














RECOMMEND THE



































































































RECOMMEND THE



















































































The Association of Dental Groups (ADG) launched a new report in September. ‘Patients First’ details seven core recommendations for Government that, “if implemented, will transform the experience for dental patients in every corner of the United Kingdom.”
The report was presented in Parliament on Wednesday 11 September to MPs and Peers from across the political aisle, as the ADG seeks to work with the new Government to improve dental care across the board. The ADG’s seven recommendations, most of which can be actioned in the short term without legislative change and with no cost to Government, are as follows:
1. Commit to support recruitment: Accelerate long-term workforce plan and unlock barriers preventing high-quality international dentists registering
2. Use commissioning solutions: To meet the needs of the population and roll out examples of successful flexible commissioning
3. Plan the workforce: Recognise the relationship between the mixed economy, skill mix and devolved nations
4. Invest in community prevention: Support water fluoridation, have policies for sugar reduction, hold Integrated Care Boards/ LA/ NHS to account for delivering community preventative schemes like supervised toothbrushing
5. Renumerate practice-based prevention: Offer realistic remuneration and promote flexible commissioning for practicebased prevention.
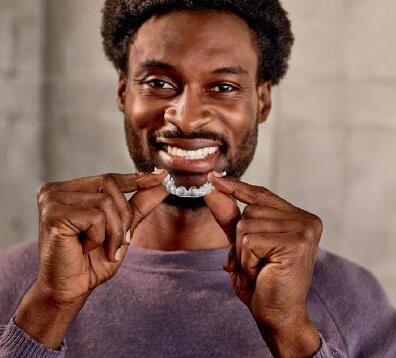
Dental teams in the UK may help to detect the early signs of Type-2 diabetes, as new research aims to validate routine screening during oral health check-ups.
Diabetes is one of the most common chronic conditions in Europe and is widely recognised to have a strong link with severe gum disease (periodontitis). An estimated one in three people living with diabetes remain undiagnosed, with over 1 million undiagnosed in the UK alone. Left untreated, diabetes can lead to long-term complications or can be life-threatening.
Recognising this link, researchers at the University of Birmingham have secured funding from Haleon, the global consumer health company which owns oral health

6. Protect the dental budget: Ringfence the budget and require ICBs to have a clear plan for dental underspend.
7. Support the retention of the workforce: Continue to reform the dental contract and ensure that pay review processes are transparent.
Neil Carmichael, Chair of the ADG and former MP explained that: “Our recommendations are centred around increasing the numbers of dentists working in order to provide better access for patients. Just 100,000 more dentists will create 750,000 more appointments, massively improving access for so many patients in dire need, and reducing pressure on NHS services elsewhere. We stand ready to support the new Government in putting patients first.”
brands like Sensodyne, Corsodyl and Polident, and the support of the National Institute for Health and Care Research (NIHR) Birmingham Biomedical Research Centre (BRC), to continue the development of a new care pathway for early case detection of Type2 diabetes and pre-diabetes in high street dental practices.
In a study published in 2023, the group at the University of Birmingham comprising Dr Zehra Yonel and Professors Iain Chapple and Thomas Dietrich teamed up with Professor Laura Gray from the University of Leicester to develop a new score called the Diabetes risk assessment in Dentistry Score (DDS), for use by dental teams to detect pre-diabetes and diabetes in dental settings.
When Parliament adjourned, the ADG was joined by MPs, representatives from various dental associations and press, for a launch event in Terrace Dining Room A of the Houses of Parliament. among the speakers was Tom Whiting, Chief Executive and Registrar of the General Dental Council (GDC). “We welcome the ADG’s discussions about access for patients, oral health and creating a sustainable dental industry,” he said. “There is evidence that the recovery of dental services after the pandemic has not only stalled but may have gone into reverse. We believe that this needs urgent attention.
“If we want more dentists and other dental professionals, there needs to be a multi-point plan for the capacity needed to train them.”
The GDC Chief Exec went to on to explain that the supply of UK qualified dentists is fixed in the short term but that inquiries have been received by the regulator from those seeking to establish new dental schools. He added that the GDC has tripled the number of places for part 1 of the ORE and increased capacity of the Part 2 exam by a third. “We are currently tendering for more capacity for next year.”
There is, however, no guarantee that increasing international registrants will solve the challenge of delivering NHS care. “Once a dentist is registered with the GDC, where and how they work and whether they provide NHS or private treatment is a matter for them,” Whiting explained.
“Furthermore, for the longer term, there’s a real need to modernise the legislation we work under – so that we can protect patients and support dental professionals effectively,” he concluded.
As part of a recent pilot study called INDICATE, funded by NIHR and Diabetes UK, the DDS was used in conjunction with a fingerprick test for diabetes, called the HbA1c test. The INDICATE trial, which engaged 13 dental practices and 805 dental patients, found that almost 15% of people walking through dental practice doors perceiving themselves to be healthy, exceeded UK pre-diabetes / diabetes thresholds (≥ 42mmol/mol HbA1c).
Now, thanks to funding from Haleon and NIHR, INDICATE-2 will work with 50 dental practices across England and Scotland to screen more than 10,000 patients and develop a care pathway that could help health services detect and treat many more people with undiagnosed diabetes in the UK.
When the result counts!




bite splints can be completed quickly and easily, guaranteeing maximum satisfaction.
Wear comfort, aesthetics and functionality are crucial factors when it comes to creating 3D-printed bite splints. Our extremely stable and flexible material LuxaPrint Ortho Comfort offers precisely these qualities. Combined with the NEW Bite Splint Workflow in the DentaMile connect software, bite splints can be completed quickly and easily, guaranteeing maximum satisfaction.
Discover more at www.dentamile.com
Discover more at www.dentamile.com




With Denplan as your partner we can help you unlock exciting opportunities to grow and develop your practice.
Welcome to a bumper issue of The Probe. Not only is this issue jam-packed with great content, such as a look into the Molar Explorer Cat Burford’s upcoming South Pole expedition, but we also have three hours of CPD tucked within these pages. In addition, those of you reading the physical, paper version of the magazine will also find a Brush Up supplement containing two more hours of CPD content. That’s five hours of CPD in total!
All CPD can be completed via our dedicated CPD platform, which was given a fresh coat of paint earlier this year, at cpd.the-probe.co.uk.
There is plenty I could signpost you to within this issue, but practice owners and managers should read Pam Swain’s piece on page 12, as from 26 October 2024, employers have a mandatory duty to prevent sexual harassment. Pam outlines everything you need to know. November, meanwhile, is Mouth Cancer Action Month. Find out how you can get involved on page 16. I’m running out of space, so enjoy the magazine and I’ll see you next time!









The Probe is published by Purple Media Solutions.
Registered in England.
Registered number 5949065
Managing Editor: James Cooke
Commercial Director: Gary Henson
Divisional Administrator: Francesca Smith







Production Designer 1 : Lorna Reekie
Production Designer 2: Rob Tremain
Digital Content Manager: Stephen Wadey
Circulation Manager: Andy Kirk
Managing Director: Ed Hunt
Regular Contributors: Lisa Bainham, Nigel Carter, Barry Cockcroft, Ollie Jupes and Pam Swain
E-mail news, stories or opinion to james.cooke@purplems.com
Circulation/Subscriptions: The Probe Subscriptions, Perception SaS, PO Box 304, Uckfield, East Sussex, TN22 9EZ, Tel: 01825 701520, https://purplems.my-subs.co.uk ©Purple
Media Solutions Ltd, 2014. All rights reserved. ISSN 0032-9185. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies, and information retrieval systems. While every effort has been made to ensure that the information in this publication is correct and accurate, the publisher cannot accept


liability for any consequential loss or damage, however caused, arising as a result of using information printed in this magazine. The views expressed in The Probe are not necessarily the views of the magazine, nor of Purple Media Solutions
Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth RCS(Eng), D’Orth RCS(Eng); Mark Wright BDS(Lon), DGDP RCS(UK), Dip Imp Dent.RCS (Eng) Adv. Cert, FICD; Dr Yasminder Virdee BDS. Readers who
















Afew years ago, while I was still a practice owner, the police came to my practice and took my fingerprints.
Although I knew I had nothing to hide, it was still a markedly unnerving and humiliating experience. Mercifully, I wasn’t alone during the psychological ordeal, since all other members of my staff similarly had to line up to have their dabs recorded for posterity.
The events that led to our prints being taken were desperately sad. A year-or-so earlier, I had taken on a new part-time dental therapist, who worked for me one day a week. Stacey (‘twas not her real name) was an excellent clinician – caring, affable and popular with patients, and I was more than happy to refer patients to her for their restorative work, and the patients in turn were very pleased with the treatment they received and the manner in which it was delivered.
After a few months, Stacey began ringing in sick a few times, usually at very short notice. At that point my practice manager began to become a tad disappointed with Stacey, but I asked her to bear with the therapist since, when she did turn up, Stacey was a clinical star.
When I took over my rural practice in 1994 from a retiring practitioner, I agreed to carry on paying his/my staff in cash. Although I wasn’t a big fan of the arrangement, the long-serving staff had it written into their contracts that they
should be paid (weekly) in cash and when I took over the business, they indicated that they would much prefer to be paid in bangers, as they were accustomed to. Since many of our patients also preferred at that time to pay their dental fees in cash (this was a VERY rural practice), my practice manager’s routine was to keep the wedges on the premises in a place even I wasn’t aware of. I was never ever accused of being a micromanager.
At the end of a week in which Stacey HAD turned up for work, my practice manager went to her cash hiding place on payday to find that all the wage money had disappeared. She immediately suspected Stacey since, in all the years she had worked with her colleagues, there had never been any discrepancies in takings (all the staff on occasions, looked after the reception desk). In fact, the only other ‘unknown’ in the place was ME. The police were called and we were advised that we would be fingerprinted shortly for ‘elimination purposes’.
At one point during questioning, a police officer asked me “How’s business going then? You’re surviving in the NHS?” I suddenly felt under suspicion.
Long story short, when the police finally managed to interview Stacey, she admitted stealing the cash and, subsequently, appeared before magistrates, where she pleaded guilty. She was ordered to pay the money back to the practice but, due to an

administrative disaster, it was nowhere near being paid fully.
It goes without saying that the therapist was dismissed with immediate effect. I later heard from another practitioner, to whom I had previously recommended Stacey, that she had stolen a dental nurse’s wages while working for him.
My reason for telling this particular tale is not to garner sympathy – I don’t deserve any because I should have actually been a boss and insisted that all cash was banked and not left lying around the practice – but to draw attention to the stress that we all felt until the real culprit admitted that she had stolen the cash (nearly £2,000). For a couple of weeks after discovering the theft until Stacey owned up, we all felt under suspicion.
Now, this sorry tale of the trials and tribulations that can pull the rug from under any incompetent and inept dental practice owner came back to me recently when I learned that the General Dental Council has in the past few weeks affirmed that it WILL continue to use ‘covert surveillance’ during its investigations during Fitness to Practise (FtP) investigations and Illegal Practise (IP) investigations.
There was no mention in Stefan Czerniawski’s announcement of the GDC’s Covert Surveillance Guidance that the regulator wouldn’t be refraining from the use of what effectively amounts to the ‘entrapment’ techniques the GDC employed a few years ago when private investigators were hired to pose as relatives of a fictitious relative – ‘Evelyn’an elderly relative who needed dentures but was too ill to attend in person, in an attempt to induce a clinical denture technician to act outside his scope of practice. In that instance, the GDC admitted to Dental Protection that it acted ‘unlawfully in undertaking an underguise operation without reasonable justification,’ through a declaration sealed by the High Court. The regulator paid about £38,000 in costs and damages as a result of the admission that it had acted unlawfully. Between 2013 and 2019, the GDC spent a total of £59,258.85 on investigators. And bear in mind that this is the same regulator that has the gall to put up articles on its website entitled ‘Transparency, trust and improving the fitness to practise process’ when talking about the stress experienced by dental professionals when under FtP investigation.
‘Transparency?’ Really? This from an organisation that wants to continue using private investigators to carry out covert ‘surveillance’ on registrants? Is it just me who doesn’t believe that ‘covert’ = ‘transparent?’
Another sub-heading from the same article by author Stefan Czerniawski, the GDC’s Executive Director of Strategy, was ‘Transparency is important to building trust.’ Isn’t it just! I personally can’t fathom the obsession with private investigators. Maybe it’s because the GDC has an address in Baker Street?
In introducing the publication of the GDC’s Covert Surveillance Guidance,
Stefan Czerniawski again uses his favourite noun ‘transparency’ when describing ‘the stringent legal and ethical framework governing covert surveillance in FtP and IP investigations.’ The GDC’s commitment to ensure all investigative activities comply with the Human Rights Act 1988 is something to behold.
Just as a reminder, the General Dental Council has STILL NOT RELEASED the number of registrants who have taken their own lives while enduring the stress of being under Fitness to Practise investigation, nearly 23 months after announcing it would publish a ‘report of this in the first half of 2023’ –AND YET – it is going to continue with the frankly, vindictive idea of continuing to pursue registrants through covert surveillance, even though it ‘will be used sparingly and only as a last resort.’ But can you imagine going through an FtP investigation and discovering the devastating news that you have been under surveillance?
With the number of complaints made to the GDC about registrants supposedly dropping - the Dental Defence Union reported the GDC ‘received 1,264 new concerns in 2022, a decrease of 6% on the previous year’ – is the GDC wanting to ensure the continuation of business by persisting in embracing covert surveillance operations? Yes – it IS an absurd question, but not as risible as a regulator that regularly receives justifiable derision for the intensity in which it pursues registrants. As an example, the GDC has been resolutely unable to accept a High Court decision made in June 2022 that overturned a previous decision by an FtP panel to erase a young dentist. The High Court found that NHS regulations do not forbid ‘top-up’ fees. Mercifully, the regulator has struggled to gain support for an appeal – probably on the grounds that it is, frankly, insane.
Despite its proclamations that it is concerned for the mental well-being of dental registrants, the actions of the General Dental Council do little to allay the suspicion that this is all lip-service. Adding to the bottom of its website’s news articles ‘Reach out if you need some support. If you are affected by the issues discussed above, please reach out to the Samaritans’ does nothing for the mental well-being of dental registrants.
Releasing the suicide figures and actually LEARNING lessons from them by not vindictively pursuing registrants until they take their own lives or have mental breakdowns would be a start. I have to go. There’s a rerun of Father Brown on. Now there IS a transparent private investigator! n
About the author ollie Jupes is the pseudonym of a former nHs dentist. He monitors dentistry on twitter X as @DentistGoneBadd



Softens plaque for easier removal
4x more effective at removing plaque than brushing alone
Significant reduction in the number of bleeding sites
Helps reverse early gum problems the main cause of bleeding gums, enabling gums to repair




















6 clinical studies
As a clinician you can select different chart types, plaque index, bleeding index or gingival index scores
Adjust between tested products across dental sites EXPLORE THE










Making better use of the existing workforce and prevention, rather than just more clinicians and more treatments, is the right way forward
Listening to the new Secretary of State talk about the challenges ahead was quite enlightening. There is hope for the future, but it is going to be difficult, and some serious vested interests will need to be challenged. I think I have said before that when I was CDO, the secondary care sector accounted for about 4% of dental services delivered but took about 20% of the overall dental budget. Some of this work is complex, urgent and very specialist, which definitely needs provision in secondary care. However, much could be commissioned in the primary care sector, saving the NHS a significant amount of revenue, providing care quicker and more conveniently for patients and, crucially, providing an attractive career pathway for clinicians in NHS primary care.
I dread to think how many third molar extractions are carried out in hospitals and at what cost. There are hundreds of oral surgeons on the specialist list, the OMFS fraternity fought long and hard to prevent them acquiring consultant status when we were reviewing the specialty of oral and maxillofacial surgery, the worst example of protectionism I came across in my time as CDO! This sort of thing has to
stop. For the NHS to be efficient (gosh that will take time) everybody needs to be working at the top of their skill set, not performing functions that can be more efficiently carried out by other members of the health care fraternity. Dentistry and its relationship with general health is a classic case study. I remember we initiated a pilot in the north of England looking to spot asymptomatic cases of chlamydia in young men. We arranged for a dental practice in a newly established Darzi centre to collect urine samples from men between the ages of 18 and 40 attending the practice and to send them for routine testing in a similar way as the GP practice located in the same building. More cases were detected in the dental practice than from the GP practice. Why? It is simple really: at the time, more men between the ages of 18 and 40 visited the dentist regularly than visited their GP. Was this a great success? Yes. Was it continued? No. Why? Because the doctors running the CCG at the time thought this was ‘their territory’.
The same thing could be done with testing for diabetes and simple BP measurement for hypertension. Ara Darzi is involved again and I hope the “Darzi centre” concept is revisited. Colocation of primary care facilities in
decent premises, in convenient sites, is surely the way forward. There is, after all, an abundance of town centre premises currently sitting empty and this would not only make services more conveniently available for the public but might address some of the neglect we currently see in our high streets.
Working in a centre like this would make many dental healthcare providers feel more a part of the NHS and might also tackle the ridiculous situation where hygienists and therapists working in hospitals and the salaried services are eligible to be members of the NHS pension scheme but not if they work in a practice setting.
My last article led to a highly placed member of the BDA messaging me and saying he was “disappointed” with the article. I replied and asked which bit of the piece was incorrect? I have not yet had a reply. When I graduated, 70% of five year old children suffered from the damage caused by dental caries. Now that has reversed. Over 70% of children are caries free – still too many but probably not related to the availability of care but more related to deprivation and its associated issues. The dental workforce is changed and our services need to recognise and reflect that now.
What is sexual harassment?
According to the Equality Act 2020, it is unwanted conduct of a sexual nature which has the purpose or effect of violating a worker’s dignity or creating an intimidating, hostile, degrading, humiliating or offensive environment for that worker.
Contrary to popular opinion, behaviour amounts to sexual harassment even if: the alleged harasser didn’t mean to cause offence or considered the behaviour to be a compliment; it was directed at someone who is the same gender as the alleged harasser; it consists of just a single comment; or it takes place outside of work.
From 26 October 2024, employers have a mandatory duty to prevent sexual harassment. If an employee raises an Employment Tribunal claim for sexual harassment and the Tribunal finds that the duty has not been fulfilled by the employer, it can increase compensation to the employee by up to 25% – and compensation for sexual harassment claims are uncapped! In addition, the
Equality & Human Rights Commission (EHRC) can take enforcement action against the employer.
If a Tribunal considers that the preventative duty has been breached, the EHRC can: investigate the employer; issue a notice confirming the breach and requiring the employer to prepare an action plan; enter into a formal, legally binding agreement with the
employer to prevent future unlawful acts; and ask the court for an injunction to restrain an employer from committing an unlawful act.
The Worker Protection (Amendment of Equality Act 2010) Act 2023 states that:
• Employers must take reasonable steps (see box below) to prevent sexual harassment of its employees in the course of their employment
What is ‘reasonable’ will vary from employer to employer, taking into account relevant factors . There are no specific criteria or minimum standards which must be met by the employer. The revised technical guidance says that employers should consider the risks of sexual harassment occurring in the course of employment, consider what steps it could take to reduce those risks and which of those steps it would be reasonable to take . The employer should then implement those reasonable steps.
Relevant factors include the size of the employer, the nature of the workplace, the risks present in that workplace, the third parties employees may have contact with, and the likelihood of employees coming into contact with such third parties.
Years ago, I was invited by a contact to apply for a board position at an NHS Trust in the Midlands. Towards the end of the interview, I was asked about the interface between private providers and the NHS. I said I was comfortable with this as long as it offered good value but I did say that I would try to introduce a way of charging private providers if one of their patients developed complications and had to be transferred to NHS intensive care. I also said that there ought to be a levy on private providers of healthcare to help fund the education and training of their NHS trained staff. I was doing ok until then but ultimately was not appointed. I found out later that the chair of the panel was also the Chief Executive of the local private hospital. I am not saying this was the reason I was not appointed but this sort of conflict at the top of our system needs to be stopped. n
About the author Dr Barry Cockcroft CBe is the former Chief Dental officer for england.

• The preventative duty is an anticipatory duty recognising the need for employers to take steps to mitigate the risk of sexual harassment occurring
• The preventative duty relates to the actions of an employer’s own workers and any third parties with whom employees come into contact during their work – in the case of dentistry this would mean patients, sales reps, etc.
• Compliance with the duty is not a one-off event – assessment, implementation, training, monitoring, etc. should all be ongoing processes with regular reviews and appropriate amendments
BADN is collaborating with the BDA to produce guidance and specimen policies for dental practices. Members should consult the BADN and BDA websites for more information. n
About the author pam swain is Chief executive of BADn

Friday 18th October is World Menopause Awareness Day, the highlight of a month of events
to get people talking about the menopause and how to support women going through this experience.
Menopausal symptoms affect many women, including patients, staff and fellow dental professionals. Whether or not you’re one of them, it makes sense to understand the impact symptoms can have on health and wellbeing, and how your practice should respond.
Research has shown that 10% of women leave their jobs and many more are reducing their hours or are not able to achieve their potential because of the menopause. Ensuring colleagues feel supported is an important way to retain valued members of the dental team and help them perform at their best.
More employers are now being taken to an employment tribunal by staff for discriminating against them because of menopause symptoms, including a teacher in Scotland who was awarded more than £60,000 in June 2024 for unfair dismissal. Another case involving a former social worker set a legal precedent when the Employment Appeal Tribunal ruled that menopause symptoms can amount to a disability under the Equality Act 2010.
In February 2024, the Equality and Human Rights Commission issued new guidance on menopause in the workplace, setting out employers’ legal obligations, including the need to make reasonable adjustments and prevent discrimination.
therefore discuss circumstances on an individual basis with their employee and consider what adjustments can be made to the workplace. For example, ensuring that there is fresh air or temperaturecontrolled spaces, comfortable desk seating, a private room or space with less distractions. If an employee is underperforming and it could be linked to menopause, look at ways that support could be provided.

Dental professionals have an ethical obligation to treat patients and colleagues fairly, and not discriminate against them. The GDC says those managing a team should ‘make sure that all team members, including those not registered with the GDC, have a work environment that is not discriminatory.’ (para 6.6.1).
So how can you ensure that your practice is menopause friendly?
Menopause policies
Having a menopause policy in place and communicating this so staff know of the support available is a good starting point. Check if your professional organisation has a menopause policy available that you can use as a template.
Make it easy to raise concerns
Fostering an open, inclusive environment where employees feel they can raise concerns about how the menopause is affecting them with no stigma or embarrassment, will help practices in becoming menopause friendly employers.
Make necessary adjustments
While menopause is not a protected characteristic, as mentioned, an employment tribunal could find that the effect of the menopause on an employee satisfies the definition of a disability under the Equality Act 2010. Where this applies, employers have a legal obligation to make reasonable adjustments to premises or to working practices.
Menopause, and perimenopause, affect people in different ways, so designing some support that is individual for the employee is advisable. Employers should
Staff training
Training managers on how to handle such matters sensitively can also be a good step to take. Having a menopause champion within the organisation might be a way to promote an inclusive environment.
DDU practice owner members get free access to an employment law advice line from Peninsula, a leading provider of employment law and health and
































































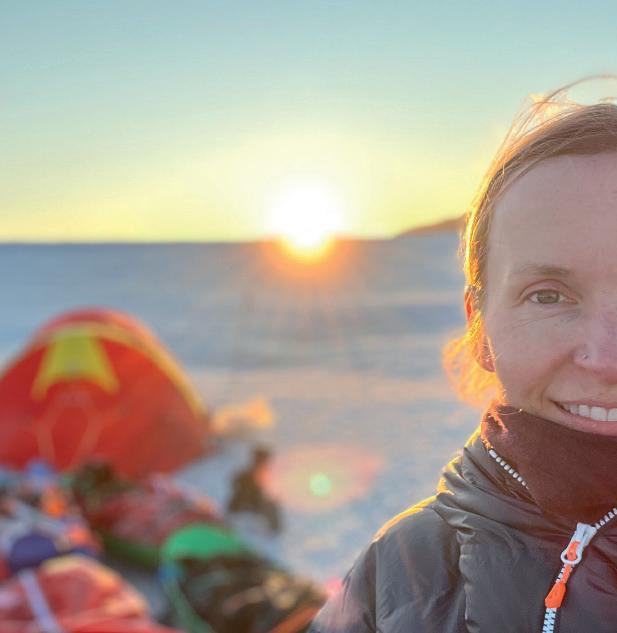
Cat Burford shares her unique journey through dentistry and the adventurous spirit that has led her to an extraordinary expedition to the South Pole
Cat Burford’s journey into dentistry began at a young age, when a bike accident that resulted in a broken front tooth introduced her to the wonders of dental care.
‘I wanted to be a dentist since I was about 10 years old,’ Cat recalls. ‘It was only when I went to the dentist that I saw the UV light, and I thought, “This looks pretty cool.”’
After graduating from the University of Liverpool in 2005, Cat faced a pivotal decision. Torn between staying close to the outdoor adventures of the Lake District or relocating to Cornwall, she let fate decide.
‘I flipped a coin and thought, “It’s only a year for training. I’ll go down to Cornwall for a year and then I can always come back.”
But it’s been my home ever since.’
In Cornwall, she found a practice that perfectly matched her adventurous spirit, allowing her the flexibility to pursue her passion for travel and volunteer work.


A life of adventure
Cat’s love for travel and exploration has been a constant companion throughout her career. Inspired by her father’s latein-life travels and the pages of National Geographic magazines that filled her childhood home, Cat’s wanderlust took her far beyond the confines of a traditional dental practice.
‘As soon as I could, when I was 19, I took a year out before going to university and took my first trip to Borneo to teach English,’ she says.
Her travels have taken her to some of the world’s most breathtaking and remote locations, including the Gobi Desert and the Himalaya, in addition to the rainforests of Borneo.
During her time practising dentistry in New Zealand and volunteering in South America, Cat combined her profession with her passion for giving back. In Bolivia, she worked with a project that trained street children to become dental hygienists, providing them with a sustainable future.
‘It was great to see how investing in these girls helped their families, and it was rewarding to be a part of that.’
Balancing dentistry and adventure
For Cat, the flexibility of a career in dentistry has been instrumental in balancing her professional and personal pursuits.
‘Dentistry is a flexible career. You’re selfemployed and, although it’s not as flexible as I thought it would be, it still allows me to work towards my next trip or adventure.’
She acknowledges the challenges, including the financial sacrifices. But believes that her travels provide a necessary perspective.
‘By going and doing the volunteer work, it helps put things in perspective and gives you a balance when you come back to work.’
“I’m still a bit short of the funds I need to reach the start line, and support from the dental community would make all the difference. I believe that this is a unique opportunity, and the backing of individuals or companies would be invaluable”
The call of Antarctica Cat’s latest and most daring challenge is a solo expedition to the South Pole.
The inspiration for this extraordinary journey can be traced back to a geography lesson in school. Her teacher, Alison Taylor, once asked, ‘What’s the largest desert on Earth?’ When she revealed it was Antarctica, Cat was captivated by the idea of this vast, white wilderness.
‘It was just something that triggered in me. I thought, “Well, I’m going to go there one day.”’
The dream of reaching Antarctica simmered in the background for years, reignited during the Covid-19 pandemic. ‘I used to do all of this exciting stuff, and the last few years, with a mortgage and daily life, I’d lost touch with that.’
A simple Google search for “Expedition to Antarctica” led her to a training course in Norway, which set the wheels in motion for her South Pole quest. She trained with notable explorers like Louis Rudd and Wendy Searle, who recognised her potential and offered mentorship.
The trek to the South Pole Cat’s journey will begin in November 2024, with a flight to Chile followed by another to Union Glacier in Antarctica.
From there, she will start her 704mile uphill ski from Hercules Inlet to the South Pole, a trek that will take approximately 50 days.
‘I’ll be skiing solo, and it’s quite an endeavour. Only 12 women have done it ever, and this year marks the 30th anniversary of the first woman to do it.’
Navigating the extreme conditions of Antarctica is no small feat. Temperatures can plummet to minus 50 degrees Celsius, and the landscape is marked by sastrugi –sharp, wave-like ridges of ice that can be up to eight metres high.
Cat’s training has been rigorous, involving everything from tyre dragging to strength training, and even practising setting up



Challenges and support
Funding the expedition has been one of Cat’s biggest challenges.
‘Raising money, fundraising, if you’ve never tried it, then you’re probably naive to think how easy it might be – because it’s not!’
Despite initial setbacks, she secured support from a few key sponsors, including AXA, Dentex and Denplan, who believed in her vision.
Cat is also using her journey to raise funds for Bridge2Aid, a charity that trains healthcare workers in developing countries. Her progress can be tracked through her website, themolarexplorer.com, where she will post daily updates via voice messages.
Looking ahead
As Cat prepares for her departure, she reflects on the impact of her journey and
the importance of following one’s dreams, no matter how daunting they may seem. I still have a final amount to raise, to fund the large logistical costs and get me to the start line. It would be great if I could get that support from individuals or companies within the dental industry and fly their flags at the South Pole in January! I do feel like this is a unique opportunity,’ she says.
Cat’s story is a testament to the power of resilience, the pursuit of adventure, and the belief that it’s never too late to chase your dreams.
For those inspired by Cat’s journey, her message is clear: ‘Go for it. Find that balance between work and passion, and don’t be afraid to step out of your comfort zone.’
As she embarks on her expedition to the South Pole, Cat Burford proves that with determination and courage, the sky – or even the South Pole – is the limit.
To donate to Bridge2Aid and support Cat’s trek to the South Pole, simply visit themolarexplorer.com




Ceramir
CAD/CAM
BLOCKS are a breakthrough in the market of CAD/CAM


Ceramir CAD/CAM BLOCKS are manufactured using a patented and highly advanced laser sintering technology. The result is a material with the strength of particle infiltrated ceramics, the aesthetics of glass-ceramics and the flexibility similar to dentin.
For more information scan the QR-code with your phone
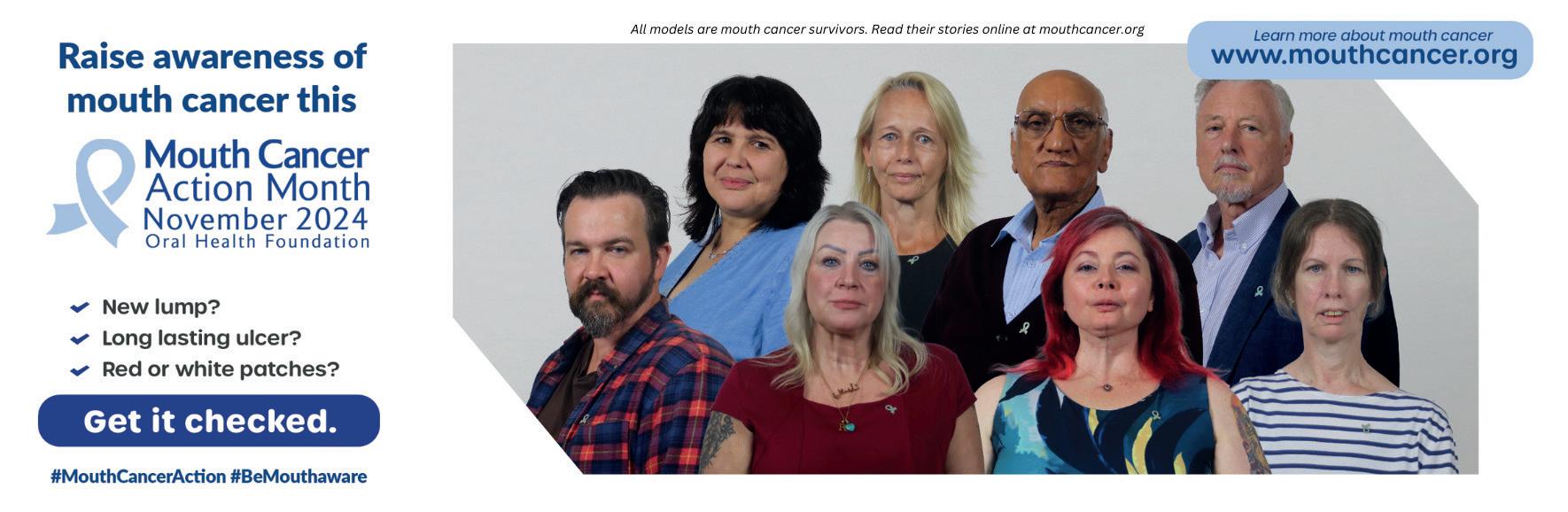
Mouth Cancer Action Month takes place every November, aiming to raise awareness about mouth cancer. For many, the word ‘cancer’ can be daunting, but increasing awareness and understanding can empower the public to take control of their oral health.
the landscape of mouth cancer in the uK
Mouth cancer, also known as oral cancer, is a significant and growing concern in the UK. In fact, we are now approaching 10,000 new cases every year – a number which has more than doubled over the past 20 years. In the last decade alone, the incidence of mouth cancer has risen by more than a third (34%).
Mouth cancer does not discriminate; it affects individuals of all ages and genders. However, it is more commonly diagnosed in men, who account for nearly two-thirds (68%) of cases. Additionally, almost two-thirds (64%)
of mouth cancer cases are diagnosed in people over the age of 60. Tragically, over 3,000 people in the UK lose their lives to mouth cancer each year, which equates to about eight deaths per day.
Why Mouth Cancer action Month is important
The primary goal of Mouth Cancer Action Month is to educate the public about the risks and signs of mouth cancer. Early detection significantly improves survival rates and outcomes. As dental professionals, you play a crucial role in this educational effort. By providing patients with the necessary information, you can help build stronger relationships within your community and make a tangible difference in people’s lives.
h ow dental professionals can support Mouth Cancer a ction Month
Dental practices are uniquely positioned to support Mouth Cancer
Action Month. Here are several ways you can get involved:
1. d isplays and chairside information
Creating informative displays in your dental practice is a simple yet effective way to raise awareness. Use posters supplied by the Oral Health Foundation and provide instructions on how to perform a mouth cancer self-check at home. Adding small pieces of bunting can make the display more visually appealing and attract attention. However, this awareness must also translate to the chairside. During consultations, identify a patient’s possible level of risk by asking about lifestyle habits that link to mouth cancer, such as smoking, alcohol consumption, and diet. As you perform a visual examination of the mouth and neck, explain what you are doing and why it is important. This not only educates the patient but also reassures them about the thoroughness of their check-up.
2. o rganise activities and events
Engaging in activities and events can be a fun and impactful way to raise awareness. Here are some ideas:
• f undraising: Fundraising is a powerful way to raise awareness and collect donations for Mouth Cancer Action Month. These donations help the Oral Health Foundation continue its vital work in raising awareness and educating the public about mouth cancer. Fundraising not only supports the campaign but also enhances your practice’s community presence, fosters team building, and boosts staff morale. On the campaign website there are lots of ideas to get you started.
• Community outreach: Going out into the local community to give talks and workshops is another impactful way to raise awareness about mouth cancer. By visiting local workplaces, sports clubs, care homes, and community centres, you can help people identify the early warning signs and understand
the risks associated with mouth cancer. These outreach efforts can significantly enhance public knowledge and encourage early detection, ultimately saving lives.
the importance of early detection
Early detection of mouth cancer can significantly improve the chances of successful treatment and recovery. Encourage your patients to look out for common signs such as:
• Persistent mouth ulcers that do not heal.
• Lumps or swellings.
• Red or white patches in the mouth.
• Unexplained pain or numbness in the mouth or lips.
By promoting awareness and education, you can help reduce the number of lives lost to mouth cancer each year.
Get involved
If you would like to get involved in Mouth Cancer Action Month, visit the Oral Health Foundation’s website at www.mouthcancer.org to find out how you can make a difference. Whether through fundraising, hosting events, or simply spreading the word, every effort counts.
Mouth Cancer Action Month is a vital campaign that brings attention to a serious health issue. As dental professionals, you have the power to make a significant impact. By participating in this campaign, you can help save lives and improve the overall health of your community.
Let’s come together this November to raise awareness, educate, and support the fight against mouth cancer. n
about the author
Karen Coates, oral health Content Specialist at the oral health foundation, and rdn


Tokuyama’s unique colourless Omnichroma composite means you don’t need to use a shade guide to identify the shade of any teeth prior to restoration. One syringe or PLT of colourless Omnichroma replaces all the shades of every other range of composite, eliminating at least one headache from your daily life. Whilst Omnichroma won’t be the answer for absolutely every single restoration it will be the answer for nearly all of them. For the others there’s Tokuyama Estelite Sigma Quick or Asteria.
Light years ahead!
When white light comprising all the spectrum of the rainbow hits most objects the object either absorbs none of the wavelengths, reflects them all back towards the observer and so appears white; absorbs some of the wavelengths, reflects the others back so that the object appears the colour of the wavelengths not absorbed and consequently reflected back; or absorbs all of the wavelengths, reflects none of them back and so appears black.
The same occurs with traditional composite restorative materials, which are made up of resins and filler particles containing pigments to give them their desired Vita shade. Some of the wavelengths contained in the white light hitting the composite’s surface are absorbed, so that only the wavelengths required to match the desired Vita shade are reflected back towards the observer.
Natural phenomenon of “structural light”
There are some objects that behave in a completely different manner, however. For example peacock’s feathers, certain breeds of butterfly, soap bubbles etc. These objects have special surfaces that exhibit the phenomenon of “structural light”. When white light hits their surfaces it is reflected off in different wavelengths depending upon the angle in which it hits the object and therefore altering the colour the observer sees. Hence the wide array of colours seen on a soap bubble’s surface when the light catches it in a certain way.
Surface texture
Another important factor is the smoothness of the surface the light reflects back off. If it is perfectly smooth then the light is reflected back in a uniform manner and the surface appears shiny and smooth. However, if the surface is rough then the light is reflected back in a haphazard manner and the surface appears dull.
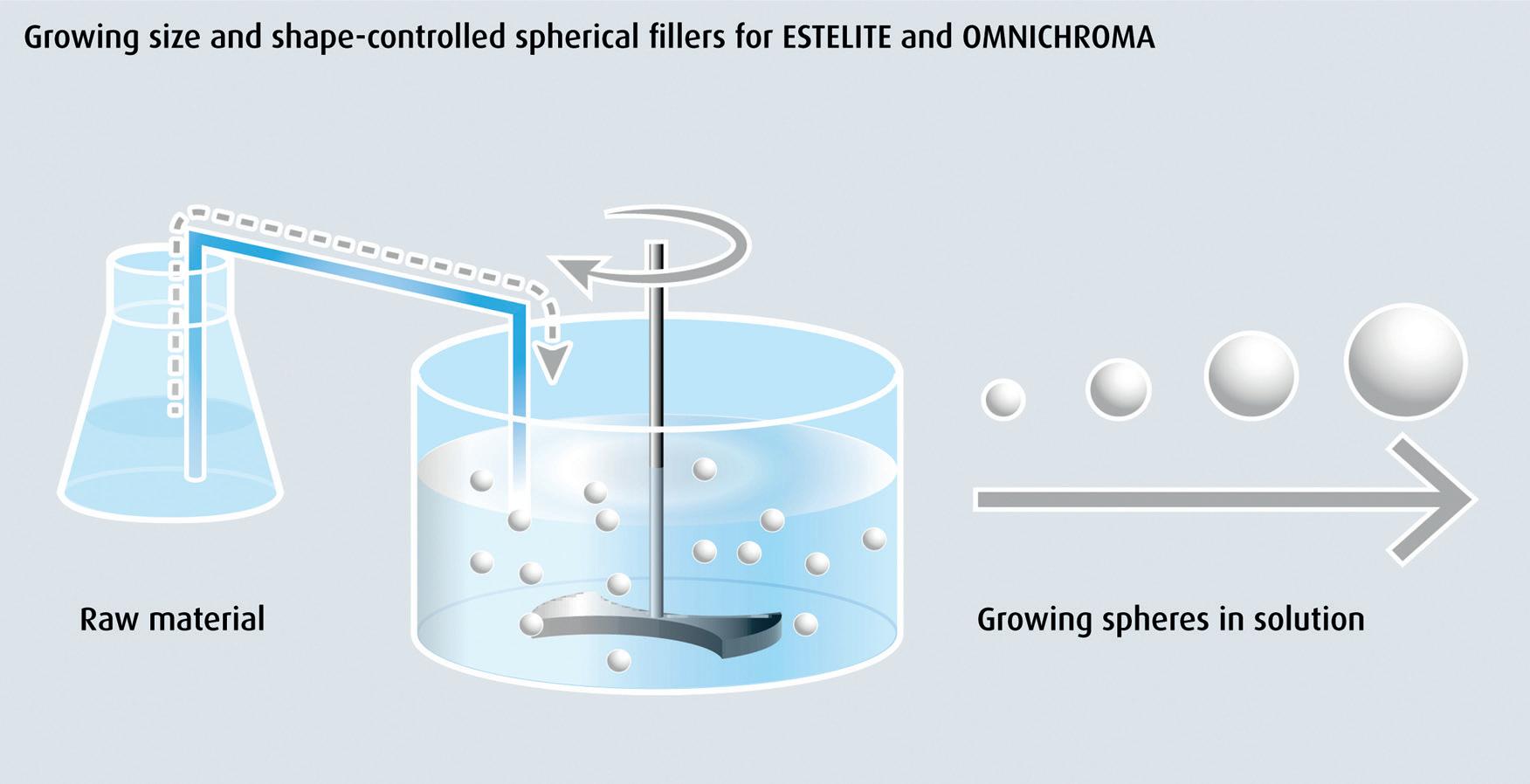
When polishing a composite the clinician is trying to reduce the irregularity of the surface so that the light is reflected back in a uniform manner and so the restoration looks natural, smooth and shiny. With composites containing irregular shaped filler particles it is extremely difficult to create such a smooth surface because some of the particles are plucked out randomly leaving an irregular crater-like surface. This is particularly the case with materials containing larger irregular shaped filler particles, see figures 1 and 2.
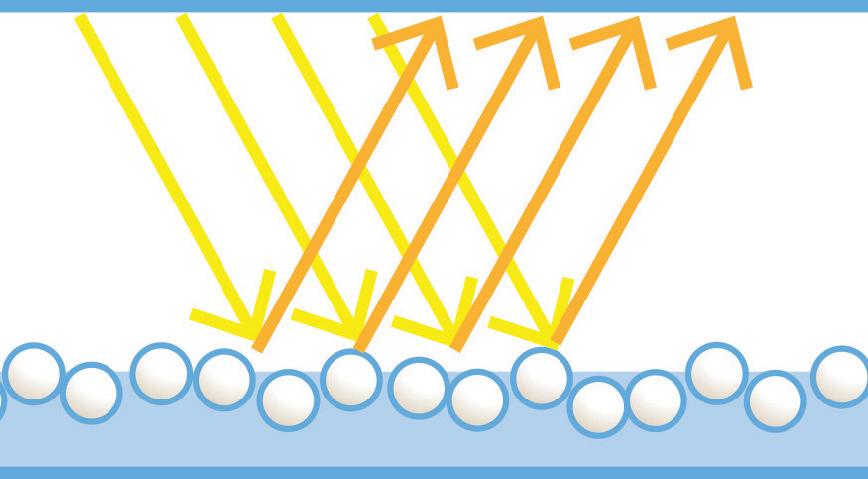

All Tokuyama composites comprise spherical filler particles, which are grown in a Sol-Gel method (figure 3) to precise dimensions depending upon the physical properties Tokuyama want their composite materials to exhibit. Because they contain spherical particles, Tokuyama composite materials are much easier and quicker to polish to a high lustre finish. This saves time and delivers a superior aesthetic result.
colourless Omnichroma –throw the shade guide away!
In Omnichroma’s case the spheres have been grown to a very consistent and precise 260nm diameter. Not only does this filler particle size provide Omnichroma with its unique physical and handling properties, but they also exhibit the natural phenomenon of “structural light”, generating light in the same red/yellow wavelengths that natural teeth reflect to give them their natural shades. Omnichroma is the world’s first and only colourless composite comprising of unpigmented filler particles and a clear resin. When white light hits an Omnichroma restoration and surrounding tooth it passes through the clear resin and bounces back from the cavity walls with the natural colour of the surrounding tooth. At the same time, the red/yellow “structural light” generated from the unpigmented spherical filler particles is reflected back too and combines with the light reflected from the surrounding tooth to perfectly match its colour, whatever its shade! This patented technology makes Tokuyama’s colourless Omnichroma unique because one syringe or PLT will match every tooth shade, eliminating the need for shade matching ever again! Figure 4 shows colourless Omnichroma inserted into teeth of an extensive range of Vita shaded teeth. Uncured it appears opaque to aid cavity placement and carving. Lightcured it becomes translucent and instantly disappears by seamlessly adopting the shade of the surrounding tooth structure. To supplement Omnichroma, Tokuyama have developed Omnichroma Blocker,
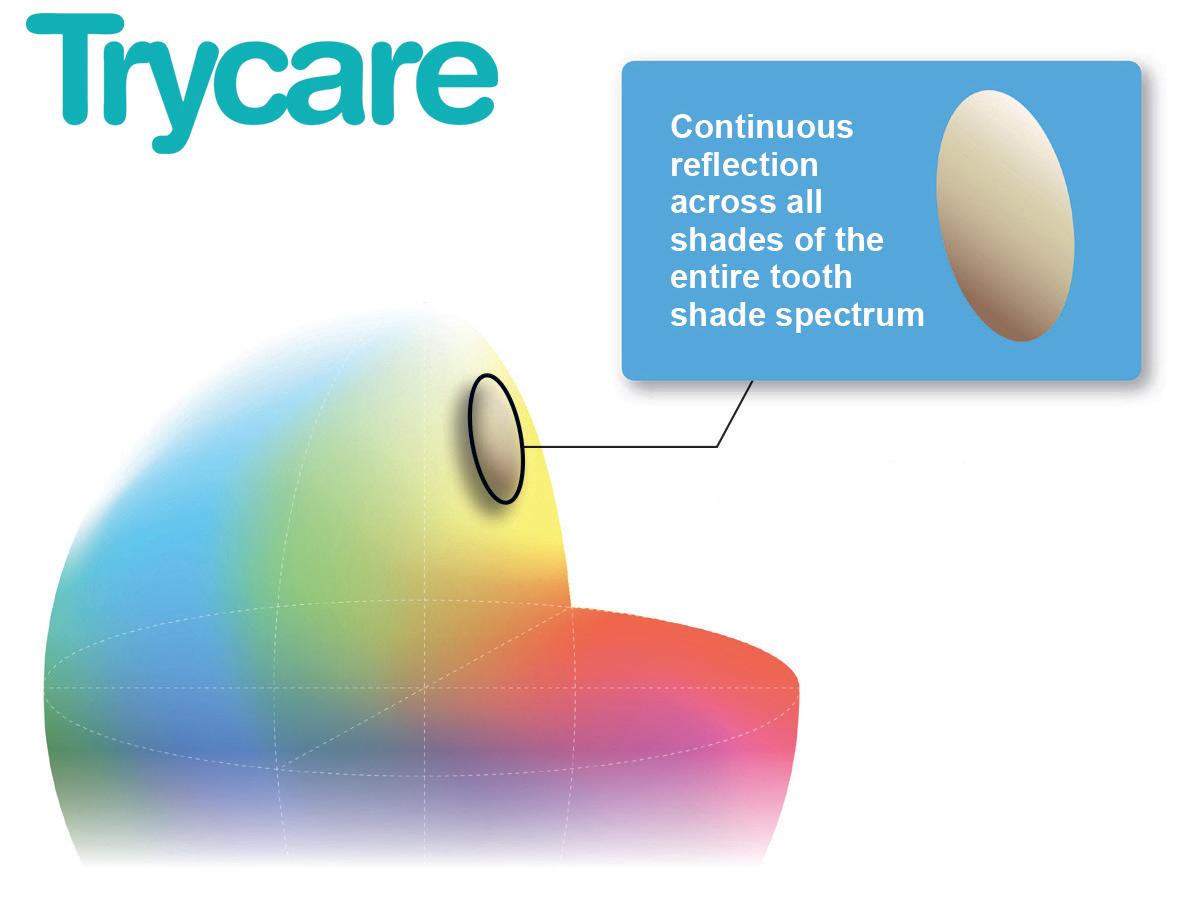
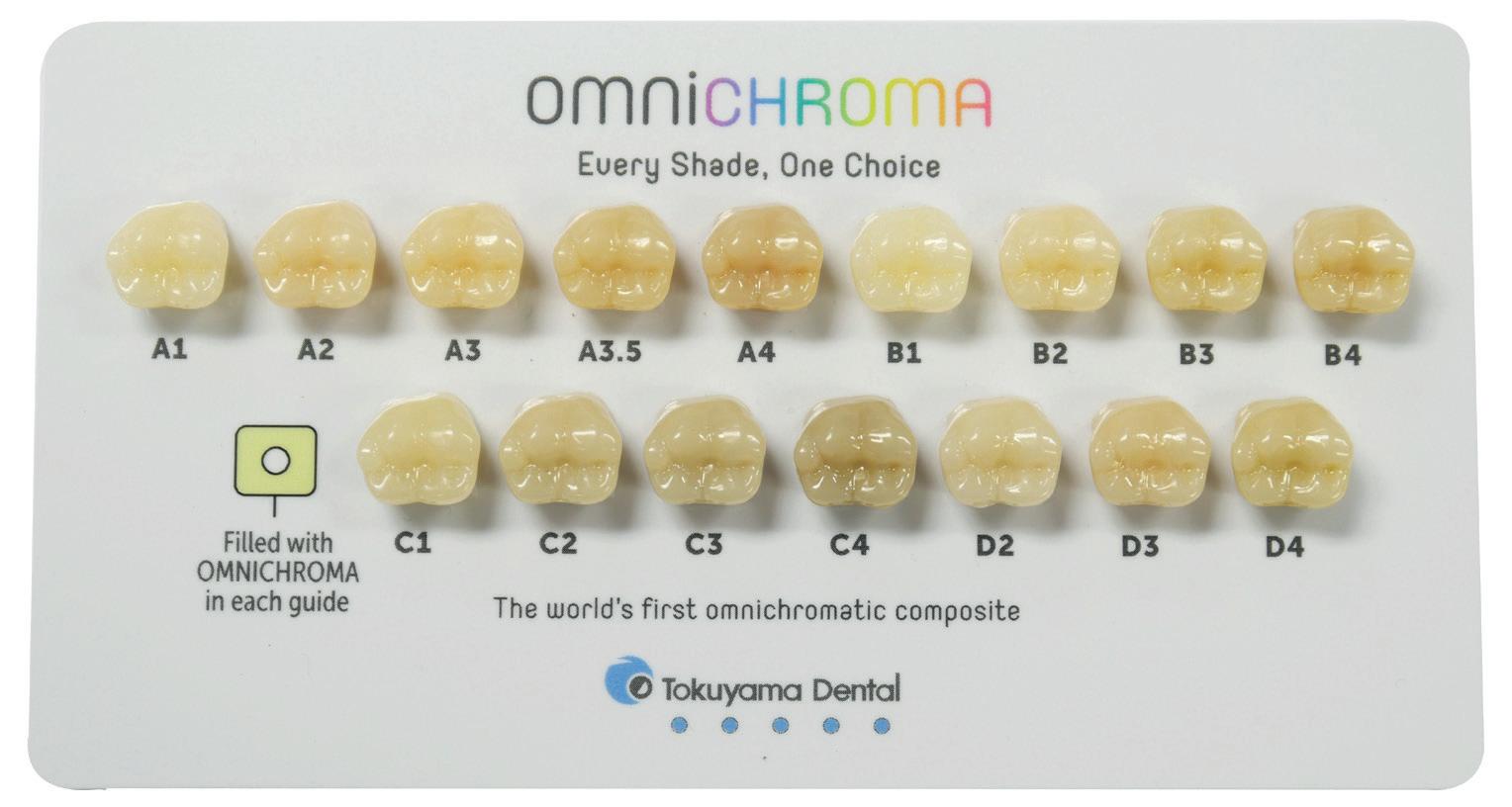
a colourless masking material which is used to hide heavy staining which could otherwise affect the overlying translucent Omnichroma restoration, affecting its ability to match perfectly the natural shade of the surrounding tooth. Omnichroma Blocker is also used to recreate palatal walls in Class IV restorations.
Experience shows that Omnichroma Blocker is required in approximately one in four restorations. However, this still means that a Practice only needs one Omnichroma and one Omnichroma Blocker to quickly and easily match every shade in the mouth. What is more, if the patient subsequently
has their teeth whitened Omnichroma restorations adapt to the new situation, unlike conventional composite materials which either stand out or need replacing. All of the above benefits are available within the complete Omnichroma range which includes Ominchroma for anterior and posterior restorations, Omnichroma Flow and Omnichroms Flow Bulk. For more information about the complete Tokuyama range, including Omnichroma, contact your local Trycare Representative, call 01274 885544 or visit www.trycare.co.uk/omnichroma or tokuyama-dental.eu/en n


Invest
Providing patients with the tools to increase their health literacy is a vital part of optimising treatment outcomes. It is recognised as the most ethical and effective way to build informed consent. However, headlines increasingly warn that patients’ ability to engage with, or to absorb information is compromised by the ubiquitous use of digital technologies in daily life.
Attention span averages are not as dire as some would have us believe – there is no reliable evidence to support the oftpublished claim that the average person now has an 8-second attention-span, for example. However, there is no doubt that the compulsive use of digital media, and repeated exposure to distractions is strongly linked to an impaired ability to concentrate. Clinicians should be cautious about assuming patients are able to engage with large amounts of information, or commit it to memory.
Sustained attention
Sustained attention (SA) is a complex field of study focusing on the ability to maintain attention while performing a mundane task.
Simple answers to the question of what modern patients can absorb – and how information is best shared during consultations in the digital age – are hard to come by.
In studies on attention-span, the simple consensus seems to be that most neurotypical people have variable capacities at various points in their lives for remembering or engaging with information.
The ability to commit information to memory and to sustain attentiveness largely depends on levels of interest as well as age.
Task-complexity has been shown to have an influence on SA, with more stimulating tasks predictably prompting more sustained and stable interest from participants.
SA between tasks, age groups and neurotype are very variable – in one single study of 262 individuals, average stable states of attention while completing a monotonous task ranged between 30 and 76 seconds. However, the overall range was very wide – between 9 seconds (the lowest result among children in the study) and 190 seconds (the highest result, from a participating young adult). Broadly, children had the lowest average attention spans, and young adults the highest.
the concerns – where patients’ concentration might be impaired
In some studies, addictive behaviour around digital technology – predominantly gaming and social media – is linked to symptoms closely resembling those associated with attention deficit hyperactivity disorder (ADHD), although there is no causal link to the condition, and the long-term effects are not clear.
Other studies have considered the risks of ‘shallow information processing’ in people overly relying on their digital devices. The availability of instant information on smartphones might be responsible for cognitive shortcuts that impair knowledgeconstruction in the brain. The phenomenon,
known as digital amnesia, refers to a decline in memory capacity due to an over-reliance on digital devices for storing and retrieving information. Patients suffering from this condition might struggle to engage deeply with information, and may have less developed critical thinking skills.
Used positively, the digital environment can enhance cognitive abilities. A number of apps, websites and games have been shown to stimulate visual attention and reaction time, as well as enhancing learning and thinking skills. One study, using magnetic resonance imaging (MRI) to track brain activity during internet searches, suggests that simply using search engines can be a form of mental exercise that can strengthen neural circuits, improving cognitive function.
Digital-era patient engagement
To ensure patients are truly engaged with information, and are genuinely able to consent to treatment, effective education resources are a must. Educators are advised to combine auditory, visual and hands-on learning to ensure patients with different processing preferences are fully engaged and able to access the information. For patients with an impaired ability to pay attention, it is advised that information is wellorganised, visual and clear, and repeated as many times as needed.
However, clinicians often find that time is limited in consultations, and that they lack the opportunity to provide bespoke learning material for patients. In a 2022 survey,
84.4% of healthcare providers believed that electronic methods made patient education faster and more efficient. Enhanced digital engagement tools have been welcomed, and continue to evolve.
At the heart of Kiroku is a genuine aim to enhance patient understanding. Kiroku produces notes 60% faster, allowing clinicians to spend more time engaging with patients, as well as significantly reducing their own screen time. Amazing new voice transcription and other innovative tools in Kiroku AI take this even further. At the touch of a button, Kiroku provides easy-to-understand information, which can be sent directly to patients, along with consultation summaries and digital consent forms, ensuring real understanding at the same time as protecting clinicians. There may well be cause for concern in terms of capturing the attention of some patients in a world full of distractions. However, used correctly, digital tools can do much to enhance learning and inspire patients. Effective tools can also save much-needed time, allowing clinicians to spend less time on screens, and more time building real connections with patients. To find out more about Kiroku, or to start your free trial, please visit trykiroku.com n
about the author Hannah Burrow, ceO of Kiroku.
Many dentists, particularly those who qualified more recently, are very familiar with using digital workflows in the dentistry they provide. Globally, digital dentistry was estimated to be worth $6.9 billion in 2024 and is expected to grow to $9.3 billion by 2029 – a compound annual growth rate (CAGR) of 6.2% in this time.
The expected drivers of growth in this market are increasing demands for same day dentistry (saving both patients and clinicians time), increased outsourcing of manufacturing to dental labs, and rising demand for advanced cosmetic dental procedures. Each of these areas are supported by some form of digital dental solution, whether it increases collaboration between practices and labs, or improves efficiency, enabling practices to offer more modalities with shorter treatment times. Particular areas driving growth are dental lasers and digital imaging, as they enhance patient care and efficiency.
So, where can we expect to see development, what impact might this have, and how might digital dental innovations impact the profession and patient care?
Digital dental imaging
Dental imaging is an area which has already been greatly impacted by digital innovation. The development of CBCT, intraoral
scanners, and digital radiographs has made in-practice dental imaging more accessible for clinicians. However, whilst this uptick in usage spurs on innovation, the current technology widely available does not always provide the best and most reliable results.
Recent research suggests that the most influential area of digital dental radiography, in particular, is artificial intelligence (AI). However, it also acknowledges the role that dental magnetic resonance imaging, stationary intraoral tomosynthesis, and second-generation cone-beam computed tomography are set to have.
The continued research and development in digital dental imaging is promising, with various solutions proving themselves to be effective in dental workflows when treating mild to moderate cases. However, current models which use AI should be approached with caution. Whilst AI is very promising for the future of the profession, it is important to note that it is still in its early stages, with research and development in the area happening at all times.
The use of AI in dental imaging shows promise for the future of diagnostic accuracy. However, current models have their limitations. One review, analysing the current applications, opportunities, and limitations of AI in dental imaging, found a
number of factors which may impact the reliability of current models. Of the issues it found, the study highlighted two key limiting areas. These were AI models being trained using a small number of images and AI models only being trained using images of patients with confirmed diseases. Because of these factors, the appraisals AI models produce may be falsely optimistic, and might result in a lack of data heterogeneity, especially where the same imaging equipment has been used to capture the training images. As such, these limitations may mean that the resulting AI models have a lack of generalisability and are less reliable as a result. If used in other settings with other variables, where clinicians are using different imaging equipment and there are different patient populations, for example, the AI models may not be effective or accurate.
With digital dental technology becoming more popular, and its value set to rise in the coming years, many clinicians will be considering which pieces of equipment to adopt in their day-to-day workflows, and which areas to watch and wait. This is an area which, at current, offers a multitude of options which promise to make workflows more efficient. As such, it is important to carefully consider which pieces would most benefit your unique setting.

It is important to remember that accuracy in assessment, diagnosis, treatment planning, and treatment provision is vital. Therefore, the equipment you use to provide patient care must meet this high standard. Whilst digital solutions show much promise for the coming years, for now conventional methods must not be overlooked. Oftentimes, only the traditional techniques used to assess and diagnose patients offer the accuracy that is absolutely essential, particularly for those providing complex care, or running a specialist clinic. Digital dentistry is now an unstoppable force, and those of us providing patient care as part of our daily workflows must embrace it for the safer and more efficient future of our profession. However, it is vital to carefully consider the equipment which we use in our practices, and how they might help or hinder patient care.
https://mimetrik.co.uk n
about the author

alyn Morgan is the immediate past president of the British endodontic Society, and the co-founder and ceO of a spin-out company from the University of Leeds, Mimetrik Solutions.
There are many factors that affect the dental patient’s experience. Though some are more important that others, all must be considered in order to curate a consistently positive, effective and efficient patient journey. The consequences of getting it right are huge for the practitioner and for the practice. Not only are happy patients more likely to develop loyalty and return time after time, they are also more likely to recommend your services to friends and family, further supporting business growth. Furthermore, there is evidence demonstrating a positive correlation between patient satisfaction and clinical effectiveness.
excellence remains king
As would be expected, one of the top contributors to a fantastic patient experience is high-quality treatment. A European study from 2023 found the quality of treatment received to impact everything from whether a patient would recommend the dentist to others to their relationship with the dentist. Interestingly, the same research found that patient satisfaction with the frequency of appointments also impacted their overall contentment with treatment and loyalty to the practice. There is also evidence to show that patient perception of pain and pain management may impact their overall experience. Efficient pain assessment and pain management options with fewer side effects have proven helpful in improving patient satisfaction with treatment. This
further supports the importance of clinical excellence in dentistry, as with careful planning that includes an effective choice of analgesic, clinicians can help to reduce post operative pain.
However, it doesn’t stop there. There are social factors at play too. For instance, patient characteristics like age and education level can affect their perceived experience in any healthcare setting. Broader influences like those from wider societal trends, or community and family contexts can also affect patient expectations and, therefore, satisfaction with the dental care they receive.
In addition, the communication between patients and healthcare professionals has been shown to influence their satisfaction with the service received. Specifically in dentistry, effective professional-patient communication has long been recognised as a cornerstone of high-quality care. Ensuring that patients understand their current oral health status and the need for recommended treatment, empowers them to be more involved in their oral health, improving their overall experience. This communication can also reduce the risk of dental anxiety among patients and increase trust in their practitioner.
However, it doesn’t stop there. A combination of staff behaviours, facilities and basic environmental needs also
influence the patient experience. Examples include practice opening hours and cleanliness. The physical environment may also impact patient outcomes and satisfaction, including the layout of the practice, room features, medical equipment visible, lighting and music.
Technology is another area that has become instrumental in delivering an excellent patient experience. Studies have touted the latest tech as having helped to enhance efficiency, safety and accessibility of dental care. Specific solutions such as intraoral scanners have also become a widespread preference among patients, who appreciate the elimination of the traditional ‘gooey’ impressions.
Of course, imaging technology isn’t the only solution making waves in the dental profession. Innovative practice management software is streamlining the entire patient experience from the moment they book an appointment, through to their treatment and beyond. AeronaDental, for example, is a next generation cloud-based software that impacts every aspect of the patient journey. Add-ons like the Patient Portal facilitates online engagement, bookings, digital form-filling and online consultations, while integration with solutions like Dojo – a flexible and secure payment provider –make paying for treatment 58% faster than the average mobile card machine. Plus, the provider offers all this alongside exceptional customer support, so you know you have the experts on your side when it comes to optimising your patient experience.

Ultimately, everything about the modern dental profession is designed to support patients to better oral health. If patients have a positive experience in the practice, this is not only good for business, but it also means they are more likely to return for on-going treatment, boosting continuity of care and their long-term health. Considering every aspect of their journey through the practice is important for a truly patient-centred approach.
For more information, please visit aerona. com or call 028 7000 2040
Follow us on LinkedIn: @AeronaDental Software and Instagram @aeronasoftware for the latest updates
Mark Garner, General Manager, Areona Dental.


















Across the profession, things continue to change. Digital dental innovations are the driving force behind many changes to workflows in practices across the country. It’s important to understand the ways in which digital solutions can be implemented, and what they mean for yourself, your team, and your patients. Digitisation within imaging, diagnosis, and communication all play a key role in streamlining workflows as well as improving your patients’ experiences. To make the very most out of a digital workflow, incorporating this technology in all aspects of the practice, including the treatment centre, will be beneficial.
Using digital solutions in your practice benefits the whole dental team. Oftentimes, less time needs to be spent on administrative tasks when a digital system is used. For example, intraoral scanner image files can be sent digitally, as opposed to sending physical impressions by post. Plus, when sharing equipment or discussing cases within the practice, digital systems accommodate this, making it far easier to collaborate with other dentists. Digital workflows are designed with easeof-use in mind, and are often time-saving solutions. This means that new systems are generally more intuitive, and easier for the whole dental team to pick up on. When a team is confident using modern technology, your practice is future-proofed, ready for any further digital technology you’d like to introduce. With this confidence, the likelihood
of errors during the patient’s journey is far reduced, for a more reliable experience.
consistency across the practice
While individuals must prioritise which areas of digital dentistry to invest in first, based on the unique requirements of the dental practice, aiming for a seamless digital workflow helps to keep all processes consistent and integrated. An intraoral scanner, for example, may be used to produce digital impressions which inform a patient’s treatment options. By having all digital imaging available in one place, as opposed to a mixture of analogue and digital variations, fewer mistakes are likely to be made, and treatment decisions will be more predictable and reliable. By incorporating digital advancements across all areas of your practice, you offer patients a seamless journey, supported by the latest technology. This is even appropriate in areas you may not immediately think of, like your treatment centre. It’s important that this key piece of equipment offers exceptional patient comfort and ergonomic working for you and your team, however, integrated technology could offer additional tools to support treatment acceptance and communication.
Digital solutions, in general, have the ability to enhance communication between patients and dentists. Imaging, in particular, allows dentists to clearly show their patients exactly what they can expect during their treatment. This makes patients feel more included in decision making, and gives them the information they need to ask questions
Dentistry often evokes a lot of emotion in people. This might be seen in the passion that dentists and their teams have to improve public health, or the wholehearted gratefulness that patients experience after their dentist has changed their life for the better. Of course, there can be some less positive emotions at times as well, especially when it comes to professionals under significant pressure. For many patients – over half the population in fact – feelings of anxiety and fear are associated with a visit to the dental practice as well, which can impact the regularity of their attendance and their oral health-related quality of life. Helping these patients to regulate and alleviate their concerns is important and involves creating the right physical environment in which to deliver their dental care.
Where does the fear come from?
Dental anxiety can develop for a number of reasons and it often has a complex aetiology. For many individuals, the fear stems from traumatic previous experiences in the dental practice, whether as children or earlier on in their adulthood. Dental anxiety can also be a learned behaviour from parents, with education level and personal traits impacting a patient’s risk of developing dental fear. This highlights the importance of effective communication with affected patients, giving them an opportunity to share their

and participate more actively in their care. Some research suggests that the use of digital solutions in the practice encourages trust. It is important to tailor every aspect of the care you provide your patients – this means selecting the best approach in each case. For some patients, using high tech solutions during their appointments will not appeal, but for others, it could be the difference between them accepting treatment or not. Clinicians should stay up to date on the latest technology – ensuring that they feel comfortable using it – and establish patient trust. This, in turn, can further boost treatment acceptance.
Implementing digital solutions across your practice is key for boosting the patient experience, and streamlining workflows - this includes your treatment centre. This piece of
equipment is at the very heart of your dental surgery, and is in the perfect place to enhance communication with your patient. Clark Dental has over 49 years of experience in dentistry, and can make choosing the perfect solution for your unique surgery easy. The advanced Dentsply Sirona Axano treatment centre offers exceptional ergonomic features in addition to integrated digital functions such as the SiroCam AF+, Sivision monitor, and Smart Touch user interface. The Axano’s design is optimised to produce excellent workflows –from the initial diagnosis to case completion. Its Sivision monitor allows you to improve communication with your patients, helping them to actively engage in their treatment. In many cases, digital solutions allow clinicians and their patients to get the most out of each appointment. Tools which enable clinicians to easily explain treatment plans to their patients are particularly helpful – enabling patients to get involved with their care. While it’s important to establish the areas which would most benefit from digital workflows in your practice, consider ways in which these solutions can boost patient satisfaction, improve treatment predictability, and increase treatment acceptance. If you’d like to find out more about Clark Dental’s solutions, call the team on 01268 733 146, email info@clarkdental.co.uk or visit www.clarkdental.co.uk. n
about the author
Stuart clark, Managing Director of clark Dental.

concerns without judgement. To optimise this exchange, it’s vital to create a warm and welcoming atmosphere within the practice, to treat them with respect and dignity and to really listen to what they say. It’s essential that these patients feel validated, cared for and supported by a clinician who is genuinely interested in making the dental experience as pleasant as possible. In the practice, nervous patients may be triggered by a number of physical aspects too, including the sounds, smells and sights of the practice. The combat these, the dental team may consider using headphones and music to calm patients in the chair, and installing fragrance solutions throughout the practice. When it comes to the aesthetic of the practice and making the physical environment more appealing, there are several areas to explore.
colour me calm
The physical environment can also have a significant impact on patients’ emotions and behavioural responses. For instance, the décor can instantly create or destroy the atmosphere within a room thanks to colour psychology. Research in this field has shown that certain colours evoke specific feelings and emotions in the majority of individuals ¬– green is often linked to nature, growth and freshness; blue with sympathy, compassion and warmth; orange with sunshine and happiness. A study in 2020
looked at this in more detail and found red is associated with anger or love, yellow with joy, brown with disgust, grey disappointment and black fear and contempt. So, choose your colour scheme wisely when it comes to decorating your practice, particularly with nervous patients in mind.
Bringing the outside in
Interior design concepts like biophilic design may further help to reduce anxiety and promote recovery from stress among patients visiting the practice. This involves incorporating elements of nature into the indoor environment, by adding plants or with views to the outdoors through strategically placed windows. In addition, the choice of materials within a space can help to reduce people’s stress levels, with glass associated with fewer feelings of isolation and enhanced relaxation compared to metal and even wood in some instances.
Another feature to think about when creating the best possible physical environment for nervous patients is ergonomics. A layout and design that facilitates patient comfort and makes their journey through the practice as simple and pleasant as possible is essential. The dental equipment selected can also play a role here, impacting the efficiency of a patient’s treatment experience.
For expert support in designing, installing and maintaining a new practice for years to come, turn to RPA Dental. Their team has decades of experience in tailoring surgery design for the benefit of patients and professionals alike, utilising their stellar knowledge of dental specific regulations and general design concepts to help you create a stunning practice you will be proud of. Known for exceptional customer service, they will help you select the right dental equipment, cabinetry and finishings for your business, and then look after them with long-term servicing and support.
It’s important that all patients feel able to access the essential dental care they need, including those that suffer with dental fear or anxiety. There is an array of steps that a dental practice can take to create a more welcoming and comfortable environment for these individuals.
For more detail about the solutions and services available from RPA Dental, please visit dental-equipment.co.uk, call 08000 933 975 or email info@rpadental.net n
about the author
adam Shaw, Sales Director at rpa Dental Ltd.

Adental practice impacts the environment, from the material waste generated by procedures to the consistent use of water and electricity. Its impact is in fact greater than that of general healthcare: across Europe, General Medical Practitioners produce 100kg of waste per year whilst General Dental Practitioners produce 260kg per year, indicating the need for more sustainable solutions to manage waste in dentistry.
One of the products found in dental waste is mercury, which comprises 50% of the dental amalgam used in restorative dentistry. Amalgam waste is generated from overproduction, drilling, and removing old fillings. Disposing of it properly is essential for the safety of the environment, wildlife, staff and patients, making it a legal, ethical and professional duty.
In optimal conditions, bacteria can convert mercury waste into methylmercury, a neurotoxin. If methylmercury integrates within the natural world – rivers, seas, soils – it is absorbed into the wildlife, potentially affecting the animals that humans may then eat. Methylmercury can cause brain, kidney and lung damage for humans, and it is alarmingly easy for people to reach high levels of exposure to this substance.
For over 150 years, mercury has been a key component used in dental amalgam, along with other metals such as silver, tin and lead. Amalgam use in primary care is high, especially in the publicly funded sector where the majority of posterior restoration provision lies. Whilst amalgam is being phased out globally, the amount of waste that is, and still will be produced, is high: dental clinics contribute between 3% and 70% of environmental mercury, with spillage, storage issues and a non-adherence to the necessary precautions being the three common explanations for this output.
Mercury can be released from autoclaving amalgam-filling dental instruments, incinerating amalgam wastes, and the uncontrolled disposal of amalgam extracted teeth. The proper management and disposal of dental amalgam can, therefore, minimise the amount of elemental mercury vapour entering the environment.
It is imperative to be up-to-date with the best practice waste disposal regulations and have an effective strategy within the dental practice setting to follow these. To avoid binning harmful substances into the sludge drum or washing them away into the water supply, practices need to educate their staff on the safe management of mercury waste. This is necessary to follow The Controlled Waste (England and Wales) Regulations 2012, the Environmental Protection Act 1990

and the Regulation (EU) 2017/852 of the European Parliament and of the Council, which dictates that amalgam separators must retain 95% of amalgam particles and these shall not be released directly or indirectly into the environment under any circumstance. For amalgam separators, meeting the British Standard Dental Equipment (BS ISO EN 11143:2000) is also essential for waste safety.
Besides harmful substances, the manufacturing and distributing of any object has an environmental impact as it requires raw materials and energy, with the added potential of releasing pollutants into the air, land or water. Research has elucidated that, since the 1970s, humanity has accumulated an ecological debt; more resources are being spent than the planet can reproduce. This is especially obvious in economically developed countries, where the amount of waste produced per person is significantly higher. By managing our resources in an environmentally friendly way, such as using recyclable products, the imbalance can be changed.
Initial Medical supports sustainable dentistry with their range of recycled dental collector cups. Ideal for capturing amalgam waste and preventing the release of mercury into the environment, the collector cups are thoroughly cleaned and returned to the original standard of a new cup by the Initial Medical service. This reduces single-use plastic consumption in the practice and offers a more cost-effective option compared to purchasing new collector cups. By replacing the collector cup after each use, the build-up of debris that can damage the dental pump is prevented, ensuring a safer workplace. Initial Medical is here to help both your practice and the planet.
As the fight to preserve the natural world becomes more and more important, incorporating sustainable solutions into the dental practice
can better manage harmful waste. Controlling amalgam waste and the mercury in it promotes a safer, greener work environment for staff and patients alike.
To find out more, get in touch at 0808 304 7411 or visit the website today www.initial.co.uk/medical n

about the author rebecca Waters has worked in the healthcare sector for the past 20 years and earned a BSc chemistry (Hons) prior to joining rentokil initial in 2003. She works within the research and Development team and keeps up-todate on all changes within the clinical waste management industry, as well as the specialist hygiene and infection control industries, and is an active member of the ciWM and HWMa Following roles as an analytical chemist and Hygiene chemist, she has worked in a variety of leading marketing roles since 2006, making her an expert within the industry. She is a Fellow at the chartered institute of Marketing, an FciM. rebecca loves spending time outdoors and in the water – whether walking, camping, or swimming – and completed a focus on environmental studies during her university degree. She is proud to be pushing a sustainability agenda throughout her work.


To learn more about our digital solutions, contact us todaymarketinguk@planmeca.com or 0800 5200 330
Embarrassment is a common and ultimately necessary part of the human experience. However, the feeling can often be overwhelming, and anxieties can develop because of it. In dental care, a patient’s embarrassment about their oral health – perhaps because of its aesthetic qualities – may lead to them developing dental anxiety, and avoiding regular appointments.
It is the responsibility of the clinician to manage patients’ dental anxiety appropriately, and treat them with kindness and compassion. Working this way makes the practice a more welcoming space for those dealing with such intense negative emotions, and allows them to access essential oral health care without shame.
It is expected that patients with dental anxiety also have worse oral health because they actively avoid dental care; this further fuels the cycle where patients can suffer psychologically and physically. Intervention is therefore of even greater importance.
Self-conscious concern
Societal standards of oral health and aesthetics may not be met by patients, becoming a key source of embarrassment. The expectation in western societies is that one’s teeth will be straight and white. When a patient’s condition deviates from this ideal, they may feel negatively about themselves, and believe that other people, including clinicians, will hold the same opinions. Some adults with dental phobia may feel this way because of poor treatment from a previous dentist. Others
may anticipate a poor reaction based on experiences outside of the dental chair, which have then been ruminated on for weeks, months and years. Situations such as these can create ‘schemas’, or psychological core beliefs that have developed over time, which could include a belief that others will view their dental health as unacceptable.
Clinicians must observe that shame is also linked to one’s core identity, and that it can affect an individual’s sense of belonging and social acceptance. Dental aesthetics also have a significant role in social interaction, with an attractive smile being of great importance for first impressions. People with favourable dentofacial aesthetics are also perceived as more intelligent and attractive, as well as more successful.
When a patient believes their condition could result in social rejection, especially from a dental professional who they presume sees exemplary dentitions on a daily basis, they may perceive that their identity as a person is at risk of being judged too.
When patients anticipate a negative response – even when it is not felt nor expressed in any way – they may avoid appointments, or respond to oral health advice and instruction with sarcasm in attempt to regain control of the situation. Patients may not even realise the latter is related to their embarrassment, and may not have malicious intent behind it. Clinicians should exercise patience and ensure individuals can receive the care they need in the moment.
The scope of the dental professional has expanded in recent years.
We now provide information and advice on so much more than just oral hygiene, including exercise and diet recommendations. Our goal is to facilitate the overall wellbeing of our patients. Plus, all these areas connect so improving one will often simultaneously enhance a person’s physical, mental and oral health. When it comes to diet, I was interested to come across an article considering supplements and their effectiveness. Are they necessary? When are they most beneficial? Should we as dental professionals be recommending them to patients? I did some reading…
The five most common supplements taken by adults in the UK are vitamin D, vitamin C, vitamin B complex, vitamin A and vitamin E, although half the population chooses a multivitamin to cover several bases at once.
Vitamin D: Approximately 1 in 6 adults have low vitamin D levels in the UK, which increases their risk of rickets. The vitamin is also important for a lowest risk of oral health concerns like dental caries and periodontitis, with research suggesting beneficial indications for endodontic treatment in patients with systemic health conditions like diabetes. The majority of vitamin D is absorbed from sunlight and there are limited dietary sources. Current
encouraging attendance
Individuals not attending appointments are a major cause for concern. They may see their oral health worsen if they do not receive timely treatment to arrest decay or infection. As their condition continues to deteriorate, the feelings of embarrassment may develop further; the individual then falls into a continuous cycle that is difficult to break.
To actively engage with embarrassed or anxious individuals, and ensure they return for treatment on a consistent basis, dental professionals must listen to their concerns and create an environment that is welcoming. Dentists should be aware of how their tone of voice and body language might be perceived. They should display emotional support to alleviate patients’ fears, placing an emphasis on developing a relationship built on mutual trust.
Ensuring patients feel some control over their care is essential. In the practice, this could include use of the tell-show-do technique or signalling when a patient needs a break from treatment.
Dentists can also empower individuals by recommending effective oral hygiene routines with easily implementable solutions, like the Cordless Advanced Water Flosser from WaterpikTM. The simpleto-use oral hygiene adjunct removes up to 99.9% of plaque from treated areas with just a 3-second application, and is 50% more effective than traditional dental floss. For the self-conscious patient, it is a straightforward step in their oral hygiene routine that can have immense benefits to the health and appearance of

their dentition, supporting the journey to restored confidence.
An individual’s oral health and appearance can be a great source of embarrassment and anxiety that stops patients from receiving timely help. Dental professionals have the opportunity to provide encouragement in both regular attendance and the maintenance of oral hygiene routines. By listening to the concerns of anxious individuals, giving them control where appropriate, and creating a welcoming environment, patients that are embarrassed about their condition may be more likely to return for future oral health care.
For more information on WaterpikTM water flosser products visit waterpik.co.uk. WaterpikTM products are available from Amazon, Costco UK, Argos, Boots and Tesco online and in stores across the UK and Ireland. n
about the author
Margaret Black works between fixed and locum hygienist posts, and secured a role as an independent contractor for Church and Dwight in 2019.

recommendations from the Department of Health and Social Care are that adults and children should consider taking 10mg supplements daily between October and March, with some at-risk groups advised to continue year-round.
Vitamin C: Around 1 in 20 people in the UK has a vitamin C deficiency, otherwise known as scurvy. The body can usually get enough vitamin C through absorbing sunlight and eating adequate fruit and vegetables. Key symptoms of scurvy include yellowing of the skin and eyes, fever and bleeding gums. NHS guidance does not suggest that additional supplements are necessary for the general population, particularly as excessive intake can cause headaches, nausea and dizziness, and increase the risk of kidney stones.
Vitamin B12: Vitamin B12 helps the body make red blood cells, keep the nervous system functioning and release energy from food. The recommended daily amounts can usually be obtained from eating normal amounts of foods like meat, fish, milk, cheese and eggs. Official advice is not to take supplements unless specified by a doctor. Taking less than 2mg a day is unlikely to cause harm, though taking too much may lead to pain, fever, itching, numbness of joints, shortness of breath, rapid weight gain or bleeding, among other adverse effects. However, there is some evidence
to suggest that older adults, vegetarians, vegans and those with pernicious anaemia or gastrointestinal disorders may be more prone to vitamin B12 deficiency and may therefore consider supplements.
Vitamin a: Supporting the immune system, aiding vision and improving skin health, vitamin A is an important retinoid for the body. It also plays a crucial role in oral leukoplakia, oral sub mucous fibrosis and wound healing in the mouth. This is another substance that daily recommended amounts should be easy to achieve through a balanced diet – food like cheese, eggs, oily fish, milk and yogurt are ideal, though supplements may be useful in those with a proven deficiency. Consuming over the advised daily 1.5mg of vitamin A over many years can reduce the health of your bones and increase the risk of fracture in older age. Excessive intake can also damage the liver.
Vitamin e: Good for healthy skin, eyes and immune response, vitamin E is another substance that can be consumed adequately through a balanced diet. Found in plant oils, nuts and seeds, it can be stored by the body until needed so does not need to be eaten every day. An overdose of vitamin E can cause internal bleeding as well as thyroid problems, emotional disorders and gastrointestinal issues – it only becomes toxic with the use of supplements and rarely if ever due to diet alone.
the verdict on dietary supplements
The above is only a snapshot of the dietary supplements available to the general population and the research surrounding it. The general consensus seems to be that supplements may be useful for some people, some of the time – although they are not needed by the majority of adults. If anything, excessive intake of certain vitamins can actually do more harm than good. There is also evidence to suggest that supplements do not lower risk of cardiovascular disease or malignancies when taken by otherwise healthy people. Like everything in healthcare, the recommendation for dietary supplements must be made on a case-by-case basis and tailored specifically to the individual’s needs. It may also be worth asking patients whether they already take extra vitamins to be included in their notes for future reference. Some food for thought! For further information please call EndoCare on 020 7224 0999 or visit www.endocare.co.uk n
about the author endoCare, led by Dr Michael Sultan, is one of the UK’s most trusted Specialist endodontist practices.

Oral cancer is a growing public health problem, with its incidence increasing worldwide and becoming more common across all demographics, including women and young people. As such, it’s important that clinicians and patients alike are familiar with its early signs and risk factors, to help limit patients risk levels, and to help detect mouth cancer in its early stages.
Increasing prevalence of oral cancer
Oral cancer is becoming more common, with an increase in new cases and deaths in recent years – in 2020 there were an estimated 377,713 new cases and 177,757 deaths. Oral cancer can affect the lips, mouth, and oropharynx, and is the 13th most common cancer worldwide, being more common in men and older people. In Europe and North America, mouth cancer is becoming more prevalent in younger people due to human papillomavirus (HPV), whilst tobacco, alcohol, and areca nut use are some of the leading risk factors for the disease. Public awareness of mouth cancer is poor meaning that many patients may not know that their habits or lifestyle may be putting them at risk of the disease. Because of this, it’s essential to educate patients when they attend their appointments, to help make them aware of the signs and the importance of attending the practice regularly. Oftentimes, a visual exam is not sufficient to detect mouth cancer in its early
stages. As such, it is important that clinicians take into account a patient’s oral health, and other risk factors, along with undertaking pre-diagnostic tests to determine a patient’s risk level for oral cancer.
Poor oral hygiene brings increased risk
There exist strong associations between mouth cancer and poor oral hygiene. Research suggests that having fewer missing teeth, regularly attending dental check-ups, and toothbrushing twice per day are associated with a reduced risk of oral cancer. Additionally, poor dental hygiene aids the cancer-causing potential of other known carcinogens – such as tobacco and alcohol, for example. However, even when adjusted for these factors, poor oral health may present a higher risk of mouth cancer. This is due to poor dental hygiene and the accumulation of plaque leading to a chronic inflammatory process. The environment promotes the development of oral cancer. A study revealed that periodontitis is an independent risk factor for mouth cancer, with the risk of oral squamous cell carcinoma increasing in the more severe stages of periodontitis. Another study found that 93.4% of patients with oral squamous cell carcinoma reported to brush their teeth only once per day, and the majority (57.85%) never attended dental appointments.
With the maintenance of dental hygiene, dentists and dental hygienists/therapists can help to prevent oral cancer. Further to this, clinicians should evaluate patients’
socioeconomic statuses and lifestyle factors to establish their level of risk. By educating patients about the relationship between oral hygiene and mouth cancer, clinicians can help to prevent the development of periodontal diseases and, in turn, reduce the risk of cancer.

Early detection for better outcomes
It can be very difficult to detect oral cancer in its early stages, with initial symptoms appearing visually similar to other common issues – like mouth ulcers, for example. However, detecting it in stages I and II is essential for giving patients the best outcomes. When diagnosed and treated in its later stages, oral cancer treatment can have a lasting effect on patients, impacting their quality of life. Further to this, survival rates significantly improve when mouth cancer is detected in the early stages. Research suggests a 95% survival rate at five years for stage I mouth cancer, with stage IV cancer having a 5% survival rate at five years. As such, to significantly improve a patient’s prognosis, early detection is essential.
A great way of doing this is by testing patients with the BeVigilant™ OraFusion™ System from Vigilant Biosciences® as part of a health check-up. The non-lesion test rapidly detects oral cancer-associated biomarkers in 15 minutes or less. It analyses the patient’s saliva for biomarkers associated with oral cancer, as well as their risk factors to produce a report of low, moderate, or high risk for cancer. Ideal for chairside use during dental appointments, it offers clinicians a straightforward and accurate way to test their patients, aiding in the early detection of mouth cancer. In order to improve outcomes for your patients, regular dental appointments, education, and improved dental hygiene is essential. With many risk factors affecting all demographics, and a rise in women and young people getting mouth cancer, it’s important to ensure clinicians are tailoring the advice they provide their patients, and carrying out thorough exams and prediagnostic testing frequently. This will allow them to detect oral cancer in its early stages, and improve survival rates for their patients. For more information, please visit www.vigilantbiosciences.com or email info@vigilantbiosciences.com
About the author Phillip
Silver, Founder of Total TMJ.




As an increasing number of adults seek orthodontic treatment for aesthetic reasons as well as to restore function, it’s important to be reminded of the relationship between orthodontic treatment and periodontal health, which is both significant and complex.
Understanding the connection is crucial for clinicians and patients, as it can impact the overall success of orthodontic procedures as well as the long-term gingival health and the supporting structures of the teeth. Poor periodontal health can lead to tooth mobility, loss of attachment, and even tooth loss.
Orthodontic treatment as a benefit to periodontal health
While there are challenges associated with orthodontic treatment and periodontal health, there are also many potential benefits. Straightening teeth can lead to a less traumatic occlusion, reducing the acceleration of bone loss in those patients suffering with periodontal disease. Addressing malocclusion has also been found to result in a reduction of periodontal pocket depths in some patients.
Once orthodontic treatment is complete, and teeth are aligned, patients can often find it easier to maintain proper oral hygiene due to improved tooth alignment, which can contribute to better long-term periodontal health.
Careful remodelling
The primary goal of orthodontic treatment is to reposition teeth. As teeth move, a complex series of changes occur around the surrounding periodontal tissues and alveolar bone. Whilst remodelling tissue
and bone is an essential part of orthodontic treatment, the process can temporarily affect the health of these tissues, and has to be managed and monitored carefully to prevent complications.
Healthy periodontal structures include a root cementum, periodontal ligament (PDL), and alveolar bone, and constitute a functional unit or organ. The PDL forms a vitally important and complex connection between teeth and the alveolar bone. Fibroblasts from the PDL maintain and repair the alveolar bone as well as the cementum of the teeth. Orthodontic treatment can result in traumatic widening of the PDL, which can cause it to thicken, affecting its function. This widening is implicated in the processes resulting in the thinning of alveolar bone as well as gingival recession, and is considered to be a warning sign of periodontal disease.
Before commencing any orthodontic treatment, a thorough periodontal assessment is essential. Clinicians should evaluate the health of the gums and supporting structures to identify any preexisting conditions. Treating periodontal issues, and evaluating patient motivation prior to orthodontic intervention is vital to ensure better outcomes and minimise risks during treatment.
Regular monitoring of periodontal health throughout orthodontic treatment is also crucial. The dental team should work collaboratively to ensure that patients maintain good oral hygiene and that any signs of periodontal disease are addressed promptly.
Patients with fixed appliances may find it challenging to maintain adequate oral hygiene

around brackets and wires to prevent the spread of harmful bacteria. The intricate surfaces of braces can create additional opportunities for food particles to accumulate, leading to the formation of biofilm, increasing the risk to periodontal health.
The antibacterial and flushing effects of saliva, as well as contact with the lips and tongue that help keep teeth and gingiva clean can be hampered during clear aligner treatment, and tight, form-fitting plastic of aligners or retainers create new surfaces for biofilm to adhere to. Keeping aligners clean is vital to protect oral health, and to prevent demineralisation, fluoride toothpaste, rinses and gels are recommended.
for patients
Regular oral health examinations with both orthodontists and dental hygienists are important for professional cleanings and monitoring periodontal health during treatment. Maintaining excellent oral hygiene is paramount to prevent periodontal complications. Patient education is essential to ensure they brush their teeth at least twice a day.
Patients with fixed appliances should also be shown how to perform interdental cleaning during treatment, and how to clean around brackets and wires effectively. Incorporating antimicrobial mouth rinses and
gels can help reduce the build-up of biofilm, protecting teeth and gingiva throughout their treatment. Enhanced oral hygiene routines are important post-treatment too, as subgingival bacteria can remain higher than average for orthodontically treated patients for up to 6 months after the removal of their fixed appliance.
Oral hygiene products like the FLEXI range of interdental brushes from TANDEX are perfect for use with orthodontic appliances. FLEXI comes in 11 different brush sizes to suit every interdental space, and is perfect for cleaning difficult-to-reach areas around brackets and wires. Extra protection can be easily achieved by adding a small amount of PREVENT Gel to FLEXI brushes. With 0.12% chlorhexidine and 900 ppm fluoride, the gel is perfect for everyday oral hygiene routines. Due to the strong links between periodontal health and orthodontic treatment, clinicians continually prioritise periodontal assessment and monitoring throughout the treatment process to ensure optimal outcomes. By understanding the interplay between orthodontics and periodontal health, both practitioners and patients can work together to achieve not only a straighter smile but also excellent overall oral health.
For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from DHB Oral Healthcare https://dhb.co.uk/ n
about the author Jacob Watwoodon on behalf of tandex.

The main functions of root canal sealers are sealing off of voids, forming a bond between the core of the filling material and the root canal wall, and acting as a lubricant while facilitating the placement of the filling core and entombing any remaining bacteria. Several types of sealers are available, which vary in formulation and properties. They are classified into five main groups according to their composition: zinc oxide eugenol (ZOE) based, calcium hydroxide based, glass ionomer-based, resin-based and bioceramic sealers.
An effective root canal sealer should be able to create a tight seal, should be radioopaque, antimicrobial, non-shrinking, nonstaining, non-irritating, insoluble in tissue fluid and biocompatible. Finding the right biomaterial to seal and fill a root canal is a hot topic, due to the exciting development of new materials, as well as the fact that inadequate obturation has been found to be the most frequent reason of treatment failure.
What are biomaterials?
Biomaterials are biological or synthetic substances which can be introduced into body tissue as part of an implanted medical device, or used to replace an organ, bodily function, developed to be compatible with existing living tissue. The technology is fastdeveloping, bringing together principles
from engineering, chemistry and biology. Metals, ceramics, polymers, glass, nanoparticles, and even living cells and tissue all can be used in creating a biomaterial. Newly developed biomaterials do more than simply coexist benignly with living tissue to restore function. More and more, biomaterials contain bioactive components that are actively able to promote wound healing and soft and hard-tissue regeneration. Inorganic bioactive materials have gained significant importance in the last two decades for the management of dental tissue loss, increasing the chances of regeneration and remineralisation.
Bioactive bioceramics
Bioceramic-based root canal sealers, have only been available for use in endodontics for the past thirty years. Bioactive materials in this category – calcium silicate, bioactive glass and ceramic, and hydroxyapatite – interact with the surrounding tissue to encourage the growth of more durable tissues.
Calcium silicate (CS) is widely used, as it has a number of advantages as sealer material. It has antibacterial properties, is highly biocompatible, its particles diffuse well into the dentinal tubules to produce mechanical interlocking bond, and silicatebased endodontic sealers exhibit superior suppression of chronic inflammation than zinc oxide-based materials. These is also
a reaction with CS in the presence of the dentine’s moisture, resulting in the formation of hydroxyapatite along the mineral infiltration zone.
Hydroxyapatite is the main structural component of tooth enamel and bone mineral that provides hardness. Due to its excellent biocompatibility and bioactivity, it’s also widely used in orthopaedic and dental implants.
the importance of biocompatibility
Biocompatibility has been defined as ‘the ability of a material to function in a specific application in the presence of an appropriate host response’, meaning the host immune response to biomaterials is a critical determinant of successful clinical outcomes. The term ‘host response’ encompasses a wide range of various biological responses from cytotoxicity and allergic reaction to biostimulatory effects on tissues.
Sealers based on bioceramic materials have been shown to be significantly less cytotoxic than other sealers. Epoxy-resin based materials cause a longer-lasting and more powerful chronic inflammatory response than all other sealers.
Intelligent biomaterials
ROEKO GuttaFlow® bioseal from COLTENE isn’t just a state-of-the art, intelligent obturation material for quickly and effectively sealing and filling root canals, it is
also an extremely bioactive material which actively contributes to the healing process. A number of studies have demonstrated that GuttaFlow® bioseal is significantly less cytotoxic than all number of other sealants due to its superior biocompatibility. GuttaFlow® bioseal is also thixotropic, meaning its viscosity diminishes under pressure so it flows into the smallest canal and isthmus. GuttaFlow® bioseal contains calcium and silicate to aid in the natural repair process. After curing, the bioseal also forms hydroxyapatite crystals to improve tissue regeneration.
Biomaterials play an integral role in dentistry and medicine today—restoring function and facilitating healing for people after injury or disease. Endodontics has significantly evolved in recent years, with advancements in biomaterials and nanomaterials science playing a pivotal role. Advanced biomaterials are transforming endodontic treatment techniques, offering improved clinical outcomes, improving healing and wellbeing and enabling a more patient-centred approach. n
about the author nicolas Coomber, Coltene national account & marketing manager.


upheaval of a patient complaint could happen to anyone. Our dentolegal experts will help get things back to normal.
Dental implantation is a longpracticed treatment for restoring function and aesthetics to the oral cavity, dating back to ancient times. For the treatment to work, a surviving implant must remain in the bone, be stable, and be functionally successful. Despite being effective as a treatment for edentulism, implant failure can occur in either short-term or long-term capacities if the risks are not reduced.
Such factors for implant failure can include selecting an alveolar bone site of inadequate quality, if the patient is a strong bruxist, or if they have poor oral hygiene. Whilst these factors can be controlled to an extent, peri-implant diseases can be a major barrier to treatment success and can be influenced by factors that are much harder to navigate or identify.
Finding the root Biology can play a major role in peri-implant diseases, with certain genetics and systemic diseases increasing the risk of peri-implant mucositis and peri-implantitis. Peri-implant diseases are long-term risk factors for treatment failure and understanding their aetiological history is essential to provide implant treatments that last.
Peri-implant diseases are inflammatory reactions from soft tissues that encircle a dental implant. They are multi-factorial, with the predominant causes being biological – (patients over the age of 60 are 3.2 times more likely to be diagnosed with them), biomechanical, clinical or relating
to the lifestyle choices of the patient.ii For example, patients who have a poor diet and fail to maintain a consistent oral hygiene routine are more at risk.
Peri-implant mucositis has a higher prevalence than peri-implantitis, ranging from 29.48% to 46.83%, but is also associated with an increased risk of becoming peri-implantitis. It is reversible through early treatment if its cause is identified and eliminated. However, dentists must work around certain biological factors to ensure treatment success.
Research into genetics as a factor for peri-implant diseases has often been inconclusive. Focus is drawn to the polymorphisms in the interleukin (IL) 1 gene cluster, with studies finding an association with periodontitis, a risk factor for peri-implant diseases. Moreover, the IL-1 genotype has a synergistic effect with cigarette use that can be detrimental to implant success. Prevalence of periimplantitis among smokers is 36.3%, almost double the rate compared to nonsmokers. It is therefore vital to discourage smoking for patients with implants as it can boost the risk of treatment failure.
As an inflammatory cytokine, the presence of IL-23 may add to the inflammation around an implant and can lead to impaired osseointegration and subsequent bone loss, undermining the stability of the implant. Cytokines may be crucial for the future as they can also act as a diagnostic tool; genetic
Avoiding overtreatment is essential for the safety of patients and the success of every dentist’s work. Overtreatment is defined as an intervention that is neither medically necessary or beneficial for a patient. Unnecessary treatments can incur higher costs and a higher risk of malpractice if the patient is harmed. As such, excessive overtreatment from practitioners is one of the major factors that can affect the public’s attitude to visiting the dentist, so it must be contained.
Understanding the aetiology of overtreatment will allow dentists to give safe, ethical care that benefits the patient. The risk of overtreatment increases if the dentist is younger, their practice is busy and they have less continuing professional education.
Overtreatment factors
A common cause of overtreatment is over-detection. Dental students have been found to consistently perform unnecessary diagnostic tests, over-thinking the process and often wasting their and, more crucially, the patient’s time. As students emerge into the professional world, they may bring an extra cautiousness to ensure that nothing is missed in the patient’s oral health.
A study of final-year dental students found that 87.8% of them proposed an overtreatment of a faulty restoration. This stems from an overdiagnosis and/or the proposal of unnecessarily invasive treatment plans. Poor communication with and education of the patient about the process can further complicate the process. This
polymorphisms are promising paths for new drugs to act on to help with treatments.
Systemic diseases
Systemic diseases have been found to have negative effects on implant success. Such diseases include diabetes mellitus, scleroderma, ectodermal disease, lichen planus, osteoporosis, rheumatoid arthritis, and Sjögren’s syndrome.
For diabetic patients, one of the more prevalent diseases, patient awareness and glycemic control should be taken into consideration when implant therapy is needed.ii By detailing the impact that diabetes can have on implant treatment, dentists can help encourage patients to maintain well-controlled insulin levels, as poor metabolic control provides more favourable environments for infection. Identifying patients with, or at risk of, systemic diseases is vital for better treatment planning so that long-term treatment success is ensured.
Alongside better implant treatment planning, complication risk can be decreased by creating an awareness of systemic issues and communicating with the patients who are more at risk of periimplant diseases. The use of more effective diagnostic tools, from instruments that assess implant stability to surgical guides, can help dentists achieve more predictable outcomes for implants that last.
Consider the W&H surgical range for an array of first-class equipment including

the Implantmed Surgical motor, Piezomed piezo surgery unit and the Osstell Beacon for measuring implant stability. From effortless bone cutting to assessing the stability of an implant, their ecosystem of innovative instruments and equipment can support your implant treatments. For over 30 years W&H has placed people as their priority. They are recognised for their quality advice and after-sales support, working with Key Opinion Leaders to run training courses and providing a team of efficient service engineers to ensure your equipment is always working at its best. By using W&H, you can revolutionise minimally invasive surgery that is maximally effective.
Peri-implant diseases can limit the lifespan of a successful implant. Whilst some of the factors for these diseases can be prevented or minimised, genetics and systemic diseases cannot. In these circumstances, raising awareness of these impacts can help secure the long-term success of implant treatment.
To find out more visit www.wh.com, call 01727 874990 or email office.uk@wh.com n
about the author Kate Scheer, marketing executive, W&H (UK) Ltd.

increases the risk of multiple restorations or re-restorations being needed, as the patient may not understand how to reduce the risk of restoration failure.
Students also tended to perform unnecessary treatments on patients with pre-existing conditions, such as those with caries. Whilst this level of care has the patient’s best interests in mind, delivering the necessary treatment details in the right way can make it easier for patients to digest the information. Patients do not have the time to listen to lots of explanations or undergo numerous unneeded treatments –most just want to hear or receive the best solution to their problem. It is important for graduates to develop a balance as they enter the professional sphere, managing well-communicated patient care without overdiagnosing and overtreating.
a matter of ethics
In healthcare, it can be hard to meet the demands of the patient, with moral dilemmas arising from the following of a strict ethical code. Patients may request treatments that they do not need, and this can lead to overtreatment. Unfulfilled expectations, especially in cosmetic dentistry, can dissatisfy patients who then seek additional treatment to achieve their vision. Some patients may also assume that the more care they receive, the better. It can be difficult to refuse a patient’s wish, creating a moral tension for dentists caught between the professional desire to meet patient expectations and avoid unethical treatment. This may cause psychological strain.
Acting ethically is vital for dental success; providing an excellent service maintains trust and loyalty from the patient, creating positive experiences and therefore return visits. Remembering that patients are not customers should always be at the forefront of a dentist’s mind. Taking preventative approaches and putting the patients’ interests before their own is crucial for dentists to comply with the GDC Standards for the Dental Team.
Dentists who clearly discuss all possible options before any treatment and offer advice and guidance on the risk, cost and effectiveness of each treatment display effective communication skills to the patient, helping them understand the options and generating trust. Clear communication and education on the patient’s additional treatment wishes can curb overtreatment by illuminating what is or isn’t necessary.
Overtreatment can be unintentional if outdated treatment techniques are used. A lack of knowledge and confidence can also encourage young dentists to undertake unnecessary treatments due to unclear diagnostics.i Radiographs are integral for identifying defects but, even for experts, analysing radiographs is an error-prone process. Undetected or misinterpreted anomalies can have serious consequences for patients.
This can be negated by incorporating effective, reliable services and equipment into your workflow that offer accurate diagnostics. By utilising more precise technologies, all dentists can avoid

an incorrect diagnostic and prevent unintentional overtreatment.
For those looking to take a first step into digital dental radiography, the RVG 5200 sensor is the economical and easy-to-use device from Carestream Dental. Small in size, the sensor produces high-quality images that inform exceptional treatment plans, all while being affordable. Image processing tools allow you to customise according to your own specifications, ensuring confidence with your diagnosis. The RVG 5200 has been tested for ten years for intense, daily use. It is also fully waterproof, allowing immersion in disinfecting solution for enhanced hygiene and safety.
Overtreatment can be risky and unappealing for patients, impacting how they perceive a dental appointment. By fusing ethically-driven dentistry with accurate diagnostic equipment, dentists can ensure that they only do what is needed, improving patient care and engagement.
For more information on the RVG 5200 visit www.carestreamdental.com n
about the author nimisha nariapara is the trade marketing manager at Carestream Dental covering the UK, middle east, nordics, South africa, russia and CIS regions

Although dentistry is, at its core, focused on oral health, clinical techniques and approaches have developed and the range of treatments that dentists are able to offer their patients has expanded. The obvious benefit being an increase in both patient choice and the ways in which dentists can assist their patients. There is certainly a great deal more interest in, and demand for, cosmetic dentistry. The online world has exposed people to ever-greater levels of expectation and pressure to look good. Attractive teeth have always been valued, and have now become even more of an aspirational commodity. This is reflected in the ways that patients seek information on and engage with dental treatment. Against this backdrop, the role of ‘treatment co-ordinator’ has become an established concept in some areas of practice.
The whole idea of treatment co-ordinators is not entirely new. They have been around in one form or another for a while now, but it’s fair to say that it is a role that has become more of a feature in recent years.
There are clearly benefits to both clinician and patient in ensuring that patients are as well-informed as they can be about treatment options. In some cases, a treatment co-ordinator can be the liaison between patient and dentist and act as a “personal guide” to assist patients with their dental journey by being able to offer explanations in patient-friendly language. They are often a first contact point with prospective patients who may be interested in exploring possibilities before organising an appointment with the dentist.
Treatment coordinators may also be involved in more traditional front-of-house tasks, such as booking appointments, and it is not unknown for the treatment co-ordinator role to be carried out by a member of the dental nurse team who works chairside as well.
There are numerous benefits to the practice in having such a role. It can allow team members to expand their skills and make the most of their experience in communicating with patients.
In terms of potential benefits for patients, having a treatment co-ordinator can allow a patient the opportunity to express their priorities and concerns, as well as obtaining a general idea of treatment possibilities and potential costs, without having to see a dentist. This can be helpful if, for example, a patient is embarrassed by their teeth and doesn’t know where to start. After speaking with the patient to establish their views and priorities, the treatment co-ordinator can book an appointment with the appropriate dentist.
Further to being seen by the dentist, the treatment co-ordinator can help with explaining the various stages of the planned treatment and clarify any outstanding questions on how long it
will take, what is involved, how much it will cost and payment options. Patients can sometimes find it easier to speak to a ‘non-dentist’ and may be less embarrassed to ask questions or seek further explanations.
The potential benefit to the dentist is that delegating some tasks can allow them to concentrate on the treatment and allow other team members to play to their strengths. Discussing payment plan options may not be the most efficient use of clinician time. From a commercial perspective, it can reduce appointment slots being used on patients who may simply be fact-finding, may help sift out patients who are only window shopping or those with unrealistic expectations in relation to timeframes or costs.
While there are many benefits, it is important to take note of potential risks. With respect to a treatment coordinator and the information presented, there is a need to ensure patient expectations are accurate. The patient needs to know that a treatment co-ordinator is not a dentist and, although able to address general questions, they will be unable to give specific details. What may be achievable, after a full clinical assessment, might be very different to theoretical options, and the patient needs to understand this. Only after the dentist has carried out an assessment will there be definitive information to indicate which options are appropriate and feasible. Unless information is delivered carefully, a meeting with a treatment coordinator may unintentionally reinforce – or generate – unrealistic expectations.
It is worth having some form of explanatory material for patients to help manage expectations. For example:
“An appointment with a treatment co-ordinator is a preliminary consultation to discuss treatments available at the practice. It is not a substitute for a clinical examination. All patients will require a full assessment examination before any decision about treatment can be made.”
“Potential options and costs given by the treatment coordinator are intended simply as a general guide. A full clinical assessment with the dentist will be required to obtain an accurate view of the possible treatment options and costs.”
The treatment coordinator may be able to identify what the patient wants but it is only the dentist who can figure out what can actually be achieved, and there is a line between outlining the types of treatment that might be possible and giving advice on actual treatment options.
Dentistry is strictly regulated, and it is important to ensure that a treatment co-ordinator does not exceed their own scope of practice.
Careful consideration must be given to ensuring an ethical approach to promoting treatments. There is a risk of enthusiasm and positive promotion
spilling into the territory of hard sell or focusing on certain treatment options whilst overlooking other, perhaps less profitable, options that the patient should be offered too.
When considering options, particularly for elective, aesthetic-based treatments, patients will need cooling-off time to reflect before committing to anything. They do sometimes change their minds. It is always better that this happens before treatment rather than during.
Good team communication is essential. If the transfer of information between the treatment co-ordinator, the dentist and the rest of the team is not clear and consistent, there is plenty of scope for misunderstandings and patient dissatisfaction.
Obtaining patient consent is an area ripe for misunderstandings. Consent is a process that involves information sharing, checking, understanding and obtaining agreement. A treatment co-ordinator can be a source of information about types of treatment, but they are not in a position to obtain valid consent to a particular type of treatment. They cannot
provide the patient with the information specific to that patient’s particular clinical presentation and individual treatment need. Only a dentist can assess the full clinical picture and be able to go over the specific risks and benefits of the various treatment options for that patient.
It is the responsibility of the treating clinician to ensure that the patient understands the information, the risks and benefits of treatment, the alternative options, and has chosen freely to proceed with the treatment. It is vital that the dentist does not abdicate responsibility for this through the view that consent is ‘taken care of’ by a treatment co-ordinator.
In summary, the use of treatment co-ordinators can bring many benefits to a practice. However it is important to understand the risks and the boundaries within which they should operate. n about the author martin Foster, Dentolegal Consultant at Dental Protection.








































The NHS recommends that patients brush their teeth thoroughly with a fluoride toothpaste to effectively prevent tooth decay. However, with many options available on the market containing varying levels of fluoride, it’s essential that clinicians are able to recommend the right solution for each patient, and understand the benefits and risks associated with it.
Fluoride is a naturally occurring mineral found in water in varying amounts, depending on where you are in the UK. It is widely accepted that fluoride plays a vital role in preventing tooth decay, and has been a standout ingredient in toothpastes since the 1970s. Because it is so widely used, it’s important to have a good understanding of the benefits it offers, as well as any potential risks, and how to use it to help your patients protect their oral health more effectively.
What are the benefits afforded by fluoride?
Fluoride prevents demineralisation by travelling into the enamel sub-surface, where it absorbs into the crystal structure, and provides protection. It promotes remineralisation as it accelerates the growth of fluorapatite crystals on partially demineralised teeth. It absorbs into the surface and attracts calcium, in turn attracting more fluoride, resulting in a fluorapatite-like surface. This makes the tooth surface less vulnerable to acid. Additionally, it hinders plaque formation. At a low pH, fluoride ions are able to travel through the cariogenic bacterial cell wall. Once inside, it acidifies the bacterial environment and inhibits the bacteria.
What are the risks of overprescribing fluoride?
Whilst fluoride offers patients countless dental health benefits, it’s important to consider the potential effects of over-use.
• Dental fluorosis
During childhood, whilst the teeth are still developing, exposure to high concentrations of fluoride can lead to mild dental fluorosis. These are small white streaks or specks on the enamel. Whilst this doesn’t affect patients’ health, the discolouration can be noticeable. To mitigate the risk, children should not use high concentrations of fluoride, and should be supervised when brushing their teeth to ensure they do not swallow their toothpaste.
• Skeletal fluorosis
Excessive exposure can impact bone health too, leading to a bone disease called skeletal fluorosis. Over time, this can cause pain and damage to bones and joints, and the risk of fractures may increase.
• Other health problems
In addition, there are a number of other conditions which may occur due to excessive fluoride exposure. These include thyroid problems, neurological problems, acne, cardiovascular problems, and reproductive issues.
What are the legal limitations surrounding fluoride?
In the UK, there is a legal limit for the maximum concentration of fluoride that over-thecounter toothpastes can contain to protect patients’ safety. This is 1,500 ppm fluoride, and is why many popular toothpastes contain
Accuracy is essential within many fields of dentistry. From fitting fixed prostheses that are properly functional to placing prosthetically-driven implants, accuracy supports treatment success and is therefore important for all practitioners to achieve. Besides treatment benefits, improving upon the accuracy of their work can help dental laboratory technicians develop positive relationships with practitioners, with enhanced communication enabling better treatment results. By doing so, greater patient satisfaction and streamlined professional workflows can be ensured.
Getting it right
With regards to dental impressions, there are two components to accuracy: precision and trueness. Precision describes the symmetry of repeated measurements whilst trueness encapsulates how close the measurements are to the real dimensions of the measured structures. The accuracy of impressions is affected by numerous factors in dentistry, such as the occlusion type of the patient and tooth placement. Steep inclines to the oral and buccal aspect of the mouth have a lower repeatability as well, leading to inaccuracy when stitching large objects together, such as full arch scans. This can make it difficult for technicians who receive the scans to effectively fabricate the needed prostheses. Highly accurate models and prosthetics are only made possible with
just under this – usually 1,450 ppm. Some patients and clinicians may assume that this is the recommended concentration for clinical benefits, however, it should instead be viewed as an absolute maximum daily dosage. Although, dentists have the ability to prescribe higher dose fluoride toothpastes to those who are susceptible to caries. However, a high concentration doesn’t necessarily mean a toothpaste offers an effective result. The fluoride contained in toothpaste is usually soluble, meaning that its effects do not last very long, washing away very quickly. As such, it’s important for clinicians to consider options that provide their patients with long-lasing results.
Low concentration and slowrelease fluoride
Clinicians may instead consider recommending a toothpaste option which contains a lower concentration of fluoride, which is released over a longer period.
BioMin® F, the innovative fluoride-containing toothpaste from BioMin®, incorporates fluoride in the structure of a bioactive glass, alongside phosphate and calcium ions. By capturing the fluoride within the toothpaste’s structure, it is able to adhere to the tooth surface and dissolve slowly – gradually releasing a continuous supply of fluoride over 12 hours. BioMin® F works with the saliva to produce fluorapatite which is deposited on the surface of the teeth and in the dentinal tubules, which strengthens and protects the tooth enamel. Additionally, BioMin® F acts as a pH buffer as it’s gradually released. This means that, when a patient consumes acidic

food or drink, the levels of acid in the mouth are kept to a minimum. By carefully considering the recommendations clinicians make to patients, taking into account all of the potential risks and shortfalls of particular fluoride toothpastes, they can offer their patients an effective, long-lasting solution. For more information about BioMin®, and the innovative range of toothpastes, please visit www.biomin.co.uk or call 0203 281 7282. n
about the author alec Hilton, CeO, Biomin technologies Ltd.

optimal scanning methods in the practice and first-class work in the laboratory. It is, therefore, essential that labs hire skilful technicians and give them access to highquality master model materials, such as addition-cured duplicating silicone, to attain accurate results.
technological trust
Technological developments in dentistry have further helped secure accurate treatment workflows and outcomes. For instance, AI can assist dental technicians by analysing digital dental impressions, generating customised designs and providing instructions for automated milling or 3D printing of the prosthetics. By improving accuracy, high quality technologies reduce the need for restorative adjustments, boosting the relationship between the technician and the practitioner, and also the overall patient experience. New technologies can improve the laboratory management system too, promoting a fair workload that doesn’t overload technicians. This can lessen the chance of systematic errors and increase the overall quality of work, creating job satisfaction and a stronger inter-professional relationship with peers.
Effective communication between members of the dental team is vital for the delivery of excellent and accurate patient care. The British Society for the Study of Prosthetic
Dentistry guidelines decree that ‘restorative work involving technical procedures requires a close relationship between clinician and technician.’ Any disruption in communication can have consequences for treatment success, potentially leading to a negative experience for the patient.
For all laboratory work, dental technicians must receive as much detail as the practitioner can provide. Minimal information, which many technicians feel they often receive, impacts workflow and the quality of results. In the case of veneer fabrication, technicians have emphasised the need for extra- and intra-oral pre-treatment photographs and precise jaw relation records to optimise their work. But miscommunication between the two professions is a globally recognised issue.
Studies have shown that 25% of dental technicians experienced a lack of involvement in the dental team, and only 31% felt they played an integral role in prosthesis fabrication. This miscommunication or feeling of isolation can stem from an uncertainty as to the job parameters: 61% of prosthodontic specialists felt that clinicians had the lead role in treating patients with fixed-implant prostheses.
Some clinicians will be guided regarding choice of materials for the prosthesis by the technician – provided the patient’s wishes are fulfilled, of course. Encouraging efficient communication can improve this process and promote better patient care,
as complications such as inadequate prescriptions, substandard impressions and missing dental records can be avoided.
Getting that accurate result
Alongside clear communications with the practitioner, having effective solutions in the laboratory ensures that technicians are able to produce the best customisable prostheses. For an addition-cured duplicating system that can meet all laboratory needs, consider Kemsil Duplicating silicone from Kemdent. Simple and reliable, mixing equal amounts of Kemsil A + B is all that is required – no messy activator needed. With an added wetting agent, Kemsil Duplicating silicone provides fantastic precision and stability, ideal for the accurate duplication of master models.
Accuracy is a cornerstone of dentistry, providing long-lasting treatments for maximum patient satisfaction. By using the latest innovations for optimum accuracy, it connects the laboratory technician with both patient and practitioner so that the practice runs smoothly and to its highest ability.
For more information about the leading solutions available from Kemdent, visit kemdent.co.uk or call 01793 770 256 n
about the author alistair mayoh, marketing Director, Kemdent.










Modern approach for prevention, cleaning and minimally invasive prophylaxis treatments.
Dental Scaler + Air Polisher


















SIMPLE & SOPHISTICATED

Ease of use, a complete unit that comes with all the tools to allow for many procedures:


AIR POLISHING + PERIODONTAL TREATMENT + ENDODONTIC TREATMENT
+ IMPLANT MAINTENANCE + EFFICIENT AND COMFORTABLE PLAQUE REMOVAL



AUTOMATIC IDENTIFICATION OF PROCEDURE MODE

Automatically recognizes which feature you require when you pick up either handpiece – scaling or air polishing.



AIR POLISHING
Compressed air precisely delivers powder and water effectively removing surface substances and polishes the tooth surface. It is less harsh on the tooth enamel with minimal abrasion. Delivers an efficient and comfortable treatment ensuring a pleasant experience for patients for supragingival and subgingival treatments.


One package with everything you need to have clinical confidence.






Implant maintenance has always been a critical aspect of dental care, especially given the complexities associated with the surfaces and structures of dental implants. Traditional methods often involved the use of bulky instruments that could potentially traumatise soft tissues and alter the delicate titanium surfaces of the implants. However, Guided Biofilm Therapy (GBT) has emerged as a game-changing, patient-centred approach, offering a minimally invasive, efficient and comfortable solution for both clinicians and patients.
What sets GBt apart?
Implants present unique challenges due to their complex surfaces, and GBT addresses these challenges head-on by focusing on biofilm removal without altering the titanium surfaces or traumatising the surrounding soft tissues. Indeed, GBT represents a significant shift from traditional implant maintenance methods, prioritising a systematic and patient-focused approach. The cornerstone of GBT is the use of erythritol powder, measuring a mere 14 microns, combined with the state-of-the-art Airflow, Perioflow and Piezon no-pain technologies. This combination allows for pain-free, efficient biofilm removal, with the added benefit of being able to use the Airflow technology up to 4mm subgingivally, making it ideal for both sub- and supra-gingival implant structures. This means that GBT’s innovative technology, coupled with disclosing solutions, ensures that every trace of biofilm is meticulously removed, and patients are actively engaged in their treatment, making oral hygiene an integral part of the process.
Powerful but gentle
At the heart of GBT’s effectiveness is Airflow technology, which combines water, air and powder in a consistent and regulated flow. This technology can be safely used on all implant surfaces and surrounding soft tissues. Erythritol powder, known for its natural antibacterial properties, plays a crucial role in this process. The combination of the powder with Airflow technology allows for thorough and quick biofilm removal without leaving residue or altering any surfaces, ensuring maximum patient comfort and optimal clinical outcomes. Perioflow, another vital component of GBT, is particularly beneficial for managing implant diseases. The flexibility and ergonomic design of the Perioflow tip allows it to adapt to the complex geometries of implants and their suprastructures. This adaptability is crucial, especially in areas where access is limited, such as posterior regions of the mouth. The Perioflow tip is designed with pressure grooves that ensure patient comfort, and its clearly marked areas at 3mm, 5mm, 7mm and 9mm allow for precise measurement and effective treatment of peri-implant pockets. The targeted delivery of erythritol powder through the Perioflow tip effectively removes biofilm from implant surfaces, threads and substructures, helping to prevent and treat peri-implant diseases. By addressing these issues early, GBT can prevent the progression of peri-implant
mucositis to more severe conditions like peri-implantitis, which could jeopardise the longevity of the implant.
early preventive care
Peri-implant mucositis, the precursor to periimplantitis, is a preventable condition that, if left untreated, can lead to implant failure. GBT plays a critical role in the early detection and treatment of peri-implant mucositis, ensuring the longterm health and longevity of the implant.
The combination of Airflow, Perioflow, and PI Max Piezon technologies allows for comprehensive biofilm management, both in the clinic and through tailored home care plans. Disclosing solutions used in GBT highlight any remaining biofilm, guiding both the clinician and patient in achieving complete biofilm removal and optimal implant health.
Patient focused
One of the most significant advantages of GBT is its minimally invasive nature. From the ultra-fine erythritol powder used in Airflow and Perioflow to the PI Max tip, every aspect of GBT is designed to ensure a pain-free, efficient treatment that leaves soft tissues, hard tissues, implant and prosthetic surfaces undamaged and free of biofilm. This approach not only enhances patient comfort but also encourages patients to return for regular maintenance, knowing that their treatment will be pleasant and effective.
Patients invest heavily in their implants, both financially and emotionally. GBT, with its focus on tailored home care plans and minimally invasive, pain-free treatment, ensures that this investment is protected. Healthy implants lead to happy patients, and GBT is setting the standard for achieving long-term implant success.
As more dental professionals adopt this revolutionary approach, GBT is poised to become the gold standard in implant maintenance, ensuring that patients enjoy healthy, long-lasting implants for years to come.
For further details about GBt, please visit www.ems-dental.com. additionally, Jolene will be speaking at the ‘Confidence in Implant Dentistry’ course on 1st november at the royal College of Physicians in London. You can find more details and register at https://bit.ly/3SJcblU. n
about the author

Jolene Pinder is a dental hygienist committed to the promotion of oral health. She qualified in the royal navy in 2002. after working throughout the UK over the last 22 years, she is currently working at the Dental Health Spa in Brighton. as a study club director for the ItI, she combines academic excellence with hands-on expertise gained from working alongside experts in implantology.
For many, mouth taping conjures up images of captive and abduction films where duct tape is used horizontally to gag the victim. Imagine what a nightmare it would be if their target had a cold – they’d really struggle to breathe!
In contrast, sleep experts such as Patrick McKeown claim that improving the quality of sleep is a dream. Simply tape the lips vertically to keep the mouth closed, preferably with use of a hypoallergenic, light surgical or athletic tape, which is porous and intended for use on human skin rather than duct tape!
Lip tape has many uses of interest to dental professionals. They include:
1. Cleft lip/palate (CLP)
A taping regimen is often used prior to a baby’s surgery to narrow the size off the gap by moving the cleft segments closer together. Using this technique, tape is placed across the cleft in order to advance direction of the tissues, e.g. in a unilateral case, pulling the tape more towards the cleft side to encourage movement in that direction. In contrast, in a bilateral case, the premaxillary segment, or ‘nub’ as its sometimes referred to, is pulled backwards.
2. Facial aesthetics
Lip taping is a lip filler trend that has been shared extensively on social media channels. The technique, often referred to as ‘butterfly lips’ because the shape is similar to butterfly wings, sees aestheticians taping lips prior to injecting vertically to give a highly defined everted lip and cupid’s bow. Taping is thought to allow the filler to settle in position and prevent migration but, unfortunately, the general consensus is that it is simply not strong enough to prevent filler from drifting. In order to achieve this, a much stronger force from both above and below the lip would be required.
It is fair to say that breathing techniques, in particular nasal breathing, have been topical since the pandemic, when it became clear that although we can live without food for weeks and water for days, we can only go minutes without oxygen. Evidence suggests that there are many advantages to nasal breathing:
• It is efficient and effective at stimulating the lower lungs, ensuring deeper, fuller breaths
• Air travelling through the nasal cavity is warmed, humidified, and filtered, thus removing dust, allergens, and other pollutants
• The parasympathetic nervous system is activated, which reduces stress and encourages relaxation, allowing nasal breathers to fall asleep quicker, stay asleep longer, and feel more energised upon waking
• Brain fog, dry mouth, halitosis, and snoring are said to be reduced
• The sinuses are naturally enabled to produce a gas called nitric oxide, which flows to the lungs and enters the bloodstream, widening blood vessels, improving blood flow, and reducing blood pressure
Adequate nasal breathing is said to be enhanced by tape as shown by the following:

Those working in sports dentistry will be aware that many athletes use tape to improve their nasal breathing and overall oxygen absorption both during training and competitions.
The purpose of taping the mouth at night is to ensure conversion from mouth to nasalbreathing during sleep, thus discouraging mouth-breathing and the snoring that may accompany it.
So, are there any proven benefits to mouth taping?
Well one study has found that snoring intensity, as reported by each participant’s bed partner, was reduced slightly with the tape in place compared with a night without it. Advocates of mouth taping claim it may help reduce the negative effects thought to be associated with mouth breathing, including snoring, fatigue, concentration issues, bad breath, excessive thirst and dry, cracked lips.
But is it safe?
Well, despite its recent popularity, mouth taping has not been extensively studied, so there is little research endorsing its use. But it is fair to say that taping is not for everyone, especially as it’s reported that most people are not ‘primary snorers’ but instead have an intrinsic reason for snoring. If a patient asks for advice about snoring, we need to establish whether they have any underlying issues, such as sleep apnoea, because this could have long-term health implications, including heart disease and stroke, as well as challenges controlling conditions such as diabetes, high blood pressure, nasal congestion, allergies, asthma, and other respiratory issues. There are also possible side effects, not least discomfort, when removing the tape, especially for those with facial hair – ouch!
In conclusion, although it is clear that lip tape does have its uses, it would seem that the recent trend of mouth taping is not one of them. There is simply insufficient evidence to support its anecdotal benefits. Dental professionals who notice any of the negative signs and symptoms of mouth breathing in a patient should recommend that they see their general practitioner, who may refer them to a specialist in this field; after all the dental team is well placed to signpost patients for an official diagnosis AND help alleviate problems caused by simple snoring. n
about the author ali Lowe is the founder of Fit Lip UK – a campaign aimed at encouraging people to wear SPF lip balm in order to protect their lips, prevent lip cancer and keep their mouth healthy.



User-friendly design eliminates operator error

A true hybrid machine, giving the same clarity on both 2D and 3D images

Perfect 3D volume allows you to see all of the dentition, but with reduced radiation dose for the patient
Reassurance of German manufacturing standards


@durr_dental_uk Duerr Dental UK

For more information visit www.duerrdental.com/en/products/imaging/x-ray-units
We catch up with Dental Nurse of the Year Brittany Pittham to find out how she juggles multiple roles and whether there is a clear career pathway for dental nurses
Brittany Pittham had twice the reason to celebrate during the 2024 Dental Awards. Not only was she named the winner of the award for Dental Nurse of the Year, but she was also listed as a finalist in the Practice Manager of the Yeat category.
How did it feel to be named Dental Nurse of the Year?
I’m just so proud!
Winning the Dental Nurse of the Year award was an incredibly rewarding experience. It was a testament to the hard work, dedication and genuine passion I bring to my role every day. I felt honoured and humbled to be recognised by the industry. It reaffirmed my commitment to providing the highest quality of care to our patients and supporting my team.
How do you define your role as a dental nurse?
It’s hard to define the role of a dental nurse, because a nurse can take on a multitude of roles within their career.
But overall, as a dental nurse, my primary role is to support the dentist in all aspects of patient care. This includes preparing the treatment room, assisting during procedures, and ensuring patients feel comfortable and informed throughout their visit. Beyond clinical duties, I also handle administrative and compliance tasks, maintain equipment, and ensure a safe and efficient practice environment. Ultimately, my goal as a nurse is to facilitate a smooth operation and contribute to the overall patient experience.
You were also a finalist in the Practice Manager of the Year category. How do you juggle your roles?
Balancing the roles of a dental nurse and practice manager requires excellent time management, organisation and a collaborative approach. I prioritise tasks based on urgency and importance, delegate when necessary, and always maintain open communication with my team on all levels.
By remaining adaptable and proactive, I ensure that both clinical and administrative responsibilities are met without compromising on the quality of care or operational efficiency.
It’s about finding a balance and leveraging the skills from both roles to enhance the practice as a whole.
Is there a clear career pathway from dental nursing into practice management?
Yes, absolutely! There is a clear career pathway from dental nursing to practice management. Many of the skills acquired as a dental nurse, such as patient care, organisational abilities and knowledge of dental procedures, are directly transferable to a practice management role.
Additional training and qualifications in management, leadership and business administration helped me to further support my transition. Mentorship and professional development opportunities also play a significant role in bridging the gap between these roles.


Does your clinical role as a dental nurse benefit your practice management responsibilities – and vice versa?
Definitely. I recently lectured on this to a group of dental nurses.
My clinical experience as a dental nurse provides me with a deep understanding of the day-to-day operations and challenges faced by the clinical team. This insight is invaluable when making management decisions that affect clinical workflows and patient care. Conversely, my practice management responsibilities have enhanced my leadership, communication and organisational skills, which I bring back to my role as a dental nurse. This dual perspective allows me to implement more effective strategies and foster a cohesive, efficient practice environment.
What you would say to dental nurses thinking of entering the awards next year, or colleagues who may want to nominate them?
I’d say go for it! Dental nurses are the heart and soul of every dental practice and, without them, there simply would be no dentistry. They deserve to be celebrated and recognised for their excellence. The efforts of the nurse can sometimes be behind the scenes, but the impact a nurse has is in every smile that walks out of the door of a dental practice.
Awards are not just about trophies, but about recognition and celebrating excellence and inspiring the best in each other. Dental nursing is so much more than just a job, it’s a commitment to patient care and continuous learning.
To those considering stepping forward for an award, I encourage you to embrace the opportunity and, for my colleagues, consider nominating a fellow nurse. We all have someone in our team who inspires us with their commitment - don’t let their brilliance go unnoticed!
What does your new role on the BADN Panel of Representatives entail and why do you think it’s important to join an association like BADN?
The BADN Panel of Representatives consists of members who represent a specific area of dentistry, either regional or professional. We act as a conduit between dental nurses across the country and the BADN executive committee. Panel representatives get involved with supporting the whole organisation and contribute to the continuous development of the dental nursing profession. I will personally be representing dental nurses that have, or want to, develop into the role of a treatment coordinator in addition to being the representative to women’s health - specifically infertility.
I have been a treatment coordinator for about four years now and thoroughly love the role, and, after gaining my formal diploma in treatment coordination, I have trained a team of dental nurses into becoming coordinators. The benefits of a TCO within a dental practice are second to none, and the job itself is

incredibly rewarding. I speak very openly about my battle with infertility and endometriosis and want to continue advocating for fellow colleagues who are struggling and are not receiving adequate support within the workplace, in addition to raising awareness of a ‘taboo’ topic. I am very excited about my new role with the BADN and can’t wait to network with nruses across the country.















Rhiannon Cullinan, Dental Nurse



Equipment, service & support you can rely on.








Our nationwide team of over 50 highly trained engineers work exclusively on Eschmann products, enabling us to provide an unparalleled level of professional support to our customers.

to unlimited spare parts & labour included in our Care & Cover


Our engineers are all equipped with the necessary tools & spare parts to ensure that your Eschmann products are working effectively & to their maximum potential. With access to unlimited spare parts & labour included in our Care & Cover service package, you can be confident that your decontamination equipment won’t let you down.
Experience Eschmann excellence at www.eschmann.co.uk, or call us on 01903 875787.











Changing your story describes a way of making a change or a series of changes that sets you on a new path or, at least, one that’s fundamentally different to the one you’re on now. People change their story usually in response to circumstances or the feeling that the life they’re living might need a shake-up. It could be health-related, a career u-turn or a sudden desire to live off-grid in a shack in the middle of nowhere. Wherever your thoughts might take you, they are always worth listening to.
Any kind of change is likely to be a big deal – but only to you and your immediate circle. There’s a great word – sonder – it reminds us that every other living person exists not only in relation to us (we are so self-absorbed!) but they have their own 360-degree life. I think to remember this gives us some perspective, tells us that our story is important, but is only of genuine significance to us and our family or close friends. Being brave enough to change your story can feel monumental but might only result in a passing comment to your friends and colleagues.
Change your narrative
What if the story you’ve been telling yourself isn’t the full picture? Have you ever paused to question the assumptions you’ve made about your career or your potential? Sometimes, the key to change is as simple as telling a different story. Instead of “I’m not ready,” try “What if I could?” Instead of “I’ve always done it this way,” how about “Why not try something new?”

When thinking about changing your story, ask yourself what genuinely excites you. Not just what you’re good at or pays the bills, but what makes you feel energised and motivated. Is there a path or new area of your career that you’ve always dreamed of tackling? Revisit that idea. It might be where your next chapter begins. Think about undertaking some training, or researching your ideas further, it could lead you to dismiss or develop that train of thought. I knew someone who gave up a very lucrative corporate position in the city to train with one of the UK’s top florists. She developed a brand, set up a
studio, launched a new business, had a van sign-written, enjoyed lots of publicity… and absolutely hated it. She returned to her former employ, unfazed, undeterred and richer for the experience. Being a florist excited her in theory but not in reality. How amazing to have been that brave and also to have had the experience.
Your life plans don’t have to be linear It’s tempting to map out the next five years in detail, but career stories often don’t follow a straight line. Have you considered letting your five-year plan be a bit more fluid? Is there a rush? Within dentistry we talk a lot about career pathways. What if,
You’re stuck in a rut and, as the saying goes, “the only difference between a rut and a grave is the depth”.
Question 1: i s this why you spent five years at university?
Question 2: Does the reality match the dream?
A frequent conversation with my brother is around the differences between the training of doctors and dentists, and how that influences their career paths. I can only talk about my experiences as an undergraduate and subsequent varied careers within the microcosm that is dentistry. He, on the other hand, gained the giddy heights of being a professor of medicine in

two different universities, albeit in his relatively small speciality (which also starts with the letters ‘de’).
What neither of us can truly understand is the other’s experience, because, as closely as we have observed it, shared notes and learned lessons, neither of us has lived it.
One thing on which we do agree is that making a decision on a lifelong career at the age of 18 or younger is questionable at the least and can lead to much of the increasing unhappiness and disillusion seen in both broader medicine and the more specialised field of dentistry. The situation is made worse in the UK because of the shift in the responsibilities of universities. Pressure to churn out medical graduates and to fund the universities has led to massive increases in undergraduate numbers. These souls, when compared with their predecessors of even 20 years ago, have much reduced patient contact and clinical experience. The tick box culture has led to a superficial education skimming across the surface.
I know this is the result of two seniors talking, both of whom want
instead of ticking off goals, you focus on building experiences, learning, and growth?
Shifting your perspective to see your career as a journey rather than a checklist can help you embrace the twists and turns along the way. You don’t have to become a florist to do it, but you could try different kinds of dentistry, in a variety of settings. I believe it adds up to a rewarding, and potentially more interesting, career.
A change-story is the narrative you create when you decide to shift the direction of your life. It’s a conscious decision to reframe your experiences and set new intentions. Whether it’s stepping into a new career, taking on a leadership role, or even just adjusting your work-life balance, your story is yours to reshape. Changing your story isn’t always easy, but it’s entirely possible. With reflection, small steps, and the courage to be brave, you can create a new narrative – one that’s fulfilling, authentic, and uniquely yours. n
About the author

Dr Dhiraj Arora has two dental practices in Twickenham and Gerards Cross. He is also a Dental foundation Training educational supervisor for Health education england, Honorary Lecturer in endodontics at QMUL Masters programme, and runs his own courses via evo endo in Central London for general dentists. His background spans nHs and private settings, from Harley street to community HealthCare.
the best for the next and subsequent generations. Neither of us wears rosetinted spectacles about our past.
I well remember that some of my teachers 40+ years ago, especially the “bullying restorative academics,” to quote Claire Nightingale’s excellent piece on gender equality in the current BDJ in Practice, were dismissive of our novice efforts and revelled in humiliation. Post-clinic tears were shed by both sexes.
That is the past and, as the trite saying goes, “we are where we are”. The career path for medics and dentists, which is not of their making, can be a minefield. Tales of couples in long-term stable relationships being separated for years by 200 miles or more on training programmes are routine.
Dentistry brings the newish graduate to the roulette table. Should they specialise without knowing what is fully involved? If they do, what is the genuine and honest career path? Can they afford it? How can they get experience in general practice, especially but certainly not exclusively, within a corporate whose eyes are mostly on survival, rapid expansion or
preparing for a sale, and whose clinical lead may be in a different part of the country? How ethical is it to expect newish graduates to be upselling with financial driven targets and where the spreadsheet has replaced the clinical journal as an accepted guideline?
”The oldest and strongest emotion of mankind is fear, and the oldest and strongest kind of fear is fear of the unknown.”
- H.p. Lovecraft
The medics are stuck for the duration, looking forward to that oneway ticket to somewhere, anywhere, overseas where their dedication is respected and rewarded.
As for dentistry, the majority still serve their patients in general practice and the good news is that all you need is a chair and the courage to do things your way. You can, and should, take control of your own destiny.
Question 3: i f not now, when? n
Carl Wood speaks with Dr Emanuele Clozza about the future of implant dentistry and the game-changing potential of digital workflows
Carl: How did you first become interested in dental implants, and what led you to focus on the ‘Complete arch of implants in a digital workflow’ at the event?
Emanuele: My interest in dental implants began in 2008 during my time as a dental student at the University of Trieste, Italy. I chose to focus on ‘Complete arch of implants in a digital workflow’ because it is a ‘hot topic’ in implant dentistry. I believe digital workflows have the potential to revolutionise the field, and I’m excited to share my insights and experiences with attendees.
Carl: Your presentation covers a paradigm shift using photogrammetry in digital workflows for complete arch implants. What inspired you to explore and advocate for this technique?
Emanuele: I was driven by the need for more efficient and precise methods for taking impressions compared to traditional techniques. Photogrammetry allows for highly accurate implant positioning, reduces the number of appointments, and eliminates costly remakes. By integrating photogrammetry with intraoral scanning, I’ve achieved a significant improvement in patient outcomes, and even my team has embraced this innovation.
Carl: What key takeaways can attendees expect from your talk about implementing photogrammetry in their practice?
Emanuele: Attendees will learn how photogrammetry provides micron-level accuracy in capturing implant positions, allowing them to skip verification steps and fully utilise digital tools already available in their practices. This leads to more predictable and streamlined workflows.
Carl: How does your topic complement or contrast with the presentations of your colleagues at this event?
Emanuele: My topic complements my colleagues’ presentations by offering a broader perspective on the latest advancements in full-arch implants. While others may present specific case studies, I’ll provide insights into the overall impact of these advancements on the field of implant dentistry.
Carl: Networking is often valuable at conferences. What opportunities do you see for attendees to connect and collaborate with you and other experts?
Emanuele: This event offers excellent networking opportunities. I’m open to scheduling one-on-one meetings with attendees to discuss collaboration opportunities and share knowledge about photogrammetry and other digital workflows.
Carl: Confidence is a significant theme of this event. Why do you believe building confidence in implant dentistry is crucial for dental professionals?
Emanuele: Confidence is essential because it impacts patient trust, the willingness to pursue advanced treatments and overall patient outcomes. This field is no longer limited to a few ‘gurus’; with confidence, dental professionals can make informed decisions, communicate effectively with patients and deliver high-quality care.
Carl: Digital workflows are transforming many areas of dentistry. How do you see photogrammetry and digital techniques evolving in implant dentistry?
Emanuele: Photogrammetry is on track to become the gold standard for complete arch implant impressions. I believe it will continue to play a significant role for at least the next decade, enhancing the accuracy and efficiency of implant planning and placement.
Carl: For dental professionals considering attending, what would you say to encourage them to sign up for this event?
Emanuele: Attendees will see clinical cases from practices using the latest workflows and technology. This event offers a chance to stay updated with the latest trends and improve your skills, ultimately benefiting your patients and practice.
Carl: You’ve placed over 11,000 implants. How has your approach evolved, and how do you stay at the forefront of this field?
Emanuele: My approach has evolved significantly, especially with advancements in restorative protocols, CAD-CAM dental software, 3D printing, and intraoral scanners. I stay at the forefront by continuously learning, attending conferences, and keeping up with the latest research and technology.
Don’t miss out on learning from Dr Emanuele Clozza and other leading experts like Dr Barry Oulton, Louise Warden, Dr Aly Virani and Jolene Pinder, who will cover everything from implant integration to maintenance. Gain the confidence and skills needed to excel in implant dentistry at the ‘Confidence in Implant Dentistry’ event on November 1st at the Royal College of Physicians, London. Register now at https://bit.ly/47dgSuz!
About the authors Dr Emanuele Clozza, a dentist who graduated from the University of Trieste, (Italy) and specialised in Periodontics at New York University (USA), has been practising in London for over 10 years and placed more than 11,000 dental implants. He has presented at international conferences, published over 20 articles in peer-reviewed journals, and served as a reviewer for 12 scientific journals. His expertise includes All-on-4 and All-on-6 treatments, aesthetic implants, gum grafting and bone regeneration.



An Xtra powerful team for direct fillings!
Perfectly coordinated products with easy and efficient application for safe and aesthetic results – that is the SHOFU X-Factor, for the added plus in your daily practice.


Carl Wood is the General Manager at Bien-Air UK Ltd, helping to lead the charge in delivering highperformance dental systems that set the standard for precision and innovation.




























For further information, please contact the SHOFU office 01732 783580 or sales@shofu.co.uk
www.shofu.co.uk

In the UK, 72% of businesses have reported an increase in cases brought against their companies in the last five years, with 60% anticipating a further rise over the next year. Dentists think the same: 98% of dental professionals believe that society is becoming more litigious.
Spurred on by the cost-of-living crisis, economic instability and a more disagreeable culture, the growing threat of litigation is a worry for dentists. To combat this, having reliable indemnity can safeguard practitioners against the financial fallout of dental malpractice claims or General Dental Council (GDC) investigations.
It is important that patients are able to obtain compensation if something goes wrong in their dental appointment. It is therefore a legal requirement that the appropriate indemnity cover is in place for all practising dental professionals, allowing a successful patient claim to be compensated.
Patients may seek compensation for several reasons. A negligence claim may transpire if a patient feels their treatment was substandard. If a patient has a communication issue, such as feeling uninformed before a dental procedure, they may make a consent dispute. Improper diagnosis or delays can also cause a patient to seek compensation if an oral health issue is worsened because of such aspects.
There are differing types of dental indemnity cover.
Personal cover is an indemnity policy that is in your name, rather than that of an employer or NHS. This can be obtained through indemnity providers. Contractual indemnity will cover you for all claims made as specified within the contract, whereas with discretionary indemnity policies it is at the provider’s discretion as to whether they will defend on against a particular claim. Run-off cover is also recommended so that there is protection after an indemnity policy has expired.
The other type of dental indemnity is for staff directly employed by the NHS, with cover included with the clinical negligence scheme. However, any dental work performed privately is not covered by this policy. It is up to you to guarantee that you are appropriately covered by the NHS indemnity across all the tasks that you do and the locations and hours that you work. It should never be assumed that you are correctly covered. NHS indemnity also does not cover fitness to practise investigations, meaning that personal insurance may still need to be taken.
Burnout is well-cited in dentistry for its impact on daily work, but the threat of litigation also affects how the dental team perform. 89% of practitioners fear legal action by patients. In a litigious society, this fear may be constant. This fear correlates with the 74% of practitioners who believe that the risk of being sued changes how they practise, leading to many more referrals.
In turn, this legal fear may undermine job satisfaction and impact mental health and performance. The risk of making a mistake and having dissatisfied patients are two of the most prominent stressors effecting a dentist’s work.
This may be avoided by having greater legal protection. Having indemnity may boost self-confidence in handling treatments, as there will be a stable, legal groundwork that safeguards your treatments and your finance.
indemnity and implants
Implant treatment has many inherent risks and complexities, such as peri-implantitis, nerve damage, and sinus issues if working in the maxilla. Failure of the treatment is the most common reason cited for successful claims, accounting for over a third of cases. Due to these risks, professionals providing implant procedures must have indemnity to cover themselves.
To have the best protection in any circumstances, it is vital that you have comprehensive clinical notes for all treatments, as it gives your indemnity company as much detail to protect you as they need.
For the legal support of implant dentists, the Association of Dental Implantology (ADI) offers members a 15% discount in indemnity insurance with Professional Dental Indemnity (PDI). This covers legal expenses and compensation payments in the wake of adverse outcomes or malpractice claims, safeguarding your reputation and finances. With ADI membership, dentists can have peace of mind, allowing them to focus and deliver exceptional implant treatment whilst being protected.
Indemnity is a necessary component for great dentistry. By shielding your work with the best indemnity providers, you can mitigate the financial impact of litigation and feel more in control of your work.
For more information visit adi.org.uk/membership/benefits/dentists n
About the author
Dr. Zaki Kanaan, ADi president.

Composite restorations are becoming increasingly popular among dentists and patients alike worldwide. They provide a minimally invasive and cost-effective solution to improve the aesthetics and function of the teeth in a wide range of clinical situations. However, like all dentistry, these procedures are not without their risks and challenges. To deliver consistent and predictable results, clinicians must be aware of the potential complications and plan to minimise them in each case.
Dr Albert Gajdos is passionate about cosmetic dentistry. Having trained with renowned clinicians himself, Albert now runs his own dental academy that teaches techniques in composite bonding and veneers.
On the main challenges that clinicians face in composite restorations, he comments:
“Getting the correct shape of the restoration is the MOST important thing and one of the main challenges. More specifically, it is being able to handle the resin to sculpt the desired anatomy, and to correctly finish and polish it. Another challenge is shade selection. All composite systems present a different selection of shades/opacities and optical properties to their composites, as well as their unique nomenclature – this can make it confusing for inexperienced operators to shade match when there are similar shades available.”
The BACD 20th Annual Conference takes place this November in London, and Albert will be presenting a hands-on workshop, entitled “Simplifi Anterior Composite with Next Generation Resin,” on Thursday 7th November. Albert details its content:

“The session aims to present clinicians with a few simple protocols for tackling clinical scenarios, such as full composite veneers for discoloured teeth or partial bonding in Class IV cases. We will introduce GC’s next generation resin materials such as Gaenial Achord, which presents unparalleled handling for straightforward resin placement and a value-based system for shade selection to simplify the process. We truly hope this simplicity of protocol and material choice will make the direct resin workflow more predictable and easier to implement. We can then achieve a beautifully natural result, even in challenging scenarios.”
Choosing the best material is crucial for
predictable and effective treatments. For Albert, there are several key considerations to account for in material selection:
“Good handling is the most important criteria in a material. If you cannot handle the material well you will not achieve the desired anatomy or form. Your restorations will be more prone to defects such as air bubbles, greatly reducing treatment success. An aesthetic composite is useless if you cannot sculpt and shape it.
“I also want good optical and colour properties in a material so that I can closely match natural enamel and dentine and also be able to blend with the natural tooth structures. In addition, materials should be chip and wear resistance and have reliable polishability and polish retention.”
If delegates take one thing away from his workshop session, Albert hopes that it is this:
“Keep your techniques and instruments as simple as possible. The fewer steps there are, the lower the chance for error.”
Albert reflects on his experience with the BACD and why the Annual Conference in November is the place to be:
“I have thoroughly enjoyed the events that the BACD puts on every year, namely the Annual Conferences. It is so great to see all the amazing speakers they bring around, as well as to catch up with familiar faces and friends and interact with other like-minded clinicians. It is a great community to be a part of. The Annual Conference this November is no exception – seeing the line-up I am truly excited! Hopefully I will see you all there!”
Albert’s brilliant workshop is just one example of what the BACD Annual Conference 2024 can offer. An immense amalgam of education, skill development and socialising, it will also celebrate the achievements of our cosmetic dentists throughout the BACD. For a superb evening event, the Gala Dinner promises to be an unmissable opportunity: a Masquerade Ball with dinner, drinks, a free bar, entertainment and dancing. This, and the various other social opportunities will be an ideal environment to relax, have fun and network with likeminded professionals. To join in on the birthday celebrations of the BACD, book your tickets today!
BACD 20th Annual Conference 7-9 november 2024 it’s our Birthday And We’ll smile if We Want To!
Book your tickets today at bacd.com n





























• Mini head: Ø 10.6x12.4mm MODEL M800L CODE P1253001 RRP £773






Optic
Power 20w
Micro head: Ø 9 x 10.8 mm MODEL Z micro (ultra-mini head) CODE PA2357001 RRP £1,173





• Lightweight external titanium body • Optic with internal water • Small head/narrow neck
• Unique spray switch on Z95L, Z45L, Z25L

• Optic • 1:5 Increasing+Spray switch • Head size ø8.9 x 13.4mm
C1034001-SW RRP £1,610

•
• Head size ø8.9 x 13.4mm

• Optic • 1:4.2 Increasing+Spray switch
• 45° head
• Head size ø9.6 x 14.5mm
• Ideal for minor oral surgery too
• For regular or extra long (25mm) FG burs
MODEL Z45L CODE C1064001 RRP £1,610


• Stainless steel • All with internal water • Choice of optic & non-optic

• Optic • 1:5 Increasing
• Head size 10 x H.14.6mm
M95L CODE C1023001 RRP £1,040
• Non-Optic
• 1:5 Increasing
• Head size 10 x H.14.6mm

•
• Optic • 1:1 Direct Drive
MODEL M25L
C1024001 RRP £842


• Non-Optic Straight • 1:1 Direct Drive
• Push button chuck
• No internal water


• Non-Optic Contra-angle • 1:1 Direct Drive
• Push button chuck



• Non-Optic • 1:1 Straight MODEL M65 CODE H1008001 RRP £541






















The British Endodontic Society (BES) is a speciality society, open to all those with an interest in endodontology. Founded in 1963, we are committed to furthering the nation’s dental health and wellbeing through pioneering, researching, and supporting members. This is demonstrated in a number of ways, including our prizes, awards, and grants which show our dedication to promote the field by investing in our colleagues.
The BES aims to support all who provide endodontic treatment, which is why we are open to all who want to gain education, experience, and connections in the field. We welcome specialists, GDPs, post-graduates, DFTs, undergraduates, and overseas dentists – enabling everyone to access the myriad of benefits we have on offer.
What do we do?
The BES hosts events each year, encouraging our members to come together to socialise and expand their knowledge of endodontology. Over the years, we’ve hosted Regional Meetings across the UK, with our Spring Scientific Meeting occurring in London each year. We have been delighted to be joined by excellent speakers from around the world at our events, presenting sessions on cutting-edge topics in the field. In fact, the recent IFEA World Endodontic Congress (WEC), hosted by the BES in Glasgow, saw speakers and delegates from around the world come together here in the UK to immerse themselves in the world of endodontics.
Members of the BES are also eligible to enter into our awards and prizes. BES prizes aim to recognise the achievements of those going above and beyond in the field of endodontology, with a wide range of prizes available. These include the Harty Essay Prize, Undergraduate Research Prize, General Dental Practitioner Prize, and BES Poster prize. These encourage a broad spectrum of our membership to get involved in research, evaluate their cases, and gain recognition amongst colleagues. The BES also presents awards for Inspirational Part/Full-time lecturers, Outstanding Clinical Cases, and Early Career Dentists.
New to endodontics?
For those who are new to endodontology, or the dental profession as a whole, there is a place for you at the BES Early Career Group (ECG). This exciting initiative enables us to engage directly with those in the early stages of their careers who share a passion for endodontics, and who wish to grow their knowledge and skills. The ECG aims to support these dentists by providing high-quality education and training, with the ultimate goal of elevating the endodontic care provided by those in the early stages of their career. The ECG hosts an annual Study Day in July, with content targeted to newly qualified dentists who are keen to improve their endodontic skills.
Why join?
Our membership benefits vary depending on the membership type, but UK Full Membership includes:
• A monthly copy of the International Endodontic Journal (IEJ) and online access to all issues of the IEJ
• Reduced rates at BES conferences and associated CPD
• Membership of the European Society of Endodontology (ESE) and reduced rates at its Congresses as ‘Ordinary Members’
• Membership of IFEA and reduced rates at its Congresses
• Opportunity to enter for BES Prizes and Research Awards
• Access to a weekly ‘In the Media’ update on issues relating to dentistry
Each of these benefits aim to enrich clinicians’ education and skills, promote a sense of community, and keep them up to date with the very latest in the profession. Each of these are essential for furthering their career, and providing the very best care to their patients.




A warm welcome
The BES welcomes all who wish to elevate the quality of their endodontics, so be sure to visit the website to find out more about the Society, its membership benefits, and awards, prizes, and initiatives tailored to your needs. For more information about the BES, or to join, please visit the website www.britishendodonticsociety.org.uk or call 07762945847









Dentistry has consistently fostered a strong need for technological advancements. The incorporation of more sophisticated technology has had many benefits: improved clinical accuracy, patient comfort, treatment success. In the Continuing Professional Development (CPD) of a dentist or dental hygienist/therapist, technology has also enriched teaching and learning experiences.

Lifelong learning is crucial for every dental professional because knowledge, skills and technology are always evolving. Whether studying the theory, obtaining the practical skills or attending seminars, there are many ways to advance your professional career in oral health. Staying up to date with the changes and developments of the industry will allow exceptional patient care to be delivered.
Curaden leads the way
Over many decades, Curaden has been dedicated to ensuring lifelong oral health for all. They have trained over 60,000 dental professionals across the globe on preventative thinking and decisive action, supporting dental teams in giving first-class treatments. Through exceptional dentistry, patient education and professional support, Curaden promotes health and happiness among the general population.
At Curaden, the mission to empower dental professionals is being achieved with specialised training and quality products. Their worldwide distribution net reflects the excellence of their service.
Checking the catalogue
Innovative products are important for treatment success and the continual growth of a dental practice. The Curaprox product range from Curaden is filled with effective products to meet every need. These include:
• Fresh breath
• Teeth whitening
• Sensitive teeth
• Braces and aligner care
• Gingival issues
• Denture and implant care
Curaprox products can revolutionise the daily oral hygiene routine for patients. The toothbrush choice is vast: the CS manual toothbrushes have unique Curen© filaments for a gentle but powerful cleaning effect, and a deliberately angled head for maximum coverage. There is also a variety in hydrosonic toothbrushes and specialised toothbrushes for implants, orthodontic appliances and sensitive gums.
For interdental cleaning, the range of CPS interdental brushes are effective and sustainable, with refill packaging meaning
only the brush tip needs replacing, reducing plastic waste. With numerous sizes available, there is an appropriate interdental brush for every interdental space.
For orthodontic patients, the Curaprox Ortho Travel Set features a unique Ortho travel toothbrush, a Be you whitening toothpaste, three CPS Ortho interdental brushes and a colourful case for the easy maintenance of oral hygiene on the go. Curaprox Aligner Foam is also ideal for safeguarding teeth when wearing plastic aligners, retainers and mouth guards, using natural minerals to shield and enrich each tooth.
The convenience of the Curaprox Implant Care Kit, which contains everything from a CS surgical toothbrush to Perio Plus Regenerate mouth rinse, means that patients can maintain post-surgery care wherever, whenever, ensuring the success of the implant treatment.
Curaprox also houses a reliable product range for babies and kids – toothpastes and toothbrushes designed to make brushing fun and enjoyable for little ones. The variety in soothers and teething rings can provide relief for parent and toddler alike. With bright colours and fruity flavours, the children’s range can increase adherence with the daily oral hygiene routine, improving their health. Becoming familiar with the extensive options available for these wants and needs can help you point patients towards the right solutions. Curaden representatives are available for lunchtime sessions at your practice to demonstrate all such products and more.

These Curaden educational sessions provide a fantastic opportunity to prevent oral health problems before they emerge, all from the comfort of your practice. As Curaprox conveniently comes to you, the relaxed atmosphere of the sessions will make them a positive environment for the whole team. Not only will products be available to try and sample, but Curaden representatives will also explore the science behind each one, and how best to use them clinically. By providing a greater understanding of each product, you can effectively communicate with patients on the benefits of using them and the problems they can prevent. Curaden seeks a healthier, smiling world. Join them in fulfilling this.
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk For more information, please visit curaprox.co.uk and curaden.co.uk n


In early 2024, Solventum, formerly 3M Health Care, was introduced to the dental field to help provide effective solutions for an endless array of patients.
Members of the Solventum team pride themselves on supporting clinicians throughout their professional journey, equipping them with breakthrough orthodontic and restorative solutions that can maximise patient satisfaction and treatment efficiency.
At its heart, Solventum is enabling better, smarter, safer healthcare to improve lives.
the solventum promise
With more than 70 years of delivering healthcare innovations behind us, Solventum continues to move industry solutions forward by listening closely to the professionals that use our products and encounter new challenges every day – you. By listening to your needs and ideas, we continue to pioneer game-changing innovations at the intersection of health, material and data sciences. As a result, we have been able to improve outcomes for individuals in every aspect of care, everywhere, from the dental chair to data centres, and from hospitals to patient homes.
Collaborative efforts
Oral care professionals need more than reliable products to ensure that patients can achieve healthy, bright smiles that restore their quality of life. They need to be able to simplify procedures, making treatment experiences more enjoyable, and provide predictable clinical outcomes that can exceed treatment expectations.
Solventum delivers solutions that promote advanced patient care and deepen the trust on which relationships with patients and other dental professionals are built. Collaboration in this manner is the key to successful and long-lasting care, which is why we encourage clinicians to reach out and learn more about how we can advance modern dental care together.
When dental professionals work with the Solventum team, we actively listen to your needs and help you find ways to improve for your workflows, whether you provide restorative, orthodontic or general dental treatment. Our awardwinning solutions* are loved by industry experts, and can help professionals in a wide range of clinical scenarios.
improving restorative treatments
For restorative care, new and effective solutions such as the Filtek Easy Match Universal Restorative ensures clinicians
can experience simplified shade selection for anterior and posterior single-shade restorations. With just three shades – Bright, Natural and Warm – you can match the classical VITA shade guide, whilst taking advantage of the same nanotechnology behind other leading Filtek Dental Restoratives. It delivers exceptional polish retention, and makes aesthetic restorations simple to achieve for maximum patient satisfaction.
Other clinically renowned solutions include the Filtek Supreme Flowable Restorative, which was crowned with a Dental Advisor Research Award* in 2024. It offers excellent adaption and versatility for a wide range of indications and techniques, including injection moulding. An updated syringe means clinicians observe virtually no bubbles or material “run-on”, making injection a comfortable and predictable experience.
deliver exceptional orthodontics Solventum also endeavours to improve orthodontic care, with a range of new products that enable orthodontists to provide fully customisable treatment. With the Clarity Aligners Flex + Force, two unique aligner materials can be combined in one treatment plan to suit each individual patient’s needs, and orthodontic plans can be designed with ease in the cloud-based Oral Care Portal.
The streamlined platform allows clinicians to plan, design, analyse and refine custom treatment options in one system, empowering them to provide their greatest level of care. As a cloudbased software, treatment designs can be accessed simply and conveniently. With the time saved, dental professionals can focus on crafting their excellent patient experience.
Join our journey
Solventum has embarked on a new journey in oral care, and we want to support as many clinicians as possible, and help provide treatments that are long-lasting and exceptionally effective.
This is just the beginning, and Solventum will continue to create and refine new treatment solutions for all dental professionals, and help them solve big healthcare challenges. We are solventum.
We never stop solving for you.
To learn more about Solventum, please visit solventum.com/en-gb/home/oral-care/ n
©Solventum 2024. Solventum, the S logo and Filtek are trademarks of Solventum and its affiliates. 3M and Clarity are trademarks of 3M.
*Dental Advisor awards 2024, https://www. dentaladvisorawards.com/manufacturer/3m
None of us know what the future holds.
Having to take time off work because of an illness or injury can have a serious effect on your finances. This is where we come in – our income protection plans can help take away the worry by replacing the income you lose, until life gets back to normal.
For over a hundred years, our members have trusted us to give them peace of mind when they need it most. Isn’t it time you did the same?
To get a quote for an income protection plan please visit www.dentistsprovident.co.uk

To discuss a new plan just for you or review your current plan please contact our member services consultants on 020 7400 5710 or memberservices@dentistsprovident.co.uk
Protecting your lifestyle. Securing your future.
Eschmann, a leading British manufacturer of decontamination products and provider of first-class support services in the field, has recently received the EU Medical Device Regulation (MDR) certification for the range of autoclaves. This achievement marks a significant milestone in ensuring the highest standards of safety and performance for medical devices within the European Union.
a long-standing commitment to quality and safety
The regulations are in place to promote patient safety, while also increasing transparency regarding the lifecycle of medical devices. Eschmann’s journey to EU MDR certification began with a comprehensive review of their existing processes and products. The organisation has always prioritised quality and safety, and this certification is a testament to their on-going work in the area. By adhering to the stringent requirements of the EU MDR, Eschmann ensures that all their autoclaves meet the highest standards of safety, performance, and reliability. The result for dental professionals is the provision of decontamination products that can be depended on to minimise the risk of infection among staff, patients and practice visitors.
Achieving EU MDR certification involved a review of the research and testing that has already contributed to the development of Eschmann’s industry-leading autoclaves. Each device underwent extensive assessment to ensure compliance with the new regulations. This included thorough evaluations of each product design and all associated manufacturing processes, as well as post-market surveillance. Eschmann’s dedication to continuous improvement and innovation played a crucial role in meeting these stringent requirements.
As part of the certification process, Eschmann has also had an opportunity to introduce several further enhancements to the autoclave range available. These improvements not only ensure compliance with the EU MDR, but also enhance the overall user experience, ensuring an even more efficient professional workflow for the dental practice team. Innovative features such as advanced cycle validation, userfriendly interfaces and improved data management capabilities have now been incorporated for the benefit of professionals, patients and businesses.


With more than 60 years of experience in designing and manufacturing autoclaves, it’s no wonder that Eschmann has become a nationally recognised expert in decontamination. The comprehensive portfolio today includes a range of Little Sister autoclaves, affording different capacities, as well as a combination of vacuum and non-vacuum options, and both ‘B’ and ‘N’ type cycles to accommodate the needs of every dental practice. Designed for reliability, efficiency and durability, the autoclaves are available with a dedicated Little Sister Autolog and e-Logbook, which provide automatic recording of cycle data for convenient compliance. Eschmann also provides an array of other decontamination solutions to complete the infection control workflow in any practice, including washer disinfectors, ultrasonic cleaners and RO water systems.
exceptional support to match
In addition to industry-leading solutions and EU MDR certified autoclaves, Eschmann delivers peace of mind to customers with exceptional technical support. The Care & Cover servicing and maintenance package gives customers access to Annual Validation
and Pressure Vessel Certification (PSSR), annual service and software upgrades, unlimited breakdown cover, unlimited Eschmann parts and labour, and Enhanced CPD user training. Fast and efficient remote support is available over the phone and a nationwide team of 50+ manufacturertrained Eschmann engineers provide on-site technical assistance whenever required. They carry Eschmann original parts in their vans as standard, helping them to resolve 91% of equipment issues in their first practice visit for unmatched efficiency.
With the EU MDR certification, Eschmann is ideally-positioned to continue providing high-quality autoclaves to dental and other healthcare facilities across Europe. This achievement reinforces their reputation as a trusted provider of dental and medical devices and support, underscoring their commitment to patient safety, product excellence and innovation.
For more information on the highly effective and affordable range of infection control products from Eschmann, please visit www.eschmann.co.uk or call 01903 753322 n
The dental therapist is a crucial member of the practice team today. There are several factors that need to be considered for individuals to fulfil their potential and build a long and successful career. These include properly utilising their full scope of practice, being valued for their skills across the practice team and having access to first-class education and training. We all have a part to play in increasing awareness of the dental therapist’s role among the professional team, ultimately improving patient care, enhancing skill mix in practices and boosting job satisfaction for individuals in this role.
Promoting a team approach
To ensure dental therapists feel valued and able to fulfil their potential, it’s important that dentists understand their clinical remit. Not only do they need to know which treatments dental therapists can provide directly to patients, but they also need to consider how they may work in tandem with dental associates. Effective collaboration between team members can facilitate smoother daily workflows, create a more
clinically diverse working day and ensure a less isolated working environment for other clinicians. It can also streamline emergency appointments and free up precious time for dentists to focus on other areas of dentistry such as implantology or endodontics.
Of course, is it just as relevant to consider how dental therapists can impact the patient experience. For a start, improved teamwork among all practice practitioners means faster, more efficient and often more effective dental care for patients. The majority of patients are already happy to see the dental therapist for a simple restoration, so there should be few barriers from them as a practice increases their dental therapy services. Patient satisfaction with treatment provided by dental therapists has been positive as well. Many of the same factors apply as would impact patient satisfaction with care from a dentist – with trust and familiarity proving essential. These can be established and developed through professional behaviours and attitudes, good communication and smooth continuity of care.
Once dentists and other colleagues really understand how the dental therapist works,
they can all operate within a workable business model that enhances patient care and boosts business profitability.
Although there has historically been a lack of understanding in the field, perceptions are gradually evolving. Regulatory changes are also being implemented that broaden the scope for both dental hygienists and therapists, who may now supply and administer specific medicines without a prescription from a dentist, once they have sufficient training and experience.
In order for dental therapists to use their entire scope of practice, they must be confident and competent in their skills. For those who are new to the profession, or who have been unable to practise dental therapy in recent years, it can be difficult to adjust. That’s why it’s beneficial to access tailored training and support that will consolidate, develop and refresh your capabilities in a positive environment.
At Clyde Munro, we strive to be the change we want to see in the profession. We understand the importance of the dental therapist role and aim to remove barriers
so that professionals may fully utilise their expertise. Our dedicated Therapist Support Programme has been designed specifically to help dental therapists to consolidate and expand their skills, covering a broad range of topics in training sessions and offering handson assistance from a clinical support team.
skill, confidence and success
For many dental therapists, the chance to fully utilise their skills is important. Not only is job satisfaction improved, so too is the quality of patient care that can be delivered by the whole practice team. If you are feeling under-utilised, now is the time to make a change.
Want to know more? Please visit the relevant webpage here, or contact us on joinus@clydemunrodental.com. n
about the author
Nora Garcia tbabaa, Marketing executive, Clyde Munro

Are you a dedicated dental professional looking for a supportive and caring workplace that offers exceptional opportunities for career growth? At Rodericks Dental Partners, we pride ourselves on fostering an environment where our team members can thrive both professionally and personally.

Dr Vanessa Caldeira, who has been part of the Rodericks Dental Partners family for the past six years, highlights the importance of a supportive work culture. After Rodericks Dental Partners acquired Chilwell Dental Practice in Nottingham three years ago, Vanessa experienced firsthand the benefits of working in a caring and understanding environment.
“I have a family, and I’ve been able to find the right balance for me with the help of Rodericks Dental Partners,” says Vanessa. “From enabling a phased return to work after having my children, to agreeing to working hours that suited my life, they have been great.”
Joining Rodericks Dental Partners means being part of a professional network that covers a wide range of dental specialties. Vanessa, with her extensive experience in restorative dentistry and her background working at the Restorative Department at the Queens Medical Centre in Nottingham, appreciates the access to different specialist teams that the group provides.
“Since joining Rodericks Dental Partners, I have appreciated the access to different specialist teams I have gained through the group’s professional networks,” Vanessa notes. “This access has allowed me to enhance my skills and provide the best possible care to my patients.”
At Rodericks Dental Partners, we believe in continuous learning and career development. We support our team members through co-funded courses and flexible working arrangements that help them achieve their professional goals. Vanessa’s journey with us exemplifies this commitment.
“I have been able to develop my career through co-funded courses, and my career growth has also been helped greatly by the group’s supportive approach to flexible working,” says Vanessa. “The team I work with are
very caring and supportive, and I am happy to recommend Rodericks Dental Partners.”
Rodericks Dental Partners is more than just a workplace; it’s a community where dental professionals can grow, learn and thrive. Whether you are just starting your career or are an experienced practitioner looking for new challenges, we offer the support and opportunities you need to succeed.
Dr Vanessa Caldeira’s story is just one example of how we empower our team members to achieve a fulfilling and balanced career. If you are passionate about dentistry and are looking for a caring and supportive work environment with access to specialist teams and professional development opportunities, Rodericks Dental Partners is the place for you.

To find out more about what it’s like to work with Rodericks Dental Partners and to discuss current vacancies, you can visit www.rodericksdentalpartners. co.uk/careers

DuraTip ® inserts deliver unprecedented like new performance for the entire life of the insert.
We have been using the Parkell DuraTip inserts for 7 months on over 200 patients and they are as efficient as when we first got them. I have seen a lot of things over the years, but nothing compares to the Parkell DuraTip insert.

— Cathy Hendrickson, RDH Watch and learn more

For information and orders contact infoeurope@parkell.com | +46 708 593481
In 1925, only half of American houses had electrical power. 100 years later, 66% of the world’s population has internet access. Technology has grown to the point that it is now capable of creating content and solving problems almost as if it is human – those 66% can access such software in an instant. We are living in a time of rapid technological change. The digital world is not just our way of working, but it is also how we communicate and what we live by.
In healthcare, technology has evolved to meet the demands of more effective and reliable treatments. For all practitioners, it is important to stay up to date with the latest developments so that the best care can be given to patients. Undertaking hands-on workshops can support you and your team so that you can keep at the forefront of your field.
education
In the late 1800s, Hermann Ebbinghaus established the Forgetting Curve, observing that, after one hour, learners forget 50% of the information presented. One day later, they forget 70%; one week later they forget 90%. Hands-on workshops are a way of learning by doing; retention of information is enhanced through experiential learning.
Workshops are successful in increasing the knowledge of the participants because they are sociable. Interaction and group discussion has a 50% rate of retention, five times higher than reading information. Even better, practicing something newly learnt has a 75% retention rate, making a hands-on workshop ideal for using new equipment or materials.
Practical environments enable participants to feel more comfortable and relaxed, increasing their engagement and better developing their problem-solving, critical thinking and concentration. By seeing the end results from their practical efforts, workshop attendees can also build their confidence, encouraging them to try it again without assistance.

As technologies become more and more sophisticated, it can seem daunting to incorporate something new into your daily workflow. Advances in the science of dental, oral and craniofacial health are constantly expanding, allowing for more effective customised care built on the latest breakthroughs. For instance, wearables linked to smartphone apps can monitor pain levels, postoperative healing and home oral health habits so that practitioners can better identify any complications or areas of improvement.
Workshops that feature product demonstration are an easy way for dental professionals to understand new technologies and consider their efficiency within their daily workflow. Such technologies may include 3D printing, which continues to become

an integral part of prosthodontics, orthodontics and oral surgery; its lower costs compared to laboratory fees making it a more financially palatable option in some circumstances.
From the perspective of public health, new technology has had an overwhelmingly positive impact. The growing popularity of patient portals and teledentistry makes dentistry more accessible to the patient, increasing their engagement. Demonstrations of these patient-facing products can show the latest ways of reaching and looking after your patients.
Getting to grips with the latest innovations in a workshop or sampling new materials can give you a foundational knowledge. It is important that new treatments and technologies improve outcomes and expand care for all, independent of social-economic status.
In-person workshops also serve as a brilliant opportunity for networking; meeting other professionals in an environment that cultivates knowledge exchange. Doing practical workshops with colleagues may act as a team building exercise, fostering greater cooperation, motivation, trust and respect among the dental team. This is beneficial for creating or supporting a positive practice atmosphere, which in turn may reduce burnout risk and nurture a more comfortable experience for patients.
For an exciting opportunity to learn new skills and enhance old ones, attend BDIA Dental Showcase 2025. The hands-on Clinical Excellence
Workshops are back by popular demand to provide an unparalleled environment for immersive education. Experts in various fields offer personalised, one-on-one training experiences in which you can refine techniques, discover new innovations and engage with exciting products. With over 150 sign-ups already, the workshops are the place to be. Cutting-edge dental equipment, materials and technologies are in your reach with BDIA Dental Showcase. Keeping up with the latest technologies can be challenging. By participating in workshops, you and your team can try new products and be educated on recent developments, all over an exciting day shared with fellow professionals.
Register now and receive an early bird discount code: dentalshowcase.com/workshops-pre-register

BDIA Dental showcase 2025 14th-15th March exCeL London dentalshowcase.com n
About the author David Hussey, event Director, MA exhibitions.









Easy & fast placement
Moisture tolerant
Proven longevity








Thixotropic viscosity
Wear resistance
Polishability & aesthetics





Reinforced with glass fibres
Perfect adaptation
Bulk fill












BOS President, n ikki Atack , discusses 30 years of the British Orthodontic Society and what it means to be involved
2024 marks 30 years since the UK’s orthodontic societies unified to form the British Orthodontic Society (BOS) – the starting point for the BOS being recognised nationally and internationally as the voice of orthodontics in the UK.
Nikki Atack is currently President of the British Orthodontic Society, having been elected in 2021. She is a full-time consultant orthodontist at University Hospitals Bristol and Weston Foundation Trust, as well as an honorary senior clinical lecturer at University of Bristol, where she is the orthodontic lead for the dental undergraduate programme. Here, Nikki reflects on 30 years of the BOS, while also looking into the future and remaining focused on the present.
how has the BOs evolved since 1994, and what remains the same?
The last 30 years have witnessed many transformations in health care delivery, and orthodontics has not been immune to this. At the same time, peoples’ perceptions and expectations have shifted. The BOS has adapted and evolved to meet these changing environments.
We recognise the importance of inclusion, listening to both our members and their patients, which have helped us to maintain our relevance.
I think the initial aspirations of the BOS have not changed and still underpins the Society today; the enthusiasm of members to volunteer and get involved in all aspects; the friendship, respect and support that members give each other; and the common goal to strive to improve and promote standards, education and research within orthodontics.
how did you come to be involved with the BOs and what does it mean to serve as President?
I started my orthodontic training in 1993 in Bristol, so I became aware of the BOS in its infancy, so to speak. Professor Chris Stephens was one of my tutors, and he was closely involved with the unification process, so it was natural for me to join the new unified Society as a trainee. I attended the1994 BOC conference in Harrogate, volunteering as a steward; interestingly this was when the first BOS Council meeting was held. Later, as a newly appointed consultant, I was invited to represent the Society as their representative with Healthcare Quality Improvement Partnership (HQIP) and I subsequently applied to become the Chair of the BOS Clinical Standards Committee. In 2015, with further re-structuring of the Society, I became its first Director of Clinical Governance. I was elected in early 2021 to be BOS President. This was a huge honour, especially as I was the first to be elected to this role. It was with a degree of trepidation that I took over in September 2021, but I was heartened knowing that I had the support of BOS members. The role brings with it the responsibility of balancing all the interests within the Society, but also challenges from external


sources. However, I am lucky enough to work with a dedicated Board of Trustees and Society volunteers, as well our amazing team at the head office.
What are some of the society’s key highlights?
Firstly, managing to achieve unification. This came about after many years of careful discussion and collaboration between the five founding orthodontic groups.
Over the 30 years, there are so many highlights across a number of fields, including education and research, it is difficult to single out a few. In the field of education, the Society developed, principally with the University of Bristol, the first national orthodontic virtual learning environment, which gives a national framework and resource for teaching.
The BOS provides expert guidance and advice for both patients, members and external bodies. We received particular praise for the information we provided during the Covid-19 pandemic and the recent guidance on teledentistry. Finally, of course, the BOS delivers a high-quality education programme for our members, the pinnacle of this being the annual British Orthodontic Conference. The ultimate recognition of the Society’s skill in this area was to be awarded the opportunity to host the 2015 World Orthodontic Conference in London.
On the research side, the BOS developed a Foundation – BOSF –which focuses on and funds orthodontic research. The BOSF has provided over £1.5 million of research funding since its inception in 1999.
Finally, there is our internationally recognised and respected journal, the Journal of Orthodontics, which recently obtained its first impact factor, being included in the Emerging Sources Citation Index with an impact factor of 1.3.
Why is it important for orthodontists to consider joining if they haven’t already?
As a BOS member, there is access to a whole range of benefits that are tailored to members’ specific needs. The BOS gives access to the right support at every stage of one’s career, whether thinking about specialising when a dental student or new graduate, or working in general or specialist practice. The Society is there for advice, education and peer-support. Many of our members have been with us throughout their entire career.
By becoming a member, you become part of a wide network of experts in the field of orthodontics. Due to our diverse wide-ranging membership, the BOS is recognised as providing a national voice for orthodontics and its views are valued by the public and professionals alike.
I would like to think that, by joining the BOS, you join a family of like-minded, keen and enthusiastic orthodontic clinicians, and, together, we will continue to promote the study, standards and practice of orthodontics.
What does the future hold?
There are huge opportunities for the whole of dentistry with innovations in technology, particularly in the digital arena. With advances comes change, and sometimes this is difficult to adapt to, but it presents us with great prospects going forward.
The BOS will continue to develop orthodontic education and research, embracing the digital world. Remote monitoring is an area that has made significant advances over the last few years, and this may provide ways for us to deliver assessments and treatment differently and more effectively. This, together with continuing to maintain and build on our close relationships with general practice and orthodontic therapist colleagues gives us the opportunity to further develop patient care in the widest sense.
It is vital to me that the BOS plays a leading role in the development of orthodontics moving forward, so that all our members and those who wish to join feel included and valued. Together, we will continue to champion the orthodontic specialty both for members and the wider public. n
In the intricate world of periodontal and oral surgery, precision and attention to detail are crucial. However, an often overlooked yet integral factor in achieving successful outcomes is the ergonomics of the dental workspace. Achieving optimal outcomes in periodontal and oral surgery relies not only on clinical expertise but also on the seamless integration of ergonomics into the dental workspace. Maintaining body posture in a neutral position as much as possible, minimising the leaning or bending towards the patient, results in fewer injuries and musculoskeletal defects. Dentistry often involves prolonged periods of repetitive tasks and precise movements, which can lead to musculoskeletal issues if proper ergonomic principles are not applied. The International Journal of Environmental Research and Public Health published a study (Jacquier-Bret, J., Gorce, P., 2003) stating that over 60% of dentists experience some form of musculoskeletal pain during their career.
Ergonomically designed seating, e.g. The Bambach Saddle Seat, enables practitioners to achieve and maintain optimal postures and creating an environment conducive to delivering precise and effective treatments. Its unique patented saddle-shaped design promotes a neutral spine, reducing strain on the lower back and providing unparalleled support for precise and intricate procedures. Most of us find ourselves with collapsing C-shaped curved spines, compressing our organs and encouraging posture-related health problems.

• Shoulders relaxed
• Straight back
• circulation in legs
• healthy hip and knee joints
• Feet flat on the floor

Maintaining the right posture and positioning during surgery is crucial for precision. The Bambach Saddle Seat promotes a neutral spine, reducing strain on the lower back and providing optimal support for precise movements. This directly translates into improved patient outcomes and procedural success. For precision and accuracy, the arm position and health of the upper body musculoskeletal system is of high importance, and the use of armrests for macro and microscopic surgery can be a helping factor.
Dental professionals spend long hours performing intricate procedures. The Bambach chair not only enhances patient care but also safeguards the health and wellbeing of the dental team. Its unique design encourages proper posture, reducing the risk of musculoskeletal issues and promoting long-term career sustainability.
Ergonomically designed dental chairs, such as the Bambach Saddle Seat, contribute to streamlined workflows. The chair’s flexibility and adjustability enable practitioners to work comfortably, with easy access to instruments and equipment, thereby minimising downtime and maximising efficiency.
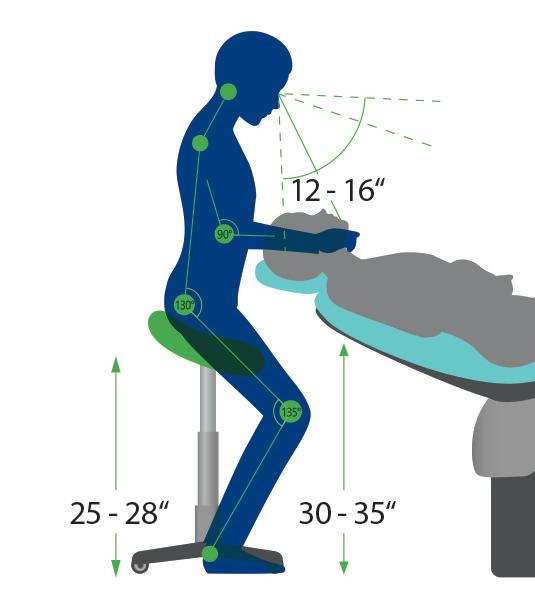

A comfortable practitioner is better equipped to ensure patient comfort. The Bambach Saddle Seat’s ergonomic design not only supports the dentist but also contributes to a more relaxed environment for the patient during surgical procedures.
Dentistry is a lifelong commitment, and the Bambach dentist chair plays a crucial role in ensuring the longevity of a practitioner’s career. By prioritising ergonomics, dental professionals can mitigate the risk of occupational hazards and continue to provide exceptional care throughout their careers.
In conclusion, the importance of ergonomics in periodontal and oral surgery, with special mention of the Bambach dentist chair, cannot be overstated. It is a holistic approach that not only benefits practitioners but also enhances the overall quality of patient care. As we navigate the complexities of dental surgery, let us remember that a well-designed, ergonomic workspace is the foundation for excellence in every procedure. n
about the author
Zerina hadžić, PhD, mSc, DDS, Specialist in Periodontology and Oral medicine.

Colin Campbell, Director at The Campbell Clinic, recalls how Planmeca has supported him in getting his purpose-built facility up and running
Colin Campbell’s relationship with Planmeca began in 2018. He is the Director & Specialist in Oral Surgery at The Campbell Clinic and Campbell Academy in Nottingham, which was in the process of being purpose built at the time. Colin and his team travelled to Helsinki to find out firsthand about the company, its culture and to see what was under production. It was there that a partnership was formed, as Colin was looking for great value and excellent service as he kitted out his new facility.
“We were looking for someone to partner with in this project, which was massive,” explains Colin. “We needed trust, excellent service and quality, which we received from Planmeca as soon as they became involved in the design process.”
It was Planmeca’s range of CBCT scanners that initially led Colin to Finland. “The thing that first drew my attention was the Ultra low dose feature,” he recalls. “The way it worked in my mind was that if you could lower the dose of CBCT, you could take more CBCT scans of patients and achieve better diagnostic quality and additional diagnostic information. For example, if I was able to cut the dosage in half, I could take twice as many scans. Cutting it in half again, I could have four times as many images for each patient.
“This means I can take pre-op and postop scans of a patient if I wanted to. But, more importantly, I can reduce the overall dose to my patients.”
Planmeca Ultra Low Dose is a unique way to capture CBCT images at patient doses comparable to or even lower than panoramic images – as proven in various scientific studies. The imaging protocol can be used with all imaging modes and voxel sizes.
Impressed with the feature for numerous reasons, Colin selected the Planmeca ProMax 3D Classic – a unit that covers the entire dentition, making it an excellent option for full arch dental 3D imaging. It includes the all-in-one imaging software Planmeca Romexis, which supports all 2D and 3D imaging as well as CAD/CAM work.
“Everybody gets obsessed with clarity of image at any price but that’s not how it

works,” says Colin. “I’ve used pretty much every software system there is, and there isn’t one better than Romexis with how intuitive it is, how clear it is, and how easy it is to plan cases. If you want to design guides, you can. If you want to import other digital media, you can. It’s all seamless and, combined with the Ultra Low Dose facility and CBCT adaptability, it’s just an extraordinary product.”
Of course, Colin needed more than a CBCT unit. He had an entire purposebuilt facility to equip. Browsing through Planmeca’s range of dental chairs, he came across the Compact i5.
Compact i5 is Planmeca’s most widely sold dental unit family, constantly updated with new features and functionalities in order to offer clinicians around the world the best possible working companion. The Planmeca Compact i5 dental unit is the culmination of five generations of continuous improvement, with a sleek and distinctive, user-centric design created to stand the test of time. Product development is guided

by what Planmeca believes contributes to good design: ergonomics, safety, comfort, and aesthetics.
“Everybody comments on the chair setup because it’s minimal – not clunky,” explains Colin Campbell. “The knee break element, for me, was really important. I don’t know why anyone wouldn’t have a knee break chair, because it creates so much room in your surgery, and it provides a normal sitting position for a patient for when you first speak with them at the start of an appointment. Their legs aren’t flat out until they lie back, it’s more comfortable.”
“What you get with Planmeca, and why we continue to work with them, is value,” says Colin. “Some people think value means the cheapest product, but it doesn’t. Value is getting more than that which you pay for, and that’s what you get back in terms of the relationship and support, in collaboration and in products that are forward thinking, innovative and always developing.”
The Planmeca Compact i5 dental unit has been designed to offer the smoothest possible workflow for the dental team and the most enjoyable treatment experience for patients of all sizes and ages, enabling the entire clinic to benefit from stress-free dentistry.
“There’s plenty of scope for adjustment on the chair,” Colin adds. “And there’s no armrests – a massive feature that some people overlook. “I do a lot of intravenous sedation, and I don’t have patients with arms falling off the side of the chair. The chairs are designed to keep everybody comfortably in the centre.”
To meet the demands of today’s dentistry – the increasing infection control and quality assurance demands, different users using the same devices, the constantly growing patient flow, just to name a few – Planmeca has created smart, customisable solutions that let dentists concentrate on patient treatment while technology takes care of the rest.
“An add-on feature that we added is this,” says Colin, patting the cushioned


seat of the chair. “I can tell you that, in our practice, from a patient perspective, that is the biggest feature we offer.”
Planmeca guarantees a long life span for the Compact i5 dental unit. It has been built to allow for upgrades, with new features and improvements coming at any time. This makes it a truly future-proof investment, with countless unique options to always choose from to match your ever-evolving preferences and needs.
“There’s also the ergonomics,” Colin adds. “It’s designed for working.”
Planmeca Compact i5 is ideal for both two-handed and four-handed dentistry. It provides plenty of working space for a dental assistant and offers easy access to suction tubes and other essential instruments. Since all the infection control functions are neatly organised in their own compartments, daily routines become more straightforward and less time-consuming.
“We have the overarm delivery, which is a little bit non-British in a lot of ways,” explains Colin of the Finnish design. “However, I would never return to cart system in a million years, and nobody else here would, because of the digital setup. It’s easy to control and program for individual clinicians. It’s also easy to interchange the componentry, which makes it easy to service. We’ve found that personally, and have had plenty of support from Planmeca and their engineers.”
To discover more features of the Planmeca Compact i5, visit https:// www.planmeca.com/dental-units/ planmeca-compact-i5/

Colin Campbell, Director at The Campbell Clinic, recalls how Planmeca has supported him in getting his purpose-built facility up and running.
Scan the QR code to watch the full interview with Colin Campbell
From Helsinki to Nottingham

Can dental professionals deliver whitening without increasing the risk of sensitive teeth?
Patients are increasingly asking dental care professionals to recommend in-clinic services or at-home products for whitening teeth. Various factors, including a raised awareness of the importance of oral hygiene, and the influence of social media and celebrity endorsement are driving the demand for whiter, brighter and more photogenic smiles.1 Teeth whitening is now the most popular elective procedure in dentistry. It offers the opportunity to enhance one’s appearance through a relatively simple and non-invasive procedure.2
In the UK, interest in tooth whitening is growing rapidly, and is now worth over an estimated £40 million annually.3 In fact, the UK is ranked second only to the United States in terms of interest and demand for teeth whitening services. 4 Often associated with health and confidence, the aesthetic appeal of whiter teeth is undeniable. However, achieving successful results can come with potential risks and undesirable effects, which patients must be made aware of.
One major source of risks is that of undertaking whitening procedures by illegal and untrained providers. Apparently, it is single adults who are driving this trade in illegal teeth whitening products and services, attracted by the offer of cheaper treatment and often unsubstantiated results.4 Only registered dental practitioners are permitted to sell or administer whitening products containing or releasing above 0.1% hydrogen peroxide. Those doing so who are not registered dental professionals are liable for prosecution.4
Even though we can only do so much to deter people from the risks associated with illegal whitening services, there are practical steps we can take to help reduce the potential risks and undesirable effects of professionally administered or at-home whitening. One of the main risks associated with teeth whitening, whether conducted professionally in-practice or self-administered at home, is increased dentine sensitivity. This is due to the key ingredients in some teeth whitening products; hydrogen peroxide or one of its precursors, hydrogen carbamide, penetrating the enamel as part of their mode of action and entering the dentine. Such bleaching agents can cause alterations on

the enamel, including depressions, porosity, and surface irregularities.5
The numbers of patients reported as experiencing some level of sensitivity during teeth whitening, either at-home or in-surgery, can vary from 54% to 80%.6–8 The sensitivity patients feel is usually described as mild but, for 10-14% of patients, this may increase to be moderate or severe in scale.7 In the case of home bleaching, this can potentially lead to a patient discontinuing the at-home whitening process and so they do not achieve the results they were hoping for.8 Some patients may also be deterred from undertaking teeth whitening due to a previous bad experience of sensitivity during the process.8
If a patient has gingival recession, there is a greater likelihood that tooth sensitivity will occur.6 Hence the need for a patient to be examined prior to embarking on a course of teeth whitening procedure. Other factors that may play a role in increasing sensitivity include the presence of adhesive restorations, or the intensity and duration of light usage during the whitening procedure.9 Studies have also suggested that the higher the concentration of hydrogen peroxide, the greater the risk of tooth sensitivity.10
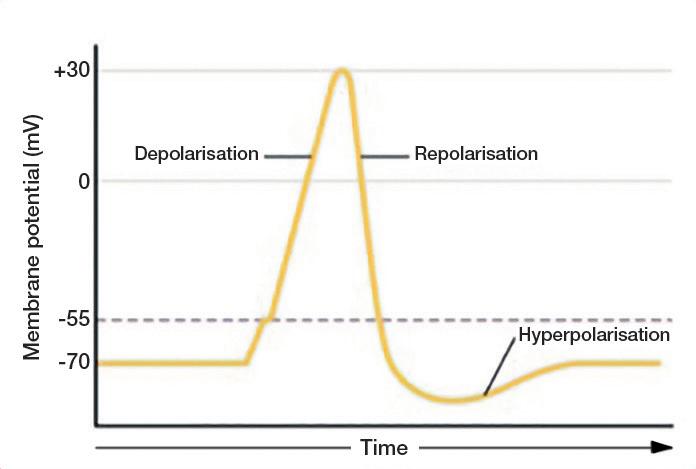
Whatever its precise prevalence, dental sensitivity is recognised as the most common undesirable effect of teeth whitening. So, whether a patient is looking for an in-clinic procedure or an at-home option, they must be made aware of the risks before they start whitening.
How can sensitivity be alleviated?
Whilst patients often recognise the risk of sensitivity, most will accept it as a small consequence to achieve their goal of a whiter smile. As dental professionals, there are options that we can employ to help minimise a patient’s risk of sensitivity or to alleviate its effect as much as possible.
The application of fluoride has traditionally been used during and after professional bleaching to help manage sensitivity as it is believed to block tubules and control the flow of pulpal fluid.2
Potassium nitrate is a desensitising agent used in the context of sensitivity. Potassium nitrate is an inorganic salt, the ions of which are important for the maintenance of cell membrane potential, particularly the potential of electrically excitable tissues, such as nerves.11 Potassium nitrate works by blocking the transmission of nerve signals in the teeth. Most cells are negatively charged relative to their surroundings, and nerve cells generate impulses by rapidly depolarising and repolarising again.12
Potassium ions can keep the intradental nerve cells in a depolarised state, preventing them from sending pain impulses.11,12
When applied topically, potassium nitrate penetrates the structure of the tooth and reduces the excitability of nerve endings and, consequently, reduces their sensitivity to external stimuli.13
Used alongside bleaching agents, such as hydrogen peroxide, potassium nitrate can help reduce sensitivity when regularly applied before, during and after teeth whitening procedures.13 Studies have shown that potassium nitrate is effective in reducing sensitivity without affecting the efficacy of whitening products.13 When formulated in
a toothpaste with whitening ingredients, a specialist toothpaste containing potassium nitrate could help prevent stains and maintain whiteness, whilst also protecting patients from dentine sensitivity. n
References:
1. Carey C. J Evid Based Dent Pract. 2014;14:70–76. doi:10.1016/j. jebdp.2014.02.006.
2. Tang B. and Millar B. BDJ. 2010;208(12):577–577.
3. Oral Health Foundation. Available at: https://www.dentalhealth.org/news/ single-adults-leading-growth-in-uksillegal-tooth-whitening-industry-studyfinds Accessed April 2024.
4. Aesthetic Medicine. Available at: https://aestheticmed.co.uk/site/ featuresdetails/brits-second-mostinterested-in-teeth-whitening Accessed April 2024.
5. Krishnakumar K, et al. Cureus 2022;14(4):e24028.
6. Jorgensen M. and Carroll W. J Am Dent Assoc. 2002;133(8):1094-1095.
7. Tredwin C, et al. BDJ. 2006;200(7):371–376.
8. Dentistry. Available at: https:// dentistry.co.uk/2006/11/22/treatmentsensitivity-during-home-bleaching/. Accessed April 2024.
9. American Dental Association. Whitening. Available at: https://www.ada.org/ resources/ada-library/oral-health-topics/ whitening Accessed April 2024.
10. Pontes M, et al. Op Dent. 2020;45(3):265-75.
11. National Center for Biotechnology Information (2023). PubChem Compound Summary for CID 24434, Potassium Nitrate. Available at: https:// pubchem.ncbi.nlm.nih.gov/compound/ Potassium-Nitrate Accessed April 2024.
12. Biology Online Dictionary: Depolarization. Available at: https:// www.biologyonline.com/dictionary/ depolarization. Accessed April 2024.
13. Pierote J, et al. Clin Cosmet Investig Dent. 2019;29(11):219-226.





The couple that helps you to achieve even better oral hygiene

FLEXI
• The special FLEXIBLE HANDLE makes it possible to angle the handle to achieve better and easier access to all interdental spaces.
• The non-slip handle ensures good grip even when fingers are wet.
• All brushes have plastic coated wire. This ensures no metal is in direct contact with teeth and gums, thus making them much more comfortable to use and preventing dental injuries.
• 11 sizes ensure that all needs are covered.


TANDEX PREVENT Gel
• Strengthens the enamel and has an anti-bacterial effect.
• 0.12% chlorhexidine and 900 ppm fluoride.
• The consistency combined with the needle shaped tube end make it easy to apply directly on the FLEXI brush and use wherever needed.
• Pleasant taste of peppermint.
• No alcohol or abrasives.
New research from Bupa Dental Care has found that nearly half the population (44%) dread visiting the dentist and 76% of those put off the visit entirely. The study reveals that a leading cause of dental anxiety stems from childhood, with nearly two-thirds suffering from dental anxiety having a family member who is anxious about going to the dentist, and 36% saying this fear has contributed to their own dread.
As a result, a cycle of dental anxiety has been perpetuating. One in five put off taking their children to the dentist and 38% of parents say their children are nervous about dental appointments.
We spoke with Bupa Dental Care’s Head of General Dentistry, Anni Seaborne, to discuss the results.
why is understanding dental anxiety so important?
Dental anxiety affects a large proportion of the population and is the cause of widespread avoidance of dental care. We know the consequences of not regularly visiting the dentist include deteriorating oral hygiene, increased health problems and, sometimes, even a need for more complex treatments, so addressing dental anxiety is crucial for improving a person’s overall wellbeing and health. By prioritising this issue and understanding the root causes, we as a profession can help patients overcome their fears.
How did expectations correlate with the findings?
We didn’t go into the research with strong assumptions; we wanted to hear directly from people who suffer from anxiety, where it stems from and the kind of support they believe would help. We were particularly interested that one of the leading causes stems from childhood, with nearly twothirds suffering from dental anxiety having a family member who is anxious about going to the dentist, and 36% saying this fear has contributed to their own dread. It seems like there’s a cycle of dental anxiety that we really need to break to ensure people aren’t deterred from getting their children the dental care they need or passing down their fears.
what are the first steps in encouraging those with severe dental anxiety to visit the dental practice?
We know that treating anxious patients can be more complex, as they may not always feel comfortable receiving routine care. Therefore, we need to reassure them that we’re in the profession because we care and want to help. Encouraging individuals with severe dental anxiety to even visit a dental practice in the first place is a big step in the right direction. We need them to know that our approach puts them first. To identify who might be an anxious patient, there can be tell-tale signs, such as someone who fails to make appointments
or cancels at the last moment, attends the appointment late or does not make recall appointments, or appears disengaged with the information or treatment being given.
As part of our research, respondents told us that being supported by a practice team who can help with dental anxiety would be the most beneficial way to help their dental anxiety.
Bupa Dental Care partnered with the Speakmans. How did that come about?
After our research revealed that nearly half the population (44%) dread visiting the dentist and 76% of those put off the visit entirely, we set out to find an expert partner who could help raise awareness of this issue and help us respond. The Speakmans are recognised life coaches and therapists who support people with a range of fears, and so could have a positive influence and strong voice on dental anxiety among their large audience. This made them the perfect partner.
what guidance has been offered to dental professionals?
In partnership with The Speakmans, we have produced a list of recommendations for practice teams to support patients with dental fear or phobia.
1. If you see signs of dental anxiety or a patient directly tells you about their anxiety, take the time to talk to them about their concerns and offer practical support – such as allocating time to discuss what they can expect from their appointment or agreeing on a signal to use if they would like a procedure to stop, such as raising their hand, so that they feel more in control.
2. Work with patients to understand whether their fear is actually of the dentist, or whether this is from another phobia or fear, such as needles. This helps you to address any specific concerns or potentially adjust how the appointment is carried out.
3. After discussing the origin of your patient’s dental phobia, help support them by reminding them that:
• If they had a difficult dental experience as a child, it’s important to know that dental procedures have come a long way with technology. We use the latest dental innovations to enhance the patient experience and provide the best care and comfort.
• As an adult, it is often easier to talk openly with their dentist, and you want to address any concerns and reassure them every step of the way.
• The dentist will be committed to providing them with the highest quality care. Their goal is to ensure that their visit is safe, painless, and as positive as possible.
• Dentists and dental professionals choose their careers because they are passionate about helping

people. They want to prevent oral health issues, alleviate pain, and support overall health and wellbeing.
4. Allow patients to visit your dental practice before the appointment to get used to the environment. This can help to address and combat any concerns they might have.
5. Following this visit, check in with the patient on whether there is anything you can do to make their visit more comfortable. For example, minimise the time they have to stay in the waiting room or allow them to wear their own personal sunglasses instead of the practice’s goggles.
6. Make a note in their file that they are nervous, so the team knows ahead of their next visit. For example, this may indicate that the team should try their best to be as on time as possible for this patient to reduce waiting time, which might otherwise heighten their nerves.
7. Talk through your patient’s fear with them to try to encourage a shift in mindset. If they are worrying about a worst-case scenario that might happen, you can help them by explaining the reality of their appointment. You can also remind them that by having regular check-ups, this allows them to keep on top of their oral health before more serious issues arise.
8. Allocate an “anxiety lead” to manage the initial contact with the patient. This
doesn’t necessarily have to be a dentist, but having one specific dentist who looks after anxious patients may also be beneficial.
tell us more about the video series you have launched with Just Ask a Question (JAAQ). As additional support for people with dental anxiety, we’re leveraging our partnership with JAAQ to support people through engaging content. JAAQ is a specialist mental health platform that addresses a range of issues through engaging video content. It means people can get help and advice from world leading clinicians and wellbeing experts whenever they need it. Working with our own dental professionals, our series is designed to help people access information to ease their fear of the dentist in a clear and easily accessible way. We address a range of challenges including the common worries associated with visiting the dentist, including how to make an appointment, what treatments are covered, and what technology we use.
To view the videos, visit: https://tinyurl.com/DentalDread n



























































































































The patented Smart Chromatic Technology in OMNICHROMA ensures infinite colour matching from A1 to D4 thanks to structural colour. Add to this 3 different viscosities for all preferences and areas of application. The OMNICHROMA family thus offers the user every conceivable option with a minimum of materials.
OMNICHROMA –is all you need for state-of-the-art filling therapy.




















































artificial colour pigments ”automatically” adapts to the tooth shade








Bis-GMA– formulation for better biocompatibility

sustainable stocking only order 1 shade & no expired special shades






Many dental manufacturers claim their products make Dentists’ lives easier, but not every manufacturer makes it their mission. That’s unless it’s Centrix, the 50-years old dental innovator which launched the first direct-to-prep delivery system back in 1970.
Centrix continues to produce singlepatient-use products designed to make dentistry easier. This includes the ubiquitous Benda Brush and Benda Micro brush; Tempit temporary filling materials; FluoroDose sodium fluoride varnish, which is now available in six patient-pleasing flavours and can be applied in less than a minute via its innovative LolliTray dispenser; NoMix moisture-activated temporary cement, which is designed for use in the surgery and at home in emergencies; Exposé disposable caries indicators which eliminate the need for measuring and mixing, and the risk of spillages; and many others.
Free sample of NeW DraganBerry flavoured FluoroDose!
Centrix have extended their range of Award Winning Fluorodose varnishes by launching NEW DraganBerry flavour! To obtain a free sample contact your local Trycare representative, telephone 01274 885544 or email dental@trycare.co.uk
Centrix’s FluoroDose 5% sodium fluoride varnish is easy to apply in less than a minute.
To make life easier, its packaging has patented features to enhance handling, comfort and patient safety. Containing a single dose of varnish, each LolliTray includes a Benda Brush applicator and is designed so that it “pops up” with one hand, making removal simple and safe. Drying in seconds when contacting saliva, FluoroDose remains in situ for up to six hours for optimum fluoride uptake. It offers a smooth non-stringy or clumpy consistency, fast application and six patient-pleasing flavours – caramel, bubble gum, mint, cherry, melon and NEW DraganBerry! It is supplied in Introductory Packs containing the five original flavours and refills of all six individual flavours. Freshly mixed prior to application it always has the optimum fluoride distribution, unlike syringes which frequently separate out leaving inconsistent mixes of ineffectively low and dangerously high fluoride concentrations.
Each LolliTray contains enough varnish to protect a full adult dentition. Non-gritty and easy to apply in undetectably thin films, it is colourless so does not affect the appearance after bleaching etc.
Quick-drying and long-lasting, FluoroDose is suitable for adults with caries risk factors and children. Applied as often as needed it is FDA-approved for treating dentinal sensitivity.
exposé
With today’s emphasis on minimally invasive dentistry, Clinicians want to ensure that their direct restorations remove as little healthy tooth tissue as possible. One thing that can help ensure this is a caries detection dye.
Exposé caries indicators make the use and application of a caries detection dye simple, mess-free and precise. Its wellknown Benda Micro brush applicator, available in either fine or extra-fine, is prefilled with a dry blue dye, which is simply touched onto a wet tooth to activate. The dye, which acts by staining caries by-products, stains active caries lesions thereby enabling the Clinician to identify precisely the tooth material to be removed. Plus, because it does not become liquid until it has touched the wet tooth there are no drips to stain clothing or soft tissue.
Benda Brush and Benda Micro brushes
While a brush is a seemingly simple tool, it’s important to have the right one for the job.
When applying a precise amount of material to a broad surface, the onepiece Benda Brush with its bendable brush head is ideal. The Benda Brush smoothly places and spreads fissure sealants, bonding and etching agents, whitening agents and other materials.
Benda Micro brushes are perfect for applying smaller amounts of materials or when precise placement is required, such as with selective etching or single point placement.
Both brush heads can be angled with ease and remain in position without bouncing back. Their chemical-resistant, non-absorbent fibres are suitable for harsh substances. Disposable for easy clean-up, Benda Brush and Benda Micro brushes are available in two sizes and assorted colours, so they can be colour-coded to avoid cross-contamination.
Freshly mixed for optimum consistency and easy to apply in less than a minute!


exposé
Drip-free caries detection –perfect for minimally invasive dentistry!
Benda Brush and Benda Micro Brushes Facilitate precision placement of fissure sealants, etching and bonding agents and much much more!

All of these exciting innovations are now available from Trycare, the UK’s fastest growing dental dealer, who have been appointed sole UK Distributors for the complete range of Centrix problem-solvers. This expands further the comprehensive range of products available from Trycare, which includes everything you
need from all the major manufacturers. Yet another reason to contact Trycare and “Discover the magic” for yourself! For further information about the complete Centrix range contact your local Trycare representative, call 01274 885544 or visit www.trycare.co.uk/centrix. n





























































































































The maxillary sinus, one of four pairs of paranasal sinuses, is a pyramid-shaped structure with its base pointing towards the nasal sidewall and its apex pointing towards the zygomatic region of the maxilla. It contains the maxillary sinus ostium, located towards the cranial side which connects it to the nasal cavity, enabling the drainage of its content.
Diseases affecting the maxillary sinus can cause a great deal of discomfort in a patient’s orofacial region. As this can present as tooth pain, dentists may often be the primary diagnostician, encountering conditions, such as sinusitis, polyps, cysts, mucocele and other lesions via radiographs.
Ear, nose and throat specialists (ENT), or otolaryngologists, are also concerned with this area, and due to their related areas of interest, oral and maxillofacial surgeons may often find themselves collaborating with ENT surgeons when planning treatment for some diseases of the maxillary sinus. An understanding of the maxillary sinus region, the neurovascular systems and alveolar bone is essential for effective surgery, as well as management of complications related to oral surgical procedures.
dental disorders and the maxillary sinus
Dental disorders can be associated with alterations of the sinus mucosa due to the close anatomical relationship between some premolars and upper molars and the maxillary sinus floor.
Maxillary sinusitis (MS) is the most common pathology of the maxillary sinus, and can be rhinogenic, traumatic, allergic or
neoplastic – but it can also be odontogenic. A significant proportion of MS is associated with odontogenic infection from posterior maxillary teeth as a result of their close proximity to the sinuses.
Odontogenic infection and sinusitis can result from dental caries, dentigerous cysts, retained tooth roots, periapical diseases, and periodontal disease. These may also result from surgery in the posterior maxilla, including the removal of teeth, sinus lift grafting and implant placement. Maxillary sinus infections of odontogenic origin are likely to be caused by the same kinds of bacteria as typically seen with dental infections.
Apical periodontitis (AP) is a major risk factor for odontogenic maxillary sinusitis (OMS). The progression of periapical lesions (PALs) from the posterior maxillary teeth can lead to inflammatory changes in the mucosal lining of the maxillary sinus, leading to OMS, as well as structural changes in the Schneiderian mucosal sinus membrane and possibly the entire sinus.
The upper second and the first molar are also more prone to furcation involvement (FI) compared to other teeth which can lead to tooth loss. The loss of the maxillary second molar, particularly, is thought to be a cause of maxillary sinus pneumatization (MSP), which in severe cases can lead to an engagement between the sinus floor and the alveolar crest.
Tooth loss can cause alveolar process resorption. When bone volume or height decreases, implant treatment becomes more complex. In addition, maxillary sinus diseases decrease the elasticity of the Schneiderian membrane. This increases the technical difficulty of surgery, as well as the risk of complications.
a multidisciplinary approach to diagnosis and management OMS and non-odontogenic MS are sometimes difficult to diagnose correctly, and one can be confused with the other. Due to the complexity of the paranasal regions, collaboration between otolaryngologists and dentists optimises outcomes once OMS, or other conditions affecting the maxillary sinus, have been diagnosed. Radiographic images, including panoramic and conebeam computed tomography (CBCT) scans which are often used in oral and maxillofacial surgery can help with the diagnosis of maxillary sinus diseases, including OMS. Surgical approaches to OMS are based essentially on dental surgery, often combined with endoscopic sinus surgery. These techniques remove any infection, and restore the drainage ability of the sinus, preventing any recurrence of sinusitis. This approach draws upon dental as well as ENT expertise, which is essential to successfully manage the dental pathology and any possible complications resulting from interventions.
ICE Postgraduate Dental Institute & Hospital and the University of Salford will address maxillary sinus anatomy, pathology, and treatment in an advanced course in bone and tissue regeneration, and sinus grafting this autumn. Led by eminent specialist oral surgeon, Professor Cemal Ucer, along with a stellar group of ENT consultants, this course will provide a deeper clinical understanding of sinus pathology and management, as well as a comprehensive combination of hands-on and theoretical training for the experienced implant surgeon in reconstructive preprosthetic oral surgery.
Dr Nisha Sisodia, a dentist who provides dental implants, has completed both the Advanced Horizontal & Vertical Augmentation course and the Soft Tissue Management Around Teeth & Implants course from the ASHA Club. She describes her experience of these courses:

“I chose to enrol on the Soft Tissue Management Around Teeth & Implants course after attending a few of Professor Giovanni Zucchelli’s masterclasses and completing an online course of his. I have been wanting to attend a soft tissue course
taught by him for a few years but hadn’t had the opportunity. I heard through one of the faculty members that there were a few places available for this year so I booked it!
“I chose the Advanced Horizontal & Vertical Augmentation course as, previously, I would refer any cases that involved significant bone and gum grafting to colleagues. I felt it was time to move to the next stage in my implant journey and improve my skills in this area. I heard about this course while attending the ASHA Soft Tissue Management Around Teeth & Implants course presented by Professor Zucchelli; as I enjoyed that course, I booked this one too.”
The Advanced Horizontal & Vertical Augmentation course is presented by ASHA founder Dr Selvaraj Balaji, whilst he also co-presents the Soft Tissue Management Around Teeth & Implants course with Professor Zucchelli. Dr Sisodia comments on the teaching in each course, and their structures:
“They both have very different teaching techniques, and both are very good teachers. The way that they simplified and explained the advanced techniques that they practise was a good way to learn. I also liked the interactive nature of their teaching, and their use of photos and videos of real clinical cases.

Identifying the relationship between dental and sinus pathologies is essential to establish the correct diagnosis, and the subsequent management of the patient experiencing maxillary sinus diseases requires close cooperation between professionals. For over eighty years, OMS has represented a positive common ground for otolaryngologists and dental surgeons. Interdisciplinary collaboration not only provides an additional medicolegal safeguard for practitioners, but offers patients the benefits of uniting two fields of knowledge and expertise. To find out more, contact Ucer Education today. Contact Professor Ucer at ucer@icedental.institute or Mel Hay at mel@mdic.co; call 01612 371842 or visit www.ucer-clinic.dental. n
about the author Professor cemal ucer (BdS, MSc, Phd, oral Surgeon, iti Fellow).

“Both of the courses were structured well. There was a flow to both parts which was logical, and aided in reinforcing the teachings as there was overlap in some of the techniques. Additionally, because there were a couple of months in between part one and two of each course, I was able to use the techniques in clinical practice before the second part began. This aided in reinforcing my learning.”
Dr Sisodia explains how she feels the courses have impacted her dentistry long-term: “Since completing the ASHA courses, I look at each case I plan very differently, and have implemented the soft and hard tissue techniques I learnt in my clinical practice. I started by practising sling sutures, then incorporated CTG, and I have now planned for some horizontal and vertical defects too.
“My confidence in the cases I take on has grown. The way I approach each case is very different now and, instead of referring cases, I am now confident in planning for them which has greatly benefited my dentistry. Because of this boost in confidence, I feel that the way I explain my skills to patients has changed and I am noticing better clinical outcomes. I can also handle complications better and, generally, the rapport I have with my patients has also increased.”
Delegates who complete courses from the ASHA Club benefit from ongoing mentoring, in addition to exclusive access to the ASHA Club WhatsApp group. Dr Sisodia describes her personal experience with this: “The sharing of cases on the ASHA Club WhatsApp group is beneficial, and the way other dentists reflect on their work – both positively and negatively – is a huge help. If I have any questions, it is also nice to have a group who understands and can help.
“I have also attended Dr Balaji’s practice to observe for a day – the benefit of this was huge. It reinforced the teachings from the ASHA courses. The way that Dr Balaji explained what he was doing and even reflected on his own work afterwards made the mentoring invaluable. I am grateful to him and his team for welcoming me and inspiring me to steer out of my comfort zone and use the techniques I learnt.
“I would 100% recommend the ASHA courses to colleagues, and I have already recommended them to some dentists who provide dental implant treatment.” n Find out more atashaclub.co.uk/courses Soft tissue Management around teeth & implants
15th & 16th november 2024
10th & 11th January 2025 to book, please call: 07974 304269 or email: info@ashaclub.co.uk
Whether you are new to dental implantology or starting to develop your skills in more advanced areas of the field, it is crucial to have access to clinical mentorship and support. This affords many advantages, from a higher quality of patient care to accelerated career progression and increased job satisfaction for clinicians.

Dr Chetan Mathias is a highly-renowned cosmetic and implant dentist based in Coventry who understands the impact that mentorship can have on an individual and the dentistry they deliver. Having placed thousands of dental implants and completed hundreds of comprehensive smile makeovers, he is ideally positioned to help colleagues broaden their skills in the field. Dr Mathias shares his thoughts on the peer-to-peer support available today:
“It’s very important to have a mentor – it’s a non-negotiable in implant dentistry. I’ve been doing implants for the last 19 years and I wish we had the mentoring programmes we have available today when I started. There weren’t many people doing implants back then so, to learn new techniques, we had to go abroad to Europe or the US.
“This hurdle no longer exists and clinicians today have plenty of colleagues they can rely on to guide them in the next stages in their professional journeys. By engaging with those who have experience in the field, dentists can fast-track their own careers. They can learn from others’ mistakes and therefore avoid making the same errors themselves. Not only does this improve their outcomes, but – most importantly – it enhances the quality of care they can deliver to patients even early on in their implant journey. That’s why mentoring is so vital for clinicians at any stage in their career.”
Dr Mathias provides mentoring to colleagues through the uniquely designed Chairside Visitation programme. This offers a fantastic opportunity for dentists to observe Dr Mathias as he plans and treats cases within their field of interest.
“For effective progression into a complex area of dentistry, it’s really important for clinicians to see planning technologies, surgical techniques and restorative workflows applied to specific cases in a practical way,” Dr Mathias continues. “The Chairside Visitation programme, therefore, gives clinicians an opportunity to observe a case first-hand, from start to finish. The clinical strategy and


techniques employed can then be more easily replicated in their own clinics.”
As Dr Mathias suggests, Chairside Visitation enables dentists to watch the entire treatment process, with the chance to ask questions for an enriched learning experience. In some instances, a second case will be discussed and observed in the afternoon. The day concludes with a presentation about the diagnosis, treatment planning and surgical protocols implemented to afford a comprehensive understanding of the workflow from start to finish. Dr Mathias adds: “The entire learning experience is tailored to the individual. The initial video call with the dentist is crucial to discuss their current expertise, competence and experience. This allows us to determine the type and complexity of case that would be most beneficial for them. I am mindful that they have sufficient surgical experience before observing a full arch or complex rehabilitation case, for example, in order to get the very most from their day with us. We have had great feedback from clinicians so far who found this format of observation and learning to be truly eye opening.
“The main difference between a Chairside Visitation and attending a training course, is that you get a more realistic understanding of the process. Many courses present some really amazing cases, but they are not always at the right level for the individual. To observe a case that has been picked specifically for your expertise, and to see it happen in real-time is a completely different experience. You develop a better
appreciation for the work that is required to achieve the very best result.”
Chairside Visitation is available to clinicians in collaboration with BioHorizons Camlog. Dr Mathias comments on why he chose to work with the leading supplier of dental implant products and education:
“I have been working with BioHorizons Camlog for the last 15 years. I’ve been part of their journey as they’ve grown into the company they are today, and they have been a pivotal part of mine. For me, the organisation is more than an implant company – they are an extension of what I do, of my team. I firmly believe that to be able to offer the service and treatment that I do, I need a company that can back me at every stage of my journey.”
Are you interested in advancing your knowledge and understanding of advanced surgical procedures with a leading clinician in the field? Getting involved with Chairside Visitation is easy. Simply complete the enquiry form on the website and BioHorizons Camlog will be in touch to discuss availability and location for your visitation with your local mentor. Please allow six weeks where possible for co-ordination of the day. For more details, please visit education.theimplanthub.com/chairsidevisitation.n








































































When patients require restorative care, they likely envisage a major transformation, with radical improvements to their smile. In reality, whilst great dentistry can have this effect, clinicians may seek to have a minimal influence on the dentition. This is especially relevant when managing a patient’s occlusion with a conformative dental approach.
This methodology looks to work with the existing dentition, and can be applied in the vast majority of restorative cases. Clinicians need to consider how to plan for and design restorative solutions that work with a patient’s present occlusion. Making a thorough assessment of the existing occlusion is key when utilising a conformative approach, or deciding whether it is even suitable in a given clinical situation. Understanding how it could be valuable, and when it may not be, is fundamental, and should be a skill that every clinician develops.
the limits of conformity
When a patient requires restorative care, dental professionals can implement a conformative or reorganised approach. In the former, the clinician will consider a patient’s existing intercuspal position, and provide new restorations that dovetail with the existing jaw relationships. Some changes may be made to the restoration, for example, through the shortening of an opposing cusp or the removal of a deflective contact on a tooth that is being restored. A reorganised approach may be necessary if the proposed restoration requires an adjustment of the occlusion. Whilst clinicians can work with the existing dentition, it’s not necessary that a restoration replicates the existing contacts. After all, treatment may be needed to improve upon this aspect of the dentition – a like-for-like restoration would defeat the object of pursuing care.
An example would be changing the design of a restored tooth to minimise the influence of a problematic cusp. Where a patient may be experiencing non-working side interference during lateral mandibular movement, a high cusp might be subject to a damaging load. The restorative solution could feature a slight reduction of height of the cusp in question, eliminating the nonworking side interference and reducing the risk of future fracture. Since the rest of the occlusion remains as the patient presented, this would be a conservative intervention. There are multiple benefits to taking a conformative approach to restorative care. It is a simpler approach to care, often not requiring orthodontic treatment, and is largely predictable. It’s also a safe and reliable strategy, and requires little or no adaption of the neuro-muscular system. Without needing to adjust the occlusion, treatment time is minimised, meaning an effective result may be achieved relatively quickly.
time to reorganise
Whilst treating patients in this manner may be favourable, clinicians must be able to recognise when it is not possible to provide care with conformative dentistry. Taking a reorganised approach may be the only way to
reach an effective result that promotes longlasting benefits, especially when the maximum interocclusal position is unsatisfactory.
Implementing orthodontic treatment to reorganise the dentition may also be necessary when an increase in vertical dimension is required, when a large fixed prosthesis is needed to replace a significant portion of the dentition, and when full mouth rehabilitation is necessary.
Clinicians should not progress with their care under the assumption that a conformative approach can and should be applied in every case, waiting to find whether the occlusion remains effective until post-restoration. It is only through pre-treatment assessments and developed knowledge that the most effective treatment can be decided upon with confidence.
it’s what you know
Every treatment decision taken by a clinician should be justifiable, and therefore dental professionals must have the skills and confidence to recognise when a conformative approach is ideal or ineffective, and when reorganisation is worthwhile for an extended treatment time, and perhaps increased treatment complexity. This requires up-to-date education, and an exploration of the current restorative solutions available to clinicians; these may produce new ways of managing cases that were previously unthinkable.
The Basics of Occlusion course from IAS Academy is a brilliant option for clinicians looking to develop their knowledge of occlusion. Dr Jaz Gulati and Dr Mahmoud Ibrahim present their unique ‘Tangible’ philosophy which ensures every concept taught, including advanced techniques in conformative dentistry and wear pattern recognition, can be implemented immediately for enhanced patient outcomes. Over two days, your understanding of occlusion will be transformed, enabling you to perform more confident and predictable treatment planning.
Conformative dentistry has its perks, but cannot be applicable in every clinical situation. Understanding when to reorganise the dentition is essential for successful outcomes, but knowing how to implement conformative care whilst also making subtle yet powerful changes to intercuspal points can make for a wider range of treatment approaches.
For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
about the author dr tif Qureshi,
Founder and a clinical director of
iaS academy.
It’s essential to consider peri-implant tissue health when devising treatment plans for successful rehabilitation. After a patient has undergone implant placement, it is then important to monitor the recovery of the soft tissue, and the quality of their oral health and hygiene in the years to come.
Peri-implantitis, the infection of the implant site that results in inflammation of the soft tissue and bone loss, is one of the most well-known risk factors for late implant failure due to biological complications.
Any dental professional treating patients with an implant must be able to recognise the presence of peri-implantitis, and action an effective treatment plan to prevent its progression that will be detrimental to the implant and/or the surrounding dentition. Better yet, clinicians should be able to recognise how peri-implant tissue care can be optimised to prevent the development of the infection in the first place.
Peri-implant disease management
Peri-implantitis affects 15-57% of patients and 8-28% of implants. The key to preventing peri-implantitis is the same as preventing other periodontal diseases like gingivitis or periodontitis – patients must exercise good oral hygiene at home. The literature cites patient-administered mechanical plaque control as the current standard of care, with oral rinses or a dentifrice having a positive, albeit limited, adjunctive effect. Clinicians can not only reinforce this habit before and after implant treatment, but can provide support by employing professional mechanical plaque debridement with different hand or powered instruments, with or without polishing tools.
A previous history of periodontal disease has been strongly associated with peri-implantitis, and active infection at the site of adjacent teeth is further considered a predictor of future peri-implantitis. In fact, patients with a history of generalised aggressive periodontitis are 5 times more prone to implant failure, and up to 14 times more susceptible to peri-implantitis. This could inform a patient’s suitability for treatment, and reinforces the need for individuals to keep an effective oral hygiene routine.
It’s of no surprise that smoking has a negative effect on peri-implant tissue, much in the same way that it affects conventional periodontal health. Smokers have almost double the risk of developing peri-implantitis compared to non-smokers, and the habit is associated with increased severity of periimplantitis lesions. Clinicians could try to help patients cease their smoking habits long before the implant is placed, which would ensure the peri-implant tissue has the greatest opportunity to be healthy. Where this is not possible, any attempts to cut back on a smoking habit should be supported and commended by dental professionals.
keratinised tissue – which, when not present, can increase the susceptibility of peri-implant tissue destruction – and gingival thickness around dental implants. However, autogenous grafts require a second surgical donor site, which is associated with increased post-operative bleeding, tissue necrosis and discomfort, and there may be a limited availability of autogenous grafts due to anatomical limitations.
Alternative solutions, such as acellular dermal matrices or xenogeneic collagen matrices, have been proven to increase keratinised mucosa width and mucosal thickness, with significant improvements when compared to non-augmented sites. Xenogeneic collagen matrices, in particular, have been recognised as advantageous due to their unlimited supply, less invasive treatments, no donor site morbidity, and reduced surgical time.
Soft tissue augmentation is a brilliant workflow to learn for clinicians who routinely provide dental implants, or have extensive experience in doing so.
developing soft-tissue skills
Clinicians that are providing dental implants or are treating patients with such restorations must be aware of how they can enhance peri-implant soft tissue health and care. By developing their knowledge in these areas, and acquiring new skills such as soft tissue augmentation, the rising demand for dental implants can be met with effective solutions.
Dental professionals could undertake Management of Soft Tissue with No Issue, a one-day course from One to One Implant Education, supported by Megagen, to further their knowledge. Delegates will develop their understanding of the anatomy of peri-implant soft tissue, as well as their ability to identify and diagnose common peri-implant diseases. They will also gain practical skills in performing procedures for soft tissue augmentation, with the ability to apply their learning in clinical practice. Led by the renowned Dr Fazeela Khan-Osborne and Dr Nikolas Vourakis, it’s the perfect opportunity to enhance their patient care. The complete success of dental implant treatment, with patients benefiting from optimal aesthetics, function and longevity, relies strongly upon soft tissue health. Clinicians should always look to develop their knowledge to ensure patients have the best possible chance of preventing peri-implantitis, or undergo soft tissue augmentation when it is most appropriate. To reserve your place or to find out more, please visit 121implanteducation.co.uk or call 020 7486 0000. n
about the authors dr Fazeela Khanosborne, Principal implant and Restorative Surgeon.

Clinicians should also explore the merits and impacts of soft tissue augmentation. Where soft tissue volume is inadequate, autogenous soft tissue grafts or effective substitutes can be utilised.
Historically, autogenous grafts have been preferred, with positive results in increasing

dr nikolas Vourakis, Senior implant and Restorative Surgeon in private clinics in London and edinburgh.



the result counts!
Wear comfort, aesthetics and functionality are crucial factors when it comes to creating 3D-printed bite splints. Our extremely stable and flexible material LuxaPrint Ortho Comfort offers precisely these qualities. It is also important for the bitesplint to be completed in a short amount of time with minimal adjustment work, which is made possible by the efficient and precise DentaMile connect software. In this way, the DentaMile 3D Bite Splint Workflow guarantees maximum satisfaction.
Find out more about DentaMile at www.dentamile.com

Why isn’t Piezotome technology being widely used by Dental Surgeons, when it’s seen as a game changer by their Rhinoplasty counterparts?
Aims
This article aims to highlight the benefits of using piezotome technology for more predictable and safer surgical outcomes that improve the user and patient experience
Objectives:
• Identify the benefits of piezotome technology over rotary instruments
• Identify the patient benefits of using piezotome technology
• Identify the applications piezotome technology can be used for
• To understand why this technology is safer for use on hard and soft tissues
Learning Outcome: C, D
The Piezotome Cube by Acteon stands out as an essential everyday piece of equipment for the dental professionals who have invested in it for extractions and implant surgery. Its blend of precision, safety, and versatility not only elevates the surgical experience for clinicians but also significantly enhances patient outcomes. In the last few years, this has become a firm favourite and a game changer when applied to rhinoplasty and cranial operations, where more and more surgeons are using our M+ device. The M+ uses the same technology as the Piezotome Cube, to further improve predictability and safety in procedures that require such precision. So, this begs us to ask the all-important question – doesn’t every dental professional want stability, predictability and better outcomes for their patients? If the answer is yes, why aren’t more people investing in this affordable and easy to use technology?
One of the standout features of the Piezotome Cube is its ability to deliver incredibly precise and controlled bone cutting. Unlike traditional rotary instruments, which can cause significant damage to soft tissues, the Cube operates through ultrasonic vibrations that selectively target hard tissues while preserving surrounding soft tissues, such as nerves, membranes, and blood vessels. This level of precision reduces the risk of intraoperative complications and supports more predictable surgical outcomes. Safety is another critical aspect where the Piezotome Cube excels. The device's automatic power regulation adjusts the ultrasonic power based on the resistance encountered during surgery. This dynamic adjustment ensures that the device remains powerful enough to cut through dense bone while minimizing the risk of damaging soft tissues. The controlled intraosseous temperature during operations further reduces the
likelihood of thermal damage, making the Piezotome Cube a safer choice for both surgeons and patients.
Enhancing Patient Comfort and Reducing Recovery Time
For patients, the Piezotome Cube offers a significantly more comfortable surgical experience compared to traditional methods. The minimally invasive nature of the technology means that procedures can be performed with less trauma to the surrounding tissues, leading to reduced postoperative pain and swelling. Clinical studies have shown that patients who undergo surgery with the Piezotome

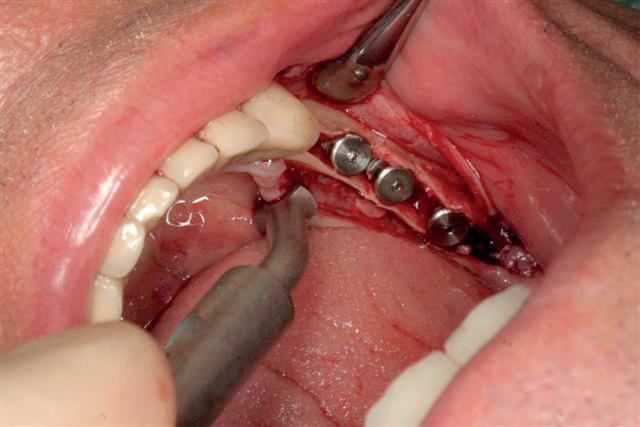


Cube experience up to 50% less postoperative discomfort and a reduction in the need for analgesics by 98%.
Additionally, the Piezotome Cube's ability to preserve the bone structure during procedures such as extractions or sinus lifts means that patients can benefit from faster recovery times. With

less bone loss and trauma, healing is quicker and more predictable, allowing patients to return to their normal activities sooner. As Dr. Marcel Wainwright from Sweden notes, “86% of the patients observed had no postsurgical swelling and 87% reported no postsurgical pain,” highlighting the device's capacity to significantly improve patient outcomes.
The Piezotome Cube’s versatility is another reason why it is indispensable
1. Clinical studies have shown that patients who undergo surgery with the Piezotome Cube experience:
a) Up to 20% less post-operative discomfort and a reduction in the need for analgesics by 98%.
b) Up to 30% less post-operative discomfort and a reduction in the need for analgesics by 98%.
c) Up to 40% less post-operative discomfort and a reduction in the need for analgesics by 98%.
d) Up to 50% less post-operative discomfort and a reduction in the need for analgesics by 98%.
2. What is a major advantage of piezo technology over conventional drilling techniques?
a) Faster procedures
b) Removal of the need for analgesics
c) Precision and safety, minimizing damage to the soft tissues
d) Elimination of postoperative infections
3. Which of the following is NOT a cited application of the Pieztome Cube?
a) Dental extractions
b) Sinus lifts and bone grafting
c) Supragingival debridement
d) Implant surgery
4. How does Piezotome technology facilitate the integrity of the extraction site?
a) It respects the four walls of the socket
b) It allows for immediate implant placement
c) It helps achieve optimal aesthetic results
d) All the above
in dental practices. The device is equipped with a wide range of surgical tips designed for various applications, including extractions, sinus lifts, osteotomies, and bone grafting. This versatility allows clinicians to expand their surgical capabilities without the need for multiple specialised instruments. Please note it is essential to use original Acteon tips, as tips from other suppliers will jeopardise the machine’s capabilities and could eventually lead to equipment failure.
For instance, the Cube's ability to perform flapless extractions with minimal bone loss has revolutionised the approach to dental extractions. By maintaining the integrity of the alveolar bone, the Piezotome Cube facilitates immediate implant placement, a significant advantage in contemporary implantology. Dr. Jeffrey Brooks, D.M.D., from the USA, underscores this by stating, “Maintaining the integrity of the extraction site and the four bony walls around allows for immediate implant placement,” which is critical for achieving optimal aesthetic and functional results in implant dentistry.
Don’t just take our word for it!
The Piezotome Cube has received
widespread acclaim from dental professionals worldwide. Dr. Sami Stagnell from the UK describes the Cube as an “absolute game changer,” praising its ability to improve patient experience, save time, and broaden the scope of treatment options available. This sentiment is echoed by numerous other practitioners who have found that the Piezotome Cube has made their surgeries more predictable, less traumatic, and ultimately more successful.
Dr. Majed Abu Arqub, a periodontist specialist from Jordan, emphasizes how the Piezotome Cube aids in achieving current implantology trends, which focus on reducing post-operative pain and improving pre-implant tissue quality. These testimonials underscore the Piezotome Cube’s role in not only enhancing surgical precision but also in delivering compassionate care that meets the evolving demands of dental surgery.
Acteon believes its Piezotome Cube is indispensable for any dental practice committed to providing the highest standard of care. The feedback received from clinicians using the system further clarifies this, with many stating simpler workflow, superior outcomes and enhanced patient satisfaction. n
J&S Davis is delighted to bring you this article, with the aim of supporting the ongoing Enhanced CPD needs of dental healthcare professionals in improving and maintaining the oral health of their patients.
Aims:
To provide a greater understanding of the science behind enamel remineralisation so that clinicians are able to make more informed decisions around the products they use to treat non-cavitated caries lesions, abrasions and erosion of the enamel as well as conditions such as hypersensitivity, MIH and fluorosis.
Objectives
• Examine the biological make-up of a tooth and the role that remineralisation can play in restoring aesthetics, strength and function to enamel
• Identify the main properties that remineralisation products need to offer for optimum treatment efficacy
• Discover new concepts and techniques in the treatment of enamel demineralisation
By achieving these objectives, clinicians will be better able to critically assess the range of remineralisation products currently available to them. They will also therefore be in a better position to be able to select the right product(s) to meet their clinical needs, and explain the scientific rationale and benefits of these products to their patients.
Learning Outcome: C
A review on the remineralisation of tooth enamel published in the Journal of Dental Research stated that the goal of modern dentistry is to manage noncavitated carious lesions non-invasively through remineralisation in an attempt to prevent disease progression and improve aesthetics, strength and function. It was in the 1970’s when Jens Andreasen began to study the biological processes that govern the reparative phases that follow a trauma. He explained how even fractured teeth have a good chance of repair that will last for a long time. Both primary and permanent teeth consist mainly of two highly mineralised tissues: the enamel and the dentine. The basic constituent of dentine, enamel and cementum is an inorganic salt arranged in hexagonal crystals that is called hydroxyapatite. From the first stage of eruption, the enamel and dental tissue are attacked daily by agents such as bacterial plaque, food, acidic substances, chewing and inappropriate oral hygiene practices. The single or combined action of these aggressive factors, if sufficiently prolonged, may lead to a loss of mineral substances from the surface of the tooth, with consequent weakening of dental structure and reduced masticatory capacity. Natural hydroxyapatite without added minerals does not have any particular capacity to remineralise.
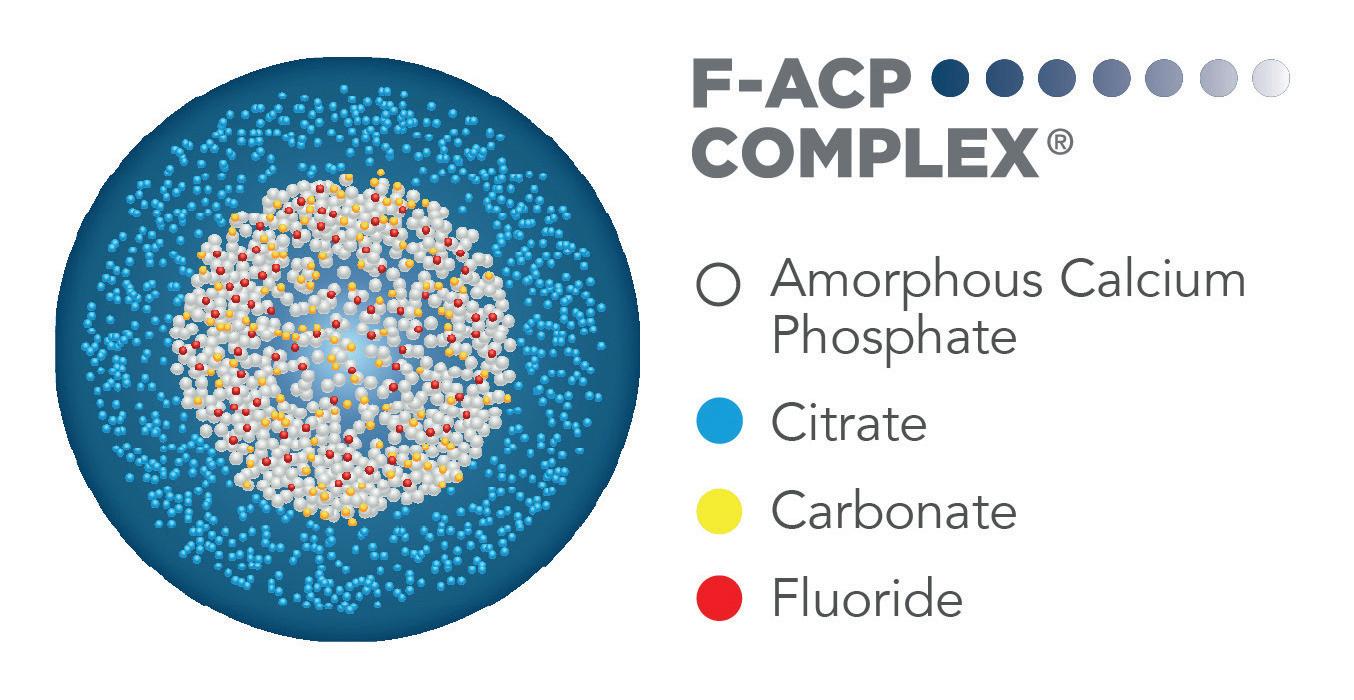
Remineralisation in the oral environment is a natural process, which is, however, limited owing to many circumstances. Nowadays, there are many products on the market that use the term 'remineralisation'. Remineralisation means that the constituent minerals of the teeth, mainly calcium and phosphate ions, can be sourced to promote ion deposition into the crystal voids of the demineralised enamel. However, the substances that can claim to have this biomimetic property must be able to interact significantly with the tooth surfaces, even if conveyed in a simple toothpaste or mouthwash.
Curasept Biosmalto ® toothpastes and mouthwashes, for children and adults, contain a mixture of two different hydroxyapatites that allow the biomimetic properties necessary for effective remineralisation to develop: a hydroxyapatite substituted with magnesium, strontium and carbonate conjugated with chitosan called Bio-active Complex, and a fluoro-hydroxyapatite. Natural hydroxyapatite is a very stable mineral and, even if it comes into contact with damaged tooth areas, it is not able to release active ions. Products that contain only this type of hydroxyapatite are not very effective at remineralising, although they can still claim desensitising properties. The substitution with magnesium, strontium and carbonate, however, makes Curasept Biosmalto ® hydroxyapatite very reactive, able to quickly release bioactive elements that lead to true remineralisation, exploiting the normal biological processes. In addition, the presence of fluoride helps to create a mineralised surface
Brought to you by

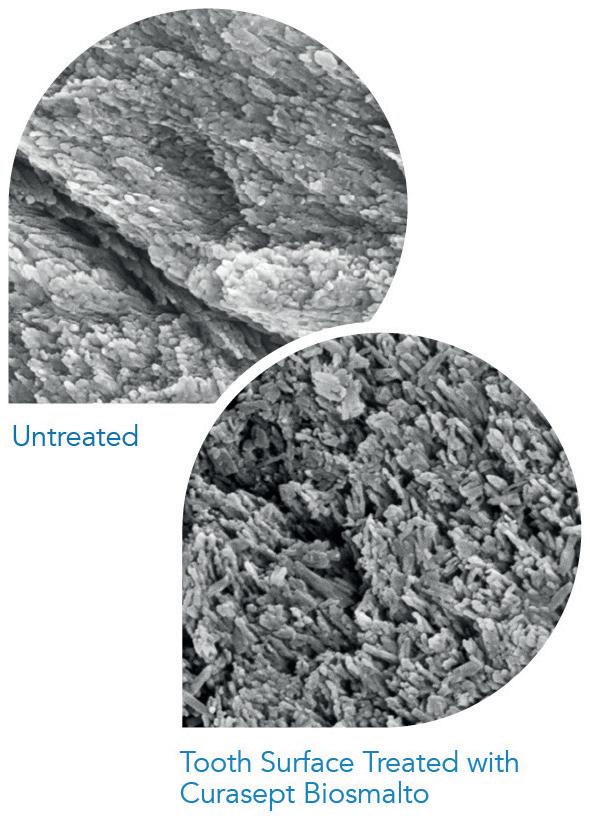
that is more resistant to acid attacks and to better protect the tooth from erosion, abrasion and brushing damage. The formulation has been further enriched with strontium salts to reduce pain rapidly in cases of dentinal sensitivity.
In subjects particularly predisposed to strong demineralisation, for example, those suffering from
Sjögren’s syndrome, diabetes or dry mouth, or undergoing chemotherapy or radiotherapy, wearers of orthodontic appliances and patients with white spots or with frequent caries, the additional use of Curasept Biosmalto ® Impact Action Mousse is recommended. It is based on amorphous calcium phosphate enriched with carbonate
1. Which set of teeth consists of the enamel and the dentine?
a. Primary
b. Permanent
c. Both
d. Neither
2. A review in the Journal of Dental Research stated that the goal of modern dentistry is to manage non-cavitated carious lesions non-invasively through remineralisation. Why?
a. To prevent disease progression
b. To improve aesthetics
c. To improve strength and function
d. To prevent disease progression and improve aesthetics, strength and function
3. Natural hydroxyapatite is a very stable mineral but what is its main disadvantage?
a. They are not able to release active ions
b. They release too few active ions
c. They release too many active ions, overloading the tissue with minerals
d. There are no disadvantages
4. Curasept Biosmalto® Impact Action Mousse is based on?
a. Natural hydroxyapatite
b. Amorphous calcium phosphate enriched with carbonate and fluoride
c. Ion deposition
d. A concentration of enamel and cementum
and fluoride and externally citratefunctionalised. In contact with saliva, the complex dissolves immediately, rapidly releasing the active substances. In this way, a large amount of calcium, phosphate and fluoride is released directly on to the dental surface and in proximity to the demineralised lesions, while citrate facilitates the penetration of
the ions into the tooth. The result is a rapid and intense remineralising action. Curasept Biosmalto ® Mousse is also recommended for children. To guarantee a correct remineralisation process, Curasept Biosmalto ® Mousse should be combined with products from the Curasept Biosmalto ® toothpaste line, selected according to the patient’s age. n

Tepe is delighted to bring you this article, with the aim of supporting the ongoing Enhanced CPD needs of dental healthcare professionals in improving and maintaining the oral health of their patients
Aims
This article highlights the importance of discussing dry mouth with patients, providing practical support to alleviate their symptoms
Learning objectives:
• To understand the wide-ranging affects that dry mouth can have on patients and their quality of life
• To explore patient understanding of the condition and how patients can be encouraged to talk about their symptoms
• To consider the suitability of different oral hygiene products for patients suffering from dry mouth
Learning Outcome: A, C
Dry mouth, or xerostomia, can have a detrimental impact on sufferers’ quality of life. Not only does the condition increase the risk of oral health problems, but several other psychological and social issues prevail too. With effective patient communication, education and rapport, the dental team can offer invaluable, practical support that helps to enhance their patients’ quality of life significantly.
Research has shown a significant correlation between dry mouth and oral health-related quality of life (OHRQoL), particularly in older people and those with a life-limiting condition.ii This makes it an important consideration within palliative care, as a way of making patients as comfortable as possible. One studyiii found that more than 80% of individuals asked reported moderate or severe dry mouth with almost 75% scoring their discomfort six or more out of 10. The same patients found the condition to interfere most with talking (56%), eating (61%) or taste (60%).
There is also evidenceiv that xerostomia impacts quality of life of those not otherwise inflicted with systemic health concerns, affecting everything from physical to emotional and social functioning. Given that someone with xerostomia may struggle to eat or speak properly, they are more likely to shy away from social interactions. This social isolation is linked with a decline in both mental and physical healthv which, in turn, further reduces quality of life. Due to this and other factors, dry mouth can affect anyone, at any stage of life. Among younger adults, researchvi has found an equally robust association between xerostomia and OHRQoL among participants aged 32. One in 10 had the condition, with 69% reporting that they experienced dry mouth occasionally. The greatest

impact this had on their lives were feelings of self-consciousness (25%) and embarrassment (20%), as well as discomfort when eating (17%).
Interestingly, this study also assessed personality traits for correlations with dry mouth and OHRQoL. Those found to have a negative emotionality – and were more likely to be stressed, restrained, cautious and prone to negative emotions like anxiety and anger – were also more strongly associated with xerostomia prevalence.
Despite so many people experiencing dry mouth at different stages of life, its actual incidence nationwide is relatively unknown. This is partly
because the parameters are unstandardised and symptoms subjective. However, it has also been found that a massive 62% of sufferers do not talk about their condition. vii
It is difficult to determine why this is, but there are various factors that are likely to be playing a role. For example, it has been postulated that patients avoid discussing symptoms or experiences that they don’t understand, as well as any that they feel their clinician won’t be interested in or might cause them embarrassment, or if they’re concerned about what their admission might lead to. viii
Of course, knowledge and education of oral health issues among the public could be contributing to the issues,
given that health literacy corresponds with health outcomes and service uptake. Public Health England ix found that more than 40% of workingage adults in England either don’t understand or don’t implement basic healthcare information. This highlights the gap in public knowledge around all health topics, no doubt including that about essential dental care. Dental fear is another aspect that is likely exacerbating the problem. An estimated 53% of the UK population are fearful or anxious about visiting the dentist, with 17% developing a level of dental phobia that they stay away completely. x If a patient is already uncomfortable during a dental review, they are probably looking
to leave as quickly as possible and therefore unlikely to bring up the topic of dry mouth.
The biggest challenge for dental professionals, therefore, is encouraging patients to talk about their symptoms. This may be achieved by enhancing the patient experience and engagement. The former relates to everything from quality of care to communication with the dental team and access to services, and can increase patient satisfaction and adherence to treatment plans, as well as health outcomes. The latter is about encouraging patients to take an active role in their oral health care, to participate in the decision-making and make informed choices. This has also been linked with better compliance and outcomes. Combining the two elements together means fostering a patient’s trust and enhancing the relationship between them and the dental team.xi Ultimately, this makes patients more comfortable in the dental setting and more likely to speak up if they are experiencing any issues – including dry mouth.
Furthermore, it is necessary for clinicians to review how they communicate with their patients. A US surveyxii from 2014 asked patients directly what would make them speak up more about their health needs. Responses included being asked more questions and feeling listened to by their practitioner, as well as eye contact when speaking. All of these are simple and easy-to-implement elements that can be incorporated into every patient interaction.
These answers also emphasise the importance of verbal and nonverbal communication, both of which must be optimised to create the best possible patient rapport. Effective communication from the dental team is more than a GDC requirement; viii it is considered integral to patientcentred care, enables more accurate diagnostics and increases efficiency of care delivered.xiv Speaking clearly, using simple language, discussing topics at the right pace for the patient and offering written or animated adjunctive aids are all advantageous.
Practical support
How you communicate is just as important as what you communicate. Patients need to understand their current oral health condition and realise that the dry mouth they are experiencing is nothing to be ashamed of. If they believe their dental practitioner is sympathetic and can help them alleviate symptoms, they are far more likely to admit to their suffering, however mild or severe.
Alongside general oral health education, the dental team can provide advice on practical steps that patients can take for xerostomia relief. Advice can be delivered on everything from
Brought to you by

hydration to diet, with emphasis placed on enhancing oral hygiene where this is found lacking. No matter what their situation, all patients experiencing xerostomia will benefit from the moisturising and soothing effects of the new Hydrate™ Mouthwashes from TePe. Alcohol-free, the solutions are available in a mild apple/peppermint flavour and non-flavoured to suit all preferences, and contain 0.2% fluoride to offer extra protection against caries. They are also complemented by the new Hydrate™ Mouth Gel, which provides immediate and long-lasting comfort in a convenient solution that can be used on-the-go.
Sometimes, even the smallest relief from dental pain and discomfort can have an extraordinary impact on patients’ quality of life. Dry mouth is no small issue and with effective communication, education and advice, dental professionals can help put a smile back on their patients’ faces. For more information on the innovative new products available from TePe, please visit www.tepedirect.com
References
i. Gerdin EW, Einarson S, Jonsson M, Aronsson K, Johansson I. Impact of dry mouth conditions on oral health-related quality of life in older people. Gerodontology. 2005 Dec;22(4):219-26. doi: 10.1111/j.1741-2358.2005.00087.x. PMID: 16329230.
ii. van der Meulen, A.I., Neis, E.P.J.G., de Nijs, E.J.M. et al. Dry mouth in patients with a life-limiting condition or frailty: a study protocol for two intervention studies and a nested qualitative sub-study (the Dry mOuth Project, DROP). BMC Palliat Care 22, 120 (2023). https://doi.org/10.1186/ s12904-023-01242-0
iii. Fleming, M., Craigs, C.L. & Bennett, M.I. Palliative care assessment of dry mouth: what matters most to patients with advanced disease?. Support Care Cancer 28, 1121–1129 (2020). https:// doi.org/10.1007/s00520-019-04908-9
iv. Gibson B, Periyakaruppiah K, Thornhill MH, Baker SR, Robinson PG. Measuring the symptomatic, physical, emotional and social impacts of dry mouth: A qualitative study. Gerodontology. 2020 Jun;37(2):132142. doi: 10.1111/ger.12433. Epub 2019 Jul 26. PMID: 31347735.
v. González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, Muñoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020 Jul;87:172-176. doi: 10.1016/j.bbi.2020.05.040. Epub 2020 May 13. PMID: 32405150; PMCID: PMC7219372.
vi. Thomson, W.M., Lawrence, H.P., Broadbent, J.M. et al. The impact of xerostomia on oral-health-related quality of life among younger adults. Health Qual Life Outcomes 4, 86 (2006). https://doi.org/10.1186/14777525-4-86
vii. Key findings within the group saying dry mouth is affecting their daily life (13%).
TePe – Mouth Dryness in UK, web panel questionnaire study with 1000 respondents, Transvector, April 2023
1. What percentage of patients receiving palliative care were found to have xerostomia according to the study cited in the article?
a) 10%
b) 60% c) 70% d) 80%
2. How many people aged 32 suffered dry mouth symptoms in the research cited in the article?
a) One in five b) One in 10
c) One in 12 d) One in 15
3. How many dry mouth sufferers are estimated to not talk about their condition?
a) 62% b) 52% c) 42% d) 32%
4. What percentage of working-age people does Public Health England suggest don’t understand or implement basic health advice?
a) 20%
b) 30% c) 40% d) 50%
5. What can practitioners do to encourage patients to speak up about their health needs?
a) Ask them more questions
b) Listen to them
c) Make eye contact d) All of the above
6. What practical support can the dental team provide patients with xerostomia to help relieve symptoms?
a) Oral health advice
b) Hydration and diet advice
c) Recommending effective products like the Hydrate™ Mouth Wash
d) All of the above
viii. Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005 Sep;1(3):189-99. PMID: 18360559; PMCID: PMC1661624.
ix. Public Health England. Local action on health inequalities. Improving health literacy to recue health inequalities. September 2015.
x. Dentalphobia.co.uk https://www. dentalphobia.co.uk/ [Accessed February 2024]
xi. Chakaipa S, Prior SJ, Pearson S, van Dam PJ. Improving Patient Experience through Meaningful Engagement: The Oral Health Patient’s Journey. Oral. 2023; 3(4):499-510. https://doi. org/10.3390/oral3040041
xii. Gold Foundation. How healthcare professionals can encourage patients to speak up. November 2014. https:// www.gold-foundation.org/newsroom/ blog/healthcare-professionals-canencourage-patients-speak/ [Accessed February 2024]
xiii. General Dental Council. Principle Two. Communicate effectively with patients. Focus on Standards. The 9 Principles. https://standards.gdc-uk. org/pages/principle2/principle2.aspx [Accessed February 2024]
xiv. Waylen, A. The Importance of Communication in Dentistry. Dental Update 2017; 44(8), 774-780. [P774]. n
About the author

Miranda has worked in dentistry for over 20 years, as a Dental Therapist in NHS practices treating the general population. Miranda volunteered at the 2012 London Olympics treating athletes. In 2016 Miranda travelled to Tanzania to treat local villages and train local clinical officers in emergency dental care. Miranda has taught at the University of Central Lancashire teaching undergraduate Dental Therapy and Postgraduate Dentistry. Working for Colosseum Dental Group Miranda help facilitate the use to Dental Therapists in their clinics and was part of the Medical Board for Colosseum Dental Group UK. Now currently working at TePe as the Clinical Education Manager, driving education and healthy smiles for life.
the Planmeca European roadshow is coming to a town near you

We are excited to announce that our expansive mobile showroom will be in the UK this Autumn! Bringing cutting-edge technology directly to your doorstep this October, the moving showroom is the perfect way to learn the unique benefits of the whole Planmeca product portfolio - digital dental units, 2D and 3D imaging devices, CAD/CAM solutions and Romexis software.
Free to attend, come and interact with members of the local Planmeca team and engage in hands-on demonstrations. If you’re interested in new equipment, come and explore our complete range of dental solutions, designed to enhance patient outcomes and streamline practice operations.
For more information on the roadshow, a full schedule and all tour stops is available on www.planmeca.com/roadshow
dublin – Monday 7th october
Leixlip – tuesday 8th october
Manchester – thursday 10th october
Birmingham – saturday 12th october
stockbridge – tuesday 15th october
twickenham – thursday 17th october n
DEXIS announced upgrades across its digital ecosystem to aid clinicians in everything from visualising progressive dental issues to designing chairside surgical guides, launching new a CBCT unit, automated surgical guide design and an IOS module to help clinicians visualize progressive dental issues. The ORTHOPANTOMOGRAPH™ OP 3D™ EX captures consistently accurate images through a straightforward, easy-tolearn workflow. The unit has a wide range of field of view sizes to support multiple clinical indications including implant placement, endodontics, periodontics, and analysis for airway and

Surrounding your professional life with other like-minded dentists means you can share ideas and support one another to better achieve your clinical goals. For members of the Association of Dental Implantologists (ADI), networking has never been so easy.
The ADI’s mission is to advance professional education in dental implantology, as well as supporting patients. The forthcoming ADI Team Congress in May 2025 is the leading event for implant dentistry in the UK, with handson sessions and world-renowned speakers sharing knowledge and experience. This offers a unique opportunity for members, new and old, to learn and socialise, building a network of contacts.
The ADI offers more exciting events
What does the future of dentistry look like to you? Do you foresee better insights into patient needs, broader treatment options, and greater engagement? Get there now with the CS 8200 3D Family of imaging technology from Carestream Dental.
The CS 8200 3D Neo Edition, a longstanding hallmark of high quality CBCT insights, is now joined by the CS 8200 3D Access. This brand-new solution is ideal for practices looking to make their first foray into owning CBCT imaging without cutting corners – it provides intuitive user interfaces for simple operation, supporting exceptionally safe, high quality and reliable imaging processes.
The CS 8200 3D Access is a 4-in-1 solution that, with the help of CS MAR
TMJ. Early adopters of the OP 3D EX have reported positive feedback:
DTX Studio™ Clinic stores and manages all patient data as well as helps clinicians execute each step of the implant process from diagnostics to delivery.
The software’s new functionality allows practitioners to plan an implant treatment and generate a surgical guide chairside – all in less than 3 minutes. Clinicians can virtually extract teeth, adjust photorealistic abutments and crowns, and create an automated surgical guide that can be sent to a lab or produced in-house for same-day delivery.
To learn more about DEXIS and the latest implant workflow upgrades, visit: https://www.dexis.com. n
throughout the year, including ADI Masterclasses and ADI Focus Meetings, and their biennial Members’ National Forum, all with discounted rates for members. The ADI Members-only Facebook Group is also accessible, promoting an easy, instant way to engage with other implant dentists and share queries and advice so all can benefit. To expand your dental network, consider the benefits of an ADI membership. For more information visit www.adi.org.uk n
Ensure your practice is equipped with the highest standard of service for your @nsk.uk dental Handpieces with Mc dental Ltd & Mc repairs Ltd.
As a Certified NSK Repair Centre, we offer expert maintenance and repair services designed to keep your tools in peak condition.
◊ Why choose Mc repairs?
• Optimized Performance: Keep your handpieces running at the most optimum performance.
• Extended Lifespan: Maximize the durability of your equipment.
• Enhanced Safety: Ensure safe and reliable operation on your patients.
• Cost Efficiency: Save on costly replacements with regular maintenance.
Regular maintenance of the suction system can not only ensure patient safety but also peak performance and increased life span of the equipment.
Unlike many competitor solutions that require separate daily and weekly cleaning solutions to target different types of contamination. Bossklein DAILYasp is a single stage, all in one solution combining the best of both into one.
Designed specifically to remove contamination and micro-organisms that can cause biofilm build up inside aspirator systems and to help prevent the transmission of disease. The low-foaming and nonabrasive formulation ensure maximum microbial effect with no risk to sensitive equipment.

Invest in preventative maintenance with MC Repairs and experience the difference in performance and reliability with our trusted services.
Request your FREEPost Packs below! https://mcrepairs.co.uk/request-freepost-packs/n

DAILYasp has the performance of a market leader with a much lower price tag. For more information call 0800 132 373 or visit www.bossklein.com n
technology, can reduce the impact of metal artifacts, helping you confirm diagnoses with a minimised risk of misinterpretation.
To learn more about your beginnings in CBCT imaging with Carestream Dental, contact the team today.

For more information on Carestream Dental visit www.carestreamdental.co.uk
For the latest news and updates, follow us on Facebook and Instagram @ carestreamdental.uk n
BDIA Dental Showcase provides an exclusive opportunity to engage with leading dental manufacturers and suppliers, with several organisations making this the only UK exhibition they attend all year.
NSK (Official Handpiece Partner 2024) returned to BDIA Dental Showcase after seven years away from all major events. Alexander Breitenbach, UK Managing Director at NSK, shared why they chose to attend this exhibition above all others:
“This event is all about BDIA member companies presenting their wares to the profession. There has been a really positive vibe from the audience and exhibitors. It’s great to come together as industry and profession to showcase what we have to
Dental cabinetry should be so much more than a simple storage solution. Your dental cabinetry should be tailored to suit your daily needs, workspace, and your brand.
Clark Dental has over 49 years’ experience working with the dental profession, and has the expertise to help you design your ideal dental practice. The team offers a wide selection of cabinetry options including the Edarredo Joy range of dental cabinets. Practical and beautiful, the Joy range combines striking design and functionality for the ultimate solution.
The Joy range also enables you to configure your cabinetry to suit your unique aesthetic and operational requirements, and the Clark Dental team are on hand to support you at every step of the way.
Please visit the website to find out more.

offer and to promote clinical excellence. The benefits of attending for dental professionals are, without any doubt, the fact that everyone is here, so you can make informed decisions when looking to buy and invest.”
To make sure you have access to the greatest number of relevant dental organisations and industry experts in 2025, don’t miss BDIA Dental Showcase! BDIA Dental Showcase 2025, 14th-15th March, ExCeL London dentalshowcase.com n
For more information call Clark Dental on
Conventional 1450ppm and above fluoride toothpastes only deliver fluoride for a maximum of 90 minutes, whatever their fluoride content and provided the patient does not rinse. Despite its lower 530ppm fluoride content, Biomin F remains active for up to 12 hours, continuously releasing fluoride to strengthen teeth and protect against decay, even if the patient’s toothbrushing is erratic and inefficient.
Available from Trycare, BioMin F contains tiny bioglass particles made up of fluoro calcium phosphosilicate bioactive glass which bonds to teeth and enters the dentinal tubules, where they gradually dissolve for up to 12 hours, slowly releasing calcium, fluoride and phosphate ions. These combine with saliva to form fluorapatite which has been clinically proven to strengthen and
Tokuyama are the only composite manufacturer to use patented spherical filler particles within their composite materials. Each variant utilising spherical particles of different diameters to maximise their optical and physical properties for the desired indication.
In addition to optimised optical properties, resulting in enhanced aesthetic restorations, Tokuyama’s spherical filler particles offer other significant advantages compared with the irregular shaped filler particles used by all other manufacturers. Quicker and easier to pack into undercuts, reducing the risk of voids; easier to sculpt and carve, producing enhanced morphology of the final restoration; and a much smoother surface finish which has a natural high sheen that requires minimal if any polishing.

protect tooth enamel. BioMin F also provides effective treatment for hypersensitivity. Patients also report that teeth feel smoother and cleaner, there is a noticeable absence of background oral sensitivity and that gums are healthier and less prone to bleeding.
A genuine Practice Builder, BioMin F enables patients to enhance their smile and improve their oral health and comfort. It is the only toothpaste approved by the Oral Health Foundation for sensitivity relief.
For further information visit the Trycare website, contact your local representative or call : 01274 885544.n
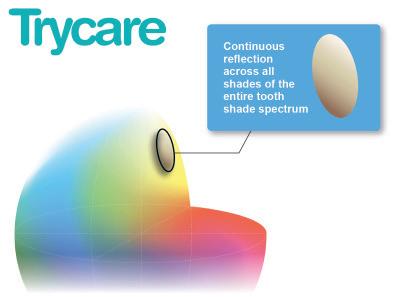
Tokuyama’s development of spherical filler particles has culminated in Omnichroma, the world’s only colourless universal composite which matches every tooth colour no matter what the shade. Omnichroma Flow Bulk is a low viscosity composite which can be placed in 3.5mm increments. Like the other Omnichroma materials it delivers unprecedented colour matching, high polishability and stain resistance. It also has low polymerization shrinkage compared with other bulk filled composite materials.
For more information call 01274 885544 or visit www.trycare.co.uk. n
trycare - free sample of new draganberry flavoured Fluorodose!
Centrix have extended their range of Award Winning Fluorodose varnishes by launching NEW DraganBerry flavour! To obtain a free sample contact your local Trycare representative, telephone 01274 885544 or email dental@ trycare.co.uk
Available from Trycare, Centrix’s FluoroDose 5% sodium fluoride varnish is easy to apply in less than a minute. FluoroDose’s packaging has patented features to enhance handling, comfort and patient safety. Containing a single dose of varnish, each LolliTray includes a Benda Brush applicator and is designed so that it “pops up” with one hand, making removal simple and safe. Drying in seconds when contacting saliva, FluoroDose remains in situ for up to six hours for optimum fluoride uptake. It offers a smooth non-
stringy or clumpy consistency, fast application and six patient-pleasing flavours – caramel, bubble gum, mint, cherry, melon and NEW DraganBerry! It is supplied in Introductory Packs containing the five original flavours and refills of all six individual flavours.
Freshly mixed prior to application, it always has the optimum fluoride distribution, unlike syringes which frequently separate out leaving inconsistent mixes of ineffectively low and dangerously high fluoride concentrations. Each LolliTray contains enough varnish to protect a full adult dentition. For information about the complete Centrix range contact your local Trycare representative, call 01274 885544 or visit www.trycare.co.uk.n
Exclusively available from Trycare, the UK’s fastest growing dental company, Tokuyama Universal Bond II is the only self-curing bonding agent that can bond any direct or indirect restorative material using the same three quick and easy steps and without the need to lightcure, agitate surfaces, use additional primers or activators or wait in between steps. Simply mix, apply, air-dry and that’s it!
Tokuyama Universal Bond II eliminates the need for technique sensitive, error-prone steps and saves valuable surgery time.
It features Borate self-cure technology (BoSE) which provides storage stability and the same bond strength as photopolymerization systems.

Its combination of Tokuyama patented 3D-SR, 10-MDP, MTU-6 monomers and a new silane coupling agent y-MPTES is more stable than conventional y-MPS, bonding tooth, zirconia, alumina, non-precious metal, precious metal, glass ceramics and resin. Featuring colour change verification that it’s completely mixed, Tokuyama Universal Bond II can be used for direct anterior and posterior restorations with light-curing, dual-curing and self-curing composite materials.
Contact your local Trycare Representative, call 01274 885544 or visit www.trycare.co.uk.n
Predicta® Bioactive Desensitizer by Parkell swiftly alleviates dentin hypersensitivity using natural tooth elements, calcium and phosphate. Upon application, it forms hydroxyapatite plugs in the dentinal tubules and adds a mineralization layer that broadens the seal, protecting pain-sensing A-delta nerve fibers. Ideal to treat sensitivity from exposed roots after perio-surgery, bleaching, scaling, root planing, and gingival recession.
Patients report immediate relief from sensitivity lasting up to six months.

Get your heavily discounted Predicta® Bioactive Desensitizer kit here: https://europe.parkell.com/predictabioactive-desensitizer-uk-proben
BDIA Dental Showcase is the annual event of choice for dental professionals, with something for every member of the dental team. It’s a golden opportunity to stay current with the latest innovations, connect with peers and professionals, and learn from the most highly respected minds working in dentistry today.
Every year, BDIA Dental Showcase provides the best experiences for dental professionals, aiming to raise the standards of oral care. The exhibition and educational programme is always relevant, provides vital updates and guidance, and includes the exclusive presence of the Chief Dental Officer.
Join thousands of dental professionals working in all areas of dentistry for the most
important event in the calendar. Find out more about BDIA Dental Showcase and book your place today! Save the date BDIA Dental Showcase 2025, 14th-15th March, ExCeL London dentalshowcase.com n
As restorative dentistry booms, having an ideal composite block for single tooth restorations is essential. For a highperformance composite material, choose BRILLIANT Crios from Coltene. Designed for fast and aesthetic restorations on a daily basis, BRILLIANT Crios offers two sizes, 3 translucencies and 15 shades, providing a wealth of options to match the natural tooth colour requirements of your patient.
It is ideal for use in both the anterior and posterior region, suitable for all conventional indications such as inlays, onlays, crowns and veneers. An effective choice for bruxism patients, BRILLIANT Crios has shock-

absorbing effects, maintaining the strength of the restoration against mechanical impacts. As more patients seek restorative work, using a high-quality composite can help you perform excellent restorative dentistry with precision and skill. With BRILLIANT Crios, you can ensure long-term restoration success. For more on COLTENE, visit www.coltene. com, email info.uk@coltene.com or call 0800 254 5115. n
When patients are undergoing dental treatments, have infections, or have caries, additional oral hygiene supplements can help to maintain their oral health and remove biofilm. Depending on their unique situation, be sure to recommend the right Perio plus mouthwash from Curaprox to each patient. Perio plus Forte is the strongest in the range, with a chlorhexidine concentration of 0.2%, recommended for use before and after invasive dental procedures. Regenerate is recommended for comprehensive protection against gum and implant-related issues, with a chlorhexidine concentration of 0.09%. Finally, Balance is designed for occasional use to offer protection against plaque, ideal for patients undergoing orthodontic treatment, containing
the lowest concentration of 0.05% chlorhexidine. Recommend Perio plus products to your patients who need an extra oral hygiene boost.

To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visit: www.curaprox.co.uk and www.curaden.co.uk n
DGSHAPE launches the DWX-53D, the nextgeneration desktop dry dental milling device, equipped with advanced Internet of Things (IoT) technology via DGSHAPE CLOUD, enabling extensive mobile management for dental laboratories, whilst providing an enhanced user experience.
A built-in camera enables remote monitoring of live production and provides recorded video for troubleshooting and maintenance oversight. The accompanying VPanel software features a streamlined interface, granting users easy access to settings, updates, support, and maintenance management, fostering seamless communication with DGSHAPE Engineers and facilitating prompt resolution of issues. An automated cleaning process simplifies
the removal of Zirconia dust and waste from the device.

Reinforced with a stronger base and spindle, the DWX-53D enables swift and precise milling for various dental applications. Utilising a four-millimetre bur expedites roughing, facilitating rapid production of PMMA applications like dentures and partials with unmatched quality. Additionally, DGSHAPE’s Milling Digital Denture Solution “DK2-53” and accompanying tools (ZRB/ZPB Series) offer highly efficient and precise denture production. n
Do you provide orthodontic treatment, dental implants, or endodontics in your practice? Would you like to improve the quality of images you produce? Upgrading your extraoral imaging system could be the solution.
The Orthophos S 2D/3D extraoral imaging system, available from Clark Dental, generates detailed images while providing comfort and ensuring optimal patient
positioning. Perfect for any dental practice, the Orthophos S produces accurate images, even in the most challenging scenarios.
To find out more, please contact the team at Clark Dental.
For more information call Clark Dental on 01268 733 146, email info@clarkdental. co.uk or visit www.clarkdental.co.ukn
When attracting new patients to join your dental practice making the experience as convenient as possible is crucial.
Conventionally, making a dental appointment requires the patient to call the practice during working hours, taking up theirs and the practice team’s time. And once they arrive for their appointment they must complete preappointment forms.
When practices implement the Sensei Cloud practice management platform, patients are able to book their appointments online at a time that’s convenient for them. Plus, they can complete pre-appointment forms in a virtual waiting room, so they spend less time in the waiting room for a more comfortable experience.
Do your patients want a brighter smile, but are worried about sensitivity? Try BRILLIANT Lumina!
The in-office brightening system, BRILLIANT Lumina from COLTENE is formulated with phthalimido-peroxy-caproic acid (PAP). It offers patients tooth brightening without sensitivity, which is extremely gentle on the tooth structure, and it is very easy to use. When prescribed by a dentist, the treatment can be provided by a dental therapist. Over 5000 treatments have already been performed with BRILLIANT Lumina, with no tooth sensitivity observed during or after the procedure. Analysis has shown that the tooth structure is not eroded following treatment with BRILLIANT Lumina. This makes the solution the ideal choice for patients who are hoping to achieve a naturally brighter smile.
Buying a dental practice can be a complex business. Having the right support in place to ensure a seamless experience, from finding the right practice, securing the right deal, to ensuring compliance with the CQC, is worth its weight in gold. Professionals with the confidence to make the process pleasant as well as efficient for all stakeholders – well that’s very special indeed!
As ‘M’ recently posted on Google Reviews: “There was amazing support throughout the process, from viewing to the whole CQC application process. We were kept updated at all times, and if we had any questions, we were quick to get a reply.
“A special thanks to Laura and Emma. Thank you for making the buying process
“I
Dr Thomas Munro shares his experience of using Kiroku, the digital note taking platform.
“I have been using Kiroku for over a year and a half, and the part I love the most about it is the fact that it’s always consistent. The treatment notes are always uniform, and the questions we’re answering for our diagnostics are always the same. This means that, no matter who’s taking the notes, or who is performing the exam, key pieces of information are being recorded for all of our patients. This is particularly useful for larger orthodontic or implant cases. I really value this.
“The program itself is really intuitive, it always makes recommendations based on things that we are changing or adding
enjoyable.”
To find out more about what Dental Elite can do for you, contact the team today!
For more information contact the Dental Elite team on 01788 545900 https://dentalelite.co.uk/ n

on a constant basis – it recommends adding information in automatically so that it is just a single touch button in order to make changes.

“I highly recommend Kiroku to anybody. If you value consistency along with saving time and making your team’s life easier in that note taking process – sign up!”
To find out more about Kiroku, or to start your free trial, please visit trykiroku.com n
For more information, please contact the team at Sensei, the practice and patient management brand from Carestream Dental. For more information on Sensei Cloud visit gosensei.co.uk
For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.ukn

To find out more about the BRILLIANT Lumina tooth brightening system from COLTENE, please contact the team.
For more on COLTENE, visit www.coltene.com, email info.uk@coltene.com or call 0800 254 5115 n

refer your endo cases to the experts
If you’re looking for expert support in providing advanced endodontics to your patients, refer them to EndoCare for exceptional outcomes and an excellent treatment experience.
We understand the high quality of service your patients expect and we will work as an extension of your team to ensure their endodontic journey is just as seamless. Our team of endodontic experts and specialists deliver world-class dentistry using state-of-the-art facilities to deliver predictable procedures and outstanding clinical results.
We also make the referral process as simple as possible – simply complete the secure online form and we will be in contact to arrange the rest. Once the referred treatment is complete, your patient will return to you for their ongoing care.
Refer your complex endodontic cases to the experts at EndoCare today.
For further information please call EndoCare on 020 7224 0999 or visit www.endocare.co.uk n

Preventive care is key for promoting long-term oral health. Interdental cleaning and using products which contain key ingredients such as fluoride and chlorhexidine are essential here, enabling patients to reduce levels of plaque and prevent future oral health issues.
As such, it’s important to recommend products which boost oral hygiene, and are easy to use, like FLEXI interdental brushes and PREVENT GEL from TANDEX. When using both of these together, patients are able to remove plaque from in between the teeth with ease, whilst also applying 0.12% chlorhexidine for an antibacterial effect, and 900ppm fluoride to help strengthen enamel.
FLEXI interdental brushes have a flexible handle, making them easy to use, and are
available in 11 different sizes, ensuring the perfect fit for each interdental space. Contact the team at TANDEX for more information.
For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from DHB Oral Healthcare https://dhb.co.uk/n

All newly qualified dentists, here’s a little gift to get you going…
Kiroku is an incredibly powerful system using AI to enable clinicians to complete notes 60% faster and then convert them instantly into documentation.
As dentists, the people behind Kiroku understand the need to get up and running as fast as possible after you qualify, and so here is some great news for graduates!
Dental professionals who graduated in 2024, working in the UK and Ireland, can benefit from a whole year for free if they make just 30 notes in 30 days. And you can get a massive 50% off any plan for the following 12 months.
If you graduated in 2023, you can get a 50% discount on any plan for the next
12 months if you subscribe now!

And last but not least, if you are a PLVE with proof of status, you can get a free 14-day trial, plus 50% off Kiroku during your first year of work.
Check the website to find out how to apply today!
To find out more about Kiroku, or to start your free trial, please visit https://www.trykiroku.com/dental-foundationtraining n
When a dental practice makes changes to their waste management workflows, they have the opportunity to become more environmentallyconscious, and make an impact on the world around them. The NHS has set a target to become net zero for the emissions it controls by 2040 – you can take active steps today to make a difference.
Solutions like the Sharpak Zero reusable sharps containers, available from Initial Medical, are exceptional at reducing the impact your practice has on the environment, and help work towards net zero dental care.
Replacing single-use sharp waste containers, Sharpak Zero solutions are collected after each use, emptied and sanitised for 10 waste cycles. Then, the plastic container is reprocessed, creating a new sharps waste container with an entirely new lease of life. This entire process is repeated 10
times over.
The Align, Bleach and Bond course from the IAS Academy is the perfect base for clinicians to introduce clear aligner orthodontics and orthorestorative care into their everyday dentistry.
Spanning over two days, delegates will first understand the workings of Inman and clear aligners, looking at appropriate case assessments and selection. Under the guidance of leading clinicians and dental educators, delegates will also explore occlusal planning and retention, before having a hands-on experience with Inman/clear aligner attachment placement.
Ortho-restorative workflows are covered comprehensively on day two, as dental professionals are presented with guidance on simple edge bonding and polishing, aesthetic tooth shaping, guidance on treatment

Where dental practitioners once employed singleuse sharps waste containers to collect and store used needles, syringes and similar equipment, they can now choose a solution that lasts a total of 100 waste cycles. The vast amount of plastic that is needed to support dental professionals across the UK can be reduced, one container at a time.
To learn more about environmentally friendly waste management with Initial Medical, contact the team today. To find out more, get in touch at 0808 304 7411 or visit the website today: www.initial.co.uk/medical n
The team at Clark Dental understands that the treatment centre is the heart of your dental practice. That’s why they support you in your decisions to find the best option for your unique practice.
The A-DEC 500 treatment centre is a fantastic choice for those looking to provide comfortable and effective patient care. This high-quality treatment centre allows you to efficiently maintain a healthy posture while carrying out daily tasks. An ergonomic design is essential, allowing you and your patient to remain comfortable, even during long procedures.
Its design allows you optimal access thanks to its ultra-thin backrest, while its stingray-shape ensures the patient is fully
supported throughout their appointment. Contact the Clark Dental team to find out more.
For more information call Clark Dental on 01268 733 146, email info@clarkdental. co.uk or visit www.clarkdental.co.uk n

Often, orthodontic aligners promote bacterial growth, leading to demineralisation of the teeth due to the weakened natural saliva defence.
Demineralisation can result in white spots forming on the teeth, frequently experienced by orthodontic patients. Aligner Foam from Curaprox naturally remineralises, fortifies, and shields your patients’ teeth – nourishing the enamel to restore calcium and phosphate. Additionally, Aligner Foam fights plaque, tackles bad breath, moisturises the teeth surfaces, and has antibacterial properties. For more information, please contact the team at Curaprox.
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@ curaden.co.uk
For more information, please visit www.curaprox. co.uk and www. curaden.co.uk n

techniques such as the Dahl Principle, and so much more.

The course is expertly led by well-regarded IAS Academy tutors such as Tif Qureshi, Geoff Stone, Seb Wilkins and Guy Wells. Delegates can approach tutors with any and all questions about orthodontic and orthorestorative care, and can receive clinical support long after the conclusion of the course.
To learn more about exceptional courses with the IAS Academy, contact the team today. For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
A cost-effective intraoral imaging system can begin to earn back its value in your practice from your very first scan. Choose the CS 7200 Neo Edition imaging plate system from Carestream Dental, and create efficient workflows in an instant.
High-resolution images can be accessed in as little as 8 seconds, as clinicians simply scan the thin, flexible and cable free imaging plates. The radiographs are then automatically recognised and distributed to the appropriate computer and patient file to reduce the potential for human error.
The compact system is a time saver, and can remain as such long into the future with the exceptionally durable imaging plates. Since they are scratchresistant, they can be reused hundreds
A service to smile for
For the smooth running of your practice it is vital that you have sufficient staffing. From illness to holiday, quickly finding locum cover for absent staff keeps the workflow efficient.
Dental Elite can be your greatest asset for getting cover sorted, removing the stress and worry from your job.
On working with one of the Dental Elite team, Chalet Hill says “I can’t say enough good things about Luke [Arnold, Locum Controller]. He has been absolutely amazing in finding locum cover for multiple sites. His response is incredibly quick, and we never have any issues or worries.
“Every time we need a locum, he manages to provide us one within a week
of times. If you find yourself in need of a replacement, they are relatively inexpensive too.
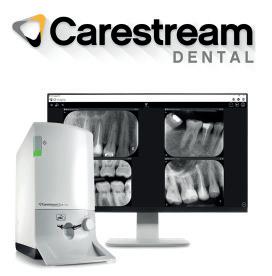
Without a continuous expenditure on film and associated chemicals, there is more to be saved than time.
To learn more about efficient imaging workflows in your practice, contact the Carestream Dental team today.
For more information on Carestream Dental visit www.carestreamdental.co.uk
For the latest news and updates, follow us on Facebook and Instagram @ carestreamdental.ukn
carestreamdental.co.uk

of asking. His efficiency and dedication make our working lives so much easier. Highly recommend!” For a consistent workflow and reliable locum cover, try Dental Elite.
For more information contact the Dental Elite team on 01788 545900 https://dentalelite.co.uk/n
Leader in decontamination, Eschmann, offers comprehensive service and support for all its customers. It is one of the only providers in the market to deliver Enhanced CPD training with new equipment as it is installed, and annually thereafter if you are one of their Care & Cover contract customers.
ECPD training ensures that all appropriate members of the dental team know how to confidently use and maintain your infection control equipment. This includes efficient daily operation, as well as knowing how to perform the necessary daily, weekly and monthly testing required for compliance with regulations and optimised product life.
All training is provided by expertly qualified

Eschmann engineers, who have extensive experience with Eschmann equipment and with dental regulations. They are also available after the training should your team have any questions.
In addition, there is a technical helpline for any enquiries regarding the equipment.
To find out more, contact Eschmann today. For more information on the highly effective and affordable range of infection control products from Eschmann, please visit www.eschmann.co.uk or call 01903 753322 n
Chris
future-mindsets in relation to

Ioften spend years talking to prospective clients about the market, their particular circumstances, and what a great plan for them to exit their dental practice would look like. It’s what we do. After all, our advice to clients is to start considering your options up to ten years before you exit. You can imagine how people are at different stages of their decision-making process. Should I sell? If so, when? What do I want the deal to look like? Do I have the experience and bandwidth to sell it myself and, if not, who am I going to appoint to act on my behalf?
Sometimes, during these conversations, I think I understand the other person’s perspective, but then I realise we are not really moving the discussion forward.
Perhaps we are not on the same time zone?
I recently read an interesting book titled The Anticipatory Organization: Turn Disruption and Change into Opportunity and Advantage by Daniel Burrus. In it, Burrus provides a framework for creating an organisation that, in mindset and culture, is future-oriented. It talks of focusing on turning change into advantage in order to exploit the future.
In his book, Burrus posits that we all sit on a spectrum with regard to our comfort level with change. This is exactly where our clients are. They are all considering or actively seeking significant change but they are not all in the same time zone.
Burrus suggests that, in general, we fall into one of three personality types. We possess either a past-, a present- or a future-oriented mindset.
Clients with a past-oriented mindset are not comfortable with change. They resist change and would prefer things stay as they were.
Clients with a present-oriented mindset acknowledge that the future is approaching at full speed but tend to view change as an unwelcome disruption rather than a creator of opportunity.
Clients with a future mindset want to jump into tomorrow with both feet as they can’t wait to seize upon the opportunities that change offers.
Taken together, buying and selling a dental practice is two halves of an act of change. An act that, by its very nature, disrupts the status quo. So, when I am talking to clients and can sense a reluctance to move forward, what are they actually saying? Are
they really going cold on the idea of selling or are they in a different time zone to me?
Perhaps the vendor knows that, ultimately, time is against them. That their peer group are exiting the profession or planning to leave practice ownership but they have a past orientated mindset. They know that they can’t stay where they are. But they’re so locked into their comfort zone that they’re turning a blind eye to the risks of standing still and putting off change as long as they can.
And here I am, with my future-mindset assuming that any logical person should be excited about the cool things we can do and the future opportunities that we can unlock for them. Instead, they’re listening or looking at me like I am a stranger from another planet. So, what do you do?
I could make the decision to park them until sometime in the future. Or, I can apply some empathy to the situation and refocus on their view of the world. When someone has what appears to be a clear need for our services but is frightened of change, what should you do?
First, I have to go back to their time zone. This could mean something as simple as forgoing the virtual meeting where I share
my screen to inviting them to one of our seminars or meeting them at their practice.
I must then confirm their time mindset. I can do that by asking discovery questions that uncover past attempts to change as well as what prevented those from materialising. Listen slowly to their answers and hear what they are saying instead of what I want to hear.
I also need to stay in their time zone. I can ask them what their vision for the business and themselves is. I can even write it down and share it with them. I look for opportunities where our services can help them achieve their vision and objectives and I am trying to connect with them on a human level at a tempo they are comfortable with. I want the client to see a way forward, to develop a shared mindset and establish a trust that will enable me to walk them into the future. n
about the author chris Mayor, commercial Director, Lily Head Dental Practice sales.


TABLETS FOR CLEANING REMOVABLE DENTAL APPLIANCES
Help your patients keep their appliances clean and bright with Effer-ves. Specially formulated to kill bacteria that can build up as well as reducing odours.
Effer-ves is easy to use and removes common stains caused by tea, coffee and some foods.



Effer-ves is suitable for all removable dental appliances
• Aligners
• Orthodontic retainers



Independently tested by Invisalign®

Scan here for more aligner related products

• URA’s (incorporating acrylic and s/s wire)
• Functional appliances
• Mouthguards
• Bruxing Appliances
• TMJ Appliances
NEW Aligner Accessories Brochure available – call us to receive a copy.




It is common for principals to offer first refusal to an associate or colleague, ahead of putting the practice on the open market. This may be with or without the help of a sales agent. Here we discuss what you need to know, do, and think about, to decide whether to purchase or not.
Get the right information
If there is a sales agent involved, they will likely have produced a sales prospectus for you to review. This should include: an income breakdown for the last 12 months, current staff costs, associate, hygienist and therapist pay terms, and the last three years’ accounts. The latest accounts will give you a good overview of the standard practice costs (premises and running costs), however you will need current income and staffing details as these are likely to have changed since the last set of accounts were produced.
You will need all this information to review how the practice is currently performing and to produce projections under your ownership. This information will also be required by lenders when approaching them for finance.
is this the right practice for you?
Practices are usually valued under two models: Associate Led and Principal Led. If the practice is valued Principal Led, you will need to be confident that you can generate the income attributed to the Principal. Take note of any specialist income to ensure that you include any additional associate fees in your personal projections, should you not be able to generate this income yourself.
Consider whether this is the right practice for you. Is the practice in the right area? Is the practice the right size for you to manage alongside your clinical work? If the practice needs financial investment, is this something you can provide? If the practice has room to expand, do you have the skills and vision to grow the practice further?
are you ready?
It is common for buyers to be offered a practice when they may not be actively looking to buy. Timing is important in practice sales, both financially and personally. You should think about if you have the right skills to take over and run a practice, as this is something the banks will ask. Do you have a cash deposit? Some banks will lend up to 100% finance if you have sufficient security, but most will require a 5-20% cash deposit. Don’t forget about buying costs in addition to your deposit as these are often between £15,000 and £20,000.
Look into finance
The principal will be excited to get started but, prior to placing an offer, you will need to look into your finance options (if needed). To help with speed, it is best to use a healthcare finance broker rather than trying to contact multiple banks alone. The broker will be able to consolidate your information and prepare a lending report to issue to multiple banks, hopefully receiving multiple offers for you to choose from within a couple of days. Once you have funding offers, you will then be in a position to offer on the practice if you wish.
speak to an accountant
You will need to look at how the practice will work financially under your ownership. A dental accountant can prepare personal projections to illustrate this for you. Accountant’s projections will also tell you how much you will take home after loan repayments and tax.
Before going to credit with a bank or starting any legal work, you will need to confirm your purchase structure, e.g. are you going to buy through a limited company or as an individual. Ask your accountant for their guidance on this to help with future tax planning.
Before starting any legal work on the purchase, you will need to agree some of the main purchase terms. Whilst discussing these with the seller and/or agent, carefully consider whether you are happy with the deal.
• What you are buying, e.g. assets or shares, if the practice is currently a limited company?
• Are you buying or leasing the property? If buying, the property should be subject to valuation in line with your bank valuation and funding. If leasing and obtaining bank funding, you will need a lease term in line with your loan term.
• Does the principal want to stay on as an associate or do you need them to leave at completion so that you can take over their income?
• What are the timescales? Perhaps the principal wants to sell immediately but you have a six-month notice period at another practice – be upfront and realistic about your timescales.
In today’s digital age, the reputation of any business, including dental practices, is heavily influenced by online reviews. Patients are more informed and selective than ever, often turning to platforms like Google and Facebook to choose their dental providers. This means that managing online reviews isn’t just important – it’s essential.
This is where review management software comes into play, offering an indispensable tool for modern dental practices to build and maintain their reputation.
enhancing patient trust and credibility
Trust is the foundation of the patient-dentist relationship. Before visiting a new dentist, patients typically research online to find out what others are saying. Positive reviews and high ratings can significantly enhance a practice’s credibility, making potential patients more likely to book an appointment. Review management software helps practices ensure that satisfied patients are encouraged to leave positive feedback, which in turn bolsters the practice’s online reputation.
increasing patient acquisition
With most potential new patients searching for dentists online, having a strong online presence is crucial. Practices with numerous positive reviews stand out in search results,
increasing the likelihood that prospective patients will choose them over competitors.
Review management software automates the process of requesting reviews from satisfied patients, thereby consistently boosting the number of positive reviews and enhancing the practice’s visibility online.
Managing and responding to negative feedback
No practice is immune to negative reviews. However, the way in which a practice responds to these reviews can make a significant difference. Review management software not only alerts practices to new reviews in real-time but also provides tools for crafting timely, professional responses. Addressing negative feedback promptly and constructively can mitigate the impact of a bad review and demonstrate to other potential patients that the practice is committed to patient satisfaction and quality care.
improving the patient experience
Feedback is a valuable tool for growth. Reviews provide insights into what a practice is doing well and where there is room for improvement. Review management software can help you analyse feedback, offering a clear view of patient opinion. This data allows practices to make informed decisions on how
to enhance patient care and improve the overall patient experience.
boosting seO and online visibility
Online reviews are not just about reputation –they’re also a critical factor in search engine optimisation (SEO). Search engines prioritise businesses with a high volume of positive reviews, making them more likely to appear at the top of local search results. Review management software helps maintain a steady flow of reviews, improving rankings on platforms like Google, which in turn drives more traffic to the practice’s website and increases appointment bookings.
Manually managing reviews across multiple platforms can be time-consuming and overwhelming. Review management software simplifies this process by centralising reviews from common platforms in one place. This allows the practice’s team members to monitor and respond to feedback efficiently, saving valuable time that can be better spent on patient care and other critical aspects of the practice.
Building long-term relationships with patients Encouraging patients to leave reviews not only helps attract new patients but also fosters long-term relationships with existing ones.

PFM Dental offers a comprehensive range of professional services exclusively for dentists. Since 1990 we have been trusted advisers to the dental profession with a hard won reputation for sound, ethical and independent advice. Our services incorporate 4 key departments: practice sales and valuations, independent financial advice, dental accountancy and dental legal services.
https://pfmdental.co.uk/
about the author samantha Hodgson is a finance broker and practice valuer at PfM Dental.

Deciding whether to buy a dental practice is a mixture of personal, professional and financial decisions. Take your time to consider all aspects of the practice on offer to ensure that you are confident this is the right move for you. n
When patients see that their feedback is valued and acted upon, they are more likely to return for future dental care and recommend the practice to friends and family. Review management software facilitates this ongoing dialogue, helping practices maintain strong, lasting relationships with their patients.
In an increasingly competitive marketplace, dental practices cannot afford to overlook the importance of online reputation management. Review management software is a powerful tool that enables practices to enhance their credibility, attract new patients, respond effectively to feedback, and ultimately provide better patient care.
By integrating review management software into their daily operations, dental practices can not only protect but actively enhance their reputation, ensuring long-term success in an ever-evolving digital landscape. n
about the author Vicki Mayson, sales & Marketing Manager at connect My Marketing.

connectmymarketing.com






It’s only natural when there’s a perceived gap in a market for new competitors and innovators to emerge, promising to be the ideal fix. The dental market is no exception, as concerns about recruitment and affordability continue to affect the industry.
The huge discounts and celebrity endorsements characteristic of some of these disruptions are hard to beat. In the face of this, how can private practices respond to attract and retain patients and ensure their business value doesn’t take a hit?
Who and what are the current disruptors?
When considering how to stay competitive, it’s important to know your market and to understand the potential appeal of disruptive innovations to patients.
The dramatic death of Smile Direct Club hasn’t been the end for directto-consumer (DTC) dental products. Despite famously letting down millions of patients, a number of other direct-toconsumer companies are still operating.
The ostensibly low up-front costs will be the greatest competitive factor that practices have to contend with.
In another high-profile example, BUPA is offering a very attractive new benefits package designed to enlist those currently subscribing to health insurance to use their dental services. It includes a free annual appointment with a BUPA dentist plus a £300 allowance to cover any clinically necessary follow-up treatment listed in the policy. The initiative represents a huge investment by BUPA, and will be
very appealing to private patients with a local BUPA practice. Could this lure private patients into a BUPA practice from another neighbouring private practice?
The health and wellness membership organisation, Until – now with Steven Bartlett’s backing to the tune of £4 million – recently announced that it is entering the dental market. This time, the disruption is aimed at professionals wanting to build an independent, stress-free practice. Until offers kitted-out facilities for rent, as well as mentoring and support training as part of its membership. The organisation currently only has one location with dental facilities, but plans to expand, providing more dental professionals with more rooms, equipment and even dental nurses. This will allow them to offer services as and when needed, for an hourly fee.
Some responses and countermoves to consider Dentists have already made the case against DTC in terms of patient safety, as well as the false economy, and practices tend to communicate this very well. This message has been strengthened by the Smile Direct Club going bust, with highly publicised legal battles. However, enhancing your patient communication is also important and the introduction of teledentistry may offer patients flexibility, but with a trusted clinician, retaining business and practice value.
The BUPA promotion is very interesting because it’s something we anticipated they’d do when they first acquired Oasis as it makes strategic sense to cross-sell. BUPA dentists and associates working alongside them may also have cause to
be grateful for the opportunities and solid private patients it could present. Despite this, it may well leave some in private practice concerned about how they will compete. Although a promotion on this scale may be well out of reach for most practitioners, a cost-benefit analysis will show you how a targeted promotion or discount might work to achieve more business for you, while also taking the pressure off your patients. If successful, it also remains to be seen how other private medical insurance providers respond, especially those who already have a foot in the dentistry door.
The offer from Until could well be appealing to some clinicians who wish to remove themselves from the hassles of being a principal without being an associate – similar to how private medical consultants work. However, operating from a rented space lacks the personal interaction you get with consistent team members and an established list of patients. Some patients may find the flexibility appealing; however, the jury is out on whether this plan will take patients away from existing practices, or if it appeals to a totally new market. Though it will be one to watch, similar initiatives haven’t significantly impacted on practice valuations across the market in the past. There is also the question over who owns the goodwill. The renting dentist, who doesn’t have a long-term lease suitable for bank lending, or Until, who benefits from rental income?
Confidence in your strengths
In all the excitement, fear can take over, and it can be easy to forget what you
£13 million a day. An eye-watering price to pay, but one that faced property insurers throughout 2023, when the industry paid out £4.86 billion to homeowners and businesses. It was the largest year of claims for weather-related damage, amassing to £573 million, a 36% greater figure than seen in 2022. Dental professionals up and down the country should heed these figures as a potential warning for the future. Extreme weather affects properties in a variety of ways, be it through high winds, rain and flooding – 1 in 6 UK properties are at risk this way – or snow and hail, amongst other problems.
Knowing this, clinicians should take action to protect their business properties and homes, which is most effectively done through building insurance. This will not stop flooding, nor put a barrier up against high winds, but if damage is caused, it is of the upmost importance to begin repairs whilst staying financially stable.
Claim values
The number of claims on building insurance is not rising – the 2023 data observed a “fairly level’ volume
according to the Association of British Insurersi – but the value of claims are. When accounting for inflation, the cost of an average claim had risen by 11% from 2022. Were your practice not insured, but succumbed to damage through an extreme weather-event, you may be out of pocket by a substantial sum. Building maintenance costs also increased by an average of 9.22% in the year leading to the first quarter of 2024 – wherever you look, building repairs look increasingly expensive.
The value of your building insurance should cover a worst-case scenario: a complete rebuild. This may feel excessive, but it means you are not left completely destitute were the worst to happen. You can find out the value you should be covered for from a recent mortgage survey, or pay a surveyor to carry out a rebuilding estimate for you.
You may be interested in how ‘at-risk’ your dental practice or private property is from a range of weather events. Some events can’t be predicted, but longterm flood risks can be assessed simply through the GOV.UK website.
are already doing that has attracted your patients to you and your practice, and what keeps them coming back.
Cost is an enormously important factor, as is accessibility and convenience. But so is the team, and building trust is one of the key factors in retaining patients, as well as getting their support in building up your base. Investing time, resources and energy in promoting staff wellbeing is also shown to pay dividends in terms of the patient experience.
Enlisting the support of experts is also essential when looking to enhance services to build and protect goodwill. Dental Elite has decades of collective experience in helping dental practices add value by improving services and optimising business fundamentals. The team works closely with clients, offering individualised support to increase the value of their practices.
Sometimes the innovations of competitors can throw a much-needed new idea into the mix – they can prevent your practice from getting left behind by sparking your imagination, inspiring the whole team to pull together to stay relevant. It can remind you what your strengths are, and what attributes you can honestly say make your practice a good choice for patients.
For more information contact the Dental Elite team on 01788 545900 https://dentalelite.co.uk/
About the author Luke Moore is one of the Founders and Directors of Dental Elite.

Winter windstorms are expected to increase in prevalence and severity across the UK in the coming years, but this prediction is not certain as some climate models differ in their forecasts. If your practice is based by a coast, be aware that flooding in your area may be more likely – even under weaker storms – due to climate change and rising sea levels. No matter the risk you perceive your practice to face, your building insurance must be able to cover your needs at any given moment. By consulting independent financial advisers, like those from the money4dentists team, you can ensure you find the optimal solution available to you. money4dentists was established to support dental professionals with a variety of business and financial needs through expert advice; the team has now supported UK dentists for two decades. You can book a free consultation to discuss your building insurance options today. Building insurance is ever-important for the protection and longevity of a practice. With the industry seeing rises in claim values, especially because of unpredictable weather, choosing the most suitable solution is essential.


We’re a specialist dental practice sales agency, so whether you are looking to sell your dental practice on the open market, selling to your associate or intrigued with Corporate interest, we’ve helped thousands of dentists like you.
You cannot be in better hands with our expert valuers, a single point of contact throughout the sale and in-house legal team, allowing us to

We work with dentists all over the UK
Our scale and reach means we’re here to help wherever you’re based
Practice sales over the past 12 months 50+
Current dental accountancy clients 1200+
Practice finance raised in the last year £15m+





Accurate valuations for associate & principal led models with advice on enhancing the practice value.

advise you from start to finish. Supportive Throughout
We liaise with solicitors, buyers, and CQC to ensure everything is in place to minimise stress and give a smooth sale.

Get access to 1000s of pre vetted purchasers, being individuals, small groups and all of the major corporates.

We have specialist dental solicitors with expertise in commercial law, property law, and CQC processes.

We will ensure your practice attracts the best possible price by negotiating the sale on your behalf.

Fee Free Sale
95% of our NHS practices sell to priority buyers meaning the purchaser covers the agency fee.
Experience exceptionally lightweight loupes with crystal clear optics, designed and optimised for you.
• Custom Measurements
• Custom Fitting
• Custom Fabrication
For a t as unique as you are.

