworks and realworld examples, the authors present practical strategies for reflective writing tailored to sonography. The article outlines a structured approach to reflection, emphasising cyclical processes such as critical incident analysis, which help identify and address gaps in knowledge, skills, and emotional responses. Practical guides, including guided prompts for reflective writing, are provided to support the implementation of these strategies in sonography.
What the article found
The article suggests that affective reflection and reflective writing can effectively support emotional resilience, self-awareness, and self-regulation among sonographers. Reflective practice allows professionals to process emotions, reframe responses, and develop coping mechanisms to manage ongoing emotional stress. The authors observed that sonographers who engage in reflective writing can better adapt to stressful situations, potentially preventing burnout and promoting empathy in patient interactions. Additionally, the article suggests that reflective practice can enhance clinical skills and decision-making by helping sonographers bridge gaps between theory and practice, creating opportunities for growth in cognitive, psychomotor, and emotional domains.
Relevance to clinical practice
This article highlights the importance of integrating reflective practices into the sonography field, emphasising their potential to foster emotional resilience and enhance patient care. By making reflection a routine part of clinical practice, sonographers may experience improved emotional stability and reduced stress reactivity, which can positively impact patient interactions and clinical outcomes. Introducing structured reflective writing and mindfulness practices can help sonographers better manage the emotional challenges of their work, ultimately contributing to their professional development and personal wellbeing.
“Given the clear link between the practice of reflection and the development of resilience in other healthcare professions, this concept can be adopted by sonographers to reduce their degree of emotional fatigue and enhance their overall wellbeing”
Ultrasound had high accuracy in measuring hip joint capsule thickness
MUSCULOSKELETAL
Reviewer: Dr Michelle Fenech, FASA
ASA SIG: Musculoskeletal
Authors: Gao G, Fang H, Zhou K, Mo Z, Liu J, Meng L, Wang J and Xu Y
Journal: BMC Musculoskeletal Disorders
Open Access: Yes
Read the full article here
Why the study was performed
The hip joint capsule plays a crucial role in hip joint stability. The iliofemoral, pubofemoral and ischiofemoral ligaments contribute to the hip joint capsule and can become thickened with various hip conditions. Ultrasound can demonstrate the anterior hip joint capsular morphology and measure the capsule thickness which can be used to diagnose hip joint pathology, guide patient management and evaluate treatment outcomes, and guide hip joint injections and aspirations. This study compared the thickness of the hip joint capsule on the same patient as measured by magnetic resonance imaging (MRI) and ultrasound to determine their correlation (Figure 1).

How the study was performed
Magnetic resonance and ultrasound imaging of the hips of 307 patients (mean age 38.6 years) was retrospectively reviewed, and the anterior hip joint capsular thickness was measured and compared using Bland-Altman analysis and two-tailed paired t-tests. The capsule thickness (depth) was measured where the anterior iliofemoral ligament folded back on itself at the junction of the femoral head and neck (Figure 2).

For MR imaging, the patient was supine with legs extended; for ultrasound imaging, the patients were positioned supine, with their leg of interest in the ‘frog leg’ position (knee flexed and externally rotated). The transducer was positioned along the long axis of the femoral neck.
What the study found
Significant correlation between MRI and ultrasound capsular thickness measurements was demonstrated (p < 0.001). The mean capsular thickness on MRI was 5.0 mm ± 1.2 mm, and on ultrasound was 5.0 ± 1.5 mm. Ultrasound is consistent with MRI for investigating the thickness of the anterior hip joint capsule.
Relevance to clinical practice
Ultrasound of the anterior hip joint can not only be used to identify fluid and pathological material within the hip joint recess but can demonstrate the capsule itself which is comprised of ligaments. It is important for sonographers to appreciate the anatomy of the iliofemoral, pubofemoral (both anterior hip) and ischiofemoral (posterior hip) ligaments, and identify their presence on imaging.
Figure 1. Ligaments that comprise the hip joint capsule demonstrated from the anterior and posterior approach (Image drawn by M Fenech).
Figure 2.A. Anatomy of the anterior hip joint demonstrating the anterior acetabular labrum and iliofemoral ligament, which comprises part of the anterior hip joint capsule. The iliofemoral ligament extends inferiorly and folds up on itself. B. Area of thickness measure of the anterior hip joint capsule (Image drawn by M Fenech).
“Ultrasound can be used clinically as a substitute for MRI in assessing hip joint capsule thickness”
High-resolution ultrasound approach to quadrangular joint in carpal boss: Everything musculoskeletal sonographer should know
Why the review was performed
A carpal boss (CB) is a rare hypertrophied bony protuberance located on the dorsal aspect of the hand at the quadrangular joint (QAJ). Symptoms of CB may include pain, swelling and restriction of hand motion. Traditionally it is imaged with plain radiographs, computerised tomography (CT) or magnetic resonance imaging (MRI). Radiographs and CT may evaluate the osseous morphology of CB but may fail to adequately image the associated soft tissue changes. MRI is costly, timeconsuming, lacks dynamic imaging and may be contraindicated in a number of patients. Ultrasound has superior spatial resolution in the near field, is low cost, and allows real-time dynamic assessment as well as contralateral comparison and Doppler imaging.
The purpose of the review is to define the pathology spectrum around and within the QAJ in CB, highlighting the role of highresolution ultrasonography (HR-US) in its assessment, with emphasis placed on normal anatomy, a description of the examination technique and the pathological finding.
What the review described
The QAJ is the dorsal four-cornered articular space of the carpometacarpal (CMC) joints between the bases of the second and third metacarpals and the trapezoid and capitate. The QAJ has a close relationship with multiple soft tissue structures including the CMC ligaments, the insertions of extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) and the tendons of extensor indicis (EI) and extensor digitorum communis (EDC) to the index finger. An accessory ossicle called an os styloideum (OS) also occurs at the QAJ. The presence of OS in the QAJ region can alter the normal biomechanics of wrist joint motion, leading to the onset of degenerative osteoarthritis and the development of an overlying ganglion or bursitis.
CB may be classified as acquired (due to trauma and/or degenerative osteophytosis), congenital (due to the OS) or mixed (caused by a combination of trauma, osteophytes and OS). On examination, the CB appears as a firm, fixed prominence at the base of the second and/or third metacarpals. It is particularly noticeable when the wrist is flexed and is tender when local pressure is applied. Clinically, it is often difficult, if not impossible, to distinguish between CB and dorsal ganglia of the wrist.
A high frequency linear or small-footprint hockey stick probe is used. Copious amounts of gel used as a stand-off can minimise artefacts in the near field. Alternatively, a stand-off pad can be utilised.
Scanning over the palpable lump will demonstrate the presence of a cystic (ganglion) or bony (CB) abnormality. If the CB is congenital, the OS can be recognised, appearing as a distinct, tiny ossicle at the QAJ (Figure 1). If acquired, local osteophytes will present as spurs originating from the dorsal aspect of bones at QAJ. In the mixed type, HR-US shows a combination of both OS and local osteophytes.
Upon establishing the diagnosis of CB, HRUS can effectively detect any concomitant soft tissue pathology including effusion, synovial thickening, ganglion cyst or bursitis, tenosynovitis, or tendinopathy of ECRB, ECRL, or EPI/EDC. It is possible to observe a snapping phenomenon caused by EI and EDC of the index finger slipping/snapping over the CB when the wrist undergoes flexion extension and ulnar-radial deviation.
Reviewer: Andrew Grant
ASA SIG: Musculoskeletal
Authors: Corvino A, Ricci V, Cocco G, Delli Pizzi A, Tafuri D, Corvino F, Nevalainen MT, Chew FS, Mespreuve M & Catalano O
Journal: Journal of Clinical Ultrasound. J Clin Ultrasound
Open Access: Yes
Read the full article here
Figure 1. Ligaments that comprise the hip joint capsule demonstrated from the anterior and posterior approach (Image drawn by M Fenech).
High-resolution ultrasound approach to quadrangular joint in carpal boss: Everything musculoskeletal sonographer should know (continued)
Relevance to clinical practice
Given that CB clinically presents with a lump on the dorsum of the wrist, US is frequently employed as the initial imaging modality, leading to a conclusive diagnosis in most cases. The differential diagnosis of CB must be considered when no dorsal wrist ganglion is identified. HR-US is crucial in assessing the QAJ in CB and should increasingly assume a primary role compared to invasive or costlier modalities such as radiography, CT and MRI, which should be considered as second-level methods and retained for patients with an unfavourable outcome following conservative management or when surgical treatment is considered.
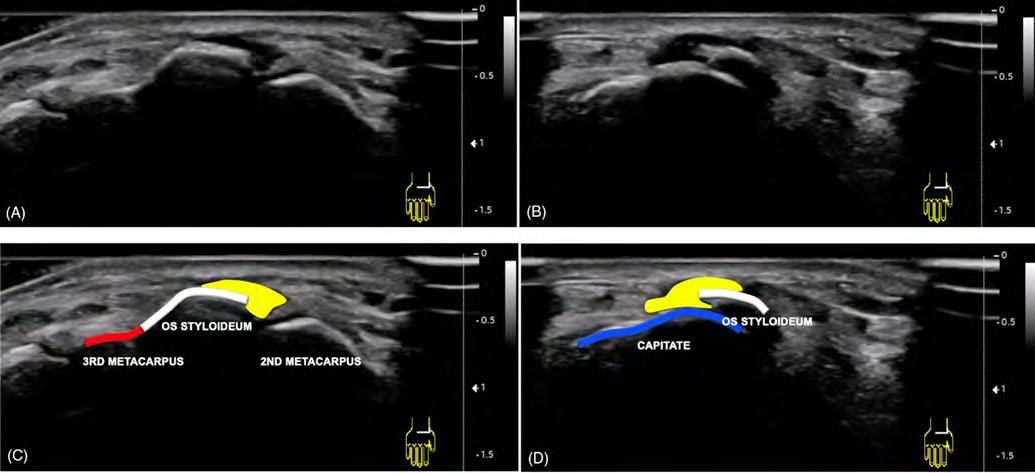
“US is crucial in assessing the QAJ in CB and should increasingly assume a primary role compared to invasive or costlier modalities such radiography, CT and MRI”
Figure 1. Axial high-resolution sonogram obtained using a 14.0 MHz linear transducer. (A, B) and corresponding schematic images (C, D) show an osseous protuberance that is fused to the base of the third metacarpal and extends over the capitate bone in keeping with an os styloideum. An overlying ganglion cyst is well demonstrated.
(C, D) Red, third metacarpal; blue, capitate; white, os styloideum; yellow, ganglion cyst.
The role of Doppler ultrasound in the evaluation of penile haemodynamics
– A sonographer’s guide to the documentation of vasculogenic erectile dysfunction
Why the guide was written
This guide aimed to educate sonographers, standardise the performance of penile Doppler ultrasound examinations and emphasise the importance of accurate diagnosis and management of vasculogenic erectile dysfunction (ED).
It provides a comprehensive guide for sonographers addressing this important aspect of men’s health, including describing the patient preparation, anatomy, physiology, interpretation of ultrasound findings and technical skills required to perform a penile Doppler ultrasound examination.
The author notes that there has been a decline in skilled sonographers who are capable of performing these examinations due to the introduction of oral phosphodiesterase inhibitors, which are used as the first-line treatment in the management of ED. These inhibitors are used to regulate blood flow and aid in muscle relaxation.
Due to this decrease in skilled professionals, there is a lack of a standard protocol for performing and interpreting the haemodynamics of penile Doppler ultrasound.
However, it is noted that despite the success of oral pharmacological treatment of ED, ultrasound remains an important assessment tool in postoperative patients, patients who have had pelvic trauma and those who don’t respond to oral phosphodiesterase inhibitors.
Key findings of the guide
The standout feature of the guide was the detailed recommendations provided for the interpretation of ultrasound findings. The guide notes that vasculogenic ED is the most common form of ED, and is primarily caused by disturbances in the arterial inflow and abnormalities in the veno-occlusive mechanism.
The guide serves as an excellent educational resource that describes five characteristic waveform stages of erection observed during penile Doppler ultrasound. These stages reflect the changes in penile blood flow and vascular dynamics as the penis transitions from a flaccid state to full erection and back to detumescence.
The author also describes the key ultrasound criteria for diagnosing vasculogenic ED, including assessment of the cavernosal artery peak systolic velocity, end-diastolic velocity and the resistive index.
Relevance to clinical practice
This guide is highly valuable, offering detailed guidance and recommendations for sonographers performing penile Doppler examinations. It is a thorough guideline that is a valuable resource for both new and experienced sonographers.
The author highlights growing evidence that suggests vasculogenic ED may be an early indicator of systemic vascular disease, which could make penile Doppler ultrasound a valuable tool for predicting future cardiovascular disease, allowing for early intervention and management. The author explains that penile arteries are smaller than the coronary arteries and therefore may show signs of disease earlier. This indicates that ED can precede the onset of more serious cardiovascular events like heart attacks and strokes due to the underlying endothelial dysfunction affecting the inner lining of blood vessels.
Both ED and cardiovascular disease significantly impact the quality of life. Addressing ED can not only improve men’s sexual health but also overall wellbeing and cardiovascular health. Improved accessibility and application of penile Doppler ultrasound could serve as an effective tool to diagnose disease. This guide serves as a significant step towards improving the diagnosis and treatment of vasculogenic ED, leading to enhanced quality of care and better patient outcomes.
GENERAL
Reviewer: Emma Jardine
ASA SIG: General
Author: Napier, D
Journal: Sonography
Open Access: Yes
Read the full article here
“Addressing erectile dysfunction can not only improve sexual health but also overall wellbeing and cardiovascular health”
Global trends in hepatocellular carcinoma epidemiology: implications for screening, prevention and therapy
Why the study was performed
Liver cancer is the sixth most commonly diagnosed cancer and the third most common cause of cancer-related deaths globally. Hepatocellular carcinoma (HCC), which accounts for more than 80% of liver cancers, is among the top three causes of cancerrelated deaths in 46 countries and among the top five in 90 countries. Primary prevention strategies offer the best hope of reducing HCC-related mortality, although surveillance for HCC can also improve patient outcomes by ensuring that the disease is detected at an early stage amenable to curative therapies.
How the study was performed
In this review, the authors discussed trends in the epidemiology of HCC and their implications for screening, prevention and therapy. A comprehensive literature review was undertaken.
What the review found
The incidence of HCC varies across regions of the world, owing to differences in the distribution of aetiological risk factors and access to screening and treatments for underlying liver diseases. HCC incidence is highest in Asia and Africa, with lower incidence in the Americas, Europe and the Middle East. More than 70% of all HCC cases occur in Asia.
The epidemiological shifts in the incidence of HCC from patients with virus-related liver disease to those with non-viral aetiologies, including alcohol-associated and metabolic dysfunction-associated steatotic liver disease, have important implications for prevention, surveillance and treatment. Hepatitis B vaccination and antiviral therapy for hepatitis B and C are effective for primary prevention of virus-related HCCs, but chemoprevention strategies for non-viral liver disease remain an unmet need. Emerging data suggest associations between aspirin, statins, metformin and coffee and reduced HCC incidence, although none has been proven to be causally related.
Secondary prevention of HCC via semiannual surveillance is associated with improvements in early detection and thus reduced mortality; however, current tools, including abdominal ultrasonography, have suboptimal sensitivity for the detection of early-stage HCC, particularly in patients with obesity and/or non-viral liver disease. From an imaging perspective, cohort studies from South Korea have suggested that two-phase low-dose CT and contrastenhanced MRI can yield superior sensitivity for early-stage HCC detection versus ultrasonography (83% and 86% versus 28–29%, respectively). However, the broad use of CT or MRI surveillance is limited by concerns over costs, radiology service capacity and potential safety risks (for example, owing to contrast and/or radiation exposure).
Although resection almost always results in complete removal of the initial tumour, HCC recurrence is common, particularly in those with multinodular disease, microvascular invasion and/or poorly differentiated tumours. Antiviral therapies are safe and can improve overall survival (OS). Although resection almost always results in complete removal of the initial tumour (or tumours), HCC recurrence is common (with 5-year rates of 50–70%), particularly in those with multinodular disease, microvascular invasion and/or poorly differentiated tumours. Antiviral therapies are safe and can improve OS in patients who have previously undergone locoregional treatment for virus-related HCCs, including resection, although the effect on short-term HCC recurrence patterns is less clear. Other adjuvant therapies failed to show a benefit in improving RFS, with the exception of the aforementioned regimen consisting of atezolizumab plus bevacizumab for up to 1 year. The improvement in postoperative recurrence observed with this regimen might prompt some centres to consider the use of surgical resection in patients previously deemed to have an unacceptably high risk of recurrence.
GENERAL
Reviewer: Marilyn Zelesco
ASA SIG: General
Authors: Singal A, Kanwal F & Llovet J
Journal: Nature Reviews Clinical Oncology
Open Access: No
Read the full article here
Global trends in hepatocellular carcinoma epidemiology: implications for screening, prevention and therapy (continued)
Relevance to clinical practice
HCC is one of the few cancers with rising incidence and increasing mortality globally. Shifts in epidemiological patterns among at-risk patients, most notably an increasing proportion of HCCs with nonviral aetiology, have important implications for primary prevention, surveillance and treatment. Unmet needs include proven chemoprevention and effective surveillance strategies in patients with non-viral liver disease, although ongoing studies are investigating promising interventions in both areas. Surgical therapies, when applicable, still provide the best long-term survival outcomes for patients with HCC, although the introduction of ICI-based regimens has substantially improved OS for patients with advanced-stage, unresectable tumours. Sonographers should be cautious when scanning patients at risk of HCC to ensure small, early lesions are not missed.
“… HCC is one of the few cancers with rising incidence and increasing mortality globally …”
The ability for teaching self-efficacy by clinical preceptors in diagnostic medical sonography
CLINICAL SUPERVISORS
Reviewer: Deanne Chester,
AFASA
ASA SIG: Clinical Supervisors
Author: Peak K
Journal: Sage Journals
Open Access: No
Read the full article here
Why the study was performed
Most clinical trainers are experienced clinicians; however, this does not equate to the skills needed to teach effectively. This research aimed to investigate the level of perceived self-efficacy of clinical tutors (preceptors) teaching sonography students and to determine if there is a difference in selfefficacy between those preceptors who had received teaching training and those who had not. Albert Bandura’s concept of self-efficacy is defined as an individual’s belief in their ability to act in the ways necessary to succeed in specific situations,[1] and consequently plays an important role in how we approach a task, goal, or challenge.
How the study was performed
A survey called the Sonography Preceptor Teaching Self-Efficacy Inventory (SPTSEI) was used to obtain quantitative data to address the aim of the study. The SPTSEI was based on two existing surveys, which were adapted with permission. A Qualtrics survey of 45 questions on a 10-point Likert scale was created and information was sought in relation to perceived ability in three areas: effective teaching; evaluation of student performance; and interpersonal relations.
Participants were clinical preceptors of sonography students enrolled in United States bachelor’s degree courses accredited by the Commission on Accreditation of Allied Health Education Programs (CAAHEP). The preceptors were invited to complete the SPTSEI via program directors of the sonography course providers including general, vascular and cardiac programs. There were 44 participants of varying ages, sonographic experience, qualification level, and time spent as a preceptor. Seventy-five per cent of the participants had received no training or professional development to prepare for their role as preceptors. The small number of participants was an acknowledged limitation to this study.
What the study found
Research question 1 found that most of the sonography preceptors surveyed had high self-efficacy levels with respect to the three areas of ability. Given most had no training, this is interesting as research indicates assurance in teaching is limited without some knowledge of learning theories and processes. Research question 2 findings correlated with the literature: formal preparation for a training role has a positive impact on self-efficacy levels. Preceptors are better able to perform their role if they can undertake formal training in educational concepts and strategies, which in turn has a direct influence on student achievements.
Relevance to clinical practice
While the study suggests sonographer preceptors have high self-efficacy in their abilities, without appropriate training this is unlikely to include evidence-based best practice. Professional development as a minimum would help to ensure reliable teaching approaches and consistent clinical practices are being experienced. Participants, regardless of whether they had undergone preceptor training, agreed with the literature that training in education for preceptors improves student outcomes and the entire experience for tutor and student. The author calls for faculty to partner with clinical supervisors to facilitate this training to benefit the sonographer community long term as a high priority. To bring this into the Australian context, the provision of specific training for tutor sonographers may be a future consideration for ASAR sonographer course accreditation.
Bandura A (1977). “Self-efficacy: Toward a unifying theory of behavioral change”. Psychological Review 84 (2): 191–215.
“A prepared and confident clinical preceptor will possess a higher level of teaching self-efficacy and will be better prepared to affect learning in their students through their teaching abilities”
Common models and approaches for the clinical educator to plan effective feedback encounters
CLINICAL SUPERVISORS
Reviewer: Jenny Parkes, FASA
ASA SIG: Clinical Supervisors
Authors: Orsini C, Rodrigues V, Tricio J and Rosel M
Journal: Journal of Educational
Evaluation for Health Professionals
Open Access: Yes
Read the full article here
The purpose of this paper
Giving feedback to a student or colleague can be very intimidating, even for those with some experience. This article reviews the wellevidenced methods and models for doing this. The paper aimed to outline common feedback models and assess how they can be used in the workplace.
What the review described
The author acknowledges that giving meaningful feedback is a learnt skill that can be developed. This article reviews the six most common feedback models that can be used in different clinical situations with each clearly summarised. The accompanying table offers a succinct outline of the strengths and weaknesses of each model, stating which approach is best suited for the different learning situations. The table was designed to be a useful resource for clinical educators.
In addition, the review discusses the use and difference between micro-feedback, informal or unplanned encounters of 1–5 minutes and macro-feedback, formal or planned encounters of 5–20 minutes.
The six feedback models are:
1. The Feedback Sandwich: Named due to the two doses of positive/reinforcement feedback with one dose of critical/corrective feedback sandwiched between to make it more palatable and acceptable. This is brief and structured for the inexperienced educator; however, it does not provide the opportunity for learner input.
2. Pendleton Rules: This model is a modification of the Feedback Sandwich. The educator’s comments are preceded by the learner’s reflections on what was good about their performance, and what were the areas for improvement.
3. One-Minute Preceptor: Useful in microfeedback encounters and busy clinical settings, the model aids the development of clinical reasoning and decision-making skills.
4. SET-GO: This model is beneficial for feedback in group encounters and encourages peer feedback; however, it
requires the time and expertise of the educator.
5. R2C2: Developed to give assessment- and performance-based feedback rather than based on daily practice or specific rostered periods. The model has a learner-centred process, requiring high level expertise of the educator in feedback provision.
6. ALOBA: Aims to establish a learnercentred conversation or interview-type feedback guided by the learners’ agenda and needs to be complemented by the educators’ view. High feedback skills and judgement are required.
Relevance to clinical practice
While the article does not apply specifically to the sonography profession, the principles of providing effective feedback are universal. As a clinical supervisor or tutor sonographer, it is important when giving feedback, irrespective of the model utilised, to establish a safe environment for the feedback encounter, base feedback on direct observation in a balanced manner (including details on what and how the learner is or is not doing to achieve their goals), provide feedback in a timely manner and check for understanding and acceptance of the feedback. Furthermore, an action plan should be agreed upon with appropriate documentation of the encounter.
This article provides an excellent review of evidence-based models for educators, providing feedback to learners, which can be readily applied during the training of sonographers by supervisors or tutor sonographers in clinical practice.
“Undoubtedly, giving (and receiving) constructive feedback is crucial for learners to bridge the gap between their current performance and the desired standards of competence”
Sonographers’ perspectives on research – A worldwide online questionnaire study
Reviewer: Assoc Prof Tristan Reddan, FASA
ASA SIG: Research
Authors: Pedersen MRV, Kraus B, Santos R, Harrison G
Journal: Radiography
Open Access: Yes
Read the full article here
Why the study was performed
The study aimed to understand sonographers’ perspectives on research. The authors recognised sonographers’ important role in research translation and implementation into clinical practice, which leads to improved patient outcomes.
How the study was performed
A cross-sectional online questionnaire was distributed via social media and research networks that the authors were involved with, over two months in 2023. After piloting with seven European sonographers in 2022, the final survey contained 21 open and closed questions. Sonographers worldwide were able to participate.
What the study found
Responses from 165 sonographers were mostly from Europe (66.1%), Africa (13.3%), and Oceania (11.5%) (Figure 1). Only 32% of respondents had performed research, while 68.5% desired more involvement. Reported research experience mostly involved the conduct of clinical examinations (42.2%) for studies. Most reported prior involvement was in quantitative studies (34.4%), while investigations into the safety of ultrasound were the lowest (10.3%). The largest proportion of respondents were from large hospitals (43.3%) with varied lengths of experience. Nearly 35% identified as sonographers despite the title not being protected in their country, some were classified as ultrasound-reporting radiographers. Most respondents hadn’t published (55.9%), though some had submitted to peer-reviewed journals (31.5%) or presented at conferences (28.7%), or locally (25.9%). Lack of time (43%), funding (30.3%), administrative (26.7%) and management (21.8%) support were the most reported barriers to participation. The top motivators for better engagement included opportunities to tackle identified problems (65.5%), develop new skills (61.2%), improve job satisfaction (59.4%), and face an intellectual challenge (57.0%).
Relevance to clinical practice
The findings align with existing literature on sonographers’ attitudes towards research,[1] identifying an underlying interest but lack of experience in research among sonographers. Sonographers have a responsibility to engage with research to improve the practice, and it is also important for workplaces to value a research-driven culture to help overcome some of those identified barriers like administrative or management support. It is often curious sonographers who view research as a means to overcome a problem or implement an improvement who will gravitate towards research.
The relatively small response size of the study limits generalisability, particularly here in Oceania. There are valuable points discussed that can help us better understand some of the perceived barriers and enablers to research for sonographers that may help influence workplace culture and future policy direction.
“There are valuable points discussed which can help us better understand some of the perceived barriers and enablers to research for sonographers, that may help influence workplace culture, and future policy direction”

Figure 1. Overview of the respondents’ countries of origin (used with permission).
McLean G, Lewis A. Building research capacity in ultrasound departments. Sonography. 2024 Sept 9;11(3): 287–9.
Barriers to reporting guideline adherence in point-of-care ultrasound research: a cross-sectional
survey of authors and journal editors
Why the study was performed
The Enhancing the Quality and Transparency of Health Research (EQUATOR) Network publishes reporting guidelines for a variety of different research methods (equatornetwork.org).[1] Reporting guidelines were borne of a desire for honest, appropriate, and transparent reporting of findings for the benefit of patients.[2] One such guideline is the Standards of Reporting of Diagnostic Studies (STARD), most recently published in 2015. The STARD guidelines are a list of items that should be included in manuscripts reporting diagnostic accuracy studies that generally adhere to the IMRaD framework (Introduction, Methods, Results, and Discussion). Given the role sonography plays in diagnostic imaging, these guidelines are particularly relevant to sonographers when reporting or reading research findings. Many journals encourage but do not mandate the use of the guidelines. With the proliferation of point-of-care ultrasound (PoCUS), there have been a proportionate number of diagnostic accuracy studies into the utility of PoCUS in various clinical settings. The authors of this study sought to determine the barriers to adhering to the STARD guidelines in the PoCUS literature.
How the study was performed
Two online surveys were used for data collection. One was sent to the authors (first and corresponding) of published diagnostic accuracy manuscripts, and the other to the editors-in-chief of the journals in which these articles were published. Publications between 2016 and 2019 were included and identified in a previous study in an acute care setting.[3] The surveys sought responses to the respondents’ knowledge, attitudes, and behaviours related to adherence to the STARD 2015 guidelines.
What the study found
Response rates were 26% (18/69) and 24% (5/21) for authors and editors, respectively. Most (67%) investigators were aware of STARD 2015. All respondents agreed incomplete reporting limited generalisability and assessment of bias. STARD being limited
to only English language submissions, and the time required to adhere to the guidelines were perceived as barriers by authors. Authors and editors both reported that peer reviewers should be responsible for complete reporting. Only one editor reported returning submissions to authors without an accompanying STARD checklist.
Relevance to clinical practice
While the study’s focus is PoCUS, this is readily generalisable to sonographers as some of us work in this professional domain, and we should be aware of the accuracy of PoCUS in developing disciplines in our respective systems. The study highlights the importance of complete reporting to prevent bias and permit the generalisability of results. Those sonographers engaged in peer review should be aware of their responsibilities in relation to reporting guidelines.
Reviewer: Assoc Prof Tristan Reddan, FASA
ASA SIG: Research
Authors: Prager R, Gagnon L, Bowdridge J, Unni RR, McGrath TA, Cobey K, Bossuyt PM & McInnes MDF
Journal: BMJ Evidence-Based Medicine
Open Access: Yes
Read the full article here
1. Altman DG, Simera I. A history of the evolution of guidelines for reporting medical research: the long road to the EQUATOR Network. J R Soc Med. 2016 Feb 15;109(2): 67–77.
2. Rennie D. A tribute to Douglas G. Altman, DSc. JAMA – J Am Med Assoc. 2019 Apr 23;321(16): 1621.
3. Prager R, Bowdridge J, Kareemi H, Wright C, McGrath TA, McInnes MDF. Adherence to the Standards for Reporting of Diagnostic Accuracy (STARD) 2015 Guidelines in Acute Point-of-Care Ultrasound Research. JAMA Netw Open. 2020 May 1;3(5): e203871–e203871.
“The study highlights the importance of complete reporting to prevent bias and permit generalisability of results”
Artificial intelligence in breast ultrasound: application in clinical practice
EMERGING TECHNOLOGIES
Reviewer: Lisa McGuire, AFASA
ASA SIG: Emerging Technologies
Authors: Brot H, Mango V
Journal: Ultrasonography
Open Access: Yes
Read the full article here
Why the study was performed
Ultrasound (US) has enormous clinical potential and economic benefits in diagnosing breast lesions when compared to other imaging modalities. This review explores the current applications of artificial intelligence (AI) in US and its potential impact on clinical practice. It discusses the impact of AI on clinical workflow and breast cancer detection, classification and diagnosis. This article also highlights the potential significance of AI in breast US for underserved areas.
How the study was performed
AI is a broad term encompassing various technologies, including machine learning (ML), deep learning (DL) and computeraided detection (CAD). Radiologists rely on qualitative visual assessment to characterise breast lesions. AI technologies analyse vast amounts of imaging data, hence assisting radiologists in identifying abnormalities and predicting outcomes, optimising the diagnostic process.
CAD is a commercially available AI software; however, there are a number of iterations. In general terms, once the lesion is identified as a region of interest, the CAD component generates a numerical assessment of the region. The software provides a BI-RADS category based on shape, orientation, margin, echo pattern and posterior features.
One DL AI model excelled in distinguishing between triple-negative breast cancer and other subtypes, significantly improving the accuracy, sensitivity, and specificity of four radiologists. The convolutional neural network multi-modal was developed by Zhou et al. and trained on combined grayscale US images together with colour Doppler and shear wave elastography features. This model surprisingly also outperformed core needle biopsy.
Another study investigated AI and deep learning radiomics (DLR) using US images in patients undergoing neoadjunctive chemotherapy (NAC). Jiang et al. developed a novel preoperative pathological complete response (pCR) prediction model, which is based on pre- and post-NAC US images, showing an AUC of 0.94 (95% CI, 0.91 to 0.77), outperforming two experienced
radiologists. Additionally, Gu et al. prospective study used two post-treatment time points to assess response to NAC. This stepwise prediction DLR model successfully identified 90% of non-responders, triaging them to a different treatment strategy.
A predictive model of lymph node metastasis in patients with breast cancer using DL was developed by Zhou et al. The best-performing CNN model was superior to a consensus of five radiologists, achieving a higher sensitivity of 85%.

What the study found
Image analysis and interpretation algorithms have the potential to automate the detection of breast lesions in US images. This paper reports sensitivity and specificity comparable to that of experienced radiologists.
The review shows the adjunct of CAD enabled faster and more accurate interpretations.
The paper states AI can assist in differentiating between benign and malignant lesions, analysing features such as shape, margin and echogenicity. Large DL models have been trained on large data sets to recognise patterns and characterisation of lesions that may indicate malignancy, providing additional diagnostic support.
Figure 1. B-mode ultrasound images of a breast mass (indicated by the red box), where the artificial intelligence displayed a high score of lesion characteristics.
Artificial intelligence in breast ultrasound: application in clinical practice (continued)
Relevance to clinical practice
The integration of AI into breast US has the potential to improve clinical outcomes through enhanced diagnostic accuracy. This review suggests AI can reduce unnecessary biopsies and, in turn, patient anxiety.
Despite the promise of AI in breast US shown in this review, several challenges remain: data quality and bias; AI models are heavily dependent on data quality and diversity of training. Inadequate datasets can lead to biased algorithms. It is also challenging to successfully integrate AI tools into existing workflows.
Most importantly, AI may improve access to healthcare and bring radiology services to underserved areas with few or no radiologists; however, further prospective studies are necessary to comprehensively assess the influence of AI in real-world clinical settings.
“An excellent diagnostic performance was obtained by the AI tool detecting malignant breast lesions with a sensitivity of 100% and specificity of 86%”
The performance of ChatGPT-4.0o in medical imaging evaluation: a cross-sectional study
EMERGING TECHNOLOGIES
Reviewer: Dr Jacqui Roots
ASA SIG: Emerging Technologies
Authors: Arruzza E, Evangelista C, Chau M
Journal: Journal of Educational Evaluation for Health Professions
Open Access: Yes
Read the full article here
Why the study was performed
A large aspect of the medical imaging profession is the evaluation of image quality and optimisation to allow for accurate diagnosis. ChatGPT-4.0o has a new feature that allows the user to upload an image for evaluation. This study investigated the accuracy of the AI’s evaluation of medical images, specifically radiographs. The authors aimed to compare the ChatGPT’s evaluation of a radiograph’s quality and positioning.
How the study was performed
Radiographs of the knee, elbow, ankle, hand, shoulder and pelvis of phantoms were used in this study. The authors created and uploaded a variety of correct and suboptimal images to ChatGPT and entered a prompt. The AI was asked “(1) to identify positioning error(s), (2) to explain the error using specific and relevant anatomical terminology, and (3) to provide a suitable radiographic method to enhance the positioning”. The answer generated was evaluated, scored and graded based on the number of errors that were correctly or incorrectly identified, as well as the presence or absence of a justification and if corrections were offered by the AI.
What the study found
The answers generated by ChatGPT-4.0o correctly recognised all errors as well as suggested improvements in 20% of cases. In almost 27% of cases, ChatGPT either could not recognise errors or incorrectly identified an error in an optimal image. The authors have demonstrated that the current ChatGPT4.0o has low accuracy in the evaluation of radiographs. While additional information and prompts provided to the AI may have increased the accuracy, there is a lot of growth required before it may eventually be used as an educational or assistive tool.
Relevance to clinical practice
From an educational point of view, the new feature of ChatGPT to evaluate medical images may be able to provide information on image quality and positioning errors. This could assist students in correcting their basic errors and increase confidence in image optimisation. For experienced staff, this feature may be useful when asked to complete an unusual or uncommon view. Currently, ChatGPT only provides low accuracy in its image evaluation and provision of corrections.
“The phantoms were purposely positioned to include a range and spectrum of positioning errors, including radiographs that were optimally positioned”
Ultrasonography of pediatric superficial soft tissue tumors and tumor-like
lesions
Reviewer: Madonna Burnett
ASA SIG: Paediatrics
Authors: Kim H, MD, Yoo S, Oh S, Jeon T, Kim J
Journal: Korean Journal of Radiology
2020
Open Access: Yes
Read the full article here
Why the study was performed
This article was written to provide insight into the many different types of paediatric superficial soft tissue tumours and tumourlike lesions. Ultrasound is usually the first examination performed to look at these palpable or visible areas of concern in a paediatric patient. Along with clinical assessments such as age on presentation, clinical course, and any visible skin discolouration, ultrasound can provide detailed information about the lesion’s location and characterisation (solid vs cystic, vascularity, compressibility). Sufficient knowledge of the normal anatomy is also required. This article reviews the techniques used and what information can be discovered about superficial, soft tissue lesions in children.
What the paper looked at
It is necessary to clinically assess the lesion before scanning and ask for relevant clinical details such as when the lesion appeared, any size increase/decrease, and/ or discolouration or other symptoms.
Ultrasound technique was discussed. Superficial lesions should be examined with a high frequency linear transducer and parameters set appropriately. A gel standoff or excess ultrasound gel can be applied so as not to compress/distort the lesion. Echogenicity, compressibility and vascularity are all assessed. Spectral Doppler recorded for vessels with velocities and resistive index performed when necessary.
The article then discusses all the different types of superficial soft tissue tumour-like lesions and tumours.
What the study found
Superficial soft tissue lesions/tumours may be any of the following:
1. Vascular anomalies – these can be broken into vascular tumours and vascular malformations. Vascular tumours include infantile haemangioma, congenital haemangioma, tufted haemangioma and lobar capillary haemangioma. Vascular malformations are categorised
histologically into lymphatic, capillary, venous, arteriovenous, or mixed malformations
2. Adipocytic tumours and other fatcontaining mass-like lesions – lipomas, lipoblastomas and subcutaneous fat necrosis
3. Fibroblastic and myofibroblastic lesions – such as nodular fasciitis, fibrous hamartoma, pericytic (perivascular) tumours such as infantile myofibroma and myofibromatosis
4. Neurogenic lesions – peripheral nerve sheath tumours, schwannomas, neurofibromas, malignant peripheral nerve sheath tumours and giant cell tumours of tendon sheath (fibrohistiocytic tumour)
5. Other benign lesions, such as ectodermal inclusion cysts, pilomatricoma, dermoid/epidermoid cysts and ganglia
6. Malignant soft tissue tumours –rhabdomyosarcoma, synovial sarcoma, infantile or congenital fibrosarcoma, subcutaneous panniculitis-like T-cell lymphoma. Multiple, subcutaneous nodules in neonates and infants should raise a concern for underlying malignancy. All the above-mentioned pathologies are discussed in detail with ultrasound and clinical findings.
Relevance to clinical practice
Ultrasound is frequently used as an initial workup of paediatric superficial soft tissue tumours and tumour-like lesions. Ultrasound can provide a specific diagnosis in certain pathologies and in others narrow the differential diagnosis. Lesions may need additional imaging or biopsy. Knowledge of ultrasound techniques and key imaging findings of these lesions in children will facilitate establishing the correct diagnosis and guiding management of the patient.
“Sufficient knowledge of the normal anatomy, proper ultrasonographic techniques, and the imaging findings of common and uncommon soft tissue lesions in children are crucial for accurate assessment and management of patients”
