Bedfordshire Hospitals Professional Midwifery Advocate Team


Booklet for Maternity Staff
The A-EQUIP Model (NHS England, 2017) Advocating for Education and Quality Improvement Image adapted for the maternity staff booklet
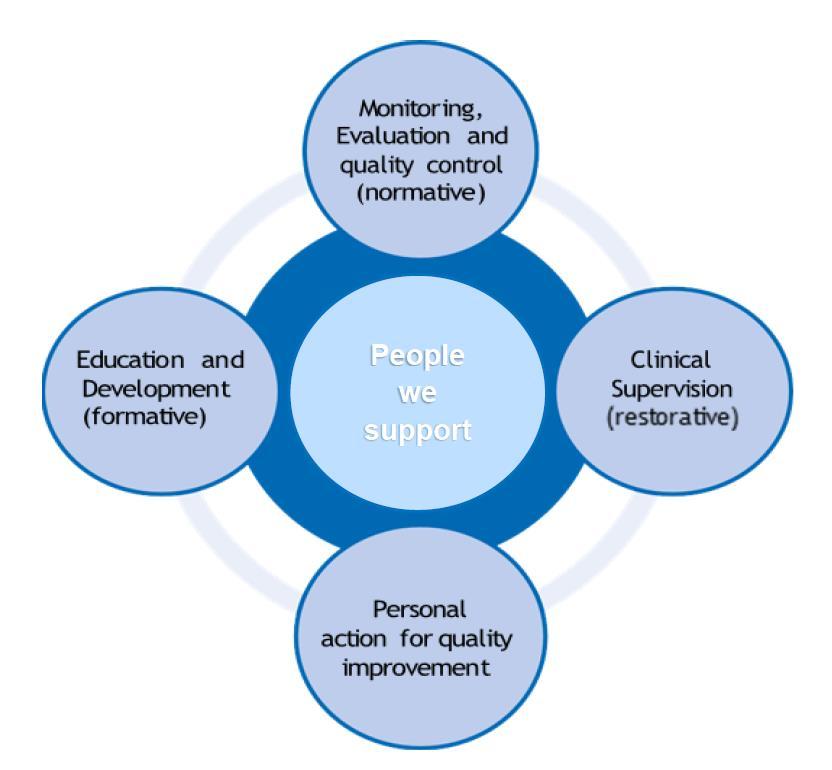





The A-EQUIP Model (NHS England, 2017) Advocating for Education and Quality Improvement Image adapted for the maternity staff booklet


In supporting midwives, preceptorship midwives, internationally recruited midwives, students and maternity support staff


Bedfordshire Hospitals NHS Foundation Trust Professional Midwifery Advocate Team are here to support staff by creating thinking space around the day-to-day demands of providing safe and appropriate care for women and babies.
The PMA Team deploy the A-EQUIP model (Advocating for Education and Quality Improvement) which aims to support YOU through a process of restorative clinical supervision (RCS) and personal action for quality improvement.

The PMA supports you in delivering good quality care when faced with complex or challenging situations. By offering opportunities to have reflective conversations, as a group or on a one to one basis, where you can contemplate different perspectives and think through changes you may be able to implement to improve the quality of care of Maternity Services and job satisfaction.
Providing support and feedback to develop progress and strengthen the capabilities of the maternity workforce by actioning themes from restorative clinical supervision (RCS) sessions.
 Bedfordshire Hospitals Professional Midwifery Advocate Team Booklet for Maternity Staff. Bedfordshire Hospitals Lead PMAs Keely Franklin & Tina McCann. May 2023, V2.
Bedfordshire Hospitals Professional Midwifery Advocate Team Booklet for Maternity Staff. Bedfordshire Hospitals Lead PMAs Keely Franklin & Tina McCann. May 2023, V2.
Benefits and how the Professional Midwifery Advocate (PMA) team can support you
Improve well-being of staff feeling valued, reducing stress levels, relieving emotional fatigue
Working relationships and team dynamics improve
Increases job satisfaction and staff retention
Supports Reflective Sessions, either as a group or individually, provision of a safe, confidential environment to talk
Supports a continuous improvement process that builds on personal and professional resilience
Enhances the quality of care for women, their babies and family through quality improvement ideas and by developing skills empowering you to become an advocate for women accessing maternity services
Supports preparedness for appraisal and professional revalidation
Supports personal action for quality improvement and continuous educational and training needs, empowering staff to continue with lifelong learning
Supports the midwives through a process of restorative clinical supervision (RCS)
Support following an incident in practice, statement writing and reflections

Support for staff on a supportive clinical practice ‘action plan’
Support when attending an HSIB (Health Service Investigation Bureau) interview

Multi-disciplinary debriefs following incidents in practice
Signpost to supportive services (well-being, education support).

An active listening ear for you

Provides a space to think and reflect on your role as a midwife, as an autonomous practitioner and being part of a multidisciplinary team
Has a positive impact on the immediate well-being of midwives
Helps midwives to feel valued by their employer leading to improved retention of midwives

A reduction in stress and an increase in resilience
Improves compassion of midwives towards others, improves relationships and team dynamics
Supports midwives to manage work life balance
Increases satisfaction relating to work (Petit & Stephen, 2015).
RCS takes place through a process of discussion and reflective conversation, supportive challenge and open and honest feedback.
What can you bring to a Restorative Clinical Supervision (RCS) session?
Any aspect of your personal or professional work life, which may be challenging
A quality improvement idea
Any successes in practice that you would like to share
Education, development and career discussions.
Confidentiality will be maintained. However, if there are clinical practice issues, safeguarding issues or well-being concerns that are disclosed, then escalation and support will be offered.

A restorative clinical supervision (RCS) session can be held as a one to one session or as a group session of 6-8 midwives, preceptees, students or maternity support staff. The PMA will facilitate the session.

You lead the RCS sessions, however we may ask you:
What would you like to achieve from today?
What have you tried before, was this successful?
How do you think you can achieve this?
Who do you think can support you with this?
To improve Maternity Services at Bedfordshire Hospitals

Through Service User surveys
Women’s experience & feedback (FFT)
Maternity Voices Partnership
Maternity Voices Partnership Coffee mornings
Walk the Patch
Whose Shoes Events
Reviewing maternity services, guidelines, policies and publications
Service User Experience Forums

Patient Experience Midwife

A structured framework for reflection
A tool for professional development
A safe place to think, reflect & learn, being listened to
Self-driven/self-owned by participants
Exploration of actions and feelings
Supportive of personal accountability
Open to questions and challenges
Supportive and inclusive
A means of checking up or judging practice
A performance management tool



Therapy/counselling/mentoring

An assessment or appraisal
A place for gossiping/moaning/snooping/blaming/personal soap box/speaking of others
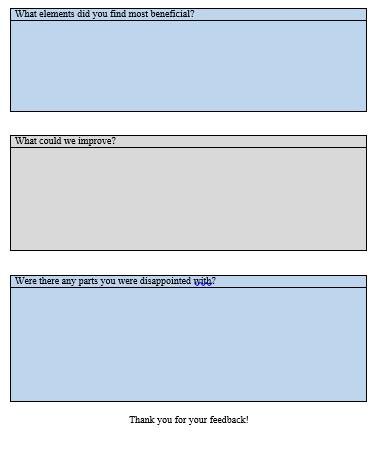
The Lead PMA maintains two separate databases. One lists themes of discussions and the other database lists the date and name of attendee. Feedback forms are given to maternity staff so that the Lead PMAs can collate information about how PMAs can improve the PMA support for YOU. The feedback remains anonymous.
The PMA Team support is a piece of a puzzle when supporting midwives and maternity support staff. Managers, Risk & Governance Team, Clinical Educators, PDM Team and other colleagues are available to support you too.




The PMA Team will ask for your feedback on the support you have been offered with deployment of the A-EQUIP Model: Quality Improvement Projects, Education & Development discussions, support with Action Plans, Restorative Clinical Supervision (RCS) support and signposting to well- being services. You will remain anonymous. Quotes or testimonials may be used for training purposes. Please do complete the feedback forms so that we can improve the PMA Service for maternity staff.




A midwife’s personal contribution to quality improvement may include:

Opportunities where they have reflected, learned and taught others about their personal action for quality improvement
Participation in audit and research and contribution to implementation of finds where appropriate
Embedding learning from incidents in practice
Contributing to service improvements made as a result of user feedback and staff feedback


Addressing public health concerns that require feedback and reassurance to the public
Facilitating the implementation of research findings, N.B. active contribution to a quality improvement activity does not need to be in a clinical setting

PMAs are qualified midwives
The structure of the PMA team may differ within organisations
PMAs deploy the A-EQUIP Model in Higher Education Institutes (HEI) and the private health sector.

From experience in the East of England Region in NHS Trust settings there tends to be a full time Lead PMA who co-ordinates the PMA Team and deploys the A-EQUIP Model.
Sessional PMAs form the rest of the team. These are midwives that have a substantive post within Bedfordshire Hospitals NHS Foundation Trust and have attended additional training to obtain a level 6 or 7 qualification as a Professional Midwifery Advocate.

The sessional PMAs are given 7.5 hours a month to deploy the A-EQUIP Model.
Linking PMAs to ward areas, a student year group, preceptorship midwives, international recruited midwives, a community team, specialist midwives…… has been beneficial from experience and gives structure to the sessional PMAs role.
Each PMA will be allocated a Link Area. However, you are most welcome to access any PMA and not just the PMA allocated to where you are working. Sessional PMAs will not be linked to the area that they work within their substantive roles.
PMAs can be invited to your team meetings or to support the team with an RCS session, QI project or education and development support. PMAs can support at 1:1 meetings and with mediation.






PDM Team
Well-being Services
Maternity drivers
CQC MIS CCG
Senior Management Team
Obstetric and Neonatal teams
East of England PMA Support Network
Risk and Governance Team
National PMA Steering Group
Staff Networks
LGBTQ+ BAME
Disability & Inclusivity
Patient Experience Midwife



Specialist Midwives
Higher Education Institutes
Service Users Communications Team
PNA Team
Revalidation is about promoting good practice, as well as strengthening public confidence in the nursing and midwifery professions. It is important to know that it’s not about making an assessment of your fitness to practise.
Revalidation helps to encourage a culture of sharing, reflection and improvement. It will provide benefits for you as a nurse, midwife or nursing associate as well as the people you care for (NMC, 2022).
www.nmc.org.uk/globalassets/sitedocuments/revalidation/howto-revalidate-booklet.pdf
by
Listening to your reflective accounts experience
Learning how you have linked your reflections to The Code
Being your confirmer
Did you know… you could pay for your NMC subscription in quarterly direct debit payments?

If you are asked to be a Confirmer, the NMC expects you to adhere to the conditions for acting as a confirmer set out in the guidance (link below), for example avoiding conflicts of interest.
https://www.nmc.org.uk/globalassets/sitedocuments/revalidation/information-for-confirmers.pdf


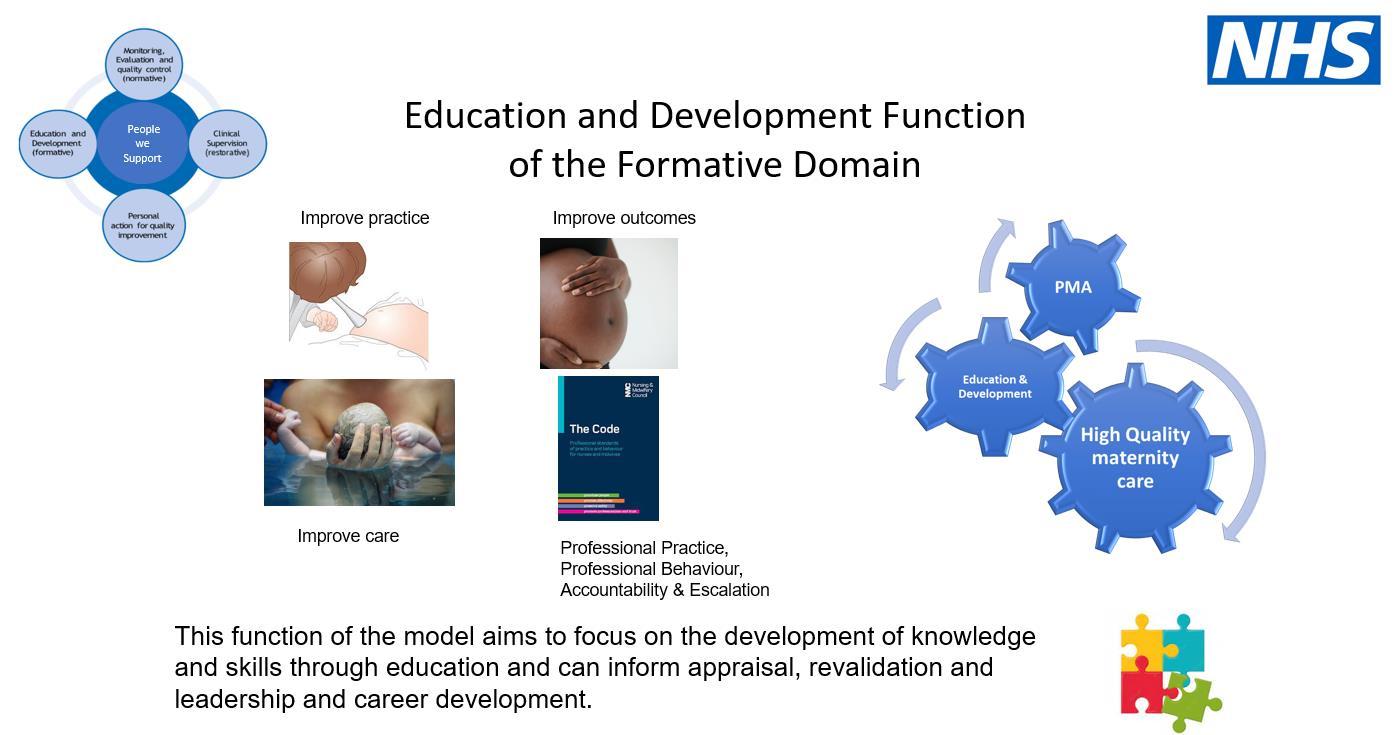
The PMA Team can support you to prepare for your appraisal through the Education and Development function of the formative domain of the A-EQUIP Model. Please contact a PMA prior to your Appraisal date with your Line Manager.
Get in the habit of filing all certificates, list training attended and the date, save feedback and thank you cards from women and families and from colleagues, including appreciative emails. Document any verbal feedback. Write your five Reflections (5 required for revalidation) as an interesting case or experience occurs or if you have been involved in writing a statement - you can reflect on this. You can increase your CPD hours by online training with the RCM, e-learning for healthcare (elfh), NHS England for example. (Please share any online training forums you access).
The Code presents the professional standards that nurses, midwives and nursing associates must uphold in order to be registered to practise in the UK.


Please download a copy of The Code and read it.
www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf
When you write your reflections, reference the paragraphs of each function of The Code instead of just referring to the function. The functions are prioritise people, practise effectively, preserve safety and promote professionalism. The paragraphs are under each function read and you will see. How your reflection relates to The Code will be more specific.
Please familiarise yourself with the NMC social media guidance that is underpinned by The Code and covers the need to use social media and social networking sites responsibly.
www.nmc.org.uk/standards/guidance/social-media-guidance/
Midwives and nurses are role models, leaders, advocates and professionals. Please see NMC guidance on Enabling Professionalism in Nursing and Midwifery Practice.
www.nmc.org.uk/globalassets/sitedocuments/other-publications/enabling-professionalism.pdf



Please escalate any concerns who have whilst you are at work. These may be:
Clinical concerns when you are concerned about the clinical picture whilst caring for a mother or baby


Non-clinical concerns which may be behaviours and attitudes of clinicians

Behaviours and attitudes of the people you are caring for
If you have escalated concerns and you do not feel that they have been addressed then do not be afraid to escalate them further, regardless of whom you escalated to. You will be expected to complete an ‘Inphase’ form (replaces Datix) if it is appropriate for the type of situation.
We work mindfully and collaboratively to create a well-organised, professional and supportive atmosphere that achieves the possible outcomes for all. We do this by:

Communicating effectively and respectfully with our colleagues
Valuing all contributions and taking the time to listen to each other
Making decisions together to provide the best possible service for all

We are open, authentic and have integrity in all we do by:
Openly sharing constructive feedback with others in a kind and empathetic way
Understanding the impact and value of our role on patients, colleagues and carers

Supporting colleagues to learn and reflect when things don’t go as expected
We respect colleagues, patients and carers by actively listening, responding, and providing everyone with a voice to create a positive work atmosphere. We do this by:
Showing empathy and understanding when communicating with others
Valuing the importance of everyone’s role within the team
Taking the time to actively listen and respond to patients, colleagues and carers
Respecting each other as equally capable, independent people
We are fair and inclusive and appreciate the diversity within our community:
Supporting the diverse communities we serve in our working life
Confidently challenging discriminative behaviour
Considering different needs in order to provide fair access to our services
Ensure that our workforce has equal access to opportunities
We value patients, colleagues and carers by showing care and empathy. We do this by:


Acknowledging everyone’s efforts and successes
Taking the time to care for our own wellbeing and check in on others
Encouraging a supportive community that enables everyone to make a difference
We share knowledge, information and support each other to develop, innovate and learn. We do this by:

Being open to challenges and improvement

Acting on and embracing constructive feedback
Collaborating with others to share innovative ideas
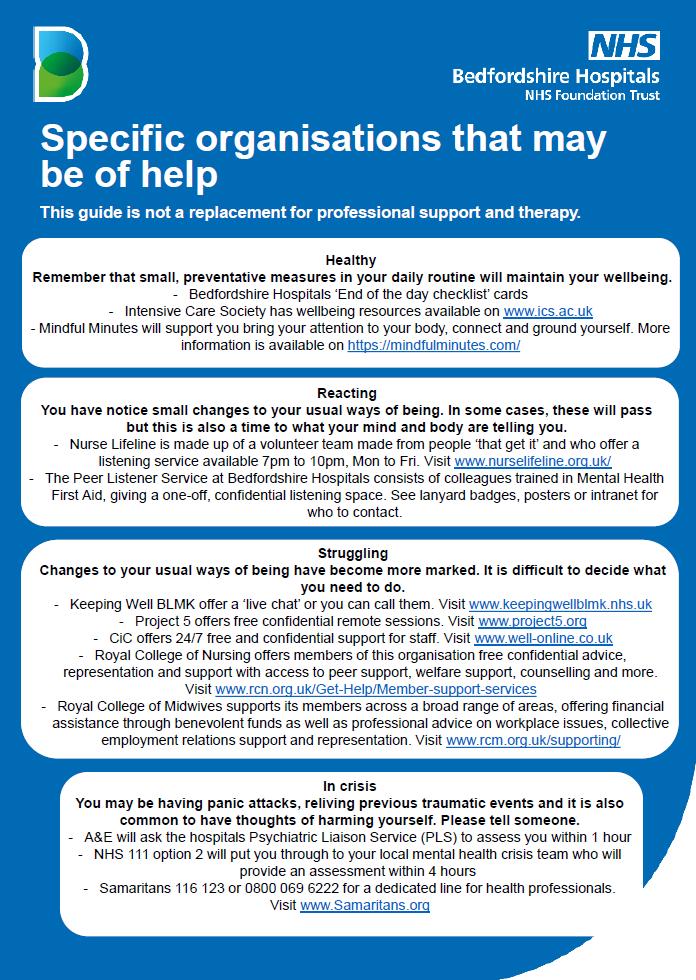
Please have a discussion with a PMA, PDM, Line Manager, colleagues, clinical tutor, university tutor, Freedom to Speak Up Guardian, Pastoral Care Team & the wellbeing team. A listening ear can be beneficial.
Organisation intranet – health & well-being services – mental health, financial support, sleep hygiene, menopause, retirement, men’s health, therapies - massage
Headspace – visit https://help.headspace.com/hc/en-us/articles/360044971154-Headspacefor-the-NHS

ShinyMind App – a gift for NHS Staff



Occupational Health
GP










Ask yourself ~ How am I doing today?
Practice being kind to yourself
Voice any anxieties you may having and difficulties you might be facing
Always remember that help & support is available
There will be difficult days, mostly positive days
Talk to your colleagues, friends and family
Rest well between shifts
Eat as healthily as possible and stay hydrated
Take a break away from your work area if possible
Growing our culture of kindness: Civility Toolkit by Capital Midwife: www.hee.nhs.uk/sites/default/files/documents/CM%20civility%20toolkit%20March%2022.p df

Find a little time each day to practice mindfulness exercise, yoga and gentle stretching
- 1 minute mindfulness exercise https://youtu.be/kI4bDaZ83g4
- 10 minute beginners yoga, gentle stretching
https://www.youtube.com/watch?v=VaoV1PrYft4

Take a moment to think about your day
Acknowledge one thing that was difficult during your workday – Let it go!
Consider three things that went well
Check on your colleagues before you leave – are they ok?
Are you ok? We are here to support you
Now switch your attention to home – Rest and recharge

1. Azarbayajni, B.F (2018) PMA Leaflet. London: Royal Free London NHS Foundation Trust.
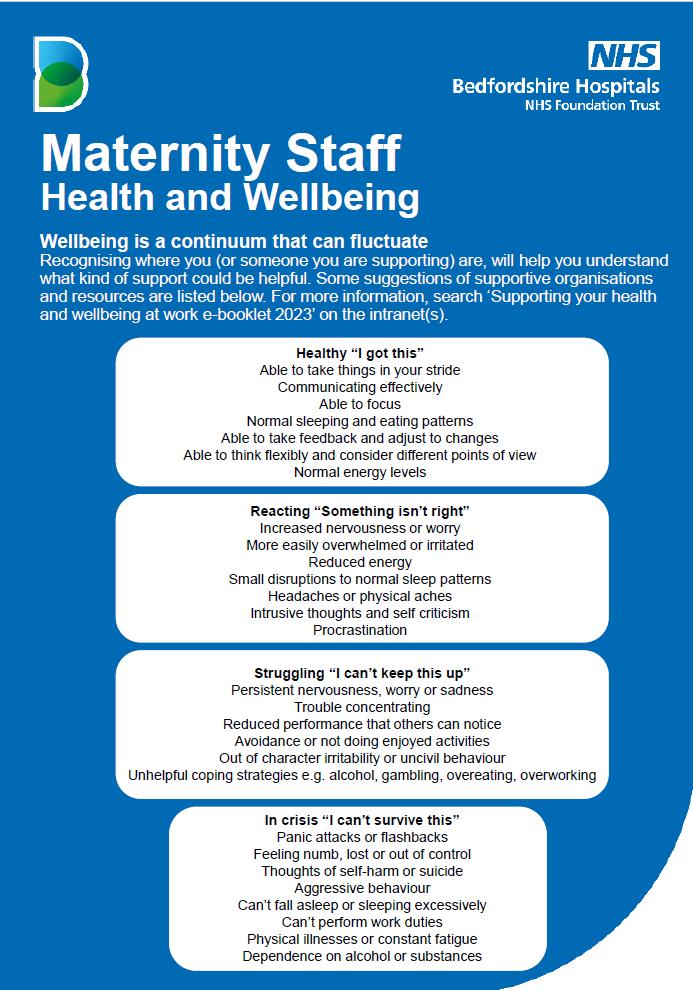
2. Bedfordshire Human Resources & Maternity Unit (2022) Maternity Staff Health and Wellbeing Poster. Bedfordshire: Bedfordshire Hospitals NHS Foundation Trust.
3. Chater, R. & Spong, A. (2020) Maternity Staff Health and Wellbeing Leaflet. Adapted May 2023 by the Communications Team. Bedfordshire Hospitals NHS Foundation Trust: Bedfordshire.
4. Franklin, K. (2018) Professional Midwifery Advocate Staff Leaflet. Watford: West Herts Teaching Hospital.
5. Franklin, K. (2018) The Professional Midwifery Advocate Team Training Presentation (revised 2022). Watford: West Hertfordshire Teaching Hospitals NHS Trust.
6. Franklin, K. & McCann, T. (2022) The Role of the PMA in Supporting Newly Qualified Midwives and International Recruited Midwives. Bedford: Bedfordshire Hospitals NHS Foundation Trust.

7. Leonard, H.; Johnson, C. & Nelson, K. (2019) The Role of the PMA at Bedfordshire Hospitals ~ Leading the Way Forward Professional Midwifery Advocates. Bedford: Bedford Hospital NHS Foundation Trust.
8. McCann, T. (2022) Professional Midwifery Advocate Staff Leaflet, adapted by T. McCann (2022). Luton: Luton and Dunstable Hospital, NHS England (2017) A-EQUIP a model of clinical supervision. London: NHSE.
9. McGrath, S. (2022) PMA Team staff referral business card. Liverpool: Liverpool Women’s Hospital PMA Team
10. Nursing and Midwifery Council (NMC).

https://www.nmc.org.uk/globalassets/sitedocuments/revalidation/how-to-revalidate-booklet.pdf Accessed 29/12/2022.
11. Nursing and Midwifery Council (NMC) (2018) https://www.nmc.org.uk/globalassets/sitedocuments/nmcpublications/nmc-code.pdf Accessed 29/12/2022.
12. Nursing and Midwifery Council (NMC). https://www.nmc.org.uk/standards/guidance/social-mediaguidance/ Accessed 30/12/2022.
13. Nursing and Midwifery Council (NMC).
https://www.nmc.org.uk/globalassets/sitedocuments/revalidation/information-for-confirmers.pdf

14. Nursing and Midwifery Council (NMC). https://www.nmc.org.uk/globalassets/sitedocuments/otherpublications/enabling-professionalism.pdf Accessed 30/12/2022.
15. Petit, A. & Stephen, R. (2015). Supporting Health Visitors and fostering resilience. London: Institute of Health Visiting.
16. Proctor, B., (1986) Supervision: A Co-operative Exercise in Accountability in: Marken, M., Payne, M. (eds.) Enabling and Ensuring – supervision in practice National Youth Bureau, Council for Education and Training in Youth and Community Work. Leicester, UK.
17. UoH (2017) PMA Bridging Course Materials. Hertfordshire: University of Hertfordshire.
18. Top tips for self-care and going home checklist. Cards handed out by Bedfordshire Hospitals Communications Team.
Bedfordshire Hospitals Professional Midwifery Advocate Team Booklet for Maternity Staff. Bedfordshire Hospitals Lead PMAs Keely Franklin & Tina McCann. May 2023, V2.