
































































































The call to put the mouth back in the body is not new. Over a decade ago the World Health Organization (WHO) acknowledged the critical link between oral health and NCDs. Since then, it has championed integrating oral health into NCD prevention frameworks and embedding oral health within universal health coverage (UHC) policies.
The urgency for action has been underscored by the recent World Economic Forum (WEF) white paper, The Economic Rationale for a Global Commitment to Invest in Oral Health (WEF 2024). The report identifies poor oral health as a significant contributor to rising healthcare costs, particularly through preventable conditions and emergency interventions. By integrating oral health into primary care and community services, the WEF demonstrates that nations can achieve substantial returns, including cost savings, driven by reduced systemic health complications, improved population health, and lower overall treatment costs, all of which contribute to healthcare sustainability. By prioritising oral health, governments and health systems unlock a powerful lever for improving health outcomes and reducing inequities at a system-wide scale.
For our new Government focused on economic growth and equity, the case for oral health is clear. Prioritising oral health would alleviate NHS pressures, reduce health disparities, and drive economic stability.
A broken system
In the UK, dental care and oral health services have been marginalised for decades, despite clear evidence of need and persistent calls for reform. Successive Secretaries of State for Health deferred decision-making, kicking the dental can down the road. This institutionalised apathy has led to stark disparities with entire regions of England, termed “dental deserts,” where accessing affordable dental care is impossible. Many local authorities have also neglected their oral health promotion responsibilities. The consequences are devastating. Childhood tooth decay remains the leading cause of hospital admissions, despite being almost entirely preventable.

Adults face insurmountable barriers to care, some resorting to DIY dentistry or forgoing treatment altogether. The insidious second order effects on systemic health multiply, for the patient and the public purse.
The current system is not just unsustainable –it is broken. Yet, I believe it is fixable, if we are prepared to reimagine dental care with the attitude and aptitude to think broadly and act boldly.
Wes Streeting's 10-Year Health Plan provides us with a unique opportunity to rethink and rebuild oral health services. We have a fresh ministerial team, and I hope for a fresh approach. One that will make oral health a cornerstone of public health and an integral element of NHS care delivery.
What’s at Stake?
Poor oral health doesn’t just affect teeth; it exacerbates NCDs like diabetes and cardiovascular conditions, amplifying the financial burden on the entire healthcare system. The effects extend beyond costs, undermining workforce productivity, quality of life, and the broader societal well-being.
Failing to act risks compounding these challenges, locking the NHS and society into a cycle of escalating costs and worsening health disparities. Now is the moment to pivot from reactive care to proactive investment in oral health, transforming it into a cornerstone of sustainable public health and equitable healthcare.
Oral health's inclusion in the 10-Year Health Plan for England isn’t just about risk management – it’s a strategic opportunity to lead the way in integrating dental care with broader healthcare frameworks. There are many strands of activity, from contracts to commissioning, business models and workforce, but the founding Three Strategic Priorities required to set the conditions for success and reshape oral health delivery are:
Treating oral health as an integral part of overall health requires system change:
• Embedding dental services and oral health care pathways within primary and community services as part of the multi-disciplinary approach.
• Commissioning oral health interventions as part of NCD prevention strategies.
• Co-locating dental services in general medical practices and community health settings.
For the NHS, this also means forwardthinking infrastructure planning. Capital projects should incorporate preventive and therapeutic dental services, improving accessibility and efficiency.
Harnessing technology can drive smarter, more effective care delivery. For oral health:
• Leveraging shared electronic health records to ensure seamless, multidisciplinary patient care.
• AI tools to enhance triage, diagnostics and monitoring.
• Real-time analytics to enable targeted interventions for at-risk populations.
• Digital outreach for residential care settings. Oral health must be embedded in every NHS digital initiative – not as an afterthought, but as a standard.
The key message is that good health starts with a healthy mouth. With
transformative public health campaigns there is potential to change behaviours by connecting oral health to systemic health benefits. This includes:
• Public messaging linking oral health to NCDs, improved quality of life and reduced healthcare costs.
• Partnering with councils and charities to address social determinants of oral health to support outreach and oral health literacy, community distribution of oral hygiene packs tailored to local design/needs.
This triad of strategies are the basis of a patient-centred oral health system designed to reduce inequities and achieve long-term cost efficiencies.
Oral Health matters to everyone
Oral health isn’t an isolated achievement or the sole responsibility of dental professionals. To shift thinking, we need a collective effort involving caregivers, educators, policymakers, public health advocates, the food industry, and every healthcare or social care professional who interacts with patients or communities. Investing in oral health for our communities means investing in a healthier, more resilient future. It is fundamentally a social, economic, and equity issue that demands collective action to challenge the orthodoxy that has siloed oral health.
By putting the mouth into the body of Wes Streeting's 10-Year Health Plan we can create a healthcare system that doesn’t just treat disease but prevents it –starting at the root, quite literally.
This is a call to action for all of us: policymakers, teachers and technologists, academics and industry leaders, media commentators and community advocates, and the public at large. We need to act now if we are to create a future where dental care and oral health are not afterthoughts but a pillar of equity, sustainability, and well-being for all.
Your advocacy and your views on oral health and dental care services need to be part of the conversation at: change.nhs.uk


We begin the year with a bang! If you’ve skipped straight to my welcome message, head back a page and don’t miss Sara Hurley’s Call to Action . The former Chief Dental Officer is calling for the government to make oral health central to the 10-year Health Plan for England and needs the help of us all – dental professionals and members of the public at large. As Sara mentions at the end of her piece, your views on oral health and dental care services can be made heard at: https://change.nhs.uk/
We here at The Probe would also like to publicly congratulate Pam Swain, Chief Executive of The British Association of Dental Nurses, on receiving a well-earned MBE as part of the New Year Honours List. We have the news covered overleaf. In addition, Pam has also provided us with a highly personal, must-read spotlight feature on bullying in the workplace, which you can find on page 38.
Before I go, here’s a quick reminder to get your entries in for the 2025 Dental Awards at the-probe.co.uk/awards before they close next month.
Happy New Year!








The Probe is published by Purple Media Solutions.
Registered in England.
Registered number 5949065
Managing Editor: James Cooke
Commercial Director: Gary Henson
Divisional Administrator: Francesca Smith





Production Designer 1 : Lorna Reekie
Production Designer 2: Rob Tremain
Digital Content Manager: Stephen Wadey
Circulation Manager: Andy Kirk
Managing Director: Ed Hunt
Regular Contributors: Lisa Bainham, Nigel Carter, Barry Cockcroft, Ollie Jupes and Pam Swain
E-mail news, stories or opinion to james.cooke@purplems.com
Circulation/Subscriptions: The Probe Subscriptions, Perception SaS, PO Box 304, Uckfield, East Sussex, TN22 9EZ, Tel: 01825 701520, https://purplems.my-subs.co.uk ©Purple
Media Solutions Ltd, 2014. All rights reserved. ISSN 0032-9185. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies, and information retrieval systems. While every effort has been made to ensure that the information in this publication is correct and accurate, the publisher cannot accept


liability for any consequential loss or damage, however caused, arising as a result of using information printed in this magazine. The views expressed in The Probe are not necessarily the views of the magazine, nor of Purple Media Solutions
Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth RCS(Eng), D’Orth RCS(Eng); Mark Wright BDS(Lon), DGDP RCS(UK), Dip Imp Dent.RCS (Eng) Adv. Cert, FICD; Dr Yasminder Virdee BDS. Readers who fall
















The General Dental Council (GDC) has met 16 out of 18 Standards of Good Regulation for 2023/24, making significant improvements that achieved the standards in registration, without meeting the standards for EDI and fitness to practise timeliness, according to the Professional Standards Authority (PSA) annual review.
The GDC successfully met the Standards for Registration this year, reducing the backlog of overseas-qualified dentists who applied as dental care professionals (DCPs) significantly. The backlog of unworked DCP applications which stood at 5,700 in April 2023 following a change in legislation has now been eliminated, with all remaining applications scheduled to undertake a panel assessment by April 2025.
Key achievements highlighted in the review include reducing the average processing time for UK graduate registration to two weeks, enhanced support systems for those involved in fitness to practise (FtP) cases and strengthened stakeholder engagement and consultation processes.
Tom Whiting, Chief Executive of the General Dental Council (GDC), said: “We welcome the PSA’s recognition of our progress across multiple areas, particularly in registration, while acknowledging there is more work to do. We remain firmly committed to improving fitness to practise processes and implementing our EDI strategy.
“Our priority is ensuring we deliver effective regulation that protects patients and supports dental professionals. We welcome close working with partners and stakeholder organisations to build trust in effective regulation and achieve a goal that we all share, which is patient safety and public confidence in the dental professions.”
The PSA commended the GDC’s work in seeking and acting on feedback from diverse stakeholder groups and its commitment to evidence-based policy development. It recognised the regulator’s efforts to improve communication with registrants during fitness to practise investigations, noting positive feedback about the more empathetic tone and improved signposting to support services.
However, the review identified ongoing challenges in the timeliness of fitness to practise cases, particularly in cases older than 156 weeks. With only nine cases older than 101 weeks, the GDC continues to reduce the number of older cases, which is more effective in FtP stages where the regulator can exert greater influence over timeliness.
The GDC has revised its fitness to practise processes to improve timeliness when investigating single patient clinical practice concerns. The move follows the successful pilot of revised processes for handling fitness to practise concerns raised about dental professionals with no allegations of impaired fitness to practise in the previous 12 months.
The regulator has plans in place to further enhance communication and support for those involved in fitness to practise cases as well as reviewing its decision-making guidance to ensure that it addresses allegations of discriminatory conduct.
The GDC recognised the PSA’s concerns that it needs to provide clearer visibility of the work underway to deliver the current EDI strategy and has published an update on the strategy that shows progress and areas where it needs to do more.
The GDC’s EDI vision and approach will be incorporated into its corporate strategy from 2026, to ensure that EDI is embedded within its broader strategic objectives. n
The British Association of Dental Nurses (BADN), the professional association for dental nurses in the UK, has announced that Chief Executive Pam Swain has been awarded an MBE in the 2025 New Year’s Honours list for services to dental nursing.
“I have known Pam for years; I have witnessed her working alongside various Presidents and the BADN Executive Committee for the empowerment and benefit of the dental nursing workforce” said BADN President Preetee Hylton. “Although not a dental nurse herself, she has demonstrated unwavering dedication to the profession. Her tenacity and passion in standing up for dental nurses is admirable. I am delighted and honoured to have her by my side as I start my tenure as BADN President.”
Pam, who has worked for the Association since 1992, has had a varied international career. Following a gap year studying German whilst selling newspapers outside Vienna’s Wien Mitte railway station and working as an au pair and English tutor in Vienna, and a brief spell at the Home Office Research Unit in the late 70s, Pam brushed up her French in the pharmaceutical/food (CPC Europe) and hotel industries (Hilton International European Office) in Brussels, before working at the NATO Headquarters in a number of posts, ranging from Electronic Warfare to Crisis Management, Exercise & Training.
In the late 80s, she moved to Bermuda to work in the Bank of Bermuda’s Investment Department, where she completed three quarters of her American Institute of Banking Diploma and several business management courses before moving on.

During this time, she trained as a hotline counsellor with the Bermuda Rape Crisis Centre, manning the phone hotline once a week; and was Vice President of the Alliance Francaise des Bermudes.
Some 15 years after her first gap year, Pam took another – spending 12 months in Boston, Massachusetts studying holistic therapy at the Massage Institute of New England and obtaining the American Massage Therapy Association certification. Pam returned to her hometown of Fleetwood in 1991 and began working for BADN (then ABDSA) in 1992, whilst running her own holistic therapy business in her spare time. As well as being BADN’s Chief Executive, Pam is Editor of the “British Dental Nurses’ Journal”, and also writes regular columns for “The Probe” and other dental publications.
Having been a member of Soroptimist International Fleetwood until it closed in 2004, Pam is now an active member of SI Blackpool & District; and was President
The Association of Dental Groups (ADG) membership is at an all-time high as a further five groups have joined over the last six months. Now a total of 28 of the UK’s dental groups, ranging from some of the largest groups of dental practices in the country to smaller providers make up the membership profile. The five new member groups to sign up recently are smaller, showing that even for groups with fewer practices, there are benefits to be gained from representation at policy level by the ADG, which is the trade association for dental group providers.
New dental groups:
1. Cwmbwrla Dentist Practice: one practice offering both NHS & private care
2. High Street Smiles: three practices offering both NHS & private care
3. Elegant Smiles Group: five practices offering both NHS & private care
4. Bessacarr Dental Practice: two practices offering both NHS & private care
5. SGA Services: three practices offering both NHS & private care
Dentsply Sirona, the world’s largest manufacturer of professional dental products and technologies, continues its support to Smile Train, the world’s largest cleft-focused organisation, starting a local partnership with Indian treatment centres, by providing funding for advanced training for Smile Train partner doctors, state-ofthe-art equipment donations to three Smile Train partner centres as well as donating oral health kits for cleft patients. This comes as the partners are announced Bronze winners of the 2024 Global Good Awards in the Community Partnership category.
of SI Blackpool 2012-2014. During her Presidential term, Pam organised various events – including a chocolate Tombola and a Meat Free Mondays piggy bank campaign – to raise money for her Presidential charities: Bridge2Aid and the Household Cavalry Occupational Casualties Fund. Another ad hoc project was the provision of filled backpacks for the Mary’s Meals Backpack Project – a number of dental companies provided children’s toothbrushes and toothpaste for inclusion in SI Blackpool’s backpacks.
Pam obtained the City & Guilds Licentiate in Management in 2005 and a Master’s degree in Business Administration in 2007. She is a Fellow of the Chartered Management Institute.
In 2012, Pam was awarded Outstanding Achievement Award at the Dental Awards, and the BADN Outstanding Contribution to Dental Nursing Award. Pam celebrated 32 years of employment with BADN in 2024 and lives in Fleetwood. n
Henry Schein UK has announced the launch of the new HenrySchein.co.uk, an eCommerce platform that demonstrates the company’s commitment to offering health care professionals a world-class online shopping experience.
Designed based on customer feedback, Henry Schein’s website now offers users a more personalised experience loaded with new features and enhanced benefits, including:
• Improved search capabilities
• Intuitive navigation
• Optimised features to make the shopping and buying experience simpler, such as:
• Redesigned product pages with multiple high-resolution images
• A new product comparison tool
• Ability to save products as favourites
• Easier ways to add items to the shopping lists and set up recurring orders
• New self-service and account management tools










■
■
■
















Afortnight before Christmas, I went to watch a gig performed by one of my favourite bands.
I say ‘I,’ I also took my wife – I’m never one to boast, but I believe I’m reasonably generous with regard to sharing the spoils of my hard-earned NHS pension.
I can’t name the band or the location of the concert for reasons which will become clear, but the evening’s entertainment was a just reward for a tough week in dental retirement. I mean, it was a double-bin week. On Tuesday the green recycling bin had to be put out before 8.00am and, on Wednesday, just 24 hours later, I had to put the garden waste bin out as well! It’s true what retired people had told me while I was still working – you have so much to do in retirement, you really won’t know how you fit it all in while you were still working. It’s exhausting to be honest. We arrived early and were first into the theatre auditorium and, aside from putting my watch and phone into airplane mode, I watched as people drifted in. I was just reflecting on the fact that even though the venue is local to where I practised, I rarely saw people we knew on these occasions, when I recognised a couple who walked in and sat a few rows in front of us, just ahead of the sound engineer’s station in the middle of the theatre. It took a couple of minutes of racking the cerebrum before it clicked that they were ex-patients - a married couple from a nearby town who followed me to a couple of practices over the years. But could I remember their names? Not a chance. I was appalled with myself, having had a very good relationship with them for nearly a quarter of a century. I always prided myself on knowing the names of all my patients when I was working, and if ever I saw patients in the streets, pubs, restaurants or, even once, in Sydney, I would go up to them and greet them by name.
I know the wife recognised me, giving a half smile in my direction, but I shamefully confess that for the rest of the evening, I deliberately didn’t look in their direction in case I caught their eye and they’d approach me and my cognitive deficiencies would finally be exposed to the world. I even directed my wife to go out a different door to the one we had come into the auditorium, despite it being much further away. She would have put it down to ‘Ollie just being weird again.’ Of course, I woke up the following morning with their names and the names of their two kids screaming at me from the core of my very being. My conscience was also yelling at me for being such an ignorant **** and not going over to say hello.
Should I have acted differently? Of course. I should have taken the decision to go over and say hello and hang the risk of social embarrassment when it became obvious that I’d completely forgotten that they had names.
But that’s me and decisions for you. It must be because it’s the end of the year – that time when endless annual reviews appear on the TV – that I descended the following morning into a review of my whole life in dentistry and, in particular, the really poor career decisions I had made
along the way. That’s pretty much been the theme of my retirement to be honest. Day after day. If I hadn’t done that, would this have happened? And would I have been a happier dental bunny?
At the time I was about to graduate, near the end of the 1980s, vocational training for prospective GDPs was optional. A number of my peers took up vocational training places but, having hit my 35th birthday a month or so before finals began, I convinced myself that I was a big boy and the idea of one more year under close supervision didn’t appeal. So, against the advice of a couple of the nice lecturers (they were scarce at my dental school), I went straight into a single-surgery practice in a designated new town, recently purchased by a lovely practitioner whose main surgery was based in the Cotswolds.
My boss, Simon (‘twas not his name), was a delight to work for. He even let me work in his main Cotswolds practice for a while. Simon had helped build up his practices by offering intravenous sedation and when I arrived and he asked, “Would you be comfortable giving IV sedation?” I naturally replied: “Yeah. I can do that.” despite the fact that Simon was some 45 miles away and could only lend a practical hand after an hour-and-fifteenminute journey.
In those pre-Poswillo days, it was perfectly acceptable to give IV sedation AND be the operator, and my first three sedation sessions (with oral surgery) went well. My fourth IV sedation session went badly wrong and, as a result, my career went off on a different geographical trajectory.
My patient was an incredibly nervous individual. She had refused referral to the local oral surgery unit and asked if I could remove her troublesome lower
retained roots and broken down lower eight because she trusted me.
When she came into my surgery, my patient seemed unusually calm and was happy to proceed. Her husband went into the waiting room while I struggled to find a suitable vein to put the midazolam into. I recall having to raise a vein by getting her to soak her hands in a warm bowl of water in the kitchen, since the antecubital fossa was having none of it.
The induction went terrifically well. I titrated the dose perfectly, until I got the classic halfclosed eyelids and we were away… that is, until I tried to access her mouth.
Would she open? No. Could I prise her mouth open? No. She slurred, ‘Go away,’ a number of times. After half an hour of trying to rouse her, it became a waiting game, since these were the days before flumazenil (the midazolam reversal agent) became available.
By this time, I was panicking. Though, mercifully, she was the last patient of the day. I rang Simon, who patiently described what to do.
“Pinch her ear on the very edge of her earlobe,” he told me. “Be ruthless!” If you’d heard that for the first time, you would have thought he was barking but, fortunately, that technique had been described to me previously by a consultant anaesthetist I had worked with during a month-long elective project at dental school.
“It’s a noxious stimulus,” he told me. “It’s a simple, effective technique.”
So, I did that – for about another half an hour. Actually, my nurse also took turns at pinching. I have a sneaking suspicion she enjoyed it. Eventually, at about 5.00pm (her appointment was at 4.00pm), the patient (a surgical theatre nurse) began to rouse. “Is it done?” she asked. I applied the mouth prop so I could at least put the
local in and we managed to complete the procedure and suture her within twenty minutes or so. When the patient was sufficiently with it to be dismissed with an escort, I went to bring her husband in. In the waiting room I double-checked that his wife hadn’t been on any other medication that we hadn’t been made aware of. “No,” he confirmed. “But she hasn’t slept AT ALL for the past three nights, worrying about today.” As soon as Jupes put the IV in, of course, it was Rip Van Winkle time.
I did no more IV sedation after that episode, referring anyone in need back to Simon. At the end of the afternoon, brutal realisation had slapped me in the face - I needed to be in the same building as other dentists for a while, at least until I had acquired enough experience to not panic when faced with the unusual. With reluctance, I resigned and found an associateship in a multi-dentist practice in another county. Suffice to say, other disasters were ubiquitous, but you can look forward to those tales another day. Since it was introduced as a crucial part of Continuing Professional Development in 2018, I was never averse to a bit of self-reflection (see above), but after the past few years and the calamities that the GDC have overseen, do you suppose they ever look back and think ‘No, shouldn’t have done that!’ No. Me neither. n
About the author ollie Jupes is the pseudonym of a former nHs dentist. He monitors dentistry on twitter X as @DentistGoneBadd

As we enter the new year, it’s time to start thinking about your goals for the 12 months ahead

As we start a new year, many dental professionals will reflect on their achievements while planning for the challenges ahead.
For practice principals, this is the ideal time to set ambitious targets – not just for personal growth, but to inspire the team and elevate the practice’s success.
why ambition matters
Ambition is more than setting a goal –it’s the driving force that pushes us to grow beyond our current limits. In dentistry, where patient care and practice management converge, ambition ensures we don’t settle for the status quo. It challenges us to improve, innovate, and explore new possibilities.
For me, ambition isn’t just about reaching targets. It’s about the ripple effect that determination can have on the people around you.
When a practice principal sets ambitious, clear, and achievable goals, it provides a framework that inspires the entire team. It creates a culture of shared purpose and commitment.
Defining your 2025 vision
The first step to setting ambitious targets is defining what success looks like for you and your practice. Is it growing your patient base? Expanding services? Enhancing your team’s skills? Whatever your priorities, ensure they align with your long-term vision and values.
For 2025, I am focusing on three core areas:
1. Empowering people: investing in the growth of your team is essential. This means creating opportunities for continuous professional development, mentoring junior staff, and recognising contributions to
build confidence and loyalty. Empowered teams drive better patient outcomes and foster innovation within the practice.
2. Enhancing patient experience: as expectations for care quality evolve, focusing on the patient journey is key. Whether through new technologies, streamlined processes, or improving communication, ambitious targets in this area will not only boost satisfaction but also strengthen your reputation in the community.
3. Business growth and sustainability: a successful practice is one that operates sustainably. For 2025, consider how you can increase profitability while reducing waste, adopting sustainable materials, and implementing smarter resource management.
Setting a vision is the easy part –execution is where the challenge lies.
To avoid feeling overwhelmed, break down each target into smaller, actionable steps.
For example, if your goal is to expand services, start by identifying what additional treatments would most benefit your patients.
Research equipment, training, and potential revenue before creating a timeline for implementation.
In my experience, involving your team in this process ensures that everyone feels invested.
Collaborative planning sessions not only generate creative solutions, but also strengthen the sense of unity within your practice.
Measuring progress
Ambitious targets require accountability. Regularly assessing progress keeps you on track and allows for adjustments where necessary.
Establish clear measurables for each goal. Whether it’s monthly revenue, patient satisfaction scores, or staff development milestones.
inspiring your team
Leadership in a dental practice extends beyond setting targets – it’s about inspiring those around you to aim higher and achieve more.
Share your vision openly and communicate why these goals matter. Transparency fosters trust, which is crucial for your team to work well together.
One of the most rewarding aspects of my role is seeing the impact that an ambitious practice culture has on individual careers.
In the past year, I’ve supported several team members in gaining advanced qualifications, empowering them to take on new responsibilities and build their confidence.
Their achievements not only benefit the practice but also reinforce the value of setting ambitious goals.
networking and collaboration
Ambition doesn’t happen in isolation. Collaborating with other dental professionals can provide fresh perspectives and open new opportunities.
Whether through local study groups, conferences and exhibitions, or online forums, engaging with peers can inspire ideas you may not have considered.
Throughout 2025, I encourage practice principals to explore partnerships that complement their goals. Connections can amplify the impact of your targets.
staying resilient
Ambition is daunting. Along the way, you’ll face setbacks and challenges. But it’s how you
respond to these moments that defines your success.
Building resilience – both for yourself and your team – is vital.
Celebrate small wins, learn from failures, and keep your focus on the bigger picture.
In my journey, one of the most important lessons is to embrace adaptability. Dentistry is constantly evolving, and ambitious targets should be flexible enough to accommodate changes in technology, patient needs, and market conditions.
Leading by example
Ultimately, positioning yourself as a leader in the dental profession means leading by example.
By setting and achieving ambitious goals, you not only elevate your own practice but also inspire others in the profession to aim higher.
This collective ambition drives the industry forward. It ensures that we continue to deliver exceptional care and make meaningful contributions to our local communities.
As we step into 2025, let’s commit to pushing boundaries, supporting one another, and striving for excellence. Whether you’re a practice principal or an aspiring dental professional, the new year presents a fresh opportunity to set your sights on success. n
For more
About the author polly Bhambra, practice principal at treetops Dental surgery.

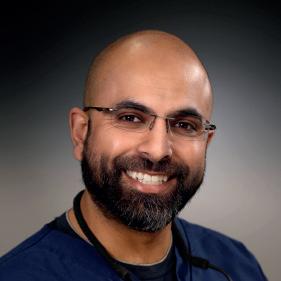
By Dr Colm Harney, Dentolegal Consultant at Dental Protection
Multiplication is the process of combining two or more quantities to find their total value or product. However, there’s one number that holds a unique significance in mathematics: zero.
Zero possesses distinct properties that set it apart from other numbers. One of its most notable characteristics is its behaviour when multiplied by other numbers. Regardless of the value of the other number involved, from one to Elon Musk-net worth numbers, that figure multiplied by zero results in zero.
This fundamental property is formally known as the zero property of multiplication.
We know that in life there are some actions that can negate everything else of meaning that we do, regardless of prior efforts, sunk costs or significance.
Gerald Ratner was the CEO of the Ratners Group, jewellers that shook up the UK jewellery market in the 1980s by aiming some of its products at the budget end of the market through a chain of high street shops. Although the chain was widely ridiculed and considered gaudy, tacky and cheap by other jewellers, many customers wanting to buy jewellery and not break the bank flocked to the stores,
turning Ratners into a household name throughout England and capturing over 50% of the UK’s jewellery market.
At the peak of his powers in April 1991, Ratner was invited to speak to the Institute of Directors about how he’d made his company so successful. The speaking engagement, which Ratner himself now refers to as “the speech”, has since gone down as one of the biggest blunders in business history.
When asked how the company was able to sell things so cheaply, he replied (later saying it was in jest): “People say, ‘How can you sell this for such a low price?’ I say, because it’s total crap.”
After the speech, the value of the Ratner Group plummeted by around £500 million, which very nearly resulted in the group’s collapse. This blunder became known as ‘doing a Ratner’.
Personal examples of multiplying by zero can be adopting healthy, wholesome living by eating organic, exercising and sleeping optimally – and then being casual about wearing a seatbelt while driving. Some ways of thinking might make it seem like this is a risk one could take on certain occasions. If we consider whether the multiplying by zero model
applies (from the risk of demerit points/ hefty fines to the risk of catastrophic injury) then maybe it’s a risk we should never take and, indeed, most don’t.
What about the practice of dentistry – where might some of the ‘zeroes’ lie in ambush?
We can have the best hands and do beautiful (by all objective measures) work, but if there is a disconnect between the understanding of the dentist and the patient in what outcome is to be achieved (mutually understood and agreed consent prior to treatment) – then it may well be a multiple of zero if the patient has not had their expectations met.
Alternatively, we might well have done the beautiful work and discussed all the material risks/gained consent – but when a lawsuit lands in the inbox years later and the records are scant or non-existent, then both practitioner and their indemnifier may be left holding ‘zero’, in terms of being able to mount a viable defence of the matter.
What about marketing and image? An architect-designed practice renovation backed up by a lavish spend on optimal branding and SEO might lead to many new patients contacting the practice. But if there is a staff member consistently
Does a rising wave of anti-fluoride
the need for a national fluoride
In recent months, the resurgence of antifluoride rhetoric has sparked concern among public health professionals. Across the Atlantic, the narrative has gained traction with figures like Robert F. Kennedy Jr., who, as a prominent political figure in the United States, has been vocally critical of water fluoridation. His claims, including assertions linking fluoride to various health issues, have amplified misinformation and driven policy debates in the US. While the structural differences between the American and British healthcare systems mean such policies are unlikely to directly affect the UK, the broader implications of anti-fluoride sentiment cannot be ignored. As dental professionals, it’s critical to examine whether this growing wave of propaganda necessitates a proactive response in the form of a national fluoride campaign. This article explores why such a campaign may be timely, the benefits it could bring, and how it can counteract the pervasive spread of misinformation.
why misinformation is a problem for the UK
In the United States, decisions about water fluoridation are made locally by municipalities or states, with public opinion often playing a significant role. By contrast, in the UK, these decisions are based on NHS-backed scientific evidence and include local public consultation as part of a structured, centralised process. Despite this, the cultural and informational closeness between the UK and the US allows anti-fluoride rhetoric to cross borders, particularly through social media platforms. A simple search for ‘fluoride’ online unveils a torrent of conspiracy theories and
pseudoscientific claims, many of which are alarmingly persuasive. Social media platforms have become fertile grounds for misinformation. Hashtags such as #fluoridefreetoothpaste amass thousands of posts, while influencers tout the supposed benefits of fluoride-free products with little regard for evidence-based science. What is particularly concerning is how these platforms blur the lines between credible information and outright falsehoods. In these spaces, it’s not the accuracy of a claim that determines its success, but how loudly and widely it is shared.
The spread of misinformation and antifluoride rhetoric can severely undermine the UK’s structured, evidence-based approach to water fluoridation decisions. As social media allows pseudoscientific claims to gain significant traction, they can erode public trust in the science supporting fluoride’s benefits. This, in turn, could distort public consultation processes, leading to decisions that are influenced more by fear and misinformation than by the robust, scientific evidence backing fluoridation. Ultimately, this undermines the integrity of the decision-making process and jeopardises public health initiatives aimed at reducing dental decay.
why a pro-fluoride campaign matters
The history of fluoride use is one of the most compelling success stories in public health. Fluoride has significantly reduced the prevalence of dental caries, improving quality of life and preventing costly dental treatments. Yet, the effectiveness of fluoride is contingent on public understanding and acceptance.
‘doing a Ratner’, with poor interpersonal skills and rude demeanour on initial patient contact, then all the efforts and pounds may degrade to zero. We all know the customer satisfaction statistics – one happy customer will, on average, tell one other person, whereas one dissatisfied customer may tell up to nine or 10 people. Cross infection control breaches also have that catastrophic ‘multiplication by zero’ potential. Consider the practitioner with the fabulous work, happy patients, great consent/records and bustling practice – it can all come unstuck very quickly if the regulator finds cross infection control breaches. It may shut the practice and suspend the practitioner (at least until issues are rectified to their satisfaction) in order to uphold the overarching duty to ensure public safety.
When we evaluate risk, we need to consider not only likelihood/frequency of occurrence but also consequences if it were to occur. The ‘zero’ model focuses on the consequences. Just because the likelihood of something happening is very slim, it does not mean that it shouldn’t be front of mind in risk assessment, especially where the possibility of the ‘multiplication by zero’ effect may be at play. n
A national fluoride campaign would serve several crucial purposes. Not only would it provide clear, evidence-based information – a campaign can also debunk myths and reassure the public about the safety and benefits of fluoride. By engaging with social media and other digital platforms, a campaign can counteract anti-fluoride narratives where they are most pervasive.
A well-crafted campaign would help, support and empower us as health professionals to confidently address patient concerns, armed with accessible resources and messaging.
The ultimate outcome is acceptance over the benefits to expand water fluoridation to more regions in the UK. We believe this would reduce oral health inequalities, particularly in underserved communities.
from the past & present
The UK has not seen a high-profile fluoride campaign in years, despite fluoride’s pivotal role in transforming oral health outcomes. Revisiting this strategy could help counter the growing social media-driven misinformation that reaches millions daily. The availability of fluoridefree toothpaste on mainstream platforms like Amazon and high street retailers underscores how easily misinformation translates into consumer behaviour.
Recent statistics reveal that social and oral health inequalities persist in the UK, with children in deprived areas experiencing higher levels of tooth decay. This is a stark reminder that public health campaigns must address not just misinformation but also the systemic barriers to oral health.
the path forward
A national fluoride campaign would require collaboration between the government, dental professionals, and oral health manufacturers. With adequate funding and strategic messaging, such a campaign could not only highlight the scientific evidence supporting fluoride, but it could address the economic benefits of reducing dental decay through fluoride use.
As professionals, we must advocate for action before misinformation gains further ground. The stakes are too high to remain passive. Fluoride has been the single most impactful intervention in reducing tooth decay, and its benefits are unequivocal. The time has come to reaffirm its value to public health through a coordinated and impactful campaign.
The rising tide of anti-fluoride propaganda poses a clear challenge, but it also presents an opportunity. By addressing misinformation head-on and promoting the undeniable benefits of fluoride, we can ensure that evidence, not ideology, shapes public health policy and consumer behaviour. For the UK, a national fluoride campaign shouldn’t be a luxury – it’s a necessity. n
About the author
Karen Coates, oral Health Content specialist at the oral Health Foundation, and RDn

The British Society of Periodontology (BSP) states that periodontal disease is the sixth most prevalent disease in the world, affecting over half the population of the UK. Dental professionals are imperative in the diagnosis, monitoring and treatment of the disease, but it is the patient who ultimately has the biggest impact on its cause and progression, as a result of their oral hygiene and habits.
One of the most important roles the treating clinician has is therefore making sure a patient is aware of the disease and its consequences, and what steps they need to take in their home dental care to prevent or manage it.
Despite being such a common condition with clear processes for diagnosis and management, claims involving periodontal disease are some of the most complex to investigate, and most expensive to settle.
DDU claims data
Over the period 2009-2023, an average of 58% of claims about periodontal disease notified to the DDU needed to be settled. In 2023 that figure was 64%. Every year from 2009-2023, a higher proportion of periodontal claims required settlement than any other type of dental claim we deal with.
• Be prepared to offer referral to a specialist if the patient’s condition does not improve despite treatment.
Periodontal e-learning
In conjunction with the BSP, the DDU has developed a free CPD e-learning


The average settlement value of a periodontal disease claim is higher than that of any other type of settled dental claim. In 2023, £2.2 million was paid out in settled claims involving periodontal disease, in both damages and the claimant’s legal costs and disbursements.
In the last few years, the DDU has begun to see a reduction in the number of periodontal disease claims notified, but it is too early to know if it represents a trend. The good news is that, if DDU members face a claim, our claims handlers and dento-legal advisers can offer expert support. Because we’re staffed by dentists with real-life experience of exactly these sorts of issues, we understand how stressful the process is and the importance of mounting a maintainable defence of your position.
Minimising risks
There are also steps you can take to reduce the risk of periodontal claims. The DDU has published a full list of recommendations in our latest DDU journal which include:
• Follow available national guidance to make sure your treatment is evidencebased – for example, the BSP’s guidance on the Basic Periodontal Examination (BPE), 6-point pocket charting, radiographs and recall periods.
• Record all your examination findings, diagnosis and recommended treatment in the patient’s clinical notes.
• Explain to the patient what periodontal disease is, if they are at risk and how they can protect themselves. Emphasise the need for good oral hygiene and more frequent visits to the hygienist, as well as the importance of stopping smoking. Make a detailed note of the conversation and any information leaflets or other resources provided.
course for dental professionals to improve their understanding of the treatment and management of periodontal disease.
The course covers both dento-legal and clinical aspects, and offers three hours of verifiable CPD. Sign up at: https://tinyurl.com/DDU-BSP


About the author
Greta Barnes, Senior Claims Handler at the Dental Defence Union.



































































Effective daily plaque control is key to tackling the causes of gum disease and stopping gingivitis in its tracks.

For patients, however, changing their oral health behaviours can be hard.
has developed a range of tools and resources for dental professionals to help power up your patients’ gum health.

Over 80% of UK adults show signs of gum disease.1 As dental professionals, you know that effective daily plaque control is key to tackling the causes of gum disease and stopping gingivitis in its tracks. Haleon recently hosted a panel of dental experts to discuss the barriers dental professionals face in encouraging behaviour change for improved gum health. Led by Professor Tim Newton, President of the Oral Health Foundation, the panel explored practical strategies for motivating patients.*
The experts included:









The panel discussion ranged over a series of different topics, with the panellists bringing their knowledge and insight to the conversation.
Topics discussed included:
Framing the issue
The role of the patient
Practical approaches
Working with commercial organisations Behaviour change


Listen to the conversation at Haleon HealthPartner
“BLEEDING GUMS IS SO NORMALISED.”
Dr.


“I THINK THERE’S A LACK OF UNDERSTANDING FROM A VERY YOUNG AGE OF ALL OF THE BENEFITS OF HAVING A HEALTHY MOUTH.”
Neha Mehta Rhiannon Jones












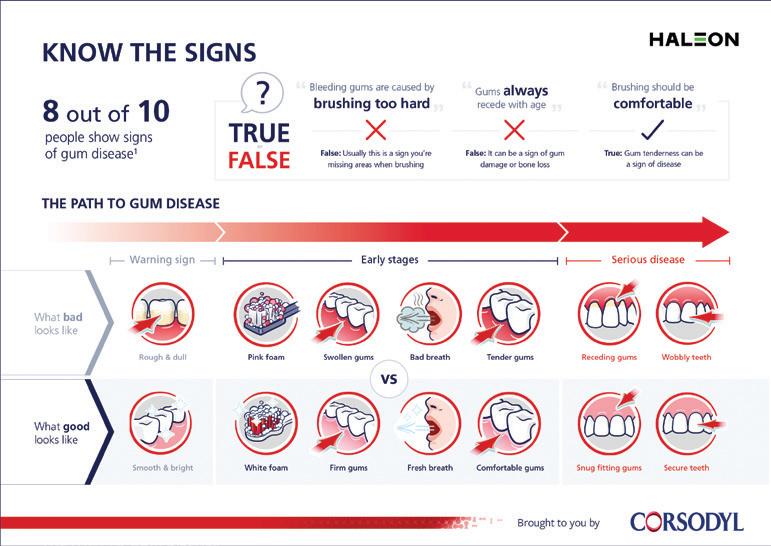





Corsodyl has developed a range of tools and resources for dental professionals to help power up your patients’ gum health.
This includes our in-surgery discussion guide, designed to support conversations about simple steps to better gum health, and to help you explain to patients the potential impacts of gum disease on overall health.
Find out more at Haleon HealthPartner

simon Cosgrove, Dental Regional Manager at Wesleyan Financial Services, shares his top tips for a strong financial start in 2025

January is the traditional time of year for the making, and almost inevitable breaking, of resolutions. The wellintentioned shiny new gym membership or a nutritious new diet is often dashed on the cliff face of the return to a normal routine.
However, financial decisions don’t have to suffer the same fate and can lead to actual life-changing outcomes.
Last year’s Autumn Budget announcement changed the goalposts in several areas for dentists and, now that the dust has settled, January is an ideal time for planning for the future based on the new landscape. There are still a couple of months until the end of the tax year and we have all had time to reflect on how the changes will affect both dentists individually and practices collectively.
The freezing of income tax bands until 2028 will mean that more dentists may find themselves being pushed into higher tax bands as their incomes increase. Making a resolution to reduce taxable income is a good way of trying to combat this.
Pension contributions are one of the most effective ways of reducing your taxable income. As an example, if you make a £1,000 gross contribution to a pension, your taxable income is reduced by £1,000. As well as the obvious long-term benefit of helping save to meet your retirement objectives, the immediate benefit of reducing your taxable income can help to reduce your tax bill. If you earn over £100,000, this can also
help to regain some or all of the Personal Allowance that you may have lost by earning over that threshold, depending on your level of income and the level of contribution.
Remember, any contributions to a pension can be made either through lump sums or monthly, so taking advice on setting up a monthly and/or lump sum contribution to a pension is a resolution that will pay dividends over the years, both before and after retirement.
As pensions are so tax efficient, there are limits to how much people are allowed to contribute each tax year. The approach of the end of the tax year at the beginning of April can provide a little more scope for those who have fallen behind on pension contributions to use their allowances over two tax years, which is also the case with the annual £20,000 ISA limit. Unused pension allowances from the three previous tax years can be utilised, whilst ISA contributions must be used by the end of a tax year or are then lost.
Another significant change that the Budget imposed was the increase in Employer National Insurance contributions. For dental practices, staff costs are among their biggest outgoings, so this increase will squeeze the profits of practices and could potentially reduce take-home pay for principals. It will also reduce the ability of practices to invest in their facilities and teams, which means fewer opportunities to grow, increase capacity and offer more services.
Here, a resolution for principals to consider their business finances as well as their personal finances would be sensible. Having a clear understanding of the practice’s finances, with an accurate assessment of anticipated costs for upcoming years, will ensure that the practice remains on solid ground. Considerations, such as the impact of the death or serious illness of a principal of the practice, should not be discounted either, as this can lead to significant problems should either scenario come to pass.
Additionally, in my experience, many practices assure their associates that they will source and pay for a locum if the associate is unable to work through accident or sickness, to maintain a good working relationship. This new stretch in practice finances may mean that this is now a less attractive solution for practices. In most associates’ contracts, it states that it is the responsibility of the associate to both source and pay for a locum, so legally practices would be within their rights to insist that the contract is followed and that the bill for the locum lies at the associate’s door. Considering an insurance policy for the associate to provide the funds for this can protect the financial security of both associates and practices.
Resolutions to review both personal and business finances with a specialist adviser is not something that should just be saved for January (or after a Budget). People’s lives and objectives change over the years, so
regular specialist financial reviews should be on everyone’s ‘to-do’ list at least once a year.
speak to a specialist Book to speak to a dental Specialist Financial Adviser at Wesleyan Financial Services by visiting our website at wesleyan.co.uk/dentists or calling 0808 149 9416.
Please note: Charges may apply. You will not be charged until you have agreed to the services you require and the associated costs.
Learn more about the charges at wesleyan.co.uk/charges.
Tax treatment depends on your individual circumstances and may be subject to change in future. n
Wesleyan Financial Services Ltd (Registered in England and Wales No. 1651212) is authorised and regulated by the Financial Conduct Authority. Registered Office: Colmore Circus, Birmingham B4 6AR. Telephone: 0345 351 2352. Calls may be recorded to help us provide, monitor and improve our services to you.

about the author simon Cosgrove is a Dental Regional Manager at wesleyan Financial services, guiding a team of Dental specialist Financial advisers to support dentists, their families, and their practices with financial planning to secure their financial future.





The couple that helps you to achieve even better oral hygiene

FLEXI
• The special FLEXIBLE HANDLE makes it possible to angle the handle to achieve better and easier access to all interdental spaces.
• The non-slip handle ensures good grip even when fingers are wet.
• All brushes have plastic coated wire. This ensures no metal is in direct contact with teeth and gums, thus making them much more comfortable to use and preventing dental injuries.
• 11 sizes ensure that all needs are covered.



TANDEX PREVENT Gel
• Strengthens the enamel and has an anti-bacterial effect.
• 0.12% chlorhexidine and 900 ppm fluoride.
• The consistency combined with the needle shaped tube end make it easy to apply directly on the FLEXI brush and use wherever needed.
• Pleasant taste of peppermint.
• No alcohol or abrasives.
With the festivities now a somewhat distant memory, normality is returning to life inside and outside of dentistry. However, the New Year presents a good opportunity to reflect on the various daily processes in the dental practice and ensure that high standards are maintained throughout. Decontamination workflows should be among those reviewed – it never hurts to double down on health and safety protocols for patients and staff alike.
All essential requirements and best practice guidelines for infection control workflows in dentistry are set by HTM 01-05 and SDCEP. Dental practices are expected to have a policy in place that details how they are moving beyond essential requirements and towards best practice standards. At present, there is no deadline for attaining best practice, given that some of the recommendations will be more challenging for some practices to achieve than others – especially smaller practices with less available space.
The plan to meet best practice should be realistic for the business, outlining key steps that would need to be taken to optimise processes. In England and Wales, for example, these may include the purchase and implementation of equipment, or changes to the design of the practice, for example. It should cover three main areas of the practice: the instrument cleaning and sterilisation workflow, the decontamination environment and the storage of reprocessed instruments.
The first step towards best practice will be largely dependent on the physical space available within the practice. Establishing a completely separate and dedicated room for decontamination minimises the risk of re-contaminating instruments or infecting staff/patients via aerosol transmission. The usual dirty-toclean workflow should be employed.
Other best practice standards are simple to achieve – just implement a washer disinfector within your instrument decontamination process. Why is this best practice? Because the washer disinfector offers a validated, automated and repeatable way to clean instruments prior to sterilisation. The variance in and subjectivity of manual washing are eliminated, and the risk of needle-stick injuries is also reduced for staff due to less handling of sharps. Washer disinfectors are already mandatory in Scotland for all these reasons.
With regards to storing instruments once reprocessed, finding an area separate from the clinical treatment area is the goal. This also further reduces the risk of instrument re-contamination.
Overcome barriers
There are a few potential barriers to best practice that may be preventing some dental teams from optimising their processes. The first and most obvious is the perceived cost of making changes or purchasing equipment. However, this should be considered an investment in the quality of patient care delivered, as well as
in the business. Not only does complying with best practice ensure the highest safety standards for everyone frequenting the premises, but it will also future-proof your workflows – no deadline exists yet, but it’s not a stretch to predict that there will be one in the future.

This is especially true when it comes to introducing new equipment like a washer disinfector. Plus, it is simple to maximise your return on investment. All you need to do is choose a robust machine that has been built to last by a reputable manufacturer. From here, it’s important to look after the equipment with the necessary in-practice testing and maintenance, as well as annual servicing and validation completed by an appropriately trained external professional.
The entire process from purchasing a reliable washer disinfector to installing and maintaining it can be made simple by working with a leading expert in decontamination such as Eschmann. All our equipment is highly effective, reliable and robust, and comes with exceptional technical support and customer service from a team of 50+ Eschmann trained engineers nationwide. The Care & Cover servicing package also affords access to unlimited breakdown cover, Annual Validation and Pressure Vessel Certification, unlimited Eschmann parts and labour. In addition, we offer enhanced CPD user training and can advise on achieving best practice.
a journey
No matter where your practice is in its journey towards best practice, it is important that you have a plan in place to achieve it in the future. This might involve bigger changes for some businesses than others, but is achievable for all with the right preparation and mindset.
Health and safety is already a priority in UK dental practices. With the additional achievement of best practice, patients and staff alike can gain confidence in the quality of service you deliver.
Want to find out more about achieving best practice in decontamination? Contact Eschmann at www.eschmann.co.uk or by calling 01903 753322 n
about the author
Nicky Varney, Senior Marketing Manager at eschmann.
Choosing sterilisation, disinfection and decontamination methods that effectively prevent and control the spread of pathogens in accordance with HTM 01-05 is an essential responsibility of every practitioner. With exposure to blood, saliva and the oral cavity – a natural habitat for a large number of microorganisms – the dental setting presents a high number of opportunities for infection.
Dental handpieces can be particularly difficult to sterilise due to the complex internal structures which are considered particularly prone to contamination. To maintain a safe practice and prevent crosscontamination, a dental autoclave is an essential commodity for any busy practice, ensuring all instruments that could present a risk are safe for reuse.
Due to other pressures on the modern dental practice, choosing the right steriliser will increasingly involve other considerations, such as energy consumption, speed and efficiency, and intuitiveness/ease of use. Ideally, any member of the dental team should be able to reprocess handpieces quickly and effectively to meet appointment schedule demands as well as the needs of patients.
The main infections that can be contracted in the environment are caused by bacteria, mycobacteria, fungi and viruses and prions – all of which can present a real danger to health. Contamination can be bidirectional, during treatment and afterwards, from patient to clinician and vice versa, and can be transmitted by inhalation, injection, ingestion, or absorption through the mucosa or skin.
Potential bloodborne diseases include human immunodeficiency virus (HIV), hepatitis B virus (HBV) and hepatitis C virus (HCV). Due to gingival bleeding, saliva should be treated with the same caution as blood. Without the proper mitigations in place, pathogens also have the potential to be transferred from patient to patient through shared access to poorly disinfected environments, as well as inadequately decontaminated devices and instruments.
autoclave types – a summary
The steriliser of choice must be fit for purpose in terms of consistent infection control.
The ‘N’ type autoclave is appropriate for flat, unwrapped, solid medical tools. It is not suitable for sterilising hollow, porous or wrapped loads, but may be useful if your practice has a large number of solid instruments to sterilise.
to keep free from infection. Once they have been cleaned and lubricated, the sterilisation process is essential to ensure they are free from infection.
‘B’ type sterilisers are considered the ideal autoclave for managing these instruments. They use a pump to create a vacuum, enabling a high-pressure environment at a temperature too high for microbial survival. The resultant pressure when introducing boiling steam into the vacuum leads to an increase in the boiling point of the water. In addition, the sudden pressure-change creates very hot steam at high speeds, forcing heat through the instrument, penetrating the interior more effectively than other methods.
Energy efficiency is a vital concern both to save money and to reduce the carbon footprint of the operation. Of equal importance to any busy practice will be the speed and efficiency of the workflow. Sterilisation must also be validated, tested, documented and audited. Sterilisers that integrate these considerations, offering ease of use as well as speedy, effective function, are hugely beneficial for the efficiency of every practice.
Choosing the right autoclave for the practice will also require consideration of the appropriate capacity and size needed for regular use. Do you have limited space, and need a compact design? Or is your operation busy and large enough to warrant a larger unit? Do you need specialised support if things go wrong? If so, is this provided by the manufacturer?
W&H has a range of sterilisers, in compact, large and extra-large sizes to meet the needs of every dental practice. The Lisa steriliser from W&H, for example, provides both ‘S’ and ‘B’ cycles for flexibility, and offers the operator intuitive control for comprehensive and reliable sterilisation. EliTrace automates the vital audit function, meaning every instrument is automatically logged and tracked, so practices know where every instrument is in its decontamination schedule. Eco Dry+ technology also reduces the cycle time, optimising energy consumption for a more cost-effective sterilisation process. And ProService from W&H provides additional peace of mind, with total technical support.
Infection control is an important concern for all dental professionals, as procedures are carried out in an environment that exposes staff and patients to significant risk.

The ‘S’ type autoclave is considered the intermediate choice between ‘B’ and ‘N’ type options for dental practices, and can be highly useful for sterilising porous, bagged products, although it can’t process textiles. The S class autoclave usually has a range of drying cycle options, and is generally very quick and straightforward to use, but not considered optimal for hollow instruments. Dental air turbines and straight and contra-angle handpieces can draw in contaminants during their operation. The small parts and long, narrow cavities make these instruments particularly challenging
Choosing a high-quality steriliser represents an opportunity to invest in the safety of your practice, as well as its overall efficiency.
To find out more visit wh.com/en_uk, call 01727 874990 or email office.uk@wh.com n
about the author
Jon Bryant, National Sales & Marketing Manager,
W&H UK.


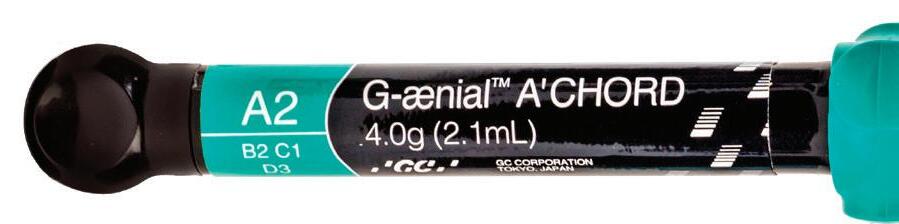
About one fourth of people are unhappy with their smile, which has a considerable psychosocial impact. Many could benefit from subtle, minimally invasive changes to their teeth that ultimately greatly improve the overall smile aesthetics. G-ænial A’CHORD and G-ænial Universal Injectable are the excellent partners herein. With remarkable shade matching, gloss and viscosities for each preferences and indications, even the highest aesthetic demands can be fulfilled.


Restorative dental care has seen a substantial shift in recent years, as professionals look to employ resin-based composite (RBC) restorations in their care more often. This could be because of the advancement of the aesthetic potential of such solutions, as well as the push to reduce amalgam use – dental professionals across the EU will have their hand forced with the amalgam ban beginning from 1st January 2025, and practitioners in the UK will likely see disruption and higher costs because of the resultant pressures on supply chains.
Many clinicians currently use RBC solutions and will likely use them more frequently in the future, which requires appropriate management of any waste created. It’s important to delve into the current understanding of the health and environmental risks of RBC use, and waste. With this knowledge, best practice workflows when discarding the material in daily care are possible.
risk management
RBC is a preferred restorative material due to its aesthetic appearance and ability to blend in with the existing dentition. In addition, it can withstand high compressive forces – necessary to bear occlusal contacts – leading to long-lasting results. As such, the material often replaces amalgam as a go-to for dental fillings.
Amalgam has been criticised as an unviable restorative material for the future of dental care, partly due to the impact of mercury on the environment. If improperly wasted, the resource could contaminate water sources, harm aquatic organisms and work its way into the food chain. If consumed in large quantities, individuals may experience reproductive problems, and liver and kidney damage.

There are issues with the alternative. RBC breaks down into microparticles when shaped, finished and polished. These microparticles can reach water sources if discarded improperly, acting as direct pollutants that can also attract and bind to biotoxins known as persistent organic pollutants (POPs). It is thought that POPs bonded to microplastics can enter the food chain through bio-accumulation, and a variety of aquatic animals have been seen to ingest microplastics. The issue of microparticle production is only exacerbated with the increased use of highly polymerised RBC for the creation of crowns, inlays and onlays through reductive CAD/CAM milling, which creates large volumes of microparticle powder.
It is important to consider the general breakdown of RBC restorations and materials in landfills, in greater volumes than ever. This occurs through the process of elution, where monomers within the RBC structure are released into a solution – typically water in landfills and the environment. The chemical durability of the composite material is then compromised, creating risks for environmental pollution.

The monomers that are commonly released through elution include bisephenol A-glycidyl methacrylate (BisGMA), urethane-dimethacrylate (UDMA) monomers and, most prominently, triethylene glycol dimethacrylate (TEGDMA). Previous studies have recognised that TEGDMA has a cytotoxic effect and can affect markers of oxidative stress, making it a threat to living beings that it come into contact with it in the environment.
conscious waste management
Unlike amalgam waste, RBC is not mentioned in Health Technical Memorandum 07-01 (HTM 07-01). However, RBC is generally designated as municipal solid waste, as it does not present the active infectious hazards of many other medical items, which may otherwise be placed in yellow or orange waste streams. This creates some issues; the typical disposal methods of municipal waste include recycling, which is preferred, or discarding the items in landfills. Here, the aforementioned risks of environmental contamination may arise.
A third option, energy from waste production, may be suitable. Whilst this process, which typically requires the combustion of waste items, produces carbon content, it is still preferable to landfills where carbon release is inevitable. Energy from waste plants can create excess energy, besides the quantity needed to run, which can support the push to reduce fossil fuel use. RBC disposed of by this method has little chance of microparticles and eluted monomers reaching key areas of the local environment.
Dental practices can ensure their RBC is managed safely and securely, through being directed towards energy production from waste processing facilities or recycling. To do this, they should work with a specialist waste management service such as Initial
Medical. With decades of experience in healthcare and dentistry, Initial Medical can help you manage your municipal waste workflows safely, and with simple and organised waste segregation. The team is on hand to provide advice and insight on how to optimise your waste workflows and ensure your practice better protects the environment.
RBC creates some risk to the environment if improperly managed in the waste workflow. Clinicians should avoid landfills where possible for this waste material, including any contaminated packaging, and work to protect the environment.
To find out more, get in touch at 0808 304 7411 or visit www.initial.co.uk/medical n
about the author rebecca Waters has worked in the healthcare sector for the past 20 years and earned a BSc chemistry (Hons) prior to joining rentokil initial in 2003. She works within the research and Development team and keeps up-todate on all changes within the clinical waste management industry, as well as the specialist hygiene and infection control industries, and is an active member of the ciWM and HWMa. Following roles as an analytical chemist and Hygiene chemist, she has worked in a variety of leading marketing roles since 2006, making her an expert within the industry. She is a Fellow at the chartered institute of Marketing, an FciM. rebecca loves spending time outdoors and in the water – whether walking, camping, or swimming – and completed a focus on environmental studies during her university degree. She is proud to be pushing a sustainability agenda throughout her work.

Missed appointments cost dental practices thousands of pounds per year. To address this problem, House of Dental, a mixed practice in Hinkley, Birmingham, set Black Ivy Design a brief to improve attendance by transforming the practice into a striking, comfortable and welcoming environment that referenced the feel of a hospitality or hotel setting – all while ensuring the space was relevant for private and NHS services.
Leanne Armstrong, Founder and Creative Director of Black Ivy Design, said: “With an even share of NHS and Private patients, it was important for House of Dental that the space should feel both accessible and subtly luxurious. They wanted the design to convey a sense of serenity, while also functioning perfectly as a busy dental practice.
“The works had to be carefully planned to ensure House of Dental remained fully operational to NHS patients throughout the process,” Leanne continued. “As much consideration had to be given the patient’s flow throughout the practice as to staff productivity.”
A timeless design concept
The interior design was centred around creating a relaxed patient experience rather than aligning with trends that might date. Leanne explained: “To put patients at immediate ease, the reception area was decorated with neutral off-white tones and marble, complemented by greenery and centrally placed dark seating. A contrasting partition with lit signage at the entrance added a touch of luxury.
“The aim was to create a more open, modern, and inviting space for patients and staff. This was achieved by extensive work, including the removal of some walls and the relocation of the staircase encased with glass. A balcony provided even more natural light to add to this sense of expansiveness.”
Judicious use of natural wood, stone and marble as well as a polished mineral composite enhanced the hospitality feeling. Feature walls with decorative mouldings painted in the same warm colours as the walls, added subtle visual interest. A few selected artworks were chosen to reflect the whole ethos of the design, featuring harmonious work to make people feel relaxed and at ease.

“These elements all work together to create a bright, welcoming, natural space with a sense of openness,” added Leanne. “They produce a refined aesthetic that feels comfortable yet elevated, helping to make patients feel at home.”
Treatment rooms – total function, enhanced relaxation and comfort
To move away from the traditional white clinical look while ensuring every surface was easy to wipe down for optimal hygiene,


polished marble was complemented by warm lighting and dark cabinets. Like the reception area, the layout of consulting rooms was planned to maximise the use of natural light.
Tactile finishes, signature scents and a sound system were incorporated to contribute to a relaxing sensory experience.
TV screens were installed in ceilings to help distract patients who might be feeling anxious or uncomfortable during long procedures. A screen was also installed at the end of the dental chairs in each surgery to make it easier to show patients their records, x-rays or to help them visualise or understand their treatment options.
Black Ivy Design meticulously planned each phase of the project to minimise disruption. This included scheduling construction activities during out-of-hours and creating temporary partitions to maintain a safe and welcoming environment.
By collaborating closely, both client and designer ensured patient care was


prioritised throughout the renovation. Temporary adjustments were made to operations, including reconfiguring patient flow and maintaining clear communication with staff and patients about any changes. This partnership allowed the dental practice to maintain high standards of care while progressing with the project.
The importance of excellent project management
Every project undertaken by the Black Ivy Design is centred around the unique needs and identity of the client. The studio offers total design and build support – from initial consultation through to realisation. House of Dental said:
“Working with Black Ivy Design has been a great experience. Their professionalism made the process smoother and more manageable. The transformation of our practice has exceeded expectations, and we’re thrilled with the results.”
“This project was exciting for us because of the challenge to create a beautiful, serene space that functions well as a clinical environment,” Leanne concluded.
“We are extremely proud of the result. The renovation has enhanced the overall patient experience, providing a calm and spacious environment that supports our commitment to excellent dental care. The engaging design has meant patients are more likely to attend appointments and feedback has been excellent.”
For more information about Black Ivy Design, visit www.blackivydesign.co.uk













Every day, frontline staff are required to ensure patients in need of an emergency appointment receive appropriate attention. Patients experiencing acute problems, like dental trauma, severe dental or facial pain, may require immediate treatment from a dental professional. However, prioritising appointments according to the urgency of cases requires a great level of skill and empowerment, which is not always present within the frontline team.
Reception staff, practice managers and/ or dental nurses are often responsible for the diary. They have a huge effect on the smooth running of a practice, and are tasked with ensuring patients are greeted appropriately, and that their expectations are met, whether in urgent need of attention or a routine check-up. Getting the balance right can be tricky.
Although recommended to assist in effectively prioritising care, there is currently no requirement for members of the wider dental team to undertake any formal training in triage. As well as potentially risking the safety of patients, this can lead to frustration – for patients and the team alike.
From covid and beyond
The recent Covid-19 pandemic forced the introduction of different processes for allocating emergency appointments, allowing for the remote triaging of patients. New technology and innovative workflows offered clinicians new opportunities for patient communication, and new approaches to patient prioritisation. Empowering the frontline dental team with flowcharts and guidelines during COVID highlighted the benefits of effective triaging in the management of emergency patients across the country. The need for triage is no less important post-Covid. In 2021, it was recognised that the backlog of treatment delayed during the pandemic would lead to a ‘tsunami’ of urgent dental problems. Indeed, in many areas, patient need currently outstrips provision, which reinforces the importance of adopting effective triaging processes across the dental team. With appropriate training, frontline staff can contribute more formally to the process of prioritising the right patients.
empowering the team
Receptionists, dental nurses and practice managers have an important role to play in urgent dental care. The addition of multiple unscheduled appointments to the diary can add a great deal of added strain to a dental professional’s working day. Research has shown that time pressure is one of the major causes of stress for dentists, and a common cause of conflict between clinicians and reception staff.
Emergency appointments can be short and are often double-booked, with limited time for the dentist to successfully diagnose and provide treatment for these patients.
However, frontline staff also feel the pressure. In a pre-Covid study, a number of dental nurses reported they were under strict instructions to ensure all patients were allocated non-scheduled appointments, regardless of the number of appointments already in the diary.
Empowering staff has long been shown to improve engagement levels and performance and a study on health care workers commissioned during Covid showed that empowering frontline staff also reduced stress levels and enhanced communication. To truly empower staff, they must be provided with the right knowledge and skills.
From triple a to complex protocols
With the appropriate training, tools and guidance, experienced dental nurses and reception staff can safely follow decision-support flowcharts to determine the urgency of a patient’s problem and triage accordingly. We already know this works. During the pandemic, guidelines and flowcharts produced by NHS England and Scottish Dental Clinical Effectiveness Programme (SDCEP), for example, allowed many patients to be successfully managed remotely by the ‘AAA’ approach of advice, analgesia and antibiotics.
Patients may present as an emergency patient for a variety of reasons, from trauma, severe pain, or orofacial swelling, to a lost crown or filling. These problems have a range of approaches and complexities, and the time required as well as the urgency of treatment for those problems can vary significantly. By following appropriate triage protocols, more information can be gathered from patients to treat them within the correct timeframe, with the right appointment length for their condition.
All members of the dental team should receive formal training to assess and interpret symptoms, assign urgency to clinical need, and provide simple, practical advice regarding oral hygiene and analgesia. For example, Orajel™ is a great oral analgesic to recommend to patients needing rapid relief from dental pain. Patients can apply Orajel™ directly using a clean finger or swab up to four times daily, giving them targeted control over pain management. This improves patient comfort while they wait for an appointment to see the dentist, relieving some of the pressure on staff.
Implementation of a formal dental triage system can help frontline staff manage diary pressures and patient expectations. Awareness of what constitutes a true emergency, and how long an emergency appointment is likely to last makes more efficient use of surgery time. Gaining the confidence and skills to improve patient comfort, and contribute to positive outcomes, can lead to a happier, more empowered team.
For more information, please visit www.orajel.co.uk n
tart reading through the General Dental Council’s “Standards for the Dental Team”, and it’s not long until you find the first mention of radiography. Standard 1.5 notes that clinicians must treat patients in a hygienic and safe environment, which necessitates reading up on the laws and regulations that will affect the practice – including legislation relating to radiography. Keeping up to date and informed on the regulatory requirements placed on practices that use dental radiographs is essential. Considering the range of health conditions that have been found to correlate with dental radiography exposure – such as brain and thyroid cancers, leukaemia and low birth weight – it is paramount to only use them in practice when justified, and be able to employ them in line with the appropriate regulations for optimal patient safety.
Some of the most paramount pieces of legislation that dental professionals must understand are the Ionising Radiation (Medical Exposure) Regulations, often referred to as IR(ME)R, which have most recently seen new amendments take effect on 1st October 2024 – referred to as IR(ME)(A)R 2024. The updated documents supersede the IR(ME)R 2017, which took effect in February 2018 and were quickly amended upon their implementation.
The new amends are recognised by the British Dental Association, who approached the UK Health Security Agency for clarification into the changes made to dentistry. Upon reviewing the amended legislation, there are few changes that will dramatically change the workflow of the average clinician. This is of little surprise considering that radiography use has been refined for safety in this field.
However, the amendments are further reaching than the 2018 update, with IR(ME) (A)R 2024 changing 17 separate regulations and schedules. Many are updates to wordage, making it more applicable to today’s practice of healthcare radiography. Notably the reference to “European” diagnostic reference levels are now “international”, and there is a conscious effort to widely include referrers and operators, as opposed to only practitioners.
One significant change requires practitioners to establish a system for the appropriate actions that should be taken when an accidental or unintended exposure occurs. Previously, the regulations only demanded that clinicians create a workflow that records the analysis of these events. It is imperative that this change is immediately implemented in the practice, and may require clinicians and radiographers to draw up an action plan that can be referred to depending on the severity of an unintended radiation exposure. This adds to the communication of review outcomes to referrers, practitioners and the affected patient. In the long term, this can prevent the repetition of mistakes and protect future patients.
Co-operation between practitioners and operators is briefly mentioned in Regulation 10 of IR(ME)R 2017, but the latest amends also reiterate this in a newly added Regulation 6A. IR(ME)(A)R 2024 formally introduces the need to share relevant patient information between practitioners,
including the justification for the exposure, to better protect individuals who are treated by multiple professionals. This can optimise the communication between the team, improving outcomes and patient safety.
The Care Quality Commission (CQC) is the enforcement body for the IR(ME)R in England. Under Regulation 8, clinicians must make their enforcing body aware of any accidental or unintended exposure that is significant or clinically significant. The differentiation between these is slight; significant accidental or unintended exposures are significantly greater than intended or perhaps as a result of equipment malfunction. Clinically significant exposures can be defined as those that create moderate harm, increasing the patient’s need for treatment through dental or general health care.
To minimise the risk of such exposures, and ensure you are compliant when proceeding with radiographic imaging in the practice in the future, it is imperative that you choose equipment you can trust. Modern systems can make image capturing simple and safe, and clinicians new to radiology should seek out solutions that eradicate any difficulties when selecting factors such as dose strength.

The CS 8200 3D Access CBCT scanner from Carestream Dental can help professionals of all experience levels optimise their in-house workflows. It features a user-friendly interface that makes CBCT, panoramic, and cephalometric image data simple to produce, analyse and share with other clinicians. A lowdose imaging mode also allows clinicians to deliver high-quality 3D images at the same or lower does as a standard panoramic exam, to protect patients further.
Keeping up to date with the regulatory changes surrounding radiographic care is essential. Clinicians should review the updated IR(ME)R with their team, to ensure the entire practice can deliver the best possible care to each and every patient. For more information on Carestream Dental visit www.carestreamdental.co.uk
For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
about the author
Nimisha Nariapara is the trade Marketing Manager at carestream Dental covering the UK, Middle east, Nordics, South africa, russia and ciS regions.


Dental practices must closely monitor bacterial levels in dental unit waterlines (DUWLs) to ensure patient safety and compliance with hygiene standards.
Justin Hind, A-dec Territory Manager for London & Southeast England, highlights the importance of addressing the often-overlooked issues relating to DUWLs and outlines essential processes for maintaining waterline cleanliness to mitigate risks and uphold practice integrity.
Why waterline maintenance matters
Patients trust the water used during their dental treatments is clean and safe. However, this is not always guaranteed if the dental practice does not implement adequate waterline maintenance.
To fully understand the best practices for DUWLs, it is crucial to understand biofilm and its impact on these systems in dental offices. Biofilm is a slimy bacterial layer that thrives within the small-diameter waterlines of dental units, typically measuring 0.5–2 mm in diameter (CDC, 2023). These narrow tubes, used with high-speed dental handpieces, ultrasonic scalers, and air/water syringes, make it challenging to eliminate bacteria due to low water flow rates.
Water from municipal systems often contains trace amounts of bacteria and
microorganisms. As it moves through the narrow DUWL tubing, the combination of low flow rates and prolonged stagnation provides ideal conditions for bacterial growth. This can lead to water exiting the dental unit heavily contaminated with microorganisms such as Legionella, Pseudomonas aeruginosa, and nontuberculous mycobacteria (CDC, 2023). Without proactive steps to prevent and eliminate microorganisms, dental units are highly susceptible to bacterial growth.
Maintain. Monitor. Shock.
Three steps to clean
How can you ensure the highest water quality for your patients? Implementing a daily waterline maintenance protocol, regularly monitoring water quality, and periodically shocking the lines to eliminate deposits and contamination is essential. It’s important to use only treatments compatible with your dental unit to prevent damage and ensure the best results. If unsure, consult the manufacturer of your dental equipment for recommendations on shock and maintenance treatments. These three steps are critical to maintaining clean dental unit waterlines:
1. Maintain
Daily maintenance is crucial. Use a specially formulated waterline treatment tablet to prevent odours, foul-tasting
bacteria, and microbial build-up, ensuring waterline effluent stays at ≤10 CFU/ml.
For example, A-dec ICX tablets are easy to use. Simply drop one tablet into an empty self-contained water bottle before each refill. As the tablet dissolves, it releases ingredients that help maintain bacteria levels at ≤10 CFU/ mL, preventing the buildup of odours and foul-tasting bacteria. ICX remains active in the system with each treatment, protecting waterlines from further contamination and minimising the need for frequent shock treatments.
2. Monitor
Regular water quality testing is vital.
Bacteria levels exceeding 100-200 CFU/ml indicate it’s time to shock the waterlines. The frequency of testing will depend on your results:
• Start by testing monthly.
• If results consistently show bacteria levels below 100-200 CFU/ml for three consecutive months, reduce testing to every three months.
For accurate readings, use a laboratory service or an in-practice water quality test kit, following the manufacturer’s instructions. When collecting samples from an individual dental unit, combine approximately equal amounts of water from each tubing (e.g., handpiece tubing and air/water syringes).
Shocking waterlines clear deposits, odours, and foul-tasting bacteria. It’s recommended to shock waterlines:
• Before the first use of a new dental unit.
• After bacterial test results exceed 100-200 CFU/ml.
Products like A-dec’s ICX Renew are effective for shocking dental unit waterlines. The A-dec ICX renew is a fast-acting liquid shock solution that effectively eliminates odours and foul-tasting bacteria in dental unit waterlines. To start with, mix the two solutions in an empty water bottle, run the mixture through the lines, and let it soak overnight. The blue colour enhances visibility, ensuring the solution is present in the waterlines. After the shock treatment is complete, flush the lines with water and return to your regular maintenance routine. Following the shock treatment, resume regular use of waterline treatment tablets like ICX for daily maintenance.
For more details on maintaining, monitoring, and shocking dental unit waterlines, download the ICX & ICX Renew Dental Waterline Treatment Brochure at https://tinyurl.com/ICX-Adec or get in touch with A-dec today by calling 0800-233-285 or emailing info@a-dec.co.uk. n
It is well known among dental practitioners that oral health has a strong association with general health, but patients may be less familiar with this. As such there is a need for patient awareness to be improved, particularly on the impact that neglecting their oral hygiene can have on the rest of the body. Among adults, strokes are one of the leading causes of disability and mortality in the UK. Over 100,000 people have a stroke each year. Of major concern to dental practitioners is the link between oral disease and strokes: patients with periodontitis are around twice as likely to have a stroke, whilst patients who have had strokes are at a greater risk of infection in the oral cavity due to inadequate hygiene. Practitioners can help with both circumstances.

raising awareness
Strokes are not curable, but the wider public awareness of FAST (Face, Arms, Speech, Time) has improved the speed in which patients can be diagnosed and treated. Whilst FAST and innovations in emergency treatments have led to a decrease in fatalities, strokes remain the fourth single leading cause of death in the UK. There are two types: haemorrhagic strokes and ischaemic strokes. The former are caused by blood vessels that burst in the brain and are associated with high mortality. Ischaemic strokes are caused by a blockage, such as a clot, which starves the brain of blood and oxygen. 85% of strokes are ischaemic strokes.
Controlling the risks
There are many risk factors for strokes, such as age, diet, education, exercise, smoking, alcohol consumption, stress, diabetes, hypertension and cardiovascular disease. For patients who are more at risk of having a stroke, periodontitis is also a concern as it heightens the risk: there is a higher prevalence rate and a lower survival rate of strokes in patients with periodontal disease compared to those with gingvitis. Periodontitis causes inflammation which affects the supporting structures of the teeth, including the gingivae, alveolar bone and periodontal ligament. Bleeding of the gingivae can be common, leading to the infectious bacteria responsible for the disease entering the bloodstream. The bacteria can also reach the circulatory system through eating, chewing and
toothbrushing.
The presence of infectious bacteria in the bloodstream causes the body to react, leading to a rise in C-Reactive proteins and IL-6 that inflame the blood vessels and reduce the blood flow to the brain. These inflammatory markers are indicators for an increased stroke risk and are also identified as biomarkers of periodontitis. A consistent and effective oral hygiene routine can prevent periodontitis, minimising the risk of inflammation in the bloodstream.
In addition to being a risk factor for strokes, periodontitis prevalence can also increase for patients who have had a stroke. There are 1.3 million stroke survivors in the UK, and many have poor oral hygiene. After a stroke, neurons begin to die within minutes when the oxygen supply is cut off, leading to brain damage and the subsequent impairment of certain bodily functions like movement, memory and speech.
Disability in the face, hands and arms can prevent stroke patients from effectively brushing their teeth. This can lead to oral health neglect, which is why support in their oral hygiene routine is needed to protect them from further complications. Moreover, inflammation may lead to stroke recurrence and less favourable outcomes; preventing gingival disease or periodontitis can help reduce this likelihood.
It is also likely that stroke survivors develop dysphagia; the reduced ability to swallow increases the risk of bacterial colonisation in the oral cavity, with saliva or bolus lingering in the oral cavity. Infection from these particles can lead to aspiration pneumonia, so maintaining a consistent oral hygiene routine can reduce the presence of harmful bacteria and prevent further health complications.
a suitable solution
An effective and reliable interdental brush can protect the teeth and gingivae from disease. The FLEXI series of interdental brushes, from TANDEX, includes 11 different sizes for optimal access. Able to clean the tooth surface and massage the gums, using FLEXI is an effective way to reduce the risk of infection. With a flexible handle and a brush that can be shaped for user preference, this is an interdental brush for comfort. Use with PREVENT Gel, from TANDEX, for an antibacterial boost and a fluoride flourish.
Chronic exposure to common infections contributes to stroke risk. Preventing oral diseases among those vulnerable to strokes can better protect them, maintaining their quality of life. Make a difference today.
For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from CTS Dental Supplies www.cts-dental.com n
about the author Jacob Watwood on behalf of tandex.
The human body is comprised of organs and bones bound together by tissue. There are four types of tissue: epithelial, muscle, nervous, and connective. If the connective tissue is damaged, basic bodily functions can be impeded.
Connective tissue disease (CTD) encompasses a range of autoimmune diseases that negatively affect the connective tissue, often leading to inflammation and pain. For dental practitioners, the damage that a CTD can cause to the temporomandibular joint (TMJ) is essential to understand. A dysfunctional TMJ can inhibit mastication and limit quality of life. A greater awareness of the types of CTD can enable clinicians to better manage patients at-risk from temporomandibular joint disorder (TMD).
CtD explained
There are more than 200 types of CTD. Some of the more prevalent examples include:
• Polymyositis and dermatomyositis
• Rheumatoid arthritis
• Scleroderma
• Systemic Lupus Erythematosus (SLE)
• Mixed connective tissue disease (MCTD)
• Sjögren’s syndrome
A CTD can be inherited, caused by environmental factors, or may have an unknown aetiology. Exposure to excessive ultraviolet light or toxic chemicals from pollution of cigarette smoke can be risk factors, as are poor nutrition and infection. The usual cessation and behavioural advice – stopping cigarette smoking, eating healthier foods – can be given to help reduce these risk factors.
Connective tissues are composed of two proteins: collagen and elastin. Collagen is found in the tendons, ligaments, cartilage, skin, bone and blood vessels. Elastin, as the name suggests, is a stretchy protein, resembling a rubber band, that is an integral part of the ligaments and skin.
A CTD inflames these proteins, and this then harms the connected body parts, such as the TMJ.
significant increase in potential TMD risk must be noted for CTD patients.
Some CTDs have a much higher prevalence in women compared to men. For instance, among SLE patients, which causes widespread inflammation, 90% are women. Another is Sjögren’s syndrome which affects 1.2% of the UK population, with the highest prevalence in women aged 40-60. Causing chronic inflammation of the exocrine glands, Sjögren’s syndrome can have multiple impacts on a patient’s oral health. The reduction in bodily fluids like saliva can lead to xerostomia and dysphagia, leaving the oral cavity vulnerable to disease. Dental caries has been reported in 56.9% of Sjögren’s syndrome patients and gingivitis in 75%.
Moreover, 91.7% of Sjögren’s syndrome patients have reported TMD symptoms –muscle pain when chewing and difficulty in mouth opening – which reinforces the impact the autoimmune disease can have on the oral cavity. Sjögren’s syndrome is therefore a condition that must be closely monitored among patients, particularly women. As it is incurable, practitioners and patients must counteract its symptoms with appropriate measures, such as chewing sugar free gum to combat xerostomia or regularly exercising the TMJ.
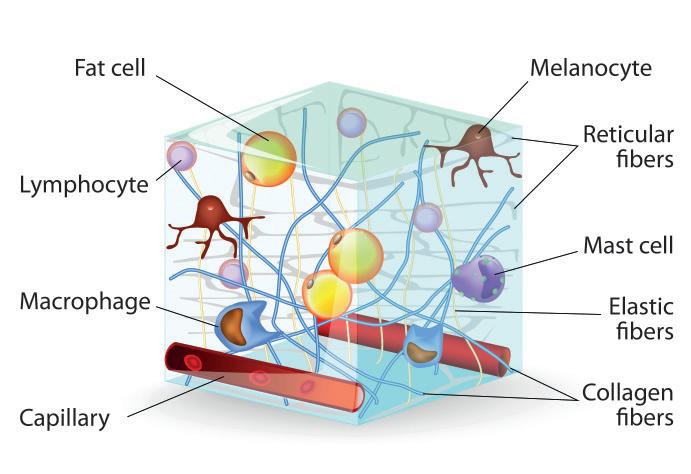
Giving patients a helping hand

85% of patients with TMD also suffer from other conditions. Many CTDs have a complex, overlapping pathogenesis with TMD; they are often comorbid. Identifying CTD patients can therefore help practitioners with managing the risk of TMD. For instance, despite its low prevalence, MCTD can massively affect jaw function due to its symptoms of polyarthritis. A study found that erosion of the TMJ was 19 times more likely in MCTD patients than those without it, as well as causing a much higher prevalence of pain from the jaw area. Whilst the strong association between CTD and TMD development is not concrete, the
To assist patients suffering from TMD, recommend the OraStretch® Press Jaw Rehab System from Total TMJ. The device is designed for simplicity – inserting the mouthpiece and squeezing the handles mobilises the jaw and stretches the mouth open. Repeated exercises with the OraStretch® Press throughout the day can assist in treating dysfunction, trismus and fibrosis. By regularly exercising the jaw muscles, patients can be on a quicker road to recovery. This ensures that patients will soon have optimal masticatory function, reduced pain and a better quality of life. CTDs cover many health conditions. Patients effected by these diseases are at a greater risk of TMD, which is why practitioners must find and encourage appropriate solutions to reduce this risk. Whilst many can’t be cured, fighting CTD symptoms is vital for the ongoing preservation of the country’s oral health. For more details about Total TMJ and the products available, please visit totaltmj.co.uk/products/orastretch n
about the author
Founded in 2018 by Phil Silver, total tMJ is a specialist provider of medical devices.






Minimise Complications and Improve Healing Conditions In Mucogingival and Implant Surgery


Leveraging the antibacterial and wound-healing properties of zinc ions, Elemental can be used post-operatively with or without a membrane.



Elemental activates when in contact with boiling water, and the resulting material, which sets rigid and stable, can be quickly and easily moulded and shaped according to the needs of the patient.


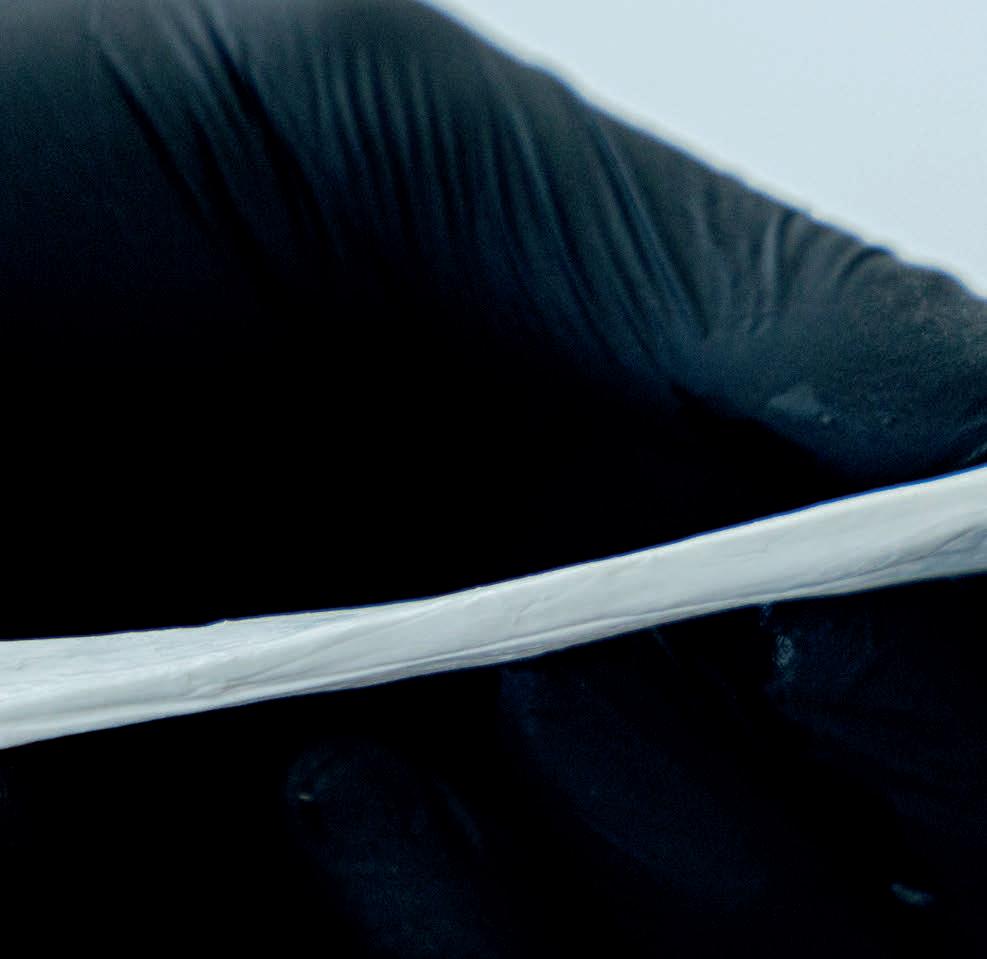























In the UK, 66 people are diagnosed with inflammatory bowel disease (IBD) every day. IBD refers to a group of disorders that inflame the colon and small intestine; ulcerative colitis and Crohn’s disease are the two most common in this category. The disease places a notable demand on healthcare resources, prompting the need for a greater awareness of its symptoms and how to manage it.
For dental practitioners, IBD’s association with oral diseases, such as dental caries and periodontitis, must be taken into consideration. As a patient with IBD is more susceptible to develop an oral disease, and as a patient with an oral disease is more likely to develop IBD, practitioners must help break this link by promoting a consistent oral hygiene routine.
Understanding IBD
The aetiology of IBD is often unknown. However, those with parents or grandparents who have IBD are more likely to develop it, with white ethnic groups having the highest prevalence of it. It is a lifelong, debilitating condition with no cure, affecting half a million Brits of varying age groups.
With IBD, the immune system attacks the bowel, causing it to inflame. Patients can greatly struggle, with common symptoms including severe stomach pain and diarrhoea. Other signs and symptoms can present, such as blood or mucus in faeces, feeling constantly tired and losing weight without trying. These symptoms can be evident up to 10 years before a diagnosis. IBD can lead to days off work or school, a withdrawal from social environments, and an inability to go about the day or perform simple tasks. As such, anxiety and depression symptoms are associated with it, emphasising the need for a multidisciplinary approach to managing IBD.
For IBD patients, the impacted immune system causes changes in the proinflammatory cytokines and oxidative status markers. This is the same cause that progresses periodontitis, leading to tissue destruction. Whilst many may associate the gut with being part of the torso, the gastrointestinal tract connects the gut with the oral cavity, increasing the spread of proinflammatory cytokines. The immune system then sends antibodies to reduce the inflammation in the gingivae, damaging the teeth’s supportive structures and increasing the risk of oral disease. As such, there is a higher prevalence of caries and periodontitis in IBD patients. Caries is notable in ulcerative colitis patients, with its dysbiosis leading to increased levels of streptococcus mutans, the microbe that contributes to enamel demineralisation and tooth decay. IBD patients are therefore at greater risk from oral disease.
A poor diet has been associated with IBD patients. The World Health Organization found that those with IBD ate more sugary foods, such as jam, sweets, and carbonated
soft drinks, like lemonade. Furthermore, 30% of IBD patients had oral lesions. Advising IBD patients to avoid sugary or processed foods and drinks can play a crucial role in reducing the prevalence of caries and managing IBD symptoms.
IBD can be treated with medication, such as steroids. A disadvantage is that these medications can cause xerostomia, stalling saliva secretion and depriving the oral cavity’s natural defence against harmful acids.vii This exposes the region to a higher chance of infection, such as the recurrent mouth ulcers found in Crohn’s and ulcerative colitis patients. Dental practitioners should recommend solutions for dry mouth, such as chewing sugar-free gum or speaking to a pharmacist.

To help IBD patients repel the threat of oral diseases, recommend using the Cordless Advanced from WaterpikTM, the leading water flosser brand. Reenergise their oral health with this innovative device that can remove up to 99.99% of plaque. The Cordless Advanced can be customised for optimal compliancy with its four tips, three pressure settings and a full 360-degree tip rotation. This helps the patient find the most comfortable and effective setting for the best results in preventing oral disease infection.
A patient’s quality of life can be reduced by IBD. With overlapping impacts on oral health, physical health and mental health, a multi-disciplinary approach is needed to manage its symptoms. Dental practitioners are a key part of this, and guiding IBD patients towards a reliable oral hygiene routine can play a big role in restoring quality of life.
For more information on WaterpikTM water flosser products visit waterpik. co.uk. WaterpikTM products are available from Amazon, Costco UK, Argos, Boots and Tesco online and in stores across the UK and Ireland. n
about the author
anne Symons is a Dental hygienist currently working in a Specialist Periodontal/ Implant practice and also a busy NhS surgery. She has previously worked in a Max Fax unit, and also taught oral health care to staff in nursing and residential homes.

Winter is the time for illness – you may have already had one of the two to three common colds that adults are expected to experience annually. As people spend longer indoors, the risk of infection increases, with viruses preferring the lower temperatures.
Among the sore throats and blocked noses, it can be easy for patients to develop sinusitis. For patients undergoing implant treatment, education on the link between implant care and sinusitis must be highlighted by the dental practitioner to minimise the chance of infection and subsequent treatment failure.
Sinusitis explained
Chronic sinusitis is experienced by 11% of UK adults. The sinuses are connected to the external environment through the nasal passages. The mucous lining and paranasal cavities – air pockets – can become inflamed. This blocks the sinus drainage and impairs the body’s natural defences, allowing mucus, bacteria, viruses or fungi to build-up in a moist, fertile environment – this causes infection.iv The symptoms are well known: a blocked or runny nose, reduced sense of smell, a high temperature. It can also cause headaches, coughs, toothaches, halitosis, and pain, swelling and tenderness around the cheeks, eyes or forehead.
Infectious implants
More than 40% of sinusitis infections in the maxillary sinuses stem from a dental infection; the close proximity of the teeth to the sinus floor allows odontogenic infections to easily enter from the oral cavity. Odontogenic sinusitis is a result of varying dental pathologies, such as recent treatments, infections, or trauma.
Implant treatments are a common cause of odontogenic sinusitis. Peri-implantitis inflames the surrounding tissue of an implant and can lead to recession of the alveolar bone and a loose implant. It is this inflammation that makes implant treatment, and poor oral hygiene, a risk hazard for sinusitis, with infectious bacteria spreading into the air cavities. Research has also found that the same cytokines found in periimplant breakdown are connected to many other systemic conditions and diseases, from periodontitis to cardiovascular disease. Limiting the chance for peri-implantitis can better protect overall health too.
Sinusitis can have several effects on oral health. It can affect other teeth, with the irritation from the maxillary sinuses radiating back to the upper teeth and causing sensitivity, toothache and pain.viii Odontogenic sinusitis can therefore cause more dental problems for patients. Further impacts on the oral cavity include halitosis. If the infection reaches the throat, it can release a foul malodour that can be hard to combat without antibiotics. Similarly, patients may take medications to treat sinusitis that can cause xerostomia.

Antihistamines are one example, drying out the oral cavity and leaving the teeth – and any recent implant – less protected without the optimal amount of saliva to buffer harmful acids. Xerostomia can increase the risk of tooth decay and yeast infection, so vulnerable patients should be encouraged to use special gels or chew sugar-free chewing gum to keep saliva levels up. Maintaining excellent oral hygiene is essential before, during and after implant treatment. Preventative measures should begin before any implant placement and persist in the following years for maximum success.
For implant patients, minimising the risk of odontogenic sinusitis can be achieved through a consistent oral hygiene routine that protects the implant. By cleaning all the surfaces and surrounding teeth and gingivae, peri-implantitis can be avoided. However, a study revealed that, whilst 90% of participants learned how to clean their implants, it was found that only 40% actually practised it whilst supervised by a practitioner. This can lead to neglect or improper cleaning methods. Practitioners must therefore demonstrate to implant patients how best to care for their implants. To protect patients who have undergone implant treatment, recommending the Curaprox REGENERATE Implant Kit can reduce the risk of infection and enhance the treatment success. It contains a variety of uniquely designed implant cleaning products, such as a CS Surgical Toothbrush, Perio plus Support toothpaste and Perio plus Regenerate rinse for an antibacterial boost. The kit also includes a CS 5460 Ultra-Soft toothbrush, a CS 708 Implant brush and five CPS mixed implant interdental brushes for maximum oral hygiene maintenance. Having the Curaprox range of effective oral hygiene products all in one kit makes this the best way to look after implants.
Sinusitis is common over the winter months. By encouraging effective oral hygiene routines, practitioners can help at-risk patients limit the risk of infection and lead a happier, healthier winter.
For more information, please visit curaprox.co.uk and curaden.co.uk n
about the author andrew turner, Curaden UK head of Marketing.

The natural mineral bone material that doesn’t wash away!

Augma’s Bond Apatite is a natural mineral bone regeneration material that does not wash away, unlike other synthetic bone materials.
Supplied in an all-in-one syringe that enables immediate dispensing directly into the bone defect, it is incredibly quick and easy to use. Simply depress the plunger to activate the ingredients, dispense it into the defect and apply pressure using a sterile gauze and it’s set. The whole process takes literally seconds.
Bond Apatite sets hard, so it won’t wash away even in the presence of blood and saliva. And, because it sets hard, there is no need for a membrane which saves additional time and unnecessary expense. There is no need to achieve tension-free closure, this is actually contra-indicated, or even complete primary closure for gaps less than 3mm. Small dehiscences can be left exposed without any risk of infection or breakdown. Larger
dehiscences can be protected by suturing an Augma Shield protective layer over it.
Formed from a patented mixture of biphasic Calcium Sulphate and Hydroxyapatite in a 2:1 ratio, Bond Apatite sets like a cement in the oral cavity, even in the presence of blood and saliva. After a few weeks it transforms into a radiolucent matrix, before calcifying and becoming radiopaque new bone. It produces 90% new bone after 3 months and over 95% new bone after 8 months. Benefits recently challenged by the distributors of another synthetic bone material, but proven histologically correct.
Full Day bond apatite Hands-on Workshop
Augma is running a Full Day Bone Cement Hands-on Workshop on Saturday 29th March at the Leonardo Royal London City hotel, near London Tower.
It will be presented by Dr Lucio Faria who has been a National and International Speaker for Nobel
Biocare since 2011, is a Surgical Master in Regenerative Implant Dentistry and has undertaken extensive Postgraduate Studies in Prosthodontics, bone and soft tissue grafting, and Zygomatic implant surgery and rehabilitation.
Dr Faria will review four of the most common surgical protocols using Bond Apatite bone grafting cement, which sets immediately and is accompanied by minimally invasive surgical procedures that do not require a membrane.
Delegates will receive practical knowledge on how to perform socket grafting without flap reflection, lateral ridge augmentation and augmentation in the aesthetic zone.
The course includes a variety of resources, such as animated videos, recorded live surgery demonstrations and clinical videos. Evidence based data histology shows how following the surgical protocols leads to clinical success and complete bone regeneration for the patient.
Lucio Faria
The course fee is £195.00 plus vat (including all course materials and lunch) with a £145.00 plus vat Early Bird for confirmed bookings before 31st January 2025.
For more information on Augma Bond Apatite or the 29th March Handson Workshop in London contact your local Trycare representative, Denise Law at the Trycare Events Team on 01274 885544 or email events@trycare.co.uk n

Dental crowns are a common and effective treatment option for individuals looking to restore the dentition. A 2021 survey revealed that 34% of people had at least one crowned tooth, with prevalence increasing with age.
Crowns can bring aesthetic and functional advantages where an existing tooth is severely caries-affected, but some of the structure is healthy enough to remain within the oral cavity. Though these indirect restorations are inherently invasive – some anatomy must be removed prior to placement – they are far more advantageous than surgical approaches including extraction and denture or implant placement.
Ensuring patients receive high-quality restorations is essential. There are a number of potential complications that may arise from controllable variables, such as material choice and adhesive approach, which can be optimised through informed clinical judgement.
made of stronger stuff
Conventional crown placement has yielded excellent long-term clinical results, and as dentistry has evolved, clinicians have been pulled away from the traditional metal caps. As with nearly every other aspect of dental care, aesthetics has played a significant role in this. Orthodontics has seen the rise of clear aligners, teeth whitening has become a popular cosmetic procedure, and so it is of little surprise that the demand for metalfree materials with increased translucency for a natural finish has escalated. However, dental professionals must find a balance. Function and oral health must also be considered. As seen in the General Dental Council’s (GDC) Standards for the Dental Team, patient expectations may need to be tempered to meet their oral health needs, and in the scenarios where a desired outcome is not in their best interests –perhaps if it is driven by aesthetics – a clinician must diligently talk through all aspects of such care.
For example, zirconia crowns are renowned for their strength and durability, but the ability to match the surrounding dentition is thought to be bested – even if only slightly – by porcelain solutions. Some clinicians may combine the two, veneering porcelain onto a zirconia structure, but chipping of the material is a commonly reported complication. This is especially present in posterior restorations. Allceramic crowns have been suggested to avoid chipping, but these instead can result in complete fracture. Bruxism, as to be expected, increases the prevalence of porcelain chipping three-fold. A zirconia solution may therefore be preferred where improved longevity is the first priority.
However, there is also the need to consider that a zirconia crown will be likely more expensive than a porcelain or even all-metal crown. Understanding that patients can be strongly influenced by the cost of each treatment, as well as the perceived functional and aesthetic benefits, is important when carefully supporting patient decisions.
The choice of adhesive material and method in which it is applied can also impact the complications associated with crown placement, including retention.
Both resin-based cements that are used in conjunction with a tooth primer and self-adhesive solutions form a hybrid layer with dentine, creating the term ‘bonding’. Laboratory studies have shown that resin cements increase the retention strength of a crown greater than glass ionomer or zinc phosphate cements, two other popular solutions.
Adhesion onto dentine is a clinical challenge due to the presence of moisture and its organic and inorganic composition, but self-adhesive resin cements have been shown to be suitable due to their acidic monomers. Glass ionomer cements can also provide a strong chemical bond to dentine, but studies have noted they can be weaker when bonding to an artificial core or coping materials.
As zirconia crowns feature a low inherent surface roughness, they must be prepared to provide ample bond strength and increase crown retention. The preparation of the indirect restoration site is in many ways as essential as the chosen adhesive material.
Self-adhesive resins are preferred by many where appropriate, as they simplify the bonding procedure. The characteristics of a cement will affect clinical performance, and so dental professionals should explore the options available to them.
materials you trust
Finding materials and adhesive solutions that you trust to deliver consistent, highquality results is key. The RelyX Universal Resin Cement from Solventum, formerly 3M Health Care, could be the pick for you, presenting brilliant outcomes for virtually all adhesive and self-adhesive indications. The cement, renowned for simplifying restorations, offers superior self-adhesive bond strength to dentine, without the need for additional adhesive or primer in both light- and self-cure workflows. Indirect restorations can be placed with confidence, delivering long-term retention and success.
Dental crowns are a mainstay in restorative dentistry, and can be optimised through material and adhesive choice. Clinicians may need to adjust their preferences dependent on clinical demands – but materials you have confidence in are paramount.
To learn more about Solventum, visit solventum.com/en-gb/home/oral-care/ n
©Solventum 2024. Solventum, the S logo and RelyX are trademarks of Solventum and its affiliates. 3M is a trademark of 3M company.

Bad habits are a defining trait of being human – even if we know something is bad for us, we often can’t help but do it anyway. Born out of repetition and impulse, we are often aware of our vices. These can include anything from smoking to unhealthy snacking or spending too much time on our phones.
The average adult will attempt to stop their bad habit twice a year, with January and New Year resolutions often viewed as an opportune moment for a fresh start. However, there are many poor habits that we may be less conscious about – these are harder to stop. For dental practitioners, a patient’s bad habits may impact the success of implant treatment. A greater awareness, both for patient and practitioner, on the consequences of certain harmful routines is needed to better prevent implant failure and optimise outcomes.
nervous ticks
A poll of the UK’s worst but most common habits had nail biting in third place. This repetitive behavioural act is difficult to suppress and has a high prevalence –20-33% – among children. Whilst the frequency of nail biting decreases in adulthood, many still continue the habit. It has many effects on the oral cavity: apical root resorption, chipping off incisal edges of the anterior teeth, temporomandibular joint dysfunction, gingival swelling, and destruction of the alveolar bone. The latter two can prevent the successful osseointegration of an implant.
The habit can vary in frequency, duration and intensity. Patients who are stressed or nervous may bite their nails without thinking about it, with higher levels of anxiety found in nail biters than those without the habit. There is also a risk of infection from placing unwashed fingers into the oral cavity, with diseases like periodontitis and periimplantitis able to manifest from the spread of harmful bacteria.
For optimal implant outcomes, identifying patients who may bite their nails and educating them on the association between that habit and implant failure is essential before any surgical procedure occurs. Encouraging solutions to destress – from breathing exercises to regular sleeping patterns – can also assist in reducing nail biting frequency.
Sleep bruxism
Some patients may not be aware of their damaging habits. Those with notable mechanical wear of the teeth, such as the flattening of the occlusal surfaces, and tender or stiff jaw muscles, among other signs and symptoms, may have bruxism. Sleep bruxism can affect 8-10% of adults; those that sleep alone may be harder to
diagnose without someone else having seen or heard them do it. As sleep bruxism occurs unconsciously, it is harder to stop. Much like nail biting, both awake and sleep bruxism can be exacerbated by stress and anxiety, whilst obstructive sleep apnoea can also be a major risk factor for the latter. Bruxism leads to excessive occlusal overload and subsequent implant and marginal bone loss. It is the leading cause of implant failure. For diagnosed patients, highlighting the importance of destressing and following a regular sleeping pattern can help minimise the risk of bruxism, but a mouth guard or mouth splint will better protect the implant from mechanical wear.
Whereas nail biting and bruxism can occur throughout the day, there are several other less common oral hygiene related habits that can reduce implant success. Overbrushing the teeth every day is damaging, with the rough abrasion wearing away the tooth enamel. This rigorous brushing can also lead to gingival recession, leaving the roots exposed to infection or damage. Similarly, using teeth as tools is another bad habit that can cause cracking and fracturing. Both can cause implant failure.
To advance your understanding of implantology and better recognise patient habits and other risks that can cause treatment failure, consider an advanced course with One to One Implant Education. The PG Diploma in Advanced Techniques in Implant Dentistry is a two-year masterclass for practitioners who want to take their skills and knowledge in implantology to the next level. Under the unparalleled tutelage of Dr Fazeela Khan-Osborne and Dr Nikolas Vourakis, practitioners can embark on an expansive journey across nine comprehensive modules, including an assessed case of a full arch reconstruction. Course delegates are also eligible for a 50% discount on ADI membership, helping form a reliable community of implant professionals. Most people have bad habits. Identifying the patients with habits that may be detrimental to their oral health is important; helping them find solutions to minimise the damage that can be dealt to an implant is even more so. By working with patients, you can keep their smiles safe.
To reserve your place on the Postgraduate Diploma in Advanced Techniques in Implant Dentistry or to find out more, please visit https://121implanteducation.co.uk or call 020 7486 0000 n
about the author
Dr Fazeela KhanOsborne, Principal Implant and restorative Surgeon.

Endodontic treatment is a predictable and effective way to treat dental infections, with treated teeth surviving for 10 years in 80-90% of cases. However, sometimes, endodontic treatment may fail, requiring further treatment.
Why might endodontic treatment fail?
Even though it is a widely successful procedure, there are a variety of reasons why endodontic treatment may fail. These include poor aseptic control during treatment, insufficient chemo-mechanical preparation, and suboptimal obturation of the canals. However, root canal anatomy is complex and, even in adequately filled teeth, infection can persist due to extra-radicular sources of infection such as periradicular biofilms, foreign body extrusions and selfsustaining cystic lesions.
Reinfection may also occur if there is a breakdown of the coronal seal, as this can result in microleakage, in addition to errors which occurred during the initial procedure such as instrument separation or perforations, as well as resistant microorganisms such as E. Faecalis.
Diagnosis and prognosis
Should an endodontically treated tooth require further treatment, it’s important to confirm the diagnosis ensuring there are no non-odontogenic causes of the patient’s symptoms, assess the likely origin of the infection, and decide whether the patient















may be a suitable candidate for nonsurgical retreatment.
As part of the clinical assessment, particular attention should be paid to the restorability of the tooth, determining whether coronal tooth structure is sufficient. However, if this is not the case, such as when there are medical contraindications to extraction, non-surgical retreatment can be performed as long as an aseptic environment can be maintained throughout the procedure.
For accuracy in diagnosis and treatment planning, it is important to carry out a thorough radiographic examination. In addition to revealing root canal morphology and periradicular radiolucency, radiographs can indicate procedural errors, the quality of obturation, and the quality of the coronal seal. The use of CBCT could also be considered pre-operatively, when justified, as it may help formulate a diagnosis and enhance the management of the tooth.
As with primary root fillings, teeth that have undergone root canal retreatment should be reviewed on an annual basis until completely healed. If teeth become symptomatic, or the lesion stays the same size or has not completely resolved within four years, apicectomy or extraction should be considered as next steps.
Because root canal treated teeth are usually restored with a permanent restoration, nonsurgical endodontic retreatment can be a more complex procedure as accessing the tooth can be a challenge. It is thus integral




















that magnification and illumination are adequate, to detect subtle colour changes between restorative materials and dentine. In addition to this, obturation material must be removed to facilitate adequate disinfection of canals.
When restoration margins are sound, access cavities can be created through the restoration. However, in many cases, the coronal restoration must be removed if it is defective (to evaluate any underlying pathology and restorability of the tooth), if locating the canals is difficult, or if underlying pathology is detected during access. If posts are present, it is advised the case is referred to a more experienced practitioner (i.e. specialist). Whilst diamond and long neck burs will help operators traverse through the majority of restorative material, ultrasonics enable the removal of subtle materials closer to the floor up the pulp chamber, reducing the risk of perforation.
Gutta-percha (GP) can be removed using hand and mechanical rotary and/ or reciprocating instruments and solvents. The technique used to remove the GP will be influenced by the obturation technique, the extent of voids, curvature of the canal, and how narrow the canals are. The preoperative radiograph should be used to determine these factors.
Following this, canal patency should be established and treatment should then follow a similar process to that of initial treatment. Clinicians should pay special attention when obturating the canals though, as cracks are more likely to occur
in retreated teeth. Achieving a restoration with a good coronal seal and resistance is essential, for long-term survival of the endodontically treated tooth.
Staying up-to-date
Up-to-date knowledge is critical when providing endodontic retreatment. As such, the British Endodontic Society (BES) is hosting the first in a series of hands-on workshops on 22nd February 2025 entitled “Endodontic Retreatment: a British Endodontic Society Hands-on Workshop”, which aims to improve delegates’ clinical and decision-making skills in this area. Furthermore, the BES has created ‘A Guide to Good Endodontic Practice’, which is a fantastic resource for clinicians to refer to. It reviews the basic principles of endodontics, and takes the reader through the decision-making process that leads to endodontic intervention.
Endodontics often offers successful outcomes, however, retreatment is sometimes necessary. Clinicians must assess cases carefully and decide whether to treat or refer to a specialist.
For more information about the BES, or to join, please visit www.britishendodonticsociety.org.uk or call 07762945847



























In 1928, pioneering dentist Charles Pincus was asked by Hollywood executives to perfect the look of an actor’s smile and the earliest form of veneers was invented. Synonymous with celebrities, demand for veneers has skyrocketed with the rise of social media and influencers; achieving the ‘Hollywood smile’ is an aesthetic goal for many.
The global dental veneers market was valued at £1.83 billion in 2023, with a compound annual growth of 7.4%. Since the wider induction of Zoom calls, Teams meetings and other video calling services since the pandemic, people have become more conscious about how they look. From observing themselves onscreen, more patients are looking to enhance their smiles. But knowing the right cosmetic treatment to get can be a hard choice.
Failing cases
For patients seeking veneers, they have two material options: porcelain or composite resin. Because of its malleable qualities that allow dentists to sculpt it directly to the tooth, composite resin is a more manageable material for veneers. Patients may prefer that no preparation of the tooth is required and that their desired aesthetics can be equally achieved with composite materials, making it an agreeable option. Moreover, composite veneers are costeffective and far less time-consuming to deliver. The short application progress can be completed in one appointment,
with minimal preparation. For patients not wanting multiple practice visits, composite veneers can provide the quick and noninvasive treatment they need. Despite the ease of composite veneers, there are drawbacks. Patients with poor dental hygiene, bruxism or who eat hard foods may find that composite veneer failure is more likely, and so other alternatives could be more effective if the lifestyle choices are not changed.
The survival rate of a composite veneer is 87% after three years and 75% after ten years. Patients may need appointments to repair, replace or remove damaged composite veneers, as the resin is porous and therefore more susceptible to wear and staining than materials like porcelain. Dentists may then have to decide the best way to repair the veneer: either to directly apply the composite resin to the broken surface or to remove the restoration and repair it in a laboratory. Repairing the broken restoration without removing it is often more satisfactory for patient and practitioner, even if durability is limited.
As porcelain is custom-made and more natural-looking, it is unsurprising that patients with composite veneers had a lower satisfaction rate (67%) than those with porcelain veneers (93%), as porcelain is more likely to survive.
As veneer demand continues to rise, and more patients seek this treatment
specifically, it is easy to rely on this as the main restorative solution. Abraham Maslow noted that “if the only tool you have is a hammer, you tend to see every problem as a nail,” when observing psychiatric treatments in 1966. For dentists, abiding by this cognitive bias would ignore other cosmetic solutions in favour of familiarity. Composite veneers may be easier to offer and do than other options, but it is important to avoid the pitfall of fitting patients into preferred treatment regimes rather than working with what is best for each individual patient.
Decision-making can be affected by numerous factors, such as costeffectiveness and professional bias. But being able to offer multiple cosmetic treatment options can both satisfy patients and minimise the risks of complications. For instance, a patient with enamel hypoplasia may prefer the minimal invasiveness of composite veneers to achieve their aesthetic desire. On the other hand, patients with severe issues like large gaps or extreme discolouration may find that composite veneers are not a viable solution.
For dentists who cannot offer the most appropriate treatment to a patient, referring them may be the in the best interests for their long-term health. Providing one cosmetic treatment option is therefore limiting for both the patient and the practice, and expanding your skills can prevent this.

The British Academy of Cosmetic Dentistry (BACD) provides the opportunity for cosmetic dentists to become Accredited members. The Accreditation process will allow dentists to show that they can diagnose, plan and execute various cosmetic dental treatment options to the highest standard of competency, ethics and safety. The skill set to be demonstrated includes composite veneers, indirect shade matching and posterior aesthetics, among others. Accredited members will have enhanced skills across the board of cosmetic dentistry, delivering first-class treatments for optimal patient care.
With veneer demand ever increasing, knowing and navigating the logistical and ethical problems that composite veneer treatment can cause is essential so that patients receive the appropriate treatment that most benefits them.
For further information and enquiries about the British Academy of Cosmetic Dentistry visit www.bacd.com n
about the author
Dr Sam Jethwa is President of the British academy of Cosmetic Dentistry.

Patients can present with different forms of malocclusion, each unique to the individual. On a caseby-case basis, clinicians will also encounter new parafunctional habits – nail biting, pen chewing, thumb sucking – that can impact occlusion over time depending on the frequency and severity of the action. With so many unique problems presenting in the dental chair, it’s important to be able to recognise when a patient can be considered ‘high-risk’ for developing a malocclusion, or when an existing condition will present future problems. Clinicians that are able to identify such problems early can begin to implement an effective treatment plan.
Posterior open bites are a rare form of malocclusion that can present a number of aesthetic and functional problems. Clinicians must assess the risk of such a condition developing early in order to provide interceptive care, and be able to aid patients that have surpassed this point to prevent damage to the dentition and general health.
Identifying causation
The aetiology of a posterior open bite could be linked to failed tooth eruption, a lateral tongue-thrusting habit, or as a result of changes to the temporomandibular joints, amongst other factors. Dissecting the balance of genetic and environmental factors is complex, as seen in a 2020 study that focused on a family with a generation of children that all exhibited posterior open bites. Despite its small sample size, it reasons that as treatment had been successful in some
of the family, failure of eruption would not be the cause in this case, ruling out ankylosis –where the cementum is fused to the alveolar bone, limiting tooth eruption – as a potential cause. Instead, it highlighted a common similarity of retruded upper and lower lips, increased muscle tones, retroclined incisors and lateral tongue thrust. Together, the case could be made that genetics had affected the increased muscle tone of the lips, which is known to cause upper incisor retroclination, reducing the anterior-posterior length of both arches and forcing the tongue to exhibit pressure laterally. Alternatively, another genetic or environmental component could have a stronger contribution to the common posterior open bites through an as yet undiscovered mechanism.
Lateral tongue thrust is a habit that has been described widely throughout the literature in connection with posterior open bites and tongue thrust is seen as a potential cause of open bites in other areas of the dentition. It creates a mechanical interference in posterior tooth eruption, which, if intercepted early, could be corrected by cessation of the habit. Without it, occlusal contacts may not meet over time. Cessation is also necessary for effective outcome retention. It must be noted that lateral tongue thrusting is commonly present alongside other known risk factors, suggesting that it could be a contributing factor that is aided by similarly detrimental dental or skeletal conditions.
There is also evidence to suggest that a posterior open bite may be caused by the use of mandibular advancement devices.

A 2014 study into the use of mandibular advancement splints to treat obstructive sleep apnoea observed 51% of participants developing a posterior open bite. The devices in question could protrude the lower incisors after prolonged treatment and regular use, causing premature anterior contacts that leave the posterior teeth unable to fully close.
the need for treatment
There are a number of ways a posterior open bite may be detrimental to the dentition. A lack of posterior support has been seen to affect anterior tooth wear, and a greater severity of it – though this is debated in some results. Patients may experience defective speech, which can be an issue in social interactions, prompting psychological issues in turn. Mastication challenges are also reported, which could affect digestion and wider general health issues. Treatment will differ depending on each case. Orthodontic care that aligns the
dentition is common, but some cases may need more invasive surgical intervention to create space. No matter the case, clinicians must exhibit a developed understanding of optimising occlusion, and create a treatment plan that considers a resolution within the existing dentition.
Dental professionals could develop their knowledge by taking the Occlusion: Basics & Beyond course from the IAS Academy, led by Dr Jaz Gulati and Dr Mahmoud Ibrahim. The online course can be accessed and taken at your desired pace, covering occlusion in comprehensive detail to inform your clinical judgements. With an OBAB Starter Kit containing an autoclavable Huffman Leaf Gauge and a pack of 8 microns Hanel Shimstock Foil, and OBAB Hardback Textbook included, it is the perfect source for clinicians looking to develop. Though posterior open bites are rare, it is essential to understand how they can occur in order to confidently provide interceptive care that restores the occlusion. This is only possible through diligent education for all practitioners. For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
about the author Dr tif Qureshi, Founder and a Clinical Director of IaS academy.

SprintRay offers the only comprehensive digital 3D printing ecosystem designed specifically for dentists. It allows the same-day design of over 15 different indications including definitive crowns, with end-to-end product possible in just 45 minutes. This is achieved while maximising precision of fit, durability and aesthetics of the restoration, as well as optimising the patient experience.
a first of its kind ceramic crown resin
Introducing the brand-new SprintRay Ceramic Crown, which is truly a first of its kind. The only complete end-to-end solution for 3D printed restorations, this is changing the game for practitioners, and for their patients.
The SprintRay Ceramic Crown is a hybrid nanoceramic that contains 51% ceramic material for high flexural strength (comparable to that of natural

The workflow-driven portfolio was recently expanded with brandnew 3D printing resins added to the already impressive range of restorative materials.

dentine) and wear resistance. This new class of resin has been shown to deliver an excellent margin fit, optimising the effectiveness and longevity of restorative treatment. As an inorganic material, it is radiopaque for easy visibility on scans, and is FDA and MDR cleared as a Class II resin for definitive crowns, partial crowns and veneers. It is also indicated for use with inlays and onlays.
Streamlining the professional workflow, the new SprintRay Ceramic Crown is easy to finish and polish to a smooth surface. It blends in with a patient’s natural dentition for seamless aesthetics that both practitioners and patients will love.
Key features of the sprintray OnX:
• Only 3D printing resin MDr-cleared for fixed hybrid dentures
• Facilitates lower-cost, same-day implant placement and restoration
• Delivers exceptional aesthetics
• simple processing and finishing
• MDr-approved, ceramic dominant formula
• radiopaque for easy visibility
• smooth surface finish for exceptional aesthetics
• Excellent margin fit, strength and wear resistance
• prints in under 15 minutes

Utilising the entire chairside digital workflow from SprintRay, clinicians can now design crowns using powerful AI-assisted technologies, 3D print crowns in as little as 10 minutes and use the most advanced post-curing system on the market to make restorations ready for fitting in the mouth in a total of just 45 minutes or less.
The SprintRay Ceramic Crown is the 3D printed chairside solution for definitive crowns, completely redefining the professional workflow. Find out more on the website.
a first for denture fabrication
When it comes to making dentures, the SprintRay OnX Tough 2 builds on the previous generation of product that was the first radiopaque nanoceramic restorative resin on the market.
OnX Tough 2 is the only 3D printing resin MDR-cleared for fixed hybrid dentures, making it ideal for implantretained prostheses in full arch rehabilitation cases. By leveraging cutting-edge NanoFusion™ technology, the denture resin sets new standards of quality and durability. It exhibits significantly higher flexural strength, flexural modulus and impact strength than other resins for dentures and implantretained prostheses on the market. This affords complete peace of mind for both practitioner and their patient that the new dentures provided will stand the test of time.
The Class II 3D printing resin is also designed to mimic natural dentition with just the right amount of translucency and opacity. This optical performance is intensified by

shade stability for uncompromising natural aesthetics. In addition, used in combination with the SprintRay Pro 2 3D printer, the Onx Tough 2 affords unparalleled accuracy and throughput, meeting the highest clinical standards and most complex patient needs. The result is a long-term provisional or even final restoration delivered on the same day as surgery, when performed using a guided approach. Patients enjoy the enormous advantage of shorter treatment times, fewer practice visits, increased convenience and the associated lowered costs. For clinicians, the speed of treatment, combined with superior outcomes, means increased efficiency and profitability – with absolutely no compromise in quality. All the details can once again be found on the SprintRay website.
3D printing reimagined

As SprintRay continues to operate in a field of its own, the goal remains the same – to help clinicians across the globe reimagine chairside 3D printing for the benefit for their patients. Chairside restorative workflows can now be implemented with no compromise in quality, accuracy, strength or aesthetics. Find out how SprintRay could help you redefine your restorative workflows today.
For more information, please visit https://sprintray.com/en-uk/ n

Removing inflamed pulp and sealing a tooth preserves its natural strength, making root canal treatment possible. This is nearly always preferrable to extracting the tooth. The apex of the tooth contains all the blood vessels and nerve fibres needed to keep the tooth alive. However, tooth decay, leaky fillings and dental trauma can damage the apex, opening it up for harmful bacteria to infect the root canal.
An open apex can prevent root canal treatment success as there is no natural barrier to contain the added filling. Because of this, closing the open tooth root is a crucial clinical challenge, one which is best aided by using a reliable electronic apex locator (EAL) to find the position of the apical foramen and work out the length of the root canal space.
the working length
Whilst radiographs are used by practitioners for diagnosis and determining the working length of the tooth root, an EAL can be more effective for the latter, with a 99.7% accuracy versus the 98.1% of a digital radiograph and 96.1% for a conventional radiograph. The working length of a tooth must be reliably determined for the success of the operation as it keeps the preparation inside the restricted radicular area; apical extrusion is then avoided and good obturation is secured. Inaccuracy in locating the apex and defining the working length can lead to damage of the apices and periapical tissues, limiting the success of post-operative healing.
Moreover, accidental overinstrumentation can result in a root canal with no apical constriction. In these instances of treatment failure, the patient will be dissatisfied, with discomfort, pain and inconvenience, surmounting to a negative experience. The importance of determining working length therefore demands a device as effective as an EAL to ensure treatment success and create a satisfying experience for the patient.
Childhood trauma is a common cause for an incompletely formed tooth root, with the highest frequency for dental trauma among children of 12-14 years. This is often attributed to the increase in participating in aggressive sports and other physical activities, whilst infants and preschool children are most likely to experience dental trauma caused by a fall at home. Paediatric dentists treating these injuries are likely to perform apexification and using an EAL can make the treatment easier – one of the major advantages of an EAL is its non-invasiveness, making it a preferrable option when delivering complex root canal therapy that requires patient compliance, especially among children. Unlike the experience of a radiograph, in which having to bite down on the intraoral film causes discomfort and can trigger the gag reflex, an EAL is more agreeable.

It connects the patient’s lip with the endodontic file in the root canal, turning the body into a minimally invasive electric circuit. A painful or uncomfortable treatment can both inhibit its success and lead to a negative experience for the young patient, with the potential to increase dental anxiety or fear; an EAL can provide greater clinical confidence whilst also being a satisfactory experience for the patient. Emetophobic adult patients may also prefer an EAL for treatment, whilst the reduction in radiation exposure compared to a radiograph makes it a more appealing alternative. Moreover, an EAL streamlines the workflow, taking less time and providing results quickly, without the practitioner having to step out of the room. Combined with its non-invasiveness, the efficiency of an EAL makes it optimal for treatment success and patient satisfaction.
For a first-class apex locator, consider the CanalPro Jeni from Coltene, an innovative endomotor that features a digital assistance system designed for root canal preparation. The angled handpiece of the integrated apex locator allows for constant, precise measurement of the working length; afterwards the machine changes to the next file size until the required preparation size has been achieved. Capable of so much more, the CanalPro Jeni assistance system uses complex algorithms to control the variable file movements in millisecond intervals by receiving feedback of the current intensity, torque and file stress, preventing overinstrumentation. This makes the system a safe, simple and effective solution. A comfortable experience and a successful treatment can improve how patients engage with the dental practice. By harnessing the best technologies, practitioners can deliver excellent endodontic work for adults and children alike, preserving the natural teeth.
For more on COLTENE, visit coltene.group/lp/canalpro-jeni-en, email info.uk@coltene.com or call 0800 254 5115. n
There is an abundance of factors that the dental professional must consider when recording impressions for indirect restorative care. Ensuring occlusal contacts are properly recorded so that a new solution works with the existing dentition is fundamental, and accurately covering the surrounding structures so that an aesthetic and harmonious restoration can be designed is also important.
In a matter that concerns both aesthetics and oral health, clinicians must make the decision to either implement a supragingival or subgingival margin. It’s important to recognise when either solution may be necessary, and ensure accuracy of the impression for a precise restoration.
When providing an indirect restoration, a subgingival margin placement is often required when covering old restorations or decay, increasing the length of the tooth structure, or enhancing the aesthetics in the anterior dentition. It can be as much of a functional decision as one to improve the aesthetic result. When working this way, however, there are risks that can compromise the viability of a solution. Without proper access to the subgingival margin and sufficient drainage of fluid at the treatment site, the impression-taking process and restoration will be impaired. Poor margin adaption is of high concern when placing a subgingival restoration. Patients risk an increase in accumulation of bacteria at the treatment site, which, if not cleaned thoroughly, can prompt gingival inflammation and an increased risk of secondary caries development.
This is one reason why a supragingival finish is preferred where at all possible. When margins are kept supragingival, the environment is optimised for an ideal patient tissue response, which could lead to more predictable treatment recovery. Such an approach to indirect restorations has also come under the umbrella of minimally invasive dentistry when used in tandem with adhesive solutions, with some professionals going as far as to suggest it should replace traditional mechanically retained restorative dentistry.
As expected, the supragingival margins present different difficulties. Primarily, there is a possible aesthetic misalignment between natural and restored tooth structure, and in these circumstances, it is recommended to limit the use of supragingival restorations to the proximal and lingual areas of the dentition. With the demand for aesthetic dental treatments growing, a compromise may have to be made.
interact with the opposite arch, requiring adequate occlusal contacts that work with the surrounding dentition, and the relationship with the teeth laterally within the same arch must also be considered for aesthetics, function, and future interdental cleaning. Where the gingival margin is unaffected, the creation of the restoration will not need an accurate impression of the sulcus at the treatment site for an effective result.
However, when an indirect restoration needs to be placed with an aspect in the subgingival margin, high-quality accuracy at this point is non-negotiable. The detection of a finish line in the subgingival margin requires a clean, healthy gingival sulcus, with proper soft tissue displacement, and clear visibility of the prepared tooth anatomy. This is the case when using both conventional and digital impression taking methods. The literature has shown that intraoral scanners struggle to accurately capture the margin where it finishes deeper into the sulcus. A 2021 study goes as far as stating that when placing a crown’s margins deep (1.5-2mm) into the sulcus, it is ill-advised to use digital impressions.
return to convention
To adequately record the subgingival margin when creating an indirect restoration with a conventional approach, it’s essential to retract and displace the adjacent soft tissue. This allows the chosen impression material to capture the features of the preparation and finish line, as well as some unprepared tooth structure apically. The margin width should be a minimum of 0.2mm in order to give the impression material enough space to develop, and not tear or distort upon removal.
Moisture control at the site is another controllable variable that may affect the outcome, but optimising the impression is also possible by choosing the bestsuited material for the task. The KemKat impression compound from Kemdent is ideal for adding to an impression tray, and its high viscosity allows for impressive recording of the full sulcal depth. Clinicians can break off only what is needed for partials or additions, but be sure to develop optimal detail for the restoration. Both subgingival and supragingival restorations have their merits. No matter the clinical need, and the preference of the patient, its essential to be able to deliver a high-quality result. This begins with an accurate impression, and ends with a restored smile.
For more information about the leading solutions available from Kemdent, please visit www.kemdent.co.uk or call 01793 770 256 n
about the author
nicolas Coomber, COLtene national account & marketing manager.

Dental professionals need an accurate representation of the dentition to prepare an indirect restoration, whether it is placed subgingivally or supragingivally. The latter approach provides the advantage of easier impression acquisition within the necessary anatomical interactions. This is understandable; the restoration will only

about the author alistair mayoh, marketing Director, Kemdent.

Is it time for mixed practices to finally cut loose from the NHS altogether? Practice Plan Regional Support Manager, Donna Hall, suggests events may be forcing the hand of some dentists
The start of a new year is a great time to make plans and changes. In between the eating, drinking and being merry, the Christmas break can often be a time to reflect on the previous year and decide what worked and what no longer serves you.
Many things of moment happened in 2024. There were general elections in 24 countries, which accounted for more than half of the global population. Our own general election in July ushered in the first Labour government for 14 years and, with it, a new Secretary of State for Health who promised to reform the NHS dental contract.
economic factors
While we still await further news about contract reform, probably the events that affected dental practices on a more fundamental level were the new Employment Rights Bill and the Chancellor of the Exchequer’s first budget. The measures announced in them made running a dental practice far more expensive thanks to the increases in the minimum wage and employer’s National Insurance contributions.
There were some winners in relation to the latter thanks to the rise from £5,000 to £10,500 for the Employment Allowance. So, if you run a mainly private practice with only a handful of employees, you may be one of the lucky ones who is better off. However, if more than 50% of your income comes from NHS treatments, you cannot benefit from this change as the public sector is excluded from claiming the allowance.
Private practices are able to pass on the increase to their patients through higher fees. However, this option is not available to NHS practitioners. The expenses element of the uplift will go nowhere near covering the increases in costs dentists are, and have been experiencing, for a few years. Fixed fees leave contract holders without a way to compensate for these spiralling costs leaving them facing the prospect of being far less profitable, or even running at a loss.
Informal cross subsidy has long been a feature of mixed practices. While retaining a small NHS contract may satisfy the social conscience of the dentist, it still leaves them subject to the bureaucracy that, in many cases, was a factor in their decision to introduce more private dentistry in the first place. As the cost v benefit calculation becomes trickier, is now the time to hand back the whole contract and find other ways, outside the NHS, to satisfy your conscience?
A dentist who did just that after many years of running a children’s NHS contract alongside his private practice is Practice Plan customer, Simon Thackeray, of Thackeray Dental in Mansfield. When Simon made the decision in 2005 to go into private practice he retained a small NHS contract for the children in his practice. However, in 2021 he finally chose to become a fully private practice and handed back his contract. “When we did the original partial conversion, I didn’t want there to be a criticism levelled at me that there would be a two-tier service for adults with some exempt NHS patients and others private,” Simon explains. “I didn’t think that was equitable. However, with the children, that was much more emotive. So, we kept them on.”
The decision to become fully private with no NHS involvement was fuelled partly by Simon’s frustration with the bureaucracy surrounding it. “It was so stressful and time-consuming that it wasn’t worth it,” he says. “It was 1% or 2% of my turnover but it was 80% of my stress. I had to fill in so many forms or complete things online, it was stopping us doing the clinical work we were supposed to be doing.”
The practice had been subsidising the cost of children’s care for many years as Simon admits, “To tell the truth we offered a private level service, and the parents seemed to realise that we were subsidising it. So, when we finally went fully private, it wasn’t such a big jump for the parents as they’d got used to having care of a particular standard, and their kids had received the same level of care too.”
early education a focus
The practice now has a children’s plan for those aged six and over. However, care for children under that age is free. His aim is to help ensure that children develop good oral health habits in the early years. As he says, “Advice is the treatment you provide at that age.” In addition, the practice has oral health educators to reinforce advice given by the dentists.
Although the practice turnover for children’s care is now lower than under the NHS contract, Simon is content

with this. “This doesn’t bother me,” he says, “Our focus on children’s oral healthcare has bolstered the reputation of the practice so much that the net gain from the additional adult patients more than compensates for this.”
What advice would he give to someone in a mixed practice unsure about whether to retain their NHS contract? “We waited quite a long time before doing away with the children’s contract. Would I do things the same way again? Probably not. I would rather have a clean break and just get rid of the whole thing at once.”
Having made the decision to return the last portion of his NHS contract Simon’s daily hassle has been reduced and he has full control of his own business. As he says himself, he has never looked back and has no regrets.

“If you have the reputation and the energy to push yourself forward then it’s a great thing to do. Going private is one of the best business decisions I have ever made.”
This year, Practice Plan celebrates 30 years of welcoming practices into the family, helping them to grow profitable businesses through the introduction of practice-branded membership plans.
With over 300 years’ dental experience in our field team, if you’re looking for a provider that has that family feel but knows a thing or two about dentistry… Be Practice Plan and get in touch. Call 01691 684165 or visit practiceplan.co.uk/be-practice-plan/ n
about the author
Donna Hall has been a regional Support Manager at practice plan for 10 years. practice plan is the UK’s leading provider of practice-branded patient membership plans, partnering with over 2,000 dental practices and offering a wide range of business support services.



2024’s Dental Hygienist of the Year, Amanda Harbrow-Harris, discusses her career, professional outlook, and the incredible extra curricula activities that led to her winning the award for a second time
You began your career as a dental nurse before transitioning to become a dental hygienist. What first attracted you to dentistry and what keeps you motivated?
I was very naughty at school and left with no GCSEs. It took me years to get to where I am now. I started university at 36 years old after gaining the required UCAS points to study.
I started as a trainee dental nurse in 1995 (I’m old!) and, from day one, I was hooked. I have always enjoyed dentistry.
There’s the obvious element of getting people out of pain and improving confidence in their smiles, but I honestly think for me the main thing is interacting with people – following their journeys in life and having a good old natter when they come in. People always seem to trust a dental nurse more, as they are their advocate in the room, and I’ve carried this ethic over to my role as a hygienist.
I had completely exhausted the role of a dental nurse, from working in NHS and private practices as a senior nurse in Harley Street, Dubai, and dental training hospitals. The natural progression for me to take my career further was to train to be a hygienist. Although, I do remind the nurses I work with that I am also still a dental nurse. I am dual qualified now.
The patients’ best interest is always paramount to me, and I will give them advice on what treatment options they have with a dentist based on their circumstances and anxiety levels.
I’m always keen to keep up to date with the latest procedures and products. This keeps me motivated. I am a self-confessed tooth geek!
Tell us a bit about your role at Sharrow Group. I am one of nine hygienists over the four practices within the group. We all get along well and have a WhatsApp chat to ask each other for advice and arrange catch-up days.
I work four days per week at Springfield Dental Care and have been there for nearly nine years now. I share the surgery with another hygienist, and we work very


well together. We each leave the room set up for the other and take on shared responsibility of ordering stock and maintaining the equipment.
How do you motivate patients to maintain good oral health habits?
By seeing them at regular intervals tailored to each individual’s needs. By not being judgemental or authoritarian but by empathising and educating them. I update every single patient’s medical history on arrival and, if there is anything relevant for oral hygiene, I will point this out to them.
I always make sure they leave my room with their mouth spotless so I can see their progress between visits.
You keep yourself busy away from the practice. What else do you get up to?
I belong to the BSDHT and am involved in a mentoring programme called Ikigai. I am a clinical educator for NSK and do presentations throughout the year, as well as running trade stands and hands-on training for other DCPs on how to use their powder therapy and Piezo equipment. I also do talks on my specialised topics, lupus in dentistry and whitening, for which I have had papers published.
In addition, I am a clinical educator, training Dental Hygienists for the University of Essex.
Becoming an educator for Ikigai has been integral to my career since winning Hygienist of the year in 2019. They approached me and I gladly joined their team. It has been a fantastic experience; I have learned so much and made some good friends. They are such a supportive non-judgemental group.
I do a lot of charity work as well. In October 2023, I raised over £2,100 for Maggie’s cancer charity by completing an open water swim every day for a month. I volunteer at local hospices to give talks on palliative care and dentistry to the health care staff and have been delving deeper into cancer care over the past couple of years due to my wife having breast cancer. I have enjoyed helping people by advising on suitable toothpaste and products to relieve their symptoms, and it has been very satisfying to pass on my knowledge.
I am planning on volunteering my services at the breast care unit as I recently made a plaster of Paris bust for someone due to have a mastectomy, which I feel it would be a great free service to offer.
I also want to help at the local chemotherapy unit, as I have been advising the oncologists on products that help relieve the chemotherapy symptoms. It has been lovely that so many of my peers have helped with advice and products.
In my personal life, I’ve lost four stone in the past year, which is great. I am supporting my partner, who is doing the London Marathon in April and, subsequently, I am now running long distance myself and completed my first parkrun on the weekend. I’ve signed myself up to do an open water


swim in June, which I am in training for, so lots to look forward to this year.
For my next adventure, I am going to Tanzania on 1st March to do some dental volunteering after raising £2,000 for Bridge 2 Aid last year.
How did it feel to be named Dental Hygienist of the Year?
Amazing! I was so happy. I feel like I manifested that I was going to win in 2024. I’d had a personally bad year in 2023 with my partner being very ill with cancer (they are ok now) and felt some good luck must be due to come my way. It is such an honour as I truly do love being a hygienist and it is 100% my vocation in life. I won it in 2019 and had massive imposter syndrome. Therefore, to win it a second time has made me feel much more confident in myself and my skills. I feel I have made it!
My friends and family are so proud of me as are my patients when I tell them. The practice was obviously thrilled and I was also really humbled when I spoke to one of the judges and she explained why they had voted for me based on my true passion for the job and not being egotistical.










You’ve got to crack a few eggs to make an omelette, so the well-worn cliché goes.
When you’re facing change, especially if it’s a big change, it can be hard to unpick some of the legacy decisions you’ve previously made. It feels conflicting and messy to turn things upside down and reconsider things from within a new context.
Last year, I rebranded one of my endodontics courses. We’d worked under the name of Endo Roots for a while but, when we stopped and really thought about it, it didn’t tell the story we wanted it to. After some thought (and a lively WhatsApp group for suggested new names), we came up with ‘Everything Endo’, with the tagline ‘The A-Z of endodontics’. It didn’t take too long to evolve the brand but it did feel a little uncomfortable as we updated the many places where it appears –course outlines, presentations, booking websites and so on.
Making change can be difficult but identifying the need and having the vision for a better outcome is a great motivator.
You could use four categories to help you navigate the messy business of change:
• Keep (it works)
• Improve (it works but needs a tweak or two)
• Replace (we need an updated approach)
• Discard (serves no purpose)
In business circles, this is sometimes referred to as DAKI (drop, add, keep, improve) and discarding is often a good place to start – it helps you clear out what’s not working so you

can start to think clearly about what needs addressing.
This kind of framing can provide a more comfortable route to reach a solution. You can even put something in a temporary category – improving something ‘for now’, knowing that it will need to be replaced in 12 months’ time, for example.
It’s also important to involve everyone in the process. How you view the way things are done are likely to affect other people within your practice, so get their views for a full 360-degree perspective.
There are always some aspects of our work life that we cling to for dear life as it’s what we’ve always done – and they are reassuringly
familiar to us. It’s particularly hard to face changing these as they might also involve a need for emotional disentanglement before you can disconnect and move on.
Making a change that involves the sacrifice of something that has gone before can feel challenging. It’s a bit like throwing something out when you remember what you originally paid for it! A good way to look at it is as an evolvement, a step up from the old regime that served its purpose – and onto something that delivers what you need now. That way, you can feel reassured that your historic decisions have played a vital part in today’s decisions and are part of an essential, natural cycle.
Whatever you happily implement, be prepared to challenge it again at some point – no decision is truly future-proof and you’ll need to face the messy business of change all over again! n
About the author Dr Dhiraj Arora BDs MJDf rCs (eng) Msc (endo) pG Cert Ce. owner of evo endo, with three practices (limited to endodontics) in Twickenham, Gerrard’s Cross and slough. Dhiraj is a passionate teacher and ambassador for all things endo. follow him on instagram: @drdij_evoendo

Iwrite these pieces to help, to try to stimulate, and occasionally to provoke. I am aware, like most writers, that these articles will not be read by all and may go unacknowledged. In spite of that, we persist.
Similarly, once I had got used to the fact that my patients rarely gave me a second thought between visits, my fragile ego was able to rest. What did my patients really want from me? First, to be there when they perceived a need or a want; in spite of the ‘BS’ spouted by some marketing people, I take need and want to have much the same

meaning. Second, to treat them well. That single statement, presuming as it does competence, caring and comprehension of their situation, could probably be expanded into a book, joining the long list of books that I will never write.
The year marks the 20th anniversary of the sale of my dental business and the start of the rest of my life, as the cliché goes. I sold because it was time, I had taken things as far as I wanted and needed new challenges. The changing face of clinical dentistry with its increasing emphasis on aesthetics was something that I was happy to leave to others. It was not why I had become a dentist in the first place and whilst I delight in the success of others, especially my clients, it didn’t float my boat. I want to share two things I thought I understood then, but have only come to truly acknowledge in the intervening years. They are simplicity and complacency, and I believe they are inexorably linked. Firstly, it is vital to keep things as simple as possible. The more you try
to show, the less people see. The more you try to say, the less they hear. The more you try to explain, the less they understand. This is true for relationships with both patients and colleagues. I know that the shadow cast by the litigators and prosecutors (I include the GDC here) is an almost permanent influence but that brings a greater requirement for clarity that is best provided with simplicity, not complexity. A recent posting by the ‘Gaping Void’ team gives the example of the London Underground map as a triumph of the simple over the complex.
Secondly comes the current state of the computer company Intel, whose most recent chief executive has recently resigned, marking another step in the gradual decline of one of the world’s most successful businesses. Their failure, to ‘completely miss mobile’ and to decide to never be a ‘player in the game’, has seen them slide from dominance. They have gone from being a top 10 chip manufacturer in terms of market capitalisation to 180th. They thought they didn’t need
to shift from what they perceived as their core business and are suffering as a consequence.
Their long-time CEO and chairman, and third employee, Andy Grove, wrote in his autobiography, “Business success contains the seeds of its own destruction. Success breeds complacency. Complacency breeds failure. Only the paranoid survive.” It is obvious that, in spite of the apparent clarity of his words, nobody listened to him.
The metaphor I use is that of a soap bubble balancing on the palm of your hand, as soon as you presume you have it and try to hold it, it has gone forever.
If you acknowledge one or both of these topics, my time has been well spent. n
references
• https://mailchi.mp/gapingvoid/ stop-being-so-right-all-thetime?e=824aedcacd
• https://daringfireball.net/2024/12/ andy_grove_was_right?utm_ source=substack&utm_ medium=email
Stem cell therapy has been explored since the 1950s, with the first bone marrow transplant occurring in 1956. The technique has been evolving ever since, with several indications in modern medicine.
A cure for type 1 diabetes?
I was interested to read recently that stem cell therapy has been used to reverse type 1 diabetes. The study, which took place in China, chemically induced fat cells from a lady with the disease to make them behave as pluripotent stem cells. This gave them the ability to develop into other types of cells, which they used to create islet cells. Islet cells are commonly found in the pancreas and are involved in the production of insulin. It is these cells that are destroyed by the immune system to develop type 1 diabetes in the first place.
For the research, the islet cells created were injected between the skin and abdominal muscles. They were able to successfully develop in the body, developing their own vasculature. Within two and a half months, the patient no longer needed insulin injections. She was able to produce enough insulin to reach her target glycaemic range 96.2% of the time – compared to just 43.2% of the time prior to the procedure. She also had lower glycated haemoglobin, indicating long-term glucose levels of a non-diabetic.
The patient in this study had already experienced two failed liver transplants and one failed pancreas transplant prior to the stem cell therapy. To find an effective and minimally invasive solution to her type 1 diabetes is fantastic.
Of course, this area of study is ongoing with a lot more to do before such a treatment concept could safely be made available to the masses. However, there is a lot of promise in the approach for a number of conditions.
Stem cell therapies are already being used in the bone marrow transplant procedure for leukaemia, skins grafts for severe burns and corneal grafts for sight loss. This is an exciting and rapidly growing area of regenerative medicine, with stem cells used to optimise cell renewal, development and healing in different clinical situations.
In dentistry, stem cell research is often focused on regenerating damaged dentine or pulp, treating resorbed teeth, periodontal regeneration or perforation repair. There is even research happening into whole tooth regeneration as a replacement for dental implant treatment – though this is still some way off being implementable. Stem cells of dental origin may also have wider medical implications. For example, they might be used in heart therapies, to regenerate brain tissue or for muscular dystrophy therapies. Again, significant study is needed for before any of these can be confirmed and utilised in a practical way, though it is exciting to consider the possibilities. n
About the author endoCare, led by Dr Michael sultan, is one of the UK’s most trusted specialist endodontist practices.

Dr Philip Mitchell is the current Vice President Elect of the British Endodontic Society (BES), and will become President Elect of the Society after the Spring Scientific Meeting next year. He shares a little bit about himself and his experience with the BES:
“I am currently the Vice President Elect of the BES, with my presidency due to take office in 2026. Previously I have acted as a council member, beginning around 15 years ago, and I was part of a specialist advisory board at the Royal College of Surgeons of Edinburgh.
“Endodontics first appealed to me as one needs to specialise in order to improve and achieve excellence. I was attracted to the biological side of things, as this is a discipline in which we treat diseases.
“I think it is obligatory for someone who is a specialist in endodontics to become a member of the BES, in order to support and promote the specialism both within general dentistry and within the population as well.
“My favourite benefit offered by BES membership is the social aspect of the annual meetings. It is great to meet up
There has been much discussion recently about expanding the roles of dental care professionals. These changes enable them to more effectively utilise their full scope of practice, and alleviate the workload of dentists to enable patients to receive the highest possible standards of care. As of July 2024, there are 10,051 dental hygienists, 6,690 dental therapists, and 64,968 dental nurses registered with the General Dental Council in the UK. By enabling these vital members of the team to work to their full capacity, expand their skillset, and lead evermore fulfilling careers, the dental practice can run more smoothly, resulting in a better experience for all patients.
new powers for dental hygienists and therapists
Previously, dental hygienists and therapists were able to administer medicines such as local anaesthetic and high-strength fluoride, but only under the prescription of a dentist. In this workflow, they were required to leave their patient to interrupt a dentist’s work to ask them to sign a prescription to enable them to continue with their own patient care. Recent changes, which came into effect in June 2024, enable dental therapists and hygienists to supply specific medications on their own. This legislative change aims to make the process more efficient for everybody, including both the practice team and their patients.
Overwhelming support was received when public consultations ran in 2023, with 97% of respondents approving of these new powers. When dental hygienists and therapists with the appropriate training use their new powers, patients will receive the primary care they need more quickly and simply, enabling dental hygienists and therapists to provide pain relief and fluoride without approval from a dentist.
However, even without these new interventions, there are a number of ways that dental practices can encourage their dental hygienists and therapists to expand their skillset, and utilise their full scope of practice. For example, dental therapists can provide restorations, carry out pulpotomies, and extract teeth, and both dental hygienists and therapists can develop additional skills to enable them to provide tooth whitening under a dentist’s prescription, administer inhalation sedation, and remove sutures.
encourage your dental nurses’ career development
It can also be extremely valuable to encourage the career development of the dental nurses in your team. By motivating your dental nurses to develop additional skills within their scope of practice, you not only provide them new career opportunities, you also help the practice to run more smoothly, freeing up your time, and that of your dental team to enable better patient care.
Just a few of the additional skills dental nurses might like to develop include oral health education, assisting in the treatment of patients who are under conscious sedation, patients with special needs, and orthodontic patients, and intra and extra oral photography. Further to this, dental nurses can undertake a range of other tasks under the prescription of another clinician – including taking radiographs.
Using high-quality equipment makes expanding dental care professionals’ skillsets easier for the whole team. The latest models will have all of the features you and your team need to inspire confidence, and ensure that things go right the first time. When selecting an imaging system, for example, choose a system which offers high-quality images, ease of use, and exceptional patient comfort. It can also be incredibly useful to acquire your equipment from a team who truly understands you and your workflow. Clark Dental has over 49 years of experience working with the dental profession, and is perfectly placed to ensure dental practices like yours receive the ideal equipment for them. Its wide range of dental imaging solutions includes the Axeos Extraoral Imaging System, the 2D/3D imaging system which can be flexibly adapted to suit the specific and evolving needs of

with old friends a couple of times a year to chat and catch up.
“Outside of work, I very much enjoy riding my bikes and swimming.”
For more information about the BES, or to join, please visit the website www.britishendodonticsociety.org.uk or call 07762945847 n

your practice. Axeos is easy to use, to help the practice team to work more efficiently, reduce errors, and provide a comfortable patient experience. The EasyPad is intuitive to use with self-explanatory symbols, and the patient positioning and image assistant enables smart height adjustment, reducing waiting times for patients, and ensuring reproduceable image quality.
By encouraging additional training and skill development in your practice, you enable your dental team to achieve their potential and develop their careers, all whilst making the patient journey smoother and helping the practice to run more efficiently. Utilising high quality equipment will help the dental team to feel more confident in using their new skills, and will reduce the risk of errors in your practice.
For more information call Clark Dental on 01268 733 146, email info@clarkdental.co.uk or visit www.clarkdental.co.uk n
About the author
stuart Clark, Managing Director of Clark Dental.

When was the last time you got out of your comfort zone? For many, it’s a rare occurrence. If it were easy, there wouldn’t be so much discussion about it. But pushing beyond what’s comfortable can also be immensely rewarding, both professionally and personally.
For dental practitioners, the daily workflow can be a comfort in its predictability. But there are many parts of the role that may be harder to embrace, such as networking events, engaging with difficult patients or making that next leap to deliver a lecture or find a mentor. Finding the confidence and motivation needed to face a challenge and do something new is therefore essential for practitioners in order to enhance their career opportunities.
Zoning in
The comfort zone is a psychological, emotional and behavioural construct, best epitomised by a person’s daily routine. It is familiar and safe, promoting security and confidence in the day-to-day dealings of life. From taking the same route to work to maintaining identical meal times, certain behaviours can become subconscious acts. In the UK, the majority of Brits stick to their daily routines and play it safe when it comes to trying new things, with 45% fearing that they may one day regret it. There are many reasons for this, varying from being worried about embarrassment to a lack of self-confidence or being afraid. By staying in the comfort zone, a wealth of knowledge and resources remains untapped, especially at social events. From missed experiences to learning something invaluable, resistance to the new can limit professional growth. For instance, dental practitioners seeking stronger relationships may wish, but be nervous about, attending a networking event. Whilst going alone can be a daunting prospect and may deter some, not going would be a missed opportunity to make the new professional connections to visit future events with. Similarly, practitioners may find engaging with certain patients difficult; they could be rude or shy, for instance. Getting to know patients is a vital aspect of a successful dental career, improving the practitionerpatient relationship and deepening the level of trust. However, many medical students have ended up distanced from their patients, highlighting how emotion is often eclipsed from the medical education discourse. Younger dental practitioners must therefore push themselves to be curious about their patients, establishing friendly connections for a better patient experience. This will also improve the confidence of the practitioner.
feel the buzz
Getting out of the comfort zone can also release adrenaline, and this can have several positive impacts. Adrenaline is the hormone that induces the fight-or-flight response and can be triggered in many ways; horror films, theme park rides, skydiving, driving fast cars. It increases blood pressure and blood sugar levels, making the brain more alert and energising the body. For a temporary amount of time, adrenaline also boosts the circulation of antioxidants, neutralising the damaging free radicals. With a surge of

adrenaline, the brain becomes fully engaged and can handle cognitive tasks much more efficiently. For some, an adrenaline rush can also release dopamine and serotonin, causing feelings of positivity and a sense of freedom. This can release any tension and serve as a distraction for those stressed or worried. A small adrenaline rush may also help practitioners open up when talking with a new professional.
Comfort outside the comfort zone
For dental practitioners, getting out of the comfort zone can release adrenaline as the fight-or-flight instinct kicks in. This can refresh the body, regulate mood and give peace of mind. An adrenaline rush can come from giving a lecture, meeting new people, going on trips or doing something adventurous.
When it comes to trying something new, consider the exciting events at Clover Dental Group. For a day of adrenaline, the Porsche Dental Roadshow in South Lakes is a perfect fusion of fast cars, fine dining and intimate networking. An hour of CPD in the form of an insightful talk will also keep things on track. Located at the stunning Gilpin Hotel & Lake House, this luxury day is an excellent ice-breaker for making long-term professional connections in an environment that champions innovation and elegance. Don’t miss out on the high-octane thrills and book with Clover Dental Group today. There are many ways for practitioners to push themselves out of their comfort zones. Those that do can unlock new levels of confidence, embracing a positive mindset that enhances their professional and personal lives.
exclusive: porsche Dental roadshow south Lakes 3 April 2025 9:00am – 5:00pm
For more information on the events available from Clover Dental Group, please visit the https://cloverdentalfitout.co.uk or call 07961 669996 n
About the author steve Kettle is a Director at Clover Dental.
As we bid farewell to 2024, it’s time to embrace the opportunities and challenges that 2025 will bring to dental practice management. The past year has taught us valuable lessons in adaptability and resilience, and as we move forward, it’s crucial to stay prepared and proactive. Let’s welcome 2025 with a commitment to excellence and a readiness to navigate the evolving landscape of dental care.
One of the significant challenges in the later part of 2024 was the noticeable decrease in patient enquiries and the uptake in treatment plans. Several factors contribute to this trend, including economic uncertainties, changes in patient priorities, and increased competition. To address this, dental practices need to adopt a patientcentric approach, emphasising the value of preventive care and regular check-ups.
Leveraging front of House teams
The front of house team plays a crucial role in managing patient interactions and ensuring a seamless experience. Efficient Front of House operations can significantly impact patient satisfaction and retention. Training staff to handle enquiries effectively, manage appointments, and provide excellent customer service is essential. Implementing a system for regular feedback and continuous improvement can help the team stay responsive to patient needs.
effective diary management
Efficient diary management is another critical aspect of handling fewer patient enquiries and maximising the use of available appointment slots. Utilising modern scheduling tools and software can help automate and optimise appointment bookings, reduce no-shows, and ensure that the practice runs smoothly. Clear communication with patients regarding appointment availability and the importance of attending scheduled visits can also help manage the diary effectively.
enhancing patient engagement
Engaging with patients through various channels, such as social media, newsletters, and direct communication, can help maintain their interest in dental care. Educational content about the benefits of regular dental visits, new treatments, and preventive care can keep patients informed and encourage them to stay committed to their oral health.
fostering a culture of continuous improvement
In the face of these challenges, fostering a culture of continuous improvement within the practice is vital. Regular training and development opportunities for staff, staying updated with industry trends, and being open to new technologies and methods can help practices adapt and thrive.
financial management and efficiency
The financial landscape for dental practices in 2025 will see increased overheads and operating costs, which may be unavoidable in some instances. However, increasing efficiencies within the practice is crucial. Ensuring that hourly targets are met, optimising the use of resources, and minimising waste can help manage these costs effectively. By focusing on efficiency, practices can maintain financial health while continuing to provide high-quality care.


Understanding the difference between “want” and “need” patients is crucial for tailoring services and communications effectively. “Need” patients require immediate dental care due to pain, infection, or urgent dental issues. They often seek treatment for essential services and may have different motivations compared to “want” patients, who seek elective or cosmetic procedures to enhance their smile. Tailoring your approach to meet the specific needs of each group can improve patient satisfaction and retention.
Being prepared for the challenges of 2025 requires a comprehensive approach that involves understanding changing patient behaviours, leveraging the Front of House team, managing the diary effectively, and continuously engaging with patients. By focusing on these areas, dental practices can navigate the evolving landscape and continue to provide excellent care to their patients. n
About the author
Lisa Bainham is president at ADAM and practice management coach at practice
Management Matters.



Dr Manraj Kalsi is a specialist periodontist and implant dentist with a special interest in prosthodontics. He graduated from Leeds Dental Institute in 2016 and completed his vocational training in West Sussex. Following this, Dr Kalsi worked across South West London and Surrey, gaining experience in NHS and private dentistry.
Dr Kalsi shares a little bit about himself and his role as Regional Rep for South East England within the Association of Dental Implantology (ADI):
“I joined the ADI straight after I qualified, meaning I have been a member since 2017/2018. Since then, I have been to all the Team Congresses and Masterclasses alongside completing a lot of postgraduate training. Attending ADI events has really complemented my learning, with the opportunity to hear from overseas speakers who have opened my eyes to developments outside of the UK. Two stand out events for me have been the ADI Team Congress in Birmingham and the Sinus Augmentation Masterclass in London.
“Last year I joined the ADI Next Gen committee, helping Dr Ricky Bhopal with planning events and masterclasses. As a part of Next Gen, we have a roadshow running throughout 2024, which has been hard work but excellent fun, allowing us to meet lots of people, and learn a lot!
“Because I joined the ADI early in my career, I was able to enjoy free and heavily discounted membership rates. This enabled me to attend all of the Team Congresses and Study Days straight away, which was a great way to learn a lot and network at these big events.
“I have attended events hosted by a couple of other dental groups in the UK, however I found the ADI to offer the best balance of academic learning and clinical experience – a great mixture of the two.
Robbie Lawson has been announced as President of the British Orthodontic Society and Roz McMullan as Honorary Patron. Both will take up their roles in January 2025.
Robbie finished his specialty training in Cardiff in 1996 and has been a Specialist Orthodontist in Edinburgh since then. As a founding partner in a busy, multi-surgery specialist practice, he has a keen understanding of the challenges in providing both NHS and Private treatment in an ever-changing environment. He has been the Chair and Co-Chair of the Scottish Orthodontic Specialist Group, President of the Royal Odontochirurgical Society of Scotland and has served on the OSG and BOC committees of BOS. He is an examiner in M Orth at the RCS (Edin).
Robbie has an enthusiasm for aesthetic treatments and lectures internationally. Obviously presenting at BOC has been a career highlight! He regularly contributes to postgraduate training programmes throughout the UK and Europe.
so freely of their time and expertise. I am sure that, together, we can ensure that the BOS continues to provide strong, relevant advocacy for all sectors of the specialty and our patients in the years ahead.”
new Honorary patron

Dr Amit Patel was the president at the last ADI Team Congress and, as a fellow periodontist, it was great to see the ADI delving into the different niches like soft tissue and sinus lifting.
“This is not to mention the social side of the events, particularly at the Team Congresses, which host the best parties!”
Discussing his appointment to the ADI Board, Dr Kalsi comments:
“I have been working with the Next Gen committee for the last year or so, and have tried to contribute as much as possible by organising events. This has been a lot of fun, and I have been able to pursue training alongside this. Currently, I am developing my teaching abilities, and running and teaching on Study Days will further my skills in this area. Additionally, it will provide the opportunity to invite others to teach, and increase the exposure of everyone involved.
“I also hope to bring a different energy to the board, having been involved in Next Gen. I think this is a great opportunity to highlight the talents of young dentists like myself, and those who are new to implantology.”
Finally, Dr Kalsi shares his advice for those who want to or already provide dental implants and are looking to improve their skills: “My key tip would be to find a good mentor. This does not necessarily mean the best clinician, but instead a good teacher. I would definitely recommend mentorship rather than just undertaking courses for dental education. Additionally, I would suggest those who are new to implants focus on learning the basics, before moving on to the ‘fancy’ aspects of the field. Get engaged in your learning at every stage, and never be afraid to ask for help, and attend as many conferences as you possibly can.”
For more information, please visit www.adi.org.uk
Become a member today n
“I am honoured to be taking on this responsibility”

Commenting on his new role as President of BOS, Robbie said: “It is daunting, but I am deeply honoured to be taking on this responsibility. I am humbled to follow such eminent colleagues who have served as executives within the BOS. I am under no illusions about the myriad of challenges that face our specialty and the Society but am heartened to know that I will be joining a wide team of dedicated colleagues who give
The new Honorary Patron of the BOS is Roz McMullan, a retired Consultant Orthodontist in the Western Health and Social Care Trust in Northern Ireland (NI). During her long and distinguished career, was a Past President of the British Dental Association (BDA) and the Northern Ireland Branch, past Chair of NI Council, BDA, and until recently, worked with the Association in matters relating to wellness and mental health. She is a Life member of the European Orthodontic Society and the NI Orthodontic Study Group. During her career, Roz was involved in Trust governance, quality improvement, audit and appraisal. She was Clinical Lead for Specialist Surgery for seven years. Roz was secretary to the Audit Committee of the BOS and chaired the Northern Ireland Hospital Training Committee NIMDTA for nine years.
Of her new role, Roz said: “I am honoured, humbled and delighted to be installed as Patron of the BOS for 2025. Every voice in this Society, no matter how quiet or lonely, is valued and valuable. As Patron I am not an elected representative, nor a voting member of the Board with all the governance responsibility that carries, but I do hope to be a connection between the quiet voices and the leaders within the BOS, while also representing the Society with the respect and gravitas it deserves. You can trust me to laud you, and the brilliant work you do every day that is so valued by your patients. I look forward to working closely with the President, Robbie Lawson.” n

Surprisingly, bullying itself is not illegal in the UK. There is no current anti-bullying legislation in this country, although 32 US states – most notably Massachusetts, New York and West Virginia – have enacted workplace bullying legislation: the Healthy Workplace Bill1
What is bullying? According to Gov.UK and ACAS2, bullying is unwanted behaviour from a person or group that is:
• Offensive, intimidating, malicious or insulting
• An abuse or misuse of power, which undermines, humiliates, or causes physical or emotional harm to someone
This might be a one-off incident, or a regular pattern of behaviour; it might take place face to face, on social media, in e-mails or during telephone calls. Most importantly, it might not be obvious to others, or even to the person being bullied.
The National Bullying Helpline3 speaks out regularly about the disturbingly high level of NHS employee calls to the helpline. Up to 80% of ‘work-related’ calls to The National Bullying Helpline are from public sector employees – predominantly NHS staff.
The Helpline website speaks scathingly about the NHS’s ‘tendency to appoint senior medical personnel into Head of Department or Team Leader posts without first ensuring they have relevant people management skills, leadership training or basic employment law training’ and the fact that the NHS is ‘notoriously slow to take relevant, timely, action. Disciplinary and Grievances Investigations have been known to take months and months to complete and are often carried out by managers who lack basic employee relations skills.’
In my opinion, this is also true in general dental practice. Employers (i.e. dentists) are not taught basic people management or leadership skills and know little of employment law. Practice managers in many cases happens to be the dental nurse who has been there longest, again without the required skills or training to manage staff. In this article, we will be looking at notimmediately-obvious forms of bullying and exploding some of the myths surrounding it.
Myth 1: Bullying is always top-down/ most bullies are managers. Not so – bullies can project horizontally, or even upwards, as well as downwards. Most managers bullied by their subordinates are loathe to admit to it, because they see being the target of bullies as a sign of weakness4
Myth 2: Bullies work alone. Again, not always true. Bullying can be undertaken by groups of people who work together to isolate their target – otherwise known as “mobbing”. We will look at this later in the article.
Myth 3: Most bullies are male. Also not true. Bullying is insidious, manipulative and emotional – it doesn’t require physical strength. Apparently, 80% of female targets are bullied by other women4
According to Pelago Health5, Queen Bee Syndrome is a term used to describe ‘a high-ranking female employee, usually a manager, (who) intimidates and excludes her female subordinates, often leading to a hostile and uncomfortable work environment.’ This can include “making disparaging remarks about other women’s looks or abilities, refusing to help or mentor other women, and actively working to undermine their success.’
Myth 4: Only weak, timid people are bullied. I know that this isn’t true, because I was bullied at work.
For those who don’t know me, I am 66 years old and not exactly backwards at coming forwards. I have been doing my job for 32 years now, and have p****d off a lot of people in dentistry by speaking up for dental nurses over those three decades. Prior to working for the Association, I lived and worked in five different countries on both sides of the Atlantic. My background includes working for the Home Office in London, selling newspapers on a street corner and as an au pair in Vienna, working for the military at the NATO HQ in Brussels, working in investment banking in Bermuda, and training as a holistic therapist in Boston, Massachusetts. A timid wallflower, I am not!
I love my job! But, some years ago, I found myself suffering from anxiety, panic attacks and insomnia – minor ailments that gave me an excuse not to go to work. I had panic attacks every Sunday evening, dreaded turning on my computer in the morning and seeing the barrage of emails from the bully, and tried to avoid answering my phone. I made an appointment with my doctor, who asked me lots of questions about work, then announced that I was being bullied and that she was sending me for counselling. My first reaction was one of disbelief – what do you mean, I am being bullied? I’m a grown up, for heaven’s sake! Not a child in a playground! But, during the six months of counselling that followed, I began to see that she was right.
According to the National Bullying Helpline, subtle bullying is ‘the actions of someone who behaves with mischief, often intentional and usually behind your back, with negative motive, i.e. to ease you out of your role or cause you professional embarrassment […] to bring you into disrepute or have you excluded in some way.’6 This behaviour ‘creeps up slowly but impacts on you negatively and leaves you questioning yourself.’
Mobbing
This is perpetrated by a group, rather than an individual, somewhat like a group of magpies surrounding a smaller bird and attacking it! Although, mobbing –orchestrated by the bully – can be much more subtle, and some of those taking part may not be aware of exactly what they are doing. Examples of mobbing include:
• Excluding you from social events – birthday celebrations, drinks after work, lunch, etc.
• Colleagues stop talking when you enter a room
• You are kept out of the loop – excluded from/not informed of meetings, for example, or not included in e-mails, WhatsApp groups, etc.
• Gossip or rumours about you are circulated
gaslighting
The term ‘gaslighting’ comes from a 1938 play, Gaslight, set in 1880s London where the husband dims the gas lights in their home and makes strange noises, removing items from the home and manipulating his wife into thinking she is insane so he can steal from her, as well as a 1944 film starring Ingrid Bergman based on the play. The term gaslighting has come to

a cocktail of practices manipulating someone into doubting their own sanity. An employee who is the target of this subtle but unhealthy manipulative behaviour will struggle to understand what is happening.
The 2017 TV drama The Replacement deals with the same subject, but in an updated workplace environment.
A target of a gaslighting bully will:
• Believe they are imagining things
• Feel non-credible
• Feel constantly undermined and/or excluded
• Start to develop trust issues
• Lose confidence in themselves and their abilities
They may also start to feel unwell, or even be signed off work by their GP with workrelated stress.
Let’s be clear about this: gaslighting is an abuse of power. It is a manipulative power game, which the bully plays with deliberate intent to control another individual.
some examples of bullying
• Constantly criticising someone’s work –and not in a constructive manner
• Deliberately giving someone a heavier workload than other staff
• Demanding that a specific staff member perform menial tasks not appropriate to their role
• Giving someone unattainable tasks and deadlines that they will fail to complete
• Withholding information – details critical to successful completion of tasks
• Withholding tasks – reassigning tasks to junior or less competent staff
• Giving the impression that a specific staff member is unskilled and incompetent
• Constantly putting someone down, devaluing their input or ridiculing their opinions
• Spreading gossip or malicious rumours about someone
• Excluding a specific staff member from team social events
Are you being bullied?
• Do you feel intimidated or threatened at work?
• Are you regularly humiliated or ridiculed or made to look incompetent in front of colleagues?
• Are your efforts consistently undervalued or disregarded?
• Do you feel sick when you work with a particular colleague?
• Do you suffer frequently from minor ailments that cause time off work?
• Do you have the Sunday night jitters because you dread going to work on Monday? If you answer yes to even some of these questions, then you are probably being bullied at work.
Why Me?
There could be several reasons, according to VeryWellMind7 p rofessional jealousy: Workplace bullies target those with talent because they either feel inferior or they worry that they are overshadowed by the other employee’s work and abilities. So, you are a likely target for a workplace bully if you:
• Are intelligent, determined, creative
• Regularly contribute new and innovative ideas
• Go the extra mile and gain recognition for your hard work
• Move through projects quickly while others are struggling
• Are a perfectionist and striving for success social Envy: As mentioned above, it is a myth that only weak, timid people are targets of bullies. In fact, targets are often popular, capable, socially adept, and experts in their own field.
Control: Are you caring, social, collaborative – all characteristics which drain a bully’s power? If you are a team player, this may be the reason for the bullying.
‘Team-building is the antithesis of what a bully wants. Bullies want to be in control and to call all the shots. So, you may be targeted by bullies because you are a team player.’7 p rejudice: You may be targeted by a bully due to race, gender, age, sexual preference, religion/beliefs or disability. If so, under UK law, this constitutes harassment under the Equality Act 2020. Your employer MUST do all they can to prevent this and MUST take any complaint seriously and investigate it thoroughly. You can take legal action against your employer if you have been harassed in the workplace.
An article in The Guardian9 by Dr Mary Lamia suggests that bullying is a response to internalised shame: bullies ‘tend to have high self-esteem and hubristic pride. They attack others to take away their shame –which allows them to remain unaware of their feelings […] bullies cause shame to others by recognising and attacking their insecurities […] Attacking others not only blots out the shame they are feeling, but it also stimulates the experience of power.’
According to VeryWellMind, bullies are insecure and bully others to make themselves feel superior. They may be resentful or jealous of the person they are targeting and lack empathy, so have no problem dominating, blaming, intimidating, or taking advantage of others, lacking the ability to relate to another person’s experience, refusing to acknowledge the repercussions of their behaviour, driven by a desire for power and attention.
A Family Lives article on Serial Bullies11 suggests that methods used by bullies to make it harder for others to recognise actual bullying include emotional blackmail, malicious gossip and one-on-one confrontations with no witnesses. The article goes on to say that when the bully realises that their target is close to complaining or exposing their misconduct, they neutralise the target by isolating them, destroying their credibility and reputation before eliminating them through dismissal or forced resignation.
According to Family Lives, bullies are often charismatic and charming, portraying themselves as clever, successful, important, wonderful, kind, caring and compassionate. In reality, they are frequently self-opinionated and arrogant with a superior sense of entitlement and an unhealthy need to feel recognised and admired. They feel no remorse and have no conscience, seeing nothing wrong with their behaviour. They are often convincing liars, particularly when asked to account for their actions, and are duplicitous, pretending to be acting in the interests of others when in fact acting in their own interests. They think of themselves as being of superior intelligence.
Bullies manage others’ attitudes and allegiances by indoctrination and manipulating emotions, through being untruthful and drawing others into believing in their false reality, using intimidation and criticism to isolate their targets, gossip, backstabbing and lies to discredit their targets, plagiarising and taking credit for others’ work, and feigning victimhood.
Family Lives sets out three stages of response when a bully is called to account: Denial: ‘Sometimes the denial is direct and robust, and sometimes it involves avoiding discussion of the matter that has been raised, never giving a straight answer, deliberately missing the point and creating distractions and diversions.’
Retaliation or counter-attack: ‘Firm criticism of the target, including counterallegations based on distortion or fabrication. Lying, deception, duplicity, hypocrisy and blame are the hallmarks of this stage’
Feigning victimhood: ‘Can include bursting into tears, indignation, pretending to be “devastated” or “deeply offended”, being histrionic, playing the martyr and generally trying to make others feel sorry for them – a “poor-me” melodrama [that] allows the bully to avoid […] accepting responsibility for what they have said or done.’
What if you are being bullied?
• Keep detailed notes: who, what, where, when. It is not necessary to ‘prove’ that you are being bullied, but if you can produce a diary, letters, e-mails etc., this will strengthen your case.
• Inform your line manager – or their manager – or the HR Department – or the boss! All you need to do is raise the issue with your employer. Once you have lodged a formal complaint through the practice grievance procedure, it is the responsibility of your employer to ensure that your concerns are thoroughly and independently investigated.
• Contact the National Bullying Helpline –www.nationalbullyinghelpline.co.uk or 0845 2255787.
• Contact ACAS (the Advisory, Conciliation and Arbitration Service) –0300 123 1100 or https://www.acas. org.uk/discrimination-and-bullying
• If you are a dental nurse (or non-clinical manager/receptionist) who is a current member of BADN, your professional association, you can contact our legal helpline for free legal advice (number in the members’ area of our website badn.org.uk), contact our counselling/ support helpline in the Health & Wellness Hub (also in the members’ area) or contact the BADN office (01253 338360).
• If you are a dental nurse (or nonclinical manager/receptionist) who is not currently a BADN member, you can join your professional association at www.badn.org.uk/join.
• Other members of the dental team can contact their own professional associations – e.g. the BDA (dentists), BSDHT (hygienist/therapists), BADT (therapists), DTA (technicians), BACDT (clinical dental technicians)
BADN survey on Abuse
This recent impromptu survey showed that over a third of dental nurses had been the target of abuse in the workplace. Examples provided by respondents revealed that the majority of the abuse was, in fact, bullying by fellow dental colleagues. BADN will be taking further action on this subject in 2025.
This article was written for Dental Review News and Dental Technician, and has been repurposed for The Probe with permission. A version will also appear in the Winte 25 edition of the British Dental Nurses’ Journal
References
1. https://healthyworkplacebill.org/
2. https://www.acas.org.uk/bullying-at-work
3. https://www.nationalbullyinghelpline.co.uk/ employees.html
4. https://www.corporatewellnessmagazine.com/ article/bullying-what-are-the-myths
5. https://www.pelagohealth.com/resources/ hr-glossary/queen-bee-syndrome/
6. www.nationalbullyinghelpline.co.uk
7. https://www.verywellmind.com/reasons-whyworkplace-bullies-target-people
8. https://www.gov.uk/workplace-bullying-andharassment
9. https://www.theguardian.com/careers/2017/ mar/28/the-psychology-of-a-workplace-bully
10. https://www.familylives.org.uk/advice/bullying/ bullying-at-work/serial-bullies-in-the-workplace
About the author pam swain is
Chief Executive of BADN









Universal all-in-one adhesive for a wide range of applications and adherends
Compatible with all etching techniques
No filler and no HEMA – protection against hydrolysis
Reliable strong bond, less technical sensitivity
Simplified procedure for any adherend surface
No additional primer ne eded
For further information, please contact the SHOFU office 01732 783580 or sales@shofu.co.uk
www.shofu.co.uk
dr Balaji presents a case of moderate complexity in which he places two implants in the difficult positions of the upper lateral incisors, utilising both hard and soft tissue augmentation techniques for the best result
Afemale 30-year-old patient presented to the practice with congenitally missing lateral incisors. She was a nonsmoker, her medical history confirmed her to be generally fit and well and her oral hygiene was in good condition. The patient had a fixed bridge in place, but reported that this was continually debonding every six months or so. Given that this type of restoration wasn’t working for her, she was seeking a more permanent solution in the form of a dental implant. The patient also informed us of her upcoming wedding, for which she hoped to have all dental treatment complete in time.
A comprehensive clinical assessment was conducted to determine suitability for implant treatment, including a full suite of clinical photographs and an intraoral impression. A medium-high lip line was noted, which would make the avoidance of black triangles important to the final outcome. It was also established that the existing spaces were very narrow, which indicated that orthodontic treatment would be required prior to implant placement. This was discussed with the patient, along with detailing the potential implant therapy options post realignment, and she was very keen to proceed. A referral was made for Invisalign treatment to widen the spaces at the lateral incisor sites and the patient returned to the practice a few months later for full implant planning.
A radiograph and CBCT image were taken to show adequate width had been obtained for the placement of two lateral implants. However, there was a lack of bone buccally, indicating that bone augmentation would be necessary for successful implant treatment. Soft tissue grafting was also recommended in order to boost gingival volume and restore any height lost post-operatively for an ideal aesthetic (which was especially important given the mediumhigh lip line in mind).
A fully digital workflow was utilised to plan the ideal position, angle and depth of the implants, as well as the accompanying restorations. It was decided to use a guided surgical approach in order to increase the accuracy, predictability and efficiency of the procedure, encouraging a faster and more comfortable patient experience. This was particularly beneficial given the narrow area in which we were placing the implants.
The diagnostic wax-up was created and shared with the patient as part of the consent process. Once the benefits, risks and limitations of treatment were discussed once again with the patient, informed consent was recorded to proceed.
The scans, diagnostic wax-up and photos were sent to the dental laboratory to fabricate the surgical guides.





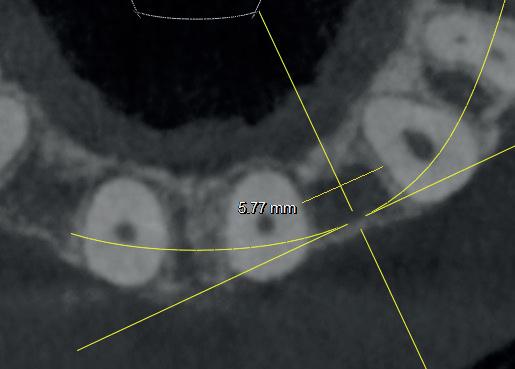

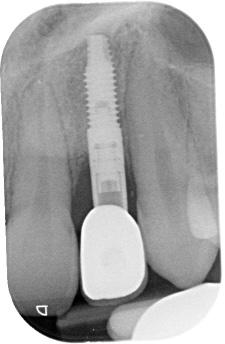

I – s urgical treatment with implant placement, soft and hard tissue augmentation
On the day of surgery, the patient was numbed with a local anaesthetic and a split-mucogingival, full thickness flap was raised. The surgical guide was fitted into the mouth and the two implants were placed through the guide to replicate the exact positions, angles and depths determined during the planning phase.
Bone was harvested from the left mandible and used to augment the implant sites. The bone grafting was performed by combining this autogenous bone with xenograft and using the ‘mini sausage’ technique. A collagen membrane was used to hold the graft material in place, secured with periosteal sutures.
Soft tissue was then harvested from the palate – enough for two connective tissue grafts (CTGs) at each lateral incisor location. The aim of these was to regain the soft tissue contour around the implant sites and build the papillae back up. This would not only reduce the soft tissue shrinkage that occurs postsurgery, but would actually increase the width of the papillae compared to where we started for optimal aesthetic results.
The flap was coronally advanced to increase root coverage and sutured closed. Upon conclusion of the surgery, the patient was given standard post-operative oral hygiene and dietary instructions, with particular focus on oral hygiene. She returned to the practice one week later for the post-surgical review, reporting no abnormal pain or discomfort. The sites also looked to be healing as expected.






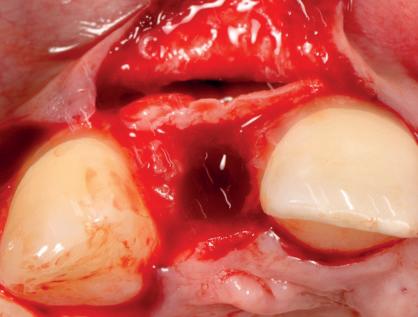

The patient returned three months later for the restorative phase of treatment. The implants were exposed and the abutments and temporary crowns were fitted. These were designed to help contour the newly enhanced soft tissue and shape the papilla accordingly. They also provide an excellent trial for the patient, ensuring she was happy with the shape and colour of the crowns before the final restorations were fabricated in zirconia.
Both the patient and I were delighted with the outcome reached in this case. The patient achieved her primary aim of restoring the lateral incisors with a fixed solution that wouldn’t require adjustments or re-bonding every six months. We were also able to deliver a highly aesthetic and functional result with the use of soft and hard tissue augmentation.
The planning for a case such as the above is crucial. It presents ‘double trouble’ in that the lateral incisor site is extremely difficult to place an implant into due to how narrow the space tends to be – and we were treating both lateral incisor sites. As such, this case was very aesthetically demanding, plus we had to consider the time restrictions imposed by the patient’s upcoming wedding. The soft tissue management was particularly important for the aesthetic outcome. This was made slightly simpler by the use of guided surgery, which ensured that the implants were placed accurately for the best results.
Fig 1 - Starting point for implant treatment post orthodontic treatment; Fig 2Retracted view of congenitally missing lateral incisors; Fig 3 - Occulsal view of lateral incisor locations; Fig 4 - Pre treatment OPG; Fig 5a - CT scan for implant planning; Fig 5b - CT scan for implant planning; Fig 6 - Assessment of space available for implant placement; Fig 7 - Surgical guide tried in mouth; Fig 8Raising flap; Fig 9 - Implant position checked after osteotomy; Fig 10 - Grafting material harvested from patient; Fig 11 - Grafting material placed; Fig 12Coronally Advanced Flap (CAF) closed; Fig 13 - Post implant placement radiograph left lateral; Fig 14 - Post implant placement radiograph right lateral; Fig 15 - Post treatment smile; Fig 16 - Post treatment upper arch
In conclusion, this type of case requires meticulous planning and sufficient skill with both bone and soft tissue grafting techniques. However, with adequate training it is possible for most dentists within the implantology field to achieve an excellent result. I would recommend that colleagues have at least five years of experience with dental implants before moving onto situations that present the complexity that a double lateral incisor restoration offers.
Dr Selvaraj Balaji presents advanced training in soft and hard tissue management alongside other world-renowned clinicians through the ASHA Club
Find out more at ashaclub.co.uk
To book or for more info, please call 07974 3024269 or email info@ashaclub.co.uk n
about the author

dr selvaraj Balaji Bds, MFds RcPs(Gla), MFd sRcs(ed), Lds Rcs(eng) since he obtained the Bds degree, dr Balaji has worked in Maxillo-facial units in the uK for several years and gained substantial experience in surgical dentistry. He is the principal dentist of the Gallery dental Group which is made up of Meadow Walk dental Practice and the Gallery dental & Implant centre. dr Balaji is also the founder of the academy of soft and Hard tissue augmentation (asHa) and runs courses, lectures and study clubs in the uK and around europe for aspiring implantologists
CPD 4 DCPs is a fully veri able ECPD programme that enables each member of the dental team to complete one year’s ECPD requirement in a highly cost-effective manner. Covering all the highly recommended subjects, each volume is specially designed to cover the ECPD needs of up to 10 DCPs.
Providing 10 hours of veri able ECPD, one Volume covers the annual veri able ECPD needs of most practices.
VAT
Subjects covered:
• Early diagnosis of oral cancer: raising awareness of symptoms to improve outcomes
• Tackling safeguarding in dentistry
• When asthma attacks!
• Quality assurance of photostimulable phosphor plates




• How to handle a GDC investigation and come out the other side intact
• Radiographs and radiation safety in clinical dentistry
• Working with bloodborne viruses
• Complaints in the dental practice
• Patient education and communication: tackling gingival disease
• How can deafness and hearing loss impact dental care?
Just one Volume per practice per year, up to 10 people
10 hours veri able CPD including all recommended subjects
Ongoing modular learning programme
The whole team learning from the same information at the same pace
Saves time and money
Can be used by GDPs
Enhanced CPD Compliant
dr Omar Iqbal replaces a patient’s failing bridge in the aesthetic zone with a new prosthesis fixed in place with two Tapered Pro Conical implants





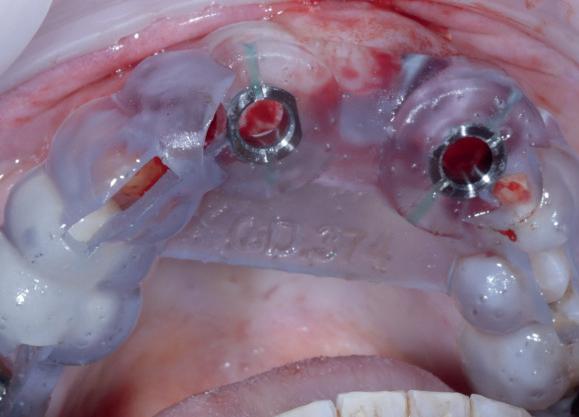




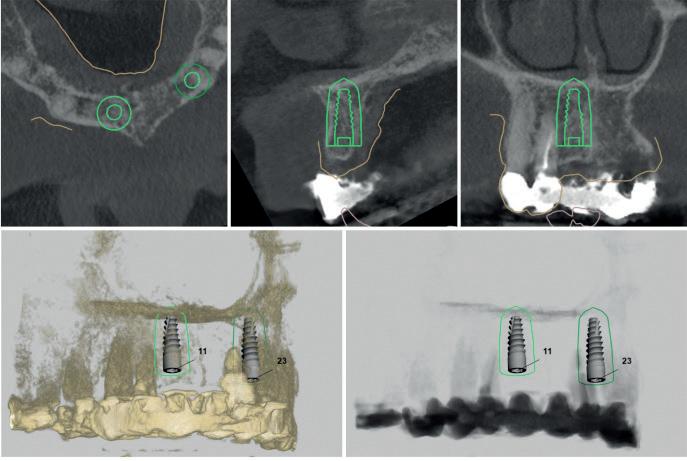
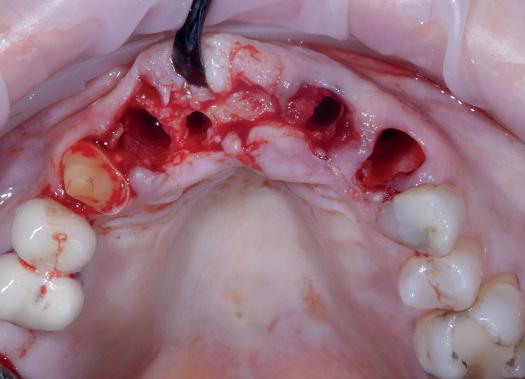
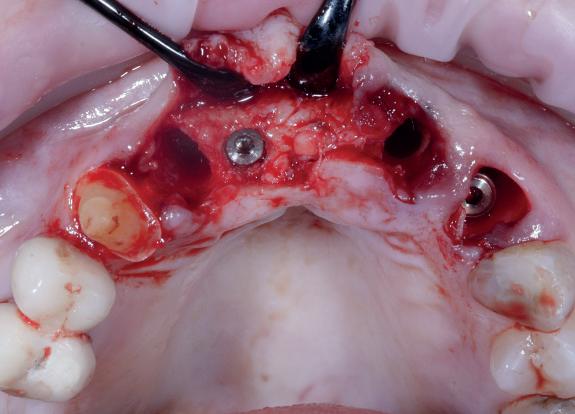
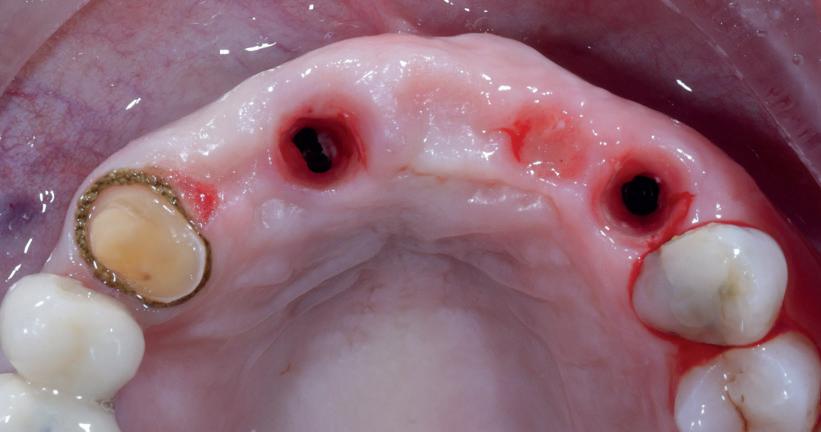
A 61-year-old female patient presented with a failing, upper 3-3, metal ceramic bridge, connected to the canines and lateral incisors on either side. The bridge had failed with caries and core fractures on both abutment teeth on the patient’s left side. As such, the patient was keen to repair or replace the bridge without the use of a removable prosthesis at any point during treatment.
A comprehensive clinical assessment was conducted to evaluate the potential treatment options. A full suite of clinical photographs was taken to assess the aesthetics, with x-rays to better understand the damage to the remaining teeth. A CT scan was also required to assess the existing bone volume.
Despite using all the available examination tools, it was still challenging to assess the level of damage to the teeth under the metal






Fig 1
and UL3 as per the digital plan; Fig 15 - Occlusal view of temporary restorations; Fig 16 - Soft tissue sutured closed without tension and temporary bridge in place; Fig 17 - 3 months post-operative review shows good soft tissue adaptation; Fig 18 - Postoperative radiograph of implant at the UL3 site; Fig 19 - Post-operative radiograph of implant showing implant at the UR1 site; Fig 20 - Temporary prosthesis removed at 3 months post-operative
ceramic bridge, because the prosthetic material obstructed the x-ray. It was confirmed that two teeth were decayed and fractured, but it was not possible to confidently diagnose the UR2.
The assessment findings were discussed with the patient in detail. This included the extraction of the UL2 and 3, which were carious and unrestorable, and the need to assess the UR2 once the bridge had been removed. The patient was informed of the potential solutions depending on the prognosis of the UR2, which included extraction should the tooth be in poor condition. With regards to the restorative options for this case, taking the patient’s preference for a fixed restoration into consideration, treatment would involve an implant-retained prosthesis. All the potential benefits, limitations and risks were explored with the patient and she was comfortable to give informed consent.
This case would be treated using a guided approach. With a greater number of implants placed, the appreciation for guided surgery has grown due to the benefits it provides. This technique helps to mitigate the potential for human error on the day of surgery, resulting in a more predictable treatment process. The literature demonstrates the increased accuracy of implant placement made possible with a fully guided technique compared to freehand surgery.
Guided surgery requires more preparatory work to be completed in the background, but this effort is worthwhile for the streamlined surgical treatment on the day of the procedure. Guided surgery is particularly ideal for immediate implant placement in fresh sockets, especially when immediate loading is planned. This approach facilitates a smoother transition from implant placement to connecting
the temporary restoration. Research supports this concept; however, factors such as clinician experience and guide fabrication methods should be optimised to achieve the best outcomes.ii
Having identified the UL3 as needing extraction, this provided an ideal site for immediate implant placement. The existing root was large with limited bone available around it, so it was crucial to ensure appropriate implant selection and precise placement for good stability. Bone grafting was also strongly indicated at this site. Whenever extracting a tooth, regardless of how atraumatic the process is designed to be, there is always the potential for bone and soft tissue loss.
Both hard and soft tissue augmentation is an absolute requirement with every immediate implant placed into a fresh extraction socket. The science shows that bone augmentation into the buccal
void between the socket and immediately placed implant surface can help to preserve volume of the alveolar ridge.iii There is also evidence that bone and soft tissue grafting around an immediate implant can increase bone stability, prevent gingival recession and improve aesthetic results.iv This was pertinent in this particular case, where the surgical sites required grafting to minimise the hard and soft tissue changes that would take place post-surgery, maximising stability and aesthetics.
For the second implant, both central incisor sites would have been suitable, but the UR1 location was selected as an ideal position to support a 4-unit bridge. Questions remained over the UR2, so preparations were made for different situations. If the tooth was found to have a poor prognosis upon assessment, a cantilever could be created on the bridge to the UR3.
Digital tools were used to plan treatment, including the precise implant positions, angulations and depths.
The new Tapered Pro Conical implants (BioHorizons Camlog) were selected for this case for several reasons. These implants integrate the best features of BioHorizons’ Tapered Pro and Camlog’s CONELOG Progressive-Line implants. The conical connection of the Tapered Pro Conical implants boasts a 13-year heritage and has demonstrated evidence of highprecision manufacturing and superior positional stability compared to other conical connections. v This new conical connection provides confidence that an optimal emergence profile will be achieved with the restoration, which is crucial when working in the aesthetic zone. The 3.3mm diameter implants were chosen; while wider implants are generally preferred, this case required a balance between utilising the available bone and adhering to natural structures, necessitating the use of narrower implants.
All the scans, planning software images and photos were sent to our lab partner – Guider Dental – for the fabrication of the guides, which is their specialist area.
surgical intervention
On the day of surgery, the first step was to carefully dismantle the bridge while avoiding any damage to the teeth we wanted to keep on the right-hand side. The prosthesis was sectioned and removed in several pieces.
The UR2 was assessed and deemed unrestorable. The UR2, UL2 and 3 were then extracted as minimally traumatically as possible.
A miniflap was raised in the upper central region for this case to enhance visualisation for implant placement and augmentation. The guide was placed in the mouth and the standard guided surgery drilling protocols were followed. The new surgical kit improves workflow and intraoperative efficiency with the removal of spoons and a guide adaptor allowing for both guided and freehand use. During this step of the procedure, the guide was temporarily removed to double check the drilling angulation and verify this lined up with the pre-fabricated temporary bridge.
The two 3.3mm diameter Tapered Pro Conical implants were then placed
through the guide at the pre-determined positions, angles and depths. Both implants achieved an insertion torque above 30Ncm.
Bone grafting was then performed, placing MinerOss X (BioHorizons Camlog) into the extraction sockets and the jump gap around the implant in the UL3 socket, to preserve the existing bone of the socket. This would help to minimise changes in the bone postsurgery and help to maintain the buccal profile of the ridge. The biomaterial is a bovine bone mineral matrix that has been proven to increase vertical bone height alongside implant placement.vi It has worked very well in my cases to date, offering a high turnover to bone for maximum stability and efficient results with immediate implant protocols.
A soft tissue graft was then performed, harvesting connective tissue from the palate and placing it in the sulcus of the UL3.
Non-engaging cylinders were placed onto the implants to connect to the prefabricated temporary bridge. A premade temporary bridge was connected, contoured and polished, with particular attention paid to the contour of the restoration and suturing with the aim of prosthetically guided soft tissue healing. Standard post-operative instructions were provided to the patient, including appropriate adjustments to diet and oral hygiene in the short-term.
Review and reflection
The patient returned to the practice for review two weeks post-surgery and to confirm successful and otherwise uneventful healing. Discomfort was minimal and she reported being very satisfied with the outcome. After a healing period of three months, the patient returned to begin making the final prosthesis. Good soft tissue adaptation was noted around the temporary prosthesis and the buccal contour was successfully maintained.
Upon professional reflection, this case went according to plan, emphasising the importance of meticulous assessment and preparation prior to implant surgery. The guided approach helped to ensure the precise positioning of the implants which facilitated connecting the temporary bridge. This, alongside the implant selection, was crucial for maximising on the limited bone available for primary stability.
The Tapered Pro Conical implant from BioHorizons Camlog is a game-changer, offering a new narrow diameter option for enhanced versatility in areas with limited bone. Its conical connection improves the implant-prosthetic interface and emergence profile, delivering optimal aesthetics, while the titanium alloy (Ti-6AL-4V ELI) delivers exceptional strength. It is indicated for use in the mandible and maxilla, single tooth replacements, fixed bridgework, and overdentures. With high insertion torque limits of up to 136 Ncm, the Tapered Pro Conical implant also ensures stability and success in a range of clinical scenarios. Since switching to BioHorizons Camlog two years ago, their invaluable support, innovative ideas, and expert guidance have streamlined my processes, relieved stress, and allowed me to focus on the clinical side.
For product information from BioHorizons Camlog, please visit https://theimplanthub.com/
References
i. Takács A, Hardi E, Cavalcante BGN, Szabó B, Kispélyi B, Joób-Fancsaly Á, Mikulás K, Varga G, Hegyi P, Kivovics M. Advancing accuracy in guided implant placement: A comprehensive meta-analysis: MetaAnalysis evaluation of the accuracy of available implant placement Methods. J Dent. 2023 Dec;139:104748. doi: 10.1016/j.jdent.2023.104748. Epub 2023 Oct 19. PMID: 37863173.
ii. Xing Q, Lin J, Lyu M. The Accuracy of Immediate Implantation Guided by Digital Templates and Potential Influencing Factors: A Systematic Review. International Dental Journal. 2024, ISSN 0020-6539, https://doi. org/10.1016/j.identj.2024.10.010.
iii. Liñares A, Dopico J, Magrin G, Blanco J. Critical review on bone grafting during immediate implant placement. Periodontol 2000. 2023; 93: 309326. doi:10.1111/prd.12516
iv. Rondone EM, Leitão-Almeida B, Pereira MS, Fernandes GVO, Borges T. The Use of Tissue Grafts Associated with Immediate Implant Placement to Achieve Better Peri-Implant Stability and Efficacy: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(3):821. https:// doi.org/10.3390/jcm13030821
v. Semper-Hogg, W et al. Analytical and experimental position stability of the abutment in different dental implant systems with a conical implant–abutment connection. Clinical Oral Investigation (2013) 17: 1017. vi. Potres Z, Deshpande S, Klöeppel H, Voss K, Klineberg I. Assisted Wound Healing and Vertical Bone Regeneration with Simultaneous Implant Placement: A Histologic Pilot Study. Int J Oral Maxillofac Implants. 2016 Jan-Feb;31(1):45-54. doi: 10.11607/jomi.3951. PMID: 26800162.



about the author dr Omar Iqbal qualified from the university of Glasgow in 2005 and has since worked to continually improve his skills. In 2008 he attained the MJdF qualification from the Royal College of Physicians and surgeons england. He has been placing dental implants since 2011, having undertaken training with an array of internationally renowned teaching institutions. Omar completed his Msc in dental implantology in 2018 and has worked with the Bristol university as a postgraduate supervisor for students conducting implant research projects.

Jocelyn Harding is an award-winning Dental Hygienist and the President Elect of the Mouth Cancer Foundation. She is passionate about helping colleagues more confidently detect and manage mouth cancer cases, enabling more patients to survive the terrible disease.
“Healthcare has moved at an astounding pace in recent times, with many areas of care becoming extremely specialised. The oral cavity can often be regarded as a separate entity to the rest of the body, so any opportunity to support healthcare professionals in dental health should be encouraged. With the current cost of living crisis and poor access to dental professionals alongside fear and financial considerations of treatment, collaborating with healthcare colleagues such as GPs, pharmacists and those working in other primary care service increases the chance of an early referral and diagnosis for mouth cancer.”
In addition to promoting more integrated health and dental care, other challenges remain for dental professionals when it comes to mouth cancer detection and management.
“One of the greatest challenges for dental professionals is creating time during the appointment – ideally when confirming a patient’s medical history, smoking status and alcohol consumption – to also discuss the risks of head and neck cancer. In this discussion, HPV should be mentioned, and this should be used as an opportunity to educate patients on the success of vaccinations.
“It’s important that all dental professionals feel comfortable with these conversations alongside undertaking intra-oral and extra-
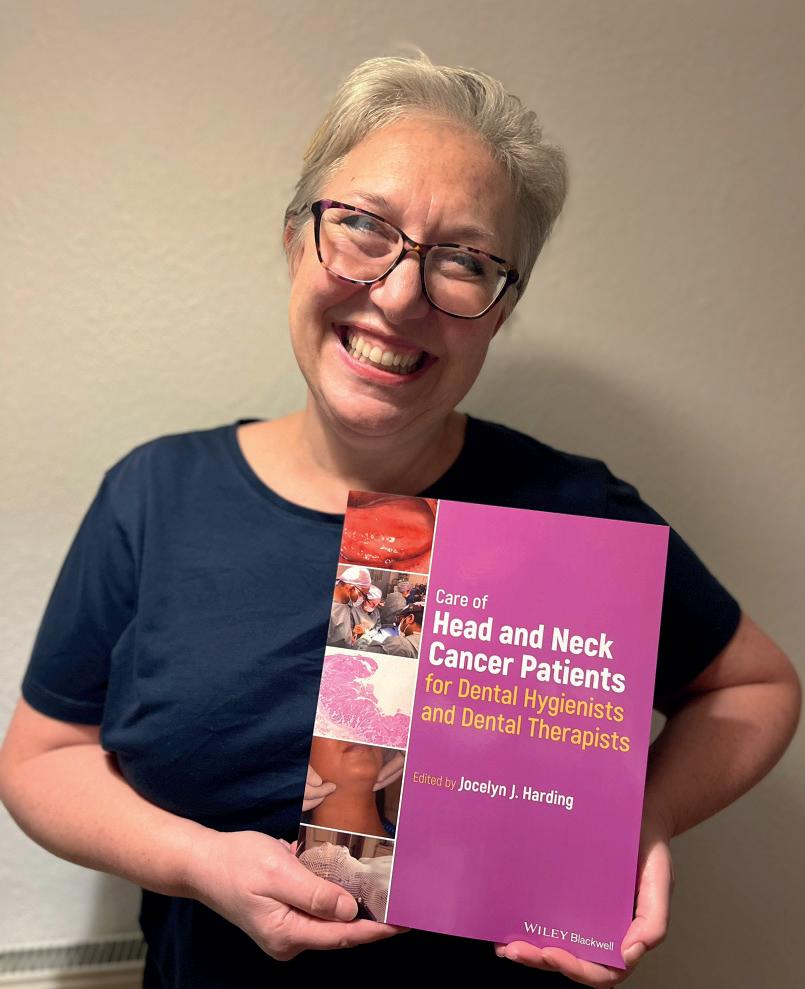
oral examinations. The examinations are far more valuable when this is combined with essential discussions and the exchange of relevant information. Many abnormalities are found at stage III or IV, so monthly self-examinations should be encouraged in patients, too.”
Aside from playing a crucial role in early mouth cancer diagnosis, dental professionals also have a role to play in managing patients’ oral health during and after cancer treatment.
“Patients’ mouths will often become tender, swollen, dry, burnt and extremely sore during treatment and for up to two weeks after completing radiotherapy. Managing their oral health can be very problematic and, at certain times, not a priority. However, oral care during cancer treatment should be encouraged where possible.
“Oral health post-treatment is vitally important as the long-term effects, also known as late effects, of which there are up to sixty, can be detrimental to a patient’s overall health. It is also important to remember that the patient bears the longterm financial implications of treatment, which can be prohibitive to any more extensive dental procedures.”
Joss will be joining other members of the Mouth Cancer Foundation team at BDIA Dental Showcase in March among the exhibition. This will be the ideal platform from which to raise awareness of the challenges and potential solutions in the field.
“The Mouth Cancer Foundation is committed to raising awareness of risk factors, signs and symptoms of mouth, throat, and head and neck cancer, alongside support for affected patients. The latter has become easier for many and their caregivers in recent years with increased access to online video meetings, a private Facebook group, a helpline and a website dedicated to the cause. It has become very apparent that these have been much-needed resources for those both in the UK and internationally. Many patients report a lack of support after cancer treatment has concluded, so the charity would like to connect with dental professionals, hospital teams, dieticians, and speech and language therapists to create a ‘go-to’ link for patient support.”
Offering further opportunities for dental professionals to advance their knowledge and confidence in supporting patients affected by mouth cancer, Joss will be presenting in the Oral Health Theatre on Friday 14th March at 2pm.
“I hope to help attendees better understand the challenges of mouth care for head and neck cancer patients before, during and after treatment. I would like colleagues to feel more supported with practical suggestions for managing longterm oral effects, while also discussing the importance of self-examination. It’s important that we all have a good understanding of a head and neck cancer patient’s journey if we are to help them. This starts by undertaking comprehensive intra-oral and extra-oral examinations and having the right discussions with patients. I will cover this and more, ensuring dental professionals feel more confident speaking to their patients.
“BDIA Dental Showcase provides a perfect opportunity to network, listen to interesting presentations and connect with sponsors – what is there not to like? It’s also ideal for keeping up with recommended CPD topics for all dental professionals. Oral cancer: early detection is a GDC recommended CPD topic. With head and neck cancer statistics increasing, all team members should keep up to date and feel better supported in this area of care.” Don’t miss this and so much more at BDIA Dental Showcase 2025! n

BDIA Dental showcase 2025 14th-15th March exCeL London dentalshowcase.com Register for your free ticket at forms.reg.buzz/BDIA-Dental-showcase
For dentists, dental hygienists and therapists, dental nurses and practice managers who support the delivery of dental implant treatment, it is crucial to remain abreast of the latest predicts, technologies and techniques in the field. This requires constantly refreshing knowledge and learning new skills according to the latest evidence-based research. The result is more predictable treatment outcomes, greater patient happiness and increased job satisfaction for professionals.
In addition to the various skills required, dental implantology also often mandates a multidisciplinary approach. This means that collaboration between dental team members must be optimised, allowing for the sharing of expertise and abilities for the benefit of the patient.
To facilitate effective collaboration amongst the dental team, it has been shown that both strong leadership and shared goals are important. So too are building a team of like-minded professionals, and effectively allocating tasks according to each individual’s skillset.
Interprofessional education has also been shown to promote collaboration between healthcare professionals, improving communication skills and helping to establish coherent teams for better health outcomes. When it comes to dental implantology,
this means enabling all members of the dental team to learn together – from general dental practitioners to restorative specialists, dental nurses, dental hygienists/therapists, treatment coordinators and more.
For these reasons, the Association of Dental Implantology (ADI) hosts a biennial Team Congress which is designed specifically for the entire dental implant team to attend. As the UK’s independent network and membership organisation for implant dentistry, the ADI is constantly striving to connect professionals with expert education, mentoring and research to support them in every stage of their careers.
The Team Congress 2025 will be no different. Entitled “The Implant Aesthetic Kaleidoscope”, the event will demonstrate the diversity of the field and the many different factors that must be considered for clinical success and career development. Not only will programmes be designed specifically for each member of the dental implant team, but there will be a dynamic array of topics discussed by nationally and internationally renowned speakers.
Among them will be Dr Telmo Iceta, Specialist Orthodontist, who says: “Interdisciplinary work is crucial in today’s dentistry. As a Specialist Orthodontist, I will talk about the benefits of orthodontics in achieving better long-term results in
complex implant cases as part of my session at the ADI Team Congress. I will also discuss the use of orthodontics as a way of facilitating implant work.
“I think that we often underestimate the potential of patients’ own teeth to facilitate the oral surgeon’s work. In many cases, orthodontics can play a role in not only improving alignment and occlusion, but also enhancing the hard and soft tissue situation. This is of particular interest when treating patients who have already had some failed implant or dental work. Colleagues attending my session will be able to take away some new ideas on alternative treatment options for these patients.
“This will be my first time at the ADI Team Congress and I am looking forward to it.”
Hands-on workshops will also be available for clinicians to advance their practical skills under the supervision of leading lights in the field. In addition, dentists who are new to dental implants can learn from young and aspiring colleagues about how they are excelling in their careers. Finding the right mentor is critical when getting started in dental implantology – the ADI is full of passionate and engaging clinicians who would be more than happy to help you take your first steps into the field.
And that’s not to mention the major exhibition or unique social programme, which
both afford opportunities to engage with the wider profession and network among likeminded professionals while having fun with friends. Further still, visitors will get a chance to enjoy all the vibrance and inclusivity that Brighton has to offer. Why not make a weekend of it with the family and enjoy some time on the famous pier, discovering the exotic and historical architecture or participating in some water sports?
The ADI Team Congress 2025 will absolutely be an event not to miss for anyone involved in dental implantology. Substantial early bird discounts are available until 1 December 2024, so register soon to take advantage of these savings and secure your place. n

ADI team Congress 2025 the Implant Aesthetic Kaleidoscope 1-3 May, the Brighton Centre For more information, visit adi.org.uk Become a member today


























































































































































































Sign up today and mark the date in your calendar!
The British Dental Conference & Dentistry Show (BDCDS) makes a welcome return next year at NEC Birmingham on 16-17 May 2025. In association with the British Dental Association, the highly anticipated event promises to be an unmissable gathering for all dental practitioners seeking to enhance their practice and personal development, expand their network, and learn more about cutting-edge products and services.
Following on from the footsteps of the phenomenal Dentistry Show London earlier this year, the event promises to be bigger and better than ever – providing an unparalleled exploration of the latest innovations in dental technology and practice, as well as the best treatments available for patients. Bringing together the entire dental community for personal and professional development, the mustattend event is the UK’s largest dental show and not to be missed. Sign up today and register your interest to receive exclusive updates and news in the lead up to May.
More than 400 exhibitors, including top dental brands and suppliers, will be showcasing a wide range of new and innovative products, plus advanced technologies, equipment and services to help attendees enhance their dental practices. From key technology providers to training course organisers and companies providing state-of-the art dental care units and scanners, there’s something for everyone.
With the floor set to be abuzz with trends, there is no better place to celebrate dynamism and creativity as well as giving valuable insights into the industry’s future. Within the fast-paced dentistry environment, it is critical to be one step ahead, and BDCDS allows you to see hundreds, if not thousands, of new products under one roof. Speak face-to-face with exhibitors about innovations of interest and leave empowered and inspired.
Leading and innovative brands will be making a return including Agilio Software, Align Technology, the BDA, Listerine, Colgate, Kent Brushes, NHS Dental Services and plenty more. Many will be offering demonstrations, showcasing the latest products they have on offer – giving you the opportunity to get hands on, learning a new skill, theory or technique by seeing it in action. Attendees can also benefit from some exclusive show offers and discounts.
For those looking to gain enhanced CPD, the event is irrefutable. 11 show theatres will host a series of insightful seminars and workshops and are set to be buzzing with the most relevant and applicable hot topics. Every dental team member will be catered for, with core clinical areas covered as well

as the most topical and current subjects affecting daily practice – ideal for personal development as well as benefiting your entire team.
From the popular BDA Theatre, which will host thought-provoking presentations from dentistry’s leading innovators and thinkers, to the BACD Aesthetic & Digital Dentist Theatre, providing a comprehensive overview of the latest treatment solutions in the world of aesthetic and digital dentistry, and the Dental Business Theatre, there’s a host of talks helping you gain a finger on the pulse, equipping you with essential knowledge and insights. Don’t miss the Speciality Interest Theatre, which will also be making a comeback in 2025 as well as many other popular show theatres.
Up to 12 enhanced CPD hours will be available across the two days, and planning is key to make the most out of your visit. 150 free eCPD hours are also available for all attendees, with BDCDS proving itself to be the hub of excellence and knowledge once again.
Senior Show Manager, Leanne Brown, comments: “Every year we aim to raise the bar for the dental industry and the 2025 show is set to be our best yet. There is no better place to come together as a team to learn, educate and inspire each other. BDCDS is set to provide a platform for dentistry to continue to excel throughout 2025 and beyond – ensuring better oral care for all.”
BDCDS doesn’t just attract top quality UK personalities. Names from across the globe will be heading to Birmingham to share their expert knowledge. Over 200 speakers will take to the stage to delight and inspire, guaranteeing you hear about the latest discoveries and insights to improve your own skills.
Speakers will be covering issues and trends affecting the whole dental community, and can help you find solutions to issues you’re facing in practice. Last year the biggest and most accomplished names took part, and 2025 promises to build upon this, providing exceptional quality to the conference programme. Keep your eyes peeled for a well-known business guru to be announced soon…
As well as inspiring speakers, the show offers an unparalleled networking opportunity – allowing you to meet with colleagues and friends, plus make new connections. The ‘who’s who’ of dentistry will be in attendance and dental experts, fellow practitioners and key opinion leaders will be on hand to share experiences, engage in meaningful conversations and discuss emerging trends, as well as potential challenges in the dental field.
Nothing beats seeing people in person, and the event allows everyone
to congregate in one place to connect and debate latest developments, plus hot topics and subjects dominating the news agenda. From the use of Artificial Intelligence to the growth of cosmetic dentistry and teledentistry, the priorities of the new government and beyond, the floor will be alight with inspiring discussions from aspirational personalities.
In addition to visiting the networking lounges and exchanging knowledge on the show floor, look out for events taking place at stands throughout the event and connect with attendees, exhibitors and speakers ahead of and during the event via the Dentistry Show Event App. Brown adds: “We’re really excited about opening our doors once again. BDCDS really is an event for every dental professional – whether you want to gain Enhanced CPD, find solutions for issues you’re facing in practice or buy revolutionary equipment, you will leave BDCDS with a whole new outlook. Make sure you block out the 16-17th May 2025 in your calendar, sign up and stay tuned for more exciting developments coming in early 2025.”
For more information and to register for free, visit birmingham.dentistryshow.co.uk/2025 as well as following @dentistryshowCS on Instagram to receive updates and exciting news about what 2025 has in store. n









How many times have I made a New Year’s resolution to get fit or focus on a healthier diet, only to find myself sitting on the sofa with a bowl of ice cream two weeks later? This in turn leads to frustration and a sense of failure. That’s why, last year, I decided to take a different approach. I took the time to carefully consider my options. I thought about what would challenge me, what new skills I could learn, and how I could contribute more to my role at Denplan and my beloved Dental Nursing profession. This reflection led me to make personal development my resolution.
My motivation stemmed from a deep sense of professional pride. Having dedicated over 20 years to my roles as a dental nurse and practice manager, I felt a strong desire to master the art of thought leadership. I wanted to share my journey and experiences, mentor fellow Dental Care Professionals from afar, and offer unwavering support. My goal is to be a voice for my peers within the dental sector, advocating for their needs and celebrating their successes.
Where to start?
I began by doing a SWOT analysis to identify my Strengths, Weaknesses, Opportunities, and Threats. While it was relatively easy to pinpoint areas for development, I found it challenging to highlight my personal strengths. This is a common struggle for many professionals, as we often focus more on our shortcomings than our achievements. To overcome this difficulty, I sought feedback from colleagues and mentors. Their insights helped me see my strengths from an external perspective. Additionally, I found it helpful to keep a journal of my accomplishments and positive feedback received. This not only boosted my confidence but also provided concrete examples of my strengths.
With this clearer understanding, I developed a robust Personal Development Plan (PDP) focusing on short-, medium-, and long-term goals. By setting these goals, I created a clear roadmap for my personal and professional growth. Each step was designed to build on the previous one, ensuring continuous development and progress. The journey was not without its challenges, but the sense of accomplishment and growth made it worthwhile.
These were the goals I set for myself:
e nhance my internal knowledge of the company.
As my short-term goal, I immersed myself in activities designed to
broaden my understanding of the business. I attended internal training sessions to learn more about our products, services, and operational processes. Participating in crossdepartmental meetings allowed me to see how different teams collaborate and contribute to our overall goals. I also made a conscious effort to engage with colleagues from different departments, learning about their roles and responsibilities. This comprehensive approach not only deepened my knowledge of the company but also fostered stronger working relationships and a more cohesive team environment.
e nhance my article writing skills. In the medium term, I committed to writing regularly, even if my work didn’t gain immediate recognition. When I wrote my first substantial article, I chose a topic I was passionate about, allowing me to infuse my voice into the piece. Drawing on my past experiences and keeping my audience front-ofmind made the process smoother. I remember the first time I shared a draft with a colleague. I was nervous about their feedback, but their constructive criticism helped me see my work from a new perspective. Now, each article I write serves as a lesson in refining my skills, and I always look forward to the insights my peers provide.
Obtain a coaching and mentoring qualification.
This long-term goal was deeply personal to me, driven by a heartfelt desire to support and guide others in their professional journeys. I wanted to gain the skills necessary to be an effective mentor and
coach, enhancing my ability to contribute meaningfully to both the organisation and my profession.
Achieving this qualification was a profound milestone in my life. The journey was challenging, filled with rigorous coursework, practical training, and moments of intense self-reflection. I vividly remember the overwhelming sense of accomplishment and pride when I finally completed the programme. It wasn’t just about earning a certificate; it was about the personal growth and transformation I experienced along the way.
looking back at 2024
Through this process, I developed a deeper understanding of how to inspire and motivate others, helping them unlock their potential and achieve their dreams. The skills I gained have allowed me to make a more meaningful impact within my organisation, fostering a culture of continuous learning and development. This accomplishment has not only enhanced my professional capabilities but also brought a profound sense of fulfilment and joy, knowing that I can now play a pivotal role in shaping the careers of my colleagues and peers.
Every time I see someone I’ve coached succeed, it fills my heart with immense pride and happiness. This journey has been about more than just professional development; it’s been about making a difference in the lives of others, and that is the most rewarding feeling of all.
Successfully developing
Personal development is a continuous journey that requires reflection,
planning, and perseverance. It’s not a destination but an ongoing process of growth and self-improvement. By conducting a SWOT analysis, we gain valuable insights into our current capabilities and areas for improvement. This self-assessment helps us to identify our strengths, which we can leverage, and our weaknesses, which we can work on.
Seeking feedback from others is another crucial component of personal development. Constructive feedback provides an external perspective on our performance and can highlight areas we might not have considered. It is important to approach feedback with an open mind and a willingness to learn, as it can be a powerful tool for growth.
Setting clear, achievable goals is essential for maintaining focus and direction in our development journey. Goals give us something to strive for and help us measure our progress. They should be specific, measurable, attainable, relevant, and time-bound (SMART) to ensure they are effective.
Overcoming the challenges of personal development requires dedication and resilience. It involves stepping out of our comfort zones, embracing new experiences, and learning from both successes and setbacks. As we move forward, it is important to embrace the opportunities for learning and development that come our way. This might involve taking on new projects, seeking out professional development courses, or simply being open to new ideas and perspectives.
Ultimately, the goal of personal development is to make meaningful contributions to our professions and communities. By continuously improving ourselves, we can better serve those around us and achieve a greater sense of fulfilment and purpose in our work. Let us commit to this journey with enthusiasm and determination, knowing that each step we take brings us closer to our full potential.
Wishing you all a very happy New Year. n

about
the author
lianne Scott-Munden, Clinical Quality and Complaints Risk Manager at denplan.





























Achieving predictable success in dental implant treatment relies on careful selection of placement and loading protocols. This summary of ITI guidelines and research findings provides clinicians with the knowledge to optimise patient outcomes and long-term stability - Dr Tom Murphy discusses
On completing this Enhanced CPD session, the reader will:
• Have a greater understanding of implant placement and loading protocols
• Gain insights into a comprehensive systematic review by Gallucci et al.
• Be equipped with practical considerations and clinical recommendations
Learning Outcome: C, D
Dental implants are an essential treatment for restoring function and aesthetics in partially edentulous patients. Selecting the appropriate implant placement and loading protocols is critical to ensuring predictable outcomes. This summary outlines key insights from the International Team for Implantology (ITI) guidelines and supporting research, including findings from systematic reviews.
Implant placement protocols are categorised based on the interval between tooth extraction and implant placement:
1. Immediate Implant Placement (Type 1): The implant is placed on the same day as the extraction. This approach shortens treatment duration but requires precise planning to ensure sufficient stability and proper site anatomy.
2. Early Implant Placement (Types 2 and 3): Placement occurs after partial healing of tissues. The process is further divided into:
• Placement after soft tissue healing (4–8 weeks post-extraction).
• Placement after partial bone healing (12–16 weeks post-extraction).
3. Late Implant Placement (Type 4): Placement occurs after full bone healing, typically six months or longer following extraction. Though this approach is the most conservative, it extends treatment duration and carries a greater risk of alveolar ridge resorption.
Each protocol has its clinical advantages and limitations. Immediate placement offers convenience but requires careful patient selection to maintain bone and soft tissue stability, particularly in the aesthetic zone. Early placement strikes a balance between reduced treatment time and allowing for partial natural healing, while late placement remains the most predictable option in cases requiring maximum bone stability.

Following implant placement, the timing of prosthetic loading is equally significant in determining success:
1. Immediate Loading: The prosthesis is connected within one week of implant placement. This protocol can enhance patient satisfaction by quickly restoring function and aesthetics but requires exceptional primary stability.
2. Early Loading: Loading occurs between one week and two months post-placement. This allows some bone healing while maintaining a shorter overall treatment timeline.
3. Conventional Loading: The prosthesis is connected more than two months after placement, providing sufficient time for osseointegration and longterm predictability.
The selection of a loading protocol depends on factors such as bone density, primary stability, and patient-specific requirements.
from Systematic Reviews
A comprehensive systematic review by Gallucci et al. evaluated combinations of placement and loading protocols, focusing on survival and success rates.
Key protocols include:
• Type 1A: Immediate placement with immediate loading.
• Type 1B: Immediate placement with early loading.
• Type 1C: Immediate placement with conventional loading.
• Type 2-3C: Early placement with conventional loading.
• Type 4A: Late placement with immediate loading.
• Type 4B: Late placement with early loading.
• Type 4C: Late placement with conventional loading.
(Yellow: Clinically Documented / Green: Clinically well documented)
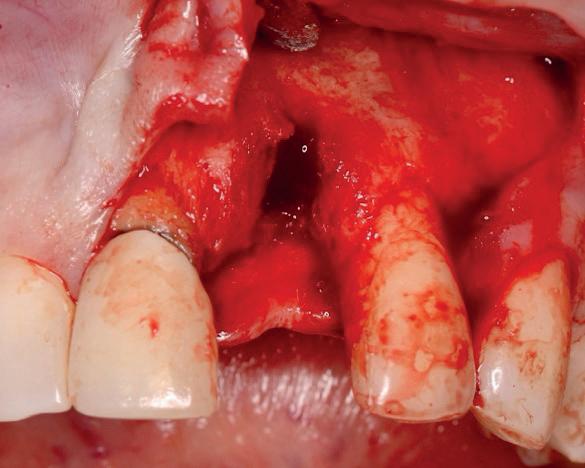

1. High Success Rates Across Protocols: Survival rates range from 96% to 100%, emphasising the reliability of current implant techniques.
2. Immediate Placement and Loading: The Type 1A protocol achieved a survival rate of 98.4%, demonstrating its viability when strict case selection and surgical expertise are applied.
3. Late Placement with Conventional Loading: Type 4C protocols reported a 97.7% survival rate, reinforcing its predictable outcomes.
4. Early Placement Benefits: Early placement (Types 2–3) combined with conventional loading offers a predictable and efficient alternative for reducing treatment duration without compromising success rates.
5. Risk Factors: Immediate placement protocols depend heavily on achieving primary stability and having adequate bone support. Insufficient bone density or compromised soft tissue may elevate failure risks, underscoring the importance of meticulous presurgical planning.
6. Aesthetic Considerations: In highly visible zones, immediate placement may deliver superior aesthetic outcomes. However, achieving natural results demands precise alignment with adjacent teeth and careful management of soft tissue.

To optimise outcomes, clinicians must carefully evaluate:
• Patient-Specific Factors: Protocols should align with bone density, periodontal health, systemic conditions, and patient preferences. Caution is advised for patients with systemic health concerns (e.g., diabetes).
• Site-Specific Challenges: Treatment in the aesthetic zone requires detailed planning and, at times, adjunct procedures like soft tissue grafting to ensure natural aesthetics and longterm stability.
• Surgical Expertise: Immediate protocols demand a high level of surgical proficiency to manage complex requirements. Comprehensive training and experience are essential for minimising risks and ensuring predictable success.
1. Plan Implant Placement and Loading Pre-Extraction: Treatment plans should address tissue stability, aesthetics, and patient/site-specific factors before tooth extraction.
2. Include Alternative Treatment Options: Prepare alternative plans, such as essix retainers or dentures, as part of the consent process in case intra-operative criteria are not met. Treatment complexity must match clinician expertise.
3. Consider Patient-Centred Benefits and Risks: Protocols should be selected
1. Which best describes an immediate placement with conventional loading?
a) 1A
b) 1C
c) 2A
d) 2C
2. How many weeks are typically required for soft tissue healing before implant placement?
a) 2-4 weeks
b) 4-8 weeks
c) 6-12 weeks
d) 12-16 weeks
3. How long after implant placement does prosthesis placement need to be to be considered conventional loading?
a) 2 days
b) 2 weeks
c) 2 months d) 2 years
4. How long is the maximum time for a prosthesis to be placed for it to be considered immediate loading?
a) 1 day
b) 1 week c) 1 month
d) 1 year
5. When should implants ideally be planned?
a) Pre Extraction
b) Immediately post extraction
c) 3 months post extraction
d) 6 months post extraction
6. Which placement carries the greatest risk of alveolar ridge resorption?
a) Immediate placement
b) Early Placement (4-8 weeks)
c) Early placement (12-16 weeks)
d) Late placement (>6 months)
based on the balance of benefits, risks, and predictable outcomes for the patient.
4. Limit Type 1A Protocol to Specific Indications: Immediate placement/ loading should only be performed for clear patient-centred advantages (e.g., aesthetics, reduced morbidity) and when strict clinical conditions are met.
5. Conventional Loading for Early Placement: Type 2-3C protocols are well-documented and recommended for early placement. Immediate and early loading are less supported and not routine.
6. Avoid Late Placement if Possible: Late placement carries a higher risk of alveolar ridge resorption. If necessary, consider ridge preservation procedures.
7. Use Reliable Protocols for Late Placement: Early (Type 4B) and conventional (Type 4C) loading are the most predictable options for late placement. Immediate loading (Type 4A) should only be applied when strict criteria are satisfied.
Conclusion
The ITI guidelines and supporting evidence emphasise the importance of
selecting appropriate placement and loading protocols based on individual patient needs and clinical conditions. By combining careful timing, thorough presurgical assessment, and evidence-based decision-making, dental professionals can consistently achieve predictable and successful outcomes.
The combination of evolving research and clinical expertise continues to advance implantology, ensuring that patients receive not only functional solutions but also optimal aesthetic results and longterm stability. n
About the author
Dr Tom Murphy BDS (QUB) MFDS (RCPSGlasg) MSc ImpSurg (Distinct.)(UCLan) DipMedEd(Distinct.)(QUB) PGDip Perio (EduQual).

• University Lecturer, University of Central Lancashire School of Medicine and Dentistry.
• Visiting Lecturer, Royal College of Surgeons England - Faculty of Dental Surgery.
• UK/IRE Committee - Association of Dental Implantology (NextGen)
Unlike most wipes which are made from polypropylene, Bossklein V-WIPE ZERO EcoXL wipes are constructed from 100% natural, biodegradable fibres. Wipes are made from renewable, plant-based viscose material and sustainably sourced.
The fast-acting Bossklein V-WIPE ZERO formulation contains no alcohol and takes advantage of safer and greener chemical components to create a simpler and more effective product. Ideal to use on the majority of wipeable surfaces, including dental chairs. Wipes have a pleasant apple aroma. Each flowpack with stay fresh lid removes the need for a dispenser tub further reducing the amount of plastic consumed. Packs contain 100 extra large wipes measuring
240x200mm each.
V-WIPE ZERO Eco-XL wipes are available now. For more information call 0800 132 373 or visit www.bossklein.com n

Are you ready to take your in-house dental imaging to the next level? Revamp the patient journey with the CS 8200 3D Access from Carestream Dental, the exceptional CBCT system that is ideal for first-time users.
With intuitive design from scanning setup to data assessment, the CS 8200 3D Access is a brilliant choice for practices looking to invest in their first high-quality CBCT system.
The solution is versatile, presenting clinicians with treatment options for CBCT imaging, 3D model scanning, panoramic technology and optional cephalometric imaging. Each can be offered with highquality results, whilst maintaining safe examinations thanks to the low-dose mode.

When activated, the low-dose modality means high-quality 3D images can be delivered at the same or lower dose as a standard panoramic exam. For patients who require multiple examinations, this allows you to provide care thoughtfully.
To learn more about how you can introduce in-house CBCT imaging seamlessly contact the Carestream Dental team today.
For more information on Carestream Dental visit the website. For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
Dr Raid Ali is a principal dentist at Restore Dental Group. He graduated in Baghdad, Iraq in 1996, then moved to the UK and finished his international qualifying exams (IQE) in 2006. Dr Ali is ambitious about his career, constantly furthering his education. His passion lies with implant dentistry and is always working to expand this knowledge as a practitioner and build on his learning.
Dr Ali has been elected as Regional Rep for Wales. He shares an insight into his career and experience with the ADI, his election to the Board, and why he believes ADI membership is important for implant dentists:
“I have been placing implants since 2013, and I joined the ADI as a member

at that time. I have attended the full range of ADI events, including Congresses and Masterclasses. They are really good, and it is the only organisation that I depend on for resources and events. I always look forward to them, they are always really well organised and the Congress in particular has always been a great event to attend.
“I wanted to get involved with a great organisation, which is why I was happy to be elected onto the Board. This will be a great learning opportunity for me, and a chance to meet lots of people.
For more information, please visit the website. Become a member today n
adi.org.uk
Lily Head Dental Practice Sales have recently released a guide for principal dentists looking to sell their dental practices, titled Maximising Your Dental Practice’s Value for a Successful Exit. Since the business was established in 2010, their team of brokers have witnessed how early planning can dramatically increase the value of a dental practice as well as ensuring a smooth and more profitable transition. You can download our guide at: www. dentalpracticesales.co.uk/exit
Written for dentists planning their exit strategy, the guide sets out the reasons why planning early puts sellers in an advantageous position, allowing them to maximise value and potentially increase returns.
Lily Head Dental Practice Sales empowers
sellers to make informed decisions, find the right buyer for a dental practice and work to negotiate the best deal. To talk to one of their experts, call +44 (0)333 772 0654 or visit dentalpracticesales.co.uk n

dentalpracticesales.co.uk
Are you looking to renovate your surgery? Work with the experts!
Clark Dental has 49 years of experience working in the dental profession, supporting practices as they upgrade their dental surgeries. Their Dental Surgery Design Service offers clinicians bespoke 3D visualisation, allowing you to see your dream practice in stunning 3D render. This ensures that you always get exactly what you want, for total peace of mind.
Clark Dental goes the extra mile at every stage of your project, sharing their expertise and innovative ideas to help you build your perfect practice.
For more information about solutions from Clark Dental, please contact the team.
Staying up to date on the best oral hygiene products ensures you can recommend the best solutions to your patients.
Since 1956, Curaden has been an innovative and supportive partner of the dental industry, designing products under Curaprox that promote oral health with lasting effects. Organising a Practice Educational Meeting with a Curaden Development Manager can provide your team with a better understanding and experience of the equipment, services and solutions available.
From gaining an insight into the Perio plus mouthwash range to learning about the many CPS interdental brush options, these sessions highlight the many advantages of
For more information call Clark Dental on 01268 733 146, email info@clarkdental. co.uk or visit www.clarkdental.co.uk n


using Curaprox products and how the oral hygiene routine of your patients can be transformed. Don’t let the latest dental products leave you behind – get familiar with Curaden today.
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visit curaprox.co.uk and www.curaden.co.ukn
Hydrogen peroxide-based toothbrightening treatments can not only look unnatural but can also irritate soft tissue, contribute to dental erosion, and cause tooth sensitivity. BRILLIANT Lumina from COLTENE is based on the active ingredient PAP (phthalimido peroxy caproic acid), which beautifully brightens teeth without compromise.
Not only is BRILLIANT Lumina painless and gentle on the tooth structure but it also follows a simple treatment protocol that can be performed by dental therapists under the prescription of a dentist.
The unique formula in BRILLIANT Lumina specifically targets enamel, leaving the dentine unaffected. The tooth shade is enhanced with a bright, natural-looking aesthetic.
If a patient presents with a complex anatomy, complications after endodontic treatment or unexplained symptoms, you need a referral practice you can trust to help.
At EndoCare, we have a team of endodontic experts and specialists with decades of experience in the field. They utilise evidence-based techniques alongside state-of-the-art materials and technologies to treat even the most advanced cases with confidence. Procedures available by referral include complex root canal solutions, endodontic re-treatment and endodontic microsurgery. We will work with you to
Find out more about the system by visiting the website today!
For more on COLTENE, visit lumina.coltene.com/email info.uk@coltene.com or call 0800 254 5115 n

diagnose the problem and then plan the best course of treatment, communicating with you every step of the way.
To find out more about how we deliver exceptional care to your patient, contact the team today.
For further information please call EndoCare on 020 7224 0999 Or visit www.endocare.co.uk n
The WRAS-approved RO Water System from expert in decontamination, Eschmann, affords several benefits for dental practices. Not only does it reliably deliver clean water on tap faster than methods such as water distillers, but it is also more sustainable than bottled water, producing significantly less plastic waste.
The 12-litre water tank comes as standard, and a 60-litre version is available to meet the needs of larger practices. Easy to connect to the mains cold water supply, the system affords a rapid return on investment, often in less than 12 months.
Plus, the equipment can be optimised under the Eschmann Care & Cover servicing and maintenance package, with comprehensive telephone support and expert engineers on hand to keep all
Discover 5 reasons why it is the ultimate choice for precision denture design and streamlined workflows.
• Precision design: EVO Fusion uses advanced digital technologies to achieve precise denture design. From initial scans to the final product, every detail is meticulously crafted, ensuring optimal fit and function for patients.
•streamlined Workflows: EVO Fusion streamlines workflows, optimising efficiency in your practice. Spend less time on manual tasks and more time focusing on patient care.
•seamless Integration: Whether you’re already using digital scanning or CAD/CAM systems, it complements your workflow, enhancing overall efficiency without disruption.
• customisation capabilities: Tailor
Pair long-lasting orthodontic solutions with life-changing restorative workflows after taking the Align, Bleach and Bond course from IAS Academy.
The two-day course explores clear aligner solutions and how they can be paired with restorative approaches such as composite bonding and tooth whitening in one seamless workflow.
Dr Tif Qureshi, the pioneer of the concept of Progressive Smile Design through the Align, Bleach and Bond principle, and Dr Guy Wells, a clinical educator with a wealth of experience in advanced courses and practice care, lead the programme. Together, they support clinicians through a comprehensive syllabus that reinforces confidence in techniques that can be immediately
your decontamination equipment running efficiently for years to come.
For more information on the highly effective and affordable range of infection control products from Eschmann, please visit eschmann.co.uk or call 01903 753322 n

dentures to meet the specific requirements of each patient, ensuring they receive personalised care and superior comfort.

• Enhanced Patient Experience: Offering precise, comfortable, and aesthetically pleasing dentures elevates patient satisfaction and builds trust in your practice, leading to positive reviews and referrals.
EVO Fusion is not just a denture solution; it’s a comprehensive approach to modern dentistry that empowers dentists to deliver exceptional care. Take your practice to new heights with EVO Fusion today. n

implemented in the practice. Former delegates are especially complimentary about the clinical support that extends beyond the course completion, with mentoring available on every case you take.
To learn more about the Align, Bleach and Bond course, contact the team today.
For more information on upcoming IAS Academy training courses, please visit iasortho.com or call 01932 336470 (Press 1) n
OrajelTM is the go-to solution to help manage tooth pain in under 2 minutes. The effective gels can be applied to affected areas with a clean finger or swab up to four times daily, giving patients total control over their own oral pain management. Rapid Toothache Relief contains 10% w/w benzocaine, a local anaesthetic, ideal for managing the pain associated with a broken tooth or a tooth requiring a filling.
OrajelTM Mouth Gel also makes use of 10% benzocaine to quickly relieve pain in gums, from mouth ulcers or dentures.
For acute dental pain, OrajelTM Extra Strength contains the maximum benzocaine allowed without a prescription – instantly blocking the pathways for pain signals along the nerves, temporarily numbing the affected area.
For fast, targeted and long-lasting relief, recommend OrajelTM!
To find out more, visit the website today. For more information, please visit: www.orajel.co.uk n
Enter the new era of digital dental care with Dentsply Sirona Primescan 2, available from Clark Dental.
The team at Clark Dental understand the needs of dental professionals, and work with clinicians to help decide on the right equipment for them. The Primescan 2 intraoral scanner is a fantastic option for those who want to take the next step in digital dentistry.
The first cloud-native intraoral scanning solution enables enhanced communication both with patients and within the dental team. Plus, the device is able to complete a full arch scan in under one minute, and can be immediately ready to scan the next patient, allowing it to be used flexibly throughout the practice.
BRILLIANT Crios from COLTENE is the reinforced CAD/CAM composite you can trust for permanent restoration.
Suitable for inlays, onlays, crowns and veneers, BRILLIANT Crios is the ideal choice for single tooth restorations, both in the anterior and posterior regions.
BRILLIANT Crios has excellent aesthetics alongside reliability and durability.
Not only does BRILLIANT Crios blend in exceptionally well, it is beautifully polishable. Crios comes in a broad spectrum of shades and 3 translucencies. It looks and behaves much like a natural tooth, with high wear resistance and low abrasion.
As tooth substance and BRILLIANT Crios have a similar modulus of elasticity,
For more information, please contact the team at Clark Dental and visit the website.
For more information call Clark Dental on 01268 733 146, email info@clarkdental.co.uk or visit: www.clarkdental.co.uk n

stress peaks are reduced during chewing, resulting in a decreased risk of material fatigue. Due to its shock absorbing effects, BRILLIANT Crios is recommended for implant-supported crowns.
Find out more about BRILLIANT Crios from COLTENE today!
For more on COLTENE, visit colteneuk.com/CRIOS email info.uk@coltene.com or call: 0800 254 5115.n
Having to repeatedly buy brand new amalgam collector cups can be costly and environmentally damaging. With a recyclable alternative your practice can help to support a greener future, whilst also saving money.
Initial Medical has an excellent range of PureGuardTM recycled dental collector cups. When you need to dispose of your used cups, Initial Medical will collect and thoroughly clean, disinfect and check the product within their specialist recycling system. This sustainable approach helps reduce the consumption of single-use plastics within your dental practice. Recycling is also cost-effective as it is a cheaper alternative compared to consistently buying brand new collector cups. The mandatory replacing of a used collector cup each time also helps to prevent the
accumulation of damaging debris in your dental pump, minimising the risk of a costly repair.

For an efficient service that helps both your practice and the planet, Initial Medical offers the best solutions in sustainable waste management. Make your practice greener today.
To find out more, get in touch at 0808 304 7411 or visit the website today www.initial.co.uk/medical n
When bacterial plaque accumulates close to the gumline, there is a risk of developing gingivitis, which, if left untreated, can significantly affect patients’ oral health. PREVENT Gel from TANDEX contains 0.12% chlorhexidine to help control the bacteria that can lead to inflammation. Adding just a small amount of PREVENT Gel to a FLEXI interdental brush can help patients protect their teeth and gingiva from harmful bacteria. PREVENT Gel is a simple but effective addition to every daily routine, and its nonabrasive texture and pleasant taste make it easy to recommend. Not only does PREVENT Gel provide excellent antibacterial effects, it also contains 900 ppm fluoride to help strengthen enamel.

Find out more about the benefits of PREVENT Gel from TANDEX today! For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from DHB Oral Healthcare https://dhb.co.uk/ n
Protecting and maintaining implants requires numerous appliances to ensure success.
With the Curaprox Implant Care Kit, patients have everything they need – all in one place. The kit contains many of Curaprox’s finest products and solutions for good oral hygiene.
The Perio plus Regenerate mouthwash is optimised for comprehensive protection against peri-implant problems, promoting the regeneration of the gingivae and mucosa. The Perio plus Support toothpaste works in tandem, without interfering with the mouthwash’s chlorhexidine.
Also included are three toothbrushes, with the CS surgical toothbrush designed for implant care, and an array of CPS implant interdental brushes designed to access the
Fiona Welsh, Senior Dental Nurse at Nash House, Ipswich, spoke about her experience with Eschmann products and the support received from engineers:
“The Eschmann solutions we have are really good. With the help of our washer disinfectors and Little Sister autoclaves, we are fully HTM 01-05 compliant in our whole decontamination process. The Little Sister autoclaves in particular are especially quick.
“We’ve always been supported by the Eschmann team. Historically, when in a different care setting, Eschmann was on the end of the phone for troubleshooting, and now that we have Eschmann solutions in the practice, we have even more support.
“We know we can reach them with an email or a phone call, and an engineer can either come in
FLEXI is a range of interdental brushes from TANDEX, recommended by dentists and dental hygienists to clean between teeth efficiently and gently, even in difficult-to-reach areas of the mouth.
The FLEXI interdental brushes come in 11 different sizes, to suit the needs of every patient.
The soft bristles comfortably clean tooth surfaces, and massage the gingiva. The brush can be shaped and reshaped to fit any interdental space perfectly, effectively reducing the build up of food particles and biofilm between the teeth.
difficult areas. With an Implant Care patient leaflet to help, everything needed is contained in one reliable kit.
To better protect patients, recommend the Curaprox Implant Care Kit and ensure the long-term success of their implant treatment.

To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visit curaprox.co.uk and www.curaden.co.uk n
For many buyers, realising the dream of owning their own dental practice can be an exciting, but daunting process. Buyers don’t want to be in any doubt that they are in good hands. With a dental specialist finance broker who completely understands the market, and is familiar with dental specialist lenders, buyers can achieve the most favourable financial terms based on a realistic budget.
With DE Finance, buyers receive a fully personalised service to support them through the whole process. The team will help you with an instant indication of your upper borrowing limit, provide a bespoke analysis of your prospective purchase to assess affordability.
The team at Dental Elite work tirelessly to support you, with a tailored application for

banks, specific to your needs, free CQC application support, full sales progression support until completion and much more – all with zero additional cost on 76% of transactions!
As Saleem Mulla says of his experience: “DE Finance got us the best market rate at very favourable terms. Thank you.” Contact the team today to take the plunge! For more information on Dental Elite visit dentalelite.co.uk, email info@dentalelite.co.uk or call 01788 545 900 n
to the practice, or we’ll be directed with some troubleshooting.
“I would definitely recommend Eschmann to practices looking to make a change in their decontamination equipment.”

Alongside a range of autoclaves, washer disinfectors, and RO water treatment systems, and so much more, Eschmann promises a bespoke, personable service whenever your practice is in need of support. Contact the team today to find out more about Eschmann Care & Cover service and maintenance package.
For more information on the highly effective and affordable range of infection control products from Eschmann, please visit the webiste or call 01903 753322 n
Growing your practice can be challenging and stressful. But with the right guidance and an effective strategy, you can fulfil your goals.
The Business and Mindset Mastery course with the IAS Academy is a fun and intensive day of training that will redefine your approach to practice and personal growth. Led by Dr Prav Solanki, a marketing scientist and dentrepreneur, you will be shown his top business coaching principles such as marketing strategies for ethically gaining and retaining more patients.
As well as the focus on business, Dr Solanki will also be championing the importance of a work-life balance and the

benefits of taking time out to declutter your mind from business. This will consider your health, wealth, career and recreational activities to maximise your well-being.
To achieve peak performance as a person and as a practice, sign up with the IAS Academy today.
For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
Contact Professor Ucer at ucer@icedental.institute or Mel Hay at mel@mdic.co. 01612 371842 www.ucer-clinic.dental n one
For additional protection, it is recommended that patients apply PREVENT GEL from TANDEX to the bristles. PREVENT GEL
In the uncertainty of the modern world and dynamic economy, life insurance is an important option for securing the financial stability of your dependents.
Having spent decades dedicated to the financial needs of the dental profession, money4dentists can provide the expert knowledge and guidance you need to navigate the intricacies of life insurance. The reliable team can develop practical strategies to effectively achieve financial goals for you and your dependents.
As a member of the Association of Specialist Providers to Dentists (ASPD) since 2004, money4dentists is respected as an honest and dependable independent financial planner. Besides life insurance the team cover many
contains fluoride to remineralise and protect teeth, and chlorhexidine to remove harmful bacteria. Find out more about FLEXI interdental brushes, and PREVENT GEL from TANDEX today.

For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from DHB Oral Healthcare https://dhb.co.uk/ n

more financial aspects, like pension planning and building insurance. Life insurance will give you and your dependents peace of mind, knowing that they will be financially safe in should the worst happen. Just let money4dentists do the work. For more information, please call 0845 345 5060 or 0754DENTIST. Email info@money4dentists.com or visit www.money4dentists.com n
money4dentists.com
Zygomatic implants are an effective option for long-term success when treating the atrophic edentulous maxilla. For patients who require this treatment, referring them to an experienced practitioner can restore their oral health-related quality of life.
The Centre for Oral, Maxillofacial & Dental Implant Reconstructive Surgery is a referral option that all clinicians can rely on. It is run by the eminent Professor Cemal Ucer, a leading figure in dental implantology and Specialist Oral Surgeon, and supported by a first-class team who provide brilliant implant treatments.
Professor Ucer’s team is driven by clear communication: the patient will be seen within 2 weeks of receiving the referral and a full written report will be sent within 7 days of
Cancer risk is a scary topic for patients to discuss with a dental practitioner. Using non-invasive equipment is more appealing for patients, improving compliance and reducing fears.
The BeVigilant™ OraFusion™ System from Vigilant Biosciences® can reliably identify the biomarkers in the mouth associated with oral cancer, doing so in 15 minutes or less. It uses a simple saliva test that is an agreeable alternative to more invasive procedures, promoting convenience and ease for patients. With a short waiting time for results that determine a low, moderate or high risk, practitioners can help organise any treatment decisions that may have to be made. This can prevent an agonising wait for patients and will empower the

the initial consultation. Referred patients will find themselves in a clinic defined by state-of-the-art surgery and innovative equipment for a comfortable patient experience.
To guarantee that your patients receive the best possible treatment, keep the Manchester Centre for Oral, Maxillofacial & Dental Implant Reconstructive Surgery in mind.

practitioner that they are doing all they can, as quickly as they can. By using simple and comfortable solutions for identifying oral cancer risk, practitioners can reduce the anxieties and fears that patients may have towards cancer, allowing both to tackle the problem together. Try the BeVigilant™ OraFusion™ System today.
For more information, visit vigilantbiosciences.com or email info@vigilantbiosciences.com n
Edentulism is a debilitating condition that can create numerous barriers for patients, affecting masticatory function, communication, self-confidence, and mental health. The ICE Postgraduate Dental Institute and Hospital offers a range of advanced courses for clinicians, including innovative techniques to provide life-changing results for their edentulous patients.
Led by eminent specialist oral surgeon Professor Cemal Ucer at ICE, a unique opportunity is available for dentists to gain hands-on surgical expertise in the use of zygomatic, nazalus, trans-sinus, and pterygoid implants for the treatment of severely atrophic maxillae.
Delegates will develop an enhanced understanding of relevant facial anatomy, delving into the benefits of different treatment approaches as well as the potential risks and evidence-based mitigations.
Contact the team to find out more today!
Please contact Professor Ucer at ucer@icedental.institute or Mel Hay at mel@mdic.co. 01612 371842 www.ucer-clinic.dental n
The right locum support can enable dental practices to offer continuity of care to patients whatever the circumstances, maintaining high standards and protecting valuable income.
Dental Elite has its finger on the pulse when it comes to the locum market. They understand the incentives that genuinely attract the best talent, and work hard to ensure the match is mutually beneficial, meeting the needs of all parties.
Clients are supported closely through completing paperwork, invoicing and compliance services. The team are on hand to offer their insights and advice to ensure the locum can hit the ground running.
As Dr Chalet Hill said: “I can’t say enough good things about Luke. He has been
absolutely amazing in finding locum cover for multiple sites. His response is incredibly quick, and we never have any issues or worries. Every time we need a locum, he manages to provide us one within a week of asking. His efficiency and dedication make our working lives so much easier. Highly recommend!”

Contact the team to find out more! For more information on Dental Elite visit www.dentalelite.co.uk, email info@dentalelite.co.uk or call 01788 545 900n ucer-clinic.dental
Ensuring everyone receives the support and guidance is our priority at Rodericks Dental Partners. Each international dentist is allocated a dedicated mentor to provide personalised day-to-day guidance .
Every new member has access to a large network of colleagues in similar situations, offering additional companionship and support. All International Dental Graduates at Rodericks Dental Partners can enjoy discounted CPD to develop their skills, including opportunities for co-investment. Rodericks Dental Partners will cover up to 50% of fees for postgraduate training courses (terms and conditions apply). This programme includes of a simple six step process to help meet requirements, and a “Clinical Passport” to document their journey and development.
No matter whether you work as a dentist, dental hygienist, dental therapist, dental nurse or reception staff, it’s important that you feel supported and part of a team.
With Clyde Munro Dental Group, this is made easier to achieve with dedicated clinical support, on-going training opportunities and a truly collaborative culture.
Nicola Logan, Chief People Officer, commented:
“There is a hugely collaborative culture at Clyde Munro and our own internal app enables each of our team members to interact and communicate within the wider group.”
If you’re looking for a new role in a supportive and collaborative environment
As Evripidis Tziokas, a Greek National dental graduate at Milehouse

Dental Practice says: “You won’t find a better introduction to dentistry anywhere. You have time to acclimatise to the system without UDA stress. It’s easy to find patients and Rodericks Dental Partners don’t expect the world.”
To find out more about what it’s like to work with Rodericks Dental Partners as an International Dental Graduate, visit: https://rodericksdentalpartners.co.uk/careers/ overseas-dentist n
Invasive procedures can make dental appointments intimidating and uncomfortable for patients, impacting their experience. Minimally invasive techniques can instead preserve the trusting relationship between practitioner and patient.
For detecting the risk of oral cancer in patients, the BeVigilant™ OraFusion™ System from Vigilant Biosciences® is designed to be as minimally invasive as possible. The innovative system uses a saliva test to detect the biomarkers associated with oral cancer in a patient. Easy to use and simple for the patient to understand too, the system provides results in 15 minutes or less, allowing for a swift procedure that will reduce the nervous waiting time that patients may have. The
that enables you to really thrive in your career, consider joining Clyde Munro. Find out more about the career opportunities and vacancies available with Clyde Munro today at careers.clydemunrodental.com or contact joinus@clydemunrodental.com for a confidential chat n

The OraStretch Press distributed by Total TMJ is a jaw motion rehabilitation system that patients can use at home.
It provides an anatomically correct stretch – even those with severely extended over or under bites, or those with missing teeth and dentures can use the OraStretch Press comfortably.
Other features:
• Easy to hold handles
• Small and light
• Improved fit – standard, extended and paediatric versions available.
The OraStretch Press can reduce swelling and pain, for example post oral-surgery or for treating trismus. Using different protocols, depending on the scenario, the
patient will feel a light stretch, helping to increase bite strength.
For details, contact the distributor today.
For more details about Total TMJ and the products available, please call 01202 313701 n

dentalelite.co.uk

speed and simplicity ensure that the practitioner and patient can appropriately act on what do to next, depending on the reported risk from the system.
To promote a comfortable experience for patients, consider the effective BeVigilant™ OraFusion™ System today and be one step ahead of oral cancer.
For more information, visit vigilantbiosciences.com or email info@vigilantbiosciences.com n
Guided implant surgery is the treatment modality of choice for an increasing number of clinicians, as they endeavour to provide precise and predictable restorations that improve patient outcomes.
Join the journey to enhanced implant care with Smop, from Swissmeda, the clinical software and services portfolio from Carestream Dental.
Smop is a cloud-based open framework application that allows clinicians to precisely devise guided implant placement workflows, improving surgery times and patient outcomes in tandem.
It is the world’s only implant planning system with true integration between lab and clinician, allowing for enhanced collaboration between each member of
Well established Dental Practice for sale based in Channel Islands with multiple Dental Practices as well as Aesthetic Practice. This is excellent opportunity for a dental professional looking to expand in thriving location.
For more details email: dentistmare@gmail.com
the dental team.

Together, surgical guides with a unique “clamp” system can be designed, featuring the ability to easily irrigate and improve visibility, in turn creating the optimal environment for precision placement.
To learn more about the guided future of implant dentistry, and how it can aid your workflows, contact the team today.
For more information on Carestream Dental visit the website.
For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
carestreamdental.co.uk

Agilio Software’s compliance experts are here to help your practice tackle the challenges of 2025 with practical advice, innovative tools and hands-on support
For dental practices, staying compliant with regulations that always have the potential to evolve is no easy task. From health and safety to fire prevention measures and HR management, plus with CQC inspections and GDC requirements to consider, managing all aspects of compliance alongside patient care and clinical responsibilities can feel overwhelming. To help practices overcome these challenges, Agilio Software is proud to introduce ‘The Compliance Hotseat’ series for 2025. This initiative will feature regular articles, webinars, and in-person discussions at events throughout the year, offering expert advice to address your compliance questions and provide practical solutions. Led by three of Agilio’s compliance specialists – Fran Sorodoc, Alex O’Neill, and Rhys Jones – the series aims to simplify complex requirements and support practices in achieving compliance while fostering efficient and safe operations.
compliance challenges
Running a dental practice already involves a delicate balance between clinical work and administrative duties. Add compliance to the mix, and many practices find themselves stretched thin. Key challenges include:
• Health and safety: staying updated on regulations to ensure the safety of staff and patients can be a timeconsuming task
• Fire regulations: meeting legal obligations for fire prevention and safety often gets overshadowed by other priorities
• HR management: navigating employment laws, creating robust policies, and handling contracts require expertise that many practices understandably lack in-house
• CQC expectations: with inspections focusing more on risk management and patient outcomes, practices must maintain consistent standards to remain compliant
• GDC requirements: ensuring compliance with the GDC’s standards for patient care and professional conduct adds another layer of responsibility for dental teams.
In 2025, practices will, of course, need to remain vigilant in managing not just compliance but also how it integrates with overall operational efficiency and staff wellbeing. This is especially true as pressures from recruitment difficulties, cost management, and new technology adoption continue to mount.
For many practices, managing compliance effectively often involves combining the right tools with expert guidance. Solutions like iComply can help streamline workflows and provide clarity around meeting CQC standards, offering practical support to reduce the pressures associated with compliance. For those needing more tailored assistance,
services such as iManage offer the option of working with a dedicated compliance manager to address specific challenges, from audits to inspections. These kinds of support systems can help practice teams establish a culture of compliance, easing the administrative load and allowing more time to focus on patient care.
At the same time, accessing expert advice can empower practice managers to address gaps in knowledge or confidence.
That’s why The Compliance Hotseat is such a valuable resource – it provides actionable insights, demystifies regulations, and helps practices create a compliance strategy that works in harmony with their operational and patient care goals.
Fran Sorodoc, Agilio’s Head of Professional Services, has extensive experience in both medical and dental practices. Fran discovered her passion for compliance in 2016 while using iComply and joined Agilio as a consultant in 2019. She believes any practice manager can become compliance savvy with the right support and is known for achieving exceptional results. Fran’s philosophy centres on streamlined operations, strong leadership, and continuous improvement.
Next up is Alex O’Neill, Managing Director – Practice Services, an expert in healthcare governance, operational excellence, and organisational culture. He has guided countless practices in
The start of a new year is the perfect time for UK dentists to reflect on their achievements, re-evaluate their strategies, and set actionable goals for the year ahead. Growing a dental practice isn’t just about increasing patient numbers – it requires clear planning, intentional goal setting, and strategic marketing to ensure long-term success. Here’s my step-by-step guide to help you effectively develop your dental practice in 2025.
1. assess your current position
Before setting new goals, take stock of where your practice currently stands. Evaluate key metrics such as patient numbers and retention rates; treatment acceptance rates; revenue and profit margins; and online visibility. Understanding your starting point allows you to identify opportunities for improvement and focus on what matters most. For instance, are you struggling to attract new patients, or are existing patients not returning? Pinpoint these challenges so you can set targeted goals.
2. set sMaRT goals
Effective goal setting revolves around the SMART framework:
• Specific: Clearly define your goals, e.g. ‘Increase new patient sign-ups by 20% in 2025’.
• Measurable: Use metrics to track progress and success.
• Achievable: Set realistic goals based on your resources.
• Relevant: Align goals with your overall growth objectives.
• Time-bound: Create a clear deadline, e.g. ‘within 12 months’.
3. focus on patient retention and experience
A strong patient base begins with delivering exceptional care and memorable experiences. Focus on developing improved communication, ensuring that follow-ups, reminders, and post-visit care instructions are timely and personalised. For patient comfort, upgrade your practice environment to make it more welcoming and modern, and regularly collect feedback through surveys to understand patient needs and concerns.
Retaining loyal patients is more costeffective than constantly acquiring new ones. Happy patients are also more likely to refer friends and family.
4. enhance your online presence
Most patients begin their search for dental care online. To ensure your practice stands out, you need to ensure your website is mobile-friendly, fast, and provides essential information (services, team profiles, booking options). Optimise your site for local keywords like “dentist in [your city]” to attract nearby patients, and leverage Google Business Profile to keep your

developing strategies to achieve compliance and operational efficiency. Alex also leads the evolution of tools like iComply and iManage, and is a trusted voice in the industry as a speaker and author. His practical, insightful advice has helped practices large and small succeed. Meanwhile, Rhys Jones, Head of Compliance at Agilio, is a specialist in health and safety, with particular expertise in fire safety, electrical safety, and radiation. With extensive knowledge of compliance requirements, Rhys is committed to providing clear, practical advice to support dental teams in navigating complex regulations. His approach focuses on demystifying topics such as COSHH and disability access while addressing common misconceptions, ensuring practices can operate safely and confidently.
The Compliance Hotseat series is your chance to get expert advice on the compliance issues that matter most to your practice. Whether it’s a specific challenge or a general query, Fran, Alex, and Rhys are here to help. Look out for the first article in an upcoming issue, join our webinars, and meet the team at key exhibitions throughout the year. Have a question? Send it to compliance.hotseat@agiliosoftware.com for your chance to have it answered – we may tackle it in The Compliance Hotseat and even get in touch to discuss it further! n
details updated and encourage satisfied patients to leave positive reviews.
Use social media marketing to share patient success stories, dental tips, and promotions to engage your audience and increase visibility.
A strong digital footprint can significantly boost your reach and credibility, attracting more patients to your practice.
5. invest in training and technology
The dental industry is constantly evolving, and this coming year we predict significant developments in both marketing and dental technology. To stay ahead of your competitors, you need to invest in ongoing team training, new technology, and digital tools, such as practice management software to streamline booking systems, reduce missed appointments, and improve communication.
6. expand your services
If you’re looking to grow revenue and attract new patients, consider expanding your offerings. Popular growth areas include cosmetic dentistry, orthodontics, dental implants, and preventive care plans. Promote your new services through targeted campaigns, email newsletters, and in-practice communication to ensure patients are aware of the value you provide.
7. Leverage strategic marketing
Strategic marketing is essential for growth, so create a cohesive plan that includes
local advertising and community events, content marketing, paid advertising, and email marketing.
With consistent marketing, you can maintain visibility, attract new patients, and retain existing ones.
8. Track your progress
Once your goals are set and strategies are implemented, it’s essential to monitor your progress regularly. Use key performance indicators (KPIs) to assess patient growth rates, revenue increases, online review scores, and marketing campaign effectiveness.
If something isn’t working, adjust your strategies and stay agile. Continuous monitoring ensures you remain on track to achieve your goals.
By following this plan – setting SMART goals, prioritising patient experiences, leveraging digital tools, and tracking progress – you’ll be well on your way to growing a successful dental practice in 2025. With careful planning and a proactive marketing strategy, you can position your practice as a trusted and thriving health service within your community. n
about the author cally Walker, founder of connect My Marketing






With a new year upon us, Martyn bradshaw, Director of PFM Dental – one of the leading dental practice sales agencies – answers the start of a Q&A series, the first being on the market and whether 2025 should be the year to sell your dental practice
What has the market been like over the last few years?
There is no doubt that the dental sales market over the last few years has had to weather some storms with Covid, an increase in bank rates (from 0.1% to 5.25%, although this has more recently reduced to 4.75%) and the struggles with associate recruitment.
However, what we have seen over this time is the robustness of the market. Whilst some Corporate groups had stopped purchasing for periods of times, others continued. Owner occupiers continued to purchase, helped by the banks’ continued support for dental practice purchases, irrespective of the increased borrowing costs.
We did see a small reduction in the multiples being used when calculating the values of the practices. However, when you consider that the EBITDA (earnings before interest, tax, depreciation and amortisation) calculations that we use removes the loan repayments, it is easy to see why such multiples could previously be achieved when the Bank of England base rate was at 0.1% and some loans were totalling less than 3%, as the affordability was easier. However, we are only talking a small reduction.
What do you expect from 2025?
The growth in the market was actually seen in the last half of 2024, and I believe that we will continue to see the same growth. We have already had a number of discussions with Corporates this year who have huge spending plans and are now looking for the right practices to fit into their structure.
Private buyer interest remains high, likely because of them seeing that the Bank of England base rate stabilised from mid-2023, then reduced in 2024. We actually saw a higher percentage of sales to private individuals last year in comparison with previous years.
Will ‘business asset Disposal Relief’ changes affect the market?
Just to reiterate what happened in the 2024 autumn budget, the new rate of tax applied to Business Asset Disposal Relief (formerly known as Entrepreneurs’ Relief – applicable to gains of up to £1.0m when you sell a business) is increasing from 10% to 14% in April 2025, and then rising to 18% in April 2026. Capital Gains Tax (above the £1.0m of gain) is now charged at a rate of 24%, which is a 4% increase from previous rates.
For any vendor who is looking to sell their dental practice in the next 12 months, it is likely that they will want to be conscious of
these increases and ensure that the sale is completed prior to the further increase in April 2026 so that they do not pay the extra tax. I don’t, however, believe that people will bring their retirements significantly forward because of this.
What about the timing for someone looking to sell?
Typically, we are finding that the legal and regulatory element of a dental practice sale can take anywhere between six and 12 months. Then, build in time for finding a suitable buyer for the practice, and I would urge anyone looking to complete before April 2026 (i.e. the increase to 18% for Business Asset Disposal Relief) to start the process now.
This should give sufficient time to consider offers from buyers and undertake the necessary legal and regulatory work. Whilst the likes of limited companies can be quicker in that the CQC timescales can be less onerous, having a £40,000 ‘penalty’ for not completing by their ideal time is something that can be easily avoided by starting the process as early as possible. Those who may be interested in Corporate buyers will also need to consider the expected tie-ins in requirements, which can be between two to four years for the selling principal, so this would need to be

factored into the planning when considering timescales to sell. n
PfM Dental offers a comprehensive range of professional services exclusively for dentists. since 1990 we have been trusted advisers to the dental profession with a hard won reputation for sound, ethical and independent advice. Our services incorporate 4 key departments: practice sales and valuations, independent financial advice, dental accountancy and dental legal services. https://pfmdental.co.uk/
about the author
Martyn bradshaw is a Director of PfM Dental and heads up the dental practice sales agency.

Employee ownership is one of the fastest growing business models in the UK. It’s been widely reported that one in 20 of all private company sales are to an employee ownership trust (or EOT). That rate is increasing in line with the growth of the employee-ownership sector. Employee ownership is not a new concept –John Lewis has been a notable flag bearer for the sector over 100 years – but government tax incentives introduced in 2014 provided a significant boost. It is now becoming an increasingly popular ownership model for companies of all shapes and sizes given the benefits for businesses, their owners and employees. The EOT model is now being adopted across a wide range and diversity of industry sectors; the dental sector is playing its part in that growth. The Gateway Dental Practice and Your New Dentist are just two dental practices which have recently embraced the EO model as a succession solution. More will surely follow.
There are plenty of reasons why a dental practice might favour an employee ownership model, but the following characteristics and themes tend to be common to most.
Employee ownership can be the right succession solution where the current practice owners are looking to retire but an exit via a third-party sale or buy-out is not desirable or achievable. This may be because:
• The concept of being acquired by a competitor or ‘big brand’ consolidator is unappealing.
• The junior practitioners do not have the appetite or financial means to structure a buy-out.
• As a family-owned practice, there may not be a next generation willing to take over the running of the business.
• The owners may struggle to secure a fair price for the practice from a third party.
Strong management, though, remains important. A leadership succession plan is needed for practice owners who are currently integral to the day-to-day operations of the business but who are looking to step back. Unlike a trade sale where change is far more rapid, under an EOT structure the retiring practice owners will be able to structure and manage the handover of responsibilities, typically over a number of years, to allow for a smooth and gradual succession.
Probably the over-riding reason to transition to employee ownership is that the model helps preserve the integrity and continuity of the practice which may have a proud history of being independent and a distinct culture that the owners have nurtured over many years. Independent practices work hard to create and instil a distinct culture and market reputation. Employee ownership can be a way to protect and enhance that culture and independence for the long term.
Tax incentives
There are key tax incentives associated with becoming employee owned. In a changing tax climate, it is notable that practice
owners selling to an EOT will have no capital gains tax to pay. Staff of employeeowned businesses also benefit through the ability to receive tax-free bonuses. The rationale of these tax benefits is often mis-understood. The favourable tax regime reflects continuing government support for employee-ownership as it helps promote stable, profitable and resilient businesses where ordinary workers have a share in their success.
An important factor is how an exit to an EOT is funded. Other than where external debt is used, the business value paid to the current owners must be funded out of the after-tax profits of the practice. The affordability for the business is therefore an important consideration and one that requires careful planning. Owners of well-run and profitable practices will see employee ownership as a more achievable and straightforward exit route compared with owners of practices facing a potentially more uncertain future.
a people-focussed practice
Employee ownership ultimately works well for businesses that put their people at the core of their organisation. Becoming employee-owned can build on an existing employee-focused culture by providing a heightened sense of well-being as well as financial rewards to staff. This, in turn, can help drive business performance with the following outcomes:
• Employee-owned businesses tend to be more innovative because managers go out of their way to consult, share information about the business and give staff responsibility.
• Staff in employee-owned businesses tend to be more entrepreneurial and committed to the practice and its success.
• Because they involve staff and give everyone a stake, employee-owned businesses are better at recruiting and retaining talented, committed staff. With a decision as important as the future succession of your practice, it is important to weigh up all the relevant factors carefully. There is an increasing number of dental practices who feel employee-ownership is the right route for them.
Brabners have supported over 50 businesses and are recognised experts on EOTs as a succession strategy with a specialised sector focus on dental services. n
about the authors stephen Hadlow is a corporate partner and eOT specialist at brabners LLP.
nicola Lomas is a corporate partner and leads the dental team at brabners LLP.
























Ergonomic

Three





















































The benefits of selling by 5th April
The idea that information is power is based upon the rationale that people can make better decisions and have more control over the outcome.
For some time, I have been talking to clients about the possible implications of changes to Government policy on Business Disposal Asset Relief (BDAR) and overall Capital Gains Tax (CGT). But, of course, we have only been able to make decisions based on expert opinion and not facts. The fact is that no changes were ever announced. That is until the first budget by the newly elected Labour government this autumn.
Now we know what their plans are. We are able to have much more detailed discussions with people and are able to drill into exactly what the implications are for our clients who are planning on exiting their dental practice.
The government announced that BDAR will gradually reduce between 6th April 2025 and 5th April 2027.
On 5th April 2025, BDAR will increase to 14%. On 5th April 2026, it will increase to 18%.
Capital Gains Tax was increased from 20% to 24% on 31st October 2024 and will remain at that level at least until 5th April 2027.
There are qualifying criteria that must be met in order for individuals to be eligible to claim BDAR. Whilst I recommend you speak to your accountant, this gives you a flavour of what HMRC will require for you to be eligible.
• The person selling the shares in the company must have owned and worked in the business for at least two years prior.
• They must sell the whole or a large part of the business.
• They must claim business asset disposal relief on the business sale to be allowed to claim the relief on any buildings.
The government has given us three milestones to consider: 5th April 2025, 5th April 2026, and 5th April 2027. We know that the tax relief will reduce, and the tax liability will increase on the first £1,000,000 of the asset disposed of in 2025 and 2026. We don’t know what will happen effective 6th April 2027. The labour government could increase or decrease the tax liability on the sale of a business. You can decide where to put your money. We have done some modelling with Nathan Poole at Ross Brooke to project what the implications are for two of our clients. Practice A has a Capital Gains Liability of £1,850,000 and Practice B has a Capital Gains Liability of £850,000. What the modelling highlights is that the changes in tax are not equitable for both practices. Practice B has a proportionally higher tax burden. This because the uplift in tax is not equitable.

Just to be clear, unless you have a sale that is well progressed, it will not be possible to complete before the end of the financial year 2025. Therefore, we projected forward to 2026 and 2027.
With Practice A, we saw that, completing a sale by the end of the financial year 2026, the vendor will have a capital gains liability (including their BDAR) of £343,280. This is a capital gains tax liability uplift of 13%.
If Practice A was to complete on a sale during the financial year ending 2027, the vendor(s) would have a capital gains tax liability of £383,280. This is a 12% increase compared to completing before the end of the 2026 financial year.
With Practice B, we saw that, completing a sale during the financial year ending 2027, the vendor(s) will have a capital gains liability of £152,460. This is a 29% increase compared to completing before the end of the 2026 financial year.
The financial burden is higher for the smaller practice because more their CGT liability falls in the £1.00 to £1,000,000 allowance, where the biggest changes have occurred.
Our modelling also projected how much extra value the principals would have to add to their dental practice values to fill the gap in their retirement funds. In Practice A, the principal would have to add £133,000 of fees if they completed after 5th April 2026. For Practice B, the principal would have to add £91,955 in fees if they completed after 5th April 2026.
My message to clients has been that if you are ready to sell, don’t delay. There is an opportunity to mitigate a significant amount of CGT by completing your sale prior to 5th April 2026.
It takes nine months from agreeing a sale to get to completion. Ahead of that, you must allow time to appoint a dental broker, launch the practice onto the market and agree a deal with a willing buyer.
There are procedural requirements for vendors, such as NHS transfer process, CQC registrations and third party landlords, which dictate the timescales.
There are also procedural requirements for buyers, such as CQC registration, funding and fulfilling the banks conditions.
But there are parts of the process which can be started at a very early stage, or even before your practice is put up for sale. For example, sorting out your lease, dealing with property regulatory standards, preparing for due diligence and having all the current and historical financial information up to date and available. Think about how you are going to conduct yourself during the sale process. Being responsive, pragmatic and goalfocused will expedite the process.
If you are not sure if you can meet any of the milestones around the CGT increases, then please contact me for a full assessment of your circumstances.
If you are not at the point of wishing to exit, then speak to your financial planner first to plan your retirement. A financial planner will look at how you are going to finance your retirement, your costs, your lifestyle, what you need and when. n
about the author abi Greenhough,
Managing Director of Lily Head Dental Practice sales.
















Guests join us from all areas of the industry to provide their own unique perspectives on a wide range of topics, from manufacturers and figureheads of various dental organisations, to those in the trenches working in practice, and more.


















Nothing is off limits in The Probe Dental Podcast, so be sure to tune in wherever you get your podcasts! The Probe Dental Podcast features discussions that explore all areas of the British dental sector.









For more information, sponsorship opportunities or to book a podcast please contact





The Autumn Budget has given the dental market a lot to talk about.
While investment in health and social care will be welcomed by many, the budget will hold consequences for dental practices due to changes in taxation thresholds and percentages, despite some measures designed to ease the financial burden for smaller businesses.
As well as the changes to Capital Gains Tax, Inheritance Tax and Business Rates
– all of which will be discussed in greater detail – of particular interest for many dental practices in the weeks following the Autumn Budget are the changes to Employer’s National Insurance Contributions (ER NIC).
Although an increased allowance for small businesses will result in many predominantly private dental practices being better off, primary care providers within the NHS have expressed concern about increases to ER NIC, combined with increased salary costs. Not eligible for relief in the form of Employers Allowance, and as yet unclear on how investment in health and social care will be allocated, some practice principals may have little option but to decrease their NHS offer in favour of private treatments.
What are the changes to ER NIC?
In her first budget as chancellor, Rachel Reeves confirmed a rise in ER NIC from 13.8% to 15% from April 6, 2025. In addition, the Employer’s Secondary Threshold will be lowered from £9,100 to £5,000. Benchmarking data produced
earlier this year gives us an annual staff cost of around £161,000 for the average UK dental practice with around £906k revenue and 6 full time equivalent (FTE) PAYE staff. This gives us an average additional cost of just under £5k in ER NIC.
To offset this, the Employment Allowance is to from £5.5k to £10.5k meaning – according to government estimates –around 865,000 employers won’t pay any Employers National Insurance at all next year. Indeed, for predominantly private practices with annual staff costs under about £180k, the cost of employing people will be slightly lower or about the same post-Budget.
The additional consideration of wage increases
Businesses have already seen considerable rises in salary costs and related NI rates since 2019. According to the Office for National Statistics, between 2019 and 2023, the average wage for business service staff increased by 25%.
National Minimum Wage (NMW) will increase from £8.60 to £10/hour. That’s almost a £4 per hour increase since 2019. Apprenticeship and under 18s pay will go up by over £1 from April 2025 – from £6.40/hour to £7.55/hour. National Living Wage (NLW) also increased between 201819 and 2024 from £7.83 to £11.44 per hour, while the statutory age dropped from 25 to 21 years. NLW will again increase to £12.21 an hour from April 2025.
Increases to NMW and NLW require a consideration of commensurate pay rises for staff earning above those on the lowest pay and, of course, this also adds to the ER NIC bill for employers.
The government has committed an annual average increase of 3.8% in funding for Health and Social Care between 202324 and 2026 totalling over £25 billion. However, at the time of writing, there is not yet any detail to confirm what investment NHS dentistry might expect.
Currently, the increase in ER NIC does mean that many NHS practices will be looking at higher employment costs next year, unless something changes. There is deep concern among those delivering NHS primary care about whether the ER NIC uplift has to come out of core budgets. In an open letter to the government, the BDA has called for the chancellor to extend Employment Allowance relief to struggling practices who are already providing NHS services at a financial loss.
Despite all this, there is reason for optimism. A recent set of statistics released by NHS Business Services Authority (NHSBSA) surprised many by demonstrating that income, courses of treatment and dental activity for NHS practices has risen in the last year, and benchmarking information demonstrates that an NHS contract can still be a key driver for practice growth.
There are few challenges that dental professionals face like setting up a squat dental practice. This endeavour into the unknown requires a great deal of time, patience, and organisation for success.
The financial aspects of a squat practice are just one part of the process to consider, alongside the hiring of a team, advertising, selecting and installing new dental chairs, and of course the actual location of the new practice. However, the costs and profits of the new business are a fundamental, and will begin to affect every other choice you make, in one way or another.
Before a clinician can begin to seek funding, it’s important to generate a cash flow forecast. Prepare a plan for the project’s financial costs set against estimated profits from, for example, the first year of providing dental care, and you begin to understand what you can feasibly afford. What treatments will you provide, how much will you charge individuals, and how many patients in the surrounding area will seek that care? It’s tough to know the entirety of your costs, but speak to colleagues who own practices, or seek specialist financial advice, to begin to understand the viability of your investment.
The income that allows you to purchase and begin building a squat practice is key. You should consider the amount of money you need from loans or third-party investments, and establish an achievable repayment plan.
The difficulty with founding a squat practice is, unlike an existing dental service, a lender (usually a bank) has little to go off of except for your skills and prospective business plan to consider whether you will be able to meet your costs. If you are purchasing a pre-existing dental centre, you might be able to use previous years’ income statements that evidence a pre-existing patient-base, with established costs and profits.
When setting up a squat practice, it’s important to have as much information to hand as possible to ensure an investor feels confident in their choices. The more you can minimise risk for a lender, the easier it becomes to secure a favourable financing option.
Take time for
Clinicians should also consider how they can be tax efficient when establishing a squat practice. By legally and thoughtfully minimising the amount of taxes you owe, for
Going back to basics can help to ensure you are maximising the value of your business. As always, maintaining a forensic understanding of your finances, and keeping abreast of market influences and trends, alongside strategic investment in growth areas for your particular practice is vitally important.
The Dental Elite Benchmarking Report 2024 revealed a pre-Budget advantage in the dental market for mixed practices. This remains the case, with the new proviso that practices will benefit from a greater that 50% emphasis on private work. For any principals looking to increase the value of their practices, or to buy or sell, Dental Elite has a team of specialist brokers and finance experts who all have an unparalleled understanding of the dental market. You don’t have to navigate your way through the twists and turns of the dental market alone. If you are considering selling or purchasing a dental practice, there are exciting opportunities available. For more information on Dental Elite visit www.dentalelite.co.uk, email info@dentalelite.co.uk or call 01788 545 900
About the author Luke Moore is one of the Founders and Directors of Dental Elite.

example, through deducting the cost of supplies and dental equipment, or even rent and utilities used to provide everyday care, you can save more money, and reinvest every penny into the new business.
Not every dentist will be an expert on tax law, or brokering for finance with lenders. That is where independent financial advisers, such as the team at money4dentists, come in. With decades of experience solely supporting dentists, the team completely understands the unique quirks of the profession. They can provide tailored support for clinicians thinking about establishing a squat practice, ensuring you are confident in your finances before making lifechanging decisions.
Setting up a squat practice is a large endeavour, but can be professionally fruitful. Seeking support for your financial management is a sure-fire way to gain confidence in the choices you make throughout this process.
For more information, please call 0845 345 5060 or 0754DENTIST.
Email info@money4dentists.com or visit www.money4dentists.com


We’re a specialist dental practice sales agency, so whether you are looking to sell your dental practice on the open market, selling to your associate or intrigued with Corporate interest, we’ve helped thousands of dentists like you.
You cannot be in better hands with our expert valuers, a single point of contact throughout the sale and in-house legal team, allowing us to

We work with dentists all over the UK
Our scale and reach means we’re here to help wherever you’re based
Practice sales over the past 12 months 50+
Current dental accountancy clients 1200+
Practice finance raised in the last year £15m+





Accurate valuations for associate & principal led models with advice on enhancing the practice value.

advise you from start to finish. Supportive Throughout
We liaise with solicitors, buyers, and CQC to ensure everything is in place to minimise stress and give a smooth sale.

Get access to 1000s of pre vetted purchasers, being individuals, small groups and all of the major corporates.

We have specialist dental solicitors with expertise in commercial law, property law, and CQC processes.

We will ensure your practice attracts the best possible price by negotiating the sale on your behalf.

Fee Free Sale
95% of our NHS practices sell to priority buyers meaning the purchaser covers the agency fee.


