Experience exceptionally lightweight loupes with crystal clear optics, designed and optimised for you.
• Custom Measurements
• Custom Fitting
• Custom Fabrication
For a t as unique as you are.



Experience exceptionally lightweight loupes with crystal clear optics, designed and optimised for you.
• Custom Measurements
• Custom Fitting
• Custom Fabrication
For a t as unique as you are.


The British Dental Association has warned unmet need for NHS dentistry in England is now at an all-time high, with official data showing no signs of recovery for the struggling service. Analysis by the professional body of dental data in the recently published GP Survey by Ipsos shows:
• Unmet need for NHS dentistry in England now stands at 13m, or well over 1 in 4 of the adult population (28%).
• This includes an estimated 5.6m adults who tried and failed to secure and appointment in the last 2 years. Nearly as many have given up trying with 5.4m not attempting to make appointments as they didn’t think they could secure care. The cost of care pushed 1.25m away, and around 780,000 indicated they were on waiting lists.
• While there has been some methodological change, with the survey moving online-first approach, this is clear growth from last year, when total figures stood at around 12m.
• Access problems predate COVID. Prior to the pandemic unmet need for NHS dentistry hovered consistently at around 4m or 1 in 10 of the adult population.
The professional body stress that the failure of dentistry to ‘bounce back’ to pre-Covid levels reflect the lacklustre policies from the last government, which failed to tackle the discredited NHS contract fuelling workforce and

access crises head on. Despite calls from the Health Committee and the Nuffield Trust for a fundamental break from this system of targets, the system has received little more than tweaks.
The BDA has been encouraged by the new Government’s new policy to view the NHS as ‘broken’, together with acknowledgement in early talks with Secretary of State Wes Streeting MP on the role the contract is playing in the current crisis. Dentist leaders have stressed the urgency here, pressing for a short-term rescue package to keep
practices afloat, ahead of longer term reform of the contract.
Shawn Charlwood, Chair of the British Dental Association’s General Dental Practice Committee, said: “NHS dentistry has effectively ceased to exist for millions across this country. A new government has inherited old problems, but luckily hasn’t followed in its predecessor’s footsteps by pretending this crisis has been solved. These numbers are stark reminder we need urgency and ambition to save this service.”
Professor Avijit Banerjee FCGDent has been appointed as the first Chair of the Board of the College of General Dentistry (CGDent) Faculty of Dentists. The Faculty of Dentists is a constituency comprising all dentist members of the College, and the Faculty Board advances the interests of dentists as a discrete professional group. The Chair is appointed for a three-year term, advises and reports to the College Council, and works closely with the President and other Faculty Board Chairs in realising College priorities.



Professor Banerjee is Professor of Cariology and Operative Dentistry, Clinical Lead for Undergraduate
Education, and Honorary Consultant and Clinical Lead for Restorative Dentistry at the Faculty of Dentistry, Oral & Craniofacial Sciences at King’s College London (KCL) and Guy’s & St Thomas’ Hospitals Trust. He is also KCL’s Head of Conservative & Minimum Intervention (MI) Dentistry, Programme Director of its distancelearning MSc in Advanced MI Dentistry, leads its Cariology & Operative Dentistry research programme, and continues to work in private practice in north London as a specialist in restorative dentistry, prosthodontics and periodontics.
School talks should involve the

Clare Callan discusses trends in Fitness to Practise, page 14

Stopping thumb sucking for over a decade, page 18

CASE STUDY
Guided implant approach for reproducible results, page 28



Whiting joins the GDC as CEO and Registrar

The summer holidays are here – although it can be easy to forget when looking out to a cloud-filled sky. Still, the importance of looking after our skin must not be forgotten – something I was reminded of recently during a skin cancer check. Thankfully, I was fine, but a lesson was learned and at the very least I’m applying SPF moisturiser. As Ali Lowe, founder of Fit-Lip reminds us on page 18, SPF lip balm is something also essential to protect the lips, which are often left exposed to the wrath of the sun’s rays.
The crucial role that dental nurses play is highlighted in this issue. Evelyn Ferguson-Williams celebrates the work of dental nurses on page 16. Meanwhile Dr Dhiraj Arora discusses the importance of building a championship-worthy tag team between dentists and dental nurses on page 40.
Before the kids head back to school, Miranda Steeples provides a practical lesson on how beneficial it is to bring different members of the dental team with you to classroom careers talks on page 12. And, on page 14, Clare Callan, Associate Director of Fitness to Practise at the GDC, notes how the regulator is seeing fewer concerns and closing more cases at the early stages of the process. There’s so much more to sink your teeth into this issue, including multiple case studies. Here’s hoping the sun makes an appearance as you read.









The Probe is published by Purple Media Solutions.
Registered in England.
Registered number 5949065
Managing Editor: James Cooke
Commercial Director: Gary Henson
Divisional Administrator: Francesca Smith




Production Designer 1 : Lorna Reekie
Production Designer 2: Rob Tremain
Digital Content Manager: Stephen Wadey
Circulation Manager: Andy Kirk
Managing Director: Ed Hunt
Regular Contributors: Lisa Bainham, Nigel Carter, Barry Cockcroft, Ollie Jupes and Pam Swain
E-mail news, stories or opinion to james.cooke@purplems.com
Circulation/Subscriptions: The Probe Subscriptions, Perception SaS, PO Box 304, Uckfield, East Sussex, TN22 9EZ, Tel: 01825 701520, https://purplems.my-subs.co.uk ©Purple
Media Solutions Ltd, 2014. All rights reserved. ISSN 0032-9185. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies, and information retrieval systems. While every effort has been made to ensure that the information in this publication is correct and accurate, the publisher cannot accept




liability for any consequential loss or damage, however caused, arising as a result of using information printed in this magazine. The views expressed in The Probe are not necessarily the views of the magazine, nor of Purple Media Solutions
Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth RCS(Eng), D’Orth RCS(Eng); Mark Wright BDS(Lon), DGDP RCS(UK), Dip Imp Dent.RCS (Eng) Adv. Cert, FICD; Dr Yasminder Virdee BDS. Readers who fall outside the terms of control may















For more information and to speak to your local representative, scan the QR code



INCREASE TREATMENT ACCEPTANCE BY YOUR PATIENTS
Better understanding of the suggested treatment plan.
INCREASE TRUST AND PATIENT CONFIDENCE
Communicate any changes from visit to visit.


ENHANCE THE VISIBILITY OF INFLAMMATION & DISEASE
Detect plaque, gingival inflammation and caries.







Ateam of six employees from Community Dental Services CIC (CDS) in Bedfordshire built a raft in their free time and took part in the Bedford River Festival’s Raft Race on Sunday 21st July to raise awareness and funds for the Mouth Cancer Foundation; a charity dedicated to helping and supporting those living with or at risk of mouth cancer, throat cancer and other head and neck cancers, as well as providing assistance and information on living with mouth cancer for families, friends and carers.

The raft race was one part of the Bedford River Festival, a biannual, twoday community event which also hosts live entertainment, music, workshops,
farming area, crazy golf, activities, a funfair, and river displays; and attracts in the region of 250,000 visitors.
Glen Taylor, Chief Operating Officer for CDS in the East of England, and one of the raft crew was delighted with the team’s efforts at the weekend: “This was our second year competing in the raft race. Our team consisted of Dental Officers, Dental Nurses, our Specialist in Special Care and our Clinical Director. Together, we spent some of our weekends building our raft; tweaking our design from valuable lessons learnt in 2022. We wanted a traditional raft but one that would be lighter and hopefully more agile, and we added a CDS flag on the back.
“We pulled together as a team when things got tough, and the cheering of the crowd provided much needed encouragement. With such amazing support we were delighted to take third place in our heat and fifth in the final – compared to our 2022 efforts

which saw us come third in our heat and sixth in the final.
“We had a lot of fun but most importantly were proud to raise awareness of mouth, throat, head and neck cancer; and we managed to not sink in front of the crowd of over 10,000 spectators, which was a welcomed bonus!”
To sponsor the team and help raise funds for the Mouth Cancer Foundation, please visit their Just Giving Page: https://tinyurl.com/CDSplash n
The contribution Dr Sejal Bhansali has made to the dental profession was recognised on 22nd June 2024, when she was inducted as a Fellow of the International College of Dentists, European Section, in Limassol, Cyprus. Sejal was one of 51 inductees from across Europe including 12 from District 5: England, Scotland and Wales.


he EFP, with the support of meridol, launches a comprehensive campaign titled “The journey to a healthy smile.” This initiative aims to promote oral health awareness and best practices by helping the public understand gingivitis and periodontitis, explain risk factors and general health implications of gum health, and provide practical tips to fit healthy behaviour in daily routines. Effective motivation strategies are essential in actively engaging and helping patients achieve and maintain a healthy smile. The campaign will provide educational videos and materials for oral health professionals to use in motivating their patients to make positive changes at different stages of their journey. The videos will cover topics such as spotting and preventing gum disease, the impact of daily habits on oral health and motivating patients on their oral health journey to a fitter and longer life.
“We are proud to partner with the European Federation of Periodontology on this innovative initiative,” said Irina Laura Chivu-Garip, Colgate-Palmolive Head of Scientific Affairs for Europe. “By leveraging the power of behavioural science, we aim to inspire lifelong healthy habits in individuals, ultimately enhancing their oral health, and impacting general health and wellbeing. This collaboration underscores our commitment to advancing health literacy and aims to engage medical and dental professionals, as well as their patients, in pursuing health goals by leveraging evidencebased approaches,” concludes. n
Operation Smile is the beneficiary of a significant legacy fund donation from The European Aligner Society (EAS). £80,000 is being paid over three years to help the charity develop and support cleft lip and palate treatment programmes which have a lasting impact in developing countries. Operation Smile carries out hundreds of surgical programmes all over the world, with the long term vision of improving the local healthcare system in the areas in which it operates. In addition to mobilising highly accredited medical volunteers, Operation Smile trains local medical professionals, and partners with hospitals, governments and ministries of health in order to ensure that safe and effective surgery is a right for everyone in need. The charity ensures that its ongoing programmes are run by local medical teams to the extent that over 85% of all programmes globally are now managed by local teams – a testament to the significance of the work it carries out with local healthcare professionals.
Dr Les Joffe, CEO of EAS, commented: “The EAS Board considered what it could do with surpluses generated by sponsorship and delegate fees from a series of highly successful congresses and meetings. EAS is a not for profit
organisation, so we created a Legacy Fund into which surpluses could be directed. This fund focuses on 3 aspects: Donating funds to worthy causes in the oral health field; Applying funds to research projects in the aligner field and; Launching ‘Summer Schools’ in aligner education for young aspiring orthodontists.”
He continued: “The EAS chose to collaborate with Operation Smile as we were particularly interested in its work on patients with cleft conditions in developing countries. Operation Smile works with clinicians to initiate the diagnosis, repair and support for patients with a cleft at the start of life. The expertise that Operation Smile brings to each country is handed onto the local clinicians so that ongoing care and support can be carried on locally and the hands-on training and support for a range of oral health projects globally meant that our legacy fund could in turn fund a significant legacy in less developed countries. This process takes funds and EAS was happy to be able to offer Operations Smile £80,000. The outcomes of Operation Smile’s work is both wonderful and heart warming. You only have to look at the organisation’s website to understand why EAS wants to support what Operation Smile is achieving – it is so worthwhile.” n

She was nominated by Sir Nairn Wilson CBE. Dr. Sejal Bhansali is a General Dental Practitioner in London and Clinical Tutor at King’s College. In addition, she set up the Kenya Division of the Dental Wellness Trust, providing oral health care to 8,000 children in Kibera, Kenya – Africa’s largest slum. n
Specialist business property adviser, Christie & Co, has expanded its dental team into the Northern Ireland market, with the appointment of Cathy Murphy as its lead agent in the region.
Cathy Murphy joined Christie & Co’s dental team in August 2023 and brought with her a wealth of market knowledge and experience in the sector. Initially covering the sale of dental businesses in the North of England, she will now also play a pivotal role in developing the company’s brokerage arm in Northern Ireland.
Christie & Co’s expansion into the Northern Ireland market reflects the growing demand for dental businesses in this part of the UK, and the company’s commitment to expanding its brokerage offering. n
Dr Laura Milby awarded MBe
Dr Laura Milby, former NHS Lanarkshire’s clinical director, general dental services, who received an MBE (Member of the Order of the British Empire) in this year’s King’s Birthday Honours in recognition of her services to dentistry.
Laura said: “To be awarded an MBE in the King’s Birthday Honours was quite a surprise and truly humbling. I’m really looking forward to attending St James’s Palace in London where I will be formally presented with my award.” n
Practice Plan is bolstering the support it offers to multi-site customers with the recruitment of a new member of the support team. Former employee of Practice Plan Group patient finance company, Medenta, James Cameron, has, as he puts it, “Come back home” after an absence of five years.n













“And there it was, hope. Running over the hill with its a*** on fire.” - Woody Allen
Over the many years I spent in dentistry, I must confess that I slowly transformed into that wretched, ‘glass half-empty’ sort of bloke. You know the type – you’d rather stand at the back of the lecture theatre and endure excruciating cramp, rather than sit for the entire CPD day on ‘Getting To Really Know The Secrets Of The BPE Probe’ next to the depressing principal from up the road who bangs on all day about how his associates are draining him of his profits because he suspects they are doing private whitening on the side and selling old crowns to the specialist scrappy.
I wasn’t quite that bad but, having entered dental school in the 80’s full of hope, the faint glimmer that was desperately clinging on for dear life at the tail end of the 2010s before I retired early was pretty much extinguished for all eternity.
Having spent well over a decade as a provincial journalist, and having suffered various indignities and insults at the hands of people like prospective Parliamentary candidates and local politicians (a district councillor once strode up and called me a ‘lackey of the local gutter-press’) I was looking forward to being held in some regard by society in general for a change, with a dental degree as my shield. But that hope quickly faded when I realised that dental school was teeming with a good number of lecturers who disparaged local practitioners, who had referred patients into Hogwarts, and certainly had no qualms about crushing the spirit of their students at every available opportunity.
I vividly remember being humiliated by one lecturer when I wasn’t quite quick enough in answering one of his questions. He was a Reader in the university and just happened to be my personal tutor. He came back to me after I failed to deliver the prompt answer he required earlier, prefacing his next question to me with, “Now, I wonder what the genius will make of this one.” You can almost certainly empathise with how I felt.
That incident typified the dismissal and contempt that lecturers would mete out to students, which plagued me and many of my peers during our long and uncomfortable journey through dental school. I believe it was only because we clung on to our hope that things would get better that any of us persevered with the course. That same dismissive attitude is very much reminiscent of the way the last government treated the dental profession.
I have mentioned previously that I have been a lifelong coward in the dental chair – a profound gagging reflex and a shouting-at by a dentist as a child that haunts me to this day.
When I moved to my last newspaper, a colleague recommended a dentist who helped with her dental phobia. I went and he literally changed my life. He treated me with nitrous oxide and kindness and patience, and it was then that I went back to evening classes at the local tech to get the ‘A’ levels I needed to get into dental school. The practice was unique.
The two partners had built everything open plan, with discreet partitions separating the dental units. I loved it and REALLY hoped to work there one day or, at least, find a practice that was on a par with it.
When I qualified, I hoped that I would find a practice that I would be comfortable and happy in. But every time I found a practice that I thought I could be happy in, my hopes were crushed like a new porcelain veneer under the wheels of an operator’s stool (I’ve done that) – usually as a result of personalities that worked in the establishment.
My first part-time practice on qualification was lovely but, since I was working alone, I felt I needed to work with other experienced practitioners and, perhaps unwisely, moved on.
I worked with one dentist who used to under-pack occlusal amalgams so he could save on the cost of materials and didn’t have to waste time on adjusting the occlusion. When I first arrived, most patients had occlusal food traps and what I felt were failing restorations until his nurse put me right.
Subsequently, I was keen to work with a laid-back practitioner who later turned out to have been banned for drink-driving and used to carry out apicectomies by extracting the tooth, filling the apex with amalgam, and then bunging the tooth back in the socket, splinting it with a bit of composite. He told his patients they were ‘implants’. His nurse told me they never worked.
When I ran my own practice, I hated it – mainly because the owner was an idiot. Even my hopes for a troublefree sale when I finally found a buyer for my practice fell by the wayside. But that is a tale for another day.
But what of the hopes that the newly elected Labour Government will save NHS dentistry?
The half-full glass in me would like to think that there IS hope. Keir Starmer’s new Secretary of State for Health and Social Care, Wes Streeting, met up with representatives from the British Dental Association on the first Monday in the job.

What of the hopes that the newly elected Labour Government will save NHS dentistry?
Dr Shawn Charlwood, Chair of the BDA’s General Dental Practice Committee, said on the BDA website: “Labour had repeatedly pledged to meet with us soon after the election on the task ahead: rescuing and reforming NHS dentistry. I am pleased to report that promise has been kept.” I am assuming Dr Charlwood meant that Labour had met up with the BDA, not that NHS dentistry had been rescued and reformed.
This was a great start, and perhaps a reflection of the fact that Labour appears to acknowledge the importance of dentistry and has more than taken note of the growing anger the public and dental health professionals feel about the demise of the NHS dental service.
On his X account, Mr Streeting said: “It is now the policy of the Government that our NHS is broken. It will be the mission of my department, every member of this government, and the 1.4 million people who work in the NHS, to turn our health service around.”
But this is a man who must also turn his attention quickly to solving the pay dispute with junior doctors who are still, at the time of writing, taking strike action in
pursuit of their pay claim. It has been reported that junior doctors in England have said their pay has been cut by more than a quarter over the last fifteen years, and have called for a 35% increase in pay. Solving that dilemma would seem a priority for the new Health Secretary, as would cutting hospital waiting lists. So, the glass half-empty part of me is dreading that the initial momentum of the Government will lose pace after being overshadowed by the needs of the general medical sector of the health service.
But with the Health Secretary’s sprint start to his new role, there appears to be some hope that the importance of dentistry in the health of the nation is no longer going to be ignored as it was with a Tory Government, which merely paid lip service to the dental service – epitomised by its risible ‘dental rescue plan’. As far as the Tories were concerned, it was ‘job done!’
Let’s all hope we don’t see hope disappearing over the horizon any time soon. n
About the author ollie Jupes is the pseudonym of a former nHs dentist. He monitors dentistry on twitter X as @DentistGoneBadd














1. Adaptable to different guided surgery protocols: piloted, semi-guided or fully guided.
2. No friction between drills and guide sleeve, no overheating and no release of particles.
3. No specific drills and a very small surgical box.
4. Full control of drilling depth.
5. Your conventional driver-guided drilling sequence.


The Tories may have given them a “nudge” in the right direction just in time
Since before I was born, the Labour Party has been the party of public services, including the NHS.
When the concept of an NHS was first proposed in the Beveridge report in 1942, it dominated British politics. In the first post war general election, Winston Churchill, who only a few months earlier had been hailed as a national hero, lost, mainly because he was opposed to the establishment of the welfare state, including the NHS. Access to dental care had previously been a choice only for the wealthy, and this was one of the main pillars of the NHS when it was founded. The people of the country have a passionate belief in the NHS, although delivery is now more complex, expensive and impactful than could ever have been imagined. Conservative policy towards NHS dentistry has always been a bit lacking in enthusiasm. I first became involved in national dental politics, joining the General Dental Services Committee of the BDA in 1990, shortly before the government of the day decided to reduce the fees paid to NHS dentists in the already disliked item of servicebased system by 7%. This was the start of the development of serious access problems, especially when combined with the effect of closing three dental schools in the mideighties. The reasoning behind this was complex but demonstrated a lack of interest, which was to continue until the election in 1997. With the change of government, there was a
clear intention to revive the system and tackle the massive access issues that had been increasing since 1992. Between then and 2015, the money spent on NHS dental services increased from around £1.4 billion to a budget of well over £3.5 billion, and access increased by 2.7 million people – all this despite a contract being in place which the BDA describes as “failed”!
Contracts usually fail if they are not implemented correctly and, since 2015, there seems to have been no attempt to maintain the progress made up until then. The situation has deteriorated with opportunities missed (or deliberately ignored?). The wider scope of practice of DCPs has been almost completely disregarded when it comes to using them more in NHS general practice; patient charges have been increased far more than inflation and contract values held down below the inflation in costs, making NHS providers feel, quite reasonably, that the aim was to drive people away from delivering NHS dental services as much as possible. No attempt has been made to use the flexibilities in the existing system and, where some commissioners have tried, they have often been discouraged from the centre.
Now, there is an opportunity again, and the roundtable meetings organised by the outgoing minister with portfolio responsibility for dentistry before the election was called might have pointed out a better way forward. Dentistry is a team-delivered service and around
the table were invited a whole range of stakeholders: the regulator, educators, local dental representatives, the BDA and representatives of all the other groups of dental care professionals who can play a part in delivering care. Some of the ideas mentioned by the minister, especially around NHS patient charges, were a little bizarre but you have to give them credit for finally driving forward on expanding water fluoridation and for bringing together such a wide-ranging and inclusive group.
As I often heard politicians say, “You should never waste a good crisis,” and that is what has been created in NHS dental services since 2015. There is now an opportunity to move forward for the benefit of our patients and the oral health of the country. To challenge the status quo, involving all parties.
The medical workforce and treatment needs have changed massively since 1948. We now replace arthritic joints with artificial ones and failing organs using transplantation. We treat many heart attack victims with same-day stents and discharge people the very same day! Babies born at 25 weeks can now survive and flourish, smallpox, polio and TB are largely things of the past, and medical education has adapted to keep pace with the changing needs. We know that some conditions that used to be treated surgically can be resolved by other means, such as physiotherapy, and that some of the procedures carried out for years were not effective. We now regularly
see practice nurses at GP practices, Advanced Nurse Practitioners work on medical rotas and carry out many procedures that used to be considered the role of doctors, and clinical pharmacists help with the quality of prescribing, diagnosing and treating minor ailments but all these extended roles must be regulated.
Dental education also needs to fundamentally change, we still train a largely similar workforce to that which we did in 1948, when the health of the nation was so much worse. Since we expanded the scope of practice of DCPs, working with the regulator, there should have been a review of the needs of the population. We have some of the lowest overall caries prevalence rates in the world but still train a workforce largely based on 1948 disease patterns.
Most dental disease is preventable but it does not need a dentist to apply fluoride varnish, fissure seal teeth where there is a high risk of caries, explain the importance of correct tooth brushing or give good dietary and lifestyle advice.
As a taxpayer now, rather than a dentist, the status quo does not seem to be a good use of my taxes. n
About the author Dr Barry Cockcroft CBe is the former Chief Dental officer for england and current chair of the British Fluoridation society.

Climate change and caring for our planet are rarely out of the news, so how can dentistry take more responsibility and become more sustainable?
According to the FDI, the healthcare sector is responsible for around 5% of global greenhouse gas emissions. The latest statistics show that the world generates around 53.85 billion tonnes of Greenhouse gas emissions. 1
The least sustainable part of dentistry is our patients and staff travelling to the dental practice. We can help to reduce this by booking families for appointments at the same time and possible staff car share arrangements. However, without the patients and staff, there is no dental practice, so it is inherently difficult to offset these.
Some of the other less environmentally friendly factors of dental treatment are the single-use items and plastics that, again, are unavoidable.
what is being done to help?
The Sustainability in Dentistry Task Team provides guidance and scientific expertise to ensure effective execution of
the Sustainability in Dentistry project. The project aims to map out strategies and implement solutions to help reduce the environmental impact of dentistry and the dental industry.
Its current goals are to:
• Increase awareness of the need to implement sustainable actions in the dental community
• To develop a guide for oral health professionals to identify actions that can lead to environmentally sustainable outcomes
• To conduct a review of the current literature and identify the current research and guidelines and to identify any gaps in the literature regarding sustainability in dentistry
This will only be successful if many dental professionals decide they care enough to put the work in to make this feasible by acting in their own dental practices. There is so much that can be done including recycling, energy usage, and other sustainable changes to the working environment.
How can i get involved?
You can get involved in several ways, including taking part in their sustainability toolkit and registering your practice to help increase interest and provide support.
Focus on the prevention of oral diseases is the best way to help not only patients but also improve carbon emissions.
If, as a practice, patients need less work done on their mouths, they will have less need to travel to see you. In today’s world, most people must travel by car or bus unless they live very near the practice. Walking or biking would be a great alternative if possible. However, in this busy world, it is not always a practical solution depending on circumstances. Cutting down on the need to travel will reduce emissions from this type of transport, leading to a healthier world.
The FDI Sustainability Award promotes sustainability in dental practice by providing the opportunity for individuals or dental practices to receive global recognition. Each year, four awards will
be granted: two for dental practice and two for individuals.
Not only is it good for the environment but you can be globally recognised as trying your best for both dentistry and the planet. Although the deadline for entry this year has now closed, the winners will be announced during the FDI World Dental Congress, held in Istanbul in September 2024.
If you are interested in taking part in this next year, you can go to https://www. fdiworlddental.org/sustainability-dentistry to find out more information. n
Research
1. https://ourworldindata.org/greenhousegas-emissions Accessed 19th July 2024 09.44
About the author Karen Coates, oral Health Content specialist at the oral Health Foundation, and RDn

As the summer holidays are upon us, a new school year beckons. Some pupils are starting to think about their university choices and career options. This is no different for the previous set of Year 12 pupils at the Victory Academy in Chatham.
Miss Layla Steeples, Head of English, helped organise an enrichment week for the pupils to listen to invited speakers share their career experiences, a taster of what their profession includes, and an overview of how they got there.
Layla understands that dentistry does not just mean dentists; there is a whole team involved in delivering oral health care and everyone works interdependently for the benefit of patients. With this in mind, she invited me – her sister – as a dental hygienist and dental therapist, to join this event. I felt it would add value to bring in additional team members, so invited Ken Binnah, dental nurse, and Rowland Gardner, a clinical dental technician.
Around 80 Year 12 pupils had listened to a morning of career options, and dentistry was the session standing between them and their lunch. I started with an overview of the whole oral health care team and briefly touched on other career options within dentistry, such as being a practice manager or a treatment coordinator. This was followed by a closer focus on dental hygienists and dental therapists, explaining their skills, scope of practice, and how they fit into an oral health care team.
I shared a personal part of my story: my journey from starting in entertainment, to being a dental nurse, to becoming a dental hygienist and therapist, to President of the BSDHT in 2022.
Next up was Rowland Gardner, who spoke about his journey to becoming a clinical dental technician. He described what he can do in his role and as a dental professional after completing formal training as
a multi-specialist, a teacher, and clinician. He is currently part of specialist hospital team, working alongside other medical and dental professionals. A key role is crafting and making smiles, literally giving people their smile back.
As he described his day-to-day work, his passion and love for his profession was evident throughout.
Rowland has worked as a dental technician for over 50 years and still loves his job, describing it as the “best job in the world”.
After Rowland, we listened to Ken Binnah, who spoke about being a dental nurse, offering an overview of how the dental nurse is integral to almost every role within dentistry. In some respects, the most important, because they take care of the cross-infection control, while supporting both the clinician and the patient.
Ken described his career journey from starting as a dental nurse to then taking on more responsibilities in becoming a dental nurse tutor and an examiner, further leading him to undertake a master’s qualification at the University of Kent. He has established a dental nurse agency and training business, which he runs alongside his day job as a dental clinical team lead to provide clinical and team management of the dental nursing and administrative staff, which supports the delivery of clinical services within a specialist dental service. Once again, Ken’s passion for his profession shone through with every word as he described his role and pathway.
At the end of the session, two pupils came and spoke to us. Both were interested in joining the oral health care team.
My message from the start was if each person in the room could tell at least one person about the day’s talk and to let them know that there are actually seven different registered dental professions, as well as many other potential


career options that one could take to be involved within dentistry. It was reinforced that whatever your grades, whatever your skill set, there is likely something in the world of dentistry for you, something that will give you as much joy in your work as described by Ken, Rowland, and myself. And then to ask that person to also tell one other person, and so on.
This is how we ensure recruitment into our wonderful profession of dentistry. So, this is a call to action, to you the reader: If you are invited to go to a school to talk about your career in dentistry, whatever your role is, please take at least one other team member with you and let the students know that there’s a whole world of opportunity for people to come in and join this fantastic profession. Thank you! n
A note from Head of english, Layla steeples:
“it was great for our Year 12 students to experience the world of dentistry without simply being told to be a dentist. For many of our students, alternative routes and courses are better suited, and understanding that they can enter the world of either dental nursing, clinical dental technology, or dental hygiene and dental therapy opened up opportunities to them that many had probably not even considered.”
About the author Miranda steeples, BsDHt president, qualified as a dental hygienist and dental therapist from the University from Leeds in 2009 having previously worked as a dental nurse.




We are seeing fewer concerns and closing more cases at the early stages of the process
No one wants to be the subject of a Fitness to Practise investigation. It’s a stressful situation for any healthcare professional and can be both concerning and frustrating if the issues raised are felt to be minor and are ultimately resolved with no case to answer.
It is sometimes suggested to us that the GDC inflates concerns out of all proportion to their seriousness, often progressing cases all the way to a hearing when they could be resolved earlier.
We recognise that this, and similar views, may lead to unnecessary stress and unintended consequences as professionals report that they are practising defensively. To protect themselves, they’re spending considerable time explaining all possible treatment options to their patients while taking copious notes to describe what they said and did and doing it in considerable detail – time that could be better spent treating and caring for patients.
We want to explain how Fitness to Practise is changing. We are seeing signs that efforts to improve complaint handling through local resolution are having an impact, and some of our more recent process improvements are starting to have an effect. The initial inquiries pilot has the potential to improve things further.
We exist to protect the public. We are not out to get professionals, but we are told that it can feel that way when an investigation is underway. We need to do more to support individuals, but we also need to start tackling some of the long-held but increasingly outdated beliefs that persist around Fitness to Practise, not least because they can have real-world effects.
we are seeing far fewer concerns than a decade ago
The number of concerns received and initially assessed has reduced by more than half over the last decade. Public confidence in the profession remains high. Over the same period, the number of people registered to practise dentistry in the UK has increased. What is behind this clear trend?
Work across the sector to emphasise the importance of good complainthandling has certainly contributed. The Dental Complaints Service has grown, helping to resolve issues raised in private practice, while reducing the number of issues they refer to us for an investigation. We have also seen new protections for whistleblowers and the introduction of the professional duty of candour.
Considerable effort has gone into ensuring that people can find guidance on how to provide feedback or make a complaint before raising it with us, and further improvements have been made in recent months. We have

also updated our processes to help make sure people are directed to the organisation best placed to resolve their issues.
the majority of cases are resolved early in the process
Our strategic priority is to ensure that concerns are addressed effectively and proportionately to protect the public. While our legislation has been constraining, progress has been made. When we receive a concern, we will make an initial assessment. That assessment will be based solely on the information we receive from the person who raised the concern. We have no further information to inform decisions at this stage. We must make further inquiries where the answer is yes to one or both of the following:
• Harm has been or may be caused to a member of the public
• Public confidence in the profession has been or may be undermined This low threshold means we need to open a case for the majority of concerns received. Typically, around 85% of all concerns considered by our Initial Assessment team are progressed for an investigation and proceed to the assessment stage.
To be able to make an assessment, we need to gather more information, including contacting the registrant to request relevant records.
Last year, almost 40% of all cases opened for an investigation fell into the category of clinical complaints raised by a single patient. In terms of seriousness, these are generally at the lower end of the scale. Our initial inquiries pilot is focusing on these types of cases to see how we can resolve them at an earlier stage. We have recently announced that we are extending the pilot and, if we get the approach right, it has the potential to deliver significant benefits, including:
• Reducing the impact of investigations on everyone involved
• Earlier outcomes and opportunities to reflect on the issues raised
• Freeing up resources to improve overall case progression and timeliness
We have already noticed some positive impacts, with only 12% of cases assessed through the pilot being progressed to case examiners. The Assessment team has reported faster responses to requests for records. Our ability to make fully informed decisions quicker and earlier in the process depends on the cooperation of dental professionals, so we are grateful for the response we have received to our requests for records in the pilot’s first six months.
Record keeping is important to ensure high standards of care and can be helpful if things do not go to plan, but we do not expect anyone in the dental team to be creating unnecessary records. That is not what we or your patients expect. We are asking for complete and accurate records that are readable and taken at the time.
Clinical advisers will review records in these cases. They are asked to determine if your records demonstrate that the standard of care delivered has met the level of professional practice reasonably expected of someone working within that discipline.
Our more recent efforts to conclude cases at an earlier stage builds on progress made as a result of reforms to legislation in 2016. The legislative changes made introduced case examiners, who were empowered to make outcome decisions in Fitness to Practise cases. Case examiners can:
• Close a case
• Issue advice or a warning
• Ask a dental professional to agree to undertakings
The change meant that cases, particularly the less serious ones, could be resolved earlier in the process without convening a panel and the parties having to attend a hearing. Clinical dental advisers were also brought into the GDC in 2016 to improve consistency in advice in clinical cases before being passed to case examiners for an outcome decision.
These changes had an impact: The number of cases progressed to a
hearing fell by a third in a single year to a little over 200 cases. The number of cases referred to a hearing has stayed around this level over more recent years but did fall to its lowest level in a decade last year.
starting to see green shoots of further improvement
We say this a lot, but the number of concerns raised with us each year is small. The number of cases referred to the Dental Professionals Hearings Service for a hearing is even smaller against a backdrop of a growing number of people working in dentistry as part of the dental team.
In 2016, 333 cases were referred for a hearing, representing about three registrants in every 1,000 (0.3%) on the register that year. Seven years later in 2023, we referred just 132 cases, or around one registrant in every 1,000 (0.11%). While the total number of cases being progressed to a hearing has remained quite static over more recent years (ranging between 132 to 176 cases over the last four years), increases in the number of professionals on the register means that the proportion of cases progressed to a hearing has reduced.
The impact of changes made over several years is now being reflected in the figures and performance. We have made a number of improvements over the past two years, including increasing our staffing in 2022, to help to ease pressure on existing colleagues, and our staff retention rates have improved. The position is shifting and, as a result, in April and May we managed to outperform our targets for cases to reach an Assessment decision for all case types. We are currently processing an active caseload at assessment of around 550 cases.
The reality of Fitness to Practise is that the number of serious concerns raised has reduced significantly over recent years and we are progressing fewer cases to the later stages. We have more to do to improve timeliness and the support provided to individuals, but the indications are that efforts across the sector to improve complaint-handling and reduce the impact of investigations are having an effect, and we are moving in the right direction. n
About the author
clare callan is the Associate director of Fitness to practise. clare joined the gdc in April 2019 as the Head of Fitness to practise case progression and helped to establish the department in Birmingham as it relocated from London. prior to joining the gdc, clare worked for nearly 20 years in legal regulation and progressed from a caseworker to various management positions.

As all Dürr Dental compressors are registered medical devices class IIa, and have been since 2015, their air quality is in accordance with ISO 22052
ULPA U16/ISO 65 U virus-bacterial filter included
No service requirement, just an annual filter change


Remote monitoring possible via VistaSoft Monitor app Up to 5-year warranty


Idon’t underestimate the challenge of reforming NHS dentistry provision; if it were straightforward to solve, it would have been done by now.
But for too long, problems in accessing an NHS dentist, caused in no small part by a funding squeeze on service providers, has pushed ever more patients and dentists to turn to the private sector. We understand that funds are limited, but too often the NHS dental budget is not diverted to those that need it most. So, now is the time for a new government to get its teeth into this important issue and take bold action, rather than overseeing more of the same slow decay.
The Labour Party’s election victory came after it campaigned in part on a Dentistry Rescue Plan, which they say is fully funded and will “make sure everyone who needs a dentist can get one”.
The new government kept its pledge to sit down with the British Dental Association in its first week in office to begin negotiations around contract reform. These are promising signs, but we need to see a fully formed plan that will get to the root of the problem sooner rather than later.
The Labour manifesto’s focus on emergency dental appointments, urgent care, and care for under 18s may suggest that its plan is to introduce some form of core service.
That might balance delivering for those most in need with some limited form of NHS care for the wider public, possibly including urgent appointments and maybe even a free examination with a focus on preventative dentistry and good oral health.
But such promises could prove to be ineffective unless the full scale of the sector’s workforce challenge is properly appreciated.
A large proportion of the profession has shifted to part-time clinical work, while a move towards defensive dentistry, with all the extensive notetaking that entails, means productivity is falling, so there is an urgent need to recruit large numbers of new dentists.
Boosting the number of graduates will help in the longer term, but we are years away from meaningful numbers being available as dental school capacity needs to increase significantly, as well as the number of people to staff them.
Recruiting dentists from overseas is an option, but this can sometimes require additional mentoring and supervision, which is expensive, time consuming and further erodes the productivity of experienced dentists already in the UK.
Loosening the qualification requirements for service providers runs the risk of compromising patient care and safety, which neither the Government nor the General Dental Council want on their watch.
promoting prevention
But while the scarcity of clinicians persists, patients will continue struggling to access the treatment they need.
This will inevitably play into the hands of those private practices that can offer dentists both the pay and conditions that NHS practices will find hard to match.
However, there is an opportunity to mitigate the pressures on dentistry by driving down demand through a focus on prevention.
While Labour’s plan to introduce supervised toothbrushing for 3-to-5year-olds was criticised as an example of ‘nanny state’ politics, I believe most dentists would approve.
This, combined with a roll out of the sugar tax that has already halved the amount of sugar consumed by children from soft drinks to cover other high sugar products, will undoubtedly pay dividends for the nation’s dental health.
Still, these are not a substitute for a contractual framework that is structured in a way that genuinely incentivises prevention. For now, it is difficult to know what additional investment can be made into dental services, which will depend on the new Government’s resources and priorities. What is clear is that any new money must come alongside contract reform that ensures valuable resources are targeted at those most in need: children, older people and vulnerable adult groups such as the working poor, who cannot afford private care. n
About the author Nigel Jones, sales Director at practice plan, part of the Wesleyan group.

Evelyn Ferguson-Williams, a registered dental nurse and Dental Case Manager at Dental Protection, highlights the key role dental nurses play in the success of a dental practice
There is a common misperception, by both patients and clinicians alike, that a dental nurse’s role is to simply pass the instruments, aspirate fluids and clean the surgery. Yet, the knowledge, experience and skills that a dental nurse requires to both qualify as a dental nurse, retain their registration and to achieve post qualification certificates is extensive!
In the past, a dental nurse’s role very much revolved around supporting the clinician. However, now we can be much more involved in the provision of patient care, treatment planning and even dental practice compliance.
With additional training, competency and qualifications, a dental nurse can bring so much more to a practice, such as taking radiographs, impressions, intraoral scans, the application of topical fluoride and so much more. The time and energy that a clinician can save by utilising their dental nurse’s skills and experience is invaluable.
Although the General Dental Council’s (GDC) Scope of Practice clearly lists the extensive additional duties that a dental nurse can offer, many clinicians remain unaware of said list or lack confidence in the role of a dental nurse.
Unfortunately, the lack of recognition and trust takes its toll on the wellbeing of dental nurses. In a recent Dental Protection survey 1, 73% of dental nurses said their clinical colleague’s negative behaviour has had a significant or moderate impact on their mental wellbeing. A further 49% of the dental nurses who took part in the survey said they are considering their future in
the dental profession, while 40% feel pessimistic about the future.
This feedback clearly demonstrates the constraints and unnecessary pressure that some dental nurses are working under and how more should be done on the regulatory landscape to properly recognise the role of dental nurses. I feel that increased specialisation opportunities and expanded scope of practice could also help to increase recognition and respect for our role.
Whilst I do appreciate that it is likely to take some time for the role of a dental nurse to be nurtured into its full potential on practice level, I would like to highlight the many benefits we bring, even if a nurse is working in a basic supportive capacity.
I am sure many clinicians reading this article have experienced working a day in a practice that is short staffed, and the chaos that can prevail. Not only is there the potential added stress and expenses involved in hiring locum nurses, but patient care can be significantly affected.
The support with surgery preparation, record keeping, decontamination, infection control, treatment planning and even management of medical emergencies is entirely absent, often resulting in cancellation of clinics or the unsafe provision of care, which, in turn, will leave a clinician extremely vulnerable to complaints. The GDC standards clearly state that: “You should work with another appropriately trained member of the dental team at all times when treating patients in a dental setting.” It is often at this point, when a dentist is left entirely unsupported, that they may recognise their nurse’s invaluable involvement.

I think that most dentists are now very appreciative of our ever-evolving role as dental nurses. Especially as we are trying to contribute more than ever before, such as meticulous record keeping, complying with the strict decontamination guidance, treatment coordination, oral hygiene instruction and even constructing study models, retainers and mouthguards. The list of potential benefits really does go on.
Alongside our clinical colleagues, the main purpose of a dental nurse is to support a practice in ensuring the safe and effective provision of patient care. To do so, dental nurses must be recognised, valued and nurtured to reach their full potential. Building professional relationships on mutual trust and understanding will also help to achieve the best patient outcomes and create a more collaborative and enjoyable environment.
Alongside a dental nurse being appropriately qualified, trained and competent to carry out these additional
duties, they must be adequately indemnified. Whilst dental nurses are in most cases an employee of the practice, meaning the practice is vicariously liable for their acts and omissions during their professional activities, it is coming to light that many dental nurses believe that the indemnity ‘umbrella’ offered as part of their role will entitle them to unconditional assistance. It is often the case that whilst they will be indemnified for any complaints and/or claims for compensation that may arise, they are left entirely without support with any GDC ‘Fitness to Practise’ investigations. Understandably, this is likely to be very distressing news, at what is likely to already be a very worrying time. Therefore, it is Dental Protection’s advice for all dental nurses who fall under their employer’s indemnity package, to request a copy of any relevant paperwork, demonstrating the level of assistance they are entitled to. Should they have any concerns, they should contact the relevant indemnity provider for more clarification. It is my conclusion that whilst dentists will naturally remain the face of dental care, the vital role of dental nurses should no longer be overlooked. They are the backbone of dental practices and show unwavering dedication and compassion to patient care. A dental nurse’s role can now thankfully extend way beyond the dental chair, making them an indispensable asset to the field of dentistry. n
References
1. Dental Protection’s wellbeing survey completed by 153 dental nurses between March and April 2023



























Thumb sucking is a habit that can be incredibly difficult to break. Even the most determined parents can find it tricky to persuade their child to stop. And some families probably don’t consider it to be a problem. But is it? The short answer is: it can be!
Prolonged and vigorous thumb sucking over a number of years can lead to a variety of issues, both physical and emotional. This article will explain in more detail what those problems are, what causes thumb sucking, and suggest some solutions.
Why do children suck their thumbs?
Like many actions, thumb sucking starts in the womb. It is a totally natural reflex which in many ways mimics breast feeding. Babies want comfort and reassurance, and thumb sucking provides an easy way for a child to self-soothe.
Ultimately, thumb sucking can often be traced back to anxiety. If a child is nervous about something – for example a new sibling – then they are likely to seek out comfort from something they find calming and reassuring. Something like thumb sucking. Many children suck their thumbs in the early years of their life, and this is typically not a problem. But if they continue to suck their thumbs beyond the age of four or five, or when the adult teeth start to emerge, more serious issues can occur.
What problems can thumb sucking cause?
There are a number of emotional challenges associated with thumb sucking: low self-
esteem, for example. But some of the most obvious side-effects are related to oral health. Two very commonly seen problems are a crossbite and an anterior open bite. When a child regularly places a thumb or finger in their mouth, their teeth can grow in an irregular pattern. This, of course, can lead to dental problems as their teeth develop.
Other common issues include lisping, imprecise pronunciation and thrusting out the tongue when talking. The shape of the palette can also change, and a child can experience frequent jaw ache and problems with chewing. These issues can all add up, and be emotionally, financially and physically challenging.
are there solutions?
Of course! We may be biased, but we think one of the best solutions is a Thumbsie. But it’s not just Thumbsie. Many parents also find that replacements work well. A comfort blanket or a favourite cuddly toy, for example. If a child focuses their attention on something else, they are less likely to suck their thumbs.
Encouragement is also key. If a child feels supported and listened to, they will feel more ready to (slowly) break the thumb sucking habit.
But what about thumbsie?
For over a decade, Thumbsie has been producing snug fabric thumb guards that fit over a child’s thumb like a glove. They serve as a reminder to a child not to suck their thumb. Most importantly, they are fun. They come in five different sizes and countless

different designs: from flowers to animals and superheroes. They can be worn for school and playtime and, best of all, they work! We are accredited by the Oral Health Foundation and have received a wide range of awards. We also have a 4.8 out of 5 rating from parents on Google Reviews. And we are especially thrilled that dentists from across the globe support Thumbsie and recommend us to their patients. Here’s a couple of brilliant reviews: Donna at iQ Orthodontics explains: “Digit sucking has a huge emotional attachment in young children and so it can be a very difficult habit to break. Thumbsie is a great way to help to stop the habit, children can choose their own design and really make the Thumbsies their own. We have had great success with patients using the Thumbsie and regularly recommend it. It often means we don’t need to use orthodontic appliances to stop a thumb or finger sucking habit.”
Dr. Andrew McGregor, Park Orthodontics, Glasgow loves Thumbsie because: “Anything that makes the process fun can be a massive help because getting a child to stop thumb sucking can be very difficult. Thumbsie has helped several of my patients to successfully kick the habit. I now recommend it to every frustrated parent!” For more information, visit our website –https://thumbsie.co.uk/
If you are a dentist that would like a sample of our gloves and our book please email Jo on hello@thumbise.co.uk. n
about the author Jo Bates, Mum of a former thumb sucker and Owner thumbsie Ltd.
A guide to SPF lip balm choice for our patients
Everybody should be wearing an SPF lip balm daily. Preferably one with a water-resistant broad-spectrum coverage, as this will not only protect against ultra-violet (UV) light but also help with both hydrating and maintaining the integrity of the lips, which is important in the fight against disease. It is a little-known fact that cold sore sufferers are at increased risk of developing lip cancer, so it makes sense to take any preventative measures we can. However, despite their frequent exposure, the lips are often forgotten when considering sun protection. Thus, it is clear that, as dental professionals, we need to empathise the importance of wearing SPF lip balm in order to protect this sensitive area from the sun’s damaging effects.
Which to choose?
SPF lip balms come in various formulations, including both physical and chemical, but just how do they differ, and which type should we be recommending to our patients?
Mineral (aKa physical)
These lip balms use more ‘natural’ ingredients that function as a barrier deflecting the sun’s ultraviolet rays. The active ingredients tend to be titanium dioxide or zinc oxide, and they generally contain occlusives such as organic beeswax or shea butter (petroleum is usually avoided as it may be contaminated) that help to lock in moisture and prevent water loss.
Because of their more ‘natural’ formulas they are often recommended for toddlers, kids, and expectant mothers to avoid them ingesting any ‘nasties’ such as pesticides. They are also better tolerated by those with sensitive lips as they are less likely to cause an allergic reaction. One disadvantage is that some formulas tend to be whiter and pastier, sitting on the lips and resisting absorption. But, on the plus side, they are active as soon as you apply them, so you do not need to wait for them to start working. Ideally all SPF lip balms (but especially mineral) should be:
• Safe for sensitive skin
• A minimum of SPF 25
• Broad spectrum
• Considered reef safe (more on that later)
Examples of mineral/physical lip balms include:
• Sun Bum mineral SPF 30 lip balm
• Coola tinted mineral sunscreen SPF 30
• Balmy Fox lip balm SPF 25
• Summer Camp Mineral BFF SPF 50
chemical lip balms
These contain synthetic compounds that absorb UV radiation and convert it into heat. Thus, they offer broad spectrum protection against UVA and UVB rays by acting like a sponge ab-sorbing the UV rays and minimising harm to the lips. As their name suggests, they contain artificial active ingredients such as avobenzone, octinoxate and oxybenzone along with other additives such as fragrances.
However, unlike mineral/physical balms, which work immedi-ately you have to wait 20 minutes before they are activated – a fact which is often unfortu-nately overlooked and needs reinforcing. Examples include:
• Coola LipLux Classic Sunscreen lip balm SPF 30
• Supergoop Play lip balm SPF 30 with mint
• Jack Black Intense Lip Therapy SPF25
Hybrid
Some SPF balms are known as ‘hybrid’ as they contain both types of filters. An example of this type of balm is:
• EltaMD UV lip balm SPF 36 are they harmful?
There has been a lot of misinformation about the risk of sun protection being carcinogenic, and patients may well ask about this. However, there is no firm evidence of SPF lip balms being linked to cancer.
What about the environment?
Zinc oxide is always considered ocean friendly as it is deemed coral reef safe. However, it is not as simple as one being ‘good’ and the other ‘bad’ although that is often how they are portrayed. Indeed, tracking down zinc often means that some is released into the environ-ment which is obviously of ecological concern. Also, the term ‘reef friendly’ has yet to be regulated so if patients are concerned, they need to check the ingredients and

avoid sub-stances such as Oxybenzone, Octinoxate, Parabens, and Triclosan as these can harm coral reefs. The take home message is that just because mineral SPF balms are considered more ‘natural’ they are not necessarily more eco-friendly.
So, what’s better mineral or chemical sunscreen?
It is really all down to personal preference. As mentioned above, just because it’s ‘natural’ it does not make it good. Similarly, ‘chemical’ does not make it bad. In fact, they are remarkably similar as both convert UV rays to energy like heat and both are safe and effective if used properly. The list of balms mentioned above is by no means exhaustive and it makes sense for patients to seek the advice of a pharmacist before purchasing their chosen prod-uct. At the end of the day, the best SPF lip balm is the one that they are happy to use every day and doesn’t spoil the taste of their lunch! References available on request. n
about the author
ali Lowe is the founder of Fit Lip UK
– a campaign aimed at encouraging people to wear SpF lip balm in order to protect their lips, prevent lip cancer and keep their mouth healthy.




























Dental anxiety, the unpleasant feeling or stress that something undesirable will happen in a dental appointment, affects 51% of the UK population. As a dental prophylaxis appointment may require periodontal probing, X-rays, and the prophylaxis itself, this can be an uncomfortable experience for anxious patients. Dental prophylaxis may need to be performed on some patients prior to impression-taking or tooth whitening. It can also be provided as an effective treatment for mildmoderate gingivitis, preventing further development of the condition. Creating a trusting environment in your practice can reduce patient anxiety and allow you to deliver such treatments with greater confidence.
a calming practice
Sound can be a key stimulant for anxiety. Maintaining a relaxing atmosphere in the dental practice by playing soft music can help. Within an appointment, pleasant music can reduce the activity of the neuroendocrine and sympathetic nervous systems, reducing stress. Whether your practice plays background music or the patient wears earphones should be up to them, promoting a feeling of control. Another aural component to consider is tone of voice: staff should use a positive, caring tone with patients that further supplements the calming environment.
Other sensory stimulants that can be controlled include the avoidance of bright lights and high temperatures, but brightly coloured rooms and posters can have a positive impact. Pleasant ambient odours in a dental practice have also been found to increase patient comfort for moderate cases of anxiety, often concealing the smells of chemicals that can trigger stress.
A calming waiting room environment can help accommodate anxious patients prior to their appointment. Once in the surgery, it is up to the practitioner to comfort the patient by communicating clearly and effectively, identifying anxieties and finding solutions around them.
Children often have a fear of the dentist and finding ways to keep them comfortable in the dental chair can be difficult. The source of fear can include many things: the shiny instruments, drilling, dentists in white uniform and even contact with a ‘stranger’. With help from a parent/guardian, finding the source of the fear can allow you to adjust your approach. For instance, if the child is fearful of the instruments, the Tell-Show-Do technique can demonstrate their harmlessness before being used. The technique is effective at reducing the heart rate, sparking the encouragement the child needs to sit and receive treatment. Having a few toys and stickers on-hand can also help increase the child’s comfort.
Another factor for dental anxiety could be experiencing sensitivity during a cleaning.
Enquiring whether patients experience sensitivity can reduce their anxiety if relief options are then offered. This can involve applying topical pastes before cleaning to plug and seal any open dentinal tubules.
tastefully done
Flavour can help make oral hygiene and treatments more agreeable for patients. We have seen how minty toothpaste is commonly used for its fresh taste, and makes brushing a more pleasant experience for those who like the flavour. 50% of adults reported that flavour influenced their choice of toothpaste. Flavour is a key factor in decision making for other oral hygiene products like mouthwash. From spicy or sour to sweet and fruity, dental health products now have expansive ranges to ensure that the patient’s taste preference is catered to.
More importantly, having an agreeable taste increases compliance with the product, with a sweet toothpaste increasing brushing times among children, for instance. For neurodivergent patients, particularly autistic individuals, sweet tastes are generally preferred over bitter flavours. Colour may also be a factor for what they would willingly try. For dental prophylaxis, sweet-flavoured options that are brightly coloured could increase compliance in neurodivergent and young patients.
tasty treatment
For dental prophylaxis, comforting uncertain patients can be achieved with
Alearning disability is a lifelong condition affecting a person’s intellectual ability and may impair their capacity to undertake everyday activities, like brushing their teeth or visiting the dentist, independently. Although individual abilities vary, people with a learning disability may need support to develop new skills, understand complicated information and interact with other people.
It is estimated that over a million people in England have a learning disability. Of those, around 905,000 are over 18, and 286,000 are children. Although services, including community dental services, exist to support adults with learning disabilities, it is estimated that only 20% of learning-disabled adults in the UK use these services, and many adults may not receive any assistance with the daily challenges they face.
People with learning disabilities have worse health outcomes in general than non-disabled people. Studies have found that people with intellectual disabilities are significantly more likely to suffer from edentulousness, and have worse oral health overall. There are several contributory factors cited; adults with learning disabilities have a lower uptake of screening services, and may struggle to adhere to treatment or hygiene recommendations where memory or cognition is affected. Some medications may be a contributory factor – antipsychotics prescribed to some people with learning disabilities may increase the risk of xerostomia, for example.
A nationally coordinated survey of specialist schools concluded that a much higher percentage of children from 5 to 12
years with Special Educational Needs in the UK had experienced dental caries than children in mainstream schools. Of these, each had on average 3.9 affected primary teeth. Six per cent of 5-year-olds had one or more teeth extracted on one or more occasions, across England. This figure is approximately double that found among children attending mainstream schools.
Degrees of impairment require different approaches or support from family or paid carers. Where individuals do have dedicated support, they may still struggle to manage their oral care, including dental visits and managing adherence to treatments. Additional support for carers is recommended.
A more person-centred approach to the treatment of learning-disabled people has emerged in the last 30 years, with the introduction of the Disabilities Discrimination Act (DDA) (1995), then the Equalities Act (2010), alongside developments in Human Rights legislation. The Mental Capacity Act 2005 outlines in its Code of Practice 2007 that although a person may lack the capacity to make certain decisions about complex matters, where they do have capacity, they should be allowed to participate in decision-making.
The social model of disability was first introduced in the 1980s, and identifies the importance of removing barriers to enable disabled people to participate in society rather than focusing on a person’s illness as the problem. Dental practices are tasked with making reasonable adjustments to remove barriers to equal treatment.
a flavoured paste. Kemdent’s range of prophylaxis pastes includes original, strawberry, bubble-gum and spearmint flavours, providing ample choice depending on a patient’s preference. Each paste has a specially designed viscosity that allows it to cling to the brush whilst its unique formulation eliminates drink and food stains. Furthermore, its thixotropic consistency makes it far more manageable for cleaning. Offering medium grit for normal use and heavy-duty grits for tougher stains, Kemdent’s range will help to provide care that meets the demands of each patient, polishing their teeth effectively. By maintaining a calm atmosphere within your practice and tailoring treatment options to appeal to patient tastes, you can create a positive experience for those that feel anxious about a dental appointment. Having open conversations and boosting trust can leave the patient feeling positive that their oral health is in good hands. For more information about the leading solutions available from Kemdent, please visit www.kemdent.co.uk or call 01793 770 256 n
about the author alistair Mayoh, Marketing Director, Kemdent.

Codes of practice around the treatment of children and adults with impaired intellectual capacity increasingly encourage seeking participation from and collaboration with the person undergoing treatment wherever possible. To support the delivery of adjusted, person-centred care, the evidence shows a need for clinicians to undertake special training, and to utilise a number of different strategies to encourage understanding and participation. This is important for family carers, paid supporters, dental professionals and their staff teams, as well as for people with learning disabilities themselves.
People with learning difficulties can experience a high level of anxiety in a consulting room, and this can be a real barrier for patients in participating in their treatment. Communication skills that help with building a rapport, and resources that provide a distraction, like workbooks or tactile objects, can be helpful.
Public Health England recommends that people with learning disabilities are involved in delivering training for the dental team. This has the additional advantage of providing teams with real-life experience.
A person must be assumed to have capacity unless it is established otherwise, but even if they don’t, their participation in decisions affecting their own welfare is still important wherever possible. According to the Mental Capacity Act 2005, efforts must be made to include people in decisions until all practicable steps have been taken without success. Consent is a process,
not a one-off event, and it is important that there is continuing discussion to reflect the evolving nature of treatment.
Clinicians can make use of technology to assist patients in understanding the nature and purpose of certain treatments. Chairsyde – a state-of-the-art patient consultation platform – helps dentists to improve patients’ understanding of treatments. The system uses patient-friendly dental animations to demonstrate the benefits as well as the risks of all treatment options. Visualising treatment additionally supports patients who might struggle with different cognitive abilities. Chairsyde is recognised and recommended by dental industry leaders to support patients in committing to and participating in ongoing dental care.
Every practitioner is required to make genuine efforts to help patients understand their options before seeking consent, at every stage of treatment. Where there are impairments in understanding, it is the responsibility of clinicians to make adjustments to enable people to participate in decisions around their own care, and there are lots of resources out there to make this easier.
For more information, or to book a Chairsyde demo, please visit www. chairsyde.com or call 020 3951 8360 n
about the author Loven Ganeswaran, ceO and founder, chairsyde.

The safety and wellbeing of patients is every clinician’s first priority.
Dental professionals do all they can to optimise conditions for successful treatment, free of complications or harm of any kind. Despite this, the fear of litigation weighs heavily. In a recent survey of dentists, it was revealed that 98% believe that society has become increasingly litigious, and 79% are concerned about the impact this is having on their welfare and the way they practice. 77% of respondents have experienced stress or anxiety connected to fear of being sued.
This fear does little to improve the quality of care. Anxiety leads to practitioners feeling less clinically confident, affects the decisionmaking process, and leads to professionals feeling less able to form a diagnosis.
The World Health Organization (WHO) and the NHS have developed recommendations and protocols to contribute to an environment that promotes patient safety. A positive patient safety culture should not just address risk management around treatments, but should also support the safety and wellbeing of clinicians, allowing them to practice and learn without fear.
Safety in practice
According to guidelines, patient safety is about maximising the things that go right and minimising the things that go wrong for people experiencing healthcare. A safe environment adopts procedures, systems and culture that reduce the occurrence of avoidable harm, making error less likely and

reducing its impact when it does occur. This is achieved by building competency through continual learning while adopting a supportive approach to teamwork. Alongside patient engagement, an emphasis on organisational strategy and systems that support excellent communication, and effective, coordinated treatment, is advised.
Only a tiny fraction of patient safety incidents occurs in primary care, but the report lists a number of factors that could potentially threaten the safety of patients in these settings. These include risks to electronic health records, communication breakdown between practitioners and other team members, limited patient health literacy, a lack of patient engagement or adherence, and the effects of clinician burnout.
The report notes that dental work historically done in secondary care, such as minor oral surgery, can increasingly be offered in a primary and community care setting, potentially increasing risk. Clinicians are advised to apply additional risk management protocols when conducting more complex
procedures, but surveys have revealed 64% of respondents feel that the fear of being sued has resulted in them making more referrals rather than attempting procedures that hold greater risk. This caution prevents clinicians from honing or developing new skills, fuelling a sense of frustration, as well as closing off potential areas of development for their business. It’s clear that further mitigation is needed to allay fears.
To protect dental professionals from the anxiety of litigation, and to maximise patient safety, the GDC – as well as the NHS –have emphasised the importance of excellent documentation and record keeping, by every clinician at every stage of treatment. Doing so builds a body of evidence to support the clinician’s approach to decision-making, and demonstrates that patients were clearly made aware of any risks as well as the benefits of all options around treatments before consenting. WHO recommends investment in the means to promote patient engagement, which, if done well, can increase the safety of patients by up to 15%. Studies show the value of clear communication in promoting trust between patients and dental professionals. When patients feel more engaged and informed, they are more likely to display autonomy in adopting healthier behaviours, and will engage more proactively in decision-making around their care, optimising outcomes. Patientcentred care – treating patients as individuals and equal partners in the business of healing
– leads to greater patient satisfaction, improved outcomes, enhanced health status, and reduced utilisation of care.
Investing in a system that boosts patient engagement as well as providing the best in contemporaneous note-taking, that can be translated into documentation instantly and effortlessly, is a game-changer in creating a safer environment for patients and clinicians. Kiroku believes clinicians can spend less time writing records with intelligent machine-learning systems, all while enhancing legal protections and patient safety. Kiroku Docs seamlessly takes information input in consultations via AI-powered, one-click notes, and converts them to any documentation clinicians need for records, referrals, treatment plans, patientfriendly information and consent forms. Now Kiroku Practice adds new features such as smart prompts and AI audits to ensure the whole team follows best practice all the time.
Maintaining a positive culture of patient safety is helped by systems that protect the wellbeing of practitioners as well as patients. Relaxed, confident clinicians feel more able to develop new skills that could open up new horizons, as well as cater to the more complex needs of their patients. When systems are improved, everybody wins.
To find out more about Kiroku, or to start your free trial, please visit trykiroku.com
About the author Hannah Burrow, CEO of Kiroku.



















They say a good worker never blames their tools, but what if the tools are not good for the worker?
Chronic back pain now afflicts over 2.8 million adults in the UK, resulting in 31 million workdays being lost due to musculoskeletal disorders (MSDs). As the country’s workplace becomes increasingly remote and computer-based, the epidemic of back-related pains grows, with 80% of cases caused by poor posture. Like all professions, dentistry has its occupational hazards. From exposure to radiation to high levels of stress, dentists have a host of variables to control in their daily work. Dentists are susceptible to MSDs, with neck, wrist and lower back pain manifesting itself in conspicuously high numbers, leading to low productivity and time off work. MSDs can develop from inadequate dental equipment; having the best technology available is crucial for maintaining a low-risk workplace and keeping yourself and your associate dentists in good physical health.
practitioner posture and practitioner pain
Treating patients for long periods of time may involve the persistent bending of the body and the constant craning of the head. The subsequently overstressed spine and peripheral nervous system causes tightening of the neck and back muscles, leading to a notable, sometimes
painful, ache for the practitioner and a risk of developing MSDs.
Despite the small number of dental posture analyses, one study ascertained that the extraction of the left and right lower jaw teeth, the extraction of the right upper jaw teeth, and restorative procedures on the upper teeth all exacerbated poor posture, putting dentists at the greatest risk while performing these treatments.
The stooped position in which standing or sitting dentists deliver lengthy procedures from can be offset through stretching and maintaining an upright posture whenever possible, but it is also important to evaluate the equipment being used.
Inadequate illumination is linked to MSDs and is an overlooked factor that the practitioner can control. Studies have shown that undergraduate students who had good illumination had a low risk of developing MSDs, as well as eye strain and fatigue. By obtaining brighter operative lighting, practitioners will not need to strain their necks as much and can mitigate the chance of developing muscle problems. In conjunction with better lighting is the use of dental loupes. It is commonly perceived that loupes exclusively aid vision, yet they are also an instrument to improve practitioner posture and working positions, removing the need for the practitioner to lean forward as much.
Sitting on a stool for extended periods of time is part of the job, but dentists are more likely to report severe back pain if they do not alternate between sitting and standing. This is because the type of stool used influences lumbar posture. Finding a supportive dental stool is therefore of paramount interest for the workplace, particularly for new dentists at the start of their career with years of sitting ahead. Rather than hunching beside a patient, using the latest ergonomically designed dental stool will promote clinician comfort by supporting the natural curve of the back. Saddle stools, in particular, are gaining traction in the profession because they open up the angle between thigh and torso, distributing weight evenly and reducing pressure on the spine. However, it is still up to the practitioner to maintain an upright posture when working, and an ergonomic stool is more assistive rather than demonstratively alleviative. Still, selecting an ergonomic stool that supports the spine should be used to prevent MSDs.
With the practitioner sitting on a more supportive stool, the patient should be in an equally supportive dental chair, not just for their own satisfaction and comfort but for the practitioner’s too. A cutting-edge ergonomic dental chair provides practitioners with the adjustable positioning range needed to undertake long procedures that do not stress the spine and neck.
Artificial intelligence (AI) is changing the status quo in dentistry and enhancing practice efficiency. It facilitates the design of restorations, highlights dental decay or the position of the ID nerve on radiographs, and streamlines dental reception management. It is such an exciting emerging field, research suggests that a third of US practices had already embraced AI by 2023. For more practices to do the same, it’s important they choose the right provider of AI-supported technology.
concerns about ai
In the aforementioned research, 67% of dentists surveyed were concerned about data privacy and security, as well as reliability and accuracy of AI systems in dentistry. And they may be right to be. When analysing x-ray images, or designing crowns from a scan, clinical data can easily be separated from the personal, anonymised and learnt from by “Narrow AI” systems, without compromising data privacy. But what happens when using “Generative AI” – Large Language Models (LLMs) that generate something new – to create clinical written records that contain sensitive information?
Some industry standards regulating the use of data are well-established. The challenge is understanding the implications of using personal, sensitive data with AI. Can you use GDPR-protected data to train AI models? Can you use ChatGPT to generate letters or does this fall foul of data privacy rules? Can Generative AI systems access the personal information needed to populate clinical records and consultation notes?
These are not easy questions, but they’re essential to build a safe future with AI-supported healthcare.
protection from within
The dental practice is a data controller and must appoint a Data Protection Officer (DPO) responsible for ensuring the privacy, security and protection of patient information. Registration with the Information Commissioner’s Officer (ICO) is also essential for practices – and for individual dentists who take patient information off-site.
Where using AI to generate written notes, the practice DPO must ensure that data is used, stored and processed in accordance with the UK regulatory framework. A Data Protection Impact Assessment (DPIA) helps to identify and minimise data protection risks and is crucial for due diligence. Patients have a right to expect their data not to be used to train LLMs without their explicit consent. Further, the creation and storage of clinical records must have a secure audit trail to demonstrate authenticity and accuracy.
Dental practices must, therefore, also ensure their AI technology provider meets the relevant standards for data privacy, security and the clinical record.
Standards for data security are wellestablished and technology providers must demonstrate compliance with one or more security standards.
Cyber Essentials is a government-backed scheme designed to prevent cyber attacks. The NHS Data Security and Protection Toolkit (DSPT) is a self-assessment solution for businesses handling NHS data,
Leading suppliers provide the latest in ergonomic dental chairs, stools and operating lights alongside efficient installation and regular servicing and support. With 50 years of experience in dentistry, RPA Dental optimises ergonomics in everything from the dental chair to the surgery layout, providing an extensive service from design to instillation and longterm maintenance. Their response time guarantee is nationwide, mobilising a first-class technical team that will support your practice by providing exceptional customer service. Offering premium brands like Stern Weber, Castellini, and Kavo, RPA Dental’s holistic focus with clients ensures that a practice can achieve its maximum potential.
With 60% of dentists reporting lower back pain each year, procuring the latest equipment from a dependable supplier will lower the risk of MSDs and improve the productivity, and therefore success, of your practice. It is time for new tools.
For more detail about the solutions and services available from RPA Dental, please visit www.dental-equipment. co.uk, call 08000 933 975 or email info@rpadental.net n
about the author adam Shaw, Sales Director at rpa Dental ltd.

necessitating an annual security penetration test. For more advanced cyber resilience, the ISO/IEC 27001 governs information security management systems.
If a technology provider uses third-party systems to perform some or all of the data processing, zero-retention agreements must be in place. The world’s first AI management system standard is the ISO/IEC 42001 promoting the responsible and effective use of AI. The US National Institute of Standards and Technology (NIST) also facilitates federal coordination of AI standards.
These standards are very new and currently focus more on AI development than usage. It’s also worth noting that these standards, while easily applied to Narrow AI (such as x-ray reporting), are much more difficult to apply to Generative AI models (those used for generating written records from a voice audio recordings).
The enormous speed of software and AI development keeps governance in a state flux, so end users may easily lag behind. Consequently, dentists should work with technology suppliers that understand the evolving field and care about keeping you and your business compliant.
When using an AI note generating software, that technology provider should provide evidence of their ICO registration and share any current certificates from programmes like Cyber Essentials and the NHS DSPT to demonstrate the data protection and security credentials necessary for compliance. You can confirm all of these by visiting the respective organisation websites. Dental practices should also ask about the data policies and processes in
place to ensure data is protected from generation to storage.
For instance, Dental Audio Notes (DAN) utilises AI algorithms to generate written records from audio records of patient consultations, and no information is ever used directly to train or build new models. It also has zero-retention policies in place with AI model providers, and offers a complete audit trail for the clinical record. Immediate end-to-end encryption further protects data. This means that DAN provides a safe way of recording patient consultations, ensuring complete, contemporaneous and accurate record keeping while also maximising data security for total peace of mind.
It is likely that specialist large language models will soon be designed to fulfil the specific data privacy and security needs of dentistry. Until then, we must continue to utilise AI capabilities carefully to avoid unintentional consequences for dentists and for the patients whose data is being processed.
Definitely do check out AI generated record keeping. But please do it safely. You want to make sure that you stay on the right side of the ICO – data protection breaches can be very expensive.
Discover Dental Audio Notes (DAN) or arrange a free demo at dentalaudionotes.com n
about the author aleksandra rozwadowska (ala) is a dentist and the co-founder of Dental audio Notes.






The couple that helps you to achieve even better oral hygiene

FLEXI
• The special FLEXIBLE HANDLE makes it possible to angle the handle to achieve better and easier access to all interdental spaces.
• The non-slip handle ensures good grip even when fingers are wet.
• All brushes have plastic coated wire. This ensures no metal is in direct contact with teeth and gums, thus making them much more comfortable to use and preventing dental injuries.
• 11 sizes ensure that all needs are covered.



TANDEX PREVENT Gel
• Strengthens the enamel and has an anti-bacterial effect.
• 0.12% chlorhexidine and 900 ppm fluoride.
• The consistency combined with the needle shaped tube end make it easy to apply directly on the FLEXI brush and use wherever needed.
• Pleasant taste of peppermint.
• No alcohol or abrasives.
Effective digital systems can help practices organise information, safeguard precious data, provide useful business metrics, streamline financial management processes, manage the team more effectively and enhance communications with patients.
If you have more than one practice, these functions need to be effective across every site you own. Gaining control of all the many complexities and variables represented by different staffing, different locations and different environments can make all the difference to the successful management of a busy multi-site business.
Why your multi-site practice needs an integrated system
Data integration involves the extraction of information from disparate sources to create new information and useful metrics, combined into a single view. A system that quickly and efficiently converts comparative data from disparate sources into a single view can enable you to perform detailed analyses on different metrics of interest to you across different locations.
For example, you can test your preconceptions on what procedures work best at different sites at different times. You will develop insight on what staff training to prioritise, and scheduling tools will help you manage working patterns remotely.
Selecting the best system for your business
If you have been dealing with a system that doesn’t match your needs, it’s easy

to be reactive, and concentrate on the gaps in the system you have rather than on the opportunities to rethink procedures and processes.
Having a set of clear criteria is vital before embarking on the process of selecting a new practice management system that better suits your particular business. Once you’ve created your wish list, it’s important to identify the business need for all the functionalities you’re hoping for, and to prioritise these throughout the process of selection.
Think about your whole business – your locations, your patients and ways of working. What are your current systems? What do users like and dislike? Try to attach a financial cost and benefit to different features of interest. For example, how do any delays in accessing patient data affect consultations, patient perceptions, clinician stress and what does this cost you? Think about your wide business development objectives and how these might change over time. Before you start – who will benefit, and how?
1. Have you identified all stakeholders? By stakeholders, we mean more than users. Yes – team members who interact with data are stakeholders, whether they are inputting medical information during patient consultations, finance management or business analysis, but so are patients, and those in the business who don’t interact with data, but who benefit from efficient systems around internal communications and staff scheduling, for example.
2. Have you consulted them? Surveying the needs and experience of stakeholders is extremely important when implementing any change that affects them. During this process, you will identify where your current systems might be working well and where they might be improved. Consultation with patients will offer useful information. What is the patient experience, and how might interactions with your practice be easier for them? Do clinicians have accurate and up to date records at their fingertips? Do patients receive relevant information promptly and in a consistent way?
From your perspective, are you certain your data management is compliant with the ICO and safe and secure from data breaches? Can appropriate information be accessed quickly and securely by those who need it?
Can you quickly analyse which treatments are most successful in each location? Can you do quick, live, dynamic comparisons on the relative performance of one location over others?
Building a good reputation, both as an individual dentist and a dental practice, is essential for acquiring new patients and ensuring they stay with you long-term. In an age where patients might choose to shop-around for their dental care, it’s important to present a good image of yourself across all aspects of your online and physical presence. In order to do this, there are a number of key things that practices can do to boost their reputation, encourage positive feedback, and ensure they continue to provide excellent standards of care to their patients. So, what should practices consider when building their reputation?
Building a positive presence
No matter how talented your dental team is, and how high-end your facilities are, you will not be able to showcase your skills if you do not attract patients. As such, a great way to let potential patients know you’re there is to create and maintain an online presence. This usually involves building a website which reflects your brand, is informative, and is user-friendly. Be sure to list the treatments you offer clearly, using patient friendly language, and feature informative blogs to ensure patients have a good understanding of the treatments they are seeking from a reliable source – you! It can also be very helpful to have a ‘team’ page, which
allows potential patients to ‘meet’ the dental team virtually, viewing information such as qualifications, specialties or areas of interest, as well as personal information, where appropriate. This can help to show that your practice is friendly and approachable. Creating a presence on social media is another great way to connect with patients in an informal way.
However, patients are unlikely to go straight to your website. Commonly, those seeking dental care will search “dentist near me” and start there. As such, put yourself on the map – literally. Ensure you are easily searchable on Google Maps, with your phone number and practice website clickable from there. Another helpful feature here is the ‘reviews’ function. This is a great place to send patients to leave feedback following their appointments, as it is a fantastic tool for patients when deciding to register with the practice.
When it comes to patient reviews and feedback, inevitably, not all will be glowing. As such, it’s important to know how to handle a bad review and, more importantly, how to learn from one. While positive reviews are fantastic, enabling you to showcase your successes, and increase your star rating, negative feedback can also be incredibly useful. Constructive criticism, in particular,
Every practice will have their own criteria, but as you go through the procurement process, don’t be afraid to ask difficult questions; for example, about scalability, data migration logistics, compatibility with other systems, or any additional costs, like licence fees, hardware or support.
AeronaDental practice management software offers full functionality to seamlessly integrate systems for any multisite dental business. Cloud-based, the system safely retains all patient information, appointment types, clinical information, recall durations, and medical histories, which are easily accessible across sites. Patient engagement is aided by powerful communications tools, including access to the appointments calendar across all sites. Professionals can use the system to communicate with others in different locations, and business metrics can be analysed instantly, putting you in control of the whole business.
When you do start your search, the product team’s response to requests to clarify details important to you will be very telling. Do be wary of the sales pitch, and be sure to keep score against your criteria as you interview and trial different systems. For more information, visit aerona.com n
about the author
Mark Garner, General Manager, aeronaDental.

can highlight areas where you could improve your practice further, be it the physical environment, patient experience, or learning experiences for the dental team. Where these reviews – positive or negative – are submitted to a public forum, responding quickly can be helpful, as this shows that your dental practice engages with its patients, even after the appointment is over. Not only is this a great way to keep current patients coming back, but it acts as an advert for new patients too.
Another fantastic way to keep patients long-term is to offer high-quality treatment types, provided by highly skilled clinicians using excellent materials and equipment. Constantly investing in your own training and education, as well as that of your team where appropriate, can be an incredibly valuable asset. When you possess an outstanding skillset, patients are far more likely to be satisfied with the high-quality treatment you provide, and choose to come back time and time again. Similarly, investing in equipment which matches these high standards will allow you to carry out your treatments to their full potential. By creating an environment that reflects your brand, you will be able to develop a consistent image of your business. Patients create an association with your practice, and high-quality treatment, with the familiarity building a sense of trust. As part
of this, it’s important to invest in high-quality equipment which sets you apart from your competitors. A chairside workflow, for example, can be a fantastic selling point when drawing in new patients. Clark Dental offers the CEREC Primescan, Primemill, and Primeprint chairside workflow, which allows clinicians to carry out entire treatments in one place, without the need to employ the services of an external dental lab in many cases. This creates a streamlined experience for the patient, allowing them to receive their restorations more quickly thanks to an entirely digital workflow. In the modern and competitive dental landscape, it’s important that dental practices have the knowledge and skills they need to stay ahead of the curve. Maintaining a good reputation can play a big part in this, enabling you to attract new patients, and encourage existing patients to keep coming back.
For more information call Clark Dental on 01268 733 146, email info@clarkdental.co.uk or visit www.clarkdental.co.uk n
about the author Stuart clark, Managing Director, clark Dentel.

Following dental implant treatment, it’s important that patients implement a stringent oral hygiene routine. Some patients may assume that, because their new tooth is artificial, it does not need the same amount of cleaning and care as a natural tooth. This is a common misconception, so it is important to ensure that patients understand how to properly take care of their dental implants to avoid infections, implant failure, and the need for further restorations.
set patients up for success
Providing implant patients with the tools they need to maintain excellent oral hygiene following treatment is a great way to set them up for success and prioritise prevention.

Supplying patients with the Implant Kit from Curaprox is the perfect solution. It contains everything patients need to keep their implants clean. For post-surgery care, the Kit contains a Curaprox Surgical Toothbrush, Perio plus Support toothpaste, a Perio plus Regenerate 0.09% or Forte 0.2% chlorhexidine mouth rinse, Perio plus Focus Gel, and a range of CPS interdental brushes in different sizes. And, for ongoing care it includes a CS5460
Ultra Soft Toothbrush, CS708 Implant & Ortho brush, and long-handle interdental brush holder.
thorough brushing
The best way for patients to keep their dental implants clean and free from bacteria is to care for them in the same way as, if not better than, their natural teeth. Making sure that patients know how to properly execute the basics is key – so it’s worthwhile demonstrating how to effectively brush every area of the mouth to remove as much plaque as possible, using the Curaprox Surgical or CS5460 Ultra Soft toothbrush.
The Surgical toothbrush is designed for special care following operations and features 12,000 ultra fine filaments, each 0.06 mm in diameter. When patients have healed and are ready to level up their oral hygiene, the CS5460 Ultra Soft toothbrush is gentle and effective thanks to 5,460 densely packed filaments, enabling patients to polish their teeth to perfection.
interdental cleaning
Preventing oral diseases around implants and the natural teeth will help patients keep more of their natural teeth for longer, preventing the need for further restorative treatment. Make sure that patients understand how to properly use their new CPS Interdental Brushes by offering a demonstration, or talking them through the process in the practice.
CPS Interdental Brushes from Curaprox can clean even the narrowest spaces and,
thanks to the click system, any Curaprox interdental brush will fit into any holder type. Patients can easily click out and discard the old brush, click the new one into the holder, and keep cleaning the interdental spaces.
Perio plus for long-term protection
Some patients may also benefit from using a mouth rinse as part of their oral care routines. Particularly helpful post-surgery to keep bacteria to a minimum, Perio plus Forte mouth rinse contains 0.2% chlorhexidine for an antibacterial effect.
For long-term use, recommend the Perio plus Regenerate oral rinse, containing 0.09% chlorhexidine, it is an ideal adjunctive solution for patients who need an extra boost. Be sure to offer individuals specific advice for use depending on their unique situation.
For targeted care, implant patients can also benefit from Perio plus Focus Gel. It contains 0.5% chlorhexidine and features hyaluronic acid for a soothing antibacterial effect. It can be applied with pinpoint accuracy for care where it’s needed most, and it adheres well to teeth, gingiva, and oral mucosa, ensuring the Gel’s active ingredients can be delivered to the area effectively.
Patients can also use the Perio plus Support toothpaste in place of their usual toothpaste for comprehensive protection when they are experiencing gingival and implant related issues.
Perio plus products contain CITROX®, a natural extract of bitter oranges, combined with polylysine amino acids which enhances

the range’s healing and protective effects. Use of CITROX® is ideal before and after oral surgery, protecting against periodontal diseases, and preventing candida infections.
tailored oral hygiene advice
Ultimately, discussing a tailored oral hygiene routine with patients is the most effective way of preventing oral diseases and infections. Demonstrating what effective cleaning and plaque removal should look and feel like, as well as supplying information to take home can ensure that patients have a good understanding of how to care for their new dental implants. Provide patients with all of the tools they need to maintain excellent oral health postsurgery and beyond with the Implant Care Kit from Curaprox.
For more information, please visit curaprox.co.uk and curaden.co.uk n

The jump from university into a practice environment can be daunting for dental students, but having the right support will make a significant difference to their learning experience. This is about more than simply being exposed to the dental system, as well as new patients, and new clinical situations.
Clyde Munro is delighted to be able to support newly graduated dentists whilst they complete their Vocational Training (VT) year. This support is packaged into a structured scheme known as the Best Foot Forward programme, which provides dedicated training events and additional support to help clinicians safely and effectively consolidate and advance their skills. It gives them access to topics that help equip them for joining general practice as an associate, as well as allowing them a chance to network with their colleagues.
The most recent programme was very well attended by Clyde Munro VTs and very

positive feedback has been received. The VTs clearly found the topics beneficial, really providing them with a deeper understanding of the opportunities available as they join the dental profession.
Dr Lucy Mason recently completed the Best Foot Forward programme with Clyde Munro, and says:
“It was really good to be involved with the programme and to have the opportunity to attend the events that were put on. These enabled me to learn new information and refresh my existing knowledge, which is helpful as a VT because you’re learning new things all the time.
“What I found most beneficial was having access to the highly knowledgeable speakers. We had a nice small group which allowed us to ask questions and learn from their expertise in an informal and productive way. The session about becoming an associate, talking through finances and the self-employed structure was really helpful as I hadn’t received much information on this previously during the VT year.
“Everyone at Clyde Munro was very supportive and there were always new opportunities to participate in. I’m looking forward to utilising the Flying Start Programme next year as I continue developing my confidence. I would encourage other VTs and young graduates to get involved in order to broaden their skills as much as possible.”
In addition to the topics Lucy mentioned, her fellow VTs also found the session
on AI (artificial intelligence) technology and the benefits of using this with radiographs and communication with patients extremely helpful. This topic also showcased Clyde Munro’s investment in innovation and newly qualified dentists, with cutting-edge technology made available to all clinicians in practice.
Nicola Logan, Chief People Officer for Clyde Munro, added: “The Best Foot Forward programme has been a great success and working with our newly qualified dentists is something that is so important to the group. We want to support the future of dentistry in Scotland and we are keen to listen and improve the programme year on year. This means developing our training within digital technology and promoting the importance of wellbeing for our newly qualified dentists. We are invested in improving the support we provide to clinicians. There is a lot of pressure put on this generation and we need to make sure, as a leader within Scottish dentistry, that we have the right mechanisms in place to help and support our dentists when they need it.”
In November 2024, we will welcome the third cohort of VT dentists joining Clyde Munro’s best Foot Forward programme. It will consist of three educational and networking sessions over the course of the year. This includes training on digital workflows, AI technology and digital 3D printing; insight into the financials of being a self-employed associate; diary
management; working with a dental therapist; and an invite to ClydeFest our very own internal group event to celebrate our newly qualified dentists. This is a dedicated networking event with a mixture of VTs from both within and outside of the Clyde Munro group.

We hope by providing this support, we can encourage many of our VT dentists to join the group and begin their career with us. Perhaps even joining us on our second internal programme; the Flying Start programme for early career dentists! Ultimately, the Best Foot Forward programme provides newly qualified dentists with an insight into the opportunities and investments they can take advantage of to further their career development. For more details, contact the team today. Find out more about the career opportunities and vacancies available with Clyde Munro today at careers. clydemunrodental.com or contact joinus@clydemunrodental.com for a confidential chat n
Afemale patient presented with severe deterioration of her dentition and the surrounding soft- and hardtissue. She had mobile teeth, and a malocclusion in class II division I, which gave a false indication of the incisal level.
Digital records were captured to inform the entire clinical team as best as possible.
A CBCT scan and a pre-operative OPG displayed severe bone atrophy due to chronic periodontal disease.
Considering treatment options
Treatment options included doing nothing at all, and using dentures to restore the dentition. The patient agreed upon a full arch rehabilitation using implant supported prosthetics.
Experienced clinicians will know that full arch surgery is a complex and demanding procedure, and efficient patient selection and communication is key to maximising success. You must understand their needs and desires, and recognise that many patients will suffer from chronic dental issues and dental anxiety: it is the clinician’s responsibility to create a predictable patient journey.
However, fixed implant prostheses routinely develop complications. Biological problems include early and late implant failures, whilst aesthetic complications are associated with miscommunication, poor planning, poor ceramic work, and misplacement of the transition zone.
The incidence of fracture of a provisional restoration in full arch cases ranges up to 30%i – time-consuming to repair, they may also shake a patient’s confidence.
These risks were communicated to the patient, who consented to the procedure and was given clear oral hygiene instructions. She was provided periodontic therapy to arrest the progression of present disease.
Perfect planning
We undertook an interdisciplinary strategy that incorporated sophisticated surgical procedures and prosthetically-driven digital treatment.
This workflow is fully digital, and keeps the final prosthesis in mind when devising the surgical steps, tailored to each patient. The surgeon and dental technician are involved in all aspects of planning, improving communication and collaboration for optimal delivery of the provisional prosthesis and final hybrid restoration.
Intraoral scans were merged with the DICOM data from the CBCT to allow for software-based planning. This ensured that all the tissue anatomy necessary for denture fabrication was captured.
Digital files and photographs were imported into EXOCAD smile design software. The desired tooth placement, shape, and length were determined, as was the ideal transition line between mucosa and prosthesis. Working closely with the dental technician informed me of any prosthetic challenges and limitations, enhancing my communication with the patient.
The implants’ positions were planned using a prosthetically-driven approach. The STL digital files of the existing dentition and the virtual plan were merged, and the DICOM data from our CBCT scans was implemented. Implant placement could then be planned for



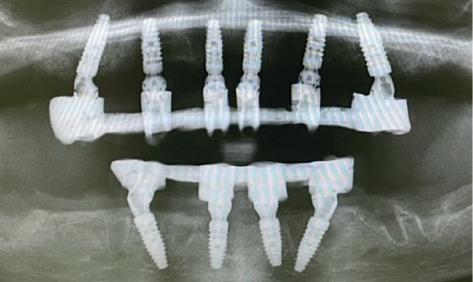


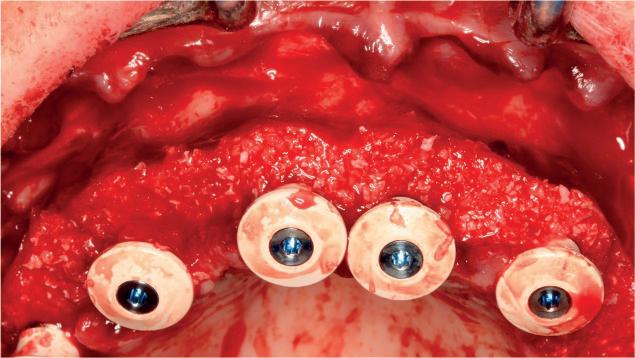

optimal recovery and success, and the teeth that would be extracted first were identified.
We created a tooth-supported surgical guide, the easiest and most accurate solution in my hands. This was designed alongside a provisional prosthesis and steps to follow during surgery, which could then commence.
effectively managed surgery
The previously identified teeth were extracted, whilst the lateral incisors, premolars, and second molars were strategically left to secure the guide support. A full thickness buccal flap was raised, and thorough degranulation of the sockets was performed.
With the surgical guide in place, the implant beds were prepared. Six CONELOG PROGRESSIVE implants, from BioHorizons Camlog, were inserted through the template, allowing precise depth and angulation control. These feature an optimal thread design and tapered figure, helping achieve high primary stability. The guide was removed, and the remaining teeth extracted – except the last two molars.
Straight multi-unit abutments were fixed and tightened with a torque value of 25 n/cm. Titanium cylinders were adjusted and fixed onto these, ready for the provisional restoration.
We used a Gallucci Prosthetic Guide. Though this looks like a normal denture, it is a 3D printed composite bridge with palatal support. The palatal support sits below the fitting surface of the bridge, and is used to locate the bridge in centric occlusion using the hard palate of the patient. The provisional restoration is an exact copy of the digital wax up that helped to plan the positions of the implants, meaning minimum adjustments were necessary. It was established using a light cured composite resin-based material and reinforced with a bent titanium wire, of 2mm diameter.



The procedure progressed in the same manner, entirely as planned, in the mandible. Our guided approach and clear communication meant that the provisional restoration in situ was easily comparable to the prosthetic plan. Post-operative X-rays demonstrated accurate implant placement in accordance with our original designs.
Post-provisional placement
Routine post-surgery advice was given to the patient. She returned a week later, smiling confidently and experiencing no major complications.
Creating the final prosthesis was simple due to our extensive planning and refinement. The chosen workflow was the digital fabrication process through the Atlantis Bridge Base System. The Bridge Base is fabricated directly from the digital impression by milling the MUA connections on a Titanium Select Laser Melted support bar. This extremely accurate support structure also acts as a support structure for the zirconia overlay. This combined the strength and biocompatibility of titanium with the biocompatibility and aesthetics of the zirconium, in a minimal number of appointments.
The patient was delighted with the treatment and the final result. We managed to improve the function of the patient by reducing the original overjet and deep bite and we managed, with the right hard and soft tissue manipulation, to improve the cleanability and thus the predictability of the therapeutic outcome.
I am equally thrilled with the outcome. With an emphasis on effective communication, my team ensured that each stage was well considered, formulating approaches that could be taken with confidence. The result – a successful full arch rehabilitation that has restored aesthetics and function – speaks for itself.



Dr Nikolas Vourakis is a tutor at One to One Implant education, where he guides clinicians of all experiences through their implant dentistry journey. To reserve your place or to find out more, please visit: https://121implanteducation.co.uk or call 020 7486 0000.
Reference
i. Lemos-Gulinelli, J., Pavani, R., NaryFilho, H., Alves-Pesqueira, A., Pessoa, J., & Santos, P. L. (2020). Incidence of surgical and prosthetic complications in total edentulous patients rehabilitated by the All-on-Four® technique: a retrospective study. International journal of interdisciplinary dentistry, 13(2), 76-79.
about the author
dr Nikolas Vourakis

is a dental implant specialist at the One to One dental Clinic in Harley street, and is also a lecturer and tutor at One to One Implant education. He supports clinicians of all experiences throughout their implant dentistry journeys on a range of informative, hands-on courses. dr Vourakis has been a practicing dental surgeon since graduating in 2005 from the prestigious Military academy Medical school at the university of thessaloniki, Greece, and spending time as a military dental surgeon in afghanistan, from 2006-07. He received his Msc degree in Oral surgery and Implantology from Goethe university








































Paste








Flow




















































































OMNICHROMA –is all you need for state-of-the-art filling therapy. Flow



The patented Smart Chromatic Technology in OMNICHROMA ensures continuous shade adjustment from A1 to D4 due to its structural colour. Add to this 3 different viscosities for all preferences and areas of application. The OMNICHROMA family thus offers the user every conceivable option with a minimum of materials.


More information: tokuyama-dental.eu/en/omnichroma






































artificial colour pigments ”automatically” adapts to the tooth shade









Bis-GMA– formulation for better biocompatibility

sustainable stocking only order 1 shade & no expired special shades






We’re living in a highly litigious world today. Therefore, when clinicians move into more complex treatments – like dental implants – they need to be confident in their skills. Only with adequate training and experience will they be able to justify the treatment they deliver, should they end up in front of the regulator.
Guided surgery supports implant outcomes and provides an extra layer of protection for clinicians. It forces practitioners to look at the threedimensional anatomy, including the volume, character, and nature of the bone, the thickness of the soft tissue, and the distances available for implant placement. If an anatomically correct diagnostic wax-up is used for the planning, the ideal implant position can be identified. In my opinion, the ideal depth of placement is an element of planning that is poorly understood.
Guided surgery, a technique that has never been more accessible, is now supported by virtually every implant company through partnered software. This widespread availability makes it easier than ever for clinicians to adopt a guided approach. For those new to the field, it’s crucial to find high-quality training that will offer a strong foundation of knowledge and skills. I invite colleagues to consider our “Level Up in Guided Surgery Level 1” course with BioHorizons Camlog, which provides comprehensive teaching and mentorship. The case presentation below demonstrates the type of patient you can expect to treat after completing the training, further highlighting the accessibility and benefits of guided surgery.
A young male presented with hypodontia and a number of missing permanent teeth. He was relatively unconcerned about his appearance and was driven more by his parents to seek treatment. As such, the patient was unsure about what he wanted from treatment and hesitant to undergo more than he absolutely needed to.
Upon assessment, it became clear that the patient’s tooth spacing was not ideal, and realignment would be necessary to create space for the lateral incisors. The patient had already been referred to me, and the option of no treatment had been discussed and ruled out. I presented the patient with two treatment options: Maryland Bridges or a combination of orthodontics and implant placement. The latter was my professional recommendation, and the patient provided informed consent to proceed, providing a clear understanding of his condition and the treatment options considered.

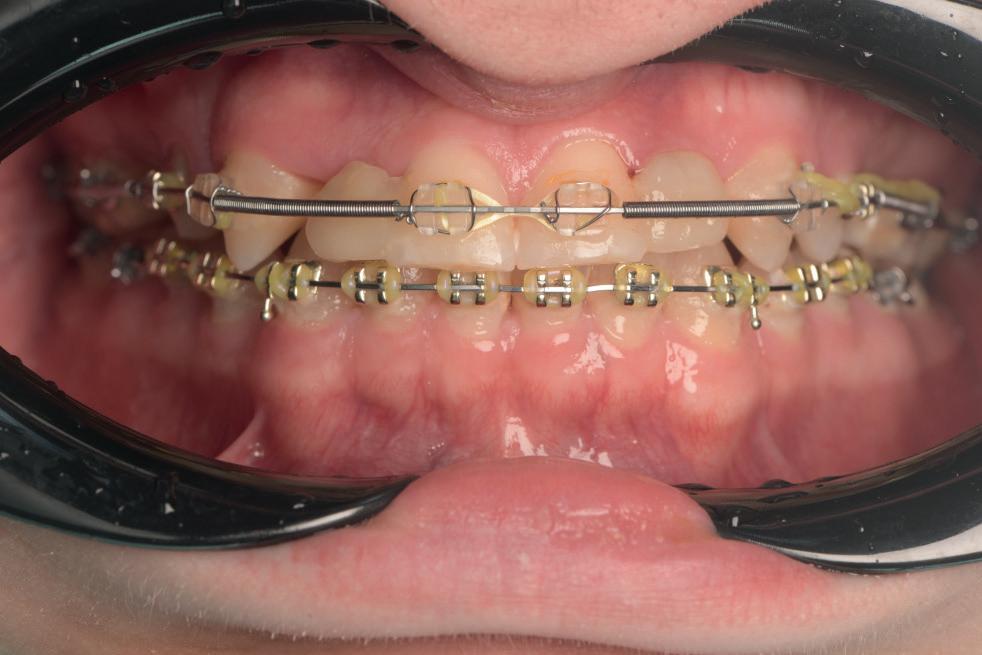











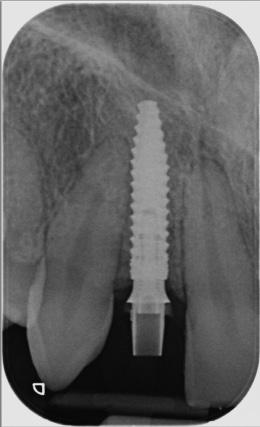







The patient visited the orthodontist for the first phase of treatment. Before the appliance was removed, I confirmed that the desired tooth positions had been achieved to ensure adequate spaces for implant placement.
A CBCT scan was taken using a Morita X800. This dataset was imported into the planning software, where it was merged with the STLs of the anatomically correct diagnostic digital wax-up and modules. With the anatomically correct diagnostic waxup, there was no ambiguity regarding planning the implant position, angle and depth with precision. I like to plan these types of cases myself, but it is possible to outsource the planning stage for clinicians who are new to the process and looking to increase their workflow efficiency. For this case, I wanted to build up the gingival thickness in order to improve the papillae around the implant sites. The surgical plan, therefore, included soft tissue grafting.
On the day of surgery, a splitthickness envelope flap was raised. Two CONELOG® Progressive-Line implants were placed through the surgical guide in the pre-determined lateral incisor positions. Soft tissue augmentation was performed simultaneously with the implant placement, and the site was sutured and closed without tension. The implants were immediately loaded using provisional crowns that were prefabricated in the lab.
The CONELOG implants were selected because they provide a very stable connection and feature a geometry that facilitates high primary stability,

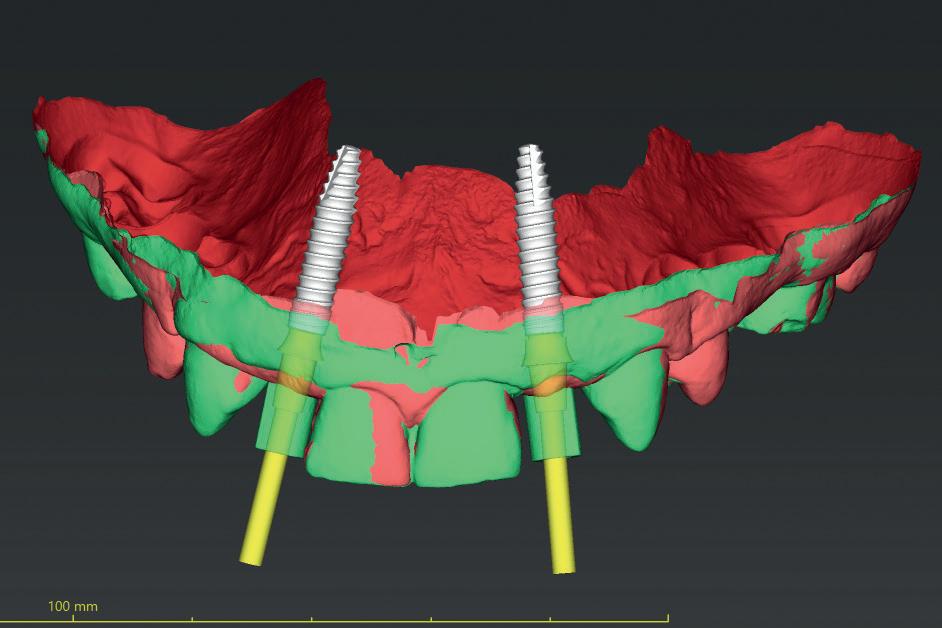

which is important when placing immediate implants. They also integrate very successfully – we have had better results with these implants than with other products that are available. I also appreciate the simplicity of the keyless guided surgery kit.
Both the patient and I were very happy with the outcome in this case. Given the patient’s reluctance towards excessive treatment, he was not willing to undergo any further procedures such as composite edge bonding or veneers, which could have enhanced the aesthetic result. However, he was more than satisfied with the replacement of his missing lateral incisors, and while he understands that more implants will be needed in the future when the remaining deciduous teeth are lost, he was happy to postpone that treatment for now. This case presentation shows a reallife result of the kind of treatment we deliver every day in our clinic. It also demonstrates how a guided workflow allows us to place implants exactly as planned, making the process easier and more efficient.
Planning using a guided surgery workflow makes it possible to carry out a virtual surgery on a patient. It does require some training and experience to achieve reproducible results, but a guided approach removes a lot of the ambiguity that implant cases can present. Once you get your head around the workflow, you won’t want to place implants any other way – and your patients won’t want it done any other way either.
When upskilling in order to move into guided surgery, it’s important to take baby steps – don’t go straight to complex cases, build up to them gradually. It is necessary to learn the materials and techniques first. Finding a good mentor is also beneficial, as you have someone to share cases with and ask questions of. Once you and your team are familiar with materials and workflow, this makes it much easier to achieve consistently good results for the patient.
For more details about the Level Up In Guided Surgery Level 1 course, please visit education.theimplanthub.com.
For product information from BioHorizons Camlog, please visit theimplanthub.com n
about the author dr Nick Fahey Bds, Mclin.dent (Pros) MRd RCs(ed), FRaCds and MFds RCs (eng.)

Nick’s professional interests include all aspects of dentistry related to dental implants and fixed and removable prosthodontics. as a pioneer in computer-guided surgery, Nick has taught a generation of dentists about guided surgery and has been a KOL in this field for many companies. He is particularly interested in computerguided surgery and guided surgical navigation for simplification of surgical placement of dental implants and has authored a textbook called “Guided surgery. Making Implant Placement simpler”. Nick is also a co-director of the FitzFahey academy. aside from his teaching and mentoring commitments, Nick works as a specialist in Prosthodontics and is the Principal dentist of Woodborough House dental Practice in West Berkshire.














I invested in the Ti-Max Z Series turbines because I wanted more consistent torque for cutting through sturdy materials.
Edward Li BDS, Clinical Director, the a.b.c. smile






“The increase in torque over previous handpieces makes a big
Alex Jones
Dental Surgeon, The Campbell Clinic
*Ti-Max Z990L with air pressure at 3 to 4.2 bar


Mojtaba Dehghanpour Principal, Yourdental Wellness Power from 30- 44W*
“The lightness and even weight distribution make a tangible difference to hand fatigue and performance.”
Turbines Ti-Max Z990L / Z890L In 5 Coupling fittings RRP £1,173 each
ULTIMATE power 30-44W*
NEW high performance turbines with 30-44W* of power



Lightweight titanium body with Duragrip coating to reduce hand fatigue
Ti-Max Z micro
In 3 Coupling fittings RRP £1,173 each
S-Max M900L / M800L In up to 5 Coupling fittings RRP £773 each
S-Max M900 / M800
Ultra-mini head for better access, uses regular burs Pana-Max2 In NSK or KaVo fittings RRP £468 In M4 or Borden Direct Connections RRP £425 each

£3,995 +£350 ** install & delivery RENT for just £155pm‡














































Brushing twice a day is only the starting point for a consistent oral hygiene routine.
Toothbrushing alone may only reach 60% of the tooth surface and removes a lowly 42% of the overall dental biofilm. Poor biofilm disruption can lead to dental caries, gingivitis and periodontal disease.
Some individuals may find oral hygiene challenging, particularly those with Developmental Coordination Disorder (DCD), often referred to as dyspraxia. This common disorder affects the motor coordination in children and adults; writing, typing, riding a bike, driving and DIY tasks are some everyday aspects that individuals with DCD may struggle with. Coordinating movements is a complex process involving many different nerves and parts of the brain, so any problems within this process can inhibit movement and coordination. According to the Dyspraxia Foundation, DCD affects up to 6% of the UK population. Those with it can often have attention deficit hyperactivity disorder (ADHD), dyslexia, autism spectrum disorder, depression and anxiety. Most of these conditions have also been connected to poor oral hygiene.
Brushing up on your oral health
Toothbrushing requires a level of coordination that individuals with DCD may struggle with, especially children. This can lead to non-compliance and the neglect of their oral health – if regular toothbrushing already misses 40% of tooth surfaces, then a poor brushing technique, common among individuals with DCD, will add to the problem. This increases the risk of gingivitis and periodontal diseases.
It is paramount that individuals with DCD protect their teeth. Brushing must be supplemented by interdental cleaning to ensure that the plaque biofilm is sufficiently disrupted. Interdental cleaning is always recommended by dentists to clean the places that toothbrushes struggle to reach. For individuals with DCD, string flossing has been reported as “near-impossible” –preparing the floss and then manipulating the floss successfully between the teeth requires the precise coordination that individuals with DCD struggle with. As such, flossing has a low compliance because of its technical difficulty.
a helping hand
Instead of flossing, interdental brushing should be recommended to individuals with DCD. Interdental brushes are more effective at removing plaque from between the teeth than toothbrushes and are as good, if not superior, to string floss at reducing plaque and the risk of gingivitis. They are especially good for periodontal patients and are the preferred method for cleaning around implants.
For individuals with DCD, interdental brushes still demand some coordination. However, only half the hands are needed when compared to string flossing and the movement of an interdental brush is like using a key, with a simple in-and-turn motion.

There is no cure for DCD and its symptoms are largely dependent on the self-management of the individual. However, with patience, encouragement and education, individuals with DCD can improve their ability with certain tasks such as interdental brushing. Not only will this be a huge victory for their oral health, but the successful completion of a coordinated task, no matter how simple or complex, will boost their self-confidence. Moreover, increased patient convenience and acceptability towards something new promotes compliance and comfort with new oral hygiene practices.
recommended action Surprisingly, there is very little research on oral care and DCD. To help raise awareness of the impacts that DCD can have on oral health, having brochures or posters highlighting some of the problems in your practice can increase the chance of a patient discussing it with you. This can therefore help you to steer DCD patients towards interdental brushes as a method of reducing biofilm that is less technically complicated than flossing.
For an ideal interdental brush, consider FLEXI interdental brushes from TANDEX. With 11 different sizes, the FLEXI reaches all the areas a toothbrush cannot, reducing plaque comfortably. The ergonomic handle is flexible and the brush can be shaped perfectly, making it easier for individuals with DCD to coordinate their brushing and achieve success. FLEXI works brilliantly with PREVENT Gel, from TANDEX, a non-abrasive substance used like toothpaste that strengthens enamel and adds an anti-bacterial effect through the application of fluoride. With the right interdental brush and gel, plaque won’t stand a chance.
The indirect health impacts of DCD make it an important condition to be aware of. By supporting DCD patients by offering manageable solutions, you can ensure that their oral health is sustained by a consistent hygiene routine.
For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from CTS Dental Supplies: www.cts-dental.com n
about the author Jacob Watwood on behalf of tandex.
Summer is finally here, and with it comes the long anticipated warm, bright weather. Your patients will have been eagerly awaiting hot afternoons in their gardens, but may not realise the impact this new wave of weather will have on their oral health.
Providing effective support can help patients recognise the good habits they need to reinforce or pick up when the summer sun makes its appearance. Whether this is through face-to-face appointments, or reminders on social media, spreading the simple messages that can have the greatest impact is key to protecting their oral health.
In the warmer months, it’s easy for patients to forget to keep on top of hydration. However, considering the impact on salivary production, it’s an important aspect of oral health care. Salivary flow rates decrease in the summer when compared to the winter months, caused by hypofunction of the salivary glands. Whilst this can be caused by anything from anxiety to acute infections, dehydration is the more likely cause at this time of year.
Studies have shown that once exposed to higher temperatures, a decrease in salivary flow rates is almost immediate. In one, patients that were subject to 37ºC temperatures for just 10 minutes – too short a period for dehydration – quickly saw decreased salivary flow. Whilst the UK is unlikely to see consistent weeks upon end of 37ºC highs, we can recognise that with longer exposures to hotter temperatures, patients are more likely to experience dry mouth.
The nutrient supply within saliva serves to maintain the presence of certain bacteria and exclude others. Saliva itself performs bacterial clearance, buffering capacities, direct antibacterial activity and remineralisation –when reduced, as seen in the heat, dental caries and infections can develop.
Patients should be reminded to keep hydrated in the summer months, emphasising the effect dehydration can have on their oral health. The Eatwell Guide encourages water, lower-fat milks, and lower-sugar or sugar-free drinks (including tea and coffee) to make up the daily fluid intake. Avoiding excessive intake of highsugar fluids, such as juices or some sodas, is key for maintaining healthy dentition.
Despite the increased risk of dehydration, summer is by no means doom and gloom for the dentition. A lack of sunlight has been connected with gum disease, and with approximately one billion people around the world being vitamin D deficient, the summer sun is an opportunity to improve the battle against oral infections.

Through sunlight exposure, 7-dehydrocholesterol in the skin absorbs UV B radiation, and is converted to previtamin D3, which in turn isomerises into vitamin D3. The effects on oral health can be profound. Vitamin D impacts bone and tooth mineralisation, and with unregulated levels patients may develop a rachitic tooth, which is highly susceptible to fracture and decay.
Many studies have also found that the presence of periodontitis is associated with lower levels of vitamin D when compared with patients without the disease. Those with the deficiency have also been observed to experience high levels inflammation, as well as increased bleeding on probing, compared to those with high levels of the vitamin.
Treatments for vitamin D deficient individuals come in the form of supplements, which can often be bought over the counter, and prescription vitamin D. Changes to a patient’s diet may be beneficial, with more fatty fish, egg yolks, and yoghurt being recommended solutions. In the summer, taking advantage of the sun will also be of use, but should be done responsibly with sunscreen and adequate hydration.
Why stop at summer?
Summer will not last forever, but patients must be informed on how best to protect their oral health in the warm weather. Hydration is essential, and safely getting enough sun should be recommended whilst the season lasts, but nothing will beat an effective year-round oral hygiene routine. Brushing twice daily, with interdental cleaning and the use of an effective toothpaste is essential, no matter the weather. Consider recommending patients use either of the specialised 100% Natural Baking Soda Toothpaste solutions from Arm & Hammer™, available to strengthen Whitening Protection or Gum Protection. Each solution utilises baking soda, which is alkaline in nature, to help return the oral pH to neutral levels within the mouth. Containing 1450ppm of fluoride, their formulas effectively remineralise and strengthen enamel, and remove more plaque around the gumline to prevent infection, when compared to nonbaking soda toothpastes.

With the warm weather incoming, patients should be aware of the ways the environment can affect them in the short term, and in turn pick up habits that will protect their oral health long into the future. For more information about the carefully formulated Arm & Hammer™ toothpaste range, please visit www.armandhammer.co.uk or email: ukenquiries@churchdwight.com n
about the author
anne Symons is a Dental hygienist currently working in a Specialist Periodontal/ Implant practice as well as a busy NhS surgery. anne is also a Professional educator for Waterpik.

Recently, headlines have reported a “very concerning” increase in the number of younger patients in the UK with mouth cancer, despite the lack of an obvious reason for a spike in cases. Traditionally, mouth cancer has been considered by many to be an “old man’s disease” – something that young people and women should be less concerned about – with research suggesting that only 20% of women think that they are at risk. Because of this, some patients in these demographics might be flying under the radar. It has been suggested that women, therefore, often miss out on an early diagnosis, in a similar way to other supposedly “male” conditions such as cardiac diseases or heart attacks. Some research suggests that, as tobacco use is decreasing, human papillomavirus (HPV) might be to blame for the increasing rates in mouth cancer in younger people.
hPV: what are the risks?
HPV is a virus and, like other viruses such as the flu, there are many different types. It can infect the mouth and throat, with some types (most often HPV 16) leading to mouth and oropharyngeal cancer. In the UK, HPV is thought to be responsible for around 25% of cancers of this kind. Whilst HPV can be contracted by anyone, with most adults having some form of the virus during their lives, and 10% of men and 5% of women having it at any given moment, it is generally associated with cervical cancer in women. This is problematic as it may mean that patients are completely unaware of their level of risk for both HPV and oral cancer, together

and separately. Because HPV increases the risk of some types of cancer, including mouth cancer, and causes almost all cases of cervical cancer, the HPV vaccination was developed to help prevent cancer caused by the virus. It is offered to all children in the UK who are between the ages of 11-13. A study from 2021 found that rates of cervical cancer were reduced by almost 90% in women in their 20s in England who were offered the vaccine at ages 12-13.
The HPV vaccine has been instrumental in reducing the rates of the virus in the UK population. However, it’s important that patients understand the risks the virus presents, and whether they are at increased risk of mouth cancer. By making patients aware of the signs and symptoms of the early stages of mouth cancer, they will feel more confident about reporting any concerns to you quickly. Because early signs can resemble benign issues, like mouth ulcers, some patients might feel that they are wasting your time by flagging the unusual lesion. As such, it’s important to reassure patients that if they notice anything out of the ordinary, and it lasts for 3 weeks or more, they should book an appointment. In addition to lingering mouth ulcers, other early signs of mouth cancer might include
a red or white patch, a lump, pain, difficulty swallowing, croaky voice, or weight loss. Dental professionals should be checking their patient’s mouth and tongue for these signs at every appointment, and it’s helpful to make patients aware of what you’re checking for so that they can monitor their own health at home when brushing their teeth.
While clinicians will carry out examinations for oral cancer at every appointment, it is important to know what to do if they find something suspicious. Because the early symptoms can be difficult to spot, some dental professionals may doubt themselves about what they’ve seen. As such, it’s important to establish a patient’s level of risk, and carry out the right tests before referring the patient for a biopsy or further testing. Additionally, carrying out effective tests will help to ensure that dental professionals do not miss anything. Biopsies are invasive procedures, so it’s important to undertake all necessary prediagnostic tests prior to referring patients.
The BeVigilant™ OraFusion™ System, available from Total TMJ, is the ideal solution here. The pre-diagnostic test is designed to be used at point of care to establish the likelihood of a cancerous lesion in 15 minutes or less. The device analyses saliva
to produce a result of high, moderate, or low level of risk, by detecting biomarkers associated with oral cancer. This is a fantastic system for clinicians who would like to feel more confident about their decision making when they spot an unusual lesion, offering improved certainty and allowing oral cancer to be detected in stages I and II.

HPV can affect anybody, so it’s important to keep patients informed about the signs and symptoms of oral cancer to help ensure any early signs of the disease are detected as early as possible.
For more details about the BeVigilant™ OraFusion™ System, visit the Total TMJ website www.totaltmj.co.uk/products/bevigilantorafusion/, or email info@totaltmj.co.uk n
about the author Phil Silver, Founder of total tMJ, which distributes innovative technologies from leading healthcare manufacturers to dentists and clinicians.

Tooth wear can be identified in over 75% of adults and 50% of children in the UK. Dental erosion works synergistically with attrition and abrasion to weaken tooth structure, affecting aesthetics, functionality and quality of life among those suffering from it. With life expectancy increasing, defending against the connected rise in tooth wear is now an urgent battle. Dental erosion is a stealthy process and patients can be unaware of it occurring. It is therefore paramount for clinicians to identify dietary habits and medical complications in patients who are showing early signs of it, with a focus on controlling exposure to intrinsic and extrinsic acids before the risk worsens.
Understanding diet control is pivotal for patients to protect their teeth. Many food and drink items are acidic and demineralise enamel, thus increasing the sensitivity of effected teeth when brushing. Strong, non-bacterial acids are commonly found in sugary carbonated drinks and these are ill-advised to be swished or retained in the mouth. Instead, they should be ideally consumed through a straw or with a meal to limit the damage.
Carbonated water may be more acidic than still water, but it is far less harmful
than other fizzy drinks unless it has been artificially sweetened. Studies have shown that carbonated drinks with calcium ions can alleviate their erosive quality – these are therefore better options than sugary, fizzy drinks.
Fruits are highly acidic. Apples, berries and citrus fruits mostly harbour a pH in the 3.0-4.0 range and teeth erode at a pH of 2.0-4.0. However, the eating of fruit should not be discouraged, with government guidelines decreeing that the majority of children and adults do not currently consume enough to have a healthy diet.
Among adults, the frequency and timing of acidic fruit consumption is significantly associated with dental erosion. A high consistency of snacking on fruit has been found to progress tooth wear, especially when compared to those who eat fruit with their meals. Instead of dissuading patients from eating fruit, promoting the consumption of acidic fruits with a meal is a more positive solution.
Defending against intrinsic acids
Some patients may be at a greater risk of tooth wear because of health complications. Frequent regurgitation of gastric contents can result in erosion, with stomach acid measuring a pH of 1.5-2.0. Tooth wear is common among people with gastroesophageal reflux disease (GERD).
The growing number of patients with eating disorders are also at great risk: over 1.25 million people in the UK have an eating disorder, with 19% of cases being bulimia. Vomiting affects the enamel in the oral cavity and the purgative subtype of bulimia has been connected to the erosion of the lingual surfaces of the maxillary teeth, with 90% of self-induced vomiting patients found to have had enamel erosion.
Many people immediately brush their teeth after vomiting, pushing non-bacterial stomach acids around and, through vigorous brushing, boosting the likelihood of abrasion too. Clinicians can help lessen the risk of erosion by advising such patients on the benefits of using either water, an alkali substance like baking soda, or a fluoride mouthwash, to clean and rinse with first, and then to brush at least 30 minutes later to promote remineralisation of the teeth.
Furthermore, 12.5% of 17 to 19-yearolds have an eating disorder. With rates among young women dramatically rising, so too will the interest in cosmetic surgery as tooth wear worsens. Eating disorders can be difficult topics to discuss, so ensuring the dental practice has a positive atmosphere that promotes awareness of eating disorders can boost confidence in patients – doing so will better inform the dentist of the patient’s dietary habits and how to better manage them.
Tooth wear is becoming an ever-growing issue for dentists, and the problems caused by intrinsic and extrinsic acids is only one facet of the triple-pronged threat of erosion, abrasion and attrition. The British Academy of Cosmetic Dentistry (BACD) offers a vast range of education on tooth wear and many other crucial topics, sharing advice and solutions. The BACD 20th Annual Conference in November 2024 will mark 20 years of excellence and promises to be an educationally beneficial networking opportunity for all.
In order to reduce and treat tooth wear, it is essential for practitioners to know the dietary habits and medical complications of their patients so that the best advice can be given. Identifying and battling tooth wear early can ensure that patients can continue to feel good about smiling.
For further information and enquiries about the British Academy of Cosmetic Dentistry visit www.bacd.com n
about the author luke hutchins, BaCD President.

Advances in implantology have transformed modern dentistry, providing an effective and increasingly long-term solution for tooth loss. However, resorption of the edentulous or partially edentulous alveolar ridge can compromise dental implant placement, and can present challenges in the rehabilitation of a severely atrophic maxilla.
Augmentation of insufficient bone volume can be required prior to or in conjunction with implant placement to ensure stability for long-term function and aesthetics. Once a patient has lost teeth, bone grafts are the only solution to reverse dental bone loss, and are used to treat resorption in about one-in-four dental implants.
Zygomatic implants are an increasingly effective solution for patients with a severely atrophic maxilla, and are used to treat patients who are unable or unwilling to undergo grafting treatments, or in cases where grafts or other interventions have failed. However, innovations in zygomatic implants have developed alongside promising new grafting techniques, biomaterials and treatments.
Patients with resorption so severe they required zygomatic implants in the past may be successfully treated today with new types of bone grafts, which are increasingly able to create a sufficient foundation for implants. In addition, growing evidence behind reduced diameter, short and ultrashort implants may have also changed what clinicians previously considered as the minimum available bone for conventional implant placement.
Advances in the use of dental cone beam CT (CBCT) scans and imaging software also allow clinicians to perform a more accurate analysis of the alveolar and midface structures, including bone quality and volumetric measurements. Outcomes have been improved by innovations in virtual planning and guided surgery.
Bones and resorption
Bones are not static, but constantly changing to better carry out their functions as storehouses for minerals, maintaining vital structure and protection for the body. Resorption is part of a normal, essential cycle in the development of living bone. However, severe gingival inflammation or periodontal disease can cause excessive bone loss due to the direct damaging effect of bacteria, as well as the production of resorbing factors by white cells. The local immune response against periodontitis disturbs the homeostatic balance of bone formation and resorption in favour of bone loss.
In addition, once edentulism occurs, whether due to infection, trauma, surgery or congenital malformation, there is rapid resorption of alveolar bone due to lack of intraosseous stimulation by periodontal ligament (PDL) fibres. This is further complicated in older patients, as the processes around bone regeneration are slowed.
Optimising the development of new bone
Bone grafting is possible because bone tissue has the ability to regenerate completely if provided the space and opportunity to grow. As natural bone grows, it should replace the

graft material completely, resulting in a fully integrated region of new bone.
The development of science around bone grafts has been phenomenal in recent years, particularly in the development of synthetic bone substitutes. Autogenous bone was always considered the gold standard for reconstructive techniques due to its biocompatibility and having osteogenic, osteoconductive, and osteoinductive properties. However, autografts present some disadvantages such as the need for an additional surgical site, associated morbidity, and rapid resorption rate.
Other natural biomaterials such as xenogenic grafts have been notable for low-content inflammatory reactions and high longevity. Synthetic biomaterials such as bioactive glasses are another promising choice for bone augmentation considering their notable neosynthesised bone and low amount of graft residue.
Bioactive glass is used in combination with polymethylmethacrylate to form bioactive bone cement. Used on metal implants as a coating to form a calcium-deficient carbonated calcium phosphate layer, it facilitates osseointegration. Calcium phosphate materials can be mixed with ions such as strontium or with bone marrow aspirate to increase biological activity. The presence of strontium can result in higher bone mineral density.
Advanced study with those at the forefront of the discipline
To assist experienced implant dentists in incorporating the latest innovations into their practice, eminent Specialist Oral Surgeon, Professor Cemal Ucer and Professor Simon Wright MBE have developed the Advanced Certificate in Full Mouth Oral Implant Rehabilitation at ICE Postgraduate Dental institute and Hospital. As part of this highly structured, comprehensive course, there will be a review of the current use of grafting techniques and biomaterials in modern implantology. Alongside excellent lectures and mentoring support, there will be hands-on training in a number of advanced surgical options for treating the atrophic/fully edentulous jaw, including short implants, zygomatic implants and 3D printed customised implants.
Oral rehabilitation for a patient with severe loss of alveolar bone presents a challenge to clinicians. In a rapidly advancing field, advanced knowledge about bone grafting as well as other cutting-edge surgical methods will enable clinicians to offer the best support for their patients through life-changing treatment. Please contact Professor Ucer at ucer@icedental.institute or Mel Hay at mel@mdic.co
Call: 01612 371842
Visit: www.ucer-clinic.dental
About the author Prof. Cemal Ucer, BDS, MSc, PhD, FDTFEd., ITI Fellow, Specialist Oral Surgeon














On Friday 5th July, the winners of the 2024 Dental Awards gathered at The Ivy in London to receive their trophies and celebrate their victories along with members of the judging panel and sponsors
Following the virtual presentation that streamed in May on The Probe website and Youtube, the winners of the 2024 Dental Awards were invited to a celebratory awards lunch to be presented with their trophies in person.
The Private Room at The Ivy (the original on West Street) set

the scene perfectly. While A-list celebrities dined on the ground floor, the best in British dentistry celebrated in style above.
After guests were greeted with a champagne reception, Dr Nigel Carter OBE, Chief Executive of the Oral Health Foundation, kicked off the proceedings with a warm welcome.


James Cooke, Editor of The Probe, presented the winners with their trophies and certificates before The Ivy’s signature savoury bowls were served.
As the plates were cleared and the dust settled, guests were treated to a performance from renowned magician and mind reader Neb, who had been
circling the room, executing closeup magic to the delight of all. His big performance for the entire room capped of the event by leaving jaws firmly on the ground.
Stay tuned in the coming weeks for details on how to enter the 2025 Dental Awards, and you too could find yourself celebrating next year!































NATIONAL SMILE MONTH












Community Dental Services CIC – Oral
Health Improvement Team at Colworth House, Sharnbrook, Bedfordshire1
Best Outreach or Charity Initiative
KeepStokeSmiling2
Website and Digital Campaign of the Year
Cheadle Hulme Dental and Cosmetics, Manchester3
Front of House
Trudy Horne, Dorset Dental Clinic, Poole4
Dental Therapist of the Year
Natalie Peary, Smile Together Dental CIC, Bodmin5
Dental Hygienist of the Year
Amanda Harbrow-Harris, Sharrow Dental Group, Chelmsford6
Dental Nurse of the Year
Brittany Pittham, Inspired Dental Care, Exeter7
Practice Manager of the Year
Amanda Reast, The Dental Architect, Leeds8
Dentist of the Year
Rachel Derby, Chapel Dental, Flackwell Heath9
Practice of the Year
Smile Together Dental CIC, Bodmin10
Young Dentist of the Year
Chloe Harrington-Taylor, Hereford Dental
Implant Clinic, Hereford
Dental Team of the Year
Glenhaven Dental, Cardiff


































This is a conversation starter around teamwork in its purest sense. We all understand the benefits of working together and building connections with the people we work with but, for me, one of the most pivotal aspects of dental teamwork is the dentist-nurse relationship.
Working with your nurse day in, day out, under pressure, in a small space, with dental health and positive outcomes at the forefront of your mind, could create issues if you’re not perfectly in sync. The work you do together should be a well-choreographed routine and, if you get it right, it’s a thing of beauty. Having someone to assist you, knowing how you do your endo (or whatever dental area you practice – for me it’s endo) anticipating your next move, with your next instrument at the ready, has a whole heap of benefits. It means the work you are doing is streamlined and efficient. The patient, possibly without realising, will pick up on the air of calm and order, which will be helpful to them, especially the more anxious patients. It helps your thought processes and allows for an energising flow whilst you are working. We all know the frustration of interruptions and distractions when we’re in the zone. But this doesn’t just happen overnight. It would be nigh on impossible to achieve the level of synchronicity needed without a Kaizen style of incremental development over time. By explaining, training, taking time and including your nurse in the process, you’ll be building a sense of agency that nurtures responsibility and ambition.

The bonds you develop will serve you, the patient, the nurse and your practice. To ignore this important part of the dental team make-up is short-sighted and careless. Away from the chair, it’s a good idea to spend time with your team. Build in social events, rewards and teambuilding days. And I don’t mean the boring sort with raft-building and executive puzzles to solve. We have
evening socials, we go into London, and we do silly stuff like mini golf. The main thing is to have fun! Alongside the laughs, also take the time to find out what your nurse is working towards. The world is made up of all kinds of working ideals –if your nurse is perfectly happy in their role and sees that as the one they want long-term, that’s great. If they want more and are interested
The ladder against the wall analogy is widespread in coaching and beyond. If you are not familiar with the concept, let me explain. Each rung on a ladder represents a crucial step along your path. An effort against the pull of gravity brings you closer to reaching your goal. Some say that an ability to see the entire ladder is a “superpower,” allowing individuals to map out a clear path to their success. Others have described scenarios where the first or middle rungs are absent and so on. I’m sure you can get the drift.

Like most metaphors it has limitations. Firstly, what do you do when you realise that your ladder is leaning against the wrong wall? How do you deal with the problem when you attain the top of the wall only to discover that the view is not what you were promised? Finally, after investing in, building, or buying what you believed to be the right ladder, it becomes clear that you have been missold and it is too short for your purpose?
My early experiences as a dentist in dental and general hospitals, followed by a number of very different practices, showed me a variety of ladders. It allowed me take a few steps up and then to safely come down to earth again. When I embarked on the seriously big wall of practice ownership, I had to be prepared to build my own ladder as I went. The top of the wall was in the clouds, the wall itself was anything but perfectly formed, and the ladder was inadequate. My son remarked, when we were comparing career notes, “Sounds more like rock climbing with
in developing their skills, support them with that. Getting to know how your nurse ticks is as important as them knowing your ways, foibles, preferences and irritating habits (we all have them!).
Once you have reached the point of having people around you that fit together, and work seamlessly and positively, we need to be wary of becoming complacent. Think about training, of course, but also the work environment itself. We need to lift our heads from the clinical work in front of us to assess our practices themselves. The level of flexibility we offer and the job satisfaction being experienced. Ask for feedback from your team; it’s incredibly valuable. And, just as we were about to start a national day in appreciation of our dental nurses, we found out that ‘National Dental Nurse Day’ is already in existence – put 22nd November in your diary and maybe that’s the day for thank you cakes or a round (or two) of drinks? n
About the author

Dr Dhiraj Arora has two dental practices in Twickenham and Gerards Cross. He is also a Dental foundation Training educational supervisor for Health education england, Honorary Lecturer in endodontics at QMUL Masters programme, and runs his own courses via evo endo in Central London for general dentists. His background spans nHs and private settings, from Harley street to community HealthCare.
dodgy gear to me, Dad.” He was quite correct, although his career path has had its own particular challenges.
One of my biggest challenges as a business coach has been to moderate between the hopes and beliefs of the ladder myths, and the reality of the rock face. It is only when the myths have been addressed – the dodgy equipment jettisoned and the off-the-shelf maps and guide books shredded – that true individual progress can be made.
In recent times, I realise that there is little point in being a sherpa on the dental version of the Everest escalator. It puts food on my table, but I eat less than I used to. Working with increasing numbers of people, many of whom seem to want the selfie at Base Camp, they then expect to be handheld to a summit. Any summit.
I’m reconsidering my own ladder.
The joy in my life is helping individuals who are halfway up someone else’s ladder, or have encountered the snake (one of the 101 things nobody mentioned at Dental School: that for

every ladder there is a snake) that brings you back down – painfully. From here on, I want to work with you if you have realised your ladder, as perfect as it may once have appeared, is leaning against the wrong wall or has run out of rungs. If you can’t find a way to move up, down or sideways and are hanging by your fingernails in quiet desperation, drop me a line. n
William McLean, President of the British Endodontic Society (BES), discusses his hopes for his presidential term and for the future of the society, and shares his excitement for events coming up in the year ahead
My presidential year has started well, with our 2024 Spring Scientific Meeting a great success. We were joined by two fantastic speakers, Sergio Kuttler and José Aranguren, who delivered excellent presentations and provoked thought amongst our delegates. There was a brilliant turn out – the best since the pandemic – and it was great to see the endodontic community supporting the Society yet again. As is customary for each presidential year, this was the first of two meetings. The second meeting for my presidential year will take the form of the IFEA World Endodontic Congress (WEC). This is to be held in Glasgow, Scotland. It has been a long time in planning, with the journey starting 8 years ago. I have been given the responsibility by the BES to deliver this highly anticipated Congress, and it is a great honour. This is an event which myself and others on behalf of the BES fought to win and I am excited to be delivering it in the year of my presidency. Preparing for the WEC has been a team effort, and I have been honoured to act on behalf of the Society and as Congress Chair to help us achieve this. This will be a truly global event with speakers from around the world presenting. The programme is
fantastic and Phil Tomson, the Chair of the Scientific Committee, has done an exceptional job in bringing this together. It has been great to see the support that the Congress has had from the industry. This reflects the positive change in the relationship between industry and organisations such as the BES.
I am excited to see that the BES Early Career Group (ECG) continues to go from strength to strength. It’s excellent to see that they have become formally organised, enabling them to run an education and support programme for those early in their careers. The ECG will be delivering a parallel educational programme at WEC under the stewardship of Dipti Mehta and Daniel Vaz de Souza. Along with this, attendees can expect a Teachers in Endodontics parallel session, organised by Professor Alison Qualtrough. This is a brilliant opportunity for teachers globally and highlights the importance of education to the BES.
Besides WEC, my key aim for the Society in the coming year is to maintain the momentum that has been developed over the past few years, thus allowing continued growth of the BES. On the back of some very positive conversations, I am keen to be more collaborative with international societies, so that our members can

truly become integrated into the wider global endodontic community. Legacy development is very important to me also. As a society, our primary goals are to promote and advance endodontology.
As part of this, I hope to facilitate the BES’s engagement with the public.
In part, I aim to do this through the Congress with the development of an exhibit at the Glasgow Science Centre exploring biofilm disease and its management and with a dental trauma activity to be held ahead of the Congress in Glasgow’s Central Station. Past-Presidents have initiated several projects over recent years, and
Dentists commit to lifelong learning when they enter the profession, and this is optimised when working within a community of peers. The formal and informal benefits of peer-to-peer learning and mentoring can be a real lifeline, both professionally and personally. For many, the special privilege to be in a field with such a richly diverse group of like-minded colleagues, who have equal passion about the science and practice of dentistry, is one of the chief benefits.
Much emphasis has been placed on the importance of mentoring to support dentists throughout the experience of qualifying and beyond. As newly qualified dentists emerge into the world of real clinical practice – perhaps working within a disciplinary team for the first time, perhaps treating vulnerable patients living with complex issues, perhaps facing difficulties in managing some patients’ expectations – a supportive network of mentors and professional peers is vital.
Individuals generously giving their time to support others contributes to a supportive culture, which improves mental health and resilience. Such a network not only keeps knowledge fresh; it enriches professions that adopt the practice.
Mentoring – a two-way street
Mentors often speak of the benefits of the relationship to their own learning. Apart from the rewards of helping someone succeed and grow, the mentee may raise awareness of new ideas that inspire a
mentor to pursue surprising and fruitful new avenues. The lines can be blurred between mentor and mentee, especially as careers develop. A positive mentoring relationship is dynamic; activity is sometimes led by mentee, sometimes by mentor.
Formal or informal career mentors can help emerging professionals set boundaries and aid understanding in developing an effective and sustainable work ethic. A mentor can model the importance of diligence and consistency in the workplace, but can be helpful also in terms of managing workload, and teaching coping skills when times get tough.
As a mentor, the relationship can build your leadership skills, helping you to become a better manager and team member. Interpersonal skill acquisition works both ways. Both parties will have a different set of experiences, may be of greatly different ages, and may have a different language or culture, all of which is beneficial when developing the flexibility to communicate with a diverse range of people as a professional.
soft skills
As a mentee, the relationship with a mentor can broaden your horizons, and offer insight into managing different situations, with an additional personal element that can be invaluable. Sometimes the ‘soft skills’ gained, such as interpersonal communication, are as valuable as information exchange. Interpersonal skills are essential when working with patients and colleagues, and are an enormous advantage in career development.
Empathetic communication and active listening are not only vital in terms of building trust and rapport with patients, resulting in greater adherence to advice and a better understanding of treatments discussed; they also improve teamwork. There’s no shame in admitting communication skills don’t always come naturally. The good news is, skills can be learned and honed throughout your career. Support from other professionals who have struggled or are still struggling can be a great bonus. And finally, many leadership qualities are defined as soft skills. These include selfawareness, courageousness, empathy, the willingness and ability to take responsibility for actions as well as the consequences, a growth mindset, the ability to remain calm under pressure, to negotiate and resolve conflict, and much more. Leaders model behaviour for team members, and so are important de facto mentors –sometimes without realising the extent of their influence.
Significant learning can be shown to take place during peer-to-peer engagements, and the benefits extend well beyond an educational setting. Co-learning deepens the value of the knowledge and understanding gained. Peer learners have a similar cognitive framework. Learning experiences are more likely to be informal, and the experience of gaining knowledge from a peer tends to feel safer; mentees can ask a question without feeling foolish.
stepping into this role, I will continue to support and develop these further. The Society recognises the challenges that may potentially arise with a one-year presidential system – understanding that there is an element of risk in terms of maintaining momentum. However, at the BES, we have a collaborative approach. Both past and future BES Presidents work together with the experience offered by our Chief Operations Officer Annabel Thomas, to ensure continuity for both the Society and its members.
In summary, I am very much looking forward to furthering the accomplishments of the BES and continuing to support our members. I encourage any dentist, no matter their level of endodontic expertise to become a member and join us at the upcoming IFEA WEC.
Register today for IFEA WEC 2024 at ifea2024glasgow.com/registration
For more information about the BES, or to join, visit britishendodonticsociety.org.uk or call 07762945847 n
About the author William McLean, president of the British endodontic society.

Learning from the best Rodericks Dental Partners recognises the importance of support through mentorship and peer to peer engagement. They have adopted a unique structure that focuses on support and development that goes beyond the foundation training year. The FD+1 programme provides dedicated support, guidance and development opportunities to facilitate a successful transition to the next stage of a rewarding career. Every cohort of FD+1 has opportunities for networking and peer review. Additionally, all dentists joining the team benefit from a dedicated clinical support lead, gain numerous growth opportunities inherent in a generous network and have the opportunity to mentor others. There are so many exciting growth opportunities through mentorship, as well as a wealth of resources in the dental community. The sharing of knowledge and experience is designed to enable the development and enrichment of professional skills. Benefitting from a large network of peers and dedicated mentors as you develop clinical as well as soft skills can be of huge benefit when launching your career. To find out more about what it’s like to work with Rodericks Dental Partners and to discuss current vacancies, visit rodericksdentalpartners.co.uk/careers n
About the author Glenn rhodes, Head of Marketing, rodericks Dental partners.

Burnout is a significant issue affecting dental professionals worldwide. Characterised by emotional exhaustion and a reduced sense of personal accomplishment, burnout can severely impact the wellbeing of dental teams and the quality of patient care. Understanding the causes and implementing effective strategies to prevent burnout is essential, and practice managers play a pivotal role in this process.
Understanding burnout
Burnout in dental teams often stems from prolonged stress and overwork. The high demands of patient care, administrative tasks, and maintaining a high standard of clinical performance can lead to physical and emotional exhaustion. Common signs of burnout include:
• e motional e xhaustion – feeling drained, cranky or emotionally detached from patients and colleagues
• reduced performance – quality of work can be affected, slower pace with lower output than normal
• Depersonalisation – forgetting that our patients and colleagues are people and have needs
• physical – headaches, lack of sleep, fatigue. In some cases, this results in too much sleep. I know that when I am burning out, all I do is sleep. It’s an escape, and can be equally as unhealthy as a lack of sleep
The role of practice managers in preventing burnout
Practice managers are in a unique position to identify and mitigate the factors contributing to burnout. Their responsibilities include overseeing the daily operations of the dental practice, managing staff, and ensuring a supportive work environment.

Here are some key strategies practice managers can employ:
• promote open communication: Encourage team members to share their concerns and feelings.
Top Tip – Regular meetings and an open-door policy can help create a safe space for discussing stressors and finding solutions.
• Monitor workloads: Ensure that workloads are manageable and evenly distributed.
Top Tip – Avoid overburdening any single team member and provide adequate support during busy periods.
• foster a positive work environment: Create a culture of appreciation and recognition.
Top Tip – Celebrate achievements, both big and small, to boost morale and motivation.
• provide professional development opportunities:
Top Tip – Offer training and development to help team members grow their skills and advance their careers. This can increase job satisfaction and reduce feelings of stagnation.
• encourage work-life balance:
Top Tip – Encourage regular breaks, flexible working hours, and time off. Ensure that team members have the opportunity to recharge and pursue personal interests.
• implement stress management programmes:
Top Tip – Introduce stress management and wellness programmes, such as mindfulness training, yoga sessions, or access to mental health resources. These can
Dentistry show London
BADN will again be exhibiting at Dentistry Show London, which is being held at ExCel London on Friday 4 and Saturday 5 October. We don’t have our stand number yet, but Honorary President Joan Hatchard, our IT & Comms person Jacek, and I will be manning the stand on both days. BADN President-elect Preetee Hylton and I will also be speaking on the Friday morning on ‘stealth bullying’ – not the obvious, in your face kind of bullying that everybody recognises as such, but more covert bullying – gaslighting, mobbing, etc. This kind of surreptitious bullying can lead to physical and mental reactions without the target realising that they are actually being bullied. We will also be busting some myths about bullying – and providing details of some resources for those who are being bullied in the workplace.
BADN members Sally Khawaja (speaker at the BADN July Coffee Catch Up), Brittany Pittham and Rebecca Silver will also be speaking at the Show.
We plan to hold the BADN Annual General Meeting at Dentistry Show London –on Saturday 5 October 2025 at 11am, courtesy of CloserStill Media, the Show’s organisers (to be confirmed).
Full details will be available soon in the members’ area of the BADN website – attendance is open to all current BADN members as at COB 4 October 2025, either in person or online, but registration is required. An invitation to register for the AGM will be published on our website, social media and e-newsletters. If you have not signed up for our e-newsletters, please do so at www.badn.org.uk/newsletter.

The Coffee Catch Up programme has been paused during the holiday month of August, but will start again in September. This is still free for BADN members, and for non-members attending the original presentation – but non-members who want the CPD certificate will have to pay a £3.50 admin fee. (So, if you are planning to attend several Coffee Catch Ups, it would be more cost effective to join BADN and take advantage of all the other membership benefits as well! www. badn.org.uk/join) Recordings of Coffee Catch Ups will shortly be available online, and we are planning other CPD online in the near future.
help team members manage stress more effectively. I am a strong believer in people owning their stress, and figuring out triggers. This might not only be a work-related issue, and that has to be addressed too.
Conclusion
Burnout in dental teams is a pressing issue that requires proactive management. Practice managers play a crucial role in preventing burnout by fostering a supportive work environment, promoting open communication, and ensuring manageable workloads. By prioritising the wellbeing of their teams, practice managers can help maintain high standards of patient care and create a more positive and productive workplace.
By addressing burnout effectively, dental practices can ensure the health and happiness of their teams, ultimately leading to better patient outcomes and a thriving practice.
What else can we do?
• Have safety nets!
• Locum cover
• Associates and owners (if they are providers too) to have adequate insurance for sickness
• Keep a close on UDAs – don’t wait for there to be an issue and panic
• Deal with issues and conflict promptly
• Effective financial planning
• Good diary maintenance
As we tell our patients – prevention is better than cure! n
About the author Lisa Bainham is president at ADAM and practice management coach at practice Management Matters.

Due to repeated requests, BADN will be shortly publishing job adverts on our website www.badn.org.uk. This will not be a job board as such – just a place for employers to advertise any vacancies. Advertising fees will be reasonable, and obviously considerably less for practices who employ BADN member dental nurses! If your practice would like to advertise a job vacancy, please email me (pam@badn.org.uk) with the details. n
About the author pam swain is Chief executive of BADn

Dental implants are a hugely successful solution for restoring aesthetics and function to edentulous patients. Although the procedure is increasingly successful, failures do still occur, and a number of factors can be to blame, including the health and age of the patient, habits like smoking or poor dental hygiene, the quality of bone and soft tissue, or systemic disease, often in combination. The leading cause of implant failure, however, is avoidable infection.
As soon as an implant surface is exposed to the oral cavity, it becomes colonised by oral microorganisms, forming a microbial biofilm. Conventional treatment for managing peri-implant diseases has in the past tended to disregard the contributory characteristics of dental implant design and materials, following evidence available for the treatment of periodontitis. However, the design of the implants, combined with various surface modifications of titanium, may foster increased plaque accumulation, resulting in faster bacterial biofilm formation than on natural teeth.
Microorganisms most commonly associated with implant failure are spirochetes and mobile forms of Gramnegative anaerobes. Diagnosis is based on colour and appearance-changes in the gingiva, bleeding and probing depth of periimplant pockets, suppuration, radiographic evidence of bone-resorption, as well as the degree and extent of gradual loss of bone height around the tooth.
Peri-implantitis, the plaque-associated, site-specific infection, is characterised by inflammation in the peri-implant mucosa and consequent gradual bone loss. The condition is a progressive and largely irreversible disease of the hard and soft tissues surrounding the implant and is accompanied with bone resorption, decreased osseointegration, increased pocket formation and the presence of purulence.

In some cases, with the correct management, it is possible to regain osseointegration non-surgically. For non-surgical treatment to be effective, early detection and accurate diagnosis makes all the difference. The prosthetic itself should be checked for any ill-fitting components or design flaws that impede oral hygiene. Effective plaque control by the patient is paramount for implant
success. If inflammation persists regardless of low plaque scores, further investigations addressing the patient’s general health may be warranted, and the prosthetic might need to be modified or replaced.
Once any contributing factors have been eliminated, like poor oral hygiene, smoking, or mechanical problems with the implant, the first priority is to control the infection. Mechanical debridement can effectively reduce bleeding on probing (BOP) by 20%–50%. In cases of mild peri-implant disease, debridement by air-polishing devices, YAG lasers, or curettes can reduce pockets by around 1mm.
The addition of antiseptic therapy to mechanical debridement has not been proven to provide additional benefits where the pocket depth is less than 4mm but may help with deeper peri-implant lesions. The addition of systemic antibiotics can also improve outcomes.
Surgical techniques for periimplantitis
In conventional surgical management of peri-implantitis, the damaged implant is thoroughly debrided and decontaminated with the use of a surgical flap. Surgery often involves using autogenous bone grafts, with a control access flap procedure.
Resective surgery has been shown to be effective in reducing symptoms of periimplantitis. This entails using ostectomy and osteoplasty techniques combined with bacterial decontamination. Outcomes are improved by combing resective therapy with implantoplasty – a process of smoothing and polishing the supracrestal implant surface.
Studies have indicated that combining resective therapy with bone grafting procedures can provide a significant improvement to peri-implant health for about 6 months to 2 years after surgery. However, over time, bone-loss can still occur.
Soft tissue grafting to manage peri-implantitis
Soft tissue grafting is not a new procedure. Invented 50 years ago, it has been increasingly used in clinical practice for augmenting tissue thickness, re-establishing an adequate width of keratinised tissue, correcting mucogingival deformities, and improving aesthetics, around teeth and dental implants.
An increasing number of studies suggest that soft tissue grafting techniques might be more effective than bone grafts in successfully preventing and treating periimplant diseases, reducing marginal bone loss, biofilm accumulation and peri-implant inflammation. The use of an autogenous connective tissue graft (CTG) can be an effective treatment for peri-implantitis when there is gingival recession and a lack of keratinised mucosa, associated with increased plaque accumulation and attachment loss.
Learn directly with the innovators World-renowned periodontologist, Professor G. Zucchelli, has published widely on soft tissue management around teeth and implants. He leads an advanced course on the subject at the Academy of Soft and Hard Tissue Augmentation (ASHA) this autumn, alongside highly respected clinician in the field, Dr Selvaraj Balaji.

This one-of-a-kind, 2-part course – entitled Soft Tissue Management Around Teeth & Implants – combines theory and practice to equip participants with the newest research, unique techniques and exciting innovations to manage soft tissue around teeth and implants.
Infection can threaten the survival of implants at any point after their placement. When preventative measures and nonsurgical therapies have not been effective, surgical intervention is the only option. By maintaining proficiency in the most advanced techniques and theory in the field, clinicians can offer their edentulous patients more support, and more options,
leading to happier and healthier outcomes. Find out more at hashaclub.co.uk/courses Soft Tissue Management Around Teeth & Implants
15th & 16th November 2024 10th & 11th January 2025
To book, please call: 07974 304269 or email: info@ashaclub.co.uk
About the author Dr Selvaraj Balaji, Founder of the Academy of Soft and Hard Tissue Augmentation (ASHA).

Most tooth extractions are relatively straightforward, nonsurgical procedures. However, they can be complex processes, in some cases requiring high levels of risk management and/or surgical intervention. Extractions may be required in a number of different circumstances, including dental caries, periodontitis, trauma, periapical disease, impaction or in preparation for orthodontic treatment.
Atraumatic, minimally invasive extraction without complications is the goal, and is of particular importance for patients requiring post-extraction treatment like immediately placed implants. Despite amazing advances in technology and procedures, complications can still arise, so clinicians must prepare careful risk assessments, maximise patient awareness of possible complications, and perform detailed diagnostic tests before proceeding.
Some possible complications
Complications vary depending on the nature of the condition affecting patients, as well as the location of the problem tooth, but an important consideration is potential damage to the complex network of nerves in the oral and maxillofacial anatomy. Risk assessments must also take into consideration any possible damage to other teeth, as well as impacts on occlusion after extraction. And soft-tissue healing should be optimised in order to minimise the risk of infection.
Oral and maxillofacial surgeons are presented with impacted lower third molars on a regular basis, many of which require surgical extraction. Post-operative pain, swelling and trismus are common yet
usually short-lived side-effects. However, dry socket (alveolar osteitis), prolonged temporomandibular joint symptoms and trigeminal nerve injuries may also occur. Mandibular fracture is rare but also a possible complication after extraction of third molars from the lower jaw. Additionally, the porous, honeycomb-like network of the mandible’s trabecular bone is less vascularised than the maxilla, tending towards more difficult extractions and a slower healing response.
Extractions in the posterior maxilla also risk nerve damage, and can lead to oro-antral communication (OAC). To avoid trauma or perforation of the maxillary sinus, a great deal of planning will be important, for example, when removing teeth with bulbous roots, or periapical abnormalities. Failure of external sinus floor elevation and/or augmentation can also lead to the formation of an OAC. The treatment of OACs varies depending on the size of the opening access. Communications less than 2 mm in diameter can close spontaneously, and therefore treatment is not necessary. However, if larger than 2 mm, OACs may require surgical interventions. The surgical closure of OACs within 48 hours is recommended. If left untreated, OACs can act as an avenue for bacteria into the maxillary sinus, causing infections, sinusitis, or delayed healing.
Special considerations for first permanent molars
Most extractions in the UK are caused by dental caries. Hospital extractions due to dental caries among children has been at the forefront of the news, as a government report demonstrated a shocking 17% increase in recent years. The decision
to remove first permanent molars (FPM) – most often affected by caries – is not straightforward, as outlined in the guidance published by the Royal College of Surgeons. Children with affected FPMs can experience a great deal of sensitivity and pain due to dental caries, and treatment can require complex restorations or extractions. When correctly planned, early extraction of an affected FPM can be followed by successful eruption of the second permanent molar (SPM) to provide a suitable replacement, ideally allowing the third molar eruption (TPM) to complete the molar dentition. FPM treatment planning decisions should ideally be made in partnership with both the general dental practitioner (GDP) or paediatric dentist and a specialist orthodontist.
atraumatic extraction
Implants are an increasingly popular treatment for edentulous adults. Increasingly, studies have shown the comparative benefits of immediate placement of implants in fresh sockets. Survival rates compare well with implants placed in fully healed sockets, and fewer interventions promote healing which is preferable for patients, and can be of benefit in the osseointegration process. Atraumatic extraction is hugely advantageous, as it minimises gingival recession and marginal bone loss. Most minimally invasive methods depend on the exertion of forces on the periodontal ligament of the tooth, which in turn creates hyaluronic acid build-up in the periodontal ligament space, supporting a hydraulic pressure release in the socket. Other techniques involve sectioning the tooth and root while taking care to preserve the alveolar bone and buccal wall.
A bladed periotome has been successfully used to detach gingival fibres, enabling an extraction by forceps with minimal laceration to the soft tissue. Slow-speed handpieces have also been used successfully in atraumatic extraction. Holes are drilled around the tooth, while progressively sliding down root surfaces. This disrupts the periodontal ligament space, reduces hydraulic pressure, and increases hyaluronic acid build-up allowing for an estimated 40% to 50% reduction in extraction trauma.
Extraction methods will be dependent on the clinician’s risk assessment. W&H offers the most advanced tools to conduct atraumatic extractions according to each patient’s needs. The Piezomed from W&H, for example, offers ultrasound technology that is shown to be minimally invasive due to the incredible power of its high-frequency micro-vibrations. This results in an incredibly precise and controlled action. Additionally, the cavitation effect leaves surgical sites almost blood-free for enhanced healing effects. Atraumatic extractions result in fewer complications, and offer more restorative options. Outcomes are optimised by advanced techniques, and the best possible tools.
To find out more visit wh.com/en_uk, call 01727 874990 or email office.uk@wh.com n
about the author Kate Scheer, marketing executive, W&H (UK) Ltd

Duses composite bonding to improve his patient’s smile aesthetics.
Patient background
A patient presented to the practice who wanted to know more about composite bonding. She wanted to improve the aesthetics of her teeth, with the aim to give her self-confidence a boost.
assessment and diagnosis
The patient’s suitability for restorative treatment was assessed. This involved carrying out a Basic Periodontal Examination (BPE) which found BPE scores of 212 in the upper dentition, and 222 in the lower. Her overall oral health and hygiene was good, and she had caries in her UL5 which had been restored using composite.
treatment planning
During the treatment planning stages, whitening and composite bonding were discussed. As the patient was particularly interested in composite bonding, planning and treatment using SmileFast was discussed, as well as the use of a trial smile, and bonding the teeth immediately afterwards.
SmileFast was used to create a 3D design. This was approved digitally, and the appearance verified with the patient with a trial smile. Once verified, a stent was fabricated that features strips which fit between the patient’s teeth. In this case,
BRILLIANT Everglow from COLTENE was used in shade Opaque Bleach (OBL) – this is the brightest white shade available whilst not to everybody’s taste, this was the patient’s preference. The stent was trialled, prior to composite placement, to ensure a good fit.
BRILLIANT Everglow was then heated to 65°C and placed inside the stent. This allows the composite material to be placed on all teeth at once. Following placement of the composite, the material was light cured through the stent first, and then through glycerin. Once cured, the stent was removed and the teeth were polished. Polishing rubber, diamond discs, and diamond polishing paste were used to achieve a nice finish.
Outcome
Both the patient and I were happy with the results of this treatment. We were able to achieve our initial goal, creating a white, bright smile to help her feel more confident.
Case appraisal
Having reflected on this case, I can appreciate that the OBL shade of the BRILLIANT

Pre-treatment upper arch

Post-treatment upper arch

Everglow composite allows you to achieve an in-your-face look. This is exactly what the patient was hoping for, and she was happy with the aesthetic result. My advice to other dentists who are looking to achieve a bright white smile is to be sure to add texture to help achieve a more natural looking finish.
COLTENE offers a wide range of restorative products to help dentists and their patients achieve their desired look. The range includes the BRILLIANT
Everglow™ composite material which is available in an array of shades, including dentine shades and the brightest white bleach shades. COLTENE aims to meet the aesthetic desires of each patient, which makes this composite the ideal choice. For more information, info.uk@coltene. com and 0800 254 5115 n
about the author Dr rajiv ruwala is a Principal Dentist and Facial aesthetics Practitioner, and currently runs 2 Green Dental Practice in Dartford.

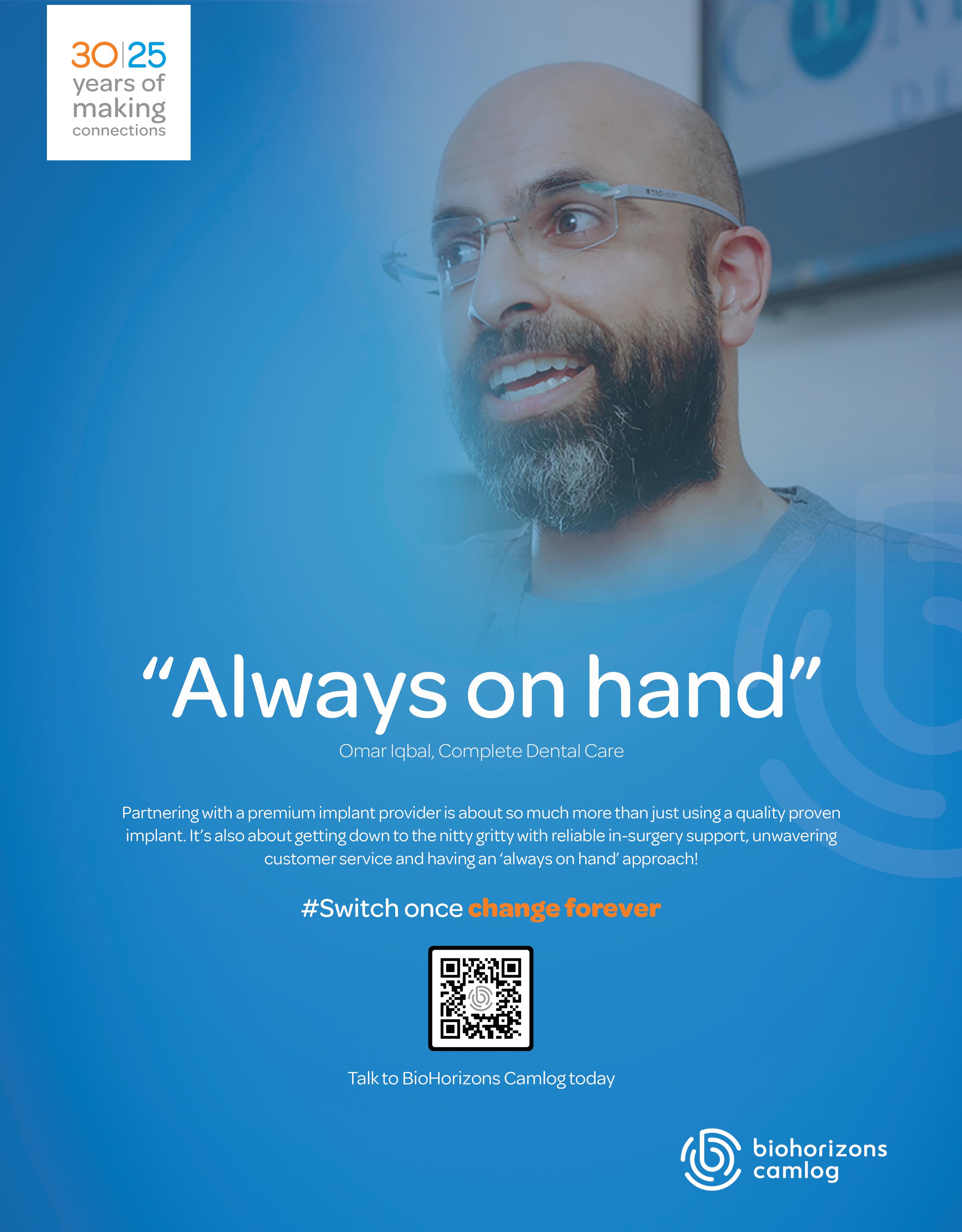
When it comes to your decontamination equipment, there is a lot to think about.
A malfunction or even complete breakdown can be costly for your business in more ways than one. Not only will you have to find the money to pay for potential repairs or replacements while experiencing loss of income and down time across the practice, but patient services could be significantly disrupted, reducing their satisfaction and causing additional stress for the professional team. That’s why it’s so important to look after your equipment and keep it running efficiently. Furthermore, both HTM 01-05 and SDCEP mandate that autoclaves be validated and maintained appropriately, with best practice recommending the use of a validated washer disinfector too.
It’s necessary to understand the different processes involved in maintaining your decontamination equipment to ensure its long-term functionality. Some steps, like daily & weekly testing, can be quickly completed in-house by staff. Others require the expertise of specially trained engineers; these include servicing and validation. So, what’s the difference? Servicing is about checking the equipment to make sure that all the mechanical and electrical parts are working correctly. The engineer performing this task will test each aspect and make any adjustments or minor repairs as they are needed. The benefit of regular servicing – usually recommended annually – is that small issues within the equipment can be identified and rectified before they affect the efficiency of equipment operation or longevity.
Validation, on the other hand, is a legal requirement and the process of confirming that specific functions are working as they should. For example, the engineer will test the steam penetration, temperature, pressure and cycle time parameters achieved by an autoclave to make sure the correct conditions are met to allow for the effective sterilisation of instruments. Annual validation is mandatory for these pieces of equipment.
the legal aspects of validation
Any technologies with pressure systems –including autoclaves – used within a place of work must comply with the Pressure Systems Safety Regulations (PSSR) 2000. The regulations state that the machine owner (the dental practice/principal) must ensure that the equipment is evaluated and certified by a ‘competent person’. This means it is vital to seek validation from a reputable provider who you can trust to send well-trained and experienced engineers to perform the task at hand. A written scheme of examination is required for every relevant piece of equipment and a copy of the most recent Report of Examination Certificate, this must be kept at or accessible from the practice. It must also be updated at a maximum interval of 14 months.
The validation process will vary slightly depending on the type of autoclave you have in practice. In every case,
maintenance and safety checks should be performed, alongside thermometric tests, an Automatic Control Test, a steam generator overheat cut-out test and the verification and calibration of the steriliser. For vacuum autoclaves, the engineer will also complete air leakage tests and a steam penetration test.
For many dental practices, it’s easiest to contact your equipment manufacturer to arrange for the annual servicing and validation. Where that’s not ideal or available for whatever reason, several other providers do offer the services independently and can help look after your equipment. It is most important that your chosen provider works with engineers who are sufficiently trained and competent in performing in the necessary tests. You will have the ultimate responsibility for correctly validating your equipment so you have to work with a team you trust completely. Another consideration is your provider’s ability to be flexible around your practice’s schedule, to offer the convenience that you need to keep your equipment running smoothly while running a busy business. Plus, you’ll want to know that the engineers who visit can make any minor adjustments and repairs to your equipment as quickly and efficiently as possible as part of the servicing process.
Leader in the field, Eschmann offers a comprehensive servicing, maintenance and validation package suitable for any brand of decontamination equipment. Highly trained engineers complete all the necessary testing and checks for complete peace of mind that your practice will be compliant. They carry Eschmann original parts to perform repairs on the spot for maximum efficiency, and with parts and labour included in the Care & Cover plan, it’s cost-effective too. In addition, Eschmann is one of the only providers to deliver Enhanced CPD accredited training with the installation of new decontamination equipment, and annually thereafter if you are one of their Care & Cover contract customers. This ensures that staff can confidently use and maintain your technologies on a daily basis too.
Avoiding problems with decontamination equipment is essential for all dental practices to help preserve an efficient professional workflow and exceptional patient experience. Equipment servicing and validation are two different, yet equally important processes that must be implemented annually. Make sure your practice is prepared with a maintenance plan in place.
For more information on the highly effective and affordable range of infection control products from Eschmann, please visit www.eschmann.co.uk or call 01903 753322 n
about the author
nicky Varney, Senior marketing manager at eschmann.
Peri-implant diseases are inflammatory conditions that affect the peri-implant tissues. They encompass two distinct conditions: peri-implant mucositis and peri-implantitis. The former is an inflammatory lesion of the peri-implant mucosa, without bone loss. It is characterised by bleeding on gentle probing, as well as redness, inflammation, and increased probing depth. Peri-implant mucositis is a reversible condition caused by a microbial disruption at the implantmucosa interface. It can be caused and progressed due to biofilm accumulation, smoking, and radiation therapy.
The latter, peri-implantitis, is a biofilmassociated pathological condition which occurs in the tissues surrounding dental implants. It is characterised by inflammation and the progressive loss of supporting bone. Signs include inflammation, bleeding on probing, increased probing depth, mucosal recession, and radiographic bone loss. Peri-implant plaque biofilm is the primary cause of peri-implantitis, with other risk factors including: a history of severe periodontitis, poor plaque control, and irregular supportive peri-implant care after treatment.
Peri-implant diseases are a growing public health concern, with a high prevalence and potentially devastating consequences (implant loss). As such, it is vital that clinicians have a good understanding of preventing and managing both peri-implant mucositis and peri-implantitis.
The BSP Implementation of Prevention and Treatment of Peri-implant Diseases – The EFP S3 Level Clinical Practice Guideline offers recommendations for the prevention and treatment of peri-implant diseases, facilitating a consistent, interdisciplinary, evidence-based approach.
Peri-implant mucositis is treatable, and can be successfully managed by carefully controlling of the peri-implant biofilm. If it is allowed to persist, however, periimplantitis will develop. It is believed that peri-implant mucositis always precedes peri-implantitis, which results in larger lesions. Peri-implantitis, without treatment, can accelerate very quickly – much faster than is commonly seen in periodontitis.
The Prevention and Treatment of Periimplant Diseases Guideline identifies best-practice interventions for preserving the health of peri-implant tissues, and therefore extending the survival of dental implants, and minimising complications. It encompasses 55 clinical recommendations for the prevention of peri-implant diseases, which are directly relevant to the UK healthcare community including the public.

periodontitis, should be addressed, to help lower the risk of complications.
Post-operatively and once the prosthesis has been placed, patients should immediately be subject to a supportive peri-implant care programme in which they are provided with professional plaque biofilm removal, oral hygiene advice and motivation, and early detection of pathological conditions. Patients should be monitored for healthy peri-implant tissues, peri-implant mucositis, and peri-implantitis, and provided with a prompt diagnosis so that appropriate treatments can commence.
Once diagnosed as peri-implantitis, clinicians must first decide whether the affected site is treatable. In the case that it is, non-surgical sub-marginal instrumentation therapy should be performed, followed by a re-assessment of the clinical situation. At this point, clinicians should decide between preventative therapy, or surgical treatment – elevating a surgical flap and performing sub-marginal instrumentation. Following successful treatment, patients should be re-enrolled for preventative therapies. Constant monitoring of peri-implant health is critical as it enables clinicians to select the best care pathway for each patient. Effective peri-implant treatment requires the successful, long-term maintenance of the tissues – encompassing behaviour, health monitoring, prevention, and careful treatment decision making.
Decision making using appropriate guidelines
As peri-implant diseases have become so widespread, it is absolutely vital that clinicians understand how to prevent, identify, and treat peri-implant issues should they arrive. This means that clinicians must offer patients appropriate advice prior to and following dental implant placement, stay vigilant when patients experience inflammation at the implant site, and decide on the best course of treatment to protect the longevity of the dental implant.
The Prevention and Treatment of Periimplant Diseases Guideline was created in collaboration with the Association of Dental Implantology (ADI), with ADI representatives including Amit Patel, Pynadath George, Paul Shenfine, Daniel Benson, Sunkanmi Oladeji Olaore, Jaimini Vadgama, Kasia GurzwaskaComis, Jiten Vaghela, Viraj Patel, Rajiv Sheth, and Nikos Donos. The ADI is passionate about educating both its members and their patients on how to maintain healthy dental implants, and guidelines which reflect best practice for managing peri-implant diseases mirror this passion.
The Guideline acknowledges that any patient receiving dental implants is automatically at risk for peri-implant diseases because, once the implant is exposed to the oral microbiome it is vulnerable to biofilm accumulation without sufficient intervention. Therefore, during the treatment planning stage, known risk factors, such as smoking, diabetes, and
As dental implant providers, we have a duty to remain educated about best practices in the field. The Prevention and Treatment of Peri-implant Diseases Guideline makes this clear, and offers sound advice to clinicians to help them offer their patients the best possible outcomes. For more information, visit adi.org.uk n
about the author Dr Zaki Kanaan,
aDI President.

Dr
A37-year-old male patient was referred to me as he was unhappy with the appearance of his smile. He was becoming increasingly concerned about the level of chipping and wear to his front teeth. He explained he had undergone orthodontic treatment as a teenager, but had relapsed due to no long-term retention.
The patient presented with good oral hygiene, no caries and good periodontal support. He was medically fit and a regular dental attender at the practice. He had mild to moderate wear, chipping and discolouration of the upper and lower central incisors, that involved classic ‘butterfly’ rotations. This was associated with a restricted envelope of function. Several treatment options were discussed with the patient.
These included:
1. Orthodontics.
2. Restorative treatment with ceramic or composite veneers. However, due to the restricted envelope of function and the irreversible nature of these treatments, these were neither viable long-term stable option’s or conducive to the patient’s desires.
3. No treatment and monitor, which was unfavourable.
The patient expressed a preference for a more conservative option, and so the orthodontic options were explored. We discussed the options of aligners, Inman Aligner and clears, fixed appliances and referral to a specialist. The patient didn’t wish to have fixed appliances and declined referral. He decided to proceed with an orthodontic assessment to explore what options were available.
Devising a treatment plan
The orthodontic assessment revealed:
• Mild class 3 skeletal relationship with normal FMPA and high LFH
• Soft tissues normal
• Class III incisal relationship
• Overjet reduced to approximately 1mm and approx. 5% overbite
• Centre lines coincident
• Molar relationship L and R class III 1/2 unit
• Canine relationship R Class 1 L Class 3 1/4 unit
• Well aligned buccal segments
• Crossbite LL6/UL56
• Mild upper and lower crowding
• Mild to moderate anterior Incisal wear and chipping
• Heavily stained teeth, mainly caused by coffee consumption
• Patient was a habitual bruxist
• Good oral hygiene
• Good bone levels
Full clinical photos were taken and an initial 2D analysis of his dentition with the Spacewize+ digital space calculator and a subsequent 3D analysis with Archwize displayed 1.7mm of crowding in the upper arch, and 1mm in the lower arch.


The 3D analysis demonstrated a potential result could be achieved using the Inman Aligner appliance for the upper and lower arches, and that a few refiners in the lower arch may be required. The Inman Aligner could give efficient movement over the incisor rotations, which are often difficult to manage, reducing treatment time and cost.
The patient was presented with 3D models of the proposed outcome, assisting informed consent. I discussed the anticipated treatment and showed the patient the type of appliance we were going to use.
In the upper arch we also opted for an integrated combined expander, engaging temporary lateral expansion to create space for the incisors to move forwards. This enabled the case to progress more efficiently, and with controlled IPR (interproximal reduction) and PPR (predictive proximal reduction), achieve an optimal aesthetic result.
A letter of quotation and consent was sent and approved.
We began with the upper arch, reducing possible interferences with the anterior teeth. Since the patient’s upper and lower central incisors were of a triangular shape, PPR was carried out to ensure even contact with the lateral incisors, reducing the chance of black triangles and improving aesthetics. IPR was completed on the straight contacts, 0.3mm between the UR3 and UR4, 0.3mm between the UL3 and UL4, and 0.3mm between the UL1 and UR1. Half of the recommended IPR was performed at the other sites. Composite button anchors were placed to engage the palatal bow on the most palatally positioned teeth. The remaining IPR was completed as the case progressed. All of this was carried out as per the 3D Archwize planner guidance. The patient was shown how to place and remove the aligner, correctly engage the bow with the composite buttons and how to turn the expander. Appliance maintenance instructions were given.


The patient was reviewed regularly and was exceptionally compliant throughout treatment. He initially had some concerns regarding speech clarity but adjusted quickly. After 12 weeks, the upper teeth were aligned. A customised fixed bonded retainer was fitted and a temporary removable vacuum formed retainer given.
The lower Inman Aligner was provided and the necessary PPR and IPR carried out, with composite buttons placed to anchor the bow. Alignment in the lower arch progressed as expected, with minimal complications. Prior to the end of treatment, to reduce treatment time, the patient also carried out some at home tooth whitening using the Philips Zoom 6% hydrogen peroxide and bleaching trays provided by the IAS Laboratory.
With the planned movements accomplished, a second Archwize assessment was performed and 3 refiners were required for final movements and optimal aesthetics. After the refinements a customised fixed bonded retainer was fitted.
Following the guidelines of the ABB (Align, Bleach, Bond) concept, composite edge bonding was carried out with A2 and OL from Venus Pearl, wrapping slightly over the labial surfaces of the teeth using the IAS reverse triangle technique, developed by Tif Qureshi. It is a simple technique involving 2 layers of composite, one dentine and one enamel shade, and offering efficiency and great aesthetics.
Upper and lower removable vacuum formed retainers were provided for night-time wear and retention.
The patient was thrilled with the results. The treatment exceeded his expectations and helped restore confidence in the ability to smile.
On reflection, I’m equally delighted with the outcome of the case. I was able to achieve a stable and aesthetic outcome in a conservative manner by using the techniques


I have learnt through attending the IAS academy.
In hindsight, it may have been an option to use the Inman Aligner in the upper arch and clear aligners in the lower arch to potentially reduce treatment time, or even upper and lower aligners. However, the benefits of the Inman Aligner providing efficient movements, especially of rotated incisors, at a low laboratory cost cannot be overlooked as a viable and successful treatment option.
A key factor to the success and efficiency of this case was the support and guidance received, specifically from Claudia Waddell and Kelly Toft, mentors at the IAS Academy.
In addition, the ongoing mentoring I receive throughout all my orthodontic cases at the academy is one of the most supportive I have experienced over 25 years of dentistry. The academy enables safe and continued development and I recommend anyone interested in developing their restorative/orthodontic skills to use the IAS academy.
For more information on upcoming IAS Academy training courses, please visit www. iasortho.com or call 01932 336470 (Press 1) n
about the author

Dr neil Fearns is a dentist practising in the northwest of england. He graduated from Leeds University in 1998 with a distinction in Child Dental Health, soon after he successfully achieved his national Board Qualification of Canada. He has completed various postgraduate qualifications in restorative dentistry as well as undergoing several restorative - Orthodontic courses and now undergoing the advanced Orthodontic Diploma at the IaS academy.
Avoiding complications in restorative dentistry is essential when providing long-lasting and effective results. Secondary or recurrent caries, in particular, are a significant risk to the success of a restoration, and clinicians must understand how they can be avoided. The pathogenesis of dentine secondary caries is near identical to any other caries lesion, involving demineralisation and enzymatic dissolution of the organic component. The presence of a restoration or sealant margin makes this a unique issue, distinct from that of primary caries. Several factors may influence the development of recurrent caries, from restorative material, to the location of restoration gaps, a patient’s caries risk or the experience of the clinician. Whilst the problem may never be completely eradicated from dentistry, understanding the steps that can be taken to minimise the risk of such complications is key.
the scale of the issue
Dental professionals must understand the extent to which secondary caries plague the success of restorative treatment. One study found that 3.6% of all observed restorations were affected by secondary caries (amongst a sample of 4036 restorations), and at least 20% of patients in the study had at least one secondary caries lesion. It is the most common diagnosis for restoration failure. When a restoration fails, a repair or replacement is needed. A repair may be preferred where at all possible, as it is often quicker and less anxiety provoking for
the patient. However, the most important clinical indicator that favours a replacement over a repair is the extent of secondary caries. One study saw that as the depth of recurrent caries increased, a complete replacement was more likely to be carried out in general dental practice. This is likely in an effort to ensure that no caries is left in situ to develop into future problems.
Minimising the need for such an intervention will always remain ideal. Clinicians need to choose the appropriate approach for a restoration, including their choice of materials, and provide effective support to high caries risk individuals.
efforts against caries development
Multiple patient factors can increase the opportunity for recurrent caries to develop. They are, in essence, the same as those for primary caries; oral hygiene, dietary and smoking habits all play a role. Clinicians can encourage patients to take up effective dental hygiene routines to minimise the risk of recurrent caries development. Whether they take the advice – such as regular brushing with a fluoridated toothpaste or ceasing a smoking habit – is entirely up to the individual. The profession’s understanding of patient motivation, and thus its efficacy, is developing with time, but clinicians cannot always have control over this aspect of recurrent caries risk reduction.
Clinicians may be able to influence, and reduce, the development of secondary caries through their choice of materials for a restoration. Direct amalgam restorations

have been observed to reduce the incidence of caries when compared to composites in some studies, however, this often requires tooth or restoration preparation, which may weaken the restored tooth. As well as this, patient chair-side time increases. In addition, amalgam restorations are considered less aesthetic than composite solutions and with the commencement of the amalgam ban in EU countries come 2025, UK dentists are expected to be hit with disruptions to supply chains and increased costs.
The predominant alternative at current is glass ionomer cements (GICs). They have good biocompatibility and bind chemically to dental hard tissues, but more importantly, release fluoride which may protect against secondary caries. High viscosity GICs have been noted to protect against secondary caries even in cases of low fluoride compliance. By choosing such a restorative material, clinicians are opting
for a solution that can actively work against secondary caries development whilst the patient is outside the practice, even if the patient does not completely adhere to effective hygiene routines. A GIC will not eliminate the risk of secondary caries development entirely, but its impact can be inarguably effective.
Avoiding secondary caries, and thus invasive repairs and replacements, is no easy feat, but can be achieved with patient compliance and an effective restoration. The choice of material –whether for a direct or indirect restoration – can play a large role.
When a patient needs an indirect restoration, whether it’s a metal crown or bridge, inlay/onlay or all zirconia crown or bridge, clinicians should choose the award-winning Ketac Cem Plus ResinModified Glass Ionomer Cement from Solventum, formerly 3M Health Care. The hybrid glass ionomer cement offers sustained fluoride release, with virtually no post-operative sensitivity for increased patient comfort. The solution is formulated to make everyday procedures faster and more reliable, with a higher bond strength than conventional glass ionomers. Secondary caries will always be a concern for dental professionals, but by implementing effective materials into the restorative workflow, there is an opportunity to reduce their incidence. n
Vertical root fracture (VRF) is a leading cause of tooth loss, especially in endodontically treated teeth. Different to cracks, which may just be coronal, VRFs extend through the pulp to the roots. They may begin as a crack, and propagate slowly down into the pulp chamber, and then the root. In my clinical experience, VRF is becoming a more common reason for tooth loss. Previously, the leading cause was caries, however, patients are now far more aware of the impact of their diet on oral health. This, combined with increased use of fluoride has begun to make caries less problematic. As such, vertical root fracture caused by tooth surface loss is likely to be the next tooth loss epidemic – with its incidence increasing in recent years.
Preventing the next tooth loss epidemic
This more frequent occurrence is problematic for a number of reasons. The loss of teeth is expensive should patients choose to replace them with dental implants. Biologically, whilst implants are good, they are not as good as natural teeth as there is no periodontal ligament. Additionally, the loss of alveolar bone associated with tooth loss is devastating for patients’ oral health.
As such, a preventative approach to VRF and tooth surface loss is essential. Tooth structure loss often leads to occlusal changes which, in turn, increases the risk of wear. In time, this increases the likelihood of cracks, VRFs, and the need for extraction and subsequentially implant supported restorations. By preventing tooth structure loss and wear in the first place, through occlusal analysis and mouth guards, for example, the patient’s risk of tooth loss is reduced significantly over time.
It’s important to note that patients presenting with VRF are younger than we would previously have expected too – with many in their 40s. Prior to now, we might have anticipated this type of fracture in patients in their 60s and 70s who have had extensive restorative treatment. VRF is also much more common in root filled teeth, and there has been an increase in frequency since COVID. Women and older patients do appear to be more at risk, and VRFs are more likely to be seen in mandibular molars and maxillary pre-molars.
Diagnosing vertical root fractures
There are numerous factors which may increase the risk of VRF but, ultimately, the two key areas are the structural integrity of the tooth, and the occlusion.
Radiographically, when assessing a tooth with a suspected fracture, circumferential
bone loss is a key indicator. Here, a CBCT scan can be helpful for identifying areas of bone loss, and communicating this with patients in a clear manner. Further to this, the “Tamse Triad” offers clinicians a number of identifying factors during the assessment. These include a sinus close to the gingival margin, a deep and narrow probing defect, and circumferential bone loss. If these are present, VRF is highly-likely, and the prognosis is usually extraction.
Communication with patients is important too, as this will allow you to more accurately assess the clinical situation. If they have minimal restorations, and are experiencing spontaneous pain, query whether this may be linked to a particular event, such as biting down on hard food, as this will help to indicate the likelihood of fracture.
How should clinicians manage these cases?
In order to recommend the most appropriate course of treatment, it is wise to undertake a restorability assessment in which the tooth is opened up, and the extent of the fracture is assessed. Using magnification and transillumination is crucial here, to enable the clinician to see whether the fracture has extended into the root canal system.
In many cases, once the fracture has extended to the roots, the tooth is not salvageable, and extraction is
recommended. This is because bone loss is still likely following root canal treatment, which could compromise the options available for restoration using dental implants down the line. However, in cases where a cracked tooth is restorable, a full coverage crown is recommended to reduce the risk of VRF going forward. The risk of tooth loss is six times higher in cases where a full crown is not provided.
Prevention is better than cure Cracks and vertical root fractures are an increasing problem, and the likelihood is that they are only going to get worse with time. Treatment options are limited for VRF, as such prevention is better than cure in many cases. This means that clinicians should incorporate occlusal analysis and tooth wear assessments into their workflows as part of their preventative strategies going forward.
https://mimetrik.co.uk n
about the author alyn morgan is the immediate Past President of the British endodontic Society, and the co-founder and CeO of a spin-out company from the University of Leeds, mimetrik Solutions.

Iwas interested to come across a news article recently suggesting that the popular Japanese tea could support the prevention of periodontal disease. It seems that matcha, which is made from the raw leaves of the tea plant gown in almost no sunlight, may be a friend to dentists everywhere.
C. sinensis – from which matcha comes – is already known for its antimicrobial properties. This research paper assessed matcha specifically for its ability to inhibit the growth of P. gingivalis, as well as two other pathogens related to oral disease (Prevotella nigrescens and Fusobacterium nucleatum). It found that matcha triggers both morphological and physiological changes in the pathogenic envelope. The substance increased membrane stiffness while decreasing membrane permeability of P. gingivalis. It also caused membrane depolarisation, all of which made the cells easier to destroy.

A dose-dependent and heat stable correlation was reported, suggesting that matcha would be effective against P. gingivalis in various conditions. Researchers also postulated a potential for the green tea to improve probing pocket depth, although further study will be required to confirm this.
These latest findings make matcha a strong potential ally in the fight against gingival diseases. It is relatively inexpensive and easy for patients to implement, while also being a natural substance with no known negative side effects when consumed in moderation.
On a side note, matcha has been linked with various other health benefits that may be of interest for the holistic dentist or any other healthcare professional. For instance, it helps to reduce stress and anxiety, improve memory and boost cognitive function. There is also some evidence to show that matcha supports sleep quality. More definitive research is still needed, but results so far certainly provide food for thought.
Back to periodontal disease, this remains a pressing concern across the country, with half of all UK adults expected to experience the condition at some point in their lives. There is also a substantial body of evidence associating periodontitis with a whole host of systemic conditions, elevating the importance of prevention.
Something as simple as a daily cup of green tea could benefit a huge number of people. Of course, there is no substitute for a highquality oral hygiene routine, but safe and effective adjunctives that protect the mouth throughout the day are always welcome.

































































We are always talking about the importance of quality over quantity, substance over form, but what does that really mean? In dentistry, this can apply to everything from the care delivered to your patients to the benefits you offer your practice team and the training courses you attend to further your clinical skills. In every situation, it’s important to consider whether the perceived value of an activity or event is accurately reflected in reality.
Though it’s difficult to define exactly what quality care is, Donabedian’s 1980s suggestion was “care which is expected to maximise an inclusive measure of patient welfare, after one has taken account of the balance of expected gains and losses that attend the process of care in all its parts”. The World Health Organization offered its own description in 2018, stating the three key components for quality patient care to be effective, evidence-based services; safe; and people-centred.
Both of these can be applied to modern dentistry, where it is more important than ever that expectations of both healthcare professionals and patients are met. A survey from 2015 found that the patient experience was often focused on access, value, health, trust, safety, technology, environment and patient-centred care. Confidence in their dentist’s skills was another major contributor to patients’ satisfaction.
From a professional perspective, treatment success rates will indicate both clinical skill and quality of care provided. Though not easy to achieve, this is much simpler to monitor compared to patient-driven factors. A clinical audit of treatment delivered can be used to demonstrate how often procedures end in the desired/expected outcome.
Most businesses talk about supporting their staff, but it is important to ensure that there is substance in what is delivered.
A benefits scheme, for example, may be considered to offer a tangible list of advantages for team members. Reports from both 2020 and 2022 suggested that employee benefits were the main reason that those surveyed would change job, other than for higher pay. The favourite benefits among UK workers are thought to include health insurance, flexible working, pension contribution matching, paid sick leave, mental health and wellbeing support, extra holiday allowance and support for parents, among others.
Supporting dental professionals with tangible education and career development opportunities is also important. This means providing access to training courses, and being flexible in allowing for time out of the practice to attend programmes. Skill advancement should also be actively discussed during annual appraisals in order to ensure that individuals feel supported in making the right career decisions for them. This is critical in dentistry right now given the challenges being faced in recruitment across the country.
An education of substance
Complementing education for all members of the dental team, and providing a platform to find the right programmes, are dental exhibitions and conferences. These make sourcing information and professional recommendations easy, with training providers on hand to offer bespoke advice and guidance. Added advantages of attending such events include being able to take the whole team, networking with the wider dental community and discovering state-of-theart innovations that will help to drive the future success of your business.
However, not all events are made equal. As with all the other areas

discussed, it is important to ensure that you select an event that will truly deliver all that you need it to.
What does this look like? A broad range of industry organisations should be in attendance ensuring you can engage with everyone necessary to make intelligent business decisions. There should be an opportunity to try products and materials for yourself, on stands and perhaps also in a practical workshop situation for an enriched learning experience. With regards to the educational programme, make sure there are appropriate lectures for all members of your team that are covering genuinely relevant topics. It is just as useful to check the speaker line-up – you need more than one main headline speaker to make your team’s visit productive and valuable. If you’re looking for an event you can rely on in 2025, take your team to BDIA Dental Showcase. This is the largest gathering of practice owners, team members and product experts in the UK, designed specifically to deliver tangible benefits that positively affect your business development and staff retention. Several brands attend BDIA Dental Showcase as their only UK event, making this an exclusive opportunity
to see them and their cutting-edge solutions. Plus, the conference programme includes a substantial range of leading speakers and relevant topics, with dedicated theatres for fast-growing disciplines such as dental implantology and cosmetic dentistry, and unique hands-on workshops for a truly comprehensive experience.
Beyond the headlines
Whether looking to deliver exceptional patient care, improve staff retention with better support or find an event that facilitates business growth, make sure you do your homework. It’s important to look beyond the headlines to make sure you are getting quality over quantity and substance over form! n
BDIA Dental showcase 2025 14th-15th March exCeL London dentalshowcase.com
About the author David Hussey, event Director, MA exhibitions.

Ideal for those who are new to endodontics, or who are early in their careers and want to find out more about the field, the British Endodontic Society (BES) is running a parallel Early Careers Group (ECG) programme at the IFEA World Endodontic Congress (WEC). Chair and Vice-Chair of the ECG, Daniel Vaz de Souza and Dipti Mehta, shared their excitement about the upcoming Congress, and described what attendees can expect. Dipti is a specialist endodontist; she works part time in private practice and teaches for the remainder of the week.
As Vice-Chair of the ECG, she shares an insight into what delegates can expect from the ECG parallel programme:
“My session, which I am co-presenting, is titled ‘The journey of an early career endodontist’. When I completed my specialist training, I remember a feeling of being underprepared, despite having these newfound skills in endodontics. The journey that we will talk about is the management of that uncertainty when we enter the

practice world, both from a clinical and a non-clinical aspect.
“So, why should you come to the WEC 2024? Attending an international congress such as this with the number of speakers and attendees that we’re going to have involved provides a huge opportunity, not only to improve your endodontic knowledge, but also to network on an international level.
I feel that this is something that’s critical

for the development and enjoyment of endodontics as we progress in our careers.”
Daniel, also a specialist in endodontics, is a member of the BES council, and Chair of the ECG. He will be co-presenting the session with Dipti, and shares his perspective of what it means to be an early career endodontist:
“As we progress in our dental careers, and particularly in endodontics, we are
faced with daily challenges and adversities, both clinical and non-clinical. Our main goal during the session is to give our own insight on these challenges and how to overcome them with some experience.
“There are a number of benefits of attending the WEC 2024. Let’s not forget this is a global event, so we are gathering hundreds, if not thousands, of dentists from different cultures and different countries. It’s interesting to find that we all face the same difficulties in endodontics, and we are all going to be in the same place learning from our own challenges, and ways of moving forward in endodontics. Not only that, but there’s also going to be a big chance to network with colleagues who we have never had the chance to meet before. So, enjoy WEC 2024!”
Register today for IFEA WEC 2024 at ifea2024glasgow.com/registration
For more information about the BES, or to join, please visit the website www.britishendodonticsociety.org.uk or call 07762945847 n












































































































































































































This October, ExCeL London will once again host one of the dental industry’s most anticipated events: Dentistry Show London.
This year’s event promises to be the best yet, offering an unparalleled exploration of the latest advancements in dental technology, practice, and patient care.
Over the course of two actionpacked days (4-5 October), attendees will have the opportunity to engage with more than 180 exhibitors and listen to inspiring talks from over 100 leading speakers covering a wide range of topical subjects.
With more than 100 hours of innovative content, there’s something for everyone – designed to inspire, inform, and invigorate the dental community.
As one of CloserStill’s premier events in the dental calendar, the show offers fantastic networking opportunities, fostering connections among dental professionals, suppliers, and educators.
It’s the perfect place to collaborate with colleagues and expand your community by sharing ideas and thoughts.
Building lasting business connections can open new doors and reveal shared interests, challenges, and potential collaboration prospects.
In addition to meeting exhibitors and making connections on the trade show floor, you can visit the networking lounges to connect with like-minded individuals or attend a stand hosting an event.
Many exhibitors also provide tickets for parties showcasing new products, technologies, equipment, or services,
offering a chance to meet a diverse range of professionals in an informal and relaxed setting.
Ahead of this free-to-attend event, you can connect with other attendees, exhibitors, and speakers via the Dentistry Shows event app, helping you prepare, network in advance, and maximise your time at the show.
This one-stop shop is the place to be for recognising and celebrating modern dentistry.
Leading exhibitors representing all aspects of dentistry, including Agilio Software, Colgate, Dental Implant Education Ltd, the GDC, Ivoclar, Listerine, MDDUS, and NHS Dental Services, will be on hand to demonstrate their latest innovations and connect with delegates.
From cutting-edge products to the latest clinical techniques and equipment, the floor will buzz with trends celebrating dynamism and creativity, providing valuable insights into the industry’s future.
Business owners looking to attend will learn resolution tactics for issues they may have noticed in their practice and find out more about the latest clinical techniques and equipment.
Attendees will have the chance to earn enhanced CPD hours during their visit.
Across the engaging theatres, the most relevant and applicable hot topics will be discussed, allowing you to gain up to 12 CPD hours over the two days. This is an excellent way for individuals to keep their professional knowledge up to date and for teams to come together and be inspired by the best the industry has to offer.


We’re thrilled about opening the doors again in October and look forward to meeting everyone, plus gaining valuable feedback from attendees, exhibitors, and speakers
Planning is key to ensure you maximise your time at the Capital’s premier dental event and leave with valuable information to help meet and maintain high professional standards.
Portfolio Director, Alex Harden, is enthusiastic about what 2024 has in store: “Every year we aim to raise the bar for the dental industry, and this year is no exception.
“With a fantastic lineup of interactive workshops, inspiring keynote speakers, and the latest innovations in dental equipment, materials, and software, we are confident that the show will be a phenomenal success.
“We hope delegates can unite and thrive over the two days, leaving feeling refreshed, inspired, and empowered.
“We are committed to providing a platform for networking, learning, and innovation within the dental community, and our London event is testament to this mission.
“We’re thrilled about opening the doors again in October and look forward to meeting everyone, plus gaining valuable feedback from attendees, exhibitors, and speakers.”
As the dental profession and industry continue to evolve, Dentistry Show London remains committed to facilitating knowledge exchange, promoting professional development, and supporting the community in delivering exceptional patient care.
The event follows the success of the British Dental Conference & Dentistry Show (BDCDS) in Birmingham, which took place earlier this year in May.
With an exceptional lineup already planned and a host of fresh opportunities on offer, London is set to follow in its footsteps. n




By updating the Ecosite Elements shade palette, we have made our established range even better. The clever shade combination is made up of three modules, which now include the two Pure shades A1 and BL1, providing a simple, aesthetic solution.
Fundamental composites - perfect results, amazing simplicity


With an innovative NC1 material structure



Exceptional handling for maximum safety and precision thanks to the push-and-flow effect
Advanced, intuitive and quick shade slection


Available Pure shades: BL1, B1, A1, A2, A3, A3.5 For more information visit uk.dmg-dental.com










Predicta® Bioactive Desensitizer by Parkell swiftly alleviates dentin hypersensitivity using natural tooth elements, calcium and phosphate. Upon application, it forms hydroxyapatite plugs in the dentinal tubules and adds a mineralization layer that broadens the seal, protecting pain-sensing A-delta nerve fibers. Ideal to treat sensitivity from exposed roots after perio-surgery, bleaching, scaling, root planing, and gingival recession.
Patients report immediate relief from sensitivity lasting up to six months.

Get your heavily discounted Predicta® Bioactive Desensitizer kit here:
https://europe.parkell.com/predictabioactive-desensitizer-uk-probe n
https://europe.parkell.com/predicta-bioactive-desensitizer-uk-probe
Using guided surgery for implant placement has become increasingly popular among Implantologists because it offers many benefits for the Clinician and patient.
For patients there is dramatically reduced surgical time, which helps improve patient comfort and reduces apprehension. Plus, it utilises flapless surgery which significantly improves the healing process and time in most cases, and minimizes risk of complications.
For the Implantologist it significantly improves placement accuracy, reduces the risk of complications and minimizes chair time leading to greater efficiency and cost savings. The adinguide™ guided surgery system delivers effortless procedures plus accurate
As peri-implant diseases have become so widespread, it is absolutely vital that clinicians understand how to prevent, identify, and treat peri-implant issues should they arrive. This means that clinicians must offer patients appropriate advice prior to and following dental implant placement, stay vigilant when patients experience inflammation at the implant site, and decide on the best course of treatment to protect the longevity of the dental implant.
The Prevention and Treatment of Periimplant Diseases Guideline was created in collaboration with the Association of Dental Implantology (ADI), with ADI representatives including Amit Patel, Pynadath George, Paul Shenfine, Daniel Benson, Sunkanmi Oladeji Olaore, Jaimini Vadgama, Kasia GurzwaskaComis, Jiten Vaghela, Viraj Patel, Rajiv Sheth,
What sets interdental brushes from Curaprox apart from string floss?
Floss is not able to clean the most critical areas, like teeth concavities and the area between the papillae. Curaprox interdental brushes have long filaments – which fill the entire interdental space, making a single movement in and out enough to thoroughly clean the interdental space.
For the most effective clean, interdental brushes from Curaprox are easy to use, and are an eco-friendly choice. The handles of Curaprox interdental brushes are reusable, meaning patients only have to replace the brush head.
IDactiv QUANTUM is the most powerful disinfectant available in the Bossklein range. Designed to remove organic debris from instrument surfaces and attack a range of micro-organisms including spores. QUANTUM leaves instrument surfaces contamination free and ready for sterilisation.
This high-powered product utilises peracetic acid to eliminate infection causing microbes and includes active colour changing properties. Immediately after mixing, the solution is dyed a deep red colour which will gradually fade over the working day to eventually be colourless and no longer active.
and predictable implant placement. It delivers everything you need in a guided surgery system. It is a keyless system which helps save surgery time, whilst ensuring accurate and predictable implant placement. It features ActiveFlow™ Irrigation Technology which delivers coolant directly to the surgical site. This helps prevent bone overheating, thereby maintaining healthy bone for optimum osteointegration and minimised risks of complications.
Call: 01274 885544 or visit the website. n

and Nikos Donos. The ADI is passionate about educating both its members and their patients on how to maintain healthy dental implants, and Guidelines which reflect best practice for managing peri-implant diseases mirror this passion.
For more information, please get in touch with the ADI team.
For more information, please visit: www.adi.org.uk Become a member today n
Discover the full range of interdental brushes by visiting the website, or getting in touch with the team.
For more information, please visit: www.curaprox.co.uk n

Featuring Tokuyama’s patented RAP monomer and aesthetic spherical filler technology, Estelite Sigma Quick delivers an extended working time in ambient light yet cures in only 10 seconds! There is also less residual monomer and minimal aftercure colour change for long-term aesthetic satisfaction.
Estelite Sigma Quick offers miracle shade matching! Its spherical filler particles offer inherent shade mimicking so that, in most cases, just one shade will blend perfectly with the natural teeth.
Estelite Sigma Quick is ideally used in combination with Tokuyama’s award-winning

The unique powder-based solution is used at an economical 2% dilution. That’s just 20g per litre of cleaning solution, so a single 700g tub can create up to 35 litres. For more information call 0800 132 373 or visit www.bossklein.com n

Universal Bond II which can be used to bond all direct and indirect restorative materials, Garrison Sectional Matrix Systems and for the ultimate aesthetic finish Eve polishers!
For more information, call Trycare Ltd on 01274 885544 or visit www.trycare.co.uk/ estelite n
When you invest in new imaging systems, you are also investing in your own skillset, and opening up your care to a wide range of new capabilities.
To maximise the opportunities that lay in front of you, consider speaking to the Carestream Dental team, who will help to provide immense insight into your new imaging systems.
No one knows the potential of our award-winning CBCT scanners better than ourselves, which is why our team is always on hand to show clinicians on how to implement our imaging systems into their daily workflows.
The Carestream Dental team can provide demos of our systems to your practice, or can be reached over the phone or via
Don’t buy off a brochure – experience our range of dental solutions first-hand with a visit from PlanDemo! An appointment with our PlanDemo mobile showroom is not only a great chance to see the full range of equipment Planmeca has to offer but it’s also an opportunity for you to plan, design and build your practice – and you can even do it in your lunch hour!
Experience the complete digital workflow and discover the latest in 3D dental Imaging with our popular ProMax 3D CBCT. See the only complete all in one digital software solution you will ever need with Planmeca’s Romexis.
Wave goodbye to messy impression materials and start scanning and milling in house with our Planmill 35 chairside Mill

email if you have any questions. Our website also features informative user guides for each of our system families, so you can better understand the unique features presented by each solution.
To learn more about how the Carestream Dental team can help your practice reach its newly expanded clinical imaging potential, contact us today.
For more information on Carestream Dental visit our website. For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
complemented by our accurate lightweight intra-oral scanner Emerald S. Experience all this for FREE. You can even meet with your local distributor at the same time, to conveniently discuss other aspects of the project with the whole picture in mind. Visit the Planmeca UK Facebook page and drop us a message @PlanmecaUK to book today.

Telephone: 0800 5200 330 Email: marketingUK@planmeca.com n
Communicating with your patients effectively is the key to avoiding missed appointments and improving your relationships with the community around you. Patient Bridge, a Sensei product from Carestream Dental, helps your practice take everyday interactions to another level.
Automated communications directly to your patients not only relieve your team of time-consuming tasks, but means you can quickly and effectively deliver appointment reminders, requests for feedback, marketing campaigns, and so much more with a simple click.
The security of your patient data is our highest priority, which is why Patient Bridge is completely GDPR compliant, but also protected in secure Microsoft Azure data
centres, which are fully audited and accredited by the NHS.

To learn more about building effective relationships with Patient Bridge, contact the Carestream Dental team today.
For more information on Sensei Cloud visit https://gosensei.co.uk/
For the latest news and updates, follow us on Facebook and Instagram @ carestreamdental.ukn
Selling a dental practice is a complex business. Dental Elite has all the specialist knowledge and dedication needed to support vendors through the whole process, from supporting them with the intricacies of complying with regulatory frameworks, to negotiating a great deal with buyers.
As Dr James Whitehead recently commented in a review: “Dental Elite handled the sale of my practice superbly from even before the sale went live. I was guided through every step and stage including the process of changing the NHS contract. They found me a really friendly couple to buy the practice, suggested a superb team of lawyers. All the while making sure momentum was
kept up. I would highly recommend Phil, Carl and their team to organise the sale of any practice.”
To find out how Dental Elite can support you with selling your dental practice, contact the team today!

For more information contact the Dental Elite team on 01788 545900 https://dentalelite.co.uk/ n
Complex endodontic re-treatment can be difficult to approach, especially when issues present after a previous root canal procedure.
For help getting your patients out of pain quickly and effectively, work with EndoCare. Our team includes a range of endodontic experts and specialists with advanced skills and experience in the field. We utilise evidence-based techniques and leading technologies to elevate the accuracy of our procedures.
As such, the team can address even the most advanced endodontic concerns and complications, ensuring your patient
receives the highest standard of treatment possible. Want to know more? Contact us today. For further information please call EndoCare on 020 7224 0999 Or visit www. endocare.co.uk n
In order to create a beautiful and resilient restoration with a straightforward workflow, clinicians should choose a highperformance composite which meets their patients’ needs.
BRILLIANT Crios from COLTENE combines all the advantages of an innovative submicron hybrid composite material with those of a CAD/CAM fabrication process. This offers reliability, aesthetics, and speed.
BRILLIANT Crios is the ideal choice for single tooth restorations in both the anterior and posterior region, including inlays, onlays, crowns, and veneers. Due to its shock absorbing properties it is also recommended for bruxism patients or implant supported crowns.
If you are looking for a solution which offers a broad range of uses in daily practice, visit the website to find out more or get in touch with the team today. For more information, info.uk@coltene. com and 0800 254 5115
COLTENE loyalty scheme https:// rewards.coltene.comn

Providing implant patients with the tools they need to maintain excellent oral hygiene following treatment is a great way to set them up for success and prioritise prevention.
Supplying patients with the Implant Kit from Curaprox is the perfect solution. It contains everything patients need to keep their implants clean.
For post-surgery care, the Kit contains a Curaprox Surgical Toothbrush, Perio plus Support toothpaste, a Perio plus Regenerate 0.09% or Forte 0.2% chlorhexidine mouth rinse, Perio plus Focus Gel, and a range of CPS interdental brushes in different sizes. And, for ongoing care it includes a CS5460 Ultra Soft
Toothbrush, CS708 Implant & Ortho brush, and long-handle interdental brush holder.
To find out more about the Kit, please contact the team at Curaprox.

For more information, please visit www.curaprox. co.uk and www.curaden.co.ukn
Eschmann engineers fix 91% of equipment issues during their first visit, demonstrating the quality of service delivered. The engineers are trained specifically on Eschmann equipment and carry original manufacturer’s parts in their vans as standard, meaning they can provide effective resolutions in a wide range of situations, quickly and efficiently.
The Eschmann team provides detailed enhanced CPD and product training to help practice teams look after their equipment. Not only does this reduce the risk of malfunctions, but it also prolongs the life of equipment.
Unlimited breakdown cover, parts and labour and Enhanced CPD training are all included in the Care & Cover servicing and

maintenance package from Eschmann. Care & Cover also includes annual service and software upgrades and on-site support from 50+ Eschmann engineers nationwide, as well as unlimited technical telephone support.
Find out more today!
For more information on the highly effective and affordable range of infection control products from Eschmann, please visit the website or call 01903 753322 n
Online learning offers convenience and flexibility for busy practitioners, but it’s important to be discerning to ensure it is of the best quality.
The IAS Academy offers excellent online education and support, delivered by the best trainers available in the field, that offer dental professionals an opportunity to learn at a time and a setting that suits them. Online learning enables delegates to spend as much time as they need with information, and has the benefit of a pause button when you need to take a break.

Find out more about the comprehensive range of top-quality online courses and webinars available today.
For more information on upcoming IAS Academy training courses, please visit the website or call 01932 336470 (Press 1) n
For example, the seemingly complex topic of occlusion is presented in an accessible and supremely practical way in Occlusion: Basics & Beyond, presented by Mahmoud Ibrahim and Jaz Gulati. This popular course offers the most tangible, real-world and comprehensive occlusion training available, and all at your own pace.
Consider the Griff Pac range from Initial Medical for solutions to help your practice fulfil its needs.
The Griff Pac containers are an eco-friendly solution for healthcare waste disposal, manufactured from lightweight corrugated polypropylene with an integral HDPE liner. This makes them brilliantly lightweight, cost-effective waste containers that are colour-coded to fit seamlessly with your waste disposal systems. A simple fold-flat design makes them easy to store before use, and their lining means they can handle both dry and some liquid waste, such as contaminated PPE, out of date medicines, suction tips and items that may puncture a clinical waste bag. Their design doesn’t just alleviate storage concerns; it also sees a 64% reduction in raw material carbon emissions and a 75% reduction in shipping carbon emissions versus standard rigid containers. This makes them an environmentally friendly and efficient option for your practice, aligning with the core principles of Initial Medical. The Griff Pac containers are available in a variety of colours, with options for clinical, infectious, anatomical and non-hazardous pharmaceutical waste. Plus, Initial Medical provides waste collection services, so we can manage your refuse when it is time to send it for onward disposal via recycling, incineration or landfill.

To find out more, get in touch at 0808 304 7411 or visit the website. n
Dental Elite delivers elite business services across the dental sector, using decades of specialist experience to meet the needs of dental practices.
As a leading dental recruiter, Dental Elite goes above and beyond to help dental practices put together their perfect team. The team works tirelessly to help talented dental candidates find the perfect fit.
Kahkshan Kanwal says in her recent review: “Huge thanks to Toni Robison for their support in finding a dental hygienist position! Their team is professional and efficient, connecting me with great opportunities. Highly recommend!”
Deeba Saaher adds: “Toni has been very helpful in my recruitment process. Immediate response and supportive with the entire hiring process. Thank you for all your efforts!”
More than a third of British adults now choose interdental brushes to clean in between their teeth rather than floss, so the products play a vital role in optimising gingival health and preventing oral disease.
The FLEXI interdental brush range from TANDEX is specifically designed to access interdental spaces and along the gingival margin. Their flexible grips enable patients to reach even difficult-to-access spaces at the back of the mouth.
The colour-coded brushes can be used to apply PREVENT GEL too, a product which contains 0.12% chlorhexidine and 900ppm fluoride known for their antibacterial and enamel strengthening properties.
To find out how the FLEXI range and PREVENT GEL can boost your patients’
Ensuring everyone receives the required support and guidance is our priority at Rodericks Dental Partners. Upon joining, each international dentist is allocated a dedicated mentor to assist them in practice day-to-day, providing personal guidance. Recognising the benefits of peer engagement, each new member has access to a large network of colleagues in similar situations, offering additional companionship and support.
All International Dental Graduates at Rodericks Dental Partners can enjoy discounted CPD to develop their skills further. Rodericks Dental Partners will cover 50% of fees for postgraduate training courses. This programme includes of a simple six step process to help meet requirements,
Finally, Shefali Patel says: “I have had the most pleasant experience with TONI. She is lovely and very helpful. She was very quick with responses and helped me reach out to different clinics by forwarding my CV to her friends and colleagues working as recruiters. I highly recommend Dental Elite to anyone looking for a job.”

To find your perfect fit, contact the team today!
For more information contact the Dental Elite team on 01788 545900 n

interdental cleaning visit the website today. For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from CTS Dental Supplies: https://www.cts-dental.com/ and DHB Oral Healthcare https://dhb.co.uk/n
Eschmann offers dental practices the choice between purchasing or leasing a range of industry-leading decontamination equipment. Which is best for you? That depends on your situation, as there are benefits to both. Purchasing outright means you own the equipment and, with proper care and support from Eschmann, can keep it operating efficiently for many years. Leasing may be more suitable if you have less capital to invest upfront and wish to spread the payment over time. This also allows you to either buy the equipment or upgrade to a newer model at the end of your lease agreement.
Whichever agreement you choose, rest assured that all Eschmann autoclaves, washer disinfectors and RO Water Systems are built
to last and make your daily workflows more efficient.

Plus, you can maximise the lifetime of your products with the Care & Cover servicing and maintenance package, offering exceptional support from 50+ Eschmann engineers, as well as Annual Validation and Pressure Vessel Certification (PSSR), annual service and software upgrades, unlimited breakdown cover, unlimited Eschmann parts and labour, and Enhanced CPD user training.
For more information please visit the webiste or call 01903 753322 n
Let’s face it, for some patients, regular flossing is simply too fiddly. So, to avoid plaque buildup, why not recommend to them a simple, easy-to-use tool for improved oral hygiene?
The Waterpik® Water Flosser is backed extensively by clinical research, demonstrating its efficacy in keeping the mouth clean and healthy. For example, studies show that the Waterpik® Water Flosser removes 99.9% of plaque biofilm after a 3-second application; it’s also over 50% more effective than string floss for reducing gingivitis. With only a minute of use, your patients can keep their interdental spaces clean and free of bacteria and plaque build-up.
To find out more, visit the website today.
For more information on Waterpik®Water Flosser products visit www.waterpik. co.uk. Waterpik® products are available from Amazon, Costco UK, Argos, Boots, Superdrug and Tesco online and in stores across the UK and Ireland. n
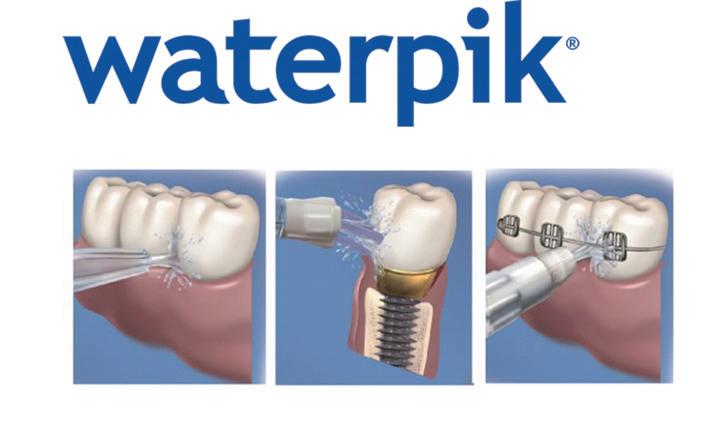
and a “Clinical Passport” to document their journey and development.

As Evripidis Tziokas, a Greek National, currently a Dental Graduate at Milehouse Dental Practice says: “You won’t find a better introduction to dentistry, anywhere. You have time to acclimatise to the system without UDA stress. It’s easy to find patients, and Rodericks Dental Partners don’t expect the world.”
Find out more about how Rodericks Dental Partners can be part of your professional journey. n
BDIA Dental Showcase provides an exclusive opportunity to engage with leading dental manufacturers and suppliers, with several organisations making this the only UK exhibition they attend all year.
SDI is one such organisation. Jayne Cahill, UK Sales Manager at SDI, said: “We’ve always supported the event and for us, it’s the most successful show. We speak to clinicians and we take orders – if you’ve got a new product to detail, this is the show to come to! We only attend one show a year, and our choice is always BDIA Dental Showcase so I would recommend anyone who hasn’t visited or exhibited to do so! To sum it up in one word, successful!”
Ideal for an associate setting up a practice! n Accelerate oral cancer detection in
Alone, smoking increases oral cancer risk by 10, and heavy alcohol consumption increases risk by a factor of five. Moreover, patients with alcohol dependency are three times more likely to smoke, and patients who are dependent on tobacco are four times more likely to be addicted to alcohol. As such, understanding a patient’s risk factors is essential in achieving better oral cancer outcomes. The next step is accurate pre-diagnostic assessments once lesions are identified. The BeVigilant™ OraFusion™ System from Vigilant Biosciences® helps providers speed up the detection of oral cancer by analysing clinical risk factors and identifying early-stage biomarkers found in saliva.

The non-invasive test is performed at the point of care and provides a result in 15 minutes or less.
For more information, please contact the team or visit the website.
For more information, please visit the website or email: info@vigilantbiosciences.comn

To make sure you have access to the greatest number of relevant dental organisations and industry experts at the largest London Show in 2025, don’t miss BDIA Dental Showcase and register at https://dentalshowcase.com/registerinterest-pr!
BDIA Dental Showcase 2025 14th-15th March, ExCeL London dentalshowcase.com n
(2 surgeries - 1 x for dentistry & 1 x surgical operations)
Customised cabinetry, scrub area, vast collection of oral surgery & implant instruments. Lab equipment, customised reception counter. Please note the inventory can be emailed. Please contact Dr Stowell to view:
Dr J Stowell
Mobile: 07734773748
woodvaleclinic@btinternet.com






















Over its 30-year history, the BORA turbine has continued to reaffirm the quality of its engineering. Its reliability and service life are self-evident. Because of the trust you have placed in it, we wanted to ensure that this legacy continues. The new design of the BORA 2 turbine provides even better performance, whilst retaining the legendary reliability which has characterised previous versions since 1991.
It was in late 2022 that I was writing about how to navigate the dental practice sales market in a recession. At that time, interest rates for buyers were rising, energy prices were increasing, buyers were being more cautious, lenders were becoming more cautious. In effect the market was rebalancing and becoming more of a buyer’s market than it had been in the past.
There was plenty of advice in the market from some respected quarters that vendors should delay in taking their practice to the market until these headwinds had subsided. That advice was fine for vendors who had time on their side. By that, I mean vendors who were not affected by the need to manage their debt, who are not near retirement age, and who do not have health or family matters demanding an injection of cash.
In March 2023, I wrote about how vendors could have more empathy with buyers in order to help them secure deals when buyers in the market were more cautious than they had been before. This was good advice and we saw vendors really changing their approaches and becoming much more collaborative in their approach to selling their practice.
All these factors combined, along with seeing valuations coming down, led
vendors to be cautious about bringing their practice(s) to market.
The key message I want to share with entrepreneurial dentists is that we are seeing the market pivot. We are seeing more investors willing to step in and buy the stock of practices we have for sale. Many of these investors are new to the market.
At a macro level, supply and demand always impacts a market. Inflation coming down to 2% and the bank rates being stable at 5.25% since July 2023 are all combining to change the mood of investors.
There is also a noticeable increase in activity from entrepreneurial micro corporates and startup investors. They are searching for sustainable practices that they can transform to great practices through organic growth and developing a healthy culture.
These investors are not buying indiscriminately simply to build EBITDA where the end goal is to sell to a body corporate.
I have observed more buyers entering the market with an entrepreneurial mindset. Recent headwinds have forced buyers into looking at ways of creating additional value in the practices they are targeting. These investor buyers are planning to stay in the market longer to build that value.
What we are seeing at a micro level is an increase in enquiries, viewings and offers on practices.
As just one example, we marketed and agreed a deal on a dental practice in March 2023. There were seven viewings and three offers. The deal never got to completion due to buyer caution.
We remarketed the same practice in early 2024. The practice was performing at the same level it was the previous year. Only, this time, there were 10 viewings and five competitive offers. These numbers may sound small but, when you contextualise them, you can see we have an uplift in viewings of 62.5% and an uplift in the number of competitive offers of 60%. This gives the vendor way more options, not just to get the best price with the best terms but also more choice of prospective purchasers to work with post sale.
There are seasonal trends in the market. The market does pick up in the spring of each year when the financial and NHS year end have concluded. However, the uptick in investor activity compared to last year is not simply down to that.
We have seen a 70% increase in buyer activity, resulting in more sales being agreed than in 2023. Anyone who pays attention to our website will see that our stock of practices for sale has gone down since its peak of 67 practices in July 2023.
In the highly competitive field of dentistry, where patient acquisition and retention are crucial for a practice’s success, call conversion plays a pivotal role. Call conversion refers to the process of turning incoming phone enquiries into scheduled appointments. For dental practices, improving call conversion rates can significantly impact revenue, patient satisfaction and long-term growth. We’re going to explore the importance of call conversion, some common challenges, and effective strategies to enhance this critical aspect of dental practice management.
understanding call conversion
Call conversion is a metric that tracks the percentage of incoming phone calls into your dental practice that result in booked appointments. This is vital because it directly correlates with a practice’s ability to attract and retain patients. A high call conversion rate shows that a dental practice effectively communicates its value to potential patients, while a low conversion rate suggests missed opportunities and potential revenue loss.
Despite its importance, many dental practices face challenges in optimising their call conversion rates. Common issues include:
• Missed Calls – High volumes of missed calls can result in lost opportunities. Practices often struggle with balancing patient care and answering phone calls during peak hours.
• Inefficient Call Handling – Without standardised procedures, call
handling can be inconsistent, leading to potential patients feeling undervalued or confused. The top three reasons patients don’t schedule appointments are, lack of attention, the receptionist didn’t listen, and that the caller felt rushed.
• Lack of Follow-Up – Failure to follow up with potential patients who did not immediately schedule an appointment can result in lost opportunities and lack of customer service. An effective system where you can record the details of any potential new patient, should be an essential part of your process.
• Poor Communication Skills – Your team may lack the necessary communication skills to effectively engage with callers and address these concerns.
Investing in comprehensive training programmes so your team can significantly improve call conversion rates. Training should focus on:
• Customer Service Excellence – teaching your team to provide a warm, welcoming and professional demeanour.
• Effective Communication – equipping team members with techniques to handle enquiries, objections and concerns efficiently.
• Appointment Setting – training your team on the importance of securing appointments and offering flexible scheduling options. call handling procedures Implementing call handling procedures ensure consistency and
Despite some of the negative press around NHS contracts, predominantly NHS practices in busy conurbations are still of real interest to the group buyers. Those investor buyers are offering between 6.5-7.0 x EBITDA.
The fact remains that NHS practices in rural and coastal locations have not seen renewed interest from investors. These practices can often be unattractive to investors because of workforce recruitment issues or the cost of retaining associate dentists is high.
For owner-operated practices where the transaction is dentist to dentist, multiples have remained stable over the last three years at 3.5 x adjusted net profit. What we are seeing is much more buyer confidence as well as different buyer profiles entering the market. Investors are confident their purchases will increase in value. Whilst I am cautious about predicting the future, we are optimistic. I invite you to get your practice valued in order to get a handle on whether you share my optimism. n
about the author abi Greenhough, Managing Director of Lily Head Dental Practice sales.

professionalism in every interaction. Procedures should include:
• Standardised Scripts – providing your team with scripts for common enquiries to ensure clear and consistent communication. But not have staff read off a sheet, as this can sound false.
• Personalised Responses –encouraging the team to personalise interactions based on a caller’s needs and concerns. A lot of potential patients will be phobic and will need a little care, compassion and attention in order for them to move forward with their treatment.
• Information Delivery – ensuring your team can provide detailed and accurate information about services and appointment availability.
Technology and tools
Leveraging technology can enhance call handling efficiency and effectiveness. Essential tools include:
• Advanced Phone Systems – utilising phone systems with call tracking, recording and analytics capabilities to monitor and improve performance.
• Customer Relationship Management (CRM) Software – implementing CRM software to manage patient information, track interactions and follow up on enquiries.
• Automated Reminders and Follow-Ups – using automated systems to send appointment reminders and follow-up messages to potential patients. enhancing availability Improving availability can reduce missed calls and increase conversion rates.
Strategies include:
• Extended Office Hours – offering extended hours or weekend availability to accommodate patients’ schedules.
• After-Hours Services – implementing after-hours call handling services or answering services to capture enquiries outside regular office hours.
• Online Scheduling – providing an online appointment scheduling option to cater to patients who prefer digital interactions.
best practices for call conversion
• Prompt Response – aim to answer calls within three rings or 30 seconds to reduce the likelihood of missed calls.
• Accurate Documentation – collect and document patient information accurately to ensure follow-up and personalised care.
• Clear Communication – provide clear and detailed explanations of services, pricing and appointment procedures.
• Flexible Scheduling – offer convenient appointment times and flexible scheduling options to meet patient needs.
• Proactive Follow-Up – follow up with potential patients who did not schedule immediately to reinforce interest and address any lingering concerns. n
about the author John Gow, account Manager at connectmymarketing.com

Before I came to work for Denplan to guide the clinical services team and share my compliance and clinical knowledge, I spent almost 20 years as a dental nurse and practice manager. I can still clearly see myself in my practice, sat in my stuffy, windowless office, surrounded by file upon file of policies and procedures, logbooks, and risk assessments that needed to be completed. My ever-growing to-do list weighed on me, and I remember wondering if the compliance treadmill would ever ease.
At some point, you have probably experienced this feeling too. Finishing up an extremely busy day in clinic only to be met with questions from the team: “When you have a moment can you…” “I know you’re about to leave but can you just…”.
This is why it’s essential to create a culture of compliance within dental teams, where the responsibility rests upon everyone’s shoulders. Not only does this maintain patient safety and uphold ethical standards, but it’s also essential for your mental wellbeing. But how do you create such a culture? Let’s explore…
Leadership plays a critical role in shaping any culture, with leaders establishing their expectations by actions and words. When a leader prioritises compliance, the team will follow. Leading by example will demonstrate adherence to the processes and regulations, and staff members will observe this behaviour and emulate their leader. As with all cultures, communication is key. As a leader you will be looked to, to provide clear guidance and support on what the compliance requirements are, explain policies in detail, listen to and address your team’s concerns. Whilst daunting, leaders will hold their team accountable for compliance, and this consistent approach will reinforce the importance of following the practice procedures.
Alongside a consistent approach to compliance comes education and training. Leaders can facilitate training sessions and provide ongoing education. Not only will this assist in the adoption of a compliance culture, but it will showcase investment in the team’s development, and increase their awareness and understanding of compliance.
But what about the team members? They may be unsure about the regulations, policies and ethical guidelines that are encased in that dreaded word, ‘compliance’. Here is where staff education and training shine. Regular, formal, and indeed informal, training, both in house and online, on aspects such as infection control, record keeping, risk assessment, audits, and other critical areas, will provide a foundation for them to feel more knowledgeable and comfortable completing the tasks asked of them. It can be helpful to embed compliance tasks into our team’s daily routine. A good example of this would be a COSHH assessment that requires reviewing. Your team may very well be using that material during their day, so ask them to check the assessment is current and correct. This not only heightens awareness
of compliance but also serves as training on document importance. Using checklists can also be helpful to ensure there’s a consistent approach to practice protocols. Could they perhaps carry out a daily audit in the surgery, so that results can be collated with ease at the six-month point? Not only will this highlight errors, but it can also help to rectify them quickly and efficiently. You can address misconceptions by sharing myth busting articles and communicate openly about the compliance expectations and consequences. Asking your team members to complete compliance tasks must come with the reassurance that they can report potential issues they may have come across without fear of reprisal. And, most importantly, celebrate success in their achievements in maintaining the practice compliance. When creating a culture of compliance, you will need to communicate to your team the reasoning behind the change, always embracing transparency. You aren’t just doing it to make your life easier; you see it as collaboration at its finest, bringing the team together and sharing the sense of achievement. Share your vision of the compelling benefits to the patients, practice, and team, whilst ensuring that you listen to the feedback supplied to you. Actively engaging the team in the change of process by seeking their input will make them feel valued and create a real sense of ownership for the individuals.
For me, the thought of handing over the compliance reins to my team was extremely daunting. I had spent a lot of time ensuring that all the policies and procedures were in place and reviewed as appropriate. All the risk assessments and audits were complete with clear action plans, all t’s crossed, and i’s dotted. I would go so far as to say the fear of not being in control was very real. However, I had carried out training sessions with my team, explained my expectations (and those of the regulators), identified the team’s strength areas as well as considering what areas they found of interest, and began delegation. Of course, for the first six months I kept a close eye on the different areas I had tasked them with, but I needn’t have worried. If ever there were concerns or questions, they always approached me for guidance and clarification of the next steps.
I saw my team begin to converse more around practice compliance, sharing “did you know…” and asking for one another’s input before approaching me. Implementing a culture of compliance gave them a sense of empowerment over other areas, not just in surgery or reception, allowing them to be subject matter experts in their allocated field of compliance and educate other members of the team.
My compliance treadmill had ceased. n
What do you do if you’ve found a practice but have no idea if the price is right, or even if the financial calculations you have been given are correct? Here’s how a valuation ahead of buying a dental practice can help you:
1. accurate assessment of value
To be accurate, a practice valuation should be based on the current income, current staff costs, current associate and hygienist/therapist costs, and standard expenditure from the latest set of accounts. It should not rely on historical data e.g. staff costs from previous accounts, or proposed future income. A valuation is the perfect time to obtain all current information. Two EBITDA (earnings before interest, tax, depreciation and amortisation) models will then be calculated (Associate Led and Principal Led), to show projected profit for a new owner.
An experienced dental practice valuer will be able to identify where costs may be too low to maintain, unwarranted costs have been removed, or if the best set of accounts have been used when the practice was valued for the seller.
A practice valuation is a detailed financial analysis that cannot be done thoroughly from just the last three years’ accounts. In an ever-changing market, only an advisor with daily experience in dental practice sales has the knowledge to ensure that you are not paying above market value for a practice.
2. identify strengths and weaknesses
Within a valuation, a valuer will highlight any areas that may need your attention as a new owner. Perhaps the practice is currently understaffed, and an additional nurse is needed to provide sufficient holiday and sickness cover. Or maybe the practice is overstaffed, and you will need to make redundancies to ensure continued profitability. It could even be as simple as the valuer advising that lab costs are higher than average, and you may wish to change provider.
Equally, the valuer may comment that everything at the practice is working great and that this isn’t a practice to miss out on.
about the author
Lianne scott-Munden, clinical Quality and complaints Risk Manager at Denplan.

Should your valuation come back lower than the seller expects for the practice, you will have a full report from an experienced practice valuer that clearly explains how the value has been calculated. With this, you can discuss each point with the seller to hopefully come to an agreement on price.
Conversely, the practice valuation may come back higher than the asking price. In this case, you can proceed with assurance that you are buying
well, hopefully being able to secure your dream practice with renewed confidence in its value.
4. financial planning and bank funding
A valuation will give you an open market assessment of the practice and the projected profit under both an Associate Led and Principal Led model. However, you will still need to factor in your personal costs, e.g. tax and loan repayments, to determine what you will have left to live on. Having a valuation ahead of personal projections will save you time and money in calculating this.
A valuation report provides the necessary financial information required by lenders to assess the viability of providing a loan for your proposed purchase. With high interest rates making borrowing tighter for buyers, being able to provide a lender with clear workings of the projected profit can often speed up the process to obtain a loan offer.
5.
As soon as your offer is accepted on a practice you will start to incur costs – a deposit, legal fees, and bankinstructed valuation are usually the first of these.
A bank valuation now costs in the region of £2,000-£3,000 and marks a crucial point in your purchase. The bank will only lend based on the value provided by their panel valuer. Therefore, should the valuation come back significantly lower than your offer, you would either need to reduce your offer for the practice, or make up any difference in cash. Should the seller choose not to accept a reduced offer and proceed with another buyer, you won’t be able to recoup the funds spent on the failed purchase. Having your own valuation ahead of the bank instructed valuation could therefore highlight potential issues in advance and save you thousands in lost fees. We know buying a dental practice is a big step. That’s why we work daily with buyers to ensure they have the information they need to proceed with confidence, in turn helping sellers find committed buyers. Contact PFM Dental Sales & Valuations to instruct your purchase valuation on 01904 670820 or email sales@pfmdental.co.uk. n
about the author s amantha Hodgson is a finance broker and practice valuer. P f M Dental are leading professional advisers to dentists for: sales and valuations of dental practices, financial advice, legal and accountancy services.


















Guests join us from all areas of the industry to provide their own unique perspectives on a wide range of topics, from manufacturers and figureheads of various dental organisations, to those in the trenches working in practice, and more.














































Nothing is off limits in The Probe Dental Podcast, so be sure to tune in wherever you get your podcasts! The Probe Dental Podcast features discussions that explore all areas of the British dental sector.














For more information, sponsorship opportunities or to book a podcast please contact














Dr James Whitehead qualified in London in 1989 at Guy’s Hospital, and remained there as a house dental surgeon in the maxillofacial surgery department for a short time before practicing in Uckfield as an associate for four years.
He joined the dental team at Elm House Dental Practice, based in West Sussex, buying it from the previous principal in 1999, together with his wife. After many years, both Dr Whitehead’s partner and a well-established associate left the practice. “That, and turning 60 this year, made me think about selling, but it wasn’t a fire sale,” he says. “I dipped my toe in the market for three or four years before making a decision. I wanted to make sure it was going to work for me.”
Being happy with his work and the practice, he was in no hurry to leave. “About eighteen months ago I had a valuation, and the price was right. The opportunity fit with the first stage of my retirement plan, so I was ready to set it all in motion.”
Finding the right buyer
“Initially I had hoped to sell the practice to my new associate. I really didn’t want to leave anyone in the lurch, as selling can
spell real trouble for associates. I didn’t want to do that to anyone, but he wasn’t keen on buying at the time.”
“To get the kind of deal that worked, I assumed I’d end up having to sell to a corporate,” says Dr Whitehead, but Dental Elite steered him in the right direction for a deal that worked in terms of pricing, but also for him and the team. “I was concerned at first that I wouldn’t get the price that I was hoping for, but thankfully that all went well. Luckily the couple who bought the practice also wanted to keep both me and my associate on. I was really happy to stay.” says Dr Whitehead. “I’ve been here for 25 years now, and I’ve agreed to stay on for at least three more years. After the three years are up, I just have to give six-month’s notice if I want to leave. I might well carry on longer – it all feels really good at the moment. I really like my job!”
Behind-the-scenes negotiations
“I went with HCR Law, a firm of solicitors recommended by Dental Elite, and they were absolutely fantastic,” says Dr Whitehead. “I actually liked them so much my family and I have taken them on to help with the sale of our house!”
“Unfortunately, the buyer’s solicitors were slow to issue the request for due diligence, which could have presented huge problems. The process is already time-consuming,” says Dr Whitehead. “There are quite a lot of detailed questions, and filling out all the paperwork alongside a busy practice was quite gruelling at times. Thankfully, Dental Elite were there to help keep everything moving, and they smoothed it all out for me. It was tough, but there were no negative consequences in the end, apart from an unavoidable delay to the completion date.”
Dr Whitehead was particularly grateful to Dental Elite for their assistance with changing the NHS contract. He had anticipated that this process might be a difficult one, until Dental Elite simply presented him with a document to sign, having sorted it all out behind the scenes. “That was it! It all happened so smoothly I hadn’t even realised it was happening. It was completely painless”, he says.
Highly recommended Dr Whitehead got talking to Phil Kolodynski, Director of Practice Sales Dental Elite Team, at an event. “I first came across Dental Elite by accident. I think it was a chance encounter at

a post-graduate meeting. I was really impressed, and we stayed in contact.
“Phil listened really well, and offered me instantly useful advice on the kinds of clients that might suit my practice. He’s the one that came through with the valuation that gave me the confidence to go ahead and press the button to get the sale going.”
“I can’t recommend them highly enough! In fact, I’ve already recommended them to a friend, who is just getting ready to sell their practice and is using them right now. That’s in the pipeline now and it all looks promising.”
For more information on Dental Elite visit www.dentalelite.co.uk, email info@dentalelite.co.uk or call 01788 545 900

Pension planning is a fundamental part of financial management that it pays to get right. The choices you make now can be extremely rewarding in the future, but many dental professionals may feel inundated with choice for pension schemes and solutions.
A stakeholder pension is one of these options, arguably the most well-known. It is a type of personal pension that is subject to specific government-imposed requirements, such as limits on charges. Some employers offer them, and you can also start one for yourself, but it’s important to understand whether it is an optimal solution for you.
The key features of a stakeholder pension are the low and flexible minimum contributions, and the legal cap on charges – 1.5 per cent a year of the value of your pension for the first decade, then 1 per cent each year. You can also stop and re-start your contributions at any time without a penalty, and they will be placed into a default investment fund if you don’t want to make any decisions on this front.
A stakeholder pension can make contributions simpler for many dental professionals, and you may be able to benefit from the limited charges. These were once some of the best options available, but now some pension funds may have even lower charges. The margin
by which a pension fund subceeds these charges is a key feature to consider.
How is your pension invested?
Another key differential between the variety of stakeholder pensions available will be their chosen investment funds. A default investment option will likely be a ‘lifestyle’ or ‘target date’ fund. These consider your expected retirement age, and change their investment choices accordingly.
When you are younger your contributions may be placed into ‘riskier’ investments – for example, company shares that are likely to see growth over time, but can fluctuate heavily in the short-term. As you reach retirement, your investments will shift to more stable assets such as bonds and cash deposits. These aren’t risk free, but may offer greater stability as you edge closer to retirement.
You may be open to assessing other options for yourself. If you don’t want to choose a default fund, but you don’t feel confident in identifying an alternative fund that will serve your contributions well, speaking with a financial advisor who is knowledgeable in the field is ideal.
Being tax efficient
Another attractive aspect of a stakeholder pension is the tax efficient advantages it offers. There is no upper limit on the amount you can pay into the scheme, but you receive a tax relief of up to 100% of
your earnings, with an annual allowance capped at £60,000.
Your contributions are entitled to immediate income tax relief at 20%. For every £80 you pay into your stakeholder pension, you will accumulate £100 in the pot. HM Revenue and Customs allow Higher Rate Tax payers to claim up to 40% tax relief directly from them.
However, above the tax relief annual allowance ceilings of £60,000, excess investments may no longer be tax efficient.
To better understand how to utilise a stakeholder pension, and whether it is an optimal solution for you as a dental professional, consider speaking to expert independent financial advisers.
The money4dentists team have these in abundance, with decades of experience solely working with dental professionals, ensuring they understand the unique financial situations of clinicians. Since merging with the talented team at Ruby Financial, they are even better equipped to help find the most efficient pension solutions for you.
The stakeholder pension is always an option dental professionals should consider, and with an in-depth understanding of how it could work for you, you will be able to make effective investment choices.
For more information, please call 0845 345 5060 or 0754DENTIST.
Email info@money4dentists.com or visit www.money4dentists.com


We’re a specialist dental practice sales agency, so whether you are looking to sell your dental practice on the open market, selling to your associate or intrigued with Corporate interest, we’ve helped thousands of dentists like you.
You cannot be in better hands with our expert valuers, a single point of contact throughout the sale and in-house legal team, allowing us to

We work with dentists all over the UK
Our scale and reach means we’re here to help wherever you’re based
Practice sales over the past 12 months 50+
Current dental accountancy clients 1200+
Practice finance raised in the last year £15m+





Accurate valuations for associate & principal led models with advice on enhancing the practice value.

advise you from start to finish. Supportive Throughout
We liaise with solicitors, buyers, and CQC to ensure everything is in place to minimise stress and give a smooth sale.

Get access to 1000s of pre vetted purchasers, being individuals, small groups and all of the major corporates.

We have specialist dental solicitors with expertise in commercial law, property law, and CQC processes.

We will ensure your practice attracts the best possible price by negotiating the sale on your behalf.

Fee Free Sale
95% of our NHS practices sell to priority buyers meaning the purchaser covers the agency fee.

Award-winning TRIOS technology distilled down to its most essential and affordable form. That’s TRIOS Core. Accurate, fast and easy, for a great send-to-lab experience.