About Sheltering Arms Institute

VISION
Reinventing rehabilitation for life beyond limits
HISTORY
MISSION
Sheltering Arms Institute, a national leader in the science of rehabilitation, delivers personalized care in an environment that supports recovery and restores possibility through the integration of collaborative science and research, inter-professional education, community engagement, and stewardship.
VALUES
Courage, Integrity, Positivity, Community, Discovery, and Accessibility
In 2016, Sheltering Arms and VCU Health System announced plans for a new, state-of-the-science physical rehabilitation hospital in Goochland County, Virginia called Sheltering Arms Institute, a collaboration with VCU Health. In 2017, the two parent organizations’ application for a certificate of public need was approved to combine 68 beds from Sheltering Arms’ two former inpatient facilities and 46 beds from the former inpatient facility operated by VCU Health System.
In June 2020, Sheltering Arms Institute opened its doors to provide care for individuals who have experienced strokes, spinal cord injuries, brain injuries, and limb loss, as well as those in need of general rehabilitation for various traumatic injuries, neurological diseases and disorders, and orthopedic or metabolic conditions. The Institute blends advanced technology, research, and evidence-based clinical care to create an innovative, transdisciplinary model of rehabilitative care that facilitates superior outcomes for patients.
As a nonprofit, 501(c)(3) organization, Sheltering Arms Institute provides a comprehensive array of physical rehabilitation services, including:
• Physician, nursing, and psychology services
• Physical, occupational, and speech therapy, including upper- and lower-extremity and assistive technology specialists
• Therapeutic recreation
• Music therapy
• Care management
• Chaplaincy
• Nutrition and dietary counseling
• Community engagement services
Sheltering Arms Institute also continually develops research and education programs intended to enhance functional outcomes for patients while training future generations of rehabilitation professionals.
SHELTERING ARMS INSTITUTE ADMISSIONS
Fiscal Year 2022 (October 1, 2021 to September 30, 2022)
Fiscal Year 2023 (October 1, 2022 to September 30, 2023)
*Sheltering Arms Institute began offering outpatient services July 1, 2022
SHELTERING ARMS INSTITUTE CONSOLIDATED FINANCIAL SUMMARY
Fiscal Year 2022 (October 1, 2021 to September 30, 2022)
Fiscal Year 2023 (October 1, 2022 to September 30, 2023)
Fiscal Year 2024 (October 1, 2023 to September 30, 2024)
Fiscal Year 2024 (October 1, 2023 to September 30, 2024)
Net Patient Revenue (Audited financial statement) $65,073,000 $79,612,000 $82,855,000
Estimated Community Benefit – Schedule H*
*Including unpaid costs of Medicare and Medicaid
Community Health Needs Assessment (CHNA) Background
The primary purpose of the Sheltering Arms Institute Community Health Needs Assessment (CHNA) process is to further address the health and wellness needs of individuals in the Central Virginia community within the general scope of physical rehabilitation.
The impetus for the CHNA process was the Patient Protection and Affordable Care Act (2010), which included a new Section 501(r)(3) in the Internal Revenue Service (IRS) Tax Code that requires charitable hospitals to conduct a CHNA that addresses the hospital’s community needs. Sheltering Arms Institute is pleased to submit this CHNA, both as a matter of compliance with Section 501(r)(3) and as an obligation to those we serve. As an organization, we have taken this change in law as an opportunity to improve our community service and continuously focus on meeting the changing health care needs of our community. Specifically, tax-exempt hospitals must:
1. Conduct a CHNA at least once every three years, integrating input from community stakeholders; 2. Adopt an Implementation Strategy (IS) to meet the community health needs identified through the CHNA; and 3. Complete a Community Health Impact Report (CHIR) on the most recently conducted CHNA and most recently adopted IS, including feedback from the community that the hospital serves to better inform future CHNAs and Implementation Strategies, to have a meaningful exchange over time between the hospital and the community it serves to improve community health.
The 2025 CHNA Report is the hospital’s second triennial report. The CHNA process undertaken in 2025 and described in this report was conducted in compliance with current federal requirements.
Part I: Community Health Needs Assessment
Section 501(r)(3) provides the following guidance on conducting a CHNA. The hospital facility must:
• Define the community it serves and assess the health needs of that community;
• Consider input from persons who represent the broad interests of their community, including those with special knowledge of or expertise in public health; and
• Assess and address the needs of the medically underserved, low-income, and minority populations in the areas it serves.
Sheltering Arms Institute’s Definition of Community Served
Sheltering Arms Institute identified the community we serve as all adolescents and adults with physical and/or cognitive disabilities as well as their caregivers who reside within the eight cities/counties of the Richmond Metro area surrounding Sheltering Arms Institute’s main hospital campus: City of Richmond, Henrico County, Chesterfield County, Hanover County, Powhatan County, Goochland County, New Kent County, and Charles City County.
The rationale for this definition is as follows:
1. Sheltering Arms Institute is a specialty hospital focused on providing physical rehabilitative care to individuals who have experienced a wide range of physical and/or cognitive disabilities and supporting their caregivers.
In the last three fiscal years, the hospital has provided inpatient physical rehabilitation services to patients with the following diagnoses specifically:
Discharges by Diagnosis Group
Rehab Impairment Category (RIC) Group
Year 2022 (October 1, 2021 to September 30, 2022)
Year 2023 (October 1, 2022 to September 30, 2023)
Year 2024 (October 1, 2023 to September 30, 2024)
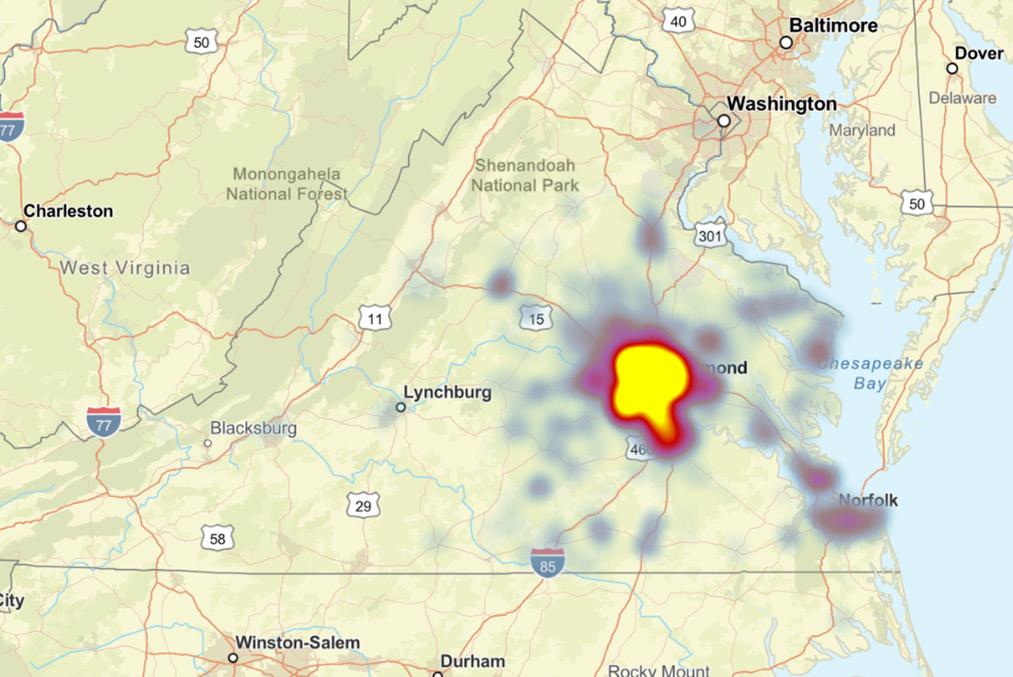
2. Sheltering Arms Institute is a nationally ranked hospital that serves individuals from across the United States; however, the hospital is located in Richmond, Virginia and approximately 70% of individuals cared for through our inpatient rehabilitation hospital are discharged to the Central Virginia region. By defining the community geographically within these eight cities/counties, we will be able to develop more meaningful implementation strategies to benefit our community.
Counties served:

Assessing the Health Needs of the Community: Process and Methodology
SURVEY CREATION
An 8-minute online survey was created to assess the health needs of the community, as defined below. The content of the survey was based on broad community health data from the following sources, with narrowing of the scope of the survey questions such that they aligned and are consistent with the mission of Sheltering Arms Institute: National: Healthy People 2030 “sets data-driven national objectives to improve health and well-being over the next decade” (health.gov/healthypeople). There are specific objectives related to people with disabilities (health.gov/ healthypeople/objectives-and-data/browse-objectives/people-disabilities).
State: The Partnership for People with Disabilities (partnership.vcu.edu) is a center within Virginia Commonwealth University’s School of Education. Its mission is to “partner with people with disabilities and others to build communities where all people can live, learn, work, and play together.” The Partnership administers several community living and health programs (partnership.vcu.edu/programs/community-living) (partnership.vcu.edu/programs/health), in addition to education and training opportunities for people with disabilities, families, providers, and students (partnership.vcu.edu/ education-and-training).
Furthermore, the Partnership publishes a Virginia Disability Status Report by Cornell University, which is based on Virginia’s data from the US Census Bureau’s American Community Survey (disabilitystatistics.org/report/2023/VA).
Local: The Virginia Department of Health—Office of Minority Health and Health Equity—developed the Virginia Health Opportunity Index (HOI) to help communities understand the many factors determining health (data.virginia.gov/ dataset/health-opportunity-index). Factors include, but are not limited to, community walkability, food accessibility, affordability, income inequality, and access to care.
See Appendix A for a copy of the survey.
Figure 1: Heat map of Sheltering Arms Institute inpatient discharges July 2024 – July 2025
METHODOLOGY
To take into account input from persons who represent the broad interests of the community we serve, including those with special knowledge of or expertise in public health, primary data were collected via surveys and structured interviews. The surveys were completed by consumers and health professionals between January 13 and February 7, 2025; the structured interviews were conducted with regional public health department officials between April 23 and May 29, 2025.
Survey Distribution
The survey was administered online via a consumer web panel to a random sample of 300 individuals in the general population of the Greater Richmond region. These individuals reside within the Central Virginia area, including the following cities/counties that Sheltering Arms Institute serves: Chesterfield, Henrico, City of Richmond, Hanover, Prince George, Petersburg, Powhatan, Dinwiddie, Goochland, New Kent, Colonial Heights, Charles City, and Hopewell. General population data were weighted by age, gender, race/ethnicity, education, and region according to U.S. Census Bureau Current Population Survey (CPS) statistics. Since this group of individuals surveyed were a random sample of the general population, they may or may not have knowledge of or an affiliation with Sheltering Arms Institute.
The same online survey was duplicated to create a second unique URL to administer via email and social media to individuals who are familiar with and/or have a relationship with Sheltering Arms Institute in some capacity (i.e., current or former patients, caregivers, team members, donors, or board members). Signs with QR codes leading to the survey were also placed throughout Sheltering Arms Institute’s eight locations for individuals to scan and complete the survey on their smartphones. Individuals in need of assistance or who did not have a smartphone were provided access to an iPad and support from a team member to complete the survey.
At the start of the survey, three screening questions served to:
1. Filter out individuals who are not classified as healthcare decision makers (those under age 26)
2. Filter out those who reside outside of the community
3. Classify respondents into the following two audiences:
a. Consumers, including current and former patients
b. Healthcare professionals
Information Gaps
Sheltering Arms Institute did not receive input directly from all members of the low-income, minority, and medically underserved populations in our community, instead obtaining input from a representative sample (see Appendix B), as well as organizations that work with those individuals on a daily basis. Although we are unable to identify any specific information gaps, we recognize that members of those populations may have provided different information if they directly participated. Additionally, we recognize that other individuals who were not invited to participate may have provided different input.
Survey Results:
• Individuals age 26+
• Reside in Greater Richmond area, including the following cities/ counties: Chesterfield, Henrico, City of Richmond, Hanover, Prince George, Petersburg, Powhatan, Dinwiddie, Goochland, New Kent, Colonial Heights, Charles City, and Hopewell
• Mix by race/ethnicity, gender, income, age, and education
Survey Results Continued:
Survey Administered to:
Sheltering Arms Institute Community
• Current or former patient
• Caregiver of current or former patient
• Donor
• Employee
• Board member
• Current or former fitness member
• Caregiver of current or former fitness member
Community Free Clinics, Disease-Specific Associations, and Community Partners
• Organizations serving individuals in the cities/counties from which the majority of Sheltering Arms Institute patients reside
Sheltering Arms Institute and Sheltering Arms Community Programs Team Members
• Physicians, therapists, nurses, care managers, exercise physiologists, community liaisons, administrative staff, etc. who care for and interact with people with disabilities
Structured Interviews Conducted With:
Public Health Departments
• Those departments in the cities/counties from which the majority of Sheltering Arms Institute patients reside
Number of Respondents
231
Total Respondents:
See Appendices B and C for survey result data.
45 respondents from organizations, including:
• 1-800-Medicare
• A private urgent care company
• ABM
• Above and Beyond Home Healthcare
• Alternative Adult Care
• Bon Secours
• Brandermill Woods
• Center for Neurorehabilitation Services
• Circle Center Adult Day Services
• Community Recreation
• Covenant Woods
• Crossover Healthcare Ministry
• Datavant
• Dermatology
71
• Foundation for Rehabilitation Equipment Endowment (F.R.E.E.)
• GoochlandCares
• Haleon Healthcare
• Hospital Corporation of America (HCA) Healthcare
• Integrated Health Services (IHS)
• Morrisons
• New Growth Behavioral Health
• Public Partnership
• Sentara Health
• Sportable
• The SPAN Center
• UnitedHealth Group
• Virginia Commonwealth University (VCU) Health
Number of Respondents
8 respondents from the following cities/counties:
• Chesterfield Health District: Chesterfield County Powhatan County
• Chickahominy Health District: Goochland County Hanover County New Kent County Charles City County
613
• Henrico Health District: Henrico County
• Richmond City Health District: Richmond City
Part II: Implementation Strategy
The second component of the CHNA process is the development and adoption of an Implementation Strategy (IS). According to Section 501(r)(3), the hospital facility must:
• Include a prioritized description of the significant health needs of the community identified though the CHNA, along with a description of the process and criteria used in prioritizing these health needs
• Include a description of the potential measures and resources identified through the CHNA to address the significant health needs by:
Addressing a health need identified through a CHNA if the written plan either: (1) describes how the hospital facility plans to meet the health need, or (2) identifies the health need as one that the hospital facility does not intend to meet with an explanation as to why the hospital facility does not intend to meet the health need; Identifying the programs and resources the hospital facility plans to commit to address the health need; and Describing, in addition to the actions the hospital facility intends to take to address the health need, the anticipated impact of these actions and the plan to evaluate such impact.
Significant Health Needs Identified
Survey and interview results were grouped into two categories: greatest needs and greatest barriers.
• Mental health services
• Medication
• Transportation for medical appointments
• Inability to pay for services
• Lack of insurance/inadequate insurance
• Transportation challenges
The abbreviated results from the 613 surveys are above; full results can be found in Appendices B and C.
Significant Health Needs Prioritized
Sheltering Arms Institute prioritized the health needs of the community based on the volume of responses for each need and by considering the feasibility of addressing each need as well as the impact our hospital—along with our community partners—could have to meaningfully impact the identified needs. Based on these considerations, the top community health need priorities for Sheltering Arms Institute are:
Potential Measures and Resources to Address Prioritized Health Needs
Sheltering Arms Institute plans to address the top community health need priorities, as described below:
Mental Health
Implementation Strategy
Continue to offer rehabilitation psychology services to patients participating in inpatient rehabilitation at Sheltering Arms Institute
As a standard of care at discharge, continue to refer appropriate and interested patients to outpatient psychology services
Update existing mental health resource guide twice annually and continue to house on our website/ distribute paper copies to patients & caregivers as needed
Share mental health resource guide with other organizations/agencies such as LeadingAge Virginia
Continue to host support groups for various diagnoses, including stroke, limb loss, concussion, Parkinson’s disease, and aphasia as well as a support group dedicated to caregivers
Anticipated Impact
Integrating mental health into physical rehab improves recovery, boosts motivation, and supports long-term well-being through a holistic healing approach
Appropriate and interested patients are referred to the resource that aligns with their needs
Increase knowledge of mental health services and available resources for the community
Cross-promotion of resource guide will help increase knowledge of mental health services and available resources amongst a larger population of the community
Support groups provide a combination of educational resources and a network of peer support during and following patients’ initial physical rehabilitation stays
Financial Barriers to Access Care
Provide nearly $2 million in community benefits annually, including the cost of providing charity care and financial assistance
Increase accessibility of physical rehabilitation and related services for patients in need
Plan to Evaluate or Measure Impact
Volume of patients who receive rehabilitation psychology services
Volume of patients referred
Webpage analytic data such as page views, time spent on page, and click-throughs
Webpage analytic data such as page views, time spent on page, and click-throughs
Volume of support group meetings; volume of attendees
Total dollar amount given in community benefits as reported in Schedule H (IRS Form 1040)
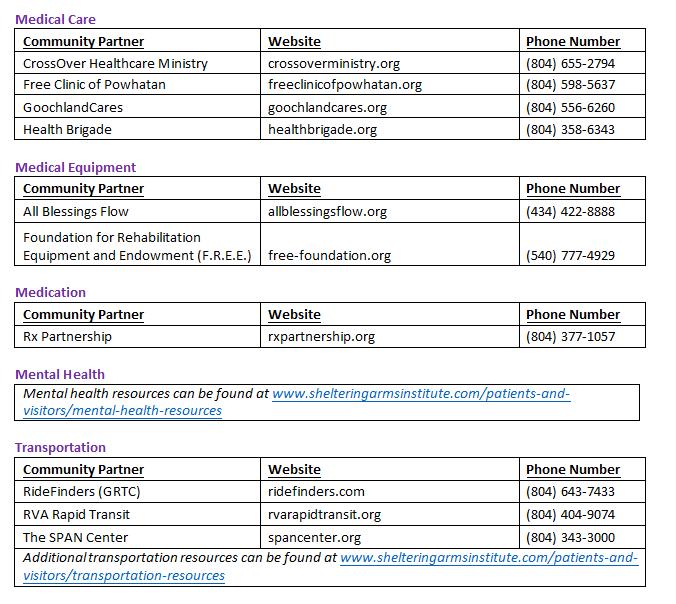
Medication
Expand Meds-to-Beds program whereby prescriptions are delivered directly to patients’ room prior to discharge
Collaborate with Sheltering Arms Foundation to make targeted grant to support the work of Rx Partnership
More timely access to medications, improved adherence, and collaboration between pharmacy and physicians to ensure medication coverage and availability
Provide operating support to Rx Partnership, an organization dedicated to increasing access to medication for vulnerable people in Virginia by coordinating the distribution of free brand and low-cost generic medications to individuals without insurance, regardless of their ability to pay
Transportation Barriers to Access Care
Implementation
Refer patients directly to organizations that offer transportation resources through UniteUs and assist patients with completing applications for transportation services as applicable
Update existing transportation resource guide twice annually and continue to house on our website/ distribute paper copies to patients & caregivers as needed
Share transportation resource guide with other organizations/agencies such as LeadingAge Virginia
Collaborate with Sheltering Arms Foundation to make targeted grants to support organizations that offer transportation resources in our community
Initiate connections to transportation resources for individuals in need of service
Patients and community members will have increased knowledge of accessible transportation vendors and available resources for patients
Cross-promotion of resource guide will help increase knowledge of accessible transportation vendors and available resources amongst a larger population of the community
Provide operating support to organizations in our community that provide transportation resources such as GRTC, RVA Rapid Transit, and The SPAN Center
Volume of patients served through Meds-to-Beds program; volume of prescriptions filled
Dollar amount of grant funding provided; volume of patients served and prescriptions filled through Rx Partnership
Volume of referrals sent to organizations offering transportation resources; volume of transportation applications completed on patients’ behalf
Webpage analytic data such as page views, time spent on page, and click-throughs
Webpage analytic data such as page views, time spent on page, and click-throughs
Dollar amount of grant funding provided; volume of individuals served/rides provided through grant-supported community organizations
Significant Health Needs Not Addressed
Section 501(r)(3) allows for hospitals to decide which identified community health needs will be addressed and those the hospital facility does not intend to address. The following community health needs will not be addressed by Sheltering Arms Institute in this cycle of the CHNA process:
Community Health Need
Reasons for Not Addressing Medical Care
This need is being addressed by other organizations in our community. For example, CrossOver Healthcare Ministry (crossoverministry.org), Free Clinic of Powhatan (freeclinicofpowhatan.org), GoochlandCares Free Clinic and Family Services (goochlandcares.org), and Health Brigade (healthbrigade.org)—all of which are supported by the Sheltering Arms Foundation Fund through grants—serve the primary care needs of the uninsured in the greater Richmond area.
Healthy Food Options
Opportunities for Social Engagements
This need is being addressed by other organizations in the community. For example, Feed More (feedmore.org) is dedicated to fighting hunger in Central Virginia.
This need is being addressed by other organizations in the community, including Sportable Adaptive Sports & Recreation (sportable.org), Sheltering Arms Community Programs (shelteringarms.com), and Community Brain Injury Services’ The Mill House Clubhouse (communitybraininjury.org), all of which are supported by the Sheltering Arms Foundation Fund through grants and provide opportunities for social engagements to individuals in Central Virginia.
2022 Community Health Impact Report
The third component of the CHNA process is the development of a Community Health Impact Report (CHIR). According to Section 501(r)(3), the hospital facility must:
• Take into account written comments received on its most recently adopted implementation strategy
• Evaluate the impact of any actions that were taken to address the significant health needs identified in the immediately preceding CHNA
Written Comments
Sheltering Arms Institute published our 2022 CHNA to the hospital’s website on September 29, 2022 (shelteringarmsinstitute.com/about-us/brochures-and-reports). Sheltering Arms Institute was willing to consider written comments related to its prior CHNA Report and Implementation Strategies, and a questionnaire was distributed to members of Sheltering Arms Institute’s Community Advisory Council and open from January 27 through February 24, 2023 to solicit comments. The comments were aggregated and are described below.
If any reader would like to provide input on this community health needs assessment, they can submit their comment(s), in writing, to Jennifer Lankford, Director of Marketing, at jennifer.lankford@sai.rehab.
Comments
Survey the general population in Central Virginia in addition to individuals who have experience or a relationship with Sheltering Arms Institute to adequately explore and identify broader community needs
Further increase the volume of healthcare professional survey responses outside of Sheltering Arms Institute employees to adequately explore and identify broader community needs
Improve survey design to include open-ended or write-in answers to questions in case the prepopulated answer selections did not align with the respondent’s answers
Expand list of services in access-related questions within survey to provide more specific categories and holistic options
How Comments Were Considered
Secured grant funding to support contracted assistance from third-party research firm to expand the scope of survey respondents to include a sample of 300 individuals from the general public in addition to respondents from the Sheltering Arms Institute community
Increased survey response volume amongst healthcare professionals outside of Sheltering Arms Institute by 29% (from 41 in 2022 to 53 in 2025)
Included answer options such as “none of the above” or “other” with an open-ended, write-in space to allow respondents to answer questions as accurately as possible
Increased volume of answer selections in accessrelated questions by 54% (6 in 2022 to 11 in 2025) to include broader health categories and greater detail
Differentiate wording in survey questions related to access versus needed services
Break out survey response data to identify any differences in needs based on specific populations (i.e., individuals with cognitive impairments; individuals with physical impairments; individuals who have experienced a stroke, spinal cord injury, brain injury, limb loss, etc.)
Utilized wording such as “issues with access to” versus “programs…your community is lacking” in questions to distinguish services that exist but are difficult to obtain versus services or programs that need to be created
Asked additional demographic questions to extrapolate any differences in themes based on criteria, including:
1) Experience or relationship with Sheltering Arms Institute versus no experience or relationship
2) Caregivers versus non-caregivers
3) Socioeconomic status
2022 Implementation Strategy Evaluation of Impact
The tables on the following pages are a report of the implementation strategies from the Sheltering Arms Institute 2022-2025 CHNA process.
1 EXERCISE, RECREATION, AND LEISURE
Implementation Strategy
Create a transportation guide to house on our website with accessible transportation resources in the Central Virginia area
Host annual community partner vendor fair on the Sheltering Arms Institute hospital campus
Educate team members and patients on Sheltering Arms’ fitness, recreation, and wellness services to refer patients to appropriate programs
Offer community partner office hours and weekly clinics with the adaptive sports organization Sportable
Create a recreation/social program resource guide to house on our website for the Central Virginia area
Collaborate with local YMCAs to share resources with patients
Demonstrate assistive technology to support social connection, recreation, and decrease isolation
Status and Impact
COMPLETE
Increased knowledge of accessible transportation vendors and available resources among patients and community members
COMPLETE
Increased knowledge of resources available in the community to engage and support patients in active lifestyles post-discharge among patients and community members
COMPLETE
Increased interdepartmental knowledge of information and resources available to patients among team members
COMPLETE
A higher volume of patients have been exposed to Sportable’s adaptive sports programs and introduced to Sportable team members
NOT COMPLETED
Insufficient resources
COMPLETE
Increased knowledge about YMCA offerings for patients to engage in healthy lifestyle post-discharge and access to pools/fitness programs among team members
COMPLETE
Patients and community members engaged in visits to the MyLife Room at Sheltering Arms Institute for assistive technology demonstrations and education; Patients and community members were loaned assistive technology devices and provided follow-up education at home through a collaboration with the Virginia Assistive Technology System (VATS)
FOOD, DIET, AND NUTRITION
Implementation Strategy
Host cooking and nutrition classes for hospital patients and caregivers to take home a cookbook to implement practices they have learned regarding nutrition and healthy cooking
Offer a vegetable cart inside Sheltering Arms Institute’s café, which is open to the public, where extra vegetables are sold at an affordable and discounted price
Offer a bi-monthly outpatient nutrition clinic on the Sheltering Arms Institute hospital campus, potentially expanding to other Sheltering Arms Institute outpatient therapy locations in the community
Host an annual community health event to include a nutrition and/or fitness topic for former patients and/or community members
Host a nutritional seminar for discharged patients and community members that provides healthy eating strategies
Enroll appropriate patients in BeatDiabetes program
Status and Imapct
COMPLETE
Patients and caregivers were able to implement lifestyle changes through healthier choices in the kitchen while preparing healthy recipes
NOT COMPLETED
Insufficient resources
COMPLETE
Hospital patients who discharged home had access to further education and counseling with a registered dietitian; flyers about the nutrition clinic were also created and distributed to patients receiving care on an outpatient basis who inquired with their therapist about nutrition services
COMPLETE
Former patients and/or the community were provided an opportunity to expand their knowledge on the benefits of a healthy lifestyle
COMPLETE
Increased knowledge about strategies and resources for healthy eating among community members
PARTIALLY COMPLETE
The BeatDiabetes program has been discontinued; however, we pivoted to directly refer patients to the Virginia Cooperative Extension Program through the Unite Us platform to support patients with diabetes management

NAVIGATION, CARE COORDINATION, AND SUPPORT
Implementation Strategy
Create a caregiver ambassador program and continuum of care partnership with Brain Injury Association of Virginia’s (BIAV) future caregiver mentoring program
As a standard of care at discharge, refer appropriate patients to physician-recommended specialist for chronic disease management and assist patients by scheduling their first appointment
Offer Stanford evidence-based chronic disease self-management course
Offer Stanford evidence-based diabetes selfmanagement course
Create guide for patients from admission to discharge, including a checklist to review with patients throughout their stay to identify potential future needs (i.e., medical devices/ equipment, fitness & wellness services, nutrition counseling)
Develop diagnosis-specific peer mentor programs to match patients with peer mentors for support
As a standard of care at discharge, connect patients in need with free or low-cost primary care resources
Complete Universal Assessment Instrument (UAI) to determine the need for a personal care aide (PCA) or skilled nursing facility (SNF)
During team rounds, screen for social determinants of health
Status and Impact
COMPLETE
Increased access to caregiver ambassadors and peer mentors to expand needed support networks
COMPLETE
Patients were connected with an appropriate specialist prior to discharge and received support in scheduling their appointment
COMPLETE
Increased accessibility of information and available resources for patients and community members with chronic disease
COMPLETE
Increased accessibility of information and available resources for patients and community members with diabetes
COMPLETE
Screening for potential future needs will connect patients and caregivers with applicable educational materials as well as instructions on where to obtain needed information in the future
COMPLETE
Patients were provided encouragement in the recovery journey
COMPLETE
Patients received access to community services for continuity of care
COMPLETE
Continuity of care has been enhanced through early identification of resources needed upon discharge
COMPLETE
Patients were referred to appropriate community partners based on individual needs
NAVIGATION, CARE COORDINATION, AND SUPPORT
Implementation Strategy
Implement Unite VA as a community-based organization referral platform to connect patients with appropriate community partners
Promote Sheltering Arms Institute support groups across the continuum of care and on social media to reach the community
Provide nearly $2 million in community benefits annually, including the cost of providing charity care and financial assistance
4
MENTAL HEALTH
Implementation Strategy
Status and Impact
COMPLETE
Patients were referred to appropriate resources and agencies to support their transition to the community
COMPLETE
Increased awareness about diagnosis-specific support groups to meet patients at the right time in their recovery for maximum engagement
COMPLETE
FY22: $3,533,000
FY23: $3,327,000
FY24: $3,709,000
Expand psychiatric support at Sheltering Arms Institute via telehealth
As a standard of care at discharge, refer appropriate and interested patients to outpatient psychology services
Create a mental health resources guide to house on our website with mental health resources in the Central Virginia area
Site-specific project of the recently re-funded TBIMS project; care transition with community health services
As a standard of care at discharge, refer appropriate patients to the Master Center for Addiction Medicine for outpatient substance abuse treatment services
Status and Impact
PARTIALLY COMPLETE
Explored expansion of psychiatric support services; however, psychiatric-specific services for our patient population were not heavily needed; guidance was provided to physicians regarding psychiatric medication management
COMPLETE
Appropriate and interested patients were referred to the resource that aligns with their needs
COMPLETE
Increased knowledge of mental health services and available resources for patients
COMPLETE
Increased access to community health services after discharge from inpatient rehabilitation for survivors of traumatic brain injury and their caregivers
COMPLETE
Increased access to community health services after discharge from inpatient rehabilitation for survivors of traumatic brain injury and their caregivers
Adoption by Sheltering Arms Institute Board of Managers
This document was adopted by the Sheltering Arms Institute Board of Managers on August 28, 2025. For questions regarding the CHNA, please contact Jennifer Lankford at jennifer.lankford@sai.rehab.
Acknowledgements
We would like to express our sincere gratitude to The Walter W. and Maria Teresa Regirer Foundation for their generous support of this project. Additionally, we would like to offer our thanks to Alan Newman Research (ANR) Market Research Consultants and CLA (CliftonLarsonAllen LLP) for their assistance in helping us assess the health needs of our community.
Appendix A:
Appendix A: CHNA
Survey Questionnaire
CHNA Survey Questionnaire
Sheltering Arms Institute
Community Health Needs Assessment
Mode: Online (consumer web panel sample)
S Sample si ze: n=300
Length: 8 minutes
Geography: Greater Richmond area, including the following counties/cities: Chesterfield, Henrico, Richmond City, Hanover, Prince George, Petersburg City, Powhatan, Dinwiddie, Goochland, New Kent, Colonial Heights, Charles City, Hopewell
T Target audience: Ages 26+; mix by race/ethnicity, gender, income, age and education
F Fielding: January 13 through February 7, 2025
S Screener
S1. In which of the following categories is your age?
1 Under 25 (Terminate)
2 26-34
3 35-44
4 45-54
5 55-64
6 65-74
7 75+
9 Prefer not to say (Terminate)
S2. What is your 5-digit home zip code? (Terminate if not in Greater Richmond Region)
S3. Do you work for a hospital, clinic, or any other type of organization that provides healthcare or healthcare-related services?
1 Yes
2 No
8 Don’t know
C Community Health Needs
Q1. Overall, how would you rate the health of the people in the community where you live? Please use a scale from 1 to 5 where 1 means “poor” and 5 means “excellent.” (Include 8=Don’t know)
Q1a. Do you feel that the health of the people in your community could be improved?
1 Yes
2 No
8 Don’t know
Q2. In your opinion, how easy or difficult is it for people in your community to access the healthcare they need? Please use a scale of 1 to 5, where 1 means “very difficult” and 5 means “very easy.” (Include 8=Don’t know)
Q3. In your opinion, does your community experience issues with access to any of the following? Please select all that apply.
(Randomize)
1 Medical care
2 Medication
3 Medical devices (such as walkers and wheelchairs)
4 Transportation for medical appointments
5 Internet and technology
6 High-quality long-term care
7 Parks and recreational activities
8 Opportunities for social engagements at places like community centers
9 Physical rehabilitation services
10 Mental health services
11 Healthy food options
98 Other, specify
99 None of the above
Q4. Which of the following programs, if any, do you feel your community is lacking? Please select all that apply.
(Randomize)
1 Medication education
2 Chronic disease management (for example diabetes, COPD, high blood pressure, etc.)
3 Nutritional education and counseling
4 Health and wellness
8 Substance abuse treatment or support services
98 Other, specify
None of the above
Q5. In the past 12 months, what challenges, if any, have you or someone in your household faced when trying to get the healthcare services needed? (Open-end)
Q6 Have you or anyone in your household experienced issues with access to any of the following? Please select all that apply.
None of the above
Q7. Was there a time in the past 12 months when you needed medical care or health care services but did not get it?
Yes
Don’t know
Q8. (If Q7= 1) What prevented you from accessing care? Please select all that apply.
6 Hours of operation or appointment times did not fit my schedule
7 Services were not available in my preferred language
8 Did not have childcare
9 Services did not meet my mobility needs
10 Could not find a provider that offered services I needed
11 Unable to leave work
98 Other, specify
99 None of the above
Q9. Is your ability to afford the medical care you need impacted by costs associated with any of the following? Please select all that apply.
1 Housing (mortgage or rent)
2 Utilities (gas, electric, and water)
3 Groceries and household necessities
4 Cell phone plan
5 Transportation costs (like gas for your car or public transportation)
8 Other, specify
9 None of the above
Q10. What, if any, relationship do you have with Sheltering Arms Institute? Please select all that apply.
(Randomize)
1 Current or former patient
2 Caregiver of current or former patient
3 Donor
4 Employee
5 Current or former fitness member
6 Caregiver of current or former fitness member
7 I have no relationship with Sheltering Arms
8 Other, specify:
9 Don’t know
H Health Demographics
We have just a few more questions to help us classify the results of our survey.
D1. Compared to other people your own age, how would you rate your health overall? Please use a scale from 1 to 5 where 1 means “poor” and 5 means “excellent.” (Include 8=Don’t know)
D2. Do you need assistance in getting your healthcare needs met? (for example finding services, filling out forms, etc.)
D3a. Do you currently provide unpaid care for an adult loved one? This may include assisting with personal needs like dressing, household chores, meals, or managing finances or medical care.
D3b. Are you currently a caregiver to someone under 18 years of age with a disability or special needs?
D4. Please select your gender below.
D5. Which of the following best describes the highest level of education that you completed?
Prefer not to
Do you consider yourself to be of Hispanic origin or Latino descent?
D7. What is your race or ethnic background? Please select the category you most closely identify with. (Accept 1 response)
5 Native Hawaiian or other Pacific Islander
8 Something else
9 Prefer not to answer
D8. In which of the following categories is your total annual household income from 2024?
1 Under $20,000
2 $20,000 to $34,999
3 $35,000 to $49,999
4 $50,000 to $74,999
5 $75,000 to $99,999
6 $100,000 to $149,999
7 $150,000 to $199,999
8 $200,000 or more
9 Prefer not to answer
D9. [S3=1] Earlier you mentioned you work in healthcare or healthcare-related services. What organization do you work for? (Open-ended, include prefer not to answer)
C Closing
Thank you for your participation in this survey. We appreciate your time and input!
Appendix B: CHNA Survey Results
Methodology & Sample Distribution

Data collection mode
Sample size
Qualifications
8-minute online survey
Greater Richmond Region General Population (Gen pop): n=303
Sheltering Arms Institute Community: n=302
• Age: 26+
• Resides in the Greater Richmond area
Timing January 13 to February 7, 2025
Weighting
Gen pop data are weighted by age, gender, race/ethnicity, education, and region according to U.S. Census Bureau CPS statistics
Maximum margin of error (95% confidence level) n=300: +5.7%
Summary of Key Findings
Community Health Needs:
Survey results demonstrate the continued need for improved access to healthcare services in Sheltering Arms Institute’s service area. Although only a small percentage of respondents in the Greater Richmond Region rated the health of their community poorly (4%), most (75%) believe the overall health of the people in their community could improve.
One-quarter (29%) of respondents reported forgoing needed medical care in the past 12 months, citing the financial burden of medical bills (47%) and/or a lack of insurance or inadequate coverage (37%).
Access to mental health services and programs was a top issue among respondents in the Greater Richmond Region.
• Respondents rated difficulty accessing mental health services as the top issue for their community (38%) and for themselves personally (22%).
• While mental health services and programs emerged as the top area for access issues, 16% feel their community experiences issues accessing physical rehabilitation.
Community Needs and Access to Healthcare
While few respondents have rated the health of people in their community poorly (4%), threequarters (75%) feel the health of the people in their community could be improved.


Significantly higher among respondents age 26-44 (85%)

COMMUNITY NEEDS
Access to Healthcare
Only half (54%) think it is easy for people in their community to access the healthcare they need. While 27% said getting healthcare is neither easy nor difficult, 12% said it is difficult to access care.

and
respondents being
likely to say
Q1.

COMMUNITY NEEDS
Access to Healthcare Services
Two in five (38%) respondents feel it is hard to access mental health services in their community. Additionally, one-quarter feel their community experiences issues accessing healthy food options (29%), medication (28%), highquality long-term care (28%), and medical care (28%).

COMMUNITY NEEDS
Central Virginians feel their community is lacking in many areas, with mental health (43%) and substance abuse treatment (37%) topping the list.
All respondents (n=303)
All respondents (n=303)

Personal Access to Healthcare
PERSONAL ACCESS
Health Services
Among the 54% of respondents who encountered an access issue, the issues most commonly cited involve mental health (40%) and medical care (35%). Further, 17% specifically said they had an issue accessing physical rehabilitation services.

COMMUNITY VS PERSONAL ACCESS
Health Services
Respondents indicated that mental health services is the top area for access issues both personally and in their community more broadly.

One-quarter (29%) reported forgoing needed medical care in the past 12 months. The top two barriers were both financial, with 47% citing the inability to pay for services and 37% reporting a lack of insurance (or inadequate coverage).


Q7.
Q8.
All respondents (n=303)
Q7=yes)
PERSONAL ACCESS
Financial Barriers to Medical Care
The primary financial burdens preventing respondents from affording needed medical care are the cost of mortgage or rent (42%) and groceries and other household necessities (40%).
Younger respondents (age 26-44) are significantly more likely to have the cost of living impact their ability to afford medical care.
Community Health Profile
Six in ten (63%) respondents rated their health highly when comparing to other people their age. Fifteen percent (15%) say they need assistance in getting their healthcare needs met.



Caregiving Status
Two in ten (20%) respondents said they are currently providing unpaid care for an adult loved one.

Caregiving Status
Eight percent (8%) of respondents are currently providing care to someone under 18 years of age with a disability or special needs.
Caregiver to Someone Under 18
Demographics
Demographics
Demographics

Sheltering Arms Institute Affiliation
Among
COMMUNITY ACCESS
Community Needs
Employees, donors and community partners of Sheltering Arms Institute are the group most likely to see the need for improved health in the community (80%).

Q1. Overall, how would you rate the health of the people in the community where you live?
Q1a. Do you feel that the health of the people in your community could be improved?
Q2. In your opinion, how easy or difficult is it for people in your community to access the healthcare they need?
Q7. Was there a time in the past 12 months when you needed medical care or health care services but did not get it? Red/blue shading indicates significantly lower/higher result
COMMUNITY ACCESS
Health Services
Employees, donors and community partners of Sheltering Arms Institute are more likely to see the need for mental health services, medications, medical care, transportation, and medical devices in the community.

Q3. In your opinion, does your community experience issues with access to any of the following? Please select all
Health Programs
Percent Selected
Chronic disease management and nutritional education and counseling are two services employees, donors and community partners of Sheltering Arms Institute are more likely to see a need for in the community.

Q4. Which of the following programs, if any, do you feel your community is lacking? Please select all that apply. Red/blue shading indicates significantly lower/higher result
Health Services
PERSONAL ACCESS Percent Selected
Current and former patients of Sheltering Arms Institute are more likely to say they have experienced issues with access to physical rehabilitation services and medical devices than employees, donors, volunteers and community partners.

Q6. Have you or anyone in your household experienced issues with access to any of the following? Please select all that apply Red/blue shading indicates significantly lower/higher result



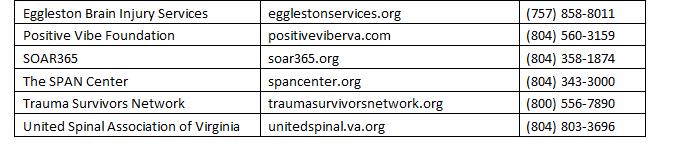
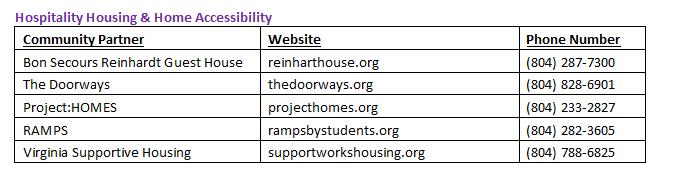
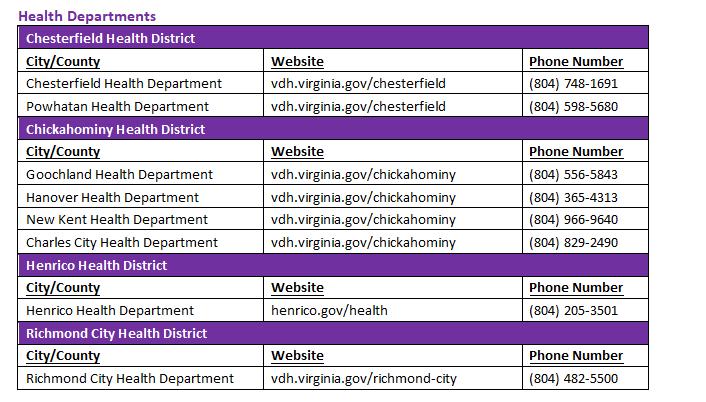
Appendix D: Community Resources
The following pages include a list of resources currently available in our community to address the significant community health needs discussed in this report. Despite our efforts, we recognize that this list may not be allinclusive and welcome any information to add available resources and increase its usefulness. Such information can be sent to the address provided on page 11 of this report.
The Virginia Department of Health’s districts in Central Virginia provide support to our community members in numerous ways. The services and programs offered by these local health departments include, but are not limited to:
• Child car seat distribution and education
• Communicable disease testing and treatment (i.e., sexually transmitted diseases, HIV testing, tuberculosis, rabies)
• Family planning
• Healthy heart blood pressure program
• Immunizations
• Long term/personal care assessment services
• Mental health first aid training
• Newcomer health for refugees
• Opioid overdose and naloxone education
• Primary care for individuals who have Medicaid, Medicare, or those who are uninsured
• Women, Infants & Children (WIC) nutritional care and food for low-income pregnant, breastfeeding, and postpartum women and children up to age five
• Women’s health services, including maternity services and breast and cervical cancer screening and diagnostic services
• Vital records
• Voter registration
For a complete list of services, we recommend visiting each department’s website and/or calling their office.
Virginia Department of Social Services provides support to our community members in numerous ways. The services and programs offered by these local departments include, but are not limited to:
• Adult Protective Services (APS)
• Child care assistance
• Child Protective Services (CPS)
• Domestic violence (DV) services
• Employment services
• Energy assistance
• Food connections
• Foster care (FC) and adoption
• Medical assistance
• Supplemental Nutrition Assistance Program (SNAP) benefits
• Temporary Assistance for Needy Families (TANF)
For a complete list of services, we recommend visiting each department’s website and/or calling their office.
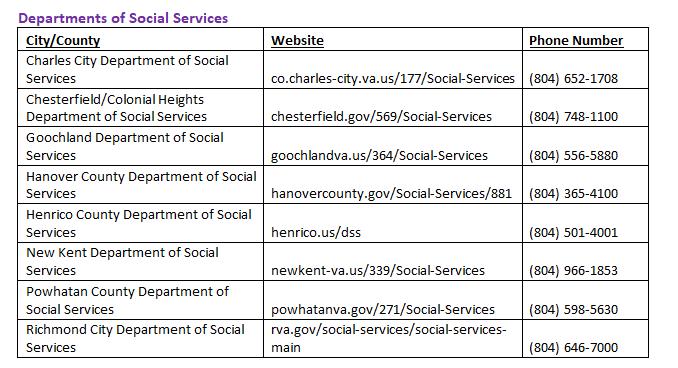
As part of our mission, we give back to the community by supporting and partnering with other local nonprofits to extend our continuum of services. Additionally, we are fortunate to welcome several of our key community partners to Sheltering Arms Institute’s main campus on a regular basis to assist in mentoring patients directly to ensure they have, or are connected with, needed resources before returning to the community.
Our partner organizations offer specialized services, accessible housing and ramps, recreation, peer mentoring and support groups, and so much more. The following organizations are official community partners of Sheltering Arms Institute and/or grant receipients of Sheltering Arms Foundation.