





































































































































































































National primary care bodies, the British Dental Association, British Medical Association, Community Pharmacy England, Optometric Fees Negotiating Committee and the Association for Primary Care Audiology Providers have joined forces to make the case for investment into primary care across Parliament.
At the “Moving from Crisis to Recovery” Future of Primary Care Parliamentary event hosted this week, MPs were reminded that primary care is the foundation of the health and care system and the front door to the NHS. It is where the public go for advice, treatment, and referrals to more specialised care if needed.
Primary care services are the place where primary patient relationships with healthcare are built, ensuring continuity of care which is critical for prevention and treatment. It is vital that this essential part of the NHS is protected and built upon for the future.
MPs were warned that if primary care continues to be under-prioritised and underfunded compared with the rest of the NHS and relative to its costs, access and patient health will continue to be put at risk.
The event, which was sponsored by Helen Maguire MP, Liberal Democrat Primary Care and Cancer Spokesperson,

was well-attended with 21MPs, peers and their staff present on the day, and many more in touch before the event.
MPs are being asked to urge Government to support these objectives and to take a series of actions to call for direct political intervention to secure a long-term sustainable future for the primary care sector.
Helen Maguire, Member of Parliament for Epsom & Ewell and Liberal Democrat
Spokesperson for Primary Care and Cancer, said: “I was delighted to sponsor this event and hear directly from organisations across primary care, all of whom underscored an important message: Primary care is the front door to our NHS, but is under increasing pressure.
“The Government must provide comprehensive investment to secure a sustainable future for the NHS and its primary care services.” ■
Agilio Software, the leading provider of healthcare software solutions, is delighted to announce the acquisition of Patient Plan Direct (PPD), a specialist dental membership plan provider that helps practices grow sustainable, recurring income and strengthen patient relationships. The deal brings together Agilio’s established
dental compliance, workforce and marketing solutions with PPD’s proven expertise in plan design, technology, training, and support to nurture strong growth and retention.
Read our interview with Andy Sloan, Agilio’s Managing Director for Dental, and Simon Reynolds, Managing Director at PPD, on page 44.

The dental community is joining together in 2026 to take part in a BIG 100km charity challenge – and now is your chance to sign up and be part of it.

Dental groups, suppliers, clinicians and energetic fundraisers are being invited to test their limits and raise money to support Dentaid The Dental Charity in its 30th anniversary year as part of Dentistry’s BIG Community Challenge.
A team with participants from across the profession is entering the ‘original’ 100km London 2 Brighton Ultra Challenge on Saturday 23rd and Sunday 24th May 2026.
For those seeking a shorter route, two one-day challenges are available on the Sunday with a marathon-distance 42km route and a 25km looped walk from Brighton Racecourse. There will be also be a Walk in a Box option for anyone unable to join the main event.
Event registration is now open and professionals from across the industry are being invited to get their best foot forward and sign up.
Registration costs £189 for the full challenge, £132 for the marathon challenge and £84 for the 25k challenge. Participants are required to raise at least £500 in sponsorship for Dentaid (£300 if taking part in the 25k event).
To sign up for the event please visit: https://tinyurl.com/Dentaid-LDN-BRN ■

As February begins, 2026 has made its intention to be as quick-paced as 2025 clear. January was a busy month for UK dentistry and the year shows no signs of slowing down.
We broke the news in early January of Agilio Software acquiring Patient Plan Direct. The implications of the deal are that Agilio’s platform now connects membership plans with compliance, practice operations and practice growth solutions. After the news broke, I conducted an interview with Agilio’s Andy Sloan and Patient Plan Direct’s Simon Reynolds for The Probe Dental Podcast, which you can watch by scanning the QR code or visiting the-probe.co.uk/podcasts. An abridged version of the interview can also be found by turning to page 44.
As usual, there is plenty more to sink your teeth into, including an in-depth look at the latest statistics that show tooth decay among adults in England has hit a low point not seen since the late 1990s. Polly Bhambra ponders whether this is just the tip of the iceberg on page 10. And, finally, don’t forget there’s still time to enter The Dental Awards before the end of February. Visit the-probe.co.uk/awards for more information, or see page 40 for details of the newest category introduced this year.









The Probe is published by Purple Media Solutions.
Registered in England.
Registered number 5949065
Managing Editor: James Cooke
Commercial Director: Gary Henson
Divisional Administrator: Francesca Smith







Production Designer 1 : Lorna Reekie
Production Designer 2: Rob Tremain
Digital Content Manager: Stephen Wadey
Circulation Manager: Andy Kirk
Managing Director: Ed Hunt
Regular Contributors: Lisa Bainham, Nigel Carter, Barry Cockcroft, Ollie Jupes and Pam Swain
E-mail news, stories or opinion to james.cooke@purplems.com
Circulation/Subscriptions: The Probe Subscriptions, Perception SaS, PO Box 304, Uckfield, East Sussex, TN22 9EZ, Tel: 01825 701520, https://purplems.my-subs.co.uk ©Purple
Media Solutions Ltd, 2014. All rights reserved. ISSN 0032-9185. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies, and information retrieval systems. While every effort has been made to ensure that the information in this publication is correct and accurate, the publisher cannot accept
liability for any consequential loss or damage, however caused, arising as a result of using information printed in this magazine. The views expressed in The Probe are not necessarily the views of the magazine, nor of Purple Media Solutions
Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth RCS(Eng), D’Orth RCS(Eng); Mark Wright BDS(Lon), DGDP RCS(UK), Dip Imp Dent.RCS (Eng) Adv. Cert, FICD; Dr Yasminder Virdee BDS. Readers who





Discover how we lead technology and patient experience
Stand F10 at the BDIA Show London 13th & 14th March
Idon’t know why this sprang into my mind – perhaps it was triggered on this January 8th by waiting with trepidation for the arrival of Storm Goretti – but I was thinking this morning about UDAs and the time I was arrested and spent a sweaty afternoon in a police ‘Black Maria.’ Anyway, I’ll leave it there.
Okay, if you insist… It was June 1978 and I was working as a press photographer for a large evening newspaper in the midlands. I was the paper’s photographer, based in a regional office on the Welsh border. My reporter colleagues and I covered the rural border area and often ventured into mid-Wales.
One afternoon I was covering an incredibly tedious church fete (the job was all glamour) just outside the small town where we were based, when an assistant to the church vicar approached and advised me there was a telephone call – these were the pre-mobile days, of course. I took the call in the parish office from our office’s chief reporter, who told me to “Get you’re a**e down to the A4* fast, there’s been a big crash! Loads killed.”
As soon as the chief uttered that, I pretty much gunned myself into reverse despite being keen to grab any opportunity to escape this ‘fete worse than death.’ I had no desire to turn up like a ghoul at a tragic accident. Firstly, I’ve always regarded it as unseemly for photographers and camera crews to record scenes of devastation at tragic events and, secondly, at the time I was an extremely squeamish individual and had never witnessed death (or even neardeath) first hand. You can imagine what I was like at my first dental school dissection session in the early 1980s.
Despite my procrastinated drive to the scene, I arrived to find body parts strewn over the carriageway. A lorry had taken out the side of a coachload of (I later found out) American tourists. I had a Nikon F1 around my neck and a camera bag over my shoulder and I was removing the camera to put it away as I approached the young trainee photographer from the local rival weekly newspaper. I was in the middle of telling the photographer not to take pictures when I became aware of a clearly traumatised senior police officer on board the coach standing next to deceased passengers screaming to his uniformed subordinates on the road to “ARREST THOSE TWO!”
I was only a skinny little bloke in those days and, within a few seconds, I found myself air-walking as two burly officers frogmarched me off to the back of an incredibly hot Black Maria to be incarcerated with the blubbing 19-year-old idiot who’d got me into the mess in the first place. We spent two-and-a-half hours in the back of the sweltering van with no word from outside. As far as we were aware, nobody from our respective publications knew where we were. Having been a court reporter for a few years before switching to photography, I did know that there had been a procedural – for the want of a better word – cockup by the police, since no rights were read to us before we were unceremoniously dumped in the back of the van. Eventually, in the nick of time before we both passed out, the doors were opened and we were let out into the scorching afternoon sun. Mercifully, one of
my reporter colleagues had witnessed us being dumped in the van and had walked a mile down the road to a nearby Little Chef to make a call to our editor in the paper’s headquarters, some 20 miles away.
After the editor finally got in touch with the Chief Constable, over two hours had elapsed. It was a completely uncomfortable afternoon. Despite knowing that I faced no charges, there was still a feeling during my incarceration that I was trapped and completely abandoned.
Talking of being trapped and completely abandoned, I wonder how NHS dental surgeons are feeling now that the government is ‘tackling the deep-rooted problems so patients can have faith in NHS dentistry.’ Yes, that’s right, Stephen Kinnock, Minister of State (Department of Health and Social Care), actually said those words in the announcement by the government that it will be ‘prioritising patients with the greatest needs’ in changes to the dental contract ‘which will be in place from April 2026.’
It makes you wonder if Mr Kinnock knows what roots actually are or is aware that lightly dusting a blossom is unlikely to cure Rose canker. Similarly, it makes you wonder if anyone in government has speculated on the notion that ‘rolling out urgent and emergency care appointments’ isn’t fixing anything. It’s like hitting someone over the head with a sledgehammer then giving them an Elastoplast and saying, “Look, we care!”
Never forget that it was Labour who introduced the UDA-based 2006 dental contract in the first place. Until the UDA is exterminated, nothing will be fixed. Calling the proposals ‘the most significant modernisation of the NHS dental contract
in years’ is absolute garbage. In April, it will have been 20 years since the NHS dental system was broken by Labour. The fee-peritem system wasn’t perfect – like the current system, it was underfunded – but it didn’t operate under some nebulous, abstract concept of units of dental activity. Has anyone ever explained to your satisfaction what a unit of dental activity is, exactly?
And before I get accused of being a Tory, as former trade unionist - the NUJ to be specific - my affinity was, for many years, for Labour, so it tears me apart to see Neil Kinnock’s son say things like, “We inherited a broken NHS dental system.” Yes, YOU LOT BROKE IT! Who says irony is dead?
So, is there an out for NHS dentists? Is there even a chink of light heralding in the foreseeable despatch of UDAs?
Shawn Charlwood, Chair of the BDA’s General Dental Practice Committee, described the package as ‘modest, marginal changes’ that won’t fix the ‘rotten foundations’ of the system, and cautioned that if government treats these tweaks as the end point, it could spell the ‘death of NHS dentistry.’
So, is it the end? I would have thought that Labour would have been driven to sort out the debacle by the SHAME of having caused the problem in the first place – but maybe the general press hasn’t stressed loudly and often enough, the original cause of the decline of the public dental health service – not that the Conservatives or the Con-Lib alliance did anything in nearly two decades to help stop the rot.
Roughly 24,000 dentists delivered some NHS activity in 2025/25 but with the numbers of practitioners reportedly taking early retirement, could this lead to
a significant decline? Anecdotally, I’m told, older practitioners were more protective of their NHS patients and contracts than their younger colleagues, so, theoretically, there will be fewer benevolent health service dentists to serve health service patients. In other words, the way to get out of a poorly recompensed health service dental contract seems to be to retire early. Bit like a gaolbreak really. n
A month or so after I was arrested, I joined another newspaper in a city still served by the same Constabulary. One day, two plain-clothed detectives appeared on my doorstep wanting to interview me. The editor of the rival weekly paper complained about the Inspector who made the arrests and the Independent Police Complaints Commission had been informed. I told them that I completely empathised with the officer who arrested us. I heard nothing more. Over the past few years, I have become friendly with a croquet buddy who is a former Detective Chief Superintendent. He happened to be a colleague of the officer who ordered my arrest. I told him of the incident and he told me that his colleague thrived, reaching the rank of Chief Superintendent. Mercifully, HE didn’t feel he had to retire early.
About the author
ollie Jupes is the pseudonym of a former nHs dentist. He monitors dentistry on twitter X as @DentistGoneBadd














































State-of-the-art restorations with our intelligent composite system: maximum control, impressive aesthetics and seamless processing.

























































































Excellent polishability & handling multiple awards from Dental Advisor



Individual possibilities of application thanks to a wide range of viscosities
High resilience due to optimally matched spherical fillers





Deep & fast curing through controlled refractive indices & RAP-Technology






































































































































Raj Rattan, Dental Director at Dental Protection, examines the influences that shape contemporary dentistry and offers a renewed sense of perspective
As we move into 2026, it is worth considering not only how dentistry is changing, but how those changes shape the way we see our work, our responsibilities, and ourselves. Some influences are obvious; others are quieter, like shadows, imperceptibly shaping how we view the world.
To explore this, it is helpful to revisit an old idea. More than 2,000 years ago, Plato illustrated how easily appearances can be mistaken for reality. In The Republic, he described prisoners chained in a cave, able to see only shadows cast on a wall by objects passing in front of a fire behind them. Having known nothing else, the prisoners believed the shadows were real. Plato’s insight was simple but enduring: our understanding is shaped – and limited – by the conditions in which we work.
Over time, entire generations of dentists have practised knowing only the present. For example, for many the shadow cast by the 2006 GDS contract is the only professional reality they have known. We are all influenced by the shadows of regulation, targets, payment systems, commercial pressures, corporate interests, technology, and digital platforms. These shadows influence what is measured, what is rewarded, and – from a dentolegal
perspective – what is feared. As the saying goes, you get what you measure for.
These are not predictions, but five features of the 2026 landscape:
1. social media
A typology of social media use among dentists has been described, including avoiders, secondary and occasional users, observers, seekers, active but cautious users, limited users, engaged users, and deleters1. Despite these differences, there is broad agreement that social media increasingly shapes how dentistry is perceived and judged. These platforms reward visibility, confidence, and certainty, often at the expense of clinical nuance or long-term outcomes. What gains attention is usually what looks good and is easy to share, creating shadows that can obscure the complexity of ethical clinical decision-making.
It is important to recognise that social media can also be a force for good. Used thoughtfully, it can support education, professional connection, patient engagement, and the sharing of good practice. The challenge lies not in its existence, but in how easily its shadows can go unnoticed.
Social media has also created a powerful arena for professional comparison, where clinicians measure their skills, careers, and even lifestyles against carefully curated portrayals of others’ success. Streams of flawless cases and ‘Instagram smiles’ cast shadows over everyday dentistry, editing out the ordinary uncertainties and incremental progress that characterise real clinical practice. Over time, this can contribute to stress, low mood, and burnout, driven by a persistent sense of never quite measuring up despite demonstrable competence.
The GDS contract has cast a 20-year shadow that is difficult to shake off – a constant presence shaping how dentists work and how patients experience care. For many dentists who have practised since 2006, these shadows have come to define the new normal.
Recent changes to the NHS dental contract are welcome and may soften some of these shadows. However, they remain cast by familiar objects: limited funding, activitybased targets, and ongoing access pressures. Without more fundamental reform, the risk is that the shadow becomes the cave wall – no longer recognised as a limitation but accepted as the boundary of what is possible.
Artificial intelligence and automated tools are the new puppeteers. Their outputs will increasingly influence diagnosis, treatment planning, record-keeping, and clinical risk assessment. These systems can highlight patterns in large datasets, but they may also embed bias or oversimplification.
Verification therefore remains critical. Conventional clinical methods – including examination, radiographic interpretation, patient history, and relevant investigations – must underpin the use of AI-generated outputs. Clinicians should adopt a process of triangulation, assessing whether algorithmic recommendations corroborate or conflict with clinical findings and the patient’s presenting concerns. This approach helps guard against
automation bias – the tendency to over-rely on algorithmic outputs simply because they appear authoritative.
4. Commoditisation and commercialism
Dentistry must operate as a business, and commercial pressures are inevitable. As Holden observes, “the rise and persistence of a commercial model of healthcare and the potential shift towards the commodification of dental services, provided to consumers, should provoke thought about the nature and purpose of dentistry and whether this paradigm is cause for concern.”2
The ethical risk lies not in commercialism, but in commodification. When care is reduced to products and patients to consumers, vulnerable individuals may be steered towards profitable interventions while more conservative, preventive options are overlooked. As I have previously argued, minimal intervention dentistry rarely looks impressive on a spreadsheet, but it often delivers the greatest benefit for patients over time.
5. A global currency
Ultimately, trust is the universal currency of dentistry – a value that transcends borders and requires no conversion. There is no border control when it comes to trust; it is recognised instantly and understood everywhere. The relationship between clinician and patient is built on this foundation.
Rather than relying on caveat emptor – “let the buyer beware” – dentistry should look beyond the shadows and aspire to caveat fides: let trust be safeguarded. That is what every patient deserves and has a right to expect. n
References available on request
About the author Raj Rattan, Dental Director at Dental protection.
This March, A-dec is set to showcase why it’s a global leader in dental manufacturing at the BDIA Dental Showcase. We invite attendees to visit Stand C10 to explore A-dec’s award-winning range of dental chair packages, delivery systems, LED lights, and dental stools. Plus, we’re excited to showcase a new solution aimed at enhancing everyday practice, safety and compliance. With three complete dental chair packages: the premium A-dec 500 Pro Chair Package, the versatile A-dec 400 Pro Chair Package, and the entry-level A-dec 300 Core to learn about and discuss with A-dec’s team of expert Territory Managers, it’s well worth taking time out of the day to drop by and see A-dec. three chair packages. one standard of excellence. Discover the perfect blend of quality and innovation with our three chair packages, each representing a standard of excellence.
At the heart of our offerings is the flagship A-dec 500 Pro Dental Package, which features the A-dec 500 Dental Chair paired with the cutting-edge 500 Pro Delivery System. This package is thoughtfully designed to fit seamlessly into your practice, promoting smarter workflows that enhance both dentist comfort and patient care.
What sets the 500 Pro apart is A-dec+ updatable software platform. Instead of needing constant hardware upgrades, A-dec+ enables practices to have ongoing software updates that introduce new features and boost performance. This forward-thinking equipment keeps your practice modern, connected, and future ready.
For those who value a mix of performance, ergonomics, and flexibility, the A-dec 400 Pro Chair Package is a great choice.
It combines the sleek A-dec 400 chair with the advanced A-dec 300 Pro Delivery System. The user-friendly interface makes daily tasks a breeze with customisable settings, intuitive instrument control, and multi-user capabilities. Thanks to A-dec+, the 400 Pro system also allows practices to keep an eye on equipment status, receive alerts, manage updates, and oversee one or multiple locations effortlessly.
Rounding up our lineup is the A-dec 300 Core, a reliable entry-level solution crafted to meet the high standards A-dec is known for. It’s the perfect option for new practices or those looking for dependable performance without any compromises. innovation beyond the chair
Alongside A-dec’s dental chair packages, the A-dec team are excited to showcase a range of delivery systems, LED dental lights, and ergonomic dental stools. This gives visitors a chance to see firsthand how a fully integrated practice can improve posture, visibility, and overall workflow efficiency.
Also featured will be A-dec’s NEW Dental Unit Waterline (DUWL) solution, created to provide best practices in waterline maintenance and compliance. With infection control being a top priority for dental practices, this solution provides a straightforward and effective way to ensure water quality and peace of mind.
Every innovation showcased reflects A-dec’s excellent manufacturing expertise, backed by an industry leading 10-year warranty and anticipated equipment lifespan of up to 20 years. Rather than resting on its laurels, A-dec is committed to evolving its products throughout that lifespan, delivering greater value to dentists over time. This long-term vision is at the heart of what A-dec calls “The A-dec Way”: a


dedication to quality, reliability, and continuous improvement that has defined the brand for over 60 years.
Live demonstration: Learn, engage, experience
On Saturday, March 14th, visitors can join a live 60-minute taster session at the A-dec stand, led by Dr Jane Lelean and Nikki Laidi, focusing on:
» The benefits of 4-handed dentistry
» Seamless instrument exchange
» Reducing physical strain
» Sharpening focus and enhancing workflow
This session provides practical insights into how thoughtful equipment design can impact dentist wellbeing and efficiency.
Beyond BDiA
For those who can’t make it to the event, simply schedule a visit to one of three A-dec’s showrooms in Bracknell, Warrington, or Nuneaton to explore the full range of solutions available for your specific needs. Go to a-dec.com/find-a-dealer for more details or to book a showroom appointment. n




New data reveals that tooth decay among adults in England has hit a low point not seen since the late 1990s. polly Bhambra explains why this is a systemic failure – and how we can fix it
If you are currently working in a dental surgery, the headlines that emerged at the end of last year likely didn’t come as a shock. They might have left you feeling disheartened, exasperated or simply nodding in tired agreement – but surprised? Certainly not.
A significant national study involving researchers from UCL has uncovered that 41% of adults in England are now living with visible tooth decay. This is a staggering climb from the 28% reported in 2009.
Essentially, we have wiped out nearly 20 years of clinical progress in oral health, sliding back to statistics last recorded in the late 90s.
While the general public and the media label this a “dental crisis,” those of us on the front lines – donning our scrubs and greeting patients (or having to turn them away) – understand the deeper reality. This isn’t merely a “tooth” problem, and it isn’t contained within dentistry.
These figures represent the painful, visible peak of a much larger iceberg, a neglected workforce and a chronic refusal to acknowledge that the mouth is an integral part of the human body.
the high cost of “cheap” dentistry
For a decade and a half, we have been told that the NHS dental budget is “ring-fenced.” When inflation is factored in, it has been decimated. We have been shackled to a contract that rewards volume over health outcomes, and we have watched as our workforce has been pushed to breaking point. The fallout is clear: a “prevention-free” void for millions of people.
When you slash investment in NHS dentistry, you don’t save a penny; you simply relocate the debt. You shift the cost from a routine £28.50 examination to a £500 emergency A&E visit. You trade a simple filling for a complex surgical extraction under general anaesthesia. We must remember that this cost the NHS £74.8 million for paediatric cases alone in 2024. However, the financial impact extends far beyond hospital wards.
Poor oral health is a thief of time and money. It drains national productivity, costing the UK economy more than £105 million annually in dentalrelated sick leave. It also clogs up GP surgeries, where family doctors are seeing thousands of patients for dental agony they are neither trained nor equipped to manage.
the mouth is not an island
The most galling aspect of the UCL report for me was the confirmation
that we continue to treat the mouth as if it were a separate entity from the rest of the body.
Dr Anja Heilmann from UCL was spot on when she noted that, “oral and general health belong together.”
We need to stop mentioning this in passing and start championing it.
We are fully aware that periodontal disease has a bi-directional relationship with diabetes. We know the documented links to heart disease, kidney issues and even dementia.
When we permit 41% of the population to live with active decay and rampant gum disease, we aren’t just failing their teeth; we are compromising their hearts, their metabolic health and their overall lifespan.
Imagine the impact of truly integrated care. Imagine if every diabetic patient’s annual check-up required a periodontal assessment. Evidence suggests this could save the NHS over £120 million by simply improving blood sugar control through better gum health. But to achieve that, you need a functioning workforce. And that brings us to the elephant in the room.
We must stop treating the symptoms and start treating the system.
the austerity legacy
A health crisis cannot be solved with a fractured workforce. The rise of “dental deserts” and the surge in decay isn’t solely down to sugar consumption. It is happening because, in many areas, there is simply no one left to provide the care.
For over 10 years, pay for dental professionals has remained stagnant. We have seen dental nurses – the very heart of patient safety and clinical support – earning barely more than minimum wage in many areas. We have seen NHS dentists endure a realterms pay drop of nearly 40%.
Is it any wonder people are walking away? When you undervalue the individuals providing the care, you inevitably devalue the care itself. We are now witnessing the true cost of “efficiency savings” that were, in fact, incredibly inefficient.
the solution is in your surgery So, is the situation hopeless? I refuse to accept that, but I do believe we need a fundamental shift in who provides care. If the crisis is one of preventable disease, the answer lies with our prevention specialists.

The UCL data shows that decay is most prevalent in our most deprived communities –the very places where finding a dentist is hardest. But do you really need a dentist to show a new parent how to navigate sugar in a toddler’s diet? Do you need a dentist to take a digital scan or apply fluoride?
No. The untapped capability of our dental nurses is the “secret weapon” we are currently wasting.
We have a dedicated workforce of registered professionals who are ready to do more. If I were sitting in the Health Secretary’s office, I wouldn’t just be tweaking the contract; I would be overhauling the skill mix:
• e mpower dental nurses: we need fully funded, dental nurseled clinics in the heart of our communities. We should be paying dental nurses properly to lead initiatives in schools and care homes, providing fluoride, education, and triage
• Make prevention pay: the 2026 contract reforms promise to remunerate preventative work. We must hold the government’s feet to the fire on this. If a practice can thrive by running a “zero-cavity” programme led by dental therapists and nurses, we will change the trajectory of the nation’s health
• i ntegrate teams: we need to bridge the gap between dental and GP surgeries. A diagnosis of Type 2 diabetes should trigger an automatic, funded referral to a dental hygienist
treat the system
The UCL findings are a source of shame for a Western nation in 2026.
A decay rate of 41% is a statistic that belongs in the Victorian era, not the present day. But let’s turn that shame into momentum.
This report is proof that the old “drill and fill” philosophy has failed. It proves that austerity was a false economy. Most importantly, it proves that ignoring the mouth-body connection is an ethical failure. to my fellow practice owners: look at your team. Are you utilising them fully? Are you enabling your nurses to be the clinicians and educators they are trained to be?
to the policy makers: stop viewing dentistry as an optional extra. It is the primary gateway to systemic wellbeing.
to the taxpayers: you are already paying for this failure through overstretched A&E departments, GP shortages and lost productivity. Wouldn’t you rather invest that money in a dental nurse helping a child stay healthy?
We can fix this. But we must stop treating the symptoms and start treating the system. n

About the author polly Bhambra, is practice owner at treetops Dental surgery, a dental nurse and passionate advocate for team culture and mental health in dentistry. she writes regularly on leadership, the elevation of nursing, and the future of holistic dental care.
Assessing dental patients’ capacity to consent is a vital part of the treatment process. sarah ide, dento-legal adviser at the Dental Defence Union (DDU), discusses what you need to know and how to assess mental capacity
Aperson may not have mental capacity for many reasons, for example a serious brain injury, an illness such as advanced dementia, or severe learning difficulties.
Mental capacity can also fluctuate. This might often be seen in dementia and some mental health conditions. A person can also recover mental capacity – for instance, following a severe stroke.
Mental capacity legislation across the UK
In England and Wales, the Mental Capacity Act 2005 (MCA) provides a legal framework, for people 16 years and over who lack capacity. The Act is supplemented by a detailed Code of Practice, with which dental professionals are expected to comply.
In Northern Ireland, the relevant legislation is the Mental Capacity Act (Northern Ireland) 2016.
Meanwhile, in Scotland, the relevant legislation is the Adults with Incapacity (Scotland) Act 2000. Under this Act, a suitably trained health professional will make an assessment of a patient’s capacity to consent to treatment. If the patient is deemed unable to consent, the health professional will complete a ‘section 47’ certificate to allow them to provide treatment.
As 16 is the legal age for capacity in Scotland, a 16 or 17-year old without capacity to consent is treated as an adult without capacity.

Assumption of capacity
There are a number of assumptions dental professionals should make when assessing the mental capacity of patients. Firstly, you should assume all adult patients have the capacity to consent to treatment, unless you determine they lack that capacity. If you decide an adult lacks capacity to consent, you should then decide if it’s in their best interests to proceed with treatment.
The fact that a person has a mental health condition or learning difficulties is not, on its own, grounds for deciding that this person does not have capacity. Nor should you assume that the patient lacks capacity by making judgments about their behaviour or appearance. If a patient appears to make an unwise or irrational decision, this is not sufficient reason to treat them as lacking capacity. If you do decide a patient lacks capacity to consent, you should be able to justify your decision.
You should take all steps practicable to help patients make decisions about their treatment before concluding they lack capacity.
When you are assessing a patient’s ability to make a decision, the patient must be able to do the following:
• Understand the information relevant to the decision. This includes information about the reasonably foreseeable consequences of deciding one way or another, or failing to make a decision
• Retain that information
• Use or weigh up that information as part of the process of making the decision
• Communicate their decision. This may be through talking, using sign language or other means of communication
A patient’s capacity may vary depending on the complexity of the decision to be made. It may also fluctuate with time.
If an adult patient lacks capacity and you are faced with providing treatment without consent, you should consider the views of relatives, carers and the patient’s previously expressed wishes in helping to determine if the treatment is in their best interests. When assessing if treatment is in the patient’s best interests, you should consider whether the patient may regain capacity later. With this in mind, if a patient has
fluctuating capacity, it would be unusual for routine dental treatment to be appropriate while the patient lacks capacity, when it could be left until the patient regains capacity and can consent.
Firstly, make sure the patient has all the information they need to make a decision about treatment.
Next, present the information in a way that is easy for the patient to understand. For example, by using simple language or visual aids. Additionally, record in the clinical notes the processes you went through in determining capacity.
Finally, if the patient lacks capacity, record in the notes the basis on which a decision to treat, or not treat, was in the patient’s best interests, and the steps you took to establish that.
To attend the DDU’s upcoming webinar on assessing capacity or to watch content on demand visit theddu.com/learn-and-develop/webinars n
About the author sarah ide, Dento-legal Adviser at the Dental Defence Union (DDU).


For so many dental practices across the UK, the issue of sustaining great quality care within the standard NHS framework is becoming increasingly challenging. Alongside the notoriously mounting waitlists is the struggle of patient retention and funding pressures, which are continuously shaping the reality of daily practice. As such, more and more practices are considering a shift towards more private care.
Of course, incorporating private care assumes a great change in costs for patients, though this is not the only concern that some patients will have. For example, many might be worried about continuity of care. With clear practice-topatient communication, the move from NHS to private care can be implemented most successfully.

The NHS is a familiar framework for many patients, representing both consistency and security. In contrast, private care has historically held the stigma of luxury, exclusivity, and something that many believe they simply couldn’t afford. With these ideals deeply ingrained among some patient groups, confusion and anxiety are hence felt when practices initiate the idea of transitioning away from NHS services. For many individuals, they want to know what the change would actually mean for them. Will they be able to see the same dentist? Will appointments be affected in the future? For families that have been associated with the same dentist for generations – with an emotional and familiar connection having developed over that time – they could rightfully expect to be kept in the loop to encourage their ongoing loyalty to the practice.
communication goes a long way
Clear communication helps to overcome these barriers, supporting patients whilst your practice focuses on the logistics. Honest, sensitive conversations before and during the transition stage can make a huge difference, helping patients understand what the change means for them in terms of increased accessibility and treatment choice. Furthermore, a huge emphasis on internal alignment is vital: the entire dental team must both deliver the same message to patients with the same level of confidence. Everyone – from the administrative and management teams to dental nurses and clinicians – should talk to patients about upcoming changes in a consistent way in order to reduce anxieties and maintain trust among patients.
accessible private care
One of the messages that will need to be communicated clearly is that of cost. Affordability maintains a great concern for many individuals, as has been seen with NHS fee increases in recent years. Due to this, the financial options offered to patients while transitioning to private services are integral to their comfort and retention. Introducing a patient plan, for example, provides the option of monthly payments that can cover an array of dental appointments like check-ups, dental hygiene visits, and preventive care. As such, they allow patients to budget for their essential dental care in a more predictable and manageable way.
The format will be familiar to many patients who use payment plans in various other areas of their lives. The reassurance of smaller but more frequent payments encourages regular attendance to the practice – which is invaluable for high-quality preventive patient care. For the practice, dental plans offer the added advantage of maintaining a steady monthly income, supporting cash flow while minimising the time and effort spent on chasing debts.
If you’re looking to introduce a new dental plan – or to switch your current offering to one that is better tailored to your patients – be sure to work with a provider you can trust.
IndepenDent Care Plans (ICP) has three decades of experience in understanding the unique challenges of transitioning from NHS to private practice. The team supports businesses with a tailored approach, aligning solutions with the identity, values, and goals of each individual practice. Making the process as seamless as possible, ICP provides the practical tools needed through bespoke dental plans and expert guidance from dedicated Business Development Consultants – including marketing and communication material, ongoing team training, and administrative support. ICP assists practices in building and maintaining trust and stability, allowing change to feel like a united progress rather than another challenge for patients to overcome.
Moving forward with confidence
Transitioning from NHS dentistry to private services involves many complexities –for both the practice and its patients. However, when handled carefully, with full team involvement, and clear patient communication, it can be used to elevate the patient experience and reinforce patientpractice relationships. This inevitably leads to improved patient retention and a more sustainable future for your practice. For more information and to book a no-obligation consultation, please visit ident/co.uk or call 01463 222 999 n
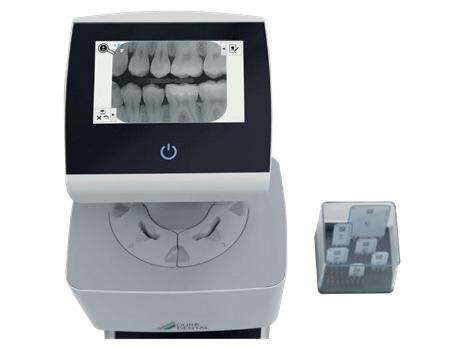
In order for practices to improve and expand on the services they provide, investing in and utilising new equipment is important. Dental professionals have a commitment to provide excellent standards of care to their patients. As such, patients must trust clinicians to maintain their oral health and therefore overall wellbeing – with the expectation of safe, effective, and long-term care. However, the ability for professionals to provide these exacting standards of care can come under pressure when balancing costs and benefits. This is because, providing top-quality care can be costly – due to the use of high-quality materials, innovative technology, and advanced skills – both for patients and practitioners.
As such, it is important that practices make smart investments in their equipment to help ensure excellent standards are maintained, whilst also being cost-effective. In-practice milling, for example, is a fantastic option for practices who are looking to expand their services, enhance their patients’ experiences, and improve efficiencies – ultimately ensuring money is saved for both their business and their patients in the long-term.
Chairside milling offers a number of benefits, reducing chair times and practice visits, and eliminating the need for cord packing, impression material, and temporary crowns in many cases. By removing the need for return visits within a single course of treatment, tooth sensitivity commonly experienced between appointments is reduced and no additional anaesthetic is required.

The chairside milling process is very efficient, incorporating the following steps:
1. The clinician uses an intraoral scanner to capture digital impressions of a patient’s mouth – removing the need for conventional impressions.
2. The digital impressions are then used to design the restoration using CAD/CAM software – often in just a few clicks. Modern solutions may utilise artificial intelligence (AI) to produce a first proposal, which can then be adjusted by the clinician if needed.
3. Finally, the restorative design is sent to the chairside milling unit, and the restoration is manufactured from a material block. This step may vary depending on the material used.
about the author
Dr robert Donald, indepenDent care plans Director.

As in any other business type, time is money in the dental practice. This means that the time it takes to produce a restoration using a chairside milling machine should be taken into account. A typical chairside milling workflow can take between 88 and 120 minutes. Milled restorations are precise and consistent, whilst eliminating the delays and potential for errors which are associated with traditional lab fabrication. With CAD/ CAM blocks available in multiple materials, chairside milling enables clinicians and patients to select the best option for them, whilst ensuring a durable final restoration. Fabrication processes should be decided on a case-by-case basis to ensure the most appropriate solution is provided for every patient, meaning that lab production may still be required in some situations. Because the initial investment in CAD/ CAM solutions can be significant, it is important to seek advice from those who can best support your practice and make appropriate recommendations for you. Practices should also consider the need for ongoing maintenance and support to ensure the longevity and effectiveness of the equipment. Whilst initial investments can be costly, chairside milling machines can soon pay themselves off, by saving in other areas such as laboratory fees and consumables.
Having worked with dental professionals for over 50 years, the experienced team at Clark Dental is best placed to support your practice in its mission to achieve excellence. Clark Dental’s high-quality portfolio of dental equipment includes the CEREC® range of chairside milling solutions: CEREC® Go, the cost-effective entry to single-visit dentistry; CEREC Primemill® Lite, which makes excellence easy; and CEREC Primemill®, which facilitates premium milling in your practice. Clark Dental is able to support you in your decision making, to ensure you can make the best investment for your unique practice, and its equipment maintenance service will keep your new equipment working long-term.
Offering single-visit dentistry by utilising high-quality dental equipment enables practices to maintain and even elevate the quality of the care they provide, whilst also minimising the time taken to achieve these results and reduce costs for themselves and their patients. In turn, this means more efficient workflows, and enhanced patient experiences. For more information call Clark Dental on 01268 733 146, email info@clarkdental.co.uk or visit www.clarkdental.co.uk n

Chairside milling offers several advantages for dental practices, one of the most significant being the speed and convenience it provides. The ability to deliver same-day dentistry significantly reduces the treatment time, therefore improving workflows for dental professionals and experience for patients.
about the author Stuart clark, Managing Director at clark Dental equipment Systems.

The modern dental practice requires constant investment to remain abreast of the latest equipment on the market. This is crucial not only for the delivery of exceptional clinical treatment and patient care, but it is also a foundation of job satisfaction among staff, which aids retention. For any principals, associates, managers or team members keen to introduce new technology, it is important to ensure the viability of the investment. This can be achieved by creating a business case for the equipment in question.
Step 1 – The why
To put an effective proposal forward, it is crucial to first outline the need for change and the potential advantages afforded by the investment. Why is this a good idea and how would this new equipment benefit the practice, the team or the patients – or all of the above? The objectives of introducing the product should be clearly defined, including a way to measure success so that it can be monitored over time. For example, if you’re looking to integrate a new CBCT machine, your business case should outline the positive impacts on patient care, treatment times, practice efficiency and productivity, and potential revenue streams.
Step 2 – Financial analysis
To determine the feasibility of any investment within the practice, thorough financial analysis is crucial. For new equipment, this should include justified
estimates for all expected outlays, from purchase price to ongoing maintenance plan costs. The approximate revenue generated should also be calculated, and this can be utilised to identify the breakeven figure. This is an important financial metric that demonstrates – in our example of a new CBCT scan – exactly how many scans would need to be performed, or how long the equipment would need to be in situ before it made back the money it cost. A calculation like this will help demonstrate when the equipment will start generating a profit, which is a powerful tool when assessing the viability of the investment.
Both in terms of finances and in relation to other aspects, it’s necessary to address all the potential risks or challenges of introducing the new equipment you are suggesting. The objective is not to highlight reasons to prevent moving forward, but to ensure you are prepared for every eventuality, increasing the chance of success.
Sticking to our example, some of the elements to review include possible difficulties in building an imaging referral network, the costs of marketing the new service, the risk of slow uptake, and the cost of unexpected equipment malfunctions or breakdowns. Each scenario should be ranked according to likelihood and impact on the business to show if and how concerning each possibility would be. Some market
research and communication with other practices may be useful in establishing these factors and their frequency.
With all this information, you’ll be equipped to develop a practical implementation plan that provides logical, step-by-step guidance for the introduction of your proposed new equipment. This plan should provide a timeframe for each step, as well as allocate responsibility for different actions to specific individuals to ensure accountability and progress. This plan will also need to address all the potential risks and challenges with detailed plans on how to prevent issues and how to manage them if they do occur.
Of course, as part of this business case, you will need to share market research on the solutions available, while also suggesting the most suitable for your practice with justification as to why. Returning to our aforementioned example, not all CBCT machines are made equal, and the exact model, brand and supplier you choose will each have a significant impact on your success.
For complete peace of mind, the expert team at Dental Directory can support such important business decisions with invaluable product insights and comparisons. They will help you explore the vast range of equipment on offer and select the most appropriate for you. You can also include

within your comprehensive business case the wide-reaching support and technical maintenance services available from Dental Directory that will allow your team to fully utilise the equipment while protecting and maximising your investment.
Continuous investment is important for the ongoing development of any dental practice, but the right investment is crucial for real success. By assessing your options carefully, analysing the potential benefits and risks, and being prepared for the practical implementation of new solutions, you will help make the right decisions for your business.
For more information on the products and maintenance services available from Dental Directory, please visit ddgroup.com or call 0800 585 586
About the author Dean Hallows, Managing Director, Dental Directory.




“ A big thank you to the Lily Head Dental Practice Sales team and especially to Tom Orchard. Tom has been very professional and a big help through the practice purchase. It was a tricky and unusual purchase but Tom’s reassurance and even-handedness during the journey was very helpful. We would highly recommend to my colleagues. ” Grace & Rosh, Farley House Dental Care





As we enter what can be an extremely busy time for many dental practices, it is important to start planning for the year ahead. Creating a 2026 budget is a massive part of this preparation, ensuring that you spend your money wisely for maximum return on investment. To achieve this, it is helpful to follow a few simple steps.
a PriMe approach
The purpose of a budget is to plan your finances for the specified time period. This might involve allocating available funds to specific operational tasks, staff salaries, marketing campaigns, equipment investments, new services or anything else you anticipate requiring. You will also then need to break the budget for each area down further, ensuring you know exactly where your money is going to ensure that it works as hard as possible. A concept often applied here to ensure effective budgeting is PRIME.
Planning – set or reflect on your business objectives and manage the budget accordingly.
Responsibility – communicate the plan to your team, clearly delegating tasks so everyone knows what they are responsible for.
Integration and coordination –the budget should align with daily operations throughout the practice, it’s a tool to keep individuals or teams within the business working together.
Motivation – the budget provides a benchmark to refer to throughout the year to ensure you are sticking to your plan and spending money in a controlled way.
Evaluation and control – once the budget is in place, it’s essential to monitor investment to ensure you remain on track.
a practical approach
A simple place to start when budgeting for the year to come is to review this year’s finances. You can expect most of your expenses to remain constant, perhaps allowing for a standard small year-on-year increase. Income can also be predicted based on the number of patients you anticipate retaining, the type of treatment you routinely offer and the predicted productivity of your team. Changes will need to implemented to outgoings and income that reflect any new equipment that you need to buy or new services you have introduced.
As a general rule of thumb, businesses will allocate 25% of revenue to staff expenses, 5% on marketing, and 5% on new equipment or other practice improvements and maintenance. Of course, the exact amounts will vary depending on your business goals, your current challenges, and recent successes. The most important thing is to analyse

your finances and create a 2026 budget – only then will you ensure that your profitability is maximised and appropriate business investment is maintained.
Looking ahead with confidence Ultimately, effective budgeting affords confidence that your business is doing well and that any investments you have been considering are feasible. For many practices, but especially larger or multi-site businesses, it can be hugely helpful to seek the support of an accountant or financial advisor to aid with budgeting for 2026. n
about the author Dr Michael Sultan, Specialist endodontist, endocare.

Every dental professional will know some of the challenges that could affect orthodontic care, dental implant placement, or root canal treatment. But each member of the team should be knowledgeable about the non-clinical waste challenges that are faced every day.
Dental waste management is a paramount aspect of daily workflows and patient safety, and clinicians should be able to confidently tackle any common problems that are encountered. In an age of climate awareness, this includes how to make the practice more environmentally friendly. Issues encountered by professionals include potential knowledge gaps, the need for infrastructural changes within the practice, and the recycling capability of the materials required in everyday care.
The growth of the dental industry, and the variety of treatments provided, has increased the volume of waste produced by the profession. With this, steps must be taken to ensure it is managed in a way that best protects patients, practitioners, and the world around us.
The first barrier to making any changes in the practice is the knowledge of the clinical team. Health Technical Memorandum 07-01 is the leading guidance for waste management in dental care, and professionals should have a thorough understanding of how it aids environmentally friendly workflows.
Throughout this guidance, clinicians are presented with ways to safely store waste based on the hazards presented. For example, it details the need for unique bins for amalgam waste. These should be sealable, made from a puncture-resistant material, and must contain mercury suppressants, alongside clearly defined dental amalgam labels. It is vital that dental professionals know this, and recognise where they can retrieve a container from,

how it should be handled once full, and how to arrange its safe removal from the site. If a clinician is unsure about how to store or segregate hazardous materials, such as amalgam-contaminated waste, there is a risk of harm to patients and the clinical team, as well as the potential for the waste to be diverted to the wrong management service.
The waste workflow is designed to be uniform across every practice, as well as other healthcare services, which ensures that professionals can easily integrate into a clinical setting and manage waste with little difficulty. However, this can only happen with appropriate levels of knowledge. Practices should consider the value of continuing professional development (CPD) around the topic for all team members, as well as reviewing in-house workflows to ensure waste is handled in line with any changes to guidance.
When thinking about waste management, recycling and reusing items is of course encouraged. It has become as important in disposal routines at home as it is
in professional settings. Unfortunately, due to the nature of dental care, it is difficult to reuse many items; the literature finds that the dental profession utilises a high volume of single-use plastics that ultimately become clinical waste, requiring landfill or incineration.
The sheer amount of such products used daily in dentistry creates a difficult challenge for professionals. A 2024 research project estimated that in the previous two years, in NHS dental appointments alone, singleuse plastics contributed the equivalent of 1.7 million tonnes of carbon dioxide to the waste workflow. To offset this carbon cost, the NHS would need to grow nearly 30 million seedlings for 10 years.
If a waste item presents a clinical hazard, it must be attributed to the correct waste stream, which can have non-environmentally friendly disposal workflows by default. Where possible, clinicians could strive for their items to go to Energy from Waste (EfW) facilities, though this is only possible for offensive and municipal waste in HTM 07-01. Investing in reusable solutions, such as specially-designed PPE, can be
effective, and helps to offset the volume of waste produced by the practice. These items may be suitable for disinfection or autoclaving, depending on the manufacturer’s instructions.
An often-forgotten part of the waste produced on a daily basis comes from the waste containers themselves. Whether using specially-designed amalgam containers, or generic clinical waste bins, each will need to be disposed of after use. To counteract the environmental impact, practices can choose solutions that are made from recycled materials, or could be recycled themselves – but these should only be chosen from a trusted supplier.
Initial Medical provides a wide array of environmentally friendly waste containers to dental practices, including Griff Pac containers. These are colour-coded in line with HTM 07-01, ensuring professionals instantly recognise their use, and are made from 70% corrugated recycled plastic. Griff Pac containers can safely store clinical, infectious, anatomical and offensive waste, meeting the demands of the colour code, suiting the needs of every dental practice. Being knowledgeable about the challenges facing dental professionals in the field of waste management is key –but recognising the potential solutions is even more important. Whether this means improving team knowledge, or changing the materials or waste containers used, the practice can be more environmentally friendly with some small changes.
To find out more, get in touch at 0808 304 7411 or visit www.initial.co.uk/medical n
about the author rebecca Waters, Head of Marketing at rentokil initial.


No dentist should face the turmoil of a claim against them alone. If it happens to you, our dentolegal experts will help keep you grounded.
Join the No.1 for protection and be ready for whatever life throws at you.
Osteoporosis is a systemic skeletal disorder categorised by low bone density and deterioration. It is one of the most prevalent diseases in older adults and particularly post-menopausal women. The disorder involves the systemic weakening of bone strength which leads to a heightened vulnerability to fractures; osteoporosis is often asymptomatic until a fracture occurs – making early intervention and detection imperative.
Fragility fractures affect almost one in three women and one in five men over the age of 50 – but the disorder impacts beyond systemic health, affecting oral health too. Ongoing research evidences the bidirectional link between osteoporosis and oral health, with reduced bone density impacting the jawbone and further affecting the surrounding periodontal tissues and tooth retention. It is therefore crucial as dental professionals to both understand and support patients experiencing the effects of this relationship through early identification and preventive strategies.
Characterised by the inflammation of the gingivae and the intensifying deterioration of the alveolar bone, periodontal disease is more prevalent in those with osteoporosis. Both diseases are inflammation-driven and associated with age-related bone diseases. Not only does this encourage weakened surrounding periodontal support, but can also compound periodontal conditions –creating an enfeebled oral environment. Contrarily, the reverse can occur, whereby periodontal disease impacts systemic inflammation – potentially affecting both osteoporosis and bone metabolism –demanding greater collective management.
Low bone density affects the strength and structure of the jawbone. The alveolar bone – which supports the teeth – uses the teeth’s movement to maintain its dynamic nature and volume. In turn, a reduced volume of the bone weakens the foundations – increasing the risk of tooth mobility and gingival recession.
Not only can the consequence of the disease be tooth loss, the weakened alveolar bone can also make prosthodontic treatments – such as implants or dentures – incredibly challenging. The frequent monitoring and early intervention of such is vital in maintaining oral health and function, as well as patient comfort long-term.
In osteoporotic women – particularly those who are post-menopausal – tooth loss may be caused by both local and systemic factors. The bidirectional relationship means periodontitis is an early indicator of osteoporosis – making it imperative for dental professionals to assist in recognising the signs, supporting through, and adapting treatment plans to the individual.
Medication & systemic considerations
The management of osteoporosis commonly involves bisphosphonates – often alendronate and risedronate –which essentially inhibit bone resorption. Reducing the rate of bone tissue breakdown, bisphosphonates maintain or increase bone density, which may assist in the prevention of tooth mobility and loss. The consistent monitoring of this treatment is necessary to manage the risk and side effects, which sometimes include osteonecrosis of the jaw (ONJ) and atypical femoral fractures in long-term use.
Other methods of medication include
hormone replacement therapy (HRT) –often oestrogen – to navigate hormonal deficiencies. Due to the importance of oestrogen in maintaining bone density, HRT is most commonly used in postmenopausal women to counteract the reduced secretion of oestrogen and counteract the bone loss caused by hormonal changes.
Patients receiving these forms of medications must be managed with a multidisciplinary approach to ensure that each element of their osteoporosis and oral health symptoms are supported properly.
Dental professionals can best assist their osteoporotic patients by recommending preventive strategies. These include the cessation of smoking, reduction of alcohol intake, increased supplements like vitamin D and calcium, and profound attention to oral care – beyond the average mechanical cleaning. Each of these changes contribute to maintaining both periodontal and bone health. Supporting great oral health involves the encouragement of a consistent and comprehensive routine. With gentle yet thorough cleaning, patients can assist with the preservation of the alveolar bone and the reduction of gingival inflammation. Older adults suffer from osteoporosis most commonly, they also often experience sensitivity and gingival recession and will require gentler cleaning techniques to target biofilm.
Alveolar bone loss most commonly begins in interdental spaces, meaning that dental professionals must recommend the best interdental cleaning methods to patients. Not only will this help minimise the reduction of bone loss, but it can prevent
Diet can define health. Consuming a consistent yet varied number of healthy foods and drinks is essential for growth and reducing the risk of many diseases. However, patients with temporomandibular joint disorder (TMD) may experience pain during mastication, causing difficulties in maintaining a balanced diet by limiting the foods that can be easily eaten. For patients with TMD, altered dietary habits can have two opposing yet notable effects. First, not being able to eat preferred foods can have a negative impact on the patient’s quality of life. However, eating certain foods can also be supportive of TMD, reducing the risk of developing associated chronic conditions and even easing the pain. Because of this, it is useful for dental practitioners to understand and encourage the nutritional strategies that can most help patients with TMD.
live, diet, repeat As the temporomandibular joint (TMJ) is an essential component for mastication, it is inevitable that those experiencing jaw pain when eating will opt for softer foods. A study found that 77.6% of patients with TMD modified their diet; 71.8% cut their food into smaller pieces, 42.4% boiled their foods until soft, and 40% mashed more of their meals. The leading three modifications each led to a reduced enjoyment of eating.
For patients who are reporting jaw pain, dental practitioners can recommend a range of dietary alternatives for a more comfortable eating experience. Hard cheeses, breads with seeds, fresh fruits with skins, sweets and fried meats are not advisable due to how much the jaw must move to consume them. Instead, smooth yoghurts, soft cheeses, soft breads without seeds, pancakes, pasta, gnocchi, rice, canned fruits, smoothies, cooked vegetables and cream-based soups are far more agreeable for the TMJ. However, whilst advising a soft (or softer) diet is useful for the short-term alleviation of TMJ pain, it may contradict the long-term success if a poor nutritional state is exacerbated.
accounting for the whole
One of the main challenges concerning the relationship between diet and TMD is the holistic impact. Whereas a change in diet may help alleviate symptoms, the same change has the possibility of effecting other parts of the body. Deficiencies in certain minerals, vitamins and more can increase the risk of disease or other health conditions elsewhere in the body. For instance, Vitamin D deficiency is implicated in the development of musculoskeletal disorders. This can complicate TMD recovery as interdisciplinary approaches that accommodate mind-body therapies (such as massages), rehabilitation exercises and diet can better manage chronic pain.
the development of other oral diseases too.

A highly effective choice is the TANDEX FLEXI interdental brushes. Specially designed to deliver an efficient and gentle cleaning aid for between teeth and along the gingival margin, the brushes come in 11 different sizes to suit each patient’s specific interdental spaces. Furthermore, the ergonomic, flexible grip makes it easy to reach interdental spaces throughout the entire mouth – even the hardest-to-reach areas at the back. Paired with the TANDEX PREVENT Gel, the brushes create the perfect preventative oral routine –non-abrasively protecting oral health with 900 ppm of fluoride to help keep caries at bay.
Working towards the best outcome
As research continues to evidence, the intersection between osteoporosis and oral health is something that patients require support with. By recognising oral manifestations, such as bone loss and tooth mobility, and recommending the best preventative strategies and tools, patients have the best chance of successful management. For more information on Tandex’s range of products, visit https://tandex.dk/ For product samples and orders, please contact DHB Oral Healthcare https://dhb.co.uk/ n
about the author
Jacob Watwood, rodericks Dental Partners associate Dentist, on behalf of tandex.

There is a limited body of evidence on nutritional approaches to chronic pain experienced by patients with TMD. However, Western diets can lead to poor dietary choices due to the volume of processed foods and high levels of salt, sugar and unhealthy fats – this can lead to various health conditions associated with TMD. This includes rheumatoid arthritis (RA), a condition that can affect the TMJ. The prevalence of TMJ involvement among patients with RA is reported as 19-86%, emphasising the correlation.
Four diets stand-out for their efficacy in reducing chronic pain from RA, headaches, musculoskeletal pain and more TMDassociated conditions: Mediterranean, vegetarian, vegan, and high protein diets. All rich in antioxidants, they can reduce proinflammatory cytokines and manage TMJ inflammation. Whilst some patients may be unwilling to switch their diets so radically, encouraging the consumption of foods with omega-3 fatty acids is a more appealing alternative. Omega-3 fatty acids alleviate chronic pain and other symptoms and are most commonly found in fish and oils – consuming them should not require too much mastication either.
empowered
Nutritional strategies for TMD can have many long-term health benefits, providing
consistent adherence and a balanced diet. An extra benefit is that it is a patientcentered approach that empowers them to take control; what a patient chooses to eat can be a vital part of TMD rehabilitation. Along with dietary changes, patients can restore strength and function to the TMJ with the OraStretch Press Rehab System from Total TMJ. A user-operated device, it is simple to use yet shows notable improvements within a week. By inserting the mouthpiece and squeezing the handles, patients mobilise the TMJ and stretch the orofacial tissues. Diligent exercises, as recommended by a healthcare professional, ultimately lead to a stronger jaw, improving mastication, speech and reducing pain for a better quality of life. Changing diets can have a tremendous impact on our health. For patients with TMD, being unable to eat certain foods should not be the be all or end all – by modifying their food they can not only enjoy eating again, but can also reap the many health benefits and reduce the symptoms of TMD. For more details about Total TMJ and the products available, please email info@totaltmj.co.uk n
about the author Karen harnott, total tMJ operations Director.







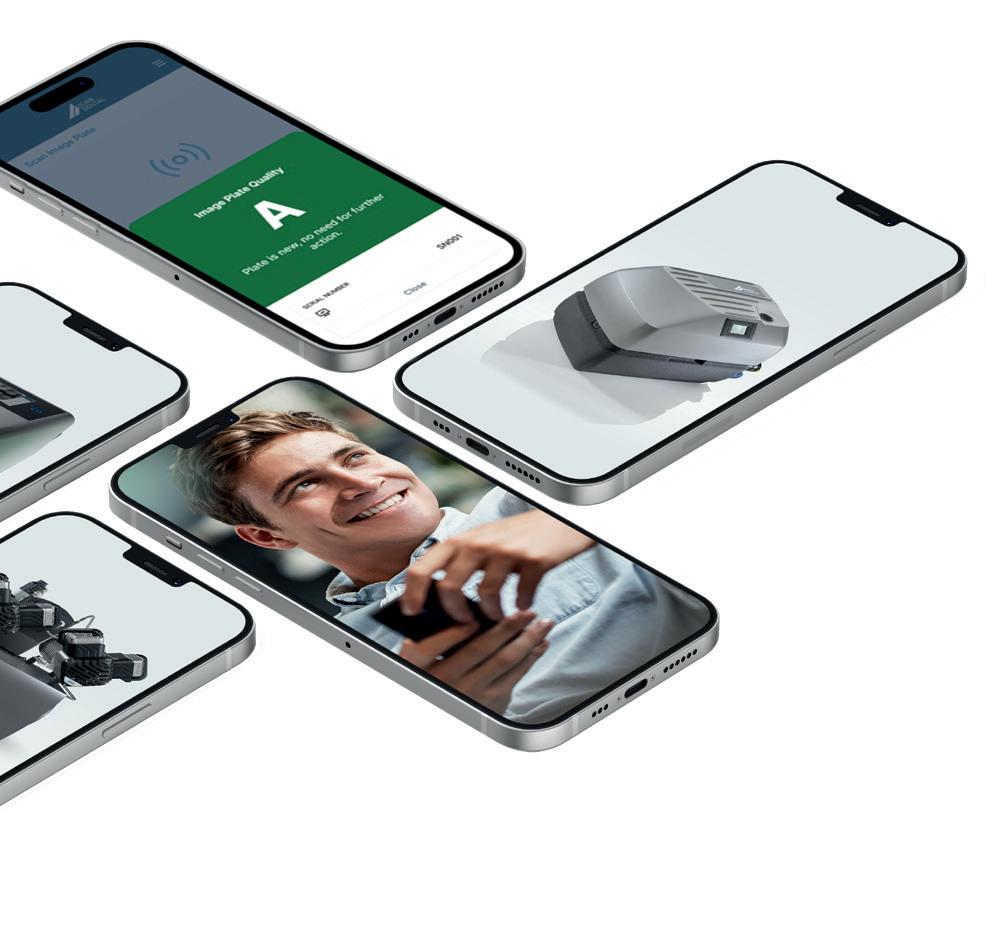
New functionality within Dürr Dental’s VistaSoft Monitor app allows users to effortlessly check a plate’s quality by simply holding a mobile phone over the plate. The app provides a clear rating – from ‘A’ for excellent condition, to ‘E’ when it’s time for a replacement, making it easy to maintain optimal imaging performance. Even those using 3rd party imaging software, instead of VistaSoft, can check the quality of their plates. Great images allow for accurate diagnostics.
For more information visit www.duerrdental.com/en/GB/products/software/ networking-for-dental-practices/vistasoft-monitor/

For consistently sharp images, you need high-quality image plates @durr_dental_uk Duerr Dental UK



Pain throughout the gingival tissue is a common symptom of periodontal disease, often accompanied by bleeding during eating or oral hygiene routines, and as well as inflammation. This discomfort can significantly impact daily life, with patients changing dietary choices or avoiding thorough interdental cleaning due to the soreness it induces.
The latter element can be particularly concerning. Pain throughout the periodontal tissue can be brought on by additional factors such as heavily abrasive brushing – a problem faced by even the most wellintentioned patient. However, avoidance of these effective oral hygiene practices can give way to an increased risk of infection and oral disease, exacerbating the very causes of gingival pain.
Clinicians should be prepared to recognise the causes of gingival sensitivity in any presenting patients. It’s also important to understand how it affects their day-today life, and professionals should be able to recommend immediate implementable changes that can improve periodontal health over time.
Behind the pain
Traditional oral hygiene routines can cause trauma to the soft tissue, creating gingival abrasions that can cause pain and encourage recession of the tissue. The literature reports that a medium-hard toothbrush is twice as likely to cause tissue damage as a soft toothbrush. In the same vein, a medium toothbrush can remove more damaging biofilm than soft toothbrushes. To minimise harm whilst maximising the ability to remove plaque and biofilm, patients need to use adopt a more careful technique; gentle, circular brushing that focuses on each tooth surface, and takes care around the

gingival margin is key. Proper interdental cleaning should support this, with a variety of solutions available, such as traditional floss or oral irrigators.
Infections linked to periodontal pain are manifold. The most prominent link is periodontal disease; almost a fifth (19%) of adults in the UK have been told they have gum disease. Gingivitis will typically present with inflammation and bleeding upon brushing or flossing, as well as dull pain, but progression to periodontitis may create a tender feeling simply upon being touched, which can be troubling for many patients. As oral hygiene routines improve, and plaque and bacteria is kept away from the gingival margin, patients can expect inflammation to subside over time, and discomfort to fade with it.
Discomfort can also be the result of gingival and periodontal abscesses, necrotising periodontal diseases, injuries related to traumas such as piercings, gingival recession, and more. Gingival recession is likely the most prevalent condition of these, and can be caused by aggressive brushing, poor oral hygiene and frequent tobacco use. The reduced width of keratinised connective tissue can once again cause inflammation, which may also increase dentine hypersensitivity.
Sensitivity and pain throughout the periodontal tissue can place a significant strain on everyday life. Patients may find certain foods being uncomfortable to eat or meals being interrupted entirely. If a patient avoids certain types of food because of this, they could encounter various issues. Harder fruits and vegetables, such as apples and carrots, often contain vital nutrients, and replacing these with unhealthy alternatives can be detrimental.
Inadequate oral hygiene routines and, in particular, interdental cleaning approaches, can be extremely detrimental to gingival health, with evidence of abrasion and physical injury in some cases. Whilst patients may be motivated to look after their oral health, and take on new routines such as conventional flossing as a result, the pain caused by this may lead to them ceasing such a behaviour. The benefits of flossing outweigh the risk of damage, but an interdental cleaning alternative that reduces any aggravation of pain would be ideal.
Conventional flossing is technique sensitive, and so alternative interdental cleaning solutions may be helpful in order to improve oral hygiene whilst managing pain. Patients rely on their dental professionals to provide effective recommendations. An oral irrigator could be an ideal solution for individuals with gingival pain, with studies showing a statistically significant reduction in bleeding on probing in just four weeks.
A solution such as the Cordless Advanced water flosser from Waterpik™ can aid patients with up to 99.9% of plaque and bacteria removed with just a three second application, reaching below the gingival margin and in the interdental spaces, where brushing alone cannot access. Patients
with sensitive gums can choose between three pressure settings, for an effective clean without compromising on comfort. Waterpik™ is the #1 water flosser brand recommended by dental professionals, and is the only water flosser brand to be approved by the Oral Health Foundation –ensure you recommend by name.

Pain and discomfort throughout the gingival tissue can be caused by a number of issues, but ensuring gentle and effective oral hygiene routines are in place will minimise risk in a number of ways. This can help patients return to smiling and living in comfort, every day.
For more information on WaterpikTM water flosser products visit waterpik.co.uk. WaterpikTM products are available from Amazon, Costco UK, Argos, Boots and Tesco online and in stores across the UK and Ireland. n
about the author rachel Bennett, Dental hygienist at Bupa Dental Care leeds and Churchview Dental Care.

Medical Device Regulation (MDR) ensures that medical devices on the UK market are safe and effective for patients, the public, and healthcare professionals. In order to comply with MDR, products must undergo independent clinical testing, which provides evidence that they are safe and effective. Following the UK’s exit from the European Union, many medical devices which were previously covered by the EU MDD are undergoing the process of achieving MDR status in the UK. Ultimately, clinicians should feel confident that the products they recommend to their patients have undergone the appropriate testing and have evidence to support this. Whilst toothpaste is not necessarily classified as a medical device – instead, many are considered ‘cosmetic’ – if it claims to have a medical function such as to treat or prevent a disease, or is intended to relieve sensitivity, it is considered as such and should undergo the appropriate testing to prove the claims.
enhanced efficiency & confidence
Evidence-based dentistry aims to provide the best possible care to a patient by considering the evidence. It is regarded as
the gold standard in health care delivery around the world. By focussing on the evidence, clinicians can more effectively select solutions that minimise the risks associated with treatment or preventative care. In doing so, both the patient and the clinician can rest assured that the treatment type has been scientifically assessed, and can be more easily trusted. As products which have undergone the MDR process are independently clinically tested, clinicians can look to this as a reflection of their reliability.
Products that promise excellent results but don’t deliver are disappointing for patients, and may lead to a negative experience, particularly if they are experiencing prolonged pain or sensitivity as a result. Instead, recommend clinically-tested products which offer predictable and repeatable results and can increase patient satisfaction. This not only helps to improve patients’ oral health, but potentially reduces pain and helps to prevent disease. In turn, this improves patients’ trust in their practitioners as they repeatedly receive successful care and treatment which meets the expectations set by their care provider.
Some patients may choose their toothpaste based on price, convenience, or because they have seen an advert for it before. However, it may be insufficient for their unique needs. By recommending patients a clinically-tested and evidence-based toothpaste by brand, clinicians can ensure patients are getting the exact formula they need to protect their teeth in-between appointments. Practitioners can be sure that products subjected to MDR testing are proven to do what they claim –for example, offering caries protection, gum health, and enamel-strengthening.
For patients, this means enhanced quality of life and reduced risk of developing dental issues and ultimately more trust in the Dental professional Recommendation. Particularly for patients who are experiencing dental sensitivity, have tooth wear, or who are undergoing tooth whitening treatment, the use of a trusted toothpaste can offer preventative effects and support their overall oral health – offering a long-term defence against attack and sensitivity in the future.
BioMin® is committed to evidence-based dentistry. We’re currently updating our medical device approval to align with the latest standards, ensuring clinicians and patients can

continue to trust and rely on our high-quality formula for lasting sensitivity protection. The comprehensive nature of this testing means that only a handful of toothpastes undergo MDR. Whilst this means that BioMin® is unavailable for now, the next time you order our toothpaste, you’ll receive one of the most thoroughly tested and endorsed sensitivity toothpastes on the market.
Evidence-based dentistry means you can feel confident in the products you use, and your patients will, ultimately, feel the benefit. The science is clear. The solution is simple. www.biomin.co.uk n
about the author alec hilton, Ceo, BioMin technologies.

Fluoride has long been recognised as a cornerstone of paediatric dental care, and its importance lies in the way it supports the development and maintenance of strong teeth during childhood. Deciduous teeth are particularly vulnerable to caries because they are softer and more porous, making additional care vital in many cases.
Despite the many benefits of fluoride use in oral hygiene, the excessive ingestion of this chemical can lead to fluorosis. For this reason, the use of fluoride in paediatric dental care should be carefully monitored and balanced between mitigating caries and avoiding fluorosis.
historic discoveries
The successful use of fluoride in the prevention of caries has been well documented for over 100 years. In 1901, dentist Dr Frederick McKay observed that many children living in a specific area of Colorado Springs presented with a unique brown staining on their teeth, but suffered with very few caries.
Upon further research, Dr McKay discovered a very high concentration of fluoride in the local water supply, prompting further research into the relationship between fluoride and its ability to mitigate of caries. By the 1940s, states in America began adding fluoride to the public water supply, and its use in dental products became widespread across the world by the 1950s
Bountiful benefits
Fluoride helps to reinforce enamel, making it more resistant to the acids that cause caries.
It does this by promoting remineralisation, and mitigating early damage.
The recommendations for fluoride use vary depending on age, and careful supervision is essential to ensure children benefit without risk of overexposure. For infants and toddlers up to three years old, only a small amount of fluoride toothpaste (the NHS references it as a smear) is advised. Parents should supervise brushing closely at this stage to prevent children from swallowing toothpaste.
From the age of three to six, the amount can be increased to a pea-sized portion, with children encouraged to spit out the toothpaste after brushing without rinsing.
Twice daily brushing at this age helps to build good habits for later life whilst protecting deciduous teeth. Professionals may find it appropriate to recommend fluoride varnish applications during routine check-ups. These varnishes provide an extra layer of protection, particularly for children at higher risk of caries or hypersensitivity. Patients of all ages can continue to benefit from these if they need extra support alongside a standard oral hygiene routine.
the need for moderation
Dental fluorosis appears as faint white streaks or spots on the teeth. As this develops, white lines in the enamel can become more pronounced, alongside cloudy aspects of the enamel, or even the entire tooth taking on a chalky white appearance, ultimately losing transparency. With prolonged exposure, the enamel can become less mineralised and more susceptible to damage.
If children ingest an excessive amount of fluoride, usually from swallowing too much toothpaste or from unnecessary doses of fluoride tablets, fluoride toxicity can occur. Nausea, vomiting, abdominal pain, and diarrhoea are some of the symptoms, and whilst rare, very high doses may even be fatal. Such issues are rare, but clinicians can support paediatric patients if they begin to notice adverse symptoms or have been exposed to high levels of fluoride.
Supervision is key
Parents play a crucial role in managing fluoride use. Supervision during brushing is vital, especially for younger children, to avoid swallowing excess toothpaste. Following age-specific guidelines and professional advice ensures that children receive the right amount of fluoride safely. Clinicians should provide the necessary support for all parents, to ensure that young patients are best supported. They can also provide assurance for concerned parents who may be aware of fluorosis, but unknowing of quite how much fluoride will trigger adverse effects.
Finding the right balance
In addition to daily routines, professional fluoride treatments can provide valuable support. 3M™ Clinpro™ Clear Fluoride Treatment from Solventum (formerly known as 3M Health Care) is one option that focuses on making the experience more pleasant for children. Unlike traditional varnishes that may feel sticky or taste unpleasant, Clinpro™


Clear Fluoride is designed to be comfortable, with a smoother application and improved taste. It is formulated to provide an effective fluoride uptake with a lower dosage, thanks to soluble fluoride ions that immediately deposit on the tooth, supporting patients experiencing hypersensitivity.
a lifetime of protection
Fluoride remains an essential ally in paediatric dentistry, offering powerful protection against caries when used responsibly. The challenge lies in striking the right balance, providing children with enough fluoride to strengthen and safeguard their teeth, while avoiding the risks of overexposure. With careful supervision, adherence to age-specific guidelines, and professional oversight, fluoride can continue to play a pivotal role in nurturing healthy, confident smiles that last a lifetime.
To learn more about Solventum, please visit solventum.com/en-gb/home/oral-care/
For more updates on trends, information and events follow us on Instagram at @solventumdentalUK and @solventumorthodonticsemea n







At Eschmann – the experts in decontamination – we offer a comprehensive range of equipment, services, and support in the field. Our heritage of almost 200 years means we understand exactly what it takes to design and manufacture equipment that is effective, efficient, and durable. As a result, we are proud to support thousands of dental practices across the UK in their pursuit of exceptional health and safety standards.
a solution for every stage
From a practical perspective, we offer equipment for each stage of the instrument decontamination workflow. Each product is extensively tested and has been proven to perform consistently, enabling practice teams to spend more time focusing on their patients.
At the start of the instrument decontamination workflow are the ultrasonic cleaner and washer disinfector. The former is available as the Little Sister UltraSONICA, which has been a trusted brand in decontamination for many decades now.
For washer disinfectors, we offer the choice of a benchtop and under bench solution, both affording an automated and validated alternative to manual cleaning. The Hydrim C61 benchtop technology is delivered in partnership with COLTENE, providing highly advanced equipment for the cleaning and disinfection of contaminated instruments that is ideal for compact spaces. The PWD 8682 under bench washer disinfector from MIELE affords increased capacity with space for up to 360 instruments. It provides heavy duty cleaning, disinfection and drying in under an hour for maximum workflow efficiency.
To perform the next step in the workflow, we provide various autoclaves that ensure fast, effective, and reliable instrument sterilisation. The range of Little Sister autoclaves includes both vacuum and nonvacuum options, ensuring the needs of every dental practice are met.
Completing the workflow, the Eschmann Reverse Osmosis (RO) Water System produces pure water free from minerals, total dissolved solids, bacteria and other microorganisms, to ensure compliance with both HTM 01-05 and SHTM 01-05.
service and support to match
To ensure that you get the very most from your Eschmann equipment, we strive to offer first-class service and support. This means there is always someone available to answer your questions, offer advice, or guide you to the most appropriate equipment for your practice.

To protect your investment and keep your equipment operating efficiently for longer, the Eschmann Care & Cover package is ideal.
This all-encompassing solution includes:
• Annual Validation and PSSR certification
• Annual service and software upgrade
• On-site support from our nationwide team of over 50 specifically trained engineers
• Unlimited breakdown cover
• Unlimited Eschmann parts and labour
• Technical telephone support
• Annual Enhanced CPD user training upon installation, with annual refresher training thereafter
The result is enhanced team compliance, with reduced risk of equipment malfunction for minimal disruption to your practice and reduced long-term costs. Equipment also lasts longer, making your investment work harder for total peace of mind.
don’t just take our word for it…
We don’t just expect you to take our word for it. A number of customers have shared their experiences regarding the quality of equipment and service delivered by Eschmann…
“We have had some of our Little Sister autoclaves for well over 10 years now and have been really happy with them. The machines are easy to use and very reliable. We protect our autoclaves with the Eschmann Care & Cover servicing and maintenance package. I would unreservedly recommend Eschmann products and the Care & Cover service package to others.” –Maxine Northall-Rollins, stock controller at Scott Arms Dental Practice.
“We really appreciate how quickly an engineer is allocated to resolve an issue – they always deal with it straight away and minimise delays within the practice. The autoclaves from Eschmann have also proven efficient and we have relied on them to ensure we are contamination free. I would certainly recommend Eschmann.” –Sharon Davies, practice manager of Rhos Cottage Dental Practice.
“I have consistently found Eschmann to provide lovely service and support, which helps my practice to run worry-free. You just know that your autoclave will be well looked after and will always be in working order. I would rate Eschmann 10 out of 10.” – Dr Kumar Thanki, Principal of Healthy Smiles Dental Practice.
For more information on the highly effective range of infection control products from Eschmann, please visit eschmann.co.uk or call 01903 753322 n
Dr Stephen Pitt has grown The Dental Studio from scratch over the last 20 years, and was considering selling as a way to drive further development.
He commented:
“I had been looking to sell intermittently for about 6 years. I felt I had taken the practice as far as I could on my own – I was hitting a ceiling and needed more knowledge and expertise to unlock the next stage of growth. I believed that selling was my only option.
“Despite starting the process a few times, I never found the right buyer or contract for me, my team, and my business. I was concerned about losing the identity of the practice and the culture we had created – it was about more than just keeping the name. In addition, I had reservations about transitioning to an associate role, effectively losing control of the business from an operational perspective and no longer having any influence on how staff and patients were treated.
“I set up The Dental Studio as a squat back in 2005 and grew it from nothing. It was important to me to protect everything we had achieved, so I needed to be sure that I was leaving it in the right hands.”
Stephen recently joined DeNovo Dental Partners, which offers a unique alternative to traditional practice sales that protects each business’ individuality, autonomy, and leadership. Stephen shares what stood out most to him:
“With DeNovo, it wasn’t about handing the practice off to a new owner, but rather, introducing an extra pair of hands to help steer the practice on the next stage of its journey. Getting to know the DeNovo team was integral to the decision-making process for me; I came to really understand who DeNovo is and who the people are.
This, combined with the opportunity to keep the identity of the practice intact and continue managing it without external pressures, tipped the scales. The latter concept I was initially hesitant about – to be honest, it sounded too good to be true. However, I was able to speak with existing Partners to find out more about their experiences, and they confirmed that everything was true; you can still be who you are as a practice, but there’s support available if you want it.
“I also appreciated that DeNovo sought practices with unique quirks and individuality. They embraced the things that we did a little differently. For example, I love teaching, and while other potential buyers were sceptical about the income this would continue to generate – despite its 10 years of success – DeNovo had a far more positive approach. They were honest, friendly, and transparent at every turn. From the moment I made the decision, the transaction moved rapidly and completed in just 2-3 months.”
DeNovo offers a distinctive shared ownership model that enables Partner principals to retain full clinical and practice autonomy, supported by dedicated central expertise across HR, marketing, procurement, and more. Practice owners

receive the full value of their business upfront, through a combination of cash and equity in the parent company, alongside multiple opportunities to benefit from long-term value creation as both the practice and the wider organisation grow. Stephen continues:
“The promises definitely translated into a post-sale reality – the current environment is one of collaboration, with support I can use as much as I want. The practice has already benefitted, with team expansion in progress and conversations about introducing new sleep dentistry services. I have also found support in areas like marketing especially useful. The whole team remains easy to work with and really approachable. All of this has been achieved, despite nothing changing for practice staff – promises of autonomy have definitely been fulfilled in this regard. I have actually been pleasantly surprised with how quickly they respond to questions and how proactive they have been in delivering the support I have requested. They are very forward-thinking.
“DeNovo provides more opportunities from a financial perspective too. I have the chance to earn more based on practice growth post-sale, and – as a shareholder in the wider company – I also benefit from the increased value in shares. This is a great model and it really incentivises investment back into the practice for continued growth and development.
“DeNovo is not for principals who want to sell their practice and walk away from dentistry completely. It is perfect for anyone who wants to continue working clinically for several years, but seeks expertise and support to unlock further practice growth. If you love the practice that you have built and wish to remain a part of its journey for a bit longer, DeNovo could be the answer you’re looking for.”
https://www.denovo.partners/ n

Through both genetic and environmental influences, many patients can develop class III malcoclussions, characterised by a mesial molar relationship, often accompanied by anterior crossbite. Studies assessing the incidence of such malocclusions in relation to different geographic regions suggest that 3-5% of people in the United Kingdom are affected. When looking to develop orthodontic skills, it’s paramount to invest time into learning how to treat such complications. This requires an understanding of how patients develop a class III malocclusion, as well as appropriate treatment approaches, whilst confidently managing other oral health needs. Clinicians will need to look to the literature for guidance, before embarking on effective training courses for expert support and hands-on training opportunities.
Clinical manifestations
Class III malocclusions can result from mandibular prognathism or maxillary hypoplasia and retrognathism, or both in equal measure. Whilst familial experience with malocclusions can indicate whether a young patient is likely to develop this occlusal complication, environmental factors from an early age can also be impactful. This could include everything from enlarged tonsils, chronic mouth breathing that leads to downward and backward growth of the mandible, abnormal tongue and mandibular posture, trauma, and prolonged sucking or resting tongue habits. The latter behaviours provide opportunity for intervention at a young age, but clinicians should expect to encounter class III malocclusions that have not been intercepted.
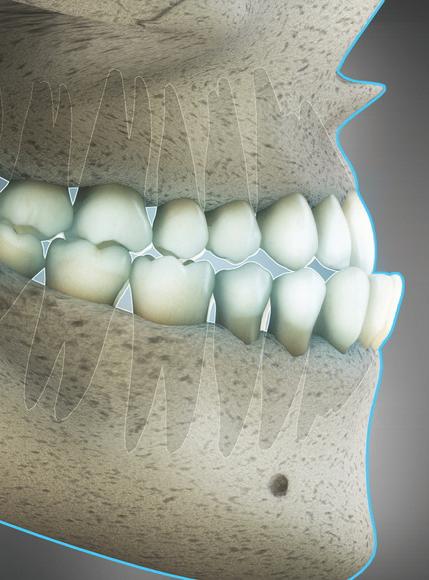
Patients may present with complications such as deteriorated chewing efficiency. Those with anterior cross bite are found to have their chewing ability reduced by half compared to those with standard occlusion. Individuals could also have issues with the articulating certain letters, such as “s” and “z”; abnormal tooth wear between incisors, prompting pulpitis, occlusal trauma, and an increased risk of periodontal disease; as well as the development of temporomandibular joint disorder. Each of these may not only have a prominent and direct impact on everyday life through increased risk of injury and pain, and difficulties communicating with others, but also on an individual’s mental health. Visually prominent occlusion is also suggested to be a risk factor for bullying among children and adolescents, creating the risk of emotional harm.
Early intervention for class III malocclusion is preferable, avoiding surgical intervention and therefore reducing the invasive nature of treatment overall. For paediatric patients, this also creates a favourable environment for growth and improves the occlusal relationship, with orthodontic care helping to guide the development of the permanent dentition as it comes through.
Results have previously shown that the early introduction of protraction headgear can successfully reduce the perceived need for orthognathic surgery, minimising instances of such intervention by 3.5 times. However, the study only made final assessments with patients at 15 years of age, and judging the need for surgery can be subjective.
Treatment can also include conventional orthodontic solutions, aiming to bring the upper anterior dentition forward, whilst retracting the lower anterior teeth. In some instances, this can be paired with surgical intervention, with the placement of metal miniplates and miniscrews into the maxilla and mandible. These can anchor elastics, enabling clinicians to exert another force on the maxillofacial structure.
The use of both straightforward and complex orthodontic approaches for class III malocclusion requires an exceptional level of care, attention to detail, and time. Dental professionals need to be able to confidently predict the effects of movements of both individual teeth, and the larger skeletal structure; this comes with engaging in effective courses, reading clinical literature, and gaining hands-on experience.
Clinical understanding
When a patient presents with class III malocclusion, no matter its stage of development, a clinician must be able to appropriately guide the individual for effective support. If the dental professional is not confident that they have the necessary training and competence to carry out effective care, they must refer the patient to an appropriately trained colleague, as per the Standards for the Dental Team laid out by the GDC.
For clinicians that want to take on such cases, training can take many forms. Most importantly, dental professionals should have the opportunity to practice with handson sessions, supported by leading tutors, whilst having a comprehensive knowledge of orthodontic treatment surrounding class III malocclusions alone.
The IAS Advanced Diploma course from IAS Academy is a comprehensive orthodontic course than enables clinicians to manage more complex malocclusions, including class I, class II div 1, class II div 2, and class III cases. Dental professionals take on 6 multi-day courses as part of the Diploma, for a total of 154 verifiable CPD hours. Teaching consists of interactive lectures, hands-on practical sessions, webinars and reviews of the literature – for a complete understanding.
Class III malocclusions are often complex cases, and require high levels of clinical knowledge. Professionals should take time to understand aetiologies, treatment options, and long-lasting care in order to support the individuals that require such great intervention. For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
about the author
Dr tif Qureshi, Founder and a Clinical Director of IaS academy.
Bone loss after losing a tooth can present a significant obstacle for patients who would like dental implant treatment. This may mean that clinicians deem implants unsuitable in these cases, only presenting options such as dentures and bridges, for example. However, clinicians should consider referring these complex cases to specialist periodontists for treatment, alongside seeking out training courses to enhance their knowledge of bone and soft augmentation as a tool to facilitate dental implant placement in these cases.
The body’s natural process of bone remodelling involves removing old bone (resorption) and replacing it where it’s needed (ossification). This, when functioning properly, is an important process for the body’s health. However, when bone is being lost at a rapid rate, bone mass decreases putting the structure at a higher risk of fracture. This process can affect the jawbone, having an impact on the health of the mouth. As such, it’s important to understand what might cause this, and how it can be managed.
Usually, the force exerted on the jawbone during chewing will send signals to osteoblasts to maintain bone strength. If a tooth is missing, whether that’s due to extraction, injury, or disease, that area of the jawbone will no longer receive stimuli, and the jawbone will break down as the rebuilding of structure is no longer a priority. Bone may still regenerate, but at a far slower rate, and dentures may exacerbate bone loss in some cases.

Dental implants offer unique benefits. They mimic the natural appearance and function of the teeth, are a permanent solution, and can be cleaned at home in a similar way to the natural teeth. However, they can also be a useful tool for preventing bone loss that occurs after a tooth is lost. Research suggests that 30% of the alveolar ridge is lost within the first 12 weeks postextraction, having a significant impact on oral health. Dental implants offer noticeable residual alveolar ridge preservation which varies from reducing the rate of resorption. Providing patients with a long-lasting and highly aesthetic option should be considered wherever possible, in order to deliver the best possible outcomes for patients.
treatment of bone recession


However, bone and soft tissue augmentation are advanced procedures, and it is essential that clinicians are appropriately trained and qualified to provide the treatments they offer. As such, clinicians must refer patients who require this treatment type to more experienced professionals until they have received adequate training and are confident, competent, and indemnified to offer bone and soft tissue augmentation treatment to facilitate dental implant placement.
ASHA Club is an excellent option for clinicians who wish to advance their skills in hard and soft tissue augmentation. For example, Dr Selvaraj Balaji is set to deliver Comprehensive Cadaver Training in Advanced Hard and Soft Tissue Augmentation (With Sinus Grafting), offering attendees the ability to develop their knowledge and skills in a supportive environment. The three-day course consists of one day of theory (for those who have not already completed the Advanced Horizontal & Vertical Augmentation) and two days of hands-on cadaver training. Plus, those who complete ASHA Club courses are eligible for mentoring opportunities from Dr Balaji. Bone loss can present a hurdle for some patients who would like a dental implant to replace a missing tooth. Whilst, initially, dental implants may not appear to be an appropriate option in these cases, it is important to consider the role that bone and soft tissue augmentation can play to facilitate this permanent option. It is absolutely crucial that professionals offering bone augmentation are confident and have received high-quality training to offer these solutions. Providing patients with highly functional, aesthetic, and long-lasting solutions for missing teeth can have a huge impact on their lives, building their confidence in their smile and reducing the risk of further risk due to increased bone loss.
Find out more at ashaclub.co.uk/courses To book, please call: 07974 304269 or email: info@ashaclub.co.uk n
about the author
Dr Selvaraj Balaji BDS, MFDS RCPS(Gla), MFD SRCS(Ed), LDS RCS(Eng)

It is for these reasons that dental implants have become an increasingly popular treatment option. As such, in patients with insufficient bone – where it may be difficult to place implants, usually – bone augmentation plays a vital role. Placing a bone graft in preparation for dental implants helps to ensure that there is optimal bone in place to support a permanent restoration long-term, for the ideal treatment outcome for the patient.
Since he obtained the BDS Degree, Dr Balaji has worked in Maxillo-facial units in the UK for several years and gained substantial experience in surgical dentistry. He is the principal dentist of The Gallery Dental Group which is made up of Meadow Walk Dental Practice and The Gallery Dental & Implant Centre. Dr Balaji is also the founder of the Academy of Soft and Hard Tissue Augmentation (ASHA) and runs courses, lectures and study clubs in the UK and around Europe for aspiring implantologists

Experience the perfect combination of adhesion, versatility, and convenience :
Truly universal: Works with all etching techniques and materials
Exceptional bond strength
Even in total dark cure mode
Ergonomic bottle design
Precise dispensing, less waste
Minimal post-op sensitivity
Better comfort for your patients
Proven OptiBond ™ GPDM technology, now enriched with MDP for a Truly Universal Bond. Claim Your Free Sample
Dental implantology remains an area of rapid growth in UK dentistry. Offering a permanent solution to partial or complete edentulism, it appeals to patients of all ages and backgrounds. Modern technologies, techniques and materials are also making the treatment modality more predictable and accessible than ever before, elevating outcomes and enabling more individuals to take advantage of the solutions available.
For clinicians offering the surgical and/or restorative stage of implantology, it is crucial to be aware of all the factors influencing success. With comprehensive training and experience, alongside meticulous treatment planning and delivery, any dentist can build a thriving dental implant business. Though much emphasis is often placed on the surgical phase of the workflow, properly preparing for and executing the restorative aspect is just as important for success.
a successful treatment option
With many tools in the armamentarium, today’s clinicians have the opportunity to consistently achieve success in the field. A systematic review found the average 5-year survival of single-unit implant-retained prosthetics to be 95.6%. Specific papers reviewed found the prosthetic survival rate to be as high as 95.2% at 10 years. This provides confidence that implants can be restored in a predictable and long-lasting way, when approached with sufficient planning, products and techniques.
All of these are essential to mitigating potential complications and increasing the chance of treatment success.
Overcoming biological complications
As with any area of dentistry, complications can occur when restoring implants. Some of the factors affecting implant success and survival are the number of implants placed in the mouth and the location of the implants.
Peri-implantitis is another leading cause of implant complications, with a prevalence of 20% at patient-level and 13% at implantlevel. Research has found several links between the development of the disease and prosthetic considerations. For example, residual cement around the restoration can induce marginal bone loss and increase the risk of peri-implantitis. A poorly designed implant-abutment interface can also increase bacterial infiltration and disease risk.
This highlights the importance of creating an effective emergence profile when designing the implant-abutmentcrown connections. Though more studies are needed to determine the impact of the emergence angle on aspects like marginal bone loss, evidence so far suggests that the right angle increases will support peri-implant tissue health and stability. For instance, emergence angles of <30 degrees and of a concave or straight design are associated with a decreased peri-implantitis risk. An effective prosthetic design is also critical in
ensuring the cleansability of the restoration and implant site, further minimising the risk of peri-implant disease.
a mechanical issue too
In addition to biological factors, there are various mechanical complications relating to implant-supported prosthetics reported in the literature as well. Some of the most common include fractures in the veneering material, loss of access hole, abutment or screw loosening and loss of retention of cemented fixed prosthetics. There is also evidence of fracturing screws, frameworks, and abutments, where the restoration is not planned and executed correctly.
Many of these challenges can be avoided with sufficient implant planning. A prostheticallydriven approach is often implemented as a way to identify the best position and angle to allow for a functional, aesthetic and durable restoration. Everything from bone quality and quantity to occlusal forces, surgical technique and prosthetic design should be taken into consideration, working together to optimise the treatment outcome.
time to be materialistic
With all of this in mind, the restorative material must also be chosen carefully to ensure that aesthetics and longevity can be achieved. Any implant-retained restorations should be created with confidence that they will reliably withstand masticatory forces, blend with the natural dentition and facilitate
For early years clinicians entering the world of dentistry, mastering the art of dental impression-taking is not merely a technical requirement, it is a cornerstone of clinical success. Impressions serve as the blueprint for a wide range of treatments, from crowns and bridges to dentures and orthodontic appliances. Inaccurate impressions can lead to ill-fitting restorations, increased chair time, patient dissatisfaction, and costly remakes. Therefore, developing precision and confidence in impression-taking is essential for clinicians in the formative stages of their careers.
a fine art
Dental impressions are a tactile and visual representation of the patient’s oral anatomy. They must capture fine details of soft and hard tissues, including margins, occlusal surfaces, and undercuts. For early years clinicians, the challenge lies not only in selecting the appropriate material but also in executing the technique with consistency. Errors in impression-taking are a common cause of prosthetic failure, particularly in general practice settings. These errors often stem from inadequate training, poor moisture control, and improper tray selection.
Improving impression techniques begins with understanding the properties of the materials in use. Alginate, for example, is widely used for preliminary impressions due to its ease of manipulation and costeffectiveness. However, its dimensional instability and susceptibility to distortion require prompt pouring and careful handling.
Elastomeric materials such as polyvinyl siloxane (PVS) and polyether offer good accuracy and tear resistance, making them ideal for impressions. Yet, their success depends heavily on proper mixing, timing, and tissue management.
moisture management
Excessive moisture such as saliva and blood can compromise the integrity of the impression material, particularly in subgingival areas. Different methods can be used to mitigate excessive oral moisture including oral evacuation systems such as saliva ejectors and high-volume evacuators (HVE).
Absorbent materials like cotton rolls or pads can be placed under the salivary duct gland to provide a temporary solution, but perhaps the most effective method of controlling excessive moisture is a dental dam to completely isolate the treatment area.
The ability to maintain a dry field is not only a technical skill but also a marker of clinical maturity. The presence of moisture during impression-taking significantly reduces the accuracy of elastomeric materials, leading to marginal discrepancies in restorations.vii
Tray selection is another critical factor. A tray that is too small may compress tissues and distort the impression, while an oversized tray can result in uneven material thickness and poor detail capture.
Custom trays, although more timeconsuming to fabricate, offer superior control and uniformity. For early years clinicians, learning to assess arch form and select the appropriate tray is a skill that improves with experience and mentorship.
Digital impression systems are becoming increasingly prevalent, offering an alternative to traditional methods. Intraoral scanners provide immediate feedback, reduce patient discomfort, and can suit clinicians in a practice that follows a more digital workflow. Some studies show that digital scanners provide a more accurate measurement than conventional impression taking methods. However, they require a different skill set and are not universally applicable, especially in cases involving subgingival margins or extensive soft tissue manipulation. For early years clinicians, exposure to both analogue and digital techniques is beneficial, allowing them to choose the most appropriate method based on clinical indications.
Patient communication also plays a vital role. Anxiety and movement during computerised optical impression scans can lead to the creation of ill-fitting prosthetics. Explaining the procedure, setting expectations, and using calming techniques can enhance cooperation and reduce the likelihood of retakes.
This is particularly important in paediatric patients, where tolerance for intraoral procedures may be limited.
Continuous education is essential. Attending workshops, seeking feedback from laboratory technicians, and reviewing clinical outcomes can help clinicians refine their technique. Higher accuracy in impression-taking is dependent on competent practical abilities. Lifelong learning and professional development are vital in achieving clinical excellence.
a good marginal seal to keep bacteria at bay for a reduced risk of peri-implant disease. The BRILLIANT Crios from COLTENE offers such a solution for single-unit implant restorations. Its outstanding bonding values, excellent marginal seal and high wear resistance all afford peace of mind in the quality and durability of the restoration it creates. Particularly important for implant-retained restorations, the material also exhibits a dentine-like modulus of elasticity, minimising stress from chewing and the risk of material fatigue.
Success in implantology relies on a number of factors, with the restorative phase having a significant impact on the long-term outcome. Prosthetic design, and material selection must be deliberate in order to reduce the risk of both biological and mechanical complications. By embracing a prostheticallydriven approach and working with trusted solutions, you too can deliver exceptional implant-retained smiles for your patients. For more information, visit colteneuk.com/CRIOS Email info.uk@coltene.com or call 0800 254 5115. n
about the author nicolas Coomber, COLtene national account & marketing manager.

Incorporating high-quality materials and equipment into daily practice can also make a tangible difference. For clinicians looking to improve their impression outcomes, using reliable products designed for ease and precision is a practical step forward. The KemKat Impression Compound from Kemdent, for instance, offers excellent flow and stability, making it ideal for border moulding and preliminary impressions in edentulous cases. When paired with the Kemdent Dental Water Bath, clinicians can achieve consistent softening temperatures and optimal handling characteristics, reducing variability and enhancing reproducibility. Impression-taking is a skill that demands attention to detail, anatomical understanding, and technical finesse. For early years clinicians, investing time and effort into mastering this foundational procedure pays dividends across all areas of restorative dentistry. By combining sound technique with quality materials and ongoing education, clinicians can ensure that their impressions lead to predictable, functional, and aesthetically pleasing outcomes, setting the stage for a successful and rewarding career.
For more information about the leading solutions available from Kemdent, visit www.kemdent.co.uk or call 01793 770 256 n
about the author alistair mayoh, marketing Director, Kemdent.












Perfectly coordinated products with easy and efficient application for safe and aesthetic results for direct restorations!
Universal all-in-one adhesive for all techniques

Fluoride-releasing composites for multiple indications

Superior finishing and polishing disks





























































Whilst implants can provide patients with a new lease of life, it is vital to promote good oral hygiene following treatment and to educate patients about effective aftercare solutions. This helps to reduce the risk of disease and prolongs the lifespan of the implant, resulting in greater patient confidence, satisfaction and trust in dental practices.
Fluctuating trends
Edentulism is characterised as the final stage of untreated dental caries or disease, but can also be caused by physical trauma, leading to tooth loss.
Whilst the prevalence of edentulism is decreasing across populations in highincome countries, the opposite trend can be observed in low-income nations due to a rise of untreated caries and disease. This is largely attributed to limited access to dental care and hygiene products, as well as the absence of fluoride in drinking water.
Medical concerns & mental well-being
The World Health Organization categorises edentulism as a disability, as tooth loss can cause a variety of debilitating medical issues from discomfort to increased rates of chronic inflammation.
Patients suffering with chronic gingival disease are also more likely to suffer from other health conditions such as non-insulindependent diabetes and kidney disease. Additionally, they are at an increased risk of developing chronic vitamin deficiencies due to difficulty consuming a varied diet including fruit and vegetables.
The absence of an aesthetically pleasing smile not only has the potential
Fto impact a patient’s medical health, but can also have a devastating effect on mental well-being. Many sufferers of tooth loss feel self-conscious and even ashamed to laugh or smile in public which can lead to mental health issues such as anxiety and depression.
Restored function
Dental implants have a variety of benefits for those suffering from partial or complete edentulism. They also foster a healthier and more positive outlook for individuals who may have previously felt discouraged or overwhelmed about their oral health.
Studies indicate that about 58% of edentulous people experience difficulties accepting tooth loss.
Potential complications
Promoting both short- and long-term aftercare is essential to ensure dental implants last their intended lifespan. It also fosters a healthier and more positive outlook for individuals who may have previously felt discouraged or overwhelmed about their oral health.
Dental implants have the potential to last as long as natural teeth, but boast an average lifespan of around 10-15 years. Poor oral hygiene can lead to serious complications for dental implant patients such as periimplantitis which is a destructive infection of the soft tissue and progressive loss of bone around the implant.
Long-term aftercare is key
Peri-implantitis is usually very preventable with adequate oral hygiene and healthy lifestyle choices. Educating patients about the importance of long-term aftercare following implant surgery is essential to
both the lifespan of the implants and the overall health and well-being of the patient.
According to Perussolo, J & Donos, N. (2024), some of the key points to discuss with your patient include:
Patient awareness: Ensure the patient understands that while implants offer a long-term solution to edentulism, their effectiveness depends on consistent home aftercare. For most cases of implant failure, the primary cause is plaque accumulation due to lack of plaque management by the patient. Ensuring that the patient fully understands that implants are not an alternative to proper dental care and hygiene is key in the prevention of disease and the potential failure of the implants.xii
Informing patients about possible complications: Dentists should explain the risks of peri-implantitis and its symptoms to help patients to seek treatment where necessary.
Encouraging oral hygiene and healthy choices: Patient-performed plaque control is vital. Recommend regular brushing, flossing, and lifestyle changes such as quitting smoking and reducing sugar intake.
Encouraging regular check-ups: Professional plaque biofilm removal is another primary preventive measure. Ensuring that the patient attends the clinic for regular plaque removal can greatly reduce the risk of disease.
These preventive measures all involve a level of patient awareness and cooperation which should be encouraged by dentists.
The British Academy of Cosmetic Dentistry (BACD) offers access to a sprawling network of dental professionals, educational programmes and mentoring.
across the world
or younger generations, travel is all the rage. 27% of Gen Z in the UK plan to travel both domestically and internationally each summer, whilst in the colder October-March months, 84% of Brits express a desire to travel. Alarmingly, only 39% keep up with health and wellness routines on holiday. This can lead to lapses in things like oral health, putting young travellers at risk.
A compact healthcare product offers enormous appeal. There is a growing demand for items that are small in size yet retain their quality – a perfect blend of affordability and convenience that can improve compliancy. In particular, the trend of “flying naked,” in which travellers go abroad without bags – just the clothes they wear and the pockets in them – highlights how space-saving solutions are immensely desirable. Those heading off to skiing trips loaded with luggage will also benefit from some packing minimalism.
Enter the Ortho Travel Kit from Curaprox, an all-in-one care set to improve the health of the teeth and gingivae during orthodontic treatment.
Due to the higher risk of oral disease, orthodontic treatment demands a consistent daily oral hygiene routine that cleans every tooth, gingival and bracket surface for optimal results. This level of comprehensive cleaning is attained with the Travel Kits five components:
• Ortho Travel toothbrush
• Curaprox Be You toothpaste
• CPS 14 ortho interdental brush
• CPS 18 ortho interdental brush
• CPS 07 prime interdental brush
A groovy brush
Toothbrushes can be awkward things to take abroad; poking out of travel bags or leaving toothpaste and water stains on clothes. The Ortho Travel toothbrush remedies these concerns as it can be parted into two pieces so as to fit into the compact case that the Ortho Travel Kit comes in. This efficiency is matched by the toothbrush’s effectiveness: it’s head incorporates a bracket groove, allowing the 5,460 ultra-fine Curen filaments to clean the tooth surfaces around each bracket. Gentle yet powerful, the brush filaments promote a comfortable experience. No toothbrush can work solo, and the Be You toothpaste is a reliable partner packed with freshness, herbs and oral health essentials. Four flavours are available, depending on the Ortho Travel Kit colour:
• Green – Peach and Apricot
• Orange – Apple and Aloe Vera
• Blue – Watermelon
• Pink – Blackberry and Liquorice
Behind each pleasant flavour is a fluoride-fix that protects against caries and strengthens the teeth.
Small but mighty
The trio of interdental brushes comes with a duo holder, enabling orthodontic patients to alternate quickly between sizes. The CPS 14 is cone-shaped to better clean around orthodontic bands, as well as accessing the interdental surfaces between the wires, teeth and around the brackets. The CPS 18 is also ideal for cleaning the wires, removing trapped food particles with ease. Finally, the CPS 07 is effective for brushing the interdental
Part of the BACD’s services include career support for dentists and exclusive educational courses to help dental professionals improve their skills via continuing professional development (CPD) courses, and to help dentists stay on trend with topics such as implant aftercare. Encouraging good patient aftercare is not only beneficial to the patient, it can also enhance the reputation and success of a dental practice:
• Improved patient outcomes lead to higher satisfaction and increased wordof-mouth referrals.
• Fewer complications mean reduced emergency visits and more predictable treatment results.
• Stronger patient relationships foster trust and loyalty, increasing the likelihood of long-term engagement.
• Professional credibility is reinforced when patients see their dentist as a proactive partner in their health journey. By embedding aftercare education into implant treatment plans, dentists can cultivate a practice culture centred on excellence, prevention, and patient empowerment. This, in turn, enhances the practice’s reputation and supports growth.
For further information and enquiries about the British Academy of Cosmetic Dentistry visit www.bacd.com
About the author Dr Carol Somerville, President of the British Academy of Cosmetic Dentistry.


spaces, optimising oral hygiene outcomes and ensuring fresh breath.





These powerful cleaning aides are contained in an aesthetically-pleasing vibrant case. It measures a compact 9.5cm x 6cm – small enough to fit in a trouser pocket. For orthodontic patients looking to travel as lightly as possible, the Travel Kit’s size is unbeatable for its practicality and its contents.
Orthodontic patients should be able to enjoy the thrill of travel without having to pack bulky hygiene solutions or neglecting their oral health. With the excellent product range from Curaprox, patients can level-up their daily dental care and lower the risk of caries and periodontitis. This means that, when the braces come off, their smile isn’t just straight – it is healthy. Recommend today.
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visitc uraprox.co.uk and curaden.co.uk
One of the most valuable aspects of dentistry is the connection between professionals, creating a network that can aid patient outcomes.
Referrals for specialist imaging needs are commonplace. It can be essential for complex work, particularly oral surgery, dental implant placement and endodontic care.
To become a go-to source for referrals, it’s important to understand current guidelines around the support provided. These can then be used to optimise business growth potential for the practice, as well as improve the team’s standing in the professional sphere as a source of reliable support.
Safely accepting referrals
‘Standards for the Dental Team’ by the General Dental Council (GDC) dictates the conversation about safe, ethical and effective referrals for dental imaging.
Clinicians are held to standard 1.7.6, which notes that referrals to another member of the dental team must be in the patient’s best interests rather than that of the referring clinician or another team member, including for financial gain or benefit. This ensures clinicians focus on providing high-quality care first and foremost, giving patients confidence that they are receiving the best possible service available.
The same guidelines also establish when referrals are warranted. Standard 6.3.3 notes that patients should be referred if their treatment is outside of the scope of the presiding clinician. This does not absolve the referring clinician of complete accountability.
Instead, they can still be held to the actions of the professional they refer to, as it is their responsibility to ensure said professional is trained, competent and indemnified.
In many cases, dental professionals will have some training in dental imaging. However, the limitations afforded by the solutions in their practice will be the prompt for a referral, and would be grounded in Standard 6.3.3 as a result.
A clinician receiving a referral must only accept if they have the knowledge and skills to complete the requested care. If a practice is trying to increase its referral services for dental imaging, a clinician must be able to safely manage radiographic and digital workflows, with this knowledge tailored to the systems that they use, and ensure patient safety is always prioritised. If a patient has a disability, they may need reasonable adjustments to their care. Where these cannot be made in order to safely treat a patient, clinicians once again have the responsibility to organise a referral. Practices looking to increase referrals should ensure their facilities are designed to accommodate as many patients as possible, and make safe and considered changes for individuals with disabilities.
Referrals can be an effective source of income for a practice. However, it’s vital that charges are ethical and appropriate when they accept a referral for dental imaging. Since the GDC demands that patients’ interests are prioritised over financial
Designed specially for individuals experiencing dry mouth, taste sensitivity, or aversions to strong flavours.


No added flavours
SLS-free and non-foaming –gentle on dry and sensitive mouths

1450ppm fluoride and xylitol to help protect teeth
gain, practices should avoid referral fees. Instead, they should only invoice the initial referring practice for treatment costs, much in the same way that they would charge any individual that they already care for at the practice. This should be reflected in the patient’s original treatment plan in order to keep them fully informed about treatment costs before they proceed with a designated route of care.
If investing in an imaging system that can increase referrals, as well as support inhouse treatments, it’s important to select a solution that produces high-quality results. A cone beam computed tomography (CBCT) system is favourable, and clinicians should look for high CBCT resolution to assess the tiniest clinical details, as well as additions such as metal artifact reduction technology, which can improve the visibility of results for patients with numerous amalgam restorations. A versatile solution would include different imaging modalities, and offer benefits for a wider range of treatment plans, increasing the number of patients that can be supported. With awareness for referrals for patients with disabilities, a system that is designed to support a variety of treatment needs is ideal compared to inflexible alternatives. The choice between solutions is made simple with the CS 8200 3D Access CBCT Scanner, from Carestream Dental. As a scalable 4-in-1 system, it can grow with your practice, and introduce CBCT imaging, 2D






panoramic and cephalometric imaging, as well as 3D model scanning to your practice’s repertoire. A low dose mode is designed to minimise risks for patients, and an ultra-compact, smart design means it can fit into smaller practices. The solution’s height is also adjustable, for patients that need to stand or stay seated during an examination.
Referrals are a key part of modern dentistry, and will continue to be in future. Choosing high-quality systems in your practice can help to establish opportunities to accept referrals, but safe treatment can only be delivered when all guidance is followed to the letter.
For more information on Carestream Dental visit www.carestreamdental.co.uk
For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk
About the author Nimisha Nariapara, Trade Marketing Manager at Carestream Dental.









Scan to request samples


Running a dental practice today means navigating a landscape where patient expectations are rising, online platforms amplify every opinion, and the smallest misstep can escalate into a reputational or regulatory headache. Complaints – whether voiced in person, emailed formally, or posted publicly as online reviews – are an inevitable part of practice life. How we manage them determines whether they become catalysts for improvement or sources of long term vulnerability.
The modern complaint
The nature of complaints has changed. It has never been easier for a patient to express dissatisfaction, and online reviews have become one of the most common outlets. With a few taps, a frustrated individual can broadcast their experience across Google, Facebook, or NHS review platforms. Over the years, I’ve seen everything, from a patient comparing a new dentist’s chest hair to Chewbacca’s, to a receptionist being described as fit for an Oompa Loompa audition. Amusing as these may be, they highlight a deeper truth: online commentary is unfiltered, public, and permanent.
A single negative review can damage trust, deter new patients, and demoralise your team. That’s why responding correctly is essential. A professional, calm, factual reply—never defensive, never personal— signals that your practice listens, cares, and takes concerns seriously. It also protects confidentiality, which is non negotiable. After responding, the next step is internal: review what happened,
identify whether systems contributed to the issue, and ensure learning is shared constructively.
supporting your team when complaints hurt
Behind every complaint or review is a human being on the receiving end. Dentists, nurses, and receptionists are often deeply affected by negative feedback, especially when it feels unfair or personal. As employers, we have a legal and moral duty of care to protect staff from harassment, discrimination, and psychological harm. This duty becomes even more significant with the new 2025 legislation, which strengthens protections for employees and extends accountability to third parties – including patients. Practices will need to demonstrate that they have taken reasonable steps to prevent harm, such as:
• Clear anti harassment policies
• Training on handling difficult interactions
• Systems for reporting and escalating concerns
• Evidence of supportive management responses If a patient’s behaviour crosses the line, practices will have greater authority – and responsibility – to intervene, restrict access, or refuse treatment where appropriate.
ending the patient–practice relationship
I’ve also seen a sharp rise in situations where a patient leaves a negative review or raises a complaint, and the practice’s immediate reaction is to end the relationship. It’s understandable as complaints can be emotionally charged, and sometimes the dynamic between patient and clinician
We started 2026 with some good news: long time BADN member and former Council member Elaine Simmons was awarded an MBE in the 2026 New Years Honours list. Congratulations, Elaine – very well deserved!

BADN will be out and about again this year with a full programme of shows to attend. First on the calendar is Dental Showcase on 13-14 March at ExCel, London. We are at stand G55, so do come along to find out about membership of your professional association, renew your membership, buy a BADN badge or merch, or just stop by to chat!
Speakers at Showcase will include BADN President Preetee Hylton RDN and Treasurer Rebecca Silver RDN MSc. Rebecca will be speaking on “The Digital Dental Nurse” in the Oral Health Theatre on Saturday at 15:45.
“I hope my session will show colleagues some of the latest advances in digital dentistry and AI,” said Rebecca. “I want to encourage dental nurses to expand and use their full scope of practice. You are a huge asset to the practice!
“I would encourage my fellow dental nurses to attend, as the British Association of Dental Nurses
genuinely breaks down. But this is an area where practices must tread very carefully.
The GDC’s Complaints Handling principles make it clear that patients should have a positive experience when raising a concern and must never be discriminated against for doing so. Ending a patient’s care solely because they complained is not only unethical, but it may breach the NHS Constitution and the Health and Social Care Act 2008, both of which emphasise fair access to care and prohibit detrimental treatment of individuals who raise concerns.
There are legitimate circumstances where a clinician may decide they can no longer provide care. The GDC’s Standards for the Dental Team states:
“You must end a professional relationship with a patient only when it is necessary to do so,” and “You must be able to justify your decision, and you must not end a relationship with a patient solely because they have made a complaint.”
I have always supported clinicians who feel they cannot continue treating a particular patient. It is their right, and sometimes their responsibility, when trust has eroded or when continuing care would compromise professional judgement. But the rationale must be transparent, documented, and clearly unrelated to the complaint itself.
When ending a relationship, the practice must:
• Explain that the decision is based on a breakdown in trust, not the act of complaining
• Provide the patient with clear information on how to seek care elsewhere
• Ensure the decision is made in the patient’s best interests
• Record the reasoning thoroughly
Handled poorly, these situations can expose a practice to allegations of discrimination or regulatory criticism. Handled well, they demonstrate professionalism, fairness, and a commitment to safe, ethical care.
A window into your systems
Every complaint, whether whispered at reception or shouted across the internet, reveals something about your processes. A delayed appointment may highlight scheduling issues. A communication breakdown may point to training needs. A personality clash may indicate a mismatch in expectations. The key is to treat complaints as data, not personal attacks.
Regularly reviewing themes, outcomes, and responses strengthens your practice’s resilience and demonstrates compliance with governance and risk management expectations.
The bottom line
Complaints and reviews are two sides of the same coin. They can sting, they can amuse, and they can expose vulnerabilities – but they also offer opportunities. When handled with professionalism, empathy, and strategic thinking, they protect your reputation, support your team, and reinforce the trust patients place in you. n
About the author Lisa Bainham is president at ADAM and practice management coach at practice Management Matters.

is always present and must for any dental nursing questions or queries. If you are undecided about attending, do it! It may change your career in ways you do not expect.”
Preetee will be speaking twice: once on Friday 13 March in the Oral Health Theatre on “Soft Skills: What the Oral Health Team can Learn from Dental Nurses” and also on Saturday 14 March in a live case study – an interactive insight into contemporary care planning for the oral healthcare team.
And then we are off to Birmingham for the Dentistry Show at the NEC on 15-16 May, where we are at stand J11, and will be chairing the Dental Nurse Forum on Friday 15 May. BADN speakers include: Decon Pete; Dr Rachael England, Director of Policy and Advocacy at the Oral Health Foundation; Janet Pickles of RA Medical Ltd; and BADN’s Preetee Hylton and Rebecca Silver.
Later in the year, we will be at the Scottish Dental Show (one of my favourite Shows – great venue, excellent organisation, friendly people!) at the Braehead Arena, Glasgow on 12-13 June; and the London Dentistry Show at ExCel on 9-10 October.
The BADN Dental Shows Portal will have up to date details at www. badn.org.uk. I will be including dates of the later shows as they become available. If you have signed up for our e-newsletters (now weekly) atbadn.org.uk/NewPublic/ Newsletter-Preferences.aspx, we will keep you up to date with news, speakers, etc of all the dental shows. See you there! n
About the author pam swain MBe is Chief executive of BADn
































Gentle yet powerful, reliable and exceptionally durable, Varios Combi Pro2 has a host of advanced features designed to improve efficiency, control and enhance patient comfort. Engineered with meticulous attention to detail, Varios Combi Pro2 is an investment in clinical excellence and in the health of your patients.
• Superbly comfortable water temperature, for both ultrasonic & powder
• Durable titanium ultrasonic handpiece
• Jet Nozzle for Perio Handpiece
• Auto Cleaning
• Removable Powder Chambers*
• Multi-functional wireless foot control
Elevate your practice and patient care with the Varios Combi Pro2 - the future of ultrasonic and powder therapy.




Heated Water
Both ultrasonic and powder handpieces inject water that is heated to the approximate temperature of the oral cavity, ensuring greater comfort, even for those patients with sensitivity.
Jet Nozzle for Perio Handpiece
Executes precise, targeted treatment to areas with staining or thick biofilm on roots or restorations.


Titanium Ultrasonic handpiece
• Durable & lightweight, with unrivaled ergonomics
• Non-slip & scratch-resistant Duragrip coating
• Slim LED handpiece enhances visibility








Watch the VCP2 demo with Cat Edney


iCart Prophy2

User-friendly and convenient trolley cart with the optional extra of a water bottle attachment, to create an independent water supply. This means that when the Varios Combi Pro2 is used with the iCart & bottle, you can treat patients without connecting to the external water mains supply.


Supragingival powder for tough stains. Used with ProphyMate or the Varios Combi Pro (Prophy Chamber).

• Calcium carbonate powder (54

Supragingival powder for moderate stains. Used with Prophy-Mate or the Varios Combi Pro (Prophy Chamber).

based powder (65
m).
soluble, making clean up easier.
Perio Mate Powder
For subgingival biofilm removal or mild supragingival stains. Used with PerioMate or the Varios Combi Pro (Perio Chamber).
• Glycine based powder (25 µm)




BUY ANY 2 PACKS OF FLASH OR SOFT pearl GET A FREE nozzle for Varios Combi Pro or Prophy-Mate 4

Available on request with Prophy-Mate neo, Perio-Mate and Varios Combi Pro purchases.





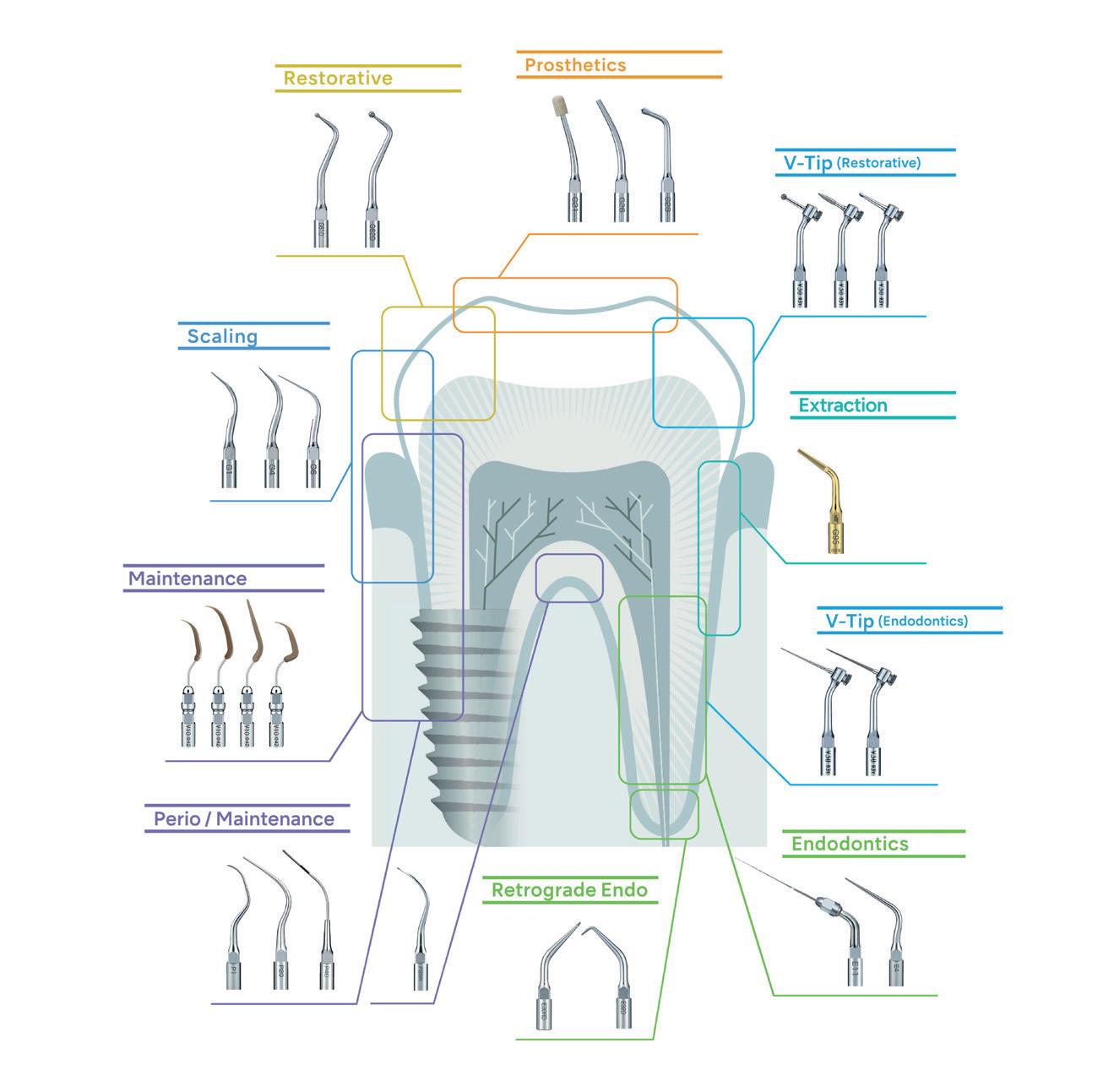



Including reciprocating and rotary Endo features
NEW compact portable electric micromotor, for general & endodontic applications with contra angles (ie speed increasing/red band, 1:1 direct drive/blue band or speed reducing/ green band).
• Lighter motor with enhanced power/torque
• Ideal for general (restorative, prophy etc) and endo applications (rotary & reciprocating** modes)
• Enhanced patient safety function indicates when the handpiece needs repair to minimise it overheating
• Versatile installation options – portable or semi












Derbys/Notts/Yorkshire/Lincs
07435 840097
786619 National
Hargreaves
Muirhead nmuirhead@nsk-uk.com 07353 969563 South Wales Robert Musgrove rmusgrove@nsk-uk.com 07798 918741
07872 824175
South West Ben Guest bguest@nsk-uk.com 07350 361543





Our diaries tell a black and white story. Our patients are booked, procedures times are allocated, and the day has a clear plan. Other days might include admin or planning, lectures or meetings. Our days and weeks take shape with easily identifiable tasks creating the structure. Yet, how much of our day is unseen? Have you even thought about the volume of work you do that can’t be so easily quantified? Dentistry contains a great deal of invisible work where effort isn’t recorded, charged for, or always consciously acknowledged, but which quietly and constantly uses our energy.
recognising our emotional investment
We know that dentistry is not just technical. Alongside the clinical work runs a constant emotional current: managing anxiety, explaining risk, breaking bad news gently, negotiating expectations, maintaining positivity, calculating procedures, assessing potential outcomes, being at our absolute best for patients and the teams around us. This emotional labour requires focus, empathy and restraint, often repeatedly. It is real work, yet it doesn’t appear on the treatment plan. This is the unseen part of what we do and it’s also exactly what we signed up for, but maybe not with our full knowledge. I don’t think you can get round it if you care – so we have to understand and navigate through it.
Carrying yesterday into today
Our work also has a habit of lingering. A difficult case, a complaint, or a patient who left unhappy can follow us home (not literally I hope!) and sometimes we can take our work hangovers back into the surgery the next morning.

Carrying the administrative load
Many dentists report that admin feels more exhausting than dentistry itself. Clinical work is structured, purposeful and familiar. Admin, by contrast, often feels fragmented, reactive and never-ending. It interrupts flow, demands context-switching, and offers little sense of completion. It’s also not very exciting or fulfilling – a set of necessary chores. We like a tangible outcome, not just orderly admin.
The weight of small stresses
It is rarely one big issue that exhausts dentists. More often, it is the cumulative effect of small, repeated stresses:
• Running behind schedule
• Equipment not quite right
• A patient misunderstanding
• A schedule with no breathing space
• Constant low-level vigilance
Individually, these are manageable. Collectively, they build up into genuine tension. Even on the best of days, it’s exhausting, especially as it isn’t even acknowledged.
I don’t restrict this viewpoint to dentistry but it’s the only one I know. Of course, the accumulative effect of the invisible work we all do adds up and takes its toll. Sustained attention, emotional regulation, personal development, decision-making and responsibility are all core components of what we do. Pinpointing your invisible work is extremely helpful in understanding yourself, your limits and preferences. It can help you to identify any feelings of negativity or resentment – maybe before they set in.
We recently had some work done here at Rees Acres. Our driveway should have been given some TLC about a decade ago. But we were always busy, then Covid came along, following which everyone was seemingly busy. Another year or two went by with proclamations of “We really must get round to…” Call it procrastination, a reluctance to spend, or not knowing anyone we liked and trusted who could do the work. Like

everything postponed, the excuses are varied, imaginative, and you’re fooling nobody but yourself.
Every time a patient used to apologise for not attending more regularly, my stock answer was, “You’re a grown up, you make your own decisions, you have other pressures on your time. There’s no need to apologise; you haven’t wasted our time at all. You’re here now, how can I help?”
It defuses a circumstance and brings things back from a potential PAC (parent, adult, child)* situation, which only ends in conflict or stalemate and lays down ground rules in order to start again.
Back to the driveway: We were given the contact details for X, who, when we rang him, said he couldn’t do it and suggested Y, who also declined but gave us the name of Z. Z turned up on our doorstep, talked non-stop, omitted to mention a price and returned the next morning with his lads and their gear.
Three days later we had a new driveway, a patio and a bill… which we paid
Making the invisible visible
Name your hidden work – make an actual list and consider how you might make life a little more comfortable. This might mean:
• Allowing recovery time between appointments. If not always then how about for any complex or emotionally demanding sessions?
• Designing diaries with realistic admin, not just clinical, capacity
• Letting an easier day be recognised as still requiring effort
• Letting go of the expectation that only challenging days justify tiredness
• Delegating some aspects of your work that could be done by someone else
When invisible work is acknowledged, it becomes easier to manage and less likely to quietly erode wellbeing.
A final reflection
What we do is demanding but it’s really valuable to take stock and look at the whole 360 shape of our days. There might be some simple daily tweaks that can make life more manageable –and sometimes it can come from just seeing the whole picture. Our mental health will certainly thank us for it! n
About the author Dr Dhiraj Arora BDs MJDf rCs (eng) Msc (endo) pG Cert Ce owner of evo endo, with three practices (limited to endodontics) in Twickenham, Gerrard’s Cross and slough. Dhiraj is a passionate teacher and ambassador for all things endo. follow him on instagram: @drdij_evoendo

in a bewildering combination of cash, cheques and money transfers.
There is a sting in the tail, as you would expect. Not the driveway or the patio (although, it is early days) but from the tidying up. The soil moved had blocked an admittedly small drain, but it meant that, when it rained, the rain had nowhere to run. This is West Cork and rain is a fact of life, so I have become a dab hand with drain rods over the years; it’s as satisfying as opening an abscessed tooth to allow a flow of pus.
I sorted it out and all has been well since but the experience has been less than optimal. Being ‘sold to’, the inability to contact Z, who has at least three names under which he trades, and the post-op lack of care leaves a bad taste.
In the reception area of our practice, adjacent to the desk – and deliberately very visible – was a framed statement, attributed to John Ruskin even though there is no proof that he actually wrote it.
It sums up what has become known as The Common Law of Business Balance:
“There is hardly anything in the world that cannot be made a little worse and sold a little cheaper, and those who consider price alone are that man’s lawful prey.
“It’s unwise to pay too much, but it’s worse to pay too little. When you pay too much, you lose a little money – that is all. When you pay too little, you sometimes lose everything, because the thing you bought was incapable of doing the thing it was bought to do.
“The common law of business balance prohibits paying a little and getting a lot – it can’t be done. If you deal with the lowest bidder, it is well to add something for the risk you run, and if you do that you will have enough to pay for something better.”
Underneath, we added:
“There is only one standard of treatment in this practice; the best that we can do.”
It’s a good way to start. n
*PAC (parent, adult, child) see I’m Ok, You’re Ok: A practical guide to Transactional Analysis by Thomas A. Harris MD.

For over 500 years, the Royal College of Physicians has continually championed breakthroughs in British medicine and healthcare. This dedication to clinical brilliance was reflected by the Association of Dental Implantology (ADI), who hosted the Members National Forum at the venue in November 2025.
A biennial celebration of implantology packed with eye-opening lectures and ground-breaking discoveries, the event lifted off with the handing over of the ADI Presidency to Dr Pynadath George. Setting tongues wagging with a teaser trailer for the ADI Team Congress 2027 in Liverpool, Dr Pynadath cemented the association’s commitment to growth and first-class events before introducing the first of 25 speakers and getting the ball rolling.
The sheer range of speakers and topics, split across two lecture theatres, enabled ADI members to enjoy a varied programme. Each talk lasted 20 minutes and, after four in a row, the speakers then engaged in a panel discussion, taking audience questions and generating thoughtful conversations.
Dr Marina George emphasised the array of subjects: “The diverse topics by the speakers were very informative and clinically relevant; an interesting mix of digital workflow and clinical cases. The highlight of the event was the lecture by Dr Jakub Batycki – the research work was very useful in understanding the role of immunological markers in implant dentistry.”
Whilst Dr Batycki explored the osteoimmunological impact of immediate versus delayed implant placements, dental technician Kristina Vaitelyte focused on digitally planning cases to save chair time – a presentation filled with innovative technological demonstrations. For Peter Cotton, having educational opportunities for dental technicians is a key reason to become an ADI member: “Being an ADI member keeps you up to date with innovative, dayto-day changes. As a dental technician there aren’t many of us [at the ADI], but it is really beneficial and good to hear the clinical aspect. For both dentists and technicians, an ADI membership is recommended.”
The clinical theatre overflowed with delegates, with many standing at the back to hear from leading clinicians. Attendees heard from Dr Sally Rayment on how Botox could be used in the dental chair. Pedestalled as a game-changing treatment for patients who break everything, Dr Rayment’s talk emphasised the simplicity of Botox and its minimally invasive, evidence-based approach. Patients with temporomandibular joint disorder (TMD) can also benefit from the treatment, helping protect implants from bruxism.

Dr Ahmed Naji’s 20 minutes on autologous platelet concentrates (APCs) provided a comprehensive review of various APCs, assessing each distinct biological composition and evaluating the research around them. By better understanding each APC, clinicians can identify the optimal clinical scenarios in which they can be applied for enhanced patient outcomes.
A line-up of implantologists would be incomplete without Dr Selvaraj Balaji, whose session revolved around “the power of not knowing”. Dr Balaji’s philosophy surprised delegates, forcing them to reflect on previous treatments and their own clinical growth over the years. By showcasing complex cases, some successful, others not, Dr Balaji gave an honest and illuminating perspective on how to manage complications such as hard and soft tissue defects.
Across the day, passion for dental implantology was high. Fervent questions, friendly disagreements and conversations around new technologies all amounted to a truly informative networking experience.
Dr Howard Stean commented: “I have been a member for 30 odd years. In this time the ADI has grown bigger and bigger, and the events more and more luxurious. The Members’ National Forum is inexpensive (free to members!) and boasts fantastic educational value – I highly recommend it for young dentists.”
It is this generational continuity that the ADI continues to look ahead to. The ADI Board Members singled out the excellent work that the Next Gen committee, led by Dr Ricky Bhopal, have been doing to engage with those at the beginning of their implant career. Uniting dental professionals across the whole spectrum of the implantology pathway, be they young or experienced, clinicians or technicians, the ADI upholds an educational legacy fitting for the Royal College of Physicians.
An ADI membership doesn’t just reduce rates for unmissable networking events – it provides access to a supportive community of likeminded dental professionals. For those set to climb the implantology ladder, those curious about what the pathway can offer, and experienced implantologists looking to share their talents, turn to the ADI for the knowledge and skills needed to flourish.
For more information about the ADI, visit www.adi.org.uk
Dental nursing provides a dynamic and rewarding career for anyone with a passion for helping people. Practices across the UK are constantly looking to complete their teams with talented and dedicated dental nurses, who can make a difference to their patients and their practices.
The role is fundamental to the delivery of exceptional patient care, having a direct impact on the patient experience, clinical outcomes, the broader professional team, and the daily operation of the business.
At a time of increasing regulatory challenges, mounting time pressures, and rising patient demand, optimising quality and efficiency throughout the practice is essential. The dental nurse is the key to achieving this and more.
The cornerstone of excellence
Among the many roles of the dental nurse, patient engagement and education are central to improving treatment outcomes and overall patient satisfaction. A simple discussion with patients can make a significant difference to their treatment experience. The dental nurse assists the dentists and can be on hand to discuss treatment or concerns with the patients, helping to put their mind at ease. There is also evidence that interaction with the dental nurse can help to reduce dental anxiety in patients and improve their oral health-related quality of life.
Beyond the patient experience, dental nurses have a direct impact on clinical outcomes. For example, research suggests that the oral health education they provide in just a single conversation with families after their children require an extraction, can reduce the risk of further tooth decay by an impressive 29%. Evidence is also available to show that effective use of skills mix in the practice – including full utilisation of the dental nurse’s abilities –supports prevention and general treatment strategies, elevating outcomes.
A powerful career opportunity
The dental nursing role not only transforms patients’ lives – it offers professionals a chance to thrive in a highly progressive career that they love. There is nothing more rewarding than actively helping a patient improve their health and their selfesteem, guiding them and their family to better oral hygiene habits.
There is always room for growth as well. Diversification is possible with the development of extended duties, which include oral health education and promotion, assisting conscious sedation, special needs dentistry, intraoral photography, shade taking, suture removal, taking radiographs, and so much more. These additional skills can be gained through postgraduate education and further training, enabling individuals to tailor their learning according to their specific interests and passions. The result is a varied and exciting job where no two days are ever the same.
Further still, dental nursing affords a good career pathway and opportunity for progression. In the current dental landscape particularly, there are multiple career pathways available and a choice of job vacancies, allowing you to select the
very best working environment for your preferences and future ambitions.
To broaden capabilities and optimise job satisfaction, it is important that dental nurses are able to use their full scope of practice. This requires structured, high-quality, and consistent training and support, ensuring that individuals have the knowledge, skills, and confidence to perform tasks to the best of their ability.
All of this is achievable in the right practice environment ¬– one that nurtures and encourages, provides opportunities to grow, and offers a strong support structure. For example, Clyde Munro has developed the STRIVE programme. This is a 12-month, fully-funded training scheme for trainee dental nurses that introduces professionals to life in the practice and helps them build solid foundations for a long and prosperous career. Extensive clinical and administrative support is included, with additional education offered from Clyde Munro’s dedicated Advanced Dentistry & Clinical Skills Centre to prepare delegates for their first weeks in the practice. Postqualification, there are various employment opportunities available with ongoing support and guidance ensured.

Dental nursing is more than supporting the dentist in delivering treatment. It is a crucial role that directly shapes the quality of the patient experience, and contributes to the performance of the wider dental team. Dental nurses are also essential in the maintenance of high clinical standards. It is a meaningful and deeply fulfilling profession that offers individuals a diverse career that is rich in opportunity and joy.
To fulfil your potential, it is crucial to be part of a supportive team that embodies a culture of kindness and growth. With the right support, a career in dental nursing has the power to transform not only your professional life, but also the experiences and outcomes of the patients and communities that you serve.
To find out more about the STRIVE programme at Clyde Munro, please visit https://careers.clydemunrodental.com/ strive-programme/
About the author
Jo Hood, Head of Clinical Recruitment & Development at Clyde
Munro Dental Group.

The dental market is shifting - and practice values are still rising. If you’re planning your next move, up-to-date data is essential.
Inside our latest Goodwill Report:
• Average sale values now exceed £1.45M
• Group and corporate buyer activity is increasing
• Private and mixed practices command premium prices
• Confidence among independent buyers is growing
Scan the QR code to download your copy now.

















SprintRay has built a flourishing reputation on designing and providing first-class digital solutions to make 3D printing a vital extension of modern dental workflows. Their entire ecosystem amalgamates intuition, innovation, and coherence to streamline treatments and offer reliability beyond measure.
The new Duo Kit from SprintRay is the latest solution for clinicians, taking workflows currently using the Pro 2 3D printer to the next level

Firstly, an indispensable attribute of the new product is beyond the functionality and efficiency it brings to practices, but how it reduces everyday disruptions.
It involves a split-build platform and a dual resin tank system that permit the printing of two different resins in just one singular print job. Due to this, clinicians no longer waste precious time having to stop and swap materials between patients. Both materials can be cured independently yet simultaneously, ensuring the accuracy that the Pro 2 has always delivered.
the future is here
This revolutionary introduction of dual-resin workflows creates time-sensitive versatility. Clinicians and technicians now have the ability to:
• Print denture bases and denture teeth in one batch
• Create models and crowns together
• Build multiple appliances incredibly fast
• Deliver two shades of resin in the same job for multi-stage planning and production
These shifts in efficiency reduce downtime immensely – with more high-quality outcomes in fewer workflows and shorter amounts of time.
The Duo Kit is specifically esteemed for practices that offer – or are looking to offer –same-day dentistry. Appointments become streamlined, with comprehensive tasks condensed, and patient expectations better met. Not only does this encourage the rhythm of treatment delivery, but augments the patient experience beyond measure, guaranteeing enhanced satisfaction. Another benefit is the ability for practices to expand in-house services, opposed to outsourcing skill. This creates greater internal communication, faster treatment times, and even reduced costs in the long run.
The Duo Kit is designed around the existing SprintRay ecosystem, supporting the entire range of SprintRay resins. Between different patients, goals and expectations

differ – from strong and durable long-term dentures using the OnX Tough 2, aesthetic hybrid crowns, patient-specific retainers, and more – the Pro 2, with the upgraded introduction of the Duo Kit, offers the same great variety with minimised interruption.

Despite vast developments in the complexities of its engineering, the userexperience remains straightforward, yet sophisticated. Remaining familiar to the Pro 2 3D printer, the Duo Kit requires minimal staff training, integrating seamlessly into current workflows.
This ease-of-use is sustained by the strong and attentive support network offered by SprintRay. Users have constant access to real-time assistance, a responsive and dependable customer service team, and training material to help you easily get to grips with new features. The Duo Kit offers revolutionary technology, without any unnecessary complexity.
upgrades
As digital dentistry continues to advance rapidly, and patient expectations accelerate at a similar pace, ensure that your practice continues to align – always leading dental innovation with SprintRay.
The Duo Kit delivers a simple and comprehensive solution, offering incredibly streamlined workflows, enhanced patient satisfaction, exciting innovatively-led opportunities, and more control over in-house production – each paramount attributes for leading practices. Without making digital dentistry overly complicated, the developments on the Pro 2 3D printer make the Duo Kit an absolute must for your practice – creating accessible and sustainable opportunities.
Find out more about advancing with SprintRay, contact the team today!
For more information on the 3D printing solutions available from SprintRay, please visit https://sprintray.com/en-uk/ n

Dental pain can have a significant impact on patients. Depending on its severity, toothache can make it difficult for patients to eat, speak, and sleep. In these cases, patients frequently contact their dental practice, seeking care to reduce their pain as soon as possible. Even though clinicians endeavour to see patients as soon as possible when they are in pain, a same day appointment may be unrealistic – potentially requiring patients to wait hours or even days to be seen. When toothache strikes, act quickly. Recommend Orajel® to patients with toothache for fast and effective relief whilst they wait for treatment. Unlike traditional pain killers, such as oral analgesics which can take up to an hour to take effect, Orajel® provides rapid relief.
Orajel® is formulated with benzocaine, a powerful local anaesthetic, which is clinically proven to relieve pain in 2 minutes or less. This means that patients can expect rapid relief from acute toothache. This is incredibly important to patients, with research suggesting that 63% of patients prioritise speed in pain relief.
targeted relief
Orajel® gives patients the power to apply the gel directly at the source of pain. This kind of precision can really make a difference. A topical gel, Orajel® delivers localised relief, ensuring effective management where it’s needed the most.
Orajel™ is effective and, importantly, safe. 87% of patients experience significant pain relief when they use Orajel® Extra Strength. It has a non-systemic formulation and minimal drug interactions. This means it is well tolerated, and a reliable choice for a broad range of patients. It also means that it can be used alongside systemic analgesics, for enhanced pain management.
Benzocaine is absorbed rapidly through the oral mucosa, allowing it to act quickly to target dental pain directly, ensuring effective pain management in less than two minutes. It reversibly binds to and inhibits sodium channels in nerve cell membranes, blocking the conduction of nerve impulses, reducing pain signal transmission.
Additionally, depending on the intensity and the cause of dental pain, clinicians can recommend the most appropriate option from the Orajel® range. This includes:
orajel™ dental Gel

For rapid relief when it’s needed most, recommend Orajel® Dental Gel. It contains 10% w/w benzocaine, ideal for reducing pain associated with a broken tooth or in a tooth that may require a filling. The topical gel puts patients in control over the product, enabling them to apply it right to the source of pain, providing targeted relief.
orajel™ extra strength

For relief of severe dental pain, Orajel® Extra Strength contains the maximum level of benzocaine available without prescription in the Orajel® range – 20% w/w benzocaine. The Orajel® Extra Strength can be applied directly to the painful area, for effective and targeted relief. The powerful local anaesthetic that works by temporarily blocking the pathway of pain signals along the nerves. This numbs the area.
orajel™ Mouth Gel

For patients with painful mouth ulcers, or denture pain, Orajel® Mouth Gel is an effective option. It provides pain relief at the source of mouth pain, giving patients control over the product for targeted relief. Orajel® Mouth Gel contains 10% w/w benzocaine, effective for targeted relief. To help patients get their dental pain under control quickly, be sure to recommend Orajel®, for the rapid relief of pain whilst they wait for treatment. Even though reducing the symptoms is not a permanent solution to a patient’s clinical issues, reducing pain and distress whilst they wait for an appointment is vital, and will improve patients’ overall experience when it comes to dental treatment.
For essential information, and to see the full range of Orajel products, please visit https://www.orajelhcp.co.uk/ n
The innovative conical brush head glides smoothly between a range of interdental spaces to remove plaque effectively – making it easy and comfortable for patients who are just starting out.
Available in sizes S/M and M/L.



For decades, the bench has been the engine room of British dentistry. While the clinical team often receives the direct applause of the patient, the intricate artistry and scientific precision occurring in laboratories across the UK are what make lifechanging smiles possible.
As we move into 2026, The Dental Awards is proud to evolve alongside the profession. We are thrilled to announce the launch of our newest category: The Technical Excellence Award. In association with the Clinical Dental Technicians Association (CDTA) and British Association of Clinical Dental Technology (BACDT), and specifically designed for GDC-registered Dental Technicians (DTs) and Clinical Dental Technicians (CDTs), this award is more than just a trophy for the mantelpiece – it is a gold standard recognition of those who are mastering the intersection of clinical integration and technical mastery.
The landscape of dentistry in the UK is changing. The rise of the Clinical Dental Technician has shifted the way patients access removable prosthetics, while the digital revolution has transformed the humble dental lab into a hub of high-tech innovation.
We recognise that a great appliance isn’t just about “making a tooth”; it’s about understanding occlusal schemes, navigating complex implant systems, and adhering to the rigorous best practice standards that keep our patients safe.
The Technical Excellence Award has been created to celebrate those who don’t just follow a prescription but enhance the entire clinical outcome through their expertise.
Two paths to excellence
This category is unique because it respects the distinct, yet overlapping, roles of the DT and the CDT. This is what our esteemed panel of judges are looking for:
1. Integrated technical and clinical mastery Excellence looks different depending on your scope of practice, and our judging panel is looking for evidence of deep, functional understanding:
• For Dental Technicians: The judges are looking for “The Clinician’s Partner”. You must demonstrate an exceptional ability to interpret and execute complex prescriptions. Whether it’s a full-arch implant-retained bridge or a delicate ceramic restoration, the judges want to see how your technical fabrication respects the referring clinician’s requirements and the patient’s biological needs.
• For Clinical Dental Technicians: Judges want to see the direct impact. As you manage the patient journey from assessment to fit, they are looking for evidence of your communication skills, the accuracy of your direct impressions, and how your clinical assessment leads to superior functional and aesthetic results.



2. Innovation in practice
We aren’t just looking for traditional skill; we are looking for the future. The 2026 Technical Excellence Award puts a spotlight on those embracing advanced techniques and digital dentistry. Are you a pioneer in digital dentures? Have you integrated 3D scanning into a seamless workflow for complex fixed/removable cases? The judges would like to see how you are using technology to enhance the patient experience, improve fit accuracy, and streamline the workflow within the scope of UK practice.
The anatomy of a winning entry
Winning a Dental Award requires more than a few nice photos. To ensure a fair and rigorous judging process, all entrants must provide:
• A comprehensive case study: This is the heart of your entry. We need to see a patient case (or a series of cases) that demonstrates the full, start-to-finish journey. From the initial prescription or assessment through to the final fit, your entry should include diagnostic records, technical stages of manufacture, and high-quality clinical photographs.
• GDC integrity: This award is a mark of professional standing. All entrants must provide their GDC registration number(s) to confirm they are operating within the UK’s regulatory framework.
• The power of the testimonial: Excellence is best described by those who experience it. Your entry must include at least one


testimonial. This could be from a UK-registered clinician who relies on your lab work, or a patient whose quality of life has been transformed by your care.
Why you should enter
The Dental Awards are the original, longest running, and most prestigious awards programme of the UK dental profession. Being a finalist or a winner in the Technical Excellence category sends a powerful message to your referring dentists and your patients. It proves that you are committed to the highest standards of UK dentistry and that your work stands up to the scrutiny of the industry’s most respected experts. It is also an incredible boost for lab morale. In an era where recruitment and retention are challenges, being a Dental Award-winning laboratory sets you apart as a leader in the field.
Step into the spotlight
The unseen work of the technician is hidden no more. Whether you are an individual DT pushing the boundaries of ceramic layering or a CDT providing bespoke denture care on the High Street, we want to see your work.
Entries for the 2026 Technical Excellence Award are now open. Don’t let your best work go unrecognised. Gather your case studies, talk to your referring dentists, and show the UK dental community what true technical excellence looks like.
Enter at the-probe.co.uk/awards, completing your entry by 28th February.

















As a full-time working mum with two wonderful children who seem to have a club or activity every evening, life can feel like a constant juggling act.
For years, I believed stress wouldn’t affect me; I thought I was resilient enough to handle anything. But as time went on, the day-to-day pressures crept in. After always putting myself last, becoming unwell in 2024 felt as though I had received a wake-up call: I needed to make space for myself and manage stress proactively. Now, I’m strict about carving out at least 30 minutes a day for exercise. I’ve even joined the ‘5am Club’, and while it’s not for everyone, there’s something incredibly calming about moving your body before the world wakes up. That quiet time sets the tone for my day and reminds me that self-care isn’t selfish, it’s essential.
My experience isn’t unique. The 2025 Health and Wellbeing at Work report, by the CIPD and Simplyhealth, highlights just how widespread workplace stress has become across industries and shows that stress remains a significant challenge for organisations. In fact, 26% of organisations report stress as one of the top three causes of shortterm absence. The most common triggers include heavy workloads (41%), personal health issues (37%), and family or relationship challenges (34%). Over the past year, 64% of HR professionals have reported stress-related absence within their organisation. Encouragingly, 64% of organisations are taking steps to identify and reduce stress, yet only half (50%) believe their efforts are truly effective, suggesting that more robust strategies are needed to tackle this growing issue. Dentistry is an inherently demanding profession. The combination of tight schedules, high patient expectations, and strict compliance requirements creates an environment where stress can easily take hold. If left unmanaged, this pressure can lead to burnout, fatigue, and increased absenteeism, while also lowering morale and heightening the risk of mistakes. These challenges don’t just affect the team, they can disrupt clinical judgment, strain team dynamics, and ultimately impact the quality of care and the patient experience within the practice.
Stress management isn’t just about coping, it’s about prevention. Here are some tried and true strategies that have worked for my colleagues and I:
Start each day by identifying your most important task – the one that will have the biggest impact – and tackle it first. This approach is known as the ‘Eat the Frog’ technique, based on the idea that if you deal with the hardest or most critical task early, the rest of the day feels easier and more productive. Combine this with a clear daily task list and avoid multitasking, which can increase stress and reduce efficiency. By focusing on what matters most, you set yourself up for success and reduce the mental load of unfinished priorities.
Short pauses between patients are an opportunity to reset your mind. The Refocus Technique involves stepping away from your current task for a few minutes and engaging in something simple and different, like stretching, deep breathing, or even looking out of a window and observing your surroundings. This brief mental shift helps break the cycle of stress, clears cognitive overload, and allows you to return to your work with renewed concentration and calm. Think of it as pressing the refresh button for your brain.
Breathing exercises or short meditation sessions can calm the nervous system during busy periods. One simple technique is Box Breathing, which helps reduce stress and improve focus:
How to do Box Breathing (4-4-4-4 method):
1. Inhale slowly through your nose for 4 seconds.
2. Hold your breath for 4 seconds.
3. Exhale gently through your mouth for 4 seconds.
4. Pause and hold for 4 seconds before the next inhale.
Repeat this cycle 4 times. It only takes a couple of minutes and can be done discreetly between patients or during a short break. This technique signals your body to relax and helps clear mental clutter.
Stay physically active
This is a personal favourite of mine! Regular, physical activity is one of the most effective ways to manage stress, as it helps release tension and boosts mood. Activities like walking, cycling, or yoga outside of work can significantly reduce stress levels and improve overall wellbeing. Of course, finding time for exercise isn’t always easy during a full day of patients, but even short bursts during a break or committing to movement at the end of the day can make a big difference.
Seek support early
Stress often builds gradually, and it’s easy to ignore the signs until it becomes overwhelming. Speaking up early can make a huge difference. If you start feeling under pressure, reach out to your manager or a trusted colleague before things escalate. Early intervention allows for practical adjustments – whether that’s redistributing workload, offering flexible scheduling, or simply a listening ear. Many organisations also provide additional resources, such as the Employee Assistance Programme (EAP) that Denplan offers for teams, giving access to confidential support, counselling, and wellbeing advice. Asking for help is not a weakness, it’s a proactive step toward maintaining your wellbeing and ensuring you can continue to deliver high-quality care.
Employers play a vital role in reducing workplace stress and fostering a healthy environment for dental teams. It starts with monitoring workloads to ensure tasks are distributed fairly and no one is overloaded, which helps prevent burnout before it begins. Equally important is promoting honest conversations, creating a culture where staff feel safe to share concerns without fear of judgment. Investing in training programmes, such as stress management and resilience workshops, equips teams with practical tools to cope with pressure effectively. Organisations should also review policies regularly, using absence data and staff feedback to refine wellbeing initiatives and keep them relevant. Finally, leaders must lead by example, demonstrating healthy work habits, taking breaks, and prioritising wellbeing themselves. By doing so, it normalises them across the team and reinforces that wellbeing is a shared priority.
Stress is not a sign of weakness; it’s a reality of modern life. For dental teams, where patient safety and quality care are paramount, addressing stress proactively is essential. My journey taught me that making time for yourself isn’t optional, it’s vital. Whether it’s a 5am workout or a mindful moment between patients, those small steps can make a big difference.
Lianne Scott-Munden, Clinical Services Lead at Denplan.






RAPID RESPONSE


Clinically proven to get to work in under , relieving acute dental pain.4
TARGETED RELIEF
Benzocaine provides effective relief right at the source of dental pain.1-3
TRUSTED TOLERANCE
Orajel’s non-systemic formula is well-tolerated with minimal risk of side effects.1,2,4


WILL ORAJEL BE YOUR RECOMMENDATION FOR TARGETED, RAPID PAIN RELIEF?









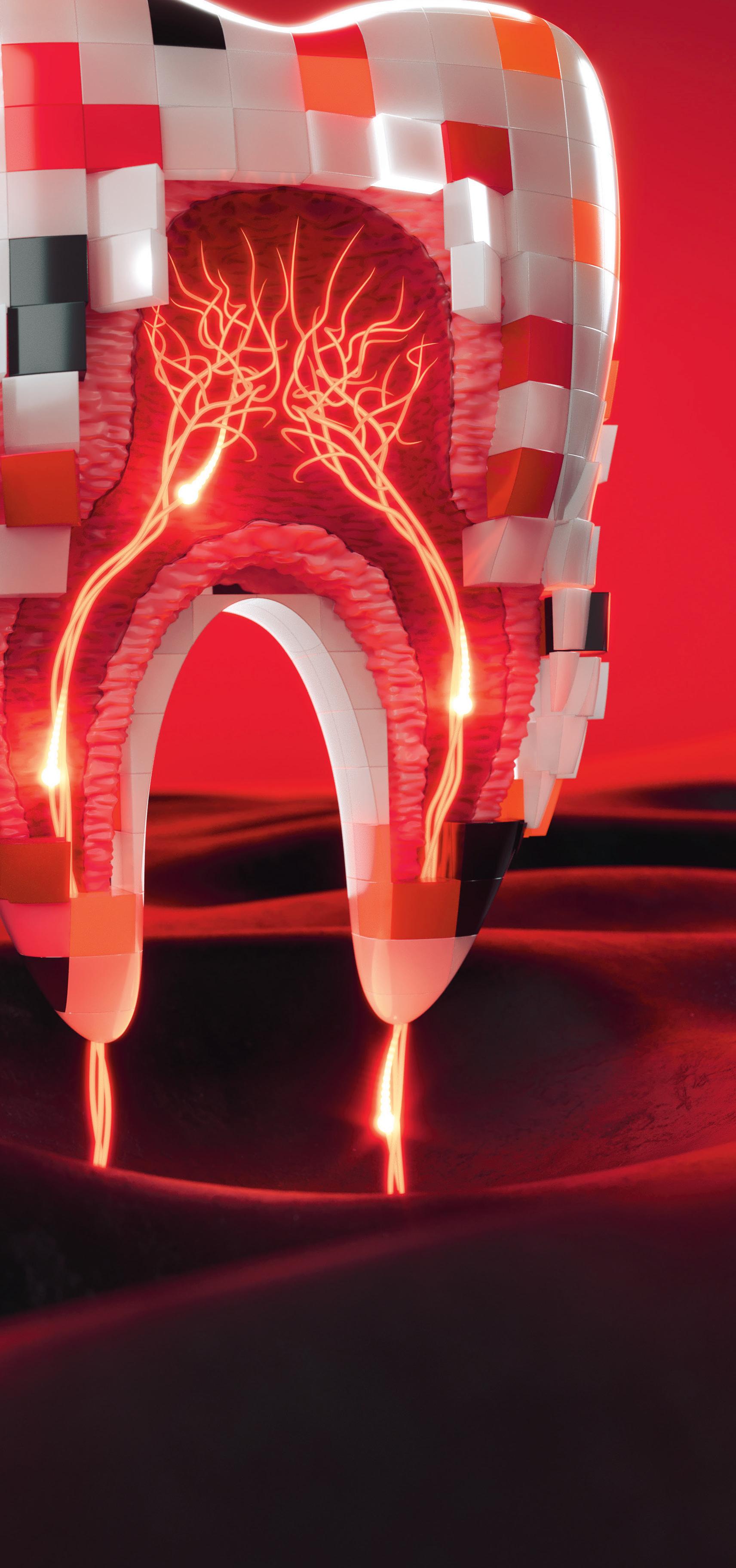

On 8th January 2026, the UK dental landscape shifted.
Agilio Software, the nation’s leading provider of healthcare operations software, officially announced its acquisition of Patient Plan Direct (PPD). This wasn’t just another corporate merger; it was a strategic alignment of two industry heavyweights, designed to create what has been described as a “powerhouse platform” for dental practices.
In a recent interview for The Probe Dental Podcast , Andy Sloan, Managing Director for Dental at Agilio Software, and Simon Reynolds, Managing Director at Patient Plan Direct, sat down to discuss the vision behind this union. Their message was clear: the future of dentistry isn’t just about clinical excellence – it’s about operational simplicity.
the right move at the right time The timing of the acquisition is no accident. Dentistry in the UK is currently navigating a significant transition, with a clear trend of practices moving from NHS contracts toward private or mixed care. In this environment, membership plans have become the bedrock of financial stability.
“Membership plans are central to that transition,” explains Andy Sloan. “By bringing PPD and Agilio together, we are combining compliance, workforce, and growth tools with a proven plan platform. This creates a joined-up solution that reduces admin overhead beyond what we could achieve before.”
For Simon Reynolds, the decision to join forces with Agilio was born from a desire to sustain and accelerate PPD’s rapid growth. “Partnering with Agilio provides that platform,” Simon notes. “We now have access to a wider pool of resource, technology expertise, and the exciting AI tools Agilio is developing.”
Curing app fatigue
One of the most persistent complaints from practice managers today is “app fatigue” – the overwhelming number of disconnected systems required to run a modern surgery.
“Imagine logging into one place to see your appointments, compliance status, plan performance, and marketing ROI,” says Andy. “We don’t want teams to be overwhelmed. We want them to have one place to manage everything, allowing them to focus on what they do best: delivering patient care.”
Data-driven growth and Ai
The vision for a modern morning routine in a dental practice involves AI doing the heavy lifting. Instead of manually auditing patient lists, the software could automatically identify growth opportunities.
“It’s about making growth more predictable,” Simon adds. “Having the infrastructure that Agilio provides means we can deliver these features faster and better than we could as an independent company.”
Despite the technological leap, both leaders emphasised that the human element remains at the core of the business. The PPD team has been fully integrated into the Agilio fold, ensuring continuity for existing clients.
“I’ve known the PPD team for a long time,” Andy remarks. “They are passionate, dedicated, and have a proven track record. Combining them with the Agilio team creates a powerhouse that can really change the game.”
Looking ahead
When asked what success looks like in three years’ time, the outlook was focused on reducing the administrative burden on clinicians and owners.
“I want to see thousands more practices running smoothly, with better patient outcomes and fewer grey hairs for the owners,” jokes Andy. Simon agrees, adding that his highlight would be “hearing from clients that this integration didn’t just make life easier, but helped them grow in ways they didn’t think were possible, backed by data to prove it”.
As 2026 begins, the Agilio Software and Patient Plan Direct partnership stands as a bold statement of intent. By bridging the gap between clinical compliance and financial growth, they are building the infrastructure for the next generation of UK dentistry. n
watch or listen to the full conversation now:

Christie & Co has observed strong demand from both independent buyers and a renewed wave of corporate interest, resulting in a highly competitive market for practice owners considering a sale.
To maximise value and secure the best possible price and terms, it is essential that sellers engage a reputable agent who can effectively explore all market opportunities.
• Advised on, agreed or sold 1,241 practices with a combined value of £1.68bn
• In addition to this we carried out 432 formal RICS Valuations with a combined value of £359,908,503
• Brought 205 practices to market
• Arranged 562 viewings
• Received 330 offers
• 6.7% increase in deals agreed compared to last year

It is vital that sellers seek trusted and professional advice when considering the sale of their practice.







Practice Plan is delighted to bring you this article, with the aim of supporting the ongoing Enhanced CPD needs of dental healthcare professionals and their teams
Objectives
By the end of this article, you should be able to:
• Explain why effective communication is essential in dental practice.
• Apply practical strategies to improve patient communication and reduce anxiety.
• Understand and implement the requirements for valid consent in line with UK law and GDC standards.
• Demonstrate how GDC Principle 2 underpins everyday patient interactions. Learning Outcome: A
“The single biggest problem in communication is the illusion that it has taken place.”
As George Bernard Shaw hints, it’s very easy for miscommunication to occur. Perhaps this explains why the General Dental Council’s (GDC) Principle 2 is: “Communicate effectively with patients.”
At first glance that sounds very simple. However, we have all been on the other end of miscommunication at some point in our lives. Communication can easily go awry if care is not taken over it. In a dental practice setting the consequences of poor communication can be dire for both the patient and the practice. For this reason, when speaking to patients, dental team members should ensure they communicate clearly at all times. This means listening carefully, explaining clearly and making sure patients understand their options before they agree to treatment.
Good communication is one of the most powerful tools in dentistry. It serves a much greater purpose than simply explaining treatment. It also helps to build trust, reduce fear and enables patients to feel confident in their decisions. The consequences of a communication breakdown include patients left feeling anxious, misunderstood or even misled, all of which can lead to complaints or legal/regulatory issues.
Why communication matters
Clear communication matters for many reasons.
Dental visits can be stressful. Patients often worry about pain, costs and outcomes. Effective communication helps to reduce anxiety by providing reassurance and clarity.
It also serves to build rapport, which is essential for developing trust. Trust is the bedrock of a successful relationship between a patient and practice. Without it, patients are less likely to take advice or accept guidance on treatment plans. Before they are likely to trust someone’s professional judgement, they need to believe that person is trustworthy and that they will be safe in their hands. Without rapport built through clear communication, they are unlikely to feel that way. Once trust and mutual respect
–
George Bernard Shaw
have been established, patients are more likely to take up suggested treatment plans or heed oral health advice, leading to better outcomes.
Great communication can also insulate the practice from complaints to a certain extent. People are generally less inclined to sue someone they like. The nature of dentistry is such that there is a possibility that something will go wrong during a dentist’s career. Those practitioners who have taken the time to make sure that they and their practice team communicate clearly with their patients are far less likely to find themselves subject to litigation or a fitness to practise complaint than those who have not.
GDC Principle 2 in practice
Principle 2 is a daily responsibility. Dental teams should ensure they give patients the information they need in a way they can understand. Treat them as individuals and take account of any cultural needs. Give them the time they need to ensure they understand what’s being said and check they really have understood before moving forward. Present all the risks, benefits and alternatives honestly, including doing nothing. Also, respect their right to make decisions about their own care.
How to communicate effectively
Here are some practical suggestions you can use every day in practice:
Listen actively
Listening actively means listening to understand, not just listening to respond. If a patient is expressing a concern, show that you value how they feel. Maintain eye contact and avoid interrupting. Demonstrate that you have heard them by reflecting back what they’ve said: “So you’re worried about the pain?”
Use plain language
Keep things simple. Use everyday language and avoid jargon. For example, instead of “You need an endodontic procedure,” say: “We need to treat the inside of your tooth to remove infection.”
empathy
A trip to the dentist can be very scary for some people. A 2024 survey [Space Dental] showed more than half of UK adults fear the dentist somewhat or a lot. This means it’s likely that a high proportion of patients visiting your practice will be feeling nervous.
If, after an examination it turns out that they need treatment, this anxiety may well heighten. Show empathy by acknowledging these feelings and take things slowly by saying something like: “I understand this feels overwhelming, but we’ll go through each step together.”
Reassurance is what’s needed when someone is feeling anxious or fearful. The Space Dental survey found that pain was what caused the biggest fear about visiting the dentist. Letting them know that their experience will be comfortable can help alleviate some of that fear and anxiety.
Pay attention to non-verbal cues
There is more to communication than just words. Your tone, posture, and facial expressions all matter too. Stay calm, confident and approachable, especially if you’re handling a complaint. Let the person have their say without interrupting and listen respectfully. Staying calm can help to diffuse a situation so that you can look at finding a way forward.
Check understanding
For consent to be valid, the patient needs to have understood what the treatment entails. To check they really
have understood, ask them to explain to you in their own words what they believe will happen. Try asking them “Can you tell me what you understand about the next step?”. This gives you the opportunity to correct any misapprehensions before going ahead. In addition to this, you should give patients a written treatment plan that they can refer to.
Many dentists adopt a shared decisionmaking approach. This is where the dentist's expertise (the various options, evidence, potential risks etc) is combined with the patient's preferences, values and personal circumstances to reach a mutually agreed-upon decision, rather than leaving the patient to simply make up their own mind.
Building trust
Trust has already been mentioned as an essential component of a successful dentist/patient relationship and it grows when patients feel respected and informed. Always introduce yourself and treat each patient as an individual. Personalise your conversations by using their name and referring to previous visits. Be transparent about how much things will cost, what risks (if any) are involved in treatments and make them aware of alternatives. You should also respect the patient’s autonomy. They have the right to make their own decisions regarding treatment so you should never pressure them into treatment. As well as being good ways to build trust, Principle 2 obliges practices to do these things anyway.
Principle Two - Communicate effectively with patients
Patients can expect:
• To receive full, clear and accurate information that they can understand, before, during and after treatment, so that they can make informed decisions in partnership with the people providing their care.
• A clear explanation of the treatment, possible outcomes and what they can expect.
• To know how much their treatment will cost before it starts and to be told about any changes.
• Communication that they can understand.
• To know the names of those providing their care.
Practice Plan has been welcoming practices into the family since 1995, helping them to grow profitable businesses through the introduction of practice-branded membership plans.
With over 300 years’ dental experience in our field team, if you’re looking for a provider that has that family feel but knows a thing or two about dentistry then you’re in safe hands. Be Practice Plan and get in touch. Call 01691 684165 or visit www.practiceplan.co.uk/be-practice-plan/

Barriers and solutions
You should make sure you communicate with patients in a way they can understand. Use interpreters or translated materials If there are language differences. Speak slowly, use visual aids and confirm understanding if your patient has hearing or cognitive issues. Be sure to allocate enough time for complex discussions if needed. Don’t rush your patients.
Valid consent: what you need to know
Consent is more than just a signature, it’s a process. UK law and GDC standards require that consent is:
1. Voluntary: The patient chooses freely.
2. Informed: They understand the nature, purpose, risks, benefits and alternatives.
3. Given by someone with capacity: They can make the decision. There are different types of consent that can be obtained and they vary according to the circumstances. These are:
• Implied: For simple checks (e.g., examination)
• Verbal: For minor treatments after a discussion
• Written: For complex or high-risk procedures.
When gaining consent, it’s essential to explain any material risks attached
Brought to you by

to the procedure. These would be risks that a reasonable patient would want to know. As well as the treatment you’re recommending, any alternatives also need to be discussed. This includes doing nothing. These discussions should all be documented in the notes.
It’s important to remember that, as well as being a legal obligation, consent is also about respecting the patient’s autonomy and dignity. Failure to obtain valid consent can lead to GDC investigations and civil claims. You should also bear in mind that consent is not infinite and we should continue to seek valid consent throughout a course of treatment, especially if anything changes.
Practical tips for gaining consent
It can be helpful to use diagrams or models to explain procedures as some people respond better to visual aids. Ensure you provide patients with written information regarding their treatment so that they can review it at home. Remember that you may need to revisit consent if treatment changes.
Conclusion
Effective communication and valid consent go hand in hand. By following GDC Principle 2, listening actively and explaining clearly, you can build trust, improve outcomes and meet your professional obligations. n
References available upon request.
1. Which of the following is NOT a principle of effective communication?
a) Active listening
b) Using jargon
c) Empathy
d) Checking understanding
2. What are the three elements of valid consent?
a) Voluntary, Informed, Capacity
b) Written, Signed, Witnessed
c) Quick, Efficient, Documented
d) Verbal, Implied, Written
3. Which of the following best describes the purpose of checking a patient’s understanding during the consent process?
a) To ensure the patient agrees with the clinician’s preferred treatment option
b) To confirm that the patient can repeat the clinical terminology accurately
c) To verify that the patient fully understands the risks, benefits and alternatives before proceeding
d) To speed up the consultation so treatment can begin sooner
Zygomatic implants are a valuable solution for patients with severe maxillary atrophy who are unsuitable for conventional implants or bone grafting. Anchored in the zygomatic bone, these implants bypass the need for vertical bone height in the posterior maxilla. While they offer high success rates and life-changing results, they also come with distinct risks and complications that clinicians must be prepared to address or refer if necessary.
Surgical complexity and anatomical risks
Placement demands precise anatomical knowledge and surgical skill. Proximity to the orbit, infraorbital nerve, and maxillary sinus increases intraoperative risk. Misplacement may cause orbital penetration, nerve damage, or sinus perforation.
Sinus complications
Sinusitis is one of the most frequently reported complications.
Sinus perforation during zygomatic implant placement typically occurs due to anatomical challenges brought about by its proximity to the surgical site. The thinness and variability of the sinus wall and Schneiderian membrane make it prone to accidental perforation.
This is particularly problematic given that patients who suffer from atrophic maxilla will typically present with a thinner wall between the sinus floor and the alveolar crest, thus the accidental breaching of the Schneiderian membrane is more likely.
Chronic sinus infections caused by sinus perforation compromise implant stability and cause significant discomfort for the patient. Some of the long-term complications include on-going nasal
congestion, nasal discharge, facial pain/ pressure, headaches, and a reduced sense of smell.
For these reasons, it is vital that clinicians are able to thoroughly analyse the anatomical characteristics of each patient using advanced imaging technologies.
Soft tissue issues
A prosthetic design which is overly bulky can cause the patient significant difficulties in their ability to maintain adequate oral hygiene, leading to the accumulation of bacterial biofilm around the implant. Controlling this is crucial to prevent the onset of peri-implantitis.
Inadequate keratinised mucosa around the implant may also contribute to long-term complications. Some studies suggest that healthy keratinised mucosa may protect the surgical site against microorganisms and subgingival plaque, thus decreasing the likelihood of peri-implantitis.
To allow for the patient to carry out adequate home-hygiene, clinicians should avoid over-contoured prosthetics that trap food and plaque, opting for smooth transitions between implant and soft tissue to reduce bacterial niches.
Prosthetic challenges
Achieving proper occlusion, aesthetics, and function requires careful coordination between surgical and prosthetic teams.
Poor implant positioning can also contribute to serious complications including orbital and ocular penetration or damage to the infraorbital nerve during the surgical drilling process due to improper preparation and lack of awareness of the patient’s anatomical features.
Prevention strategies
Effective preoperative planning is the cornerstone of successful zygomatic implant placement. It involves detailed imaging, typically with CBCT scans, to assess bone anatomy, sinus health, and proximity to critical structures like the orbit.
Digital planning tools and 3D models allow surgeons to simulate implant trajectories, anticipate challenges, and customise surgical guides, reducing intraoperative surprises and enhancing safety.
ZaGa technique
Precision in surgical technique is vital to avoid complications such as orbital penetration or sinus perforation. Surgeons must maintain correct angulation and depth during implant insertion, aided by navigation systems or custom guides.
One such system is the Zygomatic Anatomy-Guided Approach (ZAGA) technique. This is a patient-specific approach which aims to mitigate surgical risks using a variety of methods.
Firstly, the dental surgeon will use the ZAGA classification system which aims to group the anatomical evaluation of the concavity of the maxillary wall into groups ranging from ZAGA zero to four, giving the dental surgeon a clearer understanding of the individual anatomy of the maxillary wall and its relationship with the zygomatic implant’s path. This maximises the predictability and long-term success of the procedure.
Secondly, the ZAGA technique avoids the initial establishment of a window or slot into the lateral wall of the maxillary sinus before implant placement, in favour of opening a mucoperiosteal flap in the posterior maxillary wall and the superior zygomatic rim to allow complete visual control of the surgical site.
Mentors provide a key source of support to dental professionals, and can be beneficial to individuals no matter their career experience. One could seek guidance when foraying into a new clinical field, or be able to have second approval over their treatment plans when a vote of confidence is necessary. Seeking out a good coach or mentor is key, and clinicians have a number of aspects to consider. The first step, however, may simply be understanding what you want to learn from this partnership.
A mentor will be a trusted colleague who helps to progress skills and knowledge, provide new ways to assess challenges, and realise any opportunities for future training. In dentistry, the chances to develop professionally can span across many aspects of everyday care. An individual might choose a mentor that can help them tackle new clinical fields such as dental implantology, endodontics, or orthodontics, or perhaps provide new insights into how to run a practice as a business. Whilst these will be engaged with in formal educational settings, a mentor can provide
supplementary knowledge and guidance that enables clinicians to implement new approaches safely and confidently. Mentoring enables direct conversation and sharing of ideas in a way that might not always be possible in a larger classroom setting. Some mentors might also be able to work closely in person, offering shadowing opportunities if the aim is to develop clinical knowledge and skills. However, communication online now enables effective mentoring relationships to take place across the globe.
opportunities for success
Choosing the right mentor can be a considerable process. The elected individual should be knowledgeable, with an understanding of how best to support individuals by managing their own behaviours. This can enable them to adapt their teaching style where it will best help the mentee. The literature notes that some of the most important qualities of a successful mentor include approachability, communication, non-bias, patience, enthusiasm, trust and empathy. Each quality can also be used as examples of what makes a good dental professional. Alongside these, a mentor needs to realise the importance of commitment, their
Both immediate surgical complications and the long-term success of zygomatic implants depend on a variety of contributing factors, from individual patient lifestyle and oral hygiene habits to the adoption of progressive surgical techniques which mitigate the risks.
Practice makes perfect

Clinicians should seek to further their understanding of intricate surgical procedures, develop their ability to implement anatomically-specific treatment plans and master handson techniques by enrolling in training courses such as the Postgraduate Dental Institute and Hospital (ICE)’s Advanced Certificate in Full Mouth Oral Implant Rehabilitation.
This five-part programme, led by Professor Cemal Ucer and accredited by the University of Salford, includes both theoretical and practical elements including face-to-face lectures and live surgeries to help clinicians perfect their skills in this complex procedure and mitigate surgical risks.
Zygomatic implants are a challenging aspect of surgical dentistry. The successful implementation of the procedure relies on an advanced understanding of patients’ anatomy, cutting-edge surgical techniques, intricate preoperative planning and a significant level of hands-on practice. Contact Professor Ucer at ucer@icedental.institute or Mel Hay at mel@mdic.co to book your place. n
potential to network and open doors for their mentee, as well as having the relevant experience or credibility to provide support.
A dental professional may be able to learn more about a prospective mentor by finding them online, or speaking to clinicians who may also know them. A mentor may also be a clinician that one has worked with or learned from before, with the formalisation of this educational relationship building upon this prior collaboration.
Some suggest that mentoring not only has educational benefits, but can also improve morale and create a positive professional culture of communication, with the literature noting increased professional productivity from those who have been mentored in a clinical setting. Engaging in these opportunities can therefore have such a benefit on clinical care that it could be worth pursuing consistently.
To ensure mentoring remains rewarding over time, clinicians should push themselves in fields that they enjoy, find professional success in, and those that take professionals out of their comfort zones. This could include the provision of complex care, from orthodontic cases, to dental implant restorations.
One to One Implant Education offers leading mentoring opportunities through its courses, including the PG Diploma in Implant Dentistry, the ultimate entryway for any professional. A tiered peer mentor system ensures each delegate has a dedicated tutor who has previously completed the program, and is able to provide guidance and advice throughout their journey. Supported by world-class speakers, this mentoring set-up allows professionals to thrive with the support of their peers, simultaneously growing a network of confident and talented dental professionals.
Mentoring is to be embraced, but clinicians need to know what to look for in a mentor, and where to find one. By first considering how they want to progress their own path, it’s possible to develop a fruitful professional relationship.
To reserve your place or to find out more, please visit 121implanteducation.co.uk or call 020 7486 0000. n
about the author

dr Fazeela Khanosborne is the founding clinician of the Face dental implant multidisciplinary team for the one to one dental clinic, London.
Wear is real, so are our
Wear is real, so are our solutions
solutions
Pragmatic direct approaches for tooth wear from GC
Pragmatic direct approaches for tooth wear from GC



4 out of 10 patients are affected by tooth wear*
SCAN HERE to discover our wear solutions
*Azeez, A. A., Sheri f, S., & Franca, R. (2021). Statistical estimation of wear in permanent teeth: a systematic review. Dentistry Review, 1(1), 100001.
* Zielinski, G., Pajak, A., & Wojcicki, M. (2024). Global prevalence of sleep bruxism and awake bruxism in pediatric and adult populations: a systematic review and meta-analysis. Journal of Clinical Medicine, 13(14), 4259.
GC UNITED KINGDOM Ltd. info.uk@gc.dental +44 1908 218999
www.gc.dental/europe/en-GB

emma Wilks, Business Development Manager at Patient Plan Direct, challenges a common assumption
When a dental practice transitions from NHS to private dentistry, one of the most common and emotionally charged concerns raised by practice teams is about patients who are exempt from NHS charges. There is a deeply held belief that leaving the NHS means leaving behind communities on lower incomes or those relying on benefits, who need NHS dentistry the most, and won’t be able to afford private care. This concern often comes with genuine guilt. I see it time and again when working with dental teams going through an NHS-to-private conversion. Clinicians and front-ofhouse teams worry they are doing something wrong, turning their backs on the very people they trained to help. This feeling is especially strong among clinicians who themselves come from working-class or lower socio-economic backgrounds. And the idea of patients who are exempt feeling they have no option but to commit to a monthly payment for oral care from their preferred dentist can be particularly uncomfortable for these clinicians.
But what I’ve consistently witnessed during NHS conversions challenges this concern.
When practices introduce a private dental membership plan built around small, manageable monthly payments by direct debit, uptake among NHSexempt patients is often surprisingly high. Again and again, many patients who were previously exempt choose to sign up without hesitation. As

like non-exempt patients, they value continuity of care, predictable costs, and the reassurance of knowing they can access appointments when they need them. The narrative that exemption automatically equals inability or unwillingness to pay doesn’t hold up in practice.
One of the biggest issues with the NHS dental system is the treadmill it places clinicians on. Appointments may need to be rushed, treatment can be more reactive than proactive, and the focus is often on firefighting rather than prevention. Ironically, the very system designed to help exempt patients often prevents clinicians from delivering the quality of care they want and need to provide.
Dental plans change that dynamic. They allow practices to step away from volume-driven dentistry and instead focus on preventative care, regular reviews, and building trust.
For many patients, especially those who have spent years feeling rushed through appointments, this is not a luxury, it’s a relief.
There’s also a misconception that, if someone is exempt, they may not prioritise their oral health as much as other demographics, which isn’t the case. Maybe they just haven’t yet been offered a model that works for them. When private costs are spread monthly and clearly explained, dental care becomes predictable and manageable, not a sudden expense that causes stress.
Of course, it’s important to be honest: there will always be some people who genuinely can’t afford a

patientplandirect.com/nhs
about the author emma Wilks, Business development Manager at patient plan direct.
dental plan. No system can support everyone equally, and no practice should carry that burden alone. But that reality shouldn’t overshadow the many patients who can and do choose to stay with a practice when it goes private.
For that reason, I always advise practice owners going through an NHS-to-private conversion never to discount the likely uptake from patients simply because they are exempt. Time and again, we see exempt patients (and this goes for non-exempt too!) recognise the value of a private dental plan when the benefits are explained; from priority access to their preferred clinician, to preventative care, discounts on further treatment, and added benefits such as global dental cover. When the alternative is losing access altogether, many choose to stay, and they do so confidently. The reality is simple: more exempt patients join a plan than most practices ever expect.
The key message for dental teams is this: it’s okay to let go of the guilt. Choosing to work in a model that allows you to provide better care doesn’t mean abandoning your community. Often, it means serving them better, just in a different way.
For more information on NHS conversions, visit: https://patientplandirect.com/nhs n


patientplandirect.com/start
info@patientplandirect.co.uk
Ahead of her talk at the British Dental Conference & Dentistry Show in May, nina Farmer explores how dental nurses can make every contact count and how nutrition is one of the most powerful, and often underused, tools in preventative dentistry

Nutrition impacts oral health in many ways, from sugar and caries risk to more farreaching effects such as supporting periodontal outcomes and managing wider health risk factors. Yet due to time pressures and limited training, it’s often under discussed in everyday practice.
We are increasingly aware of the links between oral health and general health, but awareness alone isn’t enough. If we want to improve outcomes, we need to feel confident having conversations about diet, lifestyle and prevention in a way that is practical, safe and within our professional scope.
Making every contact count
One of the key principles I’ll be exploring in my session is ‘Making Every Contact Count’ — an NHS initiative that encourages anyone working in healthcare to use routine patient interactions to support wellbeing and lifestyle change.
In dentistry, we see patients regularly and often build long-term relationships with them. That gives us a unique opportunity to reinforce preventive messages at every appointment, whether that’s during oral health education, chairside support or routine reviews.
For me, making every contact count doesn’t mean delivering long lectures or overwhelming patients. It means using small, meaningful moments to encourage healthier choices and trusting that those small moments add up.
t he host response
I will also be exploring how nutrition supports the host response: the body’s immune and inflammatory processes.
Nutrients are essential for immune function and inflammation regulation, and it’s well established that diets low in essential nutrients are linked to a higher risk of infection and poorer healing. This has direct implications for periodontal disease, wound healing and overall treatment success.
When we understand this, nutrition stops being an ‘add-on’ and becomes a central part of clinical care.
s igns of nutritional deficiency
Many nutritional insufficiencies and deficiencies present first in the mouth, often before they are detected elsewhere in the body. Some of the key oral signs include recurrent ulcers, angular cheilitis, glossitis, dry mouth and delayed healing. These signs can be early indicators that something more systemic is happening.
Poor nutrition may also be linked to general health conditions such as anaemia, diabetes, osteoporosis, gastrointestinal disorders, hormonal imbalances and eating disorders, all of which can have oral manifestations.
One of the most common concerns I hear from dental nurses is, “I’m worried about saying the wrong thing.” That’s completely understandable and it’s something I’m keen to address.
For safe, generic advice, I always encourage focusing on adding to the diet rather than taking away. For example, never remove a food group, as this can be harmful, particularly for individuals with a difficult relationship with food.
Instead, I recommend asking open, nonjudgemental questions, framing advice positively, suggesting improvements
rather than restricting and using simple, supportive resources such as My Plate. This approach helps patients feel supported rather than criticised and is essential for lasting behaviour change.
Dental nurses are not expected to diagnose or manage complex nutritional or medical conditions, but they are ideally placed to recognise when something isn’t right. They have frequent patient contact, patients trust them, and they play a central role in preventative care pathways.
Any concerns about a patient’s general health should be signposted to their GP. This referral pathway is essential for safe, effective care and ensures patients receive the appropriate support. By understanding their role within the wider healthcare team, dental nurses can contribute to earlier intervention, better outcomes and more joined-up care.
At Dentistry Show Birmingham I’ll also be talking about practical tools that can support patient engagement, such as diet diaries. Used well, they can shift conversations from assumption to evidence and empower patients to reflect on their own habits — which is far more effective than being told what to do!
Diet diaries can increase patient awareness, help identify patterns, encourage ownership and provide a clear starting point for discussion.
thoughts
If there’s one message, I want to convey it’s this: Nutrition is a huge part of
prevention, and you have the confidence, opportunity and influence to make every contact count with your patients. By attending my session, I hope attendees will gain confidence in discussing nutrition with their patients, gain practical tools for patient engagement, clear guidance on signposting plus a deeper understanding of the role they can play in holistic care. Most importantly, they’ll leave empowered to use every patient interaction as an opportunity to improve health: in the mouth and beyond. n
Nina Farmer will be speaking at the British Dental Conference & Dentistry Show, which takes place on 15th -16th May 2026 at NEC Birmingham.
Her talk will be at the Dental Nurse Forum, hosted by the Society of British Dental Nurses, sponsored by the Ikigai Oral Hygiene programme by NSK. For further information and to register for the show visit birmingham.dentistryshow.co.uk.
About the author nina Farmer is a Dental therapist and dual-trained nutritional therapist with over 20 years’ experience in dentistry. she began her career as a Dental nurse and has since built a practice focused on prevention, holistic care and empowering patients to achieve better oral and general health outcomes.





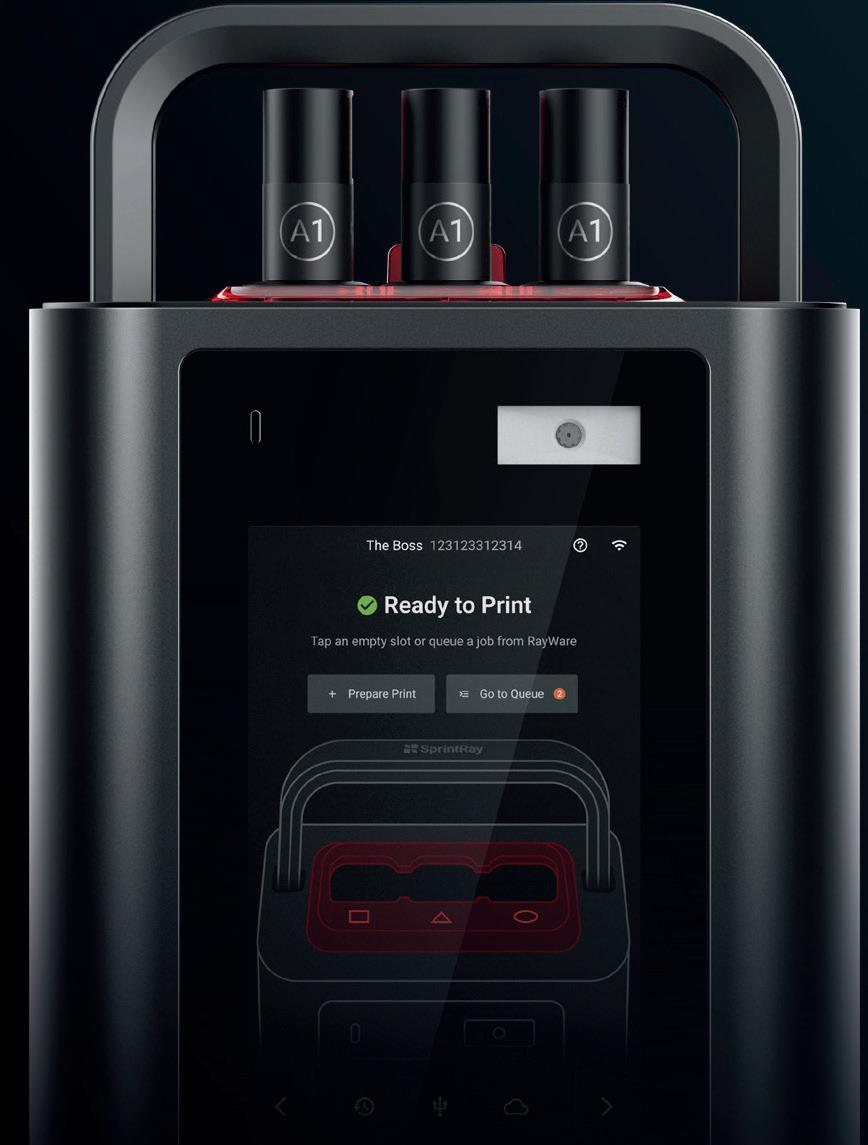

Patented Digital Press Stereolithography™ powers an all-in-one resin capsule system, printing ultra-viscous, ceramic-filled resins with unmatched precision. MDR-cleared for crowns, inlays, onlays, and veneers.
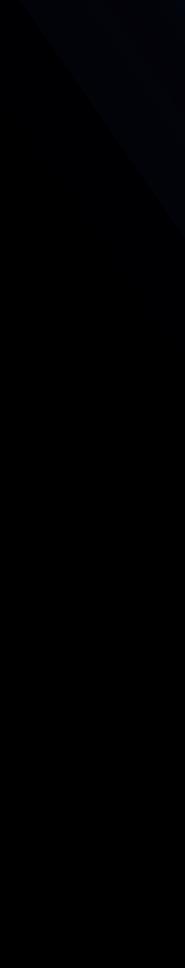

THE WORLD’S FIRST DIGITAL RESTORATION PRESS
See Midas in Action. Scan to schedule a Demo Today.



Our mobile showroom Plandemo is packed with the latest in cutting-edge technology and provides the perfect opportunity to explore our full product range at a time and location that suits you.
See the New Viso G1 CBCT imaging unit inside. Discover how easy it is to use first hand, and the high-quality clinical images it produces.
Try out our innovative Compact i5 kneebreak dental unit, with sumptuous Metallic Gold Ultra Relax upholstery.
Experience the rich selection of tools and features available in Romexis with a software demonstration, and find out how same-day dentistry can be incorporated into your surgery with the PlanMill 35 milling unit.

Want to incorporate digital dentistry into your practice? Book now at www.planmeca.com/plandemo and we’ll take care of the rest. n
• BeautiBond Xtreme: All-in-one universal adhesive with high bond strength, suitable for all etching techniques.
• BEAUTIFIL Flow Plus-X: Versatile, fluoridereleasing hybrid composite in 2 viscosities, perfect for Class I-V restorations.
• Super-Snap X-Treme Polishers: Achieve a flawless finish with our enhanced polishing disks for ultimate patient comfort. n

Improving one’s knowledge is vital to stay ahead in the field of dental implantology. As techniques, technologies, and materials evolve, clinicians must too. Due to this, access to high-grade learning opportunities is crucial in order to maintain positive confidence and a strong, updated skillset.
The Association of Dental Implantology (ADI) enriches members with a huge array of educational resources. This includes reduced fees to their world-renowned implantology conferences and £150 credit for use on the Osteocom Dental Education Platform. With webinars available too, an ADI membership encompasses every aspect of innovative learning. Each attribute delivers practical,

research-based information that is not only applicable to clinical performance, but also enhances decision-making and patient care. Discover how ADI membership can augment your role in implantology today!
For more information about the ADI, visit www.adi.org.uk Join todayn
Dental practices require support from a specialist waste management service, such as Initial Medical, to maximise the safety afforded to patients and clinical teams and ensure current regulations are met in full.
Based in the UK, Initial Medical has been an expert in hygiene and waste management for over 120 years, and today offers eco-friendly solutions to dental practices in the form of clinical waste containers. These include the Griff Pac containers, made from lightweight corrugated polypropylene, that are available in a wide range of designs to match the colour code implemented by NHS England. They also have the added benefit of a 74% reduction in weight versus rigid plastic containers, which helps reduce disposal costs overall.
Bossklein ETCHgel is perfect for all etching techniques and a vital part of restorative dentistry. It prepares the surface of the tooth, helping restorative materials adhere and ensures a longlasting result.
The 37% thixotropic phosphoric acid gel helps dissolve minerals in the outer layers of the tooth leaving behind a rougher surface. The ideal consistency and perfect texture help the etch gel stay in place on the tooth surface without collapsing. The optimum level of viscosity combined with the distinctive green colour enables accurate and unmistakable placement of the etch gel.
The Initial Medical team can also offer support for waste segregation in the practice, as well as waste collection, ensuring your items are managed in compliance with current regulations.
Simply get in touch today, or visit us online, to learn more.
To find out more, get in touch at: 0808 304 7411 or visit the website today. n

Available in 2 sizes – 12g and MAXI 60g. Each include enough bendable syringe tips for repeated applications. Available now. For more information call 0800 132 373 or visit: www.bossklein.com n
The British Endodontic Society (BES) Early Career Group (ECG) is an exciting initiative which engages with dental professionals at the early stage of their career who share a passion for endodontics.
The group supports dentists early in their endodontic journey by providing high-quality education and training for dental professionals pursuing career development in endodontics. In doing this the quality of endodontic care amongst newly qualified dentists in primary and secondary care settings is improved, and early career members are

Endodontics is a cornerstone of daily practice, yet complex cases and potential mishaps often bring clinical stress. Join The EndoGuys in London on 20th & 21st March 2026 for “The Principles of Endodontics,” a comprehensive course designed to ensure predictable, reproducible success in your surgery. Led by Specialist Endodontists Dr Ammar Al Hourani and Dr Brian Beggan, this programme offers an individualised approach tailored to your specific skill set. Through interactive lectures and intensive hands-on training with extracted teeth, you will master every step of the journey: from access cavity design to
mechanical preparation using systems like Wave One Gold and Protaper Ultimate. Covering irrigation protocols, bioceramic sealers, and pain management, the course provides 13 hours of CPD and serves as an accredited module for the ACE PG Diploma. Investment: £995 (£850 for mydentist GDPs & IDS members). to book: Email theendoguys@gmail.com. n

The Tapered Pro Conical implant from BioHorizons Camlog is designed to help optimise outcomes in immediate cases, including full-arch rehabilitation.
The product line was recently extended to include a regular platform 3.8mm implant for greater restorative flexibility. A streamlined clinical performance, with a single prosthetic platform offers simpler workflows and faster planning procedures for streamlined immediate full-arch cases.
This adds to the benefits already afforded by the Tapered Pro Conical, which include, controlled placement, excellent primary stability, reduced micromovements and surgical efficiency.
linked with more experienced endodontists for enhanced networking opportunities. For more information, please contact the team.
For more information about the BES, or to join, please visit the website www.britishendodonticsociety.org.uk or call 07762945847 n
britishendodonticsociety.org.uk

Optimise simplicity, efficiency, and clinical confidence with the Tapered Pro Conical implant from BioHorizons Camlog and unlock enhanced full-arch workflows. Find out more today. For more information on the Tapered Pro Conical implant from BioHorizons Camlog, please visit: www.theimplanthub.com/taperedproconical/ n
When seeking implant treatment, patients look for trust and reputation. How better to encompass this than by being part of a successful and professional organisation that demonstrates your commitment to excellence? The Association of Dental Implantology (ADI) offers just that – setting clinicians apart from the rest.
An ADI membership evidences quality and professionalism. Members have the opportunity to prove their pledge to ethical, evidence-based practice through the proficiency and visibility of the ADI Directory. Not only does this enhance credibility from the perspective of patients and peers, but it comes with multiple other benefits that distinguish clinicians as

excellent. Exclusive to members, clinicians are listed on the website for both member and public enquiries, and have full free access to the ADI logo – an esteemed mark within the industry.
Prove your guarantee of excellence by becoming a member of the ADI today!
For more information about the ADI, visit www.adi.org.uk
Join today n
Chairside workflows are becoming increasingly valuable, enabling practices to offer their patients the convenience of single-visit dentistry. Clark Dental has 50 years of experience working with dental professionals, providing surgery design and dental equipment.
Clark Dentals equipment portfolio includes the CEREC® Go, the costeffective entry to single-visit dentistry. Working with DS Core, CEREC® Go enables clinicians to produce dental crowns two times faster than 3D printing, offering a straightforward path for clinicians who want to achieve excellent restorative results with ease.
The Black is White Hydrosonic toothbrush harnesses the power of activated carbon to enable gentle whitening every day.
Ergonomically satisfying and visually pleasing, the stylish design of the toothbrush is matched by the aesthetic benefits it brings each smile – the brush heads are coated with activated carbon to absorb discoloured particles and brighten the teeth.
It’s not just a bright smile, but a healthy smile – the Black is White Hydrosonic toothbrush offers three different cleaning levels, reaching up to 84,000 movements a minute. This hydrosonic effects forces the toothpaste and saliva in the mouth, maximising the fluid to help push trapped food particles out from the interdental

Its super-fast grinding function enables clinicians to provide crowns, inlays, and onlays using hybrid ceramics and composites for natural-looking, strong results.
For more information, please get in touch with the helpful team.
For more information call Clark Dental on 01268 733 146, email info@clarkdental. co.uk or visit the website. n
Dr Michael Brown, 2025 winner of the British Endodontic Society (BES) General Dental Practitioner Award, shares a little bit about himself as well as his experience with the BES and preparing his entry:
“I decided to apply for the prize as I was completing more complex treatment and felt it was a good opportunity to reflect on the level of dentistry I was providing. I was delighted to gain recognition for my work, and believe there is value in self-reflection in dentistry.
“I found out that I had won the award whilst I was on holiday in France on my birthday, which was a lovely surprise. For this, I received a prize of £1,000 which was fantastic, however I found that the recognition I received and the sharing of my cases is what mattered most to me. Personally, it had a big impact on me, and
professionally it was great to share the news of this recognition with patients and referrers.
“I would absolutely encourage people in my position to enter for this award. It is a great opportunity to reflect on your cases, whether you win or not. The simple act of looking at the work you’ve completed is a great way to encourage yourself, and the process of applying is good too – just go for it!”
For more information about the BES, or to join, please visit the website or call 07762945847 n
britishendodonticsociety.org.uk
spaces, achieving a professional standard of cleanliness.
Driven by a powerful battery and stored in a sleek, compact case, the Black is White Hydrosonic toothbrush is a cuttingedge oral hygiene solution that marries the aesthetic with the functional.

To arrange a practice educational meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visit www.curaprox.co.uk and www.curaden.co.uk n
the Interim
The latest Dental Elite Interim Goodwill Report delivers vital insight into the current market, assisting principals who are planning to sell their practice – whether now or further down the line – with all the information they need.
The report demonstrates a strong market, evidenced by another increase in average deal value – from £1,276,078 in March 2025, to £1,458,050 by October 2025.
The report indicates that group buyers seek “big stock” assets, such as strong financial performance and well-established management. Independent buyers, however, prefer practices that are mixed, NHS, and then private, in that order – prioritising income stability.
In order to confidently approach the sale of

your practice, the Dental Elite Interim Goodwill Report provides essential insights to help you prepare. With live market data under constant analysis, principals can better understand buyer behaviour, divergence, and demand, enhancing their chance of a successful sale. Contact the team today to learn more about what to expect from the current and future dental market.
For more information contact Dental Elite. Visit www.dentalelite.co.uk, email info@dentalelite. co.uk or call 01788 545 900 n
To give your patients a brighter smile that they’ll love, introduce the BRILLIANT Lumina from COLTENE today. Utilising the technology of the future, the product is completely free from both hydrogen peroxide and carbamide peroxide. Containing PAP (phthalimido peroxy caproic acid) instead, it gently brightens teeth without the sensitivity often associated with traditional whitening solutions. It also requires a simple treatment protocol, involving uncomplicated application on the teeth for a smooth professional workflow. The result is happy patients and a happy team.

To see how you can give your patients a brighter smile with ease, discover the BRILLIANT Lumina from COLTENE.
For more information, visit https:// colteneuk.com/BRILLIANTLumina email info.uk@coltene.com or call 0800 254 5115. n
colteneuk.com/brillIantlumina
As an official partner of KaVo, Dental Directory is thrilled to support the innovative sustainability initiative available with KaVo treatment units.
This allows practices to trade in an old unit – any make, any model – and claim thousands off their new KaVo package. When you exchange your old treatment unit, you will receive:
• £3,000 off any KaVo uniQua package
• £2,000 off any KaVo amiQua package
• £600 off any KaVo E30 package
Further extending the green credentials of the transaction, KaVo will even plant a tree for each unit purchased, helping

to tackle the broader deforestation and climate change challenges of today.
To take advantage of this fantastic opportunity to upgrade your treatment unit in a more sustainable way, contact Dental Directory today.
For more information on the products and maintenance services available from Dental Directory, please visit ddgroup.com or call 0800 585 586 n
At DeNovo Dental Partners, caring for communities sits at the heart of who we are.Our Co-founder and Chief Executive Officer, Mark Aichroh, demonstrated this in a remarkable way. As a long-standing volunteer and First Responder with Festival Medical Services (FMS), Mark joined Nich Woolf, Chairman of FMS and retired paramedic, to deliver an ambulance filled with critical medical supplies to Ukraine. The vehicle was donated by FMS to the Ukrainian Army’s 5 Brigade and will be used in the Donbas, supporting frontline teams where resources remain desperately limited.
The ambulance was loaded with trauma packs and essential medical equipment – practical help that will make a real difference to those providing emergency care in the toughest of conditions.
When asked why they do it, Nich put it simply: “Because neither of us want to have just been a passenger in this life – we want to do something about the troubles going on around us.”

Together, Mark and Nich undertook the 1,630mile journey across Europe, delivering vital aid to Kyiv at a time when medical support is urgently needed. Their effort is a powerful reminder that meaningful contribution can start with individuals choosing to act.
Anyone wanting to get involved or support Festival Medical Services can visit the website. n
Offer your dental implant patients the optimal oral care package with the Curapox Implant Regenerate Kit, perfect for both the postsurgery window and the ongoing maintenance after restoration.
Along with the amazing CS Surgical brush for use after dental implant treatment, the kit also contains the CS 5460 Ultra soft toothbrush and CS 708 Implant toothbrush, which features a unique brush head shape and flexible neck for easy cleaning around implants. The kit also contains the Curaprox CPS Implant specific interdental brushes, and a comprehensive implant advice booklet.
To support healing, the kit includes a Perio Plus Regenerate mouthwash. Containing chlorhexidine at 0.09%, the innovative Citrox®

bioflavonoid antibacterial compound and hyaluronic acid, Regenerate helps reduce inflammation and promotes faster soft tissue healing when used along with its partner product, Perio Plus Support toothpaste.
The Implant Regenerate kit offers enhanced post-surgery healing, better protection against peri-implant disease, and helps patients ensure that their implants are long-lasting. Recommend today to elevate your dental implant patients oral health.
To arrange a practice educational meeting with your Curaden Development Manager please email us on sales@curaden.co.uk n
Clark Dental recognises the importance of choosing superior equipment. Having worked with dental professionals upgrading their practices for 50 years, Clark Dental offers a range of high-quality imaging systems, helping you to select the best option for you.
By investing in the right intraoral imaging systems for your practice, clinicians can decrease the time to diagnosis and accurate treatment. Clark Dental offers the XIOS XG Supreme AE – a leader in its class – equipped with multiple cable lengths, sensor sizes, and connectivity options, the system optimises chairside diagnosis for every patient.
Find out more about the products and services available from Clark Dental by getting in touch with the team. For more information call Clark Dental on 01268 733 146, info@clarkdental.co.uk or visit www.clarkdental.co.uk n
At Dental Directory, we are always striving to enhance the experience of every single clinician and practice team member we work with.
That’s why our comprehensive portfolio includes an array of industry-leading equipment and handpieces, as well as the servicing and maintenance support you need to keep them running smoothly for longer.
Close collaboration with various dental manufacturers means that our engineers are trained to effectively test, assess, repair and service all the equipment brands we supply. This allows us to achieve a 92% first time fix rate, giving you complete peace of mind.
EndoCare includes some of the most experienced and highly trained endodontic specialists and experts in the UK. This means you and your patients receive exceptional treatment outcomes and a smooth journey with every referral.
Introducing:
• Dr Adi Moran – Endodontic Specialist
• Dr Satinder Matharu – Endodontic Specialist
• Professor Federico Foschi –Endodontic Specialist
• Dr Michael Sultan – Endodontic Specialist
• Dr Corneliu Gherasim – Endodontic Specialist
• Supported by Beverly Street and Fiona Gore

We also offer simple annual service plans that help you budget for long-term maintenance, protecting your equipment from malfunction and your business from disruption. Find out more today. For more information on the products and maintenance services available from Dental Directory, please visit ddgroup.com or call 0800 585 586 n

With decades of combined experience in dentistry, the EndoCare clinical team offers various endodontic services, including endodontic microsurgery and retreatment. The referral process is also quick and simple – just complete the secure online form to get started. Contact us or visit the website today for more information.
For further information about the endodontic referral services available from EndoCare, please call 020 7224 0999 or visit the website. n
Recruitment remains one of the greatest challenges faced by dental practice owners in today’s industry. Dental Elite understands the importance of a strong and consistent team – supporting staff recruitment for practices and individuals job searching across the UK.
Talent shortages continue to challenge the field, which is why Dental Elite assists practices in securing durable talent through tailored recruitment and transition solutions. Adrian Byrne explains that when working with Dental Elite, he “always felt they were on his side and had his back, with regular contact and a well-fulfilled outcome”.
The supportive Dental Elite team works with you to ensure the best outcomes for your practice.
High-quality radiographic imaging is at your fingertips with the CS 8200 3D Access CBCT scanner from Carestream Dental, a solution optimised for intuitive clinical use.
Featuring a modern, user-friendly interface, the CS 8200 3D Access makes CBCT imaging simple for patient and clinician, helping to develop accurate, insightful results with minimal scanning time. The ultra-compact design is also adjustable for different patient needs, ensuring a variety of individuals can benefit from leading radiographic scanning. A low-dose imaging mode is integrated into the CS 8200 3D Access, allowing clinicians to record 3D images at the

Whether a dental practice searching for the perfect new addition, or a practitioner seeking your next new challenge, the expert consultants go beyond filling job vacancies –guaranteeing to reinforce the strong team already in place, building upon them to thrive. Find out how Dental Elite can help you build and retain the right team for lasting success!
For more information contact Dental Elite. Visit www.dentalelite.co.uk, email info@ dentalelite.co.uk or call 01788 545 900 n
How can you take your practice and business to new heights? Prav Solanki is here to show you with the Business and Mindset Mastery course from IAS Academy.
Delegates will discover the key to an effective work-life balance, whilst reaping the benefits of business growth thanks to actionable targets and goals for the entire team to embrace.
After breaking down business processes, professionals uncover the importance of storytelling in more than marketing – instead, it goes as far as everyday conversations with patients about clinical findings and treatment recommendations. All delegates build a 90-day plan
that can be immediately implemented in their practice in the hopes of positive growth, day by day. You can learn more about the course, and all available dates, by contacting the IAS Academy team today.
For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
same or lower dose as a standard panoramic examination.

Clinicians can also benefit from additions such as CS MAR (Metal Artifact Reduction) technology, which gives confidence in more diagnoses. Learn more about effective CBCT imaging by contacting Carestream Dental. For more information on Carestream Dental visit www.carestreamdental.co.uk For the latest news and updates, follow us on Facebook and Instagram @ carestreamdental.uk n
For those considering the introduction of a dental plan into their practice, IndepenDent Care Plans (ICP) is your trusted partner – providing insightful support since 1995.
Dental plans include support and marketing materials, including your logo with branded patient registration packs, brochures, and posters – delivering tailored solutions for your practice. Each plan offers flexibility, guaranteeing that all your specific needs and those of your patients are met.
Celebrating 30 years in UK dentistry, ICP is renowned for its dependability, delivering predictable outcomes by providing all the tools and expertise necessary. From streamlining workflows to enhancing
patient retention, ICP has a plethora of resources available to you, provided by the friendly and knowledgeable team.
To find out more about taking your practice to the next level, contact the ICP team today!
For more information about ICP and to book a no-obligation consultation, please visit ident.co.uk or call 01463 222 999 n
When navigating the complexities of practice valuation, the right support is vital. Dental Elite offers everything you need to make the process seamless – helping you achieve your sale ambitions.
The valuation experts guarantee clear, evidence-based guidance into the true valuation of each practice. Described as “responsive and proactive” by recent client David Cook, the Dental Elite team fulfil every promise they make – ensuring a “nonpressured approach,” and “an overall excellent experience”.
Dental Elite understands the differences that each practice offers, adjusting analysis and tailoring advice accordingly, ensuring the best outcome for you. They deliver a thorough snapshot of your business’s health
and accurate practice valuations so you know what you could achieve on the market – a precise valuation can make the difference between a smooth sale and months of delay.

Find out more about the future of your practice, from those that understand the dental market from every angle. As David said: “Go with your instinct and speak to the team today!”
For more information contact Dental Elite. Visit www.dentalelite.co.uk, email info@ dentalelite.co.uk or call 01788 545 900 n
After 20 years of building The Dental Studio from the ground up, Dr Stephen Pitt has chosen to join DeNovo Dental Partners. He shares his experience of becoming part of a shared-ownership group:
“I felt I had taken the practice as far as I could on my own – I was hitting a ceiling and needed more knowledge and expertise to unlock the next stage of growth.
“Getting to know the DeNovo team was integral to the decision-making process; I came to really understand who DeNovo is. This, combined with the opportunity to keep the identity of the practice intact and continue managing it without external pressures, tipped the scales.
Carestream Dental’s latest innovation in digital implant planning is CS 3D Implant Premium, an advanced AI-powered software solution that streamlines workflows, improves case acceptance and simplifies case sharing between professionals.
Utilise CS 3D Imaging Premium and its AI capabilities to automate routine tasks, accelerating the implant planning process. Once you merge a CBCT scan with digital impressions, the AI Auto Implant feature automatically identifies and numbers teeth. Then, select an implant from a digital library featuring more than 100 manufacturers, and the program calculates an appropriate crown position and the dimensions and position of the virtual implant, all whilst accounting for the present anatomy.
“Now, the environment is one of collaboration, with support I can use as much as I want. The whole team remains easy to work with and really approachable. All of this has been achieved, despite nothing changing for practice staff – promises of autonomy have definitely been fulfilled.
“If you love the practice that you have built and wish to remain a part of its journey for a bit longer, DeNovo could be the answer you’re looking for.” n
Successful implant practice requires the right tools, support, and knowledge.
The Association of Dental Implantology (ADI) offers its members an entire bank of useful resources that maintain confident and successful procedures. From journals, newsletters, and CPD resources, each of these offering practical guidance. Members can access exclusive discounts from industry partners, such as the International Journal of Oral Implantology (IJOI) to enhance your clinical success. From general enquiries to complex advice-seeking, having ADI to reliably resort to allows clinicians to dedicate all their time and energy into
delivering exceptional care.
With the ADI guiding them, members can flourish in every aspect of their patient-care.
Explore an ADI membership today to enhance your implantology knowledge and practice!
For more information about the ADI, visit www.adi.org.uk
Join today n
Dr Onkar Mudhar’s passion for supporting patients has been supported by the excellent range of toothbrushes from Curaprox. Driven by the desire to provide long-term support and to change public perceptions around dentistry, Dr Mudhar highlights how Curaprox products make a difference:
“I always recommend the CPS interdental brushes and the CS 5460 toothbrush to my patients – they are eye-catching and lead to excellent compliancy and oral hygiene outcomes. In particular, the soft bristles make them ideal for perio patients, promoting a comfortable clean that accommodates the sensitive gingivae.
“As well as the functional benefits, Curaprox products enliven the dental practice with their vibrancy. From the colour-coded sizes of

the CPS interdental brushes to the variety of bright handles for the CS 5460, their products are aesthetically pleasing and make the dental practice seem more inviting and less sterile. Patients will walk in and immediately notice them, sparking interest. I highly encourage fellow dental professionals to recommend Curaprox products for outstanding oral hygiene results among their patients.”
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk For more information, please visit www.curaprox.co.uk and www.curaden.co.uk n
Orthodontic patients face unique oral hygiene challenges – many of which can be solved with the Orthodontic Kit from TANDEX.
The set contains the ADVANCE toothbrush with a V-shaped cut, cleaning around braces easier and more effectively. Other features include a combination of precision tools and brushes to support patients throughout treatment; the FLEXI Lime easily removes plaque and food debris from underneath the metal wires with the conical brush design. Sensitive areas of the mouth – such as the tongue and cheeks – are protected from the sharp edges of the metal
The case plan can be exported as STL files to labs, or exported directly into Smop or BlueSkyBio software for surgical guide creation.
The Share My Case service seamlessly enables sending CBCT data and implant planning files online without manually exporting the data.
It is crucial to maintain your dental equipment, reducing the risk of breakdowns and saving your practice time, money and hassle in the long-run.
At Dental Directory, we make this easier with the availability of different service plans:
All premium features are available through a new subscription plan, but you can experience them in a free 30 day trial, simply get in touch.
For more information visit the website below.
Follow us on Facebook and Instagram @ carestreamdental.uk n
brackets by the BracketWax, whilst it soothes sore tissue. Find out more about how the Orthodontic Kit from TANDEX can revitalise the lives of your orthodontic patients today.
For more information on Tandex’s range of products, visit https://tandex.dk/
For product samples and orders, please contact DHB Oral Healthcare: https://dhb.co.uk/ n
• Option 1 is an annual solution that covers two pieces of equipment, supporting your practice compliance and minimising the risk of malfunctions
• Option 2 provides fixed costs for a longer timeframe, inclusive of all manufacturer supplied parts and labour costs
• Option 3 is for the maintenance and repair of small equipment and handpieces.
For the latter, we even strive to return them to you within 48 hours
All repairs come with a warranty as standard to offer you confidence in the quality of services delivered. Find out more by contacting the team today.

For more information on the products and maintenance services available from Dental Directory, please visit ddgroup.com or call 0800 585 586 n
Toothache can ruin anyone’s day – and for some, more than that. This National Toothache Day, OrajelTM are here as a reminder that fast and effective relief is always available – with the OrajelTM Dental Gel.
Anything can cause toothache – from ice-cold food and sweet treats to harsh pressure on the tooth. The OrajelTM Dental Gel is designed to provide targeted toothache relief exactly where and when it’s needed.
Its fast-acting 10% w/w benzocaine formulation works by temporarily blocking the pain signals along the nerves, numbing the area for rapid relief – until they can seek appropriate support from dental professionals.

Advising on the use of OrajelTM provides patients with a safe, easy, and accessible source of comfort – offering them personal and confident control over their suffering. Recommend OrajelTM Dental Gel today – delivering reassuring relief no matter when or where.
For more information, and to see the full range of Orajel products, please visit the website below. n

Attracting new patients and retaining existing ones requires a clear strategy. The good news? Impactful marketing doesn’t always require major spending. With forethought and consistency, you can strengthen patient relationships, grow revenue, and even increase the value of your practice when it’s time to sell.
Why marketing matters
Marketing is about more than advertising – it’s about building trust, visibility, and loyalty.
How a strong marketing plan helps you:
• Retain existing patients by keeping your practice top-of-mind and reinforcing value
• Attract new patients by showcasing your services and differentiating your practice
• Protect your revenue by reducing gaps in your appointment book and improving patient recall
start with what you already have Before spending a penny, maximise your existing resources:
• Your patient database: Use it to send appointment reminders, notices, and newsletters. Regular communication builds loyalty and encourages repeat visits
• Your website: Ensure it’s up to date, mobile-friendly, and easy to navigate. Include clear calls to action (e.g., “Book an appointment”)
• s ocial media: Free platforms like Facebook and Instagram allow you to share updates, oral health tips, and behind-the-scenes content to engage your community
Your strategy is your overarching goal – for example, becoming the leading dental implant provider in your area. Your tactics are the channels and actions you use to achieve that goal, such as social media campaigns, SEO, or local press advertising. If you’re preparing to sell within the next two to three years, it’s important to establish a realistic strategy and consider your approach. Implementing the strategy in stages will help you and your team build momentum and allow for meaningful wins along the way.
1. e mail marketing: Use free or lowcost tools to send newsletters and promotions. Share helpful content, such as oral health advice or seasonal offers, to keep patients engaged.
2. Google My b usiness Profile: Claim and optimise your profile. Add photos, opening hours, and encourage satisfied patients to leave reviews. Positive reviews boost credibility and local search visibility.
3. s ocial media engagement: Post consistently. Showcase your team, behind-the-scenes content, patient success stories, and testimonials (with consent), and highlight your services. Authentic content builds trust and humanises your brand.
4. c ommunity presence: Attend local events or partner with nearby businesses for cross-promotion –and don’t forget that word of mouth remains a powerful referral tool.
internal marketing: Your best ROi
Internal marketing offers the highest return on investment because it costs less to reactivate an existing patient than to acquire a new one. Tactics include:
• Reactivation campaigns: Send newsletters to patients who haven’t visited for years. A printed newsletter or targeted email can entice them back
• Welcome literature: Invest in highquality patient packs for new enquiries, making them personal and professional
external marketing: attracting new patients
New patients remain the lifeblood of any practice. Consider these approaches:
• Website optimisation: Ensure your site is mobile-friendly, easy to navigate, and optimised for search terms like “dentist near me”. Online chat features can offer instant engagement
• Local press: Don’t overlook print media, especially for reaching mature audiences. Many publications offer competitive rates as advertising shifts online
• Event marketing: Link treatments to events and specialisms. Host open days to encourage local engagement and interest
set goals and track progress
Define what success looks like before launching any campaign. For example, if you aim to attract 20 new orthodontic patients over six months, ensure your team understands the target and track progress weekly. Adjust your tactics as needed to improve results. Finding the time and resources to implement a marketing strategy can feel challenging – especially when your existing team is already operating at full capacity. However, effective marketing doesn’t always require additional headcount. With the right structure, clear responsibilities, and manageable
expectations, your current team can play a valuable role in supporting your practice’s growth.
budget wisely
Set a marketing budget as a percentage of turnover. While the exact figure depends on your objectives, remember that even large global brands invest heavily in marketing. Consistent, strategic spending will pay dividends in patient acquisition and practice value.
final thought
Marketing doesn’t have to be expensive to be effective. With a clear plan and consistent effort, you can strengthen patient relationships, attract new business, and future proof your practice, even on a limited budget. Better still, a well executed marketing strategy can significantly enhance your practice’s appeal to buyers when the time comes to sell.
Ready to position your practice for success?
At Lily Head Dental Practice Sales, we specialise in helping principal dentists maximise the value of their practices and navigate the complexities of today’s market. Whether you’re planning to sell now or in the future, our team offers trusted advice, tailored strategies, and hands on support to help you achieve the best possible outcome.
Contact us today to discuss your goals and discover how we can help you position your practice for success. dentalpracticesales.co.uk n
about the author abi Greenhough, Managing Director of Lily Head Dental Practice sales.





Hands-on Clinical Training with Guaranteed Implant Placement - 86 CPD hours (verifiable) This course exceeds any GDC Implant Training Guidelines
Hands-On Experience
Placeup to 4 implants over 2 days under direct clinical supervision, guaranteed for every delegate
Patients are triaged and provided
Treat straightforward to basic advanced level cases; single units, small gaps, non aesthetic cases and GBR where required
Build real-world competence and confidence in a safe environment
Complete Patient Pathway
Fromconsultationto restoration,including logbook completion
Restoration is advised and additional to the course; arranged direct with your Clinical Supervisor
Instruction and support in logbook completion for professional documentation
CBCT Training Included
Level 1 &2trainingfulfilsUKrequirements, no separate course needed
Duration
March 2026 –December 2026
Venue
Central London & Carlisle
Weekend Delivery
Saturdaysonly,minimisetime away from your clinic
Fee
£9,500 + VAT
CBCT Masterclass with Dr Jimmy Makdissi
Two remote/virtual learning days included in your course fees.
Laptops and cases provided No hidden extras!

Many principals may have identified that they would like to sell to a Body Corporate for the purpose of the confidentiality of the sale, the ability to continue working clinically post sale or because they deem it to be the right fit due to the size of the practice.
Often, these sales are not out in the public domain. For instance, we have agreed five sales in January alone that have never been openly marketed and have gone to a selection of suitable buyers. Good agents will have regular contact with Corporates, understand who is looking in which areas and, from your practice specifics, should be able to identify the types of buyers that would be suitable with ease.
In reality, the Corporate market is not just the handful of well-known names. The Corporate market is filled with many smaller groups that can be more competitive in their offers to establish themselves with a number of practices in a quick time, or smaller cluster groups that are looking for practices in certain areas.
The Corporate market is constantly changing. Some have stopped buying over periods of time (but may still be loosely looking to appear to still be in the market), new groups are being created constantly and smaller groups continue to expand.
ebiTDa
The well-known EBITDA (earnings before interest, tax, depreciation and amortisation) is very important for a Body Corporate. In reality, by purchasing a practice, they are looking to add profit (EBITDA) to their total position. The calculation is based under an ‘associate led’ model, meaning that the principal is costed in as an associate.
To realise the best price, the calculation of the EBITDA should be undertaken independently from the buyer, as a valuer/agent can identify costs that should be removed or a slight change in the way the practice is structured, which can have huge benefits to the EBITDA and a multiple of this. Examples can be the recharge mechanism made for associates using hygienists and making sure that this is cost neutral or lowering the principal’s new
associate rate. Also ensuring that one-off costs that have been included within the latest accounts are identified and removed with explanation. As associate-led multiples can often range between 7-8, an extra £20,000 adjustment in the EBITDA would create extra value of £140,000£160,000. Discrepancies far higher have historically been identified and show the importance of having someone on your side who is as experienced as the Corporate. I have also identified errors in Corporate calculations, which, if you did not have a comparative calculation, would never be realised.
The main consideration with a Corporate that differs from a principal buyer, is the terms that come alongside the financial offer. There are typically two main requirements:
Principal Tie-In – As a Corporate, unlike an owner occupier, they are not looking to come and work in the practice. Therefore, they require the continuation of the principal to work at the practice post-sale. The length of the tie-in can be impacted by the level of gross fees or type of treatment that the principal undertakes. A simple way to look at this may be how easy or hard the principal is to replace. Typical ties-ins can range from 2-4 years.
Guarantee of Income – Most of the larger Corporates require a turnover-based target. For example, the practice must achieve the same turnover for the following three years. Interestingly the smaller Corporates do not generally require any targets, and where there is significant competition for the practice you can find that their requirements may be more relaxed to remain a competitive offer. Payments and Deferred – Some of the larger Corporates may typically offer 80% of the sale price upfront and require 20% deferred. The deferred would then be paid over the tie-in period subject to the principal remaining at the practice and if the turnover-based target has been maintained. If a target is in place, then a mechanism will likely be in place should the practice not achieve the target – i.e. you would not wish to be £1 short of target but lose the whole of the retention.
Interestingly, smaller Corporates often do not require any tie-in, but a discussion may happen to ask how long the principal wishes to stay, with no legal tie-in. Also, targets for future performance are also not expected. Thus, they can be an attractive alternative to the larger Corporate.
summary
If you are thinking of selling your dental practice and attracted to a Corporate, then you may want to ensure that you are not limiting your choice to the handful of household names, and instructing a dental sales agent should give you far more access to other Corporates, great and small. They will also be able to ensure that any price and terms are negotiated to give you the best possible outcome.
https://pfmdental.co.uk/


Includes integrated Apex Locator
Already programmed for the new HyFlex OGSF sequence file
Continuous rotation and a reciprocation motion for all common le systems
Wireless endomotor for easy and exible operation
Integrated apex locator for safe and e cient treatments
Insulated contra angle with super mini-head and slim neck provides convenient usage and free eld of view
Intuitive control display for easy handling
Pre-programmed settings for COLTENE le systems saves preparation time



















Entering the new year places the UDA (Units of Dental Activity) deadline just two months away. Principals and dental management teams will be assessing the projected delivery against their NHS contractual expectations – and optimising UDA performance in all strategic decision-making in the coming weeks. For those with concerns about fulfilling targets, now is the time to take decision action and optimise productivity across the practice.
The challenges surrounding the uDa system
As all in the field will know, the UDA system intends to measure the access and delivery of the NHS dental system, with different measurable units for different bands of treatments, reflecting the amount of work involved.
Although the concept is straightforward, maintaining consistency in fulfilling these targets is – and continues to grow more –difficult in practice. As per the NHS dental contract management arrangement, when practices fall short, the result is financial recoupment. Furthermore, practices that repeatedly underperform risk inhibiting contract renewal and income stability. Staying on track is not always as simple as it might seem, as various complications can set back the attainment of these targets. These unanticipated circumstances can lead to mounting pressures, hindering the ability to achieve at least 90% of the allocated UDAs per year.
Such complications include: patient cancellations, clinical absence, a continuum
of recruitment difficulties, or simply operational disruptions. Many practices are at the staff-to-treatment capacity, making it difficult to overcome unforeseen shortfalls without additional support. This means practices need long-term planning, not short-term reaction to reach their goals. As such, the prompt identification of risks and setbacks can support the interventions necessary. This can be particularly beneficial when looking to be as prepared as possible for the UDA deadlines in future years.
The strain on NHS dental staff is continuously growing, with a huge 84% of practice owners reporting increasing stress, and 74% of practice owners’ concerns related to recruitment –significantly higher than practices with a greater private commitment. This figure is expedited by the feeling of falling behind on UDAs, with the fear that they’re unable to catch up. The strain that dental professionals feel between patient care and administrative load leads to extreme staff burnout, creating an even greater problem when March’s UDA deadline arrives. The consequences of these building pressures affecting performance can be solved through preparations. When practices are more prepared – with a set plan in place – stress among clinicians is significantly reduced, establishing a much more efficiently running workplace. Removing the strains of deadlines permits an improved environment for clinical excellence and higher patient satisfaction.
The power of locum support Practices experiencing the strains of workload and deadlines – looking to increase capacity without long-term staff commitment – often find effective solutions through the support of locum professionals. They can provide immediate support when it’s needed most, offering practices flexible resolutions to both patient and contractual demands. The incorporation of locum assistance not only reduces wait times and increases appointment availability, but helps meet UDA deadlines without compromising schedules.
Locums also offer the reassurance of continued aid during periods of clinician absence or more demanding seasonal periods. Though renowned for their shortterm assistance, many practice owners now use locum support proactively throughout the year, regulating workflow, enhancing patient access, and – importantly – reducing the stress build-up among core teams whilst striving towards targets.
support that truly delivers Accessing essential locum support efficiently is facilitated with the support of proficient recruitment partners. Dental Elite offers more than a decade of experience in sourcing and assisting the hiring of locum dental nurses, dental hygienists, associates, and more – understanding the nuances of UDA expectations thoroughly. Supporting practices through contractual challenges, the team at Dental Elite streamlines the administrative burden of sourcing, screening, and shortlisting
candidates – delivering peace of mind by providing direct access to a pool of skilled dental professionals.
Dental Elite’s incredible online visibility means that when complications surface, contractual targets can still be attained. As mentioned by a recent client, “Dental Elite goes above and beyond to find locum dentists… listening carefully to the specific needs to ensure the perfect match for your requirements.”
Keeping up with deadlines
With the demands of NHS treatment continuously growing, preparing for inevitable pressures beyond current capacity is vital. With the March deadline approaching, proactive support can be the difference between hitting targets and facing clawback – and locum capacity continues to be one of the most effective ways to protect both your workload and your contract.
For more information contact Dental Elite. Visit www.dentalelite.co.uk, email info@dentalelite.co.uk or call 01788 545 900 n

about the author Luke Moore, founder and Director of Dental elite.

Running a dental practice successfully involves a combination of clinical excellence, patient satisfaction, and the right tracking of appropriate metrics. Whilst the first two remain integral, long-term sustainability and growth of a practice are ultimately dependent on the utilisation of both operational and financial metrics surrounding the business.
Revenue and patient statistics are of course important to monitor practice performance. These and other key data support a better understanding of a practice’s growth potential and profitability. Principals tracking the appropriate metrics can make more informed decisions – ensuring that operational pressures never undermine clinical excellence.
Profitability per service
Not all treatment types contribute equally to a practice’s profit, meaning that understanding revenue by service is vital for maximising profitability. For example, a complex restorative procedure – though requiring substantial chair time, clinical skill, and staff – might deliver a greater margin than the accumulation of multiple routine dental hygiene
appointments. Furthermore, a popular and well-received whitening treatment might attract a significant number of patients, but generate a reduced rate of profit due to material costs. By analysing the data, principals are able to make more intentional decisions regarding marketing, staff delegation, scheduling, and treatment offerings. Furthermore, strategy in pricing can be better adapted –adjusting respective fees to represent the costs-to-return ratio. This is important as it means that higher value treatments are encouraged and supported, without dismissing low profit, routine services – these must continue to be accessible for patients. Longitudinally, the information allows practices to balance different types of treatment in a way that promotes both financial health and excellent patient outcomes.
More patients doesn’t mean greater profit
Another important understanding is the revenue achieved from a patient’s long-term association at the practice. For example, many practices will spend significant amounts on marketing to acquire new patients, without considering what will earn them worthwhile returns.
Patient lifetime value (PLV) shows the financial value of patients to your practice over time. To calculate PLV use this formula: PLV = average annual order value x annual purchase frequency x customer lifespan.
This allows principals to determine the patients that contribute the most to revenue growth, and where they came from – ultimately informing where to refocus marketing activities for greater success moving forward.
utilising metrics properly
When looking to enhance the financial security through data, partnering with experienced and knowledgeable support can offer the stability and understanding that many seek.
IndepenDent Care Plans (ICP) supports practices with their financial health planning by providing bespoke assistance with a personal Business Development Consultant – there for you every step of the way. With dental plans and guidance on team training, marketing materials, and success reports, practices can expect both growth and analytics of how to improve further. Made by dentists for dentists, ICP understands exactly how to push a practice in the direction of success, ensuring patient satisfaction
and operational success for the practice as a whole.
Utilising the right metrics properly allows principals to make confident and strategic choices for the continued success of their practice. Understanding which services encourage the highest profits and maintaining staff efficiency and understanding allows for better patient care and financial health.
Incorporating the insight gained from data analysis offers a more measurable and research-based opportunity for success – gaining clarity, reducing risk and uncertainty, and establishing the perfect environment for long-term growth.
Find out more about how ICP can support your practice – contact the team today! For more information and to book a no-obligation consultation, please visit ident/co.uk or call 01463 222 999 n
about the author
Dr Robert Donald, indepenDent care Plans Director.

























































































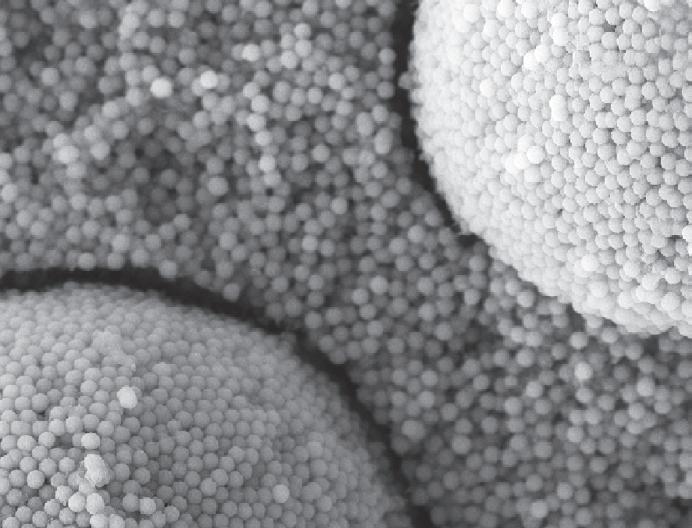
















































Bis-GMA-free formulation: for better biocompatibility
Easy stocking: only 1 shade for economic sustainability

Structural shade without artificial colour pigments: adapts seamlessly to any tooth shade from A1 to D4



Samples & More